User login
Physical activity linked to less cirrhosis-related mortality
SAN DIEGO – People who were more physically active, including those who did strength training, had significantly reduced risks of cirrhosis-related and liver cancer–related mortality, based on 26 years of prospective data from 113,000 participants in the Nurses Health Study and the Health Professionals Follow-Up Study.
Adults in the highest quintile of physical activity in the study had a 73% lower risk for cirrhosis-related death than did those in the lowest quintile, according to researchers at Massachusetts General Hospital and Harvard Medical School, Boston, who presented the study findings at Digestive Disease Week 2019.
One of the researchers, Tracey Simon, MD, MPH, of Massachusetts General Hospital, Boston, broke down the major take-home messages from the study in this video interview.
For example, vigorous activity was not necessary to improve hepatic health, she said. Walking for 4 hours per week made a big difference.
Dr. Simon has no relevant financial disclosures.
SAN DIEGO – People who were more physically active, including those who did strength training, had significantly reduced risks of cirrhosis-related and liver cancer–related mortality, based on 26 years of prospective data from 113,000 participants in the Nurses Health Study and the Health Professionals Follow-Up Study.
Adults in the highest quintile of physical activity in the study had a 73% lower risk for cirrhosis-related death than did those in the lowest quintile, according to researchers at Massachusetts General Hospital and Harvard Medical School, Boston, who presented the study findings at Digestive Disease Week 2019.
One of the researchers, Tracey Simon, MD, MPH, of Massachusetts General Hospital, Boston, broke down the major take-home messages from the study in this video interview.
For example, vigorous activity was not necessary to improve hepatic health, she said. Walking for 4 hours per week made a big difference.
Dr. Simon has no relevant financial disclosures.
SAN DIEGO – People who were more physically active, including those who did strength training, had significantly reduced risks of cirrhosis-related and liver cancer–related mortality, based on 26 years of prospective data from 113,000 participants in the Nurses Health Study and the Health Professionals Follow-Up Study.
Adults in the highest quintile of physical activity in the study had a 73% lower risk for cirrhosis-related death than did those in the lowest quintile, according to researchers at Massachusetts General Hospital and Harvard Medical School, Boston, who presented the study findings at Digestive Disease Week 2019.
One of the researchers, Tracey Simon, MD, MPH, of Massachusetts General Hospital, Boston, broke down the major take-home messages from the study in this video interview.
For example, vigorous activity was not necessary to improve hepatic health, she said. Walking for 4 hours per week made a big difference.
Dr. Simon has no relevant financial disclosures.
REPORTING FROM DDW 2019
Immunostaining boosts pathologists’ accuracy in Barrett’s esophagus
SAN DIEGO – Years of experience and an academic medical center affiliation predicted the accuracy of pathologists reviewing biopsies from patients with Barrett’s esophagus, according to the results of a multinational study.
Those with 5 or more years of experience were less likely to make major diagnostic errors in reviewing Barrett’s esophagus biopsies (odds ratio [OR], 0.48, 95% confidence interval, 0.31-0.74). Pathologists who worked in nonacademic settings were more likely to make a major diagnostic error (OR, 1.76; 95% CI, 1.15-2.69) when reviewing hematoxylin and eosin-stained slides alone, but the addition of p53 immunostaining greatly improved accuracy.
Current guidelines recommend expert evaluation of Barrett’s esophagus biopsies that show dysplasia, but exact determination of expert review status had been lacking, according to Marnix Jansen, MD, a pathologist at University College London.
“The guidelines say that biopsies with dysplasia need to be reviewed by an expert pathologist, but don’t define what makes an expert pathologist,” Dr. Jansen said in an interview at the annual Digestive Disease Week.
“We wanted to advance the field by for the first time creating objective and quantitative standards” to delineate the characteristics of an expert pathologist in reviewing Barrett’s esophagus tissue samples, said Dr. Jansen. The study’s first author is Myrtle J. van der Wel, MD, of Amsterdam University Medical Center, the Netherlands.
More than 6,000 individual case diagnoses were used in the study, which included pathologists from more than 20 countries. Before the pathologists began reviewing the case set, they answered a questionnaire about training, practice context, years of experience, case volume, and other demographic characteristics.
“We then sent those biopsies around the world to ... 55 pathologists in the U.S., in Europe, Japan, Australia, even some in South America – so really around the whole globe,” explained Dr. Jansen. Biopsies were assessed by each pathologist before and after p53 immunostaining.
“Once we had the final dataset – which is massive, because we had 6,000 case diagnoses within our dataset – we could then regress those variables back onto the consensus data,” providing a first-ever look at “clear predictors of what the pathologist looks like that will score on a par with where the experts are,” said Dr. Jansen.
The results? “You need at least 5 years of experience. On top of that, if you are a pathologist working in a [nonacademic center], you are at a slightly increased risk of making major diagnostic errors,” said Dr. Jansen. However, the analysis convincingly showed that the addition of p53 immunostaining neutralized the risk for these pathologists – a strength of having such a large dataset, he said.
The study also affirmed the safety of digital pathology for expert review, said Dr. Jansen: “One of the reassuring points of our study was that we found that the best concordance was for nondysplastic Barrett’s, and high-grade dysplasia, which really replicates known glass slide characteristics. So we can really say that digital pathology is safe for this application – which is very relevant for pathologists that are taking in cases from outside for expert review.”
Concordance rates for nondysplastic Barrett’s esophagus and high-grade dysplasia were over 70%; for low-grade dysplasia, rates were intermediate at 42%.
Going forward, the study can inform the next iteration of guidelines for pathologist review of Barrett’s dysplasia, said Dr. Jansen. Rather than just recommending expert review, the guidelines can include a quantitative assessment of what’s needed. “You need to have to have at least 5 years of experience, and if you work in a [community hospital], to use a p53, and that is collectively what amounts to expertise in Barrett’s pathology.”
A follow-up study with a similar design is planned within the United Kingdom, the Netherlands, and the United States. This study, which Dr. Jansen said would enroll hundreds of pathologists, will include an intervention arm that administers a tutorial with the aim of improving concordance scoring.
Dr. Jansen reported no relevant conflicts of interest.
SAN DIEGO – Years of experience and an academic medical center affiliation predicted the accuracy of pathologists reviewing biopsies from patients with Barrett’s esophagus, according to the results of a multinational study.
Those with 5 or more years of experience were less likely to make major diagnostic errors in reviewing Barrett’s esophagus biopsies (odds ratio [OR], 0.48, 95% confidence interval, 0.31-0.74). Pathologists who worked in nonacademic settings were more likely to make a major diagnostic error (OR, 1.76; 95% CI, 1.15-2.69) when reviewing hematoxylin and eosin-stained slides alone, but the addition of p53 immunostaining greatly improved accuracy.
Current guidelines recommend expert evaluation of Barrett’s esophagus biopsies that show dysplasia, but exact determination of expert review status had been lacking, according to Marnix Jansen, MD, a pathologist at University College London.
“The guidelines say that biopsies with dysplasia need to be reviewed by an expert pathologist, but don’t define what makes an expert pathologist,” Dr. Jansen said in an interview at the annual Digestive Disease Week.
“We wanted to advance the field by for the first time creating objective and quantitative standards” to delineate the characteristics of an expert pathologist in reviewing Barrett’s esophagus tissue samples, said Dr. Jansen. The study’s first author is Myrtle J. van der Wel, MD, of Amsterdam University Medical Center, the Netherlands.
More than 6,000 individual case diagnoses were used in the study, which included pathologists from more than 20 countries. Before the pathologists began reviewing the case set, they answered a questionnaire about training, practice context, years of experience, case volume, and other demographic characteristics.
“We then sent those biopsies around the world to ... 55 pathologists in the U.S., in Europe, Japan, Australia, even some in South America – so really around the whole globe,” explained Dr. Jansen. Biopsies were assessed by each pathologist before and after p53 immunostaining.
“Once we had the final dataset – which is massive, because we had 6,000 case diagnoses within our dataset – we could then regress those variables back onto the consensus data,” providing a first-ever look at “clear predictors of what the pathologist looks like that will score on a par with where the experts are,” said Dr. Jansen.
The results? “You need at least 5 years of experience. On top of that, if you are a pathologist working in a [nonacademic center], you are at a slightly increased risk of making major diagnostic errors,” said Dr. Jansen. However, the analysis convincingly showed that the addition of p53 immunostaining neutralized the risk for these pathologists – a strength of having such a large dataset, he said.
The study also affirmed the safety of digital pathology for expert review, said Dr. Jansen: “One of the reassuring points of our study was that we found that the best concordance was for nondysplastic Barrett’s, and high-grade dysplasia, which really replicates known glass slide characteristics. So we can really say that digital pathology is safe for this application – which is very relevant for pathologists that are taking in cases from outside for expert review.”
Concordance rates for nondysplastic Barrett’s esophagus and high-grade dysplasia were over 70%; for low-grade dysplasia, rates were intermediate at 42%.
Going forward, the study can inform the next iteration of guidelines for pathologist review of Barrett’s dysplasia, said Dr. Jansen. Rather than just recommending expert review, the guidelines can include a quantitative assessment of what’s needed. “You need to have to have at least 5 years of experience, and if you work in a [community hospital], to use a p53, and that is collectively what amounts to expertise in Barrett’s pathology.”
A follow-up study with a similar design is planned within the United Kingdom, the Netherlands, and the United States. This study, which Dr. Jansen said would enroll hundreds of pathologists, will include an intervention arm that administers a tutorial with the aim of improving concordance scoring.
Dr. Jansen reported no relevant conflicts of interest.
SAN DIEGO – Years of experience and an academic medical center affiliation predicted the accuracy of pathologists reviewing biopsies from patients with Barrett’s esophagus, according to the results of a multinational study.
Those with 5 or more years of experience were less likely to make major diagnostic errors in reviewing Barrett’s esophagus biopsies (odds ratio [OR], 0.48, 95% confidence interval, 0.31-0.74). Pathologists who worked in nonacademic settings were more likely to make a major diagnostic error (OR, 1.76; 95% CI, 1.15-2.69) when reviewing hematoxylin and eosin-stained slides alone, but the addition of p53 immunostaining greatly improved accuracy.
Current guidelines recommend expert evaluation of Barrett’s esophagus biopsies that show dysplasia, but exact determination of expert review status had been lacking, according to Marnix Jansen, MD, a pathologist at University College London.
“The guidelines say that biopsies with dysplasia need to be reviewed by an expert pathologist, but don’t define what makes an expert pathologist,” Dr. Jansen said in an interview at the annual Digestive Disease Week.
“We wanted to advance the field by for the first time creating objective and quantitative standards” to delineate the characteristics of an expert pathologist in reviewing Barrett’s esophagus tissue samples, said Dr. Jansen. The study’s first author is Myrtle J. van der Wel, MD, of Amsterdam University Medical Center, the Netherlands.
More than 6,000 individual case diagnoses were used in the study, which included pathologists from more than 20 countries. Before the pathologists began reviewing the case set, they answered a questionnaire about training, practice context, years of experience, case volume, and other demographic characteristics.
“We then sent those biopsies around the world to ... 55 pathologists in the U.S., in Europe, Japan, Australia, even some in South America – so really around the whole globe,” explained Dr. Jansen. Biopsies were assessed by each pathologist before and after p53 immunostaining.
“Once we had the final dataset – which is massive, because we had 6,000 case diagnoses within our dataset – we could then regress those variables back onto the consensus data,” providing a first-ever look at “clear predictors of what the pathologist looks like that will score on a par with where the experts are,” said Dr. Jansen.
The results? “You need at least 5 years of experience. On top of that, if you are a pathologist working in a [nonacademic center], you are at a slightly increased risk of making major diagnostic errors,” said Dr. Jansen. However, the analysis convincingly showed that the addition of p53 immunostaining neutralized the risk for these pathologists – a strength of having such a large dataset, he said.
The study also affirmed the safety of digital pathology for expert review, said Dr. Jansen: “One of the reassuring points of our study was that we found that the best concordance was for nondysplastic Barrett’s, and high-grade dysplasia, which really replicates known glass slide characteristics. So we can really say that digital pathology is safe for this application – which is very relevant for pathologists that are taking in cases from outside for expert review.”
Concordance rates for nondysplastic Barrett’s esophagus and high-grade dysplasia were over 70%; for low-grade dysplasia, rates were intermediate at 42%.
Going forward, the study can inform the next iteration of guidelines for pathologist review of Barrett’s dysplasia, said Dr. Jansen. Rather than just recommending expert review, the guidelines can include a quantitative assessment of what’s needed. “You need to have to have at least 5 years of experience, and if you work in a [community hospital], to use a p53, and that is collectively what amounts to expertise in Barrett’s pathology.”
A follow-up study with a similar design is planned within the United Kingdom, the Netherlands, and the United States. This study, which Dr. Jansen said would enroll hundreds of pathologists, will include an intervention arm that administers a tutorial with the aim of improving concordance scoring.
Dr. Jansen reported no relevant conflicts of interest.
REPORTING FROM DDW 2019
Button batteries that pass to the stomach may warrant rapid endoscopic removal
SAN DIEGO – A button battery lodged in a child’s esophagus is an acknowledged emergency, but there is less evidence about retrieval of button batteries that have passed to the stomach. Observation alone has been recommended when an x-ray determines that the button battery has passed to the stomach within 2 hours of ingestion, when the battery is less than 20 mm, and the child is aged at least 5 years.
At the annual Digestive Disease Week, Racha Khalaf, MD, and Thomas Walker, MD, both of Children’s Hospital Colorado, Aurora, presented data that call this approach into question. Their retrospective cohort study of 4 years’ worth of records from four pediatric centers in the United States identified 68 cases in which a pediatric gastroenterologist had endoscopically removed the button battery. In 60% of those cases, the battery had already caused mucosal damage varying from minor to deep necrosis and perforation.
Further, the degree of injury was not correlated with symptoms, strengthening the recommendation for retrieving the button battery from the stomach.
In our exclusive video interview, Dr. Khalaf and Dr. Walker discussed the impact of their findings for guidelines for pediatric gastroenterologists and Poison Control Center advice to parents about ingestion of button batteries.
Their study was partly supported by a Cystic Fibrosis Foundational Grant Award and by National Institutes of Health Training Grants.
SAN DIEGO – A button battery lodged in a child’s esophagus is an acknowledged emergency, but there is less evidence about retrieval of button batteries that have passed to the stomach. Observation alone has been recommended when an x-ray determines that the button battery has passed to the stomach within 2 hours of ingestion, when the battery is less than 20 mm, and the child is aged at least 5 years.
At the annual Digestive Disease Week, Racha Khalaf, MD, and Thomas Walker, MD, both of Children’s Hospital Colorado, Aurora, presented data that call this approach into question. Their retrospective cohort study of 4 years’ worth of records from four pediatric centers in the United States identified 68 cases in which a pediatric gastroenterologist had endoscopically removed the button battery. In 60% of those cases, the battery had already caused mucosal damage varying from minor to deep necrosis and perforation.
Further, the degree of injury was not correlated with symptoms, strengthening the recommendation for retrieving the button battery from the stomach.
In our exclusive video interview, Dr. Khalaf and Dr. Walker discussed the impact of their findings for guidelines for pediatric gastroenterologists and Poison Control Center advice to parents about ingestion of button batteries.
Their study was partly supported by a Cystic Fibrosis Foundational Grant Award and by National Institutes of Health Training Grants.
SAN DIEGO – A button battery lodged in a child’s esophagus is an acknowledged emergency, but there is less evidence about retrieval of button batteries that have passed to the stomach. Observation alone has been recommended when an x-ray determines that the button battery has passed to the stomach within 2 hours of ingestion, when the battery is less than 20 mm, and the child is aged at least 5 years.
At the annual Digestive Disease Week, Racha Khalaf, MD, and Thomas Walker, MD, both of Children’s Hospital Colorado, Aurora, presented data that call this approach into question. Their retrospective cohort study of 4 years’ worth of records from four pediatric centers in the United States identified 68 cases in which a pediatric gastroenterologist had endoscopically removed the button battery. In 60% of those cases, the battery had already caused mucosal damage varying from minor to deep necrosis and perforation.
Further, the degree of injury was not correlated with symptoms, strengthening the recommendation for retrieving the button battery from the stomach.
In our exclusive video interview, Dr. Khalaf and Dr. Walker discussed the impact of their findings for guidelines for pediatric gastroenterologists and Poison Control Center advice to parents about ingestion of button batteries.
Their study was partly supported by a Cystic Fibrosis Foundational Grant Award and by National Institutes of Health Training Grants.
REPORTING FROM DDW 2019
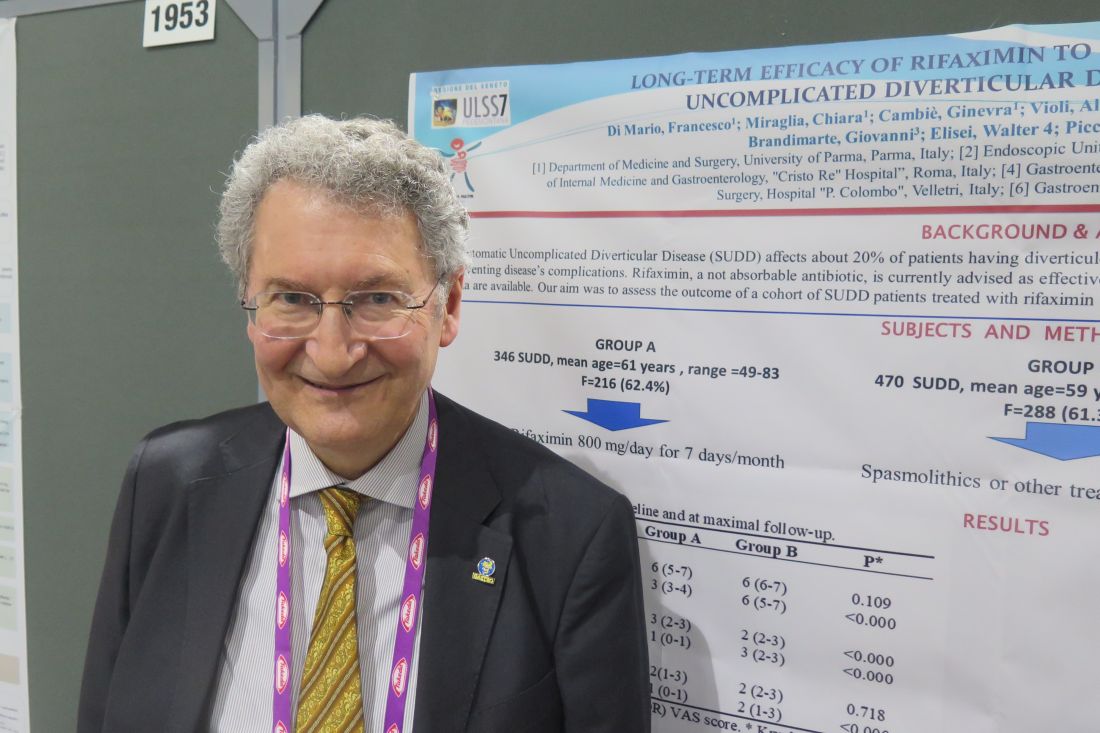
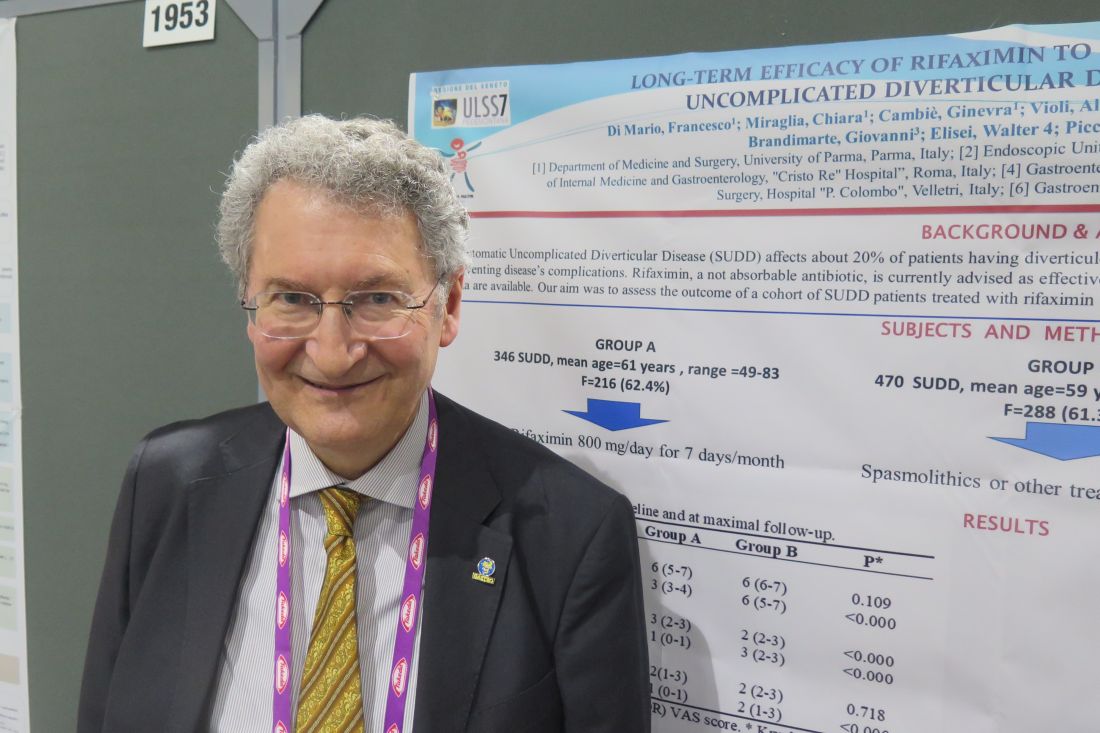
Rifaximin effective for uncomplicated diverticulitis in real-life study
SAN DIEGO – Rifaximin relieves symptoms and reduces the risk of disease-related complications in patients with symptomatic uncomplicated diverticular disease (SUDD) of the colon, results from a retrospective study showed.
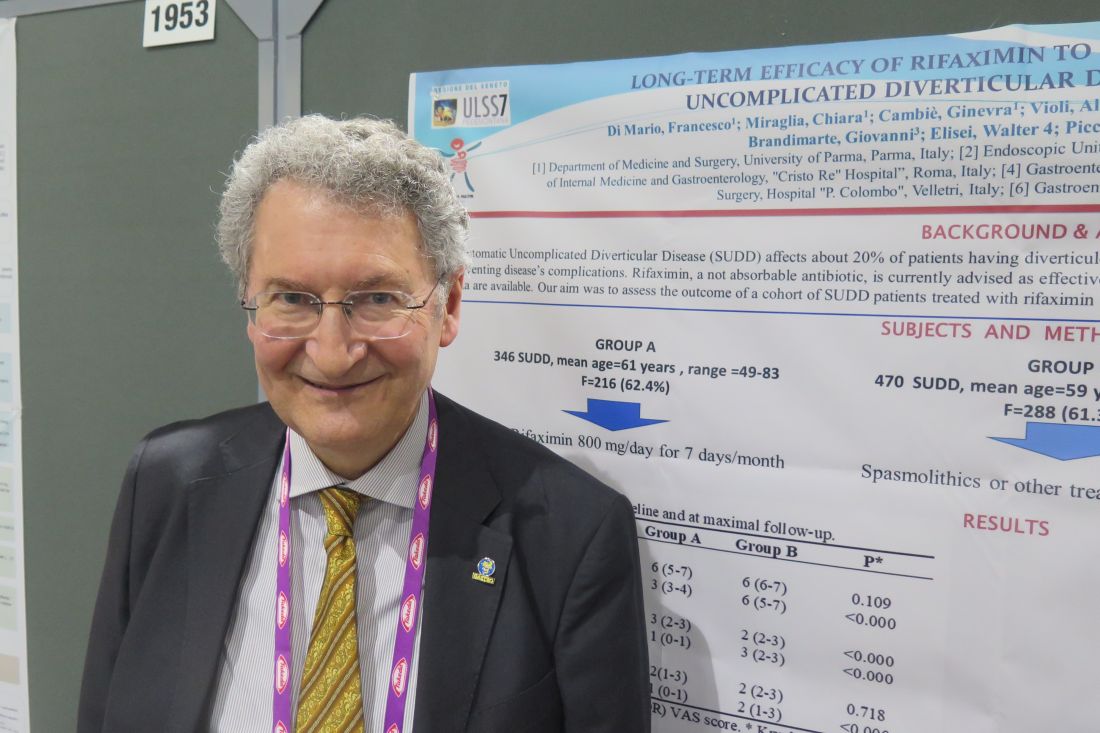
“The majority of studies published on this topic are not exactly the picture of real life, because they’re conducted on a selected sample of patients queued into the hospital,” lead study author Francesco Di Mario, MD, said at the annual Digestive Disease Week. Dr. Di Mario sought long-term data “from general practitioners – data from real life.”
For an 8-year follow-up study, Dr. Di Mario, professor of gastroenterology at the University of Parma (Italy), and colleagues at several general physician practices in Italy enrolled two groups of patients. The study group (group A) consisted of 346 SUDD patients who were treated with rifaximin 800 mg/day for 7 days every month. Their median age was 64 years, and 63% were female. The control group (group B) included 470 SUDD patients who were taking spasmolithics or any other treatment on demand. Their median age was 65 years, and 61% were female.
The researchers administered a 10-point visual analog scale (VAS) to assess left lower abdominal pain and bloating, with a score of 10 representing the most severe symptoms. Daily bowel movements were also reported.
The median baseline VAS score for pain was 6 in groups A and B. After 8 years of follow-up, the VAS scores for the two groups were 3 and 6, respectively (P less than .0001), and both bloating and daily bowel movements were significantly reduced in group A (P less than .0001).
As for the impact of rifaximin on other outcomes, acute diverticulitis occurred in 9 patients in group A (2.6%) and in 21 patients in group B (4.5%), a difference that reached statistical significance (P = .155). In addition, four patients (1.2%) in group A and nine patients (1.9%) in group B had surgery (P = .432). No disease-related deaths occurred in group A, but two patients in group B died (0.4%; P = .239). No side effects were recorded during the entire study period.
The researchers reported having no financial disclosures.
SAN DIEGO – Rifaximin relieves symptoms and reduces the risk of disease-related complications in patients with symptomatic uncomplicated diverticular disease (SUDD) of the colon, results from a retrospective study showed.
“The majority of studies published on this topic are not exactly the picture of real life, because they’re conducted on a selected sample of patients queued into the hospital,” lead study author Francesco Di Mario, MD, said at the annual Digestive Disease Week. Dr. Di Mario sought long-term data “from general practitioners – data from real life.”
For an 8-year follow-up study, Dr. Di Mario, professor of gastroenterology at the University of Parma (Italy), and colleagues at several general physician practices in Italy enrolled two groups of patients. The study group (group A) consisted of 346 SUDD patients who were treated with rifaximin 800 mg/day for 7 days every month. Their median age was 64 years, and 63% were female. The control group (group B) included 470 SUDD patients who were taking spasmolithics or any other treatment on demand. Their median age was 65 years, and 61% were female.
The researchers administered a 10-point visual analog scale (VAS) to assess left lower abdominal pain and bloating, with a score of 10 representing the most severe symptoms. Daily bowel movements were also reported.
The median baseline VAS score for pain was 6 in groups A and B. After 8 years of follow-up, the VAS scores for the two groups were 3 and 6, respectively (P less than .0001), and both bloating and daily bowel movements were significantly reduced in group A (P less than .0001).
As for the impact of rifaximin on other outcomes, acute diverticulitis occurred in 9 patients in group A (2.6%) and in 21 patients in group B (4.5%), a difference that reached statistical significance (P = .155). In addition, four patients (1.2%) in group A and nine patients (1.9%) in group B had surgery (P = .432). No disease-related deaths occurred in group A, but two patients in group B died (0.4%; P = .239). No side effects were recorded during the entire study period.
The researchers reported having no financial disclosures.
SAN DIEGO – Rifaximin relieves symptoms and reduces the risk of disease-related complications in patients with symptomatic uncomplicated diverticular disease (SUDD) of the colon, results from a retrospective study showed.
“The majority of studies published on this topic are not exactly the picture of real life, because they’re conducted on a selected sample of patients queued into the hospital,” lead study author Francesco Di Mario, MD, said at the annual Digestive Disease Week. Dr. Di Mario sought long-term data “from general practitioners – data from real life.”
For an 8-year follow-up study, Dr. Di Mario, professor of gastroenterology at the University of Parma (Italy), and colleagues at several general physician practices in Italy enrolled two groups of patients. The study group (group A) consisted of 346 SUDD patients who were treated with rifaximin 800 mg/day for 7 days every month. Their median age was 64 years, and 63% were female. The control group (group B) included 470 SUDD patients who were taking spasmolithics or any other treatment on demand. Their median age was 65 years, and 61% were female.
The researchers administered a 10-point visual analog scale (VAS) to assess left lower abdominal pain and bloating, with a score of 10 representing the most severe symptoms. Daily bowel movements were also reported.
The median baseline VAS score for pain was 6 in groups A and B. After 8 years of follow-up, the VAS scores for the two groups were 3 and 6, respectively (P less than .0001), and both bloating and daily bowel movements were significantly reduced in group A (P less than .0001).
As for the impact of rifaximin on other outcomes, acute diverticulitis occurred in 9 patients in group A (2.6%) and in 21 patients in group B (4.5%), a difference that reached statistical significance (P = .155). In addition, four patients (1.2%) in group A and nine patients (1.9%) in group B had surgery (P = .432). No disease-related deaths occurred in group A, but two patients in group B died (0.4%; P = .239). No side effects were recorded during the entire study period.
The researchers reported having no financial disclosures.
REPORTING FROM DDW 2019
Key clinical point: “Real-life” data show a benefit of rifaximin on symptoms and complications experienced by patients with symptomatic uncomplicated diverticular disease of the colon.
Major finding: Acute diverticulitis occurred in 9 patients in the rifaximin group (2.6%) and in 21 patients who did not receive rifaximin (4.5%), a difference that reached statistical significance (P = .155).
Study details: A retrospective study of 816 patients with symptomatic uncomplicated diverticular disease.
Disclosures: The researchers reported having no financial disclosures.
Opioid use associated with common bile duct dilation
SAN DIEGO – Biliary duct dilation in the setting of an intact gallbladder and normal bilirubin levels was more common among those who used opioids, based on the results of a large, retrospective, single-center cohort study.
Patients were included in the study if they had a documented measurement for the diameter of the common bile duct, with no evidence of an obstructive lesion and a normal bilirubin level. The mean common bile duct diameter was significantly higher at 8.67 mm for 867 patients who used opioids, compared with 7.24 mm for 818 similar patients who did not use opioids (P less than .001). The association was strongest among opioid users with an intact gallbladder.
“Opiate use is associated with biliary dilation in the setting of normal bilirubin,” Monique Barakat, MD, a gastroenterologist at Stanford (Calif.) University, reported at the annual Digestive Disease Week. “Known opiate users with normal LFTs [liver function tests] may not require expensive and potentially risky endoscopic evaluation for biliary dilation.”
Dr. Barakat and senior author Subhas Banerjee, MD, professor of gastroenterology and hepatology at Stanford, decided to examine a possible association between biliary duct dilation and opioid use based on previous small clinical studies that found a possible association. Along with opioid status, Dr. Barakat and her coauthor also looked at patient age, cholecystectomy status, ethnicity, weight, and height for possible associations with bile duct diameter.
The researchers took a random 20% sample of adults seen for all causes in the ED at Stanford over a 5-year period. Using a health informatic platform based on the electronic medical record, they identified all patients who had received an abdominal CT or MRI. Patients were included in the study if they had a documented measurement for the diameter of the common bile duct, with no evidence of obstructive lesion and a normal bilirubin level.
Compared with 818 patients who did not use opioids, the 867 patients who used opioids had a significantly larger common bile duct diameter. Using 7 mm as the threshold for biliary duct enlargement, 84% of patients who used opioids had an enlarged common bile duct, compared with 27% of nonopioid users (P less than .001), said Dr. Barakat, recipient of an early investigator award for the study.
“We frequently get referrals for bile duct dilation with concern for more sinister causes of biliary duct dilation – stones, strictures, and malignancy,” said Dr. Barakat. Because of the increase in cross-sectional imaging via CT or MRI, bile duct dilation is being detected at increasingly higher rates.
Dr. Barakat said that about one-third of referrals to the therapeutic endoscopy clinic at Stanford are now for patients with biliary dilation and normal liver function tests. And similar increases are being “seen across all settings – so office, primary care clinic, inpatient, and most markedly, the emergency department. Coupled with this, the population is aging, and patients who present to each of these settings are more likely, if they are older, to undergo cross-sectional imaging.”
Other contributors to higher rates of bile duct dilation include increased rates of obesity and increased prevalence of nonalcoholic steatohepatitis (NASH). About 20% of individuals with NASH will also have abnormal LFTs, she said, and NASH can be the trigger for cross-sectional imaging.
For most of these patients with biliary duct dilation and normal LFTs, no obstructive process was found on endoscopic evaluation.
Although gastroenterology textbooks may say that bile duct diameter increases with age, Dr. Barakat and colleagues didn’t find this to be the case. Among nonopioid users in the study cohort, age did not predict of common bile duct diameter. Among the entire cohort, “Advancing age weakly predicts increased common bile duct diameter,” she said, suggesting that factors other than age along may drive increased bile duct diameter.
Limitations included the retrospective nature of the study, as well as the limitations of information from the electronic medical record. Also, interobserver variability may have come into play, as bile duct diameter measurements were made by multiple radiologists in the course of clinical care.
The study was funded by the National Institutes of Health. Dr. Barakat reported no relevant financial disclosures.
SAN DIEGO – Biliary duct dilation in the setting of an intact gallbladder and normal bilirubin levels was more common among those who used opioids, based on the results of a large, retrospective, single-center cohort study.
Patients were included in the study if they had a documented measurement for the diameter of the common bile duct, with no evidence of an obstructive lesion and a normal bilirubin level. The mean common bile duct diameter was significantly higher at 8.67 mm for 867 patients who used opioids, compared with 7.24 mm for 818 similar patients who did not use opioids (P less than .001). The association was strongest among opioid users with an intact gallbladder.
“Opiate use is associated with biliary dilation in the setting of normal bilirubin,” Monique Barakat, MD, a gastroenterologist at Stanford (Calif.) University, reported at the annual Digestive Disease Week. “Known opiate users with normal LFTs [liver function tests] may not require expensive and potentially risky endoscopic evaluation for biliary dilation.”
Dr. Barakat and senior author Subhas Banerjee, MD, professor of gastroenterology and hepatology at Stanford, decided to examine a possible association between biliary duct dilation and opioid use based on previous small clinical studies that found a possible association. Along with opioid status, Dr. Barakat and her coauthor also looked at patient age, cholecystectomy status, ethnicity, weight, and height for possible associations with bile duct diameter.
The researchers took a random 20% sample of adults seen for all causes in the ED at Stanford over a 5-year period. Using a health informatic platform based on the electronic medical record, they identified all patients who had received an abdominal CT or MRI. Patients were included in the study if they had a documented measurement for the diameter of the common bile duct, with no evidence of obstructive lesion and a normal bilirubin level.
Compared with 818 patients who did not use opioids, the 867 patients who used opioids had a significantly larger common bile duct diameter. Using 7 mm as the threshold for biliary duct enlargement, 84% of patients who used opioids had an enlarged common bile duct, compared with 27% of nonopioid users (P less than .001), said Dr. Barakat, recipient of an early investigator award for the study.
“We frequently get referrals for bile duct dilation with concern for more sinister causes of biliary duct dilation – stones, strictures, and malignancy,” said Dr. Barakat. Because of the increase in cross-sectional imaging via CT or MRI, bile duct dilation is being detected at increasingly higher rates.
Dr. Barakat said that about one-third of referrals to the therapeutic endoscopy clinic at Stanford are now for patients with biliary dilation and normal liver function tests. And similar increases are being “seen across all settings – so office, primary care clinic, inpatient, and most markedly, the emergency department. Coupled with this, the population is aging, and patients who present to each of these settings are more likely, if they are older, to undergo cross-sectional imaging.”
Other contributors to higher rates of bile duct dilation include increased rates of obesity and increased prevalence of nonalcoholic steatohepatitis (NASH). About 20% of individuals with NASH will also have abnormal LFTs, she said, and NASH can be the trigger for cross-sectional imaging.
For most of these patients with biliary duct dilation and normal LFTs, no obstructive process was found on endoscopic evaluation.
Although gastroenterology textbooks may say that bile duct diameter increases with age, Dr. Barakat and colleagues didn’t find this to be the case. Among nonopioid users in the study cohort, age did not predict of common bile duct diameter. Among the entire cohort, “Advancing age weakly predicts increased common bile duct diameter,” she said, suggesting that factors other than age along may drive increased bile duct diameter.
Limitations included the retrospective nature of the study, as well as the limitations of information from the electronic medical record. Also, interobserver variability may have come into play, as bile duct diameter measurements were made by multiple radiologists in the course of clinical care.
The study was funded by the National Institutes of Health. Dr. Barakat reported no relevant financial disclosures.
SAN DIEGO – Biliary duct dilation in the setting of an intact gallbladder and normal bilirubin levels was more common among those who used opioids, based on the results of a large, retrospective, single-center cohort study.
Patients were included in the study if they had a documented measurement for the diameter of the common bile duct, with no evidence of an obstructive lesion and a normal bilirubin level. The mean common bile duct diameter was significantly higher at 8.67 mm for 867 patients who used opioids, compared with 7.24 mm for 818 similar patients who did not use opioids (P less than .001). The association was strongest among opioid users with an intact gallbladder.
“Opiate use is associated with biliary dilation in the setting of normal bilirubin,” Monique Barakat, MD, a gastroenterologist at Stanford (Calif.) University, reported at the annual Digestive Disease Week. “Known opiate users with normal LFTs [liver function tests] may not require expensive and potentially risky endoscopic evaluation for biliary dilation.”
Dr. Barakat and senior author Subhas Banerjee, MD, professor of gastroenterology and hepatology at Stanford, decided to examine a possible association between biliary duct dilation and opioid use based on previous small clinical studies that found a possible association. Along with opioid status, Dr. Barakat and her coauthor also looked at patient age, cholecystectomy status, ethnicity, weight, and height for possible associations with bile duct diameter.
The researchers took a random 20% sample of adults seen for all causes in the ED at Stanford over a 5-year period. Using a health informatic platform based on the electronic medical record, they identified all patients who had received an abdominal CT or MRI. Patients were included in the study if they had a documented measurement for the diameter of the common bile duct, with no evidence of obstructive lesion and a normal bilirubin level.
Compared with 818 patients who did not use opioids, the 867 patients who used opioids had a significantly larger common bile duct diameter. Using 7 mm as the threshold for biliary duct enlargement, 84% of patients who used opioids had an enlarged common bile duct, compared with 27% of nonopioid users (P less than .001), said Dr. Barakat, recipient of an early investigator award for the study.
“We frequently get referrals for bile duct dilation with concern for more sinister causes of biliary duct dilation – stones, strictures, and malignancy,” said Dr. Barakat. Because of the increase in cross-sectional imaging via CT or MRI, bile duct dilation is being detected at increasingly higher rates.
Dr. Barakat said that about one-third of referrals to the therapeutic endoscopy clinic at Stanford are now for patients with biliary dilation and normal liver function tests. And similar increases are being “seen across all settings – so office, primary care clinic, inpatient, and most markedly, the emergency department. Coupled with this, the population is aging, and patients who present to each of these settings are more likely, if they are older, to undergo cross-sectional imaging.”
Other contributors to higher rates of bile duct dilation include increased rates of obesity and increased prevalence of nonalcoholic steatohepatitis (NASH). About 20% of individuals with NASH will also have abnormal LFTs, she said, and NASH can be the trigger for cross-sectional imaging.
For most of these patients with biliary duct dilation and normal LFTs, no obstructive process was found on endoscopic evaluation.
Although gastroenterology textbooks may say that bile duct diameter increases with age, Dr. Barakat and colleagues didn’t find this to be the case. Among nonopioid users in the study cohort, age did not predict of common bile duct diameter. Among the entire cohort, “Advancing age weakly predicts increased common bile duct diameter,” she said, suggesting that factors other than age along may drive increased bile duct diameter.
Limitations included the retrospective nature of the study, as well as the limitations of information from the electronic medical record. Also, interobserver variability may have come into play, as bile duct diameter measurements were made by multiple radiologists in the course of clinical care.
The study was funded by the National Institutes of Health. Dr. Barakat reported no relevant financial disclosures.
REPORTING FROM DDW 2019
PPI metabolism may be altered in about one-third of bariatric surgery candidates
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
REPORTING FROM DDW 2019
Systemic anticoagulation found to benefit acute pancreatitis patients
SAN DIEGO –
“Acute pancreatitis is a very common disease,” lead study author Yan Bi, MD, PhD, a senior associate consultant and assistant professor in the department of gastroenterology and hepatology at Mayo Clinic, Jacksonville, Fla., said in an interview in advance of the annual Digestive Disease Week. “It’s the number one GI cause for hospitalization. Unfortunately, even after decades of basic science and clinical research, there’s still no cure; there’s nothing to prevent it from happening. The only treatment we can offer is supportive care, which includes fluid hydration, pain control, and nutrition support.”
The pathogenesis of acute pancreatitis (AP) is complex, she continued, and represents a sequence of distinct and interconnected pathologic events. “Both animal data and human studies have shown that acute pancreatitis is a hypercoagulable state,” she said. “We hypothesize that coagulation plays important roles in the development of pancreatitis.”
To test their hypothesis, Dr. Bi and associates performed a retrospective study. They drew from the 2014 National Inpatient Sample to evaluate the effect of systemic anticoagulation prior to AP onset on outcomes of the condition. They used ICD-9 codes to identify patients with a primary diagnosis of AP as well as those who were taking systemic anticoagulation. The primary outcome was the odds of AP in patients taking systemic anticoagulation, compared with those who were not. Secondary outcomes were mortality, morbidity, length of hospital stay, and total hospitalization charges and costs. The researchers used propensity score matching to create a 1:1 matching population for sex, age, and Charlson Comorbidity Index, and multivariate regression to adjust for patient ZIP code, income, hospital region, location, size, and teaching status.
Dr. Bi presented results from 442,535 patients with AP. Of these, 12,735 were on systemic anticoagulation prior to AP. Their mean age was 66 and 47% were female. After adjustment for confounders, patients on systemic anticoagulation prior to AP onset displayed a decreased odds of AP occurrence, compared with those who were not on anticoagulation (OR 0.56; P less than .01). In addition, patients on anticoagulation displayed improved outcomes in a number of variables, compared with their counterparts who were not on anticoagulation: mortality (OR 0.65), shock (OR 0.68), acute kidney injury (OR 0.83), ICU admission (OR 0.57), multiorgan failure (OR 0.85), and hospital charges (a mean reduction of $9,275), as well as AP induced by alcohol use (OR 0.26; P less than .01 for all associations). “These data suggest that the majority of AP associated with alcohol was prevented by anticoagulation medication,” Dr. Bi said. “This is very striking. Anticoagulation may hold promise in both the prevention and treatment of AP.”
To further prove their points, Dr. Bi teamed with Baoan Ji, MD, PhD, a basic research scientist at Mayo Clinic, and developed a humanized AP animal model. With this model, they showed that Pradaxa, a Food and Drug Administration–approved anticoagulant, is effective in experimental AP prevention and treatment. “We are currently enrolling patients into a prospective clinical trial to further prove this in humans,” Dr. Bi said. The experimental therapeutic study will be reported at DDW on May 20.
She cautioned against using systemic anticoagulants in this patient population before results of the trial currently underway at Mayo Clinic’s Florida campus are known. “That should be sometime in mid-2020,” she said. “And the bleeding risk should be carefully monitored when using anticoagulants.”
The researchers were supported by funding from the Mayo Clinic and the Department of Defense.
SOURCE: Bi Y et al. DDW 2019, Abstract Sa1381.
SAN DIEGO –
“Acute pancreatitis is a very common disease,” lead study author Yan Bi, MD, PhD, a senior associate consultant and assistant professor in the department of gastroenterology and hepatology at Mayo Clinic, Jacksonville, Fla., said in an interview in advance of the annual Digestive Disease Week. “It’s the number one GI cause for hospitalization. Unfortunately, even after decades of basic science and clinical research, there’s still no cure; there’s nothing to prevent it from happening. The only treatment we can offer is supportive care, which includes fluid hydration, pain control, and nutrition support.”
The pathogenesis of acute pancreatitis (AP) is complex, she continued, and represents a sequence of distinct and interconnected pathologic events. “Both animal data and human studies have shown that acute pancreatitis is a hypercoagulable state,” she said. “We hypothesize that coagulation plays important roles in the development of pancreatitis.”
To test their hypothesis, Dr. Bi and associates performed a retrospective study. They drew from the 2014 National Inpatient Sample to evaluate the effect of systemic anticoagulation prior to AP onset on outcomes of the condition. They used ICD-9 codes to identify patients with a primary diagnosis of AP as well as those who were taking systemic anticoagulation. The primary outcome was the odds of AP in patients taking systemic anticoagulation, compared with those who were not. Secondary outcomes were mortality, morbidity, length of hospital stay, and total hospitalization charges and costs. The researchers used propensity score matching to create a 1:1 matching population for sex, age, and Charlson Comorbidity Index, and multivariate regression to adjust for patient ZIP code, income, hospital region, location, size, and teaching status.
Dr. Bi presented results from 442,535 patients with AP. Of these, 12,735 were on systemic anticoagulation prior to AP. Their mean age was 66 and 47% were female. After adjustment for confounders, patients on systemic anticoagulation prior to AP onset displayed a decreased odds of AP occurrence, compared with those who were not on anticoagulation (OR 0.56; P less than .01). In addition, patients on anticoagulation displayed improved outcomes in a number of variables, compared with their counterparts who were not on anticoagulation: mortality (OR 0.65), shock (OR 0.68), acute kidney injury (OR 0.83), ICU admission (OR 0.57), multiorgan failure (OR 0.85), and hospital charges (a mean reduction of $9,275), as well as AP induced by alcohol use (OR 0.26; P less than .01 for all associations). “These data suggest that the majority of AP associated with alcohol was prevented by anticoagulation medication,” Dr. Bi said. “This is very striking. Anticoagulation may hold promise in both the prevention and treatment of AP.”
To further prove their points, Dr. Bi teamed with Baoan Ji, MD, PhD, a basic research scientist at Mayo Clinic, and developed a humanized AP animal model. With this model, they showed that Pradaxa, a Food and Drug Administration–approved anticoagulant, is effective in experimental AP prevention and treatment. “We are currently enrolling patients into a prospective clinical trial to further prove this in humans,” Dr. Bi said. The experimental therapeutic study will be reported at DDW on May 20.
She cautioned against using systemic anticoagulants in this patient population before results of the trial currently underway at Mayo Clinic’s Florida campus are known. “That should be sometime in mid-2020,” she said. “And the bleeding risk should be carefully monitored when using anticoagulants.”
The researchers were supported by funding from the Mayo Clinic and the Department of Defense.
SOURCE: Bi Y et al. DDW 2019, Abstract Sa1381.
SAN DIEGO –
“Acute pancreatitis is a very common disease,” lead study author Yan Bi, MD, PhD, a senior associate consultant and assistant professor in the department of gastroenterology and hepatology at Mayo Clinic, Jacksonville, Fla., said in an interview in advance of the annual Digestive Disease Week. “It’s the number one GI cause for hospitalization. Unfortunately, even after decades of basic science and clinical research, there’s still no cure; there’s nothing to prevent it from happening. The only treatment we can offer is supportive care, which includes fluid hydration, pain control, and nutrition support.”
The pathogenesis of acute pancreatitis (AP) is complex, she continued, and represents a sequence of distinct and interconnected pathologic events. “Both animal data and human studies have shown that acute pancreatitis is a hypercoagulable state,” she said. “We hypothesize that coagulation plays important roles in the development of pancreatitis.”
To test their hypothesis, Dr. Bi and associates performed a retrospective study. They drew from the 2014 National Inpatient Sample to evaluate the effect of systemic anticoagulation prior to AP onset on outcomes of the condition. They used ICD-9 codes to identify patients with a primary diagnosis of AP as well as those who were taking systemic anticoagulation. The primary outcome was the odds of AP in patients taking systemic anticoagulation, compared with those who were not. Secondary outcomes were mortality, morbidity, length of hospital stay, and total hospitalization charges and costs. The researchers used propensity score matching to create a 1:1 matching population for sex, age, and Charlson Comorbidity Index, and multivariate regression to adjust for patient ZIP code, income, hospital region, location, size, and teaching status.
Dr. Bi presented results from 442,535 patients with AP. Of these, 12,735 were on systemic anticoagulation prior to AP. Their mean age was 66 and 47% were female. After adjustment for confounders, patients on systemic anticoagulation prior to AP onset displayed a decreased odds of AP occurrence, compared with those who were not on anticoagulation (OR 0.56; P less than .01). In addition, patients on anticoagulation displayed improved outcomes in a number of variables, compared with their counterparts who were not on anticoagulation: mortality (OR 0.65), shock (OR 0.68), acute kidney injury (OR 0.83), ICU admission (OR 0.57), multiorgan failure (OR 0.85), and hospital charges (a mean reduction of $9,275), as well as AP induced by alcohol use (OR 0.26; P less than .01 for all associations). “These data suggest that the majority of AP associated with alcohol was prevented by anticoagulation medication,” Dr. Bi said. “This is very striking. Anticoagulation may hold promise in both the prevention and treatment of AP.”
To further prove their points, Dr. Bi teamed with Baoan Ji, MD, PhD, a basic research scientist at Mayo Clinic, and developed a humanized AP animal model. With this model, they showed that Pradaxa, a Food and Drug Administration–approved anticoagulant, is effective in experimental AP prevention and treatment. “We are currently enrolling patients into a prospective clinical trial to further prove this in humans,” Dr. Bi said. The experimental therapeutic study will be reported at DDW on May 20.
She cautioned against using systemic anticoagulants in this patient population before results of the trial currently underway at Mayo Clinic’s Florida campus are known. “That should be sometime in mid-2020,” she said. “And the bleeding risk should be carefully monitored when using anticoagulants.”
The researchers were supported by funding from the Mayo Clinic and the Department of Defense.
SOURCE: Bi Y et al. DDW 2019, Abstract Sa1381.
REPORTING FROM DDW 2019
Key clinical point: Anticoagulation may hold promise in both the prevention and treatment of acute pancreatitis (AP).
Major finding: Patients on systemic anticoagulation prior to AP onset displayed a decreased odds of AP occurrence, compared with those who were not on anticoagulation (OR 0.56; P less than .01).
Study details: A retrospective analysis of 442,535 patients with AP.
Disclosures: The researchers were supported by funding from the Mayo Clinic and the Department of Defense.
Source: Bi Y et al. DDW 2019, Abstract Sa1381.
Sustainable weight loss seen 5 years after endoscopic sleeve gastroplasty

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.
FROM DDW 2019
Key clinical point: Endoscopic sleeve gastroplasty is an effective, minimally invasive weight-loss procedure that results in significant total body weight loss.
Major finding: Between 1 and 5 years after endoscopic sleeve gastroplasty, patients lost 15%-20% of their total body weight.
Study details: A retrospective study of prospectively collected data on 203 patients.
Disclosures: Dr. Sharaiha reported having no financial disclosures.
Study finds link between intrahepatic cholestasis of pregnancy and risk of NAFLD
Patients with intrahepatic cholestasis of pregnancy (ICP) were nearly six times more likely to have a diagnosis of nonalcoholic fatty liver disease (NAFLD) than were controls, results from a retrospective, single-center study demonstrated.
“If this connection is confirmed with future studies, intrahepatic cholestasis of pregnancy may prove a novel model through which to investigate bile acid metabolism in patients with fatty liver disease,” one of the study authors, Tatyana Kushner, MD, MSCE, said during a media briefing in advance of the annual Digestive Disease Week. “This could have implications for future management of fatty liver disease. Additionally, these findings suggest that ICP patients should be seen by a liver specialist because they may go on to develop chronic liver disease or may already have already existing underlying liver disease.”
ICP is characterized by a build-up of bile acids during pregnancy and is associated with an increased risk of negative fetal outcomes and fetal death if left untreated, said Dr. Kushner, of the division of liver diseases at the Icahn School of Medicine at Mount Sinai, New York. The most notable symptom during pregnancy is severe pruritus. In what is believed to be the first study of its kind, Dr. Kushner and colleagues set out to evaluate the association between ICP and NAFLD and associated metabolic risk factors, including obesity, dyslipidemia, hypertension, and diabetes. Between January and December of 2017, they drew from the electronic medical records of a New York City health system to identify 149 pregnancies complicated by ICP and compared them to a control group of 200 pregnancies without an ICP diagnosis. The researchers used Pearson’s chi-square or Fisher’s exact test and Wilcoxon rank-sum tests to evaluate association of ICP with categorical variables and continuous variables, respectively, and unadjusted odds ratios to compare the ICP and control groups for clinically significant outcomes.
The median age of the study population was 30 years, their mean body mass index was 27.5 kg/m2, and there was a higher proportion of Hispanic women in the ICP group, compared with the control group (75% vs. 62%, respectively). Dr. Kushner and colleagues found that Hispanic women were nearly twice as likely to be diagnosed with ICP than non-Hispanic women (OR, 1.90; 95% confidence interval, 1.87-3.03). However, patients in both the ICP and control groups were similar for median age (OR, 1.02; 95% CI, 0.99-1.06), nulliparity (OR, 0.79; 95% CI, 0.48-1.30), and prevalence of hepatitis C (OR, 1.35; 95% CI, 0.08-21.67). The two groups were also similar for certain metabolic risk factors, including prevalence of obesity (OR, 1.01; 95% CI, 0.62-1.61), hypertension (OR, 0.69; 95% CI, 0.31-1.52), hemoglobin A1c greater than 5.5% (OR, 0.80; 95% CI, 0.34-1.9), and total cholesterol above 200 mg/dL (OR, 4.15; 95% CI, 0.83-20.84). Median bile acid levels were 30.6 micromoles (interquartile range, 11.6, 32.7) in the ICP group.
Compared with patients in the control group, those in the ICP group had higher median levels of alanine aminotransferase (ALT) (32 vs. 16 U/L; P less than .0001), alkaline phosphatase (181 vs. 128 U/L; P less than .0001), and total bilirubin (0.5 vs. 0.35 mg/dL; P less than .0001). ICP patients were also more likely than their counterparts to have ALT levels above 50 U/L (two times the upper limit of normal; OR, 3.22; 95% CI, 1.48-7.03), a history of biliary disease (OR, 3.29; 95% CI, 1.39-7.80), and to have evidence of steatosis on liver imaging (OR, 4.69; 95% CI, 1.68-13.12). When the researchers evaluated a diagnosis of NAFLD based on ICD-10 codes or evidence of steatosis on liver imaging, ICP patients were significantly more likely to have a diagnosis of NAFLD than controls (OR, 5.7; 95% CI, 2.08-15.65).
“We recommend additional research to look at differences in NAFLD progression in women who had NAFLD and were later diagnosed with ICP, compared to women with NAFLD who did not go on to develop ICP, because that may be a reflection of the role that bile acid metabolism plays in these particular patients,” Dr. Kushner said.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
The study’s primary author was Erica Monrose, MD. The researchers reported having no financial disclosures.
SOURCE: Monrose E et al. DDW 2019, Abstract Sa1562.
Patients with intrahepatic cholestasis of pregnancy (ICP) were nearly six times more likely to have a diagnosis of nonalcoholic fatty liver disease (NAFLD) than were controls, results from a retrospective, single-center study demonstrated.
“If this connection is confirmed with future studies, intrahepatic cholestasis of pregnancy may prove a novel model through which to investigate bile acid metabolism in patients with fatty liver disease,” one of the study authors, Tatyana Kushner, MD, MSCE, said during a media briefing in advance of the annual Digestive Disease Week. “This could have implications for future management of fatty liver disease. Additionally, these findings suggest that ICP patients should be seen by a liver specialist because they may go on to develop chronic liver disease or may already have already existing underlying liver disease.”
ICP is characterized by a build-up of bile acids during pregnancy and is associated with an increased risk of negative fetal outcomes and fetal death if left untreated, said Dr. Kushner, of the division of liver diseases at the Icahn School of Medicine at Mount Sinai, New York. The most notable symptom during pregnancy is severe pruritus. In what is believed to be the first study of its kind, Dr. Kushner and colleagues set out to evaluate the association between ICP and NAFLD and associated metabolic risk factors, including obesity, dyslipidemia, hypertension, and diabetes. Between January and December of 2017, they drew from the electronic medical records of a New York City health system to identify 149 pregnancies complicated by ICP and compared them to a control group of 200 pregnancies without an ICP diagnosis. The researchers used Pearson’s chi-square or Fisher’s exact test and Wilcoxon rank-sum tests to evaluate association of ICP with categorical variables and continuous variables, respectively, and unadjusted odds ratios to compare the ICP and control groups for clinically significant outcomes.
The median age of the study population was 30 years, their mean body mass index was 27.5 kg/m2, and there was a higher proportion of Hispanic women in the ICP group, compared with the control group (75% vs. 62%, respectively). Dr. Kushner and colleagues found that Hispanic women were nearly twice as likely to be diagnosed with ICP than non-Hispanic women (OR, 1.90; 95% confidence interval, 1.87-3.03). However, patients in both the ICP and control groups were similar for median age (OR, 1.02; 95% CI, 0.99-1.06), nulliparity (OR, 0.79; 95% CI, 0.48-1.30), and prevalence of hepatitis C (OR, 1.35; 95% CI, 0.08-21.67). The two groups were also similar for certain metabolic risk factors, including prevalence of obesity (OR, 1.01; 95% CI, 0.62-1.61), hypertension (OR, 0.69; 95% CI, 0.31-1.52), hemoglobin A1c greater than 5.5% (OR, 0.80; 95% CI, 0.34-1.9), and total cholesterol above 200 mg/dL (OR, 4.15; 95% CI, 0.83-20.84). Median bile acid levels were 30.6 micromoles (interquartile range, 11.6, 32.7) in the ICP group.
Compared with patients in the control group, those in the ICP group had higher median levels of alanine aminotransferase (ALT) (32 vs. 16 U/L; P less than .0001), alkaline phosphatase (181 vs. 128 U/L; P less than .0001), and total bilirubin (0.5 vs. 0.35 mg/dL; P less than .0001). ICP patients were also more likely than their counterparts to have ALT levels above 50 U/L (two times the upper limit of normal; OR, 3.22; 95% CI, 1.48-7.03), a history of biliary disease (OR, 3.29; 95% CI, 1.39-7.80), and to have evidence of steatosis on liver imaging (OR, 4.69; 95% CI, 1.68-13.12). When the researchers evaluated a diagnosis of NAFLD based on ICD-10 codes or evidence of steatosis on liver imaging, ICP patients were significantly more likely to have a diagnosis of NAFLD than controls (OR, 5.7; 95% CI, 2.08-15.65).
“We recommend additional research to look at differences in NAFLD progression in women who had NAFLD and were later diagnosed with ICP, compared to women with NAFLD who did not go on to develop ICP, because that may be a reflection of the role that bile acid metabolism plays in these particular patients,” Dr. Kushner said.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
The study’s primary author was Erica Monrose, MD. The researchers reported having no financial disclosures.
SOURCE: Monrose E et al. DDW 2019, Abstract Sa1562.
Patients with intrahepatic cholestasis of pregnancy (ICP) were nearly six times more likely to have a diagnosis of nonalcoholic fatty liver disease (NAFLD) than were controls, results from a retrospective, single-center study demonstrated.
“If this connection is confirmed with future studies, intrahepatic cholestasis of pregnancy may prove a novel model through which to investigate bile acid metabolism in patients with fatty liver disease,” one of the study authors, Tatyana Kushner, MD, MSCE, said during a media briefing in advance of the annual Digestive Disease Week. “This could have implications for future management of fatty liver disease. Additionally, these findings suggest that ICP patients should be seen by a liver specialist because they may go on to develop chronic liver disease or may already have already existing underlying liver disease.”
ICP is characterized by a build-up of bile acids during pregnancy and is associated with an increased risk of negative fetal outcomes and fetal death if left untreated, said Dr. Kushner, of the division of liver diseases at the Icahn School of Medicine at Mount Sinai, New York. The most notable symptom during pregnancy is severe pruritus. In what is believed to be the first study of its kind, Dr. Kushner and colleagues set out to evaluate the association between ICP and NAFLD and associated metabolic risk factors, including obesity, dyslipidemia, hypertension, and diabetes. Between January and December of 2017, they drew from the electronic medical records of a New York City health system to identify 149 pregnancies complicated by ICP and compared them to a control group of 200 pregnancies without an ICP diagnosis. The researchers used Pearson’s chi-square or Fisher’s exact test and Wilcoxon rank-sum tests to evaluate association of ICP with categorical variables and continuous variables, respectively, and unadjusted odds ratios to compare the ICP and control groups for clinically significant outcomes.
The median age of the study population was 30 years, their mean body mass index was 27.5 kg/m2, and there was a higher proportion of Hispanic women in the ICP group, compared with the control group (75% vs. 62%, respectively). Dr. Kushner and colleagues found that Hispanic women were nearly twice as likely to be diagnosed with ICP than non-Hispanic women (OR, 1.90; 95% confidence interval, 1.87-3.03). However, patients in both the ICP and control groups were similar for median age (OR, 1.02; 95% CI, 0.99-1.06), nulliparity (OR, 0.79; 95% CI, 0.48-1.30), and prevalence of hepatitis C (OR, 1.35; 95% CI, 0.08-21.67). The two groups were also similar for certain metabolic risk factors, including prevalence of obesity (OR, 1.01; 95% CI, 0.62-1.61), hypertension (OR, 0.69; 95% CI, 0.31-1.52), hemoglobin A1c greater than 5.5% (OR, 0.80; 95% CI, 0.34-1.9), and total cholesterol above 200 mg/dL (OR, 4.15; 95% CI, 0.83-20.84). Median bile acid levels were 30.6 micromoles (interquartile range, 11.6, 32.7) in the ICP group.
Compared with patients in the control group, those in the ICP group had higher median levels of alanine aminotransferase (ALT) (32 vs. 16 U/L; P less than .0001), alkaline phosphatase (181 vs. 128 U/L; P less than .0001), and total bilirubin (0.5 vs. 0.35 mg/dL; P less than .0001). ICP patients were also more likely than their counterparts to have ALT levels above 50 U/L (two times the upper limit of normal; OR, 3.22; 95% CI, 1.48-7.03), a history of biliary disease (OR, 3.29; 95% CI, 1.39-7.80), and to have evidence of steatosis on liver imaging (OR, 4.69; 95% CI, 1.68-13.12). When the researchers evaluated a diagnosis of NAFLD based on ICD-10 codes or evidence of steatosis on liver imaging, ICP patients were significantly more likely to have a diagnosis of NAFLD than controls (OR, 5.7; 95% CI, 2.08-15.65).
“We recommend additional research to look at differences in NAFLD progression in women who had NAFLD and were later diagnosed with ICP, compared to women with NAFLD who did not go on to develop ICP, because that may be a reflection of the role that bile acid metabolism plays in these particular patients,” Dr. Kushner said.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
The study’s primary author was Erica Monrose, MD. The researchers reported having no financial disclosures.
SOURCE: Monrose E et al. DDW 2019, Abstract Sa1562.
REPORTING FROM DDW 2019
FMT explored as a potential weight loss treatment
“Currently, fecal microbiota transplantation [FMT] can only be performed clinically in the US to treat recurrent Clostridium difficile infection,” lead study author Jessica R. Allegretti, MD, MPH, said during a media briefing in advance of the annual Digestive Disease Week.
“However, there is ongoing research to find out whether FMT works for other health conditions such as obesity, a condition which affects millions of people worldwide. [It’s] a condition that also increases the risk of developing many other illnesses, including diabetes, heart disease, and certain cancers. In my clinical practice, we regularly see patients who have not yet developed some of these other conditions related to obesity, but really do have difficulty losing weight. Through our research we wanted to focus on a population we call the medically uncompromised obese, and understand if FMT might be a viable treatment option for them,” she said.
Dr. Allegretti, director of the fecal microbiota transplant program at Brigham and Women’s Hospital, Boston, conducted a parallel study of 22 patients with a body mass index of 35 kg/m2 or higher who were metabolically healthy – defined as having no type 2 diabetes, nonalcoholic steatohepatitis (NASH), or metabolic syndrome. They randomized study participants 1:1 to receive 30 FMT capsules followed by two doses of 12 capsules over a 12-week period, or identical placebo capsules. A single healthy lean donor with a BMI of 17 kg/m2 was used.
The researchers assessed patients with a mixed meal tolerance test at baseline, week 6, and week 12 post-FMT, at which biomarkers GLP-1 and leptin were measured. Stool was collected at baseline and at one, four, six, eight, and 12 weeks post-FMT. The primary outcomes were safety and change in the area under the curve for GLP-1 at 12 weeks compared to baseline. Secondary endpoints include gut microbiome profiles and diversity as well as bile acid profiles at 12 weeks post FMT. Additional endpoints include a decrease in BMI and waist circumference at week 12. Standard stool microbiome and bile acid analysis was performed.
The mean age of the patients at baseline was 43 years, and their mean BMI was 41 kg/m2. Between baseline and week 12, the research observed no increase of GLP-1 in either group, while the change in leptin revealed an increase in the placebo group only (P less than .001). At week 12, no early changes in BMI were noted in either group (P = .51). No serious adverse events occurred in either arm.
Dr. Allegretti and her colleagues observed global signals of donor community engraftment following FMT, including an increase in alpha diversity and increased similarity to stool samples from the FMT donor – trends that were not observed in the placebo arm. In addition, bile acid analysis suggested a sustained decrease in taurocholic acid in the FMT arm, comparable with the donor – an effect that was not seen in the placebo arm. “We know that what leads to the germination of C. diff. spores is brought out by bile acids,” she said. “That’s one of the critical components of pathogenesis in that disease. My group has been able to show that after FMT, you regain bile acid homeostasis.”
Dr. Allegretti concluded her remarks by noting that the current study “adds an encouraging first step in trying to understand the role that the gut microbiome is playing in the pathogenesis of medically uncompromised obese patients. As a next step, we plan to seek more sensitive measures of GLP-1, as well as conduct additional research into varied doses of FMT capsules, as well as potentially investigating other microbial pathways to better understand the role the microbiome is playing in obesity.”
Somerville, Mass.–based Finch Therapeutics provided funding for the research. Dr. Allegretti reported having no financial disclosures.
SOURCE: Allegretti J et al. DDW 2019. Abstract 621.
“Currently, fecal microbiota transplantation [FMT] can only be performed clinically in the US to treat recurrent Clostridium difficile infection,” lead study author Jessica R. Allegretti, MD, MPH, said during a media briefing in advance of the annual Digestive Disease Week.
“However, there is ongoing research to find out whether FMT works for other health conditions such as obesity, a condition which affects millions of people worldwide. [It’s] a condition that also increases the risk of developing many other illnesses, including diabetes, heart disease, and certain cancers. In my clinical practice, we regularly see patients who have not yet developed some of these other conditions related to obesity, but really do have difficulty losing weight. Through our research we wanted to focus on a population we call the medically uncompromised obese, and understand if FMT might be a viable treatment option for them,” she said.
Dr. Allegretti, director of the fecal microbiota transplant program at Brigham and Women’s Hospital, Boston, conducted a parallel study of 22 patients with a body mass index of 35 kg/m2 or higher who were metabolically healthy – defined as having no type 2 diabetes, nonalcoholic steatohepatitis (NASH), or metabolic syndrome. They randomized study participants 1:1 to receive 30 FMT capsules followed by two doses of 12 capsules over a 12-week period, or identical placebo capsules. A single healthy lean donor with a BMI of 17 kg/m2 was used.
The researchers assessed patients with a mixed meal tolerance test at baseline, week 6, and week 12 post-FMT, at which biomarkers GLP-1 and leptin were measured. Stool was collected at baseline and at one, four, six, eight, and 12 weeks post-FMT. The primary outcomes were safety and change in the area under the curve for GLP-1 at 12 weeks compared to baseline. Secondary endpoints include gut microbiome profiles and diversity as well as bile acid profiles at 12 weeks post FMT. Additional endpoints include a decrease in BMI and waist circumference at week 12. Standard stool microbiome and bile acid analysis was performed.
The mean age of the patients at baseline was 43 years, and their mean BMI was 41 kg/m2. Between baseline and week 12, the research observed no increase of GLP-1 in either group, while the change in leptin revealed an increase in the placebo group only (P less than .001). At week 12, no early changes in BMI were noted in either group (P = .51). No serious adverse events occurred in either arm.
Dr. Allegretti and her colleagues observed global signals of donor community engraftment following FMT, including an increase in alpha diversity and increased similarity to stool samples from the FMT donor – trends that were not observed in the placebo arm. In addition, bile acid analysis suggested a sustained decrease in taurocholic acid in the FMT arm, comparable with the donor – an effect that was not seen in the placebo arm. “We know that what leads to the germination of C. diff. spores is brought out by bile acids,” she said. “That’s one of the critical components of pathogenesis in that disease. My group has been able to show that after FMT, you regain bile acid homeostasis.”
Dr. Allegretti concluded her remarks by noting that the current study “adds an encouraging first step in trying to understand the role that the gut microbiome is playing in the pathogenesis of medically uncompromised obese patients. As a next step, we plan to seek more sensitive measures of GLP-1, as well as conduct additional research into varied doses of FMT capsules, as well as potentially investigating other microbial pathways to better understand the role the microbiome is playing in obesity.”
Somerville, Mass.–based Finch Therapeutics provided funding for the research. Dr. Allegretti reported having no financial disclosures.
SOURCE: Allegretti J et al. DDW 2019. Abstract 621.
“Currently, fecal microbiota transplantation [FMT] can only be performed clinically in the US to treat recurrent Clostridium difficile infection,” lead study author Jessica R. Allegretti, MD, MPH, said during a media briefing in advance of the annual Digestive Disease Week.
“However, there is ongoing research to find out whether FMT works for other health conditions such as obesity, a condition which affects millions of people worldwide. [It’s] a condition that also increases the risk of developing many other illnesses, including diabetes, heart disease, and certain cancers. In my clinical practice, we regularly see patients who have not yet developed some of these other conditions related to obesity, but really do have difficulty losing weight. Through our research we wanted to focus on a population we call the medically uncompromised obese, and understand if FMT might be a viable treatment option for them,” she said.
Dr. Allegretti, director of the fecal microbiota transplant program at Brigham and Women’s Hospital, Boston, conducted a parallel study of 22 patients with a body mass index of 35 kg/m2 or higher who were metabolically healthy – defined as having no type 2 diabetes, nonalcoholic steatohepatitis (NASH), or metabolic syndrome. They randomized study participants 1:1 to receive 30 FMT capsules followed by two doses of 12 capsules over a 12-week period, or identical placebo capsules. A single healthy lean donor with a BMI of 17 kg/m2 was used.
The researchers assessed patients with a mixed meal tolerance test at baseline, week 6, and week 12 post-FMT, at which biomarkers GLP-1 and leptin were measured. Stool was collected at baseline and at one, four, six, eight, and 12 weeks post-FMT. The primary outcomes were safety and change in the area under the curve for GLP-1 at 12 weeks compared to baseline. Secondary endpoints include gut microbiome profiles and diversity as well as bile acid profiles at 12 weeks post FMT. Additional endpoints include a decrease in BMI and waist circumference at week 12. Standard stool microbiome and bile acid analysis was performed.
The mean age of the patients at baseline was 43 years, and their mean BMI was 41 kg/m2. Between baseline and week 12, the research observed no increase of GLP-1 in either group, while the change in leptin revealed an increase in the placebo group only (P less than .001). At week 12, no early changes in BMI were noted in either group (P = .51). No serious adverse events occurred in either arm.
Dr. Allegretti and her colleagues observed global signals of donor community engraftment following FMT, including an increase in alpha diversity and increased similarity to stool samples from the FMT donor – trends that were not observed in the placebo arm. In addition, bile acid analysis suggested a sustained decrease in taurocholic acid in the FMT arm, comparable with the donor – an effect that was not seen in the placebo arm. “We know that what leads to the germination of C. diff. spores is brought out by bile acids,” she said. “That’s one of the critical components of pathogenesis in that disease. My group has been able to show that after FMT, you regain bile acid homeostasis.”
Dr. Allegretti concluded her remarks by noting that the current study “adds an encouraging first step in trying to understand the role that the gut microbiome is playing in the pathogenesis of medically uncompromised obese patients. As a next step, we plan to seek more sensitive measures of GLP-1, as well as conduct additional research into varied doses of FMT capsules, as well as potentially investigating other microbial pathways to better understand the role the microbiome is playing in obesity.”
Somerville, Mass.–based Finch Therapeutics provided funding for the research. Dr. Allegretti reported having no financial disclosures.
SOURCE: Allegretti J et al. DDW 2019. Abstract 621.
REPORTING FROM DDW 2019
Key clinical point: Using capsules filled with fecal matter from a lean donor, researchers successfully changed some of the composition of the gut microbiota of patients with obesity.
Major finding: Following fecal microbiota transplantation, researchers detected a decrease in a specific bile acid and alterations in stool samples that showed increased similarity to those of the lean donor.
Study details: A randomized, placebo-controlled trial of 22 healthy obese patients.
Disclosures: Somerville, Mass.–based Finch Therapeutics provided funding for the research. Dr. Allegretti reported having no financial disclosures.
Source: Allegretti J et al. DDW 2019. Abstract 621.