User login
To the Editor:
Sebaceous nevus (SN) is a relatively common hamartoma that presents most often as a single congenital hairless plaque on the scalp. After puberty, histologic features characteristically include papillomatous hyperplasia of the epidermis, a large number of mature or nearly mature sebaceous glands, and a lack of terminally differentiated hair follicles; however, histologic findings can be misleading during childhood when sebaceous glands are still underdeveloped. Bright yellow dots, which are thought to indicate the presence of sebaceous glands, may be seen on dermoscopy and can be useful in differentiating SN from aplasia cutis congenita in newborns.
We report a case of an SN in an 18-year-old woman and discuss how the histology findings correlated with features seen on dermoscopy.
An 18-year-old woman presented to our dermatology clinic with an asymptomatic, hairless plaque on the right parietal scalp that had been present since birth. The patient noted that the plaque had recently become larger in size. On physical examination, an 8×3-cm plaque with a smooth, flesh-colored surface was noted with central comedolike structures and an erythematous, verrucous periphery (Figure 1).

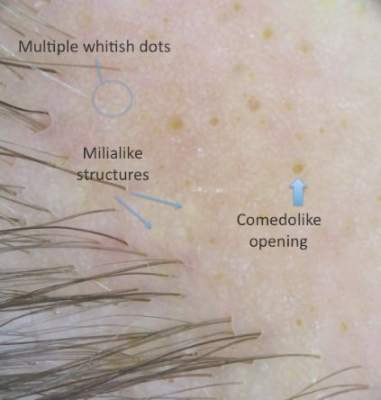
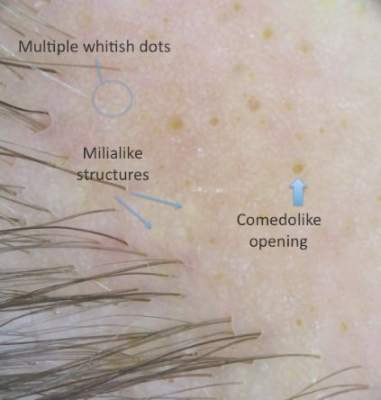
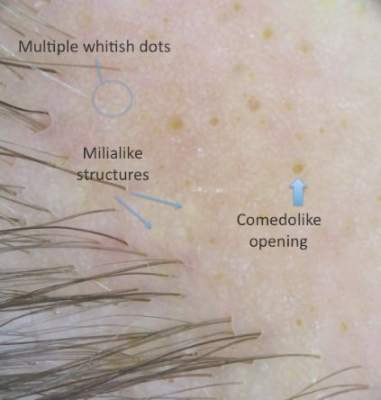
Dermoscopy (handheld dermoscope using polarized light) revealed 3 distinct types of round structures within the lesion: (1) comedolike openings (similar to those seen in seborrheic keratosis) that appeared as brownish-yellow, sharply circumscribed structures; (2) milialike cysts (also found in acanthotic seborrheic keratosis), which appeared as bright yellow structures; and (3) multiple whitish structures that were irregular in shape and size and covered the surface of the lesion where there were no other dermoscopic findings (Figure 2). The affected skin was pale to red in color and the verrucous aspect of the surface was better visualized at the edge of the lesion.
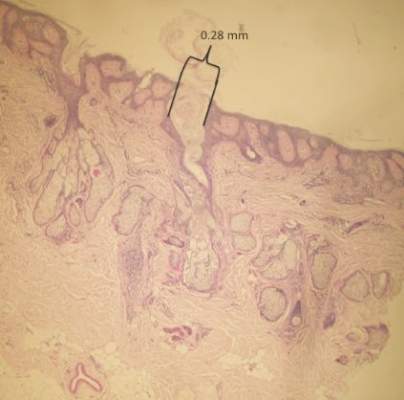
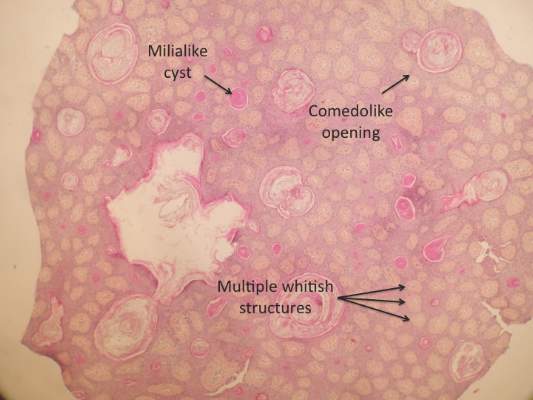
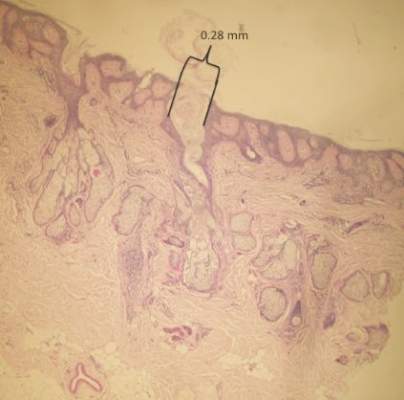
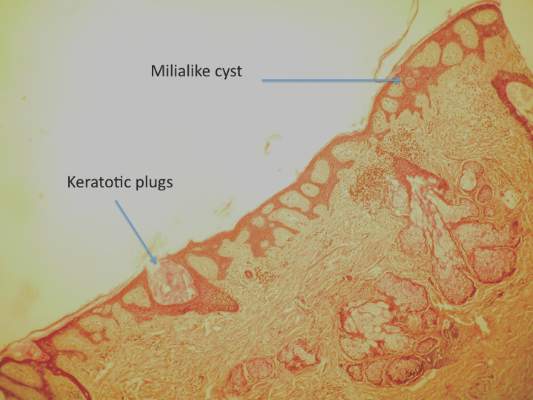
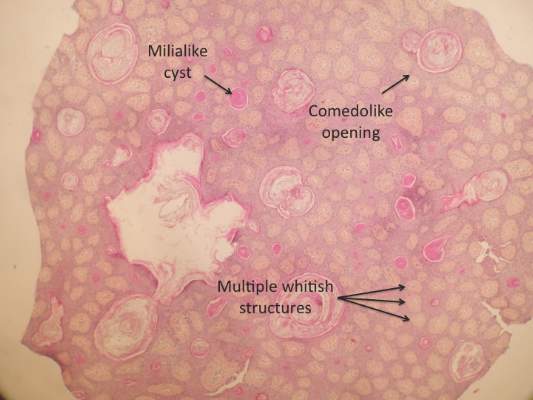
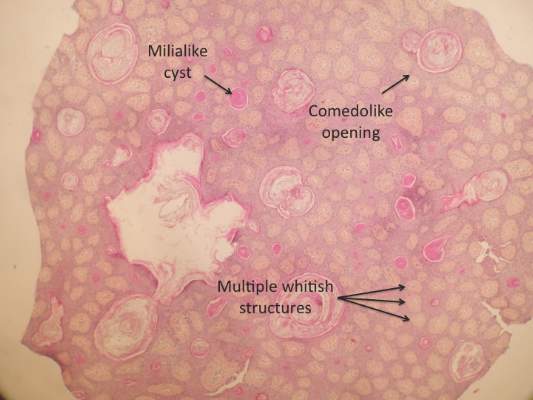
Two 4-mm punch biopsies were performed following dermoscopy: one for horizontal sectioning and one for vertical sectioning. Histologic analysis showed an acanthotic epidermis with an anastomosing network of elongated rete ridges in the superficial dermis. Numerous hyperplasic sebaceous glands were found in the mid dermis, with some also located above this level. Immature hair follicles were present and sebaceous gland ducts communicated directly with the epidermis through dilated hyperkeratinized pathways. Eccrine glands were normal, but no apocrine glands were present. A lymphocytic infiltrate was noted around the sebaceous glands and immature hair follicles and also around dilated capillaries in the superficial dermis. Moderate spongiosis and lymphocytic exocytosis were noted in the glandular epithelium and in the basal layer of the hair follicles and the epidermis. Superficial slides of horizontal sections of the biopsy specimen showed a correlation between the histology findings and dermoscopy images: multiple normal-appearing papilla surrounded by a network of anastomosing rete ridges correlated with multiple whitish structures, keratotic cysts with compact keratin corresponded to bright yellow dots, and larger conglomerates of loose lamelar keratin correlated with comedolike openings. Due to the presence of eczematous changes (eg, epithelial spongiosis, inflammatory cells) observed on histology, a diagnosis of an irritated sebaceous nevus was made, which explained the recent enlargement of the congenital lesion.
Sebaceous nevus is a benign, epidermal appendageal tumor with differentiation towards sebaceous glands that is composed of mature or nearly mature skin structures. Histologically, it is classified as a hamartoma.1 It commonly arises on the scalp as a yellowish or flesh-colored, hairless plaque of variable size. At birth, its surface is smooth and the differential diagnoses include aplasia cutis congenita, congenital triangular alopecia, and alopecia areata.2 As the patient ages, hormones stimulate the proliferation of sebaceous glands and the epidermis, and the lesion gradually acquires a verrucous, waxy surface.3 Benign appendageal tumors often develop inside SN. Basal cell epitheliomas are rarely found.4 Surgical excision is recommended for aesthetic purposes or to prevent the development of tumors.
Histology also varies with the patient’s age and can be misleading in childhood because the sebaceous glands are underdeveloped.5,6 After adrenarche, histology becomes more diagnostic, showing a dermis almost completely filled with sebaceous glands with varying degrees of maturity.2 The presence of incompletely differentiated follicles without hair shafts can be found in newborns and children and may be helpful for the correct histological diagnosis before puberty.1,5 The epidermis presents no abnormalities at birth but develops acanthosis and papillomatosis as the patient ages. Ectopic dilated apocrine glands sometimes can be found deeper in the dermis in the late stage of the lesion.5
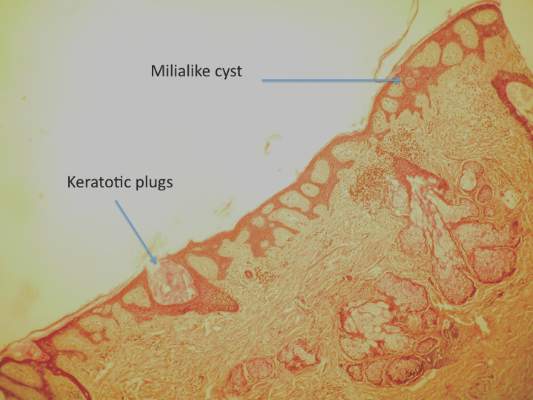
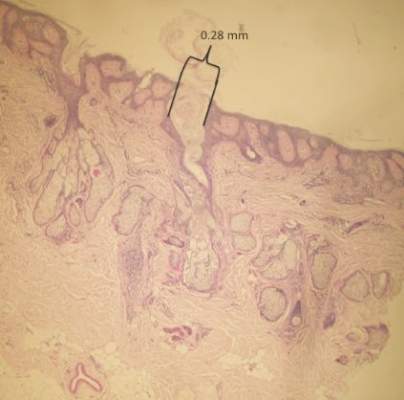
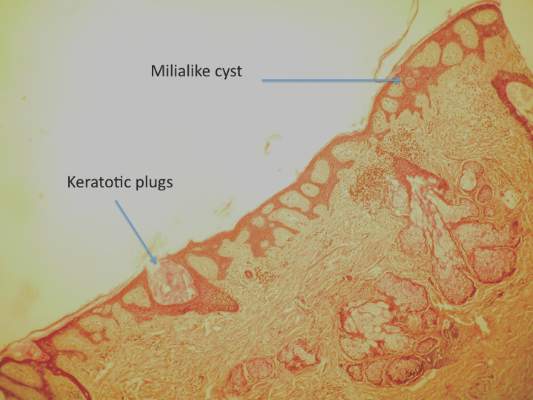
In a report by Neri et al,7 multiple bright yellow dots were noted on dermoscopy in 2 children with SN. The investigators concluded that this characteristic feature, which was thought to represent the sebaceous glands, can be useful in differentiating SN from aplasia cutis congenita in early infancy, but no histologic analyses were performed.7 In our patient, we identified 3 different dermoscopic features that correlated with histologic findings. Comedolike openings correlated with the accumulated keratin (ie, keratotic plugs) inside dilated sebaceous gland ducts directly connected to the epidermis. The brownish-yellow color of these openings observed on dermoscopy may be due to the oxidation of kerat-inous material, such as those in seborrheic keratosis lesions (Figure 3). We also noted bright yellow dots similar to those reported by Neri et al7; however, histologic analysis in our patient showed these dots more closely correlated with keratotic cysts similar to milialike structures seen in acanthotic seborrheic keratosis. The material remained lightly colored because no oxidation process had occurred (Figure 4). The third structure found on dermoscopy in our patient was multiple whitish structures that were irregular in shape and size. According to our comparison of superficial horizontal histology slides with dermoscopy images, we hypothesized this finding was the result of epidermal papillomatosis over a dermis filled with enlarged sebaceous glands (Figure 5). This finding was likely absent in the cases previously reported by Neri et al7 because epidermal and glandular changes occur later in the evolution of SN and the patients in these cases were younger than 4 months old.
Our correlation of dermoscopic features with histology findings in an 18-year-old woman with an irritated SN highlights the need for more studies needed in order to establish the prevalence of certain dermoscopic findings in this setting, particularly considering the important morphological changes that occur in these lesions as patients age as well as the histological variation among different hamartomas. Over the last decade, dermoscopy has proven to be a useful tool in the diagnosis of various hair and scalp diseases.8 Histologic correlation of dermoscopy findings is essential for more precise understanding of this new imaging technique and should be conducted whenever possible.
- Lever WF, Schaumburg-Lever G. Tumors of the epidermal appendages. In: Lever WF, Schaumburg-Lever G, eds. Histopathology of the Skin. 5th ed. Philadelphia, PA: Lippincott Co; 1975:498-502.
- Civatte J. Tumeurs du cuir chevelu. In: Bouhanna P, Reygagne P, eds. Pathologie du Cheveu et du Cuir Cheveulu. Paris, France: Masson Co; 1999:208-209.
- Gruβendorf-Conen E-I. Adnexal cysts and tumors of the scalp. In: Orfanos CE, Happle R, eds. Hair and Hair Diseases. 1st ed. Berlin Germany: Springer-Verlag Berlin Heidelberg Co; 1990:710-711.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceous: a study of 596 cases. J Am Acad Dermatol. 2000;42(2 pt 1):263-268.
- Camacho F. Tumeurs du cuir chevelu. In: Camacho F, Montagna W, eds. Trichologie: Maladie du Follicule Pilosébacé. Madrid, Spain: Grupo Aula Medica; 1997:515-516.
- Wechsler J. Hamartome sebace. In: Wechsler J, Fraitag S, Moulonguet I, eds. Pathologie Cutanee Tumorale. Montpelier, France: Sauramps Medical Co; 2009:100-102.
- Neri I, Savoia F, Giacomini F, et al. Usefulness of dermatoscopy for the early diagnosis of sebaceous naevus and differentiation from aplasia cutis congenita [published online ahead of print May 5, 2009]. Clin Exp Dermatol. 2009;34:e50-e52.
- Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;67:1040-1048.
To the Editor:
Sebaceous nevus (SN) is a relatively common hamartoma that presents most often as a single congenital hairless plaque on the scalp. After puberty, histologic features characteristically include papillomatous hyperplasia of the epidermis, a large number of mature or nearly mature sebaceous glands, and a lack of terminally differentiated hair follicles; however, histologic findings can be misleading during childhood when sebaceous glands are still underdeveloped. Bright yellow dots, which are thought to indicate the presence of sebaceous glands, may be seen on dermoscopy and can be useful in differentiating SN from aplasia cutis congenita in newborns.
We report a case of an SN in an 18-year-old woman and discuss how the histology findings correlated with features seen on dermoscopy.
An 18-year-old woman presented to our dermatology clinic with an asymptomatic, hairless plaque on the right parietal scalp that had been present since birth. The patient noted that the plaque had recently become larger in size. On physical examination, an 8×3-cm plaque with a smooth, flesh-colored surface was noted with central comedolike structures and an erythematous, verrucous periphery (Figure 1).

Dermoscopy (handheld dermoscope using polarized light) revealed 3 distinct types of round structures within the lesion: (1) comedolike openings (similar to those seen in seborrheic keratosis) that appeared as brownish-yellow, sharply circumscribed structures; (2) milialike cysts (also found in acanthotic seborrheic keratosis), which appeared as bright yellow structures; and (3) multiple whitish structures that were irregular in shape and size and covered the surface of the lesion where there were no other dermoscopic findings (Figure 2). The affected skin was pale to red in color and the verrucous aspect of the surface was better visualized at the edge of the lesion.
Two 4-mm punch biopsies were performed following dermoscopy: one for horizontal sectioning and one for vertical sectioning. Histologic analysis showed an acanthotic epidermis with an anastomosing network of elongated rete ridges in the superficial dermis. Numerous hyperplasic sebaceous glands were found in the mid dermis, with some also located above this level. Immature hair follicles were present and sebaceous gland ducts communicated directly with the epidermis through dilated hyperkeratinized pathways. Eccrine glands were normal, but no apocrine glands were present. A lymphocytic infiltrate was noted around the sebaceous glands and immature hair follicles and also around dilated capillaries in the superficial dermis. Moderate spongiosis and lymphocytic exocytosis were noted in the glandular epithelium and in the basal layer of the hair follicles and the epidermis. Superficial slides of horizontal sections of the biopsy specimen showed a correlation between the histology findings and dermoscopy images: multiple normal-appearing papilla surrounded by a network of anastomosing rete ridges correlated with multiple whitish structures, keratotic cysts with compact keratin corresponded to bright yellow dots, and larger conglomerates of loose lamelar keratin correlated with comedolike openings. Due to the presence of eczematous changes (eg, epithelial spongiosis, inflammatory cells) observed on histology, a diagnosis of an irritated sebaceous nevus was made, which explained the recent enlargement of the congenital lesion.
Sebaceous nevus is a benign, epidermal appendageal tumor with differentiation towards sebaceous glands that is composed of mature or nearly mature skin structures. Histologically, it is classified as a hamartoma.1 It commonly arises on the scalp as a yellowish or flesh-colored, hairless plaque of variable size. At birth, its surface is smooth and the differential diagnoses include aplasia cutis congenita, congenital triangular alopecia, and alopecia areata.2 As the patient ages, hormones stimulate the proliferation of sebaceous glands and the epidermis, and the lesion gradually acquires a verrucous, waxy surface.3 Benign appendageal tumors often develop inside SN. Basal cell epitheliomas are rarely found.4 Surgical excision is recommended for aesthetic purposes or to prevent the development of tumors.
Histology also varies with the patient’s age and can be misleading in childhood because the sebaceous glands are underdeveloped.5,6 After adrenarche, histology becomes more diagnostic, showing a dermis almost completely filled with sebaceous glands with varying degrees of maturity.2 The presence of incompletely differentiated follicles without hair shafts can be found in newborns and children and may be helpful for the correct histological diagnosis before puberty.1,5 The epidermis presents no abnormalities at birth but develops acanthosis and papillomatosis as the patient ages. Ectopic dilated apocrine glands sometimes can be found deeper in the dermis in the late stage of the lesion.5
In a report by Neri et al,7 multiple bright yellow dots were noted on dermoscopy in 2 children with SN. The investigators concluded that this characteristic feature, which was thought to represent the sebaceous glands, can be useful in differentiating SN from aplasia cutis congenita in early infancy, but no histologic analyses were performed.7 In our patient, we identified 3 different dermoscopic features that correlated with histologic findings. Comedolike openings correlated with the accumulated keratin (ie, keratotic plugs) inside dilated sebaceous gland ducts directly connected to the epidermis. The brownish-yellow color of these openings observed on dermoscopy may be due to the oxidation of kerat-inous material, such as those in seborrheic keratosis lesions (Figure 3). We also noted bright yellow dots similar to those reported by Neri et al7; however, histologic analysis in our patient showed these dots more closely correlated with keratotic cysts similar to milialike structures seen in acanthotic seborrheic keratosis. The material remained lightly colored because no oxidation process had occurred (Figure 4). The third structure found on dermoscopy in our patient was multiple whitish structures that were irregular in shape and size. According to our comparison of superficial horizontal histology slides with dermoscopy images, we hypothesized this finding was the result of epidermal papillomatosis over a dermis filled with enlarged sebaceous glands (Figure 5). This finding was likely absent in the cases previously reported by Neri et al7 because epidermal and glandular changes occur later in the evolution of SN and the patients in these cases were younger than 4 months old.
Our correlation of dermoscopic features with histology findings in an 18-year-old woman with an irritated SN highlights the need for more studies needed in order to establish the prevalence of certain dermoscopic findings in this setting, particularly considering the important morphological changes that occur in these lesions as patients age as well as the histological variation among different hamartomas. Over the last decade, dermoscopy has proven to be a useful tool in the diagnosis of various hair and scalp diseases.8 Histologic correlation of dermoscopy findings is essential for more precise understanding of this new imaging technique and should be conducted whenever possible.
To the Editor:
Sebaceous nevus (SN) is a relatively common hamartoma that presents most often as a single congenital hairless plaque on the scalp. After puberty, histologic features characteristically include papillomatous hyperplasia of the epidermis, a large number of mature or nearly mature sebaceous glands, and a lack of terminally differentiated hair follicles; however, histologic findings can be misleading during childhood when sebaceous glands are still underdeveloped. Bright yellow dots, which are thought to indicate the presence of sebaceous glands, may be seen on dermoscopy and can be useful in differentiating SN from aplasia cutis congenita in newborns.
We report a case of an SN in an 18-year-old woman and discuss how the histology findings correlated with features seen on dermoscopy.
An 18-year-old woman presented to our dermatology clinic with an asymptomatic, hairless plaque on the right parietal scalp that had been present since birth. The patient noted that the plaque had recently become larger in size. On physical examination, an 8×3-cm plaque with a smooth, flesh-colored surface was noted with central comedolike structures and an erythematous, verrucous periphery (Figure 1).

Dermoscopy (handheld dermoscope using polarized light) revealed 3 distinct types of round structures within the lesion: (1) comedolike openings (similar to those seen in seborrheic keratosis) that appeared as brownish-yellow, sharply circumscribed structures; (2) milialike cysts (also found in acanthotic seborrheic keratosis), which appeared as bright yellow structures; and (3) multiple whitish structures that were irregular in shape and size and covered the surface of the lesion where there were no other dermoscopic findings (Figure 2). The affected skin was pale to red in color and the verrucous aspect of the surface was better visualized at the edge of the lesion.
Two 4-mm punch biopsies were performed following dermoscopy: one for horizontal sectioning and one for vertical sectioning. Histologic analysis showed an acanthotic epidermis with an anastomosing network of elongated rete ridges in the superficial dermis. Numerous hyperplasic sebaceous glands were found in the mid dermis, with some also located above this level. Immature hair follicles were present and sebaceous gland ducts communicated directly with the epidermis through dilated hyperkeratinized pathways. Eccrine glands were normal, but no apocrine glands were present. A lymphocytic infiltrate was noted around the sebaceous glands and immature hair follicles and also around dilated capillaries in the superficial dermis. Moderate spongiosis and lymphocytic exocytosis were noted in the glandular epithelium and in the basal layer of the hair follicles and the epidermis. Superficial slides of horizontal sections of the biopsy specimen showed a correlation between the histology findings and dermoscopy images: multiple normal-appearing papilla surrounded by a network of anastomosing rete ridges correlated with multiple whitish structures, keratotic cysts with compact keratin corresponded to bright yellow dots, and larger conglomerates of loose lamelar keratin correlated with comedolike openings. Due to the presence of eczematous changes (eg, epithelial spongiosis, inflammatory cells) observed on histology, a diagnosis of an irritated sebaceous nevus was made, which explained the recent enlargement of the congenital lesion.
Sebaceous nevus is a benign, epidermal appendageal tumor with differentiation towards sebaceous glands that is composed of mature or nearly mature skin structures. Histologically, it is classified as a hamartoma.1 It commonly arises on the scalp as a yellowish or flesh-colored, hairless plaque of variable size. At birth, its surface is smooth and the differential diagnoses include aplasia cutis congenita, congenital triangular alopecia, and alopecia areata.2 As the patient ages, hormones stimulate the proliferation of sebaceous glands and the epidermis, and the lesion gradually acquires a verrucous, waxy surface.3 Benign appendageal tumors often develop inside SN. Basal cell epitheliomas are rarely found.4 Surgical excision is recommended for aesthetic purposes or to prevent the development of tumors.
Histology also varies with the patient’s age and can be misleading in childhood because the sebaceous glands are underdeveloped.5,6 After adrenarche, histology becomes more diagnostic, showing a dermis almost completely filled with sebaceous glands with varying degrees of maturity.2 The presence of incompletely differentiated follicles without hair shafts can be found in newborns and children and may be helpful for the correct histological diagnosis before puberty.1,5 The epidermis presents no abnormalities at birth but develops acanthosis and papillomatosis as the patient ages. Ectopic dilated apocrine glands sometimes can be found deeper in the dermis in the late stage of the lesion.5
In a report by Neri et al,7 multiple bright yellow dots were noted on dermoscopy in 2 children with SN. The investigators concluded that this characteristic feature, which was thought to represent the sebaceous glands, can be useful in differentiating SN from aplasia cutis congenita in early infancy, but no histologic analyses were performed.7 In our patient, we identified 3 different dermoscopic features that correlated with histologic findings. Comedolike openings correlated with the accumulated keratin (ie, keratotic plugs) inside dilated sebaceous gland ducts directly connected to the epidermis. The brownish-yellow color of these openings observed on dermoscopy may be due to the oxidation of kerat-inous material, such as those in seborrheic keratosis lesions (Figure 3). We also noted bright yellow dots similar to those reported by Neri et al7; however, histologic analysis in our patient showed these dots more closely correlated with keratotic cysts similar to milialike structures seen in acanthotic seborrheic keratosis. The material remained lightly colored because no oxidation process had occurred (Figure 4). The third structure found on dermoscopy in our patient was multiple whitish structures that were irregular in shape and size. According to our comparison of superficial horizontal histology slides with dermoscopy images, we hypothesized this finding was the result of epidermal papillomatosis over a dermis filled with enlarged sebaceous glands (Figure 5). This finding was likely absent in the cases previously reported by Neri et al7 because epidermal and glandular changes occur later in the evolution of SN and the patients in these cases were younger than 4 months old.
Our correlation of dermoscopic features with histology findings in an 18-year-old woman with an irritated SN highlights the need for more studies needed in order to establish the prevalence of certain dermoscopic findings in this setting, particularly considering the important morphological changes that occur in these lesions as patients age as well as the histological variation among different hamartomas. Over the last decade, dermoscopy has proven to be a useful tool in the diagnosis of various hair and scalp diseases.8 Histologic correlation of dermoscopy findings is essential for more precise understanding of this new imaging technique and should be conducted whenever possible.
- Lever WF, Schaumburg-Lever G. Tumors of the epidermal appendages. In: Lever WF, Schaumburg-Lever G, eds. Histopathology of the Skin. 5th ed. Philadelphia, PA: Lippincott Co; 1975:498-502.
- Civatte J. Tumeurs du cuir chevelu. In: Bouhanna P, Reygagne P, eds. Pathologie du Cheveu et du Cuir Cheveulu. Paris, France: Masson Co; 1999:208-209.
- Gruβendorf-Conen E-I. Adnexal cysts and tumors of the scalp. In: Orfanos CE, Happle R, eds. Hair and Hair Diseases. 1st ed. Berlin Germany: Springer-Verlag Berlin Heidelberg Co; 1990:710-711.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceous: a study of 596 cases. J Am Acad Dermatol. 2000;42(2 pt 1):263-268.
- Camacho F. Tumeurs du cuir chevelu. In: Camacho F, Montagna W, eds. Trichologie: Maladie du Follicule Pilosébacé. Madrid, Spain: Grupo Aula Medica; 1997:515-516.
- Wechsler J. Hamartome sebace. In: Wechsler J, Fraitag S, Moulonguet I, eds. Pathologie Cutanee Tumorale. Montpelier, France: Sauramps Medical Co; 2009:100-102.
- Neri I, Savoia F, Giacomini F, et al. Usefulness of dermatoscopy for the early diagnosis of sebaceous naevus and differentiation from aplasia cutis congenita [published online ahead of print May 5, 2009]. Clin Exp Dermatol. 2009;34:e50-e52.
- Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;67:1040-1048.
- Lever WF, Schaumburg-Lever G. Tumors of the epidermal appendages. In: Lever WF, Schaumburg-Lever G, eds. Histopathology of the Skin. 5th ed. Philadelphia, PA: Lippincott Co; 1975:498-502.
- Civatte J. Tumeurs du cuir chevelu. In: Bouhanna P, Reygagne P, eds. Pathologie du Cheveu et du Cuir Cheveulu. Paris, France: Masson Co; 1999:208-209.
- Gruβendorf-Conen E-I. Adnexal cysts and tumors of the scalp. In: Orfanos CE, Happle R, eds. Hair and Hair Diseases. 1st ed. Berlin Germany: Springer-Verlag Berlin Heidelberg Co; 1990:710-711.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceous: a study of 596 cases. J Am Acad Dermatol. 2000;42(2 pt 1):263-268.
- Camacho F. Tumeurs du cuir chevelu. In: Camacho F, Montagna W, eds. Trichologie: Maladie du Follicule Pilosébacé. Madrid, Spain: Grupo Aula Medica; 1997:515-516.
- Wechsler J. Hamartome sebace. In: Wechsler J, Fraitag S, Moulonguet I, eds. Pathologie Cutanee Tumorale. Montpelier, France: Sauramps Medical Co; 2009:100-102.
- Neri I, Savoia F, Giacomini F, et al. Usefulness of dermatoscopy for the early diagnosis of sebaceous naevus and differentiation from aplasia cutis congenita [published online ahead of print May 5, 2009]. Clin Exp Dermatol. 2009;34:e50-e52.
- Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;67:1040-1048.
