User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Staging psychiatric disorders: A clinico-biologic model
Staging of medical illness is common in oncology and cardiology, but not in psychiatry. Staging can provide important information about illness severity, appropriate therapeutic intervention for that stage, treatment outcomes, and long-term prognosis.
In psychiatry, clinicians generally give a DSM label to a disorder once symptoms emerge and if it persists, simply categorize it as chronic. It’s time for psychiatry to adopt a clinically meaningful staging schema for its major disorders. Several researchers already have proposed such staging models.
The momentum for staging major psychiatric disorders such as schizophrenia, bipolar disorder (BD), and major depressive disorder is being stoked by 2 major research advances: 1) accelerating recognition and characterization of the prodrome as a preclinical stage of psychiatric disorders, and 2) rapidly accruing neurobiologic discoveries about the deleterious biochemical and neural changes that evolve with each successive episode. However, early attempts and current proposals for staging psychiatric disorders are broadly clinical and descriptive.1-4
Clinical staging
McGorry et al5 have proposed the following staging model:
Stage 0: Increased risk of psychotic or mood disorders, although no symptoms are present.
Stage 1a: Mild, nonspecific symptoms.
Stage 1b: Moderate, subthreshold symptoms.
Stage 2: Onset of first episode of a psychotic or mood disorder.
Stage 3a: Incomplete remission from the first episode.
Stage 3b: Recurrence or relapse of a psychotic or mood disorder.
Stage 3c: Multiple relapses, worsening of clinical severity and impact of illness.
Stage 4: Severe, persistent, or unremitting illness.
Although this is a good start, it does not incorporate the emerging neurobiologic findings of progressive psychotic and mood disorders from the preclinical stage to chronic deteriorative state. These pathologies include inflammation, oxidative stress, loss of neurotropic growth factors, and impaired neuroplasticity, all of which result in deleterious neuropathologic progression of damage to key brain circuits. Acute psychotic or mood episodes are recognized to have serious neurotoxic effects, just as myocardial infarction damages the myocardium. This is why patients who experience a first episode of psychosis, mania, or depression must be protected from relapsing: evidence is mounting that second (and certainly subsequent) episodes can be more damaging to the brain than first episodes and would require more aggressive treatment, similar to more advanced cancer stages. This has been well documented clinically, with excellent response to medication and remission in two-thirds of patients with first-episode schizophrenia,6 but far lower remission rates after multiple relapses.
Consider the following advances about the adverse neurobiologic events associated with psychotic or mood episodes at various stages of the illness:
In utero, the risk genes, copy number variations, and random mutations in the thousands of genes involved in brain development probably account for smaller brain volume and hypoplasia of certain brain regions.
In the premorbid phase (childhood and early adolescence), negative symptoms and low cognition are evident as asociality and mediocre grades.
In the prodrome phase (mid-to-late adolescence), cortical changes and cognitive decline as well as mood symptoms are more apparent. Only omega-3 fatty acids—but not atypical antipsychotics—prevented a switch to psychosis better than placebo.7 This suggests the emergence of a neuroinflammatory process that may respond to omega-3 fatty acids.
In the first psychotic episode, a stunning new finding8 reveals brain edema, with a swollen brain and smaller ventricles, caused by water diffusion into extra cellular space of both gray and white matter. Such water diffusion can trigger neuroinflammation and the beginning of serious tissue damage, which can be slowed down by antipsychotics. Increased dopamine activity is associated with an increase of free radicals (oxidative stress) and suppression of growth factors. Glutamate hypofunction, another putative factor in schizophrenia, may be associated with cognitive decline and impaired neuroplasticity.
In the second episode of psychosis, recurrent water diffusion and continued neuroinflammation lead to axonal damage and more serious neurodegeneration.8 This confirms the observation of more serious clinical and functional deterioration after the second episode compared with the first, and becomes much worse if the patient does not adhere to treatment and relapses. Drug response also declines, possibly because of neurodegeneration and further oxidative stress,9 inflammation, breakdown in white matter, disruption in neuroplasticity, and further dysconnectivity across brain regions.10
In the treatment-resistant or refractory phase, clozapine is the only agent that has been shown to improve persistent psychotic symptoms. Although its exact mechanism of action remains unknown, recent studies indicate it may be exerting some of its effects by inhibiting microglial activation,11 which is the main pathway for neuroinflammation in degenerative brain disorders.
Ultimately, after multiple episodes the chromosomal telomere becomes shorter in BD and schizophrenia,12 which is known to predict mortality. This may explain premature death in chronically mentally ill patients (apart from cardiovascular risk factors caused by obesity).
Based on the above, I propose the following clinico-biologic staging model:
Stage 0: Abnormal brain development in utero due to genetic and nongenetic factors.
Stage 1a: Poor premorbid function in childhood (asociality, mediocre school performance).
Stage 1b: The prodrome, with noticeable negative symptoms, cognitive dysfunction, and gray and white matter changes.
Stage 2: First psychotic episode, with delusions and hallucinations, increasing negative symptoms, and marked cognitive decline, accompanied by frontal, parietal, and hippocampal volume losses, white matter pathology, brain edema, inflammatory markers, oxidative stress, and decreased neurotropic growth factors.
Stage 3: Second psychotic episode, with more intense psychotic and negative symptoms, cognitive dysfunction, and worsening social and vocational functioning. Biologic signs include neuroinflammation, oxidative stress and impaired neuroplasticity biomarkers, axonal degeneration and further brain tissue loss, and slower response to antipsychotics.
Stage 4: Several psychotic episodes (subchronic phase), with residual positive and negative symptoms and continued cognitive impairment especially in memory, executive function, attention and verbal learning, accompanied by glial cell death, decline in dendritic spines, retraction or neurite extension, and low response to antipsychotics, with a Global Assessment of Functioning (GAF) score of 30 to 40.
Stage 5: Refractory, unremitting psychosis (chronic phase), with poor response to antipsychotics, severe clinical, social, and functional deterioration, inability to care for oneself, severe neurodegeneration (widespread brain atrophy and dysconnectivity), and GAF score ≤30.
This staging model implies that early intervention to prevent the first or second episode may be the best approach to arrest (and perhaps reverse) psychobiologic deterioration and modify the trajectory of serious psychiatric brain disorders. More can be done to prevent a downhill course in psychosis, and emphasizing the clinical and neurobiologic features of each stage of illness may serve as a roadmap for aggressive treatment approaches early in the illness course. Until a cure is found, prevention and early intervention are the best approaches. Staging models should be incorporated in future versions of the DSM so that psychiatric practitioners can implement the optimal treatment algorithm at the earliest stage possible. Readers’ opinions are welcome!
1. Cosci F, Fava GA. Staging of mental disorders: systematic review. Psychother Psychosom. 2013;82(1):20-34.
2. Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry. 2001;50(11):884-897.
3. Agius M, Goh C, Ulhaq S, et al. The staging model in schizophrenia, and its clinical implications. Psychiatr Danub. 2010;22(2):211-220.
4. McGorry PD, Hickie IB, Yung AR, et al. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry. 2006;40(8):616-622.
5. McGorry PD, Nelson B, Goldstone S, et al. Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Can J Psychiatry. 2010;55(8):486-497.
6. Emsley R, Oosthuizen P, Koen L, et al. Remission in patients with first-episode schizophrenia receiving assured antipsychotic medication: a study with risperidone long-acting injection. Int Clin Psychopharmacol. 2008;23(6):325-331.
7. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
8. Pasternak O, Westin CF, Bouix S, et al. Excessive extracellular volume reveals a neurodegenerative pattern in schizophrenia onset. J Neurosci. 2012;32(48):17365-17372.
9. Yao JK, Reddy R. Oxidative stress in schizophrenia: pathogenetic and therapeutic implications. Antioxid Redox Signal. 2011;15(7):1999-2002.
10. Oertel-Knöchel V, Bittner RA, Knöchel C, et al. Discovery and development of integrative biological markers for schizophrenia. Prog Neurobiol. 2011;95(4):686-702.
11. Hu X, Zhou H, Zhang D, et al. Clozapine protects dopaminergic neurons from inflammation-induced damage by inhibiting microglial overactivation. J Neuroimmune Pharmacol. 2012;7(1):187-201.
12. Fries GR, Pfaffenseller B, Stertz L, et al. Staging and neuroprogression in bipolar disorder. Curr Psychiatry Rep. 2012;14(6):667-675.
Staging of medical illness is common in oncology and cardiology, but not in psychiatry. Staging can provide important information about illness severity, appropriate therapeutic intervention for that stage, treatment outcomes, and long-term prognosis.
In psychiatry, clinicians generally give a DSM label to a disorder once symptoms emerge and if it persists, simply categorize it as chronic. It’s time for psychiatry to adopt a clinically meaningful staging schema for its major disorders. Several researchers already have proposed such staging models.
The momentum for staging major psychiatric disorders such as schizophrenia, bipolar disorder (BD), and major depressive disorder is being stoked by 2 major research advances: 1) accelerating recognition and characterization of the prodrome as a preclinical stage of psychiatric disorders, and 2) rapidly accruing neurobiologic discoveries about the deleterious biochemical and neural changes that evolve with each successive episode. However, early attempts and current proposals for staging psychiatric disorders are broadly clinical and descriptive.1-4
Clinical staging
McGorry et al5 have proposed the following staging model:
Stage 0: Increased risk of psychotic or mood disorders, although no symptoms are present.
Stage 1a: Mild, nonspecific symptoms.
Stage 1b: Moderate, subthreshold symptoms.
Stage 2: Onset of first episode of a psychotic or mood disorder.
Stage 3a: Incomplete remission from the first episode.
Stage 3b: Recurrence or relapse of a psychotic or mood disorder.
Stage 3c: Multiple relapses, worsening of clinical severity and impact of illness.
Stage 4: Severe, persistent, or unremitting illness.
Although this is a good start, it does not incorporate the emerging neurobiologic findings of progressive psychotic and mood disorders from the preclinical stage to chronic deteriorative state. These pathologies include inflammation, oxidative stress, loss of neurotropic growth factors, and impaired neuroplasticity, all of which result in deleterious neuropathologic progression of damage to key brain circuits. Acute psychotic or mood episodes are recognized to have serious neurotoxic effects, just as myocardial infarction damages the myocardium. This is why patients who experience a first episode of psychosis, mania, or depression must be protected from relapsing: evidence is mounting that second (and certainly subsequent) episodes can be more damaging to the brain than first episodes and would require more aggressive treatment, similar to more advanced cancer stages. This has been well documented clinically, with excellent response to medication and remission in two-thirds of patients with first-episode schizophrenia,6 but far lower remission rates after multiple relapses.
Consider the following advances about the adverse neurobiologic events associated with psychotic or mood episodes at various stages of the illness:
In utero, the risk genes, copy number variations, and random mutations in the thousands of genes involved in brain development probably account for smaller brain volume and hypoplasia of certain brain regions.
In the premorbid phase (childhood and early adolescence), negative symptoms and low cognition are evident as asociality and mediocre grades.
In the prodrome phase (mid-to-late adolescence), cortical changes and cognitive decline as well as mood symptoms are more apparent. Only omega-3 fatty acids—but not atypical antipsychotics—prevented a switch to psychosis better than placebo.7 This suggests the emergence of a neuroinflammatory process that may respond to omega-3 fatty acids.
In the first psychotic episode, a stunning new finding8 reveals brain edema, with a swollen brain and smaller ventricles, caused by water diffusion into extra cellular space of both gray and white matter. Such water diffusion can trigger neuroinflammation and the beginning of serious tissue damage, which can be slowed down by antipsychotics. Increased dopamine activity is associated with an increase of free radicals (oxidative stress) and suppression of growth factors. Glutamate hypofunction, another putative factor in schizophrenia, may be associated with cognitive decline and impaired neuroplasticity.
In the second episode of psychosis, recurrent water diffusion and continued neuroinflammation lead to axonal damage and more serious neurodegeneration.8 This confirms the observation of more serious clinical and functional deterioration after the second episode compared with the first, and becomes much worse if the patient does not adhere to treatment and relapses. Drug response also declines, possibly because of neurodegeneration and further oxidative stress,9 inflammation, breakdown in white matter, disruption in neuroplasticity, and further dysconnectivity across brain regions.10
In the treatment-resistant or refractory phase, clozapine is the only agent that has been shown to improve persistent psychotic symptoms. Although its exact mechanism of action remains unknown, recent studies indicate it may be exerting some of its effects by inhibiting microglial activation,11 which is the main pathway for neuroinflammation in degenerative brain disorders.
Ultimately, after multiple episodes the chromosomal telomere becomes shorter in BD and schizophrenia,12 which is known to predict mortality. This may explain premature death in chronically mentally ill patients (apart from cardiovascular risk factors caused by obesity).
Based on the above, I propose the following clinico-biologic staging model:
Stage 0: Abnormal brain development in utero due to genetic and nongenetic factors.
Stage 1a: Poor premorbid function in childhood (asociality, mediocre school performance).
Stage 1b: The prodrome, with noticeable negative symptoms, cognitive dysfunction, and gray and white matter changes.
Stage 2: First psychotic episode, with delusions and hallucinations, increasing negative symptoms, and marked cognitive decline, accompanied by frontal, parietal, and hippocampal volume losses, white matter pathology, brain edema, inflammatory markers, oxidative stress, and decreased neurotropic growth factors.
Stage 3: Second psychotic episode, with more intense psychotic and negative symptoms, cognitive dysfunction, and worsening social and vocational functioning. Biologic signs include neuroinflammation, oxidative stress and impaired neuroplasticity biomarkers, axonal degeneration and further brain tissue loss, and slower response to antipsychotics.
Stage 4: Several psychotic episodes (subchronic phase), with residual positive and negative symptoms and continued cognitive impairment especially in memory, executive function, attention and verbal learning, accompanied by glial cell death, decline in dendritic spines, retraction or neurite extension, and low response to antipsychotics, with a Global Assessment of Functioning (GAF) score of 30 to 40.
Stage 5: Refractory, unremitting psychosis (chronic phase), with poor response to antipsychotics, severe clinical, social, and functional deterioration, inability to care for oneself, severe neurodegeneration (widespread brain atrophy and dysconnectivity), and GAF score ≤30.
This staging model implies that early intervention to prevent the first or second episode may be the best approach to arrest (and perhaps reverse) psychobiologic deterioration and modify the trajectory of serious psychiatric brain disorders. More can be done to prevent a downhill course in psychosis, and emphasizing the clinical and neurobiologic features of each stage of illness may serve as a roadmap for aggressive treatment approaches early in the illness course. Until a cure is found, prevention and early intervention are the best approaches. Staging models should be incorporated in future versions of the DSM so that psychiatric practitioners can implement the optimal treatment algorithm at the earliest stage possible. Readers’ opinions are welcome!
Staging of medical illness is common in oncology and cardiology, but not in psychiatry. Staging can provide important information about illness severity, appropriate therapeutic intervention for that stage, treatment outcomes, and long-term prognosis.
In psychiatry, clinicians generally give a DSM label to a disorder once symptoms emerge and if it persists, simply categorize it as chronic. It’s time for psychiatry to adopt a clinically meaningful staging schema for its major disorders. Several researchers already have proposed such staging models.
The momentum for staging major psychiatric disorders such as schizophrenia, bipolar disorder (BD), and major depressive disorder is being stoked by 2 major research advances: 1) accelerating recognition and characterization of the prodrome as a preclinical stage of psychiatric disorders, and 2) rapidly accruing neurobiologic discoveries about the deleterious biochemical and neural changes that evolve with each successive episode. However, early attempts and current proposals for staging psychiatric disorders are broadly clinical and descriptive.1-4
Clinical staging
McGorry et al5 have proposed the following staging model:
Stage 0: Increased risk of psychotic or mood disorders, although no symptoms are present.
Stage 1a: Mild, nonspecific symptoms.
Stage 1b: Moderate, subthreshold symptoms.
Stage 2: Onset of first episode of a psychotic or mood disorder.
Stage 3a: Incomplete remission from the first episode.
Stage 3b: Recurrence or relapse of a psychotic or mood disorder.
Stage 3c: Multiple relapses, worsening of clinical severity and impact of illness.
Stage 4: Severe, persistent, or unremitting illness.
Although this is a good start, it does not incorporate the emerging neurobiologic findings of progressive psychotic and mood disorders from the preclinical stage to chronic deteriorative state. These pathologies include inflammation, oxidative stress, loss of neurotropic growth factors, and impaired neuroplasticity, all of which result in deleterious neuropathologic progression of damage to key brain circuits. Acute psychotic or mood episodes are recognized to have serious neurotoxic effects, just as myocardial infarction damages the myocardium. This is why patients who experience a first episode of psychosis, mania, or depression must be protected from relapsing: evidence is mounting that second (and certainly subsequent) episodes can be more damaging to the brain than first episodes and would require more aggressive treatment, similar to more advanced cancer stages. This has been well documented clinically, with excellent response to medication and remission in two-thirds of patients with first-episode schizophrenia,6 but far lower remission rates after multiple relapses.
Consider the following advances about the adverse neurobiologic events associated with psychotic or mood episodes at various stages of the illness:
In utero, the risk genes, copy number variations, and random mutations in the thousands of genes involved in brain development probably account for smaller brain volume and hypoplasia of certain brain regions.
In the premorbid phase (childhood and early adolescence), negative symptoms and low cognition are evident as asociality and mediocre grades.
In the prodrome phase (mid-to-late adolescence), cortical changes and cognitive decline as well as mood symptoms are more apparent. Only omega-3 fatty acids—but not atypical antipsychotics—prevented a switch to psychosis better than placebo.7 This suggests the emergence of a neuroinflammatory process that may respond to omega-3 fatty acids.
In the first psychotic episode, a stunning new finding8 reveals brain edema, with a swollen brain and smaller ventricles, caused by water diffusion into extra cellular space of both gray and white matter. Such water diffusion can trigger neuroinflammation and the beginning of serious tissue damage, which can be slowed down by antipsychotics. Increased dopamine activity is associated with an increase of free radicals (oxidative stress) and suppression of growth factors. Glutamate hypofunction, another putative factor in schizophrenia, may be associated with cognitive decline and impaired neuroplasticity.
In the second episode of psychosis, recurrent water diffusion and continued neuroinflammation lead to axonal damage and more serious neurodegeneration.8 This confirms the observation of more serious clinical and functional deterioration after the second episode compared with the first, and becomes much worse if the patient does not adhere to treatment and relapses. Drug response also declines, possibly because of neurodegeneration and further oxidative stress,9 inflammation, breakdown in white matter, disruption in neuroplasticity, and further dysconnectivity across brain regions.10
In the treatment-resistant or refractory phase, clozapine is the only agent that has been shown to improve persistent psychotic symptoms. Although its exact mechanism of action remains unknown, recent studies indicate it may be exerting some of its effects by inhibiting microglial activation,11 which is the main pathway for neuroinflammation in degenerative brain disorders.
Ultimately, after multiple episodes the chromosomal telomere becomes shorter in BD and schizophrenia,12 which is known to predict mortality. This may explain premature death in chronically mentally ill patients (apart from cardiovascular risk factors caused by obesity).
Based on the above, I propose the following clinico-biologic staging model:
Stage 0: Abnormal brain development in utero due to genetic and nongenetic factors.
Stage 1a: Poor premorbid function in childhood (asociality, mediocre school performance).
Stage 1b: The prodrome, with noticeable negative symptoms, cognitive dysfunction, and gray and white matter changes.
Stage 2: First psychotic episode, with delusions and hallucinations, increasing negative symptoms, and marked cognitive decline, accompanied by frontal, parietal, and hippocampal volume losses, white matter pathology, brain edema, inflammatory markers, oxidative stress, and decreased neurotropic growth factors.
Stage 3: Second psychotic episode, with more intense psychotic and negative symptoms, cognitive dysfunction, and worsening social and vocational functioning. Biologic signs include neuroinflammation, oxidative stress and impaired neuroplasticity biomarkers, axonal degeneration and further brain tissue loss, and slower response to antipsychotics.
Stage 4: Several psychotic episodes (subchronic phase), with residual positive and negative symptoms and continued cognitive impairment especially in memory, executive function, attention and verbal learning, accompanied by glial cell death, decline in dendritic spines, retraction or neurite extension, and low response to antipsychotics, with a Global Assessment of Functioning (GAF) score of 30 to 40.
Stage 5: Refractory, unremitting psychosis (chronic phase), with poor response to antipsychotics, severe clinical, social, and functional deterioration, inability to care for oneself, severe neurodegeneration (widespread brain atrophy and dysconnectivity), and GAF score ≤30.
This staging model implies that early intervention to prevent the first or second episode may be the best approach to arrest (and perhaps reverse) psychobiologic deterioration and modify the trajectory of serious psychiatric brain disorders. More can be done to prevent a downhill course in psychosis, and emphasizing the clinical and neurobiologic features of each stage of illness may serve as a roadmap for aggressive treatment approaches early in the illness course. Until a cure is found, prevention and early intervention are the best approaches. Staging models should be incorporated in future versions of the DSM so that psychiatric practitioners can implement the optimal treatment algorithm at the earliest stage possible. Readers’ opinions are welcome!
1. Cosci F, Fava GA. Staging of mental disorders: systematic review. Psychother Psychosom. 2013;82(1):20-34.
2. Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry. 2001;50(11):884-897.
3. Agius M, Goh C, Ulhaq S, et al. The staging model in schizophrenia, and its clinical implications. Psychiatr Danub. 2010;22(2):211-220.
4. McGorry PD, Hickie IB, Yung AR, et al. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry. 2006;40(8):616-622.
5. McGorry PD, Nelson B, Goldstone S, et al. Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Can J Psychiatry. 2010;55(8):486-497.
6. Emsley R, Oosthuizen P, Koen L, et al. Remission in patients with first-episode schizophrenia receiving assured antipsychotic medication: a study with risperidone long-acting injection. Int Clin Psychopharmacol. 2008;23(6):325-331.
7. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
8. Pasternak O, Westin CF, Bouix S, et al. Excessive extracellular volume reveals a neurodegenerative pattern in schizophrenia onset. J Neurosci. 2012;32(48):17365-17372.
9. Yao JK, Reddy R. Oxidative stress in schizophrenia: pathogenetic and therapeutic implications. Antioxid Redox Signal. 2011;15(7):1999-2002.
10. Oertel-Knöchel V, Bittner RA, Knöchel C, et al. Discovery and development of integrative biological markers for schizophrenia. Prog Neurobiol. 2011;95(4):686-702.
11. Hu X, Zhou H, Zhang D, et al. Clozapine protects dopaminergic neurons from inflammation-induced damage by inhibiting microglial overactivation. J Neuroimmune Pharmacol. 2012;7(1):187-201.
12. Fries GR, Pfaffenseller B, Stertz L, et al. Staging and neuroprogression in bipolar disorder. Curr Psychiatry Rep. 2012;14(6):667-675.
1. Cosci F, Fava GA. Staging of mental disorders: systematic review. Psychother Psychosom. 2013;82(1):20-34.
2. Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry. 2001;50(11):884-897.
3. Agius M, Goh C, Ulhaq S, et al. The staging model in schizophrenia, and its clinical implications. Psychiatr Danub. 2010;22(2):211-220.
4. McGorry PD, Hickie IB, Yung AR, et al. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry. 2006;40(8):616-622.
5. McGorry PD, Nelson B, Goldstone S, et al. Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Can J Psychiatry. 2010;55(8):486-497.
6. Emsley R, Oosthuizen P, Koen L, et al. Remission in patients with first-episode schizophrenia receiving assured antipsychotic medication: a study with risperidone long-acting injection. Int Clin Psychopharmacol. 2008;23(6):325-331.
7. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
8. Pasternak O, Westin CF, Bouix S, et al. Excessive extracellular volume reveals a neurodegenerative pattern in schizophrenia onset. J Neurosci. 2012;32(48):17365-17372.
9. Yao JK, Reddy R. Oxidative stress in schizophrenia: pathogenetic and therapeutic implications. Antioxid Redox Signal. 2011;15(7):1999-2002.
10. Oertel-Knöchel V, Bittner RA, Knöchel C, et al. Discovery and development of integrative biological markers for schizophrenia. Prog Neurobiol. 2011;95(4):686-702.
11. Hu X, Zhou H, Zhang D, et al. Clozapine protects dopaminergic neurons from inflammation-induced damage by inhibiting microglial overactivation. J Neuroimmune Pharmacol. 2012;7(1):187-201.
12. Fries GR, Pfaffenseller B, Stertz L, et al. Staging and neuroprogression in bipolar disorder. Curr Psychiatry Rep. 2012;14(6):667-675.
Psychotic and sexually deviant
CASE: Paranoid and distressed
Mr. P, age 21, is a single, white college student who presents to a psychiatric emergency room with his father at his psychotherapist’s recommendation. The psychotherapist, who has been treating Mr. P for anxiety and depression, recommended he be evaluated because of increased erratic behavior and paranoia. Mr. P reports that he has been feeling increasingly “anxious” and “paranoid” and thinks the security cameras at his college have been following him. He also describes an increased connection with God and hearing God’s voice as a commentary on his behaviors. Mr. P denies euphoria, depression, increased goal-directed activities, distractibility, increased impulsivity, or rapid speech. He is admitted voluntarily to the psychiatric unit for further evaluation.
During the hospitalization, Mr. P discloses that he has been viewing child pornography for 2 years, and during the past 6 months he has been distressed by the intensity of his sexual fantasies involving sexual contact with prepubescent girls. He also continues to experience paranoia and increased religiosity.
Mr. P says he began looking at pornography on the internet at age 14. He says he was watching “regular straight porn” and he would use it to masturbate and achieve orgasm. Mr. P began looking at child pornography at age 19. He stated that “regular porn” was no longer sufficiently arousing for him. Mr. P explains, “First, I started looking for 15- or 16-year-olds. They would work for a while [referring to sexual gratification], but then I would look for younger girls.” He says the images of younger girls are sexually arousing, typically “young girls, 8 to 10 years old” who are nude or involved in sex acts.
Mr. P denies sexual contact with prepubescent individuals and says his thoughts about such contact are “distressing.” He reports that he has viewed child pornography even when he wasn’t experiencing psychotic or mood symptoms. Mr. P’s outpatient psychotherapist reports that Mr. P first disclosed viewing child pornography and his attraction to prepubescent girls 2 years before this admission.
The authors’ observations
DSM-IV-TR diagnostic criteria for pedophilia (Table 1)1 are based on a history of sexual arousal to prepubescent individuals. A subset of sex offenders meet criteria for a paraphilia (Table 2),1 an axis I disorder, and a subset of sex offenders with paraphilia meet diagnostic criteria for pedophilia. Dunsieth et al2 found that among a sample of 113 male sex offenders, 74% had a diagnosable paraphilia, and 50% of individuals with paraphilia met criteria for pedophilia.
Table 1
DSM-IV-TR diagnostic criteria for pedophilia
| A) | Over a period of ≥6 months, recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child or children (generally age ≤13) |
| B) | The person has acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty |
| C) | The person is age ≥16 and ≥5 years older than the child or children in criterion A |
| Note: Do not include an individual in late adolescence involved in an ongoing sexual relationship with a 12- or 13-year-old | |
| Source: Reference 1 | |
DSM-IV-TR diagnostic criteria for a paraphilia
| The essential features of a paraphilia are recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving: | |
| A) | nonhuman objects, the suffering or humiliation of oneself or one’s partner, or children or other nonconsenting persons that occur over a period of ≥6 months |
| B) | The behavior, sexual urges, or fantasies cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 1 | |
Although most schizophrenia patients without a history of sexual offenses do not exhibit sexual deviancy, sexual content in hallucinations and delusions is common.6 Confusion about sexual identity and the boundaries of one’s body are common and may contribute to sexual deviancy.6 Psychiatric inpatients without a history of sexual offenses—including but not limited to psychotic patients—have higher rates of sexually deviant fantasies and behaviors compared with those without psychiatric illness.6 In one survey, 15% of men with schizophrenia displayed paraphilic behaviors and 20% had atypical sexual thoughts.7
Alish et al4 found that pedophilia was not necessarily linked to psychotic behavior or antisocial personality features when comparing pedophilia rates in individuals with or without schizophrenia. In a sample of 22 adolescent males who sexually molested a child at least once, axis I morbidity was common, and 55% met criteria for bipolar disorder.8
Few experts in paraphilias
A patient who endorses deviant sexual fantasies should be evaluated by a mental health professional with specialized training in paraphilias. Although paraphilias are not recognized as a subspecialty in psychiatry, diagnosing and treating patients with a paraphilia requires additional training. There is a scarcity of psychiatrists trained to evaluate and treat patients with paraphilias.
Sexual evaluation. Evaluating a patient who presents with problematic sexual behaviors includes performing a comprehensive psychiatric history with a focus on sexual history. A psychosexual history is distinct from general psychiatric evaluations because of the level of detail regarding a sexual history (Table 3). In addition to the clinical interview, objective testing to determine sexual interests may be useful in some patients (Table 4).9
Actuarial tools—risk assessment instruments based on statistically significant risk factors—are valid tools for determining the risk of sexual reoffending. There are several validated actuarial tools in the assessment of sex offender recidivism, such as the Static-99R,10 Stable-2007,11 and the Sex Offender Risk Appraisal Guide.12 However, these tools are used for sex offenders, and would not be used for individuals who have not committed a sex offense, such as Mr. P.
Table 3
Psychosexual evaluation
| Aspect of evaluation | Measures |
| Sexual behavior history | History of sexual abuse Childhood exposure to sex Masturbation history Preferred sexual partners Kinsey Scale |
| Sexual addiction or compulsion | Total Sexual Outlet measure Amount of time in sexual fantasy Financial, legal, or social cost of sexual behavior Prior treatment of sexual behavior |
| Sexual interests | Sex, age, and number of partner(s) Review of criteria for all paraphilias (exposing, voyeurism, cross-dressing, sadistic or masochistic interests) |
Objective testing to determine sexual interests
| Test | Results |
|---|---|
| Penile plethysmograph | Measures penis circumference with a mercury-in-rubber strain gauge. Used clinically by measuring circumferential changes in the penis while the patient is listening to audio or video stimuli of various sexual vignettes |
| Abel Assessment for Sexual Interests-3 | An objective method for evaluating deviant sexual interest uses noninvasive means to achieve objective measures of sexual interest. The subject’s visual response time is measured while viewing images of males and females of varying age. Visual reaction time is correlated with sexual interests |
| Source: Reference 9 | |
Medicolegal aspects of a psychosexual evaluation may include mandated reporting, confidentiality, and documentation. Mental health professionals are mandated to report to law enforcement or child welfare agencies when they observe or suspect physical, sexual, or other types of abuse in vulnerable populations such as children. In psychosexual evaluations, the evaluator is legally required to report if a patient discloses current sexual behavior with a child with a plan to continue to engage in the behavior. In Mr. P’s case, there was no duty to report because although he described viewing child pornography and had a sexual interest in prepubescent individuals, he did not report a history of engaging in handson sexual behaviors with children or impulses to do so. When an individual has engaged in sexual contact with a prepubescent individual, reporting is not mandated unless the individual continues to engage in sexual behavior with a minor. Mental health professionals are not responsible for calling the police or alerting authorities after a crime has been committed.
The relationship between viewing child pornography and pedophilia is unclear. Some child pornography viewers are pedophilic, others are sexually compulsive, and others are viewing out of curiosity and have no sexual deviance. Seto et al13 suggested that child pornography offenders show greater sexual arousal to children than to adults. Persistent child pornography use is a stronger diagnostic indicator of pedophilia than sexually offending against child victims.13 A clinician who learns that a patient is viewing child pornography should take a detailed sexual history, including a review of criteria for paraphilias. In addition, when appropriate, the clinician should perform a risk assessment to determine the patient’s risk of engaging in sexual offenses with children.
OUTCOME: Expert consultation
We start Mr. P on risperidone, 1 mg/d, to treat his paranoia and request a consultation with an expert in paraphilias to determine if Mr. P has a paraphilia and to discuss treatment options.
Mr. P’s initial diagnosis is psychotic disorder not otherwise specified. His viewing of child pornography and sexual interest in prepubescent individuals is not limited to his current mental status, and these interests persist in the absence of mood and psychotic states. Mr. P’s viewing of child pornography and sexual attraction to prepubescent girls meet the diagnostic criteria for pedophilia. During hospitalization, we educate Mr. P about his diagnoses and need for continued treatment. We refer him to a sexual disorders outpatient clinic, which continues to address his deviant sexual interests.
The authors’ observations
A meta-analysis indicates that a combination of pharmacologic and behavioral treatments coupled with close legal supervision seems to reduce the risk of repeated sexual offenses.14 Legal supervision is a general term to describe oversight of offenders in the community by supervisory boards, such as probation or parole, and tracking devices such as GPS. Currently, pedophilia treatment focuses on minimizing deviant sexual arousal through behavioral modification, cognitive-behavioral therapies, and testosterone-lowering medications, such as medroxyprogesterone or leuprolide. The decision to prescribe testosterone-lowering medication should be based on informed consent and the patient’s risk of dangerous sexual behaviors.
- Reijnen L, Bulten E, Nijman H. Demographic and personality characteristics of internet child pornography downloaders in comparison to other offenders. J Child Sex Abus. 2009;18(6):611-622.
- Hall RC, Hall RC. A profile of pedophilia: definition, characteristics of offenders, recidivism, treatment outcomes, and forensic issues. Mayo Clin Proc. 2007;82(4):457-471.
- Leuprolide • Eligard, Lupron
- Medroxyprogesterone • Cycrin, Provera
- Risperidone • Risperdal
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Dunsieth NW, Jr, Nelson EB, Brusman-Lovins LA, et al. Psychiatric and legal features of 113 men convicted of sexual offenses. J Clin Psychiatry. 2004;65(3):293-300.
3. Wallace C, Mullen P, Burgess P, et al. Serious criminal offending and mental disorder. Case linkage study. Br J Psychiatry. 1998;172:477-484.
4. Alish Y, Birger M, Manor N, et al. Schizophrenia sex offenders: a clinical and epidemiological comparison study. Int J Law Psychiatry. 2007;30(6):459-466.
5. Smith AD, Taylor PJ. Serious sex offending against women by men with schizophrenia. Relationship of illness and psychiatric symptoms to offending. Br J Psychiatry. 1999;174:233-237.
6. Drake CR, Pathé M. Understanding sexual offending in schizophrenia. Crim Behav Ment Health. 2004;14(2):108-120.
7. Harley EW, Boardman J, Craig T. Sexual problems in schizophrenia prevalence and characteristics: a cross sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):759-766.
8. Galli V, McElroy SL, Soutullo CA, et al. The psychiatric diagnoses of twenty-two adolescents who have sexually molested other children. Compr Psychiatry. 1999;40(2):85-88.
9. Abel GG, Jordan A, Hand CG, et al. Classification models of child molesters utilizing the Abel Assessment for sexual interest. Child Abuse Negl. 2001;25(5):703-718.
10. Hanson RK, Thornton D. Improving risk assessments for sex offenders: a comparison of three actuarial scales. Law Hum Behav. 2000;24(1):119-136.
11. Hanson RK, Harris AJ, Scott TL, et al. Assessing the risk of sexual offenders on community supervision: The Dynamic Supervision Project. Vol 5. Ottawa, Canada: Public Safety Canada; 2007.
12. Quinsey VL, Harris AJ, Rice ME, et al. Violent offenders: appraising and managing risk. 2nd ed. Washington DC: American Psychological Association; 2006.
13. Seto M, Cantor JM, Blanchard R. Child pornography offenses are a valid diagnostic indicator of pedophilia. J Abnorm Psychol. 2006;115(3):610-615.
14. Thibaut F, De La Barra F, Gordon H, et al. WFSBP Task Force on Sexual Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias. World J Biol Psychiatry. 2010;11(4):604-655.
CASE: Paranoid and distressed
Mr. P, age 21, is a single, white college student who presents to a psychiatric emergency room with his father at his psychotherapist’s recommendation. The psychotherapist, who has been treating Mr. P for anxiety and depression, recommended he be evaluated because of increased erratic behavior and paranoia. Mr. P reports that he has been feeling increasingly “anxious” and “paranoid” and thinks the security cameras at his college have been following him. He also describes an increased connection with God and hearing God’s voice as a commentary on his behaviors. Mr. P denies euphoria, depression, increased goal-directed activities, distractibility, increased impulsivity, or rapid speech. He is admitted voluntarily to the psychiatric unit for further evaluation.
During the hospitalization, Mr. P discloses that he has been viewing child pornography for 2 years, and during the past 6 months he has been distressed by the intensity of his sexual fantasies involving sexual contact with prepubescent girls. He also continues to experience paranoia and increased religiosity.
Mr. P says he began looking at pornography on the internet at age 14. He says he was watching “regular straight porn” and he would use it to masturbate and achieve orgasm. Mr. P began looking at child pornography at age 19. He stated that “regular porn” was no longer sufficiently arousing for him. Mr. P explains, “First, I started looking for 15- or 16-year-olds. They would work for a while [referring to sexual gratification], but then I would look for younger girls.” He says the images of younger girls are sexually arousing, typically “young girls, 8 to 10 years old” who are nude or involved in sex acts.
Mr. P denies sexual contact with prepubescent individuals and says his thoughts about such contact are “distressing.” He reports that he has viewed child pornography even when he wasn’t experiencing psychotic or mood symptoms. Mr. P’s outpatient psychotherapist reports that Mr. P first disclosed viewing child pornography and his attraction to prepubescent girls 2 years before this admission.
The authors’ observations
DSM-IV-TR diagnostic criteria for pedophilia (Table 1)1 are based on a history of sexual arousal to prepubescent individuals. A subset of sex offenders meet criteria for a paraphilia (Table 2),1 an axis I disorder, and a subset of sex offenders with paraphilia meet diagnostic criteria for pedophilia. Dunsieth et al2 found that among a sample of 113 male sex offenders, 74% had a diagnosable paraphilia, and 50% of individuals with paraphilia met criteria for pedophilia.
Table 1
DSM-IV-TR diagnostic criteria for pedophilia
| A) | Over a period of ≥6 months, recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child or children (generally age ≤13) |
| B) | The person has acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty |
| C) | The person is age ≥16 and ≥5 years older than the child or children in criterion A |
| Note: Do not include an individual in late adolescence involved in an ongoing sexual relationship with a 12- or 13-year-old | |
| Source: Reference 1 | |
DSM-IV-TR diagnostic criteria for a paraphilia
| The essential features of a paraphilia are recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving: | |
| A) | nonhuman objects, the suffering or humiliation of oneself or one’s partner, or children or other nonconsenting persons that occur over a period of ≥6 months |
| B) | The behavior, sexual urges, or fantasies cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 1 | |
Although most schizophrenia patients without a history of sexual offenses do not exhibit sexual deviancy, sexual content in hallucinations and delusions is common.6 Confusion about sexual identity and the boundaries of one’s body are common and may contribute to sexual deviancy.6 Psychiatric inpatients without a history of sexual offenses—including but not limited to psychotic patients—have higher rates of sexually deviant fantasies and behaviors compared with those without psychiatric illness.6 In one survey, 15% of men with schizophrenia displayed paraphilic behaviors and 20% had atypical sexual thoughts.7
Alish et al4 found that pedophilia was not necessarily linked to psychotic behavior or antisocial personality features when comparing pedophilia rates in individuals with or without schizophrenia. In a sample of 22 adolescent males who sexually molested a child at least once, axis I morbidity was common, and 55% met criteria for bipolar disorder.8
Few experts in paraphilias
A patient who endorses deviant sexual fantasies should be evaluated by a mental health professional with specialized training in paraphilias. Although paraphilias are not recognized as a subspecialty in psychiatry, diagnosing and treating patients with a paraphilia requires additional training. There is a scarcity of psychiatrists trained to evaluate and treat patients with paraphilias.
Sexual evaluation. Evaluating a patient who presents with problematic sexual behaviors includes performing a comprehensive psychiatric history with a focus on sexual history. A psychosexual history is distinct from general psychiatric evaluations because of the level of detail regarding a sexual history (Table 3). In addition to the clinical interview, objective testing to determine sexual interests may be useful in some patients (Table 4).9
Actuarial tools—risk assessment instruments based on statistically significant risk factors—are valid tools for determining the risk of sexual reoffending. There are several validated actuarial tools in the assessment of sex offender recidivism, such as the Static-99R,10 Stable-2007,11 and the Sex Offender Risk Appraisal Guide.12 However, these tools are used for sex offenders, and would not be used for individuals who have not committed a sex offense, such as Mr. P.
Table 3
Psychosexual evaluation
| Aspect of evaluation | Measures |
| Sexual behavior history | History of sexual abuse Childhood exposure to sex Masturbation history Preferred sexual partners Kinsey Scale |
| Sexual addiction or compulsion | Total Sexual Outlet measure Amount of time in sexual fantasy Financial, legal, or social cost of sexual behavior Prior treatment of sexual behavior |
| Sexual interests | Sex, age, and number of partner(s) Review of criteria for all paraphilias (exposing, voyeurism, cross-dressing, sadistic or masochistic interests) |
Objective testing to determine sexual interests
| Test | Results |
|---|---|
| Penile plethysmograph | Measures penis circumference with a mercury-in-rubber strain gauge. Used clinically by measuring circumferential changes in the penis while the patient is listening to audio or video stimuli of various sexual vignettes |
| Abel Assessment for Sexual Interests-3 | An objective method for evaluating deviant sexual interest uses noninvasive means to achieve objective measures of sexual interest. The subject’s visual response time is measured while viewing images of males and females of varying age. Visual reaction time is correlated with sexual interests |
| Source: Reference 9 | |
Medicolegal aspects of a psychosexual evaluation may include mandated reporting, confidentiality, and documentation. Mental health professionals are mandated to report to law enforcement or child welfare agencies when they observe or suspect physical, sexual, or other types of abuse in vulnerable populations such as children. In psychosexual evaluations, the evaluator is legally required to report if a patient discloses current sexual behavior with a child with a plan to continue to engage in the behavior. In Mr. P’s case, there was no duty to report because although he described viewing child pornography and had a sexual interest in prepubescent individuals, he did not report a history of engaging in handson sexual behaviors with children or impulses to do so. When an individual has engaged in sexual contact with a prepubescent individual, reporting is not mandated unless the individual continues to engage in sexual behavior with a minor. Mental health professionals are not responsible for calling the police or alerting authorities after a crime has been committed.
The relationship between viewing child pornography and pedophilia is unclear. Some child pornography viewers are pedophilic, others are sexually compulsive, and others are viewing out of curiosity and have no sexual deviance. Seto et al13 suggested that child pornography offenders show greater sexual arousal to children than to adults. Persistent child pornography use is a stronger diagnostic indicator of pedophilia than sexually offending against child victims.13 A clinician who learns that a patient is viewing child pornography should take a detailed sexual history, including a review of criteria for paraphilias. In addition, when appropriate, the clinician should perform a risk assessment to determine the patient’s risk of engaging in sexual offenses with children.
OUTCOME: Expert consultation
We start Mr. P on risperidone, 1 mg/d, to treat his paranoia and request a consultation with an expert in paraphilias to determine if Mr. P has a paraphilia and to discuss treatment options.
Mr. P’s initial diagnosis is psychotic disorder not otherwise specified. His viewing of child pornography and sexual interest in prepubescent individuals is not limited to his current mental status, and these interests persist in the absence of mood and psychotic states. Mr. P’s viewing of child pornography and sexual attraction to prepubescent girls meet the diagnostic criteria for pedophilia. During hospitalization, we educate Mr. P about his diagnoses and need for continued treatment. We refer him to a sexual disorders outpatient clinic, which continues to address his deviant sexual interests.
The authors’ observations
A meta-analysis indicates that a combination of pharmacologic and behavioral treatments coupled with close legal supervision seems to reduce the risk of repeated sexual offenses.14 Legal supervision is a general term to describe oversight of offenders in the community by supervisory boards, such as probation or parole, and tracking devices such as GPS. Currently, pedophilia treatment focuses on minimizing deviant sexual arousal through behavioral modification, cognitive-behavioral therapies, and testosterone-lowering medications, such as medroxyprogesterone or leuprolide. The decision to prescribe testosterone-lowering medication should be based on informed consent and the patient’s risk of dangerous sexual behaviors.
- Reijnen L, Bulten E, Nijman H. Demographic and personality characteristics of internet child pornography downloaders in comparison to other offenders. J Child Sex Abus. 2009;18(6):611-622.
- Hall RC, Hall RC. A profile of pedophilia: definition, characteristics of offenders, recidivism, treatment outcomes, and forensic issues. Mayo Clin Proc. 2007;82(4):457-471.
- Leuprolide • Eligard, Lupron
- Medroxyprogesterone • Cycrin, Provera
- Risperidone • Risperdal
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Paranoid and distressed
Mr. P, age 21, is a single, white college student who presents to a psychiatric emergency room with his father at his psychotherapist’s recommendation. The psychotherapist, who has been treating Mr. P for anxiety and depression, recommended he be evaluated because of increased erratic behavior and paranoia. Mr. P reports that he has been feeling increasingly “anxious” and “paranoid” and thinks the security cameras at his college have been following him. He also describes an increased connection with God and hearing God’s voice as a commentary on his behaviors. Mr. P denies euphoria, depression, increased goal-directed activities, distractibility, increased impulsivity, or rapid speech. He is admitted voluntarily to the psychiatric unit for further evaluation.
During the hospitalization, Mr. P discloses that he has been viewing child pornography for 2 years, and during the past 6 months he has been distressed by the intensity of his sexual fantasies involving sexual contact with prepubescent girls. He also continues to experience paranoia and increased religiosity.
Mr. P says he began looking at pornography on the internet at age 14. He says he was watching “regular straight porn” and he would use it to masturbate and achieve orgasm. Mr. P began looking at child pornography at age 19. He stated that “regular porn” was no longer sufficiently arousing for him. Mr. P explains, “First, I started looking for 15- or 16-year-olds. They would work for a while [referring to sexual gratification], but then I would look for younger girls.” He says the images of younger girls are sexually arousing, typically “young girls, 8 to 10 years old” who are nude or involved in sex acts.
Mr. P denies sexual contact with prepubescent individuals and says his thoughts about such contact are “distressing.” He reports that he has viewed child pornography even when he wasn’t experiencing psychotic or mood symptoms. Mr. P’s outpatient psychotherapist reports that Mr. P first disclosed viewing child pornography and his attraction to prepubescent girls 2 years before this admission.
The authors’ observations
DSM-IV-TR diagnostic criteria for pedophilia (Table 1)1 are based on a history of sexual arousal to prepubescent individuals. A subset of sex offenders meet criteria for a paraphilia (Table 2),1 an axis I disorder, and a subset of sex offenders with paraphilia meet diagnostic criteria for pedophilia. Dunsieth et al2 found that among a sample of 113 male sex offenders, 74% had a diagnosable paraphilia, and 50% of individuals with paraphilia met criteria for pedophilia.
Table 1
DSM-IV-TR diagnostic criteria for pedophilia
| A) | Over a period of ≥6 months, recurrent, intense sexually arousing fantasies, sexual urges, or behaviors involving sexual activity with a prepubescent child or children (generally age ≤13) |
| B) | The person has acted on these sexual urges, or the sexual urges or fantasies cause marked distress or interpersonal difficulty |
| C) | The person is age ≥16 and ≥5 years older than the child or children in criterion A |
| Note: Do not include an individual in late adolescence involved in an ongoing sexual relationship with a 12- or 13-year-old | |
| Source: Reference 1 | |
DSM-IV-TR diagnostic criteria for a paraphilia
| The essential features of a paraphilia are recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving: | |
| A) | nonhuman objects, the suffering or humiliation of oneself or one’s partner, or children or other nonconsenting persons that occur over a period of ≥6 months |
| B) | The behavior, sexual urges, or fantasies cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 1 | |
Although most schizophrenia patients without a history of sexual offenses do not exhibit sexual deviancy, sexual content in hallucinations and delusions is common.6 Confusion about sexual identity and the boundaries of one’s body are common and may contribute to sexual deviancy.6 Psychiatric inpatients without a history of sexual offenses—including but not limited to psychotic patients—have higher rates of sexually deviant fantasies and behaviors compared with those without psychiatric illness.6 In one survey, 15% of men with schizophrenia displayed paraphilic behaviors and 20% had atypical sexual thoughts.7
Alish et al4 found that pedophilia was not necessarily linked to psychotic behavior or antisocial personality features when comparing pedophilia rates in individuals with or without schizophrenia. In a sample of 22 adolescent males who sexually molested a child at least once, axis I morbidity was common, and 55% met criteria for bipolar disorder.8
Few experts in paraphilias
A patient who endorses deviant sexual fantasies should be evaluated by a mental health professional with specialized training in paraphilias. Although paraphilias are not recognized as a subspecialty in psychiatry, diagnosing and treating patients with a paraphilia requires additional training. There is a scarcity of psychiatrists trained to evaluate and treat patients with paraphilias.
Sexual evaluation. Evaluating a patient who presents with problematic sexual behaviors includes performing a comprehensive psychiatric history with a focus on sexual history. A psychosexual history is distinct from general psychiatric evaluations because of the level of detail regarding a sexual history (Table 3). In addition to the clinical interview, objective testing to determine sexual interests may be useful in some patients (Table 4).9
Actuarial tools—risk assessment instruments based on statistically significant risk factors—are valid tools for determining the risk of sexual reoffending. There are several validated actuarial tools in the assessment of sex offender recidivism, such as the Static-99R,10 Stable-2007,11 and the Sex Offender Risk Appraisal Guide.12 However, these tools are used for sex offenders, and would not be used for individuals who have not committed a sex offense, such as Mr. P.
Table 3
Psychosexual evaluation
| Aspect of evaluation | Measures |
| Sexual behavior history | History of sexual abuse Childhood exposure to sex Masturbation history Preferred sexual partners Kinsey Scale |
| Sexual addiction or compulsion | Total Sexual Outlet measure Amount of time in sexual fantasy Financial, legal, or social cost of sexual behavior Prior treatment of sexual behavior |
| Sexual interests | Sex, age, and number of partner(s) Review of criteria for all paraphilias (exposing, voyeurism, cross-dressing, sadistic or masochistic interests) |
Objective testing to determine sexual interests
| Test | Results |
|---|---|
| Penile plethysmograph | Measures penis circumference with a mercury-in-rubber strain gauge. Used clinically by measuring circumferential changes in the penis while the patient is listening to audio or video stimuli of various sexual vignettes |
| Abel Assessment for Sexual Interests-3 | An objective method for evaluating deviant sexual interest uses noninvasive means to achieve objective measures of sexual interest. The subject’s visual response time is measured while viewing images of males and females of varying age. Visual reaction time is correlated with sexual interests |
| Source: Reference 9 | |
Medicolegal aspects of a psychosexual evaluation may include mandated reporting, confidentiality, and documentation. Mental health professionals are mandated to report to law enforcement or child welfare agencies when they observe or suspect physical, sexual, or other types of abuse in vulnerable populations such as children. In psychosexual evaluations, the evaluator is legally required to report if a patient discloses current sexual behavior with a child with a plan to continue to engage in the behavior. In Mr. P’s case, there was no duty to report because although he described viewing child pornography and had a sexual interest in prepubescent individuals, he did not report a history of engaging in handson sexual behaviors with children or impulses to do so. When an individual has engaged in sexual contact with a prepubescent individual, reporting is not mandated unless the individual continues to engage in sexual behavior with a minor. Mental health professionals are not responsible for calling the police or alerting authorities after a crime has been committed.
The relationship between viewing child pornography and pedophilia is unclear. Some child pornography viewers are pedophilic, others are sexually compulsive, and others are viewing out of curiosity and have no sexual deviance. Seto et al13 suggested that child pornography offenders show greater sexual arousal to children than to adults. Persistent child pornography use is a stronger diagnostic indicator of pedophilia than sexually offending against child victims.13 A clinician who learns that a patient is viewing child pornography should take a detailed sexual history, including a review of criteria for paraphilias. In addition, when appropriate, the clinician should perform a risk assessment to determine the patient’s risk of engaging in sexual offenses with children.
OUTCOME: Expert consultation
We start Mr. P on risperidone, 1 mg/d, to treat his paranoia and request a consultation with an expert in paraphilias to determine if Mr. P has a paraphilia and to discuss treatment options.
Mr. P’s initial diagnosis is psychotic disorder not otherwise specified. His viewing of child pornography and sexual interest in prepubescent individuals is not limited to his current mental status, and these interests persist in the absence of mood and psychotic states. Mr. P’s viewing of child pornography and sexual attraction to prepubescent girls meet the diagnostic criteria for pedophilia. During hospitalization, we educate Mr. P about his diagnoses and need for continued treatment. We refer him to a sexual disorders outpatient clinic, which continues to address his deviant sexual interests.
The authors’ observations
A meta-analysis indicates that a combination of pharmacologic and behavioral treatments coupled with close legal supervision seems to reduce the risk of repeated sexual offenses.14 Legal supervision is a general term to describe oversight of offenders in the community by supervisory boards, such as probation or parole, and tracking devices such as GPS. Currently, pedophilia treatment focuses on minimizing deviant sexual arousal through behavioral modification, cognitive-behavioral therapies, and testosterone-lowering medications, such as medroxyprogesterone or leuprolide. The decision to prescribe testosterone-lowering medication should be based on informed consent and the patient’s risk of dangerous sexual behaviors.
- Reijnen L, Bulten E, Nijman H. Demographic and personality characteristics of internet child pornography downloaders in comparison to other offenders. J Child Sex Abus. 2009;18(6):611-622.
- Hall RC, Hall RC. A profile of pedophilia: definition, characteristics of offenders, recidivism, treatment outcomes, and forensic issues. Mayo Clin Proc. 2007;82(4):457-471.
- Leuprolide • Eligard, Lupron
- Medroxyprogesterone • Cycrin, Provera
- Risperidone • Risperdal
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Dunsieth NW, Jr, Nelson EB, Brusman-Lovins LA, et al. Psychiatric and legal features of 113 men convicted of sexual offenses. J Clin Psychiatry. 2004;65(3):293-300.
3. Wallace C, Mullen P, Burgess P, et al. Serious criminal offending and mental disorder. Case linkage study. Br J Psychiatry. 1998;172:477-484.
4. Alish Y, Birger M, Manor N, et al. Schizophrenia sex offenders: a clinical and epidemiological comparison study. Int J Law Psychiatry. 2007;30(6):459-466.
5. Smith AD, Taylor PJ. Serious sex offending against women by men with schizophrenia. Relationship of illness and psychiatric symptoms to offending. Br J Psychiatry. 1999;174:233-237.
6. Drake CR, Pathé M. Understanding sexual offending in schizophrenia. Crim Behav Ment Health. 2004;14(2):108-120.
7. Harley EW, Boardman J, Craig T. Sexual problems in schizophrenia prevalence and characteristics: a cross sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):759-766.
8. Galli V, McElroy SL, Soutullo CA, et al. The psychiatric diagnoses of twenty-two adolescents who have sexually molested other children. Compr Psychiatry. 1999;40(2):85-88.
9. Abel GG, Jordan A, Hand CG, et al. Classification models of child molesters utilizing the Abel Assessment for sexual interest. Child Abuse Negl. 2001;25(5):703-718.
10. Hanson RK, Thornton D. Improving risk assessments for sex offenders: a comparison of three actuarial scales. Law Hum Behav. 2000;24(1):119-136.
11. Hanson RK, Harris AJ, Scott TL, et al. Assessing the risk of sexual offenders on community supervision: The Dynamic Supervision Project. Vol 5. Ottawa, Canada: Public Safety Canada; 2007.
12. Quinsey VL, Harris AJ, Rice ME, et al. Violent offenders: appraising and managing risk. 2nd ed. Washington DC: American Psychological Association; 2006.
13. Seto M, Cantor JM, Blanchard R. Child pornography offenses are a valid diagnostic indicator of pedophilia. J Abnorm Psychol. 2006;115(3):610-615.
14. Thibaut F, De La Barra F, Gordon H, et al. WFSBP Task Force on Sexual Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias. World J Biol Psychiatry. 2010;11(4):604-655.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Dunsieth NW, Jr, Nelson EB, Brusman-Lovins LA, et al. Psychiatric and legal features of 113 men convicted of sexual offenses. J Clin Psychiatry. 2004;65(3):293-300.
3. Wallace C, Mullen P, Burgess P, et al. Serious criminal offending and mental disorder. Case linkage study. Br J Psychiatry. 1998;172:477-484.
4. Alish Y, Birger M, Manor N, et al. Schizophrenia sex offenders: a clinical and epidemiological comparison study. Int J Law Psychiatry. 2007;30(6):459-466.
5. Smith AD, Taylor PJ. Serious sex offending against women by men with schizophrenia. Relationship of illness and psychiatric symptoms to offending. Br J Psychiatry. 1999;174:233-237.
6. Drake CR, Pathé M. Understanding sexual offending in schizophrenia. Crim Behav Ment Health. 2004;14(2):108-120.
7. Harley EW, Boardman J, Craig T. Sexual problems in schizophrenia prevalence and characteristics: a cross sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):759-766.
8. Galli V, McElroy SL, Soutullo CA, et al. The psychiatric diagnoses of twenty-two adolescents who have sexually molested other children. Compr Psychiatry. 1999;40(2):85-88.
9. Abel GG, Jordan A, Hand CG, et al. Classification models of child molesters utilizing the Abel Assessment for sexual interest. Child Abuse Negl. 2001;25(5):703-718.
10. Hanson RK, Thornton D. Improving risk assessments for sex offenders: a comparison of three actuarial scales. Law Hum Behav. 2000;24(1):119-136.
11. Hanson RK, Harris AJ, Scott TL, et al. Assessing the risk of sexual offenders on community supervision: The Dynamic Supervision Project. Vol 5. Ottawa, Canada: Public Safety Canada; 2007.
12. Quinsey VL, Harris AJ, Rice ME, et al. Violent offenders: appraising and managing risk. 2nd ed. Washington DC: American Psychological Association; 2006.
13. Seto M, Cantor JM, Blanchard R. Child pornography offenses are a valid diagnostic indicator of pedophilia. J Abnorm Psychol. 2006;115(3):610-615.
14. Thibaut F, De La Barra F, Gordon H, et al. WFSBP Task Force on Sexual Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias. World J Biol Psychiatry. 2010;11(4):604-655.
Suicide, depression, and CYP2D6: How are they linked?
Genetic variations in drug-metabolizing enzymes dramatically affect drug pharmacokinetics and can result in clinically relevant differences in drug efficacy or toxicity. Cytochrome P450 (CYP) enzymes such as CYP2D6 are involved in metabolism of antidepressants, including selective serotonin reuptake inhibitors (SSRIs), which often are a first-line choice for patients with major depressive disorder (MDD).1,2 CYP2D6 is a highly polymorphic gene with 75 allelic variants (CYP2D6*1 to *75) and >30 additional subvariants.3 These variants are associated with phenotypes where CYP2D6 activity is increased, reduced, or lost, which can increase the risk of adverse drug reactions, decrease efficacy, and possibly influence a patient’s suicide risk.
In this article, we review the pharmacogenetics of CYP2D6 and discuss a possible relationship between CYP2D6 genotype and suicidal events during antidepressant treatment for MDD.
CYP2D6: Many variants
CYP450 enzymes are a group of 57 proteins, each coded by a different gene. Five subfamilies in the CYP450 family metabolize most drugs: CYP1A2, CYP3A4, CYP2C19, CYP2E1, and CYP2D6.4
Researchers discovered CYP2D6 in studies of nonpsychotropics (Box).5-9 CYP2D6 is widely expressed in many tissues, with dominant expression in the liver. Although CYP2D6 accounts for 2% of the total CYP450 liver enzyme content, it mediates metabolism in 25% to 30% of drugs in common clinical use and has a major influence on the biotransformation of SSRIs (Table).10
I the late 1970s, 2 groups of researchers noted unexpected serious adverse reactions in studies of debrisoquine,5 a sympatholytic antihypertensive drug, and sparteine,6 an antiarrhythmic and oxytocic alkaloid drug. They observed that 5% to 10% of patients were unable to efficiently metabolize debrisoquine and sparteine and went on to define a genetic polymorphism responsible for these metabolic differences. They also observed that metabolism of antidepressants, antipsychotics, and beta blockers also was defective in these patients.
Further investigations established that the enzyme responsible for debrisoquine metabolism was a cytochrome P450 (CYP) enzyme that is now termed CYP2D6.7 In addition to biochemical evidence, the colocalization of sparteine oxidation deficiency and of the CYP2D6 locus at chromosome 22q13.1 confirmed CYP2D6 as the target gene of the debrisoquine/sparteine polymorphism.8,9
Table
CYP450 enzymes involved in biotransformation of SSRIs
| SSRI | Enzymes involved in biotransformation |
|---|---|
| Citalopram | CYP2C19, CYP2D6, CYP3A4 |
| Escitalopram | CYP2C19, CYP2D6, CYP3A4 |
| Fluoxetine | CYP2D6, CYP2C9, CYP2C19, CYP3A4 |
| Fluvoxamine | CYP1A2, CYP2D6 |
| Paroxetine | CYP2D6, CYP3A4 |
| Sertraline | CYP2C9, CYP2C19, CYP2D6, CYP3A4 |
| CYP: cytochrome P450; SSRI: selective serotonin reuptake inhibitors Source: Reference 10 | |
Approximately 100 polymorphic CYP2D6 alleles (variants) have been identified.3 These alleles are active, resulting in normal CYP2D6 enzyme activity, or inactive, leading to decreased enzyme activity. Genotyping for most common CYP2D6 alleles in ethnically defined populations can predict poor metabolizers (PMs), intermediate metabolizers (IMs), extensive metabolizers (EMs), and ultra-rapid metabolizers (UMs) with high accuracy.11 PMs are compound heterozygous for inactivating alleles or homozygous for an inactivating variant. IMs carry one functional allele and one nonfunctional allele but may demonstrate a range of enzyme activity levels. EMs have 2 functional gene copies and UMs have >2 functional genes from gene duplication, resulting in ultra-rapid metabolism.
Suicide and CYP2D6 status
The widespread use of antidepressants appears to have led to significant decline in suicide rates in many countries.12 Based on an investigation of suicide mortality in 27 countries from 1980 to 2000, Ludwig and Marcotte12 found that faster growth in SSRI sales per capita was associated with larger declines in suicide rates. This finding was not confounded by other suicide risk factors such as unemployment, sex, age, or divorce rate.12 Countries such as Germany, Austria, Estonia, Switzerland, Sweden, Denmark, Hungary, and Slovenia—which had the highest suicide rate in the world 20 years ago (20 to 46 per 100,000 per year)—have had impressive declines in suicide rates (24% to 57% in the last 2 decades) with a marked (6- to 8-fold) increase in SSRI prescriptions during the same period.13-15 On the other hand, a few countries, such as Portugal and Spain, have experienced dramatic increases (58% and 86%, respectively) in the suicide rate with a similar increase in SSRI prescribing during the same 20-year period.16
A review of the distribution of CYP2D6 genotype among countries indicates a south/north gradient of CYP2D6 gene duplications, which indicate UM status.16 The proportion of UMs increases by almost 2-fold in southern European countries (8.4% and 7% to 10% for Portugal and Spain, respectively) compared with northern European countries (1% to 2% and 3.6% for Sweden and Germany, respectively); this south/north trend extends to Africa.17 The prevalence of CYP2D6 UMs is lower in northern countries, where increased anti-depressant use appears to have reduced suicide rates, and higher in southern countries, where suicide rates increased despite higher antidepressant use.
Case reports and observational studies18-21 suggest that compared with other CYP2D6 phenotypes, UMs may need to take higher doses of antidepressants to achieve therapeutic response. In a case report, Bertilsson et al18 described 2 patients who were UMs and required high doses of nortriptyline and clomipramine to obtain appropriate plasma drug concentrations. Baumann et al19 described a depressed patient with CYP2D6 gene duplication who required higher-than-usual doses of clomipramine. Rau et al20 found a 3-fold increase in the frequency of UMs in a group of 16 depressed German patients who did not respond to SSRIs or serotonin–norepinephrine reuptake inhibitors, both of which are metabolized by CYP2D6. Kawanishi et al21 found a significantly greater prevalence of UMs among 81 Nordic patients who did not respond to SSRIs compared with the general population.
Because suicidality may be caused by inadequately treated depressive illness, MDD patients who are UMs may be more likely to commit suicide because of suboptimal antidepressant levels. In a 2010 Swedish study, Zackrisson et al22 found that compared with those who died of other causes, significantly more individuals who committed suicide had >2 active CYP2D6 genes. Stingl et al23 found that among 285 depressed German patients, UMs had an elevated risk of having a high suicidality score compared with individuals with other genotypes, after adjusting for sex, baseline score on the Hamilton Depression Rating Scale (after excluding item 3 for suicidality), and number of previous depressive episodes. Other researchers found that patients with eating disorders who are UMs have a greater risk of suicidal behavior.24 Although none of these 3 studies specified if these patients were treated with antidepressants, the association between CYP2D6 gene duplication and suicide risk suggests CYP2D6’s role in suicide risk might not be related solely to antidepressant metabolism.
Effects on serotonin, dopamine
CYP2D6 is expressed in the brain and localized primarily in large principle cells of the hippocampus and Purkinje cells of the cerebellum, with no expression in other brain regions such as glial cells.25 This heterogeneous expression among brain regions and cell types indicates that in addition to its role in metabolizing drugs, CYP2D6 might influence neurotransmitter levels. In vitro and in vivo animal studies suggest that CYP2D6 plays a role in biotransformation of serotonin and dopamine.26,27
Serotonin is likely to play a causal role in the pathophysiology of depression, and depressed patients have abnormalities in serotonin activity.28 Serotonin is generated primarily from the transformation of tryptophan by tryptophan decarboxylase and tryptamine 5-hydroxylase.29 Yu et al27 found that CYP2D6 may be an additional pathway to regenerate serotonin through O-demethylation from 5-methoxytryptamine, but it is unclear what proportion of the physiologic pool of serotonin in synaptic nerve terminals is generated through the CYP2D6 pathway. However, this discovery provides a mechanistic basis of CYP2D6 involvement in the endogenous serotonin balance and by extension, in serotonergic physiology and neuropsychiatric disorders such as depression.30 Because SSRIs target the serotonergic pathway, baseline levels of serotonin and all related components of this pathway—including CYP2D6—are likely to help determine a patient’s response to SSRIs.
Dopamine also is generated from tyramine through CYP2D6,31 and distribution of CYP2D6 in the brain follows that of dopamine nerve terminals.32 The serotonergic system has strong anatomical and functional interaction with the dopaminergic system,33 and imbalance between serotonin and dopamine activity is thought to give rise to behavioral changes,2 which play an important role in the development of anxiety and impulsivity.
CYP2D6 in clinical practice
Although research into a possible link between CYP2D6 status and suicide risk in depressed patients treated with antidepressants is ongoing, at present this connection is speculative. More studies are warranted to reveal the exact role of CYP2D6 in response to SSRI treatment and suicide risk.
Knowledge of this potential association can help clinicians keep CYP450 genotyping in mind when prescribing antidepressants to depressed patients. The FDA has approved a pharmacogenetic test to analyze polymorphisms of CYP2D6 and CYP2C19.34 The results of such testing might guide pharmacotherapy for depressed patients, including medication selection and dosing. For example, a patient who is a PM might be started at a lower antidepressant dosage to avoid potential adverse drug effects, whereas it might be appropriate to prescribe a higher starting dose for a UM patient to achieve an effective drug concentration.
Related Resources
- Peñas-Lledó EM, Blasco-Fontecilla H, Dorado P, et al. CYP2D6 and the severity of suicide attempts. Pharmacogenomics. 2012;13(2):179-184.
- Blasco-Fontecilla H, Peñas-Lledó E, Vaquero-Lorenzo C, et al. CYP2D6 polymorphism and mental and personality disorders in suicide attempters [published online February 11, 2013]. J Pers Disord. doi: 10.1521/pedi_2013_27_080.
Drug Brand Names
- Citalopram • Celexa
- Clomipramine • Anafranil
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors thank Marwah Shahid and Ijlal Yazdani for their assistance with this article.
1. Meyer UA, Amrein R, Balant LP, et al. Antidepressants and drug-metabolizing enzymes—expert group report. Acta Psychiatr Scand. 1996;93(2):71-79.
2. Kroemer HK, Eichelbaum M. “It’s the genes stupid”. Molecular bases and clinical consequences of genetic cytochrome P450 2D6 polymorphism. Life Sci. 1995;56(26):2285-2298.
3. The Human Cytochrome P450 (CYP) Allele Nomenclature Database. CYP2D6 allele nomenclature. http://www.cypalleles.ki.se/cyp2d6.htm. Accessed February 25, 2013.
4. Hemeryck A, Belpaire FM. Selective serotonin reuptake inhibitors and cytochrome P-450 mediated drug-drug interactions: an update. Curr Drug Metab. 2002;3(1):13-37.
5. Mahgoub A, Idle JR, Dring LG, et al. Polymorphic hydroxylation of debrisoquine in man. Lancet. 1977;2(8038):584-586.
6. Eichelbaum M, Spannbrucker N, Steincke B, et al. Defective N-oxidation of sparteine in man: a new pharmacogenetic defect. Eur J Clin Pharmacol. 1979;16(3):183-187.
7. Distlerath LM, Reilly PE, Martin MV, et al. Purification and characterization of the human liver cytochromes P-450 involved in debrisoquine 4-hydroxylation and phenacetin O-deethylation, two prototypes for genetic polymorphism in oxidative drug metabolism. J Biol Chem. 1985;260(15):9057-9067.
8. Eichelbaum M, Baur MP, Dengler HJ, et al. Chromosomal assignment of human cytochrome P-450 (debrisoquine/sparteine type) to chromosome 22. Br J Clin Pharmacol. 1987;23(4):455-458.
9. Gonzalez FJ, Vilbois F, Hardwick JP, et al. Human debrisoquine 4-hydroxylase (P450IID1): cDNA and deduced amino acid sequence and assignment of the CYP2D locus to chromosome 22. Geonomics. 1988;2(2):174-179.
10. Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008;30(7):1206-1227.
11. Roses AD. Pharmacogenetics and the practice of medicine. Nature. 2000;405(6788):857-865.
12. Ludwig J, Marcotte DE. Anti-depressants suicide, and drug regulation. J Policy Anal Manage. 2005;24(2):249-272.
13. Isacsson G. Suicide prevention—a medical breakthrough? Acta Psychiatr Scand. 2000;102(2):113-117.
14. Rihmer Z. Can better recognition and treatment of depression reduce suicide rates? A brief review. Eur Psychiatry. 2001;16(7):406-409.
15. Rihmer Z. Decreasing national suicide rates—fact or fiction? World J Biol Psychiatry. 2004;5(1):55-56.
16. Rihmer Z, Akiskal H. Do antidepressants t(h)reat(en) depressives? Toward a clinically judicious formulation of the antidepressant-suicidality FDA advisory in light of declining national suicide statistics from many countries. J Affect Disord. 2006;94(1-3):3-13.
17. Correia C, Santos P, Coutinho AM, et al. Characterization of pharmacogenetically relevant CYP2D6 and ABCB1 gene polymorphisms in a Portuguese population sample. Cell Biochem Funct. 2009;27(4):251-255.
18. Bertilsson L, Dahl ML, Sjöqvist F, et al. Molecular basis for rational megaprescribing in ultrarapid hydroxylators of debrisoquine. Lancet. 1993;341(8836):63.-
19. Baumann P, Broly F, Kosel M, et al. Ultrarapid metabolism of clomipramine in a therapy-resistant depressive patient, as confirmed by CYP2 D6 genotyping. Pharmacopsychiatry. 1998;31(2):72.-
20. Rau T, Wohlleben G, Wuttke H, et al. CYP2D6 genotype: impact on adverse effects and nonresponse during treatment with antidepressants-a pilot study. Clin Pharmacol Ther. 2004;75(5):386-393.
21. Kawanishi C, Lundgren S, Agren H, et al. Increased incidence of CYP2D6 gene duplication in patients with persistent mood disorders: ultrarapid metabolism of antidepressants as a cause of nonresponse. A pilot study. Eur J Clin Pharmacol. 2004;59(11):803-807.
22. Zackrisson AL, Lindblom B, Ahlner J. High frequency of occurrence of CYP2D6 gene duplication/multiduplication indicating ultrarapid metabolism among suicide cases. Clin Pharmacol Ther. 2010;88(3):354-359.
23. Stingl JC, Viviani R. CYP2D6 in the brain: impact on suicidality. Clin Pharmacol Ther. 2011;89(3):352-353.
24. Peñas-Lledó EM, Dorado P, Agüera Z, et al. High risk of lifetime history of suicide attempts among CYP2D6 ultrarapid metabolizers with eating disorders. Mol Psychiatry. 2011;16(7):691-692.
25. Siegle I, Fritz P, Eckhardt K, et al. Cellular localization and regional distribution of CYP2D6 mRNA and protein expression in human brain. Pharmacogenetics. 2001;11(3):237-245.
26. Eichelbaum M. In search of endogenous CYP2D6 substrates. Pharmacogenetics. 2003;13(6):305-306.
27. Yu AM, Idle JR, Gonzalez FJ. Polymorphic cytochrome P450 2D6: humanized mouse model and endogenous substrates. Drug Metab Rev. 2004;36(2):243-277.
28. Cowen PJ. Serotonin and depression: pathophysiological mechanism or marketing myth? Trends Pharmacol Sci. 2008;29(9):433-436.
29. Kang S, Kang K, Lee K, et al. Characterization of tryptamine 5-hydroxylase and serotonin synthesis in rice plants. Plant Cell Rep. 2007;26(11):2009-2015.
30. Yu AM, Idle JR, Herraiz T, et al. Screening for endogenous substrates reveals that CYP2D6 is a 5-methoxyindolethylamine O-demethylase. Pharmacogenetics. 2003;13(6):307-319.
31. Hiroi T, Imaoka S, Funae Y. Dopamine formation from tyramine by CYP2D6. Biochem Biophys Res Commun. 1998;249(3):838-843.
32. Niznik HB, Tyndale RF, Sallee FR, et al. The dopamine transporter and cytochrome P45OIID1 (debrisoquine 4-hydroxylase) in brain: resolution and identification of two distinct [3H]GBR-12935 binding proteins. Arch Biochem Biophys. 1990;276(2):424-432.
33. Kapur S, Remington G. Serotonin-dopamine interaction and its relevance to schizophrenia. Am J Psychiatry. 1996;153(4):466-476.
34. Jain KK. Applications of AmpliChip CYP450. Mol Diagn. 2005;9(3):119-127.
Genetic variations in drug-metabolizing enzymes dramatically affect drug pharmacokinetics and can result in clinically relevant differences in drug efficacy or toxicity. Cytochrome P450 (CYP) enzymes such as CYP2D6 are involved in metabolism of antidepressants, including selective serotonin reuptake inhibitors (SSRIs), which often are a first-line choice for patients with major depressive disorder (MDD).1,2 CYP2D6 is a highly polymorphic gene with 75 allelic variants (CYP2D6*1 to *75) and >30 additional subvariants.3 These variants are associated with phenotypes where CYP2D6 activity is increased, reduced, or lost, which can increase the risk of adverse drug reactions, decrease efficacy, and possibly influence a patient’s suicide risk.
In this article, we review the pharmacogenetics of CYP2D6 and discuss a possible relationship between CYP2D6 genotype and suicidal events during antidepressant treatment for MDD.
CYP2D6: Many variants
CYP450 enzymes are a group of 57 proteins, each coded by a different gene. Five subfamilies in the CYP450 family metabolize most drugs: CYP1A2, CYP3A4, CYP2C19, CYP2E1, and CYP2D6.4
Researchers discovered CYP2D6 in studies of nonpsychotropics (Box).5-9 CYP2D6 is widely expressed in many tissues, with dominant expression in the liver. Although CYP2D6 accounts for 2% of the total CYP450 liver enzyme content, it mediates metabolism in 25% to 30% of drugs in common clinical use and has a major influence on the biotransformation of SSRIs (Table).10
I the late 1970s, 2 groups of researchers noted unexpected serious adverse reactions in studies of debrisoquine,5 a sympatholytic antihypertensive drug, and sparteine,6 an antiarrhythmic and oxytocic alkaloid drug. They observed that 5% to 10% of patients were unable to efficiently metabolize debrisoquine and sparteine and went on to define a genetic polymorphism responsible for these metabolic differences. They also observed that metabolism of antidepressants, antipsychotics, and beta blockers also was defective in these patients.
Further investigations established that the enzyme responsible for debrisoquine metabolism was a cytochrome P450 (CYP) enzyme that is now termed CYP2D6.7 In addition to biochemical evidence, the colocalization of sparteine oxidation deficiency and of the CYP2D6 locus at chromosome 22q13.1 confirmed CYP2D6 as the target gene of the debrisoquine/sparteine polymorphism.8,9
Table
CYP450 enzymes involved in biotransformation of SSRIs
| SSRI | Enzymes involved in biotransformation |
|---|---|
| Citalopram | CYP2C19, CYP2D6, CYP3A4 |
| Escitalopram | CYP2C19, CYP2D6, CYP3A4 |
| Fluoxetine | CYP2D6, CYP2C9, CYP2C19, CYP3A4 |
| Fluvoxamine | CYP1A2, CYP2D6 |
| Paroxetine | CYP2D6, CYP3A4 |
| Sertraline | CYP2C9, CYP2C19, CYP2D6, CYP3A4 |
| CYP: cytochrome P450; SSRI: selective serotonin reuptake inhibitors Source: Reference 10 | |
Approximately 100 polymorphic CYP2D6 alleles (variants) have been identified.3 These alleles are active, resulting in normal CYP2D6 enzyme activity, or inactive, leading to decreased enzyme activity. Genotyping for most common CYP2D6 alleles in ethnically defined populations can predict poor metabolizers (PMs), intermediate metabolizers (IMs), extensive metabolizers (EMs), and ultra-rapid metabolizers (UMs) with high accuracy.11 PMs are compound heterozygous for inactivating alleles or homozygous for an inactivating variant. IMs carry one functional allele and one nonfunctional allele but may demonstrate a range of enzyme activity levels. EMs have 2 functional gene copies and UMs have >2 functional genes from gene duplication, resulting in ultra-rapid metabolism.
Suicide and CYP2D6 status
The widespread use of antidepressants appears to have led to significant decline in suicide rates in many countries.12 Based on an investigation of suicide mortality in 27 countries from 1980 to 2000, Ludwig and Marcotte12 found that faster growth in SSRI sales per capita was associated with larger declines in suicide rates. This finding was not confounded by other suicide risk factors such as unemployment, sex, age, or divorce rate.12 Countries such as Germany, Austria, Estonia, Switzerland, Sweden, Denmark, Hungary, and Slovenia—which had the highest suicide rate in the world 20 years ago (20 to 46 per 100,000 per year)—have had impressive declines in suicide rates (24% to 57% in the last 2 decades) with a marked (6- to 8-fold) increase in SSRI prescriptions during the same period.13-15 On the other hand, a few countries, such as Portugal and Spain, have experienced dramatic increases (58% and 86%, respectively) in the suicide rate with a similar increase in SSRI prescribing during the same 20-year period.16
A review of the distribution of CYP2D6 genotype among countries indicates a south/north gradient of CYP2D6 gene duplications, which indicate UM status.16 The proportion of UMs increases by almost 2-fold in southern European countries (8.4% and 7% to 10% for Portugal and Spain, respectively) compared with northern European countries (1% to 2% and 3.6% for Sweden and Germany, respectively); this south/north trend extends to Africa.17 The prevalence of CYP2D6 UMs is lower in northern countries, where increased anti-depressant use appears to have reduced suicide rates, and higher in southern countries, where suicide rates increased despite higher antidepressant use.
Case reports and observational studies18-21 suggest that compared with other CYP2D6 phenotypes, UMs may need to take higher doses of antidepressants to achieve therapeutic response. In a case report, Bertilsson et al18 described 2 patients who were UMs and required high doses of nortriptyline and clomipramine to obtain appropriate plasma drug concentrations. Baumann et al19 described a depressed patient with CYP2D6 gene duplication who required higher-than-usual doses of clomipramine. Rau et al20 found a 3-fold increase in the frequency of UMs in a group of 16 depressed German patients who did not respond to SSRIs or serotonin–norepinephrine reuptake inhibitors, both of which are metabolized by CYP2D6. Kawanishi et al21 found a significantly greater prevalence of UMs among 81 Nordic patients who did not respond to SSRIs compared with the general population.
Because suicidality may be caused by inadequately treated depressive illness, MDD patients who are UMs may be more likely to commit suicide because of suboptimal antidepressant levels. In a 2010 Swedish study, Zackrisson et al22 found that compared with those who died of other causes, significantly more individuals who committed suicide had >2 active CYP2D6 genes. Stingl et al23 found that among 285 depressed German patients, UMs had an elevated risk of having a high suicidality score compared with individuals with other genotypes, after adjusting for sex, baseline score on the Hamilton Depression Rating Scale (after excluding item 3 for suicidality), and number of previous depressive episodes. Other researchers found that patients with eating disorders who are UMs have a greater risk of suicidal behavior.24 Although none of these 3 studies specified if these patients were treated with antidepressants, the association between CYP2D6 gene duplication and suicide risk suggests CYP2D6’s role in suicide risk might not be related solely to antidepressant metabolism.
Effects on serotonin, dopamine
CYP2D6 is expressed in the brain and localized primarily in large principle cells of the hippocampus and Purkinje cells of the cerebellum, with no expression in other brain regions such as glial cells.25 This heterogeneous expression among brain regions and cell types indicates that in addition to its role in metabolizing drugs, CYP2D6 might influence neurotransmitter levels. In vitro and in vivo animal studies suggest that CYP2D6 plays a role in biotransformation of serotonin and dopamine.26,27
Serotonin is likely to play a causal role in the pathophysiology of depression, and depressed patients have abnormalities in serotonin activity.28 Serotonin is generated primarily from the transformation of tryptophan by tryptophan decarboxylase and tryptamine 5-hydroxylase.29 Yu et al27 found that CYP2D6 may be an additional pathway to regenerate serotonin through O-demethylation from 5-methoxytryptamine, but it is unclear what proportion of the physiologic pool of serotonin in synaptic nerve terminals is generated through the CYP2D6 pathway. However, this discovery provides a mechanistic basis of CYP2D6 involvement in the endogenous serotonin balance and by extension, in serotonergic physiology and neuropsychiatric disorders such as depression.30 Because SSRIs target the serotonergic pathway, baseline levels of serotonin and all related components of this pathway—including CYP2D6—are likely to help determine a patient’s response to SSRIs.
Dopamine also is generated from tyramine through CYP2D6,31 and distribution of CYP2D6 in the brain follows that of dopamine nerve terminals.32 The serotonergic system has strong anatomical and functional interaction with the dopaminergic system,33 and imbalance between serotonin and dopamine activity is thought to give rise to behavioral changes,2 which play an important role in the development of anxiety and impulsivity.
CYP2D6 in clinical practice
Although research into a possible link between CYP2D6 status and suicide risk in depressed patients treated with antidepressants is ongoing, at present this connection is speculative. More studies are warranted to reveal the exact role of CYP2D6 in response to SSRI treatment and suicide risk.
Knowledge of this potential association can help clinicians keep CYP450 genotyping in mind when prescribing antidepressants to depressed patients. The FDA has approved a pharmacogenetic test to analyze polymorphisms of CYP2D6 and CYP2C19.34 The results of such testing might guide pharmacotherapy for depressed patients, including medication selection and dosing. For example, a patient who is a PM might be started at a lower antidepressant dosage to avoid potential adverse drug effects, whereas it might be appropriate to prescribe a higher starting dose for a UM patient to achieve an effective drug concentration.
Related Resources
- Peñas-Lledó EM, Blasco-Fontecilla H, Dorado P, et al. CYP2D6 and the severity of suicide attempts. Pharmacogenomics. 2012;13(2):179-184.
- Blasco-Fontecilla H, Peñas-Lledó E, Vaquero-Lorenzo C, et al. CYP2D6 polymorphism and mental and personality disorders in suicide attempters [published online February 11, 2013]. J Pers Disord. doi: 10.1521/pedi_2013_27_080.
Drug Brand Names
- Citalopram • Celexa
- Clomipramine • Anafranil
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors thank Marwah Shahid and Ijlal Yazdani for their assistance with this article.
Genetic variations in drug-metabolizing enzymes dramatically affect drug pharmacokinetics and can result in clinically relevant differences in drug efficacy or toxicity. Cytochrome P450 (CYP) enzymes such as CYP2D6 are involved in metabolism of antidepressants, including selective serotonin reuptake inhibitors (SSRIs), which often are a first-line choice for patients with major depressive disorder (MDD).1,2 CYP2D6 is a highly polymorphic gene with 75 allelic variants (CYP2D6*1 to *75) and >30 additional subvariants.3 These variants are associated with phenotypes where CYP2D6 activity is increased, reduced, or lost, which can increase the risk of adverse drug reactions, decrease efficacy, and possibly influence a patient’s suicide risk.
In this article, we review the pharmacogenetics of CYP2D6 and discuss a possible relationship between CYP2D6 genotype and suicidal events during antidepressant treatment for MDD.
CYP2D6: Many variants
CYP450 enzymes are a group of 57 proteins, each coded by a different gene. Five subfamilies in the CYP450 family metabolize most drugs: CYP1A2, CYP3A4, CYP2C19, CYP2E1, and CYP2D6.4
Researchers discovered CYP2D6 in studies of nonpsychotropics (Box).5-9 CYP2D6 is widely expressed in many tissues, with dominant expression in the liver. Although CYP2D6 accounts for 2% of the total CYP450 liver enzyme content, it mediates metabolism in 25% to 30% of drugs in common clinical use and has a major influence on the biotransformation of SSRIs (Table).10
I the late 1970s, 2 groups of researchers noted unexpected serious adverse reactions in studies of debrisoquine,5 a sympatholytic antihypertensive drug, and sparteine,6 an antiarrhythmic and oxytocic alkaloid drug. They observed that 5% to 10% of patients were unable to efficiently metabolize debrisoquine and sparteine and went on to define a genetic polymorphism responsible for these metabolic differences. They also observed that metabolism of antidepressants, antipsychotics, and beta blockers also was defective in these patients.
Further investigations established that the enzyme responsible for debrisoquine metabolism was a cytochrome P450 (CYP) enzyme that is now termed CYP2D6.7 In addition to biochemical evidence, the colocalization of sparteine oxidation deficiency and of the CYP2D6 locus at chromosome 22q13.1 confirmed CYP2D6 as the target gene of the debrisoquine/sparteine polymorphism.8,9
Table
CYP450 enzymes involved in biotransformation of SSRIs
| SSRI | Enzymes involved in biotransformation |
|---|---|
| Citalopram | CYP2C19, CYP2D6, CYP3A4 |
| Escitalopram | CYP2C19, CYP2D6, CYP3A4 |
| Fluoxetine | CYP2D6, CYP2C9, CYP2C19, CYP3A4 |
| Fluvoxamine | CYP1A2, CYP2D6 |
| Paroxetine | CYP2D6, CYP3A4 |
| Sertraline | CYP2C9, CYP2C19, CYP2D6, CYP3A4 |
| CYP: cytochrome P450; SSRI: selective serotonin reuptake inhibitors Source: Reference 10 | |
Approximately 100 polymorphic CYP2D6 alleles (variants) have been identified.3 These alleles are active, resulting in normal CYP2D6 enzyme activity, or inactive, leading to decreased enzyme activity. Genotyping for most common CYP2D6 alleles in ethnically defined populations can predict poor metabolizers (PMs), intermediate metabolizers (IMs), extensive metabolizers (EMs), and ultra-rapid metabolizers (UMs) with high accuracy.11 PMs are compound heterozygous for inactivating alleles or homozygous for an inactivating variant. IMs carry one functional allele and one nonfunctional allele but may demonstrate a range of enzyme activity levels. EMs have 2 functional gene copies and UMs have >2 functional genes from gene duplication, resulting in ultra-rapid metabolism.
Suicide and CYP2D6 status
The widespread use of antidepressants appears to have led to significant decline in suicide rates in many countries.12 Based on an investigation of suicide mortality in 27 countries from 1980 to 2000, Ludwig and Marcotte12 found that faster growth in SSRI sales per capita was associated with larger declines in suicide rates. This finding was not confounded by other suicide risk factors such as unemployment, sex, age, or divorce rate.12 Countries such as Germany, Austria, Estonia, Switzerland, Sweden, Denmark, Hungary, and Slovenia—which had the highest suicide rate in the world 20 years ago (20 to 46 per 100,000 per year)—have had impressive declines in suicide rates (24% to 57% in the last 2 decades) with a marked (6- to 8-fold) increase in SSRI prescriptions during the same period.13-15 On the other hand, a few countries, such as Portugal and Spain, have experienced dramatic increases (58% and 86%, respectively) in the suicide rate with a similar increase in SSRI prescribing during the same 20-year period.16
A review of the distribution of CYP2D6 genotype among countries indicates a south/north gradient of CYP2D6 gene duplications, which indicate UM status.16 The proportion of UMs increases by almost 2-fold in southern European countries (8.4% and 7% to 10% for Portugal and Spain, respectively) compared with northern European countries (1% to 2% and 3.6% for Sweden and Germany, respectively); this south/north trend extends to Africa.17 The prevalence of CYP2D6 UMs is lower in northern countries, where increased anti-depressant use appears to have reduced suicide rates, and higher in southern countries, where suicide rates increased despite higher antidepressant use.
Case reports and observational studies18-21 suggest that compared with other CYP2D6 phenotypes, UMs may need to take higher doses of antidepressants to achieve therapeutic response. In a case report, Bertilsson et al18 described 2 patients who were UMs and required high doses of nortriptyline and clomipramine to obtain appropriate plasma drug concentrations. Baumann et al19 described a depressed patient with CYP2D6 gene duplication who required higher-than-usual doses of clomipramine. Rau et al20 found a 3-fold increase in the frequency of UMs in a group of 16 depressed German patients who did not respond to SSRIs or serotonin–norepinephrine reuptake inhibitors, both of which are metabolized by CYP2D6. Kawanishi et al21 found a significantly greater prevalence of UMs among 81 Nordic patients who did not respond to SSRIs compared with the general population.
Because suicidality may be caused by inadequately treated depressive illness, MDD patients who are UMs may be more likely to commit suicide because of suboptimal antidepressant levels. In a 2010 Swedish study, Zackrisson et al22 found that compared with those who died of other causes, significantly more individuals who committed suicide had >2 active CYP2D6 genes. Stingl et al23 found that among 285 depressed German patients, UMs had an elevated risk of having a high suicidality score compared with individuals with other genotypes, after adjusting for sex, baseline score on the Hamilton Depression Rating Scale (after excluding item 3 for suicidality), and number of previous depressive episodes. Other researchers found that patients with eating disorders who are UMs have a greater risk of suicidal behavior.24 Although none of these 3 studies specified if these patients were treated with antidepressants, the association between CYP2D6 gene duplication and suicide risk suggests CYP2D6’s role in suicide risk might not be related solely to antidepressant metabolism.
Effects on serotonin, dopamine
CYP2D6 is expressed in the brain and localized primarily in large principle cells of the hippocampus and Purkinje cells of the cerebellum, with no expression in other brain regions such as glial cells.25 This heterogeneous expression among brain regions and cell types indicates that in addition to its role in metabolizing drugs, CYP2D6 might influence neurotransmitter levels. In vitro and in vivo animal studies suggest that CYP2D6 plays a role in biotransformation of serotonin and dopamine.26,27
Serotonin is likely to play a causal role in the pathophysiology of depression, and depressed patients have abnormalities in serotonin activity.28 Serotonin is generated primarily from the transformation of tryptophan by tryptophan decarboxylase and tryptamine 5-hydroxylase.29 Yu et al27 found that CYP2D6 may be an additional pathway to regenerate serotonin through O-demethylation from 5-methoxytryptamine, but it is unclear what proportion of the physiologic pool of serotonin in synaptic nerve terminals is generated through the CYP2D6 pathway. However, this discovery provides a mechanistic basis of CYP2D6 involvement in the endogenous serotonin balance and by extension, in serotonergic physiology and neuropsychiatric disorders such as depression.30 Because SSRIs target the serotonergic pathway, baseline levels of serotonin and all related components of this pathway—including CYP2D6—are likely to help determine a patient’s response to SSRIs.
Dopamine also is generated from tyramine through CYP2D6,31 and distribution of CYP2D6 in the brain follows that of dopamine nerve terminals.32 The serotonergic system has strong anatomical and functional interaction with the dopaminergic system,33 and imbalance between serotonin and dopamine activity is thought to give rise to behavioral changes,2 which play an important role in the development of anxiety and impulsivity.
CYP2D6 in clinical practice
Although research into a possible link between CYP2D6 status and suicide risk in depressed patients treated with antidepressants is ongoing, at present this connection is speculative. More studies are warranted to reveal the exact role of CYP2D6 in response to SSRI treatment and suicide risk.
Knowledge of this potential association can help clinicians keep CYP450 genotyping in mind when prescribing antidepressants to depressed patients. The FDA has approved a pharmacogenetic test to analyze polymorphisms of CYP2D6 and CYP2C19.34 The results of such testing might guide pharmacotherapy for depressed patients, including medication selection and dosing. For example, a patient who is a PM might be started at a lower antidepressant dosage to avoid potential adverse drug effects, whereas it might be appropriate to prescribe a higher starting dose for a UM patient to achieve an effective drug concentration.
Related Resources
- Peñas-Lledó EM, Blasco-Fontecilla H, Dorado P, et al. CYP2D6 and the severity of suicide attempts. Pharmacogenomics. 2012;13(2):179-184.
- Blasco-Fontecilla H, Peñas-Lledó E, Vaquero-Lorenzo C, et al. CYP2D6 polymorphism and mental and personality disorders in suicide attempters [published online February 11, 2013]. J Pers Disord. doi: 10.1521/pedi_2013_27_080.
Drug Brand Names
- Citalopram • Celexa
- Clomipramine • Anafranil
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors thank Marwah Shahid and Ijlal Yazdani for their assistance with this article.
1. Meyer UA, Amrein R, Balant LP, et al. Antidepressants and drug-metabolizing enzymes—expert group report. Acta Psychiatr Scand. 1996;93(2):71-79.
2. Kroemer HK, Eichelbaum M. “It’s the genes stupid”. Molecular bases and clinical consequences of genetic cytochrome P450 2D6 polymorphism. Life Sci. 1995;56(26):2285-2298.
3. The Human Cytochrome P450 (CYP) Allele Nomenclature Database. CYP2D6 allele nomenclature. http://www.cypalleles.ki.se/cyp2d6.htm. Accessed February 25, 2013.
4. Hemeryck A, Belpaire FM. Selective serotonin reuptake inhibitors and cytochrome P-450 mediated drug-drug interactions: an update. Curr Drug Metab. 2002;3(1):13-37.
5. Mahgoub A, Idle JR, Dring LG, et al. Polymorphic hydroxylation of debrisoquine in man. Lancet. 1977;2(8038):584-586.
6. Eichelbaum M, Spannbrucker N, Steincke B, et al. Defective N-oxidation of sparteine in man: a new pharmacogenetic defect. Eur J Clin Pharmacol. 1979;16(3):183-187.
7. Distlerath LM, Reilly PE, Martin MV, et al. Purification and characterization of the human liver cytochromes P-450 involved in debrisoquine 4-hydroxylation and phenacetin O-deethylation, two prototypes for genetic polymorphism in oxidative drug metabolism. J Biol Chem. 1985;260(15):9057-9067.
8. Eichelbaum M, Baur MP, Dengler HJ, et al. Chromosomal assignment of human cytochrome P-450 (debrisoquine/sparteine type) to chromosome 22. Br J Clin Pharmacol. 1987;23(4):455-458.
9. Gonzalez FJ, Vilbois F, Hardwick JP, et al. Human debrisoquine 4-hydroxylase (P450IID1): cDNA and deduced amino acid sequence and assignment of the CYP2D locus to chromosome 22. Geonomics. 1988;2(2):174-179.
10. Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008;30(7):1206-1227.
11. Roses AD. Pharmacogenetics and the practice of medicine. Nature. 2000;405(6788):857-865.
12. Ludwig J, Marcotte DE. Anti-depressants suicide, and drug regulation. J Policy Anal Manage. 2005;24(2):249-272.
13. Isacsson G. Suicide prevention—a medical breakthrough? Acta Psychiatr Scand. 2000;102(2):113-117.
14. Rihmer Z. Can better recognition and treatment of depression reduce suicide rates? A brief review. Eur Psychiatry. 2001;16(7):406-409.
15. Rihmer Z. Decreasing national suicide rates—fact or fiction? World J Biol Psychiatry. 2004;5(1):55-56.
16. Rihmer Z, Akiskal H. Do antidepressants t(h)reat(en) depressives? Toward a clinically judicious formulation of the antidepressant-suicidality FDA advisory in light of declining national suicide statistics from many countries. J Affect Disord. 2006;94(1-3):3-13.
17. Correia C, Santos P, Coutinho AM, et al. Characterization of pharmacogenetically relevant CYP2D6 and ABCB1 gene polymorphisms in a Portuguese population sample. Cell Biochem Funct. 2009;27(4):251-255.
18. Bertilsson L, Dahl ML, Sjöqvist F, et al. Molecular basis for rational megaprescribing in ultrarapid hydroxylators of debrisoquine. Lancet. 1993;341(8836):63.-
19. Baumann P, Broly F, Kosel M, et al. Ultrarapid metabolism of clomipramine in a therapy-resistant depressive patient, as confirmed by CYP2 D6 genotyping. Pharmacopsychiatry. 1998;31(2):72.-
20. Rau T, Wohlleben G, Wuttke H, et al. CYP2D6 genotype: impact on adverse effects and nonresponse during treatment with antidepressants-a pilot study. Clin Pharmacol Ther. 2004;75(5):386-393.
21. Kawanishi C, Lundgren S, Agren H, et al. Increased incidence of CYP2D6 gene duplication in patients with persistent mood disorders: ultrarapid metabolism of antidepressants as a cause of nonresponse. A pilot study. Eur J Clin Pharmacol. 2004;59(11):803-807.
22. Zackrisson AL, Lindblom B, Ahlner J. High frequency of occurrence of CYP2D6 gene duplication/multiduplication indicating ultrarapid metabolism among suicide cases. Clin Pharmacol Ther. 2010;88(3):354-359.
23. Stingl JC, Viviani R. CYP2D6 in the brain: impact on suicidality. Clin Pharmacol Ther. 2011;89(3):352-353.
24. Peñas-Lledó EM, Dorado P, Agüera Z, et al. High risk of lifetime history of suicide attempts among CYP2D6 ultrarapid metabolizers with eating disorders. Mol Psychiatry. 2011;16(7):691-692.
25. Siegle I, Fritz P, Eckhardt K, et al. Cellular localization and regional distribution of CYP2D6 mRNA and protein expression in human brain. Pharmacogenetics. 2001;11(3):237-245.
26. Eichelbaum M. In search of endogenous CYP2D6 substrates. Pharmacogenetics. 2003;13(6):305-306.
27. Yu AM, Idle JR, Gonzalez FJ. Polymorphic cytochrome P450 2D6: humanized mouse model and endogenous substrates. Drug Metab Rev. 2004;36(2):243-277.
28. Cowen PJ. Serotonin and depression: pathophysiological mechanism or marketing myth? Trends Pharmacol Sci. 2008;29(9):433-436.
29. Kang S, Kang K, Lee K, et al. Characterization of tryptamine 5-hydroxylase and serotonin synthesis in rice plants. Plant Cell Rep. 2007;26(11):2009-2015.
30. Yu AM, Idle JR, Herraiz T, et al. Screening for endogenous substrates reveals that CYP2D6 is a 5-methoxyindolethylamine O-demethylase. Pharmacogenetics. 2003;13(6):307-319.
31. Hiroi T, Imaoka S, Funae Y. Dopamine formation from tyramine by CYP2D6. Biochem Biophys Res Commun. 1998;249(3):838-843.
32. Niznik HB, Tyndale RF, Sallee FR, et al. The dopamine transporter and cytochrome P45OIID1 (debrisoquine 4-hydroxylase) in brain: resolution and identification of two distinct [3H]GBR-12935 binding proteins. Arch Biochem Biophys. 1990;276(2):424-432.
33. Kapur S, Remington G. Serotonin-dopamine interaction and its relevance to schizophrenia. Am J Psychiatry. 1996;153(4):466-476.
34. Jain KK. Applications of AmpliChip CYP450. Mol Diagn. 2005;9(3):119-127.
1. Meyer UA, Amrein R, Balant LP, et al. Antidepressants and drug-metabolizing enzymes—expert group report. Acta Psychiatr Scand. 1996;93(2):71-79.
2. Kroemer HK, Eichelbaum M. “It’s the genes stupid”. Molecular bases and clinical consequences of genetic cytochrome P450 2D6 polymorphism. Life Sci. 1995;56(26):2285-2298.
3. The Human Cytochrome P450 (CYP) Allele Nomenclature Database. CYP2D6 allele nomenclature. http://www.cypalleles.ki.se/cyp2d6.htm. Accessed February 25, 2013.
4. Hemeryck A, Belpaire FM. Selective serotonin reuptake inhibitors and cytochrome P-450 mediated drug-drug interactions: an update. Curr Drug Metab. 2002;3(1):13-37.
5. Mahgoub A, Idle JR, Dring LG, et al. Polymorphic hydroxylation of debrisoquine in man. Lancet. 1977;2(8038):584-586.
6. Eichelbaum M, Spannbrucker N, Steincke B, et al. Defective N-oxidation of sparteine in man: a new pharmacogenetic defect. Eur J Clin Pharmacol. 1979;16(3):183-187.
7. Distlerath LM, Reilly PE, Martin MV, et al. Purification and characterization of the human liver cytochromes P-450 involved in debrisoquine 4-hydroxylation and phenacetin O-deethylation, two prototypes for genetic polymorphism in oxidative drug metabolism. J Biol Chem. 1985;260(15):9057-9067.
8. Eichelbaum M, Baur MP, Dengler HJ, et al. Chromosomal assignment of human cytochrome P-450 (debrisoquine/sparteine type) to chromosome 22. Br J Clin Pharmacol. 1987;23(4):455-458.
9. Gonzalez FJ, Vilbois F, Hardwick JP, et al. Human debrisoquine 4-hydroxylase (P450IID1): cDNA and deduced amino acid sequence and assignment of the CYP2D locus to chromosome 22. Geonomics. 1988;2(2):174-179.
10. Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008;30(7):1206-1227.
11. Roses AD. Pharmacogenetics and the practice of medicine. Nature. 2000;405(6788):857-865.
12. Ludwig J, Marcotte DE. Anti-depressants suicide, and drug regulation. J Policy Anal Manage. 2005;24(2):249-272.
13. Isacsson G. Suicide prevention—a medical breakthrough? Acta Psychiatr Scand. 2000;102(2):113-117.
14. Rihmer Z. Can better recognition and treatment of depression reduce suicide rates? A brief review. Eur Psychiatry. 2001;16(7):406-409.
15. Rihmer Z. Decreasing national suicide rates—fact or fiction? World J Biol Psychiatry. 2004;5(1):55-56.
16. Rihmer Z, Akiskal H. Do antidepressants t(h)reat(en) depressives? Toward a clinically judicious formulation of the antidepressant-suicidality FDA advisory in light of declining national suicide statistics from many countries. J Affect Disord. 2006;94(1-3):3-13.
17. Correia C, Santos P, Coutinho AM, et al. Characterization of pharmacogenetically relevant CYP2D6 and ABCB1 gene polymorphisms in a Portuguese population sample. Cell Biochem Funct. 2009;27(4):251-255.
18. Bertilsson L, Dahl ML, Sjöqvist F, et al. Molecular basis for rational megaprescribing in ultrarapid hydroxylators of debrisoquine. Lancet. 1993;341(8836):63.-
19. Baumann P, Broly F, Kosel M, et al. Ultrarapid metabolism of clomipramine in a therapy-resistant depressive patient, as confirmed by CYP2 D6 genotyping. Pharmacopsychiatry. 1998;31(2):72.-
20. Rau T, Wohlleben G, Wuttke H, et al. CYP2D6 genotype: impact on adverse effects and nonresponse during treatment with antidepressants-a pilot study. Clin Pharmacol Ther. 2004;75(5):386-393.
21. Kawanishi C, Lundgren S, Agren H, et al. Increased incidence of CYP2D6 gene duplication in patients with persistent mood disorders: ultrarapid metabolism of antidepressants as a cause of nonresponse. A pilot study. Eur J Clin Pharmacol. 2004;59(11):803-807.
22. Zackrisson AL, Lindblom B, Ahlner J. High frequency of occurrence of CYP2D6 gene duplication/multiduplication indicating ultrarapid metabolism among suicide cases. Clin Pharmacol Ther. 2010;88(3):354-359.
23. Stingl JC, Viviani R. CYP2D6 in the brain: impact on suicidality. Clin Pharmacol Ther. 2011;89(3):352-353.
24. Peñas-Lledó EM, Dorado P, Agüera Z, et al. High risk of lifetime history of suicide attempts among CYP2D6 ultrarapid metabolizers with eating disorders. Mol Psychiatry. 2011;16(7):691-692.
25. Siegle I, Fritz P, Eckhardt K, et al. Cellular localization and regional distribution of CYP2D6 mRNA and protein expression in human brain. Pharmacogenetics. 2001;11(3):237-245.
26. Eichelbaum M. In search of endogenous CYP2D6 substrates. Pharmacogenetics. 2003;13(6):305-306.
27. Yu AM, Idle JR, Gonzalez FJ. Polymorphic cytochrome P450 2D6: humanized mouse model and endogenous substrates. Drug Metab Rev. 2004;36(2):243-277.
28. Cowen PJ. Serotonin and depression: pathophysiological mechanism or marketing myth? Trends Pharmacol Sci. 2008;29(9):433-436.
29. Kang S, Kang K, Lee K, et al. Characterization of tryptamine 5-hydroxylase and serotonin synthesis in rice plants. Plant Cell Rep. 2007;26(11):2009-2015.
30. Yu AM, Idle JR, Herraiz T, et al. Screening for endogenous substrates reveals that CYP2D6 is a 5-methoxyindolethylamine O-demethylase. Pharmacogenetics. 2003;13(6):307-319.
31. Hiroi T, Imaoka S, Funae Y. Dopamine formation from tyramine by CYP2D6. Biochem Biophys Res Commun. 1998;249(3):838-843.
32. Niznik HB, Tyndale RF, Sallee FR, et al. The dopamine transporter and cytochrome P45OIID1 (debrisoquine 4-hydroxylase) in brain: resolution and identification of two distinct [3H]GBR-12935 binding proteins. Arch Biochem Biophys. 1990;276(2):424-432.
33. Kapur S, Remington G. Serotonin-dopamine interaction and its relevance to schizophrenia. Am J Psychiatry. 1996;153(4):466-476.
34. Jain KK. Applications of AmpliChip CYP450. Mol Diagn. 2005;9(3):119-127.
PSYCHIATRY UPDATE 2013
Current Psychiatry and the American Academy of Clinical Psychiatrists were pleased to host more than 550 psychiatric practitioners for this conference, led by Meeting Chair Richard Balon, MD, and Meeting Co-Chairs Donald W. Black, MD, and Nagy Youssef, MD, April 4-6, 2013 at the Swissôtel in Chicago, IL. Attendees could earn up to 18 AMA PRA Category 1 Credits™.
THURSDAY, APRIL 4, 2013
MORNING SESSIONS
Evidence-based medicine and treatment guidelines may not address complex patients with treatment-resistant depression (TRD). Andrew A. Nierenberg, MD, Massachusetts General Hospital, reviewed newer medications for TRD, including olanzapine-fluoxetine combination, ketamine, riluzole, and L-methylfolate; however, use of these medications requires careful consideration of risks and benefits.
Many FDA-approved drugs have a “black-box” warning, but still are widely used. Henry A. Nasrallah, MD, University of Cincinnati, reviewed black-box warnings for antipsychotics, antidepressants, mood stabilizers, benzodiazepines, stimulants, opiates, and hypnotics and offered strategies on how to incorporate these warnings into clinical practice.
Dr. Nierenberg discussed the outcomes of 3 published medication effectiveness studies for bipolar disorder (BD)—STEP-BD, BALANCE, and LiTMUS—and one currently underway, CHOICE. These studies examined monotherapy and combination therapy with antidepressants, anticonvulsants, antipsychotics, and psychosocial interventions.
Although there is an association between psychosis and violence, most psychotic patients are not violent. Rajiv Tandon, MD, University of Florida, reviewed modifiable and nonmodifiable risk factors for violence, key clinical questions to consider, and scales to use when assessing a patient’s risk of violence.
AFTERNOON SESSIONS
Measuring biomarkers can augment other clinical methods to help identify metabolic, structural, and functional brain changes associated with preclinical stages of cognitive disorders. James Ellison, MD, MPH, McLean Hospital, Harvard Medical School, explained how biomarkers can improve the differential diagnosis of memory impairments and aid in identifying different types of dementia.
Donald W. Black, MD, (right) receives the 2013 George Winokur Research
Award from Carol S. North, MD, for his article on pathological gambling
Case-control studies have found a strong association between schizophrenia and type II diabetes, which contributes to higher mortality among schizophrenia patients. Along with vigilant metabolic monitoring, Dr. Tandon recommended a therapeutic approach that includes changing antipsychotics, prescribing metformin, suggesting lifestyle interventions, and treating comorbid conditions.
Depressed older adults may report anxiety, hopelessness, anhedonia, or somatic symptoms, rather than sadness. Depressive symptoms may be associated with vascular disease or cognitive impairment. Dr. Ellison reviewed psychotherapeutic and pharmacologic treatments for older depressed patients.
FRIDAY, APRIL 5, 2013
MORNING SESSIONS
Many strategies exist for treating patients with TRD; adding an atypical antipsychotic has the best evidence, but there are tolerability considerations. Dr. Nierenberg suggested using a combination of treatments.
Pregnancy is inherently risky for women who take antipsychotics. In all patients of childbearing potential, take a thorough reproductive history and ask about contraception use. Marlene P. Freeman, MD, Massachusetts General Hospital, explained that psychotropics with unfavorable FDA pregnancy ratings may be among first-line choices.
George T. Grossberg, MD, (left) speaks with attendees
Clinical symptoms, cognitive deficits, psychiatric comorbidities, genetic factors, neuroimaging features, and pharmacotherapy may overlap considerably between schizophrenia and BD. Dr. Nasrallah described clinical features that differentiate the 2 disorders.
Cognitive enhancers can improve activities of daily living, behavior, and cognition in patients with Alzheimer’s disease. George T. Grossberg, MD, St. Louis University, reviewed the evidence for acetylcholinesterase inhibitors, the NMDA receptor antagonist memantine, combination therapy, and atypical antipsychotics.
Dietary consultation for older patients might help delay or decrease their risk of dementia. Patients should consume omega-3 fatty acids, whole grains, fresh fruits and vegetables, beans, legumes, and certain spices. Dr. Grossberg also suggested patients engage in physical and mental exercises, social and spiritual activities, and stress reduction, and control cardiovascular risk factors.
AFTERNOON SESSIONS
Many women experience anxiety during pregnancy, and the risk is highest during the first trimester. Dr. Freeman reviewed prevalence, diagnosis, and treatment of panic disorder, generalized anxiety disorder, obsessive-compulsive disorder, and posttraumatic stress disorder during pregnancy and postpartum.
Kathleen Brady, MD, PhD, Medical University of South Carolina, explained how methylenedioxypyrovalerone, also known as bath salts, and other designer drugs are not detectable on standard urine drug screens. Agitation, tachycardia, combative behavior, hyperthermia, and hallucinations have been reported.
Kathleen Brady, MD, MPH
Alcohol abuse and depression are highly comorbid and are associated with higher suicidality, more severe symptoms, and poorer treatment response than either disorder alone. Depressive symptoms often are seen during alcohol withdrawal, and may resolve with abstinence. Dr. Brady reviewed the evidence for treating depressed alcoholics with antidepressants, medications targeting alcohol dependence such as disulfiram and naltrexone, and psychotherapy.
Ralph Aquila, MD, Columbia College of Physicians and Surgeons, discussed risk factors for and consequences of treatment nonadherence in patients with schizophrenia. Leslie L. Citrome, MD, MPH, New York Medical College, covered strategies to improve adherence, including identifying and addressing barriers to adherence for individual patients, improving the therapeutic alliance, and considering long-acting injectable antipsychotics.
SATURDAY, APRIL 6, 2013
MORNING SESSIONS
Forty-six percent of depressed patients will stop pharmacotherapy before they have a chance to respond. To minimize short-term side effects, Andrew J. Cutler, MD, Florida Clinical Research Center, suggested educating patients and slowly titrating medications; options for reducing long-term side effects or residual symptoms include switching or augmenting pharmacotherapy.
When treating patients addicted to opioids, outcome measures go beyond general health to obtaining employment and reducing criminal activity. Pharmacotherapy options include methadone maintenance therapy, oral and injectable naltrexone, and oral, sublingual, and implantable buprenorphine. Walter Ling, MD, David Geffen School of Medicine at UCLA, described factors that may improve patient outcomes.
Geriatric BD is relatively common in clinical settings, but there is a lack of evidence-based clinical practice guidelines. James W. Jefferson, MD, University of Wisconsin School of Medicine and Public Health, recommended choosing a treatment based on the illness phase and balancing the benefit of certain pharmacotherapies against short- and long-term risks.
Most medications for treating alcohol dependence work by modulating functions of opioids, glutamate, GABA, and serotonin. Dr. Ling reviewed the evidence base, dosing guidelines, and clinical recommendations for disulfiram, oral and injectable naltrexone, and acamprosate, which are FDA-approved for treating alcohol dependence. He also recommended combining medications with nonpharmacologic treatments, such as 12-step programs.
Most people who die by suicide deny suicide ideation at their last mental health visit. Risk factors for suicide include family history of suicide, childhood or adult trauma, substance abuse, stressful life events, chronic illness, and psychiatric disorders. Dr. Jefferson described suicide rating and tracking scales and encouraged clinicians to document suicide risk evaluations.
AFTERNOON SESSION
Roger S. McIntyre, MD, FRCPCRobert M.A. Hirschfeld, MD, University of Texas Medical Branch, discussed how the concept of allostatic load—bodily “wear and tear” that emerges with sustained allostatic states—may help explain cognitive and physical decline associated with BD. Roger S. McIntyre, MD, FRCPC, University of Toronto, emphasized that BD is a progressive disorder and comorbidities such as metabolic problems may promote this progression. Terence A. Ketter, MD, Stanford School of Medicine, covered new developments in BD treatment, including certain second-generation antipsychotics, dopaminergic neurotransmission enhancers, mood stabilizers, adjunctive antidepressants, and adjunctive psychotherapy.
Current Psychiatry and the American Academy of Clinical Psychiatrists were pleased to host more than 550 psychiatric practitioners for this conference, led by Meeting Chair Richard Balon, MD, and Meeting Co-Chairs Donald W. Black, MD, and Nagy Youssef, MD, April 4-6, 2013 at the Swissôtel in Chicago, IL. Attendees could earn up to 18 AMA PRA Category 1 Credits™.
THURSDAY, APRIL 4, 2013
MORNING SESSIONS
Evidence-based medicine and treatment guidelines may not address complex patients with treatment-resistant depression (TRD). Andrew A. Nierenberg, MD, Massachusetts General Hospital, reviewed newer medications for TRD, including olanzapine-fluoxetine combination, ketamine, riluzole, and L-methylfolate; however, use of these medications requires careful consideration of risks and benefits.
Many FDA-approved drugs have a “black-box” warning, but still are widely used. Henry A. Nasrallah, MD, University of Cincinnati, reviewed black-box warnings for antipsychotics, antidepressants, mood stabilizers, benzodiazepines, stimulants, opiates, and hypnotics and offered strategies on how to incorporate these warnings into clinical practice.
Dr. Nierenberg discussed the outcomes of 3 published medication effectiveness studies for bipolar disorder (BD)—STEP-BD, BALANCE, and LiTMUS—and one currently underway, CHOICE. These studies examined monotherapy and combination therapy with antidepressants, anticonvulsants, antipsychotics, and psychosocial interventions.
Although there is an association between psychosis and violence, most psychotic patients are not violent. Rajiv Tandon, MD, University of Florida, reviewed modifiable and nonmodifiable risk factors for violence, key clinical questions to consider, and scales to use when assessing a patient’s risk of violence.
AFTERNOON SESSIONS
Measuring biomarkers can augment other clinical methods to help identify metabolic, structural, and functional brain changes associated with preclinical stages of cognitive disorders. James Ellison, MD, MPH, McLean Hospital, Harvard Medical School, explained how biomarkers can improve the differential diagnosis of memory impairments and aid in identifying different types of dementia.
Donald W. Black, MD, (right) receives the 2013 George Winokur Research
Award from Carol S. North, MD, for his article on pathological gambling
Case-control studies have found a strong association between schizophrenia and type II diabetes, which contributes to higher mortality among schizophrenia patients. Along with vigilant metabolic monitoring, Dr. Tandon recommended a therapeutic approach that includes changing antipsychotics, prescribing metformin, suggesting lifestyle interventions, and treating comorbid conditions.
Depressed older adults may report anxiety, hopelessness, anhedonia, or somatic symptoms, rather than sadness. Depressive symptoms may be associated with vascular disease or cognitive impairment. Dr. Ellison reviewed psychotherapeutic and pharmacologic treatments for older depressed patients.
FRIDAY, APRIL 5, 2013
MORNING SESSIONS
Many strategies exist for treating patients with TRD; adding an atypical antipsychotic has the best evidence, but there are tolerability considerations. Dr. Nierenberg suggested using a combination of treatments.
Pregnancy is inherently risky for women who take antipsychotics. In all patients of childbearing potential, take a thorough reproductive history and ask about contraception use. Marlene P. Freeman, MD, Massachusetts General Hospital, explained that psychotropics with unfavorable FDA pregnancy ratings may be among first-line choices.
George T. Grossberg, MD, (left) speaks with attendees
Clinical symptoms, cognitive deficits, psychiatric comorbidities, genetic factors, neuroimaging features, and pharmacotherapy may overlap considerably between schizophrenia and BD. Dr. Nasrallah described clinical features that differentiate the 2 disorders.
Cognitive enhancers can improve activities of daily living, behavior, and cognition in patients with Alzheimer’s disease. George T. Grossberg, MD, St. Louis University, reviewed the evidence for acetylcholinesterase inhibitors, the NMDA receptor antagonist memantine, combination therapy, and atypical antipsychotics.
Dietary consultation for older patients might help delay or decrease their risk of dementia. Patients should consume omega-3 fatty acids, whole grains, fresh fruits and vegetables, beans, legumes, and certain spices. Dr. Grossberg also suggested patients engage in physical and mental exercises, social and spiritual activities, and stress reduction, and control cardiovascular risk factors.
AFTERNOON SESSIONS
Many women experience anxiety during pregnancy, and the risk is highest during the first trimester. Dr. Freeman reviewed prevalence, diagnosis, and treatment of panic disorder, generalized anxiety disorder, obsessive-compulsive disorder, and posttraumatic stress disorder during pregnancy and postpartum.
Kathleen Brady, MD, PhD, Medical University of South Carolina, explained how methylenedioxypyrovalerone, also known as bath salts, and other designer drugs are not detectable on standard urine drug screens. Agitation, tachycardia, combative behavior, hyperthermia, and hallucinations have been reported.
Kathleen Brady, MD, MPH
Alcohol abuse and depression are highly comorbid and are associated with higher suicidality, more severe symptoms, and poorer treatment response than either disorder alone. Depressive symptoms often are seen during alcohol withdrawal, and may resolve with abstinence. Dr. Brady reviewed the evidence for treating depressed alcoholics with antidepressants, medications targeting alcohol dependence such as disulfiram and naltrexone, and psychotherapy.
Ralph Aquila, MD, Columbia College of Physicians and Surgeons, discussed risk factors for and consequences of treatment nonadherence in patients with schizophrenia. Leslie L. Citrome, MD, MPH, New York Medical College, covered strategies to improve adherence, including identifying and addressing barriers to adherence for individual patients, improving the therapeutic alliance, and considering long-acting injectable antipsychotics.
SATURDAY, APRIL 6, 2013
MORNING SESSIONS
Forty-six percent of depressed patients will stop pharmacotherapy before they have a chance to respond. To minimize short-term side effects, Andrew J. Cutler, MD, Florida Clinical Research Center, suggested educating patients and slowly titrating medications; options for reducing long-term side effects or residual symptoms include switching or augmenting pharmacotherapy.
When treating patients addicted to opioids, outcome measures go beyond general health to obtaining employment and reducing criminal activity. Pharmacotherapy options include methadone maintenance therapy, oral and injectable naltrexone, and oral, sublingual, and implantable buprenorphine. Walter Ling, MD, David Geffen School of Medicine at UCLA, described factors that may improve patient outcomes.
Geriatric BD is relatively common in clinical settings, but there is a lack of evidence-based clinical practice guidelines. James W. Jefferson, MD, University of Wisconsin School of Medicine and Public Health, recommended choosing a treatment based on the illness phase and balancing the benefit of certain pharmacotherapies against short- and long-term risks.
Most medications for treating alcohol dependence work by modulating functions of opioids, glutamate, GABA, and serotonin. Dr. Ling reviewed the evidence base, dosing guidelines, and clinical recommendations for disulfiram, oral and injectable naltrexone, and acamprosate, which are FDA-approved for treating alcohol dependence. He also recommended combining medications with nonpharmacologic treatments, such as 12-step programs.
Most people who die by suicide deny suicide ideation at their last mental health visit. Risk factors for suicide include family history of suicide, childhood or adult trauma, substance abuse, stressful life events, chronic illness, and psychiatric disorders. Dr. Jefferson described suicide rating and tracking scales and encouraged clinicians to document suicide risk evaluations.
AFTERNOON SESSION
Roger S. McIntyre, MD, FRCPCRobert M.A. Hirschfeld, MD, University of Texas Medical Branch, discussed how the concept of allostatic load—bodily “wear and tear” that emerges with sustained allostatic states—may help explain cognitive and physical decline associated with BD. Roger S. McIntyre, MD, FRCPC, University of Toronto, emphasized that BD is a progressive disorder and comorbidities such as metabolic problems may promote this progression. Terence A. Ketter, MD, Stanford School of Medicine, covered new developments in BD treatment, including certain second-generation antipsychotics, dopaminergic neurotransmission enhancers, mood stabilizers, adjunctive antidepressants, and adjunctive psychotherapy.
Current Psychiatry and the American Academy of Clinical Psychiatrists were pleased to host more than 550 psychiatric practitioners for this conference, led by Meeting Chair Richard Balon, MD, and Meeting Co-Chairs Donald W. Black, MD, and Nagy Youssef, MD, April 4-6, 2013 at the Swissôtel in Chicago, IL. Attendees could earn up to 18 AMA PRA Category 1 Credits™.
THURSDAY, APRIL 4, 2013
MORNING SESSIONS
Evidence-based medicine and treatment guidelines may not address complex patients with treatment-resistant depression (TRD). Andrew A. Nierenberg, MD, Massachusetts General Hospital, reviewed newer medications for TRD, including olanzapine-fluoxetine combination, ketamine, riluzole, and L-methylfolate; however, use of these medications requires careful consideration of risks and benefits.
Many FDA-approved drugs have a “black-box” warning, but still are widely used. Henry A. Nasrallah, MD, University of Cincinnati, reviewed black-box warnings for antipsychotics, antidepressants, mood stabilizers, benzodiazepines, stimulants, opiates, and hypnotics and offered strategies on how to incorporate these warnings into clinical practice.
Dr. Nierenberg discussed the outcomes of 3 published medication effectiveness studies for bipolar disorder (BD)—STEP-BD, BALANCE, and LiTMUS—and one currently underway, CHOICE. These studies examined monotherapy and combination therapy with antidepressants, anticonvulsants, antipsychotics, and psychosocial interventions.
Although there is an association between psychosis and violence, most psychotic patients are not violent. Rajiv Tandon, MD, University of Florida, reviewed modifiable and nonmodifiable risk factors for violence, key clinical questions to consider, and scales to use when assessing a patient’s risk of violence.
AFTERNOON SESSIONS
Measuring biomarkers can augment other clinical methods to help identify metabolic, structural, and functional brain changes associated with preclinical stages of cognitive disorders. James Ellison, MD, MPH, McLean Hospital, Harvard Medical School, explained how biomarkers can improve the differential diagnosis of memory impairments and aid in identifying different types of dementia.
Donald W. Black, MD, (right) receives the 2013 George Winokur Research
Award from Carol S. North, MD, for his article on pathological gambling
Case-control studies have found a strong association between schizophrenia and type II diabetes, which contributes to higher mortality among schizophrenia patients. Along with vigilant metabolic monitoring, Dr. Tandon recommended a therapeutic approach that includes changing antipsychotics, prescribing metformin, suggesting lifestyle interventions, and treating comorbid conditions.
Depressed older adults may report anxiety, hopelessness, anhedonia, or somatic symptoms, rather than sadness. Depressive symptoms may be associated with vascular disease or cognitive impairment. Dr. Ellison reviewed psychotherapeutic and pharmacologic treatments for older depressed patients.
FRIDAY, APRIL 5, 2013
MORNING SESSIONS
Many strategies exist for treating patients with TRD; adding an atypical antipsychotic has the best evidence, but there are tolerability considerations. Dr. Nierenberg suggested using a combination of treatments.
Pregnancy is inherently risky for women who take antipsychotics. In all patients of childbearing potential, take a thorough reproductive history and ask about contraception use. Marlene P. Freeman, MD, Massachusetts General Hospital, explained that psychotropics with unfavorable FDA pregnancy ratings may be among first-line choices.
George T. Grossberg, MD, (left) speaks with attendees
Clinical symptoms, cognitive deficits, psychiatric comorbidities, genetic factors, neuroimaging features, and pharmacotherapy may overlap considerably between schizophrenia and BD. Dr. Nasrallah described clinical features that differentiate the 2 disorders.
Cognitive enhancers can improve activities of daily living, behavior, and cognition in patients with Alzheimer’s disease. George T. Grossberg, MD, St. Louis University, reviewed the evidence for acetylcholinesterase inhibitors, the NMDA receptor antagonist memantine, combination therapy, and atypical antipsychotics.
Dietary consultation for older patients might help delay or decrease their risk of dementia. Patients should consume omega-3 fatty acids, whole grains, fresh fruits and vegetables, beans, legumes, and certain spices. Dr. Grossberg also suggested patients engage in physical and mental exercises, social and spiritual activities, and stress reduction, and control cardiovascular risk factors.
AFTERNOON SESSIONS
Many women experience anxiety during pregnancy, and the risk is highest during the first trimester. Dr. Freeman reviewed prevalence, diagnosis, and treatment of panic disorder, generalized anxiety disorder, obsessive-compulsive disorder, and posttraumatic stress disorder during pregnancy and postpartum.
Kathleen Brady, MD, PhD, Medical University of South Carolina, explained how methylenedioxypyrovalerone, also known as bath salts, and other designer drugs are not detectable on standard urine drug screens. Agitation, tachycardia, combative behavior, hyperthermia, and hallucinations have been reported.
Kathleen Brady, MD, MPH
Alcohol abuse and depression are highly comorbid and are associated with higher suicidality, more severe symptoms, and poorer treatment response than either disorder alone. Depressive symptoms often are seen during alcohol withdrawal, and may resolve with abstinence. Dr. Brady reviewed the evidence for treating depressed alcoholics with antidepressants, medications targeting alcohol dependence such as disulfiram and naltrexone, and psychotherapy.
Ralph Aquila, MD, Columbia College of Physicians and Surgeons, discussed risk factors for and consequences of treatment nonadherence in patients with schizophrenia. Leslie L. Citrome, MD, MPH, New York Medical College, covered strategies to improve adherence, including identifying and addressing barriers to adherence for individual patients, improving the therapeutic alliance, and considering long-acting injectable antipsychotics.
SATURDAY, APRIL 6, 2013
MORNING SESSIONS
Forty-six percent of depressed patients will stop pharmacotherapy before they have a chance to respond. To minimize short-term side effects, Andrew J. Cutler, MD, Florida Clinical Research Center, suggested educating patients and slowly titrating medications; options for reducing long-term side effects or residual symptoms include switching or augmenting pharmacotherapy.
When treating patients addicted to opioids, outcome measures go beyond general health to obtaining employment and reducing criminal activity. Pharmacotherapy options include methadone maintenance therapy, oral and injectable naltrexone, and oral, sublingual, and implantable buprenorphine. Walter Ling, MD, David Geffen School of Medicine at UCLA, described factors that may improve patient outcomes.
Geriatric BD is relatively common in clinical settings, but there is a lack of evidence-based clinical practice guidelines. James W. Jefferson, MD, University of Wisconsin School of Medicine and Public Health, recommended choosing a treatment based on the illness phase and balancing the benefit of certain pharmacotherapies against short- and long-term risks.
Most medications for treating alcohol dependence work by modulating functions of opioids, glutamate, GABA, and serotonin. Dr. Ling reviewed the evidence base, dosing guidelines, and clinical recommendations for disulfiram, oral and injectable naltrexone, and acamprosate, which are FDA-approved for treating alcohol dependence. He also recommended combining medications with nonpharmacologic treatments, such as 12-step programs.
Most people who die by suicide deny suicide ideation at their last mental health visit. Risk factors for suicide include family history of suicide, childhood or adult trauma, substance abuse, stressful life events, chronic illness, and psychiatric disorders. Dr. Jefferson described suicide rating and tracking scales and encouraged clinicians to document suicide risk evaluations.
AFTERNOON SESSION
Roger S. McIntyre, MD, FRCPCRobert M.A. Hirschfeld, MD, University of Texas Medical Branch, discussed how the concept of allostatic load—bodily “wear and tear” that emerges with sustained allostatic states—may help explain cognitive and physical decline associated with BD. Roger S. McIntyre, MD, FRCPC, University of Toronto, emphasized that BD is a progressive disorder and comorbidities such as metabolic problems may promote this progression. Terence A. Ketter, MD, Stanford School of Medicine, covered new developments in BD treatment, including certain second-generation antipsychotics, dopaminergic neurotransmission enhancers, mood stabilizers, adjunctive antidepressants, and adjunctive psychotherapy.
‘Bath salts’ abuse
“The delirious substance abuser” (Cases That Test Your Skills, Current Psychiatry, January 2012, p. 58-67) was an excellent review of the complex presentations when patients use multiple substances. Recently, we admitted a patient presenting with delirium with psychosis. She presented with similar symptoms as Ms. K in your article, with the addition of severe tactile hallucinosis that led our patient to jump out of a moving vehicle because she thought bugs were crawling over her. She eventually admitted to using “bath salts” (methylenedioxypyrovalerone) orally and her psychotic symptoms remitted in 3 days.
Vineet Mehta, MD
Consulting Psychiatrist
Health First
Melbourne, FL
Private Practice
Indialantic, FL
“The delirious substance abuser” (Cases That Test Your Skills, Current Psychiatry, January 2012, p. 58-67) was an excellent review of the complex presentations when patients use multiple substances. Recently, we admitted a patient presenting with delirium with psychosis. She presented with similar symptoms as Ms. K in your article, with the addition of severe tactile hallucinosis that led our patient to jump out of a moving vehicle because she thought bugs were crawling over her. She eventually admitted to using “bath salts” (methylenedioxypyrovalerone) orally and her psychotic symptoms remitted in 3 days.
Vineet Mehta, MD
Consulting Psychiatrist
Health First
Melbourne, FL
Private Practice
Indialantic, FL
“The delirious substance abuser” (Cases That Test Your Skills, Current Psychiatry, January 2012, p. 58-67) was an excellent review of the complex presentations when patients use multiple substances. Recently, we admitted a patient presenting with delirium with psychosis. She presented with similar symptoms as Ms. K in your article, with the addition of severe tactile hallucinosis that led our patient to jump out of a moving vehicle because she thought bugs were crawling over her. She eventually admitted to using “bath salts” (methylenedioxypyrovalerone) orally and her psychotic symptoms remitted in 3 days.
Vineet Mehta, MD
Consulting Psychiatrist
Health First
Melbourne, FL
Private Practice
Indialantic, FL
Prescribing psychologists
Because psychiatric medications are complex to manage, I oppose psychologists being certified to prescribe. During medical school, I received 4 years of advanced training in physiology and pharmacology. After medical school, I completed a full year of preliminary internal medicine and an additional 3-year psychiatry residency to further increase my knowledge in managing mental illness. I am certified by the American Board of Psychiatry and Neurology, a process that included written and oral examinations over 2 years after residency to prove my expertise in psychopharmacology, diagnosis, treatment, risk assessment, and psychotherapy. I provide medications and psychotherapy for my patients as indicated. This is the rigorous path most physicians take to becoming a psychiatrist in the United States. One of my biggest concerns about psychologists prescribing is lack of medical training to make a complete differential diagnosis that includes medical causes of a mental disturbance, limited knowledge of drug-drug interactions, and potential to harm patients because of their lack of medical training. For example, a patient taking the blood thinner warfarin may have their ability to clot fatally impaired by a psychotropic drug because of a lack of adequate medical evaluation by a “prescriber” who has limited training in medical management and pharmacology. Another example of the need for medical training to fully evaluate psychiatric patients is an apathetic, depressed patient who continues to be treated with antidepressants while his or her underlying neurologic problem, thyroid condition, or undeclared substance abuse goes undiagnosed.
Lithium is the gold standard medication for bipolar disorder, but if managed incorrectly, without considering the patient’s overall medical condition, drug interactions, and daily physical activities, this drug can lead to kidney failure, coma, brain damage, and death. Many, if not all, psychotropics require ordering and interpreting diagnostic laboratory blood testing before and after initiating treatment to monitor for life-threatening complications, including diabetes and neuroleptic malignant syndrome, and changes in white blood cell count, potassium and sodium levels, and ECG data.
Medical education is long and challenging because the human body—especially the mind—is a complex system that requires a great deal of study to comprehend. A physician’s duty is to do no harm; extensive training is the most important tool for preventing unnecessary harm.
Shalini Varma, MDPrivate PracticeKenosha, WIVernon Hills, IL
Because psychiatric medications are complex to manage, I oppose psychologists being certified to prescribe. During medical school, I received 4 years of advanced training in physiology and pharmacology. After medical school, I completed a full year of preliminary internal medicine and an additional 3-year psychiatry residency to further increase my knowledge in managing mental illness. I am certified by the American Board of Psychiatry and Neurology, a process that included written and oral examinations over 2 years after residency to prove my expertise in psychopharmacology, diagnosis, treatment, risk assessment, and psychotherapy. I provide medications and psychotherapy for my patients as indicated. This is the rigorous path most physicians take to becoming a psychiatrist in the United States. One of my biggest concerns about psychologists prescribing is lack of medical training to make a complete differential diagnosis that includes medical causes of a mental disturbance, limited knowledge of drug-drug interactions, and potential to harm patients because of their lack of medical training. For example, a patient taking the blood thinner warfarin may have their ability to clot fatally impaired by a psychotropic drug because of a lack of adequate medical evaluation by a “prescriber” who has limited training in medical management and pharmacology. Another example of the need for medical training to fully evaluate psychiatric patients is an apathetic, depressed patient who continues to be treated with antidepressants while his or her underlying neurologic problem, thyroid condition, or undeclared substance abuse goes undiagnosed.
Lithium is the gold standard medication for bipolar disorder, but if managed incorrectly, without considering the patient’s overall medical condition, drug interactions, and daily physical activities, this drug can lead to kidney failure, coma, brain damage, and death. Many, if not all, psychotropics require ordering and interpreting diagnostic laboratory blood testing before and after initiating treatment to monitor for life-threatening complications, including diabetes and neuroleptic malignant syndrome, and changes in white blood cell count, potassium and sodium levels, and ECG data.
Medical education is long and challenging because the human body—especially the mind—is a complex system that requires a great deal of study to comprehend. A physician’s duty is to do no harm; extensive training is the most important tool for preventing unnecessary harm.
Shalini Varma, MDPrivate PracticeKenosha, WIVernon Hills, IL
Because psychiatric medications are complex to manage, I oppose psychologists being certified to prescribe. During medical school, I received 4 years of advanced training in physiology and pharmacology. After medical school, I completed a full year of preliminary internal medicine and an additional 3-year psychiatry residency to further increase my knowledge in managing mental illness. I am certified by the American Board of Psychiatry and Neurology, a process that included written and oral examinations over 2 years after residency to prove my expertise in psychopharmacology, diagnosis, treatment, risk assessment, and psychotherapy. I provide medications and psychotherapy for my patients as indicated. This is the rigorous path most physicians take to becoming a psychiatrist in the United States. One of my biggest concerns about psychologists prescribing is lack of medical training to make a complete differential diagnosis that includes medical causes of a mental disturbance, limited knowledge of drug-drug interactions, and potential to harm patients because of their lack of medical training. For example, a patient taking the blood thinner warfarin may have their ability to clot fatally impaired by a psychotropic drug because of a lack of adequate medical evaluation by a “prescriber” who has limited training in medical management and pharmacology. Another example of the need for medical training to fully evaluate psychiatric patients is an apathetic, depressed patient who continues to be treated with antidepressants while his or her underlying neurologic problem, thyroid condition, or undeclared substance abuse goes undiagnosed.
Lithium is the gold standard medication for bipolar disorder, but if managed incorrectly, without considering the patient’s overall medical condition, drug interactions, and daily physical activities, this drug can lead to kidney failure, coma, brain damage, and death. Many, if not all, psychotropics require ordering and interpreting diagnostic laboratory blood testing before and after initiating treatment to monitor for life-threatening complications, including diabetes and neuroleptic malignant syndrome, and changes in white blood cell count, potassium and sodium levels, and ECG data.
Medical education is long and challenging because the human body—especially the mind—is a complex system that requires a great deal of study to comprehend. A physician’s duty is to do no harm; extensive training is the most important tool for preventing unnecessary harm.
Shalini Varma, MDPrivate PracticeKenosha, WIVernon Hills, IL
Depression in pregnancy
I would like to thank Drs. Hatters Friedman and Hall for their excellent article, “Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls” (Current Psychiatry, February 2013, p. 10-17; http://bit.ly/1EIIYvD). Their emphasis on the risks of untreated depression was much appreciated and resonated deeply with me because of my own experiences.
During the second year of my residency, I treated a 31-year-old woman who experienced depressive symptoms starting in her first trimester of pregnancy. She was suffering from major depressive disorder, single episode, mild type, and was referred to me for psychotherapy. As the therapy and her pregnancy progressed, her depression worsened and I faced the difficult decision of starting a pregnant woman on psychotropics.
Despite her worsening symptoms, I was hesitant to offer her medication because she was pregnant. My discussion with my psychotherapy supervisor was the first in a series of events that made me aware of the stigma regarding prescribing psychotropics to pregnant women. I was amazed when he expressed his views of “not exposing pregnant women to medications” without a reasonable discussion of benefits. While discussing the risks, my patient replied bitterly: “You doctors won’t even say Tylenol is safe…everybody only thinks about the baby. What about me? I stopped being a person the day I became pregnant.”
After a careful risk-benefit discussion, and with guidance from my psychopharmacology supervisor, we started my patient on sertraline. More than 6 years later, I still recall my patient’s description of her attempt to fill her prescription. She said the pharmacist refused to fill the prescription and told her that a pregnant woman should not be taking that medication, implying she was being a “bad mother.” She said to me, “I did not have the strength to walk across the road to the other pharmacy. This incident again confirmed that I don’t exist; I am just a body for the baby.” I was horrified. Are we not taught to discuss the risks and the benefits of a treatment, and then help patients make the best decision for themselves? I am amazed at how often we let our personal views bias the way we look at objective evidence and how little we think of what a patient wants or needs.
After a few weeks, my patient started sertraline and responded well. She continued to attend therapy regularly. For months after her symptoms remitted, she described how disconnected she had felt from herself and how she later grieved for the time lost. Although she never blamed me, I always felt guilty for adding a few weeks to her suffering by not starting her on medication earlier.
This experience had a lasting personal impact. I am committed to ensuring that my residents and I are up-to-date about prescribing psychotropics for pregnant patients. However, the need for these well balanced and well written articles is ongoing, because I continue to see patients whose psychosis or depression worsens dramatically because their psychiatrist abruptly stopped maintenance medications during pregnancy.
Rashi Aggarwal, MDAssistant ProfessorUMDNJ-New Jersey Medical SchoolNewark, NJ
I would like to thank Drs. Hatters Friedman and Hall for their excellent article, “Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls” (Current Psychiatry, February 2013, p. 10-17; http://bit.ly/1EIIYvD). Their emphasis on the risks of untreated depression was much appreciated and resonated deeply with me because of my own experiences.
During the second year of my residency, I treated a 31-year-old woman who experienced depressive symptoms starting in her first trimester of pregnancy. She was suffering from major depressive disorder, single episode, mild type, and was referred to me for psychotherapy. As the therapy and her pregnancy progressed, her depression worsened and I faced the difficult decision of starting a pregnant woman on psychotropics.
Despite her worsening symptoms, I was hesitant to offer her medication because she was pregnant. My discussion with my psychotherapy supervisor was the first in a series of events that made me aware of the stigma regarding prescribing psychotropics to pregnant women. I was amazed when he expressed his views of “not exposing pregnant women to medications” without a reasonable discussion of benefits. While discussing the risks, my patient replied bitterly: “You doctors won’t even say Tylenol is safe…everybody only thinks about the baby. What about me? I stopped being a person the day I became pregnant.”
After a careful risk-benefit discussion, and with guidance from my psychopharmacology supervisor, we started my patient on sertraline. More than 6 years later, I still recall my patient’s description of her attempt to fill her prescription. She said the pharmacist refused to fill the prescription and told her that a pregnant woman should not be taking that medication, implying she was being a “bad mother.” She said to me, “I did not have the strength to walk across the road to the other pharmacy. This incident again confirmed that I don’t exist; I am just a body for the baby.” I was horrified. Are we not taught to discuss the risks and the benefits of a treatment, and then help patients make the best decision for themselves? I am amazed at how often we let our personal views bias the way we look at objective evidence and how little we think of what a patient wants or needs.
After a few weeks, my patient started sertraline and responded well. She continued to attend therapy regularly. For months after her symptoms remitted, she described how disconnected she had felt from herself and how she later grieved for the time lost. Although she never blamed me, I always felt guilty for adding a few weeks to her suffering by not starting her on medication earlier.
This experience had a lasting personal impact. I am committed to ensuring that my residents and I are up-to-date about prescribing psychotropics for pregnant patients. However, the need for these well balanced and well written articles is ongoing, because I continue to see patients whose psychosis or depression worsens dramatically because their psychiatrist abruptly stopped maintenance medications during pregnancy.
Rashi Aggarwal, MDAssistant ProfessorUMDNJ-New Jersey Medical SchoolNewark, NJ
I would like to thank Drs. Hatters Friedman and Hall for their excellent article, “Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls” (Current Psychiatry, February 2013, p. 10-17; http://bit.ly/1EIIYvD). Their emphasis on the risks of untreated depression was much appreciated and resonated deeply with me because of my own experiences.
During the second year of my residency, I treated a 31-year-old woman who experienced depressive symptoms starting in her first trimester of pregnancy. She was suffering from major depressive disorder, single episode, mild type, and was referred to me for psychotherapy. As the therapy and her pregnancy progressed, her depression worsened and I faced the difficult decision of starting a pregnant woman on psychotropics.
Despite her worsening symptoms, I was hesitant to offer her medication because she was pregnant. My discussion with my psychotherapy supervisor was the first in a series of events that made me aware of the stigma regarding prescribing psychotropics to pregnant women. I was amazed when he expressed his views of “not exposing pregnant women to medications” without a reasonable discussion of benefits. While discussing the risks, my patient replied bitterly: “You doctors won’t even say Tylenol is safe…everybody only thinks about the baby. What about me? I stopped being a person the day I became pregnant.”
After a careful risk-benefit discussion, and with guidance from my psychopharmacology supervisor, we started my patient on sertraline. More than 6 years later, I still recall my patient’s description of her attempt to fill her prescription. She said the pharmacist refused to fill the prescription and told her that a pregnant woman should not be taking that medication, implying she was being a “bad mother.” She said to me, “I did not have the strength to walk across the road to the other pharmacy. This incident again confirmed that I don’t exist; I am just a body for the baby.” I was horrified. Are we not taught to discuss the risks and the benefits of a treatment, and then help patients make the best decision for themselves? I am amazed at how often we let our personal views bias the way we look at objective evidence and how little we think of what a patient wants or needs.
After a few weeks, my patient started sertraline and responded well. She continued to attend therapy regularly. For months after her symptoms remitted, she described how disconnected she had felt from herself and how she later grieved for the time lost. Although she never blamed me, I always felt guilty for adding a few weeks to her suffering by not starting her on medication earlier.
This experience had a lasting personal impact. I am committed to ensuring that my residents and I are up-to-date about prescribing psychotropics for pregnant patients. However, the need for these well balanced and well written articles is ongoing, because I continue to see patients whose psychosis or depression worsens dramatically because their psychiatrist abruptly stopped maintenance medications during pregnancy.
Rashi Aggarwal, MDAssistant ProfessorUMDNJ-New Jersey Medical SchoolNewark, NJ
Treating depression in hepatitis C patients
Sildenafil for SSRI-induced sexual dysfunction in women
- Sexual dysfunction can arise from environmental, social, medical, or drug effects and requires a multifaceted approach to treatment.
- When possible, take a baseline sexual dysfunction measurement to assess if selective serotonin reuptake inhibitor use is correlated with onset or worsening of sexual dysfunction.
- Nonpharmacologic options should be considered before and during pharmacotherapy.
- Sildenafil may be useful for treating anorgasmia in women taking serotonergic antidepressants.
- Phosphodiesterase type 5 inhibitors are not FDA-approved for sexual dysfunction in women.
Mrs. L, age 27, has a history of major depressive disorder with symptoms of anxiety. She was managed successfully for 2 years with bupropion XL, 300 mg/d, but was switched to venlafaxine, titrated to 225 mg/d, after she developed seizures secondary to a head injury sustained in a car accident. After the switch, Mrs. L’s mood deteriorated and she was hospitalized. Since then, she’s received several medication trials, including paroxetine, 30 mg/d, a selective serotonin reuptake inhibitor (SSRI), and the tricyclic antidepressant (TCA) nortriptyline, 75 mg/d, but she could not tolerate these medications because of severe xerostomia.
After taking sertraline, 150 mg/d, for 8 weeks, Mrs. L improves and has a Patient Health Questionnaire score of 6, indicating mild depression. Her initial complaints of diarrhea and nausea have resolved, but Mrs. L now reports that she and her husband are having marital difficulties because she cannot achieve orgasm during sexual intercourse. She did not have this problem when she was taking bupropion. Her husband occasionally takes the phosphodiesterase type 5 (PDE5) inhibitor sildenafil before intercourse, and Mrs. L asks you if this medication will help her achieve orgasm.
DSM-IV-TR defines sexual dysfunction as disturbances in sexual desire and/or in the sexual response cycle (excitement, plateau, orgasm, and resolution) that result in marked distress and interpersonal difficulty.1 Sexual dysfunction can occur with the use of any antidepressant with serotonergic activity; it affects an estimated 50% to 70% of patients who take SSRIs.2 Sexual dysfunction can occur with all SSRIs; however, higher rates of sexual dysfunction are found with citalopram, fluoxetine, paroxetine, and sertraline.3 Studies have suggested there may be a dose-side effect relationship with SSRI-induced sexual dysfunction.4
Several factors can increase a patient’s risk of sexual dysfunction and should be considered before prescribing an antidepressant or when a patient presents with new or worsening sexual dysfunction (Table 1).5 In general, nonserotonergic agents such as bupropion, mirtazapine, and nefazodone are associated with lower rates of sexual dysfunction. The pharmacology of these agents explains their decreased propensity to cause sexual dysfunction. These agents increase levels of dopamine in the mesolimbic dopaminergic system either by blocking reuptake (bupropion) or antagonizing the serotonin subtype-2 receptor and facilitating disinhibition of decreased dopamine downstream (nefazodone and mirtazapine).
Table 1
Risk factors for sexual dysfunction
| Sex | Risk factors |
|---|---|
| Women | History of sexual, physical, or emotional abuse, physical inactivity |
| Men | Severe hyperprolactinemia, smoking |
| Both sexes | Poor to fair health, genitourinary disease, diabetes mellitus, cardiovascular disease, hypertension, increasing age, psychiatric disorders, relationship difficulties |
| Source: Reference 5 | |
One option for treating antidepressant-induced sexual dysfunction in women is PDE5 inhibitors, which are used to treat erectile dysfunction (ED). These medications ameliorate ED by inhibiting degradation of cyclic guanosine monophosphate by PDE5, which increases blood flow to the penis during sexual stimulation. Although these medications are not FDA-approved for treating sexual dysfunction in women, adjunctive PDE5 inhibitor treatment may be beneficial for sexual dysfunction in females because similar mediators, such as nitric oxide and cyclic guanosine monophosphate, involved in the nonadrenergic-noncholinergic signaling that controls sexual stimulation in men also are found in female genital tissue.6
When treating a woman with SSRI-induced sexual dysfunction, consider nonpharmacologic treatments both before and during pharmacotherapy (Table 2).7,8 See Table 3 for a comparison of pharmacokinetics, side effects, and drug interactions of the 4 FDA-approved PDE5 inhibitors—avanafil, sildenafil, tadalafil, and vardenafil.
Table 2
Management strategies for SSRI-induced sexual dysfunction
| Intervention | Comments |
|---|---|
| Nonpharmacologic | |
| Lifestyle modifications | Encourage healthy eating, weight loss, smoking cessation, substance abuse treatment, or minimizing alcohol intake to improve patient self-image and overall health |
| Cognitive-behavioral therapy | Patients can identify coping strategies for reducing symptom severity and preventing worsening sexual dysfunction |
| Sex therapy | May benefit patients with relationship difficulties |
| ‘Watch and wait’ | Spontaneous resolving (or ‘adaptation’) of sexual dysfunction with antidepressants can take ≥6 months. Studies have found adaptation rates generally are low (~10%) |
| Pharmacologic | |
| Drug holiday | May be an option for patients taking antidepressants with shorter half-lives and patients taking lower doses. Be cautious of empowering patients to stop their own medications as needed |
| Dosage reduction | Serotonergic antidepressant-induced sexual dysfunction may be related to dose. Little research has been conducted on this method and the patient’s clinical status must be considered |
| Dose timing | Instructing a patient to take the antidepressant after his or her usual time of sexual activity (eg, patients who engage in sexual activity at night should take the antidepressant before falling asleep). This may allow the drug level to be lowest during sexual activity |
| Switching medications | Case reports, retrospective studies, and RCTs suggest switching to a different antidepressant with less serotonergic activity may be appropriate, particularly if the patient has not responded to the current antidepressant |
| Adjunctive therapy | RCTs support adjunctive bupropion (≥300 mg/d) or olanzapine (5 mg/d) as treatment for SSRI-induced sexual dysfunction in women Studies have found no improvement in sexual functioning with adjunctive buspirone, granisetron, amantadine, mirtazapine, yohimbine, ephedrine, or ginkgo biloba in women |
| RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor Source: Reference 7,8 | |
Table 3
Phosphodiesterase type 5 inhibitors: A comparison
| Medication | Dose rangea | Pharmacokinetics | Side effects | Significant drug interactions |
|---|---|---|---|---|
| Avanafil | 50 to 200 mg, 30 minutes before sexual activity | Bioavailability: N/A (high-fat meal delays Tmax by 60 minutes and reduces Cmax by 24% to 39%; clinically insignificant) Half life: 5 hours Metabolism: CYP3A4 | Headache, flushing, nasal congestion, nasopharyngitis, backache | Strong CYP3A4 inhibitors (increased avanafil levels) Contraindicated within 12 hours of nitrate use (eg, nitroglycerin) |
| Sildenafil | 25 to 100 mg, 1 to 2 hours before sexual activity | Bioavailability: 41% (food/high-fat meal delays Tmax by 60 minutes and reduces Cmax by 29%) Half life: 4 hours Metabolism: CYP3A4 | Headache, flushing, erythema, indigestion, insomnia, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased sildenafil levels) Contraindicated within 24 hours of nitrate use |
| Tadalafil | 10 to 20 mg, 30 minutes before sexual activity | Bioavailability: N/A (not affected by food) Half life: 17.5 hours (duration of action up to 36 hours) Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, myalgia, and back pain | Strong CYP3A4 inhibitors (increased tadalafil levels) Contraindicated within 48 hours of nitrate use |
| Vardenafil | 5 to 20 mg, 30 minutes to 2 hours before sexual activity | Bioavailability: 15% for film-coated tablet (high-fat meal reduces Cmax by 18% to 50%) Half life: 4 to 5 hours Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased vardenafil levels) Contraindicated within 24 hours of nitrate use |
| aTypical dose range for treatment of erectile dysfunction Cmax: maximum concentration; CYP: cytochrome P450; Tmax: time to maximum concentration Source: Micromedex® Healthcare Series [Internet database]. Greenwood Village, CO: Thomson Healthcare. Accessed October 10, 2012 | ||||
Limited evidence for sildenafil
Case reports, a few small open-label trials, and 1 prospective, randomized controlled trial (RCT) have evaluated sildenafil as an adjunctive treatment for serotonergic antidepressant-associated sexual dysfunction in women.6,9 Nurnberg et al6 examined the efficacy of adjunctive sildenafil in women with SSRI-induced sexual dysfunction. This 8-week, placebo-controlled, double-blind, RCT used a flexible dose (50 or 100 mg), intention-to-treat design to assess the effect of sildenafil on 98 premenopausal women whose depression was in remission. Ten patients were taking the serotonin-norepinephrine inhibitor venlafaxine, 1 was taking the TCA clomipramine, and 87 were receiving an SSRI. Patients were instructed to take sildenafil or placebo 1 to 2 hours before sexual activity. The primary outcome was mean change from baseline on the Clinical Global Impression-Sexual Function (CGI-SF) scale.
Women taking sildenafil showed significant improvement compared with those taking placebo, with a treatment difference between groups of 0.8 (95% CI, 0.6 to 1.0; =.001). Additionally, 23% of sildenafil-treated patients reported no improvement with the intervention, compared with 73% of patients receiving placebo. Secondary outcomes using 3 validated scales that evaluated specific phases of sexual function found that patients’ orgasmic function significantly benefited from sildenafil treatment, while desire, arousal, and overall satisfaction were not significantly different.
Although these findings seem to support sildenafil for treating serotonergic antidepressant-associated sexual dysfunction in women, the study had a relatively small treatment effect in a well-defined patient population; therefore, replication in future trials and different patient populations is warranted. Overall, sildenafil was well tolerated, despite patient reports of headaches, flushing, visual disturbances, dyspepsia, nasal congestion, and palpitations. Finally, cost vs benefit should be considered; PDE5 inhibitors may not be covered by insurance or may require prior authorization.
CASE CONTINUED: Symptoms resolve
Bupropion is not an appropriate choice for Mrs. L because of her seizure risk. Mirtazapine is ruled out because in the past she experienced excessive somnolence that impaired her ability to function. You are not comfortable prescribing nefazodone because of its risk of hepatotoxicity or suggesting that Mrs. L take a “drug holiday” (stop taking any antidepressants for a short period) because of the risk of depressive relapse. You suggest that Mrs. L continue to take sertraline because sometimes antidepressant-induced sexual dysfunction resolves after ≥6 months of treatment with the same agent, but she is adamant that her relationship with her husband will deteriorate if she waits that long. She also declines cognitive-behavioral therapy because her job doesn’t allow the time or flexibility to commit to the sessions.
You prescribe sildenafil, 50 mg, and instruct Mrs. L to take 1 tablet 1 to 2 hours before sexual activity. This treatment improves her ability to achieve orgasm. She tolerates the drug well and after 8 weeks of treatment her CGI-SF score improves from 6 at baseline, indicating extreme dysfunction, to 2, indicating normal function. Ten months into her sertraline treatment, Mrs. L discovers she no longer requires sildenafil to achieve orgasm.
Related Resources
- Nurnberg HG. An evidence-based review updating the various treatment and management approaches to serotonin reuptake inhibitor-associated sexual dysfunction. Drugs Today (Barc). 2008;44(2):147-168.
- NIH Medline Plus. Sexual problems in women. www.nlm.nih.gov/medlineplus/sexualproblemsinwomen.html.
- Sturpe DA, Mertens MK, Scoville C. What are the treatment options for SSRI-related sexual dysfunction? J Fam Pract. 2002;51(8):681.
Drug Brand Names
- Amantadine • Symadine, Symmetrel
- Avanafil • Stendra
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Granisetron • Kytril
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nitroglycerin • Nitrostat
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Sildenafil • Viagra
- Tadalafil • Cialis
- Vardenafil • Levitra
- Venlafaxine • Effexor
Disclosures
Dr. Burghardt receives grant or research support from the University of Michigan Depression Center.
Ms. Gardner reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Montejo AL, Llorca G, Izquierdo JA, et al. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62(suppl 3):10-21.
3. Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009;29(3):259-266.
4. Clayton AH, Pradko JF, Croft HA, et al. Prevalence of sexual dysfunction among newer antidepressants. J Clin Psychiatry. 2002;63(4):357-366.
5. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35-39.
6. Nurnberg HG, Hensley PL, Heiman JR, et al. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300(4):395-404.
7. Taylor MJ, Rudkin L, Hawton K. Strategies for managing antidepressant-induced sexual dysfunction: systematic review of randomised controlled trials. J Affect Disord. 2005;88(3):241-254.
8. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
9. Brown DA, Kyle JA, Ferrill MJ. Assessing the clinical efficacy of sildenafil for the treatment of female sexual dysfunction. Ann Pharmacother. 2009;43(7):1275-1285.
- Sexual dysfunction can arise from environmental, social, medical, or drug effects and requires a multifaceted approach to treatment.
- When possible, take a baseline sexual dysfunction measurement to assess if selective serotonin reuptake inhibitor use is correlated with onset or worsening of sexual dysfunction.
- Nonpharmacologic options should be considered before and during pharmacotherapy.
- Sildenafil may be useful for treating anorgasmia in women taking serotonergic antidepressants.
- Phosphodiesterase type 5 inhibitors are not FDA-approved for sexual dysfunction in women.
Mrs. L, age 27, has a history of major depressive disorder with symptoms of anxiety. She was managed successfully for 2 years with bupropion XL, 300 mg/d, but was switched to venlafaxine, titrated to 225 mg/d, after she developed seizures secondary to a head injury sustained in a car accident. After the switch, Mrs. L’s mood deteriorated and she was hospitalized. Since then, she’s received several medication trials, including paroxetine, 30 mg/d, a selective serotonin reuptake inhibitor (SSRI), and the tricyclic antidepressant (TCA) nortriptyline, 75 mg/d, but she could not tolerate these medications because of severe xerostomia.
After taking sertraline, 150 mg/d, for 8 weeks, Mrs. L improves and has a Patient Health Questionnaire score of 6, indicating mild depression. Her initial complaints of diarrhea and nausea have resolved, but Mrs. L now reports that she and her husband are having marital difficulties because she cannot achieve orgasm during sexual intercourse. She did not have this problem when she was taking bupropion. Her husband occasionally takes the phosphodiesterase type 5 (PDE5) inhibitor sildenafil before intercourse, and Mrs. L asks you if this medication will help her achieve orgasm.
DSM-IV-TR defines sexual dysfunction as disturbances in sexual desire and/or in the sexual response cycle (excitement, plateau, orgasm, and resolution) that result in marked distress and interpersonal difficulty.1 Sexual dysfunction can occur with the use of any antidepressant with serotonergic activity; it affects an estimated 50% to 70% of patients who take SSRIs.2 Sexual dysfunction can occur with all SSRIs; however, higher rates of sexual dysfunction are found with citalopram, fluoxetine, paroxetine, and sertraline.3 Studies have suggested there may be a dose-side effect relationship with SSRI-induced sexual dysfunction.4
Several factors can increase a patient’s risk of sexual dysfunction and should be considered before prescribing an antidepressant or when a patient presents with new or worsening sexual dysfunction (Table 1).5 In general, nonserotonergic agents such as bupropion, mirtazapine, and nefazodone are associated with lower rates of sexual dysfunction. The pharmacology of these agents explains their decreased propensity to cause sexual dysfunction. These agents increase levels of dopamine in the mesolimbic dopaminergic system either by blocking reuptake (bupropion) or antagonizing the serotonin subtype-2 receptor and facilitating disinhibition of decreased dopamine downstream (nefazodone and mirtazapine).
Table 1
Risk factors for sexual dysfunction
| Sex | Risk factors |
|---|---|
| Women | History of sexual, physical, or emotional abuse, physical inactivity |
| Men | Severe hyperprolactinemia, smoking |
| Both sexes | Poor to fair health, genitourinary disease, diabetes mellitus, cardiovascular disease, hypertension, increasing age, psychiatric disorders, relationship difficulties |
| Source: Reference 5 | |
One option for treating antidepressant-induced sexual dysfunction in women is PDE5 inhibitors, which are used to treat erectile dysfunction (ED). These medications ameliorate ED by inhibiting degradation of cyclic guanosine monophosphate by PDE5, which increases blood flow to the penis during sexual stimulation. Although these medications are not FDA-approved for treating sexual dysfunction in women, adjunctive PDE5 inhibitor treatment may be beneficial for sexual dysfunction in females because similar mediators, such as nitric oxide and cyclic guanosine monophosphate, involved in the nonadrenergic-noncholinergic signaling that controls sexual stimulation in men also are found in female genital tissue.6
When treating a woman with SSRI-induced sexual dysfunction, consider nonpharmacologic treatments both before and during pharmacotherapy (Table 2).7,8 See Table 3 for a comparison of pharmacokinetics, side effects, and drug interactions of the 4 FDA-approved PDE5 inhibitors—avanafil, sildenafil, tadalafil, and vardenafil.
Table 2
Management strategies for SSRI-induced sexual dysfunction
| Intervention | Comments |
|---|---|
| Nonpharmacologic | |
| Lifestyle modifications | Encourage healthy eating, weight loss, smoking cessation, substance abuse treatment, or minimizing alcohol intake to improve patient self-image and overall health |
| Cognitive-behavioral therapy | Patients can identify coping strategies for reducing symptom severity and preventing worsening sexual dysfunction |
| Sex therapy | May benefit patients with relationship difficulties |
| ‘Watch and wait’ | Spontaneous resolving (or ‘adaptation’) of sexual dysfunction with antidepressants can take ≥6 months. Studies have found adaptation rates generally are low (~10%) |
| Pharmacologic | |
| Drug holiday | May be an option for patients taking antidepressants with shorter half-lives and patients taking lower doses. Be cautious of empowering patients to stop their own medications as needed |
| Dosage reduction | Serotonergic antidepressant-induced sexual dysfunction may be related to dose. Little research has been conducted on this method and the patient’s clinical status must be considered |
| Dose timing | Instructing a patient to take the antidepressant after his or her usual time of sexual activity (eg, patients who engage in sexual activity at night should take the antidepressant before falling asleep). This may allow the drug level to be lowest during sexual activity |
| Switching medications | Case reports, retrospective studies, and RCTs suggest switching to a different antidepressant with less serotonergic activity may be appropriate, particularly if the patient has not responded to the current antidepressant |
| Adjunctive therapy | RCTs support adjunctive bupropion (≥300 mg/d) or olanzapine (5 mg/d) as treatment for SSRI-induced sexual dysfunction in women Studies have found no improvement in sexual functioning with adjunctive buspirone, granisetron, amantadine, mirtazapine, yohimbine, ephedrine, or ginkgo biloba in women |
| RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor Source: Reference 7,8 | |
Table 3
Phosphodiesterase type 5 inhibitors: A comparison
| Medication | Dose rangea | Pharmacokinetics | Side effects | Significant drug interactions |
|---|---|---|---|---|
| Avanafil | 50 to 200 mg, 30 minutes before sexual activity | Bioavailability: N/A (high-fat meal delays Tmax by 60 minutes and reduces Cmax by 24% to 39%; clinically insignificant) Half life: 5 hours Metabolism: CYP3A4 | Headache, flushing, nasal congestion, nasopharyngitis, backache | Strong CYP3A4 inhibitors (increased avanafil levels) Contraindicated within 12 hours of nitrate use (eg, nitroglycerin) |
| Sildenafil | 25 to 100 mg, 1 to 2 hours before sexual activity | Bioavailability: 41% (food/high-fat meal delays Tmax by 60 minutes and reduces Cmax by 29%) Half life: 4 hours Metabolism: CYP3A4 | Headache, flushing, erythema, indigestion, insomnia, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased sildenafil levels) Contraindicated within 24 hours of nitrate use |
| Tadalafil | 10 to 20 mg, 30 minutes before sexual activity | Bioavailability: N/A (not affected by food) Half life: 17.5 hours (duration of action up to 36 hours) Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, myalgia, and back pain | Strong CYP3A4 inhibitors (increased tadalafil levels) Contraindicated within 48 hours of nitrate use |
| Vardenafil | 5 to 20 mg, 30 minutes to 2 hours before sexual activity | Bioavailability: 15% for film-coated tablet (high-fat meal reduces Cmax by 18% to 50%) Half life: 4 to 5 hours Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased vardenafil levels) Contraindicated within 24 hours of nitrate use |
| aTypical dose range for treatment of erectile dysfunction Cmax: maximum concentration; CYP: cytochrome P450; Tmax: time to maximum concentration Source: Micromedex® Healthcare Series [Internet database]. Greenwood Village, CO: Thomson Healthcare. Accessed October 10, 2012 | ||||
Limited evidence for sildenafil
Case reports, a few small open-label trials, and 1 prospective, randomized controlled trial (RCT) have evaluated sildenafil as an adjunctive treatment for serotonergic antidepressant-associated sexual dysfunction in women.6,9 Nurnberg et al6 examined the efficacy of adjunctive sildenafil in women with SSRI-induced sexual dysfunction. This 8-week, placebo-controlled, double-blind, RCT used a flexible dose (50 or 100 mg), intention-to-treat design to assess the effect of sildenafil on 98 premenopausal women whose depression was in remission. Ten patients were taking the serotonin-norepinephrine inhibitor venlafaxine, 1 was taking the TCA clomipramine, and 87 were receiving an SSRI. Patients were instructed to take sildenafil or placebo 1 to 2 hours before sexual activity. The primary outcome was mean change from baseline on the Clinical Global Impression-Sexual Function (CGI-SF) scale.
Women taking sildenafil showed significant improvement compared with those taking placebo, with a treatment difference between groups of 0.8 (95% CI, 0.6 to 1.0; =.001). Additionally, 23% of sildenafil-treated patients reported no improvement with the intervention, compared with 73% of patients receiving placebo. Secondary outcomes using 3 validated scales that evaluated specific phases of sexual function found that patients’ orgasmic function significantly benefited from sildenafil treatment, while desire, arousal, and overall satisfaction were not significantly different.
Although these findings seem to support sildenafil for treating serotonergic antidepressant-associated sexual dysfunction in women, the study had a relatively small treatment effect in a well-defined patient population; therefore, replication in future trials and different patient populations is warranted. Overall, sildenafil was well tolerated, despite patient reports of headaches, flushing, visual disturbances, dyspepsia, nasal congestion, and palpitations. Finally, cost vs benefit should be considered; PDE5 inhibitors may not be covered by insurance or may require prior authorization.
CASE CONTINUED: Symptoms resolve
Bupropion is not an appropriate choice for Mrs. L because of her seizure risk. Mirtazapine is ruled out because in the past she experienced excessive somnolence that impaired her ability to function. You are not comfortable prescribing nefazodone because of its risk of hepatotoxicity or suggesting that Mrs. L take a “drug holiday” (stop taking any antidepressants for a short period) because of the risk of depressive relapse. You suggest that Mrs. L continue to take sertraline because sometimes antidepressant-induced sexual dysfunction resolves after ≥6 months of treatment with the same agent, but she is adamant that her relationship with her husband will deteriorate if she waits that long. She also declines cognitive-behavioral therapy because her job doesn’t allow the time or flexibility to commit to the sessions.
You prescribe sildenafil, 50 mg, and instruct Mrs. L to take 1 tablet 1 to 2 hours before sexual activity. This treatment improves her ability to achieve orgasm. She tolerates the drug well and after 8 weeks of treatment her CGI-SF score improves from 6 at baseline, indicating extreme dysfunction, to 2, indicating normal function. Ten months into her sertraline treatment, Mrs. L discovers she no longer requires sildenafil to achieve orgasm.
Related Resources
- Nurnberg HG. An evidence-based review updating the various treatment and management approaches to serotonin reuptake inhibitor-associated sexual dysfunction. Drugs Today (Barc). 2008;44(2):147-168.
- NIH Medline Plus. Sexual problems in women. www.nlm.nih.gov/medlineplus/sexualproblemsinwomen.html.
- Sturpe DA, Mertens MK, Scoville C. What are the treatment options for SSRI-related sexual dysfunction? J Fam Pract. 2002;51(8):681.
Drug Brand Names
- Amantadine • Symadine, Symmetrel
- Avanafil • Stendra
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Granisetron • Kytril
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nitroglycerin • Nitrostat
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Sildenafil • Viagra
- Tadalafil • Cialis
- Vardenafil • Levitra
- Venlafaxine • Effexor
Disclosures
Dr. Burghardt receives grant or research support from the University of Michigan Depression Center.
Ms. Gardner reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
- Sexual dysfunction can arise from environmental, social, medical, or drug effects and requires a multifaceted approach to treatment.
- When possible, take a baseline sexual dysfunction measurement to assess if selective serotonin reuptake inhibitor use is correlated with onset or worsening of sexual dysfunction.
- Nonpharmacologic options should be considered before and during pharmacotherapy.
- Sildenafil may be useful for treating anorgasmia in women taking serotonergic antidepressants.
- Phosphodiesterase type 5 inhibitors are not FDA-approved for sexual dysfunction in women.
Mrs. L, age 27, has a history of major depressive disorder with symptoms of anxiety. She was managed successfully for 2 years with bupropion XL, 300 mg/d, but was switched to venlafaxine, titrated to 225 mg/d, after she developed seizures secondary to a head injury sustained in a car accident. After the switch, Mrs. L’s mood deteriorated and she was hospitalized. Since then, she’s received several medication trials, including paroxetine, 30 mg/d, a selective serotonin reuptake inhibitor (SSRI), and the tricyclic antidepressant (TCA) nortriptyline, 75 mg/d, but she could not tolerate these medications because of severe xerostomia.
After taking sertraline, 150 mg/d, for 8 weeks, Mrs. L improves and has a Patient Health Questionnaire score of 6, indicating mild depression. Her initial complaints of diarrhea and nausea have resolved, but Mrs. L now reports that she and her husband are having marital difficulties because she cannot achieve orgasm during sexual intercourse. She did not have this problem when she was taking bupropion. Her husband occasionally takes the phosphodiesterase type 5 (PDE5) inhibitor sildenafil before intercourse, and Mrs. L asks you if this medication will help her achieve orgasm.
DSM-IV-TR defines sexual dysfunction as disturbances in sexual desire and/or in the sexual response cycle (excitement, plateau, orgasm, and resolution) that result in marked distress and interpersonal difficulty.1 Sexual dysfunction can occur with the use of any antidepressant with serotonergic activity; it affects an estimated 50% to 70% of patients who take SSRIs.2 Sexual dysfunction can occur with all SSRIs; however, higher rates of sexual dysfunction are found with citalopram, fluoxetine, paroxetine, and sertraline.3 Studies have suggested there may be a dose-side effect relationship with SSRI-induced sexual dysfunction.4
Several factors can increase a patient’s risk of sexual dysfunction and should be considered before prescribing an antidepressant or when a patient presents with new or worsening sexual dysfunction (Table 1).5 In general, nonserotonergic agents such as bupropion, mirtazapine, and nefazodone are associated with lower rates of sexual dysfunction. The pharmacology of these agents explains their decreased propensity to cause sexual dysfunction. These agents increase levels of dopamine in the mesolimbic dopaminergic system either by blocking reuptake (bupropion) or antagonizing the serotonin subtype-2 receptor and facilitating disinhibition of decreased dopamine downstream (nefazodone and mirtazapine).
Table 1
Risk factors for sexual dysfunction
| Sex | Risk factors |
|---|---|
| Women | History of sexual, physical, or emotional abuse, physical inactivity |
| Men | Severe hyperprolactinemia, smoking |
| Both sexes | Poor to fair health, genitourinary disease, diabetes mellitus, cardiovascular disease, hypertension, increasing age, psychiatric disorders, relationship difficulties |
| Source: Reference 5 | |
One option for treating antidepressant-induced sexual dysfunction in women is PDE5 inhibitors, which are used to treat erectile dysfunction (ED). These medications ameliorate ED by inhibiting degradation of cyclic guanosine monophosphate by PDE5, which increases blood flow to the penis during sexual stimulation. Although these medications are not FDA-approved for treating sexual dysfunction in women, adjunctive PDE5 inhibitor treatment may be beneficial for sexual dysfunction in females because similar mediators, such as nitric oxide and cyclic guanosine monophosphate, involved in the nonadrenergic-noncholinergic signaling that controls sexual stimulation in men also are found in female genital tissue.6
When treating a woman with SSRI-induced sexual dysfunction, consider nonpharmacologic treatments both before and during pharmacotherapy (Table 2).7,8 See Table 3 for a comparison of pharmacokinetics, side effects, and drug interactions of the 4 FDA-approved PDE5 inhibitors—avanafil, sildenafil, tadalafil, and vardenafil.
Table 2
Management strategies for SSRI-induced sexual dysfunction
| Intervention | Comments |
|---|---|
| Nonpharmacologic | |
| Lifestyle modifications | Encourage healthy eating, weight loss, smoking cessation, substance abuse treatment, or minimizing alcohol intake to improve patient self-image and overall health |
| Cognitive-behavioral therapy | Patients can identify coping strategies for reducing symptom severity and preventing worsening sexual dysfunction |
| Sex therapy | May benefit patients with relationship difficulties |
| ‘Watch and wait’ | Spontaneous resolving (or ‘adaptation’) of sexual dysfunction with antidepressants can take ≥6 months. Studies have found adaptation rates generally are low (~10%) |
| Pharmacologic | |
| Drug holiday | May be an option for patients taking antidepressants with shorter half-lives and patients taking lower doses. Be cautious of empowering patients to stop their own medications as needed |
| Dosage reduction | Serotonergic antidepressant-induced sexual dysfunction may be related to dose. Little research has been conducted on this method and the patient’s clinical status must be considered |
| Dose timing | Instructing a patient to take the antidepressant after his or her usual time of sexual activity (eg, patients who engage in sexual activity at night should take the antidepressant before falling asleep). This may allow the drug level to be lowest during sexual activity |
| Switching medications | Case reports, retrospective studies, and RCTs suggest switching to a different antidepressant with less serotonergic activity may be appropriate, particularly if the patient has not responded to the current antidepressant |
| Adjunctive therapy | RCTs support adjunctive bupropion (≥300 mg/d) or olanzapine (5 mg/d) as treatment for SSRI-induced sexual dysfunction in women Studies have found no improvement in sexual functioning with adjunctive buspirone, granisetron, amantadine, mirtazapine, yohimbine, ephedrine, or ginkgo biloba in women |
| RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor Source: Reference 7,8 | |
Table 3
Phosphodiesterase type 5 inhibitors: A comparison
| Medication | Dose rangea | Pharmacokinetics | Side effects | Significant drug interactions |
|---|---|---|---|---|
| Avanafil | 50 to 200 mg, 30 minutes before sexual activity | Bioavailability: N/A (high-fat meal delays Tmax by 60 minutes and reduces Cmax by 24% to 39%; clinically insignificant) Half life: 5 hours Metabolism: CYP3A4 | Headache, flushing, nasal congestion, nasopharyngitis, backache | Strong CYP3A4 inhibitors (increased avanafil levels) Contraindicated within 12 hours of nitrate use (eg, nitroglycerin) |
| Sildenafil | 25 to 100 mg, 1 to 2 hours before sexual activity | Bioavailability: 41% (food/high-fat meal delays Tmax by 60 minutes and reduces Cmax by 29%) Half life: 4 hours Metabolism: CYP3A4 | Headache, flushing, erythema, indigestion, insomnia, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased sildenafil levels) Contraindicated within 24 hours of nitrate use |
| Tadalafil | 10 to 20 mg, 30 minutes before sexual activity | Bioavailability: N/A (not affected by food) Half life: 17.5 hours (duration of action up to 36 hours) Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, myalgia, and back pain | Strong CYP3A4 inhibitors (increased tadalafil levels) Contraindicated within 48 hours of nitrate use |
| Vardenafil | 5 to 20 mg, 30 minutes to 2 hours before sexual activity | Bioavailability: 15% for film-coated tablet (high-fat meal reduces Cmax by 18% to 50%) Half life: 4 to 5 hours Metabolism: CYP3A4 | Headache, flushing, indigestion, nasal congestion, dizziness, visual disturbances (blue vision) | Strong CYP3A4 inhibitors (increased vardenafil levels) Contraindicated within 24 hours of nitrate use |
| aTypical dose range for treatment of erectile dysfunction Cmax: maximum concentration; CYP: cytochrome P450; Tmax: time to maximum concentration Source: Micromedex® Healthcare Series [Internet database]. Greenwood Village, CO: Thomson Healthcare. Accessed October 10, 2012 | ||||
Limited evidence for sildenafil
Case reports, a few small open-label trials, and 1 prospective, randomized controlled trial (RCT) have evaluated sildenafil as an adjunctive treatment for serotonergic antidepressant-associated sexual dysfunction in women.6,9 Nurnberg et al6 examined the efficacy of adjunctive sildenafil in women with SSRI-induced sexual dysfunction. This 8-week, placebo-controlled, double-blind, RCT used a flexible dose (50 or 100 mg), intention-to-treat design to assess the effect of sildenafil on 98 premenopausal women whose depression was in remission. Ten patients were taking the serotonin-norepinephrine inhibitor venlafaxine, 1 was taking the TCA clomipramine, and 87 were receiving an SSRI. Patients were instructed to take sildenafil or placebo 1 to 2 hours before sexual activity. The primary outcome was mean change from baseline on the Clinical Global Impression-Sexual Function (CGI-SF) scale.
Women taking sildenafil showed significant improvement compared with those taking placebo, with a treatment difference between groups of 0.8 (95% CI, 0.6 to 1.0; =.001). Additionally, 23% of sildenafil-treated patients reported no improvement with the intervention, compared with 73% of patients receiving placebo. Secondary outcomes using 3 validated scales that evaluated specific phases of sexual function found that patients’ orgasmic function significantly benefited from sildenafil treatment, while desire, arousal, and overall satisfaction were not significantly different.
Although these findings seem to support sildenafil for treating serotonergic antidepressant-associated sexual dysfunction in women, the study had a relatively small treatment effect in a well-defined patient population; therefore, replication in future trials and different patient populations is warranted. Overall, sildenafil was well tolerated, despite patient reports of headaches, flushing, visual disturbances, dyspepsia, nasal congestion, and palpitations. Finally, cost vs benefit should be considered; PDE5 inhibitors may not be covered by insurance or may require prior authorization.
CASE CONTINUED: Symptoms resolve
Bupropion is not an appropriate choice for Mrs. L because of her seizure risk. Mirtazapine is ruled out because in the past she experienced excessive somnolence that impaired her ability to function. You are not comfortable prescribing nefazodone because of its risk of hepatotoxicity or suggesting that Mrs. L take a “drug holiday” (stop taking any antidepressants for a short period) because of the risk of depressive relapse. You suggest that Mrs. L continue to take sertraline because sometimes antidepressant-induced sexual dysfunction resolves after ≥6 months of treatment with the same agent, but she is adamant that her relationship with her husband will deteriorate if she waits that long. She also declines cognitive-behavioral therapy because her job doesn’t allow the time or flexibility to commit to the sessions.
You prescribe sildenafil, 50 mg, and instruct Mrs. L to take 1 tablet 1 to 2 hours before sexual activity. This treatment improves her ability to achieve orgasm. She tolerates the drug well and after 8 weeks of treatment her CGI-SF score improves from 6 at baseline, indicating extreme dysfunction, to 2, indicating normal function. Ten months into her sertraline treatment, Mrs. L discovers she no longer requires sildenafil to achieve orgasm.
Related Resources
- Nurnberg HG. An evidence-based review updating the various treatment and management approaches to serotonin reuptake inhibitor-associated sexual dysfunction. Drugs Today (Barc). 2008;44(2):147-168.
- NIH Medline Plus. Sexual problems in women. www.nlm.nih.gov/medlineplus/sexualproblemsinwomen.html.
- Sturpe DA, Mertens MK, Scoville C. What are the treatment options for SSRI-related sexual dysfunction? J Fam Pract. 2002;51(8):681.
Drug Brand Names
- Amantadine • Symadine, Symmetrel
- Avanafil • Stendra
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Granisetron • Kytril
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nitroglycerin • Nitrostat
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Sildenafil • Viagra
- Tadalafil • Cialis
- Vardenafil • Levitra
- Venlafaxine • Effexor
Disclosures
Dr. Burghardt receives grant or research support from the University of Michigan Depression Center.
Ms. Gardner reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Montejo AL, Llorca G, Izquierdo JA, et al. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62(suppl 3):10-21.
3. Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009;29(3):259-266.
4. Clayton AH, Pradko JF, Croft HA, et al. Prevalence of sexual dysfunction among newer antidepressants. J Clin Psychiatry. 2002;63(4):357-366.
5. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35-39.
6. Nurnberg HG, Hensley PL, Heiman JR, et al. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300(4):395-404.
7. Taylor MJ, Rudkin L, Hawton K. Strategies for managing antidepressant-induced sexual dysfunction: systematic review of randomised controlled trials. J Affect Disord. 2005;88(3):241-254.
8. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
9. Brown DA, Kyle JA, Ferrill MJ. Assessing the clinical efficacy of sildenafil for the treatment of female sexual dysfunction. Ann Pharmacother. 2009;43(7):1275-1285.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Montejo AL, Llorca G, Izquierdo JA, et al. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62(suppl 3):10-21.
3. Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009;29(3):259-266.
4. Clayton AH, Pradko JF, Croft HA, et al. Prevalence of sexual dysfunction among newer antidepressants. J Clin Psychiatry. 2002;63(4):357-366.
5. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35-39.
6. Nurnberg HG, Hensley PL, Heiman JR, et al. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300(4):395-404.
7. Taylor MJ, Rudkin L, Hawton K. Strategies for managing antidepressant-induced sexual dysfunction: systematic review of randomised controlled trials. J Affect Disord. 2005;88(3):241-254.
8. Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry. 2006;163(9):1504-1509.
9. Brown DA, Kyle JA, Ferrill MJ. Assessing the clinical efficacy of sildenafil for the treatment of female sexual dysfunction. Ann Pharmacother. 2009;43(7):1275-1285.
Vitamin D deficiency and psychiatric illness
In the United States, >50% of psychiatric inpatients have vitamin D deficiency—<30 nmol/L (<12 ng/mL).1 A growing body of literature has found associations between vitamin D deficiency and psychiatric illnesses, particularly depression. Several randomized controlled trials (RCTs) have demonstrated that vitamin D supplementation can benefit depression symptoms. In this article, we discuss the current literature on vitamin D and psychiatric illness, and provide practical information for clinicians on the use of vitamin D supplementation.
Biosynthesis of vitamin D
Biosynthesis of vitamin D begins with the sterol provitamin D3 molecule 7-dehydrocholesterol (Figure).2 When skin is exposed to sunlight, 7-dehydrocholesterol absorbs UV radiation and forms provitamin D3, which undergoes rapid transformation to vitamin D3.2 Vitamin D3 is released from the plasma membrane and enters systemic circulation in a protein-bound form that has a serum half-life of 36 to 78 hours.3 Vitamin D3 can be taken up by adipocytes and stored in fat deposits, where it has a half-life of approximately 2 months.4
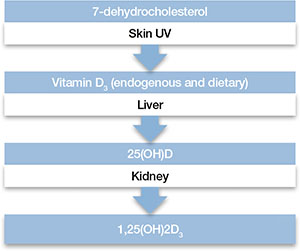
Figure: Biosynthesis of vitamin D
Provitamin D3 (7-dehydrocholesterol) in the skin absorbs UV radiation and undergoes isomerization to form vitamin D3. Endogenously produced vitamin D3 along with dietary vitamin D2 and vitamin D3 absorbed in the gastrointestinal tract are metabolized in the liver to 25-hydroxyvitamin D (25[OH]D), which re-enters the circulation and is metabolized in the kidney and other tissues to the active metabolite 1,25-dihydroxyvitamin D (1,25[OH]2D). Catabolism of 25(OH)D and 1,25(OH)2D into biologically-inactive molecules is primarily mediated by the cytochrome P450 (CYP) enzymes CYP24 and CYP3A4.
Source: Reference 2Circulating vitamin D3 is metabolized in the liver by the enzyme vitamin D-25-hydroxylase to 25-hydroxyvitamin D (25[OH]D3), which has a serum half-life of approximately 15 days.4 Circulating 25(OH)D3 is not biologically active at the physiological level, and requires activation by conversion to 1,25-dihydroxyvitamin D (1,25[OH]2D3) in the kidneys by the enzyme 25(OH)D-1α-hydroxylase. Production of 1,25(OH)2D3 is regulated by serum phosphorus and parathyroid hormone levels and other factors.5 Catabolism of 1,25(OH)2D3 is rapid, with a serum half-life of 3.5 to 21 hours.6 Vitamin D2 is structurally similar to vitamin D3, but occurs primarily in fungi, yeasts, and some invertebrates.
Risk factors for deficiency
A patient’s vitamin D status is determined by measuring 25(OH)D (Box 1). Risk factors for vitamin D deficiency include conditions that affect cutaneous production (insufficient sunlight exposure), obesity, gastrointestinal disorders, aging, renal disorders, and medications (Table 1). 2,5,7,8 The link between sunscreen use, either alone or in cosmetics, and vitamin D deficiency continues to be debated. While controlled studies have found that application of sunscreen with high sun protection factor can significantly reduce vitamin D production, 9 studies in clinical populations have failed to confirm these findings. 10,11 See Box 2 for a discussion of these risk factors and Box 3 for a discussion of acute and long-term medical manifestations of deficiency.
Although 1,25-dihydroxyvitamin D (1,25[OH]2D3) is the biologically active form of vitamin D, its circulating half-life is only 4 to 6 hours.a,b Therefore, 25-hydroxyvitamin D (25[OH]D) is the principal vitamin D metabolite measured to determine vitamin D status. Vitamin D levels commonly are expressed as ng/mL or nmol/L; the conversion factor from ng/mL to nmol/L is 2.496. The Institute of Medicine has defined vitamin D deficiency as a serum 25(OH)D level of <30 nmol/L (<12 ng/mL).c However, many experts define vitamin D insufficiency as a 25(OH)D level of 21 to 29 ng/ml, and deficiency as <20 ng/mL.a,d The upper limit is more difficult to define, but symptoms of vitamin D intoxication appear with blood levels >150 to 200 ng/mL.a
References
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81(3):353-373.
- Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73-78.
- Aloia JF. Clinical review: the 2011 report on dietary reference intake for vitamin D: where do we go from here? J Clin Endocrinol Metab. 2011;96(10):2987-2996.
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, et al. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84(1):18-28.
Table 1
Risk factors associated with vitamin D deficiency
| Age (>65) |
| Insufficient sunlight |
| Breastfeeding |
| Dark skin |
| Malabsorption diseases |
| Obesity (BMI >30 kg/m2) |
| Use of medications that alter vitamin D metabolism (eg, anticonvulsants, glucocorticoids) |
| Hepatobiliary disease |
| Renal disease |
| BMI: body mass index Source: References 2,5,7,8 |
Any factor that diminishes UV radiation penetration into the skin will affect cutaneous synthesis of vitamin D.a,b For example, sunscreen with a sun protection factor of 15 can decrease vitamin D synthesis by 98%.c Geography and its impact on yearly sunlight exposure is a well-known factor in vitamin D deficiency. Individuals who live below a latitude of approximately 35° North—approximately the southern border of Tennessee and through Albuquerque, NM—receive sufficient UV radiation exposure to ensure adequate vitamin D production throughout the year, but at higher latitudes, adequate vitamin D is not produced during winter months.d Melanin affects UV radiation absorption in a manner that prevents vitamin D production, and increased skin pigmentation markedly reduces vitamin D synthesis.e African Americans with very dark skin have significantly diminished cutaneous production of vitamin D.e,f
Renal 1α-hydroxylase activity decreases with aging in parallel with age-related decreases in glomerular filtration.g In addition, aging is associated with increased clearance of 1,25-dihydroxyvitamin D (1,25[OH]2D3).h However, vitamin D absorption generally is adequate even at older ages.i Studies have shown that obese individuals tend to have lower serum concentrations of vitamin D and 25-hydroxyvitamin D (25[OH]D) than those at a normal weight.j,k Obese patients have been shown to have lower cutaneous production of vitamin D3 and display lower bioavailability of orally administered vitamin D2.j
For patients with chronic renal insufficiency, creatinine clearance is positively correlated with serum 1,25(OH)2D levels.l Any process that results in malabsorption of intestinal fat may impair vitamin D absorption. In patients with celiac disease, biliary obstruction, or chronic pancreatitis, absorption consistently is reduced.m Individuals taking bile acid-binding medications, such as cholestyramine for hypercholesterolemia, also may have impaired vitamin D absorption.n In addition, hepatobiliary disease is associated with low levels of 25(OH)D.o Some drugs that alter hepatic metabolism are associated with vitamin D deficiency, including anticonvulsants or glucocorticoids, which can increase catabolism or vitamin D.p
References
- Holick MF. The vitamin D deficiency pandemic and consequences for nonskeletal health: mechanisms of action. Mol Aspects Med. 2008;29(6):361-368.
- Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
- Matsuoka LY, Ide L, Wortsman J, et al. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64(6):1165-1168.
- Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371.
- Clemens TL, Adams JS, Henderson SL, et al. Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet. 1982;1(8263):74-76.
- Chen TC, Chimeh F, Lu Z, et al. Factors that influence the cutaneous synthesis and dietary sources of vitamin D. Arch Biochem Biophys. 2007;460(2):213-217.
- Slovik DM, Adams JS, Neer RM, et al. Deficient production of 1,25-dihydroxyvitamin D in elderly osteoporotic patients. N Engl J Med. 1981;305(7):372-374.
- Armbrecht HJ, Zenser TV, Davis BB. Effect of age on the conversion of 25-hydroxyvitamin D3 to 1,25-dihydroxyvitamin D3 by kidney of rat. J Clin Invest. 1980;66(5):1118-1123.
- Lips P, Wiersinga A, van Ginkel FC, et al. The effect of vitamin D supplementation on vitamin D status and parathyroid function in elderly subjects. J Clin Endocrinol Metab. 1988;67(4):644-650.
- Wortsman J, Matsuoka LY, Chen TC, et al. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690-693.
- Bell NH, Epstein S, Greene A, et al. Evidence for alteration of the vitamin D-endocrine system in obese subjects. J Clin Invest. 1985;76(1):370-373.
- Pitts TO, Piraino BH, Mitro R, et al. Hyperparathyroidism and 1,25-dihydroxyvitamin D deficiency in mild, moderate, and severe renal failure. J Clin Endocrinol Metab. 1988;67(5):876-881.
- Thompson GR, Lewis B, Booth CC. Absorption of vitamin D3-3H in control subjects and patients with intestinal malabsorption. J Clin Invest. 1966;45(1):94-102.
- Lo CW, Paris PW, Clemens TL, et al. Vitamin D absorption in healthy subjects and in patients with intestinal malabsorption syndromes. Am J Clin Nutr. 1985;42(4):644-649.
- Pappa HM, Bern E, Kamin D, et al. Vitamin D status in gastrointestinal and liver disease. Curr Opin Gastroenterol. 2008;24(2):176-183.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
Acute effects. Vitamin D deficiency produces a range of clinical effects.a-c One well-documented consequence of vitamin D deficiency is osteomalacia—bone demineralization—which produces characteristic bone deformity and growth retardation in children.d,e In adults, osteomalacia may manifest as diffuse pain bone discomfort and muscle aches that may resemble fibromyalgia or arthritis.f Because vitamin D receptors are present in skeletal muscle, deficiency also may lead to proximal muscle weakness; an increased risk of falls; global bone discomfort, often elicited with pressure over the sternum or tibia; and low back pain in older women.c,f
Long-term effects. A large epidemiologic study found that adults with 25-hydroxyvitamin D (25[OH]D) levels <21 ng/mL had an increased risk of hypertension, diabetes, obesity, and dyslipidemia.g Cardiovascular mortality was higher in individuals with 25(OH)D levels <10 ng/mL compared with those with >40 ng/mL.h Adolescents in the National Health and Nutrition Examination Survey-III with serum 25(OH)D levels <15 ng/mL were more likely to have elevated blood glucose levels than those with >26 ng/mL.i Other epidemiologic data have demonstrated associations of vitamin D deficiency with multiple sclerosis, seasonal allergies, asthma, and various infectious diseases.j,k
Because vitamin D is known to promote cellular differentiation and inhibit cellular proliferation, its role in cancer has been studied extensively. A recent meta-analysis of case-control studies found that the odds of colon cancer were reduced by >40% for each 20 ng/mL increase in serum 25(OH)D levels.l Another meta-analysis reported a lower risk of breast cancer among women in the highest quartile of 25(OH)D values compared with the lowest quartile.m
References
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81(3):353-373.
- Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73-78.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
- Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
- Bordelon P, Ghetu MV, Langan RC. Recognition and management of vitamin D deficiency. Am Fam Physician. 2009;80(8):841-846.
- Hicks GE, Shardell M, Miller RR, et al. Associations between vitamin D status and pain in older adults: the Invecchiare in Chianti study. J Am Geriatr Soc. 2008;56(5):785-791.
- Martins D, Wolf M, Pan D, et al. Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2007;167(11):1159-1165.
- Ginde AA, Scragg R, Schwartz RS, et al. Prospective study of serum 25-hydroxyvitamin D level, cardiovascular disease mortality, and all-cause mortality in older U.S. adults. J Am Geriatr Soc. 2009;57(9):1595-1603.
- Reis JP, von Mühlen D, Miller ER 3rd, et al. Vitamin D status and cardiometabolic risk factors in the United States adolescent population. Pediatrics. 2009;124(3):e371-379.
- Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86(1):50-60.
- Munger KL, Levin LI, Hollis BW, et al. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296(23):2832-2838.
- Yin L, Grandi N, Raum E, et al. Meta-analysis: longitudinal studies of serum vitamin D and colorectal cancer risk. Aliment Pharmacol Ther. 2009;30(2):113-125.
- Chen P, Hu P, Xie D, et al. Meta-analysis of vitamin D, calcium and the prevention of breast cancer. Breast Cancer Res Treat. 2010;121(2):469-477.
Vitamin D’s role in the brain
Vitamin D’s role in psychiatric illnesses is suggested by region-specific expression of vitamin D receptors (VDR) in the cingulate cortex, thalamus, cerebellum, amygdala, and hippocampus.12 Most of these regions also express 1α-hydroxylase enzymes capable of metabolizing 25(OH)D to 1,25(OH)2D3, which suggests that vitamin D may have an autocrine or paracrine function in brain.13
Vitamin D regulates expression of tyrosine hydroxylase, the rate-limiting enzyme in the biosynthesis of dopamine, norepinephrine, and epinephrine.14 Vitamin D also promotes survival of monoaminergic neurons through upregulation of glial cell line-derived neurotrophic factor, which supports survival of midbrain dopaminergic neurons and confers resistance to neurotoxins that deplete dopaminergic neurons in Parkinson’s disease.15 Vitamin D also promotes neuronal survival by inhibiting oxidative pathways in the brain through inhibition of inducible nitric oxide synthase (reducing free radical formation)16 and upregulation of γ-glutamyl transpeptidase (increasing antioxidant production).17 Vitamin D may play a neuroprotective role through regulation of calcium channels. In vitro studies have shown that vitamin D downregulates expression of L-type calcium channels, conferring protection against excitatory neurotoxins in cultured neurons.18 Proteomic analysis of brain tissue in a rat model of developmental vitamin D revealed dysregulation of 36 brain proteins involved in many biologic pathways involved in calcium homeostasis, synaptic plasticity, and neurotransmission.19 Taken together, these findings suggest vitamin D has a neurosteroid-like role in the CNS.
Psychotic disorders
Several epidemiologic studies have linked low vitamin D levels to schizophrenia and other psychotic disorders. Researchers in Norway who used a structured clinical interview to identify psychosis consistently found low levels of 25(OH)D among immigrants and native Norwegians with psychotic symptoms.20 A study of 8,411 Swedish women found low vitamin D levels were associated with psychotic symptoms.21 The Finnish birth cohort study found that use of vitamin D supplementation during the first year of life reduced the incidence of schizophrenia.22 In another pilot study, researchers measured third-trimester serum 25(OH)D levels and found that low levels of maternal vitamin D may be associated with an increased risk of schizophrenia.23 These studies suggest that low prenatal vitamin D levels may adversely impact the developing brain, increasing the risk for adult-onset schizophrenia.
Cognitive dysfunction
Low vitamin D concentrations have been associated with impairments in cognitive functions such as memory and orientation,24 executive function impairments,25 and Alzheimer’s disease (AD).26 A large study conducted from 1998 to 2006 in Italy concluded that persons with severe vitamin D deficiency (<25 nmol/L) had a higher risk of substantial decline on Mini-Mental State Examination than those with sufficient levels (≥75 nmol/L).27 Other studies have linked low vitamin D levels to poor cognitive performance in depressed older adults.28 Low vitamin D levels in older women have been associated with risk of AD, but not with other dementias.29 Polymorphisms of VDR have been associated with depression and poor cognitive performance.30
Depression
Epidemiologic studies evaluating vitamin D deficiency have had conflicting results. The Third National Health and Nutrition Examination Survey, which used a sample of 7,970 non-institutionalized U.S. residents age 15 to 39, demonstrated that individuals with serum vitamin D ≤50 nmol/L are at a significantly higher risk of developing depression than those with vitamin D ≥75 nmol/L.31 A study of 1,282 adults age 65 to 95 in the Netherlands found that 25(OH)D levels were 14% lower in depressed patients compared with controls.32 However, a large epidemiologic study in China did not detect a relationship between vitamin D and depression in 3,262 men and women age 50 to 70.33 After researchers adjusted for geography, body mass index, physical activity, and smoking, 25(OH)D levels did not correlate significantly with the presence or severity of depression. In a case series,34 after 48 vitamin D-deficient depressed adolescents were given vitamin D3 over 3 months, there was a significant improvement in well-being, depressive symptoms, irritability, and fatigue.34 Other small, cross-sectional studies have examined associations between vitamin D status and depression with divergent results, which may reflect differences in population and methodology.
Prospective interventional studies. Although direct causal relationships are difficult to establish, several prospective studies have tested the hypothesis that treating vitamin D deficiency can improve depressive symptoms.
In a double-blind, controlled trial, Jorde et al35 randomized 441 individuals age 21 to 70 to vitamin D, 20,000 IU per week; vitamin D, 40,000 IU per week; or placebo for 1 year. Individuals with serum 25(OH)D levels <40 nmol/L scored significantly higher on depression rating scales than those with serum 25(OH)D levels ≥40 nmol/L at the end of the study. There was no significant improvement in depression ratings in the placebo group (Table 2).35 These results must be interpreted with care because depressive symptoms were secondary endpoints in this study.
Table 2
Effect of vitamin D supplementation on depressive symptoms in a controlled trial
| Vitamin D Supplementation | Serum 25(OH)D levels at baseline | BDI total score, Median and range at end of study | After 1 year of vitamin D supplementation |
|---|---|---|---|
| 20,000 IU/week | <40 nmol/L | Significantly higher (more depressive traits), 6.0 (0 to 23) | Significantly improved BDI score |
| 40,000 IU/week | ≥40 nmol/L | 4.5 (0 to 28) | Significantly improved BDI score |
| Placebo | - | - | No improvement in BDI score |
| 25(OH)D: 25-hydroxyvitamin D; BDI: Beck Depression Inventory Source: Reference 35 | |||
Kjærgaard et al36 systematically examined vitamin D levels in a case-control study followed by a randomized controlled trial (RCT) of vitamin D supplementation. In the case-control phase, participants with low 25(OH)D levels at baseline were significantly more depressed than participants with high 25(OH)D levels. Participants with low 25(OH)D levels were randomized to placebo or 40,000 IU vitamin D3 per week for 6 months. Low levels of vitamin D were strongly associated with depressive symptoms, but vitamin D supplementation did not have a significant effect on depressive symptom scores.
Seasonal affective disorder (SAD). Seasonal variation in vitamin D levels suggests that supplementation may help patients who have seasonal mood disturbances. In a randomized, double-blind study, 44 healthy individuals received vitamin D3, 400 IU/d, 800 IU/d, or no vitamin D3 for 5 days during late winter. Based on self-reports, vitamin D3 significantly enhanced positive affect and there was some evidence it reduced negative affect.37 In a pilot study of 9 women with serum vitamin D levels <40 ng/ml, vitamin D supplementation during winter was associated with an average 10-point decline in Beck Depression Inventory-II scores.38 In a prospective RCT of 15 individuals with SAD, all patients who received vitamin D improved in all outcome measures.39 Vieth40 randomized 82 adults with vitamin D deficiency to 600 IU/d or 4,000 IU/d of vitamin D3 for 3 months over 2 consecutive winters. Patients taking the higher dose showed some evidence of improved well-being compared with those taking the lower dose, although results were not significant for all comparisons. Two other trials did not observe any improvement in SAD symptoms with vitamin D treatment.41,42
Treating vitamin D deficiency
The Endocrine Society recently developed consensus guidelines for diagnosing and managing vitamin D deficiency.43 In addition, the Institute of Medicine of the National Academies recommends daily vitamin D supplementation to prevent deficiency:
- age <70: 400 IU/d
- age >70: 800 IU/d
- pregnant or lactating women: 600 IU/d
- upper limit: 4,000 IU/d.7
Higher doses may be used for patients deprived of sun exposure.8 A typical replacement regimen consists of oral ergocalciferol, 50,000 IU per week for 8 weeks.44 The optimal time for rechecking serum levels after repletion has not been clearly defined, but serum 25(OH)D levels should be measured again after therapy is completed. If values have not reached or exceeded 20 ng/mL, consider a second 8-week course of ergocalciferol (see the Box 1 for a discussion of measuring vitamin D levels). If serum 25(OH)D levels have not increased, the most likely cause is nonadherence or malabsorption.
Contraindications and toxicity. Contraindications to vitamin D supplementation include granulomatous diseases, sarcoidosis, metastatic bone disease, and Williams syndrome.45Table 345 lists signs of vitamin D toxicity. There is little risk of toxicity at dosages of up to 2,000 IU/d.46
Table 3
Signs of vitamin D toxicity
| Headache |
| Metallic taste |
| Nephrocalcinosis or vascular calcinosis |
| Pancreatitis |
| Nausea |
| Vomiting |
| Source: Reference 45 |
Related Resources
- LaFerney MC. Vitamin D deficiency in older adults. Current Psychiatry. 2012;11(11):63.
- National Institutes of Health Office of Dietary Supplements. Dietary supplement fact sheet: vitamin D. http://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional.
Drug Brand Names
- Cholestyramine • Questran
- Ergocalciferol • Calciferol, Drisdol
Disclosures
Dr. Harris is an employee of Rho, Chapel Hill, NC.
Dr. Jaiswal reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Holmes receives research support from Bristol-Myers Squibb, Elan, Merck, Otsuka, Shire, Takeda, and Theravance, and is on the speaker’s bureau for Forest Pharmaceuticals and PamLab.
Dr. Patkar is a consultant for Dey Pharmaceuticals, Forest, Gilead, and TTK Pharma and is on the speaker’s bureau and received honoraria from Alkermes, Bristol-Myers Squibb, Dey Pharmaceuticals, Pfizer, and Sunovion; and has received grant support from the Duke Endowment, Dey Pharmaceuticals, Envivo, Forest, Janssen, Lundbeck, The National Institutes of Health, the National Institute on Drug Abuse, National Institute on Alcohol Abuse and Alcoholism, Pfizer Inc., Shire, Sunovion, and Titan.
Dr. Weisler has been a consultant to, on the speaker’s bureaus of, and/or received research support from Abbott, Agency for Toxic Substances and Disease Registry, AstraZeneca, Biovail, Bristol-Myers Squibb, Burroughs Wellcome, Cenerx, Centers for Disease Control and Prevention, Cephalon, Ciba Geigy, CoMentis, Corcept, Cortex, Dainippon Sumitomo Pharma America, Eisai, Elan, Eli Lilly and Company, Forest Pharmaceuticals, GlaxoSmithKline, Janssen, Johnson & Johnson, Lundbeck, McNeil Pharmaceuticals, Medicinova, Medscape Advisory Board, Merck, National Institute of Mental Health, Neurochem, New River Pharmaceuticals, Novartis, Organon, Otsuka America Pharma, Pfizer Inc., Pharmacia, Repligen, Saegis, Sandoz, Sanofi, Sanofi-Synthelabo, Schwabe/Ingenix, Sepracor, Shire, Solvay, Sunovion, Synaptic, Takeda, TAP, Theravance, Transcept Pharma, TransTech, UCB Pharma, Validus, Vela, and Wyeth.
1. McCue RE, Charles RA, Orendain GC, et al. Vitamin D deficiency among psychiatric inpatients [published online April 19, 2012]. Prim Care Companion CNS Disord. doi: 10.4088/PCC.11m01230.
2. Tsiaras WG, Weinstock MA. Factors influencing vitamin D status. Acta Derm Venereol. 2011;91(2):115-124.
3. Adams JS, Clemens TL, Parrish JA, et al. Vitamin-D synthesis and metabolism after ultraviolet irradiation of normal and vitamin-D-deficient subjects. N Engl J Med. 1982;306(12):722-725.
4. Jones G. Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr. 2008;88(2):582S-586S.
5. Holick MF. Vitamin D: importance in the prevention of cancers type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371.
6. Fakih MG, Trump DL, Muindi JR, et al. A phase I pharmacokinetic and pharmacodynamic study of intravenous calcitriol in combination with oral gefitinib in patients with advanced solid tumors. Clin Cancer Res. 2007;13(4):1216-1223.
7. Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
8. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
9. Matsuoka LY, Ide L, Wortsman J, et al. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64(6):1165-1168.
10. Norval M, Wulf HC. Does chronic sunscreen use reduce vitamin D production to insufficient levels? Br J Dermatol. 2009;161(4):732-736.
11. Linos E, Keiser E, Kanzler M, et al. Sun protective behaviors and vitamin D levels in the US population: NHANES 2003-2006. Cancer Causes Control. 2012;23(1):133-140.
12. Prüfer K, Veenstra TD, Jirikowski GF, et al. Distribution of 1,25-dihydroxyvitamin D3 receptor immunoreactivity in the rat brain and spinal cord. J Chem Neuroanat. 1999;16(2):135-145.
13. Eyles DW, Smith S, Kinobe R, et al. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat. 2005;29(1):21-30.
14. Garcion E, Wion-Barbot N, Montero-Menei CN, et al. New clues about vitamin D functions in the nervous system. Trends Endocrinol Metab. 2002;13(3):100-105.
15. Smith MP, Fletcher-Turner A, Yurek DM, et al. Calcitriol protection against dopamine loss induced by intracerebroventricular administration of 6-hydroxydopamine. Neurochem Res. 2006;31(4):533-539.
16. Garcion E, Nataf S, Berod A, et al. 1,25-dihydroxyvitamin D3 inhibits the expression of inducible nitric oxide synthase in rat central nervous system during experimental allergic encephalomyelitis. Brain Res Mol Brain Res. 1997;45(2):255-267.
17. Baas D, Prüfer K, Ittel ME, et al. Rat oligodendrocytes express the vitamin D(3) receptor and respond to 1,25-dihydroxyvitamin D(3). Glia. 2000;31(1):59-68.
18. Brewer LD, Thibault V, Chen KC, et al. Vitamin D hormone confers neuroprotection in parallel with downregulation of L-type calcium channel expression in hippocampal neurons. J Neurosci. 2001;21(1):98-108.
19. Almeras L, Eyles D, Benech P, et al. Developmental vitamin D deficiency alters brain protein expression in the adult rat: implications for neuropsychiatric disorders. Proteomics. 2007;7(5):769-780.
20. Berg AO, Melle I, Torjesen PA, et al. A cross-sectional study of vitamin D deficiency among immigrants and Norwegians with psychosis compared to the general population. J Clin Psychiatry. 2010;71(12):1598-1604.
21. Hedelin M, Löf M, Olsson M, et al. Dietary intake of fish, omega-3, omega-6 polyunsaturated fatty acids and vitamin D and the prevalence of psychotic-like symptoms in a cohort of 33,000 women from the general population. BMC Psychiatry. 2010;10:38.-
22. McGrath J, Saari K, Hakko H, et al. Vitamin D supplementation during the first year of life and risk of schizophrenia: a Finnish birth cohort study. Schizophr Res. 2004;67(2-3):237-245.
23. McGrath J, Eyles D, Mowry B, et al. Low maternal vitamin D as a risk factor for schizophrenia: a pilot study using banked sera. Schizophr Res. 2003;63(1-2):73-78.
24. Przybelski RJ, Binkley NC. Is vitamin D important for preserving cognition? A positive correlation of serum 25-hydroxyvitamin D concentration with cognitive function. Arch Biochem Biophys. 2007;460(2):202-205.
25. Lee DM, Tajar A, Ulubaev A, et al. Association between 25-hydroxyvitamin D levels and cognitive performance in middle-aged and older European men. J Neurol Neurosurg Psychiatry. 2009;80(7):722-729.
26. Buell JS, Dawson-Hughes B, Scott TM, et al. 25-hydroxyvitamin D, dementia, and cerebrovascular pathology in elders receiving home services. Neurology. 2010;74(1):18-26.
27. Llewellyn DJ, Lang IA, Langa KM, et al. Vitamin D and risk of cognitive decline in elderly persons. Arch Intern Med. 2010;170(13):1135-1141.
28. Wilkins CH, Sheline YI, Roe CM, et al. Vitamin D deficiency is associated with low mood and worse cognitive performance in older adults. Am J Geriatr Psychiatry. 2006;14(12):1032-1040.
29. Annweiler C, Rolland Y, Schott AM, et al. Higher vitamin D dietary intake is associated with lower risk of Alzheimer’s disease: a 7-year follow-up. J Gerontol A Biol Sci Med Sci. 2012;67(11):1205-1211.
30. Kuningas M, Mooijaart SP, Jolles J, et al. VDR gene variants associate with cognitive function and depressive symptoms in old age. Neurobiol Aging. 2009;30(3):466-473.
31. Ganji V, Milone C, Cody MM, et al. Serum vitamin D concentrations are related to depression in young adult US population: the Third National Health and Nutrition Examination Survey. Int Arch Med. 2010;3:29.-
32. Hoogendijk WJ, Lips P, Dik MG, et al. Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Arch Gen Psychiatry. 2008;65(5):508-512.
33. Pan A, Lu L, Franco OH, et al. Association between depressive symptoms and 25-hydroxyvitamin D in middle-aged and elderly Chinese. J Affect Disord. 2009;118(1-3):240-243.
34. Högberg G, Gustafsson SA, Hällström T, et al. Depressed adolescents in a case-series were low in vitamin D and depression was ameliorated by vitamin D supplementation. Acta Paediatr. 2012;101(7):779-783.
35. Jorde R, Sneve M, Figenschau Y, et al. Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trial. J Intern Med. 2008;264(6):599-609.
36. Kjærgaard M, Waterloo K, Wang CE, et al. Effect of vitamin D supplement on depression scores in people with low levels of serum 25-hydroxyvitamin D: nested case-control study and randomised clinical trial. Br J Psychiatry. 2012;201(5):360-368.
37. Lansdowne AT, Provost SC. Vitamin D3 enhances mood in healthy subjects during winter. Psychopharmacology (Berl). 1998;135(4):319-223.
38. Shipowick CD, Moore CB, Corbett C, et al. Vitamin D and depressive symptoms in women during the winter: a pilot study. Appl Nurs Res. 2009;22(3):221-225.
39. Gloth FM 3rd, Alam W, Hollis B. Vitamin D vs broad spectrum phototherapy in the treatment of seasonal affective disorder. J Nutr Health Aging. 1999;3(1):5-7.
40. Vieth R, Kimball S, Hu A, et al. Randomized comparison of the effects of the vitamin D3 adequate intake versus 100 mcg (4000 IU) per day on biochemical responses and the wellbeing of patients. Nutr J. 2004;3:8.-
41. Harris S, Dawson-Hughes B. Seasonal mood changes in 250 normal women. Psychiatry Res. 1993;49(1):77-87.
42. Dumville JC, Miles JN, Porthouse J, et al. Can vitamin D supplementation prevent winter-time blues? A randomised trial among older women. J Nutr Health Aging. 2006;10(2):151-153.
43. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930.
44. Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86(1):50-60.
45. Schwalfenberg G. Not enough vitamin D: health consequences for Canadians. Can Fam Physician. 2007;53(5):841-854.
46. Norman AW, Bouillon R, Whiting SJ, et al. 13th Workshop consensus for vitamin D nutritional guidelines. J Steroid Biochem Mol Biol. 2007;103(3-5):204-205.
In the United States, >50% of psychiatric inpatients have vitamin D deficiency—<30 nmol/L (<12 ng/mL).1 A growing body of literature has found associations between vitamin D deficiency and psychiatric illnesses, particularly depression. Several randomized controlled trials (RCTs) have demonstrated that vitamin D supplementation can benefit depression symptoms. In this article, we discuss the current literature on vitamin D and psychiatric illness, and provide practical information for clinicians on the use of vitamin D supplementation.
Biosynthesis of vitamin D
Biosynthesis of vitamin D begins with the sterol provitamin D3 molecule 7-dehydrocholesterol (Figure).2 When skin is exposed to sunlight, 7-dehydrocholesterol absorbs UV radiation and forms provitamin D3, which undergoes rapid transformation to vitamin D3.2 Vitamin D3 is released from the plasma membrane and enters systemic circulation in a protein-bound form that has a serum half-life of 36 to 78 hours.3 Vitamin D3 can be taken up by adipocytes and stored in fat deposits, where it has a half-life of approximately 2 months.4
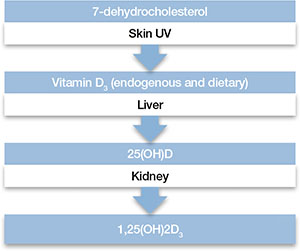
Figure: Biosynthesis of vitamin D
Provitamin D3 (7-dehydrocholesterol) in the skin absorbs UV radiation and undergoes isomerization to form vitamin D3. Endogenously produced vitamin D3 along with dietary vitamin D2 and vitamin D3 absorbed in the gastrointestinal tract are metabolized in the liver to 25-hydroxyvitamin D (25[OH]D), which re-enters the circulation and is metabolized in the kidney and other tissues to the active metabolite 1,25-dihydroxyvitamin D (1,25[OH]2D). Catabolism of 25(OH)D and 1,25(OH)2D into biologically-inactive molecules is primarily mediated by the cytochrome P450 (CYP) enzymes CYP24 and CYP3A4.
Source: Reference 2Circulating vitamin D3 is metabolized in the liver by the enzyme vitamin D-25-hydroxylase to 25-hydroxyvitamin D (25[OH]D3), which has a serum half-life of approximately 15 days.4 Circulating 25(OH)D3 is not biologically active at the physiological level, and requires activation by conversion to 1,25-dihydroxyvitamin D (1,25[OH]2D3) in the kidneys by the enzyme 25(OH)D-1α-hydroxylase. Production of 1,25(OH)2D3 is regulated by serum phosphorus and parathyroid hormone levels and other factors.5 Catabolism of 1,25(OH)2D3 is rapid, with a serum half-life of 3.5 to 21 hours.6 Vitamin D2 is structurally similar to vitamin D3, but occurs primarily in fungi, yeasts, and some invertebrates.
Risk factors for deficiency
A patient’s vitamin D status is determined by measuring 25(OH)D (Box 1). Risk factors for vitamin D deficiency include conditions that affect cutaneous production (insufficient sunlight exposure), obesity, gastrointestinal disorders, aging, renal disorders, and medications (Table 1). 2,5,7,8 The link between sunscreen use, either alone or in cosmetics, and vitamin D deficiency continues to be debated. While controlled studies have found that application of sunscreen with high sun protection factor can significantly reduce vitamin D production, 9 studies in clinical populations have failed to confirm these findings. 10,11 See Box 2 for a discussion of these risk factors and Box 3 for a discussion of acute and long-term medical manifestations of deficiency.
Although 1,25-dihydroxyvitamin D (1,25[OH]2D3) is the biologically active form of vitamin D, its circulating half-life is only 4 to 6 hours.a,b Therefore, 25-hydroxyvitamin D (25[OH]D) is the principal vitamin D metabolite measured to determine vitamin D status. Vitamin D levels commonly are expressed as ng/mL or nmol/L; the conversion factor from ng/mL to nmol/L is 2.496. The Institute of Medicine has defined vitamin D deficiency as a serum 25(OH)D level of <30 nmol/L (<12 ng/mL).c However, many experts define vitamin D insufficiency as a 25(OH)D level of 21 to 29 ng/ml, and deficiency as <20 ng/mL.a,d The upper limit is more difficult to define, but symptoms of vitamin D intoxication appear with blood levels >150 to 200 ng/mL.a
References
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81(3):353-373.
- Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73-78.
- Aloia JF. Clinical review: the 2011 report on dietary reference intake for vitamin D: where do we go from here? J Clin Endocrinol Metab. 2011;96(10):2987-2996.
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, et al. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84(1):18-28.
Table 1
Risk factors associated with vitamin D deficiency
| Age (>65) |
| Insufficient sunlight |
| Breastfeeding |
| Dark skin |
| Malabsorption diseases |
| Obesity (BMI >30 kg/m2) |
| Use of medications that alter vitamin D metabolism (eg, anticonvulsants, glucocorticoids) |
| Hepatobiliary disease |
| Renal disease |
| BMI: body mass index Source: References 2,5,7,8 |
Any factor that diminishes UV radiation penetration into the skin will affect cutaneous synthesis of vitamin D.a,b For example, sunscreen with a sun protection factor of 15 can decrease vitamin D synthesis by 98%.c Geography and its impact on yearly sunlight exposure is a well-known factor in vitamin D deficiency. Individuals who live below a latitude of approximately 35° North—approximately the southern border of Tennessee and through Albuquerque, NM—receive sufficient UV radiation exposure to ensure adequate vitamin D production throughout the year, but at higher latitudes, adequate vitamin D is not produced during winter months.d Melanin affects UV radiation absorption in a manner that prevents vitamin D production, and increased skin pigmentation markedly reduces vitamin D synthesis.e African Americans with very dark skin have significantly diminished cutaneous production of vitamin D.e,f
Renal 1α-hydroxylase activity decreases with aging in parallel with age-related decreases in glomerular filtration.g In addition, aging is associated with increased clearance of 1,25-dihydroxyvitamin D (1,25[OH]2D3).h However, vitamin D absorption generally is adequate even at older ages.i Studies have shown that obese individuals tend to have lower serum concentrations of vitamin D and 25-hydroxyvitamin D (25[OH]D) than those at a normal weight.j,k Obese patients have been shown to have lower cutaneous production of vitamin D3 and display lower bioavailability of orally administered vitamin D2.j
For patients with chronic renal insufficiency, creatinine clearance is positively correlated with serum 1,25(OH)2D levels.l Any process that results in malabsorption of intestinal fat may impair vitamin D absorption. In patients with celiac disease, biliary obstruction, or chronic pancreatitis, absorption consistently is reduced.m Individuals taking bile acid-binding medications, such as cholestyramine for hypercholesterolemia, also may have impaired vitamin D absorption.n In addition, hepatobiliary disease is associated with low levels of 25(OH)D.o Some drugs that alter hepatic metabolism are associated with vitamin D deficiency, including anticonvulsants or glucocorticoids, which can increase catabolism or vitamin D.p
References
- Holick MF. The vitamin D deficiency pandemic and consequences for nonskeletal health: mechanisms of action. Mol Aspects Med. 2008;29(6):361-368.
- Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
- Matsuoka LY, Ide L, Wortsman J, et al. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64(6):1165-1168.
- Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371.
- Clemens TL, Adams JS, Henderson SL, et al. Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet. 1982;1(8263):74-76.
- Chen TC, Chimeh F, Lu Z, et al. Factors that influence the cutaneous synthesis and dietary sources of vitamin D. Arch Biochem Biophys. 2007;460(2):213-217.
- Slovik DM, Adams JS, Neer RM, et al. Deficient production of 1,25-dihydroxyvitamin D in elderly osteoporotic patients. N Engl J Med. 1981;305(7):372-374.
- Armbrecht HJ, Zenser TV, Davis BB. Effect of age on the conversion of 25-hydroxyvitamin D3 to 1,25-dihydroxyvitamin D3 by kidney of rat. J Clin Invest. 1980;66(5):1118-1123.
- Lips P, Wiersinga A, van Ginkel FC, et al. The effect of vitamin D supplementation on vitamin D status and parathyroid function in elderly subjects. J Clin Endocrinol Metab. 1988;67(4):644-650.
- Wortsman J, Matsuoka LY, Chen TC, et al. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690-693.
- Bell NH, Epstein S, Greene A, et al. Evidence for alteration of the vitamin D-endocrine system in obese subjects. J Clin Invest. 1985;76(1):370-373.
- Pitts TO, Piraino BH, Mitro R, et al. Hyperparathyroidism and 1,25-dihydroxyvitamin D deficiency in mild, moderate, and severe renal failure. J Clin Endocrinol Metab. 1988;67(5):876-881.
- Thompson GR, Lewis B, Booth CC. Absorption of vitamin D3-3H in control subjects and patients with intestinal malabsorption. J Clin Invest. 1966;45(1):94-102.
- Lo CW, Paris PW, Clemens TL, et al. Vitamin D absorption in healthy subjects and in patients with intestinal malabsorption syndromes. Am J Clin Nutr. 1985;42(4):644-649.
- Pappa HM, Bern E, Kamin D, et al. Vitamin D status in gastrointestinal and liver disease. Curr Opin Gastroenterol. 2008;24(2):176-183.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
Acute effects. Vitamin D deficiency produces a range of clinical effects.a-c One well-documented consequence of vitamin D deficiency is osteomalacia—bone demineralization—which produces characteristic bone deformity and growth retardation in children.d,e In adults, osteomalacia may manifest as diffuse pain bone discomfort and muscle aches that may resemble fibromyalgia or arthritis.f Because vitamin D receptors are present in skeletal muscle, deficiency also may lead to proximal muscle weakness; an increased risk of falls; global bone discomfort, often elicited with pressure over the sternum or tibia; and low back pain in older women.c,f
Long-term effects. A large epidemiologic study found that adults with 25-hydroxyvitamin D (25[OH]D) levels <21 ng/mL had an increased risk of hypertension, diabetes, obesity, and dyslipidemia.g Cardiovascular mortality was higher in individuals with 25(OH)D levels <10 ng/mL compared with those with >40 ng/mL.h Adolescents in the National Health and Nutrition Examination Survey-III with serum 25(OH)D levels <15 ng/mL were more likely to have elevated blood glucose levels than those with >26 ng/mL.i Other epidemiologic data have demonstrated associations of vitamin D deficiency with multiple sclerosis, seasonal allergies, asthma, and various infectious diseases.j,k
Because vitamin D is known to promote cellular differentiation and inhibit cellular proliferation, its role in cancer has been studied extensively. A recent meta-analysis of case-control studies found that the odds of colon cancer were reduced by >40% for each 20 ng/mL increase in serum 25(OH)D levels.l Another meta-analysis reported a lower risk of breast cancer among women in the highest quartile of 25(OH)D values compared with the lowest quartile.m
References
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81(3):353-373.
- Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73-78.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
- Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
- Bordelon P, Ghetu MV, Langan RC. Recognition and management of vitamin D deficiency. Am Fam Physician. 2009;80(8):841-846.
- Hicks GE, Shardell M, Miller RR, et al. Associations between vitamin D status and pain in older adults: the Invecchiare in Chianti study. J Am Geriatr Soc. 2008;56(5):785-791.
- Martins D, Wolf M, Pan D, et al. Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2007;167(11):1159-1165.
- Ginde AA, Scragg R, Schwartz RS, et al. Prospective study of serum 25-hydroxyvitamin D level, cardiovascular disease mortality, and all-cause mortality in older U.S. adults. J Am Geriatr Soc. 2009;57(9):1595-1603.
- Reis JP, von Mühlen D, Miller ER 3rd, et al. Vitamin D status and cardiometabolic risk factors in the United States adolescent population. Pediatrics. 2009;124(3):e371-379.
- Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86(1):50-60.
- Munger KL, Levin LI, Hollis BW, et al. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296(23):2832-2838.
- Yin L, Grandi N, Raum E, et al. Meta-analysis: longitudinal studies of serum vitamin D and colorectal cancer risk. Aliment Pharmacol Ther. 2009;30(2):113-125.
- Chen P, Hu P, Xie D, et al. Meta-analysis of vitamin D, calcium and the prevention of breast cancer. Breast Cancer Res Treat. 2010;121(2):469-477.
Vitamin D’s role in the brain
Vitamin D’s role in psychiatric illnesses is suggested by region-specific expression of vitamin D receptors (VDR) in the cingulate cortex, thalamus, cerebellum, amygdala, and hippocampus.12 Most of these regions also express 1α-hydroxylase enzymes capable of metabolizing 25(OH)D to 1,25(OH)2D3, which suggests that vitamin D may have an autocrine or paracrine function in brain.13
Vitamin D regulates expression of tyrosine hydroxylase, the rate-limiting enzyme in the biosynthesis of dopamine, norepinephrine, and epinephrine.14 Vitamin D also promotes survival of monoaminergic neurons through upregulation of glial cell line-derived neurotrophic factor, which supports survival of midbrain dopaminergic neurons and confers resistance to neurotoxins that deplete dopaminergic neurons in Parkinson’s disease.15 Vitamin D also promotes neuronal survival by inhibiting oxidative pathways in the brain through inhibition of inducible nitric oxide synthase (reducing free radical formation)16 and upregulation of γ-glutamyl transpeptidase (increasing antioxidant production).17 Vitamin D may play a neuroprotective role through regulation of calcium channels. In vitro studies have shown that vitamin D downregulates expression of L-type calcium channels, conferring protection against excitatory neurotoxins in cultured neurons.18 Proteomic analysis of brain tissue in a rat model of developmental vitamin D revealed dysregulation of 36 brain proteins involved in many biologic pathways involved in calcium homeostasis, synaptic plasticity, and neurotransmission.19 Taken together, these findings suggest vitamin D has a neurosteroid-like role in the CNS.
Psychotic disorders
Several epidemiologic studies have linked low vitamin D levels to schizophrenia and other psychotic disorders. Researchers in Norway who used a structured clinical interview to identify psychosis consistently found low levels of 25(OH)D among immigrants and native Norwegians with psychotic symptoms.20 A study of 8,411 Swedish women found low vitamin D levels were associated with psychotic symptoms.21 The Finnish birth cohort study found that use of vitamin D supplementation during the first year of life reduced the incidence of schizophrenia.22 In another pilot study, researchers measured third-trimester serum 25(OH)D levels and found that low levels of maternal vitamin D may be associated with an increased risk of schizophrenia.23 These studies suggest that low prenatal vitamin D levels may adversely impact the developing brain, increasing the risk for adult-onset schizophrenia.
Cognitive dysfunction
Low vitamin D concentrations have been associated with impairments in cognitive functions such as memory and orientation,24 executive function impairments,25 and Alzheimer’s disease (AD).26 A large study conducted from 1998 to 2006 in Italy concluded that persons with severe vitamin D deficiency (<25 nmol/L) had a higher risk of substantial decline on Mini-Mental State Examination than those with sufficient levels (≥75 nmol/L).27 Other studies have linked low vitamin D levels to poor cognitive performance in depressed older adults.28 Low vitamin D levels in older women have been associated with risk of AD, but not with other dementias.29 Polymorphisms of VDR have been associated with depression and poor cognitive performance.30
Depression
Epidemiologic studies evaluating vitamin D deficiency have had conflicting results. The Third National Health and Nutrition Examination Survey, which used a sample of 7,970 non-institutionalized U.S. residents age 15 to 39, demonstrated that individuals with serum vitamin D ≤50 nmol/L are at a significantly higher risk of developing depression than those with vitamin D ≥75 nmol/L.31 A study of 1,282 adults age 65 to 95 in the Netherlands found that 25(OH)D levels were 14% lower in depressed patients compared with controls.32 However, a large epidemiologic study in China did not detect a relationship between vitamin D and depression in 3,262 men and women age 50 to 70.33 After researchers adjusted for geography, body mass index, physical activity, and smoking, 25(OH)D levels did not correlate significantly with the presence or severity of depression. In a case series,34 after 48 vitamin D-deficient depressed adolescents were given vitamin D3 over 3 months, there was a significant improvement in well-being, depressive symptoms, irritability, and fatigue.34 Other small, cross-sectional studies have examined associations between vitamin D status and depression with divergent results, which may reflect differences in population and methodology.
Prospective interventional studies. Although direct causal relationships are difficult to establish, several prospective studies have tested the hypothesis that treating vitamin D deficiency can improve depressive symptoms.
In a double-blind, controlled trial, Jorde et al35 randomized 441 individuals age 21 to 70 to vitamin D, 20,000 IU per week; vitamin D, 40,000 IU per week; or placebo for 1 year. Individuals with serum 25(OH)D levels <40 nmol/L scored significantly higher on depression rating scales than those with serum 25(OH)D levels ≥40 nmol/L at the end of the study. There was no significant improvement in depression ratings in the placebo group (Table 2).35 These results must be interpreted with care because depressive symptoms were secondary endpoints in this study.
Table 2
Effect of vitamin D supplementation on depressive symptoms in a controlled trial
| Vitamin D Supplementation | Serum 25(OH)D levels at baseline | BDI total score, Median and range at end of study | After 1 year of vitamin D supplementation |
|---|---|---|---|
| 20,000 IU/week | <40 nmol/L | Significantly higher (more depressive traits), 6.0 (0 to 23) | Significantly improved BDI score |
| 40,000 IU/week | ≥40 nmol/L | 4.5 (0 to 28) | Significantly improved BDI score |
| Placebo | - | - | No improvement in BDI score |
| 25(OH)D: 25-hydroxyvitamin D; BDI: Beck Depression Inventory Source: Reference 35 | |||
Kjærgaard et al36 systematically examined vitamin D levels in a case-control study followed by a randomized controlled trial (RCT) of vitamin D supplementation. In the case-control phase, participants with low 25(OH)D levels at baseline were significantly more depressed than participants with high 25(OH)D levels. Participants with low 25(OH)D levels were randomized to placebo or 40,000 IU vitamin D3 per week for 6 months. Low levels of vitamin D were strongly associated with depressive symptoms, but vitamin D supplementation did not have a significant effect on depressive symptom scores.
Seasonal affective disorder (SAD). Seasonal variation in vitamin D levels suggests that supplementation may help patients who have seasonal mood disturbances. In a randomized, double-blind study, 44 healthy individuals received vitamin D3, 400 IU/d, 800 IU/d, or no vitamin D3 for 5 days during late winter. Based on self-reports, vitamin D3 significantly enhanced positive affect and there was some evidence it reduced negative affect.37 In a pilot study of 9 women with serum vitamin D levels <40 ng/ml, vitamin D supplementation during winter was associated with an average 10-point decline in Beck Depression Inventory-II scores.38 In a prospective RCT of 15 individuals with SAD, all patients who received vitamin D improved in all outcome measures.39 Vieth40 randomized 82 adults with vitamin D deficiency to 600 IU/d or 4,000 IU/d of vitamin D3 for 3 months over 2 consecutive winters. Patients taking the higher dose showed some evidence of improved well-being compared with those taking the lower dose, although results were not significant for all comparisons. Two other trials did not observe any improvement in SAD symptoms with vitamin D treatment.41,42
Treating vitamin D deficiency
The Endocrine Society recently developed consensus guidelines for diagnosing and managing vitamin D deficiency.43 In addition, the Institute of Medicine of the National Academies recommends daily vitamin D supplementation to prevent deficiency:
- age <70: 400 IU/d
- age >70: 800 IU/d
- pregnant or lactating women: 600 IU/d
- upper limit: 4,000 IU/d.7
Higher doses may be used for patients deprived of sun exposure.8 A typical replacement regimen consists of oral ergocalciferol, 50,000 IU per week for 8 weeks.44 The optimal time for rechecking serum levels after repletion has not been clearly defined, but serum 25(OH)D levels should be measured again after therapy is completed. If values have not reached or exceeded 20 ng/mL, consider a second 8-week course of ergocalciferol (see the Box 1 for a discussion of measuring vitamin D levels). If serum 25(OH)D levels have not increased, the most likely cause is nonadherence or malabsorption.
Contraindications and toxicity. Contraindications to vitamin D supplementation include granulomatous diseases, sarcoidosis, metastatic bone disease, and Williams syndrome.45Table 345 lists signs of vitamin D toxicity. There is little risk of toxicity at dosages of up to 2,000 IU/d.46
Table 3
Signs of vitamin D toxicity
| Headache |
| Metallic taste |
| Nephrocalcinosis or vascular calcinosis |
| Pancreatitis |
| Nausea |
| Vomiting |
| Source: Reference 45 |
Related Resources
- LaFerney MC. Vitamin D deficiency in older adults. Current Psychiatry. 2012;11(11):63.
- National Institutes of Health Office of Dietary Supplements. Dietary supplement fact sheet: vitamin D. http://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional.
Drug Brand Names
- Cholestyramine • Questran
- Ergocalciferol • Calciferol, Drisdol
Disclosures
Dr. Harris is an employee of Rho, Chapel Hill, NC.
Dr. Jaiswal reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Holmes receives research support from Bristol-Myers Squibb, Elan, Merck, Otsuka, Shire, Takeda, and Theravance, and is on the speaker’s bureau for Forest Pharmaceuticals and PamLab.
Dr. Patkar is a consultant for Dey Pharmaceuticals, Forest, Gilead, and TTK Pharma and is on the speaker’s bureau and received honoraria from Alkermes, Bristol-Myers Squibb, Dey Pharmaceuticals, Pfizer, and Sunovion; and has received grant support from the Duke Endowment, Dey Pharmaceuticals, Envivo, Forest, Janssen, Lundbeck, The National Institutes of Health, the National Institute on Drug Abuse, National Institute on Alcohol Abuse and Alcoholism, Pfizer Inc., Shire, Sunovion, and Titan.
Dr. Weisler has been a consultant to, on the speaker’s bureaus of, and/or received research support from Abbott, Agency for Toxic Substances and Disease Registry, AstraZeneca, Biovail, Bristol-Myers Squibb, Burroughs Wellcome, Cenerx, Centers for Disease Control and Prevention, Cephalon, Ciba Geigy, CoMentis, Corcept, Cortex, Dainippon Sumitomo Pharma America, Eisai, Elan, Eli Lilly and Company, Forest Pharmaceuticals, GlaxoSmithKline, Janssen, Johnson & Johnson, Lundbeck, McNeil Pharmaceuticals, Medicinova, Medscape Advisory Board, Merck, National Institute of Mental Health, Neurochem, New River Pharmaceuticals, Novartis, Organon, Otsuka America Pharma, Pfizer Inc., Pharmacia, Repligen, Saegis, Sandoz, Sanofi, Sanofi-Synthelabo, Schwabe/Ingenix, Sepracor, Shire, Solvay, Sunovion, Synaptic, Takeda, TAP, Theravance, Transcept Pharma, TransTech, UCB Pharma, Validus, Vela, and Wyeth.
In the United States, >50% of psychiatric inpatients have vitamin D deficiency—<30 nmol/L (<12 ng/mL).1 A growing body of literature has found associations between vitamin D deficiency and psychiatric illnesses, particularly depression. Several randomized controlled trials (RCTs) have demonstrated that vitamin D supplementation can benefit depression symptoms. In this article, we discuss the current literature on vitamin D and psychiatric illness, and provide practical information for clinicians on the use of vitamin D supplementation.
Biosynthesis of vitamin D
Biosynthesis of vitamin D begins with the sterol provitamin D3 molecule 7-dehydrocholesterol (Figure).2 When skin is exposed to sunlight, 7-dehydrocholesterol absorbs UV radiation and forms provitamin D3, which undergoes rapid transformation to vitamin D3.2 Vitamin D3 is released from the plasma membrane and enters systemic circulation in a protein-bound form that has a serum half-life of 36 to 78 hours.3 Vitamin D3 can be taken up by adipocytes and stored in fat deposits, where it has a half-life of approximately 2 months.4
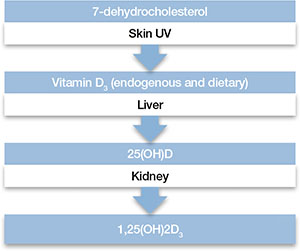
Figure: Biosynthesis of vitamin D
Provitamin D3 (7-dehydrocholesterol) in the skin absorbs UV radiation and undergoes isomerization to form vitamin D3. Endogenously produced vitamin D3 along with dietary vitamin D2 and vitamin D3 absorbed in the gastrointestinal tract are metabolized in the liver to 25-hydroxyvitamin D (25[OH]D), which re-enters the circulation and is metabolized in the kidney and other tissues to the active metabolite 1,25-dihydroxyvitamin D (1,25[OH]2D). Catabolism of 25(OH)D and 1,25(OH)2D into biologically-inactive molecules is primarily mediated by the cytochrome P450 (CYP) enzymes CYP24 and CYP3A4.
Source: Reference 2Circulating vitamin D3 is metabolized in the liver by the enzyme vitamin D-25-hydroxylase to 25-hydroxyvitamin D (25[OH]D3), which has a serum half-life of approximately 15 days.4 Circulating 25(OH)D3 is not biologically active at the physiological level, and requires activation by conversion to 1,25-dihydroxyvitamin D (1,25[OH]2D3) in the kidneys by the enzyme 25(OH)D-1α-hydroxylase. Production of 1,25(OH)2D3 is regulated by serum phosphorus and parathyroid hormone levels and other factors.5 Catabolism of 1,25(OH)2D3 is rapid, with a serum half-life of 3.5 to 21 hours.6 Vitamin D2 is structurally similar to vitamin D3, but occurs primarily in fungi, yeasts, and some invertebrates.
Risk factors for deficiency
A patient’s vitamin D status is determined by measuring 25(OH)D (Box 1). Risk factors for vitamin D deficiency include conditions that affect cutaneous production (insufficient sunlight exposure), obesity, gastrointestinal disorders, aging, renal disorders, and medications (Table 1). 2,5,7,8 The link between sunscreen use, either alone or in cosmetics, and vitamin D deficiency continues to be debated. While controlled studies have found that application of sunscreen with high sun protection factor can significantly reduce vitamin D production, 9 studies in clinical populations have failed to confirm these findings. 10,11 See Box 2 for a discussion of these risk factors and Box 3 for a discussion of acute and long-term medical manifestations of deficiency.
Although 1,25-dihydroxyvitamin D (1,25[OH]2D3) is the biologically active form of vitamin D, its circulating half-life is only 4 to 6 hours.a,b Therefore, 25-hydroxyvitamin D (25[OH]D) is the principal vitamin D metabolite measured to determine vitamin D status. Vitamin D levels commonly are expressed as ng/mL or nmol/L; the conversion factor from ng/mL to nmol/L is 2.496. The Institute of Medicine has defined vitamin D deficiency as a serum 25(OH)D level of <30 nmol/L (<12 ng/mL).c However, many experts define vitamin D insufficiency as a 25(OH)D level of 21 to 29 ng/ml, and deficiency as <20 ng/mL.a,d The upper limit is more difficult to define, but symptoms of vitamin D intoxication appear with blood levels >150 to 200 ng/mL.a
References
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81(3):353-373.
- Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73-78.
- Aloia JF. Clinical review: the 2011 report on dietary reference intake for vitamin D: where do we go from here? J Clin Endocrinol Metab. 2011;96(10):2987-2996.
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, et al. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84(1):18-28.
Table 1
Risk factors associated with vitamin D deficiency
| Age (>65) |
| Insufficient sunlight |
| Breastfeeding |
| Dark skin |
| Malabsorption diseases |
| Obesity (BMI >30 kg/m2) |
| Use of medications that alter vitamin D metabolism (eg, anticonvulsants, glucocorticoids) |
| Hepatobiliary disease |
| Renal disease |
| BMI: body mass index Source: References 2,5,7,8 |
Any factor that diminishes UV radiation penetration into the skin will affect cutaneous synthesis of vitamin D.a,b For example, sunscreen with a sun protection factor of 15 can decrease vitamin D synthesis by 98%.c Geography and its impact on yearly sunlight exposure is a well-known factor in vitamin D deficiency. Individuals who live below a latitude of approximately 35° North—approximately the southern border of Tennessee and through Albuquerque, NM—receive sufficient UV radiation exposure to ensure adequate vitamin D production throughout the year, but at higher latitudes, adequate vitamin D is not produced during winter months.d Melanin affects UV radiation absorption in a manner that prevents vitamin D production, and increased skin pigmentation markedly reduces vitamin D synthesis.e African Americans with very dark skin have significantly diminished cutaneous production of vitamin D.e,f
Renal 1α-hydroxylase activity decreases with aging in parallel with age-related decreases in glomerular filtration.g In addition, aging is associated with increased clearance of 1,25-dihydroxyvitamin D (1,25[OH]2D3).h However, vitamin D absorption generally is adequate even at older ages.i Studies have shown that obese individuals tend to have lower serum concentrations of vitamin D and 25-hydroxyvitamin D (25[OH]D) than those at a normal weight.j,k Obese patients have been shown to have lower cutaneous production of vitamin D3 and display lower bioavailability of orally administered vitamin D2.j
For patients with chronic renal insufficiency, creatinine clearance is positively correlated with serum 1,25(OH)2D levels.l Any process that results in malabsorption of intestinal fat may impair vitamin D absorption. In patients with celiac disease, biliary obstruction, or chronic pancreatitis, absorption consistently is reduced.m Individuals taking bile acid-binding medications, such as cholestyramine for hypercholesterolemia, also may have impaired vitamin D absorption.n In addition, hepatobiliary disease is associated with low levels of 25(OH)D.o Some drugs that alter hepatic metabolism are associated with vitamin D deficiency, including anticonvulsants or glucocorticoids, which can increase catabolism or vitamin D.p
References
- Holick MF. The vitamin D deficiency pandemic and consequences for nonskeletal health: mechanisms of action. Mol Aspects Med. 2008;29(6):361-368.
- Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
- Matsuoka LY, Ide L, Wortsman J, et al. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64(6):1165-1168.
- Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371.
- Clemens TL, Adams JS, Henderson SL, et al. Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet. 1982;1(8263):74-76.
- Chen TC, Chimeh F, Lu Z, et al. Factors that influence the cutaneous synthesis and dietary sources of vitamin D. Arch Biochem Biophys. 2007;460(2):213-217.
- Slovik DM, Adams JS, Neer RM, et al. Deficient production of 1,25-dihydroxyvitamin D in elderly osteoporotic patients. N Engl J Med. 1981;305(7):372-374.
- Armbrecht HJ, Zenser TV, Davis BB. Effect of age on the conversion of 25-hydroxyvitamin D3 to 1,25-dihydroxyvitamin D3 by kidney of rat. J Clin Invest. 1980;66(5):1118-1123.
- Lips P, Wiersinga A, van Ginkel FC, et al. The effect of vitamin D supplementation on vitamin D status and parathyroid function in elderly subjects. J Clin Endocrinol Metab. 1988;67(4):644-650.
- Wortsman J, Matsuoka LY, Chen TC, et al. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690-693.
- Bell NH, Epstein S, Greene A, et al. Evidence for alteration of the vitamin D-endocrine system in obese subjects. J Clin Invest. 1985;76(1):370-373.
- Pitts TO, Piraino BH, Mitro R, et al. Hyperparathyroidism and 1,25-dihydroxyvitamin D deficiency in mild, moderate, and severe renal failure. J Clin Endocrinol Metab. 1988;67(5):876-881.
- Thompson GR, Lewis B, Booth CC. Absorption of vitamin D3-3H in control subjects and patients with intestinal malabsorption. J Clin Invest. 1966;45(1):94-102.
- Lo CW, Paris PW, Clemens TL, et al. Vitamin D absorption in healthy subjects and in patients with intestinal malabsorption syndromes. Am J Clin Nutr. 1985;42(4):644-649.
- Pappa HM, Bern E, Kamin D, et al. Vitamin D status in gastrointestinal and liver disease. Curr Opin Gastroenterol. 2008;24(2):176-183.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
Acute effects. Vitamin D deficiency produces a range of clinical effects.a-c One well-documented consequence of vitamin D deficiency is osteomalacia—bone demineralization—which produces characteristic bone deformity and growth retardation in children.d,e In adults, osteomalacia may manifest as diffuse pain bone discomfort and muscle aches that may resemble fibromyalgia or arthritis.f Because vitamin D receptors are present in skeletal muscle, deficiency also may lead to proximal muscle weakness; an increased risk of falls; global bone discomfort, often elicited with pressure over the sternum or tibia; and low back pain in older women.c,f
Long-term effects. A large epidemiologic study found that adults with 25-hydroxyvitamin D (25[OH]D) levels <21 ng/mL had an increased risk of hypertension, diabetes, obesity, and dyslipidemia.g Cardiovascular mortality was higher in individuals with 25(OH)D levels <10 ng/mL compared with those with >40 ng/mL.h Adolescents in the National Health and Nutrition Examination Survey-III with serum 25(OH)D levels <15 ng/mL were more likely to have elevated blood glucose levels than those with >26 ng/mL.i Other epidemiologic data have demonstrated associations of vitamin D deficiency with multiple sclerosis, seasonal allergies, asthma, and various infectious diseases.j,k
Because vitamin D is known to promote cellular differentiation and inhibit cellular proliferation, its role in cancer has been studied extensively. A recent meta-analysis of case-control studies found that the odds of colon cancer were reduced by >40% for each 20 ng/mL increase in serum 25(OH)D levels.l Another meta-analysis reported a lower risk of breast cancer among women in the highest quartile of 25(OH)D values compared with the lowest quartile.m
References
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81(3):353-373.
- Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73-78.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
- Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
- Bordelon P, Ghetu MV, Langan RC. Recognition and management of vitamin D deficiency. Am Fam Physician. 2009;80(8):841-846.
- Hicks GE, Shardell M, Miller RR, et al. Associations between vitamin D status and pain in older adults: the Invecchiare in Chianti study. J Am Geriatr Soc. 2008;56(5):785-791.
- Martins D, Wolf M, Pan D, et al. Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2007;167(11):1159-1165.
- Ginde AA, Scragg R, Schwartz RS, et al. Prospective study of serum 25-hydroxyvitamin D level, cardiovascular disease mortality, and all-cause mortality in older U.S. adults. J Am Geriatr Soc. 2009;57(9):1595-1603.
- Reis JP, von Mühlen D, Miller ER 3rd, et al. Vitamin D status and cardiometabolic risk factors in the United States adolescent population. Pediatrics. 2009;124(3):e371-379.
- Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86(1):50-60.
- Munger KL, Levin LI, Hollis BW, et al. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296(23):2832-2838.
- Yin L, Grandi N, Raum E, et al. Meta-analysis: longitudinal studies of serum vitamin D and colorectal cancer risk. Aliment Pharmacol Ther. 2009;30(2):113-125.
- Chen P, Hu P, Xie D, et al. Meta-analysis of vitamin D, calcium and the prevention of breast cancer. Breast Cancer Res Treat. 2010;121(2):469-477.
Vitamin D’s role in the brain
Vitamin D’s role in psychiatric illnesses is suggested by region-specific expression of vitamin D receptors (VDR) in the cingulate cortex, thalamus, cerebellum, amygdala, and hippocampus.12 Most of these regions also express 1α-hydroxylase enzymes capable of metabolizing 25(OH)D to 1,25(OH)2D3, which suggests that vitamin D may have an autocrine or paracrine function in brain.13
Vitamin D regulates expression of tyrosine hydroxylase, the rate-limiting enzyme in the biosynthesis of dopamine, norepinephrine, and epinephrine.14 Vitamin D also promotes survival of monoaminergic neurons through upregulation of glial cell line-derived neurotrophic factor, which supports survival of midbrain dopaminergic neurons and confers resistance to neurotoxins that deplete dopaminergic neurons in Parkinson’s disease.15 Vitamin D also promotes neuronal survival by inhibiting oxidative pathways in the brain through inhibition of inducible nitric oxide synthase (reducing free radical formation)16 and upregulation of γ-glutamyl transpeptidase (increasing antioxidant production).17 Vitamin D may play a neuroprotective role through regulation of calcium channels. In vitro studies have shown that vitamin D downregulates expression of L-type calcium channels, conferring protection against excitatory neurotoxins in cultured neurons.18 Proteomic analysis of brain tissue in a rat model of developmental vitamin D revealed dysregulation of 36 brain proteins involved in many biologic pathways involved in calcium homeostasis, synaptic plasticity, and neurotransmission.19 Taken together, these findings suggest vitamin D has a neurosteroid-like role in the CNS.
Psychotic disorders
Several epidemiologic studies have linked low vitamin D levels to schizophrenia and other psychotic disorders. Researchers in Norway who used a structured clinical interview to identify psychosis consistently found low levels of 25(OH)D among immigrants and native Norwegians with psychotic symptoms.20 A study of 8,411 Swedish women found low vitamin D levels were associated with psychotic symptoms.21 The Finnish birth cohort study found that use of vitamin D supplementation during the first year of life reduced the incidence of schizophrenia.22 In another pilot study, researchers measured third-trimester serum 25(OH)D levels and found that low levels of maternal vitamin D may be associated with an increased risk of schizophrenia.23 These studies suggest that low prenatal vitamin D levels may adversely impact the developing brain, increasing the risk for adult-onset schizophrenia.
Cognitive dysfunction
Low vitamin D concentrations have been associated with impairments in cognitive functions such as memory and orientation,24 executive function impairments,25 and Alzheimer’s disease (AD).26 A large study conducted from 1998 to 2006 in Italy concluded that persons with severe vitamin D deficiency (<25 nmol/L) had a higher risk of substantial decline on Mini-Mental State Examination than those with sufficient levels (≥75 nmol/L).27 Other studies have linked low vitamin D levels to poor cognitive performance in depressed older adults.28 Low vitamin D levels in older women have been associated with risk of AD, but not with other dementias.29 Polymorphisms of VDR have been associated with depression and poor cognitive performance.30
Depression
Epidemiologic studies evaluating vitamin D deficiency have had conflicting results. The Third National Health and Nutrition Examination Survey, which used a sample of 7,970 non-institutionalized U.S. residents age 15 to 39, demonstrated that individuals with serum vitamin D ≤50 nmol/L are at a significantly higher risk of developing depression than those with vitamin D ≥75 nmol/L.31 A study of 1,282 adults age 65 to 95 in the Netherlands found that 25(OH)D levels were 14% lower in depressed patients compared with controls.32 However, a large epidemiologic study in China did not detect a relationship between vitamin D and depression in 3,262 men and women age 50 to 70.33 After researchers adjusted for geography, body mass index, physical activity, and smoking, 25(OH)D levels did not correlate significantly with the presence or severity of depression. In a case series,34 after 48 vitamin D-deficient depressed adolescents were given vitamin D3 over 3 months, there was a significant improvement in well-being, depressive symptoms, irritability, and fatigue.34 Other small, cross-sectional studies have examined associations between vitamin D status and depression with divergent results, which may reflect differences in population and methodology.
Prospective interventional studies. Although direct causal relationships are difficult to establish, several prospective studies have tested the hypothesis that treating vitamin D deficiency can improve depressive symptoms.
In a double-blind, controlled trial, Jorde et al35 randomized 441 individuals age 21 to 70 to vitamin D, 20,000 IU per week; vitamin D, 40,000 IU per week; or placebo for 1 year. Individuals with serum 25(OH)D levels <40 nmol/L scored significantly higher on depression rating scales than those with serum 25(OH)D levels ≥40 nmol/L at the end of the study. There was no significant improvement in depression ratings in the placebo group (Table 2).35 These results must be interpreted with care because depressive symptoms were secondary endpoints in this study.
Table 2
Effect of vitamin D supplementation on depressive symptoms in a controlled trial
| Vitamin D Supplementation | Serum 25(OH)D levels at baseline | BDI total score, Median and range at end of study | After 1 year of vitamin D supplementation |
|---|---|---|---|
| 20,000 IU/week | <40 nmol/L | Significantly higher (more depressive traits), 6.0 (0 to 23) | Significantly improved BDI score |
| 40,000 IU/week | ≥40 nmol/L | 4.5 (0 to 28) | Significantly improved BDI score |
| Placebo | - | - | No improvement in BDI score |
| 25(OH)D: 25-hydroxyvitamin D; BDI: Beck Depression Inventory Source: Reference 35 | |||
Kjærgaard et al36 systematically examined vitamin D levels in a case-control study followed by a randomized controlled trial (RCT) of vitamin D supplementation. In the case-control phase, participants with low 25(OH)D levels at baseline were significantly more depressed than participants with high 25(OH)D levels. Participants with low 25(OH)D levels were randomized to placebo or 40,000 IU vitamin D3 per week for 6 months. Low levels of vitamin D were strongly associated with depressive symptoms, but vitamin D supplementation did not have a significant effect on depressive symptom scores.
Seasonal affective disorder (SAD). Seasonal variation in vitamin D levels suggests that supplementation may help patients who have seasonal mood disturbances. In a randomized, double-blind study, 44 healthy individuals received vitamin D3, 400 IU/d, 800 IU/d, or no vitamin D3 for 5 days during late winter. Based on self-reports, vitamin D3 significantly enhanced positive affect and there was some evidence it reduced negative affect.37 In a pilot study of 9 women with serum vitamin D levels <40 ng/ml, vitamin D supplementation during winter was associated with an average 10-point decline in Beck Depression Inventory-II scores.38 In a prospective RCT of 15 individuals with SAD, all patients who received vitamin D improved in all outcome measures.39 Vieth40 randomized 82 adults with vitamin D deficiency to 600 IU/d or 4,000 IU/d of vitamin D3 for 3 months over 2 consecutive winters. Patients taking the higher dose showed some evidence of improved well-being compared with those taking the lower dose, although results were not significant for all comparisons. Two other trials did not observe any improvement in SAD symptoms with vitamin D treatment.41,42
Treating vitamin D deficiency
The Endocrine Society recently developed consensus guidelines for diagnosing and managing vitamin D deficiency.43 In addition, the Institute of Medicine of the National Academies recommends daily vitamin D supplementation to prevent deficiency:
- age <70: 400 IU/d
- age >70: 800 IU/d
- pregnant or lactating women: 600 IU/d
- upper limit: 4,000 IU/d.7
Higher doses may be used for patients deprived of sun exposure.8 A typical replacement regimen consists of oral ergocalciferol, 50,000 IU per week for 8 weeks.44 The optimal time for rechecking serum levels after repletion has not been clearly defined, but serum 25(OH)D levels should be measured again after therapy is completed. If values have not reached or exceeded 20 ng/mL, consider a second 8-week course of ergocalciferol (see the Box 1 for a discussion of measuring vitamin D levels). If serum 25(OH)D levels have not increased, the most likely cause is nonadherence or malabsorption.
Contraindications and toxicity. Contraindications to vitamin D supplementation include granulomatous diseases, sarcoidosis, metastatic bone disease, and Williams syndrome.45Table 345 lists signs of vitamin D toxicity. There is little risk of toxicity at dosages of up to 2,000 IU/d.46
Table 3
Signs of vitamin D toxicity
| Headache |
| Metallic taste |
| Nephrocalcinosis or vascular calcinosis |
| Pancreatitis |
| Nausea |
| Vomiting |
| Source: Reference 45 |
Related Resources
- LaFerney MC. Vitamin D deficiency in older adults. Current Psychiatry. 2012;11(11):63.
- National Institutes of Health Office of Dietary Supplements. Dietary supplement fact sheet: vitamin D. http://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional.
Drug Brand Names
- Cholestyramine • Questran
- Ergocalciferol • Calciferol, Drisdol
Disclosures
Dr. Harris is an employee of Rho, Chapel Hill, NC.
Dr. Jaiswal reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Holmes receives research support from Bristol-Myers Squibb, Elan, Merck, Otsuka, Shire, Takeda, and Theravance, and is on the speaker’s bureau for Forest Pharmaceuticals and PamLab.
Dr. Patkar is a consultant for Dey Pharmaceuticals, Forest, Gilead, and TTK Pharma and is on the speaker’s bureau and received honoraria from Alkermes, Bristol-Myers Squibb, Dey Pharmaceuticals, Pfizer, and Sunovion; and has received grant support from the Duke Endowment, Dey Pharmaceuticals, Envivo, Forest, Janssen, Lundbeck, The National Institutes of Health, the National Institute on Drug Abuse, National Institute on Alcohol Abuse and Alcoholism, Pfizer Inc., Shire, Sunovion, and Titan.
Dr. Weisler has been a consultant to, on the speaker’s bureaus of, and/or received research support from Abbott, Agency for Toxic Substances and Disease Registry, AstraZeneca, Biovail, Bristol-Myers Squibb, Burroughs Wellcome, Cenerx, Centers for Disease Control and Prevention, Cephalon, Ciba Geigy, CoMentis, Corcept, Cortex, Dainippon Sumitomo Pharma America, Eisai, Elan, Eli Lilly and Company, Forest Pharmaceuticals, GlaxoSmithKline, Janssen, Johnson & Johnson, Lundbeck, McNeil Pharmaceuticals, Medicinova, Medscape Advisory Board, Merck, National Institute of Mental Health, Neurochem, New River Pharmaceuticals, Novartis, Organon, Otsuka America Pharma, Pfizer Inc., Pharmacia, Repligen, Saegis, Sandoz, Sanofi, Sanofi-Synthelabo, Schwabe/Ingenix, Sepracor, Shire, Solvay, Sunovion, Synaptic, Takeda, TAP, Theravance, Transcept Pharma, TransTech, UCB Pharma, Validus, Vela, and Wyeth.
1. McCue RE, Charles RA, Orendain GC, et al. Vitamin D deficiency among psychiatric inpatients [published online April 19, 2012]. Prim Care Companion CNS Disord. doi: 10.4088/PCC.11m01230.
2. Tsiaras WG, Weinstock MA. Factors influencing vitamin D status. Acta Derm Venereol. 2011;91(2):115-124.
3. Adams JS, Clemens TL, Parrish JA, et al. Vitamin-D synthesis and metabolism after ultraviolet irradiation of normal and vitamin-D-deficient subjects. N Engl J Med. 1982;306(12):722-725.
4. Jones G. Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr. 2008;88(2):582S-586S.
5. Holick MF. Vitamin D: importance in the prevention of cancers type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371.
6. Fakih MG, Trump DL, Muindi JR, et al. A phase I pharmacokinetic and pharmacodynamic study of intravenous calcitriol in combination with oral gefitinib in patients with advanced solid tumors. Clin Cancer Res. 2007;13(4):1216-1223.
7. Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
8. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
9. Matsuoka LY, Ide L, Wortsman J, et al. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64(6):1165-1168.
10. Norval M, Wulf HC. Does chronic sunscreen use reduce vitamin D production to insufficient levels? Br J Dermatol. 2009;161(4):732-736.
11. Linos E, Keiser E, Kanzler M, et al. Sun protective behaviors and vitamin D levels in the US population: NHANES 2003-2006. Cancer Causes Control. 2012;23(1):133-140.
12. Prüfer K, Veenstra TD, Jirikowski GF, et al. Distribution of 1,25-dihydroxyvitamin D3 receptor immunoreactivity in the rat brain and spinal cord. J Chem Neuroanat. 1999;16(2):135-145.
13. Eyles DW, Smith S, Kinobe R, et al. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat. 2005;29(1):21-30.
14. Garcion E, Wion-Barbot N, Montero-Menei CN, et al. New clues about vitamin D functions in the nervous system. Trends Endocrinol Metab. 2002;13(3):100-105.
15. Smith MP, Fletcher-Turner A, Yurek DM, et al. Calcitriol protection against dopamine loss induced by intracerebroventricular administration of 6-hydroxydopamine. Neurochem Res. 2006;31(4):533-539.
16. Garcion E, Nataf S, Berod A, et al. 1,25-dihydroxyvitamin D3 inhibits the expression of inducible nitric oxide synthase in rat central nervous system during experimental allergic encephalomyelitis. Brain Res Mol Brain Res. 1997;45(2):255-267.
17. Baas D, Prüfer K, Ittel ME, et al. Rat oligodendrocytes express the vitamin D(3) receptor and respond to 1,25-dihydroxyvitamin D(3). Glia. 2000;31(1):59-68.
18. Brewer LD, Thibault V, Chen KC, et al. Vitamin D hormone confers neuroprotection in parallel with downregulation of L-type calcium channel expression in hippocampal neurons. J Neurosci. 2001;21(1):98-108.
19. Almeras L, Eyles D, Benech P, et al. Developmental vitamin D deficiency alters brain protein expression in the adult rat: implications for neuropsychiatric disorders. Proteomics. 2007;7(5):769-780.
20. Berg AO, Melle I, Torjesen PA, et al. A cross-sectional study of vitamin D deficiency among immigrants and Norwegians with psychosis compared to the general population. J Clin Psychiatry. 2010;71(12):1598-1604.
21. Hedelin M, Löf M, Olsson M, et al. Dietary intake of fish, omega-3, omega-6 polyunsaturated fatty acids and vitamin D and the prevalence of psychotic-like symptoms in a cohort of 33,000 women from the general population. BMC Psychiatry. 2010;10:38.-
22. McGrath J, Saari K, Hakko H, et al. Vitamin D supplementation during the first year of life and risk of schizophrenia: a Finnish birth cohort study. Schizophr Res. 2004;67(2-3):237-245.
23. McGrath J, Eyles D, Mowry B, et al. Low maternal vitamin D as a risk factor for schizophrenia: a pilot study using banked sera. Schizophr Res. 2003;63(1-2):73-78.
24. Przybelski RJ, Binkley NC. Is vitamin D important for preserving cognition? A positive correlation of serum 25-hydroxyvitamin D concentration with cognitive function. Arch Biochem Biophys. 2007;460(2):202-205.
25. Lee DM, Tajar A, Ulubaev A, et al. Association between 25-hydroxyvitamin D levels and cognitive performance in middle-aged and older European men. J Neurol Neurosurg Psychiatry. 2009;80(7):722-729.
26. Buell JS, Dawson-Hughes B, Scott TM, et al. 25-hydroxyvitamin D, dementia, and cerebrovascular pathology in elders receiving home services. Neurology. 2010;74(1):18-26.
27. Llewellyn DJ, Lang IA, Langa KM, et al. Vitamin D and risk of cognitive decline in elderly persons. Arch Intern Med. 2010;170(13):1135-1141.
28. Wilkins CH, Sheline YI, Roe CM, et al. Vitamin D deficiency is associated with low mood and worse cognitive performance in older adults. Am J Geriatr Psychiatry. 2006;14(12):1032-1040.
29. Annweiler C, Rolland Y, Schott AM, et al. Higher vitamin D dietary intake is associated with lower risk of Alzheimer’s disease: a 7-year follow-up. J Gerontol A Biol Sci Med Sci. 2012;67(11):1205-1211.
30. Kuningas M, Mooijaart SP, Jolles J, et al. VDR gene variants associate with cognitive function and depressive symptoms in old age. Neurobiol Aging. 2009;30(3):466-473.
31. Ganji V, Milone C, Cody MM, et al. Serum vitamin D concentrations are related to depression in young adult US population: the Third National Health and Nutrition Examination Survey. Int Arch Med. 2010;3:29.-
32. Hoogendijk WJ, Lips P, Dik MG, et al. Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Arch Gen Psychiatry. 2008;65(5):508-512.
33. Pan A, Lu L, Franco OH, et al. Association between depressive symptoms and 25-hydroxyvitamin D in middle-aged and elderly Chinese. J Affect Disord. 2009;118(1-3):240-243.
34. Högberg G, Gustafsson SA, Hällström T, et al. Depressed adolescents in a case-series were low in vitamin D and depression was ameliorated by vitamin D supplementation. Acta Paediatr. 2012;101(7):779-783.
35. Jorde R, Sneve M, Figenschau Y, et al. Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trial. J Intern Med. 2008;264(6):599-609.
36. Kjærgaard M, Waterloo K, Wang CE, et al. Effect of vitamin D supplement on depression scores in people with low levels of serum 25-hydroxyvitamin D: nested case-control study and randomised clinical trial. Br J Psychiatry. 2012;201(5):360-368.
37. Lansdowne AT, Provost SC. Vitamin D3 enhances mood in healthy subjects during winter. Psychopharmacology (Berl). 1998;135(4):319-223.
38. Shipowick CD, Moore CB, Corbett C, et al. Vitamin D and depressive symptoms in women during the winter: a pilot study. Appl Nurs Res. 2009;22(3):221-225.
39. Gloth FM 3rd, Alam W, Hollis B. Vitamin D vs broad spectrum phototherapy in the treatment of seasonal affective disorder. J Nutr Health Aging. 1999;3(1):5-7.
40. Vieth R, Kimball S, Hu A, et al. Randomized comparison of the effects of the vitamin D3 adequate intake versus 100 mcg (4000 IU) per day on biochemical responses and the wellbeing of patients. Nutr J. 2004;3:8.-
41. Harris S, Dawson-Hughes B. Seasonal mood changes in 250 normal women. Psychiatry Res. 1993;49(1):77-87.
42. Dumville JC, Miles JN, Porthouse J, et al. Can vitamin D supplementation prevent winter-time blues? A randomised trial among older women. J Nutr Health Aging. 2006;10(2):151-153.
43. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930.
44. Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86(1):50-60.
45. Schwalfenberg G. Not enough vitamin D: health consequences for Canadians. Can Fam Physician. 2007;53(5):841-854.
46. Norman AW, Bouillon R, Whiting SJ, et al. 13th Workshop consensus for vitamin D nutritional guidelines. J Steroid Biochem Mol Biol. 2007;103(3-5):204-205.
1. McCue RE, Charles RA, Orendain GC, et al. Vitamin D deficiency among psychiatric inpatients [published online April 19, 2012]. Prim Care Companion CNS Disord. doi: 10.4088/PCC.11m01230.
2. Tsiaras WG, Weinstock MA. Factors influencing vitamin D status. Acta Derm Venereol. 2011;91(2):115-124.
3. Adams JS, Clemens TL, Parrish JA, et al. Vitamin-D synthesis and metabolism after ultraviolet irradiation of normal and vitamin-D-deficient subjects. N Engl J Med. 1982;306(12):722-725.
4. Jones G. Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr. 2008;88(2):582S-586S.
5. Holick MF. Vitamin D: importance in the prevention of cancers type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371.
6. Fakih MG, Trump DL, Muindi JR, et al. A phase I pharmacokinetic and pharmacodynamic study of intravenous calcitriol in combination with oral gefitinib in patients with advanced solid tumors. Clin Cancer Res. 2007;13(4):1216-1223.
7. Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S-1086S.
8. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281.
9. Matsuoka LY, Ide L, Wortsman J, et al. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64(6):1165-1168.
10. Norval M, Wulf HC. Does chronic sunscreen use reduce vitamin D production to insufficient levels? Br J Dermatol. 2009;161(4):732-736.
11. Linos E, Keiser E, Kanzler M, et al. Sun protective behaviors and vitamin D levels in the US population: NHANES 2003-2006. Cancer Causes Control. 2012;23(1):133-140.
12. Prüfer K, Veenstra TD, Jirikowski GF, et al. Distribution of 1,25-dihydroxyvitamin D3 receptor immunoreactivity in the rat brain and spinal cord. J Chem Neuroanat. 1999;16(2):135-145.
13. Eyles DW, Smith S, Kinobe R, et al. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat. 2005;29(1):21-30.
14. Garcion E, Wion-Barbot N, Montero-Menei CN, et al. New clues about vitamin D functions in the nervous system. Trends Endocrinol Metab. 2002;13(3):100-105.
15. Smith MP, Fletcher-Turner A, Yurek DM, et al. Calcitriol protection against dopamine loss induced by intracerebroventricular administration of 6-hydroxydopamine. Neurochem Res. 2006;31(4):533-539.
16. Garcion E, Nataf S, Berod A, et al. 1,25-dihydroxyvitamin D3 inhibits the expression of inducible nitric oxide synthase in rat central nervous system during experimental allergic encephalomyelitis. Brain Res Mol Brain Res. 1997;45(2):255-267.
17. Baas D, Prüfer K, Ittel ME, et al. Rat oligodendrocytes express the vitamin D(3) receptor and respond to 1,25-dihydroxyvitamin D(3). Glia. 2000;31(1):59-68.
18. Brewer LD, Thibault V, Chen KC, et al. Vitamin D hormone confers neuroprotection in parallel with downregulation of L-type calcium channel expression in hippocampal neurons. J Neurosci. 2001;21(1):98-108.
19. Almeras L, Eyles D, Benech P, et al. Developmental vitamin D deficiency alters brain protein expression in the adult rat: implications for neuropsychiatric disorders. Proteomics. 2007;7(5):769-780.
20. Berg AO, Melle I, Torjesen PA, et al. A cross-sectional study of vitamin D deficiency among immigrants and Norwegians with psychosis compared to the general population. J Clin Psychiatry. 2010;71(12):1598-1604.
21. Hedelin M, Löf M, Olsson M, et al. Dietary intake of fish, omega-3, omega-6 polyunsaturated fatty acids and vitamin D and the prevalence of psychotic-like symptoms in a cohort of 33,000 women from the general population. BMC Psychiatry. 2010;10:38.-
22. McGrath J, Saari K, Hakko H, et al. Vitamin D supplementation during the first year of life and risk of schizophrenia: a Finnish birth cohort study. Schizophr Res. 2004;67(2-3):237-245.
23. McGrath J, Eyles D, Mowry B, et al. Low maternal vitamin D as a risk factor for schizophrenia: a pilot study using banked sera. Schizophr Res. 2003;63(1-2):73-78.
24. Przybelski RJ, Binkley NC. Is vitamin D important for preserving cognition? A positive correlation of serum 25-hydroxyvitamin D concentration with cognitive function. Arch Biochem Biophys. 2007;460(2):202-205.
25. Lee DM, Tajar A, Ulubaev A, et al. Association between 25-hydroxyvitamin D levels and cognitive performance in middle-aged and older European men. J Neurol Neurosurg Psychiatry. 2009;80(7):722-729.
26. Buell JS, Dawson-Hughes B, Scott TM, et al. 25-hydroxyvitamin D, dementia, and cerebrovascular pathology in elders receiving home services. Neurology. 2010;74(1):18-26.
27. Llewellyn DJ, Lang IA, Langa KM, et al. Vitamin D and risk of cognitive decline in elderly persons. Arch Intern Med. 2010;170(13):1135-1141.
28. Wilkins CH, Sheline YI, Roe CM, et al. Vitamin D deficiency is associated with low mood and worse cognitive performance in older adults. Am J Geriatr Psychiatry. 2006;14(12):1032-1040.
29. Annweiler C, Rolland Y, Schott AM, et al. Higher vitamin D dietary intake is associated with lower risk of Alzheimer’s disease: a 7-year follow-up. J Gerontol A Biol Sci Med Sci. 2012;67(11):1205-1211.
30. Kuningas M, Mooijaart SP, Jolles J, et al. VDR gene variants associate with cognitive function and depressive symptoms in old age. Neurobiol Aging. 2009;30(3):466-473.
31. Ganji V, Milone C, Cody MM, et al. Serum vitamin D concentrations are related to depression in young adult US population: the Third National Health and Nutrition Examination Survey. Int Arch Med. 2010;3:29.-
32. Hoogendijk WJ, Lips P, Dik MG, et al. Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Arch Gen Psychiatry. 2008;65(5):508-512.
33. Pan A, Lu L, Franco OH, et al. Association between depressive symptoms and 25-hydroxyvitamin D in middle-aged and elderly Chinese. J Affect Disord. 2009;118(1-3):240-243.
34. Högberg G, Gustafsson SA, Hällström T, et al. Depressed adolescents in a case-series were low in vitamin D and depression was ameliorated by vitamin D supplementation. Acta Paediatr. 2012;101(7):779-783.
35. Jorde R, Sneve M, Figenschau Y, et al. Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trial. J Intern Med. 2008;264(6):599-609.
36. Kjærgaard M, Waterloo K, Wang CE, et al. Effect of vitamin D supplement on depression scores in people with low levels of serum 25-hydroxyvitamin D: nested case-control study and randomised clinical trial. Br J Psychiatry. 2012;201(5):360-368.
37. Lansdowne AT, Provost SC. Vitamin D3 enhances mood in healthy subjects during winter. Psychopharmacology (Berl). 1998;135(4):319-223.
38. Shipowick CD, Moore CB, Corbett C, et al. Vitamin D and depressive symptoms in women during the winter: a pilot study. Appl Nurs Res. 2009;22(3):221-225.
39. Gloth FM 3rd, Alam W, Hollis B. Vitamin D vs broad spectrum phototherapy in the treatment of seasonal affective disorder. J Nutr Health Aging. 1999;3(1):5-7.
40. Vieth R, Kimball S, Hu A, et al. Randomized comparison of the effects of the vitamin D3 adequate intake versus 100 mcg (4000 IU) per day on biochemical responses and the wellbeing of patients. Nutr J. 2004;3:8.-
41. Harris S, Dawson-Hughes B. Seasonal mood changes in 250 normal women. Psychiatry Res. 1993;49(1):77-87.
42. Dumville JC, Miles JN, Porthouse J, et al. Can vitamin D supplementation prevent winter-time blues? A randomised trial among older women. J Nutr Health Aging. 2006;10(2):151-153.
43. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930.
44. Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86(1):50-60.
45. Schwalfenberg G. Not enough vitamin D: health consequences for Canadians. Can Fam Physician. 2007;53(5):841-854.
46. Norman AW, Bouillon R, Whiting SJ, et al. 13th Workshop consensus for vitamin D nutritional guidelines. J Steroid Biochem Mol Biol. 2007;103(3-5):204-205.








