User login
Transitions of care from hospital to home are high‐risk times for patients.[1, 2] Increasing complexity of hospital admissions and shorter lengths of stay demand more effective coordination of care between hospitalists and outpatient clinicians.[3, 4, 5] Inaccurate, delayed, or incomplete clinical handoversthat is, transfer of information and professional responsibility and accountability[6]can lead to patient harm, and has been recognized as a key cause of preventable morbidity by the World Health Organization and The Joint Commission.[6, 7, 8] Conversely, when done effectively, transitions can result in improved patient health outcomes, reduced readmission rates, and higher patient and provider satisfaction.3
Previous studies note deficits in communication at discharge and primary care provider (PCP) dissatisfaction with discharge practices.[4, 9, 10, 11, 12, 13] In studies at academic medical centers, there were low rates of direct communication between inpatient and outpatient providers, mainly because of providers' belief that the discharge summary was adequate and the presence of significant barriers to direct communication.[14, 15] However, studies have shown that discharge summaries often omit critical information, and often are not available to PCPs in a timely manner.[10, 11, 12, 16] In response, the Society of Hospital Medicine developed a discharge checklist to aide in standardization of safe discharge practices.[1, 5] Discharge summary templates further attempt to improve documentation of patients' hospital courses. An electronic medical record (EMR) system shared by both inpatient and outpatient clinicians should impart several advantages: (1) automated alerts provide timely notification to PCPs regarding admission and discharge, (2) discharge summaries are available to the PCP as soon as they are written, and (3) all patient information pertaining to the hospitalization is available to the PCP.
Although it is plausible that shared EMRs should facilitate transitions of care by streamlining communication between hospitalists and PCPs, guidelines on format and content of PCP communication at discharge in the era of a shared EMR have yet to be defined. In this study, we sought to understand current discharge communication practices and PCP satisfaction within a shared EMR at our institution, and to identify key areas in which communication can be improved.
METHODS
Participants and Setting
We surveyed all resident and attending PCPs (n=124) working in the Division of General Internal Medicine (DGIM) Outpatient Practice at the University of California, San Francisco (UCSF). In June 2012, the outpatient and inpatient practices of UCSF transitioned from having separate medical record systems to a shared EMR (Epic Systems Corp., Verona, WI) where all informationboth inpatient and outpatientis accessible among healthcare professionals. The EMR provides automated notifications of admission and discharge to PCPs, allows for review of inpatient notes, labs, and studies, and immediate access to templated discharge summaries (see Supporting Information, Appendix 1, in the online version of this article). The EMR also enables secure communication between clinicians. At our institution, over 90% of discharge summaries are completed within 24 hours of discharge.[17]
Study Design and Analysis
We developed a survey about the discharge communication practices of inpatient medicine patients based on a previously described survey in the literature (see Supporting Information, Appendix 2, in the online version of this article).[9] The anonymous, 17‐question survey was electronically distributed to resident and attending PCPs at the DGIM practice. The survey was designed to determine: (1) overall PCP satisfaction with current communication practices from the inpatient team at patient discharge, (2) perceived adequacy of automatic discharge notifications, and (3) perception of the types of patients and hospitalizations requiring additional high‐touch communication at discharge.
We analyzed results of our survey using descriptive statistics. Differences in resident and attending responses were analyzed by 2tests.
RESULTS
Seventy‐five of 124 (60%) clinicians (46% residents, 54% attendings) completed the survey. Thirty‐nine (52%) PCPs were satisfied or very satisfied with communication at patient discharge. Although most reported receiving automated discharge notifications (71%), only 39% felt that the notifications plus the discharge summaries were adequate communication for safe transition of care from hospital to community. Fifty‐one percent desired direct contact beyond a discharge summary. There were no differences in preferences on discharge communication between resident and attending PCPs (P>0.05).
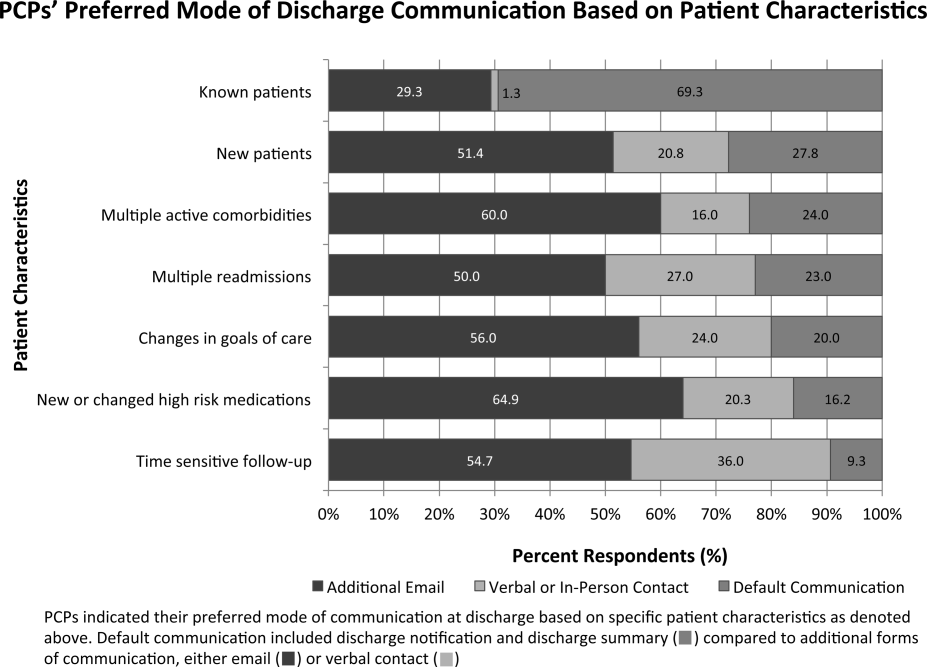
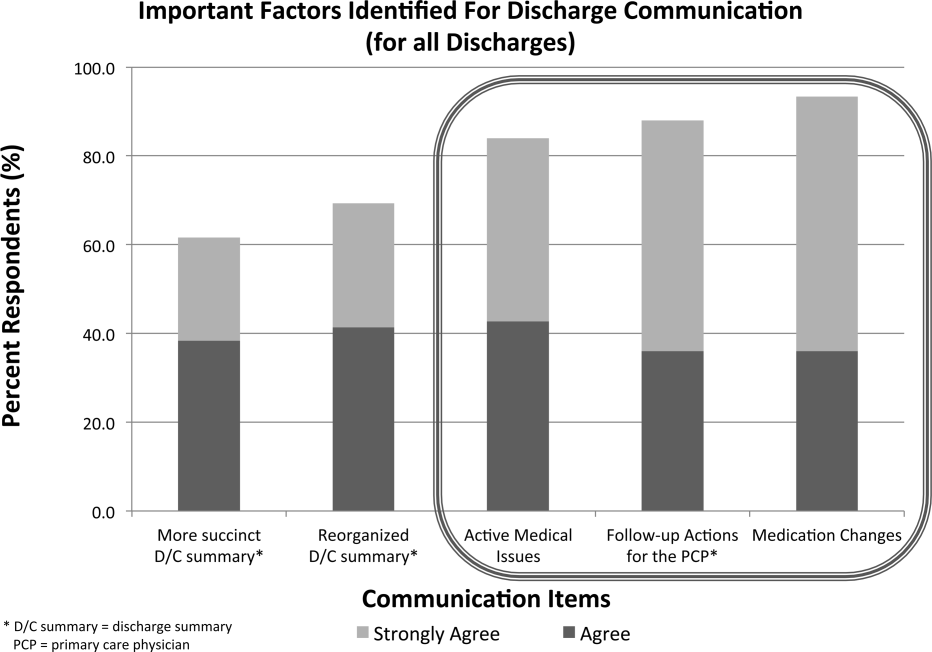
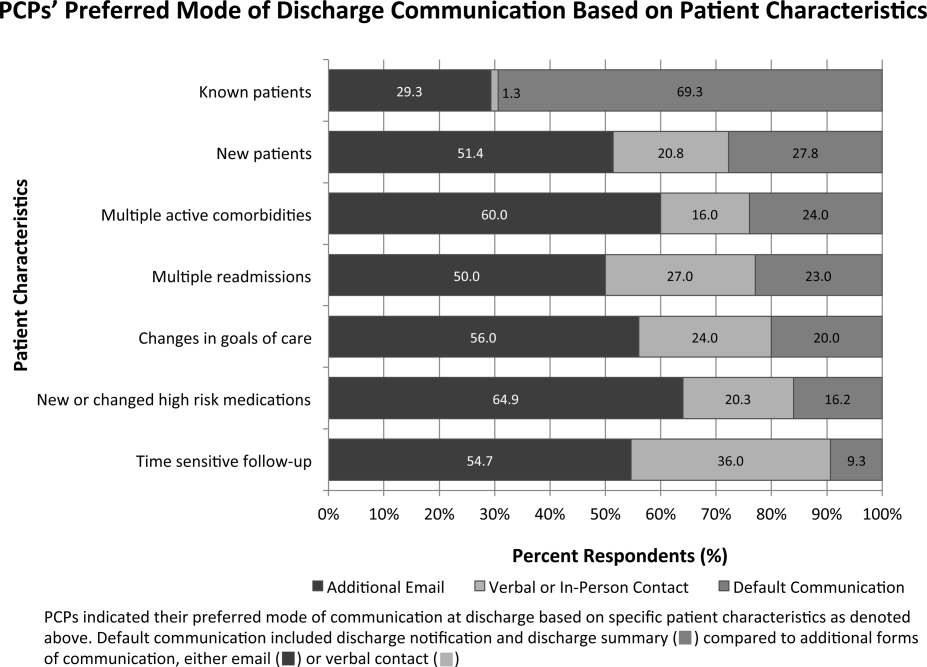
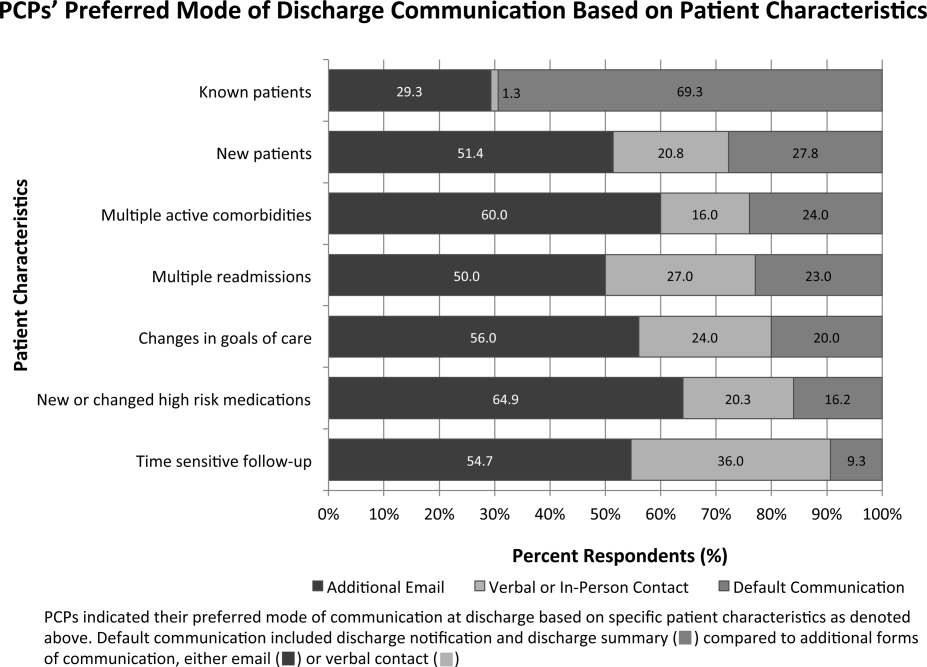
Over three‐fourths of PCPs surveyed preferred that for patients with complex hospitalizations (multiple readmissions, multiple active comorbidities, goals of care changes, high‐risk medication changes, time‐sensitive follow‐up needs), an additional e‐mail or verbal communication was needed to augment the information in the discharge summary (Figure 1). Only 31% reported receiving such communication.
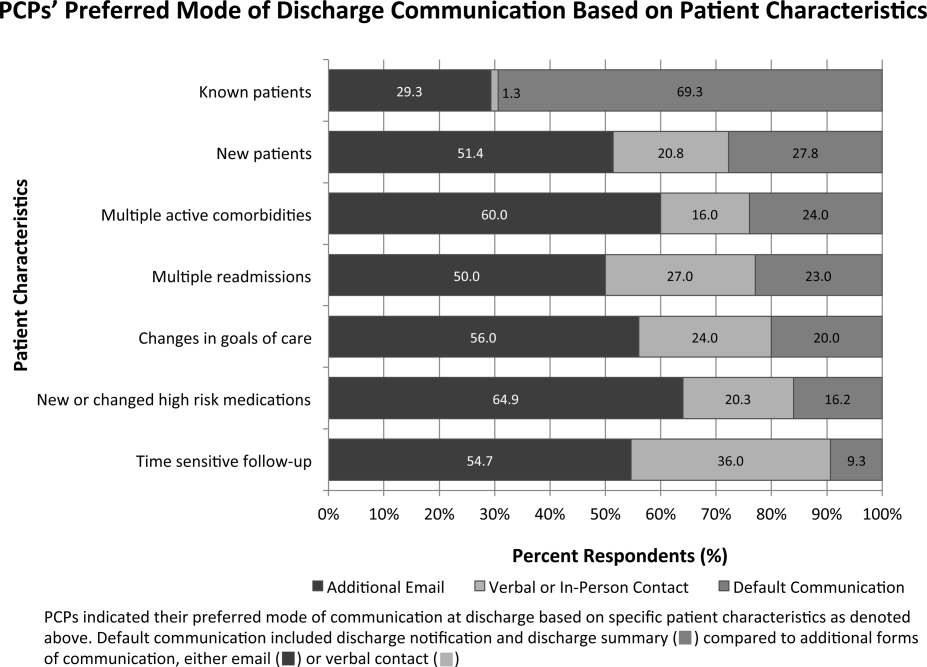
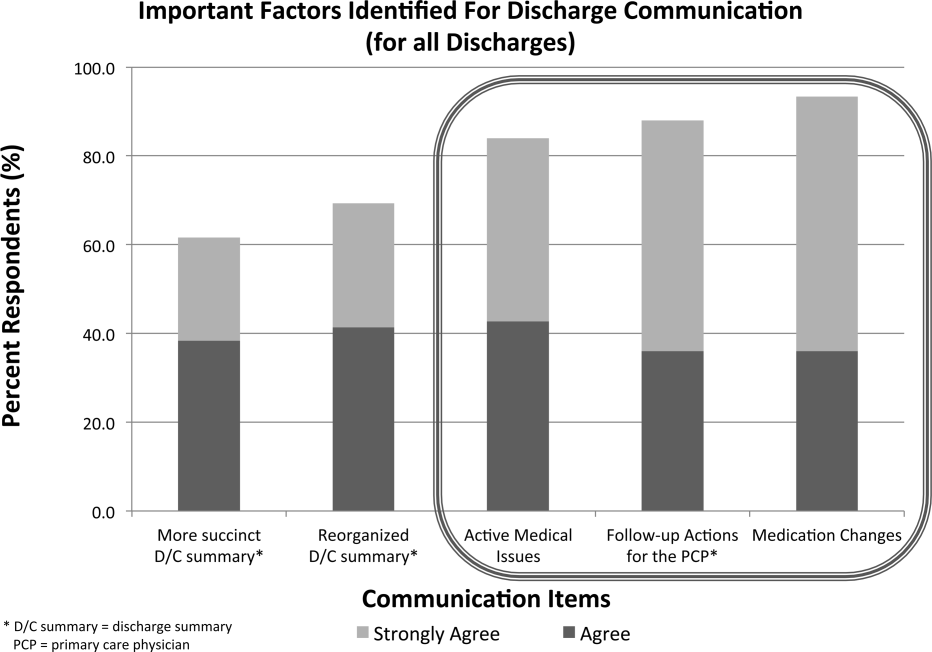
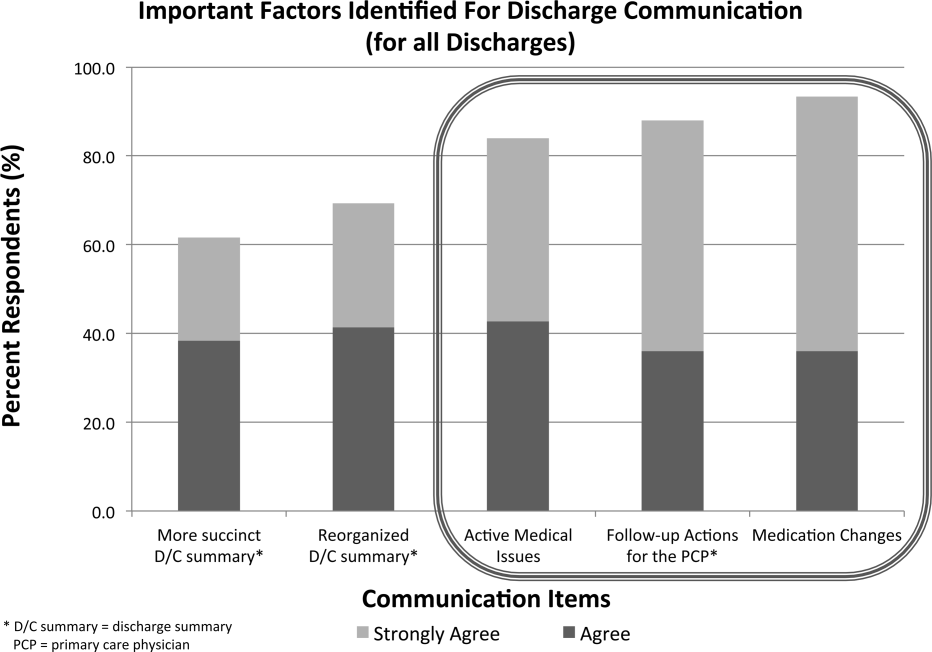
When asked about important items to communicate for safer transitions of care, PCPs reported finding the following elements most critical: (1) medication changes (93%), (2) follow‐up actions for the PCP (88%), and (3) active medical issues (84%) (Figure 2).
CONCLUSIONS
In the era of shared EMRs, real‐time access to medication lists, pending test results, and discharge summaries should facilitate care transitions at discharge.[18, 19] We conducted a study to determine PCP perceptions of discharge communication after implementation of a shared EMR. We found that although PCPs largely acknowledged timely receipt of automated discharge notifications and discharge summaries, the majority of PCPs felt that most discharges required additional communication to ensure safe transition of care.
Guidelines for discharge communication emphasize timely communication with the PCP, primarily through discharge summaries containing key safety elements.[1, 5, 10] At our institution, we have improved the timeliness and quality of discharge summaries according to guideline recommendations,[17] and conducted quality improvement projects to improve rates of direct communication with PCPs.[9] In addition, the shared EMR provides automated notifications to PCPs when their patients are discharged. Despite these interventions, our survey shows that PCP satisfaction with discharge communication is still inadequate. PCPs desired direct communication that highlights active medical issues, medication changes, and specific follow‐up actions. Although all of these topics are included in our discharge summary template (see Supporting Information, Appendix 1, in the online version of this article), it is possible that the templated discharge summaries lend themselves to longer documents and information overload, as prior studies have documented the desire for more succinct discharge summaries.[18] We also found that automated notifications of discharge were less reliable and useful for PCPs than anticipated. There were several reasons for this: (1) discharge summaries sometimes were sent to PCPs uncoupled from the discharge notification, (2) there were errors with the generation and delivery of automated messages at the rollout of the new system, and (3) PCPs received many other automated system messages, meaning that discharge notifications could be easily missed. These factors all likely contribute to PCPs' desire for high‐touch communication that highlights the most salient aspects of each patient's hospitalization. It is also possible that automated notifications and depersonalized discharge summaries create distance and a less‐collaborative feeling to patient care. PCPs want more direct communication, and desire to play a more active role in inpatient management, especially for complex hospitalizations.[18] This emphasis on direct communication resonates with previous studies conducted before shared EMRs existed.[9, 12, 19]
Our study had several limitations. First, because this is a single‐institution study at a tertiary care academic setting, the results may not be generalizable to all shared EMR settings, and may not reflect all the challenges of communication with the wider community of outpatient providers. One can postulate that inpatient and outpatient clinician relationships are stronger in an academic setting than in other more disparate environments, where direct communication may happen even less frequently. Of note, our low rates of direct communication are consistent with other single‐ and multi‐institution studies, suggesting that our findings are generalizable.[14, 15] Second, our survey is limited in its ability to distinguish those patients who require high‐touch communication and those who do not. Third, although we have used the survey to assess PCP satisfaction in previous studies, it is not a validated instrument, and therefore we cannot reliably say that increasing direct PCP communication would increase their satisfaction around discharge. Last, the PCP‐reported rates of discharge communication are subjective and may be influenced by recall bias. We did not have a systematic way to confirm the actual rates of communication at discharge, which could have occurred through EMR messages, e‐mails, phone calls, or pages.
Although a shared EMR allows for real‐time access to patient data, it does not eliminate PCPs' desire for direct 2‐way dialogue at discharge, especially for complex patients. Key information desired in such communication should include active medical issues, medication changes, and follow‐up needs, which is consistent with prior studies. Standardizing this direct communication process in an efficient way can be challenging. Further elucidation of PCP preferences around which patients necessitate higher‐level communication and preferred methods and timing of communication is needed, as well as determining the most efficient and effective method for hospitalists to provide such communication. Improving communication between hospitalists and PCPs requires not just the presence of a shared EMR, but additional, systematic efforts to engage both inpatient and outpatient clinicians in collaborative care.
Disclosure
Nothing to report.
- , , , et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444–449.
- , , , , The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417–428.
- , , , , “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354−660.
- , , , , Improving measurement in clinical handover. Qual Saf Health Care. 2009;18:272–277.
- World Health Organization. Patient safety: action on patient safety: high 5s. 2007. Available at: http://www.who.int/patientsafety/implementation/solutions/high5s/en/index.html. Accessed January 28, 2015.
- The Joint Commission Center for Transforming Healthcare. Hand‐off communications. 2012. Available at: http://www.centerfortransforminghealthcare.org/projects/detail.aspx?Project=1. Accessed January 28, 2015.
- , , , et al. The effect of a resident‐led quality improvement project on improving communication between hospital‐based and outpatient physicians. Am J Med Qual. 2013;28(6):472–479.
- , , , Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323.
- , , , , , Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21:i97–i105.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA. 2013;173(8):624–629.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , The Housestaff Incentive Program: improving the timeliness and quality of discharge summaries by engaging residents in quality improvement. BMJ Qual Saf. 2013;22(9):768–774.
- , , , et al. A Failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations [published online ahead of print October 15, 2014]. J Gen Intern Med. doi: 10.1007/s11606-014-3056-x.
- , , , et al. Pediatric hospitalists and primary care providers: a communication needs assessment. J Hosp Med. 2009;4(3):187–193.
Transitions of care from hospital to home are high‐risk times for patients.[1, 2] Increasing complexity of hospital admissions and shorter lengths of stay demand more effective coordination of care between hospitalists and outpatient clinicians.[3, 4, 5] Inaccurate, delayed, or incomplete clinical handoversthat is, transfer of information and professional responsibility and accountability[6]can lead to patient harm, and has been recognized as a key cause of preventable morbidity by the World Health Organization and The Joint Commission.[6, 7, 8] Conversely, when done effectively, transitions can result in improved patient health outcomes, reduced readmission rates, and higher patient and provider satisfaction.3
Previous studies note deficits in communication at discharge and primary care provider (PCP) dissatisfaction with discharge practices.[4, 9, 10, 11, 12, 13] In studies at academic medical centers, there were low rates of direct communication between inpatient and outpatient providers, mainly because of providers' belief that the discharge summary was adequate and the presence of significant barriers to direct communication.[14, 15] However, studies have shown that discharge summaries often omit critical information, and often are not available to PCPs in a timely manner.[10, 11, 12, 16] In response, the Society of Hospital Medicine developed a discharge checklist to aide in standardization of safe discharge practices.[1, 5] Discharge summary templates further attempt to improve documentation of patients' hospital courses. An electronic medical record (EMR) system shared by both inpatient and outpatient clinicians should impart several advantages: (1) automated alerts provide timely notification to PCPs regarding admission and discharge, (2) discharge summaries are available to the PCP as soon as they are written, and (3) all patient information pertaining to the hospitalization is available to the PCP.
Although it is plausible that shared EMRs should facilitate transitions of care by streamlining communication between hospitalists and PCPs, guidelines on format and content of PCP communication at discharge in the era of a shared EMR have yet to be defined. In this study, we sought to understand current discharge communication practices and PCP satisfaction within a shared EMR at our institution, and to identify key areas in which communication can be improved.
METHODS
Participants and Setting
We surveyed all resident and attending PCPs (n=124) working in the Division of General Internal Medicine (DGIM) Outpatient Practice at the University of California, San Francisco (UCSF). In June 2012, the outpatient and inpatient practices of UCSF transitioned from having separate medical record systems to a shared EMR (Epic Systems Corp., Verona, WI) where all informationboth inpatient and outpatientis accessible among healthcare professionals. The EMR provides automated notifications of admission and discharge to PCPs, allows for review of inpatient notes, labs, and studies, and immediate access to templated discharge summaries (see Supporting Information, Appendix 1, in the online version of this article). The EMR also enables secure communication between clinicians. At our institution, over 90% of discharge summaries are completed within 24 hours of discharge.[17]
Study Design and Analysis
We developed a survey about the discharge communication practices of inpatient medicine patients based on a previously described survey in the literature (see Supporting Information, Appendix 2, in the online version of this article).[9] The anonymous, 17‐question survey was electronically distributed to resident and attending PCPs at the DGIM practice. The survey was designed to determine: (1) overall PCP satisfaction with current communication practices from the inpatient team at patient discharge, (2) perceived adequacy of automatic discharge notifications, and (3) perception of the types of patients and hospitalizations requiring additional high‐touch communication at discharge.
We analyzed results of our survey using descriptive statistics. Differences in resident and attending responses were analyzed by 2tests.
RESULTS
Seventy‐five of 124 (60%) clinicians (46% residents, 54% attendings) completed the survey. Thirty‐nine (52%) PCPs were satisfied or very satisfied with communication at patient discharge. Although most reported receiving automated discharge notifications (71%), only 39% felt that the notifications plus the discharge summaries were adequate communication for safe transition of care from hospital to community. Fifty‐one percent desired direct contact beyond a discharge summary. There were no differences in preferences on discharge communication between resident and attending PCPs (P>0.05).
Over three‐fourths of PCPs surveyed preferred that for patients with complex hospitalizations (multiple readmissions, multiple active comorbidities, goals of care changes, high‐risk medication changes, time‐sensitive follow‐up needs), an additional e‐mail or verbal communication was needed to augment the information in the discharge summary (Figure 1). Only 31% reported receiving such communication.
When asked about important items to communicate for safer transitions of care, PCPs reported finding the following elements most critical: (1) medication changes (93%), (2) follow‐up actions for the PCP (88%), and (3) active medical issues (84%) (Figure 2).
CONCLUSIONS
In the era of shared EMRs, real‐time access to medication lists, pending test results, and discharge summaries should facilitate care transitions at discharge.[18, 19] We conducted a study to determine PCP perceptions of discharge communication after implementation of a shared EMR. We found that although PCPs largely acknowledged timely receipt of automated discharge notifications and discharge summaries, the majority of PCPs felt that most discharges required additional communication to ensure safe transition of care.
Guidelines for discharge communication emphasize timely communication with the PCP, primarily through discharge summaries containing key safety elements.[1, 5, 10] At our institution, we have improved the timeliness and quality of discharge summaries according to guideline recommendations,[17] and conducted quality improvement projects to improve rates of direct communication with PCPs.[9] In addition, the shared EMR provides automated notifications to PCPs when their patients are discharged. Despite these interventions, our survey shows that PCP satisfaction with discharge communication is still inadequate. PCPs desired direct communication that highlights active medical issues, medication changes, and specific follow‐up actions. Although all of these topics are included in our discharge summary template (see Supporting Information, Appendix 1, in the online version of this article), it is possible that the templated discharge summaries lend themselves to longer documents and information overload, as prior studies have documented the desire for more succinct discharge summaries.[18] We also found that automated notifications of discharge were less reliable and useful for PCPs than anticipated. There were several reasons for this: (1) discharge summaries sometimes were sent to PCPs uncoupled from the discharge notification, (2) there were errors with the generation and delivery of automated messages at the rollout of the new system, and (3) PCPs received many other automated system messages, meaning that discharge notifications could be easily missed. These factors all likely contribute to PCPs' desire for high‐touch communication that highlights the most salient aspects of each patient's hospitalization. It is also possible that automated notifications and depersonalized discharge summaries create distance and a less‐collaborative feeling to patient care. PCPs want more direct communication, and desire to play a more active role in inpatient management, especially for complex hospitalizations.[18] This emphasis on direct communication resonates with previous studies conducted before shared EMRs existed.[9, 12, 19]
Our study had several limitations. First, because this is a single‐institution study at a tertiary care academic setting, the results may not be generalizable to all shared EMR settings, and may not reflect all the challenges of communication with the wider community of outpatient providers. One can postulate that inpatient and outpatient clinician relationships are stronger in an academic setting than in other more disparate environments, where direct communication may happen even less frequently. Of note, our low rates of direct communication are consistent with other single‐ and multi‐institution studies, suggesting that our findings are generalizable.[14, 15] Second, our survey is limited in its ability to distinguish those patients who require high‐touch communication and those who do not. Third, although we have used the survey to assess PCP satisfaction in previous studies, it is not a validated instrument, and therefore we cannot reliably say that increasing direct PCP communication would increase their satisfaction around discharge. Last, the PCP‐reported rates of discharge communication are subjective and may be influenced by recall bias. We did not have a systematic way to confirm the actual rates of communication at discharge, which could have occurred through EMR messages, e‐mails, phone calls, or pages.
Although a shared EMR allows for real‐time access to patient data, it does not eliminate PCPs' desire for direct 2‐way dialogue at discharge, especially for complex patients. Key information desired in such communication should include active medical issues, medication changes, and follow‐up needs, which is consistent with prior studies. Standardizing this direct communication process in an efficient way can be challenging. Further elucidation of PCP preferences around which patients necessitate higher‐level communication and preferred methods and timing of communication is needed, as well as determining the most efficient and effective method for hospitalists to provide such communication. Improving communication between hospitalists and PCPs requires not just the presence of a shared EMR, but additional, systematic efforts to engage both inpatient and outpatient clinicians in collaborative care.
Disclosure
Nothing to report.
Transitions of care from hospital to home are high‐risk times for patients.[1, 2] Increasing complexity of hospital admissions and shorter lengths of stay demand more effective coordination of care between hospitalists and outpatient clinicians.[3, 4, 5] Inaccurate, delayed, or incomplete clinical handoversthat is, transfer of information and professional responsibility and accountability[6]can lead to patient harm, and has been recognized as a key cause of preventable morbidity by the World Health Organization and The Joint Commission.[6, 7, 8] Conversely, when done effectively, transitions can result in improved patient health outcomes, reduced readmission rates, and higher patient and provider satisfaction.3
Previous studies note deficits in communication at discharge and primary care provider (PCP) dissatisfaction with discharge practices.[4, 9, 10, 11, 12, 13] In studies at academic medical centers, there were low rates of direct communication between inpatient and outpatient providers, mainly because of providers' belief that the discharge summary was adequate and the presence of significant barriers to direct communication.[14, 15] However, studies have shown that discharge summaries often omit critical information, and often are not available to PCPs in a timely manner.[10, 11, 12, 16] In response, the Society of Hospital Medicine developed a discharge checklist to aide in standardization of safe discharge practices.[1, 5] Discharge summary templates further attempt to improve documentation of patients' hospital courses. An electronic medical record (EMR) system shared by both inpatient and outpatient clinicians should impart several advantages: (1) automated alerts provide timely notification to PCPs regarding admission and discharge, (2) discharge summaries are available to the PCP as soon as they are written, and (3) all patient information pertaining to the hospitalization is available to the PCP.
Although it is plausible that shared EMRs should facilitate transitions of care by streamlining communication between hospitalists and PCPs, guidelines on format and content of PCP communication at discharge in the era of a shared EMR have yet to be defined. In this study, we sought to understand current discharge communication practices and PCP satisfaction within a shared EMR at our institution, and to identify key areas in which communication can be improved.
METHODS
Participants and Setting
We surveyed all resident and attending PCPs (n=124) working in the Division of General Internal Medicine (DGIM) Outpatient Practice at the University of California, San Francisco (UCSF). In June 2012, the outpatient and inpatient practices of UCSF transitioned from having separate medical record systems to a shared EMR (Epic Systems Corp., Verona, WI) where all informationboth inpatient and outpatientis accessible among healthcare professionals. The EMR provides automated notifications of admission and discharge to PCPs, allows for review of inpatient notes, labs, and studies, and immediate access to templated discharge summaries (see Supporting Information, Appendix 1, in the online version of this article). The EMR also enables secure communication between clinicians. At our institution, over 90% of discharge summaries are completed within 24 hours of discharge.[17]
Study Design and Analysis
We developed a survey about the discharge communication practices of inpatient medicine patients based on a previously described survey in the literature (see Supporting Information, Appendix 2, in the online version of this article).[9] The anonymous, 17‐question survey was electronically distributed to resident and attending PCPs at the DGIM practice. The survey was designed to determine: (1) overall PCP satisfaction with current communication practices from the inpatient team at patient discharge, (2) perceived adequacy of automatic discharge notifications, and (3) perception of the types of patients and hospitalizations requiring additional high‐touch communication at discharge.
We analyzed results of our survey using descriptive statistics. Differences in resident and attending responses were analyzed by 2tests.
RESULTS
Seventy‐five of 124 (60%) clinicians (46% residents, 54% attendings) completed the survey. Thirty‐nine (52%) PCPs were satisfied or very satisfied with communication at patient discharge. Although most reported receiving automated discharge notifications (71%), only 39% felt that the notifications plus the discharge summaries were adequate communication for safe transition of care from hospital to community. Fifty‐one percent desired direct contact beyond a discharge summary. There were no differences in preferences on discharge communication between resident and attending PCPs (P>0.05).
Over three‐fourths of PCPs surveyed preferred that for patients with complex hospitalizations (multiple readmissions, multiple active comorbidities, goals of care changes, high‐risk medication changes, time‐sensitive follow‐up needs), an additional e‐mail or verbal communication was needed to augment the information in the discharge summary (Figure 1). Only 31% reported receiving such communication.
When asked about important items to communicate for safer transitions of care, PCPs reported finding the following elements most critical: (1) medication changes (93%), (2) follow‐up actions for the PCP (88%), and (3) active medical issues (84%) (Figure 2).
CONCLUSIONS
In the era of shared EMRs, real‐time access to medication lists, pending test results, and discharge summaries should facilitate care transitions at discharge.[18, 19] We conducted a study to determine PCP perceptions of discharge communication after implementation of a shared EMR. We found that although PCPs largely acknowledged timely receipt of automated discharge notifications and discharge summaries, the majority of PCPs felt that most discharges required additional communication to ensure safe transition of care.
Guidelines for discharge communication emphasize timely communication with the PCP, primarily through discharge summaries containing key safety elements.[1, 5, 10] At our institution, we have improved the timeliness and quality of discharge summaries according to guideline recommendations,[17] and conducted quality improvement projects to improve rates of direct communication with PCPs.[9] In addition, the shared EMR provides automated notifications to PCPs when their patients are discharged. Despite these interventions, our survey shows that PCP satisfaction with discharge communication is still inadequate. PCPs desired direct communication that highlights active medical issues, medication changes, and specific follow‐up actions. Although all of these topics are included in our discharge summary template (see Supporting Information, Appendix 1, in the online version of this article), it is possible that the templated discharge summaries lend themselves to longer documents and information overload, as prior studies have documented the desire for more succinct discharge summaries.[18] We also found that automated notifications of discharge were less reliable and useful for PCPs than anticipated. There were several reasons for this: (1) discharge summaries sometimes were sent to PCPs uncoupled from the discharge notification, (2) there were errors with the generation and delivery of automated messages at the rollout of the new system, and (3) PCPs received many other automated system messages, meaning that discharge notifications could be easily missed. These factors all likely contribute to PCPs' desire for high‐touch communication that highlights the most salient aspects of each patient's hospitalization. It is also possible that automated notifications and depersonalized discharge summaries create distance and a less‐collaborative feeling to patient care. PCPs want more direct communication, and desire to play a more active role in inpatient management, especially for complex hospitalizations.[18] This emphasis on direct communication resonates with previous studies conducted before shared EMRs existed.[9, 12, 19]
Our study had several limitations. First, because this is a single‐institution study at a tertiary care academic setting, the results may not be generalizable to all shared EMR settings, and may not reflect all the challenges of communication with the wider community of outpatient providers. One can postulate that inpatient and outpatient clinician relationships are stronger in an academic setting than in other more disparate environments, where direct communication may happen even less frequently. Of note, our low rates of direct communication are consistent with other single‐ and multi‐institution studies, suggesting that our findings are generalizable.[14, 15] Second, our survey is limited in its ability to distinguish those patients who require high‐touch communication and those who do not. Third, although we have used the survey to assess PCP satisfaction in previous studies, it is not a validated instrument, and therefore we cannot reliably say that increasing direct PCP communication would increase their satisfaction around discharge. Last, the PCP‐reported rates of discharge communication are subjective and may be influenced by recall bias. We did not have a systematic way to confirm the actual rates of communication at discharge, which could have occurred through EMR messages, e‐mails, phone calls, or pages.
Although a shared EMR allows for real‐time access to patient data, it does not eliminate PCPs' desire for direct 2‐way dialogue at discharge, especially for complex patients. Key information desired in such communication should include active medical issues, medication changes, and follow‐up needs, which is consistent with prior studies. Standardizing this direct communication process in an efficient way can be challenging. Further elucidation of PCP preferences around which patients necessitate higher‐level communication and preferred methods and timing of communication is needed, as well as determining the most efficient and effective method for hospitalists to provide such communication. Improving communication between hospitalists and PCPs requires not just the presence of a shared EMR, but additional, systematic efforts to engage both inpatient and outpatient clinicians in collaborative care.
Disclosure
Nothing to report.
- , , , et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444–449.
- , , , , The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417–428.
- , , , , “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354−660.
- , , , , Improving measurement in clinical handover. Qual Saf Health Care. 2009;18:272–277.
- World Health Organization. Patient safety: action on patient safety: high 5s. 2007. Available at: http://www.who.int/patientsafety/implementation/solutions/high5s/en/index.html. Accessed January 28, 2015.
- The Joint Commission Center for Transforming Healthcare. Hand‐off communications. 2012. Available at: http://www.centerfortransforminghealthcare.org/projects/detail.aspx?Project=1. Accessed January 28, 2015.
- , , , et al. The effect of a resident‐led quality improvement project on improving communication between hospital‐based and outpatient physicians. Am J Med Qual. 2013;28(6):472–479.
- , , , Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323.
- , , , , , Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21:i97–i105.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA. 2013;173(8):624–629.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , The Housestaff Incentive Program: improving the timeliness and quality of discharge summaries by engaging residents in quality improvement. BMJ Qual Saf. 2013;22(9):768–774.
- , , , et al. A Failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations [published online ahead of print October 15, 2014]. J Gen Intern Med. doi: 10.1007/s11606-014-3056-x.
- , , , et al. Pediatric hospitalists and primary care providers: a communication needs assessment. J Hosp Med. 2009;4(3):187–193.
- , , , et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444–449.
- , , , , The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417–428.
- , , , , “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354−660.
- , , , , Improving measurement in clinical handover. Qual Saf Health Care. 2009;18:272–277.
- World Health Organization. Patient safety: action on patient safety: high 5s. 2007. Available at: http://www.who.int/patientsafety/implementation/solutions/high5s/en/index.html. Accessed January 28, 2015.
- The Joint Commission Center for Transforming Healthcare. Hand‐off communications. 2012. Available at: http://www.centerfortransforminghealthcare.org/projects/detail.aspx?Project=1. Accessed January 28, 2015.
- , , , et al. The effect of a resident‐led quality improvement project on improving communication between hospital‐based and outpatient physicians. Am J Med Qual. 2013;28(6):472–479.
- , , , Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323.
- , , , , , Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21:i97–i105.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA. 2013;173(8):624–629.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , The Housestaff Incentive Program: improving the timeliness and quality of discharge summaries by engaging residents in quality improvement. BMJ Qual Saf. 2013;22(9):768–774.
- , , , et al. A Failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations [published online ahead of print October 15, 2014]. J Gen Intern Med. doi: 10.1007/s11606-014-3056-x.
- , , , et al. Pediatric hospitalists and primary care providers: a communication needs assessment. J Hosp Med. 2009;4(3):187–193.