User login
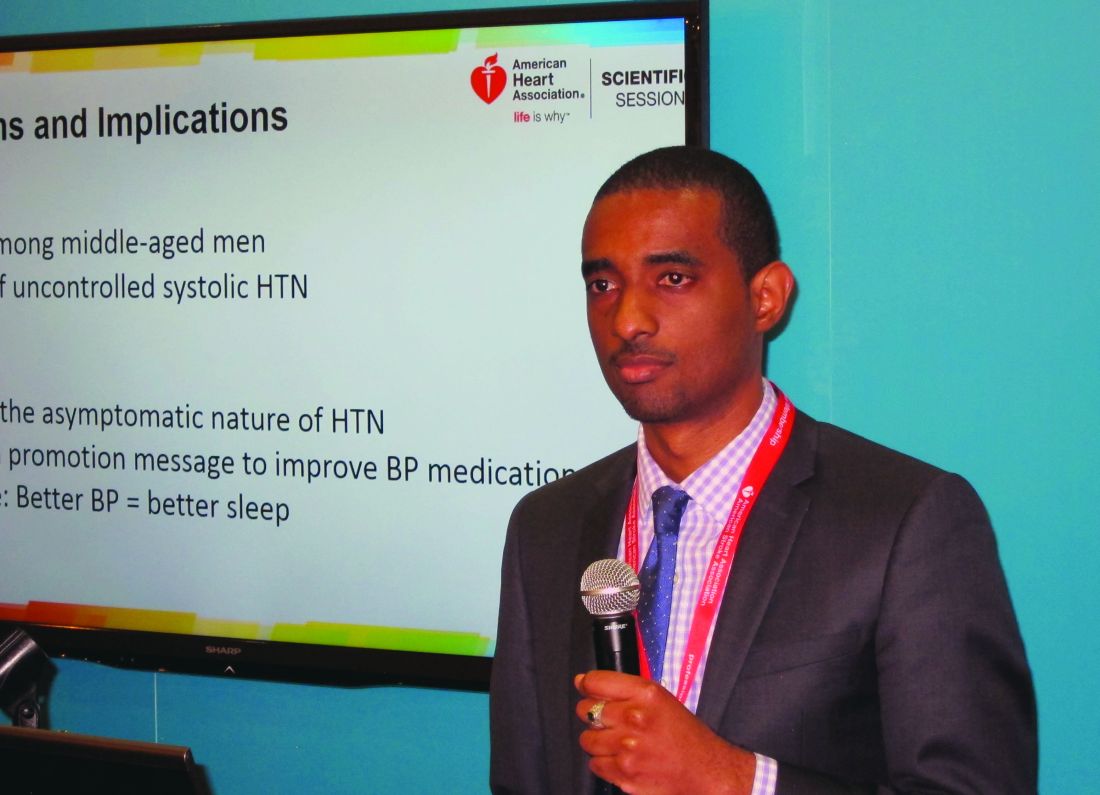
NEW ORLEANS – Uncontrolled systolic hypertension is a strong independent determinant of nocturia in middle-aged African American men, O’Neil Mason, MD, reported at the American Heart Association scientific sessions.
This finding from the ongoing National Heart, Lung, and Blood Institute–sponsored Barbershop Study challenges the traditional notion of hypertension as an asymptomatic disease. It also provides a novel health promotion message aimed at improving compliance with blood pressure medication.
The Barbershop Study is a hypertension intervention trial that’s being conducted in Los Angeles barbershops frequented by black men. In the initial screening phase for study eligibility, 2,577 African American men aged 35-79 years underwent highly accurate blood pressure measurements using an average of three readings taken via an oscillometric monitor.
The mean age of the men was 53 years. It was an obese group, with a mean body mass index of 30 kg/m2. Fifty percent of the men had hypertension, and among that cohort fully one-third weren’t on antihypertensive medication and another 28% were treated but uncontrolled, with on-treatment blood pressures of 140/90 mm Hg or more. Thus, only 39% of these middle-aged African American men with high blood pressure were treated and controlled at baseline.
Seventy-seven percent of the screened men reported awakening once or more per night to urinate. A progressive increase in nocturia severity was seen with increasing systolic blood pressure. The prevalence of nocturia ranged from 68% among normotensive men to 91% among those with treated but uncontrolled hypertension, Dr. Mason reported.
In a multivariate logistic regression analysis controlling for the standard risk factors for nocturia – including advancing age, an enlarged prostate, and diabetes, which was present in 16% of the men – stage 1 systolic hypertension in the range of 140-159 mm Hg was independently associated with a 1.57-fold increased likelihood of nocturia, compared with normotensive subjects. Stage 2 hypertension, with a systolic blood pressure of 160 mm Hg or more, was associated with a 2.32-fold increased risk; that’s in the same ballpark as having an enlarged prostate, which carried a 2.1-fold increased risk. Prehypertension – that is, a systolic pressure of 120-139 mm Hg – was associated with a nonsignificant 1.18-fold risk.
Diastolic blood pressure wasn’t an independent determinant of nocturia.
In a similar multivariate analysis focused on severe nocturia, defined as three or more episodes per night, stage 1 systolic hypertension was independently associated with a 2.29-fold increased risk, compared with normotension, and stage 2 systolic hypertension carried a 2.77-fold increased risk.
Audience members were clearly intrigued by this novel finding. They were quick to speculate as to potential underlying pathophysiologic mechanisms, including atrial stretch, increased renal blood flow, or perhaps a side effect of diuretic therapy. However, Dr. Mason and his coinvestigators favor another possibility: “African Americans have more salt-sensitive hypertension and they have less nocturnal blood pressure dipping,” he noted. “So if nighttime blood pressure is high it could lead through increased pressure natriuresis to increased urine production. More activity in getting up to go to the bathroom increases the blood pressure and creates a cycle that begets more urine.”
Asked if uncontrolled systolic hypertension is also a determinant of nocturia in African American women, Dr. Mason replied that he would assume so. But that question hasn’t ever been studied. The Barbershop Study is restricted to African American men with hypertension because studies have shown they have a particularly low rate of controlled hypertension. In contrast, the controlled hypertension rate among hypertensive African American women is comparable with their white counterparts.
In the next phase of the Barbershop Study, participants’ use of various classes of antihypertensive medication will be prospectively tracked. Among other things, this will enable investigators to determine whether diuretics contribute to nocturia.
Dr. Mason reported having no conflicts of interest regarding the study.
NEW ORLEANS – Uncontrolled systolic hypertension is a strong independent determinant of nocturia in middle-aged African American men, O’Neil Mason, MD, reported at the American Heart Association scientific sessions.
This finding from the ongoing National Heart, Lung, and Blood Institute–sponsored Barbershop Study challenges the traditional notion of hypertension as an asymptomatic disease. It also provides a novel health promotion message aimed at improving compliance with blood pressure medication.
The Barbershop Study is a hypertension intervention trial that’s being conducted in Los Angeles barbershops frequented by black men. In the initial screening phase for study eligibility, 2,577 African American men aged 35-79 years underwent highly accurate blood pressure measurements using an average of three readings taken via an oscillometric monitor.
The mean age of the men was 53 years. It was an obese group, with a mean body mass index of 30 kg/m2. Fifty percent of the men had hypertension, and among that cohort fully one-third weren’t on antihypertensive medication and another 28% were treated but uncontrolled, with on-treatment blood pressures of 140/90 mm Hg or more. Thus, only 39% of these middle-aged African American men with high blood pressure were treated and controlled at baseline.
Seventy-seven percent of the screened men reported awakening once or more per night to urinate. A progressive increase in nocturia severity was seen with increasing systolic blood pressure. The prevalence of nocturia ranged from 68% among normotensive men to 91% among those with treated but uncontrolled hypertension, Dr. Mason reported.
In a multivariate logistic regression analysis controlling for the standard risk factors for nocturia – including advancing age, an enlarged prostate, and diabetes, which was present in 16% of the men – stage 1 systolic hypertension in the range of 140-159 mm Hg was independently associated with a 1.57-fold increased likelihood of nocturia, compared with normotensive subjects. Stage 2 hypertension, with a systolic blood pressure of 160 mm Hg or more, was associated with a 2.32-fold increased risk; that’s in the same ballpark as having an enlarged prostate, which carried a 2.1-fold increased risk. Prehypertension – that is, a systolic pressure of 120-139 mm Hg – was associated with a nonsignificant 1.18-fold risk.
Diastolic blood pressure wasn’t an independent determinant of nocturia.
In a similar multivariate analysis focused on severe nocturia, defined as three or more episodes per night, stage 1 systolic hypertension was independently associated with a 2.29-fold increased risk, compared with normotension, and stage 2 systolic hypertension carried a 2.77-fold increased risk.
Audience members were clearly intrigued by this novel finding. They were quick to speculate as to potential underlying pathophysiologic mechanisms, including atrial stretch, increased renal blood flow, or perhaps a side effect of diuretic therapy. However, Dr. Mason and his coinvestigators favor another possibility: “African Americans have more salt-sensitive hypertension and they have less nocturnal blood pressure dipping,” he noted. “So if nighttime blood pressure is high it could lead through increased pressure natriuresis to increased urine production. More activity in getting up to go to the bathroom increases the blood pressure and creates a cycle that begets more urine.”
Asked if uncontrolled systolic hypertension is also a determinant of nocturia in African American women, Dr. Mason replied that he would assume so. But that question hasn’t ever been studied. The Barbershop Study is restricted to African American men with hypertension because studies have shown they have a particularly low rate of controlled hypertension. In contrast, the controlled hypertension rate among hypertensive African American women is comparable with their white counterparts.
In the next phase of the Barbershop Study, participants’ use of various classes of antihypertensive medication will be prospectively tracked. Among other things, this will enable investigators to determine whether diuretics contribute to nocturia.
Dr. Mason reported having no conflicts of interest regarding the study.
NEW ORLEANS – Uncontrolled systolic hypertension is a strong independent determinant of nocturia in middle-aged African American men, O’Neil Mason, MD, reported at the American Heart Association scientific sessions.
This finding from the ongoing National Heart, Lung, and Blood Institute–sponsored Barbershop Study challenges the traditional notion of hypertension as an asymptomatic disease. It also provides a novel health promotion message aimed at improving compliance with blood pressure medication.
The Barbershop Study is a hypertension intervention trial that’s being conducted in Los Angeles barbershops frequented by black men. In the initial screening phase for study eligibility, 2,577 African American men aged 35-79 years underwent highly accurate blood pressure measurements using an average of three readings taken via an oscillometric monitor.
The mean age of the men was 53 years. It was an obese group, with a mean body mass index of 30 kg/m2. Fifty percent of the men had hypertension, and among that cohort fully one-third weren’t on antihypertensive medication and another 28% were treated but uncontrolled, with on-treatment blood pressures of 140/90 mm Hg or more. Thus, only 39% of these middle-aged African American men with high blood pressure were treated and controlled at baseline.
Seventy-seven percent of the screened men reported awakening once or more per night to urinate. A progressive increase in nocturia severity was seen with increasing systolic blood pressure. The prevalence of nocturia ranged from 68% among normotensive men to 91% among those with treated but uncontrolled hypertension, Dr. Mason reported.
In a multivariate logistic regression analysis controlling for the standard risk factors for nocturia – including advancing age, an enlarged prostate, and diabetes, which was present in 16% of the men – stage 1 systolic hypertension in the range of 140-159 mm Hg was independently associated with a 1.57-fold increased likelihood of nocturia, compared with normotensive subjects. Stage 2 hypertension, with a systolic blood pressure of 160 mm Hg or more, was associated with a 2.32-fold increased risk; that’s in the same ballpark as having an enlarged prostate, which carried a 2.1-fold increased risk. Prehypertension – that is, a systolic pressure of 120-139 mm Hg – was associated with a nonsignificant 1.18-fold risk.
Diastolic blood pressure wasn’t an independent determinant of nocturia.
In a similar multivariate analysis focused on severe nocturia, defined as three or more episodes per night, stage 1 systolic hypertension was independently associated with a 2.29-fold increased risk, compared with normotension, and stage 2 systolic hypertension carried a 2.77-fold increased risk.
Audience members were clearly intrigued by this novel finding. They were quick to speculate as to potential underlying pathophysiologic mechanisms, including atrial stretch, increased renal blood flow, or perhaps a side effect of diuretic therapy. However, Dr. Mason and his coinvestigators favor another possibility: “African Americans have more salt-sensitive hypertension and they have less nocturnal blood pressure dipping,” he noted. “So if nighttime blood pressure is high it could lead through increased pressure natriuresis to increased urine production. More activity in getting up to go to the bathroom increases the blood pressure and creates a cycle that begets more urine.”
Asked if uncontrolled systolic hypertension is also a determinant of nocturia in African American women, Dr. Mason replied that he would assume so. But that question hasn’t ever been studied. The Barbershop Study is restricted to African American men with hypertension because studies have shown they have a particularly low rate of controlled hypertension. In contrast, the controlled hypertension rate among hypertensive African American women is comparable with their white counterparts.
In the next phase of the Barbershop Study, participants’ use of various classes of antihypertensive medication will be prospectively tracked. Among other things, this will enable investigators to determine whether diuretics contribute to nocturia.
Dr. Mason reported having no conflicts of interest regarding the study.
Key clinical point:
Major finding: A systolic blood pressure of 140-159 mm Hg was independently associated with a 2.29-fold increased risk of severe nocturia, compared with normotension in middle-aged African American men, while a pressure of 160 mm Hg or more conferred a 2.77-fold increased risk.
Data source: A report on the initial cross-sectional screening phase of the Barbershop Study, in which 2,577 middle-aged African American men underwent blood pressure measurements in Los Angeles barbershops.
Disclosures: The Barbershop Study is funded by the National Heart, Lung, and Blood Institute. The presenter reported having no financial conflicts.