User login
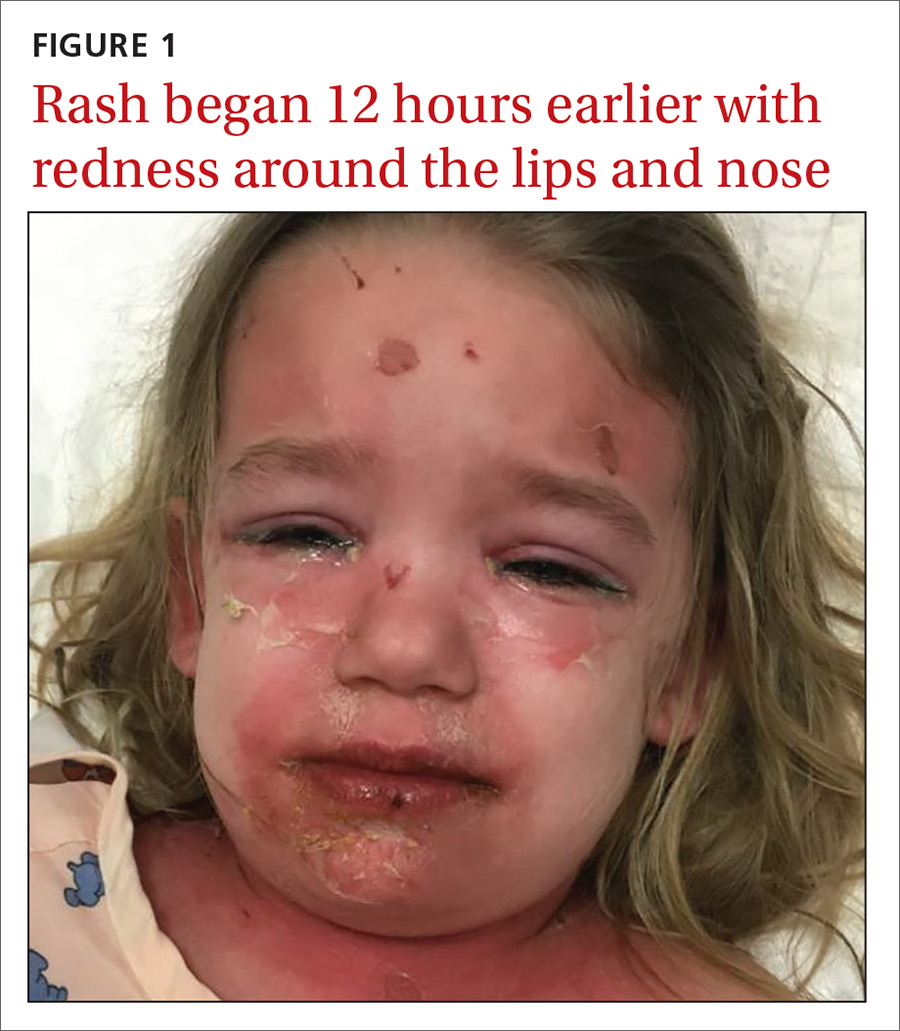
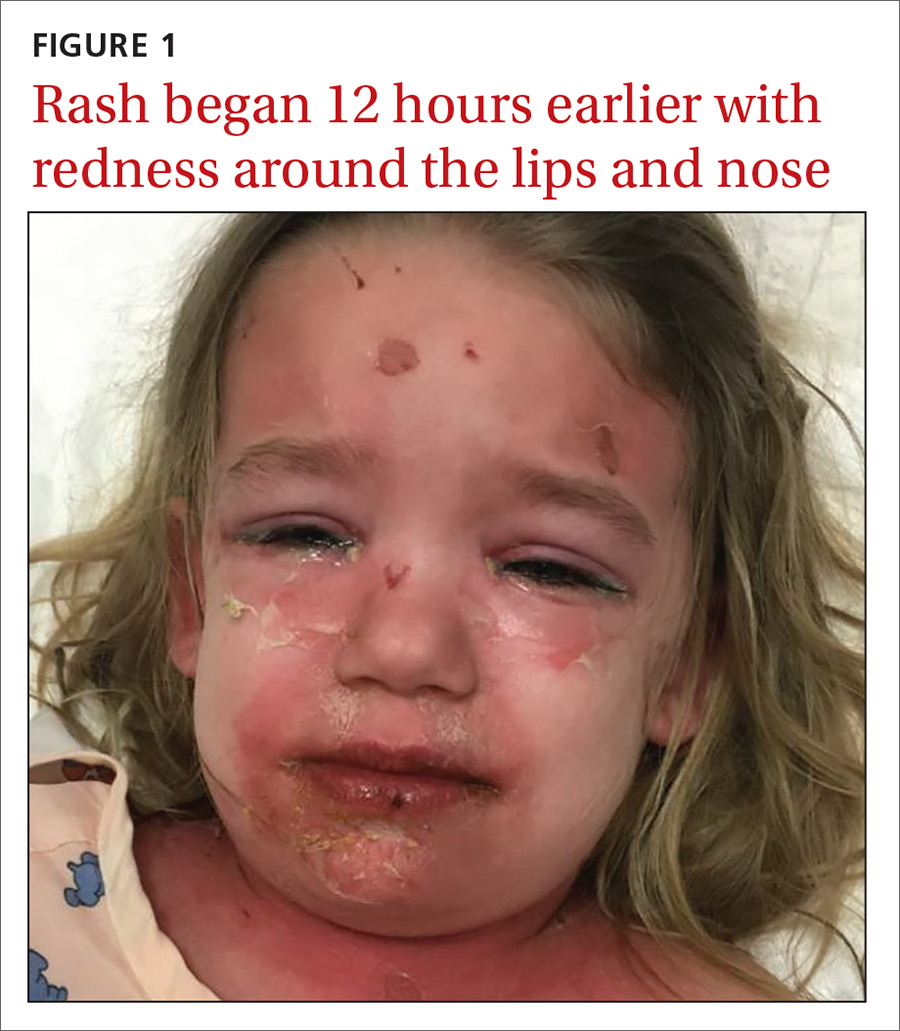
A 3-year-old girl presented with a rapidly progressing rash. The rash began the previous day with redness around her lips and nose (FIGURE 1). Twelve hours later, the rash had progressed to involve her neck, trunk, and inguinal area (FIGURE 2). The child’s parents reported that she had no recent illnesses or treatment with antibiotics.
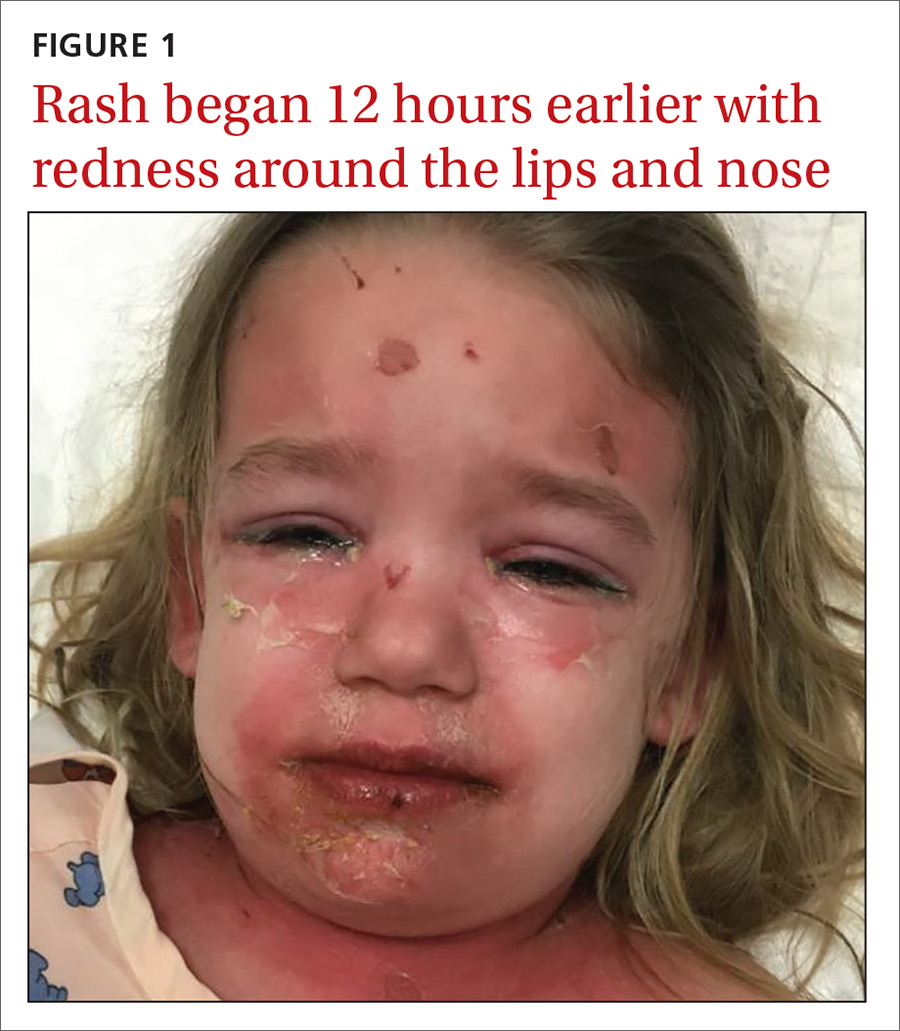
On physical examination, she was febrile (101.8° F) and irritable throughout the encounter. She had perioral and nasolabial erythema and dryness. Her lips were dry with no intraoral mucosal lesions, and her conjunctiva was clear.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Staphylococcal scalded skin syndrome
Based on the patient’s classic presentation and exam findings, the physician suspected staphylococcal scalded skin syndrome. SSSS is a rare but serious condition that progresses quickly with high fevers and diffuse painful erythema. The exact epidemiology of SSSS is unclear; some articles report incidences between 0.09 and 0.13 cases per 1 million people.1 The mortality rate is about 5% due to complications of sepsis, superinfection, and electrolyte disturbances.2
SSSS is caused by Staphylococcus aureus from a localized source that produces exfoliative toxins A and B that spread hematogenously, causing extensive epidermal damage. Exotoxins bind to desmosomes, causing skin cells to lose adherence.3 Histopathology shows intraepidermal cleavage through the stratum granulosum.
Infants and younger children appear more likely to be affected by SSSS, although it may occur in older children or adults who are immunocompromised. It may be that younger children are most susceptible due to a lack of antibodies to the toxin produced or because of a delayed clearance of the toxin-antibody complex from an immature renal system.
What you’ll see. Patients with SSSS may have a prodrome of irritability, malaise, and fever. The rash is first noticeable as erythema in the flexural areas.4 The erythematous tender patches spread and coalesce into a scarlatiniform erythema. Fragile bullae become large sheets of epidermis that slough (a positive Nikolsky’s sign).5 The desquamated areas can exhibit a scalded appearance.3
Differential diagnosis includes TEN and SJS
There is a broad differential for vesiculobullous rashes, ranging from self-limiting conditions to those that are life threatening.
Toxic epidermal necrolysis (TEN), Stevens-Johnson Syndrome (SJS), and erythema multiforme major (EMM) are immunological reactions to certain drugs or infections varying in the severity of their presentation. EMM, SJS, and TEN involve the mucosal surfaces, while SSSS does not. The histopathology of these conditions also differs from SSSS as they have keratinocyte necrosis of varying levels of the skin, whereas SSSS only involves the epidermis.
SSSS also may be confused with drug reactions, such as DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. DRESS typically is associated with anticonvulsants and sulfonamides and may have peripheral eosinophilia and a transaminitis.4
Continue to: Other more self-limited vesiculobullous rashes...
Other more self-limited vesiculobullous rashes include human enteroviruses such as coxsackie virus (hand-foot-mouth disease), echovirus, and enterovirus. However, unlike SSSS, which only affects the epidermis, these disorders may produce epidermal necrosis resulting in epidermal-dermal separation and mucocutaneous blistering.4
Making the diagnosis
When a patient has classic SSSS, the diagnosis can be made based on exam findings and the patient’s history. Families will usually report a generalized rash in neonates with desquamation of the entire skin. Fever is often present. Recent exposures to other family members with skin and soft-tissue infections is a possibility. If there is doubt, a skin biopsy can be obtained for histology. Lab work may reveal an elevated white blood cell count; blood culture is often negative.
The primary site of S aureus infection is usually the nasopharynx, causing a mild upper respiratory tract infection; therefore, nasopharyngeal cultures may be positive.4 Cultures can also be drawn from blood, wounds, nares, and ocular exudates if there is suspicion. Cultures from the actual blisters are typically negative, as the toxin—not the actual bacteria—is responsible for the blistering. Unlike adults who experience SSSS, children typically have negative blood cultures.4
Prompt treatment is essential
Swift diagnosis and management of SSSS is important due to the risk of severe disease. It is important to start antibiotics early because methicillin-sensitive S aureus is a predominant cause of SSSS.2 The epidemiology of methicillin-sensitive and methicillin-resistant S aureus (MRSA) continues to shift. A recent study suggests that empiric therapy with penicillinase-resistant penicillins, along with clindamycin, be employed until culture sensitivities are available to guide therapy.2 Local resistance patterns to S aureus should help guide initial empiric antibiotic treatment. Patients should receive intravenous (IV) fluids to compensate for insensible fluid losses similar to an extensive burn wound. Wound dressings placed over sloughed skin can help prevent secondary infection.2 Lastly, the use of anti-inflammatory drugs and opiates often depends upon the extent of pain the patient experiences.
Our patient was immediately started on IV clindamycin 10 mg/kg tid and IV fluids. She was given morphine 0.01 mg/kg for pain control. As expected, cultures of her nasopharynx, blood, and vulva did not grow S aureus. Although no organism was isolated, her rash rapidly improved, and she was discharged home to complete a 10-day oral course of clindamycin 10 mg/kg tid.
CORRESPONDENCE
Nicholas M. Potisek, MD, Wake Forest School of Medicine, Department of Pediatrics, Medical Center Blvd, Winston-Salem, NC 27157; [email protected]
1. Mockenhaupt M, Idzko M, Grosber M, et al. Epidemiology of staphylococcal scalded skin syndrome in Germany. J Invest Dermatol. 2005;124:700-703.
2. Braunstein I, Wanat K, Abuabara K, et al. Antibiotic sensitivity and resistance patterns in pediatric staphylococcal scalded skin syndrome. Pediatr Dermatol. 2014;31:305-308.
3. Mishra AK, Yadav, P, Mishra A. A systemic review on Staphylococcal Scalded Skin Syndrome (SSSS): A rare and critical disease of neonates. Open Microbiol J. 2016;10: 150-159.
4. Handler MZ, Schwarz RA. Staphylococcal scalded skin syndrome: diagnosis and management in children and adults. J Eur Acad Dermatol Venereol. 2014;28:1418-1423.
5. Franco L, Pereira P. Staphylococcal scalded skin syndrome. Indian Pediatr. 2016. 53:939.
A 3-year-old girl presented with a rapidly progressing rash. The rash began the previous day with redness around her lips and nose (FIGURE 1). Twelve hours later, the rash had progressed to involve her neck, trunk, and inguinal area (FIGURE 2). The child’s parents reported that she had no recent illnesses or treatment with antibiotics.
On physical examination, she was febrile (101.8° F) and irritable throughout the encounter. She had perioral and nasolabial erythema and dryness. Her lips were dry with no intraoral mucosal lesions, and her conjunctiva was clear.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Staphylococcal scalded skin syndrome
Based on the patient’s classic presentation and exam findings, the physician suspected staphylococcal scalded skin syndrome. SSSS is a rare but serious condition that progresses quickly with high fevers and diffuse painful erythema. The exact epidemiology of SSSS is unclear; some articles report incidences between 0.09 and 0.13 cases per 1 million people.1 The mortality rate is about 5% due to complications of sepsis, superinfection, and electrolyte disturbances.2
SSSS is caused by Staphylococcus aureus from a localized source that produces exfoliative toxins A and B that spread hematogenously, causing extensive epidermal damage. Exotoxins bind to desmosomes, causing skin cells to lose adherence.3 Histopathology shows intraepidermal cleavage through the stratum granulosum.
Infants and younger children appear more likely to be affected by SSSS, although it may occur in older children or adults who are immunocompromised. It may be that younger children are most susceptible due to a lack of antibodies to the toxin produced or because of a delayed clearance of the toxin-antibody complex from an immature renal system.
What you’ll see. Patients with SSSS may have a prodrome of irritability, malaise, and fever. The rash is first noticeable as erythema in the flexural areas.4 The erythematous tender patches spread and coalesce into a scarlatiniform erythema. Fragile bullae become large sheets of epidermis that slough (a positive Nikolsky’s sign).5 The desquamated areas can exhibit a scalded appearance.3
Differential diagnosis includes TEN and SJS
There is a broad differential for vesiculobullous rashes, ranging from self-limiting conditions to those that are life threatening.
Toxic epidermal necrolysis (TEN), Stevens-Johnson Syndrome (SJS), and erythema multiforme major (EMM) are immunological reactions to certain drugs or infections varying in the severity of their presentation. EMM, SJS, and TEN involve the mucosal surfaces, while SSSS does not. The histopathology of these conditions also differs from SSSS as they have keratinocyte necrosis of varying levels of the skin, whereas SSSS only involves the epidermis.
SSSS also may be confused with drug reactions, such as DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. DRESS typically is associated with anticonvulsants and sulfonamides and may have peripheral eosinophilia and a transaminitis.4
Continue to: Other more self-limited vesiculobullous rashes...
Other more self-limited vesiculobullous rashes include human enteroviruses such as coxsackie virus (hand-foot-mouth disease), echovirus, and enterovirus. However, unlike SSSS, which only affects the epidermis, these disorders may produce epidermal necrosis resulting in epidermal-dermal separation and mucocutaneous blistering.4
Making the diagnosis
When a patient has classic SSSS, the diagnosis can be made based on exam findings and the patient’s history. Families will usually report a generalized rash in neonates with desquamation of the entire skin. Fever is often present. Recent exposures to other family members with skin and soft-tissue infections is a possibility. If there is doubt, a skin biopsy can be obtained for histology. Lab work may reveal an elevated white blood cell count; blood culture is often negative.
The primary site of S aureus infection is usually the nasopharynx, causing a mild upper respiratory tract infection; therefore, nasopharyngeal cultures may be positive.4 Cultures can also be drawn from blood, wounds, nares, and ocular exudates if there is suspicion. Cultures from the actual blisters are typically negative, as the toxin—not the actual bacteria—is responsible for the blistering. Unlike adults who experience SSSS, children typically have negative blood cultures.4
Prompt treatment is essential
Swift diagnosis and management of SSSS is important due to the risk of severe disease. It is important to start antibiotics early because methicillin-sensitive S aureus is a predominant cause of SSSS.2 The epidemiology of methicillin-sensitive and methicillin-resistant S aureus (MRSA) continues to shift. A recent study suggests that empiric therapy with penicillinase-resistant penicillins, along with clindamycin, be employed until culture sensitivities are available to guide therapy.2 Local resistance patterns to S aureus should help guide initial empiric antibiotic treatment. Patients should receive intravenous (IV) fluids to compensate for insensible fluid losses similar to an extensive burn wound. Wound dressings placed over sloughed skin can help prevent secondary infection.2 Lastly, the use of anti-inflammatory drugs and opiates often depends upon the extent of pain the patient experiences.
Our patient was immediately started on IV clindamycin 10 mg/kg tid and IV fluids. She was given morphine 0.01 mg/kg for pain control. As expected, cultures of her nasopharynx, blood, and vulva did not grow S aureus. Although no organism was isolated, her rash rapidly improved, and she was discharged home to complete a 10-day oral course of clindamycin 10 mg/kg tid.
CORRESPONDENCE
Nicholas M. Potisek, MD, Wake Forest School of Medicine, Department of Pediatrics, Medical Center Blvd, Winston-Salem, NC 27157; [email protected]
A 3-year-old girl presented with a rapidly progressing rash. The rash began the previous day with redness around her lips and nose (FIGURE 1). Twelve hours later, the rash had progressed to involve her neck, trunk, and inguinal area (FIGURE 2). The child’s parents reported that she had no recent illnesses or treatment with antibiotics.
On physical examination, she was febrile (101.8° F) and irritable throughout the encounter. She had perioral and nasolabial erythema and dryness. Her lips were dry with no intraoral mucosal lesions, and her conjunctiva was clear.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Staphylococcal scalded skin syndrome
Based on the patient’s classic presentation and exam findings, the physician suspected staphylococcal scalded skin syndrome. SSSS is a rare but serious condition that progresses quickly with high fevers and diffuse painful erythema. The exact epidemiology of SSSS is unclear; some articles report incidences between 0.09 and 0.13 cases per 1 million people.1 The mortality rate is about 5% due to complications of sepsis, superinfection, and electrolyte disturbances.2
SSSS is caused by Staphylococcus aureus from a localized source that produces exfoliative toxins A and B that spread hematogenously, causing extensive epidermal damage. Exotoxins bind to desmosomes, causing skin cells to lose adherence.3 Histopathology shows intraepidermal cleavage through the stratum granulosum.
Infants and younger children appear more likely to be affected by SSSS, although it may occur in older children or adults who are immunocompromised. It may be that younger children are most susceptible due to a lack of antibodies to the toxin produced or because of a delayed clearance of the toxin-antibody complex from an immature renal system.
What you’ll see. Patients with SSSS may have a prodrome of irritability, malaise, and fever. The rash is first noticeable as erythema in the flexural areas.4 The erythematous tender patches spread and coalesce into a scarlatiniform erythema. Fragile bullae become large sheets of epidermis that slough (a positive Nikolsky’s sign).5 The desquamated areas can exhibit a scalded appearance.3
Differential diagnosis includes TEN and SJS
There is a broad differential for vesiculobullous rashes, ranging from self-limiting conditions to those that are life threatening.
Toxic epidermal necrolysis (TEN), Stevens-Johnson Syndrome (SJS), and erythema multiforme major (EMM) are immunological reactions to certain drugs or infections varying in the severity of their presentation. EMM, SJS, and TEN involve the mucosal surfaces, while SSSS does not. The histopathology of these conditions also differs from SSSS as they have keratinocyte necrosis of varying levels of the skin, whereas SSSS only involves the epidermis.
SSSS also may be confused with drug reactions, such as DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. DRESS typically is associated with anticonvulsants and sulfonamides and may have peripheral eosinophilia and a transaminitis.4
Continue to: Other more self-limited vesiculobullous rashes...
Other more self-limited vesiculobullous rashes include human enteroviruses such as coxsackie virus (hand-foot-mouth disease), echovirus, and enterovirus. However, unlike SSSS, which only affects the epidermis, these disorders may produce epidermal necrosis resulting in epidermal-dermal separation and mucocutaneous blistering.4
Making the diagnosis
When a patient has classic SSSS, the diagnosis can be made based on exam findings and the patient’s history. Families will usually report a generalized rash in neonates with desquamation of the entire skin. Fever is often present. Recent exposures to other family members with skin and soft-tissue infections is a possibility. If there is doubt, a skin biopsy can be obtained for histology. Lab work may reveal an elevated white blood cell count; blood culture is often negative.
The primary site of S aureus infection is usually the nasopharynx, causing a mild upper respiratory tract infection; therefore, nasopharyngeal cultures may be positive.4 Cultures can also be drawn from blood, wounds, nares, and ocular exudates if there is suspicion. Cultures from the actual blisters are typically negative, as the toxin—not the actual bacteria—is responsible for the blistering. Unlike adults who experience SSSS, children typically have negative blood cultures.4
Prompt treatment is essential
Swift diagnosis and management of SSSS is important due to the risk of severe disease. It is important to start antibiotics early because methicillin-sensitive S aureus is a predominant cause of SSSS.2 The epidemiology of methicillin-sensitive and methicillin-resistant S aureus (MRSA) continues to shift. A recent study suggests that empiric therapy with penicillinase-resistant penicillins, along with clindamycin, be employed until culture sensitivities are available to guide therapy.2 Local resistance patterns to S aureus should help guide initial empiric antibiotic treatment. Patients should receive intravenous (IV) fluids to compensate for insensible fluid losses similar to an extensive burn wound. Wound dressings placed over sloughed skin can help prevent secondary infection.2 Lastly, the use of anti-inflammatory drugs and opiates often depends upon the extent of pain the patient experiences.
Our patient was immediately started on IV clindamycin 10 mg/kg tid and IV fluids. She was given morphine 0.01 mg/kg for pain control. As expected, cultures of her nasopharynx, blood, and vulva did not grow S aureus. Although no organism was isolated, her rash rapidly improved, and she was discharged home to complete a 10-day oral course of clindamycin 10 mg/kg tid.
CORRESPONDENCE
Nicholas M. Potisek, MD, Wake Forest School of Medicine, Department of Pediatrics, Medical Center Blvd, Winston-Salem, NC 27157; [email protected]
1. Mockenhaupt M, Idzko M, Grosber M, et al. Epidemiology of staphylococcal scalded skin syndrome in Germany. J Invest Dermatol. 2005;124:700-703.
2. Braunstein I, Wanat K, Abuabara K, et al. Antibiotic sensitivity and resistance patterns in pediatric staphylococcal scalded skin syndrome. Pediatr Dermatol. 2014;31:305-308.
3. Mishra AK, Yadav, P, Mishra A. A systemic review on Staphylococcal Scalded Skin Syndrome (SSSS): A rare and critical disease of neonates. Open Microbiol J. 2016;10: 150-159.
4. Handler MZ, Schwarz RA. Staphylococcal scalded skin syndrome: diagnosis and management in children and adults. J Eur Acad Dermatol Venereol. 2014;28:1418-1423.
5. Franco L, Pereira P. Staphylococcal scalded skin syndrome. Indian Pediatr. 2016. 53:939.
1. Mockenhaupt M, Idzko M, Grosber M, et al. Epidemiology of staphylococcal scalded skin syndrome in Germany. J Invest Dermatol. 2005;124:700-703.
2. Braunstein I, Wanat K, Abuabara K, et al. Antibiotic sensitivity and resistance patterns in pediatric staphylococcal scalded skin syndrome. Pediatr Dermatol. 2014;31:305-308.
3. Mishra AK, Yadav, P, Mishra A. A systemic review on Staphylococcal Scalded Skin Syndrome (SSSS): A rare and critical disease of neonates. Open Microbiol J. 2016;10: 150-159.
4. Handler MZ, Schwarz RA. Staphylococcal scalded skin syndrome: diagnosis and management in children and adults. J Eur Acad Dermatol Venereol. 2014;28:1418-1423.
5. Franco L, Pereira P. Staphylococcal scalded skin syndrome. Indian Pediatr. 2016. 53:939.
