User login
Nausea and Vomiting in Cancer: It's Not Always the Chemotherapy
Nausea and vomiting is common in cancer patients and a frequent presentation in the ED. When evaluating nausea and vomiting, the clinician should be aware that the two are not always linked—nausea may present without vomiting and vice versa. Nausea is “an unpleasant sensation of the need to vomit and is associated with autonomic symptoms,” whereas vomiting is “the forceful propulsion of abdominal contents via the contraction of the abdominal musculature and diaphragm.”1 Whether these symptoms present together or independently of each other, both can result in serious metabolic disturbances, internal injury, malnutrition, and poor quality of life. In addition, nausea and vomiting can result in patient withdrawal from potentially beneficial treatment.2 Based on the current literature, this article reviews and provides recommendations on appropriate assessment and treatment of the cancer patient presenting to the ED with nausea and/or vomiting.
Epidemiology
In 2007, the US Nationwide Emergency Department Sample database noted 122 million ED visits, 1.6 million of which were due to nausea and vomiting.3 In contrast, a small study from the United Kingdom cited 18% of ED visits in one of its centers were due to nausea and/or vomiting, demonstrating that the percentage of patients presenting with these symptoms can vary greatly.4
The incidence of cancer-related nausea and vomiting in the ED is unknown. Although EDs affiliated with large cancer centers see many cases of cancer-associated nausea and vomiting, presentations to noncancer-center EDs are becoming more prevalent due to increases in community-based cancer care.5 While the number of cancer patients is rising and the general population is aging,6 there is now less incidence of breakthrough chemotherapy-induced nausea and vomiting (CINV), which is a common cause of cancer-related nausea and vomiting. Older studies quote a 40% to 60% rate of breakthrough CINV; however, with the advent of newer antiemetic prophylaxis, by 2013 the incidence had decreased to about 28%.7 As such, the net effect may be a stable or decreased number of ED visits. In one study of patients with breakthrough CINV, 64% were treated inpatient, 26% outpatient, and 10% in the ED. The study, however, does not note how many of these inpatient visits originated in the ED, highlighting that this is an area in need of further study.8
Current knowledge about the epidemiology and etiology of non-CINV comes from end-of-life (EOL) palliative-care literature treatment guidelines, which are organized by cause (etiology-based antiemetic treatment [EBAT]).9-11 Although one systematic review found that the EBAT approach “cannot be shown to be more effective than using a single antiemetic at effective doses,”12 the etiologic framework is useful and can be applied to non-EOL patients. According to a systematic review on the prevalence of symptoms, nausea in advanced cancer patients ranged from 6% to 68%.6 Another review on cancer-related nausea and vomiting that cited studies conducted in the 1990s showed patients had increased nausea and vomiting as they approach EOL—ranging from 36% upon entering palliative-care programs to 71% in the final week of life.13 However, another systematic review citing more recent studies contradicts these findings, stating that in the last 2 weeks of life, nausea was less common (17%) than in patients who were not at the last 2 weeks of life (31%);14 the same was true of vomiting (20% vs 13%). This data perhaps implies that treatment of nausea and vomiting has improved over time for EOL patients. The same review also found that women were more likely to experience nausea and vomiting than men,14 a finding also seen in a 2011 prospective study of antiemetics for breakthrough CINV vomiting.15
When evaluating patients with cancer-associated nausea and vomiting, it is important to remember that these symptoms rarely occur in isolation. Most patients present with between seven and 15 other complaints, such as pain, weakness, fatigue, anorexia, constipation, dry mouth, early satiety, and dyspnea.16
Pathophysiology
To understand nausea and vomiting, it is helpful to review the emetic pathway. There are four areas that stimulate the central vomiting center located in the medulla oblongata. These are the cerebral cortex, the vestibular nucleus, the intestinal tract, and the chemoreceptor trigger zone (located on the floor of the fourth ventricle). With sufficient input from any of these to the vomiting center, nausea occurs, followed by the vomiting reflex. It is known that each of the input zones, as well as the vomiting center itself, have receptors for various substances, including the following:1,13,17-20
· Cerebral cortex: gamma-aminobutyric acid, histamine type 1 (H1)
· Vestibular nucleus: muscarinic acetylcholine receptor (AChM), H1
· Intestinal tract: 5 hydroxytryptamine type 3 (5-HT3) or serotonin type 3 receptors, 5 hydroxytryptamine type 4 (5-HT4) or serotonin type 3 receptors, dopamine type 2 (D2)
· Chemoreceptor trigger zone: 5 hydroxytryptamine type 2 (5-HT2) or serotonin type 2; D2, neurokinin-1 (NK1), or substance P
· Vomiting center: AChM, H1, 5-HT2, D2, NK1, ([GK mµ] opioid receptors), and cannabinoid (CB) receptors
Each of the aforementioned substances in turn stimulate receptors in the intestinal tract and in the chemoreceptor trigger zone, triggering the vomiting center.1,13,17 Most antiemetic agents block the receptors for one or more of these mediators and are discussed later in more detail. Chemotherapeutic agents specifically cause the release 5-HT and NK1 in the gut, which contains over 90% of the body’s serotonin. This knowledge has led to the development of newer 5-HT3 and NK1 antagonists for CINV. Unlike the other mediators, cannabinoids cause an antiemetic effect when they bind to CB receptors.13,17,19 This finding has led to the development of specific pharmacologic treatment agents.
Etiology and Differential Diagnosis
Perhaps the best way for the emergency physician (EP) to assess the cancer patient with nausea or vomiting is to determine whether the cause is treatment- or nontreatment-related. Treatment-related causes are due to chemotherapy or radiotherapy, and any other causes would be considered nontreatment related. It is, however, wise for the EP to remember that a patient who has had recent chemotherapy can still be at risk for nontreatment etiologies.
Treatment-Related Nausea and Vomiting
Chemotherapy-Induced
Chemotherapy-induced nausea and vomiting has been well-studied in the literature. Chemotherapy is classified as highly, moderately, low, and minimally emetogenic.18,19 Nausea itself is classified as acute (onset within 24 hours), delayed (onset after 24 hours), and anticipatory (prior to the chemotherapy, usually due to anxiety over previous unpleasant experiences). Breakthrough vomiting occurs despite the use of antiemetics and may be acute or delayed up to 5 days.
When evaluating the patient with recent chemotherapy and vomiting, it is prudent to find out if the agent is expected to cause vomiting. For example, a patient on cladribine, which is classified as minimally emetogenic, who experiences significant nausea and vomiting should likely be worked up for another etiology. Even when vomiting is controlled, a significant number of patients still experience nausea without vomiting, which in turn has a negative impact on quality of life.
Even though prophylactic regimens of 5-HT3 and NK1 receptor antagonists have led to improved rates of CINV control,18,19,21 both persistent nausea without vomiting and breakthrough vomiting remain problematic,18 and little scientific work has been done on breakthrough treatment. A small prospective pilot study of the efficacy of prochlorperazine versus serotonin 5-HT3 receptor antagonists for breakthrough vomiting found both medications reduced nausea by 75% at 4 hours.15 In contrast, randomized controlled trials comparing olanzapine to metoclopramide and prochlorperazine for breakthrough vomiting found that at 3 days, olanzapine consistently achieved total relief of vomiting 66% to 70%, while the success rates of the other agents ranged from 20% to 37%.18
Radiotherapy-Induced
Radiotherapy has long been known to adversely affect the gastrointestinal (GI) tract. 5-HT3 (ie, serotonin) is released from the gut enterochromaffin cells, in a manner similar to chemotherapy. A 2015 review on the subject showed that radiotherapy to the upper abdomen is most likely to lead to nausea and vomiting, with 50% to 67% of patients reporting nausea and 21% to 38% reporting vomiting.20 Recommended prophylaxis and treatment regimens are based on consensus expert opinion, highlighting the lack of quality evidence that is seen with CINV. Prophylaxis regimens use 5-HT3 antagonists prior to every session, plus dexamethasone for the first 5 days. Rescue from breakthrough is also treated with 5-HT3 antagonists. The use of daily 5-HT3 antagonists for a long course of radiotherapy, however, can be very expensive and unnecessary.
In addition, there is a delayed nausea and vomiting phenomena that may be due to substances other than serotonin, since 5-HT3 depletes a few days after radiotherapy is begun, and may explain why 5-HT3 antagonists are less effective after the first few days of radiotherapy. Nonpharmacologic treatments such as acupuncture, acupressure, hydrogen therapy, and ginger have been used or proposed as treatments for nausea, with mild benefit and little toxicity, so they should be studied further.20
Nontreatment-Related Nausea or Vomiting
Again, much of what is known about nontreatment cancer-related nausea and/or vomiting comes from the palliative-care literature. It is estimated that 60% of advanced cancer patients experience nontreatment-related nausea, and 30% experience vomiting.1,11 One study of 61 hospice patients showed nausea or vomiting occurred due to the following (listed in order from most to least frequent):
· Impaired gastric emptying due to tumor or hepatomegaly, bowel obstruction, metabolic problems (eg, renal failure, liver failure, hypercalcemia, hyponatremia, ketoacidosis)
· infection
· drugs
· increased intracranial pressure (ICP)
· anxiety
The above causes of nausea and vomiting accounted for 85% of the cases in the study.9 Similar results were found in another study, showing that impaired gastric emptying and metabolic/drugs each caused about one third of the cases.10
Nontreatment-related causes of nausea and vomiting are traditionally divided into the following six broad etiological categories by palliative care practitioners9,10,13:
1. Biochemical: medications, tumor products, metabolic derangements, comorbidities, including systemic infections, noncancer abdominal illnesses; and silent cardiac ischemia
2. Gastric stasis: tumor, neuropathy, hepatomegaly, ascites
3. Bowel dysmotility/obstruction: tumor, metastases, adhesions, ileus, constipation
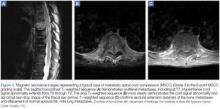
4. Intracranial pressure: tumor edema, bleeding, hydrocephalus, leptomeningeal disease
5. Vestibular: opioids, comorbid vestibular problems, brainstem metastases
6. Miscellaneous: anxiety, pain
These classification schemes are designed to help guide the treatment of palliative-care patients (EBAT),9-11 but very little evidence supports the recommendations.11-13,17 Expert opinion consensus guidelines favor haloperidol for biochemical etiology and metoclopramide for impaired gastric emptying. In intestinal obstruction, the H1-blocking antihistamine cyclizine and the anticholinergic hyoscine butylbromide (scopoloamine) are the preferred agents, but dexamethasone and haloperidol are also favored by some. It is believed that increased ICP nausea is best treated with cyclizine and dexamethasone. Vestibular etiologies are treated with cyclizine, and anxiety-mediated nausea should be treated with benzodiazepines.9,17 As there are often multiple etiologies in a given patient, selection of one agent can be problematic.13 Furthermore, no studies have applied these guidelines to ED cancer patients. This framework, however, can assist the EP in forming a differential diagnosis and appropriate workup. On history and physical examination, the EP should look for and consider the following:13,16
· Small-volume undigested emesis shortly after eating, suggesting gastric emptying impairment
· Bilious or feculent vomitus, large volumes, constipation, and obstipation, suggesting bowel obstruction (evaluate via X-ray or computed tomographic imaging)
· Early morning nausea and headache, suggesting increased ICP
· Nausea associated with head movement or motion, with or without vertigo, (suggesting vestibular disease)
· Current or recent use of opioids, antibiotics, antifungals, anticonvulsants, vitamins, ethanol, and selective serotonin reuptake inhibitors
· Infection, sepsis
· Metabolic abnormalities found on blood tests (for example, renal failure, liver failure, hypercalcemia, hyponatremia, ketoacidosis, osmolar gap, toxins/poisons, Addisonian crisis from steroid withdrawal or adrenal metastases); and/or
· Silent cardiac ischemia (evaluate via electrocardiography and cardiac enzymes)
· Careful consideration of each of the above possibilities will make one less likely to miss other serious causes of nausea and vomiting in the cancer patient with recent chemotherapy.
Opioid-Induced Nausea
Forty percent of cancer patients taking opioids experience nausea, which can adversely impact pain control.22 Opioid-induced nausea is due to constipation, gastroparesis, stimulation of the chemoreceptor trigger zone, and sensitization of the labyrinth, all of which can in turn stimulate the vomiting center.
Regarding the treatment of opioid-induced nausea and vomiting, there is no evidence to support the use of one antiemetic over another. Some weak evidence-based recommendations suggest either changing the medication to a different opioid, or changing the route of administration from oral to subcutaneous and adding coanalgesics such as gabapentin or ketamine to reduce opioid dosages. Though these strategies may be helpful in practice, none of the studies was large enough or thorough enough to support or warrant any formal recommendations in this systematic review.22
Initial Management and Treatment
As always, attention to the patient’s airway, breathing, and circulation is of utmost importance. Endotracheal intubation should be considered in patients at risk for aspiration—unless a living will or do-not-resuscitate order exists. Maneuvers such as raising the head of the bed or turning the patient on his or her side may help avoid aspiration.
Intravenous (IV) hydration is generally beneficial. The choice and amount of fluid should be based on clinical judgment. Electrolyte imbalances should be corrected. The mainstay of treatment for nausea and/or vomiting is pharmacologic, which is the focus of the next section.
Pharmacologic Management
Prokinetic Agents
Prokinetic agents increase peristalsis and exert an antiemetic effect. Metoclopramide is the best known and most widely available prokinetic agent. Since it is both inexpensive and very effective as an antiemetic, its use in the ED is widespread. Etiology-based antiemetic treatment guidelines list metoclopramide as the antiemetic of choice when gastroparesis or other gastric emptying problems are diagnosed9,10,13,17 as it exerts both D2 and 5-HT3 central nervous system (CNS) antiemetic effects, relaxes pyloric tone (D2), and increases peristalsis by stimulating 5-HT4 serotonin receptors in the gut.
The main limitation of metoclopramide is its extrapyramidal side effects (eg, akathisia, dystonia, psuedoparkinsonism, dyskinesia). Akathisias (ie, restlessness) is a particularly common phenomenon in patients taking metoclopramide. Patients experiencing extrapyramidal reactions are typically treated with diphenhydramine. In addition to the extrapyramidal side effects, metoclopramide is relatively contraindicated in patients with complete bowel obstruction.13,17
In addition to metoclopramide, erythromycin and mirtazapine are other prokinetic agents used in palliative care. Erythromycin has mainly been used for diabetic gastroparesis due to its stimulatory effect on motilin receptors in the GI tract.13,23 Mirtazapine is an antidepressant with both 5-HT3 and 5-HT4 receptor activity. In one case report it was used to treat gastroparesis refractory to all other therapies, including metoclopramide and erythromycin.23
Dopamine-Receptor Antagonists
This category includes many agents, most which are known for their antipsychotic effects. The primary mode of action of dopamine-receptor antagonists is to block D2 receptors in the vomiting center. Etiology-based antiemetic treatment guidelines list these drugs as the first choice in patients with a biochemical-based etiology for nausea, though there is little-to-no evidence to support this recommendation.9,10,12,13,17
While a review on haloperidol use in cancer found its effects better than placebo for CINV and postoperative nausea, studies in the review were small and the evidence weak.24 Due to its low cost, and comparatively favorable side-effect profile, haloperidol is a reasonable alternative to metoclopramide. Indeed, if palliative-care models are used, haloperidol would be preferred over metoclopramide since biochemical nausea is probably more prevalent in the general ED cancer patient than gastroparesis.
Regarding route of administration, olanzapine can be given orally or intramuscularly, making it potentially useful in the ED setting for those who cannot keep pills down and have poor venous access. When used in the supportive care setting, however, olanzapine is typically given at bedtime due to its sedative effects. As such, this agent may be best given to those who will be admitted or placed on observation status, since some patients may not be able to be discharged even if nausea resolves.
Antihistamine Agents
Cyclizine, diphenhydramine, hydroxyzine, meclozine, and promethazine, are all piperazine H1-receptor blockers that work in the vomiting center, vestibular nucleus, and chemoreceptor trigger zone. In addition to its properties as an H1-receptor antagonist, cyclizine also exhibits some anticholinergic activity that decreases bowel secretions, thus making it theoretically beneficial in patients with bowel obstruction. Each of these antihistamines are considered beneficial in treating nausea due to vestibular dysfunction and in motion sickness, and may be helpful in patients with increased ICP. Heavy sedation, anticholinergic, and extrapyramidal side effects may occur with these drugs, especially in elderly patients.1,13,17
Serotonin 5-HT3 Receptor Antagonists
Dolasetron, granisetron, ondansetron, palonosetron, and tropisetron are among the 5-HT3 (serotonin type 3) receptor antagonists used to treat nausea and vomiting. As previously stated, chemotherapy stimulates release of 5-HT from the gut, which in turn stimulates 5-HT3 receptors in the gut, vagus nerve, and the chemotherapy trigger zone—all of which in turn stimulate the vomiting center, leading to the vomiting reflex.1,13,17,19,21 The blocking action of these drugs on the 5-HT3 receptors is the basis of the antiemetic effect. Palonosetron, with its long 40-hour half-life, has become the preferred prophylactic agent for CINV. The most common adverse events with 5-HT3 antagonists include mild headache, transient elevation of hepatic aminotransferase levels, and constipation.19,21 The use of ondansetron for emesis in the ED is becoming more established both for CINV and non-CINV—mainly due to its high efficacy and favorable side-effect profile compared to metoclopramide and the dopamine antagonists.
Substance P Antagonists (NK1-Receptor Antagonists)
Oral aprepitant, injectable fosaprepitant, and netupitant are some of the Substance P (NK1) antagonists used to treat nausea and vomiting. In a manner similar to 5-HT release, chemotherapeutic agents stimulate the cellular release of NK1 in the gut. This reaction in turn activates receptors in the vagus nerve and the chemotherapy trigger zone, which stimulates the vomiting center. The NK1 receptors are blocked by these agents. The main use of these medications has been to complement the 5-HT3 antagonists for prophylaxis prior to administration of chemotherapy. Neurokinin-1receptor antagonists have not been studied in the setting of breakthrough nausea and vomiting but they are being used to treat delayed phase breakthrough CINV by the authors at their institution’s ED. The agents have been shown to be more effective than 5-HT3 agents in preventing delayed phase nausea and vomiting.25 As such, the possibility they may also be effective in treating delayed phase breakthrough CINV has led to this use. Recent studies have found these agents highly effective in the treatment of postoperative nausea and vomiting in high-risk patients.26
The standard in recent years for prophylaxis has been combining 5-HT3 antagonists, NK1 inhibitors, and dexamethasone. Netupitant/palonosetron (commonly referred to as NEPA) is a novel oral agent combining a long-acting 5-HT3 antagonist, and a long-acting NK1 inhibitor for CINV prophylaxis.27 Its use in treating delayed breakthrough vomiting remains to be seen.
Corticosteroids
Based on its antiemetic properties, the corticosteroid dexamethasone increases the effects of antiemetics (ie, metoclopramide and more recently 5-HT3 and NK1 receptor antagonists) in preventing CINV, perhaps by reducing the blood-brain barrier permeability to emetogenic substances. There are also some evidence-based benefits in using dexamethasone in patients with bowel obstruction. It is also used to reduce ICP from cerebral edema.1,11,13,17,19
Benzodiazepines
The benzodiazepines are best given to enhance the antiemetic effects of other drugs, especially in patients experiencing anxiety-related side effects. The benzodiazepines work well for anticipatory nausea. Lorazepam is the preferred drug of choice due to the lack of active metabolites. However, the clinician should always exercise caution when using benzodiazepines in elderly patients due to the increased risk of falls and cognitive impairment.13,17,19
Cannabinoids
The observation that the incidence of CINV decreased in marijuana smokers led to the exploration of cannabinoids for the treatment of nausea and vomiting. Tetrahydrocannabinol, the psychoactive substance in marijuana, is a phytocannabinoid. Its receptor, CB1, exists throughout the brain. Synthetic cannabinoids such as oral dronabinol, oral nabilone, and intramuscular levonantradol have been used with antiemetic success superior to chlorpromazine, haloperidol, metoclopramide, and prochlorperazine, but at the cost of unpleasant CNS effects and postural hypotension in elderly patients.1,13,17
As cited in a systematic review, cannabinoids appear to inhibit growth of glioblastoma multiforme, breast, prostate, and thyroid cancer, colon carcinoma, leukemia, and lymphomas. Cannabinoids can also benefit cancer patients by stimulating appetite, elevating mood, and inhibiting pain.28 Clearly, more oncologic research needs to be done on the topic. As such, this class of medication is years, if not decades, away from use in the ED.
Nonpharmacologic Treatments
Acupuncture and Acupressure
A 2006 Cochrane systematic review and meta-analysis showed that acupuncture helped with acute CINV but not with delayed CINV.29 Acupuncture was shown to work best with electro-acupuncture needles. Acupressure without needles helped nausea but not vomiting.29 A more recent review on the specific P6 acupuncture area on the wrist near the median nerve found that electroacupuncture, but not manual acupuncture, was beneficial for first-day vomiting, and acupressure was effective for first-day nausea but not vomiting. Neither acupuncture nor acupressure was shown to help delayed nausea or vomiting.30
Ginger
Ginger has been shown to help with CINV and anticipatory nausea, but not with other types of nausea.13 Supplementing routine antiemetics with 0.5 to 1.5 g of ginger per day for 6 days (beginning 3 days before chemotherapy) was shown to reduce the severity of nausea on the day of chemotherapy, but did not affect vomiting.21
Percutaneous Gastrostomy, Stenting, and Laser Therapy
Several strategies have been developed for palliation of intestinal obstruction when surgery is not warranted. Percutaneous gastrostomy tubes (PEG) are used to vent GI secretions that would otherwise build up. Esophageal, colorectal, and gastric outlet obstructions can be palliated by endoscopically placed stenting devices. Argon beam plasma coagulation laser therapy can be used for gastric outlet as well as colonic obstruction.13,31 One review evaluating the benefits of colonic obstruction stenting found an 89% success rate in symptom relief. This same review noted that venting the PEG tube placement had an 84% rate of symptom relief.31
Selecting an Agent in the ED: the Evidence (or Lack Thereof)
Nontreatment-Related Nausea and Vomiting
A 2011 systematic review of cancer nausea unrelated to chemotherapy or radiotherapy found level B evidence that metoclopramide is the most effective first-line empiric agent. In patients with bowel obstruction, dexamethasone, hyoscine butylbromide (scopolamine), and octreotide are effective. While dexamethasone is often thought to improve the effects of antiemetic drugs, this review showed it did not improve nausea when added to chlorpromazine or metoclopramide. Furthermore, neither metoclopramide nor ondansetron were shown to reduce opioid-induced emesis.13 The review further pointed out the lack of good evidence for expert opinion guideline recommendations in breakthrough vomiting—eg, dose titration of the same drug, switching to a different drug class, or using two or more drugs together at once.13
Another review had similar findings, while pointing out that an “absence of evidence is not evidence of absence,” and noting that many of these treatments have been used for years—ie, the problem is lack of evidence, but not negative evidence.17 Both studies are notable in that they were all done in palliative-care units in which time to relief from nausea and/or vomiting was typically measured in days, not hours, making their application to the emergency setting—where time is a factor—difficult.
Due to the potential for drug toxicity, using the same antiemetic drug repeatedly within a short amount of time in a patient refractory to therapy may not be the best strategy in the ED. It is most likely more beneficial and effective to switch drugs or use a combination of drugs right away—though this approach has theoretical concerns with drug-drug interactions. Again, this is an area in which further study is needed.
Treatment-Related Nausea and Vomiting
A recent review on breakthrough CINV again cited the paucity of clinical trials for this entity. Based on few studies, olanzapine and metoclopramide seem to be of value when prophylactic antiemetic regimens have failed. The review further noted that treatment of breakthrough CINV with an agent from same drug class as that used in the prophylactic regimen (usually 5-HT3 and NK1 antagonists) is unlikely to be successful.32 This review also mentioned an interesting phase 2 study using a transdermal gel consisting of diphenhydramine, haloperidol, and lorazepam to the wrist, in which 27 of 33 patients in the study reported a decrease in nausea within a 4-hour period.33 The same combination of drugs in IV form (lorazepam 0.5 mg, diphenhydramine 12.5 mg, and haloperidol 1 mg) is frequently used in the ED at the authors’ institution to treat breakthrough vomiting refractory to metoclopramide, antihistamines, or 5-HT3 antagonists. To the authors’ knowledge, this combination treatment has not been previously cited in the medical literature.
Recommendations and Summary
Cancer patients presenting to the ED with nausea and vomiting should be thoroughly evaluated regarding the possible etiology of their symptoms. A careful history must include recent chemotherapy, radiation, medications, as well as knowledge of the potential complications associated with the specific type of cancer. The EP also should keep in mind that delayed nausea and vomiting can be present several days after chemotherapy, and that CINV may not manifest until after the initial prophylactic medications have worn off. Moreover, he or she should be aware that some individuals have unique responses to chemotherapy and radiation and may experience more nausea and vomiting symptoms than is considered typical.
In addition to CINV, other etiologies, including GI issues such as delayed gastric emptying, partial bowel obstruction, and constipation should also be carefully considered. When evaluating the patient, the EP should also consider non-GI causes such as elevated ICP, kidney obstruction, infection, silent cardiac ischemia, steroid withdrawal, Addisonian crisis, and electrolyte abnormalities.
The lack of conclusive evidence for the treatment of cancer-related nausea and vomiting in any circumstance—except for prophylaxis prior to chemotherapy—precludes the recommendation of a specific treatment algorithm. However, the evidence is abundant that there are multiple effective agents with different, if not overlapping, mechanisms of action available. The EP, therefore, should be familiar with the most commonly used antiemetic drugs from several different categories and their side effects, and tailor the approach based on the assumed etiology of the symptoms. When treating CINV or cancer-related nausea and vomiting, it is not uncommon that patients may require multiple agents, either simultaneously or in sequence, to obtain symptom resolution.
Dr Sandoval is an assistant professor, department of emergency medicine, division of internal medicine at The University of Texas MD Anderson Cancer Center, Houston. Dr Rice is an assistant professor and clinical medical director in the department of emergency medicine, division of internal medicine at The University of Texas MD Anderson Cancer Center, Houston.
- Davis M, Walsh D. Treatment of nausea and vomiting in advanced cancer. Support Care Cancer. 2000;8(6):444-452.
- Abernethy AP, Wheeler JL, Zafar SY. Detailing of gastrointestinal symptoms in cancer patients with advanced disease: new methodologies, new insights, and a proposed approach. Curr Opin Support Palliat Care. 2009;3(1):41-49.
- Myer PA, Mannalithara A, Singh G, Singh G, Pasricha PJ, Ladabaum U. Clinical and economic burden of emergency department visits due to gastrointestinal diseases in the United States. Am J Gastroenterol. 2013;108(9):1496-1507.
- Body R, Kaide E, Kendal S, Foex B. Not all suffering is pain: sources of patients’ suffering in the emergency department call for improvements in communication from practitioners. Emerg Med J. 2015;32(1):15-20.
- National Chemotherapy Advisory Group. Chemotherapy Services in England: ensuring quality and safety. London, England: Department of Health; 2009. http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_104501.pdf. Accessed July 17, 2015.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Carlotto A, Hogsett VL, Maiorini EM, Razulis JG, Sonis ST. The economic burden of toxicities associated with cancer treatment: review of the literature and analysis of nausea and vomiting, diarrhoea, oral mucositis and fatigue. Pharmacoeconomics. 2013;31(9):753-766.
- Burke TA, Wisniewski T, Ernst FR. Resource utilization and costs associated with chemotherapy-induced nausea and vomiting (CINV) following highly or moderately emetogenic chemotherapy administered in the US outpatient hospital setting. Support Care Cancer. 2011;19(1):131-140.
- Stephenson J. Davies A. An assessment of aetiology-based guidelines for the management of nausea and vomiting in patients with advanced cancer. Support Care Cancer. 2006;14(4):348-353.
- Bentley A, Boyd K. Use of clinical pictures in the management of nausea and vomiting: a prospective audit. Palliat Med. 2001;15(3):247–253.
- Glare P, Pereira G, Kristjanson LJ, Stockler M, Tattersall M. Systematic review of the efficacy of antiemetics in the treatment of nausea in patients with far-advanced cancer. Support Care Cancer. 2004;12(6):432–440.
- Davis MP, Hallerberg G; Palliative Medicine Study Group of the Multinational Association of Supportive Care in Cancer. A systematic review of the treatment of nausea and/or vomiting in cancer unrelated to chemotherapy or radiation. J Pain Symptom Manage. 2010;39(4):756-767.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Teunissen, S, Wesker W, Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manage. 2007;34(1):94-104.
- Jones JM, Qin R, Bardia A, Linquist B, Wolf S, Loprinzi CL. Antiemetics for chemotherapy-induced nausea and vomiting occurring despite prophylactic antiemetic therapy. J Palliat Med. 2011;14(7):810-814.
- Shoemaker LK, Estfan B, Induru R, Walsh TD. Symptom management: an important part of cancer care. Cleve Clin J Med. 2011;78(1):25-34.
- Harris DG. Nausea and vomiting in advanced cancer. Br Med Bull. 2010;96:175-185.
- Hocking CM, Kichenadasse G. Olanzapine for chemotherapy-induced nausea and vomiting: a systematic review. Support Care Cancer. 2014;22(4):1143-1151.
- Hesketh PJ. Chemotherapy-induced nausea and vomiting. N Engl J Med. 2008;358(23):2482-2494.
- Dennis K, Poon M, Chow E. Nausea and vomiting induced by gastrointestinal radiation therapy: current status and future directions. Curr Opin Support Palliat Care. 2015;9(2):182-188.
- Rangwala F, Zafar SY, Abernethy AP. Gastrointestinal symptoms in cancer patients with advanced disease: new methodologies, insights, and a proposed approach. Curr Opin Support Palliat Care. 2012;6(1):69-76.
- Laugsand EA, Kaasa S, Klepstad P. Management of opioid-induced nausea and vomiting in cancer patients: systematic review and evidence-based recommendations. Palliat Med. 2011;25(5):442-453.
- Kim SW, Shin IS, Kim JM, et al. Mirtazapine for severe gastroparesis unresponsive to conventional prokinetic treatment. Psychosomatics. 2006;47(5):440-442.
- McLean SL, Blenkinsopp A, Bennett MI. Using haloperidol as an antiemetic in palliative care: informing practice through evidence from cancer treatment and postoperative contexts. J Pain Palliat Care Pharmacother. 2013;27(2):132-135.
- Aapro M, Carides A, Rapoport BL, Schmoll HJ, Zhang L, Warr D. Aprepitant and fosaprepitant: a 10-year review of efficacy and safety. Oncologist. 2015;20(4)450-458.
- Soga T, Kume K, Kakuta N, et al. Fosaprepitant versus ondansetron for the prevention of postoperative nausea and vomiting in patients who undergo gynecologic abdominal surgery with patient-controlled epidural analgesia: a prospective, randomized, double-blind study. J Anesth. 2015;29(5):696-701.
- Abramovitz RB, Gaertner KM. The role of netupitant and palonosetron in chemotherapy-induced nausea and vomiting [published online ahead of print April 24, 2015]. J Oncol Pharm Pract. doi:10.1177/1078155215581525.
- Pisanti S, Malfitano AM, Grimaldi C, et al. Use of cannabinoid receptor agonists in cancer therapy as palliative and curative agents. Best Pract Res Clin Endocrinol Metab. 2009;23(1):117-131.
- Ezzo JM, Richardson MA, Vickers A, et al: Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database Syst Rev. 2006;19(2):CD002285.
- Ezzo J, Streitberger K, Schneider A. Cochrane systematic reviews examine P6 acupuncture-point stimulation for nausea and vomiting. J Altern Complement Med. 2006;12(5):489-495.
- Laval G, Marcelin-Benazech B, Guirimand F, et al; French Society for Palliative Care; French Society for Digestive Surgery; French Society for Gastroenterology; French Association for Supportive Care in Oncology; French Society for Digestive Cancer. Recommendations for bowel obstruction with peritoneal carcinomatosis. J Pain Symptom Manage. 2014;48(1):75-91.
- Navari RM. Treatment of breakthrough and refractory chemotherapy-induced nausea and vomiting. Biomed Res Int. 2015;2015:595894.
- Bleicher J, Bhaskara A, Huyck T, Constantino S, Bardia A, Loprinzi CL, et al. Lorazepam, diphenhydramine, and haloperidol transdermal gel for rescue from chemotherapy-induced nausea/vomiting: results of two pilot trials. J Support Oncol. 2008;6(1):27-32.
Nausea and vomiting is common in cancer patients and a frequent presentation in the ED. When evaluating nausea and vomiting, the clinician should be aware that the two are not always linked—nausea may present without vomiting and vice versa. Nausea is “an unpleasant sensation of the need to vomit and is associated with autonomic symptoms,” whereas vomiting is “the forceful propulsion of abdominal contents via the contraction of the abdominal musculature and diaphragm.”1 Whether these symptoms present together or independently of each other, both can result in serious metabolic disturbances, internal injury, malnutrition, and poor quality of life. In addition, nausea and vomiting can result in patient withdrawal from potentially beneficial treatment.2 Based on the current literature, this article reviews and provides recommendations on appropriate assessment and treatment of the cancer patient presenting to the ED with nausea and/or vomiting.
Epidemiology
In 2007, the US Nationwide Emergency Department Sample database noted 122 million ED visits, 1.6 million of which were due to nausea and vomiting.3 In contrast, a small study from the United Kingdom cited 18% of ED visits in one of its centers were due to nausea and/or vomiting, demonstrating that the percentage of patients presenting with these symptoms can vary greatly.4
The incidence of cancer-related nausea and vomiting in the ED is unknown. Although EDs affiliated with large cancer centers see many cases of cancer-associated nausea and vomiting, presentations to noncancer-center EDs are becoming more prevalent due to increases in community-based cancer care.5 While the number of cancer patients is rising and the general population is aging,6 there is now less incidence of breakthrough chemotherapy-induced nausea and vomiting (CINV), which is a common cause of cancer-related nausea and vomiting. Older studies quote a 40% to 60% rate of breakthrough CINV; however, with the advent of newer antiemetic prophylaxis, by 2013 the incidence had decreased to about 28%.7 As such, the net effect may be a stable or decreased number of ED visits. In one study of patients with breakthrough CINV, 64% were treated inpatient, 26% outpatient, and 10% in the ED. The study, however, does not note how many of these inpatient visits originated in the ED, highlighting that this is an area in need of further study.8
Current knowledge about the epidemiology and etiology of non-CINV comes from end-of-life (EOL) palliative-care literature treatment guidelines, which are organized by cause (etiology-based antiemetic treatment [EBAT]).9-11 Although one systematic review found that the EBAT approach “cannot be shown to be more effective than using a single antiemetic at effective doses,”12 the etiologic framework is useful and can be applied to non-EOL patients. According to a systematic review on the prevalence of symptoms, nausea in advanced cancer patients ranged from 6% to 68%.6 Another review on cancer-related nausea and vomiting that cited studies conducted in the 1990s showed patients had increased nausea and vomiting as they approach EOL—ranging from 36% upon entering palliative-care programs to 71% in the final week of life.13 However, another systematic review citing more recent studies contradicts these findings, stating that in the last 2 weeks of life, nausea was less common (17%) than in patients who were not at the last 2 weeks of life (31%);14 the same was true of vomiting (20% vs 13%). This data perhaps implies that treatment of nausea and vomiting has improved over time for EOL patients. The same review also found that women were more likely to experience nausea and vomiting than men,14 a finding also seen in a 2011 prospective study of antiemetics for breakthrough CINV vomiting.15
When evaluating patients with cancer-associated nausea and vomiting, it is important to remember that these symptoms rarely occur in isolation. Most patients present with between seven and 15 other complaints, such as pain, weakness, fatigue, anorexia, constipation, dry mouth, early satiety, and dyspnea.16
Pathophysiology
To understand nausea and vomiting, it is helpful to review the emetic pathway. There are four areas that stimulate the central vomiting center located in the medulla oblongata. These are the cerebral cortex, the vestibular nucleus, the intestinal tract, and the chemoreceptor trigger zone (located on the floor of the fourth ventricle). With sufficient input from any of these to the vomiting center, nausea occurs, followed by the vomiting reflex. It is known that each of the input zones, as well as the vomiting center itself, have receptors for various substances, including the following:1,13,17-20
· Cerebral cortex: gamma-aminobutyric acid, histamine type 1 (H1)
· Vestibular nucleus: muscarinic acetylcholine receptor (AChM), H1
· Intestinal tract: 5 hydroxytryptamine type 3 (5-HT3) or serotonin type 3 receptors, 5 hydroxytryptamine type 4 (5-HT4) or serotonin type 3 receptors, dopamine type 2 (D2)
· Chemoreceptor trigger zone: 5 hydroxytryptamine type 2 (5-HT2) or serotonin type 2; D2, neurokinin-1 (NK1), or substance P
· Vomiting center: AChM, H1, 5-HT2, D2, NK1, ([GK mµ] opioid receptors), and cannabinoid (CB) receptors
Each of the aforementioned substances in turn stimulate receptors in the intestinal tract and in the chemoreceptor trigger zone, triggering the vomiting center.1,13,17 Most antiemetic agents block the receptors for one or more of these mediators and are discussed later in more detail. Chemotherapeutic agents specifically cause the release 5-HT and NK1 in the gut, which contains over 90% of the body’s serotonin. This knowledge has led to the development of newer 5-HT3 and NK1 antagonists for CINV. Unlike the other mediators, cannabinoids cause an antiemetic effect when they bind to CB receptors.13,17,19 This finding has led to the development of specific pharmacologic treatment agents.
Etiology and Differential Diagnosis
Perhaps the best way for the emergency physician (EP) to assess the cancer patient with nausea or vomiting is to determine whether the cause is treatment- or nontreatment-related. Treatment-related causes are due to chemotherapy or radiotherapy, and any other causes would be considered nontreatment related. It is, however, wise for the EP to remember that a patient who has had recent chemotherapy can still be at risk for nontreatment etiologies.
Treatment-Related Nausea and Vomiting
Chemotherapy-Induced
Chemotherapy-induced nausea and vomiting has been well-studied in the literature. Chemotherapy is classified as highly, moderately, low, and minimally emetogenic.18,19 Nausea itself is classified as acute (onset within 24 hours), delayed (onset after 24 hours), and anticipatory (prior to the chemotherapy, usually due to anxiety over previous unpleasant experiences). Breakthrough vomiting occurs despite the use of antiemetics and may be acute or delayed up to 5 days.
When evaluating the patient with recent chemotherapy and vomiting, it is prudent to find out if the agent is expected to cause vomiting. For example, a patient on cladribine, which is classified as minimally emetogenic, who experiences significant nausea and vomiting should likely be worked up for another etiology. Even when vomiting is controlled, a significant number of patients still experience nausea without vomiting, which in turn has a negative impact on quality of life.
Even though prophylactic regimens of 5-HT3 and NK1 receptor antagonists have led to improved rates of CINV control,18,19,21 both persistent nausea without vomiting and breakthrough vomiting remain problematic,18 and little scientific work has been done on breakthrough treatment. A small prospective pilot study of the efficacy of prochlorperazine versus serotonin 5-HT3 receptor antagonists for breakthrough vomiting found both medications reduced nausea by 75% at 4 hours.15 In contrast, randomized controlled trials comparing olanzapine to metoclopramide and prochlorperazine for breakthrough vomiting found that at 3 days, olanzapine consistently achieved total relief of vomiting 66% to 70%, while the success rates of the other agents ranged from 20% to 37%.18
Radiotherapy-Induced
Radiotherapy has long been known to adversely affect the gastrointestinal (GI) tract. 5-HT3 (ie, serotonin) is released from the gut enterochromaffin cells, in a manner similar to chemotherapy. A 2015 review on the subject showed that radiotherapy to the upper abdomen is most likely to lead to nausea and vomiting, with 50% to 67% of patients reporting nausea and 21% to 38% reporting vomiting.20 Recommended prophylaxis and treatment regimens are based on consensus expert opinion, highlighting the lack of quality evidence that is seen with CINV. Prophylaxis regimens use 5-HT3 antagonists prior to every session, plus dexamethasone for the first 5 days. Rescue from breakthrough is also treated with 5-HT3 antagonists. The use of daily 5-HT3 antagonists for a long course of radiotherapy, however, can be very expensive and unnecessary.
In addition, there is a delayed nausea and vomiting phenomena that may be due to substances other than serotonin, since 5-HT3 depletes a few days after radiotherapy is begun, and may explain why 5-HT3 antagonists are less effective after the first few days of radiotherapy. Nonpharmacologic treatments such as acupuncture, acupressure, hydrogen therapy, and ginger have been used or proposed as treatments for nausea, with mild benefit and little toxicity, so they should be studied further.20
Nontreatment-Related Nausea or Vomiting
Again, much of what is known about nontreatment cancer-related nausea and/or vomiting comes from the palliative-care literature. It is estimated that 60% of advanced cancer patients experience nontreatment-related nausea, and 30% experience vomiting.1,11 One study of 61 hospice patients showed nausea or vomiting occurred due to the following (listed in order from most to least frequent):
· Impaired gastric emptying due to tumor or hepatomegaly, bowel obstruction, metabolic problems (eg, renal failure, liver failure, hypercalcemia, hyponatremia, ketoacidosis)
· infection
· drugs
· increased intracranial pressure (ICP)
· anxiety
The above causes of nausea and vomiting accounted for 85% of the cases in the study.9 Similar results were found in another study, showing that impaired gastric emptying and metabolic/drugs each caused about one third of the cases.10
Nontreatment-related causes of nausea and vomiting are traditionally divided into the following six broad etiological categories by palliative care practitioners9,10,13:
1. Biochemical: medications, tumor products, metabolic derangements, comorbidities, including systemic infections, noncancer abdominal illnesses; and silent cardiac ischemia
2. Gastric stasis: tumor, neuropathy, hepatomegaly, ascites
3. Bowel dysmotility/obstruction: tumor, metastases, adhesions, ileus, constipation
4. Intracranial pressure: tumor edema, bleeding, hydrocephalus, leptomeningeal disease
5. Vestibular: opioids, comorbid vestibular problems, brainstem metastases
6. Miscellaneous: anxiety, pain
These classification schemes are designed to help guide the treatment of palliative-care patients (EBAT),9-11 but very little evidence supports the recommendations.11-13,17 Expert opinion consensus guidelines favor haloperidol for biochemical etiology and metoclopramide for impaired gastric emptying. In intestinal obstruction, the H1-blocking antihistamine cyclizine and the anticholinergic hyoscine butylbromide (scopoloamine) are the preferred agents, but dexamethasone and haloperidol are also favored by some. It is believed that increased ICP nausea is best treated with cyclizine and dexamethasone. Vestibular etiologies are treated with cyclizine, and anxiety-mediated nausea should be treated with benzodiazepines.9,17 As there are often multiple etiologies in a given patient, selection of one agent can be problematic.13 Furthermore, no studies have applied these guidelines to ED cancer patients. This framework, however, can assist the EP in forming a differential diagnosis and appropriate workup. On history and physical examination, the EP should look for and consider the following:13,16
· Small-volume undigested emesis shortly after eating, suggesting gastric emptying impairment
· Bilious or feculent vomitus, large volumes, constipation, and obstipation, suggesting bowel obstruction (evaluate via X-ray or computed tomographic imaging)
· Early morning nausea and headache, suggesting increased ICP
· Nausea associated with head movement or motion, with or without vertigo, (suggesting vestibular disease)
· Current or recent use of opioids, antibiotics, antifungals, anticonvulsants, vitamins, ethanol, and selective serotonin reuptake inhibitors
· Infection, sepsis
· Metabolic abnormalities found on blood tests (for example, renal failure, liver failure, hypercalcemia, hyponatremia, ketoacidosis, osmolar gap, toxins/poisons, Addisonian crisis from steroid withdrawal or adrenal metastases); and/or
· Silent cardiac ischemia (evaluate via electrocardiography and cardiac enzymes)
· Careful consideration of each of the above possibilities will make one less likely to miss other serious causes of nausea and vomiting in the cancer patient with recent chemotherapy.
Opioid-Induced Nausea
Forty percent of cancer patients taking opioids experience nausea, which can adversely impact pain control.22 Opioid-induced nausea is due to constipation, gastroparesis, stimulation of the chemoreceptor trigger zone, and sensitization of the labyrinth, all of which can in turn stimulate the vomiting center.
Regarding the treatment of opioid-induced nausea and vomiting, there is no evidence to support the use of one antiemetic over another. Some weak evidence-based recommendations suggest either changing the medication to a different opioid, or changing the route of administration from oral to subcutaneous and adding coanalgesics such as gabapentin or ketamine to reduce opioid dosages. Though these strategies may be helpful in practice, none of the studies was large enough or thorough enough to support or warrant any formal recommendations in this systematic review.22
Initial Management and Treatment
As always, attention to the patient’s airway, breathing, and circulation is of utmost importance. Endotracheal intubation should be considered in patients at risk for aspiration—unless a living will or do-not-resuscitate order exists. Maneuvers such as raising the head of the bed or turning the patient on his or her side may help avoid aspiration.
Intravenous (IV) hydration is generally beneficial. The choice and amount of fluid should be based on clinical judgment. Electrolyte imbalances should be corrected. The mainstay of treatment for nausea and/or vomiting is pharmacologic, which is the focus of the next section.
Pharmacologic Management
Prokinetic Agents
Prokinetic agents increase peristalsis and exert an antiemetic effect. Metoclopramide is the best known and most widely available prokinetic agent. Since it is both inexpensive and very effective as an antiemetic, its use in the ED is widespread. Etiology-based antiemetic treatment guidelines list metoclopramide as the antiemetic of choice when gastroparesis or other gastric emptying problems are diagnosed9,10,13,17 as it exerts both D2 and 5-HT3 central nervous system (CNS) antiemetic effects, relaxes pyloric tone (D2), and increases peristalsis by stimulating 5-HT4 serotonin receptors in the gut.
The main limitation of metoclopramide is its extrapyramidal side effects (eg, akathisia, dystonia, psuedoparkinsonism, dyskinesia). Akathisias (ie, restlessness) is a particularly common phenomenon in patients taking metoclopramide. Patients experiencing extrapyramidal reactions are typically treated with diphenhydramine. In addition to the extrapyramidal side effects, metoclopramide is relatively contraindicated in patients with complete bowel obstruction.13,17
In addition to metoclopramide, erythromycin and mirtazapine are other prokinetic agents used in palliative care. Erythromycin has mainly been used for diabetic gastroparesis due to its stimulatory effect on motilin receptors in the GI tract.13,23 Mirtazapine is an antidepressant with both 5-HT3 and 5-HT4 receptor activity. In one case report it was used to treat gastroparesis refractory to all other therapies, including metoclopramide and erythromycin.23
Dopamine-Receptor Antagonists
This category includes many agents, most which are known for their antipsychotic effects. The primary mode of action of dopamine-receptor antagonists is to block D2 receptors in the vomiting center. Etiology-based antiemetic treatment guidelines list these drugs as the first choice in patients with a biochemical-based etiology for nausea, though there is little-to-no evidence to support this recommendation.9,10,12,13,17
While a review on haloperidol use in cancer found its effects better than placebo for CINV and postoperative nausea, studies in the review were small and the evidence weak.24 Due to its low cost, and comparatively favorable side-effect profile, haloperidol is a reasonable alternative to metoclopramide. Indeed, if palliative-care models are used, haloperidol would be preferred over metoclopramide since biochemical nausea is probably more prevalent in the general ED cancer patient than gastroparesis.
Regarding route of administration, olanzapine can be given orally or intramuscularly, making it potentially useful in the ED setting for those who cannot keep pills down and have poor venous access. When used in the supportive care setting, however, olanzapine is typically given at bedtime due to its sedative effects. As such, this agent may be best given to those who will be admitted or placed on observation status, since some patients may not be able to be discharged even if nausea resolves.
Antihistamine Agents
Cyclizine, diphenhydramine, hydroxyzine, meclozine, and promethazine, are all piperazine H1-receptor blockers that work in the vomiting center, vestibular nucleus, and chemoreceptor trigger zone. In addition to its properties as an H1-receptor antagonist, cyclizine also exhibits some anticholinergic activity that decreases bowel secretions, thus making it theoretically beneficial in patients with bowel obstruction. Each of these antihistamines are considered beneficial in treating nausea due to vestibular dysfunction and in motion sickness, and may be helpful in patients with increased ICP. Heavy sedation, anticholinergic, and extrapyramidal side effects may occur with these drugs, especially in elderly patients.1,13,17
Serotonin 5-HT3 Receptor Antagonists
Dolasetron, granisetron, ondansetron, palonosetron, and tropisetron are among the 5-HT3 (serotonin type 3) receptor antagonists used to treat nausea and vomiting. As previously stated, chemotherapy stimulates release of 5-HT from the gut, which in turn stimulates 5-HT3 receptors in the gut, vagus nerve, and the chemotherapy trigger zone—all of which in turn stimulate the vomiting center, leading to the vomiting reflex.1,13,17,19,21 The blocking action of these drugs on the 5-HT3 receptors is the basis of the antiemetic effect. Palonosetron, with its long 40-hour half-life, has become the preferred prophylactic agent for CINV. The most common adverse events with 5-HT3 antagonists include mild headache, transient elevation of hepatic aminotransferase levels, and constipation.19,21 The use of ondansetron for emesis in the ED is becoming more established both for CINV and non-CINV—mainly due to its high efficacy and favorable side-effect profile compared to metoclopramide and the dopamine antagonists.
Substance P Antagonists (NK1-Receptor Antagonists)
Oral aprepitant, injectable fosaprepitant, and netupitant are some of the Substance P (NK1) antagonists used to treat nausea and vomiting. In a manner similar to 5-HT release, chemotherapeutic agents stimulate the cellular release of NK1 in the gut. This reaction in turn activates receptors in the vagus nerve and the chemotherapy trigger zone, which stimulates the vomiting center. The NK1 receptors are blocked by these agents. The main use of these medications has been to complement the 5-HT3 antagonists for prophylaxis prior to administration of chemotherapy. Neurokinin-1receptor antagonists have not been studied in the setting of breakthrough nausea and vomiting but they are being used to treat delayed phase breakthrough CINV by the authors at their institution’s ED. The agents have been shown to be more effective than 5-HT3 agents in preventing delayed phase nausea and vomiting.25 As such, the possibility they may also be effective in treating delayed phase breakthrough CINV has led to this use. Recent studies have found these agents highly effective in the treatment of postoperative nausea and vomiting in high-risk patients.26
The standard in recent years for prophylaxis has been combining 5-HT3 antagonists, NK1 inhibitors, and dexamethasone. Netupitant/palonosetron (commonly referred to as NEPA) is a novel oral agent combining a long-acting 5-HT3 antagonist, and a long-acting NK1 inhibitor for CINV prophylaxis.27 Its use in treating delayed breakthrough vomiting remains to be seen.
Corticosteroids
Based on its antiemetic properties, the corticosteroid dexamethasone increases the effects of antiemetics (ie, metoclopramide and more recently 5-HT3 and NK1 receptor antagonists) in preventing CINV, perhaps by reducing the blood-brain barrier permeability to emetogenic substances. There are also some evidence-based benefits in using dexamethasone in patients with bowel obstruction. It is also used to reduce ICP from cerebral edema.1,11,13,17,19
Benzodiazepines
The benzodiazepines are best given to enhance the antiemetic effects of other drugs, especially in patients experiencing anxiety-related side effects. The benzodiazepines work well for anticipatory nausea. Lorazepam is the preferred drug of choice due to the lack of active metabolites. However, the clinician should always exercise caution when using benzodiazepines in elderly patients due to the increased risk of falls and cognitive impairment.13,17,19
Cannabinoids
The observation that the incidence of CINV decreased in marijuana smokers led to the exploration of cannabinoids for the treatment of nausea and vomiting. Tetrahydrocannabinol, the psychoactive substance in marijuana, is a phytocannabinoid. Its receptor, CB1, exists throughout the brain. Synthetic cannabinoids such as oral dronabinol, oral nabilone, and intramuscular levonantradol have been used with antiemetic success superior to chlorpromazine, haloperidol, metoclopramide, and prochlorperazine, but at the cost of unpleasant CNS effects and postural hypotension in elderly patients.1,13,17
As cited in a systematic review, cannabinoids appear to inhibit growth of glioblastoma multiforme, breast, prostate, and thyroid cancer, colon carcinoma, leukemia, and lymphomas. Cannabinoids can also benefit cancer patients by stimulating appetite, elevating mood, and inhibiting pain.28 Clearly, more oncologic research needs to be done on the topic. As such, this class of medication is years, if not decades, away from use in the ED.
Nonpharmacologic Treatments
Acupuncture and Acupressure
A 2006 Cochrane systematic review and meta-analysis showed that acupuncture helped with acute CINV but not with delayed CINV.29 Acupuncture was shown to work best with electro-acupuncture needles. Acupressure without needles helped nausea but not vomiting.29 A more recent review on the specific P6 acupuncture area on the wrist near the median nerve found that electroacupuncture, but not manual acupuncture, was beneficial for first-day vomiting, and acupressure was effective for first-day nausea but not vomiting. Neither acupuncture nor acupressure was shown to help delayed nausea or vomiting.30
Ginger
Ginger has been shown to help with CINV and anticipatory nausea, but not with other types of nausea.13 Supplementing routine antiemetics with 0.5 to 1.5 g of ginger per day for 6 days (beginning 3 days before chemotherapy) was shown to reduce the severity of nausea on the day of chemotherapy, but did not affect vomiting.21
Percutaneous Gastrostomy, Stenting, and Laser Therapy
Several strategies have been developed for palliation of intestinal obstruction when surgery is not warranted. Percutaneous gastrostomy tubes (PEG) are used to vent GI secretions that would otherwise build up. Esophageal, colorectal, and gastric outlet obstructions can be palliated by endoscopically placed stenting devices. Argon beam plasma coagulation laser therapy can be used for gastric outlet as well as colonic obstruction.13,31 One review evaluating the benefits of colonic obstruction stenting found an 89% success rate in symptom relief. This same review noted that venting the PEG tube placement had an 84% rate of symptom relief.31
Selecting an Agent in the ED: the Evidence (or Lack Thereof)
Nontreatment-Related Nausea and Vomiting
A 2011 systematic review of cancer nausea unrelated to chemotherapy or radiotherapy found level B evidence that metoclopramide is the most effective first-line empiric agent. In patients with bowel obstruction, dexamethasone, hyoscine butylbromide (scopolamine), and octreotide are effective. While dexamethasone is often thought to improve the effects of antiemetic drugs, this review showed it did not improve nausea when added to chlorpromazine or metoclopramide. Furthermore, neither metoclopramide nor ondansetron were shown to reduce opioid-induced emesis.13 The review further pointed out the lack of good evidence for expert opinion guideline recommendations in breakthrough vomiting—eg, dose titration of the same drug, switching to a different drug class, or using two or more drugs together at once.13
Another review had similar findings, while pointing out that an “absence of evidence is not evidence of absence,” and noting that many of these treatments have been used for years—ie, the problem is lack of evidence, but not negative evidence.17 Both studies are notable in that they were all done in palliative-care units in which time to relief from nausea and/or vomiting was typically measured in days, not hours, making their application to the emergency setting—where time is a factor—difficult.
Due to the potential for drug toxicity, using the same antiemetic drug repeatedly within a short amount of time in a patient refractory to therapy may not be the best strategy in the ED. It is most likely more beneficial and effective to switch drugs or use a combination of drugs right away—though this approach has theoretical concerns with drug-drug interactions. Again, this is an area in which further study is needed.
Treatment-Related Nausea and Vomiting
A recent review on breakthrough CINV again cited the paucity of clinical trials for this entity. Based on few studies, olanzapine and metoclopramide seem to be of value when prophylactic antiemetic regimens have failed. The review further noted that treatment of breakthrough CINV with an agent from same drug class as that used in the prophylactic regimen (usually 5-HT3 and NK1 antagonists) is unlikely to be successful.32 This review also mentioned an interesting phase 2 study using a transdermal gel consisting of diphenhydramine, haloperidol, and lorazepam to the wrist, in which 27 of 33 patients in the study reported a decrease in nausea within a 4-hour period.33 The same combination of drugs in IV form (lorazepam 0.5 mg, diphenhydramine 12.5 mg, and haloperidol 1 mg) is frequently used in the ED at the authors’ institution to treat breakthrough vomiting refractory to metoclopramide, antihistamines, or 5-HT3 antagonists. To the authors’ knowledge, this combination treatment has not been previously cited in the medical literature.
Recommendations and Summary
Cancer patients presenting to the ED with nausea and vomiting should be thoroughly evaluated regarding the possible etiology of their symptoms. A careful history must include recent chemotherapy, radiation, medications, as well as knowledge of the potential complications associated with the specific type of cancer. The EP also should keep in mind that delayed nausea and vomiting can be present several days after chemotherapy, and that CINV may not manifest until after the initial prophylactic medications have worn off. Moreover, he or she should be aware that some individuals have unique responses to chemotherapy and radiation and may experience more nausea and vomiting symptoms than is considered typical.
In addition to CINV, other etiologies, including GI issues such as delayed gastric emptying, partial bowel obstruction, and constipation should also be carefully considered. When evaluating the patient, the EP should also consider non-GI causes such as elevated ICP, kidney obstruction, infection, silent cardiac ischemia, steroid withdrawal, Addisonian crisis, and electrolyte abnormalities.
The lack of conclusive evidence for the treatment of cancer-related nausea and vomiting in any circumstance—except for prophylaxis prior to chemotherapy—precludes the recommendation of a specific treatment algorithm. However, the evidence is abundant that there are multiple effective agents with different, if not overlapping, mechanisms of action available. The EP, therefore, should be familiar with the most commonly used antiemetic drugs from several different categories and their side effects, and tailor the approach based on the assumed etiology of the symptoms. When treating CINV or cancer-related nausea and vomiting, it is not uncommon that patients may require multiple agents, either simultaneously or in sequence, to obtain symptom resolution.
Dr Sandoval is an assistant professor, department of emergency medicine, division of internal medicine at The University of Texas MD Anderson Cancer Center, Houston. Dr Rice is an assistant professor and clinical medical director in the department of emergency medicine, division of internal medicine at The University of Texas MD Anderson Cancer Center, Houston.
Nausea and vomiting is common in cancer patients and a frequent presentation in the ED. When evaluating nausea and vomiting, the clinician should be aware that the two are not always linked—nausea may present without vomiting and vice versa. Nausea is “an unpleasant sensation of the need to vomit and is associated with autonomic symptoms,” whereas vomiting is “the forceful propulsion of abdominal contents via the contraction of the abdominal musculature and diaphragm.”1 Whether these symptoms present together or independently of each other, both can result in serious metabolic disturbances, internal injury, malnutrition, and poor quality of life. In addition, nausea and vomiting can result in patient withdrawal from potentially beneficial treatment.2 Based on the current literature, this article reviews and provides recommendations on appropriate assessment and treatment of the cancer patient presenting to the ED with nausea and/or vomiting.
Epidemiology
In 2007, the US Nationwide Emergency Department Sample database noted 122 million ED visits, 1.6 million of which were due to nausea and vomiting.3 In contrast, a small study from the United Kingdom cited 18% of ED visits in one of its centers were due to nausea and/or vomiting, demonstrating that the percentage of patients presenting with these symptoms can vary greatly.4
The incidence of cancer-related nausea and vomiting in the ED is unknown. Although EDs affiliated with large cancer centers see many cases of cancer-associated nausea and vomiting, presentations to noncancer-center EDs are becoming more prevalent due to increases in community-based cancer care.5 While the number of cancer patients is rising and the general population is aging,6 there is now less incidence of breakthrough chemotherapy-induced nausea and vomiting (CINV), which is a common cause of cancer-related nausea and vomiting. Older studies quote a 40% to 60% rate of breakthrough CINV; however, with the advent of newer antiemetic prophylaxis, by 2013 the incidence had decreased to about 28%.7 As such, the net effect may be a stable or decreased number of ED visits. In one study of patients with breakthrough CINV, 64% were treated inpatient, 26% outpatient, and 10% in the ED. The study, however, does not note how many of these inpatient visits originated in the ED, highlighting that this is an area in need of further study.8
Current knowledge about the epidemiology and etiology of non-CINV comes from end-of-life (EOL) palliative-care literature treatment guidelines, which are organized by cause (etiology-based antiemetic treatment [EBAT]).9-11 Although one systematic review found that the EBAT approach “cannot be shown to be more effective than using a single antiemetic at effective doses,”12 the etiologic framework is useful and can be applied to non-EOL patients. According to a systematic review on the prevalence of symptoms, nausea in advanced cancer patients ranged from 6% to 68%.6 Another review on cancer-related nausea and vomiting that cited studies conducted in the 1990s showed patients had increased nausea and vomiting as they approach EOL—ranging from 36% upon entering palliative-care programs to 71% in the final week of life.13 However, another systematic review citing more recent studies contradicts these findings, stating that in the last 2 weeks of life, nausea was less common (17%) than in patients who were not at the last 2 weeks of life (31%);14 the same was true of vomiting (20% vs 13%). This data perhaps implies that treatment of nausea and vomiting has improved over time for EOL patients. The same review also found that women were more likely to experience nausea and vomiting than men,14 a finding also seen in a 2011 prospective study of antiemetics for breakthrough CINV vomiting.15
When evaluating patients with cancer-associated nausea and vomiting, it is important to remember that these symptoms rarely occur in isolation. Most patients present with between seven and 15 other complaints, such as pain, weakness, fatigue, anorexia, constipation, dry mouth, early satiety, and dyspnea.16
Pathophysiology
To understand nausea and vomiting, it is helpful to review the emetic pathway. There are four areas that stimulate the central vomiting center located in the medulla oblongata. These are the cerebral cortex, the vestibular nucleus, the intestinal tract, and the chemoreceptor trigger zone (located on the floor of the fourth ventricle). With sufficient input from any of these to the vomiting center, nausea occurs, followed by the vomiting reflex. It is known that each of the input zones, as well as the vomiting center itself, have receptors for various substances, including the following:1,13,17-20
· Cerebral cortex: gamma-aminobutyric acid, histamine type 1 (H1)
· Vestibular nucleus: muscarinic acetylcholine receptor (AChM), H1
· Intestinal tract: 5 hydroxytryptamine type 3 (5-HT3) or serotonin type 3 receptors, 5 hydroxytryptamine type 4 (5-HT4) or serotonin type 3 receptors, dopamine type 2 (D2)
· Chemoreceptor trigger zone: 5 hydroxytryptamine type 2 (5-HT2) or serotonin type 2; D2, neurokinin-1 (NK1), or substance P
· Vomiting center: AChM, H1, 5-HT2, D2, NK1, ([GK mµ] opioid receptors), and cannabinoid (CB) receptors
Each of the aforementioned substances in turn stimulate receptors in the intestinal tract and in the chemoreceptor trigger zone, triggering the vomiting center.1,13,17 Most antiemetic agents block the receptors for one or more of these mediators and are discussed later in more detail. Chemotherapeutic agents specifically cause the release 5-HT and NK1 in the gut, which contains over 90% of the body’s serotonin. This knowledge has led to the development of newer 5-HT3 and NK1 antagonists for CINV. Unlike the other mediators, cannabinoids cause an antiemetic effect when they bind to CB receptors.13,17,19 This finding has led to the development of specific pharmacologic treatment agents.
Etiology and Differential Diagnosis
Perhaps the best way for the emergency physician (EP) to assess the cancer patient with nausea or vomiting is to determine whether the cause is treatment- or nontreatment-related. Treatment-related causes are due to chemotherapy or radiotherapy, and any other causes would be considered nontreatment related. It is, however, wise for the EP to remember that a patient who has had recent chemotherapy can still be at risk for nontreatment etiologies.
Treatment-Related Nausea and Vomiting
Chemotherapy-Induced
Chemotherapy-induced nausea and vomiting has been well-studied in the literature. Chemotherapy is classified as highly, moderately, low, and minimally emetogenic.18,19 Nausea itself is classified as acute (onset within 24 hours), delayed (onset after 24 hours), and anticipatory (prior to the chemotherapy, usually due to anxiety over previous unpleasant experiences). Breakthrough vomiting occurs despite the use of antiemetics and may be acute or delayed up to 5 days.
When evaluating the patient with recent chemotherapy and vomiting, it is prudent to find out if the agent is expected to cause vomiting. For example, a patient on cladribine, which is classified as minimally emetogenic, who experiences significant nausea and vomiting should likely be worked up for another etiology. Even when vomiting is controlled, a significant number of patients still experience nausea without vomiting, which in turn has a negative impact on quality of life.
Even though prophylactic regimens of 5-HT3 and NK1 receptor antagonists have led to improved rates of CINV control,18,19,21 both persistent nausea without vomiting and breakthrough vomiting remain problematic,18 and little scientific work has been done on breakthrough treatment. A small prospective pilot study of the efficacy of prochlorperazine versus serotonin 5-HT3 receptor antagonists for breakthrough vomiting found both medications reduced nausea by 75% at 4 hours.15 In contrast, randomized controlled trials comparing olanzapine to metoclopramide and prochlorperazine for breakthrough vomiting found that at 3 days, olanzapine consistently achieved total relief of vomiting 66% to 70%, while the success rates of the other agents ranged from 20% to 37%.18
Radiotherapy-Induced
Radiotherapy has long been known to adversely affect the gastrointestinal (GI) tract. 5-HT3 (ie, serotonin) is released from the gut enterochromaffin cells, in a manner similar to chemotherapy. A 2015 review on the subject showed that radiotherapy to the upper abdomen is most likely to lead to nausea and vomiting, with 50% to 67% of patients reporting nausea and 21% to 38% reporting vomiting.20 Recommended prophylaxis and treatment regimens are based on consensus expert opinion, highlighting the lack of quality evidence that is seen with CINV. Prophylaxis regimens use 5-HT3 antagonists prior to every session, plus dexamethasone for the first 5 days. Rescue from breakthrough is also treated with 5-HT3 antagonists. The use of daily 5-HT3 antagonists for a long course of radiotherapy, however, can be very expensive and unnecessary.
In addition, there is a delayed nausea and vomiting phenomena that may be due to substances other than serotonin, since 5-HT3 depletes a few days after radiotherapy is begun, and may explain why 5-HT3 antagonists are less effective after the first few days of radiotherapy. Nonpharmacologic treatments such as acupuncture, acupressure, hydrogen therapy, and ginger have been used or proposed as treatments for nausea, with mild benefit and little toxicity, so they should be studied further.20
Nontreatment-Related Nausea or Vomiting
Again, much of what is known about nontreatment cancer-related nausea and/or vomiting comes from the palliative-care literature. It is estimated that 60% of advanced cancer patients experience nontreatment-related nausea, and 30% experience vomiting.1,11 One study of 61 hospice patients showed nausea or vomiting occurred due to the following (listed in order from most to least frequent):
· Impaired gastric emptying due to tumor or hepatomegaly, bowel obstruction, metabolic problems (eg, renal failure, liver failure, hypercalcemia, hyponatremia, ketoacidosis)
· infection
· drugs
· increased intracranial pressure (ICP)
· anxiety
The above causes of nausea and vomiting accounted for 85% of the cases in the study.9 Similar results were found in another study, showing that impaired gastric emptying and metabolic/drugs each caused about one third of the cases.10
Nontreatment-related causes of nausea and vomiting are traditionally divided into the following six broad etiological categories by palliative care practitioners9,10,13:
1. Biochemical: medications, tumor products, metabolic derangements, comorbidities, including systemic infections, noncancer abdominal illnesses; and silent cardiac ischemia
2. Gastric stasis: tumor, neuropathy, hepatomegaly, ascites
3. Bowel dysmotility/obstruction: tumor, metastases, adhesions, ileus, constipation
4. Intracranial pressure: tumor edema, bleeding, hydrocephalus, leptomeningeal disease
5. Vestibular: opioids, comorbid vestibular problems, brainstem metastases
6. Miscellaneous: anxiety, pain
These classification schemes are designed to help guide the treatment of palliative-care patients (EBAT),9-11 but very little evidence supports the recommendations.11-13,17 Expert opinion consensus guidelines favor haloperidol for biochemical etiology and metoclopramide for impaired gastric emptying. In intestinal obstruction, the H1-blocking antihistamine cyclizine and the anticholinergic hyoscine butylbromide (scopoloamine) are the preferred agents, but dexamethasone and haloperidol are also favored by some. It is believed that increased ICP nausea is best treated with cyclizine and dexamethasone. Vestibular etiologies are treated with cyclizine, and anxiety-mediated nausea should be treated with benzodiazepines.9,17 As there are often multiple etiologies in a given patient, selection of one agent can be problematic.13 Furthermore, no studies have applied these guidelines to ED cancer patients. This framework, however, can assist the EP in forming a differential diagnosis and appropriate workup. On history and physical examination, the EP should look for and consider the following:13,16
· Small-volume undigested emesis shortly after eating, suggesting gastric emptying impairment
· Bilious or feculent vomitus, large volumes, constipation, and obstipation, suggesting bowel obstruction (evaluate via X-ray or computed tomographic imaging)
· Early morning nausea and headache, suggesting increased ICP
· Nausea associated with head movement or motion, with or without vertigo, (suggesting vestibular disease)
· Current or recent use of opioids, antibiotics, antifungals, anticonvulsants, vitamins, ethanol, and selective serotonin reuptake inhibitors
· Infection, sepsis
· Metabolic abnormalities found on blood tests (for example, renal failure, liver failure, hypercalcemia, hyponatremia, ketoacidosis, osmolar gap, toxins/poisons, Addisonian crisis from steroid withdrawal or adrenal metastases); and/or
· Silent cardiac ischemia (evaluate via electrocardiography and cardiac enzymes)
· Careful consideration of each of the above possibilities will make one less likely to miss other serious causes of nausea and vomiting in the cancer patient with recent chemotherapy.
Opioid-Induced Nausea
Forty percent of cancer patients taking opioids experience nausea, which can adversely impact pain control.22 Opioid-induced nausea is due to constipation, gastroparesis, stimulation of the chemoreceptor trigger zone, and sensitization of the labyrinth, all of which can in turn stimulate the vomiting center.
Regarding the treatment of opioid-induced nausea and vomiting, there is no evidence to support the use of one antiemetic over another. Some weak evidence-based recommendations suggest either changing the medication to a different opioid, or changing the route of administration from oral to subcutaneous and adding coanalgesics such as gabapentin or ketamine to reduce opioid dosages. Though these strategies may be helpful in practice, none of the studies was large enough or thorough enough to support or warrant any formal recommendations in this systematic review.22
Initial Management and Treatment
As always, attention to the patient’s airway, breathing, and circulation is of utmost importance. Endotracheal intubation should be considered in patients at risk for aspiration—unless a living will or do-not-resuscitate order exists. Maneuvers such as raising the head of the bed or turning the patient on his or her side may help avoid aspiration.
Intravenous (IV) hydration is generally beneficial. The choice and amount of fluid should be based on clinical judgment. Electrolyte imbalances should be corrected. The mainstay of treatment for nausea and/or vomiting is pharmacologic, which is the focus of the next section.
Pharmacologic Management
Prokinetic Agents
Prokinetic agents increase peristalsis and exert an antiemetic effect. Metoclopramide is the best known and most widely available prokinetic agent. Since it is both inexpensive and very effective as an antiemetic, its use in the ED is widespread. Etiology-based antiemetic treatment guidelines list metoclopramide as the antiemetic of choice when gastroparesis or other gastric emptying problems are diagnosed9,10,13,17 as it exerts both D2 and 5-HT3 central nervous system (CNS) antiemetic effects, relaxes pyloric tone (D2), and increases peristalsis by stimulating 5-HT4 serotonin receptors in the gut.
The main limitation of metoclopramide is its extrapyramidal side effects (eg, akathisia, dystonia, psuedoparkinsonism, dyskinesia). Akathisias (ie, restlessness) is a particularly common phenomenon in patients taking metoclopramide. Patients experiencing extrapyramidal reactions are typically treated with diphenhydramine. In addition to the extrapyramidal side effects, metoclopramide is relatively contraindicated in patients with complete bowel obstruction.13,17
In addition to metoclopramide, erythromycin and mirtazapine are other prokinetic agents used in palliative care. Erythromycin has mainly been used for diabetic gastroparesis due to its stimulatory effect on motilin receptors in the GI tract.13,23 Mirtazapine is an antidepressant with both 5-HT3 and 5-HT4 receptor activity. In one case report it was used to treat gastroparesis refractory to all other therapies, including metoclopramide and erythromycin.23
Dopamine-Receptor Antagonists
This category includes many agents, most which are known for their antipsychotic effects. The primary mode of action of dopamine-receptor antagonists is to block D2 receptors in the vomiting center. Etiology-based antiemetic treatment guidelines list these drugs as the first choice in patients with a biochemical-based etiology for nausea, though there is little-to-no evidence to support this recommendation.9,10,12,13,17
While a review on haloperidol use in cancer found its effects better than placebo for CINV and postoperative nausea, studies in the review were small and the evidence weak.24 Due to its low cost, and comparatively favorable side-effect profile, haloperidol is a reasonable alternative to metoclopramide. Indeed, if palliative-care models are used, haloperidol would be preferred over metoclopramide since biochemical nausea is probably more prevalent in the general ED cancer patient than gastroparesis.
Regarding route of administration, olanzapine can be given orally or intramuscularly, making it potentially useful in the ED setting for those who cannot keep pills down and have poor venous access. When used in the supportive care setting, however, olanzapine is typically given at bedtime due to its sedative effects. As such, this agent may be best given to those who will be admitted or placed on observation status, since some patients may not be able to be discharged even if nausea resolves.
Antihistamine Agents
Cyclizine, diphenhydramine, hydroxyzine, meclozine, and promethazine, are all piperazine H1-receptor blockers that work in the vomiting center, vestibular nucleus, and chemoreceptor trigger zone. In addition to its properties as an H1-receptor antagonist, cyclizine also exhibits some anticholinergic activity that decreases bowel secretions, thus making it theoretically beneficial in patients with bowel obstruction. Each of these antihistamines are considered beneficial in treating nausea due to vestibular dysfunction and in motion sickness, and may be helpful in patients with increased ICP. Heavy sedation, anticholinergic, and extrapyramidal side effects may occur with these drugs, especially in elderly patients.1,13,17
Serotonin 5-HT3 Receptor Antagonists
Dolasetron, granisetron, ondansetron, palonosetron, and tropisetron are among the 5-HT3 (serotonin type 3) receptor antagonists used to treat nausea and vomiting. As previously stated, chemotherapy stimulates release of 5-HT from the gut, which in turn stimulates 5-HT3 receptors in the gut, vagus nerve, and the chemotherapy trigger zone—all of which in turn stimulate the vomiting center, leading to the vomiting reflex.1,13,17,19,21 The blocking action of these drugs on the 5-HT3 receptors is the basis of the antiemetic effect. Palonosetron, with its long 40-hour half-life, has become the preferred prophylactic agent for CINV. The most common adverse events with 5-HT3 antagonists include mild headache, transient elevation of hepatic aminotransferase levels, and constipation.19,21 The use of ondansetron for emesis in the ED is becoming more established both for CINV and non-CINV—mainly due to its high efficacy and favorable side-effect profile compared to metoclopramide and the dopamine antagonists.
Substance P Antagonists (NK1-Receptor Antagonists)
Oral aprepitant, injectable fosaprepitant, and netupitant are some of the Substance P (NK1) antagonists used to treat nausea and vomiting. In a manner similar to 5-HT release, chemotherapeutic agents stimulate the cellular release of NK1 in the gut. This reaction in turn activates receptors in the vagus nerve and the chemotherapy trigger zone, which stimulates the vomiting center. The NK1 receptors are blocked by these agents. The main use of these medications has been to complement the 5-HT3 antagonists for prophylaxis prior to administration of chemotherapy. Neurokinin-1receptor antagonists have not been studied in the setting of breakthrough nausea and vomiting but they are being used to treat delayed phase breakthrough CINV by the authors at their institution’s ED. The agents have been shown to be more effective than 5-HT3 agents in preventing delayed phase nausea and vomiting.25 As such, the possibility they may also be effective in treating delayed phase breakthrough CINV has led to this use. Recent studies have found these agents highly effective in the treatment of postoperative nausea and vomiting in high-risk patients.26
The standard in recent years for prophylaxis has been combining 5-HT3 antagonists, NK1 inhibitors, and dexamethasone. Netupitant/palonosetron (commonly referred to as NEPA) is a novel oral agent combining a long-acting 5-HT3 antagonist, and a long-acting NK1 inhibitor for CINV prophylaxis.27 Its use in treating delayed breakthrough vomiting remains to be seen.
Corticosteroids
Based on its antiemetic properties, the corticosteroid dexamethasone increases the effects of antiemetics (ie, metoclopramide and more recently 5-HT3 and NK1 receptor antagonists) in preventing CINV, perhaps by reducing the blood-brain barrier permeability to emetogenic substances. There are also some evidence-based benefits in using dexamethasone in patients with bowel obstruction. It is also used to reduce ICP from cerebral edema.1,11,13,17,19
Benzodiazepines
The benzodiazepines are best given to enhance the antiemetic effects of other drugs, especially in patients experiencing anxiety-related side effects. The benzodiazepines work well for anticipatory nausea. Lorazepam is the preferred drug of choice due to the lack of active metabolites. However, the clinician should always exercise caution when using benzodiazepines in elderly patients due to the increased risk of falls and cognitive impairment.13,17,19
Cannabinoids
The observation that the incidence of CINV decreased in marijuana smokers led to the exploration of cannabinoids for the treatment of nausea and vomiting. Tetrahydrocannabinol, the psychoactive substance in marijuana, is a phytocannabinoid. Its receptor, CB1, exists throughout the brain. Synthetic cannabinoids such as oral dronabinol, oral nabilone, and intramuscular levonantradol have been used with antiemetic success superior to chlorpromazine, haloperidol, metoclopramide, and prochlorperazine, but at the cost of unpleasant CNS effects and postural hypotension in elderly patients.1,13,17
As cited in a systematic review, cannabinoids appear to inhibit growth of glioblastoma multiforme, breast, prostate, and thyroid cancer, colon carcinoma, leukemia, and lymphomas. Cannabinoids can also benefit cancer patients by stimulating appetite, elevating mood, and inhibiting pain.28 Clearly, more oncologic research needs to be done on the topic. As such, this class of medication is years, if not decades, away from use in the ED.
Nonpharmacologic Treatments
Acupuncture and Acupressure
A 2006 Cochrane systematic review and meta-analysis showed that acupuncture helped with acute CINV but not with delayed CINV.29 Acupuncture was shown to work best with electro-acupuncture needles. Acupressure without needles helped nausea but not vomiting.29 A more recent review on the specific P6 acupuncture area on the wrist near the median nerve found that electroacupuncture, but not manual acupuncture, was beneficial for first-day vomiting, and acupressure was effective for first-day nausea but not vomiting. Neither acupuncture nor acupressure was shown to help delayed nausea or vomiting.30
Ginger
Ginger has been shown to help with CINV and anticipatory nausea, but not with other types of nausea.13 Supplementing routine antiemetics with 0.5 to 1.5 g of ginger per day for 6 days (beginning 3 days before chemotherapy) was shown to reduce the severity of nausea on the day of chemotherapy, but did not affect vomiting.21
Percutaneous Gastrostomy, Stenting, and Laser Therapy
Several strategies have been developed for palliation of intestinal obstruction when surgery is not warranted. Percutaneous gastrostomy tubes (PEG) are used to vent GI secretions that would otherwise build up. Esophageal, colorectal, and gastric outlet obstructions can be palliated by endoscopically placed stenting devices. Argon beam plasma coagulation laser therapy can be used for gastric outlet as well as colonic obstruction.13,31 One review evaluating the benefits of colonic obstruction stenting found an 89% success rate in symptom relief. This same review noted that venting the PEG tube placement had an 84% rate of symptom relief.31
Selecting an Agent in the ED: the Evidence (or Lack Thereof)
Nontreatment-Related Nausea and Vomiting
A 2011 systematic review of cancer nausea unrelated to chemotherapy or radiotherapy found level B evidence that metoclopramide is the most effective first-line empiric agent. In patients with bowel obstruction, dexamethasone, hyoscine butylbromide (scopolamine), and octreotide are effective. While dexamethasone is often thought to improve the effects of antiemetic drugs, this review showed it did not improve nausea when added to chlorpromazine or metoclopramide. Furthermore, neither metoclopramide nor ondansetron were shown to reduce opioid-induced emesis.13 The review further pointed out the lack of good evidence for expert opinion guideline recommendations in breakthrough vomiting—eg, dose titration of the same drug, switching to a different drug class, or using two or more drugs together at once.13
Another review had similar findings, while pointing out that an “absence of evidence is not evidence of absence,” and noting that many of these treatments have been used for years—ie, the problem is lack of evidence, but not negative evidence.17 Both studies are notable in that they were all done in palliative-care units in which time to relief from nausea and/or vomiting was typically measured in days, not hours, making their application to the emergency setting—where time is a factor—difficult.
Due to the potential for drug toxicity, using the same antiemetic drug repeatedly within a short amount of time in a patient refractory to therapy may not be the best strategy in the ED. It is most likely more beneficial and effective to switch drugs or use a combination of drugs right away—though this approach has theoretical concerns with drug-drug interactions. Again, this is an area in which further study is needed.
Treatment-Related Nausea and Vomiting
A recent review on breakthrough CINV again cited the paucity of clinical trials for this entity. Based on few studies, olanzapine and metoclopramide seem to be of value when prophylactic antiemetic regimens have failed. The review further noted that treatment of breakthrough CINV with an agent from same drug class as that used in the prophylactic regimen (usually 5-HT3 and NK1 antagonists) is unlikely to be successful.32 This review also mentioned an interesting phase 2 study using a transdermal gel consisting of diphenhydramine, haloperidol, and lorazepam to the wrist, in which 27 of 33 patients in the study reported a decrease in nausea within a 4-hour period.33 The same combination of drugs in IV form (lorazepam 0.5 mg, diphenhydramine 12.5 mg, and haloperidol 1 mg) is frequently used in the ED at the authors’ institution to treat breakthrough vomiting refractory to metoclopramide, antihistamines, or 5-HT3 antagonists. To the authors’ knowledge, this combination treatment has not been previously cited in the medical literature.
Recommendations and Summary
Cancer patients presenting to the ED with nausea and vomiting should be thoroughly evaluated regarding the possible etiology of their symptoms. A careful history must include recent chemotherapy, radiation, medications, as well as knowledge of the potential complications associated with the specific type of cancer. The EP also should keep in mind that delayed nausea and vomiting can be present several days after chemotherapy, and that CINV may not manifest until after the initial prophylactic medications have worn off. Moreover, he or she should be aware that some individuals have unique responses to chemotherapy and radiation and may experience more nausea and vomiting symptoms than is considered typical.
In addition to CINV, other etiologies, including GI issues such as delayed gastric emptying, partial bowel obstruction, and constipation should also be carefully considered. When evaluating the patient, the EP should also consider non-GI causes such as elevated ICP, kidney obstruction, infection, silent cardiac ischemia, steroid withdrawal, Addisonian crisis, and electrolyte abnormalities.
The lack of conclusive evidence for the treatment of cancer-related nausea and vomiting in any circumstance—except for prophylaxis prior to chemotherapy—precludes the recommendation of a specific treatment algorithm. However, the evidence is abundant that there are multiple effective agents with different, if not overlapping, mechanisms of action available. The EP, therefore, should be familiar with the most commonly used antiemetic drugs from several different categories and their side effects, and tailor the approach based on the assumed etiology of the symptoms. When treating CINV or cancer-related nausea and vomiting, it is not uncommon that patients may require multiple agents, either simultaneously or in sequence, to obtain symptom resolution.
Dr Sandoval is an assistant professor, department of emergency medicine, division of internal medicine at The University of Texas MD Anderson Cancer Center, Houston. Dr Rice is an assistant professor and clinical medical director in the department of emergency medicine, division of internal medicine at The University of Texas MD Anderson Cancer Center, Houston.
- Davis M, Walsh D. Treatment of nausea and vomiting in advanced cancer. Support Care Cancer. 2000;8(6):444-452.
- Abernethy AP, Wheeler JL, Zafar SY. Detailing of gastrointestinal symptoms in cancer patients with advanced disease: new methodologies, new insights, and a proposed approach. Curr Opin Support Palliat Care. 2009;3(1):41-49.
- Myer PA, Mannalithara A, Singh G, Singh G, Pasricha PJ, Ladabaum U. Clinical and economic burden of emergency department visits due to gastrointestinal diseases in the United States. Am J Gastroenterol. 2013;108(9):1496-1507.
- Body R, Kaide E, Kendal S, Foex B. Not all suffering is pain: sources of patients’ suffering in the emergency department call for improvements in communication from practitioners. Emerg Med J. 2015;32(1):15-20.
- National Chemotherapy Advisory Group. Chemotherapy Services in England: ensuring quality and safety. London, England: Department of Health; 2009. http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_104501.pdf. Accessed July 17, 2015.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Carlotto A, Hogsett VL, Maiorini EM, Razulis JG, Sonis ST. The economic burden of toxicities associated with cancer treatment: review of the literature and analysis of nausea and vomiting, diarrhoea, oral mucositis and fatigue. Pharmacoeconomics. 2013;31(9):753-766.
- Burke TA, Wisniewski T, Ernst FR. Resource utilization and costs associated with chemotherapy-induced nausea and vomiting (CINV) following highly or moderately emetogenic chemotherapy administered in the US outpatient hospital setting. Support Care Cancer. 2011;19(1):131-140.
- Stephenson J. Davies A. An assessment of aetiology-based guidelines for the management of nausea and vomiting in patients with advanced cancer. Support Care Cancer. 2006;14(4):348-353.
- Bentley A, Boyd K. Use of clinical pictures in the management of nausea and vomiting: a prospective audit. Palliat Med. 2001;15(3):247–253.
- Glare P, Pereira G, Kristjanson LJ, Stockler M, Tattersall M. Systematic review of the efficacy of antiemetics in the treatment of nausea in patients with far-advanced cancer. Support Care Cancer. 2004;12(6):432–440.
- Davis MP, Hallerberg G; Palliative Medicine Study Group of the Multinational Association of Supportive Care in Cancer. A systematic review of the treatment of nausea and/or vomiting in cancer unrelated to chemotherapy or radiation. J Pain Symptom Manage. 2010;39(4):756-767.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Teunissen, S, Wesker W, Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manage. 2007;34(1):94-104.
- Jones JM, Qin R, Bardia A, Linquist B, Wolf S, Loprinzi CL. Antiemetics for chemotherapy-induced nausea and vomiting occurring despite prophylactic antiemetic therapy. J Palliat Med. 2011;14(7):810-814.
- Shoemaker LK, Estfan B, Induru R, Walsh TD. Symptom management: an important part of cancer care. Cleve Clin J Med. 2011;78(1):25-34.
- Harris DG. Nausea and vomiting in advanced cancer. Br Med Bull. 2010;96:175-185.
- Hocking CM, Kichenadasse G. Olanzapine for chemotherapy-induced nausea and vomiting: a systematic review. Support Care Cancer. 2014;22(4):1143-1151.
- Hesketh PJ. Chemotherapy-induced nausea and vomiting. N Engl J Med. 2008;358(23):2482-2494.
- Dennis K, Poon M, Chow E. Nausea and vomiting induced by gastrointestinal radiation therapy: current status and future directions. Curr Opin Support Palliat Care. 2015;9(2):182-188.
- Rangwala F, Zafar SY, Abernethy AP. Gastrointestinal symptoms in cancer patients with advanced disease: new methodologies, insights, and a proposed approach. Curr Opin Support Palliat Care. 2012;6(1):69-76.
- Laugsand EA, Kaasa S, Klepstad P. Management of opioid-induced nausea and vomiting in cancer patients: systematic review and evidence-based recommendations. Palliat Med. 2011;25(5):442-453.
- Kim SW, Shin IS, Kim JM, et al. Mirtazapine for severe gastroparesis unresponsive to conventional prokinetic treatment. Psychosomatics. 2006;47(5):440-442.
- McLean SL, Blenkinsopp A, Bennett MI. Using haloperidol as an antiemetic in palliative care: informing practice through evidence from cancer treatment and postoperative contexts. J Pain Palliat Care Pharmacother. 2013;27(2):132-135.
- Aapro M, Carides A, Rapoport BL, Schmoll HJ, Zhang L, Warr D. Aprepitant and fosaprepitant: a 10-year review of efficacy and safety. Oncologist. 2015;20(4)450-458.
- Soga T, Kume K, Kakuta N, et al. Fosaprepitant versus ondansetron for the prevention of postoperative nausea and vomiting in patients who undergo gynecologic abdominal surgery with patient-controlled epidural analgesia: a prospective, randomized, double-blind study. J Anesth. 2015;29(5):696-701.
- Abramovitz RB, Gaertner KM. The role of netupitant and palonosetron in chemotherapy-induced nausea and vomiting [published online ahead of print April 24, 2015]. J Oncol Pharm Pract. doi:10.1177/1078155215581525.
- Pisanti S, Malfitano AM, Grimaldi C, et al. Use of cannabinoid receptor agonists in cancer therapy as palliative and curative agents. Best Pract Res Clin Endocrinol Metab. 2009;23(1):117-131.
- Ezzo JM, Richardson MA, Vickers A, et al: Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database Syst Rev. 2006;19(2):CD002285.
- Ezzo J, Streitberger K, Schneider A. Cochrane systematic reviews examine P6 acupuncture-point stimulation for nausea and vomiting. J Altern Complement Med. 2006;12(5):489-495.
- Laval G, Marcelin-Benazech B, Guirimand F, et al; French Society for Palliative Care; French Society for Digestive Surgery; French Society for Gastroenterology; French Association for Supportive Care in Oncology; French Society for Digestive Cancer. Recommendations for bowel obstruction with peritoneal carcinomatosis. J Pain Symptom Manage. 2014;48(1):75-91.
- Navari RM. Treatment of breakthrough and refractory chemotherapy-induced nausea and vomiting. Biomed Res Int. 2015;2015:595894.
- Bleicher J, Bhaskara A, Huyck T, Constantino S, Bardia A, Loprinzi CL, et al. Lorazepam, diphenhydramine, and haloperidol transdermal gel for rescue from chemotherapy-induced nausea/vomiting: results of two pilot trials. J Support Oncol. 2008;6(1):27-32.
- Davis M, Walsh D. Treatment of nausea and vomiting in advanced cancer. Support Care Cancer. 2000;8(6):444-452.
- Abernethy AP, Wheeler JL, Zafar SY. Detailing of gastrointestinal symptoms in cancer patients with advanced disease: new methodologies, new insights, and a proposed approach. Curr Opin Support Palliat Care. 2009;3(1):41-49.
- Myer PA, Mannalithara A, Singh G, Singh G, Pasricha PJ, Ladabaum U. Clinical and economic burden of emergency department visits due to gastrointestinal diseases in the United States. Am J Gastroenterol. 2013;108(9):1496-1507.
- Body R, Kaide E, Kendal S, Foex B. Not all suffering is pain: sources of patients’ suffering in the emergency department call for improvements in communication from practitioners. Emerg Med J. 2015;32(1):15-20.
- National Chemotherapy Advisory Group. Chemotherapy Services in England: ensuring quality and safety. London, England: Department of Health; 2009. http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_104501.pdf. Accessed July 17, 2015.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Carlotto A, Hogsett VL, Maiorini EM, Razulis JG, Sonis ST. The economic burden of toxicities associated with cancer treatment: review of the literature and analysis of nausea and vomiting, diarrhoea, oral mucositis and fatigue. Pharmacoeconomics. 2013;31(9):753-766.
- Burke TA, Wisniewski T, Ernst FR. Resource utilization and costs associated with chemotherapy-induced nausea and vomiting (CINV) following highly or moderately emetogenic chemotherapy administered in the US outpatient hospital setting. Support Care Cancer. 2011;19(1):131-140.
- Stephenson J. Davies A. An assessment of aetiology-based guidelines for the management of nausea and vomiting in patients with advanced cancer. Support Care Cancer. 2006;14(4):348-353.
- Bentley A, Boyd K. Use of clinical pictures in the management of nausea and vomiting: a prospective audit. Palliat Med. 2001;15(3):247–253.
- Glare P, Pereira G, Kristjanson LJ, Stockler M, Tattersall M. Systematic review of the efficacy of antiemetics in the treatment of nausea in patients with far-advanced cancer. Support Care Cancer. 2004;12(6):432–440.
- Davis MP, Hallerberg G; Palliative Medicine Study Group of the Multinational Association of Supportive Care in Cancer. A systematic review of the treatment of nausea and/or vomiting in cancer unrelated to chemotherapy or radiation. J Pain Symptom Manage. 2010;39(4):756-767.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Teunissen, S, Wesker W, Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manage. 2007;34(1):94-104.
- Jones JM, Qin R, Bardia A, Linquist B, Wolf S, Loprinzi CL. Antiemetics for chemotherapy-induced nausea and vomiting occurring despite prophylactic antiemetic therapy. J Palliat Med. 2011;14(7):810-814.
- Shoemaker LK, Estfan B, Induru R, Walsh TD. Symptom management: an important part of cancer care. Cleve Clin J Med. 2011;78(1):25-34.
- Harris DG. Nausea and vomiting in advanced cancer. Br Med Bull. 2010;96:175-185.
- Hocking CM, Kichenadasse G. Olanzapine for chemotherapy-induced nausea and vomiting: a systematic review. Support Care Cancer. 2014;22(4):1143-1151.
- Hesketh PJ. Chemotherapy-induced nausea and vomiting. N Engl J Med. 2008;358(23):2482-2494.
- Dennis K, Poon M, Chow E. Nausea and vomiting induced by gastrointestinal radiation therapy: current status and future directions. Curr Opin Support Palliat Care. 2015;9(2):182-188.
- Rangwala F, Zafar SY, Abernethy AP. Gastrointestinal symptoms in cancer patients with advanced disease: new methodologies, insights, and a proposed approach. Curr Opin Support Palliat Care. 2012;6(1):69-76.
- Laugsand EA, Kaasa S, Klepstad P. Management of opioid-induced nausea and vomiting in cancer patients: systematic review and evidence-based recommendations. Palliat Med. 2011;25(5):442-453.
- Kim SW, Shin IS, Kim JM, et al. Mirtazapine for severe gastroparesis unresponsive to conventional prokinetic treatment. Psychosomatics. 2006;47(5):440-442.
- McLean SL, Blenkinsopp A, Bennett MI. Using haloperidol as an antiemetic in palliative care: informing practice through evidence from cancer treatment and postoperative contexts. J Pain Palliat Care Pharmacother. 2013;27(2):132-135.
- Aapro M, Carides A, Rapoport BL, Schmoll HJ, Zhang L, Warr D. Aprepitant and fosaprepitant: a 10-year review of efficacy and safety. Oncologist. 2015;20(4)450-458.
- Soga T, Kume K, Kakuta N, et al. Fosaprepitant versus ondansetron for the prevention of postoperative nausea and vomiting in patients who undergo gynecologic abdominal surgery with patient-controlled epidural analgesia: a prospective, randomized, double-blind study. J Anesth. 2015;29(5):696-701.
- Abramovitz RB, Gaertner KM. The role of netupitant and palonosetron in chemotherapy-induced nausea and vomiting [published online ahead of print April 24, 2015]. J Oncol Pharm Pract. doi:10.1177/1078155215581525.
- Pisanti S, Malfitano AM, Grimaldi C, et al. Use of cannabinoid receptor agonists in cancer therapy as palliative and curative agents. Best Pract Res Clin Endocrinol Metab. 2009;23(1):117-131.
- Ezzo JM, Richardson MA, Vickers A, et al: Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database Syst Rev. 2006;19(2):CD002285.
- Ezzo J, Streitberger K, Schneider A. Cochrane systematic reviews examine P6 acupuncture-point stimulation for nausea and vomiting. J Altern Complement Med. 2006;12(5):489-495.
- Laval G, Marcelin-Benazech B, Guirimand F, et al; French Society for Palliative Care; French Society for Digestive Surgery; French Society for Gastroenterology; French Association for Supportive Care in Oncology; French Society for Digestive Cancer. Recommendations for bowel obstruction with peritoneal carcinomatosis. J Pain Symptom Manage. 2014;48(1):75-91.
- Navari RM. Treatment of breakthrough and refractory chemotherapy-induced nausea and vomiting. Biomed Res Int. 2015;2015:595894.
- Bleicher J, Bhaskara A, Huyck T, Constantino S, Bardia A, Loprinzi CL, et al. Lorazepam, diphenhydramine, and haloperidol transdermal gel for rescue from chemotherapy-induced nausea/vomiting: results of two pilot trials. J Support Oncol. 2008;6(1):27-32.
Metastatic Spinal Cord Compression: A Review
Case
A 60-year-old man with stage IV hormoneindependent prostate cancer, with widely metastatic disease to the bone, presents to the ED with increased weakness and new onset of numbness in the lower extremities, which he states began earlier that day. After failing several lines of chemotherapy, he is currently being treated with hormonal therapy alone. Patient first noted weakness in the left lower extremity 5 days before presentation, which progressed to bilateral involvement, making ambulation difficult and requiring the use of a walker. He denies back pain or urinary or fecal incontinence. Regarding pain management, he had been recently treated at one of the pain clinics in the hospital and has continued on opioid medication at another institution. Until the past week, he states he had back pain without neurological deficits.
His vital signs are stable at presentation. Patient is obese but in no acute distress. His cardiopulmonary examination is unremarkable; abdominal examination is benign; and back examination is normal. On neurological examination, iliopsoas flexion is 4/5 bilaterally; the rest of the motor examination is normal, with toes downgoing bilaterally upon plantar stimulation. Diminished sensation to light touch is noted at the T4-T6 sensory level and below; patient also has diminished proprioception in his lower extremities.
Patient had undergone a whole body scan one month prior to presentation, which revealed increased tracer uptake of Technetium-99m in multiple areas in the thoracic and lumbar spine. The radiologist also reported bilateral involvement in the wrists, femurs, tibias, and humeri—all in concordance with multifocal bone disease noted in previous computed tomography scans.
How should you approach this case?
Overview of Metastatic Spinal Cord Compression
Malignant or metastatic spinal cord compression (MSCC) of the thecal sac is an ominous complication of advanced cancer and an oncologic emergency presenting clinically in approximately 3% to 10% of cancer-related deaths.1,2 Cancer patients have a median survival of 3 to 6 months from diagnosis of MSCC.1,3,4 This disease causes significant disability due to paralysis, sensory loss, protracted pain, and sphincter dysfunction.5 If left untreated, MSCC has the potential to cause paraplegia in almost all affected patients; therefore, prompt recognition and treatment are essential to maintain mobility and neurological function. Generally speaking, any cancer patient who presents with new or worsening back pain—even in the absence of neurological deficits—merits evaluation for spinal cord compression.6 Nevertheless, individual risk assessment is warranted.7
Epidemiology
In the United States, more than 20,000 cases of MSCC are reported each year.8 According to postmortem studies, this condition affects 5% to 36% of cancer patients.9,10 In a US nationwide study of 15,367 cases of MSCC,2 the mean age at hospitalization was 62 years, with 37% of cases occurring in women. In approximately 20% of cases, MSCC was the initial presentation of cancer4; this has been reflected in our experience at MD Anderson Cancer Center.
Cancers of the breast, lung, prostate, and multiple myeloma are the most frequent underlying conditions in MSCC.2,8 Its prevalence varies depending on tumor type, occurring in 0.2% of pancreatic cancers; however, MSCC may affect up to 7.9% to 15% of myelomas1,2 and 13% of lymphomas.2 Interestingly, 5.5% of patients with prostate cancer develop MSCC.2 According to a study by Lu et al,11 historical risk factors include known nonvertebral bony metastases and stage IV disease at the time of diagnosis.
The most common location of MSCC is the thoracic spine (69% of cases); 29% of cases occur at the lumbosacral level and 10% at the cervical area.12 Most likely this pattern follows the lymphatic drainage, as metastases from breast and lung cancers tend to be found in the thoracic spine. Pelvic and intra-abdominal malignancies most commonly migrate to the lumbar spine. Multiple spinal epidural metastases were noted in 31% of those who underwent complete imaging of the spine.12
Pathophysiology
Most cases of MSCC are epidural in origin, arising from the vertebral column in 85% of patients.8 Epidural spread is caused mainly by hematogenous mechanism through the Batson venous plexus,13 debilitating the bone and eventually causing vertebral collapse with compression of the spinal canal. Epidural spread is less likely caused by direct tumor extension (ie, erosion through the bone) or by direct deposition of tumor cells into the epidural space.14 Ultimate neuronal injury is thought to involve vasogenic edema,15 leading to ischemia13 through venous infarction, but there has been debate regarding this last phenomenon.16 In cases of paralysis, demyelination is striking.16
Clinical Presentation
Even though cancer accounts for less than 1% of episodes of low back pain, it is the most common systemic disease affecting the spine.17 An important clinical inquiry is to determine whether back pain in an established cancer patient can be ruled out without extensive imaging. Unfortunately, clinical examination alone cannot exclude MSCC. Because of the high specificity (0.98), any cancer patient with new back pain should be considered to have metastasis until proven otherwise.17
Symptoms in MSCC at presentation can be motor, sensory, and/or autonomic. Back pain varies depending on the site of metastasis, which can be referred, local, radicular, or a combination of all three.18 The primary complaint is pain in 83% to 96% of cases,19,20 though this is a nonspecific sign.
Previous studies have shown 40% to 64% of patients were not ambulatory at the time of diagnosis.19,25 Recent case series, however, report an increased number of ambulatory patients—possibly due to increased clinician awareness.26 In other cases, only 9% of patients were able to walk independently without aid.27 Loss of sensation, dense paraplegia, and incontinence are late findings and likely signal some degree of permanent disability.19
Misdiagnosis is a common issue in the ED setting. In an interesting retrospective study of 63 patients with spinal cord compression28 (not necessarily malignant), 18 (29%) were misdiagnosed.28 Consequently, there was a significant delay in diagnosis despite obvious neurological deficits at presentation.
Evaluation and Imaging
A detailed physical examination is essential to diagnosing MSCC. A thorough neurological examination, including sensation, strength, and reflexes should be carefully documented. If spinal instability is suspected, range-of-motion testing is contraindicated. The modified Frankel classification,29 adapted from the traumatic spine cord injury work by Frankel, et al,30 may be used to assess the degree of disability (Table).
Lu et al11 noted hyperreflexia and upward going Babinski reflex as common findings. Moreover, risk factors of decreased rectal sphincter tone and bladder were determinant for poor outcomes.
MRI studies should include the entire spine—not just the perceived area of interest— as up to 38% of patients have multiple-site metastases12 (Figure 1). Sensory deficits and mechanical pain may be present two to four vertebral levels away from the actual lesion.11 If MRI suggests cord compression, severity can be graded using the MSCC scale34 (Figure 2). Several scoring systems have been developed to aid in decision making concerning surgical treatment.
Management and Outcomes
The goal of therapy is symptom control and preservation of function. This requires a multidisciplinary approach and may involve radiation therapy and surgery, as well as medical efforts. Upon diagnosis and initiation of therapy, serial neurological evaluation should be undertaken. Neurovital signs should be scheduled to coincide with other nursing efforts to ease the burden of care and minimize patient discomfort.
The mainstay of medical therapy is treatment with corticosteroids.35 Initial trials have demonstrated that corticosteroids improve functional status in MSCC, but controversy exists regarding the effective dose. In a randomized, controlled trial by Sorensen et al,36 which sought to evaluate functional outcomes of highdose corticosteroids as an adjunct to radiotherapy, 57 patients received either high-dose dexamethasone or no corticosteroid therapy. Fifty-nine percent of patients in the dexamethasone group were ambulatory 6 months after treatment compared to 39% in the group who did not receive steroids.36
A patient without a biopsy-confirmed cancer diagnosis in need of corticosteroid treatment presents a dilemma. Plasmacytomas, thymomas, lymphomas, multiple myeloma, germ-cell tumors are very sensitive to corticosteroid therapy in patients with MSCC.38 However, corticosteroids given before tissue samples are obtained may hinder proper diagnosis and complicate future management.39,40 In the absence of neurological deficit, corticosteroids may be withheld and emergent consultation with neurosurgery and oncology should be obtained. If there is any question regarding the nature of the lesion, tissue diagnosis must be obtained without delay.
Strict bed rest (including logroll and bedpan use) should be instituted if there is suspicion of spinal cord instability. Patients with suspected involvement of the cervical spine should have a Philadelphia collar placed until spinal stability has been confirmed. In the United Kingdom, the National Institutes for Health Care Excellence guidelines recommend all patients with suspected cord compression be nursed in a flat position.22 Other institutions, however, do not believe that strict bed rest is necessary, as it is presumed that MSCC is inherently different from that caused by trauma. Authors supporting this position contend that the increased incidence of deep vein thrombosis, infection (particularly from the urinary tract), and decubitus ulcers outweighs the benefit of bed rest. Patient preference should be taken into consideration as those with good functional status may be quite resistant to bed rest. In cases where cord compression is strongly suspected, these patients should be educated on proper bed rest. The greatest predictors of outcome are ambulatory and functional status at the time of diagnosis (generally based on an Eastern Cooperative Oncology Group scale). Patients with a good functional status, limited disease, and a life expectancy of greater than 3 to 6 months may benefit from surgery.41 However, emergent surgical evaluation is required in patients not responding to radiotherapy or who received received only limited doses of radiotherapy, as well as those with spinal instability, direct cord compression due to a bony fragment, impending sphincter dysfunction, unknown primary tumor, or no paraplegia for >48 hours.15
Unfortunately, surgery is only indicated in 10% to 15% of MSCC cases.42 In the past two decades, significant improvements regarding new aggressive surgical techniques have been made, and include circumferential decompression of the spine and staged or single stage anterior posterior surgery with stabilization. 43 Additionally, the combination of surgery with radiotherapy has improved outcomes.44
Most patients benefit from short-course radiotherapy45 even when given palliatively. 46 Longer courses of radiotherapy are highly recommended for patients with a more favorable prognosis.47 Up to 10% of patients diagnosed with spinal cord compression will require treatment for disease recurrence.42 There is a limited role for chemotherapy, and in seminomas and lymphomas, results can be quite dramatic.38
Prevention
Lu et al11 found that only 54% of patients were aware that back pain should be reported to their physician. Delays in diagnosis and treatment are common and well described in the literature.21 Patients should be instructed to call their physician within 24 hours from the development of any new or worsening back pain, and should be advised to seek immediate care if they develop any neurological symptoms. To facilitate appropriate and prompt management of MSCC, hospitals should develop diagnostic algorithms to minimize delays in referral to a comprehensive center for further treatment.
Case Conclusion
Based on this patient’s symptoms and status at presentation, the emergency team determined he was at high risk for MSCC. An initial dosage of 10 mg dexamethasone was administered intravenously (IV), followed by 4 mg IV every 6 hours prior to imaging. An MRI without contrast of the cervical, thoracic, and lumbar spine showed cord compression with mild cord edema at T4 level, along with diffused osseous metastasis.
Upon diagnosis, patient was referred to radiation oncology for radiotherapy of the T2-T6 vertebral bodies. Three days after initiation of radiation therapy, his neurological function deteriorated with paraplegia and incontinence, and he was emergently evaluated for neurosurgery. Although T4 laminectomy and decompression of the spinal cord were performed without complication, patient did not recover neurological function. His hospital course was complicated by Ogilvie syndrome and episodes of delirium, and he was discharged to a rehabilitation facility 23 days after admission; paraplegia and urinary and bowel incontinence remained unchanged.
- Loblaw DA, Laperriere NJ, Mackillop WJ. A population-based study of malignant spinal cord compression in Ontario. Clin Oncol (R Coll Radiol). 2003;15(4):211-217.
- Mak KS, Lee LK, Mak RH, et al. Incidence and treatment patterns in hospitalizations for malignant spinal cord compression in the United States, 1998-2006. Int J Radiat Oncol Biol Phys. 2011;80(3):824-831.
- Constans JP, de Divitiis E, Donzelli R, Spaziante R, Meder JF, Haye C. Spinal metastases with
- neurological manifestations. Review of 600 cases. J Neurosurg. 1983;59(1):111-118.
- Schiff D, O’Neill BP, Suman VJ. Spinal epidural metastasis as the initial manifestation of malignancy: clinical features and diagnostic approach. Neurology. 1997;49(2):452-456.
- Loblaw DA, Perry J, Chambers A, Laperriere NJ. Systematic review of the diagnosis and management of malignant extradural spinal cord compression: the Cancer Care Ontario Practice Guidelines Initiative’s Neuro-Oncology Disease Site Group. J Clin Oncol. 2005;23(9):2028-2037.
- Levack P, Graham J, Collie D, et al. Don’t wait for a sensory level—listen to the symptoms: a prospective audit of the delays in diagnosis of malignant cord compression. Clin Oncol (R Coll Radiol). 2002;14(6):472-480.
- Talcott JA, Stomper PC, Drislane FW, et al. Assessing suspected spinal cord compression: a multidisciplinary outcomes analysis of 342 episodes. Support Care Cancer. 1999;7(1):31-38.
- Byrne TN. Spinal cord compression from epidural metastases. N Engl J Med. 1992;327(9):614-619.
- Abrams HL, Spiro R, Goldstein N. Metastases in carcinoma; analysis of 1000 autopsied cases. Cancer. 1950;3(1):74-85.
- Wong DA, Fornasier VL, MacNab I. Spinal metastases: the obvious, the occult, and the impostors. Spine (Phila Pa 1976). 1990;15(1):1-4.
- Lu C, Gonzalez RG, Jolesz FA, Wen PY, Talcott JA. Suspected spinal cord compression in cancer patients: a multidisciplinary risk assessment. J Support Oncol. 2005;3(4):305-312.
- Schiff D, O’Neill BP, Wang CH, O’Fallon JR. Neuroimaging and treatment implications of patients with multiple epidural spinal metastases. Cancer. 1998;83(8):1593-1601.
- Arguello F, Baggs RB, Duerst RE, Johnstone L, McQueen K, Frantz CN. Pathogenesis of vertebral metastasis and epidural spinal cord compression. Cancer. 1990;65(1):98-106.
- Schiff D. Spinal cord compression. Neurol Clin. 2003;21(1):67-86, viii.
- Prasad D, Schiff D. Malignant spinal-cord compression. Lancet Oncol. 2005;6(1):15-24.
- Helweg-Larsen S, Laursen H. Clinical and autopsy findings in spinal cord compression due to metastatic disease. Eur J Neurol. 1998;5(6):587-592.
- Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 199218. Abrahm JL, Banffy MB, Harris MB. Spinal cord compression in patients with advanced metastatic cancer: "all I care about is walking and living my life." JAMA. 2008;299(8):937-946.
- Bach F, Larsen BH, Rohde K, et al. Metastatic spinal cord compression. Occurrence, symptoms, clinical presentations and prognosis in 398 patients with spinal cord compression. Acta Neurochir (Wien). 1990;107(1-2):37-43.
- Gilbert RW, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: diagnosis and treatment. Ann Neurol. 1978;3(1):40-51.
- Husband DJ. Malignant spinal cord compression: prospective study of delays in referral and treatment. BMJ. 1998;317(7150):18-21.
- Metastatic Spinal Cord Compression: Diagnosis and Management of Patients at Risk of or with Metastatic Spinal Cord Compression. Cardiff UK: National Collaborating Centre for Cancer; 2008.
- Shiue K, Sahgal A, Chow E, et al. Management of metastatic spinal cord compression. Expert Rev Anticancer Ther. 2010;10(5):697-708.
- Hammack JE. Spinal cord disease in patients with cancer. Continuum (Minneap Minn). 2012;18(2):312-327.
- Helweg-Larsen S. Clinical outcome in metastatic spinal cord compression. A prospective study of 153 patients. Acta Neurol Scand. 1996;94(4):269-275.
- Rades D, Fehlauer F, Schulte R, et al. Prognostic factors for local control and survival after radiotherapy of metastatic spinal cord compression. J Clin Oncol. 2006;24(21):3388-3393.
- McLinton A, Hutchison C. Malignant spinal cord compression: a retrospective audit of clinical practice at a UK regional cancer centre. Br J Cancer. 2006;94(4):486-491.
- Dugas AF, Lucas JM, Edlow JA. Diagnosis of spinal cord compression in nontrauma patients in the emergency department. Acad Emerg Med. 2011;18(7):719-725.
- Ditunno JF, Jr, Young W, Donovan WH, Creasey metastatic spinal CORD compression 18 EMERGENCY MEDICINE I january 2014 www.emed-journal.com G. American Spinal Surgery Association. The international standards booklet for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Paraplegia. 1994;32(2):70-80.
- Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7(3):179-192.
- Portenoy RK, Galer BS, Salamon O, et al. Identification of epidural neoplasm. Radiography and bone scintigraphy in the symptomatic and asymptomatic spine. Cancer. 1989;64(11):2207-2213.
- Husband DJ, Grant KA, Romaniuk CS. MRI in the diagnosis and treatment of suspected malignant spinal cord compression. Br J Radiol. 2001;74(877):15-23.
- Carmody RF, Yang PJ, Seeley GW, Seeger JF, Unger EC, Johnson JE. Spinal cord compression due to metastatic disease: diagnosis with MR imaging versus myelography. Radiology. 1989;173(1):225-229.
- Bilsky MH, Laufer I, Fourney DR, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13(3):324-328.
- Loblaw DA, Mitera G, Ford M, Laperriere NJ. A 2011 updated systematic review and clinical practice guideline for the management of malignant extradural spinal cord compression. Int J Radiat Oncol Biol Phys. 2012;84(2):312-317.
- Sorensen S, Helweg-Larsen S, Mouridsen H, Hansen HH. Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: a randomised trial. Eur J Cancer. 1994;30A(1):22-27.
- Heimdal K, Hirschberg H, Slettebo H, Watne K, Nome O. High incidence of serious side effects of high-dose dexamethasone treatment in patients with epidural spinal cord compression. J Neurooncol. 1992;12(2):141-144.
- Posner JB, Howieson J, Cvitkovic E. "Disappearing" spinal cord compression: oncolytic effect of glucocorticoids (and other chemotherapeutic agents) on epidural metastases. Ann Neurol. 1977;2(5):409-413.
- Kan E, Levi I, Benharroch D. Alterations in the primary diagnosis of lymphomas pretreated with corticosteroid agents. Leuk Lymphoma. 2011;52(3):425-428.
- Borenstein SH, Gerstle T, Malkin D, Thorner P, Filler RM. The effects of prebiopsy cortico-steroid treatment on the diagnosis of mediastinal lymphoma. J Pediatr Surg. 2000;35(6):973-976.
- Akram H, Allibone J. Spinal surgery for palliation in malignant spinal cord compression. Clin Oncol (R Coll Radiol). 2010;22(9):792-800.
- Rades D, Abrahm JL. The role of radiotherapy for metastatic epidural spinal cord compression. Nat Rev Clin Oncol. 2010;7(10):590-598.
- Sundaresan N, Sachdev VP, Holland JF, et al. Surgical treatment of spinal cord compression from epidural metastasis. J Clin Oncol. 1995;13(9):2330-2335.
- Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643-648.
- Rades D, Dahm-Daphi J, Rudat V, et al. Is shortcourse radiotherapy with high doses per fraction the appropriate regimen for metastatic spinal cord compression in colorectal cancer patients? Strahlenther Onkol. 2006;182(12):708-712.
- van den Hout WB, van der Linden YM, Steenland E, et al. Single- versus multiple-fraction radiotherapy in patients with painful bone metastases: cost-utility analysis based on a randomized trial. J Natl Cancer Inst. 2003;95(3):222-229.
- Steenland E, Leer JW, van Houwelingen H, et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: a global analysis of the Dutch Bone Metastasis Study. Radiother Oncol. 1999;52(2):101-109.
- Rades D, Hueppe M, Schild SE. A score to identify patients with metastatic spinal cord compression who may be candidates for best supportive care. Cancer. 2013;119(4):897-903.
- Guo Y, Palmer JL, Bianty J, Konzen B, Shin K, Bruera E. Advance directives and do-not-resuscitate orders in patients with cancer with metastatic spinal cord compression: advanced care planning implications. J Palliat Med. 2010;13(5):513-517.
Case
A 60-year-old man with stage IV hormoneindependent prostate cancer, with widely metastatic disease to the bone, presents to the ED with increased weakness and new onset of numbness in the lower extremities, which he states began earlier that day. After failing several lines of chemotherapy, he is currently being treated with hormonal therapy alone. Patient first noted weakness in the left lower extremity 5 days before presentation, which progressed to bilateral involvement, making ambulation difficult and requiring the use of a walker. He denies back pain or urinary or fecal incontinence. Regarding pain management, he had been recently treated at one of the pain clinics in the hospital and has continued on opioid medication at another institution. Until the past week, he states he had back pain without neurological deficits.
His vital signs are stable at presentation. Patient is obese but in no acute distress. His cardiopulmonary examination is unremarkable; abdominal examination is benign; and back examination is normal. On neurological examination, iliopsoas flexion is 4/5 bilaterally; the rest of the motor examination is normal, with toes downgoing bilaterally upon plantar stimulation. Diminished sensation to light touch is noted at the T4-T6 sensory level and below; patient also has diminished proprioception in his lower extremities.
Patient had undergone a whole body scan one month prior to presentation, which revealed increased tracer uptake of Technetium-99m in multiple areas in the thoracic and lumbar spine. The radiologist also reported bilateral involvement in the wrists, femurs, tibias, and humeri—all in concordance with multifocal bone disease noted in previous computed tomography scans.
How should you approach this case?
Overview of Metastatic Spinal Cord Compression
Malignant or metastatic spinal cord compression (MSCC) of the thecal sac is an ominous complication of advanced cancer and an oncologic emergency presenting clinically in approximately 3% to 10% of cancer-related deaths.1,2 Cancer patients have a median survival of 3 to 6 months from diagnosis of MSCC.1,3,4 This disease causes significant disability due to paralysis, sensory loss, protracted pain, and sphincter dysfunction.5 If left untreated, MSCC has the potential to cause paraplegia in almost all affected patients; therefore, prompt recognition and treatment are essential to maintain mobility and neurological function. Generally speaking, any cancer patient who presents with new or worsening back pain—even in the absence of neurological deficits—merits evaluation for spinal cord compression.6 Nevertheless, individual risk assessment is warranted.7
Epidemiology
In the United States, more than 20,000 cases of MSCC are reported each year.8 According to postmortem studies, this condition affects 5% to 36% of cancer patients.9,10 In a US nationwide study of 15,367 cases of MSCC,2 the mean age at hospitalization was 62 years, with 37% of cases occurring in women. In approximately 20% of cases, MSCC was the initial presentation of cancer4; this has been reflected in our experience at MD Anderson Cancer Center.
Cancers of the breast, lung, prostate, and multiple myeloma are the most frequent underlying conditions in MSCC.2,8 Its prevalence varies depending on tumor type, occurring in 0.2% of pancreatic cancers; however, MSCC may affect up to 7.9% to 15% of myelomas1,2 and 13% of lymphomas.2 Interestingly, 5.5% of patients with prostate cancer develop MSCC.2 According to a study by Lu et al,11 historical risk factors include known nonvertebral bony metastases and stage IV disease at the time of diagnosis.
The most common location of MSCC is the thoracic spine (69% of cases); 29% of cases occur at the lumbosacral level and 10% at the cervical area.12 Most likely this pattern follows the lymphatic drainage, as metastases from breast and lung cancers tend to be found in the thoracic spine. Pelvic and intra-abdominal malignancies most commonly migrate to the lumbar spine. Multiple spinal epidural metastases were noted in 31% of those who underwent complete imaging of the spine.12
Pathophysiology
Most cases of MSCC are epidural in origin, arising from the vertebral column in 85% of patients.8 Epidural spread is caused mainly by hematogenous mechanism through the Batson venous plexus,13 debilitating the bone and eventually causing vertebral collapse with compression of the spinal canal. Epidural spread is less likely caused by direct tumor extension (ie, erosion through the bone) or by direct deposition of tumor cells into the epidural space.14 Ultimate neuronal injury is thought to involve vasogenic edema,15 leading to ischemia13 through venous infarction, but there has been debate regarding this last phenomenon.16 In cases of paralysis, demyelination is striking.16
Clinical Presentation
Even though cancer accounts for less than 1% of episodes of low back pain, it is the most common systemic disease affecting the spine.17 An important clinical inquiry is to determine whether back pain in an established cancer patient can be ruled out without extensive imaging. Unfortunately, clinical examination alone cannot exclude MSCC. Because of the high specificity (0.98), any cancer patient with new back pain should be considered to have metastasis until proven otherwise.17
Symptoms in MSCC at presentation can be motor, sensory, and/or autonomic. Back pain varies depending on the site of metastasis, which can be referred, local, radicular, or a combination of all three.18 The primary complaint is pain in 83% to 96% of cases,19,20 though this is a nonspecific sign.
Previous studies have shown 40% to 64% of patients were not ambulatory at the time of diagnosis.19,25 Recent case series, however, report an increased number of ambulatory patients—possibly due to increased clinician awareness.26 In other cases, only 9% of patients were able to walk independently without aid.27 Loss of sensation, dense paraplegia, and incontinence are late findings and likely signal some degree of permanent disability.19
Misdiagnosis is a common issue in the ED setting. In an interesting retrospective study of 63 patients with spinal cord compression28 (not necessarily malignant), 18 (29%) were misdiagnosed.28 Consequently, there was a significant delay in diagnosis despite obvious neurological deficits at presentation.
Evaluation and Imaging
A detailed physical examination is essential to diagnosing MSCC. A thorough neurological examination, including sensation, strength, and reflexes should be carefully documented. If spinal instability is suspected, range-of-motion testing is contraindicated. The modified Frankel classification,29 adapted from the traumatic spine cord injury work by Frankel, et al,30 may be used to assess the degree of disability (Table).
Lu et al11 noted hyperreflexia and upward going Babinski reflex as common findings. Moreover, risk factors of decreased rectal sphincter tone and bladder were determinant for poor outcomes.
MRI studies should include the entire spine—not just the perceived area of interest— as up to 38% of patients have multiple-site metastases12 (Figure 1). Sensory deficits and mechanical pain may be present two to four vertebral levels away from the actual lesion.11 If MRI suggests cord compression, severity can be graded using the MSCC scale34 (Figure 2). Several scoring systems have been developed to aid in decision making concerning surgical treatment.
Management and Outcomes
The goal of therapy is symptom control and preservation of function. This requires a multidisciplinary approach and may involve radiation therapy and surgery, as well as medical efforts. Upon diagnosis and initiation of therapy, serial neurological evaluation should be undertaken. Neurovital signs should be scheduled to coincide with other nursing efforts to ease the burden of care and minimize patient discomfort.
The mainstay of medical therapy is treatment with corticosteroids.35 Initial trials have demonstrated that corticosteroids improve functional status in MSCC, but controversy exists regarding the effective dose. In a randomized, controlled trial by Sorensen et al,36 which sought to evaluate functional outcomes of highdose corticosteroids as an adjunct to radiotherapy, 57 patients received either high-dose dexamethasone or no corticosteroid therapy. Fifty-nine percent of patients in the dexamethasone group were ambulatory 6 months after treatment compared to 39% in the group who did not receive steroids.36
A patient without a biopsy-confirmed cancer diagnosis in need of corticosteroid treatment presents a dilemma. Plasmacytomas, thymomas, lymphomas, multiple myeloma, germ-cell tumors are very sensitive to corticosteroid therapy in patients with MSCC.38 However, corticosteroids given before tissue samples are obtained may hinder proper diagnosis and complicate future management.39,40 In the absence of neurological deficit, corticosteroids may be withheld and emergent consultation with neurosurgery and oncology should be obtained. If there is any question regarding the nature of the lesion, tissue diagnosis must be obtained without delay.
Strict bed rest (including logroll and bedpan use) should be instituted if there is suspicion of spinal cord instability. Patients with suspected involvement of the cervical spine should have a Philadelphia collar placed until spinal stability has been confirmed. In the United Kingdom, the National Institutes for Health Care Excellence guidelines recommend all patients with suspected cord compression be nursed in a flat position.22 Other institutions, however, do not believe that strict bed rest is necessary, as it is presumed that MSCC is inherently different from that caused by trauma. Authors supporting this position contend that the increased incidence of deep vein thrombosis, infection (particularly from the urinary tract), and decubitus ulcers outweighs the benefit of bed rest. Patient preference should be taken into consideration as those with good functional status may be quite resistant to bed rest. In cases where cord compression is strongly suspected, these patients should be educated on proper bed rest. The greatest predictors of outcome are ambulatory and functional status at the time of diagnosis (generally based on an Eastern Cooperative Oncology Group scale). Patients with a good functional status, limited disease, and a life expectancy of greater than 3 to 6 months may benefit from surgery.41 However, emergent surgical evaluation is required in patients not responding to radiotherapy or who received received only limited doses of radiotherapy, as well as those with spinal instability, direct cord compression due to a bony fragment, impending sphincter dysfunction, unknown primary tumor, or no paraplegia for >48 hours.15
Unfortunately, surgery is only indicated in 10% to 15% of MSCC cases.42 In the past two decades, significant improvements regarding new aggressive surgical techniques have been made, and include circumferential decompression of the spine and staged or single stage anterior posterior surgery with stabilization. 43 Additionally, the combination of surgery with radiotherapy has improved outcomes.44
Most patients benefit from short-course radiotherapy45 even when given palliatively. 46 Longer courses of radiotherapy are highly recommended for patients with a more favorable prognosis.47 Up to 10% of patients diagnosed with spinal cord compression will require treatment for disease recurrence.42 There is a limited role for chemotherapy, and in seminomas and lymphomas, results can be quite dramatic.38
Prevention
Lu et al11 found that only 54% of patients were aware that back pain should be reported to their physician. Delays in diagnosis and treatment are common and well described in the literature.21 Patients should be instructed to call their physician within 24 hours from the development of any new or worsening back pain, and should be advised to seek immediate care if they develop any neurological symptoms. To facilitate appropriate and prompt management of MSCC, hospitals should develop diagnostic algorithms to minimize delays in referral to a comprehensive center for further treatment.
Case Conclusion
Based on this patient’s symptoms and status at presentation, the emergency team determined he was at high risk for MSCC. An initial dosage of 10 mg dexamethasone was administered intravenously (IV), followed by 4 mg IV every 6 hours prior to imaging. An MRI without contrast of the cervical, thoracic, and lumbar spine showed cord compression with mild cord edema at T4 level, along with diffused osseous metastasis.
Upon diagnosis, patient was referred to radiation oncology for radiotherapy of the T2-T6 vertebral bodies. Three days after initiation of radiation therapy, his neurological function deteriorated with paraplegia and incontinence, and he was emergently evaluated for neurosurgery. Although T4 laminectomy and decompression of the spinal cord were performed without complication, patient did not recover neurological function. His hospital course was complicated by Ogilvie syndrome and episodes of delirium, and he was discharged to a rehabilitation facility 23 days after admission; paraplegia and urinary and bowel incontinence remained unchanged.
Case
A 60-year-old man with stage IV hormoneindependent prostate cancer, with widely metastatic disease to the bone, presents to the ED with increased weakness and new onset of numbness in the lower extremities, which he states began earlier that day. After failing several lines of chemotherapy, he is currently being treated with hormonal therapy alone. Patient first noted weakness in the left lower extremity 5 days before presentation, which progressed to bilateral involvement, making ambulation difficult and requiring the use of a walker. He denies back pain or urinary or fecal incontinence. Regarding pain management, he had been recently treated at one of the pain clinics in the hospital and has continued on opioid medication at another institution. Until the past week, he states he had back pain without neurological deficits.
His vital signs are stable at presentation. Patient is obese but in no acute distress. His cardiopulmonary examination is unremarkable; abdominal examination is benign; and back examination is normal. On neurological examination, iliopsoas flexion is 4/5 bilaterally; the rest of the motor examination is normal, with toes downgoing bilaterally upon plantar stimulation. Diminished sensation to light touch is noted at the T4-T6 sensory level and below; patient also has diminished proprioception in his lower extremities.
Patient had undergone a whole body scan one month prior to presentation, which revealed increased tracer uptake of Technetium-99m in multiple areas in the thoracic and lumbar spine. The radiologist also reported bilateral involvement in the wrists, femurs, tibias, and humeri—all in concordance with multifocal bone disease noted in previous computed tomography scans.
How should you approach this case?
Overview of Metastatic Spinal Cord Compression
Malignant or metastatic spinal cord compression (MSCC) of the thecal sac is an ominous complication of advanced cancer and an oncologic emergency presenting clinically in approximately 3% to 10% of cancer-related deaths.1,2 Cancer patients have a median survival of 3 to 6 months from diagnosis of MSCC.1,3,4 This disease causes significant disability due to paralysis, sensory loss, protracted pain, and sphincter dysfunction.5 If left untreated, MSCC has the potential to cause paraplegia in almost all affected patients; therefore, prompt recognition and treatment are essential to maintain mobility and neurological function. Generally speaking, any cancer patient who presents with new or worsening back pain—even in the absence of neurological deficits—merits evaluation for spinal cord compression.6 Nevertheless, individual risk assessment is warranted.7
Epidemiology
In the United States, more than 20,000 cases of MSCC are reported each year.8 According to postmortem studies, this condition affects 5% to 36% of cancer patients.9,10 In a US nationwide study of 15,367 cases of MSCC,2 the mean age at hospitalization was 62 years, with 37% of cases occurring in women. In approximately 20% of cases, MSCC was the initial presentation of cancer4; this has been reflected in our experience at MD Anderson Cancer Center.
Cancers of the breast, lung, prostate, and multiple myeloma are the most frequent underlying conditions in MSCC.2,8 Its prevalence varies depending on tumor type, occurring in 0.2% of pancreatic cancers; however, MSCC may affect up to 7.9% to 15% of myelomas1,2 and 13% of lymphomas.2 Interestingly, 5.5% of patients with prostate cancer develop MSCC.2 According to a study by Lu et al,11 historical risk factors include known nonvertebral bony metastases and stage IV disease at the time of diagnosis.
The most common location of MSCC is the thoracic spine (69% of cases); 29% of cases occur at the lumbosacral level and 10% at the cervical area.12 Most likely this pattern follows the lymphatic drainage, as metastases from breast and lung cancers tend to be found in the thoracic spine. Pelvic and intra-abdominal malignancies most commonly migrate to the lumbar spine. Multiple spinal epidural metastases were noted in 31% of those who underwent complete imaging of the spine.12
Pathophysiology
Most cases of MSCC are epidural in origin, arising from the vertebral column in 85% of patients.8 Epidural spread is caused mainly by hematogenous mechanism through the Batson venous plexus,13 debilitating the bone and eventually causing vertebral collapse with compression of the spinal canal. Epidural spread is less likely caused by direct tumor extension (ie, erosion through the bone) or by direct deposition of tumor cells into the epidural space.14 Ultimate neuronal injury is thought to involve vasogenic edema,15 leading to ischemia13 through venous infarction, but there has been debate regarding this last phenomenon.16 In cases of paralysis, demyelination is striking.16
Clinical Presentation
Even though cancer accounts for less than 1% of episodes of low back pain, it is the most common systemic disease affecting the spine.17 An important clinical inquiry is to determine whether back pain in an established cancer patient can be ruled out without extensive imaging. Unfortunately, clinical examination alone cannot exclude MSCC. Because of the high specificity (0.98), any cancer patient with new back pain should be considered to have metastasis until proven otherwise.17
Symptoms in MSCC at presentation can be motor, sensory, and/or autonomic. Back pain varies depending on the site of metastasis, which can be referred, local, radicular, or a combination of all three.18 The primary complaint is pain in 83% to 96% of cases,19,20 though this is a nonspecific sign.
Previous studies have shown 40% to 64% of patients were not ambulatory at the time of diagnosis.19,25 Recent case series, however, report an increased number of ambulatory patients—possibly due to increased clinician awareness.26 In other cases, only 9% of patients were able to walk independently without aid.27 Loss of sensation, dense paraplegia, and incontinence are late findings and likely signal some degree of permanent disability.19
Misdiagnosis is a common issue in the ED setting. In an interesting retrospective study of 63 patients with spinal cord compression28 (not necessarily malignant), 18 (29%) were misdiagnosed.28 Consequently, there was a significant delay in diagnosis despite obvious neurological deficits at presentation.
Evaluation and Imaging
A detailed physical examination is essential to diagnosing MSCC. A thorough neurological examination, including sensation, strength, and reflexes should be carefully documented. If spinal instability is suspected, range-of-motion testing is contraindicated. The modified Frankel classification,29 adapted from the traumatic spine cord injury work by Frankel, et al,30 may be used to assess the degree of disability (Table).
Lu et al11 noted hyperreflexia and upward going Babinski reflex as common findings. Moreover, risk factors of decreased rectal sphincter tone and bladder were determinant for poor outcomes.
MRI studies should include the entire spine—not just the perceived area of interest— as up to 38% of patients have multiple-site metastases12 (Figure 1). Sensory deficits and mechanical pain may be present two to four vertebral levels away from the actual lesion.11 If MRI suggests cord compression, severity can be graded using the MSCC scale34 (Figure 2). Several scoring systems have been developed to aid in decision making concerning surgical treatment.
Management and Outcomes
The goal of therapy is symptom control and preservation of function. This requires a multidisciplinary approach and may involve radiation therapy and surgery, as well as medical efforts. Upon diagnosis and initiation of therapy, serial neurological evaluation should be undertaken. Neurovital signs should be scheduled to coincide with other nursing efforts to ease the burden of care and minimize patient discomfort.
The mainstay of medical therapy is treatment with corticosteroids.35 Initial trials have demonstrated that corticosteroids improve functional status in MSCC, but controversy exists regarding the effective dose. In a randomized, controlled trial by Sorensen et al,36 which sought to evaluate functional outcomes of highdose corticosteroids as an adjunct to radiotherapy, 57 patients received either high-dose dexamethasone or no corticosteroid therapy. Fifty-nine percent of patients in the dexamethasone group were ambulatory 6 months after treatment compared to 39% in the group who did not receive steroids.36
A patient without a biopsy-confirmed cancer diagnosis in need of corticosteroid treatment presents a dilemma. Plasmacytomas, thymomas, lymphomas, multiple myeloma, germ-cell tumors are very sensitive to corticosteroid therapy in patients with MSCC.38 However, corticosteroids given before tissue samples are obtained may hinder proper diagnosis and complicate future management.39,40 In the absence of neurological deficit, corticosteroids may be withheld and emergent consultation with neurosurgery and oncology should be obtained. If there is any question regarding the nature of the lesion, tissue diagnosis must be obtained without delay.
Strict bed rest (including logroll and bedpan use) should be instituted if there is suspicion of spinal cord instability. Patients with suspected involvement of the cervical spine should have a Philadelphia collar placed until spinal stability has been confirmed. In the United Kingdom, the National Institutes for Health Care Excellence guidelines recommend all patients with suspected cord compression be nursed in a flat position.22 Other institutions, however, do not believe that strict bed rest is necessary, as it is presumed that MSCC is inherently different from that caused by trauma. Authors supporting this position contend that the increased incidence of deep vein thrombosis, infection (particularly from the urinary tract), and decubitus ulcers outweighs the benefit of bed rest. Patient preference should be taken into consideration as those with good functional status may be quite resistant to bed rest. In cases where cord compression is strongly suspected, these patients should be educated on proper bed rest. The greatest predictors of outcome are ambulatory and functional status at the time of diagnosis (generally based on an Eastern Cooperative Oncology Group scale). Patients with a good functional status, limited disease, and a life expectancy of greater than 3 to 6 months may benefit from surgery.41 However, emergent surgical evaluation is required in patients not responding to radiotherapy or who received received only limited doses of radiotherapy, as well as those with spinal instability, direct cord compression due to a bony fragment, impending sphincter dysfunction, unknown primary tumor, or no paraplegia for >48 hours.15
Unfortunately, surgery is only indicated in 10% to 15% of MSCC cases.42 In the past two decades, significant improvements regarding new aggressive surgical techniques have been made, and include circumferential decompression of the spine and staged or single stage anterior posterior surgery with stabilization. 43 Additionally, the combination of surgery with radiotherapy has improved outcomes.44
Most patients benefit from short-course radiotherapy45 even when given palliatively. 46 Longer courses of radiotherapy are highly recommended for patients with a more favorable prognosis.47 Up to 10% of patients diagnosed with spinal cord compression will require treatment for disease recurrence.42 There is a limited role for chemotherapy, and in seminomas and lymphomas, results can be quite dramatic.38
Prevention
Lu et al11 found that only 54% of patients were aware that back pain should be reported to their physician. Delays in diagnosis and treatment are common and well described in the literature.21 Patients should be instructed to call their physician within 24 hours from the development of any new or worsening back pain, and should be advised to seek immediate care if they develop any neurological symptoms. To facilitate appropriate and prompt management of MSCC, hospitals should develop diagnostic algorithms to minimize delays in referral to a comprehensive center for further treatment.
Case Conclusion
Based on this patient’s symptoms and status at presentation, the emergency team determined he was at high risk for MSCC. An initial dosage of 10 mg dexamethasone was administered intravenously (IV), followed by 4 mg IV every 6 hours prior to imaging. An MRI without contrast of the cervical, thoracic, and lumbar spine showed cord compression with mild cord edema at T4 level, along with diffused osseous metastasis.
Upon diagnosis, patient was referred to radiation oncology for radiotherapy of the T2-T6 vertebral bodies. Three days after initiation of radiation therapy, his neurological function deteriorated with paraplegia and incontinence, and he was emergently evaluated for neurosurgery. Although T4 laminectomy and decompression of the spinal cord were performed without complication, patient did not recover neurological function. His hospital course was complicated by Ogilvie syndrome and episodes of delirium, and he was discharged to a rehabilitation facility 23 days after admission; paraplegia and urinary and bowel incontinence remained unchanged.
- Loblaw DA, Laperriere NJ, Mackillop WJ. A population-based study of malignant spinal cord compression in Ontario. Clin Oncol (R Coll Radiol). 2003;15(4):211-217.
- Mak KS, Lee LK, Mak RH, et al. Incidence and treatment patterns in hospitalizations for malignant spinal cord compression in the United States, 1998-2006. Int J Radiat Oncol Biol Phys. 2011;80(3):824-831.
- Constans JP, de Divitiis E, Donzelli R, Spaziante R, Meder JF, Haye C. Spinal metastases with
- neurological manifestations. Review of 600 cases. J Neurosurg. 1983;59(1):111-118.
- Schiff D, O’Neill BP, Suman VJ. Spinal epidural metastasis as the initial manifestation of malignancy: clinical features and diagnostic approach. Neurology. 1997;49(2):452-456.
- Loblaw DA, Perry J, Chambers A, Laperriere NJ. Systematic review of the diagnosis and management of malignant extradural spinal cord compression: the Cancer Care Ontario Practice Guidelines Initiative’s Neuro-Oncology Disease Site Group. J Clin Oncol. 2005;23(9):2028-2037.
- Levack P, Graham J, Collie D, et al. Don’t wait for a sensory level—listen to the symptoms: a prospective audit of the delays in diagnosis of malignant cord compression. Clin Oncol (R Coll Radiol). 2002;14(6):472-480.
- Talcott JA, Stomper PC, Drislane FW, et al. Assessing suspected spinal cord compression: a multidisciplinary outcomes analysis of 342 episodes. Support Care Cancer. 1999;7(1):31-38.
- Byrne TN. Spinal cord compression from epidural metastases. N Engl J Med. 1992;327(9):614-619.
- Abrams HL, Spiro R, Goldstein N. Metastases in carcinoma; analysis of 1000 autopsied cases. Cancer. 1950;3(1):74-85.
- Wong DA, Fornasier VL, MacNab I. Spinal metastases: the obvious, the occult, and the impostors. Spine (Phila Pa 1976). 1990;15(1):1-4.
- Lu C, Gonzalez RG, Jolesz FA, Wen PY, Talcott JA. Suspected spinal cord compression in cancer patients: a multidisciplinary risk assessment. J Support Oncol. 2005;3(4):305-312.
- Schiff D, O’Neill BP, Wang CH, O’Fallon JR. Neuroimaging and treatment implications of patients with multiple epidural spinal metastases. Cancer. 1998;83(8):1593-1601.
- Arguello F, Baggs RB, Duerst RE, Johnstone L, McQueen K, Frantz CN. Pathogenesis of vertebral metastasis and epidural spinal cord compression. Cancer. 1990;65(1):98-106.
- Schiff D. Spinal cord compression. Neurol Clin. 2003;21(1):67-86, viii.
- Prasad D, Schiff D. Malignant spinal-cord compression. Lancet Oncol. 2005;6(1):15-24.
- Helweg-Larsen S, Laursen H. Clinical and autopsy findings in spinal cord compression due to metastatic disease. Eur J Neurol. 1998;5(6):587-592.
- Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 199218. Abrahm JL, Banffy MB, Harris MB. Spinal cord compression in patients with advanced metastatic cancer: "all I care about is walking and living my life." JAMA. 2008;299(8):937-946.
- Bach F, Larsen BH, Rohde K, et al. Metastatic spinal cord compression. Occurrence, symptoms, clinical presentations and prognosis in 398 patients with spinal cord compression. Acta Neurochir (Wien). 1990;107(1-2):37-43.
- Gilbert RW, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: diagnosis and treatment. Ann Neurol. 1978;3(1):40-51.
- Husband DJ. Malignant spinal cord compression: prospective study of delays in referral and treatment. BMJ. 1998;317(7150):18-21.
- Metastatic Spinal Cord Compression: Diagnosis and Management of Patients at Risk of or with Metastatic Spinal Cord Compression. Cardiff UK: National Collaborating Centre for Cancer; 2008.
- Shiue K, Sahgal A, Chow E, et al. Management of metastatic spinal cord compression. Expert Rev Anticancer Ther. 2010;10(5):697-708.
- Hammack JE. Spinal cord disease in patients with cancer. Continuum (Minneap Minn). 2012;18(2):312-327.
- Helweg-Larsen S. Clinical outcome in metastatic spinal cord compression. A prospective study of 153 patients. Acta Neurol Scand. 1996;94(4):269-275.
- Rades D, Fehlauer F, Schulte R, et al. Prognostic factors for local control and survival after radiotherapy of metastatic spinal cord compression. J Clin Oncol. 2006;24(21):3388-3393.
- McLinton A, Hutchison C. Malignant spinal cord compression: a retrospective audit of clinical practice at a UK regional cancer centre. Br J Cancer. 2006;94(4):486-491.
- Dugas AF, Lucas JM, Edlow JA. Diagnosis of spinal cord compression in nontrauma patients in the emergency department. Acad Emerg Med. 2011;18(7):719-725.
- Ditunno JF, Jr, Young W, Donovan WH, Creasey metastatic spinal CORD compression 18 EMERGENCY MEDICINE I january 2014 www.emed-journal.com G. American Spinal Surgery Association. The international standards booklet for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Paraplegia. 1994;32(2):70-80.
- Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7(3):179-192.
- Portenoy RK, Galer BS, Salamon O, et al. Identification of epidural neoplasm. Radiography and bone scintigraphy in the symptomatic and asymptomatic spine. Cancer. 1989;64(11):2207-2213.
- Husband DJ, Grant KA, Romaniuk CS. MRI in the diagnosis and treatment of suspected malignant spinal cord compression. Br J Radiol. 2001;74(877):15-23.
- Carmody RF, Yang PJ, Seeley GW, Seeger JF, Unger EC, Johnson JE. Spinal cord compression due to metastatic disease: diagnosis with MR imaging versus myelography. Radiology. 1989;173(1):225-229.
- Bilsky MH, Laufer I, Fourney DR, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13(3):324-328.
- Loblaw DA, Mitera G, Ford M, Laperriere NJ. A 2011 updated systematic review and clinical practice guideline for the management of malignant extradural spinal cord compression. Int J Radiat Oncol Biol Phys. 2012;84(2):312-317.
- Sorensen S, Helweg-Larsen S, Mouridsen H, Hansen HH. Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: a randomised trial. Eur J Cancer. 1994;30A(1):22-27.
- Heimdal K, Hirschberg H, Slettebo H, Watne K, Nome O. High incidence of serious side effects of high-dose dexamethasone treatment in patients with epidural spinal cord compression. J Neurooncol. 1992;12(2):141-144.
- Posner JB, Howieson J, Cvitkovic E. "Disappearing" spinal cord compression: oncolytic effect of glucocorticoids (and other chemotherapeutic agents) on epidural metastases. Ann Neurol. 1977;2(5):409-413.
- Kan E, Levi I, Benharroch D. Alterations in the primary diagnosis of lymphomas pretreated with corticosteroid agents. Leuk Lymphoma. 2011;52(3):425-428.
- Borenstein SH, Gerstle T, Malkin D, Thorner P, Filler RM. The effects of prebiopsy cortico-steroid treatment on the diagnosis of mediastinal lymphoma. J Pediatr Surg. 2000;35(6):973-976.
- Akram H, Allibone J. Spinal surgery for palliation in malignant spinal cord compression. Clin Oncol (R Coll Radiol). 2010;22(9):792-800.
- Rades D, Abrahm JL. The role of radiotherapy for metastatic epidural spinal cord compression. Nat Rev Clin Oncol. 2010;7(10):590-598.
- Sundaresan N, Sachdev VP, Holland JF, et al. Surgical treatment of spinal cord compression from epidural metastasis. J Clin Oncol. 1995;13(9):2330-2335.
- Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643-648.
- Rades D, Dahm-Daphi J, Rudat V, et al. Is shortcourse radiotherapy with high doses per fraction the appropriate regimen for metastatic spinal cord compression in colorectal cancer patients? Strahlenther Onkol. 2006;182(12):708-712.
- van den Hout WB, van der Linden YM, Steenland E, et al. Single- versus multiple-fraction radiotherapy in patients with painful bone metastases: cost-utility analysis based on a randomized trial. J Natl Cancer Inst. 2003;95(3):222-229.
- Steenland E, Leer JW, van Houwelingen H, et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: a global analysis of the Dutch Bone Metastasis Study. Radiother Oncol. 1999;52(2):101-109.
- Rades D, Hueppe M, Schild SE. A score to identify patients with metastatic spinal cord compression who may be candidates for best supportive care. Cancer. 2013;119(4):897-903.
- Guo Y, Palmer JL, Bianty J, Konzen B, Shin K, Bruera E. Advance directives and do-not-resuscitate orders in patients with cancer with metastatic spinal cord compression: advanced care planning implications. J Palliat Med. 2010;13(5):513-517.
- Loblaw DA, Laperriere NJ, Mackillop WJ. A population-based study of malignant spinal cord compression in Ontario. Clin Oncol (R Coll Radiol). 2003;15(4):211-217.
- Mak KS, Lee LK, Mak RH, et al. Incidence and treatment patterns in hospitalizations for malignant spinal cord compression in the United States, 1998-2006. Int J Radiat Oncol Biol Phys. 2011;80(3):824-831.
- Constans JP, de Divitiis E, Donzelli R, Spaziante R, Meder JF, Haye C. Spinal metastases with
- neurological manifestations. Review of 600 cases. J Neurosurg. 1983;59(1):111-118.
- Schiff D, O’Neill BP, Suman VJ. Spinal epidural metastasis as the initial manifestation of malignancy: clinical features and diagnostic approach. Neurology. 1997;49(2):452-456.
- Loblaw DA, Perry J, Chambers A, Laperriere NJ. Systematic review of the diagnosis and management of malignant extradural spinal cord compression: the Cancer Care Ontario Practice Guidelines Initiative’s Neuro-Oncology Disease Site Group. J Clin Oncol. 2005;23(9):2028-2037.
- Levack P, Graham J, Collie D, et al. Don’t wait for a sensory level—listen to the symptoms: a prospective audit of the delays in diagnosis of malignant cord compression. Clin Oncol (R Coll Radiol). 2002;14(6):472-480.
- Talcott JA, Stomper PC, Drislane FW, et al. Assessing suspected spinal cord compression: a multidisciplinary outcomes analysis of 342 episodes. Support Care Cancer. 1999;7(1):31-38.
- Byrne TN. Spinal cord compression from epidural metastases. N Engl J Med. 1992;327(9):614-619.
- Abrams HL, Spiro R, Goldstein N. Metastases in carcinoma; analysis of 1000 autopsied cases. Cancer. 1950;3(1):74-85.
- Wong DA, Fornasier VL, MacNab I. Spinal metastases: the obvious, the occult, and the impostors. Spine (Phila Pa 1976). 1990;15(1):1-4.
- Lu C, Gonzalez RG, Jolesz FA, Wen PY, Talcott JA. Suspected spinal cord compression in cancer patients: a multidisciplinary risk assessment. J Support Oncol. 2005;3(4):305-312.
- Schiff D, O’Neill BP, Wang CH, O’Fallon JR. Neuroimaging and treatment implications of patients with multiple epidural spinal metastases. Cancer. 1998;83(8):1593-1601.
- Arguello F, Baggs RB, Duerst RE, Johnstone L, McQueen K, Frantz CN. Pathogenesis of vertebral metastasis and epidural spinal cord compression. Cancer. 1990;65(1):98-106.
- Schiff D. Spinal cord compression. Neurol Clin. 2003;21(1):67-86, viii.
- Prasad D, Schiff D. Malignant spinal-cord compression. Lancet Oncol. 2005;6(1):15-24.
- Helweg-Larsen S, Laursen H. Clinical and autopsy findings in spinal cord compression due to metastatic disease. Eur J Neurol. 1998;5(6):587-592.
- Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 199218. Abrahm JL, Banffy MB, Harris MB. Spinal cord compression in patients with advanced metastatic cancer: "all I care about is walking and living my life." JAMA. 2008;299(8):937-946.
- Bach F, Larsen BH, Rohde K, et al. Metastatic spinal cord compression. Occurrence, symptoms, clinical presentations and prognosis in 398 patients with spinal cord compression. Acta Neurochir (Wien). 1990;107(1-2):37-43.
- Gilbert RW, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: diagnosis and treatment. Ann Neurol. 1978;3(1):40-51.
- Husband DJ. Malignant spinal cord compression: prospective study of delays in referral and treatment. BMJ. 1998;317(7150):18-21.
- Metastatic Spinal Cord Compression: Diagnosis and Management of Patients at Risk of or with Metastatic Spinal Cord Compression. Cardiff UK: National Collaborating Centre for Cancer; 2008.
- Shiue K, Sahgal A, Chow E, et al. Management of metastatic spinal cord compression. Expert Rev Anticancer Ther. 2010;10(5):697-708.
- Hammack JE. Spinal cord disease in patients with cancer. Continuum (Minneap Minn). 2012;18(2):312-327.
- Helweg-Larsen S. Clinical outcome in metastatic spinal cord compression. A prospective study of 153 patients. Acta Neurol Scand. 1996;94(4):269-275.
- Rades D, Fehlauer F, Schulte R, et al. Prognostic factors for local control and survival after radiotherapy of metastatic spinal cord compression. J Clin Oncol. 2006;24(21):3388-3393.
- McLinton A, Hutchison C. Malignant spinal cord compression: a retrospective audit of clinical practice at a UK regional cancer centre. Br J Cancer. 2006;94(4):486-491.
- Dugas AF, Lucas JM, Edlow JA. Diagnosis of spinal cord compression in nontrauma patients in the emergency department. Acad Emerg Med. 2011;18(7):719-725.
- Ditunno JF, Jr, Young W, Donovan WH, Creasey metastatic spinal CORD compression 18 EMERGENCY MEDICINE I january 2014 www.emed-journal.com G. American Spinal Surgery Association. The international standards booklet for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Paraplegia. 1994;32(2):70-80.
- Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7(3):179-192.
- Portenoy RK, Galer BS, Salamon O, et al. Identification of epidural neoplasm. Radiography and bone scintigraphy in the symptomatic and asymptomatic spine. Cancer. 1989;64(11):2207-2213.
- Husband DJ, Grant KA, Romaniuk CS. MRI in the diagnosis and treatment of suspected malignant spinal cord compression. Br J Radiol. 2001;74(877):15-23.
- Carmody RF, Yang PJ, Seeley GW, Seeger JF, Unger EC, Johnson JE. Spinal cord compression due to metastatic disease: diagnosis with MR imaging versus myelography. Radiology. 1989;173(1):225-229.
- Bilsky MH, Laufer I, Fourney DR, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13(3):324-328.
- Loblaw DA, Mitera G, Ford M, Laperriere NJ. A 2011 updated systematic review and clinical practice guideline for the management of malignant extradural spinal cord compression. Int J Radiat Oncol Biol Phys. 2012;84(2):312-317.
- Sorensen S, Helweg-Larsen S, Mouridsen H, Hansen HH. Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: a randomised trial. Eur J Cancer. 1994;30A(1):22-27.
- Heimdal K, Hirschberg H, Slettebo H, Watne K, Nome O. High incidence of serious side effects of high-dose dexamethasone treatment in patients with epidural spinal cord compression. J Neurooncol. 1992;12(2):141-144.
- Posner JB, Howieson J, Cvitkovic E. "Disappearing" spinal cord compression: oncolytic effect of glucocorticoids (and other chemotherapeutic agents) on epidural metastases. Ann Neurol. 1977;2(5):409-413.
- Kan E, Levi I, Benharroch D. Alterations in the primary diagnosis of lymphomas pretreated with corticosteroid agents. Leuk Lymphoma. 2011;52(3):425-428.
- Borenstein SH, Gerstle T, Malkin D, Thorner P, Filler RM. The effects of prebiopsy cortico-steroid treatment on the diagnosis of mediastinal lymphoma. J Pediatr Surg. 2000;35(6):973-976.
- Akram H, Allibone J. Spinal surgery for palliation in malignant spinal cord compression. Clin Oncol (R Coll Radiol). 2010;22(9):792-800.
- Rades D, Abrahm JL. The role of radiotherapy for metastatic epidural spinal cord compression. Nat Rev Clin Oncol. 2010;7(10):590-598.
- Sundaresan N, Sachdev VP, Holland JF, et al. Surgical treatment of spinal cord compression from epidural metastasis. J Clin Oncol. 1995;13(9):2330-2335.
- Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643-648.
- Rades D, Dahm-Daphi J, Rudat V, et al. Is shortcourse radiotherapy with high doses per fraction the appropriate regimen for metastatic spinal cord compression in colorectal cancer patients? Strahlenther Onkol. 2006;182(12):708-712.
- van den Hout WB, van der Linden YM, Steenland E, et al. Single- versus multiple-fraction radiotherapy in patients with painful bone metastases: cost-utility analysis based on a randomized trial. J Natl Cancer Inst. 2003;95(3):222-229.
- Steenland E, Leer JW, van Houwelingen H, et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: a global analysis of the Dutch Bone Metastasis Study. Radiother Oncol. 1999;52(2):101-109.
- Rades D, Hueppe M, Schild SE. A score to identify patients with metastatic spinal cord compression who may be candidates for best supportive care. Cancer. 2013;119(4):897-903.
- Guo Y, Palmer JL, Bianty J, Konzen B, Shin K, Bruera E. Advance directives and do-not-resuscitate orders in patients with cancer with metastatic spinal cord compression: advanced care planning implications. J Palliat Med. 2010;13(5):513-517.