User login
CASE 1 ›
A 3-year-old boy was brought to our emergency department for evaluation of skin lesions that he’d had for 7 days. The boy would sometimes scratch the lesions, which began on his right flank as erythematous micropapules and later spread to his right lateral thigh and inner arm (FIGURE 1). His lymph nodes were not palpable.
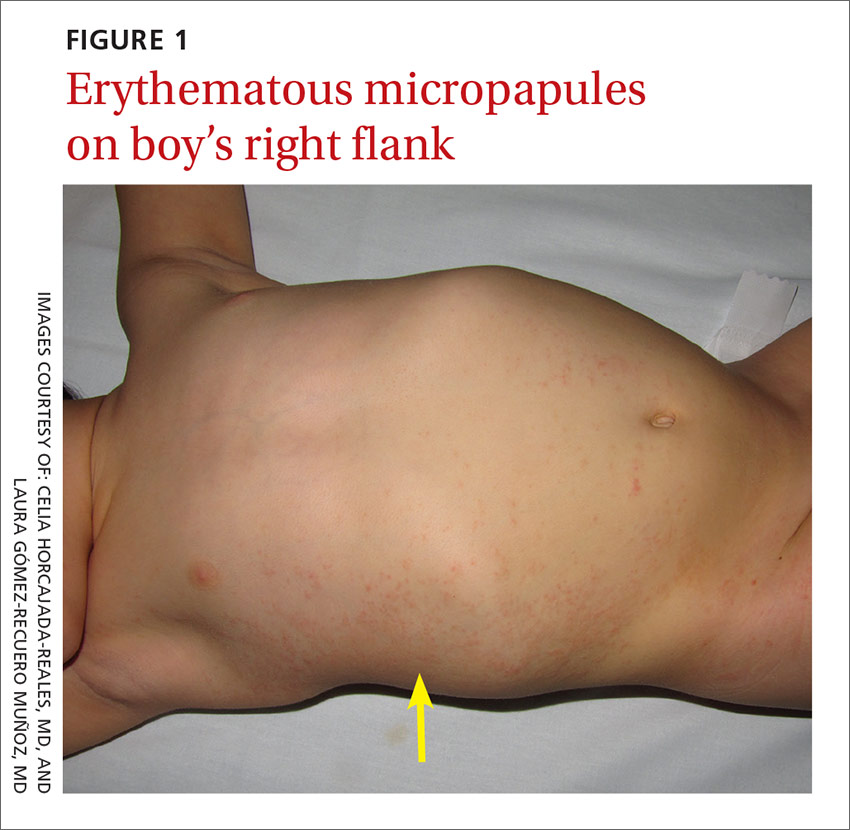
The boy’s parents had been told to use a topical corticosteroid, but the rash did not improve. His family denied fever or other previous infectious or systemic symptoms, and said that he hadn’t come into contact with any irritants or allergenic substances.
CASE 2 ›
A 13-year-old girl came to our emergency department with a pruriginous rash on her right leg and abdomen that she’d had for 4 days (FIGURE 2). The millimetric papules had also spread to the right side of her trunk, her right arm and armpit, and her inner thigh. Before the rash, she’d had a fever, otalgia, and conjunctivitis. We noted redness of her left conjunctiva, eardrum, and pharynx. The girl’s lymph nodes were not palpable. Serologic examinations for Epstein-Barr virus, cytomegalovirus, rubella, parvovirus B19, and Mycoplasma were negative.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Asymmetric periflexural exanthem of childhood
Both of these patients were given a diagnosis of asymmetric periflexural exanthem of childhood (APEC), based on the appearance and distribution of the rashes.
A rare condition that mostly affects young children
APEC is a rash of unknown cause, although epidemiologic and clinical findings support a viral etiology. Cases of this rash were first reported in 1992 by Bodemer et al, and a year later, Taïeb et al reported new cases, establishing the term “asymmetric periflexural exanthem.”1,2 Several viruses have been related to APEC (including adenovirus, parvovirus B19, parainfluenza 2 and 3, and human herpesvirus 7), but none of these has been consistently associated with the rash.3-5
APEC tends to affect children between one and 5 years of age, but adult cases have been reported.6,7 The condition occurs slightly more frequently among females and more often in winter and spring.8,9 APEC is a rare condition; since 1992, there have only been about 300 cases reported in the literature.10
What you’ll see. The erythematous rash appears as an asymmetrical or unilateral papular, scarlatiniform, or eczematous exanthema. It initially affects the axilla or groin and may then progress to the extremities and trunk. Minor lesions infrequently present on the contralateral side. Most children who are affected by APEC are otherwise healthy and asymptomatic at presentation. The exanthem is occasionally pruritic and can be preceded by short respiratory or gastrointestinal prodromes or a low-grade fever.2,9 If the rash predominantly affects the lateral thoracic wall, it may be referred to as unilateral laterothoracic exanthem.11 Regional lymphadenopathies can often be found, and there is no systemic involvement.
The distribution of the rash helps to distinguish the condition
The differential diagnosis for this type of exanthem includes drug eruptions, pityriasis rosea, miliaria, scarlet fever, papular acrodermatitis of childhood, and other viral rashes. The asymmetric distribution of APEC helps to distinguish the condition. Other possible asymmetric skin lesions, such as contact dermatitis, tinea corporis, or lichen striatus, can be differentiated by the characteristics of the cutaneous lesions. Contact dermatitis lesions are more vesicular, pruritic, and related to the contact area. Tinea corporis lesions tend to be smaller, circular, well-limited, and often have pustules. Lichen striatus starts as small pink-, red-, or flesh-colored spots that join together to form a dull red and slightly scaly linear band over the course of one or 2 weeks.12 Because APEC is self-limiting, a skin biopsy is usually not necessary.13
Lesions usually persist for one to 6 weeks and resolve with no sequelae. Only symptomatic treatment is required.9 Topical emollients, topical corticosteroids, or oral antihistamines can be used, if necessary.
Our patients. Both patients were treated with oral antihistamines and the rashes completely resolved within 2 to 3 weeks.
CORRESPONDENCE
Celia Horcajada-Reales, MD, Hospital Gregorio Marañón, Calle del Dr. Esquerdo, 46, 28007 Madrid, Spain; [email protected].
1. Bodemer C, de Prost Y. Unilateral laterothoracic exanthem in children: a new disease? J Am Acad Dermatol. 1992;27:693-696.
2. Taïeb A, Mégraud F, Legrain V, et al. Asymmetric periflexural exanthem of childhood. J Am Acad Dermatol. 1993;29:391-393.
3. Al Yousef Ali A, Farhi D, De Maricourt S, et al. Asymmetric periflexural exanthema associated with HHV7 infection. Eur J Dermatol. 2010;20:230-231.
4. Coustou D, Masquelier B, Lafon ME, et al. Asymmetric periflexural exanthem of childhood: microbiologic case-control study. Pediatr Dermatol. 2000;17:169-173.
5. Harangi F, Várszegi D, Szücs G. Asymmetric periflexural exanthem of childhood and viral examinations. Pediatr Dermatol. 1995;12:112-115.
6. Zawar VP. Asymmetric periflexural exanthema: a report in an adult patient. Indian J Dermatol Venereol Leprol. 2003;69:401-404.
7. Pauluzzi P, Festini G, Gelmetti C. Asymmetric periflexural exanthem of childhood in an adult patient with parvovirus B19. J Eur Acad Dermatol Venereol. 2001;15:372-374.
8. McCuaig CC, Russo P, Powell J, et al. Unilateral laterothoracic exanthem. A clinicopathologic study of forty-eight patients. J Am Acad Dermatol. 1996;34:979-984.
9. Coustou D, Léauté-Labrèze C, Bioulac-Sage P, et al. Asymmetric periflexural exanthem of childhood: a clinical, pathologic, and epidemiologic prospective study. Arch Dermatol. 1999;135:799-803.
10. Mejía-Rodríguez SA, Ramírez-Romero VS, Valencia-Herrera A, et al. Unilateral laterothoracic exanthema of childhood. An infrequently diagnosed disease entity. Bol Med Hosp Infant Mex. 2007;64:65-68.
11. Chuh AA, Chan HH. Unilateral mediothoracic exanthem: a variant of unilateral laterothoracic exanthem. Cutis. 2006;77:29-32.
12. Chuh A, Zawar V, Law M, et al. Gianotti-Crosti syndrome, pityriasis rosea, asymmetrical periflexural exanthem, unilateral mediothoracic exanthem, eruptive pseudoangiomatosis, and papular-purpuric gloves and socks syndrome: a brief review and arguments for diagnostic criteria. Infect Dis Rep. 2012;4:e12.
13. Gelmetti C, Caputo R. Asymmetric periflexural exanthem of childhood: who are you? J Eur Acad Dermatol Venereol. 2001;15:293-294.
CASE 1 ›
A 3-year-old boy was brought to our emergency department for evaluation of skin lesions that he’d had for 7 days. The boy would sometimes scratch the lesions, which began on his right flank as erythematous micropapules and later spread to his right lateral thigh and inner arm (FIGURE 1). His lymph nodes were not palpable.
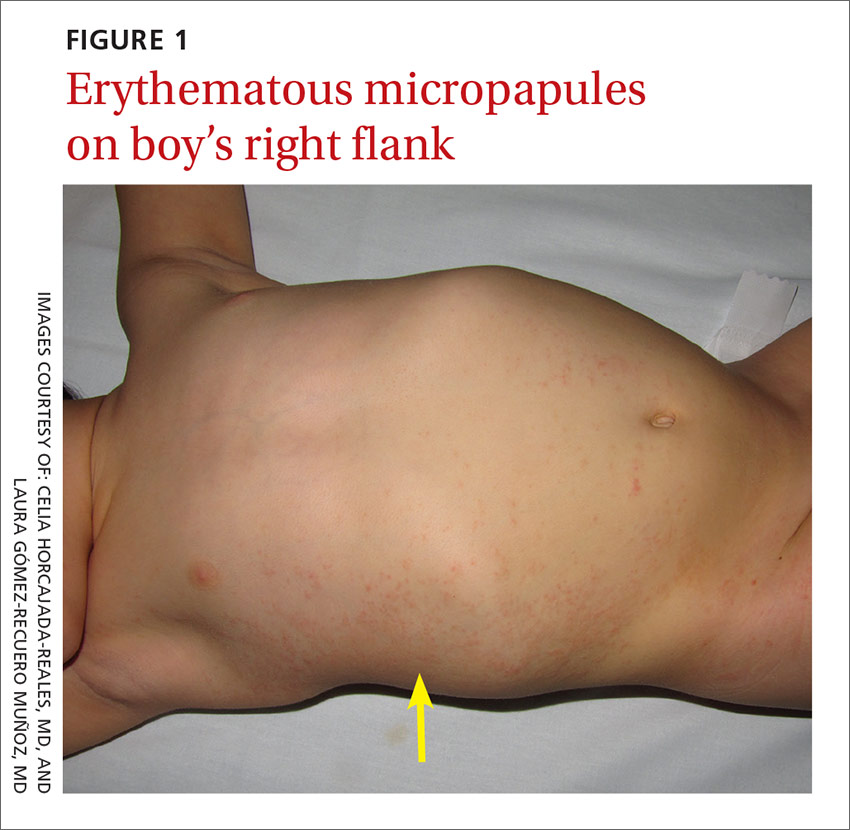
The boy’s parents had been told to use a topical corticosteroid, but the rash did not improve. His family denied fever or other previous infectious or systemic symptoms, and said that he hadn’t come into contact with any irritants or allergenic substances.
CASE 2 ›
A 13-year-old girl came to our emergency department with a pruriginous rash on her right leg and abdomen that she’d had for 4 days (FIGURE 2). The millimetric papules had also spread to the right side of her trunk, her right arm and armpit, and her inner thigh. Before the rash, she’d had a fever, otalgia, and conjunctivitis. We noted redness of her left conjunctiva, eardrum, and pharynx. The girl’s lymph nodes were not palpable. Serologic examinations for Epstein-Barr virus, cytomegalovirus, rubella, parvovirus B19, and Mycoplasma were negative.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Asymmetric periflexural exanthem of childhood
Both of these patients were given a diagnosis of asymmetric periflexural exanthem of childhood (APEC), based on the appearance and distribution of the rashes.
A rare condition that mostly affects young children
APEC is a rash of unknown cause, although epidemiologic and clinical findings support a viral etiology. Cases of this rash were first reported in 1992 by Bodemer et al, and a year later, Taïeb et al reported new cases, establishing the term “asymmetric periflexural exanthem.”1,2 Several viruses have been related to APEC (including adenovirus, parvovirus B19, parainfluenza 2 and 3, and human herpesvirus 7), but none of these has been consistently associated with the rash.3-5
APEC tends to affect children between one and 5 years of age, but adult cases have been reported.6,7 The condition occurs slightly more frequently among females and more often in winter and spring.8,9 APEC is a rare condition; since 1992, there have only been about 300 cases reported in the literature.10
What you’ll see. The erythematous rash appears as an asymmetrical or unilateral papular, scarlatiniform, or eczematous exanthema. It initially affects the axilla or groin and may then progress to the extremities and trunk. Minor lesions infrequently present on the contralateral side. Most children who are affected by APEC are otherwise healthy and asymptomatic at presentation. The exanthem is occasionally pruritic and can be preceded by short respiratory or gastrointestinal prodromes or a low-grade fever.2,9 If the rash predominantly affects the lateral thoracic wall, it may be referred to as unilateral laterothoracic exanthem.11 Regional lymphadenopathies can often be found, and there is no systemic involvement.
The distribution of the rash helps to distinguish the condition
The differential diagnosis for this type of exanthem includes drug eruptions, pityriasis rosea, miliaria, scarlet fever, papular acrodermatitis of childhood, and other viral rashes. The asymmetric distribution of APEC helps to distinguish the condition. Other possible asymmetric skin lesions, such as contact dermatitis, tinea corporis, or lichen striatus, can be differentiated by the characteristics of the cutaneous lesions. Contact dermatitis lesions are more vesicular, pruritic, and related to the contact area. Tinea corporis lesions tend to be smaller, circular, well-limited, and often have pustules. Lichen striatus starts as small pink-, red-, or flesh-colored spots that join together to form a dull red and slightly scaly linear band over the course of one or 2 weeks.12 Because APEC is self-limiting, a skin biopsy is usually not necessary.13
Lesions usually persist for one to 6 weeks and resolve with no sequelae. Only symptomatic treatment is required.9 Topical emollients, topical corticosteroids, or oral antihistamines can be used, if necessary.
Our patients. Both patients were treated with oral antihistamines and the rashes completely resolved within 2 to 3 weeks.
CORRESPONDENCE
Celia Horcajada-Reales, MD, Hospital Gregorio Marañón, Calle del Dr. Esquerdo, 46, 28007 Madrid, Spain; [email protected].
CASE 1 ›
A 3-year-old boy was brought to our emergency department for evaluation of skin lesions that he’d had for 7 days. The boy would sometimes scratch the lesions, which began on his right flank as erythematous micropapules and later spread to his right lateral thigh and inner arm (FIGURE 1). His lymph nodes were not palpable.
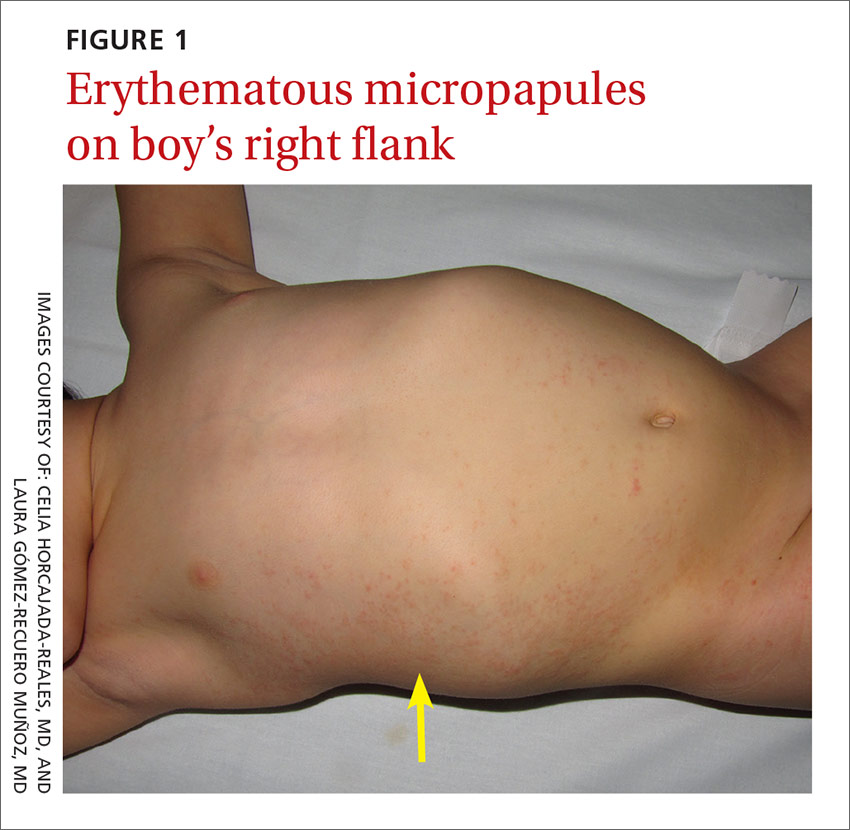
The boy’s parents had been told to use a topical corticosteroid, but the rash did not improve. His family denied fever or other previous infectious or systemic symptoms, and said that he hadn’t come into contact with any irritants or allergenic substances.
CASE 2 ›
A 13-year-old girl came to our emergency department with a pruriginous rash on her right leg and abdomen that she’d had for 4 days (FIGURE 2). The millimetric papules had also spread to the right side of her trunk, her right arm and armpit, and her inner thigh. Before the rash, she’d had a fever, otalgia, and conjunctivitis. We noted redness of her left conjunctiva, eardrum, and pharynx. The girl’s lymph nodes were not palpable. Serologic examinations for Epstein-Barr virus, cytomegalovirus, rubella, parvovirus B19, and Mycoplasma were negative.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Asymmetric periflexural exanthem of childhood
Both of these patients were given a diagnosis of asymmetric periflexural exanthem of childhood (APEC), based on the appearance and distribution of the rashes.
A rare condition that mostly affects young children
APEC is a rash of unknown cause, although epidemiologic and clinical findings support a viral etiology. Cases of this rash were first reported in 1992 by Bodemer et al, and a year later, Taïeb et al reported new cases, establishing the term “asymmetric periflexural exanthem.”1,2 Several viruses have been related to APEC (including adenovirus, parvovirus B19, parainfluenza 2 and 3, and human herpesvirus 7), but none of these has been consistently associated with the rash.3-5
APEC tends to affect children between one and 5 years of age, but adult cases have been reported.6,7 The condition occurs slightly more frequently among females and more often in winter and spring.8,9 APEC is a rare condition; since 1992, there have only been about 300 cases reported in the literature.10
What you’ll see. The erythematous rash appears as an asymmetrical or unilateral papular, scarlatiniform, or eczematous exanthema. It initially affects the axilla or groin and may then progress to the extremities and trunk. Minor lesions infrequently present on the contralateral side. Most children who are affected by APEC are otherwise healthy and asymptomatic at presentation. The exanthem is occasionally pruritic and can be preceded by short respiratory or gastrointestinal prodromes or a low-grade fever.2,9 If the rash predominantly affects the lateral thoracic wall, it may be referred to as unilateral laterothoracic exanthem.11 Regional lymphadenopathies can often be found, and there is no systemic involvement.
The distribution of the rash helps to distinguish the condition
The differential diagnosis for this type of exanthem includes drug eruptions, pityriasis rosea, miliaria, scarlet fever, papular acrodermatitis of childhood, and other viral rashes. The asymmetric distribution of APEC helps to distinguish the condition. Other possible asymmetric skin lesions, such as contact dermatitis, tinea corporis, or lichen striatus, can be differentiated by the characteristics of the cutaneous lesions. Contact dermatitis lesions are more vesicular, pruritic, and related to the contact area. Tinea corporis lesions tend to be smaller, circular, well-limited, and often have pustules. Lichen striatus starts as small pink-, red-, or flesh-colored spots that join together to form a dull red and slightly scaly linear band over the course of one or 2 weeks.12 Because APEC is self-limiting, a skin biopsy is usually not necessary.13
Lesions usually persist for one to 6 weeks and resolve with no sequelae. Only symptomatic treatment is required.9 Topical emollients, topical corticosteroids, or oral antihistamines can be used, if necessary.
Our patients. Both patients were treated with oral antihistamines and the rashes completely resolved within 2 to 3 weeks.
CORRESPONDENCE
Celia Horcajada-Reales, MD, Hospital Gregorio Marañón, Calle del Dr. Esquerdo, 46, 28007 Madrid, Spain; [email protected].
1. Bodemer C, de Prost Y. Unilateral laterothoracic exanthem in children: a new disease? J Am Acad Dermatol. 1992;27:693-696.
2. Taïeb A, Mégraud F, Legrain V, et al. Asymmetric periflexural exanthem of childhood. J Am Acad Dermatol. 1993;29:391-393.
3. Al Yousef Ali A, Farhi D, De Maricourt S, et al. Asymmetric periflexural exanthema associated with HHV7 infection. Eur J Dermatol. 2010;20:230-231.
4. Coustou D, Masquelier B, Lafon ME, et al. Asymmetric periflexural exanthem of childhood: microbiologic case-control study. Pediatr Dermatol. 2000;17:169-173.
5. Harangi F, Várszegi D, Szücs G. Asymmetric periflexural exanthem of childhood and viral examinations. Pediatr Dermatol. 1995;12:112-115.
6. Zawar VP. Asymmetric periflexural exanthema: a report in an adult patient. Indian J Dermatol Venereol Leprol. 2003;69:401-404.
7. Pauluzzi P, Festini G, Gelmetti C. Asymmetric periflexural exanthem of childhood in an adult patient with parvovirus B19. J Eur Acad Dermatol Venereol. 2001;15:372-374.
8. McCuaig CC, Russo P, Powell J, et al. Unilateral laterothoracic exanthem. A clinicopathologic study of forty-eight patients. J Am Acad Dermatol. 1996;34:979-984.
9. Coustou D, Léauté-Labrèze C, Bioulac-Sage P, et al. Asymmetric periflexural exanthem of childhood: a clinical, pathologic, and epidemiologic prospective study. Arch Dermatol. 1999;135:799-803.
10. Mejía-Rodríguez SA, Ramírez-Romero VS, Valencia-Herrera A, et al. Unilateral laterothoracic exanthema of childhood. An infrequently diagnosed disease entity. Bol Med Hosp Infant Mex. 2007;64:65-68.
11. Chuh AA, Chan HH. Unilateral mediothoracic exanthem: a variant of unilateral laterothoracic exanthem. Cutis. 2006;77:29-32.
12. Chuh A, Zawar V, Law M, et al. Gianotti-Crosti syndrome, pityriasis rosea, asymmetrical periflexural exanthem, unilateral mediothoracic exanthem, eruptive pseudoangiomatosis, and papular-purpuric gloves and socks syndrome: a brief review and arguments for diagnostic criteria. Infect Dis Rep. 2012;4:e12.
13. Gelmetti C, Caputo R. Asymmetric periflexural exanthem of childhood: who are you? J Eur Acad Dermatol Venereol. 2001;15:293-294.
1. Bodemer C, de Prost Y. Unilateral laterothoracic exanthem in children: a new disease? J Am Acad Dermatol. 1992;27:693-696.
2. Taïeb A, Mégraud F, Legrain V, et al. Asymmetric periflexural exanthem of childhood. J Am Acad Dermatol. 1993;29:391-393.
3. Al Yousef Ali A, Farhi D, De Maricourt S, et al. Asymmetric periflexural exanthema associated with HHV7 infection. Eur J Dermatol. 2010;20:230-231.
4. Coustou D, Masquelier B, Lafon ME, et al. Asymmetric periflexural exanthem of childhood: microbiologic case-control study. Pediatr Dermatol. 2000;17:169-173.
5. Harangi F, Várszegi D, Szücs G. Asymmetric periflexural exanthem of childhood and viral examinations. Pediatr Dermatol. 1995;12:112-115.
6. Zawar VP. Asymmetric periflexural exanthema: a report in an adult patient. Indian J Dermatol Venereol Leprol. 2003;69:401-404.
7. Pauluzzi P, Festini G, Gelmetti C. Asymmetric periflexural exanthem of childhood in an adult patient with parvovirus B19. J Eur Acad Dermatol Venereol. 2001;15:372-374.
8. McCuaig CC, Russo P, Powell J, et al. Unilateral laterothoracic exanthem. A clinicopathologic study of forty-eight patients. J Am Acad Dermatol. 1996;34:979-984.
9. Coustou D, Léauté-Labrèze C, Bioulac-Sage P, et al. Asymmetric periflexural exanthem of childhood: a clinical, pathologic, and epidemiologic prospective study. Arch Dermatol. 1999;135:799-803.
10. Mejía-Rodríguez SA, Ramírez-Romero VS, Valencia-Herrera A, et al. Unilateral laterothoracic exanthema of childhood. An infrequently diagnosed disease entity. Bol Med Hosp Infant Mex. 2007;64:65-68.
11. Chuh AA, Chan HH. Unilateral mediothoracic exanthem: a variant of unilateral laterothoracic exanthem. Cutis. 2006;77:29-32.
12. Chuh A, Zawar V, Law M, et al. Gianotti-Crosti syndrome, pityriasis rosea, asymmetrical periflexural exanthem, unilateral mediothoracic exanthem, eruptive pseudoangiomatosis, and papular-purpuric gloves and socks syndrome: a brief review and arguments for diagnostic criteria. Infect Dis Rep. 2012;4:e12.
13. Gelmetti C, Caputo R. Asymmetric periflexural exanthem of childhood: who are you? J Eur Acad Dermatol Venereol. 2001;15:293-294.
