User login
Don’t bypass breasts and nipples in routine skin exams
ORLANDO – As dermatologists do their routine skin checks, they also should pay attention to the breast and the nipple, Dr. David T. Harvey advised in a presentation at the annual meeting of the Florida Society of Dermatologic Surgeons.
Although nipple and areolar tumors are relatively rare, “we have an important role in their evaluation and a wonderful opportunity to impact breast cancer awareness and detection,” said Dr. Harvey, a dermatologist and cosmetic surgeon in Newnan, Ga.
Literature on nipple tumors is limited, but in general, benign breast lesions are much more frequent than the malignant ones. The differential diagnosis can be confusing, “so you don’t want to over or underreact,” while still giving patients the best advice, Dr. Harvey said.
Begin with history
The first step in assessing a lesion on the nipple or areola is to take a thorough history and physical.
The questions to ask include: Is there a discharge? Is there atrophy? Is there a cutaneous erosion? Has the lesion been changing in size? Is the patient pregnant? Is the lesion painful? Perform a visual inspection of the breast and areolar skin, looking for unusual lumps and masses. If the patient will allow, cursory palpation of the breast tissue is helpful.
Ask patients if they have a record of their latest mammograms or MRI. “Get on the phone if you’re not sure. Call a trusted breast specialist, general plastic surgeon, or a surgical oncologist,” he said.
If there’s a lesion that’s erosive and has been there for 6 or 7 months, get a full-thickness incisional biopsy. It also is important to document the presence or absence of axillary lymphadenopathy.
The nipple discharge can be cultured, although most times cultures don’t yield specific data.
And finally, educate patients about the benefits and risks of undergoing regular breast cancer screenings.
Benign tumors
Common benign tumors of the nipple and areola include leiomyoma, erosive adenomatosis, angiolipoma, glomus tumor, neurofibromas, cherry angioma, tags, and epidermal nevus.
Hyperkeratosis around the nipple is another benign condition and can be caused by lack of hygiene. “In these cases, education about how to clean and care for this area is helpful,” Dr. Harvey said.
Erosive adenoma of the nipple is another rare condition. It is usually 0.5-1.5 cm in diameter and arises from apocrine sweat ducts of the nipple’s epithelium. Its clinical symptoms include serosanguinous discharge, bleeding, crusting, erythema, swelling, ulceration, and, in some cases, recurrence because of incomplete removal. This tumor usually occurs in middle-aged women and sometimes is associated with fibrocystic breast disease, breast cancer, and supernumerary nipple. It also can be bilateral. The best treatment is Mohs micrographic surgery.
Malignant tumors
Malignant tumors of the breast and nipple usually present as a lump, hard knot, or thickening inside the breast or underarm area. There’s usually swelling, warmth, redness, or skin hyperpigmentation, in addition to change in the size or shape of the breast.
Other clinical features include dimpling and puckering of the skin and an itchy, scaling sore or rash on the nipple, said Dr. Harvey.
Look for the “pulling in” of the nipple or other parts of the breast, nipple discharge, and discomfort in the breast that doesn’t resolve, he said.
Examples of malignant tumors of the nipple include intraductal breast carcinoma, well-differentiated adenocarcinoma, melanoma, leiomyosarcoma, and squamous cell carcinoma.
Paget’s disease (PD), another breast malignancy, is rare and can mimic eczema or dermatitis. In PD, the nipple may be flattened or eroded. This condition often presents with a discharge and affects older women.
Between 50% and 70% of patients with biopsy-proven mammary PD show positive findings on mammography. The majority of patients who have biopsy-proven Paget’s disease of the nipple as the only physical finding have an underlying deeper breast carcinoma, said Dr. Harvey.
Negative preoperative mammography findings do not reliably exclude an underlying carcinoma. “MRI of the involved breast is a more sensitive way to detect occult PD and is an important tool to help with treatment planning for patients with PD,” he said.
The treatment is radical or modified mastectomy, and lymph node clearance for mammary PD with a palpable mass and underlying invasive breast carcinoma. Estrogen receptor antagonists also can be used in selected cases.
In summary, Dr. Harvey said that it is vital to biopsy a nipple or areolar lesion that is not responding to traditional therapies.
And don’t limit your examination to women
Dr. Christopher Moeller of Wichita, Kan., said that he had diagnosed three men with breast cancer, none of whom where aware of it. One patient had a retracted nipple, another had one breast larger than the other, and he found another lump through palpation.
“Always ask patients,” about their breast health and examine the area, he advised.
Dr. Harvey and Dr. Moeller had no relevant financial disclosures.
ORLANDO – As dermatologists do their routine skin checks, they also should pay attention to the breast and the nipple, Dr. David T. Harvey advised in a presentation at the annual meeting of the Florida Society of Dermatologic Surgeons.
Although nipple and areolar tumors are relatively rare, “we have an important role in their evaluation and a wonderful opportunity to impact breast cancer awareness and detection,” said Dr. Harvey, a dermatologist and cosmetic surgeon in Newnan, Ga.
Literature on nipple tumors is limited, but in general, benign breast lesions are much more frequent than the malignant ones. The differential diagnosis can be confusing, “so you don’t want to over or underreact,” while still giving patients the best advice, Dr. Harvey said.
Begin with history
The first step in assessing a lesion on the nipple or areola is to take a thorough history and physical.
The questions to ask include: Is there a discharge? Is there atrophy? Is there a cutaneous erosion? Has the lesion been changing in size? Is the patient pregnant? Is the lesion painful? Perform a visual inspection of the breast and areolar skin, looking for unusual lumps and masses. If the patient will allow, cursory palpation of the breast tissue is helpful.
Ask patients if they have a record of their latest mammograms or MRI. “Get on the phone if you’re not sure. Call a trusted breast specialist, general plastic surgeon, or a surgical oncologist,” he said.
If there’s a lesion that’s erosive and has been there for 6 or 7 months, get a full-thickness incisional biopsy. It also is important to document the presence or absence of axillary lymphadenopathy.
The nipple discharge can be cultured, although most times cultures don’t yield specific data.
And finally, educate patients about the benefits and risks of undergoing regular breast cancer screenings.
Benign tumors
Common benign tumors of the nipple and areola include leiomyoma, erosive adenomatosis, angiolipoma, glomus tumor, neurofibromas, cherry angioma, tags, and epidermal nevus.
Hyperkeratosis around the nipple is another benign condition and can be caused by lack of hygiene. “In these cases, education about how to clean and care for this area is helpful,” Dr. Harvey said.
Erosive adenoma of the nipple is another rare condition. It is usually 0.5-1.5 cm in diameter and arises from apocrine sweat ducts of the nipple’s epithelium. Its clinical symptoms include serosanguinous discharge, bleeding, crusting, erythema, swelling, ulceration, and, in some cases, recurrence because of incomplete removal. This tumor usually occurs in middle-aged women and sometimes is associated with fibrocystic breast disease, breast cancer, and supernumerary nipple. It also can be bilateral. The best treatment is Mohs micrographic surgery.
Malignant tumors
Malignant tumors of the breast and nipple usually present as a lump, hard knot, or thickening inside the breast or underarm area. There’s usually swelling, warmth, redness, or skin hyperpigmentation, in addition to change in the size or shape of the breast.
Other clinical features include dimpling and puckering of the skin and an itchy, scaling sore or rash on the nipple, said Dr. Harvey.
Look for the “pulling in” of the nipple or other parts of the breast, nipple discharge, and discomfort in the breast that doesn’t resolve, he said.
Examples of malignant tumors of the nipple include intraductal breast carcinoma, well-differentiated adenocarcinoma, melanoma, leiomyosarcoma, and squamous cell carcinoma.
Paget’s disease (PD), another breast malignancy, is rare and can mimic eczema or dermatitis. In PD, the nipple may be flattened or eroded. This condition often presents with a discharge and affects older women.
Between 50% and 70% of patients with biopsy-proven mammary PD show positive findings on mammography. The majority of patients who have biopsy-proven Paget’s disease of the nipple as the only physical finding have an underlying deeper breast carcinoma, said Dr. Harvey.
Negative preoperative mammography findings do not reliably exclude an underlying carcinoma. “MRI of the involved breast is a more sensitive way to detect occult PD and is an important tool to help with treatment planning for patients with PD,” he said.
The treatment is radical or modified mastectomy, and lymph node clearance for mammary PD with a palpable mass and underlying invasive breast carcinoma. Estrogen receptor antagonists also can be used in selected cases.
In summary, Dr. Harvey said that it is vital to biopsy a nipple or areolar lesion that is not responding to traditional therapies.
And don’t limit your examination to women
Dr. Christopher Moeller of Wichita, Kan., said that he had diagnosed three men with breast cancer, none of whom where aware of it. One patient had a retracted nipple, another had one breast larger than the other, and he found another lump through palpation.
“Always ask patients,” about their breast health and examine the area, he advised.
Dr. Harvey and Dr. Moeller had no relevant financial disclosures.
ORLANDO – As dermatologists do their routine skin checks, they also should pay attention to the breast and the nipple, Dr. David T. Harvey advised in a presentation at the annual meeting of the Florida Society of Dermatologic Surgeons.
Although nipple and areolar tumors are relatively rare, “we have an important role in their evaluation and a wonderful opportunity to impact breast cancer awareness and detection,” said Dr. Harvey, a dermatologist and cosmetic surgeon in Newnan, Ga.
Literature on nipple tumors is limited, but in general, benign breast lesions are much more frequent than the malignant ones. The differential diagnosis can be confusing, “so you don’t want to over or underreact,” while still giving patients the best advice, Dr. Harvey said.
Begin with history
The first step in assessing a lesion on the nipple or areola is to take a thorough history and physical.
The questions to ask include: Is there a discharge? Is there atrophy? Is there a cutaneous erosion? Has the lesion been changing in size? Is the patient pregnant? Is the lesion painful? Perform a visual inspection of the breast and areolar skin, looking for unusual lumps and masses. If the patient will allow, cursory palpation of the breast tissue is helpful.
Ask patients if they have a record of their latest mammograms or MRI. “Get on the phone if you’re not sure. Call a trusted breast specialist, general plastic surgeon, or a surgical oncologist,” he said.
If there’s a lesion that’s erosive and has been there for 6 or 7 months, get a full-thickness incisional biopsy. It also is important to document the presence or absence of axillary lymphadenopathy.
The nipple discharge can be cultured, although most times cultures don’t yield specific data.
And finally, educate patients about the benefits and risks of undergoing regular breast cancer screenings.
Benign tumors
Common benign tumors of the nipple and areola include leiomyoma, erosive adenomatosis, angiolipoma, glomus tumor, neurofibromas, cherry angioma, tags, and epidermal nevus.
Hyperkeratosis around the nipple is another benign condition and can be caused by lack of hygiene. “In these cases, education about how to clean and care for this area is helpful,” Dr. Harvey said.
Erosive adenoma of the nipple is another rare condition. It is usually 0.5-1.5 cm in diameter and arises from apocrine sweat ducts of the nipple’s epithelium. Its clinical symptoms include serosanguinous discharge, bleeding, crusting, erythema, swelling, ulceration, and, in some cases, recurrence because of incomplete removal. This tumor usually occurs in middle-aged women and sometimes is associated with fibrocystic breast disease, breast cancer, and supernumerary nipple. It also can be bilateral. The best treatment is Mohs micrographic surgery.
Malignant tumors
Malignant tumors of the breast and nipple usually present as a lump, hard knot, or thickening inside the breast or underarm area. There’s usually swelling, warmth, redness, or skin hyperpigmentation, in addition to change in the size or shape of the breast.
Other clinical features include dimpling and puckering of the skin and an itchy, scaling sore or rash on the nipple, said Dr. Harvey.
Look for the “pulling in” of the nipple or other parts of the breast, nipple discharge, and discomfort in the breast that doesn’t resolve, he said.
Examples of malignant tumors of the nipple include intraductal breast carcinoma, well-differentiated adenocarcinoma, melanoma, leiomyosarcoma, and squamous cell carcinoma.
Paget’s disease (PD), another breast malignancy, is rare and can mimic eczema or dermatitis. In PD, the nipple may be flattened or eroded. This condition often presents with a discharge and affects older women.
Between 50% and 70% of patients with biopsy-proven mammary PD show positive findings on mammography. The majority of patients who have biopsy-proven Paget’s disease of the nipple as the only physical finding have an underlying deeper breast carcinoma, said Dr. Harvey.
Negative preoperative mammography findings do not reliably exclude an underlying carcinoma. “MRI of the involved breast is a more sensitive way to detect occult PD and is an important tool to help with treatment planning for patients with PD,” he said.
The treatment is radical or modified mastectomy, and lymph node clearance for mammary PD with a palpable mass and underlying invasive breast carcinoma. Estrogen receptor antagonists also can be used in selected cases.
In summary, Dr. Harvey said that it is vital to biopsy a nipple or areolar lesion that is not responding to traditional therapies.
And don’t limit your examination to women
Dr. Christopher Moeller of Wichita, Kan., said that he had diagnosed three men with breast cancer, none of whom where aware of it. One patient had a retracted nipple, another had one breast larger than the other, and he found another lump through palpation.
“Always ask patients,” about their breast health and examine the area, he advised.
Dr. Harvey and Dr. Moeller had no relevant financial disclosures.
EXPERT ANALYSIS FROM THE FSDS ANNUAL MEETING
Positive CvLPRIT Results Lead ACC to Change Guidelines
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
AT THE ESC CONGRESS 2014
Positive CvLPRIT results lead ACC to change guidelines
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
On Twitter @naseemmiller
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
On Twitter @naseemmiller
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
On Twitter @naseemmiller
AT THE ESC CONGRESS 2014
Key clinical point: Complete revascularization at the time of primary PCI may be considered by future STEMI guidelines committees.
Major finding: There was a 55% reduction in MACE among heart attack patients who received complete revascularization at the time of primary PCI.
Data source: An open-label, randomized trial of 296 heart attack patients.
Disclosures: Dr. Gershlick and Dr. Mehta had no disclosures.
MULTIMEDIA: Guide to being a good intern
The first year of residency can be overwhelming. Just ask Dr. Anneliese Beaubrun, an intern at the University of Central Florida College of Medicine’s internal medicine residency program in Orlando.
You’re suddenly responsible for patients, and you definitely don’t want to be the one asking what you think is the wrong question, she says.
But the professors and program directors have a different view.
In a video interview, Dr. Abdo Asmar, associate director of the internal medicine residency program at UCF, shares his advice to first-year residents. Chief resident Olga Karasik, too, looks back at her first year and shares what she’s learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
And there’s more.
In her blog, Wellness Rounds, Dr. Mary L. Brandt, professor of surgery, pediatrics and medical ethics and interim senior associate dean of Medical Education at Baylor College of Medicine, Houston, takes a holistic approach to medical school and residency. Her posts cover a wide range of topics, from the type of shoes to wear at the hospital, to advice on preparing for residency interviews.
Being a good intern is among the popular posts on her blog, and in a phone interview she shared some of her top tips and advice for first-year residents.
What are your tips and advice for interns? Leave us a comment.
On Twitter @naseemmiller
The first year of residency can be overwhelming. Just ask Dr. Anneliese Beaubrun, an intern at the University of Central Florida College of Medicine’s internal medicine residency program in Orlando.
You’re suddenly responsible for patients, and you definitely don’t want to be the one asking what you think is the wrong question, she says.
But the professors and program directors have a different view.
In a video interview, Dr. Abdo Asmar, associate director of the internal medicine residency program at UCF, shares his advice to first-year residents. Chief resident Olga Karasik, too, looks back at her first year and shares what she’s learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
And there’s more.
In her blog, Wellness Rounds, Dr. Mary L. Brandt, professor of surgery, pediatrics and medical ethics and interim senior associate dean of Medical Education at Baylor College of Medicine, Houston, takes a holistic approach to medical school and residency. Her posts cover a wide range of topics, from the type of shoes to wear at the hospital, to advice on preparing for residency interviews.
Being a good intern is among the popular posts on her blog, and in a phone interview she shared some of her top tips and advice for first-year residents.
What are your tips and advice for interns? Leave us a comment.
On Twitter @naseemmiller
The first year of residency can be overwhelming. Just ask Dr. Anneliese Beaubrun, an intern at the University of Central Florida College of Medicine’s internal medicine residency program in Orlando.
You’re suddenly responsible for patients, and you definitely don’t want to be the one asking what you think is the wrong question, she says.
But the professors and program directors have a different view.
In a video interview, Dr. Abdo Asmar, associate director of the internal medicine residency program at UCF, shares his advice to first-year residents. Chief resident Olga Karasik, too, looks back at her first year and shares what she’s learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
And there’s more.
In her blog, Wellness Rounds, Dr. Mary L. Brandt, professor of surgery, pediatrics and medical ethics and interim senior associate dean of Medical Education at Baylor College of Medicine, Houston, takes a holistic approach to medical school and residency. Her posts cover a wide range of topics, from the type of shoes to wear at the hospital, to advice on preparing for residency interviews.
Being a good intern is among the popular posts on her blog, and in a phone interview she shared some of her top tips and advice for first-year residents.
What are your tips and advice for interns? Leave us a comment.
On Twitter @naseemmiller
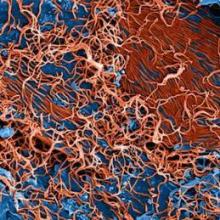
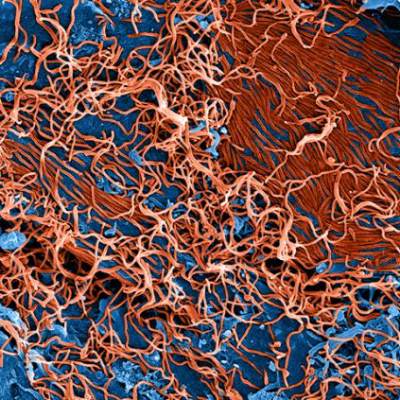
To stop Ebola, think about it, identify, isolate, diagnose
Thomas Eric Duncan, a Liberian man who has become the face of Ebola in the United States, died on Wednesday morning at Texas Health Presbyterian Hospital, more than a week after he became the first person to be diagnosed with the virus here.
His body will be handled and cremated in accordance to the Centers for Disease Control and Prevention guidelines, said the Texas Department of State Health Services in a statement.
Mr. Duncan’s death further highlights “what a deadly enemy Ebola is and how important it is to protect Americans and to stop Ebola at its source in West Africa,” said CDC Director Dr. Thomas Frieden, in an afternoon news briefing on Wednesday.
Like more than 36,000 individuals leaving West Africa in the last 2 months, Mr. Duncan filled out a questionnaire and had his temperature taken before he boarded a plane to visit his family in Dallas.
For more layers of protection, federal officials ramped up their efforts on Wednesday by adding entry screening for those arriving from the affected West African countries at five U.S. airports
New York’s JFK International Airport, Washington-Dulles, Newark, Chicago-O’Hare, and Atlanta International airports receive more than 94% of travelers from Guinea, Liberia, and Sierra Leone. Passengers arriving from the three affected countries to these airports will be screened there. If they have symptoms or are suspected of having exposure to Ebola, they will be referred to a public health authority. Travelers with no symptoms will be asked to provide contact information and to complete a daily temperature log. The screening will begin as early as this Saturday.
CDC has also issued level 3 travel advisories for Guinea, Liberia, Sierra Leone, asking Americans to avoid nonessential trips to these regions.
Meanwhile, health professionals should be thinking about the possibility of Ebola and be able to identify who might have it and isolate and test them.
“Identification, diagnosis, and safe care needs to be on top of the minds right now for health care professionals,” said Dr. Frieden.
The American freelance journalist who contracted the virus in Liberia and is hospitalized in Nebraska has received blood transfusion from another American, Dr. Kent Brantly, who survived the virus.
Another patient who was suspected of having Ebola and was hospitalized at the National Institutes of Health Clinical Center was released on Tuesday, October 7, without a positive diagnosis. He continues to be monitored.
Nearly 50 individuals in Texas who have had definite or possible contact with Mr. Duncan will continue to be monitored for 21 days. None have shown any symptoms.
Since March, there have been 8,033 cases of Ebola in Guinea, Liberia, Nigeria, Senegal, Sierra Leone, and the United States, including 3,879 deaths, according to the latest numbers from the World Health Organization.
Dr. Frieden once again emphasized that isolating the affected West African countries is not the answer to stopping the Ebola threat.
“As long as Ebola is spreading in Africa, it will remain a risk in the United States,” he said.
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
Thomas Eric Duncan, a Liberian man who has become the face of Ebola in the United States, died on Wednesday morning at Texas Health Presbyterian Hospital, more than a week after he became the first person to be diagnosed with the virus here.
His body will be handled and cremated in accordance to the Centers for Disease Control and Prevention guidelines, said the Texas Department of State Health Services in a statement.
Mr. Duncan’s death further highlights “what a deadly enemy Ebola is and how important it is to protect Americans and to stop Ebola at its source in West Africa,” said CDC Director Dr. Thomas Frieden, in an afternoon news briefing on Wednesday.
Like more than 36,000 individuals leaving West Africa in the last 2 months, Mr. Duncan filled out a questionnaire and had his temperature taken before he boarded a plane to visit his family in Dallas.
For more layers of protection, federal officials ramped up their efforts on Wednesday by adding entry screening for those arriving from the affected West African countries at five U.S. airports
New York’s JFK International Airport, Washington-Dulles, Newark, Chicago-O’Hare, and Atlanta International airports receive more than 94% of travelers from Guinea, Liberia, and Sierra Leone. Passengers arriving from the three affected countries to these airports will be screened there. If they have symptoms or are suspected of having exposure to Ebola, they will be referred to a public health authority. Travelers with no symptoms will be asked to provide contact information and to complete a daily temperature log. The screening will begin as early as this Saturday.
CDC has also issued level 3 travel advisories for Guinea, Liberia, Sierra Leone, asking Americans to avoid nonessential trips to these regions.
Meanwhile, health professionals should be thinking about the possibility of Ebola and be able to identify who might have it and isolate and test them.
“Identification, diagnosis, and safe care needs to be on top of the minds right now for health care professionals,” said Dr. Frieden.
The American freelance journalist who contracted the virus in Liberia and is hospitalized in Nebraska has received blood transfusion from another American, Dr. Kent Brantly, who survived the virus.
Another patient who was suspected of having Ebola and was hospitalized at the National Institutes of Health Clinical Center was released on Tuesday, October 7, without a positive diagnosis. He continues to be monitored.
Nearly 50 individuals in Texas who have had definite or possible contact with Mr. Duncan will continue to be monitored for 21 days. None have shown any symptoms.
Since March, there have been 8,033 cases of Ebola in Guinea, Liberia, Nigeria, Senegal, Sierra Leone, and the United States, including 3,879 deaths, according to the latest numbers from the World Health Organization.
Dr. Frieden once again emphasized that isolating the affected West African countries is not the answer to stopping the Ebola threat.
“As long as Ebola is spreading in Africa, it will remain a risk in the United States,” he said.
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
Thomas Eric Duncan, a Liberian man who has become the face of Ebola in the United States, died on Wednesday morning at Texas Health Presbyterian Hospital, more than a week after he became the first person to be diagnosed with the virus here.
His body will be handled and cremated in accordance to the Centers for Disease Control and Prevention guidelines, said the Texas Department of State Health Services in a statement.
Mr. Duncan’s death further highlights “what a deadly enemy Ebola is and how important it is to protect Americans and to stop Ebola at its source in West Africa,” said CDC Director Dr. Thomas Frieden, in an afternoon news briefing on Wednesday.
Like more than 36,000 individuals leaving West Africa in the last 2 months, Mr. Duncan filled out a questionnaire and had his temperature taken before he boarded a plane to visit his family in Dallas.
For more layers of protection, federal officials ramped up their efforts on Wednesday by adding entry screening for those arriving from the affected West African countries at five U.S. airports
New York’s JFK International Airport, Washington-Dulles, Newark, Chicago-O’Hare, and Atlanta International airports receive more than 94% of travelers from Guinea, Liberia, and Sierra Leone. Passengers arriving from the three affected countries to these airports will be screened there. If they have symptoms or are suspected of having exposure to Ebola, they will be referred to a public health authority. Travelers with no symptoms will be asked to provide contact information and to complete a daily temperature log. The screening will begin as early as this Saturday.
CDC has also issued level 3 travel advisories for Guinea, Liberia, Sierra Leone, asking Americans to avoid nonessential trips to these regions.
Meanwhile, health professionals should be thinking about the possibility of Ebola and be able to identify who might have it and isolate and test them.
“Identification, diagnosis, and safe care needs to be on top of the minds right now for health care professionals,” said Dr. Frieden.
The American freelance journalist who contracted the virus in Liberia and is hospitalized in Nebraska has received blood transfusion from another American, Dr. Kent Brantly, who survived the virus.
Another patient who was suspected of having Ebola and was hospitalized at the National Institutes of Health Clinical Center was released on Tuesday, October 7, without a positive diagnosis. He continues to be monitored.
Nearly 50 individuals in Texas who have had definite or possible contact with Mr. Duncan will continue to be monitored for 21 days. None have shown any symptoms.
Since March, there have been 8,033 cases of Ebola in Guinea, Liberia, Nigeria, Senegal, Sierra Leone, and the United States, including 3,879 deaths, according to the latest numbers from the World Health Organization.
Dr. Frieden once again emphasized that isolating the affected West African countries is not the answer to stopping the Ebola threat.
“As long as Ebola is spreading in Africa, it will remain a risk in the United States,” he said.
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
FROM A CDC TELEBRIEFING
VIDEO: A new system for staging squamous cell carcinoma
ORLANDO – Squamous cell carcinoma has a direct cost of nearly $300 million a year. Although squamous cell carcinoma (SCC) is not as deadly as other forms of skin cancer, it is a serious public health issue, according to Dr. Chrysalyne D. Schmults.
Dr. Schmults of Harvard Medical School and the Brigham and Women’s Hospital, Boston, published a study earlier this year introducing a new staging system for SCC, called the Brigham and Women’s Hospital (BWH) tumor staging system.
The BWH system, Dr. Schmults and her colleagues wrote, “offers improved distinctiveness, homogeneity, and monotonicity” over both the American Joint Committee on Cancer and International Union Against Cancer staging systems, although larger studies are needed.
In a video interview at the annual meeting of the Florida Society of Dermatologic Surgeons, Dr. Schmults explained the BWH staging system and shared her clinical advice and recommendations for managing SCC.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
ORLANDO – Squamous cell carcinoma has a direct cost of nearly $300 million a year. Although squamous cell carcinoma (SCC) is not as deadly as other forms of skin cancer, it is a serious public health issue, according to Dr. Chrysalyne D. Schmults.
Dr. Schmults of Harvard Medical School and the Brigham and Women’s Hospital, Boston, published a study earlier this year introducing a new staging system for SCC, called the Brigham and Women’s Hospital (BWH) tumor staging system.
The BWH system, Dr. Schmults and her colleagues wrote, “offers improved distinctiveness, homogeneity, and monotonicity” over both the American Joint Committee on Cancer and International Union Against Cancer staging systems, although larger studies are needed.
In a video interview at the annual meeting of the Florida Society of Dermatologic Surgeons, Dr. Schmults explained the BWH staging system and shared her clinical advice and recommendations for managing SCC.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
ORLANDO – Squamous cell carcinoma has a direct cost of nearly $300 million a year. Although squamous cell carcinoma (SCC) is not as deadly as other forms of skin cancer, it is a serious public health issue, according to Dr. Chrysalyne D. Schmults.
Dr. Schmults of Harvard Medical School and the Brigham and Women’s Hospital, Boston, published a study earlier this year introducing a new staging system for SCC, called the Brigham and Women’s Hospital (BWH) tumor staging system.
The BWH system, Dr. Schmults and her colleagues wrote, “offers improved distinctiveness, homogeneity, and monotonicity” over both the American Joint Committee on Cancer and International Union Against Cancer staging systems, although larger studies are needed.
In a video interview at the annual meeting of the Florida Society of Dermatologic Surgeons, Dr. Schmults explained the BWH staging system and shared her clinical advice and recommendations for managing SCC.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT FSDS 2014
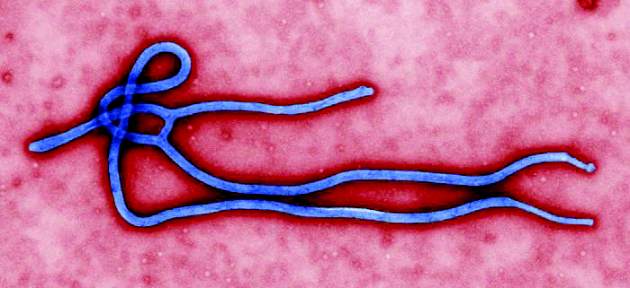
CDC director: Expect long Ebola fight
The enemy is a virus, and the fight will be long and hard, but the tried and true public health measures will stop the spread of Ebola, said Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention.
“The main point is to suspect Ebola and isolate it,” said Dr. Frieden during an Oct. 7 news briefing. You don’t need a fancy unit for infection control, he said. All you need is a private room with its own bathroom, and meticulous attention to details and protocols.
Federal officials are also planning to announce increased safety measures for travelers in the upcoming days.
In the past 2 months, CDC teams have screened more than 36,000 airplane passengers coming from West Africa, officials said. More than 70 have been stopped from boarding the planes, although there are no signs that any of them developed Ebola.
Meanwhile, Thomas Eric Duncan, the first person to be diagnosed with Ebola in the United States, remains in critical but stable condition. “He is on a ventilator and receiving kidney dialysis. His liver function, which declined over the weekend, has improved, but doctors caution that this could vary in coming days,” according to a statement from Texas Health Presbyterian Hospital, Dallas, where he is in isolation. He is still receiving the investigational drug brincidofovir.
Another American, a freelance journalist who tested positive for Ebola in Liberia and is now in isolation in Omaha, Nebraska, also is receiving the investigational drug.
Dr. Frieden said that no more ZMapp is available.
Federal and Texas health officials continue to monitor 48 individuals, 10 of whom have had definite contact with Mr. Duncan. None have shown any signs or symptoms of Ebola so far.
In Spain, a nurse who was caring for Ebola patients there became the first patient to contract Ebola outside of the affected West African countries. U.S. health officials said Oct. 7 that the case highlights the importance of meticulous attention to detail, teamwork, and careful attention to protocols.
Dr. Frieden said that there are some signs of progress in West Africa. The number of cases in some parts of Liberia has dropped, partly because there are enough isolation beds and because of improvements in burial practice safety, but there’s no way to know when the epidemic will be under control and come to an end.
So far, there’s no sign that the Ebola Zaire virus strain has mutated or become airborne, officials said.
Since Mr. Duncan was diagnosed with Ebola in Texas last week, federal health officials and President Barack Obama have stressed that isolating the affected West African countries is not the answer.
“One of our cardinal rules in medicine is do no harm,” said Dr. Frieden. Impeding the ability to control Ebola in West Africa will only increase the challenge of controlling the spread of the virus, he said.
On Twitter @naseemmiller
The enemy is a virus, and the fight will be long and hard, but the tried and true public health measures will stop the spread of Ebola, said Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention.
“The main point is to suspect Ebola and isolate it,” said Dr. Frieden during an Oct. 7 news briefing. You don’t need a fancy unit for infection control, he said. All you need is a private room with its own bathroom, and meticulous attention to details and protocols.
Federal officials are also planning to announce increased safety measures for travelers in the upcoming days.
In the past 2 months, CDC teams have screened more than 36,000 airplane passengers coming from West Africa, officials said. More than 70 have been stopped from boarding the planes, although there are no signs that any of them developed Ebola.
Meanwhile, Thomas Eric Duncan, the first person to be diagnosed with Ebola in the United States, remains in critical but stable condition. “He is on a ventilator and receiving kidney dialysis. His liver function, which declined over the weekend, has improved, but doctors caution that this could vary in coming days,” according to a statement from Texas Health Presbyterian Hospital, Dallas, where he is in isolation. He is still receiving the investigational drug brincidofovir.
Another American, a freelance journalist who tested positive for Ebola in Liberia and is now in isolation in Omaha, Nebraska, also is receiving the investigational drug.
Dr. Frieden said that no more ZMapp is available.
Federal and Texas health officials continue to monitor 48 individuals, 10 of whom have had definite contact with Mr. Duncan. None have shown any signs or symptoms of Ebola so far.
In Spain, a nurse who was caring for Ebola patients there became the first patient to contract Ebola outside of the affected West African countries. U.S. health officials said Oct. 7 that the case highlights the importance of meticulous attention to detail, teamwork, and careful attention to protocols.
Dr. Frieden said that there are some signs of progress in West Africa. The number of cases in some parts of Liberia has dropped, partly because there are enough isolation beds and because of improvements in burial practice safety, but there’s no way to know when the epidemic will be under control and come to an end.
So far, there’s no sign that the Ebola Zaire virus strain has mutated or become airborne, officials said.
Since Mr. Duncan was diagnosed with Ebola in Texas last week, federal health officials and President Barack Obama have stressed that isolating the affected West African countries is not the answer.
“One of our cardinal rules in medicine is do no harm,” said Dr. Frieden. Impeding the ability to control Ebola in West Africa will only increase the challenge of controlling the spread of the virus, he said.
On Twitter @naseemmiller
The enemy is a virus, and the fight will be long and hard, but the tried and true public health measures will stop the spread of Ebola, said Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention.
“The main point is to suspect Ebola and isolate it,” said Dr. Frieden during an Oct. 7 news briefing. You don’t need a fancy unit for infection control, he said. All you need is a private room with its own bathroom, and meticulous attention to details and protocols.
Federal officials are also planning to announce increased safety measures for travelers in the upcoming days.
In the past 2 months, CDC teams have screened more than 36,000 airplane passengers coming from West Africa, officials said. More than 70 have been stopped from boarding the planes, although there are no signs that any of them developed Ebola.
Meanwhile, Thomas Eric Duncan, the first person to be diagnosed with Ebola in the United States, remains in critical but stable condition. “He is on a ventilator and receiving kidney dialysis. His liver function, which declined over the weekend, has improved, but doctors caution that this could vary in coming days,” according to a statement from Texas Health Presbyterian Hospital, Dallas, where he is in isolation. He is still receiving the investigational drug brincidofovir.
Another American, a freelance journalist who tested positive for Ebola in Liberia and is now in isolation in Omaha, Nebraska, also is receiving the investigational drug.
Dr. Frieden said that no more ZMapp is available.
Federal and Texas health officials continue to monitor 48 individuals, 10 of whom have had definite contact with Mr. Duncan. None have shown any signs or symptoms of Ebola so far.
In Spain, a nurse who was caring for Ebola patients there became the first patient to contract Ebola outside of the affected West African countries. U.S. health officials said Oct. 7 that the case highlights the importance of meticulous attention to detail, teamwork, and careful attention to protocols.
Dr. Frieden said that there are some signs of progress in West Africa. The number of cases in some parts of Liberia has dropped, partly because there are enough isolation beds and because of improvements in burial practice safety, but there’s no way to know when the epidemic will be under control and come to an end.
So far, there’s no sign that the Ebola Zaire virus strain has mutated or become airborne, officials said.
Since Mr. Duncan was diagnosed with Ebola in Texas last week, federal health officials and President Barack Obama have stressed that isolating the affected West African countries is not the answer.
“One of our cardinal rules in medicine is do no harm,” said Dr. Frieden. Impeding the ability to control Ebola in West Africa will only increase the challenge of controlling the spread of the virus, he said.
On Twitter @naseemmiller
FROM A CDC TELEBRIEFING
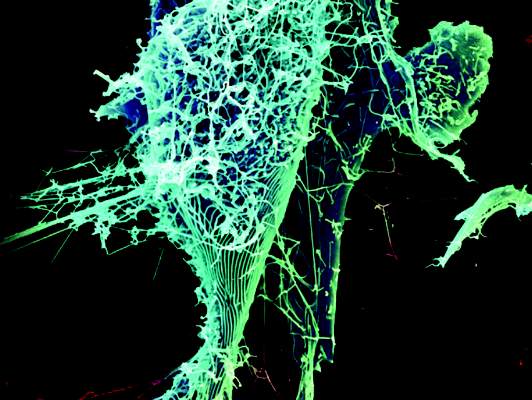
Meticulous attention to detail key in Ebola crisis
It is important for health care providers to stay informed about Ebola, to make sure they have the right information, and to strictly follow all relevant protocols, said President Barack Obama in brief comments to the press on Oct. 6.
The importance of such diligence was further highlighted the same day when a Spanish nurse who was caring for an Ebola patient tested positive for Ebola in Madrid, marking the first case of Ebola virus transmission outside of West Africa.
Meanwhile, Thomas Eric Duncan, the 42-year-old Liberian man who was diagnosed with the Ebola virus in Texas Sept. 30, began receiving the investigational drug brincidofovir on Oct. 4, according to a statement from the Texas Health Presbyterian Hospital, where he’s in an isolation unit. He is still in critical but stable condition. Brincidofovir is an oral antiviral drug that works by keeping viruses from creating additional copies of themselves, according to its maker, Chimerix.
Federal and Texas officials continue to closely monitor 10 people who have had contact with Mr. Duncan. Another 38 individuals also are being monitored for fever. No one has showed any signs or symptoms so far.
Since the outbreak of Ebola in West Africa, there have been more than 7,400 cases and 3,400 deaths in Guinea, Sierra Leone, and Liberia, according to the CDC.
Meanwhile, there are examples of a successful fight against the spread of the virus. The World Health Organization recently highlighted the example of a Guinean district that stopped the spread of Ebola. Guinea has had more than 1,200 cases of Ebola so far and more than 700 deaths.
“Ebola represents a pressing global health crisis, but more are certain to follow,” wrote Dr. Andrew S. Boozary and his colleagues in a commentary in JAMA.
“The outcomes of the next several months will reveal the capacity to forge effective partnerships across borders and disciplines, and the extent of the commitment to value all human lives equally,” they wrote.
In another perspective, policy experts at the Kaiser Family Foundation expressed their concern with the growth of the Ebola epidemic in West Africa.
###break###
“Unfortunately, the story these estimates and projections tell is an exceedingly grim one, and should create an even greater incentive for the world as a whole to respond to this still-growing crisis,” they wrote. “The numbers are stark enough, but they only hint at the full weight of the massive and growing toll that Ebola has inflicted on the people in affected countries and communities.”
In his Oct. 6 comments, President Obama said the chances of an epidemic in the United States are “extraordinarily low,” because “we know what has to be done, and we’ve got the medical infrastructure to do it.”
He said that protocols are in the works to do additional passenger screening at the source (affected West African countries) and in the United States, adding that he looked forward to the collaboration from other countries in stopping the epidemic in West Africa.
“Let’s keep in mind that as we speak there are children on the streets dying. Thousands of them,” he said. “Obviously, my first job is to make sure that we’re taking care of the American people, but we have a larger role than that. We also have an obligation that those children and their families are safe as well, because ultimately the best thing we can do for our public health is also to extend the kind of empathy, compassion, and effort so that folks in those countries as well can get rid of this disease.”
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
It is important for health care providers to stay informed about Ebola, to make sure they have the right information, and to strictly follow all relevant protocols, said President Barack Obama in brief comments to the press on Oct. 6.
The importance of such diligence was further highlighted the same day when a Spanish nurse who was caring for an Ebola patient tested positive for Ebola in Madrid, marking the first case of Ebola virus transmission outside of West Africa.
Meanwhile, Thomas Eric Duncan, the 42-year-old Liberian man who was diagnosed with the Ebola virus in Texas Sept. 30, began receiving the investigational drug brincidofovir on Oct. 4, according to a statement from the Texas Health Presbyterian Hospital, where he’s in an isolation unit. He is still in critical but stable condition. Brincidofovir is an oral antiviral drug that works by keeping viruses from creating additional copies of themselves, according to its maker, Chimerix.
Federal and Texas officials continue to closely monitor 10 people who have had contact with Mr. Duncan. Another 38 individuals also are being monitored for fever. No one has showed any signs or symptoms so far.
Since the outbreak of Ebola in West Africa, there have been more than 7,400 cases and 3,400 deaths in Guinea, Sierra Leone, and Liberia, according to the CDC.
Meanwhile, there are examples of a successful fight against the spread of the virus. The World Health Organization recently highlighted the example of a Guinean district that stopped the spread of Ebola. Guinea has had more than 1,200 cases of Ebola so far and more than 700 deaths.
“Ebola represents a pressing global health crisis, but more are certain to follow,” wrote Dr. Andrew S. Boozary and his colleagues in a commentary in JAMA.
“The outcomes of the next several months will reveal the capacity to forge effective partnerships across borders and disciplines, and the extent of the commitment to value all human lives equally,” they wrote.
In another perspective, policy experts at the Kaiser Family Foundation expressed their concern with the growth of the Ebola epidemic in West Africa.
###break###
“Unfortunately, the story these estimates and projections tell is an exceedingly grim one, and should create an even greater incentive for the world as a whole to respond to this still-growing crisis,” they wrote. “The numbers are stark enough, but they only hint at the full weight of the massive and growing toll that Ebola has inflicted on the people in affected countries and communities.”
In his Oct. 6 comments, President Obama said the chances of an epidemic in the United States are “extraordinarily low,” because “we know what has to be done, and we’ve got the medical infrastructure to do it.”
He said that protocols are in the works to do additional passenger screening at the source (affected West African countries) and in the United States, adding that he looked forward to the collaboration from other countries in stopping the epidemic in West Africa.
“Let’s keep in mind that as we speak there are children on the streets dying. Thousands of them,” he said. “Obviously, my first job is to make sure that we’re taking care of the American people, but we have a larger role than that. We also have an obligation that those children and their families are safe as well, because ultimately the best thing we can do for our public health is also to extend the kind of empathy, compassion, and effort so that folks in those countries as well can get rid of this disease.”
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
It is important for health care providers to stay informed about Ebola, to make sure they have the right information, and to strictly follow all relevant protocols, said President Barack Obama in brief comments to the press on Oct. 6.
The importance of such diligence was further highlighted the same day when a Spanish nurse who was caring for an Ebola patient tested positive for Ebola in Madrid, marking the first case of Ebola virus transmission outside of West Africa.
Meanwhile, Thomas Eric Duncan, the 42-year-old Liberian man who was diagnosed with the Ebola virus in Texas Sept. 30, began receiving the investigational drug brincidofovir on Oct. 4, according to a statement from the Texas Health Presbyterian Hospital, where he’s in an isolation unit. He is still in critical but stable condition. Brincidofovir is an oral antiviral drug that works by keeping viruses from creating additional copies of themselves, according to its maker, Chimerix.
Federal and Texas officials continue to closely monitor 10 people who have had contact with Mr. Duncan. Another 38 individuals also are being monitored for fever. No one has showed any signs or symptoms so far.
Since the outbreak of Ebola in West Africa, there have been more than 7,400 cases and 3,400 deaths in Guinea, Sierra Leone, and Liberia, according to the CDC.
Meanwhile, there are examples of a successful fight against the spread of the virus. The World Health Organization recently highlighted the example of a Guinean district that stopped the spread of Ebola. Guinea has had more than 1,200 cases of Ebola so far and more than 700 deaths.
“Ebola represents a pressing global health crisis, but more are certain to follow,” wrote Dr. Andrew S. Boozary and his colleagues in a commentary in JAMA.
“The outcomes of the next several months will reveal the capacity to forge effective partnerships across borders and disciplines, and the extent of the commitment to value all human lives equally,” they wrote.
In another perspective, policy experts at the Kaiser Family Foundation expressed their concern with the growth of the Ebola epidemic in West Africa.
###break###
“Unfortunately, the story these estimates and projections tell is an exceedingly grim one, and should create an even greater incentive for the world as a whole to respond to this still-growing crisis,” they wrote. “The numbers are stark enough, but they only hint at the full weight of the massive and growing toll that Ebola has inflicted on the people in affected countries and communities.”
In his Oct. 6 comments, President Obama said the chances of an epidemic in the United States are “extraordinarily low,” because “we know what has to be done, and we’ve got the medical infrastructure to do it.”
He said that protocols are in the works to do additional passenger screening at the source (affected West African countries) and in the United States, adding that he looked forward to the collaboration from other countries in stopping the epidemic in West Africa.
“Let’s keep in mind that as we speak there are children on the streets dying. Thousands of them,” he said. “Obviously, my first job is to make sure that we’re taking care of the American people, but we have a larger role than that. We also have an obligation that those children and their families are safe as well, because ultimately the best thing we can do for our public health is also to extend the kind of empathy, compassion, and effort so that folks in those countries as well can get rid of this disease.”
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
Daily Ebola update: 50 monitored; 9 high risk
It’s been 5 days since a 42-year old Liberian man became the first patient to be diagnosed with Ebola in the United States, and the main message that health officials stress daily is this: take the travel history and communicate it with your staff.
The travel history for Ebola is very specific and currently is limited to Guinea, Liberia, Sierra Leone, and Nigeria.
“We’ve produced checklists and flowcharts and we encourage hospitals to use them,” said Dr. Thomas Frieden, director of Centers for Disease Control and Prevention, in a news conference Oct. 4.
Public health officials have so far assessed 114 individuals in Texas who may have had contact with the patient, Thomas Eric Duncan. They have ruled out about half of them, and are now monitoring 50 individuals, 9 of whom had definite contact with Mr. Duncan.
Among the 9 are 4 individuals who were in the same apartment as Mr. Duncan. On Friday, they were moved to an undisclosed location provided by a member of their faith community, Texas officials said.
All 50 individuals will be monitored for 21 days since the day they potentially came in contact with Mr. Duncan after he became ill and infectious. No one has reported a fever so far. Mr. Duncan remains in serious condition.
Dr. Frieden said that tracing those who may have had contact with Mr. Duncan, monitoring them, and isolating them if they become symptomatic are the core of public health practice and that’s “why we’re confident that we’ll stop this in its tracks in Texas.”
Questions, however, remain as to why Mr. Duncan was initially sent home from his first visit to Texas Health Presbyterian Hospital’s emergency department.
Hospital officials added to the confusion late on Oct. 3, when they retracted an earlier statement, which had pointed to a flaw in the electronic health records as the culprit.
In a clarification, officials said, “As a standard part of the nursing process, the patient’s travel history was documented and available to the full care team in the electronic health record (EHR), including within the physician’s workflow. There was no flaw in the EHR in the way the physician and nursing portions interacted related to this event.”
Officials didn’t provide an explanation for the change in the hospital’s statement and said that the broader point is communicating the travel history with all staff.
CDC has received more than 100 Ebola-related inquiries so far and all the specimen have been negative except for Mr. Duncan’s case.
“We expect more rumors about possible cases, but until there’s a positive result, they are just rumors and concerns,” Dr. Frieden said. More than a dozen laboratories around the nation are equipped to conduct high quality testing for Ebola. The test takes a few hours, but with the added shipping time, the process can take up to 24 hours.
Meanwhile, trained CDC staff are screening individuals who are boarding planes from the affected countries and so far 77 people have been prevented from boarding the plane although it’s not clear if they had Ebola.
There are also quarantine stations at all major U.S. airport, but no suspected Ebola cases have been referred to them so far, Dr. Frieden said.
“We’re all connected,” he said. “And we’re not going to get to zero risk until we can control the outbreak in Africa. It’s going to be a long, hard road.”
[email protected]
On Twitter @naseemmiller
It’s been 5 days since a 42-year old Liberian man became the first patient to be diagnosed with Ebola in the United States, and the main message that health officials stress daily is this: take the travel history and communicate it with your staff.
The travel history for Ebola is very specific and currently is limited to Guinea, Liberia, Sierra Leone, and Nigeria.
“We’ve produced checklists and flowcharts and we encourage hospitals to use them,” said Dr. Thomas Frieden, director of Centers for Disease Control and Prevention, in a news conference Oct. 4.
Public health officials have so far assessed 114 individuals in Texas who may have had contact with the patient, Thomas Eric Duncan. They have ruled out about half of them, and are now monitoring 50 individuals, 9 of whom had definite contact with Mr. Duncan.
Among the 9 are 4 individuals who were in the same apartment as Mr. Duncan. On Friday, they were moved to an undisclosed location provided by a member of their faith community, Texas officials said.
All 50 individuals will be monitored for 21 days since the day they potentially came in contact with Mr. Duncan after he became ill and infectious. No one has reported a fever so far. Mr. Duncan remains in serious condition.
Dr. Frieden said that tracing those who may have had contact with Mr. Duncan, monitoring them, and isolating them if they become symptomatic are the core of public health practice and that’s “why we’re confident that we’ll stop this in its tracks in Texas.”
Questions, however, remain as to why Mr. Duncan was initially sent home from his first visit to Texas Health Presbyterian Hospital’s emergency department.
Hospital officials added to the confusion late on Oct. 3, when they retracted an earlier statement, which had pointed to a flaw in the electronic health records as the culprit.
In a clarification, officials said, “As a standard part of the nursing process, the patient’s travel history was documented and available to the full care team in the electronic health record (EHR), including within the physician’s workflow. There was no flaw in the EHR in the way the physician and nursing portions interacted related to this event.”
Officials didn’t provide an explanation for the change in the hospital’s statement and said that the broader point is communicating the travel history with all staff.
CDC has received more than 100 Ebola-related inquiries so far and all the specimen have been negative except for Mr. Duncan’s case.
“We expect more rumors about possible cases, but until there’s a positive result, they are just rumors and concerns,” Dr. Frieden said. More than a dozen laboratories around the nation are equipped to conduct high quality testing for Ebola. The test takes a few hours, but with the added shipping time, the process can take up to 24 hours.
Meanwhile, trained CDC staff are screening individuals who are boarding planes from the affected countries and so far 77 people have been prevented from boarding the plane although it’s not clear if they had Ebola.
There are also quarantine stations at all major U.S. airport, but no suspected Ebola cases have been referred to them so far, Dr. Frieden said.
“We’re all connected,” he said. “And we’re not going to get to zero risk until we can control the outbreak in Africa. It’s going to be a long, hard road.”
[email protected]
On Twitter @naseemmiller
It’s been 5 days since a 42-year old Liberian man became the first patient to be diagnosed with Ebola in the United States, and the main message that health officials stress daily is this: take the travel history and communicate it with your staff.
The travel history for Ebola is very specific and currently is limited to Guinea, Liberia, Sierra Leone, and Nigeria.
“We’ve produced checklists and flowcharts and we encourage hospitals to use them,” said Dr. Thomas Frieden, director of Centers for Disease Control and Prevention, in a news conference Oct. 4.
Public health officials have so far assessed 114 individuals in Texas who may have had contact with the patient, Thomas Eric Duncan. They have ruled out about half of them, and are now monitoring 50 individuals, 9 of whom had definite contact with Mr. Duncan.
Among the 9 are 4 individuals who were in the same apartment as Mr. Duncan. On Friday, they were moved to an undisclosed location provided by a member of their faith community, Texas officials said.
All 50 individuals will be monitored for 21 days since the day they potentially came in contact with Mr. Duncan after he became ill and infectious. No one has reported a fever so far. Mr. Duncan remains in serious condition.
Dr. Frieden said that tracing those who may have had contact with Mr. Duncan, monitoring them, and isolating them if they become symptomatic are the core of public health practice and that’s “why we’re confident that we’ll stop this in its tracks in Texas.”
Questions, however, remain as to why Mr. Duncan was initially sent home from his first visit to Texas Health Presbyterian Hospital’s emergency department.
Hospital officials added to the confusion late on Oct. 3, when they retracted an earlier statement, which had pointed to a flaw in the electronic health records as the culprit.
In a clarification, officials said, “As a standard part of the nursing process, the patient’s travel history was documented and available to the full care team in the electronic health record (EHR), including within the physician’s workflow. There was no flaw in the EHR in the way the physician and nursing portions interacted related to this event.”
Officials didn’t provide an explanation for the change in the hospital’s statement and said that the broader point is communicating the travel history with all staff.
CDC has received more than 100 Ebola-related inquiries so far and all the specimen have been negative except for Mr. Duncan’s case.
“We expect more rumors about possible cases, but until there’s a positive result, they are just rumors and concerns,” Dr. Frieden said. More than a dozen laboratories around the nation are equipped to conduct high quality testing for Ebola. The test takes a few hours, but with the added shipping time, the process can take up to 24 hours.
Meanwhile, trained CDC staff are screening individuals who are boarding planes from the affected countries and so far 77 people have been prevented from boarding the plane although it’s not clear if they had Ebola.
There are also quarantine stations at all major U.S. airport, but no suspected Ebola cases have been referred to them so far, Dr. Frieden said.
“We’re all connected,” he said. “And we’re not going to get to zero risk until we can control the outbreak in Africa. It’s going to be a long, hard road.”
[email protected]
On Twitter @naseemmiller
FROM A CDC TELEBRIEFING
Daily Ebola Update: 50 people followed daily; 10 high risk
After casting a wide net to assess 100 people who may have come in contact with the man who has Ebola, federal and Texas state officials have narrowed down the number to 50 people, 10 of whom are considered high risk, including the patient’s four family members who are quarantined in their apartment.
The patient, 42-year-old Thomas Eric Duncan, remains in serious but stable condition. Among the 50 are a number of at-risk hospital workers and staff. All individuals are doing well and have reported no symptoms so far, Texas health officials reported during an afternoon news conference Oct. 3.
Late in the day on Oct. 2, CDC issued an updated advisory for health care professionals on evaluating patients for Ebola, asking them to increase their vigilance in taking travel history; to isolate patients who fit the precautionary criteria for Ebola; and to immediately notify local and state health departments.
“We’ve been redoubling out efforts to sensitize health care providers on how to correctly identify and safely deal with Ebola patients,” said Dr. Beth P. Bell, director of the National Center for Emerging and Zoonotic Infectious Diseases at the Centers for Disease Control and Prevention.
Meanwhile, Texas Health Presbyterian Hospital, which initially sent Mr. Duncan home with antibiotics, released more details about that encounter.
In an Oct. 2 statement, the hospital noted that physician and nursing workflows were separate in the electronic health records, such that “the travel history would not automatically appear in the physician’s standard workflow.”
On his first visit to the emergency department, Mr. Duncan presented with a temperature of 100.1° F, abdominal pain for 2 days, a sharp headache, and decreased urination, although no symptoms were severe, the hospital reported. He reported no nausea, vomiting, or diarrhea. Mr. Duncan also said that he had not been around any sick individuals and that he had been in Africa.
The hospital said that the travel history documentation has now been relocated “to a portion of the EHR that is part of both [nursing and physician] workflows. It also has been modified to specifically reference Ebola-endemic regions in Africa.”
Dr. Kristi L. Koenig, director of Center for Disaster Medical Sciences at University of California, Irvine, said that its important for physicians to be aware of infectious diseases worldwide. She urged her peers to be up to date and pay attention to credible authorities, so that they can rapidly identify and isolate potentially infected patients.
"You have to be prepared regardless of health care setting," Dr. Koenig, a national spokesperson for the American College of Emergency Physicians, said in an interview.
In a paper, Dr. Koenig and colleagues list several actions that emergency physicians should take when treating febrile travelers and remind their peers that several factors, including the globalization of health care, climate change, and rapid international travel "means that microbial threat to the population have increased."
The number of Ebola cases in West Africa continues to grow, according to the latest information from the World Health Organization. A total of 7,470 confirmed cases and 3,431 deaths have been reported in in Guinea, Liberia, and Sierra Leone, according to the World Health Organization.
Dr. Bell of the CDC said that a couple of Ebola vaccines are in early phases of human trials. “We’re working very hard to accelerate this, but we need to be sure that the vaccines are safe and effective. But this is a very high priority for us.”
Helpful Links:
Information for health-care workers
Latest outbreak information in West Africa
World Health Organization Ebola page
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
After casting a wide net to assess 100 people who may have come in contact with the man who has Ebola, federal and Texas state officials have narrowed down the number to 50 people, 10 of whom are considered high risk, including the patient’s four family members who are quarantined in their apartment.
The patient, 42-year-old Thomas Eric Duncan, remains in serious but stable condition. Among the 50 are a number of at-risk hospital workers and staff. All individuals are doing well and have reported no symptoms so far, Texas health officials reported during an afternoon news conference Oct. 3.
Late in the day on Oct. 2, CDC issued an updated advisory for health care professionals on evaluating patients for Ebola, asking them to increase their vigilance in taking travel history; to isolate patients who fit the precautionary criteria for Ebola; and to immediately notify local and state health departments.
“We’ve been redoubling out efforts to sensitize health care providers on how to correctly identify and safely deal with Ebola patients,” said Dr. Beth P. Bell, director of the National Center for Emerging and Zoonotic Infectious Diseases at the Centers for Disease Control and Prevention.
Meanwhile, Texas Health Presbyterian Hospital, which initially sent Mr. Duncan home with antibiotics, released more details about that encounter.
In an Oct. 2 statement, the hospital noted that physician and nursing workflows were separate in the electronic health records, such that “the travel history would not automatically appear in the physician’s standard workflow.”
On his first visit to the emergency department, Mr. Duncan presented with a temperature of 100.1° F, abdominal pain for 2 days, a sharp headache, and decreased urination, although no symptoms were severe, the hospital reported. He reported no nausea, vomiting, or diarrhea. Mr. Duncan also said that he had not been around any sick individuals and that he had been in Africa.
The hospital said that the travel history documentation has now been relocated “to a portion of the EHR that is part of both [nursing and physician] workflows. It also has been modified to specifically reference Ebola-endemic regions in Africa.”
Dr. Kristi L. Koenig, director of Center for Disaster Medical Sciences at University of California, Irvine, said that its important for physicians to be aware of infectious diseases worldwide. She urged her peers to be up to date and pay attention to credible authorities, so that they can rapidly identify and isolate potentially infected patients.
"You have to be prepared regardless of health care setting," Dr. Koenig, a national spokesperson for the American College of Emergency Physicians, said in an interview.
In a paper, Dr. Koenig and colleagues list several actions that emergency physicians should take when treating febrile travelers and remind their peers that several factors, including the globalization of health care, climate change, and rapid international travel "means that microbial threat to the population have increased."
The number of Ebola cases in West Africa continues to grow, according to the latest information from the World Health Organization. A total of 7,470 confirmed cases and 3,431 deaths have been reported in in Guinea, Liberia, and Sierra Leone, according to the World Health Organization.
Dr. Bell of the CDC said that a couple of Ebola vaccines are in early phases of human trials. “We’re working very hard to accelerate this, but we need to be sure that the vaccines are safe and effective. But this is a very high priority for us.”
Helpful Links:
Information for health-care workers
Latest outbreak information in West Africa
World Health Organization Ebola page
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
After casting a wide net to assess 100 people who may have come in contact with the man who has Ebola, federal and Texas state officials have narrowed down the number to 50 people, 10 of whom are considered high risk, including the patient’s four family members who are quarantined in their apartment.
The patient, 42-year-old Thomas Eric Duncan, remains in serious but stable condition. Among the 50 are a number of at-risk hospital workers and staff. All individuals are doing well and have reported no symptoms so far, Texas health officials reported during an afternoon news conference Oct. 3.
Late in the day on Oct. 2, CDC issued an updated advisory for health care professionals on evaluating patients for Ebola, asking them to increase their vigilance in taking travel history; to isolate patients who fit the precautionary criteria for Ebola; and to immediately notify local and state health departments.
“We’ve been redoubling out efforts to sensitize health care providers on how to correctly identify and safely deal with Ebola patients,” said Dr. Beth P. Bell, director of the National Center for Emerging and Zoonotic Infectious Diseases at the Centers for Disease Control and Prevention.
Meanwhile, Texas Health Presbyterian Hospital, which initially sent Mr. Duncan home with antibiotics, released more details about that encounter.
In an Oct. 2 statement, the hospital noted that physician and nursing workflows were separate in the electronic health records, such that “the travel history would not automatically appear in the physician’s standard workflow.”
On his first visit to the emergency department, Mr. Duncan presented with a temperature of 100.1° F, abdominal pain for 2 days, a sharp headache, and decreased urination, although no symptoms were severe, the hospital reported. He reported no nausea, vomiting, or diarrhea. Mr. Duncan also said that he had not been around any sick individuals and that he had been in Africa.
The hospital said that the travel history documentation has now been relocated “to a portion of the EHR that is part of both [nursing and physician] workflows. It also has been modified to specifically reference Ebola-endemic regions in Africa.”
Dr. Kristi L. Koenig, director of Center for Disaster Medical Sciences at University of California, Irvine, said that its important for physicians to be aware of infectious diseases worldwide. She urged her peers to be up to date and pay attention to credible authorities, so that they can rapidly identify and isolate potentially infected patients.
"You have to be prepared regardless of health care setting," Dr. Koenig, a national spokesperson for the American College of Emergency Physicians, said in an interview.
In a paper, Dr. Koenig and colleagues list several actions that emergency physicians should take when treating febrile travelers and remind their peers that several factors, including the globalization of health care, climate change, and rapid international travel "means that microbial threat to the population have increased."
The number of Ebola cases in West Africa continues to grow, according to the latest information from the World Health Organization. A total of 7,470 confirmed cases and 3,431 deaths have been reported in in Guinea, Liberia, and Sierra Leone, according to the World Health Organization.
Dr. Bell of the CDC said that a couple of Ebola vaccines are in early phases of human trials. “We’re working very hard to accelerate this, but we need to be sure that the vaccines are safe and effective. But this is a very high priority for us.”
Helpful Links:
Information for health-care workers
Latest outbreak information in West Africa
World Health Organization Ebola page
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
FROM A CDC TELEBRIEFING