User login
Top 10 things physician advisors want hospitalists to know
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
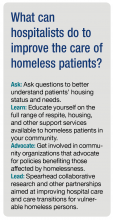
Homelessness: Whose job is it?
Despite programs to end homelessness, it remains a substantial and growing problem in many cities in the United States.1,2 In 2016, there were an estimated 10,550 homeless people living in my home state of Colorado, a 6% increase from the prior year.2 A recent point-estimate study found that there were more than 5,000 homeless individuals in the Denver metropolitan area on a single night in January 2017.3 Because of the relative scarcity of housing, a growing number of cities like Denver now utilize a practice known as vulnerability indexing to prioritize homeless persons at high risk of mortality from medical conditions for placement in permanent supportive housing.4
Although hospitalists like myself frequently care for vulnerable homeless patients in the hospital, most have little formal training in how best to care for and advocate for these individuals beyond treating their acute medical need, and little direct contact with community organizations with expertise in doing so. Instead, we have learned informally through experience. Hospital providers are often frustrated by the perceived lack of services and support available to these patients, and there is substantial variability in the extent to which providers engage patients and community partners during and after hospitalization. Despite the growing practice of vulnerability indexing in the community, hospital-based providers do not routinely assess vulnerability with respect to housing. Previous research indicates that housing status is assessed in only a minority of homeless patients during their hospital stay.12 Thus, hospitalization often represents a missed opportunity to identify vulnerability and utilize it to connect patients with housing and other resources.
Addressing the significant known health disparities faced by homeless persons is one of the greatest health equity challenges of our time.13 We need better ways of understanding, identifying, and addressing vulnerability among homeless patients who are hospitalized, paired with improved integration with local community organizations. This will require moving beyond the idea that homelessness is the social worker’s job to one of shared responsibility and advocacy.
Collaborative research and other partnerships that engage both community organizations and individuals affected by homelessness are crucial to further understand the specific needs, barriers, challenges, and opportunities for improving hospital care and care transitions in this population. As well-respected community members and systems thinkers who witness these inequities on a daily basis, hospitalists are well positioned to help lead this work.
Dr. Stella is a hospitalist at Denver Health and Hospital Authority, and an associate professor of medicine at the University of Colorado. She is a member of The Hospitalist editorial advisory board.
References
1. Ending Chronic Homelessness. (Aug 2017). U.S. Interagency Council on Homelessness. Available at: https://www.usich.gov/goals/chronicsness. Accessed: Oct 21, 2017.
2. 2016 Annual Homeless Assessment Report (AHAR) to Congress. (Nov 2016). U.S. Department of Housing and Urban Development Office of Community Planning and Development, Part 1. Available at: https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Accessed: Oct 21, 2017.
3. 2017 Point-In-Time Report, Seven-County Metro Denver Region. Metro Denver Homeless Initiative. Available at: http://www.mdhi.org/2017_pit. Accessed Oct 22, 2017.
4. Henwood BF et al. Examining mortality among formerly homeless adults enrolled in Housing First: An observational study. BMC Public Health. 2015;15:1209.
5. Weinstein LC et al. Moving from street to home: Health status of entrants to a Housing First program. J Prim Care Community Health. 2011;2:11–5.
6. Kushel MB et al. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200-6.
7. Kushel MB et al. Emergency department use among the homeless and marginally housed: Results from a community-based study. Am J Public Health. 2002;92(5):778-84.
8. Baggett TP et al. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Intern Med. 2013 Feb 11;173(3):189–95.
9. Johnson et al. For many patients who use large amounts of health care services, the need is intense yet temporary. Health Aff (Millwood). 2015 Aug;34(8):1312-9.
10. Durfee J et al. The impact of tailored intervention services on charges and mortality for adult super-utilizers. Healthc (Amst). 2017 Aug 25. pii: S2213-0764(17)30057-X. doi: 10.1016/j.hjdsi.2017.08.004. [Epub ahead of print]
11. Rinehart DJ et al. Identifying subgroups of adult super utilizers in an urban safety-net system using latent class analysis: Implications for clinical practice. Med Care. 2016 Sep 14. doi: 10.1097/MLR.0000000000000628. [Epub ahead of print]
12. Greysen RS et al. Understanding transitions of care from hospital to homeless shelter: A mixed-methods, community-based participatory approach. J Gen Intern Med. 2012;27(11):1484-91.
13. National Health Care for the Homeless Council. (Oct 2012). Improving Care Transitions for People Experiencing Homelessness. (Lead author: Sabrina Edgington, policy and program specialist.) Available at: www.nhchc.org/wp-content/uploads/2012/12/Policy_Brief_Care_Transitions.pdf. Accessed Oct 21, 2017.
14. Koh HK et al. Improving healthcare for homeless people. JAMA. 2016;316(24):2586-7.
Despite programs to end homelessness, it remains a substantial and growing problem in many cities in the United States.1,2 In 2016, there were an estimated 10,550 homeless people living in my home state of Colorado, a 6% increase from the prior year.2 A recent point-estimate study found that there were more than 5,000 homeless individuals in the Denver metropolitan area on a single night in January 2017.3 Because of the relative scarcity of housing, a growing number of cities like Denver now utilize a practice known as vulnerability indexing to prioritize homeless persons at high risk of mortality from medical conditions for placement in permanent supportive housing.4
Although hospitalists like myself frequently care for vulnerable homeless patients in the hospital, most have little formal training in how best to care for and advocate for these individuals beyond treating their acute medical need, and little direct contact with community organizations with expertise in doing so. Instead, we have learned informally through experience. Hospital providers are often frustrated by the perceived lack of services and support available to these patients, and there is substantial variability in the extent to which providers engage patients and community partners during and after hospitalization. Despite the growing practice of vulnerability indexing in the community, hospital-based providers do not routinely assess vulnerability with respect to housing. Previous research indicates that housing status is assessed in only a minority of homeless patients during their hospital stay.12 Thus, hospitalization often represents a missed opportunity to identify vulnerability and utilize it to connect patients with housing and other resources.
Addressing the significant known health disparities faced by homeless persons is one of the greatest health equity challenges of our time.13 We need better ways of understanding, identifying, and addressing vulnerability among homeless patients who are hospitalized, paired with improved integration with local community organizations. This will require moving beyond the idea that homelessness is the social worker’s job to one of shared responsibility and advocacy.
Collaborative research and other partnerships that engage both community organizations and individuals affected by homelessness are crucial to further understand the specific needs, barriers, challenges, and opportunities for improving hospital care and care transitions in this population. As well-respected community members and systems thinkers who witness these inequities on a daily basis, hospitalists are well positioned to help lead this work.
Dr. Stella is a hospitalist at Denver Health and Hospital Authority, and an associate professor of medicine at the University of Colorado. She is a member of The Hospitalist editorial advisory board.
References
1. Ending Chronic Homelessness. (Aug 2017). U.S. Interagency Council on Homelessness. Available at: https://www.usich.gov/goals/chronicsness. Accessed: Oct 21, 2017.
2. 2016 Annual Homeless Assessment Report (AHAR) to Congress. (Nov 2016). U.S. Department of Housing and Urban Development Office of Community Planning and Development, Part 1. Available at: https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Accessed: Oct 21, 2017.
3. 2017 Point-In-Time Report, Seven-County Metro Denver Region. Metro Denver Homeless Initiative. Available at: http://www.mdhi.org/2017_pit. Accessed Oct 22, 2017.
4. Henwood BF et al. Examining mortality among formerly homeless adults enrolled in Housing First: An observational study. BMC Public Health. 2015;15:1209.
5. Weinstein LC et al. Moving from street to home: Health status of entrants to a Housing First program. J Prim Care Community Health. 2011;2:11–5.
6. Kushel MB et al. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200-6.
7. Kushel MB et al. Emergency department use among the homeless and marginally housed: Results from a community-based study. Am J Public Health. 2002;92(5):778-84.
8. Baggett TP et al. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Intern Med. 2013 Feb 11;173(3):189–95.
9. Johnson et al. For many patients who use large amounts of health care services, the need is intense yet temporary. Health Aff (Millwood). 2015 Aug;34(8):1312-9.
10. Durfee J et al. The impact of tailored intervention services on charges and mortality for adult super-utilizers. Healthc (Amst). 2017 Aug 25. pii: S2213-0764(17)30057-X. doi: 10.1016/j.hjdsi.2017.08.004. [Epub ahead of print]
11. Rinehart DJ et al. Identifying subgroups of adult super utilizers in an urban safety-net system using latent class analysis: Implications for clinical practice. Med Care. 2016 Sep 14. doi: 10.1097/MLR.0000000000000628. [Epub ahead of print]
12. Greysen RS et al. Understanding transitions of care from hospital to homeless shelter: A mixed-methods, community-based participatory approach. J Gen Intern Med. 2012;27(11):1484-91.
13. National Health Care for the Homeless Council. (Oct 2012). Improving Care Transitions for People Experiencing Homelessness. (Lead author: Sabrina Edgington, policy and program specialist.) Available at: www.nhchc.org/wp-content/uploads/2012/12/Policy_Brief_Care_Transitions.pdf. Accessed Oct 21, 2017.
14. Koh HK et al. Improving healthcare for homeless people. JAMA. 2016;316(24):2586-7.
Despite programs to end homelessness, it remains a substantial and growing problem in many cities in the United States.1,2 In 2016, there were an estimated 10,550 homeless people living in my home state of Colorado, a 6% increase from the prior year.2 A recent point-estimate study found that there were more than 5,000 homeless individuals in the Denver metropolitan area on a single night in January 2017.3 Because of the relative scarcity of housing, a growing number of cities like Denver now utilize a practice known as vulnerability indexing to prioritize homeless persons at high risk of mortality from medical conditions for placement in permanent supportive housing.4
Although hospitalists like myself frequently care for vulnerable homeless patients in the hospital, most have little formal training in how best to care for and advocate for these individuals beyond treating their acute medical need, and little direct contact with community organizations with expertise in doing so. Instead, we have learned informally through experience. Hospital providers are often frustrated by the perceived lack of services and support available to these patients, and there is substantial variability in the extent to which providers engage patients and community partners during and after hospitalization. Despite the growing practice of vulnerability indexing in the community, hospital-based providers do not routinely assess vulnerability with respect to housing. Previous research indicates that housing status is assessed in only a minority of homeless patients during their hospital stay.12 Thus, hospitalization often represents a missed opportunity to identify vulnerability and utilize it to connect patients with housing and other resources.
Addressing the significant known health disparities faced by homeless persons is one of the greatest health equity challenges of our time.13 We need better ways of understanding, identifying, and addressing vulnerability among homeless patients who are hospitalized, paired with improved integration with local community organizations. This will require moving beyond the idea that homelessness is the social worker’s job to one of shared responsibility and advocacy.
Collaborative research and other partnerships that engage both community organizations and individuals affected by homelessness are crucial to further understand the specific needs, barriers, challenges, and opportunities for improving hospital care and care transitions in this population. As well-respected community members and systems thinkers who witness these inequities on a daily basis, hospitalists are well positioned to help lead this work.
Dr. Stella is a hospitalist at Denver Health and Hospital Authority, and an associate professor of medicine at the University of Colorado. She is a member of The Hospitalist editorial advisory board.
References
1. Ending Chronic Homelessness. (Aug 2017). U.S. Interagency Council on Homelessness. Available at: https://www.usich.gov/goals/chronicsness. Accessed: Oct 21, 2017.
2. 2016 Annual Homeless Assessment Report (AHAR) to Congress. (Nov 2016). U.S. Department of Housing and Urban Development Office of Community Planning and Development, Part 1. Available at: https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Accessed: Oct 21, 2017.
3. 2017 Point-In-Time Report, Seven-County Metro Denver Region. Metro Denver Homeless Initiative. Available at: http://www.mdhi.org/2017_pit. Accessed Oct 22, 2017.
4. Henwood BF et al. Examining mortality among formerly homeless adults enrolled in Housing First: An observational study. BMC Public Health. 2015;15:1209.
5. Weinstein LC et al. Moving from street to home: Health status of entrants to a Housing First program. J Prim Care Community Health. 2011;2:11–5.
6. Kushel MB et al. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200-6.
7. Kushel MB et al. Emergency department use among the homeless and marginally housed: Results from a community-based study. Am J Public Health. 2002;92(5):778-84.
8. Baggett TP et al. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Intern Med. 2013 Feb 11;173(3):189–95.
9. Johnson et al. For many patients who use large amounts of health care services, the need is intense yet temporary. Health Aff (Millwood). 2015 Aug;34(8):1312-9.
10. Durfee J et al. The impact of tailored intervention services on charges and mortality for adult super-utilizers. Healthc (Amst). 2017 Aug 25. pii: S2213-0764(17)30057-X. doi: 10.1016/j.hjdsi.2017.08.004. [Epub ahead of print]
11. Rinehart DJ et al. Identifying subgroups of adult super utilizers in an urban safety-net system using latent class analysis: Implications for clinical practice. Med Care. 2016 Sep 14. doi: 10.1097/MLR.0000000000000628. [Epub ahead of print]
12. Greysen RS et al. Understanding transitions of care from hospital to homeless shelter: A mixed-methods, community-based participatory approach. J Gen Intern Med. 2012;27(11):1484-91.
13. National Health Care for the Homeless Council. (Oct 2012). Improving Care Transitions for People Experiencing Homelessness. (Lead author: Sabrina Edgington, policy and program specialist.) Available at: www.nhchc.org/wp-content/uploads/2012/12/Policy_Brief_Care_Transitions.pdf. Accessed Oct 21, 2017.
14. Koh HK et al. Improving healthcare for homeless people. JAMA. 2016;316(24):2586-7.
HM17 session summary: Hospitalists as leaders in patient flow and hospital throughput
Presenters
Gaby Berger, MD; Aaron Hamilton, MD, FHM; Christopher Kim, MD, SFHM; Eduardo Margo, MD; Vikas Parekh, MD, FACP, SFHM; Anneliese Schleyer, MD, SFHM; Emily Wang, MD
Session Summary
This HM17 workshop brought together academic and community hospitalists to share effective strategies for improving hospital patient flow.
This was followed by a break-out session, in which hospitalists were encouraged to further explore these and other strategies for improving patient flow.
Key takeaways for HM
- Expedited discharge: Identify patients who can be safely discharged before noon. Consider creating standard work to ensure that key steps in discharge planning process, such as completion of medication reconciliation and discharge instructions and communication with patient and families and the interdisciplinary team, occur the day prior to discharge.
- Length of stay reduction strategies: Partner with utilization management to identify and develop a strategy to actively manage patients with long length of stay. Several institutions have set up committees to review such cases and address barriers, escalating requests for resources to executive leadership as needed.
- Facilitate transfers: Develop a standard process that is streamlined and patient-centered and includes established criteria for deciding whether interhospital transfers are appropriate.
- Short Stay Units: Some hospitals have had success with hospitalist-run short stay units as a strategy to decrease length of stay in observation patients. This strategy is most ideal for patients with a predictable length of stay. If you are thinking of starting an observation unit at your hospital, consider establishing criteria and protocols to expedite care.
- Hospitalist Quarterback: Given their broad perspective and clinical knowledge, hospitalists are uniquely positioned to help manage hospital, and even system-wide, capacity in real time. Some hospitals have successfully employed this strategy in some form to improve throughput. However, hospitalists need tools to help them electronically track incoming patients, integration with utilization management resources, and support from executive leadership to be successful.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.
Presenters
Gaby Berger, MD; Aaron Hamilton, MD, FHM; Christopher Kim, MD, SFHM; Eduardo Margo, MD; Vikas Parekh, MD, FACP, SFHM; Anneliese Schleyer, MD, SFHM; Emily Wang, MD
Session Summary
This HM17 workshop brought together academic and community hospitalists to share effective strategies for improving hospital patient flow.
This was followed by a break-out session, in which hospitalists were encouraged to further explore these and other strategies for improving patient flow.
Key takeaways for HM
- Expedited discharge: Identify patients who can be safely discharged before noon. Consider creating standard work to ensure that key steps in discharge planning process, such as completion of medication reconciliation and discharge instructions and communication with patient and families and the interdisciplinary team, occur the day prior to discharge.
- Length of stay reduction strategies: Partner with utilization management to identify and develop a strategy to actively manage patients with long length of stay. Several institutions have set up committees to review such cases and address barriers, escalating requests for resources to executive leadership as needed.
- Facilitate transfers: Develop a standard process that is streamlined and patient-centered and includes established criteria for deciding whether interhospital transfers are appropriate.
- Short Stay Units: Some hospitals have had success with hospitalist-run short stay units as a strategy to decrease length of stay in observation patients. This strategy is most ideal for patients with a predictable length of stay. If you are thinking of starting an observation unit at your hospital, consider establishing criteria and protocols to expedite care.
- Hospitalist Quarterback: Given their broad perspective and clinical knowledge, hospitalists are uniquely positioned to help manage hospital, and even system-wide, capacity in real time. Some hospitals have successfully employed this strategy in some form to improve throughput. However, hospitalists need tools to help them electronically track incoming patients, integration with utilization management resources, and support from executive leadership to be successful.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.
Presenters
Gaby Berger, MD; Aaron Hamilton, MD, FHM; Christopher Kim, MD, SFHM; Eduardo Margo, MD; Vikas Parekh, MD, FACP, SFHM; Anneliese Schleyer, MD, SFHM; Emily Wang, MD
Session Summary
This HM17 workshop brought together academic and community hospitalists to share effective strategies for improving hospital patient flow.
This was followed by a break-out session, in which hospitalists were encouraged to further explore these and other strategies for improving patient flow.
Key takeaways for HM
- Expedited discharge: Identify patients who can be safely discharged before noon. Consider creating standard work to ensure that key steps in discharge planning process, such as completion of medication reconciliation and discharge instructions and communication with patient and families and the interdisciplinary team, occur the day prior to discharge.
- Length of stay reduction strategies: Partner with utilization management to identify and develop a strategy to actively manage patients with long length of stay. Several institutions have set up committees to review such cases and address barriers, escalating requests for resources to executive leadership as needed.
- Facilitate transfers: Develop a standard process that is streamlined and patient-centered and includes established criteria for deciding whether interhospital transfers are appropriate.
- Short Stay Units: Some hospitals have had success with hospitalist-run short stay units as a strategy to decrease length of stay in observation patients. This strategy is most ideal for patients with a predictable length of stay. If you are thinking of starting an observation unit at your hospital, consider establishing criteria and protocols to expedite care.
- Hospitalist Quarterback: Given their broad perspective and clinical knowledge, hospitalists are uniquely positioned to help manage hospital, and even system-wide, capacity in real time. Some hospitals have successfully employed this strategy in some form to improve throughput. However, hospitalists need tools to help them electronically track incoming patients, integration with utilization management resources, and support from executive leadership to be successful.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.
HM17 session summary: The hospitalist’s role in the opioid epidemic
Presenters
Shoshana J. Herzig, MD, MPH, and Hillary J. Mosher, MFA, MD, FHM
Summary
The growth in opiate prescribing and associated increases in adverse events has created unique challenges for hospitalists, including how best to assess pain and opiate use disorders and how to safely prescribe opiates during hospitalization and at discharge.
These challenges are compounded by patient and system factors and a paucity of evidence-based guidelines to help guide safe administration of opiates in hospitalized patients. This can mean frustration for hospitalists and harm for patients.
Key takeaways for HM
- When assessing patients’ pain, it is crucial to differentiate between acute and chronic pain (or both) and whether it is nociceptive or neuropathic. Misclassification of pain contributes to inappropriate exposure and escalation of opiate therapy during hospitalization.
- Always consider nonopioid analgesics such as NSAIDs first and pair them with opiates. Studies in a variety of conditions have demonstrated that these are equally, if not more, effective, even for severe pain, such as with renal colic. Reserve opiates for moderate to severe pain.
- Always assess whether the benefits of initiating or continuing opioid therapy outweigh the risks for individual patients. There is no validated tool to predict risk for adverse events and/or opioid abuse disorder but a careful review of patient history can identify established risk factors (such as a history of mental illness or substance abuse disorders, renal impairment, or other comorbidities). In addition, nearly all states now have Prescription Drug Monitoring Programs, and hospitalists should consult these routinely when prescribing opiates.
- Always clearly discuss expectations and risks of opioid therapy, including the potential for development of opioid use disorders with hospitalized patients prior to initiation. Emphasize pain reduction rather than elimination and focus on functional goals such as improved mobility. Also, set expectations for stepping down treatment up front.
- Use the lowest effective dose of immediate-release opioids (preferably oral route) for shortest duration possible. Long acting opiates are associated with increased risk of adverse events, and their initiation should generally be avoided in hospitalized patients with noncancer pain.
- Minimize risk by avoiding concurrent administration of other medications with sedative properties, especially benzodiazepines, which have been found to significantly increase the risk of adverse events, including overdose.
- Recognize that chronic opioid use often begins with treatment of acute pain during hospitalization. Adopt best practice for discharge, including prescribing shorter courses whenever possible, discussing initiation, and changes or modifications in opiate therapy with patients’ primary care provider, and ensure timely postdischarge follow-up. Also consider coprescription of naloxone at discharge for higher risk patients.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.
Presenters
Shoshana J. Herzig, MD, MPH, and Hillary J. Mosher, MFA, MD, FHM
Summary
The growth in opiate prescribing and associated increases in adverse events has created unique challenges for hospitalists, including how best to assess pain and opiate use disorders and how to safely prescribe opiates during hospitalization and at discharge.
These challenges are compounded by patient and system factors and a paucity of evidence-based guidelines to help guide safe administration of opiates in hospitalized patients. This can mean frustration for hospitalists and harm for patients.
Key takeaways for HM
- When assessing patients’ pain, it is crucial to differentiate between acute and chronic pain (or both) and whether it is nociceptive or neuropathic. Misclassification of pain contributes to inappropriate exposure and escalation of opiate therapy during hospitalization.
- Always consider nonopioid analgesics such as NSAIDs first and pair them with opiates. Studies in a variety of conditions have demonstrated that these are equally, if not more, effective, even for severe pain, such as with renal colic. Reserve opiates for moderate to severe pain.
- Always assess whether the benefits of initiating or continuing opioid therapy outweigh the risks for individual patients. There is no validated tool to predict risk for adverse events and/or opioid abuse disorder but a careful review of patient history can identify established risk factors (such as a history of mental illness or substance abuse disorders, renal impairment, or other comorbidities). In addition, nearly all states now have Prescription Drug Monitoring Programs, and hospitalists should consult these routinely when prescribing opiates.
- Always clearly discuss expectations and risks of opioid therapy, including the potential for development of opioid use disorders with hospitalized patients prior to initiation. Emphasize pain reduction rather than elimination and focus on functional goals such as improved mobility. Also, set expectations for stepping down treatment up front.
- Use the lowest effective dose of immediate-release opioids (preferably oral route) for shortest duration possible. Long acting opiates are associated with increased risk of adverse events, and their initiation should generally be avoided in hospitalized patients with noncancer pain.
- Minimize risk by avoiding concurrent administration of other medications with sedative properties, especially benzodiazepines, which have been found to significantly increase the risk of adverse events, including overdose.
- Recognize that chronic opioid use often begins with treatment of acute pain during hospitalization. Adopt best practice for discharge, including prescribing shorter courses whenever possible, discussing initiation, and changes or modifications in opiate therapy with patients’ primary care provider, and ensure timely postdischarge follow-up. Also consider coprescription of naloxone at discharge for higher risk patients.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.
Presenters
Shoshana J. Herzig, MD, MPH, and Hillary J. Mosher, MFA, MD, FHM
Summary
The growth in opiate prescribing and associated increases in adverse events has created unique challenges for hospitalists, including how best to assess pain and opiate use disorders and how to safely prescribe opiates during hospitalization and at discharge.
These challenges are compounded by patient and system factors and a paucity of evidence-based guidelines to help guide safe administration of opiates in hospitalized patients. This can mean frustration for hospitalists and harm for patients.
Key takeaways for HM
- When assessing patients’ pain, it is crucial to differentiate between acute and chronic pain (or both) and whether it is nociceptive or neuropathic. Misclassification of pain contributes to inappropriate exposure and escalation of opiate therapy during hospitalization.
- Always consider nonopioid analgesics such as NSAIDs first and pair them with opiates. Studies in a variety of conditions have demonstrated that these are equally, if not more, effective, even for severe pain, such as with renal colic. Reserve opiates for moderate to severe pain.
- Always assess whether the benefits of initiating or continuing opioid therapy outweigh the risks for individual patients. There is no validated tool to predict risk for adverse events and/or opioid abuse disorder but a careful review of patient history can identify established risk factors (such as a history of mental illness or substance abuse disorders, renal impairment, or other comorbidities). In addition, nearly all states now have Prescription Drug Monitoring Programs, and hospitalists should consult these routinely when prescribing opiates.
- Always clearly discuss expectations and risks of opioid therapy, including the potential for development of opioid use disorders with hospitalized patients prior to initiation. Emphasize pain reduction rather than elimination and focus on functional goals such as improved mobility. Also, set expectations for stepping down treatment up front.
- Use the lowest effective dose of immediate-release opioids (preferably oral route) for shortest duration possible. Long acting opiates are associated with increased risk of adverse events, and their initiation should generally be avoided in hospitalized patients with noncancer pain.
- Minimize risk by avoiding concurrent administration of other medications with sedative properties, especially benzodiazepines, which have been found to significantly increase the risk of adverse events, including overdose.
- Recognize that chronic opioid use often begins with treatment of acute pain during hospitalization. Adopt best practice for discharge, including prescribing shorter courses whenever possible, discussing initiation, and changes or modifications in opiate therapy with patients’ primary care provider, and ensure timely postdischarge follow-up. Also consider coprescription of naloxone at discharge for higher risk patients.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.