User login
The Diagnosis: Hypopigmented Mycosis Fungoides
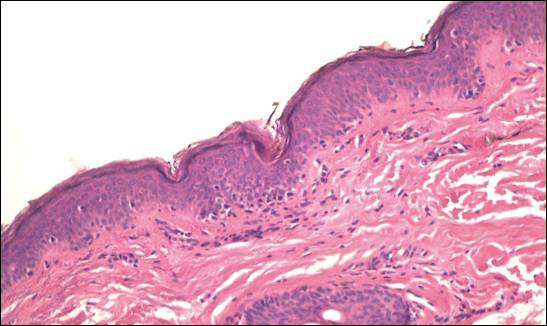
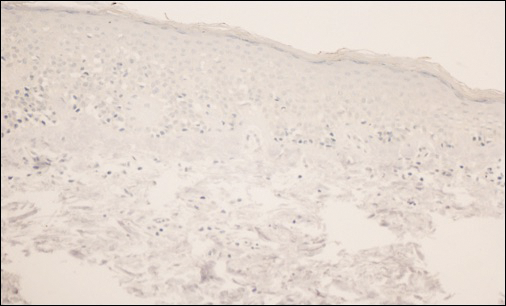
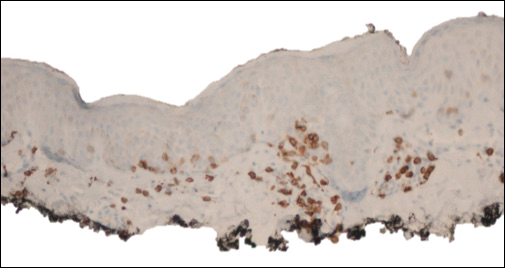
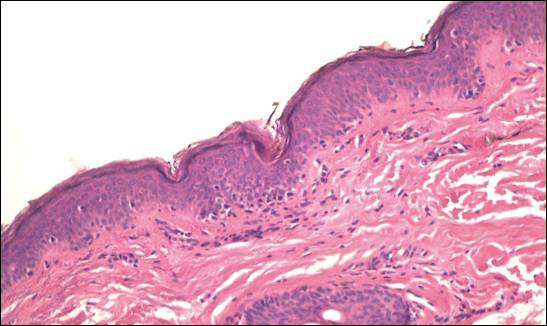
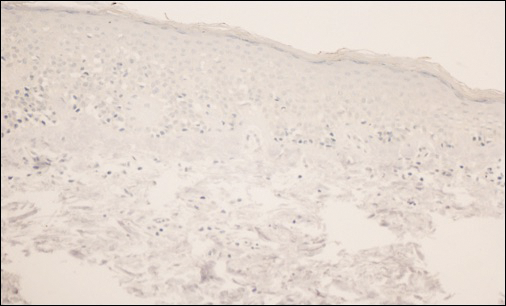
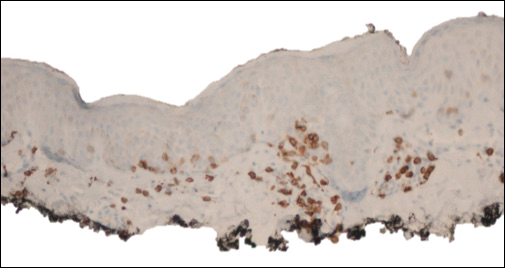
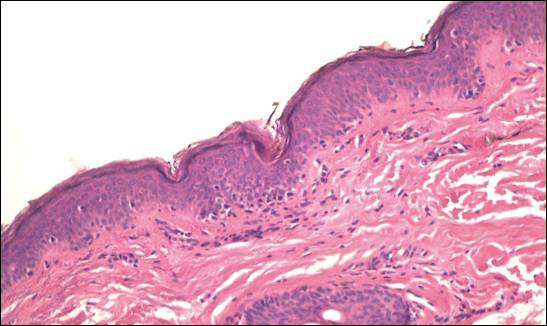
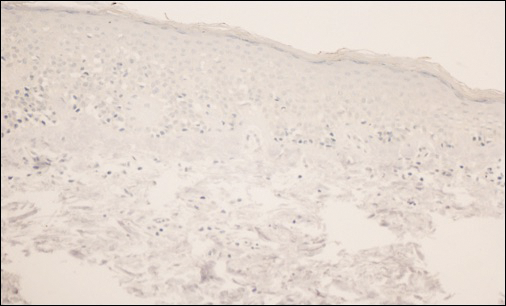
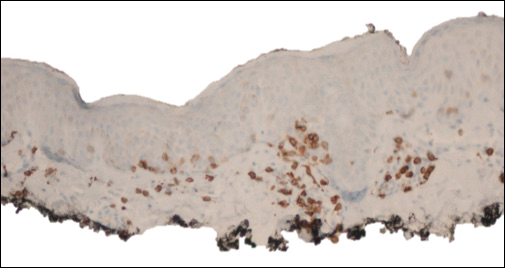
The patient was started on clobetasol dipropionate cream 0.05% twice daily, which she did not tolerate due to a burning sensation on application. She then was started on narrowband UVB phototherapy 2 to 3 times weekly, and the hypopigmented areas began to improve. Narrowband UVB phototherapy was discontinued after 7 weeks due to the high cost to the patient, but the hypopigmented patches on the left thigh appeared to remit, and the patient did not return to the clinic for 6 months. She returned when the areas on the left thigh reappeared, along with new areas on the right buttock and right medial upper arm. Serial biopsies of the new patches also revealed a CD8+ atypical lymphocytic infiltrate consistent with hypopigmented patch-stage mycosis fungoides (MF). She was started on halobetasol ointment 0.05% twice daily to affected areas, which she tolerated well. Complete blood count and peripheral blood smear were unremarkable, and the patient continued to deny systemic symptoms. Over the next year, the patient's cutaneous findings continued to wax and wane with topical treatment, and she was referred to a regional cancer treatment center for a second opinion from a hematopathologist. Hematopathologic and dermatopathologic review of the case, including hematoxylin and eosin and immunohistochemical staining, was highly consistent with hypopigmented MF (Figures 1-3).
Mycosis fungoides is an uncommon disease characterized by atypical clonal T cells exhibiting epidermotropism. Most commonly, MF is characterized by a CD4+ lymphocytic infiltrate. Mycosis fungoides can be difficult to diagnose in its early stages, as it may resemble benign inflammatory conditions (eg, chronic atopic dermatitis, nummular eczema) and often requires biopsy and additional studies, such as immunohistochemistry, to secure a diagnosis. Hypopigmented MF is regarded as a subtype of MF, as it can exhibit different clinical and pathologic characteristics from classical MF. In particular, the lymphocytic phenotype in hypopigmented MF is more likely to be CD8+.
In general, the progression of MF is characterized as stage IA (patches or plaques involving less than 10% body surface area [BSA]), IB (patches or plaques involving ≥10% BSA without lymph node or visceral involvement), IIA (patches or plaques of any percentage of BSA with lymph node involvement), IIB (cutaneous tumors with or without lymph node involvement), III (erythroderma with low blood tumor burden), or IV (erythroderma with high blood tumor burden with or without visceral involvement). Hypopigmented MF generally presents in early patch stage and rarely progresses past stage IB, and thus generally has a favorable prognosis.1,2 Kim et al3 demonstrated that evolution from patch to plaque stage MF is accompanied by a shift in lymphocytes from the T helper 1 (Th1) to T helper 2 phenotype; therefore the Th1 phenotype, CD8+ T cells are associated with lower risk for disease progression. Other investigators also have hypothesized that predominance of Th1 phenotype, CD8+ T cells may have an immunoregulatory effect, thus preventing evolution of disease from patch to plaque stage and explaining why hypopigmented MF, with a predominantly CD8+ phenotype, confers better prognosis with less chance for disease progression than classical MF.4,5 The patch- or plaque-stage lesions of classical MF have a predilection for non-sun exposed areas (eg, buttocks, medial thighs, breasts),2 whereas hypopigmented MF tends to present with hypopigmented or depigmented lesions mainly distributed on the trunk, arms, and legs. These lesions may become more visible following sun exposure.1 The size of the hypopigmented lesions can vary, and patients may complain of pruritus with variable intensity.
Hypopigmented MF presents more commonly in younger populations, in contrast to classical MF.6-8 However, like classical MF, hypopigmented MF appears to more frequently affect individuals with darker Fitzpatrick skin types.1,9,10 Although it generally is accepted that hypopigmented MF does not favor either sex, some studies suggest that hypopigmented MF has a female predominance.6,10
Classical MF is characterized by an epidermotropic infiltrate of CD4+ T helper cells,10 whereas CD8+ epidermotropism is considered hallmark in hypopigmented MF.10-12 The other typical histopathologic features of hypopigmented MF generally are identical to those of classical MF, with solitary or small groups of atypical haloed lymphocytes within the basal layer, exocytosis of lymphocytes out of proportion to spongiosis, and papillary dermal fibrosis. Immunohistochemistry generally is helpful in distinguishing between classical MF and hypopigmented MF.
The clinical differential diagnosis for hypopigmented MF includes the early (inflammatory) stage of vitiligo, postinflammatory hypopigmentation, lichen sclerosus, pityriasis alba, and leprosy.
First-line treatment for hypopigmented MF consists of phototherapy/photochemotherapy and topical steroids.9,13 Narrowband UVB phototherapy has been used with good success in pediatric patients.14 However, narrowband UVB may not be as effective in darker-skinned individuals; it has been hypothesized that this lack of efficacy could be due to the protective effects of increased melanin in the skin.1 Other topical therapies may include topical carmustine and topical nitrogen mustard.
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Girardi M, Heald PW, Wilson LD. The pathogenesis of mycosis fungoides. N Engl J Med. 2004;350:1978-1988.
- Kim EJ, Hess S, Richardson SK, et al. Immunopathogenesis and therapy of cutaneous T cell lymphoma. J Clin Invest. 2005;115:798-812.
- Stone ML, Styles AR, Cockerell CJ, et al. Hypopigmented report of 7 cases and review of the literature. Cutis. 2001;67:133-138.
- Volkenandt M, Soyer HP, Cerroni L, et al. Molecular detection of clone-specific DNA in hypopigmented lesions of a patient with early evolving mycosis fungoides. Br J Dermatol. 1993;128:423-428.
- Furlan FC, Pereira BA, Sotto MN, et al. Hypopigmented mycosis fungoides versus mycosis fungoides with concomitant hypopigmented lesions: same disease or different variants of mycosis fungoides? Dermatology. 2014;229:271-274.
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270.
- Boulos S, Vaid R, Aladily TN, et al. Clinical presentation, immunopathology, and treatment of juvenile-onset mycosis fungoides: a case series of 34 patients. J Am Acad Dermatol. 2014;71:1117-1126.
- Lambroza E, Cohen SR, Phelps R, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- El-Shabrawi-Caelen L, Cerroni L, Medeiros LJ, et al. Hypopigmented mycosis fungoides: Frequent expression of a CD8+ T-cell phenotype. Am J Surg Pathol. 2002;26:450-457.
- Furlan FC, de Paula Pereira BA, da Silva LF, et al. Loss of melanocytes in hypopigmented mycosis fungoides: a study of 18 patients. J Cutan Pathol. 2014;41:101-107.
- Tolkachjov SN, Comfere NI. Hypopigmented mycosis fungoides: a clinical mimicker of vitiligo. J Drugs Dermatol. 2015;14:193-194.
- Duarte I, Bedrikow, R, Aoki S. Mycosis fungoides: epidemiologic study of 17 cases and evaluation of PUVA photochemotherapy. An Bras Dermatol. 2006;81:40-45.
- Onsun N, Kural Y, Su O, et al. Hypopigmented mycosis fungoides associated with atopy in two children. Pediatr Dermatol. 2006;23:493-496.
The Diagnosis: Hypopigmented Mycosis Fungoides
The patient was started on clobetasol dipropionate cream 0.05% twice daily, which she did not tolerate due to a burning sensation on application. She then was started on narrowband UVB phototherapy 2 to 3 times weekly, and the hypopigmented areas began to improve. Narrowband UVB phototherapy was discontinued after 7 weeks due to the high cost to the patient, but the hypopigmented patches on the left thigh appeared to remit, and the patient did not return to the clinic for 6 months. She returned when the areas on the left thigh reappeared, along with new areas on the right buttock and right medial upper arm. Serial biopsies of the new patches also revealed a CD8+ atypical lymphocytic infiltrate consistent with hypopigmented patch-stage mycosis fungoides (MF). She was started on halobetasol ointment 0.05% twice daily to affected areas, which she tolerated well. Complete blood count and peripheral blood smear were unremarkable, and the patient continued to deny systemic symptoms. Over the next year, the patient's cutaneous findings continued to wax and wane with topical treatment, and she was referred to a regional cancer treatment center for a second opinion from a hematopathologist. Hematopathologic and dermatopathologic review of the case, including hematoxylin and eosin and immunohistochemical staining, was highly consistent with hypopigmented MF (Figures 1-3).
Mycosis fungoides is an uncommon disease characterized by atypical clonal T cells exhibiting epidermotropism. Most commonly, MF is characterized by a CD4+ lymphocytic infiltrate. Mycosis fungoides can be difficult to diagnose in its early stages, as it may resemble benign inflammatory conditions (eg, chronic atopic dermatitis, nummular eczema) and often requires biopsy and additional studies, such as immunohistochemistry, to secure a diagnosis. Hypopigmented MF is regarded as a subtype of MF, as it can exhibit different clinical and pathologic characteristics from classical MF. In particular, the lymphocytic phenotype in hypopigmented MF is more likely to be CD8+.
In general, the progression of MF is characterized as stage IA (patches or plaques involving less than 10% body surface area [BSA]), IB (patches or plaques involving ≥10% BSA without lymph node or visceral involvement), IIA (patches or plaques of any percentage of BSA with lymph node involvement), IIB (cutaneous tumors with or without lymph node involvement), III (erythroderma with low blood tumor burden), or IV (erythroderma with high blood tumor burden with or without visceral involvement). Hypopigmented MF generally presents in early patch stage and rarely progresses past stage IB, and thus generally has a favorable prognosis.1,2 Kim et al3 demonstrated that evolution from patch to plaque stage MF is accompanied by a shift in lymphocytes from the T helper 1 (Th1) to T helper 2 phenotype; therefore the Th1 phenotype, CD8+ T cells are associated with lower risk for disease progression. Other investigators also have hypothesized that predominance of Th1 phenotype, CD8+ T cells may have an immunoregulatory effect, thus preventing evolution of disease from patch to plaque stage and explaining why hypopigmented MF, with a predominantly CD8+ phenotype, confers better prognosis with less chance for disease progression than classical MF.4,5 The patch- or plaque-stage lesions of classical MF have a predilection for non-sun exposed areas (eg, buttocks, medial thighs, breasts),2 whereas hypopigmented MF tends to present with hypopigmented or depigmented lesions mainly distributed on the trunk, arms, and legs. These lesions may become more visible following sun exposure.1 The size of the hypopigmented lesions can vary, and patients may complain of pruritus with variable intensity.
Hypopigmented MF presents more commonly in younger populations, in contrast to classical MF.6-8 However, like classical MF, hypopigmented MF appears to more frequently affect individuals with darker Fitzpatrick skin types.1,9,10 Although it generally is accepted that hypopigmented MF does not favor either sex, some studies suggest that hypopigmented MF has a female predominance.6,10
Classical MF is characterized by an epidermotropic infiltrate of CD4+ T helper cells,10 whereas CD8+ epidermotropism is considered hallmark in hypopigmented MF.10-12 The other typical histopathologic features of hypopigmented MF generally are identical to those of classical MF, with solitary or small groups of atypical haloed lymphocytes within the basal layer, exocytosis of lymphocytes out of proportion to spongiosis, and papillary dermal fibrosis. Immunohistochemistry generally is helpful in distinguishing between classical MF and hypopigmented MF.
The clinical differential diagnosis for hypopigmented MF includes the early (inflammatory) stage of vitiligo, postinflammatory hypopigmentation, lichen sclerosus, pityriasis alba, and leprosy.
First-line treatment for hypopigmented MF consists of phototherapy/photochemotherapy and topical steroids.9,13 Narrowband UVB phototherapy has been used with good success in pediatric patients.14 However, narrowband UVB may not be as effective in darker-skinned individuals; it has been hypothesized that this lack of efficacy could be due to the protective effects of increased melanin in the skin.1 Other topical therapies may include topical carmustine and topical nitrogen mustard.
The Diagnosis: Hypopigmented Mycosis Fungoides
The patient was started on clobetasol dipropionate cream 0.05% twice daily, which she did not tolerate due to a burning sensation on application. She then was started on narrowband UVB phototherapy 2 to 3 times weekly, and the hypopigmented areas began to improve. Narrowband UVB phototherapy was discontinued after 7 weeks due to the high cost to the patient, but the hypopigmented patches on the left thigh appeared to remit, and the patient did not return to the clinic for 6 months. She returned when the areas on the left thigh reappeared, along with new areas on the right buttock and right medial upper arm. Serial biopsies of the new patches also revealed a CD8+ atypical lymphocytic infiltrate consistent with hypopigmented patch-stage mycosis fungoides (MF). She was started on halobetasol ointment 0.05% twice daily to affected areas, which she tolerated well. Complete blood count and peripheral blood smear were unremarkable, and the patient continued to deny systemic symptoms. Over the next year, the patient's cutaneous findings continued to wax and wane with topical treatment, and she was referred to a regional cancer treatment center for a second opinion from a hematopathologist. Hematopathologic and dermatopathologic review of the case, including hematoxylin and eosin and immunohistochemical staining, was highly consistent with hypopigmented MF (Figures 1-3).
Mycosis fungoides is an uncommon disease characterized by atypical clonal T cells exhibiting epidermotropism. Most commonly, MF is characterized by a CD4+ lymphocytic infiltrate. Mycosis fungoides can be difficult to diagnose in its early stages, as it may resemble benign inflammatory conditions (eg, chronic atopic dermatitis, nummular eczema) and often requires biopsy and additional studies, such as immunohistochemistry, to secure a diagnosis. Hypopigmented MF is regarded as a subtype of MF, as it can exhibit different clinical and pathologic characteristics from classical MF. In particular, the lymphocytic phenotype in hypopigmented MF is more likely to be CD8+.
In general, the progression of MF is characterized as stage IA (patches or plaques involving less than 10% body surface area [BSA]), IB (patches or plaques involving ≥10% BSA without lymph node or visceral involvement), IIA (patches or plaques of any percentage of BSA with lymph node involvement), IIB (cutaneous tumors with or without lymph node involvement), III (erythroderma with low blood tumor burden), or IV (erythroderma with high blood tumor burden with or without visceral involvement). Hypopigmented MF generally presents in early patch stage and rarely progresses past stage IB, and thus generally has a favorable prognosis.1,2 Kim et al3 demonstrated that evolution from patch to plaque stage MF is accompanied by a shift in lymphocytes from the T helper 1 (Th1) to T helper 2 phenotype; therefore the Th1 phenotype, CD8+ T cells are associated with lower risk for disease progression. Other investigators also have hypothesized that predominance of Th1 phenotype, CD8+ T cells may have an immunoregulatory effect, thus preventing evolution of disease from patch to plaque stage and explaining why hypopigmented MF, with a predominantly CD8+ phenotype, confers better prognosis with less chance for disease progression than classical MF.4,5 The patch- or plaque-stage lesions of classical MF have a predilection for non-sun exposed areas (eg, buttocks, medial thighs, breasts),2 whereas hypopigmented MF tends to present with hypopigmented or depigmented lesions mainly distributed on the trunk, arms, and legs. These lesions may become more visible following sun exposure.1 The size of the hypopigmented lesions can vary, and patients may complain of pruritus with variable intensity.
Hypopigmented MF presents more commonly in younger populations, in contrast to classical MF.6-8 However, like classical MF, hypopigmented MF appears to more frequently affect individuals with darker Fitzpatrick skin types.1,9,10 Although it generally is accepted that hypopigmented MF does not favor either sex, some studies suggest that hypopigmented MF has a female predominance.6,10
Classical MF is characterized by an epidermotropic infiltrate of CD4+ T helper cells,10 whereas CD8+ epidermotropism is considered hallmark in hypopigmented MF.10-12 The other typical histopathologic features of hypopigmented MF generally are identical to those of classical MF, with solitary or small groups of atypical haloed lymphocytes within the basal layer, exocytosis of lymphocytes out of proportion to spongiosis, and papillary dermal fibrosis. Immunohistochemistry generally is helpful in distinguishing between classical MF and hypopigmented MF.
The clinical differential diagnosis for hypopigmented MF includes the early (inflammatory) stage of vitiligo, postinflammatory hypopigmentation, lichen sclerosus, pityriasis alba, and leprosy.
First-line treatment for hypopigmented MF consists of phototherapy/photochemotherapy and topical steroids.9,13 Narrowband UVB phototherapy has been used with good success in pediatric patients.14 However, narrowband UVB may not be as effective in darker-skinned individuals; it has been hypothesized that this lack of efficacy could be due to the protective effects of increased melanin in the skin.1 Other topical therapies may include topical carmustine and topical nitrogen mustard.
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Girardi M, Heald PW, Wilson LD. The pathogenesis of mycosis fungoides. N Engl J Med. 2004;350:1978-1988.
- Kim EJ, Hess S, Richardson SK, et al. Immunopathogenesis and therapy of cutaneous T cell lymphoma. J Clin Invest. 2005;115:798-812.
- Stone ML, Styles AR, Cockerell CJ, et al. Hypopigmented report of 7 cases and review of the literature. Cutis. 2001;67:133-138.
- Volkenandt M, Soyer HP, Cerroni L, et al. Molecular detection of clone-specific DNA in hypopigmented lesions of a patient with early evolving mycosis fungoides. Br J Dermatol. 1993;128:423-428.
- Furlan FC, Pereira BA, Sotto MN, et al. Hypopigmented mycosis fungoides versus mycosis fungoides with concomitant hypopigmented lesions: same disease or different variants of mycosis fungoides? Dermatology. 2014;229:271-274.
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270.
- Boulos S, Vaid R, Aladily TN, et al. Clinical presentation, immunopathology, and treatment of juvenile-onset mycosis fungoides: a case series of 34 patients. J Am Acad Dermatol. 2014;71:1117-1126.
- Lambroza E, Cohen SR, Phelps R, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- El-Shabrawi-Caelen L, Cerroni L, Medeiros LJ, et al. Hypopigmented mycosis fungoides: Frequent expression of a CD8+ T-cell phenotype. Am J Surg Pathol. 2002;26:450-457.
- Furlan FC, de Paula Pereira BA, da Silva LF, et al. Loss of melanocytes in hypopigmented mycosis fungoides: a study of 18 patients. J Cutan Pathol. 2014;41:101-107.
- Tolkachjov SN, Comfere NI. Hypopigmented mycosis fungoides: a clinical mimicker of vitiligo. J Drugs Dermatol. 2015;14:193-194.
- Duarte I, Bedrikow, R, Aoki S. Mycosis fungoides: epidemiologic study of 17 cases and evaluation of PUVA photochemotherapy. An Bras Dermatol. 2006;81:40-45.
- Onsun N, Kural Y, Su O, et al. Hypopigmented mycosis fungoides associated with atopy in two children. Pediatr Dermatol. 2006;23:493-496.
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Girardi M, Heald PW, Wilson LD. The pathogenesis of mycosis fungoides. N Engl J Med. 2004;350:1978-1988.
- Kim EJ, Hess S, Richardson SK, et al. Immunopathogenesis and therapy of cutaneous T cell lymphoma. J Clin Invest. 2005;115:798-812.
- Stone ML, Styles AR, Cockerell CJ, et al. Hypopigmented report of 7 cases and review of the literature. Cutis. 2001;67:133-138.
- Volkenandt M, Soyer HP, Cerroni L, et al. Molecular detection of clone-specific DNA in hypopigmented lesions of a patient with early evolving mycosis fungoides. Br J Dermatol. 1993;128:423-428.
- Furlan FC, Pereira BA, Sotto MN, et al. Hypopigmented mycosis fungoides versus mycosis fungoides with concomitant hypopigmented lesions: same disease or different variants of mycosis fungoides? Dermatology. 2014;229:271-274.
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270.
- Boulos S, Vaid R, Aladily TN, et al. Clinical presentation, immunopathology, and treatment of juvenile-onset mycosis fungoides: a case series of 34 patients. J Am Acad Dermatol. 2014;71:1117-1126.
- Lambroza E, Cohen SR, Phelps R, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- El-Shabrawi-Caelen L, Cerroni L, Medeiros LJ, et al. Hypopigmented mycosis fungoides: Frequent expression of a CD8+ T-cell phenotype. Am J Surg Pathol. 2002;26:450-457.
- Furlan FC, de Paula Pereira BA, da Silva LF, et al. Loss of melanocytes in hypopigmented mycosis fungoides: a study of 18 patients. J Cutan Pathol. 2014;41:101-107.
- Tolkachjov SN, Comfere NI. Hypopigmented mycosis fungoides: a clinical mimicker of vitiligo. J Drugs Dermatol. 2015;14:193-194.
- Duarte I, Bedrikow, R, Aoki S. Mycosis fungoides: epidemiologic study of 17 cases and evaluation of PUVA photochemotherapy. An Bras Dermatol. 2006;81:40-45.
- Onsun N, Kural Y, Su O, et al. Hypopigmented mycosis fungoides associated with atopy in two children. Pediatr Dermatol. 2006;23:493-496.

A 39-year-old woman presented with 2 areas of hypopigmented discoloration on the left thigh of 6 months' duration. The hypopigmentation was more visible following sun exposure because the areas did not tan. The patient had not sought prior treatment for the discoloration and denied any previous rash or trauma to the area. Her medical history was remarkable for hypothyroidism associated with mild and transient alopecia, acne, and xerosis. Her daily medications included oral contraceptive pills (norgestimate/ethinyl estradiol), oral levothyroxine/liothyronine, and sulfacetamide lotion 10%. She denied any allergies, and the remainder of her medical, surgical, social, and family history was unremarkable. A review of systems was negative for enlarged lymph nodes, fever, night sweats, and fatigue. Physical examination revealed 2 subtle hypopigmented patches with fine, atrophic, cigarette paper-like wrinkling distributed on the left medial and posterior upper thigh. Initial biopsy of the hypopigmented patches revealed a CD8+ lymphocytic infiltrate with an atypical interface.
