User login
Early phase III data positive for adalimumab biosimilar, for both psoriasis and PsA
MADRID – To date, an adalimumab biosimilar has proven itself in a large, phase III trial of patients with psoriasis, including a subset with mild to moderate psoriatic arthritis (PsA).
The biosimilar, known as CHS-1420, cleared psoriatic plaques and improved health-related quality of life just as well as adalimumab after 12 weeks of treatment, Barbara Finck, MD, said at the European Congress of Rheumatology. It also suppressed high-sensitivity C-reactive protein (CRP) as well as the originator molecule, she said.
Dr. Finck, the chief medical officer of Coherus Biosciences, the developer of CHS-1420, reported results from the first 16-week phase of the 48-week study. Data are still to come on a 6-week period during which half those taking adalimumab switched to CHS-1420 in a blinded fashion, and 26 weeks of open-label CHS-1420 for all patients.
The study’s primary endpoint was a 75% reduction in the Psoriasis Area and Severity Index (PASI) score (PASI 75) Two additional endpoints were evaluated in patients with PsA: change in the Health Assessment Questionnaire-Disability Index (HAQ-DI) and changes in CRP.
Dr. Finck bemoaned the lack of the clinical rheumatologic endpoint, tender and swollen joint count. “I advocated for this but was unable to convince our dermatology colleagues” to conduct this exam, she said. “I think we have a ways to go to educate our colleagues in this regard.”
The study comprised 545 patients with mild to moderate psoriasis; of these, 127 had PsA. They received subcutaneous injections of either CHS-1420 or adalimumab at identical doses (80 mg at week 1, followed by 40 mg every other week). They were a mean of 44 years o
In the entire study population, treatment with CHS-1420 and adalimumab followed almost identical response curves. By week 4, 22% of the CHS-1420 group and 20% of the adalimumab group had reached a PASI75 response. By week 8, those numbers were 57% and 61%, respectively, and by week 12, they were 69% and 72% – not significantly different.
Response was similar in the subgroup of PsA patients: By week 12, 82% of the CHS-1420 group and 77% of the adalimumab group had reached a PASI 75. PsA patients also responded equally well to both medications on the HAQ-DI by week 12. At baseline, the mean HAQ-DI was about 1 in each group. At 12 weeks, it was reduced by about half a point in both groups. High-sensitivity CRP decreased similarly in the CHS-1420 and adalimumab groups as well (reductions of 8.9 mg/L and 6.3 mg/L, respectively).
Adalimumab, a tumor necrosis factor blocker, is a highly immunogenic molecule, and as such, many patients developed antibodies to both it and to CHS-1420. By week 12, 84% of both treatment groups had developed anti-drug antibodies and 32%, neutralizing antibodies. Among those with PsA, 82% taking CHS-1420 and 88% of those taking adalimumab developed antidrug antibodies. Neutralizing antibodies developed in 33% and 30%, respectively. Neither of these differences was statistically significant.
Other adverse events were similar, Dr. Finck noted. These included nasopharyngitis (9% of both groups), upper respiratory tract infection (6%), injection site reaction (4%), headache (3%), and worsening of psoriasis (1% for CHS-1420, and 3% for adalimumab).
If the switching study data are similarly positive, Coherus expects to file a Biologics License Application with the Food and Drug Administration in early 2018, Dr. Finck said.
[email protected]
On Twitter @Alz_gal
MADRID – To date, an adalimumab biosimilar has proven itself in a large, phase III trial of patients with psoriasis, including a subset with mild to moderate psoriatic arthritis (PsA).
The biosimilar, known as CHS-1420, cleared psoriatic plaques and improved health-related quality of life just as well as adalimumab after 12 weeks of treatment, Barbara Finck, MD, said at the European Congress of Rheumatology. It also suppressed high-sensitivity C-reactive protein (CRP) as well as the originator molecule, she said.
Dr. Finck, the chief medical officer of Coherus Biosciences, the developer of CHS-1420, reported results from the first 16-week phase of the 48-week study. Data are still to come on a 6-week period during which half those taking adalimumab switched to CHS-1420 in a blinded fashion, and 26 weeks of open-label CHS-1420 for all patients.
The study’s primary endpoint was a 75% reduction in the Psoriasis Area and Severity Index (PASI) score (PASI 75) Two additional endpoints were evaluated in patients with PsA: change in the Health Assessment Questionnaire-Disability Index (HAQ-DI) and changes in CRP.
Dr. Finck bemoaned the lack of the clinical rheumatologic endpoint, tender and swollen joint count. “I advocated for this but was unable to convince our dermatology colleagues” to conduct this exam, she said. “I think we have a ways to go to educate our colleagues in this regard.”
The study comprised 545 patients with mild to moderate psoriasis; of these, 127 had PsA. They received subcutaneous injections of either CHS-1420 or adalimumab at identical doses (80 mg at week 1, followed by 40 mg every other week). They were a mean of 44 years o
In the entire study population, treatment with CHS-1420 and adalimumab followed almost identical response curves. By week 4, 22% of the CHS-1420 group and 20% of the adalimumab group had reached a PASI75 response. By week 8, those numbers were 57% and 61%, respectively, and by week 12, they were 69% and 72% – not significantly different.
Response was similar in the subgroup of PsA patients: By week 12, 82% of the CHS-1420 group and 77% of the adalimumab group had reached a PASI 75. PsA patients also responded equally well to both medications on the HAQ-DI by week 12. At baseline, the mean HAQ-DI was about 1 in each group. At 12 weeks, it was reduced by about half a point in both groups. High-sensitivity CRP decreased similarly in the CHS-1420 and adalimumab groups as well (reductions of 8.9 mg/L and 6.3 mg/L, respectively).
Adalimumab, a tumor necrosis factor blocker, is a highly immunogenic molecule, and as such, many patients developed antibodies to both it and to CHS-1420. By week 12, 84% of both treatment groups had developed anti-drug antibodies and 32%, neutralizing antibodies. Among those with PsA, 82% taking CHS-1420 and 88% of those taking adalimumab developed antidrug antibodies. Neutralizing antibodies developed in 33% and 30%, respectively. Neither of these differences was statistically significant.
Other adverse events were similar, Dr. Finck noted. These included nasopharyngitis (9% of both groups), upper respiratory tract infection (6%), injection site reaction (4%), headache (3%), and worsening of psoriasis (1% for CHS-1420, and 3% for adalimumab).
If the switching study data are similarly positive, Coherus expects to file a Biologics License Application with the Food and Drug Administration in early 2018, Dr. Finck said.
[email protected]
On Twitter @Alz_gal
MADRID – To date, an adalimumab biosimilar has proven itself in a large, phase III trial of patients with psoriasis, including a subset with mild to moderate psoriatic arthritis (PsA).
The biosimilar, known as CHS-1420, cleared psoriatic plaques and improved health-related quality of life just as well as adalimumab after 12 weeks of treatment, Barbara Finck, MD, said at the European Congress of Rheumatology. It also suppressed high-sensitivity C-reactive protein (CRP) as well as the originator molecule, she said.
Dr. Finck, the chief medical officer of Coherus Biosciences, the developer of CHS-1420, reported results from the first 16-week phase of the 48-week study. Data are still to come on a 6-week period during which half those taking adalimumab switched to CHS-1420 in a blinded fashion, and 26 weeks of open-label CHS-1420 for all patients.
The study’s primary endpoint was a 75% reduction in the Psoriasis Area and Severity Index (PASI) score (PASI 75) Two additional endpoints were evaluated in patients with PsA: change in the Health Assessment Questionnaire-Disability Index (HAQ-DI) and changes in CRP.
Dr. Finck bemoaned the lack of the clinical rheumatologic endpoint, tender and swollen joint count. “I advocated for this but was unable to convince our dermatology colleagues” to conduct this exam, she said. “I think we have a ways to go to educate our colleagues in this regard.”
The study comprised 545 patients with mild to moderate psoriasis; of these, 127 had PsA. They received subcutaneous injections of either CHS-1420 or adalimumab at identical doses (80 mg at week 1, followed by 40 mg every other week). They were a mean of 44 years o
In the entire study population, treatment with CHS-1420 and adalimumab followed almost identical response curves. By week 4, 22% of the CHS-1420 group and 20% of the adalimumab group had reached a PASI75 response. By week 8, those numbers were 57% and 61%, respectively, and by week 12, they were 69% and 72% – not significantly different.
Response was similar in the subgroup of PsA patients: By week 12, 82% of the CHS-1420 group and 77% of the adalimumab group had reached a PASI 75. PsA patients also responded equally well to both medications on the HAQ-DI by week 12. At baseline, the mean HAQ-DI was about 1 in each group. At 12 weeks, it was reduced by about half a point in both groups. High-sensitivity CRP decreased similarly in the CHS-1420 and adalimumab groups as well (reductions of 8.9 mg/L and 6.3 mg/L, respectively).
Adalimumab, a tumor necrosis factor blocker, is a highly immunogenic molecule, and as such, many patients developed antibodies to both it and to CHS-1420. By week 12, 84% of both treatment groups had developed anti-drug antibodies and 32%, neutralizing antibodies. Among those with PsA, 82% taking CHS-1420 and 88% of those taking adalimumab developed antidrug antibodies. Neutralizing antibodies developed in 33% and 30%, respectively. Neither of these differences was statistically significant.
Other adverse events were similar, Dr. Finck noted. These included nasopharyngitis (9% of both groups), upper respiratory tract infection (6%), injection site reaction (4%), headache (3%), and worsening of psoriasis (1% for CHS-1420, and 3% for adalimumab).
If the switching study data are similarly positive, Coherus expects to file a Biologics License Application with the Food and Drug Administration in early 2018, Dr. Finck said.
[email protected]
On Twitter @Alz_gal
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: By week 12, 69% of those who received CHS-1420 and 72% of those who received adalimumab had reached a PASI75, response rates that were not significantly different.
Data source: The phase III trial randomized 545 patients with psoriasis, including 127 with PsA, to treatment with adalimumab or the biosimilar.
Disclosures: Dr. Finck is chief medical officer of Coherus Biosciences, which is developing CHS-1420.
Nurses help more rheumatic disease patients get vaccinated
MADRID – A nurse-led program successfully increased the uptake of pneumococcal vaccination among patients with chronic inflammatory rheumatic diseases in a single-center study.
From the start to the end of a 4-month evaluation period, the rate of vaccination of at-risk patients increased from 17.1% (13/76) to 77.6% (59/76; P less than .001).
It is well known that patients with inflammatory rheumatic diseases, such as systemic lupus erythematous (SLE) and systemic vasculitis, are at high risk for contracting pneumococcal disease, reported Tiphaine Goulenok, MD, of Bichat Hospital, Paris, at the European Congress of Rheumatology. This is particularly the case if they are receiving immunosuppressive treatments.
Although French national guidelines were introduced in 2011 that recommend that such patients routinely receive pneumococcal vaccination, the vaccination rate is often lower than is desirable, Dr. Goulenok observed at a press briefing. Her prior research suggests that only 16.2% of patients with an indication for the PCV13 vaccine actually received it.
In the current study, 126 patients with inflammatory rheumatic diseases were consecutively recruited and seen at the day unit of Bichat Hospital. Of these patients, 76 were candidates for pneumococcal vaccination because they were receiving steroids or other immunosuppressive drugs. Of these patients, 13 were already vaccinated, and, of the 63 who were not, nurses correctly identified 56 (88.9%) who needed to be vaccinated, of whom 46 agreed and 10 refused.
“We found a low rate of pneumococcal vaccination among patients,” said Dr. Goulenok, “but, thanks to high screening by the nurses, vaccination coverage was increased and the nurse-led vaccination program was very efficient”.
Robert Landewé, MD, who chaired the press briefing, observed that, despite being in an “era of guidelines,” ways of successfully implementing them in practice remained a challenge. The nurse-led program appeared to be one way to increase pneumococcal vaccination uptake, but perhaps other ways need to be sought, especially as there may be substantial resistance to vaccination among patients, he said.
“Patients are sometimes more afraid of the consequences of vaccination than [of] the disease that is prevented by vaccination,” said Dr. Landewé, who is professor of rheumatology at the Academic Medical Center in Amsterdam (the Netherlands).
Dr. Goulenok and Dr. Landewé reported no disclosures.
MADRID – A nurse-led program successfully increased the uptake of pneumococcal vaccination among patients with chronic inflammatory rheumatic diseases in a single-center study.
From the start to the end of a 4-month evaluation period, the rate of vaccination of at-risk patients increased from 17.1% (13/76) to 77.6% (59/76; P less than .001).
It is well known that patients with inflammatory rheumatic diseases, such as systemic lupus erythematous (SLE) and systemic vasculitis, are at high risk for contracting pneumococcal disease, reported Tiphaine Goulenok, MD, of Bichat Hospital, Paris, at the European Congress of Rheumatology. This is particularly the case if they are receiving immunosuppressive treatments.
Although French national guidelines were introduced in 2011 that recommend that such patients routinely receive pneumococcal vaccination, the vaccination rate is often lower than is desirable, Dr. Goulenok observed at a press briefing. Her prior research suggests that only 16.2% of patients with an indication for the PCV13 vaccine actually received it.
In the current study, 126 patients with inflammatory rheumatic diseases were consecutively recruited and seen at the day unit of Bichat Hospital. Of these patients, 76 were candidates for pneumococcal vaccination because they were receiving steroids or other immunosuppressive drugs. Of these patients, 13 were already vaccinated, and, of the 63 who were not, nurses correctly identified 56 (88.9%) who needed to be vaccinated, of whom 46 agreed and 10 refused.
“We found a low rate of pneumococcal vaccination among patients,” said Dr. Goulenok, “but, thanks to high screening by the nurses, vaccination coverage was increased and the nurse-led vaccination program was very efficient”.
Robert Landewé, MD, who chaired the press briefing, observed that, despite being in an “era of guidelines,” ways of successfully implementing them in practice remained a challenge. The nurse-led program appeared to be one way to increase pneumococcal vaccination uptake, but perhaps other ways need to be sought, especially as there may be substantial resistance to vaccination among patients, he said.
“Patients are sometimes more afraid of the consequences of vaccination than [of] the disease that is prevented by vaccination,” said Dr. Landewé, who is professor of rheumatology at the Academic Medical Center in Amsterdam (the Netherlands).
Dr. Goulenok and Dr. Landewé reported no disclosures.
MADRID – A nurse-led program successfully increased the uptake of pneumococcal vaccination among patients with chronic inflammatory rheumatic diseases in a single-center study.
From the start to the end of a 4-month evaluation period, the rate of vaccination of at-risk patients increased from 17.1% (13/76) to 77.6% (59/76; P less than .001).
It is well known that patients with inflammatory rheumatic diseases, such as systemic lupus erythematous (SLE) and systemic vasculitis, are at high risk for contracting pneumococcal disease, reported Tiphaine Goulenok, MD, of Bichat Hospital, Paris, at the European Congress of Rheumatology. This is particularly the case if they are receiving immunosuppressive treatments.
Although French national guidelines were introduced in 2011 that recommend that such patients routinely receive pneumococcal vaccination, the vaccination rate is often lower than is desirable, Dr. Goulenok observed at a press briefing. Her prior research suggests that only 16.2% of patients with an indication for the PCV13 vaccine actually received it.
In the current study, 126 patients with inflammatory rheumatic diseases were consecutively recruited and seen at the day unit of Bichat Hospital. Of these patients, 76 were candidates for pneumococcal vaccination because they were receiving steroids or other immunosuppressive drugs. Of these patients, 13 were already vaccinated, and, of the 63 who were not, nurses correctly identified 56 (88.9%) who needed to be vaccinated, of whom 46 agreed and 10 refused.
“We found a low rate of pneumococcal vaccination among patients,” said Dr. Goulenok, “but, thanks to high screening by the nurses, vaccination coverage was increased and the nurse-led vaccination program was very efficient”.
Robert Landewé, MD, who chaired the press briefing, observed that, despite being in an “era of guidelines,” ways of successfully implementing them in practice remained a challenge. The nurse-led program appeared to be one way to increase pneumococcal vaccination uptake, but perhaps other ways need to be sought, especially as there may be substantial resistance to vaccination among patients, he said.
“Patients are sometimes more afraid of the consequences of vaccination than [of] the disease that is prevented by vaccination,” said Dr. Landewé, who is professor of rheumatology at the Academic Medical Center in Amsterdam (the Netherlands).
Dr. Goulenok and Dr. Landewé reported no disclosures.
AT THE EULAR 2017 CONGRESS
Key clinical point: A nurse-led program increased the uptake of a guideline-recommended vaccination in patients with chronic inflammatory rheumatic diseases.
Major finding: The pre- and postintervention pneumococcal vaccination rates were 17.1% (13/76) and 77.6% (59/76) of at-risk patients (P less than .001).
Data source: A 4-month, prospective pilot study of 126 consecutively recruited patients with chronic inflammatory rheumatic diseases.
Disclosures: The presenter and commentator had no disclosures to report.
Study validates EULAR definition of arthralgia suspicious for progression to RA
Results of a longitudinal study have confirmed that the recently established EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis can help to distinguish patients who are at highest risk for progression from those who do not progress to RA.
Patients clinically suspected of arthralgia who met the definition for arthralgia suspicious for progression to RA displayed an increased risk for arthritis development, compared with patients who did not meet the EULAR definition (hazard ratio, 2.1; 95% confidence interval, 0.9-4.7). The approach had a sensitivity of 83% and positive predictive value of 30%, study head Annette van der Helm–van Mil, MD, reported at the European Congress of Rheumatology in Madrid.
The findings should help investigators looking at early arthritis progression to design better clinical trials by enabling more homogeneous populations of patients to be included, said Dr. van der Helm–van Mil, professor of rheumatology at Leiden University Medical Center and at Erasmus Medical Center in Rotterdam, both in the Netherlands.
“Previous data have shown that rheumatologists do recognize patients at risk for RA based on their clinical expertise and pattern recognition. So, they do recognize patients who have a combination of clinical characteristics that characterize the symptomatic prearthritis stage of RA. (This pattern is also called clinically suspect arthralgia,)” Dr. van der Helm–van Mil said in an interview.
However, the disadvantage of rheumatologists’ use of pattern recognition to identify patients at risk for RA is that it can be subjective, she said.
Several proof-of-concept trials are testing the hypothesis that the disease is more susceptible to disease-modifying treatment in the symptomatic prearthritis phase and that such early treatment might even prevent progression to chronic RA. But, selecting the “correct symptomatic patient” for early treatment with disease-modifying antirheumatic drugs is important, she said. Such a patient does not have clinical arthritis but is truly at risk for RA. Not all arthralgia patients are similar, and the type of arthralgia that is the hallmark for a heightened risk of progression to RA had not been defined formally prior to the EULAR definition.
A EULAR task force sought to provide some objective clarity by defining arthralgia at risk for RA (Ann Rheum Dis. 2017;76:491-6). The process relied on clinical expertise at all stages. However, until now, the definition had not been validated longitudinally. The current study used progression from arthralgia to clinical arthritis or RA as the outcome.
The definition of arthralgia at risk for RA hinges on seven parameters: symptom duration less than 1 year, symptoms in metacarpophalangeal joints, morning stiffness lasting an hour or more, symptoms that are worst in the morning, family history of RA, difficulty forming a fist, and positive squeeze test of metacarpophalangeal joints.
The researchers used those seven parameters to follow 241 Dutch patients considered likely to develop RA and 113 patients with recent-onset arthralgia in small joints who had not been evaluated by rheumatologists and who were referred to secondary care.
“The EULAR definition was developed for use in scientific studies and this definition is immediately applicable for this purpose,” Dr. van der Helm–van Mil said.
“With regards to application in daily practice, the clinical definition should be combined with results of additional investigations to accurately identify imminent RA in the phase of arthralgia. Which combination of markers yields the best accuracy is a subject for further studies,” Dr. van der Helm–van Mil said.
An important aspect of the task force’s definition is that rheumatologists should use it in patients in whom they consider imminent RA more likely than other diagnoses. The definition was not discriminative for RA when the investigators of the current study ignored this entry criterion, leading to a sensitivity of just 10% and positive predictive value of 3%.
“This suggests that the definition should be used in secondary care but may not be useful in primary care. However, more research is needed here,” Dr. van der Helm–van Mil said.
The authors reported no disclosures of interest.
Results of a longitudinal study have confirmed that the recently established EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis can help to distinguish patients who are at highest risk for progression from those who do not progress to RA.
Patients clinically suspected of arthralgia who met the definition for arthralgia suspicious for progression to RA displayed an increased risk for arthritis development, compared with patients who did not meet the EULAR definition (hazard ratio, 2.1; 95% confidence interval, 0.9-4.7). The approach had a sensitivity of 83% and positive predictive value of 30%, study head Annette van der Helm–van Mil, MD, reported at the European Congress of Rheumatology in Madrid.
The findings should help investigators looking at early arthritis progression to design better clinical trials by enabling more homogeneous populations of patients to be included, said Dr. van der Helm–van Mil, professor of rheumatology at Leiden University Medical Center and at Erasmus Medical Center in Rotterdam, both in the Netherlands.
“Previous data have shown that rheumatologists do recognize patients at risk for RA based on their clinical expertise and pattern recognition. So, they do recognize patients who have a combination of clinical characteristics that characterize the symptomatic prearthritis stage of RA. (This pattern is also called clinically suspect arthralgia,)” Dr. van der Helm–van Mil said in an interview.
However, the disadvantage of rheumatologists’ use of pattern recognition to identify patients at risk for RA is that it can be subjective, she said.
Several proof-of-concept trials are testing the hypothesis that the disease is more susceptible to disease-modifying treatment in the symptomatic prearthritis phase and that such early treatment might even prevent progression to chronic RA. But, selecting the “correct symptomatic patient” for early treatment with disease-modifying antirheumatic drugs is important, she said. Such a patient does not have clinical arthritis but is truly at risk for RA. Not all arthralgia patients are similar, and the type of arthralgia that is the hallmark for a heightened risk of progression to RA had not been defined formally prior to the EULAR definition.
A EULAR task force sought to provide some objective clarity by defining arthralgia at risk for RA (Ann Rheum Dis. 2017;76:491-6). The process relied on clinical expertise at all stages. However, until now, the definition had not been validated longitudinally. The current study used progression from arthralgia to clinical arthritis or RA as the outcome.
The definition of arthralgia at risk for RA hinges on seven parameters: symptom duration less than 1 year, symptoms in metacarpophalangeal joints, morning stiffness lasting an hour or more, symptoms that are worst in the morning, family history of RA, difficulty forming a fist, and positive squeeze test of metacarpophalangeal joints.
The researchers used those seven parameters to follow 241 Dutch patients considered likely to develop RA and 113 patients with recent-onset arthralgia in small joints who had not been evaluated by rheumatologists and who were referred to secondary care.
“The EULAR definition was developed for use in scientific studies and this definition is immediately applicable for this purpose,” Dr. van der Helm–van Mil said.
“With regards to application in daily practice, the clinical definition should be combined with results of additional investigations to accurately identify imminent RA in the phase of arthralgia. Which combination of markers yields the best accuracy is a subject for further studies,” Dr. van der Helm–van Mil said.
An important aspect of the task force’s definition is that rheumatologists should use it in patients in whom they consider imminent RA more likely than other diagnoses. The definition was not discriminative for RA when the investigators of the current study ignored this entry criterion, leading to a sensitivity of just 10% and positive predictive value of 3%.
“This suggests that the definition should be used in secondary care but may not be useful in primary care. However, more research is needed here,” Dr. van der Helm–van Mil said.
The authors reported no disclosures of interest.
Results of a longitudinal study have confirmed that the recently established EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis can help to distinguish patients who are at highest risk for progression from those who do not progress to RA.
Patients clinically suspected of arthralgia who met the definition for arthralgia suspicious for progression to RA displayed an increased risk for arthritis development, compared with patients who did not meet the EULAR definition (hazard ratio, 2.1; 95% confidence interval, 0.9-4.7). The approach had a sensitivity of 83% and positive predictive value of 30%, study head Annette van der Helm–van Mil, MD, reported at the European Congress of Rheumatology in Madrid.
The findings should help investigators looking at early arthritis progression to design better clinical trials by enabling more homogeneous populations of patients to be included, said Dr. van der Helm–van Mil, professor of rheumatology at Leiden University Medical Center and at Erasmus Medical Center in Rotterdam, both in the Netherlands.
“Previous data have shown that rheumatologists do recognize patients at risk for RA based on their clinical expertise and pattern recognition. So, they do recognize patients who have a combination of clinical characteristics that characterize the symptomatic prearthritis stage of RA. (This pattern is also called clinically suspect arthralgia,)” Dr. van der Helm–van Mil said in an interview.
However, the disadvantage of rheumatologists’ use of pattern recognition to identify patients at risk for RA is that it can be subjective, she said.
Several proof-of-concept trials are testing the hypothesis that the disease is more susceptible to disease-modifying treatment in the symptomatic prearthritis phase and that such early treatment might even prevent progression to chronic RA. But, selecting the “correct symptomatic patient” for early treatment with disease-modifying antirheumatic drugs is important, she said. Such a patient does not have clinical arthritis but is truly at risk for RA. Not all arthralgia patients are similar, and the type of arthralgia that is the hallmark for a heightened risk of progression to RA had not been defined formally prior to the EULAR definition.
A EULAR task force sought to provide some objective clarity by defining arthralgia at risk for RA (Ann Rheum Dis. 2017;76:491-6). The process relied on clinical expertise at all stages. However, until now, the definition had not been validated longitudinally. The current study used progression from arthralgia to clinical arthritis or RA as the outcome.
The definition of arthralgia at risk for RA hinges on seven parameters: symptom duration less than 1 year, symptoms in metacarpophalangeal joints, morning stiffness lasting an hour or more, symptoms that are worst in the morning, family history of RA, difficulty forming a fist, and positive squeeze test of metacarpophalangeal joints.
The researchers used those seven parameters to follow 241 Dutch patients considered likely to develop RA and 113 patients with recent-onset arthralgia in small joints who had not been evaluated by rheumatologists and who were referred to secondary care.
“The EULAR definition was developed for use in scientific studies and this definition is immediately applicable for this purpose,” Dr. van der Helm–van Mil said.
“With regards to application in daily practice, the clinical definition should be combined with results of additional investigations to accurately identify imminent RA in the phase of arthralgia. Which combination of markers yields the best accuracy is a subject for further studies,” Dr. van der Helm–van Mil said.
An important aspect of the task force’s definition is that rheumatologists should use it in patients in whom they consider imminent RA more likely than other diagnoses. The definition was not discriminative for RA when the investigators of the current study ignored this entry criterion, leading to a sensitivity of just 10% and positive predictive value of 3%.
“This suggests that the definition should be used in secondary care but may not be useful in primary care. However, more research is needed here,” Dr. van der Helm–van Mil said.
The authors reported no disclosures of interest.
FROM THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: Patients clinically suspected of arthralgia who met the EULAR definition were twice as likely to develop RA at 2 years than were those who did not meet the definition (hazard ratio, 2.1; 95% confidence interval, 0.9–4.7).
Data source: Longitudinal study of 241 patients considered likely to develop RA and 113 patients with recent-onset arthralgia in small joints who had not been evaluated by rheumatologists and who were referred to secondary care.
Disclosures: The authors reported no disclosures of interest.
Add-on tofacitinib as good as adalimumab for active RA
MADRID – When it comes to patients with rheumatoid arthritis who are responding inadequately to methotrexate therapy, results of the Oral Rheumatoid Arthritis triaL (ORAL) Strategy study suggest that adding the Janus kinase inhibitor tofacitinib is just as effective as adding the tumor necrosis factor inhibitor adalimumab.
At 6 months’ follow-up, 46% of patients randomized to tofacitinib (Xeljanz) plus methotrexate met the trial’s primary endpoint of an American College of Rheumatology response of at least 50% (ACR50), compared with 44% of those who were given adalimumab (Humira) plus methotrexate. This result met the trial’s prespecified criteria for noninferiority. An ACR50 response means that there was at least 50% improvement in tender or swollen joint counts as well as a 50% improvement in at least three of the other five criteria (acute phase reactant, such as erythrocyte sedimentation rate; patient assessment; physician assessment; pain scale; and disability/functional questionnaire).
Nevertheless, “in circumstances where methotrexate is precluded, tofacitinib monotherapy is a clinically viable option,” lead study author Roy Fleischmann, MD, said at the European Congress of Rheumatology.
“This actually substantiates what I’ve done in clinical practice since [tofacitinib] was approved,” said Dr. Fleischmann, a rheumatologist in group practice in Dallas. “If I have patients on methotrexate and they show an incomplete response, I add tofacitinib; I don’t switch, I add. Then if the patient has a good response – a really good response – then I discontinue [methotrexate].”
Dr. Fleischmann said he does the same when adding a tumor necrosis factor inhibitor to methotrexate and that there are some patients who just do better with combination treatment.
ORAL Strategy was a phase IIIB/IV study that randomized 1,152 adults with active RA, despite treatment for more than 4 months with 15-25 mg/kg of methotrexate per week. Patients had to have four or more painful or tender joints and four or more swollen joints at baseline, and a high-sensitivity C-reactive protein level of 3 mg/L or more.
Patients were randomized to one of the study’s three treatment arms: tofacitinib 5 mg twice daily as monotherapy (n = 384), the same regimen of tofacitinib added to methotrexate (n = 376), or adalimumab 40 mg every 2 weeks added to methotrexate (n = 386). (Two patients in each group did not receive their assigned treatment.) Treatment was for 1 year, and concomitant treatment with nonsteroidal anti-inflammatory drugs, oral glucocorticoids, or both was allowed so long as their doses remained stable and no dose adjustments were necessary.
ACR20 responses were also recorded and were achieved by 65% with tofacitinib monotherapy, 73% with tofacitinib plus methotrexate, and 71% with adalimumab plus methotrexate, and ACR70 responses were 18%, 25%, and 21%, respectively. Comparable improvements from baseline to the end of the study were also seen for Simple Disease Activity Index, Clinical Disease Activity Index, Disease Activity Score in 28 joints using erythrocyte sedimentation rate, and Health Assessment Questionnaire scores in patients given the combination treatments.
The study’s findings were published online (Lancet. 2017 Jun 16. doi: 10.1016/S0140-6736[17]31618-5) to coincide with their presentation in a late-breaking abstract at the meeting.
“The ORAL Strategy trial highlights three benefits from the combination of tofacitinib and methotrexate in active rheumatoid arthritis,” independent commentators David Scott, MD, and Matt D. Stevenson, PhD, wrote in an editorial (Lancet. 2017 Jun 16. doi: 10.1016/S0140-6736[17]31659-8).
“First, this combination’s efficacy and toxicity are similar to injectable biologics such as adalimumab,” said Dr. Scott of King’s College London and Dr. Stevenson of the University of Sheffield (England). Indeed, no new side effects were seen, and side effects were consistent with those seen in previous studies.
“Second,” they wrote, “the onset of action of these drugs seems equally rapid. Third, most patients are able to remain on tofacitinib therapy for 12 months.”
Dr. Scott and Dr. Stevenson suggested these findings are “extremely encouraging” as “they show the ongoing benefits of innovation in drug treatment.”
The findings support the previous RA-BEAM trial (N Engl J Med. 2017;376:652-62) with another Janus kinase inhibitor, baricitinib, Dr. Fleischmann said during his presentation, which had also shown combination therapy with methotrexate was perhaps more beneficial than adding adalimumab.
In the Lancet editorial, Dr. Scott and Dr. Stevenson wrote: “Although a combination of [Janus kinase] inhibitors with methotrexate is likely to be the way they are used in clinical practice, monotherapy results in clinical and functional responses, as shown in the ORAL Strategy trial, and thus might be appropriate in some patients.”
The study was funded by Pfizer. Dr. Fleischmann has received research grants, research support, and consultancy fees from Pfizer and from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, GlaxoSmithKline, Janssen, Novartis, Sanofi-Genzyme, and UCB. Dr. Scott has advised Eli Lilly, Roche Products, Napp Pharmaceuticals, Baxalta, and Novartis. Dr. Stevenson did not have any industry disclosures.
MADRID – When it comes to patients with rheumatoid arthritis who are responding inadequately to methotrexate therapy, results of the Oral Rheumatoid Arthritis triaL (ORAL) Strategy study suggest that adding the Janus kinase inhibitor tofacitinib is just as effective as adding the tumor necrosis factor inhibitor adalimumab.
At 6 months’ follow-up, 46% of patients randomized to tofacitinib (Xeljanz) plus methotrexate met the trial’s primary endpoint of an American College of Rheumatology response of at least 50% (ACR50), compared with 44% of those who were given adalimumab (Humira) plus methotrexate. This result met the trial’s prespecified criteria for noninferiority. An ACR50 response means that there was at least 50% improvement in tender or swollen joint counts as well as a 50% improvement in at least three of the other five criteria (acute phase reactant, such as erythrocyte sedimentation rate; patient assessment; physician assessment; pain scale; and disability/functional questionnaire).
Nevertheless, “in circumstances where methotrexate is precluded, tofacitinib monotherapy is a clinically viable option,” lead study author Roy Fleischmann, MD, said at the European Congress of Rheumatology.
“This actually substantiates what I’ve done in clinical practice since [tofacitinib] was approved,” said Dr. Fleischmann, a rheumatologist in group practice in Dallas. “If I have patients on methotrexate and they show an incomplete response, I add tofacitinib; I don’t switch, I add. Then if the patient has a good response – a really good response – then I discontinue [methotrexate].”
Dr. Fleischmann said he does the same when adding a tumor necrosis factor inhibitor to methotrexate and that there are some patients who just do better with combination treatment.
ORAL Strategy was a phase IIIB/IV study that randomized 1,152 adults with active RA, despite treatment for more than 4 months with 15-25 mg/kg of methotrexate per week. Patients had to have four or more painful or tender joints and four or more swollen joints at baseline, and a high-sensitivity C-reactive protein level of 3 mg/L or more.
Patients were randomized to one of the study’s three treatment arms: tofacitinib 5 mg twice daily as monotherapy (n = 384), the same regimen of tofacitinib added to methotrexate (n = 376), or adalimumab 40 mg every 2 weeks added to methotrexate (n = 386). (Two patients in each group did not receive their assigned treatment.) Treatment was for 1 year, and concomitant treatment with nonsteroidal anti-inflammatory drugs, oral glucocorticoids, or both was allowed so long as their doses remained stable and no dose adjustments were necessary.
ACR20 responses were also recorded and were achieved by 65% with tofacitinib monotherapy, 73% with tofacitinib plus methotrexate, and 71% with adalimumab plus methotrexate, and ACR70 responses were 18%, 25%, and 21%, respectively. Comparable improvements from baseline to the end of the study were also seen for Simple Disease Activity Index, Clinical Disease Activity Index, Disease Activity Score in 28 joints using erythrocyte sedimentation rate, and Health Assessment Questionnaire scores in patients given the combination treatments.
The study’s findings were published online (Lancet. 2017 Jun 16. doi: 10.1016/S0140-6736[17]31618-5) to coincide with their presentation in a late-breaking abstract at the meeting.
“The ORAL Strategy trial highlights three benefits from the combination of tofacitinib and methotrexate in active rheumatoid arthritis,” independent commentators David Scott, MD, and Matt D. Stevenson, PhD, wrote in an editorial (Lancet. 2017 Jun 16. doi: 10.1016/S0140-6736[17]31659-8).
“First, this combination’s efficacy and toxicity are similar to injectable biologics such as adalimumab,” said Dr. Scott of King’s College London and Dr. Stevenson of the University of Sheffield (England). Indeed, no new side effects were seen, and side effects were consistent with those seen in previous studies.
“Second,” they wrote, “the onset of action of these drugs seems equally rapid. Third, most patients are able to remain on tofacitinib therapy for 12 months.”
Dr. Scott and Dr. Stevenson suggested these findings are “extremely encouraging” as “they show the ongoing benefits of innovation in drug treatment.”
The findings support the previous RA-BEAM trial (N Engl J Med. 2017;376:652-62) with another Janus kinase inhibitor, baricitinib, Dr. Fleischmann said during his presentation, which had also shown combination therapy with methotrexate was perhaps more beneficial than adding adalimumab.
In the Lancet editorial, Dr. Scott and Dr. Stevenson wrote: “Although a combination of [Janus kinase] inhibitors with methotrexate is likely to be the way they are used in clinical practice, monotherapy results in clinical and functional responses, as shown in the ORAL Strategy trial, and thus might be appropriate in some patients.”
The study was funded by Pfizer. Dr. Fleischmann has received research grants, research support, and consultancy fees from Pfizer and from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, GlaxoSmithKline, Janssen, Novartis, Sanofi-Genzyme, and UCB. Dr. Scott has advised Eli Lilly, Roche Products, Napp Pharmaceuticals, Baxalta, and Novartis. Dr. Stevenson did not have any industry disclosures.
MADRID – When it comes to patients with rheumatoid arthritis who are responding inadequately to methotrexate therapy, results of the Oral Rheumatoid Arthritis triaL (ORAL) Strategy study suggest that adding the Janus kinase inhibitor tofacitinib is just as effective as adding the tumor necrosis factor inhibitor adalimumab.
At 6 months’ follow-up, 46% of patients randomized to tofacitinib (Xeljanz) plus methotrexate met the trial’s primary endpoint of an American College of Rheumatology response of at least 50% (ACR50), compared with 44% of those who were given adalimumab (Humira) plus methotrexate. This result met the trial’s prespecified criteria for noninferiority. An ACR50 response means that there was at least 50% improvement in tender or swollen joint counts as well as a 50% improvement in at least three of the other five criteria (acute phase reactant, such as erythrocyte sedimentation rate; patient assessment; physician assessment; pain scale; and disability/functional questionnaire).
Nevertheless, “in circumstances where methotrexate is precluded, tofacitinib monotherapy is a clinically viable option,” lead study author Roy Fleischmann, MD, said at the European Congress of Rheumatology.
“This actually substantiates what I’ve done in clinical practice since [tofacitinib] was approved,” said Dr. Fleischmann, a rheumatologist in group practice in Dallas. “If I have patients on methotrexate and they show an incomplete response, I add tofacitinib; I don’t switch, I add. Then if the patient has a good response – a really good response – then I discontinue [methotrexate].”
Dr. Fleischmann said he does the same when adding a tumor necrosis factor inhibitor to methotrexate and that there are some patients who just do better with combination treatment.
ORAL Strategy was a phase IIIB/IV study that randomized 1,152 adults with active RA, despite treatment for more than 4 months with 15-25 mg/kg of methotrexate per week. Patients had to have four or more painful or tender joints and four or more swollen joints at baseline, and a high-sensitivity C-reactive protein level of 3 mg/L or more.
Patients were randomized to one of the study’s three treatment arms: tofacitinib 5 mg twice daily as monotherapy (n = 384), the same regimen of tofacitinib added to methotrexate (n = 376), or adalimumab 40 mg every 2 weeks added to methotrexate (n = 386). (Two patients in each group did not receive their assigned treatment.) Treatment was for 1 year, and concomitant treatment with nonsteroidal anti-inflammatory drugs, oral glucocorticoids, or both was allowed so long as their doses remained stable and no dose adjustments were necessary.
ACR20 responses were also recorded and were achieved by 65% with tofacitinib monotherapy, 73% with tofacitinib plus methotrexate, and 71% with adalimumab plus methotrexate, and ACR70 responses were 18%, 25%, and 21%, respectively. Comparable improvements from baseline to the end of the study were also seen for Simple Disease Activity Index, Clinical Disease Activity Index, Disease Activity Score in 28 joints using erythrocyte sedimentation rate, and Health Assessment Questionnaire scores in patients given the combination treatments.
The study’s findings were published online (Lancet. 2017 Jun 16. doi: 10.1016/S0140-6736[17]31618-5) to coincide with their presentation in a late-breaking abstract at the meeting.
“The ORAL Strategy trial highlights three benefits from the combination of tofacitinib and methotrexate in active rheumatoid arthritis,” independent commentators David Scott, MD, and Matt D. Stevenson, PhD, wrote in an editorial (Lancet. 2017 Jun 16. doi: 10.1016/S0140-6736[17]31659-8).
“First, this combination’s efficacy and toxicity are similar to injectable biologics such as adalimumab,” said Dr. Scott of King’s College London and Dr. Stevenson of the University of Sheffield (England). Indeed, no new side effects were seen, and side effects were consistent with those seen in previous studies.
“Second,” they wrote, “the onset of action of these drugs seems equally rapid. Third, most patients are able to remain on tofacitinib therapy for 12 months.”
Dr. Scott and Dr. Stevenson suggested these findings are “extremely encouraging” as “they show the ongoing benefits of innovation in drug treatment.”
The findings support the previous RA-BEAM trial (N Engl J Med. 2017;376:652-62) with another Janus kinase inhibitor, baricitinib, Dr. Fleischmann said during his presentation, which had also shown combination therapy with methotrexate was perhaps more beneficial than adding adalimumab.
In the Lancet editorial, Dr. Scott and Dr. Stevenson wrote: “Although a combination of [Janus kinase] inhibitors with methotrexate is likely to be the way they are used in clinical practice, monotherapy results in clinical and functional responses, as shown in the ORAL Strategy trial, and thus might be appropriate in some patients.”
The study was funded by Pfizer. Dr. Fleischmann has received research grants, research support, and consultancy fees from Pfizer and from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, GlaxoSmithKline, Janssen, Novartis, Sanofi-Genzyme, and UCB. Dr. Scott has advised Eli Lilly, Roche Products, Napp Pharmaceuticals, Baxalta, and Novartis. Dr. Stevenson did not have any industry disclosures.
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: The primary endpoint of an ACR50 was met by 46% of patients randomized to tofacitinib plus methotrexate vs. 44% of those who were given adalimumab plus methotrexate. This result met the trial’s prespecified criteria for noninferiority.
Data source: ORAL Strategy: A phase IIIB/IV, double-blind, head-to-head, noninferiority, randomized, controlled trial of tofacitinib with or without methotrexate, and adalimumab with methotrexate, in 1,152 RA patients inadequately responding to methotrexate.
Disclosures: The study was funded by Pfizer. The study presenter has received research grants, research support, and consultancy fees from Pfizer and from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, GlaxoSmithKline, Janssen, Novartis, Sanofi-Genzyme, and UCB. One independent commentator has advised Eli Lilly, Roche Products, Napp Pharmaceuticals, Baxalta, and Novartis, while the other did not have any industry disclosures.
VIDEO: Hip, knee replacements fall in Danish RA patients
MADRID – The rates of both total hip and total knee replacement surgeries dropped among Danish patients with rheumatoid arthritis since the mid-1990s, reductions that were coincident with more widespread use of biologic drugs as well as with other improvements in care, according to analyses of Danish national health records.
“The introduction of guidelines [on biologic drug use] in 2002 and increasing use of biologic drugs [as a result] may have contributed to this positive development,” Lene Dreyer, MD, said at the European Congress of Rheumatology. Other factors that may have also contributed include widespread use of conventional disease-modifying antirheumatic drugs (DMARDs) and adoption of a treat-to-target strategy by many clinicians.
In 1996, the first year studied and before any biologic DMARDs were routinely used for rheumatoid arthritis, the rate of total knee replacement was nearly 6/1,000 person-years among RA patients, compared with a 0.42/1,000 person-years rate in the general adult Danish population, a roughly 14-fold excess among the RA patients, Dr. Dreyer reported. But by 2016, ”this gap had almost disappeared,” she said in a video interview. “It seems like rheumatologists in Denmark are doing a good job” treating RA patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
That may have been especially true subsequent to 2002, when the Danish Institute for Rational Pharmacotherapy issued recommendations that opened the door to wider use of biologic DMARDs, such as tumor necrosis factor inhibitors, to treat RA patients, noted Dr. Dreyer of Gentofte University Hospital, Copenhagen. During 2003-2011, use of total knee replacement surgery in RA patients fell by an average annualized rate of 0.2 surgeries/1,000 person-years. But among the general Danish population the average annualized rate of knee surgeries rose by 0.08/1,000 person-years.
“This is a very important finding,” commented Robert Landewé, MD, PhD, professor of rheumatology at the Academic Medical Center in Amsterdam. “It is extremely difficult to test the effect of the introduction of the [biologic DMARD] guidelines,” he cautioned. But he highlighted the positive finding that the excess of hip and knee replacement surgeries in patients with RA, compared with the general population, had recently narrowed.
Dr. Dreyer and her associates used records from the Danish National Patient Register to compare 29,427 patients with incident RA during 1996-2011 with more than 290,000 matched control individuals. All people studied had not undergone knee or hip replacement surgery prior to their entry into the study. The researchers used an “interrupted time series analysis” to examine the possible impact of the introduction of widespread access to biologic DMARDs starting in 2003.
The analysis showed that the rate of total hip replacements in 1996 was nearly 9 surgeries/1,000 person-years among RA patients and nearly 3/1,000 person-years in the general population, a threefold excess for RA patients. This rate fell by an average annual rate of 0.38/1,000 person-years among RA patients both before and after 2002, so that by 2011 the rate was roughly half the 1996 rate, about 4.5/1,000 patient-years. The rate in the general population rose during 1996-2011, and by 2011 was nearly 4/1,000 person-years and so nearly the same as RA patients. Wider availability of biologic DMARDs for RA patients starting in 2003 did not have an apparent impact on the rate of total hip replacement.
In contrast, wider use of biologic DMARDs appeared to have an effect on the rate of total knee surgeries among RA patients. During 1996-2001, the rate rose by an annual average of 0.19/1,000 person-years, very similar to the 0.21/1,000 person-years annual rise in the general Danish population. However, during 2003-2011, the average annual rate of total knee surgery fell by 0.20/1,000 person-years in the RA patients but continued to rise at an annual average rate of 0.08/1,000 person-years in the general population, Dr. Dreyer reported.
Additional Danish registry data exist for patients who received biologic DMARDs, and Dr. Dreyer said that she and her associates hope to use this to further examine the impact of these drugs on patient outcomes.
Dr. Dreyer has received lecture fees from Merck Sharp & Dohme and UCB. Dr. Landewé has received consulting fees from several drug companies.
[email protected]
On Twitter @mitchelzoler
MADRID – The rates of both total hip and total knee replacement surgeries dropped among Danish patients with rheumatoid arthritis since the mid-1990s, reductions that were coincident with more widespread use of biologic drugs as well as with other improvements in care, according to analyses of Danish national health records.
“The introduction of guidelines [on biologic drug use] in 2002 and increasing use of biologic drugs [as a result] may have contributed to this positive development,” Lene Dreyer, MD, said at the European Congress of Rheumatology. Other factors that may have also contributed include widespread use of conventional disease-modifying antirheumatic drugs (DMARDs) and adoption of a treat-to-target strategy by many clinicians.
In 1996, the first year studied and before any biologic DMARDs were routinely used for rheumatoid arthritis, the rate of total knee replacement was nearly 6/1,000 person-years among RA patients, compared with a 0.42/1,000 person-years rate in the general adult Danish population, a roughly 14-fold excess among the RA patients, Dr. Dreyer reported. But by 2016, ”this gap had almost disappeared,” she said in a video interview. “It seems like rheumatologists in Denmark are doing a good job” treating RA patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
That may have been especially true subsequent to 2002, when the Danish Institute for Rational Pharmacotherapy issued recommendations that opened the door to wider use of biologic DMARDs, such as tumor necrosis factor inhibitors, to treat RA patients, noted Dr. Dreyer of Gentofte University Hospital, Copenhagen. During 2003-2011, use of total knee replacement surgery in RA patients fell by an average annualized rate of 0.2 surgeries/1,000 person-years. But among the general Danish population the average annualized rate of knee surgeries rose by 0.08/1,000 person-years.
“This is a very important finding,” commented Robert Landewé, MD, PhD, professor of rheumatology at the Academic Medical Center in Amsterdam. “It is extremely difficult to test the effect of the introduction of the [biologic DMARD] guidelines,” he cautioned. But he highlighted the positive finding that the excess of hip and knee replacement surgeries in patients with RA, compared with the general population, had recently narrowed.
Dr. Dreyer and her associates used records from the Danish National Patient Register to compare 29,427 patients with incident RA during 1996-2011 with more than 290,000 matched control individuals. All people studied had not undergone knee or hip replacement surgery prior to their entry into the study. The researchers used an “interrupted time series analysis” to examine the possible impact of the introduction of widespread access to biologic DMARDs starting in 2003.
The analysis showed that the rate of total hip replacements in 1996 was nearly 9 surgeries/1,000 person-years among RA patients and nearly 3/1,000 person-years in the general population, a threefold excess for RA patients. This rate fell by an average annual rate of 0.38/1,000 person-years among RA patients both before and after 2002, so that by 2011 the rate was roughly half the 1996 rate, about 4.5/1,000 patient-years. The rate in the general population rose during 1996-2011, and by 2011 was nearly 4/1,000 person-years and so nearly the same as RA patients. Wider availability of biologic DMARDs for RA patients starting in 2003 did not have an apparent impact on the rate of total hip replacement.
In contrast, wider use of biologic DMARDs appeared to have an effect on the rate of total knee surgeries among RA patients. During 1996-2001, the rate rose by an annual average of 0.19/1,000 person-years, very similar to the 0.21/1,000 person-years annual rise in the general Danish population. However, during 2003-2011, the average annual rate of total knee surgery fell by 0.20/1,000 person-years in the RA patients but continued to rise at an annual average rate of 0.08/1,000 person-years in the general population, Dr. Dreyer reported.
Additional Danish registry data exist for patients who received biologic DMARDs, and Dr. Dreyer said that she and her associates hope to use this to further examine the impact of these drugs on patient outcomes.
Dr. Dreyer has received lecture fees from Merck Sharp & Dohme and UCB. Dr. Landewé has received consulting fees from several drug companies.
[email protected]
On Twitter @mitchelzoler
MADRID – The rates of both total hip and total knee replacement surgeries dropped among Danish patients with rheumatoid arthritis since the mid-1990s, reductions that were coincident with more widespread use of biologic drugs as well as with other improvements in care, according to analyses of Danish national health records.
“The introduction of guidelines [on biologic drug use] in 2002 and increasing use of biologic drugs [as a result] may have contributed to this positive development,” Lene Dreyer, MD, said at the European Congress of Rheumatology. Other factors that may have also contributed include widespread use of conventional disease-modifying antirheumatic drugs (DMARDs) and adoption of a treat-to-target strategy by many clinicians.
In 1996, the first year studied and before any biologic DMARDs were routinely used for rheumatoid arthritis, the rate of total knee replacement was nearly 6/1,000 person-years among RA patients, compared with a 0.42/1,000 person-years rate in the general adult Danish population, a roughly 14-fold excess among the RA patients, Dr. Dreyer reported. But by 2016, ”this gap had almost disappeared,” she said in a video interview. “It seems like rheumatologists in Denmark are doing a good job” treating RA patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
That may have been especially true subsequent to 2002, when the Danish Institute for Rational Pharmacotherapy issued recommendations that opened the door to wider use of biologic DMARDs, such as tumor necrosis factor inhibitors, to treat RA patients, noted Dr. Dreyer of Gentofte University Hospital, Copenhagen. During 2003-2011, use of total knee replacement surgery in RA patients fell by an average annualized rate of 0.2 surgeries/1,000 person-years. But among the general Danish population the average annualized rate of knee surgeries rose by 0.08/1,000 person-years.
“This is a very important finding,” commented Robert Landewé, MD, PhD, professor of rheumatology at the Academic Medical Center in Amsterdam. “It is extremely difficult to test the effect of the introduction of the [biologic DMARD] guidelines,” he cautioned. But he highlighted the positive finding that the excess of hip and knee replacement surgeries in patients with RA, compared with the general population, had recently narrowed.
Dr. Dreyer and her associates used records from the Danish National Patient Register to compare 29,427 patients with incident RA during 1996-2011 with more than 290,000 matched control individuals. All people studied had not undergone knee or hip replacement surgery prior to their entry into the study. The researchers used an “interrupted time series analysis” to examine the possible impact of the introduction of widespread access to biologic DMARDs starting in 2003.
The analysis showed that the rate of total hip replacements in 1996 was nearly 9 surgeries/1,000 person-years among RA patients and nearly 3/1,000 person-years in the general population, a threefold excess for RA patients. This rate fell by an average annual rate of 0.38/1,000 person-years among RA patients both before and after 2002, so that by 2011 the rate was roughly half the 1996 rate, about 4.5/1,000 patient-years. The rate in the general population rose during 1996-2011, and by 2011 was nearly 4/1,000 person-years and so nearly the same as RA patients. Wider availability of biologic DMARDs for RA patients starting in 2003 did not have an apparent impact on the rate of total hip replacement.
In contrast, wider use of biologic DMARDs appeared to have an effect on the rate of total knee surgeries among RA patients. During 1996-2001, the rate rose by an annual average of 0.19/1,000 person-years, very similar to the 0.21/1,000 person-years annual rise in the general Danish population. However, during 2003-2011, the average annual rate of total knee surgery fell by 0.20/1,000 person-years in the RA patients but continued to rise at an annual average rate of 0.08/1,000 person-years in the general population, Dr. Dreyer reported.
Additional Danish registry data exist for patients who received biologic DMARDs, and Dr. Dreyer said that she and her associates hope to use this to further examine the impact of these drugs on patient outcomes.
Dr. Dreyer has received lecture fees from Merck Sharp & Dohme and UCB. Dr. Landewé has received consulting fees from several drug companies.
[email protected]
On Twitter @mitchelzoler
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: RA patient hip replacements fell from nearly 9/1,000 person-years in 1996 to about 4.5/1,000 person-years in 2011.
Data source: Records from more than 300,000 people in the Danish National Patient Register.
Disclosures: Dr. Dreyer has received lecture fees from Merck Sharp & Dohme and UCB. Dr. Landewé has received consulting fees from several drug companies.
Obesity blunts TNFi response in axial spondyloarthritis
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
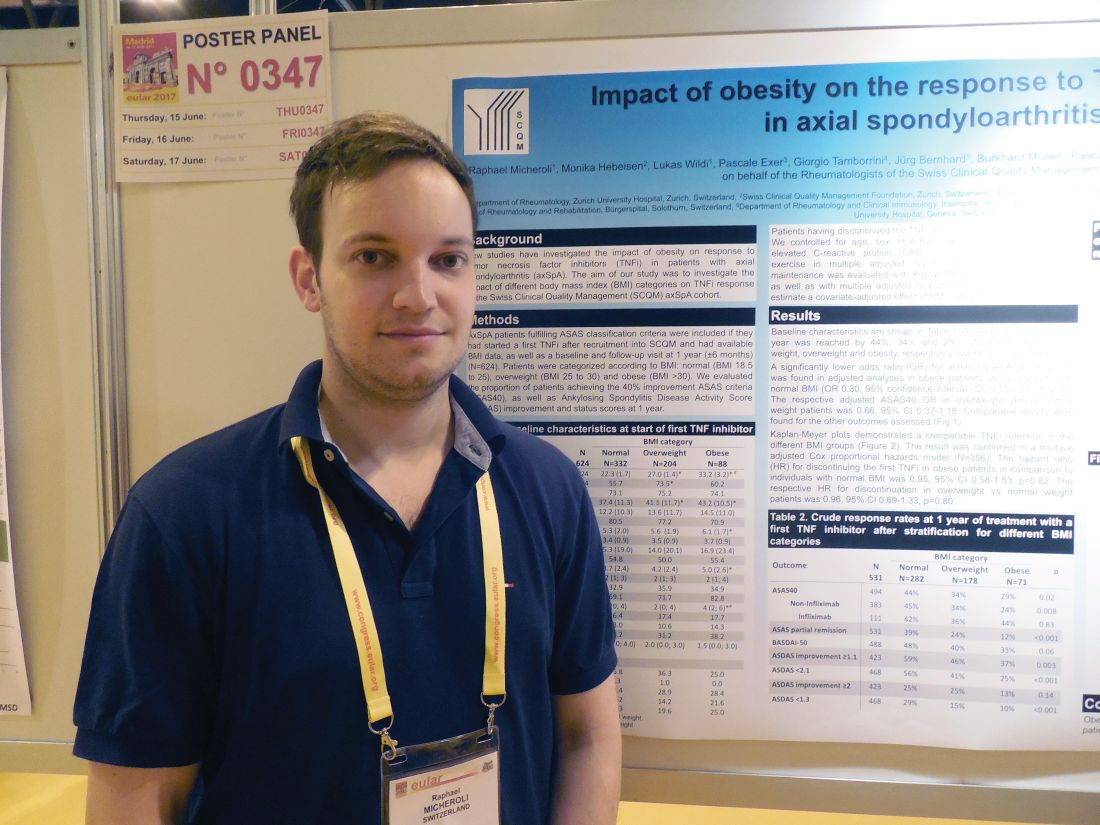
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
[email protected]
On Twitter @mitchelzoler
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
[email protected]
On Twitter @mitchelzoler
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: Obese patients had a 70% lower response rate to a tumor necrosis factor inhibitor, compared with healthy-weight patients.
Data source: A cohort of 531 axial spondyloarthritis patients enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases program.
Disclosures: Dr. Micheroli had no disclosures.
VIDEO: Does biologic immunogenicity matter in daily practice?
MADRID – Measuring the formation of antibodies against biologic agents has no real value in daily practice as their presence or absence does not really change how patients are likely to be treated, Johannes W.J. Bijlsma, MD, observed at the European Congress of Rheumatology.
Consider a female patient who is 59 years old, diagnosed with rheumatoid arthritis (RA) in 2014, he said. She was being treated with methotrexate at a dose of 20 mg with additional glucocorticoids, initially given at a dose of 10 mg, reduced to 5 mg after 2 years, and then stopped. The patient experiences a disease flare, however, and for various other reasons is given a tumor necrosis factor inhibitor (TNFi). She does well initially but then has another flare, so would there be any point of measuring anti-drug antibodies (ADAbs) as this point? Not really, Dr. Bijlsma suggested, as the same decision to change the biologic agent would probably result if ADAbs were detected or not.
“If I do not measure them, I decide to change the biological. If I measure them and they are present, I change the biological, and if they are absent, I still change the biological,” said Dr. Bijlsma, professor and head of the department of rheumatology and clinical immunology at University Medical Center Utrecht (the Netherlands).
Following the European League Against Rheumatism (EULAR) recommendations for biologic disease-modifying antirheumatic drug (bDMARD) use (Ann Rheum Dis. 2017;76:960-77) would then mean that the first bDMARD, in this case adalimumab (Humira), would be replaced by another biologic with a different mechanism of action or a second TNFi.
“The immune response is always there,” Dr. Bijlsma said. It does not matter what or how it is administered, introducing any foreign protein, humanized or not, will instigate some kind of immune reaction, he said. The extent to which an immune reaction is raised might vary between biologic agents, but it will be there. He cited a review paper (Rheumatology [Oxford]. 2016;55:210-20) showing that the mean estimated occurrence of ADAbs in patients with RA ranges from 0.6% with the interleukin-6-targeting agent tocilizumab (Actemra) to 30% with infliximab (Remicade).
Measuring the level of ADAbs becomes problematic when considering that different biologics will induce different levels of immune response. The level of detection also will be dependent on which of three current types of assays are used. In addition, “humanization of biological agents is not the key point in preventing anti-drug antibodies,” Dr. Bijlsma said, pointing out that the prevalence of ADAbs against adalimumab did not appear to by any lower than ADAbs against infliximab.
Preventing ADAbs can be achieved by co-administering methotrexate or alternating the treatment schedule, Dr. Bijlsma said. Treatment with methotrexate, which is usually continued when patients start a biologic, “diminishes the immune response,” he noted. Indeed, while 50% of patients who are not treated with this conventional DMARD develop ADAbs, only 14%-35% develop them while taking methotrexate, depending on the dose used.
It is likely to be more useful in clinical practice to measure individual patients’ drug trough levels than to measure ADAb levels, he suggested, with dosing continued or adjusted accordingly for each patient. Using drug trough levels to personalize adalimumab treatment has been tested (Ann Rheum Dis. 2015;74:361-8) using a theoretical algorithm based on whether patients achieve a EULAR response at 6 months. If they do achieve a EULAR response and drug trough levels are between 5 and 12 mg/L or greater than 12 mg/L, then adalimumab treatment should continue. However, if the trough levels fall below 5 mg/L, there is probably no point in continuing treatment and this TNFi should be stopped. If patients do not respond and drug testing shows a trough level above 5 mg/L, then a switch to infliximab might be advantageous, while a trough level below this threshold could indicated that a TNFi with a lower immunogenic potential such as etanercept might be a better choice.
Using drug trough levels is still very much research based right now and is not ready for clinical practice just yet, but the theory is that it could help decide if patients should continue, stop, or perhaps switch their biologic, Dr. Bijlsma said.
Dr. Bijlsma spoke about these issues in a video interview at the congress.
Dr. Bijlsma has worked with many of the pharmaceutical companies that produce biologic agents for the management of rheumatic diseases but had no specific disclosures in relation to his comments.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MADRID – Measuring the formation of antibodies against biologic agents has no real value in daily practice as their presence or absence does not really change how patients are likely to be treated, Johannes W.J. Bijlsma, MD, observed at the European Congress of Rheumatology.
Consider a female patient who is 59 years old, diagnosed with rheumatoid arthritis (RA) in 2014, he said. She was being treated with methotrexate at a dose of 20 mg with additional glucocorticoids, initially given at a dose of 10 mg, reduced to 5 mg after 2 years, and then stopped. The patient experiences a disease flare, however, and for various other reasons is given a tumor necrosis factor inhibitor (TNFi). She does well initially but then has another flare, so would there be any point of measuring anti-drug antibodies (ADAbs) as this point? Not really, Dr. Bijlsma suggested, as the same decision to change the biologic agent would probably result if ADAbs were detected or not.
“If I do not measure them, I decide to change the biological. If I measure them and they are present, I change the biological, and if they are absent, I still change the biological,” said Dr. Bijlsma, professor and head of the department of rheumatology and clinical immunology at University Medical Center Utrecht (the Netherlands).
Following the European League Against Rheumatism (EULAR) recommendations for biologic disease-modifying antirheumatic drug (bDMARD) use (Ann Rheum Dis. 2017;76:960-77) would then mean that the first bDMARD, in this case adalimumab (Humira), would be replaced by another biologic with a different mechanism of action or a second TNFi.
“The immune response is always there,” Dr. Bijlsma said. It does not matter what or how it is administered, introducing any foreign protein, humanized or not, will instigate some kind of immune reaction, he said. The extent to which an immune reaction is raised might vary between biologic agents, but it will be there. He cited a review paper (Rheumatology [Oxford]. 2016;55:210-20) showing that the mean estimated occurrence of ADAbs in patients with RA ranges from 0.6% with the interleukin-6-targeting agent tocilizumab (Actemra) to 30% with infliximab (Remicade).
Measuring the level of ADAbs becomes problematic when considering that different biologics will induce different levels of immune response. The level of detection also will be dependent on which of three current types of assays are used. In addition, “humanization of biological agents is not the key point in preventing anti-drug antibodies,” Dr. Bijlsma said, pointing out that the prevalence of ADAbs against adalimumab did not appear to by any lower than ADAbs against infliximab.
Preventing ADAbs can be achieved by co-administering methotrexate or alternating the treatment schedule, Dr. Bijlsma said. Treatment with methotrexate, which is usually continued when patients start a biologic, “diminishes the immune response,” he noted. Indeed, while 50% of patients who are not treated with this conventional DMARD develop ADAbs, only 14%-35% develop them while taking methotrexate, depending on the dose used.
It is likely to be more useful in clinical practice to measure individual patients’ drug trough levels than to measure ADAb levels, he suggested, with dosing continued or adjusted accordingly for each patient. Using drug trough levels to personalize adalimumab treatment has been tested (Ann Rheum Dis. 2015;74:361-8) using a theoretical algorithm based on whether patients achieve a EULAR response at 6 months. If they do achieve a EULAR response and drug trough levels are between 5 and 12 mg/L or greater than 12 mg/L, then adalimumab treatment should continue. However, if the trough levels fall below 5 mg/L, there is probably no point in continuing treatment and this TNFi should be stopped. If patients do not respond and drug testing shows a trough level above 5 mg/L, then a switch to infliximab might be advantageous, while a trough level below this threshold could indicated that a TNFi with a lower immunogenic potential such as etanercept might be a better choice.
Using drug trough levels is still very much research based right now and is not ready for clinical practice just yet, but the theory is that it could help decide if patients should continue, stop, or perhaps switch their biologic, Dr. Bijlsma said.
Dr. Bijlsma spoke about these issues in a video interview at the congress.
Dr. Bijlsma has worked with many of the pharmaceutical companies that produce biologic agents for the management of rheumatic diseases but had no specific disclosures in relation to his comments.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MADRID – Measuring the formation of antibodies against biologic agents has no real value in daily practice as their presence or absence does not really change how patients are likely to be treated, Johannes W.J. Bijlsma, MD, observed at the European Congress of Rheumatology.
Consider a female patient who is 59 years old, diagnosed with rheumatoid arthritis (RA) in 2014, he said. She was being treated with methotrexate at a dose of 20 mg with additional glucocorticoids, initially given at a dose of 10 mg, reduced to 5 mg after 2 years, and then stopped. The patient experiences a disease flare, however, and for various other reasons is given a tumor necrosis factor inhibitor (TNFi). She does well initially but then has another flare, so would there be any point of measuring anti-drug antibodies (ADAbs) as this point? Not really, Dr. Bijlsma suggested, as the same decision to change the biologic agent would probably result if ADAbs were detected or not.
“If I do not measure them, I decide to change the biological. If I measure them and they are present, I change the biological, and if they are absent, I still change the biological,” said Dr. Bijlsma, professor and head of the department of rheumatology and clinical immunology at University Medical Center Utrecht (the Netherlands).
Following the European League Against Rheumatism (EULAR) recommendations for biologic disease-modifying antirheumatic drug (bDMARD) use (Ann Rheum Dis. 2017;76:960-77) would then mean that the first bDMARD, in this case adalimumab (Humira), would be replaced by another biologic with a different mechanism of action or a second TNFi.
“The immune response is always there,” Dr. Bijlsma said. It does not matter what or how it is administered, introducing any foreign protein, humanized or not, will instigate some kind of immune reaction, he said. The extent to which an immune reaction is raised might vary between biologic agents, but it will be there. He cited a review paper (Rheumatology [Oxford]. 2016;55:210-20) showing that the mean estimated occurrence of ADAbs in patients with RA ranges from 0.6% with the interleukin-6-targeting agent tocilizumab (Actemra) to 30% with infliximab (Remicade).
Measuring the level of ADAbs becomes problematic when considering that different biologics will induce different levels of immune response. The level of detection also will be dependent on which of three current types of assays are used. In addition, “humanization of biological agents is not the key point in preventing anti-drug antibodies,” Dr. Bijlsma said, pointing out that the prevalence of ADAbs against adalimumab did not appear to by any lower than ADAbs against infliximab.
Preventing ADAbs can be achieved by co-administering methotrexate or alternating the treatment schedule, Dr. Bijlsma said. Treatment with methotrexate, which is usually continued when patients start a biologic, “diminishes the immune response,” he noted. Indeed, while 50% of patients who are not treated with this conventional DMARD develop ADAbs, only 14%-35% develop them while taking methotrexate, depending on the dose used.
It is likely to be more useful in clinical practice to measure individual patients’ drug trough levels than to measure ADAb levels, he suggested, with dosing continued or adjusted accordingly for each patient. Using drug trough levels to personalize adalimumab treatment has been tested (Ann Rheum Dis. 2015;74:361-8) using a theoretical algorithm based on whether patients achieve a EULAR response at 6 months. If they do achieve a EULAR response and drug trough levels are between 5 and 12 mg/L or greater than 12 mg/L, then adalimumab treatment should continue. However, if the trough levels fall below 5 mg/L, there is probably no point in continuing treatment and this TNFi should be stopped. If patients do not respond and drug testing shows a trough level above 5 mg/L, then a switch to infliximab might be advantageous, while a trough level below this threshold could indicated that a TNFi with a lower immunogenic potential such as etanercept might be a better choice.
Using drug trough levels is still very much research based right now and is not ready for clinical practice just yet, but the theory is that it could help decide if patients should continue, stop, or perhaps switch their biologic, Dr. Bijlsma said.
Dr. Bijlsma spoke about these issues in a video interview at the congress.
Dr. Bijlsma has worked with many of the pharmaceutical companies that produce biologic agents for the management of rheumatic diseases but had no specific disclosures in relation to his comments.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE EULAR 2017 CONGRESS
VIDEO: Cancer immunotherapies activate rheumatologic adverse effects
MADRID – The introduction of immune checkpoint inhibitor drugs has “been great for cancer but bad for rheumatology.”
That’s the gist of the immunologic adverse effect fallout from the immunomodulatory revolution that’s recently swept oncology, Leonard Calabrese, DO, said in a video interview during the European Congress of Rheumatology.
Results from a recent survey of U.S. rheumatologists run by Dr. Calabrese and his associates showed that “more than a quarter” now have seen at least one patient who experienced activation of a rheumatologic disease after starting treatment with an immune checkpoint inhibitor, said Dr. Calabrese, head of the section of clinical immunology at the Cleveland Clinic in Ohio.
Unlike most other immunological adverse effects caused by immune checkpoint inhibitors, the rheumatologic complications usually don’t resolve when treatment stops, he added.
These adverse effects represent a new wrinkle for the practice of rheumatology and are now something that clinicians must familiarize themselves with, Dr. Calabrese advised.
Dr. Calabrese reported that he is a consultant to Bristol-Myers Squibb.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
MADRID – The introduction of immune checkpoint inhibitor drugs has “been great for cancer but bad for rheumatology.”
That’s the gist of the immunologic adverse effect fallout from the immunomodulatory revolution that’s recently swept oncology, Leonard Calabrese, DO, said in a video interview during the European Congress of Rheumatology.
Results from a recent survey of U.S. rheumatologists run by Dr. Calabrese and his associates showed that “more than a quarter” now have seen at least one patient who experienced activation of a rheumatologic disease after starting treatment with an immune checkpoint inhibitor, said Dr. Calabrese, head of the section of clinical immunology at the Cleveland Clinic in Ohio.
Unlike most other immunological adverse effects caused by immune checkpoint inhibitors, the rheumatologic complications usually don’t resolve when treatment stops, he added.
These adverse effects represent a new wrinkle for the practice of rheumatology and are now something that clinicians must familiarize themselves with, Dr. Calabrese advised.
Dr. Calabrese reported that he is a consultant to Bristol-Myers Squibb.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
MADRID – The introduction of immune checkpoint inhibitor drugs has “been great for cancer but bad for rheumatology.”
That’s the gist of the immunologic adverse effect fallout from the immunomodulatory revolution that’s recently swept oncology, Leonard Calabrese, DO, said in a video interview during the European Congress of Rheumatology.
Results from a recent survey of U.S. rheumatologists run by Dr. Calabrese and his associates showed that “more than a quarter” now have seen at least one patient who experienced activation of a rheumatologic disease after starting treatment with an immune checkpoint inhibitor, said Dr. Calabrese, head of the section of clinical immunology at the Cleveland Clinic in Ohio.
Unlike most other immunological adverse effects caused by immune checkpoint inhibitors, the rheumatologic complications usually don’t resolve when treatment stops, he added.
These adverse effects represent a new wrinkle for the practice of rheumatology and are now something that clinicians must familiarize themselves with, Dr. Calabrese advised.
Dr. Calabrese reported that he is a consultant to Bristol-Myers Squibb.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE EULAR 2017 CONGRESS
Mesenchymal precursor cells simmer down rheumatoid arthritis
MADRID – A single injection of allogeneic mesenchymal precursor cells was apparently both safe and effective for relieving some symptoms of rheumatoid arthritis in biological-refractory patients in a phase II randomized trial with 48 patients.
Most of the efficacy measures ran out to 12 weeks, but researchers followed one measure, the American College of Rheumatology N (ACR-N) index of improvement, out to 39 weeks after a single infusion, and this measure showed a statistically significant, durable benefit from the higher tested dose of mesenchymal precursor cells (MPC) when compared with placebo, Suzanne Kafaja, MD, said while presenting a poster at the European Congress of Rheumatology.
“The trial met its primary endpoints, and so far the data look pretty encouraging, but it’s still pretty early,” she said.
“I was surprised by the durability” of the anti-inflammatory effect of the MPC at 39 weeks, Dr. Kafaja added in an interview.
The study, run at 16 U.S. centers and 2 sites in Australia, enrolled 48 patients with rheumatoid arthritis and on a stable methotrexate regimen for at least 4 months who had a history of failing to adequately respond to at least one biological disease-modifying drug, most commonly a tumor necrosis factor inhibitor. The average age of the enrolled patients was 55 years; nearly three-quarters were women. The patients had been diagnosed with rheumatoid arthritis for an average of 13 years, and more than one-third of the patients had a history of inadequate response to three or more biological agents.
Thirty-six of the patients received a single infusion of a preparation of MPC taken from the bone marrow of healthy donors and isolated and expanded ex vivo. Half the patients in the active-treatment group received 1 million MPC per kg, and the other half received 2 million MPC per kg. An additional 16 patients received placebo. The researchers obtained the MPC from Mesoblast Limited, an Australia-based company that sponsored the study and uses a proprietary method for MPC processing to produce an “off-the-shelf” product.
The allogeneic MPC used in the study is a homogeneous population of cells that respond to pro-inflammatory cytokines by releasing cytokines of their own that induce monocytes and T-cells into an anti-inflammatory state.
The treatment groups showed no difference, compared with the placebo group, for the ACR20, ACR50, and ACR70 measurements, but for two other measures, the Health Assessment Questionnaire and the 28-joint Disease Activity Score, the results showed trends toward dose-related improvements following MPC treatment. The results showed statistically significant improvements after 12 and 39 weeks in average ACR-N in the patients who received 2 million MPC per kg. After 39 weeks, the average ACR-N improvement rate was about 35% among patients who had received 2 million MPC per kg, about 10% among those who received 1 million cells per kg, and about 8% among placebo patients, Dr. Kafaja reported.
Mesoblast funded the study. Dr. Kafaja had no other disclosures.
[email protected]
On Twitter @mitchelzoler
MADRID – A single injection of allogeneic mesenchymal precursor cells was apparently both safe and effective for relieving some symptoms of rheumatoid arthritis in biological-refractory patients in a phase II randomized trial with 48 patients.
Most of the efficacy measures ran out to 12 weeks, but researchers followed one measure, the American College of Rheumatology N (ACR-N) index of improvement, out to 39 weeks after a single infusion, and this measure showed a statistically significant, durable benefit from the higher tested dose of mesenchymal precursor cells (MPC) when compared with placebo, Suzanne Kafaja, MD, said while presenting a poster at the European Congress of Rheumatology.
“The trial met its primary endpoints, and so far the data look pretty encouraging, but it’s still pretty early,” she said.
“I was surprised by the durability” of the anti-inflammatory effect of the MPC at 39 weeks, Dr. Kafaja added in an interview.
The study, run at 16 U.S. centers and 2 sites in Australia, enrolled 48 patients with rheumatoid arthritis and on a stable methotrexate regimen for at least 4 months who had a history of failing to adequately respond to at least one biological disease-modifying drug, most commonly a tumor necrosis factor inhibitor. The average age of the enrolled patients was 55 years; nearly three-quarters were women. The patients had been diagnosed with rheumatoid arthritis for an average of 13 years, and more than one-third of the patients had a history of inadequate response to three or more biological agents.
Thirty-six of the patients received a single infusion of a preparation of MPC taken from the bone marrow of healthy donors and isolated and expanded ex vivo. Half the patients in the active-treatment group received 1 million MPC per kg, and the other half received 2 million MPC per kg. An additional 16 patients received placebo. The researchers obtained the MPC from Mesoblast Limited, an Australia-based company that sponsored the study and uses a proprietary method for MPC processing to produce an “off-the-shelf” product.
The allogeneic MPC used in the study is a homogeneous population of cells that respond to pro-inflammatory cytokines by releasing cytokines of their own that induce monocytes and T-cells into an anti-inflammatory state.
The treatment groups showed no difference, compared with the placebo group, for the ACR20, ACR50, and ACR70 measurements, but for two other measures, the Health Assessment Questionnaire and the 28-joint Disease Activity Score, the results showed trends toward dose-related improvements following MPC treatment. The results showed statistically significant improvements after 12 and 39 weeks in average ACR-N in the patients who received 2 million MPC per kg. After 39 weeks, the average ACR-N improvement rate was about 35% among patients who had received 2 million MPC per kg, about 10% among those who received 1 million cells per kg, and about 8% among placebo patients, Dr. Kafaja reported.
Mesoblast funded the study. Dr. Kafaja had no other disclosures.
[email protected]
On Twitter @mitchelzoler
MADRID – A single injection of allogeneic mesenchymal precursor cells was apparently both safe and effective for relieving some symptoms of rheumatoid arthritis in biological-refractory patients in a phase II randomized trial with 48 patients.
Most of the efficacy measures ran out to 12 weeks, but researchers followed one measure, the American College of Rheumatology N (ACR-N) index of improvement, out to 39 weeks after a single infusion, and this measure showed a statistically significant, durable benefit from the higher tested dose of mesenchymal precursor cells (MPC) when compared with placebo, Suzanne Kafaja, MD, said while presenting a poster at the European Congress of Rheumatology.
“The trial met its primary endpoints, and so far the data look pretty encouraging, but it’s still pretty early,” she said.
“I was surprised by the durability” of the anti-inflammatory effect of the MPC at 39 weeks, Dr. Kafaja added in an interview.
The study, run at 16 U.S. centers and 2 sites in Australia, enrolled 48 patients with rheumatoid arthritis and on a stable methotrexate regimen for at least 4 months who had a history of failing to adequately respond to at least one biological disease-modifying drug, most commonly a tumor necrosis factor inhibitor. The average age of the enrolled patients was 55 years; nearly three-quarters were women. The patients had been diagnosed with rheumatoid arthritis for an average of 13 years, and more than one-third of the patients had a history of inadequate response to three or more biological agents.
Thirty-six of the patients received a single infusion of a preparation of MPC taken from the bone marrow of healthy donors and isolated and expanded ex vivo. Half the patients in the active-treatment group received 1 million MPC per kg, and the other half received 2 million MPC per kg. An additional 16 patients received placebo. The researchers obtained the MPC from Mesoblast Limited, an Australia-based company that sponsored the study and uses a proprietary method for MPC processing to produce an “off-the-shelf” product.
The allogeneic MPC used in the study is a homogeneous population of cells that respond to pro-inflammatory cytokines by releasing cytokines of their own that induce monocytes and T-cells into an anti-inflammatory state.
The treatment groups showed no difference, compared with the placebo group, for the ACR20, ACR50, and ACR70 measurements, but for two other measures, the Health Assessment Questionnaire and the 28-joint Disease Activity Score, the results showed trends toward dose-related improvements following MPC treatment. The results showed statistically significant improvements after 12 and 39 weeks in average ACR-N in the patients who received 2 million MPC per kg. After 39 weeks, the average ACR-N improvement rate was about 35% among patients who had received 2 million MPC per kg, about 10% among those who received 1 million cells per kg, and about 8% among placebo patients, Dr. Kafaja reported.
Mesoblast funded the study. Dr. Kafaja had no other disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: Mesenchymal precursor cells led to an average 35% ACR-N improvement, compared with 8% in placebo-treated patients.
Data source: A multicenter, dose-ranging phase II study with 48 rheumatoid arthritis patients.
Disclosures: Mesoblast funded the study. Dr. Kafaja had no other disclosures.
IL-6 nanobody vobarilizumab advances despite equivocal phase II data
MADRID – Despite failing its phase II primary endpoint, the single-domain antibody vobarilizumab, being developed for rheumatoid arthritis, will advance to phase III studies.
A robust placebo response obscured the strength of clinical response to vobarilizumab, a nanobody that blocks the soluble interleukin-6 receptor, Thomas Dorner, MD, said at the European Congress of Rheumatology. But by 24 weeks of treatment, vobarilizumab effected a deep, sustained response in up to half of patients with rheumatoid arthritis who responded inadequately to methotrexate.
The safety profile was encouraging, Dr. Dorner said, with just one case of gastrointestinal perforation. These events have been a problem in some IL-6 blockade studies; the protein stimulates repair of the intestinal epithelium and blocking it leaves the tissue vulnerable to injury. The single case in this trial occurred 17 days after the patient withdrew from the study for other reasons, so it was not considered to be related to the study medication, Dr. Dorner said.
Vobarilizumab is composed of two heavy chains, lacking the two light-chain arms of a full antibody. It is minuscule – just 10% of the molecular weight of a conventional antibody. One chain targets human serum albumin and is designed to prolong the molecule’s half-life by up to 14 days; the other chain targets the soluble IL-6 receptor.
The phase IIb study comprised 345 patients with active RA despite treatment with methotrexate (mean dose 16 mg/week). While staying on their methotrexate, they were equally assigned to five treatment groups: placebo or vobarilizumab at 75 mg every 4 weeks; 150 mg every 4 weeks; 150 mg every 2 weeks; or 225 mg every 2 weeks.
The primary endpoint was the difference in ACR20 response at week 12 between placebo and the four dosing groups. While the majority of patients taking vobarilizumab met that endpoint, the percentages did not significantly differ from each other, nor from placebo. ACR20 was met by 62% of the placebo group and 81%-72% of the vobarilizumab groups. ACR50 was met by 28% of the placebo group and 45%-29% of the vobarilizumab groups and ACR70 by 9% of the placebo group and 21%-14% of the vobarilizumab groups.
However, Dr. Dorner said, response in the placebo group tended to tail off as the study progressed, while staying significantly stronger in the higher-dose vobarilizumab groups. By week 24, 16% of the placebo group still had an ACR50 – significantly less than in the vobarilizumab 150 mg/2 weeks and 225 mg/2 weeks groups (31%, 39%, respectively).
On a measure of remission that combined C-reactive protein of less than 2.6 mg/L and low disease activity, vobarilizumab looked much better at week 24. At that point, 16% of placebo patients met the endpoint, compared to 39% of the 150 mg/4 weeks and 150 mg/2 weeks vobarilizumab groups, and 51% of the 225 mg/2 weeks group.
Adverse events occurred in 36% of placebo patients and about 44% of vobarilizumab patients and did not show any dose-response relationship. About 38% of these were considered treatment related; 7% of the cohort withdrew due to an adverse event. There were seven serious infections among those taking vobarilizumab (three pneumonia, and one each herpes zoster, ear infection, staphylococcus sepsis, and bacterial arthritis). One patient died of a myocardial infarction, but she had experienced a previous heart attack and undergone percutaneous coronary intervention. The single gastrointestinal perforation occurred in a woman taking the highest dose of vobarilizumab, more than 2 weeks after she stopped taking it.
Vobarilizumab will continue into a phase III study, according to the Ablynx website. The company is seeking an industry partner. AbbVie had an option to license vobarilizumab, but declined last fall on the mixed results of Ablynx’s phase II studies.
[email protected]
On Twitter @Alz_gal
MADRID – Despite failing its phase II primary endpoint, the single-domain antibody vobarilizumab, being developed for rheumatoid arthritis, will advance to phase III studies.
A robust placebo response obscured the strength of clinical response to vobarilizumab, a nanobody that blocks the soluble interleukin-6 receptor, Thomas Dorner, MD, said at the European Congress of Rheumatology. But by 24 weeks of treatment, vobarilizumab effected a deep, sustained response in up to half of patients with rheumatoid arthritis who responded inadequately to methotrexate.
The safety profile was encouraging, Dr. Dorner said, with just one case of gastrointestinal perforation. These events have been a problem in some IL-6 blockade studies; the protein stimulates repair of the intestinal epithelium and blocking it leaves the tissue vulnerable to injury. The single case in this trial occurred 17 days after the patient withdrew from the study for other reasons, so it was not considered to be related to the study medication, Dr. Dorner said.
Vobarilizumab is composed of two heavy chains, lacking the two light-chain arms of a full antibody. It is minuscule – just 10% of the molecular weight of a conventional antibody. One chain targets human serum albumin and is designed to prolong the molecule’s half-life by up to 14 days; the other chain targets the soluble IL-6 receptor.
The phase IIb study comprised 345 patients with active RA despite treatment with methotrexate (mean dose 16 mg/week). While staying on their methotrexate, they were equally assigned to five treatment groups: placebo or vobarilizumab at 75 mg every 4 weeks; 150 mg every 4 weeks; 150 mg every 2 weeks; or 225 mg every 2 weeks.
The primary endpoint was the difference in ACR20 response at week 12 between placebo and the four dosing groups. While the majority of patients taking vobarilizumab met that endpoint, the percentages did not significantly differ from each other, nor from placebo. ACR20 was met by 62% of the placebo group and 81%-72% of the vobarilizumab groups. ACR50 was met by 28% of the placebo group and 45%-29% of the vobarilizumab groups and ACR70 by 9% of the placebo group and 21%-14% of the vobarilizumab groups.
However, Dr. Dorner said, response in the placebo group tended to tail off as the study progressed, while staying significantly stronger in the higher-dose vobarilizumab groups. By week 24, 16% of the placebo group still had an ACR50 – significantly less than in the vobarilizumab 150 mg/2 weeks and 225 mg/2 weeks groups (31%, 39%, respectively).
On a measure of remission that combined C-reactive protein of less than 2.6 mg/L and low disease activity, vobarilizumab looked much better at week 24. At that point, 16% of placebo patients met the endpoint, compared to 39% of the 150 mg/4 weeks and 150 mg/2 weeks vobarilizumab groups, and 51% of the 225 mg/2 weeks group.
Adverse events occurred in 36% of placebo patients and about 44% of vobarilizumab patients and did not show any dose-response relationship. About 38% of these were considered treatment related; 7% of the cohort withdrew due to an adverse event. There were seven serious infections among those taking vobarilizumab (three pneumonia, and one each herpes zoster, ear infection, staphylococcus sepsis, and bacterial arthritis). One patient died of a myocardial infarction, but she had experienced a previous heart attack and undergone percutaneous coronary intervention. The single gastrointestinal perforation occurred in a woman taking the highest dose of vobarilizumab, more than 2 weeks after she stopped taking it.
Vobarilizumab will continue into a phase III study, according to the Ablynx website. The company is seeking an industry partner. AbbVie had an option to license vobarilizumab, but declined last fall on the mixed results of Ablynx’s phase II studies.
[email protected]
On Twitter @Alz_gal
MADRID – Despite failing its phase II primary endpoint, the single-domain antibody vobarilizumab, being developed for rheumatoid arthritis, will advance to phase III studies.
A robust placebo response obscured the strength of clinical response to vobarilizumab, a nanobody that blocks the soluble interleukin-6 receptor, Thomas Dorner, MD, said at the European Congress of Rheumatology. But by 24 weeks of treatment, vobarilizumab effected a deep, sustained response in up to half of patients with rheumatoid arthritis who responded inadequately to methotrexate.
The safety profile was encouraging, Dr. Dorner said, with just one case of gastrointestinal perforation. These events have been a problem in some IL-6 blockade studies; the protein stimulates repair of the intestinal epithelium and blocking it leaves the tissue vulnerable to injury. The single case in this trial occurred 17 days after the patient withdrew from the study for other reasons, so it was not considered to be related to the study medication, Dr. Dorner said.
Vobarilizumab is composed of two heavy chains, lacking the two light-chain arms of a full antibody. It is minuscule – just 10% of the molecular weight of a conventional antibody. One chain targets human serum albumin and is designed to prolong the molecule’s half-life by up to 14 days; the other chain targets the soluble IL-6 receptor.
The phase IIb study comprised 345 patients with active RA despite treatment with methotrexate (mean dose 16 mg/week). While staying on their methotrexate, they were equally assigned to five treatment groups: placebo or vobarilizumab at 75 mg every 4 weeks; 150 mg every 4 weeks; 150 mg every 2 weeks; or 225 mg every 2 weeks.
The primary endpoint was the difference in ACR20 response at week 12 between placebo and the four dosing groups. While the majority of patients taking vobarilizumab met that endpoint, the percentages did not significantly differ from each other, nor from placebo. ACR20 was met by 62% of the placebo group and 81%-72% of the vobarilizumab groups. ACR50 was met by 28% of the placebo group and 45%-29% of the vobarilizumab groups and ACR70 by 9% of the placebo group and 21%-14% of the vobarilizumab groups.
However, Dr. Dorner said, response in the placebo group tended to tail off as the study progressed, while staying significantly stronger in the higher-dose vobarilizumab groups. By week 24, 16% of the placebo group still had an ACR50 – significantly less than in the vobarilizumab 150 mg/2 weeks and 225 mg/2 weeks groups (31%, 39%, respectively).
On a measure of remission that combined C-reactive protein of less than 2.6 mg/L and low disease activity, vobarilizumab looked much better at week 24. At that point, 16% of placebo patients met the endpoint, compared to 39% of the 150 mg/4 weeks and 150 mg/2 weeks vobarilizumab groups, and 51% of the 225 mg/2 weeks group.
Adverse events occurred in 36% of placebo patients and about 44% of vobarilizumab patients and did not show any dose-response relationship. About 38% of these were considered treatment related; 7% of the cohort withdrew due to an adverse event. There were seven serious infections among those taking vobarilizumab (three pneumonia, and one each herpes zoster, ear infection, staphylococcus sepsis, and bacterial arthritis). One patient died of a myocardial infarction, but she had experienced a previous heart attack and undergone percutaneous coronary intervention. The single gastrointestinal perforation occurred in a woman taking the highest dose of vobarilizumab, more than 2 weeks after she stopped taking it.
Vobarilizumab will continue into a phase III study, according to the Ablynx website. The company is seeking an industry partner. AbbVie had an option to license vobarilizumab, but declined last fall on the mixed results of Ablynx’s phase II studies.
[email protected]
On Twitter @Alz_gal
AT EULAR 2017