User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Sleep terrors in adults: How to help control this potentially dangerous condition
Sleep terrors (STs)—also known as night terrors—are characterized by sudden arousal accompanied by a piercing scream or cry in the first few hours after falling asleep. These parasomnias arise out of slow-wave sleep (stages 3 and 4 of nonrapid eye movement [non-REM] sleep) and affect approximately 5% of adults.1 The condition is twice as common in men than women, and usually affects children but may not develop until adulthood.1
During STs, a patient may act scared, afraid, agitated, anxious, or panicky without being fully aware of his or her surroundings. The episode may last 30 seconds to 5 minutes; most patients don’t remember the event the next morning. STs may leave individuals feeling exhausted and perplexed the next day. Verbalization during the episode is incoherent and a patient’s perception of the environment seems altered. Tachycardia, tachypnea, sweating, flushed skin, or mydriasis are prominent. When ST patients walk, they may do so violently and can cause harm to themselves or others.
The differential diagnosis of STs includes posttraumatic stress disorder; nocturnal seizures characterized by excessive motor activity and organic CNS lesions; REM sleep behavior disorder; sleep choking syndrome; and nocturnal panic attacks. Patients with STs report high rates of stressful events—eg, divorce or bereavement—in the previous year. They are more likely to have a history of mood and anxiety disorders and high levels of depression, anxiety, and obsessive-compulsive and phobic traits. One study found patients with STs were 4.3 times more likely to have had a car accident in the past year.2
Evaluating and treating STs
Rule out comorbid conditions such as obstructive sleep apnea and periodic limb movement disorder. Encourage your patient to improve his or her sleep hygiene by maintaining a regular sleep/wake cycle, exercising, and limiting caffeine and alcohol and exposure to bright light before bedtime.
Self-help techniques. To avoid injury, encourage your patient to remove dangerous objects from their sleeping area. Suggest locking the doors to the room or home, and putting medications in a secure place. Patients also may consider keeping their mattress close to the floor to limit the risk of injury.
Pharmacotherapy and psychotherapy. Along with counseling and support, your patient may benefit from cognitive-behavioral therapy, relaxation therapy, or hypnosis.3 Anticipatory arousal therapy may help by interrupting the altered underlying electrophysiology of partial arousal.
If your patient is concerned about physical injury during STs, consider prescribing clonazepam, temazepam, or diazepam.4 Trazodone and selective serotonin reuptake inhibitors such as paroxetine5 also have been used to treat STs.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Crisp AH. The sleepwalking/night terrors syndrome in adults. Postgrad Med J. 1996;72(852):599-604.
2. Oudiette D, Leu S, Pottier M, et al. Dreamlike mentations during sleepwalking and sleep terrors in adults. Sleep. 2009;32(12):1621-1627.
3. Lowe P, Humphreys C, Williams SJ. Night terrors: women’s experiences of (not) sleeping where there is domestic violence. Violence Against Women. 2007;13(6):549-561.
4. Schenck CH, Mahowald MW. Long-term nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med. 1996;100(3):333-337.
5. Lillywhite AR, Wilson SJ, Nutt DJ. Successful treatment of night terrors and somnambulism with paroxetine. Br J Psychiatry. 1994;164(4):551-554.
Sleep terrors (STs)—also known as night terrors—are characterized by sudden arousal accompanied by a piercing scream or cry in the first few hours after falling asleep. These parasomnias arise out of slow-wave sleep (stages 3 and 4 of nonrapid eye movement [non-REM] sleep) and affect approximately 5% of adults.1 The condition is twice as common in men than women, and usually affects children but may not develop until adulthood.1
During STs, a patient may act scared, afraid, agitated, anxious, or panicky without being fully aware of his or her surroundings. The episode may last 30 seconds to 5 minutes; most patients don’t remember the event the next morning. STs may leave individuals feeling exhausted and perplexed the next day. Verbalization during the episode is incoherent and a patient’s perception of the environment seems altered. Tachycardia, tachypnea, sweating, flushed skin, or mydriasis are prominent. When ST patients walk, they may do so violently and can cause harm to themselves or others.
The differential diagnosis of STs includes posttraumatic stress disorder; nocturnal seizures characterized by excessive motor activity and organic CNS lesions; REM sleep behavior disorder; sleep choking syndrome; and nocturnal panic attacks. Patients with STs report high rates of stressful events—eg, divorce or bereavement—in the previous year. They are more likely to have a history of mood and anxiety disorders and high levels of depression, anxiety, and obsessive-compulsive and phobic traits. One study found patients with STs were 4.3 times more likely to have had a car accident in the past year.2
Evaluating and treating STs
Rule out comorbid conditions such as obstructive sleep apnea and periodic limb movement disorder. Encourage your patient to improve his or her sleep hygiene by maintaining a regular sleep/wake cycle, exercising, and limiting caffeine and alcohol and exposure to bright light before bedtime.
Self-help techniques. To avoid injury, encourage your patient to remove dangerous objects from their sleeping area. Suggest locking the doors to the room or home, and putting medications in a secure place. Patients also may consider keeping their mattress close to the floor to limit the risk of injury.
Pharmacotherapy and psychotherapy. Along with counseling and support, your patient may benefit from cognitive-behavioral therapy, relaxation therapy, or hypnosis.3 Anticipatory arousal therapy may help by interrupting the altered underlying electrophysiology of partial arousal.
If your patient is concerned about physical injury during STs, consider prescribing clonazepam, temazepam, or diazepam.4 Trazodone and selective serotonin reuptake inhibitors such as paroxetine5 also have been used to treat STs.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Sleep terrors (STs)—also known as night terrors—are characterized by sudden arousal accompanied by a piercing scream or cry in the first few hours after falling asleep. These parasomnias arise out of slow-wave sleep (stages 3 and 4 of nonrapid eye movement [non-REM] sleep) and affect approximately 5% of adults.1 The condition is twice as common in men than women, and usually affects children but may not develop until adulthood.1
During STs, a patient may act scared, afraid, agitated, anxious, or panicky without being fully aware of his or her surroundings. The episode may last 30 seconds to 5 minutes; most patients don’t remember the event the next morning. STs may leave individuals feeling exhausted and perplexed the next day. Verbalization during the episode is incoherent and a patient’s perception of the environment seems altered. Tachycardia, tachypnea, sweating, flushed skin, or mydriasis are prominent. When ST patients walk, they may do so violently and can cause harm to themselves or others.
The differential diagnosis of STs includes posttraumatic stress disorder; nocturnal seizures characterized by excessive motor activity and organic CNS lesions; REM sleep behavior disorder; sleep choking syndrome; and nocturnal panic attacks. Patients with STs report high rates of stressful events—eg, divorce or bereavement—in the previous year. They are more likely to have a history of mood and anxiety disorders and high levels of depression, anxiety, and obsessive-compulsive and phobic traits. One study found patients with STs were 4.3 times more likely to have had a car accident in the past year.2
Evaluating and treating STs
Rule out comorbid conditions such as obstructive sleep apnea and periodic limb movement disorder. Encourage your patient to improve his or her sleep hygiene by maintaining a regular sleep/wake cycle, exercising, and limiting caffeine and alcohol and exposure to bright light before bedtime.
Self-help techniques. To avoid injury, encourage your patient to remove dangerous objects from their sleeping area. Suggest locking the doors to the room or home, and putting medications in a secure place. Patients also may consider keeping their mattress close to the floor to limit the risk of injury.
Pharmacotherapy and psychotherapy. Along with counseling and support, your patient may benefit from cognitive-behavioral therapy, relaxation therapy, or hypnosis.3 Anticipatory arousal therapy may help by interrupting the altered underlying electrophysiology of partial arousal.
If your patient is concerned about physical injury during STs, consider prescribing clonazepam, temazepam, or diazepam.4 Trazodone and selective serotonin reuptake inhibitors such as paroxetine5 also have been used to treat STs.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Crisp AH. The sleepwalking/night terrors syndrome in adults. Postgrad Med J. 1996;72(852):599-604.
2. Oudiette D, Leu S, Pottier M, et al. Dreamlike mentations during sleepwalking and sleep terrors in adults. Sleep. 2009;32(12):1621-1627.
3. Lowe P, Humphreys C, Williams SJ. Night terrors: women’s experiences of (not) sleeping where there is domestic violence. Violence Against Women. 2007;13(6):549-561.
4. Schenck CH, Mahowald MW. Long-term nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med. 1996;100(3):333-337.
5. Lillywhite AR, Wilson SJ, Nutt DJ. Successful treatment of night terrors and somnambulism with paroxetine. Br J Psychiatry. 1994;164(4):551-554.
1. Crisp AH. The sleepwalking/night terrors syndrome in adults. Postgrad Med J. 1996;72(852):599-604.
2. Oudiette D, Leu S, Pottier M, et al. Dreamlike mentations during sleepwalking and sleep terrors in adults. Sleep. 2009;32(12):1621-1627.
3. Lowe P, Humphreys C, Williams SJ. Night terrors: women’s experiences of (not) sleeping where there is domestic violence. Violence Against Women. 2007;13(6):549-561.
4. Schenck CH, Mahowald MW. Long-term nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med. 1996;100(3):333-337.
5. Lillywhite AR, Wilson SJ, Nutt DJ. Successful treatment of night terrors and somnambulism with paroxetine. Br J Psychiatry. 1994;164(4):551-554.
Omega-3 fatty acids for psychiatric illness
Discuss this article at www.facebook.com/CurrentPsychiatry
Epidemiologic data suggest that people who consume diets rich in omega-3 fatty acids (FAs)—long-chain polyunsaturated FAs such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)—have a decreased risk of major depressive disorder (MDD), postpartum depression, and bipolar disorder (BD).1-5 Omega-3 FA concentration may impact serotonin and dopamine transmission via effects on cell membrane fluidity.6 Therefore, decreased intake may increase the risk of several psychiatric disorders. As the average Western diet has changed over the last 2 centuries, omega-3 FA consumption has decreased.7 Omega-3 FAs cannot be synthesized by the body and must come from exogenous sources, such as fish and nuts. For a discussion of different types of dietary fats, see Box 1.8
Should we advise our patients to increase their omega-3 FA consumption? The American Psychiatric Association (APA) and the American Heart Association (AHA) recommend omega-3 FA consumption for the general population and in some cases, supplementation for specific disorders (Box 2).9-12 New data has been published since Current Psychiatry last reviewed the evidence for using omega-3 FAs for psychiatric conditions in 2004.8 This article looks at the latest evidence on the use of omega-3 FAs to treat mood disorders, schizophrenia, dementia, and other psychiatric conditions.
Dietary fat is saturated or unsaturated. Unsaturated fats are further categorized as monounsaturated or polyunsaturated (PUFA). PUFAs contain a hydrocarbon chain with ≥2 double bonds.8 The position of this double bond relative to the methyl end carbon—or “omega” carbon—groups the PUFAs into 2 categories:8
- omega-6 fatty acids, including arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids, including eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA). ALA is a metabolic precursor to EPA and DHA.
PUFAs—in particular AA and DHA—are thought to contribute to cell membrane fluidity, modulation of neurotransmitters, and signal transduction pathways. As precursors to eicosanoids and cytokines, PUFAs may affect anti-inflammatory response systems.
Consumption of omega-3 fatty acids (FAs) reduces risk for arrhythmia, thrombosis, and atherosclerotic plaque, according to American Heart Association (AHA) guidelines. Omega-3 FA intake also may improve endothelial function, slightly lower blood pressure, and reduce inflammatory response. Replacing dietary saturated fat with polyunsaturated fat reduces coronary heart disease risk by 19%.9 The AHA recommends that all adults eat fish, particularly oily fish such as salmon or tuna, ≥2 times per week. Patients with documented coronary heart disease should consume 1 g/d eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) combined10 either via oily fish or omega-3 FA capsules. Side effects of omega-3 FA supplements are minor and include mild gastrointestinal discomfort, mostly burping or an unpleasant aftertaste; no cases of bleeding have been reported.11
For patients with hypertriglyceridemia, 2 to 4 g/d may be useful. Because of a theoretical risk of bleeding, doses >3 g/d should be supervised by a physician.
Because psychiatric illnesses and cardiovascular disease may be comorbid, the Omega-3 FA Subcommittee of the American Psychiatric Association supports the AHA’s guidelines regarding fish consumption, and further recommends that patients with mood, impulse control, or psychotic disorders consume ≥1 g/d of combined EPA and DHA.12
Limitations of the data
Reviewing the literature on omega-3 FAs to treat psychiatric disorders is hampered by several difficulties:13
- studies may evaluate the use of EPA alone, EPA combined with DHA, or DHA alone
- the doses of EPA and DHA and ratio of EPA to DHA of the supplements used in clinical trials varies greatly
- patients’ dietary consumption of omega-3 FAs is difficult to control
- DSM diagnostic criteria, as well as severity of illness, differ within studies.
In addition, studies may use omega-3 FAs as monotherapy or as adjuncts. All of these factors lead to difficulty interpreting the literature, as well as trouble in extracting data for meta-analysis.
Omega-3 FAs for mood disorders
MDD and other depressive diagnoses. Several meta-analyses examining the use of omega-3 FAs for treating depressive disorders have had equivocal findings. Variability in results might be partially explained by differences in the severity of baseline depression among diverse study populations, diagnostic variation, differing omega-3 supplementation protocols, or other issues.13 In addition, publication bias also may affect results.
In a 2011 literature review and meta-analysis of omega-3 FAs as monotherapy or an adjunct to antidepressants to treat MDD, Bloch and Hannestad6 concluded that omega-3 FAs offer a small but nonsignificant benefit in treating MDD. This review suggested that omega-3 FAs may be more effective in patients with more severe depression. The effects of varying levels of EPA vs DHA were not examined.
In a systematic review and meta-analysis, Appleton et al14 concluded that omega-3 FA supplements have little beneficial effect on depressed mood in individuals who do not have a depressive illness diagnosis (eg, MDD). However, this study did not consider the differential effects of EPA vs DHA on treatment response. Patients diagnosed with a depressive illness received greater benefits from omega-3 FA supplementation, although the patients in this study were heterogeneous. Similar to Bloch and Hannestad, Appleton et al14 found that omega-3 FA supplementation may be most beneficial for depressed patients with more severe symptoms, but is unlikely to help those with mild-to-moderate symptoms or individuals without symptoms who aim to prevent depression.
A meta-analysis by Martins15 looked at EPA vs DHA to treat depressive illness and found that only supplements that were mostly or completely EPA effectively treated depressive symptoms. Martins also found that severity of illness is key for positive treatment outcomes; there was a significant relationship between higher baseline depression levels and efficacy.15 Martins noted that omega-3 FA therapy was more effective as a treatment than a preventive strategy, and that adding omega-3 FAs to antidepressants was more efficacious than omega-3 FAs alone.15
A meta-analysis of clinical trials of omega-3 FAs for depressive illness suggested EPA should be ≥60% of total EPA + DHA.16
BD. A recent meta-analysis of 6 randomized controlled trials (RCTs) found that adding omega-3 supplements to mood stabilizers in patients with BD was associated with a statistically significant reduction of depressive symptoms, but was not effective for treating mania.17 The authors suggested patients with BD—especially those with comorbid cardiovascular or metabolic conditions— increase their dietary consumption of foods containing omega-3 FAs (Table)18 and, if necessary, take a supplement of 1 to 1.5 g/d of mixed EPA and DHA, with a higher ratio of EPA.19 See Box 3 for a box on how to read omega-3 supplement labels.
In a small RCT of 51 children and adolescents (age 6 to 17) with symptomatic bipolar I or bipolar II disorder, supplementation with flax oil (alpha-linolenic acid, a polyunsaturated omega-3 FA that is a precursor to EPA and DHA) did not affect symptoms as measured by several rating scales.20
Perinatal and postpartum depression. Omega-3 FAs are considered a safe treatment for depressive disorders during pregnancy because they provide neurodevelopmental benefits for neonates and have few contraindications during pregnancy.21 RCTs of omega-3 FA monotherapy for perinatal depression have been small (≤51 patients) and produced mixed findings.21 A pilot study (N = 16) of patients with postpartum depression found a significant decrease in depressive symptoms with EPA treatment.22 More research is needed before omega-3 FA supplementation can be recommended during pregnancy.
Table
Foods with healthy fats: From best to worst
| Polyunsaturated fats | Omega-3 | Fish-based: oily fish, including salmon, tuna, mackerel, lake trout, herring, and sardines Plant-based: tofu and other forms of soybeans; walnuts and flaxseed and their oils, and canola oil |
| Omega-6 | Only available in plant-based form: corn, soy, and safflower oil | |
| Monosaturated fats | Olive and peanut oil | |
| Saturated fats | Red meats, high-fat dairy, and partially hydrogenated oils | |
| Source: Reference 18 | ||
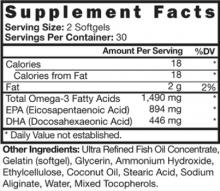
Because nutritional supplements vary, advise patients to look at the supplement facts on the back of a bottle of omega-3 fatty acids. The American Psychiatric Association recommends patients take a total eicosapentaenoic acid (EPA) + docosahexaenoic acid (DHA) of 1 g/d; EPA should be ≥60% of total EPA + DHA.
This image is an example of a label that would meet the appropriate criteria. Total EPA + DHA = 1,490 mg and EPA is 60% of this combined total.
Source: Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584
Schizophrenia
In a Cochrane review of 8 studies of patients with schizophrenia, adjunctive treatment with omega-3 FAs led to >25% reduction in the Positive and Negative Syndrome Scale, but this improvement was not statistically significant.23 Omega-3 FAs did not decrease tardive dyskinesia symptoms as measured by the Abnormal Involuntary Movement Scale. The authors stated that results were inconclusive, and use of omega-3 FAs in patients with schizophrenia remains experimental. In a separate meta-analysis that included 335 patients with schizophrenia, EPA augmentation had no beneficial effect on psychotic symptoms.24
In a double-blind RCT of 81 adolescents and young adults (age 13 to 25) at ultra-high risk of psychotic illness, 5% of patients who received 1.2 g/d of omega-3 FAs developed a psychotic disorder compared with 28% of patients receiving placebo.25 The authors concluded that supplementation with omega-3 FAs may be a safe and effective strategy for young patients with subthreshold psychotic symptoms.
Dementia
Studies evaluating the relationship between omega-3 FAs and dementia risk have revealed mixed findings.26,27 In a pilot study of 10 geriatric patients with moderately severe dementia related to thrombotic cerebrovascular disorder, DHA supplementation led to improved Hamilton Depression Rating Scale and Mini-Mental State Examination (MMSE) scores compared with controls.28 In another study, administering EPA to 64 patients with Alzheimer’s disease significantly improved MMSE scores, with maximum improvement at 3 months, but this benefit dissipated after 6 months of treatment.29 In a study of 22 patients with various types of dementia, Suzuki et al30 found that DHA supplementation improved scores on a Japanese dementia scale. These studies show promise, but more evidence is necessary before recommendations can be made.
Other psychiatric disorders
Omega-3 FAs as monotherapy or an adjunct to psychostimulants does not seem to improve symptoms in children who meet DSM-IV-TR criteria for attention-deficit/hyperactivity disorder (ADHD).31-33 Studies of omega-3 FAs as treatment for anxiety and personality disorders are limited. To date, omega-3 FAs as adjunctive treatment in obsessive-compulsive disorder (OCD) and monotherapy in borderline personality disorder have not shown efficacy.34,35
Using omega-3 FAs in practice
Based on new data and several recent meta-analyses, clinical recommendations have emerged. Sarris et al17 suggested patients with BD increase dietary intake of omega-3 FAs or take a supplement with 1 to 1.5 g/d of mixed EPA and DHA (with a higher ratio of EPA). In MDD, the type of omega-3 FA supplementation seems to be important; EPA seems to be the primary component for efficacy.15,19 Additionally, the more severe the depression, the more likely symptoms will respond to omega-3 FAs.6,14,15 Omega-3 FAs are not effective at preventing depression14,15 and evidence is equivocal for treating perinatal depression.21 Omega-3 FA supplementation has not shown efficacy for patients with schizophrenia,23,24 although it may prevent transition to psychosis in adolescents and young adults at ultra-high risk for a psychotic disorder.25 Data examining omega-3 FA supplementation in postpartum depression22 and dementia28,29 are limited but show promise. Omega-3 FAs appear to lack efficacy in ADHD,31-33 OCD,34 and borderline personality disorder.35
Related Resources
- National Center for Complementary and Alternative Medicine. Omega-3 fatty acids. http://nccam.nih.gov/health/omega3.
- National Institutes of Health. Office of Dietary Supplements. Working group report: Omega-3 fatty acids and cardiovascular disease. http://ods.od.nih.gov/Health_Information/omega_3_fatty_acids.aspx.
Disclosure
Dr. Morreale reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv. 2001;52(4):529-531.
3. Silvers KM, Scott KM. Fish consumption and self-reported physical and mental health status. Public Health Nutr. 2002;5(3):427-431.
4. Timonen M, Horrobin DF, Jokelaienen J, et al. Fish consumption and depression: the northern Finland 1966 birth cohort study. J Affect Disord. 2004;82(3):447-452.
5. Freeman MP, Rapaport MH. Omega-3 fatty acids and depression: from cellular mechanisms to clinical care. J Clin Psychiatry. 2011;72(2):258-259.
6. Bloch MH, Hannestad J. Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis [published online ahead of print September 20 2011]. Mol Psychiatry. doi: 10.1038/mp.2011.100.
7. Parker G, Gibson NA, Brotchie H, et al. Omega-3 fatty acids and mood disorders. Am J Psychiatry. 2006;163(6):969-978.
8. Martinez JM, Marangell LB. Omega-3 fatty acids: do ‘fish oils’ have a therapeutic role in psychiatry? Current Psychiatry. 2004;3(1):25-52.
9. Mozaffarian D, Micha R, Wallace S. Effects of coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252.-
10. Kris-Etherton PM, Harris WS, Appel LJ. AHA Nutrition Committee. American Heart Association. Omega-3 fatty acids and cardiovascular disease: new recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol. 2003;23(2):151-152.
11. Freeman MP, Fava M, Lake J, et al. Complementary and alternative medicine in major depressive disorder: the American Psychiatric Association Task Force report. J Clin Psychiatry. 2010;71(6):669-681.
12. Freeman MP, Hibbeln J, Wisner KL, et al. Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry. 2006;67(12):1954-1967.
13. Mischoulon D. The impact of omega-3 fatty acids on depressive disorders and suicidality: can we reconcile 2 studies with seemingly contradictory results? J Clin Psychiatry. 2011;72(12):1574-1576.
14. Appleton KM, Rogers PJ, Andrew RN. Updated systematic review and meta-analysis of the effects of n-3 long-chain polyunsaturated fatty acids on depressed mood. Am J Clin Nutr. 2010;91(31):757-770.
15. Martins JG. EPA but not DHA appears to be responsible for the efficacy of omega-3 long chain polyunsaturated fatty acid supplementation in depression: evidence from a meta-analysis of randomized controlled trials. J Am Coll Nutr. 2009;28(5):525-542.
16. Young G, Conquer J. Omega-3 fatty acids and neuropsychiatric disorders. Reprod Nutr Dev. 2005;45(1):1-28.
17. Sarris J, Mischoulon D, Schweitzer I. Omega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depression. J Clin Psychiatry. 2012;73(1):81-86.
18. Sacks F. Ask the expert: omega-3 fatty acids. The Nutrition Source.http://www.hsph.harvard.edu/nutritionsource/questions/omega-3/index.html. Accessed July 23 2012.
19. Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584.
20. Gracious BL, Chirieac MC, Costescu S, et al. Randomized, placebo-controlled trial of flax oil in pediatric bipolar disorder. Bipolar Disord. 2010;12(2):142-154.
21. Freeman MP. Omega-3 fatty acids in major depressive disorder. J Clin Psychiatry. 2009;70(suppl 5):7-11.
22. Freeman MP, Hibbeln JR, Wisner KL, et al. Randomized dose-ranging pilot trial of omega-3 fatty acids for postpartum depression. Acta Psychiatr Scand. 2006;113(1):31-35.
23. Joy CB, Mumby-Croft R, Joy LA. Polyunsaturated fatty acid supplementation for schizophrenia. Cochrane Database Syst Rev. 2006;(3):CD001257.-
24. Fusar-Poli P, Berger G. Eicosapentaenoic acid interventions in schizophrenia: meta-analysis of randomized placebo-controlled studies. J Clin Psychopharmacol. 2012;32(2):179-185.
25. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
26. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol. 2003;60(7):940-946.
27. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology. 2002;59(12):1915-1921.
28. Terano T, Fujishiro S, Ban T, et al. Docosahexaenoic acid supplementation improves the moderately severe dementia from thrombotic cerebrovascular diseases. Lipids. 1999;34 suppl:S345-S346.
29. Otsuka M. Analysis of dietary factors in Alzheimer’s disease: clinical use of nutritional intervention for prevention and treatment of dementia [in Japanese]. Nihon Ronen Igakkai Zasshi. 2000;37(12):970-973.
30. Suzuki H, Morikawa Y, Takahashi H. Effect of DHA oil supplementation in intelligence and visual acuity in the elderly. World Rev Nutr Diet. 2001;88:68-71.
31. Joshi K, Lad S, Kale M, et al. Supplementation with flax oil and vitamin C improves the outcome of attention deficit hyperactivity disorder (ADHD). Prostaglandins Leukot Essent Fatty Acids. 2006;74(1):17-21.
32. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr. 2001;139(2):189-196.
33. Hirayama S, Hamazaki T, Terasawa K. Effect of docosahexaenoic acid-containing food administration on symptoms of attention-deficit/hyperactivity disorder - a placebo-controlled double-blind study. Eur J Clin Nutr. 2004;58(3):467-473.
34. Fux M, Benjamin J, Nemets B. A placebo-controlled cross-over trial of adjunctive EPA in OCD. J Psychiatr Res. 2004;38(3):323-325.
35. Zanarini MC, Frankenburg FR. Omega-3 Fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
Discuss this article at www.facebook.com/CurrentPsychiatry
Epidemiologic data suggest that people who consume diets rich in omega-3 fatty acids (FAs)—long-chain polyunsaturated FAs such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)—have a decreased risk of major depressive disorder (MDD), postpartum depression, and bipolar disorder (BD).1-5 Omega-3 FA concentration may impact serotonin and dopamine transmission via effects on cell membrane fluidity.6 Therefore, decreased intake may increase the risk of several psychiatric disorders. As the average Western diet has changed over the last 2 centuries, omega-3 FA consumption has decreased.7 Omega-3 FAs cannot be synthesized by the body and must come from exogenous sources, such as fish and nuts. For a discussion of different types of dietary fats, see Box 1.8
Should we advise our patients to increase their omega-3 FA consumption? The American Psychiatric Association (APA) and the American Heart Association (AHA) recommend omega-3 FA consumption for the general population and in some cases, supplementation for specific disorders (Box 2).9-12 New data has been published since Current Psychiatry last reviewed the evidence for using omega-3 FAs for psychiatric conditions in 2004.8 This article looks at the latest evidence on the use of omega-3 FAs to treat mood disorders, schizophrenia, dementia, and other psychiatric conditions.
Dietary fat is saturated or unsaturated. Unsaturated fats are further categorized as monounsaturated or polyunsaturated (PUFA). PUFAs contain a hydrocarbon chain with ≥2 double bonds.8 The position of this double bond relative to the methyl end carbon—or “omega” carbon—groups the PUFAs into 2 categories:8
- omega-6 fatty acids, including arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids, including eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA). ALA is a metabolic precursor to EPA and DHA.
PUFAs—in particular AA and DHA—are thought to contribute to cell membrane fluidity, modulation of neurotransmitters, and signal transduction pathways. As precursors to eicosanoids and cytokines, PUFAs may affect anti-inflammatory response systems.
Consumption of omega-3 fatty acids (FAs) reduces risk for arrhythmia, thrombosis, and atherosclerotic plaque, according to American Heart Association (AHA) guidelines. Omega-3 FA intake also may improve endothelial function, slightly lower blood pressure, and reduce inflammatory response. Replacing dietary saturated fat with polyunsaturated fat reduces coronary heart disease risk by 19%.9 The AHA recommends that all adults eat fish, particularly oily fish such as salmon or tuna, ≥2 times per week. Patients with documented coronary heart disease should consume 1 g/d eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) combined10 either via oily fish or omega-3 FA capsules. Side effects of omega-3 FA supplements are minor and include mild gastrointestinal discomfort, mostly burping or an unpleasant aftertaste; no cases of bleeding have been reported.11
For patients with hypertriglyceridemia, 2 to 4 g/d may be useful. Because of a theoretical risk of bleeding, doses >3 g/d should be supervised by a physician.
Because psychiatric illnesses and cardiovascular disease may be comorbid, the Omega-3 FA Subcommittee of the American Psychiatric Association supports the AHA’s guidelines regarding fish consumption, and further recommends that patients with mood, impulse control, or psychotic disorders consume ≥1 g/d of combined EPA and DHA.12
Limitations of the data
Reviewing the literature on omega-3 FAs to treat psychiatric disorders is hampered by several difficulties:13
- studies may evaluate the use of EPA alone, EPA combined with DHA, or DHA alone
- the doses of EPA and DHA and ratio of EPA to DHA of the supplements used in clinical trials varies greatly
- patients’ dietary consumption of omega-3 FAs is difficult to control
- DSM diagnostic criteria, as well as severity of illness, differ within studies.
In addition, studies may use omega-3 FAs as monotherapy or as adjuncts. All of these factors lead to difficulty interpreting the literature, as well as trouble in extracting data for meta-analysis.
Omega-3 FAs for mood disorders
MDD and other depressive diagnoses. Several meta-analyses examining the use of omega-3 FAs for treating depressive disorders have had equivocal findings. Variability in results might be partially explained by differences in the severity of baseline depression among diverse study populations, diagnostic variation, differing omega-3 supplementation protocols, or other issues.13 In addition, publication bias also may affect results.
In a 2011 literature review and meta-analysis of omega-3 FAs as monotherapy or an adjunct to antidepressants to treat MDD, Bloch and Hannestad6 concluded that omega-3 FAs offer a small but nonsignificant benefit in treating MDD. This review suggested that omega-3 FAs may be more effective in patients with more severe depression. The effects of varying levels of EPA vs DHA were not examined.
In a systematic review and meta-analysis, Appleton et al14 concluded that omega-3 FA supplements have little beneficial effect on depressed mood in individuals who do not have a depressive illness diagnosis (eg, MDD). However, this study did not consider the differential effects of EPA vs DHA on treatment response. Patients diagnosed with a depressive illness received greater benefits from omega-3 FA supplementation, although the patients in this study were heterogeneous. Similar to Bloch and Hannestad, Appleton et al14 found that omega-3 FA supplementation may be most beneficial for depressed patients with more severe symptoms, but is unlikely to help those with mild-to-moderate symptoms or individuals without symptoms who aim to prevent depression.
A meta-analysis by Martins15 looked at EPA vs DHA to treat depressive illness and found that only supplements that were mostly or completely EPA effectively treated depressive symptoms. Martins also found that severity of illness is key for positive treatment outcomes; there was a significant relationship between higher baseline depression levels and efficacy.15 Martins noted that omega-3 FA therapy was more effective as a treatment than a preventive strategy, and that adding omega-3 FAs to antidepressants was more efficacious than omega-3 FAs alone.15
A meta-analysis of clinical trials of omega-3 FAs for depressive illness suggested EPA should be ≥60% of total EPA + DHA.16
BD. A recent meta-analysis of 6 randomized controlled trials (RCTs) found that adding omega-3 supplements to mood stabilizers in patients with BD was associated with a statistically significant reduction of depressive symptoms, but was not effective for treating mania.17 The authors suggested patients with BD—especially those with comorbid cardiovascular or metabolic conditions— increase their dietary consumption of foods containing omega-3 FAs (Table)18 and, if necessary, take a supplement of 1 to 1.5 g/d of mixed EPA and DHA, with a higher ratio of EPA.19 See Box 3 for a box on how to read omega-3 supplement labels.
In a small RCT of 51 children and adolescents (age 6 to 17) with symptomatic bipolar I or bipolar II disorder, supplementation with flax oil (alpha-linolenic acid, a polyunsaturated omega-3 FA that is a precursor to EPA and DHA) did not affect symptoms as measured by several rating scales.20
Perinatal and postpartum depression. Omega-3 FAs are considered a safe treatment for depressive disorders during pregnancy because they provide neurodevelopmental benefits for neonates and have few contraindications during pregnancy.21 RCTs of omega-3 FA monotherapy for perinatal depression have been small (≤51 patients) and produced mixed findings.21 A pilot study (N = 16) of patients with postpartum depression found a significant decrease in depressive symptoms with EPA treatment.22 More research is needed before omega-3 FA supplementation can be recommended during pregnancy.
Table
Foods with healthy fats: From best to worst
| Polyunsaturated fats | Omega-3 | Fish-based: oily fish, including salmon, tuna, mackerel, lake trout, herring, and sardines Plant-based: tofu and other forms of soybeans; walnuts and flaxseed and their oils, and canola oil |
| Omega-6 | Only available in plant-based form: corn, soy, and safflower oil | |
| Monosaturated fats | Olive and peanut oil | |
| Saturated fats | Red meats, high-fat dairy, and partially hydrogenated oils | |
| Source: Reference 18 | ||
Because nutritional supplements vary, advise patients to look at the supplement facts on the back of a bottle of omega-3 fatty acids. The American Psychiatric Association recommends patients take a total eicosapentaenoic acid (EPA) + docosahexaenoic acid (DHA) of 1 g/d; EPA should be ≥60% of total EPA + DHA.
This image is an example of a label that would meet the appropriate criteria. Total EPA + DHA = 1,490 mg and EPA is 60% of this combined total.
Source: Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584
Schizophrenia
In a Cochrane review of 8 studies of patients with schizophrenia, adjunctive treatment with omega-3 FAs led to >25% reduction in the Positive and Negative Syndrome Scale, but this improvement was not statistically significant.23 Omega-3 FAs did not decrease tardive dyskinesia symptoms as measured by the Abnormal Involuntary Movement Scale. The authors stated that results were inconclusive, and use of omega-3 FAs in patients with schizophrenia remains experimental. In a separate meta-analysis that included 335 patients with schizophrenia, EPA augmentation had no beneficial effect on psychotic symptoms.24
In a double-blind RCT of 81 adolescents and young adults (age 13 to 25) at ultra-high risk of psychotic illness, 5% of patients who received 1.2 g/d of omega-3 FAs developed a psychotic disorder compared with 28% of patients receiving placebo.25 The authors concluded that supplementation with omega-3 FAs may be a safe and effective strategy for young patients with subthreshold psychotic symptoms.
Dementia
Studies evaluating the relationship between omega-3 FAs and dementia risk have revealed mixed findings.26,27 In a pilot study of 10 geriatric patients with moderately severe dementia related to thrombotic cerebrovascular disorder, DHA supplementation led to improved Hamilton Depression Rating Scale and Mini-Mental State Examination (MMSE) scores compared with controls.28 In another study, administering EPA to 64 patients with Alzheimer’s disease significantly improved MMSE scores, with maximum improvement at 3 months, but this benefit dissipated after 6 months of treatment.29 In a study of 22 patients with various types of dementia, Suzuki et al30 found that DHA supplementation improved scores on a Japanese dementia scale. These studies show promise, but more evidence is necessary before recommendations can be made.
Other psychiatric disorders
Omega-3 FAs as monotherapy or an adjunct to psychostimulants does not seem to improve symptoms in children who meet DSM-IV-TR criteria for attention-deficit/hyperactivity disorder (ADHD).31-33 Studies of omega-3 FAs as treatment for anxiety and personality disorders are limited. To date, omega-3 FAs as adjunctive treatment in obsessive-compulsive disorder (OCD) and monotherapy in borderline personality disorder have not shown efficacy.34,35
Using omega-3 FAs in practice
Based on new data and several recent meta-analyses, clinical recommendations have emerged. Sarris et al17 suggested patients with BD increase dietary intake of omega-3 FAs or take a supplement with 1 to 1.5 g/d of mixed EPA and DHA (with a higher ratio of EPA). In MDD, the type of omega-3 FA supplementation seems to be important; EPA seems to be the primary component for efficacy.15,19 Additionally, the more severe the depression, the more likely symptoms will respond to omega-3 FAs.6,14,15 Omega-3 FAs are not effective at preventing depression14,15 and evidence is equivocal for treating perinatal depression.21 Omega-3 FA supplementation has not shown efficacy for patients with schizophrenia,23,24 although it may prevent transition to psychosis in adolescents and young adults at ultra-high risk for a psychotic disorder.25 Data examining omega-3 FA supplementation in postpartum depression22 and dementia28,29 are limited but show promise. Omega-3 FAs appear to lack efficacy in ADHD,31-33 OCD,34 and borderline personality disorder.35
Related Resources
- National Center for Complementary and Alternative Medicine. Omega-3 fatty acids. http://nccam.nih.gov/health/omega3.
- National Institutes of Health. Office of Dietary Supplements. Working group report: Omega-3 fatty acids and cardiovascular disease. http://ods.od.nih.gov/Health_Information/omega_3_fatty_acids.aspx.
Disclosure
Dr. Morreale reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Epidemiologic data suggest that people who consume diets rich in omega-3 fatty acids (FAs)—long-chain polyunsaturated FAs such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)—have a decreased risk of major depressive disorder (MDD), postpartum depression, and bipolar disorder (BD).1-5 Omega-3 FA concentration may impact serotonin and dopamine transmission via effects on cell membrane fluidity.6 Therefore, decreased intake may increase the risk of several psychiatric disorders. As the average Western diet has changed over the last 2 centuries, omega-3 FA consumption has decreased.7 Omega-3 FAs cannot be synthesized by the body and must come from exogenous sources, such as fish and nuts. For a discussion of different types of dietary fats, see Box 1.8
Should we advise our patients to increase their omega-3 FA consumption? The American Psychiatric Association (APA) and the American Heart Association (AHA) recommend omega-3 FA consumption for the general population and in some cases, supplementation for specific disorders (Box 2).9-12 New data has been published since Current Psychiatry last reviewed the evidence for using omega-3 FAs for psychiatric conditions in 2004.8 This article looks at the latest evidence on the use of omega-3 FAs to treat mood disorders, schizophrenia, dementia, and other psychiatric conditions.
Dietary fat is saturated or unsaturated. Unsaturated fats are further categorized as monounsaturated or polyunsaturated (PUFA). PUFAs contain a hydrocarbon chain with ≥2 double bonds.8 The position of this double bond relative to the methyl end carbon—or “omega” carbon—groups the PUFAs into 2 categories:8
- omega-6 fatty acids, including arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids, including eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA). ALA is a metabolic precursor to EPA and DHA.
PUFAs—in particular AA and DHA—are thought to contribute to cell membrane fluidity, modulation of neurotransmitters, and signal transduction pathways. As precursors to eicosanoids and cytokines, PUFAs may affect anti-inflammatory response systems.
Consumption of omega-3 fatty acids (FAs) reduces risk for arrhythmia, thrombosis, and atherosclerotic plaque, according to American Heart Association (AHA) guidelines. Omega-3 FA intake also may improve endothelial function, slightly lower blood pressure, and reduce inflammatory response. Replacing dietary saturated fat with polyunsaturated fat reduces coronary heart disease risk by 19%.9 The AHA recommends that all adults eat fish, particularly oily fish such as salmon or tuna, ≥2 times per week. Patients with documented coronary heart disease should consume 1 g/d eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) combined10 either via oily fish or omega-3 FA capsules. Side effects of omega-3 FA supplements are minor and include mild gastrointestinal discomfort, mostly burping or an unpleasant aftertaste; no cases of bleeding have been reported.11
For patients with hypertriglyceridemia, 2 to 4 g/d may be useful. Because of a theoretical risk of bleeding, doses >3 g/d should be supervised by a physician.
Because psychiatric illnesses and cardiovascular disease may be comorbid, the Omega-3 FA Subcommittee of the American Psychiatric Association supports the AHA’s guidelines regarding fish consumption, and further recommends that patients with mood, impulse control, or psychotic disorders consume ≥1 g/d of combined EPA and DHA.12
Limitations of the data
Reviewing the literature on omega-3 FAs to treat psychiatric disorders is hampered by several difficulties:13
- studies may evaluate the use of EPA alone, EPA combined with DHA, or DHA alone
- the doses of EPA and DHA and ratio of EPA to DHA of the supplements used in clinical trials varies greatly
- patients’ dietary consumption of omega-3 FAs is difficult to control
- DSM diagnostic criteria, as well as severity of illness, differ within studies.
In addition, studies may use omega-3 FAs as monotherapy or as adjuncts. All of these factors lead to difficulty interpreting the literature, as well as trouble in extracting data for meta-analysis.
Omega-3 FAs for mood disorders
MDD and other depressive diagnoses. Several meta-analyses examining the use of omega-3 FAs for treating depressive disorders have had equivocal findings. Variability in results might be partially explained by differences in the severity of baseline depression among diverse study populations, diagnostic variation, differing omega-3 supplementation protocols, or other issues.13 In addition, publication bias also may affect results.
In a 2011 literature review and meta-analysis of omega-3 FAs as monotherapy or an adjunct to antidepressants to treat MDD, Bloch and Hannestad6 concluded that omega-3 FAs offer a small but nonsignificant benefit in treating MDD. This review suggested that omega-3 FAs may be more effective in patients with more severe depression. The effects of varying levels of EPA vs DHA were not examined.
In a systematic review and meta-analysis, Appleton et al14 concluded that omega-3 FA supplements have little beneficial effect on depressed mood in individuals who do not have a depressive illness diagnosis (eg, MDD). However, this study did not consider the differential effects of EPA vs DHA on treatment response. Patients diagnosed with a depressive illness received greater benefits from omega-3 FA supplementation, although the patients in this study were heterogeneous. Similar to Bloch and Hannestad, Appleton et al14 found that omega-3 FA supplementation may be most beneficial for depressed patients with more severe symptoms, but is unlikely to help those with mild-to-moderate symptoms or individuals without symptoms who aim to prevent depression.
A meta-analysis by Martins15 looked at EPA vs DHA to treat depressive illness and found that only supplements that were mostly or completely EPA effectively treated depressive symptoms. Martins also found that severity of illness is key for positive treatment outcomes; there was a significant relationship between higher baseline depression levels and efficacy.15 Martins noted that omega-3 FA therapy was more effective as a treatment than a preventive strategy, and that adding omega-3 FAs to antidepressants was more efficacious than omega-3 FAs alone.15
A meta-analysis of clinical trials of omega-3 FAs for depressive illness suggested EPA should be ≥60% of total EPA + DHA.16
BD. A recent meta-analysis of 6 randomized controlled trials (RCTs) found that adding omega-3 supplements to mood stabilizers in patients with BD was associated with a statistically significant reduction of depressive symptoms, but was not effective for treating mania.17 The authors suggested patients with BD—especially those with comorbid cardiovascular or metabolic conditions— increase their dietary consumption of foods containing omega-3 FAs (Table)18 and, if necessary, take a supplement of 1 to 1.5 g/d of mixed EPA and DHA, with a higher ratio of EPA.19 See Box 3 for a box on how to read omega-3 supplement labels.
In a small RCT of 51 children and adolescents (age 6 to 17) with symptomatic bipolar I or bipolar II disorder, supplementation with flax oil (alpha-linolenic acid, a polyunsaturated omega-3 FA that is a precursor to EPA and DHA) did not affect symptoms as measured by several rating scales.20
Perinatal and postpartum depression. Omega-3 FAs are considered a safe treatment for depressive disorders during pregnancy because they provide neurodevelopmental benefits for neonates and have few contraindications during pregnancy.21 RCTs of omega-3 FA monotherapy for perinatal depression have been small (≤51 patients) and produced mixed findings.21 A pilot study (N = 16) of patients with postpartum depression found a significant decrease in depressive symptoms with EPA treatment.22 More research is needed before omega-3 FA supplementation can be recommended during pregnancy.
Table
Foods with healthy fats: From best to worst
| Polyunsaturated fats | Omega-3 | Fish-based: oily fish, including salmon, tuna, mackerel, lake trout, herring, and sardines Plant-based: tofu and other forms of soybeans; walnuts and flaxseed and their oils, and canola oil |
| Omega-6 | Only available in plant-based form: corn, soy, and safflower oil | |
| Monosaturated fats | Olive and peanut oil | |
| Saturated fats | Red meats, high-fat dairy, and partially hydrogenated oils | |
| Source: Reference 18 | ||
Because nutritional supplements vary, advise patients to look at the supplement facts on the back of a bottle of omega-3 fatty acids. The American Psychiatric Association recommends patients take a total eicosapentaenoic acid (EPA) + docosahexaenoic acid (DHA) of 1 g/d; EPA should be ≥60% of total EPA + DHA.
This image is an example of a label that would meet the appropriate criteria. Total EPA + DHA = 1,490 mg and EPA is 60% of this combined total.
Source: Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584
Schizophrenia
In a Cochrane review of 8 studies of patients with schizophrenia, adjunctive treatment with omega-3 FAs led to >25% reduction in the Positive and Negative Syndrome Scale, but this improvement was not statistically significant.23 Omega-3 FAs did not decrease tardive dyskinesia symptoms as measured by the Abnormal Involuntary Movement Scale. The authors stated that results were inconclusive, and use of omega-3 FAs in patients with schizophrenia remains experimental. In a separate meta-analysis that included 335 patients with schizophrenia, EPA augmentation had no beneficial effect on psychotic symptoms.24
In a double-blind RCT of 81 adolescents and young adults (age 13 to 25) at ultra-high risk of psychotic illness, 5% of patients who received 1.2 g/d of omega-3 FAs developed a psychotic disorder compared with 28% of patients receiving placebo.25 The authors concluded that supplementation with omega-3 FAs may be a safe and effective strategy for young patients with subthreshold psychotic symptoms.
Dementia
Studies evaluating the relationship between omega-3 FAs and dementia risk have revealed mixed findings.26,27 In a pilot study of 10 geriatric patients with moderately severe dementia related to thrombotic cerebrovascular disorder, DHA supplementation led to improved Hamilton Depression Rating Scale and Mini-Mental State Examination (MMSE) scores compared with controls.28 In another study, administering EPA to 64 patients with Alzheimer’s disease significantly improved MMSE scores, with maximum improvement at 3 months, but this benefit dissipated after 6 months of treatment.29 In a study of 22 patients with various types of dementia, Suzuki et al30 found that DHA supplementation improved scores on a Japanese dementia scale. These studies show promise, but more evidence is necessary before recommendations can be made.
Other psychiatric disorders
Omega-3 FAs as monotherapy or an adjunct to psychostimulants does not seem to improve symptoms in children who meet DSM-IV-TR criteria for attention-deficit/hyperactivity disorder (ADHD).31-33 Studies of omega-3 FAs as treatment for anxiety and personality disorders are limited. To date, omega-3 FAs as adjunctive treatment in obsessive-compulsive disorder (OCD) and monotherapy in borderline personality disorder have not shown efficacy.34,35
Using omega-3 FAs in practice
Based on new data and several recent meta-analyses, clinical recommendations have emerged. Sarris et al17 suggested patients with BD increase dietary intake of omega-3 FAs or take a supplement with 1 to 1.5 g/d of mixed EPA and DHA (with a higher ratio of EPA). In MDD, the type of omega-3 FA supplementation seems to be important; EPA seems to be the primary component for efficacy.15,19 Additionally, the more severe the depression, the more likely symptoms will respond to omega-3 FAs.6,14,15 Omega-3 FAs are not effective at preventing depression14,15 and evidence is equivocal for treating perinatal depression.21 Omega-3 FA supplementation has not shown efficacy for patients with schizophrenia,23,24 although it may prevent transition to psychosis in adolescents and young adults at ultra-high risk for a psychotic disorder.25 Data examining omega-3 FA supplementation in postpartum depression22 and dementia28,29 are limited but show promise. Omega-3 FAs appear to lack efficacy in ADHD,31-33 OCD,34 and borderline personality disorder.35
Related Resources
- National Center for Complementary and Alternative Medicine. Omega-3 fatty acids. http://nccam.nih.gov/health/omega3.
- National Institutes of Health. Office of Dietary Supplements. Working group report: Omega-3 fatty acids and cardiovascular disease. http://ods.od.nih.gov/Health_Information/omega_3_fatty_acids.aspx.
Disclosure
Dr. Morreale reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv. 2001;52(4):529-531.
3. Silvers KM, Scott KM. Fish consumption and self-reported physical and mental health status. Public Health Nutr. 2002;5(3):427-431.
4. Timonen M, Horrobin DF, Jokelaienen J, et al. Fish consumption and depression: the northern Finland 1966 birth cohort study. J Affect Disord. 2004;82(3):447-452.
5. Freeman MP, Rapaport MH. Omega-3 fatty acids and depression: from cellular mechanisms to clinical care. J Clin Psychiatry. 2011;72(2):258-259.
6. Bloch MH, Hannestad J. Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis [published online ahead of print September 20 2011]. Mol Psychiatry. doi: 10.1038/mp.2011.100.
7. Parker G, Gibson NA, Brotchie H, et al. Omega-3 fatty acids and mood disorders. Am J Psychiatry. 2006;163(6):969-978.
8. Martinez JM, Marangell LB. Omega-3 fatty acids: do ‘fish oils’ have a therapeutic role in psychiatry? Current Psychiatry. 2004;3(1):25-52.
9. Mozaffarian D, Micha R, Wallace S. Effects of coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252.-
10. Kris-Etherton PM, Harris WS, Appel LJ. AHA Nutrition Committee. American Heart Association. Omega-3 fatty acids and cardiovascular disease: new recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol. 2003;23(2):151-152.
11. Freeman MP, Fava M, Lake J, et al. Complementary and alternative medicine in major depressive disorder: the American Psychiatric Association Task Force report. J Clin Psychiatry. 2010;71(6):669-681.
12. Freeman MP, Hibbeln J, Wisner KL, et al. Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry. 2006;67(12):1954-1967.
13. Mischoulon D. The impact of omega-3 fatty acids on depressive disorders and suicidality: can we reconcile 2 studies with seemingly contradictory results? J Clin Psychiatry. 2011;72(12):1574-1576.
14. Appleton KM, Rogers PJ, Andrew RN. Updated systematic review and meta-analysis of the effects of n-3 long-chain polyunsaturated fatty acids on depressed mood. Am J Clin Nutr. 2010;91(31):757-770.
15. Martins JG. EPA but not DHA appears to be responsible for the efficacy of omega-3 long chain polyunsaturated fatty acid supplementation in depression: evidence from a meta-analysis of randomized controlled trials. J Am Coll Nutr. 2009;28(5):525-542.
16. Young G, Conquer J. Omega-3 fatty acids and neuropsychiatric disorders. Reprod Nutr Dev. 2005;45(1):1-28.
17. Sarris J, Mischoulon D, Schweitzer I. Omega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depression. J Clin Psychiatry. 2012;73(1):81-86.
18. Sacks F. Ask the expert: omega-3 fatty acids. The Nutrition Source.http://www.hsph.harvard.edu/nutritionsource/questions/omega-3/index.html. Accessed July 23 2012.
19. Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584.
20. Gracious BL, Chirieac MC, Costescu S, et al. Randomized, placebo-controlled trial of flax oil in pediatric bipolar disorder. Bipolar Disord. 2010;12(2):142-154.
21. Freeman MP. Omega-3 fatty acids in major depressive disorder. J Clin Psychiatry. 2009;70(suppl 5):7-11.
22. Freeman MP, Hibbeln JR, Wisner KL, et al. Randomized dose-ranging pilot trial of omega-3 fatty acids for postpartum depression. Acta Psychiatr Scand. 2006;113(1):31-35.
23. Joy CB, Mumby-Croft R, Joy LA. Polyunsaturated fatty acid supplementation for schizophrenia. Cochrane Database Syst Rev. 2006;(3):CD001257.-
24. Fusar-Poli P, Berger G. Eicosapentaenoic acid interventions in schizophrenia: meta-analysis of randomized placebo-controlled studies. J Clin Psychopharmacol. 2012;32(2):179-185.
25. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
26. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol. 2003;60(7):940-946.
27. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology. 2002;59(12):1915-1921.
28. Terano T, Fujishiro S, Ban T, et al. Docosahexaenoic acid supplementation improves the moderately severe dementia from thrombotic cerebrovascular diseases. Lipids. 1999;34 suppl:S345-S346.
29. Otsuka M. Analysis of dietary factors in Alzheimer’s disease: clinical use of nutritional intervention for prevention and treatment of dementia [in Japanese]. Nihon Ronen Igakkai Zasshi. 2000;37(12):970-973.
30. Suzuki H, Morikawa Y, Takahashi H. Effect of DHA oil supplementation in intelligence and visual acuity in the elderly. World Rev Nutr Diet. 2001;88:68-71.
31. Joshi K, Lad S, Kale M, et al. Supplementation with flax oil and vitamin C improves the outcome of attention deficit hyperactivity disorder (ADHD). Prostaglandins Leukot Essent Fatty Acids. 2006;74(1):17-21.
32. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr. 2001;139(2):189-196.
33. Hirayama S, Hamazaki T, Terasawa K. Effect of docosahexaenoic acid-containing food administration on symptoms of attention-deficit/hyperactivity disorder - a placebo-controlled double-blind study. Eur J Clin Nutr. 2004;58(3):467-473.
34. Fux M, Benjamin J, Nemets B. A placebo-controlled cross-over trial of adjunctive EPA in OCD. J Psychiatr Res. 2004;38(3):323-325.
35. Zanarini MC, Frankenburg FR. Omega-3 Fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
1. Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv. 2001;52(4):529-531.
3. Silvers KM, Scott KM. Fish consumption and self-reported physical and mental health status. Public Health Nutr. 2002;5(3):427-431.
4. Timonen M, Horrobin DF, Jokelaienen J, et al. Fish consumption and depression: the northern Finland 1966 birth cohort study. J Affect Disord. 2004;82(3):447-452.
5. Freeman MP, Rapaport MH. Omega-3 fatty acids and depression: from cellular mechanisms to clinical care. J Clin Psychiatry. 2011;72(2):258-259.
6. Bloch MH, Hannestad J. Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis [published online ahead of print September 20 2011]. Mol Psychiatry. doi: 10.1038/mp.2011.100.
7. Parker G, Gibson NA, Brotchie H, et al. Omega-3 fatty acids and mood disorders. Am J Psychiatry. 2006;163(6):969-978.
8. Martinez JM, Marangell LB. Omega-3 fatty acids: do ‘fish oils’ have a therapeutic role in psychiatry? Current Psychiatry. 2004;3(1):25-52.
9. Mozaffarian D, Micha R, Wallace S. Effects of coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252.-
10. Kris-Etherton PM, Harris WS, Appel LJ. AHA Nutrition Committee. American Heart Association. Omega-3 fatty acids and cardiovascular disease: new recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol. 2003;23(2):151-152.
11. Freeman MP, Fava M, Lake J, et al. Complementary and alternative medicine in major depressive disorder: the American Psychiatric Association Task Force report. J Clin Psychiatry. 2010;71(6):669-681.
12. Freeman MP, Hibbeln J, Wisner KL, et al. Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry. 2006;67(12):1954-1967.
13. Mischoulon D. The impact of omega-3 fatty acids on depressive disorders and suicidality: can we reconcile 2 studies with seemingly contradictory results? J Clin Psychiatry. 2011;72(12):1574-1576.
14. Appleton KM, Rogers PJ, Andrew RN. Updated systematic review and meta-analysis of the effects of n-3 long-chain polyunsaturated fatty acids on depressed mood. Am J Clin Nutr. 2010;91(31):757-770.
15. Martins JG. EPA but not DHA appears to be responsible for the efficacy of omega-3 long chain polyunsaturated fatty acid supplementation in depression: evidence from a meta-analysis of randomized controlled trials. J Am Coll Nutr. 2009;28(5):525-542.
16. Young G, Conquer J. Omega-3 fatty acids and neuropsychiatric disorders. Reprod Nutr Dev. 2005;45(1):1-28.
17. Sarris J, Mischoulon D, Schweitzer I. Omega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depression. J Clin Psychiatry. 2012;73(1):81-86.
18. Sacks F. Ask the expert: omega-3 fatty acids. The Nutrition Source.http://www.hsph.harvard.edu/nutritionsource/questions/omega-3/index.html. Accessed July 23 2012.
19. Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584.
20. Gracious BL, Chirieac MC, Costescu S, et al. Randomized, placebo-controlled trial of flax oil in pediatric bipolar disorder. Bipolar Disord. 2010;12(2):142-154.
21. Freeman MP. Omega-3 fatty acids in major depressive disorder. J Clin Psychiatry. 2009;70(suppl 5):7-11.
22. Freeman MP, Hibbeln JR, Wisner KL, et al. Randomized dose-ranging pilot trial of omega-3 fatty acids for postpartum depression. Acta Psychiatr Scand. 2006;113(1):31-35.
23. Joy CB, Mumby-Croft R, Joy LA. Polyunsaturated fatty acid supplementation for schizophrenia. Cochrane Database Syst Rev. 2006;(3):CD001257.-
24. Fusar-Poli P, Berger G. Eicosapentaenoic acid interventions in schizophrenia: meta-analysis of randomized placebo-controlled studies. J Clin Psychopharmacol. 2012;32(2):179-185.
25. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
26. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol. 2003;60(7):940-946.
27. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology. 2002;59(12):1915-1921.
28. Terano T, Fujishiro S, Ban T, et al. Docosahexaenoic acid supplementation improves the moderately severe dementia from thrombotic cerebrovascular diseases. Lipids. 1999;34 suppl:S345-S346.
29. Otsuka M. Analysis of dietary factors in Alzheimer’s disease: clinical use of nutritional intervention for prevention and treatment of dementia [in Japanese]. Nihon Ronen Igakkai Zasshi. 2000;37(12):970-973.
30. Suzuki H, Morikawa Y, Takahashi H. Effect of DHA oil supplementation in intelligence and visual acuity in the elderly. World Rev Nutr Diet. 2001;88:68-71.
31. Joshi K, Lad S, Kale M, et al. Supplementation with flax oil and vitamin C improves the outcome of attention deficit hyperactivity disorder (ADHD). Prostaglandins Leukot Essent Fatty Acids. 2006;74(1):17-21.
32. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr. 2001;139(2):189-196.
33. Hirayama S, Hamazaki T, Terasawa K. Effect of docosahexaenoic acid-containing food administration on symptoms of attention-deficit/hyperactivity disorder - a placebo-controlled double-blind study. Eur J Clin Nutr. 2004;58(3):467-473.
34. Fux M, Benjamin J, Nemets B. A placebo-controlled cross-over trial of adjunctive EPA in OCD. J Psychiatr Res. 2004;38(3):323-325.
35. Zanarini MC, Frankenburg FR. Omega-3 Fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
How to target psychiatric symptoms of Huntington’s disease
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatric symptoms are a common and debilitating manifestation of Huntington’s disease (HD), a progressive, inherited neurodegenerative disorder also characterized by chorea (involuntary, nonrepetitive movements) and cognitive decline. The prevalence of HD is 4 to 8 patients per 100,000 persons in most populations of European descent, with lower prevalence among non-Europeans.1 HD is caused by an abnormal expansion of a trinucleotide (CAG) repeat sequence on chromosome 4, and is inherited in an autosomal dominant fashion, meaning a HD patient’s child has a 50% chance of inheriting the mutation. The expansion is located in the gene that encodes the “huntingtin” protein, the normal function of which is not well understood.
There’s no cure for HD, and treatments primarily are directed at symptom control. Psychiatric symptoms include depression, apathy, anxiety, and psychosis (Table).2-4 Treating patients with HD can be challenging because most psychiatrists will see only a handful of patients with this multifaceted illness during their careers. See Box 1 for a case study of a patient with HD.
Table
Psychiatric symptoms of HD
| Anxiety |
| Apathy |
| Delusions |
| Disinhibitions, impulsivity, aggressive behavior |
| Dysphoria |
| Euphoria |
| Hallucinations |
| Irritability |
| Obsessions and compulsions |
| HD: Huntington’s disease Source: References 2-4 |
Mr. M, age 50, was diagnosed with Huntington’s disease (HD) 1 year ago. He returns to our psychiatric clinic for treatment of depressive symptoms and temper. Previously, he was prescribed citalopram, 40 mg/d; eventually low-dose olanzapine, 2.5 mg at night, was added. Mr. M reported better temper control, but his low mood, irritability, hopelessness, and amotivation were not significantly improved.
Mr. M left his job at a software company because he had difficulty completing tasks as the result of mood and cognitive changes. He wants to return to work, but feels that he would be unable to complete his job duties.
He begins a trial of bupropion, 150 mg/d, to improve the vegetative component of his mood symptoms to help him return to work. Mr. M now complains of worsening chorea, irritability, and insomnia, with continued difficulty completing tasks. He is intermittently tearful throughout the interview.
Mr. M continues to struggle with mood symptoms that likely are related to the stressful experience of declining function and the intrinsic evolution of HD. His chorea worsens on bupropion; this agent is discontinued and replaced with mirtazapine, 15 mg at night, for his depressive symptoms and insomnia. Citalopram and olanzapine are unchanged. Mr. M is advised to follow up with our HD psychiatry team in 1 month, and is referred for brief psychotherapy. We remind him—as we do for all of our HD patients—to call the HD clinic or 911 if he becomes suicidal. Ongoing treatment efforts likely will be complex, given the multifaceted and progressive nature of his disease.
Psychiatric sequelae
In general, psychiatric symptoms of HD become increasingly prevalent over time (Box 2).3,5 In a 2001 study of 52 HD patients by Paulsen et al,2 51 patients had ≥1 psychiatric symptom, such as dysphoria (69.2%), agitation (67.3%), irritability (65.4%), apathy (55.8%), and anxiety (51.9%); delusions (11.5%) and hallucinations (1.9%) were less prevalent.2 Similarly, Thompson et al3 followed 111 HD patients for ≥3 years and all experienced psychiatric symptoms.
According to Thompson et al,3 the presence and severity of apathy, irritability, and depression trend differently across the course of Huntington’s disease (HD). Apathy worsens with disease progression, closely following cognitive and motor symptoms. Irritability increases significantly, but this effect seems confined to early stages of HD. Depressive symptoms appear to decline slightly as HD advances, although it is unclear if this is because of antidepressants’ effects, increasing emotional blunting, and waning insight in later stages of HD, or another unknown factor.3 This study did not examine psychotic symptoms over time because few patients were experiencing delusions or hallucinations.
Similar to Thompson et al, Naarding et al5 found that apathy and depression in HD follow distinct time courses. Depression is a feature of early HD and apathy worsens with overall disease progression.
Depressed mood and functional ability—not cognitive or motor symptoms6—are the 2 most critical factors linked to health-related quality of life in HD. Hamilton et al7 found that apathy or executive dysfunction in HD patients is strongly related to decline in ability to complete activities of daily living, and may be severely debilitating.
Apathy. Often mistaken for a symptom of depression, apathy’s presentation may resemble anhedonia or fatigue; however, research suggests that depression and apathy are distinct conditions. Naarding et al
5 noted that apathy is more common than depressive symptoms in HD patients and may be a hallmark symptom of HD.
Depression affects most HD patients, and often is most severe early in the disease course. Hubers et al8 found that 20% of 100 HD patients had suicidal ideation. The strongest predictor was depressed mood.
Sleep disturbances and daytime somnolence are common among HD patients, and patients with comorbid depression report more disturbed sleep. Managing disturbed sleep and daytime somnolence in HD, with emphasis on comorbid depression, may improve the quality of life of patients and their caregivers.9
Anxiety was present in >50% of HD patients in a study by Paulsen et al2 and 37% evaluated by Craufurd et al.10 Craufurd et al10 also reported that 61% of patients were “physically tense and unable to relax.”
Among HD patients, 5% report obsessions and 10% report compulsive behaviors; these symptoms appear to become increasingly common as HD progresses.4,10
Impulsivity and disinhibition. Craufurd et al10 found that 71% of HD patients experienced poor judgment and self-monitoring, 40% had poor temper control and verbal outbursts, 22% exhibited threatening behavior or violence, and 6% had disinhibited or inappropriate sexual behavior.10
Recent studies have shown higher rates of disinhibition in “presymptomatic” gene-positive subjects vs gene-negative controls, suggesting that these symptoms may arise early in HD.11 Further, researchers demonstrated that patients lack symptom awareness and rate themselves as less impaired than their caregivers do.11
In our clinical experience, impulsivity frequently is encountered and creates significant conflict between patients and their caregivers. We speculate that when coupled with depressive symptoms of HD, impulsivity and disinhibition may play an important role in the high rates of suicidality seen in these patients.
Psychosis. Delusions and hallucinations are less common in HD than other psychiatric symptoms. Craufurd et al10 reported 3% of HD patients had delusions, 3% had auditory hallucinations, 2% had tactile hallucinations, and no patients had visual hallucinations.
A few case reports and a small study by Tsuang et al12 suggested that psychotic features in HD may be similar to those seen in paranoid schizophrenia. Tsuang et al12 also noted that more severe HD-related psychosis tends to cluster in families, which suggests that susceptibility to HD psychosis may be heritable.
Treating psychiatric symptoms
High-quality randomized controlled trials of pharmacotherapies for psychiatric symptoms in HD patients are lacking. Decisions regarding which agents to use often are based on case reports or clinical experience. The suggestions below are based on available evidence and our clinical experience.
Depression. Depressive symptoms in HD seem to respond to conventional pharmacologic treatments for major depressive disorder (MDD). A small trial of venlafaxine extended-release (XR) in 26 HD patients with MDD showed statistically significant improvements in depressive symptoms; however, this trial was not blinded and did not have a placebo group.13 In addition, 1 in 5 patients developed significant side effects—nausea, irritability, or worsening chorea.13
Evidence for selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants (TCAs) is lacking. Antidepressant choice should be based on patient response, side effect profile, and the need for secondary therapeutic effects.14
We often prescribe sertraline, citalopram, or escitalopram for our HD patients because of the relative absence of drug-drug interactions and favorable safety profile in medically and surgically ill patients. However, it’s important to tailor the treatment approach to your patient’s needs—eg, patients prone to forgetting their medicine may benefit from a drug with a longer half-life, such as fluoxetine. We avoid TCAs because of their anticholinergic effects, which may worsen dementia symptoms. Because HD patients have high rates of suicidality, agents that are highly toxic when taken in overdose should be used with caution.
One small study of HD patients with MDD or bipolar disorder showed clinical improvement in depressive symptoms after electroconvulsive therapy (ECT).15 Patients who suffered from comorbid delusions had the best improvements in mood.15 ECT likely is a good choice for HD patients who have failed several antidepressants, are suicidal, or who have depression with psychotic features.16
Apathy. A 2011 review concluded that no evidence-based recommendations regarding pharmacologic treatment for apathy in HD can be made because of lack of research.7 The Huntington’s Disease Society of America’s (HDSA) A Physician’s Guide to Managing Huntington’s Disease includes recommendations for treating apathy based on clinical experience.16 It suggests a nonsedating SSRI, followed by a trial of methylphenidate, pemoline, or dextroamphetamine if SSRIs were unsuccessful.
16 The HDSA guide notes psychostimulants may worsen irritability in HD and have a high potential for abuse. ECT appears to have little effect on apathy.15
Anxiety. A small, open-label study of 11 patients found that olanzapine, 5 mg/d, significantly improved depression, anxiety, irritability, and obsessive behavior in HD patients.17
The HDSA guide suggests treating anxiety and obsessive-compulsive symptoms as you would in patients without HD. For anxiety, SSRIs and possibly a short-term trial of a low-dose benzodiazepine (ie, lorazepam, clonazepam) are suggested.16 Benzodiazepines may increase the risk of falls and delirium in this population. Anecdotally, buspirone is helpful in some patients, with a starting dose of 5 mg 2 to 3 times per day and increased to 20 to 30 mg/d in divided doses.16 For obsessive-compulsive symptoms, SSRIs are recommended; atypical antipsychotics are reserved for severe or refractory symptoms.16
Disinhibition and impulsivity. There’s no research on treating disinhibition and impulsivity in HD. In our clinical experience, atypical antipsychotics are the most helpful. Factors regarding choosing an agent and dosing levels are similar to those for psychotic symptoms.
Psychotic symptoms. Most studies of typical and atypical antipsychotics for HD psychosis have shown beneficial effects.14,16-21 Neurologists frequently use these agents for managing chorea. Both neurologic and psychiatric features of the patient’s presentation must be considered when selecting a drug because treatment directed at 1 component of the disease may inadvertently exacerbate another. Specifically, higher potency antipsychotics (eg, haloperidol) are effective for chorea but can dramatically worsen bradykinesia; lower potency agents (eg, quetiapine) are less helpful for chorea but do not significantly worsen rigidity symptoms.
Olanzapine has been shown to improve chorea, anxiety, irritability, depression, sleep dysfunction, and weight loss in addition to psychotic symptoms.14,17 We find that olanzapine treats a constellation of symptoms common among HD patients, and we prescribe it frequently. Because olanzapine is considered a mid-potency agent, we find it’s best suited for concurrent control of psychotic symptoms and mild to moderate chorea in patients with minimal bradykinesia. Start olanzapine at 2.5 mg/d and gradually increase to 5 to 10 mg/d as tolerated.14
Risperidone is effective for treating psychosis and chorea. It can be started at 0.5 to 1 mg/d, and gradually increased to 6 to 8 mg/d.14 The depot formulation of risperidone has been shown to be effective in HD, which may help patients adhere to their medication.18 Risperidone is a mid-high potency antipsychotic, and in our experience is best used to control psychotic symptoms in patients with moderate chorea and few or no symptoms of bradykinesia or rigidity.
Quetiapine reduces psychotic symptoms, agitation, irritability, and insomnia without worsening bradykinesia or rigidity,19 but it is not beneficial for chorea. It can be started at 12.5 mg/d and gradually increased for effect as tolerated, up to 600 mg/d (depending on indication), in 2 or 3 divided doses.14
Haloperidol is a high-potency typical antipsychotic and may help psychotic patients with severe chorea; it should not be used in patients with bradykinesia. Start haloperidol at 0.5 to 1 mg/d and gradually increase to 6 to 8 mg/d as tolerated.14 Because of higher likelihood of side effects with typical antipsychotics, we often reserve its use for patients whose psychosis does not respond to atypical agents.
Other antipsychotics. Aripiprazole in HD has been examined in only 2 single- patient case reports20,21; the drug appeared to reduce psychosis and possibly chorea. Clozapine’s effectiveness for HD psychosis is not well known. It does not appear to be helpful for chorea and can cause agranulocytosis.22
Because one of the hallmarks of HD is dementia, it is worth noting that the FDA has issued a “black-box” warning on the use of antipsychotic drugs in patients with dementia because of concerns regarding increased mortality. However, drawing specific conclusions is difficult because the FDA warning is based on studies that looked primarily at Alzheimer’s disease and vascular dementia, not HD.
Other pharmacotherapies
Tetrabenazine is the only FDA-approved drug for treating HD. However, it carries a “black-box” warning for increased risk of depression and suicidal ideation and is contraindicated in suicidal patients and those with untreated or inadequately treated depression.
Although several small trials have had conflicting results regarding its benefit, amantadine sometimes is used to treat chorea.23-25 For more information about tetrabenazine and amantadine, see Box 3.
Tetrabenazine, the only FDA-approved drug for treating Huntington’s disease (HD), is a dopamine-depleting agent given to control chorea. In a 12-week, randomized, double-blind, placebo-controlled clinical trial, tetrabenazine was shown to be effective in HD patients.a Treatment with tetrabenazine results in symptomatic improvement of chorea, but does not slow or alter the course of the disease. Tetrabenazine can provide relief from choreiform movements, but these benefits should be balanced with the risks of depression and suicidality.a Tetrabenazine is known to prolong QTc interval, and should be used with caution in combination with other drugs that have the potential to do the same (eg, antipsychotics).a
Several case reports have found an association between tetrabenazine and development of neuroleptic malignant syndrome (NMS).b-d Be aware of the clinical characteristics of NMS—mental status change, rigidity, fever, and dysautonomia—and use caution when starting patients taking tetrabenazine on antipsychotics or other agents known to cause NMS.
Amantadine also has been used to treat chorea in HD patients who are unable to tolerate tetrabenazine or antipsychotics. Our neurologists sometimes have found it to be beneficial in patients with juvenile-onset HD because these patients often have debilitating dystonia. Be aware that amantadine is known to precipitate or worsen psychosis.e
References
- Food and Drug Administration. NDA 21-894 Xenazine® (tetrabenazine). Risk evaluation and mitigation strategy (REMS). Click here. Published August 15, 2008. Updated April 2011. Accessed June 20, 2012.
- Stevens E, Roman A, Houa M, et al. Severe hyperthermia during tetrabenazine therapy for tardive dyskinesia. Intensive Care Med. 1998;24(4):369-371.
- Petzinger GM, Bressman SB. A case of tetrabenazine-induced neuroleptic malignant syndrome after prolonged treatment. Mov Disord. 1997;12(2):246-248.
- Ossemann M, Sindic CJ, Laterre C. Tetrabenazine as a cause of neuroleptic malignant syndrome. Mov Disord. 1996;11(1):95.
- Wolters EC. Dopaminomimetic psychosis in Parkinson’s disease patients: diagnosis and treatment. Neurology. 1999;52 (7 suppl 3):S10-S13.
Related Resources
- Huntington’s Disease Society of America. www.hdsa.org.
- Family Caregiver Alliance. Huntington’s disease. www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=574.
- Huntington Study Group. www.huntington-study-group.org.
- Huntington’s Disease Advocacy Center. www.hdac.org.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Wellbutrin XL, others
- Buspirone • BuSpar
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Dextroamphetamine • Dexedrine
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
- Methylphenidate • Concerta, Ritalin, others
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Tetrabenazine • Xenazine
- Venlafaxine XR • Effexor XR
Disclosures
Dr. Scher is a consultant to the advisory board for Lundbeck.
Ms. Kocsis reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Harper PS. The epidemiology of Huntington’s disease. Hum Genet. 1992;89(4):365-376.
2. Paulsen JS, Ready RE, Hamilton JM, et al. Neuropsychiatric aspects of Huntington’s disease. J Neurol Neurosurg Psychiatry. 2001;71(3):310-314.
3. Thompson JC, Harris J, Sollom AC, et al. Longitudinal evaluation of neuropsychiatric symptoms in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2012;24(1):53-60.
4. Beglinger LJ, Langbehn DR, Duff K, et al. Probability of obsessive and compulsive symptoms in Huntington’s disease. Biol Psychiatry. 2007;61(3):415-418.
5. Naarding P, Janzing JG, Eling P, et al. Apathy is not depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2009;21(3):266-270.
6. Ho AK, Gilbert AS, Mason SL, et al. Health-related quality of life in Huntington’s disease: which factors matter most? Mov Disord. 2009;24(4):574-578.
7. Hamilton JM, Salmon DP, Corey-Bloom J, et al. Behavioural abnormalities contribute to functional decline in Huntington’s disease. J Neurol Neurosurg Psychiatry. 2003;74(1):120-122.
8. Hubers AA, Reedeker N, Giltay EJ, et al. Suicidality in Huntington’s disease. J Affect Disord. 2012;136(3):550-557.
9. Videnovic A, Leurgans S, Fan W, et al. Daytime somnolence and nocturnal sleep disturbances in Huntington disease. Parkinsonism Relat Disord. 2009;15(6):471-474.
10. Craufurd D, Thompson JC, Snowden JS. Behavioral changes in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(4):219-226.
11. Duff K, Paulsen JS, Beglinger LJ, et al. “Frontal” behaviors before the diagnosis of Huntington’s disease and their relationship to markers of disease progression: evidence of early lack of awareness. J Neuropsychiatry Clin Neurosci. 2010;22(2):196-207.
12. Tsuang D, Almqvist EW, Lipe H, et al. Familial aggregation of psychotic symptoms in Huntington’s disease. Am J Psychiatry. 2000;157(12):1955-1959.
13. Holl AK, Wilkinson L, Painold A, et al. Combating depression in Huntington’s disease: effective antidepressive treatment with venlafaxine XR. Int Clin Psychopharmacol. 2010;25(1):46-50.
14. Killoran A, Biglan KM. Therapeutics in Huntington’s disease. Curr Treat Options Neurol. 2012;14(2):137-149.
15. Ranen NG, Peyser CE, Folstein SE. ECT as a treatment for depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 1994;6(2):154-159.
16. Rosenblatt A, Ranen NG, Nance MA, et al. A physician’s guide to the management of Huntington’s disease. 2nd edition. http://www.hdsa.org/images/content/1/1/11289.pdf. Published 1999. Accessed July 27, 2012.
17. Squitieri F, Cannella M, Piorcellini A, et al. Short-term effects of olanzapine in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(1):69-72.
18. Johnston TG. Risperidone long-acting injection and Huntington’s disease: case series with significant psychiatric and behavioural symptoms. Int Clin Psychopharmacol. 2011;26(2):114-119.
19. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
20. Lin WC, Chou YH. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
21. Oulis P, Mourikis I, Konstantakopoulos G, et al. Aripiprazole in the treatment of olanzapine-resistant psychotic and motor symptoms of Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2010;22(3):352c.e4-352c.e5.
22. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomised comparative study. J Neurol Neurosurg Psychiatry. 1997;63(1):35-39.
23. Verhagen Metman L, Morris MJ, Farmer C, et al. Huntington’s disease: a randomized, controlled trial using the NMDA-antagonist amantadine. Neurology. 2002;59(5):694-699.
24. Lucetti C, Del Dotto P, Gambaccini G, et al. IV amantadine improves chorea in Huntington’s disease: an acute randomized, controlled study. Neurology. 2003;60(12):1995-1997.
25. O’Suilleabhain P, Dewey RB, Jr. A randomized trial of amantadine in Huntington disease. Arch Neurol. 2003;60(7):996-998.
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatric symptoms are a common and debilitating manifestation of Huntington’s disease (HD), a progressive, inherited neurodegenerative disorder also characterized by chorea (involuntary, nonrepetitive movements) and cognitive decline. The prevalence of HD is 4 to 8 patients per 100,000 persons in most populations of European descent, with lower prevalence among non-Europeans.1 HD is caused by an abnormal expansion of a trinucleotide (CAG) repeat sequence on chromosome 4, and is inherited in an autosomal dominant fashion, meaning a HD patient’s child has a 50% chance of inheriting the mutation. The expansion is located in the gene that encodes the “huntingtin” protein, the normal function of which is not well understood.
There’s no cure for HD, and treatments primarily are directed at symptom control. Psychiatric symptoms include depression, apathy, anxiety, and psychosis (Table).2-4 Treating patients with HD can be challenging because most psychiatrists will see only a handful of patients with this multifaceted illness during their careers. See Box 1 for a case study of a patient with HD.
Table
Psychiatric symptoms of HD
| Anxiety |
| Apathy |
| Delusions |
| Disinhibitions, impulsivity, aggressive behavior |
| Dysphoria |
| Euphoria |
| Hallucinations |
| Irritability |
| Obsessions and compulsions |
| HD: Huntington’s disease Source: References 2-4 |
Mr. M, age 50, was diagnosed with Huntington’s disease (HD) 1 year ago. He returns to our psychiatric clinic for treatment of depressive symptoms and temper. Previously, he was prescribed citalopram, 40 mg/d; eventually low-dose olanzapine, 2.5 mg at night, was added. Mr. M reported better temper control, but his low mood, irritability, hopelessness, and amotivation were not significantly improved.
Mr. M left his job at a software company because he had difficulty completing tasks as the result of mood and cognitive changes. He wants to return to work, but feels that he would be unable to complete his job duties.
He begins a trial of bupropion, 150 mg/d, to improve the vegetative component of his mood symptoms to help him return to work. Mr. M now complains of worsening chorea, irritability, and insomnia, with continued difficulty completing tasks. He is intermittently tearful throughout the interview.
Mr. M continues to struggle with mood symptoms that likely are related to the stressful experience of declining function and the intrinsic evolution of HD. His chorea worsens on bupropion; this agent is discontinued and replaced with mirtazapine, 15 mg at night, for his depressive symptoms and insomnia. Citalopram and olanzapine are unchanged. Mr. M is advised to follow up with our HD psychiatry team in 1 month, and is referred for brief psychotherapy. We remind him—as we do for all of our HD patients—to call the HD clinic or 911 if he becomes suicidal. Ongoing treatment efforts likely will be complex, given the multifaceted and progressive nature of his disease.
Psychiatric sequelae
In general, psychiatric symptoms of HD become increasingly prevalent over time (Box 2).3,5 In a 2001 study of 52 HD patients by Paulsen et al,2 51 patients had ≥1 psychiatric symptom, such as dysphoria (69.2%), agitation (67.3%), irritability (65.4%), apathy (55.8%), and anxiety (51.9%); delusions (11.5%) and hallucinations (1.9%) were less prevalent.2 Similarly, Thompson et al3 followed 111 HD patients for ≥3 years and all experienced psychiatric symptoms.
According to Thompson et al,3 the presence and severity of apathy, irritability, and depression trend differently across the course of Huntington’s disease (HD). Apathy worsens with disease progression, closely following cognitive and motor symptoms. Irritability increases significantly, but this effect seems confined to early stages of HD. Depressive symptoms appear to decline slightly as HD advances, although it is unclear if this is because of antidepressants’ effects, increasing emotional blunting, and waning insight in later stages of HD, or another unknown factor.3 This study did not examine psychotic symptoms over time because few patients were experiencing delusions or hallucinations.
Similar to Thompson et al, Naarding et al5 found that apathy and depression in HD follow distinct time courses. Depression is a feature of early HD and apathy worsens with overall disease progression.
Depressed mood and functional ability—not cognitive or motor symptoms6—are the 2 most critical factors linked to health-related quality of life in HD. Hamilton et al7 found that apathy or executive dysfunction in HD patients is strongly related to decline in ability to complete activities of daily living, and may be severely debilitating.
Apathy. Often mistaken for a symptom of depression, apathy’s presentation may resemble anhedonia or fatigue; however, research suggests that depression and apathy are distinct conditions. Naarding et al
5 noted that apathy is more common than depressive symptoms in HD patients and may be a hallmark symptom of HD.
Depression affects most HD patients, and often is most severe early in the disease course. Hubers et al8 found that 20% of 100 HD patients had suicidal ideation. The strongest predictor was depressed mood.
Sleep disturbances and daytime somnolence are common among HD patients, and patients with comorbid depression report more disturbed sleep. Managing disturbed sleep and daytime somnolence in HD, with emphasis on comorbid depression, may improve the quality of life of patients and their caregivers.9
Anxiety was present in >50% of HD patients in a study by Paulsen et al2 and 37% evaluated by Craufurd et al.10 Craufurd et al10 also reported that 61% of patients were “physically tense and unable to relax.”
Among HD patients, 5% report obsessions and 10% report compulsive behaviors; these symptoms appear to become increasingly common as HD progresses.4,10
Impulsivity and disinhibition. Craufurd et al10 found that 71% of HD patients experienced poor judgment and self-monitoring, 40% had poor temper control and verbal outbursts, 22% exhibited threatening behavior or violence, and 6% had disinhibited or inappropriate sexual behavior.10
Recent studies have shown higher rates of disinhibition in “presymptomatic” gene-positive subjects vs gene-negative controls, suggesting that these symptoms may arise early in HD.11 Further, researchers demonstrated that patients lack symptom awareness and rate themselves as less impaired than their caregivers do.11
In our clinical experience, impulsivity frequently is encountered and creates significant conflict between patients and their caregivers. We speculate that when coupled with depressive symptoms of HD, impulsivity and disinhibition may play an important role in the high rates of suicidality seen in these patients.
Psychosis. Delusions and hallucinations are less common in HD than other psychiatric symptoms. Craufurd et al10 reported 3% of HD patients had delusions, 3% had auditory hallucinations, 2% had tactile hallucinations, and no patients had visual hallucinations.
A few case reports and a small study by Tsuang et al12 suggested that psychotic features in HD may be similar to those seen in paranoid schizophrenia. Tsuang et al12 also noted that more severe HD-related psychosis tends to cluster in families, which suggests that susceptibility to HD psychosis may be heritable.
Treating psychiatric symptoms
High-quality randomized controlled trials of pharmacotherapies for psychiatric symptoms in HD patients are lacking. Decisions regarding which agents to use often are based on case reports or clinical experience. The suggestions below are based on available evidence and our clinical experience.
Depression. Depressive symptoms in HD seem to respond to conventional pharmacologic treatments for major depressive disorder (MDD). A small trial of venlafaxine extended-release (XR) in 26 HD patients with MDD showed statistically significant improvements in depressive symptoms; however, this trial was not blinded and did not have a placebo group.13 In addition, 1 in 5 patients developed significant side effects—nausea, irritability, or worsening chorea.13
Evidence for selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants (TCAs) is lacking. Antidepressant choice should be based on patient response, side effect profile, and the need for secondary therapeutic effects.14
We often prescribe sertraline, citalopram, or escitalopram for our HD patients because of the relative absence of drug-drug interactions and favorable safety profile in medically and surgically ill patients. However, it’s important to tailor the treatment approach to your patient’s needs—eg, patients prone to forgetting their medicine may benefit from a drug with a longer half-life, such as fluoxetine. We avoid TCAs because of their anticholinergic effects, which may worsen dementia symptoms. Because HD patients have high rates of suicidality, agents that are highly toxic when taken in overdose should be used with caution.
One small study of HD patients with MDD or bipolar disorder showed clinical improvement in depressive symptoms after electroconvulsive therapy (ECT).15 Patients who suffered from comorbid delusions had the best improvements in mood.15 ECT likely is a good choice for HD patients who have failed several antidepressants, are suicidal, or who have depression with psychotic features.16
Apathy. A 2011 review concluded that no evidence-based recommendations regarding pharmacologic treatment for apathy in HD can be made because of lack of research.7 The Huntington’s Disease Society of America’s (HDSA) A Physician’s Guide to Managing Huntington’s Disease includes recommendations for treating apathy based on clinical experience.16 It suggests a nonsedating SSRI, followed by a trial of methylphenidate, pemoline, or dextroamphetamine if SSRIs were unsuccessful.
16 The HDSA guide notes psychostimulants may worsen irritability in HD and have a high potential for abuse. ECT appears to have little effect on apathy.15
Anxiety. A small, open-label study of 11 patients found that olanzapine, 5 mg/d, significantly improved depression, anxiety, irritability, and obsessive behavior in HD patients.17
The HDSA guide suggests treating anxiety and obsessive-compulsive symptoms as you would in patients without HD. For anxiety, SSRIs and possibly a short-term trial of a low-dose benzodiazepine (ie, lorazepam, clonazepam) are suggested.16 Benzodiazepines may increase the risk of falls and delirium in this population. Anecdotally, buspirone is helpful in some patients, with a starting dose of 5 mg 2 to 3 times per day and increased to 20 to 30 mg/d in divided doses.16 For obsessive-compulsive symptoms, SSRIs are recommended; atypical antipsychotics are reserved for severe or refractory symptoms.16
Disinhibition and impulsivity. There’s no research on treating disinhibition and impulsivity in HD. In our clinical experience, atypical antipsychotics are the most helpful. Factors regarding choosing an agent and dosing levels are similar to those for psychotic symptoms.
Psychotic symptoms. Most studies of typical and atypical antipsychotics for HD psychosis have shown beneficial effects.14,16-21 Neurologists frequently use these agents for managing chorea. Both neurologic and psychiatric features of the patient’s presentation must be considered when selecting a drug because treatment directed at 1 component of the disease may inadvertently exacerbate another. Specifically, higher potency antipsychotics (eg, haloperidol) are effective for chorea but can dramatically worsen bradykinesia; lower potency agents (eg, quetiapine) are less helpful for chorea but do not significantly worsen rigidity symptoms.
Olanzapine has been shown to improve chorea, anxiety, irritability, depression, sleep dysfunction, and weight loss in addition to psychotic symptoms.14,17 We find that olanzapine treats a constellation of symptoms common among HD patients, and we prescribe it frequently. Because olanzapine is considered a mid-potency agent, we find it’s best suited for concurrent control of psychotic symptoms and mild to moderate chorea in patients with minimal bradykinesia. Start olanzapine at 2.5 mg/d and gradually increase to 5 to 10 mg/d as tolerated.14
Risperidone is effective for treating psychosis and chorea. It can be started at 0.5 to 1 mg/d, and gradually increased to 6 to 8 mg/d.14 The depot formulation of risperidone has been shown to be effective in HD, which may help patients adhere to their medication.18 Risperidone is a mid-high potency antipsychotic, and in our experience is best used to control psychotic symptoms in patients with moderate chorea and few or no symptoms of bradykinesia or rigidity.
Quetiapine reduces psychotic symptoms, agitation, irritability, and insomnia without worsening bradykinesia or rigidity,19 but it is not beneficial for chorea. It can be started at 12.5 mg/d and gradually increased for effect as tolerated, up to 600 mg/d (depending on indication), in 2 or 3 divided doses.14
Haloperidol is a high-potency typical antipsychotic and may help psychotic patients with severe chorea; it should not be used in patients with bradykinesia. Start haloperidol at 0.5 to 1 mg/d and gradually increase to 6 to 8 mg/d as tolerated.14 Because of higher likelihood of side effects with typical antipsychotics, we often reserve its use for patients whose psychosis does not respond to atypical agents.
Other antipsychotics. Aripiprazole in HD has been examined in only 2 single- patient case reports20,21; the drug appeared to reduce psychosis and possibly chorea. Clozapine’s effectiveness for HD psychosis is not well known. It does not appear to be helpful for chorea and can cause agranulocytosis.22
Because one of the hallmarks of HD is dementia, it is worth noting that the FDA has issued a “black-box” warning on the use of antipsychotic drugs in patients with dementia because of concerns regarding increased mortality. However, drawing specific conclusions is difficult because the FDA warning is based on studies that looked primarily at Alzheimer’s disease and vascular dementia, not HD.
Other pharmacotherapies
Tetrabenazine is the only FDA-approved drug for treating HD. However, it carries a “black-box” warning for increased risk of depression and suicidal ideation and is contraindicated in suicidal patients and those with untreated or inadequately treated depression.
Although several small trials have had conflicting results regarding its benefit, amantadine sometimes is used to treat chorea.23-25 For more information about tetrabenazine and amantadine, see Box 3.
Tetrabenazine, the only FDA-approved drug for treating Huntington’s disease (HD), is a dopamine-depleting agent given to control chorea. In a 12-week, randomized, double-blind, placebo-controlled clinical trial, tetrabenazine was shown to be effective in HD patients.a Treatment with tetrabenazine results in symptomatic improvement of chorea, but does not slow or alter the course of the disease. Tetrabenazine can provide relief from choreiform movements, but these benefits should be balanced with the risks of depression and suicidality.a Tetrabenazine is known to prolong QTc interval, and should be used with caution in combination with other drugs that have the potential to do the same (eg, antipsychotics).a
Several case reports have found an association between tetrabenazine and development of neuroleptic malignant syndrome (NMS).b-d Be aware of the clinical characteristics of NMS—mental status change, rigidity, fever, and dysautonomia—and use caution when starting patients taking tetrabenazine on antipsychotics or other agents known to cause NMS.
Amantadine also has been used to treat chorea in HD patients who are unable to tolerate tetrabenazine or antipsychotics. Our neurologists sometimes have found it to be beneficial in patients with juvenile-onset HD because these patients often have debilitating dystonia. Be aware that amantadine is known to precipitate or worsen psychosis.e
References
- Food and Drug Administration. NDA 21-894 Xenazine® (tetrabenazine). Risk evaluation and mitigation strategy (REMS). Click here. Published August 15, 2008. Updated April 2011. Accessed June 20, 2012.
- Stevens E, Roman A, Houa M, et al. Severe hyperthermia during tetrabenazine therapy for tardive dyskinesia. Intensive Care Med. 1998;24(4):369-371.
- Petzinger GM, Bressman SB. A case of tetrabenazine-induced neuroleptic malignant syndrome after prolonged treatment. Mov Disord. 1997;12(2):246-248.
- Ossemann M, Sindic CJ, Laterre C. Tetrabenazine as a cause of neuroleptic malignant syndrome. Mov Disord. 1996;11(1):95.
- Wolters EC. Dopaminomimetic psychosis in Parkinson’s disease patients: diagnosis and treatment. Neurology. 1999;52 (7 suppl 3):S10-S13.
Related Resources
- Huntington’s Disease Society of America. www.hdsa.org.
- Family Caregiver Alliance. Huntington’s disease. www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=574.
- Huntington Study Group. www.huntington-study-group.org.
- Huntington’s Disease Advocacy Center. www.hdac.org.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Wellbutrin XL, others
- Buspirone • BuSpar
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Dextroamphetamine • Dexedrine
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
- Methylphenidate • Concerta, Ritalin, others
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Tetrabenazine • Xenazine
- Venlafaxine XR • Effexor XR
Disclosures
Dr. Scher is a consultant to the advisory board for Lundbeck.
Ms. Kocsis reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatric symptoms are a common and debilitating manifestation of Huntington’s disease (HD), a progressive, inherited neurodegenerative disorder also characterized by chorea (involuntary, nonrepetitive movements) and cognitive decline. The prevalence of HD is 4 to 8 patients per 100,000 persons in most populations of European descent, with lower prevalence among non-Europeans.1 HD is caused by an abnormal expansion of a trinucleotide (CAG) repeat sequence on chromosome 4, and is inherited in an autosomal dominant fashion, meaning a HD patient’s child has a 50% chance of inheriting the mutation. The expansion is located in the gene that encodes the “huntingtin” protein, the normal function of which is not well understood.
There’s no cure for HD, and treatments primarily are directed at symptom control. Psychiatric symptoms include depression, apathy, anxiety, and psychosis (Table).2-4 Treating patients with HD can be challenging because most psychiatrists will see only a handful of patients with this multifaceted illness during their careers. See Box 1 for a case study of a patient with HD.
Table
Psychiatric symptoms of HD
| Anxiety |
| Apathy |
| Delusions |
| Disinhibitions, impulsivity, aggressive behavior |
| Dysphoria |
| Euphoria |
| Hallucinations |
| Irritability |
| Obsessions and compulsions |
| HD: Huntington’s disease Source: References 2-4 |
Mr. M, age 50, was diagnosed with Huntington’s disease (HD) 1 year ago. He returns to our psychiatric clinic for treatment of depressive symptoms and temper. Previously, he was prescribed citalopram, 40 mg/d; eventually low-dose olanzapine, 2.5 mg at night, was added. Mr. M reported better temper control, but his low mood, irritability, hopelessness, and amotivation were not significantly improved.
Mr. M left his job at a software company because he had difficulty completing tasks as the result of mood and cognitive changes. He wants to return to work, but feels that he would be unable to complete his job duties.
He begins a trial of bupropion, 150 mg/d, to improve the vegetative component of his mood symptoms to help him return to work. Mr. M now complains of worsening chorea, irritability, and insomnia, with continued difficulty completing tasks. He is intermittently tearful throughout the interview.
Mr. M continues to struggle with mood symptoms that likely are related to the stressful experience of declining function and the intrinsic evolution of HD. His chorea worsens on bupropion; this agent is discontinued and replaced with mirtazapine, 15 mg at night, for his depressive symptoms and insomnia. Citalopram and olanzapine are unchanged. Mr. M is advised to follow up with our HD psychiatry team in 1 month, and is referred for brief psychotherapy. We remind him—as we do for all of our HD patients—to call the HD clinic or 911 if he becomes suicidal. Ongoing treatment efforts likely will be complex, given the multifaceted and progressive nature of his disease.
Psychiatric sequelae
In general, psychiatric symptoms of HD become increasingly prevalent over time (Box 2).3,5 In a 2001 study of 52 HD patients by Paulsen et al,2 51 patients had ≥1 psychiatric symptom, such as dysphoria (69.2%), agitation (67.3%), irritability (65.4%), apathy (55.8%), and anxiety (51.9%); delusions (11.5%) and hallucinations (1.9%) were less prevalent.2 Similarly, Thompson et al3 followed 111 HD patients for ≥3 years and all experienced psychiatric symptoms.
According to Thompson et al,3 the presence and severity of apathy, irritability, and depression trend differently across the course of Huntington’s disease (HD). Apathy worsens with disease progression, closely following cognitive and motor symptoms. Irritability increases significantly, but this effect seems confined to early stages of HD. Depressive symptoms appear to decline slightly as HD advances, although it is unclear if this is because of antidepressants’ effects, increasing emotional blunting, and waning insight in later stages of HD, or another unknown factor.3 This study did not examine psychotic symptoms over time because few patients were experiencing delusions or hallucinations.
Similar to Thompson et al, Naarding et al5 found that apathy and depression in HD follow distinct time courses. Depression is a feature of early HD and apathy worsens with overall disease progression.
Depressed mood and functional ability—not cognitive or motor symptoms6—are the 2 most critical factors linked to health-related quality of life in HD. Hamilton et al7 found that apathy or executive dysfunction in HD patients is strongly related to decline in ability to complete activities of daily living, and may be severely debilitating.
Apathy. Often mistaken for a symptom of depression, apathy’s presentation may resemble anhedonia or fatigue; however, research suggests that depression and apathy are distinct conditions. Naarding et al
5 noted that apathy is more common than depressive symptoms in HD patients and may be a hallmark symptom of HD.
Depression affects most HD patients, and often is most severe early in the disease course. Hubers et al8 found that 20% of 100 HD patients had suicidal ideation. The strongest predictor was depressed mood.
Sleep disturbances and daytime somnolence are common among HD patients, and patients with comorbid depression report more disturbed sleep. Managing disturbed sleep and daytime somnolence in HD, with emphasis on comorbid depression, may improve the quality of life of patients and their caregivers.9
Anxiety was present in >50% of HD patients in a study by Paulsen et al2 and 37% evaluated by Craufurd et al.10 Craufurd et al10 also reported that 61% of patients were “physically tense and unable to relax.”
Among HD patients, 5% report obsessions and 10% report compulsive behaviors; these symptoms appear to become increasingly common as HD progresses.4,10
Impulsivity and disinhibition. Craufurd et al10 found that 71% of HD patients experienced poor judgment and self-monitoring, 40% had poor temper control and verbal outbursts, 22% exhibited threatening behavior or violence, and 6% had disinhibited or inappropriate sexual behavior.10
Recent studies have shown higher rates of disinhibition in “presymptomatic” gene-positive subjects vs gene-negative controls, suggesting that these symptoms may arise early in HD.11 Further, researchers demonstrated that patients lack symptom awareness and rate themselves as less impaired than their caregivers do.11
In our clinical experience, impulsivity frequently is encountered and creates significant conflict between patients and their caregivers. We speculate that when coupled with depressive symptoms of HD, impulsivity and disinhibition may play an important role in the high rates of suicidality seen in these patients.
Psychosis. Delusions and hallucinations are less common in HD than other psychiatric symptoms. Craufurd et al10 reported 3% of HD patients had delusions, 3% had auditory hallucinations, 2% had tactile hallucinations, and no patients had visual hallucinations.
A few case reports and a small study by Tsuang et al12 suggested that psychotic features in HD may be similar to those seen in paranoid schizophrenia. Tsuang et al12 also noted that more severe HD-related psychosis tends to cluster in families, which suggests that susceptibility to HD psychosis may be heritable.
Treating psychiatric symptoms
High-quality randomized controlled trials of pharmacotherapies for psychiatric symptoms in HD patients are lacking. Decisions regarding which agents to use often are based on case reports or clinical experience. The suggestions below are based on available evidence and our clinical experience.
Depression. Depressive symptoms in HD seem to respond to conventional pharmacologic treatments for major depressive disorder (MDD). A small trial of venlafaxine extended-release (XR) in 26 HD patients with MDD showed statistically significant improvements in depressive symptoms; however, this trial was not blinded and did not have a placebo group.13 In addition, 1 in 5 patients developed significant side effects—nausea, irritability, or worsening chorea.13
Evidence for selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants (TCAs) is lacking. Antidepressant choice should be based on patient response, side effect profile, and the need for secondary therapeutic effects.14
We often prescribe sertraline, citalopram, or escitalopram for our HD patients because of the relative absence of drug-drug interactions and favorable safety profile in medically and surgically ill patients. However, it’s important to tailor the treatment approach to your patient’s needs—eg, patients prone to forgetting their medicine may benefit from a drug with a longer half-life, such as fluoxetine. We avoid TCAs because of their anticholinergic effects, which may worsen dementia symptoms. Because HD patients have high rates of suicidality, agents that are highly toxic when taken in overdose should be used with caution.
One small study of HD patients with MDD or bipolar disorder showed clinical improvement in depressive symptoms after electroconvulsive therapy (ECT).15 Patients who suffered from comorbid delusions had the best improvements in mood.15 ECT likely is a good choice for HD patients who have failed several antidepressants, are suicidal, or who have depression with psychotic features.16
Apathy. A 2011 review concluded that no evidence-based recommendations regarding pharmacologic treatment for apathy in HD can be made because of lack of research.7 The Huntington’s Disease Society of America’s (HDSA) A Physician’s Guide to Managing Huntington’s Disease includes recommendations for treating apathy based on clinical experience.16 It suggests a nonsedating SSRI, followed by a trial of methylphenidate, pemoline, or dextroamphetamine if SSRIs were unsuccessful.
16 The HDSA guide notes psychostimulants may worsen irritability in HD and have a high potential for abuse. ECT appears to have little effect on apathy.15
Anxiety. A small, open-label study of 11 patients found that olanzapine, 5 mg/d, significantly improved depression, anxiety, irritability, and obsessive behavior in HD patients.17
The HDSA guide suggests treating anxiety and obsessive-compulsive symptoms as you would in patients without HD. For anxiety, SSRIs and possibly a short-term trial of a low-dose benzodiazepine (ie, lorazepam, clonazepam) are suggested.16 Benzodiazepines may increase the risk of falls and delirium in this population. Anecdotally, buspirone is helpful in some patients, with a starting dose of 5 mg 2 to 3 times per day and increased to 20 to 30 mg/d in divided doses.16 For obsessive-compulsive symptoms, SSRIs are recommended; atypical antipsychotics are reserved for severe or refractory symptoms.16
Disinhibition and impulsivity. There’s no research on treating disinhibition and impulsivity in HD. In our clinical experience, atypical antipsychotics are the most helpful. Factors regarding choosing an agent and dosing levels are similar to those for psychotic symptoms.
Psychotic symptoms. Most studies of typical and atypical antipsychotics for HD psychosis have shown beneficial effects.14,16-21 Neurologists frequently use these agents for managing chorea. Both neurologic and psychiatric features of the patient’s presentation must be considered when selecting a drug because treatment directed at 1 component of the disease may inadvertently exacerbate another. Specifically, higher potency antipsychotics (eg, haloperidol) are effective for chorea but can dramatically worsen bradykinesia; lower potency agents (eg, quetiapine) are less helpful for chorea but do not significantly worsen rigidity symptoms.
Olanzapine has been shown to improve chorea, anxiety, irritability, depression, sleep dysfunction, and weight loss in addition to psychotic symptoms.14,17 We find that olanzapine treats a constellation of symptoms common among HD patients, and we prescribe it frequently. Because olanzapine is considered a mid-potency agent, we find it’s best suited for concurrent control of psychotic symptoms and mild to moderate chorea in patients with minimal bradykinesia. Start olanzapine at 2.5 mg/d and gradually increase to 5 to 10 mg/d as tolerated.14
Risperidone is effective for treating psychosis and chorea. It can be started at 0.5 to 1 mg/d, and gradually increased to 6 to 8 mg/d.14 The depot formulation of risperidone has been shown to be effective in HD, which may help patients adhere to their medication.18 Risperidone is a mid-high potency antipsychotic, and in our experience is best used to control psychotic symptoms in patients with moderate chorea and few or no symptoms of bradykinesia or rigidity.
Quetiapine reduces psychotic symptoms, agitation, irritability, and insomnia without worsening bradykinesia or rigidity,19 but it is not beneficial for chorea. It can be started at 12.5 mg/d and gradually increased for effect as tolerated, up to 600 mg/d (depending on indication), in 2 or 3 divided doses.14
Haloperidol is a high-potency typical antipsychotic and may help psychotic patients with severe chorea; it should not be used in patients with bradykinesia. Start haloperidol at 0.5 to 1 mg/d and gradually increase to 6 to 8 mg/d as tolerated.14 Because of higher likelihood of side effects with typical antipsychotics, we often reserve its use for patients whose psychosis does not respond to atypical agents.
Other antipsychotics. Aripiprazole in HD has been examined in only 2 single- patient case reports20,21; the drug appeared to reduce psychosis and possibly chorea. Clozapine’s effectiveness for HD psychosis is not well known. It does not appear to be helpful for chorea and can cause agranulocytosis.22
Because one of the hallmarks of HD is dementia, it is worth noting that the FDA has issued a “black-box” warning on the use of antipsychotic drugs in patients with dementia because of concerns regarding increased mortality. However, drawing specific conclusions is difficult because the FDA warning is based on studies that looked primarily at Alzheimer’s disease and vascular dementia, not HD.
Other pharmacotherapies
Tetrabenazine is the only FDA-approved drug for treating HD. However, it carries a “black-box” warning for increased risk of depression and suicidal ideation and is contraindicated in suicidal patients and those with untreated or inadequately treated depression.
Although several small trials have had conflicting results regarding its benefit, amantadine sometimes is used to treat chorea.23-25 For more information about tetrabenazine and amantadine, see Box 3.
Tetrabenazine, the only FDA-approved drug for treating Huntington’s disease (HD), is a dopamine-depleting agent given to control chorea. In a 12-week, randomized, double-blind, placebo-controlled clinical trial, tetrabenazine was shown to be effective in HD patients.a Treatment with tetrabenazine results in symptomatic improvement of chorea, but does not slow or alter the course of the disease. Tetrabenazine can provide relief from choreiform movements, but these benefits should be balanced with the risks of depression and suicidality.a Tetrabenazine is known to prolong QTc interval, and should be used with caution in combination with other drugs that have the potential to do the same (eg, antipsychotics).a
Several case reports have found an association between tetrabenazine and development of neuroleptic malignant syndrome (NMS).b-d Be aware of the clinical characteristics of NMS—mental status change, rigidity, fever, and dysautonomia—and use caution when starting patients taking tetrabenazine on antipsychotics or other agents known to cause NMS.
Amantadine also has been used to treat chorea in HD patients who are unable to tolerate tetrabenazine or antipsychotics. Our neurologists sometimes have found it to be beneficial in patients with juvenile-onset HD because these patients often have debilitating dystonia. Be aware that amantadine is known to precipitate or worsen psychosis.e
References
- Food and Drug Administration. NDA 21-894 Xenazine® (tetrabenazine). Risk evaluation and mitigation strategy (REMS). Click here. Published August 15, 2008. Updated April 2011. Accessed June 20, 2012.
- Stevens E, Roman A, Houa M, et al. Severe hyperthermia during tetrabenazine therapy for tardive dyskinesia. Intensive Care Med. 1998;24(4):369-371.
- Petzinger GM, Bressman SB. A case of tetrabenazine-induced neuroleptic malignant syndrome after prolonged treatment. Mov Disord. 1997;12(2):246-248.
- Ossemann M, Sindic CJ, Laterre C. Tetrabenazine as a cause of neuroleptic malignant syndrome. Mov Disord. 1996;11(1):95.
- Wolters EC. Dopaminomimetic psychosis in Parkinson’s disease patients: diagnosis and treatment. Neurology. 1999;52 (7 suppl 3):S10-S13.
Related Resources
- Huntington’s Disease Society of America. www.hdsa.org.
- Family Caregiver Alliance. Huntington’s disease. www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=574.
- Huntington Study Group. www.huntington-study-group.org.
- Huntington’s Disease Advocacy Center. www.hdac.org.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Wellbutrin XL, others
- Buspirone • BuSpar
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Dextroamphetamine • Dexedrine
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
- Methylphenidate • Concerta, Ritalin, others
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Tetrabenazine • Xenazine
- Venlafaxine XR • Effexor XR
Disclosures
Dr. Scher is a consultant to the advisory board for Lundbeck.
Ms. Kocsis reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Harper PS. The epidemiology of Huntington’s disease. Hum Genet. 1992;89(4):365-376.
2. Paulsen JS, Ready RE, Hamilton JM, et al. Neuropsychiatric aspects of Huntington’s disease. J Neurol Neurosurg Psychiatry. 2001;71(3):310-314.
3. Thompson JC, Harris J, Sollom AC, et al. Longitudinal evaluation of neuropsychiatric symptoms in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2012;24(1):53-60.
4. Beglinger LJ, Langbehn DR, Duff K, et al. Probability of obsessive and compulsive symptoms in Huntington’s disease. Biol Psychiatry. 2007;61(3):415-418.
5. Naarding P, Janzing JG, Eling P, et al. Apathy is not depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2009;21(3):266-270.
6. Ho AK, Gilbert AS, Mason SL, et al. Health-related quality of life in Huntington’s disease: which factors matter most? Mov Disord. 2009;24(4):574-578.
7. Hamilton JM, Salmon DP, Corey-Bloom J, et al. Behavioural abnormalities contribute to functional decline in Huntington’s disease. J Neurol Neurosurg Psychiatry. 2003;74(1):120-122.
8. Hubers AA, Reedeker N, Giltay EJ, et al. Suicidality in Huntington’s disease. J Affect Disord. 2012;136(3):550-557.
9. Videnovic A, Leurgans S, Fan W, et al. Daytime somnolence and nocturnal sleep disturbances in Huntington disease. Parkinsonism Relat Disord. 2009;15(6):471-474.
10. Craufurd D, Thompson JC, Snowden JS. Behavioral changes in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(4):219-226.
11. Duff K, Paulsen JS, Beglinger LJ, et al. “Frontal” behaviors before the diagnosis of Huntington’s disease and their relationship to markers of disease progression: evidence of early lack of awareness. J Neuropsychiatry Clin Neurosci. 2010;22(2):196-207.
12. Tsuang D, Almqvist EW, Lipe H, et al. Familial aggregation of psychotic symptoms in Huntington’s disease. Am J Psychiatry. 2000;157(12):1955-1959.
13. Holl AK, Wilkinson L, Painold A, et al. Combating depression in Huntington’s disease: effective antidepressive treatment with venlafaxine XR. Int Clin Psychopharmacol. 2010;25(1):46-50.
14. Killoran A, Biglan KM. Therapeutics in Huntington’s disease. Curr Treat Options Neurol. 2012;14(2):137-149.
15. Ranen NG, Peyser CE, Folstein SE. ECT as a treatment for depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 1994;6(2):154-159.
16. Rosenblatt A, Ranen NG, Nance MA, et al. A physician’s guide to the management of Huntington’s disease. 2nd edition. http://www.hdsa.org/images/content/1/1/11289.pdf. Published 1999. Accessed July 27, 2012.
17. Squitieri F, Cannella M, Piorcellini A, et al. Short-term effects of olanzapine in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(1):69-72.
18. Johnston TG. Risperidone long-acting injection and Huntington’s disease: case series with significant psychiatric and behavioural symptoms. Int Clin Psychopharmacol. 2011;26(2):114-119.
19. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
20. Lin WC, Chou YH. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
21. Oulis P, Mourikis I, Konstantakopoulos G, et al. Aripiprazole in the treatment of olanzapine-resistant psychotic and motor symptoms of Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2010;22(3):352c.e4-352c.e5.
22. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomised comparative study. J Neurol Neurosurg Psychiatry. 1997;63(1):35-39.
23. Verhagen Metman L, Morris MJ, Farmer C, et al. Huntington’s disease: a randomized, controlled trial using the NMDA-antagonist amantadine. Neurology. 2002;59(5):694-699.
24. Lucetti C, Del Dotto P, Gambaccini G, et al. IV amantadine improves chorea in Huntington’s disease: an acute randomized, controlled study. Neurology. 2003;60(12):1995-1997.
25. O’Suilleabhain P, Dewey RB, Jr. A randomized trial of amantadine in Huntington disease. Arch Neurol. 2003;60(7):996-998.
1. Harper PS. The epidemiology of Huntington’s disease. Hum Genet. 1992;89(4):365-376.
2. Paulsen JS, Ready RE, Hamilton JM, et al. Neuropsychiatric aspects of Huntington’s disease. J Neurol Neurosurg Psychiatry. 2001;71(3):310-314.
3. Thompson JC, Harris J, Sollom AC, et al. Longitudinal evaluation of neuropsychiatric symptoms in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2012;24(1):53-60.
4. Beglinger LJ, Langbehn DR, Duff K, et al. Probability of obsessive and compulsive symptoms in Huntington’s disease. Biol Psychiatry. 2007;61(3):415-418.
5. Naarding P, Janzing JG, Eling P, et al. Apathy is not depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2009;21(3):266-270.
6. Ho AK, Gilbert AS, Mason SL, et al. Health-related quality of life in Huntington’s disease: which factors matter most? Mov Disord. 2009;24(4):574-578.
7. Hamilton JM, Salmon DP, Corey-Bloom J, et al. Behavioural abnormalities contribute to functional decline in Huntington’s disease. J Neurol Neurosurg Psychiatry. 2003;74(1):120-122.
8. Hubers AA, Reedeker N, Giltay EJ, et al. Suicidality in Huntington’s disease. J Affect Disord. 2012;136(3):550-557.
9. Videnovic A, Leurgans S, Fan W, et al. Daytime somnolence and nocturnal sleep disturbances in Huntington disease. Parkinsonism Relat Disord. 2009;15(6):471-474.
10. Craufurd D, Thompson JC, Snowden JS. Behavioral changes in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(4):219-226.
11. Duff K, Paulsen JS, Beglinger LJ, et al. “Frontal” behaviors before the diagnosis of Huntington’s disease and their relationship to markers of disease progression: evidence of early lack of awareness. J Neuropsychiatry Clin Neurosci. 2010;22(2):196-207.
12. Tsuang D, Almqvist EW, Lipe H, et al. Familial aggregation of psychotic symptoms in Huntington’s disease. Am J Psychiatry. 2000;157(12):1955-1959.
13. Holl AK, Wilkinson L, Painold A, et al. Combating depression in Huntington’s disease: effective antidepressive treatment with venlafaxine XR. Int Clin Psychopharmacol. 2010;25(1):46-50.
14. Killoran A, Biglan KM. Therapeutics in Huntington’s disease. Curr Treat Options Neurol. 2012;14(2):137-149.
15. Ranen NG, Peyser CE, Folstein SE. ECT as a treatment for depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 1994;6(2):154-159.
16. Rosenblatt A, Ranen NG, Nance MA, et al. A physician’s guide to the management of Huntington’s disease. 2nd edition. http://www.hdsa.org/images/content/1/1/11289.pdf. Published 1999. Accessed July 27, 2012.
17. Squitieri F, Cannella M, Piorcellini A, et al. Short-term effects of olanzapine in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(1):69-72.
18. Johnston TG. Risperidone long-acting injection and Huntington’s disease: case series with significant psychiatric and behavioural symptoms. Int Clin Psychopharmacol. 2011;26(2):114-119.
19. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
20. Lin WC, Chou YH. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
21. Oulis P, Mourikis I, Konstantakopoulos G, et al. Aripiprazole in the treatment of olanzapine-resistant psychotic and motor symptoms of Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2010;22(3):352c.e4-352c.e5.
22. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomised comparative study. J Neurol Neurosurg Psychiatry. 1997;63(1):35-39.
23. Verhagen Metman L, Morris MJ, Farmer C, et al. Huntington’s disease: a randomized, controlled trial using the NMDA-antagonist amantadine. Neurology. 2002;59(5):694-699.
24. Lucetti C, Del Dotto P, Gambaccini G, et al. IV amantadine improves chorea in Huntington’s disease: an acute randomized, controlled study. Neurology. 2003;60(12):1995-1997.
25. O’Suilleabhain P, Dewey RB, Jr. A randomized trial of amantadine in Huntington disease. Arch Neurol. 2003;60(7):996-998.
Psychiatric advance directives: May you disregard them?
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient stopped antipsychotic medication, experienced a recurrence of paranoid schizophrenia, and now is involuntarily hospitalized. During her admission assessment, she said she had a “psychiatric advance directive.” I obtained the document, which says she refuses psychopharmacologic treatment under any circumstances. Without medication, she might take years to recover. How should I proceed?
Submitted by “Dr. Y”
Most psychiatrists who regularly practice hospital-based care know their state’s legal procedures for forcing psychotic, civilly committed patients to take medication to relieve their acute symptoms. In most jurisdictions, courts will order medication over a patient’s objection after finding that the patient lacks competence to refuse antipsychotic therapy and that the proposed treatment is in the patient’s best interest.1
But if a patient has a psychiatric advance directive (PAD) that opposes psychotropic medication, things may become complicated. To decide what to do if a patient’s PAD precludes administering a treatment you think is necessary, you should understand:
- what PADs do
- what courts have said about PADs
- what your state’s laws say about PADs
- where and when to seek legal advice.
What are advance directives?
An advance directive (or “declaration”) for health care (ADHC) is a legal document executed by a competent individual that states preferences regarding medical treatment should that individual become incapable of making or expressing decisions.2-4 An ADHC may be a “living will” that lays out instructions for specific health care situations or a “durable power of attorney” (DPOA) that designates a proxy decision maker, or it may include elements of both. In 1990, the U.S. Congress passed the Patient Self-Determination Act,5 which required health care institutions that receive Medicare or Medicaid to ask patients whether they have ADHCs and to give patients information about state laws governing ADHCs.
Modeled after medical advance directives, PADs let competent individuals declare their wishes should they need psychiatric treatment during a period of decision-making incapacity.3,4 At least 25 states have advance directive statutes specific to psychiatry.6 Depending on the state, PADs may allow individuals to assert their preferences regarding psychotropic medication, electroconvulsive therapy (ECT), alternatives to hospitalization, location and length of voluntary hospitalization, the treating psychiatrist, seclusion and restraint, emergency medications, and visitors.
Prevalence and praise
The prevalence of PADs is unknown. A 2006 survey of 1,011 psychiatric outpatients in California, Florida, Illinois, Massachusetts, and North Carolina by Swanson et al7 found only 4% to 13% of patients previously executed a PAD. However, most participants said that if given the opportunity and assistance, they would create a PAD.7
Psychiatric advocacy groups have lauded the development of PADs. For example, the National Alliance on Mental Illness’ position is that “PADs should be considered as a way to empower consumers to take a more active role in their treatment, and as a way to avoid conflicts over treatment and medication issues.”8 Proponents suggest that PADs:
- promote autonomy
- foster communication between patients and treatment providers
- increase compliance with medication
- reduce involuntary treatment and judicial involvement.4,8
Mental Health America launched My Plan, My Life: My Psychiatric Advance Directive in September 2011 to increase public awareness of the availability of PADs.9 Therefore, it is safe to assume that most psychiatrists will encounter patients with PADs.
What if a PAD blocks treatment?
What happens when an adult such as Dr. Y’s patient has a PAD that precludes effective treatment? A similar situation led to Hargrave v Vermont.10
Nancy Hargrave, a Vermont woman with schizophrenia and a history of psychiatric hospitalizations, executed a DPOA—Vermont does not have a separate statute for PADs—in which she explicitly refused “any and all anti-psychotic, neuroleptic, psychotropic, or psychoactive medications,” and ECT.10
In anticipation of situations like this, Vermont’s legislature passed Act 114, a 1998 state law that required caregivers to abide by the DPOAs of civilly committed individuals and mentally ill prisoners for 45 days.10 After this time, a court may override the advance directive and allow involuntary medication administration if a patient “ha[d] not experienced a significant clinical improvement in his or her mental state, and remain[ed] incompetent.”10
In 1999, Hargrave sued the state of Vermont and other parties in federal court, alleging that Act 114 constituted discrimination under Title II of the Americans with Disabilities Act11 because Act 114 excluded her from participating in the “services, programs, or activities of a public entity,” namely, the use of her DPOA under Vermont state law.10 The federal district court sided with Hargrave, concluding that “Act 114 was facially discriminatory against mentally disabled individuals.” One year later, the U.S. Court of Appeals for the Second Circuit affirmed the district court’s ruling.
Surprisingly, no other court has adjudicated this issue. However, in Second Circuit states—Vermont, New York, and Connecticut—DPOAs of mentally ill patients cannot be abrogated. This is an unsettling notion for many psychiatrists, because, as Paul Appelbaum, MD, explains, “Advance directives may now constitute an ironclad bulwark against future involuntary treatment with medication—except in emergencies—even for incompetent, committed patients and even when the alternative is long-term institutional care.”12 Other scholars have pointed out that giving physicians an avenue to override or disregard patients’ directives would negate their intended purpose, which is to have one’s competently expressed wishes followed when one’s decision-making capacity is compromised.6,13
Doctors’ duties
How you should respond to an involuntary patient’s PAD depends on which state you practice in. A physician’s obligation to comply with a patient’s PAD depends on state law, and most states with PAD laws provide some latitude or options if physicians believe they should not comply with a patient’s wishes.6,13Table 114-18 cites examples of statutory language regarding a physician’s duty to comply with a PAD.
A survey of 164 psychiatrists in North Carolina provides some insight into psychiatrists’ perceptions of PADs.19 After reading a hypothetical scenario about a mentally ill individual whose PAD expressed refusal of hospitalization or treatment with antipsychotics, 47% of the psychiatrists chose to override the PAD. The authors found that “PAD override was more likely among psychiatrists who worked in hospital emergency departments; those who were concerned about patients’ violence risk and lack of insight; and those who were legally defensive.”
In addition to addressing conflicts between patients’ PADs and doctors’ views about proper treatment, some state laws also contain clauses that spell out the limits of physician liability in cases of physician compliance or noncompliance with PADs. Excerpts from 2 such laws appear in Table 2.16-17
Table 1
Examples of state laws on compliance with psychiatric advance directives
| State | Provider compliance |
|---|---|
| Kentucky14 | Providers must provide mental health treatment that complies with the instructions in an advance directive to the fullest extent possible when the instructions are within standards for mental and physical health care and permitted by state and federal law. Providers may override expressed refusals of treatment only if a court order contradicts the advance directive or an emergency endangers a patient’s life or poses a serious risk to physical health |
| Ohio15 | A provider who does not wish to comply with a patient’s declaration must notify the patient and any proxy and document the notification. The provider may not interfere with the patient’s transfer to another provider who is willing to follow the patient’s declaration. Providers may subject a patient to treatment contrary to a declaration only if:
|
| Oklahoma16 | Physicians and psychologists must follow as closely as possible the terms of a patient’s declaration. A provider who cannot comply with the terms of the patient’s declaration must make arrangements to transfer the patient and the appropriate medical records without delay to another physician or psychologist |
| Pennsylvania17 | If a provider cannot in good conscience comply with a patient’s declaration because the instructions are contrary to accepted clinical practice and medical standards, the provider must make every reasonable effort to help transfer care to another provider who will comply with the declaration. While the transfer is pending, the provider must provide treatment in a way that is consistent with the declaration. If reasonable efforts to transfer fail, the patient may be discharged |
| Utah18 | A physician must comply with a declaration to the fullest extent possible, consistent with reasonable medical practice, the availability of treatments requested, and applicable law. A physician may subject a patient to treatment contrary to wishes expressed in a declaration if:
|
Table 2
Excerpts from state laws on PAD-related liability
| State | Liability or immunity |
|---|---|
| Oklahoma16 | A provider who transfers the patient without unreasonable delay to another provider or who makes a good faith attempt to do so may not be subject to criminal prosecution or civil liability. The provider may not be found to have committed an act of unprofessional conduct for refusal to comply with the terms of the declaration, and transfer under such circumstances shall not constitute abandonment. However, the failure of a provider to transfer in accordance with this subsection shall constitute professional misconduct |
| Pennsylvania17 | A provider who acts in good faith and consistent with the statute may not be subject to criminal or civil liability, discipline for unprofessional conduct, or administrative sanctions. A provider may not be found to have committed an act of unprofessional conduct by the relevant state professional board because the provider refused to comply with:
|
| PAD: psychiatric advance directive | |
Related Resources
- National Resource Center on Psychiatric Advance Directives. www.nrc-pad.org.
- Duke University Program on Psychiatric Advance Directives. http://pad.duhs.duke.edu.
- Hung EK, McNiel DE, Binder RL. Covert medication in psychiatric emergencies: is it ever ethically permissible? J Am Acad Psychiatry Law. 2012;40(2):239-245.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Eclavea RP, Martin LD. State-created right to refuse medication. 53 Am. Jur. 2d Mentally Impaired Persons § 111 (West 2012).
2. Aitken PV, Jr. Incorporating advance care planning into family practice. Am Fam Physician. 1999;59(3):605-614, 617–620.
3. Gallagher EM. Advance directives for psychiatric care: a theoretical and practical overview for legal professionals. Psychol Public Policy Law. 1998;4(3):746-787.
4. DeWolf Bosek MS, Ring ME, Cady RF. Do psychiatric advance directives protect autonomy? JONAS Healthc Law Ethics Regul. 2008;10(1):17-24.
5. Patient Self Determination Act 42 USC § 1395cc 1396a (1994)
6. Swanson JW, McCrary SV, Swartz MS, et al. Superseding psychiatric advance directives: ethical and legal considerations. J Am Acad Psychiatry Law. 2006;34(3):385-394.
7. Swanson J, Swartz M, Ferron J, et al. Psychiatric advance directives among public mental health consumers in five U.S. cities: prevalence, demand, and correlates. J Am Acad Psychiatry Law. 2006;34(1):43-57.
8. National Alliance on Mental Illness. Psychiatric advance directives. http://www.nami.org/Template.cfm?Section=Issue_Spotlights&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=5&ContentID=8217. Accessed July 11, 2012.
9. Mental Health America. My plan, my life: my psychiatric advance directive. http://www.myplanmylife.com. Accessed July 23, 2012.
10. Hargrave v Vermont 340 F3d 27 (2d Cir Vt 2003).
11. Americans with Disabilities Act, 42 USCA § 12132
12. Appelbaum PS. Law & psychiatry: psychiatric advance directives and the treatment of committed patients. Psychiatr Serv. 2004;55(7):751-752, 763.
13. Appelbaum PS. Commentary: psychiatric advance directives at a crossroads—when can PADs be overridden? J Am Acad Psychiatry Law. 2006;34(3):395-397.
14. Ky Rev State § 202A.426 (Michie 2012).
15. Ohio Rev Code § 2135.07 (Page 2012).
16. 43A Okla. St.§ 11-110 (Lexis 2012).
17. 20 Pa. Cons. Stat. §5804.
18. Utah Code Ann. § 62A-15-1003 (Lexis, 2012).
19. Swanson JW, Van McCrary S, Swartz MS, et al. Overriding psychiatric advance directives: factors associated with psychiatrists’ decisions to preempt patients’ advance refusal of hospitalization and medication. Law Hum Behav. 2007;31(1):77-90.
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient stopped antipsychotic medication, experienced a recurrence of paranoid schizophrenia, and now is involuntarily hospitalized. During her admission assessment, she said she had a “psychiatric advance directive.” I obtained the document, which says she refuses psychopharmacologic treatment under any circumstances. Without medication, she might take years to recover. How should I proceed?
Submitted by “Dr. Y”
Most psychiatrists who regularly practice hospital-based care know their state’s legal procedures for forcing psychotic, civilly committed patients to take medication to relieve their acute symptoms. In most jurisdictions, courts will order medication over a patient’s objection after finding that the patient lacks competence to refuse antipsychotic therapy and that the proposed treatment is in the patient’s best interest.1
But if a patient has a psychiatric advance directive (PAD) that opposes psychotropic medication, things may become complicated. To decide what to do if a patient’s PAD precludes administering a treatment you think is necessary, you should understand:
- what PADs do
- what courts have said about PADs
- what your state’s laws say about PADs
- where and when to seek legal advice.
What are advance directives?
An advance directive (or “declaration”) for health care (ADHC) is a legal document executed by a competent individual that states preferences regarding medical treatment should that individual become incapable of making or expressing decisions.2-4 An ADHC may be a “living will” that lays out instructions for specific health care situations or a “durable power of attorney” (DPOA) that designates a proxy decision maker, or it may include elements of both. In 1990, the U.S. Congress passed the Patient Self-Determination Act,5 which required health care institutions that receive Medicare or Medicaid to ask patients whether they have ADHCs and to give patients information about state laws governing ADHCs.
Modeled after medical advance directives, PADs let competent individuals declare their wishes should they need psychiatric treatment during a period of decision-making incapacity.3,4 At least 25 states have advance directive statutes specific to psychiatry.6 Depending on the state, PADs may allow individuals to assert their preferences regarding psychotropic medication, electroconvulsive therapy (ECT), alternatives to hospitalization, location and length of voluntary hospitalization, the treating psychiatrist, seclusion and restraint, emergency medications, and visitors.
Prevalence and praise
The prevalence of PADs is unknown. A 2006 survey of 1,011 psychiatric outpatients in California, Florida, Illinois, Massachusetts, and North Carolina by Swanson et al7 found only 4% to 13% of patients previously executed a PAD. However, most participants said that if given the opportunity and assistance, they would create a PAD.7
Psychiatric advocacy groups have lauded the development of PADs. For example, the National Alliance on Mental Illness’ position is that “PADs should be considered as a way to empower consumers to take a more active role in their treatment, and as a way to avoid conflicts over treatment and medication issues.”8 Proponents suggest that PADs:
- promote autonomy
- foster communication between patients and treatment providers
- increase compliance with medication
- reduce involuntary treatment and judicial involvement.4,8
Mental Health America launched My Plan, My Life: My Psychiatric Advance Directive in September 2011 to increase public awareness of the availability of PADs.9 Therefore, it is safe to assume that most psychiatrists will encounter patients with PADs.
What if a PAD blocks treatment?
What happens when an adult such as Dr. Y’s patient has a PAD that precludes effective treatment? A similar situation led to Hargrave v Vermont.10
Nancy Hargrave, a Vermont woman with schizophrenia and a history of psychiatric hospitalizations, executed a DPOA—Vermont does not have a separate statute for PADs—in which she explicitly refused “any and all anti-psychotic, neuroleptic, psychotropic, or psychoactive medications,” and ECT.10
In anticipation of situations like this, Vermont’s legislature passed Act 114, a 1998 state law that required caregivers to abide by the DPOAs of civilly committed individuals and mentally ill prisoners for 45 days.10 After this time, a court may override the advance directive and allow involuntary medication administration if a patient “ha[d] not experienced a significant clinical improvement in his or her mental state, and remain[ed] incompetent.”10
In 1999, Hargrave sued the state of Vermont and other parties in federal court, alleging that Act 114 constituted discrimination under Title II of the Americans with Disabilities Act11 because Act 114 excluded her from participating in the “services, programs, or activities of a public entity,” namely, the use of her DPOA under Vermont state law.10 The federal district court sided with Hargrave, concluding that “Act 114 was facially discriminatory against mentally disabled individuals.” One year later, the U.S. Court of Appeals for the Second Circuit affirmed the district court’s ruling.
Surprisingly, no other court has adjudicated this issue. However, in Second Circuit states—Vermont, New York, and Connecticut—DPOAs of mentally ill patients cannot be abrogated. This is an unsettling notion for many psychiatrists, because, as Paul Appelbaum, MD, explains, “Advance directives may now constitute an ironclad bulwark against future involuntary treatment with medication—except in emergencies—even for incompetent, committed patients and even when the alternative is long-term institutional care.”12 Other scholars have pointed out that giving physicians an avenue to override or disregard patients’ directives would negate their intended purpose, which is to have one’s competently expressed wishes followed when one’s decision-making capacity is compromised.6,13
Doctors’ duties
How you should respond to an involuntary patient’s PAD depends on which state you practice in. A physician’s obligation to comply with a patient’s PAD depends on state law, and most states with PAD laws provide some latitude or options if physicians believe they should not comply with a patient’s wishes.6,13Table 114-18 cites examples of statutory language regarding a physician’s duty to comply with a PAD.
A survey of 164 psychiatrists in North Carolina provides some insight into psychiatrists’ perceptions of PADs.19 After reading a hypothetical scenario about a mentally ill individual whose PAD expressed refusal of hospitalization or treatment with antipsychotics, 47% of the psychiatrists chose to override the PAD. The authors found that “PAD override was more likely among psychiatrists who worked in hospital emergency departments; those who were concerned about patients’ violence risk and lack of insight; and those who were legally defensive.”
In addition to addressing conflicts between patients’ PADs and doctors’ views about proper treatment, some state laws also contain clauses that spell out the limits of physician liability in cases of physician compliance or noncompliance with PADs. Excerpts from 2 such laws appear in Table 2.16-17
Table 1
Examples of state laws on compliance with psychiatric advance directives
| State | Provider compliance |
|---|---|
| Kentucky14 | Providers must provide mental health treatment that complies with the instructions in an advance directive to the fullest extent possible when the instructions are within standards for mental and physical health care and permitted by state and federal law. Providers may override expressed refusals of treatment only if a court order contradicts the advance directive or an emergency endangers a patient’s life or poses a serious risk to physical health |
| Ohio15 | A provider who does not wish to comply with a patient’s declaration must notify the patient and any proxy and document the notification. The provider may not interfere with the patient’s transfer to another provider who is willing to follow the patient’s declaration. Providers may subject a patient to treatment contrary to a declaration only if:
|
| Oklahoma16 | Physicians and psychologists must follow as closely as possible the terms of a patient’s declaration. A provider who cannot comply with the terms of the patient’s declaration must make arrangements to transfer the patient and the appropriate medical records without delay to another physician or psychologist |
| Pennsylvania17 | If a provider cannot in good conscience comply with a patient’s declaration because the instructions are contrary to accepted clinical practice and medical standards, the provider must make every reasonable effort to help transfer care to another provider who will comply with the declaration. While the transfer is pending, the provider must provide treatment in a way that is consistent with the declaration. If reasonable efforts to transfer fail, the patient may be discharged |
| Utah18 | A physician must comply with a declaration to the fullest extent possible, consistent with reasonable medical practice, the availability of treatments requested, and applicable law. A physician may subject a patient to treatment contrary to wishes expressed in a declaration if:
|
Table 2
Excerpts from state laws on PAD-related liability
| State | Liability or immunity |
|---|---|
| Oklahoma16 | A provider who transfers the patient without unreasonable delay to another provider or who makes a good faith attempt to do so may not be subject to criminal prosecution or civil liability. The provider may not be found to have committed an act of unprofessional conduct for refusal to comply with the terms of the declaration, and transfer under such circumstances shall not constitute abandonment. However, the failure of a provider to transfer in accordance with this subsection shall constitute professional misconduct |
| Pennsylvania17 | A provider who acts in good faith and consistent with the statute may not be subject to criminal or civil liability, discipline for unprofessional conduct, or administrative sanctions. A provider may not be found to have committed an act of unprofessional conduct by the relevant state professional board because the provider refused to comply with:
|
| PAD: psychiatric advance directive | |
Related Resources
- National Resource Center on Psychiatric Advance Directives. www.nrc-pad.org.
- Duke University Program on Psychiatric Advance Directives. http://pad.duhs.duke.edu.
- Hung EK, McNiel DE, Binder RL. Covert medication in psychiatric emergencies: is it ever ethically permissible? J Am Acad Psychiatry Law. 2012;40(2):239-245.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient stopped antipsychotic medication, experienced a recurrence of paranoid schizophrenia, and now is involuntarily hospitalized. During her admission assessment, she said she had a “psychiatric advance directive.” I obtained the document, which says she refuses psychopharmacologic treatment under any circumstances. Without medication, she might take years to recover. How should I proceed?
Submitted by “Dr. Y”
Most psychiatrists who regularly practice hospital-based care know their state’s legal procedures for forcing psychotic, civilly committed patients to take medication to relieve their acute symptoms. In most jurisdictions, courts will order medication over a patient’s objection after finding that the patient lacks competence to refuse antipsychotic therapy and that the proposed treatment is in the patient’s best interest.1
But if a patient has a psychiatric advance directive (PAD) that opposes psychotropic medication, things may become complicated. To decide what to do if a patient’s PAD precludes administering a treatment you think is necessary, you should understand:
- what PADs do
- what courts have said about PADs
- what your state’s laws say about PADs
- where and when to seek legal advice.
What are advance directives?
An advance directive (or “declaration”) for health care (ADHC) is a legal document executed by a competent individual that states preferences regarding medical treatment should that individual become incapable of making or expressing decisions.2-4 An ADHC may be a “living will” that lays out instructions for specific health care situations or a “durable power of attorney” (DPOA) that designates a proxy decision maker, or it may include elements of both. In 1990, the U.S. Congress passed the Patient Self-Determination Act,5 which required health care institutions that receive Medicare or Medicaid to ask patients whether they have ADHCs and to give patients information about state laws governing ADHCs.
Modeled after medical advance directives, PADs let competent individuals declare their wishes should they need psychiatric treatment during a period of decision-making incapacity.3,4 At least 25 states have advance directive statutes specific to psychiatry.6 Depending on the state, PADs may allow individuals to assert their preferences regarding psychotropic medication, electroconvulsive therapy (ECT), alternatives to hospitalization, location and length of voluntary hospitalization, the treating psychiatrist, seclusion and restraint, emergency medications, and visitors.
Prevalence and praise
The prevalence of PADs is unknown. A 2006 survey of 1,011 psychiatric outpatients in California, Florida, Illinois, Massachusetts, and North Carolina by Swanson et al7 found only 4% to 13% of patients previously executed a PAD. However, most participants said that if given the opportunity and assistance, they would create a PAD.7
Psychiatric advocacy groups have lauded the development of PADs. For example, the National Alliance on Mental Illness’ position is that “PADs should be considered as a way to empower consumers to take a more active role in their treatment, and as a way to avoid conflicts over treatment and medication issues.”8 Proponents suggest that PADs:
- promote autonomy
- foster communication between patients and treatment providers
- increase compliance with medication
- reduce involuntary treatment and judicial involvement.4,8
Mental Health America launched My Plan, My Life: My Psychiatric Advance Directive in September 2011 to increase public awareness of the availability of PADs.9 Therefore, it is safe to assume that most psychiatrists will encounter patients with PADs.
What if a PAD blocks treatment?
What happens when an adult such as Dr. Y’s patient has a PAD that precludes effective treatment? A similar situation led to Hargrave v Vermont.10
Nancy Hargrave, a Vermont woman with schizophrenia and a history of psychiatric hospitalizations, executed a DPOA—Vermont does not have a separate statute for PADs—in which she explicitly refused “any and all anti-psychotic, neuroleptic, psychotropic, or psychoactive medications,” and ECT.10
In anticipation of situations like this, Vermont’s legislature passed Act 114, a 1998 state law that required caregivers to abide by the DPOAs of civilly committed individuals and mentally ill prisoners for 45 days.10 After this time, a court may override the advance directive and allow involuntary medication administration if a patient “ha[d] not experienced a significant clinical improvement in his or her mental state, and remain[ed] incompetent.”10
In 1999, Hargrave sued the state of Vermont and other parties in federal court, alleging that Act 114 constituted discrimination under Title II of the Americans with Disabilities Act11 because Act 114 excluded her from participating in the “services, programs, or activities of a public entity,” namely, the use of her DPOA under Vermont state law.10 The federal district court sided with Hargrave, concluding that “Act 114 was facially discriminatory against mentally disabled individuals.” One year later, the U.S. Court of Appeals for the Second Circuit affirmed the district court’s ruling.
Surprisingly, no other court has adjudicated this issue. However, in Second Circuit states—Vermont, New York, and Connecticut—DPOAs of mentally ill patients cannot be abrogated. This is an unsettling notion for many psychiatrists, because, as Paul Appelbaum, MD, explains, “Advance directives may now constitute an ironclad bulwark against future involuntary treatment with medication—except in emergencies—even for incompetent, committed patients and even when the alternative is long-term institutional care.”12 Other scholars have pointed out that giving physicians an avenue to override or disregard patients’ directives would negate their intended purpose, which is to have one’s competently expressed wishes followed when one’s decision-making capacity is compromised.6,13
Doctors’ duties
How you should respond to an involuntary patient’s PAD depends on which state you practice in. A physician’s obligation to comply with a patient’s PAD depends on state law, and most states with PAD laws provide some latitude or options if physicians believe they should not comply with a patient’s wishes.6,13Table 114-18 cites examples of statutory language regarding a physician’s duty to comply with a PAD.
A survey of 164 psychiatrists in North Carolina provides some insight into psychiatrists’ perceptions of PADs.19 After reading a hypothetical scenario about a mentally ill individual whose PAD expressed refusal of hospitalization or treatment with antipsychotics, 47% of the psychiatrists chose to override the PAD. The authors found that “PAD override was more likely among psychiatrists who worked in hospital emergency departments; those who were concerned about patients’ violence risk and lack of insight; and those who were legally defensive.”
In addition to addressing conflicts between patients’ PADs and doctors’ views about proper treatment, some state laws also contain clauses that spell out the limits of physician liability in cases of physician compliance or noncompliance with PADs. Excerpts from 2 such laws appear in Table 2.16-17
Table 1
Examples of state laws on compliance with psychiatric advance directives
| State | Provider compliance |
|---|---|
| Kentucky14 | Providers must provide mental health treatment that complies with the instructions in an advance directive to the fullest extent possible when the instructions are within standards for mental and physical health care and permitted by state and federal law. Providers may override expressed refusals of treatment only if a court order contradicts the advance directive or an emergency endangers a patient’s life or poses a serious risk to physical health |
| Ohio15 | A provider who does not wish to comply with a patient’s declaration must notify the patient and any proxy and document the notification. The provider may not interfere with the patient’s transfer to another provider who is willing to follow the patient’s declaration. Providers may subject a patient to treatment contrary to a declaration only if:
|
| Oklahoma16 | Physicians and psychologists must follow as closely as possible the terms of a patient’s declaration. A provider who cannot comply with the terms of the patient’s declaration must make arrangements to transfer the patient and the appropriate medical records without delay to another physician or psychologist |
| Pennsylvania17 | If a provider cannot in good conscience comply with a patient’s declaration because the instructions are contrary to accepted clinical practice and medical standards, the provider must make every reasonable effort to help transfer care to another provider who will comply with the declaration. While the transfer is pending, the provider must provide treatment in a way that is consistent with the declaration. If reasonable efforts to transfer fail, the patient may be discharged |
| Utah18 | A physician must comply with a declaration to the fullest extent possible, consistent with reasonable medical practice, the availability of treatments requested, and applicable law. A physician may subject a patient to treatment contrary to wishes expressed in a declaration if:
|
Table 2
Excerpts from state laws on PAD-related liability
| State | Liability or immunity |
|---|---|
| Oklahoma16 | A provider who transfers the patient without unreasonable delay to another provider or who makes a good faith attempt to do so may not be subject to criminal prosecution or civil liability. The provider may not be found to have committed an act of unprofessional conduct for refusal to comply with the terms of the declaration, and transfer under such circumstances shall not constitute abandonment. However, the failure of a provider to transfer in accordance with this subsection shall constitute professional misconduct |
| Pennsylvania17 | A provider who acts in good faith and consistent with the statute may not be subject to criminal or civil liability, discipline for unprofessional conduct, or administrative sanctions. A provider may not be found to have committed an act of unprofessional conduct by the relevant state professional board because the provider refused to comply with:
|
| PAD: psychiatric advance directive | |
Related Resources
- National Resource Center on Psychiatric Advance Directives. www.nrc-pad.org.
- Duke University Program on Psychiatric Advance Directives. http://pad.duhs.duke.edu.
- Hung EK, McNiel DE, Binder RL. Covert medication in psychiatric emergencies: is it ever ethically permissible? J Am Acad Psychiatry Law. 2012;40(2):239-245.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Eclavea RP, Martin LD. State-created right to refuse medication. 53 Am. Jur. 2d Mentally Impaired Persons § 111 (West 2012).
2. Aitken PV, Jr. Incorporating advance care planning into family practice. Am Fam Physician. 1999;59(3):605-614, 617–620.
3. Gallagher EM. Advance directives for psychiatric care: a theoretical and practical overview for legal professionals. Psychol Public Policy Law. 1998;4(3):746-787.
4. DeWolf Bosek MS, Ring ME, Cady RF. Do psychiatric advance directives protect autonomy? JONAS Healthc Law Ethics Regul. 2008;10(1):17-24.
5. Patient Self Determination Act 42 USC § 1395cc 1396a (1994)
6. Swanson JW, McCrary SV, Swartz MS, et al. Superseding psychiatric advance directives: ethical and legal considerations. J Am Acad Psychiatry Law. 2006;34(3):385-394.
7. Swanson J, Swartz M, Ferron J, et al. Psychiatric advance directives among public mental health consumers in five U.S. cities: prevalence, demand, and correlates. J Am Acad Psychiatry Law. 2006;34(1):43-57.
8. National Alliance on Mental Illness. Psychiatric advance directives. http://www.nami.org/Template.cfm?Section=Issue_Spotlights&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=5&ContentID=8217. Accessed July 11, 2012.
9. Mental Health America. My plan, my life: my psychiatric advance directive. http://www.myplanmylife.com. Accessed July 23, 2012.
10. Hargrave v Vermont 340 F3d 27 (2d Cir Vt 2003).
11. Americans with Disabilities Act, 42 USCA § 12132
12. Appelbaum PS. Law & psychiatry: psychiatric advance directives and the treatment of committed patients. Psychiatr Serv. 2004;55(7):751-752, 763.
13. Appelbaum PS. Commentary: psychiatric advance directives at a crossroads—when can PADs be overridden? J Am Acad Psychiatry Law. 2006;34(3):395-397.
14. Ky Rev State § 202A.426 (Michie 2012).
15. Ohio Rev Code § 2135.07 (Page 2012).
16. 43A Okla. St.§ 11-110 (Lexis 2012).
17. 20 Pa. Cons. Stat. §5804.
18. Utah Code Ann. § 62A-15-1003 (Lexis, 2012).
19. Swanson JW, Van McCrary S, Swartz MS, et al. Overriding psychiatric advance directives: factors associated with psychiatrists’ decisions to preempt patients’ advance refusal of hospitalization and medication. Law Hum Behav. 2007;31(1):77-90.
1. Eclavea RP, Martin LD. State-created right to refuse medication. 53 Am. Jur. 2d Mentally Impaired Persons § 111 (West 2012).
2. Aitken PV, Jr. Incorporating advance care planning into family practice. Am Fam Physician. 1999;59(3):605-614, 617–620.
3. Gallagher EM. Advance directives for psychiatric care: a theoretical and practical overview for legal professionals. Psychol Public Policy Law. 1998;4(3):746-787.
4. DeWolf Bosek MS, Ring ME, Cady RF. Do psychiatric advance directives protect autonomy? JONAS Healthc Law Ethics Regul. 2008;10(1):17-24.
5. Patient Self Determination Act 42 USC § 1395cc 1396a (1994)
6. Swanson JW, McCrary SV, Swartz MS, et al. Superseding psychiatric advance directives: ethical and legal considerations. J Am Acad Psychiatry Law. 2006;34(3):385-394.
7. Swanson J, Swartz M, Ferron J, et al. Psychiatric advance directives among public mental health consumers in five U.S. cities: prevalence, demand, and correlates. J Am Acad Psychiatry Law. 2006;34(1):43-57.
8. National Alliance on Mental Illness. Psychiatric advance directives. http://www.nami.org/Template.cfm?Section=Issue_Spotlights&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=5&ContentID=8217. Accessed July 11, 2012.
9. Mental Health America. My plan, my life: my psychiatric advance directive. http://www.myplanmylife.com. Accessed July 23, 2012.
10. Hargrave v Vermont 340 F3d 27 (2d Cir Vt 2003).
11. Americans with Disabilities Act, 42 USCA § 12132
12. Appelbaum PS. Law & psychiatry: psychiatric advance directives and the treatment of committed patients. Psychiatr Serv. 2004;55(7):751-752, 763.
13. Appelbaum PS. Commentary: psychiatric advance directives at a crossroads—when can PADs be overridden? J Am Acad Psychiatry Law. 2006;34(3):395-397.
14. Ky Rev State § 202A.426 (Michie 2012).
15. Ohio Rev Code § 2135.07 (Page 2012).
16. 43A Okla. St.§ 11-110 (Lexis 2012).
17. 20 Pa. Cons. Stat. §5804.
18. Utah Code Ann. § 62A-15-1003 (Lexis, 2012).
19. Swanson JW, Van McCrary S, Swartz MS, et al. Overriding psychiatric advance directives: factors associated with psychiatrists’ decisions to preempt patients’ advance refusal of hospitalization and medication. Law Hum Behav. 2007;31(1):77-90.
Understanding PTSD
How to distinguish complicated grief from "normal" grief
The avoidant psychotherapy patient
CASE: Unexplained panic
Mr. J, age 35, is a married, unemployed musician who presents for outpatient treatment for panic attacks. He experienced his first panic attack at his oldest son’s baptism 12 years ago, but does not know why it occurred at that moment. He rarely has panic attacks now, but wants to continue medication management. He denies depressive symptoms, saying, “I’m the most optimistic person in the world.” Mr. J tried several medications for his panic attacks before clonazepam, 2 mg/d, proved effective, but always has been vehemently opposed to antidepressants. Despite his insistence that he needs only medication management, Mr. J chooses to enroll in a resident-run psychotherapy clinic.
In sessions, Mr. J describes his father, who also has panic disorder, as a powerful figure who is physically and emotionally abusive, but also charismatic, charming, and “impossible not to love.” However, Mr. J felt his father was impossible to live with, and moved out at age 18 to marry his high school sweetheart. They have 3 children, ages 12, 10, and 8. Mr. J worked for his father at his construction company, but was not able to satisfy him or live up to his standards so he quit because he was tired of being cut down and emasculated.
Mr. J’s parents divorced 15 years ago after his mother had an affair with her husband’s friend. His father learned of the affair and threatened his wife with a handgun. Although Mr. J and his mother were close before her affair, he has been unable to forgive or empathize with her, and rarely speaks to her. Mr. J’s mother could not protect him from his father’s abuse, and later compounded her failure by abandoning her husband and son through her sexual affair. Growing up with a father he did not respect or get comfort from and sharing a common fear and alliance with his mother likely made it difficult for Mr. J to navigate his Oedipal phase,1 and made her abandonment even more painful.
When Mr. J was 6 years old, he was molested by one of his father’s friends. His father stabbed the man in the shoulder when he found out about the molestation and received probation. Although Mr. J knows he was molested, he does not remember it and has repressed most of his childhood.
The authors’ observations
I (JF) wanted to discuss with Mr. J why his first panic attack occurred during such a symbolic occasion. His panic could be the result of a struggle between a murderous wish toward his father and paternal protective instinct toward his son. The baptism placed his son in a highly vulnerable position, which reminded Mr. J of his own vulnerability and impotent rage toward his father. Anxiety often results when an individual has 2 opposing wishes,2 and a murderous wish often is involved when anxiety progresses to panic. Getting to the root of this with Mr. J could allow for further psychological growth.3 His murderous wishes and fantasies are ego-dystonic, and panic could be a way of punishing himself for these thoughts. When Mr. J identified himself as his son during the baptism, he likely was flooded with thoughts that his defenses were no longer able to repress. Seeing his son submerged in the baptismal font brought back an aspect of his own life that he had completely split off from consciousness, and likely will take time to process. Considering the current therapeutic dynamic, I decided that it was not the best time to address this potential conflict; however, I could have chosen a manualized form of psychodynamic psychotherapy for panic disorder.4 See Table 1 for an outline of the phases of psychodynamic psychotherapy for panic disorder.
Although Mr. J’s initial willingness to discuss his past was encouraging, he refused to schedule more than 1 session every 4 weeks. He also began to keep the content of our sessions superficial, which caused me angst because he seemed to be withholding information and would not come more frequently. Although I was not proud of my feelings, I had to be honest with myself that I had started to dislike Mr. J.
Table 1
Psychodynamic psychotherapy for panic disorder
| Phase | Comments |
|---|---|
| Treatment of acute panic | Therapy focuses on discovering the conscious and unconscious meaning of panic symptoms |
| Treatment of panic vulnerability | Core dynamic conflicts related to panic are understood and altered. Tasks include addressing the nature of the transference and working through them |
| Termination | The therapist directly addresses patients’ difficulties with separation and independence as they emerge in treatment. After treatment, patients may be better able to manage separations, anger, and independence |
| Source: Adapted from reference 4 | |
Countertransference reactions
Countertransference is a therapist's emotional reaction to a patient. Just as patients form reactions based on past relationships brought to present, therapists develop similar reactions.5 Noting one’s countertransference provides a window into how the patient’s thoughts and actions evoke feelings in others. It also can shed light on an aspect of the doctor-patient relationship that may have gone unnoticed.2
Countertransference hatred can occur when a therapist begins to dislike a patient. Typically, patients with borderline personality disorder, masochistic tendencies, or suicidality arouse strong countertransference reactions6; however, any patient can evoke these emotions. This type of hateful patient can precipitate antitherapeutic feelings such as aversion or malice that can be a major obstacle to treatment.7 Aversion leads the therapist to withdraw from the patient, and malice can trigger cruel impulses.
Maltsberger and Buie7 identified 5 defenses therapists may use to combat countertransference hatred (Table 2). When treating Mr. J, I used several of these defenses, including projection and turning against the self to protect myself from this challenging patient. In turning against the self, I became doubtful and critical of my skills and increasingly submissive to Mr. J. Additionally, I projected this countertransference hatred onto Mr. J, focusing on the negative transference that he brought to our therapeutic encounters. On an unconscious level, I may have feared retribution from Mr. J.
I became so frustrated with Mr. J that I reduced the frequency of our sessions to once every 6 weeks, which I realized could be evidence of my feelings regarding Mr. J’s minimization and avoidant style.
Table 2
Defenses against countertransference hate
| Defense mechanism | Description |
|---|---|
| Repression | Remaining unconscious of feelings of hate; may manifest as difficulty paying attention to what the patient is saying or feeling bored or tired |
| Turning against oneself | Doubting one’s capacity to help the patient; may feel inadequate, helpless, and hopeless. May lead to giving up on the patient because the therapist feels incompetent |
| Reaction formation | Turning hatred into the opposite emotion. The therapist may be too preoccupied with being helpful or overly concerned about the patient’s welfare and comfort |
| Projection | Feeling that the patient hates the therapist, leading to feelings of dread and fear |
| Distortion of reality | Devaluing the patient and seeing the patient as a hopeless case or a dangerous person. The therapist may feel indifference, pity, or anger toward the patient |
| Source: Reference 7 | |
TREATMENT: A breakthrough
Mr. J presents with obvious unease at the first visit after we had decreased the frequency of our sessions. At this point, Mr. J opens up to me. He says he has not been truthful with me, and has had worsening depression, anhedonia, and agoraphobia over the past year. He also reveals that he has homosexual fantasies that he cannot stop, which disturb him because he says he is heterosexual. He agrees to come once a week, and reluctantly admits that he desperately needs help.
Although Mr. J only takes clonazepam and citalopram, 20 mg/d, which I prescribed after he admitted to depression and anxiety, he has hyperlipidemia and a family history of heart disease. In addition to being a musician and working at his father’s construction company, he has worked as a security guard, bounty hunter, and computer technician. His careers have been solitary in nature, and, with the exception of computer work, permitted an outlet for aggression. However, he recently started taking online college classes and wants to become a music teacher because he feels he has a lot to offer children as a result of his life experiences. His fantasy of being a teacher shows considerably less aggression, and could be a sign of psychological growth.
Mr. J is struggling financially and his home is on the verge of foreclosure. Early in treatment he told me that he stopped paying his mortgage, but demonstrated blind optimism that things would “work out.” I asked if this was a wise decision, but he seemed confident and dismissive of my concerns. Although he now struggles with this situation, I consider this healthier than his constant pseudo-happy state, and a sign of psychological development.8 Despite his financial stressors, he wants to pursue his dream of being a famous musician, and says he “could never work a 9-to-5 job in a cubicle.”
The authors’ observations
I do not think it’s a coincidence that Mr. J stopped minimizing his symptoms when we decreased the frequency of his sessions. I had viewed our sessions as unproductive and blamed Mr. J for wasting both of our time with his resistance and minimization and had begun to dislike him. I felt impotent because he had been controlling each session with long, elaborate stories that had little relevance to his panic attacks, and I could not redirect him or get him to focus on pertinent issues. It was as if I was an audience for him, and provided nothing useful. However, I was interested in these superficial stories because Mr. J was charming and engaging. He likely reenacted his relationship with his father with me. Mr. J’s superficial relationship with me caused me to dislike him, and, similar to his father, reject him. This rejection likely was damaging because I was unable to anticipate his needs, which would have been to increase—rather than decrease—the frequency of our sessions. Just like his father, I was not able to take care of him.
Mr. J is deeply conflicted about his father. He states that his father “is a monster who instills fear and intimidation into everyone around him, but he’s charismatic, and I’ll always love him.” His view of his domineering father likely developed into a castration anxiety because he was afraid of competing for his mother’s love, contributing to a muddled sexual identity. This was intensified when Mr. J was sexually abused; he may have been stimulated by the molestation, adding to his confusion. Although Mr. J has repressed the abuse and split off most of his childhood, he suffers from shame, guilt, and depression because of his ego-dystonic homosexual fantasies. Homosexuality is at odds with his self-image and contributes to his anxiety and panic attacks. He cannot adequately discharge this dangerous libidinal energy, and as he becomes more conscious of it, his anxiety intensifies.
OUTCOME: Overcoming fear
As Mr. J sits crying in my office, he says he hasn’t cried in front of another man in years. I wonder aloud what his father would think of this situation. His states that his father does not respect any type of weakness and probably would “knock his teeth in.” Overcoming this fear of opening up will be a goal of Mr. J’s treatment. His unbridled optimism borders on pathologic, and is a defense against reality.8 Additionally, his reluctance to accept that he is suffering from depression, which he perceives as a weakness, will be a struggle throughout therapy. He likely will continue to minimize his symptoms when possible, making the true depths of his illness difficult to grasp.
Related Resources
- Waska R. Using countertransference: analytic contact, projective identification, and transference phantasy states. Am J Psychother. 2008;62(4):333-351.
- Gabbard GO, Litowitz BE, Williams P. Textbook of psychoanalysis. Arlington, VA: American Psychiatric Publishing, Inc; 2011.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Blos P. Son and father: before and beyond the Oedipus complex. New York NY: Free Press/Macmillan; 1985.
2. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington VA: American Psychiatric Publishing; 2004.
3. Akhtar S. Comprehensive dictionary of psychoanalysis. London United Kingdom: Kamac Books; 2009.
4. Busch FN, Milrod BL, Singer MB. Theory and technique in psychodynamic treatment of panic disorder. J Psychother Pract Res. 1999;8(3):234-242.
5. Freud S. The future prospects of psycho-analytic therapy. The standard edition of the complete psychological works of Sigmund Freud volume XI (1910): five lectures on psycho-analysis, Leonardo da Vinci and other works. London, United Kingdom: Hogarth Press; 1957:139–152.
6. Winnicott DW. Hate in the counter-transference. J Psychother Pract Res. 1994;3(4):348-356.
7. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
8. Akhtar S. “Someday…” and “if only…” fantasies: pathological optimism and inordinate nostalgia as related forms of idealization. J Am Psychoanal Assoc. 1996;44(3):723-753.
CASE: Unexplained panic
Mr. J, age 35, is a married, unemployed musician who presents for outpatient treatment for panic attacks. He experienced his first panic attack at his oldest son’s baptism 12 years ago, but does not know why it occurred at that moment. He rarely has panic attacks now, but wants to continue medication management. He denies depressive symptoms, saying, “I’m the most optimistic person in the world.” Mr. J tried several medications for his panic attacks before clonazepam, 2 mg/d, proved effective, but always has been vehemently opposed to antidepressants. Despite his insistence that he needs only medication management, Mr. J chooses to enroll in a resident-run psychotherapy clinic.
In sessions, Mr. J describes his father, who also has panic disorder, as a powerful figure who is physically and emotionally abusive, but also charismatic, charming, and “impossible not to love.” However, Mr. J felt his father was impossible to live with, and moved out at age 18 to marry his high school sweetheart. They have 3 children, ages 12, 10, and 8. Mr. J worked for his father at his construction company, but was not able to satisfy him or live up to his standards so he quit because he was tired of being cut down and emasculated.
Mr. J’s parents divorced 15 years ago after his mother had an affair with her husband’s friend. His father learned of the affair and threatened his wife with a handgun. Although Mr. J and his mother were close before her affair, he has been unable to forgive or empathize with her, and rarely speaks to her. Mr. J’s mother could not protect him from his father’s abuse, and later compounded her failure by abandoning her husband and son through her sexual affair. Growing up with a father he did not respect or get comfort from and sharing a common fear and alliance with his mother likely made it difficult for Mr. J to navigate his Oedipal phase,1 and made her abandonment even more painful.
When Mr. J was 6 years old, he was molested by one of his father’s friends. His father stabbed the man in the shoulder when he found out about the molestation and received probation. Although Mr. J knows he was molested, he does not remember it and has repressed most of his childhood.
The authors’ observations
I (JF) wanted to discuss with Mr. J why his first panic attack occurred during such a symbolic occasion. His panic could be the result of a struggle between a murderous wish toward his father and paternal protective instinct toward his son. The baptism placed his son in a highly vulnerable position, which reminded Mr. J of his own vulnerability and impotent rage toward his father. Anxiety often results when an individual has 2 opposing wishes,2 and a murderous wish often is involved when anxiety progresses to panic. Getting to the root of this with Mr. J could allow for further psychological growth.3 His murderous wishes and fantasies are ego-dystonic, and panic could be a way of punishing himself for these thoughts. When Mr. J identified himself as his son during the baptism, he likely was flooded with thoughts that his defenses were no longer able to repress. Seeing his son submerged in the baptismal font brought back an aspect of his own life that he had completely split off from consciousness, and likely will take time to process. Considering the current therapeutic dynamic, I decided that it was not the best time to address this potential conflict; however, I could have chosen a manualized form of psychodynamic psychotherapy for panic disorder.4 See Table 1 for an outline of the phases of psychodynamic psychotherapy for panic disorder.
Although Mr. J’s initial willingness to discuss his past was encouraging, he refused to schedule more than 1 session every 4 weeks. He also began to keep the content of our sessions superficial, which caused me angst because he seemed to be withholding information and would not come more frequently. Although I was not proud of my feelings, I had to be honest with myself that I had started to dislike Mr. J.
Table 1
Psychodynamic psychotherapy for panic disorder
| Phase | Comments |
|---|---|
| Treatment of acute panic | Therapy focuses on discovering the conscious and unconscious meaning of panic symptoms |
| Treatment of panic vulnerability | Core dynamic conflicts related to panic are understood and altered. Tasks include addressing the nature of the transference and working through them |
| Termination | The therapist directly addresses patients’ difficulties with separation and independence as they emerge in treatment. After treatment, patients may be better able to manage separations, anger, and independence |
| Source: Adapted from reference 4 | |
Countertransference reactions
Countertransference is a therapist's emotional reaction to a patient. Just as patients form reactions based on past relationships brought to present, therapists develop similar reactions.5 Noting one’s countertransference provides a window into how the patient’s thoughts and actions evoke feelings in others. It also can shed light on an aspect of the doctor-patient relationship that may have gone unnoticed.2
Countertransference hatred can occur when a therapist begins to dislike a patient. Typically, patients with borderline personality disorder, masochistic tendencies, or suicidality arouse strong countertransference reactions6; however, any patient can evoke these emotions. This type of hateful patient can precipitate antitherapeutic feelings such as aversion or malice that can be a major obstacle to treatment.7 Aversion leads the therapist to withdraw from the patient, and malice can trigger cruel impulses.
Maltsberger and Buie7 identified 5 defenses therapists may use to combat countertransference hatred (Table 2). When treating Mr. J, I used several of these defenses, including projection and turning against the self to protect myself from this challenging patient. In turning against the self, I became doubtful and critical of my skills and increasingly submissive to Mr. J. Additionally, I projected this countertransference hatred onto Mr. J, focusing on the negative transference that he brought to our therapeutic encounters. On an unconscious level, I may have feared retribution from Mr. J.
I became so frustrated with Mr. J that I reduced the frequency of our sessions to once every 6 weeks, which I realized could be evidence of my feelings regarding Mr. J’s minimization and avoidant style.
Table 2
Defenses against countertransference hate
| Defense mechanism | Description |
|---|---|
| Repression | Remaining unconscious of feelings of hate; may manifest as difficulty paying attention to what the patient is saying or feeling bored or tired |
| Turning against oneself | Doubting one’s capacity to help the patient; may feel inadequate, helpless, and hopeless. May lead to giving up on the patient because the therapist feels incompetent |
| Reaction formation | Turning hatred into the opposite emotion. The therapist may be too preoccupied with being helpful or overly concerned about the patient’s welfare and comfort |
| Projection | Feeling that the patient hates the therapist, leading to feelings of dread and fear |
| Distortion of reality | Devaluing the patient and seeing the patient as a hopeless case or a dangerous person. The therapist may feel indifference, pity, or anger toward the patient |
| Source: Reference 7 | |
TREATMENT: A breakthrough
Mr. J presents with obvious unease at the first visit after we had decreased the frequency of our sessions. At this point, Mr. J opens up to me. He says he has not been truthful with me, and has had worsening depression, anhedonia, and agoraphobia over the past year. He also reveals that he has homosexual fantasies that he cannot stop, which disturb him because he says he is heterosexual. He agrees to come once a week, and reluctantly admits that he desperately needs help.
Although Mr. J only takes clonazepam and citalopram, 20 mg/d, which I prescribed after he admitted to depression and anxiety, he has hyperlipidemia and a family history of heart disease. In addition to being a musician and working at his father’s construction company, he has worked as a security guard, bounty hunter, and computer technician. His careers have been solitary in nature, and, with the exception of computer work, permitted an outlet for aggression. However, he recently started taking online college classes and wants to become a music teacher because he feels he has a lot to offer children as a result of his life experiences. His fantasy of being a teacher shows considerably less aggression, and could be a sign of psychological growth.
Mr. J is struggling financially and his home is on the verge of foreclosure. Early in treatment he told me that he stopped paying his mortgage, but demonstrated blind optimism that things would “work out.” I asked if this was a wise decision, but he seemed confident and dismissive of my concerns. Although he now struggles with this situation, I consider this healthier than his constant pseudo-happy state, and a sign of psychological development.8 Despite his financial stressors, he wants to pursue his dream of being a famous musician, and says he “could never work a 9-to-5 job in a cubicle.”
The authors’ observations
I do not think it’s a coincidence that Mr. J stopped minimizing his symptoms when we decreased the frequency of his sessions. I had viewed our sessions as unproductive and blamed Mr. J for wasting both of our time with his resistance and minimization and had begun to dislike him. I felt impotent because he had been controlling each session with long, elaborate stories that had little relevance to his panic attacks, and I could not redirect him or get him to focus on pertinent issues. It was as if I was an audience for him, and provided nothing useful. However, I was interested in these superficial stories because Mr. J was charming and engaging. He likely reenacted his relationship with his father with me. Mr. J’s superficial relationship with me caused me to dislike him, and, similar to his father, reject him. This rejection likely was damaging because I was unable to anticipate his needs, which would have been to increase—rather than decrease—the frequency of our sessions. Just like his father, I was not able to take care of him.
Mr. J is deeply conflicted about his father. He states that his father “is a monster who instills fear and intimidation into everyone around him, but he’s charismatic, and I’ll always love him.” His view of his domineering father likely developed into a castration anxiety because he was afraid of competing for his mother’s love, contributing to a muddled sexual identity. This was intensified when Mr. J was sexually abused; he may have been stimulated by the molestation, adding to his confusion. Although Mr. J has repressed the abuse and split off most of his childhood, he suffers from shame, guilt, and depression because of his ego-dystonic homosexual fantasies. Homosexuality is at odds with his self-image and contributes to his anxiety and panic attacks. He cannot adequately discharge this dangerous libidinal energy, and as he becomes more conscious of it, his anxiety intensifies.
OUTCOME: Overcoming fear
As Mr. J sits crying in my office, he says he hasn’t cried in front of another man in years. I wonder aloud what his father would think of this situation. His states that his father does not respect any type of weakness and probably would “knock his teeth in.” Overcoming this fear of opening up will be a goal of Mr. J’s treatment. His unbridled optimism borders on pathologic, and is a defense against reality.8 Additionally, his reluctance to accept that he is suffering from depression, which he perceives as a weakness, will be a struggle throughout therapy. He likely will continue to minimize his symptoms when possible, making the true depths of his illness difficult to grasp.
Related Resources
- Waska R. Using countertransference: analytic contact, projective identification, and transference phantasy states. Am J Psychother. 2008;62(4):333-351.
- Gabbard GO, Litowitz BE, Williams P. Textbook of psychoanalysis. Arlington, VA: American Psychiatric Publishing, Inc; 2011.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Unexplained panic
Mr. J, age 35, is a married, unemployed musician who presents for outpatient treatment for panic attacks. He experienced his first panic attack at his oldest son’s baptism 12 years ago, but does not know why it occurred at that moment. He rarely has panic attacks now, but wants to continue medication management. He denies depressive symptoms, saying, “I’m the most optimistic person in the world.” Mr. J tried several medications for his panic attacks before clonazepam, 2 mg/d, proved effective, but always has been vehemently opposed to antidepressants. Despite his insistence that he needs only medication management, Mr. J chooses to enroll in a resident-run psychotherapy clinic.
In sessions, Mr. J describes his father, who also has panic disorder, as a powerful figure who is physically and emotionally abusive, but also charismatic, charming, and “impossible not to love.” However, Mr. J felt his father was impossible to live with, and moved out at age 18 to marry his high school sweetheart. They have 3 children, ages 12, 10, and 8. Mr. J worked for his father at his construction company, but was not able to satisfy him or live up to his standards so he quit because he was tired of being cut down and emasculated.
Mr. J’s parents divorced 15 years ago after his mother had an affair with her husband’s friend. His father learned of the affair and threatened his wife with a handgun. Although Mr. J and his mother were close before her affair, he has been unable to forgive or empathize with her, and rarely speaks to her. Mr. J’s mother could not protect him from his father’s abuse, and later compounded her failure by abandoning her husband and son through her sexual affair. Growing up with a father he did not respect or get comfort from and sharing a common fear and alliance with his mother likely made it difficult for Mr. J to navigate his Oedipal phase,1 and made her abandonment even more painful.
When Mr. J was 6 years old, he was molested by one of his father’s friends. His father stabbed the man in the shoulder when he found out about the molestation and received probation. Although Mr. J knows he was molested, he does not remember it and has repressed most of his childhood.
The authors’ observations
I (JF) wanted to discuss with Mr. J why his first panic attack occurred during such a symbolic occasion. His panic could be the result of a struggle between a murderous wish toward his father and paternal protective instinct toward his son. The baptism placed his son in a highly vulnerable position, which reminded Mr. J of his own vulnerability and impotent rage toward his father. Anxiety often results when an individual has 2 opposing wishes,2 and a murderous wish often is involved when anxiety progresses to panic. Getting to the root of this with Mr. J could allow for further psychological growth.3 His murderous wishes and fantasies are ego-dystonic, and panic could be a way of punishing himself for these thoughts. When Mr. J identified himself as his son during the baptism, he likely was flooded with thoughts that his defenses were no longer able to repress. Seeing his son submerged in the baptismal font brought back an aspect of his own life that he had completely split off from consciousness, and likely will take time to process. Considering the current therapeutic dynamic, I decided that it was not the best time to address this potential conflict; however, I could have chosen a manualized form of psychodynamic psychotherapy for panic disorder.4 See Table 1 for an outline of the phases of psychodynamic psychotherapy for panic disorder.
Although Mr. J’s initial willingness to discuss his past was encouraging, he refused to schedule more than 1 session every 4 weeks. He also began to keep the content of our sessions superficial, which caused me angst because he seemed to be withholding information and would not come more frequently. Although I was not proud of my feelings, I had to be honest with myself that I had started to dislike Mr. J.
Table 1
Psychodynamic psychotherapy for panic disorder
| Phase | Comments |
|---|---|
| Treatment of acute panic | Therapy focuses on discovering the conscious and unconscious meaning of panic symptoms |
| Treatment of panic vulnerability | Core dynamic conflicts related to panic are understood and altered. Tasks include addressing the nature of the transference and working through them |
| Termination | The therapist directly addresses patients’ difficulties with separation and independence as they emerge in treatment. After treatment, patients may be better able to manage separations, anger, and independence |
| Source: Adapted from reference 4 | |
Countertransference reactions
Countertransference is a therapist's emotional reaction to a patient. Just as patients form reactions based on past relationships brought to present, therapists develop similar reactions.5 Noting one’s countertransference provides a window into how the patient’s thoughts and actions evoke feelings in others. It also can shed light on an aspect of the doctor-patient relationship that may have gone unnoticed.2
Countertransference hatred can occur when a therapist begins to dislike a patient. Typically, patients with borderline personality disorder, masochistic tendencies, or suicidality arouse strong countertransference reactions6; however, any patient can evoke these emotions. This type of hateful patient can precipitate antitherapeutic feelings such as aversion or malice that can be a major obstacle to treatment.7 Aversion leads the therapist to withdraw from the patient, and malice can trigger cruel impulses.
Maltsberger and Buie7 identified 5 defenses therapists may use to combat countertransference hatred (Table 2). When treating Mr. J, I used several of these defenses, including projection and turning against the self to protect myself from this challenging patient. In turning against the self, I became doubtful and critical of my skills and increasingly submissive to Mr. J. Additionally, I projected this countertransference hatred onto Mr. J, focusing on the negative transference that he brought to our therapeutic encounters. On an unconscious level, I may have feared retribution from Mr. J.
I became so frustrated with Mr. J that I reduced the frequency of our sessions to once every 6 weeks, which I realized could be evidence of my feelings regarding Mr. J’s minimization and avoidant style.
Table 2
Defenses against countertransference hate
| Defense mechanism | Description |
|---|---|
| Repression | Remaining unconscious of feelings of hate; may manifest as difficulty paying attention to what the patient is saying or feeling bored or tired |
| Turning against oneself | Doubting one’s capacity to help the patient; may feel inadequate, helpless, and hopeless. May lead to giving up on the patient because the therapist feels incompetent |
| Reaction formation | Turning hatred into the opposite emotion. The therapist may be too preoccupied with being helpful or overly concerned about the patient’s welfare and comfort |
| Projection | Feeling that the patient hates the therapist, leading to feelings of dread and fear |
| Distortion of reality | Devaluing the patient and seeing the patient as a hopeless case or a dangerous person. The therapist may feel indifference, pity, or anger toward the patient |
| Source: Reference 7 | |
TREATMENT: A breakthrough
Mr. J presents with obvious unease at the first visit after we had decreased the frequency of our sessions. At this point, Mr. J opens up to me. He says he has not been truthful with me, and has had worsening depression, anhedonia, and agoraphobia over the past year. He also reveals that he has homosexual fantasies that he cannot stop, which disturb him because he says he is heterosexual. He agrees to come once a week, and reluctantly admits that he desperately needs help.
Although Mr. J only takes clonazepam and citalopram, 20 mg/d, which I prescribed after he admitted to depression and anxiety, he has hyperlipidemia and a family history of heart disease. In addition to being a musician and working at his father’s construction company, he has worked as a security guard, bounty hunter, and computer technician. His careers have been solitary in nature, and, with the exception of computer work, permitted an outlet for aggression. However, he recently started taking online college classes and wants to become a music teacher because he feels he has a lot to offer children as a result of his life experiences. His fantasy of being a teacher shows considerably less aggression, and could be a sign of psychological growth.
Mr. J is struggling financially and his home is on the verge of foreclosure. Early in treatment he told me that he stopped paying his mortgage, but demonstrated blind optimism that things would “work out.” I asked if this was a wise decision, but he seemed confident and dismissive of my concerns. Although he now struggles with this situation, I consider this healthier than his constant pseudo-happy state, and a sign of psychological development.8 Despite his financial stressors, he wants to pursue his dream of being a famous musician, and says he “could never work a 9-to-5 job in a cubicle.”
The authors’ observations
I do not think it’s a coincidence that Mr. J stopped minimizing his symptoms when we decreased the frequency of his sessions. I had viewed our sessions as unproductive and blamed Mr. J for wasting both of our time with his resistance and minimization and had begun to dislike him. I felt impotent because he had been controlling each session with long, elaborate stories that had little relevance to his panic attacks, and I could not redirect him or get him to focus on pertinent issues. It was as if I was an audience for him, and provided nothing useful. However, I was interested in these superficial stories because Mr. J was charming and engaging. He likely reenacted his relationship with his father with me. Mr. J’s superficial relationship with me caused me to dislike him, and, similar to his father, reject him. This rejection likely was damaging because I was unable to anticipate his needs, which would have been to increase—rather than decrease—the frequency of our sessions. Just like his father, I was not able to take care of him.
Mr. J is deeply conflicted about his father. He states that his father “is a monster who instills fear and intimidation into everyone around him, but he’s charismatic, and I’ll always love him.” His view of his domineering father likely developed into a castration anxiety because he was afraid of competing for his mother’s love, contributing to a muddled sexual identity. This was intensified when Mr. J was sexually abused; he may have been stimulated by the molestation, adding to his confusion. Although Mr. J has repressed the abuse and split off most of his childhood, he suffers from shame, guilt, and depression because of his ego-dystonic homosexual fantasies. Homosexuality is at odds with his self-image and contributes to his anxiety and panic attacks. He cannot adequately discharge this dangerous libidinal energy, and as he becomes more conscious of it, his anxiety intensifies.
OUTCOME: Overcoming fear
As Mr. J sits crying in my office, he says he hasn’t cried in front of another man in years. I wonder aloud what his father would think of this situation. His states that his father does not respect any type of weakness and probably would “knock his teeth in.” Overcoming this fear of opening up will be a goal of Mr. J’s treatment. His unbridled optimism borders on pathologic, and is a defense against reality.8 Additionally, his reluctance to accept that he is suffering from depression, which he perceives as a weakness, will be a struggle throughout therapy. He likely will continue to minimize his symptoms when possible, making the true depths of his illness difficult to grasp.
Related Resources
- Waska R. Using countertransference: analytic contact, projective identification, and transference phantasy states. Am J Psychother. 2008;62(4):333-351.
- Gabbard GO, Litowitz BE, Williams P. Textbook of psychoanalysis. Arlington, VA: American Psychiatric Publishing, Inc; 2011.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Blos P. Son and father: before and beyond the Oedipus complex. New York NY: Free Press/Macmillan; 1985.
2. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington VA: American Psychiatric Publishing; 2004.
3. Akhtar S. Comprehensive dictionary of psychoanalysis. London United Kingdom: Kamac Books; 2009.
4. Busch FN, Milrod BL, Singer MB. Theory and technique in psychodynamic treatment of panic disorder. J Psychother Pract Res. 1999;8(3):234-242.
5. Freud S. The future prospects of psycho-analytic therapy. The standard edition of the complete psychological works of Sigmund Freud volume XI (1910): five lectures on psycho-analysis, Leonardo da Vinci and other works. London, United Kingdom: Hogarth Press; 1957:139–152.
6. Winnicott DW. Hate in the counter-transference. J Psychother Pract Res. 1994;3(4):348-356.
7. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
8. Akhtar S. “Someday…” and “if only…” fantasies: pathological optimism and inordinate nostalgia as related forms of idealization. J Am Psychoanal Assoc. 1996;44(3):723-753.
1. Blos P. Son and father: before and beyond the Oedipus complex. New York NY: Free Press/Macmillan; 1985.
2. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington VA: American Psychiatric Publishing; 2004.
3. Akhtar S. Comprehensive dictionary of psychoanalysis. London United Kingdom: Kamac Books; 2009.
4. Busch FN, Milrod BL, Singer MB. Theory and technique in psychodynamic treatment of panic disorder. J Psychother Pract Res. 1999;8(3):234-242.
5. Freud S. The future prospects of psycho-analytic therapy. The standard edition of the complete psychological works of Sigmund Freud volume XI (1910): five lectures on psycho-analysis, Leonardo da Vinci and other works. London, United Kingdom: Hogarth Press; 1957:139–152.
6. Winnicott DW. Hate in the counter-transference. J Psychother Pract Res. 1994;3(4):348-356.
7. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
8. Akhtar S. “Someday…” and “if only…” fantasies: pathological optimism and inordinate nostalgia as related forms of idealization. J Am Psychoanal Assoc. 1996;44(3):723-753.
Biopsychosocial psychiatry
With all of the discussion about a truly comprehensive and inclusive psychiatry, it was sad to see the emptiness and one-sidedness of Dr. Nasrallah’s June editorial (“Innovative approaches to treatment-resistant depression,” From the Editor, Current Psychiatry, June 2012, p. 4-5; http://bit.ly/1GM92oV). Depression certainly is not a unified diagnosis such as measles or appendicitis. In the face of so-called treatment-resistance, the first step is to review the psychological and biologic formulation of the patient and the reasons for his or her depression. Dr. Nasrallah does not mention the need for a review of all aspects of the patient’s life. The approaches he suggests are dreary, dull, ineffective, and unchanging. It proves that patients are best cared for by psychiatrists who practice biopsychosocial psychiatry and not merely to pay lip service to it.
Arnold Robbins, MD
Private Practice
Cambridge, MA
Clinical Professor of Psychiatry
Boston University School of Medicine
Boston, MA
Dr. Nasrallah responds
I thank Dr. Robbins for his letter. As someone trained by the father of biopsychosocial psychiatry—George Engel, MD, at the University of Rochester—I agree that it is the optimal practice of psychiatry and I practice that approach with all my patients. However, I was describing innovative interventions and paradigm shifts for truly end-of-the-road refractory depression, where all psychosocial and pharmacotherapy treatments have failed and the patient is desperate, disabled, and at high risk for suicide. None of the available interventions work with such individuals and that’s why I regard the innovative breakthroughs I described in my editorial as a promise of hope, thanks to dedicated psychiatric neuroscientists. I hope psychotherapy researchers can achieve breakthroughs for these patients as well.
Henry A. Nasrallah, MD
Editor-in-Chief
Psychotherapy for GAD
I appreciated Dr. Barry’s in-depth review of current diagnostic criteria and therapy for generalized anxiety disorder (GAD) (“Generalized anxiety disorder: Helping patients overcome worry,” Current Psychiatry, May 2012, p. 40-44; http://bit.ly/1oUymyJ). However, I want to point out an error under the “Evidence-based treatments” section labeled “Psychotherapy.” Dr. Barry states that cognitive-behavioral therapy (CBT) is the preferred form of psychotherapy for GAD. In my 40 years of practice, I have found a combination of medication—preferably selective serotonin reuptake inhibitors—and psychodynamic psychotherapy is the most effective treatment for GAD and provides more enduring relief.
Jonathan Shedler, PhD, of the University of Colorado Denver School of Medicine reported on the efficacy of psychodynamic psychotherapy vs behavioral therapy.1 He compiled the results of meta-analyses of psychotherapy efficacy by 18 investigators covering 792 studies. The findings show a superior result for psychodynamic psychotherapy over behavioral therapy and the effects are more lasting.
Edward L. Parsons, MD
Private Practice
Westfield, NJ
The author responds
I appreciate Dr. Parsons’ comments and his valuable contribution to the dialogue on GAD. Dr. Parsons reemphasizes the importance of psychotherapy in this chronic condition. As demonstrated by the meta-analyses reviewed by Dr. Shedler, there is sufficient evidence in the medical literature to support either psychodynamic psychotherapy or CBT. The specific therapeutic recommendation should consider unique patient variables, such as therapist availability and expertise, the presence of co-occurring conditions or dynamics that would better align with a specific modality, and patient preference and psychological mindedness, to name a few. Regardless, psychotherapy is indicated in the treatment of GAD, and both CBT and psychodynamic psychotherapy are well-supported interventions.
Matthew J. Barry, DO
Lead Psychiatrist
Rochester Veterans Affairs Outpatient Clinic
Canandaigua Veterans Affairs Medical Center
Canandaigua, NY
Caution with prazosin
We welcome the article discussing the use of prazosin and antipsychotics for posttraumatic stress disorder (PTSD)-related nightmares (Graham RL, Leckband SG, Endow-Eyer RA. “PTSD nightmares: Prazosin and atypical antipsychotics,” Current Psychiatry, June 2012, p. 59-62; http://bit.ly/LVAlSo). The favorable outcomes associated with prazosin use combined with its low cost and general tolerability give it considerable potential. Prazosin may be particularly valuable given the unfavorable cardiometabolic risks associated with antipsychotic use, especially because evidence suggests individuals with PTSD have higher rates of cardiovascular disease.1
We believe the occurrence of adverse cardiovascular effects when starting prazosin requires further attention. As an α1-adrenergic receptor antagonist, it has been linked to orthostatic hypotension and syncope.2,3 Its cardiovascular effects may be further complicated by concomitant use of other antihypertensive medications. Therefore, we suggest a low initiation dose and gradual titration of prazosin. In individuals who initially were normotensive but then experienced hypotension following prazosin administration, we successfully used short-term sodium chloride tablets, 4 g/d. We discontinued sodium chloride after titration was completed and no postural hypotension was evident.
To minimize polypharmacy, individuals on multiple agents for hypertension may benefit from substituting prazosin for 1 of their regular anti- hypertensives. Despite the mounting evidence supporting prazosin use, it is not indicated for PTSD.
This material is the result of work supported with resources and the use of facilities of the Mental Health and Research and Development Service Lines, Atlanta Veterans Affairs Medical Center, Decatur, GA.
Arshya Vahabzadeh, MD
PGY-2, Resident Psychiatrist
Emory University School of Medicine
Erica Duncan, MD
Attending Psychiatrist
and Associate Professor
Mental Health Service Line
Atlanta Veterans Affairs Medical Center
Decatur, GA
Department of Psychiatry and Behavioral
Sciences
Emory University School of Medicine
Atlanta, GA
The authors respond
We agree with the comments by Drs. Vahabzadeh and Duncan regarding the cardiovascular adverse effects of prazosin. It is important to assess the hemodynamic status of the patient before initiating prazosin therapy, and usually, initiation is attempted only if a patient is normotensive or hypertensive because of potential orthostatic hypotension and syncope, which can occur in up to 4% of patients.1 As noted by Drs. Vahabzadeh and Duncan, prazosin often is viewed as a dual treatment for both nightmares and blood pressure in individuals who are hypertensive prior to initiation. Prazosin therapy usually is initiated at 1 mg at bedtime and titrated by 1 to 2 mg every 3 to 5 days.2 The average dose was approximately 3 mg in studies evaluating prazosin for treating PTSD-associated nightmares (dose range: 1 to 10 mg).2 Until the patient is stabilized on a prazosin dose, blood pressure should be monitored daily for inpatients. Outpatients should be educated regarding the signs and symptoms of hypotension, especially dizziness and light-headedness upon standing, along with monitoring blood pressure at his or her next clinic appointment.
Prazosin does not carry an FDA indication for PTSD. Although this is important to consider, the level of evidence in terms of treatment of nightmares also is key. Aurora et al found prazosin was the only medication with a level A rating for treating PTSD-associated nightmares, indicating it as a recommended therapy option.2 Because we do not have any medications indicated for PTSD-associated nightmares, it is crucial to practice evidence-based medicine and base therapy choices on available literature supporting the most effective and safe options.
Safety is an issue in many clinicians’ minds, especially when treating geriatric patients with PTSD because of the risk of hypotensive effects with prazosin leading to negative outcomes, such as falls. In Peskind et al’s open-label study of 9 older patients (mean age: 76) with intractable PTSD-associated nightmares treated with prazosin (mean dose: 2.3 mg; increased by 1 mg per week to a maximum dose of 4 mg), 8 patients experienced >50% reduction in nightmares after 8 weeks of treatment, and 1 patient experienced transient orthostasis when starting prazosin that resolved spontaneously with only mild decreases in blood pressure noted otherwise (<20 mm Hg decrease in systolic blood pressure upon standing).3 Although this study was small, it provides evidence that prazosin can be an effective and safe treatment option in geriatric patients and is devoid of the highly sedating side effects of some other treatment options.
Rebecca L. Graham, PharmD
Second-Year Psychiatric Pharmacy Resident
Veterans Affairs San Diego Healthcare System
(VASDHS)
Susan G. Leckband, RPh, BCPP
Clinical Psychiatric Pharmacist Specialist
VASDHS
Assistant Clinical Professor
Skaggs School of Pharmacy and
Pharmaceutical Sciences
Department of Psychiatry
University of California, San Diego
Rene A. Endow-Eyer, PharmD, BCPP
Psychiatric Clinical Pharmacy Specialist
VASDHS
Assistant Clinical Professor
Skaggs School of Pharmacy and
Pharmaceutical Sciences
Department of Psychiatry
University of California, San Diego
San Diego, CA
With all of the discussion about a truly comprehensive and inclusive psychiatry, it was sad to see the emptiness and one-sidedness of Dr. Nasrallah’s June editorial (“Innovative approaches to treatment-resistant depression,” From the Editor, Current Psychiatry, June 2012, p. 4-5; http://bit.ly/1GM92oV). Depression certainly is not a unified diagnosis such as measles or appendicitis. In the face of so-called treatment-resistance, the first step is to review the psychological and biologic formulation of the patient and the reasons for his or her depression. Dr. Nasrallah does not mention the need for a review of all aspects of the patient’s life. The approaches he suggests are dreary, dull, ineffective, and unchanging. It proves that patients are best cared for by psychiatrists who practice biopsychosocial psychiatry and not merely to pay lip service to it.
Arnold Robbins, MD
Private Practice
Cambridge, MA
Clinical Professor of Psychiatry
Boston University School of Medicine
Boston, MA
Dr. Nasrallah responds
I thank Dr. Robbins for his letter. As someone trained by the father of biopsychosocial psychiatry—George Engel, MD, at the University of Rochester—I agree that it is the optimal practice of psychiatry and I practice that approach with all my patients. However, I was describing innovative interventions and paradigm shifts for truly end-of-the-road refractory depression, where all psychosocial and pharmacotherapy treatments have failed and the patient is desperate, disabled, and at high risk for suicide. None of the available interventions work with such individuals and that’s why I regard the innovative breakthroughs I described in my editorial as a promise of hope, thanks to dedicated psychiatric neuroscientists. I hope psychotherapy researchers can achieve breakthroughs for these patients as well.
Henry A. Nasrallah, MD
Editor-in-Chief
Psychotherapy for GAD
I appreciated Dr. Barry’s in-depth review of current diagnostic criteria and therapy for generalized anxiety disorder (GAD) (“Generalized anxiety disorder: Helping patients overcome worry,” Current Psychiatry, May 2012, p. 40-44; http://bit.ly/1oUymyJ). However, I want to point out an error under the “Evidence-based treatments” section labeled “Psychotherapy.” Dr. Barry states that cognitive-behavioral therapy (CBT) is the preferred form of psychotherapy for GAD. In my 40 years of practice, I have found a combination of medication—preferably selective serotonin reuptake inhibitors—and psychodynamic psychotherapy is the most effective treatment for GAD and provides more enduring relief.
Jonathan Shedler, PhD, of the University of Colorado Denver School of Medicine reported on the efficacy of psychodynamic psychotherapy vs behavioral therapy.1 He compiled the results of meta-analyses of psychotherapy efficacy by 18 investigators covering 792 studies. The findings show a superior result for psychodynamic psychotherapy over behavioral therapy and the effects are more lasting.
Edward L. Parsons, MD
Private Practice
Westfield, NJ
The author responds
I appreciate Dr. Parsons’ comments and his valuable contribution to the dialogue on GAD. Dr. Parsons reemphasizes the importance of psychotherapy in this chronic condition. As demonstrated by the meta-analyses reviewed by Dr. Shedler, there is sufficient evidence in the medical literature to support either psychodynamic psychotherapy or CBT. The specific therapeutic recommendation should consider unique patient variables, such as therapist availability and expertise, the presence of co-occurring conditions or dynamics that would better align with a specific modality, and patient preference and psychological mindedness, to name a few. Regardless, psychotherapy is indicated in the treatment of GAD, and both CBT and psychodynamic psychotherapy are well-supported interventions.
Matthew J. Barry, DO
Lead Psychiatrist
Rochester Veterans Affairs Outpatient Clinic
Canandaigua Veterans Affairs Medical Center
Canandaigua, NY
Caution with prazosin
We welcome the article discussing the use of prazosin and antipsychotics for posttraumatic stress disorder (PTSD)-related nightmares (Graham RL, Leckband SG, Endow-Eyer RA. “PTSD nightmares: Prazosin and atypical antipsychotics,” Current Psychiatry, June 2012, p. 59-62; http://bit.ly/LVAlSo). The favorable outcomes associated with prazosin use combined with its low cost and general tolerability give it considerable potential. Prazosin may be particularly valuable given the unfavorable cardiometabolic risks associated with antipsychotic use, especially because evidence suggests individuals with PTSD have higher rates of cardiovascular disease.1
We believe the occurrence of adverse cardiovascular effects when starting prazosin requires further attention. As an α1-adrenergic receptor antagonist, it has been linked to orthostatic hypotension and syncope.2,3 Its cardiovascular effects may be further complicated by concomitant use of other antihypertensive medications. Therefore, we suggest a low initiation dose and gradual titration of prazosin. In individuals who initially were normotensive but then experienced hypotension following prazosin administration, we successfully used short-term sodium chloride tablets, 4 g/d. We discontinued sodium chloride after titration was completed and no postural hypotension was evident.
To minimize polypharmacy, individuals on multiple agents for hypertension may benefit from substituting prazosin for 1 of their regular anti- hypertensives. Despite the mounting evidence supporting prazosin use, it is not indicated for PTSD.
This material is the result of work supported with resources and the use of facilities of the Mental Health and Research and Development Service Lines, Atlanta Veterans Affairs Medical Center, Decatur, GA.
Arshya Vahabzadeh, MD
PGY-2, Resident Psychiatrist
Emory University School of Medicine
Erica Duncan, MD
Attending Psychiatrist
and Associate Professor
Mental Health Service Line
Atlanta Veterans Affairs Medical Center
Decatur, GA
Department of Psychiatry and Behavioral
Sciences
Emory University School of Medicine
Atlanta, GA
The authors respond
We agree with the comments by Drs. Vahabzadeh and Duncan regarding the cardiovascular adverse effects of prazosin. It is important to assess the hemodynamic status of the patient before initiating prazosin therapy, and usually, initiation is attempted only if a patient is normotensive or hypertensive because of potential orthostatic hypotension and syncope, which can occur in up to 4% of patients.1 As noted by Drs. Vahabzadeh and Duncan, prazosin often is viewed as a dual treatment for both nightmares and blood pressure in individuals who are hypertensive prior to initiation. Prazosin therapy usually is initiated at 1 mg at bedtime and titrated by 1 to 2 mg every 3 to 5 days.2 The average dose was approximately 3 mg in studies evaluating prazosin for treating PTSD-associated nightmares (dose range: 1 to 10 mg).2 Until the patient is stabilized on a prazosin dose, blood pressure should be monitored daily for inpatients. Outpatients should be educated regarding the signs and symptoms of hypotension, especially dizziness and light-headedness upon standing, along with monitoring blood pressure at his or her next clinic appointment.
Prazosin does not carry an FDA indication for PTSD. Although this is important to consider, the level of evidence in terms of treatment of nightmares also is key. Aurora et al found prazosin was the only medication with a level A rating for treating PTSD-associated nightmares, indicating it as a recommended therapy option.2 Because we do not have any medications indicated for PTSD-associated nightmares, it is crucial to practice evidence-based medicine and base therapy choices on available literature supporting the most effective and safe options.
Safety is an issue in many clinicians’ minds, especially when treating geriatric patients with PTSD because of the risk of hypotensive effects with prazosin leading to negative outcomes, such as falls. In Peskind et al’s open-label study of 9 older patients (mean age: 76) with intractable PTSD-associated nightmares treated with prazosin (mean dose: 2.3 mg; increased by 1 mg per week to a maximum dose of 4 mg), 8 patients experienced >50% reduction in nightmares after 8 weeks of treatment, and 1 patient experienced transient orthostasis when starting prazosin that resolved spontaneously with only mild decreases in blood pressure noted otherwise (<20 mm Hg decrease in systolic blood pressure upon standing).3 Although this study was small, it provides evidence that prazosin can be an effective and safe treatment option in geriatric patients and is devoid of the highly sedating side effects of some other treatment options.
Rebecca L. Graham, PharmD
Second-Year Psychiatric Pharmacy Resident
Veterans Affairs San Diego Healthcare System
(VASDHS)
Susan G. Leckband, RPh, BCPP
Clinical Psychiatric Pharmacist Specialist
VASDHS
Assistant Clinical Professor
Skaggs School of Pharmacy and
Pharmaceutical Sciences
Department of Psychiatry
University of California, San Diego
Rene A. Endow-Eyer, PharmD, BCPP
Psychiatric Clinical Pharmacy Specialist
VASDHS
Assistant Clinical Professor
Skaggs School of Pharmacy and
Pharmaceutical Sciences
Department of Psychiatry
University of California, San Diego
San Diego, CA
With all of the discussion about a truly comprehensive and inclusive psychiatry, it was sad to see the emptiness and one-sidedness of Dr. Nasrallah’s June editorial (“Innovative approaches to treatment-resistant depression,” From the Editor, Current Psychiatry, June 2012, p. 4-5; http://bit.ly/1GM92oV). Depression certainly is not a unified diagnosis such as measles or appendicitis. In the face of so-called treatment-resistance, the first step is to review the psychological and biologic formulation of the patient and the reasons for his or her depression. Dr. Nasrallah does not mention the need for a review of all aspects of the patient’s life. The approaches he suggests are dreary, dull, ineffective, and unchanging. It proves that patients are best cared for by psychiatrists who practice biopsychosocial psychiatry and not merely to pay lip service to it.
Arnold Robbins, MD
Private Practice
Cambridge, MA
Clinical Professor of Psychiatry
Boston University School of Medicine
Boston, MA
Dr. Nasrallah responds
I thank Dr. Robbins for his letter. As someone trained by the father of biopsychosocial psychiatry—George Engel, MD, at the University of Rochester—I agree that it is the optimal practice of psychiatry and I practice that approach with all my patients. However, I was describing innovative interventions and paradigm shifts for truly end-of-the-road refractory depression, where all psychosocial and pharmacotherapy treatments have failed and the patient is desperate, disabled, and at high risk for suicide. None of the available interventions work with such individuals and that’s why I regard the innovative breakthroughs I described in my editorial as a promise of hope, thanks to dedicated psychiatric neuroscientists. I hope psychotherapy researchers can achieve breakthroughs for these patients as well.
Henry A. Nasrallah, MD
Editor-in-Chief
Psychotherapy for GAD
I appreciated Dr. Barry’s in-depth review of current diagnostic criteria and therapy for generalized anxiety disorder (GAD) (“Generalized anxiety disorder: Helping patients overcome worry,” Current Psychiatry, May 2012, p. 40-44; http://bit.ly/1oUymyJ). However, I want to point out an error under the “Evidence-based treatments” section labeled “Psychotherapy.” Dr. Barry states that cognitive-behavioral therapy (CBT) is the preferred form of psychotherapy for GAD. In my 40 years of practice, I have found a combination of medication—preferably selective serotonin reuptake inhibitors—and psychodynamic psychotherapy is the most effective treatment for GAD and provides more enduring relief.
Jonathan Shedler, PhD, of the University of Colorado Denver School of Medicine reported on the efficacy of psychodynamic psychotherapy vs behavioral therapy.1 He compiled the results of meta-analyses of psychotherapy efficacy by 18 investigators covering 792 studies. The findings show a superior result for psychodynamic psychotherapy over behavioral therapy and the effects are more lasting.
Edward L. Parsons, MD
Private Practice
Westfield, NJ
The author responds
I appreciate Dr. Parsons’ comments and his valuable contribution to the dialogue on GAD. Dr. Parsons reemphasizes the importance of psychotherapy in this chronic condition. As demonstrated by the meta-analyses reviewed by Dr. Shedler, there is sufficient evidence in the medical literature to support either psychodynamic psychotherapy or CBT. The specific therapeutic recommendation should consider unique patient variables, such as therapist availability and expertise, the presence of co-occurring conditions or dynamics that would better align with a specific modality, and patient preference and psychological mindedness, to name a few. Regardless, psychotherapy is indicated in the treatment of GAD, and both CBT and psychodynamic psychotherapy are well-supported interventions.
Matthew J. Barry, DO
Lead Psychiatrist
Rochester Veterans Affairs Outpatient Clinic
Canandaigua Veterans Affairs Medical Center
Canandaigua, NY
Caution with prazosin
We welcome the article discussing the use of prazosin and antipsychotics for posttraumatic stress disorder (PTSD)-related nightmares (Graham RL, Leckband SG, Endow-Eyer RA. “PTSD nightmares: Prazosin and atypical antipsychotics,” Current Psychiatry, June 2012, p. 59-62; http://bit.ly/LVAlSo). The favorable outcomes associated with prazosin use combined with its low cost and general tolerability give it considerable potential. Prazosin may be particularly valuable given the unfavorable cardiometabolic risks associated with antipsychotic use, especially because evidence suggests individuals with PTSD have higher rates of cardiovascular disease.1
We believe the occurrence of adverse cardiovascular effects when starting prazosin requires further attention. As an α1-adrenergic receptor antagonist, it has been linked to orthostatic hypotension and syncope.2,3 Its cardiovascular effects may be further complicated by concomitant use of other antihypertensive medications. Therefore, we suggest a low initiation dose and gradual titration of prazosin. In individuals who initially were normotensive but then experienced hypotension following prazosin administration, we successfully used short-term sodium chloride tablets, 4 g/d. We discontinued sodium chloride after titration was completed and no postural hypotension was evident.
To minimize polypharmacy, individuals on multiple agents for hypertension may benefit from substituting prazosin for 1 of their regular anti- hypertensives. Despite the mounting evidence supporting prazosin use, it is not indicated for PTSD.
This material is the result of work supported with resources and the use of facilities of the Mental Health and Research and Development Service Lines, Atlanta Veterans Affairs Medical Center, Decatur, GA.
Arshya Vahabzadeh, MD
PGY-2, Resident Psychiatrist
Emory University School of Medicine
Erica Duncan, MD
Attending Psychiatrist
and Associate Professor
Mental Health Service Line
Atlanta Veterans Affairs Medical Center
Decatur, GA
Department of Psychiatry and Behavioral
Sciences
Emory University School of Medicine
Atlanta, GA
The authors respond
We agree with the comments by Drs. Vahabzadeh and Duncan regarding the cardiovascular adverse effects of prazosin. It is important to assess the hemodynamic status of the patient before initiating prazosin therapy, and usually, initiation is attempted only if a patient is normotensive or hypertensive because of potential orthostatic hypotension and syncope, which can occur in up to 4% of patients.1 As noted by Drs. Vahabzadeh and Duncan, prazosin often is viewed as a dual treatment for both nightmares and blood pressure in individuals who are hypertensive prior to initiation. Prazosin therapy usually is initiated at 1 mg at bedtime and titrated by 1 to 2 mg every 3 to 5 days.2 The average dose was approximately 3 mg in studies evaluating prazosin for treating PTSD-associated nightmares (dose range: 1 to 10 mg).2 Until the patient is stabilized on a prazosin dose, blood pressure should be monitored daily for inpatients. Outpatients should be educated regarding the signs and symptoms of hypotension, especially dizziness and light-headedness upon standing, along with monitoring blood pressure at his or her next clinic appointment.
Prazosin does not carry an FDA indication for PTSD. Although this is important to consider, the level of evidence in terms of treatment of nightmares also is key. Aurora et al found prazosin was the only medication with a level A rating for treating PTSD-associated nightmares, indicating it as a recommended therapy option.2 Because we do not have any medications indicated for PTSD-associated nightmares, it is crucial to practice evidence-based medicine and base therapy choices on available literature supporting the most effective and safe options.
Safety is an issue in many clinicians’ minds, especially when treating geriatric patients with PTSD because of the risk of hypotensive effects with prazosin leading to negative outcomes, such as falls. In Peskind et al’s open-label study of 9 older patients (mean age: 76) with intractable PTSD-associated nightmares treated with prazosin (mean dose: 2.3 mg; increased by 1 mg per week to a maximum dose of 4 mg), 8 patients experienced >50% reduction in nightmares after 8 weeks of treatment, and 1 patient experienced transient orthostasis when starting prazosin that resolved spontaneously with only mild decreases in blood pressure noted otherwise (<20 mm Hg decrease in systolic blood pressure upon standing).3 Although this study was small, it provides evidence that prazosin can be an effective and safe treatment option in geriatric patients and is devoid of the highly sedating side effects of some other treatment options.
Rebecca L. Graham, PharmD
Second-Year Psychiatric Pharmacy Resident
Veterans Affairs San Diego Healthcare System
(VASDHS)
Susan G. Leckband, RPh, BCPP
Clinical Psychiatric Pharmacist Specialist
VASDHS
Assistant Clinical Professor
Skaggs School of Pharmacy and
Pharmaceutical Sciences
Department of Psychiatry
University of California, San Diego
Rene A. Endow-Eyer, PharmD, BCPP
Psychiatric Clinical Pharmacy Specialist
VASDHS
Assistant Clinical Professor
Skaggs School of Pharmacy and
Pharmaceutical Sciences
Department of Psychiatry
University of California, San Diego
San Diego, CA
Treating ‘depression’ in patients with schizophrenia
Discuss this article at www.facebook.com/CurrentPsychiatry
Approximately 25% of schizophrenia patients experience course-related depression.1-4 Depression in patients with schizophrenia is linked to reduced social and vocational functioning, increased likelihood of psychotic relapse and rehospitalization, and other problems.2-4 Depression in patients with schizophrenia also has been linked to undesirable life events, especially “exit events” such as losing people in their lives, as well as suicidal ideation, suicide attempts, and completed suicides. Overall, it has been noted that approximately 10% of patients with schizophrenia commit suicide.5 Depressed schizophrenia patients are at particularly high risk for suicide the first few months after diagnosis and after hospital discharge.
Confirm the diagnosis
The best approach to treating depressive symptoms in schizophrenia patients is to formulate a thorough differential diagnosis (Table 1).
Table 1
Differential diagnosis of ‘depression’ in schizophrenia
| Organic factors |
| Antipsychotic-induced dysphoria |
| Akinesia |
| Akathisia |
| Negative symptoms |
| Acute disappointment reactions |
| Chronic disappointment reactions |
| Prodrome of psychotic relapse |
| Depression |
Antipsychotic-induced dysphoria. Blockade of dopamine receptors is an important feature of all antipsychotics; however, dopamine neurotransmission also is involved in the brain’s “pleasure” pathways. Individuals who take antipsychotics may experience reduced joy from once-pleasurable activities. Results of studies on the link between depression and antipsychotics have been mixed.2,4 Although some researchers have found depressed mood common among patients receiving antipsychotics, others have failed to show differences between patients treated with antipsychotics and those randomized to placebo.
Akinesia, a parkinsonian side effect of antipsychotics, can be blatant or subtle. The blatant form involves large muscle groups; these patients present with diminished arm swing, stooped posture, and parkinsonian gait. Easily spotted, such patients are unlikely to be considered depressed.
The more subtle form of akinesia is easier to confuse with depression. It can affect small muscle groups, such as in the face or vocal cords. Lack of responsiveness of facial expression is easily confused with blunted affect, low mood, lack of interest, or emotional unresponsiveness. Subtle akinesia also can impair a patient’s ability to initiate or sustain motor behavior. Many activities, from striking up a conversation to changing television channels, involve initiating and sustaining motor behavior, which these patients’ basal ganglia are underequipped to do. Life becomes boring and patients criticize themselves for “being lazy.” Patients with akinesia also are prone to dysphoria.6,7 When the lack of spontaneous motor behavior found in subtle akinesia is combined with diminished experience of pleasure due to antipsychotic blockade of dopamine, a patient may feel that “nothing is worth the effort.”
Akathisia is another movement disorder of the basal ganglia that can be triggered by antipsychotics. Whereas a patient with akinesia experiences having a “broken starter motor,” the akathisia patient experiences “a starter motor that won’t turn off.” Akathisia can be blatant or subtle. A patient with blatant akathisia has difficulty remaining seated and often paces. In subtle akathisia, increased motor activity is less dramatic, and patients may simply wander or talk excessively. Akathisia also has a dysphoric component that, when the movement is interpreted as restlessness or agitation, may look like depression.8
Negative symptoms. Primary negative symptoms in schizophrenia have several features in common with depression, which can create diagnostic challenges.9 These include anhedonia, social withdrawal, lack of initiative, lowered energy, diminished expectations and/or self confidence, and reduced speech or activity. The main feature that distinguishes the primary negative symptom syndrome from depression is prominent blue mood, which is present in depression but not in negative symptoms. Cognitive features—such as guilt, pessimism, and suicidal thoughts—are common in depression, but usually are absent in negative symptoms.
4 While the acute disappointment reaction is ongoing, the emotional burden may be substantial. With bereavement or grief reactions the loss is clear; however, be vigilant for situations where the patient’s loss may be idiosyncratic or symbolic.
Chronic disappointment reactions, also known as the demoralization syndrome, involve long-term convictions of defeat, despair, incompetence, and loss of control.10 These reactions can be devastating and prolonged. These reactions are important to identify because they may be ameliorated by rehabilitative interventions or other psychosocial supports.
Prodrome of psychotic relapse. Longitudinal observations of patients with schizophrenia have found depressive symptoms may occur during the early stages of psychotic decompensation.4,11,12 These symptoms include dysphoria, anxiety, agitation, sleep and/or appetite disturbances, impaired concentration, hopelessness, helplessness, feelings of loss of control or alienation, and social withdrawal. These features usually last a few days to a couple of weeks before they are overtaken by psychotic phenomena.
Treatment: A suggested approach
Based on my clinical experience in managing newly emergent “depression” episodes in patients correctly diagnosed with schizophrenia, I suggest the following approach:
First, assess the patient for medical disorders that could present with depressive features. Collaborate with the patient’s primary care physician to determine which medications the patient is taking and whether there have been any recent changes in these agents or their doses, including adherence issues, potential substance use or abuse, and changes between brand name and generic agents. Thoroughly evaluate the patient’s psychiatric status, including symptoms, suicidal risk, and changes in life circumstances. A patient who is at high risk of suicide may require hospitalization. Also assess for the presence of extrapyramidal side effects.
Do not change your patient’s medication regimen at this early stage, but provide him or her structure and support, and schedule an early appointment for the next visit (eg, 1 week later). A planned telephone call before the appointment may be helpful as well. If the “depression” is an acute disappointment reaction, it may run its course and resolve. However, if your patient’s depressive symptoms are a prodrome of psychotic relapse, the quick follow-up contact will improve the chances of preventing a psychotic episode by increasing the antipsychotic dosage or making other reasonable changes in pharmacotherapy.
If at the follow-up visit the patient’s psychotic symptoms have not progressed but depressive symptoms persist, evaluate for the possibility of parkinsonian symptoms, which may be subtle and difficult to rule out. If your patient is restless or tends to be physically active, a trial of a benzodiazepine can be added to treat akathisia. If the patient is underactive, consider a trial of an anticholinergic antiparkinsonian agent, such as benztropine, for akinesia. Dosages of benztropine can be raised in a stepwise manner up to 6 mg/d if there are no side effects, such as constipation, dry mouth, blurry vision, or memory impairment. Advantages of treating extrapyramidal side effects first include:
- response to antiparkinsonian medications occurs rapidly—if your patient shows no response within a week, future response at this dose is unlikely
- the presence of anticholinergic side effects is a biologic marker indicating that the treatment dose is adequate
- the clinician has more time to get to know the patient and his or her condition before committing to lowering, raising, or changing the antipsychotic dosage.
Table 2
Antidepressant effects of antipsychotics in schizophrenia patients
| Study | Design | Results |
|---|---|---|
| Marder et al, 199714 | In 2 double-blind trials, 513 patients with chronic schizophrenia received risperidone (2, 6, 10, or 16 mg/d), haloperidol (20 mg/d), or placebo for 8 weeks | Patients receiving risperidone showed greater reductions in anxiety and depression symptoms as measured by PANSS scores than patients receiving haloperidol or placebo |
| Tollefson et al, 199815 | In a prospective, blinded trial, 1,996 patients with schizophrenia received olanzapine (5 to 20 mg/d) or haloperidol (5 to 20 mg/d) | Among patients with depressive signs and symptoms, those who received olanzapine showed better improvement in MADRS scores than patients receiving haloperidol |
| Emsley et al, 200316 | Patients with schizophrenia (N = 269) who had not responded to 4 weeks of fluphenazine (20 mg/d) were randomized to receive quetiapine (600 mg/d) or haloperidol (20 mg/d) for 8 weeks | Quetiapine produced greater reduction on PANSS depression scores than haloperidol |
| Mauri et al, 200817 | In a retrospective study, 222 patients in the reexacerbation phase of schizophrenia received fluphenazine, haloperidol decanoate, haloperidol, clozapine, olanzapine, quetiapine, risperidone, or L-sulpiride monotherapy | All antipsychotics led to improvements in depressive symptoms as measured by the BPRS scale, but improvements were statistically significant only with fluphenazine, haloperidol, olanzapine, risperidone, and L-sulpiride |
| BPRS: Brief Psychiatric Rating Scale; MADRS: Montgomery-Åsberg Depression Rating Scale; PANSS: Positive and Negative Syndrome Scale | ||
Antidepressants. If depressive symptoms persist after lowering or changing the antipsychotic, consider a trial of an adjunctive antidepressant. Titrate antidepressants to the recommended dose over 1 month, and continue antiparkinsonian medications. See patients frequently, and ensure that they receive psychosocial support.
No randomized trials have compared the efficacy of antidepressants for treating patients with schizophrenia; therefore, it is unclear if there is a preferred agent. Newer antidepressants often are used in depressed patients with schizophrenia because they are less likely to cause anticholinergic side effects. However, anticholinergic activity may be desirable, eg, for patients with akinesia. Caution is required when combining a selective serotonin reuptake inhibitor with clozapine because metabolism interactions could lead to toxic clozapine levels in some patients.19
If your patient’s depressive symptoms improve after adding an antidepressant, continue that agent along with the antipsychotic and any antiparkinsonian medications. Only 1 study has evaluated maintenance adjunctive antidepressant therapy for depressed patients with schizophrenia who initially responded to antidepressants. It found that imipramine appeared to protect patients from depressive relapse, and patients who received maintenance adjunctive imipramine were less likely to experience worsening psychotic symptoms.20
Depressed schizophrenia patients are most likely to improve if they receive optimal psychosocial intervention,21 which consists of nonspecific support and, when indicated, psychosocial rehabilitation services. Change, even positive change, can be stressful, and patients with schizophrenia need every advantage they can get to be successful in moving their lives in a positive direction.
- Rybakowski JK, Vansteelandt K, Szafranski T, et al. Treatment of depression in first episode of schizophrenia: Results from EUFEST [published online ahead of print May 22, 2012]. Eur Neuropsychopharmacol. doi:10.1016/j.euroneuro.2012.04.001.
- Addington D, Addington J. Calgary Depression Scale for Schizophrenia. www.ucalgary.ca/cdss.
- Benztropine • Cogentin
- Clozapine • Clozaril
- Fluphenazine • Permitil, Prolixin
- Haloperidol • Haldol
- Imipramine • Tofranil
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
Dr. Siris reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Möller HJ. Drug treatment of depressive symptoms in schizophrenia. Clin Schizophr Relat Psychoses. 2008;1(4):328-340.
2. Buckley PF, Miller BJ, Lehrer DS, et al. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35(2):383-402.
3. Hausmann A, Fleischhacker WW. Differential diagnosis of depressed mood in patients with schizophrenia: a diagnostic algorithm based on a review. Acta Psychiatr Scand. 2002;106(2):83-96.
4. Siris SG, Bench C. Depression and schizophrenia. In: Schizophrenia. Hirsch SR Weinberger DR, eds. Malden, MA: Blackwell Publishing Company; 2003:142-167.
5. Hawton K, Sutton L, Haw C, et al. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187:9-20.
6. Rifkin A, Quitkin F, Klein DF. Akinesia: a poorly recognized drug-induced extrapyramidal behavioral disorder. Arch Gen Psychiatry. 1975;32(5):672-674.
7. Van Putten T, May RP. “Akinetic depression” in schizophrenia. Arch Gen Psychiatry. 1978;35(9):1101-1107.
8. Van Putten T. The many faces of akathisia. Compr Psychiatry. 1975;16(1):43-47.
9. Bermanzohn PC, Siris SG. Akinesia: a syndrome common to parkinsonism retarded depression, and negative symptoms of schizophrenia. Compr Psychiatry. 1992;33(4):221-232.
10. Clarke DM, Kissame DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry. 2002;36(6):733-742.
11. Herz MI, Melville C. Relapse in schizophrenia. Am J Psychiatry. 1980;137(7):801-805.
12. Rosen JL, Miller TJ, D’Andrea JT, et al. Comorbid diagnoses in patients meeting criteria for the schizophrenia prodrome. Schizophr Res. 2006;85(1-3):124-131.
13. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
14. Marder SR, Davis JM, Chouinard G. The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: combined results of the North American trials. J Clin Psychiatry. 1997;58(12):538-546.
15. Tollefson GD, Sanger TM, Lu Y, et al. Depressive signs and symptoms in schizophrenia: a prospective blinded trial of olanzapine and haloperidol. Arch Gen Psychiatry. 1998;55(3):250-258.
16. Emsley RA, Buckley P, Jones AM, et al. Differential effect of quetiapine on depressive symptoms in patients with partially responsive schizophrenia. J Psychopharmacol. 2003;17(2):210-215.
17. Mauri MC, Moliterno D, Rossattini M, et al. Depression in schizophrenia: comparison of first- and second-generation antipsychotic drugs. Schizophr Res. 2008;99(1-3):7-12.
18. Siris SG. Depression in schizophrenia: perspective in the era of “atypical” antipsychotic agents. Am J Psychiatry. 2000;157(9):1379-1389.
19. Centorrino F, Baldessarini RJ, Frankenburg FR, et al. Serum levels of clozapine and norclozapine in patients treated with selective serotonin reuptake inhibitors. Am J Psychiatry. 1996;153(6):820-822.
20. Siris SG, Bermanzohn PC, Mason SE, et al. Maintenance imipramine therapy for secondary depression in schizophrenia. A controlled trial. Arch Gen Psychiatry. 1994;51(2):109-115.
21. Bustillo J, Lauriello J, Horan W, et al. The psychosocial treatment of schizophrenia: an update. Am J Psychiatry. 2001;158(2):163-175.
Discuss this article at www.facebook.com/CurrentPsychiatry
Approximately 25% of schizophrenia patients experience course-related depression.1-4 Depression in patients with schizophrenia is linked to reduced social and vocational functioning, increased likelihood of psychotic relapse and rehospitalization, and other problems.2-4 Depression in patients with schizophrenia also has been linked to undesirable life events, especially “exit events” such as losing people in their lives, as well as suicidal ideation, suicide attempts, and completed suicides. Overall, it has been noted that approximately 10% of patients with schizophrenia commit suicide.5 Depressed schizophrenia patients are at particularly high risk for suicide the first few months after diagnosis and after hospital discharge.
Confirm the diagnosis
The best approach to treating depressive symptoms in schizophrenia patients is to formulate a thorough differential diagnosis (Table 1).
Table 1
Differential diagnosis of ‘depression’ in schizophrenia
| Organic factors |
| Antipsychotic-induced dysphoria |
| Akinesia |
| Akathisia |
| Negative symptoms |
| Acute disappointment reactions |
| Chronic disappointment reactions |
| Prodrome of psychotic relapse |
| Depression |
Antipsychotic-induced dysphoria. Blockade of dopamine receptors is an important feature of all antipsychotics; however, dopamine neurotransmission also is involved in the brain’s “pleasure” pathways. Individuals who take antipsychotics may experience reduced joy from once-pleasurable activities. Results of studies on the link between depression and antipsychotics have been mixed.2,4 Although some researchers have found depressed mood common among patients receiving antipsychotics, others have failed to show differences between patients treated with antipsychotics and those randomized to placebo.
Akinesia, a parkinsonian side effect of antipsychotics, can be blatant or subtle. The blatant form involves large muscle groups; these patients present with diminished arm swing, stooped posture, and parkinsonian gait. Easily spotted, such patients are unlikely to be considered depressed.
The more subtle form of akinesia is easier to confuse with depression. It can affect small muscle groups, such as in the face or vocal cords. Lack of responsiveness of facial expression is easily confused with blunted affect, low mood, lack of interest, or emotional unresponsiveness. Subtle akinesia also can impair a patient’s ability to initiate or sustain motor behavior. Many activities, from striking up a conversation to changing television channels, involve initiating and sustaining motor behavior, which these patients’ basal ganglia are underequipped to do. Life becomes boring and patients criticize themselves for “being lazy.” Patients with akinesia also are prone to dysphoria.6,7 When the lack of spontaneous motor behavior found in subtle akinesia is combined with diminished experience of pleasure due to antipsychotic blockade of dopamine, a patient may feel that “nothing is worth the effort.”
Akathisia is another movement disorder of the basal ganglia that can be triggered by antipsychotics. Whereas a patient with akinesia experiences having a “broken starter motor,” the akathisia patient experiences “a starter motor that won’t turn off.” Akathisia can be blatant or subtle. A patient with blatant akathisia has difficulty remaining seated and often paces. In subtle akathisia, increased motor activity is less dramatic, and patients may simply wander or talk excessively. Akathisia also has a dysphoric component that, when the movement is interpreted as restlessness or agitation, may look like depression.8
Negative symptoms. Primary negative symptoms in schizophrenia have several features in common with depression, which can create diagnostic challenges.9 These include anhedonia, social withdrawal, lack of initiative, lowered energy, diminished expectations and/or self confidence, and reduced speech or activity. The main feature that distinguishes the primary negative symptom syndrome from depression is prominent blue mood, which is present in depression but not in negative symptoms. Cognitive features—such as guilt, pessimism, and suicidal thoughts—are common in depression, but usually are absent in negative symptoms.
4 While the acute disappointment reaction is ongoing, the emotional burden may be substantial. With bereavement or grief reactions the loss is clear; however, be vigilant for situations where the patient’s loss may be idiosyncratic or symbolic.
Chronic disappointment reactions, also known as the demoralization syndrome, involve long-term convictions of defeat, despair, incompetence, and loss of control.10 These reactions can be devastating and prolonged. These reactions are important to identify because they may be ameliorated by rehabilitative interventions or other psychosocial supports.
Prodrome of psychotic relapse. Longitudinal observations of patients with schizophrenia have found depressive symptoms may occur during the early stages of psychotic decompensation.4,11,12 These symptoms include dysphoria, anxiety, agitation, sleep and/or appetite disturbances, impaired concentration, hopelessness, helplessness, feelings of loss of control or alienation, and social withdrawal. These features usually last a few days to a couple of weeks before they are overtaken by psychotic phenomena.
Treatment: A suggested approach
Based on my clinical experience in managing newly emergent “depression” episodes in patients correctly diagnosed with schizophrenia, I suggest the following approach:
First, assess the patient for medical disorders that could present with depressive features. Collaborate with the patient’s primary care physician to determine which medications the patient is taking and whether there have been any recent changes in these agents or their doses, including adherence issues, potential substance use or abuse, and changes between brand name and generic agents. Thoroughly evaluate the patient’s psychiatric status, including symptoms, suicidal risk, and changes in life circumstances. A patient who is at high risk of suicide may require hospitalization. Also assess for the presence of extrapyramidal side effects.
Do not change your patient’s medication regimen at this early stage, but provide him or her structure and support, and schedule an early appointment for the next visit (eg, 1 week later). A planned telephone call before the appointment may be helpful as well. If the “depression” is an acute disappointment reaction, it may run its course and resolve. However, if your patient’s depressive symptoms are a prodrome of psychotic relapse, the quick follow-up contact will improve the chances of preventing a psychotic episode by increasing the antipsychotic dosage or making other reasonable changes in pharmacotherapy.
If at the follow-up visit the patient’s psychotic symptoms have not progressed but depressive symptoms persist, evaluate for the possibility of parkinsonian symptoms, which may be subtle and difficult to rule out. If your patient is restless or tends to be physically active, a trial of a benzodiazepine can be added to treat akathisia. If the patient is underactive, consider a trial of an anticholinergic antiparkinsonian agent, such as benztropine, for akinesia. Dosages of benztropine can be raised in a stepwise manner up to 6 mg/d if there are no side effects, such as constipation, dry mouth, blurry vision, or memory impairment. Advantages of treating extrapyramidal side effects first include:
- response to antiparkinsonian medications occurs rapidly—if your patient shows no response within a week, future response at this dose is unlikely
- the presence of anticholinergic side effects is a biologic marker indicating that the treatment dose is adequate
- the clinician has more time to get to know the patient and his or her condition before committing to lowering, raising, or changing the antipsychotic dosage.
Table 2
Antidepressant effects of antipsychotics in schizophrenia patients
| Study | Design | Results |
|---|---|---|
| Marder et al, 199714 | In 2 double-blind trials, 513 patients with chronic schizophrenia received risperidone (2, 6, 10, or 16 mg/d), haloperidol (20 mg/d), or placebo for 8 weeks | Patients receiving risperidone showed greater reductions in anxiety and depression symptoms as measured by PANSS scores than patients receiving haloperidol or placebo |
| Tollefson et al, 199815 | In a prospective, blinded trial, 1,996 patients with schizophrenia received olanzapine (5 to 20 mg/d) or haloperidol (5 to 20 mg/d) | Among patients with depressive signs and symptoms, those who received olanzapine showed better improvement in MADRS scores than patients receiving haloperidol |
| Emsley et al, 200316 | Patients with schizophrenia (N = 269) who had not responded to 4 weeks of fluphenazine (20 mg/d) were randomized to receive quetiapine (600 mg/d) or haloperidol (20 mg/d) for 8 weeks | Quetiapine produced greater reduction on PANSS depression scores than haloperidol |
| Mauri et al, 200817 | In a retrospective study, 222 patients in the reexacerbation phase of schizophrenia received fluphenazine, haloperidol decanoate, haloperidol, clozapine, olanzapine, quetiapine, risperidone, or L-sulpiride monotherapy | All antipsychotics led to improvements in depressive symptoms as measured by the BPRS scale, but improvements were statistically significant only with fluphenazine, haloperidol, olanzapine, risperidone, and L-sulpiride |
| BPRS: Brief Psychiatric Rating Scale; MADRS: Montgomery-Åsberg Depression Rating Scale; PANSS: Positive and Negative Syndrome Scale | ||
Antidepressants. If depressive symptoms persist after lowering or changing the antipsychotic, consider a trial of an adjunctive antidepressant. Titrate antidepressants to the recommended dose over 1 month, and continue antiparkinsonian medications. See patients frequently, and ensure that they receive psychosocial support.
No randomized trials have compared the efficacy of antidepressants for treating patients with schizophrenia; therefore, it is unclear if there is a preferred agent. Newer antidepressants often are used in depressed patients with schizophrenia because they are less likely to cause anticholinergic side effects. However, anticholinergic activity may be desirable, eg, for patients with akinesia. Caution is required when combining a selective serotonin reuptake inhibitor with clozapine because metabolism interactions could lead to toxic clozapine levels in some patients.19
If your patient’s depressive symptoms improve after adding an antidepressant, continue that agent along with the antipsychotic and any antiparkinsonian medications. Only 1 study has evaluated maintenance adjunctive antidepressant therapy for depressed patients with schizophrenia who initially responded to antidepressants. It found that imipramine appeared to protect patients from depressive relapse, and patients who received maintenance adjunctive imipramine were less likely to experience worsening psychotic symptoms.20
Depressed schizophrenia patients are most likely to improve if they receive optimal psychosocial intervention,21 which consists of nonspecific support and, when indicated, psychosocial rehabilitation services. Change, even positive change, can be stressful, and patients with schizophrenia need every advantage they can get to be successful in moving their lives in a positive direction.
- Rybakowski JK, Vansteelandt K, Szafranski T, et al. Treatment of depression in first episode of schizophrenia: Results from EUFEST [published online ahead of print May 22, 2012]. Eur Neuropsychopharmacol. doi:10.1016/j.euroneuro.2012.04.001.
- Addington D, Addington J. Calgary Depression Scale for Schizophrenia. www.ucalgary.ca/cdss.
- Benztropine • Cogentin
- Clozapine • Clozaril
- Fluphenazine • Permitil, Prolixin
- Haloperidol • Haldol
- Imipramine • Tofranil
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
Dr. Siris reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Approximately 25% of schizophrenia patients experience course-related depression.1-4 Depression in patients with schizophrenia is linked to reduced social and vocational functioning, increased likelihood of psychotic relapse and rehospitalization, and other problems.2-4 Depression in patients with schizophrenia also has been linked to undesirable life events, especially “exit events” such as losing people in their lives, as well as suicidal ideation, suicide attempts, and completed suicides. Overall, it has been noted that approximately 10% of patients with schizophrenia commit suicide.5 Depressed schizophrenia patients are at particularly high risk for suicide the first few months after diagnosis and after hospital discharge.
Confirm the diagnosis
The best approach to treating depressive symptoms in schizophrenia patients is to formulate a thorough differential diagnosis (Table 1).
Table 1
Differential diagnosis of ‘depression’ in schizophrenia
| Organic factors |
| Antipsychotic-induced dysphoria |
| Akinesia |
| Akathisia |
| Negative symptoms |
| Acute disappointment reactions |
| Chronic disappointment reactions |
| Prodrome of psychotic relapse |
| Depression |
Antipsychotic-induced dysphoria. Blockade of dopamine receptors is an important feature of all antipsychotics; however, dopamine neurotransmission also is involved in the brain’s “pleasure” pathways. Individuals who take antipsychotics may experience reduced joy from once-pleasurable activities. Results of studies on the link between depression and antipsychotics have been mixed.2,4 Although some researchers have found depressed mood common among patients receiving antipsychotics, others have failed to show differences between patients treated with antipsychotics and those randomized to placebo.
Akinesia, a parkinsonian side effect of antipsychotics, can be blatant or subtle. The blatant form involves large muscle groups; these patients present with diminished arm swing, stooped posture, and parkinsonian gait. Easily spotted, such patients are unlikely to be considered depressed.
The more subtle form of akinesia is easier to confuse with depression. It can affect small muscle groups, such as in the face or vocal cords. Lack of responsiveness of facial expression is easily confused with blunted affect, low mood, lack of interest, or emotional unresponsiveness. Subtle akinesia also can impair a patient’s ability to initiate or sustain motor behavior. Many activities, from striking up a conversation to changing television channels, involve initiating and sustaining motor behavior, which these patients’ basal ganglia are underequipped to do. Life becomes boring and patients criticize themselves for “being lazy.” Patients with akinesia also are prone to dysphoria.6,7 When the lack of spontaneous motor behavior found in subtle akinesia is combined with diminished experience of pleasure due to antipsychotic blockade of dopamine, a patient may feel that “nothing is worth the effort.”
Akathisia is another movement disorder of the basal ganglia that can be triggered by antipsychotics. Whereas a patient with akinesia experiences having a “broken starter motor,” the akathisia patient experiences “a starter motor that won’t turn off.” Akathisia can be blatant or subtle. A patient with blatant akathisia has difficulty remaining seated and often paces. In subtle akathisia, increased motor activity is less dramatic, and patients may simply wander or talk excessively. Akathisia also has a dysphoric component that, when the movement is interpreted as restlessness or agitation, may look like depression.8
Negative symptoms. Primary negative symptoms in schizophrenia have several features in common with depression, which can create diagnostic challenges.9 These include anhedonia, social withdrawal, lack of initiative, lowered energy, diminished expectations and/or self confidence, and reduced speech or activity. The main feature that distinguishes the primary negative symptom syndrome from depression is prominent blue mood, which is present in depression but not in negative symptoms. Cognitive features—such as guilt, pessimism, and suicidal thoughts—are common in depression, but usually are absent in negative symptoms.
4 While the acute disappointment reaction is ongoing, the emotional burden may be substantial. With bereavement or grief reactions the loss is clear; however, be vigilant for situations where the patient’s loss may be idiosyncratic or symbolic.
Chronic disappointment reactions, also known as the demoralization syndrome, involve long-term convictions of defeat, despair, incompetence, and loss of control.10 These reactions can be devastating and prolonged. These reactions are important to identify because they may be ameliorated by rehabilitative interventions or other psychosocial supports.
Prodrome of psychotic relapse. Longitudinal observations of patients with schizophrenia have found depressive symptoms may occur during the early stages of psychotic decompensation.4,11,12 These symptoms include dysphoria, anxiety, agitation, sleep and/or appetite disturbances, impaired concentration, hopelessness, helplessness, feelings of loss of control or alienation, and social withdrawal. These features usually last a few days to a couple of weeks before they are overtaken by psychotic phenomena.
Treatment: A suggested approach
Based on my clinical experience in managing newly emergent “depression” episodes in patients correctly diagnosed with schizophrenia, I suggest the following approach:
First, assess the patient for medical disorders that could present with depressive features. Collaborate with the patient’s primary care physician to determine which medications the patient is taking and whether there have been any recent changes in these agents or their doses, including adherence issues, potential substance use or abuse, and changes between brand name and generic agents. Thoroughly evaluate the patient’s psychiatric status, including symptoms, suicidal risk, and changes in life circumstances. A patient who is at high risk of suicide may require hospitalization. Also assess for the presence of extrapyramidal side effects.
Do not change your patient’s medication regimen at this early stage, but provide him or her structure and support, and schedule an early appointment for the next visit (eg, 1 week later). A planned telephone call before the appointment may be helpful as well. If the “depression” is an acute disappointment reaction, it may run its course and resolve. However, if your patient’s depressive symptoms are a prodrome of psychotic relapse, the quick follow-up contact will improve the chances of preventing a psychotic episode by increasing the antipsychotic dosage or making other reasonable changes in pharmacotherapy.
If at the follow-up visit the patient’s psychotic symptoms have not progressed but depressive symptoms persist, evaluate for the possibility of parkinsonian symptoms, which may be subtle and difficult to rule out. If your patient is restless or tends to be physically active, a trial of a benzodiazepine can be added to treat akathisia. If the patient is underactive, consider a trial of an anticholinergic antiparkinsonian agent, such as benztropine, for akinesia. Dosages of benztropine can be raised in a stepwise manner up to 6 mg/d if there are no side effects, such as constipation, dry mouth, blurry vision, or memory impairment. Advantages of treating extrapyramidal side effects first include:
- response to antiparkinsonian medications occurs rapidly—if your patient shows no response within a week, future response at this dose is unlikely
- the presence of anticholinergic side effects is a biologic marker indicating that the treatment dose is adequate
- the clinician has more time to get to know the patient and his or her condition before committing to lowering, raising, or changing the antipsychotic dosage.
Table 2
Antidepressant effects of antipsychotics in schizophrenia patients
| Study | Design | Results |
|---|---|---|
| Marder et al, 199714 | In 2 double-blind trials, 513 patients with chronic schizophrenia received risperidone (2, 6, 10, or 16 mg/d), haloperidol (20 mg/d), or placebo for 8 weeks | Patients receiving risperidone showed greater reductions in anxiety and depression symptoms as measured by PANSS scores than patients receiving haloperidol or placebo |
| Tollefson et al, 199815 | In a prospective, blinded trial, 1,996 patients with schizophrenia received olanzapine (5 to 20 mg/d) or haloperidol (5 to 20 mg/d) | Among patients with depressive signs and symptoms, those who received olanzapine showed better improvement in MADRS scores than patients receiving haloperidol |
| Emsley et al, 200316 | Patients with schizophrenia (N = 269) who had not responded to 4 weeks of fluphenazine (20 mg/d) were randomized to receive quetiapine (600 mg/d) or haloperidol (20 mg/d) for 8 weeks | Quetiapine produced greater reduction on PANSS depression scores than haloperidol |
| Mauri et al, 200817 | In a retrospective study, 222 patients in the reexacerbation phase of schizophrenia received fluphenazine, haloperidol decanoate, haloperidol, clozapine, olanzapine, quetiapine, risperidone, or L-sulpiride monotherapy | All antipsychotics led to improvements in depressive symptoms as measured by the BPRS scale, but improvements were statistically significant only with fluphenazine, haloperidol, olanzapine, risperidone, and L-sulpiride |
| BPRS: Brief Psychiatric Rating Scale; MADRS: Montgomery-Åsberg Depression Rating Scale; PANSS: Positive and Negative Syndrome Scale | ||
Antidepressants. If depressive symptoms persist after lowering or changing the antipsychotic, consider a trial of an adjunctive antidepressant. Titrate antidepressants to the recommended dose over 1 month, and continue antiparkinsonian medications. See patients frequently, and ensure that they receive psychosocial support.
No randomized trials have compared the efficacy of antidepressants for treating patients with schizophrenia; therefore, it is unclear if there is a preferred agent. Newer antidepressants often are used in depressed patients with schizophrenia because they are less likely to cause anticholinergic side effects. However, anticholinergic activity may be desirable, eg, for patients with akinesia. Caution is required when combining a selective serotonin reuptake inhibitor with clozapine because metabolism interactions could lead to toxic clozapine levels in some patients.19
If your patient’s depressive symptoms improve after adding an antidepressant, continue that agent along with the antipsychotic and any antiparkinsonian medications. Only 1 study has evaluated maintenance adjunctive antidepressant therapy for depressed patients with schizophrenia who initially responded to antidepressants. It found that imipramine appeared to protect patients from depressive relapse, and patients who received maintenance adjunctive imipramine were less likely to experience worsening psychotic symptoms.20
Depressed schizophrenia patients are most likely to improve if they receive optimal psychosocial intervention,21 which consists of nonspecific support and, when indicated, psychosocial rehabilitation services. Change, even positive change, can be stressful, and patients with schizophrenia need every advantage they can get to be successful in moving their lives in a positive direction.
- Rybakowski JK, Vansteelandt K, Szafranski T, et al. Treatment of depression in first episode of schizophrenia: Results from EUFEST [published online ahead of print May 22, 2012]. Eur Neuropsychopharmacol. doi:10.1016/j.euroneuro.2012.04.001.
- Addington D, Addington J. Calgary Depression Scale for Schizophrenia. www.ucalgary.ca/cdss.
- Benztropine • Cogentin
- Clozapine • Clozaril
- Fluphenazine • Permitil, Prolixin
- Haloperidol • Haldol
- Imipramine • Tofranil
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
Dr. Siris reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Möller HJ. Drug treatment of depressive symptoms in schizophrenia. Clin Schizophr Relat Psychoses. 2008;1(4):328-340.
2. Buckley PF, Miller BJ, Lehrer DS, et al. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35(2):383-402.
3. Hausmann A, Fleischhacker WW. Differential diagnosis of depressed mood in patients with schizophrenia: a diagnostic algorithm based on a review. Acta Psychiatr Scand. 2002;106(2):83-96.
4. Siris SG, Bench C. Depression and schizophrenia. In: Schizophrenia. Hirsch SR Weinberger DR, eds. Malden, MA: Blackwell Publishing Company; 2003:142-167.
5. Hawton K, Sutton L, Haw C, et al. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187:9-20.
6. Rifkin A, Quitkin F, Klein DF. Akinesia: a poorly recognized drug-induced extrapyramidal behavioral disorder. Arch Gen Psychiatry. 1975;32(5):672-674.
7. Van Putten T, May RP. “Akinetic depression” in schizophrenia. Arch Gen Psychiatry. 1978;35(9):1101-1107.
8. Van Putten T. The many faces of akathisia. Compr Psychiatry. 1975;16(1):43-47.
9. Bermanzohn PC, Siris SG. Akinesia: a syndrome common to parkinsonism retarded depression, and negative symptoms of schizophrenia. Compr Psychiatry. 1992;33(4):221-232.
10. Clarke DM, Kissame DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry. 2002;36(6):733-742.
11. Herz MI, Melville C. Relapse in schizophrenia. Am J Psychiatry. 1980;137(7):801-805.
12. Rosen JL, Miller TJ, D’Andrea JT, et al. Comorbid diagnoses in patients meeting criteria for the schizophrenia prodrome. Schizophr Res. 2006;85(1-3):124-131.
13. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
14. Marder SR, Davis JM, Chouinard G. The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: combined results of the North American trials. J Clin Psychiatry. 1997;58(12):538-546.
15. Tollefson GD, Sanger TM, Lu Y, et al. Depressive signs and symptoms in schizophrenia: a prospective blinded trial of olanzapine and haloperidol. Arch Gen Psychiatry. 1998;55(3):250-258.
16. Emsley RA, Buckley P, Jones AM, et al. Differential effect of quetiapine on depressive symptoms in patients with partially responsive schizophrenia. J Psychopharmacol. 2003;17(2):210-215.
17. Mauri MC, Moliterno D, Rossattini M, et al. Depression in schizophrenia: comparison of first- and second-generation antipsychotic drugs. Schizophr Res. 2008;99(1-3):7-12.
18. Siris SG. Depression in schizophrenia: perspective in the era of “atypical” antipsychotic agents. Am J Psychiatry. 2000;157(9):1379-1389.
19. Centorrino F, Baldessarini RJ, Frankenburg FR, et al. Serum levels of clozapine and norclozapine in patients treated with selective serotonin reuptake inhibitors. Am J Psychiatry. 1996;153(6):820-822.
20. Siris SG, Bermanzohn PC, Mason SE, et al. Maintenance imipramine therapy for secondary depression in schizophrenia. A controlled trial. Arch Gen Psychiatry. 1994;51(2):109-115.
21. Bustillo J, Lauriello J, Horan W, et al. The psychosocial treatment of schizophrenia: an update. Am J Psychiatry. 2001;158(2):163-175.
1. Möller HJ. Drug treatment of depressive symptoms in schizophrenia. Clin Schizophr Relat Psychoses. 2008;1(4):328-340.
2. Buckley PF, Miller BJ, Lehrer DS, et al. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35(2):383-402.
3. Hausmann A, Fleischhacker WW. Differential diagnosis of depressed mood in patients with schizophrenia: a diagnostic algorithm based on a review. Acta Psychiatr Scand. 2002;106(2):83-96.
4. Siris SG, Bench C. Depression and schizophrenia. In: Schizophrenia. Hirsch SR Weinberger DR, eds. Malden, MA: Blackwell Publishing Company; 2003:142-167.
5. Hawton K, Sutton L, Haw C, et al. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187:9-20.
6. Rifkin A, Quitkin F, Klein DF. Akinesia: a poorly recognized drug-induced extrapyramidal behavioral disorder. Arch Gen Psychiatry. 1975;32(5):672-674.
7. Van Putten T, May RP. “Akinetic depression” in schizophrenia. Arch Gen Psychiatry. 1978;35(9):1101-1107.
8. Van Putten T. The many faces of akathisia. Compr Psychiatry. 1975;16(1):43-47.
9. Bermanzohn PC, Siris SG. Akinesia: a syndrome common to parkinsonism retarded depression, and negative symptoms of schizophrenia. Compr Psychiatry. 1992;33(4):221-232.
10. Clarke DM, Kissame DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry. 2002;36(6):733-742.
11. Herz MI, Melville C. Relapse in schizophrenia. Am J Psychiatry. 1980;137(7):801-805.
12. Rosen JL, Miller TJ, D’Andrea JT, et al. Comorbid diagnoses in patients meeting criteria for the schizophrenia prodrome. Schizophr Res. 2006;85(1-3):124-131.
13. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
14. Marder SR, Davis JM, Chouinard G. The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: combined results of the North American trials. J Clin Psychiatry. 1997;58(12):538-546.
15. Tollefson GD, Sanger TM, Lu Y, et al. Depressive signs and symptoms in schizophrenia: a prospective blinded trial of olanzapine and haloperidol. Arch Gen Psychiatry. 1998;55(3):250-258.
16. Emsley RA, Buckley P, Jones AM, et al. Differential effect of quetiapine on depressive symptoms in patients with partially responsive schizophrenia. J Psychopharmacol. 2003;17(2):210-215.
17. Mauri MC, Moliterno D, Rossattini M, et al. Depression in schizophrenia: comparison of first- and second-generation antipsychotic drugs. Schizophr Res. 2008;99(1-3):7-12.
18. Siris SG. Depression in schizophrenia: perspective in the era of “atypical” antipsychotic agents. Am J Psychiatry. 2000;157(9):1379-1389.
19. Centorrino F, Baldessarini RJ, Frankenburg FR, et al. Serum levels of clozapine and norclozapine in patients treated with selective serotonin reuptake inhibitors. Am J Psychiatry. 1996;153(6):820-822.
20. Siris SG, Bermanzohn PC, Mason SE, et al. Maintenance imipramine therapy for secondary depression in schizophrenia. A controlled trial. Arch Gen Psychiatry. 1994;51(2):109-115.
21. Bustillo J, Lauriello J, Horan W, et al. The psychosocial treatment of schizophrenia: an update. Am J Psychiatry. 2001;158(2):163-175.
Recognizing and treating complicated grief
Nearly 2.5 million persons die each year in the United States.1 For the bereaved, these deaths may be among the most painful and disruptive events they will experience. In this article, we evaluate the growing body of research on complicated grief (CG)—which also has been called prolonged grief, chronic grief, traumatic grief, and pathological grief—with an emphasis on how to identify CG and distinguish it from other adaptive and maladaptive reactions to the loss of a loved one. In addition, we review empirical evidence on treating CG, including psychotherapy, pharmacotherapy, and combined treatment approaches.
The bereavement-specific syndrome we refer to as CG currently is being reviewed for possible inclusion in DSM-5 as an official diagnosis. At press time, proposals for DSM-5 included a bereavement-related adjustment disorder within the new Trauma- and Stressor-Related Disorders category, as well as a provisional diagnosis of CG entitled Persistent Complex Bereavement-Related Disorder, which, upon acceptance, would be listed in Section III.2
What is ‘normal’ grief?
Grief is highly variable across individuals and time and may range from an absence of distress to severe and persistent pain and anguish. There’s no simple definition of “normal grief.” However, as clinicians, it’s necessary to understand the range of usual reactions. We recommend 2 considerations when evaluating grief reactions.
First, be aware that grief encompasses a range of cognitions, emotions, and behaviors. It may range from a relative lack of painful thoughts and emotions to intense and disruptive sadness, loneliness, anger, guilt, intrusive thoughts, difficulty concentrating, preoccupation with loss, social withdrawal, and a sense of being overwhelmed by the loss and its consequences. In the months after a loss, bereaved individuals may look for the deceased in a crowd, speak to them, or even experience auditory or visual hallucinations of the deceased. Nonetheless, positive feelings such as relief, peace, and happiness also are common following a loss.3 Moreover, laughter and smiling when discussing a lost loved one predicts reductions in grief symptoms over time.4 Overall, grief research suggests that, far from proceeding along standard and uniform stages,5 grief is complex and comprises a broad spectrum of thoughts, feelings, and behaviors that vary within and among individuals.
Second, note that in the absence of complications, grief progresses. For those who experience elevated levels of distress, the pain and disruption of loss initially may feel overwhelming but will subside in intensity over time for most individuals.5 This is not to say that an individual will never again feel sadness or longing for the deceased; elements of grief are likely to remain. Although the trajectory of grief symptoms varies among individuals and may progress in fits and starts, over time grief becomes more intermittent, less interfering, and is balanced with a sense of interest and purpose in life.
What is CG?
As research on grief experiences has grown, there’s increasing recognition that a minority of bereaved individuals experience more extreme grief symptoms that cause substantial, persistent distress and impairment despite the passage of many months or years. Shear et al6 proposed a set of CG diagnostic criteria (Table) in which a cluster of symptoms of intense and persistent separation distress are defined as core symptoms. Similar to other psychiatric diagnoses, the symptoms must be associated with significant distress or impairment.
Table
Proposed diagnostic criteria for complicated grief
| Symptom domain | Criteria |
|---|---|
| Separation distress | The patient has ≥1 of the following 4 symptoms: 1) Persistent, intense yearning or longing for the deceased 2) Frequent feelings of intense loneliness or emptiness 3) Recurrent negative thoughts about life without the deceased or recurrent urge to join the deceased 4) Preoccupying thoughts about the deceased that impair daily functioning |
| Thoughts | The patient has ≥2 of the following 8 symptoms: 1) Rumination about circumstances of the death 2) Frequent disbelief or inability to accept the death |
| Feelings | 3) Persistent feeling of being shocked, stunned, or emotionally numb since the death 4) Recurrent feelings of anger or bitterness regarding the death 5) Difficulty trusting or caring about others since the loss 6) Experiencing pain or other somatic symptoms the deceased person had, hearing the voice of the deceased, or seeing the deceased person 7) Intense emotional reactions to memories of the deceased |
| Behaviors | 8) Excessive avoidance or excessive preoccupation with places, people, and things related to the deceased or death |
| Source: Adapted from reference 6 | |
Assessing CG symptoms
Among those with persistent elevated distress, a CG diagnosis must be considered in the context of the individual’s social and cultural environment, time since the loss, and duration of symptoms. The hallmark symptom of CG is separation distress with a focus of cognitive, behavioral, and emotional symptoms on the loss and its consequences. CG is associated with substantial distress, functional impairment, and an increased risk for suicide. See the Box for a case study.
Many individuals with CG remain undiagnosed and untreated for years despite high levels of distress and impairment and high risk for negative consequences such as suicide.7 Accordingly, there’s a need for greater CG screening. Clinically useful tools for assessing CG include a brief, 5-item dimensional screening assessment6 and the patient-rated Inventory of Complicated Grief.8
Distinguishing complicated and uncomplicated grief. Exhibiting CG symptoms in the first several months after a loss does not mean an individual has or will develop CG. Most bereaved adults report painful thoughts and emotions in the weeks and months following the loss, including distressed yearning, waves of intense grief, persistent and intrusive thoughts, images related to the death, somatic distress, and a feeling of being disconnected from others. For most individuals, the intensity of this response diminishes within 6 to 18 months after the loved one’s death.5 Although the optimal length of time to wait before establishing a diagnosis remains debatable, the earliest CG should be diagnosed is 6 months after a loss.
It’s common for grief to occasionally rise in intensity for days or weeks. This surge may occur many months or years after the loss, even in people who exhibited relatively little distress or impairment. In particular, anniversaries, holidays, or periods of stress may trigger increased grief intensity. However, these surges typically subside naturally within a short time. Accordingly, CG should be diagnosed only when symptoms persist for >1 month.
CG vs other post-loss disorders. CG, major depressive disorder (MDD), and posttraumatic stress disorder (PTSD) often are comorbid in bereaved adults. Simon et al9 found 72% of CG patients in a treatment- seeking sample reported a lifetime history of MDD and 53% reported a lifetime history of PTSD. However, CG can be distinguished from these disorders. In the same study, 25% of CG patients had no other axis I diagnosis.9 After accounting for comorbid disorders, researchers associated CG severity with work and social impairment. These findings provide clear evidence for the incremental validity of CG—ie, a CG diagnosis gives clinicians additional information that predicts impairment above and beyond other disorders. However, future research needs to further examine CG and its overlap and differentiation from MDD and PTSD.
Distinguishing CG and MDD. Intense yearning or preoccupation with the deceased is a common symptom of CG but not MDD. In addition, CG symptoms possess intentionality. For example, emotional distress such as sadness and anger are prominent features of both CG and MDD. However, in CG, these symptoms are specific to the loss or circumstances of the loss, whereas in MDD they generally are more nebulous and generalized. Similarly, CG entails proximity seeking related to the deceased, and avoidance of reminders of the deceased, whereas MDD includes a more general social withdrawal and anhedonia.
Distinguishing CG and PTSD. CG and loss-related PTSD are distinguished by the predominant emotions and focus of concern associated with each disorder. The predominant emotion in PTSD is fear, whereas in CG it is sadness and longing. In PTSD, intrusive thoughts and memories associated with the trauma generally are associated with the event itself and produce an ongoing sense of threat.10 Avoidance in PTSD is intended to reduce this threat feeling. By contrast, in CG, intrusive memories focus on the deceased or the circumstances of the death, and avoidance is aimed at preventing painful reminders of the loss or its permanence. Importantly, both syndromes may be present.
Mr. C, age 67, presents to a local emergency department (ED) with his daughter. His daughter reports that he has not been himself since his wife died in a car accident 2 years ago. He continues to live in the house he shared with his wife, despite not needing the extra space and being unable to maintain it. Although Mr. C and his daughter used to talk about her mother a great deal, she says she now tries to avoid the subject because it upsets him. More recently she became concerned when Mr. C began to tell her that his life was meaningless without his wife. He said he frequently thinks about taking his own life to end his pain and loneliness.
Mr. C tells the ED psychiatrist he feels an intense wave of grief and loneliness every morning when he realizes his wife is not with him. He often stays in bed for hours, longing for her and thinking about their time together. At times, he thinks he hears her voice downstairs but when he searches for her, she is not there. Mr. C has been unable to go through his wife’s belongings, and feels nothing should be moved in their home. He will look at her photos, yet avoids other reminders of her (eg, partaking in their favorite hobbies, going to their favorite restaurants). He feels bitter and angry about his wife’s death, and becomes agitated when describing the car accident that took her life. Mr. C feels guilty for not being with his wife when she died. He assures the psychiatrist that he loves his children, but says he feels increasingly distant from them and doesn’t understand how they can move on after their mother’s death.
Mr. C reports symptoms consistent with a diagnosis of complicated grief. Further assessment is appropriate to determine if his symptoms are severe enough to warrant treatment.
Treating CG
When is treatment indicated? For years, bereavement theorists emphasized the need to work through emotions and memories related to the deceased with particular focus on negative material. However, evidence suggests that universal application of treatment to all bereaved individuals is unhelpful. In a recent meta-analysis, Neimeyer et al11 found that the outcomes of grief therapy applied indiscriminately to all bereaved adults or all members of high-risk populations—such as parents whose child experienced a violent death—were no better than would be expected by the passage of time. In contrast, grief therapy applied only to those who develop elevated and persistent distress (eg, CG) led to greater and more enduring improvement in post-loss distress than was observed in control conditions.
These results suggest that most grieving individuals who do not meet criteria for CG (or other psychiatric disorders) will not require intervention. Those who do seek treatment for grief-related distress in the acute grief period should be assessed for bereavement-related depression, anxiety, and suicidality, and treated or referred to professional or community-based resources for support or counseling as clinically indicated.
Evidence for psychotherapy. For those who meet CG criteria, psychotherapy targeting the specific symptoms of CG is helpful. The evidence is strongest for CG treatment (CGT), a 16-session, manualized psychotherapy developed by M. Katherine Shear, MD.12 CGT is based on an attachment model and cognitive-behavioral therapy (CBT) principles, and is informed by the dual-process theory proposed by Stroebe et al.13 According to this theory, natural healing following loss comprises 2 processes:
- a loss-oriented process in which the patient comes to terms with the loss, and
- a restoration-oriented process in which the patient reinvigorates a sense of purpose and meaning in life without the deceased.
CGT focuses on both processes. To address the former, it includes clinician-guided exercises in which the patient revisits the time of the death and planned activities in which the patient reengages with people, places, or thoughts that remind him or her of the deceased. CGT aims to allow the patient to gain an increased tolerance of the distressing thoughts and emotions associated with the loss so that these thoughts can be processed and the finality of the death and its circumstances can be accepted.
The restoration process is addressed by having patients generate and discuss personal goals and aspirations for the near and distant future, as well as scheduling pleasurable and rewarding events. This is accomplished by having patients imagine what they would want for themselves if their grief was less intense and planning concrete steps to take toward these goals. The restoration-oriented process is addressed concurrent with the loss-oriented process to encourage the oscillation between processes thought to be characteristic of a natural healing process following the loss of a loved one.
Other psychotherapy approaches (eg, support groups) may have a role for some individuals, and future research may suggest alternative approaches to CGT. To date, CGT is the most targeted evidence-based psychotherapy with randomized controlled data supporting its use in CG.
Pharmacotherapy for CG. Early research suggested that antidepressants—in particular tricyclics—may effectively reduce depressive symptoms in bereavement-related depression; their effect on CG symptoms, however, may not be as strong.14 Research on pharmacologic treatment that targets CG symptoms is developing. Because of the overlap between CG, PTSD, and MDD, researchers have hypothesized that antidepressants may be effective. Two open-label studies reported that the selective serotonin reuptake inhibitor (SSRI) escitalopram may be effective for CG.15,16 Although a post-hoc comparison of paroxetine and nortriptyline17 showed significant reduction in CG and depressive symptoms with both agents, effects could not be separated from concomitant psychotherapy. Furthermore, an examination of naturalistic data on combining antidepressants with CGT suggested that antidepressants may improve outcomes for individuals receiving CGT.18 A multicenter, randomized controlled trial funded by the National Institute of Mental Health is examining the potential efficacy of citalopram, an SSRI, alone or in combination with CGT.19
The efficacy of benzodiazepines, which commonly are prescribed for bereaved individuals, has not been assessed in CG. However, recent research suggests they may not be useful for medically managing recent grief20 and that their use in the aftermath of a loss may lead to long-term dependence in geriatric patients.21
Related Resources
- Center for Anxiety and Traumatic Stress Disorders. Massachusetts General Hospital. www.bostongrief.com.
- Zisook S, Shear K. Grief and bereavement: what psychiatrists need to know. World Psychiatry. 2009;8(2):67-74.
- Bonanno G. The other side of sadness: what the new science of bereavement tells us about loss. New York, NY: Basic Books; 2009.
Drug Brand Names
- Citalopram • Celexa
- Nortriptyline • Aventyl, Pamelor
- Escitalopram • Lexapro
- Paroxetine • Paxil
Disclosures
Dr. Simon receives grant or research support from the American Cancer Society, the American Foundation for Suicide Prevention, the Department of Defense, Forest Laboratories, and the National Institute of Mental Health.
1. Kochanek KD, Xu J, Murphy SL, et al. U.S. Department of Health and Human Services. Deaths: preliminary data for 2009. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_04.pdf. Published March 16 2011. Accessed June 19, 2012.
2. American Psychiatric Association. Trauma- and stressor-related disorders. http://www.dsm5.org/ProposedRevision/Pages/TraumaandStressorRelatedDisorders.aspx. Accessed June 19 2012.
3. Bonanno GA, Kaltman S. Toward an integrative perspective on bereavement. Psychol Bull. 1999;125(6):760-776.
4. Bonanno GA, Keltner D. Facial expressions of emotion and the course of conjugal bereavement. J Abnorm Psychol. 1997;106(1):126-137.
5. Bonanno GA, Wortman CB, Lehman DR, et al. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. J Pers Soc Psychol. 2002;83(5):1150-1164.
6. Shear MK, Simon N, Wall M, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety. 2011;28(2):103-117.
7. Boelen PA, Prigerson HG. The influence of symptoms of prolonged grief disorder depression, and anxiety on quality of life among bereaved adults: a prospective study. Eur Arch Psychiatry Clin Neurosci. 2007;257(8):444-452.
8. Prigerson HG, Maciejewski PK, Reynolds CF, 3rd, et al. Inventory of Complicated Grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res. 1995;59 (1-2):65-79.
9. Simon NM, Shear KM, Thompson EH, et al. The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Compr Psychiatry. 2007;48(5):395-399.
10. Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clin Psychol Rev. 2003;23(3):339-376.
11. Neimeyer RA, Currier JM. Grief therapy: evidence of efficacy and emerging directions. Curr Dir Psychol Sci. 2009;18(6):352-356.
12. Shear K, Frank E, Houck PR, et al. Treatment of complicated grief: a randomized controlled trial. JAMA. 2005;293(21):2601-2608.
13. Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud. 1999;23(3):197-224.
14. Reynolds CF, 3rd, Miller MD, Pasternak RE, et al. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatry. 1999;156(2):202-208.
15. Simon NM, Thompson EH, Pollack MH, et al. Complicated grief: a case series using escitalopram. Am J Psychiatry. 2007;164(11):1760-1761.
16. Hensley PL, Slonimski CK, Uhlenhuth EH, et al. Escitalopram: an open-label study of bereavement-related depression and grief. J Affect Disord. 2009;113(1-2):142-149.
17. Zygmont M, Prigerson HG, Houck PR, et al. A post hoc comparison of paroxetine and nortriptyline for symptoms of traumatic grief. J Clin Psychiatry. 1998;59(5):241-245.
18. Simon NM, Shear MK, Fagiolini A, et al. Impact of concurrent naturalistic pharmacotherapy on psychotherapy of complicated grief. Psychiatry Res. 2008;159(1-2):31-36.
19. U.S. National Institutes of Health. A study of medication with or without psychotherapy for complicated grief (HEAL). http://clinicaltrials.gov/ct2/show/NCT01179568. Published June 24, 2012. Accessed June 25, 2012.
20. Warner J, Metcalfe C, King M. Evaluating the use of benzodiazepines following recent bereavement. Br J Psychiatry. 2001;178(1):36-41.
21. Cook JM, Biyanova T, Marshall R. Medicating grief with benzodiazepines: physician and patient perspectives. Arch Intern Med. 2007;167(18):2006-2007.
Nearly 2.5 million persons die each year in the United States.1 For the bereaved, these deaths may be among the most painful and disruptive events they will experience. In this article, we evaluate the growing body of research on complicated grief (CG)—which also has been called prolonged grief, chronic grief, traumatic grief, and pathological grief—with an emphasis on how to identify CG and distinguish it from other adaptive and maladaptive reactions to the loss of a loved one. In addition, we review empirical evidence on treating CG, including psychotherapy, pharmacotherapy, and combined treatment approaches.
The bereavement-specific syndrome we refer to as CG currently is being reviewed for possible inclusion in DSM-5 as an official diagnosis. At press time, proposals for DSM-5 included a bereavement-related adjustment disorder within the new Trauma- and Stressor-Related Disorders category, as well as a provisional diagnosis of CG entitled Persistent Complex Bereavement-Related Disorder, which, upon acceptance, would be listed in Section III.2
What is ‘normal’ grief?
Grief is highly variable across individuals and time and may range from an absence of distress to severe and persistent pain and anguish. There’s no simple definition of “normal grief.” However, as clinicians, it’s necessary to understand the range of usual reactions. We recommend 2 considerations when evaluating grief reactions.
First, be aware that grief encompasses a range of cognitions, emotions, and behaviors. It may range from a relative lack of painful thoughts and emotions to intense and disruptive sadness, loneliness, anger, guilt, intrusive thoughts, difficulty concentrating, preoccupation with loss, social withdrawal, and a sense of being overwhelmed by the loss and its consequences. In the months after a loss, bereaved individuals may look for the deceased in a crowd, speak to them, or even experience auditory or visual hallucinations of the deceased. Nonetheless, positive feelings such as relief, peace, and happiness also are common following a loss.3 Moreover, laughter and smiling when discussing a lost loved one predicts reductions in grief symptoms over time.4 Overall, grief research suggests that, far from proceeding along standard and uniform stages,5 grief is complex and comprises a broad spectrum of thoughts, feelings, and behaviors that vary within and among individuals.
Second, note that in the absence of complications, grief progresses. For those who experience elevated levels of distress, the pain and disruption of loss initially may feel overwhelming but will subside in intensity over time for most individuals.5 This is not to say that an individual will never again feel sadness or longing for the deceased; elements of grief are likely to remain. Although the trajectory of grief symptoms varies among individuals and may progress in fits and starts, over time grief becomes more intermittent, less interfering, and is balanced with a sense of interest and purpose in life.
What is CG?
As research on grief experiences has grown, there’s increasing recognition that a minority of bereaved individuals experience more extreme grief symptoms that cause substantial, persistent distress and impairment despite the passage of many months or years. Shear et al6 proposed a set of CG diagnostic criteria (Table) in which a cluster of symptoms of intense and persistent separation distress are defined as core symptoms. Similar to other psychiatric diagnoses, the symptoms must be associated with significant distress or impairment.
Table
Proposed diagnostic criteria for complicated grief
| Symptom domain | Criteria |
|---|---|
| Separation distress | The patient has ≥1 of the following 4 symptoms: 1) Persistent, intense yearning or longing for the deceased 2) Frequent feelings of intense loneliness or emptiness 3) Recurrent negative thoughts about life without the deceased or recurrent urge to join the deceased 4) Preoccupying thoughts about the deceased that impair daily functioning |
| Thoughts | The patient has ≥2 of the following 8 symptoms: 1) Rumination about circumstances of the death 2) Frequent disbelief or inability to accept the death |
| Feelings | 3) Persistent feeling of being shocked, stunned, or emotionally numb since the death 4) Recurrent feelings of anger or bitterness regarding the death 5) Difficulty trusting or caring about others since the loss 6) Experiencing pain or other somatic symptoms the deceased person had, hearing the voice of the deceased, or seeing the deceased person 7) Intense emotional reactions to memories of the deceased |
| Behaviors | 8) Excessive avoidance or excessive preoccupation with places, people, and things related to the deceased or death |
| Source: Adapted from reference 6 | |
Assessing CG symptoms
Among those with persistent elevated distress, a CG diagnosis must be considered in the context of the individual’s social and cultural environment, time since the loss, and duration of symptoms. The hallmark symptom of CG is separation distress with a focus of cognitive, behavioral, and emotional symptoms on the loss and its consequences. CG is associated with substantial distress, functional impairment, and an increased risk for suicide. See the Box for a case study.
Many individuals with CG remain undiagnosed and untreated for years despite high levels of distress and impairment and high risk for negative consequences such as suicide.7 Accordingly, there’s a need for greater CG screening. Clinically useful tools for assessing CG include a brief, 5-item dimensional screening assessment6 and the patient-rated Inventory of Complicated Grief.8
Distinguishing complicated and uncomplicated grief. Exhibiting CG symptoms in the first several months after a loss does not mean an individual has or will develop CG. Most bereaved adults report painful thoughts and emotions in the weeks and months following the loss, including distressed yearning, waves of intense grief, persistent and intrusive thoughts, images related to the death, somatic distress, and a feeling of being disconnected from others. For most individuals, the intensity of this response diminishes within 6 to 18 months after the loved one’s death.5 Although the optimal length of time to wait before establishing a diagnosis remains debatable, the earliest CG should be diagnosed is 6 months after a loss.
It’s common for grief to occasionally rise in intensity for days or weeks. This surge may occur many months or years after the loss, even in people who exhibited relatively little distress or impairment. In particular, anniversaries, holidays, or periods of stress may trigger increased grief intensity. However, these surges typically subside naturally within a short time. Accordingly, CG should be diagnosed only when symptoms persist for >1 month.
CG vs other post-loss disorders. CG, major depressive disorder (MDD), and posttraumatic stress disorder (PTSD) often are comorbid in bereaved adults. Simon et al9 found 72% of CG patients in a treatment- seeking sample reported a lifetime history of MDD and 53% reported a lifetime history of PTSD. However, CG can be distinguished from these disorders. In the same study, 25% of CG patients had no other axis I diagnosis.9 After accounting for comorbid disorders, researchers associated CG severity with work and social impairment. These findings provide clear evidence for the incremental validity of CG—ie, a CG diagnosis gives clinicians additional information that predicts impairment above and beyond other disorders. However, future research needs to further examine CG and its overlap and differentiation from MDD and PTSD.
Distinguishing CG and MDD. Intense yearning or preoccupation with the deceased is a common symptom of CG but not MDD. In addition, CG symptoms possess intentionality. For example, emotional distress such as sadness and anger are prominent features of both CG and MDD. However, in CG, these symptoms are specific to the loss or circumstances of the loss, whereas in MDD they generally are more nebulous and generalized. Similarly, CG entails proximity seeking related to the deceased, and avoidance of reminders of the deceased, whereas MDD includes a more general social withdrawal and anhedonia.
Distinguishing CG and PTSD. CG and loss-related PTSD are distinguished by the predominant emotions and focus of concern associated with each disorder. The predominant emotion in PTSD is fear, whereas in CG it is sadness and longing. In PTSD, intrusive thoughts and memories associated with the trauma generally are associated with the event itself and produce an ongoing sense of threat.10 Avoidance in PTSD is intended to reduce this threat feeling. By contrast, in CG, intrusive memories focus on the deceased or the circumstances of the death, and avoidance is aimed at preventing painful reminders of the loss or its permanence. Importantly, both syndromes may be present.
Mr. C, age 67, presents to a local emergency department (ED) with his daughter. His daughter reports that he has not been himself since his wife died in a car accident 2 years ago. He continues to live in the house he shared with his wife, despite not needing the extra space and being unable to maintain it. Although Mr. C and his daughter used to talk about her mother a great deal, she says she now tries to avoid the subject because it upsets him. More recently she became concerned when Mr. C began to tell her that his life was meaningless without his wife. He said he frequently thinks about taking his own life to end his pain and loneliness.
Mr. C tells the ED psychiatrist he feels an intense wave of grief and loneliness every morning when he realizes his wife is not with him. He often stays in bed for hours, longing for her and thinking about their time together. At times, he thinks he hears her voice downstairs but when he searches for her, she is not there. Mr. C has been unable to go through his wife’s belongings, and feels nothing should be moved in their home. He will look at her photos, yet avoids other reminders of her (eg, partaking in their favorite hobbies, going to their favorite restaurants). He feels bitter and angry about his wife’s death, and becomes agitated when describing the car accident that took her life. Mr. C feels guilty for not being with his wife when she died. He assures the psychiatrist that he loves his children, but says he feels increasingly distant from them and doesn’t understand how they can move on after their mother’s death.
Mr. C reports symptoms consistent with a diagnosis of complicated grief. Further assessment is appropriate to determine if his symptoms are severe enough to warrant treatment.
Treating CG
When is treatment indicated? For years, bereavement theorists emphasized the need to work through emotions and memories related to the deceased with particular focus on negative material. However, evidence suggests that universal application of treatment to all bereaved individuals is unhelpful. In a recent meta-analysis, Neimeyer et al11 found that the outcomes of grief therapy applied indiscriminately to all bereaved adults or all members of high-risk populations—such as parents whose child experienced a violent death—were no better than would be expected by the passage of time. In contrast, grief therapy applied only to those who develop elevated and persistent distress (eg, CG) led to greater and more enduring improvement in post-loss distress than was observed in control conditions.
These results suggest that most grieving individuals who do not meet criteria for CG (or other psychiatric disorders) will not require intervention. Those who do seek treatment for grief-related distress in the acute grief period should be assessed for bereavement-related depression, anxiety, and suicidality, and treated or referred to professional or community-based resources for support or counseling as clinically indicated.
Evidence for psychotherapy. For those who meet CG criteria, psychotherapy targeting the specific symptoms of CG is helpful. The evidence is strongest for CG treatment (CGT), a 16-session, manualized psychotherapy developed by M. Katherine Shear, MD.12 CGT is based on an attachment model and cognitive-behavioral therapy (CBT) principles, and is informed by the dual-process theory proposed by Stroebe et al.13 According to this theory, natural healing following loss comprises 2 processes:
- a loss-oriented process in which the patient comes to terms with the loss, and
- a restoration-oriented process in which the patient reinvigorates a sense of purpose and meaning in life without the deceased.
CGT focuses on both processes. To address the former, it includes clinician-guided exercises in which the patient revisits the time of the death and planned activities in which the patient reengages with people, places, or thoughts that remind him or her of the deceased. CGT aims to allow the patient to gain an increased tolerance of the distressing thoughts and emotions associated with the loss so that these thoughts can be processed and the finality of the death and its circumstances can be accepted.
The restoration process is addressed by having patients generate and discuss personal goals and aspirations for the near and distant future, as well as scheduling pleasurable and rewarding events. This is accomplished by having patients imagine what they would want for themselves if their grief was less intense and planning concrete steps to take toward these goals. The restoration-oriented process is addressed concurrent with the loss-oriented process to encourage the oscillation between processes thought to be characteristic of a natural healing process following the loss of a loved one.
Other psychotherapy approaches (eg, support groups) may have a role for some individuals, and future research may suggest alternative approaches to CGT. To date, CGT is the most targeted evidence-based psychotherapy with randomized controlled data supporting its use in CG.
Pharmacotherapy for CG. Early research suggested that antidepressants—in particular tricyclics—may effectively reduce depressive symptoms in bereavement-related depression; their effect on CG symptoms, however, may not be as strong.14 Research on pharmacologic treatment that targets CG symptoms is developing. Because of the overlap between CG, PTSD, and MDD, researchers have hypothesized that antidepressants may be effective. Two open-label studies reported that the selective serotonin reuptake inhibitor (SSRI) escitalopram may be effective for CG.15,16 Although a post-hoc comparison of paroxetine and nortriptyline17 showed significant reduction in CG and depressive symptoms with both agents, effects could not be separated from concomitant psychotherapy. Furthermore, an examination of naturalistic data on combining antidepressants with CGT suggested that antidepressants may improve outcomes for individuals receiving CGT.18 A multicenter, randomized controlled trial funded by the National Institute of Mental Health is examining the potential efficacy of citalopram, an SSRI, alone or in combination with CGT.19
The efficacy of benzodiazepines, which commonly are prescribed for bereaved individuals, has not been assessed in CG. However, recent research suggests they may not be useful for medically managing recent grief20 and that their use in the aftermath of a loss may lead to long-term dependence in geriatric patients.21
Related Resources
- Center for Anxiety and Traumatic Stress Disorders. Massachusetts General Hospital. www.bostongrief.com.
- Zisook S, Shear K. Grief and bereavement: what psychiatrists need to know. World Psychiatry. 2009;8(2):67-74.
- Bonanno G. The other side of sadness: what the new science of bereavement tells us about loss. New York, NY: Basic Books; 2009.
Drug Brand Names
- Citalopram • Celexa
- Nortriptyline • Aventyl, Pamelor
- Escitalopram • Lexapro
- Paroxetine • Paxil
Disclosures
Dr. Simon receives grant or research support from the American Cancer Society, the American Foundation for Suicide Prevention, the Department of Defense, Forest Laboratories, and the National Institute of Mental Health.
Nearly 2.5 million persons die each year in the United States.1 For the bereaved, these deaths may be among the most painful and disruptive events they will experience. In this article, we evaluate the growing body of research on complicated grief (CG)—which also has been called prolonged grief, chronic grief, traumatic grief, and pathological grief—with an emphasis on how to identify CG and distinguish it from other adaptive and maladaptive reactions to the loss of a loved one. In addition, we review empirical evidence on treating CG, including psychotherapy, pharmacotherapy, and combined treatment approaches.
The bereavement-specific syndrome we refer to as CG currently is being reviewed for possible inclusion in DSM-5 as an official diagnosis. At press time, proposals for DSM-5 included a bereavement-related adjustment disorder within the new Trauma- and Stressor-Related Disorders category, as well as a provisional diagnosis of CG entitled Persistent Complex Bereavement-Related Disorder, which, upon acceptance, would be listed in Section III.2
What is ‘normal’ grief?
Grief is highly variable across individuals and time and may range from an absence of distress to severe and persistent pain and anguish. There’s no simple definition of “normal grief.” However, as clinicians, it’s necessary to understand the range of usual reactions. We recommend 2 considerations when evaluating grief reactions.
First, be aware that grief encompasses a range of cognitions, emotions, and behaviors. It may range from a relative lack of painful thoughts and emotions to intense and disruptive sadness, loneliness, anger, guilt, intrusive thoughts, difficulty concentrating, preoccupation with loss, social withdrawal, and a sense of being overwhelmed by the loss and its consequences. In the months after a loss, bereaved individuals may look for the deceased in a crowd, speak to them, or even experience auditory or visual hallucinations of the deceased. Nonetheless, positive feelings such as relief, peace, and happiness also are common following a loss.3 Moreover, laughter and smiling when discussing a lost loved one predicts reductions in grief symptoms over time.4 Overall, grief research suggests that, far from proceeding along standard and uniform stages,5 grief is complex and comprises a broad spectrum of thoughts, feelings, and behaviors that vary within and among individuals.
Second, note that in the absence of complications, grief progresses. For those who experience elevated levels of distress, the pain and disruption of loss initially may feel overwhelming but will subside in intensity over time for most individuals.5 This is not to say that an individual will never again feel sadness or longing for the deceased; elements of grief are likely to remain. Although the trajectory of grief symptoms varies among individuals and may progress in fits and starts, over time grief becomes more intermittent, less interfering, and is balanced with a sense of interest and purpose in life.
What is CG?
As research on grief experiences has grown, there’s increasing recognition that a minority of bereaved individuals experience more extreme grief symptoms that cause substantial, persistent distress and impairment despite the passage of many months or years. Shear et al6 proposed a set of CG diagnostic criteria (Table) in which a cluster of symptoms of intense and persistent separation distress are defined as core symptoms. Similar to other psychiatric diagnoses, the symptoms must be associated with significant distress or impairment.
Table
Proposed diagnostic criteria for complicated grief
| Symptom domain | Criteria |
|---|---|
| Separation distress | The patient has ≥1 of the following 4 symptoms: 1) Persistent, intense yearning or longing for the deceased 2) Frequent feelings of intense loneliness or emptiness 3) Recurrent negative thoughts about life without the deceased or recurrent urge to join the deceased 4) Preoccupying thoughts about the deceased that impair daily functioning |
| Thoughts | The patient has ≥2 of the following 8 symptoms: 1) Rumination about circumstances of the death 2) Frequent disbelief or inability to accept the death |
| Feelings | 3) Persistent feeling of being shocked, stunned, or emotionally numb since the death 4) Recurrent feelings of anger or bitterness regarding the death 5) Difficulty trusting or caring about others since the loss 6) Experiencing pain or other somatic symptoms the deceased person had, hearing the voice of the deceased, or seeing the deceased person 7) Intense emotional reactions to memories of the deceased |
| Behaviors | 8) Excessive avoidance or excessive preoccupation with places, people, and things related to the deceased or death |
| Source: Adapted from reference 6 | |
Assessing CG symptoms
Among those with persistent elevated distress, a CG diagnosis must be considered in the context of the individual’s social and cultural environment, time since the loss, and duration of symptoms. The hallmark symptom of CG is separation distress with a focus of cognitive, behavioral, and emotional symptoms on the loss and its consequences. CG is associated with substantial distress, functional impairment, and an increased risk for suicide. See the Box for a case study.
Many individuals with CG remain undiagnosed and untreated for years despite high levels of distress and impairment and high risk for negative consequences such as suicide.7 Accordingly, there’s a need for greater CG screening. Clinically useful tools for assessing CG include a brief, 5-item dimensional screening assessment6 and the patient-rated Inventory of Complicated Grief.8
Distinguishing complicated and uncomplicated grief. Exhibiting CG symptoms in the first several months after a loss does not mean an individual has or will develop CG. Most bereaved adults report painful thoughts and emotions in the weeks and months following the loss, including distressed yearning, waves of intense grief, persistent and intrusive thoughts, images related to the death, somatic distress, and a feeling of being disconnected from others. For most individuals, the intensity of this response diminishes within 6 to 18 months after the loved one’s death.5 Although the optimal length of time to wait before establishing a diagnosis remains debatable, the earliest CG should be diagnosed is 6 months after a loss.
It’s common for grief to occasionally rise in intensity for days or weeks. This surge may occur many months or years after the loss, even in people who exhibited relatively little distress or impairment. In particular, anniversaries, holidays, or periods of stress may trigger increased grief intensity. However, these surges typically subside naturally within a short time. Accordingly, CG should be diagnosed only when symptoms persist for >1 month.
CG vs other post-loss disorders. CG, major depressive disorder (MDD), and posttraumatic stress disorder (PTSD) often are comorbid in bereaved adults. Simon et al9 found 72% of CG patients in a treatment- seeking sample reported a lifetime history of MDD and 53% reported a lifetime history of PTSD. However, CG can be distinguished from these disorders. In the same study, 25% of CG patients had no other axis I diagnosis.9 After accounting for comorbid disorders, researchers associated CG severity with work and social impairment. These findings provide clear evidence for the incremental validity of CG—ie, a CG diagnosis gives clinicians additional information that predicts impairment above and beyond other disorders. However, future research needs to further examine CG and its overlap and differentiation from MDD and PTSD.
Distinguishing CG and MDD. Intense yearning or preoccupation with the deceased is a common symptom of CG but not MDD. In addition, CG symptoms possess intentionality. For example, emotional distress such as sadness and anger are prominent features of both CG and MDD. However, in CG, these symptoms are specific to the loss or circumstances of the loss, whereas in MDD they generally are more nebulous and generalized. Similarly, CG entails proximity seeking related to the deceased, and avoidance of reminders of the deceased, whereas MDD includes a more general social withdrawal and anhedonia.
Distinguishing CG and PTSD. CG and loss-related PTSD are distinguished by the predominant emotions and focus of concern associated with each disorder. The predominant emotion in PTSD is fear, whereas in CG it is sadness and longing. In PTSD, intrusive thoughts and memories associated with the trauma generally are associated with the event itself and produce an ongoing sense of threat.10 Avoidance in PTSD is intended to reduce this threat feeling. By contrast, in CG, intrusive memories focus on the deceased or the circumstances of the death, and avoidance is aimed at preventing painful reminders of the loss or its permanence. Importantly, both syndromes may be present.
Mr. C, age 67, presents to a local emergency department (ED) with his daughter. His daughter reports that he has not been himself since his wife died in a car accident 2 years ago. He continues to live in the house he shared with his wife, despite not needing the extra space and being unable to maintain it. Although Mr. C and his daughter used to talk about her mother a great deal, she says she now tries to avoid the subject because it upsets him. More recently she became concerned when Mr. C began to tell her that his life was meaningless without his wife. He said he frequently thinks about taking his own life to end his pain and loneliness.
Mr. C tells the ED psychiatrist he feels an intense wave of grief and loneliness every morning when he realizes his wife is not with him. He often stays in bed for hours, longing for her and thinking about their time together. At times, he thinks he hears her voice downstairs but when he searches for her, she is not there. Mr. C has been unable to go through his wife’s belongings, and feels nothing should be moved in their home. He will look at her photos, yet avoids other reminders of her (eg, partaking in their favorite hobbies, going to their favorite restaurants). He feels bitter and angry about his wife’s death, and becomes agitated when describing the car accident that took her life. Mr. C feels guilty for not being with his wife when she died. He assures the psychiatrist that he loves his children, but says he feels increasingly distant from them and doesn’t understand how they can move on after their mother’s death.
Mr. C reports symptoms consistent with a diagnosis of complicated grief. Further assessment is appropriate to determine if his symptoms are severe enough to warrant treatment.
Treating CG
When is treatment indicated? For years, bereavement theorists emphasized the need to work through emotions and memories related to the deceased with particular focus on negative material. However, evidence suggests that universal application of treatment to all bereaved individuals is unhelpful. In a recent meta-analysis, Neimeyer et al11 found that the outcomes of grief therapy applied indiscriminately to all bereaved adults or all members of high-risk populations—such as parents whose child experienced a violent death—were no better than would be expected by the passage of time. In contrast, grief therapy applied only to those who develop elevated and persistent distress (eg, CG) led to greater and more enduring improvement in post-loss distress than was observed in control conditions.
These results suggest that most grieving individuals who do not meet criteria for CG (or other psychiatric disorders) will not require intervention. Those who do seek treatment for grief-related distress in the acute grief period should be assessed for bereavement-related depression, anxiety, and suicidality, and treated or referred to professional or community-based resources for support or counseling as clinically indicated.
Evidence for psychotherapy. For those who meet CG criteria, psychotherapy targeting the specific symptoms of CG is helpful. The evidence is strongest for CG treatment (CGT), a 16-session, manualized psychotherapy developed by M. Katherine Shear, MD.12 CGT is based on an attachment model and cognitive-behavioral therapy (CBT) principles, and is informed by the dual-process theory proposed by Stroebe et al.13 According to this theory, natural healing following loss comprises 2 processes:
- a loss-oriented process in which the patient comes to terms with the loss, and
- a restoration-oriented process in which the patient reinvigorates a sense of purpose and meaning in life without the deceased.
CGT focuses on both processes. To address the former, it includes clinician-guided exercises in which the patient revisits the time of the death and planned activities in which the patient reengages with people, places, or thoughts that remind him or her of the deceased. CGT aims to allow the patient to gain an increased tolerance of the distressing thoughts and emotions associated with the loss so that these thoughts can be processed and the finality of the death and its circumstances can be accepted.
The restoration process is addressed by having patients generate and discuss personal goals and aspirations for the near and distant future, as well as scheduling pleasurable and rewarding events. This is accomplished by having patients imagine what they would want for themselves if their grief was less intense and planning concrete steps to take toward these goals. The restoration-oriented process is addressed concurrent with the loss-oriented process to encourage the oscillation between processes thought to be characteristic of a natural healing process following the loss of a loved one.
Other psychotherapy approaches (eg, support groups) may have a role for some individuals, and future research may suggest alternative approaches to CGT. To date, CGT is the most targeted evidence-based psychotherapy with randomized controlled data supporting its use in CG.
Pharmacotherapy for CG. Early research suggested that antidepressants—in particular tricyclics—may effectively reduce depressive symptoms in bereavement-related depression; their effect on CG symptoms, however, may not be as strong.14 Research on pharmacologic treatment that targets CG symptoms is developing. Because of the overlap between CG, PTSD, and MDD, researchers have hypothesized that antidepressants may be effective. Two open-label studies reported that the selective serotonin reuptake inhibitor (SSRI) escitalopram may be effective for CG.15,16 Although a post-hoc comparison of paroxetine and nortriptyline17 showed significant reduction in CG and depressive symptoms with both agents, effects could not be separated from concomitant psychotherapy. Furthermore, an examination of naturalistic data on combining antidepressants with CGT suggested that antidepressants may improve outcomes for individuals receiving CGT.18 A multicenter, randomized controlled trial funded by the National Institute of Mental Health is examining the potential efficacy of citalopram, an SSRI, alone or in combination with CGT.19
The efficacy of benzodiazepines, which commonly are prescribed for bereaved individuals, has not been assessed in CG. However, recent research suggests they may not be useful for medically managing recent grief20 and that their use in the aftermath of a loss may lead to long-term dependence in geriatric patients.21
Related Resources
- Center for Anxiety and Traumatic Stress Disorders. Massachusetts General Hospital. www.bostongrief.com.
- Zisook S, Shear K. Grief and bereavement: what psychiatrists need to know. World Psychiatry. 2009;8(2):67-74.
- Bonanno G. The other side of sadness: what the new science of bereavement tells us about loss. New York, NY: Basic Books; 2009.
Drug Brand Names
- Citalopram • Celexa
- Nortriptyline • Aventyl, Pamelor
- Escitalopram • Lexapro
- Paroxetine • Paxil
Disclosures
Dr. Simon receives grant or research support from the American Cancer Society, the American Foundation for Suicide Prevention, the Department of Defense, Forest Laboratories, and the National Institute of Mental Health.
1. Kochanek KD, Xu J, Murphy SL, et al. U.S. Department of Health and Human Services. Deaths: preliminary data for 2009. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_04.pdf. Published March 16 2011. Accessed June 19, 2012.
2. American Psychiatric Association. Trauma- and stressor-related disorders. http://www.dsm5.org/ProposedRevision/Pages/TraumaandStressorRelatedDisorders.aspx. Accessed June 19 2012.
3. Bonanno GA, Kaltman S. Toward an integrative perspective on bereavement. Psychol Bull. 1999;125(6):760-776.
4. Bonanno GA, Keltner D. Facial expressions of emotion and the course of conjugal bereavement. J Abnorm Psychol. 1997;106(1):126-137.
5. Bonanno GA, Wortman CB, Lehman DR, et al. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. J Pers Soc Psychol. 2002;83(5):1150-1164.
6. Shear MK, Simon N, Wall M, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety. 2011;28(2):103-117.
7. Boelen PA, Prigerson HG. The influence of symptoms of prolonged grief disorder depression, and anxiety on quality of life among bereaved adults: a prospective study. Eur Arch Psychiatry Clin Neurosci. 2007;257(8):444-452.
8. Prigerson HG, Maciejewski PK, Reynolds CF, 3rd, et al. Inventory of Complicated Grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res. 1995;59 (1-2):65-79.
9. Simon NM, Shear KM, Thompson EH, et al. The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Compr Psychiatry. 2007;48(5):395-399.
10. Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clin Psychol Rev. 2003;23(3):339-376.
11. Neimeyer RA, Currier JM. Grief therapy: evidence of efficacy and emerging directions. Curr Dir Psychol Sci. 2009;18(6):352-356.
12. Shear K, Frank E, Houck PR, et al. Treatment of complicated grief: a randomized controlled trial. JAMA. 2005;293(21):2601-2608.
13. Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud. 1999;23(3):197-224.
14. Reynolds CF, 3rd, Miller MD, Pasternak RE, et al. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatry. 1999;156(2):202-208.
15. Simon NM, Thompson EH, Pollack MH, et al. Complicated grief: a case series using escitalopram. Am J Psychiatry. 2007;164(11):1760-1761.
16. Hensley PL, Slonimski CK, Uhlenhuth EH, et al. Escitalopram: an open-label study of bereavement-related depression and grief. J Affect Disord. 2009;113(1-2):142-149.
17. Zygmont M, Prigerson HG, Houck PR, et al. A post hoc comparison of paroxetine and nortriptyline for symptoms of traumatic grief. J Clin Psychiatry. 1998;59(5):241-245.
18. Simon NM, Shear MK, Fagiolini A, et al. Impact of concurrent naturalistic pharmacotherapy on psychotherapy of complicated grief. Psychiatry Res. 2008;159(1-2):31-36.
19. U.S. National Institutes of Health. A study of medication with or without psychotherapy for complicated grief (HEAL). http://clinicaltrials.gov/ct2/show/NCT01179568. Published June 24, 2012. Accessed June 25, 2012.
20. Warner J, Metcalfe C, King M. Evaluating the use of benzodiazepines following recent bereavement. Br J Psychiatry. 2001;178(1):36-41.
21. Cook JM, Biyanova T, Marshall R. Medicating grief with benzodiazepines: physician and patient perspectives. Arch Intern Med. 2007;167(18):2006-2007.
1. Kochanek KD, Xu J, Murphy SL, et al. U.S. Department of Health and Human Services. Deaths: preliminary data for 2009. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_04.pdf. Published March 16 2011. Accessed June 19, 2012.
2. American Psychiatric Association. Trauma- and stressor-related disorders. http://www.dsm5.org/ProposedRevision/Pages/TraumaandStressorRelatedDisorders.aspx. Accessed June 19 2012.
3. Bonanno GA, Kaltman S. Toward an integrative perspective on bereavement. Psychol Bull. 1999;125(6):760-776.
4. Bonanno GA, Keltner D. Facial expressions of emotion and the course of conjugal bereavement. J Abnorm Psychol. 1997;106(1):126-137.
5. Bonanno GA, Wortman CB, Lehman DR, et al. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. J Pers Soc Psychol. 2002;83(5):1150-1164.
6. Shear MK, Simon N, Wall M, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety. 2011;28(2):103-117.
7. Boelen PA, Prigerson HG. The influence of symptoms of prolonged grief disorder depression, and anxiety on quality of life among bereaved adults: a prospective study. Eur Arch Psychiatry Clin Neurosci. 2007;257(8):444-452.
8. Prigerson HG, Maciejewski PK, Reynolds CF, 3rd, et al. Inventory of Complicated Grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res. 1995;59 (1-2):65-79.
9. Simon NM, Shear KM, Thompson EH, et al. The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Compr Psychiatry. 2007;48(5):395-399.
10. Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clin Psychol Rev. 2003;23(3):339-376.
11. Neimeyer RA, Currier JM. Grief therapy: evidence of efficacy and emerging directions. Curr Dir Psychol Sci. 2009;18(6):352-356.
12. Shear K, Frank E, Houck PR, et al. Treatment of complicated grief: a randomized controlled trial. JAMA. 2005;293(21):2601-2608.
13. Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud. 1999;23(3):197-224.
14. Reynolds CF, 3rd, Miller MD, Pasternak RE, et al. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatry. 1999;156(2):202-208.
15. Simon NM, Thompson EH, Pollack MH, et al. Complicated grief: a case series using escitalopram. Am J Psychiatry. 2007;164(11):1760-1761.
16. Hensley PL, Slonimski CK, Uhlenhuth EH, et al. Escitalopram: an open-label study of bereavement-related depression and grief. J Affect Disord. 2009;113(1-2):142-149.
17. Zygmont M, Prigerson HG, Houck PR, et al. A post hoc comparison of paroxetine and nortriptyline for symptoms of traumatic grief. J Clin Psychiatry. 1998;59(5):241-245.
18. Simon NM, Shear MK, Fagiolini A, et al. Impact of concurrent naturalistic pharmacotherapy on psychotherapy of complicated grief. Psychiatry Res. 2008;159(1-2):31-36.
19. U.S. National Institutes of Health. A study of medication with or without psychotherapy for complicated grief (HEAL). http://clinicaltrials.gov/ct2/show/NCT01179568. Published June 24, 2012. Accessed June 25, 2012.
20. Warner J, Metcalfe C, King M. Evaluating the use of benzodiazepines following recent bereavement. Br J Psychiatry. 2001;178(1):36-41.
21. Cook JM, Biyanova T, Marshall R. Medicating grief with benzodiazepines: physician and patient perspectives. Arch Intern Med. 2007;167(18):2006-2007.