User login
How to use the core competencies in hospital medicine: A framework for curriculum development
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
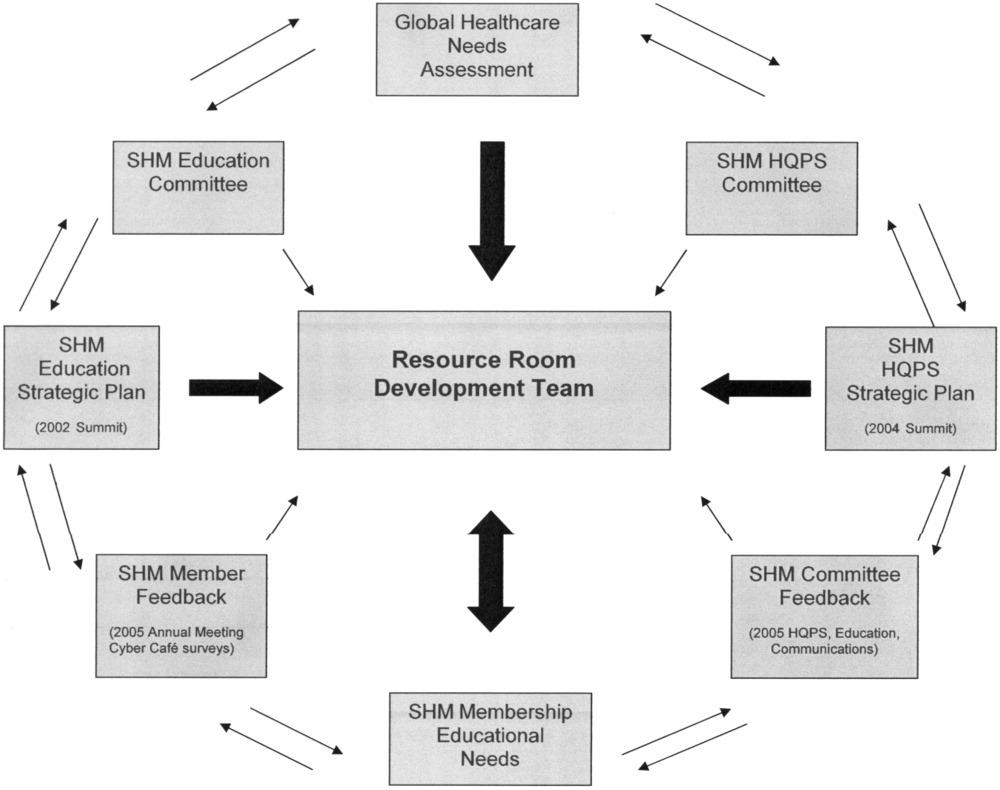
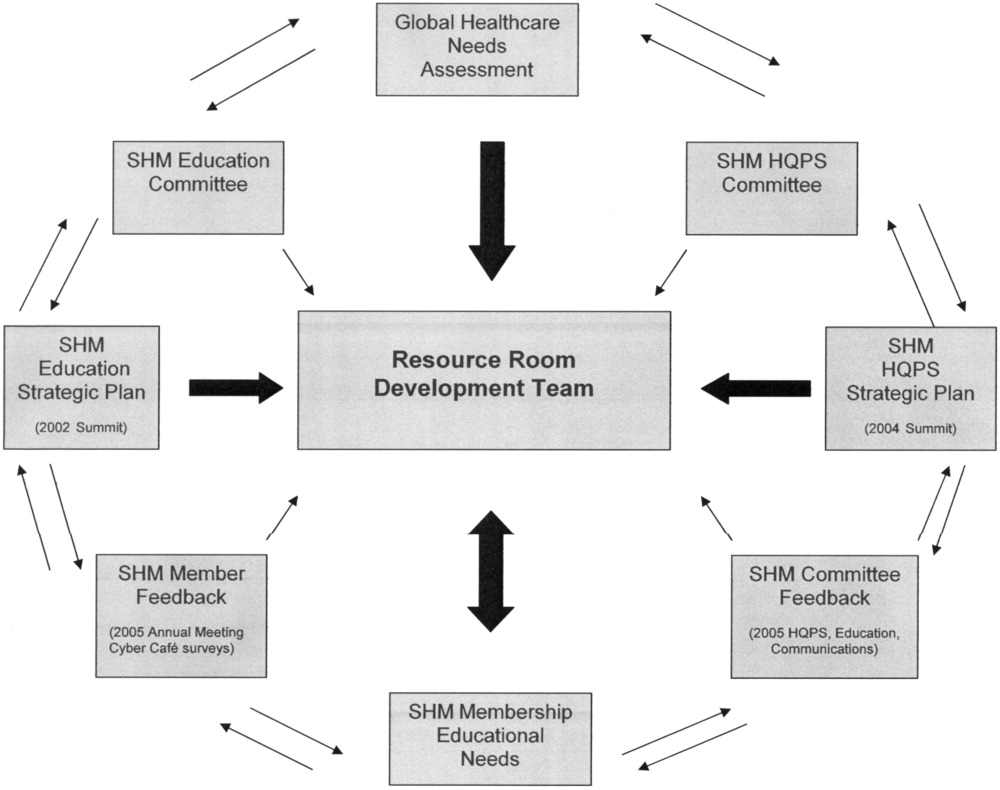
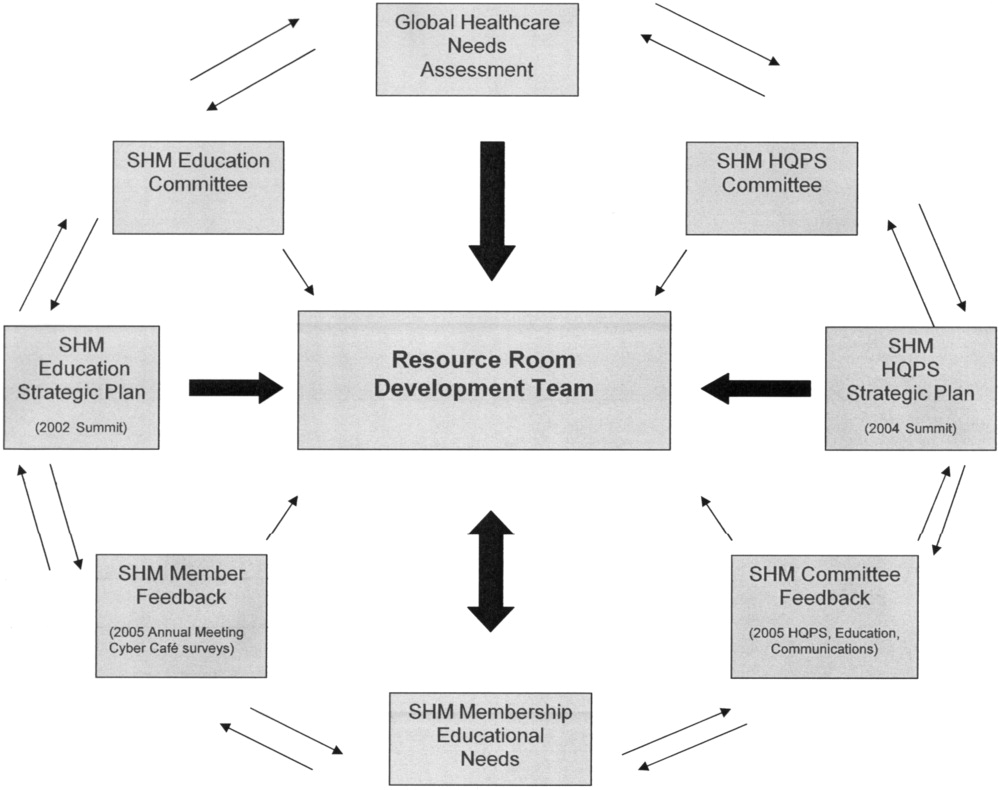
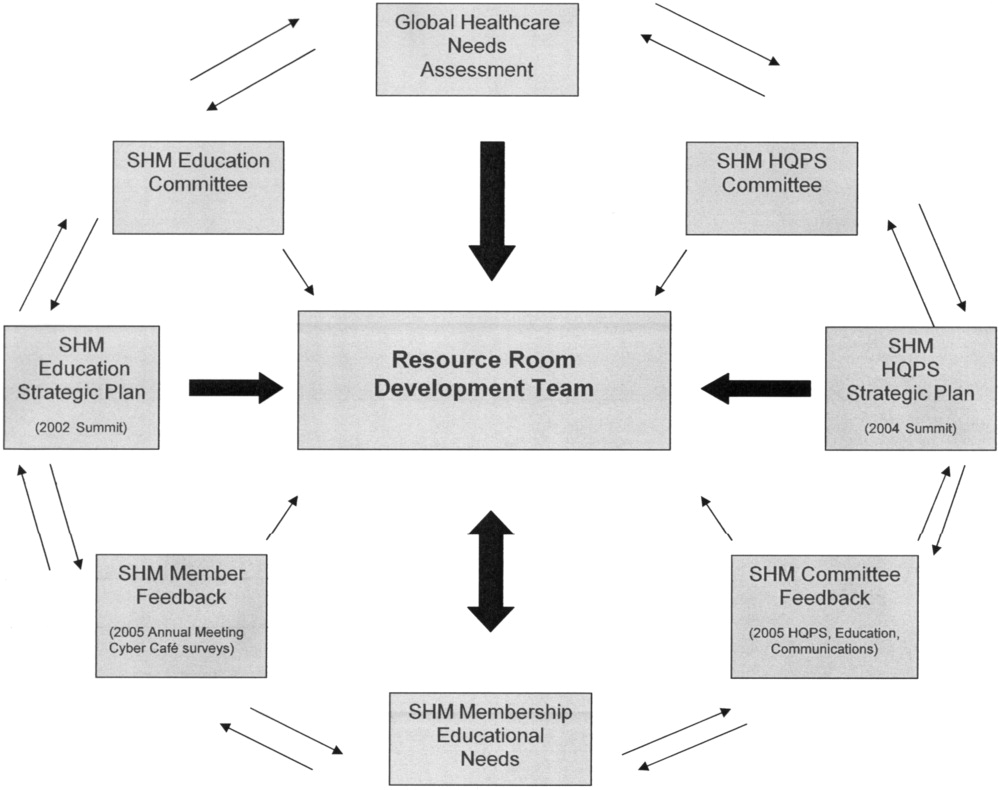
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: The focus of traditional medical education. |
| How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. | |
| Didactic lectures on the pathophysiology of VTE .rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional research | Research Questions |
| Identifying barriers to VTE prophylaxis in the hospital setting. | |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for improvement | Quality issues in the transfer of care. |
| Failure to review radiographic study. | |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other members of the inpatient team | The Current Approach: Inherent discontinuities of inpatient care. |
| ACGME legislated work hours: resident shifts. | |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for additional research | Research Questions |
| What are the key components of the sign‐out process? | |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: Problems with the work environment |
| Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. | |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org [accessed November2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org [accessed November2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL: http://www.med‐ed‐online.org/pdf/f0000040.pdf [accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org [accessed November2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: The focus of traditional medical education. |
| How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. | |
| Didactic lectures on the pathophysiology of VTE .rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional research | Research Questions |
| Identifying barriers to VTE prophylaxis in the hospital setting. | |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for improvement | Quality issues in the transfer of care. |
| Failure to review radiographic study. | |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other members of the inpatient team | The Current Approach: Inherent discontinuities of inpatient care. |
| ACGME legislated work hours: resident shifts. | |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for additional research | Research Questions |
| What are the key components of the sign‐out process? | |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: Problems with the work environment |
| Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. | |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
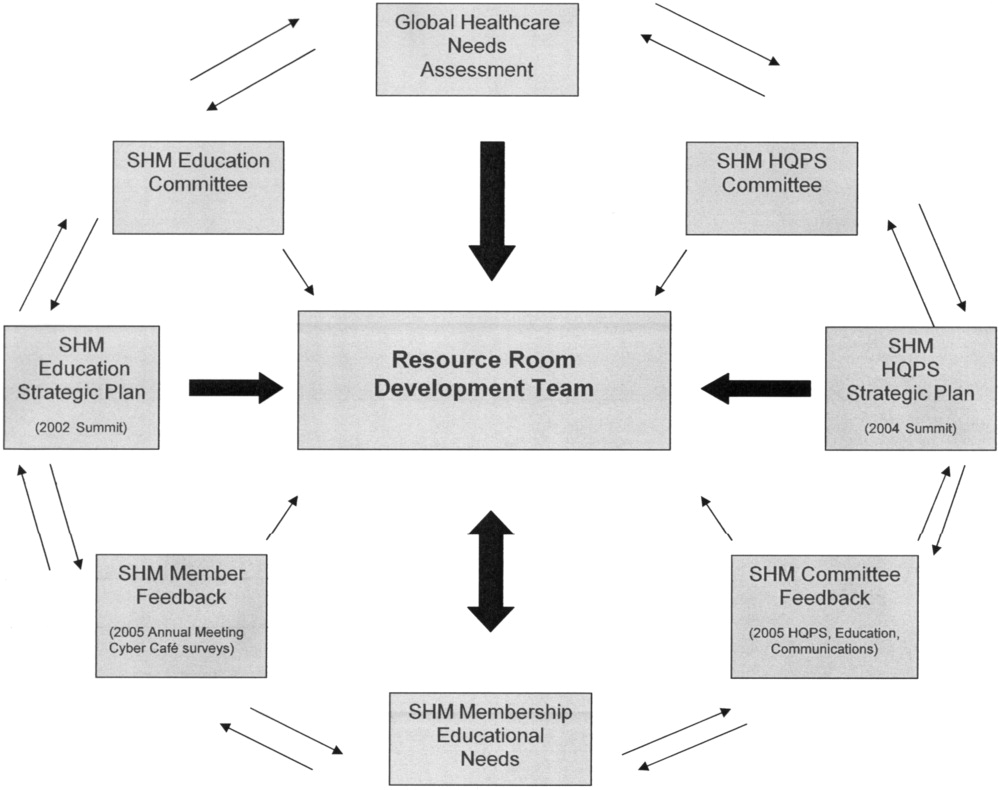
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: The focus of traditional medical education. |
| How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. | |
| Didactic lectures on the pathophysiology of VTE .rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional research | Research Questions |
| Identifying barriers to VTE prophylaxis in the hospital setting. | |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for improvement | Quality issues in the transfer of care. |
| Failure to review radiographic study. | |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other members of the inpatient team | The Current Approach: Inherent discontinuities of inpatient care. |
| ACGME legislated work hours: resident shifts. | |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for additional research | Research Questions |
| What are the key components of the sign‐out process? | |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: Problems with the work environment |
| Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. | |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org [accessed November2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org [accessed November2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL: http://www.med‐ed‐online.org/pdf/f0000040.pdf [accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org [accessed November2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org [accessed November2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org [accessed November2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL: http://www.med‐ed‐online.org/pdf/f0000040.pdf [accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org [accessed November2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
Copyright © 2006 Society of Hospital Medicine
Core competencies in hospital medicine: Development and methodology
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
| Acute Coronary Syndrome | Arthrocentesis | Care of the Elderly Patient |
| Acute Renal Failure | Chest Radiograph Interpretation | Care of Vulnerable Populations |
| Alcohol and Drug Withdrawal | Electrocardiogram Interpretation | Communication |
| Asthma | Emergency Procedures | Diagnostic Decision Making |
| Cardiac Arrhythmia | Lumbar Puncture | Drug Safety, Pharmacoeconomics and Pharmacoepidemiology |
| Cellulitis | Paracentesis | Equitable Allocation of Resources |
| Chronic Obstructive Pulmonary Disease | Thoracentesis | Evidence‐Based Medicine |
| Community‐Acquired Pneumonia | Vascular Access | Hospitalist as Consultant |
| Congestive Heart Failure | Hospitalist as Teacher | |
| Delirium and Dementia | Information Management | |
| Diabetes Mellitus | Leadership | |
| Gastrointestinal Bleed | Management Practices | |
| Hospital‐Acquired Pneumonia | Nutrition and the Hospitalized Patient | |
| Pain Management | Palliative Care | |
| Perioperative Medicine | Patient Education | |
| Sepsis Syndrome | Patient Handoff | |
| Stroke | Patient Safety | |
| Urinary Tract Infection | Practice‐Based Learning and Improvement | |
| Venous Thromboembolism | Prevention of HealthcareAssociated Infections and Antimicrobial Resistance | |
| Professionalism and Medical Ethics | ||
| Quality Improvement | ||
| Risk Management | ||
| Team Approach and Multidisciplinary Care | ||
| Transitions of Care | ||
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org [accessed July 22,2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
| Acute Coronary Syndrome | Arthrocentesis | Care of the Elderly Patient |
| Acute Renal Failure | Chest Radiograph Interpretation | Care of Vulnerable Populations |
| Alcohol and Drug Withdrawal | Electrocardiogram Interpretation | Communication |
| Asthma | Emergency Procedures | Diagnostic Decision Making |
| Cardiac Arrhythmia | Lumbar Puncture | Drug Safety, Pharmacoeconomics and Pharmacoepidemiology |
| Cellulitis | Paracentesis | Equitable Allocation of Resources |
| Chronic Obstructive Pulmonary Disease | Thoracentesis | Evidence‐Based Medicine |
| Community‐Acquired Pneumonia | Vascular Access | Hospitalist as Consultant |
| Congestive Heart Failure | Hospitalist as Teacher | |
| Delirium and Dementia | Information Management | |
| Diabetes Mellitus | Leadership | |
| Gastrointestinal Bleed | Management Practices | |
| Hospital‐Acquired Pneumonia | Nutrition and the Hospitalized Patient | |
| Pain Management | Palliative Care | |
| Perioperative Medicine | Patient Education | |
| Sepsis Syndrome | Patient Handoff | |
| Stroke | Patient Safety | |
| Urinary Tract Infection | Practice‐Based Learning and Improvement | |
| Venous Thromboembolism | Prevention of HealthcareAssociated Infections and Antimicrobial Resistance | |
| Professionalism and Medical Ethics | ||
| Quality Improvement | ||
| Risk Management | ||
| Team Approach and Multidisciplinary Care | ||
| Transitions of Care | ||
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
| Acute Coronary Syndrome | Arthrocentesis | Care of the Elderly Patient |
| Acute Renal Failure | Chest Radiograph Interpretation | Care of Vulnerable Populations |
| Alcohol and Drug Withdrawal | Electrocardiogram Interpretation | Communication |
| Asthma | Emergency Procedures | Diagnostic Decision Making |
| Cardiac Arrhythmia | Lumbar Puncture | Drug Safety, Pharmacoeconomics and Pharmacoepidemiology |
| Cellulitis | Paracentesis | Equitable Allocation of Resources |
| Chronic Obstructive Pulmonary Disease | Thoracentesis | Evidence‐Based Medicine |
| Community‐Acquired Pneumonia | Vascular Access | Hospitalist as Consultant |
| Congestive Heart Failure | Hospitalist as Teacher | |
| Delirium and Dementia | Information Management | |
| Diabetes Mellitus | Leadership | |
| Gastrointestinal Bleed | Management Practices | |
| Hospital‐Acquired Pneumonia | Nutrition and the Hospitalized Patient | |
| Pain Management | Palliative Care | |
| Perioperative Medicine | Patient Education | |
| Sepsis Syndrome | Patient Handoff | |
| Stroke | Patient Safety | |
| Urinary Tract Infection | Practice‐Based Learning and Improvement | |
| Venous Thromboembolism | Prevention of HealthcareAssociated Infections and Antimicrobial Resistance | |
| Professionalism and Medical Ethics | ||
| Quality Improvement | ||
| Risk Management | ||
| Team Approach and Multidisciplinary Care | ||
| Transitions of Care | ||
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org [accessed July 22,2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org [accessed July 22,2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
Copyright © 2006 Society of Hospital Medicine
How to Use The Core Competencies
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
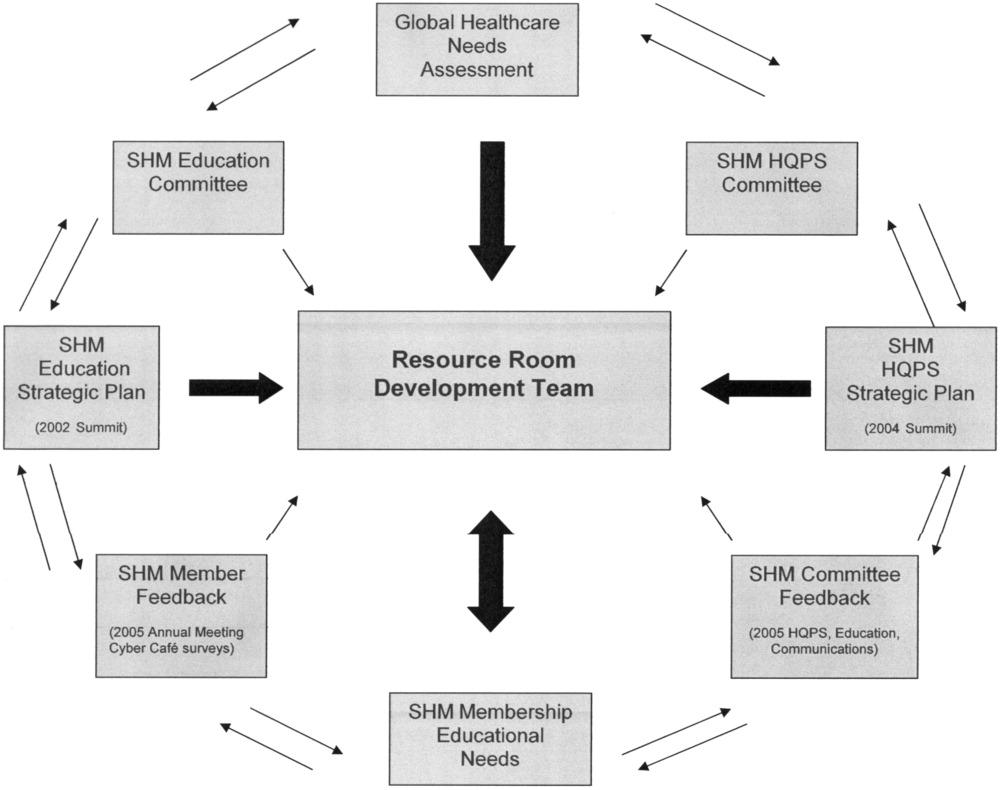
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other | The Current Approach: The focus of traditional medical education. |
| members of the inpatient team | How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. |
| Didactic lectures on the pathophysiology of VTE. rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional | Research Questions |
| research | Identifying barriers to VTE prophylaxis in the hospital setting. |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for | Quality issues in the transfer of care. |
| improvement | Failure to review radiographic study. |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other | The Current Approach: Inherent discontinuities of inpatient care. |
| embers of the inpatient team | ACGME legislated work hours: resident shifts. |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for | Research Questions |
| additional research | What are the key components of the sign‐out process? |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members | The Current Approach: Problems with the work environment |
| of the inpatient team | Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org[accessed November 2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org[accessed November 2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL:http://www.med‐ed‐online.org/pdf/f0000040.pdf[accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org[accessed November 2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
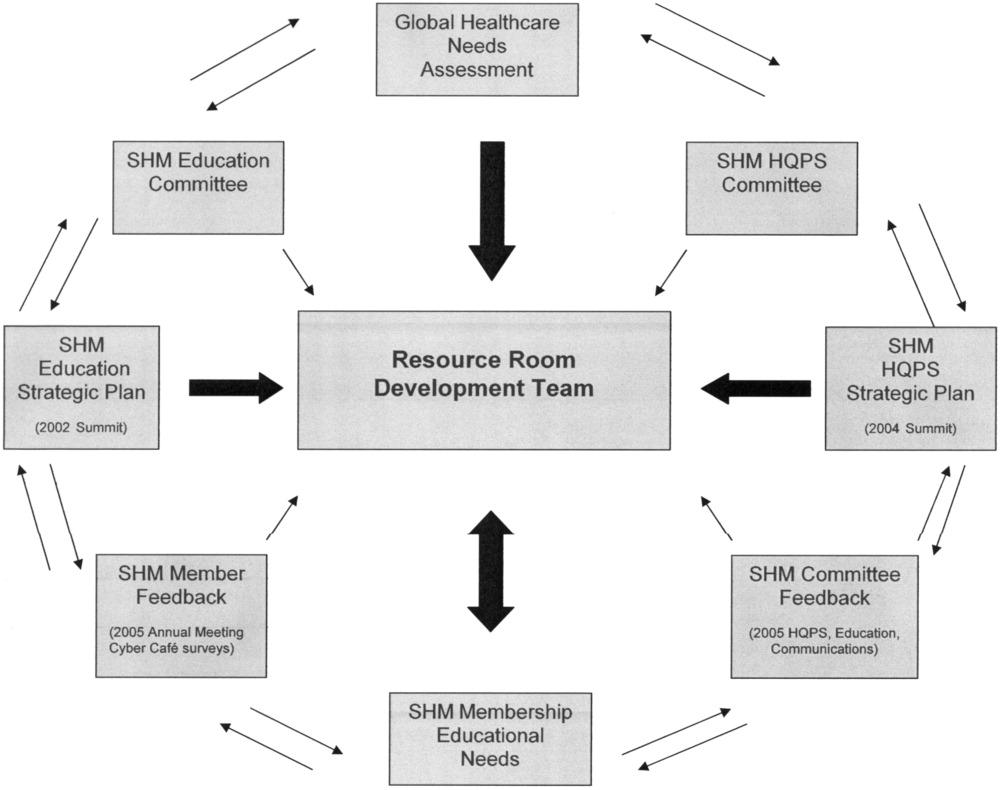
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other | The Current Approach: The focus of traditional medical education. |
| members of the inpatient team | How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. |
| Didactic lectures on the pathophysiology of VTE. rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional | Research Questions |
| research | Identifying barriers to VTE prophylaxis in the hospital setting. |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for | Quality issues in the transfer of care. |
| improvement | Failure to review radiographic study. |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other | The Current Approach: Inherent discontinuities of inpatient care. |
| embers of the inpatient team | ACGME legislated work hours: resident shifts. |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for | Research Questions |
| additional research | What are the key components of the sign‐out process? |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members | The Current Approach: Problems with the work environment |
| of the inpatient team | Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
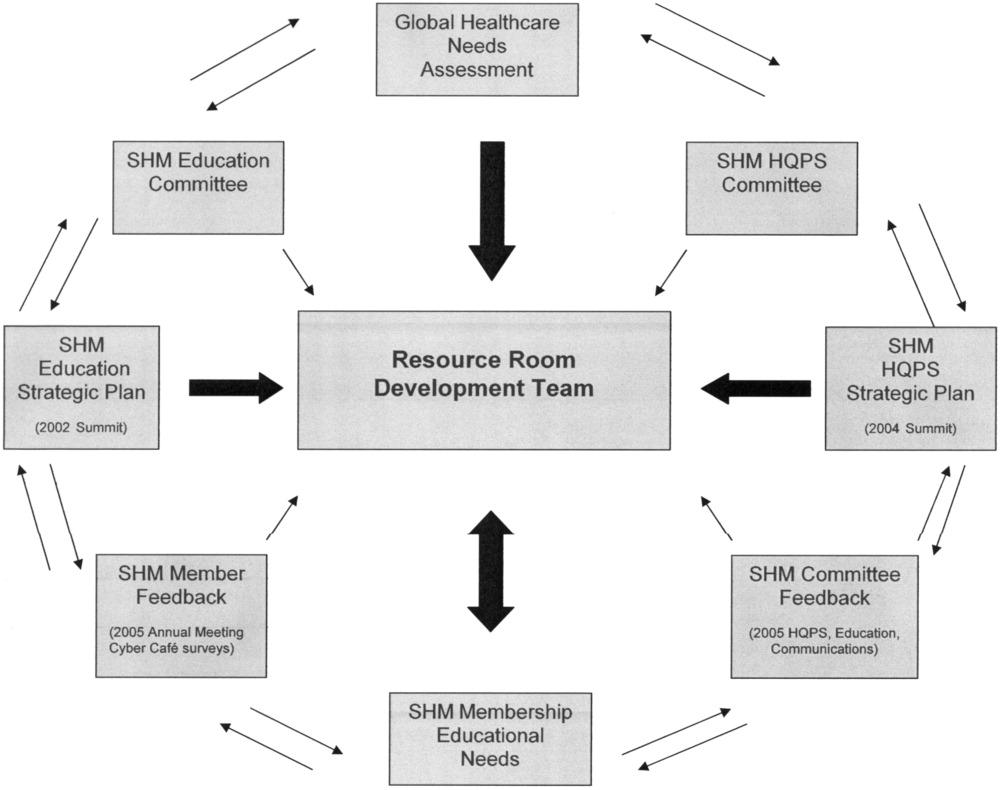
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other | The Current Approach: The focus of traditional medical education. |
| members of the inpatient team | How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. |
| Didactic lectures on the pathophysiology of VTE. rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional | Research Questions |
| research | Identifying barriers to VTE prophylaxis in the hospital setting. |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for | Quality issues in the transfer of care. |
| improvement | Failure to review radiographic study. |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other | The Current Approach: Inherent discontinuities of inpatient care. |
| embers of the inpatient team | ACGME legislated work hours: resident shifts. |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for | Research Questions |
| additional research | What are the key components of the sign‐out process? |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members | The Current Approach: Problems with the work environment |
| of the inpatient team | Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org[accessed November 2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org[accessed November 2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL:http://www.med‐ed‐online.org/pdf/f0000040.pdf[accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org[accessed November 2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org[accessed November 2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org[accessed November 2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL:http://www.med‐ed‐online.org/pdf/f0000040.pdf[accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org[accessed November 2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
Copyright © 2006 Society of Hospital Medicine
Core Competencies: Development and Methodology
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
|
|
|
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org[accessed July 22, 2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
|
|
|
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
|
|
|
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org[accessed July 22, 2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org[accessed July 22, 2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
Copyright © 2006 Society of Hospital Medicine