User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Ending a physician/patient relationship
HIV: How to provide compassionate care
The prevalence of HIV in persons with untreated psychiatric illness may be 10 to 20 times that of the general population.1 The U.S. Preventive Services Task Force has recommended HIV screening of all persons age 15 to 65 because 20% to 25% of individuals with HIV infection are unaware that they are HIV-positive.2 Because >20% of new HIV infections in the United States are undiagnosed,3 it is crucial to educate patients with mental illness about HIV prevention, make condoms available, and offer HIV testing.
As psychiatrists, we have a unique role in caring for patients at risk for or infected with HIV because in addition to comprehensive medical and psychiatric histories, we routinely take histories of substance use, sexual activities, relationships, and trauma, including childhood neglect and emotional, physical, and sexual abuse. We develop long-term, trusting relationships and work with individuals to change behaviors and maximize life potential.
Increasing awareness of stigma, discrimination, and psychiatric factors involved with the HIV pandemic can lead to decreased transmission of HIV infection and early diagnosis and treatment. Compassionate medical and psychiatric care can mitigate suffering in persons at risk for, infected with, or affected by HIV.
Preventing HIV transmission
AIDS differs from other complex, severe illnesses in 2 ways that are relevant to psychiatrists:
• it is almost entirely preventable
• HIV and AIDS are associated with sex, drugs, and AIDS-associated stigma and discrimination (“AIDSism”).4-6
Unsafe exposure of mucosal surfaces to the virus—primarily from exchanging body fluids in unprotected sexual encounters—accounts for 80% of new HIV infections.7 HIV transmission via sexual encounters is preventable with condoms. Percutaneous or intravenous infection with HIV—primarily from sharing needles in injection drug use—accounts for 20% of new infections.7 Use of alcohol or other substances can lead to sexual coercion, unprotected sex, and exchange of sex for drugs or money. Hence, treating substance use disorders can prevent HIV transmission.
Early diagnosis of HIV can lead to appropriate medical care, quicker onset of antiretroviral (ARV) treatment, and better outcomes. Recent research has shown that pre-exposure prophylaxis with ARV treatment can prevent transmission of HIV8; therefore, becoming aware of risk behaviors and prevention can be lifesaving for serodiscordant couples.
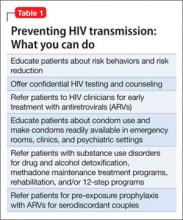
One of the most important ways to prevent HIV’s impact on the brain and CNS is to diagnose HIV shortly after transmission at onset of acute infection. If HIV is diagnosed very early—preferably as soon as possible after inoculation with HIV or at onset of the first flu-like symptoms—and treated with ARVs, the brain has less of an opportunity to act as an independent reservoir for HIV-infected cells and therefore to develop HIV-associated neurocognitive disorders.9,10Table 1 outlines steps psychiatrists can take to help prevent HIV transmission.
Psychiatric disorders and HIV
Psychiatric disorders and distress play a significant role in transmission of, exposure to, and infection with HIV (Table 2).4-6,11 They are relevant for prevention, clinical care, and adherence throughout every aspect of illness.
Comprehensive, compassionate, nonjudgmental care of persons at risk for or infected with HIV begins with a thorough psychiatric evaluation designed to provide an ego-supportive, sensitive, and comprehensive assessment that can guide other clinicians in providing care.12 Setting the tone and demonstrating compassion and respect includes shaking hands, which takes on special relevance in the context of AIDSism and stigma. Assessing the impact of HIV seropositivity or AIDS is best done by asking about the individual’s understanding of his or her diagnosis or illness and its impact. For some persons with HIV, verbalizing this understanding can be relieving as well as revealing. It is a chance for the patient to reveal painful experiences encountered in the home, school, camp, workplace, or community and the anguish of AIDSism and stigma.
Pay attention to sensitive and sometimes painful issues related to sexual history and sexuality. Questions related to sexual history and sexuality in heterosexual men and women as well as gay, lesbian, bisexual, and transgender individuals—such as “What is your sexual function like since you have been ill?” “Do feelings about your sexual identity play a role in your current level of distress?” and “What kind of barrier contraception are you using?”—are included in the comprehensive assessment described by Cohen et al.12
Comprehensive psychiatric evaluations can provide diagnoses, inform treatment, and mitigate anguish, distress, depression, anxiety, and substance use in persons with HIV and AIDS.12 A thorough and comprehensive assessment is crucial because HIV has an affinity for brain and neural tissue and can cause CNS complications such as HIV-associated neurocognitive disorders (HAND), even in otherwise healthy HIV-seropositive individuals. See this article at CurrentPsychiatry.com for a discussion of HAND and delirium in patients with HIV.
Some persons with HIV and AIDS do not have a psychiatric disorder, while others have multiple complex psychiatric disorders that are responses to illness or treatments or are associated with HIV/AIDS (such as HAND) or other medical illnesses and treatments (such as hepatitis C, cirrhosis, end-stage liver disease, HIV nephropathy, end-stage renal disease, anemia, coronary artery disease, and cancer). See this article at CurrentPsychiatry.com for case studies of HIV patients with delirium, depression, posttraumatic stress disorder (PTSD), and substance dependence.
Mood disorders. Depression is common among persons with HIV. Demoralization and bereavement may masquerade as depression and can complicate diagnosis and treatment. Depression and other mood disorders may be related to stigma and AIDSism as well as to biologic, psychological, social, and genetic factors. Because suicide is prevalent among persons with HIV and AIDS,13 every patient with HIV should be evaluated for depression and suicidal ideation.
PTSD is prevalent among persons with HIV. It is a risky diagnosis because it is associated with a sense of a foreshortened future, which leads to a lack of adequate self-care, poor adherence to medical care, risky behaviors, and comorbid substance dependence to help numb the pain of trauma.14,15 Persons with PTSD may have difficulty trusting clinicians and other authority figures if their trauma was a high-betrayal trauma, such as incest or military trauma.14,15
In patients with HIV, PTSD often is overlooked because it may be overshadowed by other psychiatric diagnoses. Intimate partner violence, history of childhood trauma, and childhood sexual abuse are risk factors for HIV infection and PTSD. Increased severity of HIV-related PTSD symptoms is associated with having a greater number of HIV-related physical symptoms, history of pre-HIV trauma, decreased social support, increased perception of stigma, and negative life events.
PTSD also is associated with nonadherence to risk reduction strategies and medical care.14,15 Diagnosis is further complicated by repression or retrograde amnesia of traumatic events and difficulties forming trusting relationships and disclosing HIV status to sexual partners or potential sexual partners because of fear of rejection.
Substance use disorders. Dependence on alcohol and other drugs complicates and perpetuates the HIV pandemic. Sharing needles and other drug paraphernalia is instrumental in HIV transmission. The indirect effects of alcohol and substance abuse include:
• the impact of intimate partner violence, child abuse, neglect, and/or abandonment
• development of PTSD in adults, with early childhood trauma leading to repeating their own history
• lack of self-care
• unhealthy partner choices
• use of drugs and alcohol to numb the pain associated with trauma.
Persons who are using alcohol or other drugs may have difficulty attending to their health, and substance dependence may prevent persons at risk from seeking HIV testing.
Intoxication from alcohol and drug use frequently leads to inappropriate partner choice, violent and coercive sexual behaviors, and lack of condom use. Substance dependence also may lead individuals to exchange sex for drugs and to fail to adhere to safer sexual practices or use sterile drug paraphernalia.
Treating persons with HIV/AIDS
Several organizations publish evidence-based clinical guidelines for treating depression, anxiety, substance abuse, and other psychiatric disorders in patients with HIV/AIDS. One such set of guidelines is available from the New York State Department of Health AIDS Institute at www.hivguidelines.org. As is the case with patients who do not have HIV, psychotherapy and pharmacotherapy are common first-line treatments.
Psychotherapy. Patients with HIV/AIDS with psychiatric comorbidities generally respond well to psychotherapeutic treatments.16,17 The choice of therapy needs to be tailored to the needs of individuals, couples, and families coping with AIDS. Options include:
• individual, couple, family, and group psychotherapy
• crisis intervention
• 12-step programs (Alcohol Anonymous, Narcotics Anonymous, etc.)
• adult survivors of child abuse programs (www.ascasupport.org), groups, and workbooks
• palliative psychiatry
• bereavement therapy
• spiritual support
• relaxation response
• wellness interventions such as exercise, yoga, keeping a journal, writing a life narrative, reading, artwork, movement therapy, listening to music or books on tape, and working on crossword puzzles and jigsaw puzzles.
Psychopharmacotherapy. Accurate diagnosis and awareness of drug-drug and drug-illness interactions are important when treating patients with HIV/AIDS; consult resources in the literature18 and online resources that are updated regularly (see Related Resources). Because persons with AIDS are particularly vulnerable to extrapyramidal and anticholinergic side effects of psychotropics, the principle start very low and go very slow is critical. For patients who are opioid-dependent, be cautious when prescribing medications that are cytochrome P450 3A4 inducers—such as carbamazepine, efavirenz, nevirapine, and ritonavir—because these medications can lower methadone levels in persons receiving agonist treatment and might lead to opioid withdrawal symptoms, discontinuation of ARVs, or relapse to opioids.18 When a person with AIDS is experiencing pain and is on a maintenance dose of methadone for heroin withdrawal, pain should be treated as a separate problem with additional opioids. Methadone for relapse prevention will target opioid tolerance needs and prevent withdrawal but will not provide analgesia for pain.
HIV through the life cycle
From prevention of prenatal transmission to the care of children with HIV to reproductive issues in serodiscordant couples, HIV complicates patients’ development. Table 3 outlines concerns regarding HIV transmission and treatment at different stages of a patient’s life.
Bottom Line
HIV transmission and effective treatment are complicated by a high prevalence of psychiatric comorbidities, including depression and other mood disorders, posttraumatic stress disorder, substance use disorders, and cognitive disorders. With an increased understanding of the issues faced by patients at risk for or infected with HIV, psychiatrists can help prevent HIV transmission, improve adherence to medical care, and diminish suffering, morbidity, and mortality.
Related Resources
- Academy of Psychosomatic Medicine HIV/AIDS Psychiatry Special Interest Group. www.apm.org/sigs/oap.
- New York State Department of Health AIDS Institute. HIV Clinical Resource. www.hivguidelines.org.
- University of Liverpool. HIV drug interactions list. www.hiv-druginteractions.org.
- Toronto General Hospital Immunodeficiency Clinic. Drug interactions tables. www.hivclinic.ca/main/drugs_interact.html.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Nevirapine • Viramune
Carbamazepine • Carbatrol, Tegretol, others
Olanzapine • Zyprexa
Quetiapine • Seroquel
Clonazepam • Klonopin
Ritonavir • Norvir
Efavirenz • Sustiva
Venlafaxine • Effexor
Escitalopram • Lexapro
Disclosure
Dr. Cohen reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Blank MB, Mandell DS, Aiken L, et al. Co-occurrence of HIV and serious mental illness among Medicaid recipients. Psychiatr Serv. 2002;53(7):868-873.
2.Moyer VA, on behalf of the U.S. Preventive Services Task Force. Screening for HIV: U.S. Preventive Services Task Force recommendation statement [published online April 30, 2013]. Ann Intern Med. doi:10.7326/0003-4819-159-1-201307020-00645.
3. Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520-529.
4. Cohen MA. AIDSism, a new form of discrimination. Am Med News. 1989;32:43.
5. Cohen MA, Gorman JM. Comprehensive textbook of AIDS psychiatry. New York, NY: Oxford University Press; 2008.
6. Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010.
7. World Health Organization, United Nations Children’s Fund, Joint United Nations Programme on HIV/AIDS. Global HIV/AIDS response. Epidemic update and health sector progress towards universal access. Progress report 2011. http://www.unaids.org/en/media/unaids/
contentassets/documents/unaidspublication/2011/
20111130_UA_Report_en.pdf. Accessed April 25, 2013.
8. Centers for Disease Control and Prevention (CDC). Interim guidance for clinicians considering the use of preexposure prophylaxis for the prevention of HIV infection in heterosexually active adults. MMWR Morb Mortal Wkly Rep. 2012;61(31):586-589.
9. Cysique LA, Murray JM, Dunbar M, et al. A screening algorithm for HIV-associated neurocognitive disorders. HIV Med. 2010;11(10):642-649.
10. Simioni S, Cavassini M, Annoni JM, et al. Cognitive dysfunction in HIV patients despite long-standing suppression of viremia. AIDS. 2010;24(9):1243-1250.
11. Cohen M, Hoffman RG, Cromwell C, et al. The prevalence of distress in persons with human immunodeficiency virus infection. Psychosomatics. 2002;43(1):10-15.
12. Cohen MA, Batista SM, Lux JZ. A biopsychosocial approach to psychiatric consultation in persons with HIV and AIDS. In: Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010:33-60.
13. Carrico AW. Elevated suicide rate among HIV-positive persons despite benefits of antiretroviral therapy: implications for a stress and coping model of suicide. Am J Psychiatry. 2010;167(2):117-119.
14. Cohen MA, Alfonso CA, Hoffman RG, et al. The impact of PTSD on treatment adherence in persons with HIV infection. Gen Hosp Psychiatry. 2001;23(5):294-296.
15. Boarts JM, Sledjeski EM, Bogart LM, et al. The differential impact of PTSD and depression on HIV disease markers and adherence to HAART in people living with HIV. AIDS Behav. 2006;10(3):253-261.
16. Sikkema KJ, Hansen NB, Ghebremichael M, et al. A randomized controlled trial of a coping group intervention for adults with HIV who are AIDS bereaved: longitudinal effects on grief. Health Psychol. 2006;25(5):563-570.
17. Cohen MA. Psychodynamic psychotherapy in an AIDS nursing home. J Am Acad Psychoanal. 1999;27(1):121-133.
18. Cozza KL, Goforth HW, Batista SM. Psychopharmacologic treatment issues in AIDS psychiatry. In: Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010:147-199.
The prevalence of HIV in persons with untreated psychiatric illness may be 10 to 20 times that of the general population.1 The U.S. Preventive Services Task Force has recommended HIV screening of all persons age 15 to 65 because 20% to 25% of individuals with HIV infection are unaware that they are HIV-positive.2 Because >20% of new HIV infections in the United States are undiagnosed,3 it is crucial to educate patients with mental illness about HIV prevention, make condoms available, and offer HIV testing.
As psychiatrists, we have a unique role in caring for patients at risk for or infected with HIV because in addition to comprehensive medical and psychiatric histories, we routinely take histories of substance use, sexual activities, relationships, and trauma, including childhood neglect and emotional, physical, and sexual abuse. We develop long-term, trusting relationships and work with individuals to change behaviors and maximize life potential.
Increasing awareness of stigma, discrimination, and psychiatric factors involved with the HIV pandemic can lead to decreased transmission of HIV infection and early diagnosis and treatment. Compassionate medical and psychiatric care can mitigate suffering in persons at risk for, infected with, or affected by HIV.
Preventing HIV transmission
AIDS differs from other complex, severe illnesses in 2 ways that are relevant to psychiatrists:
• it is almost entirely preventable
• HIV and AIDS are associated with sex, drugs, and AIDS-associated stigma and discrimination (“AIDSism”).4-6
Unsafe exposure of mucosal surfaces to the virus—primarily from exchanging body fluids in unprotected sexual encounters—accounts for 80% of new HIV infections.7 HIV transmission via sexual encounters is preventable with condoms. Percutaneous or intravenous infection with HIV—primarily from sharing needles in injection drug use—accounts for 20% of new infections.7 Use of alcohol or other substances can lead to sexual coercion, unprotected sex, and exchange of sex for drugs or money. Hence, treating substance use disorders can prevent HIV transmission.
Early diagnosis of HIV can lead to appropriate medical care, quicker onset of antiretroviral (ARV) treatment, and better outcomes. Recent research has shown that pre-exposure prophylaxis with ARV treatment can prevent transmission of HIV8; therefore, becoming aware of risk behaviors and prevention can be lifesaving for serodiscordant couples.
One of the most important ways to prevent HIV’s impact on the brain and CNS is to diagnose HIV shortly after transmission at onset of acute infection. If HIV is diagnosed very early—preferably as soon as possible after inoculation with HIV or at onset of the first flu-like symptoms—and treated with ARVs, the brain has less of an opportunity to act as an independent reservoir for HIV-infected cells and therefore to develop HIV-associated neurocognitive disorders.9,10Table 1 outlines steps psychiatrists can take to help prevent HIV transmission.
Psychiatric disorders and HIV
Psychiatric disorders and distress play a significant role in transmission of, exposure to, and infection with HIV (Table 2).4-6,11 They are relevant for prevention, clinical care, and adherence throughout every aspect of illness.
Comprehensive, compassionate, nonjudgmental care of persons at risk for or infected with HIV begins with a thorough psychiatric evaluation designed to provide an ego-supportive, sensitive, and comprehensive assessment that can guide other clinicians in providing care.12 Setting the tone and demonstrating compassion and respect includes shaking hands, which takes on special relevance in the context of AIDSism and stigma. Assessing the impact of HIV seropositivity or AIDS is best done by asking about the individual’s understanding of his or her diagnosis or illness and its impact. For some persons with HIV, verbalizing this understanding can be relieving as well as revealing. It is a chance for the patient to reveal painful experiences encountered in the home, school, camp, workplace, or community and the anguish of AIDSism and stigma.
Pay attention to sensitive and sometimes painful issues related to sexual history and sexuality. Questions related to sexual history and sexuality in heterosexual men and women as well as gay, lesbian, bisexual, and transgender individuals—such as “What is your sexual function like since you have been ill?” “Do feelings about your sexual identity play a role in your current level of distress?” and “What kind of barrier contraception are you using?”—are included in the comprehensive assessment described by Cohen et al.12
Comprehensive psychiatric evaluations can provide diagnoses, inform treatment, and mitigate anguish, distress, depression, anxiety, and substance use in persons with HIV and AIDS.12 A thorough and comprehensive assessment is crucial because HIV has an affinity for brain and neural tissue and can cause CNS complications such as HIV-associated neurocognitive disorders (HAND), even in otherwise healthy HIV-seropositive individuals. See this article at CurrentPsychiatry.com for a discussion of HAND and delirium in patients with HIV.
Some persons with HIV and AIDS do not have a psychiatric disorder, while others have multiple complex psychiatric disorders that are responses to illness or treatments or are associated with HIV/AIDS (such as HAND) or other medical illnesses and treatments (such as hepatitis C, cirrhosis, end-stage liver disease, HIV nephropathy, end-stage renal disease, anemia, coronary artery disease, and cancer). See this article at CurrentPsychiatry.com for case studies of HIV patients with delirium, depression, posttraumatic stress disorder (PTSD), and substance dependence.
Mood disorders. Depression is common among persons with HIV. Demoralization and bereavement may masquerade as depression and can complicate diagnosis and treatment. Depression and other mood disorders may be related to stigma and AIDSism as well as to biologic, psychological, social, and genetic factors. Because suicide is prevalent among persons with HIV and AIDS,13 every patient with HIV should be evaluated for depression and suicidal ideation.
PTSD is prevalent among persons with HIV. It is a risky diagnosis because it is associated with a sense of a foreshortened future, which leads to a lack of adequate self-care, poor adherence to medical care, risky behaviors, and comorbid substance dependence to help numb the pain of trauma.14,15 Persons with PTSD may have difficulty trusting clinicians and other authority figures if their trauma was a high-betrayal trauma, such as incest or military trauma.14,15
In patients with HIV, PTSD often is overlooked because it may be overshadowed by other psychiatric diagnoses. Intimate partner violence, history of childhood trauma, and childhood sexual abuse are risk factors for HIV infection and PTSD. Increased severity of HIV-related PTSD symptoms is associated with having a greater number of HIV-related physical symptoms, history of pre-HIV trauma, decreased social support, increased perception of stigma, and negative life events.
PTSD also is associated with nonadherence to risk reduction strategies and medical care.14,15 Diagnosis is further complicated by repression or retrograde amnesia of traumatic events and difficulties forming trusting relationships and disclosing HIV status to sexual partners or potential sexual partners because of fear of rejection.
Substance use disorders. Dependence on alcohol and other drugs complicates and perpetuates the HIV pandemic. Sharing needles and other drug paraphernalia is instrumental in HIV transmission. The indirect effects of alcohol and substance abuse include:
• the impact of intimate partner violence, child abuse, neglect, and/or abandonment
• development of PTSD in adults, with early childhood trauma leading to repeating their own history
• lack of self-care
• unhealthy partner choices
• use of drugs and alcohol to numb the pain associated with trauma.
Persons who are using alcohol or other drugs may have difficulty attending to their health, and substance dependence may prevent persons at risk from seeking HIV testing.
Intoxication from alcohol and drug use frequently leads to inappropriate partner choice, violent and coercive sexual behaviors, and lack of condom use. Substance dependence also may lead individuals to exchange sex for drugs and to fail to adhere to safer sexual practices or use sterile drug paraphernalia.
Treating persons with HIV/AIDS
Several organizations publish evidence-based clinical guidelines for treating depression, anxiety, substance abuse, and other psychiatric disorders in patients with HIV/AIDS. One such set of guidelines is available from the New York State Department of Health AIDS Institute at www.hivguidelines.org. As is the case with patients who do not have HIV, psychotherapy and pharmacotherapy are common first-line treatments.
Psychotherapy. Patients with HIV/AIDS with psychiatric comorbidities generally respond well to psychotherapeutic treatments.16,17 The choice of therapy needs to be tailored to the needs of individuals, couples, and families coping with AIDS. Options include:
• individual, couple, family, and group psychotherapy
• crisis intervention
• 12-step programs (Alcohol Anonymous, Narcotics Anonymous, etc.)
• adult survivors of child abuse programs (www.ascasupport.org), groups, and workbooks
• palliative psychiatry
• bereavement therapy
• spiritual support
• relaxation response
• wellness interventions such as exercise, yoga, keeping a journal, writing a life narrative, reading, artwork, movement therapy, listening to music or books on tape, and working on crossword puzzles and jigsaw puzzles.
Psychopharmacotherapy. Accurate diagnosis and awareness of drug-drug and drug-illness interactions are important when treating patients with HIV/AIDS; consult resources in the literature18 and online resources that are updated regularly (see Related Resources). Because persons with AIDS are particularly vulnerable to extrapyramidal and anticholinergic side effects of psychotropics, the principle start very low and go very slow is critical. For patients who are opioid-dependent, be cautious when prescribing medications that are cytochrome P450 3A4 inducers—such as carbamazepine, efavirenz, nevirapine, and ritonavir—because these medications can lower methadone levels in persons receiving agonist treatment and might lead to opioid withdrawal symptoms, discontinuation of ARVs, or relapse to opioids.18 When a person with AIDS is experiencing pain and is on a maintenance dose of methadone for heroin withdrawal, pain should be treated as a separate problem with additional opioids. Methadone for relapse prevention will target opioid tolerance needs and prevent withdrawal but will not provide analgesia for pain.
HIV through the life cycle
From prevention of prenatal transmission to the care of children with HIV to reproductive issues in serodiscordant couples, HIV complicates patients’ development. Table 3 outlines concerns regarding HIV transmission and treatment at different stages of a patient’s life.
Bottom Line
HIV transmission and effective treatment are complicated by a high prevalence of psychiatric comorbidities, including depression and other mood disorders, posttraumatic stress disorder, substance use disorders, and cognitive disorders. With an increased understanding of the issues faced by patients at risk for or infected with HIV, psychiatrists can help prevent HIV transmission, improve adherence to medical care, and diminish suffering, morbidity, and mortality.
Related Resources
- Academy of Psychosomatic Medicine HIV/AIDS Psychiatry Special Interest Group. www.apm.org/sigs/oap.
- New York State Department of Health AIDS Institute. HIV Clinical Resource. www.hivguidelines.org.
- University of Liverpool. HIV drug interactions list. www.hiv-druginteractions.org.
- Toronto General Hospital Immunodeficiency Clinic. Drug interactions tables. www.hivclinic.ca/main/drugs_interact.html.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Nevirapine • Viramune
Carbamazepine • Carbatrol, Tegretol, others
Olanzapine • Zyprexa
Quetiapine • Seroquel
Clonazepam • Klonopin
Ritonavir • Norvir
Efavirenz • Sustiva
Venlafaxine • Effexor
Escitalopram • Lexapro
Disclosure
Dr. Cohen reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Blank MB, Mandell DS, Aiken L, et al. Co-occurrence of HIV and serious mental illness among Medicaid recipients. Psychiatr Serv. 2002;53(7):868-873.
2.Moyer VA, on behalf of the U.S. Preventive Services Task Force. Screening for HIV: U.S. Preventive Services Task Force recommendation statement [published online April 30, 2013]. Ann Intern Med. doi:10.7326/0003-4819-159-1-201307020-00645.
3. Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520-529.
4. Cohen MA. AIDSism, a new form of discrimination. Am Med News. 1989;32:43.
5. Cohen MA, Gorman JM. Comprehensive textbook of AIDS psychiatry. New York, NY: Oxford University Press; 2008.
6. Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010.
7. World Health Organization, United Nations Children’s Fund, Joint United Nations Programme on HIV/AIDS. Global HIV/AIDS response. Epidemic update and health sector progress towards universal access. Progress report 2011. http://www.unaids.org/en/media/unaids/
contentassets/documents/unaidspublication/2011/
20111130_UA_Report_en.pdf. Accessed April 25, 2013.
8. Centers for Disease Control and Prevention (CDC). Interim guidance for clinicians considering the use of preexposure prophylaxis for the prevention of HIV infection in heterosexually active adults. MMWR Morb Mortal Wkly Rep. 2012;61(31):586-589.
9. Cysique LA, Murray JM, Dunbar M, et al. A screening algorithm for HIV-associated neurocognitive disorders. HIV Med. 2010;11(10):642-649.
10. Simioni S, Cavassini M, Annoni JM, et al. Cognitive dysfunction in HIV patients despite long-standing suppression of viremia. AIDS. 2010;24(9):1243-1250.
11. Cohen M, Hoffman RG, Cromwell C, et al. The prevalence of distress in persons with human immunodeficiency virus infection. Psychosomatics. 2002;43(1):10-15.
12. Cohen MA, Batista SM, Lux JZ. A biopsychosocial approach to psychiatric consultation in persons with HIV and AIDS. In: Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010:33-60.
13. Carrico AW. Elevated suicide rate among HIV-positive persons despite benefits of antiretroviral therapy: implications for a stress and coping model of suicide. Am J Psychiatry. 2010;167(2):117-119.
14. Cohen MA, Alfonso CA, Hoffman RG, et al. The impact of PTSD on treatment adherence in persons with HIV infection. Gen Hosp Psychiatry. 2001;23(5):294-296.
15. Boarts JM, Sledjeski EM, Bogart LM, et al. The differential impact of PTSD and depression on HIV disease markers and adherence to HAART in people living with HIV. AIDS Behav. 2006;10(3):253-261.
16. Sikkema KJ, Hansen NB, Ghebremichael M, et al. A randomized controlled trial of a coping group intervention for adults with HIV who are AIDS bereaved: longitudinal effects on grief. Health Psychol. 2006;25(5):563-570.
17. Cohen MA. Psychodynamic psychotherapy in an AIDS nursing home. J Am Acad Psychoanal. 1999;27(1):121-133.
18. Cozza KL, Goforth HW, Batista SM. Psychopharmacologic treatment issues in AIDS psychiatry. In: Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010:147-199.
The prevalence of HIV in persons with untreated psychiatric illness may be 10 to 20 times that of the general population.1 The U.S. Preventive Services Task Force has recommended HIV screening of all persons age 15 to 65 because 20% to 25% of individuals with HIV infection are unaware that they are HIV-positive.2 Because >20% of new HIV infections in the United States are undiagnosed,3 it is crucial to educate patients with mental illness about HIV prevention, make condoms available, and offer HIV testing.
As psychiatrists, we have a unique role in caring for patients at risk for or infected with HIV because in addition to comprehensive medical and psychiatric histories, we routinely take histories of substance use, sexual activities, relationships, and trauma, including childhood neglect and emotional, physical, and sexual abuse. We develop long-term, trusting relationships and work with individuals to change behaviors and maximize life potential.
Increasing awareness of stigma, discrimination, and psychiatric factors involved with the HIV pandemic can lead to decreased transmission of HIV infection and early diagnosis and treatment. Compassionate medical and psychiatric care can mitigate suffering in persons at risk for, infected with, or affected by HIV.
Preventing HIV transmission
AIDS differs from other complex, severe illnesses in 2 ways that are relevant to psychiatrists:
• it is almost entirely preventable
• HIV and AIDS are associated with sex, drugs, and AIDS-associated stigma and discrimination (“AIDSism”).4-6
Unsafe exposure of mucosal surfaces to the virus—primarily from exchanging body fluids in unprotected sexual encounters—accounts for 80% of new HIV infections.7 HIV transmission via sexual encounters is preventable with condoms. Percutaneous or intravenous infection with HIV—primarily from sharing needles in injection drug use—accounts for 20% of new infections.7 Use of alcohol or other substances can lead to sexual coercion, unprotected sex, and exchange of sex for drugs or money. Hence, treating substance use disorders can prevent HIV transmission.
Early diagnosis of HIV can lead to appropriate medical care, quicker onset of antiretroviral (ARV) treatment, and better outcomes. Recent research has shown that pre-exposure prophylaxis with ARV treatment can prevent transmission of HIV8; therefore, becoming aware of risk behaviors and prevention can be lifesaving for serodiscordant couples.
One of the most important ways to prevent HIV’s impact on the brain and CNS is to diagnose HIV shortly after transmission at onset of acute infection. If HIV is diagnosed very early—preferably as soon as possible after inoculation with HIV or at onset of the first flu-like symptoms—and treated with ARVs, the brain has less of an opportunity to act as an independent reservoir for HIV-infected cells and therefore to develop HIV-associated neurocognitive disorders.9,10Table 1 outlines steps psychiatrists can take to help prevent HIV transmission.
Psychiatric disorders and HIV
Psychiatric disorders and distress play a significant role in transmission of, exposure to, and infection with HIV (Table 2).4-6,11 They are relevant for prevention, clinical care, and adherence throughout every aspect of illness.
Comprehensive, compassionate, nonjudgmental care of persons at risk for or infected with HIV begins with a thorough psychiatric evaluation designed to provide an ego-supportive, sensitive, and comprehensive assessment that can guide other clinicians in providing care.12 Setting the tone and demonstrating compassion and respect includes shaking hands, which takes on special relevance in the context of AIDSism and stigma. Assessing the impact of HIV seropositivity or AIDS is best done by asking about the individual’s understanding of his or her diagnosis or illness and its impact. For some persons with HIV, verbalizing this understanding can be relieving as well as revealing. It is a chance for the patient to reveal painful experiences encountered in the home, school, camp, workplace, or community and the anguish of AIDSism and stigma.
Pay attention to sensitive and sometimes painful issues related to sexual history and sexuality. Questions related to sexual history and sexuality in heterosexual men and women as well as gay, lesbian, bisexual, and transgender individuals—such as “What is your sexual function like since you have been ill?” “Do feelings about your sexual identity play a role in your current level of distress?” and “What kind of barrier contraception are you using?”—are included in the comprehensive assessment described by Cohen et al.12
Comprehensive psychiatric evaluations can provide diagnoses, inform treatment, and mitigate anguish, distress, depression, anxiety, and substance use in persons with HIV and AIDS.12 A thorough and comprehensive assessment is crucial because HIV has an affinity for brain and neural tissue and can cause CNS complications such as HIV-associated neurocognitive disorders (HAND), even in otherwise healthy HIV-seropositive individuals. See this article at CurrentPsychiatry.com for a discussion of HAND and delirium in patients with HIV.
Some persons with HIV and AIDS do not have a psychiatric disorder, while others have multiple complex psychiatric disorders that are responses to illness or treatments or are associated with HIV/AIDS (such as HAND) or other medical illnesses and treatments (such as hepatitis C, cirrhosis, end-stage liver disease, HIV nephropathy, end-stage renal disease, anemia, coronary artery disease, and cancer). See this article at CurrentPsychiatry.com for case studies of HIV patients with delirium, depression, posttraumatic stress disorder (PTSD), and substance dependence.
Mood disorders. Depression is common among persons with HIV. Demoralization and bereavement may masquerade as depression and can complicate diagnosis and treatment. Depression and other mood disorders may be related to stigma and AIDSism as well as to biologic, psychological, social, and genetic factors. Because suicide is prevalent among persons with HIV and AIDS,13 every patient with HIV should be evaluated for depression and suicidal ideation.
PTSD is prevalent among persons with HIV. It is a risky diagnosis because it is associated with a sense of a foreshortened future, which leads to a lack of adequate self-care, poor adherence to medical care, risky behaviors, and comorbid substance dependence to help numb the pain of trauma.14,15 Persons with PTSD may have difficulty trusting clinicians and other authority figures if their trauma was a high-betrayal trauma, such as incest or military trauma.14,15
In patients with HIV, PTSD often is overlooked because it may be overshadowed by other psychiatric diagnoses. Intimate partner violence, history of childhood trauma, and childhood sexual abuse are risk factors for HIV infection and PTSD. Increased severity of HIV-related PTSD symptoms is associated with having a greater number of HIV-related physical symptoms, history of pre-HIV trauma, decreased social support, increased perception of stigma, and negative life events.
PTSD also is associated with nonadherence to risk reduction strategies and medical care.14,15 Diagnosis is further complicated by repression or retrograde amnesia of traumatic events and difficulties forming trusting relationships and disclosing HIV status to sexual partners or potential sexual partners because of fear of rejection.
Substance use disorders. Dependence on alcohol and other drugs complicates and perpetuates the HIV pandemic. Sharing needles and other drug paraphernalia is instrumental in HIV transmission. The indirect effects of alcohol and substance abuse include:
• the impact of intimate partner violence, child abuse, neglect, and/or abandonment
• development of PTSD in adults, with early childhood trauma leading to repeating their own history
• lack of self-care
• unhealthy partner choices
• use of drugs and alcohol to numb the pain associated with trauma.
Persons who are using alcohol or other drugs may have difficulty attending to their health, and substance dependence may prevent persons at risk from seeking HIV testing.
Intoxication from alcohol and drug use frequently leads to inappropriate partner choice, violent and coercive sexual behaviors, and lack of condom use. Substance dependence also may lead individuals to exchange sex for drugs and to fail to adhere to safer sexual practices or use sterile drug paraphernalia.
Treating persons with HIV/AIDS
Several organizations publish evidence-based clinical guidelines for treating depression, anxiety, substance abuse, and other psychiatric disorders in patients with HIV/AIDS. One such set of guidelines is available from the New York State Department of Health AIDS Institute at www.hivguidelines.org. As is the case with patients who do not have HIV, psychotherapy and pharmacotherapy are common first-line treatments.
Psychotherapy. Patients with HIV/AIDS with psychiatric comorbidities generally respond well to psychotherapeutic treatments.16,17 The choice of therapy needs to be tailored to the needs of individuals, couples, and families coping with AIDS. Options include:
• individual, couple, family, and group psychotherapy
• crisis intervention
• 12-step programs (Alcohol Anonymous, Narcotics Anonymous, etc.)
• adult survivors of child abuse programs (www.ascasupport.org), groups, and workbooks
• palliative psychiatry
• bereavement therapy
• spiritual support
• relaxation response
• wellness interventions such as exercise, yoga, keeping a journal, writing a life narrative, reading, artwork, movement therapy, listening to music or books on tape, and working on crossword puzzles and jigsaw puzzles.
Psychopharmacotherapy. Accurate diagnosis and awareness of drug-drug and drug-illness interactions are important when treating patients with HIV/AIDS; consult resources in the literature18 and online resources that are updated regularly (see Related Resources). Because persons with AIDS are particularly vulnerable to extrapyramidal and anticholinergic side effects of psychotropics, the principle start very low and go very slow is critical. For patients who are opioid-dependent, be cautious when prescribing medications that are cytochrome P450 3A4 inducers—such as carbamazepine, efavirenz, nevirapine, and ritonavir—because these medications can lower methadone levels in persons receiving agonist treatment and might lead to opioid withdrawal symptoms, discontinuation of ARVs, or relapse to opioids.18 When a person with AIDS is experiencing pain and is on a maintenance dose of methadone for heroin withdrawal, pain should be treated as a separate problem with additional opioids. Methadone for relapse prevention will target opioid tolerance needs and prevent withdrawal but will not provide analgesia for pain.
HIV through the life cycle
From prevention of prenatal transmission to the care of children with HIV to reproductive issues in serodiscordant couples, HIV complicates patients’ development. Table 3 outlines concerns regarding HIV transmission and treatment at different stages of a patient’s life.
Bottom Line
HIV transmission and effective treatment are complicated by a high prevalence of psychiatric comorbidities, including depression and other mood disorders, posttraumatic stress disorder, substance use disorders, and cognitive disorders. With an increased understanding of the issues faced by patients at risk for or infected with HIV, psychiatrists can help prevent HIV transmission, improve adherence to medical care, and diminish suffering, morbidity, and mortality.
Related Resources
- Academy of Psychosomatic Medicine HIV/AIDS Psychiatry Special Interest Group. www.apm.org/sigs/oap.
- New York State Department of Health AIDS Institute. HIV Clinical Resource. www.hivguidelines.org.
- University of Liverpool. HIV drug interactions list. www.hiv-druginteractions.org.
- Toronto General Hospital Immunodeficiency Clinic. Drug interactions tables. www.hivclinic.ca/main/drugs_interact.html.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Nevirapine • Viramune
Carbamazepine • Carbatrol, Tegretol, others
Olanzapine • Zyprexa
Quetiapine • Seroquel
Clonazepam • Klonopin
Ritonavir • Norvir
Efavirenz • Sustiva
Venlafaxine • Effexor
Escitalopram • Lexapro
Disclosure
Dr. Cohen reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Blank MB, Mandell DS, Aiken L, et al. Co-occurrence of HIV and serious mental illness among Medicaid recipients. Psychiatr Serv. 2002;53(7):868-873.
2.Moyer VA, on behalf of the U.S. Preventive Services Task Force. Screening for HIV: U.S. Preventive Services Task Force recommendation statement [published online April 30, 2013]. Ann Intern Med. doi:10.7326/0003-4819-159-1-201307020-00645.
3. Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520-529.
4. Cohen MA. AIDSism, a new form of discrimination. Am Med News. 1989;32:43.
5. Cohen MA, Gorman JM. Comprehensive textbook of AIDS psychiatry. New York, NY: Oxford University Press; 2008.
6. Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010.
7. World Health Organization, United Nations Children’s Fund, Joint United Nations Programme on HIV/AIDS. Global HIV/AIDS response. Epidemic update and health sector progress towards universal access. Progress report 2011. http://www.unaids.org/en/media/unaids/
contentassets/documents/unaidspublication/2011/
20111130_UA_Report_en.pdf. Accessed April 25, 2013.
8. Centers for Disease Control and Prevention (CDC). Interim guidance for clinicians considering the use of preexposure prophylaxis for the prevention of HIV infection in heterosexually active adults. MMWR Morb Mortal Wkly Rep. 2012;61(31):586-589.
9. Cysique LA, Murray JM, Dunbar M, et al. A screening algorithm for HIV-associated neurocognitive disorders. HIV Med. 2010;11(10):642-649.
10. Simioni S, Cavassini M, Annoni JM, et al. Cognitive dysfunction in HIV patients despite long-standing suppression of viremia. AIDS. 2010;24(9):1243-1250.
11. Cohen M, Hoffman RG, Cromwell C, et al. The prevalence of distress in persons with human immunodeficiency virus infection. Psychosomatics. 2002;43(1):10-15.
12. Cohen MA, Batista SM, Lux JZ. A biopsychosocial approach to psychiatric consultation in persons with HIV and AIDS. In: Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010:33-60.
13. Carrico AW. Elevated suicide rate among HIV-positive persons despite benefits of antiretroviral therapy: implications for a stress and coping model of suicide. Am J Psychiatry. 2010;167(2):117-119.
14. Cohen MA, Alfonso CA, Hoffman RG, et al. The impact of PTSD on treatment adherence in persons with HIV infection. Gen Hosp Psychiatry. 2001;23(5):294-296.
15. Boarts JM, Sledjeski EM, Bogart LM, et al. The differential impact of PTSD and depression on HIV disease markers and adherence to HAART in people living with HIV. AIDS Behav. 2006;10(3):253-261.
16. Sikkema KJ, Hansen NB, Ghebremichael M, et al. A randomized controlled trial of a coping group intervention for adults with HIV who are AIDS bereaved: longitudinal effects on grief. Health Psychol. 2006;25(5):563-570.
17. Cohen MA. Psychodynamic psychotherapy in an AIDS nursing home. J Am Acad Psychoanal. 1999;27(1):121-133.
18. Cozza KL, Goforth HW, Batista SM. Psychopharmacologic treatment issues in AIDS psychiatry. In: Cohen MA, Goforth HW, Lux JZ, et al, eds. Handbook of AIDS psychiatry. New York, NY: Oxford University Press; 2010:147-199.
Evaluating psychotic patients' risk of violence
Understanding psychosis
PSYCHIATRY UPDATE 2014
Current Psychiatry and the American Academy of Clinical Psychiatrists welcomed more than 550 psychiatric practitioners from across the United States and abroad to this annual conference, which was headed by Meeting Chair Richard Balon, MD, and Co-chairs Donald W. Black, MD, and Nagy Youssef, MD, March 27-29, 2014 at the Hilton Chicago in Chicago, Illinois. Attendees earned as many as 10 AMA PRA Category 1 Credits™.
Thursday, March 27, 2014
MORNING SESSION
Obsessive-compulsive disorder can be misdiagnosed as psychosis, anxiety, or a sexual disorder. In addition to contamination, patients can present with pathologic doubt, somatic obsessions, or obsessions about taboo or symmetry. Among FDA-approved medications, clomipramine might be more effective than selective serotonin reuptake inhibitors (SSRIs). Exposure response prevention therapy shows better response than pharmacotherapy, but best outcomes are seen with combination therapy. Jon E. Grant, JD, MD, MPH, University of Chicago, also discussed obsessive-compulsive personality disorder, body dysmorphic disorder, hoarding, trichotillomania, and excoriation disorder—as well as changes in DSM-5 that cover this group of disorders.
Patients with schizophrenia are at higher risk of death from cardiac and pulmonary disease than the general population. The quality of care of patients with psychosis generally is poor, because of lack of recognition, time, and resources, as well as systematic barriers to accessing health care. Questions about weight gain, lethargy, infections, and sexual functioning can help the practitioner assess a patient’s general health. When appropriate, Henry A. Nasrallah, MD, St. Louis University School of Medicine, recommends, consider switching antipsychotics, which might reverse adverse metabolic events.
Nonpharmacologic treatment goals include improving sleep, educating patients, providing them with tools for improving sleep, and creating an opportunity for patient-practitioner discussion. Stimulus control and sleep restriction are primary therapeutic techniques to improve sleep quality and reduce non-sleeping time in bed. Thomas Roth, PhD, Henry Ford Hospital, also discussed how to modify sleep hygiene techniques for pediatric, adolescent, and geriatric patients.
Donald W. Black, MD, University of Iowa, says that work groups for DSM-5 were asked to consider dimensionality and culture and gender issues. New diagnostic categories include obsessive-compulsive and related disorders and trauma and stressor-related disorders. Some diagnoses were reformulated or introduced, including autism spectrum disorder and disruptive mood dysregulation disorder. The multi-axial system was discontinued in DSM-5. He also reviewed coding issues.
In a sponsored symposium, Prakash S. Masand, MD, Global Medical Education, Inc., looked at the clinical challenges of addressing all 3 symptom domains that characterize depression (emotional, physical, and cognitive) as an introduction to reviewing the efficacy, mechanism of action, and side effects of vortioxetine (Brintellix), a new serotonergic agent for treating major depressive disorder (MDD). In all studies submitted to the FDA, vortioxetine was found to be superior to placebo, in at least 1 dosage group, for alleviating depressive symptoms and for reducing the risk of depressive recurrence.
AFTERNOON SESSION
Oppositional defiant disorder is more common in boys (onset at age 6 to 10) and is associated with inconsistent and neglectful parenting. Treatment modalities, including educational training, anticonvulsants, and lithium, do not have a strong evidence base. Intermittent explosive disorder is characterized by short-lived but frequent behavioral outbursts and often begins in adolescence. Dr. Grant also reviewed the evidence on conduct disorder, pyromania, and kleptomania.
Cognitive symptoms of schizophrenia often appear before psychotic symptoms and remain stable across the lifespan. There are no pharmacologic treatments for cognitive deficits in schizophrenia; however, Dr. Nasrallah listed tactics to improve cognitive function, including regular aerobic exercise. These cognitive deficits can be categorized as neurocognitive (memory, learning, executive function) and social (social skills, theory of mind, social cues) and contribute to functional decline and often prevent patients from working and going to school. Dr. Nasrallah described how bipolar disorder (BD) overlaps with schizophrenia in terms of cognitive dysfunction.
Henry Nasrallah, MD
Psychiatric disorders exhibit specific sleep/ wake impairments. Sleep disorders can mimic psychiatric symptoms, such as fatigue, cognitive problems, and depression. Sleep disturbances, including insomnia, obstructive sleep apnea, and decreased need for sleep, often coexist with depression, generalized anxiety disorder, posttraumatic stress disorder, and BD, and insomnia is associated with a greater risk of suicide. With antidepressant treatment, sleep in depressed patients improves but does not normalize. Dr. Roth also reviewed pharmacotherapeutic options and non-drug modalities to improve patients’ sleep.
Antidepressants have no efficacy in treating acute episodes of bipolar depression, and using such agents might yield a poor long-term outcome in BD, according to Robert M. Post, MD, George Washington University School of Medicine, Michael J. Ostacher, MD, MPH, MMSc, Stanford University, and Vivek Singh, MD, University of Texas Health Science Center at San Antonio, in an interactive faculty discussion. For patients with bipolar I disorder, lithium monotherapy or the combination of lithium and valproate is more effective than valproate alone; evidence does not support valproate as a maintenance treatment. When a patient with BD shows partial response, attendees at this sponsored symposium were advised, consider adding psychotherapy and psycho-education. Combining a mood stabilizer and an antipsychotic might be more effective than monotherapy and safer, by allowing lower dosages. The only 3 treatments FDA-approved for bipolar depression are the olanzapine-fluoxetine combination, quetiapine, and lurasidone.
Boaz Levy, PhD, (left) receives the 2014 George Winokur Research Award from Carol S. North, MD, for his article on recovery of cognitive function in patients with co-occuring bipolar disorder and alcohol dependence.
Friday, March 28, 2014
MORNING SESSION
Carmen Pinto, MD, at a sponsored symposium, reviewed the utility and safety of
long-acting injectable (LAI) antipsychotics for treating schizophrenia, with a focus on LAI aripiprazole, a partial HT-receptor agonist/partial HT-receptor antagonist. Four monthly injections (400 mg/injection) of the drug are needed to reach steady state; each injection reaches peak level in 5 to 7 days. LAI aripiprazole has been shown to delay time to relapse due to nonadherence and onset of nonresponse to the drug, and has high patient acceptance—even in those who already stable. Safety and side effects with LAI aripiprazole are the same as seen with the oral formulation.
In multimodal therapy for chronic pain, psychiatrists have a role in assessing
psychiatric comorbidities, coping ability, social functioning, and other life functions, including work and personal relationships. Cognitive-behavioral therapy can be particularly useful for chronic pain by helping patients reframe their pain experiences. Raphael J. Leo, MA, MD, FAPM, University at Buffalo, reviewed non-opioid co-analgesics that can be used for patients with comorbid pain and a substance use disorder. If opioids are necessary, consider “weak” or long-acting opioids. Monitor patients for aberrant, drug-seeking behavior.
In the second part of his overview, Dr. Black highlighted specific changes to DSM-5 of particular concern to clinicians. New chapters were created and disorders were consolidated, he explained, such as autism spectrum disorder, somatic symptom disorder, and major neurocognitive disorder. New diagnoses include hoarding disorder and binge eating disorder. Subtypes of schizophrenia were dropped. Pathologic gambling was renamed gambling disorder and gender dysphoria is now called gender identity disorder. The bereavement exclusion of a major depressive episode was dropped.
Antidepressants are effective in mitigating pain in neuropathy, headache, fibromyalgia, and chronic musculoskeletal pain, and have been advocated for other pain syndromes. Selection of an antidepressant depends on the type of pain condition, comorbid depression or anxiety, tolerability, and medical comorbidities. Dr. Leo presented prescribing strategies for tricyclics, serotoninnorepinephrine
reuptake inhibitors, SSRIs, and other antidepressants.
Treating of BD in geriatric patients becomes complicated because therapeutic choices are narrowed and response to therapy is less successful with age, according to George T. Grossberg, MD, St. Louis University. Rapid cycling tends to be the norm in geriatric BD patients. Look for agitation and irritability, rather than full-blown mania; grandiose delusions; psychiatric comorbidity, especially anxiety disorder; and sexually inappropriate behavior. Pharmacotherapeutic options include: mood stabilizers, atypical antipsychotics, and antidepressants (specifically, bupropion and SSRIs—not TCAs, venlafaxine, or duloxetine—and over the short term only). Consider divalproex for mania and hypomania, used cautiously because of its adverse side-effect potential.
George T. Grossberg, MD
AFTERNOON SESSION
Often, BD is misdiagnosed as unipolar depression, or the correct diagnosis of BD is delayed, according to Gustavo Alva, MD, ATP Clinical Research. Comorbid substance use disorder or an anxiety disorder is common. Comorbid cardiovascular disease brings a greater risk of mortality in patients with BD than suicide. Approximately two-thirds of patients with BD are taking adjunctive medications; however, antidepressants are no more effective than placebo in treating bipolar depression. At this sponsored symposium, Vladimir Maletic, MD, University of South Carolina, described a 6-week trial in which lurasidone plus lithium or divalporex was more effective in reducing depression, as measured by MADRS, than placebo plus lithium or akathisia, somnolence, and extrapyramidal symptoms.
When assessing an older patient with psychosis, first establish the cause of the symptoms, such as Alzheimer’s disease, affective disorder, substance use, or hallucinations associated with grief. Older patients with schizophrenia who have been taking typical antipsychotics for years might benefit from a switch to an atypical or a dosage reduction. Dr. Grossberg recommends considering antipsychotics for older patients when symptoms cause severe emotional distress that does not respond to other interventions or an acute episode that poses a safety risk for patients or others. Choose an antipsychotic based on side effects, and “start low and go slow,” when possible. The goal is to reduce agitation and distress—not necessarily to resolve psychotic symptoms.
Anita H. Clayton, MD, University of Virginia Health System, provided a review of sexual function from puberty through midlife and older years. Social factors play a role in sexual satisfaction, such as gender expectations, religious beliefs, and the influence of reporting in the media. Sexual dysfunction becomes worse in men after age 29; in women, the rate of sexual dysfunction appears to be consistent across the lifespan. Cardiovascular disease is a significant risk factor for sexual dysfunction in men, but not in women. Sexual function and depression have a bidirectional relationship; sexual dysfunction may be a symptom or cause of depression and antidepressants may affect desire and function. Medications, including psychotropics, oral contraceptives, and opioids, can cause sexual dysfunction.
Providers often are reluctant to bring up sexual issues with their patients, Dr. Clayton says, but patients often want to talk about their sexual problems. In reproductive-age women, look for hypoactive sexual desire disorder and pain. In men, assess for erectile dysfunction or premature ejaculation. Inquire about every phase of the sexual response cycle. When managing sexual dysfunction, aim to minimize contributing factors such as illness or medication, consider FDA-approved medications, encourage a healthy lifestyle, and employ psychological interventions when appropriate. In patients with antidepressant-associated sexual dysfunction, consider switching medications or adding an antidote, such as bupropion, buspirone, or sildenafil.
Saturday, March 29, 2014
MORNING SESSION
Because of the lack of double-blind, placebo-controlled trials, the risks of untreated depression vs the risks of antidepressant use in pregnancy are unclear. Marlene P. Freeman, MD, Massachusetts General Hospital, described the limited, long-term data on tricyclics and fluoxetine. Some studies have shown a small risk of birth defects with SSRIs; others did not find an association. For moderate or severe depression, use antidepressants at the lowest dosage and try non-medication options, such as psychotherapy and complementary and alternative medicine. During the third trimester, women may need a higher dosage to maintain therapeutic drug levels. Data indicates that folic acid use during pregnancy is associated with a decreased risk of autism and schizophrenia.
James W. Jefferson, MD, University of Wisconsin School of Medicine and Public Health, recommends ruling out medical conditions, such as cancer, that might be causing your patients’ fatigue or depression. Many medications, including over-the-counter agents and supplements, can cause fatigue. Bupropion was more effective than placebo and SSRIs in treating depressed patients with sleepiness and fatigue. Adding a psychostimulant to an SSRI does not have a significantly better effect than placebo on depressive symptoms. Adjunctive modafanil may improve depression and fatigue. Data for dopamine agonists are limited.
Lithium should be used with caution in pregnant women because of the risk of congenital malformations. Dr. Freeman also discussed the potential risks to the fetus with the mother’s use of valproate and lamotrigine (with the latter, a small increase in oral clefting). High-potency typical antipsychotics are considered safe; low-potency drugs have a higher risk of major malformations. For atypicals, the risk of malformations appears minimal; newborns might display extrapyramidal effects and withdrawal symptoms. Infants exposed to psychostimulants may have lower birth weight, but are not at increased risk of birth defects.
Dr. Jefferson reviewed the efficacy, pharmacokinetics, and adverse effects of vilazodone, levomilnacipran, and vortioxetine, which are antidepressants new to the market. Dr. Jefferson recommends reading package inserts to become familiar with new drugs. He also described studies of medications that were not FDA-approved, including edivoxetine, quetiapine XR monotherapy for MDD, and agomelatine. Agents under investigation include onabotulinumtoxin A injections, ketamine, and lanicemine.
Katherine E. Burdick, PhD, Mount Sinai School of Medicine, defined cognitive domains. First-episode MDD patients perform worse in psychomotor speed and attention than healthy controls. Late-onset depression (after age 60) is associated with worse performance on processing speed and verbal memory. Cognitive deficits in depressed patients range from mild to moderate and are influenced by symptom status and duration of illness. Treating cognitive deficits begins with prevention. Cholinesterase inhibitors are not effective for improving cognition in MDD. Antidepressants, including SSRIs, do not adequately treat cognitive deficits, Roger S. McIntyre, MD, FRCPC, University of Toronto, explained.
Current Psychiatry and the American Academy of Clinical Psychiatrists welcomed more than 550 psychiatric practitioners from across the United States and abroad to this annual conference, which was headed by Meeting Chair Richard Balon, MD, and Co-chairs Donald W. Black, MD, and Nagy Youssef, MD, March 27-29, 2014 at the Hilton Chicago in Chicago, Illinois. Attendees earned as many as 10 AMA PRA Category 1 Credits™.
Thursday, March 27, 2014
MORNING SESSION
Obsessive-compulsive disorder can be misdiagnosed as psychosis, anxiety, or a sexual disorder. In addition to contamination, patients can present with pathologic doubt, somatic obsessions, or obsessions about taboo or symmetry. Among FDA-approved medications, clomipramine might be more effective than selective serotonin reuptake inhibitors (SSRIs). Exposure response prevention therapy shows better response than pharmacotherapy, but best outcomes are seen with combination therapy. Jon E. Grant, JD, MD, MPH, University of Chicago, also discussed obsessive-compulsive personality disorder, body dysmorphic disorder, hoarding, trichotillomania, and excoriation disorder—as well as changes in DSM-5 that cover this group of disorders.
Patients with schizophrenia are at higher risk of death from cardiac and pulmonary disease than the general population. The quality of care of patients with psychosis generally is poor, because of lack of recognition, time, and resources, as well as systematic barriers to accessing health care. Questions about weight gain, lethargy, infections, and sexual functioning can help the practitioner assess a patient’s general health. When appropriate, Henry A. Nasrallah, MD, St. Louis University School of Medicine, recommends, consider switching antipsychotics, which might reverse adverse metabolic events.
Nonpharmacologic treatment goals include improving sleep, educating patients, providing them with tools for improving sleep, and creating an opportunity for patient-practitioner discussion. Stimulus control and sleep restriction are primary therapeutic techniques to improve sleep quality and reduce non-sleeping time in bed. Thomas Roth, PhD, Henry Ford Hospital, also discussed how to modify sleep hygiene techniques for pediatric, adolescent, and geriatric patients.
Donald W. Black, MD, University of Iowa, says that work groups for DSM-5 were asked to consider dimensionality and culture and gender issues. New diagnostic categories include obsessive-compulsive and related disorders and trauma and stressor-related disorders. Some diagnoses were reformulated or introduced, including autism spectrum disorder and disruptive mood dysregulation disorder. The multi-axial system was discontinued in DSM-5. He also reviewed coding issues.
In a sponsored symposium, Prakash S. Masand, MD, Global Medical Education, Inc., looked at the clinical challenges of addressing all 3 symptom domains that characterize depression (emotional, physical, and cognitive) as an introduction to reviewing the efficacy, mechanism of action, and side effects of vortioxetine (Brintellix), a new serotonergic agent for treating major depressive disorder (MDD). In all studies submitted to the FDA, vortioxetine was found to be superior to placebo, in at least 1 dosage group, for alleviating depressive symptoms and for reducing the risk of depressive recurrence.
AFTERNOON SESSION
Oppositional defiant disorder is more common in boys (onset at age 6 to 10) and is associated with inconsistent and neglectful parenting. Treatment modalities, including educational training, anticonvulsants, and lithium, do not have a strong evidence base. Intermittent explosive disorder is characterized by short-lived but frequent behavioral outbursts and often begins in adolescence. Dr. Grant also reviewed the evidence on conduct disorder, pyromania, and kleptomania.
Cognitive symptoms of schizophrenia often appear before psychotic symptoms and remain stable across the lifespan. There are no pharmacologic treatments for cognitive deficits in schizophrenia; however, Dr. Nasrallah listed tactics to improve cognitive function, including regular aerobic exercise. These cognitive deficits can be categorized as neurocognitive (memory, learning, executive function) and social (social skills, theory of mind, social cues) and contribute to functional decline and often prevent patients from working and going to school. Dr. Nasrallah described how bipolar disorder (BD) overlaps with schizophrenia in terms of cognitive dysfunction.
Henry Nasrallah, MD
Psychiatric disorders exhibit specific sleep/ wake impairments. Sleep disorders can mimic psychiatric symptoms, such as fatigue, cognitive problems, and depression. Sleep disturbances, including insomnia, obstructive sleep apnea, and decreased need for sleep, often coexist with depression, generalized anxiety disorder, posttraumatic stress disorder, and BD, and insomnia is associated with a greater risk of suicide. With antidepressant treatment, sleep in depressed patients improves but does not normalize. Dr. Roth also reviewed pharmacotherapeutic options and non-drug modalities to improve patients’ sleep.
Antidepressants have no efficacy in treating acute episodes of bipolar depression, and using such agents might yield a poor long-term outcome in BD, according to Robert M. Post, MD, George Washington University School of Medicine, Michael J. Ostacher, MD, MPH, MMSc, Stanford University, and Vivek Singh, MD, University of Texas Health Science Center at San Antonio, in an interactive faculty discussion. For patients with bipolar I disorder, lithium monotherapy or the combination of lithium and valproate is more effective than valproate alone; evidence does not support valproate as a maintenance treatment. When a patient with BD shows partial response, attendees at this sponsored symposium were advised, consider adding psychotherapy and psycho-education. Combining a mood stabilizer and an antipsychotic might be more effective than monotherapy and safer, by allowing lower dosages. The only 3 treatments FDA-approved for bipolar depression are the olanzapine-fluoxetine combination, quetiapine, and lurasidone.
Boaz Levy, PhD, (left) receives the 2014 George Winokur Research Award from Carol S. North, MD, for his article on recovery of cognitive function in patients with co-occuring bipolar disorder and alcohol dependence.
Friday, March 28, 2014
MORNING SESSION
Carmen Pinto, MD, at a sponsored symposium, reviewed the utility and safety of
long-acting injectable (LAI) antipsychotics for treating schizophrenia, with a focus on LAI aripiprazole, a partial HT-receptor agonist/partial HT-receptor antagonist. Four monthly injections (400 mg/injection) of the drug are needed to reach steady state; each injection reaches peak level in 5 to 7 days. LAI aripiprazole has been shown to delay time to relapse due to nonadherence and onset of nonresponse to the drug, and has high patient acceptance—even in those who already stable. Safety and side effects with LAI aripiprazole are the same as seen with the oral formulation.
In multimodal therapy for chronic pain, psychiatrists have a role in assessing
psychiatric comorbidities, coping ability, social functioning, and other life functions, including work and personal relationships. Cognitive-behavioral therapy can be particularly useful for chronic pain by helping patients reframe their pain experiences. Raphael J. Leo, MA, MD, FAPM, University at Buffalo, reviewed non-opioid co-analgesics that can be used for patients with comorbid pain and a substance use disorder. If opioids are necessary, consider “weak” or long-acting opioids. Monitor patients for aberrant, drug-seeking behavior.
In the second part of his overview, Dr. Black highlighted specific changes to DSM-5 of particular concern to clinicians. New chapters were created and disorders were consolidated, he explained, such as autism spectrum disorder, somatic symptom disorder, and major neurocognitive disorder. New diagnoses include hoarding disorder and binge eating disorder. Subtypes of schizophrenia were dropped. Pathologic gambling was renamed gambling disorder and gender dysphoria is now called gender identity disorder. The bereavement exclusion of a major depressive episode was dropped.
Antidepressants are effective in mitigating pain in neuropathy, headache, fibromyalgia, and chronic musculoskeletal pain, and have been advocated for other pain syndromes. Selection of an antidepressant depends on the type of pain condition, comorbid depression or anxiety, tolerability, and medical comorbidities. Dr. Leo presented prescribing strategies for tricyclics, serotoninnorepinephrine
reuptake inhibitors, SSRIs, and other antidepressants.
Treating of BD in geriatric patients becomes complicated because therapeutic choices are narrowed and response to therapy is less successful with age, according to George T. Grossberg, MD, St. Louis University. Rapid cycling tends to be the norm in geriatric BD patients. Look for agitation and irritability, rather than full-blown mania; grandiose delusions; psychiatric comorbidity, especially anxiety disorder; and sexually inappropriate behavior. Pharmacotherapeutic options include: mood stabilizers, atypical antipsychotics, and antidepressants (specifically, bupropion and SSRIs—not TCAs, venlafaxine, or duloxetine—and over the short term only). Consider divalproex for mania and hypomania, used cautiously because of its adverse side-effect potential.
George T. Grossberg, MD
AFTERNOON SESSION
Often, BD is misdiagnosed as unipolar depression, or the correct diagnosis of BD is delayed, according to Gustavo Alva, MD, ATP Clinical Research. Comorbid substance use disorder or an anxiety disorder is common. Comorbid cardiovascular disease brings a greater risk of mortality in patients with BD than suicide. Approximately two-thirds of patients with BD are taking adjunctive medications; however, antidepressants are no more effective than placebo in treating bipolar depression. At this sponsored symposium, Vladimir Maletic, MD, University of South Carolina, described a 6-week trial in which lurasidone plus lithium or divalporex was more effective in reducing depression, as measured by MADRS, than placebo plus lithium or akathisia, somnolence, and extrapyramidal symptoms.
When assessing an older patient with psychosis, first establish the cause of the symptoms, such as Alzheimer’s disease, affective disorder, substance use, or hallucinations associated with grief. Older patients with schizophrenia who have been taking typical antipsychotics for years might benefit from a switch to an atypical or a dosage reduction. Dr. Grossberg recommends considering antipsychotics for older patients when symptoms cause severe emotional distress that does not respond to other interventions or an acute episode that poses a safety risk for patients or others. Choose an antipsychotic based on side effects, and “start low and go slow,” when possible. The goal is to reduce agitation and distress—not necessarily to resolve psychotic symptoms.
Anita H. Clayton, MD, University of Virginia Health System, provided a review of sexual function from puberty through midlife and older years. Social factors play a role in sexual satisfaction, such as gender expectations, religious beliefs, and the influence of reporting in the media. Sexual dysfunction becomes worse in men after age 29; in women, the rate of sexual dysfunction appears to be consistent across the lifespan. Cardiovascular disease is a significant risk factor for sexual dysfunction in men, but not in women. Sexual function and depression have a bidirectional relationship; sexual dysfunction may be a symptom or cause of depression and antidepressants may affect desire and function. Medications, including psychotropics, oral contraceptives, and opioids, can cause sexual dysfunction.
Providers often are reluctant to bring up sexual issues with their patients, Dr. Clayton says, but patients often want to talk about their sexual problems. In reproductive-age women, look for hypoactive sexual desire disorder and pain. In men, assess for erectile dysfunction or premature ejaculation. Inquire about every phase of the sexual response cycle. When managing sexual dysfunction, aim to minimize contributing factors such as illness or medication, consider FDA-approved medications, encourage a healthy lifestyle, and employ psychological interventions when appropriate. In patients with antidepressant-associated sexual dysfunction, consider switching medications or adding an antidote, such as bupropion, buspirone, or sildenafil.
Saturday, March 29, 2014
MORNING SESSION
Because of the lack of double-blind, placebo-controlled trials, the risks of untreated depression vs the risks of antidepressant use in pregnancy are unclear. Marlene P. Freeman, MD, Massachusetts General Hospital, described the limited, long-term data on tricyclics and fluoxetine. Some studies have shown a small risk of birth defects with SSRIs; others did not find an association. For moderate or severe depression, use antidepressants at the lowest dosage and try non-medication options, such as psychotherapy and complementary and alternative medicine. During the third trimester, women may need a higher dosage to maintain therapeutic drug levels. Data indicates that folic acid use during pregnancy is associated with a decreased risk of autism and schizophrenia.
James W. Jefferson, MD, University of Wisconsin School of Medicine and Public Health, recommends ruling out medical conditions, such as cancer, that might be causing your patients’ fatigue or depression. Many medications, including over-the-counter agents and supplements, can cause fatigue. Bupropion was more effective than placebo and SSRIs in treating depressed patients with sleepiness and fatigue. Adding a psychostimulant to an SSRI does not have a significantly better effect than placebo on depressive symptoms. Adjunctive modafanil may improve depression and fatigue. Data for dopamine agonists are limited.
Lithium should be used with caution in pregnant women because of the risk of congenital malformations. Dr. Freeman also discussed the potential risks to the fetus with the mother’s use of valproate and lamotrigine (with the latter, a small increase in oral clefting). High-potency typical antipsychotics are considered safe; low-potency drugs have a higher risk of major malformations. For atypicals, the risk of malformations appears minimal; newborns might display extrapyramidal effects and withdrawal symptoms. Infants exposed to psychostimulants may have lower birth weight, but are not at increased risk of birth defects.
Dr. Jefferson reviewed the efficacy, pharmacokinetics, and adverse effects of vilazodone, levomilnacipran, and vortioxetine, which are antidepressants new to the market. Dr. Jefferson recommends reading package inserts to become familiar with new drugs. He also described studies of medications that were not FDA-approved, including edivoxetine, quetiapine XR monotherapy for MDD, and agomelatine. Agents under investigation include onabotulinumtoxin A injections, ketamine, and lanicemine.
Katherine E. Burdick, PhD, Mount Sinai School of Medicine, defined cognitive domains. First-episode MDD patients perform worse in psychomotor speed and attention than healthy controls. Late-onset depression (after age 60) is associated with worse performance on processing speed and verbal memory. Cognitive deficits in depressed patients range from mild to moderate and are influenced by symptom status and duration of illness. Treating cognitive deficits begins with prevention. Cholinesterase inhibitors are not effective for improving cognition in MDD. Antidepressants, including SSRIs, do not adequately treat cognitive deficits, Roger S. McIntyre, MD, FRCPC, University of Toronto, explained.
Current Psychiatry and the American Academy of Clinical Psychiatrists welcomed more than 550 psychiatric practitioners from across the United States and abroad to this annual conference, which was headed by Meeting Chair Richard Balon, MD, and Co-chairs Donald W. Black, MD, and Nagy Youssef, MD, March 27-29, 2014 at the Hilton Chicago in Chicago, Illinois. Attendees earned as many as 10 AMA PRA Category 1 Credits™.
Thursday, March 27, 2014
MORNING SESSION
Obsessive-compulsive disorder can be misdiagnosed as psychosis, anxiety, or a sexual disorder. In addition to contamination, patients can present with pathologic doubt, somatic obsessions, or obsessions about taboo or symmetry. Among FDA-approved medications, clomipramine might be more effective than selective serotonin reuptake inhibitors (SSRIs). Exposure response prevention therapy shows better response than pharmacotherapy, but best outcomes are seen with combination therapy. Jon E. Grant, JD, MD, MPH, University of Chicago, also discussed obsessive-compulsive personality disorder, body dysmorphic disorder, hoarding, trichotillomania, and excoriation disorder—as well as changes in DSM-5 that cover this group of disorders.
Patients with schizophrenia are at higher risk of death from cardiac and pulmonary disease than the general population. The quality of care of patients with psychosis generally is poor, because of lack of recognition, time, and resources, as well as systematic barriers to accessing health care. Questions about weight gain, lethargy, infections, and sexual functioning can help the practitioner assess a patient’s general health. When appropriate, Henry A. Nasrallah, MD, St. Louis University School of Medicine, recommends, consider switching antipsychotics, which might reverse adverse metabolic events.
Nonpharmacologic treatment goals include improving sleep, educating patients, providing them with tools for improving sleep, and creating an opportunity for patient-practitioner discussion. Stimulus control and sleep restriction are primary therapeutic techniques to improve sleep quality and reduce non-sleeping time in bed. Thomas Roth, PhD, Henry Ford Hospital, also discussed how to modify sleep hygiene techniques for pediatric, adolescent, and geriatric patients.
Donald W. Black, MD, University of Iowa, says that work groups for DSM-5 were asked to consider dimensionality and culture and gender issues. New diagnostic categories include obsessive-compulsive and related disorders and trauma and stressor-related disorders. Some diagnoses were reformulated or introduced, including autism spectrum disorder and disruptive mood dysregulation disorder. The multi-axial system was discontinued in DSM-5. He also reviewed coding issues.
In a sponsored symposium, Prakash S. Masand, MD, Global Medical Education, Inc., looked at the clinical challenges of addressing all 3 symptom domains that characterize depression (emotional, physical, and cognitive) as an introduction to reviewing the efficacy, mechanism of action, and side effects of vortioxetine (Brintellix), a new serotonergic agent for treating major depressive disorder (MDD). In all studies submitted to the FDA, vortioxetine was found to be superior to placebo, in at least 1 dosage group, for alleviating depressive symptoms and for reducing the risk of depressive recurrence.
AFTERNOON SESSION
Oppositional defiant disorder is more common in boys (onset at age 6 to 10) and is associated with inconsistent and neglectful parenting. Treatment modalities, including educational training, anticonvulsants, and lithium, do not have a strong evidence base. Intermittent explosive disorder is characterized by short-lived but frequent behavioral outbursts and often begins in adolescence. Dr. Grant also reviewed the evidence on conduct disorder, pyromania, and kleptomania.
Cognitive symptoms of schizophrenia often appear before psychotic symptoms and remain stable across the lifespan. There are no pharmacologic treatments for cognitive deficits in schizophrenia; however, Dr. Nasrallah listed tactics to improve cognitive function, including regular aerobic exercise. These cognitive deficits can be categorized as neurocognitive (memory, learning, executive function) and social (social skills, theory of mind, social cues) and contribute to functional decline and often prevent patients from working and going to school. Dr. Nasrallah described how bipolar disorder (BD) overlaps with schizophrenia in terms of cognitive dysfunction.
Henry Nasrallah, MD
Psychiatric disorders exhibit specific sleep/ wake impairments. Sleep disorders can mimic psychiatric symptoms, such as fatigue, cognitive problems, and depression. Sleep disturbances, including insomnia, obstructive sleep apnea, and decreased need for sleep, often coexist with depression, generalized anxiety disorder, posttraumatic stress disorder, and BD, and insomnia is associated with a greater risk of suicide. With antidepressant treatment, sleep in depressed patients improves but does not normalize. Dr. Roth also reviewed pharmacotherapeutic options and non-drug modalities to improve patients’ sleep.
Antidepressants have no efficacy in treating acute episodes of bipolar depression, and using such agents might yield a poor long-term outcome in BD, according to Robert M. Post, MD, George Washington University School of Medicine, Michael J. Ostacher, MD, MPH, MMSc, Stanford University, and Vivek Singh, MD, University of Texas Health Science Center at San Antonio, in an interactive faculty discussion. For patients with bipolar I disorder, lithium monotherapy or the combination of lithium and valproate is more effective than valproate alone; evidence does not support valproate as a maintenance treatment. When a patient with BD shows partial response, attendees at this sponsored symposium were advised, consider adding psychotherapy and psycho-education. Combining a mood stabilizer and an antipsychotic might be more effective than monotherapy and safer, by allowing lower dosages. The only 3 treatments FDA-approved for bipolar depression are the olanzapine-fluoxetine combination, quetiapine, and lurasidone.
Boaz Levy, PhD, (left) receives the 2014 George Winokur Research Award from Carol S. North, MD, for his article on recovery of cognitive function in patients with co-occuring bipolar disorder and alcohol dependence.
Friday, March 28, 2014
MORNING SESSION
Carmen Pinto, MD, at a sponsored symposium, reviewed the utility and safety of
long-acting injectable (LAI) antipsychotics for treating schizophrenia, with a focus on LAI aripiprazole, a partial HT-receptor agonist/partial HT-receptor antagonist. Four monthly injections (400 mg/injection) of the drug are needed to reach steady state; each injection reaches peak level in 5 to 7 days. LAI aripiprazole has been shown to delay time to relapse due to nonadherence and onset of nonresponse to the drug, and has high patient acceptance—even in those who already stable. Safety and side effects with LAI aripiprazole are the same as seen with the oral formulation.
In multimodal therapy for chronic pain, psychiatrists have a role in assessing
psychiatric comorbidities, coping ability, social functioning, and other life functions, including work and personal relationships. Cognitive-behavioral therapy can be particularly useful for chronic pain by helping patients reframe their pain experiences. Raphael J. Leo, MA, MD, FAPM, University at Buffalo, reviewed non-opioid co-analgesics that can be used for patients with comorbid pain and a substance use disorder. If opioids are necessary, consider “weak” or long-acting opioids. Monitor patients for aberrant, drug-seeking behavior.
In the second part of his overview, Dr. Black highlighted specific changes to DSM-5 of particular concern to clinicians. New chapters were created and disorders were consolidated, he explained, such as autism spectrum disorder, somatic symptom disorder, and major neurocognitive disorder. New diagnoses include hoarding disorder and binge eating disorder. Subtypes of schizophrenia were dropped. Pathologic gambling was renamed gambling disorder and gender dysphoria is now called gender identity disorder. The bereavement exclusion of a major depressive episode was dropped.
Antidepressants are effective in mitigating pain in neuropathy, headache, fibromyalgia, and chronic musculoskeletal pain, and have been advocated for other pain syndromes. Selection of an antidepressant depends on the type of pain condition, comorbid depression or anxiety, tolerability, and medical comorbidities. Dr. Leo presented prescribing strategies for tricyclics, serotoninnorepinephrine
reuptake inhibitors, SSRIs, and other antidepressants.
Treating of BD in geriatric patients becomes complicated because therapeutic choices are narrowed and response to therapy is less successful with age, according to George T. Grossberg, MD, St. Louis University. Rapid cycling tends to be the norm in geriatric BD patients. Look for agitation and irritability, rather than full-blown mania; grandiose delusions; psychiatric comorbidity, especially anxiety disorder; and sexually inappropriate behavior. Pharmacotherapeutic options include: mood stabilizers, atypical antipsychotics, and antidepressants (specifically, bupropion and SSRIs—not TCAs, venlafaxine, or duloxetine—and over the short term only). Consider divalproex for mania and hypomania, used cautiously because of its adverse side-effect potential.
George T. Grossberg, MD
AFTERNOON SESSION
Often, BD is misdiagnosed as unipolar depression, or the correct diagnosis of BD is delayed, according to Gustavo Alva, MD, ATP Clinical Research. Comorbid substance use disorder or an anxiety disorder is common. Comorbid cardiovascular disease brings a greater risk of mortality in patients with BD than suicide. Approximately two-thirds of patients with BD are taking adjunctive medications; however, antidepressants are no more effective than placebo in treating bipolar depression. At this sponsored symposium, Vladimir Maletic, MD, University of South Carolina, described a 6-week trial in which lurasidone plus lithium or divalporex was more effective in reducing depression, as measured by MADRS, than placebo plus lithium or akathisia, somnolence, and extrapyramidal symptoms.
When assessing an older patient with psychosis, first establish the cause of the symptoms, such as Alzheimer’s disease, affective disorder, substance use, or hallucinations associated with grief. Older patients with schizophrenia who have been taking typical antipsychotics for years might benefit from a switch to an atypical or a dosage reduction. Dr. Grossberg recommends considering antipsychotics for older patients when symptoms cause severe emotional distress that does not respond to other interventions or an acute episode that poses a safety risk for patients or others. Choose an antipsychotic based on side effects, and “start low and go slow,” when possible. The goal is to reduce agitation and distress—not necessarily to resolve psychotic symptoms.
Anita H. Clayton, MD, University of Virginia Health System, provided a review of sexual function from puberty through midlife and older years. Social factors play a role in sexual satisfaction, such as gender expectations, religious beliefs, and the influence of reporting in the media. Sexual dysfunction becomes worse in men after age 29; in women, the rate of sexual dysfunction appears to be consistent across the lifespan. Cardiovascular disease is a significant risk factor for sexual dysfunction in men, but not in women. Sexual function and depression have a bidirectional relationship; sexual dysfunction may be a symptom or cause of depression and antidepressants may affect desire and function. Medications, including psychotropics, oral contraceptives, and opioids, can cause sexual dysfunction.
Providers often are reluctant to bring up sexual issues with their patients, Dr. Clayton says, but patients often want to talk about their sexual problems. In reproductive-age women, look for hypoactive sexual desire disorder and pain. In men, assess for erectile dysfunction or premature ejaculation. Inquire about every phase of the sexual response cycle. When managing sexual dysfunction, aim to minimize contributing factors such as illness or medication, consider FDA-approved medications, encourage a healthy lifestyle, and employ psychological interventions when appropriate. In patients with antidepressant-associated sexual dysfunction, consider switching medications or adding an antidote, such as bupropion, buspirone, or sildenafil.
Saturday, March 29, 2014
MORNING SESSION
Because of the lack of double-blind, placebo-controlled trials, the risks of untreated depression vs the risks of antidepressant use in pregnancy are unclear. Marlene P. Freeman, MD, Massachusetts General Hospital, described the limited, long-term data on tricyclics and fluoxetine. Some studies have shown a small risk of birth defects with SSRIs; others did not find an association. For moderate or severe depression, use antidepressants at the lowest dosage and try non-medication options, such as psychotherapy and complementary and alternative medicine. During the third trimester, women may need a higher dosage to maintain therapeutic drug levels. Data indicates that folic acid use during pregnancy is associated with a decreased risk of autism and schizophrenia.
James W. Jefferson, MD, University of Wisconsin School of Medicine and Public Health, recommends ruling out medical conditions, such as cancer, that might be causing your patients’ fatigue or depression. Many medications, including over-the-counter agents and supplements, can cause fatigue. Bupropion was more effective than placebo and SSRIs in treating depressed patients with sleepiness and fatigue. Adding a psychostimulant to an SSRI does not have a significantly better effect than placebo on depressive symptoms. Adjunctive modafanil may improve depression and fatigue. Data for dopamine agonists are limited.
Lithium should be used with caution in pregnant women because of the risk of congenital malformations. Dr. Freeman also discussed the potential risks to the fetus with the mother’s use of valproate and lamotrigine (with the latter, a small increase in oral clefting). High-potency typical antipsychotics are considered safe; low-potency drugs have a higher risk of major malformations. For atypicals, the risk of malformations appears minimal; newborns might display extrapyramidal effects and withdrawal symptoms. Infants exposed to psychostimulants may have lower birth weight, but are not at increased risk of birth defects.
Dr. Jefferson reviewed the efficacy, pharmacokinetics, and adverse effects of vilazodone, levomilnacipran, and vortioxetine, which are antidepressants new to the market. Dr. Jefferson recommends reading package inserts to become familiar with new drugs. He also described studies of medications that were not FDA-approved, including edivoxetine, quetiapine XR monotherapy for MDD, and agomelatine. Agents under investigation include onabotulinumtoxin A injections, ketamine, and lanicemine.
Katherine E. Burdick, PhD, Mount Sinai School of Medicine, defined cognitive domains. First-episode MDD patients perform worse in psychomotor speed and attention than healthy controls. Late-onset depression (after age 60) is associated with worse performance on processing speed and verbal memory. Cognitive deficits in depressed patients range from mild to moderate and are influenced by symptom status and duration of illness. Treating cognitive deficits begins with prevention. Cholinesterase inhibitors are not effective for improving cognition in MDD. Antidepressants, including SSRIs, do not adequately treat cognitive deficits, Roger S. McIntyre, MD, FRCPC, University of Toronto, explained.
Evaluating psychotic patients' risk of violence: A practical guide
When evaluating a patient’s risk of violence, the presence of psychosis is a crucial concern. Douglas et al1 found that psychosis was the most important predictor of violent behavior in an analysis of 204 studies examining the relationship between psychopathology and aggression. Clinicians need to be familiar with aspects of persecutory delusions and command auditory hallucinations that are associated with an increased risk of aggression because accurately assessing patients who are experiencing these 2 symptoms is an important part of a comprehensive violence risk assessment.
This article highlights the importance of investigating persecutory delusions and command auditory hallucinations when evaluating a psychotic patient’s risk for violence. We provide specific questions to ask to help gauge risk associated with these 2 symptoms.
Evaluating persecutory delusions
Do persecutory delusions increase the risk that a person will behave violently? Research examining delusions’ contribution to violent behavior does not provide a clear answer. Earlier studies suggested that persecutory delusions were associated with an increased risk of aggression.2 Delusions noted to increase the risk of violence were characterized by threat/control-override (TCO) symptoms. TCO symptoms are beliefs that one is being threatened (eg, being followed or poisoned) or is losing control to an external source (eg, one’s mind is dominated by forces beyond his or her control).3 Similarly, using data from the Epidemiologic Catchment Area surveys, Swanson et al4 found that patients who reported TCO symptoms were approximately twice as likely to engage in assaultive behavior compared with patients with other psychotic symptoms.
In contrast, the MacArthur Study of Mental Disorder and Violence5,6 showed that the presence of delusions did not predict higher rates of violence among recently discharged psychiatric patients. In particular, researchers did not find a relationship between the presence of TCO delusions and violent behavior. In a study comparing male criminal offenders with schizophrenia found not guilty by reason of insanity with matched non-offending schizophrenia patients, Stompe et al7 found no significant association between TCO symptoms and severity of violent behavior; prevalence of TCO symptoms did not differ between the 2 groups. However, nondelusional suspiciousness—such as misperceiving others’ behavior as indicating hostile intent—was associated with subsequent violence.6
Nederlof et al8 conducted a cross-sectional multicenter study to further examine whether TCO symptoms are related to aggressive behavior. Their study included 124 patients (88% men) who had paranoid schizophrenia (70%), “other forms” of schizophrenia (16%), schizoaffective disorder (3%), delusional disorder (1%), and psychosis not otherwise specified (10%). To measure TCO symptoms in a more detailed manner than in previous research, these researchers developed the Threat/Control-Override Questionnaire (TCOQ), a 14-item, self-report scale. The 7 threat items specific to the TCOQ are:8
- I am under the control of an external force that determines my actions.
- Other people have tried to poison me or to do me harm.
- Someone has deliberately tried to make me ill.
- Other people have been secretly plotting to ruin me.
- Someone has had evil intentions against me.
- I have the thought that I was being followed for a special reason.
- People have tried to drive me insane.
The 7 control-override items on the TCOQ are:8
- Other people control my way of movements.
- Other people can insert thoughts into my head.
- My thoughts are dominated by an external force.
- I have the feeling that other people can determine my thoughts.
- Other people can insert thoughts into my mind.
- I have the feeling that other people have control over me.
- My life is being determined by something or someone except for myself.
Nederlof et al8 determined that TCO symptoms were a significant correlate of aggression in their study sample. When the 2 domains of TCO symptoms were evaluated separately, only threat symptoms made a significant contribution to aggressive behavior. These researchers suggested that varying methods of measuring TCO symptoms may underlie previous studies’ seemingly contradictory findings.8 These recent findings indicate that the debate regarding the contribution of TCO symptoms, particularly threat symptoms, to future violence remains active.
Appelbaum et al9 used the MacArthur-Maudsley Delusions Assessment Schedule to examine the contribution of non-content-related delusional material to violence in interviews with 328 delusional hospitalized psychiatric patients. The 7 dimensions of the MacArthur-Maudsley Delusions Assessment Schedule are:
- Conviction—the degree of certainty about the delusional belief
- Negative affect—whether the delusional belief makes the patient unhappy, frightened, anxious, or angry
- Action—the extent to which the patient’s actions are motivated by the delusional belief
- Inaction—whether the patient has refrained from any action as a result of the delusional belief
- Preoccupation—the extent to which the patient indicates his or her thoughts focus exclusively on the delusion
- Pervasiveness—the degree to which the delusional belief penetrates all aspects of the patient’s experiences
- Fluidity—the degree to which the delusional belief changed frequently during the interview.
Patients with persecutory delusions had significantly higher scores on “action” and “negative affect” dimensions, indicating that those with persecutory delusions may be more likely to react in response to the dysphoric aspects of their symptoms.9 Subsequent research has demonstrated that patients who suffer from persecutory delusions and negative affect are more likely to act on their delusions2,10 and to act violently11 than patients without these symptoms.
When evaluating a patient who experiences persecutory delusions, inquire if he or she has employed “safety actions.” These are specific behaviors—such as avoiding a perceived persecutor or escaping a fearful situation—the individual has employed with the intention of minimizing a misperceived threat. In a study of 100 patients with persecutory delusions, 96% reported using safety behaviors in the past month.12 In this study, individuals with a history of violence reported a greater use of safety behaviors.
Table 1 lists 10 questions to ask patients to explore persecutory delusions and associated risk factors for aggression.
Table 1
Evaluating persecutory delusions: 10 questions
| 1. | Who or what do you believe wants to harm you? |
| 2. | How is this person attempting to harm you? (Ask about specific threat/control-override beliefs) |
| 3. | How certain are you that this is happening? |
| 4. | Is there anything that could convince you that this isn’t true? |
| 5. | How does your belief make you feel (eg, unhappy, frightened, anxious, or angry)? |
| 6. | Have you thought about any actions to take as a result of these beliefs? If so, what? |
| 7. | Have you taken any action as a result of your beliefs? If so, what specific actions? |
| 8. | Has your concern about being harmed stopped you from doing any action that you would normally do? Have you changed your routine in any way? |
| 9. | How much time do you spend thinking about this each day? |
| 10. | In what ways have these beliefs impacted your life? |
Assessing auditory hallucinations
A careful inquiry about hallucinations can help determine whether their presence increases a patient’s risk of committing a violent act. Command hallucinations provide some type of directive to the patient. Approximately 50% of hallucinating psychiatric patients experience command hallucinations.13 Most command hallucinations are nonviolent, and patients are more likely to obey nonviolent instructions than violent commands.14
Research on factors associated with a patient acting on harmful command hallucinations has been mixed. In a review of 7 controlled studies, no study demonstrated a positive relationship between command hallucinations and violence, and 1 found an inverse relationship.15 In contrast, in a study of 103 psychiatric inpatients, McNiel et al16 found 30% reported having command hallucinations to harm others during the past year and 22% reported they complied with such commands. These researchers concluded that compared with those without command hallucinations, patients in their study who experienced command hallucinations to harm others were more than twice as likely to be violent.
Much of the literature examining the relationship between a patient’s actions and command hallucinations has examined the patient’s response to all command hallucinations, without delineating factors specific to violent commands. Seven factors are associated with acting on command hallucinations:13
- the presence of coexisting delusions17
- having delusions that relate to the hallucination18
- knowing the voice’s identity18
- believing the voices to be real19
- believing that the voices are benevolent20
- having few coping strategies to deal with the voices17
- not feeling in control over the voices.20
These factors also have been found to indicate increased compliance with acting on violent command hallucinations.18,20 Studies that have examined compliance specific to harmful command hallucinations provide additional guidance when evaluating the patient’s risk of harm. Aspects relevant to increased compliance to violent command hallucinations include a belief that the voice is powerful,13,21 a patient’s sense of personal superiority,21 a belief that command hallucinations benefit the patient,13 delusions that were congruent with the action described,13 and hallucinations that generate negative emotions such as anger, anxiety, and sadness.11
Table 2 lists 10 questions to ask to further investigate general command auditory hallucinations and violent command auditory hallucinations.
Table 2
Evaluating command auditory hallucinations: 10 questions
| 1. | What are the voices telling you to do? |
| 2. | Do you have any thoughts or beliefs that are associated with what you are hearing? If so, what are they? |
| 3. | Do you know the voice’s identity? If so, who is it? |
| 4. | How convinced are you that these voices are real? |
| 5. | Are these voices wishing you well or do you think that they wish you harm? |
| 6. | Have you done anything to help make the voices go away? If so, what? |
| 7. | Do you feel you have control of the voices or do you feel they control you? |
| 8. | Do you believe the voice is powerful? |
| 9. | How do the voices make you feel? |
| 10. | Have you ever done what the voice has told you to do? If so, describe what you did. |
Related Resources
- MacArthur Research Network on Mental Health and the Law. The MacArthur Violence Risk Assessment Study.http://macarthur.virginia.edu/risk.html.
- Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies [published online February 13, 2013]. PLoS One. 2013;8(2):e55942. doi: 10.1371/journal.pone.0055942.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Douglas KS, Guy LS, Hart SD. Psychosis as a risk factor for violence to others: a meta-analysis. Psychol Bull. 2009;135(5):679-706.
2. Wessely S, Buchanan A, Reed A, et al. Acting on delusions. I: Prevalence. Br J Psychiatry. 1993;163:69-76.
3. Link BG, Stueve A. Evidence bearing on mental illness as a possible cause of violent behavior. Epidemiol Rev. 1995;17(1):172-181.
4. Swanson JW, Borum R, Swartz MS, et al. Psychotic symptoms and disorders and the risk of violent behaviour in the community. Crim Behav Ment Health. 1996;6(4):309-329.
5. MacArthur Research Network on Mental Health and the Law. The MacArthur Violence Risk Assessment Study. http://macarthur.virginia.edu/risk.html. Published April 2001. Accessed March 21 2013.
6. Monahan J, Steadman HJ, Silver E, et al. Rethinking risk assessment: the MacArthur study of mental disorder and violence. New York, NY: Oxford University Press, Inc.; 2001.
7. Stompe T, Ortwein-Swoboda G, Schanda H. Schizophrenia delusional symptoms, and violence: the threat/control override concept reexamined. Schizophr Bull. 2004;30(1):31-44.
8. Nederlof AF, Muris P, Hovens JE. Threat/control-override symptoms and emotional reactions to positive symptoms as correlates of aggressive behavior in psychotic patients. J Nerv Ment Dis. 2011;199(5):342-347.
9. Appelbaum PS, Robbins PC, Roth LH. Dimensional approach to delusions: comparison across types and diagnoses. Am J Psychiatry. 1999;156(12):1938-1943.
10. Buchanan A, Reed A, Wessely S, et al. Acting on delusions. II: The phenomenological correlates of acting on delusions. Br J Psychiatry. 1993;163:77-81.
11. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res. 1997;26(2-3):181-190.
12. Freeman D, Garety PA, Kuipers E, et al. Acting on persecutory delusions: the importance of safety seeking. Behav Res Ther. 2007;45(1):89-99.
13. Shawyer F, MacKinnon A, Farhall J, et al. Command hallucinations and violence: implications for detention and treatment. Psychiatr Psychol Law. 2003;10(1):97-107.
14. Chadwick P, Birchwood M. The omnipotence of voices. A cognitive approach to auditory hallucinations. Br J Psychiatry. 1994;164(2):190-201.
15. Rudnick A. Relation between command hallucinations and dangerous behavior. J Am Acad Psychiatry Law. 1999;27(2):253-257.
16. McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatr Serv. 2000;51(10):1288-1292.
17. Mackinnon A, Copolov DL, Trauer T. Factors associated with compliance and resistance to command hallucinations. J Nerv Ment Dis. 2004;192(5):357-362.
18. Junginger J. Predicting compliance with command hallucinations. Am J Psychiatry. 1990;147(2):245-247.
19. Erkwoh R, Willmes K, Eming-Erdmann A, et al. Command hallucinations: who obeys and who resists when? Psychopathology. 2002;35(5):272-279.
20. Beck-Sander A, Birchwood M, Chadwick P. Acting on command hallucinations: a cognitive approach. Br J Clin Psychol. 1997;36(pt 1):139-148.
21. Fox JRE, Gray NS, Lewis H. Factors determining compliance with command hallucinations with violent content: the role of social rank perceived power of the voice and voice malevolence. J Forens Psychiatry Psychol. 2004;15(3):511-531.
When evaluating a patient’s risk of violence, the presence of psychosis is a crucial concern. Douglas et al1 found that psychosis was the most important predictor of violent behavior in an analysis of 204 studies examining the relationship between psychopathology and aggression. Clinicians need to be familiar with aspects of persecutory delusions and command auditory hallucinations that are associated with an increased risk of aggression because accurately assessing patients who are experiencing these 2 symptoms is an important part of a comprehensive violence risk assessment.
This article highlights the importance of investigating persecutory delusions and command auditory hallucinations when evaluating a psychotic patient’s risk for violence. We provide specific questions to ask to help gauge risk associated with these 2 symptoms.
Evaluating persecutory delusions
Do persecutory delusions increase the risk that a person will behave violently? Research examining delusions’ contribution to violent behavior does not provide a clear answer. Earlier studies suggested that persecutory delusions were associated with an increased risk of aggression.2 Delusions noted to increase the risk of violence were characterized by threat/control-override (TCO) symptoms. TCO symptoms are beliefs that one is being threatened (eg, being followed or poisoned) or is losing control to an external source (eg, one’s mind is dominated by forces beyond his or her control).3 Similarly, using data from the Epidemiologic Catchment Area surveys, Swanson et al4 found that patients who reported TCO symptoms were approximately twice as likely to engage in assaultive behavior compared with patients with other psychotic symptoms.
In contrast, the MacArthur Study of Mental Disorder and Violence5,6 showed that the presence of delusions did not predict higher rates of violence among recently discharged psychiatric patients. In particular, researchers did not find a relationship between the presence of TCO delusions and violent behavior. In a study comparing male criminal offenders with schizophrenia found not guilty by reason of insanity with matched non-offending schizophrenia patients, Stompe et al7 found no significant association between TCO symptoms and severity of violent behavior; prevalence of TCO symptoms did not differ between the 2 groups. However, nondelusional suspiciousness—such as misperceiving others’ behavior as indicating hostile intent—was associated with subsequent violence.6
Nederlof et al8 conducted a cross-sectional multicenter study to further examine whether TCO symptoms are related to aggressive behavior. Their study included 124 patients (88% men) who had paranoid schizophrenia (70%), “other forms” of schizophrenia (16%), schizoaffective disorder (3%), delusional disorder (1%), and psychosis not otherwise specified (10%). To measure TCO symptoms in a more detailed manner than in previous research, these researchers developed the Threat/Control-Override Questionnaire (TCOQ), a 14-item, self-report scale. The 7 threat items specific to the TCOQ are:8
- I am under the control of an external force that determines my actions.
- Other people have tried to poison me or to do me harm.
- Someone has deliberately tried to make me ill.
- Other people have been secretly plotting to ruin me.
- Someone has had evil intentions against me.
- I have the thought that I was being followed for a special reason.
- People have tried to drive me insane.
The 7 control-override items on the TCOQ are:8
- Other people control my way of movements.
- Other people can insert thoughts into my head.
- My thoughts are dominated by an external force.
- I have the feeling that other people can determine my thoughts.
- Other people can insert thoughts into my mind.
- I have the feeling that other people have control over me.
- My life is being determined by something or someone except for myself.
Nederlof et al8 determined that TCO symptoms were a significant correlate of aggression in their study sample. When the 2 domains of TCO symptoms were evaluated separately, only threat symptoms made a significant contribution to aggressive behavior. These researchers suggested that varying methods of measuring TCO symptoms may underlie previous studies’ seemingly contradictory findings.8 These recent findings indicate that the debate regarding the contribution of TCO symptoms, particularly threat symptoms, to future violence remains active.
Appelbaum et al9 used the MacArthur-Maudsley Delusions Assessment Schedule to examine the contribution of non-content-related delusional material to violence in interviews with 328 delusional hospitalized psychiatric patients. The 7 dimensions of the MacArthur-Maudsley Delusions Assessment Schedule are:
- Conviction—the degree of certainty about the delusional belief
- Negative affect—whether the delusional belief makes the patient unhappy, frightened, anxious, or angry
- Action—the extent to which the patient’s actions are motivated by the delusional belief
- Inaction—whether the patient has refrained from any action as a result of the delusional belief
- Preoccupation—the extent to which the patient indicates his or her thoughts focus exclusively on the delusion
- Pervasiveness—the degree to which the delusional belief penetrates all aspects of the patient’s experiences
- Fluidity—the degree to which the delusional belief changed frequently during the interview.
Patients with persecutory delusions had significantly higher scores on “action” and “negative affect” dimensions, indicating that those with persecutory delusions may be more likely to react in response to the dysphoric aspects of their symptoms.9 Subsequent research has demonstrated that patients who suffer from persecutory delusions and negative affect are more likely to act on their delusions2,10 and to act violently11 than patients without these symptoms.
When evaluating a patient who experiences persecutory delusions, inquire if he or she has employed “safety actions.” These are specific behaviors—such as avoiding a perceived persecutor or escaping a fearful situation—the individual has employed with the intention of minimizing a misperceived threat. In a study of 100 patients with persecutory delusions, 96% reported using safety behaviors in the past month.12 In this study, individuals with a history of violence reported a greater use of safety behaviors.
Table 1 lists 10 questions to ask patients to explore persecutory delusions and associated risk factors for aggression.
Table 1
Evaluating persecutory delusions: 10 questions
| 1. | Who or what do you believe wants to harm you? |
| 2. | How is this person attempting to harm you? (Ask about specific threat/control-override beliefs) |
| 3. | How certain are you that this is happening? |
| 4. | Is there anything that could convince you that this isn’t true? |
| 5. | How does your belief make you feel (eg, unhappy, frightened, anxious, or angry)? |
| 6. | Have you thought about any actions to take as a result of these beliefs? If so, what? |
| 7. | Have you taken any action as a result of your beliefs? If so, what specific actions? |
| 8. | Has your concern about being harmed stopped you from doing any action that you would normally do? Have you changed your routine in any way? |
| 9. | How much time do you spend thinking about this each day? |
| 10. | In what ways have these beliefs impacted your life? |
Assessing auditory hallucinations
A careful inquiry about hallucinations can help determine whether their presence increases a patient’s risk of committing a violent act. Command hallucinations provide some type of directive to the patient. Approximately 50% of hallucinating psychiatric patients experience command hallucinations.13 Most command hallucinations are nonviolent, and patients are more likely to obey nonviolent instructions than violent commands.14
Research on factors associated with a patient acting on harmful command hallucinations has been mixed. In a review of 7 controlled studies, no study demonstrated a positive relationship between command hallucinations and violence, and 1 found an inverse relationship.15 In contrast, in a study of 103 psychiatric inpatients, McNiel et al16 found 30% reported having command hallucinations to harm others during the past year and 22% reported they complied with such commands. These researchers concluded that compared with those without command hallucinations, patients in their study who experienced command hallucinations to harm others were more than twice as likely to be violent.
Much of the literature examining the relationship between a patient’s actions and command hallucinations has examined the patient’s response to all command hallucinations, without delineating factors specific to violent commands. Seven factors are associated with acting on command hallucinations:13
- the presence of coexisting delusions17
- having delusions that relate to the hallucination18
- knowing the voice’s identity18
- believing the voices to be real19
- believing that the voices are benevolent20
- having few coping strategies to deal with the voices17
- not feeling in control over the voices.20
These factors also have been found to indicate increased compliance with acting on violent command hallucinations.18,20 Studies that have examined compliance specific to harmful command hallucinations provide additional guidance when evaluating the patient’s risk of harm. Aspects relevant to increased compliance to violent command hallucinations include a belief that the voice is powerful,13,21 a patient’s sense of personal superiority,21 a belief that command hallucinations benefit the patient,13 delusions that were congruent with the action described,13 and hallucinations that generate negative emotions such as anger, anxiety, and sadness.11
Table 2 lists 10 questions to ask to further investigate general command auditory hallucinations and violent command auditory hallucinations.
Table 2
Evaluating command auditory hallucinations: 10 questions
| 1. | What are the voices telling you to do? |
| 2. | Do you have any thoughts or beliefs that are associated with what you are hearing? If so, what are they? |
| 3. | Do you know the voice’s identity? If so, who is it? |
| 4. | How convinced are you that these voices are real? |
| 5. | Are these voices wishing you well or do you think that they wish you harm? |
| 6. | Have you done anything to help make the voices go away? If so, what? |
| 7. | Do you feel you have control of the voices or do you feel they control you? |
| 8. | Do you believe the voice is powerful? |
| 9. | How do the voices make you feel? |
| 10. | Have you ever done what the voice has told you to do? If so, describe what you did. |
Related Resources
- MacArthur Research Network on Mental Health and the Law. The MacArthur Violence Risk Assessment Study.http://macarthur.virginia.edu/risk.html.
- Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies [published online February 13, 2013]. PLoS One. 2013;8(2):e55942. doi: 10.1371/journal.pone.0055942.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
When evaluating a patient’s risk of violence, the presence of psychosis is a crucial concern. Douglas et al1 found that psychosis was the most important predictor of violent behavior in an analysis of 204 studies examining the relationship between psychopathology and aggression. Clinicians need to be familiar with aspects of persecutory delusions and command auditory hallucinations that are associated with an increased risk of aggression because accurately assessing patients who are experiencing these 2 symptoms is an important part of a comprehensive violence risk assessment.
This article highlights the importance of investigating persecutory delusions and command auditory hallucinations when evaluating a psychotic patient’s risk for violence. We provide specific questions to ask to help gauge risk associated with these 2 symptoms.
Evaluating persecutory delusions
Do persecutory delusions increase the risk that a person will behave violently? Research examining delusions’ contribution to violent behavior does not provide a clear answer. Earlier studies suggested that persecutory delusions were associated with an increased risk of aggression.2 Delusions noted to increase the risk of violence were characterized by threat/control-override (TCO) symptoms. TCO symptoms are beliefs that one is being threatened (eg, being followed or poisoned) or is losing control to an external source (eg, one’s mind is dominated by forces beyond his or her control).3 Similarly, using data from the Epidemiologic Catchment Area surveys, Swanson et al4 found that patients who reported TCO symptoms were approximately twice as likely to engage in assaultive behavior compared with patients with other psychotic symptoms.
In contrast, the MacArthur Study of Mental Disorder and Violence5,6 showed that the presence of delusions did not predict higher rates of violence among recently discharged psychiatric patients. In particular, researchers did not find a relationship between the presence of TCO delusions and violent behavior. In a study comparing male criminal offenders with schizophrenia found not guilty by reason of insanity with matched non-offending schizophrenia patients, Stompe et al7 found no significant association between TCO symptoms and severity of violent behavior; prevalence of TCO symptoms did not differ between the 2 groups. However, nondelusional suspiciousness—such as misperceiving others’ behavior as indicating hostile intent—was associated with subsequent violence.6
Nederlof et al8 conducted a cross-sectional multicenter study to further examine whether TCO symptoms are related to aggressive behavior. Their study included 124 patients (88% men) who had paranoid schizophrenia (70%), “other forms” of schizophrenia (16%), schizoaffective disorder (3%), delusional disorder (1%), and psychosis not otherwise specified (10%). To measure TCO symptoms in a more detailed manner than in previous research, these researchers developed the Threat/Control-Override Questionnaire (TCOQ), a 14-item, self-report scale. The 7 threat items specific to the TCOQ are:8
- I am under the control of an external force that determines my actions.
- Other people have tried to poison me or to do me harm.
- Someone has deliberately tried to make me ill.
- Other people have been secretly plotting to ruin me.
- Someone has had evil intentions against me.
- I have the thought that I was being followed for a special reason.
- People have tried to drive me insane.
The 7 control-override items on the TCOQ are:8
- Other people control my way of movements.
- Other people can insert thoughts into my head.
- My thoughts are dominated by an external force.
- I have the feeling that other people can determine my thoughts.
- Other people can insert thoughts into my mind.
- I have the feeling that other people have control over me.
- My life is being determined by something or someone except for myself.
Nederlof et al8 determined that TCO symptoms were a significant correlate of aggression in their study sample. When the 2 domains of TCO symptoms were evaluated separately, only threat symptoms made a significant contribution to aggressive behavior. These researchers suggested that varying methods of measuring TCO symptoms may underlie previous studies’ seemingly contradictory findings.8 These recent findings indicate that the debate regarding the contribution of TCO symptoms, particularly threat symptoms, to future violence remains active.
Appelbaum et al9 used the MacArthur-Maudsley Delusions Assessment Schedule to examine the contribution of non-content-related delusional material to violence in interviews with 328 delusional hospitalized psychiatric patients. The 7 dimensions of the MacArthur-Maudsley Delusions Assessment Schedule are:
- Conviction—the degree of certainty about the delusional belief
- Negative affect—whether the delusional belief makes the patient unhappy, frightened, anxious, or angry
- Action—the extent to which the patient’s actions are motivated by the delusional belief
- Inaction—whether the patient has refrained from any action as a result of the delusional belief
- Preoccupation—the extent to which the patient indicates his or her thoughts focus exclusively on the delusion
- Pervasiveness—the degree to which the delusional belief penetrates all aspects of the patient’s experiences
- Fluidity—the degree to which the delusional belief changed frequently during the interview.
Patients with persecutory delusions had significantly higher scores on “action” and “negative affect” dimensions, indicating that those with persecutory delusions may be more likely to react in response to the dysphoric aspects of their symptoms.9 Subsequent research has demonstrated that patients who suffer from persecutory delusions and negative affect are more likely to act on their delusions2,10 and to act violently11 than patients without these symptoms.
When evaluating a patient who experiences persecutory delusions, inquire if he or she has employed “safety actions.” These are specific behaviors—such as avoiding a perceived persecutor or escaping a fearful situation—the individual has employed with the intention of minimizing a misperceived threat. In a study of 100 patients with persecutory delusions, 96% reported using safety behaviors in the past month.12 In this study, individuals with a history of violence reported a greater use of safety behaviors.
Table 1 lists 10 questions to ask patients to explore persecutory delusions and associated risk factors for aggression.
Table 1
Evaluating persecutory delusions: 10 questions
| 1. | Who or what do you believe wants to harm you? |
| 2. | How is this person attempting to harm you? (Ask about specific threat/control-override beliefs) |
| 3. | How certain are you that this is happening? |
| 4. | Is there anything that could convince you that this isn’t true? |
| 5. | How does your belief make you feel (eg, unhappy, frightened, anxious, or angry)? |
| 6. | Have you thought about any actions to take as a result of these beliefs? If so, what? |
| 7. | Have you taken any action as a result of your beliefs? If so, what specific actions? |
| 8. | Has your concern about being harmed stopped you from doing any action that you would normally do? Have you changed your routine in any way? |
| 9. | How much time do you spend thinking about this each day? |
| 10. | In what ways have these beliefs impacted your life? |
Assessing auditory hallucinations
A careful inquiry about hallucinations can help determine whether their presence increases a patient’s risk of committing a violent act. Command hallucinations provide some type of directive to the patient. Approximately 50% of hallucinating psychiatric patients experience command hallucinations.13 Most command hallucinations are nonviolent, and patients are more likely to obey nonviolent instructions than violent commands.14
Research on factors associated with a patient acting on harmful command hallucinations has been mixed. In a review of 7 controlled studies, no study demonstrated a positive relationship between command hallucinations and violence, and 1 found an inverse relationship.15 In contrast, in a study of 103 psychiatric inpatients, McNiel et al16 found 30% reported having command hallucinations to harm others during the past year and 22% reported they complied with such commands. These researchers concluded that compared with those without command hallucinations, patients in their study who experienced command hallucinations to harm others were more than twice as likely to be violent.
Much of the literature examining the relationship between a patient’s actions and command hallucinations has examined the patient’s response to all command hallucinations, without delineating factors specific to violent commands. Seven factors are associated with acting on command hallucinations:13
- the presence of coexisting delusions17
- having delusions that relate to the hallucination18
- knowing the voice’s identity18
- believing the voices to be real19
- believing that the voices are benevolent20
- having few coping strategies to deal with the voices17
- not feeling in control over the voices.20
These factors also have been found to indicate increased compliance with acting on violent command hallucinations.18,20 Studies that have examined compliance specific to harmful command hallucinations provide additional guidance when evaluating the patient’s risk of harm. Aspects relevant to increased compliance to violent command hallucinations include a belief that the voice is powerful,13,21 a patient’s sense of personal superiority,21 a belief that command hallucinations benefit the patient,13 delusions that were congruent with the action described,13 and hallucinations that generate negative emotions such as anger, anxiety, and sadness.11
Table 2 lists 10 questions to ask to further investigate general command auditory hallucinations and violent command auditory hallucinations.
Table 2
Evaluating command auditory hallucinations: 10 questions
| 1. | What are the voices telling you to do? |
| 2. | Do you have any thoughts or beliefs that are associated with what you are hearing? If so, what are they? |
| 3. | Do you know the voice’s identity? If so, who is it? |
| 4. | How convinced are you that these voices are real? |
| 5. | Are these voices wishing you well or do you think that they wish you harm? |
| 6. | Have you done anything to help make the voices go away? If so, what? |
| 7. | Do you feel you have control of the voices or do you feel they control you? |
| 8. | Do you believe the voice is powerful? |
| 9. | How do the voices make you feel? |
| 10. | Have you ever done what the voice has told you to do? If so, describe what you did. |
Related Resources
- MacArthur Research Network on Mental Health and the Law. The MacArthur Violence Risk Assessment Study.http://macarthur.virginia.edu/risk.html.
- Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies [published online February 13, 2013]. PLoS One. 2013;8(2):e55942. doi: 10.1371/journal.pone.0055942.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Douglas KS, Guy LS, Hart SD. Psychosis as a risk factor for violence to others: a meta-analysis. Psychol Bull. 2009;135(5):679-706.
2. Wessely S, Buchanan A, Reed A, et al. Acting on delusions. I: Prevalence. Br J Psychiatry. 1993;163:69-76.
3. Link BG, Stueve A. Evidence bearing on mental illness as a possible cause of violent behavior. Epidemiol Rev. 1995;17(1):172-181.
4. Swanson JW, Borum R, Swartz MS, et al. Psychotic symptoms and disorders and the risk of violent behaviour in the community. Crim Behav Ment Health. 1996;6(4):309-329.
5. MacArthur Research Network on Mental Health and the Law. The MacArthur Violence Risk Assessment Study. http://macarthur.virginia.edu/risk.html. Published April 2001. Accessed March 21 2013.
6. Monahan J, Steadman HJ, Silver E, et al. Rethinking risk assessment: the MacArthur study of mental disorder and violence. New York, NY: Oxford University Press, Inc.; 2001.
7. Stompe T, Ortwein-Swoboda G, Schanda H. Schizophrenia delusional symptoms, and violence: the threat/control override concept reexamined. Schizophr Bull. 2004;30(1):31-44.
8. Nederlof AF, Muris P, Hovens JE. Threat/control-override symptoms and emotional reactions to positive symptoms as correlates of aggressive behavior in psychotic patients. J Nerv Ment Dis. 2011;199(5):342-347.
9. Appelbaum PS, Robbins PC, Roth LH. Dimensional approach to delusions: comparison across types and diagnoses. Am J Psychiatry. 1999;156(12):1938-1943.
10. Buchanan A, Reed A, Wessely S, et al. Acting on delusions. II: The phenomenological correlates of acting on delusions. Br J Psychiatry. 1993;163:77-81.
11. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res. 1997;26(2-3):181-190.
12. Freeman D, Garety PA, Kuipers E, et al. Acting on persecutory delusions: the importance of safety seeking. Behav Res Ther. 2007;45(1):89-99.
13. Shawyer F, MacKinnon A, Farhall J, et al. Command hallucinations and violence: implications for detention and treatment. Psychiatr Psychol Law. 2003;10(1):97-107.
14. Chadwick P, Birchwood M. The omnipotence of voices. A cognitive approach to auditory hallucinations. Br J Psychiatry. 1994;164(2):190-201.
15. Rudnick A. Relation between command hallucinations and dangerous behavior. J Am Acad Psychiatry Law. 1999;27(2):253-257.
16. McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatr Serv. 2000;51(10):1288-1292.
17. Mackinnon A, Copolov DL, Trauer T. Factors associated with compliance and resistance to command hallucinations. J Nerv Ment Dis. 2004;192(5):357-362.
18. Junginger J. Predicting compliance with command hallucinations. Am J Psychiatry. 1990;147(2):245-247.
19. Erkwoh R, Willmes K, Eming-Erdmann A, et al. Command hallucinations: who obeys and who resists when? Psychopathology. 2002;35(5):272-279.
20. Beck-Sander A, Birchwood M, Chadwick P. Acting on command hallucinations: a cognitive approach. Br J Clin Psychol. 1997;36(pt 1):139-148.
21. Fox JRE, Gray NS, Lewis H. Factors determining compliance with command hallucinations with violent content: the role of social rank perceived power of the voice and voice malevolence. J Forens Psychiatry Psychol. 2004;15(3):511-531.
1. Douglas KS, Guy LS, Hart SD. Psychosis as a risk factor for violence to others: a meta-analysis. Psychol Bull. 2009;135(5):679-706.
2. Wessely S, Buchanan A, Reed A, et al. Acting on delusions. I: Prevalence. Br J Psychiatry. 1993;163:69-76.
3. Link BG, Stueve A. Evidence bearing on mental illness as a possible cause of violent behavior. Epidemiol Rev. 1995;17(1):172-181.
4. Swanson JW, Borum R, Swartz MS, et al. Psychotic symptoms and disorders and the risk of violent behaviour in the community. Crim Behav Ment Health. 1996;6(4):309-329.
5. MacArthur Research Network on Mental Health and the Law. The MacArthur Violence Risk Assessment Study. http://macarthur.virginia.edu/risk.html. Published April 2001. Accessed March 21 2013.
6. Monahan J, Steadman HJ, Silver E, et al. Rethinking risk assessment: the MacArthur study of mental disorder and violence. New York, NY: Oxford University Press, Inc.; 2001.
7. Stompe T, Ortwein-Swoboda G, Schanda H. Schizophrenia delusional symptoms, and violence: the threat/control override concept reexamined. Schizophr Bull. 2004;30(1):31-44.
8. Nederlof AF, Muris P, Hovens JE. Threat/control-override symptoms and emotional reactions to positive symptoms as correlates of aggressive behavior in psychotic patients. J Nerv Ment Dis. 2011;199(5):342-347.
9. Appelbaum PS, Robbins PC, Roth LH. Dimensional approach to delusions: comparison across types and diagnoses. Am J Psychiatry. 1999;156(12):1938-1943.
10. Buchanan A, Reed A, Wessely S, et al. Acting on delusions. II: The phenomenological correlates of acting on delusions. Br J Psychiatry. 1993;163:77-81.
11. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res. 1997;26(2-3):181-190.
12. Freeman D, Garety PA, Kuipers E, et al. Acting on persecutory delusions: the importance of safety seeking. Behav Res Ther. 2007;45(1):89-99.
13. Shawyer F, MacKinnon A, Farhall J, et al. Command hallucinations and violence: implications for detention and treatment. Psychiatr Psychol Law. 2003;10(1):97-107.
14. Chadwick P, Birchwood M. The omnipotence of voices. A cognitive approach to auditory hallucinations. Br J Psychiatry. 1994;164(2):190-201.
15. Rudnick A. Relation between command hallucinations and dangerous behavior. J Am Acad Psychiatry Law. 1999;27(2):253-257.
16. McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatr Serv. 2000;51(10):1288-1292.
17. Mackinnon A, Copolov DL, Trauer T. Factors associated with compliance and resistance to command hallucinations. J Nerv Ment Dis. 2004;192(5):357-362.
18. Junginger J. Predicting compliance with command hallucinations. Am J Psychiatry. 1990;147(2):245-247.
19. Erkwoh R, Willmes K, Eming-Erdmann A, et al. Command hallucinations: who obeys and who resists when? Psychopathology. 2002;35(5):272-279.
20. Beck-Sander A, Birchwood M, Chadwick P. Acting on command hallucinations: a cognitive approach. Br J Clin Psychol. 1997;36(pt 1):139-148.
21. Fox JRE, Gray NS, Lewis H. Factors determining compliance with command hallucinations with violent content: the role of social rank perceived power of the voice and voice malevolence. J Forens Psychiatry Psychol. 2004;15(3):511-531.
How we can improve end-of-life care
My mother and I were in the hospital lobby waiting for my father. My normally upbeat, sharp, energetic mom looked sick, weak, and confused. She had just been discharged from the hospital after experiencing a seizure caused by brain metastasis from long-standing breast cancer. Although we had discussed hospice care during my mother’s admission, we left the hospital without setting up the service because we wanted more time to see if she could recover. Two days later, we arranged hospice because of my mother’s rapidly deteriorating condition and our inability to manage her illness on our own. Five days later, she passed away at home surrounded by loved ones.
I am bewildered that my family did not transition my mother to end-of-life care earlier. Several family members and I work in the medical field. Being resourceful, we chose treatment at a large medical center that was a 3-hour drive from our home. Also, we were familiar with palliative care because other family members had died with hospice. Yet, in those last precious moments, we did not initiate end-of-life care for my mother until it became an emergency. This experience cultivated my interest in palliative care and hospice, specifically, in barriers to access and better ways to transition from life-saving treatment to end-of-life care. As a psychiatry resident, I feel it is important to expand opportunities for psychiatrists to participate in palliative care teams.
Barriers to end-of-life care
Poor physician-patient communication near the end of life can be a major barrier to care. Studies suggest that patients and physicians are ambivalent about end-of-life discussions and tend to avoid them.1 Communication is crucial to helping patients prepare to die well. Researchers have found that end-of-life discussions between patients and physicians can result in fewer aggressive interventions and better quality of life near death.2 These discussions did not increase emotional distress and were associated with lower rates of ventilation, resuscitation, and intensive care unit admissions.2 End-of-life discussions between physicians and patients also lead to earlier hospice enrollment and improve the quality of end-of-life care.2
Approximately one-third of patients spend <1 week in hospice.3 Studies have suggested that patients who receive >1 week of hospice care have improved quality of life compared with patients who do not receive hospice care.1 Addressing end-of-life issues early in treatment of terminally ill patients allows them to become familiar with their options as their disease progresses.
Lack of integration between hospice and the medical community is another barrier. According to Medicare guidelines,4 to be eligible for hospice a patient must have a terminal illness with a prognosis of ≤6 months. The patient must agree to give up curative treatment. If a patient lives >6 months, hospice benefits can be renewed as long as the patient has shown a persistent decline. Patients must desire and accept a palliative approach rather than a curative focus and agree to have all care provided by Medicare-certified hospices.5 These eligibility requirements may give patients and their families a sense that they are losing the forms of health care they had been using, physicians they know, and treatments they had become accustomed to, and are transferring their medical care to a unknown entity. This transition occurs when diseases are progressing and patients may feel vulnerable. In this way, end-of-life care is segregated from the rest of the medical system and can feel foreign and frightening to patients.6
Lack of palliative care specialists. The U.S. population is aging, and more people are living longer with chronic illness. Although the palliative care field is growing, only 60% of U.S. hospitals have palliative care programs and there is a shortage of palliative care clinicians.7
Psychiatry and end-of-life care
Psychiatry and psycho-oncology can help address these barriers by providing resources and expertise to palliative care teams. Psychiatrists can facilitate communication between families and primary clinicians and help patients mentally prepare for end-of-life options.
The dying process may uncover psychological, psychosocial, and existential suffering in patients and their families that often is underdiagnosed and undertreated.8 Psychiatrists can:
- diagnose and treat psychiatric disorders that surface under the stress of a new diagnosis
- aid in the psychodynamics of coping with terminal illness
- assess decision-making capacity
- recognize and treat staff stress
- provide bereavement care.
Because many clinicians believe that mood or anxiety symptoms are “normal reactions” in individuals struggling with end-of-life issues, these patients may not receive psychiatric treatment. However, treating mood and anxiety disorders can improve quality of life in palliative care patients.9
In terminally ill patients, psychological pain often manifests as symptoms of depression and anxiety. Diagnostic criteria for depression may need to be reconsidered because in patients with terminal illness depressive symptoms commonly are associated with functional decline. For example, restrictions on a patient’s ability to participate in activities and disengagement from some areas of interest are common among individuals facing the end of life, but if a patient is unable to find pleasure in any event or activity, he or she may meet criteria for depression. Endicott10 proposed a list of substitute symptoms of depression in terminally ill patients:
- weight loss or gain is substituted with depressed appearance
- loss of energy is substituted with brooding and self-pity
- insomnia or hypersomnia is substituted with social withdrawal
- loss of concentration is substituted with lack of reactivity or inability to be cheered up.
These substitutions are not in DSM-IV-TR but should be considered when assessing a terminally ill patient.
Most recommendations for pharmacologic treatment of depression in terminally ill patients are based on depression treatments for the general population. Selective serotonin reuptake inhibitors are commonly prescribed for terminally ill patients. Mirtazapine, a noradrenergic and serotonergic antidepressant, has been shown to effectively treat adjustment, mood, and anxiety disorders in patients with breast or gynecological cancer.11 Its major side effects—sedation and weight gain—might be beneficial in patients with terminal illness. Psychostimulants also have been shown to elevate mood in patients with advanced malignancies.12
Potential triggers for anxiety in terminally ill patients include chemotherapy, radiation therapy, or acute pain. Also consider anxiety related to death and dying. Certain drugs commonly used in palliative care—such as corticosteroids and psychostimulants—may contribute to anxiety and restlessness. Cancer patients may develop posttraumatic stress disorder symptoms, including re-experiencing frightening aspects of their diagnosis and treatment, nightmares, hypervigilance, and autonomic hyperactivity.13 Pharmacologic treatment of anxiety in dying patients is similar to that in the general population; benzodiazepines and antidepressants are first-line agents.
Several forms of psychotherapy can help terminally ill patients address existential issues (Box).14-16
Dignity therapy is a form of brief individual therapy developed by Chochinov et al14 that focuses on existential distress to help patients feel that their lives have been worthwhile. The goal is to have patients describe what they are most proud of, what they want to be remembered for, and what is most meaningful to them.
Viederman et al15 characterized a type of therapy known as the psychodynamic life narrative. Palliative care psychiatrists use this technique to examine patients’ lives and take stock of successes and failures. The narrative attempts to create a new perspective within terminally ill patients that increases self-esteem by emphasizing past strengths and coping mechanisms that have been successful.
Meaning-centered group therapy, developed by Breitbart,16 emphasizes group didactics, discussion, and experiential exercises, with a focus on themes related to advanced cancer.
A need for training
In a survey of psychiatry residents, 97% of respondents believed psychiatrists should be trained in end-of-life care and 94% felt there should be formal education on palliative care during residency.17 A study evaluating psychiatry residents’ attitudes, perceived preparedness, experiences, and needs in end-of-life care education found that residents felt least prepared when dealing with cultural and spiritual aspects of dying and helping patients with reconciliation and saying goodbye.18 These residents also expressed a desire for more longitudinal exposure to palliative care.
A dedicated palliative care rotation during psychiatry residency training would help build a foundation of knowledge in this field. Residency programs should make a greater effort to incorporate end-of-life issues into consultation-liaison and geriatric rotations. Education on psychosocial, existential, and spiritual distress should be highlighted, with an emphasis on integrating specific psychotherapy techniques into training. These opportunities would provide residents with necessary skills to help patients cope with end-of-life issues.
As a psychiatry resident, I believe training in this field is one way to decrease barriers for patients to access end-of-life care. End-of-life psychiatric training could help build a culture where end-of-life care is integrated into the medical care system, with the goal of helping terminally ill patients die well.
Related Resources
- Chochinov H, Breitbart W. Handbook of psychiatry in palliative medicine. New York, NY: Oxford University Press; 2009.
- Harvard Medical School Center for Palliative Care. www.hms.harvard.edu/pallcare.
Drug Brand Name
- Mirtazapine • Remeron
Disclosure
Dr. Kester reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Leydon GM, Boulton M, Moynihan C, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ. 2000;320(7239):909-913.
2. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673.
3. Harrington S, Smith T. The role of chemotherapy at the end of life: when is enough enough? JAMA. 2008;299(22):2667-2678.
4. U.S. Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare hospice benefits. http://www.medicare.gov/Pubs/pdf/02154.pdf. Revised January 2013. Accessed March 1, 2013.
5. Meier DE, Isaacs SL, Hughes RG. eds. Palliative care: transforming the care of serious illness. San Francisco, CA: Jossey-Bass; 2010.
6. Rhymes JA. Barriers to effective palliative care of terminal patients. An international perspective. Clin Geriatr Med. 1996;12(2):407-416.
7. Center to Advance Palliative Care. America’s care of serious illness: a state-by-state report card on access to palliative care in our nation’s hospitals. 2011. http://reportcard-live.capc.stackop.com/pdf/state-by-state-report-card.pdf. Accessed March 1, 2013.
8. Söllner W, DeVries A, Steixner E, et al. How successful are oncologists in identifying patient distress, perceived social support, and need for psychosocial counseling? Br J Cancer. 2001;84(2):179-185.
9. Billings JA, Block S. Integrating psychiatry and palliative medicine: the challenges and opportunities. In: Chochinov HM Breitbart W, eds. Handbook of psychiatry in palliative medicine. New York, NY: Oxford University Press; 2009:13–19.
10. Endicott J. Measurement of depression in patients with cancer. Cancer. 1984;53(10 suppl):2243-2249.
11. Thompson DS. Mirtazapine for the treatment of depression and nausea in breast and gynecological oncology. Psychosomatics. 2000;41(4):356-359.
12. Macleod AD. Methylphenidate in terminal depression. J Pain Symptom Manage. 1998;16(3):193-198.
13. Alter CL, Pelcovitz D, Axelrod A, et al. Identification of PTSD in cancer survivors. Psychosomatics. 1996;37(2):137-143.
14. Chochinov HM, Hack T, Hassard T, et al. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol. 2005;23(24):5520-5525.
15. Viederman M, Perry SW, 3rd. Use of a psychodynamic life narrative in the treatment of depression in the physically ill. Gen Hosp Psychiatry. 1980;2(3):177-185.
16. Breitbart W. Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer. 2002;10(4):272-280.
17. Irwin SA, Montross LP, Bhat RG, et al. Psychiatry resident education in palliative care: opportunities, desired training, and outcomes of a targeted educational intervention. Psychosomatics. 2011;52(6):530-536.
18. Tait GR, Hodges BD. End-of-life care education for psychiatric residents: attitudes preparedness, and conceptualizations of dignity. Acad Psychiatry. 2009;33(6):451-456.
My mother and I were in the hospital lobby waiting for my father. My normally upbeat, sharp, energetic mom looked sick, weak, and confused. She had just been discharged from the hospital after experiencing a seizure caused by brain metastasis from long-standing breast cancer. Although we had discussed hospice care during my mother’s admission, we left the hospital without setting up the service because we wanted more time to see if she could recover. Two days later, we arranged hospice because of my mother’s rapidly deteriorating condition and our inability to manage her illness on our own. Five days later, she passed away at home surrounded by loved ones.
I am bewildered that my family did not transition my mother to end-of-life care earlier. Several family members and I work in the medical field. Being resourceful, we chose treatment at a large medical center that was a 3-hour drive from our home. Also, we were familiar with palliative care because other family members had died with hospice. Yet, in those last precious moments, we did not initiate end-of-life care for my mother until it became an emergency. This experience cultivated my interest in palliative care and hospice, specifically, in barriers to access and better ways to transition from life-saving treatment to end-of-life care. As a psychiatry resident, I feel it is important to expand opportunities for psychiatrists to participate in palliative care teams.
Barriers to end-of-life care
Poor physician-patient communication near the end of life can be a major barrier to care. Studies suggest that patients and physicians are ambivalent about end-of-life discussions and tend to avoid them.1 Communication is crucial to helping patients prepare to die well. Researchers have found that end-of-life discussions between patients and physicians can result in fewer aggressive interventions and better quality of life near death.2 These discussions did not increase emotional distress and were associated with lower rates of ventilation, resuscitation, and intensive care unit admissions.2 End-of-life discussions between physicians and patients also lead to earlier hospice enrollment and improve the quality of end-of-life care.2
Approximately one-third of patients spend <1 week in hospice.3 Studies have suggested that patients who receive >1 week of hospice care have improved quality of life compared with patients who do not receive hospice care.1 Addressing end-of-life issues early in treatment of terminally ill patients allows them to become familiar with their options as their disease progresses.
Lack of integration between hospice and the medical community is another barrier. According to Medicare guidelines,4 to be eligible for hospice a patient must have a terminal illness with a prognosis of ≤6 months. The patient must agree to give up curative treatment. If a patient lives >6 months, hospice benefits can be renewed as long as the patient has shown a persistent decline. Patients must desire and accept a palliative approach rather than a curative focus and agree to have all care provided by Medicare-certified hospices.5 These eligibility requirements may give patients and their families a sense that they are losing the forms of health care they had been using, physicians they know, and treatments they had become accustomed to, and are transferring their medical care to a unknown entity. This transition occurs when diseases are progressing and patients may feel vulnerable. In this way, end-of-life care is segregated from the rest of the medical system and can feel foreign and frightening to patients.6
Lack of palliative care specialists. The U.S. population is aging, and more people are living longer with chronic illness. Although the palliative care field is growing, only 60% of U.S. hospitals have palliative care programs and there is a shortage of palliative care clinicians.7
Psychiatry and end-of-life care
Psychiatry and psycho-oncology can help address these barriers by providing resources and expertise to palliative care teams. Psychiatrists can facilitate communication between families and primary clinicians and help patients mentally prepare for end-of-life options.
The dying process may uncover psychological, psychosocial, and existential suffering in patients and their families that often is underdiagnosed and undertreated.8 Psychiatrists can:
- diagnose and treat psychiatric disorders that surface under the stress of a new diagnosis
- aid in the psychodynamics of coping with terminal illness
- assess decision-making capacity
- recognize and treat staff stress
- provide bereavement care.
Because many clinicians believe that mood or anxiety symptoms are “normal reactions” in individuals struggling with end-of-life issues, these patients may not receive psychiatric treatment. However, treating mood and anxiety disorders can improve quality of life in palliative care patients.9
In terminally ill patients, psychological pain often manifests as symptoms of depression and anxiety. Diagnostic criteria for depression may need to be reconsidered because in patients with terminal illness depressive symptoms commonly are associated with functional decline. For example, restrictions on a patient’s ability to participate in activities and disengagement from some areas of interest are common among individuals facing the end of life, but if a patient is unable to find pleasure in any event or activity, he or she may meet criteria for depression. Endicott10 proposed a list of substitute symptoms of depression in terminally ill patients:
- weight loss or gain is substituted with depressed appearance
- loss of energy is substituted with brooding and self-pity
- insomnia or hypersomnia is substituted with social withdrawal
- loss of concentration is substituted with lack of reactivity or inability to be cheered up.
These substitutions are not in DSM-IV-TR but should be considered when assessing a terminally ill patient.
Most recommendations for pharmacologic treatment of depression in terminally ill patients are based on depression treatments for the general population. Selective serotonin reuptake inhibitors are commonly prescribed for terminally ill patients. Mirtazapine, a noradrenergic and serotonergic antidepressant, has been shown to effectively treat adjustment, mood, and anxiety disorders in patients with breast or gynecological cancer.11 Its major side effects—sedation and weight gain—might be beneficial in patients with terminal illness. Psychostimulants also have been shown to elevate mood in patients with advanced malignancies.12
Potential triggers for anxiety in terminally ill patients include chemotherapy, radiation therapy, or acute pain. Also consider anxiety related to death and dying. Certain drugs commonly used in palliative care—such as corticosteroids and psychostimulants—may contribute to anxiety and restlessness. Cancer patients may develop posttraumatic stress disorder symptoms, including re-experiencing frightening aspects of their diagnosis and treatment, nightmares, hypervigilance, and autonomic hyperactivity.13 Pharmacologic treatment of anxiety in dying patients is similar to that in the general population; benzodiazepines and antidepressants are first-line agents.
Several forms of psychotherapy can help terminally ill patients address existential issues (Box).14-16
Dignity therapy is a form of brief individual therapy developed by Chochinov et al14 that focuses on existential distress to help patients feel that their lives have been worthwhile. The goal is to have patients describe what they are most proud of, what they want to be remembered for, and what is most meaningful to them.
Viederman et al15 characterized a type of therapy known as the psychodynamic life narrative. Palliative care psychiatrists use this technique to examine patients’ lives and take stock of successes and failures. The narrative attempts to create a new perspective within terminally ill patients that increases self-esteem by emphasizing past strengths and coping mechanisms that have been successful.
Meaning-centered group therapy, developed by Breitbart,16 emphasizes group didactics, discussion, and experiential exercises, with a focus on themes related to advanced cancer.
A need for training
In a survey of psychiatry residents, 97% of respondents believed psychiatrists should be trained in end-of-life care and 94% felt there should be formal education on palliative care during residency.17 A study evaluating psychiatry residents’ attitudes, perceived preparedness, experiences, and needs in end-of-life care education found that residents felt least prepared when dealing with cultural and spiritual aspects of dying and helping patients with reconciliation and saying goodbye.18 These residents also expressed a desire for more longitudinal exposure to palliative care.
A dedicated palliative care rotation during psychiatry residency training would help build a foundation of knowledge in this field. Residency programs should make a greater effort to incorporate end-of-life issues into consultation-liaison and geriatric rotations. Education on psychosocial, existential, and spiritual distress should be highlighted, with an emphasis on integrating specific psychotherapy techniques into training. These opportunities would provide residents with necessary skills to help patients cope with end-of-life issues.
As a psychiatry resident, I believe training in this field is one way to decrease barriers for patients to access end-of-life care. End-of-life psychiatric training could help build a culture where end-of-life care is integrated into the medical care system, with the goal of helping terminally ill patients die well.
Related Resources
- Chochinov H, Breitbart W. Handbook of psychiatry in palliative medicine. New York, NY: Oxford University Press; 2009.
- Harvard Medical School Center for Palliative Care. www.hms.harvard.edu/pallcare.
Drug Brand Name
- Mirtazapine • Remeron
Disclosure
Dr. Kester reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
My mother and I were in the hospital lobby waiting for my father. My normally upbeat, sharp, energetic mom looked sick, weak, and confused. She had just been discharged from the hospital after experiencing a seizure caused by brain metastasis from long-standing breast cancer. Although we had discussed hospice care during my mother’s admission, we left the hospital without setting up the service because we wanted more time to see if she could recover. Two days later, we arranged hospice because of my mother’s rapidly deteriorating condition and our inability to manage her illness on our own. Five days later, she passed away at home surrounded by loved ones.
I am bewildered that my family did not transition my mother to end-of-life care earlier. Several family members and I work in the medical field. Being resourceful, we chose treatment at a large medical center that was a 3-hour drive from our home. Also, we were familiar with palliative care because other family members had died with hospice. Yet, in those last precious moments, we did not initiate end-of-life care for my mother until it became an emergency. This experience cultivated my interest in palliative care and hospice, specifically, in barriers to access and better ways to transition from life-saving treatment to end-of-life care. As a psychiatry resident, I feel it is important to expand opportunities for psychiatrists to participate in palliative care teams.
Barriers to end-of-life care
Poor physician-patient communication near the end of life can be a major barrier to care. Studies suggest that patients and physicians are ambivalent about end-of-life discussions and tend to avoid them.1 Communication is crucial to helping patients prepare to die well. Researchers have found that end-of-life discussions between patients and physicians can result in fewer aggressive interventions and better quality of life near death.2 These discussions did not increase emotional distress and were associated with lower rates of ventilation, resuscitation, and intensive care unit admissions.2 End-of-life discussions between physicians and patients also lead to earlier hospice enrollment and improve the quality of end-of-life care.2
Approximately one-third of patients spend <1 week in hospice.3 Studies have suggested that patients who receive >1 week of hospice care have improved quality of life compared with patients who do not receive hospice care.1 Addressing end-of-life issues early in treatment of terminally ill patients allows them to become familiar with their options as their disease progresses.
Lack of integration between hospice and the medical community is another barrier. According to Medicare guidelines,4 to be eligible for hospice a patient must have a terminal illness with a prognosis of ≤6 months. The patient must agree to give up curative treatment. If a patient lives >6 months, hospice benefits can be renewed as long as the patient has shown a persistent decline. Patients must desire and accept a palliative approach rather than a curative focus and agree to have all care provided by Medicare-certified hospices.5 These eligibility requirements may give patients and their families a sense that they are losing the forms of health care they had been using, physicians they know, and treatments they had become accustomed to, and are transferring their medical care to a unknown entity. This transition occurs when diseases are progressing and patients may feel vulnerable. In this way, end-of-life care is segregated from the rest of the medical system and can feel foreign and frightening to patients.6
Lack of palliative care specialists. The U.S. population is aging, and more people are living longer with chronic illness. Although the palliative care field is growing, only 60% of U.S. hospitals have palliative care programs and there is a shortage of palliative care clinicians.7
Psychiatry and end-of-life care
Psychiatry and psycho-oncology can help address these barriers by providing resources and expertise to palliative care teams. Psychiatrists can facilitate communication between families and primary clinicians and help patients mentally prepare for end-of-life options.
The dying process may uncover psychological, psychosocial, and existential suffering in patients and their families that often is underdiagnosed and undertreated.8 Psychiatrists can:
- diagnose and treat psychiatric disorders that surface under the stress of a new diagnosis
- aid in the psychodynamics of coping with terminal illness
- assess decision-making capacity
- recognize and treat staff stress
- provide bereavement care.
Because many clinicians believe that mood or anxiety symptoms are “normal reactions” in individuals struggling with end-of-life issues, these patients may not receive psychiatric treatment. However, treating mood and anxiety disorders can improve quality of life in palliative care patients.9
In terminally ill patients, psychological pain often manifests as symptoms of depression and anxiety. Diagnostic criteria for depression may need to be reconsidered because in patients with terminal illness depressive symptoms commonly are associated with functional decline. For example, restrictions on a patient’s ability to participate in activities and disengagement from some areas of interest are common among individuals facing the end of life, but if a patient is unable to find pleasure in any event or activity, he or she may meet criteria for depression. Endicott10 proposed a list of substitute symptoms of depression in terminally ill patients:
- weight loss or gain is substituted with depressed appearance
- loss of energy is substituted with brooding and self-pity
- insomnia or hypersomnia is substituted with social withdrawal
- loss of concentration is substituted with lack of reactivity or inability to be cheered up.
These substitutions are not in DSM-IV-TR but should be considered when assessing a terminally ill patient.
Most recommendations for pharmacologic treatment of depression in terminally ill patients are based on depression treatments for the general population. Selective serotonin reuptake inhibitors are commonly prescribed for terminally ill patients. Mirtazapine, a noradrenergic and serotonergic antidepressant, has been shown to effectively treat adjustment, mood, and anxiety disorders in patients with breast or gynecological cancer.11 Its major side effects—sedation and weight gain—might be beneficial in patients with terminal illness. Psychostimulants also have been shown to elevate mood in patients with advanced malignancies.12
Potential triggers for anxiety in terminally ill patients include chemotherapy, radiation therapy, or acute pain. Also consider anxiety related to death and dying. Certain drugs commonly used in palliative care—such as corticosteroids and psychostimulants—may contribute to anxiety and restlessness. Cancer patients may develop posttraumatic stress disorder symptoms, including re-experiencing frightening aspects of their diagnosis and treatment, nightmares, hypervigilance, and autonomic hyperactivity.13 Pharmacologic treatment of anxiety in dying patients is similar to that in the general population; benzodiazepines and antidepressants are first-line agents.
Several forms of psychotherapy can help terminally ill patients address existential issues (Box).14-16
Dignity therapy is a form of brief individual therapy developed by Chochinov et al14 that focuses on existential distress to help patients feel that their lives have been worthwhile. The goal is to have patients describe what they are most proud of, what they want to be remembered for, and what is most meaningful to them.
Viederman et al15 characterized a type of therapy known as the psychodynamic life narrative. Palliative care psychiatrists use this technique to examine patients’ lives and take stock of successes and failures. The narrative attempts to create a new perspective within terminally ill patients that increases self-esteem by emphasizing past strengths and coping mechanisms that have been successful.
Meaning-centered group therapy, developed by Breitbart,16 emphasizes group didactics, discussion, and experiential exercises, with a focus on themes related to advanced cancer.
A need for training
In a survey of psychiatry residents, 97% of respondents believed psychiatrists should be trained in end-of-life care and 94% felt there should be formal education on palliative care during residency.17 A study evaluating psychiatry residents’ attitudes, perceived preparedness, experiences, and needs in end-of-life care education found that residents felt least prepared when dealing with cultural and spiritual aspects of dying and helping patients with reconciliation and saying goodbye.18 These residents also expressed a desire for more longitudinal exposure to palliative care.
A dedicated palliative care rotation during psychiatry residency training would help build a foundation of knowledge in this field. Residency programs should make a greater effort to incorporate end-of-life issues into consultation-liaison and geriatric rotations. Education on psychosocial, existential, and spiritual distress should be highlighted, with an emphasis on integrating specific psychotherapy techniques into training. These opportunities would provide residents with necessary skills to help patients cope with end-of-life issues.
As a psychiatry resident, I believe training in this field is one way to decrease barriers for patients to access end-of-life care. End-of-life psychiatric training could help build a culture where end-of-life care is integrated into the medical care system, with the goal of helping terminally ill patients die well.
Related Resources
- Chochinov H, Breitbart W. Handbook of psychiatry in palliative medicine. New York, NY: Oxford University Press; 2009.
- Harvard Medical School Center for Palliative Care. www.hms.harvard.edu/pallcare.
Drug Brand Name
- Mirtazapine • Remeron
Disclosure
Dr. Kester reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Leydon GM, Boulton M, Moynihan C, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ. 2000;320(7239):909-913.
2. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673.
3. Harrington S, Smith T. The role of chemotherapy at the end of life: when is enough enough? JAMA. 2008;299(22):2667-2678.
4. U.S. Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare hospice benefits. http://www.medicare.gov/Pubs/pdf/02154.pdf. Revised January 2013. Accessed March 1, 2013.
5. Meier DE, Isaacs SL, Hughes RG. eds. Palliative care: transforming the care of serious illness. San Francisco, CA: Jossey-Bass; 2010.
6. Rhymes JA. Barriers to effective palliative care of terminal patients. An international perspective. Clin Geriatr Med. 1996;12(2):407-416.
7. Center to Advance Palliative Care. America’s care of serious illness: a state-by-state report card on access to palliative care in our nation’s hospitals. 2011. http://reportcard-live.capc.stackop.com/pdf/state-by-state-report-card.pdf. Accessed March 1, 2013.
8. Söllner W, DeVries A, Steixner E, et al. How successful are oncologists in identifying patient distress, perceived social support, and need for psychosocial counseling? Br J Cancer. 2001;84(2):179-185.
9. Billings JA, Block S. Integrating psychiatry and palliative medicine: the challenges and opportunities. In: Chochinov HM Breitbart W, eds. Handbook of psychiatry in palliative medicine. New York, NY: Oxford University Press; 2009:13–19.
10. Endicott J. Measurement of depression in patients with cancer. Cancer. 1984;53(10 suppl):2243-2249.
11. Thompson DS. Mirtazapine for the treatment of depression and nausea in breast and gynecological oncology. Psychosomatics. 2000;41(4):356-359.
12. Macleod AD. Methylphenidate in terminal depression. J Pain Symptom Manage. 1998;16(3):193-198.
13. Alter CL, Pelcovitz D, Axelrod A, et al. Identification of PTSD in cancer survivors. Psychosomatics. 1996;37(2):137-143.
14. Chochinov HM, Hack T, Hassard T, et al. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol. 2005;23(24):5520-5525.
15. Viederman M, Perry SW, 3rd. Use of a psychodynamic life narrative in the treatment of depression in the physically ill. Gen Hosp Psychiatry. 1980;2(3):177-185.
16. Breitbart W. Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer. 2002;10(4):272-280.
17. Irwin SA, Montross LP, Bhat RG, et al. Psychiatry resident education in palliative care: opportunities, desired training, and outcomes of a targeted educational intervention. Psychosomatics. 2011;52(6):530-536.
18. Tait GR, Hodges BD. End-of-life care education for psychiatric residents: attitudes preparedness, and conceptualizations of dignity. Acad Psychiatry. 2009;33(6):451-456.
1. Leydon GM, Boulton M, Moynihan C, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ. 2000;320(7239):909-913.
2. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673.
3. Harrington S, Smith T. The role of chemotherapy at the end of life: when is enough enough? JAMA. 2008;299(22):2667-2678.
4. U.S. Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare hospice benefits. http://www.medicare.gov/Pubs/pdf/02154.pdf. Revised January 2013. Accessed March 1, 2013.
5. Meier DE, Isaacs SL, Hughes RG. eds. Palliative care: transforming the care of serious illness. San Francisco, CA: Jossey-Bass; 2010.
6. Rhymes JA. Barriers to effective palliative care of terminal patients. An international perspective. Clin Geriatr Med. 1996;12(2):407-416.
7. Center to Advance Palliative Care. America’s care of serious illness: a state-by-state report card on access to palliative care in our nation’s hospitals. 2011. http://reportcard-live.capc.stackop.com/pdf/state-by-state-report-card.pdf. Accessed March 1, 2013.
8. Söllner W, DeVries A, Steixner E, et al. How successful are oncologists in identifying patient distress, perceived social support, and need for psychosocial counseling? Br J Cancer. 2001;84(2):179-185.
9. Billings JA, Block S. Integrating psychiatry and palliative medicine: the challenges and opportunities. In: Chochinov HM Breitbart W, eds. Handbook of psychiatry in palliative medicine. New York, NY: Oxford University Press; 2009:13–19.
10. Endicott J. Measurement of depression in patients with cancer. Cancer. 1984;53(10 suppl):2243-2249.
11. Thompson DS. Mirtazapine for the treatment of depression and nausea in breast and gynecological oncology. Psychosomatics. 2000;41(4):356-359.
12. Macleod AD. Methylphenidate in terminal depression. J Pain Symptom Manage. 1998;16(3):193-198.
13. Alter CL, Pelcovitz D, Axelrod A, et al. Identification of PTSD in cancer survivors. Psychosomatics. 1996;37(2):137-143.
14. Chochinov HM, Hack T, Hassard T, et al. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol. 2005;23(24):5520-5525.
15. Viederman M, Perry SW, 3rd. Use of a psychodynamic life narrative in the treatment of depression in the physically ill. Gen Hosp Psychiatry. 1980;2(3):177-185.
16. Breitbart W. Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer. 2002;10(4):272-280.
17. Irwin SA, Montross LP, Bhat RG, et al. Psychiatry resident education in palliative care: opportunities, desired training, and outcomes of a targeted educational intervention. Psychosomatics. 2011;52(6):530-536.
18. Tait GR, Hodges BD. End-of-life care education for psychiatric residents: attitudes preparedness, and conceptualizations of dignity. Acad Psychiatry. 2009;33(6):451-456.
Treating a patient who has ‘everything’
Patients who endorse multiple psychiatric symptoms and meet criteria for several DSM diagnoses pose diagnostic and therapeutic challenges. In community samples, approximately 40% of patients with a DSM diagnosis have >1 illness, and comorbidity is more frequent in clinical trials.1 We highlight things to consider when managing a patient who has “everything.”
Endorsing ‘everything’ means something in itself. Patients with borderline personality disorder often present with myriad, disparate diagnoses and urgent requests for care.2 Also consider primary or secondary gain, particularly if the patient’s descriptions of symptoms are unusual. Saying “yes” to every question or endorsing highly unusual symptoms described by the interviewer may represent suggestibility related to catatonia or confabulation.
Focus on the most impairing symptom. This may help put other symptoms in context and focus treatment.
Find a common goal. If you can’t pick a simple symptom, move on to helping the patient identify his or her goals by asking questions such as, “Four weeks from now, what would you like to be doing?” Picking an achievable, measurable goal may be therapeutic.
Are the symptoms valid? Examine individual symptoms for validity using the SAFER criteria (Table).3
Table
SAFER criteria for symptom validity
| State vs trait: has the symptom lasted <12 weeks? |
| Assessable: can the symptom be measured? |
| Face validity: does the symptom clearly affect the patient’s behavior and functioning? |
| Ecological validity: is the symptom valid with our knowledge of its occurrence? |
| Rule of the 3Ps: is the symptom Persistent; Pathologically disruptive and different than usual; and Pervasive across normal domains? |
| Source: Reference 3 |
Multiple diagnoses may be in play, but start by treating one. Many patients meet criteria for multiple diagnoses. There is little evidence about which diagnosis should be treated first. Use your judgment in picking “the best first step” and treat accordingly.
Resist polypharmacy. Target specific symptoms or goals until a clear diagnostic picture emerges.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
2. Gunderson JG. Borderline personality disorder: ontogeny of a diagnosis. Am J Psychiatry. 2009;166(5):530-539.
3. Targum SD, Pollack MH, Fava M. Redefining affective disorders: relevance for drug development. CNS Neurosci Ther. 2008;14(1):2-9.
Patients who endorse multiple psychiatric symptoms and meet criteria for several DSM diagnoses pose diagnostic and therapeutic challenges. In community samples, approximately 40% of patients with a DSM diagnosis have >1 illness, and comorbidity is more frequent in clinical trials.1 We highlight things to consider when managing a patient who has “everything.”
Endorsing ‘everything’ means something in itself. Patients with borderline personality disorder often present with myriad, disparate diagnoses and urgent requests for care.2 Also consider primary or secondary gain, particularly if the patient’s descriptions of symptoms are unusual. Saying “yes” to every question or endorsing highly unusual symptoms described by the interviewer may represent suggestibility related to catatonia or confabulation.
Focus on the most impairing symptom. This may help put other symptoms in context and focus treatment.
Find a common goal. If you can’t pick a simple symptom, move on to helping the patient identify his or her goals by asking questions such as, “Four weeks from now, what would you like to be doing?” Picking an achievable, measurable goal may be therapeutic.
Are the symptoms valid? Examine individual symptoms for validity using the SAFER criteria (Table).3
Table
SAFER criteria for symptom validity
| State vs trait: has the symptom lasted <12 weeks? |
| Assessable: can the symptom be measured? |
| Face validity: does the symptom clearly affect the patient’s behavior and functioning? |
| Ecological validity: is the symptom valid with our knowledge of its occurrence? |
| Rule of the 3Ps: is the symptom Persistent; Pathologically disruptive and different than usual; and Pervasive across normal domains? |
| Source: Reference 3 |
Multiple diagnoses may be in play, but start by treating one. Many patients meet criteria for multiple diagnoses. There is little evidence about which diagnosis should be treated first. Use your judgment in picking “the best first step” and treat accordingly.
Resist polypharmacy. Target specific symptoms or goals until a clear diagnostic picture emerges.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Patients who endorse multiple psychiatric symptoms and meet criteria for several DSM diagnoses pose diagnostic and therapeutic challenges. In community samples, approximately 40% of patients with a DSM diagnosis have >1 illness, and comorbidity is more frequent in clinical trials.1 We highlight things to consider when managing a patient who has “everything.”
Endorsing ‘everything’ means something in itself. Patients with borderline personality disorder often present with myriad, disparate diagnoses and urgent requests for care.2 Also consider primary or secondary gain, particularly if the patient’s descriptions of symptoms are unusual. Saying “yes” to every question or endorsing highly unusual symptoms described by the interviewer may represent suggestibility related to catatonia or confabulation.
Focus on the most impairing symptom. This may help put other symptoms in context and focus treatment.
Find a common goal. If you can’t pick a simple symptom, move on to helping the patient identify his or her goals by asking questions such as, “Four weeks from now, what would you like to be doing?” Picking an achievable, measurable goal may be therapeutic.
Are the symptoms valid? Examine individual symptoms for validity using the SAFER criteria (Table).3
Table
SAFER criteria for symptom validity
| State vs trait: has the symptom lasted <12 weeks? |
| Assessable: can the symptom be measured? |
| Face validity: does the symptom clearly affect the patient’s behavior and functioning? |
| Ecological validity: is the symptom valid with our knowledge of its occurrence? |
| Rule of the 3Ps: is the symptom Persistent; Pathologically disruptive and different than usual; and Pervasive across normal domains? |
| Source: Reference 3 |
Multiple diagnoses may be in play, but start by treating one. Many patients meet criteria for multiple diagnoses. There is little evidence about which diagnosis should be treated first. Use your judgment in picking “the best first step” and treat accordingly.
Resist polypharmacy. Target specific symptoms or goals until a clear diagnostic picture emerges.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
2. Gunderson JG. Borderline personality disorder: ontogeny of a diagnosis. Am J Psychiatry. 2009;166(5):530-539.
3. Targum SD, Pollack MH, Fava M. Redefining affective disorders: relevance for drug development. CNS Neurosci Ther. 2008;14(1):2-9.
1. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
2. Gunderson JG. Borderline personality disorder: ontogeny of a diagnosis. Am J Psychiatry. 2009;166(5):530-539.
3. Targum SD, Pollack MH, Fava M. Redefining affective disorders: relevance for drug development. CNS Neurosci Ther. 2008;14(1):2-9.
Depressive recurrence on antidepressant treatment (DRAT): 4 next-step options
“Poop-out” and “tachyphylaxis” are terms used to describe loss of antidepressant response after initial benefit, but both descriptors are problematic. Poop-out carries a mildly offensive aura that conveys a lack of seriousness about the patient’s suffering. Tachyphylaxis is a pharmacologic term describing rapid or acute reduction in response to a drug after administration; it is not appropriate for antidepressant loss of response, which typically occurs months to years after treatment initiation.1
Depressive recurrence on antidepressant treatment (DRAT) is a better term to describe recurrence of a major depressive episode despite sustained treatment with an antidepressant that had induced remission. Maintenance studies of antidepressant treatment indicate DRAT occurs in approximately 10% of patients at 6 months and 20% at 2 years.2
Despite this high prevalence, there is little clinical trial data on which to base treatment decisions for patients who experience DRAT. There are 4 options:
1. Raise the dose. In small studies, doubling the dose of fluoxetine or duloxetine led to regaining response in approximately 60% of patients.3 However, these studies lacked a placebo comparison arm, so the specific benefit derived from the dose increase is unknown. Improvement with a dose increase is somewhat at odds with the known mechanism of action of selective serotonin reuptake inhibitors (SSRIs), which are thought to have a flat dose-response curve. That is, once an SSRI blocks approximately 80% of the serotonin transporters, further dose increases produce minimal further blockade and, presumably, little clinical benefit via this mechanism.4
2. Switch medication. No studies have examined switching antidepressants after DRAT. Switching to a medication with a different mechanism may be justified based on the results of treatment-resistant depression (TRD) trials, in which patients who failed to respond to an initial medication—typically an SSRI—improved after switching to an antidepressant from a different class. However, the biology of DRAT may differ from that of SSRI nonresponse. Unlike many patients with TRD, patients who experience DRAT while taking an SSRI have demonstrated previous response to serotonergic modulation.
3. Augmentation. Similar to switching, this approach has not been studied specifically for DRAT. This approach is derived from trials in which patients who did not attain response after treatment with a single antidepressant had a second medication added. Again, the biology of these patients may differ from those with DRAT, who at one point did remit with antidepressant treatment.
4. Psychotherapy. This addition is a low-risk option for patients who previously have not received evidence-based psychotherapy for depression.
Clinicians have scant evidence on which to base their decisions for this common and important problem. Dose increase after DRAT represents the best supported, simplest, and perhaps least costly next step in treatment.
Disclosure
Dr. Dunlop receives grant or research support from Bristol-Myers Squibb, Forest Pharmaceuticals, and GlaxoSmithKline, and is a consultant to MedAvante and Roche.
1. Rothschild AJ, Dunlop BW, Dunner DL, et al. Assessing rates and predictors of tachyphylaxis during the prevention of recurrent episodes of depression with venlafaxine ER for two years (PREVENT) study. Psychopharmacol Bull. 2009;42(3):5-20.
2. Hansen R, Gaynes B, Thieda P, et al. Meta-analysis of major depressive disorder relapse and recurrence with second-generation antidepressants. Psychiatr Serv. 2008;59(10):1121-1130.
3. Schmidt ME, Fava M, Zhang S, et al. Treatment approaches to major depressive disorder relapse. Part 1: dose increase. Psychother Psychosom. 2002;71(4):190-194.
4. Meyer JH, Wilson AA, Sagrati S, et al. Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry. 2004;161(5):826-835.
“Poop-out” and “tachyphylaxis” are terms used to describe loss of antidepressant response after initial benefit, but both descriptors are problematic. Poop-out carries a mildly offensive aura that conveys a lack of seriousness about the patient’s suffering. Tachyphylaxis is a pharmacologic term describing rapid or acute reduction in response to a drug after administration; it is not appropriate for antidepressant loss of response, which typically occurs months to years after treatment initiation.1
Depressive recurrence on antidepressant treatment (DRAT) is a better term to describe recurrence of a major depressive episode despite sustained treatment with an antidepressant that had induced remission. Maintenance studies of antidepressant treatment indicate DRAT occurs in approximately 10% of patients at 6 months and 20% at 2 years.2
Despite this high prevalence, there is little clinical trial data on which to base treatment decisions for patients who experience DRAT. There are 4 options:
1. Raise the dose. In small studies, doubling the dose of fluoxetine or duloxetine led to regaining response in approximately 60% of patients.3 However, these studies lacked a placebo comparison arm, so the specific benefit derived from the dose increase is unknown. Improvement with a dose increase is somewhat at odds with the known mechanism of action of selective serotonin reuptake inhibitors (SSRIs), which are thought to have a flat dose-response curve. That is, once an SSRI blocks approximately 80% of the serotonin transporters, further dose increases produce minimal further blockade and, presumably, little clinical benefit via this mechanism.4
2. Switch medication. No studies have examined switching antidepressants after DRAT. Switching to a medication with a different mechanism may be justified based on the results of treatment-resistant depression (TRD) trials, in which patients who failed to respond to an initial medication—typically an SSRI—improved after switching to an antidepressant from a different class. However, the biology of DRAT may differ from that of SSRI nonresponse. Unlike many patients with TRD, patients who experience DRAT while taking an SSRI have demonstrated previous response to serotonergic modulation.
3. Augmentation. Similar to switching, this approach has not been studied specifically for DRAT. This approach is derived from trials in which patients who did not attain response after treatment with a single antidepressant had a second medication added. Again, the biology of these patients may differ from those with DRAT, who at one point did remit with antidepressant treatment.
4. Psychotherapy. This addition is a low-risk option for patients who previously have not received evidence-based psychotherapy for depression.
Clinicians have scant evidence on which to base their decisions for this common and important problem. Dose increase after DRAT represents the best supported, simplest, and perhaps least costly next step in treatment.
Disclosure
Dr. Dunlop receives grant or research support from Bristol-Myers Squibb, Forest Pharmaceuticals, and GlaxoSmithKline, and is a consultant to MedAvante and Roche.
“Poop-out” and “tachyphylaxis” are terms used to describe loss of antidepressant response after initial benefit, but both descriptors are problematic. Poop-out carries a mildly offensive aura that conveys a lack of seriousness about the patient’s suffering. Tachyphylaxis is a pharmacologic term describing rapid or acute reduction in response to a drug after administration; it is not appropriate for antidepressant loss of response, which typically occurs months to years after treatment initiation.1
Depressive recurrence on antidepressant treatment (DRAT) is a better term to describe recurrence of a major depressive episode despite sustained treatment with an antidepressant that had induced remission. Maintenance studies of antidepressant treatment indicate DRAT occurs in approximately 10% of patients at 6 months and 20% at 2 years.2
Despite this high prevalence, there is little clinical trial data on which to base treatment decisions for patients who experience DRAT. There are 4 options:
1. Raise the dose. In small studies, doubling the dose of fluoxetine or duloxetine led to regaining response in approximately 60% of patients.3 However, these studies lacked a placebo comparison arm, so the specific benefit derived from the dose increase is unknown. Improvement with a dose increase is somewhat at odds with the known mechanism of action of selective serotonin reuptake inhibitors (SSRIs), which are thought to have a flat dose-response curve. That is, once an SSRI blocks approximately 80% of the serotonin transporters, further dose increases produce minimal further blockade and, presumably, little clinical benefit via this mechanism.4
2. Switch medication. No studies have examined switching antidepressants after DRAT. Switching to a medication with a different mechanism may be justified based on the results of treatment-resistant depression (TRD) trials, in which patients who failed to respond to an initial medication—typically an SSRI—improved after switching to an antidepressant from a different class. However, the biology of DRAT may differ from that of SSRI nonresponse. Unlike many patients with TRD, patients who experience DRAT while taking an SSRI have demonstrated previous response to serotonergic modulation.
3. Augmentation. Similar to switching, this approach has not been studied specifically for DRAT. This approach is derived from trials in which patients who did not attain response after treatment with a single antidepressant had a second medication added. Again, the biology of these patients may differ from those with DRAT, who at one point did remit with antidepressant treatment.
4. Psychotherapy. This addition is a low-risk option for patients who previously have not received evidence-based psychotherapy for depression.
Clinicians have scant evidence on which to base their decisions for this common and important problem. Dose increase after DRAT represents the best supported, simplest, and perhaps least costly next step in treatment.
Disclosure
Dr. Dunlop receives grant or research support from Bristol-Myers Squibb, Forest Pharmaceuticals, and GlaxoSmithKline, and is a consultant to MedAvante and Roche.
1. Rothschild AJ, Dunlop BW, Dunner DL, et al. Assessing rates and predictors of tachyphylaxis during the prevention of recurrent episodes of depression with venlafaxine ER for two years (PREVENT) study. Psychopharmacol Bull. 2009;42(3):5-20.
2. Hansen R, Gaynes B, Thieda P, et al. Meta-analysis of major depressive disorder relapse and recurrence with second-generation antidepressants. Psychiatr Serv. 2008;59(10):1121-1130.
3. Schmidt ME, Fava M, Zhang S, et al. Treatment approaches to major depressive disorder relapse. Part 1: dose increase. Psychother Psychosom. 2002;71(4):190-194.
4. Meyer JH, Wilson AA, Sagrati S, et al. Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry. 2004;161(5):826-835.
1. Rothschild AJ, Dunlop BW, Dunner DL, et al. Assessing rates and predictors of tachyphylaxis during the prevention of recurrent episodes of depression with venlafaxine ER for two years (PREVENT) study. Psychopharmacol Bull. 2009;42(3):5-20.
2. Hansen R, Gaynes B, Thieda P, et al. Meta-analysis of major depressive disorder relapse and recurrence with second-generation antidepressants. Psychiatr Serv. 2008;59(10):1121-1130.
3. Schmidt ME, Fava M, Zhang S, et al. Treatment approaches to major depressive disorder relapse. Part 1: dose increase. Psychother Psychosom. 2002;71(4):190-194.
4. Meyer JH, Wilson AA, Sagrati S, et al. Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry. 2004;161(5):826-835.
Long-acting injectable aripiprazole for adult schizophrenia
In February 2013, the FDA approved a long-acting IM aripiprazole formulation for treating adult schizophrenia (Table 1).1 It is the fourth second-generation antipsychotic (SGA) depot formulation approved for treating schizophrenia, and the sixth depot antipsychotic if haloperidol and fluphenazine decanoate are considered.
Table 1
Depot aripiprazole: Fast facts
| Brand name: Abilify Maintena |
| Class: Atypical antipsychotic |
| Indication: Adult schizophrenia |
| Approval date: February 28, 2013 |
| Availability date: March 18, 2013 |
| Manufacturer: Otsuka Pharmaceutical and Lundbeck |
| Dosing form: IM long-acting injection |
| Recommended dosage: 400 mg IM once a month; 200 to 300 mg IM if drug-drug interactions, poor cytochrome P450 2D6 metabolism, or adverse effects |
| Source: Reference 1 |
Clinical implications
Depot medications can improve treatment adherence2; however, long-term antipsychotic use can lead to irreversible adverse effects (dyskinesias), which in some cases were reduced by using newer antipsychotics.3
How it works
Similar to other SGAs, aripiprazole’s mechanism of action is unknown. Aripiprazole was developed based on the dopamine theory, in which dopamine hyperactivity in mesolimbic pathways of the brain leads to hallucinations, delusions, disorganization, and catatonia, and dopamine hypoactivity in mesocortical pathways and the prefrontal cortex causes alogia, anhedonia, autism, avolition, and problems with attention and abstract thinking.
Aripiprazole’s proposed mechanism of action on dopamine receptors is that of partial agonism,1 rather than antagonism, as is the case for other SGAs. In theory, aripiprazole antagonizes postsynaptic D2 receptors and activates presynaptic D2 autoreceptors, with subsequently decreased dopamine production and further stabilization of the dopamine system.4 Its antagonism of 5-HT2A is similar to other SGAs.5
Pharmacokinetics
After depot aripiprazole is injected into the gluteal muscle, the active moiety slowly is released into circulation. The effectiveness of depot aripiprazole is attributable to its active parent drug, aripiprazole monohydrate, and its active metabolite, dehydro-aripiprazole, which is the same as oral aripiprazole. Depot aripiprazole reaches maximum concentration in 5 to 7 days. The elimination half-life of depot aripiprazole is 29.9 days for a 300-mg dose and 46.5 days for a 400-mg dose if administered monthly.1
Aripiprazole does not undergo direct glucuronidation. It is metabolized predominantly through cytochrome P450 (CYP) 2D6 and 3A4 enzymes, which predisposes it to significant drug-drug interactions and may require dose adjustment (Table 2).1
Table 2
Dose adjustments of depot aripiprazole
| Drug-drug interaction | Adjusted dose |
|---|---|
| CYP2D6 poor metabolizers | 300 mg |
| CYP2D6 poor metabolizers taking CYP3A4 inhibitors (ketoconazole, itraconazole, erythromycin, grapefruit juice) | 200 mg |
| Lithium, valproate, desvenlafaxine, venlafaxine, escitalopram, dextromethorphan, omeprazole, warfarin | No significant interaction No dose adjustment |
| Sex, race, liver impairment, renal impairment, tobacco smokers | No dose adjustment |
| Patients taking 400 mg of depot aripiprazole with: | |
| 300 mg |
| 200 mg |
| Avoid use |
| Patients taking 300 mg of depot aripiprazole with: | |
| 200 mg |
| 160 mg |
| Avoid use |
| CYP: cytochrome P450 Source: Adapted from reference 1 | |
Efficacy
The ability of depot aripiprazole to sustain long-term symptom control in adult patients with schizophrenia was demonstrated in a randomized-withdrawal, double-blind, placebo-controlled trial.1 Adults included had a DSM-IV-TR diagnosis of schizophrenia, had ≥3-year history of the illness, had undergone treatment with ≥1 antipsychotic, and had a history of relapse or symptom exacerbation when not receiving antipsychotics. Psychopathology was measured by the Positive and Negative Syndrome Scale (PANSS), the Clinical Global Impression-Severity scale, the Clinical Global Impression-Improvement (CGI-I) scale, and the Clinical Global Impression-Severity of Suicide (CGI-SS) scale.1
The trial lasted 52 weeks, was divided into 4 phases, and concluded early because of demonstrated efficacy.
Phase I: Conversion phase switched patients from a different antipsychotic to oral aripiprazole. This phase lasted 4 to 6 weeks and included 633 patients. An additional 210 patients already receiving aripiprazole were entered directly into Phase II.
Phase II: Open-label, oral stabilization phase included 710 patients (60% males) age 18 to 60 who had a mean PANSS score 66. Patients received 10 to 20 mg/d of oral aripiprazole until they achieved stabilization, defined as PANSS score
Phase III: IM depot stabilization (uncontrolled single blind) included 576 patients. Patients were started on depot aripiprazole, 400 mg monthly, and continued to take 10 to 20 mg/d of oral aripiprazole for 14 consecutive days. Depot aripiprazole was decreased to 300 mg monthly if a patient developed adverse effects. Patients continued to the double-blind phase when stabilization was achieved, as evidenced by PANSS score
Phase IV: Maintenance (double-blind, randomized, placebo-controlled) included 403 patients. Two-thirds of patients continued to take the same dose of depot aripiprazole they took in Phase III. One-third of patients were switched to placebo. The primary efficacy endpoint was time to impending relapse, defined as the first occurrence of ≥1 criteria: hospitalization due to psychosis; violence toward self, others, or property; CGI-SS score ≥4 on part I or ≥7 on part II; or CGI-I score ≥5 and any individual PANSS score >4 for disorganization, hallucinations, suspiciousness, or abnormal thought content.1
Patients randomized to continue depot aripiprazole took longer to relapse or worsening of symptoms compared with the placebo group. Of 403 patients, 10% taking an active drug and 39.6% taking placebo relapsed within 360 days of randomization. This difference was statistically significant (P 1
Tolerability
One possible problem with any long-acting medication is increased duration of adverse effects (AEs), if they develop. Therefore, assessment of safety and tolerability is more important in depot formulations than in oral drugs. During the clinical trial, depot aripiprazole was well tolerated.6
During clinical trials, the most common AEs—insomnia (>5%), anxiety, and tremors—were mild to moderate and occurred within the first 4 weeks. Discontinuation of the medication because of AEs was low, and pain at the injection site was minimal.6 There were 2 deaths during the trial, which were unrelated to depot aripiprazole.6
Aripiprazole’s activity on the D2 receptor can cause extrapyramidal AEs. In head-to-head trials, patients taking aripiprazole had fewer extrapyramidal AEs than those taking risperidone or ziprasidone, but more than patients receiving olanzapine.7 Its moderate antagonism on α-adrenergic and histamine 1 (H1) receptors translates to low orthostatic hypotension, H1-mediated weight gain, and sedation. In clinical trials, weight gain and metabolic changes were comparable with placebo. In head-to-head trials, aripiprazole caused less weight gain and a higher incidence of increased cholesterol than olanzapine and risperidone, and less increase in blood glucose than olanzapine, but more than risperidone.8 Muscarinic 1-mediated cognitive impairment, dry mouth, constipation, urinary retention, and increased intraocular pressure were low.8 See Table 3 for aripiprazole's receptor binding profile.
Table 3
Aripiprazole’s receptor binding profile
| Affinity | Ki (nM)a | Effects associated with activity on the receptor | |
|---|---|---|---|
| D2 | High | 0.34 | Partial agonist |
| D3 | High | 0.8 | Partial agonist |
| 5-HT1A | High | 1.7 | Partial agonist |
| 5-HT2A | High | 3.4 | Antagonist |
| 5-HT2C | Moderate | 15 | Partial agonist |
| 5-HT7 | Moderate | 39 | Antagonist |
| D4 | Moderate | 44 | Partial agonist |
| α1-adrenergic | Moderate | 57 | Antagonist |
| H1 | Moderate | 61 | Antagonist |
| M1 | No appreciable activity | >1,000 | No appreciable activity |
| aKi dissociation constant: lower numbers indicate higher affinity of the compound for the receptor H1: histamine 1; M1: muscarinic 1 Source: References 1,6 | |||
Unique clinical issues
Clinical features for depot aripiprazole can be partially deduced based on data on oral aripiprazole. Advantages over other depot SGAs might include aripiprazole’s more favorable weight and metabolic profile.
Contraindications
Depot aripiprazole is contraindicated in patients with known sensitivity to aripiprazole or other components of the formulation. Because of pharmacokinetic drug-drug interactions, using depot aripiprazole should be avoided in patients taking strong CYP3A4 inducers (eg, rifampin and carbamazepine). Dose adjustment is recommended in patients who are taking moderate CYP2D6 and 3A4 inhibitors, such as paroxetine, fluoxetine, ketoconazole, or erythromycin.1 A “black-box” warning of increased mortality in older patients with dementia-related psychosis applies for depot aripiprazole as well as for other atypical antipsychotics.1
Depot aripiprazole is pregnancy category C and should be used in pregnant or breastfeeding mothers only when benefits outweigh the risks. Use of depot aripiprazole in geriatric and pediatric populations has not been studied; however, patients age ≥65 who received oral aripiprazole, 15 mg/d, showed decreased clearance by 20%.1
Dosing
Depot aripiprazole is available as a lyophilized powder that needs to be reconstituted in sterile water. The drug can be stored at room temperature. The kit includes two 21-gauge needles, a 1.5-inch needle for non-obese patients and a 2-inch needle for obese patients. Depot aripiprazole should be given to patients who demonstrate tolerability to oral aripiprazole. The starting and maintenance dose of depot aripiprazole is 400 mg injected into the gluteal muscle, once a month. If a patient develops an AE, decrease the monthly dose to 300 mg. Rotate the injection site between gluteal muscles to reduce AEs from injection.
Because of the potential for significant pharmacokinetic drug-drug interactions, dose adjustment is recommended for patients who are CYP2D6 poor metabolizers and those taking certain other medications (Table 4).1 See Table 4 for the recommended dosage adjustment in the case of missed doses.
Table 4
Adjusting depot aripiprazole after missed doses
| Doses missed since last injection | ||||
|---|---|---|---|---|
| Second or third dose | Fourth or subsequent dose | |||
| >4 weeks and | >5 weeks | >4 weeks and | >6 weeks | |
| Oral aripiprazole | Administer for 14 days | Administer for 14 days | ||
| Depot aripiprazole | Administer as soon as possible | Administer next injection | Administer as soon as possible | Administer next injection |
| Source: Reference 1 | ||||
After depot aripiprazole is injected into the gluteal muscle, the patient receives 10 to 20 mg/d of oral aripiprazole for 14 consecutive days to avoid a drop in plasma concentrations into subtherapeutic levels.
Related Resource
- Abilify Maintena [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Company; 2013.
Drug Brand Names
- Aripiprazole • Abilify
- Aripiprazole depot • Maintena
- Carbamazepine • Tegretol
- Desvenlafaxine • Pristiq
- Dextromethorphan • Delsym
- Erythromycin • E-Mycin
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Itraconazole • Sporanox
- Ketoconazole • Nizoral
- Lithium • Eskalith, Lithobid
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Paliperidone • Invega
- Paroxetine • Paxil
- Quinidine • Quinidex
- Rifampin • Rifadin
- Risperidone • Risperdal
- Valproate • Depakote
- Venlafaxine • Effexor
- Warfarin • Coumadin
- Ziprasidone • Geodon
Disclosure
Dr. Lincoln receives grant or research support from the Wichita Center for Graduate Medical Education.
1. Abilify Maintena [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Company; 2013.
2. Leucht C, Heres S, Kane JM, et al. Oral versus depot antipsychotic drugs for schizophrenia—a critical systematic review and meta-analysis of randomized long-term trials. Schizophr Res. 2011;127(1-3):83-92.
3. de Araújo AN, de Sena EP, de Oliveira IR, et al. Antipsychotic agents: efficacy and safety in schizophrenia. Drug Healthc Patient Saf. 2012;4:173-180.
4. Mailman RB, Murty V. Third generation antipsychotic drugs: partial agonism or receptor functional selectivity? Curr Pharm Des. 2010;16(5):488-501.
5. Roth BL, Meltzer HY. The role of serotonin in schizophrenia. http://www.acnp.org/g4/GN401000117/CH115.html. Published 2000. Accessed March 27 2013.
6. Kane JM, Sanchez R, Perry PP, et al. Aripiprazole intramuscular depot as maintenance treatment in patients with schizophrenia: a 52-week, multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2012;73(5):617-624.
7. Rummel-Kluge C, Komossa K, Schwarz S, et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr Bull. 2012;38(1):167-177.
8. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2-3):225-233.
In February 2013, the FDA approved a long-acting IM aripiprazole formulation for treating adult schizophrenia (Table 1).1 It is the fourth second-generation antipsychotic (SGA) depot formulation approved for treating schizophrenia, and the sixth depot antipsychotic if haloperidol and fluphenazine decanoate are considered.
Table 1
Depot aripiprazole: Fast facts
| Brand name: Abilify Maintena |
| Class: Atypical antipsychotic |
| Indication: Adult schizophrenia |
| Approval date: February 28, 2013 |
| Availability date: March 18, 2013 |
| Manufacturer: Otsuka Pharmaceutical and Lundbeck |
| Dosing form: IM long-acting injection |
| Recommended dosage: 400 mg IM once a month; 200 to 300 mg IM if drug-drug interactions, poor cytochrome P450 2D6 metabolism, or adverse effects |
| Source: Reference 1 |
Clinical implications
Depot medications can improve treatment adherence2; however, long-term antipsychotic use can lead to irreversible adverse effects (dyskinesias), which in some cases were reduced by using newer antipsychotics.3
How it works
Similar to other SGAs, aripiprazole’s mechanism of action is unknown. Aripiprazole was developed based on the dopamine theory, in which dopamine hyperactivity in mesolimbic pathways of the brain leads to hallucinations, delusions, disorganization, and catatonia, and dopamine hypoactivity in mesocortical pathways and the prefrontal cortex causes alogia, anhedonia, autism, avolition, and problems with attention and abstract thinking.
Aripiprazole’s proposed mechanism of action on dopamine receptors is that of partial agonism,1 rather than antagonism, as is the case for other SGAs. In theory, aripiprazole antagonizes postsynaptic D2 receptors and activates presynaptic D2 autoreceptors, with subsequently decreased dopamine production and further stabilization of the dopamine system.4 Its antagonism of 5-HT2A is similar to other SGAs.5
Pharmacokinetics
After depot aripiprazole is injected into the gluteal muscle, the active moiety slowly is released into circulation. The effectiveness of depot aripiprazole is attributable to its active parent drug, aripiprazole monohydrate, and its active metabolite, dehydro-aripiprazole, which is the same as oral aripiprazole. Depot aripiprazole reaches maximum concentration in 5 to 7 days. The elimination half-life of depot aripiprazole is 29.9 days for a 300-mg dose and 46.5 days for a 400-mg dose if administered monthly.1
Aripiprazole does not undergo direct glucuronidation. It is metabolized predominantly through cytochrome P450 (CYP) 2D6 and 3A4 enzymes, which predisposes it to significant drug-drug interactions and may require dose adjustment (Table 2).1
Table 2
Dose adjustments of depot aripiprazole
| Drug-drug interaction | Adjusted dose |
|---|---|
| CYP2D6 poor metabolizers | 300 mg |
| CYP2D6 poor metabolizers taking CYP3A4 inhibitors (ketoconazole, itraconazole, erythromycin, grapefruit juice) | 200 mg |
| Lithium, valproate, desvenlafaxine, venlafaxine, escitalopram, dextromethorphan, omeprazole, warfarin | No significant interaction No dose adjustment |
| Sex, race, liver impairment, renal impairment, tobacco smokers | No dose adjustment |
| Patients taking 400 mg of depot aripiprazole with: | |
| 300 mg |
| 200 mg |
| Avoid use |
| Patients taking 300 mg of depot aripiprazole with: | |
| 200 mg |
| 160 mg |
| Avoid use |
| CYP: cytochrome P450 Source: Adapted from reference 1 | |
Efficacy
The ability of depot aripiprazole to sustain long-term symptom control in adult patients with schizophrenia was demonstrated in a randomized-withdrawal, double-blind, placebo-controlled trial.1 Adults included had a DSM-IV-TR diagnosis of schizophrenia, had ≥3-year history of the illness, had undergone treatment with ≥1 antipsychotic, and had a history of relapse or symptom exacerbation when not receiving antipsychotics. Psychopathology was measured by the Positive and Negative Syndrome Scale (PANSS), the Clinical Global Impression-Severity scale, the Clinical Global Impression-Improvement (CGI-I) scale, and the Clinical Global Impression-Severity of Suicide (CGI-SS) scale.1
The trial lasted 52 weeks, was divided into 4 phases, and concluded early because of demonstrated efficacy.
Phase I: Conversion phase switched patients from a different antipsychotic to oral aripiprazole. This phase lasted 4 to 6 weeks and included 633 patients. An additional 210 patients already receiving aripiprazole were entered directly into Phase II.
Phase II: Open-label, oral stabilization phase included 710 patients (60% males) age 18 to 60 who had a mean PANSS score 66. Patients received 10 to 20 mg/d of oral aripiprazole until they achieved stabilization, defined as PANSS score
Phase III: IM depot stabilization (uncontrolled single blind) included 576 patients. Patients were started on depot aripiprazole, 400 mg monthly, and continued to take 10 to 20 mg/d of oral aripiprazole for 14 consecutive days. Depot aripiprazole was decreased to 300 mg monthly if a patient developed adverse effects. Patients continued to the double-blind phase when stabilization was achieved, as evidenced by PANSS score
Phase IV: Maintenance (double-blind, randomized, placebo-controlled) included 403 patients. Two-thirds of patients continued to take the same dose of depot aripiprazole they took in Phase III. One-third of patients were switched to placebo. The primary efficacy endpoint was time to impending relapse, defined as the first occurrence of ≥1 criteria: hospitalization due to psychosis; violence toward self, others, or property; CGI-SS score ≥4 on part I or ≥7 on part II; or CGI-I score ≥5 and any individual PANSS score >4 for disorganization, hallucinations, suspiciousness, or abnormal thought content.1
Patients randomized to continue depot aripiprazole took longer to relapse or worsening of symptoms compared with the placebo group. Of 403 patients, 10% taking an active drug and 39.6% taking placebo relapsed within 360 days of randomization. This difference was statistically significant (P 1
Tolerability
One possible problem with any long-acting medication is increased duration of adverse effects (AEs), if they develop. Therefore, assessment of safety and tolerability is more important in depot formulations than in oral drugs. During the clinical trial, depot aripiprazole was well tolerated.6
During clinical trials, the most common AEs—insomnia (>5%), anxiety, and tremors—were mild to moderate and occurred within the first 4 weeks. Discontinuation of the medication because of AEs was low, and pain at the injection site was minimal.6 There were 2 deaths during the trial, which were unrelated to depot aripiprazole.6
Aripiprazole’s activity on the D2 receptor can cause extrapyramidal AEs. In head-to-head trials, patients taking aripiprazole had fewer extrapyramidal AEs than those taking risperidone or ziprasidone, but more than patients receiving olanzapine.7 Its moderate antagonism on α-adrenergic and histamine 1 (H1) receptors translates to low orthostatic hypotension, H1-mediated weight gain, and sedation. In clinical trials, weight gain and metabolic changes were comparable with placebo. In head-to-head trials, aripiprazole caused less weight gain and a higher incidence of increased cholesterol than olanzapine and risperidone, and less increase in blood glucose than olanzapine, but more than risperidone.8 Muscarinic 1-mediated cognitive impairment, dry mouth, constipation, urinary retention, and increased intraocular pressure were low.8 See Table 3 for aripiprazole's receptor binding profile.
Table 3
Aripiprazole’s receptor binding profile
| Affinity | Ki (nM)a | Effects associated with activity on the receptor | |
|---|---|---|---|
| D2 | High | 0.34 | Partial agonist |
| D3 | High | 0.8 | Partial agonist |
| 5-HT1A | High | 1.7 | Partial agonist |
| 5-HT2A | High | 3.4 | Antagonist |
| 5-HT2C | Moderate | 15 | Partial agonist |
| 5-HT7 | Moderate | 39 | Antagonist |
| D4 | Moderate | 44 | Partial agonist |
| α1-adrenergic | Moderate | 57 | Antagonist |
| H1 | Moderate | 61 | Antagonist |
| M1 | No appreciable activity | >1,000 | No appreciable activity |
| aKi dissociation constant: lower numbers indicate higher affinity of the compound for the receptor H1: histamine 1; M1: muscarinic 1 Source: References 1,6 | |||
Unique clinical issues
Clinical features for depot aripiprazole can be partially deduced based on data on oral aripiprazole. Advantages over other depot SGAs might include aripiprazole’s more favorable weight and metabolic profile.
Contraindications
Depot aripiprazole is contraindicated in patients with known sensitivity to aripiprazole or other components of the formulation. Because of pharmacokinetic drug-drug interactions, using depot aripiprazole should be avoided in patients taking strong CYP3A4 inducers (eg, rifampin and carbamazepine). Dose adjustment is recommended in patients who are taking moderate CYP2D6 and 3A4 inhibitors, such as paroxetine, fluoxetine, ketoconazole, or erythromycin.1 A “black-box” warning of increased mortality in older patients with dementia-related psychosis applies for depot aripiprazole as well as for other atypical antipsychotics.1
Depot aripiprazole is pregnancy category C and should be used in pregnant or breastfeeding mothers only when benefits outweigh the risks. Use of depot aripiprazole in geriatric and pediatric populations has not been studied; however, patients age ≥65 who received oral aripiprazole, 15 mg/d, showed decreased clearance by 20%.1
Dosing
Depot aripiprazole is available as a lyophilized powder that needs to be reconstituted in sterile water. The drug can be stored at room temperature. The kit includes two 21-gauge needles, a 1.5-inch needle for non-obese patients and a 2-inch needle for obese patients. Depot aripiprazole should be given to patients who demonstrate tolerability to oral aripiprazole. The starting and maintenance dose of depot aripiprazole is 400 mg injected into the gluteal muscle, once a month. If a patient develops an AE, decrease the monthly dose to 300 mg. Rotate the injection site between gluteal muscles to reduce AEs from injection.
Because of the potential for significant pharmacokinetic drug-drug interactions, dose adjustment is recommended for patients who are CYP2D6 poor metabolizers and those taking certain other medications (Table 4).1 See Table 4 for the recommended dosage adjustment in the case of missed doses.
Table 4
Adjusting depot aripiprazole after missed doses
| Doses missed since last injection | ||||
|---|---|---|---|---|
| Second or third dose | Fourth or subsequent dose | |||
| >4 weeks and | >5 weeks | >4 weeks and | >6 weeks | |
| Oral aripiprazole | Administer for 14 days | Administer for 14 days | ||
| Depot aripiprazole | Administer as soon as possible | Administer next injection | Administer as soon as possible | Administer next injection |
| Source: Reference 1 | ||||
After depot aripiprazole is injected into the gluteal muscle, the patient receives 10 to 20 mg/d of oral aripiprazole for 14 consecutive days to avoid a drop in plasma concentrations into subtherapeutic levels.
Related Resource
- Abilify Maintena [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Company; 2013.
Drug Brand Names
- Aripiprazole • Abilify
- Aripiprazole depot • Maintena
- Carbamazepine • Tegretol
- Desvenlafaxine • Pristiq
- Dextromethorphan • Delsym
- Erythromycin • E-Mycin
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Itraconazole • Sporanox
- Ketoconazole • Nizoral
- Lithium • Eskalith, Lithobid
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Paliperidone • Invega
- Paroxetine • Paxil
- Quinidine • Quinidex
- Rifampin • Rifadin
- Risperidone • Risperdal
- Valproate • Depakote
- Venlafaxine • Effexor
- Warfarin • Coumadin
- Ziprasidone • Geodon
Disclosure
Dr. Lincoln receives grant or research support from the Wichita Center for Graduate Medical Education.
In February 2013, the FDA approved a long-acting IM aripiprazole formulation for treating adult schizophrenia (Table 1).1 It is the fourth second-generation antipsychotic (SGA) depot formulation approved for treating schizophrenia, and the sixth depot antipsychotic if haloperidol and fluphenazine decanoate are considered.
Table 1
Depot aripiprazole: Fast facts
| Brand name: Abilify Maintena |
| Class: Atypical antipsychotic |
| Indication: Adult schizophrenia |
| Approval date: February 28, 2013 |
| Availability date: March 18, 2013 |
| Manufacturer: Otsuka Pharmaceutical and Lundbeck |
| Dosing form: IM long-acting injection |
| Recommended dosage: 400 mg IM once a month; 200 to 300 mg IM if drug-drug interactions, poor cytochrome P450 2D6 metabolism, or adverse effects |
| Source: Reference 1 |
Clinical implications
Depot medications can improve treatment adherence2; however, long-term antipsychotic use can lead to irreversible adverse effects (dyskinesias), which in some cases were reduced by using newer antipsychotics.3
How it works
Similar to other SGAs, aripiprazole’s mechanism of action is unknown. Aripiprazole was developed based on the dopamine theory, in which dopamine hyperactivity in mesolimbic pathways of the brain leads to hallucinations, delusions, disorganization, and catatonia, and dopamine hypoactivity in mesocortical pathways and the prefrontal cortex causes alogia, anhedonia, autism, avolition, and problems with attention and abstract thinking.
Aripiprazole’s proposed mechanism of action on dopamine receptors is that of partial agonism,1 rather than antagonism, as is the case for other SGAs. In theory, aripiprazole antagonizes postsynaptic D2 receptors and activates presynaptic D2 autoreceptors, with subsequently decreased dopamine production and further stabilization of the dopamine system.4 Its antagonism of 5-HT2A is similar to other SGAs.5
Pharmacokinetics
After depot aripiprazole is injected into the gluteal muscle, the active moiety slowly is released into circulation. The effectiveness of depot aripiprazole is attributable to its active parent drug, aripiprazole monohydrate, and its active metabolite, dehydro-aripiprazole, which is the same as oral aripiprazole. Depot aripiprazole reaches maximum concentration in 5 to 7 days. The elimination half-life of depot aripiprazole is 29.9 days for a 300-mg dose and 46.5 days for a 400-mg dose if administered monthly.1
Aripiprazole does not undergo direct glucuronidation. It is metabolized predominantly through cytochrome P450 (CYP) 2D6 and 3A4 enzymes, which predisposes it to significant drug-drug interactions and may require dose adjustment (Table 2).1
Table 2
Dose adjustments of depot aripiprazole
| Drug-drug interaction | Adjusted dose |
|---|---|
| CYP2D6 poor metabolizers | 300 mg |
| CYP2D6 poor metabolizers taking CYP3A4 inhibitors (ketoconazole, itraconazole, erythromycin, grapefruit juice) | 200 mg |
| Lithium, valproate, desvenlafaxine, venlafaxine, escitalopram, dextromethorphan, omeprazole, warfarin | No significant interaction No dose adjustment |
| Sex, race, liver impairment, renal impairment, tobacco smokers | No dose adjustment |
| Patients taking 400 mg of depot aripiprazole with: | |
| 300 mg |
| 200 mg |
| Avoid use |
| Patients taking 300 mg of depot aripiprazole with: | |
| 200 mg |
| 160 mg |
| Avoid use |
| CYP: cytochrome P450 Source: Adapted from reference 1 | |
Efficacy
The ability of depot aripiprazole to sustain long-term symptom control in adult patients with schizophrenia was demonstrated in a randomized-withdrawal, double-blind, placebo-controlled trial.1 Adults included had a DSM-IV-TR diagnosis of schizophrenia, had ≥3-year history of the illness, had undergone treatment with ≥1 antipsychotic, and had a history of relapse or symptom exacerbation when not receiving antipsychotics. Psychopathology was measured by the Positive and Negative Syndrome Scale (PANSS), the Clinical Global Impression-Severity scale, the Clinical Global Impression-Improvement (CGI-I) scale, and the Clinical Global Impression-Severity of Suicide (CGI-SS) scale.1
The trial lasted 52 weeks, was divided into 4 phases, and concluded early because of demonstrated efficacy.
Phase I: Conversion phase switched patients from a different antipsychotic to oral aripiprazole. This phase lasted 4 to 6 weeks and included 633 patients. An additional 210 patients already receiving aripiprazole were entered directly into Phase II.
Phase II: Open-label, oral stabilization phase included 710 patients (60% males) age 18 to 60 who had a mean PANSS score 66. Patients received 10 to 20 mg/d of oral aripiprazole until they achieved stabilization, defined as PANSS score
Phase III: IM depot stabilization (uncontrolled single blind) included 576 patients. Patients were started on depot aripiprazole, 400 mg monthly, and continued to take 10 to 20 mg/d of oral aripiprazole for 14 consecutive days. Depot aripiprazole was decreased to 300 mg monthly if a patient developed adverse effects. Patients continued to the double-blind phase when stabilization was achieved, as evidenced by PANSS score
Phase IV: Maintenance (double-blind, randomized, placebo-controlled) included 403 patients. Two-thirds of patients continued to take the same dose of depot aripiprazole they took in Phase III. One-third of patients were switched to placebo. The primary efficacy endpoint was time to impending relapse, defined as the first occurrence of ≥1 criteria: hospitalization due to psychosis; violence toward self, others, or property; CGI-SS score ≥4 on part I or ≥7 on part II; or CGI-I score ≥5 and any individual PANSS score >4 for disorganization, hallucinations, suspiciousness, or abnormal thought content.1
Patients randomized to continue depot aripiprazole took longer to relapse or worsening of symptoms compared with the placebo group. Of 403 patients, 10% taking an active drug and 39.6% taking placebo relapsed within 360 days of randomization. This difference was statistically significant (P 1
Tolerability
One possible problem with any long-acting medication is increased duration of adverse effects (AEs), if they develop. Therefore, assessment of safety and tolerability is more important in depot formulations than in oral drugs. During the clinical trial, depot aripiprazole was well tolerated.6
During clinical trials, the most common AEs—insomnia (>5%), anxiety, and tremors—were mild to moderate and occurred within the first 4 weeks. Discontinuation of the medication because of AEs was low, and pain at the injection site was minimal.6 There were 2 deaths during the trial, which were unrelated to depot aripiprazole.6
Aripiprazole’s activity on the D2 receptor can cause extrapyramidal AEs. In head-to-head trials, patients taking aripiprazole had fewer extrapyramidal AEs than those taking risperidone or ziprasidone, but more than patients receiving olanzapine.7 Its moderate antagonism on α-adrenergic and histamine 1 (H1) receptors translates to low orthostatic hypotension, H1-mediated weight gain, and sedation. In clinical trials, weight gain and metabolic changes were comparable with placebo. In head-to-head trials, aripiprazole caused less weight gain and a higher incidence of increased cholesterol than olanzapine and risperidone, and less increase in blood glucose than olanzapine, but more than risperidone.8 Muscarinic 1-mediated cognitive impairment, dry mouth, constipation, urinary retention, and increased intraocular pressure were low.8 See Table 3 for aripiprazole's receptor binding profile.
Table 3
Aripiprazole’s receptor binding profile
| Affinity | Ki (nM)a | Effects associated with activity on the receptor | |
|---|---|---|---|
| D2 | High | 0.34 | Partial agonist |
| D3 | High | 0.8 | Partial agonist |
| 5-HT1A | High | 1.7 | Partial agonist |
| 5-HT2A | High | 3.4 | Antagonist |
| 5-HT2C | Moderate | 15 | Partial agonist |
| 5-HT7 | Moderate | 39 | Antagonist |
| D4 | Moderate | 44 | Partial agonist |
| α1-adrenergic | Moderate | 57 | Antagonist |
| H1 | Moderate | 61 | Antagonist |
| M1 | No appreciable activity | >1,000 | No appreciable activity |
| aKi dissociation constant: lower numbers indicate higher affinity of the compound for the receptor H1: histamine 1; M1: muscarinic 1 Source: References 1,6 | |||
Unique clinical issues
Clinical features for depot aripiprazole can be partially deduced based on data on oral aripiprazole. Advantages over other depot SGAs might include aripiprazole’s more favorable weight and metabolic profile.
Contraindications
Depot aripiprazole is contraindicated in patients with known sensitivity to aripiprazole or other components of the formulation. Because of pharmacokinetic drug-drug interactions, using depot aripiprazole should be avoided in patients taking strong CYP3A4 inducers (eg, rifampin and carbamazepine). Dose adjustment is recommended in patients who are taking moderate CYP2D6 and 3A4 inhibitors, such as paroxetine, fluoxetine, ketoconazole, or erythromycin.1 A “black-box” warning of increased mortality in older patients with dementia-related psychosis applies for depot aripiprazole as well as for other atypical antipsychotics.1
Depot aripiprazole is pregnancy category C and should be used in pregnant or breastfeeding mothers only when benefits outweigh the risks. Use of depot aripiprazole in geriatric and pediatric populations has not been studied; however, patients age ≥65 who received oral aripiprazole, 15 mg/d, showed decreased clearance by 20%.1
Dosing
Depot aripiprazole is available as a lyophilized powder that needs to be reconstituted in sterile water. The drug can be stored at room temperature. The kit includes two 21-gauge needles, a 1.5-inch needle for non-obese patients and a 2-inch needle for obese patients. Depot aripiprazole should be given to patients who demonstrate tolerability to oral aripiprazole. The starting and maintenance dose of depot aripiprazole is 400 mg injected into the gluteal muscle, once a month. If a patient develops an AE, decrease the monthly dose to 300 mg. Rotate the injection site between gluteal muscles to reduce AEs from injection.
Because of the potential for significant pharmacokinetic drug-drug interactions, dose adjustment is recommended for patients who are CYP2D6 poor metabolizers and those taking certain other medications (Table 4).1 See Table 4 for the recommended dosage adjustment in the case of missed doses.
Table 4
Adjusting depot aripiprazole after missed doses
| Doses missed since last injection | ||||
|---|---|---|---|---|
| Second or third dose | Fourth or subsequent dose | |||
| >4 weeks and | >5 weeks | >4 weeks and | >6 weeks | |
| Oral aripiprazole | Administer for 14 days | Administer for 14 days | ||
| Depot aripiprazole | Administer as soon as possible | Administer next injection | Administer as soon as possible | Administer next injection |
| Source: Reference 1 | ||||
After depot aripiprazole is injected into the gluteal muscle, the patient receives 10 to 20 mg/d of oral aripiprazole for 14 consecutive days to avoid a drop in plasma concentrations into subtherapeutic levels.
Related Resource
- Abilify Maintena [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Company; 2013.
Drug Brand Names
- Aripiprazole • Abilify
- Aripiprazole depot • Maintena
- Carbamazepine • Tegretol
- Desvenlafaxine • Pristiq
- Dextromethorphan • Delsym
- Erythromycin • E-Mycin
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Itraconazole • Sporanox
- Ketoconazole • Nizoral
- Lithium • Eskalith, Lithobid
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Paliperidone • Invega
- Paroxetine • Paxil
- Quinidine • Quinidex
- Rifampin • Rifadin
- Risperidone • Risperdal
- Valproate • Depakote
- Venlafaxine • Effexor
- Warfarin • Coumadin
- Ziprasidone • Geodon
Disclosure
Dr. Lincoln receives grant or research support from the Wichita Center for Graduate Medical Education.
1. Abilify Maintena [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Company; 2013.
2. Leucht C, Heres S, Kane JM, et al. Oral versus depot antipsychotic drugs for schizophrenia—a critical systematic review and meta-analysis of randomized long-term trials. Schizophr Res. 2011;127(1-3):83-92.
3. de Araújo AN, de Sena EP, de Oliveira IR, et al. Antipsychotic agents: efficacy and safety in schizophrenia. Drug Healthc Patient Saf. 2012;4:173-180.
4. Mailman RB, Murty V. Third generation antipsychotic drugs: partial agonism or receptor functional selectivity? Curr Pharm Des. 2010;16(5):488-501.
5. Roth BL, Meltzer HY. The role of serotonin in schizophrenia. http://www.acnp.org/g4/GN401000117/CH115.html. Published 2000. Accessed March 27 2013.
6. Kane JM, Sanchez R, Perry PP, et al. Aripiprazole intramuscular depot as maintenance treatment in patients with schizophrenia: a 52-week, multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2012;73(5):617-624.
7. Rummel-Kluge C, Komossa K, Schwarz S, et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr Bull. 2012;38(1):167-177.
8. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2-3):225-233.
1. Abilify Maintena [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Company; 2013.
2. Leucht C, Heres S, Kane JM, et al. Oral versus depot antipsychotic drugs for schizophrenia—a critical systematic review and meta-analysis of randomized long-term trials. Schizophr Res. 2011;127(1-3):83-92.
3. de Araújo AN, de Sena EP, de Oliveira IR, et al. Antipsychotic agents: efficacy and safety in schizophrenia. Drug Healthc Patient Saf. 2012;4:173-180.
4. Mailman RB, Murty V. Third generation antipsychotic drugs: partial agonism or receptor functional selectivity? Curr Pharm Des. 2010;16(5):488-501.
5. Roth BL, Meltzer HY. The role of serotonin in schizophrenia. http://www.acnp.org/g4/GN401000117/CH115.html. Published 2000. Accessed March 27 2013.
6. Kane JM, Sanchez R, Perry PP, et al. Aripiprazole intramuscular depot as maintenance treatment in patients with schizophrenia: a 52-week, multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2012;73(5):617-624.
7. Rummel-Kluge C, Komossa K, Schwarz S, et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr Bull. 2012;38(1):167-177.
8. Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2-3):225-233.