User login
In today’s global society, smartphones are ubiquitous, used by >2.5 billion people.1 They provide limitless availability of on-demand services and resources, unparalleled computing power by size, and the ability to connect with anyone in the world.
Digital applications and new mobile technologies can be used to change the nature of the psychiatrist–patient relationship. The future of clinical practice is changing with the help of smartphones and apps. Diagnosis, follow-up, and treatment will never look the same as we come to better understand and apply emerging technologies.2
Both Android and iOS—the 2 largest mobile operating systems by market share3—provide outlets for the dissemination of mobile applications. There are currently >10,000 mental health–related apps available for download.4 One particular use case of mental health–related apps is digital phenotyping.
In this article, we aim to:
- define digital phenotyping
- explore the potential advances in patient care afforded by emerging technology
- discuss the ethical dilemmas and future of mental health apps.
The possibilities of digital phenotyping
Digital phenotyping is capturing a patient’s real-time clinical state using digital technology to better understand the patient’s state outside of the clinic. While digital phenotyping may seem new, the concepts behind it are grounded in good clinical care.
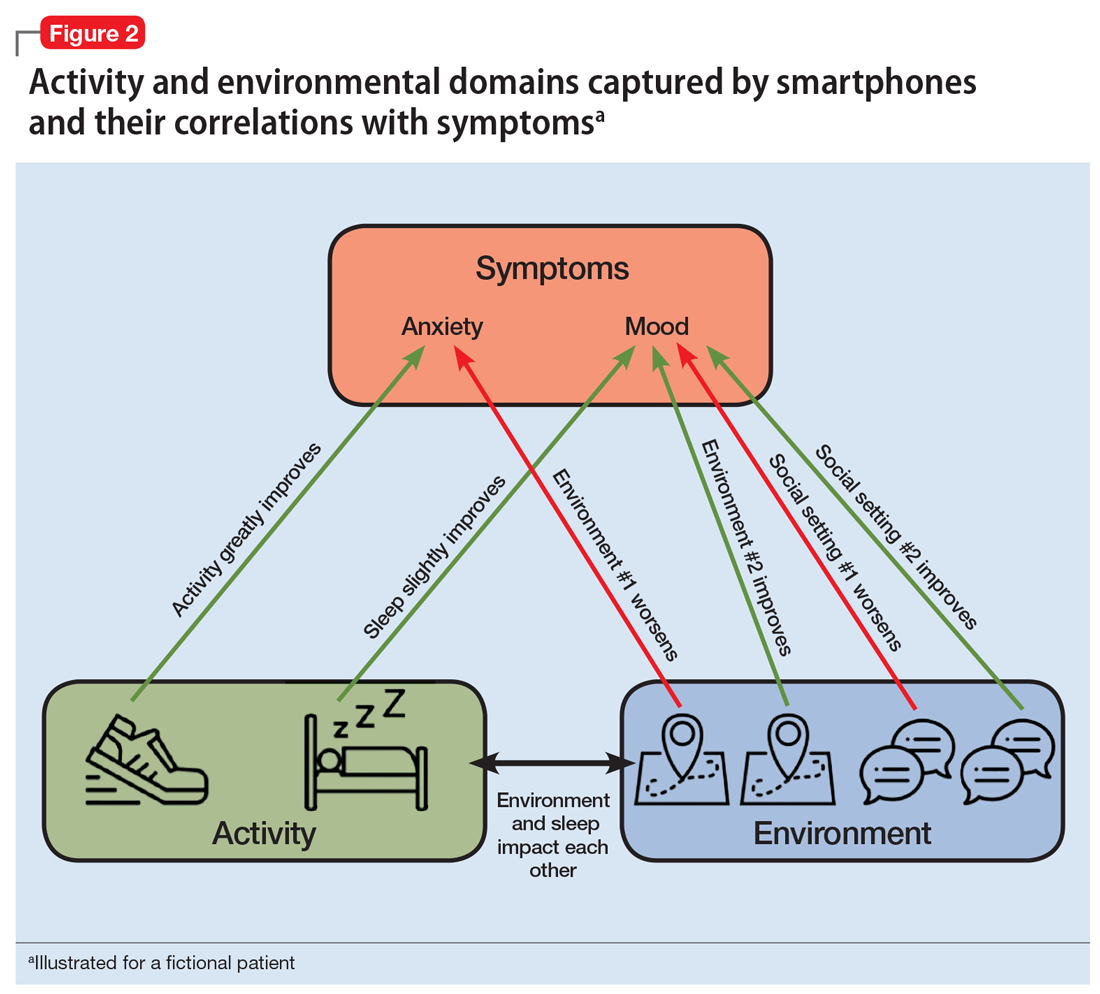
For example, it is important to assess sleep and physical activity for nearly all patients, regardless of diagnosis. However, the patient’s retrospective recollection of sleep, mood, and other clinically relevant metrics is often unreliable, especially when visits are months apart. With smartphones, it is possible to automatically collect metrics for sleep, activity, mood, and much more in real time from the convenience of our patients’ personal devices (Figure 1).
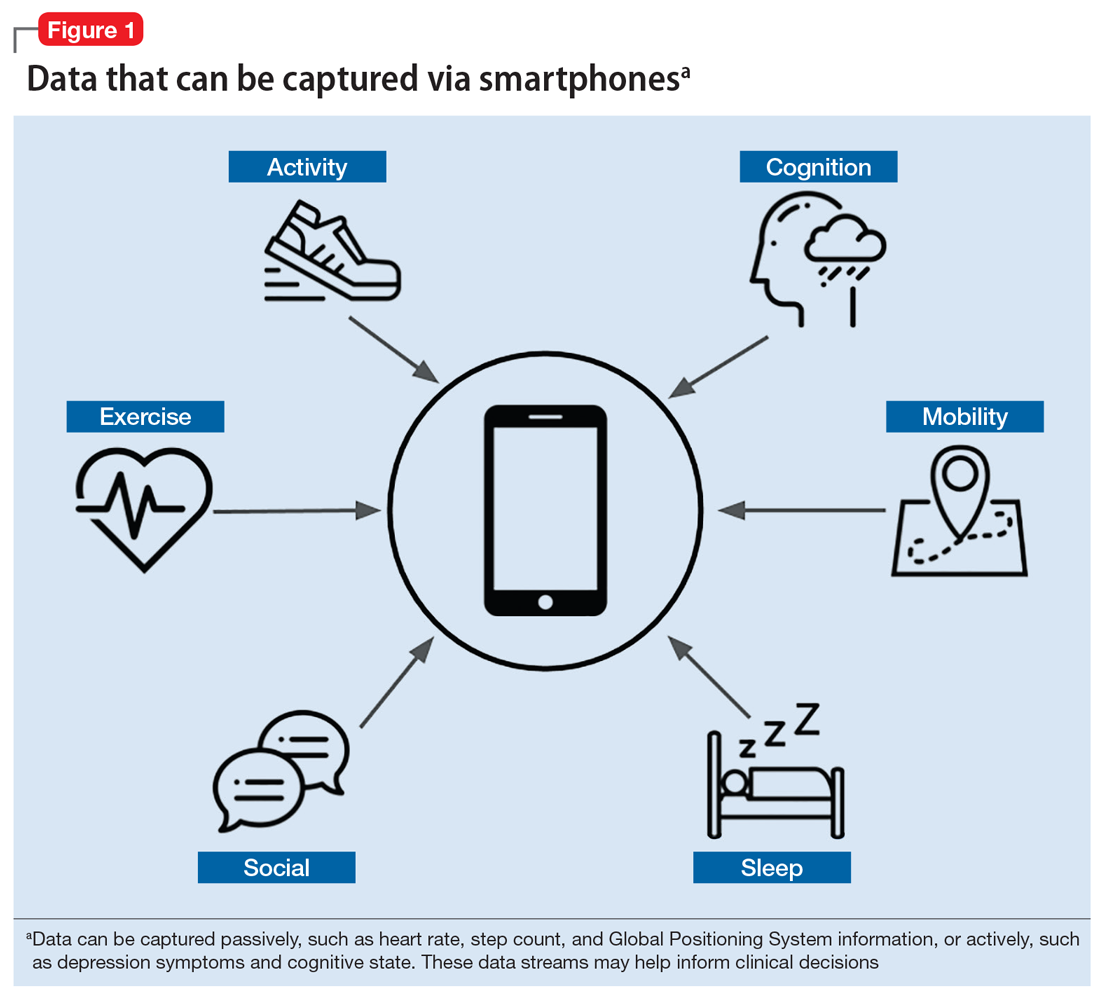
Smartphones can capture a seemingly endless number of data streams, from patient-interfacing active data, such as journal entries, messaging, and games, to data that is captured passively, such as screen time, Global Positioning System information, and step count. Clinicians can work with patients to customize which digital phenotyping data they would like to capture. In one study, researchers worked with 17 patients with schizophrenia by capturing self-reported surveys, anonymized phone call logs, and location data to see if they could predict relapse by observing variations in how patients interact with their smartphones.5 They observed that the rate of behavioral anomalies was 71% higher in the 2 weeks prior to relapse than during other periods. The data captured by the smartphone will depend on the patient and the clinical needs. Some clinicians may only want to collect data on step count and screen time to learn if a patient is overusing his or her smartphone, which might be related to becoming less physically active.
Continue to: One novel data stream...
One novel data stream offered by smartphone digital phenotyping is cognition. While we know that impaired cognition is a core symptom of schizophrenia, and that cognition is affected by depression and anxiety, cognitive symptoms are clinically challenging to quantify. Thus, the cognitive burden of mental illness and the cognitive effects of treatment are often overlooked. However, smartphones are beginning to offer a novel means of capturing a patient’s cognitive state through the use of common clinical tests. For example, the Trail Making Test measures visual attention and executive function by having participants connect dots that differ in number, color, or shape in an ascending pattern.6 By having patients perform this test on a smartphone, clinicians can utilize the touchscreen to capture the user’s discrete actions, such as time to completion and misclicks. These data can be used to build novel measures of cognitive performance that can account for learning bias and other confounding variables.7 While these digital cognitive biomarkers are still in active research, it is likely that they will quickly be developed for broad clinical use.
In addition to the novel data offered by digital phenotyping, another benefit is the low cost and ease of use. Unlike wearable devices such as smartwatches, which can also offer data on steps and sleep, smartphone-based digital phenotyping does not require patients to purchase or use additional devices. Running on patients’ smartphones, digital phenotyping offers the ability to capture rich and continuous health data without added effort or cost. Given that the average person interacts with their phone more than 2,600 times per day,8 smartphones are well suited for capturing large amounts of information that may provide insights into patients’ mental health.
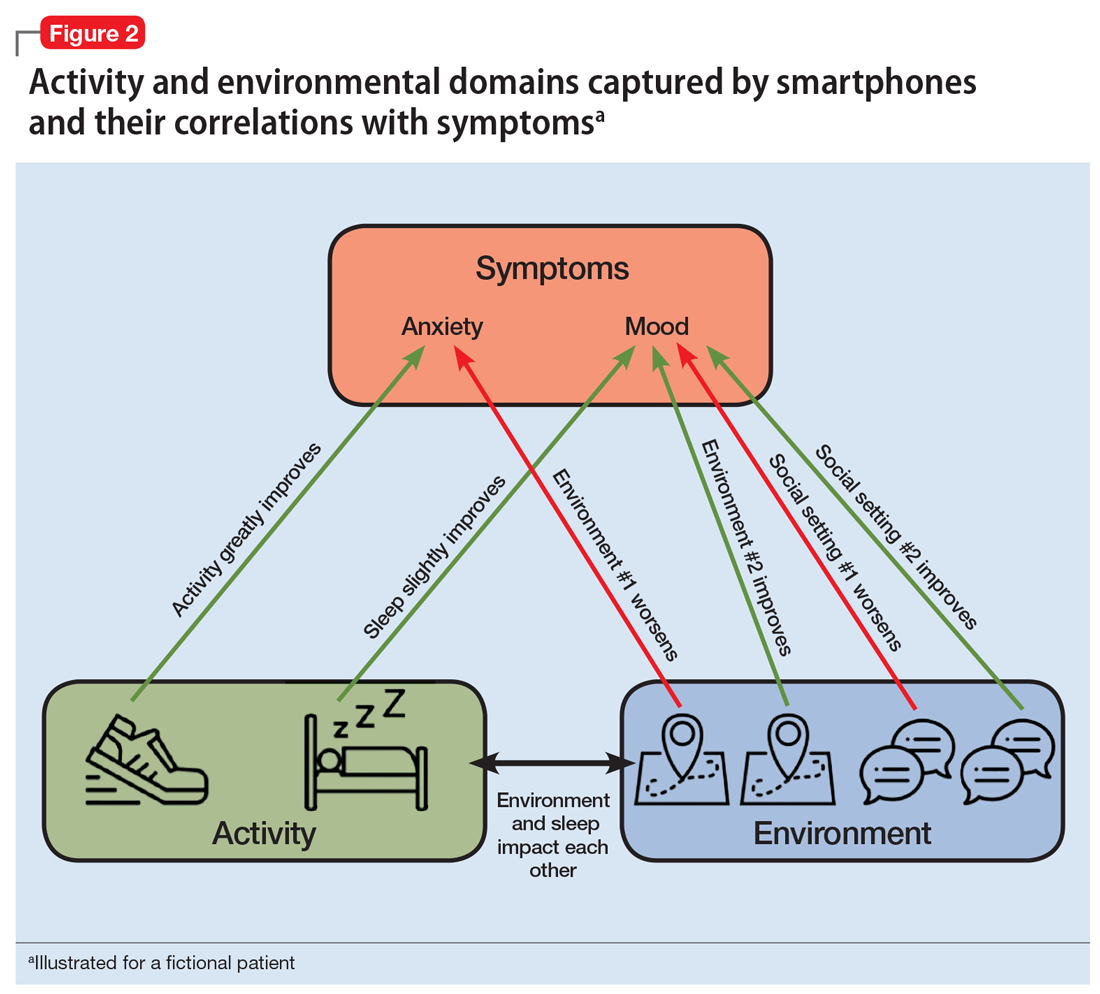
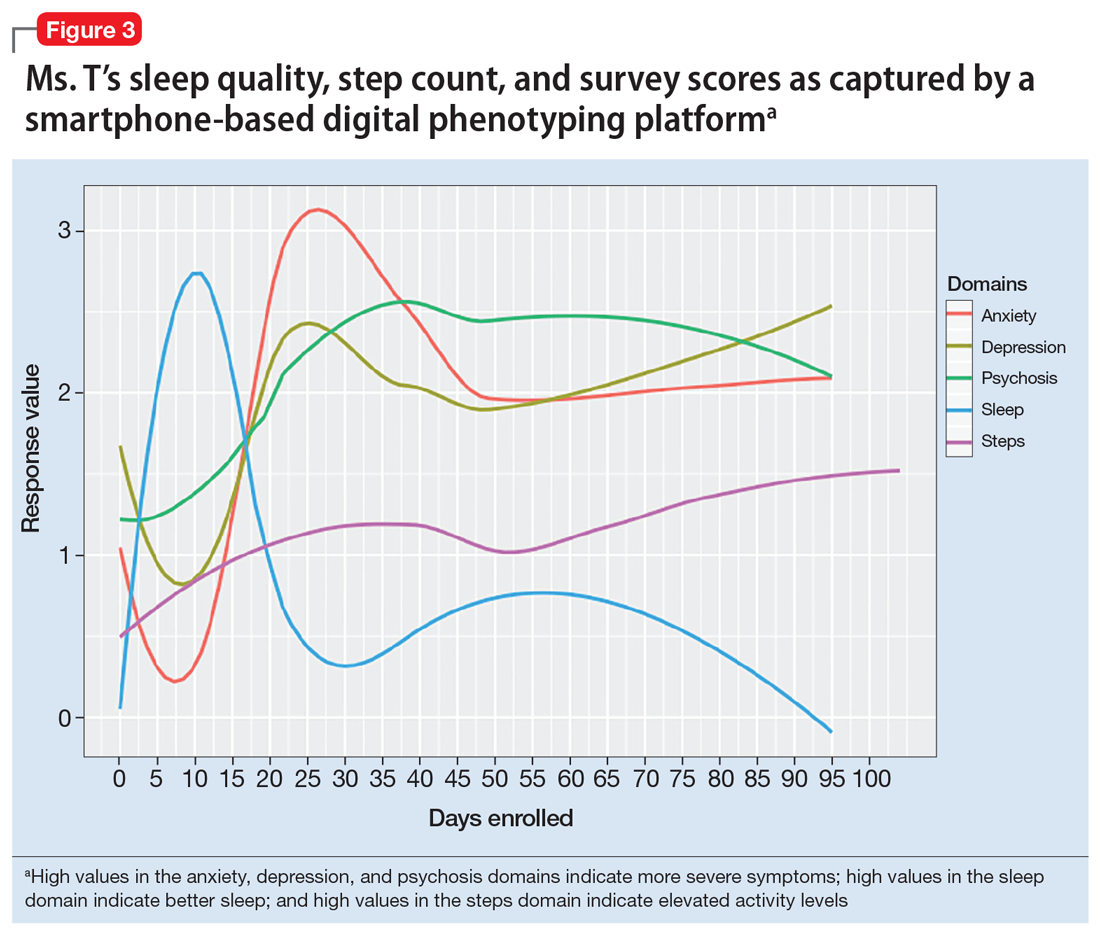
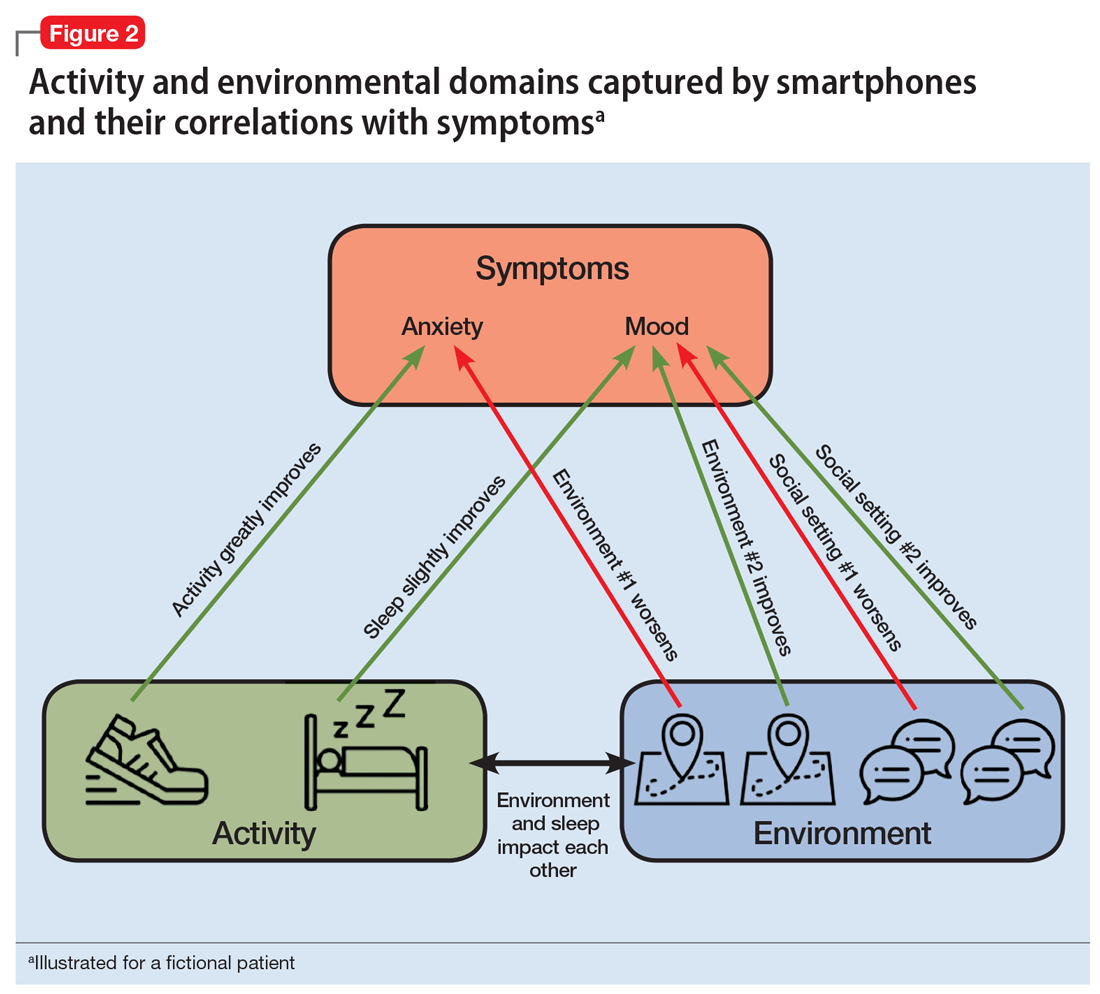
For illnesses such as depression and anxiety, the clinical relevance of digital phenotyping is in the ability to capture symptoms as they occur in context. Figure 2 provides a simplified example of how we can learn that for this fictitious patient, exercise greatly improves anxiety, whereas being in a certain environment worsens it. Other insights about sleep and social settings could also provide further information about the context of the patient’s symptoms. While these correlations alone will not lead to better clinical outcomes, it is easy to imagine how such data could help a patient and clinician start a conversation about making impactful changes.
Continue to: Case report...
Case report: Digital phenotyping
To illustrate how digital phenotyping could be put to clinical use, we created the following case report of a fictional patient who agrees to be monitored via her smartphone.
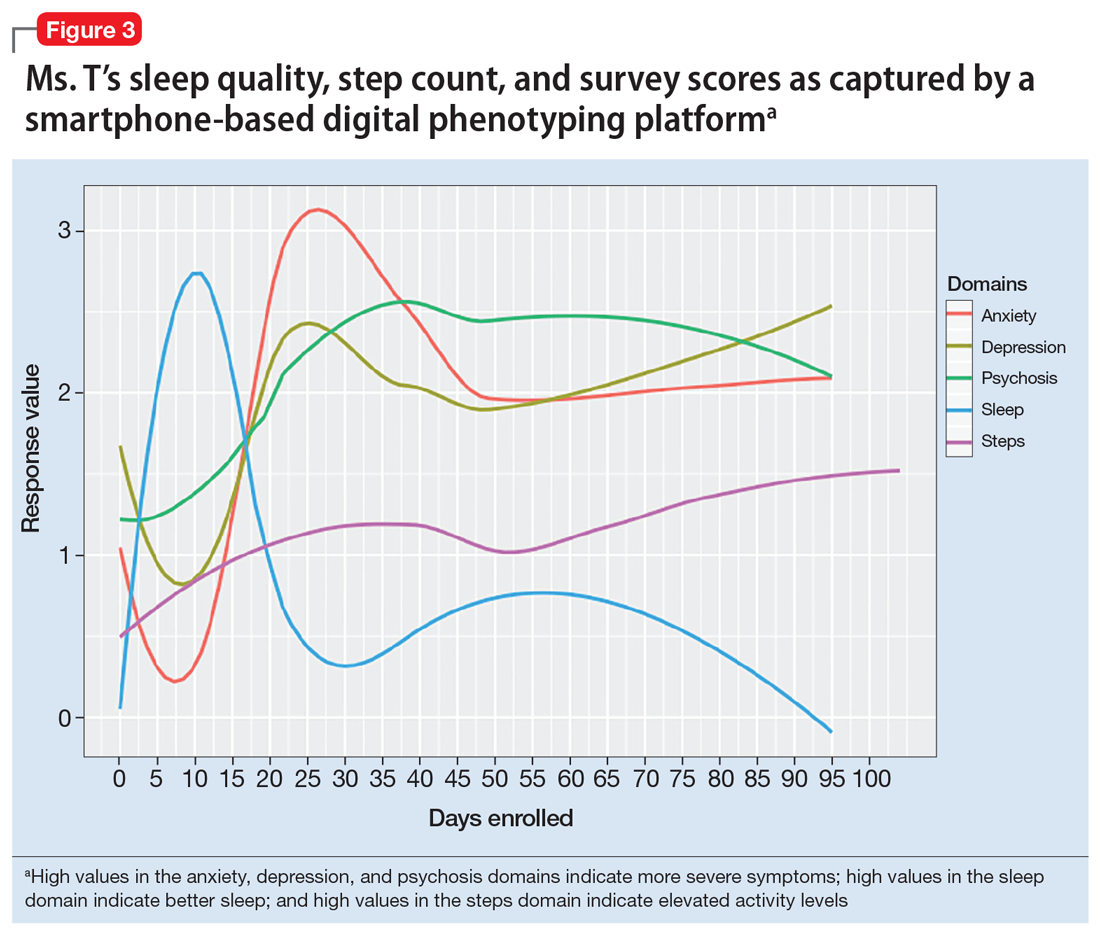
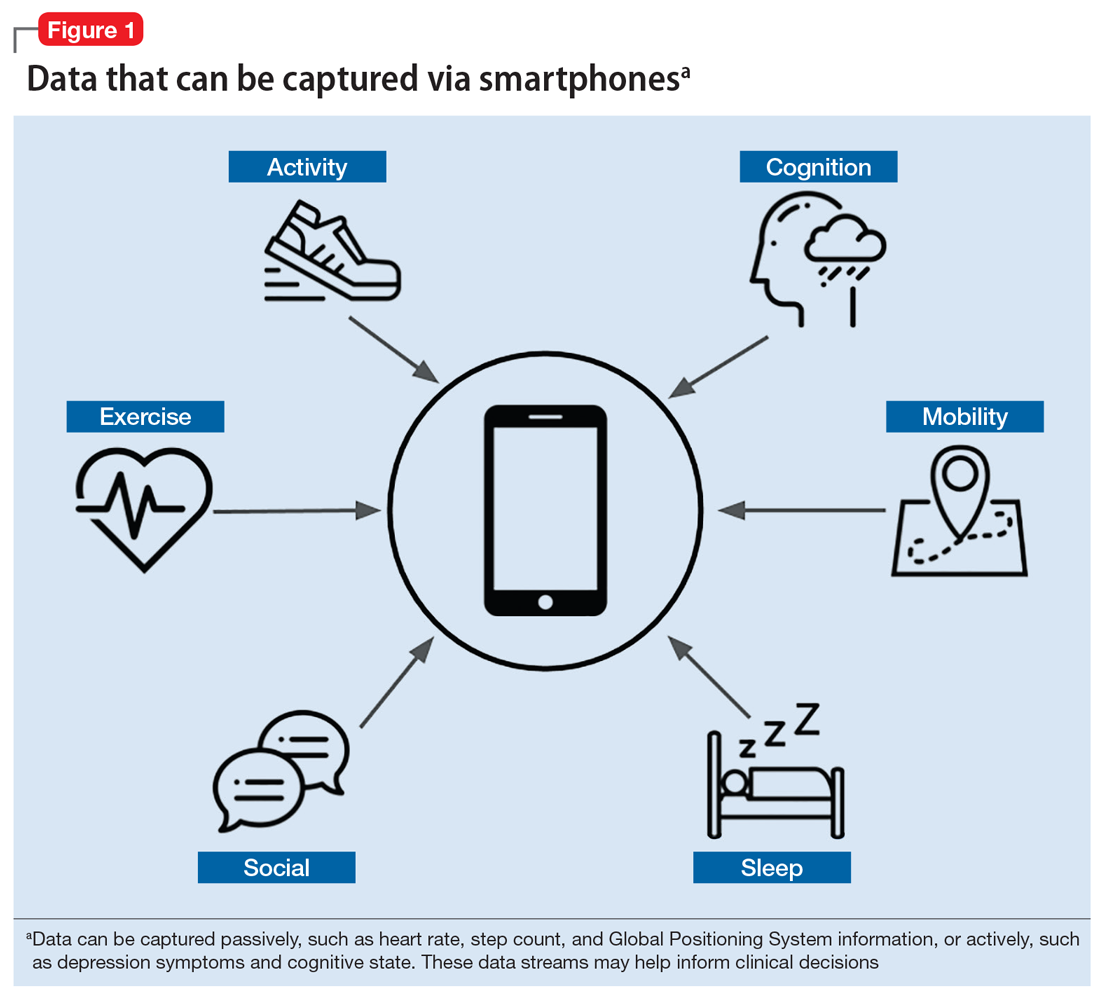
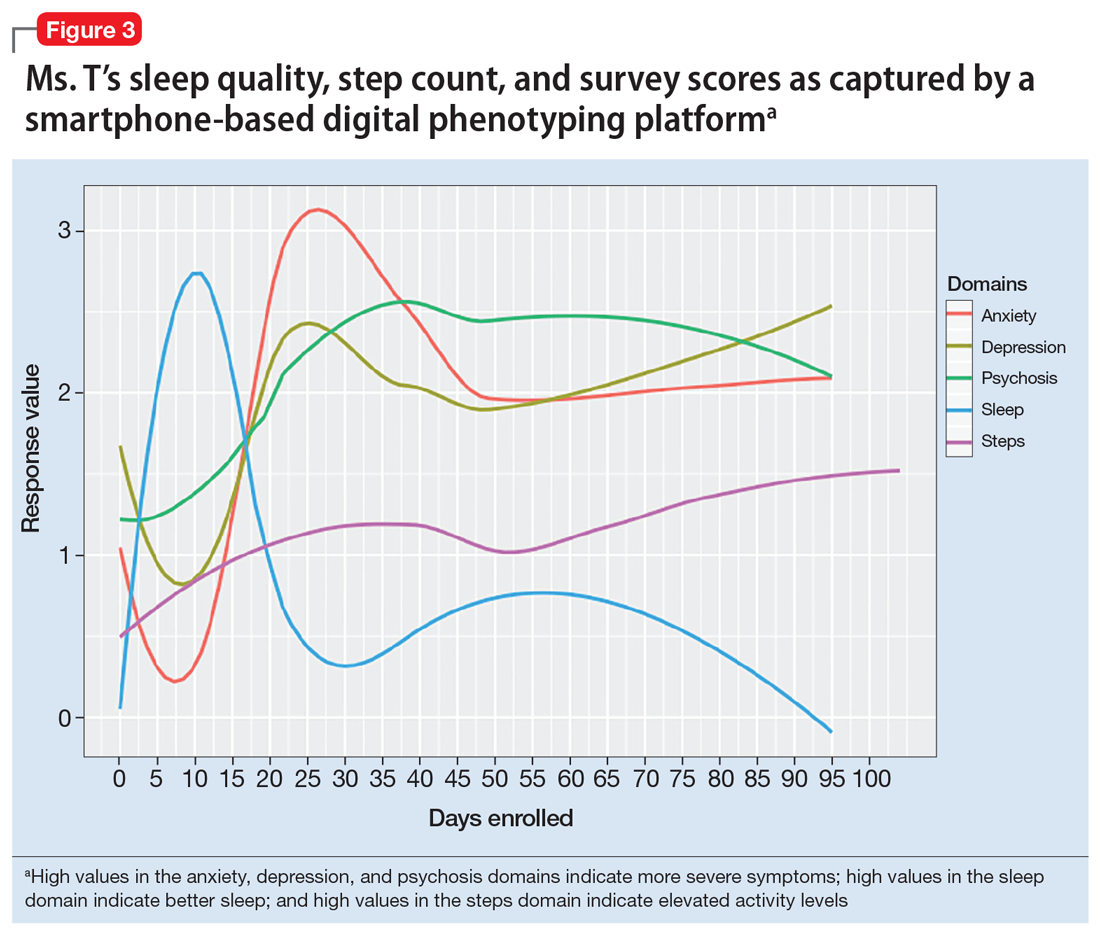
Consider a hypothetical patient we will call Ms. T who is in her mid-20s and has been diagnosed with schizophrenia. On a follow-up visit, she says she has insomnia. She also reports having a recent loss of appetite and higher levels of anxiety. After reviewing her smartphone data (Figure 3), the clinician sees an inversely proportional relationship between her sleep quality and symptoms of anxiety, psychosis, and depression, which suggests that these symptoms might be due to poor sleep. Her step count has been fairly stable, indicating that there is no significant correlation between physical activity and her other symptoms.
Continue to: The clinician shows...
The clinician shows Ms. T the data to help her understand why a trial of cognitive-behavioral therapy for insomnia, or at least improving sleep hygiene, may offer several benefits. The clinician advises her to continue to use the app to help assess her response to these interventions and monitor her progress in real time.
Dilemma: The ethics of continuous observation
The rich data captured by digital phenotyping afford many clinical opportunities, but also raise concerns. Among these are 3 significant ethical implications.
Firstly, the same data that may help a clinician learn about what environments are associated with less anxiety for the patient may also reveal personal details about where that patient has been or with whom they have interacted. In the wrong hands, such personal data could cause harm. And even in the hands of a trusted clinician, a breach in the patient’s privacy begs the question: “Should such information be anyone’s business at all?”
Secondly, many apps that offer digital phenotyping could also store patient data—something that currently pervades social media and causes reasonable discomfort for many people. You might have personally encountered this with social media platforms such as Facebook. When it comes to mobile mental health apps, clinicians should carefully understand the data usage agreement of any digital phenotyping app they wish to use and then share this information with their patients.
Finally, while it is possible to collect the types of data outlined in this article, less is known about how to use it directly in clinical care. Understanding for each patient which data streams are most meaningful and which data streams are noise that should be ignored is an area of ongoing research. A good first step may be to begin with data streams that are known to be clinically relevant and valuable, such as sleep and physical activity.9-11
Continue to: Discussion...
Discussion: Genomic sequencing and digital phenotyping
Although smartphones can gather a wide range of active and passive data, other data streams hold potential for predicting relapse and performing other clinically relevant actions. One data stream that could be of clinical use is genomic sequencing.12 The genotyping of patients provides a wealth of information about the underlying biology, and genomic sequencing has never been cheaper.13
Combining the data gathered via digital phenotyping with that of genotyping could help elucidate the mechanisms by which specific diseases and symptoms occur. This could be very promising to better understand and treat our patients. However, as is the case with genomics, digital phenotyping has important ethical implications. If used in the proper way to benefit our patients, the future for this new method is bright.
1. Statista. Number of smartphone users worldwide from 2014 to 2020 (in billions). https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Accessed April 29, 2019.
2. Thibaut F. Digital applications: the future in psychiatry? Dialogues Clin Neurosci. 2016;18(2):123.
3. Statista. Global market share held by the leading smartphone operating systems in sales to end users from 1st quarter 2009 to 2nd quarter 2018. https://www.statista.com/statistics/266136/global-market-share-held-by-smartphone-operating-systems/. Accessed April 19, 2019.
4. Torous J, Roberts L. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74(5):437-438.
5. Barnett I, Torous J, Staples P, et al. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018;43(8):1660-1666.
6. Arnett JA, Labovitz SS. Effect of physical layout in performance of the Trail Making Test. Psychological Assessment. 1995;7(2):220-221.
7. Brouillette RM, Foil H, Fontenot S, et al. Feasibility, reliability, and validity of a smartphone based application for the assessment of cognitive function in the elderly. PloS One. 2013;8(6):e65925. doi: 10.1371/journal.pone.0065925.
8. Winnick W. Putting a finger on our phone obsession. dscout. https://blog.dscout.com/mobile-touches. Published June 16, 2016. Accessed April 29, 2019.
9. Waite F, Myers E, Harvey AG, et al. Treating sleep problems in patients with schizophrenia. Behav Cogn Psychother. 2016;44(3):273-287.
10. Mcgurk SR, Mueser KT, Xie H, et al. (2015). Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial. Am J Psychiatry. 2015;172(9):852-861.
11. Firth J, Stubbs B, Rosenbaum S, et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2017;43(3):546-556.
12. Manolio TA, Chisholm RL, Ozenberger B, et al. Implementing genomic medicine in the clinic: the future is here. Genet Med. 2013;15(4):258-267.
13. National Human Genome Research Institute. The cost of sequencing a human genome. https://www.genome.gov/27565109/the-cost-of-sequencing-a-human-genome/. Updated July 6, 2016. Accessed April 29, 2019.
In today’s global society, smartphones are ubiquitous, used by >2.5 billion people.1 They provide limitless availability of on-demand services and resources, unparalleled computing power by size, and the ability to connect with anyone in the world.
Digital applications and new mobile technologies can be used to change the nature of the psychiatrist–patient relationship. The future of clinical practice is changing with the help of smartphones and apps. Diagnosis, follow-up, and treatment will never look the same as we come to better understand and apply emerging technologies.2
Both Android and iOS—the 2 largest mobile operating systems by market share3—provide outlets for the dissemination of mobile applications. There are currently >10,000 mental health–related apps available for download.4 One particular use case of mental health–related apps is digital phenotyping.
In this article, we aim to:
- define digital phenotyping
- explore the potential advances in patient care afforded by emerging technology
- discuss the ethical dilemmas and future of mental health apps.
The possibilities of digital phenotyping
Digital phenotyping is capturing a patient’s real-time clinical state using digital technology to better understand the patient’s state outside of the clinic. While digital phenotyping may seem new, the concepts behind it are grounded in good clinical care.
For example, it is important to assess sleep and physical activity for nearly all patients, regardless of diagnosis. However, the patient’s retrospective recollection of sleep, mood, and other clinically relevant metrics is often unreliable, especially when visits are months apart. With smartphones, it is possible to automatically collect metrics for sleep, activity, mood, and much more in real time from the convenience of our patients’ personal devices (Figure 1).
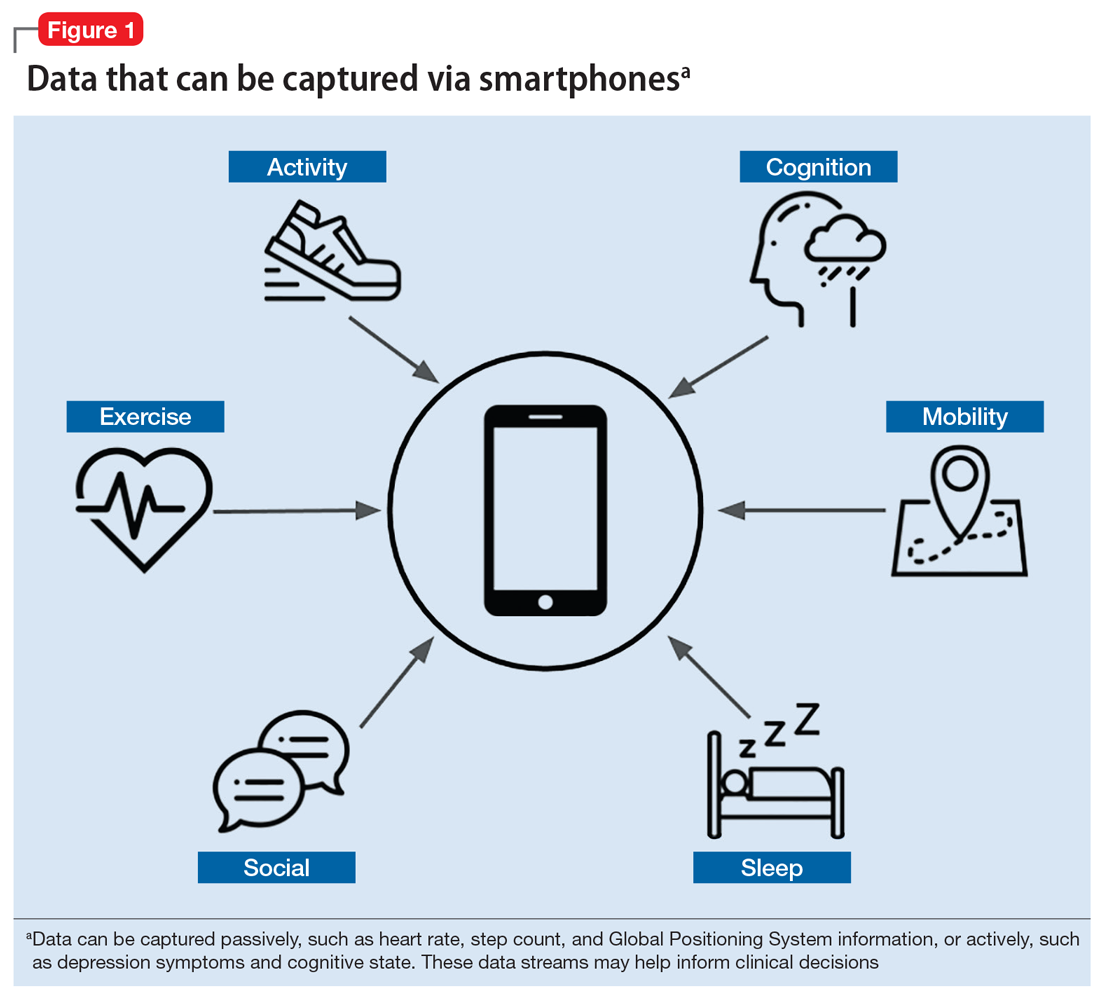
Smartphones can capture a seemingly endless number of data streams, from patient-interfacing active data, such as journal entries, messaging, and games, to data that is captured passively, such as screen time, Global Positioning System information, and step count. Clinicians can work with patients to customize which digital phenotyping data they would like to capture. In one study, researchers worked with 17 patients with schizophrenia by capturing self-reported surveys, anonymized phone call logs, and location data to see if they could predict relapse by observing variations in how patients interact with their smartphones.5 They observed that the rate of behavioral anomalies was 71% higher in the 2 weeks prior to relapse than during other periods. The data captured by the smartphone will depend on the patient and the clinical needs. Some clinicians may only want to collect data on step count and screen time to learn if a patient is overusing his or her smartphone, which might be related to becoming less physically active.
Continue to: One novel data stream...
One novel data stream offered by smartphone digital phenotyping is cognition. While we know that impaired cognition is a core symptom of schizophrenia, and that cognition is affected by depression and anxiety, cognitive symptoms are clinically challenging to quantify. Thus, the cognitive burden of mental illness and the cognitive effects of treatment are often overlooked. However, smartphones are beginning to offer a novel means of capturing a patient’s cognitive state through the use of common clinical tests. For example, the Trail Making Test measures visual attention and executive function by having participants connect dots that differ in number, color, or shape in an ascending pattern.6 By having patients perform this test on a smartphone, clinicians can utilize the touchscreen to capture the user’s discrete actions, such as time to completion and misclicks. These data can be used to build novel measures of cognitive performance that can account for learning bias and other confounding variables.7 While these digital cognitive biomarkers are still in active research, it is likely that they will quickly be developed for broad clinical use.
In addition to the novel data offered by digital phenotyping, another benefit is the low cost and ease of use. Unlike wearable devices such as smartwatches, which can also offer data on steps and sleep, smartphone-based digital phenotyping does not require patients to purchase or use additional devices. Running on patients’ smartphones, digital phenotyping offers the ability to capture rich and continuous health data without added effort or cost. Given that the average person interacts with their phone more than 2,600 times per day,8 smartphones are well suited for capturing large amounts of information that may provide insights into patients’ mental health.
For illnesses such as depression and anxiety, the clinical relevance of digital phenotyping is in the ability to capture symptoms as they occur in context. Figure 2 provides a simplified example of how we can learn that for this fictitious patient, exercise greatly improves anxiety, whereas being in a certain environment worsens it. Other insights about sleep and social settings could also provide further information about the context of the patient’s symptoms. While these correlations alone will not lead to better clinical outcomes, it is easy to imagine how such data could help a patient and clinician start a conversation about making impactful changes.
Continue to: Case report...
Case report: Digital phenotyping
To illustrate how digital phenotyping could be put to clinical use, we created the following case report of a fictional patient who agrees to be monitored via her smartphone.
Consider a hypothetical patient we will call Ms. T who is in her mid-20s and has been diagnosed with schizophrenia. On a follow-up visit, she says she has insomnia. She also reports having a recent loss of appetite and higher levels of anxiety. After reviewing her smartphone data (Figure 3), the clinician sees an inversely proportional relationship between her sleep quality and symptoms of anxiety, psychosis, and depression, which suggests that these symptoms might be due to poor sleep. Her step count has been fairly stable, indicating that there is no significant correlation between physical activity and her other symptoms.
Continue to: The clinician shows...
The clinician shows Ms. T the data to help her understand why a trial of cognitive-behavioral therapy for insomnia, or at least improving sleep hygiene, may offer several benefits. The clinician advises her to continue to use the app to help assess her response to these interventions and monitor her progress in real time.
Dilemma: The ethics of continuous observation
The rich data captured by digital phenotyping afford many clinical opportunities, but also raise concerns. Among these are 3 significant ethical implications.
Firstly, the same data that may help a clinician learn about what environments are associated with less anxiety for the patient may also reveal personal details about where that patient has been or with whom they have interacted. In the wrong hands, such personal data could cause harm. And even in the hands of a trusted clinician, a breach in the patient’s privacy begs the question: “Should such information be anyone’s business at all?”
Secondly, many apps that offer digital phenotyping could also store patient data—something that currently pervades social media and causes reasonable discomfort for many people. You might have personally encountered this with social media platforms such as Facebook. When it comes to mobile mental health apps, clinicians should carefully understand the data usage agreement of any digital phenotyping app they wish to use and then share this information with their patients.
Finally, while it is possible to collect the types of data outlined in this article, less is known about how to use it directly in clinical care. Understanding for each patient which data streams are most meaningful and which data streams are noise that should be ignored is an area of ongoing research. A good first step may be to begin with data streams that are known to be clinically relevant and valuable, such as sleep and physical activity.9-11
Continue to: Discussion...
Discussion: Genomic sequencing and digital phenotyping
Although smartphones can gather a wide range of active and passive data, other data streams hold potential for predicting relapse and performing other clinically relevant actions. One data stream that could be of clinical use is genomic sequencing.12 The genotyping of patients provides a wealth of information about the underlying biology, and genomic sequencing has never been cheaper.13
Combining the data gathered via digital phenotyping with that of genotyping could help elucidate the mechanisms by which specific diseases and symptoms occur. This could be very promising to better understand and treat our patients. However, as is the case with genomics, digital phenotyping has important ethical implications. If used in the proper way to benefit our patients, the future for this new method is bright.
In today’s global society, smartphones are ubiquitous, used by >2.5 billion people.1 They provide limitless availability of on-demand services and resources, unparalleled computing power by size, and the ability to connect with anyone in the world.
Digital applications and new mobile technologies can be used to change the nature of the psychiatrist–patient relationship. The future of clinical practice is changing with the help of smartphones and apps. Diagnosis, follow-up, and treatment will never look the same as we come to better understand and apply emerging technologies.2
Both Android and iOS—the 2 largest mobile operating systems by market share3—provide outlets for the dissemination of mobile applications. There are currently >10,000 mental health–related apps available for download.4 One particular use case of mental health–related apps is digital phenotyping.
In this article, we aim to:
- define digital phenotyping
- explore the potential advances in patient care afforded by emerging technology
- discuss the ethical dilemmas and future of mental health apps.
The possibilities of digital phenotyping
Digital phenotyping is capturing a patient’s real-time clinical state using digital technology to better understand the patient’s state outside of the clinic. While digital phenotyping may seem new, the concepts behind it are grounded in good clinical care.
For example, it is important to assess sleep and physical activity for nearly all patients, regardless of diagnosis. However, the patient’s retrospective recollection of sleep, mood, and other clinically relevant metrics is often unreliable, especially when visits are months apart. With smartphones, it is possible to automatically collect metrics for sleep, activity, mood, and much more in real time from the convenience of our patients’ personal devices (Figure 1).
Smartphones can capture a seemingly endless number of data streams, from patient-interfacing active data, such as journal entries, messaging, and games, to data that is captured passively, such as screen time, Global Positioning System information, and step count. Clinicians can work with patients to customize which digital phenotyping data they would like to capture. In one study, researchers worked with 17 patients with schizophrenia by capturing self-reported surveys, anonymized phone call logs, and location data to see if they could predict relapse by observing variations in how patients interact with their smartphones.5 They observed that the rate of behavioral anomalies was 71% higher in the 2 weeks prior to relapse than during other periods. The data captured by the smartphone will depend on the patient and the clinical needs. Some clinicians may only want to collect data on step count and screen time to learn if a patient is overusing his or her smartphone, which might be related to becoming less physically active.
Continue to: One novel data stream...
One novel data stream offered by smartphone digital phenotyping is cognition. While we know that impaired cognition is a core symptom of schizophrenia, and that cognition is affected by depression and anxiety, cognitive symptoms are clinically challenging to quantify. Thus, the cognitive burden of mental illness and the cognitive effects of treatment are often overlooked. However, smartphones are beginning to offer a novel means of capturing a patient’s cognitive state through the use of common clinical tests. For example, the Trail Making Test measures visual attention and executive function by having participants connect dots that differ in number, color, or shape in an ascending pattern.6 By having patients perform this test on a smartphone, clinicians can utilize the touchscreen to capture the user’s discrete actions, such as time to completion and misclicks. These data can be used to build novel measures of cognitive performance that can account for learning bias and other confounding variables.7 While these digital cognitive biomarkers are still in active research, it is likely that they will quickly be developed for broad clinical use.
In addition to the novel data offered by digital phenotyping, another benefit is the low cost and ease of use. Unlike wearable devices such as smartwatches, which can also offer data on steps and sleep, smartphone-based digital phenotyping does not require patients to purchase or use additional devices. Running on patients’ smartphones, digital phenotyping offers the ability to capture rich and continuous health data without added effort or cost. Given that the average person interacts with their phone more than 2,600 times per day,8 smartphones are well suited for capturing large amounts of information that may provide insights into patients’ mental health.
For illnesses such as depression and anxiety, the clinical relevance of digital phenotyping is in the ability to capture symptoms as they occur in context. Figure 2 provides a simplified example of how we can learn that for this fictitious patient, exercise greatly improves anxiety, whereas being in a certain environment worsens it. Other insights about sleep and social settings could also provide further information about the context of the patient’s symptoms. While these correlations alone will not lead to better clinical outcomes, it is easy to imagine how such data could help a patient and clinician start a conversation about making impactful changes.
Continue to: Case report...
Case report: Digital phenotyping
To illustrate how digital phenotyping could be put to clinical use, we created the following case report of a fictional patient who agrees to be monitored via her smartphone.
Consider a hypothetical patient we will call Ms. T who is in her mid-20s and has been diagnosed with schizophrenia. On a follow-up visit, she says she has insomnia. She also reports having a recent loss of appetite and higher levels of anxiety. After reviewing her smartphone data (Figure 3), the clinician sees an inversely proportional relationship between her sleep quality and symptoms of anxiety, psychosis, and depression, which suggests that these symptoms might be due to poor sleep. Her step count has been fairly stable, indicating that there is no significant correlation between physical activity and her other symptoms.
Continue to: The clinician shows...
The clinician shows Ms. T the data to help her understand why a trial of cognitive-behavioral therapy for insomnia, or at least improving sleep hygiene, may offer several benefits. The clinician advises her to continue to use the app to help assess her response to these interventions and monitor her progress in real time.
Dilemma: The ethics of continuous observation
The rich data captured by digital phenotyping afford many clinical opportunities, but also raise concerns. Among these are 3 significant ethical implications.
Firstly, the same data that may help a clinician learn about what environments are associated with less anxiety for the patient may also reveal personal details about where that patient has been or with whom they have interacted. In the wrong hands, such personal data could cause harm. And even in the hands of a trusted clinician, a breach in the patient’s privacy begs the question: “Should such information be anyone’s business at all?”
Secondly, many apps that offer digital phenotyping could also store patient data—something that currently pervades social media and causes reasonable discomfort for many people. You might have personally encountered this with social media platforms such as Facebook. When it comes to mobile mental health apps, clinicians should carefully understand the data usage agreement of any digital phenotyping app they wish to use and then share this information with their patients.
Finally, while it is possible to collect the types of data outlined in this article, less is known about how to use it directly in clinical care. Understanding for each patient which data streams are most meaningful and which data streams are noise that should be ignored is an area of ongoing research. A good first step may be to begin with data streams that are known to be clinically relevant and valuable, such as sleep and physical activity.9-11
Continue to: Discussion...
Discussion: Genomic sequencing and digital phenotyping
Although smartphones can gather a wide range of active and passive data, other data streams hold potential for predicting relapse and performing other clinically relevant actions. One data stream that could be of clinical use is genomic sequencing.12 The genotyping of patients provides a wealth of information about the underlying biology, and genomic sequencing has never been cheaper.13
Combining the data gathered via digital phenotyping with that of genotyping could help elucidate the mechanisms by which specific diseases and symptoms occur. This could be very promising to better understand and treat our patients. However, as is the case with genomics, digital phenotyping has important ethical implications. If used in the proper way to benefit our patients, the future for this new method is bright.
1. Statista. Number of smartphone users worldwide from 2014 to 2020 (in billions). https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Accessed April 29, 2019.
2. Thibaut F. Digital applications: the future in psychiatry? Dialogues Clin Neurosci. 2016;18(2):123.
3. Statista. Global market share held by the leading smartphone operating systems in sales to end users from 1st quarter 2009 to 2nd quarter 2018. https://www.statista.com/statistics/266136/global-market-share-held-by-smartphone-operating-systems/. Accessed April 19, 2019.
4. Torous J, Roberts L. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74(5):437-438.
5. Barnett I, Torous J, Staples P, et al. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018;43(8):1660-1666.
6. Arnett JA, Labovitz SS. Effect of physical layout in performance of the Trail Making Test. Psychological Assessment. 1995;7(2):220-221.
7. Brouillette RM, Foil H, Fontenot S, et al. Feasibility, reliability, and validity of a smartphone based application for the assessment of cognitive function in the elderly. PloS One. 2013;8(6):e65925. doi: 10.1371/journal.pone.0065925.
8. Winnick W. Putting a finger on our phone obsession. dscout. https://blog.dscout.com/mobile-touches. Published June 16, 2016. Accessed April 29, 2019.
9. Waite F, Myers E, Harvey AG, et al. Treating sleep problems in patients with schizophrenia. Behav Cogn Psychother. 2016;44(3):273-287.
10. Mcgurk SR, Mueser KT, Xie H, et al. (2015). Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial. Am J Psychiatry. 2015;172(9):852-861.
11. Firth J, Stubbs B, Rosenbaum S, et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2017;43(3):546-556.
12. Manolio TA, Chisholm RL, Ozenberger B, et al. Implementing genomic medicine in the clinic: the future is here. Genet Med. 2013;15(4):258-267.
13. National Human Genome Research Institute. The cost of sequencing a human genome. https://www.genome.gov/27565109/the-cost-of-sequencing-a-human-genome/. Updated July 6, 2016. Accessed April 29, 2019.
1. Statista. Number of smartphone users worldwide from 2014 to 2020 (in billions). https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Accessed April 29, 2019.
2. Thibaut F. Digital applications: the future in psychiatry? Dialogues Clin Neurosci. 2016;18(2):123.
3. Statista. Global market share held by the leading smartphone operating systems in sales to end users from 1st quarter 2009 to 2nd quarter 2018. https://www.statista.com/statistics/266136/global-market-share-held-by-smartphone-operating-systems/. Accessed April 19, 2019.
4. Torous J, Roberts L. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74(5):437-438.
5. Barnett I, Torous J, Staples P, et al. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018;43(8):1660-1666.
6. Arnett JA, Labovitz SS. Effect of physical layout in performance of the Trail Making Test. Psychological Assessment. 1995;7(2):220-221.
7. Brouillette RM, Foil H, Fontenot S, et al. Feasibility, reliability, and validity of a smartphone based application for the assessment of cognitive function in the elderly. PloS One. 2013;8(6):e65925. doi: 10.1371/journal.pone.0065925.
8. Winnick W. Putting a finger on our phone obsession. dscout. https://blog.dscout.com/mobile-touches. Published June 16, 2016. Accessed April 29, 2019.
9. Waite F, Myers E, Harvey AG, et al. Treating sleep problems in patients with schizophrenia. Behav Cogn Psychother. 2016;44(3):273-287.
10. Mcgurk SR, Mueser KT, Xie H, et al. (2015). Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial. Am J Psychiatry. 2015;172(9):852-861.
11. Firth J, Stubbs B, Rosenbaum S, et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2017;43(3):546-556.
12. Manolio TA, Chisholm RL, Ozenberger B, et al. Implementing genomic medicine in the clinic: the future is here. Genet Med. 2013;15(4):258-267.
13. National Human Genome Research Institute. The cost of sequencing a human genome. https://www.genome.gov/27565109/the-cost-of-sequencing-a-human-genome/. Updated July 6, 2016. Accessed April 29, 2019.
