User login
Peer Technical Consultant: Veteran-Centric Technical Support Model for VA Home-Based Telehealth Programs
With an increasing demand for mental health services for veterans in rural clinics, telehealth can deliver services to veterans at home or in other nonclinic settings. Telehealth can reduce demands on VA clinic space and staff required for traditional videoconferencing.
Clinic-based telemental health started at the VA in 2003 and has provided access to more than 1 million appointments.1 Despite the great strides in accessibility, logistic barriers limit expansion of clinic-based telehealth appointments. A VA staff member at the patient site must be available to “greet and seat” the veteran; scheduling requires 2 separate appointments (on patient and provider sites); and limited telehealth equipment and clinic space need to be reserved ahead of time.
The first known use of telehealth technologies to deliver mental health services within the VA network information technology system to at-home veterans occurred in 2009 at the VA Portland Health Care System (VAPORHCS) in Oregon. Between 2010 and 2013, the VAPORHCS Home-Based Telemental Health (HBTMH) pilot served about 82 veterans through about 740 appointments. The HBTMH pilot transitioned from a single facility to a regional implementation model under an Office of Innovation Grant Innovation #669: Home-Based Telemental Health (Innovation), which served about 84 veterans from 2013 to 2014.
In 2014, about 4,200 veterans accessed some health care via the national Clinical Video Telehealth–Into the Home (CVT-IH) program, with all 21 VISNs participating (John Peters, e-mail communication, February 2014). In all 3 implementation models (HBTMH pilot, Innovation, and CVT-IH), the veteran can receive health services via videoconferencing in real time, on personal or loaned computers, at home or in another nonclinic setting.
As the VA’s use of telehealth services grows in non-VA settings, technical support remains a significant challenge.2 Increased use of CVT-IH through veterans’ personal computers and devices has generated a corresponding need for technical support. The National Telehealth Technical Help Desk (NTTHD), which supports the national CVT-IH program, does not provide technical support directly to veterans. Instead, recommendations are given to the providers who are expected to transmit and implement the technical solutions with the veterans. Similarly, HBTMH pilot providers were initially responsible for all technical issues for home-based telehealth work, including helping patients with software installation and subsequent troubleshooting.
Providers participating in the HBTMH pilot project encountered veterans with all levels of comfort and skill with the required technology. Some veterans have never used a personal computer, e-mail, and/or webcam. Addressing technical issues often required up to 15 to 20 minutes during an HBTMH pilot session; some cases took hours spread over several days. In VISN 20, providers in Oregon and Washington have reported discontinuation of treatment of veterans enrolled in CVT-IH for technical reasons, including poor connections, lack of timely technical support, and incompatibility of veteran-owned computers with VA-approved third-party software (Anders Goranson, Sara Smucker Barnwell, Kathleen Woodside, e-mail communication, December 2013).
A peer technical consultant (PTC) who directly serves patients and providers may be better positioned to meet the technical needs of everyone involved in a home-based telehealth program. The PTC role was developed for the HBTMH Pilot and expanded during the Innovation program. The authors describe the role of the PTC, outline key responsibilities, and highlight how the PTC can provide effective technical support and improve provider and patient access and engagement with nonclinic-based telehealth services.
Methods
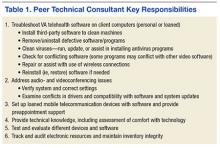
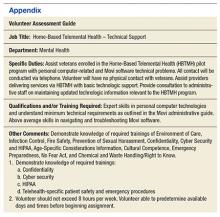
Lessons from the initial phases of the HBTMH pilot strongly suggested that technical barriers had to be reduced. In 2010, a former patient in the HBTMH pilot who had a background in information technology and computer systems and interest in helping other veterans contacted Dr. Peter Shore. They developed the novel role of a PTC, focused on delivering technical support with compassion (Table 1). A functional statement and position description were submitted to volunteer services at the VAPORHCS (Appendix). With the regionwide expansion of the HBTMH pilot into the Innovation program, the PTC was hired as a full-time contract employee to increase the availability of technical support.
The PTC assumed responsibility for installations and troubleshooting for both providers and veterans enrolled in the HBTMH pilot. The PTC, who was based at the VAPORHCS, received referrals, contacted veterans by telephone, addressed technical problems, and reported the result to the provider. No face-to-face contact occurred between the PTC and the veterans. The PTC received regular supervision from the project director. Starting in mid-2012, local providers who were using the national CVT-IH program also requested PTC services. The PTC was able to add technical support for veterans beyond the NTTHD model, allowing for immediate in-session attention in some cases.
For the Innovation program, which loaned devices (netbooks or iPads) and connectivity (mobile broadband Internet access) to veterans who needed them, the role of PTC expanded to become a technology concierge, helping to set up and manage all mobile telecommunication devices. The PTC phoned veterans when they received their device and provided a virtual tour, helped familiarize them with the technology by using test calls, and guided them in the use of relevant mobile applications installed on the device. During treatment, the PTC called enrolled veterans to follow up and to answer additional questions. The PTC also provided assistance to veterans interested in enrolling in the patient online portal My HealtheVet to access health information, communicate with providers, and request medication refills.
The VAPORHCS received institutional review board approval to present HBTMH pilot research data and program evaluation data for Innovation (as a quality improvement project). An initial evaluation of the position was completed through review of PTC workload and productivity, informal feedback from telehealth providers, and veteran and provider surveys during and after treatment.
Results
From March 2010 through April 2012, the PTC logged more than 2,500 hours of volunteer service on behalf of the HBTMH pilot (before the Innovation expansion). The dropout rate due to nonclinical reasons for veterans enrolled in the HBTMH pilot was 11%.3 During the HBTMH pilot, 78% of veterans reported that they had enough technical support (ie, from the volunteer PTC), whereas among veterans receiving clinic-based videoconferencing sessions, 61% reported having adequate technical support (ie, from telehealth clinical technicians employed by the VA).3
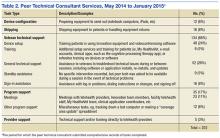
During 2013 to 2014, veterans and providers were surveyed during and after Innovation program treatment. Eighty percent of participants stated that the PTC was prompt in resolving any issues (20% reported “neutral”). One hundred percent of providers indicated that the PTC was able to resolve the technical issues and that they were “very likely” to continue participating in HBTMH if the PTC was involved. Eighty-nine percent of veterans reported they felt there was enough technical support, and 11% responded “neutral” to this question. Table 2 describes typical PTC services provided during the Innovation program.
Informal summary observations from the PTC confirmed that the most frequent interventions were device and software orientation, assessment of audio and/or video disruptions during sessions, and software log-in configuration and support. Common technical issues included audio and video bandwidth limitations and the need to clean up veterans’ personal computers to restore functionality or improve performance (eg, problems due to malware and viruses; e-mail communication, various dates, William Cannon).
Troubleshooting was performed immediately during a session about half the time (vs between sessions) and initiated by veterans about half the time (vs by providers on their behalf) according to informal observations. The average length of a technical support appointment was about 30 minutes for veterans who were comfortable with technology; in contrast, appointments with veterans who were unfamiliar with technology averaged about 90 minutes.
The task logs recorded instances where flexibility and availability were needed for optimal task completion. Although many tasks seemed to be routine, others showed considerable use of the PTC’s time or direct participation during a session.
One PTC noted, “Client called around 9:30 and had me put [provider’s name] info into Jabber. Also Jabber had an issue of being stuck but forced a call and issue cleared up. 15 min. Stayed online with client to ensure appointment connection went well. 5 min.”
Malware, although not the most common issue, seemed to be time consuming. A task that required 4 hours for resolution of multiple issues was described as “requested outside assist due to drivers. Troubleshooting discovered 240 plus malware and numerous Trojan [horses].”
Another time-consuming issue involved software or updates to existing software interfering with the videoconferencing program, with the following example logged for 90 minutes: “Jabber will not store contacts. Updated IOS. Deleted games. Deleted and reinstalled Jabber. Re-updated Jabber. Problem finally resolved” (December 19, 2014). Other patients simply needed more time to familiarize themselves with the technology, as in this example: “2.5 hours of training and using the iPad” (November 25, 2014).
Informal feedback from providers as well as formal feedback from a program audit indicated appreciation for the PTC’s ability to facilitate engagement and surmount technical hurdles. One provider reflected on a particular instance in which the PTC worked with both the veteran and the provider over the phone and webchat to teach them to use the equipment. “[Veteran] and the peer technician developed a friendly rapport and [veteran] expressed gratitude for the team’s efforts to deliver treatment that he would not have had otherwise.” Another provider commented, “The [National] Help Desk is almost too general. You have to explain who you are each time, and never get to explain who [the] veteran is. … They are aware of national problems. Otherwise, they can’t help out much.”
In 2012, the Office of Telehealth Services completed its Conditions of Participation review of all VISN 20 Telehealth programs and in their final report commended the practices of the HBTMH program, highlighting the associated peer-to-peer volunteer program.4
Discussion
The number of technical issues addressed by the PTC demonstrates the versatility and potential impact of this role. In each case, the PTC accommodates the specific needs of the veteran and any factors that might impact their technology use (eg, low cognitive functioning, hyperarousal, slowed processing speed, low frustration tolerance, or paranoia). This model could be expanded within or outside the VA, although due to the limited scope of the evaluation and the unique qualifications of the individual who filled the PTC role, generalizability remains to be established.
By providing direct support, the PTC attempts to meet veterans where they are and helps them become comfortable with the technology so they are not preoccupied with technical problems while receiving health care. In doing so, engagement in telehealth care is enhanced for patients and providers, and dropouts due to technologic problems may be prevented. Initial program evaluation of this role also suggests considerable provider and veteran satisfaction.
The PTC’s interactions help minimize potential frustrations related to technology use for the delivery of mental health care. Frequently, veterans using in-home telehealth have little experience with technology. Moreover, technology use has been found to be lower for rural dwelling adults.5 Other populations (eg, geriatric) may have greater technology challenges and need additional support.6 When patients start CVT services, there is a potential for dropout if there are initial connection problems, particularly among patients who may have low stress tolerance. The PTC can develop an ongoing relationship with veterans who have a history of technologic difficulties and help monitor them.
Technology barriers and limited support are also a documented barrier to provider engagement.7 Given the inherent limitations and reported provider discouragement with the NTTHD model, more directed technical support may enhance provider engagement and efficiency. With the immediate and one-on-one support given by the PTC, this concern has been assertively addressed. In VISN 20 some mental health care providers elected not to use the CVT-IH program technical support system of the and chose instead to work with the Innovation PTC.
Programmatically, the PTC role is consistent with the VA Office of Mental Health Services and the VA Central Office initiative to increase involvement of peer support programs. From a recovery model perspective, the role of the PTC goes beyond technical support in connecting veterans to other veterans who are encouraged to take control of their health care by making self-directed choices. They can experience empowerment through interactions with another veteran who may share some of their experiences. Further investigation into the effects of using a peer technical support system on veterans, providers, and PTCs compared with the existing national VA technical support help desk system might be useful, particularly with regard to rates of initiation of care or dropouts.
Integration of this role should be done in a purposeful and direct manner, defining peer roles and establishing clear policies and practices. Logistically, the transition of the PTC from a volunteer to a contract employee afforded increased credentialing to allow for improved integration with the other HBTMH team members. The PTC was able to effectively coordinate with clinical, support and administrative staff to share information, resolve issues collaboratively, and bridge gaps in technology knowledge.
Conclusion
Between the HBTMH pilot and the Innovation program, the authors have demonstrated the growing need for personalized and attentive technical support for patients enrolled in home-based telehealth services. Under a current call center help desk model, satisfaction and services may be inadequate for some veterans’ needs. The authors contend that the PTC is an effective way to deliver the necessary specialized technical assistance to veterans and providers and encourage further implementation and evaluation of this approach.
There is preliminary evidence suggesting that this support can have a beneficial impact on provider and veteran engagement in telehealth services. The PTC offers much needed support to providers who frequently do not have the time or knowledge to address all the technical issues that arise during telehealth care. Veterans helping veterans is a powerful alternative deserving of national resources and policy change. Although this case developed in a very VA-specific context, peer technical support may be applicable to other organizations as well.
Acknowledgements
Being the first to do anything in the VA takes courage, tenacity, and luck. The following individuals greatly assisted with the HBTMH pilot and the subsequent Innovation: William “Bear” Cannon, David Greaves, Tracy Dekelboum, William Minium, Sean O’Connor, Joe Ronzio, Kit Teague, and Mark Ward. For assistance with data entry and analysis, the authors thank Athalia White. For help with administrative approvals, the authors thank Bradford Felker and Carol Simons.
This article is dedicated to William “Bear” Cannon, who reinvented himself while serving as the PTC and saved his life along the way. His unwavering commitment to serve his fellow veterans is unheralded. May he be the shining light to those who follow him.
1. Darkins A. The growth of telehealth services in the Veterans Health Administration between 1994 and 2014: a study in the diffusion of innovation. Telemed J E Health. 2014;20(9):761-768.
2. Ronzio JL, Tuerk PW, Shore P. Technology and clinical videoconferencing infrastructures: a guide to selecting appropriate system. In: Tuerk PW, Shore P, eds. Clinical Video Teleconferencing: Program Development and Practice. New York, NY: Springer;2015:3-22.
3. Shore P, Goranson A, Ward MF, Lu MW. Meeting veterans where they're @: a VA home-based telemental health (HBTMH) pilot program. Int J Psychiatry Med. 2014;48(1):5-17.
4. U.S. Department of Veterans Affairs, Veterans Health Administration. Telehealth Conditions of Participation: Final Core and Modality-Specific Standards. Washington, DC: Veterans Health Administration; 2014.
5. Calvert JF Jr, Kaye J, Leahy M, Hexem K, Carlson N. Technology use by rural and urban oldest old. Technol Health Care. 2009;17(1):1-11.
6. Kang HG, Mahoney DF, Hoenig H, et al; Center for Integration of Medicine and Innovative Technology Working Group on Advanced Approaches to Physiologic Monitoring for the Aged. In situ monitoring of health in older adults: technologies and issues. J Am Geriatr Soc. 2010;58(8):1579-1586.
7. Brooks E, Turvey C, Augusterfer EF. Provider barriers to telemental health: obstacles overcome, obstacles remain. Telemed J E Health. 2013;19(6):433-437.
With an increasing demand for mental health services for veterans in rural clinics, telehealth can deliver services to veterans at home or in other nonclinic settings. Telehealth can reduce demands on VA clinic space and staff required for traditional videoconferencing.
Clinic-based telemental health started at the VA in 2003 and has provided access to more than 1 million appointments.1 Despite the great strides in accessibility, logistic barriers limit expansion of clinic-based telehealth appointments. A VA staff member at the patient site must be available to “greet and seat” the veteran; scheduling requires 2 separate appointments (on patient and provider sites); and limited telehealth equipment and clinic space need to be reserved ahead of time.
The first known use of telehealth technologies to deliver mental health services within the VA network information technology system to at-home veterans occurred in 2009 at the VA Portland Health Care System (VAPORHCS) in Oregon. Between 2010 and 2013, the VAPORHCS Home-Based Telemental Health (HBTMH) pilot served about 82 veterans through about 740 appointments. The HBTMH pilot transitioned from a single facility to a regional implementation model under an Office of Innovation Grant Innovation #669: Home-Based Telemental Health (Innovation), which served about 84 veterans from 2013 to 2014.
In 2014, about 4,200 veterans accessed some health care via the national Clinical Video Telehealth–Into the Home (CVT-IH) program, with all 21 VISNs participating (John Peters, e-mail communication, February 2014). In all 3 implementation models (HBTMH pilot, Innovation, and CVT-IH), the veteran can receive health services via videoconferencing in real time, on personal or loaned computers, at home or in another nonclinic setting.
As the VA’s use of telehealth services grows in non-VA settings, technical support remains a significant challenge.2 Increased use of CVT-IH through veterans’ personal computers and devices has generated a corresponding need for technical support. The National Telehealth Technical Help Desk (NTTHD), which supports the national CVT-IH program, does not provide technical support directly to veterans. Instead, recommendations are given to the providers who are expected to transmit and implement the technical solutions with the veterans. Similarly, HBTMH pilot providers were initially responsible for all technical issues for home-based telehealth work, including helping patients with software installation and subsequent troubleshooting.
Providers participating in the HBTMH pilot project encountered veterans with all levels of comfort and skill with the required technology. Some veterans have never used a personal computer, e-mail, and/or webcam. Addressing technical issues often required up to 15 to 20 minutes during an HBTMH pilot session; some cases took hours spread over several days. In VISN 20, providers in Oregon and Washington have reported discontinuation of treatment of veterans enrolled in CVT-IH for technical reasons, including poor connections, lack of timely technical support, and incompatibility of veteran-owned computers with VA-approved third-party software (Anders Goranson, Sara Smucker Barnwell, Kathleen Woodside, e-mail communication, December 2013).
A peer technical consultant (PTC) who directly serves patients and providers may be better positioned to meet the technical needs of everyone involved in a home-based telehealth program. The PTC role was developed for the HBTMH Pilot and expanded during the Innovation program. The authors describe the role of the PTC, outline key responsibilities, and highlight how the PTC can provide effective technical support and improve provider and patient access and engagement with nonclinic-based telehealth services.
Methods
Lessons from the initial phases of the HBTMH pilot strongly suggested that technical barriers had to be reduced. In 2010, a former patient in the HBTMH pilot who had a background in information technology and computer systems and interest in helping other veterans contacted Dr. Peter Shore. They developed the novel role of a PTC, focused on delivering technical support with compassion (Table 1). A functional statement and position description were submitted to volunteer services at the VAPORHCS (Appendix). With the regionwide expansion of the HBTMH pilot into the Innovation program, the PTC was hired as a full-time contract employee to increase the availability of technical support.
The PTC assumed responsibility for installations and troubleshooting for both providers and veterans enrolled in the HBTMH pilot. The PTC, who was based at the VAPORHCS, received referrals, contacted veterans by telephone, addressed technical problems, and reported the result to the provider. No face-to-face contact occurred between the PTC and the veterans. The PTC received regular supervision from the project director. Starting in mid-2012, local providers who were using the national CVT-IH program also requested PTC services. The PTC was able to add technical support for veterans beyond the NTTHD model, allowing for immediate in-session attention in some cases.
For the Innovation program, which loaned devices (netbooks or iPads) and connectivity (mobile broadband Internet access) to veterans who needed them, the role of PTC expanded to become a technology concierge, helping to set up and manage all mobile telecommunication devices. The PTC phoned veterans when they received their device and provided a virtual tour, helped familiarize them with the technology by using test calls, and guided them in the use of relevant mobile applications installed on the device. During treatment, the PTC called enrolled veterans to follow up and to answer additional questions. The PTC also provided assistance to veterans interested in enrolling in the patient online portal My HealtheVet to access health information, communicate with providers, and request medication refills.
The VAPORHCS received institutional review board approval to present HBTMH pilot research data and program evaluation data for Innovation (as a quality improvement project). An initial evaluation of the position was completed through review of PTC workload and productivity, informal feedback from telehealth providers, and veteran and provider surveys during and after treatment.
Results
From March 2010 through April 2012, the PTC logged more than 2,500 hours of volunteer service on behalf of the HBTMH pilot (before the Innovation expansion). The dropout rate due to nonclinical reasons for veterans enrolled in the HBTMH pilot was 11%.3 During the HBTMH pilot, 78% of veterans reported that they had enough technical support (ie, from the volunteer PTC), whereas among veterans receiving clinic-based videoconferencing sessions, 61% reported having adequate technical support (ie, from telehealth clinical technicians employed by the VA).3
During 2013 to 2014, veterans and providers were surveyed during and after Innovation program treatment. Eighty percent of participants stated that the PTC was prompt in resolving any issues (20% reported “neutral”). One hundred percent of providers indicated that the PTC was able to resolve the technical issues and that they were “very likely” to continue participating in HBTMH if the PTC was involved. Eighty-nine percent of veterans reported they felt there was enough technical support, and 11% responded “neutral” to this question. Table 2 describes typical PTC services provided during the Innovation program.
Informal summary observations from the PTC confirmed that the most frequent interventions were device and software orientation, assessment of audio and/or video disruptions during sessions, and software log-in configuration and support. Common technical issues included audio and video bandwidth limitations and the need to clean up veterans’ personal computers to restore functionality or improve performance (eg, problems due to malware and viruses; e-mail communication, various dates, William Cannon).
Troubleshooting was performed immediately during a session about half the time (vs between sessions) and initiated by veterans about half the time (vs by providers on their behalf) according to informal observations. The average length of a technical support appointment was about 30 minutes for veterans who were comfortable with technology; in contrast, appointments with veterans who were unfamiliar with technology averaged about 90 minutes.
The task logs recorded instances where flexibility and availability were needed for optimal task completion. Although many tasks seemed to be routine, others showed considerable use of the PTC’s time or direct participation during a session.
One PTC noted, “Client called around 9:30 and had me put [provider’s name] info into Jabber. Also Jabber had an issue of being stuck but forced a call and issue cleared up. 15 min. Stayed online with client to ensure appointment connection went well. 5 min.”
Malware, although not the most common issue, seemed to be time consuming. A task that required 4 hours for resolution of multiple issues was described as “requested outside assist due to drivers. Troubleshooting discovered 240 plus malware and numerous Trojan [horses].”
Another time-consuming issue involved software or updates to existing software interfering with the videoconferencing program, with the following example logged for 90 minutes: “Jabber will not store contacts. Updated IOS. Deleted games. Deleted and reinstalled Jabber. Re-updated Jabber. Problem finally resolved” (December 19, 2014). Other patients simply needed more time to familiarize themselves with the technology, as in this example: “2.5 hours of training and using the iPad” (November 25, 2014).
Informal feedback from providers as well as formal feedback from a program audit indicated appreciation for the PTC’s ability to facilitate engagement and surmount technical hurdles. One provider reflected on a particular instance in which the PTC worked with both the veteran and the provider over the phone and webchat to teach them to use the equipment. “[Veteran] and the peer technician developed a friendly rapport and [veteran] expressed gratitude for the team’s efforts to deliver treatment that he would not have had otherwise.” Another provider commented, “The [National] Help Desk is almost too general. You have to explain who you are each time, and never get to explain who [the] veteran is. … They are aware of national problems. Otherwise, they can’t help out much.”
In 2012, the Office of Telehealth Services completed its Conditions of Participation review of all VISN 20 Telehealth programs and in their final report commended the practices of the HBTMH program, highlighting the associated peer-to-peer volunteer program.4
Discussion
The number of technical issues addressed by the PTC demonstrates the versatility and potential impact of this role. In each case, the PTC accommodates the specific needs of the veteran and any factors that might impact their technology use (eg, low cognitive functioning, hyperarousal, slowed processing speed, low frustration tolerance, or paranoia). This model could be expanded within or outside the VA, although due to the limited scope of the evaluation and the unique qualifications of the individual who filled the PTC role, generalizability remains to be established.
By providing direct support, the PTC attempts to meet veterans where they are and helps them become comfortable with the technology so they are not preoccupied with technical problems while receiving health care. In doing so, engagement in telehealth care is enhanced for patients and providers, and dropouts due to technologic problems may be prevented. Initial program evaluation of this role also suggests considerable provider and veteran satisfaction.
The PTC’s interactions help minimize potential frustrations related to technology use for the delivery of mental health care. Frequently, veterans using in-home telehealth have little experience with technology. Moreover, technology use has been found to be lower for rural dwelling adults.5 Other populations (eg, geriatric) may have greater technology challenges and need additional support.6 When patients start CVT services, there is a potential for dropout if there are initial connection problems, particularly among patients who may have low stress tolerance. The PTC can develop an ongoing relationship with veterans who have a history of technologic difficulties and help monitor them.
Technology barriers and limited support are also a documented barrier to provider engagement.7 Given the inherent limitations and reported provider discouragement with the NTTHD model, more directed technical support may enhance provider engagement and efficiency. With the immediate and one-on-one support given by the PTC, this concern has been assertively addressed. In VISN 20 some mental health care providers elected not to use the CVT-IH program technical support system of the and chose instead to work with the Innovation PTC.
Programmatically, the PTC role is consistent with the VA Office of Mental Health Services and the VA Central Office initiative to increase involvement of peer support programs. From a recovery model perspective, the role of the PTC goes beyond technical support in connecting veterans to other veterans who are encouraged to take control of their health care by making self-directed choices. They can experience empowerment through interactions with another veteran who may share some of their experiences. Further investigation into the effects of using a peer technical support system on veterans, providers, and PTCs compared with the existing national VA technical support help desk system might be useful, particularly with regard to rates of initiation of care or dropouts.
Integration of this role should be done in a purposeful and direct manner, defining peer roles and establishing clear policies and practices. Logistically, the transition of the PTC from a volunteer to a contract employee afforded increased credentialing to allow for improved integration with the other HBTMH team members. The PTC was able to effectively coordinate with clinical, support and administrative staff to share information, resolve issues collaboratively, and bridge gaps in technology knowledge.
Conclusion
Between the HBTMH pilot and the Innovation program, the authors have demonstrated the growing need for personalized and attentive technical support for patients enrolled in home-based telehealth services. Under a current call center help desk model, satisfaction and services may be inadequate for some veterans’ needs. The authors contend that the PTC is an effective way to deliver the necessary specialized technical assistance to veterans and providers and encourage further implementation and evaluation of this approach.
There is preliminary evidence suggesting that this support can have a beneficial impact on provider and veteran engagement in telehealth services. The PTC offers much needed support to providers who frequently do not have the time or knowledge to address all the technical issues that arise during telehealth care. Veterans helping veterans is a powerful alternative deserving of national resources and policy change. Although this case developed in a very VA-specific context, peer technical support may be applicable to other organizations as well.
Acknowledgements
Being the first to do anything in the VA takes courage, tenacity, and luck. The following individuals greatly assisted with the HBTMH pilot and the subsequent Innovation: William “Bear” Cannon, David Greaves, Tracy Dekelboum, William Minium, Sean O’Connor, Joe Ronzio, Kit Teague, and Mark Ward. For assistance with data entry and analysis, the authors thank Athalia White. For help with administrative approvals, the authors thank Bradford Felker and Carol Simons.
This article is dedicated to William “Bear” Cannon, who reinvented himself while serving as the PTC and saved his life along the way. His unwavering commitment to serve his fellow veterans is unheralded. May he be the shining light to those who follow him.
With an increasing demand for mental health services for veterans in rural clinics, telehealth can deliver services to veterans at home or in other nonclinic settings. Telehealth can reduce demands on VA clinic space and staff required for traditional videoconferencing.
Clinic-based telemental health started at the VA in 2003 and has provided access to more than 1 million appointments.1 Despite the great strides in accessibility, logistic barriers limit expansion of clinic-based telehealth appointments. A VA staff member at the patient site must be available to “greet and seat” the veteran; scheduling requires 2 separate appointments (on patient and provider sites); and limited telehealth equipment and clinic space need to be reserved ahead of time.
The first known use of telehealth technologies to deliver mental health services within the VA network information technology system to at-home veterans occurred in 2009 at the VA Portland Health Care System (VAPORHCS) in Oregon. Between 2010 and 2013, the VAPORHCS Home-Based Telemental Health (HBTMH) pilot served about 82 veterans through about 740 appointments. The HBTMH pilot transitioned from a single facility to a regional implementation model under an Office of Innovation Grant Innovation #669: Home-Based Telemental Health (Innovation), which served about 84 veterans from 2013 to 2014.
In 2014, about 4,200 veterans accessed some health care via the national Clinical Video Telehealth–Into the Home (CVT-IH) program, with all 21 VISNs participating (John Peters, e-mail communication, February 2014). In all 3 implementation models (HBTMH pilot, Innovation, and CVT-IH), the veteran can receive health services via videoconferencing in real time, on personal or loaned computers, at home or in another nonclinic setting.
As the VA’s use of telehealth services grows in non-VA settings, technical support remains a significant challenge.2 Increased use of CVT-IH through veterans’ personal computers and devices has generated a corresponding need for technical support. The National Telehealth Technical Help Desk (NTTHD), which supports the national CVT-IH program, does not provide technical support directly to veterans. Instead, recommendations are given to the providers who are expected to transmit and implement the technical solutions with the veterans. Similarly, HBTMH pilot providers were initially responsible for all technical issues for home-based telehealth work, including helping patients with software installation and subsequent troubleshooting.
Providers participating in the HBTMH pilot project encountered veterans with all levels of comfort and skill with the required technology. Some veterans have never used a personal computer, e-mail, and/or webcam. Addressing technical issues often required up to 15 to 20 minutes during an HBTMH pilot session; some cases took hours spread over several days. In VISN 20, providers in Oregon and Washington have reported discontinuation of treatment of veterans enrolled in CVT-IH for technical reasons, including poor connections, lack of timely technical support, and incompatibility of veteran-owned computers with VA-approved third-party software (Anders Goranson, Sara Smucker Barnwell, Kathleen Woodside, e-mail communication, December 2013).
A peer technical consultant (PTC) who directly serves patients and providers may be better positioned to meet the technical needs of everyone involved in a home-based telehealth program. The PTC role was developed for the HBTMH Pilot and expanded during the Innovation program. The authors describe the role of the PTC, outline key responsibilities, and highlight how the PTC can provide effective technical support and improve provider and patient access and engagement with nonclinic-based telehealth services.
Methods
Lessons from the initial phases of the HBTMH pilot strongly suggested that technical barriers had to be reduced. In 2010, a former patient in the HBTMH pilot who had a background in information technology and computer systems and interest in helping other veterans contacted Dr. Peter Shore. They developed the novel role of a PTC, focused on delivering technical support with compassion (Table 1). A functional statement and position description were submitted to volunteer services at the VAPORHCS (Appendix). With the regionwide expansion of the HBTMH pilot into the Innovation program, the PTC was hired as a full-time contract employee to increase the availability of technical support.
The PTC assumed responsibility for installations and troubleshooting for both providers and veterans enrolled in the HBTMH pilot. The PTC, who was based at the VAPORHCS, received referrals, contacted veterans by telephone, addressed technical problems, and reported the result to the provider. No face-to-face contact occurred between the PTC and the veterans. The PTC received regular supervision from the project director. Starting in mid-2012, local providers who were using the national CVT-IH program also requested PTC services. The PTC was able to add technical support for veterans beyond the NTTHD model, allowing for immediate in-session attention in some cases.
For the Innovation program, which loaned devices (netbooks or iPads) and connectivity (mobile broadband Internet access) to veterans who needed them, the role of PTC expanded to become a technology concierge, helping to set up and manage all mobile telecommunication devices. The PTC phoned veterans when they received their device and provided a virtual tour, helped familiarize them with the technology by using test calls, and guided them in the use of relevant mobile applications installed on the device. During treatment, the PTC called enrolled veterans to follow up and to answer additional questions. The PTC also provided assistance to veterans interested in enrolling in the patient online portal My HealtheVet to access health information, communicate with providers, and request medication refills.
The VAPORHCS received institutional review board approval to present HBTMH pilot research data and program evaluation data for Innovation (as a quality improvement project). An initial evaluation of the position was completed through review of PTC workload and productivity, informal feedback from telehealth providers, and veteran and provider surveys during and after treatment.
Results
From March 2010 through April 2012, the PTC logged more than 2,500 hours of volunteer service on behalf of the HBTMH pilot (before the Innovation expansion). The dropout rate due to nonclinical reasons for veterans enrolled in the HBTMH pilot was 11%.3 During the HBTMH pilot, 78% of veterans reported that they had enough technical support (ie, from the volunteer PTC), whereas among veterans receiving clinic-based videoconferencing sessions, 61% reported having adequate technical support (ie, from telehealth clinical technicians employed by the VA).3
During 2013 to 2014, veterans and providers were surveyed during and after Innovation program treatment. Eighty percent of participants stated that the PTC was prompt in resolving any issues (20% reported “neutral”). One hundred percent of providers indicated that the PTC was able to resolve the technical issues and that they were “very likely” to continue participating in HBTMH if the PTC was involved. Eighty-nine percent of veterans reported they felt there was enough technical support, and 11% responded “neutral” to this question. Table 2 describes typical PTC services provided during the Innovation program.
Informal summary observations from the PTC confirmed that the most frequent interventions were device and software orientation, assessment of audio and/or video disruptions during sessions, and software log-in configuration and support. Common technical issues included audio and video bandwidth limitations and the need to clean up veterans’ personal computers to restore functionality or improve performance (eg, problems due to malware and viruses; e-mail communication, various dates, William Cannon).
Troubleshooting was performed immediately during a session about half the time (vs between sessions) and initiated by veterans about half the time (vs by providers on their behalf) according to informal observations. The average length of a technical support appointment was about 30 minutes for veterans who were comfortable with technology; in contrast, appointments with veterans who were unfamiliar with technology averaged about 90 minutes.
The task logs recorded instances where flexibility and availability were needed for optimal task completion. Although many tasks seemed to be routine, others showed considerable use of the PTC’s time or direct participation during a session.
One PTC noted, “Client called around 9:30 and had me put [provider’s name] info into Jabber. Also Jabber had an issue of being stuck but forced a call and issue cleared up. 15 min. Stayed online with client to ensure appointment connection went well. 5 min.”
Malware, although not the most common issue, seemed to be time consuming. A task that required 4 hours for resolution of multiple issues was described as “requested outside assist due to drivers. Troubleshooting discovered 240 plus malware and numerous Trojan [horses].”
Another time-consuming issue involved software or updates to existing software interfering with the videoconferencing program, with the following example logged for 90 minutes: “Jabber will not store contacts. Updated IOS. Deleted games. Deleted and reinstalled Jabber. Re-updated Jabber. Problem finally resolved” (December 19, 2014). Other patients simply needed more time to familiarize themselves with the technology, as in this example: “2.5 hours of training and using the iPad” (November 25, 2014).
Informal feedback from providers as well as formal feedback from a program audit indicated appreciation for the PTC’s ability to facilitate engagement and surmount technical hurdles. One provider reflected on a particular instance in which the PTC worked with both the veteran and the provider over the phone and webchat to teach them to use the equipment. “[Veteran] and the peer technician developed a friendly rapport and [veteran] expressed gratitude for the team’s efforts to deliver treatment that he would not have had otherwise.” Another provider commented, “The [National] Help Desk is almost too general. You have to explain who you are each time, and never get to explain who [the] veteran is. … They are aware of national problems. Otherwise, they can’t help out much.”
In 2012, the Office of Telehealth Services completed its Conditions of Participation review of all VISN 20 Telehealth programs and in their final report commended the practices of the HBTMH program, highlighting the associated peer-to-peer volunteer program.4
Discussion
The number of technical issues addressed by the PTC demonstrates the versatility and potential impact of this role. In each case, the PTC accommodates the specific needs of the veteran and any factors that might impact their technology use (eg, low cognitive functioning, hyperarousal, slowed processing speed, low frustration tolerance, or paranoia). This model could be expanded within or outside the VA, although due to the limited scope of the evaluation and the unique qualifications of the individual who filled the PTC role, generalizability remains to be established.
By providing direct support, the PTC attempts to meet veterans where they are and helps them become comfortable with the technology so they are not preoccupied with technical problems while receiving health care. In doing so, engagement in telehealth care is enhanced for patients and providers, and dropouts due to technologic problems may be prevented. Initial program evaluation of this role also suggests considerable provider and veteran satisfaction.
The PTC’s interactions help minimize potential frustrations related to technology use for the delivery of mental health care. Frequently, veterans using in-home telehealth have little experience with technology. Moreover, technology use has been found to be lower for rural dwelling adults.5 Other populations (eg, geriatric) may have greater technology challenges and need additional support.6 When patients start CVT services, there is a potential for dropout if there are initial connection problems, particularly among patients who may have low stress tolerance. The PTC can develop an ongoing relationship with veterans who have a history of technologic difficulties and help monitor them.
Technology barriers and limited support are also a documented barrier to provider engagement.7 Given the inherent limitations and reported provider discouragement with the NTTHD model, more directed technical support may enhance provider engagement and efficiency. With the immediate and one-on-one support given by the PTC, this concern has been assertively addressed. In VISN 20 some mental health care providers elected not to use the CVT-IH program technical support system of the and chose instead to work with the Innovation PTC.
Programmatically, the PTC role is consistent with the VA Office of Mental Health Services and the VA Central Office initiative to increase involvement of peer support programs. From a recovery model perspective, the role of the PTC goes beyond technical support in connecting veterans to other veterans who are encouraged to take control of their health care by making self-directed choices. They can experience empowerment through interactions with another veteran who may share some of their experiences. Further investigation into the effects of using a peer technical support system on veterans, providers, and PTCs compared with the existing national VA technical support help desk system might be useful, particularly with regard to rates of initiation of care or dropouts.
Integration of this role should be done in a purposeful and direct manner, defining peer roles and establishing clear policies and practices. Logistically, the transition of the PTC from a volunteer to a contract employee afforded increased credentialing to allow for improved integration with the other HBTMH team members. The PTC was able to effectively coordinate with clinical, support and administrative staff to share information, resolve issues collaboratively, and bridge gaps in technology knowledge.
Conclusion
Between the HBTMH pilot and the Innovation program, the authors have demonstrated the growing need for personalized and attentive technical support for patients enrolled in home-based telehealth services. Under a current call center help desk model, satisfaction and services may be inadequate for some veterans’ needs. The authors contend that the PTC is an effective way to deliver the necessary specialized technical assistance to veterans and providers and encourage further implementation and evaluation of this approach.
There is preliminary evidence suggesting that this support can have a beneficial impact on provider and veteran engagement in telehealth services. The PTC offers much needed support to providers who frequently do not have the time or knowledge to address all the technical issues that arise during telehealth care. Veterans helping veterans is a powerful alternative deserving of national resources and policy change. Although this case developed in a very VA-specific context, peer technical support may be applicable to other organizations as well.
Acknowledgements
Being the first to do anything in the VA takes courage, tenacity, and luck. The following individuals greatly assisted with the HBTMH pilot and the subsequent Innovation: William “Bear” Cannon, David Greaves, Tracy Dekelboum, William Minium, Sean O’Connor, Joe Ronzio, Kit Teague, and Mark Ward. For assistance with data entry and analysis, the authors thank Athalia White. For help with administrative approvals, the authors thank Bradford Felker and Carol Simons.
This article is dedicated to William “Bear” Cannon, who reinvented himself while serving as the PTC and saved his life along the way. His unwavering commitment to serve his fellow veterans is unheralded. May he be the shining light to those who follow him.
1. Darkins A. The growth of telehealth services in the Veterans Health Administration between 1994 and 2014: a study in the diffusion of innovation. Telemed J E Health. 2014;20(9):761-768.
2. Ronzio JL, Tuerk PW, Shore P. Technology and clinical videoconferencing infrastructures: a guide to selecting appropriate system. In: Tuerk PW, Shore P, eds. Clinical Video Teleconferencing: Program Development and Practice. New York, NY: Springer;2015:3-22.
3. Shore P, Goranson A, Ward MF, Lu MW. Meeting veterans where they're @: a VA home-based telemental health (HBTMH) pilot program. Int J Psychiatry Med. 2014;48(1):5-17.
4. U.S. Department of Veterans Affairs, Veterans Health Administration. Telehealth Conditions of Participation: Final Core and Modality-Specific Standards. Washington, DC: Veterans Health Administration; 2014.
5. Calvert JF Jr, Kaye J, Leahy M, Hexem K, Carlson N. Technology use by rural and urban oldest old. Technol Health Care. 2009;17(1):1-11.
6. Kang HG, Mahoney DF, Hoenig H, et al; Center for Integration of Medicine and Innovative Technology Working Group on Advanced Approaches to Physiologic Monitoring for the Aged. In situ monitoring of health in older adults: technologies and issues. J Am Geriatr Soc. 2010;58(8):1579-1586.
7. Brooks E, Turvey C, Augusterfer EF. Provider barriers to telemental health: obstacles overcome, obstacles remain. Telemed J E Health. 2013;19(6):433-437.
1. Darkins A. The growth of telehealth services in the Veterans Health Administration between 1994 and 2014: a study in the diffusion of innovation. Telemed J E Health. 2014;20(9):761-768.
2. Ronzio JL, Tuerk PW, Shore P. Technology and clinical videoconferencing infrastructures: a guide to selecting appropriate system. In: Tuerk PW, Shore P, eds. Clinical Video Teleconferencing: Program Development and Practice. New York, NY: Springer;2015:3-22.
3. Shore P, Goranson A, Ward MF, Lu MW. Meeting veterans where they're @: a VA home-based telemental health (HBTMH) pilot program. Int J Psychiatry Med. 2014;48(1):5-17.
4. U.S. Department of Veterans Affairs, Veterans Health Administration. Telehealth Conditions of Participation: Final Core and Modality-Specific Standards. Washington, DC: Veterans Health Administration; 2014.
5. Calvert JF Jr, Kaye J, Leahy M, Hexem K, Carlson N. Technology use by rural and urban oldest old. Technol Health Care. 2009;17(1):1-11.
6. Kang HG, Mahoney DF, Hoenig H, et al; Center for Integration of Medicine and Innovative Technology Working Group on Advanced Approaches to Physiologic Monitoring for the Aged. In situ monitoring of health in older adults: technologies and issues. J Am Geriatr Soc. 2010;58(8):1579-1586.
7. Brooks E, Turvey C, Augusterfer EF. Provider barriers to telemental health: obstacles overcome, obstacles remain. Telemed J E Health. 2013;19(6):433-437.
Telejustice: Reaching Incarcerated Veterans via Telehealth
The mission of the veterans justice programs (VJPs), which began in 2007 with the initiation of Health Care for Re-entry Veterans (HCRV) and expanded in 2009 to include Veterans Justice Outreach (VJO), is to prevent homelessness and provide justice-involved veterans with timely access to mental health and substance abuse services or other VA benefits.1 About 50% of homeless veterans have a history with the criminal justice system, and about 10% of all individuals incarcerated in the U.S. are veterans.2
Related: Redesign of a Screening Process for VA Homeless Housing
As the VA’ s use of telehealth services increases at non-VA settings, new opportunities emerge to reach veterans. One such population is incarcerated veterans, who can receive VJO and HCRV services. This article focuses primarily on the implementation of jail/prison outreach via clinical video telehealth (CVT) by VJO, which has already expanded to court liaison work (also provided by VJO) and may further expand to jail/prison outreach by HCRV. The article also describes the development and implementation of the VA’ s first telejustice program (TJP) at the VA Portland Health Care System (HCS) and briefly presents a second TJP at the VA New Jersey HCS Lyons Campus. Currently, there are about 15 known telejustice programs across the VA (Table 1).
Background
Overall, there were about 57,000 veterans seen in VJPs in fiscal year (FY) 2014, an estimated 11% increase over the previous year and an estimated 45% increase from FY12.3 Until November 2012, incarcerated veterans were able to access VJO services only by a face-to-face visit with traveling VA providers. Clinical video telehealth, conducted between a patient and a provider through real-time two-way communication, is a viable option to help improve access to care. In FY14, there were about 248,000 unique veterans who used CVT technologies to access about 660,000 appointments.4
Telemental health (TMH) via clinic-based CVT was first implemented in the VA in 2003. To date, more than 500,000 TMH encounters have occurred. Clinical video telehealth into the home (CVT-IH), which is focused on nonclinic settings was implemented nationally by VHA telehealth services in February 2013. Utilization of CVT-IH has increased from about 1,300 veterans seen (about 6,900 visits) in FY12 to about 4,200 veterans seen (about 20,000 visits) in FY14.4 Nationally, from June 2011 to April 2014, about 150 veterans received some form of VJO services via telehealth through a total of about 500 visits.
Each VAMC has a VJO specialist who serves as a liaison between the VA and law enforcement, court (particularly Veterans Treatment Courts and other collaborative treatment courts), and jails. About 225 VJO specialists provide a variety of services, including outreach, treatment matching/linkage assessment, court liaison and court team participation, and education/training to law enforcement on veteran-centric issues such as posttraumatic stress disorder (PTSD) and traumatic brain injury. Specialists spend significant time traveling to provide these jail/prison
outreach services.
The VA Portland HCS specialist, a licensed clinical social worker, had been in contact with representatives at the Deschutes County Adult Jail in Oregon and had determined there were veterans who could benefit from VA services, but she was unable to make the 322-mile round-trip in 1 day to conduct her visits. She contacted Peter Shore, PsyD, in 2010, then a clinical psychologist at the same VA who was conducting home-based TMH visits, and inquired whether it would be possible to see veterans in the jail via a webcam and personal computer. That was the start of the first VA telejustice program.
Portland Pilot
The VJO specialist at the VA Portland HCS initiated this project in early 2012. The Portland TJP used the same technology, staff, and approach that had been implemented in December 2009 through the Home-Based TMH (HBTMH) pilot. The HBTMH pilot (2009-2012), which predated the national CVT-IH program, included about 40 mental health care providers. It was the first VA pilot to successfully connect providers with veterans in their homes via Internet, webcam, and personal computer. During this period, about 250 veterans were seen in an estimated 750 clinical encounters. About 80% of those enrolled indicated they would not have received any mental health treatment were it not for the availability of HBMTH.
In May 2012, Dr. Shore was awarded a VHA Innovation grant through the VA Office for Innovation to expand the HBTMH pilot to VISN 20 via VHA Innovation 669. The Portland TJP was able to expedite implementation through the grant. In addition to continuing the mission of the HBTMH pilot to deliver behavioral health services into the homes of veterans, the Innovation 669 program was established to focus on the advancement of clinical video visits into a variety of non-VA settings, using alternative technologies, including iPads, netbooks, and alternatives to Cisco Jabber (San Jose, CA), the VA-approved videoconferencing software.
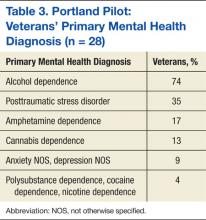
The Portland VJO specialist saw the first veteran on November 27, 2012. Through May 28, 2015, she has conducted 28 assessments with incarcerated veterans via CVT. Among the 28 individuals were 15 army, 11 navy, and 2 marine
veterans aged 24 to 70 years (mean 49.6 y). All 28 veterans were identified as male and white (non-Hispanic). Fifty percent of the veterans seen had at least 1 service-connected disability, and all 28 veterans had at least 1 recorded mental health diagnosis (Tables 2 and 3) (Belinda Maddy, LCSW, written communication, June 9, 2015).
Many of the veterans enrolled in the Portland pilot were able to successfully access services at the VA for substance abuse treatment, PTSD treatment, other mental health services, and/or medical services (Belinda Maddy, LCSW, written communication, June 9, 2015). Like the HBTMH pilot, the Portland VJO pilot has also yielded numerous unexpected patient outcomes, including access to services otherwise not available, access to community resources, enrollment in VA services, and an increase in social connectedness.
“This saved my life,” said one veteran in a testimonial. “Now I have a chance to get treatment instead of prison.” Another veteran noted, “I need to not live in this area to be able to learn how to be sober. Going to a long-term treatment program will help me learn how to live sober so I can stay out of trouble.”
New Jersey Pilot
Similar to the Portland pilot, the VA New Jersey HCS VJP specialist spearheaded the pilot and in June 2013 visited with the warden at the Mercer County Correction Center. In November 2014, a year and a half later and with numerous steps in between, a memorandum of understanding (MOU) and telehealth service agreement (TSA) were signed (Mark Correale, LICSW, written communication, June 10, 2015).
For documentation, the New Jersey specialist established a VA MOU and a TSA; whereas the Portland pilot used documentation specific to the Innovation 669 program (http://vaww.visn20.portal.va.gov/sites/clinical/TH/TeleJustice/SitePages/Home.aspx). From the outset, the specialist explored the CVT-IH model of using an Internet connection, Jabber software, and webcam. According to Mr. Correale (June 10, 2015), VA telehealth-issued webcams and Jabber video used on a VA campus did not work. In testing, it failed to provide synced video and audio but was successful after switching to the Cisco EX90 (San Jose, CA).
Mr. Correale was able to get access to desktop technology in the jail, where a stand-alone monitor was connected to a network inside the facility. As of June 2015, the New Jersey pilot has successfully made 9 videoconferencing connections in Monmouth County and has an additional signed MOU for Hudson County.
Related: Using Life Stories to Connect Veterans and Providers
Mr. Correale (June 10, 2015) indicated, “Dialing into a web-based system from the VA would have been outside the traditional VA telehealth arrangement and was therefore not pursued further.” This indicated that the web-based system used by the Portland VJO specialist may not be accepted at all VA facilities.
In the New Jersey pilot, a video-telephone booth was used, which had an EX90 desktop monitor and connection to the jail’s network. The VA information technology (IT) personnel obtained contact numbers for videoconferencing locations within the New Jersey justice system through an arrangement with the New Jersey State Parole Board. The specialist coordinated with the correctional officers (COs) responsible for escorting veterans to the chosen locations regarding privacy and visit scheduling. The CO would escort the veteran to the video-telephone booth in the jail. For scheduling and completing the encounter, the specialist scheduled the appointment time in VISTA, as did the specialist in Portland.
Discussion
A key element of the Portland pilot was autonomy. The pilot was implemented in the context of a VHA Innovation grant, which reduced a number of required approvals. Utilizing a web-based solution also eliminated significant technical obstacles. A peer technical consultant was on-call during each scheduled appointment and provided all technical support. The peer technical consultant, who had logged 2,500 hours of volunteer services in the HBTMH pilot and who worked full-time as a contractor in the Innovation 669 program, was a critical component to the success of the Portland pilot. The Portland pilot demonstrated an effective, simple, and cost-responsible clinical pathway to connect VA providers with incarcerated veterans through telehealth technologies.
The New Jersey pilot also demonstrated a feasible pathway to connect with incarcerated veterans, achieved through a different approach. The New Jersey pilot accessed incarcerated veterans through the correction center’s internal videoconferencing system, whereas the Portland pilot used VA-approved software over the Internet.
In both cases, the driver for success was the VJO specialist. The New Jersey specialist, Mr. Correale (June 10, 2015) suggested, “It’s helpful to find out what works locally and try to adapt the telehealth model that’s already working.” It is also important for the VJO specialist to get to know local and VISN telehealth staff, as they potentially could provide access to a variety of resources, including assistance with the TSA, locating appropriate equipment, etc. In both pilots, the specialists were very flexible in amending their protocols, documentation, and/or clinic times.
Related: Funding for Innovative Federal Employees
Although there is no national mandate to establish TJPs, there is support from VJO leadership for specialists to investigate the need in their local communities. Information contained in this article and supporting documentation and resources available on the Tele-Justice SharePoint site can provide an adequate starting point for any VJO specialist to initiate their own pilot. Communication through the various VJO listservs is also another mode of acquiring information for those interested in pursuing similar telejustice services.
Compensation and Pension (C&P) examinations for mental health provide a rich opportunity for further exploration. Much of the same operational guidance in this article may be applied to a C&P for mental health clinics. The only significant difference would be the referral source and how the encounter is charted.
Program Launch
A successful telehealth program launch is achieved through distinct development, planning, and implementation stages. Embedded throughout the process are building good relationships, consistent and transparent communication, and coordination. Clinical services drive the need for telehealth; telehealth should not drive the need for clinical services.
A descriptive analysis was approved as a quality improvement project by the institutional review board of the VA Portland HCS. Using information from the 2 pilot projects, the intent is to furnish practical guidance for those developing a TJP. If there is anything the reader should take away from the following guide, it is that implementing a VA TJP is very possible.
Development
Identify the need. With every telehealth program comes a fundamental question: Is there a need to deliver clinical services from a distance? The need can be viewed in many ways, but at the core is access. Identifying a need can be any of the following: travel burden, a judge interested in addressing the increasing number of veterans on their docket, limited resources at the jail/prison for transporting veterans to court hearings, inability to identify a C&P examiner willing to see a veteran in a correctional facility, or a need for the VJP to increase the number of veterans served. In the New Jersey pilot, the local VJO specialist spent time with the New Jersey County Jail Wardens Association to describe how screening justice-involved veterans via telehealth may create more opportunities for veterans and positively impact recidivism.
Evaluate feasibility. Is there buy-in from local leadership and local telehealth personnel? Does the distant site (non-VA) administration agree to a telehealth program? Does the technology at the distant site permit a videoconferencing connection? Are there individuals at the court/jail/prison who can serve as points of contact to assist with a variety of tasks?
Planning
Coordinate with the local facility telehealth coordinator (FTC). All VAMCs have an FTC whose primary role is to implement telehealth programs at the facility. As with any relatively new initiative, the FTC may be unfamiliar with the feasibility of a TJP. It is important to work closely with the FTC to ensure all necessary steps are taken, consistent with national policy regarding telehealth in non-VA settings. For most, the national CVT-IH platform will be the logical approach to establishing a TJP. In some instances, involvement with either the VISN telehealth program manager and/or the VISN behavioral health director may be recommended in addition to the VJP specialist’s supervisor.
In general, the FTC will assist with all required documentation, establishment of a clinic, and ongoing technical support. The FTC may also provide needed guidance with logistics around technical specifications at the distant site.
Conduct a site visit. Meeting with administrative and technology decision makers at the site is an important part of the process and is an opportunity to alleviate any apprehension. They may want to hear more about how telehealth is used at the VA, telehealth research in general, and/or other active TJPs.
Identify a suitable space. There will be a variety of appointments that may be considered for the TJP. If the appointment is an encounter between the provider and veteran, it is recommended to find a space at the detention facility that is as private as possible. The law library, which has windows and a cage, was the designated space for the Portland pilot. The desktop computer and webcam were situated on the outside of the cage. The veteran entered the cage with the correctional officer, who established the Internet connection (Figure).
Identify a point of contact and staff at the distant site. As feasibility is evaluated, identifying a point of contact at the distant site is vital. During the site visit, it is important to meet with the point of contact to review any ongoing logistic issues. One or more staff members should be available to escort the veteran into the space where the telehealth appointment will occur. In some cases, a correctional officer will be on standby during the appointment to address any technical issues with the VA provider and/or in case of a medical or behavioral emergency. In most if not all cases, it is important for the staff member at the distant site to have telephone contact information for the VA provider and/or their respective technical support contact person.
Evaluate technology. Does the distant site facility have Internet access for the space under consideration? If it does, it is likely the FTC will follow the protocols outlined in the CVT-IH platform. Although Jabber is currently the only nationally accepted video teleconferencing software, VISN 20 has successfully used Vidyo (Hackensack, NJ) and VSee (Sunnyvale, CA) on iPads for VISN 20 mobile telehealth programs and is in the process to deploy alternative software solutions and iPads for all VISN 20 TJPs. If the jail/prison facility is open to discussing using their own videoconferencing technologies to bridge into the VA system, these efforts should be coordinated through the FTC. In some cases, the correctional facility will request a desktop computer or laptop with Internet access. The most common issue that prevents a program from being further developed is the lack of viable technology.
VA facility preparation. After the site visit is complete, the FTC should assist with the planning process. This will include identifying a telehealth clinical technician on the VA side and development of appropriate documentation and emergency management protocols. The planning package will also include a MOU between the local VA program leadership representatives and the institution/justice entity where the veteran is being served.
Emergency management protocols must include, at a minimum, a point of contact at the distant site and a contingency point of contact. Phone numbers for each should be acquired well in advance. At the beginning of each session, the provider should have access to those names and numbers in case an emergency arises during the session. At the same time, the VA provider should communicate the emergency protocols to the veteran receiving the services. In the event of an emergency, the provider should do whatever possible to remain connected via video with the veteran and call the distant site point of contact to assist with the emergency. Importantly, participants should follow emergency protocols as outlined by the correctional facility. Readers may contact the author at
[email protected] for a copy of the Portland pilot emergency protocol.
A telehealth clinic will need to be built to capture workload. In most cases, this will be a CVT-IH clinic at the facility. Typically, the FTC will initiate the process with the facility clinical applications coordinator to establish the appropriate clinic build. As the program begins to take shape, an operations manual or practice guidelines will need to be created and updated regularly.
Implementation
After the setup documentation has been completed and before the first appointment, the technology support person and the distant site point of contact should be contacted to confirm the appointment and assist in establishing the Internet connection. (An implementation checklist is available at http://wp.me/p6jTLD-5.)
As the TJP grows, it will be important to evaluate and test the technology, technical support, staffing, and modifications to local protocols to ensure the safety and welfare of the veteran and the provider. Also consider whether the program will collect data and if so, what type.
The Portland pilot collected a variety of data sets, including provider and veteran perspectives on their experiences with the technology. The VHA Innovation 669 program used a brief technology impact questionnaire, designed to monitor how technology has impacted quality of care.5 Data was collected iteratively and used in part to improve aspects of the program. This included both veteran and provider satisfaction, clinical outcomes, quality of life, and levels of occupational and social functioning.
Conclusion
Reaching incarcerated veterans sends an important message: The VA will go to great lengths to ensure that veterans have access to services to help ease the transition back into the community. Connecting with incarcerated veterans via telehealth takes the VA mission to a new level.
Given the wide array of technical solutions currently being used in correctional facilities, VA TJPs may benefit from exploring a consumer-based technology solution. However, one factor in expanding VA TJPs is that current telehealth systems rely on VA Office of Information and Technology resources that build systems within the VA network. There are privacy and security standards the VA adheres to in order to maintain a safe clinical video connection.
There are private sector companies that offer Internet-based access to secure video to connect physicians and mental health professionals. Given the significant variability in IT across correctional facilities, VA TJPs could expand their access into correctional facilities by deploying a web-based clinical video solution, similar to those currently available in the private sector. The technology already exists, and although taking this approach would need to be thoroughly vetted, it could significantly expand VA TJPs and eliminate several obstacles outlined in
this article.
Acknowledgments
Joel Rosenthal, PhD, national training director for Veterans Justice Outreach programs, has provided enduring support to VJPs. To Linda Maddy, the Portland VJO specialist—Being the first to do anything in the VA takes courage and tenacity. To Mark Correale, the NJ VJO specialist, for his tireless efforts. A special thanks to the VHA Innovation 669 team: Chuck Brown, Kit Teague, Trevor Davis, Sean O’Connor, Tracy Dekelboum, and William “Bear” Cannon for providing ongoing support to the Portland telejustice providers and distant jail staff. Mary Lu is providing editorial and research support on this and other telehealth-related projects. This article is dedicated to justice-involved men and women who have served our nation and to those VA employees who dare to be disruptive in order to reach them.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. McGuire J, Clark S. Veterans Justice Outreach Initiative (VJO). Washington, DC: Veterans Health Administration; 2009.
2. U.S. Department of Veterans Affairs. Veterans Health Administration Fact Sheet. VA Services for Veterans Involved in the Justice System: VA’s Veterans Justice Outreach Program. Washington, DC: Veterans Health Administration; 2011.
3. Veterans Health Administration Support Service Center. Homeless Services Briefing Book. Veterans Affairs Intranet Website. http://vaww.fcdm.med.va.gov/pas/en/src/Proclarity.asp. Accessed June 8, 2015.
4. Veterans Health Administration Support Service Center. Virtual care and telehealth report. https://securereports2.vssc.med.va.gov/Reports/Pages/Folder.aspx?ViewMode=Detail. Accessed June 8, 2015.
5. Shore P, Davis T. Technology Impact Questionnaire (TIQ). http://wp.me/p2toog-1f. Published 2014. Accessed June 8, 2015.
The mission of the veterans justice programs (VJPs), which began in 2007 with the initiation of Health Care for Re-entry Veterans (HCRV) and expanded in 2009 to include Veterans Justice Outreach (VJO), is to prevent homelessness and provide justice-involved veterans with timely access to mental health and substance abuse services or other VA benefits.1 About 50% of homeless veterans have a history with the criminal justice system, and about 10% of all individuals incarcerated in the U.S. are veterans.2
Related: Redesign of a Screening Process for VA Homeless Housing
As the VA’ s use of telehealth services increases at non-VA settings, new opportunities emerge to reach veterans. One such population is incarcerated veterans, who can receive VJO and HCRV services. This article focuses primarily on the implementation of jail/prison outreach via clinical video telehealth (CVT) by VJO, which has already expanded to court liaison work (also provided by VJO) and may further expand to jail/prison outreach by HCRV. The article also describes the development and implementation of the VA’ s first telejustice program (TJP) at the VA Portland Health Care System (HCS) and briefly presents a second TJP at the VA New Jersey HCS Lyons Campus. Currently, there are about 15 known telejustice programs across the VA (Table 1).
Background
Overall, there were about 57,000 veterans seen in VJPs in fiscal year (FY) 2014, an estimated 11% increase over the previous year and an estimated 45% increase from FY12.3 Until November 2012, incarcerated veterans were able to access VJO services only by a face-to-face visit with traveling VA providers. Clinical video telehealth, conducted between a patient and a provider through real-time two-way communication, is a viable option to help improve access to care. In FY14, there were about 248,000 unique veterans who used CVT technologies to access about 660,000 appointments.4
Telemental health (TMH) via clinic-based CVT was first implemented in the VA in 2003. To date, more than 500,000 TMH encounters have occurred. Clinical video telehealth into the home (CVT-IH), which is focused on nonclinic settings was implemented nationally by VHA telehealth services in February 2013. Utilization of CVT-IH has increased from about 1,300 veterans seen (about 6,900 visits) in FY12 to about 4,200 veterans seen (about 20,000 visits) in FY14.4 Nationally, from June 2011 to April 2014, about 150 veterans received some form of VJO services via telehealth through a total of about 500 visits.
Each VAMC has a VJO specialist who serves as a liaison between the VA and law enforcement, court (particularly Veterans Treatment Courts and other collaborative treatment courts), and jails. About 225 VJO specialists provide a variety of services, including outreach, treatment matching/linkage assessment, court liaison and court team participation, and education/training to law enforcement on veteran-centric issues such as posttraumatic stress disorder (PTSD) and traumatic brain injury. Specialists spend significant time traveling to provide these jail/prison
outreach services.
The VA Portland HCS specialist, a licensed clinical social worker, had been in contact with representatives at the Deschutes County Adult Jail in Oregon and had determined there were veterans who could benefit from VA services, but she was unable to make the 322-mile round-trip in 1 day to conduct her visits. She contacted Peter Shore, PsyD, in 2010, then a clinical psychologist at the same VA who was conducting home-based TMH visits, and inquired whether it would be possible to see veterans in the jail via a webcam and personal computer. That was the start of the first VA telejustice program.
Portland Pilot
The VJO specialist at the VA Portland HCS initiated this project in early 2012. The Portland TJP used the same technology, staff, and approach that had been implemented in December 2009 through the Home-Based TMH (HBTMH) pilot. The HBTMH pilot (2009-2012), which predated the national CVT-IH program, included about 40 mental health care providers. It was the first VA pilot to successfully connect providers with veterans in their homes via Internet, webcam, and personal computer. During this period, about 250 veterans were seen in an estimated 750 clinical encounters. About 80% of those enrolled indicated they would not have received any mental health treatment were it not for the availability of HBMTH.
In May 2012, Dr. Shore was awarded a VHA Innovation grant through the VA Office for Innovation to expand the HBTMH pilot to VISN 20 via VHA Innovation 669. The Portland TJP was able to expedite implementation through the grant. In addition to continuing the mission of the HBTMH pilot to deliver behavioral health services into the homes of veterans, the Innovation 669 program was established to focus on the advancement of clinical video visits into a variety of non-VA settings, using alternative technologies, including iPads, netbooks, and alternatives to Cisco Jabber (San Jose, CA), the VA-approved videoconferencing software.
The Portland VJO specialist saw the first veteran on November 27, 2012. Through May 28, 2015, she has conducted 28 assessments with incarcerated veterans via CVT. Among the 28 individuals were 15 army, 11 navy, and 2 marine
veterans aged 24 to 70 years (mean 49.6 y). All 28 veterans were identified as male and white (non-Hispanic). Fifty percent of the veterans seen had at least 1 service-connected disability, and all 28 veterans had at least 1 recorded mental health diagnosis (Tables 2 and 3) (Belinda Maddy, LCSW, written communication, June 9, 2015).
Many of the veterans enrolled in the Portland pilot were able to successfully access services at the VA for substance abuse treatment, PTSD treatment, other mental health services, and/or medical services (Belinda Maddy, LCSW, written communication, June 9, 2015). Like the HBTMH pilot, the Portland VJO pilot has also yielded numerous unexpected patient outcomes, including access to services otherwise not available, access to community resources, enrollment in VA services, and an increase in social connectedness.
“This saved my life,” said one veteran in a testimonial. “Now I have a chance to get treatment instead of prison.” Another veteran noted, “I need to not live in this area to be able to learn how to be sober. Going to a long-term treatment program will help me learn how to live sober so I can stay out of trouble.”
New Jersey Pilot
Similar to the Portland pilot, the VA New Jersey HCS VJP specialist spearheaded the pilot and in June 2013 visited with the warden at the Mercer County Correction Center. In November 2014, a year and a half later and with numerous steps in between, a memorandum of understanding (MOU) and telehealth service agreement (TSA) were signed (Mark Correale, LICSW, written communication, June 10, 2015).
For documentation, the New Jersey specialist established a VA MOU and a TSA; whereas the Portland pilot used documentation specific to the Innovation 669 program (http://vaww.visn20.portal.va.gov/sites/clinical/TH/TeleJustice/SitePages/Home.aspx). From the outset, the specialist explored the CVT-IH model of using an Internet connection, Jabber software, and webcam. According to Mr. Correale (June 10, 2015), VA telehealth-issued webcams and Jabber video used on a VA campus did not work. In testing, it failed to provide synced video and audio but was successful after switching to the Cisco EX90 (San Jose, CA).
Mr. Correale was able to get access to desktop technology in the jail, where a stand-alone monitor was connected to a network inside the facility. As of June 2015, the New Jersey pilot has successfully made 9 videoconferencing connections in Monmouth County and has an additional signed MOU for Hudson County.
Related: Using Life Stories to Connect Veterans and Providers
Mr. Correale (June 10, 2015) indicated, “Dialing into a web-based system from the VA would have been outside the traditional VA telehealth arrangement and was therefore not pursued further.” This indicated that the web-based system used by the Portland VJO specialist may not be accepted at all VA facilities.
In the New Jersey pilot, a video-telephone booth was used, which had an EX90 desktop monitor and connection to the jail’s network. The VA information technology (IT) personnel obtained contact numbers for videoconferencing locations within the New Jersey justice system through an arrangement with the New Jersey State Parole Board. The specialist coordinated with the correctional officers (COs) responsible for escorting veterans to the chosen locations regarding privacy and visit scheduling. The CO would escort the veteran to the video-telephone booth in the jail. For scheduling and completing the encounter, the specialist scheduled the appointment time in VISTA, as did the specialist in Portland.
Discussion
A key element of the Portland pilot was autonomy. The pilot was implemented in the context of a VHA Innovation grant, which reduced a number of required approvals. Utilizing a web-based solution also eliminated significant technical obstacles. A peer technical consultant was on-call during each scheduled appointment and provided all technical support. The peer technical consultant, who had logged 2,500 hours of volunteer services in the HBTMH pilot and who worked full-time as a contractor in the Innovation 669 program, was a critical component to the success of the Portland pilot. The Portland pilot demonstrated an effective, simple, and cost-responsible clinical pathway to connect VA providers with incarcerated veterans through telehealth technologies.
The New Jersey pilot also demonstrated a feasible pathway to connect with incarcerated veterans, achieved through a different approach. The New Jersey pilot accessed incarcerated veterans through the correction center’s internal videoconferencing system, whereas the Portland pilot used VA-approved software over the Internet.
In both cases, the driver for success was the VJO specialist. The New Jersey specialist, Mr. Correale (June 10, 2015) suggested, “It’s helpful to find out what works locally and try to adapt the telehealth model that’s already working.” It is also important for the VJO specialist to get to know local and VISN telehealth staff, as they potentially could provide access to a variety of resources, including assistance with the TSA, locating appropriate equipment, etc. In both pilots, the specialists were very flexible in amending their protocols, documentation, and/or clinic times.
Related: Funding for Innovative Federal Employees
Although there is no national mandate to establish TJPs, there is support from VJO leadership for specialists to investigate the need in their local communities. Information contained in this article and supporting documentation and resources available on the Tele-Justice SharePoint site can provide an adequate starting point for any VJO specialist to initiate their own pilot. Communication through the various VJO listservs is also another mode of acquiring information for those interested in pursuing similar telejustice services.
Compensation and Pension (C&P) examinations for mental health provide a rich opportunity for further exploration. Much of the same operational guidance in this article may be applied to a C&P for mental health clinics. The only significant difference would be the referral source and how the encounter is charted.
Program Launch
A successful telehealth program launch is achieved through distinct development, planning, and implementation stages. Embedded throughout the process are building good relationships, consistent and transparent communication, and coordination. Clinical services drive the need for telehealth; telehealth should not drive the need for clinical services.
A descriptive analysis was approved as a quality improvement project by the institutional review board of the VA Portland HCS. Using information from the 2 pilot projects, the intent is to furnish practical guidance for those developing a TJP. If there is anything the reader should take away from the following guide, it is that implementing a VA TJP is very possible.
Development
Identify the need. With every telehealth program comes a fundamental question: Is there a need to deliver clinical services from a distance? The need can be viewed in many ways, but at the core is access. Identifying a need can be any of the following: travel burden, a judge interested in addressing the increasing number of veterans on their docket, limited resources at the jail/prison for transporting veterans to court hearings, inability to identify a C&P examiner willing to see a veteran in a correctional facility, or a need for the VJP to increase the number of veterans served. In the New Jersey pilot, the local VJO specialist spent time with the New Jersey County Jail Wardens Association to describe how screening justice-involved veterans via telehealth may create more opportunities for veterans and positively impact recidivism.
Evaluate feasibility. Is there buy-in from local leadership and local telehealth personnel? Does the distant site (non-VA) administration agree to a telehealth program? Does the technology at the distant site permit a videoconferencing connection? Are there individuals at the court/jail/prison who can serve as points of contact to assist with a variety of tasks?
Planning
Coordinate with the local facility telehealth coordinator (FTC). All VAMCs have an FTC whose primary role is to implement telehealth programs at the facility. As with any relatively new initiative, the FTC may be unfamiliar with the feasibility of a TJP. It is important to work closely with the FTC to ensure all necessary steps are taken, consistent with national policy regarding telehealth in non-VA settings. For most, the national CVT-IH platform will be the logical approach to establishing a TJP. In some instances, involvement with either the VISN telehealth program manager and/or the VISN behavioral health director may be recommended in addition to the VJP specialist’s supervisor.
In general, the FTC will assist with all required documentation, establishment of a clinic, and ongoing technical support. The FTC may also provide needed guidance with logistics around technical specifications at the distant site.
Conduct a site visit. Meeting with administrative and technology decision makers at the site is an important part of the process and is an opportunity to alleviate any apprehension. They may want to hear more about how telehealth is used at the VA, telehealth research in general, and/or other active TJPs.
Identify a suitable space. There will be a variety of appointments that may be considered for the TJP. If the appointment is an encounter between the provider and veteran, it is recommended to find a space at the detention facility that is as private as possible. The law library, which has windows and a cage, was the designated space for the Portland pilot. The desktop computer and webcam were situated on the outside of the cage. The veteran entered the cage with the correctional officer, who established the Internet connection (Figure).
Identify a point of contact and staff at the distant site. As feasibility is evaluated, identifying a point of contact at the distant site is vital. During the site visit, it is important to meet with the point of contact to review any ongoing logistic issues. One or more staff members should be available to escort the veteran into the space where the telehealth appointment will occur. In some cases, a correctional officer will be on standby during the appointment to address any technical issues with the VA provider and/or in case of a medical or behavioral emergency. In most if not all cases, it is important for the staff member at the distant site to have telephone contact information for the VA provider and/or their respective technical support contact person.
Evaluate technology. Does the distant site facility have Internet access for the space under consideration? If it does, it is likely the FTC will follow the protocols outlined in the CVT-IH platform. Although Jabber is currently the only nationally accepted video teleconferencing software, VISN 20 has successfully used Vidyo (Hackensack, NJ) and VSee (Sunnyvale, CA) on iPads for VISN 20 mobile telehealth programs and is in the process to deploy alternative software solutions and iPads for all VISN 20 TJPs. If the jail/prison facility is open to discussing using their own videoconferencing technologies to bridge into the VA system, these efforts should be coordinated through the FTC. In some cases, the correctional facility will request a desktop computer or laptop with Internet access. The most common issue that prevents a program from being further developed is the lack of viable technology.
VA facility preparation. After the site visit is complete, the FTC should assist with the planning process. This will include identifying a telehealth clinical technician on the VA side and development of appropriate documentation and emergency management protocols. The planning package will also include a MOU between the local VA program leadership representatives and the institution/justice entity where the veteran is being served.
Emergency management protocols must include, at a minimum, a point of contact at the distant site and a contingency point of contact. Phone numbers for each should be acquired well in advance. At the beginning of each session, the provider should have access to those names and numbers in case an emergency arises during the session. At the same time, the VA provider should communicate the emergency protocols to the veteran receiving the services. In the event of an emergency, the provider should do whatever possible to remain connected via video with the veteran and call the distant site point of contact to assist with the emergency. Importantly, participants should follow emergency protocols as outlined by the correctional facility. Readers may contact the author at
[email protected] for a copy of the Portland pilot emergency protocol.
A telehealth clinic will need to be built to capture workload. In most cases, this will be a CVT-IH clinic at the facility. Typically, the FTC will initiate the process with the facility clinical applications coordinator to establish the appropriate clinic build. As the program begins to take shape, an operations manual or practice guidelines will need to be created and updated regularly.
Implementation
After the setup documentation has been completed and before the first appointment, the technology support person and the distant site point of contact should be contacted to confirm the appointment and assist in establishing the Internet connection. (An implementation checklist is available at http://wp.me/p6jTLD-5.)
As the TJP grows, it will be important to evaluate and test the technology, technical support, staffing, and modifications to local protocols to ensure the safety and welfare of the veteran and the provider. Also consider whether the program will collect data and if so, what type.
The Portland pilot collected a variety of data sets, including provider and veteran perspectives on their experiences with the technology. The VHA Innovation 669 program used a brief technology impact questionnaire, designed to monitor how technology has impacted quality of care.5 Data was collected iteratively and used in part to improve aspects of the program. This included both veteran and provider satisfaction, clinical outcomes, quality of life, and levels of occupational and social functioning.
Conclusion
Reaching incarcerated veterans sends an important message: The VA will go to great lengths to ensure that veterans have access to services to help ease the transition back into the community. Connecting with incarcerated veterans via telehealth takes the VA mission to a new level.
Given the wide array of technical solutions currently being used in correctional facilities, VA TJPs may benefit from exploring a consumer-based technology solution. However, one factor in expanding VA TJPs is that current telehealth systems rely on VA Office of Information and Technology resources that build systems within the VA network. There are privacy and security standards the VA adheres to in order to maintain a safe clinical video connection.
There are private sector companies that offer Internet-based access to secure video to connect physicians and mental health professionals. Given the significant variability in IT across correctional facilities, VA TJPs could expand their access into correctional facilities by deploying a web-based clinical video solution, similar to those currently available in the private sector. The technology already exists, and although taking this approach would need to be thoroughly vetted, it could significantly expand VA TJPs and eliminate several obstacles outlined in
this article.
Acknowledgments
Joel Rosenthal, PhD, national training director for Veterans Justice Outreach programs, has provided enduring support to VJPs. To Linda Maddy, the Portland VJO specialist—Being the first to do anything in the VA takes courage and tenacity. To Mark Correale, the NJ VJO specialist, for his tireless efforts. A special thanks to the VHA Innovation 669 team: Chuck Brown, Kit Teague, Trevor Davis, Sean O’Connor, Tracy Dekelboum, and William “Bear” Cannon for providing ongoing support to the Portland telejustice providers and distant jail staff. Mary Lu is providing editorial and research support on this and other telehealth-related projects. This article is dedicated to justice-involved men and women who have served our nation and to those VA employees who dare to be disruptive in order to reach them.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
The mission of the veterans justice programs (VJPs), which began in 2007 with the initiation of Health Care for Re-entry Veterans (HCRV) and expanded in 2009 to include Veterans Justice Outreach (VJO), is to prevent homelessness and provide justice-involved veterans with timely access to mental health and substance abuse services or other VA benefits.1 About 50% of homeless veterans have a history with the criminal justice system, and about 10% of all individuals incarcerated in the U.S. are veterans.2
Related: Redesign of a Screening Process for VA Homeless Housing
As the VA’ s use of telehealth services increases at non-VA settings, new opportunities emerge to reach veterans. One such population is incarcerated veterans, who can receive VJO and HCRV services. This article focuses primarily on the implementation of jail/prison outreach via clinical video telehealth (CVT) by VJO, which has already expanded to court liaison work (also provided by VJO) and may further expand to jail/prison outreach by HCRV. The article also describes the development and implementation of the VA’ s first telejustice program (TJP) at the VA Portland Health Care System (HCS) and briefly presents a second TJP at the VA New Jersey HCS Lyons Campus. Currently, there are about 15 known telejustice programs across the VA (Table 1).
Background
Overall, there were about 57,000 veterans seen in VJPs in fiscal year (FY) 2014, an estimated 11% increase over the previous year and an estimated 45% increase from FY12.3 Until November 2012, incarcerated veterans were able to access VJO services only by a face-to-face visit with traveling VA providers. Clinical video telehealth, conducted between a patient and a provider through real-time two-way communication, is a viable option to help improve access to care. In FY14, there were about 248,000 unique veterans who used CVT technologies to access about 660,000 appointments.4
Telemental health (TMH) via clinic-based CVT was first implemented in the VA in 2003. To date, more than 500,000 TMH encounters have occurred. Clinical video telehealth into the home (CVT-IH), which is focused on nonclinic settings was implemented nationally by VHA telehealth services in February 2013. Utilization of CVT-IH has increased from about 1,300 veterans seen (about 6,900 visits) in FY12 to about 4,200 veterans seen (about 20,000 visits) in FY14.4 Nationally, from June 2011 to April 2014, about 150 veterans received some form of VJO services via telehealth through a total of about 500 visits.
Each VAMC has a VJO specialist who serves as a liaison between the VA and law enforcement, court (particularly Veterans Treatment Courts and other collaborative treatment courts), and jails. About 225 VJO specialists provide a variety of services, including outreach, treatment matching/linkage assessment, court liaison and court team participation, and education/training to law enforcement on veteran-centric issues such as posttraumatic stress disorder (PTSD) and traumatic brain injury. Specialists spend significant time traveling to provide these jail/prison
outreach services.
The VA Portland HCS specialist, a licensed clinical social worker, had been in contact with representatives at the Deschutes County Adult Jail in Oregon and had determined there were veterans who could benefit from VA services, but she was unable to make the 322-mile round-trip in 1 day to conduct her visits. She contacted Peter Shore, PsyD, in 2010, then a clinical psychologist at the same VA who was conducting home-based TMH visits, and inquired whether it would be possible to see veterans in the jail via a webcam and personal computer. That was the start of the first VA telejustice program.
Portland Pilot
The VJO specialist at the VA Portland HCS initiated this project in early 2012. The Portland TJP used the same technology, staff, and approach that had been implemented in December 2009 through the Home-Based TMH (HBTMH) pilot. The HBTMH pilot (2009-2012), which predated the national CVT-IH program, included about 40 mental health care providers. It was the first VA pilot to successfully connect providers with veterans in their homes via Internet, webcam, and personal computer. During this period, about 250 veterans were seen in an estimated 750 clinical encounters. About 80% of those enrolled indicated they would not have received any mental health treatment were it not for the availability of HBMTH.
In May 2012, Dr. Shore was awarded a VHA Innovation grant through the VA Office for Innovation to expand the HBTMH pilot to VISN 20 via VHA Innovation 669. The Portland TJP was able to expedite implementation through the grant. In addition to continuing the mission of the HBTMH pilot to deliver behavioral health services into the homes of veterans, the Innovation 669 program was established to focus on the advancement of clinical video visits into a variety of non-VA settings, using alternative technologies, including iPads, netbooks, and alternatives to Cisco Jabber (San Jose, CA), the VA-approved videoconferencing software.
The Portland VJO specialist saw the first veteran on November 27, 2012. Through May 28, 2015, she has conducted 28 assessments with incarcerated veterans via CVT. Among the 28 individuals were 15 army, 11 navy, and 2 marine
veterans aged 24 to 70 years (mean 49.6 y). All 28 veterans were identified as male and white (non-Hispanic). Fifty percent of the veterans seen had at least 1 service-connected disability, and all 28 veterans had at least 1 recorded mental health diagnosis (Tables 2 and 3) (Belinda Maddy, LCSW, written communication, June 9, 2015).
Many of the veterans enrolled in the Portland pilot were able to successfully access services at the VA for substance abuse treatment, PTSD treatment, other mental health services, and/or medical services (Belinda Maddy, LCSW, written communication, June 9, 2015). Like the HBTMH pilot, the Portland VJO pilot has also yielded numerous unexpected patient outcomes, including access to services otherwise not available, access to community resources, enrollment in VA services, and an increase in social connectedness.
“This saved my life,” said one veteran in a testimonial. “Now I have a chance to get treatment instead of prison.” Another veteran noted, “I need to not live in this area to be able to learn how to be sober. Going to a long-term treatment program will help me learn how to live sober so I can stay out of trouble.”
New Jersey Pilot
Similar to the Portland pilot, the VA New Jersey HCS VJP specialist spearheaded the pilot and in June 2013 visited with the warden at the Mercer County Correction Center. In November 2014, a year and a half later and with numerous steps in between, a memorandum of understanding (MOU) and telehealth service agreement (TSA) were signed (Mark Correale, LICSW, written communication, June 10, 2015).
For documentation, the New Jersey specialist established a VA MOU and a TSA; whereas the Portland pilot used documentation specific to the Innovation 669 program (http://vaww.visn20.portal.va.gov/sites/clinical/TH/TeleJustice/SitePages/Home.aspx). From the outset, the specialist explored the CVT-IH model of using an Internet connection, Jabber software, and webcam. According to Mr. Correale (June 10, 2015), VA telehealth-issued webcams and Jabber video used on a VA campus did not work. In testing, it failed to provide synced video and audio but was successful after switching to the Cisco EX90 (San Jose, CA).
Mr. Correale was able to get access to desktop technology in the jail, where a stand-alone monitor was connected to a network inside the facility. As of June 2015, the New Jersey pilot has successfully made 9 videoconferencing connections in Monmouth County and has an additional signed MOU for Hudson County.
Related: Using Life Stories to Connect Veterans and Providers
Mr. Correale (June 10, 2015) indicated, “Dialing into a web-based system from the VA would have been outside the traditional VA telehealth arrangement and was therefore not pursued further.” This indicated that the web-based system used by the Portland VJO specialist may not be accepted at all VA facilities.
In the New Jersey pilot, a video-telephone booth was used, which had an EX90 desktop monitor and connection to the jail’s network. The VA information technology (IT) personnel obtained contact numbers for videoconferencing locations within the New Jersey justice system through an arrangement with the New Jersey State Parole Board. The specialist coordinated with the correctional officers (COs) responsible for escorting veterans to the chosen locations regarding privacy and visit scheduling. The CO would escort the veteran to the video-telephone booth in the jail. For scheduling and completing the encounter, the specialist scheduled the appointment time in VISTA, as did the specialist in Portland.
Discussion
A key element of the Portland pilot was autonomy. The pilot was implemented in the context of a VHA Innovation grant, which reduced a number of required approvals. Utilizing a web-based solution also eliminated significant technical obstacles. A peer technical consultant was on-call during each scheduled appointment and provided all technical support. The peer technical consultant, who had logged 2,500 hours of volunteer services in the HBTMH pilot and who worked full-time as a contractor in the Innovation 669 program, was a critical component to the success of the Portland pilot. The Portland pilot demonstrated an effective, simple, and cost-responsible clinical pathway to connect VA providers with incarcerated veterans through telehealth technologies.
The New Jersey pilot also demonstrated a feasible pathway to connect with incarcerated veterans, achieved through a different approach. The New Jersey pilot accessed incarcerated veterans through the correction center’s internal videoconferencing system, whereas the Portland pilot used VA-approved software over the Internet.
In both cases, the driver for success was the VJO specialist. The New Jersey specialist, Mr. Correale (June 10, 2015) suggested, “It’s helpful to find out what works locally and try to adapt the telehealth model that’s already working.” It is also important for the VJO specialist to get to know local and VISN telehealth staff, as they potentially could provide access to a variety of resources, including assistance with the TSA, locating appropriate equipment, etc. In both pilots, the specialists were very flexible in amending their protocols, documentation, and/or clinic times.
Related: Funding for Innovative Federal Employees
Although there is no national mandate to establish TJPs, there is support from VJO leadership for specialists to investigate the need in their local communities. Information contained in this article and supporting documentation and resources available on the Tele-Justice SharePoint site can provide an adequate starting point for any VJO specialist to initiate their own pilot. Communication through the various VJO listservs is also another mode of acquiring information for those interested in pursuing similar telejustice services.
Compensation and Pension (C&P) examinations for mental health provide a rich opportunity for further exploration. Much of the same operational guidance in this article may be applied to a C&P for mental health clinics. The only significant difference would be the referral source and how the encounter is charted.
Program Launch
A successful telehealth program launch is achieved through distinct development, planning, and implementation stages. Embedded throughout the process are building good relationships, consistent and transparent communication, and coordination. Clinical services drive the need for telehealth; telehealth should not drive the need for clinical services.
A descriptive analysis was approved as a quality improvement project by the institutional review board of the VA Portland HCS. Using information from the 2 pilot projects, the intent is to furnish practical guidance for those developing a TJP. If there is anything the reader should take away from the following guide, it is that implementing a VA TJP is very possible.
Development
Identify the need. With every telehealth program comes a fundamental question: Is there a need to deliver clinical services from a distance? The need can be viewed in many ways, but at the core is access. Identifying a need can be any of the following: travel burden, a judge interested in addressing the increasing number of veterans on their docket, limited resources at the jail/prison for transporting veterans to court hearings, inability to identify a C&P examiner willing to see a veteran in a correctional facility, or a need for the VJP to increase the number of veterans served. In the New Jersey pilot, the local VJO specialist spent time with the New Jersey County Jail Wardens Association to describe how screening justice-involved veterans via telehealth may create more opportunities for veterans and positively impact recidivism.
Evaluate feasibility. Is there buy-in from local leadership and local telehealth personnel? Does the distant site (non-VA) administration agree to a telehealth program? Does the technology at the distant site permit a videoconferencing connection? Are there individuals at the court/jail/prison who can serve as points of contact to assist with a variety of tasks?
Planning
Coordinate with the local facility telehealth coordinator (FTC). All VAMCs have an FTC whose primary role is to implement telehealth programs at the facility. As with any relatively new initiative, the FTC may be unfamiliar with the feasibility of a TJP. It is important to work closely with the FTC to ensure all necessary steps are taken, consistent with national policy regarding telehealth in non-VA settings. For most, the national CVT-IH platform will be the logical approach to establishing a TJP. In some instances, involvement with either the VISN telehealth program manager and/or the VISN behavioral health director may be recommended in addition to the VJP specialist’s supervisor.
In general, the FTC will assist with all required documentation, establishment of a clinic, and ongoing technical support. The FTC may also provide needed guidance with logistics around technical specifications at the distant site.
Conduct a site visit. Meeting with administrative and technology decision makers at the site is an important part of the process and is an opportunity to alleviate any apprehension. They may want to hear more about how telehealth is used at the VA, telehealth research in general, and/or other active TJPs.
Identify a suitable space. There will be a variety of appointments that may be considered for the TJP. If the appointment is an encounter between the provider and veteran, it is recommended to find a space at the detention facility that is as private as possible. The law library, which has windows and a cage, was the designated space for the Portland pilot. The desktop computer and webcam were situated on the outside of the cage. The veteran entered the cage with the correctional officer, who established the Internet connection (Figure).
Identify a point of contact and staff at the distant site. As feasibility is evaluated, identifying a point of contact at the distant site is vital. During the site visit, it is important to meet with the point of contact to review any ongoing logistic issues. One or more staff members should be available to escort the veteran into the space where the telehealth appointment will occur. In some cases, a correctional officer will be on standby during the appointment to address any technical issues with the VA provider and/or in case of a medical or behavioral emergency. In most if not all cases, it is important for the staff member at the distant site to have telephone contact information for the VA provider and/or their respective technical support contact person.
Evaluate technology. Does the distant site facility have Internet access for the space under consideration? If it does, it is likely the FTC will follow the protocols outlined in the CVT-IH platform. Although Jabber is currently the only nationally accepted video teleconferencing software, VISN 20 has successfully used Vidyo (Hackensack, NJ) and VSee (Sunnyvale, CA) on iPads for VISN 20 mobile telehealth programs and is in the process to deploy alternative software solutions and iPads for all VISN 20 TJPs. If the jail/prison facility is open to discussing using their own videoconferencing technologies to bridge into the VA system, these efforts should be coordinated through the FTC. In some cases, the correctional facility will request a desktop computer or laptop with Internet access. The most common issue that prevents a program from being further developed is the lack of viable technology.
VA facility preparation. After the site visit is complete, the FTC should assist with the planning process. This will include identifying a telehealth clinical technician on the VA side and development of appropriate documentation and emergency management protocols. The planning package will also include a MOU between the local VA program leadership representatives and the institution/justice entity where the veteran is being served.
Emergency management protocols must include, at a minimum, a point of contact at the distant site and a contingency point of contact. Phone numbers for each should be acquired well in advance. At the beginning of each session, the provider should have access to those names and numbers in case an emergency arises during the session. At the same time, the VA provider should communicate the emergency protocols to the veteran receiving the services. In the event of an emergency, the provider should do whatever possible to remain connected via video with the veteran and call the distant site point of contact to assist with the emergency. Importantly, participants should follow emergency protocols as outlined by the correctional facility. Readers may contact the author at
[email protected] for a copy of the Portland pilot emergency protocol.
A telehealth clinic will need to be built to capture workload. In most cases, this will be a CVT-IH clinic at the facility. Typically, the FTC will initiate the process with the facility clinical applications coordinator to establish the appropriate clinic build. As the program begins to take shape, an operations manual or practice guidelines will need to be created and updated regularly.
Implementation
After the setup documentation has been completed and before the first appointment, the technology support person and the distant site point of contact should be contacted to confirm the appointment and assist in establishing the Internet connection. (An implementation checklist is available at http://wp.me/p6jTLD-5.)
As the TJP grows, it will be important to evaluate and test the technology, technical support, staffing, and modifications to local protocols to ensure the safety and welfare of the veteran and the provider. Also consider whether the program will collect data and if so, what type.
The Portland pilot collected a variety of data sets, including provider and veteran perspectives on their experiences with the technology. The VHA Innovation 669 program used a brief technology impact questionnaire, designed to monitor how technology has impacted quality of care.5 Data was collected iteratively and used in part to improve aspects of the program. This included both veteran and provider satisfaction, clinical outcomes, quality of life, and levels of occupational and social functioning.
Conclusion
Reaching incarcerated veterans sends an important message: The VA will go to great lengths to ensure that veterans have access to services to help ease the transition back into the community. Connecting with incarcerated veterans via telehealth takes the VA mission to a new level.
Given the wide array of technical solutions currently being used in correctional facilities, VA TJPs may benefit from exploring a consumer-based technology solution. However, one factor in expanding VA TJPs is that current telehealth systems rely on VA Office of Information and Technology resources that build systems within the VA network. There are privacy and security standards the VA adheres to in order to maintain a safe clinical video connection.
There are private sector companies that offer Internet-based access to secure video to connect physicians and mental health professionals. Given the significant variability in IT across correctional facilities, VA TJPs could expand their access into correctional facilities by deploying a web-based clinical video solution, similar to those currently available in the private sector. The technology already exists, and although taking this approach would need to be thoroughly vetted, it could significantly expand VA TJPs and eliminate several obstacles outlined in
this article.
Acknowledgments
Joel Rosenthal, PhD, national training director for Veterans Justice Outreach programs, has provided enduring support to VJPs. To Linda Maddy, the Portland VJO specialist—Being the first to do anything in the VA takes courage and tenacity. To Mark Correale, the NJ VJO specialist, for his tireless efforts. A special thanks to the VHA Innovation 669 team: Chuck Brown, Kit Teague, Trevor Davis, Sean O’Connor, Tracy Dekelboum, and William “Bear” Cannon for providing ongoing support to the Portland telejustice providers and distant jail staff. Mary Lu is providing editorial and research support on this and other telehealth-related projects. This article is dedicated to justice-involved men and women who have served our nation and to those VA employees who dare to be disruptive in order to reach them.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. McGuire J, Clark S. Veterans Justice Outreach Initiative (VJO). Washington, DC: Veterans Health Administration; 2009.
2. U.S. Department of Veterans Affairs. Veterans Health Administration Fact Sheet. VA Services for Veterans Involved in the Justice System: VA’s Veterans Justice Outreach Program. Washington, DC: Veterans Health Administration; 2011.
3. Veterans Health Administration Support Service Center. Homeless Services Briefing Book. Veterans Affairs Intranet Website. http://vaww.fcdm.med.va.gov/pas/en/src/Proclarity.asp. Accessed June 8, 2015.
4. Veterans Health Administration Support Service Center. Virtual care and telehealth report. https://securereports2.vssc.med.va.gov/Reports/Pages/Folder.aspx?ViewMode=Detail. Accessed June 8, 2015.
5. Shore P, Davis T. Technology Impact Questionnaire (TIQ). http://wp.me/p2toog-1f. Published 2014. Accessed June 8, 2015.
1. McGuire J, Clark S. Veterans Justice Outreach Initiative (VJO). Washington, DC: Veterans Health Administration; 2009.
2. U.S. Department of Veterans Affairs. Veterans Health Administration Fact Sheet. VA Services for Veterans Involved in the Justice System: VA’s Veterans Justice Outreach Program. Washington, DC: Veterans Health Administration; 2011.
3. Veterans Health Administration Support Service Center. Homeless Services Briefing Book. Veterans Affairs Intranet Website. http://vaww.fcdm.med.va.gov/pas/en/src/Proclarity.asp. Accessed June 8, 2015.
4. Veterans Health Administration Support Service Center. Virtual care and telehealth report. https://securereports2.vssc.med.va.gov/Reports/Pages/Folder.aspx?ViewMode=Detail. Accessed June 8, 2015.
5. Shore P, Davis T. Technology Impact Questionnaire (TIQ). http://wp.me/p2toog-1f. Published 2014. Accessed June 8, 2015.