User login
• When you suspect an infectious cause of hip pain, immediately order laboratory studies, blood cultures, and hip radiographs to rule out septic arthritis. A
• When you suspect avascular necrosis of the femoral head, instruct the patient to remain non-weight bearing and provide a referral to an orthopedist. A
• Stabilization with in situ pinning is the gold standard treatment for slipped capital femoral epiphysis, whether the slip is stable or unstable. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Sean L, a 12-year-old middle school student in the 90th percentile for weight, limps into your office and reports that it hurts to put his full weight down on his right leg. The pain just started, Sean says, but he began limping a day or 2 earlier. Sean plays on his school’s football team, and he wants to know what you can give him to relieve the pain so he won’t have to miss any games. What can you tell him?
Family physicians are increasingly likely to see children and adolescents with hip pain, the combined result of greater sports participation and a surge in childhood obesity. Diagnosing pediatric hip pain can be a daunting task, not only because of the complexity of the hip joint, but because of the need to consider bone, joint, tendon, muscle, bursa, and referred pain in the differential diagnosis.
But it doesn’t have to be. Being familiar with the major causes of pediatric hip pain, the diagnostic tests and maneuvers that are part of a comprehensive work-up, and the conditions that require rapid referral to an orthopedist makes it possible to adopt a straightforward approach. We’ve developed this review with that goal in mind.
Assess pain and movement with these maneuvers and tests
Begin with a pain history, determining the location of the hip pain—anterior, lateral, or posterior. Ask the patient to describe the pain and its quality: Is it diffuse, localized, or radiating? Identify any aggravating or relieving factors, and question the patient (or parents) about the onset, reproducibility, and timing of the pain, including the presence or absence of nighttime pain.
Find out, too, whether the pain is causing a limp; what effect, if any, the pain has had on the patient’s ability to bear weight; and to what extent the patient’s activity level has been affected. Then move on to the physical examination.
Begin with the patient standing up. Observe his or her gait, posture, and alignment. Check for Trendelenburg’s sign, in which the ipsilateral hip drops when the patient raises the unaffected leg. Its presence indicates a weakness of the opposite hip abductor.
With the patient in a supine position, inspect the hip for swelling, erythema, and warmth. Palpate the affected area, but keep in mind that palpation may not always reveal much because of the depth of the hip joint. If the patient is overweight, palpation of the muscles, tendons, or bones may be particularly difficult.
Test active and passive range of motion (ROM) and muscle strength of the hip in all directions. (Patients who are unable to tolerate lying down can undergo most of the ROM and strength tests in a seated position.) Check for a discrepancy in leg length, not only by visual inspection, but by measuring from the anterior superior iliac spine (ASIS) to the lateral malleoli.
Perform more focused maneuvers, as needed. If lumbar radiculopathy is a possibility, for example, do a straight leg raise, lifting the leg on the affected side in full extension with the ankle dorsiflexed, and repeat with the leg on the unaffected side. The test is positive if radiating pain down the affected leg and buttock is reproduced at ≤60° of leg elevation (or leg extension if the patient is seated). Conduct Ober’s test (FIGURE 1) to check for iliotibial band syndrome.
Follow with a system review, asking about recent conditions, including fever and infection, trauma, and constitutional, abdominal, and genitourinary symptoms. Perform an abdominal exam, and, if indicated, a pelvic or hernia exam. Check reflexes and sensation, as warranted, and examine the spine and knee.
CASE Sean is a healthy boy with no known medical problems. He has not been ill recently, and has not had any unexplained weight loss. His vital signs are normal, and he does not appear ill. He walks with a limp.
On examination, Sean has no palpable area of tenderness, swelling, or ecchymosis. His right hip has limited and painful internal rotation and, when flexed, it falls out to the side in external rotation.
FIGURE 1
Ober’s test for iliotibial band syndrome
With the patient lying on the unaffected side, passively extend the affected leg and allow the knee to drop. The test is positive if the patient experiences pain along the lateral side of the thigh or the knee does not drop down to the table.
Hip pain and infection? Consider septic arthritis
Is your patient febrile or recovering from an infection? When you suspect an acute infectious cause of hip pain, there are 2 disorders to consider in the differential diagnosis: transient synovitis (TS) and septic arthritis. Both are associated with an acute onset of pain and limping or non-weight bearing, and generally affect young children: Septic arthritis is most common in children between the age of 3 and 6 years, while the typical age range for TS is 3 through 8.1-4
There are other important differences. TS is a benign, self-limited, and common cause of hip pain in young children,5 which may be preceded by a viral infection.1 Septic arthritis is a serious condition that requires rapid identification; a delay in treatment can cause significant long-term morbidity. Complications may include early arthritis, shortened limb, dislocation, and osteonecrosis.
Because it can be difficult to distinguish between septic arthritis and TS, multiple studies have looked at the best way to make that determination. 1-7
The criteria most commonly used to identify septic arthritis are:
- fever
- refusal to bear weight
- erythrocyte sedimentation rate (ESR) >40 mm/h
- white blood cell count >12,000 mm3.
One study showed a predictive probability of 97% for septic arthritis when 3 of the 4 above criteria were present, and 99% if the patient had all 4.2,4 Other studies added 2 additional criteria—C-reactive protein (CRP) >1 mg/dL and medial joint space widening of >2 mm—with similar predictive probabilities (93% and 99%, respectively, if 3 or 4 of the 6 criteria were positive).2,4,6
Order lab work (ESR, CRP, complete blood count, and blood cultures) for any young patient whose hip pain is thought to be associated with an infectious process. Obtain hip anterior/posterior (AP) and frog lateral radiographs to look for joint space widening, as well.1-4
In addition to the above criteria, suspect septic arthritis in a child who presents with acute onset of hip pain, looks ill, and has limited ROM—particularly with internal rotation. In contrast, children with TS do not look sick and, while they often have limited ROM, it is primarily just at extremes. A modified log roll test can be used to assess the rotation of the hip.
An ultrasound-guided aspiration of fluid is the gold standard for septic arthritis diagnosis. Treatment is emergent surgical drainage and parenteral antibiotics, which should be withheld until fluid is aspirated or the joint is surgically drained. The most common causative organism is Staphylococcus aureus.3,7
It is reasonable to withhold joint aspiration for patients who don’t look sick and have normal labs and reliable follow-up, and to watch closely, with conservative management including nonsteroidal anti-inflammatory drugs (NSAIDs) and activity, as tolerated, instead.
There is some concern that TS may lead to Legg-Calves-Perthe’s disease, also known as avascular necrosis of the femoral head, although there is no strong evidence to support it. To be safe, however, obtain radiographs 2 to 18 months after TS resolves to check for further damage or complications.1,8
Femoral head disorders: When x-rays help, when they don’t
There are 2 femoral head disorders that commonly affect children and adolescents: Avascular necrosis of the femoral head and slipped capital femoral epiphysis (SCFE). Age alone is a clue to detection; children with avascular necrosis tend to be younger than those with SCFE.
Avascular necrosis of the femoral head is most commonly seen in children between the ages of 4 and 8 years, and occurs more frequently in boys than in girls. Although there is disagreement about the etiology of avascular necrosis, the condition is thought to result from a disruption in femoral blood supply, leading to osteonecrosis and flattening of the weight-bearing surface of the femoral head. One study found that structural abnormalities in the epiphyseal cartilage may lead to collapse.9
The condition often begins with a painless limp that develops—typically in 1 to 3 months—into groin, thigh, or knee pain; worsens with activity; and is relieved with rest.5 Abduction and internal rotation are limited on exam.
In patients with avascular necrosis, hip AP and frog lateral radiographs are diagnostic, with evidence of increased density of 1 epiphysis and flattening or fragmentation of the femoral head.7 When you suspect avascular necrosis, advise the patient to avoid weight bearing—and provide a referral to a pediatric orthopedist.
Treatment has consisted of containment of the femoral head with the use of splints, although there is little evidence that this treatment alters outcomes.9,10 One study found conflicting evidence that it improved results and does not support its use.9 This is why having a pediatric orthopedist involved in these cases is important.
Long-term prognosis is closely related to the degree of involvement of the femoral head and to the age at onset. Those who are younger than 6 to 8 years typically have the best outcomes, with less hip pain and dysfunction later in life.9,10
SCFE, the most common hip disorder in adolescents, can be easily missed. SCFE has a strong correlation with obesity and is especially common in obese males between the ages of 10 and 16 years who have delayed secondary sex characteristics.2,11 SCFE is generally a mechanical disorder, but in children who are younger than 10 or have low weight or height for their age, an endocrine work-up is indicated.
Symptoms include a painful limp and nonspecific knee, anterior thigh, or groin pain. A delay in diagnosis has a significant effect on complications. Prognosis is also related to the stability of the slip.11,12 An unstable slip is defined as the inability to bear weight.13 The risk of osteonecrosis, a complication of SCFE, is negligible if the slip is stable, but may be as high as 50% when the slip is unstable.2
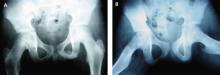
On examination, internal rotation is painful and limited, and flexion of the hip will lead to simultaneous external rotation. Leg length discrepancy or a positive Trendelenburg’s sign may be present. Diagnosis may be made with bilateral AP (FIGURES 2A AND 2B) and frog lateral radiographic views, looking for growth plate widening.12 Klein’s line—the line that would intersect the epiphysis when drawn along the anterior neck of the femur of an AP view of a normal hip13—is abnormal in a hip with SCFE.
CT or MRI can be performed in patients who have clinical evidence of SCFE but normal radiographs. Treatment is the same regardless of whether the slip is stable or unstable—patients are told to avoid weight bearing and are sent to an orthopedist. Stabilization with in situ pinning is the gold standard, regardless of severity.9,10,12
CASE AP x-rays of Sean’s right hip are abnormal, showing that the femoral epiphysis is not aligned with the femoral neck correctly when compared with the opposite side. You advise the patient and his parents that he has a serious condition called SCFE, which can lead to long-term problems if not treated surgically. You recommend that he start using crutches and remain fully non-weight bearing on his right leg, and refer him to a pediatric orthopedist.
FIGURE 2
Bilateral AP views reveal slipped capital femoral epiphysis
X-rays show the pelvic widening of the physis on the right (A) and the epiphysis slipping posteriorly and inferiorly (B).
Suspect these hip disorders in young athletes
Femoral stress fractures are particularly common in adolescents who are runners or endurance athletes. The classic history is gradual onset of anterior thigh pain, beginning during physical activity and progressing to pain at rest. Risk factors for femoral stress fractures include the female athlete triad (amenorrhea, eating disorder, and osteoporosis), a recent change in training, poor biomechanics, and underlying bone or metabolic disease.14
A positive hop test. The physical exam in a patient with a femoral stress fracture is likely to be normal, with the possible exception of limitation in hip ROM at the extremes. Pain may be reproduced with hopping (a positive result) on the affected leg; 1 study noted that 70% of patients with femoral stress fractures had a positive hop test.15
Hip radiographs should be done, but may not be helpful. In initial x-rays, sensitivity may be as low as 15%; delayed x-rays, taken 2 to 4 weeks later, have a sensitivity of about 50% for findings suggestive of a stress fracture.16
Although bone scan and MRI have approximately equal sensitivity, bone scan is less specific for detecting early stress fractures, so MRI has become the gold standard for diagnosing femoral stress fractures.14 Treatment depends on the location of the fracture. A compression stress fracture on the inferior surface of the femoral neck has a good prognosis when the patient remains non-weight bearing for 6 to 8 weeks, then gradually returns to activity.14
Tension stress fractures are on the superior surface, and patients need to be sent to an orthopedist for internal fixation.14,16 A tension-sided fracture can progress to non-union or avascular necrosis. Training and diet should be modified as indicated to promote healing and prevent recurrence.
Does the patient’s hip make a snapping sound?
Patients with snapping of the hip can be categorized into those whose injuries are painful, and those whose injuries are not. Reassure patients with pain-free snapping that there is no reason to be concerned.
External snapping is usually related to the iliotibial band moving over the greater trochanteric bursa, which can lead to a painful bursa.17 The key symptom, in addition to the snapping, is lateral hip pain of gradual onset. Examination reproduces the pain with the snapping hip maneuver (FIGURES 3A AND 3B).
Internal snapping is related to the iliopsoas tendon passing over the femoral head and hip capsule or over the iliopectineal eminence and bony ridge of the lesser trochanter.17 Inflammation of the iliopsoas bursa may lead to painful snapping. This pain is anterior in location, and the snap can be reproduced with the patient lying on the unaffected side, bringing the affected hip passively from flexed, abducted, and externally rotated to a medial position of extension, adduction, and internal rotation.
Internal and external snapping usually occurs in patients whose activities involve the repetitive motions done in the exam maneuvers. Intra-articular snapping is due to loose bodies or acetabular labral tears.
Imaging for the patient with painful hip snapping consists of hip radiographs—usually negative—and ultrasound. MRI is done if intra-articular pathology is suspected.17 Treatment of snapping hips includes activity modification, NSAIDs, physical therapy, and possible steroid injection. Rarely is the condition surgically treated.
FIGURE 3
Snapping maneuver can help identify source of pain
With the patient lying with the unaffected side down, passively abduct the affected hip (A), then move from full extension to 90° of flexion (B). External snapping is usually related to the iliotibial band moving over the greater trochanter, which can lead to a painful bursa.
Avulsion fractures, acetabular tears, and bursitis
Avulsion fractures are a separation of the secondary growth center, the apophyses, from the underlying bone in skeletally immature athletes. They occur because the athlete’s tendons are stronger than the cartilaginous growth centers,10,11,16,18 and are produced by sudden forceful contraction of the muscle. The patient will complain of acute pain and swelling. The exam will be positive for palpable tenderness at the bony site and for muscle weakness. The most common sites of avulsion fractures causing hip pain are the sartorius attachment at the ASIS, the rectus femoris attachment at the anterior inferior iliac spine, and the hamstring attachment onto the ischial tuberosity.10 Radiographs are diagnostic.16,18
Treatment is conservative, including rest, ice, analgesics, and ROM exercises. Advise the patient to refrain from stretching the injured muscle attachment for 6 weeks, then gradually return to activity. Surgery is needed only if there is a large separation (>2 cm).
Acetabular labral tears are seen in athletes of all ages. Pain may be acute from a traumatic event or insidious from repetitive trauma.10 Structural or developmental abnormalities may also predispose certain athletes to injury.10 Patients will complain of pain, snapping, or a “giving way” sensation in the anteromedial area of the hip. On examination, the impingement test—forced flexion/adduction and internal rotation— may reproduce the groin pain, or the snapping maneuver may produce an audible sound.10,16,19
Radiographs are obtained initially to rule out other causes of hip pain and to assess for predisposing abnormalities, such as femoroacetabular impingement. Magnetic resonance arthrogram is a highly sensitive test for labral tears and is usually diagnostic.10 Labral tears are rarely an isolated event, however, and are usually seen in combination with a chondral injury, ligamentum teres tear, synovitis, or loose bodies.10
After diagnosis, a trial of activity modification, NSAIDs, and physical therapy is acceptable. If there is no improvement after 4 to 6 weeks, patients should be referred to an orthopedist for hip arthroscopy. A few studies have found that arthroscopy provides excellent symptom relief in 70% to 90% of patients,10,19 with a return to full activity in 6 to 12 weeks.
Trochanteric bursitis is commonly seen in older adults, but can occur in children. It has been associated with leg length discrepancy and obesity—and, in younger athletes, it is often linked to running and climbing.
The condition is caused by repetitive trauma from contraction of the muscles inserting on the greater trochanter. Patients develop chronic, intermittent lateral hip pain, which may be worse with direct pressure. The predominant physical exam finding is pain with direct pressure over the greater trochanter. One study reported that >50% of patients with trochanteric bursitis had a positive Patrick’s test—the presence of pain with Flexion, ABduction, and External Rotation (FABER) of the affected hip.20
ROM and hip radiographs are typically normal. Diagnosis is clinical, although there is a spectrum of disorders that present with lateral hip pain. The exact source of pain is often unknown and can be from bone, tendon, or bursa. In patients with trochanteric bursitis, gluteus medius tendinopathy or syndrome should also be considered.
Treatment begins with conservative management—starting with heat and NSAIDs for the first 4 weeks, restriction of repetitive motion, correction of any underlying gait disturbance, and performance of passive stretching exercises. If no improvement occurs, a local corticosteroid injection into the point of maximum tenderness can be therapeutic. It can also be diagnostic for trochanteric bursitis if symptom relief is achieved. One study showed a 90% improvement rate with 1 to 3 injections.21,22 More recent studies show the average improvement in symptom relief is in the range of 70% to 100%, but long-term follow-up varies.20
Is an osteoid osteoma to blame?
Osteoid osteomas are common benign skeletal lesions seen in young adults with hip pain, but may be an incidental finding. The average patient age is 10 to 20 years, with males affected more than females. Pain is the predominant symptom, starting as mild and intermittent and progressing to constant and severe. Night pain is common.23 Other symptoms are swelling, deformity, or limp.
Dramatic relief of pain with aspirin or NSAIDs is a diagnostic sign of osteoid osteoma. Diagnosis is made by radiographs. Treatment is surgical excision of the osteoid osteoma nidus, resulting in a good long-term prognosis.23
CORRESPONDENCE Janna Johanns, MD, Montana Family Medicine Residency, 123 South 27th Street, Billings, MT 59101; [email protected]
1. Haueisen DC, Weiner DS, Weiner SD. The characterization of “transient synovitis of the hip” in children. J Pediatr Orthop. 1986;6:11-17.
2. Frick S. Evaluation of the child who has hip pain. Orthop Clin North Am. 2006;37:133-140.
3. Bennett OM, Namnyak SS. Acute septic arthritis of the hip joint in infancy and childhood. Clin Orthop Relat Res. 1992;281:123-132.
4. Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction alogrithm. J Bone Joint. 1999;81:1662-1670.
5. Adkins SB, III, Figler RA. Hip pain in athletes. Am Fam Physician. 2000;61:2109-2118.
6. Liu RW, Abaza H, Gilmore A. The limping child in the urgent care center. J Urgent Care Med. 2007;2:11-22.
7. Leet AI, Skaggs DL. Evaluation of the acutely limping child. Am Fam Physician. 2000;61:1011-1018.
8. Landin LA, Danielson LG, Wattsgard CW. Transient synovitis of the hip. Its incidence, epidemiology, and relation to Perthes’ disease. J Bone Joint Surg. 1987;69:238-242.
9. Weinstein SL. Bristol-Myers Squibb/Zimmer award for distinguished achievement in orthopaedic research. Long term follow-up of pediatric orthopedic conditions. J Bone Joint Surg. 2000;82-A:980-990.
10. Kocher MS, Tucker R. Pediatric athlete hip disorders. Clin Sports Med. 2006;25:241-253.
11. Lacroix VJ. A complete approach to groin pain. Phys Sportsmed. 2000;28:66-86.
12. Tokmakova KP, Stanton RP, Mason DE. Factors influencing the development of osteonecrosis in patients treated for slipped capital femoral epiphysis. J Bone Joint Surg Am. 2003;85:798-801.
13. Reynolds R. Diagnosis and treatment of slipped capital femoral epiphysis. Curr Opin Pediatr. 1999;11:80-83.
14. Heyworth BE, Green DW. Lower extremity stress fractures in pediatric and adolescent athletes. Curr Opin Pediatr. 2008;20:58-61.
15. Clement DB, Ammann W, Taunton JE, et al. Exercise-induced stress injuries to the femur. Int J Sports Med. 1993;14:347-352.
16. Ecklund K. Magnetic resonance imaging of pediatric musculoskeletal trauma. Top Magn Reson Imaging. 2002;13:203-217.
17. Idjadi J, Meislin R. Symptomatic snapping hip. Phys Sportsmed. 2004;32:25-31.
18. Paluska SA. An overview of hip injuries in running. Sports Med. 2005;35:991-1014.
19. Larson C, Swaringen J, Morrison G. Evaluation and management of hip pain. The emerging role of hip arthroscopy. Phys Sportsmed. 2005;33:26-32.
20. Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanteric pain syndrome). Mayo Clin Proc. 1996;71:565-569.
21. Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehab. 1986;67:815-817.
22. Ege Rasmussen KJ, Fano N. Trochanteric bursitis. Treatment by corticosteroid injection. Scand J Rheumatol. 1985;14:417-420.
23. Kransdorf MJ, Stull MA, Gilkey FW, et al. Osteoid osteoma. Radiographics. 1991;11:671-696.
• When you suspect an infectious cause of hip pain, immediately order laboratory studies, blood cultures, and hip radiographs to rule out septic arthritis. A
• When you suspect avascular necrosis of the femoral head, instruct the patient to remain non-weight bearing and provide a referral to an orthopedist. A
• Stabilization with in situ pinning is the gold standard treatment for slipped capital femoral epiphysis, whether the slip is stable or unstable. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Sean L, a 12-year-old middle school student in the 90th percentile for weight, limps into your office and reports that it hurts to put his full weight down on his right leg. The pain just started, Sean says, but he began limping a day or 2 earlier. Sean plays on his school’s football team, and he wants to know what you can give him to relieve the pain so he won’t have to miss any games. What can you tell him?
Family physicians are increasingly likely to see children and adolescents with hip pain, the combined result of greater sports participation and a surge in childhood obesity. Diagnosing pediatric hip pain can be a daunting task, not only because of the complexity of the hip joint, but because of the need to consider bone, joint, tendon, muscle, bursa, and referred pain in the differential diagnosis.
But it doesn’t have to be. Being familiar with the major causes of pediatric hip pain, the diagnostic tests and maneuvers that are part of a comprehensive work-up, and the conditions that require rapid referral to an orthopedist makes it possible to adopt a straightforward approach. We’ve developed this review with that goal in mind.
Assess pain and movement with these maneuvers and tests
Begin with a pain history, determining the location of the hip pain—anterior, lateral, or posterior. Ask the patient to describe the pain and its quality: Is it diffuse, localized, or radiating? Identify any aggravating or relieving factors, and question the patient (or parents) about the onset, reproducibility, and timing of the pain, including the presence or absence of nighttime pain.
Find out, too, whether the pain is causing a limp; what effect, if any, the pain has had on the patient’s ability to bear weight; and to what extent the patient’s activity level has been affected. Then move on to the physical examination.
Begin with the patient standing up. Observe his or her gait, posture, and alignment. Check for Trendelenburg’s sign, in which the ipsilateral hip drops when the patient raises the unaffected leg. Its presence indicates a weakness of the opposite hip abductor.
With the patient in a supine position, inspect the hip for swelling, erythema, and warmth. Palpate the affected area, but keep in mind that palpation may not always reveal much because of the depth of the hip joint. If the patient is overweight, palpation of the muscles, tendons, or bones may be particularly difficult.
Test active and passive range of motion (ROM) and muscle strength of the hip in all directions. (Patients who are unable to tolerate lying down can undergo most of the ROM and strength tests in a seated position.) Check for a discrepancy in leg length, not only by visual inspection, but by measuring from the anterior superior iliac spine (ASIS) to the lateral malleoli.
Perform more focused maneuvers, as needed. If lumbar radiculopathy is a possibility, for example, do a straight leg raise, lifting the leg on the affected side in full extension with the ankle dorsiflexed, and repeat with the leg on the unaffected side. The test is positive if radiating pain down the affected leg and buttock is reproduced at ≤60° of leg elevation (or leg extension if the patient is seated). Conduct Ober’s test (FIGURE 1) to check for iliotibial band syndrome.
Follow with a system review, asking about recent conditions, including fever and infection, trauma, and constitutional, abdominal, and genitourinary symptoms. Perform an abdominal exam, and, if indicated, a pelvic or hernia exam. Check reflexes and sensation, as warranted, and examine the spine and knee.
CASE Sean is a healthy boy with no known medical problems. He has not been ill recently, and has not had any unexplained weight loss. His vital signs are normal, and he does not appear ill. He walks with a limp.
On examination, Sean has no palpable area of tenderness, swelling, or ecchymosis. His right hip has limited and painful internal rotation and, when flexed, it falls out to the side in external rotation.
FIGURE 1
Ober’s test for iliotibial band syndrome
With the patient lying on the unaffected side, passively extend the affected leg and allow the knee to drop. The test is positive if the patient experiences pain along the lateral side of the thigh or the knee does not drop down to the table.
Hip pain and infection? Consider septic arthritis
Is your patient febrile or recovering from an infection? When you suspect an acute infectious cause of hip pain, there are 2 disorders to consider in the differential diagnosis: transient synovitis (TS) and septic arthritis. Both are associated with an acute onset of pain and limping or non-weight bearing, and generally affect young children: Septic arthritis is most common in children between the age of 3 and 6 years, while the typical age range for TS is 3 through 8.1-4
There are other important differences. TS is a benign, self-limited, and common cause of hip pain in young children,5 which may be preceded by a viral infection.1 Septic arthritis is a serious condition that requires rapid identification; a delay in treatment can cause significant long-term morbidity. Complications may include early arthritis, shortened limb, dislocation, and osteonecrosis.
Because it can be difficult to distinguish between septic arthritis and TS, multiple studies have looked at the best way to make that determination. 1-7
The criteria most commonly used to identify septic arthritis are:
- fever
- refusal to bear weight
- erythrocyte sedimentation rate (ESR) >40 mm/h
- white blood cell count >12,000 mm3.
One study showed a predictive probability of 97% for septic arthritis when 3 of the 4 above criteria were present, and 99% if the patient had all 4.2,4 Other studies added 2 additional criteria—C-reactive protein (CRP) >1 mg/dL and medial joint space widening of >2 mm—with similar predictive probabilities (93% and 99%, respectively, if 3 or 4 of the 6 criteria were positive).2,4,6
Order lab work (ESR, CRP, complete blood count, and blood cultures) for any young patient whose hip pain is thought to be associated with an infectious process. Obtain hip anterior/posterior (AP) and frog lateral radiographs to look for joint space widening, as well.1-4
In addition to the above criteria, suspect septic arthritis in a child who presents with acute onset of hip pain, looks ill, and has limited ROM—particularly with internal rotation. In contrast, children with TS do not look sick and, while they often have limited ROM, it is primarily just at extremes. A modified log roll test can be used to assess the rotation of the hip.
An ultrasound-guided aspiration of fluid is the gold standard for septic arthritis diagnosis. Treatment is emergent surgical drainage and parenteral antibiotics, which should be withheld until fluid is aspirated or the joint is surgically drained. The most common causative organism is Staphylococcus aureus.3,7
It is reasonable to withhold joint aspiration for patients who don’t look sick and have normal labs and reliable follow-up, and to watch closely, with conservative management including nonsteroidal anti-inflammatory drugs (NSAIDs) and activity, as tolerated, instead.
There is some concern that TS may lead to Legg-Calves-Perthe’s disease, also known as avascular necrosis of the femoral head, although there is no strong evidence to support it. To be safe, however, obtain radiographs 2 to 18 months after TS resolves to check for further damage or complications.1,8
Femoral head disorders: When x-rays help, when they don’t
There are 2 femoral head disorders that commonly affect children and adolescents: Avascular necrosis of the femoral head and slipped capital femoral epiphysis (SCFE). Age alone is a clue to detection; children with avascular necrosis tend to be younger than those with SCFE.
Avascular necrosis of the femoral head is most commonly seen in children between the ages of 4 and 8 years, and occurs more frequently in boys than in girls. Although there is disagreement about the etiology of avascular necrosis, the condition is thought to result from a disruption in femoral blood supply, leading to osteonecrosis and flattening of the weight-bearing surface of the femoral head. One study found that structural abnormalities in the epiphyseal cartilage may lead to collapse.9
The condition often begins with a painless limp that develops—typically in 1 to 3 months—into groin, thigh, or knee pain; worsens with activity; and is relieved with rest.5 Abduction and internal rotation are limited on exam.
In patients with avascular necrosis, hip AP and frog lateral radiographs are diagnostic, with evidence of increased density of 1 epiphysis and flattening or fragmentation of the femoral head.7 When you suspect avascular necrosis, advise the patient to avoid weight bearing—and provide a referral to a pediatric orthopedist.
Treatment has consisted of containment of the femoral head with the use of splints, although there is little evidence that this treatment alters outcomes.9,10 One study found conflicting evidence that it improved results and does not support its use.9 This is why having a pediatric orthopedist involved in these cases is important.
Long-term prognosis is closely related to the degree of involvement of the femoral head and to the age at onset. Those who are younger than 6 to 8 years typically have the best outcomes, with less hip pain and dysfunction later in life.9,10
SCFE, the most common hip disorder in adolescents, can be easily missed. SCFE has a strong correlation with obesity and is especially common in obese males between the ages of 10 and 16 years who have delayed secondary sex characteristics.2,11 SCFE is generally a mechanical disorder, but in children who are younger than 10 or have low weight or height for their age, an endocrine work-up is indicated.
Symptoms include a painful limp and nonspecific knee, anterior thigh, or groin pain. A delay in diagnosis has a significant effect on complications. Prognosis is also related to the stability of the slip.11,12 An unstable slip is defined as the inability to bear weight.13 The risk of osteonecrosis, a complication of SCFE, is negligible if the slip is stable, but may be as high as 50% when the slip is unstable.2
On examination, internal rotation is painful and limited, and flexion of the hip will lead to simultaneous external rotation. Leg length discrepancy or a positive Trendelenburg’s sign may be present. Diagnosis may be made with bilateral AP (FIGURES 2A AND 2B) and frog lateral radiographic views, looking for growth plate widening.12 Klein’s line—the line that would intersect the epiphysis when drawn along the anterior neck of the femur of an AP view of a normal hip13—is abnormal in a hip with SCFE.
CT or MRI can be performed in patients who have clinical evidence of SCFE but normal radiographs. Treatment is the same regardless of whether the slip is stable or unstable—patients are told to avoid weight bearing and are sent to an orthopedist. Stabilization with in situ pinning is the gold standard, regardless of severity.9,10,12
CASE AP x-rays of Sean’s right hip are abnormal, showing that the femoral epiphysis is not aligned with the femoral neck correctly when compared with the opposite side. You advise the patient and his parents that he has a serious condition called SCFE, which can lead to long-term problems if not treated surgically. You recommend that he start using crutches and remain fully non-weight bearing on his right leg, and refer him to a pediatric orthopedist.
FIGURE 2
Bilateral AP views reveal slipped capital femoral epiphysis
X-rays show the pelvic widening of the physis on the right (A) and the epiphysis slipping posteriorly and inferiorly (B).
Suspect these hip disorders in young athletes
Femoral stress fractures are particularly common in adolescents who are runners or endurance athletes. The classic history is gradual onset of anterior thigh pain, beginning during physical activity and progressing to pain at rest. Risk factors for femoral stress fractures include the female athlete triad (amenorrhea, eating disorder, and osteoporosis), a recent change in training, poor biomechanics, and underlying bone or metabolic disease.14
A positive hop test. The physical exam in a patient with a femoral stress fracture is likely to be normal, with the possible exception of limitation in hip ROM at the extremes. Pain may be reproduced with hopping (a positive result) on the affected leg; 1 study noted that 70% of patients with femoral stress fractures had a positive hop test.15
Hip radiographs should be done, but may not be helpful. In initial x-rays, sensitivity may be as low as 15%; delayed x-rays, taken 2 to 4 weeks later, have a sensitivity of about 50% for findings suggestive of a stress fracture.16
Although bone scan and MRI have approximately equal sensitivity, bone scan is less specific for detecting early stress fractures, so MRI has become the gold standard for diagnosing femoral stress fractures.14 Treatment depends on the location of the fracture. A compression stress fracture on the inferior surface of the femoral neck has a good prognosis when the patient remains non-weight bearing for 6 to 8 weeks, then gradually returns to activity.14
Tension stress fractures are on the superior surface, and patients need to be sent to an orthopedist for internal fixation.14,16 A tension-sided fracture can progress to non-union or avascular necrosis. Training and diet should be modified as indicated to promote healing and prevent recurrence.
Does the patient’s hip make a snapping sound?
Patients with snapping of the hip can be categorized into those whose injuries are painful, and those whose injuries are not. Reassure patients with pain-free snapping that there is no reason to be concerned.
External snapping is usually related to the iliotibial band moving over the greater trochanteric bursa, which can lead to a painful bursa.17 The key symptom, in addition to the snapping, is lateral hip pain of gradual onset. Examination reproduces the pain with the snapping hip maneuver (FIGURES 3A AND 3B).
Internal snapping is related to the iliopsoas tendon passing over the femoral head and hip capsule or over the iliopectineal eminence and bony ridge of the lesser trochanter.17 Inflammation of the iliopsoas bursa may lead to painful snapping. This pain is anterior in location, and the snap can be reproduced with the patient lying on the unaffected side, bringing the affected hip passively from flexed, abducted, and externally rotated to a medial position of extension, adduction, and internal rotation.
Internal and external snapping usually occurs in patients whose activities involve the repetitive motions done in the exam maneuvers. Intra-articular snapping is due to loose bodies or acetabular labral tears.
Imaging for the patient with painful hip snapping consists of hip radiographs—usually negative—and ultrasound. MRI is done if intra-articular pathology is suspected.17 Treatment of snapping hips includes activity modification, NSAIDs, physical therapy, and possible steroid injection. Rarely is the condition surgically treated.
FIGURE 3
Snapping maneuver can help identify source of pain
With the patient lying with the unaffected side down, passively abduct the affected hip (A), then move from full extension to 90° of flexion (B). External snapping is usually related to the iliotibial band moving over the greater trochanter, which can lead to a painful bursa.
Avulsion fractures, acetabular tears, and bursitis
Avulsion fractures are a separation of the secondary growth center, the apophyses, from the underlying bone in skeletally immature athletes. They occur because the athlete’s tendons are stronger than the cartilaginous growth centers,10,11,16,18 and are produced by sudden forceful contraction of the muscle. The patient will complain of acute pain and swelling. The exam will be positive for palpable tenderness at the bony site and for muscle weakness. The most common sites of avulsion fractures causing hip pain are the sartorius attachment at the ASIS, the rectus femoris attachment at the anterior inferior iliac spine, and the hamstring attachment onto the ischial tuberosity.10 Radiographs are diagnostic.16,18
Treatment is conservative, including rest, ice, analgesics, and ROM exercises. Advise the patient to refrain from stretching the injured muscle attachment for 6 weeks, then gradually return to activity. Surgery is needed only if there is a large separation (>2 cm).
Acetabular labral tears are seen in athletes of all ages. Pain may be acute from a traumatic event or insidious from repetitive trauma.10 Structural or developmental abnormalities may also predispose certain athletes to injury.10 Patients will complain of pain, snapping, or a “giving way” sensation in the anteromedial area of the hip. On examination, the impingement test—forced flexion/adduction and internal rotation— may reproduce the groin pain, or the snapping maneuver may produce an audible sound.10,16,19
Radiographs are obtained initially to rule out other causes of hip pain and to assess for predisposing abnormalities, such as femoroacetabular impingement. Magnetic resonance arthrogram is a highly sensitive test for labral tears and is usually diagnostic.10 Labral tears are rarely an isolated event, however, and are usually seen in combination with a chondral injury, ligamentum teres tear, synovitis, or loose bodies.10
After diagnosis, a trial of activity modification, NSAIDs, and physical therapy is acceptable. If there is no improvement after 4 to 6 weeks, patients should be referred to an orthopedist for hip arthroscopy. A few studies have found that arthroscopy provides excellent symptom relief in 70% to 90% of patients,10,19 with a return to full activity in 6 to 12 weeks.
Trochanteric bursitis is commonly seen in older adults, but can occur in children. It has been associated with leg length discrepancy and obesity—and, in younger athletes, it is often linked to running and climbing.
The condition is caused by repetitive trauma from contraction of the muscles inserting on the greater trochanter. Patients develop chronic, intermittent lateral hip pain, which may be worse with direct pressure. The predominant physical exam finding is pain with direct pressure over the greater trochanter. One study reported that >50% of patients with trochanteric bursitis had a positive Patrick’s test—the presence of pain with Flexion, ABduction, and External Rotation (FABER) of the affected hip.20
ROM and hip radiographs are typically normal. Diagnosis is clinical, although there is a spectrum of disorders that present with lateral hip pain. The exact source of pain is often unknown and can be from bone, tendon, or bursa. In patients with trochanteric bursitis, gluteus medius tendinopathy or syndrome should also be considered.
Treatment begins with conservative management—starting with heat and NSAIDs for the first 4 weeks, restriction of repetitive motion, correction of any underlying gait disturbance, and performance of passive stretching exercises. If no improvement occurs, a local corticosteroid injection into the point of maximum tenderness can be therapeutic. It can also be diagnostic for trochanteric bursitis if symptom relief is achieved. One study showed a 90% improvement rate with 1 to 3 injections.21,22 More recent studies show the average improvement in symptom relief is in the range of 70% to 100%, but long-term follow-up varies.20
Is an osteoid osteoma to blame?
Osteoid osteomas are common benign skeletal lesions seen in young adults with hip pain, but may be an incidental finding. The average patient age is 10 to 20 years, with males affected more than females. Pain is the predominant symptom, starting as mild and intermittent and progressing to constant and severe. Night pain is common.23 Other symptoms are swelling, deformity, or limp.
Dramatic relief of pain with aspirin or NSAIDs is a diagnostic sign of osteoid osteoma. Diagnosis is made by radiographs. Treatment is surgical excision of the osteoid osteoma nidus, resulting in a good long-term prognosis.23
CORRESPONDENCE Janna Johanns, MD, Montana Family Medicine Residency, 123 South 27th Street, Billings, MT 59101; [email protected]
• When you suspect an infectious cause of hip pain, immediately order laboratory studies, blood cultures, and hip radiographs to rule out septic arthritis. A
• When you suspect avascular necrosis of the femoral head, instruct the patient to remain non-weight bearing and provide a referral to an orthopedist. A
• Stabilization with in situ pinning is the gold standard treatment for slipped capital femoral epiphysis, whether the slip is stable or unstable. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Sean L, a 12-year-old middle school student in the 90th percentile for weight, limps into your office and reports that it hurts to put his full weight down on his right leg. The pain just started, Sean says, but he began limping a day or 2 earlier. Sean plays on his school’s football team, and he wants to know what you can give him to relieve the pain so he won’t have to miss any games. What can you tell him?
Family physicians are increasingly likely to see children and adolescents with hip pain, the combined result of greater sports participation and a surge in childhood obesity. Diagnosing pediatric hip pain can be a daunting task, not only because of the complexity of the hip joint, but because of the need to consider bone, joint, tendon, muscle, bursa, and referred pain in the differential diagnosis.
But it doesn’t have to be. Being familiar with the major causes of pediatric hip pain, the diagnostic tests and maneuvers that are part of a comprehensive work-up, and the conditions that require rapid referral to an orthopedist makes it possible to adopt a straightforward approach. We’ve developed this review with that goal in mind.
Assess pain and movement with these maneuvers and tests
Begin with a pain history, determining the location of the hip pain—anterior, lateral, or posterior. Ask the patient to describe the pain and its quality: Is it diffuse, localized, or radiating? Identify any aggravating or relieving factors, and question the patient (or parents) about the onset, reproducibility, and timing of the pain, including the presence or absence of nighttime pain.
Find out, too, whether the pain is causing a limp; what effect, if any, the pain has had on the patient’s ability to bear weight; and to what extent the patient’s activity level has been affected. Then move on to the physical examination.
Begin with the patient standing up. Observe his or her gait, posture, and alignment. Check for Trendelenburg’s sign, in which the ipsilateral hip drops when the patient raises the unaffected leg. Its presence indicates a weakness of the opposite hip abductor.
With the patient in a supine position, inspect the hip for swelling, erythema, and warmth. Palpate the affected area, but keep in mind that palpation may not always reveal much because of the depth of the hip joint. If the patient is overweight, palpation of the muscles, tendons, or bones may be particularly difficult.
Test active and passive range of motion (ROM) and muscle strength of the hip in all directions. (Patients who are unable to tolerate lying down can undergo most of the ROM and strength tests in a seated position.) Check for a discrepancy in leg length, not only by visual inspection, but by measuring from the anterior superior iliac spine (ASIS) to the lateral malleoli.
Perform more focused maneuvers, as needed. If lumbar radiculopathy is a possibility, for example, do a straight leg raise, lifting the leg on the affected side in full extension with the ankle dorsiflexed, and repeat with the leg on the unaffected side. The test is positive if radiating pain down the affected leg and buttock is reproduced at ≤60° of leg elevation (or leg extension if the patient is seated). Conduct Ober’s test (FIGURE 1) to check for iliotibial band syndrome.
Follow with a system review, asking about recent conditions, including fever and infection, trauma, and constitutional, abdominal, and genitourinary symptoms. Perform an abdominal exam, and, if indicated, a pelvic or hernia exam. Check reflexes and sensation, as warranted, and examine the spine and knee.
CASE Sean is a healthy boy with no known medical problems. He has not been ill recently, and has not had any unexplained weight loss. His vital signs are normal, and he does not appear ill. He walks with a limp.
On examination, Sean has no palpable area of tenderness, swelling, or ecchymosis. His right hip has limited and painful internal rotation and, when flexed, it falls out to the side in external rotation.
FIGURE 1
Ober’s test for iliotibial band syndrome
With the patient lying on the unaffected side, passively extend the affected leg and allow the knee to drop. The test is positive if the patient experiences pain along the lateral side of the thigh or the knee does not drop down to the table.
Hip pain and infection? Consider septic arthritis
Is your patient febrile or recovering from an infection? When you suspect an acute infectious cause of hip pain, there are 2 disorders to consider in the differential diagnosis: transient synovitis (TS) and septic arthritis. Both are associated with an acute onset of pain and limping or non-weight bearing, and generally affect young children: Septic arthritis is most common in children between the age of 3 and 6 years, while the typical age range for TS is 3 through 8.1-4
There are other important differences. TS is a benign, self-limited, and common cause of hip pain in young children,5 which may be preceded by a viral infection.1 Septic arthritis is a serious condition that requires rapid identification; a delay in treatment can cause significant long-term morbidity. Complications may include early arthritis, shortened limb, dislocation, and osteonecrosis.
Because it can be difficult to distinguish between septic arthritis and TS, multiple studies have looked at the best way to make that determination. 1-7
The criteria most commonly used to identify septic arthritis are:
- fever
- refusal to bear weight
- erythrocyte sedimentation rate (ESR) >40 mm/h
- white blood cell count >12,000 mm3.
One study showed a predictive probability of 97% for septic arthritis when 3 of the 4 above criteria were present, and 99% if the patient had all 4.2,4 Other studies added 2 additional criteria—C-reactive protein (CRP) >1 mg/dL and medial joint space widening of >2 mm—with similar predictive probabilities (93% and 99%, respectively, if 3 or 4 of the 6 criteria were positive).2,4,6
Order lab work (ESR, CRP, complete blood count, and blood cultures) for any young patient whose hip pain is thought to be associated with an infectious process. Obtain hip anterior/posterior (AP) and frog lateral radiographs to look for joint space widening, as well.1-4
In addition to the above criteria, suspect septic arthritis in a child who presents with acute onset of hip pain, looks ill, and has limited ROM—particularly with internal rotation. In contrast, children with TS do not look sick and, while they often have limited ROM, it is primarily just at extremes. A modified log roll test can be used to assess the rotation of the hip.
An ultrasound-guided aspiration of fluid is the gold standard for septic arthritis diagnosis. Treatment is emergent surgical drainage and parenteral antibiotics, which should be withheld until fluid is aspirated or the joint is surgically drained. The most common causative organism is Staphylococcus aureus.3,7
It is reasonable to withhold joint aspiration for patients who don’t look sick and have normal labs and reliable follow-up, and to watch closely, with conservative management including nonsteroidal anti-inflammatory drugs (NSAIDs) and activity, as tolerated, instead.
There is some concern that TS may lead to Legg-Calves-Perthe’s disease, also known as avascular necrosis of the femoral head, although there is no strong evidence to support it. To be safe, however, obtain radiographs 2 to 18 months after TS resolves to check for further damage or complications.1,8
Femoral head disorders: When x-rays help, when they don’t
There are 2 femoral head disorders that commonly affect children and adolescents: Avascular necrosis of the femoral head and slipped capital femoral epiphysis (SCFE). Age alone is a clue to detection; children with avascular necrosis tend to be younger than those with SCFE.
Avascular necrosis of the femoral head is most commonly seen in children between the ages of 4 and 8 years, and occurs more frequently in boys than in girls. Although there is disagreement about the etiology of avascular necrosis, the condition is thought to result from a disruption in femoral blood supply, leading to osteonecrosis and flattening of the weight-bearing surface of the femoral head. One study found that structural abnormalities in the epiphyseal cartilage may lead to collapse.9
The condition often begins with a painless limp that develops—typically in 1 to 3 months—into groin, thigh, or knee pain; worsens with activity; and is relieved with rest.5 Abduction and internal rotation are limited on exam.
In patients with avascular necrosis, hip AP and frog lateral radiographs are diagnostic, with evidence of increased density of 1 epiphysis and flattening or fragmentation of the femoral head.7 When you suspect avascular necrosis, advise the patient to avoid weight bearing—and provide a referral to a pediatric orthopedist.
Treatment has consisted of containment of the femoral head with the use of splints, although there is little evidence that this treatment alters outcomes.9,10 One study found conflicting evidence that it improved results and does not support its use.9 This is why having a pediatric orthopedist involved in these cases is important.
Long-term prognosis is closely related to the degree of involvement of the femoral head and to the age at onset. Those who are younger than 6 to 8 years typically have the best outcomes, with less hip pain and dysfunction later in life.9,10
SCFE, the most common hip disorder in adolescents, can be easily missed. SCFE has a strong correlation with obesity and is especially common in obese males between the ages of 10 and 16 years who have delayed secondary sex characteristics.2,11 SCFE is generally a mechanical disorder, but in children who are younger than 10 or have low weight or height for their age, an endocrine work-up is indicated.
Symptoms include a painful limp and nonspecific knee, anterior thigh, or groin pain. A delay in diagnosis has a significant effect on complications. Prognosis is also related to the stability of the slip.11,12 An unstable slip is defined as the inability to bear weight.13 The risk of osteonecrosis, a complication of SCFE, is negligible if the slip is stable, but may be as high as 50% when the slip is unstable.2
On examination, internal rotation is painful and limited, and flexion of the hip will lead to simultaneous external rotation. Leg length discrepancy or a positive Trendelenburg’s sign may be present. Diagnosis may be made with bilateral AP (FIGURES 2A AND 2B) and frog lateral radiographic views, looking for growth plate widening.12 Klein’s line—the line that would intersect the epiphysis when drawn along the anterior neck of the femur of an AP view of a normal hip13—is abnormal in a hip with SCFE.
CT or MRI can be performed in patients who have clinical evidence of SCFE but normal radiographs. Treatment is the same regardless of whether the slip is stable or unstable—patients are told to avoid weight bearing and are sent to an orthopedist. Stabilization with in situ pinning is the gold standard, regardless of severity.9,10,12
CASE AP x-rays of Sean’s right hip are abnormal, showing that the femoral epiphysis is not aligned with the femoral neck correctly when compared with the opposite side. You advise the patient and his parents that he has a serious condition called SCFE, which can lead to long-term problems if not treated surgically. You recommend that he start using crutches and remain fully non-weight bearing on his right leg, and refer him to a pediatric orthopedist.
FIGURE 2
Bilateral AP views reveal slipped capital femoral epiphysis
X-rays show the pelvic widening of the physis on the right (A) and the epiphysis slipping posteriorly and inferiorly (B).
Suspect these hip disorders in young athletes
Femoral stress fractures are particularly common in adolescents who are runners or endurance athletes. The classic history is gradual onset of anterior thigh pain, beginning during physical activity and progressing to pain at rest. Risk factors for femoral stress fractures include the female athlete triad (amenorrhea, eating disorder, and osteoporosis), a recent change in training, poor biomechanics, and underlying bone or metabolic disease.14
A positive hop test. The physical exam in a patient with a femoral stress fracture is likely to be normal, with the possible exception of limitation in hip ROM at the extremes. Pain may be reproduced with hopping (a positive result) on the affected leg; 1 study noted that 70% of patients with femoral stress fractures had a positive hop test.15
Hip radiographs should be done, but may not be helpful. In initial x-rays, sensitivity may be as low as 15%; delayed x-rays, taken 2 to 4 weeks later, have a sensitivity of about 50% for findings suggestive of a stress fracture.16
Although bone scan and MRI have approximately equal sensitivity, bone scan is less specific for detecting early stress fractures, so MRI has become the gold standard for diagnosing femoral stress fractures.14 Treatment depends on the location of the fracture. A compression stress fracture on the inferior surface of the femoral neck has a good prognosis when the patient remains non-weight bearing for 6 to 8 weeks, then gradually returns to activity.14
Tension stress fractures are on the superior surface, and patients need to be sent to an orthopedist for internal fixation.14,16 A tension-sided fracture can progress to non-union or avascular necrosis. Training and diet should be modified as indicated to promote healing and prevent recurrence.
Does the patient’s hip make a snapping sound?
Patients with snapping of the hip can be categorized into those whose injuries are painful, and those whose injuries are not. Reassure patients with pain-free snapping that there is no reason to be concerned.
External snapping is usually related to the iliotibial band moving over the greater trochanteric bursa, which can lead to a painful bursa.17 The key symptom, in addition to the snapping, is lateral hip pain of gradual onset. Examination reproduces the pain with the snapping hip maneuver (FIGURES 3A AND 3B).
Internal snapping is related to the iliopsoas tendon passing over the femoral head and hip capsule or over the iliopectineal eminence and bony ridge of the lesser trochanter.17 Inflammation of the iliopsoas bursa may lead to painful snapping. This pain is anterior in location, and the snap can be reproduced with the patient lying on the unaffected side, bringing the affected hip passively from flexed, abducted, and externally rotated to a medial position of extension, adduction, and internal rotation.
Internal and external snapping usually occurs in patients whose activities involve the repetitive motions done in the exam maneuvers. Intra-articular snapping is due to loose bodies or acetabular labral tears.
Imaging for the patient with painful hip snapping consists of hip radiographs—usually negative—and ultrasound. MRI is done if intra-articular pathology is suspected.17 Treatment of snapping hips includes activity modification, NSAIDs, physical therapy, and possible steroid injection. Rarely is the condition surgically treated.
FIGURE 3
Snapping maneuver can help identify source of pain
With the patient lying with the unaffected side down, passively abduct the affected hip (A), then move from full extension to 90° of flexion (B). External snapping is usually related to the iliotibial band moving over the greater trochanter, which can lead to a painful bursa.
Avulsion fractures, acetabular tears, and bursitis
Avulsion fractures are a separation of the secondary growth center, the apophyses, from the underlying bone in skeletally immature athletes. They occur because the athlete’s tendons are stronger than the cartilaginous growth centers,10,11,16,18 and are produced by sudden forceful contraction of the muscle. The patient will complain of acute pain and swelling. The exam will be positive for palpable tenderness at the bony site and for muscle weakness. The most common sites of avulsion fractures causing hip pain are the sartorius attachment at the ASIS, the rectus femoris attachment at the anterior inferior iliac spine, and the hamstring attachment onto the ischial tuberosity.10 Radiographs are diagnostic.16,18
Treatment is conservative, including rest, ice, analgesics, and ROM exercises. Advise the patient to refrain from stretching the injured muscle attachment for 6 weeks, then gradually return to activity. Surgery is needed only if there is a large separation (>2 cm).
Acetabular labral tears are seen in athletes of all ages. Pain may be acute from a traumatic event or insidious from repetitive trauma.10 Structural or developmental abnormalities may also predispose certain athletes to injury.10 Patients will complain of pain, snapping, or a “giving way” sensation in the anteromedial area of the hip. On examination, the impingement test—forced flexion/adduction and internal rotation— may reproduce the groin pain, or the snapping maneuver may produce an audible sound.10,16,19
Radiographs are obtained initially to rule out other causes of hip pain and to assess for predisposing abnormalities, such as femoroacetabular impingement. Magnetic resonance arthrogram is a highly sensitive test for labral tears and is usually diagnostic.10 Labral tears are rarely an isolated event, however, and are usually seen in combination with a chondral injury, ligamentum teres tear, synovitis, or loose bodies.10
After diagnosis, a trial of activity modification, NSAIDs, and physical therapy is acceptable. If there is no improvement after 4 to 6 weeks, patients should be referred to an orthopedist for hip arthroscopy. A few studies have found that arthroscopy provides excellent symptom relief in 70% to 90% of patients,10,19 with a return to full activity in 6 to 12 weeks.
Trochanteric bursitis is commonly seen in older adults, but can occur in children. It has been associated with leg length discrepancy and obesity—and, in younger athletes, it is often linked to running and climbing.
The condition is caused by repetitive trauma from contraction of the muscles inserting on the greater trochanter. Patients develop chronic, intermittent lateral hip pain, which may be worse with direct pressure. The predominant physical exam finding is pain with direct pressure over the greater trochanter. One study reported that >50% of patients with trochanteric bursitis had a positive Patrick’s test—the presence of pain with Flexion, ABduction, and External Rotation (FABER) of the affected hip.20
ROM and hip radiographs are typically normal. Diagnosis is clinical, although there is a spectrum of disorders that present with lateral hip pain. The exact source of pain is often unknown and can be from bone, tendon, or bursa. In patients with trochanteric bursitis, gluteus medius tendinopathy or syndrome should also be considered.
Treatment begins with conservative management—starting with heat and NSAIDs for the first 4 weeks, restriction of repetitive motion, correction of any underlying gait disturbance, and performance of passive stretching exercises. If no improvement occurs, a local corticosteroid injection into the point of maximum tenderness can be therapeutic. It can also be diagnostic for trochanteric bursitis if symptom relief is achieved. One study showed a 90% improvement rate with 1 to 3 injections.21,22 More recent studies show the average improvement in symptom relief is in the range of 70% to 100%, but long-term follow-up varies.20
Is an osteoid osteoma to blame?
Osteoid osteomas are common benign skeletal lesions seen in young adults with hip pain, but may be an incidental finding. The average patient age is 10 to 20 years, with males affected more than females. Pain is the predominant symptom, starting as mild and intermittent and progressing to constant and severe. Night pain is common.23 Other symptoms are swelling, deformity, or limp.
Dramatic relief of pain with aspirin or NSAIDs is a diagnostic sign of osteoid osteoma. Diagnosis is made by radiographs. Treatment is surgical excision of the osteoid osteoma nidus, resulting in a good long-term prognosis.23
CORRESPONDENCE Janna Johanns, MD, Montana Family Medicine Residency, 123 South 27th Street, Billings, MT 59101; [email protected]
1. Haueisen DC, Weiner DS, Weiner SD. The characterization of “transient synovitis of the hip” in children. J Pediatr Orthop. 1986;6:11-17.
2. Frick S. Evaluation of the child who has hip pain. Orthop Clin North Am. 2006;37:133-140.
3. Bennett OM, Namnyak SS. Acute septic arthritis of the hip joint in infancy and childhood. Clin Orthop Relat Res. 1992;281:123-132.
4. Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction alogrithm. J Bone Joint. 1999;81:1662-1670.
5. Adkins SB, III, Figler RA. Hip pain in athletes. Am Fam Physician. 2000;61:2109-2118.
6. Liu RW, Abaza H, Gilmore A. The limping child in the urgent care center. J Urgent Care Med. 2007;2:11-22.
7. Leet AI, Skaggs DL. Evaluation of the acutely limping child. Am Fam Physician. 2000;61:1011-1018.
8. Landin LA, Danielson LG, Wattsgard CW. Transient synovitis of the hip. Its incidence, epidemiology, and relation to Perthes’ disease. J Bone Joint Surg. 1987;69:238-242.
9. Weinstein SL. Bristol-Myers Squibb/Zimmer award for distinguished achievement in orthopaedic research. Long term follow-up of pediatric orthopedic conditions. J Bone Joint Surg. 2000;82-A:980-990.
10. Kocher MS, Tucker R. Pediatric athlete hip disorders. Clin Sports Med. 2006;25:241-253.
11. Lacroix VJ. A complete approach to groin pain. Phys Sportsmed. 2000;28:66-86.
12. Tokmakova KP, Stanton RP, Mason DE. Factors influencing the development of osteonecrosis in patients treated for slipped capital femoral epiphysis. J Bone Joint Surg Am. 2003;85:798-801.
13. Reynolds R. Diagnosis and treatment of slipped capital femoral epiphysis. Curr Opin Pediatr. 1999;11:80-83.
14. Heyworth BE, Green DW. Lower extremity stress fractures in pediatric and adolescent athletes. Curr Opin Pediatr. 2008;20:58-61.
15. Clement DB, Ammann W, Taunton JE, et al. Exercise-induced stress injuries to the femur. Int J Sports Med. 1993;14:347-352.
16. Ecklund K. Magnetic resonance imaging of pediatric musculoskeletal trauma. Top Magn Reson Imaging. 2002;13:203-217.
17. Idjadi J, Meislin R. Symptomatic snapping hip. Phys Sportsmed. 2004;32:25-31.
18. Paluska SA. An overview of hip injuries in running. Sports Med. 2005;35:991-1014.
19. Larson C, Swaringen J, Morrison G. Evaluation and management of hip pain. The emerging role of hip arthroscopy. Phys Sportsmed. 2005;33:26-32.
20. Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanteric pain syndrome). Mayo Clin Proc. 1996;71:565-569.
21. Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehab. 1986;67:815-817.
22. Ege Rasmussen KJ, Fano N. Trochanteric bursitis. Treatment by corticosteroid injection. Scand J Rheumatol. 1985;14:417-420.
23. Kransdorf MJ, Stull MA, Gilkey FW, et al. Osteoid osteoma. Radiographics. 1991;11:671-696.
1. Haueisen DC, Weiner DS, Weiner SD. The characterization of “transient synovitis of the hip” in children. J Pediatr Orthop. 1986;6:11-17.
2. Frick S. Evaluation of the child who has hip pain. Orthop Clin North Am. 2006;37:133-140.
3. Bennett OM, Namnyak SS. Acute septic arthritis of the hip joint in infancy and childhood. Clin Orthop Relat Res. 1992;281:123-132.
4. Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction alogrithm. J Bone Joint. 1999;81:1662-1670.
5. Adkins SB, III, Figler RA. Hip pain in athletes. Am Fam Physician. 2000;61:2109-2118.
6. Liu RW, Abaza H, Gilmore A. The limping child in the urgent care center. J Urgent Care Med. 2007;2:11-22.
7. Leet AI, Skaggs DL. Evaluation of the acutely limping child. Am Fam Physician. 2000;61:1011-1018.
8. Landin LA, Danielson LG, Wattsgard CW. Transient synovitis of the hip. Its incidence, epidemiology, and relation to Perthes’ disease. J Bone Joint Surg. 1987;69:238-242.
9. Weinstein SL. Bristol-Myers Squibb/Zimmer award for distinguished achievement in orthopaedic research. Long term follow-up of pediatric orthopedic conditions. J Bone Joint Surg. 2000;82-A:980-990.
10. Kocher MS, Tucker R. Pediatric athlete hip disorders. Clin Sports Med. 2006;25:241-253.
11. Lacroix VJ. A complete approach to groin pain. Phys Sportsmed. 2000;28:66-86.
12. Tokmakova KP, Stanton RP, Mason DE. Factors influencing the development of osteonecrosis in patients treated for slipped capital femoral epiphysis. J Bone Joint Surg Am. 2003;85:798-801.
13. Reynolds R. Diagnosis and treatment of slipped capital femoral epiphysis. Curr Opin Pediatr. 1999;11:80-83.
14. Heyworth BE, Green DW. Lower extremity stress fractures in pediatric and adolescent athletes. Curr Opin Pediatr. 2008;20:58-61.
15. Clement DB, Ammann W, Taunton JE, et al. Exercise-induced stress injuries to the femur. Int J Sports Med. 1993;14:347-352.
16. Ecklund K. Magnetic resonance imaging of pediatric musculoskeletal trauma. Top Magn Reson Imaging. 2002;13:203-217.
17. Idjadi J, Meislin R. Symptomatic snapping hip. Phys Sportsmed. 2004;32:25-31.
18. Paluska SA. An overview of hip injuries in running. Sports Med. 2005;35:991-1014.
19. Larson C, Swaringen J, Morrison G. Evaluation and management of hip pain. The emerging role of hip arthroscopy. Phys Sportsmed. 2005;33:26-32.
20. Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanteric pain syndrome). Mayo Clin Proc. 1996;71:565-569.
21. Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehab. 1986;67:815-817.
22. Ege Rasmussen KJ, Fano N. Trochanteric bursitis. Treatment by corticosteroid injection. Scand J Rheumatol. 1985;14:417-420.
23. Kransdorf MJ, Stull MA, Gilkey FW, et al. Osteoid osteoma. Radiographics. 1991;11:671-696.