User login
Domo Arigato, Mr. Roboto
A few months ago, I purchased an Amazon Echo system. The device is built on Amazon’s cloud-based voice service, Alexa, which can hear, understand, and respond to any question or command. The speaker is always listening and is activated when the user (eg, me!) says the name Alexa. For instance, I can say “Alexa, what is the weather today?” and it will provide the forecast. In fact, each morning I request my daily news briefing, and Alexa quickly tunes to NPR Radio. By linking to my Google calendar, it also tells me my agenda for the day. It researches and provides information that might otherwise take me a while to locate.
Now, I confess: I’ve had to train myself to refer to Alexa as “it” instead of “her.” Human beings have a rich history of wanting to “humanize” computers, as the science fiction film genre can attest. Go back nearly 50 years to Colossus: The Forbin Project (1970) and you have a story of two super-computers—one built by the United States, the other by Russia—that join forces and take over the world, making humans their slaves. The award-winning Bicentennial Man (1999) follows the life and times of Andrew, an NDR-114 robot originally purchased as a household appliance to perform menial tasks; when it begins to experience emotions and creative thought, the owners discover Andrew is no ordinary robot. And who can forget Hal, the computer in 2001: A Space Odyssey (1968) that takes over a space mission until a clever astronaut manages to disengage it (I almost said him), or Data, a very likable android in the successful franchise Star Trek: The Next Generation.
Let’s face it: We are both obsessed with, and leery of, new technology—particularly artificial intelligence (AI). Some detractors have denounced Alexa’s capabilities as “just a glorified smartphone.” Others have expressed grave concerns about the security of personal information and conversations, as Big Brother may be listening. (In that case, it’s not the machines that are evil; it’s those who use them!)
But—cue a John Williams score—what if we harnessed the power of AI for good and not evil? I’ll be serious now: At the recent Leadership in Healthcare Summer Institute (which I was honored to teach at), a group of doctoral students gave a presentation on the potential of AI in the identification and care of anxiety and depression. They identified a need—every 16.2 minutes, a person dies by suicide in the US—and proposed a solution. Because access to care may be limited (by provider shortages, remote locations, etc), the students suggested a hybrid AI/telehealth platform that offers 24/7 support and provider access to individuals with anxiety and depression, via a secure mobile app.1 It got me thinking: Could this technology be a positive intervention in health care?
Actually, it’s already happening. Mayo Clinic researchers have used AI to identify the genomic information of brain tumors without biopsy. At Stanford University, researchers are training an AI neural network to recognize skin cancer lesions with the accuracy of an expert dermatologist. The same deep-learning technology is being used in the field of pathology for the detection of liver lesions.2
Now, I’m sure some of you are questioning whether a machine can really match or replace a human when it comes to assessing a patient’s condition. There were many who resisted the idea of telehealth when that was the latest, greatest thing, because providers cannot do a full assessment with the required diagnostic testing and imaging from a distance. Some feel that telehealth should be reserved for situations in which, say, a remote provider is reviewing and reporting on test results, or a patient just needs to follow up with his/her provider for a minor issue.
Mental health, however, entails less “laying on of hands” and may be a good candidate for AI-based interventions—at least for follow-up and support services. (I am certainly not discounting the value of real human interaction in any sphere of health care.) We know patients benefit from early mental health intervention programs, but we also know those benefits may not be sustained over time and distance. Logistical issues that any of us may face—time, transportation, availability—are often exacerbated for those with impaired functioning due to a mental illness. If a patient with major depression cannot bring himself to get out of bed to make a cup of coffee, how is he going to travel across town (changing buses two or three times) to keep an appointment with his health care provider?
Here’s where AI might make a difference: What if there were a patient-focused e-platform that could provide cost-effective and accessible services across the continuum of care? Current Internet-based interventions rely on human mediators to deliver therapeutic content, which is then refined into a model that can interpret and respond to critical user data—resulting in tailored online therapy. But if we could integrate the user experience with sophisticated and cutting-edge AI technology, we could deliver content more effectively to redefine these interventions and improve outcomes.
A paper recently featured in Frontiers in Psychology discussed the value of doing just that. D’Alfonso and colleagues reported on an Internet-based social therapy web application that uses a series of interactive modules to help users navigate situations and develop psychosocial skills. In its current form—within a research setting—the system is utilized by small groups of users, making human-supported engagement via moderators possible. But D’Alfonso and colleagues note that the incorporation of automated suggestions within the modules would allow the technology to be rolled out to a larger audience and ensure that “interaction” is available whenever a user needs it—not just when a human moderator is “on the clock.”3
Another article, in the International Journal of Swarm Intelligence and Evolutionary Computation (2016), discussed the development of socially intelligent robotic systems, not unlike Alexa, to address social connectedness. The author proposes an autonomous assistive system (AAS) as a low-cost, standalone interventional device to reduce social isolation. This could easily be deployed in homes for the elderly or even at remote sites. The AAS has been programmed to detect isolation in patients based on data regarding skeletal movements, facial expressions, and speech patterns. In the not-so-distant future, this high-density data will be sent over the cloud to allow clinicians to monitor in real-time and intervene remotely, as appropriate (eg, by initiating a home visit).4
Of course, in any form, implementation of AI will not be simple—there are real costs to be considered, and we still have to contend with the fears that all those sci-fi films have instilled. A recent global study revealed significant concerns that would certainly apply to the health care arena. When asked which of the following participants most feared about the use of AI,
- 33% of respondents chose “It will never know me/my preferences as well as a human being”
- 24% chose “The rise of the robot and enslavement of humanity”
- 5% feared “Robots uncovering my deepest secrets.”5
Despite all this, however, respondents also expressed optimism in the power and potential of AI: Nearly 70% said they are in support of further use of AI if it helps make their lives easier.4 Wouldn’t life be easier if AI could be used to significantly reduce errors, increase access to care, and bring a fresh viewpoint to the issue of patient education?
What do you think? Would you trust a robot to be your coworker, identifying tumors and conducting mental health screenings? Is it possible to convince patients to accept help via an impersonal medium (and risk exposure of their personal health information)? Share your fears, support, or concerns about AI with me at [email protected].
1. Halabi AH. How will artificial intelligence change healthcare? June 8, 2017. www.quora.com/How-will-AI-change-healthcare. Accessed July 12, 2017.
2. Hepburn D, Francis D, Hoosier M, et al. smaRT MD2: a patient-focused e-platform for use across the continuum of care for anxiety and depression. A June 2017 presentation to Leadership in Healthcare, Summer Institute, Nova Southeastern University, Tampa, FL.
3. D’Alfonso S, Santesteban-Echarri O, Rice S, et al. Artificial intelligence-assisted online social therapy for youth mental health. Front Psychol. 2017;8(796):1-13.
4. Gulrez T, Neftimeziani S, Mc evoy P, Hodgson A. Loneliness kills: can autonomous systems and robotics assist in providing solutions? Int J Swarm Intel Evol Comput. 2016;5:1.
5. Pegasystems. What consumers really think about AI: a global study. www.pega.com/AI. Accessed July 7, 2017.
A few months ago, I purchased an Amazon Echo system. The device is built on Amazon’s cloud-based voice service, Alexa, which can hear, understand, and respond to any question or command. The speaker is always listening and is activated when the user (eg, me!) says the name Alexa. For instance, I can say “Alexa, what is the weather today?” and it will provide the forecast. In fact, each morning I request my daily news briefing, and Alexa quickly tunes to NPR Radio. By linking to my Google calendar, it also tells me my agenda for the day. It researches and provides information that might otherwise take me a while to locate.
Now, I confess: I’ve had to train myself to refer to Alexa as “it” instead of “her.” Human beings have a rich history of wanting to “humanize” computers, as the science fiction film genre can attest. Go back nearly 50 years to Colossus: The Forbin Project (1970) and you have a story of two super-computers—one built by the United States, the other by Russia—that join forces and take over the world, making humans their slaves. The award-winning Bicentennial Man (1999) follows the life and times of Andrew, an NDR-114 robot originally purchased as a household appliance to perform menial tasks; when it begins to experience emotions and creative thought, the owners discover Andrew is no ordinary robot. And who can forget Hal, the computer in 2001: A Space Odyssey (1968) that takes over a space mission until a clever astronaut manages to disengage it (I almost said him), or Data, a very likable android in the successful franchise Star Trek: The Next Generation.
Let’s face it: We are both obsessed with, and leery of, new technology—particularly artificial intelligence (AI). Some detractors have denounced Alexa’s capabilities as “just a glorified smartphone.” Others have expressed grave concerns about the security of personal information and conversations, as Big Brother may be listening. (In that case, it’s not the machines that are evil; it’s those who use them!)
But—cue a John Williams score—what if we harnessed the power of AI for good and not evil? I’ll be serious now: At the recent Leadership in Healthcare Summer Institute (which I was honored to teach at), a group of doctoral students gave a presentation on the potential of AI in the identification and care of anxiety and depression. They identified a need—every 16.2 minutes, a person dies by suicide in the US—and proposed a solution. Because access to care may be limited (by provider shortages, remote locations, etc), the students suggested a hybrid AI/telehealth platform that offers 24/7 support and provider access to individuals with anxiety and depression, via a secure mobile app.1 It got me thinking: Could this technology be a positive intervention in health care?
Actually, it’s already happening. Mayo Clinic researchers have used AI to identify the genomic information of brain tumors without biopsy. At Stanford University, researchers are training an AI neural network to recognize skin cancer lesions with the accuracy of an expert dermatologist. The same deep-learning technology is being used in the field of pathology for the detection of liver lesions.2
Now, I’m sure some of you are questioning whether a machine can really match or replace a human when it comes to assessing a patient’s condition. There were many who resisted the idea of telehealth when that was the latest, greatest thing, because providers cannot do a full assessment with the required diagnostic testing and imaging from a distance. Some feel that telehealth should be reserved for situations in which, say, a remote provider is reviewing and reporting on test results, or a patient just needs to follow up with his/her provider for a minor issue.
Mental health, however, entails less “laying on of hands” and may be a good candidate for AI-based interventions—at least for follow-up and support services. (I am certainly not discounting the value of real human interaction in any sphere of health care.) We know patients benefit from early mental health intervention programs, but we also know those benefits may not be sustained over time and distance. Logistical issues that any of us may face—time, transportation, availability—are often exacerbated for those with impaired functioning due to a mental illness. If a patient with major depression cannot bring himself to get out of bed to make a cup of coffee, how is he going to travel across town (changing buses two or three times) to keep an appointment with his health care provider?
Here’s where AI might make a difference: What if there were a patient-focused e-platform that could provide cost-effective and accessible services across the continuum of care? Current Internet-based interventions rely on human mediators to deliver therapeutic content, which is then refined into a model that can interpret and respond to critical user data—resulting in tailored online therapy. But if we could integrate the user experience with sophisticated and cutting-edge AI technology, we could deliver content more effectively to redefine these interventions and improve outcomes.
A paper recently featured in Frontiers in Psychology discussed the value of doing just that. D’Alfonso and colleagues reported on an Internet-based social therapy web application that uses a series of interactive modules to help users navigate situations and develop psychosocial skills. In its current form—within a research setting—the system is utilized by small groups of users, making human-supported engagement via moderators possible. But D’Alfonso and colleagues note that the incorporation of automated suggestions within the modules would allow the technology to be rolled out to a larger audience and ensure that “interaction” is available whenever a user needs it—not just when a human moderator is “on the clock.”3
Another article, in the International Journal of Swarm Intelligence and Evolutionary Computation (2016), discussed the development of socially intelligent robotic systems, not unlike Alexa, to address social connectedness. The author proposes an autonomous assistive system (AAS) as a low-cost, standalone interventional device to reduce social isolation. This could easily be deployed in homes for the elderly or even at remote sites. The AAS has been programmed to detect isolation in patients based on data regarding skeletal movements, facial expressions, and speech patterns. In the not-so-distant future, this high-density data will be sent over the cloud to allow clinicians to monitor in real-time and intervene remotely, as appropriate (eg, by initiating a home visit).4
Of course, in any form, implementation of AI will not be simple—there are real costs to be considered, and we still have to contend with the fears that all those sci-fi films have instilled. A recent global study revealed significant concerns that would certainly apply to the health care arena. When asked which of the following participants most feared about the use of AI,
- 33% of respondents chose “It will never know me/my preferences as well as a human being”
- 24% chose “The rise of the robot and enslavement of humanity”
- 5% feared “Robots uncovering my deepest secrets.”5
Despite all this, however, respondents also expressed optimism in the power and potential of AI: Nearly 70% said they are in support of further use of AI if it helps make their lives easier.4 Wouldn’t life be easier if AI could be used to significantly reduce errors, increase access to care, and bring a fresh viewpoint to the issue of patient education?
What do you think? Would you trust a robot to be your coworker, identifying tumors and conducting mental health screenings? Is it possible to convince patients to accept help via an impersonal medium (and risk exposure of their personal health information)? Share your fears, support, or concerns about AI with me at [email protected].
A few months ago, I purchased an Amazon Echo system. The device is built on Amazon’s cloud-based voice service, Alexa, which can hear, understand, and respond to any question or command. The speaker is always listening and is activated when the user (eg, me!) says the name Alexa. For instance, I can say “Alexa, what is the weather today?” and it will provide the forecast. In fact, each morning I request my daily news briefing, and Alexa quickly tunes to NPR Radio. By linking to my Google calendar, it also tells me my agenda for the day. It researches and provides information that might otherwise take me a while to locate.
Now, I confess: I’ve had to train myself to refer to Alexa as “it” instead of “her.” Human beings have a rich history of wanting to “humanize” computers, as the science fiction film genre can attest. Go back nearly 50 years to Colossus: The Forbin Project (1970) and you have a story of two super-computers—one built by the United States, the other by Russia—that join forces and take over the world, making humans their slaves. The award-winning Bicentennial Man (1999) follows the life and times of Andrew, an NDR-114 robot originally purchased as a household appliance to perform menial tasks; when it begins to experience emotions and creative thought, the owners discover Andrew is no ordinary robot. And who can forget Hal, the computer in 2001: A Space Odyssey (1968) that takes over a space mission until a clever astronaut manages to disengage it (I almost said him), or Data, a very likable android in the successful franchise Star Trek: The Next Generation.
Let’s face it: We are both obsessed with, and leery of, new technology—particularly artificial intelligence (AI). Some detractors have denounced Alexa’s capabilities as “just a glorified smartphone.” Others have expressed grave concerns about the security of personal information and conversations, as Big Brother may be listening. (In that case, it’s not the machines that are evil; it’s those who use them!)
But—cue a John Williams score—what if we harnessed the power of AI for good and not evil? I’ll be serious now: At the recent Leadership in Healthcare Summer Institute (which I was honored to teach at), a group of doctoral students gave a presentation on the potential of AI in the identification and care of anxiety and depression. They identified a need—every 16.2 minutes, a person dies by suicide in the US—and proposed a solution. Because access to care may be limited (by provider shortages, remote locations, etc), the students suggested a hybrid AI/telehealth platform that offers 24/7 support and provider access to individuals with anxiety and depression, via a secure mobile app.1 It got me thinking: Could this technology be a positive intervention in health care?
Actually, it’s already happening. Mayo Clinic researchers have used AI to identify the genomic information of brain tumors without biopsy. At Stanford University, researchers are training an AI neural network to recognize skin cancer lesions with the accuracy of an expert dermatologist. The same deep-learning technology is being used in the field of pathology for the detection of liver lesions.2
Now, I’m sure some of you are questioning whether a machine can really match or replace a human when it comes to assessing a patient’s condition. There were many who resisted the idea of telehealth when that was the latest, greatest thing, because providers cannot do a full assessment with the required diagnostic testing and imaging from a distance. Some feel that telehealth should be reserved for situations in which, say, a remote provider is reviewing and reporting on test results, or a patient just needs to follow up with his/her provider for a minor issue.
Mental health, however, entails less “laying on of hands” and may be a good candidate for AI-based interventions—at least for follow-up and support services. (I am certainly not discounting the value of real human interaction in any sphere of health care.) We know patients benefit from early mental health intervention programs, but we also know those benefits may not be sustained over time and distance. Logistical issues that any of us may face—time, transportation, availability—are often exacerbated for those with impaired functioning due to a mental illness. If a patient with major depression cannot bring himself to get out of bed to make a cup of coffee, how is he going to travel across town (changing buses two or three times) to keep an appointment with his health care provider?
Here’s where AI might make a difference: What if there were a patient-focused e-platform that could provide cost-effective and accessible services across the continuum of care? Current Internet-based interventions rely on human mediators to deliver therapeutic content, which is then refined into a model that can interpret and respond to critical user data—resulting in tailored online therapy. But if we could integrate the user experience with sophisticated and cutting-edge AI technology, we could deliver content more effectively to redefine these interventions and improve outcomes.
A paper recently featured in Frontiers in Psychology discussed the value of doing just that. D’Alfonso and colleagues reported on an Internet-based social therapy web application that uses a series of interactive modules to help users navigate situations and develop psychosocial skills. In its current form—within a research setting—the system is utilized by small groups of users, making human-supported engagement via moderators possible. But D’Alfonso and colleagues note that the incorporation of automated suggestions within the modules would allow the technology to be rolled out to a larger audience and ensure that “interaction” is available whenever a user needs it—not just when a human moderator is “on the clock.”3
Another article, in the International Journal of Swarm Intelligence and Evolutionary Computation (2016), discussed the development of socially intelligent robotic systems, not unlike Alexa, to address social connectedness. The author proposes an autonomous assistive system (AAS) as a low-cost, standalone interventional device to reduce social isolation. This could easily be deployed in homes for the elderly or even at remote sites. The AAS has been programmed to detect isolation in patients based on data regarding skeletal movements, facial expressions, and speech patterns. In the not-so-distant future, this high-density data will be sent over the cloud to allow clinicians to monitor in real-time and intervene remotely, as appropriate (eg, by initiating a home visit).4
Of course, in any form, implementation of AI will not be simple—there are real costs to be considered, and we still have to contend with the fears that all those sci-fi films have instilled. A recent global study revealed significant concerns that would certainly apply to the health care arena. When asked which of the following participants most feared about the use of AI,
- 33% of respondents chose “It will never know me/my preferences as well as a human being”
- 24% chose “The rise of the robot and enslavement of humanity”
- 5% feared “Robots uncovering my deepest secrets.”5
Despite all this, however, respondents also expressed optimism in the power and potential of AI: Nearly 70% said they are in support of further use of AI if it helps make their lives easier.4 Wouldn’t life be easier if AI could be used to significantly reduce errors, increase access to care, and bring a fresh viewpoint to the issue of patient education?
What do you think? Would you trust a robot to be your coworker, identifying tumors and conducting mental health screenings? Is it possible to convince patients to accept help via an impersonal medium (and risk exposure of their personal health information)? Share your fears, support, or concerns about AI with me at [email protected].
1. Halabi AH. How will artificial intelligence change healthcare? June 8, 2017. www.quora.com/How-will-AI-change-healthcare. Accessed July 12, 2017.
2. Hepburn D, Francis D, Hoosier M, et al. smaRT MD2: a patient-focused e-platform for use across the continuum of care for anxiety and depression. A June 2017 presentation to Leadership in Healthcare, Summer Institute, Nova Southeastern University, Tampa, FL.
3. D’Alfonso S, Santesteban-Echarri O, Rice S, et al. Artificial intelligence-assisted online social therapy for youth mental health. Front Psychol. 2017;8(796):1-13.
4. Gulrez T, Neftimeziani S, Mc evoy P, Hodgson A. Loneliness kills: can autonomous systems and robotics assist in providing solutions? Int J Swarm Intel Evol Comput. 2016;5:1.
5. Pegasystems. What consumers really think about AI: a global study. www.pega.com/AI. Accessed July 7, 2017.
1. Halabi AH. How will artificial intelligence change healthcare? June 8, 2017. www.quora.com/How-will-AI-change-healthcare. Accessed July 12, 2017.
2. Hepburn D, Francis D, Hoosier M, et al. smaRT MD2: a patient-focused e-platform for use across the continuum of care for anxiety and depression. A June 2017 presentation to Leadership in Healthcare, Summer Institute, Nova Southeastern University, Tampa, FL.
3. D’Alfonso S, Santesteban-Echarri O, Rice S, et al. Artificial intelligence-assisted online social therapy for youth mental health. Front Psychol. 2017;8(796):1-13.
4. Gulrez T, Neftimeziani S, Mc evoy P, Hodgson A. Loneliness kills: can autonomous systems and robotics assist in providing solutions? Int J Swarm Intel Evol Comput. 2016;5:1.
5. Pegasystems. What consumers really think about AI: a global study. www.pega.com/AI. Accessed July 7, 2017.
The Professional Doctorate: What Are We Waiting for?
The increasingly complex health care system in the United States relies heavily on quality improvement, interprofessional collaboration, patient outcomes, health policy legislation, and advocacy. While important, most of these factors are outside the scope of the traditional master’s-level education program—necessitating the development of methods to help advanced practice providers, including NPs and PAs, obtain additional skills. The solution of choice, for many professions, has been the introduction of the “professional doctorate” as a complementary alternative to the typical research-focused doctoral program, such as the PhD.
Traditional PhD curricula prepare individuals to perform research that is typically specialized and confined to their field of study.1 While this research does produce new knowledge, it usually remains in the realm of academia and often does not address any specific “real-world” problem.2 But to be recognized, compensated, and identified as a full professional in modern societ
Analysis by Taylor and Maxwell and by Lee, Green, and Brennan has shown that, rather than theory, the workplace demands the application of knowledge geared toward daily professional duties.3,4 They envisioned a doctorate-prepared practitioner who had less skill in pure research but who would be able to apply theory to everyday problems in the workplace.4,5 Rather than devalue the contributions of classical PhD training, this model proposed the creation of a hybrid curriculum that would prepare individuals to use “applied research.”3 As the professional doctorate gained acceptance, it matured from the “first-generation” concept (which was quite similar to the PhD in structure) to “second-generation,” which is more focused on discipline and workplace realities.3,5 In general, these professional doctorates can be earned in less time than a PhD and do not require original research.
Over the past two decades, more than 500 unique professional practice doctorate programs have emerged across the US, in fields ranging from nursing to bioethics. One of the most prominent is the Doctor of Nursing Practice (DNP), designed for RNs seeking a post-professional degree in nursing. In 2004, following three years of research by a task force, the American Association of Colleges of Nursing (AACN) endorsed the DNP, with the goal that it would become the minimum educational standard for advanced practice nurses by 2015.6 According to the AACN, there are 289 DNP programs in the US, with an additional 128 in development.6
The PA profession has lagged behind not only our NP colleagues, but also many other health professions, in the adoption of a discipline-specific, doctoral-level degree. Our counterparts in audiology, physical therapy, occupational therapy, and athletic training have been part of the exponential growth in second-generation health care doctorates.7 While these programs may differ in concept, they share several similarities: They do not require original research; they include a clinical component; and they promote knowledge in the context of the workplace.5-8
In the past five years, PAs have started considering (or debating, depending on your perspective) a professional/clinical doctorate as the next step in our post-professional journey. It’s about time, when you consider that 16.8% of newly certified PAs intend to pursue additional education or clinical training, according to a recent report from the National Commission on Certification of Physician Assistants.9
There are already a few doctoral programs for PAs. Among the earliest clinically focused doctorate programs was the US Army/Air Force-Baylor DScPAS-EM program, designed to educate military PAs at the doctoral level upon completion of an 18-month emergency medicine residency.10 Lincoln Memorial University has a Doctor of Medical Science (DMS) program, comprised of one year of online advanced clinical medicine coursework and one year of online coursework focused on primary care, hospital medicine, emergency medicine, or education.11 And Lynchburg College in Virginia has just launched a post-professional doctoral program for PAs; this DMS program includes a clinical fellowship, as well as coursework in leadership training, health care management and law, organizational behavior, disaster medicine, and global health.12
While not strictly created for PAs, the Doctor of Health Science programs at Nova Southeastern University and A.T. Still University have been educating PAs at the doctoral level for more than 10 years.13,14 Later this year, A.T. Still University plans to introduce a post-professional Doctor of Physician Assistant Studies that will provide a pathway for PAs wishing to become leaders and scholar-practitioners, develop core leadership abilities, and/or enter PA education without the location-specific requirement of a clinical or academic residency.
When the push for professional practice doctorates started, pundits claimed they were just an attempt at a “cash grab” by universities looking to bolster their rosters (and their coffers). But advocates have long argued that these degrees provide practitioners with the knowledge and training required to offer advanced services in increasingly complex social and technologic environments.7 No less than The Institute of Medicine, The Joint Commission, and the Robert Wood Johnson Foundation have called for the reinvention of education programs to equip today’s health professionals
Why? First and foremost, to ensure quality patient outcomes. Beyond that, better prepared clinicians can help to address provider shortages. Those with doctorates can also serve as faculty, educating the next generation of health care providers. And practically speaking, for those seeking advanced education, holding a doctorate will create opportunities for increased decision-making and upward mobility in the workplace.
There is no question that our current health care environment is driven by the regulations and costs of the Affordable Care Act, as well as quality management systems and strategies. NPs and PAs are in a unique position to cost-effectively direct the care of, and advocate for, diverse patient populations. NPs and PAs who recognize this opportunity to serve need doctoral-level training tailored to this milieu.
Do you agree? Share your thoughts on professional doctorates with me at [email protected].
1. Carnegie Project on the Education Doctorate. Founding literature. www.cpedinitiative.org/?. Accessed May 8, 2017.
2. Costley C, Lester S. Work-based doctorates: professional extension at the highest levels. Studies in Higher Education. 2012;37(3):257-269.
3. Taylor N, Maxwell T. Enhancing the relevance of a professional doctorate: the case of the doctor of education degree at the University of New England. Asia-Pacific J Coop Edu. 2004;5(1):60-69.
4. Lee A, Green B, Brennan M. Organisational knowledge, professional practice and the professional doctorate at work. In: Garrick J, Rhodes C (eds). Research and Knowledge at Work. Perspectives, Case-studies and Innovative Strategies. London: Routledge; 2000.
5. Maxwell T. From first to second generation professional doctorate. Studies in Higher Education. 2003;28(3):279-291.
6. American Association of Colleges of Nursing. DNP fact sheet. www.aacn.nche.edu/media-relations/fact-sheets/dnp. Accessed May 8, 2017.
7. Zusman A. Degrees of change: how new kinds of professional doctorates are changing higher education institutions. Research and Occasional Paper Series. 2013;8(13):1-20.
8. Kumar S, Dawson K. Exploring the impact of a professional practice education doctorate in educational environments. Studies in Continuing Education. 2013;35(2):165-178.
9. National Commission on Certification of Physician Assistants. 2014 statistical profile of recently certified physician assistants: an annual report of the NCCPA. www.nccpa.net/Uploads/docs/RecentlyCertifiedReport2014.pdf. Accessed May 8, 2017.
10. Baylor University. Army-Baylor emergency medicine physician assistant (EMPA) program. www.baylor.edu/graduate/pa/index.php?id=936090. Accessed May 8, 2017.
11. Lincoln Memorial University. Doctor of medical science announcement. www.lmunet.edu/academics/schools/debusk-college-of-osteopathic-medicine/dms. Accessed May 8, 2017.
12. Lynchburg College. Doctor of medical science. www.lynchburg.edu/graduate/physician-assistant-medicine/doctor-of-medical-science/. Accessed May 8, 2017.
13. Nova Southeastern University. Doctor of health science program. http://healthsciences.nova.edu/healthsciences/dhs/. Accessed May 8, 2017.
14. A.T. Still University. About the college of graduate health studies – online. www.atsu.edu/college-of-graduate-health-studies. Accessed May 8, 2017.
The increasingly complex health care system in the United States relies heavily on quality improvement, interprofessional collaboration, patient outcomes, health policy legislation, and advocacy. While important, most of these factors are outside the scope of the traditional master’s-level education program—necessitating the development of methods to help advanced practice providers, including NPs and PAs, obtain additional skills. The solution of choice, for many professions, has been the introduction of the “professional doctorate” as a complementary alternative to the typical research-focused doctoral program, such as the PhD.
Traditional PhD curricula prepare individuals to perform research that is typically specialized and confined to their field of study.1 While this research does produce new knowledge, it usually remains in the realm of academia and often does not address any specific “real-world” problem.2 But to be recognized, compensated, and identified as a full professional in modern societ
Analysis by Taylor and Maxwell and by Lee, Green, and Brennan has shown that, rather than theory, the workplace demands the application of knowledge geared toward daily professional duties.3,4 They envisioned a doctorate-prepared practitioner who had less skill in pure research but who would be able to apply theory to everyday problems in the workplace.4,5 Rather than devalue the contributions of classical PhD training, this model proposed the creation of a hybrid curriculum that would prepare individuals to use “applied research.”3 As the professional doctorate gained acceptance, it matured from the “first-generation” concept (which was quite similar to the PhD in structure) to “second-generation,” which is more focused on discipline and workplace realities.3,5 In general, these professional doctorates can be earned in less time than a PhD and do not require original research.
Over the past two decades, more than 500 unique professional practice doctorate programs have emerged across the US, in fields ranging from nursing to bioethics. One of the most prominent is the Doctor of Nursing Practice (DNP), designed for RNs seeking a post-professional degree in nursing. In 2004, following three years of research by a task force, the American Association of Colleges of Nursing (AACN) endorsed the DNP, with the goal that it would become the minimum educational standard for advanced practice nurses by 2015.6 According to the AACN, there are 289 DNP programs in the US, with an additional 128 in development.6
The PA profession has lagged behind not only our NP colleagues, but also many other health professions, in the adoption of a discipline-specific, doctoral-level degree. Our counterparts in audiology, physical therapy, occupational therapy, and athletic training have been part of the exponential growth in second-generation health care doctorates.7 While these programs may differ in concept, they share several similarities: They do not require original research; they include a clinical component; and they promote knowledge in the context of the workplace.5-8
In the past five years, PAs have started considering (or debating, depending on your perspective) a professional/clinical doctorate as the next step in our post-professional journey. It’s about time, when you consider that 16.8% of newly certified PAs intend to pursue additional education or clinical training, according to a recent report from the National Commission on Certification of Physician Assistants.9
There are already a few doctoral programs for PAs. Among the earliest clinically focused doctorate programs was the US Army/Air Force-Baylor DScPAS-EM program, designed to educate military PAs at the doctoral level upon completion of an 18-month emergency medicine residency.10 Lincoln Memorial University has a Doctor of Medical Science (DMS) program, comprised of one year of online advanced clinical medicine coursework and one year of online coursework focused on primary care, hospital medicine, emergency medicine, or education.11 And Lynchburg College in Virginia has just launched a post-professional doctoral program for PAs; this DMS program includes a clinical fellowship, as well as coursework in leadership training, health care management and law, organizational behavior, disaster medicine, and global health.12
While not strictly created for PAs, the Doctor of Health Science programs at Nova Southeastern University and A.T. Still University have been educating PAs at the doctoral level for more than 10 years.13,14 Later this year, A.T. Still University plans to introduce a post-professional Doctor of Physician Assistant Studies that will provide a pathway for PAs wishing to become leaders and scholar-practitioners, develop core leadership abilities, and/or enter PA education without the location-specific requirement of a clinical or academic residency.
When the push for professional practice doctorates started, pundits claimed they were just an attempt at a “cash grab” by universities looking to bolster their rosters (and their coffers). But advocates have long argued that these degrees provide practitioners with the knowledge and training required to offer advanced services in increasingly complex social and technologic environments.7 No less than The Institute of Medicine, The Joint Commission, and the Robert Wood Johnson Foundation have called for the reinvention of education programs to equip today’s health professionals
Why? First and foremost, to ensure quality patient outcomes. Beyond that, better prepared clinicians can help to address provider shortages. Those with doctorates can also serve as faculty, educating the next generation of health care providers. And practically speaking, for those seeking advanced education, holding a doctorate will create opportunities for increased decision-making and upward mobility in the workplace.
There is no question that our current health care environment is driven by the regulations and costs of the Affordable Care Act, as well as quality management systems and strategies. NPs and PAs are in a unique position to cost-effectively direct the care of, and advocate for, diverse patient populations. NPs and PAs who recognize this opportunity to serve need doctoral-level training tailored to this milieu.
Do you agree? Share your thoughts on professional doctorates with me at [email protected].
The increasingly complex health care system in the United States relies heavily on quality improvement, interprofessional collaboration, patient outcomes, health policy legislation, and advocacy. While important, most of these factors are outside the scope of the traditional master’s-level education program—necessitating the development of methods to help advanced practice providers, including NPs and PAs, obtain additional skills. The solution of choice, for many professions, has been the introduction of the “professional doctorate” as a complementary alternative to the typical research-focused doctoral program, such as the PhD.
Traditional PhD curricula prepare individuals to perform research that is typically specialized and confined to their field of study.1 While this research does produce new knowledge, it usually remains in the realm of academia and often does not address any specific “real-world” problem.2 But to be recognized, compensated, and identified as a full professional in modern societ
Analysis by Taylor and Maxwell and by Lee, Green, and Brennan has shown that, rather than theory, the workplace demands the application of knowledge geared toward daily professional duties.3,4 They envisioned a doctorate-prepared practitioner who had less skill in pure research but who would be able to apply theory to everyday problems in the workplace.4,5 Rather than devalue the contributions of classical PhD training, this model proposed the creation of a hybrid curriculum that would prepare individuals to use “applied research.”3 As the professional doctorate gained acceptance, it matured from the “first-generation” concept (which was quite similar to the PhD in structure) to “second-generation,” which is more focused on discipline and workplace realities.3,5 In general, these professional doctorates can be earned in less time than a PhD and do not require original research.
Over the past two decades, more than 500 unique professional practice doctorate programs have emerged across the US, in fields ranging from nursing to bioethics. One of the most prominent is the Doctor of Nursing Practice (DNP), designed for RNs seeking a post-professional degree in nursing. In 2004, following three years of research by a task force, the American Association of Colleges of Nursing (AACN) endorsed the DNP, with the goal that it would become the minimum educational standard for advanced practice nurses by 2015.6 According to the AACN, there are 289 DNP programs in the US, with an additional 128 in development.6
The PA profession has lagged behind not only our NP colleagues, but also many other health professions, in the adoption of a discipline-specific, doctoral-level degree. Our counterparts in audiology, physical therapy, occupational therapy, and athletic training have been part of the exponential growth in second-generation health care doctorates.7 While these programs may differ in concept, they share several similarities: They do not require original research; they include a clinical component; and they promote knowledge in the context of the workplace.5-8
In the past five years, PAs have started considering (or debating, depending on your perspective) a professional/clinical doctorate as the next step in our post-professional journey. It’s about time, when you consider that 16.8% of newly certified PAs intend to pursue additional education or clinical training, according to a recent report from the National Commission on Certification of Physician Assistants.9
There are already a few doctoral programs for PAs. Among the earliest clinically focused doctorate programs was the US Army/Air Force-Baylor DScPAS-EM program, designed to educate military PAs at the doctoral level upon completion of an 18-month emergency medicine residency.10 Lincoln Memorial University has a Doctor of Medical Science (DMS) program, comprised of one year of online advanced clinical medicine coursework and one year of online coursework focused on primary care, hospital medicine, emergency medicine, or education.11 And Lynchburg College in Virginia has just launched a post-professional doctoral program for PAs; this DMS program includes a clinical fellowship, as well as coursework in leadership training, health care management and law, organizational behavior, disaster medicine, and global health.12
While not strictly created for PAs, the Doctor of Health Science programs at Nova Southeastern University and A.T. Still University have been educating PAs at the doctoral level for more than 10 years.13,14 Later this year, A.T. Still University plans to introduce a post-professional Doctor of Physician Assistant Studies that will provide a pathway for PAs wishing to become leaders and scholar-practitioners, develop core leadership abilities, and/or enter PA education without the location-specific requirement of a clinical or academic residency.
When the push for professional practice doctorates started, pundits claimed they were just an attempt at a “cash grab” by universities looking to bolster their rosters (and their coffers). But advocates have long argued that these degrees provide practitioners with the knowledge and training required to offer advanced services in increasingly complex social and technologic environments.7 No less than The Institute of Medicine, The Joint Commission, and the Robert Wood Johnson Foundation have called for the reinvention of education programs to equip today’s health professionals
Why? First and foremost, to ensure quality patient outcomes. Beyond that, better prepared clinicians can help to address provider shortages. Those with doctorates can also serve as faculty, educating the next generation of health care providers. And practically speaking, for those seeking advanced education, holding a doctorate will create opportunities for increased decision-making and upward mobility in the workplace.
There is no question that our current health care environment is driven by the regulations and costs of the Affordable Care Act, as well as quality management systems and strategies. NPs and PAs are in a unique position to cost-effectively direct the care of, and advocate for, diverse patient populations. NPs and PAs who recognize this opportunity to serve need doctoral-level training tailored to this milieu.
Do you agree? Share your thoughts on professional doctorates with me at [email protected].
1. Carnegie Project on the Education Doctorate. Founding literature. www.cpedinitiative.org/?. Accessed May 8, 2017.
2. Costley C, Lester S. Work-based doctorates: professional extension at the highest levels. Studies in Higher Education. 2012;37(3):257-269.
3. Taylor N, Maxwell T. Enhancing the relevance of a professional doctorate: the case of the doctor of education degree at the University of New England. Asia-Pacific J Coop Edu. 2004;5(1):60-69.
4. Lee A, Green B, Brennan M. Organisational knowledge, professional practice and the professional doctorate at work. In: Garrick J, Rhodes C (eds). Research and Knowledge at Work. Perspectives, Case-studies and Innovative Strategies. London: Routledge; 2000.
5. Maxwell T. From first to second generation professional doctorate. Studies in Higher Education. 2003;28(3):279-291.
6. American Association of Colleges of Nursing. DNP fact sheet. www.aacn.nche.edu/media-relations/fact-sheets/dnp. Accessed May 8, 2017.
7. Zusman A. Degrees of change: how new kinds of professional doctorates are changing higher education institutions. Research and Occasional Paper Series. 2013;8(13):1-20.
8. Kumar S, Dawson K. Exploring the impact of a professional practice education doctorate in educational environments. Studies in Continuing Education. 2013;35(2):165-178.
9. National Commission on Certification of Physician Assistants. 2014 statistical profile of recently certified physician assistants: an annual report of the NCCPA. www.nccpa.net/Uploads/docs/RecentlyCertifiedReport2014.pdf. Accessed May 8, 2017.
10. Baylor University. Army-Baylor emergency medicine physician assistant (EMPA) program. www.baylor.edu/graduate/pa/index.php?id=936090. Accessed May 8, 2017.
11. Lincoln Memorial University. Doctor of medical science announcement. www.lmunet.edu/academics/schools/debusk-college-of-osteopathic-medicine/dms. Accessed May 8, 2017.
12. Lynchburg College. Doctor of medical science. www.lynchburg.edu/graduate/physician-assistant-medicine/doctor-of-medical-science/. Accessed May 8, 2017.
13. Nova Southeastern University. Doctor of health science program. http://healthsciences.nova.edu/healthsciences/dhs/. Accessed May 8, 2017.
14. A.T. Still University. About the college of graduate health studies – online. www.atsu.edu/college-of-graduate-health-studies. Accessed May 8, 2017.
1. Carnegie Project on the Education Doctorate. Founding literature. www.cpedinitiative.org/?. Accessed May 8, 2017.
2. Costley C, Lester S. Work-based doctorates: professional extension at the highest levels. Studies in Higher Education. 2012;37(3):257-269.
3. Taylor N, Maxwell T. Enhancing the relevance of a professional doctorate: the case of the doctor of education degree at the University of New England. Asia-Pacific J Coop Edu. 2004;5(1):60-69.
4. Lee A, Green B, Brennan M. Organisational knowledge, professional practice and the professional doctorate at work. In: Garrick J, Rhodes C (eds). Research and Knowledge at Work. Perspectives, Case-studies and Innovative Strategies. London: Routledge; 2000.
5. Maxwell T. From first to second generation professional doctorate. Studies in Higher Education. 2003;28(3):279-291.
6. American Association of Colleges of Nursing. DNP fact sheet. www.aacn.nche.edu/media-relations/fact-sheets/dnp. Accessed May 8, 2017.
7. Zusman A. Degrees of change: how new kinds of professional doctorates are changing higher education institutions. Research and Occasional Paper Series. 2013;8(13):1-20.
8. Kumar S, Dawson K. Exploring the impact of a professional practice education doctorate in educational environments. Studies in Continuing Education. 2013;35(2):165-178.
9. National Commission on Certification of Physician Assistants. 2014 statistical profile of recently certified physician assistants: an annual report of the NCCPA. www.nccpa.net/Uploads/docs/RecentlyCertifiedReport2014.pdf. Accessed May 8, 2017.
10. Baylor University. Army-Baylor emergency medicine physician assistant (EMPA) program. www.baylor.edu/graduate/pa/index.php?id=936090. Accessed May 8, 2017.
11. Lincoln Memorial University. Doctor of medical science announcement. www.lmunet.edu/academics/schools/debusk-college-of-osteopathic-medicine/dms. Accessed May 8, 2017.
12. Lynchburg College. Doctor of medical science. www.lynchburg.edu/graduate/physician-assistant-medicine/doctor-of-medical-science/. Accessed May 8, 2017.
13. Nova Southeastern University. Doctor of health science program. http://healthsciences.nova.edu/healthsciences/dhs/. Accessed May 8, 2017.
14. A.T. Still University. About the college of graduate health studies – online. www.atsu.edu/college-of-graduate-health-studies. Accessed May 8, 2017.
Clinician Reviews: What’s In It for You
Dynamic Duos: Professional Mentorship
Mentorship, whether through a formal or informal system, plays a significant role in a professional’s life; it fosters the development of professional expertise and is associated with increased job satisfaction. An effective mentor guides a less-experienced colleague by modeling positive behaviors and building trust, while being cognizant that his or her role is to be dependable, engaged, authentic, and attuned to the needs of the mentee. You can probably name one of your mentors off the top of your head right now!
The original “mentor” was a character of that name in Homer’s epic poem The Odyssey, but the word is now used to refer to a trusted advisor, friend, teacher, or wise person. In the story, Mentor served as a friend and advocate to Telemachus, the son of the king of Ithaca, while his father, Odysseus, was away fighting in the Trojan War. In 1699, the novel The Adventures of Telemachus portrayed Mentor as Telemachus’ tutor, and he became the hero of the story.1,2
History holds many examples of mentoring relationships: Socrates and Plato, Haydn and Beethoven, and Freud and Jung. Modern-day duos include Kobe Bryant and Shaquille O’Neal, Kirk and Spock, and—dare I say it?—Brady and Belichick. During the Middle Ages, mentorship—particularly in medicine and nursing—was practiced via apprenticeship, which incorporated support, guidance, socialization, well-being, empowerment, education, and career progression.3
Throughout my career as a PA, I have been fortunate to be guided by competent and willing mentors. What have they had in common? For starters, an internal desire (sometimes called generosity of spirit) to mentor and a commitment to my growth and development as their mentee. Successful professional mentors must also possess the necessary knowledge to help effectively develop their mentee’s skills. Discussions with my colleagues and previous mentors inspired the following compilation of the essential responsibilities and traits of a mentor.
Initiating new ideas. A main aspect of a mentor’s role involves assisting in acquiring the confidence and tools to function and excel in our competitive professional world.4-6 In the early 1970s, when I was a young PA, a wonderful physician and friend, Dr. Burton Brasher, took me under his wing and exemplified what it means to be a clinician. I learned from him that it was also my obligation to mentor others, and I have tried to do this frequently in my four decades as a PA. Through his example, I was shown the importance of cultivating emotional intelligence and sensitivity while still providing an honest assessment of strengths and weaknesses. Here was a physician who was unencumbered by ego. We met often to discuss the care of both of our patients.
Staying the course. In 1995, I mentored James Cannon—a young financial comptroller who desperately wanted to be a PA. I’ve (hopefully) helped him navigate PA school, our mutual time in the military, his time in academia, and his introduction to professional volunteer work. In each stage of his career, we had lengthy conversations about the pros and cons of his decisions. Now, 22 years later, he has become my mentor; he has matured in the profession and is at the forefront of taking it to the next level. It is now very common for me to call on him for his advice as I move into the home stretch of my career. A few years ago, he became a trustee of our university and his skills have advanced the success of our programs. Indeed, the student becomes the teacher.
Networking and articulating cultural norms. Dave Mittman, the co-founder and original publisher of Clinician Reviews, had the experience of hiring his very close friend and PA school classmate, Tom Yackeren. In 1985, Dave was publisher of Physician Assistant Journal (at that time, the official journal of the AAPA). Dave and Tom were business partners and relied on each other’s skills to grow their business. They shared trust, friendship, and a mutual knowledge of professional “culture.” They understood each other and how they could each contribute to their success. Their partnership maintained a complementary balance, each of them able to play to his
Demonstrating honesty, integrity, and enthusiasm. Marie-Eileen Onieal, our NP editor-in-chief, grew up in a household where her father was a firefighter and union organizer. He taught her the value of always paying it forward. While she has mentored many people in her career, she fondly remembers mentoring Lori Fritz through her transition into academia—what Marie-Eileen calls “the precarious journey of an educator.” When she met Lori, she says, they just “clicked,” and that bond has survived to this day. Lori is now an established academician, mentoring new students and professionals, and modeling her experience with Marie-Eileen’s involvement in the profession.
These are examples of when it works. But what happens when the relationship doesn’t “click”? Unfortunately, not all mentorships are fruitful. When mentor and mentee clash, it is paramount to acknowledge that the relationship is not working and to back away appropriately, without regard to ego. No one benefits when the parties are at odds—and this may explain why some of the greatest partnerships form organically.
Above all, in order for a mentorship to be prosperous, mentors must express compassion and remain genuine throughout all interactions with their mentee. It is a long-term commitment. Without this generosity of spirit, the influence and benefit of a professional mentor would be lost. If you have other ideas about what makes a great mentor, or how to foster a more satisfying mentor/mentee relationship, please share them with me at [email protected].
1. Anderson E. 5 Qualities to look for in a mentor. Forbes. www.forbes.com/sites/erikaandersen/2014/09/29/5-qualities-to-look-for-in-a-mentor/#389c58743021. Accessed March 8, 2017.
2. The National Academies Press. Adviser, Teacher, Role Model, Friend: On Being a Mentor to Students in Science and Engineering.
3. Kim YJ. The Odyssey and mentorship today. The Stanford Daily. www.stanforddaily.com/2016/10/27/the-iliad-and-mentorship-today. Accessed March 16, 2017.
4. Wagner AL, Seymour ME. A model of caring mentorship for nursing. J Nurses Staff Dev. 2007;23(5):201-211.
5. University of Wolverhampton Business School. A Managers’ & Mentors Handbook on Mentoring. www2.wlv.ac.uk/registry/qasd/RandV/R&V%2009-10/UWBS/Collab%20Mentoring%20Handbook.pdf. Accessed March 8, 2017.
6. Vivier J, Dana K. The value of mentorship: personal journeys inspired by the teaching philosophy of Chuck Jones. Voice and Speech Review. 2014;8(3):224-249.
Mentorship, whether through a formal or informal system, plays a significant role in a professional’s life; it fosters the development of professional expertise and is associated with increased job satisfaction. An effective mentor guides a less-experienced colleague by modeling positive behaviors and building trust, while being cognizant that his or her role is to be dependable, engaged, authentic, and attuned to the needs of the mentee. You can probably name one of your mentors off the top of your head right now!
The original “mentor” was a character of that name in Homer’s epic poem The Odyssey, but the word is now used to refer to a trusted advisor, friend, teacher, or wise person. In the story, Mentor served as a friend and advocate to Telemachus, the son of the king of Ithaca, while his father, Odysseus, was away fighting in the Trojan War. In 1699, the novel The Adventures of Telemachus portrayed Mentor as Telemachus’ tutor, and he became the hero of the story.1,2
History holds many examples of mentoring relationships: Socrates and Plato, Haydn and Beethoven, and Freud and Jung. Modern-day duos include Kobe Bryant and Shaquille O’Neal, Kirk and Spock, and—dare I say it?—Brady and Belichick. During the Middle Ages, mentorship—particularly in medicine and nursing—was practiced via apprenticeship, which incorporated support, guidance, socialization, well-being, empowerment, education, and career progression.3
Throughout my career as a PA, I have been fortunate to be guided by competent and willing mentors. What have they had in common? For starters, an internal desire (sometimes called generosity of spirit) to mentor and a commitment to my growth and development as their mentee. Successful professional mentors must also possess the necessary knowledge to help effectively develop their mentee’s skills. Discussions with my colleagues and previous mentors inspired the following compilation of the essential responsibilities and traits of a mentor.
Initiating new ideas. A main aspect of a mentor’s role involves assisting in acquiring the confidence and tools to function and excel in our competitive professional world.4-6 In the early 1970s, when I was a young PA, a wonderful physician and friend, Dr. Burton Brasher, took me under his wing and exemplified what it means to be a clinician. I learned from him that it was also my obligation to mentor others, and I have tried to do this frequently in my four decades as a PA. Through his example, I was shown the importance of cultivating emotional intelligence and sensitivity while still providing an honest assessment of strengths and weaknesses. Here was a physician who was unencumbered by ego. We met often to discuss the care of both of our patients.
Staying the course. In 1995, I mentored James Cannon—a young financial comptroller who desperately wanted to be a PA. I’ve (hopefully) helped him navigate PA school, our mutual time in the military, his time in academia, and his introduction to professional volunteer work. In each stage of his career, we had lengthy conversations about the pros and cons of his decisions. Now, 22 years later, he has become my mentor; he has matured in the profession and is at the forefront of taking it to the next level. It is now very common for me to call on him for his advice as I move into the home stretch of my career. A few years ago, he became a trustee of our university and his skills have advanced the success of our programs. Indeed, the student becomes the teacher.
Networking and articulating cultural norms. Dave Mittman, the co-founder and original publisher of Clinician Reviews, had the experience of hiring his very close friend and PA school classmate, Tom Yackeren. In 1985, Dave was publisher of Physician Assistant Journal (at that time, the official journal of the AAPA). Dave and Tom were business partners and relied on each other’s skills to grow their business. They shared trust, friendship, and a mutual knowledge of professional “culture.” They understood each other and how they could each contribute to their success. Their partnership maintained a complementary balance, each of them able to play to his
Demonstrating honesty, integrity, and enthusiasm. Marie-Eileen Onieal, our NP editor-in-chief, grew up in a household where her father was a firefighter and union organizer. He taught her the value of always paying it forward. While she has mentored many people in her career, she fondly remembers mentoring Lori Fritz through her transition into academia—what Marie-Eileen calls “the precarious journey of an educator.” When she met Lori, she says, they just “clicked,” and that bond has survived to this day. Lori is now an established academician, mentoring new students and professionals, and modeling her experience with Marie-Eileen’s involvement in the profession.
These are examples of when it works. But what happens when the relationship doesn’t “click”? Unfortunately, not all mentorships are fruitful. When mentor and mentee clash, it is paramount to acknowledge that the relationship is not working and to back away appropriately, without regard to ego. No one benefits when the parties are at odds—and this may explain why some of the greatest partnerships form organically.
Above all, in order for a mentorship to be prosperous, mentors must express compassion and remain genuine throughout all interactions with their mentee. It is a long-term commitment. Without this generosity of spirit, the influence and benefit of a professional mentor would be lost. If you have other ideas about what makes a great mentor, or how to foster a more satisfying mentor/mentee relationship, please share them with me at [email protected].
Mentorship, whether through a formal or informal system, plays a significant role in a professional’s life; it fosters the development of professional expertise and is associated with increased job satisfaction. An effective mentor guides a less-experienced colleague by modeling positive behaviors and building trust, while being cognizant that his or her role is to be dependable, engaged, authentic, and attuned to the needs of the mentee. You can probably name one of your mentors off the top of your head right now!
The original “mentor” was a character of that name in Homer’s epic poem The Odyssey, but the word is now used to refer to a trusted advisor, friend, teacher, or wise person. In the story, Mentor served as a friend and advocate to Telemachus, the son of the king of Ithaca, while his father, Odysseus, was away fighting in the Trojan War. In 1699, the novel The Adventures of Telemachus portrayed Mentor as Telemachus’ tutor, and he became the hero of the story.1,2
History holds many examples of mentoring relationships: Socrates and Plato, Haydn and Beethoven, and Freud and Jung. Modern-day duos include Kobe Bryant and Shaquille O’Neal, Kirk and Spock, and—dare I say it?—Brady and Belichick. During the Middle Ages, mentorship—particularly in medicine and nursing—was practiced via apprenticeship, which incorporated support, guidance, socialization, well-being, empowerment, education, and career progression.3
Throughout my career as a PA, I have been fortunate to be guided by competent and willing mentors. What have they had in common? For starters, an internal desire (sometimes called generosity of spirit) to mentor and a commitment to my growth and development as their mentee. Successful professional mentors must also possess the necessary knowledge to help effectively develop their mentee’s skills. Discussions with my colleagues and previous mentors inspired the following compilation of the essential responsibilities and traits of a mentor.
Initiating new ideas. A main aspect of a mentor’s role involves assisting in acquiring the confidence and tools to function and excel in our competitive professional world.4-6 In the early 1970s, when I was a young PA, a wonderful physician and friend, Dr. Burton Brasher, took me under his wing and exemplified what it means to be a clinician. I learned from him that it was also my obligation to mentor others, and I have tried to do this frequently in my four decades as a PA. Through his example, I was shown the importance of cultivating emotional intelligence and sensitivity while still providing an honest assessment of strengths and weaknesses. Here was a physician who was unencumbered by ego. We met often to discuss the care of both of our patients.
Staying the course. In 1995, I mentored James Cannon—a young financial comptroller who desperately wanted to be a PA. I’ve (hopefully) helped him navigate PA school, our mutual time in the military, his time in academia, and his introduction to professional volunteer work. In each stage of his career, we had lengthy conversations about the pros and cons of his decisions. Now, 22 years later, he has become my mentor; he has matured in the profession and is at the forefront of taking it to the next level. It is now very common for me to call on him for his advice as I move into the home stretch of my career. A few years ago, he became a trustee of our university and his skills have advanced the success of our programs. Indeed, the student becomes the teacher.
Networking and articulating cultural norms. Dave Mittman, the co-founder and original publisher of Clinician Reviews, had the experience of hiring his very close friend and PA school classmate, Tom Yackeren. In 1985, Dave was publisher of Physician Assistant Journal (at that time, the official journal of the AAPA). Dave and Tom were business partners and relied on each other’s skills to grow their business. They shared trust, friendship, and a mutual knowledge of professional “culture.” They understood each other and how they could each contribute to their success. Their partnership maintained a complementary balance, each of them able to play to his
Demonstrating honesty, integrity, and enthusiasm. Marie-Eileen Onieal, our NP editor-in-chief, grew up in a household where her father was a firefighter and union organizer. He taught her the value of always paying it forward. While she has mentored many people in her career, she fondly remembers mentoring Lori Fritz through her transition into academia—what Marie-Eileen calls “the precarious journey of an educator.” When she met Lori, she says, they just “clicked,” and that bond has survived to this day. Lori is now an established academician, mentoring new students and professionals, and modeling her experience with Marie-Eileen’s involvement in the profession.
These are examples of when it works. But what happens when the relationship doesn’t “click”? Unfortunately, not all mentorships are fruitful. When mentor and mentee clash, it is paramount to acknowledge that the relationship is not working and to back away appropriately, without regard to ego. No one benefits when the parties are at odds—and this may explain why some of the greatest partnerships form organically.
Above all, in order for a mentorship to be prosperous, mentors must express compassion and remain genuine throughout all interactions with their mentee. It is a long-term commitment. Without this generosity of spirit, the influence and benefit of a professional mentor would be lost. If you have other ideas about what makes a great mentor, or how to foster a more satisfying mentor/mentee relationship, please share them with me at [email protected].
1. Anderson E. 5 Qualities to look for in a mentor. Forbes. www.forbes.com/sites/erikaandersen/2014/09/29/5-qualities-to-look-for-in-a-mentor/#389c58743021. Accessed March 8, 2017.
2. The National Academies Press. Adviser, Teacher, Role Model, Friend: On Being a Mentor to Students in Science and Engineering.
3. Kim YJ. The Odyssey and mentorship today. The Stanford Daily. www.stanforddaily.com/2016/10/27/the-iliad-and-mentorship-today. Accessed March 16, 2017.
4. Wagner AL, Seymour ME. A model of caring mentorship for nursing. J Nurses Staff Dev. 2007;23(5):201-211.
5. University of Wolverhampton Business School. A Managers’ & Mentors Handbook on Mentoring. www2.wlv.ac.uk/registry/qasd/RandV/R&V%2009-10/UWBS/Collab%20Mentoring%20Handbook.pdf. Accessed March 8, 2017.
6. Vivier J, Dana K. The value of mentorship: personal journeys inspired by the teaching philosophy of Chuck Jones. Voice and Speech Review. 2014;8(3):224-249.
1. Anderson E. 5 Qualities to look for in a mentor. Forbes. www.forbes.com/sites/erikaandersen/2014/09/29/5-qualities-to-look-for-in-a-mentor/#389c58743021. Accessed March 8, 2017.
2. The National Academies Press. Adviser, Teacher, Role Model, Friend: On Being a Mentor to Students in Science and Engineering.
3. Kim YJ. The Odyssey and mentorship today. The Stanford Daily. www.stanforddaily.com/2016/10/27/the-iliad-and-mentorship-today. Accessed March 16, 2017.
4. Wagner AL, Seymour ME. A model of caring mentorship for nursing. J Nurses Staff Dev. 2007;23(5):201-211.
5. University of Wolverhampton Business School. A Managers’ & Mentors Handbook on Mentoring. www2.wlv.ac.uk/registry/qasd/RandV/R&V%2009-10/UWBS/Collab%20Mentoring%20Handbook.pdf. Accessed March 8, 2017.
6. Vivier J, Dana K. The value of mentorship: personal journeys inspired by the teaching philosophy of Chuck Jones. Voice and Speech Review. 2014;8(3):224-249.
Putting the “PA” in “FPA”
The term full practice authority (FPA) means different things to different clinicians. Some think it is a code phrase for “independent practice,” while others regard it as the ability to practice to the fullest extent of their education and licensure. The American Association of Nurse Practitioners (AANP) defines FPA as the “collection of state practice and licensure laws that allow for NPs to evaluate patients, diagnose, order and interpret tests, initiate and manage treatments—including prescribe medications—under the exclusive licensure authority of the state board of nursing.”1 Whatever the definition, it is an emotionally packed phrase for NPs, PAs, and our physician colleagues.
While NP and PA scope of practice is largely dictated by state laws and regulations, it is also impacted by other factors, including employment agreements, practice setting, and billing requirements of Medicare and other third-party payers.2 In the past decade, there has been increasing support for eliminating barriers to practice. Advocates say the current supply of health care services is unnecessarily limited—a problem that will increase as our population ages and people live longer with chronic conditions. With the health care system under constant pressure, many believe that all clinicians should be able to provide care to the full scope of their education and expertise.
Proponents of FPA, including the Institute of Medicine and the National Governors Association, cite improved access to and efficiency of care and reduced costs as the main motivations for lifting practice restrictions.3,4 In an extensive document, the RAND Corporation called for states to relax scope-of-practice restrictions for NPs.5 Findings from the Federal Trade Commission assert that NPs are safe and effective as independent providers of health care services within the scope of their training and licensure.6
Meanwhile, opponents—such as the American Academy of Family Physicians (AAFP) and the American Medical Association—express concerns about the lack of clinical education compared to physicians, as well as patient choice and fragmentation of care.7 Back in 2010, the AAFP objected to statements from the National Board of Medical Examiners (NBME), which alleged that physicians and nurse clinicians have comparable scopes of practice; NBME further suggested that licensing authorities for both professions “should be required to create common means of assessing proficiency for entry to and continuation in practice.”8 Osteopathic physicians pushed back on FPA, worried that NPs would be confused with physicians.9 But as NPs have clarified, their license is an extension of their RN license; they do not need physician endorsement for the advanced component.
What goes without saying is that NPs and PAs play a large and expanding role in the American health care delivery system. NPs constitute the fastest-growing segment of the primary care workforce in the United States. And because they are proven to be highly educated clinicians who take responsibility for their clinical decisions, many states are relaxing scope-of-practice restrictions to allow them to provide more extensive services to their patients. Currently, 21 states and the District of Columbia allow FPA for NPs.10 Furthermore, in a recent landmark decision, the US Department of Veterans Affairs (VA) announced new rules granting Advanced Practice Registered Nurses (APRNs) FPA within the VA system.11
In contrast to the varying degrees of autonomy with which NPs practice, PAs provide medical services exclusively under the delegation of physicians. Although many function in autonomous practices, PAs have no authority to function independently or to provide services unless assigned by and under the auspices of a supervising physician.12 This should not come as a surprise, since PAs have always touted that the profession was created for physicians, by physicians.
But as NPs have advanced their FPA agenda, many PAs have asked, “What about us?” Brian Sady, a PA from Nevada, has been advocating FPA for many years to enhance the accessibility and quality of care in his rural state.13
In fact, the American Academy of Physician Assistants has been lobbying the VA to grant FPA to PAs in parity with their recent action regarding NPs.14 And now, the Academy has gone a step further with the creation of the Joint Task Force on PA Practice Authority. Their raison d’etre is to develop a proposal that supports the elimination of regulations that require PAs to have and/or report supervisory, collaborating, or other specific relationships with a physician in order to practice.15 This is a significant change of direction for the PA profession and is stimulating a great deal of discussion.
In order to accomplish their goal, the task force must emphasize the PA profession’s continued commitment to team-based practice. Interestingly, Michigan recently enacted a law that distinguishes participating physicians from supervising physicians in order to better reflect the PA and physician roles within the team. The law removes physician responsibility for PA practice, making each member of the health care team responsible for his or her own decisions. It also removes the ratio restriction that limited the number of PAs with whom a physician may practice. By recognizing PAs as full prescribers, rather than limiting their care to “delegated prescriptive authority,” the law grants PAs more autonomy to serve patients.16
PAs are regulated by the state medical board or a subset of it—only five states have a PA-specific board—whereas NPs have always practiced under the auspices of their state nursing board. If the task force proposals are adopted by the AAPA House of Delegates, they will support the creation of autonomous state boards with a majority of PA members to regulate practice. (Iowa is currently the only state PA board that has a majority of PA members.)
Some argue that FPA for PAs would disrupt the current PA-physician relationship. Others contend that FPA for PAs will strengthen that relationship and balance the respect, support, and professionalism that enable PAs to consistently provide high-quality care.
Both NPs and PAs assert that they have, throughout 50 years, demonstrated a commitment to competent, quality care for patients. By defining the future of our professions, we make our professions more accountable, preserve our positive relationships with physicians and other members of the health care team, decrease unnecessary administrative burdens on physicians and employers, and most importantly, increase access to quality care for our patients. Share your expectations and opinions regarding professional autonomy with me at [email protected].
1. American Association of Nurse Practitioners. Issues at-a glance: full practice authority. www.aanp.org/aanpqa2/images/documents/policy-toolbox/fullpracticeauthority.pdf. Accessed January 9, 2017.
2. ECRI Institute. Scope of practice laws for nurse practitioners and physician assistants. www.ecri.org/components/PPRM/Pages/LB5.aspx. Accessed January 9, 2017.
3. Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2010/The-Future-of-Nursing/Future%20of%20Nursing%202010%20Recommendations.pdf. Accessed January 9, 2017.
4. National Governors Association. The role of nurse practitioners in meeting increasing demand for primary care. www.nga.org/cms/home/nga-center-for-best-practices/center-publications/page-health-publications/col2-content/main-content-list/the-role-of-nurse-practitioners.html. Accessed January 9, 2017.
5. Martsolf GR, Auerbach DI, Arifkhanova A. The impact of full practice authority for nurse practitioners and other advanced practice registered nurses in Ohio. www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR848/RAND_RR848.pdf. Accessed January 9, 2017.
6. Gilman DJ, Koslov TI. Policy perspectives: competition advocacy and the regulation of advanced practice nurses. www.aacn.nche.edu/government-affairs/APRN-Policy-Paper.pdf. Accessed January 9, 2017.
7. American Academy of Family Physicians. AAFP, others protest VA’s attempt to expand APRNs’ scope of practice. www.aafp.org/news/government-medicine/20131122valetteraprn.html. Accessed January 9, 2017.
8. American Academy of Family Physicians. AAFP to NBME: cease claims of equivalence between FPs and Advanced Practice Nurses. www.aafp.org/news/professional-issues/20100811nbmeletter.html. Accessed January 9, 2017.
9. Schierhorn C. As NPs push for expanded practice rights, physicians push back. http://thedo.osteopathic.org/2010/03/as-nps-push-for-expanded-practice-rights-physicians-push-back. Accessed January 9, 2017.
10. Doble M. Keep a positive spin on the progress of full practice authority for NPs. www.nursingcenter.com/ncblog/july-2015/keep-a-positive-spin-on-the-progress-of-full-pract. Accessed January 9, 2017.
11. The Department of Veterans Affairs. VA grants full practice authority to advance practice registered nurses. www.va.gov/opa/pressrel/pressrelease.cfm?id=2847. Accessed January 9, 2017.
12. Benesch K, Hyman DJ. Nonphysician practitioners: more care, less cost, different law? www.healthlawyers.org/Events/Programs/Materials/Documents/ArchivedProgramMaterialFolders2009-2011/PHY09/benesch_hyman.pdf. Accessed January 9, 2017.
13. Sady B. Autonomy now! Why PAs, like NPs, need full practice authority. Clinician Reviews. 2015;25(10):6-8.
14. American Academy of Physician Assistants. AAPA urged VA to grant full practice authority to PAs; VA extended authority only to APRNs. www.aapa.org/twocolumn.aspx?id= 6442451796. Accessed January 9, 2017.
15. American Academy of Physician Assistants. Full practice authority and responsibility. http://news-center.aapa.org/wp-content/uploads/sites/2/2016/12/FAQ-Final_12_15.pdf. Accessed January 9, 2017.
16. American Academy of Physician Assistants. Major PA victory in Michigan. www.aapa.org/twocolumn.aspx?id=6442451808. Accessed January 9, 2017.
The term full practice authority (FPA) means different things to different clinicians. Some think it is a code phrase for “independent practice,” while others regard it as the ability to practice to the fullest extent of their education and licensure. The American Association of Nurse Practitioners (AANP) defines FPA as the “collection of state practice and licensure laws that allow for NPs to evaluate patients, diagnose, order and interpret tests, initiate and manage treatments—including prescribe medications—under the exclusive licensure authority of the state board of nursing.”1 Whatever the definition, it is an emotionally packed phrase for NPs, PAs, and our physician colleagues.
While NP and PA scope of practice is largely dictated by state laws and regulations, it is also impacted by other factors, including employment agreements, practice setting, and billing requirements of Medicare and other third-party payers.2 In the past decade, there has been increasing support for eliminating barriers to practice. Advocates say the current supply of health care services is unnecessarily limited—a problem that will increase as our population ages and people live longer with chronic conditions. With the health care system under constant pressure, many believe that all clinicians should be able to provide care to the full scope of their education and expertise.
Proponents of FPA, including the Institute of Medicine and the National Governors Association, cite improved access to and efficiency of care and reduced costs as the main motivations for lifting practice restrictions.3,4 In an extensive document, the RAND Corporation called for states to relax scope-of-practice restrictions for NPs.5 Findings from the Federal Trade Commission assert that NPs are safe and effective as independent providers of health care services within the scope of their training and licensure.6
Meanwhile, opponents—such as the American Academy of Family Physicians (AAFP) and the American Medical Association—express concerns about the lack of clinical education compared to physicians, as well as patient choice and fragmentation of care.7 Back in 2010, the AAFP objected to statements from the National Board of Medical Examiners (NBME), which alleged that physicians and nurse clinicians have comparable scopes of practice; NBME further suggested that licensing authorities for both professions “should be required to create common means of assessing proficiency for entry to and continuation in practice.”8 Osteopathic physicians pushed back on FPA, worried that NPs would be confused with physicians.9 But as NPs have clarified, their license is an extension of their RN license; they do not need physician endorsement for the advanced component.
What goes without saying is that NPs and PAs play a large and expanding role in the American health care delivery system. NPs constitute the fastest-growing segment of the primary care workforce in the United States. And because they are proven to be highly educated clinicians who take responsibility for their clinical decisions, many states are relaxing scope-of-practice restrictions to allow them to provide more extensive services to their patients. Currently, 21 states and the District of Columbia allow FPA for NPs.10 Furthermore, in a recent landmark decision, the US Department of Veterans Affairs (VA) announced new rules granting Advanced Practice Registered Nurses (APRNs) FPA within the VA system.11
In contrast to the varying degrees of autonomy with which NPs practice, PAs provide medical services exclusively under the delegation of physicians. Although many function in autonomous practices, PAs have no authority to function independently or to provide services unless assigned by and under the auspices of a supervising physician.12 This should not come as a surprise, since PAs have always touted that the profession was created for physicians, by physicians.
But as NPs have advanced their FPA agenda, many PAs have asked, “What about us?” Brian Sady, a PA from Nevada, has been advocating FPA for many years to enhance the accessibility and quality of care in his rural state.13
In fact, the American Academy of Physician Assistants has been lobbying the VA to grant FPA to PAs in parity with their recent action regarding NPs.14 And now, the Academy has gone a step further with the creation of the Joint Task Force on PA Practice Authority. Their raison d’etre is to develop a proposal that supports the elimination of regulations that require PAs to have and/or report supervisory, collaborating, or other specific relationships with a physician in order to practice.15 This is a significant change of direction for the PA profession and is stimulating a great deal of discussion.
In order to accomplish their goal, the task force must emphasize the PA profession’s continued commitment to team-based practice. Interestingly, Michigan recently enacted a law that distinguishes participating physicians from supervising physicians in order to better reflect the PA and physician roles within the team. The law removes physician responsibility for PA practice, making each member of the health care team responsible for his or her own decisions. It also removes the ratio restriction that limited the number of PAs with whom a physician may practice. By recognizing PAs as full prescribers, rather than limiting their care to “delegated prescriptive authority,” the law grants PAs more autonomy to serve patients.16
PAs are regulated by the state medical board or a subset of it—only five states have a PA-specific board—whereas NPs have always practiced under the auspices of their state nursing board. If the task force proposals are adopted by the AAPA House of Delegates, they will support the creation of autonomous state boards with a majority of PA members to regulate practice. (Iowa is currently the only state PA board that has a majority of PA members.)
Some argue that FPA for PAs would disrupt the current PA-physician relationship. Others contend that FPA for PAs will strengthen that relationship and balance the respect, support, and professionalism that enable PAs to consistently provide high-quality care.
Both NPs and PAs assert that they have, throughout 50 years, demonstrated a commitment to competent, quality care for patients. By defining the future of our professions, we make our professions more accountable, preserve our positive relationships with physicians and other members of the health care team, decrease unnecessary administrative burdens on physicians and employers, and most importantly, increase access to quality care for our patients. Share your expectations and opinions regarding professional autonomy with me at [email protected].
The term full practice authority (FPA) means different things to different clinicians. Some think it is a code phrase for “independent practice,” while others regard it as the ability to practice to the fullest extent of their education and licensure. The American Association of Nurse Practitioners (AANP) defines FPA as the “collection of state practice and licensure laws that allow for NPs to evaluate patients, diagnose, order and interpret tests, initiate and manage treatments—including prescribe medications—under the exclusive licensure authority of the state board of nursing.”1 Whatever the definition, it is an emotionally packed phrase for NPs, PAs, and our physician colleagues.
While NP and PA scope of practice is largely dictated by state laws and regulations, it is also impacted by other factors, including employment agreements, practice setting, and billing requirements of Medicare and other third-party payers.2 In the past decade, there has been increasing support for eliminating barriers to practice. Advocates say the current supply of health care services is unnecessarily limited—a problem that will increase as our population ages and people live longer with chronic conditions. With the health care system under constant pressure, many believe that all clinicians should be able to provide care to the full scope of their education and expertise.
Proponents of FPA, including the Institute of Medicine and the National Governors Association, cite improved access to and efficiency of care and reduced costs as the main motivations for lifting practice restrictions.3,4 In an extensive document, the RAND Corporation called for states to relax scope-of-practice restrictions for NPs.5 Findings from the Federal Trade Commission assert that NPs are safe and effective as independent providers of health care services within the scope of their training and licensure.6
Meanwhile, opponents—such as the American Academy of Family Physicians (AAFP) and the American Medical Association—express concerns about the lack of clinical education compared to physicians, as well as patient choice and fragmentation of care.7 Back in 2010, the AAFP objected to statements from the National Board of Medical Examiners (NBME), which alleged that physicians and nurse clinicians have comparable scopes of practice; NBME further suggested that licensing authorities for both professions “should be required to create common means of assessing proficiency for entry to and continuation in practice.”8 Osteopathic physicians pushed back on FPA, worried that NPs would be confused with physicians.9 But as NPs have clarified, their license is an extension of their RN license; they do not need physician endorsement for the advanced component.
What goes without saying is that NPs and PAs play a large and expanding role in the American health care delivery system. NPs constitute the fastest-growing segment of the primary care workforce in the United States. And because they are proven to be highly educated clinicians who take responsibility for their clinical decisions, many states are relaxing scope-of-practice restrictions to allow them to provide more extensive services to their patients. Currently, 21 states and the District of Columbia allow FPA for NPs.10 Furthermore, in a recent landmark decision, the US Department of Veterans Affairs (VA) announced new rules granting Advanced Practice Registered Nurses (APRNs) FPA within the VA system.11
In contrast to the varying degrees of autonomy with which NPs practice, PAs provide medical services exclusively under the delegation of physicians. Although many function in autonomous practices, PAs have no authority to function independently or to provide services unless assigned by and under the auspices of a supervising physician.12 This should not come as a surprise, since PAs have always touted that the profession was created for physicians, by physicians.
But as NPs have advanced their FPA agenda, many PAs have asked, “What about us?” Brian Sady, a PA from Nevada, has been advocating FPA for many years to enhance the accessibility and quality of care in his rural state.13
In fact, the American Academy of Physician Assistants has been lobbying the VA to grant FPA to PAs in parity with their recent action regarding NPs.14 And now, the Academy has gone a step further with the creation of the Joint Task Force on PA Practice Authority. Their raison d’etre is to develop a proposal that supports the elimination of regulations that require PAs to have and/or report supervisory, collaborating, or other specific relationships with a physician in order to practice.15 This is a significant change of direction for the PA profession and is stimulating a great deal of discussion.
In order to accomplish their goal, the task force must emphasize the PA profession’s continued commitment to team-based practice. Interestingly, Michigan recently enacted a law that distinguishes participating physicians from supervising physicians in order to better reflect the PA and physician roles within the team. The law removes physician responsibility for PA practice, making each member of the health care team responsible for his or her own decisions. It also removes the ratio restriction that limited the number of PAs with whom a physician may practice. By recognizing PAs as full prescribers, rather than limiting their care to “delegated prescriptive authority,” the law grants PAs more autonomy to serve patients.16
PAs are regulated by the state medical board or a subset of it—only five states have a PA-specific board—whereas NPs have always practiced under the auspices of their state nursing board. If the task force proposals are adopted by the AAPA House of Delegates, they will support the creation of autonomous state boards with a majority of PA members to regulate practice. (Iowa is currently the only state PA board that has a majority of PA members.)
Some argue that FPA for PAs would disrupt the current PA-physician relationship. Others contend that FPA for PAs will strengthen that relationship and balance the respect, support, and professionalism that enable PAs to consistently provide high-quality care.
Both NPs and PAs assert that they have, throughout 50 years, demonstrated a commitment to competent, quality care for patients. By defining the future of our professions, we make our professions more accountable, preserve our positive relationships with physicians and other members of the health care team, decrease unnecessary administrative burdens on physicians and employers, and most importantly, increase access to quality care for our patients. Share your expectations and opinions regarding professional autonomy with me at [email protected].
1. American Association of Nurse Practitioners. Issues at-a glance: full practice authority. www.aanp.org/aanpqa2/images/documents/policy-toolbox/fullpracticeauthority.pdf. Accessed January 9, 2017.
2. ECRI Institute. Scope of practice laws for nurse practitioners and physician assistants. www.ecri.org/components/PPRM/Pages/LB5.aspx. Accessed January 9, 2017.
3. Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2010/The-Future-of-Nursing/Future%20of%20Nursing%202010%20Recommendations.pdf. Accessed January 9, 2017.
4. National Governors Association. The role of nurse practitioners in meeting increasing demand for primary care. www.nga.org/cms/home/nga-center-for-best-practices/center-publications/page-health-publications/col2-content/main-content-list/the-role-of-nurse-practitioners.html. Accessed January 9, 2017.
5. Martsolf GR, Auerbach DI, Arifkhanova A. The impact of full practice authority for nurse practitioners and other advanced practice registered nurses in Ohio. www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR848/RAND_RR848.pdf. Accessed January 9, 2017.
6. Gilman DJ, Koslov TI. Policy perspectives: competition advocacy and the regulation of advanced practice nurses. www.aacn.nche.edu/government-affairs/APRN-Policy-Paper.pdf. Accessed January 9, 2017.
7. American Academy of Family Physicians. AAFP, others protest VA’s attempt to expand APRNs’ scope of practice. www.aafp.org/news/government-medicine/20131122valetteraprn.html. Accessed January 9, 2017.
8. American Academy of Family Physicians. AAFP to NBME: cease claims of equivalence between FPs and Advanced Practice Nurses. www.aafp.org/news/professional-issues/20100811nbmeletter.html. Accessed January 9, 2017.
9. Schierhorn C. As NPs push for expanded practice rights, physicians push back. http://thedo.osteopathic.org/2010/03/as-nps-push-for-expanded-practice-rights-physicians-push-back. Accessed January 9, 2017.
10. Doble M. Keep a positive spin on the progress of full practice authority for NPs. www.nursingcenter.com/ncblog/july-2015/keep-a-positive-spin-on-the-progress-of-full-pract. Accessed January 9, 2017.
11. The Department of Veterans Affairs. VA grants full practice authority to advance practice registered nurses. www.va.gov/opa/pressrel/pressrelease.cfm?id=2847. Accessed January 9, 2017.
12. Benesch K, Hyman DJ. Nonphysician practitioners: more care, less cost, different law? www.healthlawyers.org/Events/Programs/Materials/Documents/ArchivedProgramMaterialFolders2009-2011/PHY09/benesch_hyman.pdf. Accessed January 9, 2017.
13. Sady B. Autonomy now! Why PAs, like NPs, need full practice authority. Clinician Reviews. 2015;25(10):6-8.
14. American Academy of Physician Assistants. AAPA urged VA to grant full practice authority to PAs; VA extended authority only to APRNs. www.aapa.org/twocolumn.aspx?id= 6442451796. Accessed January 9, 2017.
15. American Academy of Physician Assistants. Full practice authority and responsibility. http://news-center.aapa.org/wp-content/uploads/sites/2/2016/12/FAQ-Final_12_15.pdf. Accessed January 9, 2017.
16. American Academy of Physician Assistants. Major PA victory in Michigan. www.aapa.org/twocolumn.aspx?id=6442451808. Accessed January 9, 2017.
1. American Association of Nurse Practitioners. Issues at-a glance: full practice authority. www.aanp.org/aanpqa2/images/documents/policy-toolbox/fullpracticeauthority.pdf. Accessed January 9, 2017.
2. ECRI Institute. Scope of practice laws for nurse practitioners and physician assistants. www.ecri.org/components/PPRM/Pages/LB5.aspx. Accessed January 9, 2017.
3. Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2010/The-Future-of-Nursing/Future%20of%20Nursing%202010%20Recommendations.pdf. Accessed January 9, 2017.
4. National Governors Association. The role of nurse practitioners in meeting increasing demand for primary care. www.nga.org/cms/home/nga-center-for-best-practices/center-publications/page-health-publications/col2-content/main-content-list/the-role-of-nurse-practitioners.html. Accessed January 9, 2017.
5. Martsolf GR, Auerbach DI, Arifkhanova A. The impact of full practice authority for nurse practitioners and other advanced practice registered nurses in Ohio. www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR848/RAND_RR848.pdf. Accessed January 9, 2017.
6. Gilman DJ, Koslov TI. Policy perspectives: competition advocacy and the regulation of advanced practice nurses. www.aacn.nche.edu/government-affairs/APRN-Policy-Paper.pdf. Accessed January 9, 2017.
7. American Academy of Family Physicians. AAFP, others protest VA’s attempt to expand APRNs’ scope of practice. www.aafp.org/news/government-medicine/20131122valetteraprn.html. Accessed January 9, 2017.
8. American Academy of Family Physicians. AAFP to NBME: cease claims of equivalence between FPs and Advanced Practice Nurses. www.aafp.org/news/professional-issues/20100811nbmeletter.html. Accessed January 9, 2017.
9. Schierhorn C. As NPs push for expanded practice rights, physicians push back. http://thedo.osteopathic.org/2010/03/as-nps-push-for-expanded-practice-rights-physicians-push-back. Accessed January 9, 2017.
10. Doble M. Keep a positive spin on the progress of full practice authority for NPs. www.nursingcenter.com/ncblog/july-2015/keep-a-positive-spin-on-the-progress-of-full-pract. Accessed January 9, 2017.
11. The Department of Veterans Affairs. VA grants full practice authority to advance practice registered nurses. www.va.gov/opa/pressrel/pressrelease.cfm?id=2847. Accessed January 9, 2017.
12. Benesch K, Hyman DJ. Nonphysician practitioners: more care, less cost, different law? www.healthlawyers.org/Events/Programs/Materials/Documents/ArchivedProgramMaterialFolders2009-2011/PHY09/benesch_hyman.pdf. Accessed January 9, 2017.
13. Sady B. Autonomy now! Why PAs, like NPs, need full practice authority. Clinician Reviews. 2015;25(10):6-8.
14. American Academy of Physician Assistants. AAPA urged VA to grant full practice authority to PAs; VA extended authority only to APRNs. www.aapa.org/twocolumn.aspx?id= 6442451796. Accessed January 9, 2017.
15. American Academy of Physician Assistants. Full practice authority and responsibility. http://news-center.aapa.org/wp-content/uploads/sites/2/2016/12/FAQ-Final_12_15.pdf. Accessed January 9, 2017.
16. American Academy of Physician Assistants. Major PA victory in Michigan. www.aapa.org/twocolumn.aspx?id=6442451808. Accessed January 9, 2017.
Negotiating The Professional Contract
For the freshly minted NP or PA, finding the right place to practice and negotiating a reasonable professional contract can be a challenge. The keys to successful negotiation are similar to those for attaining proficiency in your clinical practice—providing insight into your personality, an evaluation of your personal and professional goals, and a commitment of time for preparation. For most NPs and PAs, employment opportunities do not just happen. Preparation, persistence, and personal contacts are basic requirements for finding the right position.
Of great interest to NPs and PAs—especially those with looming loan payments—is the compensation package. There are many important questions and topics to discuss regarding compensation (see Table 1). However, salaries are often determined by the “going rate” for particular services in your geographic region, in addition to your specialty, experience, and credentials. Your professional association (AAPA for PAs, AANP for NPs) has robust data on salaries in your particular specialty, practice setting, and geographic region; the average salary for both professions is currently about $97,000.1,2
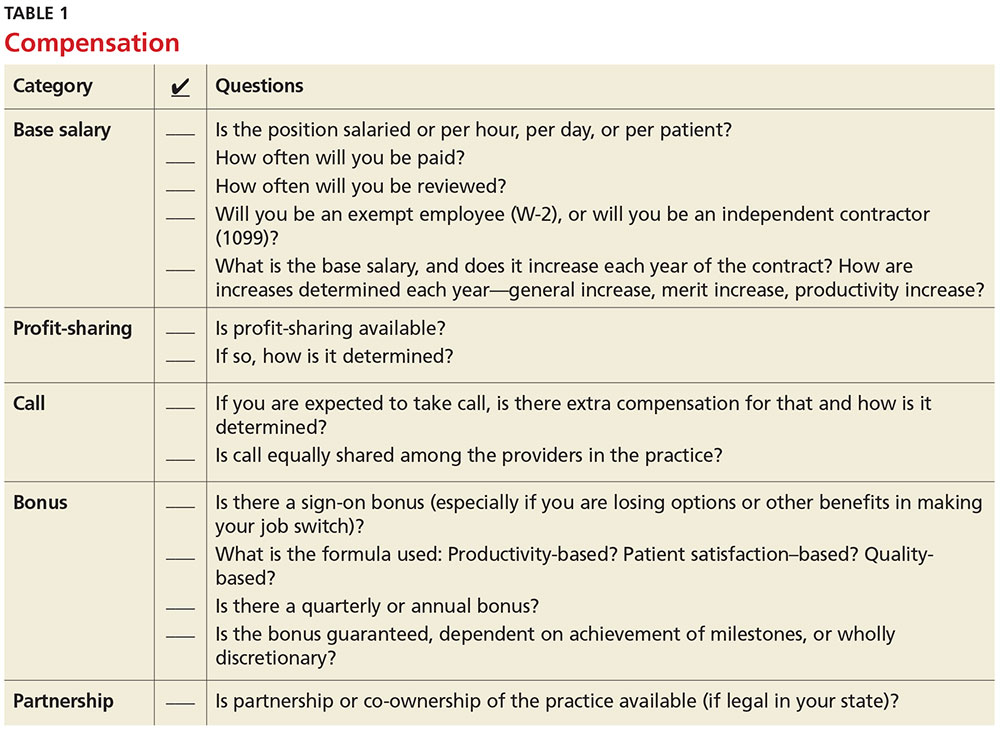
Familiarize yourself with the statutes and regulations that govern the scope of practice in your state—this is especially important if there are specific supervision or collaboration rules. Be prepared to present applicable statutes, rules, and regulations to the physician and/or office manager. Know whether any reimbursement restrictions exist. Be sure to review IRS guidelines for employee status versus independent contractor status.
The diversity of NP and PA practices means one size does not fit all, so it is best to identify the practice that complements your own personality. So, before you open negotiations, it is important that you research the practice. (For suggestions on what to inquire about, see Table 2). It is also a good idea to check the Docinfo website (http://docinfo.org/#/search/query), sponsored by the Federation of State Medical Boards, to research disciplinary records of the physician(s). Additional information can be acquired at each state regulatory board site.
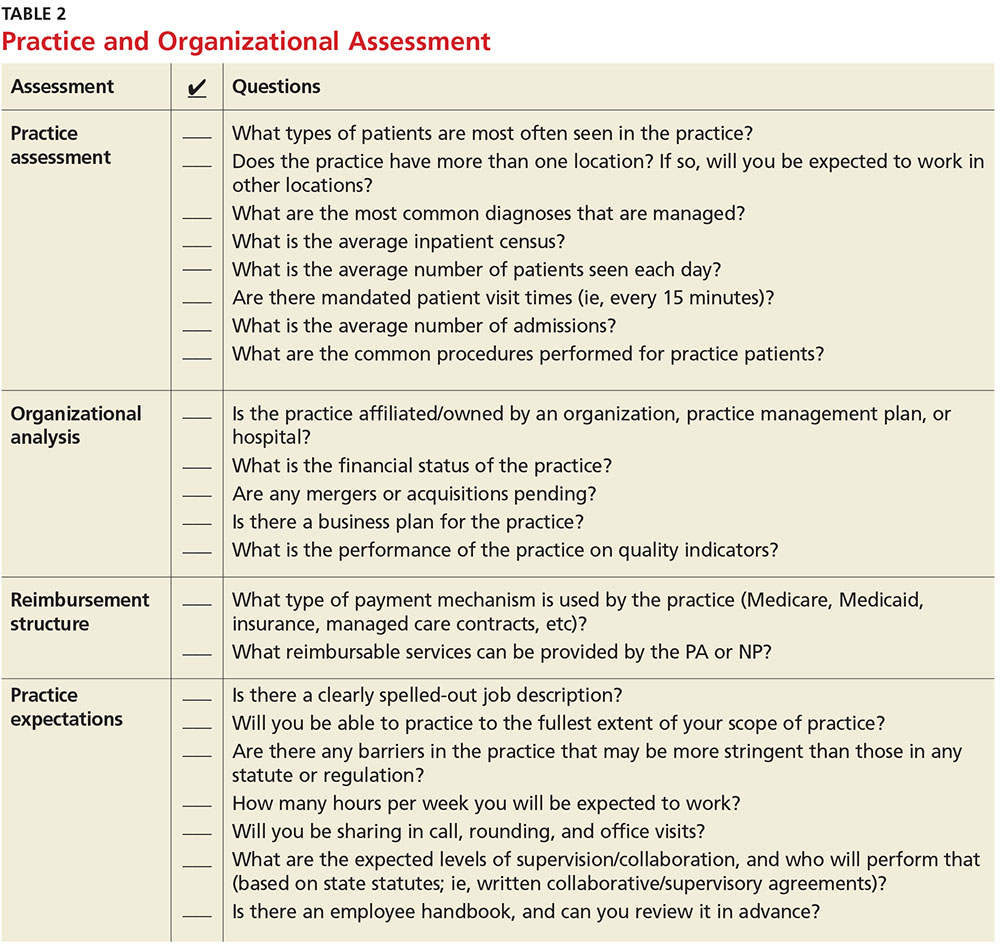
NEGOTIATION
When you’ve decided which employment offer to pursue, it’s time to think about how you want to negotiate your contract. Many people feel that negotiation is equivalent to confrontation, inevitably leading to an awkward disagreement with the practice. This is rarely the case; negotiation is simply a professional conversation, best had one-on-one with the key decision maker, rather than a group.
Never assume that your compensation package is predetermined. Whether you are starting a new job or looking to enhance your current situation, you can make a difference by asking for what you need.3 Knowing the local market and data is essential. Research the average salary in the region (for experienced versus new NP or PA). Be sure to think beyond salary and evaluate which benefits you’d like to have as part of your compensation package (see Table 3, as well as our survey results).
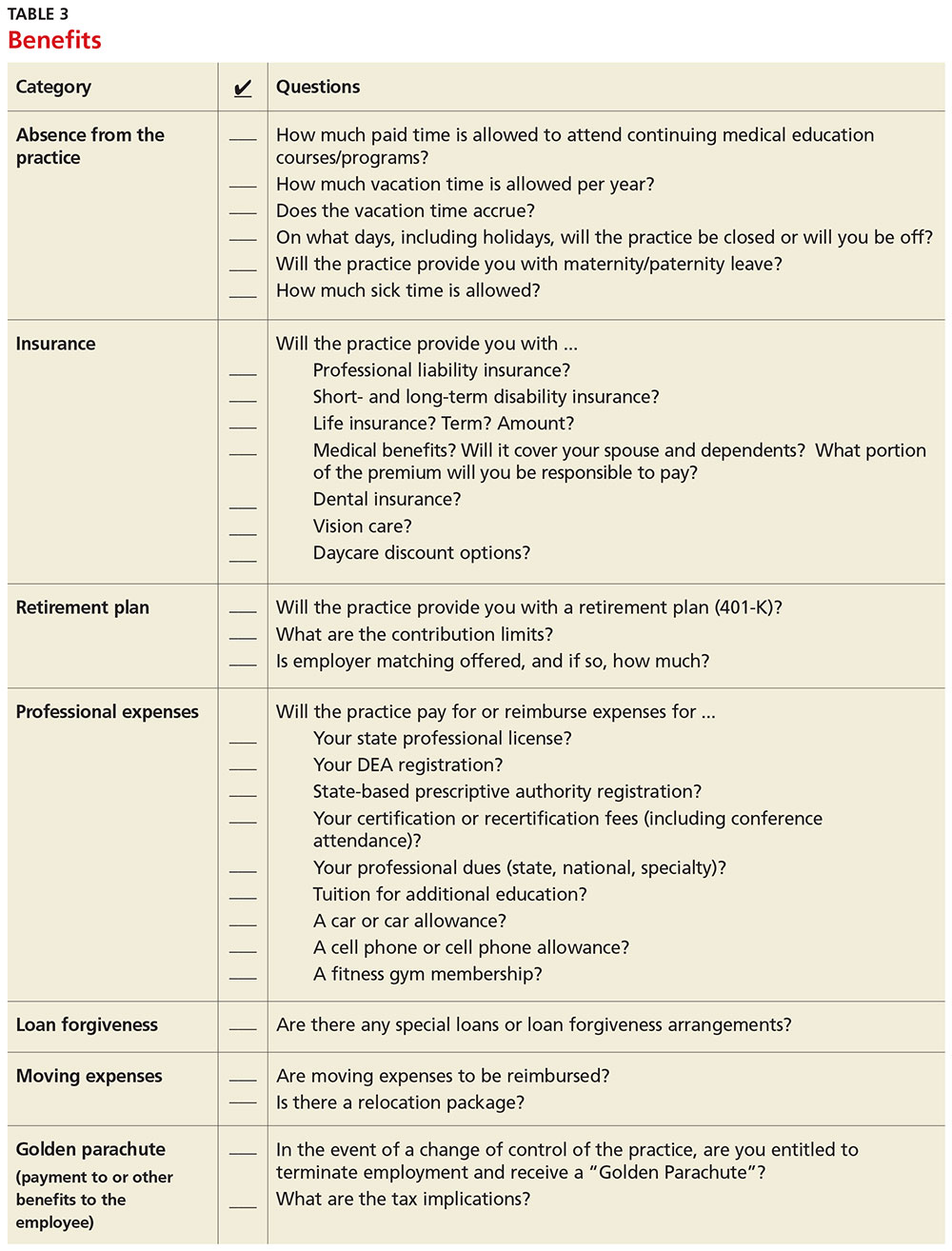
Carolyn Buppert, a specialist in legal and reimbursement issues for NPs and PAs, suggests three “P’s” of negotiation: Prepare, probe, and propose.4
Prepare. Learn how to calculate the projected revenue you would bring into a practice. You can determine the profit you generate by asking the practice administrator for data, noting Current Procedural Terminology codes and dates and becoming familiar with the fee schedule. According to Buppert, your salary and benefits should amount to about one-third of your total billings, and the benefits should equate to about 25% of your base salary.4 It is worthwhile to discuss nonmonetary contributions to the practice, such as improvements in patient satisfaction or reduction in no-shows.
Probe. Ask about the practice’s financial health during your interview and determine employer expectations for profits.
Propose. Once your prospective employer proves their value to you and after you have done due diligence researching the practice, do not hesitate to ask for what you deserve. When doing this, it is important to maintain neutral body language, keep an unemotional tone of voice, and convey an understanding of the employer’s point of view.4
Most successful negotiations occur over a couple of meetings. Careful listening is essential to avoid misunderstandings and false assumptions. By listening intently, you can identify the issues most important to the employer (eg, pay may be negotiable, but moonlighting not; or control over shift schedules is a hot button, but pay is not). Evaluating and weighing those against your own requirements may avoid an unnecessary impasse and result in a better outcome for you.
One question lives at the heart of negotiations: Should agreements be in writing? Written agreements carry more weight and prevent misunderstandings, a benefit to both parties involved. Formal, written negotiation of a contract forces the parties to discuss issues and provides a record for future reference.5
CONTRACTS
Because courses in negotiations, contract law, and business principles are rarely taught in educational programs, you should consider consulting an attorney who is familiar with contract and business issues. Avoid attorneys who have to research the laws regarding NP and PA practice—there are many who are well versed in these contracts. It is also usually more acceptable to conduct initial negotiations yourself, rather than through an attorney.
First, ask the attorney to review the contract and advise you of any troublesome provision or obvious omissions (see Table 4; a sample contract is also available on our website).6-8 Many attorneys with experience reviewing and negotiating such contracts will be willing to do an initial read and consultation for a fixed, predetermined fee. Following that consultation, it is best to discuss your concerns and questions directly with your potential employer. If you can come to a general agreement on revisions, either your lawyer or the employer’s can make the necessary changes.
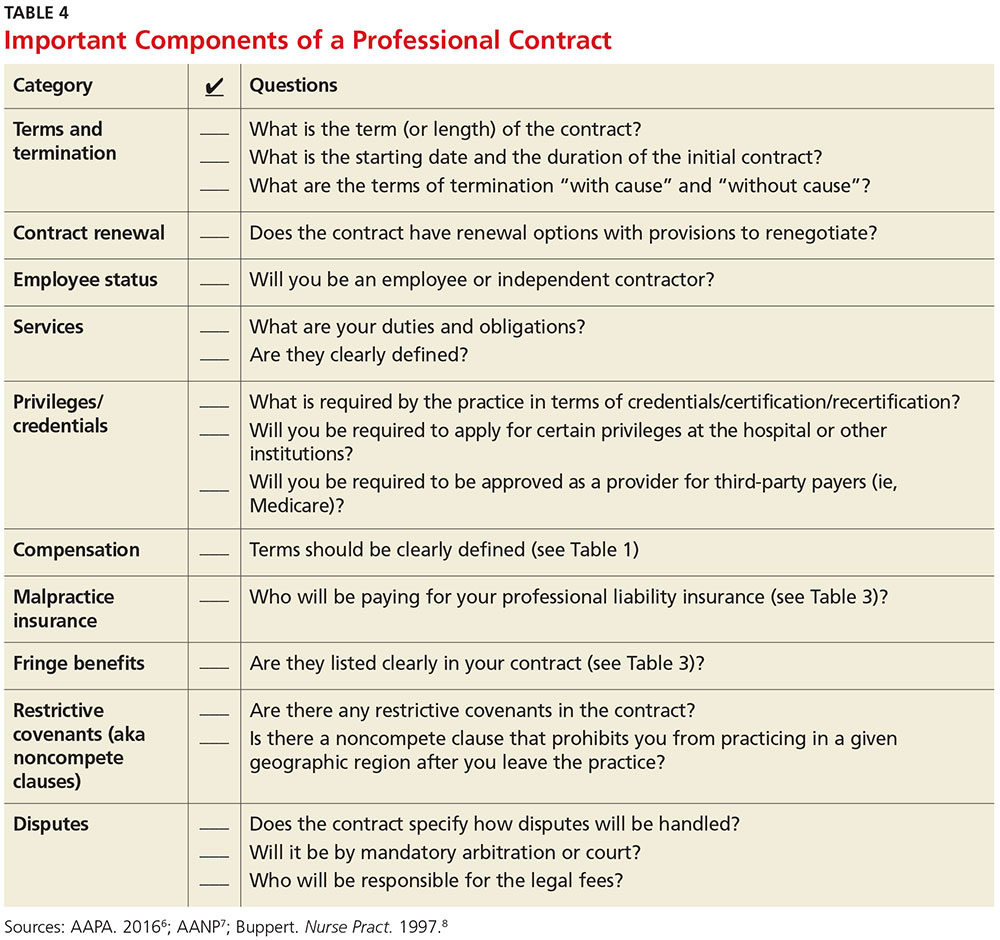
When considering an employment agreement, there are specific issues and potential hurdles to look out for. Following is a brief discussion of some of them.
Liability insurance
Find out which type of liability insurance is offered (occurrence-based or claims-made), as well as the limits of liability. Occurrence-based insurance is usually recommended. However, if the policy is claims-made, it’s important to know if the tail coverage will be paid by the employer, or if there is a rider on the physician’s policy. Determine if your contract will allow for the cost of the tail to be deducted from final amounts that may be owed to you upon termination. Be prepared to acquire the tail, if needed, to ensure coverage.
Restrictive covenants (noncompete clauses)
Unfortunately, not all employment relationships work out in the long term. In recognition of this, many professional contracts contain an agreement known as a restrictive covenant, which impedes the NP’s or PA’s ability to practice in the community following a relationship cessation. Depending on where the practice is located, such restrictions can be devastating and may even require the NP or PA to move in order to pursue a career. The law of restrictive covenants varies greatly from state to state. Your attorney can help you evaluate the enforceability and effect of a restrictive covenant, advise you on what is or isn’t reasonable in the community, and give you suggestions on how to negotiate a more reasonable one.
Moonlighting
Whether or not you can moonlight—and where—is often negotiable. An employer certainly has the right to require that moonlighting not interfere with your regular duties or schedule; endorse competitors of your employer or potentially divert patients; or expose the employer to malpractice liability. If you can assure your employer that these three situations will not transpire, then moonlighting (with advance scheduling notice and permission) should be acceptable.
Training/continuing education
It is typical for the employer to reimburse some or all of the cost of continuing education, up to a maximum annual amount. It is also reasonable for the employer (if paying for the CME) to pre-approve the curriculum, as well as the timing to avoid scheduling problems.
Salary and bonus
Compensation systems can be entirely objective (ie, production based), subjective (entirely up to the discretion of the employer based on internal criteria), or a combination of both. It is important to get a clear understanding of the system so that you know what is expected of you and what the rewards are for meeting performance goals.
Income guarantee/advanced expenses/repayment obligation
It is not uncommon for a local hospital to help a medical practice by guaranteeing the salary for a certain period of time. In this situation, the guarantee can be structured in a number of different ways—but it typically involves an obligation to repay a predetermined amount if you leave the practice area before the expiration of the term. Often, the practice will seek to pass that liability on to you. The same may apply for advanced moving expenses, CME, etc. A practice may require you to be employed for a specified amount of time to “earn” those advanced expenses, or to pay them back if an early termination occurs. In any case, it is important to know what the expectations are, and what circumstances could lead to an early termination and/or repayment obligation.
Terms and termination
Pay particular attention to the terms of your agreement. In one paragraph, it may say that the contract is for one year with annual renewals, but later on it explains that it can be terminated by either party upon 30 days notice. In that case, it is not a one-year contract; it is a 30-day contract. If there is a possibility of early termination and a restrictive covenant, or even a repayment obligation, you could really be at risk. Pay attention to whether early termination is “for cause” or “without cause.” If it is only for cause, inquire what constitutes a cause and whether there are any opportunities to rectify a perceived problem.
CONCLUSION
Constant changes in the health care marketplace will continue to generate opportunities for NPs and PAs. This is especially true for clinicians who demonstrate competence, enthusiasm, and commitment to quality patient care. The same clinical skills you learned in school and practice will help you find a clinical position and negotiate a good professional contract. Attention to detail, evidence-based research, and excellent communication skills will enable you to land a position beneficial to both parties.
1. American Academy of Physician Assistants. 2016 AAPA Salary Report. www.aapa.org/research/salary-report. Accessed November 4, 2016.
2. American Academy of Nurse Practitioners. Annual income for full-time nurse practitioners up 10% since 2011. www.aanp.org/press-room/press-releases/166-press-room/2015-press-releases/1803-annual- income-for-full-time-nurse-practitioners-up-10-since-2011. Accessed November 4, 2016.
3. Bourne H. A Great Deal! Compensation Negotiation for Nurse Practitioners & Physician Assistants. 3rd ed. Arcata, CA: Open Spaces; 1998.
4. Buppert C. Nurse Practitioner’s Business Practice and Legal Guide. 5th ed. Burlington, MA: Jones & Bartlett Learning; 2015.
5. Henley MB. Finding your ideal job and negotiating your contract: where to get the information and numbers you need to know. J Orthop Trauma. 2012;26(1):S9-S13.
6. AAPA. Contacts and contracts: a guide to your PA career. www.aapa.org/WorkArea/DownloadAsset.aspx?id=2147486883. Accessed November 4, 2016.
7. AANP. Employment negotiations. www.aanp.org/practice/reimbursement/68-articles/579-employment-negotiations. Accessed November 4, 2016.
8. Buppert C. Employment agreements: clauses that can change an NP’s life. Nurse Pract. 1997;22(8):108-109.
For the freshly minted NP or PA, finding the right place to practice and negotiating a reasonable professional contract can be a challenge. The keys to successful negotiation are similar to those for attaining proficiency in your clinical practice—providing insight into your personality, an evaluation of your personal and professional goals, and a commitment of time for preparation. For most NPs and PAs, employment opportunities do not just happen. Preparation, persistence, and personal contacts are basic requirements for finding the right position.
Of great interest to NPs and PAs—especially those with looming loan payments—is the compensation package. There are many important questions and topics to discuss regarding compensation (see Table 1). However, salaries are often determined by the “going rate” for particular services in your geographic region, in addition to your specialty, experience, and credentials. Your professional association (AAPA for PAs, AANP for NPs) has robust data on salaries in your particular specialty, practice setting, and geographic region; the average salary for both professions is currently about $97,000.1,2
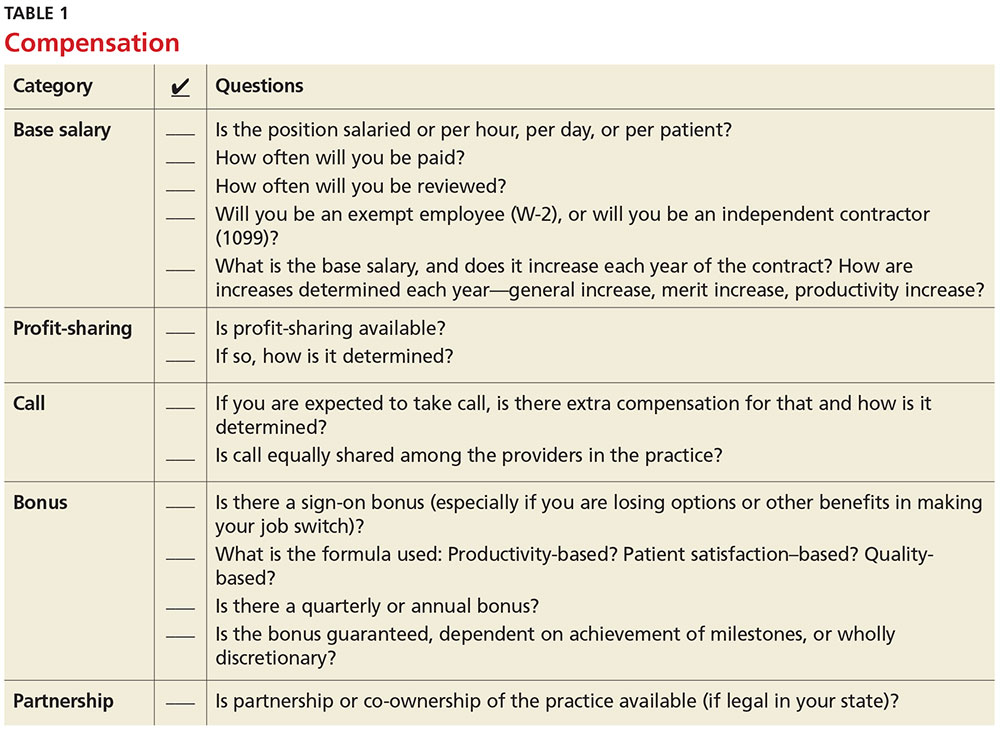
Familiarize yourself with the statutes and regulations that govern the scope of practice in your state—this is especially important if there are specific supervision or collaboration rules. Be prepared to present applicable statutes, rules, and regulations to the physician and/or office manager. Know whether any reimbursement restrictions exist. Be sure to review IRS guidelines for employee status versus independent contractor status.
The diversity of NP and PA practices means one size does not fit all, so it is best to identify the practice that complements your own personality. So, before you open negotiations, it is important that you research the practice. (For suggestions on what to inquire about, see Table 2). It is also a good idea to check the Docinfo website (http://docinfo.org/#/search/query), sponsored by the Federation of State Medical Boards, to research disciplinary records of the physician(s). Additional information can be acquired at each state regulatory board site.
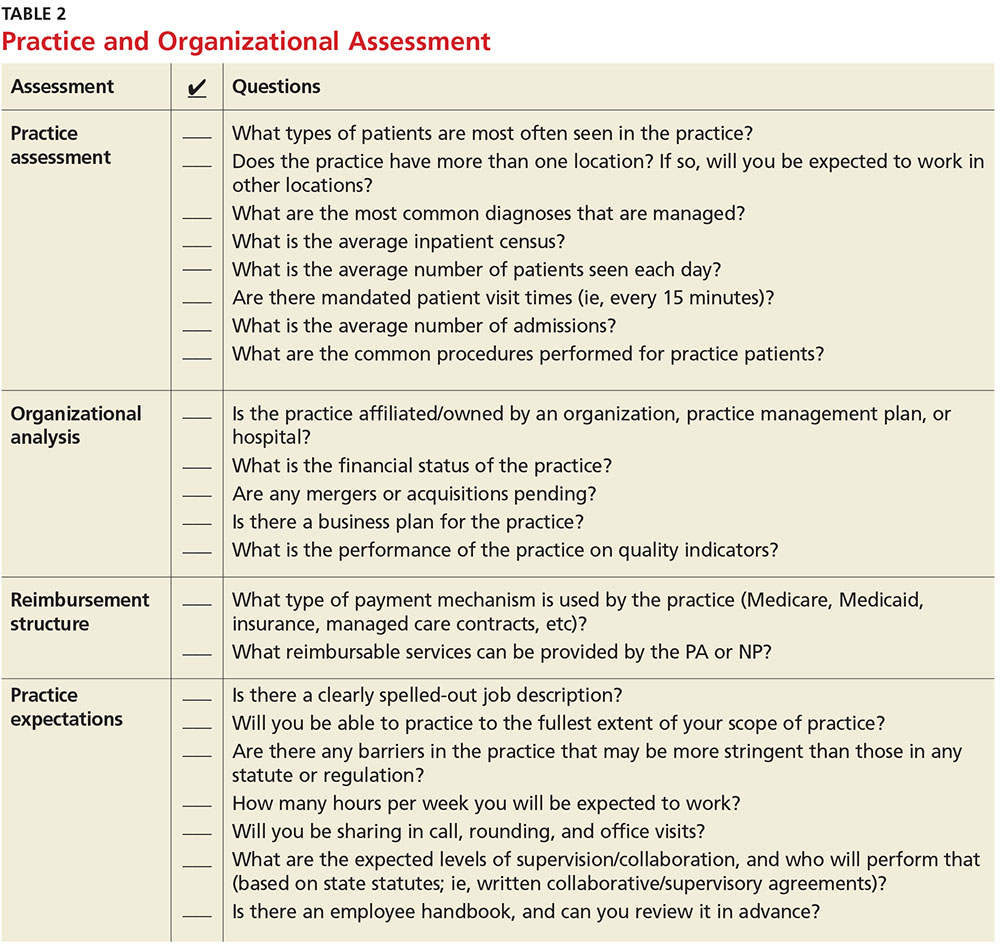
NEGOTIATION
When you’ve decided which employment offer to pursue, it’s time to think about how you want to negotiate your contract. Many people feel that negotiation is equivalent to confrontation, inevitably leading to an awkward disagreement with the practice. This is rarely the case; negotiation is simply a professional conversation, best had one-on-one with the key decision maker, rather than a group.
Never assume that your compensation package is predetermined. Whether you are starting a new job or looking to enhance your current situation, you can make a difference by asking for what you need.3 Knowing the local market and data is essential. Research the average salary in the region (for experienced versus new NP or PA). Be sure to think beyond salary and evaluate which benefits you’d like to have as part of your compensation package (see Table 3, as well as our survey results).
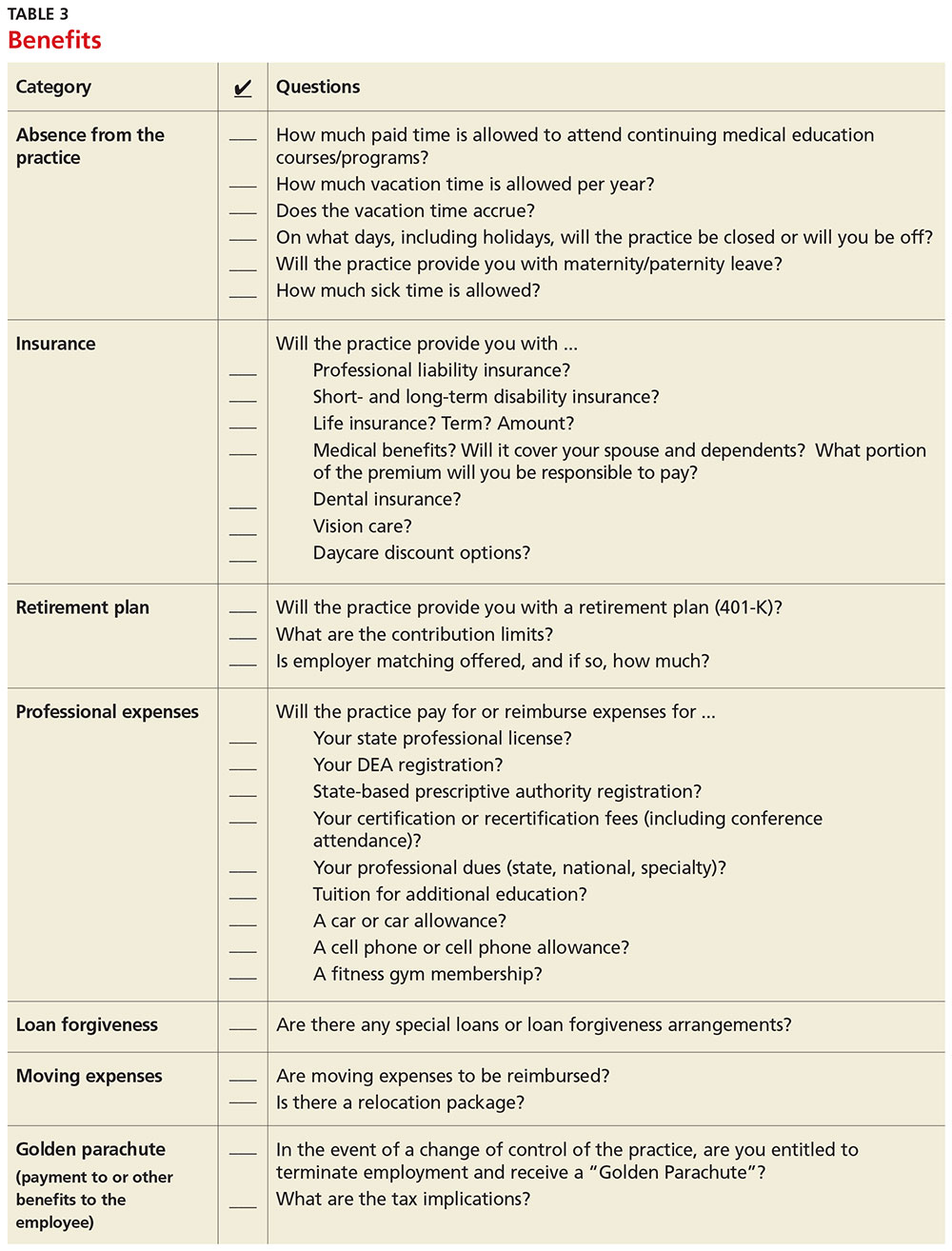
Carolyn Buppert, a specialist in legal and reimbursement issues for NPs and PAs, suggests three “P’s” of negotiation: Prepare, probe, and propose.4
Prepare. Learn how to calculate the projected revenue you would bring into a practice. You can determine the profit you generate by asking the practice administrator for data, noting Current Procedural Terminology codes and dates and becoming familiar with the fee schedule. According to Buppert, your salary and benefits should amount to about one-third of your total billings, and the benefits should equate to about 25% of your base salary.4 It is worthwhile to discuss nonmonetary contributions to the practice, such as improvements in patient satisfaction or reduction in no-shows.
Probe. Ask about the practice’s financial health during your interview and determine employer expectations for profits.
Propose. Once your prospective employer proves their value to you and after you have done due diligence researching the practice, do not hesitate to ask for what you deserve. When doing this, it is important to maintain neutral body language, keep an unemotional tone of voice, and convey an understanding of the employer’s point of view.4
Most successful negotiations occur over a couple of meetings. Careful listening is essential to avoid misunderstandings and false assumptions. By listening intently, you can identify the issues most important to the employer (eg, pay may be negotiable, but moonlighting not; or control over shift schedules is a hot button, but pay is not). Evaluating and weighing those against your own requirements may avoid an unnecessary impasse and result in a better outcome for you.
One question lives at the heart of negotiations: Should agreements be in writing? Written agreements carry more weight and prevent misunderstandings, a benefit to both parties involved. Formal, written negotiation of a contract forces the parties to discuss issues and provides a record for future reference.5
CONTRACTS
Because courses in negotiations, contract law, and business principles are rarely taught in educational programs, you should consider consulting an attorney who is familiar with contract and business issues. Avoid attorneys who have to research the laws regarding NP and PA practice—there are many who are well versed in these contracts. It is also usually more acceptable to conduct initial negotiations yourself, rather than through an attorney.
First, ask the attorney to review the contract and advise you of any troublesome provision or obvious omissions (see Table 4; a sample contract is also available on our website).6-8 Many attorneys with experience reviewing and negotiating such contracts will be willing to do an initial read and consultation for a fixed, predetermined fee. Following that consultation, it is best to discuss your concerns and questions directly with your potential employer. If you can come to a general agreement on revisions, either your lawyer or the employer’s can make the necessary changes.
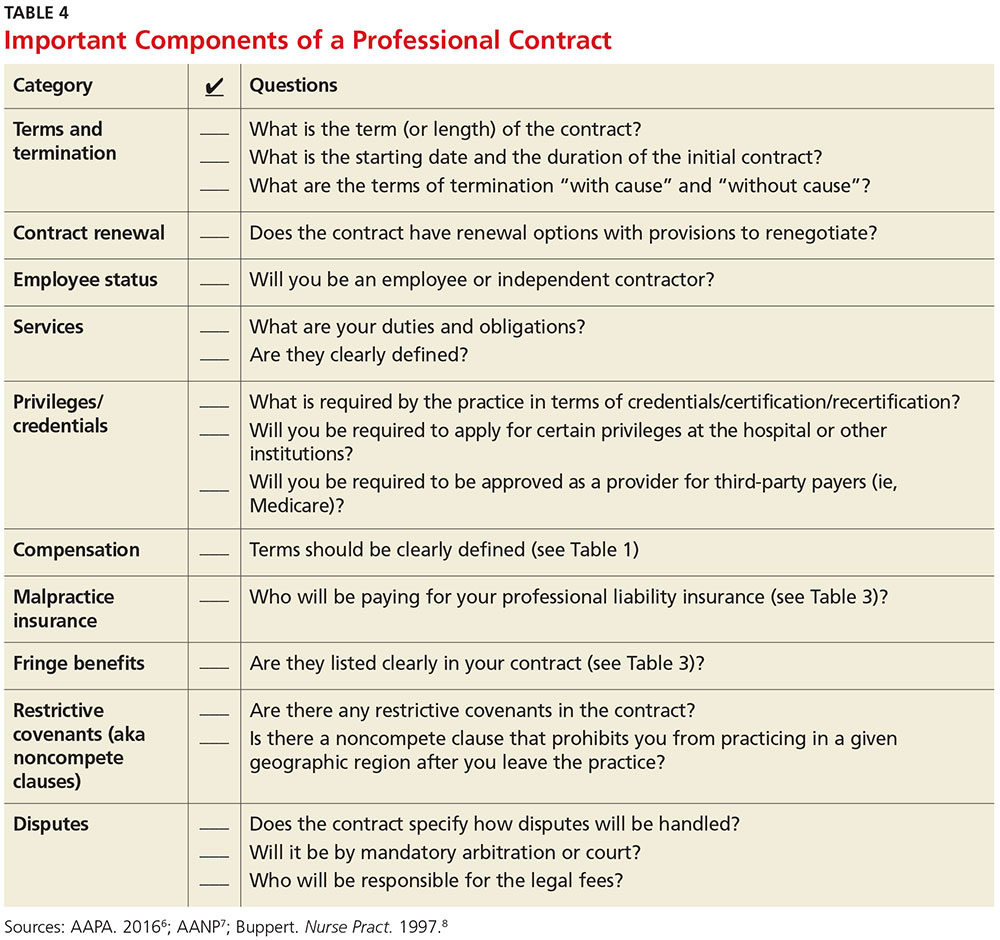
When considering an employment agreement, there are specific issues and potential hurdles to look out for. Following is a brief discussion of some of them.
Liability insurance
Find out which type of liability insurance is offered (occurrence-based or claims-made), as well as the limits of liability. Occurrence-based insurance is usually recommended. However, if the policy is claims-made, it’s important to know if the tail coverage will be paid by the employer, or if there is a rider on the physician’s policy. Determine if your contract will allow for the cost of the tail to be deducted from final amounts that may be owed to you upon termination. Be prepared to acquire the tail, if needed, to ensure coverage.
Restrictive covenants (noncompete clauses)
Unfortunately, not all employment relationships work out in the long term. In recognition of this, many professional contracts contain an agreement known as a restrictive covenant, which impedes the NP’s or PA’s ability to practice in the community following a relationship cessation. Depending on where the practice is located, such restrictions can be devastating and may even require the NP or PA to move in order to pursue a career. The law of restrictive covenants varies greatly from state to state. Your attorney can help you evaluate the enforceability and effect of a restrictive covenant, advise you on what is or isn’t reasonable in the community, and give you suggestions on how to negotiate a more reasonable one.
Moonlighting
Whether or not you can moonlight—and where—is often negotiable. An employer certainly has the right to require that moonlighting not interfere with your regular duties or schedule; endorse competitors of your employer or potentially divert patients; or expose the employer to malpractice liability. If you can assure your employer that these three situations will not transpire, then moonlighting (with advance scheduling notice and permission) should be acceptable.
Training/continuing education
It is typical for the employer to reimburse some or all of the cost of continuing education, up to a maximum annual amount. It is also reasonable for the employer (if paying for the CME) to pre-approve the curriculum, as well as the timing to avoid scheduling problems.
Salary and bonus
Compensation systems can be entirely objective (ie, production based), subjective (entirely up to the discretion of the employer based on internal criteria), or a combination of both. It is important to get a clear understanding of the system so that you know what is expected of you and what the rewards are for meeting performance goals.
Income guarantee/advanced expenses/repayment obligation
It is not uncommon for a local hospital to help a medical practice by guaranteeing the salary for a certain period of time. In this situation, the guarantee can be structured in a number of different ways—but it typically involves an obligation to repay a predetermined amount if you leave the practice area before the expiration of the term. Often, the practice will seek to pass that liability on to you. The same may apply for advanced moving expenses, CME, etc. A practice may require you to be employed for a specified amount of time to “earn” those advanced expenses, or to pay them back if an early termination occurs. In any case, it is important to know what the expectations are, and what circumstances could lead to an early termination and/or repayment obligation.
Terms and termination
Pay particular attention to the terms of your agreement. In one paragraph, it may say that the contract is for one year with annual renewals, but later on it explains that it can be terminated by either party upon 30 days notice. In that case, it is not a one-year contract; it is a 30-day contract. If there is a possibility of early termination and a restrictive covenant, or even a repayment obligation, you could really be at risk. Pay attention to whether early termination is “for cause” or “without cause.” If it is only for cause, inquire what constitutes a cause and whether there are any opportunities to rectify a perceived problem.
CONCLUSION
Constant changes in the health care marketplace will continue to generate opportunities for NPs and PAs. This is especially true for clinicians who demonstrate competence, enthusiasm, and commitment to quality patient care. The same clinical skills you learned in school and practice will help you find a clinical position and negotiate a good professional contract. Attention to detail, evidence-based research, and excellent communication skills will enable you to land a position beneficial to both parties.
For the freshly minted NP or PA, finding the right place to practice and negotiating a reasonable professional contract can be a challenge. The keys to successful negotiation are similar to those for attaining proficiency in your clinical practice—providing insight into your personality, an evaluation of your personal and professional goals, and a commitment of time for preparation. For most NPs and PAs, employment opportunities do not just happen. Preparation, persistence, and personal contacts are basic requirements for finding the right position.
Of great interest to NPs and PAs—especially those with looming loan payments—is the compensation package. There are many important questions and topics to discuss regarding compensation (see Table 1). However, salaries are often determined by the “going rate” for particular services in your geographic region, in addition to your specialty, experience, and credentials. Your professional association (AAPA for PAs, AANP for NPs) has robust data on salaries in your particular specialty, practice setting, and geographic region; the average salary for both professions is currently about $97,000.1,2
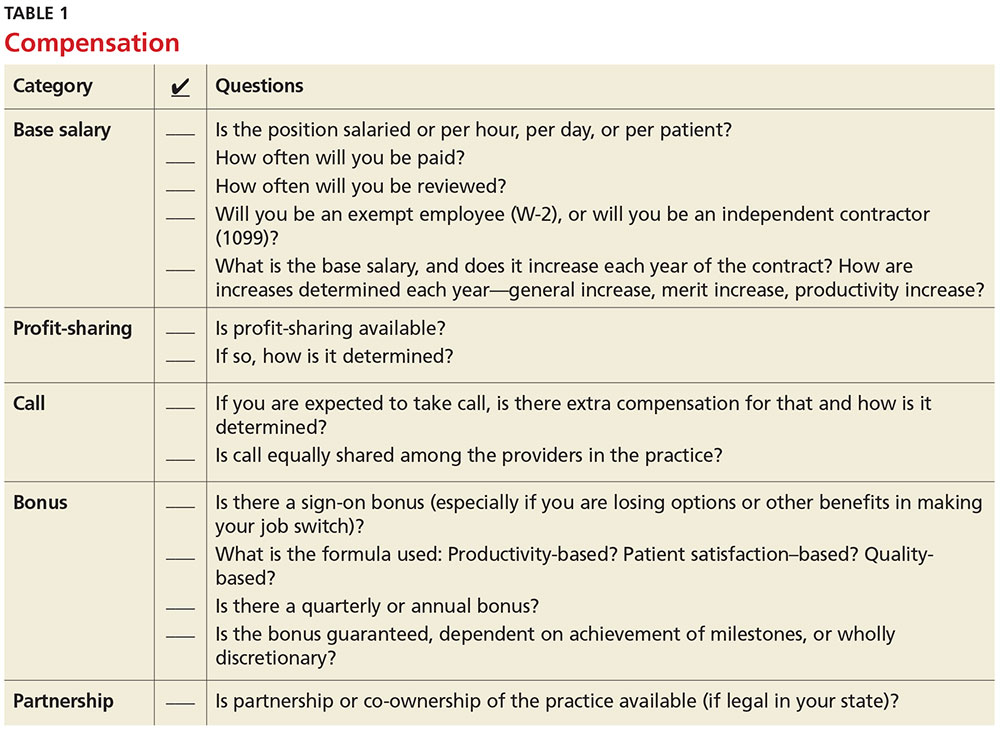
Familiarize yourself with the statutes and regulations that govern the scope of practice in your state—this is especially important if there are specific supervision or collaboration rules. Be prepared to present applicable statutes, rules, and regulations to the physician and/or office manager. Know whether any reimbursement restrictions exist. Be sure to review IRS guidelines for employee status versus independent contractor status.
The diversity of NP and PA practices means one size does not fit all, so it is best to identify the practice that complements your own personality. So, before you open negotiations, it is important that you research the practice. (For suggestions on what to inquire about, see Table 2). It is also a good idea to check the Docinfo website (http://docinfo.org/#/search/query), sponsored by the Federation of State Medical Boards, to research disciplinary records of the physician(s). Additional information can be acquired at each state regulatory board site.
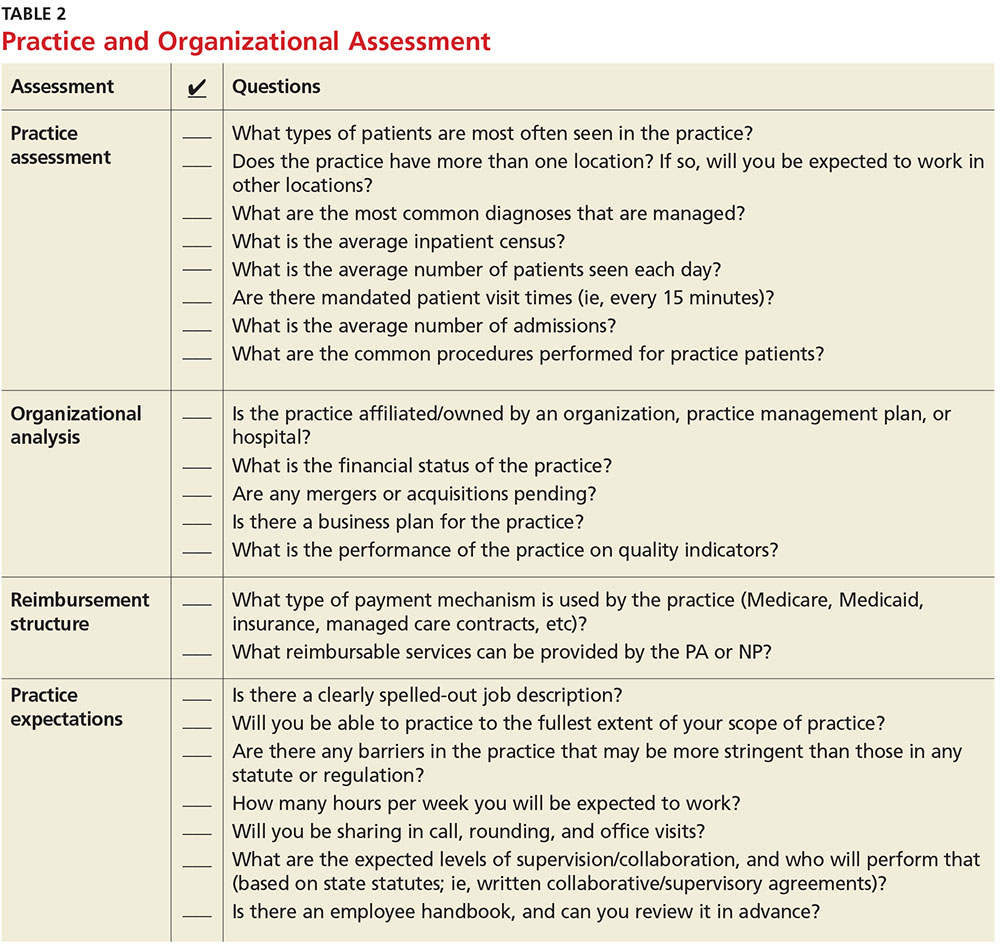
NEGOTIATION
When you’ve decided which employment offer to pursue, it’s time to think about how you want to negotiate your contract. Many people feel that negotiation is equivalent to confrontation, inevitably leading to an awkward disagreement with the practice. This is rarely the case; negotiation is simply a professional conversation, best had one-on-one with the key decision maker, rather than a group.
Never assume that your compensation package is predetermined. Whether you are starting a new job or looking to enhance your current situation, you can make a difference by asking for what you need.3 Knowing the local market and data is essential. Research the average salary in the region (for experienced versus new NP or PA). Be sure to think beyond salary and evaluate which benefits you’d like to have as part of your compensation package (see Table 3, as well as our survey results).
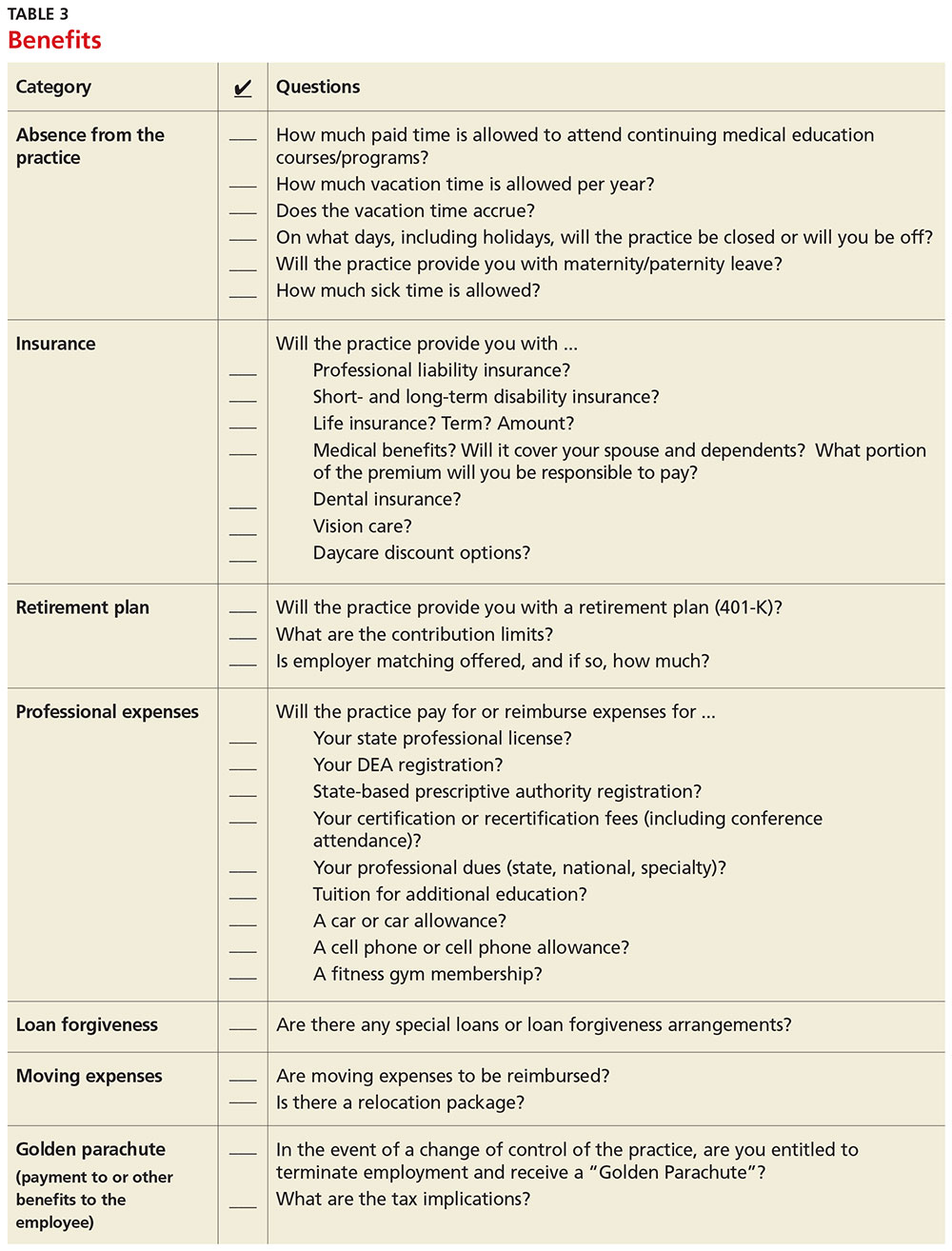
Carolyn Buppert, a specialist in legal and reimbursement issues for NPs and PAs, suggests three “P’s” of negotiation: Prepare, probe, and propose.4
Prepare. Learn how to calculate the projected revenue you would bring into a practice. You can determine the profit you generate by asking the practice administrator for data, noting Current Procedural Terminology codes and dates and becoming familiar with the fee schedule. According to Buppert, your salary and benefits should amount to about one-third of your total billings, and the benefits should equate to about 25% of your base salary.4 It is worthwhile to discuss nonmonetary contributions to the practice, such as improvements in patient satisfaction or reduction in no-shows.
Probe. Ask about the practice’s financial health during your interview and determine employer expectations for profits.
Propose. Once your prospective employer proves their value to you and after you have done due diligence researching the practice, do not hesitate to ask for what you deserve. When doing this, it is important to maintain neutral body language, keep an unemotional tone of voice, and convey an understanding of the employer’s point of view.4
Most successful negotiations occur over a couple of meetings. Careful listening is essential to avoid misunderstandings and false assumptions. By listening intently, you can identify the issues most important to the employer (eg, pay may be negotiable, but moonlighting not; or control over shift schedules is a hot button, but pay is not). Evaluating and weighing those against your own requirements may avoid an unnecessary impasse and result in a better outcome for you.
One question lives at the heart of negotiations: Should agreements be in writing? Written agreements carry more weight and prevent misunderstandings, a benefit to both parties involved. Formal, written negotiation of a contract forces the parties to discuss issues and provides a record for future reference.5
CONTRACTS
Because courses in negotiations, contract law, and business principles are rarely taught in educational programs, you should consider consulting an attorney who is familiar with contract and business issues. Avoid attorneys who have to research the laws regarding NP and PA practice—there are many who are well versed in these contracts. It is also usually more acceptable to conduct initial negotiations yourself, rather than through an attorney.
First, ask the attorney to review the contract and advise you of any troublesome provision or obvious omissions (see Table 4; a sample contract is also available on our website).6-8 Many attorneys with experience reviewing and negotiating such contracts will be willing to do an initial read and consultation for a fixed, predetermined fee. Following that consultation, it is best to discuss your concerns and questions directly with your potential employer. If you can come to a general agreement on revisions, either your lawyer or the employer’s can make the necessary changes.
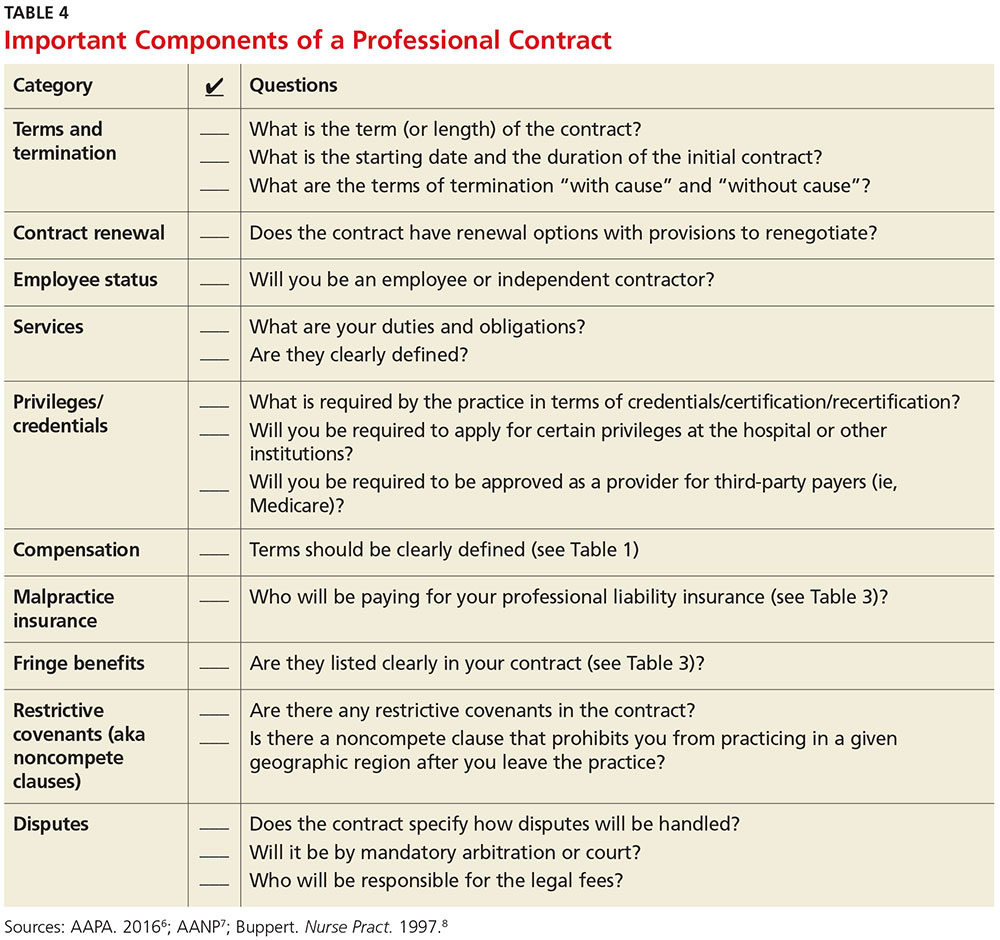
When considering an employment agreement, there are specific issues and potential hurdles to look out for. Following is a brief discussion of some of them.
Liability insurance
Find out which type of liability insurance is offered (occurrence-based or claims-made), as well as the limits of liability. Occurrence-based insurance is usually recommended. However, if the policy is claims-made, it’s important to know if the tail coverage will be paid by the employer, or if there is a rider on the physician’s policy. Determine if your contract will allow for the cost of the tail to be deducted from final amounts that may be owed to you upon termination. Be prepared to acquire the tail, if needed, to ensure coverage.
Restrictive covenants (noncompete clauses)
Unfortunately, not all employment relationships work out in the long term. In recognition of this, many professional contracts contain an agreement known as a restrictive covenant, which impedes the NP’s or PA’s ability to practice in the community following a relationship cessation. Depending on where the practice is located, such restrictions can be devastating and may even require the NP or PA to move in order to pursue a career. The law of restrictive covenants varies greatly from state to state. Your attorney can help you evaluate the enforceability and effect of a restrictive covenant, advise you on what is or isn’t reasonable in the community, and give you suggestions on how to negotiate a more reasonable one.
Moonlighting
Whether or not you can moonlight—and where—is often negotiable. An employer certainly has the right to require that moonlighting not interfere with your regular duties or schedule; endorse competitors of your employer or potentially divert patients; or expose the employer to malpractice liability. If you can assure your employer that these three situations will not transpire, then moonlighting (with advance scheduling notice and permission) should be acceptable.
Training/continuing education
It is typical for the employer to reimburse some or all of the cost of continuing education, up to a maximum annual amount. It is also reasonable for the employer (if paying for the CME) to pre-approve the curriculum, as well as the timing to avoid scheduling problems.
Salary and bonus
Compensation systems can be entirely objective (ie, production based), subjective (entirely up to the discretion of the employer based on internal criteria), or a combination of both. It is important to get a clear understanding of the system so that you know what is expected of you and what the rewards are for meeting performance goals.
Income guarantee/advanced expenses/repayment obligation
It is not uncommon for a local hospital to help a medical practice by guaranteeing the salary for a certain period of time. In this situation, the guarantee can be structured in a number of different ways—but it typically involves an obligation to repay a predetermined amount if you leave the practice area before the expiration of the term. Often, the practice will seek to pass that liability on to you. The same may apply for advanced moving expenses, CME, etc. A practice may require you to be employed for a specified amount of time to “earn” those advanced expenses, or to pay them back if an early termination occurs. In any case, it is important to know what the expectations are, and what circumstances could lead to an early termination and/or repayment obligation.
Terms and termination
Pay particular attention to the terms of your agreement. In one paragraph, it may say that the contract is for one year with annual renewals, but later on it explains that it can be terminated by either party upon 30 days notice. In that case, it is not a one-year contract; it is a 30-day contract. If there is a possibility of early termination and a restrictive covenant, or even a repayment obligation, you could really be at risk. Pay attention to whether early termination is “for cause” or “without cause.” If it is only for cause, inquire what constitutes a cause and whether there are any opportunities to rectify a perceived problem.
CONCLUSION
Constant changes in the health care marketplace will continue to generate opportunities for NPs and PAs. This is especially true for clinicians who demonstrate competence, enthusiasm, and commitment to quality patient care. The same clinical skills you learned in school and practice will help you find a clinical position and negotiate a good professional contract. Attention to detail, evidence-based research, and excellent communication skills will enable you to land a position beneficial to both parties.
1. American Academy of Physician Assistants. 2016 AAPA Salary Report. www.aapa.org/research/salary-report. Accessed November 4, 2016.
2. American Academy of Nurse Practitioners. Annual income for full-time nurse practitioners up 10% since 2011. www.aanp.org/press-room/press-releases/166-press-room/2015-press-releases/1803-annual- income-for-full-time-nurse-practitioners-up-10-since-2011. Accessed November 4, 2016.
3. Bourne H. A Great Deal! Compensation Negotiation for Nurse Practitioners & Physician Assistants. 3rd ed. Arcata, CA: Open Spaces; 1998.
4. Buppert C. Nurse Practitioner’s Business Practice and Legal Guide. 5th ed. Burlington, MA: Jones & Bartlett Learning; 2015.
5. Henley MB. Finding your ideal job and negotiating your contract: where to get the information and numbers you need to know. J Orthop Trauma. 2012;26(1):S9-S13.
6. AAPA. Contacts and contracts: a guide to your PA career. www.aapa.org/WorkArea/DownloadAsset.aspx?id=2147486883. Accessed November 4, 2016.
7. AANP. Employment negotiations. www.aanp.org/practice/reimbursement/68-articles/579-employment-negotiations. Accessed November 4, 2016.
8. Buppert C. Employment agreements: clauses that can change an NP’s life. Nurse Pract. 1997;22(8):108-109.
1. American Academy of Physician Assistants. 2016 AAPA Salary Report. www.aapa.org/research/salary-report. Accessed November 4, 2016.
2. American Academy of Nurse Practitioners. Annual income for full-time nurse practitioners up 10% since 2011. www.aanp.org/press-room/press-releases/166-press-room/2015-press-releases/1803-annual- income-for-full-time-nurse-practitioners-up-10-since-2011. Accessed November 4, 2016.
3. Bourne H. A Great Deal! Compensation Negotiation for Nurse Practitioners & Physician Assistants. 3rd ed. Arcata, CA: Open Spaces; 1998.
4. Buppert C. Nurse Practitioner’s Business Practice and Legal Guide. 5th ed. Burlington, MA: Jones & Bartlett Learning; 2015.
5. Henley MB. Finding your ideal job and negotiating your contract: where to get the information and numbers you need to know. J Orthop Trauma. 2012;26(1):S9-S13.
6. AAPA. Contacts and contracts: a guide to your PA career. www.aapa.org/WorkArea/DownloadAsset.aspx?id=2147486883. Accessed November 4, 2016.
7. AANP. Employment negotiations. www.aanp.org/practice/reimbursement/68-articles/579-employment-negotiations. Accessed November 4, 2016.
8. Buppert C. Employment agreements: clauses that can change an NP’s life. Nurse Pract. 1997;22(8):108-109.
Mental Health: A Forgotten Facet of Primary Care
One of the biggest disparities in health care today is the separate treatment of mind and body, despite their known integration.1 While mental and behavioral health conditions are frequently diagnosed and treated within primary care settings, fragmentation persists between the mental and physical health care systems—creating barriers in the quality, outcome, and efficiency of care.2 Since half of Americans with mental health conditions go without essential care, reform of our nation’s mental health system is a priority issue for NPs and PAs and the patients we serve.
Some progress has been made to implement change—the Now Is the Time initiative, launched in 2013, increased federal funding for behavioral health care workforce training in an effort to support more providers in mental and substance use disorder treatment. The Affordable Care Act (ACA) has worked to improve behavioral health coverage for Americans in three ways: ending insurance company discrimination based on pre-existing conditions, requiring health insurance coverage for mental and substance use disorder services, and expanding mental health parity. This has improved coverage and access to mental and substance abuse services for more than 60 million Americans.3 In January 2016, President Obama proposed a $500 million investment to increase access to mental health care.4 The most recent presidential election creates an uncertain future for
Regardless, more work has to be done to guarantee that Americans have the access they need. Sadly, even with these advancements in behavioral health coverage, only about half of children and less than half of adults with diagnosable mental health disorders get the treatment they need.4 A 2016 report from the Rural Health Research Center revealed that more than 15 million Americans face behavioral health issues without access to the necessary care.5
Psychiatric providers (like most other specialists) tend to be located in urban areas, limiting access in rural areas and even some underserved urban communities. Only 43% of family physicians in this country provide mental health care.6 The team-based care that NPs and PAs provide has great potential for bridging this gap in mental health coverage.
NPs and PAs are an important but underutilized resource for improving mental health care access—but how can primary care NPs and PAs work to enhance the delivery of mental health care in our country? In the preprofessional area, it would be prudent to entice qualified individuals in the mental health field—particularly those who are licensed clinical social workers, licensed professional counselors, or marriage and family therapists—into NP and PA programs with preference.
Clinical rotations in behavioral health (BH)/psychiatry should be encouraged—even mandated—in professional education. We should ensure this content is taught in the didactic portion of NP/PA professional education, as well as bolstering psychiatric pharmacology in coursework.
Postprofessional education should encourage primary care NPs and PAs to gain additional self-directed education in BH/psychiatry. This can be achieved via a focused psychiatry “boot camp” (for PAs following the CAQ blueprint, found at www.nccpa.net/psychiatry) or a competency-based online postprofessional certificate in BH/psychiatry (such as—shameless plug—the one offered at my institution; www.atsu.edu/postgraduate-certificate-in-psychiatry-and-behavioral-health-online).7,8
This psychiatric background is fundamental throughout primary care but is crucial in community health centers, correctional health care centers, and Veterans Administration hospitals. Of course, in order to make a difference, we must remove the barriers that prevent psychiatric NPs and PAs from being considered mental health providers and adjust reimbursement accordingly.
Do you have ideas on how to increase the knowledge base of primary care NPs and PAs and enhance the provision of mental health services in this country? Will the political change in leadership in January 2017 increase opportunities to make a difference in mental health care? Please share your thoughts by contacting me at [email protected].
1. deGruy F. Mental health care in the primary care setting. In: Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Primary Care: America’s Health in a New Era. Washington, DC: Institute of Medicine; 1996.
2. Simon GE, Katon WJ, VonKorff M, et al. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. Am J Psychiatry. 2001;158(10): 1638-1644.
3. Enomoto K. Improving access to mental health services - President’s FY 2017 Budget proposes new investments to increase access. http://abilitychicagoinfo.blogspot.com/2016/02/improving-access-to-mental-health.html. Accessed November 3, 2016.
4. Enomoto K. Improving access to mental health services. www.hhs.gov/blog/2016/02/09/improving-access-mental-health-services.html. Accessed November 3, 2016.
5. Rural Health Research Center. Supply and distribution of the behavioral health workforce in rural America. http://depts.washington.edu/fammed/rhrc/wp-content/uploads/sites/4/2016/09/RHRC_DB160_Larson.pdf. Accessed November 3, 2016.
6. Miller BF, Druss B. The role of family physicians in mental health care delivery in the United States: implications for health reform. J Am Board Fam Med. 2013;26(2): 111-113.
7. National Commission on Certification of Physician Assistants. Psychiatry CAQ. www.nccpa.net/psychiatry. Accessed November 3, 2016.
8. A.T. Still University. Postgraduate certificate in psychiatry and behavioral health online. www.atsu.edu/postgraduate-certificate-in-psychiatry-and-behavioral-health-online. Accessed November 3, 2016.
One of the biggest disparities in health care today is the separate treatment of mind and body, despite their known integration.1 While mental and behavioral health conditions are frequently diagnosed and treated within primary care settings, fragmentation persists between the mental and physical health care systems—creating barriers in the quality, outcome, and efficiency of care.2 Since half of Americans with mental health conditions go without essential care, reform of our nation’s mental health system is a priority issue for NPs and PAs and the patients we serve.
Some progress has been made to implement change—the Now Is the Time initiative, launched in 2013, increased federal funding for behavioral health care workforce training in an effort to support more providers in mental and substance use disorder treatment. The Affordable Care Act (ACA) has worked to improve behavioral health coverage for Americans in three ways: ending insurance company discrimination based on pre-existing conditions, requiring health insurance coverage for mental and substance use disorder services, and expanding mental health parity. This has improved coverage and access to mental and substance abuse services for more than 60 million Americans.3 In January 2016, President Obama proposed a $500 million investment to increase access to mental health care.4 The most recent presidential election creates an uncertain future for
Regardless, more work has to be done to guarantee that Americans have the access they need. Sadly, even with these advancements in behavioral health coverage, only about half of children and less than half of adults with diagnosable mental health disorders get the treatment they need.4 A 2016 report from the Rural Health Research Center revealed that more than 15 million Americans face behavioral health issues without access to the necessary care.5
Psychiatric providers (like most other specialists) tend to be located in urban areas, limiting access in rural areas and even some underserved urban communities. Only 43% of family physicians in this country provide mental health care.6 The team-based care that NPs and PAs provide has great potential for bridging this gap in mental health coverage.
NPs and PAs are an important but underutilized resource for improving mental health care access—but how can primary care NPs and PAs work to enhance the delivery of mental health care in our country? In the preprofessional area, it would be prudent to entice qualified individuals in the mental health field—particularly those who are licensed clinical social workers, licensed professional counselors, or marriage and family therapists—into NP and PA programs with preference.
Clinical rotations in behavioral health (BH)/psychiatry should be encouraged—even mandated—in professional education. We should ensure this content is taught in the didactic portion of NP/PA professional education, as well as bolstering psychiatric pharmacology in coursework.
Postprofessional education should encourage primary care NPs and PAs to gain additional self-directed education in BH/psychiatry. This can be achieved via a focused psychiatry “boot camp” (for PAs following the CAQ blueprint, found at www.nccpa.net/psychiatry) or a competency-based online postprofessional certificate in BH/psychiatry (such as—shameless plug—the one offered at my institution; www.atsu.edu/postgraduate-certificate-in-psychiatry-and-behavioral-health-online).7,8
This psychiatric background is fundamental throughout primary care but is crucial in community health centers, correctional health care centers, and Veterans Administration hospitals. Of course, in order to make a difference, we must remove the barriers that prevent psychiatric NPs and PAs from being considered mental health providers and adjust reimbursement accordingly.
Do you have ideas on how to increase the knowledge base of primary care NPs and PAs and enhance the provision of mental health services in this country? Will the political change in leadership in January 2017 increase opportunities to make a difference in mental health care? Please share your thoughts by contacting me at [email protected].
One of the biggest disparities in health care today is the separate treatment of mind and body, despite their known integration.1 While mental and behavioral health conditions are frequently diagnosed and treated within primary care settings, fragmentation persists between the mental and physical health care systems—creating barriers in the quality, outcome, and efficiency of care.2 Since half of Americans with mental health conditions go without essential care, reform of our nation’s mental health system is a priority issue for NPs and PAs and the patients we serve.
Some progress has been made to implement change—the Now Is the Time initiative, launched in 2013, increased federal funding for behavioral health care workforce training in an effort to support more providers in mental and substance use disorder treatment. The Affordable Care Act (ACA) has worked to improve behavioral health coverage for Americans in three ways: ending insurance company discrimination based on pre-existing conditions, requiring health insurance coverage for mental and substance use disorder services, and expanding mental health parity. This has improved coverage and access to mental and substance abuse services for more than 60 million Americans.3 In January 2016, President Obama proposed a $500 million investment to increase access to mental health care.4 The most recent presidential election creates an uncertain future for
Regardless, more work has to be done to guarantee that Americans have the access they need. Sadly, even with these advancements in behavioral health coverage, only about half of children and less than half of adults with diagnosable mental health disorders get the treatment they need.4 A 2016 report from the Rural Health Research Center revealed that more than 15 million Americans face behavioral health issues without access to the necessary care.5
Psychiatric providers (like most other specialists) tend to be located in urban areas, limiting access in rural areas and even some underserved urban communities. Only 43% of family physicians in this country provide mental health care.6 The team-based care that NPs and PAs provide has great potential for bridging this gap in mental health coverage.
NPs and PAs are an important but underutilized resource for improving mental health care access—but how can primary care NPs and PAs work to enhance the delivery of mental health care in our country? In the preprofessional area, it would be prudent to entice qualified individuals in the mental health field—particularly those who are licensed clinical social workers, licensed professional counselors, or marriage and family therapists—into NP and PA programs with preference.
Clinical rotations in behavioral health (BH)/psychiatry should be encouraged—even mandated—in professional education. We should ensure this content is taught in the didactic portion of NP/PA professional education, as well as bolstering psychiatric pharmacology in coursework.
Postprofessional education should encourage primary care NPs and PAs to gain additional self-directed education in BH/psychiatry. This can be achieved via a focused psychiatry “boot camp” (for PAs following the CAQ blueprint, found at www.nccpa.net/psychiatry) or a competency-based online postprofessional certificate in BH/psychiatry (such as—shameless plug—the one offered at my institution; www.atsu.edu/postgraduate-certificate-in-psychiatry-and-behavioral-health-online).7,8
This psychiatric background is fundamental throughout primary care but is crucial in community health centers, correctional health care centers, and Veterans Administration hospitals. Of course, in order to make a difference, we must remove the barriers that prevent psychiatric NPs and PAs from being considered mental health providers and adjust reimbursement accordingly.
Do you have ideas on how to increase the knowledge base of primary care NPs and PAs and enhance the provision of mental health services in this country? Will the political change in leadership in January 2017 increase opportunities to make a difference in mental health care? Please share your thoughts by contacting me at [email protected].
1. deGruy F. Mental health care in the primary care setting. In: Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Primary Care: America’s Health in a New Era. Washington, DC: Institute of Medicine; 1996.
2. Simon GE, Katon WJ, VonKorff M, et al. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. Am J Psychiatry. 2001;158(10): 1638-1644.
3. Enomoto K. Improving access to mental health services - President’s FY 2017 Budget proposes new investments to increase access. http://abilitychicagoinfo.blogspot.com/2016/02/improving-access-to-mental-health.html. Accessed November 3, 2016.
4. Enomoto K. Improving access to mental health services. www.hhs.gov/blog/2016/02/09/improving-access-mental-health-services.html. Accessed November 3, 2016.
5. Rural Health Research Center. Supply and distribution of the behavioral health workforce in rural America. http://depts.washington.edu/fammed/rhrc/wp-content/uploads/sites/4/2016/09/RHRC_DB160_Larson.pdf. Accessed November 3, 2016.
6. Miller BF, Druss B. The role of family physicians in mental health care delivery in the United States: implications for health reform. J Am Board Fam Med. 2013;26(2): 111-113.
7. National Commission on Certification of Physician Assistants. Psychiatry CAQ. www.nccpa.net/psychiatry. Accessed November 3, 2016.
8. A.T. Still University. Postgraduate certificate in psychiatry and behavioral health online. www.atsu.edu/postgraduate-certificate-in-psychiatry-and-behavioral-health-online. Accessed November 3, 2016.
1. deGruy F. Mental health care in the primary care setting. In: Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Primary Care: America’s Health in a New Era. Washington, DC: Institute of Medicine; 1996.
2. Simon GE, Katon WJ, VonKorff M, et al. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. Am J Psychiatry. 2001;158(10): 1638-1644.
3. Enomoto K. Improving access to mental health services - President’s FY 2017 Budget proposes new investments to increase access. http://abilitychicagoinfo.blogspot.com/2016/02/improving-access-to-mental-health.html. Accessed November 3, 2016.
4. Enomoto K. Improving access to mental health services. www.hhs.gov/blog/2016/02/09/improving-access-mental-health-services.html. Accessed November 3, 2016.
5. Rural Health Research Center. Supply and distribution of the behavioral health workforce in rural America. http://depts.washington.edu/fammed/rhrc/wp-content/uploads/sites/4/2016/09/RHRC_DB160_Larson.pdf. Accessed November 3, 2016.
6. Miller BF, Druss B. The role of family physicians in mental health care delivery in the United States: implications for health reform. J Am Board Fam Med. 2013;26(2): 111-113.
7. National Commission on Certification of Physician Assistants. Psychiatry CAQ. www.nccpa.net/psychiatry. Accessed November 3, 2016.
8. A.T. Still University. Postgraduate certificate in psychiatry and behavioral health online. www.atsu.edu/postgraduate-certificate-in-psychiatry-and-behavioral-health-online. Accessed November 3, 2016.
Who’s On First: A Look at Workforce Projections
Predicting the future, particularly in the ever-changing realm of health care, is always a gamble. The variables with the potential to impact health care—among them, unpredictable political agendas, unforeseen economic upheaval, and technological issues—make it difficult to identify one “expected” outcome. However, one forecasted trend will certainly make a difference: the quantity of well-educated health care practitioners.
This factor will be one of the most important determinants of our ability to deliver quality, accessible health care in a diverse society with increasingly complex medical needs. Some may say that this is an irrational fear—the US health care system is remarkably adaptable, and as far as we can tell, no serious problems have arisen due to a shortage of providers. So are we overreacting, or is there a viable reason for concern?
While more and more Americans are covered by health insurance thanks to the Affordable Care Act, fewer physicians are entering primary care. The Association of American Medical Colleges (AAMC) has projected a shortage of between 46,000 and 90,000 physicians by 2025. AAMC forecasts a shortage of 12,500 to 31,100 primary care physicians and 21,200 to 63,700 non–primary care physicians; much of the latter deficit will be in the surgical specialties.1 The report emphasizes the need for immediate action because it takes almost a decade to educate a physician for entry into the workforce.
On the surface, these numbers are quite staggering. They may even elicit a sense of doom about access to quality (or even simply adequate) health care in the next decade. To put these projections in context, here are some key statistics
- About 915,000 physicians actively practice in the US.2
- Each year, about 20,000 medical school students graduate and enter postgraduate education.3
- Thirty percent of physicians are older than 60.2
- In 2015, there were 100,000 practicing PAs, with an average age of 38.4
- As of 2016, there are 222,000 practicing NPs, with an average age of 49.5
The US population is projected to increase from 310 million in 2015 to 335 million in 2025.6 There are approximately 45 million Americans older than 65, a number that is projected to increase to almost 70 million by 2025.7,8
This inverse relationship—more potential patients and fewer people to care for them—suggests perilous changes for our health care system. Some anticipated changes—longer wait times for care, increased costs, and more opportunities for error—are real and have already been quantified in reports.9 But with the year 2025 less than a decade away, where is our sense of urgency? Even if we implement changes immediately, they are unlikely to offset the consequences of the workforce shortage. Yet to do nothing will lead to a rapid decline in quality of life for many Americans.
In theory, there are two ways to address this pending “crisis.” We can decrease demand and/or increase supply. In the next few decades, achieving the former will be difficult, because of the unavoidable toll of an aging population. Public health and preventive services may have some impact and deserve increased attention. New and improved modes of treatment offer the potential to ameliorate the impact of chronic diseases such as diabetes and cardiovascular disease. This method, while a noble goal, is also less predictable and harder to “plan” for.
The most direct approach (but certainly not the only one) is to increase the supply of health care providers—specifically, NPs and PAs—in order to meet the rising demand. The professions have long been touted as a solution to problems of access to care in both rural and urban areas. About 83% of NPs are certified in primary care; we cannot ignore the fact that only 24% of PAs practice in primary care while the rest have chosen specialties. But (another plus) patients tend to be as satisfied with care provided by NPs and PAs as by physicians.10,11
Increasing the supply of NPs and PAs requires educating more individuals to enter the professions. Education programs need to do a critical analysis of their curricula to ensure that what happens in the classroom matches real-world needs. If graduates enter the workforce unprepared for the demands of the job, no progress will be made. (For a vigorous discussion on the current state of professional education, please visit www.mdedge.com/clinicianreviews/commentary).
One significant limitation to the growth of the PA supply is the accreditation process, which now takes almost three years from the start of the process until the initial approval of a class (and five years until the first class graduates). This process adds time and expense to the creation of new education programs, many of which await approval and lack the resources to bring the program to maturity. While no one would argue the value of the ARC-PA accreditation, the process should be critically examined to identify any areas that can be streamlined without decreasing the quality of the product.
Which brings us to perhaps the most important aspect of this discussion: What actions need to be taken to mitigate the possible damage of a physician shortage? Here are some recommendations for a variety of stakeholders:
Educators should enhance their competency-based curriculum to enable NPs and PAs to move through their programs at a faster stride (again, without sacrificing valuable learning time) and get into practice sooner.
Accreditors should review current standards and remove barriers to allow education programs to create innovative curricula that help NPs and PAs gain the knowledge (and experience) they need to move into practice.
Regulators should ensure that NPs and PAs are able to practice to the fullest extent of their license and scope of practice (ie, full practice authority, scope of practice determined at the practice level). Barriers should be removed to allow these clinicians to function in rural and underserved regions of the country (eg, adaptable collaboration requirements).10 (For a different perspective on PA autonomy, see here.)
Policymakers should rally around the removal of barriers to postgraduate residencies, which would sustain and possibly increase the physician supply. Reimbursement, particularly in Medicare, should be re-evaluated to assure that all providers are reimbursed for same services. Lack of parity in reimbursement infers a difference in quality that is just not the case.
Practicing NPs and PAs should step up to the plate and volunteer as preceptors to give NP and PA students the opportunity to learn from the best and most experienced.
Physicians should seek out alternatives to retirement from medicine (ie working part-time, becoming an educator). Expanding the period of clinical practice may forestall, or even prevent, some of the shortage—at least, in the short-term.
There are those who say that a provider shortage does not exist and that those crying out about it have a vested interest in expanding medical school output. Others acknowledge the shortage but worry that increasing the supply of NPs and PAs will ultimately “devalue” individual providers (ie, drive down salaries). One thing, however, is certain: As Danish physicist Niels Bohr said, “Prediction is very difficult, especially if it’s about the future.”
What are your thoughts and ideas about the health care workforce and the increasing demand for care? Please share them with us by writing to [email protected].
1. Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2013 to 2025. Washington, DC: HIS, Inc; 2015. www.aamc.org/download/426242/data/ihsreportdownload.pdf. Accessed September 8, 2016.
2. Young A, Chaudhry HJ, Pei X, et al. A census of actively licensed physicians in the United States, 2014. J Med Regulation. 2014;96(4): 10-20.
3. Association of American Medical Colleges. Table B-2.2: total graduates by US medical school and sex, 2010-2011 through 2014-2015. www.aamc.org/download/321532/data/factstableb2-2.pdf. Accessed September 8, 2016.
4. National Commission on Certification of Physician Assistants. 2015 statistical profile of certified physician assistants. www.nccpa.net/Uploads/docs/2015StatisticalProfileofCertifiedPhysicianAssistants.pdf. Accessed September 8, 2016.
5. American Association of Nurse Practitioners. NP fact sheet. www.aanp.org/all-about-nps/np-fact-sheet. Accessed September 8, 2016.
6. US Department of Commerce. Population projections of the United States by age, sex, race, and hispanic origin: 1995 to 2050. www.census.gov/prod/1/pop/p25-1130.pdf. Accessed September 8, 2016.
7. Mather M, Jacobsen LA, Pollard KP. Aging in the United States. Popul Bull. 2015;70:1-23.
8. Ortman JM, Velkoff VA, Hogan HH. An aging nation: the older population in the United States. US Census Bureau. 2014;P25-1140.
9. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. www.nap.edu/books/0309072808/html. Accessed September 8, 2016.
10. Garment V. Nurse practitioners and physician assistants: why you should hire one (or the other). The Profitable Practice blog. 2013. http://profitable-practice.softwareadvice.com/nurse-practitioners-and-physician-assistants-why-you-should-hire-one-or-the-other-0513. Accessed September 8, 2016.
11. American Academy of Physician Assistants. Six key elements. www.aapa.org/six-key-elements. Accessed September 8, 2016.
Predicting the future, particularly in the ever-changing realm of health care, is always a gamble. The variables with the potential to impact health care—among them, unpredictable political agendas, unforeseen economic upheaval, and technological issues—make it difficult to identify one “expected” outcome. However, one forecasted trend will certainly make a difference: the quantity of well-educated health care practitioners.
This factor will be one of the most important determinants of our ability to deliver quality, accessible health care in a diverse society with increasingly complex medical needs. Some may say that this is an irrational fear—the US health care system is remarkably adaptable, and as far as we can tell, no serious problems have arisen due to a shortage of providers. So are we overreacting, or is there a viable reason for concern?
While more and more Americans are covered by health insurance thanks to the Affordable Care Act, fewer physicians are entering primary care. The Association of American Medical Colleges (AAMC) has projected a shortage of between 46,000 and 90,000 physicians by 2025. AAMC forecasts a shortage of 12,500 to 31,100 primary care physicians and 21,200 to 63,700 non–primary care physicians; much of the latter deficit will be in the surgical specialties.1 The report emphasizes the need for immediate action because it takes almost a decade to educate a physician for entry into the workforce.
On the surface, these numbers are quite staggering. They may even elicit a sense of doom about access to quality (or even simply adequate) health care in the next decade. To put these projections in context, here are some key statistics
- About 915,000 physicians actively practice in the US.2
- Each year, about 20,000 medical school students graduate and enter postgraduate education.3
- Thirty percent of physicians are older than 60.2
- In 2015, there were 100,000 practicing PAs, with an average age of 38.4
- As of 2016, there are 222,000 practicing NPs, with an average age of 49.5
The US population is projected to increase from 310 million in 2015 to 335 million in 2025.6 There are approximately 45 million Americans older than 65, a number that is projected to increase to almost 70 million by 2025.7,8
This inverse relationship—more potential patients and fewer people to care for them—suggests perilous changes for our health care system. Some anticipated changes—longer wait times for care, increased costs, and more opportunities for error—are real and have already been quantified in reports.9 But with the year 2025 less than a decade away, where is our sense of urgency? Even if we implement changes immediately, they are unlikely to offset the consequences of the workforce shortage. Yet to do nothing will lead to a rapid decline in quality of life for many Americans.
In theory, there are two ways to address this pending “crisis.” We can decrease demand and/or increase supply. In the next few decades, achieving the former will be difficult, because of the unavoidable toll of an aging population. Public health and preventive services may have some impact and deserve increased attention. New and improved modes of treatment offer the potential to ameliorate the impact of chronic diseases such as diabetes and cardiovascular disease. This method, while a noble goal, is also less predictable and harder to “plan” for.
The most direct approach (but certainly not the only one) is to increase the supply of health care providers—specifically, NPs and PAs—in order to meet the rising demand. The professions have long been touted as a solution to problems of access to care in both rural and urban areas. About 83% of NPs are certified in primary care; we cannot ignore the fact that only 24% of PAs practice in primary care while the rest have chosen specialties. But (another plus) patients tend to be as satisfied with care provided by NPs and PAs as by physicians.10,11
Increasing the supply of NPs and PAs requires educating more individuals to enter the professions. Education programs need to do a critical analysis of their curricula to ensure that what happens in the classroom matches real-world needs. If graduates enter the workforce unprepared for the demands of the job, no progress will be made. (For a vigorous discussion on the current state of professional education, please visit www.mdedge.com/clinicianreviews/commentary).
One significant limitation to the growth of the PA supply is the accreditation process, which now takes almost three years from the start of the process until the initial approval of a class (and five years until the first class graduates). This process adds time and expense to the creation of new education programs, many of which await approval and lack the resources to bring the program to maturity. While no one would argue the value of the ARC-PA accreditation, the process should be critically examined to identify any areas that can be streamlined without decreasing the quality of the product.
Which brings us to perhaps the most important aspect of this discussion: What actions need to be taken to mitigate the possible damage of a physician shortage? Here are some recommendations for a variety of stakeholders:
Educators should enhance their competency-based curriculum to enable NPs and PAs to move through their programs at a faster stride (again, without sacrificing valuable learning time) and get into practice sooner.
Accreditors should review current standards and remove barriers to allow education programs to create innovative curricula that help NPs and PAs gain the knowledge (and experience) they need to move into practice.
Regulators should ensure that NPs and PAs are able to practice to the fullest extent of their license and scope of practice (ie, full practice authority, scope of practice determined at the practice level). Barriers should be removed to allow these clinicians to function in rural and underserved regions of the country (eg, adaptable collaboration requirements).10 (For a different perspective on PA autonomy, see here.)
Policymakers should rally around the removal of barriers to postgraduate residencies, which would sustain and possibly increase the physician supply. Reimbursement, particularly in Medicare, should be re-evaluated to assure that all providers are reimbursed for same services. Lack of parity in reimbursement infers a difference in quality that is just not the case.
Practicing NPs and PAs should step up to the plate and volunteer as preceptors to give NP and PA students the opportunity to learn from the best and most experienced.
Physicians should seek out alternatives to retirement from medicine (ie working part-time, becoming an educator). Expanding the period of clinical practice may forestall, or even prevent, some of the shortage—at least, in the short-term.
There are those who say that a provider shortage does not exist and that those crying out about it have a vested interest in expanding medical school output. Others acknowledge the shortage but worry that increasing the supply of NPs and PAs will ultimately “devalue” individual providers (ie, drive down salaries). One thing, however, is certain: As Danish physicist Niels Bohr said, “Prediction is very difficult, especially if it’s about the future.”
What are your thoughts and ideas about the health care workforce and the increasing demand for care? Please share them with us by writing to [email protected].
Predicting the future, particularly in the ever-changing realm of health care, is always a gamble. The variables with the potential to impact health care—among them, unpredictable political agendas, unforeseen economic upheaval, and technological issues—make it difficult to identify one “expected” outcome. However, one forecasted trend will certainly make a difference: the quantity of well-educated health care practitioners.
This factor will be one of the most important determinants of our ability to deliver quality, accessible health care in a diverse society with increasingly complex medical needs. Some may say that this is an irrational fear—the US health care system is remarkably adaptable, and as far as we can tell, no serious problems have arisen due to a shortage of providers. So are we overreacting, or is there a viable reason for concern?
While more and more Americans are covered by health insurance thanks to the Affordable Care Act, fewer physicians are entering primary care. The Association of American Medical Colleges (AAMC) has projected a shortage of between 46,000 and 90,000 physicians by 2025. AAMC forecasts a shortage of 12,500 to 31,100 primary care physicians and 21,200 to 63,700 non–primary care physicians; much of the latter deficit will be in the surgical specialties.1 The report emphasizes the need for immediate action because it takes almost a decade to educate a physician for entry into the workforce.
On the surface, these numbers are quite staggering. They may even elicit a sense of doom about access to quality (or even simply adequate) health care in the next decade. To put these projections in context, here are some key statistics
- About 915,000 physicians actively practice in the US.2
- Each year, about 20,000 medical school students graduate and enter postgraduate education.3
- Thirty percent of physicians are older than 60.2
- In 2015, there were 100,000 practicing PAs, with an average age of 38.4
- As of 2016, there are 222,000 practicing NPs, with an average age of 49.5
The US population is projected to increase from 310 million in 2015 to 335 million in 2025.6 There are approximately 45 million Americans older than 65, a number that is projected to increase to almost 70 million by 2025.7,8
This inverse relationship—more potential patients and fewer people to care for them—suggests perilous changes for our health care system. Some anticipated changes—longer wait times for care, increased costs, and more opportunities for error—are real and have already been quantified in reports.9 But with the year 2025 less than a decade away, where is our sense of urgency? Even if we implement changes immediately, they are unlikely to offset the consequences of the workforce shortage. Yet to do nothing will lead to a rapid decline in quality of life for many Americans.
In theory, there are two ways to address this pending “crisis.” We can decrease demand and/or increase supply. In the next few decades, achieving the former will be difficult, because of the unavoidable toll of an aging population. Public health and preventive services may have some impact and deserve increased attention. New and improved modes of treatment offer the potential to ameliorate the impact of chronic diseases such as diabetes and cardiovascular disease. This method, while a noble goal, is also less predictable and harder to “plan” for.
The most direct approach (but certainly not the only one) is to increase the supply of health care providers—specifically, NPs and PAs—in order to meet the rising demand. The professions have long been touted as a solution to problems of access to care in both rural and urban areas. About 83% of NPs are certified in primary care; we cannot ignore the fact that only 24% of PAs practice in primary care while the rest have chosen specialties. But (another plus) patients tend to be as satisfied with care provided by NPs and PAs as by physicians.10,11
Increasing the supply of NPs and PAs requires educating more individuals to enter the professions. Education programs need to do a critical analysis of their curricula to ensure that what happens in the classroom matches real-world needs. If graduates enter the workforce unprepared for the demands of the job, no progress will be made. (For a vigorous discussion on the current state of professional education, please visit www.mdedge.com/clinicianreviews/commentary).
One significant limitation to the growth of the PA supply is the accreditation process, which now takes almost three years from the start of the process until the initial approval of a class (and five years until the first class graduates). This process adds time and expense to the creation of new education programs, many of which await approval and lack the resources to bring the program to maturity. While no one would argue the value of the ARC-PA accreditation, the process should be critically examined to identify any areas that can be streamlined without decreasing the quality of the product.
Which brings us to perhaps the most important aspect of this discussion: What actions need to be taken to mitigate the possible damage of a physician shortage? Here are some recommendations for a variety of stakeholders:
Educators should enhance their competency-based curriculum to enable NPs and PAs to move through their programs at a faster stride (again, without sacrificing valuable learning time) and get into practice sooner.
Accreditors should review current standards and remove barriers to allow education programs to create innovative curricula that help NPs and PAs gain the knowledge (and experience) they need to move into practice.
Regulators should ensure that NPs and PAs are able to practice to the fullest extent of their license and scope of practice (ie, full practice authority, scope of practice determined at the practice level). Barriers should be removed to allow these clinicians to function in rural and underserved regions of the country (eg, adaptable collaboration requirements).10 (For a different perspective on PA autonomy, see here.)
Policymakers should rally around the removal of barriers to postgraduate residencies, which would sustain and possibly increase the physician supply. Reimbursement, particularly in Medicare, should be re-evaluated to assure that all providers are reimbursed for same services. Lack of parity in reimbursement infers a difference in quality that is just not the case.
Practicing NPs and PAs should step up to the plate and volunteer as preceptors to give NP and PA students the opportunity to learn from the best and most experienced.
Physicians should seek out alternatives to retirement from medicine (ie working part-time, becoming an educator). Expanding the period of clinical practice may forestall, or even prevent, some of the shortage—at least, in the short-term.
There are those who say that a provider shortage does not exist and that those crying out about it have a vested interest in expanding medical school output. Others acknowledge the shortage but worry that increasing the supply of NPs and PAs will ultimately “devalue” individual providers (ie, drive down salaries). One thing, however, is certain: As Danish physicist Niels Bohr said, “Prediction is very difficult, especially if it’s about the future.”
What are your thoughts and ideas about the health care workforce and the increasing demand for care? Please share them with us by writing to [email protected].
1. Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2013 to 2025. Washington, DC: HIS, Inc; 2015. www.aamc.org/download/426242/data/ihsreportdownload.pdf. Accessed September 8, 2016.
2. Young A, Chaudhry HJ, Pei X, et al. A census of actively licensed physicians in the United States, 2014. J Med Regulation. 2014;96(4): 10-20.
3. Association of American Medical Colleges. Table B-2.2: total graduates by US medical school and sex, 2010-2011 through 2014-2015. www.aamc.org/download/321532/data/factstableb2-2.pdf. Accessed September 8, 2016.
4. National Commission on Certification of Physician Assistants. 2015 statistical profile of certified physician assistants. www.nccpa.net/Uploads/docs/2015StatisticalProfileofCertifiedPhysicianAssistants.pdf. Accessed September 8, 2016.
5. American Association of Nurse Practitioners. NP fact sheet. www.aanp.org/all-about-nps/np-fact-sheet. Accessed September 8, 2016.
6. US Department of Commerce. Population projections of the United States by age, sex, race, and hispanic origin: 1995 to 2050. www.census.gov/prod/1/pop/p25-1130.pdf. Accessed September 8, 2016.
7. Mather M, Jacobsen LA, Pollard KP. Aging in the United States. Popul Bull. 2015;70:1-23.
8. Ortman JM, Velkoff VA, Hogan HH. An aging nation: the older population in the United States. US Census Bureau. 2014;P25-1140.
9. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. www.nap.edu/books/0309072808/html. Accessed September 8, 2016.
10. Garment V. Nurse practitioners and physician assistants: why you should hire one (or the other). The Profitable Practice blog. 2013. http://profitable-practice.softwareadvice.com/nurse-practitioners-and-physician-assistants-why-you-should-hire-one-or-the-other-0513. Accessed September 8, 2016.
11. American Academy of Physician Assistants. Six key elements. www.aapa.org/six-key-elements. Accessed September 8, 2016.
1. Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2013 to 2025. Washington, DC: HIS, Inc; 2015. www.aamc.org/download/426242/data/ihsreportdownload.pdf. Accessed September 8, 2016.
2. Young A, Chaudhry HJ, Pei X, et al. A census of actively licensed physicians in the United States, 2014. J Med Regulation. 2014;96(4): 10-20.
3. Association of American Medical Colleges. Table B-2.2: total graduates by US medical school and sex, 2010-2011 through 2014-2015. www.aamc.org/download/321532/data/factstableb2-2.pdf. Accessed September 8, 2016.
4. National Commission on Certification of Physician Assistants. 2015 statistical profile of certified physician assistants. www.nccpa.net/Uploads/docs/2015StatisticalProfileofCertifiedPhysicianAssistants.pdf. Accessed September 8, 2016.
5. American Association of Nurse Practitioners. NP fact sheet. www.aanp.org/all-about-nps/np-fact-sheet. Accessed September 8, 2016.
6. US Department of Commerce. Population projections of the United States by age, sex, race, and hispanic origin: 1995 to 2050. www.census.gov/prod/1/pop/p25-1130.pdf. Accessed September 8, 2016.
7. Mather M, Jacobsen LA, Pollard KP. Aging in the United States. Popul Bull. 2015;70:1-23.
8. Ortman JM, Velkoff VA, Hogan HH. An aging nation: the older population in the United States. US Census Bureau. 2014;P25-1140.
9. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. www.nap.edu/books/0309072808/html. Accessed September 8, 2016.
10. Garment V. Nurse practitioners and physician assistants: why you should hire one (or the other). The Profitable Practice blog. 2013. http://profitable-practice.softwareadvice.com/nurse-practitioners-and-physician-assistants-why-you-should-hire-one-or-the-other-0513. Accessed September 8, 2016.
11. American Academy of Physician Assistants. Six key elements. www.aapa.org/six-key-elements. Accessed September 8, 2016.
Terrorist Activity: Are You Ready?
I was relaxing after work in my local American Legion a few weeks ago when a quiet young man entered with a backpack. He set it down to use the restroom, and when he returned a few minutes later, he picked up the backpack and walked away. After he left, a group of us discussed how lax we were about this situation. Yes, it was probably innocent—but what if it wasn’t? A sign over the bar reads, “Don’t let anyone leave a stranger.” The purpose of that sign is, of course, to make everyone feel welcome, but these days I think it also means to be aware of your surroundings. I have seen too many American flags at half-staff this year to overlook a potential tragedy.
Today, clinicians must be prepared for all possible emergencies, including terrorism. Acts of terrorism (as the word implies) are designed to instill terror and panic, disrupt security and communication systems, destroy property, and kill or injure innocent civilians.
Recent terrorist attacks in 2016, while shocking in their brutality, were not inconceivable—public locations where large groups gather are logical targets. Terrorists often target high-traffic areas, such as airports or shopping malls, where they can quickly disappear into a crowd if necessary (hence the concern circling the Olympic Games to be held in Brazil this month).
Attacks at restaurants, airports, and other public “hot spots” are especially frightening. With terrorist attack locations in the past year ranging from nightclubs (the Pulse Nightclub shooting in Orlando, Florida, left 49 dead) to restaurants (a bomb in Dhaka, Bangladesh, killed 20) to conference rooms (a shooting in San Bernardino, California, left 14 dead and 21 injured), it’s clear that the fundamental message terrorists want to send is: You are not safe—anywhere!
While organized events and big crowds are a bull’s-eye for terrorists, our personal surroundings have risk factors, too. Because a terrorist attack can happen anywhere at any time, you need to be prepared by knowing what to do and how to maximize your chances of survival.
As this year’s attacks exemplify, we shouldn’t assume we understand the “logic” or thinking of terrorist organizations or individuals. Preparation for a terrorist attack boils down to being aware of the warning signs and being cautious and alert. Terrorists use a range of weapons and tactics, including bombs, arson, hijacking, and kidnapping (see Table).1,2
According to Dr. Howard Mell, an EMS director in North Carolina, the overwhelming majority of gunfire in the emergency department—or anywhere—is not the result of an active shooter. Most gunfire is targeted at a specific goal (ie, escaping or avoiding capture) or person. However, should there be an active shooter, he recommends three steps to take: Run (if the path is open), hide (if your exit is blocked), or fight (if there are no other alternatives).3
Wherever you are, always have multiple potential escape routes in mind. If you run, leave all belongings behind. Help others escape if possible, and take steps to prevent others from entering once you have left the area.
If you are unable to run, decide where to hide. If possible, barricade the area; if you are in a room, turn out the lights and stay away from the door. Be silent and put your cell phone on silent. While you are hiding, prepare to fight.
Fighting is the last resort. Act aggressively and improvise weapons to use against the assailant. If you have family, friends, or colleagues with you, put them to work!
When law enforcement officers arrive, understand that their job is to go right to the source and contain the danger. Keep your hands visible at all times, with fingers spread. Do not grab them for protection, and avoid yelling or pointing. Be prepared to give the authorities any pertinent information (eg, shooter description, last known location, direction of travel, or weapons seen).
Many health care facilities and organizations have valuable disaster and terrorism training programs, which include emergency evacuation procedures. I encourage you to take advantage of them, particularly if you travel internationally.4
Continue for personal preparedness >>
This is about personal preparedness. While I am not promoting paranoia, I do believe the risk for terrorist activity has increased in recent years.
I therefore urge you to have a healthy suspicion when you see or hear people
• Asking unusual questions about safety procedures at work
• Engaging in behaviors that provoke suspicion
• Loitering, parking, or standing in the same area over multiple days
• Attempting to disguise themselves from visit to visit
• Obtaining unusual quantities of weapons, ammunition, or explosive precursors
• Wearing clothing not appropriate for the season
• Leaving items, including backpacks or packages, unattended
• Leaving anonymous threats via telephone or e-mail
If after conducting a risk assessment of your surroundings, you believe you could (directly or indirectly) be impacted by terrorism, you must implement evacuation plans, notification of appropriate personnel, and personal safety measures.
In the event of a terrorist incident, remain calm, follow the advice of local emergency officials, and follow radio, television, and cell phone updates for news and instructions. 5
If an attack occurs near you or your home, here are practical steps you can take: Check for injuries. Give first aid and get help for seriously injured people. Check for damage using a flashlight—do not light matches or candles, or use electrical switches. Check for fires, fire hazards, and other household hazards. Sniff for gas leaks, starting at the water heater. If you smell gas or suspect a leak, turn off the main gas valve, open windows, and evacuate quickly. Shut off any damaged utilities, and confine or secure your pets. Call your family contact—but do not use the telephone again unless it is a life-threatening emergency. Cell phones may or may not be working. Check on your neighbors, especially those who are elderly or disabled.
Terrorist attacks leave citizens concerned about future incidents of terrorism in the United States and their potential impact. They raise ambiguity about what might happen next and increase stress levels. You can take steps to prepare for terrorist attacks and reduce the stress you may feel, now and later, should an emergency arise. Taking preparatory action can reassure you, your family, and your children that you have a measure of control—even in the face of terrorism. If you have additional suggestions for terrorist defense preparation, you can email your ideas to [email protected].
References
1. Dworkin RW. Preparing hospitals, doctors, and nurses for a terrorist attack. Hudson Institute. www.hudson.org/content/researchattach ments/attachment/291/dworkin_white_paper.pdf. Accessed July 6, 2016.
2. Markenson F, DiMaggio C, Redlener I. Preparing health professions students for terrorism, disaster, and public health emergencies: core competencies. Acad Med. 2005;80(6):517-526.
3. Mell HK. Run, hide, fight: how to react when there’s gunfire in the emergency department. ACEP NOW. June 21, 2016. www.acepnow.com/react-theres-gunfire-emergency-department/?elq_mid=10369&elq_cid=5274988. Accessed July 6, 2016.
4. Uniformed Services University of the Health Sciences, Center for the Study of Traumatic Stress. Workplace preparedness for terrorism. www.cstsonline.org/assets/media/docu ments/CSTS_report_sloan_workplace_prepare_terrorism_preparedness.pdf. Accessed July 6, 2016.
5. American Red Cross. Terrorism Preparedness. www.redcross.org/prepare/disaster/terrorism. Accessed July 6, 2016.
I was relaxing after work in my local American Legion a few weeks ago when a quiet young man entered with a backpack. He set it down to use the restroom, and when he returned a few minutes later, he picked up the backpack and walked away. After he left, a group of us discussed how lax we were about this situation. Yes, it was probably innocent—but what if it wasn’t? A sign over the bar reads, “Don’t let anyone leave a stranger.” The purpose of that sign is, of course, to make everyone feel welcome, but these days I think it also means to be aware of your surroundings. I have seen too many American flags at half-staff this year to overlook a potential tragedy.
Today, clinicians must be prepared for all possible emergencies, including terrorism. Acts of terrorism (as the word implies) are designed to instill terror and panic, disrupt security and communication systems, destroy property, and kill or injure innocent civilians.
Recent terrorist attacks in 2016, while shocking in their brutality, were not inconceivable—public locations where large groups gather are logical targets. Terrorists often target high-traffic areas, such as airports or shopping malls, where they can quickly disappear into a crowd if necessary (hence the concern circling the Olympic Games to be held in Brazil this month).
Attacks at restaurants, airports, and other public “hot spots” are especially frightening. With terrorist attack locations in the past year ranging from nightclubs (the Pulse Nightclub shooting in Orlando, Florida, left 49 dead) to restaurants (a bomb in Dhaka, Bangladesh, killed 20) to conference rooms (a shooting in San Bernardino, California, left 14 dead and 21 injured), it’s clear that the fundamental message terrorists want to send is: You are not safe—anywhere!
While organized events and big crowds are a bull’s-eye for terrorists, our personal surroundings have risk factors, too. Because a terrorist attack can happen anywhere at any time, you need to be prepared by knowing what to do and how to maximize your chances of survival.
As this year’s attacks exemplify, we shouldn’t assume we understand the “logic” or thinking of terrorist organizations or individuals. Preparation for a terrorist attack boils down to being aware of the warning signs and being cautious and alert. Terrorists use a range of weapons and tactics, including bombs, arson, hijacking, and kidnapping (see Table).1,2
According to Dr. Howard Mell, an EMS director in North Carolina, the overwhelming majority of gunfire in the emergency department—or anywhere—is not the result of an active shooter. Most gunfire is targeted at a specific goal (ie, escaping or avoiding capture) or person. However, should there be an active shooter, he recommends three steps to take: Run (if the path is open), hide (if your exit is blocked), or fight (if there are no other alternatives).3
Wherever you are, always have multiple potential escape routes in mind. If you run, leave all belongings behind. Help others escape if possible, and take steps to prevent others from entering once you have left the area.
If you are unable to run, decide where to hide. If possible, barricade the area; if you are in a room, turn out the lights and stay away from the door. Be silent and put your cell phone on silent. While you are hiding, prepare to fight.
Fighting is the last resort. Act aggressively and improvise weapons to use against the assailant. If you have family, friends, or colleagues with you, put them to work!
When law enforcement officers arrive, understand that their job is to go right to the source and contain the danger. Keep your hands visible at all times, with fingers spread. Do not grab them for protection, and avoid yelling or pointing. Be prepared to give the authorities any pertinent information (eg, shooter description, last known location, direction of travel, or weapons seen).
Many health care facilities and organizations have valuable disaster and terrorism training programs, which include emergency evacuation procedures. I encourage you to take advantage of them, particularly if you travel internationally.4
Continue for personal preparedness >>
This is about personal preparedness. While I am not promoting paranoia, I do believe the risk for terrorist activity has increased in recent years.
I therefore urge you to have a healthy suspicion when you see or hear people
• Asking unusual questions about safety procedures at work
• Engaging in behaviors that provoke suspicion
• Loitering, parking, or standing in the same area over multiple days
• Attempting to disguise themselves from visit to visit
• Obtaining unusual quantities of weapons, ammunition, or explosive precursors
• Wearing clothing not appropriate for the season
• Leaving items, including backpacks or packages, unattended
• Leaving anonymous threats via telephone or e-mail
If after conducting a risk assessment of your surroundings, you believe you could (directly or indirectly) be impacted by terrorism, you must implement evacuation plans, notification of appropriate personnel, and personal safety measures.
In the event of a terrorist incident, remain calm, follow the advice of local emergency officials, and follow radio, television, and cell phone updates for news and instructions. 5
If an attack occurs near you or your home, here are practical steps you can take: Check for injuries. Give first aid and get help for seriously injured people. Check for damage using a flashlight—do not light matches or candles, or use electrical switches. Check for fires, fire hazards, and other household hazards. Sniff for gas leaks, starting at the water heater. If you smell gas or suspect a leak, turn off the main gas valve, open windows, and evacuate quickly. Shut off any damaged utilities, and confine or secure your pets. Call your family contact—but do not use the telephone again unless it is a life-threatening emergency. Cell phones may or may not be working. Check on your neighbors, especially those who are elderly or disabled.
Terrorist attacks leave citizens concerned about future incidents of terrorism in the United States and their potential impact. They raise ambiguity about what might happen next and increase stress levels. You can take steps to prepare for terrorist attacks and reduce the stress you may feel, now and later, should an emergency arise. Taking preparatory action can reassure you, your family, and your children that you have a measure of control—even in the face of terrorism. If you have additional suggestions for terrorist defense preparation, you can email your ideas to [email protected].
References
1. Dworkin RW. Preparing hospitals, doctors, and nurses for a terrorist attack. Hudson Institute. www.hudson.org/content/researchattach ments/attachment/291/dworkin_white_paper.pdf. Accessed July 6, 2016.
2. Markenson F, DiMaggio C, Redlener I. Preparing health professions students for terrorism, disaster, and public health emergencies: core competencies. Acad Med. 2005;80(6):517-526.
3. Mell HK. Run, hide, fight: how to react when there’s gunfire in the emergency department. ACEP NOW. June 21, 2016. www.acepnow.com/react-theres-gunfire-emergency-department/?elq_mid=10369&elq_cid=5274988. Accessed July 6, 2016.
4. Uniformed Services University of the Health Sciences, Center for the Study of Traumatic Stress. Workplace preparedness for terrorism. www.cstsonline.org/assets/media/docu ments/CSTS_report_sloan_workplace_prepare_terrorism_preparedness.pdf. Accessed July 6, 2016.
5. American Red Cross. Terrorism Preparedness. www.redcross.org/prepare/disaster/terrorism. Accessed July 6, 2016.
I was relaxing after work in my local American Legion a few weeks ago when a quiet young man entered with a backpack. He set it down to use the restroom, and when he returned a few minutes later, he picked up the backpack and walked away. After he left, a group of us discussed how lax we were about this situation. Yes, it was probably innocent—but what if it wasn’t? A sign over the bar reads, “Don’t let anyone leave a stranger.” The purpose of that sign is, of course, to make everyone feel welcome, but these days I think it also means to be aware of your surroundings. I have seen too many American flags at half-staff this year to overlook a potential tragedy.
Today, clinicians must be prepared for all possible emergencies, including terrorism. Acts of terrorism (as the word implies) are designed to instill terror and panic, disrupt security and communication systems, destroy property, and kill or injure innocent civilians.
Recent terrorist attacks in 2016, while shocking in their brutality, were not inconceivable—public locations where large groups gather are logical targets. Terrorists often target high-traffic areas, such as airports or shopping malls, where they can quickly disappear into a crowd if necessary (hence the concern circling the Olympic Games to be held in Brazil this month).
Attacks at restaurants, airports, and other public “hot spots” are especially frightening. With terrorist attack locations in the past year ranging from nightclubs (the Pulse Nightclub shooting in Orlando, Florida, left 49 dead) to restaurants (a bomb in Dhaka, Bangladesh, killed 20) to conference rooms (a shooting in San Bernardino, California, left 14 dead and 21 injured), it’s clear that the fundamental message terrorists want to send is: You are not safe—anywhere!
While organized events and big crowds are a bull’s-eye for terrorists, our personal surroundings have risk factors, too. Because a terrorist attack can happen anywhere at any time, you need to be prepared by knowing what to do and how to maximize your chances of survival.
As this year’s attacks exemplify, we shouldn’t assume we understand the “logic” or thinking of terrorist organizations or individuals. Preparation for a terrorist attack boils down to being aware of the warning signs and being cautious and alert. Terrorists use a range of weapons and tactics, including bombs, arson, hijacking, and kidnapping (see Table).1,2
According to Dr. Howard Mell, an EMS director in North Carolina, the overwhelming majority of gunfire in the emergency department—or anywhere—is not the result of an active shooter. Most gunfire is targeted at a specific goal (ie, escaping or avoiding capture) or person. However, should there be an active shooter, he recommends three steps to take: Run (if the path is open), hide (if your exit is blocked), or fight (if there are no other alternatives).3
Wherever you are, always have multiple potential escape routes in mind. If you run, leave all belongings behind. Help others escape if possible, and take steps to prevent others from entering once you have left the area.
If you are unable to run, decide where to hide. If possible, barricade the area; if you are in a room, turn out the lights and stay away from the door. Be silent and put your cell phone on silent. While you are hiding, prepare to fight.
Fighting is the last resort. Act aggressively and improvise weapons to use against the assailant. If you have family, friends, or colleagues with you, put them to work!
When law enforcement officers arrive, understand that their job is to go right to the source and contain the danger. Keep your hands visible at all times, with fingers spread. Do not grab them for protection, and avoid yelling or pointing. Be prepared to give the authorities any pertinent information (eg, shooter description, last known location, direction of travel, or weapons seen).
Many health care facilities and organizations have valuable disaster and terrorism training programs, which include emergency evacuation procedures. I encourage you to take advantage of them, particularly if you travel internationally.4
Continue for personal preparedness >>
This is about personal preparedness. While I am not promoting paranoia, I do believe the risk for terrorist activity has increased in recent years.
I therefore urge you to have a healthy suspicion when you see or hear people
• Asking unusual questions about safety procedures at work
• Engaging in behaviors that provoke suspicion
• Loitering, parking, or standing in the same area over multiple days
• Attempting to disguise themselves from visit to visit
• Obtaining unusual quantities of weapons, ammunition, or explosive precursors
• Wearing clothing not appropriate for the season
• Leaving items, including backpacks or packages, unattended
• Leaving anonymous threats via telephone or e-mail
If after conducting a risk assessment of your surroundings, you believe you could (directly or indirectly) be impacted by terrorism, you must implement evacuation plans, notification of appropriate personnel, and personal safety measures.
In the event of a terrorist incident, remain calm, follow the advice of local emergency officials, and follow radio, television, and cell phone updates for news and instructions. 5
If an attack occurs near you or your home, here are practical steps you can take: Check for injuries. Give first aid and get help for seriously injured people. Check for damage using a flashlight—do not light matches or candles, or use electrical switches. Check for fires, fire hazards, and other household hazards. Sniff for gas leaks, starting at the water heater. If you smell gas or suspect a leak, turn off the main gas valve, open windows, and evacuate quickly. Shut off any damaged utilities, and confine or secure your pets. Call your family contact—but do not use the telephone again unless it is a life-threatening emergency. Cell phones may or may not be working. Check on your neighbors, especially those who are elderly or disabled.
Terrorist attacks leave citizens concerned about future incidents of terrorism in the United States and their potential impact. They raise ambiguity about what might happen next and increase stress levels. You can take steps to prepare for terrorist attacks and reduce the stress you may feel, now and later, should an emergency arise. Taking preparatory action can reassure you, your family, and your children that you have a measure of control—even in the face of terrorism. If you have additional suggestions for terrorist defense preparation, you can email your ideas to [email protected].
References
1. Dworkin RW. Preparing hospitals, doctors, and nurses for a terrorist attack. Hudson Institute. www.hudson.org/content/researchattach ments/attachment/291/dworkin_white_paper.pdf. Accessed July 6, 2016.
2. Markenson F, DiMaggio C, Redlener I. Preparing health professions students for terrorism, disaster, and public health emergencies: core competencies. Acad Med. 2005;80(6):517-526.
3. Mell HK. Run, hide, fight: how to react when there’s gunfire in the emergency department. ACEP NOW. June 21, 2016. www.acepnow.com/react-theres-gunfire-emergency-department/?elq_mid=10369&elq_cid=5274988. Accessed July 6, 2016.
4. Uniformed Services University of the Health Sciences, Center for the Study of Traumatic Stress. Workplace preparedness for terrorism. www.cstsonline.org/assets/media/docu ments/CSTS_report_sloan_workplace_prepare_terrorism_preparedness.pdf. Accessed July 6, 2016.
5. American Red Cross. Terrorism Preparedness. www.redcross.org/prepare/disaster/terrorism. Accessed July 6, 2016.
Vaping: Are Its “Benefits” a Lot of Hot Air?
I was sitting in a restaurant bar a few days ago when a huge puff of cherry-scented smoke engulfed the area. As a former firefighter, I immediately looked around to find the source. You guessed it: a group of young adults were “vaping” nearby. This method of smoking is accomplished with an electronic “cigarette.” A sensor inside the e-cigarette detects airflow and initiates a heating element that vaporizes a liquid solution containing propylene glycol (organic compound with the chemical formula C₃H₈O₂), the flavoring of choice, and nicotine.1
I knew of this fad but didn’t give it much thought until recently, when I realized how pervasive it has become. Frankly, I have always thought, At least they are not smoking cigarettes and inhaling all that benzene, carbon dioxide, and formaldehyde.
We all know smoking cessation is valuable to the health of the population, but what do we know about the effects of vaping? For one thing, use of e-cigarettes (vapes) has increased considerably since they were first introduced (0.3% to 6.8% between 2007 and 2010).This is cause for concern, because while some research on e-cigarettes has emerged since their appearance, there are few definitive answers regarding their effect on human health.2
We also know that nicotine is addictive and toxic (in high doses), but we do not know the effects of propylene glycol, although it is generally recognized as “safe.” Symptoms that may occur as a result of vaporized propylene glycol inhalation include throat and ocular irritation, cough, mild airway obstruction, throat and vocal cord inflammation, headache, and dizziness. In spite of this, since the manufacturers of e-cigarettes have not made any therapeutic claims about their products, the FDA initially did not regulate them.
With e-cigarettes appearing in vaping shops, gas stations, and convenience stores—alongside advertising copy that claims vaping can help smokers curtail their habit by inhaling “harmless water vapor”—what should we tell our patients? These advertisements tout vaping as the “lesser of two evils” when compared to cigarettes. How can you knock that logic when we know cigarette smoking causes one in five deaths in the US each year and is a leading risk factor for COPD?3
Continue for the conundrum >>
The conundrum, as I see it, is threefold. The first step is to determine if vaping is a significant alternative to smoking cessation. The second is to determine if any components of vaping (nicotine, propylene glycol, or combustion) are safe for humans. Lastly, we must establish how to regulate e-cigarettes, given scientific uncertainty as to their therapeutic effects.4
In 2013, Palazzolo did a literature review of 66 articles related to e-cigarettes and vaping. He found that, when compared to the effects of smoking, vaping could be a substitute for smoking and a conceivable means for smoking reduction. It was unclear, however, if vaping could reduce nicotine addiction. He reported that the effects of vaping on human health are questionable, due to the extreme scarcity of empiric research.5
Although there has been a paucity of research on this topic, a study by Goniewicz and colleagues reports on the toxicants emitted by tobacco cigarettes and e-cigarettes.6 Their results indicate that e-cigarettes emit fewer toxicants than traditional tobacco cigarettes (formaldehyde, 0.20-5.61 µg and 1.6-52 µg, respectively; acetaldehyde, 0.11-1.36 µg and 52-140 µg).7 Despite this evidence, more studies need to be done on the effects of propylene glycol inhalation to determine the safety of e-cigarettes.
Another concern has been the lack of an age restriction on e-cigarettes and their growing popularity among grade and high school students.E-cigarette use doubled among US middle and high school students from 2011 to 2012, resulting in an estimated 1.78 million students who have used e-cigarettes as of 2012. There is serious concern about the possible harmful impact of nicotine on adolescent brain development,as well as the risk for nicotine addiction.8
Amid these growing questions and concerns, the FDA issued a warning that e-cigarettes may be as bad as the real thing and has recommended against their use.9 Just last month, the agency finalized a regulation on all tobacco products, including vaporizers, vape pens, hookah pens, e-cigs, and e-pipes. They will now regulate the manufacturing, import, packaging, labeling, and distribution of e-cigarettes to ensure that ingredients are assessed and determined to be safe for human use.FDA Commissioner Robert M. Califf, MD, said, “We must do our job under the Tobacco Control Act to reduce the harms caused by tobacco. That includes ensuring that consumers have the information they need to make informed decisions about tobacco use and making sure that new tobacco products for purchase come under comprehensive FDA review.”10,11
Well, is it just a bunch of smoke, or are the new regulations and health warnings about e-cigarettes long overdue? I would love to hear your experiences and additional advice for our colleagues and patients regarding the use of e-cigarettes and vaping. You can reach me at [email protected].
References
1. Jerry JM, Collins GB, Streem D. E-cigarettes: safe to recommend to patients? Cleve Clin J Med. 2015;82(8):521-526.
2. McMillen RC, Gottlieb MA, Shaefer RMW, et al. Trends in electronic cigarette use among US adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;17:1195-1202.
3. National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. www.ncbi.nlm.nih.gov/pubmed/24455788. Accessed May 10, 2016.
4. Gostin LO, Glasner AY. E-cigarettes, vaping, and youth. JAMA. 2014;312(6):595-596.
5. Palazzolo DL. Electronic cigarettes and vaping: a new challenge in clinical medicine and public health. A literature review. Front Public Health. 2013;1(56):1-20.
6. Goniewicz ML, Hajek P, McRobbie H. Nicotine content of electronic cigarettes, its release in vapour and its consistency across batches: regulatory implications. Addiction. 2014;109(3):500-507.
7. Arnold C. Vaping and health: what do we know about e-cigarettes? Environ Health Perspect. 2014;122(9):A244-A249. http://ehp.niehs.nih.gov/122-a244. Accessed May 10, 2016.
8. Electronic cigarette use among middle and high school students. Medscape. September 6, 2013. www.medscape.com/viewarticle/811008. Accessed May 10, 2016.
9. FDA: E-cigarettes may be as bad as real thing. NBC Nightly News. July 22, 2015. www.nbcnews.com/video/nightly-news/32091534#32091534. Accessed May 10, 2016.
10. Caudle J. Why we need new rules on e-cigs. CNN. May 6, 2016. www.cnn.com/2016/05/06/opinions/fda-electronic-cigarettes-caudle. Accessed May 10, 2016.
11. FDA. FDA takes significant steps to protect Americans from dangers of tobacco through new regulation [news release]. May 5, 2016. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm499234.htm. Accessed May 10, 2016.
I was sitting in a restaurant bar a few days ago when a huge puff of cherry-scented smoke engulfed the area. As a former firefighter, I immediately looked around to find the source. You guessed it: a group of young adults were “vaping” nearby. This method of smoking is accomplished with an electronic “cigarette.” A sensor inside the e-cigarette detects airflow and initiates a heating element that vaporizes a liquid solution containing propylene glycol (organic compound with the chemical formula C₃H₈O₂), the flavoring of choice, and nicotine.1
I knew of this fad but didn’t give it much thought until recently, when I realized how pervasive it has become. Frankly, I have always thought, At least they are not smoking cigarettes and inhaling all that benzene, carbon dioxide, and formaldehyde.
We all know smoking cessation is valuable to the health of the population, but what do we know about the effects of vaping? For one thing, use of e-cigarettes (vapes) has increased considerably since they were first introduced (0.3% to 6.8% between 2007 and 2010).This is cause for concern, because while some research on e-cigarettes has emerged since their appearance, there are few definitive answers regarding their effect on human health.2
We also know that nicotine is addictive and toxic (in high doses), but we do not know the effects of propylene glycol, although it is generally recognized as “safe.” Symptoms that may occur as a result of vaporized propylene glycol inhalation include throat and ocular irritation, cough, mild airway obstruction, throat and vocal cord inflammation, headache, and dizziness. In spite of this, since the manufacturers of e-cigarettes have not made any therapeutic claims about their products, the FDA initially did not regulate them.
With e-cigarettes appearing in vaping shops, gas stations, and convenience stores—alongside advertising copy that claims vaping can help smokers curtail their habit by inhaling “harmless water vapor”—what should we tell our patients? These advertisements tout vaping as the “lesser of two evils” when compared to cigarettes. How can you knock that logic when we know cigarette smoking causes one in five deaths in the US each year and is a leading risk factor for COPD?3
Continue for the conundrum >>
The conundrum, as I see it, is threefold. The first step is to determine if vaping is a significant alternative to smoking cessation. The second is to determine if any components of vaping (nicotine, propylene glycol, or combustion) are safe for humans. Lastly, we must establish how to regulate e-cigarettes, given scientific uncertainty as to their therapeutic effects.4
In 2013, Palazzolo did a literature review of 66 articles related to e-cigarettes and vaping. He found that, when compared to the effects of smoking, vaping could be a substitute for smoking and a conceivable means for smoking reduction. It was unclear, however, if vaping could reduce nicotine addiction. He reported that the effects of vaping on human health are questionable, due to the extreme scarcity of empiric research.5
Although there has been a paucity of research on this topic, a study by Goniewicz and colleagues reports on the toxicants emitted by tobacco cigarettes and e-cigarettes.6 Their results indicate that e-cigarettes emit fewer toxicants than traditional tobacco cigarettes (formaldehyde, 0.20-5.61 µg and 1.6-52 µg, respectively; acetaldehyde, 0.11-1.36 µg and 52-140 µg).7 Despite this evidence, more studies need to be done on the effects of propylene glycol inhalation to determine the safety of e-cigarettes.
Another concern has been the lack of an age restriction on e-cigarettes and their growing popularity among grade and high school students.E-cigarette use doubled among US middle and high school students from 2011 to 2012, resulting in an estimated 1.78 million students who have used e-cigarettes as of 2012. There is serious concern about the possible harmful impact of nicotine on adolescent brain development,as well as the risk for nicotine addiction.8
Amid these growing questions and concerns, the FDA issued a warning that e-cigarettes may be as bad as the real thing and has recommended against their use.9 Just last month, the agency finalized a regulation on all tobacco products, including vaporizers, vape pens, hookah pens, e-cigs, and e-pipes. They will now regulate the manufacturing, import, packaging, labeling, and distribution of e-cigarettes to ensure that ingredients are assessed and determined to be safe for human use.FDA Commissioner Robert M. Califf, MD, said, “We must do our job under the Tobacco Control Act to reduce the harms caused by tobacco. That includes ensuring that consumers have the information they need to make informed decisions about tobacco use and making sure that new tobacco products for purchase come under comprehensive FDA review.”10,11
Well, is it just a bunch of smoke, or are the new regulations and health warnings about e-cigarettes long overdue? I would love to hear your experiences and additional advice for our colleagues and patients regarding the use of e-cigarettes and vaping. You can reach me at [email protected].
References
1. Jerry JM, Collins GB, Streem D. E-cigarettes: safe to recommend to patients? Cleve Clin J Med. 2015;82(8):521-526.
2. McMillen RC, Gottlieb MA, Shaefer RMW, et al. Trends in electronic cigarette use among US adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;17:1195-1202.
3. National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. www.ncbi.nlm.nih.gov/pubmed/24455788. Accessed May 10, 2016.
4. Gostin LO, Glasner AY. E-cigarettes, vaping, and youth. JAMA. 2014;312(6):595-596.
5. Palazzolo DL. Electronic cigarettes and vaping: a new challenge in clinical medicine and public health. A literature review. Front Public Health. 2013;1(56):1-20.
6. Goniewicz ML, Hajek P, McRobbie H. Nicotine content of electronic cigarettes, its release in vapour and its consistency across batches: regulatory implications. Addiction. 2014;109(3):500-507.
7. Arnold C. Vaping and health: what do we know about e-cigarettes? Environ Health Perspect. 2014;122(9):A244-A249. http://ehp.niehs.nih.gov/122-a244. Accessed May 10, 2016.
8. Electronic cigarette use among middle and high school students. Medscape. September 6, 2013. www.medscape.com/viewarticle/811008. Accessed May 10, 2016.
9. FDA: E-cigarettes may be as bad as real thing. NBC Nightly News. July 22, 2015. www.nbcnews.com/video/nightly-news/32091534#32091534. Accessed May 10, 2016.
10. Caudle J. Why we need new rules on e-cigs. CNN. May 6, 2016. www.cnn.com/2016/05/06/opinions/fda-electronic-cigarettes-caudle. Accessed May 10, 2016.
11. FDA. FDA takes significant steps to protect Americans from dangers of tobacco through new regulation [news release]. May 5, 2016. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm499234.htm. Accessed May 10, 2016.
I was sitting in a restaurant bar a few days ago when a huge puff of cherry-scented smoke engulfed the area. As a former firefighter, I immediately looked around to find the source. You guessed it: a group of young adults were “vaping” nearby. This method of smoking is accomplished with an electronic “cigarette.” A sensor inside the e-cigarette detects airflow and initiates a heating element that vaporizes a liquid solution containing propylene glycol (organic compound with the chemical formula C₃H₈O₂), the flavoring of choice, and nicotine.1
I knew of this fad but didn’t give it much thought until recently, when I realized how pervasive it has become. Frankly, I have always thought, At least they are not smoking cigarettes and inhaling all that benzene, carbon dioxide, and formaldehyde.
We all know smoking cessation is valuable to the health of the population, but what do we know about the effects of vaping? For one thing, use of e-cigarettes (vapes) has increased considerably since they were first introduced (0.3% to 6.8% between 2007 and 2010).This is cause for concern, because while some research on e-cigarettes has emerged since their appearance, there are few definitive answers regarding their effect on human health.2
We also know that nicotine is addictive and toxic (in high doses), but we do not know the effects of propylene glycol, although it is generally recognized as “safe.” Symptoms that may occur as a result of vaporized propylene glycol inhalation include throat and ocular irritation, cough, mild airway obstruction, throat and vocal cord inflammation, headache, and dizziness. In spite of this, since the manufacturers of e-cigarettes have not made any therapeutic claims about their products, the FDA initially did not regulate them.
With e-cigarettes appearing in vaping shops, gas stations, and convenience stores—alongside advertising copy that claims vaping can help smokers curtail their habit by inhaling “harmless water vapor”—what should we tell our patients? These advertisements tout vaping as the “lesser of two evils” when compared to cigarettes. How can you knock that logic when we know cigarette smoking causes one in five deaths in the US each year and is a leading risk factor for COPD?3
Continue for the conundrum >>
The conundrum, as I see it, is threefold. The first step is to determine if vaping is a significant alternative to smoking cessation. The second is to determine if any components of vaping (nicotine, propylene glycol, or combustion) are safe for humans. Lastly, we must establish how to regulate e-cigarettes, given scientific uncertainty as to their therapeutic effects.4
In 2013, Palazzolo did a literature review of 66 articles related to e-cigarettes and vaping. He found that, when compared to the effects of smoking, vaping could be a substitute for smoking and a conceivable means for smoking reduction. It was unclear, however, if vaping could reduce nicotine addiction. He reported that the effects of vaping on human health are questionable, due to the extreme scarcity of empiric research.5
Although there has been a paucity of research on this topic, a study by Goniewicz and colleagues reports on the toxicants emitted by tobacco cigarettes and e-cigarettes.6 Their results indicate that e-cigarettes emit fewer toxicants than traditional tobacco cigarettes (formaldehyde, 0.20-5.61 µg and 1.6-52 µg, respectively; acetaldehyde, 0.11-1.36 µg and 52-140 µg).7 Despite this evidence, more studies need to be done on the effects of propylene glycol inhalation to determine the safety of e-cigarettes.
Another concern has been the lack of an age restriction on e-cigarettes and their growing popularity among grade and high school students.E-cigarette use doubled among US middle and high school students from 2011 to 2012, resulting in an estimated 1.78 million students who have used e-cigarettes as of 2012. There is serious concern about the possible harmful impact of nicotine on adolescent brain development,as well as the risk for nicotine addiction.8
Amid these growing questions and concerns, the FDA issued a warning that e-cigarettes may be as bad as the real thing and has recommended against their use.9 Just last month, the agency finalized a regulation on all tobacco products, including vaporizers, vape pens, hookah pens, e-cigs, and e-pipes. They will now regulate the manufacturing, import, packaging, labeling, and distribution of e-cigarettes to ensure that ingredients are assessed and determined to be safe for human use.FDA Commissioner Robert M. Califf, MD, said, “We must do our job under the Tobacco Control Act to reduce the harms caused by tobacco. That includes ensuring that consumers have the information they need to make informed decisions about tobacco use and making sure that new tobacco products for purchase come under comprehensive FDA review.”10,11
Well, is it just a bunch of smoke, or are the new regulations and health warnings about e-cigarettes long overdue? I would love to hear your experiences and additional advice for our colleagues and patients regarding the use of e-cigarettes and vaping. You can reach me at [email protected].
References
1. Jerry JM, Collins GB, Streem D. E-cigarettes: safe to recommend to patients? Cleve Clin J Med. 2015;82(8):521-526.
2. McMillen RC, Gottlieb MA, Shaefer RMW, et al. Trends in electronic cigarette use among US adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;17:1195-1202.
3. National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. www.ncbi.nlm.nih.gov/pubmed/24455788. Accessed May 10, 2016.
4. Gostin LO, Glasner AY. E-cigarettes, vaping, and youth. JAMA. 2014;312(6):595-596.
5. Palazzolo DL. Electronic cigarettes and vaping: a new challenge in clinical medicine and public health. A literature review. Front Public Health. 2013;1(56):1-20.
6. Goniewicz ML, Hajek P, McRobbie H. Nicotine content of electronic cigarettes, its release in vapour and its consistency across batches: regulatory implications. Addiction. 2014;109(3):500-507.
7. Arnold C. Vaping and health: what do we know about e-cigarettes? Environ Health Perspect. 2014;122(9):A244-A249. http://ehp.niehs.nih.gov/122-a244. Accessed May 10, 2016.
8. Electronic cigarette use among middle and high school students. Medscape. September 6, 2013. www.medscape.com/viewarticle/811008. Accessed May 10, 2016.
9. FDA: E-cigarettes may be as bad as real thing. NBC Nightly News. July 22, 2015. www.nbcnews.com/video/nightly-news/32091534#32091534. Accessed May 10, 2016.
10. Caudle J. Why we need new rules on e-cigs. CNN. May 6, 2016. www.cnn.com/2016/05/06/opinions/fda-electronic-cigarettes-caudle. Accessed May 10, 2016.
11. FDA. FDA takes significant steps to protect Americans from dangers of tobacco through new regulation [news release]. May 5, 2016. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm499234.htm. Accessed May 10, 2016.