User login
American Thyroid Association (ATA): Annual Meeting
Study aims to determine prognostic factors for subset of thyroid cancer patients
CORONADO, CALIF. – In patients with radioactive iodine–refractory differentiated thyroid cancer, those with target lesions less than 1.5 cm in size appeared to derive less benefit from sorafenib in terms of progression-free survival, results from an international study showed.
In addition, papillary histology was a positive predictive factor and a predictive factor for benefit from sorafenib.
“Patients with radioactive iodine–refractory differentiated thyroid cancer have a poor prognosis, and there is a lack of effective treatments,” Dr. Martin Schlumberger said at the annual meeting of the American Thyroid Association. “The median survival for this subset is estimated to be 2.5-5 years.”
Sorafenib was approved by the Food and Drug Administration in November 2013 for the treatment of radioactive iodine–refractory differentiated thyroid cancer based on results from the randomized, controlled, double-blind phase III DECISION trial (Lancet 2014;384:319-28). Investigators found that the use of sorafenib extended median progression-free survival by 5 months, compared with placebo (10.8 vs 5.8 months; P < .0001). The purpose of the current analysis was to determine which demographic baseline or disease-related characteristics are prognostic for better outcomes in this patient population. To do so, Dr. Schlumberger of the department of nuclear medicine and endocrine oncology at Gustave Roussy, Villejuif, France, and his associates performed multivariate Cox proportional hazards models adjusted for treatment effect.
He reported findings from 417 patients. Of these, 210 were randomized to receive placebo and 207 were randomized to receive sorafenib. Variables found to be prognostic factors for progression-free survival in placebo patients, and in all patients when adjusted for sorafenib treatment, included papillary histology, lower targeted tumor size, baseline thyroglobulin less than 486 ng/mL, lower number of lesions, and residing in Asia vs. Europe and North America. Subgroup analyses of patients in the sorafenib arm revealed that the following baseline or disease-related variables were predictive of progression-free survival: papillary histology, tumor size of at least 1.5 cm, and having only lung metastases.
In a post-hoc exploratory analysis of progression-free survival by thyroid cancer symptoms among all 417 patients at study entry, the researchers found that both symptomatic and asymptomatic patients had improved progression-free survival following treatment with sorafenib.
On the basis of these findings, radioactive iodine–refractory differentiated thyroid cancer patients with no progressive disease and a tumor size of less than 1.5 cm “appear to have a good prognosis and may be candidates for a ‘watch and wait’ approach before initiating treatment with sorafenib,” Dr. Schlumberger concluded.
Dr. Schlumberger is an adviser to AstraZeneca, Bayer, Eisai, Exelixis, and Genzyme. He has also received research support from Genzyme and Bayer.
On Twitter @dougbrunk
CORONADO, CALIF. – In patients with radioactive iodine–refractory differentiated thyroid cancer, those with target lesions less than 1.5 cm in size appeared to derive less benefit from sorafenib in terms of progression-free survival, results from an international study showed.
In addition, papillary histology was a positive predictive factor and a predictive factor for benefit from sorafenib.
“Patients with radioactive iodine–refractory differentiated thyroid cancer have a poor prognosis, and there is a lack of effective treatments,” Dr. Martin Schlumberger said at the annual meeting of the American Thyroid Association. “The median survival for this subset is estimated to be 2.5-5 years.”
Sorafenib was approved by the Food and Drug Administration in November 2013 for the treatment of radioactive iodine–refractory differentiated thyroid cancer based on results from the randomized, controlled, double-blind phase III DECISION trial (Lancet 2014;384:319-28). Investigators found that the use of sorafenib extended median progression-free survival by 5 months, compared with placebo (10.8 vs 5.8 months; P < .0001). The purpose of the current analysis was to determine which demographic baseline or disease-related characteristics are prognostic for better outcomes in this patient population. To do so, Dr. Schlumberger of the department of nuclear medicine and endocrine oncology at Gustave Roussy, Villejuif, France, and his associates performed multivariate Cox proportional hazards models adjusted for treatment effect.
He reported findings from 417 patients. Of these, 210 were randomized to receive placebo and 207 were randomized to receive sorafenib. Variables found to be prognostic factors for progression-free survival in placebo patients, and in all patients when adjusted for sorafenib treatment, included papillary histology, lower targeted tumor size, baseline thyroglobulin less than 486 ng/mL, lower number of lesions, and residing in Asia vs. Europe and North America. Subgroup analyses of patients in the sorafenib arm revealed that the following baseline or disease-related variables were predictive of progression-free survival: papillary histology, tumor size of at least 1.5 cm, and having only lung metastases.
In a post-hoc exploratory analysis of progression-free survival by thyroid cancer symptoms among all 417 patients at study entry, the researchers found that both symptomatic and asymptomatic patients had improved progression-free survival following treatment with sorafenib.
On the basis of these findings, radioactive iodine–refractory differentiated thyroid cancer patients with no progressive disease and a tumor size of less than 1.5 cm “appear to have a good prognosis and may be candidates for a ‘watch and wait’ approach before initiating treatment with sorafenib,” Dr. Schlumberger concluded.
Dr. Schlumberger is an adviser to AstraZeneca, Bayer, Eisai, Exelixis, and Genzyme. He has also received research support from Genzyme and Bayer.
On Twitter @dougbrunk
CORONADO, CALIF. – In patients with radioactive iodine–refractory differentiated thyroid cancer, those with target lesions less than 1.5 cm in size appeared to derive less benefit from sorafenib in terms of progression-free survival, results from an international study showed.
In addition, papillary histology was a positive predictive factor and a predictive factor for benefit from sorafenib.
“Patients with radioactive iodine–refractory differentiated thyroid cancer have a poor prognosis, and there is a lack of effective treatments,” Dr. Martin Schlumberger said at the annual meeting of the American Thyroid Association. “The median survival for this subset is estimated to be 2.5-5 years.”
Sorafenib was approved by the Food and Drug Administration in November 2013 for the treatment of radioactive iodine–refractory differentiated thyroid cancer based on results from the randomized, controlled, double-blind phase III DECISION trial (Lancet 2014;384:319-28). Investigators found that the use of sorafenib extended median progression-free survival by 5 months, compared with placebo (10.8 vs 5.8 months; P < .0001). The purpose of the current analysis was to determine which demographic baseline or disease-related characteristics are prognostic for better outcomes in this patient population. To do so, Dr. Schlumberger of the department of nuclear medicine and endocrine oncology at Gustave Roussy, Villejuif, France, and his associates performed multivariate Cox proportional hazards models adjusted for treatment effect.
He reported findings from 417 patients. Of these, 210 were randomized to receive placebo and 207 were randomized to receive sorafenib. Variables found to be prognostic factors for progression-free survival in placebo patients, and in all patients when adjusted for sorafenib treatment, included papillary histology, lower targeted tumor size, baseline thyroglobulin less than 486 ng/mL, lower number of lesions, and residing in Asia vs. Europe and North America. Subgroup analyses of patients in the sorafenib arm revealed that the following baseline or disease-related variables were predictive of progression-free survival: papillary histology, tumor size of at least 1.5 cm, and having only lung metastases.
In a post-hoc exploratory analysis of progression-free survival by thyroid cancer symptoms among all 417 patients at study entry, the researchers found that both symptomatic and asymptomatic patients had improved progression-free survival following treatment with sorafenib.
On the basis of these findings, radioactive iodine–refractory differentiated thyroid cancer patients with no progressive disease and a tumor size of less than 1.5 cm “appear to have a good prognosis and may be candidates for a ‘watch and wait’ approach before initiating treatment with sorafenib,” Dr. Schlumberger concluded.
Dr. Schlumberger is an adviser to AstraZeneca, Bayer, Eisai, Exelixis, and Genzyme. He has also received research support from Genzyme and Bayer.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Radioactive iodine–refractory differentiated thyroid cancer patients with no progressive disease and a tumor size of less than 1.5 cm may be candidates for a “watch and wait” approach before initiating treatment with sorafenib.
Major finding: Baseline or disease-related variables found to be prognostic factors for progression-free survival in placebo patients and in all patients when adjusted for sorafenib treatment included papillary histology, lower targeted tumor size, baseline thyroglobulin less than 486 ng/mL, lower number of lesions, and residing in Asia versus Europe and North America.
Data source: An analysis of 417 patients from the randomized, controlled, double-blind, phase III DECISION trial.
Disclosures: Dr. Schlumberger is an adviser to AstraZeneca, Bayer, Eisai, Exelixis, and Genzyme. He has also received research support from Genzyme and Bayer.
Altered mental state is key feature of thyroid storm
CORONADO, CALIF. – The presence of an altered mental state was the only feature associated with the clinical diagnosis of thyroid storm, compared with patients who had compensated thyrotoxicosis, results from a retrospective study demonstrated.
“Thyroid storm is a rare diagnosis, but it’s something that can cause mortality [of] 10% or more,” lead study author Dr. Melissa G. Lechner said in an interview during the annual meeting of the American Thyroid Association. “Though the existing Burch-Wartofsky (Endocrinol. Metab. Clin. North Am. 1993;22:263-77) and Akamizu (Thyroid 2012;22:661-79) scoring systems can help guide clinicians in the diagnosis of thyroid storm, they have not been applied to inpatient populations,” said Dr. Lechner, who is an internal medicine resident at Brigham and Women’s Faulkner Hospital, Boston. “Our question was, in an inpatient setting, and among patients who are acutely ill, how do you distinguish the patients who are hyperthyroid and going to have bad outcomes from the patient who just has sepsis and hyperthyroidism? Who do we need to be aware of in terms of being aggressive with treatment?”
To find out, she and her associates retrospectively evaluated the records of 150 patients who were admitted at Los Angeles County–University of Southern California Medical Center between Jan. 1, 2008 and Dec. 31, 2013, with a thyroid-stimulating hormone (TSH) level of less than .01 mIU/L. They evaluated patients with thyroid storm and those with compensated thyrotoxicosis for differences in clinical and laboratory characteristics, and in hospital outcomes of inpatient mortality, hospital length of stay, ICU admission, ICU length of stay, intubation, and duration of mechanical ventilation. Patients were retrospectively categorized by Burch-Wartofsky score (BWS less than 25, 25-44, or 45 and greater) and Akamizu categories (AkTS1/2). They excluded non-thyrotoxic causes of TSH suppression and those with inadequate medical records.
The researchers found that the following clinical features helped to differentiate thyroid storm from compensated thyrotoxicosis in the clinical hospital setting: fever of greater than 100.4 degrees F, heart rate of greater than 100 beats per minute, altered mentation, and precipitating event (P less than .05 for all). Altered mentation was the was only clinical feature that distinguished thyroid storm from compensated thyrotoxicosis for patients with a BWS score of greater than 45 and in patients with AkTS1/2 (P less than .001). In addition, patients diagnosed with thyroid storm had greater mortality and worse outcomes over all measures. The findings “have been useful, especially from an internal medicine perspective, because often we’re the first to see these patients,” noted Dr. Lechner, who began the study while a medical student at USC.
She and her associates concluded that patients with suspected thyroid storm who have altered mental state as a recognized feature may be at greater risk for adverse outcomes and may derive the greatest benefit from early and/or aggressive therapeutic intervention.
Dr. Lechner reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – The presence of an altered mental state was the only feature associated with the clinical diagnosis of thyroid storm, compared with patients who had compensated thyrotoxicosis, results from a retrospective study demonstrated.
“Thyroid storm is a rare diagnosis, but it’s something that can cause mortality [of] 10% or more,” lead study author Dr. Melissa G. Lechner said in an interview during the annual meeting of the American Thyroid Association. “Though the existing Burch-Wartofsky (Endocrinol. Metab. Clin. North Am. 1993;22:263-77) and Akamizu (Thyroid 2012;22:661-79) scoring systems can help guide clinicians in the diagnosis of thyroid storm, they have not been applied to inpatient populations,” said Dr. Lechner, who is an internal medicine resident at Brigham and Women’s Faulkner Hospital, Boston. “Our question was, in an inpatient setting, and among patients who are acutely ill, how do you distinguish the patients who are hyperthyroid and going to have bad outcomes from the patient who just has sepsis and hyperthyroidism? Who do we need to be aware of in terms of being aggressive with treatment?”
To find out, she and her associates retrospectively evaluated the records of 150 patients who were admitted at Los Angeles County–University of Southern California Medical Center between Jan. 1, 2008 and Dec. 31, 2013, with a thyroid-stimulating hormone (TSH) level of less than .01 mIU/L. They evaluated patients with thyroid storm and those with compensated thyrotoxicosis for differences in clinical and laboratory characteristics, and in hospital outcomes of inpatient mortality, hospital length of stay, ICU admission, ICU length of stay, intubation, and duration of mechanical ventilation. Patients were retrospectively categorized by Burch-Wartofsky score (BWS less than 25, 25-44, or 45 and greater) and Akamizu categories (AkTS1/2). They excluded non-thyrotoxic causes of TSH suppression and those with inadequate medical records.
The researchers found that the following clinical features helped to differentiate thyroid storm from compensated thyrotoxicosis in the clinical hospital setting: fever of greater than 100.4 degrees F, heart rate of greater than 100 beats per minute, altered mentation, and precipitating event (P less than .05 for all). Altered mentation was the was only clinical feature that distinguished thyroid storm from compensated thyrotoxicosis for patients with a BWS score of greater than 45 and in patients with AkTS1/2 (P less than .001). In addition, patients diagnosed with thyroid storm had greater mortality and worse outcomes over all measures. The findings “have been useful, especially from an internal medicine perspective, because often we’re the first to see these patients,” noted Dr. Lechner, who began the study while a medical student at USC.
She and her associates concluded that patients with suspected thyroid storm who have altered mental state as a recognized feature may be at greater risk for adverse outcomes and may derive the greatest benefit from early and/or aggressive therapeutic intervention.
Dr. Lechner reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – The presence of an altered mental state was the only feature associated with the clinical diagnosis of thyroid storm, compared with patients who had compensated thyrotoxicosis, results from a retrospective study demonstrated.
“Thyroid storm is a rare diagnosis, but it’s something that can cause mortality [of] 10% or more,” lead study author Dr. Melissa G. Lechner said in an interview during the annual meeting of the American Thyroid Association. “Though the existing Burch-Wartofsky (Endocrinol. Metab. Clin. North Am. 1993;22:263-77) and Akamizu (Thyroid 2012;22:661-79) scoring systems can help guide clinicians in the diagnosis of thyroid storm, they have not been applied to inpatient populations,” said Dr. Lechner, who is an internal medicine resident at Brigham and Women’s Faulkner Hospital, Boston. “Our question was, in an inpatient setting, and among patients who are acutely ill, how do you distinguish the patients who are hyperthyroid and going to have bad outcomes from the patient who just has sepsis and hyperthyroidism? Who do we need to be aware of in terms of being aggressive with treatment?”
To find out, she and her associates retrospectively evaluated the records of 150 patients who were admitted at Los Angeles County–University of Southern California Medical Center between Jan. 1, 2008 and Dec. 31, 2013, with a thyroid-stimulating hormone (TSH) level of less than .01 mIU/L. They evaluated patients with thyroid storm and those with compensated thyrotoxicosis for differences in clinical and laboratory characteristics, and in hospital outcomes of inpatient mortality, hospital length of stay, ICU admission, ICU length of stay, intubation, and duration of mechanical ventilation. Patients were retrospectively categorized by Burch-Wartofsky score (BWS less than 25, 25-44, or 45 and greater) and Akamizu categories (AkTS1/2). They excluded non-thyrotoxic causes of TSH suppression and those with inadequate medical records.
The researchers found that the following clinical features helped to differentiate thyroid storm from compensated thyrotoxicosis in the clinical hospital setting: fever of greater than 100.4 degrees F, heart rate of greater than 100 beats per minute, altered mentation, and precipitating event (P less than .05 for all). Altered mentation was the was only clinical feature that distinguished thyroid storm from compensated thyrotoxicosis for patients with a BWS score of greater than 45 and in patients with AkTS1/2 (P less than .001). In addition, patients diagnosed with thyroid storm had greater mortality and worse outcomes over all measures. The findings “have been useful, especially from an internal medicine perspective, because often we’re the first to see these patients,” noted Dr. Lechner, who began the study while a medical student at USC.
She and her associates concluded that patients with suspected thyroid storm who have altered mental state as a recognized feature may be at greater risk for adverse outcomes and may derive the greatest benefit from early and/or aggressive therapeutic intervention.
Dr. Lechner reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Patients with suspected thyroid storm who present with an altered mental state should be treated aggressively.
Major finding: Altered mentation was the was only clinical feature that distinguished thyroid storm from compensated thyrotoxicosis for patients with a Burch-Wartofsky score of greater than 45 and in patients with thyroid storm grades 1 and 2 based on Akamizu criteria (P less than .001).
Data source: A retrospective review of 150 patients who were admitted at Los Angeles County-University of Southern California Medical Center between Jan. 1, 2008 and Dec. 31, 2013 with a TSH level of less than .01 mIU/L.
Disclosures: Dr. Lechner reported having no financial disclosures.
Robotic thyroidectomy outcomes better in high-volume centers
CORONADO, CALIF. – Robotic thyroid surgery performed at the highest-volume center had a lower complication rate and shorter hospital stays than did the other hospitals in the study, results from a study of national data showed.
The Food and Drug Administration suspended its approval of robotic thyroidectomy in October 2011, citing risks and lack of adequate safety and outcomes research. The researchers observed a drop in the number of robotic thyroidectomies performed in the United States after the FDA issued its restriction in 2011. “That move appears to have made a pretty large impact on the projected growth of this procedure,” Dr. Hinson said at the annual meeting of the American Thyroid Association.
In Korea, where the procedure gained recognition in the early 2000s, “a lot of people cite cultural factors, such as aversion to neck scars, lean body habitus, and low body mass index make the procedure more feasible, so it’s a very popular approach there,” said Dr. Hinson, a research fellow at the University of Arkansas for Medical Sciences, Little Rock. In addition, until recently, there were financial incentives to do thyroid surgery with robotic assistance in the Korean health care system. “That said, in the United States, the cultural forces are distinct, our patients are larger and heavier on average, and most patients don’t have a strong aversion to a neck scar. The procedure is paid the same with or without the robot, but takes on average three times as long with the robot. Surgeons have such great results with open techniques that it’s very hard to make an argument that robotic surgery improves outcomes that much.”
In what is believed to be the largest study of its kind in the United States, Dr. Hinson and his associates evaluated data from the University HealthSystem Consortium (UHC) and an additional academic center which did not participate in the UHC discharge database. The study included 484 patients who underwent robotic thyroidectomy in the United States between 2009 and 2013. Data were compiled from discharge summaries at 110 university medical centers and another 140 of their affiliated hospitals. The researchers collected data on age, gender, race, insurance, comorbidities, complications, discharge status, length of stay, and ICU admission.
Dr. Hinson and his associates found that, compared with outpatients, inpatients had significantly greater numbers of comorbidities and complications. The most common comorbidity was hypertension (12 cases), followed by chronic pulmonary disease (8 cases) and diabetes with complications and comorbidities (6 cases). The median hospital length of stay was 1 day for inpatients, and 57% of outpatients stayed overnight. In addition, 8% of inpatients required an ICU stay, while 99% of outpatients and 97% of inpatients were discharged to home. The highest-volume institution in the data set performed most of the outpatient cases and had a lower rate of complications. “That makes sense,” Dr. Hinson said. “If you’re proficient, you’re more likely to have learned how to avoid complications.
“The approach to the neck has largely been unchanged over the last 100 years,” he said. While several other surgical fields have found highly successful and popular niches for endoscopic and/or robotic technology, the uses for these services has been largely limited in head and neck surgery. The da Vinci system was largely created with abdominal surgery in mind. As surgical techniques and robotic technology develop, systemic applications for this technology, previously unrecognized, may emerge. A lot of academic centers were/are hopeful that robotic thyroid surgery may provide the gateway for advancement of such techniques in the head and neck region.”
He reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Robotic thyroid surgery performed at the highest-volume center had a lower complication rate and shorter hospital stays than did the other hospitals in the study, results from a study of national data showed.
The Food and Drug Administration suspended its approval of robotic thyroidectomy in October 2011, citing risks and lack of adequate safety and outcomes research. The researchers observed a drop in the number of robotic thyroidectomies performed in the United States after the FDA issued its restriction in 2011. “That move appears to have made a pretty large impact on the projected growth of this procedure,” Dr. Hinson said at the annual meeting of the American Thyroid Association.
In Korea, where the procedure gained recognition in the early 2000s, “a lot of people cite cultural factors, such as aversion to neck scars, lean body habitus, and low body mass index make the procedure more feasible, so it’s a very popular approach there,” said Dr. Hinson, a research fellow at the University of Arkansas for Medical Sciences, Little Rock. In addition, until recently, there were financial incentives to do thyroid surgery with robotic assistance in the Korean health care system. “That said, in the United States, the cultural forces are distinct, our patients are larger and heavier on average, and most patients don’t have a strong aversion to a neck scar. The procedure is paid the same with or without the robot, but takes on average three times as long with the robot. Surgeons have such great results with open techniques that it’s very hard to make an argument that robotic surgery improves outcomes that much.”
In what is believed to be the largest study of its kind in the United States, Dr. Hinson and his associates evaluated data from the University HealthSystem Consortium (UHC) and an additional academic center which did not participate in the UHC discharge database. The study included 484 patients who underwent robotic thyroidectomy in the United States between 2009 and 2013. Data were compiled from discharge summaries at 110 university medical centers and another 140 of their affiliated hospitals. The researchers collected data on age, gender, race, insurance, comorbidities, complications, discharge status, length of stay, and ICU admission.
Dr. Hinson and his associates found that, compared with outpatients, inpatients had significantly greater numbers of comorbidities and complications. The most common comorbidity was hypertension (12 cases), followed by chronic pulmonary disease (8 cases) and diabetes with complications and comorbidities (6 cases). The median hospital length of stay was 1 day for inpatients, and 57% of outpatients stayed overnight. In addition, 8% of inpatients required an ICU stay, while 99% of outpatients and 97% of inpatients were discharged to home. The highest-volume institution in the data set performed most of the outpatient cases and had a lower rate of complications. “That makes sense,” Dr. Hinson said. “If you’re proficient, you’re more likely to have learned how to avoid complications.
“The approach to the neck has largely been unchanged over the last 100 years,” he said. While several other surgical fields have found highly successful and popular niches for endoscopic and/or robotic technology, the uses for these services has been largely limited in head and neck surgery. The da Vinci system was largely created with abdominal surgery in mind. As surgical techniques and robotic technology develop, systemic applications for this technology, previously unrecognized, may emerge. A lot of academic centers were/are hopeful that robotic thyroid surgery may provide the gateway for advancement of such techniques in the head and neck region.”
He reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Robotic thyroid surgery performed at the highest-volume center had a lower complication rate and shorter hospital stays than did the other hospitals in the study, results from a study of national data showed.
The Food and Drug Administration suspended its approval of robotic thyroidectomy in October 2011, citing risks and lack of adequate safety and outcomes research. The researchers observed a drop in the number of robotic thyroidectomies performed in the United States after the FDA issued its restriction in 2011. “That move appears to have made a pretty large impact on the projected growth of this procedure,” Dr. Hinson said at the annual meeting of the American Thyroid Association.
In Korea, where the procedure gained recognition in the early 2000s, “a lot of people cite cultural factors, such as aversion to neck scars, lean body habitus, and low body mass index make the procedure more feasible, so it’s a very popular approach there,” said Dr. Hinson, a research fellow at the University of Arkansas for Medical Sciences, Little Rock. In addition, until recently, there were financial incentives to do thyroid surgery with robotic assistance in the Korean health care system. “That said, in the United States, the cultural forces are distinct, our patients are larger and heavier on average, and most patients don’t have a strong aversion to a neck scar. The procedure is paid the same with or without the robot, but takes on average three times as long with the robot. Surgeons have such great results with open techniques that it’s very hard to make an argument that robotic surgery improves outcomes that much.”
In what is believed to be the largest study of its kind in the United States, Dr. Hinson and his associates evaluated data from the University HealthSystem Consortium (UHC) and an additional academic center which did not participate in the UHC discharge database. The study included 484 patients who underwent robotic thyroidectomy in the United States between 2009 and 2013. Data were compiled from discharge summaries at 110 university medical centers and another 140 of their affiliated hospitals. The researchers collected data on age, gender, race, insurance, comorbidities, complications, discharge status, length of stay, and ICU admission.
Dr. Hinson and his associates found that, compared with outpatients, inpatients had significantly greater numbers of comorbidities and complications. The most common comorbidity was hypertension (12 cases), followed by chronic pulmonary disease (8 cases) and diabetes with complications and comorbidities (6 cases). The median hospital length of stay was 1 day for inpatients, and 57% of outpatients stayed overnight. In addition, 8% of inpatients required an ICU stay, while 99% of outpatients and 97% of inpatients were discharged to home. The highest-volume institution in the data set performed most of the outpatient cases and had a lower rate of complications. “That makes sense,” Dr. Hinson said. “If you’re proficient, you’re more likely to have learned how to avoid complications.
“The approach to the neck has largely been unchanged over the last 100 years,” he said. While several other surgical fields have found highly successful and popular niches for endoscopic and/or robotic technology, the uses for these services has been largely limited in head and neck surgery. The da Vinci system was largely created with abdominal surgery in mind. As surgical techniques and robotic technology develop, systemic applications for this technology, previously unrecognized, may emerge. A lot of academic centers were/are hopeful that robotic thyroid surgery may provide the gateway for advancement of such techniques in the head and neck region.”
He reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Robotic thyroid surgery performed by higher-volume surgeons is associated with lower complications and shorter hospital stays.
Major finding: Compared with outpatients, inpatients had a significantly greater number of comorbidities (P < .001) and complications (P =.005). In addition, the highest-volume institution in the data set performed most of the outpatient cases and had a lower rate of complications.
Data source: A study of 484 patients from the University HealthSystem Consortium who underwent robotic thyroidectomy in the United States between 2009 and 2013.
Disclosures:Dr. Hinson reported having no financial disclosures.
Autoantibodies not predictive of surgery for Graves’ disease
CORONADO, CALIF.– Measurement of thyroid antibodies had no impact on the clinical features of Graves’ disease best treated with surgery, results from a single-center retrospective study showed.
The findings are part of a larger study meant to develop ways to help patients decide between surgery and radioactive iodine for their Graves’ disease. “We know that certain clinical features make patients lean toward surgery instead of radioactive iodine, including severe ophthalmopathy and young women who have concerns about family planning,” Dr. Dawn M. Elfenbein said in an interview during the annual meeting of the American Thyroid Association. “In the long-term picture, I think that a lot of provider preferences go into this decision, but we’d like to move this to being more of a patient-centered decision. So we’re trying to see if there are biochemical factors about patients that can help us recommend one treatment versus the other.”
Dr. Elfenbein of the section of endocrine surgery in the department of surgery at the University of Wisconsin, Madison, and her associates reviewed the records of 469 patients treated with radioactive iodine (RAI) or surgery for Graves’ disease at the institution during August 2008-September 2013. They excluded patients with contraindications to RAI or those with other indications for surgery or who previously failed either treatment.
Of the 469 patients, 78% were women, and their mean age was 40 years. Most (71%) underwent RAI while 29% underwent surgery. The percentage of patients who opted for surgery increased each year of the study, from 14% in the first year to 52% in the final year.
More than half of the patients (52%) had thyroid peroxidase (TPO) measured prior to treatment, while 44% had thyroglobulin antibodies (TgAb) and 45% had either thyroid simulating immunoglobulin (TSIg) or thyrotropin receptor antibody (TRAb) measured.
Dr. Elfenbein and her associates found that clinical features such as ophthalmopathy or a compressive goiter appeared to influence a patient’s decision to choose surgery over RAI. On bivariate analysis, patients with a positive TSIg or TRAb were significantly more likely to have ophthalmopathy (41% vs. 25%) while patients with positive TgAb were significantly more likely to have goiter (71% vs. 55%). On multivariate analysis, however, antibody positivity was not predictive of ophthalmopathy or goiter.
“Surgery became the primary definitive treatment of choice over RAI for Graves’ disease at our institution over the study period, particularly for younger women,” the researchers wrote in their abstract. The concluded that measurement of thyroid-specific antibodies “does not independently predict those clinical features best treated with surgery. Clinical features and patient preferences should be considered independently from autoantibody levels.”
Dr. Elfenbein acknowledged certain limitations of the study, including its retrospective design and that fact that autoantibody levels were not measured after treatment. “What would be more helpful is to measure antibodies in everyone before they undergo treatment and measure those same antibodies after treatment to see what happens; to see if there are any differences in recurrence rates with higher antibodies,” she said. “We can be more deliberate moving forward.” She reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF.– Measurement of thyroid antibodies had no impact on the clinical features of Graves’ disease best treated with surgery, results from a single-center retrospective study showed.
The findings are part of a larger study meant to develop ways to help patients decide between surgery and radioactive iodine for their Graves’ disease. “We know that certain clinical features make patients lean toward surgery instead of radioactive iodine, including severe ophthalmopathy and young women who have concerns about family planning,” Dr. Dawn M. Elfenbein said in an interview during the annual meeting of the American Thyroid Association. “In the long-term picture, I think that a lot of provider preferences go into this decision, but we’d like to move this to being more of a patient-centered decision. So we’re trying to see if there are biochemical factors about patients that can help us recommend one treatment versus the other.”
Dr. Elfenbein of the section of endocrine surgery in the department of surgery at the University of Wisconsin, Madison, and her associates reviewed the records of 469 patients treated with radioactive iodine (RAI) or surgery for Graves’ disease at the institution during August 2008-September 2013. They excluded patients with contraindications to RAI or those with other indications for surgery or who previously failed either treatment.
Of the 469 patients, 78% were women, and their mean age was 40 years. Most (71%) underwent RAI while 29% underwent surgery. The percentage of patients who opted for surgery increased each year of the study, from 14% in the first year to 52% in the final year.
More than half of the patients (52%) had thyroid peroxidase (TPO) measured prior to treatment, while 44% had thyroglobulin antibodies (TgAb) and 45% had either thyroid simulating immunoglobulin (TSIg) or thyrotropin receptor antibody (TRAb) measured.
Dr. Elfenbein and her associates found that clinical features such as ophthalmopathy or a compressive goiter appeared to influence a patient’s decision to choose surgery over RAI. On bivariate analysis, patients with a positive TSIg or TRAb were significantly more likely to have ophthalmopathy (41% vs. 25%) while patients with positive TgAb were significantly more likely to have goiter (71% vs. 55%). On multivariate analysis, however, antibody positivity was not predictive of ophthalmopathy or goiter.
“Surgery became the primary definitive treatment of choice over RAI for Graves’ disease at our institution over the study period, particularly for younger women,” the researchers wrote in their abstract. The concluded that measurement of thyroid-specific antibodies “does not independently predict those clinical features best treated with surgery. Clinical features and patient preferences should be considered independently from autoantibody levels.”
Dr. Elfenbein acknowledged certain limitations of the study, including its retrospective design and that fact that autoantibody levels were not measured after treatment. “What would be more helpful is to measure antibodies in everyone before they undergo treatment and measure those same antibodies after treatment to see what happens; to see if there are any differences in recurrence rates with higher antibodies,” she said. “We can be more deliberate moving forward.” She reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF.– Measurement of thyroid antibodies had no impact on the clinical features of Graves’ disease best treated with surgery, results from a single-center retrospective study showed.
The findings are part of a larger study meant to develop ways to help patients decide between surgery and radioactive iodine for their Graves’ disease. “We know that certain clinical features make patients lean toward surgery instead of radioactive iodine, including severe ophthalmopathy and young women who have concerns about family planning,” Dr. Dawn M. Elfenbein said in an interview during the annual meeting of the American Thyroid Association. “In the long-term picture, I think that a lot of provider preferences go into this decision, but we’d like to move this to being more of a patient-centered decision. So we’re trying to see if there are biochemical factors about patients that can help us recommend one treatment versus the other.”
Dr. Elfenbein of the section of endocrine surgery in the department of surgery at the University of Wisconsin, Madison, and her associates reviewed the records of 469 patients treated with radioactive iodine (RAI) or surgery for Graves’ disease at the institution during August 2008-September 2013. They excluded patients with contraindications to RAI or those with other indications for surgery or who previously failed either treatment.
Of the 469 patients, 78% were women, and their mean age was 40 years. Most (71%) underwent RAI while 29% underwent surgery. The percentage of patients who opted for surgery increased each year of the study, from 14% in the first year to 52% in the final year.
More than half of the patients (52%) had thyroid peroxidase (TPO) measured prior to treatment, while 44% had thyroglobulin antibodies (TgAb) and 45% had either thyroid simulating immunoglobulin (TSIg) or thyrotropin receptor antibody (TRAb) measured.
Dr. Elfenbein and her associates found that clinical features such as ophthalmopathy or a compressive goiter appeared to influence a patient’s decision to choose surgery over RAI. On bivariate analysis, patients with a positive TSIg or TRAb were significantly more likely to have ophthalmopathy (41% vs. 25%) while patients with positive TgAb were significantly more likely to have goiter (71% vs. 55%). On multivariate analysis, however, antibody positivity was not predictive of ophthalmopathy or goiter.
“Surgery became the primary definitive treatment of choice over RAI for Graves’ disease at our institution over the study period, particularly for younger women,” the researchers wrote in their abstract. The concluded that measurement of thyroid-specific antibodies “does not independently predict those clinical features best treated with surgery. Clinical features and patient preferences should be considered independently from autoantibody levels.”
Dr. Elfenbein acknowledged certain limitations of the study, including its retrospective design and that fact that autoantibody levels were not measured after treatment. “What would be more helpful is to measure antibodies in everyone before they undergo treatment and measure those same antibodies after treatment to see what happens; to see if there are any differences in recurrence rates with higher antibodies,” she said. “We can be more deliberate moving forward.” She reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Measuring thyroid antibodies adds no value in predicting clinical features of Graves’ disease best treated with surgery.
Major finding: On bivariate analysis, patients with a positive TSIg or TRAb were more likely to have ophthalmopathy (41% vs. 25%; P = .04) while patients with positive TgAb were more likely to have goiter (71% vs. 55%; P = .03). On multivariate analysis, however, antibody positivity was not predictive of ophthalmopathy or goiter.
Data source: A retrospective analysis of 469 patients treated with radioactive iodine (RAI) or surgery for Graves’ disease at the University of Wisconsin, Madison, during August 2008-September 2013.
Disclosures:Dr. Elfenbein reported having no financial disclosures.
Ultrasound bests elastography for specificity of thyroid cancer diagnosis
CORONADO, CALIF.– Compared with elastography, ultrasound predictors of malignancy were more specific for presurgical diagnosis and in differentiating between benign and malignant thyroid nodules, results from a pooled analysis showed.
“Elastography is controversial,” Dr. Parisha Bhatia said in an interview during the annual meeting of the American Thyroid Association. “Some studies have reported that it has better sensitivity and specificity, compared with conventional ultrasound, but others have found it not to be helpful.”
In an effort to compare the efficacy of elastography and ultrasound in determining benign and malignant thyroid nodules, and to determine if elastography has a complementary role to fine needle aspiration (FNA), Dr. Bhatia and her associates searched Embase and PubMed databases for articles involving more than 50 nodules using specimen histology as the reference standard. They discovered 14 prospective studies and organized them into one of two groups. Group 1 included nodules with FNA cytology–proven “benign/malignant” result. Group 2 included nodules with FNA cytology as “intermediate.” The elasticity score was compared with ultrasound features such as taller than wide, irregular margins, internal vascularity, calcification, and absence of halo to determine validity measures and likelihood ratios.
Dr. Bhatia, an endocrine surgeon at Tulane University, New Orleans, reported on findings from 2,732 nodules in the pooled analysis. Of these, 64% were benign, 25% were malignant, and 11% were indeterminate.
In group 1, elastography showed a sensitivity of 75%, a specificity of 80%, a positive predictive value (PPV) of 61%, a negative predictive value (NPV) of 89%, and a likelihood ratio of 5.7, with a higher predictive value for nodules smaller than 1 cm in diameter (PPV of 79% and NPV of 83%). The strongest ultrasound-related predictor of malignancies was “taller than wide” (a specificity of 92%, a NPV of 51%, yet a sensitivity of only 24%), followed by irregular margins (a specificity of 91%, sensitivity of 48%, and a PPV of 64%). Combination of elastography and ultrasound had the highest sensitivity (96%) and NPV (96%), yet lower specificity (46%) and PPV (46%).
In group 2, elastography yielded a higher sensitivity (90%) and NPV (92%), while ultrasound features were highly specific, with the highest values for “taller than wide” shape (85%) in these thyroid nodules.
“Ultrasound predictors of malignancy prove to be more specific for presurgical diagnosis and differentiation of benign and malignant thyroid nodules,” the researchers wrote in their abstract. “When used as an adjunct, the higher sensitivity and NPV of combination of both the techniques can lead to better selection of candidates for FNA.”
Dr. Bhatia acknowledged certain limitations of the study, including the fact that the pooled data contained little information on indeterminate thyroid nodules. She reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF.– Compared with elastography, ultrasound predictors of malignancy were more specific for presurgical diagnosis and in differentiating between benign and malignant thyroid nodules, results from a pooled analysis showed.
“Elastography is controversial,” Dr. Parisha Bhatia said in an interview during the annual meeting of the American Thyroid Association. “Some studies have reported that it has better sensitivity and specificity, compared with conventional ultrasound, but others have found it not to be helpful.”
In an effort to compare the efficacy of elastography and ultrasound in determining benign and malignant thyroid nodules, and to determine if elastography has a complementary role to fine needle aspiration (FNA), Dr. Bhatia and her associates searched Embase and PubMed databases for articles involving more than 50 nodules using specimen histology as the reference standard. They discovered 14 prospective studies and organized them into one of two groups. Group 1 included nodules with FNA cytology–proven “benign/malignant” result. Group 2 included nodules with FNA cytology as “intermediate.” The elasticity score was compared with ultrasound features such as taller than wide, irregular margins, internal vascularity, calcification, and absence of halo to determine validity measures and likelihood ratios.
Dr. Bhatia, an endocrine surgeon at Tulane University, New Orleans, reported on findings from 2,732 nodules in the pooled analysis. Of these, 64% were benign, 25% were malignant, and 11% were indeterminate.
In group 1, elastography showed a sensitivity of 75%, a specificity of 80%, a positive predictive value (PPV) of 61%, a negative predictive value (NPV) of 89%, and a likelihood ratio of 5.7, with a higher predictive value for nodules smaller than 1 cm in diameter (PPV of 79% and NPV of 83%). The strongest ultrasound-related predictor of malignancies was “taller than wide” (a specificity of 92%, a NPV of 51%, yet a sensitivity of only 24%), followed by irregular margins (a specificity of 91%, sensitivity of 48%, and a PPV of 64%). Combination of elastography and ultrasound had the highest sensitivity (96%) and NPV (96%), yet lower specificity (46%) and PPV (46%).
In group 2, elastography yielded a higher sensitivity (90%) and NPV (92%), while ultrasound features were highly specific, with the highest values for “taller than wide” shape (85%) in these thyroid nodules.
“Ultrasound predictors of malignancy prove to be more specific for presurgical diagnosis and differentiation of benign and malignant thyroid nodules,” the researchers wrote in their abstract. “When used as an adjunct, the higher sensitivity and NPV of combination of both the techniques can lead to better selection of candidates for FNA.”
Dr. Bhatia acknowledged certain limitations of the study, including the fact that the pooled data contained little information on indeterminate thyroid nodules. She reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF.– Compared with elastography, ultrasound predictors of malignancy were more specific for presurgical diagnosis and in differentiating between benign and malignant thyroid nodules, results from a pooled analysis showed.
“Elastography is controversial,” Dr. Parisha Bhatia said in an interview during the annual meeting of the American Thyroid Association. “Some studies have reported that it has better sensitivity and specificity, compared with conventional ultrasound, but others have found it not to be helpful.”
In an effort to compare the efficacy of elastography and ultrasound in determining benign and malignant thyroid nodules, and to determine if elastography has a complementary role to fine needle aspiration (FNA), Dr. Bhatia and her associates searched Embase and PubMed databases for articles involving more than 50 nodules using specimen histology as the reference standard. They discovered 14 prospective studies and organized them into one of two groups. Group 1 included nodules with FNA cytology–proven “benign/malignant” result. Group 2 included nodules with FNA cytology as “intermediate.” The elasticity score was compared with ultrasound features such as taller than wide, irregular margins, internal vascularity, calcification, and absence of halo to determine validity measures and likelihood ratios.
Dr. Bhatia, an endocrine surgeon at Tulane University, New Orleans, reported on findings from 2,732 nodules in the pooled analysis. Of these, 64% were benign, 25% were malignant, and 11% were indeterminate.
In group 1, elastography showed a sensitivity of 75%, a specificity of 80%, a positive predictive value (PPV) of 61%, a negative predictive value (NPV) of 89%, and a likelihood ratio of 5.7, with a higher predictive value for nodules smaller than 1 cm in diameter (PPV of 79% and NPV of 83%). The strongest ultrasound-related predictor of malignancies was “taller than wide” (a specificity of 92%, a NPV of 51%, yet a sensitivity of only 24%), followed by irregular margins (a specificity of 91%, sensitivity of 48%, and a PPV of 64%). Combination of elastography and ultrasound had the highest sensitivity (96%) and NPV (96%), yet lower specificity (46%) and PPV (46%).
In group 2, elastography yielded a higher sensitivity (90%) and NPV (92%), while ultrasound features were highly specific, with the highest values for “taller than wide” shape (85%) in these thyroid nodules.
“Ultrasound predictors of malignancy prove to be more specific for presurgical diagnosis and differentiation of benign and malignant thyroid nodules,” the researchers wrote in their abstract. “When used as an adjunct, the higher sensitivity and NPV of combination of both the techniques can lead to better selection of candidates for FNA.”
Dr. Bhatia acknowledged certain limitations of the study, including the fact that the pooled data contained little information on indeterminate thyroid nodules. She reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Ultrasound is more specific than elastography in helping clinicians make a presurgical diagnosis of thyroid cancer.
Major finding: Compared with elastography, ultrasound was more specific in presurgical diagnosis and in differentiating between benign and malignant thyroid nodules (specificity of 92% vs. 80%, respectively).
Data source: A pooled analysis of 14 prospective studies involving findings from 2,732 thyroid nodules.
Disclosures: Dr. Bhatia reported having no financial disclosures.
Shoulder morbidity common after thyroid cancer surgery
CORONADO, CALIF. – More than 50% of patients who underwent surgery for differentiated thyroid cancer experienced shoulder morbidity up to 10 years after the procedure, results from a Dutch study showed.
“What’s causing the pain?” Dr. Romana T. Netea-Maier asked in an interview at the annual meeting of the American Thyroid Association. “It may be that the spinal accessory nerve or other nerves have been injured during the surgery. We don’t know.”
In what she said is the first study of its kind, Dr. Netea-Maier and her associates compared the prevalence of shoulder morbidity and its relation to clinical characteristics and quality of life in 109 patients who underwent surgery for differentiated thyroid cancer at Radboud University Medical Center, Nijmegen, the Netherlands, with a group of 81 healthy controls and a group of 59 patients who underwent surgery for benign thyroid pathology. Main outcome measures were the prevalence of shoulder complaints based on results of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and the European Organization for Research and Treatment of Cancer, Quality of Life Questionnaire-C-30 (EORTC QLQ-C30).
Dr. Netea-Maier, of the department of medicine at the university, reported that the mean age of patients in the two surgery groups was 46 years, and 73% were women. During an average of 10 years following surgery, 59% of patients in the thyroid cancer group and 49% of patients in the benign thyroid pathology group reported shoulder morbidity, compared with 14% of controls (P < .01). The chief complaints among patients in the thyroid cancer group were pain (25%), muscle weakness (8%), and tingling (8%), while the main complaints among those with benign thyroid pathology were pain (38%), and tingling (7%).
Compared with healthy controls, patients in the thyroid cancer group scored worse on all subscales of the DASH and the EORTC QLQ-C30. On bivariate analysis, level V neck dissection, spinal accessory nerve damage, and employment status were associated with the prevalence of shoulder complaints and DASH scores, while the prevalence of shoulder complaints and DASH scores correlated significantly with EORTC QLQ-C30 scores.
The researchers found that only 12% of patients in the thyroid cancer group received preoperative information on the potential for shoulder morbidity and 35% received additional care for postoperative shoulder complaints.
“The take-home message would be to inform your patients of the potential for shoulder comorbidity, because what we have shown here is that patients do not recall being informed about this possible complication before the surgery,” Dr. Netea-Maier said. “If they have complaints, start with physiotherapy early on.”
Dr. Netea-Maier reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – More than 50% of patients who underwent surgery for differentiated thyroid cancer experienced shoulder morbidity up to 10 years after the procedure, results from a Dutch study showed.
“What’s causing the pain?” Dr. Romana T. Netea-Maier asked in an interview at the annual meeting of the American Thyroid Association. “It may be that the spinal accessory nerve or other nerves have been injured during the surgery. We don’t know.”
In what she said is the first study of its kind, Dr. Netea-Maier and her associates compared the prevalence of shoulder morbidity and its relation to clinical characteristics and quality of life in 109 patients who underwent surgery for differentiated thyroid cancer at Radboud University Medical Center, Nijmegen, the Netherlands, with a group of 81 healthy controls and a group of 59 patients who underwent surgery for benign thyroid pathology. Main outcome measures were the prevalence of shoulder complaints based on results of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and the European Organization for Research and Treatment of Cancer, Quality of Life Questionnaire-C-30 (EORTC QLQ-C30).
Dr. Netea-Maier, of the department of medicine at the university, reported that the mean age of patients in the two surgery groups was 46 years, and 73% were women. During an average of 10 years following surgery, 59% of patients in the thyroid cancer group and 49% of patients in the benign thyroid pathology group reported shoulder morbidity, compared with 14% of controls (P < .01). The chief complaints among patients in the thyroid cancer group were pain (25%), muscle weakness (8%), and tingling (8%), while the main complaints among those with benign thyroid pathology were pain (38%), and tingling (7%).
Compared with healthy controls, patients in the thyroid cancer group scored worse on all subscales of the DASH and the EORTC QLQ-C30. On bivariate analysis, level V neck dissection, spinal accessory nerve damage, and employment status were associated with the prevalence of shoulder complaints and DASH scores, while the prevalence of shoulder complaints and DASH scores correlated significantly with EORTC QLQ-C30 scores.
The researchers found that only 12% of patients in the thyroid cancer group received preoperative information on the potential for shoulder morbidity and 35% received additional care for postoperative shoulder complaints.
“The take-home message would be to inform your patients of the potential for shoulder comorbidity, because what we have shown here is that patients do not recall being informed about this possible complication before the surgery,” Dr. Netea-Maier said. “If they have complaints, start with physiotherapy early on.”
Dr. Netea-Maier reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – More than 50% of patients who underwent surgery for differentiated thyroid cancer experienced shoulder morbidity up to 10 years after the procedure, results from a Dutch study showed.
“What’s causing the pain?” Dr. Romana T. Netea-Maier asked in an interview at the annual meeting of the American Thyroid Association. “It may be that the spinal accessory nerve or other nerves have been injured during the surgery. We don’t know.”
In what she said is the first study of its kind, Dr. Netea-Maier and her associates compared the prevalence of shoulder morbidity and its relation to clinical characteristics and quality of life in 109 patients who underwent surgery for differentiated thyroid cancer at Radboud University Medical Center, Nijmegen, the Netherlands, with a group of 81 healthy controls and a group of 59 patients who underwent surgery for benign thyroid pathology. Main outcome measures were the prevalence of shoulder complaints based on results of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and the European Organization for Research and Treatment of Cancer, Quality of Life Questionnaire-C-30 (EORTC QLQ-C30).
Dr. Netea-Maier, of the department of medicine at the university, reported that the mean age of patients in the two surgery groups was 46 years, and 73% were women. During an average of 10 years following surgery, 59% of patients in the thyroid cancer group and 49% of patients in the benign thyroid pathology group reported shoulder morbidity, compared with 14% of controls (P < .01). The chief complaints among patients in the thyroid cancer group were pain (25%), muscle weakness (8%), and tingling (8%), while the main complaints among those with benign thyroid pathology were pain (38%), and tingling (7%).
Compared with healthy controls, patients in the thyroid cancer group scored worse on all subscales of the DASH and the EORTC QLQ-C30. On bivariate analysis, level V neck dissection, spinal accessory nerve damage, and employment status were associated with the prevalence of shoulder complaints and DASH scores, while the prevalence of shoulder complaints and DASH scores correlated significantly with EORTC QLQ-C30 scores.
The researchers found that only 12% of patients in the thyroid cancer group received preoperative information on the potential for shoulder morbidity and 35% received additional care for postoperative shoulder complaints.
“The take-home message would be to inform your patients of the potential for shoulder comorbidity, because what we have shown here is that patients do not recall being informed about this possible complication before the surgery,” Dr. Netea-Maier said. “If they have complaints, start with physiotherapy early on.”
Dr. Netea-Maier reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Postoperative shoulder morbidity is highly prevalent in patients who undergo surgery for thyroid cancer.
Major finding: During an average of 10 years following surgery, 59% of patients in the thyroid cancer group and 49% of patients in the benign thyroid pathology group reported shoulder morbidity, compared with 14% of controls (P < .01).
Data source: A Dutch study of 109 patients who underwent surgery for differentiated thyroid cancer, compared with 81 healthy controls and 59 patients who underwent surgery for benign thyroid pathology.
Disclosures: Dr. Netea-Maier reported having no financial disclosures.
Radioactive iodine may boost survival in papillary thyroid cancer
CORONADO, CALIF. – The use of radioactive iodine in patients with papillary thyroid cancer showed a small but statistically significant survival benefit for all tumor size categories, a long-term analysis of national data suggested.
“The incidence of papillary thyroid carcinoma is rapidly rising, but the survival advantage of radioactive iodine ablation has not been confirmed,” Dr. Paritosh Suman said at the annual meeting of the American Thyroid Association.
To investigate the effect of radioactive iodine (RAI) on papillary thyroid cancer mortality, Dr. Suman and his associates identified 108,565 patients from the National Cancer Data Base who were diagnosed with papillary thyroid cancer and underwent total or near total thyroidectomy between 1998 and 2006.
The investigators classified tumors into one of four groups by diameter size: 10 mm or less, 11-20 mm, 21-40 mm, and greater than 40 mm. The study researchers used Cox regression analysis to quantify the effect of radioactive iodine, adjusting for clinicopathologic, demographic, and socioeconomic variables. A total of 52% of the patients were older than 45 years, 77% were female, and 54% received RAI.
Factors predicting the use of RAI were being male, having positive margins, having cervical lymph node involvement, and having a tumor size greater than 4 cm in diameter, said Dr. Suman, an endocrinology surgery fellow at North Shore University Health System in Evanston, Ill. The 10-year overall survival rate was 90% in those who received RAI, compared with 87.4% among those who did not, for a small but statistically significant survival advantage (P < .0001).
Among patients who received RAI, the 10-year survival advantage by diameter of tumor was 3.4% for those with tumors 10 mm or less; 2.8% with 11-20 mm; 3.3% with 21-40 mm, and 5.7% with greater than 40 mm.
Age also played a factor, with a 10-year survival advantage of 0.5% for those aged 18-35 years; 1.5% for those aged 36-45 years; 0.9% for those aged 46-55 years; 0.6% for those aged 56-65 years; and 2.1% for those older than 65 years. Both men and women who received RAI had a statistically significant survival advantage at 10 years (3.9% and 1.6%, respectively).
When the researchers assessed the 10-year survival advantage by lymph node category of patients who received RAI, the rates were 2.9% for N-0, 4.2% for N-1, 5.2% for N-1A, and 5.8% for N-1B. By margin status, the 10-year survival advantage was 3.1% for negative margins, 3.6% for positive margins, 3.5% for microscopic margins, and 8.8% for gross margins.
In an analysis of all patients with very low-risk, low-risk, and high-risk papillary thyroid carcinoma according to ATA guidelines for the use of RAI, the study authors found a 10-year survival advantage of RAI in each of the three categories.
Among patients with very low-risk papillary thyroid carcinoma, the rate of 10-year survival was 92.2% among those who received RAI, compared with 89% among those who did not (hazard ratio, 0.74). Similar associations were observed in those with low-risk carcinoma (91.8% vs. 89%; HR, 0.80) and in those with high-risk carcinoma (86.2% vs. 79.2%; HR, 0.71).
“RAI is associated with a statistically significant but small overall survival advantage for most patients,” Dr. Suman said. “High-risk patients, defined by large tumor size, lymph node involvement, and gross margins, achieve the greatest benefit with RAI ablation.”
Dr. Suman reported having no relevant financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – The use of radioactive iodine in patients with papillary thyroid cancer showed a small but statistically significant survival benefit for all tumor size categories, a long-term analysis of national data suggested.
“The incidence of papillary thyroid carcinoma is rapidly rising, but the survival advantage of radioactive iodine ablation has not been confirmed,” Dr. Paritosh Suman said at the annual meeting of the American Thyroid Association.
To investigate the effect of radioactive iodine (RAI) on papillary thyroid cancer mortality, Dr. Suman and his associates identified 108,565 patients from the National Cancer Data Base who were diagnosed with papillary thyroid cancer and underwent total or near total thyroidectomy between 1998 and 2006.
The investigators classified tumors into one of four groups by diameter size: 10 mm or less, 11-20 mm, 21-40 mm, and greater than 40 mm. The study researchers used Cox regression analysis to quantify the effect of radioactive iodine, adjusting for clinicopathologic, demographic, and socioeconomic variables. A total of 52% of the patients were older than 45 years, 77% were female, and 54% received RAI.
Factors predicting the use of RAI were being male, having positive margins, having cervical lymph node involvement, and having a tumor size greater than 4 cm in diameter, said Dr. Suman, an endocrinology surgery fellow at North Shore University Health System in Evanston, Ill. The 10-year overall survival rate was 90% in those who received RAI, compared with 87.4% among those who did not, for a small but statistically significant survival advantage (P < .0001).
Among patients who received RAI, the 10-year survival advantage by diameter of tumor was 3.4% for those with tumors 10 mm or less; 2.8% with 11-20 mm; 3.3% with 21-40 mm, and 5.7% with greater than 40 mm.
Age also played a factor, with a 10-year survival advantage of 0.5% for those aged 18-35 years; 1.5% for those aged 36-45 years; 0.9% for those aged 46-55 years; 0.6% for those aged 56-65 years; and 2.1% for those older than 65 years. Both men and women who received RAI had a statistically significant survival advantage at 10 years (3.9% and 1.6%, respectively).
When the researchers assessed the 10-year survival advantage by lymph node category of patients who received RAI, the rates were 2.9% for N-0, 4.2% for N-1, 5.2% for N-1A, and 5.8% for N-1B. By margin status, the 10-year survival advantage was 3.1% for negative margins, 3.6% for positive margins, 3.5% for microscopic margins, and 8.8% for gross margins.
In an analysis of all patients with very low-risk, low-risk, and high-risk papillary thyroid carcinoma according to ATA guidelines for the use of RAI, the study authors found a 10-year survival advantage of RAI in each of the three categories.
Among patients with very low-risk papillary thyroid carcinoma, the rate of 10-year survival was 92.2% among those who received RAI, compared with 89% among those who did not (hazard ratio, 0.74). Similar associations were observed in those with low-risk carcinoma (91.8% vs. 89%; HR, 0.80) and in those with high-risk carcinoma (86.2% vs. 79.2%; HR, 0.71).
“RAI is associated with a statistically significant but small overall survival advantage for most patients,” Dr. Suman said. “High-risk patients, defined by large tumor size, lymph node involvement, and gross margins, achieve the greatest benefit with RAI ablation.”
Dr. Suman reported having no relevant financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – The use of radioactive iodine in patients with papillary thyroid cancer showed a small but statistically significant survival benefit for all tumor size categories, a long-term analysis of national data suggested.
“The incidence of papillary thyroid carcinoma is rapidly rising, but the survival advantage of radioactive iodine ablation has not been confirmed,” Dr. Paritosh Suman said at the annual meeting of the American Thyroid Association.
To investigate the effect of radioactive iodine (RAI) on papillary thyroid cancer mortality, Dr. Suman and his associates identified 108,565 patients from the National Cancer Data Base who were diagnosed with papillary thyroid cancer and underwent total or near total thyroidectomy between 1998 and 2006.
The investigators classified tumors into one of four groups by diameter size: 10 mm or less, 11-20 mm, 21-40 mm, and greater than 40 mm. The study researchers used Cox regression analysis to quantify the effect of radioactive iodine, adjusting for clinicopathologic, demographic, and socioeconomic variables. A total of 52% of the patients were older than 45 years, 77% were female, and 54% received RAI.
Factors predicting the use of RAI were being male, having positive margins, having cervical lymph node involvement, and having a tumor size greater than 4 cm in diameter, said Dr. Suman, an endocrinology surgery fellow at North Shore University Health System in Evanston, Ill. The 10-year overall survival rate was 90% in those who received RAI, compared with 87.4% among those who did not, for a small but statistically significant survival advantage (P < .0001).
Among patients who received RAI, the 10-year survival advantage by diameter of tumor was 3.4% for those with tumors 10 mm or less; 2.8% with 11-20 mm; 3.3% with 21-40 mm, and 5.7% with greater than 40 mm.
Age also played a factor, with a 10-year survival advantage of 0.5% for those aged 18-35 years; 1.5% for those aged 36-45 years; 0.9% for those aged 46-55 years; 0.6% for those aged 56-65 years; and 2.1% for those older than 65 years. Both men and women who received RAI had a statistically significant survival advantage at 10 years (3.9% and 1.6%, respectively).
When the researchers assessed the 10-year survival advantage by lymph node category of patients who received RAI, the rates were 2.9% for N-0, 4.2% for N-1, 5.2% for N-1A, and 5.8% for N-1B. By margin status, the 10-year survival advantage was 3.1% for negative margins, 3.6% for positive margins, 3.5% for microscopic margins, and 8.8% for gross margins.
In an analysis of all patients with very low-risk, low-risk, and high-risk papillary thyroid carcinoma according to ATA guidelines for the use of RAI, the study authors found a 10-year survival advantage of RAI in each of the three categories.
Among patients with very low-risk papillary thyroid carcinoma, the rate of 10-year survival was 92.2% among those who received RAI, compared with 89% among those who did not (hazard ratio, 0.74). Similar associations were observed in those with low-risk carcinoma (91.8% vs. 89%; HR, 0.80) and in those with high-risk carcinoma (86.2% vs. 79.2%; HR, 0.71).
“RAI is associated with a statistically significant but small overall survival advantage for most patients,” Dr. Suman said. “High-risk patients, defined by large tumor size, lymph node involvement, and gross margins, achieve the greatest benefit with RAI ablation.”
Dr. Suman reported having no relevant financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: The use of radioactive iodine is associated with a small but statistically significant increase in overall survival in most patients with papillary thyroid carcinoma.
Major finding: The 10-year overall survival rate was 90% in patients who received RAI, compared with 87.4% among those who did not, a small but statistically significant difference (P < .0001).
Data source: An analysis of 108,565 patients from the National Cancer Data Base who were diagnosed with papillary thyroid cancer and underwent total or near total thyroidectomy between 1998 and 2006.
Disclosures: Dr. Suman reported having no relevant financial disclosures.
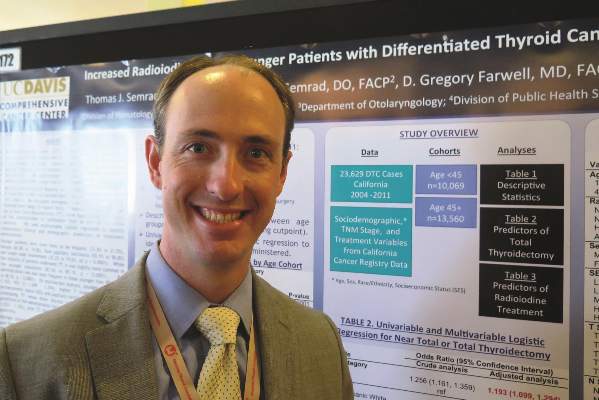
Total Thyroidectomy More Likely With Younger Thyroid Cancer Patients
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
AT THE ATA ANNUAL MEETING
Total thyroidectomy more likely with younger thyroid cancer patients
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Younger patients with differentiated thyroid cancer were more likely to undergo total thyroidectomy and receive radioactive iodine.
Major finding: Total or near-total thyroidectomy was slightly more common in patients younger than age 45 years, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients were also more likely to receive RAI (55% vs. 49%, P < .0001).
Data source: A study of 23,629 patients from the California Cancer Registry who were diagnosed with differentiated thyroid cancer between 2004 and 2011.
Disclosures: The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
Enhanced thyroid cancer guidelines expected in 2015
CORONADO, CALIF. – Expect significant enhancements to the updated thyroid cancer management guidelines from the American Thyroid Association, due to be released in early 2015.
Last updated in 2009, the goal of the new guidelines is to “be evidence based and helpful,” guidelines task force chair Dr. Bryan R. Haugen said at the annual meeting of the American Thyroid Association. For example, the new guidelines will contain 101 recommendations, up from 80 in the 2009 version; 175 subrecommendations, up from 103; and 998 references, up from 437. “Still, 59 of the existing 80 recommendations are not substantially changed, showing a general stability in our field over the past 5 to 6 years,” he said.
One enhancement is a definition of risk of structural disease recurrence in patients without structurally identifiable disease after initial therapy for thyroid cancer. Low risk is defined as intrathyroidal differentiated thyroid cancer involving up to five metastases less than 0.2 cm in size. Intermediate risk is defined as the presence of aggressive histology, minor extrathyroidal extension, vascular invasion, or more than five involved lymph nodes with metastases 0.2-0.3 cm in size. High risk is defined as the presence of gross extrathyroidal extension, incomplete tumor resection, distant metastases, or lymph node metastases greater than 3 cm in size.
The guidelines also include a table that defines a patient’s response to therapy as a dynamic risk assessment. “This best applies to the low- to intermediate-risk patients, although it definitely applies to high risk as well,” said Dr. Haugen, who heads the division of endocrinology, metabolism, and diabetes at the University of Colorado Health Sciences Center, Denver. “It’s [a] strong recommendation based on low-quality evidence to use this risk-based response to therapy. A lot of this data is generated from patients who’ve had a thyroidectomy and have received radioiodine. So we’re on a bit more shaky ground right now in a patient who’s had a thyroidectomy but no radioiodine, or a patient who’s had a lobectomy.”
Other changes include the concept that it’s not necessary to biopsy every nodule more than 1 cm in size. “We’re going to be guided by the sonographic pattern in who we biopsy and how we monitor them,” Dr. Haugen explained. “A new recommendation adds follow-up guidance for nodules that do not meet FNA [fine-needle aspiration] criteria. We’re also recommending use of the Bethesda Cytology Classification System for cytology.”
Changes in the initial management of thyroid cancer include a recommendation for cross-sectional imaging with contrast for higher-risk disease and the consideration of lobectomy for some patients with tumors 1-4 cm in size. “This is a controversial recommendation,” Dr. Haugen said. “We got some feedback from members asking if you do it, what’s the TSH target? Should we give them synthetic levothyroxine? We are revising the guidelines based on this feedback to help guide clinicians.”
The new guidelines also call for more detailed/standardized pathology reports, with inclusion of lymph node size, extranodal invasion, and the number of invaded vessels. “I’ve talked to a number of pathologists and clinicians who are very happy about this guidance,” he said. “We also need to look at tumor stage, recurrence risk, and response to therapy in our patients, and the use of selective radioiodine. There is some more information on considering lower administered activities, especially in the lower-risk patients.”
For the first time, the guidelines include a section on radioiodine treatment for refractory differentiated thyroid cancer, including tips on directed therapy, clinical trials, systemic therapy, and bone-specific therapy.
Dr. Haugen disclosed that he has received grants and research support from Veracyte and Genzyme.
On Twitter @dougbrunk
CORONADO, CALIF. – Expect significant enhancements to the updated thyroid cancer management guidelines from the American Thyroid Association, due to be released in early 2015.
Last updated in 2009, the goal of the new guidelines is to “be evidence based and helpful,” guidelines task force chair Dr. Bryan R. Haugen said at the annual meeting of the American Thyroid Association. For example, the new guidelines will contain 101 recommendations, up from 80 in the 2009 version; 175 subrecommendations, up from 103; and 998 references, up from 437. “Still, 59 of the existing 80 recommendations are not substantially changed, showing a general stability in our field over the past 5 to 6 years,” he said.
One enhancement is a definition of risk of structural disease recurrence in patients without structurally identifiable disease after initial therapy for thyroid cancer. Low risk is defined as intrathyroidal differentiated thyroid cancer involving up to five metastases less than 0.2 cm in size. Intermediate risk is defined as the presence of aggressive histology, minor extrathyroidal extension, vascular invasion, or more than five involved lymph nodes with metastases 0.2-0.3 cm in size. High risk is defined as the presence of gross extrathyroidal extension, incomplete tumor resection, distant metastases, or lymph node metastases greater than 3 cm in size.
The guidelines also include a table that defines a patient’s response to therapy as a dynamic risk assessment. “This best applies to the low- to intermediate-risk patients, although it definitely applies to high risk as well,” said Dr. Haugen, who heads the division of endocrinology, metabolism, and diabetes at the University of Colorado Health Sciences Center, Denver. “It’s [a] strong recommendation based on low-quality evidence to use this risk-based response to therapy. A lot of this data is generated from patients who’ve had a thyroidectomy and have received radioiodine. So we’re on a bit more shaky ground right now in a patient who’s had a thyroidectomy but no radioiodine, or a patient who’s had a lobectomy.”
Other changes include the concept that it’s not necessary to biopsy every nodule more than 1 cm in size. “We’re going to be guided by the sonographic pattern in who we biopsy and how we monitor them,” Dr. Haugen explained. “A new recommendation adds follow-up guidance for nodules that do not meet FNA [fine-needle aspiration] criteria. We’re also recommending use of the Bethesda Cytology Classification System for cytology.”
Changes in the initial management of thyroid cancer include a recommendation for cross-sectional imaging with contrast for higher-risk disease and the consideration of lobectomy for some patients with tumors 1-4 cm in size. “This is a controversial recommendation,” Dr. Haugen said. “We got some feedback from members asking if you do it, what’s the TSH target? Should we give them synthetic levothyroxine? We are revising the guidelines based on this feedback to help guide clinicians.”
The new guidelines also call for more detailed/standardized pathology reports, with inclusion of lymph node size, extranodal invasion, and the number of invaded vessels. “I’ve talked to a number of pathologists and clinicians who are very happy about this guidance,” he said. “We also need to look at tumor stage, recurrence risk, and response to therapy in our patients, and the use of selective radioiodine. There is some more information on considering lower administered activities, especially in the lower-risk patients.”
For the first time, the guidelines include a section on radioiodine treatment for refractory differentiated thyroid cancer, including tips on directed therapy, clinical trials, systemic therapy, and bone-specific therapy.
Dr. Haugen disclosed that he has received grants and research support from Veracyte and Genzyme.
On Twitter @dougbrunk
CORONADO, CALIF. – Expect significant enhancements to the updated thyroid cancer management guidelines from the American Thyroid Association, due to be released in early 2015.
Last updated in 2009, the goal of the new guidelines is to “be evidence based and helpful,” guidelines task force chair Dr. Bryan R. Haugen said at the annual meeting of the American Thyroid Association. For example, the new guidelines will contain 101 recommendations, up from 80 in the 2009 version; 175 subrecommendations, up from 103; and 998 references, up from 437. “Still, 59 of the existing 80 recommendations are not substantially changed, showing a general stability in our field over the past 5 to 6 years,” he said.
One enhancement is a definition of risk of structural disease recurrence in patients without structurally identifiable disease after initial therapy for thyroid cancer. Low risk is defined as intrathyroidal differentiated thyroid cancer involving up to five metastases less than 0.2 cm in size. Intermediate risk is defined as the presence of aggressive histology, minor extrathyroidal extension, vascular invasion, or more than five involved lymph nodes with metastases 0.2-0.3 cm in size. High risk is defined as the presence of gross extrathyroidal extension, incomplete tumor resection, distant metastases, or lymph node metastases greater than 3 cm in size.
The guidelines also include a table that defines a patient’s response to therapy as a dynamic risk assessment. “This best applies to the low- to intermediate-risk patients, although it definitely applies to high risk as well,” said Dr. Haugen, who heads the division of endocrinology, metabolism, and diabetes at the University of Colorado Health Sciences Center, Denver. “It’s [a] strong recommendation based on low-quality evidence to use this risk-based response to therapy. A lot of this data is generated from patients who’ve had a thyroidectomy and have received radioiodine. So we’re on a bit more shaky ground right now in a patient who’s had a thyroidectomy but no radioiodine, or a patient who’s had a lobectomy.”
Other changes include the concept that it’s not necessary to biopsy every nodule more than 1 cm in size. “We’re going to be guided by the sonographic pattern in who we biopsy and how we monitor them,” Dr. Haugen explained. “A new recommendation adds follow-up guidance for nodules that do not meet FNA [fine-needle aspiration] criteria. We’re also recommending use of the Bethesda Cytology Classification System for cytology.”
Changes in the initial management of thyroid cancer include a recommendation for cross-sectional imaging with contrast for higher-risk disease and the consideration of lobectomy for some patients with tumors 1-4 cm in size. “This is a controversial recommendation,” Dr. Haugen said. “We got some feedback from members asking if you do it, what’s the TSH target? Should we give them synthetic levothyroxine? We are revising the guidelines based on this feedback to help guide clinicians.”
The new guidelines also call for more detailed/standardized pathology reports, with inclusion of lymph node size, extranodal invasion, and the number of invaded vessels. “I’ve talked to a number of pathologists and clinicians who are very happy about this guidance,” he said. “We also need to look at tumor stage, recurrence risk, and response to therapy in our patients, and the use of selective radioiodine. There is some more information on considering lower administered activities, especially in the lower-risk patients.”
For the first time, the guidelines include a section on radioiodine treatment for refractory differentiated thyroid cancer, including tips on directed therapy, clinical trials, systemic therapy, and bone-specific therapy.
Dr. Haugen disclosed that he has received grants and research support from Veracyte and Genzyme.
On Twitter @dougbrunk
EXPERT ANALYSIS FROM THE ATA ANNUAL MEETING