User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Ending a physician/patient relationship: 8 tips for writing a termination letter
For many valid reasons, a physician-patient relationship may need to end before treatment is completed. When terminating a clinical relationship, send a letter to the patient, even if the patient initiated the termination. Here are 8 tips for writing and sending a termination letter:
1. Don’t send a form letter. Start with a standard letter but personalize it for each patient. Address the patient by name and, if possible, allude to specifics of the patient’s situation.
2. Wish the patient well, but avoid hyperbole, such as “It truly has been an honor and a privilege to participate in your treatment.” Also, be unambiguous in stating that the treatment relationship is terminated.
3. Don’t mention confidential information. Because someone other than the patient may open the letter, do not include confidential information.
4. Provide appropriate notice. Specify a date after which you can no longer provide care. A reasonable period is 30 days from the date of the letter, but if you expect the patient will need more time to find an appropriate clinician, a longer period may be necessary.1,2 Occasionally, a patient’s care may need to be terminated immediately because of a serious problem such as actual or threatened violence. Even in these cases, communicate and document how the patient can obtain emergency psychiatric care.
5. State the reason for termination. Although you are not required legally to do so, briefly state the reason for terminating the relationship, although you should never use emotional or harshly critical language. Use nonjudgmental language and avoid referring to your “policy,” which can imply unthinking application of rigid rules.
6. Recommend continued treatment. Make a clear recommendation that the patient continue treatment elsewhere. Provide a list of mental health professionals with whom the patient could continue treatment or offer to provide referrals. Offer to send a copy of your records to the patient’s new clinician. Consider enclosing a blank copy of the release form you use so that the patient can mail it to you to request his or her records.
7. Sign the letter yourself. Don’t have a staff member sign the letter or use a stamp.
8. Send the letter by certified mail. Request a return receipt and put a copy of the letter, along with the certified mail form, in the patient’s chart. When the return receipt is received, put it in the chart. If a certified letter is returned to you, put the undelivered letter and envelope in the chart, then send a copy of the letter through regular mail and document that you did so.
If the patient requests an appointment after the notice period is over, including saying that he or she did not receive the letter, you are not legally obligated to resume his or her care.2
1. The Psychiatrist’s Program. Termination of the psychiatrist-patient relationship dos and donts. http://www.psychprogram.com/risk-management/tip-termination.html. Accessed February 1, 2013.
2. Willis DR, Zerr A. Terminating a patient: is it time to part ways? Fam Pract Manag. 2005;12(8):34-38.
For many valid reasons, a physician-patient relationship may need to end before treatment is completed. When terminating a clinical relationship, send a letter to the patient, even if the patient initiated the termination. Here are 8 tips for writing and sending a termination letter:
1. Don’t send a form letter. Start with a standard letter but personalize it for each patient. Address the patient by name and, if possible, allude to specifics of the patient’s situation.
2. Wish the patient well, but avoid hyperbole, such as “It truly has been an honor and a privilege to participate in your treatment.” Also, be unambiguous in stating that the treatment relationship is terminated.
3. Don’t mention confidential information. Because someone other than the patient may open the letter, do not include confidential information.
4. Provide appropriate notice. Specify a date after which you can no longer provide care. A reasonable period is 30 days from the date of the letter, but if you expect the patient will need more time to find an appropriate clinician, a longer period may be necessary.1,2 Occasionally, a patient’s care may need to be terminated immediately because of a serious problem such as actual or threatened violence. Even in these cases, communicate and document how the patient can obtain emergency psychiatric care.
5. State the reason for termination. Although you are not required legally to do so, briefly state the reason for terminating the relationship, although you should never use emotional or harshly critical language. Use nonjudgmental language and avoid referring to your “policy,” which can imply unthinking application of rigid rules.
6. Recommend continued treatment. Make a clear recommendation that the patient continue treatment elsewhere. Provide a list of mental health professionals with whom the patient could continue treatment or offer to provide referrals. Offer to send a copy of your records to the patient’s new clinician. Consider enclosing a blank copy of the release form you use so that the patient can mail it to you to request his or her records.
7. Sign the letter yourself. Don’t have a staff member sign the letter or use a stamp.
8. Send the letter by certified mail. Request a return receipt and put a copy of the letter, along with the certified mail form, in the patient’s chart. When the return receipt is received, put it in the chart. If a certified letter is returned to you, put the undelivered letter and envelope in the chart, then send a copy of the letter through regular mail and document that you did so.
If the patient requests an appointment after the notice period is over, including saying that he or she did not receive the letter, you are not legally obligated to resume his or her care.2
For many valid reasons, a physician-patient relationship may need to end before treatment is completed. When terminating a clinical relationship, send a letter to the patient, even if the patient initiated the termination. Here are 8 tips for writing and sending a termination letter:
1. Don’t send a form letter. Start with a standard letter but personalize it for each patient. Address the patient by name and, if possible, allude to specifics of the patient’s situation.
2. Wish the patient well, but avoid hyperbole, such as “It truly has been an honor and a privilege to participate in your treatment.” Also, be unambiguous in stating that the treatment relationship is terminated.
3. Don’t mention confidential information. Because someone other than the patient may open the letter, do not include confidential information.
4. Provide appropriate notice. Specify a date after which you can no longer provide care. A reasonable period is 30 days from the date of the letter, but if you expect the patient will need more time to find an appropriate clinician, a longer period may be necessary.1,2 Occasionally, a patient’s care may need to be terminated immediately because of a serious problem such as actual or threatened violence. Even in these cases, communicate and document how the patient can obtain emergency psychiatric care.
5. State the reason for termination. Although you are not required legally to do so, briefly state the reason for terminating the relationship, although you should never use emotional or harshly critical language. Use nonjudgmental language and avoid referring to your “policy,” which can imply unthinking application of rigid rules.
6. Recommend continued treatment. Make a clear recommendation that the patient continue treatment elsewhere. Provide a list of mental health professionals with whom the patient could continue treatment or offer to provide referrals. Offer to send a copy of your records to the patient’s new clinician. Consider enclosing a blank copy of the release form you use so that the patient can mail it to you to request his or her records.
7. Sign the letter yourself. Don’t have a staff member sign the letter or use a stamp.
8. Send the letter by certified mail. Request a return receipt and put a copy of the letter, along with the certified mail form, in the patient’s chart. When the return receipt is received, put it in the chart. If a certified letter is returned to you, put the undelivered letter and envelope in the chart, then send a copy of the letter through regular mail and document that you did so.
If the patient requests an appointment after the notice period is over, including saying that he or she did not receive the letter, you are not legally obligated to resume his or her care.2
1. The Psychiatrist’s Program. Termination of the psychiatrist-patient relationship dos and donts. http://www.psychprogram.com/risk-management/tip-termination.html. Accessed February 1, 2013.
2. Willis DR, Zerr A. Terminating a patient: is it time to part ways? Fam Pract Manag. 2005;12(8):34-38.
1. The Psychiatrist’s Program. Termination of the psychiatrist-patient relationship dos and donts. http://www.psychprogram.com/risk-management/tip-termination.html. Accessed February 1, 2013.
2. Willis DR, Zerr A. Terminating a patient: is it time to part ways? Fam Pract Manag. 2005;12(8):34-38.
A teen who is wasting away
CASE: Weak and passive
Cassandra, age 17, recently was discharged from a medical rehabilitation facility with a diagnosis of conversion disorder. Her school performance and attendance had been steadily declining for the last 6 months as she lost strength and motivation to take care of herself. Cassandra lives with her father, who is her primary caretaker. Her parents are separated and her mother has fibromyalgia and chronic fatigue syndrome, which leaves her unable to care for her daughter or participate in appointments.
Now lethargic and wasting away physically, Cassandra is pushed in a wheelchair by her weary father into a child psychiatrist’s office. She does not look up or make eye contact. Her father says “the doctors didn’t know what they were doing. That needle test, a nerve conduction study they did, is what made her worse.” Although Cassandra moves her arms to adjust herself in the wheelchair, she does not move her legs or try to move the wheelchair.
Cassandra’s father states that she has “congenital neuromyopathy. Her mother gave it to her in utero. But nobody listens to me or orders the tests that will prove I am right.” He insists on obscure and specialized blood tests and immune function panels to prove that a congenital condition is causing his daughter’s deterioration and physical debility. He is unwilling to accept that there is any other cause of her condition.
Cassandra’s father is unemployed and has no social contacts or supports. He asserts that “the medical system” is against him, and he believes medical interventions are harming his daughter. He keeps Cassandra isolated from friends and other family members.
How would you proceed?
a) separate Cassandra from her father during the interview
b) contact Cassandra’s mother for collateral information
c) assure Cassandra that there is no medical cause for her physical condition
d) order the testing her father requests
EVALUATION: Demoralized, hopeless
Cassandra is uncooperative with the interview and answers questions with one-word answers. Her affect is irritable and her demeanor is frustrated. She does not seem concerned that she needs assistance with eating and toileting.
When outpatient treatment with her primary care physician did not stop her physical deterioration, she was referred to a tertiary care academic medical center for a complete medical and neurologic workup. The workup, including an MRI, electroencephalogram, nerve conduction studies, and full immunologic panels, was negative for any physical illness, including neuromuscular degenerative disease. A muscle biopsy was considered, but not ordered because Cassandra and her father resisted.
During this hospitalization, she was diagnosed with conversion disorder by the psychiatry consultation service, and transferred to a physical rehabilitation facility for further care. At the rehab facility, Cassandra’s father interfered with her care, arguing constantly with the medical team. Cassandra demonstrated no effort to work with physical or occupational therapy and was discharged after 2 weeks because of noncompliance with treatment. Cassandra and her father are resentful that no physical cause was found and feel that the medical workup and time at the rehabilitation facility made her condition worse. The rehabilitation hospital referred Cassandra to an outpatient child psychiatrist for follow-up.
During the intake evaluation and follow-up appointments with the child psychiatrist, her affect is negativistic and restrictive. She is resistant to talking about her condition and accepting psychotherapeutic interventions. She is quick to blame others for her lack of progress and unable to take responsibility for working on her treatment plan. Cassandra feels demoralized, depressed, and hopeless about her situation and prospects for recovery. She feels that no one is listening to her father and if “they did just the tests he wants, we will know what is wrong with me and that he is right.”
The author’s observations
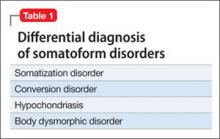
Table 1 lists conditions to consider in the differential diagnosis of conversion disorder. Although Cassandra’s conversion disorder diagnosis appears to be appropriate, it is important to consider 2 other possibilities: delusional disorder, somatic type with familial features, and Munchausen syndrome by proxy. An underlying depressive or anxiety disorder also should be considered and treated appropriately.
Conversion disorder has a challenging and often complex presentation in children and adolescents. Conversion disorders in children commonly are associated with stressful family situations including divorce, marital conflict, or loss of a close family member.1 An overbearing and conflict-prone parenting style also is associated with childhood conversion disorders.2 Common physical symptoms in conversion disorder are functional abdominal pain, partial paralysis, numbness, or seizures. Individuals such as Cassandra who are unable to express or verbalize their emotional distress are vulnerable to expressing their distress in somatic symptoms. Cassandra demonstrates La belle indifference, the characteristic attitude of not being overly concerned about what others would consider an alarming functional impairment.
Delusional disorder. A diagnosis of delusional disorder, somatic type with familial features was considered because Cassandra and her father shared persecutory and paranoid beliefs that her condition was brought on by some hidden, unrecognized medical condition. A delusional disorder with shared or “familial” features develops when a parent has strongly held delusional beliefs that are transferred to the child. Typically, it develops within the context of a close relationship with the parent, is similar in content to the parent’s belief, and is not preceded by psychosis or prodromal to schizophrenia.3
Because Cassandra’s father transferred his delusional system to his daughter, she clung to the belief that her physical symptoms and immobility were caused by medical misdiagnosis and failure to recognize her illness. Cassandra’s father strongly resisted and defended against accepting his role in her medical condition.
Munchausen by proxy. Because Cassandra and her father share a delusional system that prevented her from accepting and following treatment recommendations, it is possible that her father created her condition. Munchausen syndrome by proxy is a condition whereby illness-producing behavior in a child is exaggerated, fabricated, or induced by a parent or guardian.4 Separating Cassandra from her father and initiating antipsychotic treatment for him are critical considerations for her recovery.
How would you treat Cassandra?
a) call Child Protective Services (CPS) to remove Cassandra from her father’s custody
b) hospitalize Cassandra for intensive treatment of conversion disorder
c) start Cassandra on an atypical antipsychotic
d) begin cognitive-behavioral therapy (CBT) and an antidepressant
Treatment approach
Treating a patient with a conversion disorder, somatic type starts with validating that the patient’s and parent’s distress is real to them (Table 2).5 The clinician acknowledges that no physical evidence of physiological dysfunction has been found, which can be reassuring to the patient and family. The clinician then states that the patient’s condition and the physical manifestation of the symptoms are real. A patient’s or parent’s resistance to this reassurance may indicate that they have a large investment in the symptoms and perpetuating the dysfunction.
Taking a mind-body approach—explaining that the child’s condition is created and perpetuated by a mind-body connection and is not under their voluntary control—often is well received by patients and parents. The treating clinician emphasizes that the condition is physically disabling and that careful, appropriate, and intensive treatment is necessary.
A rehabilitation model has power for patients with conversion disorder because it acknowledges the patient’s discomfort and loss of function while shifting the focus away from finding what is wrong. The goal is to actively engage patients in their own care to help them return to normal functioning.6
Cassandra was encouraged to participate in physical therapy, go to school, and take care of herself. Actively participating in her care and recovery meant that Cassandra had to leave the sick role behind, which was impossible for her father, who saw her as passive, helpless, and fragile.
TREATMENT: Pharmacotherapy, CBT
During psychiatric evaluation, it becomes clear that in addition to her physical debility, Cassandra has major depressive disorder, moderate without psychotic features. Her depression contributes to her hopelessness and lack of participation in treatment. After discussion with her family about how her depressive symptoms are preventing her recovery, Cassandra is started on escitalopram, 10 mg/d. CBT helps her manage her depressive symptoms, prevent further somatization, and correct misperceptions about her body function and disabilities.
For conversion disorder patients, physical therapy can be combined with incentives tied to improvements in functioning. Cassandra has overwhelming anxiety while attempting physical therapy, which interferes with her participation in the therapy. Lorazepam, 0.5 mg/d, is prescribed for her intense anxiety and panic attacks, which led her to avoid physical therapy.
Staff at the rehabilitation hospital calls CPS because Cassandra’s father interferes with her care and treatment plan. CPS continues to monitor Cassandra’s progress through outpatient care. An individualized education plan and psychoeducational testing help determine a school placement to meet Cassandra’s educational needs.
CPS directs Cassandra to stay with her mother for alternating weeks. While at her mother’s, Cassandra is more interested in taking care of herself. She helps with getting herself into bed and to the toilet. Upon returning to her father’s home, these gains are lost.
The author’s observations
Psychodynamic and unconscious motivators for conversion disorder operate on a deeper, hidden level. The underlying primary conflict in pseudoseizures—a more common conversion disorder—has been described as an inability to express negative emotions such as anger. Social problems, conflict with parents, learning disorders,7 or sexual abuse8 produce the negative emotions caused by the primary conflict. Cassandra yearned for a closer relationship with her mother, yet she remained enmeshed with poor intrapsychic boundaries with her father. The fact that he assisted his 17-year-old daughter with toileting raised the possibility of sexual abuse. Sexual abuse could have led to her depression and physical decline. Cassandra’s physical debility also may have been her way to foster dependency on her father and protect him from perceived persecution.
Conversion disorder may have been a result of Cassandra’s defense mechanisms against admitting abuse and protecting against abandonment. Establishing a therapeutic alliance with Cassandra is essential to allow a graceful exit from the conversion disorder symptoms and her father’s hold on her thinking about her illness. However, this alliance may seem to threaten the child’s special connection with the parent. A therapeutic alliance was elusive in Cassandra’s case and likely nearly impossible.
Both parents underwent court-ordered psychological testing as part of the CPS evaluation. Testing on Cassandra’s father indicated a rigid personality structure with long-standing paranoia and mistrust of authority. Because Cassandra endorsed his delusional system completely, it is likely that her father inculcated her into believing his beliefs and transmitted his delusions to her by their close proximity and time together. Based upon this delusional belief system, Cassandra gave up trying to move her legs and her muscles atrophied. Her legs were so weak that she stopped trying to walk or move, illustrating the power of the mind-body connection to produce functional and physiological changes.
Children who live with a mother with chronic illness are at risk of developing psychosomatic disorders.9 Cassandra’s mother had fibromyalgia and chronic pain with symptoms of headache, weakness, and muscle pain and frequent medical office visits and tests without definitive results or symptom relief. Although Cassandra did not live with her mother, Cassandra’s somatization symptoms may be a result of modeling or observational learning within her family.9 Cassandra may have unconsciously adopted her mother’s symptoms and behaviors as a way to cope with stress and gain attention to her needs.
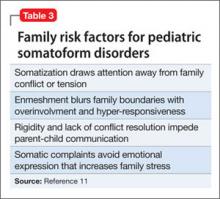
Cassandra’s negative affect, sensitivity to change, and lack of resiliency were further risk factors for developing a somatoform illness.10 She resisted and would not follow through with physical therapy. Krisnakumar10 also reported that an inability to persist in completing tasks is a risk factor for somatoform disorder. Family dynamics of problematic parental interactions also played a role in her somatoform disorder (Table 3).11
OUTCOME: Foster care, improvement
Cassandra receives weekly CBT and biweekly medication monitoring and demonstrates a moderate improvement in mood with less negativity and irritability. Her anxiety symptoms gradually respond to treatment. However, her emotional gains are not matched with improvement in her physical functioning or participation in physical therapy. Cassandra does not recover her muscular strength or control and shows little improvement in her physical capacity and independence.
After 3 months of treatment, Cassandra does not make sufficient progress or actively participate in treatment. Because her father continues to interfere with the treatment plan and does not receive treatment himself, CPS obtains a court order to prevent her father from directing her medical care and telling her treating physicians which tests to order.
Because these interventions do not improve her treatment response, Cassandra is removed from her parents’ care and placed in a therapeutic foster care home, thereby improving her independence and chances for recovery. After 3 months in foster care, she more actively participates in her physical rehabilitation. Water therapy, with the buoyancy and support in water, helps her regain muscle strength and control of her lower extremities.
Bottom Line
Patients with conversion disorder present with functional impairment and physical symptoms without clear physiological causes. Parents have a strong influence on the presentation and course of conversion disorder in children and adolescents. Parents’ mental and physical illnesses are independent risk factors for childhood somatoform disorders. Evaluation of parents’ psychological and psychiatric state is essential to determine intervention.
Related Resource
- Seltzer WJ. Conversion disorder in childhood and adolescence: a familial/cultural approach. Family Systems Medicine. 1985;3(3):261-280.
Drug Brand Names
Escitalopram • Lexapro
Lorazepam • Ativan
Disclosure
Dr. Leipsic reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Wyllie E, Glazer JP, Benbadis S, et al. Psychiatric features of children and adolescents with pseudoseizures. Arch Pediatr Adolesc Med. 1999;153(3):244-248.
2. Salmon P, Al-Marzooqi SM, Baker G, et al. Childhood family dysfunction and associated abuse in patients with nonepileptic seizures: towards a casual model. Psychosom Med. 2003;65(4):695-700.
3. Manschreck T. Delusional disorder and shared psychotic disorder. In: Sadock BJ, Sadock VA, eds. Kaplan & Sadock’s comprehensive textbook of psychiatry. 7th ed.
Philadelphia, PA: Lippincott Williams & Wilkins; 2000: 1243-1264.
4. Meadow R. Munchausen syndrome by proxy. The hinterland of child abuse. Lancet. 1977;2(8033):343-345.
5. Campo JV, Fritsch SL. Somatization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1994; 33(9):1223-1235.
6. Campo JV, Fritz G. A management model for pediatric somatization. Psychosomatics. 2001;42(6):467-476.
7. Silver LB. Conversion disorder with pseudoseizures in adolescence: a stress reaction to unrecognized and untreated learning disabilities. J Am Accad Child Psychiatry. 1982; 21(5):508-512.
8. AlperK,DevinskyO,PerrineK,etal.Nonepilepticseizures and childhood sexual and physical abuse. Neurology. 1993; 43(10):1950-1953.
9. Jamison RN, Walker LS. Illness behavior in children of chronic pain patients. Int J Psychiatry Med. 1992;22(4): 329-342.
10. Krisnakumar P, Sumesh P, Mathews L. Tempermental traits associated with conversion disorder. Indian Pediatr. 2006;43(10):895-899.
11. Minuchin S, Rosman BL, Baker L. Psychosomatic families: anorexia nervosa in context. Cambridge, MA: Harvard University Press; 1978.
CASE: Weak and passive
Cassandra, age 17, recently was discharged from a medical rehabilitation facility with a diagnosis of conversion disorder. Her school performance and attendance had been steadily declining for the last 6 months as she lost strength and motivation to take care of herself. Cassandra lives with her father, who is her primary caretaker. Her parents are separated and her mother has fibromyalgia and chronic fatigue syndrome, which leaves her unable to care for her daughter or participate in appointments.
Now lethargic and wasting away physically, Cassandra is pushed in a wheelchair by her weary father into a child psychiatrist’s office. She does not look up or make eye contact. Her father says “the doctors didn’t know what they were doing. That needle test, a nerve conduction study they did, is what made her worse.” Although Cassandra moves her arms to adjust herself in the wheelchair, she does not move her legs or try to move the wheelchair.
Cassandra’s father states that she has “congenital neuromyopathy. Her mother gave it to her in utero. But nobody listens to me or orders the tests that will prove I am right.” He insists on obscure and specialized blood tests and immune function panels to prove that a congenital condition is causing his daughter’s deterioration and physical debility. He is unwilling to accept that there is any other cause of her condition.
Cassandra’s father is unemployed and has no social contacts or supports. He asserts that “the medical system” is against him, and he believes medical interventions are harming his daughter. He keeps Cassandra isolated from friends and other family members.
How would you proceed?
a) separate Cassandra from her father during the interview
b) contact Cassandra’s mother for collateral information
c) assure Cassandra that there is no medical cause for her physical condition
d) order the testing her father requests
EVALUATION: Demoralized, hopeless
Cassandra is uncooperative with the interview and answers questions with one-word answers. Her affect is irritable and her demeanor is frustrated. She does not seem concerned that she needs assistance with eating and toileting.
When outpatient treatment with her primary care physician did not stop her physical deterioration, she was referred to a tertiary care academic medical center for a complete medical and neurologic workup. The workup, including an MRI, electroencephalogram, nerve conduction studies, and full immunologic panels, was negative for any physical illness, including neuromuscular degenerative disease. A muscle biopsy was considered, but not ordered because Cassandra and her father resisted.
During this hospitalization, she was diagnosed with conversion disorder by the psychiatry consultation service, and transferred to a physical rehabilitation facility for further care. At the rehab facility, Cassandra’s father interfered with her care, arguing constantly with the medical team. Cassandra demonstrated no effort to work with physical or occupational therapy and was discharged after 2 weeks because of noncompliance with treatment. Cassandra and her father are resentful that no physical cause was found and feel that the medical workup and time at the rehabilitation facility made her condition worse. The rehabilitation hospital referred Cassandra to an outpatient child psychiatrist for follow-up.
During the intake evaluation and follow-up appointments with the child psychiatrist, her affect is negativistic and restrictive. She is resistant to talking about her condition and accepting psychotherapeutic interventions. She is quick to blame others for her lack of progress and unable to take responsibility for working on her treatment plan. Cassandra feels demoralized, depressed, and hopeless about her situation and prospects for recovery. She feels that no one is listening to her father and if “they did just the tests he wants, we will know what is wrong with me and that he is right.”
The author’s observations
Table 1 lists conditions to consider in the differential diagnosis of conversion disorder. Although Cassandra’s conversion disorder diagnosis appears to be appropriate, it is important to consider 2 other possibilities: delusional disorder, somatic type with familial features, and Munchausen syndrome by proxy. An underlying depressive or anxiety disorder also should be considered and treated appropriately.
Conversion disorder has a challenging and often complex presentation in children and adolescents. Conversion disorders in children commonly are associated with stressful family situations including divorce, marital conflict, or loss of a close family member.1 An overbearing and conflict-prone parenting style also is associated with childhood conversion disorders.2 Common physical symptoms in conversion disorder are functional abdominal pain, partial paralysis, numbness, or seizures. Individuals such as Cassandra who are unable to express or verbalize their emotional distress are vulnerable to expressing their distress in somatic symptoms. Cassandra demonstrates La belle indifference, the characteristic attitude of not being overly concerned about what others would consider an alarming functional impairment.
Delusional disorder. A diagnosis of delusional disorder, somatic type with familial features was considered because Cassandra and her father shared persecutory and paranoid beliefs that her condition was brought on by some hidden, unrecognized medical condition. A delusional disorder with shared or “familial” features develops when a parent has strongly held delusional beliefs that are transferred to the child. Typically, it develops within the context of a close relationship with the parent, is similar in content to the parent’s belief, and is not preceded by psychosis or prodromal to schizophrenia.3
Because Cassandra’s father transferred his delusional system to his daughter, she clung to the belief that her physical symptoms and immobility were caused by medical misdiagnosis and failure to recognize her illness. Cassandra’s father strongly resisted and defended against accepting his role in her medical condition.
Munchausen by proxy. Because Cassandra and her father share a delusional system that prevented her from accepting and following treatment recommendations, it is possible that her father created her condition. Munchausen syndrome by proxy is a condition whereby illness-producing behavior in a child is exaggerated, fabricated, or induced by a parent or guardian.4 Separating Cassandra from her father and initiating antipsychotic treatment for him are critical considerations for her recovery.
How would you treat Cassandra?
a) call Child Protective Services (CPS) to remove Cassandra from her father’s custody
b) hospitalize Cassandra for intensive treatment of conversion disorder
c) start Cassandra on an atypical antipsychotic
d) begin cognitive-behavioral therapy (CBT) and an antidepressant
Treatment approach
Treating a patient with a conversion disorder, somatic type starts with validating that the patient’s and parent’s distress is real to them (Table 2).5 The clinician acknowledges that no physical evidence of physiological dysfunction has been found, which can be reassuring to the patient and family. The clinician then states that the patient’s condition and the physical manifestation of the symptoms are real. A patient’s or parent’s resistance to this reassurance may indicate that they have a large investment in the symptoms and perpetuating the dysfunction.
Taking a mind-body approach—explaining that the child’s condition is created and perpetuated by a mind-body connection and is not under their voluntary control—often is well received by patients and parents. The treating clinician emphasizes that the condition is physically disabling and that careful, appropriate, and intensive treatment is necessary.
A rehabilitation model has power for patients with conversion disorder because it acknowledges the patient’s discomfort and loss of function while shifting the focus away from finding what is wrong. The goal is to actively engage patients in their own care to help them return to normal functioning.6
Cassandra was encouraged to participate in physical therapy, go to school, and take care of herself. Actively participating in her care and recovery meant that Cassandra had to leave the sick role behind, which was impossible for her father, who saw her as passive, helpless, and fragile.
TREATMENT: Pharmacotherapy, CBT
During psychiatric evaluation, it becomes clear that in addition to her physical debility, Cassandra has major depressive disorder, moderate without psychotic features. Her depression contributes to her hopelessness and lack of participation in treatment. After discussion with her family about how her depressive symptoms are preventing her recovery, Cassandra is started on escitalopram, 10 mg/d. CBT helps her manage her depressive symptoms, prevent further somatization, and correct misperceptions about her body function and disabilities.
For conversion disorder patients, physical therapy can be combined with incentives tied to improvements in functioning. Cassandra has overwhelming anxiety while attempting physical therapy, which interferes with her participation in the therapy. Lorazepam, 0.5 mg/d, is prescribed for her intense anxiety and panic attacks, which led her to avoid physical therapy.
Staff at the rehabilitation hospital calls CPS because Cassandra’s father interferes with her care and treatment plan. CPS continues to monitor Cassandra’s progress through outpatient care. An individualized education plan and psychoeducational testing help determine a school placement to meet Cassandra’s educational needs.
CPS directs Cassandra to stay with her mother for alternating weeks. While at her mother’s, Cassandra is more interested in taking care of herself. She helps with getting herself into bed and to the toilet. Upon returning to her father’s home, these gains are lost.
The author’s observations
Psychodynamic and unconscious motivators for conversion disorder operate on a deeper, hidden level. The underlying primary conflict in pseudoseizures—a more common conversion disorder—has been described as an inability to express negative emotions such as anger. Social problems, conflict with parents, learning disorders,7 or sexual abuse8 produce the negative emotions caused by the primary conflict. Cassandra yearned for a closer relationship with her mother, yet she remained enmeshed with poor intrapsychic boundaries with her father. The fact that he assisted his 17-year-old daughter with toileting raised the possibility of sexual abuse. Sexual abuse could have led to her depression and physical decline. Cassandra’s physical debility also may have been her way to foster dependency on her father and protect him from perceived persecution.
Conversion disorder may have been a result of Cassandra’s defense mechanisms against admitting abuse and protecting against abandonment. Establishing a therapeutic alliance with Cassandra is essential to allow a graceful exit from the conversion disorder symptoms and her father’s hold on her thinking about her illness. However, this alliance may seem to threaten the child’s special connection with the parent. A therapeutic alliance was elusive in Cassandra’s case and likely nearly impossible.
Both parents underwent court-ordered psychological testing as part of the CPS evaluation. Testing on Cassandra’s father indicated a rigid personality structure with long-standing paranoia and mistrust of authority. Because Cassandra endorsed his delusional system completely, it is likely that her father inculcated her into believing his beliefs and transmitted his delusions to her by their close proximity and time together. Based upon this delusional belief system, Cassandra gave up trying to move her legs and her muscles atrophied. Her legs were so weak that she stopped trying to walk or move, illustrating the power of the mind-body connection to produce functional and physiological changes.
Children who live with a mother with chronic illness are at risk of developing psychosomatic disorders.9 Cassandra’s mother had fibromyalgia and chronic pain with symptoms of headache, weakness, and muscle pain and frequent medical office visits and tests without definitive results or symptom relief. Although Cassandra did not live with her mother, Cassandra’s somatization symptoms may be a result of modeling or observational learning within her family.9 Cassandra may have unconsciously adopted her mother’s symptoms and behaviors as a way to cope with stress and gain attention to her needs.
Cassandra’s negative affect, sensitivity to change, and lack of resiliency were further risk factors for developing a somatoform illness.10 She resisted and would not follow through with physical therapy. Krisnakumar10 also reported that an inability to persist in completing tasks is a risk factor for somatoform disorder. Family dynamics of problematic parental interactions also played a role in her somatoform disorder (Table 3).11
OUTCOME: Foster care, improvement
Cassandra receives weekly CBT and biweekly medication monitoring and demonstrates a moderate improvement in mood with less negativity and irritability. Her anxiety symptoms gradually respond to treatment. However, her emotional gains are not matched with improvement in her physical functioning or participation in physical therapy. Cassandra does not recover her muscular strength or control and shows little improvement in her physical capacity and independence.
After 3 months of treatment, Cassandra does not make sufficient progress or actively participate in treatment. Because her father continues to interfere with the treatment plan and does not receive treatment himself, CPS obtains a court order to prevent her father from directing her medical care and telling her treating physicians which tests to order.
Because these interventions do not improve her treatment response, Cassandra is removed from her parents’ care and placed in a therapeutic foster care home, thereby improving her independence and chances for recovery. After 3 months in foster care, she more actively participates in her physical rehabilitation. Water therapy, with the buoyancy and support in water, helps her regain muscle strength and control of her lower extremities.
Bottom Line
Patients with conversion disorder present with functional impairment and physical symptoms without clear physiological causes. Parents have a strong influence on the presentation and course of conversion disorder in children and adolescents. Parents’ mental and physical illnesses are independent risk factors for childhood somatoform disorders. Evaluation of parents’ psychological and psychiatric state is essential to determine intervention.
Related Resource
- Seltzer WJ. Conversion disorder in childhood and adolescence: a familial/cultural approach. Family Systems Medicine. 1985;3(3):261-280.
Drug Brand Names
Escitalopram • Lexapro
Lorazepam • Ativan
Disclosure
Dr. Leipsic reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Weak and passive
Cassandra, age 17, recently was discharged from a medical rehabilitation facility with a diagnosis of conversion disorder. Her school performance and attendance had been steadily declining for the last 6 months as she lost strength and motivation to take care of herself. Cassandra lives with her father, who is her primary caretaker. Her parents are separated and her mother has fibromyalgia and chronic fatigue syndrome, which leaves her unable to care for her daughter or participate in appointments.
Now lethargic and wasting away physically, Cassandra is pushed in a wheelchair by her weary father into a child psychiatrist’s office. She does not look up or make eye contact. Her father says “the doctors didn’t know what they were doing. That needle test, a nerve conduction study they did, is what made her worse.” Although Cassandra moves her arms to adjust herself in the wheelchair, she does not move her legs or try to move the wheelchair.
Cassandra’s father states that she has “congenital neuromyopathy. Her mother gave it to her in utero. But nobody listens to me or orders the tests that will prove I am right.” He insists on obscure and specialized blood tests and immune function panels to prove that a congenital condition is causing his daughter’s deterioration and physical debility. He is unwilling to accept that there is any other cause of her condition.
Cassandra’s father is unemployed and has no social contacts or supports. He asserts that “the medical system” is against him, and he believes medical interventions are harming his daughter. He keeps Cassandra isolated from friends and other family members.
How would you proceed?
a) separate Cassandra from her father during the interview
b) contact Cassandra’s mother for collateral information
c) assure Cassandra that there is no medical cause for her physical condition
d) order the testing her father requests
EVALUATION: Demoralized, hopeless
Cassandra is uncooperative with the interview and answers questions with one-word answers. Her affect is irritable and her demeanor is frustrated. She does not seem concerned that she needs assistance with eating and toileting.
When outpatient treatment with her primary care physician did not stop her physical deterioration, she was referred to a tertiary care academic medical center for a complete medical and neurologic workup. The workup, including an MRI, electroencephalogram, nerve conduction studies, and full immunologic panels, was negative for any physical illness, including neuromuscular degenerative disease. A muscle biopsy was considered, but not ordered because Cassandra and her father resisted.
During this hospitalization, she was diagnosed with conversion disorder by the psychiatry consultation service, and transferred to a physical rehabilitation facility for further care. At the rehab facility, Cassandra’s father interfered with her care, arguing constantly with the medical team. Cassandra demonstrated no effort to work with physical or occupational therapy and was discharged after 2 weeks because of noncompliance with treatment. Cassandra and her father are resentful that no physical cause was found and feel that the medical workup and time at the rehabilitation facility made her condition worse. The rehabilitation hospital referred Cassandra to an outpatient child psychiatrist for follow-up.
During the intake evaluation and follow-up appointments with the child psychiatrist, her affect is negativistic and restrictive. She is resistant to talking about her condition and accepting psychotherapeutic interventions. She is quick to blame others for her lack of progress and unable to take responsibility for working on her treatment plan. Cassandra feels demoralized, depressed, and hopeless about her situation and prospects for recovery. She feels that no one is listening to her father and if “they did just the tests he wants, we will know what is wrong with me and that he is right.”
The author’s observations
Table 1 lists conditions to consider in the differential diagnosis of conversion disorder. Although Cassandra’s conversion disorder diagnosis appears to be appropriate, it is important to consider 2 other possibilities: delusional disorder, somatic type with familial features, and Munchausen syndrome by proxy. An underlying depressive or anxiety disorder also should be considered and treated appropriately.
Conversion disorder has a challenging and often complex presentation in children and adolescents. Conversion disorders in children commonly are associated with stressful family situations including divorce, marital conflict, or loss of a close family member.1 An overbearing and conflict-prone parenting style also is associated with childhood conversion disorders.2 Common physical symptoms in conversion disorder are functional abdominal pain, partial paralysis, numbness, or seizures. Individuals such as Cassandra who are unable to express or verbalize their emotional distress are vulnerable to expressing their distress in somatic symptoms. Cassandra demonstrates La belle indifference, the characteristic attitude of not being overly concerned about what others would consider an alarming functional impairment.
Delusional disorder. A diagnosis of delusional disorder, somatic type with familial features was considered because Cassandra and her father shared persecutory and paranoid beliefs that her condition was brought on by some hidden, unrecognized medical condition. A delusional disorder with shared or “familial” features develops when a parent has strongly held delusional beliefs that are transferred to the child. Typically, it develops within the context of a close relationship with the parent, is similar in content to the parent’s belief, and is not preceded by psychosis or prodromal to schizophrenia.3
Because Cassandra’s father transferred his delusional system to his daughter, she clung to the belief that her physical symptoms and immobility were caused by medical misdiagnosis and failure to recognize her illness. Cassandra’s father strongly resisted and defended against accepting his role in her medical condition.
Munchausen by proxy. Because Cassandra and her father share a delusional system that prevented her from accepting and following treatment recommendations, it is possible that her father created her condition. Munchausen syndrome by proxy is a condition whereby illness-producing behavior in a child is exaggerated, fabricated, or induced by a parent or guardian.4 Separating Cassandra from her father and initiating antipsychotic treatment for him are critical considerations for her recovery.
How would you treat Cassandra?
a) call Child Protective Services (CPS) to remove Cassandra from her father’s custody
b) hospitalize Cassandra for intensive treatment of conversion disorder
c) start Cassandra on an atypical antipsychotic
d) begin cognitive-behavioral therapy (CBT) and an antidepressant
Treatment approach
Treating a patient with a conversion disorder, somatic type starts with validating that the patient’s and parent’s distress is real to them (Table 2).5 The clinician acknowledges that no physical evidence of physiological dysfunction has been found, which can be reassuring to the patient and family. The clinician then states that the patient’s condition and the physical manifestation of the symptoms are real. A patient’s or parent’s resistance to this reassurance may indicate that they have a large investment in the symptoms and perpetuating the dysfunction.
Taking a mind-body approach—explaining that the child’s condition is created and perpetuated by a mind-body connection and is not under their voluntary control—often is well received by patients and parents. The treating clinician emphasizes that the condition is physically disabling and that careful, appropriate, and intensive treatment is necessary.
A rehabilitation model has power for patients with conversion disorder because it acknowledges the patient’s discomfort and loss of function while shifting the focus away from finding what is wrong. The goal is to actively engage patients in their own care to help them return to normal functioning.6
Cassandra was encouraged to participate in physical therapy, go to school, and take care of herself. Actively participating in her care and recovery meant that Cassandra had to leave the sick role behind, which was impossible for her father, who saw her as passive, helpless, and fragile.
TREATMENT: Pharmacotherapy, CBT
During psychiatric evaluation, it becomes clear that in addition to her physical debility, Cassandra has major depressive disorder, moderate without psychotic features. Her depression contributes to her hopelessness and lack of participation in treatment. After discussion with her family about how her depressive symptoms are preventing her recovery, Cassandra is started on escitalopram, 10 mg/d. CBT helps her manage her depressive symptoms, prevent further somatization, and correct misperceptions about her body function and disabilities.
For conversion disorder patients, physical therapy can be combined with incentives tied to improvements in functioning. Cassandra has overwhelming anxiety while attempting physical therapy, which interferes with her participation in the therapy. Lorazepam, 0.5 mg/d, is prescribed for her intense anxiety and panic attacks, which led her to avoid physical therapy.
Staff at the rehabilitation hospital calls CPS because Cassandra’s father interferes with her care and treatment plan. CPS continues to monitor Cassandra’s progress through outpatient care. An individualized education plan and psychoeducational testing help determine a school placement to meet Cassandra’s educational needs.
CPS directs Cassandra to stay with her mother for alternating weeks. While at her mother’s, Cassandra is more interested in taking care of herself. She helps with getting herself into bed and to the toilet. Upon returning to her father’s home, these gains are lost.
The author’s observations
Psychodynamic and unconscious motivators for conversion disorder operate on a deeper, hidden level. The underlying primary conflict in pseudoseizures—a more common conversion disorder—has been described as an inability to express negative emotions such as anger. Social problems, conflict with parents, learning disorders,7 or sexual abuse8 produce the negative emotions caused by the primary conflict. Cassandra yearned for a closer relationship with her mother, yet she remained enmeshed with poor intrapsychic boundaries with her father. The fact that he assisted his 17-year-old daughter with toileting raised the possibility of sexual abuse. Sexual abuse could have led to her depression and physical decline. Cassandra’s physical debility also may have been her way to foster dependency on her father and protect him from perceived persecution.
Conversion disorder may have been a result of Cassandra’s defense mechanisms against admitting abuse and protecting against abandonment. Establishing a therapeutic alliance with Cassandra is essential to allow a graceful exit from the conversion disorder symptoms and her father’s hold on her thinking about her illness. However, this alliance may seem to threaten the child’s special connection with the parent. A therapeutic alliance was elusive in Cassandra’s case and likely nearly impossible.
Both parents underwent court-ordered psychological testing as part of the CPS evaluation. Testing on Cassandra’s father indicated a rigid personality structure with long-standing paranoia and mistrust of authority. Because Cassandra endorsed his delusional system completely, it is likely that her father inculcated her into believing his beliefs and transmitted his delusions to her by their close proximity and time together. Based upon this delusional belief system, Cassandra gave up trying to move her legs and her muscles atrophied. Her legs were so weak that she stopped trying to walk or move, illustrating the power of the mind-body connection to produce functional and physiological changes.
Children who live with a mother with chronic illness are at risk of developing psychosomatic disorders.9 Cassandra’s mother had fibromyalgia and chronic pain with symptoms of headache, weakness, and muscle pain and frequent medical office visits and tests without definitive results or symptom relief. Although Cassandra did not live with her mother, Cassandra’s somatization symptoms may be a result of modeling or observational learning within her family.9 Cassandra may have unconsciously adopted her mother’s symptoms and behaviors as a way to cope with stress and gain attention to her needs.
Cassandra’s negative affect, sensitivity to change, and lack of resiliency were further risk factors for developing a somatoform illness.10 She resisted and would not follow through with physical therapy. Krisnakumar10 also reported that an inability to persist in completing tasks is a risk factor for somatoform disorder. Family dynamics of problematic parental interactions also played a role in her somatoform disorder (Table 3).11
OUTCOME: Foster care, improvement
Cassandra receives weekly CBT and biweekly medication monitoring and demonstrates a moderate improvement in mood with less negativity and irritability. Her anxiety symptoms gradually respond to treatment. However, her emotional gains are not matched with improvement in her physical functioning or participation in physical therapy. Cassandra does not recover her muscular strength or control and shows little improvement in her physical capacity and independence.
After 3 months of treatment, Cassandra does not make sufficient progress or actively participate in treatment. Because her father continues to interfere with the treatment plan and does not receive treatment himself, CPS obtains a court order to prevent her father from directing her medical care and telling her treating physicians which tests to order.
Because these interventions do not improve her treatment response, Cassandra is removed from her parents’ care and placed in a therapeutic foster care home, thereby improving her independence and chances for recovery. After 3 months in foster care, she more actively participates in her physical rehabilitation. Water therapy, with the buoyancy and support in water, helps her regain muscle strength and control of her lower extremities.
Bottom Line
Patients with conversion disorder present with functional impairment and physical symptoms without clear physiological causes. Parents have a strong influence on the presentation and course of conversion disorder in children and adolescents. Parents’ mental and physical illnesses are independent risk factors for childhood somatoform disorders. Evaluation of parents’ psychological and psychiatric state is essential to determine intervention.
Related Resource
- Seltzer WJ. Conversion disorder in childhood and adolescence: a familial/cultural approach. Family Systems Medicine. 1985;3(3):261-280.
Drug Brand Names
Escitalopram • Lexapro
Lorazepam • Ativan
Disclosure
Dr. Leipsic reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Wyllie E, Glazer JP, Benbadis S, et al. Psychiatric features of children and adolescents with pseudoseizures. Arch Pediatr Adolesc Med. 1999;153(3):244-248.
2. Salmon P, Al-Marzooqi SM, Baker G, et al. Childhood family dysfunction and associated abuse in patients with nonepileptic seizures: towards a casual model. Psychosom Med. 2003;65(4):695-700.
3. Manschreck T. Delusional disorder and shared psychotic disorder. In: Sadock BJ, Sadock VA, eds. Kaplan & Sadock’s comprehensive textbook of psychiatry. 7th ed.
Philadelphia, PA: Lippincott Williams & Wilkins; 2000: 1243-1264.
4. Meadow R. Munchausen syndrome by proxy. The hinterland of child abuse. Lancet. 1977;2(8033):343-345.
5. Campo JV, Fritsch SL. Somatization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1994; 33(9):1223-1235.
6. Campo JV, Fritz G. A management model for pediatric somatization. Psychosomatics. 2001;42(6):467-476.
7. Silver LB. Conversion disorder with pseudoseizures in adolescence: a stress reaction to unrecognized and untreated learning disabilities. J Am Accad Child Psychiatry. 1982; 21(5):508-512.
8. AlperK,DevinskyO,PerrineK,etal.Nonepilepticseizures and childhood sexual and physical abuse. Neurology. 1993; 43(10):1950-1953.
9. Jamison RN, Walker LS. Illness behavior in children of chronic pain patients. Int J Psychiatry Med. 1992;22(4): 329-342.
10. Krisnakumar P, Sumesh P, Mathews L. Tempermental traits associated with conversion disorder. Indian Pediatr. 2006;43(10):895-899.
11. Minuchin S, Rosman BL, Baker L. Psychosomatic families: anorexia nervosa in context. Cambridge, MA: Harvard University Press; 1978.
1. Wyllie E, Glazer JP, Benbadis S, et al. Psychiatric features of children and adolescents with pseudoseizures. Arch Pediatr Adolesc Med. 1999;153(3):244-248.
2. Salmon P, Al-Marzooqi SM, Baker G, et al. Childhood family dysfunction and associated abuse in patients with nonepileptic seizures: towards a casual model. Psychosom Med. 2003;65(4):695-700.
3. Manschreck T. Delusional disorder and shared psychotic disorder. In: Sadock BJ, Sadock VA, eds. Kaplan & Sadock’s comprehensive textbook of psychiatry. 7th ed.
Philadelphia, PA: Lippincott Williams & Wilkins; 2000: 1243-1264.
4. Meadow R. Munchausen syndrome by proxy. The hinterland of child abuse. Lancet. 1977;2(8033):343-345.
5. Campo JV, Fritsch SL. Somatization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1994; 33(9):1223-1235.
6. Campo JV, Fritz G. A management model for pediatric somatization. Psychosomatics. 2001;42(6):467-476.
7. Silver LB. Conversion disorder with pseudoseizures in adolescence: a stress reaction to unrecognized and untreated learning disabilities. J Am Accad Child Psychiatry. 1982; 21(5):508-512.
8. AlperK,DevinskyO,PerrineK,etal.Nonepilepticseizures and childhood sexual and physical abuse. Neurology. 1993; 43(10):1950-1953.
9. Jamison RN, Walker LS. Illness behavior in children of chronic pain patients. Int J Psychiatry Med. 1992;22(4): 329-342.
10. Krisnakumar P, Sumesh P, Mathews L. Tempermental traits associated with conversion disorder. Indian Pediatr. 2006;43(10):895-899.
11. Minuchin S, Rosman BL, Baker L. Psychosomatic families: anorexia nervosa in context. Cambridge, MA: Harvard University Press; 1978.
Respondeat superior: What are your responsibilities?
Dear Dr. Mossman:
In my residency program, we cover the psychiatric emergency room (ER) overnight, and we admit, discharge, and make treatment recommendations without calling the attending psychiatrists about every decision. But if something goes wrong—eg, a discharged patient later commits suicide—I’ve heard that the faculty psychiatrist may be held liable despite never having met the patient. Should we awaken our attendings to discuss every major treatment decision?
Submitted by “Dr. R”
Postgraduate medical training programs in all specialties let interns and residents make judgments and decisions outside the direct supervision of board-certified faculty members. Medical education cannot occur unless doctors learn to take independent responsibility for patients. But if poor decisions by physicians-in-training lead to bad outcomes, might their teachers and training institutions share the blame—and the legal liability for damages?
The answer is “yes.” To understand why, and to learn about how Dr. R’s residency program should address this possibility, we’ll cover:
• the theory of respondeat superior
• factors affecting potential vicarious liability
• how postgraduate training balances supervision needs with letting residents get real-world treatment experience.
Vicarious liability
In general, if Person A injures Person B, Person B may initiate a tort action against Person A to seek monetary compensation. If the injury occurred while Person A was working for Person C, then under a legal doctrine called respondeat superior (Latin for “let the master answer”), courts may allow Person B to sue Person C, too, even if Person C wasn’t present when the injury occurred and did nothing that harmed Person B directly.
Respondeat superior imposes vicarious liability on an employer for negligent acts by employees who are “performing work assigned by the employer or engaging in a course of conduct subject to the employer’s control.”1 The doctrine extends back to 17th-century English courts and originated under the theory that, during a servant’s employment, one may presume that the servant acted by his master’s authority.2
Modern authors state that the justification for imposing vicarious liability “is largely one of public or social policy under which it has been determined that, irrespective of fault, a party should be held to respond for the acts of another.”3 Employers usually have more resources to pay damages than their employees do,4 and “in hard fact, the reason for the employers’ liability is the damages are taken from a deep pocket.”5
Determining potential responsibility
In Dr. R’s scenario, an adverse event follows the actions of a psychiatry resident who is performing a training activity at a hospital ER. Whether an attorney acting on behalf of an injured client can bring a claim of respondeat superior against the hospital, the resident’s academic institution, or the attending psychiatrist will depend on the nature of the relationships among these parties. This often becomes a complex legal matter that involves examining the residency program’s educational arrangements, official training documents (eg, affiliation agreements between a university and a hospital), employment contracts, and supervisory policies. In addition, statutes and legal precedents governing vicarious liability vary from state to state. Although an initial malpractice filing may name several individuals and institutions as defendants, courts eventually must apply their jurisdictions’ rules governing vicarious liability to determine which parties can lawfully bear potential liability.
Some courts have held that a private hospital generally is not responsible for negligent actions by attending physicians because the hospital does not control patient care decisions and physicians are not the hospital’s employees.6-8 Physicians in training, however, usually are employees of hospitals or their training institutions. Residents and attending physicians in many psychiatry training programs work at hospitals where patients reasonably believe that the doctors function as part of the hospital’s larger service enterprise. In some jurisdictions, this makes the hospitals potentially liable for their doctors’ acts,9 even when the doctors, as public employees, may have statutory immunity from being sued as individuals.10
Reuter11 has suggested that other agency theories may allow a resident’s error to create liability for an attending physician or medical school. The resident may be viewed as a “borrowed servant” such that, although a hospital was the resident’s general employer, the attending physician still exercised sufficient control with respect to the faulty act in question. A medical school faculty physician also may be liable along with the hospital under a joint employment theory based upon the faculty member’s “right to control” how the resident cares for the attending’s patient.11
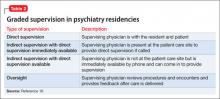
Taking into account recent cases and trends in public expectations, Kachalia and Studdert12 suggest that potential liability of attending physicians rests on 2 factors: whether the treatment context and structure of supervisory obligations establishes a patient-physician relationship between the attending physician and the injured patient, and whether the attending physician has provided adequate supervision. Details of these 2 factors appear in Table 1.12-14
Independence vs oversight
Potential malpractice liability is one of many factors that postgraduate psychiatry programs consider when titrating the amount and intensity of supervision against letting residents make independent decisions and take on clinical responsibility for patients. Patients deserve good care and protection from mistakes that inexperienced physicians may make. At the same time, society recognizes that educating future physicians requires allowing residents to get real-world experiences in evaluating and treating patients.
These ideas are expressed in the “Program Requirements” for psychiatry residencies promulgated by the Accreditation Council for Graduate Medical Education (ACGME).15 According to the ACGME, the “essential learning activity” that teaches physicians how to provide medical care is “interaction with patients under the guidance and supervision of faculty members” who let residents “exercise those skills with greater independence.”15
Psychiatry residencies must fashion learning experiences and supervisory schemes that give residents “graded and progressive responsibility” for providing care. Although each patient should have “an identifiable, appropriately-credentialed and privileged attending physician,” residents may provide substantial services under various levels of supervision described in Table 2.16
Deciding when and what kinds of patient care may be delegated to residents is the responsibility of residency program directors, who should base their judgments on explicit, prespecified criteria using information provided by supervising faculty members. Before letting first-year residents see patients on their own, psychiatry programs must determine that the residents can:
• take a history accurately
• do emergency psychiatric assessments
• present findings and data accurately to supervisors.
Physicians at all levels need to recognize when they should ask for help. The most important ACGME criterion for allowing a psychiatry resident to work under less stringent supervision is that the resident has demonstrated an “ability and willingness to ask for help when indicated.”16
Getting specifics
One way to respond Dr. R’s questions is to ask, “Do you know when you need help, and will you ask for it?” But her concerns deserve a more detailed (and more thoughtful) response that inquires about details of her training program and its specific educational experiences. Although it would be impossible to list everything to consider, some possible topics include:
• At what level of experience and training do residents assume this coverage responsibility?
• What kind of preparation do residents receive?
• What range of problems and conditions do the patients present?
• What level of clinical support is available on site—eg, experienced psychiatric nurses, other mental health staff, or other medical specialists?
• What has the program’s experience shown about residents’ actual readiness to handle these coverage duties?
• What guidelines have faculty members provided about when to call an attending physician or request a faculty member’s presence? Do these guidelines seem sound, given the above considerations?
Bottom Line
Psychiatry residents have supervisee relationships that create potential vicarious liability for institutions and faculty members. Residency training programs address these concerns by implementing adequate preparation for advanced responsibility, developing evaluative criteria and supervisory guidelines, and making sure that residents will ask for help when they need it.
Related Resources
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. South Med J. 2002;95(5):545-548.
- Winrow B, Winrow AR. Personal protection: vicarious liability as applied to the various business structures. J Midwifery Womens Health. 2008;53(2):146-149.
- Pozgar GD. Legal aspects of health care administration. 11th edition. Sudbury, MA: Jones & Bartlett Learning, LLC; 2012.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Restatement of the law of agency. 3rd ed. §7.07(2). Philadelphia, PA: American Law Institute; 2006.
2. Baty T. Vicarious liability: a short history of the liability of employers, principals, partners, associations and trade-union members. Oxford, England: Clarendon Press; 1916.
3. Dessauer v Memorial General Hosp, 628 P.2d 337 (N.M. 1981).
4. Firestone MH. Agency. In: Sandbar SS, Firestone MH, eds. Legal medicine. 7th ed. Philadelphia, PA: Mosby Elsevier; 2007:43-47.
5. Dobbs D, Keeton RE, Owen DG. Prosser and Keaton on torts. 5th ed. St. Paul, MN: West Publishing Co; 1984.
6. Austin v Litvak, 682 P.2d 41 (Colo. 1984).
7. Kirk v Michael Reese Hospital and Medical Center, 513 N.E.2d 387 (Ill. 1987).
8. Gregg v National Medical Health Care Services, Inc., 499 P.2d 925 (Ariz. App. 1985).
9. Adamski v Tacoma General Hospital, 579 P.2d 970 (Wash. App. 1978).
10. Johnson v LeBonheur Children’s Medical Center, 74 S.W.3d 338 (Tenn. 2002).
11. Reuter SR. Professional liability in postgraduate medical education. Who is liable for resident negligence? J Leg Med. 1994;15(4):485-531.
12. Kachalia A, Studdert DM. Professional liability issues in graduate medical education. JAMA. 2004;292(9):1051-1056.
13. Lownsbury v VanBuren, 762 N.E.2d 354 (Ohio 2002).
14. Sterling v Johns Hopkins Hospital, 802 A.2d 440 (Md Ct Spec App 2002).
15. Accreditation Council for Graduate Medical Education. Program and institutional guidelines. https://www.acgme.org/acgmeweb/tabid/147/ProgramandInstitutional Guidelines/MedicalAccreditation/Psychiatry.aspx. Accessed April 8, 2013.
16. Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in psychiatry. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/400_psychiatry_07012007_u04122008.pdf. Published July 1, 2007. Accessed April 8, 2013.
Dear Dr. Mossman:
In my residency program, we cover the psychiatric emergency room (ER) overnight, and we admit, discharge, and make treatment recommendations without calling the attending psychiatrists about every decision. But if something goes wrong—eg, a discharged patient later commits suicide—I’ve heard that the faculty psychiatrist may be held liable despite never having met the patient. Should we awaken our attendings to discuss every major treatment decision?
Submitted by “Dr. R”
Postgraduate medical training programs in all specialties let interns and residents make judgments and decisions outside the direct supervision of board-certified faculty members. Medical education cannot occur unless doctors learn to take independent responsibility for patients. But if poor decisions by physicians-in-training lead to bad outcomes, might their teachers and training institutions share the blame—and the legal liability for damages?
The answer is “yes.” To understand why, and to learn about how Dr. R’s residency program should address this possibility, we’ll cover:
• the theory of respondeat superior
• factors affecting potential vicarious liability
• how postgraduate training balances supervision needs with letting residents get real-world treatment experience.
Vicarious liability
In general, if Person A injures Person B, Person B may initiate a tort action against Person A to seek monetary compensation. If the injury occurred while Person A was working for Person C, then under a legal doctrine called respondeat superior (Latin for “let the master answer”), courts may allow Person B to sue Person C, too, even if Person C wasn’t present when the injury occurred and did nothing that harmed Person B directly.
Respondeat superior imposes vicarious liability on an employer for negligent acts by employees who are “performing work assigned by the employer or engaging in a course of conduct subject to the employer’s control.”1 The doctrine extends back to 17th-century English courts and originated under the theory that, during a servant’s employment, one may presume that the servant acted by his master’s authority.2
Modern authors state that the justification for imposing vicarious liability “is largely one of public or social policy under which it has been determined that, irrespective of fault, a party should be held to respond for the acts of another.”3 Employers usually have more resources to pay damages than their employees do,4 and “in hard fact, the reason for the employers’ liability is the damages are taken from a deep pocket.”5
Determining potential responsibility
In Dr. R’s scenario, an adverse event follows the actions of a psychiatry resident who is performing a training activity at a hospital ER. Whether an attorney acting on behalf of an injured client can bring a claim of respondeat superior against the hospital, the resident’s academic institution, or the attending psychiatrist will depend on the nature of the relationships among these parties. This often becomes a complex legal matter that involves examining the residency program’s educational arrangements, official training documents (eg, affiliation agreements between a university and a hospital), employment contracts, and supervisory policies. In addition, statutes and legal precedents governing vicarious liability vary from state to state. Although an initial malpractice filing may name several individuals and institutions as defendants, courts eventually must apply their jurisdictions’ rules governing vicarious liability to determine which parties can lawfully bear potential liability.
Some courts have held that a private hospital generally is not responsible for negligent actions by attending physicians because the hospital does not control patient care decisions and physicians are not the hospital’s employees.6-8 Physicians in training, however, usually are employees of hospitals or their training institutions. Residents and attending physicians in many psychiatry training programs work at hospitals where patients reasonably believe that the doctors function as part of the hospital’s larger service enterprise. In some jurisdictions, this makes the hospitals potentially liable for their doctors’ acts,9 even when the doctors, as public employees, may have statutory immunity from being sued as individuals.10
Reuter11 has suggested that other agency theories may allow a resident’s error to create liability for an attending physician or medical school. The resident may be viewed as a “borrowed servant” such that, although a hospital was the resident’s general employer, the attending physician still exercised sufficient control with respect to the faulty act in question. A medical school faculty physician also may be liable along with the hospital under a joint employment theory based upon the faculty member’s “right to control” how the resident cares for the attending’s patient.11
Taking into account recent cases and trends in public expectations, Kachalia and Studdert12 suggest that potential liability of attending physicians rests on 2 factors: whether the treatment context and structure of supervisory obligations establishes a patient-physician relationship between the attending physician and the injured patient, and whether the attending physician has provided adequate supervision. Details of these 2 factors appear in Table 1.12-14
Independence vs oversight
Potential malpractice liability is one of many factors that postgraduate psychiatry programs consider when titrating the amount and intensity of supervision against letting residents make independent decisions and take on clinical responsibility for patients. Patients deserve good care and protection from mistakes that inexperienced physicians may make. At the same time, society recognizes that educating future physicians requires allowing residents to get real-world experiences in evaluating and treating patients.
These ideas are expressed in the “Program Requirements” for psychiatry residencies promulgated by the Accreditation Council for Graduate Medical Education (ACGME).15 According to the ACGME, the “essential learning activity” that teaches physicians how to provide medical care is “interaction with patients under the guidance and supervision of faculty members” who let residents “exercise those skills with greater independence.”15
Psychiatry residencies must fashion learning experiences and supervisory schemes that give residents “graded and progressive responsibility” for providing care. Although each patient should have “an identifiable, appropriately-credentialed and privileged attending physician,” residents may provide substantial services under various levels of supervision described in Table 2.16
Deciding when and what kinds of patient care may be delegated to residents is the responsibility of residency program directors, who should base their judgments on explicit, prespecified criteria using information provided by supervising faculty members. Before letting first-year residents see patients on their own, psychiatry programs must determine that the residents can:
• take a history accurately
• do emergency psychiatric assessments
• present findings and data accurately to supervisors.
Physicians at all levels need to recognize when they should ask for help. The most important ACGME criterion for allowing a psychiatry resident to work under less stringent supervision is that the resident has demonstrated an “ability and willingness to ask for help when indicated.”16
Getting specifics
One way to respond Dr. R’s questions is to ask, “Do you know when you need help, and will you ask for it?” But her concerns deserve a more detailed (and more thoughtful) response that inquires about details of her training program and its specific educational experiences. Although it would be impossible to list everything to consider, some possible topics include:
• At what level of experience and training do residents assume this coverage responsibility?
• What kind of preparation do residents receive?
• What range of problems and conditions do the patients present?
• What level of clinical support is available on site—eg, experienced psychiatric nurses, other mental health staff, or other medical specialists?
• What has the program’s experience shown about residents’ actual readiness to handle these coverage duties?
• What guidelines have faculty members provided about when to call an attending physician or request a faculty member’s presence? Do these guidelines seem sound, given the above considerations?
Bottom Line
Psychiatry residents have supervisee relationships that create potential vicarious liability for institutions and faculty members. Residency training programs address these concerns by implementing adequate preparation for advanced responsibility, developing evaluative criteria and supervisory guidelines, and making sure that residents will ask for help when they need it.
Related Resources
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. South Med J. 2002;95(5):545-548.
- Winrow B, Winrow AR. Personal protection: vicarious liability as applied to the various business structures. J Midwifery Womens Health. 2008;53(2):146-149.
- Pozgar GD. Legal aspects of health care administration. 11th edition. Sudbury, MA: Jones & Bartlett Learning, LLC; 2012.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Restatement of the law of agency. 3rd ed. §7.07(2). Philadelphia, PA: American Law Institute; 2006.
2. Baty T. Vicarious liability: a short history of the liability of employers, principals, partners, associations and trade-union members. Oxford, England: Clarendon Press; 1916.
3. Dessauer v Memorial General Hosp, 628 P.2d 337 (N.M. 1981).
4. Firestone MH. Agency. In: Sandbar SS, Firestone MH, eds. Legal medicine. 7th ed. Philadelphia, PA: Mosby Elsevier; 2007:43-47.
5. Dobbs D, Keeton RE, Owen DG. Prosser and Keaton on torts. 5th ed. St. Paul, MN: West Publishing Co; 1984.
6. Austin v Litvak, 682 P.2d 41 (Colo. 1984).
7. Kirk v Michael Reese Hospital and Medical Center, 513 N.E.2d 387 (Ill. 1987).
8. Gregg v National Medical Health Care Services, Inc., 499 P.2d 925 (Ariz. App. 1985).
9. Adamski v Tacoma General Hospital, 579 P.2d 970 (Wash. App. 1978).
10. Johnson v LeBonheur Children’s Medical Center, 74 S.W.3d 338 (Tenn. 2002).
11. Reuter SR. Professional liability in postgraduate medical education. Who is liable for resident negligence? J Leg Med. 1994;15(4):485-531.
12. Kachalia A, Studdert DM. Professional liability issues in graduate medical education. JAMA. 2004;292(9):1051-1056.
13. Lownsbury v VanBuren, 762 N.E.2d 354 (Ohio 2002).
14. Sterling v Johns Hopkins Hospital, 802 A.2d 440 (Md Ct Spec App 2002).
15. Accreditation Council for Graduate Medical Education. Program and institutional guidelines. https://www.acgme.org/acgmeweb/tabid/147/ProgramandInstitutional Guidelines/MedicalAccreditation/Psychiatry.aspx. Accessed April 8, 2013.
16. Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in psychiatry. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/400_psychiatry_07012007_u04122008.pdf. Published July 1, 2007. Accessed April 8, 2013.
Dear Dr. Mossman:
In my residency program, we cover the psychiatric emergency room (ER) overnight, and we admit, discharge, and make treatment recommendations without calling the attending psychiatrists about every decision. But if something goes wrong—eg, a discharged patient later commits suicide—I’ve heard that the faculty psychiatrist may be held liable despite never having met the patient. Should we awaken our attendings to discuss every major treatment decision?
Submitted by “Dr. R”
Postgraduate medical training programs in all specialties let interns and residents make judgments and decisions outside the direct supervision of board-certified faculty members. Medical education cannot occur unless doctors learn to take independent responsibility for patients. But if poor decisions by physicians-in-training lead to bad outcomes, might their teachers and training institutions share the blame—and the legal liability for damages?
The answer is “yes.” To understand why, and to learn about how Dr. R’s residency program should address this possibility, we’ll cover:
• the theory of respondeat superior
• factors affecting potential vicarious liability
• how postgraduate training balances supervision needs with letting residents get real-world treatment experience.
Vicarious liability
In general, if Person A injures Person B, Person B may initiate a tort action against Person A to seek monetary compensation. If the injury occurred while Person A was working for Person C, then under a legal doctrine called respondeat superior (Latin for “let the master answer”), courts may allow Person B to sue Person C, too, even if Person C wasn’t present when the injury occurred and did nothing that harmed Person B directly.
Respondeat superior imposes vicarious liability on an employer for negligent acts by employees who are “performing work assigned by the employer or engaging in a course of conduct subject to the employer’s control.”1 The doctrine extends back to 17th-century English courts and originated under the theory that, during a servant’s employment, one may presume that the servant acted by his master’s authority.2
Modern authors state that the justification for imposing vicarious liability “is largely one of public or social policy under which it has been determined that, irrespective of fault, a party should be held to respond for the acts of another.”3 Employers usually have more resources to pay damages than their employees do,4 and “in hard fact, the reason for the employers’ liability is the damages are taken from a deep pocket.”5
Determining potential responsibility
In Dr. R’s scenario, an adverse event follows the actions of a psychiatry resident who is performing a training activity at a hospital ER. Whether an attorney acting on behalf of an injured client can bring a claim of respondeat superior against the hospital, the resident’s academic institution, or the attending psychiatrist will depend on the nature of the relationships among these parties. This often becomes a complex legal matter that involves examining the residency program’s educational arrangements, official training documents (eg, affiliation agreements between a university and a hospital), employment contracts, and supervisory policies. In addition, statutes and legal precedents governing vicarious liability vary from state to state. Although an initial malpractice filing may name several individuals and institutions as defendants, courts eventually must apply their jurisdictions’ rules governing vicarious liability to determine which parties can lawfully bear potential liability.
Some courts have held that a private hospital generally is not responsible for negligent actions by attending physicians because the hospital does not control patient care decisions and physicians are not the hospital’s employees.6-8 Physicians in training, however, usually are employees of hospitals or their training institutions. Residents and attending physicians in many psychiatry training programs work at hospitals where patients reasonably believe that the doctors function as part of the hospital’s larger service enterprise. In some jurisdictions, this makes the hospitals potentially liable for their doctors’ acts,9 even when the doctors, as public employees, may have statutory immunity from being sued as individuals.10
Reuter11 has suggested that other agency theories may allow a resident’s error to create liability for an attending physician or medical school. The resident may be viewed as a “borrowed servant” such that, although a hospital was the resident’s general employer, the attending physician still exercised sufficient control with respect to the faulty act in question. A medical school faculty physician also may be liable along with the hospital under a joint employment theory based upon the faculty member’s “right to control” how the resident cares for the attending’s patient.11
Taking into account recent cases and trends in public expectations, Kachalia and Studdert12 suggest that potential liability of attending physicians rests on 2 factors: whether the treatment context and structure of supervisory obligations establishes a patient-physician relationship between the attending physician and the injured patient, and whether the attending physician has provided adequate supervision. Details of these 2 factors appear in Table 1.12-14
Independence vs oversight
Potential malpractice liability is one of many factors that postgraduate psychiatry programs consider when titrating the amount and intensity of supervision against letting residents make independent decisions and take on clinical responsibility for patients. Patients deserve good care and protection from mistakes that inexperienced physicians may make. At the same time, society recognizes that educating future physicians requires allowing residents to get real-world experiences in evaluating and treating patients.
These ideas are expressed in the “Program Requirements” for psychiatry residencies promulgated by the Accreditation Council for Graduate Medical Education (ACGME).15 According to the ACGME, the “essential learning activity” that teaches physicians how to provide medical care is “interaction with patients under the guidance and supervision of faculty members” who let residents “exercise those skills with greater independence.”15
Psychiatry residencies must fashion learning experiences and supervisory schemes that give residents “graded and progressive responsibility” for providing care. Although each patient should have “an identifiable, appropriately-credentialed and privileged attending physician,” residents may provide substantial services under various levels of supervision described in Table 2.16
Deciding when and what kinds of patient care may be delegated to residents is the responsibility of residency program directors, who should base their judgments on explicit, prespecified criteria using information provided by supervising faculty members. Before letting first-year residents see patients on their own, psychiatry programs must determine that the residents can:
• take a history accurately
• do emergency psychiatric assessments
• present findings and data accurately to supervisors.
Physicians at all levels need to recognize when they should ask for help. The most important ACGME criterion for allowing a psychiatry resident to work under less stringent supervision is that the resident has demonstrated an “ability and willingness to ask for help when indicated.”16
Getting specifics
One way to respond Dr. R’s questions is to ask, “Do you know when you need help, and will you ask for it?” But her concerns deserve a more detailed (and more thoughtful) response that inquires about details of her training program and its specific educational experiences. Although it would be impossible to list everything to consider, some possible topics include:
• At what level of experience and training do residents assume this coverage responsibility?
• What kind of preparation do residents receive?
• What range of problems and conditions do the patients present?
• What level of clinical support is available on site—eg, experienced psychiatric nurses, other mental health staff, or other medical specialists?
• What has the program’s experience shown about residents’ actual readiness to handle these coverage duties?
• What guidelines have faculty members provided about when to call an attending physician or request a faculty member’s presence? Do these guidelines seem sound, given the above considerations?
Bottom Line
Psychiatry residents have supervisee relationships that create potential vicarious liability for institutions and faculty members. Residency training programs address these concerns by implementing adequate preparation for advanced responsibility, developing evaluative criteria and supervisory guidelines, and making sure that residents will ask for help when they need it.
Related Resources
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. South Med J. 2002;95(5):545-548.
- Winrow B, Winrow AR. Personal protection: vicarious liability as applied to the various business structures. J Midwifery Womens Health. 2008;53(2):146-149.
- Pozgar GD. Legal aspects of health care administration. 11th edition. Sudbury, MA: Jones & Bartlett Learning, LLC; 2012.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Restatement of the law of agency. 3rd ed. §7.07(2). Philadelphia, PA: American Law Institute; 2006.
2. Baty T. Vicarious liability: a short history of the liability of employers, principals, partners, associations and trade-union members. Oxford, England: Clarendon Press; 1916.
3. Dessauer v Memorial General Hosp, 628 P.2d 337 (N.M. 1981).
4. Firestone MH. Agency. In: Sandbar SS, Firestone MH, eds. Legal medicine. 7th ed. Philadelphia, PA: Mosby Elsevier; 2007:43-47.
5. Dobbs D, Keeton RE, Owen DG. Prosser and Keaton on torts. 5th ed. St. Paul, MN: West Publishing Co; 1984.
6. Austin v Litvak, 682 P.2d 41 (Colo. 1984).
7. Kirk v Michael Reese Hospital and Medical Center, 513 N.E.2d 387 (Ill. 1987).
8. Gregg v National Medical Health Care Services, Inc., 499 P.2d 925 (Ariz. App. 1985).
9. Adamski v Tacoma General Hospital, 579 P.2d 970 (Wash. App. 1978).
10. Johnson v LeBonheur Children’s Medical Center, 74 S.W.3d 338 (Tenn. 2002).
11. Reuter SR. Professional liability in postgraduate medical education. Who is liable for resident negligence? J Leg Med. 1994;15(4):485-531.
12. Kachalia A, Studdert DM. Professional liability issues in graduate medical education. JAMA. 2004;292(9):1051-1056.
13. Lownsbury v VanBuren, 762 N.E.2d 354 (Ohio 2002).
14. Sterling v Johns Hopkins Hospital, 802 A.2d 440 (Md Ct Spec App 2002).
15. Accreditation Council for Graduate Medical Education. Program and institutional guidelines. https://www.acgme.org/acgmeweb/tabid/147/ProgramandInstitutional Guidelines/MedicalAccreditation/Psychiatry.aspx. Accessed April 8, 2013.
16. Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in psychiatry. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/400_psychiatry_07012007_u04122008.pdf. Published July 1, 2007. Accessed April 8, 2013.
Beyond dopamine: The ‘other’ effects of antipsychotics
This mechanism of action (MOA) has been elevated to dogma because no agent has been approved for treating psychosis that does not exert a dopamine D2 receptor antagonist effect. However, as advances in the neurobiology of psychosis accelerate, several other functions of APs have been identified, which can be considered additional MOAs that may help mitigate psychosis’ deleterious effect on brain tissue.
Consider the following beneficial effects of APs (especially second-generation APs [SGAs]) of which many clinicians are unaware:
APs suppress induction of pro-inflammatory cytokines.1 It is well established that psychotic episodes of schizophrenia are associated with neuroinflammation and elevations of cytokines such as interleukin 1 (IL-1), IL-6, tumor necrosis factor (TNF-α), and interferon gamma (IFN-α). These inflammatory biomarkers are released by microglia, which are rapidly activated by psychosis2 and mediate brain tissue damage during psychosis. APs’ rapid inhibitory action on pro-inflammatory cytokines obviously is neuroprotective.
APs suppress immune-inflammatory pathways.3 This occurs with atypical agents but not haloperidol4 and results in decreased IL-1â and IL-6 and transforming growth factor-α.
APs significantly decrease levels of neurotoxic tryptophan catabolites (TRYCATS) such as 3-OHK and QUIN, which mediate the immune-inflammatory effects on neuronal activity. APs also increase levels of neuroprotective TRYCATS such as kynurenic acid.5
APs activate cholesterol-transport proteins such as apolipoprotein E (APOE).6 This implies that APs may improve low levels of APOE observed during psychosis and decrease myelination abnormalities and mitigate impairment of synaptic plasticity.7,8
APs increase neurotrophic growth factors that plummet during psychosis, such as brain-derived neurotrophic factor (BDNF) and nerve growth factor.9 This beneficial effect is seen with SGAs but not first-generation APs (FGAs) and is attributed to strong serotonin 5HT-2A receptor antagonism by SGAs.10
SGAs but not FGAs significantly increase the number of newly divided cells in the subventricular zone by 200% to 300%. This enhancement of neurogenesis and increased production of progenitor cells that differentiate into neurons and glia may help regenerate brain tissue lost during psychotic episodes.
Various SGAs have neuroprotective effects:
• Clozapine has neuroprotective effects against liposaccharide-induced neurodegeneration and reduces microglial activation by limiting production of reactive oxygen species (free radicals).11
• Aripiprazole inhibits glutamate-induced neurotoxicity and, in contrast to haloperidol, increases BDNF, glycogen synthase kinase (GSK)-α, and the anti-apoptotic protein Bcl-2.
• Olanzapine increases BDNF, GSK-3α, and α-catenin, increases mitosis in neuronal cell culture, and protects against neuronal death in cell cultures that lack nutrients (which fluphenazine or risperidone do not).
• Paliperidone demonstrates a higher antioxidant effect than any other SGA and clearly is better than haloperidol, olanzapine, or risperidone in preventing neuronal death when exposed to hydrogen peroxide.
• Quetiapine, ziprasidone, and lurasidone have inhibitory effects on nitric oxide release. Quetiapine, but not ziprasidone, inhibits TNF-α.
• Ziprasidone inhibits apoptosis and microglial activation and synthesis of nitric oxide and other free radicals.
• Lurasidone increases BDNF expression in the prefrontal cortex of rodents.13
Although most clinicians uphold the dopamine neurotransmitter model of schizophrenia (ie, a hyperdopaminergic state that requires treatment with dopamine antagonists), research is moving toward a multi-faceted neurotoxicity and neuroprogression model of impaired neuroplasticity, neuroinflammation, immune dysfunction, oxidative stress, nitrosative stress, apoptosis, and mitochondrial dysfunction.12 This complex model is shaping not only etio-pathological research in schizophrenia but also its future management, including treatment of negative symptoms and cognitive deficits, not just delusions and hallucinations. Interestingly, the only treatment superior to placebo in preventing conversion to psychosis in ultra high-risk prodrome patients is omega-3 fatty acid, a strong anti-inflammatory agent,14 which suggests that neuroinflammation may precede dopamine overactivity associated with the first psychotic episode. Future treatments of schizophrenia, mania, and depression may focus on more aggressively diminishing inflammation and oxidative/nitrosative stress, not just modulating dopamine or other neurotransmitters, because progressive major psychiatric disorders have been associated with destructive neuroinflammation and an abundance of reactive oxygen species.
References
1. Drzyzga L, Obuchowicz E, Marcinowska A, et al. Cytokines in schizophrenia and the effects of antipsychotic drugs. Brain Behav Immun. 2006;20(6):532-545.
2. Monji A, Kato TA, Mizoguchi Y, et al. Neuro-inflammation in schizophrenia especially focused on the role of microglia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:115-121.
3. Miller BJ, Buckley P, Seabolt W, et al. Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry. 2011;70(7):663-671.
4. Chen SL, Lee SY, Chang YH, et al. Inflammation in patients with schizophrenia: the therapeutic benefits of risperidone plus add-on dextromethorphan.
J Neuroimmune Pharmacol. 2012;7(3):656-664.
5. Myint AM, Schwarz MJ, Verkerk R, et al. Reversal of imbalance between kynurenic acid and 3-hydroxykynurenine by antipsychotics in medication-naïve and medication-free schizophrenic patients. Brain Behav Immun. 2011;25(8):1576-1581.
6. Vik-Mo AO, Fernø J, Skrede S, et al. Psychotropic drugs up-regulate the expression of cholesterol transport proteins including ApoE in cultured human CNS and liver cells. BMC Pharmacol. 2009;9:10.
7. Dean B, Digney A, Sundram S, et al. Plasma apolipoprotein E is decreased in schizophrenia spectrum and bipolar disorder. Psychiatry Res. 2008; 158(1):75-78.
8. Garver DL, Holcomb JA, Christensen JD. Compromised myelin integrity during psychosis with repair during remission in drug-responding schizophrenia. Int J Neuropsychopharmacol. 2008; 11(1):49-61.
9. Chen CC, Huang TL. Effects of antipsychotics on the serum BDNF levels in schizophrenia. Psychiatry Res. 2011;189(3):327-330.
10. Vaidya VA, Marek GJ, Aghajanian GK, et al. 5-HT2A receptor-mediated regulation of brain-derived neurotrophic factor mRNA in the hippocampus and the neocortex. J Neurosci. 1997;17(8):2785-2795.
11. Hu X, Zhou H, Zhang D, et al. Clozapine protects dopaminergic neurons from inflammation-induced damage by inhibiting microglial overactivation. J Neuroimmune Pharmacol. 2012;7(1):187-201.
12. Anderson G, Berk M, Dodd S, et al. Immuno-inflammatory, oxidative and nitrosative stress, and neuroprogressive pathways in the etiology, course and treatment of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:1-4.
13. Dodd S, Maes M, Anderson G, et al. Putative neuroprotective agents in neuropsychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:135-145.
14. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
This mechanism of action (MOA) has been elevated to dogma because no agent has been approved for treating psychosis that does not exert a dopamine D2 receptor antagonist effect. However, as advances in the neurobiology of psychosis accelerate, several other functions of APs have been identified, which can be considered additional MOAs that may help mitigate psychosis’ deleterious effect on brain tissue.
Consider the following beneficial effects of APs (especially second-generation APs [SGAs]) of which many clinicians are unaware:
APs suppress induction of pro-inflammatory cytokines.1 It is well established that psychotic episodes of schizophrenia are associated with neuroinflammation and elevations of cytokines such as interleukin 1 (IL-1), IL-6, tumor necrosis factor (TNF-α), and interferon gamma (IFN-α). These inflammatory biomarkers are released by microglia, which are rapidly activated by psychosis2 and mediate brain tissue damage during psychosis. APs’ rapid inhibitory action on pro-inflammatory cytokines obviously is neuroprotective.
APs suppress immune-inflammatory pathways.3 This occurs with atypical agents but not haloperidol4 and results in decreased IL-1â and IL-6 and transforming growth factor-α.
APs significantly decrease levels of neurotoxic tryptophan catabolites (TRYCATS) such as 3-OHK and QUIN, which mediate the immune-inflammatory effects on neuronal activity. APs also increase levels of neuroprotective TRYCATS such as kynurenic acid.5
APs activate cholesterol-transport proteins such as apolipoprotein E (APOE).6 This implies that APs may improve low levels of APOE observed during psychosis and decrease myelination abnormalities and mitigate impairment of synaptic plasticity.7,8
APs increase neurotrophic growth factors that plummet during psychosis, such as brain-derived neurotrophic factor (BDNF) and nerve growth factor.9 This beneficial effect is seen with SGAs but not first-generation APs (FGAs) and is attributed to strong serotonin 5HT-2A receptor antagonism by SGAs.10
SGAs but not FGAs significantly increase the number of newly divided cells in the subventricular zone by 200% to 300%. This enhancement of neurogenesis and increased production of progenitor cells that differentiate into neurons and glia may help regenerate brain tissue lost during psychotic episodes.
Various SGAs have neuroprotective effects:
• Clozapine has neuroprotective effects against liposaccharide-induced neurodegeneration and reduces microglial activation by limiting production of reactive oxygen species (free radicals).11
• Aripiprazole inhibits glutamate-induced neurotoxicity and, in contrast to haloperidol, increases BDNF, glycogen synthase kinase (GSK)-α, and the anti-apoptotic protein Bcl-2.
• Olanzapine increases BDNF, GSK-3α, and α-catenin, increases mitosis in neuronal cell culture, and protects against neuronal death in cell cultures that lack nutrients (which fluphenazine or risperidone do not).
• Paliperidone demonstrates a higher antioxidant effect than any other SGA and clearly is better than haloperidol, olanzapine, or risperidone in preventing neuronal death when exposed to hydrogen peroxide.
• Quetiapine, ziprasidone, and lurasidone have inhibitory effects on nitric oxide release. Quetiapine, but not ziprasidone, inhibits TNF-α.
• Ziprasidone inhibits apoptosis and microglial activation and synthesis of nitric oxide and other free radicals.
• Lurasidone increases BDNF expression in the prefrontal cortex of rodents.13
Although most clinicians uphold the dopamine neurotransmitter model of schizophrenia (ie, a hyperdopaminergic state that requires treatment with dopamine antagonists), research is moving toward a multi-faceted neurotoxicity and neuroprogression model of impaired neuroplasticity, neuroinflammation, immune dysfunction, oxidative stress, nitrosative stress, apoptosis, and mitochondrial dysfunction.12 This complex model is shaping not only etio-pathological research in schizophrenia but also its future management, including treatment of negative symptoms and cognitive deficits, not just delusions and hallucinations. Interestingly, the only treatment superior to placebo in preventing conversion to psychosis in ultra high-risk prodrome patients is omega-3 fatty acid, a strong anti-inflammatory agent,14 which suggests that neuroinflammation may precede dopamine overactivity associated with the first psychotic episode. Future treatments of schizophrenia, mania, and depression may focus on more aggressively diminishing inflammation and oxidative/nitrosative stress, not just modulating dopamine or other neurotransmitters, because progressive major psychiatric disorders have been associated with destructive neuroinflammation and an abundance of reactive oxygen species.
References
1. Drzyzga L, Obuchowicz E, Marcinowska A, et al. Cytokines in schizophrenia and the effects of antipsychotic drugs. Brain Behav Immun. 2006;20(6):532-545.
2. Monji A, Kato TA, Mizoguchi Y, et al. Neuro-inflammation in schizophrenia especially focused on the role of microglia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:115-121.
3. Miller BJ, Buckley P, Seabolt W, et al. Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry. 2011;70(7):663-671.
4. Chen SL, Lee SY, Chang YH, et al. Inflammation in patients with schizophrenia: the therapeutic benefits of risperidone plus add-on dextromethorphan.
J Neuroimmune Pharmacol. 2012;7(3):656-664.
5. Myint AM, Schwarz MJ, Verkerk R, et al. Reversal of imbalance between kynurenic acid and 3-hydroxykynurenine by antipsychotics in medication-naïve and medication-free schizophrenic patients. Brain Behav Immun. 2011;25(8):1576-1581.
6. Vik-Mo AO, Fernø J, Skrede S, et al. Psychotropic drugs up-regulate the expression of cholesterol transport proteins including ApoE in cultured human CNS and liver cells. BMC Pharmacol. 2009;9:10.
7. Dean B, Digney A, Sundram S, et al. Plasma apolipoprotein E is decreased in schizophrenia spectrum and bipolar disorder. Psychiatry Res. 2008; 158(1):75-78.
8. Garver DL, Holcomb JA, Christensen JD. Compromised myelin integrity during psychosis with repair during remission in drug-responding schizophrenia. Int J Neuropsychopharmacol. 2008; 11(1):49-61.
9. Chen CC, Huang TL. Effects of antipsychotics on the serum BDNF levels in schizophrenia. Psychiatry Res. 2011;189(3):327-330.
10. Vaidya VA, Marek GJ, Aghajanian GK, et al. 5-HT2A receptor-mediated regulation of brain-derived neurotrophic factor mRNA in the hippocampus and the neocortex. J Neurosci. 1997;17(8):2785-2795.
11. Hu X, Zhou H, Zhang D, et al. Clozapine protects dopaminergic neurons from inflammation-induced damage by inhibiting microglial overactivation. J Neuroimmune Pharmacol. 2012;7(1):187-201.
12. Anderson G, Berk M, Dodd S, et al. Immuno-inflammatory, oxidative and nitrosative stress, and neuroprogressive pathways in the etiology, course and treatment of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:1-4.
13. Dodd S, Maes M, Anderson G, et al. Putative neuroprotective agents in neuropsychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:135-145.
14. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
This mechanism of action (MOA) has been elevated to dogma because no agent has been approved for treating psychosis that does not exert a dopamine D2 receptor antagonist effect. However, as advances in the neurobiology of psychosis accelerate, several other functions of APs have been identified, which can be considered additional MOAs that may help mitigate psychosis’ deleterious effect on brain tissue.
Consider the following beneficial effects of APs (especially second-generation APs [SGAs]) of which many clinicians are unaware:
APs suppress induction of pro-inflammatory cytokines.1 It is well established that psychotic episodes of schizophrenia are associated with neuroinflammation and elevations of cytokines such as interleukin 1 (IL-1), IL-6, tumor necrosis factor (TNF-α), and interferon gamma (IFN-α). These inflammatory biomarkers are released by microglia, which are rapidly activated by psychosis2 and mediate brain tissue damage during psychosis. APs’ rapid inhibitory action on pro-inflammatory cytokines obviously is neuroprotective.
APs suppress immune-inflammatory pathways.3 This occurs with atypical agents but not haloperidol4 and results in decreased IL-1â and IL-6 and transforming growth factor-α.
APs significantly decrease levels of neurotoxic tryptophan catabolites (TRYCATS) such as 3-OHK and QUIN, which mediate the immune-inflammatory effects on neuronal activity. APs also increase levels of neuroprotective TRYCATS such as kynurenic acid.5
APs activate cholesterol-transport proteins such as apolipoprotein E (APOE).6 This implies that APs may improve low levels of APOE observed during psychosis and decrease myelination abnormalities and mitigate impairment of synaptic plasticity.7,8
APs increase neurotrophic growth factors that plummet during psychosis, such as brain-derived neurotrophic factor (BDNF) and nerve growth factor.9 This beneficial effect is seen with SGAs but not first-generation APs (FGAs) and is attributed to strong serotonin 5HT-2A receptor antagonism by SGAs.10
SGAs but not FGAs significantly increase the number of newly divided cells in the subventricular zone by 200% to 300%. This enhancement of neurogenesis and increased production of progenitor cells that differentiate into neurons and glia may help regenerate brain tissue lost during psychotic episodes.
Various SGAs have neuroprotective effects:
• Clozapine has neuroprotective effects against liposaccharide-induced neurodegeneration and reduces microglial activation by limiting production of reactive oxygen species (free radicals).11
• Aripiprazole inhibits glutamate-induced neurotoxicity and, in contrast to haloperidol, increases BDNF, glycogen synthase kinase (GSK)-α, and the anti-apoptotic protein Bcl-2.
• Olanzapine increases BDNF, GSK-3α, and α-catenin, increases mitosis in neuronal cell culture, and protects against neuronal death in cell cultures that lack nutrients (which fluphenazine or risperidone do not).
• Paliperidone demonstrates a higher antioxidant effect than any other SGA and clearly is better than haloperidol, olanzapine, or risperidone in preventing neuronal death when exposed to hydrogen peroxide.
• Quetiapine, ziprasidone, and lurasidone have inhibitory effects on nitric oxide release. Quetiapine, but not ziprasidone, inhibits TNF-α.
• Ziprasidone inhibits apoptosis and microglial activation and synthesis of nitric oxide and other free radicals.
• Lurasidone increases BDNF expression in the prefrontal cortex of rodents.13
Although most clinicians uphold the dopamine neurotransmitter model of schizophrenia (ie, a hyperdopaminergic state that requires treatment with dopamine antagonists), research is moving toward a multi-faceted neurotoxicity and neuroprogression model of impaired neuroplasticity, neuroinflammation, immune dysfunction, oxidative stress, nitrosative stress, apoptosis, and mitochondrial dysfunction.12 This complex model is shaping not only etio-pathological research in schizophrenia but also its future management, including treatment of negative symptoms and cognitive deficits, not just delusions and hallucinations. Interestingly, the only treatment superior to placebo in preventing conversion to psychosis in ultra high-risk prodrome patients is omega-3 fatty acid, a strong anti-inflammatory agent,14 which suggests that neuroinflammation may precede dopamine overactivity associated with the first psychotic episode. Future treatments of schizophrenia, mania, and depression may focus on more aggressively diminishing inflammation and oxidative/nitrosative stress, not just modulating dopamine or other neurotransmitters, because progressive major psychiatric disorders have been associated with destructive neuroinflammation and an abundance of reactive oxygen species.
References
1. Drzyzga L, Obuchowicz E, Marcinowska A, et al. Cytokines in schizophrenia and the effects of antipsychotic drugs. Brain Behav Immun. 2006;20(6):532-545.
2. Monji A, Kato TA, Mizoguchi Y, et al. Neuro-inflammation in schizophrenia especially focused on the role of microglia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:115-121.
3. Miller BJ, Buckley P, Seabolt W, et al. Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry. 2011;70(7):663-671.
4. Chen SL, Lee SY, Chang YH, et al. Inflammation in patients with schizophrenia: the therapeutic benefits of risperidone plus add-on dextromethorphan.
J Neuroimmune Pharmacol. 2012;7(3):656-664.
5. Myint AM, Schwarz MJ, Verkerk R, et al. Reversal of imbalance between kynurenic acid and 3-hydroxykynurenine by antipsychotics in medication-naïve and medication-free schizophrenic patients. Brain Behav Immun. 2011;25(8):1576-1581.
6. Vik-Mo AO, Fernø J, Skrede S, et al. Psychotropic drugs up-regulate the expression of cholesterol transport proteins including ApoE in cultured human CNS and liver cells. BMC Pharmacol. 2009;9:10.
7. Dean B, Digney A, Sundram S, et al. Plasma apolipoprotein E is decreased in schizophrenia spectrum and bipolar disorder. Psychiatry Res. 2008; 158(1):75-78.
8. Garver DL, Holcomb JA, Christensen JD. Compromised myelin integrity during psychosis with repair during remission in drug-responding schizophrenia. Int J Neuropsychopharmacol. 2008; 11(1):49-61.
9. Chen CC, Huang TL. Effects of antipsychotics on the serum BDNF levels in schizophrenia. Psychiatry Res. 2011;189(3):327-330.
10. Vaidya VA, Marek GJ, Aghajanian GK, et al. 5-HT2A receptor-mediated regulation of brain-derived neurotrophic factor mRNA in the hippocampus and the neocortex. J Neurosci. 1997;17(8):2785-2795.
11. Hu X, Zhou H, Zhang D, et al. Clozapine protects dopaminergic neurons from inflammation-induced damage by inhibiting microglial overactivation. J Neuroimmune Pharmacol. 2012;7(1):187-201.
12. Anderson G, Berk M, Dodd S, et al. Immuno-inflammatory, oxidative and nitrosative stress, and neuroprogressive pathways in the etiology, course and treatment of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:1-4.
13. Dodd S, Maes M, Anderson G, et al. Putative neuroprotective agents in neuropsychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2013;42:135-145.
14. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
Depression and inflammation: Examining the link
Sneezing, coughing, and a sore throat are hallmark symptoms of a common cold, but what keeps you in bed are the accompanying fatigue, inattentiveness, loss of appetite, change in sleep pattern, heightened perception of pain, and apathetic withdrawal. This “sickness behavior” is induced by inflammatory markers released in response to illness.1,2 These symptoms are similar to the constellation of symptoms that define depression. Within the inflammatory response to illness, we see the shadow of depression, but the precise relationship remains murky.
Is depression part of a normal somatic inflammatory response run amok? Some researchers have argued that “sickness behavior” is adaptive, forcing the body into a constricted pattern in order to funnel energy into healing.1,3 If depression and inflammation are related, depression pushes past these adaptive roots and is less a forced pause than a debilitating withdrawal. Perhaps depression, or a subtype, is a sign of inflammation along with heat, pain, redness, and swelling. In some instances, depression may be a sign of an underlying inflammatory process.4
In our progression toward understanding depression’s pathophysiology, we see factors that point to a relationship between depression and inflammation:
• depression frequently is comorbid with many inflammatory illnesses
• increased inflammatory biomarkers are associated with major depressive disorder (MDD)
• exposure to immunomodulating agents may increase the risk of developing depression
• stress can activate proinflammatory pathways
• antidepressants can decrease inflammatory response
• inhibition of inflammatory pathways can improve mood.
Exploring these factors and a possible pathway linking inflammation and neurobiologic changes found in depression allows us to look closer at the possible integration of the inflammatory process and depressive symptoms.
Illness and depression rates
Individuals with inflammatory illnesses—autoimmune diseases, cardiovascular disease, diabetes, and cancer—often struggle with depression. Nearly 1 in 5 persons with cardiovascular disease experiences MDD.5 A diabetes diagnosis doubles the odds of having depression.6 Up to 70% of patients with autoimmune diseases, such as rheumatoid arthritis or systemic lupus erythematosus, experience depression.7,8 In a large-scale longitudinal study, having a prior autoimmune disease increased the risk of depression by 45% and history of hospitalization with infection increased a patient’s risk by 62%; the risk more than doubled in individuals with both.9 Several studies show that 15% to 25% of cancer patients experience depression,10 compared with 9% in the general population.11
Role of inflammatory markers
During an inflammatory episode the body releases cytokines, which are small, cell-signaling protein molecules. These inflammatory markers launch signaling cascades that incite the immune system into action. Type 1 cytokines (interferon-ã, tumor necrosis factor-á [TNF-á], interleukin [IL]-1) enhance cellular immune responses, and type 2 cytokines (IL-6, IL-10, IL-13) engage antibody responses. These cytokines also induce acute phase proteins, such as C-reactive protein (CRP), which can activate the immune system. Significantly higher levels of inflammatory markers are associated with a range of depressive symptoms, which grants insight into disease severity and treatment response.3,12,13
Multiple studies have explored the link between depression and inflammatory markers (Table).14-21 Peripheral inflammatory markers such as IL-6, IL-1â, CRP, and TNF-á are elevated in inflammatory diseases and in otherwise healthy individuals with MDD.12 In a meta-analysis of 24 studies measuring cytokines in depressed patients, Dowlati et al14 found individuals with MDD had significantly higher concentrations of TNF-á and IL-6 compared with controls. Increased peripheral inflammatory markers were found among antidepressant nonresponders more often than those who responded to treatment.15,22
Cytokines and depression risk
Administering immunomodulating agents has been shown to increase the risk of developing depression. Injecting animals with IL-1â or TNF-á causes sickness behavior in a dose- and time-related manner.1 As these inflammatory signaling proteins increase, sickness behaviors become more pronounced.
In humans, a natural model arises in the use of the cytokine interferon-á (INF-á) for treating hepatitis C, multiple sclerosis, malignant melanoma, and some blood cancers. Patients receiving INF-á have higher rates of depression than those not administered interferon.16 Patients receiving chronic immunotherapy treatment show long-term changes in monoamine neurotransmitters and along the HPA axis; these changes mimic those seen in depressed individuals.17,23 Acutely administered immunotherapeutic agents, such as the typhoid vaccine, have led to depressive symptoms with brain changes similar to those seen in MDD.18 Low levels of IL-6 and CRP independently predicted development of depression over several years.19
Immunotherapy-induced depression looks similar to any other major depressive episode through our current diagnostic framework and at the molecular and anatomical level.
Stress and inflammation
Depression can develop in the absence of inflammatory illness. Knowing that depressive symptoms may be associated with increased peripheral inflammatory markers, what induces the inflammatory process in some persons who are depressed but medically healthy? One theory is that psychological stress can activate inflammation.
Acute and chronic stress is associated with increased availability of proinflammatory cytokines and decreases in anti-inflammatory cytokines.3,24 One theory looks to glucocorticoid response to stress as an explanation. Miller et al25 found glucocorticoid sensitivity decreased among depressed women after exposure to a mock job interview stressor and increased among nondepressed controls. Because glucocorticoids normally stop the inflammatory cascade, this finding suggests depressed individuals may not be able to control inflammation during stress.26 At the level of genetic expression, there is increased transcription of proinflammatory genes in response to stress as a result of increased activation of nuclear factor kappa B.3,27
Shared pathways
If there is a relationship between inflammation and depression, what is the possible shared pathway?
There are 4 pathways by which cytokines effect changes in the CNS:12
• cytokines can activate primary afferent neurons (eg, vagal nerve)
• cytokines, released by macrophage-like cells in response to pathogens, diffuse through the brain’s circumventricular organs
• cytokine transporters saturate the blood-brain barrier
• cytokine IL-1 activates receptors on perivascular macrophages and endothelial cells of brain venules, causing local release of prostaglandin E2.
Through these pathways, cytokines initiate a cascade of reactions that lower serotonin levels and boost glutamatergic actions, possibly contributing to development of depressive symptoms. Depression correlates with a deficiency in serotonergic neurotransmission and increased glutamate receptor N-methyl-d-aspartate (NMDA) activation.28
Proinflammatory cytokines activate theextrahepatic enzyme indoleamine 2,3-dioxygenase (IDO), which degrades tryptophan, a precursor to serotonin (Figure 1). Tryptophan is channeled increasingly toward production of kynurenine via IDO degradation, competing with the serotonin pathway. Within the microglia, which are preferentially activated over astrocytes during inflammatory states, kynurenine is metabolized into quinolinic acid, which is an agonist of glutamatergic NMDA receptors.28 Therefore, there is a serotonergic deficiency and glutamatergic overdrive in proinflammatory states that paves the way toward a likely depressive syndrome (Figure 2).
Antidepressants’ effects
The symptoms of cytokine-induced depression are no different from MDD with unknown etiology29 and both are effectively treated with antidepressants. Even sickness behavior can be improved with antidepressant treatment.30
Antidepressants not only decrease immunotherapy-induced depressive symptoms but have been shown to decrease inflammatory response and lower proinflammatory factors (IL-2, IL-6, TNF-á, and INF-ã).31-33 Electroconvulsive therapy has been shown to normalize elevated TNF-á levels.34
Enhancing depression treatment
Researchers are investigating whether treatment with anti-inflammatory agents can ease depressive symptoms. In animal studies, normal behavioral reactions to a stressor—similar to sickness behavior and overlapping with several features of depression—were reduced with administration of cytokine antagonists or anti-inflammatory cytokines directly into the brain.35 However, there have been few successful trials in humans. Both anti-inflammatory agents such as cyclooxygenase-2 (COX-2) inhibitors, acetylsalicylic acid (aspirin), and TNF receptor antagonists can enhance depression treatments. Persoons et al36 found that Crohn’s disease patients who had higher pretreatment CRP levels and MDD had greater remission of depressive symptoms after treatment with the TNF-á antagonist infliximab. In studies, depression within the context of other autoimmune disorders or any condition with increased inflammation has responded to treatment with TNF-á antagonists.37,38 COX-2 inhibitors added to a standard antidepressant regimen improved depressive symptoms in medically healthy individuals during an acute depressive episode.39 Aspirin has shown some benefits as an adjuvant agent in persons who have failed selective serotonin reuptake inhibitor monotherapy.40,41
These anti-inflammatory agents have shown benefits in treating depression in some persons, but not in all. The key difference between those subsets of patients is elusive, mired in the complex interactions of the many systems that contribute to the symptoms we label as depression.
Future clinical applications
The association between depression and inflammation raises the possibility of a tantalizing line of future theories and treatment options. However, when considered individually, these pieces are limited in defining the precise relationship - a task nearly impossible for such a diffuse symptom as inflammation and such a complex disease as depression.
It is evident that inflammation and depression form a strong relationship to each other in individuals, which suggests the possibility of an inflammatory subtype of depression. At least within that limited group, there is the possibility of successful intervention and treatment of depression by directly treating inflammation with anti-inflammatory agents.
Perhaps once the relationship between depression and inflammation is further defined and a high-risk population identified—maybe even by genotype—depressive symptoms might be used to flag a provider’s attention to a possible disease process and serve as a new tool for identifying dangerous inflammatory activity at an early stage. Managing stress and depression may become the next tool to prevent inflammatory diseases.
Given our current knowledge, clinicians treating patients with inflammatory conditions should be aware of the increased risk of depression and ensure that depression screening is routinely completed and treatment is initiated or referrals made as needed. Ensuring appropriate depression treatment may help improve patients’ quality of life and ease the inflammatory response itself.
For psychiatrists seeing patients with an inflammatory condition, brief explanations of the known links between depression and inflammation can provide patients—particularly those ambivalent about seeking mental health care—support for engaging in treatment and adhering to medication. Describing the links between inflammation and depression also can help encourage regular exercise and healthy diets rich in fruits, vegetables, and omega-3 fatty acids. In cases of treatment-resistant depression, particularly in those with known high inflammatory factors, it may be worthwhile to consider anti-inflammatory agents, such as infliximab, as an adjuvant treatment.
The relationship between inflammation and depression is rapidly unfolding, but the full intricacies have not yet described. However, this beginning awareness of the interplay among stress, inflammation, and depression can broaden our approach to care and treatment.
Bottom Line
Depression and inflammation are linked in many ways, although neither appears to be wholly necessary or sufficient for the other. Most likely there exists a particular subset of patients for whom inflammation will precipitate and perpetuate depression.
Related Resources
- The Emory University Mind-Body Program. www.
psychiatry.emory.edu/PROGRAMS/mindbody/index.html. - Gabriel B. The evolutionary advantage of depression. The Atlantic. October 2, 2012. www.theatlantic.com/health/archive/2012/10/the-evolutionary-advantage-of-depression/263124.
Drug Brand Names
Infliximab • Remicade Ribavirin • Rebetol, Virazole
Interferon-α • Intron
Disclosure
Dr. Almond reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Dantzer R, O’Connor JC, Freund GG, et al. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46-56.
2. Hart BL. Biological basis of the behavior of sick animals. Neurosci Biobehav Rev. 1988;12(2):123-137.
3. Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27(1):24-31.
4. Lamers F, Vogelzangs N, Merikangas KR, et al. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression [published online October 23, 2012]. Mol Psychiatry. doi: 10.1038/mp.2012.144.
5. Hoen P, Kupper N, de Jonge P. Depression and cardiovascular disease progression: epidemiology, mechanisms and treatment. In: Hjemdahl P, Rosengren A, Steptoe A, eds. Stress and cardiovascular disease. London, United Kingdom: Springer; 2012:211-233.
6. Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069-1078.
7. Bachen EA, Chesney MA, Criswell LA. Prevalence of mood and anxiety disorders in women with systemic lupus erythematosus. Arthritis Rheum. 2009;61(6):822-829.
8. Dickens C, McGowan L, Clark-Carter D, et al. Depression in rheumatoid arthritis: a systematic review of the literature with meta-analysis. Psychosom Med. 2002;64(1):52-60.
9. Benros ME, Waltoft BL, Nordentoft M, et al. Autoimmunity and infections as risk factors for depression and other severe mental illnesses. Neurology, Psychiatry and Brain Research. 2012;18(2):40-41.
10. National Cancer Institute. Depression (PDQ). http://www.cancer.gov/cancertopics/pdq/supportivecare/depression/HealthProfessional/page1. Updated January 9, 2013. Accessed April 23, 2013.
11. Centers for Disease Control and Prevention. Current depression among adults—United States, 2006 and 2008. Morb Mortal Wkly Rep. 2010;59(38):1229-1235.
12. Krishnadas R, Cavanagh J. Depression: an inflammatory illness? J Neurol Neurosurg Psychiatry. 2012;83(5):495-502.
13. Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732-741.
14. Dowlati Y, Herrmann N, Swardfager W, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67(5):446-457.
15. Maes M, Bosmans E, De Jongh R, et al. Increased serum IL-6 and IL-1 receptor antagonist concentrations in major depression and treatment resistant depression. Cytokine. 1997;9(11):853-858.
16. Raison CL, Borisov AS, Broadwell SD, et al. Depression during pegylated interferon-alpha plus ribavirin therapy: prevalence and prediction. J Clin Psychiatry. 2005;66(1):41-48.
17. Capuron L, Raison CL, Musselman DL, et al. Association of exaggerated HPA axis response to the initial injection of interferon-alpha with development of depression during interferon-alpha therapy. Am J Psychiatry. 2003;160(7):1342-1345.
18. Eisenberger NI, Berkman ET, Inagaki TK, et al. Inflammation-induced anhedonia: endotoxin reduces ventral striatum responses to reward. Biol Psychiatry. 2010;68(8):748-754.
19. Pasco JA, Nicholson GC, Williams LJ, et al. Association of high-sensitivity C-reactive protein with de novo major depression. Br J Psychiatry. 2010;197(5):372-377.
20. Raison CL, Rutherford RE, Woolwine BJ, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70(1):31-41.
21. Martinez JM, Garakani A, Yehuda R, et al. Proinflammatory and “resiliency” proteins in the CSF of patients with major depression. Depress Anxiety. 2012;29(1):32-38.
22. Lanquillon S, Krieg JC, Bening-Abu-Shach U, et al. Cytokine production and treatment response in major depressive disorder. Neuropsychopharmacology. 2000;22(4):370-379.
23. Raison CL, Miller AH. Is depression an inflammatory disorder? Curr Psychiatry Rep. 2011;13(6):467-775.
24. Maes M, Song C, Lin A, et al. The effects of psychological stress on humans: increased production of pro-inflammatory cytokines and Th1-like response in stress-induced anxiety. Cytokine. 1998;10(4):313-318.
25. Miller GE, Rohleder N, Stetler C, et al. Clinical depression and regulation of the inflammatory response during acute stress. Psychosom Med. 2005;67(5):679-687.
26. Raison CL, Miller AH. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry. 2003;160(9):1554-1565.
27. Tak PP, Firestein GS. NF-êB: a key role in inflammatory diseases. J Clin Invest. 2001;107(1):7-12.
28. Müller N, Schwarz MJ. The immune-mediated alteration of serotonin and glutamate: towards an integrated view of depression. Mol Psychiatry. 2007;12(11):988-1000.
29. Capuron L, Fornwalt FB, Knight BT, et al. Does cytokine-induced depression differ from idiopathic major depression in medically healthy individuals? J Affect Disord. 2009;119(1-3):181-185.
30. Yirmiya R, Pollak Y, Morag M, et al. Illness, cytokines, and depression. Ann N Y Acad Sci. 2000;917(1):478-487.
31. Maes M. The immunoregulatory effects of antidepressants. Hum Psychopharmacol. 2001;16(1):95-103.
32. Szuster-Ciesielska A, Tustanowska-Stachura A, Słotwin`ska M, et al. In vitro immunoregulatory effects of antidepressants in healthy volunteers. Pol J Pharmacol. 2003;55(3):353-362.
33. Maes M, Berk M, Goehler L, et al. Depression and sickness behavior are Janus-faced responses to shared inflammatory pathways. BMC Med. 2012;10(1):66.
34. Hestad KA, Tønseth S, Støen CD, et al. Raised plasma levels of tumor necrosis factor [alpha] in patients with depression: normalization during electroconvulsive therapy. J ECT. 2003;19(4):183-188.
35. Maier SF, Watkins LR. Intracerebroventricular interleukin-1 receptor antagonist blocks the enhancement of fear conditioning and interference with escape produced by inescapable shock. Brain Res. 1995;695(2):279-282.
36. Persoons P, Vermeire S, Demyttenaere K, et al. The impact of major depressive disorder on the short- and long-term outcome of Crohn’s disease treatment with infliximab. Aliment Pharmacol Ther. 2005;22(2):101-110.
37. Mathias SD, Colwell HH, Miller DP, et al. Health-related quality of life and functional status of patients with rheumatoid arthritis randomly assigned to receive etanercept or placebo. Clin Ther. 2000;22(1):128-139.
38. Raison C, Rutherford RE, Woolwine B, et al. The tumor necrosis factor-alpha antagonist infliximab reduces depressive symptoms in patients with treatment resistant depression and high inflammation. Brain, Behavior, and Immunity. 2012;26(suppl 1):S49.
39. Müller N, Schwarz MJ, Dehning S, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. 2006;11(7):680-684.
40. Mendlewicz J, Kriwin P, Oswald P, et al. Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study. Int Clin Psychopharmacol. 2006;21(4):227-231.
41. Brunello N, Alboni S, Capone G, et al. Acetylsalicylic acid accelerates the antidepressant effect of fluoxetine in the chronic escape deficit model of depression. Int Clin Psychopharmacol. 2006;21(4):219-225.
Sneezing, coughing, and a sore throat are hallmark symptoms of a common cold, but what keeps you in bed are the accompanying fatigue, inattentiveness, loss of appetite, change in sleep pattern, heightened perception of pain, and apathetic withdrawal. This “sickness behavior” is induced by inflammatory markers released in response to illness.1,2 These symptoms are similar to the constellation of symptoms that define depression. Within the inflammatory response to illness, we see the shadow of depression, but the precise relationship remains murky.
Is depression part of a normal somatic inflammatory response run amok? Some researchers have argued that “sickness behavior” is adaptive, forcing the body into a constricted pattern in order to funnel energy into healing.1,3 If depression and inflammation are related, depression pushes past these adaptive roots and is less a forced pause than a debilitating withdrawal. Perhaps depression, or a subtype, is a sign of inflammation along with heat, pain, redness, and swelling. In some instances, depression may be a sign of an underlying inflammatory process.4
In our progression toward understanding depression’s pathophysiology, we see factors that point to a relationship between depression and inflammation:
• depression frequently is comorbid with many inflammatory illnesses
• increased inflammatory biomarkers are associated with major depressive disorder (MDD)
• exposure to immunomodulating agents may increase the risk of developing depression
• stress can activate proinflammatory pathways
• antidepressants can decrease inflammatory response
• inhibition of inflammatory pathways can improve mood.
Exploring these factors and a possible pathway linking inflammation and neurobiologic changes found in depression allows us to look closer at the possible integration of the inflammatory process and depressive symptoms.
Illness and depression rates
Individuals with inflammatory illnesses—autoimmune diseases, cardiovascular disease, diabetes, and cancer—often struggle with depression. Nearly 1 in 5 persons with cardiovascular disease experiences MDD.5 A diabetes diagnosis doubles the odds of having depression.6 Up to 70% of patients with autoimmune diseases, such as rheumatoid arthritis or systemic lupus erythematosus, experience depression.7,8 In a large-scale longitudinal study, having a prior autoimmune disease increased the risk of depression by 45% and history of hospitalization with infection increased a patient’s risk by 62%; the risk more than doubled in individuals with both.9 Several studies show that 15% to 25% of cancer patients experience depression,10 compared with 9% in the general population.11
Role of inflammatory markers
During an inflammatory episode the body releases cytokines, which are small, cell-signaling protein molecules. These inflammatory markers launch signaling cascades that incite the immune system into action. Type 1 cytokines (interferon-ã, tumor necrosis factor-á [TNF-á], interleukin [IL]-1) enhance cellular immune responses, and type 2 cytokines (IL-6, IL-10, IL-13) engage antibody responses. These cytokines also induce acute phase proteins, such as C-reactive protein (CRP), which can activate the immune system. Significantly higher levels of inflammatory markers are associated with a range of depressive symptoms, which grants insight into disease severity and treatment response.3,12,13
Multiple studies have explored the link between depression and inflammatory markers (Table).14-21 Peripheral inflammatory markers such as IL-6, IL-1â, CRP, and TNF-á are elevated in inflammatory diseases and in otherwise healthy individuals with MDD.12 In a meta-analysis of 24 studies measuring cytokines in depressed patients, Dowlati et al14 found individuals with MDD had significantly higher concentrations of TNF-á and IL-6 compared with controls. Increased peripheral inflammatory markers were found among antidepressant nonresponders more often than those who responded to treatment.15,22
Cytokines and depression risk
Administering immunomodulating agents has been shown to increase the risk of developing depression. Injecting animals with IL-1â or TNF-á causes sickness behavior in a dose- and time-related manner.1 As these inflammatory signaling proteins increase, sickness behaviors become more pronounced.
In humans, a natural model arises in the use of the cytokine interferon-á (INF-á) for treating hepatitis C, multiple sclerosis, malignant melanoma, and some blood cancers. Patients receiving INF-á have higher rates of depression than those not administered interferon.16 Patients receiving chronic immunotherapy treatment show long-term changes in monoamine neurotransmitters and along the HPA axis; these changes mimic those seen in depressed individuals.17,23 Acutely administered immunotherapeutic agents, such as the typhoid vaccine, have led to depressive symptoms with brain changes similar to those seen in MDD.18 Low levels of IL-6 and CRP independently predicted development of depression over several years.19
Immunotherapy-induced depression looks similar to any other major depressive episode through our current diagnostic framework and at the molecular and anatomical level.
Stress and inflammation
Depression can develop in the absence of inflammatory illness. Knowing that depressive symptoms may be associated with increased peripheral inflammatory markers, what induces the inflammatory process in some persons who are depressed but medically healthy? One theory is that psychological stress can activate inflammation.
Acute and chronic stress is associated with increased availability of proinflammatory cytokines and decreases in anti-inflammatory cytokines.3,24 One theory looks to glucocorticoid response to stress as an explanation. Miller et al25 found glucocorticoid sensitivity decreased among depressed women after exposure to a mock job interview stressor and increased among nondepressed controls. Because glucocorticoids normally stop the inflammatory cascade, this finding suggests depressed individuals may not be able to control inflammation during stress.26 At the level of genetic expression, there is increased transcription of proinflammatory genes in response to stress as a result of increased activation of nuclear factor kappa B.3,27
Shared pathways
If there is a relationship between inflammation and depression, what is the possible shared pathway?
There are 4 pathways by which cytokines effect changes in the CNS:12
• cytokines can activate primary afferent neurons (eg, vagal nerve)
• cytokines, released by macrophage-like cells in response to pathogens, diffuse through the brain’s circumventricular organs
• cytokine transporters saturate the blood-brain barrier
• cytokine IL-1 activates receptors on perivascular macrophages and endothelial cells of brain venules, causing local release of prostaglandin E2.
Through these pathways, cytokines initiate a cascade of reactions that lower serotonin levels and boost glutamatergic actions, possibly contributing to development of depressive symptoms. Depression correlates with a deficiency in serotonergic neurotransmission and increased glutamate receptor N-methyl-d-aspartate (NMDA) activation.28
Proinflammatory cytokines activate theextrahepatic enzyme indoleamine 2,3-dioxygenase (IDO), which degrades tryptophan, a precursor to serotonin (Figure 1). Tryptophan is channeled increasingly toward production of kynurenine via IDO degradation, competing with the serotonin pathway. Within the microglia, which are preferentially activated over astrocytes during inflammatory states, kynurenine is metabolized into quinolinic acid, which is an agonist of glutamatergic NMDA receptors.28 Therefore, there is a serotonergic deficiency and glutamatergic overdrive in proinflammatory states that paves the way toward a likely depressive syndrome (Figure 2).
Antidepressants’ effects
The symptoms of cytokine-induced depression are no different from MDD with unknown etiology29 and both are effectively treated with antidepressants. Even sickness behavior can be improved with antidepressant treatment.30
Antidepressants not only decrease immunotherapy-induced depressive symptoms but have been shown to decrease inflammatory response and lower proinflammatory factors (IL-2, IL-6, TNF-á, and INF-ã).31-33 Electroconvulsive therapy has been shown to normalize elevated TNF-á levels.34
Enhancing depression treatment
Researchers are investigating whether treatment with anti-inflammatory agents can ease depressive symptoms. In animal studies, normal behavioral reactions to a stressor—similar to sickness behavior and overlapping with several features of depression—were reduced with administration of cytokine antagonists or anti-inflammatory cytokines directly into the brain.35 However, there have been few successful trials in humans. Both anti-inflammatory agents such as cyclooxygenase-2 (COX-2) inhibitors, acetylsalicylic acid (aspirin), and TNF receptor antagonists can enhance depression treatments. Persoons et al36 found that Crohn’s disease patients who had higher pretreatment CRP levels and MDD had greater remission of depressive symptoms after treatment with the TNF-á antagonist infliximab. In studies, depression within the context of other autoimmune disorders or any condition with increased inflammation has responded to treatment with TNF-á antagonists.37,38 COX-2 inhibitors added to a standard antidepressant regimen improved depressive symptoms in medically healthy individuals during an acute depressive episode.39 Aspirin has shown some benefits as an adjuvant agent in persons who have failed selective serotonin reuptake inhibitor monotherapy.40,41
These anti-inflammatory agents have shown benefits in treating depression in some persons, but not in all. The key difference between those subsets of patients is elusive, mired in the complex interactions of the many systems that contribute to the symptoms we label as depression.
Future clinical applications
The association between depression and inflammation raises the possibility of a tantalizing line of future theories and treatment options. However, when considered individually, these pieces are limited in defining the precise relationship - a task nearly impossible for such a diffuse symptom as inflammation and such a complex disease as depression.
It is evident that inflammation and depression form a strong relationship to each other in individuals, which suggests the possibility of an inflammatory subtype of depression. At least within that limited group, there is the possibility of successful intervention and treatment of depression by directly treating inflammation with anti-inflammatory agents.
Perhaps once the relationship between depression and inflammation is further defined and a high-risk population identified—maybe even by genotype—depressive symptoms might be used to flag a provider’s attention to a possible disease process and serve as a new tool for identifying dangerous inflammatory activity at an early stage. Managing stress and depression may become the next tool to prevent inflammatory diseases.
Given our current knowledge, clinicians treating patients with inflammatory conditions should be aware of the increased risk of depression and ensure that depression screening is routinely completed and treatment is initiated or referrals made as needed. Ensuring appropriate depression treatment may help improve patients’ quality of life and ease the inflammatory response itself.
For psychiatrists seeing patients with an inflammatory condition, brief explanations of the known links between depression and inflammation can provide patients—particularly those ambivalent about seeking mental health care—support for engaging in treatment and adhering to medication. Describing the links between inflammation and depression also can help encourage regular exercise and healthy diets rich in fruits, vegetables, and omega-3 fatty acids. In cases of treatment-resistant depression, particularly in those with known high inflammatory factors, it may be worthwhile to consider anti-inflammatory agents, such as infliximab, as an adjuvant treatment.
The relationship between inflammation and depression is rapidly unfolding, but the full intricacies have not yet described. However, this beginning awareness of the interplay among stress, inflammation, and depression can broaden our approach to care and treatment.
Bottom Line
Depression and inflammation are linked in many ways, although neither appears to be wholly necessary or sufficient for the other. Most likely there exists a particular subset of patients for whom inflammation will precipitate and perpetuate depression.
Related Resources
- The Emory University Mind-Body Program. www.
psychiatry.emory.edu/PROGRAMS/mindbody/index.html. - Gabriel B. The evolutionary advantage of depression. The Atlantic. October 2, 2012. www.theatlantic.com/health/archive/2012/10/the-evolutionary-advantage-of-depression/263124.
Drug Brand Names
Infliximab • Remicade Ribavirin • Rebetol, Virazole
Interferon-α • Intron
Disclosure
Dr. Almond reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Dantzer R, O’Connor JC, Freund GG, et al. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46-56.
2. Hart BL. Biological basis of the behavior of sick animals. Neurosci Biobehav Rev. 1988;12(2):123-137.
3. Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27(1):24-31.
4. Lamers F, Vogelzangs N, Merikangas KR, et al. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression [published online October 23, 2012]. Mol Psychiatry. doi: 10.1038/mp.2012.144.
5. Hoen P, Kupper N, de Jonge P. Depression and cardiovascular disease progression: epidemiology, mechanisms and treatment. In: Hjemdahl P, Rosengren A, Steptoe A, eds. Stress and cardiovascular disease. London, United Kingdom: Springer; 2012:211-233.
6. Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069-1078.
7. Bachen EA, Chesney MA, Criswell LA. Prevalence of mood and anxiety disorders in women with systemic lupus erythematosus. Arthritis Rheum. 2009;61(6):822-829.
8. Dickens C, McGowan L, Clark-Carter D, et al. Depression in rheumatoid arthritis: a systematic review of the literature with meta-analysis. Psychosom Med. 2002;64(1):52-60.
9. Benros ME, Waltoft BL, Nordentoft M, et al. Autoimmunity and infections as risk factors for depression and other severe mental illnesses. Neurology, Psychiatry and Brain Research. 2012;18(2):40-41.
10. National Cancer Institute. Depression (PDQ). http://www.cancer.gov/cancertopics/pdq/supportivecare/depression/HealthProfessional/page1. Updated January 9, 2013. Accessed April 23, 2013.
11. Centers for Disease Control and Prevention. Current depression among adults—United States, 2006 and 2008. Morb Mortal Wkly Rep. 2010;59(38):1229-1235.
12. Krishnadas R, Cavanagh J. Depression: an inflammatory illness? J Neurol Neurosurg Psychiatry. 2012;83(5):495-502.
13. Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732-741.
14. Dowlati Y, Herrmann N, Swardfager W, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67(5):446-457.
15. Maes M, Bosmans E, De Jongh R, et al. Increased serum IL-6 and IL-1 receptor antagonist concentrations in major depression and treatment resistant depression. Cytokine. 1997;9(11):853-858.
16. Raison CL, Borisov AS, Broadwell SD, et al. Depression during pegylated interferon-alpha plus ribavirin therapy: prevalence and prediction. J Clin Psychiatry. 2005;66(1):41-48.
17. Capuron L, Raison CL, Musselman DL, et al. Association of exaggerated HPA axis response to the initial injection of interferon-alpha with development of depression during interferon-alpha therapy. Am J Psychiatry. 2003;160(7):1342-1345.
18. Eisenberger NI, Berkman ET, Inagaki TK, et al. Inflammation-induced anhedonia: endotoxin reduces ventral striatum responses to reward. Biol Psychiatry. 2010;68(8):748-754.
19. Pasco JA, Nicholson GC, Williams LJ, et al. Association of high-sensitivity C-reactive protein with de novo major depression. Br J Psychiatry. 2010;197(5):372-377.
20. Raison CL, Rutherford RE, Woolwine BJ, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70(1):31-41.
21. Martinez JM, Garakani A, Yehuda R, et al. Proinflammatory and “resiliency” proteins in the CSF of patients with major depression. Depress Anxiety. 2012;29(1):32-38.
22. Lanquillon S, Krieg JC, Bening-Abu-Shach U, et al. Cytokine production and treatment response in major depressive disorder. Neuropsychopharmacology. 2000;22(4):370-379.
23. Raison CL, Miller AH. Is depression an inflammatory disorder? Curr Psychiatry Rep. 2011;13(6):467-775.
24. Maes M, Song C, Lin A, et al. The effects of psychological stress on humans: increased production of pro-inflammatory cytokines and Th1-like response in stress-induced anxiety. Cytokine. 1998;10(4):313-318.
25. Miller GE, Rohleder N, Stetler C, et al. Clinical depression and regulation of the inflammatory response during acute stress. Psychosom Med. 2005;67(5):679-687.
26. Raison CL, Miller AH. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry. 2003;160(9):1554-1565.
27. Tak PP, Firestein GS. NF-êB: a key role in inflammatory diseases. J Clin Invest. 2001;107(1):7-12.
28. Müller N, Schwarz MJ. The immune-mediated alteration of serotonin and glutamate: towards an integrated view of depression. Mol Psychiatry. 2007;12(11):988-1000.
29. Capuron L, Fornwalt FB, Knight BT, et al. Does cytokine-induced depression differ from idiopathic major depression in medically healthy individuals? J Affect Disord. 2009;119(1-3):181-185.
30. Yirmiya R, Pollak Y, Morag M, et al. Illness, cytokines, and depression. Ann N Y Acad Sci. 2000;917(1):478-487.
31. Maes M. The immunoregulatory effects of antidepressants. Hum Psychopharmacol. 2001;16(1):95-103.
32. Szuster-Ciesielska A, Tustanowska-Stachura A, Słotwin`ska M, et al. In vitro immunoregulatory effects of antidepressants in healthy volunteers. Pol J Pharmacol. 2003;55(3):353-362.
33. Maes M, Berk M, Goehler L, et al. Depression and sickness behavior are Janus-faced responses to shared inflammatory pathways. BMC Med. 2012;10(1):66.
34. Hestad KA, Tønseth S, Støen CD, et al. Raised plasma levels of tumor necrosis factor [alpha] in patients with depression: normalization during electroconvulsive therapy. J ECT. 2003;19(4):183-188.
35. Maier SF, Watkins LR. Intracerebroventricular interleukin-1 receptor antagonist blocks the enhancement of fear conditioning and interference with escape produced by inescapable shock. Brain Res. 1995;695(2):279-282.
36. Persoons P, Vermeire S, Demyttenaere K, et al. The impact of major depressive disorder on the short- and long-term outcome of Crohn’s disease treatment with infliximab. Aliment Pharmacol Ther. 2005;22(2):101-110.
37. Mathias SD, Colwell HH, Miller DP, et al. Health-related quality of life and functional status of patients with rheumatoid arthritis randomly assigned to receive etanercept or placebo. Clin Ther. 2000;22(1):128-139.
38. Raison C, Rutherford RE, Woolwine B, et al. The tumor necrosis factor-alpha antagonist infliximab reduces depressive symptoms in patients with treatment resistant depression and high inflammation. Brain, Behavior, and Immunity. 2012;26(suppl 1):S49.
39. Müller N, Schwarz MJ, Dehning S, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. 2006;11(7):680-684.
40. Mendlewicz J, Kriwin P, Oswald P, et al. Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study. Int Clin Psychopharmacol. 2006;21(4):227-231.
41. Brunello N, Alboni S, Capone G, et al. Acetylsalicylic acid accelerates the antidepressant effect of fluoxetine in the chronic escape deficit model of depression. Int Clin Psychopharmacol. 2006;21(4):219-225.
Sneezing, coughing, and a sore throat are hallmark symptoms of a common cold, but what keeps you in bed are the accompanying fatigue, inattentiveness, loss of appetite, change in sleep pattern, heightened perception of pain, and apathetic withdrawal. This “sickness behavior” is induced by inflammatory markers released in response to illness.1,2 These symptoms are similar to the constellation of symptoms that define depression. Within the inflammatory response to illness, we see the shadow of depression, but the precise relationship remains murky.
Is depression part of a normal somatic inflammatory response run amok? Some researchers have argued that “sickness behavior” is adaptive, forcing the body into a constricted pattern in order to funnel energy into healing.1,3 If depression and inflammation are related, depression pushes past these adaptive roots and is less a forced pause than a debilitating withdrawal. Perhaps depression, or a subtype, is a sign of inflammation along with heat, pain, redness, and swelling. In some instances, depression may be a sign of an underlying inflammatory process.4
In our progression toward understanding depression’s pathophysiology, we see factors that point to a relationship between depression and inflammation:
• depression frequently is comorbid with many inflammatory illnesses
• increased inflammatory biomarkers are associated with major depressive disorder (MDD)
• exposure to immunomodulating agents may increase the risk of developing depression
• stress can activate proinflammatory pathways
• antidepressants can decrease inflammatory response
• inhibition of inflammatory pathways can improve mood.
Exploring these factors and a possible pathway linking inflammation and neurobiologic changes found in depression allows us to look closer at the possible integration of the inflammatory process and depressive symptoms.
Illness and depression rates
Individuals with inflammatory illnesses—autoimmune diseases, cardiovascular disease, diabetes, and cancer—often struggle with depression. Nearly 1 in 5 persons with cardiovascular disease experiences MDD.5 A diabetes diagnosis doubles the odds of having depression.6 Up to 70% of patients with autoimmune diseases, such as rheumatoid arthritis or systemic lupus erythematosus, experience depression.7,8 In a large-scale longitudinal study, having a prior autoimmune disease increased the risk of depression by 45% and history of hospitalization with infection increased a patient’s risk by 62%; the risk more than doubled in individuals with both.9 Several studies show that 15% to 25% of cancer patients experience depression,10 compared with 9% in the general population.11
Role of inflammatory markers
During an inflammatory episode the body releases cytokines, which are small, cell-signaling protein molecules. These inflammatory markers launch signaling cascades that incite the immune system into action. Type 1 cytokines (interferon-ã, tumor necrosis factor-á [TNF-á], interleukin [IL]-1) enhance cellular immune responses, and type 2 cytokines (IL-6, IL-10, IL-13) engage antibody responses. These cytokines also induce acute phase proteins, such as C-reactive protein (CRP), which can activate the immune system. Significantly higher levels of inflammatory markers are associated with a range of depressive symptoms, which grants insight into disease severity and treatment response.3,12,13
Multiple studies have explored the link between depression and inflammatory markers (Table).14-21 Peripheral inflammatory markers such as IL-6, IL-1â, CRP, and TNF-á are elevated in inflammatory diseases and in otherwise healthy individuals with MDD.12 In a meta-analysis of 24 studies measuring cytokines in depressed patients, Dowlati et al14 found individuals with MDD had significantly higher concentrations of TNF-á and IL-6 compared with controls. Increased peripheral inflammatory markers were found among antidepressant nonresponders more often than those who responded to treatment.15,22
Cytokines and depression risk
Administering immunomodulating agents has been shown to increase the risk of developing depression. Injecting animals with IL-1â or TNF-á causes sickness behavior in a dose- and time-related manner.1 As these inflammatory signaling proteins increase, sickness behaviors become more pronounced.
In humans, a natural model arises in the use of the cytokine interferon-á (INF-á) for treating hepatitis C, multiple sclerosis, malignant melanoma, and some blood cancers. Patients receiving INF-á have higher rates of depression than those not administered interferon.16 Patients receiving chronic immunotherapy treatment show long-term changes in monoamine neurotransmitters and along the HPA axis; these changes mimic those seen in depressed individuals.17,23 Acutely administered immunotherapeutic agents, such as the typhoid vaccine, have led to depressive symptoms with brain changes similar to those seen in MDD.18 Low levels of IL-6 and CRP independently predicted development of depression over several years.19
Immunotherapy-induced depression looks similar to any other major depressive episode through our current diagnostic framework and at the molecular and anatomical level.
Stress and inflammation
Depression can develop in the absence of inflammatory illness. Knowing that depressive symptoms may be associated with increased peripheral inflammatory markers, what induces the inflammatory process in some persons who are depressed but medically healthy? One theory is that psychological stress can activate inflammation.
Acute and chronic stress is associated with increased availability of proinflammatory cytokines and decreases in anti-inflammatory cytokines.3,24 One theory looks to glucocorticoid response to stress as an explanation. Miller et al25 found glucocorticoid sensitivity decreased among depressed women after exposure to a mock job interview stressor and increased among nondepressed controls. Because glucocorticoids normally stop the inflammatory cascade, this finding suggests depressed individuals may not be able to control inflammation during stress.26 At the level of genetic expression, there is increased transcription of proinflammatory genes in response to stress as a result of increased activation of nuclear factor kappa B.3,27
Shared pathways
If there is a relationship between inflammation and depression, what is the possible shared pathway?
There are 4 pathways by which cytokines effect changes in the CNS:12
• cytokines can activate primary afferent neurons (eg, vagal nerve)
• cytokines, released by macrophage-like cells in response to pathogens, diffuse through the brain’s circumventricular organs
• cytokine transporters saturate the blood-brain barrier
• cytokine IL-1 activates receptors on perivascular macrophages and endothelial cells of brain venules, causing local release of prostaglandin E2.
Through these pathways, cytokines initiate a cascade of reactions that lower serotonin levels and boost glutamatergic actions, possibly contributing to development of depressive symptoms. Depression correlates with a deficiency in serotonergic neurotransmission and increased glutamate receptor N-methyl-d-aspartate (NMDA) activation.28
Proinflammatory cytokines activate theextrahepatic enzyme indoleamine 2,3-dioxygenase (IDO), which degrades tryptophan, a precursor to serotonin (Figure 1). Tryptophan is channeled increasingly toward production of kynurenine via IDO degradation, competing with the serotonin pathway. Within the microglia, which are preferentially activated over astrocytes during inflammatory states, kynurenine is metabolized into quinolinic acid, which is an agonist of glutamatergic NMDA receptors.28 Therefore, there is a serotonergic deficiency and glutamatergic overdrive in proinflammatory states that paves the way toward a likely depressive syndrome (Figure 2).
Antidepressants’ effects
The symptoms of cytokine-induced depression are no different from MDD with unknown etiology29 and both are effectively treated with antidepressants. Even sickness behavior can be improved with antidepressant treatment.30
Antidepressants not only decrease immunotherapy-induced depressive symptoms but have been shown to decrease inflammatory response and lower proinflammatory factors (IL-2, IL-6, TNF-á, and INF-ã).31-33 Electroconvulsive therapy has been shown to normalize elevated TNF-á levels.34
Enhancing depression treatment
Researchers are investigating whether treatment with anti-inflammatory agents can ease depressive symptoms. In animal studies, normal behavioral reactions to a stressor—similar to sickness behavior and overlapping with several features of depression—were reduced with administration of cytokine antagonists or anti-inflammatory cytokines directly into the brain.35 However, there have been few successful trials in humans. Both anti-inflammatory agents such as cyclooxygenase-2 (COX-2) inhibitors, acetylsalicylic acid (aspirin), and TNF receptor antagonists can enhance depression treatments. Persoons et al36 found that Crohn’s disease patients who had higher pretreatment CRP levels and MDD had greater remission of depressive symptoms after treatment with the TNF-á antagonist infliximab. In studies, depression within the context of other autoimmune disorders or any condition with increased inflammation has responded to treatment with TNF-á antagonists.37,38 COX-2 inhibitors added to a standard antidepressant regimen improved depressive symptoms in medically healthy individuals during an acute depressive episode.39 Aspirin has shown some benefits as an adjuvant agent in persons who have failed selective serotonin reuptake inhibitor monotherapy.40,41
These anti-inflammatory agents have shown benefits in treating depression in some persons, but not in all. The key difference between those subsets of patients is elusive, mired in the complex interactions of the many systems that contribute to the symptoms we label as depression.
Future clinical applications
The association between depression and inflammation raises the possibility of a tantalizing line of future theories and treatment options. However, when considered individually, these pieces are limited in defining the precise relationship - a task nearly impossible for such a diffuse symptom as inflammation and such a complex disease as depression.
It is evident that inflammation and depression form a strong relationship to each other in individuals, which suggests the possibility of an inflammatory subtype of depression. At least within that limited group, there is the possibility of successful intervention and treatment of depression by directly treating inflammation with anti-inflammatory agents.
Perhaps once the relationship between depression and inflammation is further defined and a high-risk population identified—maybe even by genotype—depressive symptoms might be used to flag a provider’s attention to a possible disease process and serve as a new tool for identifying dangerous inflammatory activity at an early stage. Managing stress and depression may become the next tool to prevent inflammatory diseases.
Given our current knowledge, clinicians treating patients with inflammatory conditions should be aware of the increased risk of depression and ensure that depression screening is routinely completed and treatment is initiated or referrals made as needed. Ensuring appropriate depression treatment may help improve patients’ quality of life and ease the inflammatory response itself.
For psychiatrists seeing patients with an inflammatory condition, brief explanations of the known links between depression and inflammation can provide patients—particularly those ambivalent about seeking mental health care—support for engaging in treatment and adhering to medication. Describing the links between inflammation and depression also can help encourage regular exercise and healthy diets rich in fruits, vegetables, and omega-3 fatty acids. In cases of treatment-resistant depression, particularly in those with known high inflammatory factors, it may be worthwhile to consider anti-inflammatory agents, such as infliximab, as an adjuvant treatment.
The relationship between inflammation and depression is rapidly unfolding, but the full intricacies have not yet described. However, this beginning awareness of the interplay among stress, inflammation, and depression can broaden our approach to care and treatment.
Bottom Line
Depression and inflammation are linked in many ways, although neither appears to be wholly necessary or sufficient for the other. Most likely there exists a particular subset of patients for whom inflammation will precipitate and perpetuate depression.
Related Resources
- The Emory University Mind-Body Program. www.
psychiatry.emory.edu/PROGRAMS/mindbody/index.html. - Gabriel B. The evolutionary advantage of depression. The Atlantic. October 2, 2012. www.theatlantic.com/health/archive/2012/10/the-evolutionary-advantage-of-depression/263124.
Drug Brand Names
Infliximab • Remicade Ribavirin • Rebetol, Virazole
Interferon-α • Intron
Disclosure
Dr. Almond reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Dantzer R, O’Connor JC, Freund GG, et al. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46-56.
2. Hart BL. Biological basis of the behavior of sick animals. Neurosci Biobehav Rev. 1988;12(2):123-137.
3. Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27(1):24-31.
4. Lamers F, Vogelzangs N, Merikangas KR, et al. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression [published online October 23, 2012]. Mol Psychiatry. doi: 10.1038/mp.2012.144.
5. Hoen P, Kupper N, de Jonge P. Depression and cardiovascular disease progression: epidemiology, mechanisms and treatment. In: Hjemdahl P, Rosengren A, Steptoe A, eds. Stress and cardiovascular disease. London, United Kingdom: Springer; 2012:211-233.
6. Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069-1078.
7. Bachen EA, Chesney MA, Criswell LA. Prevalence of mood and anxiety disorders in women with systemic lupus erythematosus. Arthritis Rheum. 2009;61(6):822-829.
8. Dickens C, McGowan L, Clark-Carter D, et al. Depression in rheumatoid arthritis: a systematic review of the literature with meta-analysis. Psychosom Med. 2002;64(1):52-60.
9. Benros ME, Waltoft BL, Nordentoft M, et al. Autoimmunity and infections as risk factors for depression and other severe mental illnesses. Neurology, Psychiatry and Brain Research. 2012;18(2):40-41.
10. National Cancer Institute. Depression (PDQ). http://www.cancer.gov/cancertopics/pdq/supportivecare/depression/HealthProfessional/page1. Updated January 9, 2013. Accessed April 23, 2013.
11. Centers for Disease Control and Prevention. Current depression among adults—United States, 2006 and 2008. Morb Mortal Wkly Rep. 2010;59(38):1229-1235.
12. Krishnadas R, Cavanagh J. Depression: an inflammatory illness? J Neurol Neurosurg Psychiatry. 2012;83(5):495-502.
13. Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732-741.
14. Dowlati Y, Herrmann N, Swardfager W, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67(5):446-457.
15. Maes M, Bosmans E, De Jongh R, et al. Increased serum IL-6 and IL-1 receptor antagonist concentrations in major depression and treatment resistant depression. Cytokine. 1997;9(11):853-858.
16. Raison CL, Borisov AS, Broadwell SD, et al. Depression during pegylated interferon-alpha plus ribavirin therapy: prevalence and prediction. J Clin Psychiatry. 2005;66(1):41-48.
17. Capuron L, Raison CL, Musselman DL, et al. Association of exaggerated HPA axis response to the initial injection of interferon-alpha with development of depression during interferon-alpha therapy. Am J Psychiatry. 2003;160(7):1342-1345.
18. Eisenberger NI, Berkman ET, Inagaki TK, et al. Inflammation-induced anhedonia: endotoxin reduces ventral striatum responses to reward. Biol Psychiatry. 2010;68(8):748-754.
19. Pasco JA, Nicholson GC, Williams LJ, et al. Association of high-sensitivity C-reactive protein with de novo major depression. Br J Psychiatry. 2010;197(5):372-377.
20. Raison CL, Rutherford RE, Woolwine BJ, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70(1):31-41.
21. Martinez JM, Garakani A, Yehuda R, et al. Proinflammatory and “resiliency” proteins in the CSF of patients with major depression. Depress Anxiety. 2012;29(1):32-38.
22. Lanquillon S, Krieg JC, Bening-Abu-Shach U, et al. Cytokine production and treatment response in major depressive disorder. Neuropsychopharmacology. 2000;22(4):370-379.
23. Raison CL, Miller AH. Is depression an inflammatory disorder? Curr Psychiatry Rep. 2011;13(6):467-775.
24. Maes M, Song C, Lin A, et al. The effects of psychological stress on humans: increased production of pro-inflammatory cytokines and Th1-like response in stress-induced anxiety. Cytokine. 1998;10(4):313-318.
25. Miller GE, Rohleder N, Stetler C, et al. Clinical depression and regulation of the inflammatory response during acute stress. Psychosom Med. 2005;67(5):679-687.
26. Raison CL, Miller AH. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry. 2003;160(9):1554-1565.
27. Tak PP, Firestein GS. NF-êB: a key role in inflammatory diseases. J Clin Invest. 2001;107(1):7-12.
28. Müller N, Schwarz MJ. The immune-mediated alteration of serotonin and glutamate: towards an integrated view of depression. Mol Psychiatry. 2007;12(11):988-1000.
29. Capuron L, Fornwalt FB, Knight BT, et al. Does cytokine-induced depression differ from idiopathic major depression in medically healthy individuals? J Affect Disord. 2009;119(1-3):181-185.
30. Yirmiya R, Pollak Y, Morag M, et al. Illness, cytokines, and depression. Ann N Y Acad Sci. 2000;917(1):478-487.
31. Maes M. The immunoregulatory effects of antidepressants. Hum Psychopharmacol. 2001;16(1):95-103.
32. Szuster-Ciesielska A, Tustanowska-Stachura A, Słotwin`ska M, et al. In vitro immunoregulatory effects of antidepressants in healthy volunteers. Pol J Pharmacol. 2003;55(3):353-362.
33. Maes M, Berk M, Goehler L, et al. Depression and sickness behavior are Janus-faced responses to shared inflammatory pathways. BMC Med. 2012;10(1):66.
34. Hestad KA, Tønseth S, Støen CD, et al. Raised plasma levels of tumor necrosis factor [alpha] in patients with depression: normalization during electroconvulsive therapy. J ECT. 2003;19(4):183-188.
35. Maier SF, Watkins LR. Intracerebroventricular interleukin-1 receptor antagonist blocks the enhancement of fear conditioning and interference with escape produced by inescapable shock. Brain Res. 1995;695(2):279-282.
36. Persoons P, Vermeire S, Demyttenaere K, et al. The impact of major depressive disorder on the short- and long-term outcome of Crohn’s disease treatment with infliximab. Aliment Pharmacol Ther. 2005;22(2):101-110.
37. Mathias SD, Colwell HH, Miller DP, et al. Health-related quality of life and functional status of patients with rheumatoid arthritis randomly assigned to receive etanercept or placebo. Clin Ther. 2000;22(1):128-139.
38. Raison C, Rutherford RE, Woolwine B, et al. The tumor necrosis factor-alpha antagonist infliximab reduces depressive symptoms in patients with treatment resistant depression and high inflammation. Brain, Behavior, and Immunity. 2012;26(suppl 1):S49.
39. Müller N, Schwarz MJ, Dehning S, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. 2006;11(7):680-684.
40. Mendlewicz J, Kriwin P, Oswald P, et al. Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study. Int Clin Psychopharmacol. 2006;21(4):227-231.
41. Brunello N, Alboni S, Capone G, et al. Acetylsalicylic acid accelerates the antidepressant effect of fluoxetine in the chronic escape deficit model of depression. Int Clin Psychopharmacol. 2006;21(4):219-225.
Scientific journalism: The dangers of misinformation
The 2011 movie Contagion portrays chaos resulting from the emergence of a highly lethal, rapidly progressing virus threatening to end civilization. One of the characters, a freelance journalist with a blog followed by 15 million people, directs his readers to ignore an effective vaccine the CDC has developed, assigning conspiratorial motives to the CDC’s efforts.
During a nationally televised 2011 presidential candidate debate, Representative Michele Bachmann created a controversy when she stated fellow candidate Texas Governor Rick Perry’s policy requiring sixth-grade girls to get vaccinated against the human papillomavirus exposed them to potential dangers.
Much has been written about the potential influence politicians and mass media have on the public’s understanding of scientific knowledge. Carvalho wrote, “The media have a crucial responsibility as a source of information and opinions about science and technology for citizens. Public perception and attitudes with regard to those domains are significantly influenced by representations of scientific knowledge conveyed by the press and other mass means of communication.”1
Recently, media attention generated by some critics—eg, professional journalists, nonmedical academics, and nonpsychiatric physicians—has questioned the effectiveness of antidepressants. These individuals are affecting public understanding of the issue.
Scientific journalism vs scientific discovery
Journalism exists in many forms—eg, advocacy, scientific, investigative—and has led to positive and negative social and cultural changes. Scientific journalism interprets information to make it interesting and understandable to readers. Ideally, journalists select what is newsworthy and provide balance to disputed themes with careful attention to the facts. Sometimes, a scientific journalist may render his or her opinion on the topic, explicitly or implicitly. When this occurs, the journalist may reflect the state-of-the-art accurately, or he or she may present biased journalism.
Although the modus operandi of a journalist can differ significantly from that of an expert conducting scientific inquiry, I do not intend to render a judgment about the superiority or inferiority of either group. Both groups have the ability to impact discovery, negatively and positively.
Scientific experts acquire and report scientific evidence regarding depression. Additionally, they develop professional guidelines to provide practical advice to clinicians who wrestle with the challenges of treating depression. Journalists are not trained to render medical judgments about the data; they simply report it.
Experts rely on pure transparency from the initial hypothesis through the design, methods, results, and conclusions. In contrast, journalists enjoy the time-honored privilege of hiding sources’ identities.
Before a scientific expert’s paper is published, he or she must negotiate a peer review process in which his or her writing is subjected to the scrutiny of qualified experts in the same field, a process that can last months to years. Journalistic methodologies also include editorial oversight, but it’s fair to say that the peer review process for scientific publication generally is more rigorous than editorial reviews of journalism, because the journalistic review process serves the goal of generating “news” for a hungry marketplace of ideas. Journalists pick and chose their content, hopefully in a balanced fashion, but at the discretion of the journalist and his or her editor. It’s relatively quick and easy for journalists to publish a book or newspaper article, and even easier to publish a blog.
Experts submitting manuscripts to peer-reviewed journals are not paid based on sales or impact factor. The literary style of the expert often is dry and technical compared with journalistic style. Academic authors are interested in promoting ideas that ultimately benefit the patients’ welfare. In contrast, most journalists have an invested interest in selling their work or increasing their blog following. Sustaining book sales can be a powerful personal incentive to cast the discourse in a compelling way, one that may counter prevailing medical opinion.
Of course, academic authors can benefit from publications in the form of grant support, scholarly authority, and notoriety. At times, these benefits can lead to personal financial gain, eg, collaborations with industry or compensation as a part of the scope of their work in their academic institution. This leads to the issue of disclosure. Disclosure has been a hot topic in medicine, and has led to the creation of the Physician Payment Sunshine Act,2 which is set to take effect August 1, 2013. Contained within the Affordable Care Act, this law will require pharmaceutical companies and other medical industries to report all direct payments or gifts to physicians >$10. With such disclosure, readers can judge the experts’ work with knowledge of what financial relationships may be in place.
No disclosure laws for journalists
In contrast, the public is not privy to journalists’ potential conflicts of interest. Although journalism has no “Sunshine” equivalent, there’s a culture of disclosure3 that is followed rigorously by some publishers and less rigorously by others. Disclosing conflicts of interest in journalism occurs internally as a function of an individual publisher’s policy. Would a “Sunshine” law applied to journalism affect how readers interpret a journalist’s rejection of the validity of prevailing expert views? Would such articles be more understandable if the public sees the amounts of journalists’ royalty checks, their collected fees for participation in their blogs or related advertising, or contributions from organizations that are against psychiatry?
Skewed coverage of psychotropics
There are well known cases in which a scientific journalist has been criticized for conveying speculation as fact, eg, global warming1 and immunizations.4 I am concerned we are experiencing this problem in the case of antidepressants and other psychiatric medications.
Depression poses an extraordinary public health problem and there’s a tremendous need for innovation in treatment and improved patient outcomes. Most scientific experts agree that we do not understand the pathophysiology underlying depression nor the mechanisms of action of antidepressants. But, as with many other medical disorders that are not yet clearly understood, clear professional guidelines for depression treatment are in place.5 These guidelines testify to the complexity of treating depression and unambiguously support the value of antidepressants as a major component of treatment. Guidelines such as these are derived from careful interpretation—a vetting process—of data. Participation in this process should not be limited to scientific experts, but the interactions required in the vetting process should be subject to rules of scientific inquiry.
A scientific journalist usually chooses his or her experts and sources at his or her discretion, free of the vetting practice described above. There are recent instances in which journalists have formulated innuendos drawing upon published research and “connected dots” that may not coincide with prevailing expert opinion.6 This kind of journalism poses profound implications for the public, especially when it runs counter to prevailing professional opinion.
One example can be seen in a blog from The Chronicle of Higher Education.7 John Horgan, a professional journalist, describes a friend who has a depressed teenage son and refers to the work of other journalists and selected experts to discredit antidepressants’ benefits. A quick review of readers’ comments demonstrates how articles like this one can mislead consumers to reject what may be the best treatment option for depression. When journalists draw their own scientific conclusions, rather than simply report on the conclusions reached by scientists, there’s a potential for misinformation and confusion.
Guidelines may help
What can be done about the potential impact of unvetted journalism on individual patients? I am not against an open dialogue about the risks and benefits of antidepressants, but given the complexity of the issue, I argue that anyone who wishes to voice an opinion via scientific journalism is obligated to follow the rules of the scientist—not the rules of the journalist—and participate in a thoughtful, balanced, and logical process that keeps the patient’s interests closely in mind. In Horgan’s case, he might have acknowledged that his friend’s son’s antidepressant discontinuation carried a risk of a negative outcome. That is, he could have mentioned the benefit side of the risk-benefit calculation.
Journalists should follow guidelines to prevent scaring readers into jumping to unilateral conclusions, stopping their needed medications and relapsing, or worse. There’s precedent for such guidelines. In 2001, several organizations collaborated to release “Reporting on Suicide: Recommendations for the Media.”8 A recent study found that these guidelines impacted journalists’ behavior.9 Similar guidelines should be developed for journalists who report on scientific studies related to psychiatric treatments. I welcome hearing case examples in which patients decided inappropriately to discontinue medications in response to reading news articles.
Bottom Line
By interpreting medical data to make it more interesting and understandable to readers instead of reporting on it, scientific journalists are affecting the public’s understanding of mental health issues, most notably the effect of antidepressants. Scientific journalists who wish to voice their opinion should be obligated to follow the rules of the scientist, not the journalist. Guidelines for journalists who report on psychiatric scientific studies should be developed.
Related Resources
- U.S. Department of Health & Human Services. The Affordable Care Act, section by section.
www.healthcare.gov/law/full/index.html. - The New York Times Company policy on ethics in journalism. www.nytco.com/press/ethics.html.
- Pew Research Center’s Project for Excellence in Journalism. Ethics codes. www.journalism.org/resources/ethics_codes.
Disclosure
Dr. Glazer is a speaker for Merck and Otsuka America Pharmaceutical, Inc.
References
1. Carvalho A. Ideological cultures and media discourses on scientific knowledge: re-reading news on climate change. Public Underst Sci. 2007;16(2):223-243.
2. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare, Medicaid, Children’s Health Insurance Programs; transparency reports and reporting of physician ownership or investment interests. Final rule. Fed Regist. 2013;78(27):9457-9528.
3. Pew Research Center’s Project for Excellence in Journalism. Ethics codes. http://www.journalism.org/resources/ethics_codes. Accessed November 21, 2012.
4. Smith MJ, Ellenberg SS, Bell LM, et al. Media coverage of the measles-mumps-rubella vaccine and autism controversy and its relationship to MMR immunization rates in the United States. Pediatrics. 2008;121(4):e836-e843.
5. American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder, third edition. http://psychiatryonline.org/content.aspx?bookid=28§ionid=1667485. Published October 2010. Accessed November 21, 2012.
6. Glazer WM. Rebuttal: questioning the validity of ‘anatomy of an epidemic’ (part 1). Behav Healthc. 2011; 31(7):42, 44-45.
7. Horgan J. Are psychiatric medications making us sicker? The Chronicle of Higher Education. September 12, 2011. http://chronicle.com/article/Are-Psychiatric-Medications/128976. Accessed November 21, 2012.
8. Centers for Disease Control and Prevention, National Institute of Mental Health, Office of the Surgeon General, Substance Abuse and Mental Health Services Administration, American Foundation for Suicide Prevention, American Association of Suicidology, Annenberg Public Policy Center. Reporting on suicide: recommendations for the media. http://www.sprc.org/sites/sprc.org/files/library/sreporting.pdf. Accessed March 21, 2013.
9. Tatum PT, Canetto SS, Slater MD. Suicide coverage in U.S. newspapers following the publication of the media guidelines. Suicide Life Threat Behav. 2010;40(5):524-534.
The 2011 movie Contagion portrays chaos resulting from the emergence of a highly lethal, rapidly progressing virus threatening to end civilization. One of the characters, a freelance journalist with a blog followed by 15 million people, directs his readers to ignore an effective vaccine the CDC has developed, assigning conspiratorial motives to the CDC’s efforts.
During a nationally televised 2011 presidential candidate debate, Representative Michele Bachmann created a controversy when she stated fellow candidate Texas Governor Rick Perry’s policy requiring sixth-grade girls to get vaccinated against the human papillomavirus exposed them to potential dangers.
Much has been written about the potential influence politicians and mass media have on the public’s understanding of scientific knowledge. Carvalho wrote, “The media have a crucial responsibility as a source of information and opinions about science and technology for citizens. Public perception and attitudes with regard to those domains are significantly influenced by representations of scientific knowledge conveyed by the press and other mass means of communication.”1
Recently, media attention generated by some critics—eg, professional journalists, nonmedical academics, and nonpsychiatric physicians—has questioned the effectiveness of antidepressants. These individuals are affecting public understanding of the issue.
Scientific journalism vs scientific discovery
Journalism exists in many forms—eg, advocacy, scientific, investigative—and has led to positive and negative social and cultural changes. Scientific journalism interprets information to make it interesting and understandable to readers. Ideally, journalists select what is newsworthy and provide balance to disputed themes with careful attention to the facts. Sometimes, a scientific journalist may render his or her opinion on the topic, explicitly or implicitly. When this occurs, the journalist may reflect the state-of-the-art accurately, or he or she may present biased journalism.
Although the modus operandi of a journalist can differ significantly from that of an expert conducting scientific inquiry, I do not intend to render a judgment about the superiority or inferiority of either group. Both groups have the ability to impact discovery, negatively and positively.
Scientific experts acquire and report scientific evidence regarding depression. Additionally, they develop professional guidelines to provide practical advice to clinicians who wrestle with the challenges of treating depression. Journalists are not trained to render medical judgments about the data; they simply report it.
Experts rely on pure transparency from the initial hypothesis through the design, methods, results, and conclusions. In contrast, journalists enjoy the time-honored privilege of hiding sources’ identities.
Before a scientific expert’s paper is published, he or she must negotiate a peer review process in which his or her writing is subjected to the scrutiny of qualified experts in the same field, a process that can last months to years. Journalistic methodologies also include editorial oversight, but it’s fair to say that the peer review process for scientific publication generally is more rigorous than editorial reviews of journalism, because the journalistic review process serves the goal of generating “news” for a hungry marketplace of ideas. Journalists pick and chose their content, hopefully in a balanced fashion, but at the discretion of the journalist and his or her editor. It’s relatively quick and easy for journalists to publish a book or newspaper article, and even easier to publish a blog.
Experts submitting manuscripts to peer-reviewed journals are not paid based on sales or impact factor. The literary style of the expert often is dry and technical compared with journalistic style. Academic authors are interested in promoting ideas that ultimately benefit the patients’ welfare. In contrast, most journalists have an invested interest in selling their work or increasing their blog following. Sustaining book sales can be a powerful personal incentive to cast the discourse in a compelling way, one that may counter prevailing medical opinion.
Of course, academic authors can benefit from publications in the form of grant support, scholarly authority, and notoriety. At times, these benefits can lead to personal financial gain, eg, collaborations with industry or compensation as a part of the scope of their work in their academic institution. This leads to the issue of disclosure. Disclosure has been a hot topic in medicine, and has led to the creation of the Physician Payment Sunshine Act,2 which is set to take effect August 1, 2013. Contained within the Affordable Care Act, this law will require pharmaceutical companies and other medical industries to report all direct payments or gifts to physicians >$10. With such disclosure, readers can judge the experts’ work with knowledge of what financial relationships may be in place.
No disclosure laws for journalists
In contrast, the public is not privy to journalists’ potential conflicts of interest. Although journalism has no “Sunshine” equivalent, there’s a culture of disclosure3 that is followed rigorously by some publishers and less rigorously by others. Disclosing conflicts of interest in journalism occurs internally as a function of an individual publisher’s policy. Would a “Sunshine” law applied to journalism affect how readers interpret a journalist’s rejection of the validity of prevailing expert views? Would such articles be more understandable if the public sees the amounts of journalists’ royalty checks, their collected fees for participation in their blogs or related advertising, or contributions from organizations that are against psychiatry?
Skewed coverage of psychotropics
There are well known cases in which a scientific journalist has been criticized for conveying speculation as fact, eg, global warming1 and immunizations.4 I am concerned we are experiencing this problem in the case of antidepressants and other psychiatric medications.
Depression poses an extraordinary public health problem and there’s a tremendous need for innovation in treatment and improved patient outcomes. Most scientific experts agree that we do not understand the pathophysiology underlying depression nor the mechanisms of action of antidepressants. But, as with many other medical disorders that are not yet clearly understood, clear professional guidelines for depression treatment are in place.5 These guidelines testify to the complexity of treating depression and unambiguously support the value of antidepressants as a major component of treatment. Guidelines such as these are derived from careful interpretation—a vetting process—of data. Participation in this process should not be limited to scientific experts, but the interactions required in the vetting process should be subject to rules of scientific inquiry.
A scientific journalist usually chooses his or her experts and sources at his or her discretion, free of the vetting practice described above. There are recent instances in which journalists have formulated innuendos drawing upon published research and “connected dots” that may not coincide with prevailing expert opinion.6 This kind of journalism poses profound implications for the public, especially when it runs counter to prevailing professional opinion.
One example can be seen in a blog from The Chronicle of Higher Education.7 John Horgan, a professional journalist, describes a friend who has a depressed teenage son and refers to the work of other journalists and selected experts to discredit antidepressants’ benefits. A quick review of readers’ comments demonstrates how articles like this one can mislead consumers to reject what may be the best treatment option for depression. When journalists draw their own scientific conclusions, rather than simply report on the conclusions reached by scientists, there’s a potential for misinformation and confusion.
Guidelines may help
What can be done about the potential impact of unvetted journalism on individual patients? I am not against an open dialogue about the risks and benefits of antidepressants, but given the complexity of the issue, I argue that anyone who wishes to voice an opinion via scientific journalism is obligated to follow the rules of the scientist—not the rules of the journalist—and participate in a thoughtful, balanced, and logical process that keeps the patient’s interests closely in mind. In Horgan’s case, he might have acknowledged that his friend’s son’s antidepressant discontinuation carried a risk of a negative outcome. That is, he could have mentioned the benefit side of the risk-benefit calculation.
Journalists should follow guidelines to prevent scaring readers into jumping to unilateral conclusions, stopping their needed medications and relapsing, or worse. There’s precedent for such guidelines. In 2001, several organizations collaborated to release “Reporting on Suicide: Recommendations for the Media.”8 A recent study found that these guidelines impacted journalists’ behavior.9 Similar guidelines should be developed for journalists who report on scientific studies related to psychiatric treatments. I welcome hearing case examples in which patients decided inappropriately to discontinue medications in response to reading news articles.
Bottom Line
By interpreting medical data to make it more interesting and understandable to readers instead of reporting on it, scientific journalists are affecting the public’s understanding of mental health issues, most notably the effect of antidepressants. Scientific journalists who wish to voice their opinion should be obligated to follow the rules of the scientist, not the journalist. Guidelines for journalists who report on psychiatric scientific studies should be developed.
Related Resources
- U.S. Department of Health & Human Services. The Affordable Care Act, section by section.
www.healthcare.gov/law/full/index.html. - The New York Times Company policy on ethics in journalism. www.nytco.com/press/ethics.html.
- Pew Research Center’s Project for Excellence in Journalism. Ethics codes. www.journalism.org/resources/ethics_codes.
Disclosure
Dr. Glazer is a speaker for Merck and Otsuka America Pharmaceutical, Inc.
References
1. Carvalho A. Ideological cultures and media discourses on scientific knowledge: re-reading news on climate change. Public Underst Sci. 2007;16(2):223-243.
2. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare, Medicaid, Children’s Health Insurance Programs; transparency reports and reporting of physician ownership or investment interests. Final rule. Fed Regist. 2013;78(27):9457-9528.
3. Pew Research Center’s Project for Excellence in Journalism. Ethics codes. http://www.journalism.org/resources/ethics_codes. Accessed November 21, 2012.
4. Smith MJ, Ellenberg SS, Bell LM, et al. Media coverage of the measles-mumps-rubella vaccine and autism controversy and its relationship to MMR immunization rates in the United States. Pediatrics. 2008;121(4):e836-e843.
5. American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder, third edition. http://psychiatryonline.org/content.aspx?bookid=28§ionid=1667485. Published October 2010. Accessed November 21, 2012.
6. Glazer WM. Rebuttal: questioning the validity of ‘anatomy of an epidemic’ (part 1). Behav Healthc. 2011; 31(7):42, 44-45.
7. Horgan J. Are psychiatric medications making us sicker? The Chronicle of Higher Education. September 12, 2011. http://chronicle.com/article/Are-Psychiatric-Medications/128976. Accessed November 21, 2012.
8. Centers for Disease Control and Prevention, National Institute of Mental Health, Office of the Surgeon General, Substance Abuse and Mental Health Services Administration, American Foundation for Suicide Prevention, American Association of Suicidology, Annenberg Public Policy Center. Reporting on suicide: recommendations for the media. http://www.sprc.org/sites/sprc.org/files/library/sreporting.pdf. Accessed March 21, 2013.
9. Tatum PT, Canetto SS, Slater MD. Suicide coverage in U.S. newspapers following the publication of the media guidelines. Suicide Life Threat Behav. 2010;40(5):524-534.
The 2011 movie Contagion portrays chaos resulting from the emergence of a highly lethal, rapidly progressing virus threatening to end civilization. One of the characters, a freelance journalist with a blog followed by 15 million people, directs his readers to ignore an effective vaccine the CDC has developed, assigning conspiratorial motives to the CDC’s efforts.
During a nationally televised 2011 presidential candidate debate, Representative Michele Bachmann created a controversy when she stated fellow candidate Texas Governor Rick Perry’s policy requiring sixth-grade girls to get vaccinated against the human papillomavirus exposed them to potential dangers.
Much has been written about the potential influence politicians and mass media have on the public’s understanding of scientific knowledge. Carvalho wrote, “The media have a crucial responsibility as a source of information and opinions about science and technology for citizens. Public perception and attitudes with regard to those domains are significantly influenced by representations of scientific knowledge conveyed by the press and other mass means of communication.”1
Recently, media attention generated by some critics—eg, professional journalists, nonmedical academics, and nonpsychiatric physicians—has questioned the effectiveness of antidepressants. These individuals are affecting public understanding of the issue.
Scientific journalism vs scientific discovery
Journalism exists in many forms—eg, advocacy, scientific, investigative—and has led to positive and negative social and cultural changes. Scientific journalism interprets information to make it interesting and understandable to readers. Ideally, journalists select what is newsworthy and provide balance to disputed themes with careful attention to the facts. Sometimes, a scientific journalist may render his or her opinion on the topic, explicitly or implicitly. When this occurs, the journalist may reflect the state-of-the-art accurately, or he or she may present biased journalism.
Although the modus operandi of a journalist can differ significantly from that of an expert conducting scientific inquiry, I do not intend to render a judgment about the superiority or inferiority of either group. Both groups have the ability to impact discovery, negatively and positively.
Scientific experts acquire and report scientific evidence regarding depression. Additionally, they develop professional guidelines to provide practical advice to clinicians who wrestle with the challenges of treating depression. Journalists are not trained to render medical judgments about the data; they simply report it.
Experts rely on pure transparency from the initial hypothesis through the design, methods, results, and conclusions. In contrast, journalists enjoy the time-honored privilege of hiding sources’ identities.
Before a scientific expert’s paper is published, he or she must negotiate a peer review process in which his or her writing is subjected to the scrutiny of qualified experts in the same field, a process that can last months to years. Journalistic methodologies also include editorial oversight, but it’s fair to say that the peer review process for scientific publication generally is more rigorous than editorial reviews of journalism, because the journalistic review process serves the goal of generating “news” for a hungry marketplace of ideas. Journalists pick and chose their content, hopefully in a balanced fashion, but at the discretion of the journalist and his or her editor. It’s relatively quick and easy for journalists to publish a book or newspaper article, and even easier to publish a blog.
Experts submitting manuscripts to peer-reviewed journals are not paid based on sales or impact factor. The literary style of the expert often is dry and technical compared with journalistic style. Academic authors are interested in promoting ideas that ultimately benefit the patients’ welfare. In contrast, most journalists have an invested interest in selling their work or increasing their blog following. Sustaining book sales can be a powerful personal incentive to cast the discourse in a compelling way, one that may counter prevailing medical opinion.
Of course, academic authors can benefit from publications in the form of grant support, scholarly authority, and notoriety. At times, these benefits can lead to personal financial gain, eg, collaborations with industry or compensation as a part of the scope of their work in their academic institution. This leads to the issue of disclosure. Disclosure has been a hot topic in medicine, and has led to the creation of the Physician Payment Sunshine Act,2 which is set to take effect August 1, 2013. Contained within the Affordable Care Act, this law will require pharmaceutical companies and other medical industries to report all direct payments or gifts to physicians >$10. With such disclosure, readers can judge the experts’ work with knowledge of what financial relationships may be in place.
No disclosure laws for journalists
In contrast, the public is not privy to journalists’ potential conflicts of interest. Although journalism has no “Sunshine” equivalent, there’s a culture of disclosure3 that is followed rigorously by some publishers and less rigorously by others. Disclosing conflicts of interest in journalism occurs internally as a function of an individual publisher’s policy. Would a “Sunshine” law applied to journalism affect how readers interpret a journalist’s rejection of the validity of prevailing expert views? Would such articles be more understandable if the public sees the amounts of journalists’ royalty checks, their collected fees for participation in their blogs or related advertising, or contributions from organizations that are against psychiatry?
Skewed coverage of psychotropics
There are well known cases in which a scientific journalist has been criticized for conveying speculation as fact, eg, global warming1 and immunizations.4 I am concerned we are experiencing this problem in the case of antidepressants and other psychiatric medications.
Depression poses an extraordinary public health problem and there’s a tremendous need for innovation in treatment and improved patient outcomes. Most scientific experts agree that we do not understand the pathophysiology underlying depression nor the mechanisms of action of antidepressants. But, as with many other medical disorders that are not yet clearly understood, clear professional guidelines for depression treatment are in place.5 These guidelines testify to the complexity of treating depression and unambiguously support the value of antidepressants as a major component of treatment. Guidelines such as these are derived from careful interpretation—a vetting process—of data. Participation in this process should not be limited to scientific experts, but the interactions required in the vetting process should be subject to rules of scientific inquiry.
A scientific journalist usually chooses his or her experts and sources at his or her discretion, free of the vetting practice described above. There are recent instances in which journalists have formulated innuendos drawing upon published research and “connected dots” that may not coincide with prevailing expert opinion.6 This kind of journalism poses profound implications for the public, especially when it runs counter to prevailing professional opinion.
One example can be seen in a blog from The Chronicle of Higher Education.7 John Horgan, a professional journalist, describes a friend who has a depressed teenage son and refers to the work of other journalists and selected experts to discredit antidepressants’ benefits. A quick review of readers’ comments demonstrates how articles like this one can mislead consumers to reject what may be the best treatment option for depression. When journalists draw their own scientific conclusions, rather than simply report on the conclusions reached by scientists, there’s a potential for misinformation and confusion.
Guidelines may help
What can be done about the potential impact of unvetted journalism on individual patients? I am not against an open dialogue about the risks and benefits of antidepressants, but given the complexity of the issue, I argue that anyone who wishes to voice an opinion via scientific journalism is obligated to follow the rules of the scientist—not the rules of the journalist—and participate in a thoughtful, balanced, and logical process that keeps the patient’s interests closely in mind. In Horgan’s case, he might have acknowledged that his friend’s son’s antidepressant discontinuation carried a risk of a negative outcome. That is, he could have mentioned the benefit side of the risk-benefit calculation.
Journalists should follow guidelines to prevent scaring readers into jumping to unilateral conclusions, stopping their needed medications and relapsing, or worse. There’s precedent for such guidelines. In 2001, several organizations collaborated to release “Reporting on Suicide: Recommendations for the Media.”8 A recent study found that these guidelines impacted journalists’ behavior.9 Similar guidelines should be developed for journalists who report on scientific studies related to psychiatric treatments. I welcome hearing case examples in which patients decided inappropriately to discontinue medications in response to reading news articles.
Bottom Line
By interpreting medical data to make it more interesting and understandable to readers instead of reporting on it, scientific journalists are affecting the public’s understanding of mental health issues, most notably the effect of antidepressants. Scientific journalists who wish to voice their opinion should be obligated to follow the rules of the scientist, not the journalist. Guidelines for journalists who report on psychiatric scientific studies should be developed.
Related Resources
- U.S. Department of Health & Human Services. The Affordable Care Act, section by section.
www.healthcare.gov/law/full/index.html. - The New York Times Company policy on ethics in journalism. www.nytco.com/press/ethics.html.
- Pew Research Center’s Project for Excellence in Journalism. Ethics codes. www.journalism.org/resources/ethics_codes.
Disclosure
Dr. Glazer is a speaker for Merck and Otsuka America Pharmaceutical, Inc.
References
1. Carvalho A. Ideological cultures and media discourses on scientific knowledge: re-reading news on climate change. Public Underst Sci. 2007;16(2):223-243.
2. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare, Medicaid, Children’s Health Insurance Programs; transparency reports and reporting of physician ownership or investment interests. Final rule. Fed Regist. 2013;78(27):9457-9528.
3. Pew Research Center’s Project for Excellence in Journalism. Ethics codes. http://www.journalism.org/resources/ethics_codes. Accessed November 21, 2012.
4. Smith MJ, Ellenberg SS, Bell LM, et al. Media coverage of the measles-mumps-rubella vaccine and autism controversy and its relationship to MMR immunization rates in the United States. Pediatrics. 2008;121(4):e836-e843.
5. American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder, third edition. http://psychiatryonline.org/content.aspx?bookid=28§ionid=1667485. Published October 2010. Accessed November 21, 2012.
6. Glazer WM. Rebuttal: questioning the validity of ‘anatomy of an epidemic’ (part 1). Behav Healthc. 2011; 31(7):42, 44-45.
7. Horgan J. Are psychiatric medications making us sicker? The Chronicle of Higher Education. September 12, 2011. http://chronicle.com/article/Are-Psychiatric-Medications/128976. Accessed November 21, 2012.
8. Centers for Disease Control and Prevention, National Institute of Mental Health, Office of the Surgeon General, Substance Abuse and Mental Health Services Administration, American Foundation for Suicide Prevention, American Association of Suicidology, Annenberg Public Policy Center. Reporting on suicide: recommendations for the media. http://www.sprc.org/sites/sprc.org/files/library/sreporting.pdf. Accessed March 21, 2013.
9. Tatum PT, Canetto SS, Slater MD. Suicide coverage in U.S. newspapers following the publication of the media guidelines. Suicide Life Threat Behav. 2010;40(5):524-534.
An inspiring vision
We read with considerable interest Dr. Nasrallah’s April editorial (“Pleiotropy of psychiatric disorders will reinvent DSM,” Current Psychiatry, April 2013, p. 6-7; http://bit.ly/1DPgxZ7) that outlined his inspiring vision for the future of psychiatric diagnosis and assessment. We agree that by unraveling the neurobiologic underpinnings of psychiatric brain disorders, we will not only uncover the pleiotropic nature of these conditions but also transform our field into a clinical neuroscience.
In any given year, >1 in 4 Americans will have a diagnosable psychiatric condition.1 Psychiatric disorders remain the most prevalent cause of disability in the United States,2 and their enormous personal, economic, and societal impact fuels the tremendous impetus to seek scientific advances in diagnosis and treatment.
Many have suggested that the mind is too complex to undergo formal scientific study, but it is the nuanced appreciation of the elegant, yet complex workings of the brain that attracts brilliant minds to psychiatry and neuroscience. The leading neuroscientific advances in fields such as optogenetics, epigenetics, psychoneuroimmunology, and psychopharmacology continue to be spearheaded by psychiatrist-scientists. Understanding brain function continues to be a high priority, exampled by the April 2013 announcement of $100 million for President Obama’s BRAIN (Brain Research through Advancing Innovative Neurotechnologies) initiative.3
All of our psychiatric treatment modalities—including psychotropics, neuromodulation, and psychotherapy—are believed to promote synaptic plasticity, neurogenesis, and alterations in neuronal circuitry. Ensuring these concepts and advances are communicated to our residents, medical students, and patients remains paramount. Psychiatry has an immense and flourishing scientific and societal impact. Millions of people are affected by brain disorders, including autism, schizophrenia, and dementia. These patients and their families are counting on psychiatrists to elucidate the workings of the body’s most complex organ.
Arshya Vahabzadeh, MD
Laughlin Fellow, American College of Psychiatrists
Chicago, IL
PGY-3 Resident
Emory University School of Medicine
Atlanta, GA
Mizrab Khan, MRCPsych
Psychiatry Trainee, National Health Service
London, UK
David Buxton, MD
Fellow, Child and Adolescent Psychiatry
Massachusetts General Hospital
McLean Hospital
Harvard Medical School
Boston, MA
Leadership Fellow, American Psychiatric Association
Arlington, VA
References
1. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):
617-627.
2. World Health Organization [WHO]. The global burden of disease: 2004 update, table A2: Burden of disease in DALYs [disability-adjusted life year] by cause, sex and income group in WHO regions, estimates for 2004. http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_AnnexA.pdf. Accessed April 23, 2013.
3. The White House. Brain initiative. http://www.whitehouse.gov/infographics/brain-initiative. Accessed April 23, 2013.
We read with considerable interest Dr. Nasrallah’s April editorial (“Pleiotropy of psychiatric disorders will reinvent DSM,” Current Psychiatry, April 2013, p. 6-7; http://bit.ly/1DPgxZ7) that outlined his inspiring vision for the future of psychiatric diagnosis and assessment. We agree that by unraveling the neurobiologic underpinnings of psychiatric brain disorders, we will not only uncover the pleiotropic nature of these conditions but also transform our field into a clinical neuroscience.
In any given year, >1 in 4 Americans will have a diagnosable psychiatric condition.1 Psychiatric disorders remain the most prevalent cause of disability in the United States,2 and their enormous personal, economic, and societal impact fuels the tremendous impetus to seek scientific advances in diagnosis and treatment.
Many have suggested that the mind is too complex to undergo formal scientific study, but it is the nuanced appreciation of the elegant, yet complex workings of the brain that attracts brilliant minds to psychiatry and neuroscience. The leading neuroscientific advances in fields such as optogenetics, epigenetics, psychoneuroimmunology, and psychopharmacology continue to be spearheaded by psychiatrist-scientists. Understanding brain function continues to be a high priority, exampled by the April 2013 announcement of $100 million for President Obama’s BRAIN (Brain Research through Advancing Innovative Neurotechnologies) initiative.3
All of our psychiatric treatment modalities—including psychotropics, neuromodulation, and psychotherapy—are believed to promote synaptic plasticity, neurogenesis, and alterations in neuronal circuitry. Ensuring these concepts and advances are communicated to our residents, medical students, and patients remains paramount. Psychiatry has an immense and flourishing scientific and societal impact. Millions of people are affected by brain disorders, including autism, schizophrenia, and dementia. These patients and their families are counting on psychiatrists to elucidate the workings of the body’s most complex organ.
Arshya Vahabzadeh, MD
Laughlin Fellow, American College of Psychiatrists
Chicago, IL
PGY-3 Resident
Emory University School of Medicine
Atlanta, GA
Mizrab Khan, MRCPsych
Psychiatry Trainee, National Health Service
London, UK
David Buxton, MD
Fellow, Child and Adolescent Psychiatry
Massachusetts General Hospital
McLean Hospital
Harvard Medical School
Boston, MA
Leadership Fellow, American Psychiatric Association
Arlington, VA
References
1. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):
617-627.
2. World Health Organization [WHO]. The global burden of disease: 2004 update, table A2: Burden of disease in DALYs [disability-adjusted life year] by cause, sex and income group in WHO regions, estimates for 2004. http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_AnnexA.pdf. Accessed April 23, 2013.
3. The White House. Brain initiative. http://www.whitehouse.gov/infographics/brain-initiative. Accessed April 23, 2013.
We read with considerable interest Dr. Nasrallah’s April editorial (“Pleiotropy of psychiatric disorders will reinvent DSM,” Current Psychiatry, April 2013, p. 6-7; http://bit.ly/1DPgxZ7) that outlined his inspiring vision for the future of psychiatric diagnosis and assessment. We agree that by unraveling the neurobiologic underpinnings of psychiatric brain disorders, we will not only uncover the pleiotropic nature of these conditions but also transform our field into a clinical neuroscience.
In any given year, >1 in 4 Americans will have a diagnosable psychiatric condition.1 Psychiatric disorders remain the most prevalent cause of disability in the United States,2 and their enormous personal, economic, and societal impact fuels the tremendous impetus to seek scientific advances in diagnosis and treatment.
Many have suggested that the mind is too complex to undergo formal scientific study, but it is the nuanced appreciation of the elegant, yet complex workings of the brain that attracts brilliant minds to psychiatry and neuroscience. The leading neuroscientific advances in fields such as optogenetics, epigenetics, psychoneuroimmunology, and psychopharmacology continue to be spearheaded by psychiatrist-scientists. Understanding brain function continues to be a high priority, exampled by the April 2013 announcement of $100 million for President Obama’s BRAIN (Brain Research through Advancing Innovative Neurotechnologies) initiative.3
All of our psychiatric treatment modalities—including psychotropics, neuromodulation, and psychotherapy—are believed to promote synaptic plasticity, neurogenesis, and alterations in neuronal circuitry. Ensuring these concepts and advances are communicated to our residents, medical students, and patients remains paramount. Psychiatry has an immense and flourishing scientific and societal impact. Millions of people are affected by brain disorders, including autism, schizophrenia, and dementia. These patients and their families are counting on psychiatrists to elucidate the workings of the body’s most complex organ.
Arshya Vahabzadeh, MD
Laughlin Fellow, American College of Psychiatrists
Chicago, IL
PGY-3 Resident
Emory University School of Medicine
Atlanta, GA
Mizrab Khan, MRCPsych
Psychiatry Trainee, National Health Service
London, UK
David Buxton, MD
Fellow, Child and Adolescent Psychiatry
Massachusetts General Hospital
McLean Hospital
Harvard Medical School
Boston, MA
Leadership Fellow, American Psychiatric Association
Arlington, VA
References
1. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):
617-627.
2. World Health Organization [WHO]. The global burden of disease: 2004 update, table A2: Burden of disease in DALYs [disability-adjusted life year] by cause, sex and income group in WHO regions, estimates for 2004. http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_AnnexA.pdf. Accessed April 23, 2013.
3. The White House. Brain initiative. http://www.whitehouse.gov/infographics/brain-initiative. Accessed April 23, 2013.
Genetic risk factors
I was pleased to see Dr. Nasrallah’s April editorial (“Pleiotropy of psychiatric disorders will reinvent DSM,” Current Psychiatry, April 2013, p. 6-7; http://bit.ly/1DPgxZ7). It’s ironic that there is a growing realization of general genetic risk factors for psychiatric disorders with such different phenotypes even before DSM-5 has been published. This certainly thickens the plot; I’m glad Dr. Nasrallah made it clear to Current Psychiatry readers.
Samuel Barondes, MD
Professor
Jeanne and Sanford Robertson Endowed Chair in Neurobiology and Psychiatry
University of California, San Francisco
San Francisco, CA
I was pleased to see Dr. Nasrallah’s April editorial (“Pleiotropy of psychiatric disorders will reinvent DSM,” Current Psychiatry, April 2013, p. 6-7; http://bit.ly/1DPgxZ7). It’s ironic that there is a growing realization of general genetic risk factors for psychiatric disorders with such different phenotypes even before DSM-5 has been published. This certainly thickens the plot; I’m glad Dr. Nasrallah made it clear to Current Psychiatry readers.
Samuel Barondes, MD
Professor
Jeanne and Sanford Robertson Endowed Chair in Neurobiology and Psychiatry
University of California, San Francisco
San Francisco, CA
I was pleased to see Dr. Nasrallah’s April editorial (“Pleiotropy of psychiatric disorders will reinvent DSM,” Current Psychiatry, April 2013, p. 6-7; http://bit.ly/1DPgxZ7). It’s ironic that there is a growing realization of general genetic risk factors for psychiatric disorders with such different phenotypes even before DSM-5 has been published. This certainly thickens the plot; I’m glad Dr. Nasrallah made it clear to Current Psychiatry readers.
Samuel Barondes, MD
Professor
Jeanne and Sanford Robertson Endowed Chair in Neurobiology and Psychiatry
University of California, San Francisco
San Francisco, CA
SSRIs and sexual health
I appreciated the pertinent article by Dr. Burghardt and Ms. Gardner, “Sildenafil for SSRI-induced sexual dysfunction in women” (Current Psychiatry, April 2013, p. 29-32; http://bit.ly/1GCtLZR). Evidence for alternative adjunctive medications for selective serotonin reuptake inhibitor (SSRI)-induced sexual dysfunction is lacking.
There is some support for bethanechol in reversing dysfunction caused by other antidepressants. Bethanechol reversed anorgasmia in a woman receiving amoxapine and eliminated erectile dysfunction in men receiving monoamine oxidase inhibitors or tricyclic antidepressants.1-3 The only trial evaluating the efficacy of bethanechol for antidepressant-induced sexual dysfunction found it effective for men receiving clomipramine.4 Evidence is limited to patients receiving older antidepressants, and there is only 1 report of efficacy in a female patient.
It would be interesting to see whether bethanechol is effective for SSRI-induced dysfunction in controlled trials, because it may be a practical option for patients with sexual dysfunction and urinary retention.
Jonathan R. Scarff, MD
PGY-4 Resident
University of Louisville
Louisville, KY
References
1. Gross MD. Reversal by bethanechol of sexual
dysfunction caused by anticholinergic anti-depressants. Am J Psychiatry. 1982;139(9):1193-1194.
2. Segraves RT. Reversal by bethanechol of imipramine-induced ejaculatory dysfunction. Am J Psychiatry. 1987;144(9):1243-1244.
3. Yager J. Bethanechol chloride can reverse erectile and ejaculatory dysfunction induced by tricyclic antidepressants and mazindol: case report. J Clin Psychiatry. 1986;47(4):210-211.
4. Bernik M, Vieira AH, Nunes PV. Bethanecol chloride for treatment of clomipramine-induced orgasmic dysfunction in males. Rev Hosp Clin Fac Med Sao Paulo. 2004;59(6):357-360.
I appreciated the pertinent article by Dr. Burghardt and Ms. Gardner, “Sildenafil for SSRI-induced sexual dysfunction in women” (Current Psychiatry, April 2013, p. 29-32; http://bit.ly/1GCtLZR). Evidence for alternative adjunctive medications for selective serotonin reuptake inhibitor (SSRI)-induced sexual dysfunction is lacking.
There is some support for bethanechol in reversing dysfunction caused by other antidepressants. Bethanechol reversed anorgasmia in a woman receiving amoxapine and eliminated erectile dysfunction in men receiving monoamine oxidase inhibitors or tricyclic antidepressants.1-3 The only trial evaluating the efficacy of bethanechol for antidepressant-induced sexual dysfunction found it effective for men receiving clomipramine.4 Evidence is limited to patients receiving older antidepressants, and there is only 1 report of efficacy in a female patient.
It would be interesting to see whether bethanechol is effective for SSRI-induced dysfunction in controlled trials, because it may be a practical option for patients with sexual dysfunction and urinary retention.
Jonathan R. Scarff, MD
PGY-4 Resident
University of Louisville
Louisville, KY
References
1. Gross MD. Reversal by bethanechol of sexual
dysfunction caused by anticholinergic anti-depressants. Am J Psychiatry. 1982;139(9):1193-1194.
2. Segraves RT. Reversal by bethanechol of imipramine-induced ejaculatory dysfunction. Am J Psychiatry. 1987;144(9):1243-1244.
3. Yager J. Bethanechol chloride can reverse erectile and ejaculatory dysfunction induced by tricyclic antidepressants and mazindol: case report. J Clin Psychiatry. 1986;47(4):210-211.
4. Bernik M, Vieira AH, Nunes PV. Bethanecol chloride for treatment of clomipramine-induced orgasmic dysfunction in males. Rev Hosp Clin Fac Med Sao Paulo. 2004;59(6):357-360.
I appreciated the pertinent article by Dr. Burghardt and Ms. Gardner, “Sildenafil for SSRI-induced sexual dysfunction in women” (Current Psychiatry, April 2013, p. 29-32; http://bit.ly/1GCtLZR). Evidence for alternative adjunctive medications for selective serotonin reuptake inhibitor (SSRI)-induced sexual dysfunction is lacking.
There is some support for bethanechol in reversing dysfunction caused by other antidepressants. Bethanechol reversed anorgasmia in a woman receiving amoxapine and eliminated erectile dysfunction in men receiving monoamine oxidase inhibitors or tricyclic antidepressants.1-3 The only trial evaluating the efficacy of bethanechol for antidepressant-induced sexual dysfunction found it effective for men receiving clomipramine.4 Evidence is limited to patients receiving older antidepressants, and there is only 1 report of efficacy in a female patient.
It would be interesting to see whether bethanechol is effective for SSRI-induced dysfunction in controlled trials, because it may be a practical option for patients with sexual dysfunction and urinary retention.
Jonathan R. Scarff, MD
PGY-4 Resident
University of Louisville
Louisville, KY
References
1. Gross MD. Reversal by bethanechol of sexual
dysfunction caused by anticholinergic anti-depressants. Am J Psychiatry. 1982;139(9):1193-1194.
2. Segraves RT. Reversal by bethanechol of imipramine-induced ejaculatory dysfunction. Am J Psychiatry. 1987;144(9):1243-1244.
3. Yager J. Bethanechol chloride can reverse erectile and ejaculatory dysfunction induced by tricyclic antidepressants and mazindol: case report. J Clin Psychiatry. 1986;47(4):210-211.
4. Bernik M, Vieira AH, Nunes PV. Bethanecol chloride for treatment of clomipramine-induced orgasmic dysfunction in males. Rev Hosp Clin Fac Med Sao Paulo. 2004;59(6):357-360.