User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Antipsychotics ineffective for symptoms of delirium in palliative care
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
A little rivaroxaban goes a long way
In patients with venous thromboembolism at equipoise for further anticoagulation therapy, treatment with a 10-mg dose of rivaroxaban (Xarelto) had comparable efficacy to a 20-mg dose, with both leading to fewer recurrences than treatment with aspirin. There were no statistically significant differences in clinically relevant nonmajor bleeding between the three groups.
The study’s conclusions are limited to relatively healthy patients such as the ones who were selected for the study.
The findings were presented at the annual meeting of the American College of Cardiology and published simultaneously in the New England Journal of Medicine (N Engl J Med 2017 March 18. doi: 10.1056/NEJMoa1700518).
Anticoagulants are the primary treatment for prevention of venous thromboembolism recurrences, but the medications are often stopped after 6-12 months because of concerns about bleeding. To counter that issue, physicians may prescribe lower doses of anticoagulants such as rivaroxaban, or substitute aspirin.
The work follows another recent study of apixaban (Eliquis), which showed that a 2.5-mg twice-daily dose performed the same as did a 5.0-mg twice-daily dose in the prevention of venous thromboembolism recurrence (N Engl J Med. 2013;368[8]:699-708).
“I think the story is kind of the same here,” said David Garcia, MD, professor of hematology at the University of Washington, Seattle, who was one of the principal investigators in the trial.
Patients with unprompted venous thromboembolism are increasingly being offered anticoagulant therapy to prevent recurrences. Those drugs have inherent bleeding risks, but the newer drugs and even warfarin are becoming safer. Even so, “as we embark on that, one has to remember that the risk of anticoagulants is cumulative. It may only carry a risk of 1% per year of major hemorrhage, but if the patient has to take it for 10 or 20 or 30 years, it’s a nontrivial risk of major bleeding over that time,” said Dr. Garcia.
The researchers conducted the Reduced-Dose Rivaroxaban in the Long-Term Prevention of Recurrent Symptomatic Venous Thromboembolism (EINSTEIN CHOICE) trial, in which 3,365 patients from 24 sites were randomized to receive 20 mg rivaroxaban, 10 mg rivaroxaban, or 100 mg aspirin for up to 1 year following an initial 6-12 months of treatment with anticoagulation therapy.
During a median follow-up of 1 year, 4.4% of patients on aspirin experienced a recurrence, compared with 1.5% of patients in the 20-mg rivaroxaban group (hazard ratio versus aspirin, 0.34; 95% confidence interval, 0.20-0.59; P less than .001), and 1.2% in the 10-mg rivaroxaban group (HR versus aspirin, 0.26; 95% CI, 0.14-0.47; P less than .001). There was no statistical significance between the two doses of rivaroxaban.
The rates of fatal thromboembolism were similar, at 0.2% in the 20-mg rivaroxaban group, 0% in the 10-mg group, and 0.2% in the aspirin group.
Major bleeding occurred in 0.5% of patients in the 20-mg rivaroxaban group, in 0.4% of the 10-mg rivaroxaban group, and 0.3% in the aspirin group. Nonmajor, clinically relevant bleeding was also similar between groups, at 2.7% in the 20-mg group, 2.0% in the 10-mg group, and 1.8% in the aspirin group. These differences were not statistically significant.
The study is good news for clinicians as they help patients decide whether to undergo preventive therapy. “Even before the newer agents arrived on the market, we had moved the needle a lot in terms of maximizing the safety of warfarin. I think these drugs take it to yet another level,” said Dr. Garcia.
Bayer Pharmaceuticals funded the study. Dr. Garcia has received honoraria from Bristol-Meyers Squibb, Pfizer, and Boehringer Ingelheim.
“Given the protection from recurrent venous thromboembolism afforded by reduced-dose rivaroxaban, extending treatment beyond 3 months could be considered in patients with provoked venous thromboembolism who are at average risk for bleeding and who are strongly averse to having another episode of venous thromboembolism. In light of the safety profile of low-dose rivaroxaban, the benefit of this strategy does not need to be large in order to justify the extension of therapy.
“This trial suggests that it would be helpful to evaluate the effects of reduced doses of rivaroxaban within 6 months after an episode of venous thromboembolism.
“For patients without cancer, the use of direct oral anticoagulant agents might be considered as first-line treatment for those with acute venous thromboembolism. Full-dose treatment could be continued for a minimum of 3-6 months. In patients in whom there is equipoise with respect to continuing anticoagulant therapy beyond this period, the use of a reduced-intensity direct oral anticoagulant agent might be considered. Clinicians who choose this strategy can be confident of excellent efficacy and low bleeding risk similar to that observed with aspirin or placebo” (N Engl J Med 2017 March 18. doi: 10.1056/NEJMe1701628).
Mark Crowther, MD, is professor of medicine at McMaster University, Hamilton, Ont. Adam Cuker is assistant professor of medicine at the hospital of the University of Pennsylvania, Philadelphia.
“Given the protection from recurrent venous thromboembolism afforded by reduced-dose rivaroxaban, extending treatment beyond 3 months could be considered in patients with provoked venous thromboembolism who are at average risk for bleeding and who are strongly averse to having another episode of venous thromboembolism. In light of the safety profile of low-dose rivaroxaban, the benefit of this strategy does not need to be large in order to justify the extension of therapy.
“This trial suggests that it would be helpful to evaluate the effects of reduced doses of rivaroxaban within 6 months after an episode of venous thromboembolism.
“For patients without cancer, the use of direct oral anticoagulant agents might be considered as first-line treatment for those with acute venous thromboembolism. Full-dose treatment could be continued for a minimum of 3-6 months. In patients in whom there is equipoise with respect to continuing anticoagulant therapy beyond this period, the use of a reduced-intensity direct oral anticoagulant agent might be considered. Clinicians who choose this strategy can be confident of excellent efficacy and low bleeding risk similar to that observed with aspirin or placebo” (N Engl J Med 2017 March 18. doi: 10.1056/NEJMe1701628).
Mark Crowther, MD, is professor of medicine at McMaster University, Hamilton, Ont. Adam Cuker is assistant professor of medicine at the hospital of the University of Pennsylvania, Philadelphia.
“Given the protection from recurrent venous thromboembolism afforded by reduced-dose rivaroxaban, extending treatment beyond 3 months could be considered in patients with provoked venous thromboembolism who are at average risk for bleeding and who are strongly averse to having another episode of venous thromboembolism. In light of the safety profile of low-dose rivaroxaban, the benefit of this strategy does not need to be large in order to justify the extension of therapy.
“This trial suggests that it would be helpful to evaluate the effects of reduced doses of rivaroxaban within 6 months after an episode of venous thromboembolism.
“For patients without cancer, the use of direct oral anticoagulant agents might be considered as first-line treatment for those with acute venous thromboembolism. Full-dose treatment could be continued for a minimum of 3-6 months. In patients in whom there is equipoise with respect to continuing anticoagulant therapy beyond this period, the use of a reduced-intensity direct oral anticoagulant agent might be considered. Clinicians who choose this strategy can be confident of excellent efficacy and low bleeding risk similar to that observed with aspirin or placebo” (N Engl J Med 2017 March 18. doi: 10.1056/NEJMe1701628).
Mark Crowther, MD, is professor of medicine at McMaster University, Hamilton, Ont. Adam Cuker is assistant professor of medicine at the hospital of the University of Pennsylvania, Philadelphia.
In patients with venous thromboembolism at equipoise for further anticoagulation therapy, treatment with a 10-mg dose of rivaroxaban (Xarelto) had comparable efficacy to a 20-mg dose, with both leading to fewer recurrences than treatment with aspirin. There were no statistically significant differences in clinically relevant nonmajor bleeding between the three groups.
The study’s conclusions are limited to relatively healthy patients such as the ones who were selected for the study.
The findings were presented at the annual meeting of the American College of Cardiology and published simultaneously in the New England Journal of Medicine (N Engl J Med 2017 March 18. doi: 10.1056/NEJMoa1700518).
Anticoagulants are the primary treatment for prevention of venous thromboembolism recurrences, but the medications are often stopped after 6-12 months because of concerns about bleeding. To counter that issue, physicians may prescribe lower doses of anticoagulants such as rivaroxaban, or substitute aspirin.
The work follows another recent study of apixaban (Eliquis), which showed that a 2.5-mg twice-daily dose performed the same as did a 5.0-mg twice-daily dose in the prevention of venous thromboembolism recurrence (N Engl J Med. 2013;368[8]:699-708).
“I think the story is kind of the same here,” said David Garcia, MD, professor of hematology at the University of Washington, Seattle, who was one of the principal investigators in the trial.
Patients with unprompted venous thromboembolism are increasingly being offered anticoagulant therapy to prevent recurrences. Those drugs have inherent bleeding risks, but the newer drugs and even warfarin are becoming safer. Even so, “as we embark on that, one has to remember that the risk of anticoagulants is cumulative. It may only carry a risk of 1% per year of major hemorrhage, but if the patient has to take it for 10 or 20 or 30 years, it’s a nontrivial risk of major bleeding over that time,” said Dr. Garcia.
The researchers conducted the Reduced-Dose Rivaroxaban in the Long-Term Prevention of Recurrent Symptomatic Venous Thromboembolism (EINSTEIN CHOICE) trial, in which 3,365 patients from 24 sites were randomized to receive 20 mg rivaroxaban, 10 mg rivaroxaban, or 100 mg aspirin for up to 1 year following an initial 6-12 months of treatment with anticoagulation therapy.
During a median follow-up of 1 year, 4.4% of patients on aspirin experienced a recurrence, compared with 1.5% of patients in the 20-mg rivaroxaban group (hazard ratio versus aspirin, 0.34; 95% confidence interval, 0.20-0.59; P less than .001), and 1.2% in the 10-mg rivaroxaban group (HR versus aspirin, 0.26; 95% CI, 0.14-0.47; P less than .001). There was no statistical significance between the two doses of rivaroxaban.
The rates of fatal thromboembolism were similar, at 0.2% in the 20-mg rivaroxaban group, 0% in the 10-mg group, and 0.2% in the aspirin group.
Major bleeding occurred in 0.5% of patients in the 20-mg rivaroxaban group, in 0.4% of the 10-mg rivaroxaban group, and 0.3% in the aspirin group. Nonmajor, clinically relevant bleeding was also similar between groups, at 2.7% in the 20-mg group, 2.0% in the 10-mg group, and 1.8% in the aspirin group. These differences were not statistically significant.
The study is good news for clinicians as they help patients decide whether to undergo preventive therapy. “Even before the newer agents arrived on the market, we had moved the needle a lot in terms of maximizing the safety of warfarin. I think these drugs take it to yet another level,” said Dr. Garcia.
Bayer Pharmaceuticals funded the study. Dr. Garcia has received honoraria from Bristol-Meyers Squibb, Pfizer, and Boehringer Ingelheim.
In patients with venous thromboembolism at equipoise for further anticoagulation therapy, treatment with a 10-mg dose of rivaroxaban (Xarelto) had comparable efficacy to a 20-mg dose, with both leading to fewer recurrences than treatment with aspirin. There were no statistically significant differences in clinically relevant nonmajor bleeding between the three groups.
The study’s conclusions are limited to relatively healthy patients such as the ones who were selected for the study.
The findings were presented at the annual meeting of the American College of Cardiology and published simultaneously in the New England Journal of Medicine (N Engl J Med 2017 March 18. doi: 10.1056/NEJMoa1700518).
Anticoagulants are the primary treatment for prevention of venous thromboembolism recurrences, but the medications are often stopped after 6-12 months because of concerns about bleeding. To counter that issue, physicians may prescribe lower doses of anticoagulants such as rivaroxaban, or substitute aspirin.
The work follows another recent study of apixaban (Eliquis), which showed that a 2.5-mg twice-daily dose performed the same as did a 5.0-mg twice-daily dose in the prevention of venous thromboembolism recurrence (N Engl J Med. 2013;368[8]:699-708).
“I think the story is kind of the same here,” said David Garcia, MD, professor of hematology at the University of Washington, Seattle, who was one of the principal investigators in the trial.
Patients with unprompted venous thromboembolism are increasingly being offered anticoagulant therapy to prevent recurrences. Those drugs have inherent bleeding risks, but the newer drugs and even warfarin are becoming safer. Even so, “as we embark on that, one has to remember that the risk of anticoagulants is cumulative. It may only carry a risk of 1% per year of major hemorrhage, but if the patient has to take it for 10 or 20 or 30 years, it’s a nontrivial risk of major bleeding over that time,” said Dr. Garcia.
The researchers conducted the Reduced-Dose Rivaroxaban in the Long-Term Prevention of Recurrent Symptomatic Venous Thromboembolism (EINSTEIN CHOICE) trial, in which 3,365 patients from 24 sites were randomized to receive 20 mg rivaroxaban, 10 mg rivaroxaban, or 100 mg aspirin for up to 1 year following an initial 6-12 months of treatment with anticoagulation therapy.
During a median follow-up of 1 year, 4.4% of patients on aspirin experienced a recurrence, compared with 1.5% of patients in the 20-mg rivaroxaban group (hazard ratio versus aspirin, 0.34; 95% confidence interval, 0.20-0.59; P less than .001), and 1.2% in the 10-mg rivaroxaban group (HR versus aspirin, 0.26; 95% CI, 0.14-0.47; P less than .001). There was no statistical significance between the two doses of rivaroxaban.
The rates of fatal thromboembolism were similar, at 0.2% in the 20-mg rivaroxaban group, 0% in the 10-mg group, and 0.2% in the aspirin group.
Major bleeding occurred in 0.5% of patients in the 20-mg rivaroxaban group, in 0.4% of the 10-mg rivaroxaban group, and 0.3% in the aspirin group. Nonmajor, clinically relevant bleeding was also similar between groups, at 2.7% in the 20-mg group, 2.0% in the 10-mg group, and 1.8% in the aspirin group. These differences were not statistically significant.
The study is good news for clinicians as they help patients decide whether to undergo preventive therapy. “Even before the newer agents arrived on the market, we had moved the needle a lot in terms of maximizing the safety of warfarin. I think these drugs take it to yet another level,” said Dr. Garcia.
Bayer Pharmaceuticals funded the study. Dr. Garcia has received honoraria from Bristol-Meyers Squibb, Pfizer, and Boehringer Ingelheim.
FROM ACC 17
Key clinical point: In venous thromboembolism prevention, a 10-mg dose matched 20 mg.
Major finding: The recurrence rates were 1.2% at 10 mg versus 4.4% with aspirin.
Data source: Randomized comparison trial of 3,365 patients.
Disclosures: Bayer Pharmaceuticals funded the study. Dr. Garcia has received honoraria from Bristol-Meyers Squibb, Pfizer, and Boehringer Ingelheim.
What are indications, complications of acute blood transfusions in sickle cell anemia? Key Points Additional Reading
Case
A 19-year-old female with a history of sickle cell anemia and hemoglobin SS, presents with a 2-day history of worsening lower back pain and dyspnea. Physical exam reveals oxygen saturation of 87% on room air, a temperature of 39.2° C, respiratory rate of 24 breaths per minute, and right-sided rales. Her hemoglobin is 5.3 g/dL (baseline hemoglobin of 7.8 g/dL). Chest radiograph reveals a right upper lobe pneumonia, and she is diagnosed with acute chest syndrome.
What are indications and complications of acute transfusion in sickle cell anemia?
Background
Chronic hemolytic anemia is a trademark of sickle cell anemia (SCA) or hemoglobin (Hb) SS as is acute anemia during illness or vaso-occlusive crises. Blood transfusions were the first therapy used in sickle cell disease, long before the pathophysiology was understood. Transfusion of red blood cells (RBC) increases the percentage of circulating normal Hb A, thereby decreasing the percentage of abnormal, sickled cells. This increases the oxygen-carrying capacity of the patient’s RBCs, improves organ perfusion, prevents organ damage, and can be life saving. SCA patients are the largest users of the United States rare donor blood bank registry.1
Unfortunately, transfusion comes with many risks including infection, transfusion reactions, alloimmunization, iron overload, hyperviscosity, and volume overload.
As SCA is a low-prevalence disease in a minority population, very few studies have been performed. Currently, the guidance available regarding blood transfusion is primarily based on expert opinion.
What to transfuse
Leukoreduced and intensive phenotypically matched RBC are not possible in many medical centers. Previous studies have noted decreased incidence of febrile nonhemolytic anemia transfusion reactions, cytomegalovirus transmission, and human leukocyte antigen alloimmunization in leukoreduced blood transfusions, however, these studies did not include SCA patients.2
Complications from transfusion
Complications from blood transfusions include febrile nonhemolytic transfusion reaction, acute hemolytic transfusion reaction (ABO incompatibility), transfusion-associated lung injury (TRALI), transfusion-associated circulatory overload (TACO), infections, and anaphylaxis. The National Heart, Lung, and Blood Institute guidelines specifically highlight the complications of delayed hemolytic transfusion reaction, iron overload, and hyperviscosity in SCA.Approximately 30% of SCA patients have alloantibodies.2 SCA patients may also develop autoimmunization, an immune response to their own RBC, particularly if the patient has multiple autoantibodies.
Infection is a risk for all individuals receiving transfusion. Screening for hepatitis B, hepatitis C, HIV, human T-cell lymphotropic virus, syphilis, West Nile virus, Trympanosoma, and bacteria are routinely performed but not 100% conclusive. Other diseases not routinely screened for include Creutzfeldt-Jakob disease, Babesia, human herpesvirus-8, dengue fever, malaria, and newer concerns such as Zika virus. 2,3
Febrile nonhemolytic transfusion reactions present as an increase in body temperature of more than 1° C during or shortly after receiving a blood transfusion in the absence of other pyrexic stimulus. Febrile nonhemolytic transfusion reaction occurs more frequently in patients with a previous history of transfusions. The use of leukoreduced RBCs reduces the occurrence to less than 1%.2
TRALI presents with the acute onset of hypoxemia and noncardiogenic pulmonary edema within 6 hours of a blood transfusion in the absence of other etiologies. The mechanism of TRALI is caused by an inflammatory response causing injury to the alveolar capillary membrane and the development of pulmonary edema.1
TACO presents with cardiogenic pulmonary edema not from another etiology. This is usually seen after transfusion of excessive volumes of blood or after excessively rapid rates of transfusion.1
Delayed hemolytic transfusion reaction (DHTR) may be a life-threatening immune response to donor cell antigens. The reaction is identified by a drop in the patient’s hemoglobin below the pretransfusion level, reticulocytopenia, a positive direct Coombs test, and occasionally jaundice on physical exam.2 Patients may have an unexpectedly high hemoglobin S% after transfusion from the hemolysis of donor cells. The pathognomonic feature is development of a new alloantibody. DHTR occurs more often in individuals who have received recurrent transfusions and has been reported in 4%-11% of transfused SCA patients.3 Donor and native cells hemolyze intra- and extravascularly 5-20 days after receiving a transfusion.2 DHTR is likely underestimated in SCA as it may be confused for a vaso-occlusive crisis.
Iron overload from recurrent transfusions is a slow, chronic process resulting in end organ damage of the heart, liver, and pancreas. It is associated with more frequent hospitalizations and higher mortality in SCA.3 The average person has 4-5 g of iron with no process to remove the excess. One unit of packed red blood cells adds 250-300 mg of iron.2 Ferritin somewhat correlates to iron overload but is not a reliable method because it is an acute-phase reactant. Liver biopsy is the current diagnostic gold standard, however, noninvasive MRI is gaining diagnostic credibility.
Hb SS blood has up to 10 times higher viscosity than does non–sickle cell blood at the same hemoglobin level. RBC transfusion increases the already hyperviscous state of SCA resulting in slow blood flow through vessels. The slow flow through small vessels from hyperviscosity may result in additional sickling and trigger or worsen a vaso-occlusive crisis. Avascular necrosis is theorized to be a result of hyperviscosity as it occurs more commonly in sickle cell patients with higher hemoglobin. It is important not to transfuse to baseline or above a hemoglobin of 10 g/dL to avoid worsening hyperviscosity.2
When to consider transfusion
Unfortunately, there are no strong randomized controlled trials to definitively dictate when simple transfusions or exchange transfusions are indicated. Acute simple transfusions should be considered in certain circumstances including acute chest syndrome, acute stroke, aplastic anemia, preoperative transfusion, splenic sequestration plus severe anemia, acute hepatic sequestration, and severe acute intrahepatic cholestasis.2
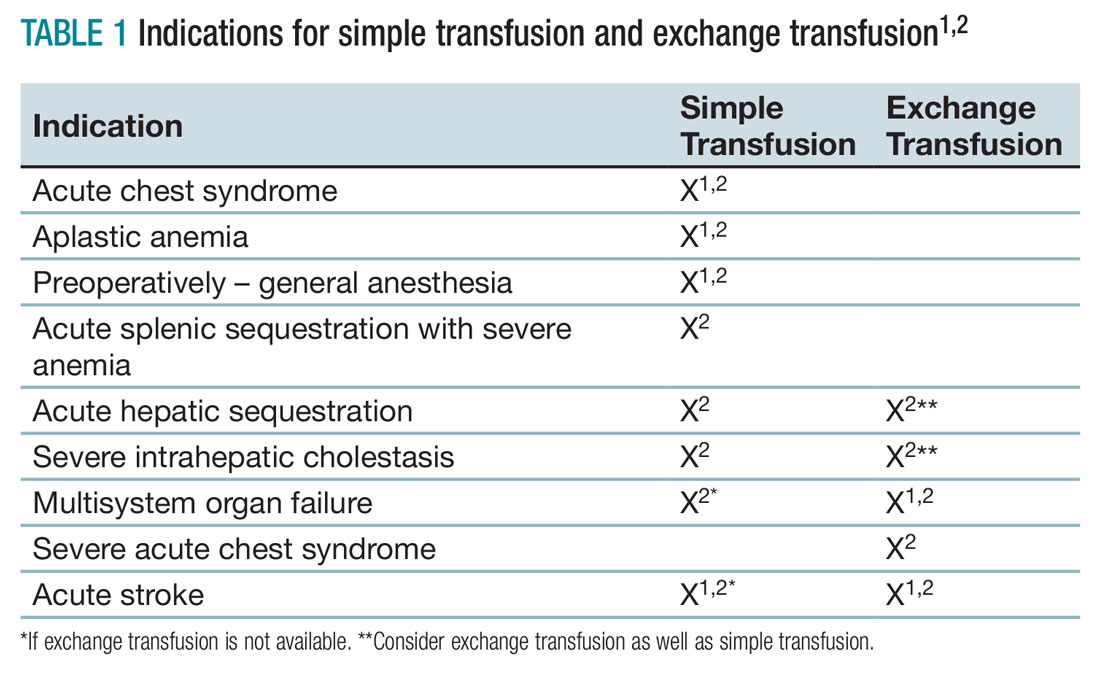
Few studies compare simple transfusion and exchange transfusion.2 The decision to use exchange transfusion over simple transfusion often is based on availability of exchange transfusion, ability of simple transfusion to decrease the percentage of hemoglobin S, and/or the patient’s current hemoglobin to avoid hyperviscosity from simple transfusion.3 Exchange transfusion should be considered for hemoglobin greater than 8-9 g/dL.2
Acute hepatic sequestration (AHS) occurs with the sequestration of RBCs in the liver and is marked by greater than 2 g/dL decrease in hemoglobin and hepatic enlargement, compared with baseline. The stretching of the hepatic capsule results in right upper quadrant pain. AHS often develops over a few hours to a few days with only mild elevation of liver function tests. AHS may be underestimated as two-thirds of SCA patients have hepatomegaly. Unless the hepatomegaly is radiographically monitored it may not be possible to determine an acute increase in liver size.2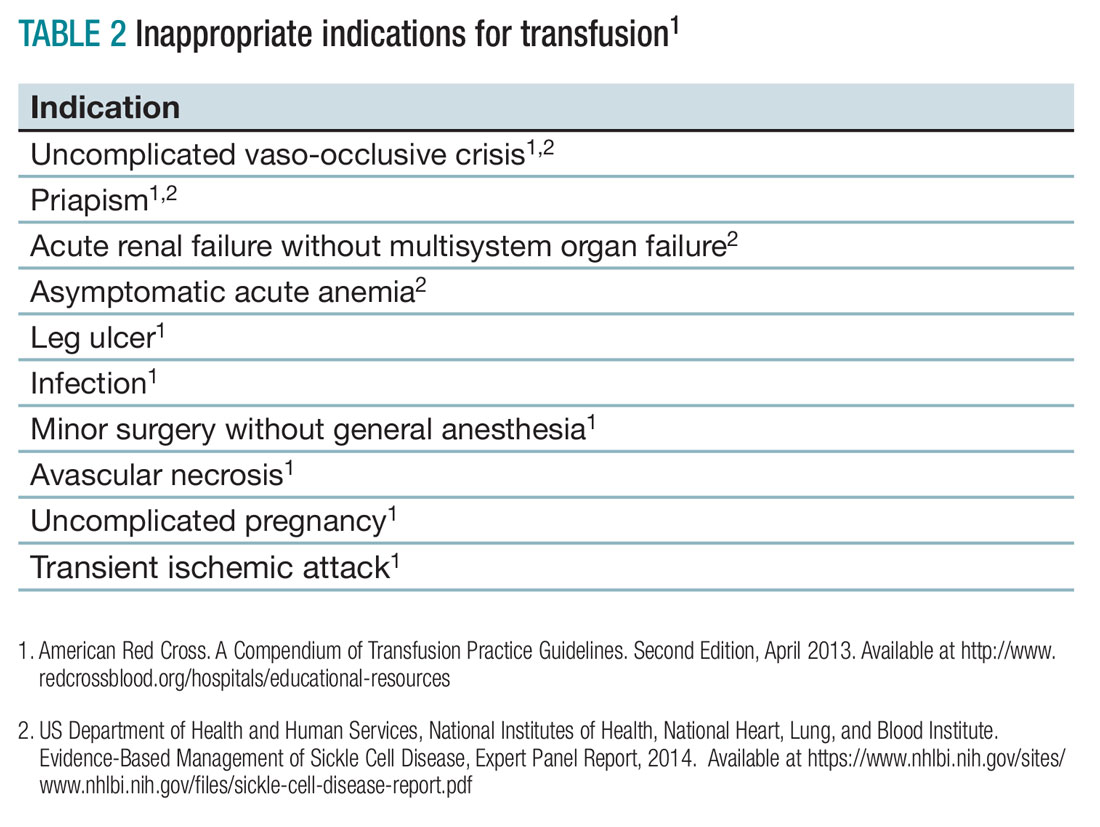
Aplastic crisis presents as a gradual onset of fatigue, shortness of breath, and sometimes syncope or fever. Physical examination may reveal tachycardia and occasionally frank heart failure. The hemoglobin is usually far below the patient’s baseline level with an inappropriate, severely low reticulocyte count. Aplastic crisis should be transfused immediately because of the markedly short life expectancy of hemoglobin S RBCs, but does not need to be transfused to baseline.2
Acute splenic sequestration presents as a decrease in hemoglobin by greater than 2 g/dL, elevated reticulocyte count and circulating nucleated red blood cells, thrombocytopenia, and sudden splenomegaly.2 The goal of transfusion is for partial correction because of the risk of hyperviscosity when the spleen releases the sequestered RBCs.
Acute chest syndrome (ACS) presents as a pneumonia radiographically consistent with a respiratory tract infection caused by cough, shortness of breath, retractions, and/or rales. ACS is the most common cause of death in SCA. ACS is usually from infection but may be because of fat embolism, intrapulmonary aggregates of sickled cells, atelectasis, or pulmonary edema.2 If ACS has a hemoglobin decrease of greater than 1g/dL, consider transfusion.1,2
Severe acute chest syndrome is distinguished by radiographic evidence of multilobe pneumonia, increased work of breathing, pleural effusions, and oxygen saturation below 95% with supplemental oxygen. Severe ACS may have a decrease in hemoglobin despite receiving transfusion. Exchange transfusion is recommended because of the high mortality in severe ACS.2
Preoperative transfusion is used to decrease the incidence of postoperative vaso-occlusive crisis, acute stroke, or ACS for patients receiving general anesthesia. The goal for transfusion hemoglobin is 10g/dL. In SCA patients with a hemoglobin greater than 9g/dL, exchange transfusion may be considered to avoid hyperviscosity.1,2
Multisystem organ failure (MSOF) is severe and life-threatening lung, liver, and/or kidney failure. MSOF may occur after several days of hospitalization. It is often unanticipated and swift, frequently presenting with fever, a rapid increase in anemia, thrombocytopenia, and altered mental status. Lung failure often presents as ACS. Liver failure is marked by hyperbilirubinemia, elevated transaminases, and coagulopathy. Kidney failure is marked by elevated creatinine, with or without change in urine output and hyperkalemia. Rapid treatment with transfusion or exchange transfusion reduces mortality.
The incidence of acute ischemic stroke in SCA decreases with prophylactic transfusion of patients with elevated transcranial Dopplers. Acute stroke is usually secondary to stenosis or an occlusion of the internal carotid or middle cerebral artery. Acute hemorrhagic stroke may present as severe headache and loss of consciousness. Acute stroke should be confirmed radiographically, then exchange transfusion instituted rapidly.2
When not to transfuse
- Do not transfuse for simple vaso-occlusive crisis in the absence of symptoms attributable to acute anemia.1-3
- Do not transfuse for priapism.2
- Do not transfuse for acute renal failure unless there is MSOF.2
Back to the case
The patient was admitted for vaso-occlusive crisis and was started on patient-controlled analgesia with hydromorphone and IV fluids. Azithromycin and ceftriaxone were initiated empirically for community-acquired pneumonia. She was given one unit of phenotypically matched, leukoreduced RBCs for acute chest syndrome. Her hemoglobin increased to 6.1 g/dL. Her fever resolved on day 2, and her dyspnea improved on day 3 of hospitalization. She was weaned off of her patient-controlled analgesia on day 4 and discharged home on day 5 with moxifloxacin to complete 7 days of antibiotics.
Bottom line
Acute simple transfusions and exchange transfusions are indicated for multiple serious and life-threatening complications in SCA. However, transfusion has many serious and life-threatening potential adverse effects. It is essential to conduct a thorough risk-benefit analysis for each individual SCA patient. Whenever possible, intensive phenotypically matched and leukoreduced RBCs should be used. TH
References
1. American Red Cross. A Compendium of Transfusion Practice Guidelines. Second Edition, April 2013.
2. US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute. Evidence-Based Management of Sickle Cell Disease, Expert Panel Report, 2014.
3. Smith-Whitely, K and Thompson, AA. Indications and complications of transfusions in sickle cell disease. Pediatr Blood Cancer. 2012;59(2):358-64.
- SCA patients are at risk for serious transfusion complications including iron overload, delayed hemolytic transfusion reaction, and hyperviscosity in addition to the usual transfusion risks.
- Do not transfuse an uncomplicated vaso-occlusive crisis without symptomatic anemia.1-3
- Repeated transfusions create alloimmunization in SCA patients increasing risk for life-threatening transfusion reactions and difficulty locating phenotypically matched RBCs.
- Transfusion should be considered in SCA patients experiencing acute chest syndrome, aplastic anemia, splenic sequestration with acute anemia, acute hepatic sequestration, and severe intrahepatic cholestasis.1,2
- If available, exchange transfusion should be considered for SCA patients experiencing multisystem organ failure, acute stroke, and severe acute chest syndrome.1,2
- American Red Cross. A Compendium of Transfusion Practice Guidelines. Second Edition, April 2013.
Case
A 19-year-old female with a history of sickle cell anemia and hemoglobin SS, presents with a 2-day history of worsening lower back pain and dyspnea. Physical exam reveals oxygen saturation of 87% on room air, a temperature of 39.2° C, respiratory rate of 24 breaths per minute, and right-sided rales. Her hemoglobin is 5.3 g/dL (baseline hemoglobin of 7.8 g/dL). Chest radiograph reveals a right upper lobe pneumonia, and she is diagnosed with acute chest syndrome.
What are indications and complications of acute transfusion in sickle cell anemia?
Background
Chronic hemolytic anemia is a trademark of sickle cell anemia (SCA) or hemoglobin (Hb) SS as is acute anemia during illness or vaso-occlusive crises. Blood transfusions were the first therapy used in sickle cell disease, long before the pathophysiology was understood. Transfusion of red blood cells (RBC) increases the percentage of circulating normal Hb A, thereby decreasing the percentage of abnormal, sickled cells. This increases the oxygen-carrying capacity of the patient’s RBCs, improves organ perfusion, prevents organ damage, and can be life saving. SCA patients are the largest users of the United States rare donor blood bank registry.1
Unfortunately, transfusion comes with many risks including infection, transfusion reactions, alloimmunization, iron overload, hyperviscosity, and volume overload.
As SCA is a low-prevalence disease in a minority population, very few studies have been performed. Currently, the guidance available regarding blood transfusion is primarily based on expert opinion.
What to transfuse
Leukoreduced and intensive phenotypically matched RBC are not possible in many medical centers. Previous studies have noted decreased incidence of febrile nonhemolytic anemia transfusion reactions, cytomegalovirus transmission, and human leukocyte antigen alloimmunization in leukoreduced blood transfusions, however, these studies did not include SCA patients.2
Complications from transfusion
Complications from blood transfusions include febrile nonhemolytic transfusion reaction, acute hemolytic transfusion reaction (ABO incompatibility), transfusion-associated lung injury (TRALI), transfusion-associated circulatory overload (TACO), infections, and anaphylaxis. The National Heart, Lung, and Blood Institute guidelines specifically highlight the complications of delayed hemolytic transfusion reaction, iron overload, and hyperviscosity in SCA.Approximately 30% of SCA patients have alloantibodies.2 SCA patients may also develop autoimmunization, an immune response to their own RBC, particularly if the patient has multiple autoantibodies.
Infection is a risk for all individuals receiving transfusion. Screening for hepatitis B, hepatitis C, HIV, human T-cell lymphotropic virus, syphilis, West Nile virus, Trympanosoma, and bacteria are routinely performed but not 100% conclusive. Other diseases not routinely screened for include Creutzfeldt-Jakob disease, Babesia, human herpesvirus-8, dengue fever, malaria, and newer concerns such as Zika virus. 2,3
Febrile nonhemolytic transfusion reactions present as an increase in body temperature of more than 1° C during or shortly after receiving a blood transfusion in the absence of other pyrexic stimulus. Febrile nonhemolytic transfusion reaction occurs more frequently in patients with a previous history of transfusions. The use of leukoreduced RBCs reduces the occurrence to less than 1%.2
TRALI presents with the acute onset of hypoxemia and noncardiogenic pulmonary edema within 6 hours of a blood transfusion in the absence of other etiologies. The mechanism of TRALI is caused by an inflammatory response causing injury to the alveolar capillary membrane and the development of pulmonary edema.1
TACO presents with cardiogenic pulmonary edema not from another etiology. This is usually seen after transfusion of excessive volumes of blood or after excessively rapid rates of transfusion.1
Delayed hemolytic transfusion reaction (DHTR) may be a life-threatening immune response to donor cell antigens. The reaction is identified by a drop in the patient’s hemoglobin below the pretransfusion level, reticulocytopenia, a positive direct Coombs test, and occasionally jaundice on physical exam.2 Patients may have an unexpectedly high hemoglobin S% after transfusion from the hemolysis of donor cells. The pathognomonic feature is development of a new alloantibody. DHTR occurs more often in individuals who have received recurrent transfusions and has been reported in 4%-11% of transfused SCA patients.3 Donor and native cells hemolyze intra- and extravascularly 5-20 days after receiving a transfusion.2 DHTR is likely underestimated in SCA as it may be confused for a vaso-occlusive crisis.
Iron overload from recurrent transfusions is a slow, chronic process resulting in end organ damage of the heart, liver, and pancreas. It is associated with more frequent hospitalizations and higher mortality in SCA.3 The average person has 4-5 g of iron with no process to remove the excess. One unit of packed red blood cells adds 250-300 mg of iron.2 Ferritin somewhat correlates to iron overload but is not a reliable method because it is an acute-phase reactant. Liver biopsy is the current diagnostic gold standard, however, noninvasive MRI is gaining diagnostic credibility.
Hb SS blood has up to 10 times higher viscosity than does non–sickle cell blood at the same hemoglobin level. RBC transfusion increases the already hyperviscous state of SCA resulting in slow blood flow through vessels. The slow flow through small vessels from hyperviscosity may result in additional sickling and trigger or worsen a vaso-occlusive crisis. Avascular necrosis is theorized to be a result of hyperviscosity as it occurs more commonly in sickle cell patients with higher hemoglobin. It is important not to transfuse to baseline or above a hemoglobin of 10 g/dL to avoid worsening hyperviscosity.2
When to consider transfusion
Unfortunately, there are no strong randomized controlled trials to definitively dictate when simple transfusions or exchange transfusions are indicated. Acute simple transfusions should be considered in certain circumstances including acute chest syndrome, acute stroke, aplastic anemia, preoperative transfusion, splenic sequestration plus severe anemia, acute hepatic sequestration, and severe acute intrahepatic cholestasis.2
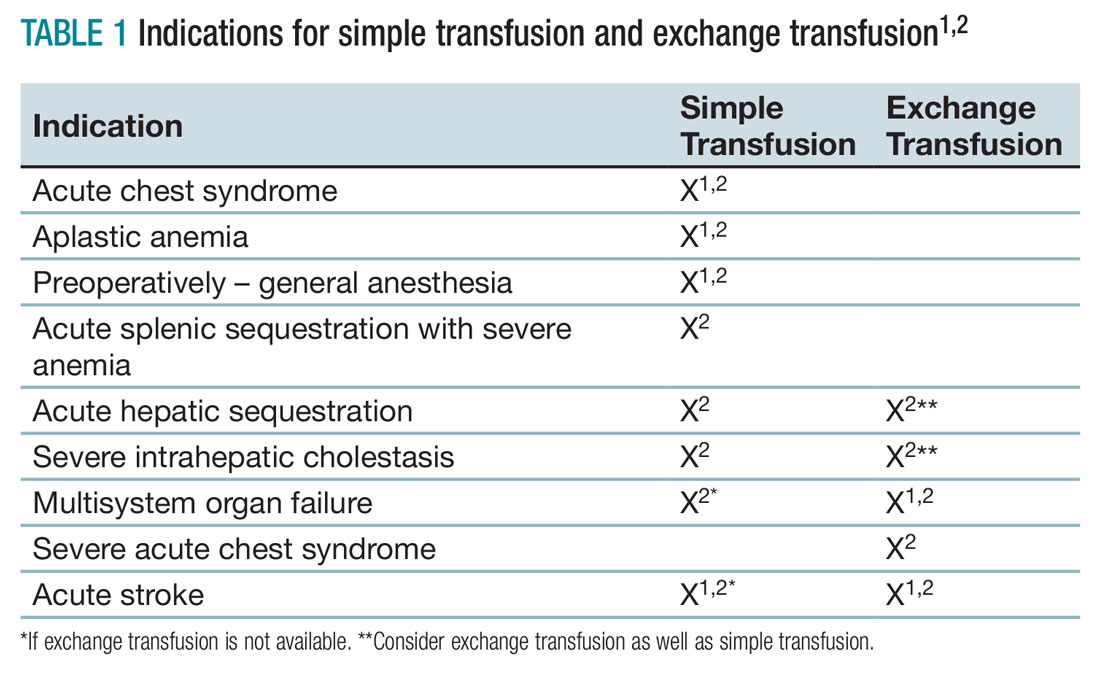
Few studies compare simple transfusion and exchange transfusion.2 The decision to use exchange transfusion over simple transfusion often is based on availability of exchange transfusion, ability of simple transfusion to decrease the percentage of hemoglobin S, and/or the patient’s current hemoglobin to avoid hyperviscosity from simple transfusion.3 Exchange transfusion should be considered for hemoglobin greater than 8-9 g/dL.2
Acute hepatic sequestration (AHS) occurs with the sequestration of RBCs in the liver and is marked by greater than 2 g/dL decrease in hemoglobin and hepatic enlargement, compared with baseline. The stretching of the hepatic capsule results in right upper quadrant pain. AHS often develops over a few hours to a few days with only mild elevation of liver function tests. AHS may be underestimated as two-thirds of SCA patients have hepatomegaly. Unless the hepatomegaly is radiographically monitored it may not be possible to determine an acute increase in liver size.2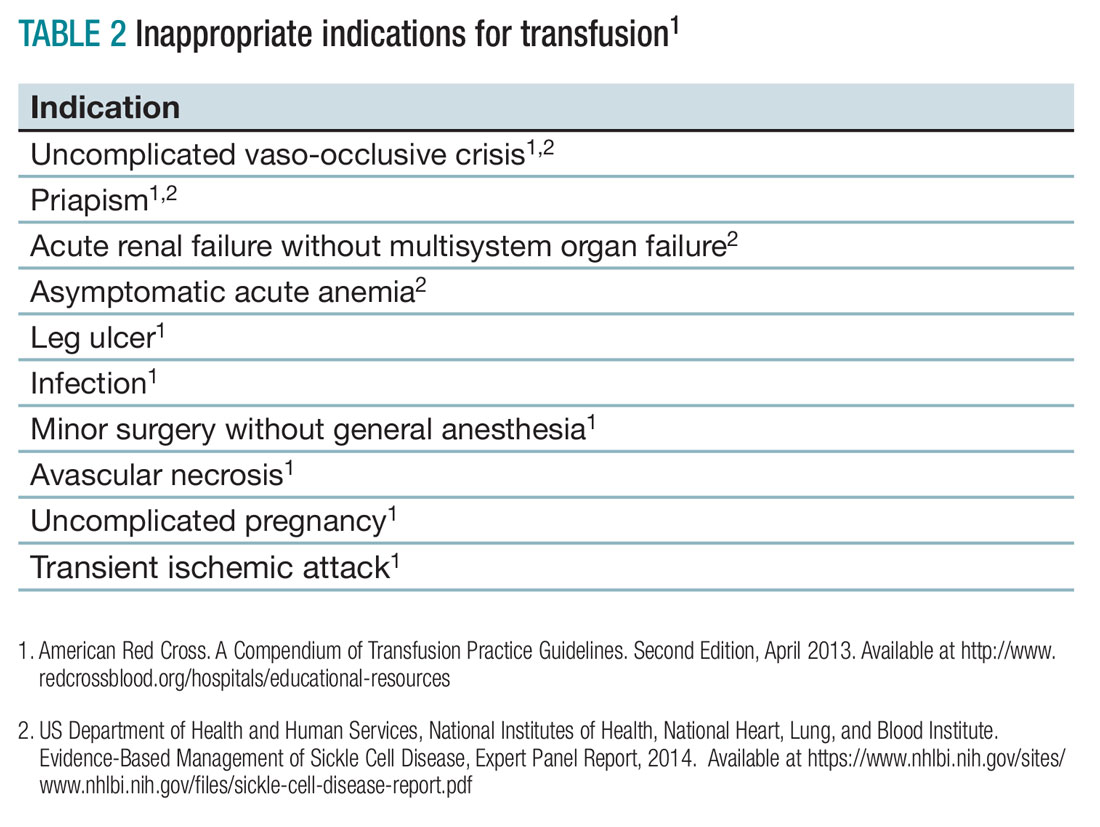
Aplastic crisis presents as a gradual onset of fatigue, shortness of breath, and sometimes syncope or fever. Physical examination may reveal tachycardia and occasionally frank heart failure. The hemoglobin is usually far below the patient’s baseline level with an inappropriate, severely low reticulocyte count. Aplastic crisis should be transfused immediately because of the markedly short life expectancy of hemoglobin S RBCs, but does not need to be transfused to baseline.2
Acute splenic sequestration presents as a decrease in hemoglobin by greater than 2 g/dL, elevated reticulocyte count and circulating nucleated red blood cells, thrombocytopenia, and sudden splenomegaly.2 The goal of transfusion is for partial correction because of the risk of hyperviscosity when the spleen releases the sequestered RBCs.
Acute chest syndrome (ACS) presents as a pneumonia radiographically consistent with a respiratory tract infection caused by cough, shortness of breath, retractions, and/or rales. ACS is the most common cause of death in SCA. ACS is usually from infection but may be because of fat embolism, intrapulmonary aggregates of sickled cells, atelectasis, or pulmonary edema.2 If ACS has a hemoglobin decrease of greater than 1g/dL, consider transfusion.1,2
Severe acute chest syndrome is distinguished by radiographic evidence of multilobe pneumonia, increased work of breathing, pleural effusions, and oxygen saturation below 95% with supplemental oxygen. Severe ACS may have a decrease in hemoglobin despite receiving transfusion. Exchange transfusion is recommended because of the high mortality in severe ACS.2
Preoperative transfusion is used to decrease the incidence of postoperative vaso-occlusive crisis, acute stroke, or ACS for patients receiving general anesthesia. The goal for transfusion hemoglobin is 10g/dL. In SCA patients with a hemoglobin greater than 9g/dL, exchange transfusion may be considered to avoid hyperviscosity.1,2
Multisystem organ failure (MSOF) is severe and life-threatening lung, liver, and/or kidney failure. MSOF may occur after several days of hospitalization. It is often unanticipated and swift, frequently presenting with fever, a rapid increase in anemia, thrombocytopenia, and altered mental status. Lung failure often presents as ACS. Liver failure is marked by hyperbilirubinemia, elevated transaminases, and coagulopathy. Kidney failure is marked by elevated creatinine, with or without change in urine output and hyperkalemia. Rapid treatment with transfusion or exchange transfusion reduces mortality.
The incidence of acute ischemic stroke in SCA decreases with prophylactic transfusion of patients with elevated transcranial Dopplers. Acute stroke is usually secondary to stenosis or an occlusion of the internal carotid or middle cerebral artery. Acute hemorrhagic stroke may present as severe headache and loss of consciousness. Acute stroke should be confirmed radiographically, then exchange transfusion instituted rapidly.2
When not to transfuse
- Do not transfuse for simple vaso-occlusive crisis in the absence of symptoms attributable to acute anemia.1-3
- Do not transfuse for priapism.2
- Do not transfuse for acute renal failure unless there is MSOF.2
Back to the case
The patient was admitted for vaso-occlusive crisis and was started on patient-controlled analgesia with hydromorphone and IV fluids. Azithromycin and ceftriaxone were initiated empirically for community-acquired pneumonia. She was given one unit of phenotypically matched, leukoreduced RBCs for acute chest syndrome. Her hemoglobin increased to 6.1 g/dL. Her fever resolved on day 2, and her dyspnea improved on day 3 of hospitalization. She was weaned off of her patient-controlled analgesia on day 4 and discharged home on day 5 with moxifloxacin to complete 7 days of antibiotics.
Bottom line
Acute simple transfusions and exchange transfusions are indicated for multiple serious and life-threatening complications in SCA. However, transfusion has many serious and life-threatening potential adverse effects. It is essential to conduct a thorough risk-benefit analysis for each individual SCA patient. Whenever possible, intensive phenotypically matched and leukoreduced RBCs should be used. TH
References
1. American Red Cross. A Compendium of Transfusion Practice Guidelines. Second Edition, April 2013.
2. US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute. Evidence-Based Management of Sickle Cell Disease, Expert Panel Report, 2014.
3. Smith-Whitely, K and Thompson, AA. Indications and complications of transfusions in sickle cell disease. Pediatr Blood Cancer. 2012;59(2):358-64.
- SCA patients are at risk for serious transfusion complications including iron overload, delayed hemolytic transfusion reaction, and hyperviscosity in addition to the usual transfusion risks.
- Do not transfuse an uncomplicated vaso-occlusive crisis without symptomatic anemia.1-3
- Repeated transfusions create alloimmunization in SCA patients increasing risk for life-threatening transfusion reactions and difficulty locating phenotypically matched RBCs.
- Transfusion should be considered in SCA patients experiencing acute chest syndrome, aplastic anemia, splenic sequestration with acute anemia, acute hepatic sequestration, and severe intrahepatic cholestasis.1,2
- If available, exchange transfusion should be considered for SCA patients experiencing multisystem organ failure, acute stroke, and severe acute chest syndrome.1,2
- American Red Cross. A Compendium of Transfusion Practice Guidelines. Second Edition, April 2013.
Case
A 19-year-old female with a history of sickle cell anemia and hemoglobin SS, presents with a 2-day history of worsening lower back pain and dyspnea. Physical exam reveals oxygen saturation of 87% on room air, a temperature of 39.2° C, respiratory rate of 24 breaths per minute, and right-sided rales. Her hemoglobin is 5.3 g/dL (baseline hemoglobin of 7.8 g/dL). Chest radiograph reveals a right upper lobe pneumonia, and she is diagnosed with acute chest syndrome.
What are indications and complications of acute transfusion in sickle cell anemia?
Background
Chronic hemolytic anemia is a trademark of sickle cell anemia (SCA) or hemoglobin (Hb) SS as is acute anemia during illness or vaso-occlusive crises. Blood transfusions were the first therapy used in sickle cell disease, long before the pathophysiology was understood. Transfusion of red blood cells (RBC) increases the percentage of circulating normal Hb A, thereby decreasing the percentage of abnormal, sickled cells. This increases the oxygen-carrying capacity of the patient’s RBCs, improves organ perfusion, prevents organ damage, and can be life saving. SCA patients are the largest users of the United States rare donor blood bank registry.1
Unfortunately, transfusion comes with many risks including infection, transfusion reactions, alloimmunization, iron overload, hyperviscosity, and volume overload.
As SCA is a low-prevalence disease in a minority population, very few studies have been performed. Currently, the guidance available regarding blood transfusion is primarily based on expert opinion.
What to transfuse
Leukoreduced and intensive phenotypically matched RBC are not possible in many medical centers. Previous studies have noted decreased incidence of febrile nonhemolytic anemia transfusion reactions, cytomegalovirus transmission, and human leukocyte antigen alloimmunization in leukoreduced blood transfusions, however, these studies did not include SCA patients.2
Complications from transfusion
Complications from blood transfusions include febrile nonhemolytic transfusion reaction, acute hemolytic transfusion reaction (ABO incompatibility), transfusion-associated lung injury (TRALI), transfusion-associated circulatory overload (TACO), infections, and anaphylaxis. The National Heart, Lung, and Blood Institute guidelines specifically highlight the complications of delayed hemolytic transfusion reaction, iron overload, and hyperviscosity in SCA.Approximately 30% of SCA patients have alloantibodies.2 SCA patients may also develop autoimmunization, an immune response to their own RBC, particularly if the patient has multiple autoantibodies.
Infection is a risk for all individuals receiving transfusion. Screening for hepatitis B, hepatitis C, HIV, human T-cell lymphotropic virus, syphilis, West Nile virus, Trympanosoma, and bacteria are routinely performed but not 100% conclusive. Other diseases not routinely screened for include Creutzfeldt-Jakob disease, Babesia, human herpesvirus-8, dengue fever, malaria, and newer concerns such as Zika virus. 2,3
Febrile nonhemolytic transfusion reactions present as an increase in body temperature of more than 1° C during or shortly after receiving a blood transfusion in the absence of other pyrexic stimulus. Febrile nonhemolytic transfusion reaction occurs more frequently in patients with a previous history of transfusions. The use of leukoreduced RBCs reduces the occurrence to less than 1%.2
TRALI presents with the acute onset of hypoxemia and noncardiogenic pulmonary edema within 6 hours of a blood transfusion in the absence of other etiologies. The mechanism of TRALI is caused by an inflammatory response causing injury to the alveolar capillary membrane and the development of pulmonary edema.1
TACO presents with cardiogenic pulmonary edema not from another etiology. This is usually seen after transfusion of excessive volumes of blood or after excessively rapid rates of transfusion.1
Delayed hemolytic transfusion reaction (DHTR) may be a life-threatening immune response to donor cell antigens. The reaction is identified by a drop in the patient’s hemoglobin below the pretransfusion level, reticulocytopenia, a positive direct Coombs test, and occasionally jaundice on physical exam.2 Patients may have an unexpectedly high hemoglobin S% after transfusion from the hemolysis of donor cells. The pathognomonic feature is development of a new alloantibody. DHTR occurs more often in individuals who have received recurrent transfusions and has been reported in 4%-11% of transfused SCA patients.3 Donor and native cells hemolyze intra- and extravascularly 5-20 days after receiving a transfusion.2 DHTR is likely underestimated in SCA as it may be confused for a vaso-occlusive crisis.
Iron overload from recurrent transfusions is a slow, chronic process resulting in end organ damage of the heart, liver, and pancreas. It is associated with more frequent hospitalizations and higher mortality in SCA.3 The average person has 4-5 g of iron with no process to remove the excess. One unit of packed red blood cells adds 250-300 mg of iron.2 Ferritin somewhat correlates to iron overload but is not a reliable method because it is an acute-phase reactant. Liver biopsy is the current diagnostic gold standard, however, noninvasive MRI is gaining diagnostic credibility.
Hb SS blood has up to 10 times higher viscosity than does non–sickle cell blood at the same hemoglobin level. RBC transfusion increases the already hyperviscous state of SCA resulting in slow blood flow through vessels. The slow flow through small vessels from hyperviscosity may result in additional sickling and trigger or worsen a vaso-occlusive crisis. Avascular necrosis is theorized to be a result of hyperviscosity as it occurs more commonly in sickle cell patients with higher hemoglobin. It is important not to transfuse to baseline or above a hemoglobin of 10 g/dL to avoid worsening hyperviscosity.2
When to consider transfusion
Unfortunately, there are no strong randomized controlled trials to definitively dictate when simple transfusions or exchange transfusions are indicated. Acute simple transfusions should be considered in certain circumstances including acute chest syndrome, acute stroke, aplastic anemia, preoperative transfusion, splenic sequestration plus severe anemia, acute hepatic sequestration, and severe acute intrahepatic cholestasis.2
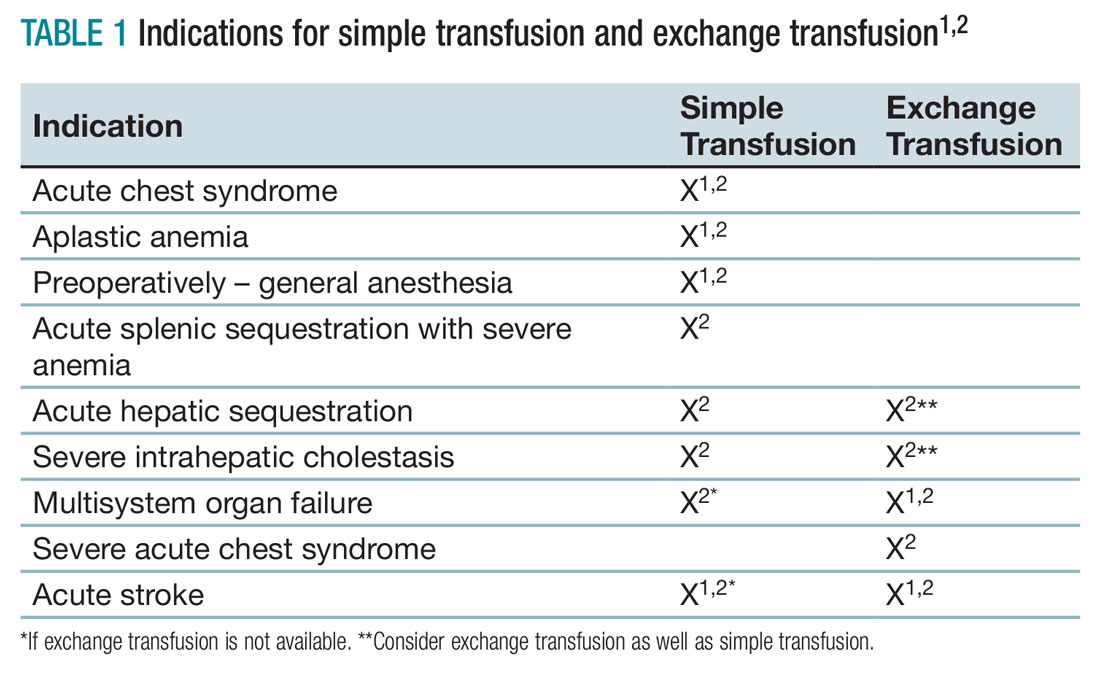
Few studies compare simple transfusion and exchange transfusion.2 The decision to use exchange transfusion over simple transfusion often is based on availability of exchange transfusion, ability of simple transfusion to decrease the percentage of hemoglobin S, and/or the patient’s current hemoglobin to avoid hyperviscosity from simple transfusion.3 Exchange transfusion should be considered for hemoglobin greater than 8-9 g/dL.2
Acute hepatic sequestration (AHS) occurs with the sequestration of RBCs in the liver and is marked by greater than 2 g/dL decrease in hemoglobin and hepatic enlargement, compared with baseline. The stretching of the hepatic capsule results in right upper quadrant pain. AHS often develops over a few hours to a few days with only mild elevation of liver function tests. AHS may be underestimated as two-thirds of SCA patients have hepatomegaly. Unless the hepatomegaly is radiographically monitored it may not be possible to determine an acute increase in liver size.2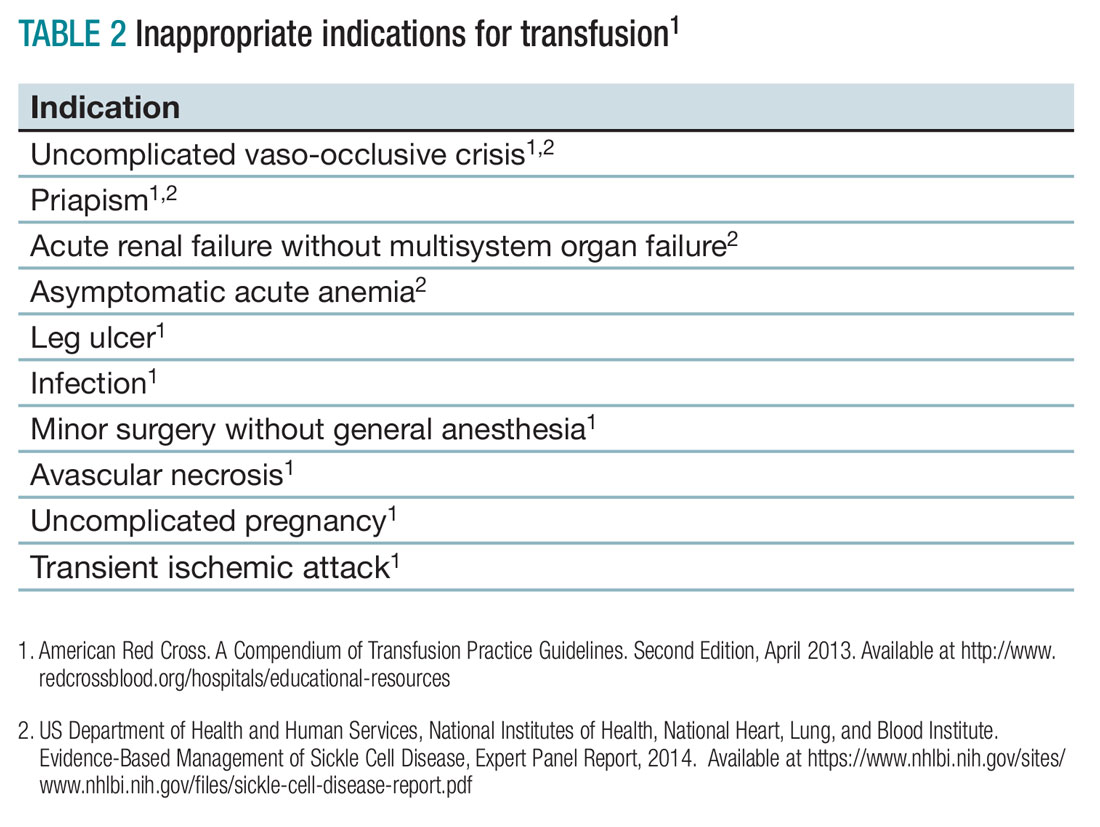
Aplastic crisis presents as a gradual onset of fatigue, shortness of breath, and sometimes syncope or fever. Physical examination may reveal tachycardia and occasionally frank heart failure. The hemoglobin is usually far below the patient’s baseline level with an inappropriate, severely low reticulocyte count. Aplastic crisis should be transfused immediately because of the markedly short life expectancy of hemoglobin S RBCs, but does not need to be transfused to baseline.2
Acute splenic sequestration presents as a decrease in hemoglobin by greater than 2 g/dL, elevated reticulocyte count and circulating nucleated red blood cells, thrombocytopenia, and sudden splenomegaly.2 The goal of transfusion is for partial correction because of the risk of hyperviscosity when the spleen releases the sequestered RBCs.
Acute chest syndrome (ACS) presents as a pneumonia radiographically consistent with a respiratory tract infection caused by cough, shortness of breath, retractions, and/or rales. ACS is the most common cause of death in SCA. ACS is usually from infection but may be because of fat embolism, intrapulmonary aggregates of sickled cells, atelectasis, or pulmonary edema.2 If ACS has a hemoglobin decrease of greater than 1g/dL, consider transfusion.1,2
Severe acute chest syndrome is distinguished by radiographic evidence of multilobe pneumonia, increased work of breathing, pleural effusions, and oxygen saturation below 95% with supplemental oxygen. Severe ACS may have a decrease in hemoglobin despite receiving transfusion. Exchange transfusion is recommended because of the high mortality in severe ACS.2
Preoperative transfusion is used to decrease the incidence of postoperative vaso-occlusive crisis, acute stroke, or ACS for patients receiving general anesthesia. The goal for transfusion hemoglobin is 10g/dL. In SCA patients with a hemoglobin greater than 9g/dL, exchange transfusion may be considered to avoid hyperviscosity.1,2
Multisystem organ failure (MSOF) is severe and life-threatening lung, liver, and/or kidney failure. MSOF may occur after several days of hospitalization. It is often unanticipated and swift, frequently presenting with fever, a rapid increase in anemia, thrombocytopenia, and altered mental status. Lung failure often presents as ACS. Liver failure is marked by hyperbilirubinemia, elevated transaminases, and coagulopathy. Kidney failure is marked by elevated creatinine, with or without change in urine output and hyperkalemia. Rapid treatment with transfusion or exchange transfusion reduces mortality.
The incidence of acute ischemic stroke in SCA decreases with prophylactic transfusion of patients with elevated transcranial Dopplers. Acute stroke is usually secondary to stenosis or an occlusion of the internal carotid or middle cerebral artery. Acute hemorrhagic stroke may present as severe headache and loss of consciousness. Acute stroke should be confirmed radiographically, then exchange transfusion instituted rapidly.2
When not to transfuse
- Do not transfuse for simple vaso-occlusive crisis in the absence of symptoms attributable to acute anemia.1-3
- Do not transfuse for priapism.2
- Do not transfuse for acute renal failure unless there is MSOF.2
Back to the case
The patient was admitted for vaso-occlusive crisis and was started on patient-controlled analgesia with hydromorphone and IV fluids. Azithromycin and ceftriaxone were initiated empirically for community-acquired pneumonia. She was given one unit of phenotypically matched, leukoreduced RBCs for acute chest syndrome. Her hemoglobin increased to 6.1 g/dL. Her fever resolved on day 2, and her dyspnea improved on day 3 of hospitalization. She was weaned off of her patient-controlled analgesia on day 4 and discharged home on day 5 with moxifloxacin to complete 7 days of antibiotics.
Bottom line
Acute simple transfusions and exchange transfusions are indicated for multiple serious and life-threatening complications in SCA. However, transfusion has many serious and life-threatening potential adverse effects. It is essential to conduct a thorough risk-benefit analysis for each individual SCA patient. Whenever possible, intensive phenotypically matched and leukoreduced RBCs should be used. TH
References
1. American Red Cross. A Compendium of Transfusion Practice Guidelines. Second Edition, April 2013.
2. US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute. Evidence-Based Management of Sickle Cell Disease, Expert Panel Report, 2014.
3. Smith-Whitely, K and Thompson, AA. Indications and complications of transfusions in sickle cell disease. Pediatr Blood Cancer. 2012;59(2):358-64.
- SCA patients are at risk for serious transfusion complications including iron overload, delayed hemolytic transfusion reaction, and hyperviscosity in addition to the usual transfusion risks.
- Do not transfuse an uncomplicated vaso-occlusive crisis without symptomatic anemia.1-3
- Repeated transfusions create alloimmunization in SCA patients increasing risk for life-threatening transfusion reactions and difficulty locating phenotypically matched RBCs.
- Transfusion should be considered in SCA patients experiencing acute chest syndrome, aplastic anemia, splenic sequestration with acute anemia, acute hepatic sequestration, and severe intrahepatic cholestasis.1,2
- If available, exchange transfusion should be considered for SCA patients experiencing multisystem organ failure, acute stroke, and severe acute chest syndrome.1,2
- American Red Cross. A Compendium of Transfusion Practice Guidelines. Second Edition, April 2013.
2016 Updates to AASLD Guidance Document on gastroesophageal bleeding in decompensated cirrhosis
Clinical question: What is appropriate inpatient management of a cirrhotic patient with acute esophageal or gastric variceal bleeding?
Study design: Guidance document developed by expert panel based on literature review, consensus conferences and authors’ clinical experience.
Background: Practice guidelines for the diagnosis and treatment of gastroesophageal hemorrhage were last published in 2007 and endorsed by several major professional societies. Since then, there have been a number of randomized controlled trials (RCTs) and consensus conferences. The American Association for the Study of Liver Diseases (AASLD) published updated practice guidelines in 2016 that encompass pathophysiology, monitoring, diagnosis, and treatment of gastroesophageal hemorrhage in cirrhotic patients. This summary will focus on inpatient management for active gastroesophageal hemorrhage.
Synopsis of Inpatient Management for Esophageal Variceal Hemorrhage: The authors suggest that all VH requires ICU admission with the goal of acute control of bleeding, prevention of early recurrence, and reduction in 6-week mortality. Imaging to rule out portal vein thrombosis and HCC should be considered. Hepatic-Venous Pressure Gradient (HVPG) greater than 20 mm Hg is the strongest predictor of early rebleeding and death. However, catheter measurements of portal pressure are not available at most centers. As with any critically ill patient, stabilization of respiratory status and ensuring hemodynamic stability with volume resuscitation is paramount. RCTs evaluating transfusion goals suggest that a restrictive transfusion goal of HgB 7 g/dL is superior to a liberal goal of 9 g/dL. The authors hypothesize this may be related to lower HVPG observed with lower transfusion thresholds. In terms of treating coagulopathy, RCTs evaluating recombinant VIIa have not shown clear benefit. Correction of INR with FFPs similarly not recommended. No recommendations are made regarding utility of platelet transfusions. Vasoactive drugs should be administered when VH is suspected with the goal of decreasing splanchnic blood flow. Octreotide is the only vasoactive drug available in the United States. RCTs show that antibiotics administered prophylactically decrease infections, recurrent hemorrhage, and death. Ceftriaxone 1 g daily is the drug of choice in the United States and should be given up to a maximum of 7 days. A reasonable strategy is discontinuation of prophylaxis concurrently with discontinuation of vasoactive agents. After stabilization of hemodynamics, patients should proceed to endoscopy no more than 12 hours after presentation. Endoscopic Variceal Ligation (EVL) should be done if signs of active or recent variceal bleeding are found. After EVL, select patients at high risk of rebleeding (Child-Pugh B with active bleeding seen on endoscopy or Child-Pugh C patients) may benefit from TIPS within 72 hours. If TIPS is done, vasoactive agents can be discontinued. Otherwise, vasoactive agents should continue for 2-5 days with subsequent transition to nonselective beta blockers (NSBB) such as nadolol or propranolol. For secondary prophylaxis of esophageal bleeding, combination EVL and NSBB is first-line therapy. If recurrent hemorrhage occurs while on secondary prophylaxis, rescue TIPS is recommended.
Synopsis of Inpatient Management for Gastric Variceal Hemorrhage: Management of Gastric Variceal Hemorrhage is similar to Esophageal Variceal (EV) Hemorrhage and encompasses volume resuscitation, vasoactive drugs, and antibiotics with endoscopy shortly thereafter. Balloon tamponade can be used as a bridge to endoscopy in massive bleeds. In addition to the above, anatomic location of Gastric Varices (GV) affects choice of intervention. GOV1 varices extend from the gastric cardia to the lesser curvature and represent 75% of GV. If these are small, they can be managed with EVL. Otherwise these can be managed with injection of cyanoacrylate glue. GOV2 varices extend from the gastric cardia into the fundus. Isolated GV type 1 varices (IGV1) are located entirely in the fundus and have the highest propensity for bleeding. For these latter two types of “cardio-fundal varices” TIPS is the preferred intervention to control acute bleeding. Data on the efficacy of secondary prophylaxis for GV bleeding is limited. A combination of NSBB, cyanoacrylate injection, or TIPS can be considered. Balloon Occluded Retrograde Transvenous Obliteration (BRTO) can be considered if fundal varices are associated with a large gastrorenal or splenorenal collateral. However, no RCTs have compared BRTO with other strategies. Isolated GV type 2 (IGV2) varices are not localized to the esophageal or gastric cardio-fundal region and are rare in cirrhotic patients but tend to occur in pre-hepatic portal hypertension. Management requires multidisciplinary input from endoscopists, hepatologists, interventional radiologists, and surgeons.
Bottom line: For esophageal variceal bleeding related to cirrhosis: volume resuscitation, antibiotic prophylaxis, and vasoactive agents are mainstays of therapy to stabilize patient for endoscopic intervention within 12 hours. This should be followed by early TIPS within 72 hours in high risk patients.
A similar approach applies to gastric variceal bleeding, but interventional management is dependent on the anatomic location of the varices in question.
Citations: Garcia-Tsao G et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis and management – 2016 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2017 Jan;65[1]:310-35.
Dr. Lu is a hospitalist at Cooper University Hospital in Camden, N.J.
Clinical question: What is appropriate inpatient management of a cirrhotic patient with acute esophageal or gastric variceal bleeding?
Study design: Guidance document developed by expert panel based on literature review, consensus conferences and authors’ clinical experience.
Background: Practice guidelines for the diagnosis and treatment of gastroesophageal hemorrhage were last published in 2007 and endorsed by several major professional societies. Since then, there have been a number of randomized controlled trials (RCTs) and consensus conferences. The American Association for the Study of Liver Diseases (AASLD) published updated practice guidelines in 2016 that encompass pathophysiology, monitoring, diagnosis, and treatment of gastroesophageal hemorrhage in cirrhotic patients. This summary will focus on inpatient management for active gastroesophageal hemorrhage.
Synopsis of Inpatient Management for Esophageal Variceal Hemorrhage: The authors suggest that all VH requires ICU admission with the goal of acute control of bleeding, prevention of early recurrence, and reduction in 6-week mortality. Imaging to rule out portal vein thrombosis and HCC should be considered. Hepatic-Venous Pressure Gradient (HVPG) greater than 20 mm Hg is the strongest predictor of early rebleeding and death. However, catheter measurements of portal pressure are not available at most centers. As with any critically ill patient, stabilization of respiratory status and ensuring hemodynamic stability with volume resuscitation is paramount. RCTs evaluating transfusion goals suggest that a restrictive transfusion goal of HgB 7 g/dL is superior to a liberal goal of 9 g/dL. The authors hypothesize this may be related to lower HVPG observed with lower transfusion thresholds. In terms of treating coagulopathy, RCTs evaluating recombinant VIIa have not shown clear benefit. Correction of INR with FFPs similarly not recommended. No recommendations are made regarding utility of platelet transfusions. Vasoactive drugs should be administered when VH is suspected with the goal of decreasing splanchnic blood flow. Octreotide is the only vasoactive drug available in the United States. RCTs show that antibiotics administered prophylactically decrease infections, recurrent hemorrhage, and death. Ceftriaxone 1 g daily is the drug of choice in the United States and should be given up to a maximum of 7 days. A reasonable strategy is discontinuation of prophylaxis concurrently with discontinuation of vasoactive agents. After stabilization of hemodynamics, patients should proceed to endoscopy no more than 12 hours after presentation. Endoscopic Variceal Ligation (EVL) should be done if signs of active or recent variceal bleeding are found. After EVL, select patients at high risk of rebleeding (Child-Pugh B with active bleeding seen on endoscopy or Child-Pugh C patients) may benefit from TIPS within 72 hours. If TIPS is done, vasoactive agents can be discontinued. Otherwise, vasoactive agents should continue for 2-5 days with subsequent transition to nonselective beta blockers (NSBB) such as nadolol or propranolol. For secondary prophylaxis of esophageal bleeding, combination EVL and NSBB is first-line therapy. If recurrent hemorrhage occurs while on secondary prophylaxis, rescue TIPS is recommended.
Synopsis of Inpatient Management for Gastric Variceal Hemorrhage: Management of Gastric Variceal Hemorrhage is similar to Esophageal Variceal (EV) Hemorrhage and encompasses volume resuscitation, vasoactive drugs, and antibiotics with endoscopy shortly thereafter. Balloon tamponade can be used as a bridge to endoscopy in massive bleeds. In addition to the above, anatomic location of Gastric Varices (GV) affects choice of intervention. GOV1 varices extend from the gastric cardia to the lesser curvature and represent 75% of GV. If these are small, they can be managed with EVL. Otherwise these can be managed with injection of cyanoacrylate glue. GOV2 varices extend from the gastric cardia into the fundus. Isolated GV type 1 varices (IGV1) are located entirely in the fundus and have the highest propensity for bleeding. For these latter two types of “cardio-fundal varices” TIPS is the preferred intervention to control acute bleeding. Data on the efficacy of secondary prophylaxis for GV bleeding is limited. A combination of NSBB, cyanoacrylate injection, or TIPS can be considered. Balloon Occluded Retrograde Transvenous Obliteration (BRTO) can be considered if fundal varices are associated with a large gastrorenal or splenorenal collateral. However, no RCTs have compared BRTO with other strategies. Isolated GV type 2 (IGV2) varices are not localized to the esophageal or gastric cardio-fundal region and are rare in cirrhotic patients but tend to occur in pre-hepatic portal hypertension. Management requires multidisciplinary input from endoscopists, hepatologists, interventional radiologists, and surgeons.
Bottom line: For esophageal variceal bleeding related to cirrhosis: volume resuscitation, antibiotic prophylaxis, and vasoactive agents are mainstays of therapy to stabilize patient for endoscopic intervention within 12 hours. This should be followed by early TIPS within 72 hours in high risk patients.
A similar approach applies to gastric variceal bleeding, but interventional management is dependent on the anatomic location of the varices in question.
Citations: Garcia-Tsao G et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis and management – 2016 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2017 Jan;65[1]:310-35.
Dr. Lu is a hospitalist at Cooper University Hospital in Camden, N.J.
Clinical question: What is appropriate inpatient management of a cirrhotic patient with acute esophageal or gastric variceal bleeding?
Study design: Guidance document developed by expert panel based on literature review, consensus conferences and authors’ clinical experience.
Background: Practice guidelines for the diagnosis and treatment of gastroesophageal hemorrhage were last published in 2007 and endorsed by several major professional societies. Since then, there have been a number of randomized controlled trials (RCTs) and consensus conferences. The American Association for the Study of Liver Diseases (AASLD) published updated practice guidelines in 2016 that encompass pathophysiology, monitoring, diagnosis, and treatment of gastroesophageal hemorrhage in cirrhotic patients. This summary will focus on inpatient management for active gastroesophageal hemorrhage.
Synopsis of Inpatient Management for Esophageal Variceal Hemorrhage: The authors suggest that all VH requires ICU admission with the goal of acute control of bleeding, prevention of early recurrence, and reduction in 6-week mortality. Imaging to rule out portal vein thrombosis and HCC should be considered. Hepatic-Venous Pressure Gradient (HVPG) greater than 20 mm Hg is the strongest predictor of early rebleeding and death. However, catheter measurements of portal pressure are not available at most centers. As with any critically ill patient, stabilization of respiratory status and ensuring hemodynamic stability with volume resuscitation is paramount. RCTs evaluating transfusion goals suggest that a restrictive transfusion goal of HgB 7 g/dL is superior to a liberal goal of 9 g/dL. The authors hypothesize this may be related to lower HVPG observed with lower transfusion thresholds. In terms of treating coagulopathy, RCTs evaluating recombinant VIIa have not shown clear benefit. Correction of INR with FFPs similarly not recommended. No recommendations are made regarding utility of platelet transfusions. Vasoactive drugs should be administered when VH is suspected with the goal of decreasing splanchnic blood flow. Octreotide is the only vasoactive drug available in the United States. RCTs show that antibiotics administered prophylactically decrease infections, recurrent hemorrhage, and death. Ceftriaxone 1 g daily is the drug of choice in the United States and should be given up to a maximum of 7 days. A reasonable strategy is discontinuation of prophylaxis concurrently with discontinuation of vasoactive agents. After stabilization of hemodynamics, patients should proceed to endoscopy no more than 12 hours after presentation. Endoscopic Variceal Ligation (EVL) should be done if signs of active or recent variceal bleeding are found. After EVL, select patients at high risk of rebleeding (Child-Pugh B with active bleeding seen on endoscopy or Child-Pugh C patients) may benefit from TIPS within 72 hours. If TIPS is done, vasoactive agents can be discontinued. Otherwise, vasoactive agents should continue for 2-5 days with subsequent transition to nonselective beta blockers (NSBB) such as nadolol or propranolol. For secondary prophylaxis of esophageal bleeding, combination EVL and NSBB is first-line therapy. If recurrent hemorrhage occurs while on secondary prophylaxis, rescue TIPS is recommended.
Synopsis of Inpatient Management for Gastric Variceal Hemorrhage: Management of Gastric Variceal Hemorrhage is similar to Esophageal Variceal (EV) Hemorrhage and encompasses volume resuscitation, vasoactive drugs, and antibiotics with endoscopy shortly thereafter. Balloon tamponade can be used as a bridge to endoscopy in massive bleeds. In addition to the above, anatomic location of Gastric Varices (GV) affects choice of intervention. GOV1 varices extend from the gastric cardia to the lesser curvature and represent 75% of GV. If these are small, they can be managed with EVL. Otherwise these can be managed with injection of cyanoacrylate glue. GOV2 varices extend from the gastric cardia into the fundus. Isolated GV type 1 varices (IGV1) are located entirely in the fundus and have the highest propensity for bleeding. For these latter two types of “cardio-fundal varices” TIPS is the preferred intervention to control acute bleeding. Data on the efficacy of secondary prophylaxis for GV bleeding is limited. A combination of NSBB, cyanoacrylate injection, or TIPS can be considered. Balloon Occluded Retrograde Transvenous Obliteration (BRTO) can be considered if fundal varices are associated with a large gastrorenal or splenorenal collateral. However, no RCTs have compared BRTO with other strategies. Isolated GV type 2 (IGV2) varices are not localized to the esophageal or gastric cardio-fundal region and are rare in cirrhotic patients but tend to occur in pre-hepatic portal hypertension. Management requires multidisciplinary input from endoscopists, hepatologists, interventional radiologists, and surgeons.
Bottom line: For esophageal variceal bleeding related to cirrhosis: volume resuscitation, antibiotic prophylaxis, and vasoactive agents are mainstays of therapy to stabilize patient for endoscopic intervention within 12 hours. This should be followed by early TIPS within 72 hours in high risk patients.
A similar approach applies to gastric variceal bleeding, but interventional management is dependent on the anatomic location of the varices in question.
Citations: Garcia-Tsao G et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis and management – 2016 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2017 Jan;65[1]:310-35.
Dr. Lu is a hospitalist at Cooper University Hospital in Camden, N.J.
Set a goal, or two, or three
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
2016 Humanitarian Award
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
Hospitalist movers and shakers
O’Neil Pike, MD, SFHM, has been promoted to chief medical officer with healthcare staffing company Medicus Healthcare Solutions (MHS) of Windham, N.H. Formerly a hospitalist consultant and chief practice advisor with MHS, Dr. Pike is a practicing hospitalist and serves as an assistant professor of medicine at Geisinger Commonwealth School of Medicine in Scranton, Pa.
Timothy D. Bode, MD, MBA, SFHM, has been named appointed medical officer at Saint Thomas Rutherford Hospital in Murfreesboro, Tenn., as well as several regional hospitals in the Saint Thomas system. Previously, Dr. Bode served as senior vice president and CMO at Memorial Health in Jacksonville, Fla.
Joseph Perras, MD, has been named chief executive officer at Mt. Ascutney Hospital and Health Center (MAHHC) in Windsor, Vt. Dr. Perras will continue as the center’s CMO, as well. He previously held the role of MAHHC’s director of hospital medicine.
Alamjit Virk, MD, has been promoted to medical director of Emergency Medicine and Hospitalist Services at Martha’s Vineyard Hospital in Oak Bluffs, Mass. Dr. Virk was a MVH staff physician for a year and half prior to the elevation, and he previously served as an attending physician in emergency medicine at Emerson Hospital in Concord, Mass.
Business Moves
Dearborn County Hospital (DCH) in Lawrenceburg, Ind., has partnered with TriHealth to provide hospitalist services for its inpatients. TriHealth’s team of more than 30 hospitalists is led by chief of hospital medicine Bryan Strader, MD. TriHealth also provides care for patients at Ohio’s Bethesda North, Good Samaritan and Bethesda Butler Hospitals.
MidMichigan Medical Centers in Alma, Gladwin, and Midland have been recognized with Five Star Excellence Awards by national health care research leader Professional Research Consultants. Awards were received for excellence in providing patients discharge information and pain management.
Pediatric Associates, located in Broward County, Fla., has expanded its pediatric hospitalist program thanks to the success of a pilot program run at Palm Beach Children’s Hospital at St. Mary’s Medical Center (West Palm Beach). Jamilah Grant-Guimaraes, MD, FAAP, and Nina Phillips Bernstein, DO, FAAP, will provide care to Pediatrics Associates patients at Broward General Medical Center.
The University of Pennsylvania Health System announced that it will add Princeton HealthCare System (PHCS) to the UPHS family. Located just 40 miles from Philadelphia, PHCS serves more than 1.3 million people in central New Jersey and includes the University Medical Center of Princeton, which opened in 2012 in Plainsboro, N.J.
Lehigh Valley Health Network, based out of Allentown, Pa., has absorbed Pocono Health System (East Stroudsburg, Pa.) in a move effective Jan. 1. Under the deal’s terms, Pocono Medical Center (the system’s only hospital) now will be known as Lehigh Valley Hospital–Pocono. LVH also absorbs Pocono’s three health centers. LVH now operates 8 hospital campuses and 19 health centers.
O’Neil Pike, MD, SFHM, has been promoted to chief medical officer with healthcare staffing company Medicus Healthcare Solutions (MHS) of Windham, N.H. Formerly a hospitalist consultant and chief practice advisor with MHS, Dr. Pike is a practicing hospitalist and serves as an assistant professor of medicine at Geisinger Commonwealth School of Medicine in Scranton, Pa.
Timothy D. Bode, MD, MBA, SFHM, has been named appointed medical officer at Saint Thomas Rutherford Hospital in Murfreesboro, Tenn., as well as several regional hospitals in the Saint Thomas system. Previously, Dr. Bode served as senior vice president and CMO at Memorial Health in Jacksonville, Fla.
Joseph Perras, MD, has been named chief executive officer at Mt. Ascutney Hospital and Health Center (MAHHC) in Windsor, Vt. Dr. Perras will continue as the center’s CMO, as well. He previously held the role of MAHHC’s director of hospital medicine.
Alamjit Virk, MD, has been promoted to medical director of Emergency Medicine and Hospitalist Services at Martha’s Vineyard Hospital in Oak Bluffs, Mass. Dr. Virk was a MVH staff physician for a year and half prior to the elevation, and he previously served as an attending physician in emergency medicine at Emerson Hospital in Concord, Mass.
Business Moves
Dearborn County Hospital (DCH) in Lawrenceburg, Ind., has partnered with TriHealth to provide hospitalist services for its inpatients. TriHealth’s team of more than 30 hospitalists is led by chief of hospital medicine Bryan Strader, MD. TriHealth also provides care for patients at Ohio’s Bethesda North, Good Samaritan and Bethesda Butler Hospitals.
MidMichigan Medical Centers in Alma, Gladwin, and Midland have been recognized with Five Star Excellence Awards by national health care research leader Professional Research Consultants. Awards were received for excellence in providing patients discharge information and pain management.
Pediatric Associates, located in Broward County, Fla., has expanded its pediatric hospitalist program thanks to the success of a pilot program run at Palm Beach Children’s Hospital at St. Mary’s Medical Center (West Palm Beach). Jamilah Grant-Guimaraes, MD, FAAP, and Nina Phillips Bernstein, DO, FAAP, will provide care to Pediatrics Associates patients at Broward General Medical Center.
The University of Pennsylvania Health System announced that it will add Princeton HealthCare System (PHCS) to the UPHS family. Located just 40 miles from Philadelphia, PHCS serves more than 1.3 million people in central New Jersey and includes the University Medical Center of Princeton, which opened in 2012 in Plainsboro, N.J.
Lehigh Valley Health Network, based out of Allentown, Pa., has absorbed Pocono Health System (East Stroudsburg, Pa.) in a move effective Jan. 1. Under the deal’s terms, Pocono Medical Center (the system’s only hospital) now will be known as Lehigh Valley Hospital–Pocono. LVH also absorbs Pocono’s three health centers. LVH now operates 8 hospital campuses and 19 health centers.
O’Neil Pike, MD, SFHM, has been promoted to chief medical officer with healthcare staffing company Medicus Healthcare Solutions (MHS) of Windham, N.H. Formerly a hospitalist consultant and chief practice advisor with MHS, Dr. Pike is a practicing hospitalist and serves as an assistant professor of medicine at Geisinger Commonwealth School of Medicine in Scranton, Pa.
Timothy D. Bode, MD, MBA, SFHM, has been named appointed medical officer at Saint Thomas Rutherford Hospital in Murfreesboro, Tenn., as well as several regional hospitals in the Saint Thomas system. Previously, Dr. Bode served as senior vice president and CMO at Memorial Health in Jacksonville, Fla.
Joseph Perras, MD, has been named chief executive officer at Mt. Ascutney Hospital and Health Center (MAHHC) in Windsor, Vt. Dr. Perras will continue as the center’s CMO, as well. He previously held the role of MAHHC’s director of hospital medicine.
Alamjit Virk, MD, has been promoted to medical director of Emergency Medicine and Hospitalist Services at Martha’s Vineyard Hospital in Oak Bluffs, Mass. Dr. Virk was a MVH staff physician for a year and half prior to the elevation, and he previously served as an attending physician in emergency medicine at Emerson Hospital in Concord, Mass.
Business Moves
Dearborn County Hospital (DCH) in Lawrenceburg, Ind., has partnered with TriHealth to provide hospitalist services for its inpatients. TriHealth’s team of more than 30 hospitalists is led by chief of hospital medicine Bryan Strader, MD. TriHealth also provides care for patients at Ohio’s Bethesda North, Good Samaritan and Bethesda Butler Hospitals.
MidMichigan Medical Centers in Alma, Gladwin, and Midland have been recognized with Five Star Excellence Awards by national health care research leader Professional Research Consultants. Awards were received for excellence in providing patients discharge information and pain management.
Pediatric Associates, located in Broward County, Fla., has expanded its pediatric hospitalist program thanks to the success of a pilot program run at Palm Beach Children’s Hospital at St. Mary’s Medical Center (West Palm Beach). Jamilah Grant-Guimaraes, MD, FAAP, and Nina Phillips Bernstein, DO, FAAP, will provide care to Pediatrics Associates patients at Broward General Medical Center.
The University of Pennsylvania Health System announced that it will add Princeton HealthCare System (PHCS) to the UPHS family. Located just 40 miles from Philadelphia, PHCS serves more than 1.3 million people in central New Jersey and includes the University Medical Center of Princeton, which opened in 2012 in Plainsboro, N.J.
Lehigh Valley Health Network, based out of Allentown, Pa., has absorbed Pocono Health System (East Stroudsburg, Pa.) in a move effective Jan. 1. Under the deal’s terms, Pocono Medical Center (the system’s only hospital) now will be known as Lehigh Valley Hospital–Pocono. LVH also absorbs Pocono’s three health centers. LVH now operates 8 hospital campuses and 19 health centers.
Trending at the Society of Hospital Medicine
Calling all pediatric hospitalists
Register for Pediatric Hospital Medicine 2017 (PHM17), the premier educational conference for pediatric hospitalists and other clinicians who care for hospitalized children. Re-energize your practice with the latest research, best practices, innovations, and more.
Register before June 7 to receive the early-bird rates. Visit www.peds2017.org for more information.
SHM can prepare you for MACRA
Visit www.macraforhm.org for general information and details in the MACRA FAQ and MIPS Tips links.
Don’t miss five new tracks at HM17
- Learn how to avoid diagnostic and therapeutic overuse, and how to move towards the right care for every hospital medicine patient with the High Value Care Track.
- Don’t miss the Clinical Updates Track, which provides evidence-based updates from recent literature published in medicine subspecialty fields and specific topic areas that all hospitalists need to know.
- Accurate and timely diagnosis are the two cornerstones of high-quality patient care. Find out what topics are in the Diagnostic Reasoning Track.
- Learn from experts during the Health Policy Track who will discuss the most current health care policy issues as they impact hospitalists and what we can expect from a new Presidential administration and changes in Congress.
- The Mini Medical Education Track is for hospitalists who are interested in improving their teaching skills.
Learn more about the HM17 schedule and offerings at www.hospitalmedicine2017.org/schedule.
Prepare for the entire Focused Practice in Hospital Medicine (FPHM) exam with SPARK ONE
This self-paced study guide engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points and define individual areas of strengths and weaknesses. SHM members Save $150! Learn more at www.hospitalmedicine.org/sparkone.
Improve your treatment of VTE during Blood Clot Awareness Month
March is Blood Clot Awareness Month, and SHM recently introduced a new toolkit and guide surrounding treatment of venous thromboembolism (VTE) in the hospital setting. SHM has a history of providing cutting-edge resources in this space, and Steven B. Deitelzweig, MD, MMM, SFHM, FACP, FACC, system chairman of hospital medicine at Oschner Health System in New Orleans, was integral in editing SHM’s VTE treatment mentored implementation guide and online toolkit.
“SHM has an established track record of implementing evidence-based and guideline-driven learnings successfully, and we continue to see improvement across multiple facilities based on this work with this disease,” Dr. Deitelzweig says. “Whenever possible, I would strongly recommend taking full advantage of SHM’s outstanding programs as they are intensely developed by experts for adoption at hospitals of different sizes, including community and academic centers.”
SHM can help you and your hospital improve treatment of VTE as well – learn how at www.hospitalmedicine.org/vtetreatment.
Share patient experience success stories
Our Patient Experience Committee wants to showcase stories of when care teams or their counterparts in the hospital made a notable shift in a patient’s experience: a special moment or interaction; a successful improvement project; an award for excellence in practice; a memo of commendation; a letter from a patient. Email examples of success to Claudia Stahl at [email protected] by May 11. Submissions can include photos, letters, or videos. SHM will share these moments that “made all the difference” with members on its website via other channels soon to be announced.
Brett Radler is SHM’s communications specialist.
Not a member? Know someone who should be? Visit www.joinshm.org to learn about the opportunities we can offer hospital medicine professionals.
Calling all pediatric hospitalists
Register for Pediatric Hospital Medicine 2017 (PHM17), the premier educational conference for pediatric hospitalists and other clinicians who care for hospitalized children. Re-energize your practice with the latest research, best practices, innovations, and more.
Register before June 7 to receive the early-bird rates. Visit www.peds2017.org for more information.
SHM can prepare you for MACRA
Visit www.macraforhm.org for general information and details in the MACRA FAQ and MIPS Tips links.
Don’t miss five new tracks at HM17
- Learn how to avoid diagnostic and therapeutic overuse, and how to move towards the right care for every hospital medicine patient with the High Value Care Track.
- Don’t miss the Clinical Updates Track, which provides evidence-based updates from recent literature published in medicine subspecialty fields and specific topic areas that all hospitalists need to know.
- Accurate and timely diagnosis are the two cornerstones of high-quality patient care. Find out what topics are in the Diagnostic Reasoning Track.
- Learn from experts during the Health Policy Track who will discuss the most current health care policy issues as they impact hospitalists and what we can expect from a new Presidential administration and changes in Congress.
- The Mini Medical Education Track is for hospitalists who are interested in improving their teaching skills.
Learn more about the HM17 schedule and offerings at www.hospitalmedicine2017.org/schedule.
Prepare for the entire Focused Practice in Hospital Medicine (FPHM) exam with SPARK ONE
This self-paced study guide engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points and define individual areas of strengths and weaknesses. SHM members Save $150! Learn more at www.hospitalmedicine.org/sparkone.
Improve your treatment of VTE during Blood Clot Awareness Month
March is Blood Clot Awareness Month, and SHM recently introduced a new toolkit and guide surrounding treatment of venous thromboembolism (VTE) in the hospital setting. SHM has a history of providing cutting-edge resources in this space, and Steven B. Deitelzweig, MD, MMM, SFHM, FACP, FACC, system chairman of hospital medicine at Oschner Health System in New Orleans, was integral in editing SHM’s VTE treatment mentored implementation guide and online toolkit.
“SHM has an established track record of implementing evidence-based and guideline-driven learnings successfully, and we continue to see improvement across multiple facilities based on this work with this disease,” Dr. Deitelzweig says. “Whenever possible, I would strongly recommend taking full advantage of SHM’s outstanding programs as they are intensely developed by experts for adoption at hospitals of different sizes, including community and academic centers.”
SHM can help you and your hospital improve treatment of VTE as well – learn how at www.hospitalmedicine.org/vtetreatment.
Share patient experience success stories
Our Patient Experience Committee wants to showcase stories of when care teams or their counterparts in the hospital made a notable shift in a patient’s experience: a special moment or interaction; a successful improvement project; an award for excellence in practice; a memo of commendation; a letter from a patient. Email examples of success to Claudia Stahl at [email protected] by May 11. Submissions can include photos, letters, or videos. SHM will share these moments that “made all the difference” with members on its website via other channels soon to be announced.
Brett Radler is SHM’s communications specialist.
Not a member? Know someone who should be? Visit www.joinshm.org to learn about the opportunities we can offer hospital medicine professionals.
Calling all pediatric hospitalists
Register for Pediatric Hospital Medicine 2017 (PHM17), the premier educational conference for pediatric hospitalists and other clinicians who care for hospitalized children. Re-energize your practice with the latest research, best practices, innovations, and more.
Register before June 7 to receive the early-bird rates. Visit www.peds2017.org for more information.
SHM can prepare you for MACRA
Visit www.macraforhm.org for general information and details in the MACRA FAQ and MIPS Tips links.
Don’t miss five new tracks at HM17
- Learn how to avoid diagnostic and therapeutic overuse, and how to move towards the right care for every hospital medicine patient with the High Value Care Track.
- Don’t miss the Clinical Updates Track, which provides evidence-based updates from recent literature published in medicine subspecialty fields and specific topic areas that all hospitalists need to know.
- Accurate and timely diagnosis are the two cornerstones of high-quality patient care. Find out what topics are in the Diagnostic Reasoning Track.
- Learn from experts during the Health Policy Track who will discuss the most current health care policy issues as they impact hospitalists and what we can expect from a new Presidential administration and changes in Congress.
- The Mini Medical Education Track is for hospitalists who are interested in improving their teaching skills.
Learn more about the HM17 schedule and offerings at www.hospitalmedicine2017.org/schedule.
Prepare for the entire Focused Practice in Hospital Medicine (FPHM) exam with SPARK ONE
This self-paced study guide engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points and define individual areas of strengths and weaknesses. SHM members Save $150! Learn more at www.hospitalmedicine.org/sparkone.
Improve your treatment of VTE during Blood Clot Awareness Month
March is Blood Clot Awareness Month, and SHM recently introduced a new toolkit and guide surrounding treatment of venous thromboembolism (VTE) in the hospital setting. SHM has a history of providing cutting-edge resources in this space, and Steven B. Deitelzweig, MD, MMM, SFHM, FACP, FACC, system chairman of hospital medicine at Oschner Health System in New Orleans, was integral in editing SHM’s VTE treatment mentored implementation guide and online toolkit.
“SHM has an established track record of implementing evidence-based and guideline-driven learnings successfully, and we continue to see improvement across multiple facilities based on this work with this disease,” Dr. Deitelzweig says. “Whenever possible, I would strongly recommend taking full advantage of SHM’s outstanding programs as they are intensely developed by experts for adoption at hospitals of different sizes, including community and academic centers.”
SHM can help you and your hospital improve treatment of VTE as well – learn how at www.hospitalmedicine.org/vtetreatment.
Share patient experience success stories
Our Patient Experience Committee wants to showcase stories of when care teams or their counterparts in the hospital made a notable shift in a patient’s experience: a special moment or interaction; a successful improvement project; an award for excellence in practice; a memo of commendation; a letter from a patient. Email examples of success to Claudia Stahl at [email protected] by May 11. Submissions can include photos, letters, or videos. SHM will share these moments that “made all the difference” with members on its website via other channels soon to be announced.
Brett Radler is SHM’s communications specialist.
Not a member? Know someone who should be? Visit www.joinshm.org to learn about the opportunities we can offer hospital medicine professionals.
Are you getting the most out of your EHR?
Sparrow Health System in Lansing, Mich., went live with its electronic health record (EHR) system at its main hospital on Dec. 1, 2012. For a year and a half, the system was untapped, innovation-wise. Very few features were turned on, and it sat relatively idle with regard to quality improvement. Hospitalists and others used the EHR, but not ambitiously. Everyone, essentially, used the post-launch period to catch their breath. Some even decided it would be the perfect time to retire, rather than confront the new reality of the EHR.
“It took a good 6 months, probably longer for some, for people to feel comfortable, to start smiling again and really feel like, ‘This isn’t so bad and actually might be working for us,’ ” said Carol Nwelue, MD, medical director of Sparrow’s adult hospitalist service.
Although Sparrow is now probably ahead of the curve when it comes to maximizing its EHR use, its story carries themes that are familiar to hospitalists and to the medical field: The beginning is scary and bumpy; there typically is a long getting-used-to period; and then some hospitalists get ansty and try to get more out of the system, but only gradually – and not without pain.
The bottom line is that most hospitals have a long way to go, said Venkataraman Palabindala, MD, a hospitalist and assistant professor of medicine at the University of Mississippi Medical Center in Jackson.
“We are nowhere close to using the technology to maximum benefit,” said Dr. Palabindala, also a member of the Society of Hospital Medicine’s information technology committee.
How well hospitalists are maximizing their use of EHRs varies from center to center and doctor to doctor. But, for those that are more advanced, Dr. Palabindala and other advocates of better EHR use mention these characteristics that drive the change:
- They have hospitalist leaders with a strong interest in IT who like to tinker and refine – and then share the tricks that work with others at their center.
- They belong to EHR-related committees or work at centers with hospitalists with a big presence in those committees.
- They keep their eyes on what other centers are doing with EHRs and use those projects as models for projects at their own centers.
- They are willing to make changes in their own processes, when feasible, so that they can better dovetail with the EHR.
- They keep their lines of communication open with their EHR vendors.
- They attend user meetings to get questions answered and share information and experiences.
At Sparrow, two committees – one nurse-led and one physician-led – guide EHR enhancement. The committees are a place where, yes, doctors can vent about the EHR (the phrase they use is “pain points”), but also a place where they can get constructive feedback. The committees also keep an eye out for EHR projects elsewhere that they might be able to do themselves.
EHR: a CAUTI example
In 2014, Sparrow doctors and nurses wanted to lower their number of catheter-associated urinary tract infections (CAUTI). With the EHR that had gone live 2 years before, they had the data that they needed. They just had to figure out how to turn the data into a workable plan. Ah, if only things were so simple with EHRs. As any health center that has gone through the great transition from paper to digital can attest, having the data only puts you at the foot of the mountain.
But using a program that Texas Health System had developed as a model, Sparrow got its CAUTI program up and running. The new system included not just a placement order, but the discontinuation order, too. Advisories on best practice were built into the work flow, including alerts on when catheters had been in for 48 hours, and metrics were created to track how well the whole thing worked.
“Once the data [were] obtained and validated, it was quickly shown that more needed to be done within this clinical program to impact our CAUTI numbers,” she said. “With collaboration from end users, the system was tweaked more and BPAs (best practice advisories) were added and removed in certain areas and shifted the focus from physician-facing to nursing-facing in most areas.”
It appears to be working: CAUTI incidence at 836-bed Sparrow Hospital has dropped from a total of 52 in 2014 to 11 over the first 3 quarters of 2016.
Sparrow has also built programs to better use its EHR for sepsis, medical reconciliation, and methicillin-resistant Staphylococcus aureus screening, and one is being developed for heart failure.
Vendor engagement = QI opportunity
Sparrow and many other health systems are motivated to use more of Epic’s features and to innovate through an Epic rewards program that gives rebates for advanced use that can total hundreds of thousands of dollars. That innovation helps Epic problem solve and it can then point to that innovation in its marketing.
Almost all hospitals, and their hospitalists, are using the EHR for such basics as reducing unnecessary testing, medical reconciliation, and to document more accurately, said Eric Helsher, vice president of client success at Epic, whose job is to foster the spread of new and better ways to use the EHR. Most hospitals use the EHR, to at least some degree, for targeted quality improvement (QI) and patient safety programs, he said.
Dr. Palabindala pointed to record-sharing features as a way clinicians can share records within minutes without having to bother with faxing or emailing. Integrating smart-paging into the EHR is another way for doctors to communicate – it may not be as good as a phone call, but it’s less disruptive during a workday, he notes.
Epic is just now rolling out a secure text-messaging system hospitalists and others can use to communicate with one another – the header of the text thread clearly shows the patient it is referencing, Mr. Helsher said. Other EHR uses, such as telemedicine, are being used around the country but are far less widespread. But users are generally becoming more ambitious, he said.
“For the last 5-10 years, we’ve been in such an implementation rush,” Mr. Helsher explained. “ Now, at much more of a macro scale, the mentality has changed to ‘OK, we have these systems, let’s go from the implementation era to the value era.’ ”
Corinne Boudreau, senior marketing manager of physician experience at Meditech, said their sepsis tool has been very popular, while messaging features and shortcut commands for simpler charting are gradually coming into wider use. Meditech also expects their Web-based EHR – designed to give patients access on their mobile devices – will give doctors the mobility they want.
Still, there’s a wide range in how much hospitalists and other doctors are using even the fundamental tools that are available to them.
“I think that between implementation and maximization there is a period of adoption, and I think that that’s where a lot of folks are these days,” she said.
As “physician engagement” has become a buzzword in the industry, Meditech has worked with physician leaders on how to get doctors to absorb the message that the EHR really can help them do their jobs better.
“If you get [doctors] at the right time, you show them how it can make things easier or take time off their workload,” Ms. Boudreau said. “For some physicians that time to get them might be first thing in the morning before they see patients. Another physician might want to do it in the evening. If you hit that evening physician in the morning, you’ve missed that window of opportunity.”
Given the demands on doctors’ time and either an inability or unwillingness to put the time in that’s needed to learn about all functions the EHR can offer, there’s a growing acknowledgment that doctors often can’t simply do this on their own.
“There’s more recognition that this is a project that needs to be resourced,” Ms. Boudreau said. “They’re already strapped for time; to put something additional on top of it needs to be accommodated for. It needs to be resourced in terms of time, it needs to be resourced in terms of compensation. There need to be governance and support of that.”
Early adopters vs. late bloomers
Many hospitalists and HM groups have advanced, but some places have lagged behind, said John Nelson, MD, MHM, a veteran hospitalist, practice management consultant, and longtime columnist with The Hospitalist.
“We find it’s reasonably common to go to a place where they’re still keeping their census in an Excel spreadsheet,” he said. “Last year, we found people who do billing on paper and index cards.”
He said that often, a failure to adopt new EHR functionality isn’t because hospitals and HM groups are avoiding it. He said he sees IT shortcomings as a major blocker.
“They want to use it,” he said. “Inertia might be part of the reason people are failing to fully capture the benefit the EHR could offer, [but] the bigger reason is local IT configurations and support.”
As an example, Dr. Nelson explained that at some of the centers he has worked with the name of the attending physician is not always reflected in the EHR. That’s a big no-no, he said. The problem, he’s sometimes found, isn’t really the EHR, but quirks in the hospital system: The EHR is locked down for that information and can be changed only by a person in the admitting department.
“It would require the hospitalist to call down [to admissions] and get someone else to make that change – and that’s tedious a big headache. They give up and don’t do it anymore,” he said. “Ideally, you’d want to make it so the hospitalists can make the change themselves.”
At his center, Overlake Hospital Medical Center in Bellevue, Wash., a go-to hospitalist is David Chu, MD, who has gone through Epic training and shares tips with colleagues. He is one of a relatively few physicians there who has taken the time to use the drop-down menu feature for putting information into a chart.
That might sound like a fairly basic use for a multimillion-dollar EHR system. But it still can take hours and hours to get it right.
“The way to do it is a little bit of a programmer’s way of looking at things,” Dr. Chu said, noting it involves programming-style language with double colons, commas, and quotations marks.
“For me, I think it took a good 10, 12, 15 hours on my part to get things going,” he said. “It was a good time investment up front to help me on that end, but it’s just hard getting people to want to commit that time, especially if they’re not that savvy with computers.”
His hospitalist colleague, Ryan Chew, MD, is more advanced – he has a taxonomy-like shorthand he uses to give him the right set of basic fields for a given type of case. For someone admitted with pneumonia, he’d want to know certain things all the time. Were they short of breath? Did they have chest pain? What were their vital signs? What about inflammatory markers?
Dr. Chew can get all of those fields to pop up by typing “.rchppneumonia.” The “.” means that a special code is to follow. The “rc” is for Ryan Chew, the “hp” is for history and physical, and “pneumonia,” is the type of case. For cases that require other information to be entered, he can add that as needed.
Hospitalists might try to write shortcut phrases, but unless they have a well-defined system, it won’t be helpful over the long run, he said.
“If you don’t have a good organization system … you’ll never remember it,” Dr. Chew said.
But even he hasn’t created the drop-down menus. He said he just hasn’t been willing to take the time, especially since he feels his own way of doing things seems to be working just fine.
Effort is essential
Expanding the functionalities of the EHR takes effort, no doubt. As a result, some physicians and hospitalist groups have not been open-minded to the idea – and opportunities – of the EHR as a database.
“I think for some people, even still, working with the EHR, it’s become more something they’ve learned to get used to rather than something that they sought to take advantage of, in terms of helping things,” Dr. Chew said. “They’re still working against the EHR a little bit.”
Dr. Palabindala agreed, and said that regardless of resistance or complaint, EHRs work.
“No matter how much we argue, it is proven in multiple studies that EHRs showed increased patient safety and better documentation and better transfer of the data,” he said.
He suggests hospitalists make more of an effort.
“I strongly encourage hospitalists to be part of the every EHR-related committee, including CPOE [computerized physician order entry], analytics, and utilization-review committees,” he said. “Learning about the upgrades and learning about all the possible options, exploring clinical informatics on a regular basis is important. I also encourage [hospitalists] to participate in online, EHR-related surveys to learn more about the EHR utility and what is missing in their home institution.”
He acknowledges that it’s “hard to develop a passion.” Then he put it in terms he thought might resonate: “Think of it like a new version of smart phone. Show the enthusiasm as if you are ready for next version of iPhone or Pixel.” TH
Is hospitalists’ EHR efficiency taken advantage of?
Even though their level of EHR use can be hit or miss, hospitalists tend to be ahead of the game, many agree. But that can come with some drawbacks. They’re often the go-to people everyone else in the hospital relies on to handle the system that some think is too unwieldy to bother with.
“One thing that really distinguishes hospitalists from many other providers, particularly on the inpatient side, is just the frequency with which they use the EHR,” said Eric Helsher of Epic. Many hospitalists are chosen by administrators to test pilot projects for that reason, he adds. “They want to get it out there with a group who they know will have a lot of exposure to the system and may be more willing to make those changes for long-term gain.”
Sometimes that expertise leads to situations that go beyond the hospitalist simply being leaders of change – they’re doing work they were never really intended to do.
John Nelson, MD, MHM, a hospitalist consultant based in Seattle, said hospitalists tell him that a subspecialist might handle a case but will not want to be the attending physician specifically so they don’t have to deal with the EHR. He said the specialist in such cases will say something along the lines of, “You can call me, I’ll help you, and I’ll come by and say hello to the patient and make the care decisions, but I need you to be the attending so you can document in the chart and you can do the med rec because ‘I can’t figure out how to do those buttons right.’ ”
Some will ask hospitalists “for a hand” with a case when really all they want is for the hospitalist to enter information into the system. It’s a tricky situation for the hospitalist, Dr. Nelson said.
“Some will be transparent and say I don’t really have a medical question – I just can’t figure out how to do the med rec and the discharge, so would you do it?” he said, adding the systems issues are largely because of new rounding patterns sparked by HM’s expanding role in-hospital. “I think it meaningfully contributes to what I perceive to be a decline in hospitalist morale in the last 2 or 3 years.”
Tom Collins is a freelance writer in South Florida.
Sparrow Health System in Lansing, Mich., went live with its electronic health record (EHR) system at its main hospital on Dec. 1, 2012. For a year and a half, the system was untapped, innovation-wise. Very few features were turned on, and it sat relatively idle with regard to quality improvement. Hospitalists and others used the EHR, but not ambitiously. Everyone, essentially, used the post-launch period to catch their breath. Some even decided it would be the perfect time to retire, rather than confront the new reality of the EHR.
“It took a good 6 months, probably longer for some, for people to feel comfortable, to start smiling again and really feel like, ‘This isn’t so bad and actually might be working for us,’ ” said Carol Nwelue, MD, medical director of Sparrow’s adult hospitalist service.
Although Sparrow is now probably ahead of the curve when it comes to maximizing its EHR use, its story carries themes that are familiar to hospitalists and to the medical field: The beginning is scary and bumpy; there typically is a long getting-used-to period; and then some hospitalists get ansty and try to get more out of the system, but only gradually – and not without pain.
The bottom line is that most hospitals have a long way to go, said Venkataraman Palabindala, MD, a hospitalist and assistant professor of medicine at the University of Mississippi Medical Center in Jackson.
“We are nowhere close to using the technology to maximum benefit,” said Dr. Palabindala, also a member of the Society of Hospital Medicine’s information technology committee.
How well hospitalists are maximizing their use of EHRs varies from center to center and doctor to doctor. But, for those that are more advanced, Dr. Palabindala and other advocates of better EHR use mention these characteristics that drive the change:
- They have hospitalist leaders with a strong interest in IT who like to tinker and refine – and then share the tricks that work with others at their center.
- They belong to EHR-related committees or work at centers with hospitalists with a big presence in those committees.
- They keep their eyes on what other centers are doing with EHRs and use those projects as models for projects at their own centers.
- They are willing to make changes in their own processes, when feasible, so that they can better dovetail with the EHR.
- They keep their lines of communication open with their EHR vendors.
- They attend user meetings to get questions answered and share information and experiences.
At Sparrow, two committees – one nurse-led and one physician-led – guide EHR enhancement. The committees are a place where, yes, doctors can vent about the EHR (the phrase they use is “pain points”), but also a place where they can get constructive feedback. The committees also keep an eye out for EHR projects elsewhere that they might be able to do themselves.
EHR: a CAUTI example
In 2014, Sparrow doctors and nurses wanted to lower their number of catheter-associated urinary tract infections (CAUTI). With the EHR that had gone live 2 years before, they had the data that they needed. They just had to figure out how to turn the data into a workable plan. Ah, if only things were so simple with EHRs. As any health center that has gone through the great transition from paper to digital can attest, having the data only puts you at the foot of the mountain.
But using a program that Texas Health System had developed as a model, Sparrow got its CAUTI program up and running. The new system included not just a placement order, but the discontinuation order, too. Advisories on best practice were built into the work flow, including alerts on when catheters had been in for 48 hours, and metrics were created to track how well the whole thing worked.
“Once the data [were] obtained and validated, it was quickly shown that more needed to be done within this clinical program to impact our CAUTI numbers,” she said. “With collaboration from end users, the system was tweaked more and BPAs (best practice advisories) were added and removed in certain areas and shifted the focus from physician-facing to nursing-facing in most areas.”
It appears to be working: CAUTI incidence at 836-bed Sparrow Hospital has dropped from a total of 52 in 2014 to 11 over the first 3 quarters of 2016.
Sparrow has also built programs to better use its EHR for sepsis, medical reconciliation, and methicillin-resistant Staphylococcus aureus screening, and one is being developed for heart failure.
Vendor engagement = QI opportunity
Sparrow and many other health systems are motivated to use more of Epic’s features and to innovate through an Epic rewards program that gives rebates for advanced use that can total hundreds of thousands of dollars. That innovation helps Epic problem solve and it can then point to that innovation in its marketing.
Almost all hospitals, and their hospitalists, are using the EHR for such basics as reducing unnecessary testing, medical reconciliation, and to document more accurately, said Eric Helsher, vice president of client success at Epic, whose job is to foster the spread of new and better ways to use the EHR. Most hospitals use the EHR, to at least some degree, for targeted quality improvement (QI) and patient safety programs, he said.
Dr. Palabindala pointed to record-sharing features as a way clinicians can share records within minutes without having to bother with faxing or emailing. Integrating smart-paging into the EHR is another way for doctors to communicate – it may not be as good as a phone call, but it’s less disruptive during a workday, he notes.
Epic is just now rolling out a secure text-messaging system hospitalists and others can use to communicate with one another – the header of the text thread clearly shows the patient it is referencing, Mr. Helsher said. Other EHR uses, such as telemedicine, are being used around the country but are far less widespread. But users are generally becoming more ambitious, he said.
“For the last 5-10 years, we’ve been in such an implementation rush,” Mr. Helsher explained. “ Now, at much more of a macro scale, the mentality has changed to ‘OK, we have these systems, let’s go from the implementation era to the value era.’ ”
Corinne Boudreau, senior marketing manager of physician experience at Meditech, said their sepsis tool has been very popular, while messaging features and shortcut commands for simpler charting are gradually coming into wider use. Meditech also expects their Web-based EHR – designed to give patients access on their mobile devices – will give doctors the mobility they want.
Still, there’s a wide range in how much hospitalists and other doctors are using even the fundamental tools that are available to them.
“I think that between implementation and maximization there is a period of adoption, and I think that that’s where a lot of folks are these days,” she said.
As “physician engagement” has become a buzzword in the industry, Meditech has worked with physician leaders on how to get doctors to absorb the message that the EHR really can help them do their jobs better.
“If you get [doctors] at the right time, you show them how it can make things easier or take time off their workload,” Ms. Boudreau said. “For some physicians that time to get them might be first thing in the morning before they see patients. Another physician might want to do it in the evening. If you hit that evening physician in the morning, you’ve missed that window of opportunity.”
Given the demands on doctors’ time and either an inability or unwillingness to put the time in that’s needed to learn about all functions the EHR can offer, there’s a growing acknowledgment that doctors often can’t simply do this on their own.
“There’s more recognition that this is a project that needs to be resourced,” Ms. Boudreau said. “They’re already strapped for time; to put something additional on top of it needs to be accommodated for. It needs to be resourced in terms of time, it needs to be resourced in terms of compensation. There need to be governance and support of that.”
Early adopters vs. late bloomers
Many hospitalists and HM groups have advanced, but some places have lagged behind, said John Nelson, MD, MHM, a veteran hospitalist, practice management consultant, and longtime columnist with The Hospitalist.
“We find it’s reasonably common to go to a place where they’re still keeping their census in an Excel spreadsheet,” he said. “Last year, we found people who do billing on paper and index cards.”
He said that often, a failure to adopt new EHR functionality isn’t because hospitals and HM groups are avoiding it. He said he sees IT shortcomings as a major blocker.
“They want to use it,” he said. “Inertia might be part of the reason people are failing to fully capture the benefit the EHR could offer, [but] the bigger reason is local IT configurations and support.”
As an example, Dr. Nelson explained that at some of the centers he has worked with the name of the attending physician is not always reflected in the EHR. That’s a big no-no, he said. The problem, he’s sometimes found, isn’t really the EHR, but quirks in the hospital system: The EHR is locked down for that information and can be changed only by a person in the admitting department.
“It would require the hospitalist to call down [to admissions] and get someone else to make that change – and that’s tedious a big headache. They give up and don’t do it anymore,” he said. “Ideally, you’d want to make it so the hospitalists can make the change themselves.”
At his center, Overlake Hospital Medical Center in Bellevue, Wash., a go-to hospitalist is David Chu, MD, who has gone through Epic training and shares tips with colleagues. He is one of a relatively few physicians there who has taken the time to use the drop-down menu feature for putting information into a chart.
That might sound like a fairly basic use for a multimillion-dollar EHR system. But it still can take hours and hours to get it right.
“The way to do it is a little bit of a programmer’s way of looking at things,” Dr. Chu said, noting it involves programming-style language with double colons, commas, and quotations marks.
“For me, I think it took a good 10, 12, 15 hours on my part to get things going,” he said. “It was a good time investment up front to help me on that end, but it’s just hard getting people to want to commit that time, especially if they’re not that savvy with computers.”
His hospitalist colleague, Ryan Chew, MD, is more advanced – he has a taxonomy-like shorthand he uses to give him the right set of basic fields for a given type of case. For someone admitted with pneumonia, he’d want to know certain things all the time. Were they short of breath? Did they have chest pain? What were their vital signs? What about inflammatory markers?
Dr. Chew can get all of those fields to pop up by typing “.rchppneumonia.” The “.” means that a special code is to follow. The “rc” is for Ryan Chew, the “hp” is for history and physical, and “pneumonia,” is the type of case. For cases that require other information to be entered, he can add that as needed.
Hospitalists might try to write shortcut phrases, but unless they have a well-defined system, it won’t be helpful over the long run, he said.
“If you don’t have a good organization system … you’ll never remember it,” Dr. Chew said.
But even he hasn’t created the drop-down menus. He said he just hasn’t been willing to take the time, especially since he feels his own way of doing things seems to be working just fine.
Effort is essential
Expanding the functionalities of the EHR takes effort, no doubt. As a result, some physicians and hospitalist groups have not been open-minded to the idea – and opportunities – of the EHR as a database.
“I think for some people, even still, working with the EHR, it’s become more something they’ve learned to get used to rather than something that they sought to take advantage of, in terms of helping things,” Dr. Chew said. “They’re still working against the EHR a little bit.”
Dr. Palabindala agreed, and said that regardless of resistance or complaint, EHRs work.
“No matter how much we argue, it is proven in multiple studies that EHRs showed increased patient safety and better documentation and better transfer of the data,” he said.
He suggests hospitalists make more of an effort.
“I strongly encourage hospitalists to be part of the every EHR-related committee, including CPOE [computerized physician order entry], analytics, and utilization-review committees,” he said. “Learning about the upgrades and learning about all the possible options, exploring clinical informatics on a regular basis is important. I also encourage [hospitalists] to participate in online, EHR-related surveys to learn more about the EHR utility and what is missing in their home institution.”
He acknowledges that it’s “hard to develop a passion.” Then he put it in terms he thought might resonate: “Think of it like a new version of smart phone. Show the enthusiasm as if you are ready for next version of iPhone or Pixel.” TH
Is hospitalists’ EHR efficiency taken advantage of?
Even though their level of EHR use can be hit or miss, hospitalists tend to be ahead of the game, many agree. But that can come with some drawbacks. They’re often the go-to people everyone else in the hospital relies on to handle the system that some think is too unwieldy to bother with.
“One thing that really distinguishes hospitalists from many other providers, particularly on the inpatient side, is just the frequency with which they use the EHR,” said Eric Helsher of Epic. Many hospitalists are chosen by administrators to test pilot projects for that reason, he adds. “They want to get it out there with a group who they know will have a lot of exposure to the system and may be more willing to make those changes for long-term gain.”
Sometimes that expertise leads to situations that go beyond the hospitalist simply being leaders of change – they’re doing work they were never really intended to do.
John Nelson, MD, MHM, a hospitalist consultant based in Seattle, said hospitalists tell him that a subspecialist might handle a case but will not want to be the attending physician specifically so they don’t have to deal with the EHR. He said the specialist in such cases will say something along the lines of, “You can call me, I’ll help you, and I’ll come by and say hello to the patient and make the care decisions, but I need you to be the attending so you can document in the chart and you can do the med rec because ‘I can’t figure out how to do those buttons right.’ ”
Some will ask hospitalists “for a hand” with a case when really all they want is for the hospitalist to enter information into the system. It’s a tricky situation for the hospitalist, Dr. Nelson said.
“Some will be transparent and say I don’t really have a medical question – I just can’t figure out how to do the med rec and the discharge, so would you do it?” he said, adding the systems issues are largely because of new rounding patterns sparked by HM’s expanding role in-hospital. “I think it meaningfully contributes to what I perceive to be a decline in hospitalist morale in the last 2 or 3 years.”
Tom Collins is a freelance writer in South Florida.
Sparrow Health System in Lansing, Mich., went live with its electronic health record (EHR) system at its main hospital on Dec. 1, 2012. For a year and a half, the system was untapped, innovation-wise. Very few features were turned on, and it sat relatively idle with regard to quality improvement. Hospitalists and others used the EHR, but not ambitiously. Everyone, essentially, used the post-launch period to catch their breath. Some even decided it would be the perfect time to retire, rather than confront the new reality of the EHR.
“It took a good 6 months, probably longer for some, for people to feel comfortable, to start smiling again and really feel like, ‘This isn’t so bad and actually might be working for us,’ ” said Carol Nwelue, MD, medical director of Sparrow’s adult hospitalist service.
Although Sparrow is now probably ahead of the curve when it comes to maximizing its EHR use, its story carries themes that are familiar to hospitalists and to the medical field: The beginning is scary and bumpy; there typically is a long getting-used-to period; and then some hospitalists get ansty and try to get more out of the system, but only gradually – and not without pain.
The bottom line is that most hospitals have a long way to go, said Venkataraman Palabindala, MD, a hospitalist and assistant professor of medicine at the University of Mississippi Medical Center in Jackson.
“We are nowhere close to using the technology to maximum benefit,” said Dr. Palabindala, also a member of the Society of Hospital Medicine’s information technology committee.
How well hospitalists are maximizing their use of EHRs varies from center to center and doctor to doctor. But, for those that are more advanced, Dr. Palabindala and other advocates of better EHR use mention these characteristics that drive the change:
- They have hospitalist leaders with a strong interest in IT who like to tinker and refine – and then share the tricks that work with others at their center.
- They belong to EHR-related committees or work at centers with hospitalists with a big presence in those committees.
- They keep their eyes on what other centers are doing with EHRs and use those projects as models for projects at their own centers.
- They are willing to make changes in their own processes, when feasible, so that they can better dovetail with the EHR.
- They keep their lines of communication open with their EHR vendors.
- They attend user meetings to get questions answered and share information and experiences.
At Sparrow, two committees – one nurse-led and one physician-led – guide EHR enhancement. The committees are a place where, yes, doctors can vent about the EHR (the phrase they use is “pain points”), but also a place where they can get constructive feedback. The committees also keep an eye out for EHR projects elsewhere that they might be able to do themselves.
EHR: a CAUTI example
In 2014, Sparrow doctors and nurses wanted to lower their number of catheter-associated urinary tract infections (CAUTI). With the EHR that had gone live 2 years before, they had the data that they needed. They just had to figure out how to turn the data into a workable plan. Ah, if only things were so simple with EHRs. As any health center that has gone through the great transition from paper to digital can attest, having the data only puts you at the foot of the mountain.
But using a program that Texas Health System had developed as a model, Sparrow got its CAUTI program up and running. The new system included not just a placement order, but the discontinuation order, too. Advisories on best practice were built into the work flow, including alerts on when catheters had been in for 48 hours, and metrics were created to track how well the whole thing worked.
“Once the data [were] obtained and validated, it was quickly shown that more needed to be done within this clinical program to impact our CAUTI numbers,” she said. “With collaboration from end users, the system was tweaked more and BPAs (best practice advisories) were added and removed in certain areas and shifted the focus from physician-facing to nursing-facing in most areas.”
It appears to be working: CAUTI incidence at 836-bed Sparrow Hospital has dropped from a total of 52 in 2014 to 11 over the first 3 quarters of 2016.
Sparrow has also built programs to better use its EHR for sepsis, medical reconciliation, and methicillin-resistant Staphylococcus aureus screening, and one is being developed for heart failure.
Vendor engagement = QI opportunity
Sparrow and many other health systems are motivated to use more of Epic’s features and to innovate through an Epic rewards program that gives rebates for advanced use that can total hundreds of thousands of dollars. That innovation helps Epic problem solve and it can then point to that innovation in its marketing.
Almost all hospitals, and their hospitalists, are using the EHR for such basics as reducing unnecessary testing, medical reconciliation, and to document more accurately, said Eric Helsher, vice president of client success at Epic, whose job is to foster the spread of new and better ways to use the EHR. Most hospitals use the EHR, to at least some degree, for targeted quality improvement (QI) and patient safety programs, he said.
Dr. Palabindala pointed to record-sharing features as a way clinicians can share records within minutes without having to bother with faxing or emailing. Integrating smart-paging into the EHR is another way for doctors to communicate – it may not be as good as a phone call, but it’s less disruptive during a workday, he notes.
Epic is just now rolling out a secure text-messaging system hospitalists and others can use to communicate with one another – the header of the text thread clearly shows the patient it is referencing, Mr. Helsher said. Other EHR uses, such as telemedicine, are being used around the country but are far less widespread. But users are generally becoming more ambitious, he said.
“For the last 5-10 years, we’ve been in such an implementation rush,” Mr. Helsher explained. “ Now, at much more of a macro scale, the mentality has changed to ‘OK, we have these systems, let’s go from the implementation era to the value era.’ ”
Corinne Boudreau, senior marketing manager of physician experience at Meditech, said their sepsis tool has been very popular, while messaging features and shortcut commands for simpler charting are gradually coming into wider use. Meditech also expects their Web-based EHR – designed to give patients access on their mobile devices – will give doctors the mobility they want.
Still, there’s a wide range in how much hospitalists and other doctors are using even the fundamental tools that are available to them.
“I think that between implementation and maximization there is a period of adoption, and I think that that’s where a lot of folks are these days,” she said.
As “physician engagement” has become a buzzword in the industry, Meditech has worked with physician leaders on how to get doctors to absorb the message that the EHR really can help them do their jobs better.
“If you get [doctors] at the right time, you show them how it can make things easier or take time off their workload,” Ms. Boudreau said. “For some physicians that time to get them might be first thing in the morning before they see patients. Another physician might want to do it in the evening. If you hit that evening physician in the morning, you’ve missed that window of opportunity.”
Given the demands on doctors’ time and either an inability or unwillingness to put the time in that’s needed to learn about all functions the EHR can offer, there’s a growing acknowledgment that doctors often can’t simply do this on their own.
“There’s more recognition that this is a project that needs to be resourced,” Ms. Boudreau said. “They’re already strapped for time; to put something additional on top of it needs to be accommodated for. It needs to be resourced in terms of time, it needs to be resourced in terms of compensation. There need to be governance and support of that.”
Early adopters vs. late bloomers
Many hospitalists and HM groups have advanced, but some places have lagged behind, said John Nelson, MD, MHM, a veteran hospitalist, practice management consultant, and longtime columnist with The Hospitalist.
“We find it’s reasonably common to go to a place where they’re still keeping their census in an Excel spreadsheet,” he said. “Last year, we found people who do billing on paper and index cards.”
He said that often, a failure to adopt new EHR functionality isn’t because hospitals and HM groups are avoiding it. He said he sees IT shortcomings as a major blocker.
“They want to use it,” he said. “Inertia might be part of the reason people are failing to fully capture the benefit the EHR could offer, [but] the bigger reason is local IT configurations and support.”
As an example, Dr. Nelson explained that at some of the centers he has worked with the name of the attending physician is not always reflected in the EHR. That’s a big no-no, he said. The problem, he’s sometimes found, isn’t really the EHR, but quirks in the hospital system: The EHR is locked down for that information and can be changed only by a person in the admitting department.
“It would require the hospitalist to call down [to admissions] and get someone else to make that change – and that’s tedious a big headache. They give up and don’t do it anymore,” he said. “Ideally, you’d want to make it so the hospitalists can make the change themselves.”
At his center, Overlake Hospital Medical Center in Bellevue, Wash., a go-to hospitalist is David Chu, MD, who has gone through Epic training and shares tips with colleagues. He is one of a relatively few physicians there who has taken the time to use the drop-down menu feature for putting information into a chart.
That might sound like a fairly basic use for a multimillion-dollar EHR system. But it still can take hours and hours to get it right.
“The way to do it is a little bit of a programmer’s way of looking at things,” Dr. Chu said, noting it involves programming-style language with double colons, commas, and quotations marks.
“For me, I think it took a good 10, 12, 15 hours on my part to get things going,” he said. “It was a good time investment up front to help me on that end, but it’s just hard getting people to want to commit that time, especially if they’re not that savvy with computers.”
His hospitalist colleague, Ryan Chew, MD, is more advanced – he has a taxonomy-like shorthand he uses to give him the right set of basic fields for a given type of case. For someone admitted with pneumonia, he’d want to know certain things all the time. Were they short of breath? Did they have chest pain? What were their vital signs? What about inflammatory markers?
Dr. Chew can get all of those fields to pop up by typing “.rchppneumonia.” The “.” means that a special code is to follow. The “rc” is for Ryan Chew, the “hp” is for history and physical, and “pneumonia,” is the type of case. For cases that require other information to be entered, he can add that as needed.
Hospitalists might try to write shortcut phrases, but unless they have a well-defined system, it won’t be helpful over the long run, he said.
“If you don’t have a good organization system … you’ll never remember it,” Dr. Chew said.
But even he hasn’t created the drop-down menus. He said he just hasn’t been willing to take the time, especially since he feels his own way of doing things seems to be working just fine.
Effort is essential
Expanding the functionalities of the EHR takes effort, no doubt. As a result, some physicians and hospitalist groups have not been open-minded to the idea – and opportunities – of the EHR as a database.
“I think for some people, even still, working with the EHR, it’s become more something they’ve learned to get used to rather than something that they sought to take advantage of, in terms of helping things,” Dr. Chew said. “They’re still working against the EHR a little bit.”
Dr. Palabindala agreed, and said that regardless of resistance or complaint, EHRs work.
“No matter how much we argue, it is proven in multiple studies that EHRs showed increased patient safety and better documentation and better transfer of the data,” he said.
He suggests hospitalists make more of an effort.
“I strongly encourage hospitalists to be part of the every EHR-related committee, including CPOE [computerized physician order entry], analytics, and utilization-review committees,” he said. “Learning about the upgrades and learning about all the possible options, exploring clinical informatics on a regular basis is important. I also encourage [hospitalists] to participate in online, EHR-related surveys to learn more about the EHR utility and what is missing in their home institution.”
He acknowledges that it’s “hard to develop a passion.” Then he put it in terms he thought might resonate: “Think of it like a new version of smart phone. Show the enthusiasm as if you are ready for next version of iPhone or Pixel.” TH
Is hospitalists’ EHR efficiency taken advantage of?
Even though their level of EHR use can be hit or miss, hospitalists tend to be ahead of the game, many agree. But that can come with some drawbacks. They’re often the go-to people everyone else in the hospital relies on to handle the system that some think is too unwieldy to bother with.
“One thing that really distinguishes hospitalists from many other providers, particularly on the inpatient side, is just the frequency with which they use the EHR,” said Eric Helsher of Epic. Many hospitalists are chosen by administrators to test pilot projects for that reason, he adds. “They want to get it out there with a group who they know will have a lot of exposure to the system and may be more willing to make those changes for long-term gain.”
Sometimes that expertise leads to situations that go beyond the hospitalist simply being leaders of change – they’re doing work they were never really intended to do.
John Nelson, MD, MHM, a hospitalist consultant based in Seattle, said hospitalists tell him that a subspecialist might handle a case but will not want to be the attending physician specifically so they don’t have to deal with the EHR. He said the specialist in such cases will say something along the lines of, “You can call me, I’ll help you, and I’ll come by and say hello to the patient and make the care decisions, but I need you to be the attending so you can document in the chart and you can do the med rec because ‘I can’t figure out how to do those buttons right.’ ”
Some will ask hospitalists “for a hand” with a case when really all they want is for the hospitalist to enter information into the system. It’s a tricky situation for the hospitalist, Dr. Nelson said.
“Some will be transparent and say I don’t really have a medical question – I just can’t figure out how to do the med rec and the discharge, so would you do it?” he said, adding the systems issues are largely because of new rounding patterns sparked by HM’s expanding role in-hospital. “I think it meaningfully contributes to what I perceive to be a decline in hospitalist morale in the last 2 or 3 years.”
Tom Collins is a freelance writer in South Florida.
MACRA: What every hospitalist needs to know
In April 2015, President Obama signed the bipartisan Medicare Access and CHIP Reauthorization Act (MACRA) into law, effectively altering the future of the Medicare payment system for providers. MACRA not only removed the Sustainable Growth Rate, but also encouraged quality measure development, expanded the use of Medicare data, and locked provider payment rates to near zero growth.
For Medicare payments, MACRA created the Quality Payment Program, which breaks down clinical payments into two pathways: the Merit-Based Incentive Payment System (MIPS) combining current pay-for-performance programs into one consolidated payment system, and Alternative Payment Models (APMs), incentivizing payment models that move away from a fee-for-service system.
Both pathways incur risk, as well as rewards:
• MIPS. –4% penalty up to 12% positive adjustment in year 1 based on 2017 data reported and collected by the CMS, growing over time to include payment adjustments from –9% to +27% in future years.
• APMs. If the provider is eligible, a 5% payment increase from 2019 to 2024, with no reporting requirements, and exemption from MIPS.
Who is included in the program?
All clinicians who receive Medicare Physician Fee Schedule payments, including physicians, physician assistants, and nurse practitioners, will be affected by this program. The only providers who are exempt from the program are those who fall under low-volume thresholds (either less than $30,000 in Medicare Part B charges or less than 101 Medicare patients) or those in their first year with Medicare.
What is MIPS?
MIPS requires reporting in four categories that determine a physician’s payment adjustment:
• Quality, which replaces the Physician Quality Reporting System (PQRS).
• Cost, which replaces the value-based modifier.
• Advancing Care Information (ACI), which replaces the meaningful use program.
• Improvement activities, a new category, but one in which hospitalists should excel, as they are already participating in many of the activities.
Each category is given relative weight, which the CMS will adjust in the first few years of the program.
Note that in the first year (2017), cost will be calculated, but not used to determine payment amount, hence this category gets a 0% weighting. Also, there are significant differences between how most providers’ MIPS score will be calculated with respect to category weights, and how this will be done for hospitalists.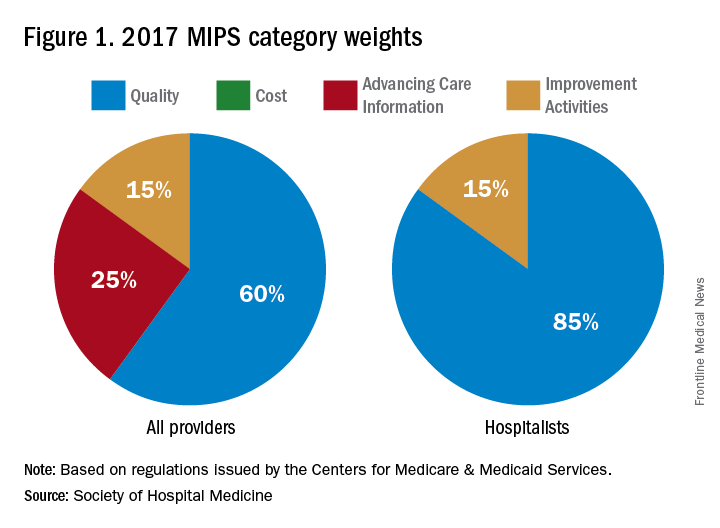
In addition to cost, the ACI will not play a role in the 2019 performance scores for hospitalists. However, hospitalists who practice in noninpatient settings, such as skilled nursing facilities or ambulatory clinics, will be subject to the ACI unless they apply for exceptions.
The quality category requires physicians to report on 6 of the 271 measures available. Hospitalists can report from the hospitalist-specific specialty set for which the Society of Hospital Medicine (SHM) was successful in advocating. Although continued cooperation between the CMS and SHM is necessary to fine-tune the measures, below are those that the SHM believes are reportable by, and most relevant to, hospitalists.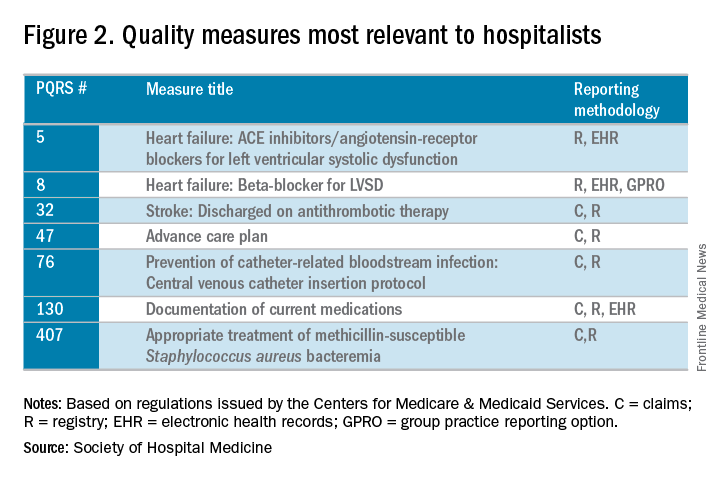
The improvement activities category will determine 15% of hospitalists’ performance in the MIPS. To receive full credit for this category, hospitalists must report on activities totaling 40 points. There are 92 available activities across eight different categories – 20 points for those that have a “high” weight determination and 10 points for those with medium weight.
In 2017, the CMS will calculate the cost category for providers, but it will not be counted toward the overall score. The data will still be collected based on Medicare Part A and Part B costs and will be reported to groups. Over time, this category will increase in scoring weight.
The Advancing Care Information category replaces the meaningful use program. This category will still promote EHR use, but hospitalists should be exempt from this category because of their “hospital-based” practice setting. This exemption is the reason why the quality category counts for 85% of the hospitalists’ score.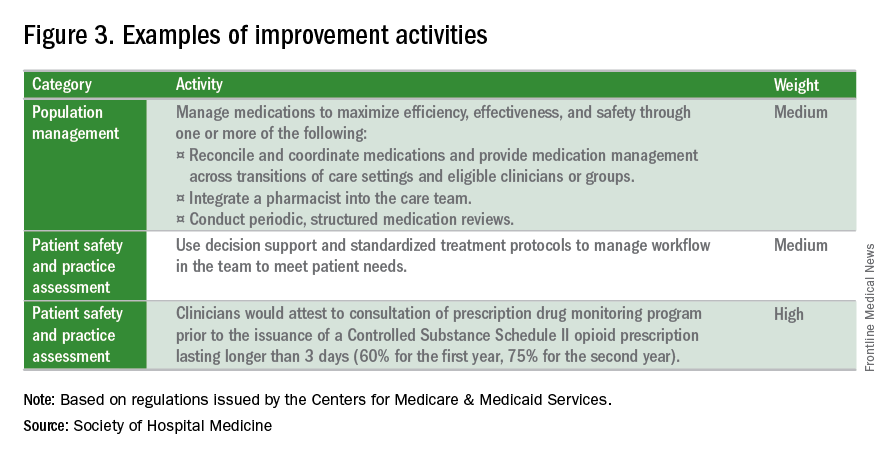
What is the APM Track?
The Alternative Payment Model pathway will be difficult for hospitalists to participate in, given its current criteria. Only advanced APMs will qualify, and for an APM to qualify as advanced, its clinicians/groups must use certified EHR technology, tie clinician payments to quality measures, and bear greater than nominal financial risk for outcomes and expenses, or qualify as a medical home. A provider must also meet rather high patient or payment thresholds coming from the model (greater than 25% of Medicare payments or greater than 20% of patients as part of an APM) in order to qualify.
Nominal financial risk is defined as either meeting revenue standards (at risk of losing 7% of its own revenues when Medicare expenditures are higher than expected) or benchmark-based standards (at risk of repaying the CMS up to a maximum of 3% of total Medicare expenditures).
Many hospitalists are participating in the Bundled Payments for Care Improvement (BPCI) model, but in its current form, it does not qualify as an APM for 2017 reporting.
The CMS has indicated that new voluntary bundled payment models that meet advanced APM criteria will be developed, but as of 2017, the list of APMs is slim, including only the Comprehensive ESRD Care, Comprehensive Primary Care Plus, Next Generation ACO, Shared Savings Program Tracks 2 and 3, and Oncology Care models.
Interested in learning more?
The SHM is working relentlessly in advocating on the behalf of hospitalists, and is constantly developing resources that will better prepare hospitalists for success within this program. If you are interested in learning more, check out the following resources:
• The SHM’s MACRA for Hospitalists website. Learn more about MACRA and its impact on hospitalists at www.macraforhm.org.
• The SHM’s annual meeting. A health policy track has been approved for HM17, including two sessions May 4 from 7:45 a.m.–8:35 a.m., “Hot Topics in Health Policy for Hospitalists,” and from 8:45 a.m.–9:40 a.m., “The Impact of the New Administration on Health Care Reform.” A MACRA-specific session will be held May 4 from 9:50 a.m.–10:45 a.m., “Tips for MIPS and Beyond,” as well as an Advocacy and Public Policy Special Interest Forum on May 2 from 4:30 p.m.–5:25 p.m.
• HMX. Join the advocacy and public policy community on HMX to learn more about dynamic changes in public policy and be a part of the conversation.
• Connect with SHM staff. Email Josh Boswell, SHM’s director of government relations, at [email protected].
• The CMS website. An easy to navigate site, the CMS’s MACRA-specific site, qpp.cms.gov, has additional resources and educational tools.
Dr. Lenchus is associate professor of clinical medicine, anesthesiology, and radiology, University of Miami Miller School of Medicine, and associate director, University of Miami/Jackson Memorial Hospital Center for Patient Safety, Miami.
Dr. Dutta is interim division chief, division of hospital medicine; medical director, attending/APP directed services; and assistant professor, department of internal medicine, Rush Medical College in Chicago.
Dr. Afsar-Manesh is chief quality officer, department of medicine, UCLA Health in Los Angeles, and treasurer of SHM’s board of directors.
All three are members of SHM’s Public Policy Committee.
In April 2015, President Obama signed the bipartisan Medicare Access and CHIP Reauthorization Act (MACRA) into law, effectively altering the future of the Medicare payment system for providers. MACRA not only removed the Sustainable Growth Rate, but also encouraged quality measure development, expanded the use of Medicare data, and locked provider payment rates to near zero growth.
For Medicare payments, MACRA created the Quality Payment Program, which breaks down clinical payments into two pathways: the Merit-Based Incentive Payment System (MIPS) combining current pay-for-performance programs into one consolidated payment system, and Alternative Payment Models (APMs), incentivizing payment models that move away from a fee-for-service system.
Both pathways incur risk, as well as rewards:
• MIPS. –4% penalty up to 12% positive adjustment in year 1 based on 2017 data reported and collected by the CMS, growing over time to include payment adjustments from –9% to +27% in future years.
• APMs. If the provider is eligible, a 5% payment increase from 2019 to 2024, with no reporting requirements, and exemption from MIPS.
Who is included in the program?
All clinicians who receive Medicare Physician Fee Schedule payments, including physicians, physician assistants, and nurse practitioners, will be affected by this program. The only providers who are exempt from the program are those who fall under low-volume thresholds (either less than $30,000 in Medicare Part B charges or less than 101 Medicare patients) or those in their first year with Medicare.
What is MIPS?
MIPS requires reporting in four categories that determine a physician’s payment adjustment:
• Quality, which replaces the Physician Quality Reporting System (PQRS).
• Cost, which replaces the value-based modifier.
• Advancing Care Information (ACI), which replaces the meaningful use program.
• Improvement activities, a new category, but one in which hospitalists should excel, as they are already participating in many of the activities.
Each category is given relative weight, which the CMS will adjust in the first few years of the program.
Note that in the first year (2017), cost will be calculated, but not used to determine payment amount, hence this category gets a 0% weighting. Also, there are significant differences between how most providers’ MIPS score will be calculated with respect to category weights, and how this will be done for hospitalists.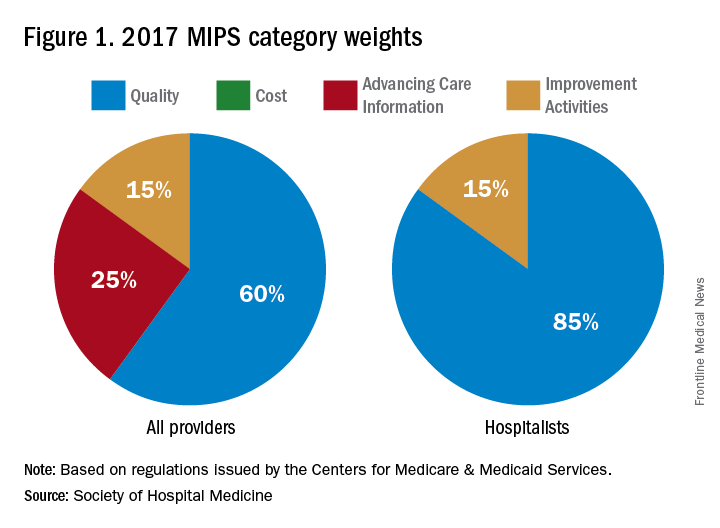
In addition to cost, the ACI will not play a role in the 2019 performance scores for hospitalists. However, hospitalists who practice in noninpatient settings, such as skilled nursing facilities or ambulatory clinics, will be subject to the ACI unless they apply for exceptions.
The quality category requires physicians to report on 6 of the 271 measures available. Hospitalists can report from the hospitalist-specific specialty set for which the Society of Hospital Medicine (SHM) was successful in advocating. Although continued cooperation between the CMS and SHM is necessary to fine-tune the measures, below are those that the SHM believes are reportable by, and most relevant to, hospitalists.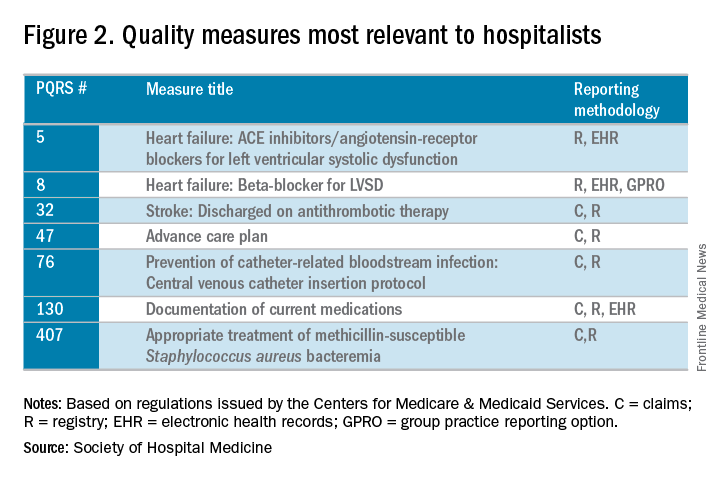
The improvement activities category will determine 15% of hospitalists’ performance in the MIPS. To receive full credit for this category, hospitalists must report on activities totaling 40 points. There are 92 available activities across eight different categories – 20 points for those that have a “high” weight determination and 10 points for those with medium weight.
In 2017, the CMS will calculate the cost category for providers, but it will not be counted toward the overall score. The data will still be collected based on Medicare Part A and Part B costs and will be reported to groups. Over time, this category will increase in scoring weight.
The Advancing Care Information category replaces the meaningful use program. This category will still promote EHR use, but hospitalists should be exempt from this category because of their “hospital-based” practice setting. This exemption is the reason why the quality category counts for 85% of the hospitalists’ score.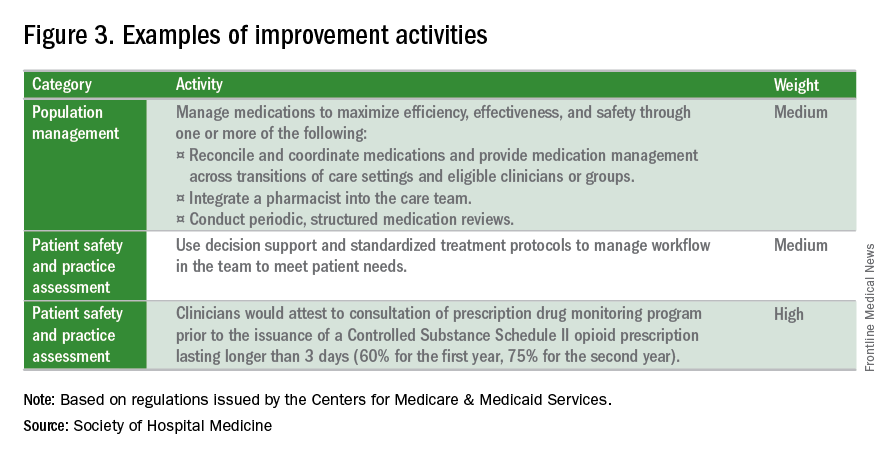
What is the APM Track?
The Alternative Payment Model pathway will be difficult for hospitalists to participate in, given its current criteria. Only advanced APMs will qualify, and for an APM to qualify as advanced, its clinicians/groups must use certified EHR technology, tie clinician payments to quality measures, and bear greater than nominal financial risk for outcomes and expenses, or qualify as a medical home. A provider must also meet rather high patient or payment thresholds coming from the model (greater than 25% of Medicare payments or greater than 20% of patients as part of an APM) in order to qualify.
Nominal financial risk is defined as either meeting revenue standards (at risk of losing 7% of its own revenues when Medicare expenditures are higher than expected) or benchmark-based standards (at risk of repaying the CMS up to a maximum of 3% of total Medicare expenditures).
Many hospitalists are participating in the Bundled Payments for Care Improvement (BPCI) model, but in its current form, it does not qualify as an APM for 2017 reporting.
The CMS has indicated that new voluntary bundled payment models that meet advanced APM criteria will be developed, but as of 2017, the list of APMs is slim, including only the Comprehensive ESRD Care, Comprehensive Primary Care Plus, Next Generation ACO, Shared Savings Program Tracks 2 and 3, and Oncology Care models.
Interested in learning more?
The SHM is working relentlessly in advocating on the behalf of hospitalists, and is constantly developing resources that will better prepare hospitalists for success within this program. If you are interested in learning more, check out the following resources:
• The SHM’s MACRA for Hospitalists website. Learn more about MACRA and its impact on hospitalists at www.macraforhm.org.
• The SHM’s annual meeting. A health policy track has been approved for HM17, including two sessions May 4 from 7:45 a.m.–8:35 a.m., “Hot Topics in Health Policy for Hospitalists,” and from 8:45 a.m.–9:40 a.m., “The Impact of the New Administration on Health Care Reform.” A MACRA-specific session will be held May 4 from 9:50 a.m.–10:45 a.m., “Tips for MIPS and Beyond,” as well as an Advocacy and Public Policy Special Interest Forum on May 2 from 4:30 p.m.–5:25 p.m.
• HMX. Join the advocacy and public policy community on HMX to learn more about dynamic changes in public policy and be a part of the conversation.
• Connect with SHM staff. Email Josh Boswell, SHM’s director of government relations, at [email protected].
• The CMS website. An easy to navigate site, the CMS’s MACRA-specific site, qpp.cms.gov, has additional resources and educational tools.
Dr. Lenchus is associate professor of clinical medicine, anesthesiology, and radiology, University of Miami Miller School of Medicine, and associate director, University of Miami/Jackson Memorial Hospital Center for Patient Safety, Miami.
Dr. Dutta is interim division chief, division of hospital medicine; medical director, attending/APP directed services; and assistant professor, department of internal medicine, Rush Medical College in Chicago.
Dr. Afsar-Manesh is chief quality officer, department of medicine, UCLA Health in Los Angeles, and treasurer of SHM’s board of directors.
All three are members of SHM’s Public Policy Committee.
In April 2015, President Obama signed the bipartisan Medicare Access and CHIP Reauthorization Act (MACRA) into law, effectively altering the future of the Medicare payment system for providers. MACRA not only removed the Sustainable Growth Rate, but also encouraged quality measure development, expanded the use of Medicare data, and locked provider payment rates to near zero growth.
For Medicare payments, MACRA created the Quality Payment Program, which breaks down clinical payments into two pathways: the Merit-Based Incentive Payment System (MIPS) combining current pay-for-performance programs into one consolidated payment system, and Alternative Payment Models (APMs), incentivizing payment models that move away from a fee-for-service system.
Both pathways incur risk, as well as rewards:
• MIPS. –4% penalty up to 12% positive adjustment in year 1 based on 2017 data reported and collected by the CMS, growing over time to include payment adjustments from –9% to +27% in future years.
• APMs. If the provider is eligible, a 5% payment increase from 2019 to 2024, with no reporting requirements, and exemption from MIPS.
Who is included in the program?
All clinicians who receive Medicare Physician Fee Schedule payments, including physicians, physician assistants, and nurse practitioners, will be affected by this program. The only providers who are exempt from the program are those who fall under low-volume thresholds (either less than $30,000 in Medicare Part B charges or less than 101 Medicare patients) or those in their first year with Medicare.
What is MIPS?
MIPS requires reporting in four categories that determine a physician’s payment adjustment:
• Quality, which replaces the Physician Quality Reporting System (PQRS).
• Cost, which replaces the value-based modifier.
• Advancing Care Information (ACI), which replaces the meaningful use program.
• Improvement activities, a new category, but one in which hospitalists should excel, as they are already participating in many of the activities.
Each category is given relative weight, which the CMS will adjust in the first few years of the program.
Note that in the first year (2017), cost will be calculated, but not used to determine payment amount, hence this category gets a 0% weighting. Also, there are significant differences between how most providers’ MIPS score will be calculated with respect to category weights, and how this will be done for hospitalists.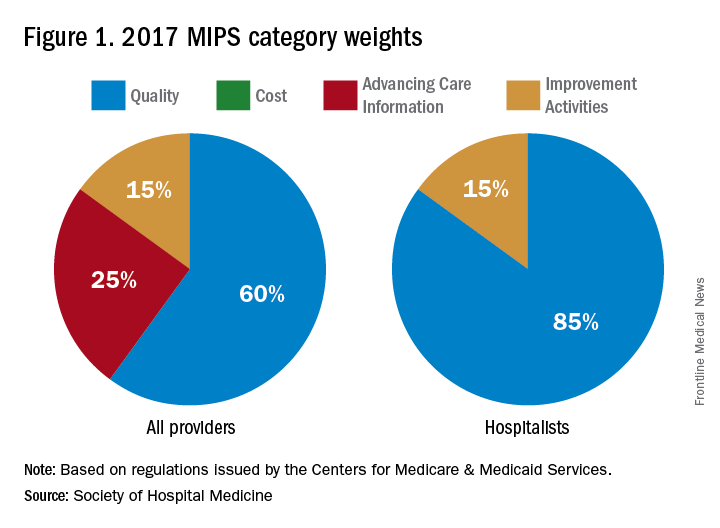
In addition to cost, the ACI will not play a role in the 2019 performance scores for hospitalists. However, hospitalists who practice in noninpatient settings, such as skilled nursing facilities or ambulatory clinics, will be subject to the ACI unless they apply for exceptions.
The quality category requires physicians to report on 6 of the 271 measures available. Hospitalists can report from the hospitalist-specific specialty set for which the Society of Hospital Medicine (SHM) was successful in advocating. Although continued cooperation between the CMS and SHM is necessary to fine-tune the measures, below are those that the SHM believes are reportable by, and most relevant to, hospitalists.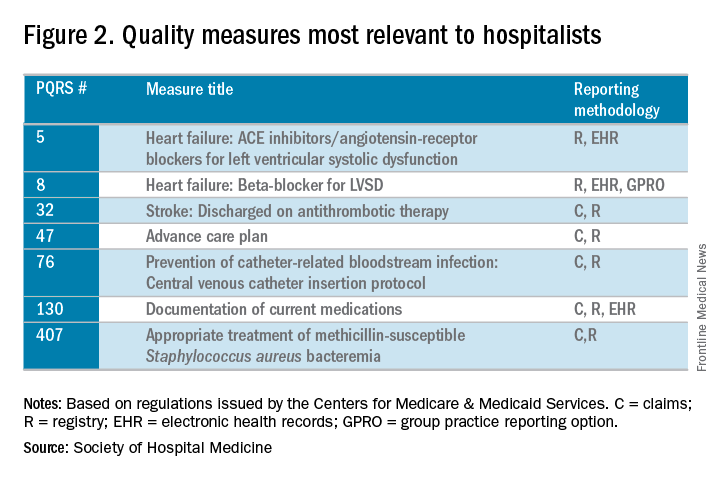
The improvement activities category will determine 15% of hospitalists’ performance in the MIPS. To receive full credit for this category, hospitalists must report on activities totaling 40 points. There are 92 available activities across eight different categories – 20 points for those that have a “high” weight determination and 10 points for those with medium weight.
In 2017, the CMS will calculate the cost category for providers, but it will not be counted toward the overall score. The data will still be collected based on Medicare Part A and Part B costs and will be reported to groups. Over time, this category will increase in scoring weight.
The Advancing Care Information category replaces the meaningful use program. This category will still promote EHR use, but hospitalists should be exempt from this category because of their “hospital-based” practice setting. This exemption is the reason why the quality category counts for 85% of the hospitalists’ score.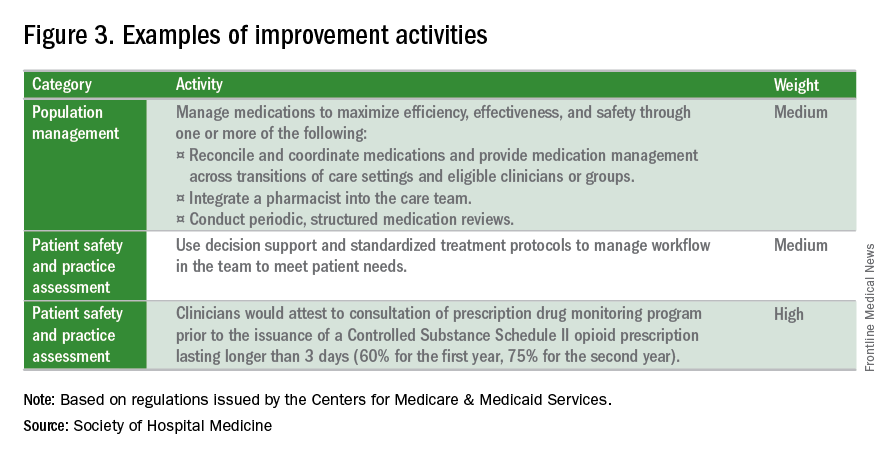
What is the APM Track?
The Alternative Payment Model pathway will be difficult for hospitalists to participate in, given its current criteria. Only advanced APMs will qualify, and for an APM to qualify as advanced, its clinicians/groups must use certified EHR technology, tie clinician payments to quality measures, and bear greater than nominal financial risk for outcomes and expenses, or qualify as a medical home. A provider must also meet rather high patient or payment thresholds coming from the model (greater than 25% of Medicare payments or greater than 20% of patients as part of an APM) in order to qualify.
Nominal financial risk is defined as either meeting revenue standards (at risk of losing 7% of its own revenues when Medicare expenditures are higher than expected) or benchmark-based standards (at risk of repaying the CMS up to a maximum of 3% of total Medicare expenditures).
Many hospitalists are participating in the Bundled Payments for Care Improvement (BPCI) model, but in its current form, it does not qualify as an APM for 2017 reporting.
The CMS has indicated that new voluntary bundled payment models that meet advanced APM criteria will be developed, but as of 2017, the list of APMs is slim, including only the Comprehensive ESRD Care, Comprehensive Primary Care Plus, Next Generation ACO, Shared Savings Program Tracks 2 and 3, and Oncology Care models.
Interested in learning more?
The SHM is working relentlessly in advocating on the behalf of hospitalists, and is constantly developing resources that will better prepare hospitalists for success within this program. If you are interested in learning more, check out the following resources:
• The SHM’s MACRA for Hospitalists website. Learn more about MACRA and its impact on hospitalists at www.macraforhm.org.
• The SHM’s annual meeting. A health policy track has been approved for HM17, including two sessions May 4 from 7:45 a.m.–8:35 a.m., “Hot Topics in Health Policy for Hospitalists,” and from 8:45 a.m.–9:40 a.m., “The Impact of the New Administration on Health Care Reform.” A MACRA-specific session will be held May 4 from 9:50 a.m.–10:45 a.m., “Tips for MIPS and Beyond,” as well as an Advocacy and Public Policy Special Interest Forum on May 2 from 4:30 p.m.–5:25 p.m.
• HMX. Join the advocacy and public policy community on HMX to learn more about dynamic changes in public policy and be a part of the conversation.
• Connect with SHM staff. Email Josh Boswell, SHM’s director of government relations, at [email protected].
• The CMS website. An easy to navigate site, the CMS’s MACRA-specific site, qpp.cms.gov, has additional resources and educational tools.
Dr. Lenchus is associate professor of clinical medicine, anesthesiology, and radiology, University of Miami Miller School of Medicine, and associate director, University of Miami/Jackson Memorial Hospital Center for Patient Safety, Miami.
Dr. Dutta is interim division chief, division of hospital medicine; medical director, attending/APP directed services; and assistant professor, department of internal medicine, Rush Medical College in Chicago.
Dr. Afsar-Manesh is chief quality officer, department of medicine, UCLA Health in Los Angeles, and treasurer of SHM’s board of directors.
All three are members of SHM’s Public Policy Committee.