User login
How well do physician and patient visit priorities align?
ABSTRACT
Purpose We undertook this study to explore the factors associated with differences between patients’ stated main reasons for outpatient visits and physicians’ main concerns at those same visits.
Methods This cross-sectional, mixed-methods study examined 192 outpatient visits with 4 physicians at 4 diverse primary care practices. During each visit, participating physicians elicited the patient’s main reason for the visit. Immediately after each visit, physicians documented 1) their understanding of the patient’s stated reason and 2) their main concern for the patient during that visit, and 3) assessed the extent of their alignment with the patient’s reason for visit. We assessed bivariate and multivariable associations of patient and visit characteristics with alignment, and further examined cases with unaligned physician-patient priorities to identify patterns.
Results In 69% of visits, the patient’s stated reason for the visit was completely aligned with the physician’s main concern. In 12% of visits, we observed totally unaligned priorities; 19% were only partially aligned. Uninsured or publicly-insured patients and visits with more problems addressed were less likely to be fully aligned. In many visits with unaligned priorities, patients’ stated reason for the visit was a self-limiting, symptomatic concern while physicians prioritized potentially dangerous asymptomatic conditions or ill-managed chronic conditions.
Conclusions In diverse family medicine practices, lack of alignment between physician and patient visit priorities reflects differing prioritization processes. Patients presenting with concerns unaligned with their physician’s priorities may require more time or different approaches to ensure the relevance and patient-centeredness of their care. These findings may inform the design of systems of care that promote mindful attention to patients’ priorities while addressing medically urgent or preventive services delivery.
T oday’s family physicians must balance patient’s acute concerns with chronic disease management, health promotion, and disease prevention. It’s not easy. As the content of outpatient visits expands and available time contracts,1 patients’, clinicians’, and payers’ agendas compete for attention. From a patient experience perspective, the health care encounter may seem diminished when guideline-driven agendas championing chronic disease management and preventive service delivery appear to take precedence over their personal concerns.2-4
In the matter of physician-patient alignment of visit priorities, prior research5,6 inadequately reflects current practice realities such as increased time pressure,7 greater chronic disease prevalence,8 growing expectations for preventive care,1 and increasing physician proactivity in longitudinal care.9-12 With so much to do and so little time and mounting pressure to deliver patient-centered care and patient satisfaction, it would be helpful to have a better understanding of how often and with whom physicians choose to depart from a patient’s explicitly stated reasons for a visit and instead prioritize other concerns.
We sought to examine alignment between patients’ stated main reasons for a visit as understood by the physician and the physician’s main concern during that same visit. Using a diverse sample of family physician-researchers to serve as data collectors and analysts, this study aimed to identify patient and visit characteristics associated with differing physician-patient visit priorities.
METHODS
Study design and sample
Four family physicians participating in a research fellowship undertook this cross- sectional descriptive study of a sample of their outpatient encounters. Each physician’s practice was unique: a free clinic, an inner city family practice within a teaching hospital, a geriatric home visit practice, and a suburban pediatric practice. Using the card study method pioneered by the Ambulatory Sentinel Practice Network,13,14 physicians collected observational and reflective data on a sample of 50 consecutive patients seen at his or her primary care practice. The University Hospitals Case Medical Center Institutional Review Board approved the study protocol.
Measures
Immediately following each patient visit, physicians recorded on a standardized data card the patient’s characteristics, visit characteristics, the reason for the visit provided to the office staff, the reason for visit reported by the patient at the beginning of the visit, and the physician’s own main concern for the patient during the visit. Patient characteristics included gender, age, race, type of insurance, and number of chronic conditions on the problem list. Visit characteristics included the total number of problems addressed, whether a second person (eg, family member, caregiver) was present in the exam room during the visit, and visit duration. To elicit the patient’s reason for the visit, physicians systematically asked, “How can I help you today?” If more than one problem was elicited from this prompt, the concern expressed as most important by the patient was noted.
In completing the data card, physicians also reflected on the extent to which the patient’s stated reason for the visit aligned with their own main concern for the patient during the visit, rating the relationship between their respective priorities as fully aligned, partially aligned, or totally unaligned. Visits were considered fully aligned if the patient’s reason for the visit and the physician’s concern were the same, or if the patient’s expressed concern was determined to be a symptom related to the physician’s main concern. Partial alignment occurred when the patient’s concern was shared by the physician but was not the physician’s main concern. Visit priorities were rated as totally unaligned if patient and physician concerns were different and determined not to be medically related.
Data analysis
We computed descriptive statistics and performed bivariate tests of association between physician-patient alignment of priorities and patient/visit characteristics, using chi-square statistics for categorical variables and analysis of variance (ANOVA) for continuous variables. We used logistic regression analysis to identify characteristics independently associated with either partially aligned or totally unaligned visit priorities, vs fully aligned priorities.
To better understand the unaligned cases, the study team examined all of the data cards identified as either only partially aligned or totally unaligned and categorized the nature of the disparate prioritization in each case. Study team members (PT, AW, MR, and PDG) individually reviewed and sorted the cards into similar observed patterns and wrote brief descriptions of those patterns. The group refined the preliminary descriptions of the overarching patterns and selected several cases to represent the patterns.
RESULTS
Quantitative findings
We collected data on 192 patients (TABLE 1). Median patient age was 47. Median number of prescription medications and chronic medical conditions were 3 and 2, respectively. Most patients (80%) primarily spoke English, 58% were female, and 59% were Caucasian. Insurance status was equally distributed among patients: 33% held private insurance, 33% had public insurance, and 34% were uninsured.
The majority of cases showed physician- patient priorities that were fully aligned (69%); only 12% were totally unaligned. TABLE 1 shows the associations between level of alignment and patient and visit characteristics. Patients whose expressed reason for their visit was less than fully aligned with their physicians’ primary concern were more likely to be older, with more chronic conditions, of Hispanic ethnicity, and either publicly insured or uninsured. Patients with some degree of unaligned concerns also tended to have greater numbers of prescribed medications and had a primary language other than English. Unaligned visit priorities were also observed more often when greater numbers of problems were addressed during the visit. Patients familiar to the physician were also more likely to express a reason for their visit that differed in some way from the primary concern of their family physician.
Multivariable logistic regression analyses showed that having more problems addressed during a visit and being publicly insured or uninsured (compared with having private insurance) were each independently associated with less than fully aligned visit priorities (indicated by § in TABLE 1).
Qualitative findings
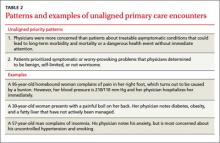
Cases classified as partially or totally unaligned showed 2 main patterns that reflect differences in the ways that patients and physicians prioritize problems. First, when physician priorities were unaligned with the patient’s stated reason for a visit, physicians typically focused on treatable, asymptomatic conditions that could lead to long-term morbidity and mortality or, absent immediate attention, to a dangerous event. Examples include chronic disease management (eg, hypertension, diabetes, asthma) and disease prevention (eg, smoking cessation, cholesterol level monitoring, cardiac disease risk reduction). Second, in those visits that were unaligned, patients tended to show more initial concern about symptomatic problems (eg, skin rash, upper respiratory infection) that would likely resolve with minimal or no medical intervention. Most of these conditions were determined by the physician to be benign, self-limited, or not worrisome (TABLE 2).
DISCUSSION
This study examined the alignment between a patient’s stated reason for a visit and the physician’s main concern. Physician-patient alignment was common, with 69% of visits showing full alignment between the patient’s reason for the visit and the physician’s main concern. While this rate is higher than that seen in prior studies,5 our method for data collection uniquely reflected how information actually is elicited and received during outpatient encounters, which likely yielded more accurate results. Also, in contrast to past approaches, our study equated patients’ symptoms to the underlying diagnosis for purposes of determining alignment.
Similar to previous studies, alignment between patient and physician concerns was less likely when the number of items addressed during the visit increased.5,6 Interestingly, physician-perceived time pressure during the visit and lack of an established patient-physician relationship were not observed to influence alignment. When time is limited, physicians may choose to prioritize the patient’s verbalized concern to avoid more complex negotiations about the agenda. In addition, during an encounter with an unfamiliar patient, prevention and chronic illness care may be deferred until the relationship becomes established.15-18
Patient insurance status was also observed to influence alignment. This finding could reflect socioeconomic or access issues among uninsured or publicly-insured patients that contribute to more complex visits.19-21 To shed further light on this finding, further research is needed that includes indicators of education or income and that separately examines Medicaid vs Medicare enrollees.
Possible study weaknesses. A potential weakness of this study is that alignment was rated by the physicians who elicited and recorded their patients’ reasons for the visit. It is possible that the central role of the physician as observer and analyst may have introduced bias and that an outside observer may have come to different conclusions about the extent to which priorities were aligned. However, by placing the physician-researcher at the center of both data collection and analysis, our study method reflects the realistic constraints of limited information on the processes of clinical discovery and sense-making that physicians regularly undertake with their patients, which we believe to be a strength of this study. While the inclusion of pediatric visits in the sample is another possible weakness, we believe that the diverse clinical settings and diverse patient populations potentially strengthen the findings. Replication with different samples of clinicians and patients is needed to assess the robustness of the findings.
Root differences in physician and patient perspectives. Collectively, these findings suggest that patients’ and physicians’ differing approaches to prioritization may limit alignment. In general, physicians tend to evaluate the full scope of the patient’s health and risk factors for future disease, while patients more often focus on symptomatically troublesome—though often self-limiting— conditions. Physicians have the knowledge and clinical experience to prioritize or deprioritize patient concerns based on an assessment of long-term risks of morbidity and mortality, yet the future-orientation of treatments and surveillance for insensible conditions (like hypertension) is less likely to align with the immediately painful or worrisome symptoms of patients. This highlights the importance of patient education on chronic disease management and disease prevention, and cooperative agenda-setting. Further work needs to be done to examine the differences in patients’ and physicians’ cognitive processes of prioritization, with the ultimate goal of providing patient-centered care through shared decision-making.
Take-home messages for all stakeholders. Amidst growing time pressures and guideline-driven protocols for care, it is important to attend to the intersecting and diverging patient, physician, and payer agendas that drive the content of the visit. Patients who are less likely to share the physician’s prioritization of their concerns—including individuals with no insurance or public insurance and those with multiple medical problems—may require more time and additional effort on the part of the physician to create a mutually acceptable agenda for the visit. Attempts at pay-for-performance should consider patients’ priorities and preferences for care, particularly when those preferences differ from the priorities of physicians or health insurance plans. A more thorough understanding of patient and physician prioritization during primary care visits could potentially guide the organization of outpatient care and inform the mindful physician’s patient-centered practice to maximize patient benefit.
CORRESPONDENCE
Susan A. Flocke, PhD, Family Medicine Research Division, Case Western Reserve University, 11000 Cedar Avenue, Suite 402, Cleveland, OH 44106; [email protected]
ACKNOWLEDGEMENTS
This study was completed as part of the culture of inquiry fellowship, supported by Academic Administrative Units in primary care Grant #D54HP05444 from the Health Resources and Services Administration, US Department of Health and Human Services. Dr. Stange’s time is supported in part by a clinical research professorship from the American Cancer Society.
1. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
2. Weyer SM, Bobiak S, Stange KC. Possible unintended consequences of a focus on performance: insights over time from the research association of practices network. Qual Manag Health Care. 2008;17:47-52.
3. Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med. 2008;6:228-234.
4. Casalino LP. The unintended consequences of measuring quality on the quality of medical care. N Engl J Med. 1999;341:1147-1150.
5. Friedin RB, Goldman L, Cecil RR. Patient-physician concordance in problem identification in the primary care setting. Ann Intern Med. 1980;93:490-493.
6. Boland BJ, Scheitel SM, Wollan PC, et al. Patient-physician agreement on reasons for ambulatory general medical examinations. Mayo Clin Proc. 1998;73:109-117.
7. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065.
8. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209-214.
9. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511-544.
10. Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4:12-25.
11. Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q. 2001;79:579-612,iv-v.
12. Wagner EH, Bennett SM, Austin BT, et al. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11(suppl 1):S7-S15.
13. Green LA. The weekly return as a practical instrument for data collection in office based research. Fam Med. 1988;20:182-184.
14. Green LA, Reed FM, Miller RS, et al. Verification of data reported by practices for a study of spontaneous abortion. Fam Med. 1988;20:189-191.
15. Ettner SL. The relationship between continuity of care and the health behaviors of patients: Does having a usual physician make a difference? Med Care. 1999;37:547-555.
16. Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004;36:22-27.
17. Blewett LA, Johnson PJ, Lee B, et al. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. 2008;23:1354-1360.
18. Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(8 suppl):AS21-AS30.
19. Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061-2069.
20. Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79:1139-1147.
21. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443-494.
ABSTRACT
Purpose We undertook this study to explore the factors associated with differences between patients’ stated main reasons for outpatient visits and physicians’ main concerns at those same visits.
Methods This cross-sectional, mixed-methods study examined 192 outpatient visits with 4 physicians at 4 diverse primary care practices. During each visit, participating physicians elicited the patient’s main reason for the visit. Immediately after each visit, physicians documented 1) their understanding of the patient’s stated reason and 2) their main concern for the patient during that visit, and 3) assessed the extent of their alignment with the patient’s reason for visit. We assessed bivariate and multivariable associations of patient and visit characteristics with alignment, and further examined cases with unaligned physician-patient priorities to identify patterns.
Results In 69% of visits, the patient’s stated reason for the visit was completely aligned with the physician’s main concern. In 12% of visits, we observed totally unaligned priorities; 19% were only partially aligned. Uninsured or publicly-insured patients and visits with more problems addressed were less likely to be fully aligned. In many visits with unaligned priorities, patients’ stated reason for the visit was a self-limiting, symptomatic concern while physicians prioritized potentially dangerous asymptomatic conditions or ill-managed chronic conditions.
Conclusions In diverse family medicine practices, lack of alignment between physician and patient visit priorities reflects differing prioritization processes. Patients presenting with concerns unaligned with their physician’s priorities may require more time or different approaches to ensure the relevance and patient-centeredness of their care. These findings may inform the design of systems of care that promote mindful attention to patients’ priorities while addressing medically urgent or preventive services delivery.
T oday’s family physicians must balance patient’s acute concerns with chronic disease management, health promotion, and disease prevention. It’s not easy. As the content of outpatient visits expands and available time contracts,1 patients’, clinicians’, and payers’ agendas compete for attention. From a patient experience perspective, the health care encounter may seem diminished when guideline-driven agendas championing chronic disease management and preventive service delivery appear to take precedence over their personal concerns.2-4
In the matter of physician-patient alignment of visit priorities, prior research5,6 inadequately reflects current practice realities such as increased time pressure,7 greater chronic disease prevalence,8 growing expectations for preventive care,1 and increasing physician proactivity in longitudinal care.9-12 With so much to do and so little time and mounting pressure to deliver patient-centered care and patient satisfaction, it would be helpful to have a better understanding of how often and with whom physicians choose to depart from a patient’s explicitly stated reasons for a visit and instead prioritize other concerns.
We sought to examine alignment between patients’ stated main reasons for a visit as understood by the physician and the physician’s main concern during that same visit. Using a diverse sample of family physician-researchers to serve as data collectors and analysts, this study aimed to identify patient and visit characteristics associated with differing physician-patient visit priorities.
METHODS
Study design and sample
Four family physicians participating in a research fellowship undertook this cross- sectional descriptive study of a sample of their outpatient encounters. Each physician’s practice was unique: a free clinic, an inner city family practice within a teaching hospital, a geriatric home visit practice, and a suburban pediatric practice. Using the card study method pioneered by the Ambulatory Sentinel Practice Network,13,14 physicians collected observational and reflective data on a sample of 50 consecutive patients seen at his or her primary care practice. The University Hospitals Case Medical Center Institutional Review Board approved the study protocol.
Measures
Immediately following each patient visit, physicians recorded on a standardized data card the patient’s characteristics, visit characteristics, the reason for the visit provided to the office staff, the reason for visit reported by the patient at the beginning of the visit, and the physician’s own main concern for the patient during the visit. Patient characteristics included gender, age, race, type of insurance, and number of chronic conditions on the problem list. Visit characteristics included the total number of problems addressed, whether a second person (eg, family member, caregiver) was present in the exam room during the visit, and visit duration. To elicit the patient’s reason for the visit, physicians systematically asked, “How can I help you today?” If more than one problem was elicited from this prompt, the concern expressed as most important by the patient was noted.
In completing the data card, physicians also reflected on the extent to which the patient’s stated reason for the visit aligned with their own main concern for the patient during the visit, rating the relationship between their respective priorities as fully aligned, partially aligned, or totally unaligned. Visits were considered fully aligned if the patient’s reason for the visit and the physician’s concern were the same, or if the patient’s expressed concern was determined to be a symptom related to the physician’s main concern. Partial alignment occurred when the patient’s concern was shared by the physician but was not the physician’s main concern. Visit priorities were rated as totally unaligned if patient and physician concerns were different and determined not to be medically related.
Data analysis
We computed descriptive statistics and performed bivariate tests of association between physician-patient alignment of priorities and patient/visit characteristics, using chi-square statistics for categorical variables and analysis of variance (ANOVA) for continuous variables. We used logistic regression analysis to identify characteristics independently associated with either partially aligned or totally unaligned visit priorities, vs fully aligned priorities.
To better understand the unaligned cases, the study team examined all of the data cards identified as either only partially aligned or totally unaligned and categorized the nature of the disparate prioritization in each case. Study team members (PT, AW, MR, and PDG) individually reviewed and sorted the cards into similar observed patterns and wrote brief descriptions of those patterns. The group refined the preliminary descriptions of the overarching patterns and selected several cases to represent the patterns.
RESULTS
Quantitative findings
We collected data on 192 patients (TABLE 1). Median patient age was 47. Median number of prescription medications and chronic medical conditions were 3 and 2, respectively. Most patients (80%) primarily spoke English, 58% were female, and 59% were Caucasian. Insurance status was equally distributed among patients: 33% held private insurance, 33% had public insurance, and 34% were uninsured.
The majority of cases showed physician- patient priorities that were fully aligned (69%); only 12% were totally unaligned. TABLE 1 shows the associations between level of alignment and patient and visit characteristics. Patients whose expressed reason for their visit was less than fully aligned with their physicians’ primary concern were more likely to be older, with more chronic conditions, of Hispanic ethnicity, and either publicly insured or uninsured. Patients with some degree of unaligned concerns also tended to have greater numbers of prescribed medications and had a primary language other than English. Unaligned visit priorities were also observed more often when greater numbers of problems were addressed during the visit. Patients familiar to the physician were also more likely to express a reason for their visit that differed in some way from the primary concern of their family physician.
Multivariable logistic regression analyses showed that having more problems addressed during a visit and being publicly insured or uninsured (compared with having private insurance) were each independently associated with less than fully aligned visit priorities (indicated by § in TABLE 1).
Qualitative findings
Cases classified as partially or totally unaligned showed 2 main patterns that reflect differences in the ways that patients and physicians prioritize problems. First, when physician priorities were unaligned with the patient’s stated reason for a visit, physicians typically focused on treatable, asymptomatic conditions that could lead to long-term morbidity and mortality or, absent immediate attention, to a dangerous event. Examples include chronic disease management (eg, hypertension, diabetes, asthma) and disease prevention (eg, smoking cessation, cholesterol level monitoring, cardiac disease risk reduction). Second, in those visits that were unaligned, patients tended to show more initial concern about symptomatic problems (eg, skin rash, upper respiratory infection) that would likely resolve with minimal or no medical intervention. Most of these conditions were determined by the physician to be benign, self-limited, or not worrisome (TABLE 2).
DISCUSSION
This study examined the alignment between a patient’s stated reason for a visit and the physician’s main concern. Physician-patient alignment was common, with 69% of visits showing full alignment between the patient’s reason for the visit and the physician’s main concern. While this rate is higher than that seen in prior studies,5 our method for data collection uniquely reflected how information actually is elicited and received during outpatient encounters, which likely yielded more accurate results. Also, in contrast to past approaches, our study equated patients’ symptoms to the underlying diagnosis for purposes of determining alignment.
Similar to previous studies, alignment between patient and physician concerns was less likely when the number of items addressed during the visit increased.5,6 Interestingly, physician-perceived time pressure during the visit and lack of an established patient-physician relationship were not observed to influence alignment. When time is limited, physicians may choose to prioritize the patient’s verbalized concern to avoid more complex negotiations about the agenda. In addition, during an encounter with an unfamiliar patient, prevention and chronic illness care may be deferred until the relationship becomes established.15-18
Patient insurance status was also observed to influence alignment. This finding could reflect socioeconomic or access issues among uninsured or publicly-insured patients that contribute to more complex visits.19-21 To shed further light on this finding, further research is needed that includes indicators of education or income and that separately examines Medicaid vs Medicare enrollees.
Possible study weaknesses. A potential weakness of this study is that alignment was rated by the physicians who elicited and recorded their patients’ reasons for the visit. It is possible that the central role of the physician as observer and analyst may have introduced bias and that an outside observer may have come to different conclusions about the extent to which priorities were aligned. However, by placing the physician-researcher at the center of both data collection and analysis, our study method reflects the realistic constraints of limited information on the processes of clinical discovery and sense-making that physicians regularly undertake with their patients, which we believe to be a strength of this study. While the inclusion of pediatric visits in the sample is another possible weakness, we believe that the diverse clinical settings and diverse patient populations potentially strengthen the findings. Replication with different samples of clinicians and patients is needed to assess the robustness of the findings.
Root differences in physician and patient perspectives. Collectively, these findings suggest that patients’ and physicians’ differing approaches to prioritization may limit alignment. In general, physicians tend to evaluate the full scope of the patient’s health and risk factors for future disease, while patients more often focus on symptomatically troublesome—though often self-limiting— conditions. Physicians have the knowledge and clinical experience to prioritize or deprioritize patient concerns based on an assessment of long-term risks of morbidity and mortality, yet the future-orientation of treatments and surveillance for insensible conditions (like hypertension) is less likely to align with the immediately painful or worrisome symptoms of patients. This highlights the importance of patient education on chronic disease management and disease prevention, and cooperative agenda-setting. Further work needs to be done to examine the differences in patients’ and physicians’ cognitive processes of prioritization, with the ultimate goal of providing patient-centered care through shared decision-making.
Take-home messages for all stakeholders. Amidst growing time pressures and guideline-driven protocols for care, it is important to attend to the intersecting and diverging patient, physician, and payer agendas that drive the content of the visit. Patients who are less likely to share the physician’s prioritization of their concerns—including individuals with no insurance or public insurance and those with multiple medical problems—may require more time and additional effort on the part of the physician to create a mutually acceptable agenda for the visit. Attempts at pay-for-performance should consider patients’ priorities and preferences for care, particularly when those preferences differ from the priorities of physicians or health insurance plans. A more thorough understanding of patient and physician prioritization during primary care visits could potentially guide the organization of outpatient care and inform the mindful physician’s patient-centered practice to maximize patient benefit.
CORRESPONDENCE
Susan A. Flocke, PhD, Family Medicine Research Division, Case Western Reserve University, 11000 Cedar Avenue, Suite 402, Cleveland, OH 44106; [email protected]
ACKNOWLEDGEMENTS
This study was completed as part of the culture of inquiry fellowship, supported by Academic Administrative Units in primary care Grant #D54HP05444 from the Health Resources and Services Administration, US Department of Health and Human Services. Dr. Stange’s time is supported in part by a clinical research professorship from the American Cancer Society.
ABSTRACT
Purpose We undertook this study to explore the factors associated with differences between patients’ stated main reasons for outpatient visits and physicians’ main concerns at those same visits.
Methods This cross-sectional, mixed-methods study examined 192 outpatient visits with 4 physicians at 4 diverse primary care practices. During each visit, participating physicians elicited the patient’s main reason for the visit. Immediately after each visit, physicians documented 1) their understanding of the patient’s stated reason and 2) their main concern for the patient during that visit, and 3) assessed the extent of their alignment with the patient’s reason for visit. We assessed bivariate and multivariable associations of patient and visit characteristics with alignment, and further examined cases with unaligned physician-patient priorities to identify patterns.
Results In 69% of visits, the patient’s stated reason for the visit was completely aligned with the physician’s main concern. In 12% of visits, we observed totally unaligned priorities; 19% were only partially aligned. Uninsured or publicly-insured patients and visits with more problems addressed were less likely to be fully aligned. In many visits with unaligned priorities, patients’ stated reason for the visit was a self-limiting, symptomatic concern while physicians prioritized potentially dangerous asymptomatic conditions or ill-managed chronic conditions.
Conclusions In diverse family medicine practices, lack of alignment between physician and patient visit priorities reflects differing prioritization processes. Patients presenting with concerns unaligned with their physician’s priorities may require more time or different approaches to ensure the relevance and patient-centeredness of their care. These findings may inform the design of systems of care that promote mindful attention to patients’ priorities while addressing medically urgent or preventive services delivery.
T oday’s family physicians must balance patient’s acute concerns with chronic disease management, health promotion, and disease prevention. It’s not easy. As the content of outpatient visits expands and available time contracts,1 patients’, clinicians’, and payers’ agendas compete for attention. From a patient experience perspective, the health care encounter may seem diminished when guideline-driven agendas championing chronic disease management and preventive service delivery appear to take precedence over their personal concerns.2-4
In the matter of physician-patient alignment of visit priorities, prior research5,6 inadequately reflects current practice realities such as increased time pressure,7 greater chronic disease prevalence,8 growing expectations for preventive care,1 and increasing physician proactivity in longitudinal care.9-12 With so much to do and so little time and mounting pressure to deliver patient-centered care and patient satisfaction, it would be helpful to have a better understanding of how often and with whom physicians choose to depart from a patient’s explicitly stated reasons for a visit and instead prioritize other concerns.
We sought to examine alignment between patients’ stated main reasons for a visit as understood by the physician and the physician’s main concern during that same visit. Using a diverse sample of family physician-researchers to serve as data collectors and analysts, this study aimed to identify patient and visit characteristics associated with differing physician-patient visit priorities.
METHODS
Study design and sample
Four family physicians participating in a research fellowship undertook this cross- sectional descriptive study of a sample of their outpatient encounters. Each physician’s practice was unique: a free clinic, an inner city family practice within a teaching hospital, a geriatric home visit practice, and a suburban pediatric practice. Using the card study method pioneered by the Ambulatory Sentinel Practice Network,13,14 physicians collected observational and reflective data on a sample of 50 consecutive patients seen at his or her primary care practice. The University Hospitals Case Medical Center Institutional Review Board approved the study protocol.
Measures
Immediately following each patient visit, physicians recorded on a standardized data card the patient’s characteristics, visit characteristics, the reason for the visit provided to the office staff, the reason for visit reported by the patient at the beginning of the visit, and the physician’s own main concern for the patient during the visit. Patient characteristics included gender, age, race, type of insurance, and number of chronic conditions on the problem list. Visit characteristics included the total number of problems addressed, whether a second person (eg, family member, caregiver) was present in the exam room during the visit, and visit duration. To elicit the patient’s reason for the visit, physicians systematically asked, “How can I help you today?” If more than one problem was elicited from this prompt, the concern expressed as most important by the patient was noted.
In completing the data card, physicians also reflected on the extent to which the patient’s stated reason for the visit aligned with their own main concern for the patient during the visit, rating the relationship between their respective priorities as fully aligned, partially aligned, or totally unaligned. Visits were considered fully aligned if the patient’s reason for the visit and the physician’s concern were the same, or if the patient’s expressed concern was determined to be a symptom related to the physician’s main concern. Partial alignment occurred when the patient’s concern was shared by the physician but was not the physician’s main concern. Visit priorities were rated as totally unaligned if patient and physician concerns were different and determined not to be medically related.
Data analysis
We computed descriptive statistics and performed bivariate tests of association between physician-patient alignment of priorities and patient/visit characteristics, using chi-square statistics for categorical variables and analysis of variance (ANOVA) for continuous variables. We used logistic regression analysis to identify characteristics independently associated with either partially aligned or totally unaligned visit priorities, vs fully aligned priorities.
To better understand the unaligned cases, the study team examined all of the data cards identified as either only partially aligned or totally unaligned and categorized the nature of the disparate prioritization in each case. Study team members (PT, AW, MR, and PDG) individually reviewed and sorted the cards into similar observed patterns and wrote brief descriptions of those patterns. The group refined the preliminary descriptions of the overarching patterns and selected several cases to represent the patterns.
RESULTS
Quantitative findings
We collected data on 192 patients (TABLE 1). Median patient age was 47. Median number of prescription medications and chronic medical conditions were 3 and 2, respectively. Most patients (80%) primarily spoke English, 58% were female, and 59% were Caucasian. Insurance status was equally distributed among patients: 33% held private insurance, 33% had public insurance, and 34% were uninsured.
The majority of cases showed physician- patient priorities that were fully aligned (69%); only 12% were totally unaligned. TABLE 1 shows the associations between level of alignment and patient and visit characteristics. Patients whose expressed reason for their visit was less than fully aligned with their physicians’ primary concern were more likely to be older, with more chronic conditions, of Hispanic ethnicity, and either publicly insured or uninsured. Patients with some degree of unaligned concerns also tended to have greater numbers of prescribed medications and had a primary language other than English. Unaligned visit priorities were also observed more often when greater numbers of problems were addressed during the visit. Patients familiar to the physician were also more likely to express a reason for their visit that differed in some way from the primary concern of their family physician.
Multivariable logistic regression analyses showed that having more problems addressed during a visit and being publicly insured or uninsured (compared with having private insurance) were each independently associated with less than fully aligned visit priorities (indicated by § in TABLE 1).
Qualitative findings
Cases classified as partially or totally unaligned showed 2 main patterns that reflect differences in the ways that patients and physicians prioritize problems. First, when physician priorities were unaligned with the patient’s stated reason for a visit, physicians typically focused on treatable, asymptomatic conditions that could lead to long-term morbidity and mortality or, absent immediate attention, to a dangerous event. Examples include chronic disease management (eg, hypertension, diabetes, asthma) and disease prevention (eg, smoking cessation, cholesterol level monitoring, cardiac disease risk reduction). Second, in those visits that were unaligned, patients tended to show more initial concern about symptomatic problems (eg, skin rash, upper respiratory infection) that would likely resolve with minimal or no medical intervention. Most of these conditions were determined by the physician to be benign, self-limited, or not worrisome (TABLE 2).
DISCUSSION
This study examined the alignment between a patient’s stated reason for a visit and the physician’s main concern. Physician-patient alignment was common, with 69% of visits showing full alignment between the patient’s reason for the visit and the physician’s main concern. While this rate is higher than that seen in prior studies,5 our method for data collection uniquely reflected how information actually is elicited and received during outpatient encounters, which likely yielded more accurate results. Also, in contrast to past approaches, our study equated patients’ symptoms to the underlying diagnosis for purposes of determining alignment.
Similar to previous studies, alignment between patient and physician concerns was less likely when the number of items addressed during the visit increased.5,6 Interestingly, physician-perceived time pressure during the visit and lack of an established patient-physician relationship were not observed to influence alignment. When time is limited, physicians may choose to prioritize the patient’s verbalized concern to avoid more complex negotiations about the agenda. In addition, during an encounter with an unfamiliar patient, prevention and chronic illness care may be deferred until the relationship becomes established.15-18
Patient insurance status was also observed to influence alignment. This finding could reflect socioeconomic or access issues among uninsured or publicly-insured patients that contribute to more complex visits.19-21 To shed further light on this finding, further research is needed that includes indicators of education or income and that separately examines Medicaid vs Medicare enrollees.
Possible study weaknesses. A potential weakness of this study is that alignment was rated by the physicians who elicited and recorded their patients’ reasons for the visit. It is possible that the central role of the physician as observer and analyst may have introduced bias and that an outside observer may have come to different conclusions about the extent to which priorities were aligned. However, by placing the physician-researcher at the center of both data collection and analysis, our study method reflects the realistic constraints of limited information on the processes of clinical discovery and sense-making that physicians regularly undertake with their patients, which we believe to be a strength of this study. While the inclusion of pediatric visits in the sample is another possible weakness, we believe that the diverse clinical settings and diverse patient populations potentially strengthen the findings. Replication with different samples of clinicians and patients is needed to assess the robustness of the findings.
Root differences in physician and patient perspectives. Collectively, these findings suggest that patients’ and physicians’ differing approaches to prioritization may limit alignment. In general, physicians tend to evaluate the full scope of the patient’s health and risk factors for future disease, while patients more often focus on symptomatically troublesome—though often self-limiting— conditions. Physicians have the knowledge and clinical experience to prioritize or deprioritize patient concerns based on an assessment of long-term risks of morbidity and mortality, yet the future-orientation of treatments and surveillance for insensible conditions (like hypertension) is less likely to align with the immediately painful or worrisome symptoms of patients. This highlights the importance of patient education on chronic disease management and disease prevention, and cooperative agenda-setting. Further work needs to be done to examine the differences in patients’ and physicians’ cognitive processes of prioritization, with the ultimate goal of providing patient-centered care through shared decision-making.
Take-home messages for all stakeholders. Amidst growing time pressures and guideline-driven protocols for care, it is important to attend to the intersecting and diverging patient, physician, and payer agendas that drive the content of the visit. Patients who are less likely to share the physician’s prioritization of their concerns—including individuals with no insurance or public insurance and those with multiple medical problems—may require more time and additional effort on the part of the physician to create a mutually acceptable agenda for the visit. Attempts at pay-for-performance should consider patients’ priorities and preferences for care, particularly when those preferences differ from the priorities of physicians or health insurance plans. A more thorough understanding of patient and physician prioritization during primary care visits could potentially guide the organization of outpatient care and inform the mindful physician’s patient-centered practice to maximize patient benefit.
CORRESPONDENCE
Susan A. Flocke, PhD, Family Medicine Research Division, Case Western Reserve University, 11000 Cedar Avenue, Suite 402, Cleveland, OH 44106; [email protected]
ACKNOWLEDGEMENTS
This study was completed as part of the culture of inquiry fellowship, supported by Academic Administrative Units in primary care Grant #D54HP05444 from the Health Resources and Services Administration, US Department of Health and Human Services. Dr. Stange’s time is supported in part by a clinical research professorship from the American Cancer Society.
1. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
2. Weyer SM, Bobiak S, Stange KC. Possible unintended consequences of a focus on performance: insights over time from the research association of practices network. Qual Manag Health Care. 2008;17:47-52.
3. Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med. 2008;6:228-234.
4. Casalino LP. The unintended consequences of measuring quality on the quality of medical care. N Engl J Med. 1999;341:1147-1150.
5. Friedin RB, Goldman L, Cecil RR. Patient-physician concordance in problem identification in the primary care setting. Ann Intern Med. 1980;93:490-493.
6. Boland BJ, Scheitel SM, Wollan PC, et al. Patient-physician agreement on reasons for ambulatory general medical examinations. Mayo Clin Proc. 1998;73:109-117.
7. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065.
8. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209-214.
9. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511-544.
10. Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4:12-25.
11. Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q. 2001;79:579-612,iv-v.
12. Wagner EH, Bennett SM, Austin BT, et al. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11(suppl 1):S7-S15.
13. Green LA. The weekly return as a practical instrument for data collection in office based research. Fam Med. 1988;20:182-184.
14. Green LA, Reed FM, Miller RS, et al. Verification of data reported by practices for a study of spontaneous abortion. Fam Med. 1988;20:189-191.
15. Ettner SL. The relationship between continuity of care and the health behaviors of patients: Does having a usual physician make a difference? Med Care. 1999;37:547-555.
16. Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004;36:22-27.
17. Blewett LA, Johnson PJ, Lee B, et al. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. 2008;23:1354-1360.
18. Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(8 suppl):AS21-AS30.
19. Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061-2069.
20. Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79:1139-1147.
21. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443-494.
1. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
2. Weyer SM, Bobiak S, Stange KC. Possible unintended consequences of a focus on performance: insights over time from the research association of practices network. Qual Manag Health Care. 2008;17:47-52.
3. Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med. 2008;6:228-234.
4. Casalino LP. The unintended consequences of measuring quality on the quality of medical care. N Engl J Med. 1999;341:1147-1150.
5. Friedin RB, Goldman L, Cecil RR. Patient-physician concordance in problem identification in the primary care setting. Ann Intern Med. 1980;93:490-493.
6. Boland BJ, Scheitel SM, Wollan PC, et al. Patient-physician agreement on reasons for ambulatory general medical examinations. Mayo Clin Proc. 1998;73:109-117.
7. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065.
8. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209-214.
9. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511-544.
10. Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4:12-25.
11. Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q. 2001;79:579-612,iv-v.
12. Wagner EH, Bennett SM, Austin BT, et al. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11(suppl 1):S7-S15.
13. Green LA. The weekly return as a practical instrument for data collection in office based research. Fam Med. 1988;20:182-184.
14. Green LA, Reed FM, Miller RS, et al. Verification of data reported by practices for a study of spontaneous abortion. Fam Med. 1988;20:189-191.
15. Ettner SL. The relationship between continuity of care and the health behaviors of patients: Does having a usual physician make a difference? Med Care. 1999;37:547-555.
16. Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004;36:22-27.
17. Blewett LA, Johnson PJ, Lee B, et al. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. 2008;23:1354-1360.
18. Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(8 suppl):AS21-AS30.
19. Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061-2069.
20. Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79:1139-1147.
21. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443-494.