User login
Brain abscesses in a 60-year-old man
A 60-year-old man with hypertension and persistent atrial fibrillation refractory to radiofrequency ablation was brought to the hospital in status epilepticus requiring intubation. His wife said that during the past month he had experienced a number of episodic seizures, but due to his busy work schedule he had not sought medical attention. He had also been hospitalized 3 times during the past week for chills, tremors, and fevers with temperatures up to 101°F (38.3°C), and his symptoms had been ascribed to the amiodarone he had been taking for the past 11 days for atrial fibrillation. The amiodarone dose had been decreased to half a tablet after the first 7 days, but his symptoms had continued.
When the patient was able to speak, he denied intravenous drug abuse and claimed to be up to date with vaccinations. Colonoscopy 10 years earlier had been negative. He has no pets, but says that there are stray cats around his home and that he has had contact with cat feces while gardening. He works as a diesel mechanic and is exposed to motor oil and diesel fuel, but denies any direct exposure to carcinogenic chemicals.
On admission, his temperature was 37.7°C (99.9°F), blood pressure 92/69 mm Hg, heart rate 96 beats per minute, respiratory rate 21 per minute, and oxygen saturation 95% on room air and 100% on oxygen at 2 L per minute.
Decerebrate posturing and forced left visual gaze deviation was observed. Oral examination revealed severe decay of multiple teeth, with some teeth broken down to the level of the gingiva, and moderate generalized periodontal disease with heavy plaque and calculi in the gingiva.
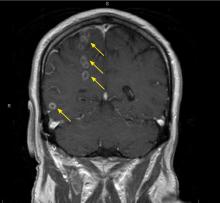
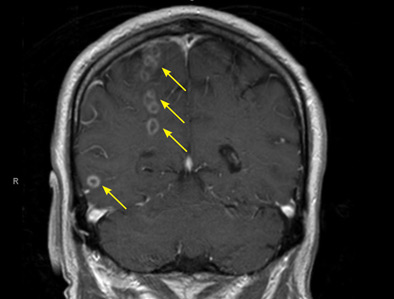
The differential diagnosis for intracranial ring-enhancing lesions includes metastasis, abscess, infection in an immunocompromised state (eg, toxoplasmosis), glioblastoma, subacute infarct, neurocysticercosis, lymphoma, demyelination, and resolving hematoma. In our patient, further testing to narrow the differential included lumbar puncture, with results within normal limits, and transthoracic echocardiography, which was negative for endocarditis. A biopsy obtained by craniotomy confirmed the diagnosis of abscess surrounded by reactive glioses.
During his hospitalization, the patient’s antiseizure regimen was lorazepam 1 to 2 mg as needed, levetiracetam 1,500 mg twice daily, and fosphenytoin infusion at 100 mg phenytoin sodium equivalents per minute. Initial antibiotic therapy included ampicillin 2 g intravenously (IV) 4 times daily.
Because of persistent nocturnal fevers with temperatures ranging from 37.8°C (100°F) to 41.2°C (106.2°F), antibiotic coverage was broadened to meropenem 2 g IV every 8 hours. Testing for Toxoplasma gondii, human immunodeficiency virus, and JC polyomavirus was negative. Cerebrospinal fluid culture and abscess cultures were also negative. Blood cultures were eventually positive for Peptostreptococcus micros and Streptococcus constellatus. Based on review of culture results, antibiotic therapy was switched to ceftriaxone 2 g IV twice daily and metronidazole 500 mg IV 3 times daily.
For the dental infection, the patient underwent surgical irrigation and debridement with full dental extraction for multiple dental abscesses.
His regimen for seizure control was changed to phenytoin and valproic acid, and he was discharged in stable condition on the following drug regimen: ceftriaxone 2 g IV twice daily, metronidazole 500 mg IV 3 times daily for 6 weeks, levetiracetam 1,500 mg twice daily, and valproic acid 750 mg 3 times daily.
At a 3-month follow-up visit, he reported no seizure-like activity but demonstrated persistent neurologic deficits (dysdiadochokinesia and mild ataxia).
A LESS COMMON CAUSE OF BRAIN ABSCESS
In the United States, 1,500 to 2,000 cases of brain abscess are diagnosed every year, and this condition is responsible for an estimated 1 in 10,000 hospitalizations. Most patients hospitalized are men over age 60 or children. Most patients with hematogenous or embolic spread of infection from a primary infection source are immunocompromised.
However, the lesions in our patient were not from compromised immunity, but rather from septic hematogenous spread of an odontogenic infection. Odontogenic bacteria are a common cause of pyogenic orofascial infection, including periapical abscess and infection of adjoining fascial spaces of the head and neck.1
P micros and S constellatus have been commonly found in many types of odontogenic infection, including dentoalveolar infection, periodontitis, and pericoronitis.2 Our patient was found to have several periodontal abscesses with bacteremia and spread to the brain. Although transthoracic echocardiography was negative for vegetations or patent foramen ovale, the quality and location of the brain abscesses suggested embolic spread of infection. Most of the suspected septic emboli were in the right hemisphere, consistent with patterns seen with cardioembolic phenomena, and a number of lesions appeared to be within the distribution of the right anterior cerebral artery and the middle cerebral artery.
EMPIRIC AND SPECIFIC THERAPIES
Empiric antibiotic therapy for local odontogenic infection includes amoxicillin with clavulanic acid and metronidazole.1 Our patient’s treatment with ceftriaxone and metronidazole was based on the species and sensitivities of the bacteria in blood cultures.
Surgical irrigation with debridement is considered first-line therapy for local dental infection, with antimicrobials as adjunctive therapy. Initiation of antibiotic therapy before surgery has been associated with a shortened duration of infection and a reduced risk of bacteremia.3
First-line therapy for cerebral abscess is typically antibiotics, specifically ceftriaxone and metronidazole as in our patient. Ceftriaxone is selected for coverage against streptococci, enterobacteriacae, and most common anaerobes, whereas metronidazole is chosen for its efficacy against Bacteroides fragilis.
Computed tomography-guided stereotactic aspiration and open drainage are viable options for solitary and surgically accessible abscesses—typically those greater than 2 cm. Our patient had multiple small septic emboli in the right hemisphere, with the largest lesion measuring 1.5 cm, thus limiting the effectiveness of surgical intervention.
Some patients with mass effect or other evidence of increased intracranial pressure may benefit from high doses of a corticosteroid such as dexamethasone. However, since our patient had no clinical or diagnostic findings suggesting elevated intracranial pressure, we opted for nonsurgical management of the brain abscesses, with 6 weeks of intravenous antibiotics, an antiseizure regimen, and plans for repeat imaging in the outpatient setting.
- Bahl R, Sandhu S, Singh K, Sahai N, Gupta M. Odontogenic infections: microbiology and management. Contemp Clin Dent 2014; 5(3):307–311. doi:10.4103/0976-237X.137921
- Kuriyama T, Karasawa T, Nakagawa K, Yamamoto E, Nakamura S. Bacteriology and antimicrobial susceptibility of gram-positive cocci isolated from pus specimens of orofacial odontogenic infections. Oral Microbiol Immunol 2002; 17(2):132–135. pmid:11929563
- Peedikayil FC. Antibiotics in odontogenic infections—an update. J Antimicro 2016; 2:(2)117. doi:10.4172/2472-1212.1000117
A 60-year-old man with hypertension and persistent atrial fibrillation refractory to radiofrequency ablation was brought to the hospital in status epilepticus requiring intubation. His wife said that during the past month he had experienced a number of episodic seizures, but due to his busy work schedule he had not sought medical attention. He had also been hospitalized 3 times during the past week for chills, tremors, and fevers with temperatures up to 101°F (38.3°C), and his symptoms had been ascribed to the amiodarone he had been taking for the past 11 days for atrial fibrillation. The amiodarone dose had been decreased to half a tablet after the first 7 days, but his symptoms had continued.
When the patient was able to speak, he denied intravenous drug abuse and claimed to be up to date with vaccinations. Colonoscopy 10 years earlier had been negative. He has no pets, but says that there are stray cats around his home and that he has had contact with cat feces while gardening. He works as a diesel mechanic and is exposed to motor oil and diesel fuel, but denies any direct exposure to carcinogenic chemicals.
On admission, his temperature was 37.7°C (99.9°F), blood pressure 92/69 mm Hg, heart rate 96 beats per minute, respiratory rate 21 per minute, and oxygen saturation 95% on room air and 100% on oxygen at 2 L per minute.
Decerebrate posturing and forced left visual gaze deviation was observed. Oral examination revealed severe decay of multiple teeth, with some teeth broken down to the level of the gingiva, and moderate generalized periodontal disease with heavy plaque and calculi in the gingiva.
The differential diagnosis for intracranial ring-enhancing lesions includes metastasis, abscess, infection in an immunocompromised state (eg, toxoplasmosis), glioblastoma, subacute infarct, neurocysticercosis, lymphoma, demyelination, and resolving hematoma. In our patient, further testing to narrow the differential included lumbar puncture, with results within normal limits, and transthoracic echocardiography, which was negative for endocarditis. A biopsy obtained by craniotomy confirmed the diagnosis of abscess surrounded by reactive glioses.
During his hospitalization, the patient’s antiseizure regimen was lorazepam 1 to 2 mg as needed, levetiracetam 1,500 mg twice daily, and fosphenytoin infusion at 100 mg phenytoin sodium equivalents per minute. Initial antibiotic therapy included ampicillin 2 g intravenously (IV) 4 times daily.
Because of persistent nocturnal fevers with temperatures ranging from 37.8°C (100°F) to 41.2°C (106.2°F), antibiotic coverage was broadened to meropenem 2 g IV every 8 hours. Testing for Toxoplasma gondii, human immunodeficiency virus, and JC polyomavirus was negative. Cerebrospinal fluid culture and abscess cultures were also negative. Blood cultures were eventually positive for Peptostreptococcus micros and Streptococcus constellatus. Based on review of culture results, antibiotic therapy was switched to ceftriaxone 2 g IV twice daily and metronidazole 500 mg IV 3 times daily.
For the dental infection, the patient underwent surgical irrigation and debridement with full dental extraction for multiple dental abscesses.
His regimen for seizure control was changed to phenytoin and valproic acid, and he was discharged in stable condition on the following drug regimen: ceftriaxone 2 g IV twice daily, metronidazole 500 mg IV 3 times daily for 6 weeks, levetiracetam 1,500 mg twice daily, and valproic acid 750 mg 3 times daily.
At a 3-month follow-up visit, he reported no seizure-like activity but demonstrated persistent neurologic deficits (dysdiadochokinesia and mild ataxia).
A LESS COMMON CAUSE OF BRAIN ABSCESS
In the United States, 1,500 to 2,000 cases of brain abscess are diagnosed every year, and this condition is responsible for an estimated 1 in 10,000 hospitalizations. Most patients hospitalized are men over age 60 or children. Most patients with hematogenous or embolic spread of infection from a primary infection source are immunocompromised.
However, the lesions in our patient were not from compromised immunity, but rather from septic hematogenous spread of an odontogenic infection. Odontogenic bacteria are a common cause of pyogenic orofascial infection, including periapical abscess and infection of adjoining fascial spaces of the head and neck.1
P micros and S constellatus have been commonly found in many types of odontogenic infection, including dentoalveolar infection, periodontitis, and pericoronitis.2 Our patient was found to have several periodontal abscesses with bacteremia and spread to the brain. Although transthoracic echocardiography was negative for vegetations or patent foramen ovale, the quality and location of the brain abscesses suggested embolic spread of infection. Most of the suspected septic emboli were in the right hemisphere, consistent with patterns seen with cardioembolic phenomena, and a number of lesions appeared to be within the distribution of the right anterior cerebral artery and the middle cerebral artery.
EMPIRIC AND SPECIFIC THERAPIES
Empiric antibiotic therapy for local odontogenic infection includes amoxicillin with clavulanic acid and metronidazole.1 Our patient’s treatment with ceftriaxone and metronidazole was based on the species and sensitivities of the bacteria in blood cultures.
Surgical irrigation with debridement is considered first-line therapy for local dental infection, with antimicrobials as adjunctive therapy. Initiation of antibiotic therapy before surgery has been associated with a shortened duration of infection and a reduced risk of bacteremia.3
First-line therapy for cerebral abscess is typically antibiotics, specifically ceftriaxone and metronidazole as in our patient. Ceftriaxone is selected for coverage against streptococci, enterobacteriacae, and most common anaerobes, whereas metronidazole is chosen for its efficacy against Bacteroides fragilis.
Computed tomography-guided stereotactic aspiration and open drainage are viable options for solitary and surgically accessible abscesses—typically those greater than 2 cm. Our patient had multiple small septic emboli in the right hemisphere, with the largest lesion measuring 1.5 cm, thus limiting the effectiveness of surgical intervention.
Some patients with mass effect or other evidence of increased intracranial pressure may benefit from high doses of a corticosteroid such as dexamethasone. However, since our patient had no clinical or diagnostic findings suggesting elevated intracranial pressure, we opted for nonsurgical management of the brain abscesses, with 6 weeks of intravenous antibiotics, an antiseizure regimen, and plans for repeat imaging in the outpatient setting.
A 60-year-old man with hypertension and persistent atrial fibrillation refractory to radiofrequency ablation was brought to the hospital in status epilepticus requiring intubation. His wife said that during the past month he had experienced a number of episodic seizures, but due to his busy work schedule he had not sought medical attention. He had also been hospitalized 3 times during the past week for chills, tremors, and fevers with temperatures up to 101°F (38.3°C), and his symptoms had been ascribed to the amiodarone he had been taking for the past 11 days for atrial fibrillation. The amiodarone dose had been decreased to half a tablet after the first 7 days, but his symptoms had continued.
When the patient was able to speak, he denied intravenous drug abuse and claimed to be up to date with vaccinations. Colonoscopy 10 years earlier had been negative. He has no pets, but says that there are stray cats around his home and that he has had contact with cat feces while gardening. He works as a diesel mechanic and is exposed to motor oil and diesel fuel, but denies any direct exposure to carcinogenic chemicals.
On admission, his temperature was 37.7°C (99.9°F), blood pressure 92/69 mm Hg, heart rate 96 beats per minute, respiratory rate 21 per minute, and oxygen saturation 95% on room air and 100% on oxygen at 2 L per minute.
Decerebrate posturing and forced left visual gaze deviation was observed. Oral examination revealed severe decay of multiple teeth, with some teeth broken down to the level of the gingiva, and moderate generalized periodontal disease with heavy plaque and calculi in the gingiva.
The differential diagnosis for intracranial ring-enhancing lesions includes metastasis, abscess, infection in an immunocompromised state (eg, toxoplasmosis), glioblastoma, subacute infarct, neurocysticercosis, lymphoma, demyelination, and resolving hematoma. In our patient, further testing to narrow the differential included lumbar puncture, with results within normal limits, and transthoracic echocardiography, which was negative for endocarditis. A biopsy obtained by craniotomy confirmed the diagnosis of abscess surrounded by reactive glioses.
During his hospitalization, the patient’s antiseizure regimen was lorazepam 1 to 2 mg as needed, levetiracetam 1,500 mg twice daily, and fosphenytoin infusion at 100 mg phenytoin sodium equivalents per minute. Initial antibiotic therapy included ampicillin 2 g intravenously (IV) 4 times daily.
Because of persistent nocturnal fevers with temperatures ranging from 37.8°C (100°F) to 41.2°C (106.2°F), antibiotic coverage was broadened to meropenem 2 g IV every 8 hours. Testing for Toxoplasma gondii, human immunodeficiency virus, and JC polyomavirus was negative. Cerebrospinal fluid culture and abscess cultures were also negative. Blood cultures were eventually positive for Peptostreptococcus micros and Streptococcus constellatus. Based on review of culture results, antibiotic therapy was switched to ceftriaxone 2 g IV twice daily and metronidazole 500 mg IV 3 times daily.
For the dental infection, the patient underwent surgical irrigation and debridement with full dental extraction for multiple dental abscesses.
His regimen for seizure control was changed to phenytoin and valproic acid, and he was discharged in stable condition on the following drug regimen: ceftriaxone 2 g IV twice daily, metronidazole 500 mg IV 3 times daily for 6 weeks, levetiracetam 1,500 mg twice daily, and valproic acid 750 mg 3 times daily.
At a 3-month follow-up visit, he reported no seizure-like activity but demonstrated persistent neurologic deficits (dysdiadochokinesia and mild ataxia).
A LESS COMMON CAUSE OF BRAIN ABSCESS
In the United States, 1,500 to 2,000 cases of brain abscess are diagnosed every year, and this condition is responsible for an estimated 1 in 10,000 hospitalizations. Most patients hospitalized are men over age 60 or children. Most patients with hematogenous or embolic spread of infection from a primary infection source are immunocompromised.
However, the lesions in our patient were not from compromised immunity, but rather from septic hematogenous spread of an odontogenic infection. Odontogenic bacteria are a common cause of pyogenic orofascial infection, including periapical abscess and infection of adjoining fascial spaces of the head and neck.1
P micros and S constellatus have been commonly found in many types of odontogenic infection, including dentoalveolar infection, periodontitis, and pericoronitis.2 Our patient was found to have several periodontal abscesses with bacteremia and spread to the brain. Although transthoracic echocardiography was negative for vegetations or patent foramen ovale, the quality and location of the brain abscesses suggested embolic spread of infection. Most of the suspected septic emboli were in the right hemisphere, consistent with patterns seen with cardioembolic phenomena, and a number of lesions appeared to be within the distribution of the right anterior cerebral artery and the middle cerebral artery.
EMPIRIC AND SPECIFIC THERAPIES
Empiric antibiotic therapy for local odontogenic infection includes amoxicillin with clavulanic acid and metronidazole.1 Our patient’s treatment with ceftriaxone and metronidazole was based on the species and sensitivities of the bacteria in blood cultures.
Surgical irrigation with debridement is considered first-line therapy for local dental infection, with antimicrobials as adjunctive therapy. Initiation of antibiotic therapy before surgery has been associated with a shortened duration of infection and a reduced risk of bacteremia.3
First-line therapy for cerebral abscess is typically antibiotics, specifically ceftriaxone and metronidazole as in our patient. Ceftriaxone is selected for coverage against streptococci, enterobacteriacae, and most common anaerobes, whereas metronidazole is chosen for its efficacy against Bacteroides fragilis.
Computed tomography-guided stereotactic aspiration and open drainage are viable options for solitary and surgically accessible abscesses—typically those greater than 2 cm. Our patient had multiple small septic emboli in the right hemisphere, with the largest lesion measuring 1.5 cm, thus limiting the effectiveness of surgical intervention.
Some patients with mass effect or other evidence of increased intracranial pressure may benefit from high doses of a corticosteroid such as dexamethasone. However, since our patient had no clinical or diagnostic findings suggesting elevated intracranial pressure, we opted for nonsurgical management of the brain abscesses, with 6 weeks of intravenous antibiotics, an antiseizure regimen, and plans for repeat imaging in the outpatient setting.
- Bahl R, Sandhu S, Singh K, Sahai N, Gupta M. Odontogenic infections: microbiology and management. Contemp Clin Dent 2014; 5(3):307–311. doi:10.4103/0976-237X.137921
- Kuriyama T, Karasawa T, Nakagawa K, Yamamoto E, Nakamura S. Bacteriology and antimicrobial susceptibility of gram-positive cocci isolated from pus specimens of orofacial odontogenic infections. Oral Microbiol Immunol 2002; 17(2):132–135. pmid:11929563
- Peedikayil FC. Antibiotics in odontogenic infections—an update. J Antimicro 2016; 2:(2)117. doi:10.4172/2472-1212.1000117
- Bahl R, Sandhu S, Singh K, Sahai N, Gupta M. Odontogenic infections: microbiology and management. Contemp Clin Dent 2014; 5(3):307–311. doi:10.4103/0976-237X.137921
- Kuriyama T, Karasawa T, Nakagawa K, Yamamoto E, Nakamura S. Bacteriology and antimicrobial susceptibility of gram-positive cocci isolated from pus specimens of orofacial odontogenic infections. Oral Microbiol Immunol 2002; 17(2):132–135. pmid:11929563
- Peedikayil FC. Antibiotics in odontogenic infections—an update. J Antimicro 2016; 2:(2)117. doi:10.4172/2472-1212.1000117