User login
Muscle cramps/pain • weakness • muscle twitching • Dx?
THE CASE
A 39-year-old man who worked in construction presented to our clinic with complaints of muscle cramps and muscle pain that had been bothering him for several months. The cramps and pain started in both of his arms and subsequently became diffuse and generalized. He also reported an unintentional 15-pound weight loss.
His exam at that time was unremarkable. He was diagnosed with dehydration and cramping due to overexertion at work. A basic metabolic panel, hemogram, lipid panel, and thyroid stimulating hormone level were ordered. The patient’s triglyceride level, which was 227 mg/dL, was the only significant result (normal level: <150 mg/dL).
The patient’s symptoms continued to worsen until he returned to the clinic 6 months later, again complaining of muscle cramps and pain throughout his body. At that second visit, he also reported profound overall weakness and the development of diffuse muscle twitching, which his wife had observed while he was sleeping. As a result of these worrisome symptoms, he had become anxious and depressed.
A review of his medical record revealed a weight loss of about 20 pounds over the previous year. On exam, he had diffuse fasciculations in all the major muscle groups, including his tongue. The patient’s strength was 4/5 in all muscle groups. His deep tendon reflexes were 3+. He had a negative Babinski reflex (ie, he had downward facing toes with plantar stimulation), and cranial nerves II to XII were all intact. His rapid alternating movements and gait were slow.
THE DIAGNOSIS
Based on the exam, the primary diagnostic consideration for the patient was amyotrophic lateral sclerosis (ALS). Lab tests were ordered and revealed normal calcium and electrolyte levels, a normal erythrocyte sedimentation rate, a normal C-reactive protein level, and a negative test for acetylcholine receptor antibodies. However, the patient had an elevated creatine kinase level of 664 U/L (normal: 30-200 U/L). The patient was sent to a neuromuscular specialist, who identified signs of upper and lower motor neuron disease in all 4 of the patient’s extremities (he had foot drop that had not been present previously) and a very brisk jaw jerk. Along with the tongue fasciculations, the results of the specialist’s physical exam suggested ALS. Four-limb electromyography (EMG) showed widespread fasciculations and some large motor unit potentials and recruitment abnormalities, which were also consistent with ALS. It appeared that the patient’s weight loss was due to both muscle atrophy and the amount of calories burned from his constant twitching.
Extensive testing was done to rule out other potential causes of the patient’s symptoms, including magnetic resonance imaging (MRI) of the spine and brain (which was normal). In addition, the patient’s aldolase level and antineutrophil cytoplasmic antibodies were normal. The patient tested negative for human immunodeficiency virus and antibodies to double-stranded DNA. After serial neurologic exams, the final diagnosis of ALS was made.
DISCUSSION
ALS, also known as Lou Gehrig’s disease, is a degenerative motor neuron disease.1-3 The incidence in North America is 1.5 to 2.7 per 100,000 per year, and the prevalence is 2.7 to 7.4 per 100,000.4 The incidence of ALS increases with each decade of life, especially after age 40, and peaks at 74 years of age.4 The male to female ratio is 1:1.5-2.4 ALS affects upper and lower motor neurons and is progressive; however, the rate of progression and phenotype vary greatly between individuals.2 Most patients with ALS die within 2 to 5 years of onset.5
There is no specific test for ALS; the diagnosis is made clinically based on the revised El Escorial World Federation of Neurology criteria, also known as the Airlie House criteria.2,6,7 These criteria include evidence of lower motor neuron degeneration by clinical, electrophysiologic, or neuropathologic exam; evidence of upper motor neuron disease by clinical exam; progressive spread of symptoms or signs within a region or to other regions (by history or exam); and the absence of electrophysiologic, neuroimaging, or pathologic evidence of other disease processes that could explain the symptoms. If patients have evidence of upper and lower motor neuron disease, they should be reevaluated in 4 weeks to see if symptoms are improving or progressing.
Like our patient, many patients will have an elevated creatine kinase level (some with levels as high as 1000 U/L), and calcium may also be elevated because, rarely, ALS is associated with primary hyperparathyroidism.8 Electrophysiologic studies can be helpful in identifying active denervation of lower motor neurons.4,6,7
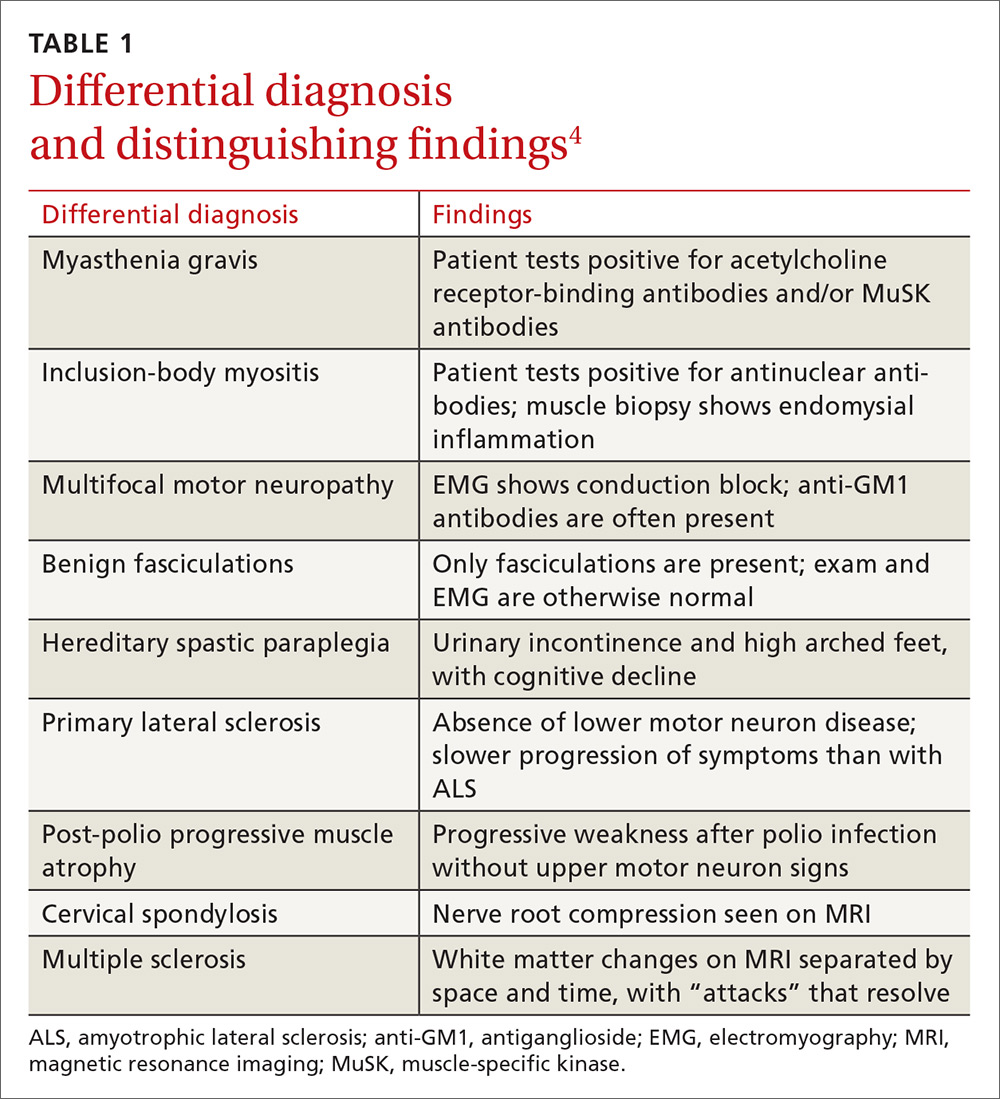
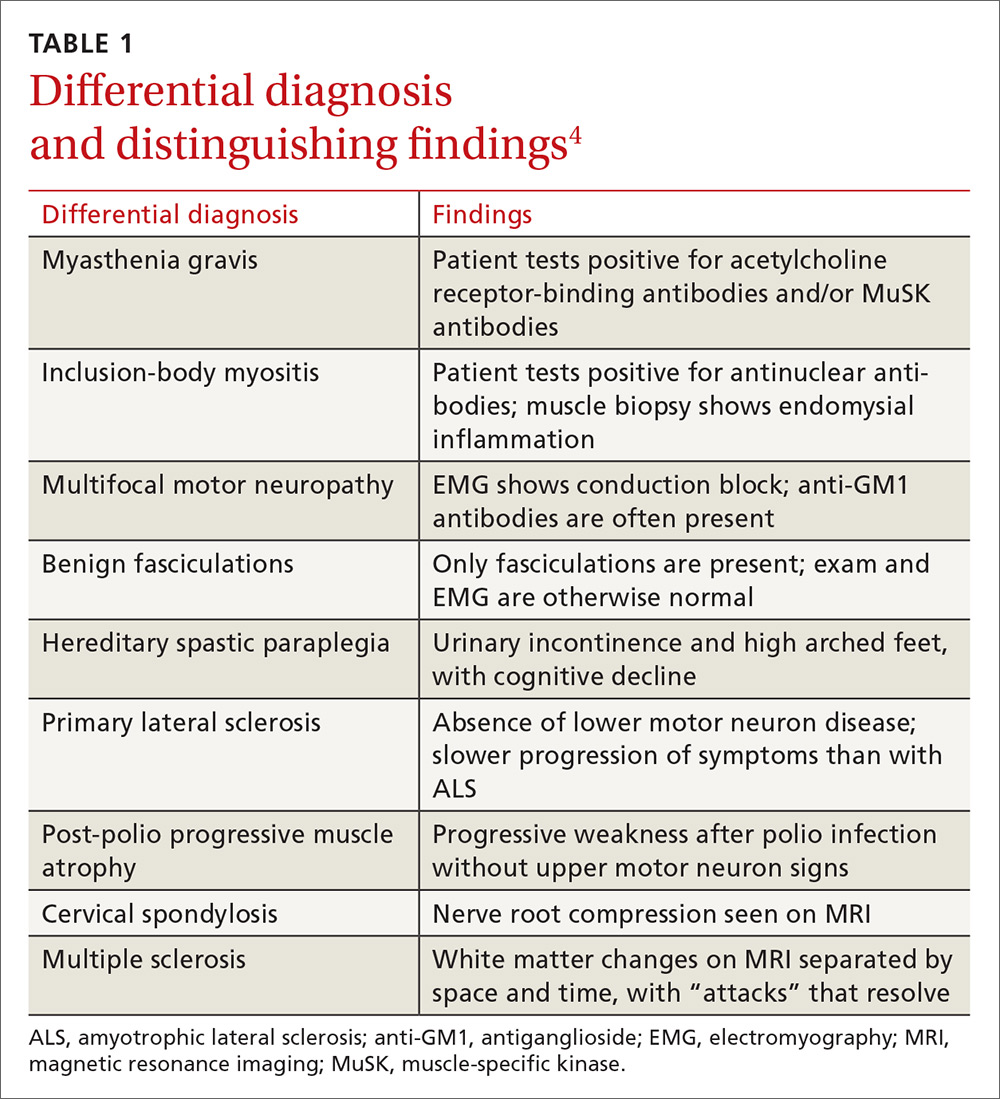
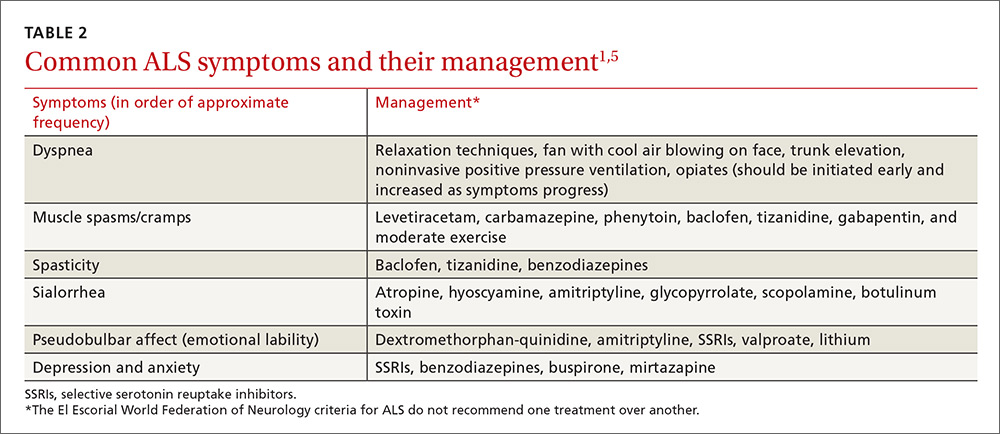
The differential diagnosis for ALS includes myasthenia gravis, inclusion-body myositis, multifocal motor neuropathy, benign fasciculations, hereditary spastic paraplegia, primary lateral sclerosis, post-polio progressive muscle atrophy, cervical spondylosis, and multiple sclerosis. A negative acetylcholine receptor antibody test will rule out myasthenia gravis, imaging of the spine can rule out cervical spondylosis, and electrophysiologic testing helps eliminate the other conditions (TABLE 14).
Treatment in specialty clinics can prolong survival
The mainstays of treatment are symptom management, multidisciplinary care (by physicians, physical/occupational/speech therapists, nutritionists, psychologists, psychotherapists, and genetic counselors), palliative care, and counseling about end-of-life issues for patients and family.1,5 Utilization of an ALS specialty clinic can provide access to all of these services and should be considered, as there is evidence that treatment in such clinics can prolong survival.5 The location of ALS specialty clinics can be found on the ALS Association’s Web site at http://www.alsa.org/community/.
Despite treatment, however, ALS is a progressive disease. The prognosis is poor, with a median survival of 2 to 5 years after diagnosis.9
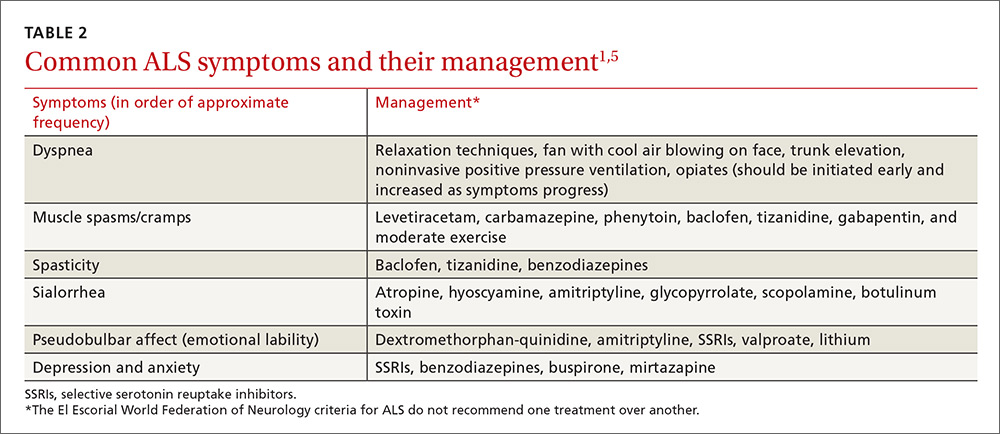
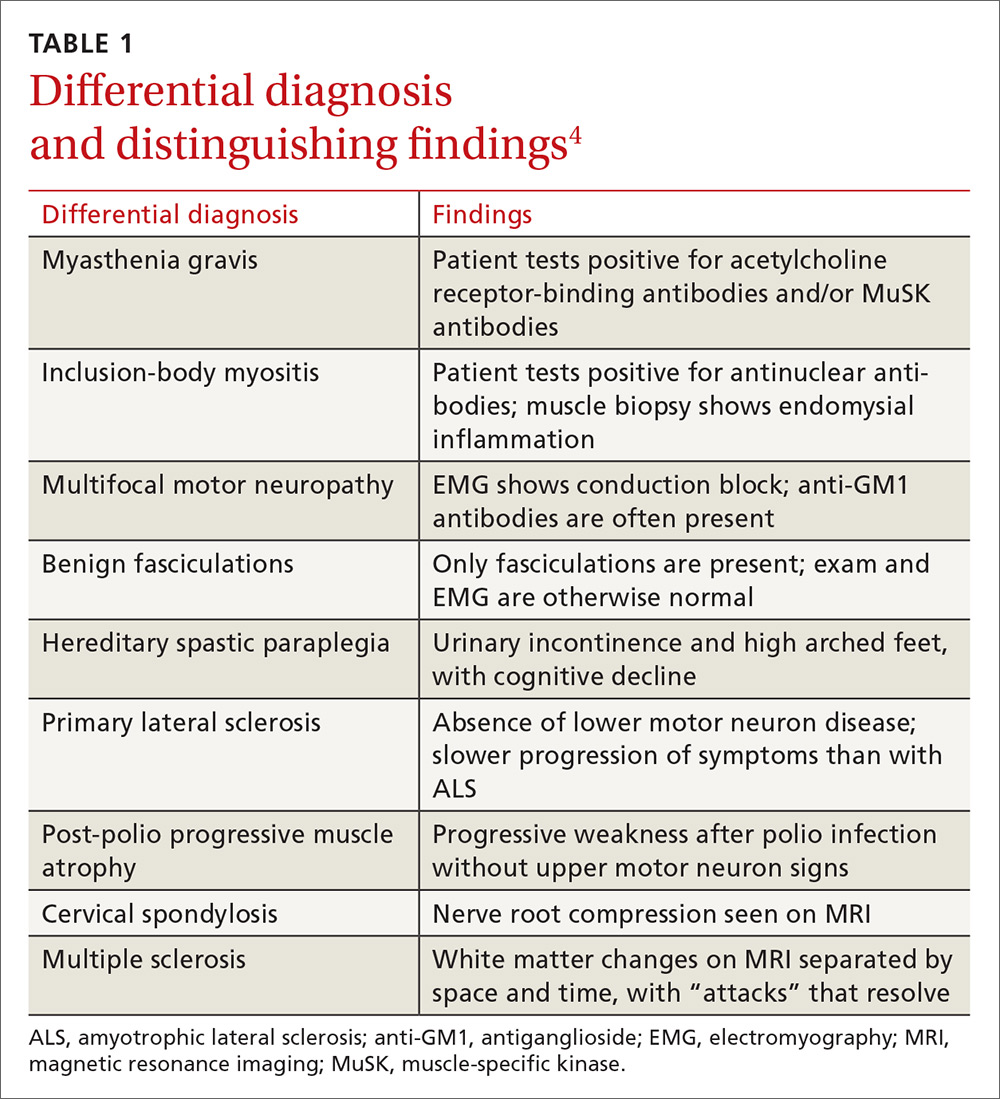
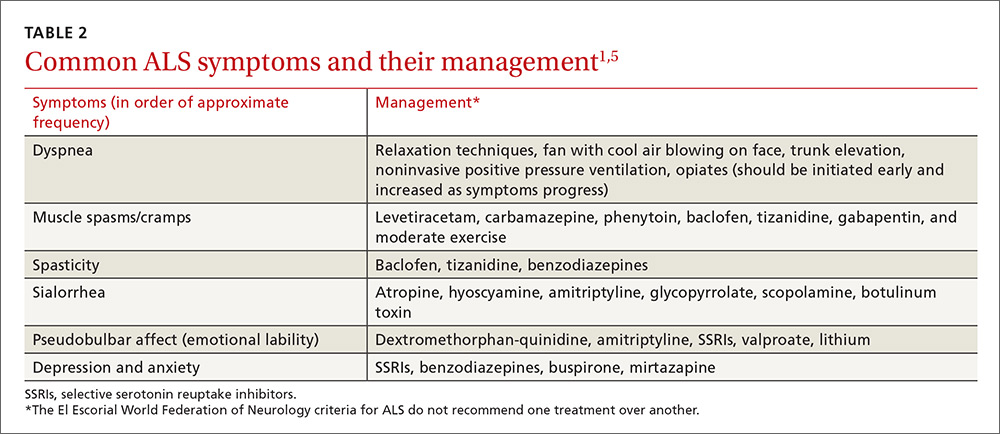
The El Escorial World Federation of Neurology criteria for the diagnosis of ALS address how to treat the most common symptoms of ALS that occur as the disease progresses. These symptoms include dyspnea, muscle spasms, spasticity, sialorrhea, and pseudobulbar affect (TABLE 21,5).
Our patient was started on baclofen 10 mg 3 times per day (titrated up as needed) for muscle spasms and cramps, which resulted in some improvement of his cramps, but no improvement in the spasms. He was also started on sertraline 50 mg for anxiety and depression. His overall weakness continued to progress, and we recommended that the patient get ankle-foot orthosis braces to help with the mobility impairment caused by foot drop.
We then referred him to an ALS specialty clinic recommended by the neuromuscular specialist. The patient is now enrolled in a clinical trial designed to test a cerebrospinal fluid marker for diagnosis and for a new drug aimed at symptom management.
THE TAKEAWAY
Muscle cramps and pain are early signs of ALS. Although ALS is uncommon, patients who present with muscle cramps and muscle pain should have a creatine kinase test ordered (which, if elevated, should prompt further investigation into ALS as the possible cause). Patients should also undergo a neurologic examination to seek evidence of upper and lower motor neuron disease. They should then be reevaluated in 4 weeks to see if symptoms are improving or progressing. If no improvement is seen and symptoms are progressive, a work-up for ALS should be considered.
The mainstay of treatment for patients with ALS is multidisciplinary symptom management and palliative care. Utilization of an ALS specialty clinic should also be recommended, as it can improve survival.5
1. Miller RG, Gelinas D, O’Connor P. Amyotrophic Lateral Sclerosis: American Academy of Neurology Press Quality of Life Guide Series. Demos Medical Publishing; 2004.
2. Simon NG, Turner MR, Vucic S, et al. Quantifying disease progression in amyotrophic lateral sclerosis. Ann Neurol. 2014;76:643-657.
3. Worms PM. The epidemiology of motor neuron diseases: a review of recent studies. J Neurol Sci. 2001;191:3-9.
4. Shaw PJ. ALS and other motor neuron diseases. In: Goldman L, Schafer AI, eds. Goldman’s Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 418.
5. Miller RG, Jackson CE, Kasarskis EJ, et al. Practice Parameter update: The Care of the Patient with Amyotrophic Lateral Sclerosis: Multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2009;73:1227-1233.
6. Brooks BR. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial “Clinical limits of amyotrophic lateral sclerosis” workshop contributors. J Neurol Sci. 1994;124:96-107.
7. Brooks BR, Miller RG, Swash M, et al; World Federation of Neurology Research Group on Motor Neuron Diseases. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293-299.
8. Jackson CE, Amato AA, Bryan WW, et al. Primary hyperparathyroidism and ALS: is there a relation? Neurology. 1998;50:1795-1799.
9. Jablecki CK, Berry C, Leach J. Survival prediction in amyotrophic lateral sclerosis. Muscle Nerve. 1989;12:833-841.
THE CASE
A 39-year-old man who worked in construction presented to our clinic with complaints of muscle cramps and muscle pain that had been bothering him for several months. The cramps and pain started in both of his arms and subsequently became diffuse and generalized. He also reported an unintentional 15-pound weight loss.
His exam at that time was unremarkable. He was diagnosed with dehydration and cramping due to overexertion at work. A basic metabolic panel, hemogram, lipid panel, and thyroid stimulating hormone level were ordered. The patient’s triglyceride level, which was 227 mg/dL, was the only significant result (normal level: <150 mg/dL).
The patient’s symptoms continued to worsen until he returned to the clinic 6 months later, again complaining of muscle cramps and pain throughout his body. At that second visit, he also reported profound overall weakness and the development of diffuse muscle twitching, which his wife had observed while he was sleeping. As a result of these worrisome symptoms, he had become anxious and depressed.
A review of his medical record revealed a weight loss of about 20 pounds over the previous year. On exam, he had diffuse fasciculations in all the major muscle groups, including his tongue. The patient’s strength was 4/5 in all muscle groups. His deep tendon reflexes were 3+. He had a negative Babinski reflex (ie, he had downward facing toes with plantar stimulation), and cranial nerves II to XII were all intact. His rapid alternating movements and gait were slow.
THE DIAGNOSIS
Based on the exam, the primary diagnostic consideration for the patient was amyotrophic lateral sclerosis (ALS). Lab tests were ordered and revealed normal calcium and electrolyte levels, a normal erythrocyte sedimentation rate, a normal C-reactive protein level, and a negative test for acetylcholine receptor antibodies. However, the patient had an elevated creatine kinase level of 664 U/L (normal: 30-200 U/L). The patient was sent to a neuromuscular specialist, who identified signs of upper and lower motor neuron disease in all 4 of the patient’s extremities (he had foot drop that had not been present previously) and a very brisk jaw jerk. Along with the tongue fasciculations, the results of the specialist’s physical exam suggested ALS. Four-limb electromyography (EMG) showed widespread fasciculations and some large motor unit potentials and recruitment abnormalities, which were also consistent with ALS. It appeared that the patient’s weight loss was due to both muscle atrophy and the amount of calories burned from his constant twitching.
Extensive testing was done to rule out other potential causes of the patient’s symptoms, including magnetic resonance imaging (MRI) of the spine and brain (which was normal). In addition, the patient’s aldolase level and antineutrophil cytoplasmic antibodies were normal. The patient tested negative for human immunodeficiency virus and antibodies to double-stranded DNA. After serial neurologic exams, the final diagnosis of ALS was made.
DISCUSSION
ALS, also known as Lou Gehrig’s disease, is a degenerative motor neuron disease.1-3 The incidence in North America is 1.5 to 2.7 per 100,000 per year, and the prevalence is 2.7 to 7.4 per 100,000.4 The incidence of ALS increases with each decade of life, especially after age 40, and peaks at 74 years of age.4 The male to female ratio is 1:1.5-2.4 ALS affects upper and lower motor neurons and is progressive; however, the rate of progression and phenotype vary greatly between individuals.2 Most patients with ALS die within 2 to 5 years of onset.5
There is no specific test for ALS; the diagnosis is made clinically based on the revised El Escorial World Federation of Neurology criteria, also known as the Airlie House criteria.2,6,7 These criteria include evidence of lower motor neuron degeneration by clinical, electrophysiologic, or neuropathologic exam; evidence of upper motor neuron disease by clinical exam; progressive spread of symptoms or signs within a region or to other regions (by history or exam); and the absence of electrophysiologic, neuroimaging, or pathologic evidence of other disease processes that could explain the symptoms. If patients have evidence of upper and lower motor neuron disease, they should be reevaluated in 4 weeks to see if symptoms are improving or progressing.
Like our patient, many patients will have an elevated creatine kinase level (some with levels as high as 1000 U/L), and calcium may also be elevated because, rarely, ALS is associated with primary hyperparathyroidism.8 Electrophysiologic studies can be helpful in identifying active denervation of lower motor neurons.4,6,7
The differential diagnosis for ALS includes myasthenia gravis, inclusion-body myositis, multifocal motor neuropathy, benign fasciculations, hereditary spastic paraplegia, primary lateral sclerosis, post-polio progressive muscle atrophy, cervical spondylosis, and multiple sclerosis. A negative acetylcholine receptor antibody test will rule out myasthenia gravis, imaging of the spine can rule out cervical spondylosis, and electrophysiologic testing helps eliminate the other conditions (TABLE 14).
Treatment in specialty clinics can prolong survival
The mainstays of treatment are symptom management, multidisciplinary care (by physicians, physical/occupational/speech therapists, nutritionists, psychologists, psychotherapists, and genetic counselors), palliative care, and counseling about end-of-life issues for patients and family.1,5 Utilization of an ALS specialty clinic can provide access to all of these services and should be considered, as there is evidence that treatment in such clinics can prolong survival.5 The location of ALS specialty clinics can be found on the ALS Association’s Web site at http://www.alsa.org/community/.
Despite treatment, however, ALS is a progressive disease. The prognosis is poor, with a median survival of 2 to 5 years after diagnosis.9
The El Escorial World Federation of Neurology criteria for the diagnosis of ALS address how to treat the most common symptoms of ALS that occur as the disease progresses. These symptoms include dyspnea, muscle spasms, spasticity, sialorrhea, and pseudobulbar affect (TABLE 21,5).
Our patient was started on baclofen 10 mg 3 times per day (titrated up as needed) for muscle spasms and cramps, which resulted in some improvement of his cramps, but no improvement in the spasms. He was also started on sertraline 50 mg for anxiety and depression. His overall weakness continued to progress, and we recommended that the patient get ankle-foot orthosis braces to help with the mobility impairment caused by foot drop.
We then referred him to an ALS specialty clinic recommended by the neuromuscular specialist. The patient is now enrolled in a clinical trial designed to test a cerebrospinal fluid marker for diagnosis and for a new drug aimed at symptom management.
THE TAKEAWAY
Muscle cramps and pain are early signs of ALS. Although ALS is uncommon, patients who present with muscle cramps and muscle pain should have a creatine kinase test ordered (which, if elevated, should prompt further investigation into ALS as the possible cause). Patients should also undergo a neurologic examination to seek evidence of upper and lower motor neuron disease. They should then be reevaluated in 4 weeks to see if symptoms are improving or progressing. If no improvement is seen and symptoms are progressive, a work-up for ALS should be considered.
The mainstay of treatment for patients with ALS is multidisciplinary symptom management and palliative care. Utilization of an ALS specialty clinic should also be recommended, as it can improve survival.5
THE CASE
A 39-year-old man who worked in construction presented to our clinic with complaints of muscle cramps and muscle pain that had been bothering him for several months. The cramps and pain started in both of his arms and subsequently became diffuse and generalized. He also reported an unintentional 15-pound weight loss.
His exam at that time was unremarkable. He was diagnosed with dehydration and cramping due to overexertion at work. A basic metabolic panel, hemogram, lipid panel, and thyroid stimulating hormone level were ordered. The patient’s triglyceride level, which was 227 mg/dL, was the only significant result (normal level: <150 mg/dL).
The patient’s symptoms continued to worsen until he returned to the clinic 6 months later, again complaining of muscle cramps and pain throughout his body. At that second visit, he also reported profound overall weakness and the development of diffuse muscle twitching, which his wife had observed while he was sleeping. As a result of these worrisome symptoms, he had become anxious and depressed.
A review of his medical record revealed a weight loss of about 20 pounds over the previous year. On exam, he had diffuse fasciculations in all the major muscle groups, including his tongue. The patient’s strength was 4/5 in all muscle groups. His deep tendon reflexes were 3+. He had a negative Babinski reflex (ie, he had downward facing toes with plantar stimulation), and cranial nerves II to XII were all intact. His rapid alternating movements and gait were slow.
THE DIAGNOSIS
Based on the exam, the primary diagnostic consideration for the patient was amyotrophic lateral sclerosis (ALS). Lab tests were ordered and revealed normal calcium and electrolyte levels, a normal erythrocyte sedimentation rate, a normal C-reactive protein level, and a negative test for acetylcholine receptor antibodies. However, the patient had an elevated creatine kinase level of 664 U/L (normal: 30-200 U/L). The patient was sent to a neuromuscular specialist, who identified signs of upper and lower motor neuron disease in all 4 of the patient’s extremities (he had foot drop that had not been present previously) and a very brisk jaw jerk. Along with the tongue fasciculations, the results of the specialist’s physical exam suggested ALS. Four-limb electromyography (EMG) showed widespread fasciculations and some large motor unit potentials and recruitment abnormalities, which were also consistent with ALS. It appeared that the patient’s weight loss was due to both muscle atrophy and the amount of calories burned from his constant twitching.
Extensive testing was done to rule out other potential causes of the patient’s symptoms, including magnetic resonance imaging (MRI) of the spine and brain (which was normal). In addition, the patient’s aldolase level and antineutrophil cytoplasmic antibodies were normal. The patient tested negative for human immunodeficiency virus and antibodies to double-stranded DNA. After serial neurologic exams, the final diagnosis of ALS was made.
DISCUSSION
ALS, also known as Lou Gehrig’s disease, is a degenerative motor neuron disease.1-3 The incidence in North America is 1.5 to 2.7 per 100,000 per year, and the prevalence is 2.7 to 7.4 per 100,000.4 The incidence of ALS increases with each decade of life, especially after age 40, and peaks at 74 years of age.4 The male to female ratio is 1:1.5-2.4 ALS affects upper and lower motor neurons and is progressive; however, the rate of progression and phenotype vary greatly between individuals.2 Most patients with ALS die within 2 to 5 years of onset.5
There is no specific test for ALS; the diagnosis is made clinically based on the revised El Escorial World Federation of Neurology criteria, also known as the Airlie House criteria.2,6,7 These criteria include evidence of lower motor neuron degeneration by clinical, electrophysiologic, or neuropathologic exam; evidence of upper motor neuron disease by clinical exam; progressive spread of symptoms or signs within a region or to other regions (by history or exam); and the absence of electrophysiologic, neuroimaging, or pathologic evidence of other disease processes that could explain the symptoms. If patients have evidence of upper and lower motor neuron disease, they should be reevaluated in 4 weeks to see if symptoms are improving or progressing.
Like our patient, many patients will have an elevated creatine kinase level (some with levels as high as 1000 U/L), and calcium may also be elevated because, rarely, ALS is associated with primary hyperparathyroidism.8 Electrophysiologic studies can be helpful in identifying active denervation of lower motor neurons.4,6,7
The differential diagnosis for ALS includes myasthenia gravis, inclusion-body myositis, multifocal motor neuropathy, benign fasciculations, hereditary spastic paraplegia, primary lateral sclerosis, post-polio progressive muscle atrophy, cervical spondylosis, and multiple sclerosis. A negative acetylcholine receptor antibody test will rule out myasthenia gravis, imaging of the spine can rule out cervical spondylosis, and electrophysiologic testing helps eliminate the other conditions (TABLE 14).
Treatment in specialty clinics can prolong survival
The mainstays of treatment are symptom management, multidisciplinary care (by physicians, physical/occupational/speech therapists, nutritionists, psychologists, psychotherapists, and genetic counselors), palliative care, and counseling about end-of-life issues for patients and family.1,5 Utilization of an ALS specialty clinic can provide access to all of these services and should be considered, as there is evidence that treatment in such clinics can prolong survival.5 The location of ALS specialty clinics can be found on the ALS Association’s Web site at http://www.alsa.org/community/.
Despite treatment, however, ALS is a progressive disease. The prognosis is poor, with a median survival of 2 to 5 years after diagnosis.9
The El Escorial World Federation of Neurology criteria for the diagnosis of ALS address how to treat the most common symptoms of ALS that occur as the disease progresses. These symptoms include dyspnea, muscle spasms, spasticity, sialorrhea, and pseudobulbar affect (TABLE 21,5).
Our patient was started on baclofen 10 mg 3 times per day (titrated up as needed) for muscle spasms and cramps, which resulted in some improvement of his cramps, but no improvement in the spasms. He was also started on sertraline 50 mg for anxiety and depression. His overall weakness continued to progress, and we recommended that the patient get ankle-foot orthosis braces to help with the mobility impairment caused by foot drop.
We then referred him to an ALS specialty clinic recommended by the neuromuscular specialist. The patient is now enrolled in a clinical trial designed to test a cerebrospinal fluid marker for diagnosis and for a new drug aimed at symptom management.
THE TAKEAWAY
Muscle cramps and pain are early signs of ALS. Although ALS is uncommon, patients who present with muscle cramps and muscle pain should have a creatine kinase test ordered (which, if elevated, should prompt further investigation into ALS as the possible cause). Patients should also undergo a neurologic examination to seek evidence of upper and lower motor neuron disease. They should then be reevaluated in 4 weeks to see if symptoms are improving or progressing. If no improvement is seen and symptoms are progressive, a work-up for ALS should be considered.
The mainstay of treatment for patients with ALS is multidisciplinary symptom management and palliative care. Utilization of an ALS specialty clinic should also be recommended, as it can improve survival.5
1. Miller RG, Gelinas D, O’Connor P. Amyotrophic Lateral Sclerosis: American Academy of Neurology Press Quality of Life Guide Series. Demos Medical Publishing; 2004.
2. Simon NG, Turner MR, Vucic S, et al. Quantifying disease progression in amyotrophic lateral sclerosis. Ann Neurol. 2014;76:643-657.
3. Worms PM. The epidemiology of motor neuron diseases: a review of recent studies. J Neurol Sci. 2001;191:3-9.
4. Shaw PJ. ALS and other motor neuron diseases. In: Goldman L, Schafer AI, eds. Goldman’s Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 418.
5. Miller RG, Jackson CE, Kasarskis EJ, et al. Practice Parameter update: The Care of the Patient with Amyotrophic Lateral Sclerosis: Multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2009;73:1227-1233.
6. Brooks BR. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial “Clinical limits of amyotrophic lateral sclerosis” workshop contributors. J Neurol Sci. 1994;124:96-107.
7. Brooks BR, Miller RG, Swash M, et al; World Federation of Neurology Research Group on Motor Neuron Diseases. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293-299.
8. Jackson CE, Amato AA, Bryan WW, et al. Primary hyperparathyroidism and ALS: is there a relation? Neurology. 1998;50:1795-1799.
9. Jablecki CK, Berry C, Leach J. Survival prediction in amyotrophic lateral sclerosis. Muscle Nerve. 1989;12:833-841.
1. Miller RG, Gelinas D, O’Connor P. Amyotrophic Lateral Sclerosis: American Academy of Neurology Press Quality of Life Guide Series. Demos Medical Publishing; 2004.
2. Simon NG, Turner MR, Vucic S, et al. Quantifying disease progression in amyotrophic lateral sclerosis. Ann Neurol. 2014;76:643-657.
3. Worms PM. The epidemiology of motor neuron diseases: a review of recent studies. J Neurol Sci. 2001;191:3-9.
4. Shaw PJ. ALS and other motor neuron diseases. In: Goldman L, Schafer AI, eds. Goldman’s Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 418.
5. Miller RG, Jackson CE, Kasarskis EJ, et al. Practice Parameter update: The Care of the Patient with Amyotrophic Lateral Sclerosis: Multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2009;73:1227-1233.
6. Brooks BR. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial “Clinical limits of amyotrophic lateral sclerosis” workshop contributors. J Neurol Sci. 1994;124:96-107.
7. Brooks BR, Miller RG, Swash M, et al; World Federation of Neurology Research Group on Motor Neuron Diseases. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293-299.
8. Jackson CE, Amato AA, Bryan WW, et al. Primary hyperparathyroidism and ALS: is there a relation? Neurology. 1998;50:1795-1799.
9. Jablecki CK, Berry C, Leach J. Survival prediction in amyotrophic lateral sclerosis. Muscle Nerve. 1989;12:833-841.