User login
American Academy of Child and Adolescent Psychiatry (AACAP): Annual Meeting
Telepsychiatry effective for ADHD treatment in rural areas
ORLANDO – Telepsychiatry in rural areas is beneficial for children with attention-deficit/hyperactivity disorder and their parents, according to one of the largest randomized controlled trials of its kind.
During the 22 weeks of the study, children who received telemental health (TMH) improved significantly in ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning, based on the ratings provided by their parents.
The study is yet another piece of evidence that telemedicine can play a role in closing the mental health gap.
"Our study shows that with modern technology, we have the opportunity to reach out to underserved areas and provide care," said Dr. William P. French of the University of Washington, Seattle. "And the care is good care and can improve the health of the patients at least as well as the local providers."
Dr. French and his colleagues used the Children’s ADHD Telemental Health Treatment Study, or CATTS, to assess the impact of telemental health on children’s inattention, hyperactivity, opposition, school performance, and impairment. They also evaluated the telepsychiatrists’ and therapists’ adherence to evidence-based treatment protocols implemented within the TMH model.
CATTS includes 223 English-speaking children aged 5.5-12 years with ADHD, along with their parents. The children were recruited from several local primary care practices in seven rural areas in Washington and Oregon between November 2009 and August 2012.
The children were randomly assigned to two groups. Group A, or the intervention group, received six teleconferencing sessions over a 22-week period. Their medication and education were delivered via videoconferencing by a child and adolescent psychiatrist. Their parents’ behavior training, which also occurred in six sessions, was provided in person by a community therapist. The local therapists already had been trained in treatment protocols and were supervised remotely.
Group B, or the active control group, received one video conferencing session with the child and adolescent psychiatrist, who gave the primary care providers treatment recommendations. For the rest of the trial period, this group received the standard of care, which was mainly treatment by their primary care provider.
The primary outcome included the Vanderbilt ADHD Rating Scales (VADRS) and the Columbia Impairment Scale–Parent Version (CIS-P), both of which were filled out by parents. Teachers assessed the ADHD and oppositional defiant disorder symptoms using VADRS.
Assessments were conducted at baseline, 4, 10, and 19 weeks, and at 25 weeks post randomization.
Results showed that during the 22 weeks, children receiving TMH had significantly better responses than the control group, the researchers found. Their parent-rated ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning improved, as did their teacher-rated ADHD inattention and school performance.
However, no effect was shown in the teacher-rated hyperactivity or oppositional defiant disorder. Dr. French said this could be attributable to the contextual demands of school versus home, or a change in teacher with kids moved to the next grade during the study period.
The study also showed that telepsychiatrists and therapists adhered to the evidence-based treatment protocols more than 90% of the time. Researchers said that TMH can be effective in training community therapists in evidence-based treatment behavioral management.
Barriers still exist to widespread implementation and adoption of telepsychiatry– with privacy concerns and lack of reimbursement just to name two – but advancement in technology is making the service more readily available, said Dr. French, who presented his findings in a poster at the American Academy of Child and Adolescent Psychiatry meeting.
"Telemedicine is going to be mostly Internet based," he said, "and this opens the potential to anyone with Internet access and a mobile device that has a camera and audio capabilities."
The study was supported by the National Institute of Mental Health. Researchers reported no relevant financial disclosures.
On Twitter @naseemsmiller
ORLANDO – Telepsychiatry in rural areas is beneficial for children with attention-deficit/hyperactivity disorder and their parents, according to one of the largest randomized controlled trials of its kind.
During the 22 weeks of the study, children who received telemental health (TMH) improved significantly in ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning, based on the ratings provided by their parents.
The study is yet another piece of evidence that telemedicine can play a role in closing the mental health gap.
"Our study shows that with modern technology, we have the opportunity to reach out to underserved areas and provide care," said Dr. William P. French of the University of Washington, Seattle. "And the care is good care and can improve the health of the patients at least as well as the local providers."
Dr. French and his colleagues used the Children’s ADHD Telemental Health Treatment Study, or CATTS, to assess the impact of telemental health on children’s inattention, hyperactivity, opposition, school performance, and impairment. They also evaluated the telepsychiatrists’ and therapists’ adherence to evidence-based treatment protocols implemented within the TMH model.
CATTS includes 223 English-speaking children aged 5.5-12 years with ADHD, along with their parents. The children were recruited from several local primary care practices in seven rural areas in Washington and Oregon between November 2009 and August 2012.
The children were randomly assigned to two groups. Group A, or the intervention group, received six teleconferencing sessions over a 22-week period. Their medication and education were delivered via videoconferencing by a child and adolescent psychiatrist. Their parents’ behavior training, which also occurred in six sessions, was provided in person by a community therapist. The local therapists already had been trained in treatment protocols and were supervised remotely.
Group B, or the active control group, received one video conferencing session with the child and adolescent psychiatrist, who gave the primary care providers treatment recommendations. For the rest of the trial period, this group received the standard of care, which was mainly treatment by their primary care provider.
The primary outcome included the Vanderbilt ADHD Rating Scales (VADRS) and the Columbia Impairment Scale–Parent Version (CIS-P), both of which were filled out by parents. Teachers assessed the ADHD and oppositional defiant disorder symptoms using VADRS.
Assessments were conducted at baseline, 4, 10, and 19 weeks, and at 25 weeks post randomization.
Results showed that during the 22 weeks, children receiving TMH had significantly better responses than the control group, the researchers found. Their parent-rated ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning improved, as did their teacher-rated ADHD inattention and school performance.
However, no effect was shown in the teacher-rated hyperactivity or oppositional defiant disorder. Dr. French said this could be attributable to the contextual demands of school versus home, or a change in teacher with kids moved to the next grade during the study period.
The study also showed that telepsychiatrists and therapists adhered to the evidence-based treatment protocols more than 90% of the time. Researchers said that TMH can be effective in training community therapists in evidence-based treatment behavioral management.
Barriers still exist to widespread implementation and adoption of telepsychiatry– with privacy concerns and lack of reimbursement just to name two – but advancement in technology is making the service more readily available, said Dr. French, who presented his findings in a poster at the American Academy of Child and Adolescent Psychiatry meeting.
"Telemedicine is going to be mostly Internet based," he said, "and this opens the potential to anyone with Internet access and a mobile device that has a camera and audio capabilities."
The study was supported by the National Institute of Mental Health. Researchers reported no relevant financial disclosures.
On Twitter @naseemsmiller
ORLANDO – Telepsychiatry in rural areas is beneficial for children with attention-deficit/hyperactivity disorder and their parents, according to one of the largest randomized controlled trials of its kind.
During the 22 weeks of the study, children who received telemental health (TMH) improved significantly in ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning, based on the ratings provided by their parents.
The study is yet another piece of evidence that telemedicine can play a role in closing the mental health gap.
"Our study shows that with modern technology, we have the opportunity to reach out to underserved areas and provide care," said Dr. William P. French of the University of Washington, Seattle. "And the care is good care and can improve the health of the patients at least as well as the local providers."
Dr. French and his colleagues used the Children’s ADHD Telemental Health Treatment Study, or CATTS, to assess the impact of telemental health on children’s inattention, hyperactivity, opposition, school performance, and impairment. They also evaluated the telepsychiatrists’ and therapists’ adherence to evidence-based treatment protocols implemented within the TMH model.
CATTS includes 223 English-speaking children aged 5.5-12 years with ADHD, along with their parents. The children were recruited from several local primary care practices in seven rural areas in Washington and Oregon between November 2009 and August 2012.
The children were randomly assigned to two groups. Group A, or the intervention group, received six teleconferencing sessions over a 22-week period. Their medication and education were delivered via videoconferencing by a child and adolescent psychiatrist. Their parents’ behavior training, which also occurred in six sessions, was provided in person by a community therapist. The local therapists already had been trained in treatment protocols and were supervised remotely.
Group B, or the active control group, received one video conferencing session with the child and adolescent psychiatrist, who gave the primary care providers treatment recommendations. For the rest of the trial period, this group received the standard of care, which was mainly treatment by their primary care provider.
The primary outcome included the Vanderbilt ADHD Rating Scales (VADRS) and the Columbia Impairment Scale–Parent Version (CIS-P), both of which were filled out by parents. Teachers assessed the ADHD and oppositional defiant disorder symptoms using VADRS.
Assessments were conducted at baseline, 4, 10, and 19 weeks, and at 25 weeks post randomization.
Results showed that during the 22 weeks, children receiving TMH had significantly better responses than the control group, the researchers found. Their parent-rated ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning improved, as did their teacher-rated ADHD inattention and school performance.
However, no effect was shown in the teacher-rated hyperactivity or oppositional defiant disorder. Dr. French said this could be attributable to the contextual demands of school versus home, or a change in teacher with kids moved to the next grade during the study period.
The study also showed that telepsychiatrists and therapists adhered to the evidence-based treatment protocols more than 90% of the time. Researchers said that TMH can be effective in training community therapists in evidence-based treatment behavioral management.
Barriers still exist to widespread implementation and adoption of telepsychiatry– with privacy concerns and lack of reimbursement just to name two – but advancement in technology is making the service more readily available, said Dr. French, who presented his findings in a poster at the American Academy of Child and Adolescent Psychiatry meeting.
"Telemedicine is going to be mostly Internet based," he said, "and this opens the potential to anyone with Internet access and a mobile device that has a camera and audio capabilities."
The study was supported by the National Institute of Mental Health. Researchers reported no relevant financial disclosures.
On Twitter @naseemsmiller
AT THE AACAP ANNUAL MEETING
Major finding: During the 22 weeks of the study, children who received telemental health improved significantly in attention-deficit/hyperactivity disorder inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning.
Data source: The results are based on 223 English-speaking children aged 5.5-12 years with ADHD, along with their parents, who were recruited from local primary care practices in seven rural areas in Washington and Oregon between November 2009 and August 2012.
Disclosures: The study was supported by the National Institute of Mental Health. The researchers said they had no relevant financial disclosures.
Ohio Medicaid data document rising polypharmacy in foster children
ORLANDO – Prescribing of three or more psychotropic medications has increased among foster children enrolled in Medicaid, based on an analysis of claims data in Ohio. The findings of polypharmacy are raising red flags about oversight and monitoring of psychotropic medication use among high-risk youth.
By 2008, nearly a quarter of foster care and disabled children in the Ohio Medicaid program were prescribed three or more psychiatric medications. Nearly one-fifth of them were prescribed medications from three or more drug classes, with the most common combination being stimulants, antipsychotics, and alpha-agonists.
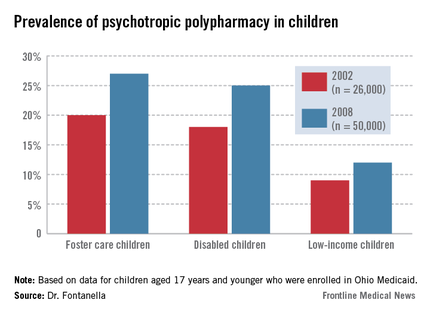
The findings make a powerful case for system-wide oversight and monitoring of psychotropic prescribing practices in the Medicaid population, especially for children in foster care, said Cynthia A. Fontanella, Ph.D., of the Ohio State University, Columbus, who led the study and presented her findings at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "We don’t know if these kids are doing better ... The increase has "occurred despite lack of data on safety and efficacy of multiple drug combination and existing concerns about adverse effects of drug-drug interactions."
A 2012 report by the Government Accountability Office that showed 18% of foster children were taking psychotropic medications. That report additionally noted, however, that 30% of the children who may have needed mental health services hadn't received them.
The rising rates of polypharmacy, especially in children enrolled in Medicaid, have been documented in other studies. But the accumulating data implies polypharmacy is pervasive in at-risk children. "It’s a growing trend," said Susan dosReis, Ph.D., associate professor at the University of Maryland School of Pharmacy, Baltimore, who has studied psychiatric prescription patterns among youth. She was not involved in the study.
Dr. dosReis acknowledged that the issue is complex, especially in the cases of children with severe conditions. Clinicians face families who are looking for a way to manage their child or to keep them in school. "And once you have a child on a combination, and there’s improvement, the thought of taking away the medications is hard to accept, because [the family is] afraid that the condition will worsen again."
Also, follow-up has been problematic, with data that don’t clearly indicate whether the children were on several medications for a short period of time until they were stabilized, or the whether the polypharmacy lasted longer. Data for children enrolled in private insurance are lacking, and prescribing is difficult to track for children in foster care because they move frequently.
Dr. Fontanella and her colleagues compared polypharmacy patterns and rates in foster care, disabled, and low-income youth aged 17 years and younger enrolled in Ohio Medicaid between 2002 (n = 26,000) and 2008 (n = 50,000).
The two outcome measures — any polypharmacy (three or more medications) — and multiclass polypharmacy (three or more medications from different drug classes) increased over time across all three groups. Polypharmacy increased from 9% to 12% for low-income youth; from 18% to 25% in disabled youth; and from 20% to 27% in foster care youth.
Combination therapies that increased the most during the time of the study were prescriptions of two or more antipsychotics, two or more stimulants, and antipsychotics with stimulants and other psychotropic medications excluding antidepressants.
The percentage of foster children who were prescribed two or more antipsychotics increased from 5% in 2002 to 10% in 2008, compared with 6% to 9% among children with disabilities, and 3% to 5% among low-income children.
The percentage of foster children who were prescribed two or more stimulants also showed a bigger jump – from 1.5% in 2002 to 8% in 2008 – compared with 1.5% to 6% among children with disabilities, and 3% to 7% among low-income children.
Meanwhile, multiclass polypharmacy has been increasing over the years, from 14% during 1996-1999 to 20% during 2004-2007. Even when it’s indicated, polypharmacy increases the risk for adverse events and drug-drug interactions, creates a complicated drug regimen and the need for more medication, and leads to higher costs, the researchers said.
Researchers also found some within class and between-class prescribing trends.
While the prescription rates for two or more antipsychotics and stimulants increased, the rate of combination antidepressant prescribing decreased.
It’s not clear if the findings can be generalized to other states and to non-Medicaid populations, the researchers noted. Also, a 30-day window as a measure of prevalence may lead to overestimation of polypharmacy, and, prescriptions don’t necessarily translate to adherence.
Dr. Fontanella and Dr. dosReis had no disclosures.
On Twitter @NaseemSMiller
ORLANDO – Prescribing of three or more psychotropic medications has increased among foster children enrolled in Medicaid, based on an analysis of claims data in Ohio. The findings of polypharmacy are raising red flags about oversight and monitoring of psychotropic medication use among high-risk youth.
By 2008, nearly a quarter of foster care and disabled children in the Ohio Medicaid program were prescribed three or more psychiatric medications. Nearly one-fifth of them were prescribed medications from three or more drug classes, with the most common combination being stimulants, antipsychotics, and alpha-agonists.
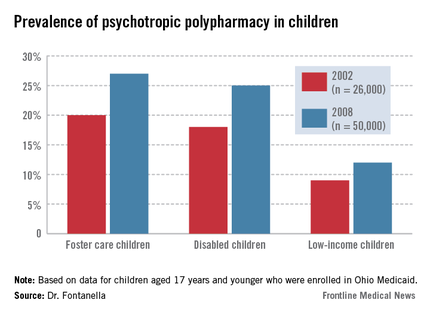
The findings make a powerful case for system-wide oversight and monitoring of psychotropic prescribing practices in the Medicaid population, especially for children in foster care, said Cynthia A. Fontanella, Ph.D., of the Ohio State University, Columbus, who led the study and presented her findings at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "We don’t know if these kids are doing better ... The increase has "occurred despite lack of data on safety and efficacy of multiple drug combination and existing concerns about adverse effects of drug-drug interactions."
A 2012 report by the Government Accountability Office that showed 18% of foster children were taking psychotropic medications. That report additionally noted, however, that 30% of the children who may have needed mental health services hadn't received them.
The rising rates of polypharmacy, especially in children enrolled in Medicaid, have been documented in other studies. But the accumulating data implies polypharmacy is pervasive in at-risk children. "It’s a growing trend," said Susan dosReis, Ph.D., associate professor at the University of Maryland School of Pharmacy, Baltimore, who has studied psychiatric prescription patterns among youth. She was not involved in the study.
Dr. dosReis acknowledged that the issue is complex, especially in the cases of children with severe conditions. Clinicians face families who are looking for a way to manage their child or to keep them in school. "And once you have a child on a combination, and there’s improvement, the thought of taking away the medications is hard to accept, because [the family is] afraid that the condition will worsen again."
Also, follow-up has been problematic, with data that don’t clearly indicate whether the children were on several medications for a short period of time until they were stabilized, or the whether the polypharmacy lasted longer. Data for children enrolled in private insurance are lacking, and prescribing is difficult to track for children in foster care because they move frequently.
Dr. Fontanella and her colleagues compared polypharmacy patterns and rates in foster care, disabled, and low-income youth aged 17 years and younger enrolled in Ohio Medicaid between 2002 (n = 26,000) and 2008 (n = 50,000).
The two outcome measures — any polypharmacy (three or more medications) — and multiclass polypharmacy (three or more medications from different drug classes) increased over time across all three groups. Polypharmacy increased from 9% to 12% for low-income youth; from 18% to 25% in disabled youth; and from 20% to 27% in foster care youth.
Combination therapies that increased the most during the time of the study were prescriptions of two or more antipsychotics, two or more stimulants, and antipsychotics with stimulants and other psychotropic medications excluding antidepressants.
The percentage of foster children who were prescribed two or more antipsychotics increased from 5% in 2002 to 10% in 2008, compared with 6% to 9% among children with disabilities, and 3% to 5% among low-income children.
The percentage of foster children who were prescribed two or more stimulants also showed a bigger jump – from 1.5% in 2002 to 8% in 2008 – compared with 1.5% to 6% among children with disabilities, and 3% to 7% among low-income children.
Meanwhile, multiclass polypharmacy has been increasing over the years, from 14% during 1996-1999 to 20% during 2004-2007. Even when it’s indicated, polypharmacy increases the risk for adverse events and drug-drug interactions, creates a complicated drug regimen and the need for more medication, and leads to higher costs, the researchers said.
Researchers also found some within class and between-class prescribing trends.
While the prescription rates for two or more antipsychotics and stimulants increased, the rate of combination antidepressant prescribing decreased.
It’s not clear if the findings can be generalized to other states and to non-Medicaid populations, the researchers noted. Also, a 30-day window as a measure of prevalence may lead to overestimation of polypharmacy, and, prescriptions don’t necessarily translate to adherence.
Dr. Fontanella and Dr. dosReis had no disclosures.
On Twitter @NaseemSMiller
ORLANDO – Prescribing of three or more psychotropic medications has increased among foster children enrolled in Medicaid, based on an analysis of claims data in Ohio. The findings of polypharmacy are raising red flags about oversight and monitoring of psychotropic medication use among high-risk youth.
By 2008, nearly a quarter of foster care and disabled children in the Ohio Medicaid program were prescribed three or more psychiatric medications. Nearly one-fifth of them were prescribed medications from three or more drug classes, with the most common combination being stimulants, antipsychotics, and alpha-agonists.
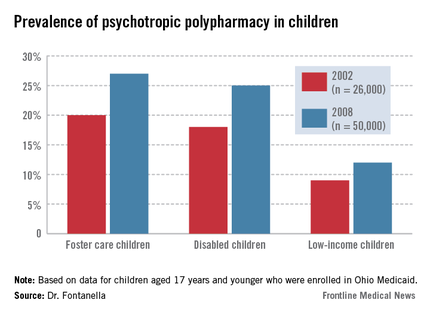
The findings make a powerful case for system-wide oversight and monitoring of psychotropic prescribing practices in the Medicaid population, especially for children in foster care, said Cynthia A. Fontanella, Ph.D., of the Ohio State University, Columbus, who led the study and presented her findings at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "We don’t know if these kids are doing better ... The increase has "occurred despite lack of data on safety and efficacy of multiple drug combination and existing concerns about adverse effects of drug-drug interactions."
A 2012 report by the Government Accountability Office that showed 18% of foster children were taking psychotropic medications. That report additionally noted, however, that 30% of the children who may have needed mental health services hadn't received them.
The rising rates of polypharmacy, especially in children enrolled in Medicaid, have been documented in other studies. But the accumulating data implies polypharmacy is pervasive in at-risk children. "It’s a growing trend," said Susan dosReis, Ph.D., associate professor at the University of Maryland School of Pharmacy, Baltimore, who has studied psychiatric prescription patterns among youth. She was not involved in the study.
Dr. dosReis acknowledged that the issue is complex, especially in the cases of children with severe conditions. Clinicians face families who are looking for a way to manage their child or to keep them in school. "And once you have a child on a combination, and there’s improvement, the thought of taking away the medications is hard to accept, because [the family is] afraid that the condition will worsen again."
Also, follow-up has been problematic, with data that don’t clearly indicate whether the children were on several medications for a short period of time until they were stabilized, or the whether the polypharmacy lasted longer. Data for children enrolled in private insurance are lacking, and prescribing is difficult to track for children in foster care because they move frequently.
Dr. Fontanella and her colleagues compared polypharmacy patterns and rates in foster care, disabled, and low-income youth aged 17 years and younger enrolled in Ohio Medicaid between 2002 (n = 26,000) and 2008 (n = 50,000).
The two outcome measures — any polypharmacy (three or more medications) — and multiclass polypharmacy (three or more medications from different drug classes) increased over time across all three groups. Polypharmacy increased from 9% to 12% for low-income youth; from 18% to 25% in disabled youth; and from 20% to 27% in foster care youth.
Combination therapies that increased the most during the time of the study were prescriptions of two or more antipsychotics, two or more stimulants, and antipsychotics with stimulants and other psychotropic medications excluding antidepressants.
The percentage of foster children who were prescribed two or more antipsychotics increased from 5% in 2002 to 10% in 2008, compared with 6% to 9% among children with disabilities, and 3% to 5% among low-income children.
The percentage of foster children who were prescribed two or more stimulants also showed a bigger jump – from 1.5% in 2002 to 8% in 2008 – compared with 1.5% to 6% among children with disabilities, and 3% to 7% among low-income children.
Meanwhile, multiclass polypharmacy has been increasing over the years, from 14% during 1996-1999 to 20% during 2004-2007. Even when it’s indicated, polypharmacy increases the risk for adverse events and drug-drug interactions, creates a complicated drug regimen and the need for more medication, and leads to higher costs, the researchers said.
Researchers also found some within class and between-class prescribing trends.
While the prescription rates for two or more antipsychotics and stimulants increased, the rate of combination antidepressant prescribing decreased.
It’s not clear if the findings can be generalized to other states and to non-Medicaid populations, the researchers noted. Also, a 30-day window as a measure of prevalence may lead to overestimation of polypharmacy, and, prescriptions don’t necessarily translate to adherence.
Dr. Fontanella and Dr. dosReis had no disclosures.
On Twitter @NaseemSMiller
AT THE AACAP ANNUAL MEETING
Major finding: Based on 2008 Medicaid data, the rate of polypharmacy was 27% in foster children.
Data source: Foster care, disabled, and low income youth aged 17 years and younger enrolled in Ohio Medicaid between 2002 (n = 26,000) and 2008 (n = 50,000).
Disclosures: Dr. Fontanella and Dr. dosReis had no disclosures.
Ask young patients about social media use
ORLANDO – Half of the teens who made comments on social media about their feelings and caused concern among those who saw the comments were brought to the hospital for assessment, according to a small survey of adolescents admitted to the child and adolescent psychiatry unit of Ohio State University Harding Hospital, Columbus.
Tragic suicides or homicides after social media use have gained national attention in recent years, but studies like this highlight the flip side of social media platforms: They can make it easier to find out when teens are in distress and help them access timely treatment and support.
The fact that these teens turned to social media to express emotional stress, "shows that [they] are having trouble conveying emotions to parents, counselors, or friends, so they’re finding a different avenue," said Dr. Sathyan Gurumurthy, who presented the unpublished study at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "So, as professionals, we have to gain a better understanding of how they convey emotions."
And given the generalized use of social media today, it is important for clinicians to ask children and adolescents about social media use during initial assessment, advised Dr. Gurumurthy, a resident physician at OSU’s Wexner Medical Center. "Talk to them about social media: how they use it and what sites they’re using," he said in an interview.
The results of the yearlong study are based on the 6-month data from an eight-question survey. Researchers were able to collect 32% of the surveys that were handed out to teens and their families at the time of admission.
Of the 82 patients who completed the survey, 54 (66%) said they had made a comment on social media about their emotional disturbance. Of those patients, 32 (60%) said their comments caused a concern, and 16 of those patients (50%) were brought to the hospital for assessment because of their comments.
Seventy-three teens were hospitalized for suicidal ideation; and they had confided mostly in friends, parents, or counselors (around 25 each). Six of the patients said that they had confided in an "Internet friend."
Half of these teens also said they preferred to communicate their suicidal thoughts in person, while 15% said they preferred social sites, and 9% preferred texts. Of the social sites, Facebook was the most popular (41%) among teens.
Of note was that only 25% circled "parent" as the person aware of their social media comments, said Dr. Gurumurthy.
"Many parents have minimal monitoring of their kids’ social media, and they have to be more involved in social media," he advised.
Dr. Gurumurthy said the group is still gathering data and hopes to increase the number of survey respondents. He said future studies gathering social media use data from outpatient and emergency department visits could reveal other possible correlations.
The authors had nothing to disclose.
On Twitter @NaseemSMiller
ORLANDO – Half of the teens who made comments on social media about their feelings and caused concern among those who saw the comments were brought to the hospital for assessment, according to a small survey of adolescents admitted to the child and adolescent psychiatry unit of Ohio State University Harding Hospital, Columbus.
Tragic suicides or homicides after social media use have gained national attention in recent years, but studies like this highlight the flip side of social media platforms: They can make it easier to find out when teens are in distress and help them access timely treatment and support.
The fact that these teens turned to social media to express emotional stress, "shows that [they] are having trouble conveying emotions to parents, counselors, or friends, so they’re finding a different avenue," said Dr. Sathyan Gurumurthy, who presented the unpublished study at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "So, as professionals, we have to gain a better understanding of how they convey emotions."
And given the generalized use of social media today, it is important for clinicians to ask children and adolescents about social media use during initial assessment, advised Dr. Gurumurthy, a resident physician at OSU’s Wexner Medical Center. "Talk to them about social media: how they use it and what sites they’re using," he said in an interview.
The results of the yearlong study are based on the 6-month data from an eight-question survey. Researchers were able to collect 32% of the surveys that were handed out to teens and their families at the time of admission.
Of the 82 patients who completed the survey, 54 (66%) said they had made a comment on social media about their emotional disturbance. Of those patients, 32 (60%) said their comments caused a concern, and 16 of those patients (50%) were brought to the hospital for assessment because of their comments.
Seventy-three teens were hospitalized for suicidal ideation; and they had confided mostly in friends, parents, or counselors (around 25 each). Six of the patients said that they had confided in an "Internet friend."
Half of these teens also said they preferred to communicate their suicidal thoughts in person, while 15% said they preferred social sites, and 9% preferred texts. Of the social sites, Facebook was the most popular (41%) among teens.
Of note was that only 25% circled "parent" as the person aware of their social media comments, said Dr. Gurumurthy.
"Many parents have minimal monitoring of their kids’ social media, and they have to be more involved in social media," he advised.
Dr. Gurumurthy said the group is still gathering data and hopes to increase the number of survey respondents. He said future studies gathering social media use data from outpatient and emergency department visits could reveal other possible correlations.
The authors had nothing to disclose.
On Twitter @NaseemSMiller
ORLANDO – Half of the teens who made comments on social media about their feelings and caused concern among those who saw the comments were brought to the hospital for assessment, according to a small survey of adolescents admitted to the child and adolescent psychiatry unit of Ohio State University Harding Hospital, Columbus.
Tragic suicides or homicides after social media use have gained national attention in recent years, but studies like this highlight the flip side of social media platforms: They can make it easier to find out when teens are in distress and help them access timely treatment and support.
The fact that these teens turned to social media to express emotional stress, "shows that [they] are having trouble conveying emotions to parents, counselors, or friends, so they’re finding a different avenue," said Dr. Sathyan Gurumurthy, who presented the unpublished study at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "So, as professionals, we have to gain a better understanding of how they convey emotions."
And given the generalized use of social media today, it is important for clinicians to ask children and adolescents about social media use during initial assessment, advised Dr. Gurumurthy, a resident physician at OSU’s Wexner Medical Center. "Talk to them about social media: how they use it and what sites they’re using," he said in an interview.
The results of the yearlong study are based on the 6-month data from an eight-question survey. Researchers were able to collect 32% of the surveys that were handed out to teens and their families at the time of admission.
Of the 82 patients who completed the survey, 54 (66%) said they had made a comment on social media about their emotional disturbance. Of those patients, 32 (60%) said their comments caused a concern, and 16 of those patients (50%) were brought to the hospital for assessment because of their comments.
Seventy-three teens were hospitalized for suicidal ideation; and they had confided mostly in friends, parents, or counselors (around 25 each). Six of the patients said that they had confided in an "Internet friend."
Half of these teens also said they preferred to communicate their suicidal thoughts in person, while 15% said they preferred social sites, and 9% preferred texts. Of the social sites, Facebook was the most popular (41%) among teens.
Of note was that only 25% circled "parent" as the person aware of their social media comments, said Dr. Gurumurthy.
"Many parents have minimal monitoring of their kids’ social media, and they have to be more involved in social media," he advised.
Dr. Gurumurthy said the group is still gathering data and hopes to increase the number of survey respondents. He said future studies gathering social media use data from outpatient and emergency department visits could reveal other possible correlations.
The authors had nothing to disclose.
On Twitter @NaseemSMiller
AT THE AACAP ANNUAL MEETING
Major finding: Fifty percent of patients whose social media comments caused concern were hospitalized for assessment.
Data source: Data from 82 patients who responded to an eight-question survey.
Disclosures: The authors had nothing to disclose.
E-cigarettes gaining popularity in high schools
ORLANDO – When it comes to popularity and use, e-cigarettes are finding their place in high schools, and some teens believe that the product is safer than other forms of tobacco, according to a survey in an urban North Carolina county, which attempted to get a snapshot of teenagers’ beliefs and attitudes toward this growing trend.
Proponents of e-cigarettes say that the product is safer than tobacco smoking and can be used for smoking cessation, but opponents say that they’re a gateway to nicotine addiction. There are no long-term data on their safety, and it’s still not clear if they’re effective for smoking cessation.
But the use of e-cigarettes has doubled among high school students between 2011 and 2012, wrote Dr. Vivek Anand of East Carolina University, Greenville, N.C., and his colleagues, who presented their unpublished study at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Researchers surveyed 3,200 high school students in an urban county in North Carolina about the use, knowledge, attitudes, and beliefs about e-cigarettes.
Roughly 85% of the students completed the survey. The mean age was 16.4 years old, the majority (44%) were black, 38% white, and 8.2% Mexican American.
About 15% of the students said they had used e-cigarettes in their lifetime, compared with 25% who had smoked cigarettes, and 13% who used smokeless tobacco. Meanwhile, 7.4% said they had used e-cigarettes during the past 30 days, compared with 15% who had smoked cigarettes, and 10% who had used smokeless tobacco.
Also, friends were the most common source of e-cigarettes (36%), compared with 24% from a tobacco store, 17% from a gas station, and 2% from a pharmacy. Meanwhile, having a family member who used tobacco products was associated with increased risk of using e-cigarettes, while being female, planning to graduate, and not knowing any e-cigarette users had a protective effect.
Significantly more e-cigarette users also found the product to be a safer route of nicotine administration, compared with teens who did not use e-cigarettes (35% v. 3%).
Researchers also found that a majority of respondents weren’t aware of quitting resources available through their high school. “This is alarming, given that e-cigarettes are perceived as healthier than other tobacco products,” Dr. Anand and his colleagues wrote. “E-cigarette users may be trying to stop smoking and could be an important population to target for evidence-based tobacco treatment interventions.”
E-cigarettes, which are powered by batteries, have a sensor that detects airflow and activates a heating element, which then vaporizes a nicotine solution.
Both the World Health Organization and the Food and Drug Administration have said that evidence about the safety of e-cigarettes is lacking, and they’ve encouraged the makers to stop making therapeutic claims. Dozens of states have banned e-cigarette sale to minors, and more are working on posing similar laws.
Dr. Anand and his colleagues said that their survey was the first large-scale study of high school students’ knowledge, attitudes, perceptions, and beliefs about e-cigarettes.
“Identification of subgroups of adolescents at highest risk for e-cigarette use, such as those whose family and friends use tobacco could guide early identification of youth at risk,” they wrote.
Dr. Anand and his colleagues had nothing to disclosure. Their study was funded by the National Institute on Drug Abuse.
ORLANDO – When it comes to popularity and use, e-cigarettes are finding their place in high schools, and some teens believe that the product is safer than other forms of tobacco, according to a survey in an urban North Carolina county, which attempted to get a snapshot of teenagers’ beliefs and attitudes toward this growing trend.
Proponents of e-cigarettes say that the product is safer than tobacco smoking and can be used for smoking cessation, but opponents say that they’re a gateway to nicotine addiction. There are no long-term data on their safety, and it’s still not clear if they’re effective for smoking cessation.
But the use of e-cigarettes has doubled among high school students between 2011 and 2012, wrote Dr. Vivek Anand of East Carolina University, Greenville, N.C., and his colleagues, who presented their unpublished study at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Researchers surveyed 3,200 high school students in an urban county in North Carolina about the use, knowledge, attitudes, and beliefs about e-cigarettes.
Roughly 85% of the students completed the survey. The mean age was 16.4 years old, the majority (44%) were black, 38% white, and 8.2% Mexican American.
About 15% of the students said they had used e-cigarettes in their lifetime, compared with 25% who had smoked cigarettes, and 13% who used smokeless tobacco. Meanwhile, 7.4% said they had used e-cigarettes during the past 30 days, compared with 15% who had smoked cigarettes, and 10% who had used smokeless tobacco.
Also, friends were the most common source of e-cigarettes (36%), compared with 24% from a tobacco store, 17% from a gas station, and 2% from a pharmacy. Meanwhile, having a family member who used tobacco products was associated with increased risk of using e-cigarettes, while being female, planning to graduate, and not knowing any e-cigarette users had a protective effect.
Significantly more e-cigarette users also found the product to be a safer route of nicotine administration, compared with teens who did not use e-cigarettes (35% v. 3%).
Researchers also found that a majority of respondents weren’t aware of quitting resources available through their high school. “This is alarming, given that e-cigarettes are perceived as healthier than other tobacco products,” Dr. Anand and his colleagues wrote. “E-cigarette users may be trying to stop smoking and could be an important population to target for evidence-based tobacco treatment interventions.”
E-cigarettes, which are powered by batteries, have a sensor that detects airflow and activates a heating element, which then vaporizes a nicotine solution.
Both the World Health Organization and the Food and Drug Administration have said that evidence about the safety of e-cigarettes is lacking, and they’ve encouraged the makers to stop making therapeutic claims. Dozens of states have banned e-cigarette sale to minors, and more are working on posing similar laws.
Dr. Anand and his colleagues said that their survey was the first large-scale study of high school students’ knowledge, attitudes, perceptions, and beliefs about e-cigarettes.
“Identification of subgroups of adolescents at highest risk for e-cigarette use, such as those whose family and friends use tobacco could guide early identification of youth at risk,” they wrote.
Dr. Anand and his colleagues had nothing to disclosure. Their study was funded by the National Institute on Drug Abuse.
ORLANDO – When it comes to popularity and use, e-cigarettes are finding their place in high schools, and some teens believe that the product is safer than other forms of tobacco, according to a survey in an urban North Carolina county, which attempted to get a snapshot of teenagers’ beliefs and attitudes toward this growing trend.
Proponents of e-cigarettes say that the product is safer than tobacco smoking and can be used for smoking cessation, but opponents say that they’re a gateway to nicotine addiction. There are no long-term data on their safety, and it’s still not clear if they’re effective for smoking cessation.
But the use of e-cigarettes has doubled among high school students between 2011 and 2012, wrote Dr. Vivek Anand of East Carolina University, Greenville, N.C., and his colleagues, who presented their unpublished study at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Researchers surveyed 3,200 high school students in an urban county in North Carolina about the use, knowledge, attitudes, and beliefs about e-cigarettes.
Roughly 85% of the students completed the survey. The mean age was 16.4 years old, the majority (44%) were black, 38% white, and 8.2% Mexican American.
About 15% of the students said they had used e-cigarettes in their lifetime, compared with 25% who had smoked cigarettes, and 13% who used smokeless tobacco. Meanwhile, 7.4% said they had used e-cigarettes during the past 30 days, compared with 15% who had smoked cigarettes, and 10% who had used smokeless tobacco.
Also, friends were the most common source of e-cigarettes (36%), compared with 24% from a tobacco store, 17% from a gas station, and 2% from a pharmacy. Meanwhile, having a family member who used tobacco products was associated with increased risk of using e-cigarettes, while being female, planning to graduate, and not knowing any e-cigarette users had a protective effect.
Significantly more e-cigarette users also found the product to be a safer route of nicotine administration, compared with teens who did not use e-cigarettes (35% v. 3%).
Researchers also found that a majority of respondents weren’t aware of quitting resources available through their high school. “This is alarming, given that e-cigarettes are perceived as healthier than other tobacco products,” Dr. Anand and his colleagues wrote. “E-cigarette users may be trying to stop smoking and could be an important population to target for evidence-based tobacco treatment interventions.”
E-cigarettes, which are powered by batteries, have a sensor that detects airflow and activates a heating element, which then vaporizes a nicotine solution.
Both the World Health Organization and the Food and Drug Administration have said that evidence about the safety of e-cigarettes is lacking, and they’ve encouraged the makers to stop making therapeutic claims. Dozens of states have banned e-cigarette sale to minors, and more are working on posing similar laws.
Dr. Anand and his colleagues said that their survey was the first large-scale study of high school students’ knowledge, attitudes, perceptions, and beliefs about e-cigarettes.
“Identification of subgroups of adolescents at highest risk for e-cigarette use, such as those whose family and friends use tobacco could guide early identification of youth at risk,” they wrote.
Dr. Anand and his colleagues had nothing to disclosure. Their study was funded by the National Institute on Drug Abuse.
AT THE AACAP ANNUAL MEETING
Major finding: Thirty-five percent of e-cigarette users said the product was a safer route of nicotine administration, compared with 3% of teens who did not use e-cigarettes (P less than .05).
Data source: Survey of 3,200 high-school students in an urban county in North Carolina.
Disclosures: Dr. Anand and colleagues had nothing to disclosure. Their study was funded by the National Institute on Drug Abuse.
Don’t ignore headaches in teens with bipolar disorder
ORLANDO – Canadian teenagers with bipolar disorder who reported having headaches also had more severe disease symptoms than did those who did not have headaches, according to an unpublished study.
"We echo previous calls for screening and identification of impairing headaches, such as migraines, among people with mood disorders for two reasons," Dr. Benjamin I. Goldstein, the study’s senior author, said in an interview.
"First, presence of impairing headaches may represent a subtype of bipolar disorder with unique course, characteristics, and perhaps treatment. Second, underrecognition and undertreatment of impairing headaches is well documented among adults with bipolar disorder, and our findings suggest the potential importance of treating these headaches among youth with bipolar disorder as well," said Dr. Goldstein, of Sunnybrook Health Sciences Centre, Toronto, whose poster was presented at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Most of the studies so far have been done on adults, and not much is known about this possible association among teens, noted Dr. Goldstein and his coinvestigators.
They studied 55 outpatients aged between 13 and 19 years, with bipolar disorder I, II, or not otherwise specified (NOS). Roughly 60% of the patients were female.
Thirty-three of the teens, or 60%, reported headaches, and these individuals had significantly higher rates of intake depressions score, intake mania score, and global functioning score, the researchers found.
Also, these teens had significantly greater identity confusion, anger/depression, and disinhibition/persistence.
Meanwhile, nearly half of patients with BP-II reported headaches, compared with 18% of the patients with BP-I, and 36% of those with BP-NOS.
But psychiatric hospitalizations and psychosis rates showed an opposite trend. Teens without headaches had a significantly higher rate in both categories, compared with those who had headaches.
"This was a somewhat counterintuitive finding, given the other findings of increased illness severity among youth with headaches," Dr. Goldstein wrote. "Bipolar disorder shares numerous features with psychotic disorders as well as affective disorders, such as unipolar depression and anxiety. We could speculate that whatever causal factors are implicated in headaches among youth with bipolar disorder may be more closely linked with the depression and anxiety than they are with psychosis, which is a frequent precipitant of hospitalization."
The researchers wrote that there’s a need for longitudinal studies to identify specific BP symptoms most associated with headaches, in addition to identifying biomarkers that might help with understanding the pathophysiology. There’s also a need to "identify the possible need of specific treatments for youth with BP [who] suffer from comorbid headaches."
One of the study’s limitations was its cross-sectional design and lack of a comparison group, according to the authors.
Dr. Goldstein is a consultant for Bristol-Myers Squibb and has received honoraria from Purdue Pharma.
On Twitter @NaseemSMiller
ORLANDO – Canadian teenagers with bipolar disorder who reported having headaches also had more severe disease symptoms than did those who did not have headaches, according to an unpublished study.
"We echo previous calls for screening and identification of impairing headaches, such as migraines, among people with mood disorders for two reasons," Dr. Benjamin I. Goldstein, the study’s senior author, said in an interview.
"First, presence of impairing headaches may represent a subtype of bipolar disorder with unique course, characteristics, and perhaps treatment. Second, underrecognition and undertreatment of impairing headaches is well documented among adults with bipolar disorder, and our findings suggest the potential importance of treating these headaches among youth with bipolar disorder as well," said Dr. Goldstein, of Sunnybrook Health Sciences Centre, Toronto, whose poster was presented at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Most of the studies so far have been done on adults, and not much is known about this possible association among teens, noted Dr. Goldstein and his coinvestigators.
They studied 55 outpatients aged between 13 and 19 years, with bipolar disorder I, II, or not otherwise specified (NOS). Roughly 60% of the patients were female.
Thirty-three of the teens, or 60%, reported headaches, and these individuals had significantly higher rates of intake depressions score, intake mania score, and global functioning score, the researchers found.
Also, these teens had significantly greater identity confusion, anger/depression, and disinhibition/persistence.
Meanwhile, nearly half of patients with BP-II reported headaches, compared with 18% of the patients with BP-I, and 36% of those with BP-NOS.
But psychiatric hospitalizations and psychosis rates showed an opposite trend. Teens without headaches had a significantly higher rate in both categories, compared with those who had headaches.
"This was a somewhat counterintuitive finding, given the other findings of increased illness severity among youth with headaches," Dr. Goldstein wrote. "Bipolar disorder shares numerous features with psychotic disorders as well as affective disorders, such as unipolar depression and anxiety. We could speculate that whatever causal factors are implicated in headaches among youth with bipolar disorder may be more closely linked with the depression and anxiety than they are with psychosis, which is a frequent precipitant of hospitalization."
The researchers wrote that there’s a need for longitudinal studies to identify specific BP symptoms most associated with headaches, in addition to identifying biomarkers that might help with understanding the pathophysiology. There’s also a need to "identify the possible need of specific treatments for youth with BP [who] suffer from comorbid headaches."
One of the study’s limitations was its cross-sectional design and lack of a comparison group, according to the authors.
Dr. Goldstein is a consultant for Bristol-Myers Squibb and has received honoraria from Purdue Pharma.
On Twitter @NaseemSMiller
ORLANDO – Canadian teenagers with bipolar disorder who reported having headaches also had more severe disease symptoms than did those who did not have headaches, according to an unpublished study.
"We echo previous calls for screening and identification of impairing headaches, such as migraines, among people with mood disorders for two reasons," Dr. Benjamin I. Goldstein, the study’s senior author, said in an interview.
"First, presence of impairing headaches may represent a subtype of bipolar disorder with unique course, characteristics, and perhaps treatment. Second, underrecognition and undertreatment of impairing headaches is well documented among adults with bipolar disorder, and our findings suggest the potential importance of treating these headaches among youth with bipolar disorder as well," said Dr. Goldstein, of Sunnybrook Health Sciences Centre, Toronto, whose poster was presented at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Most of the studies so far have been done on adults, and not much is known about this possible association among teens, noted Dr. Goldstein and his coinvestigators.
They studied 55 outpatients aged between 13 and 19 years, with bipolar disorder I, II, or not otherwise specified (NOS). Roughly 60% of the patients were female.
Thirty-three of the teens, or 60%, reported headaches, and these individuals had significantly higher rates of intake depressions score, intake mania score, and global functioning score, the researchers found.
Also, these teens had significantly greater identity confusion, anger/depression, and disinhibition/persistence.
Meanwhile, nearly half of patients with BP-II reported headaches, compared with 18% of the patients with BP-I, and 36% of those with BP-NOS.
But psychiatric hospitalizations and psychosis rates showed an opposite trend. Teens without headaches had a significantly higher rate in both categories, compared with those who had headaches.
"This was a somewhat counterintuitive finding, given the other findings of increased illness severity among youth with headaches," Dr. Goldstein wrote. "Bipolar disorder shares numerous features with psychotic disorders as well as affective disorders, such as unipolar depression and anxiety. We could speculate that whatever causal factors are implicated in headaches among youth with bipolar disorder may be more closely linked with the depression and anxiety than they are with psychosis, which is a frequent precipitant of hospitalization."
The researchers wrote that there’s a need for longitudinal studies to identify specific BP symptoms most associated with headaches, in addition to identifying biomarkers that might help with understanding the pathophysiology. There’s also a need to "identify the possible need of specific treatments for youth with BP [who] suffer from comorbid headaches."
One of the study’s limitations was its cross-sectional design and lack of a comparison group, according to the authors.
Dr. Goldstein is a consultant for Bristol-Myers Squibb and has received honoraria from Purdue Pharma.
On Twitter @NaseemSMiller
AT THE AACAP ANNUAL MEETING
Major finding: Teenagers with headaches had significantly greater identity confusion (P = .026) as measured by the LPI, and anger/depression (P = .024) and disinhibition/persistence (P = .007).
Data source: Study of 55 outpatients aged between 13 and 19 years with bipolar disorder I, II or not otherwise specified (NOS).
Disclosures: Dr. Goldstein is a consultant for BMS, and has received honoraria from Purdue Pharma.
Two factors predict suicide in teens with bipolar disorder
ORLANDO – History of self-harm and suicidal ideation are two strong indicators that a teen with bipolar disorder might attempt suicide, according to an unpublished Canadian study presented at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Identifying such clinical features is important as they can help with intervention and prevention of suicide among teens with bipolar disorder, the researchers wrote.
Previous studies have shown that adults with bipolar disorder (BD) are at a higher risk of completing suicide – as many as 25%-50% of them make at least one suicide attempt in their lifetime, and up to 20% complete the attempt.
Meanwhile, studies of pediatric patients have shown a lifetime suicide attempt rate of 20%-50%. Yet there is limited research on teens, Dr. Benjamin I. Goldstein of Sunnybrook Health Sciences Centre, Toronto, and his colleagues wrote in their poster.
A 2013 systemic review of suicidal ideation and suicide attempts by children and teenagers with bipolar disorder showed that the issue is underinvestigated. "Exploration of predictors and protective factors is imperative for the establishment of effective preventive and intervention strategies, which are urgently needed," researchers at Zucker Hillside Hospital, Glen Oaks, N.Y., wrote (Bipolar Disord. 2013;15:507-23).
Dr. Goldstein and his colleagues studied 72 teenagers aged 13-19 years who had bipolar I disorder, bipolar II disorder, or bipolar disorder not otherwise specified.
The 20% of patients who reported having attempted suicide were significantly more likely to be female and to have lower socioeconomic status, more self-harm behavior, suicide ideation, a lifetime history of conduct disorder, bulimia nervosa, lifetime lamotrigine use, and a family history of suicide attempts. That’s compared with teens who did not attempt a suicide.
The multivariate analyses showed that history of self-injurious behavior and family history of suicide attempts was strongly associated with suicide attempts. And when comparing the findings from previous studies and the current study, the researchers found that they all shared history of self-injurious behavior and suicidal ideation.
The analyses had limited power to detect small effect sizes, and "the cross-sectional methodology precludes conclusions regarding the directionality of the observed associations," Dr. Goldstein and his colleagues wrote.
They added that future studies should examine whether the characteristics found in the study can be incorporated in assessment and treatment of youth with bipolar disorder to help reduce the risk of suicide in this high-risk population.
Dr. Goldstein is a consultant for Bristol-Myers Squibb and has received honoraria from Purdue Pharma.
On Twitter @NaseemSMiller
ORLANDO – History of self-harm and suicidal ideation are two strong indicators that a teen with bipolar disorder might attempt suicide, according to an unpublished Canadian study presented at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Identifying such clinical features is important as they can help with intervention and prevention of suicide among teens with bipolar disorder, the researchers wrote.
Previous studies have shown that adults with bipolar disorder (BD) are at a higher risk of completing suicide – as many as 25%-50% of them make at least one suicide attempt in their lifetime, and up to 20% complete the attempt.
Meanwhile, studies of pediatric patients have shown a lifetime suicide attempt rate of 20%-50%. Yet there is limited research on teens, Dr. Benjamin I. Goldstein of Sunnybrook Health Sciences Centre, Toronto, and his colleagues wrote in their poster.
A 2013 systemic review of suicidal ideation and suicide attempts by children and teenagers with bipolar disorder showed that the issue is underinvestigated. "Exploration of predictors and protective factors is imperative for the establishment of effective preventive and intervention strategies, which are urgently needed," researchers at Zucker Hillside Hospital, Glen Oaks, N.Y., wrote (Bipolar Disord. 2013;15:507-23).
Dr. Goldstein and his colleagues studied 72 teenagers aged 13-19 years who had bipolar I disorder, bipolar II disorder, or bipolar disorder not otherwise specified.
The 20% of patients who reported having attempted suicide were significantly more likely to be female and to have lower socioeconomic status, more self-harm behavior, suicide ideation, a lifetime history of conduct disorder, bulimia nervosa, lifetime lamotrigine use, and a family history of suicide attempts. That’s compared with teens who did not attempt a suicide.
The multivariate analyses showed that history of self-injurious behavior and family history of suicide attempts was strongly associated with suicide attempts. And when comparing the findings from previous studies and the current study, the researchers found that they all shared history of self-injurious behavior and suicidal ideation.
The analyses had limited power to detect small effect sizes, and "the cross-sectional methodology precludes conclusions regarding the directionality of the observed associations," Dr. Goldstein and his colleagues wrote.
They added that future studies should examine whether the characteristics found in the study can be incorporated in assessment and treatment of youth with bipolar disorder to help reduce the risk of suicide in this high-risk population.
Dr. Goldstein is a consultant for Bristol-Myers Squibb and has received honoraria from Purdue Pharma.
On Twitter @NaseemSMiller
ORLANDO – History of self-harm and suicidal ideation are two strong indicators that a teen with bipolar disorder might attempt suicide, according to an unpublished Canadian study presented at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Identifying such clinical features is important as they can help with intervention and prevention of suicide among teens with bipolar disorder, the researchers wrote.
Previous studies have shown that adults with bipolar disorder (BD) are at a higher risk of completing suicide – as many as 25%-50% of them make at least one suicide attempt in their lifetime, and up to 20% complete the attempt.
Meanwhile, studies of pediatric patients have shown a lifetime suicide attempt rate of 20%-50%. Yet there is limited research on teens, Dr. Benjamin I. Goldstein of Sunnybrook Health Sciences Centre, Toronto, and his colleagues wrote in their poster.
A 2013 systemic review of suicidal ideation and suicide attempts by children and teenagers with bipolar disorder showed that the issue is underinvestigated. "Exploration of predictors and protective factors is imperative for the establishment of effective preventive and intervention strategies, which are urgently needed," researchers at Zucker Hillside Hospital, Glen Oaks, N.Y., wrote (Bipolar Disord. 2013;15:507-23).
Dr. Goldstein and his colleagues studied 72 teenagers aged 13-19 years who had bipolar I disorder, bipolar II disorder, or bipolar disorder not otherwise specified.
The 20% of patients who reported having attempted suicide were significantly more likely to be female and to have lower socioeconomic status, more self-harm behavior, suicide ideation, a lifetime history of conduct disorder, bulimia nervosa, lifetime lamotrigine use, and a family history of suicide attempts. That’s compared with teens who did not attempt a suicide.
The multivariate analyses showed that history of self-injurious behavior and family history of suicide attempts was strongly associated with suicide attempts. And when comparing the findings from previous studies and the current study, the researchers found that they all shared history of self-injurious behavior and suicidal ideation.
The analyses had limited power to detect small effect sizes, and "the cross-sectional methodology precludes conclusions regarding the directionality of the observed associations," Dr. Goldstein and his colleagues wrote.
They added that future studies should examine whether the characteristics found in the study can be incorporated in assessment and treatment of youth with bipolar disorder to help reduce the risk of suicide in this high-risk population.
Dr. Goldstein is a consultant for Bristol-Myers Squibb and has received honoraria from Purdue Pharma.
On Twitter @NaseemSMiller
AT THE AACAP ANNUAL MEETING
Major finding: Teens with bipolar disorder who attempted suicide were significantly more likely to have a history of self-harm (P less than .001) and suicidal ideation (P = .001)
Data source: The results are based on a study of 72 teenagers with bipolar I disorder, bipolar II disorder, or bipolar disorder not otherwise specified, aged between 13 and 19 years.
Disclosures: Dr. Goldstein is a consultant for Bristol-Myers Squibb and has received honoraria from Purdue Pharma.











