User login
Relapsed MCL: Options for treatment
CHICAGO – according to Kristie A. Blum, MD.
Venetoclax and lenalidomide can also be considered in the relapsed mantle cell lymphoma (MCL) setting, Dr. Blum, a professor in the department of hematology and medical oncology at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“I tend to favor BTK inhibitors as my first line of therapy,” she said, later qualifying that this applies when clinical trial enrollment is unavailable.
Ibrutinib
The BTK inhibitor ibrutinib is well established as a treatment for MCL and for use in the relapsed setting, she said, noting that pooled data from the phase 2 CYC-1104 trial, the phase 2 MCL 2001 (SPARK) trial, and the phase 3 MCL3001 (RAY) trial showed an overall response (OR) rate of 66% in 370 patients and a complete response (CR) rate of 20%.
The median duration of response (DOR) was 18.6 months, median progression-free survival (PFS) was 12.8 months, and median overall survival (OS) was 25 months (Br J Haematol. 2017 Nov;179[3]:430-8).
Adding rituximab to ibrutinib (R-ibrutinib) improved outcomes, at least in one single center phase 2 trial of 50 relapsed patients with a median of three prior therapies, she said. The OR rate in that study was 88%, and the CR rate was 58% (Br J Haematol. 2018 May;182[3]:404-11).
“What was really impressive to me was that the median duration of response was about 46 months. PFS was 43 months, and patients were on [treatment] as long as 56 cycles,” she said.
Acalabrutinib
The newer BTK inhibitor acalabrutinib also shows benefit in the relapsed MCL setting, Dr. Blum said.
In a recent multicenter, open-label, phase 2 study of 124 patients with a median age of 68 years and a median of two prior therapies, acalabrutinib at a dose of 100 mg twice daily was associated with an OR rate of 81% and a CR rate of 40% (Lancet. 2018 Feb 17;391:659-67).
“Seems a little better than what you’d expect with single agent ibrutinib,” she said, noting that median DOR and PFS have not been reached in that study.
The main toxicities have been “headache and some diarrhea,” but follow-up is currently only about 15 months, she added.
Venetoclax
Another option in this setting is the B-cell lymphoma 2 (BCL-2) inhibitor venetoclax, which was shown in a recent phase 1 study of patients with various lymphoma subtypes to have activity in relapsed MCL, Dr. Blum said.
The OR rate in 28 relapsed MCL patients in that study was 75%, and the median PFS was 14 months (J Clin Oncol. 2017 Mar;35:826-33).
Additionally, an “intriguing combination study of venetoclax and ibrutinib” was recently published in the New England Journal of Medicine, she noted.
That study included only 23 patients with relapsed MCL, but they were a “pretty high-risk” group with a median age of 68 years, about half having a TP53 abnormality, and 30% having a prior transplant.
The OR and CR rates at 16 weeks by positron emission tomography were 71% and 62%, respectively (N Engl J Med. 2018 Mar 29;378:1211-23).
“Actually, about 40% achieved [minimal residual disease] negativity, but this was only checked in about half the patients,” she said. “So this is an intriguing combination and hopefully something we’ll see more of in the upcoming years.”
Lenalidomide
In the randomized phase 2 SPRINT study, patients received either single-agent lenolidamine or the investigator’s choice of single-agent rituximab, gemcitabine, fludarabine, chlorambucil, or cytarabine.
The expected OR rate in 170 patients treated with lenalidomide was 40% versus 11% in 84 patients treated with investigator’s choice of treatment, and the respective CR rates were 5% and 0% (Lancet Oncol. 2016 Mar 1;17(3):319-31).
Median DOR was 16 months versus 10.4 months, PFS was 8.7 versus 5.2 months, and median OS was 27.9 versus 21.1 months in the groups, respectively.
Other options
Combination regimens, such as R-CHOP and R-bendamustine, are also options for the treatment of relapsed MCL patients who haven’t received combination therapy in the past, Dr. Blum said. Transplant is another option in some patients.
“I will consider transplants for younger patients if they come to me and they actually hadn’t had one in [their] first CR,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – according to Kristie A. Blum, MD.
Venetoclax and lenalidomide can also be considered in the relapsed mantle cell lymphoma (MCL) setting, Dr. Blum, a professor in the department of hematology and medical oncology at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“I tend to favor BTK inhibitors as my first line of therapy,” she said, later qualifying that this applies when clinical trial enrollment is unavailable.
Ibrutinib
The BTK inhibitor ibrutinib is well established as a treatment for MCL and for use in the relapsed setting, she said, noting that pooled data from the phase 2 CYC-1104 trial, the phase 2 MCL 2001 (SPARK) trial, and the phase 3 MCL3001 (RAY) trial showed an overall response (OR) rate of 66% in 370 patients and a complete response (CR) rate of 20%.
The median duration of response (DOR) was 18.6 months, median progression-free survival (PFS) was 12.8 months, and median overall survival (OS) was 25 months (Br J Haematol. 2017 Nov;179[3]:430-8).
Adding rituximab to ibrutinib (R-ibrutinib) improved outcomes, at least in one single center phase 2 trial of 50 relapsed patients with a median of three prior therapies, she said. The OR rate in that study was 88%, and the CR rate was 58% (Br J Haematol. 2018 May;182[3]:404-11).
“What was really impressive to me was that the median duration of response was about 46 months. PFS was 43 months, and patients were on [treatment] as long as 56 cycles,” she said.
Acalabrutinib
The newer BTK inhibitor acalabrutinib also shows benefit in the relapsed MCL setting, Dr. Blum said.
In a recent multicenter, open-label, phase 2 study of 124 patients with a median age of 68 years and a median of two prior therapies, acalabrutinib at a dose of 100 mg twice daily was associated with an OR rate of 81% and a CR rate of 40% (Lancet. 2018 Feb 17;391:659-67).
“Seems a little better than what you’d expect with single agent ibrutinib,” she said, noting that median DOR and PFS have not been reached in that study.
The main toxicities have been “headache and some diarrhea,” but follow-up is currently only about 15 months, she added.
Venetoclax
Another option in this setting is the B-cell lymphoma 2 (BCL-2) inhibitor venetoclax, which was shown in a recent phase 1 study of patients with various lymphoma subtypes to have activity in relapsed MCL, Dr. Blum said.
The OR rate in 28 relapsed MCL patients in that study was 75%, and the median PFS was 14 months (J Clin Oncol. 2017 Mar;35:826-33).
Additionally, an “intriguing combination study of venetoclax and ibrutinib” was recently published in the New England Journal of Medicine, she noted.
That study included only 23 patients with relapsed MCL, but they were a “pretty high-risk” group with a median age of 68 years, about half having a TP53 abnormality, and 30% having a prior transplant.
The OR and CR rates at 16 weeks by positron emission tomography were 71% and 62%, respectively (N Engl J Med. 2018 Mar 29;378:1211-23).
“Actually, about 40% achieved [minimal residual disease] negativity, but this was only checked in about half the patients,” she said. “So this is an intriguing combination and hopefully something we’ll see more of in the upcoming years.”
Lenalidomide
In the randomized phase 2 SPRINT study, patients received either single-agent lenolidamine or the investigator’s choice of single-agent rituximab, gemcitabine, fludarabine, chlorambucil, or cytarabine.
The expected OR rate in 170 patients treated with lenalidomide was 40% versus 11% in 84 patients treated with investigator’s choice of treatment, and the respective CR rates were 5% and 0% (Lancet Oncol. 2016 Mar 1;17(3):319-31).
Median DOR was 16 months versus 10.4 months, PFS was 8.7 versus 5.2 months, and median OS was 27.9 versus 21.1 months in the groups, respectively.
Other options
Combination regimens, such as R-CHOP and R-bendamustine, are also options for the treatment of relapsed MCL patients who haven’t received combination therapy in the past, Dr. Blum said. Transplant is another option in some patients.
“I will consider transplants for younger patients if they come to me and they actually hadn’t had one in [their] first CR,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – according to Kristie A. Blum, MD.
Venetoclax and lenalidomide can also be considered in the relapsed mantle cell lymphoma (MCL) setting, Dr. Blum, a professor in the department of hematology and medical oncology at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“I tend to favor BTK inhibitors as my first line of therapy,” she said, later qualifying that this applies when clinical trial enrollment is unavailable.
Ibrutinib
The BTK inhibitor ibrutinib is well established as a treatment for MCL and for use in the relapsed setting, she said, noting that pooled data from the phase 2 CYC-1104 trial, the phase 2 MCL 2001 (SPARK) trial, and the phase 3 MCL3001 (RAY) trial showed an overall response (OR) rate of 66% in 370 patients and a complete response (CR) rate of 20%.
The median duration of response (DOR) was 18.6 months, median progression-free survival (PFS) was 12.8 months, and median overall survival (OS) was 25 months (Br J Haematol. 2017 Nov;179[3]:430-8).
Adding rituximab to ibrutinib (R-ibrutinib) improved outcomes, at least in one single center phase 2 trial of 50 relapsed patients with a median of three prior therapies, she said. The OR rate in that study was 88%, and the CR rate was 58% (Br J Haematol. 2018 May;182[3]:404-11).
“What was really impressive to me was that the median duration of response was about 46 months. PFS was 43 months, and patients were on [treatment] as long as 56 cycles,” she said.
Acalabrutinib
The newer BTK inhibitor acalabrutinib also shows benefit in the relapsed MCL setting, Dr. Blum said.
In a recent multicenter, open-label, phase 2 study of 124 patients with a median age of 68 years and a median of two prior therapies, acalabrutinib at a dose of 100 mg twice daily was associated with an OR rate of 81% and a CR rate of 40% (Lancet. 2018 Feb 17;391:659-67).
“Seems a little better than what you’d expect with single agent ibrutinib,” she said, noting that median DOR and PFS have not been reached in that study.
The main toxicities have been “headache and some diarrhea,” but follow-up is currently only about 15 months, she added.
Venetoclax
Another option in this setting is the B-cell lymphoma 2 (BCL-2) inhibitor venetoclax, which was shown in a recent phase 1 study of patients with various lymphoma subtypes to have activity in relapsed MCL, Dr. Blum said.
The OR rate in 28 relapsed MCL patients in that study was 75%, and the median PFS was 14 months (J Clin Oncol. 2017 Mar;35:826-33).
Additionally, an “intriguing combination study of venetoclax and ibrutinib” was recently published in the New England Journal of Medicine, she noted.
That study included only 23 patients with relapsed MCL, but they were a “pretty high-risk” group with a median age of 68 years, about half having a TP53 abnormality, and 30% having a prior transplant.
The OR and CR rates at 16 weeks by positron emission tomography were 71% and 62%, respectively (N Engl J Med. 2018 Mar 29;378:1211-23).
“Actually, about 40% achieved [minimal residual disease] negativity, but this was only checked in about half the patients,” she said. “So this is an intriguing combination and hopefully something we’ll see more of in the upcoming years.”
Lenalidomide
In the randomized phase 2 SPRINT study, patients received either single-agent lenolidamine or the investigator’s choice of single-agent rituximab, gemcitabine, fludarabine, chlorambucil, or cytarabine.
The expected OR rate in 170 patients treated with lenalidomide was 40% versus 11% in 84 patients treated with investigator’s choice of treatment, and the respective CR rates were 5% and 0% (Lancet Oncol. 2016 Mar 1;17(3):319-31).
Median DOR was 16 months versus 10.4 months, PFS was 8.7 versus 5.2 months, and median OS was 27.9 versus 21.1 months in the groups, respectively.
Other options
Combination regimens, such as R-CHOP and R-bendamustine, are also options for the treatment of relapsed MCL patients who haven’t received combination therapy in the past, Dr. Blum said. Transplant is another option in some patients.
“I will consider transplants for younger patients if they come to me and they actually hadn’t had one in [their] first CR,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
EXPERT ANALYSIS FROM MHM 2018
Consider treatment, testing when CLL symptoms emerge
CHICAGO – said Paul M. Barr, MD.
He described a patient who had been observed for 7 years when he began to complain of increasing fatigue and lost work time. A complete blood count (CBC) showed thrombocytopenia.
The recently updated International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines state that assessments before treatment in this type of patient should include history and physical, evaluation of infectious disease status, and routine laboratory testing – including CBC and differential, chemistry, serum immunoglobulin, and direct antiglobulin test.
“Bone marrow biopsies and [computed tomography] scans are listed as ‘not necessarily required,’ ” Dr. Barr, medical director of the Clinical Trials Office for Wilmot Cancer Institute at the University of Rochester (N.Y.) said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
He added that he opts for CT scans prior to therapy “to understand the patient’s disease burden and potentially to compare to later” and that bone marrow biopsy is “still very reasonable” for understanding the source of a patient’s cytopenias.
“Is it marrow failure or [immune thrombocytopenia]? Could the patient have [myelodysplastic syndrome]? All important considerations,” he said.
Positron emission tomography (PET) scans, however, are only considered when there is concern about transformation, he noted.
Predictive tests that should be conducted before initiating therapy, and that could help in guiding therapy decisions, include TP53 mutation testing and immunoglobulin heavy chain variable region gene (IGHV) mutational status testing (although this doesn’t need to be repeated if it was done at diagnosis because mutational status doesn’t change). Another helpful test is molecular cytogenetics using fluorescence in situ hybridization (FISH) for del(13q), del(17p), and trisomy 12 in peripheral blood lymphocytes. This should be repeated even it was done at diagnosis because patients can acquire additional molecular aberrations over time, Dr. Barr said.
Among the data that justify this advice for predictive testing are studies showing the curative potential of fludarabine/cyclophosphamide/rituximab (FCR) in mutated IGHV CLL, the progression-free survival (PFS) benefits of ibrutinib for patients with del(17p), and the activity of idelalisib in relapsed/refractory CLL patients, including those with TP53 dysfunction.
“The IGHV mutation status is useful to know what to expect from chemoimmunotherapy over time,” Dr. Barr said, explaining that several analyses demonstrate that patients with mutated IGHV genes (patients with low-risk disease) respond exceptionally well to chemoimmunotherapy, especially FCR.
In fact, studies, including a 2016 study by Philip A. Thompson and his colleagues and another by Kirsten Fischer and her colleagues, show that nearly 60% of patients with IGHV mutation remain in remission 10 years after FCR treatment, he said. However, the same is not necessarily true for bendamustine/rituximab (BR); the CLL10 study showed a significantly greater PFS with FCR, compared with that seen with BR.
Unmutated patients in that study had lower PFS, but the outcomes were still better with FCR than with BR, he said.
Studies of novel agents, including ibrutinib and idelalisib, suggest they may have particular benefit in higher-risk patients.
Ibrutinib was shown in a phase 2 study to be of benefit regardless of IGHV status, and this was replicated in the first-line RESONATE 2 study, which compared ibrutinib with chlorambucil and showed it had better PFS than that seen in unmutated patients treated with FCR in other studies, said Dr. Barr, the first author on that study.
“So you can see how the treatment paradigms are starting to evolve. It does look like ... comparing across trials, that ibrutinib leads to better remission durations, compared to chemoimmunotherapy, so far,” he said.
Ibrutinib has also been shown to be of benefit for patients with del(17p). A single-arm phase 2 study showed 79% PFS in relapsed, high-risk patients, which is much better than has been seen with chemoimmunotherapy, he noted.
“Venetoclax is also a very good option for this patient population in the relapse setting,” he said, adding that the PFS with venetoclax has been shown to be very similar to that with ibrutinib.
Similarly, idelalisib has been shown to provide comparable benefit in relapsed/refractory CLL patients, with and without del(17p)/TP53 mutation, he said.
Dr. Barr is a consultant for Pharmacyclics, AbbVie, Celgene, Gilead, Infinity, Novartis, and Seattle Genetics and has received research funding from Pharmacyclics and AbbVie.
CHICAGO – said Paul M. Barr, MD.
He described a patient who had been observed for 7 years when he began to complain of increasing fatigue and lost work time. A complete blood count (CBC) showed thrombocytopenia.
The recently updated International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines state that assessments before treatment in this type of patient should include history and physical, evaluation of infectious disease status, and routine laboratory testing – including CBC and differential, chemistry, serum immunoglobulin, and direct antiglobulin test.
“Bone marrow biopsies and [computed tomography] scans are listed as ‘not necessarily required,’ ” Dr. Barr, medical director of the Clinical Trials Office for Wilmot Cancer Institute at the University of Rochester (N.Y.) said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
He added that he opts for CT scans prior to therapy “to understand the patient’s disease burden and potentially to compare to later” and that bone marrow biopsy is “still very reasonable” for understanding the source of a patient’s cytopenias.
“Is it marrow failure or [immune thrombocytopenia]? Could the patient have [myelodysplastic syndrome]? All important considerations,” he said.
Positron emission tomography (PET) scans, however, are only considered when there is concern about transformation, he noted.
Predictive tests that should be conducted before initiating therapy, and that could help in guiding therapy decisions, include TP53 mutation testing and immunoglobulin heavy chain variable region gene (IGHV) mutational status testing (although this doesn’t need to be repeated if it was done at diagnosis because mutational status doesn’t change). Another helpful test is molecular cytogenetics using fluorescence in situ hybridization (FISH) for del(13q), del(17p), and trisomy 12 in peripheral blood lymphocytes. This should be repeated even it was done at diagnosis because patients can acquire additional molecular aberrations over time, Dr. Barr said.
Among the data that justify this advice for predictive testing are studies showing the curative potential of fludarabine/cyclophosphamide/rituximab (FCR) in mutated IGHV CLL, the progression-free survival (PFS) benefits of ibrutinib for patients with del(17p), and the activity of idelalisib in relapsed/refractory CLL patients, including those with TP53 dysfunction.
“The IGHV mutation status is useful to know what to expect from chemoimmunotherapy over time,” Dr. Barr said, explaining that several analyses demonstrate that patients with mutated IGHV genes (patients with low-risk disease) respond exceptionally well to chemoimmunotherapy, especially FCR.
In fact, studies, including a 2016 study by Philip A. Thompson and his colleagues and another by Kirsten Fischer and her colleagues, show that nearly 60% of patients with IGHV mutation remain in remission 10 years after FCR treatment, he said. However, the same is not necessarily true for bendamustine/rituximab (BR); the CLL10 study showed a significantly greater PFS with FCR, compared with that seen with BR.
Unmutated patients in that study had lower PFS, but the outcomes were still better with FCR than with BR, he said.
Studies of novel agents, including ibrutinib and idelalisib, suggest they may have particular benefit in higher-risk patients.
Ibrutinib was shown in a phase 2 study to be of benefit regardless of IGHV status, and this was replicated in the first-line RESONATE 2 study, which compared ibrutinib with chlorambucil and showed it had better PFS than that seen in unmutated patients treated with FCR in other studies, said Dr. Barr, the first author on that study.
“So you can see how the treatment paradigms are starting to evolve. It does look like ... comparing across trials, that ibrutinib leads to better remission durations, compared to chemoimmunotherapy, so far,” he said.
Ibrutinib has also been shown to be of benefit for patients with del(17p). A single-arm phase 2 study showed 79% PFS in relapsed, high-risk patients, which is much better than has been seen with chemoimmunotherapy, he noted.
“Venetoclax is also a very good option for this patient population in the relapse setting,” he said, adding that the PFS with venetoclax has been shown to be very similar to that with ibrutinib.
Similarly, idelalisib has been shown to provide comparable benefit in relapsed/refractory CLL patients, with and without del(17p)/TP53 mutation, he said.
Dr. Barr is a consultant for Pharmacyclics, AbbVie, Celgene, Gilead, Infinity, Novartis, and Seattle Genetics and has received research funding from Pharmacyclics and AbbVie.
CHICAGO – said Paul M. Barr, MD.
He described a patient who had been observed for 7 years when he began to complain of increasing fatigue and lost work time. A complete blood count (CBC) showed thrombocytopenia.
The recently updated International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines state that assessments before treatment in this type of patient should include history and physical, evaluation of infectious disease status, and routine laboratory testing – including CBC and differential, chemistry, serum immunoglobulin, and direct antiglobulin test.
“Bone marrow biopsies and [computed tomography] scans are listed as ‘not necessarily required,’ ” Dr. Barr, medical director of the Clinical Trials Office for Wilmot Cancer Institute at the University of Rochester (N.Y.) said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
He added that he opts for CT scans prior to therapy “to understand the patient’s disease burden and potentially to compare to later” and that bone marrow biopsy is “still very reasonable” for understanding the source of a patient’s cytopenias.
“Is it marrow failure or [immune thrombocytopenia]? Could the patient have [myelodysplastic syndrome]? All important considerations,” he said.
Positron emission tomography (PET) scans, however, are only considered when there is concern about transformation, he noted.
Predictive tests that should be conducted before initiating therapy, and that could help in guiding therapy decisions, include TP53 mutation testing and immunoglobulin heavy chain variable region gene (IGHV) mutational status testing (although this doesn’t need to be repeated if it was done at diagnosis because mutational status doesn’t change). Another helpful test is molecular cytogenetics using fluorescence in situ hybridization (FISH) for del(13q), del(17p), and trisomy 12 in peripheral blood lymphocytes. This should be repeated even it was done at diagnosis because patients can acquire additional molecular aberrations over time, Dr. Barr said.
Among the data that justify this advice for predictive testing are studies showing the curative potential of fludarabine/cyclophosphamide/rituximab (FCR) in mutated IGHV CLL, the progression-free survival (PFS) benefits of ibrutinib for patients with del(17p), and the activity of idelalisib in relapsed/refractory CLL patients, including those with TP53 dysfunction.
“The IGHV mutation status is useful to know what to expect from chemoimmunotherapy over time,” Dr. Barr said, explaining that several analyses demonstrate that patients with mutated IGHV genes (patients with low-risk disease) respond exceptionally well to chemoimmunotherapy, especially FCR.
In fact, studies, including a 2016 study by Philip A. Thompson and his colleagues and another by Kirsten Fischer and her colleagues, show that nearly 60% of patients with IGHV mutation remain in remission 10 years after FCR treatment, he said. However, the same is not necessarily true for bendamustine/rituximab (BR); the CLL10 study showed a significantly greater PFS with FCR, compared with that seen with BR.
Unmutated patients in that study had lower PFS, but the outcomes were still better with FCR than with BR, he said.
Studies of novel agents, including ibrutinib and idelalisib, suggest they may have particular benefit in higher-risk patients.
Ibrutinib was shown in a phase 2 study to be of benefit regardless of IGHV status, and this was replicated in the first-line RESONATE 2 study, which compared ibrutinib with chlorambucil and showed it had better PFS than that seen in unmutated patients treated with FCR in other studies, said Dr. Barr, the first author on that study.
“So you can see how the treatment paradigms are starting to evolve. It does look like ... comparing across trials, that ibrutinib leads to better remission durations, compared to chemoimmunotherapy, so far,” he said.
Ibrutinib has also been shown to be of benefit for patients with del(17p). A single-arm phase 2 study showed 79% PFS in relapsed, high-risk patients, which is much better than has been seen with chemoimmunotherapy, he noted.
“Venetoclax is also a very good option for this patient population in the relapse setting,” he said, adding that the PFS with venetoclax has been shown to be very similar to that with ibrutinib.
Similarly, idelalisib has been shown to provide comparable benefit in relapsed/refractory CLL patients, with and without del(17p)/TP53 mutation, he said.
Dr. Barr is a consultant for Pharmacyclics, AbbVie, Celgene, Gilead, Infinity, Novartis, and Seattle Genetics and has received research funding from Pharmacyclics and AbbVie.
EXPERT ANALYSIS FROM MHM 2018
CLL: The initial work-up
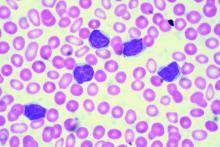
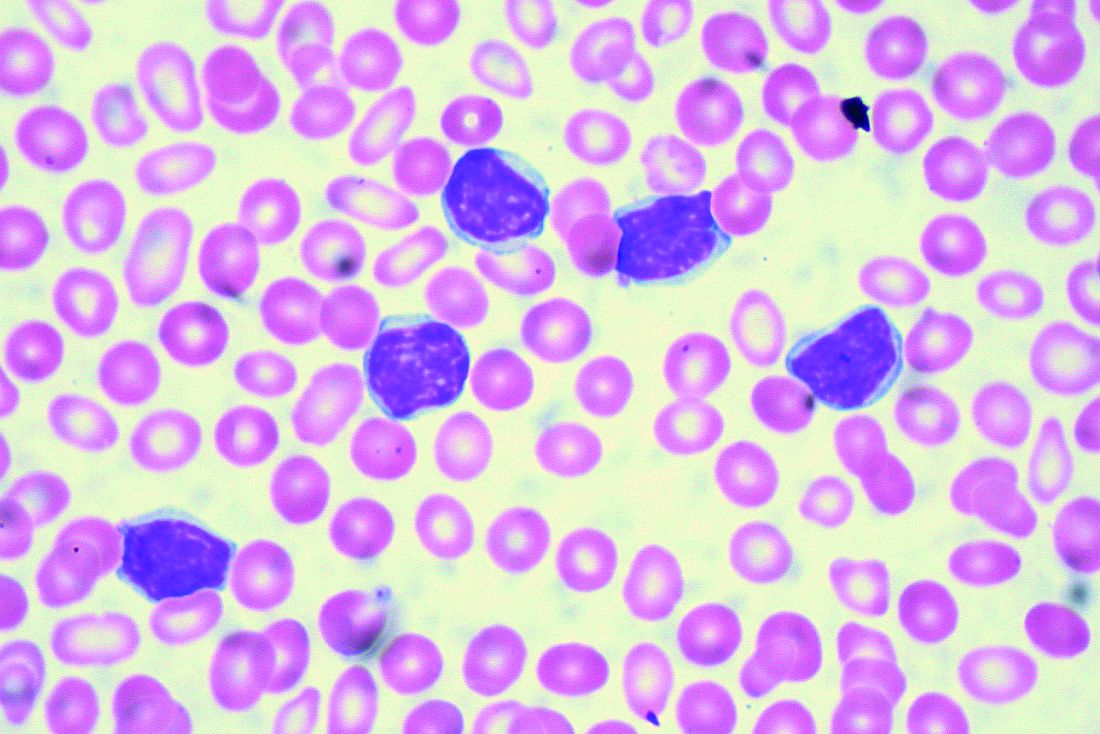
CHICAGO – A 50-year old otherwise healthy man was found on routine history and physical to have lymphocytosis and was referred for additional work-up. He denied recent infection, had no lymphadenopathy, organomegaly, or rash or other concerning skin lesions. A complete blood count showed a white cell count of 23 x 109/Land absolute lymphocyte count of 19 x 109/L and normal hemoglobin and platelets.
Based on recently updated International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines, additional work-up for this patient might include peripheral smear and flow cytometry, according to Paul Barr, MD.
“A peripheral smear is still useful in this day and age just to ensure that a patient has a typical look under the microscope. We expect to see small mature lymphocytes, smudge cells, and perhaps a smaller number of prolymphocytes. But to mark CLL based on flow cytometry we need to see greater than 5 x 109/L clonal B lymphocytes in the peripheral blood sustained over time,” Dr. Barr, medical director of the clinical trials office for Wilmot Cancer Institute at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
A nuance in the iwCLL guidelines is that CLL also can be defined by a cytopenia caused by a typical marrow infiltrate, regardless of the number of circulating B lymphocytes, he noted.
Immunophenotype
As for CLL immunophenotype, the cells are CD5- and CD23-positive, and additional B cell markers like CD20 are “often dim, and – understandably – the cells are light-chain restricted,” he said.
A subtle difference between the World Health Organization classification of CLL and the iwCLL guidelines is that, by the former, patients can have “a somewhat atypical immunophenotype.”
“So our pathologists, I like to think, use a commonsense approach where, if there are very minor differences, they will still call it CLL, but not if there are major differences in the immunophenotype,” Dr. Barr said.
Patients with lymphadenopathy, without the critical threshold of circulating B lymphocytes, are considered to have small lymphocytic lymphoma (SLL).
“In this day and age we treat CLL and SLL relatively similarly, however, monoclonal B lymphocytosis (MBL) is the precursor lesion to CLL where we see less than 5 x 109/L of circulating B lymphocytes and an absence of adenopathy and disease-related cytopenias,” he noted.
Staging
It is still common practice to stage patients given the prognostic value of staging and given that treatment is provided in advanced disease, Dr. Barr said.
“This is simple, easy to apply, applicable worldwide, and only requires laboratory testing and a physical exam,” he said.
The stages include:
- Stage 0: Lymphocytosis, peripheral lymphocyte count greater than 15,000/mcL and greater than 40% lymphocytes in bone marrow (low-risk disease status).
- Stage I: Stage 0 disease plus enlarged lymph nodes (intermediate-risk disease status).
- Stage II: Stage 0-I disease with splenomegaly and/or hepatomegaly (intermediate-risk disease status).
- Stage III: Stage 0-II disease with hemoglobin less than 11g/dL or hematocrit less than 33% (high-risk disease status).
- Stage IV: Stage 0-III disease with platelet count less than 100,000/mcL (high-risk disease status).
Prognostic testing
Once a patient is diagnosed with CLL, as was the case with the 50-year-old patient Dr. Barr described, a number of tests can be considered to assess prognosis.
There’s no “perfect answer” when it comes to which tests are considered a reasonable standard of care, he noted.
“I would typically perform [immunoglobulin variable heavy-chain gene] mutation testing, a [fluorescence in situ hybridization] panel, and TP53 mutation testing,” he said.
Scoring systems such as CLL-IPI, which combine prognostic factors to divide patients into various risk categories, can be useful.
For example, such systems may identify high-risk patients who might be appropriate candidates for clinical trials, or low-risk patients who could be expected to do well over time despite having advanced stage disease, he explained.
“I do think it’s a useful process to go through to understand a patient’s risk over time,” he added.
However, treatment for CLL still is not based on molecular aberrations/prognostic features. In fact, the treatment indications according to the updated iwCLL guidelines remain exactly the same, he said.
Therefore, the case of the 50-year-old man described earlier would be observed as long as he remained asymptomatic.
Dr. Barr is a consultant for Pharmacyclics, AbbVie, Celgene, Gilead, Infinity, Novartis, and Seattle Genetics and has received research funding from Pharmacyclics and AbbVie.
CHICAGO – A 50-year old otherwise healthy man was found on routine history and physical to have lymphocytosis and was referred for additional work-up. He denied recent infection, had no lymphadenopathy, organomegaly, or rash or other concerning skin lesions. A complete blood count showed a white cell count of 23 x 109/Land absolute lymphocyte count of 19 x 109/L and normal hemoglobin and platelets.
Based on recently updated International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines, additional work-up for this patient might include peripheral smear and flow cytometry, according to Paul Barr, MD.
“A peripheral smear is still useful in this day and age just to ensure that a patient has a typical look under the microscope. We expect to see small mature lymphocytes, smudge cells, and perhaps a smaller number of prolymphocytes. But to mark CLL based on flow cytometry we need to see greater than 5 x 109/L clonal B lymphocytes in the peripheral blood sustained over time,” Dr. Barr, medical director of the clinical trials office for Wilmot Cancer Institute at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
A nuance in the iwCLL guidelines is that CLL also can be defined by a cytopenia caused by a typical marrow infiltrate, regardless of the number of circulating B lymphocytes, he noted.
Immunophenotype
As for CLL immunophenotype, the cells are CD5- and CD23-positive, and additional B cell markers like CD20 are “often dim, and – understandably – the cells are light-chain restricted,” he said.
A subtle difference between the World Health Organization classification of CLL and the iwCLL guidelines is that, by the former, patients can have “a somewhat atypical immunophenotype.”
“So our pathologists, I like to think, use a commonsense approach where, if there are very minor differences, they will still call it CLL, but not if there are major differences in the immunophenotype,” Dr. Barr said.
Patients with lymphadenopathy, without the critical threshold of circulating B lymphocytes, are considered to have small lymphocytic lymphoma (SLL).
“In this day and age we treat CLL and SLL relatively similarly, however, monoclonal B lymphocytosis (MBL) is the precursor lesion to CLL where we see less than 5 x 109/L of circulating B lymphocytes and an absence of adenopathy and disease-related cytopenias,” he noted.
Staging
It is still common practice to stage patients given the prognostic value of staging and given that treatment is provided in advanced disease, Dr. Barr said.
“This is simple, easy to apply, applicable worldwide, and only requires laboratory testing and a physical exam,” he said.
The stages include:
- Stage 0: Lymphocytosis, peripheral lymphocyte count greater than 15,000/mcL and greater than 40% lymphocytes in bone marrow (low-risk disease status).
- Stage I: Stage 0 disease plus enlarged lymph nodes (intermediate-risk disease status).
- Stage II: Stage 0-I disease with splenomegaly and/or hepatomegaly (intermediate-risk disease status).
- Stage III: Stage 0-II disease with hemoglobin less than 11g/dL or hematocrit less than 33% (high-risk disease status).
- Stage IV: Stage 0-III disease with platelet count less than 100,000/mcL (high-risk disease status).
Prognostic testing
Once a patient is diagnosed with CLL, as was the case with the 50-year-old patient Dr. Barr described, a number of tests can be considered to assess prognosis.
There’s no “perfect answer” when it comes to which tests are considered a reasonable standard of care, he noted.
“I would typically perform [immunoglobulin variable heavy-chain gene] mutation testing, a [fluorescence in situ hybridization] panel, and TP53 mutation testing,” he said.
Scoring systems such as CLL-IPI, which combine prognostic factors to divide patients into various risk categories, can be useful.
For example, such systems may identify high-risk patients who might be appropriate candidates for clinical trials, or low-risk patients who could be expected to do well over time despite having advanced stage disease, he explained.
“I do think it’s a useful process to go through to understand a patient’s risk over time,” he added.
However, treatment for CLL still is not based on molecular aberrations/prognostic features. In fact, the treatment indications according to the updated iwCLL guidelines remain exactly the same, he said.
Therefore, the case of the 50-year-old man described earlier would be observed as long as he remained asymptomatic.
Dr. Barr is a consultant for Pharmacyclics, AbbVie, Celgene, Gilead, Infinity, Novartis, and Seattle Genetics and has received research funding from Pharmacyclics and AbbVie.
CHICAGO – A 50-year old otherwise healthy man was found on routine history and physical to have lymphocytosis and was referred for additional work-up. He denied recent infection, had no lymphadenopathy, organomegaly, or rash or other concerning skin lesions. A complete blood count showed a white cell count of 23 x 109/Land absolute lymphocyte count of 19 x 109/L and normal hemoglobin and platelets.
Based on recently updated International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines, additional work-up for this patient might include peripheral smear and flow cytometry, according to Paul Barr, MD.
“A peripheral smear is still useful in this day and age just to ensure that a patient has a typical look under the microscope. We expect to see small mature lymphocytes, smudge cells, and perhaps a smaller number of prolymphocytes. But to mark CLL based on flow cytometry we need to see greater than 5 x 109/L clonal B lymphocytes in the peripheral blood sustained over time,” Dr. Barr, medical director of the clinical trials office for Wilmot Cancer Institute at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
A nuance in the iwCLL guidelines is that CLL also can be defined by a cytopenia caused by a typical marrow infiltrate, regardless of the number of circulating B lymphocytes, he noted.
Immunophenotype
As for CLL immunophenotype, the cells are CD5- and CD23-positive, and additional B cell markers like CD20 are “often dim, and – understandably – the cells are light-chain restricted,” he said.
A subtle difference between the World Health Organization classification of CLL and the iwCLL guidelines is that, by the former, patients can have “a somewhat atypical immunophenotype.”
“So our pathologists, I like to think, use a commonsense approach where, if there are very minor differences, they will still call it CLL, but not if there are major differences in the immunophenotype,” Dr. Barr said.
Patients with lymphadenopathy, without the critical threshold of circulating B lymphocytes, are considered to have small lymphocytic lymphoma (SLL).
“In this day and age we treat CLL and SLL relatively similarly, however, monoclonal B lymphocytosis (MBL) is the precursor lesion to CLL where we see less than 5 x 109/L of circulating B lymphocytes and an absence of adenopathy and disease-related cytopenias,” he noted.
Staging
It is still common practice to stage patients given the prognostic value of staging and given that treatment is provided in advanced disease, Dr. Barr said.
“This is simple, easy to apply, applicable worldwide, and only requires laboratory testing and a physical exam,” he said.
The stages include:
- Stage 0: Lymphocytosis, peripheral lymphocyte count greater than 15,000/mcL and greater than 40% lymphocytes in bone marrow (low-risk disease status).
- Stage I: Stage 0 disease plus enlarged lymph nodes (intermediate-risk disease status).
- Stage II: Stage 0-I disease with splenomegaly and/or hepatomegaly (intermediate-risk disease status).
- Stage III: Stage 0-II disease with hemoglobin less than 11g/dL or hematocrit less than 33% (high-risk disease status).
- Stage IV: Stage 0-III disease with platelet count less than 100,000/mcL (high-risk disease status).
Prognostic testing
Once a patient is diagnosed with CLL, as was the case with the 50-year-old patient Dr. Barr described, a number of tests can be considered to assess prognosis.
There’s no “perfect answer” when it comes to which tests are considered a reasonable standard of care, he noted.
“I would typically perform [immunoglobulin variable heavy-chain gene] mutation testing, a [fluorescence in situ hybridization] panel, and TP53 mutation testing,” he said.
Scoring systems such as CLL-IPI, which combine prognostic factors to divide patients into various risk categories, can be useful.
For example, such systems may identify high-risk patients who might be appropriate candidates for clinical trials, or low-risk patients who could be expected to do well over time despite having advanced stage disease, he explained.
“I do think it’s a useful process to go through to understand a patient’s risk over time,” he added.
However, treatment for CLL still is not based on molecular aberrations/prognostic features. In fact, the treatment indications according to the updated iwCLL guidelines remain exactly the same, he said.
Therefore, the case of the 50-year-old man described earlier would be observed as long as he remained asymptomatic.
Dr. Barr is a consultant for Pharmacyclics, AbbVie, Celgene, Gilead, Infinity, Novartis, and Seattle Genetics and has received research funding from Pharmacyclics and AbbVie.
EXPERT ANALYSIS FROM MHM 2018
Prognostic features could improve ALL outcomes
CHICAGO – New recognition of the prognostic value of cytogenetic factors, minimal residual disease activity, and Philadelphia chromosome–like signature could improve the treatment and outcomes of acute lymphoblastic leukemia (ALL), according to Anjali Advani, MD.
CD20
About 80% of ALL is B-cell ALL and the majority of patients have pre–B-cell ALL, Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“And on the B lymphoblast, many antigens are expressed, including CD19, CD20, and CD52,” she said.
Rituximab, a drug often used for the treatment of lymphoma, is a chimeric monoclonal antibody against the protein CD20, which is expressed in 41% of ALL patients.
“Interestingly, CD20 expression in ALL has been associated with an adverse prognostic impact, which suggests that targeting this may potentially improve outcomes in these patients,” Dr. Advani said.
In fact, a recent randomized study by Sébastien Maury, MD, of the University of Paris-Est, and his colleagues, demonstrated that adding 16-18 doses of rituximab to a Berlin-Frankfurt-Münster (BFM)–based chemotherapy in Philadelphia chromosome (Ph)–negative patients aged 18-59 years with CD20-positive pre–B-cell ALL improved 2-year event-free survival from 52% to 65%. The data are consistent with those from prior studies, including a German study that showed a higher degree of minimal residual disease (MRD) negativity in patients treated with rituximab, she noted (N Engl J Med 2016;375:1044-53).
While the study by Dr. Maury and his colleagues didn’t look at MRD, that may offer an explanation for the improved event-free survival in their study, Dr. Advani suggested.
MRD
Minimal residual disease has become a standard part of practice in ALL, but pediatric ALL led the way in using early MRD measurement for risk-stratifying therapy, and it has taken a bit longer for it to be incorporated in the adult disease realm, Dr. Advani said.
Either flow cytometry or polymerase chain reaction (PCR) amplification can be used to measure MRD, she noted.
In one of the larger studies done in adults, researchers used PCR to look at MRD at two time points and stratified patients into three risk groups, including low, intermediate, and high risk (Blood. 2006 Feb 1;107:1116-23).
Measuring MRD at those two time points “clearly separated the prognosis of patients not only in terms of disease-free survival but [in] overall survival,” she said. “So that’s why, for ALL, this has really become very important.”
In the United States, where flow-based cytometry is used more, it is necessary to find a properly equipped laboratory that can provide reliable results, she added. “For example, at our center we actually send our MRD to Fred Hutchinson [Cancer Center in Seattle].”
Johns Hopkins [Baltimore] also has such a lab, and both can arrange to accept send-outs, she said.
The other “really exciting thing” in regard to MRD in ALL is the recent approval of blinatumomab for MRD-positive ALL, she said.
In a study of 113 evaluable patients who were treated with the monoclonal antibody, 78% achieved complete molecular response (Blood. 2018 Apr 5;131:1522-31).
“And probably most importantly, when they looked at those patients who responded to blinatumomab in terms of MRD, these patients had, again, not only improved relapse-free survival but also increased overall survival,” she said. “I think this really explains why in ALL, we are measuring MRD and how it can really impact these patients.”
One of the remaining questions that will be important to address going forward is whether patients with MRD-positive ALL should continue to be considered for transplant; some of these studies have shown “very, very good outcomes” in patients who have not been transplanted, she noted.
Ph-like signature
Another important new prognostic feature in ALL is the presence of the Ph-like signature, a gene expression signature that was initially described in children with poor-risk ALL, and which looks a lot like Ph-positive disease.
“When they delved in further, they identified that this signature actually correlated with multiple different [kinase] fusions ... and it turns out that 20%-25% of young adults have this signature,” she said.
Since event-free survival in young adults with ALL is usually in the 65%-70% range, most of the remaining 30%-35% likely have this signature, she explained.
The kinase fusions associated with the Ph-like signature retain intact tyrosine kinase domains, and the spectrum of the fusions changes across age groups.
Treatments targeting some of these – for example, dasatinib for patients with a Ph-like dasatinib-sensitive kinase mutation – are being investigated.
Additionally, the Children’s Oncology Group has developed a clinically adaptable screening assay to identify the signature, she noted.
“So I would say that, and there is probably some difference in opinion, it is now becoming fairly standard that at diagnosis in an adult with ALL we’re sending the Ph-like signature,” she said. “And again, usually you’re going to have to send this out, and at our center we send it out to [Nationwide Children’s Hospital] in Columbus [Ohio].”
As important as it is to identify the Ph-like signature, given its association with poor prognosis, a number of questions remain, including whether transplant improves outcomes.
“The hope is it probably does, and that’s something that’s being evaluated in studies,” she said, noting that clinical studies are also specifically targeting these patients.
“So these patients should probably be enrolled on a clinical trial, because their outcome is clearly inferior,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
CHICAGO – New recognition of the prognostic value of cytogenetic factors, minimal residual disease activity, and Philadelphia chromosome–like signature could improve the treatment and outcomes of acute lymphoblastic leukemia (ALL), according to Anjali Advani, MD.
CD20
About 80% of ALL is B-cell ALL and the majority of patients have pre–B-cell ALL, Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“And on the B lymphoblast, many antigens are expressed, including CD19, CD20, and CD52,” she said.
Rituximab, a drug often used for the treatment of lymphoma, is a chimeric monoclonal antibody against the protein CD20, which is expressed in 41% of ALL patients.
“Interestingly, CD20 expression in ALL has been associated with an adverse prognostic impact, which suggests that targeting this may potentially improve outcomes in these patients,” Dr. Advani said.
In fact, a recent randomized study by Sébastien Maury, MD, of the University of Paris-Est, and his colleagues, demonstrated that adding 16-18 doses of rituximab to a Berlin-Frankfurt-Münster (BFM)–based chemotherapy in Philadelphia chromosome (Ph)–negative patients aged 18-59 years with CD20-positive pre–B-cell ALL improved 2-year event-free survival from 52% to 65%. The data are consistent with those from prior studies, including a German study that showed a higher degree of minimal residual disease (MRD) negativity in patients treated with rituximab, she noted (N Engl J Med 2016;375:1044-53).
While the study by Dr. Maury and his colleagues didn’t look at MRD, that may offer an explanation for the improved event-free survival in their study, Dr. Advani suggested.
MRD
Minimal residual disease has become a standard part of practice in ALL, but pediatric ALL led the way in using early MRD measurement for risk-stratifying therapy, and it has taken a bit longer for it to be incorporated in the adult disease realm, Dr. Advani said.
Either flow cytometry or polymerase chain reaction (PCR) amplification can be used to measure MRD, she noted.
In one of the larger studies done in adults, researchers used PCR to look at MRD at two time points and stratified patients into three risk groups, including low, intermediate, and high risk (Blood. 2006 Feb 1;107:1116-23).
Measuring MRD at those two time points “clearly separated the prognosis of patients not only in terms of disease-free survival but [in] overall survival,” she said. “So that’s why, for ALL, this has really become very important.”
In the United States, where flow-based cytometry is used more, it is necessary to find a properly equipped laboratory that can provide reliable results, she added. “For example, at our center we actually send our MRD to Fred Hutchinson [Cancer Center in Seattle].”
Johns Hopkins [Baltimore] also has such a lab, and both can arrange to accept send-outs, she said.
The other “really exciting thing” in regard to MRD in ALL is the recent approval of blinatumomab for MRD-positive ALL, she said.
In a study of 113 evaluable patients who were treated with the monoclonal antibody, 78% achieved complete molecular response (Blood. 2018 Apr 5;131:1522-31).
“And probably most importantly, when they looked at those patients who responded to blinatumomab in terms of MRD, these patients had, again, not only improved relapse-free survival but also increased overall survival,” she said. “I think this really explains why in ALL, we are measuring MRD and how it can really impact these patients.”
One of the remaining questions that will be important to address going forward is whether patients with MRD-positive ALL should continue to be considered for transplant; some of these studies have shown “very, very good outcomes” in patients who have not been transplanted, she noted.
Ph-like signature
Another important new prognostic feature in ALL is the presence of the Ph-like signature, a gene expression signature that was initially described in children with poor-risk ALL, and which looks a lot like Ph-positive disease.
“When they delved in further, they identified that this signature actually correlated with multiple different [kinase] fusions ... and it turns out that 20%-25% of young adults have this signature,” she said.
Since event-free survival in young adults with ALL is usually in the 65%-70% range, most of the remaining 30%-35% likely have this signature, she explained.
The kinase fusions associated with the Ph-like signature retain intact tyrosine kinase domains, and the spectrum of the fusions changes across age groups.
Treatments targeting some of these – for example, dasatinib for patients with a Ph-like dasatinib-sensitive kinase mutation – are being investigated.
Additionally, the Children’s Oncology Group has developed a clinically adaptable screening assay to identify the signature, she noted.
“So I would say that, and there is probably some difference in opinion, it is now becoming fairly standard that at diagnosis in an adult with ALL we’re sending the Ph-like signature,” she said. “And again, usually you’re going to have to send this out, and at our center we send it out to [Nationwide Children’s Hospital] in Columbus [Ohio].”
As important as it is to identify the Ph-like signature, given its association with poor prognosis, a number of questions remain, including whether transplant improves outcomes.
“The hope is it probably does, and that’s something that’s being evaluated in studies,” she said, noting that clinical studies are also specifically targeting these patients.
“So these patients should probably be enrolled on a clinical trial, because their outcome is clearly inferior,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
CHICAGO – New recognition of the prognostic value of cytogenetic factors, minimal residual disease activity, and Philadelphia chromosome–like signature could improve the treatment and outcomes of acute lymphoblastic leukemia (ALL), according to Anjali Advani, MD.
CD20
About 80% of ALL is B-cell ALL and the majority of patients have pre–B-cell ALL, Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“And on the B lymphoblast, many antigens are expressed, including CD19, CD20, and CD52,” she said.
Rituximab, a drug often used for the treatment of lymphoma, is a chimeric monoclonal antibody against the protein CD20, which is expressed in 41% of ALL patients.
“Interestingly, CD20 expression in ALL has been associated with an adverse prognostic impact, which suggests that targeting this may potentially improve outcomes in these patients,” Dr. Advani said.
In fact, a recent randomized study by Sébastien Maury, MD, of the University of Paris-Est, and his colleagues, demonstrated that adding 16-18 doses of rituximab to a Berlin-Frankfurt-Münster (BFM)–based chemotherapy in Philadelphia chromosome (Ph)–negative patients aged 18-59 years with CD20-positive pre–B-cell ALL improved 2-year event-free survival from 52% to 65%. The data are consistent with those from prior studies, including a German study that showed a higher degree of minimal residual disease (MRD) negativity in patients treated with rituximab, she noted (N Engl J Med 2016;375:1044-53).
While the study by Dr. Maury and his colleagues didn’t look at MRD, that may offer an explanation for the improved event-free survival in their study, Dr. Advani suggested.
MRD
Minimal residual disease has become a standard part of practice in ALL, but pediatric ALL led the way in using early MRD measurement for risk-stratifying therapy, and it has taken a bit longer for it to be incorporated in the adult disease realm, Dr. Advani said.
Either flow cytometry or polymerase chain reaction (PCR) amplification can be used to measure MRD, she noted.
In one of the larger studies done in adults, researchers used PCR to look at MRD at two time points and stratified patients into three risk groups, including low, intermediate, and high risk (Blood. 2006 Feb 1;107:1116-23).
Measuring MRD at those two time points “clearly separated the prognosis of patients not only in terms of disease-free survival but [in] overall survival,” she said. “So that’s why, for ALL, this has really become very important.”
In the United States, where flow-based cytometry is used more, it is necessary to find a properly equipped laboratory that can provide reliable results, she added. “For example, at our center we actually send our MRD to Fred Hutchinson [Cancer Center in Seattle].”
Johns Hopkins [Baltimore] also has such a lab, and both can arrange to accept send-outs, she said.
The other “really exciting thing” in regard to MRD in ALL is the recent approval of blinatumomab for MRD-positive ALL, she said.
In a study of 113 evaluable patients who were treated with the monoclonal antibody, 78% achieved complete molecular response (Blood. 2018 Apr 5;131:1522-31).
“And probably most importantly, when they looked at those patients who responded to blinatumomab in terms of MRD, these patients had, again, not only improved relapse-free survival but also increased overall survival,” she said. “I think this really explains why in ALL, we are measuring MRD and how it can really impact these patients.”
One of the remaining questions that will be important to address going forward is whether patients with MRD-positive ALL should continue to be considered for transplant; some of these studies have shown “very, very good outcomes” in patients who have not been transplanted, she noted.
Ph-like signature
Another important new prognostic feature in ALL is the presence of the Ph-like signature, a gene expression signature that was initially described in children with poor-risk ALL, and which looks a lot like Ph-positive disease.
“When they delved in further, they identified that this signature actually correlated with multiple different [kinase] fusions ... and it turns out that 20%-25% of young adults have this signature,” she said.
Since event-free survival in young adults with ALL is usually in the 65%-70% range, most of the remaining 30%-35% likely have this signature, she explained.
The kinase fusions associated with the Ph-like signature retain intact tyrosine kinase domains, and the spectrum of the fusions changes across age groups.
Treatments targeting some of these – for example, dasatinib for patients with a Ph-like dasatinib-sensitive kinase mutation – are being investigated.
Additionally, the Children’s Oncology Group has developed a clinically adaptable screening assay to identify the signature, she noted.
“So I would say that, and there is probably some difference in opinion, it is now becoming fairly standard that at diagnosis in an adult with ALL we’re sending the Ph-like signature,” she said. “And again, usually you’re going to have to send this out, and at our center we send it out to [Nationwide Children’s Hospital] in Columbus [Ohio].”
As important as it is to identify the Ph-like signature, given its association with poor prognosis, a number of questions remain, including whether transplant improves outcomes.
“The hope is it probably does, and that’s something that’s being evaluated in studies,” she said, noting that clinical studies are also specifically targeting these patients.
“So these patients should probably be enrolled on a clinical trial, because their outcome is clearly inferior,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
EXPERT ANALYSIS FROM MHM 2018
Researchers consider R/R ALL drugs in the first-line setting
CHICAGO – Novel antibodies are improving outcomes in relapsed and refractory acute lymphoblastic leukemia (ALL), and the hope is that they will also show benefit in the up-front treatment setting and thereby improve overall outcomes, according to Anjali Advani, MD.
“It has been a really exciting time in ALL because several drugs have now been FDA approved: blinatumomab, inotuzumab, and now – for patients who are less than 26 years of age – we actually have CAR [chimeric antigen receptor] T cells that have been approved,” Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic said at the American Society of Hematology Meeting on Hematologic Malignancies.
At the time of relapse, however, the only known cure is allogeneic bone marrow transplant. That may change as more data regarding CAR T cells become available, but the typical goal at this time is to get patients into remission and then to transplant, she said.
Blinatumomab
“Blinatumomab is a very interesting antibody,” Dr. Advani said, explaining that it is a bispecific, T cell–engaging antibody with an anti-CD3 arm that engages the T cell and an anti-CD19 antibody that engages the B lymphoblast.
“Basically this drug then acts as a bridge between the lymphoblast and the T cell to lead to proliferation of the cytotoxic T cell and apoptosis of the lymphoblast,” she said. “It’s interesting because it’s an antibody but it actually works through the immune system through the T cells.”
The largest study to date of blinatumomab in the relapsed/refractory ALL setting showed a 43% complete remission (CR) or CR with partial hematological recovery of peripheral blood counts (CRi) in 189 treated patients with Philadelphia chromosome–negative ALL. It also demonstrated and a 39% rate of salvage status 2 or higher, she said, noting that the response was impressive given that about 30% of participants had a prior transplant (Lancet. 2015 Jan 1;16[1]:57-66).
Of the responders, 40% went on to allogeneic transplant. This was a “fairly impressive” rate given the 30% prior-transplant rate, Dr. Advani said.
“There also was a high minimal residual disease response in those patients achieving CR,” she said, adding that the only significant predictor of response was bone marrow blast count; patients with 50% or more blasts in the bone marrow had a reduced likelihood of responding to blinatumomab.
The agent was approved by the Food and Drug Administration in December 2014 based on these phase 2 findings.
Adverse events mainly included toxicities that are expected in leukemia patients; the most frequent were febrile neutropenia, neutropenia, and anemia. Two patients developed cytokine release syndrome, and about half of the blinatumomab-treated patients experienced neurological events, although the majority of those were grade 1 or 2 and were easily manageable, she noted.
Blinatumomab was further evaluated in the phase 3 TOWER study (NCT02013167), which compared it with standard-of-care chemotherapy regimens. This study showed much higher response rates with blinatumomab than with the chemotherapy regimens (CR with full, partial, or incomplete hematologic recovery, 44% vs. 25%, respectively), Dr. Advani said (N Engl J Med. 2017 Mar 2;376[9]:836-47).
“The main things to remember [are that blinatumomab is] generally very well tolerated and it has been shown to be superior over standard chemotherapy,” she said. “I think it’s a very good drug to use as a bridge to transplant.”
One setting where blinatumomab perhaps should not be used is in patients with central nervous system disease, she noted.
“There is some concern, at least theoretically, that if you have to use concurrent intrathecal chemo along with blinatumomab, there could be some neurotoxicity,” Dr. Advani said, adding that there are no clear data in that setting because patients with CNS disease were not included in the trials.
Patients with high tumor burden may also be poor candidates for blinatumomab because they tend to have lower response rates.
“That doesn’t mean you can’t use it, but you have to kind of think about what the best option would be,” she said.
Additionally, patients treated with CAR T-cell therapy may develop CD19 loss or CD19-negative disease, and blinatumomab should be avoided in these patients.
“The nice thing ... is you don’t have to worry about veno-occlusive disease [VOD] in patients who are proceeding to transplant,” she said, explaining that no increased risk of VOD was seen in these trials.
Inotuzumab
Inotuzumab, which was approved in 2017, differs from blinatumomab in that it is an anti-CD22-calicheamicin conjugate; however, it also showed high response rates in the initial phase 2 trial in relapsed/refractory ALL. The overall response rate was 57%, with 18% achieving a complete response and 63% achieving complete molecular remission.
Of 49 treated patients, 22 patients proceeded to allogeneic transplant, and 5 of those developed VOD.
“Interestingly, four out of five of these patients had received a clofarabine-based preparative regimen, and this likely explains why there was a higher risk of VOD in this study,” she said, noting that the VOD risk has been lower in subsequent studies of inotuzumab.
The international INO-VATE ALL study (NCT01564784) that led to FDA approval was similar in design to the TOWER study in that it compared inotuzumab with standard chemotherapy regimens, and response rates were clearly higher (81% vs. 33%) with inotuzumab (N Engl J Med. 2016 Aug 25;375[8]:740-53).
The VOD risk in the INO-VATE trial was 11%, and it seemed to be higher in those who received dual alkylator–conditioning regimens, which are commonly used in Europe.
Longer-term outcomes after transplant in INO-VATE participants show that median survival has not been reached.
“It’s encouraging that with longer follow-up these patients actually look like they’re doing well,” Dr. Advani said, adding that inotuzumab is a good treatment option for relapsed patients with high disease burden or with CNS disease.
The continuous hookup required for this treatment may be problematic for some younger and older patients, but it is generally not an issue, she noted.
It is important, though, to give as few cycles prior to transplant as possible and to “really think about the preparative regimen to decrease the risk of VOD.”
CAR T-cell therapy
As for CAR T-cell therapy in the relapsed/refractory ALL setting, tisagenlecleucel was approved in 2017 for those up to age 25 years with B-cell precursor ALL that is refractory or in second or later relapse.
Approval was based on a single-arm trial of 63 patients with relapsed or refractory pediatric precursor B-cell ALL, including 35 patients who had prior transplant. The confirmed overall remission rate was 82%, with a 63% CR rate and 19% CRi rate.
“This is a very exciting area,” Dr. Advani said. “There are multiple trials being done in adults with ALL to really look at the older subgroup of patients.”
Overall outcomes
“These treatments we have now really seem to be effective in the relapse setting, but the problem is that once patients relapse and then go to transplant, their overall survival is still poor,” Dr. Advani said. “So the question is how can we improve the up-front treatment of patients so that hopefully they don’t relapse, and hopefully we also can send a smaller number of patients to transplant.”
Two trials seek to address this, she said.
The A041501 study (NCT03150693) is comparing C10403 chemotherapy with C10403 induction followed by two cycles of inotuzumab before continuing with chemotherapy in adults under age 40 years with previously untreated B ALL.
The primary objective is improved 3-year event-free survival, she said, adding that minimal residual disease (MRD) testing will be used and that CD20-positive patients will receive rituximab, as is now standard.
The phase 3 E1910 study (NCT02003222) is evaluating up-front blinatumomab in patients aged 30-70 years with newly diagnosed BCR-ABL–negative B-lineage ALL. This trial was complicated by the recent approval of blinatumomab for MRD-positive disease, which rendered randomization of MRD-positive patients unethical. MRD-negative patients will be randomized, however.
“The hope is that, by incorporating blinatumomab up front, this will again improve outcomes for patients,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
CHICAGO – Novel antibodies are improving outcomes in relapsed and refractory acute lymphoblastic leukemia (ALL), and the hope is that they will also show benefit in the up-front treatment setting and thereby improve overall outcomes, according to Anjali Advani, MD.
“It has been a really exciting time in ALL because several drugs have now been FDA approved: blinatumomab, inotuzumab, and now – for patients who are less than 26 years of age – we actually have CAR [chimeric antigen receptor] T cells that have been approved,” Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic said at the American Society of Hematology Meeting on Hematologic Malignancies.
At the time of relapse, however, the only known cure is allogeneic bone marrow transplant. That may change as more data regarding CAR T cells become available, but the typical goal at this time is to get patients into remission and then to transplant, she said.
Blinatumomab
“Blinatumomab is a very interesting antibody,” Dr. Advani said, explaining that it is a bispecific, T cell–engaging antibody with an anti-CD3 arm that engages the T cell and an anti-CD19 antibody that engages the B lymphoblast.
“Basically this drug then acts as a bridge between the lymphoblast and the T cell to lead to proliferation of the cytotoxic T cell and apoptosis of the lymphoblast,” she said. “It’s interesting because it’s an antibody but it actually works through the immune system through the T cells.”
The largest study to date of blinatumomab in the relapsed/refractory ALL setting showed a 43% complete remission (CR) or CR with partial hematological recovery of peripheral blood counts (CRi) in 189 treated patients with Philadelphia chromosome–negative ALL. It also demonstrated and a 39% rate of salvage status 2 or higher, she said, noting that the response was impressive given that about 30% of participants had a prior transplant (Lancet. 2015 Jan 1;16[1]:57-66).
Of the responders, 40% went on to allogeneic transplant. This was a “fairly impressive” rate given the 30% prior-transplant rate, Dr. Advani said.
“There also was a high minimal residual disease response in those patients achieving CR,” she said, adding that the only significant predictor of response was bone marrow blast count; patients with 50% or more blasts in the bone marrow had a reduced likelihood of responding to blinatumomab.
The agent was approved by the Food and Drug Administration in December 2014 based on these phase 2 findings.
Adverse events mainly included toxicities that are expected in leukemia patients; the most frequent were febrile neutropenia, neutropenia, and anemia. Two patients developed cytokine release syndrome, and about half of the blinatumomab-treated patients experienced neurological events, although the majority of those were grade 1 or 2 and were easily manageable, she noted.
Blinatumomab was further evaluated in the phase 3 TOWER study (NCT02013167), which compared it with standard-of-care chemotherapy regimens. This study showed much higher response rates with blinatumomab than with the chemotherapy regimens (CR with full, partial, or incomplete hematologic recovery, 44% vs. 25%, respectively), Dr. Advani said (N Engl J Med. 2017 Mar 2;376[9]:836-47).
“The main things to remember [are that blinatumomab is] generally very well tolerated and it has been shown to be superior over standard chemotherapy,” she said. “I think it’s a very good drug to use as a bridge to transplant.”
One setting where blinatumomab perhaps should not be used is in patients with central nervous system disease, she noted.
“There is some concern, at least theoretically, that if you have to use concurrent intrathecal chemo along with blinatumomab, there could be some neurotoxicity,” Dr. Advani said, adding that there are no clear data in that setting because patients with CNS disease were not included in the trials.
Patients with high tumor burden may also be poor candidates for blinatumomab because they tend to have lower response rates.
“That doesn’t mean you can’t use it, but you have to kind of think about what the best option would be,” she said.
Additionally, patients treated with CAR T-cell therapy may develop CD19 loss or CD19-negative disease, and blinatumomab should be avoided in these patients.
“The nice thing ... is you don’t have to worry about veno-occlusive disease [VOD] in patients who are proceeding to transplant,” she said, explaining that no increased risk of VOD was seen in these trials.
Inotuzumab
Inotuzumab, which was approved in 2017, differs from blinatumomab in that it is an anti-CD22-calicheamicin conjugate; however, it also showed high response rates in the initial phase 2 trial in relapsed/refractory ALL. The overall response rate was 57%, with 18% achieving a complete response and 63% achieving complete molecular remission.
Of 49 treated patients, 22 patients proceeded to allogeneic transplant, and 5 of those developed VOD.
“Interestingly, four out of five of these patients had received a clofarabine-based preparative regimen, and this likely explains why there was a higher risk of VOD in this study,” she said, noting that the VOD risk has been lower in subsequent studies of inotuzumab.
The international INO-VATE ALL study (NCT01564784) that led to FDA approval was similar in design to the TOWER study in that it compared inotuzumab with standard chemotherapy regimens, and response rates were clearly higher (81% vs. 33%) with inotuzumab (N Engl J Med. 2016 Aug 25;375[8]:740-53).
The VOD risk in the INO-VATE trial was 11%, and it seemed to be higher in those who received dual alkylator–conditioning regimens, which are commonly used in Europe.
Longer-term outcomes after transplant in INO-VATE participants show that median survival has not been reached.
“It’s encouraging that with longer follow-up these patients actually look like they’re doing well,” Dr. Advani said, adding that inotuzumab is a good treatment option for relapsed patients with high disease burden or with CNS disease.
The continuous hookup required for this treatment may be problematic for some younger and older patients, but it is generally not an issue, she noted.
It is important, though, to give as few cycles prior to transplant as possible and to “really think about the preparative regimen to decrease the risk of VOD.”
CAR T-cell therapy
As for CAR T-cell therapy in the relapsed/refractory ALL setting, tisagenlecleucel was approved in 2017 for those up to age 25 years with B-cell precursor ALL that is refractory or in second or later relapse.
Approval was based on a single-arm trial of 63 patients with relapsed or refractory pediatric precursor B-cell ALL, including 35 patients who had prior transplant. The confirmed overall remission rate was 82%, with a 63% CR rate and 19% CRi rate.
“This is a very exciting area,” Dr. Advani said. “There are multiple trials being done in adults with ALL to really look at the older subgroup of patients.”
Overall outcomes
“These treatments we have now really seem to be effective in the relapse setting, but the problem is that once patients relapse and then go to transplant, their overall survival is still poor,” Dr. Advani said. “So the question is how can we improve the up-front treatment of patients so that hopefully they don’t relapse, and hopefully we also can send a smaller number of patients to transplant.”
Two trials seek to address this, she said.
The A041501 study (NCT03150693) is comparing C10403 chemotherapy with C10403 induction followed by two cycles of inotuzumab before continuing with chemotherapy in adults under age 40 years with previously untreated B ALL.
The primary objective is improved 3-year event-free survival, she said, adding that minimal residual disease (MRD) testing will be used and that CD20-positive patients will receive rituximab, as is now standard.
The phase 3 E1910 study (NCT02003222) is evaluating up-front blinatumomab in patients aged 30-70 years with newly diagnosed BCR-ABL–negative B-lineage ALL. This trial was complicated by the recent approval of blinatumomab for MRD-positive disease, which rendered randomization of MRD-positive patients unethical. MRD-negative patients will be randomized, however.
“The hope is that, by incorporating blinatumomab up front, this will again improve outcomes for patients,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
CHICAGO – Novel antibodies are improving outcomes in relapsed and refractory acute lymphoblastic leukemia (ALL), and the hope is that they will also show benefit in the up-front treatment setting and thereby improve overall outcomes, according to Anjali Advani, MD.
“It has been a really exciting time in ALL because several drugs have now been FDA approved: blinatumomab, inotuzumab, and now – for patients who are less than 26 years of age – we actually have CAR [chimeric antigen receptor] T cells that have been approved,” Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic said at the American Society of Hematology Meeting on Hematologic Malignancies.
At the time of relapse, however, the only known cure is allogeneic bone marrow transplant. That may change as more data regarding CAR T cells become available, but the typical goal at this time is to get patients into remission and then to transplant, she said.
Blinatumomab
“Blinatumomab is a very interesting antibody,” Dr. Advani said, explaining that it is a bispecific, T cell–engaging antibody with an anti-CD3 arm that engages the T cell and an anti-CD19 antibody that engages the B lymphoblast.
“Basically this drug then acts as a bridge between the lymphoblast and the T cell to lead to proliferation of the cytotoxic T cell and apoptosis of the lymphoblast,” she said. “It’s interesting because it’s an antibody but it actually works through the immune system through the T cells.”
The largest study to date of blinatumomab in the relapsed/refractory ALL setting showed a 43% complete remission (CR) or CR with partial hematological recovery of peripheral blood counts (CRi) in 189 treated patients with Philadelphia chromosome–negative ALL. It also demonstrated and a 39% rate of salvage status 2 or higher, she said, noting that the response was impressive given that about 30% of participants had a prior transplant (Lancet. 2015 Jan 1;16[1]:57-66).
Of the responders, 40% went on to allogeneic transplant. This was a “fairly impressive” rate given the 30% prior-transplant rate, Dr. Advani said.
“There also was a high minimal residual disease response in those patients achieving CR,” she said, adding that the only significant predictor of response was bone marrow blast count; patients with 50% or more blasts in the bone marrow had a reduced likelihood of responding to blinatumomab.
The agent was approved by the Food and Drug Administration in December 2014 based on these phase 2 findings.
Adverse events mainly included toxicities that are expected in leukemia patients; the most frequent were febrile neutropenia, neutropenia, and anemia. Two patients developed cytokine release syndrome, and about half of the blinatumomab-treated patients experienced neurological events, although the majority of those were grade 1 or 2 and were easily manageable, she noted.
Blinatumomab was further evaluated in the phase 3 TOWER study (NCT02013167), which compared it with standard-of-care chemotherapy regimens. This study showed much higher response rates with blinatumomab than with the chemotherapy regimens (CR with full, partial, or incomplete hematologic recovery, 44% vs. 25%, respectively), Dr. Advani said (N Engl J Med. 2017 Mar 2;376[9]:836-47).
“The main things to remember [are that blinatumomab is] generally very well tolerated and it has been shown to be superior over standard chemotherapy,” she said. “I think it’s a very good drug to use as a bridge to transplant.”
One setting where blinatumomab perhaps should not be used is in patients with central nervous system disease, she noted.
“There is some concern, at least theoretically, that if you have to use concurrent intrathecal chemo along with blinatumomab, there could be some neurotoxicity,” Dr. Advani said, adding that there are no clear data in that setting because patients with CNS disease were not included in the trials.
Patients with high tumor burden may also be poor candidates for blinatumomab because they tend to have lower response rates.
“That doesn’t mean you can’t use it, but you have to kind of think about what the best option would be,” she said.
Additionally, patients treated with CAR T-cell therapy may develop CD19 loss or CD19-negative disease, and blinatumomab should be avoided in these patients.
“The nice thing ... is you don’t have to worry about veno-occlusive disease [VOD] in patients who are proceeding to transplant,” she said, explaining that no increased risk of VOD was seen in these trials.
Inotuzumab
Inotuzumab, which was approved in 2017, differs from blinatumomab in that it is an anti-CD22-calicheamicin conjugate; however, it also showed high response rates in the initial phase 2 trial in relapsed/refractory ALL. The overall response rate was 57%, with 18% achieving a complete response and 63% achieving complete molecular remission.
Of 49 treated patients, 22 patients proceeded to allogeneic transplant, and 5 of those developed VOD.
“Interestingly, four out of five of these patients had received a clofarabine-based preparative regimen, and this likely explains why there was a higher risk of VOD in this study,” she said, noting that the VOD risk has been lower in subsequent studies of inotuzumab.
The international INO-VATE ALL study (NCT01564784) that led to FDA approval was similar in design to the TOWER study in that it compared inotuzumab with standard chemotherapy regimens, and response rates were clearly higher (81% vs. 33%) with inotuzumab (N Engl J Med. 2016 Aug 25;375[8]:740-53).
The VOD risk in the INO-VATE trial was 11%, and it seemed to be higher in those who received dual alkylator–conditioning regimens, which are commonly used in Europe.
Longer-term outcomes after transplant in INO-VATE participants show that median survival has not been reached.
“It’s encouraging that with longer follow-up these patients actually look like they’re doing well,” Dr. Advani said, adding that inotuzumab is a good treatment option for relapsed patients with high disease burden or with CNS disease.
The continuous hookup required for this treatment may be problematic for some younger and older patients, but it is generally not an issue, she noted.
It is important, though, to give as few cycles prior to transplant as possible and to “really think about the preparative regimen to decrease the risk of VOD.”
CAR T-cell therapy
As for CAR T-cell therapy in the relapsed/refractory ALL setting, tisagenlecleucel was approved in 2017 for those up to age 25 years with B-cell precursor ALL that is refractory or in second or later relapse.
Approval was based on a single-arm trial of 63 patients with relapsed or refractory pediatric precursor B-cell ALL, including 35 patients who had prior transplant. The confirmed overall remission rate was 82%, with a 63% CR rate and 19% CRi rate.
“This is a very exciting area,” Dr. Advani said. “There are multiple trials being done in adults with ALL to really look at the older subgroup of patients.”
Overall outcomes
“These treatments we have now really seem to be effective in the relapse setting, but the problem is that once patients relapse and then go to transplant, their overall survival is still poor,” Dr. Advani said. “So the question is how can we improve the up-front treatment of patients so that hopefully they don’t relapse, and hopefully we also can send a smaller number of patients to transplant.”
Two trials seek to address this, she said.
The A041501 study (NCT03150693) is comparing C10403 chemotherapy with C10403 induction followed by two cycles of inotuzumab before continuing with chemotherapy in adults under age 40 years with previously untreated B ALL.
The primary objective is improved 3-year event-free survival, she said, adding that minimal residual disease (MRD) testing will be used and that CD20-positive patients will receive rituximab, as is now standard.
The phase 3 E1910 study (NCT02003222) is evaluating up-front blinatumomab in patients aged 30-70 years with newly diagnosed BCR-ABL–negative B-lineage ALL. This trial was complicated by the recent approval of blinatumomab for MRD-positive disease, which rendered randomization of MRD-positive patients unethical. MRD-negative patients will be randomized, however.
“The hope is that, by incorporating blinatumomab up front, this will again improve outcomes for patients,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
EXPERT ANALYSIS FROM MHM 2018
MCL treatment choices depend partly on age
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
EXPERT ANALYSIS FROM MHM 2018
Some mutation testing can be useful at CLL diagnosis
CHICAGO – A number of mutation tests – including immunoglobulin heavy chain gene (IgVH), fluorescence in situ hybridization (FISH), and TP53 – provide useful prognostic information at the time of chronic lymphocytic leukemia (CLL) diagnosis, according to Paul M. Barr, MD.
“It’s understood that IgVH mutation status is certainly prognostic,” Dr. Barr, associate professor of hematology/oncology at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
The B-cell receptor of the CLL cells uses IgVH genes that may or may not have undergone somatic mutations, with unmutated being defined as 98% or more sequence homology to germline.
“This is indicative of stronger signaling through the B-cell receptor and, as we all know, predicts for an inferior prognosis,” he explained, citing a study that demonstrated superior survival rates with mutated IgVH genes (Blood. 1999;94[6]:1840-7).
“It’s also well understood and accepted that we should perform a FISH panel; we should look for interphase cytogenetics based on FISH in our patients,” Dr. Barr said. “Having said that, we, as medical oncologists, do not do a very good job of using this testing appropriately. Patterns of care studies have suggested that a significant number of patients don’t get FISH testing at diagnosis or before first-line therapy.”
In fact, a typical interphase FISH panel identifies cytogenetic lesions, including del(17p), del(11q), del(13q), and trisomy 12 in more than 80% of CLL cases, with del(13q) being the most common.
Another marker that can be assessed in CLL patients and has maintained prognostic value across multiple analyses is serum beta-2 microglobulin, Dr. Barr noted.
TP53 sequencing is valuable as well and has been associated with outcomes similar to those seen in patients with del(17p), he said, citing data from a study that found similarly poor outcomes with TP53 mutations or deletions and del(17p), even when minor subclones are identified using next-generation sequencing (Blood. 2014;123:2139-47).
“One of the primary reasons for this is that the two aberrations go together. Most often, if you have del(17p) you’re also going to find a TP53 mutation, but in about 30% of patients or so, only one allele is affected, so this is why it’s still important to test for TP53 mutations when you’re looking for a 17p deletion,” he said.
Numerous other recurrent mutations in CLL have been associated with poor overall survival and/or progression-free survival, including SF3B1, ATM, NOTCH1, POT1, BIRC3, and NFKBIE.
“The gut instinct is that maybe we should start testing for all of these mutations now, but I would caution everybody that we still need further validation before we can apply these to the majority of patients,” Dr. Barr said. “We still don’t know exactly what to do with all of these mutations – when and how often we should test for them, if the novel agents are truly better – so while, again, they can predict for inferior outcomes, I would say these are not yet standard of care to be tested in all patients.”
It is likely, though, that new prognostic systems will evolve as more is learned about how to use these molecular aberrations. Attempts are already being made to incorporate novel mutations into a prognostic system. Dr. Barr pointed to a report that looked at the integration of mutations and cytogenetic lesions to improve the accuracy of survival prediction in CLL (Blood. 2013;121:1403-12).
“But this still requires prospective testing, especially in patients getting the novel agents,” he said.
Conventional karyotyping also has potential, though a limited role in this setting, he said, noting that it can be reliably performed with stimulation of CLL cells.
“We also know additional aberrations are prognostic and that a complex karyotype predicts for a very poor outcome,” he said. The International Workshop on CLL (iwCLL) guidelines, which were recently updated for the first time in a decade, state that further validation is needed.
“I think it’s potentially useful in a very young patient you are considering taking to transplant, but again, I agree with the stance that this is not something that should be performed in every patient across the board,” he said.
The tests currently recommended by iwCLL before CLL treatment include IgVH mutation status; FISH for del(13q), del(11q), del(17p), and trisomy 12 in peripheral blood lymphocytes; and TP53.
“Some folks... don’t check a lot of these markers at diagnosis, but wait for patients to require therapy, and that’s a reasonable way to practice,” Dr. Barr said, noting, however, that he prefers knowing patients’ risk up front – especially for those patients he will see just once before they are “managed closer to home for the majority of their course.
“But if you [wait], then knowing what to repeat later is important,” he added. Namely, the FISH and TP53 tests are worth repeating as patients can acquire additional molecular aberrations over time.
Dr. Barr reported serving as a consultant for Pharmacyclics, AbbVie, Celgene, Gilead Sciences, Infinity Pharmaceuticals, Novartis, and Seattle Genetics. He also reported receiving research funding from Pharmacyclics and AbbVie.
CHICAGO – A number of mutation tests – including immunoglobulin heavy chain gene (IgVH), fluorescence in situ hybridization (FISH), and TP53 – provide useful prognostic information at the time of chronic lymphocytic leukemia (CLL) diagnosis, according to Paul M. Barr, MD.
“It’s understood that IgVH mutation status is certainly prognostic,” Dr. Barr, associate professor of hematology/oncology at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
The B-cell receptor of the CLL cells uses IgVH genes that may or may not have undergone somatic mutations, with unmutated being defined as 98% or more sequence homology to germline.
“This is indicative of stronger signaling through the B-cell receptor and, as we all know, predicts for an inferior prognosis,” he explained, citing a study that demonstrated superior survival rates with mutated IgVH genes (Blood. 1999;94[6]:1840-7).
“It’s also well understood and accepted that we should perform a FISH panel; we should look for interphase cytogenetics based on FISH in our patients,” Dr. Barr said. “Having said that, we, as medical oncologists, do not do a very good job of using this testing appropriately. Patterns of care studies have suggested that a significant number of patients don’t get FISH testing at diagnosis or before first-line therapy.”
In fact, a typical interphase FISH panel identifies cytogenetic lesions, including del(17p), del(11q), del(13q), and trisomy 12 in more than 80% of CLL cases, with del(13q) being the most common.
Another marker that can be assessed in CLL patients and has maintained prognostic value across multiple analyses is serum beta-2 microglobulin, Dr. Barr noted.
TP53 sequencing is valuable as well and has been associated with outcomes similar to those seen in patients with del(17p), he said, citing data from a study that found similarly poor outcomes with TP53 mutations or deletions and del(17p), even when minor subclones are identified using next-generation sequencing (Blood. 2014;123:2139-47).
“One of the primary reasons for this is that the two aberrations go together. Most often, if you have del(17p) you’re also going to find a TP53 mutation, but in about 30% of patients or so, only one allele is affected, so this is why it’s still important to test for TP53 mutations when you’re looking for a 17p deletion,” he said.
Numerous other recurrent mutations in CLL have been associated with poor overall survival and/or progression-free survival, including SF3B1, ATM, NOTCH1, POT1, BIRC3, and NFKBIE.
“The gut instinct is that maybe we should start testing for all of these mutations now, but I would caution everybody that we still need further validation before we can apply these to the majority of patients,” Dr. Barr said. “We still don’t know exactly what to do with all of these mutations – when and how often we should test for them, if the novel agents are truly better – so while, again, they can predict for inferior outcomes, I would say these are not yet standard of care to be tested in all patients.”
It is likely, though, that new prognostic systems will evolve as more is learned about how to use these molecular aberrations. Attempts are already being made to incorporate novel mutations into a prognostic system. Dr. Barr pointed to a report that looked at the integration of mutations and cytogenetic lesions to improve the accuracy of survival prediction in CLL (Blood. 2013;121:1403-12).
“But this still requires prospective testing, especially in patients getting the novel agents,” he said.
Conventional karyotyping also has potential, though a limited role in this setting, he said, noting that it can be reliably performed with stimulation of CLL cells.
“We also know additional aberrations are prognostic and that a complex karyotype predicts for a very poor outcome,” he said. The International Workshop on CLL (iwCLL) guidelines, which were recently updated for the first time in a decade, state that further validation is needed.
“I think it’s potentially useful in a very young patient you are considering taking to transplant, but again, I agree with the stance that this is not something that should be performed in every patient across the board,” he said.
The tests currently recommended by iwCLL before CLL treatment include IgVH mutation status; FISH for del(13q), del(11q), del(17p), and trisomy 12 in peripheral blood lymphocytes; and TP53.
“Some folks... don’t check a lot of these markers at diagnosis, but wait for patients to require therapy, and that’s a reasonable way to practice,” Dr. Barr said, noting, however, that he prefers knowing patients’ risk up front – especially for those patients he will see just once before they are “managed closer to home for the majority of their course.
“But if you [wait], then knowing what to repeat later is important,” he added. Namely, the FISH and TP53 tests are worth repeating as patients can acquire additional molecular aberrations over time.
Dr. Barr reported serving as a consultant for Pharmacyclics, AbbVie, Celgene, Gilead Sciences, Infinity Pharmaceuticals, Novartis, and Seattle Genetics. He also reported receiving research funding from Pharmacyclics and AbbVie.
CHICAGO – A number of mutation tests – including immunoglobulin heavy chain gene (IgVH), fluorescence in situ hybridization (FISH), and TP53 – provide useful prognostic information at the time of chronic lymphocytic leukemia (CLL) diagnosis, according to Paul M. Barr, MD.
“It’s understood that IgVH mutation status is certainly prognostic,” Dr. Barr, associate professor of hematology/oncology at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
The B-cell receptor of the CLL cells uses IgVH genes that may or may not have undergone somatic mutations, with unmutated being defined as 98% or more sequence homology to germline.
“This is indicative of stronger signaling through the B-cell receptor and, as we all know, predicts for an inferior prognosis,” he explained, citing a study that demonstrated superior survival rates with mutated IgVH genes (Blood. 1999;94[6]:1840-7).
“It’s also well understood and accepted that we should perform a FISH panel; we should look for interphase cytogenetics based on FISH in our patients,” Dr. Barr said. “Having said that, we, as medical oncologists, do not do a very good job of using this testing appropriately. Patterns of care studies have suggested that a significant number of patients don’t get FISH testing at diagnosis or before first-line therapy.”
In fact, a typical interphase FISH panel identifies cytogenetic lesions, including del(17p), del(11q), del(13q), and trisomy 12 in more than 80% of CLL cases, with del(13q) being the most common.
Another marker that can be assessed in CLL patients and has maintained prognostic value across multiple analyses is serum beta-2 microglobulin, Dr. Barr noted.
TP53 sequencing is valuable as well and has been associated with outcomes similar to those seen in patients with del(17p), he said, citing data from a study that found similarly poor outcomes with TP53 mutations or deletions and del(17p), even when minor subclones are identified using next-generation sequencing (Blood. 2014;123:2139-47).
“One of the primary reasons for this is that the two aberrations go together. Most often, if you have del(17p) you’re also going to find a TP53 mutation, but in about 30% of patients or so, only one allele is affected, so this is why it’s still important to test for TP53 mutations when you’re looking for a 17p deletion,” he said.
Numerous other recurrent mutations in CLL have been associated with poor overall survival and/or progression-free survival, including SF3B1, ATM, NOTCH1, POT1, BIRC3, and NFKBIE.
“The gut instinct is that maybe we should start testing for all of these mutations now, but I would caution everybody that we still need further validation before we can apply these to the majority of patients,” Dr. Barr said. “We still don’t know exactly what to do with all of these mutations – when and how often we should test for them, if the novel agents are truly better – so while, again, they can predict for inferior outcomes, I would say these are not yet standard of care to be tested in all patients.”
It is likely, though, that new prognostic systems will evolve as more is learned about how to use these molecular aberrations. Attempts are already being made to incorporate novel mutations into a prognostic system. Dr. Barr pointed to a report that looked at the integration of mutations and cytogenetic lesions to improve the accuracy of survival prediction in CLL (Blood. 2013;121:1403-12).
“But this still requires prospective testing, especially in patients getting the novel agents,” he said.
Conventional karyotyping also has potential, though a limited role in this setting, he said, noting that it can be reliably performed with stimulation of CLL cells.
“We also know additional aberrations are prognostic and that a complex karyotype predicts for a very poor outcome,” he said. The International Workshop on CLL (iwCLL) guidelines, which were recently updated for the first time in a decade, state that further validation is needed.
“I think it’s potentially useful in a very young patient you are considering taking to transplant, but again, I agree with the stance that this is not something that should be performed in every patient across the board,” he said.
The tests currently recommended by iwCLL before CLL treatment include IgVH mutation status; FISH for del(13q), del(11q), del(17p), and trisomy 12 in peripheral blood lymphocytes; and TP53.
“Some folks... don’t check a lot of these markers at diagnosis, but wait for patients to require therapy, and that’s a reasonable way to practice,” Dr. Barr said, noting, however, that he prefers knowing patients’ risk up front – especially for those patients he will see just once before they are “managed closer to home for the majority of their course.
“But if you [wait], then knowing what to repeat later is important,” he added. Namely, the FISH and TP53 tests are worth repeating as patients can acquire additional molecular aberrations over time.
Dr. Barr reported serving as a consultant for Pharmacyclics, AbbVie, Celgene, Gilead Sciences, Infinity Pharmaceuticals, Novartis, and Seattle Genetics. He also reported receiving research funding from Pharmacyclics and AbbVie.
EXPERT ANALYSIS FROM MHM 2018
Prognostic factors guide mantle cell treatment decisions
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
REPORTING FROM MHM 2018