User login
Biologics options for pediatric asthma continue to grow
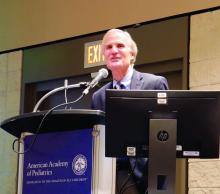
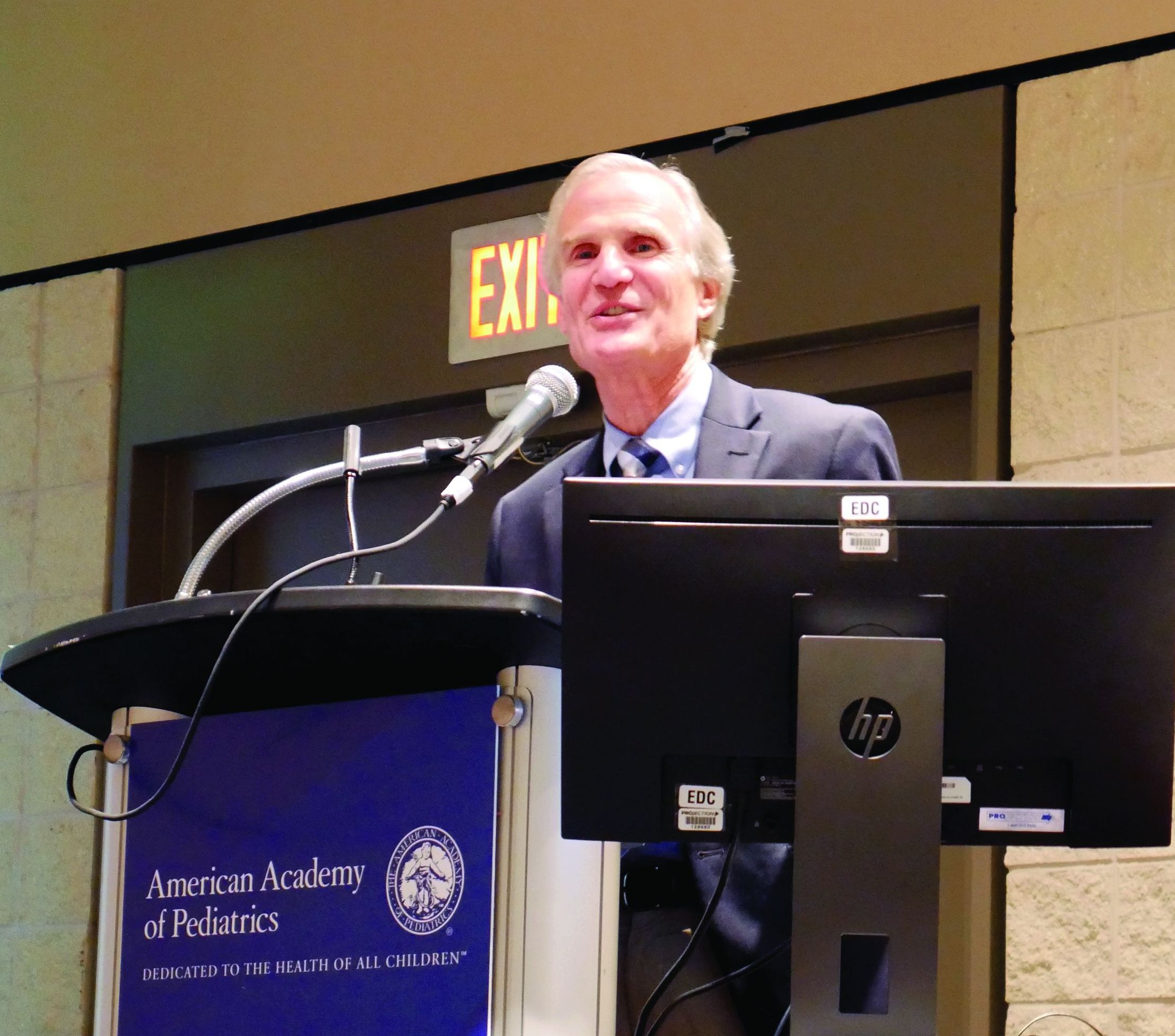
ORLANDO – The goal of treatment is the same for all asthma cases, regardless of severity: “to enable a patient to achieve and maintain control over their asthma,” according to Stanley J. Szefler, MD, a professor of pediatrics at the University of Colorado at Denver, Aurora.
That goal includes “reducing the risk of exacerbations, emergency department visits, hospitalizations, and progression as well as reducing impairments, including symptoms, functional limitations, poor quality of life, and other manifestations of asthma,” Dr. Szefler, also director of the Children’s Hospital of Colorado pediatric asthma research program, told colleagues at the annual meeting of the American Academy of Pediatrics.
Severe asthma challenges
These aims are more difficult with severe asthma, defined by the World Health Organization as “the current level of clinical control and risks which can result in frequent severe exacerbations and/or adverse reactions to medications and/or chronic morbidity,” Dr. Szefler explained. Severe asthma includes untreated severe asthma, difficult-to-treat asthma, and treatment-resistant severe asthma, whether controlled on high-dose medication or not.
Allergen sensitization, viral respiratory infections, and respiratory irritants (such as air pollution and smoking) are common features of severe asthma in children. Also common are challenges specific to management: poor medication adherence, poor technique for inhaled medications, and undertreatment. Poor management can lead to repeated exacerbations, adverse effects from drugs, disease progression, possible development of chronic obstructive pulmonary disease (COPD), and early mortality.
The National Heart, Lung, and Blood Institute EPR-3 guidelines for treatment of pediatric asthma recommend a stepwise approach to therapy, starting with short-acting beta2-agonists as needed (SABA p.r.n.). The clinician then assesses the patient’s symptoms, exacerbations, side effects, quality of life, and lung function to determine whether the asthma is well managed or requires inhaled corticosteroids, or another therapy in moving through the steps. Each step also involves patient education, environmental control, and management of the child’s comorbidities.
It is not until steps 5 and 6 that the guidelines advise considering the biologic omalizumab for patients who have allergies. But other biologic options exist as well. Four biologics currently approved for treating asthma include omalizumab, mepolizumab, benralizumab, and reslizumab, but reslizumab is approved only for patients at least 18 years old.
Biologics for pediatric asthma
Omalizumab, which targets IgE, is appropriate for patients at least 6 years old in whom inhaled corticosteroids could not adequately control the symptoms of moderate to-severe persistent asthma. Dosing of omalizumab is a subcutaneous injection every 2-4 weeks based on pretreatment serum IgE and body weight using a dosing table that starts at 0.016 mg/kg/IgE (IU/mL). Maximum dose is 375 mg every 2 weeks in the United States and 600 mg every 2 weeks in the European Union.
The advantages of an anti-IgE drug are its use only once a month and its substantial effect on reducing exacerbations in a clearly identified population. However, these drugs are costly and require supervised administration, Dr. Szefler noted. They also carry a risk of anaphylaxis in less than 0.2% of patients, requiring the patient to be monitored after first administration and to carry an injectable epinephrine after omalizumab administration as a precaution for late-occurring anaphylaxis.
Mepolizumab is an anti–interleukin (IL)–5 drug used in patients at least 12 years old with severe persistent asthma that’s inadequately controlled with inhaled corticosteroids. Peripheral blood counts of eosinophilia determine if a patient has an eosinophilic phenotype, which has the best response to mepolizumab. People with at least 150 cells per microliter at baseline or at least 300 cells per microliter within the past year have shown a good response to mepolizumab. Dosing is 100 mg subcutaneously every 4 weeks.
For patients with atopic asthma, mepolizumab is effective in reducing the daily oral corticosteroid dose and the number of both annual exacerbations and exacerbations requiring hospitalization or an emergency visit. Other benefits of mepolizumab include increasing the time to a first exacerbation, the pre- and postbronchodilator forced expiratory volume in one second (FEV1) and overall quality of life.
Patient reductions in exacerbations while taking mepolizumab were associated with eosinophil count but not IgE, atopic status, FEV1 or bronchodilator response in the DREAM study (Lancet. 2012 Aug 18;380[9842]:651-9.).
Two safety considerations with mepolizumab include an increased risk of shingles and the risk of a preexisting helminth infection getting worse. Providers should screen for helminth infection and might consider a herpes zoster vaccination prior to starting therapy, Dr. Szefler said.
Benralizumab is an anti-IL5Ra for use in people at least 12 years old with severe persistent asthma and an eosinophilic phenotype (at least 300 cells per microliter). Dosing begins with three subcutaneous injections of 30 mg every 4 weeks, followed by administration every 8 weeks thereafter.
Benralizumab’s clinical effects include reduced exacerbations and oral corticosteroid use, and improved asthma symptom scores and prebronchodilator FEV1. Higher serum eosinophils and a history of more frequent exacerbations are both biomarkers for reduced exacerbations with benralizumab treatment.
Dupilumab: New kid on the block
The newest biologic for asthma is dupilumab, approved Oct. 19, 2018, by the Food and Drug Administration as the only asthma biologic that patients can administer at home. Dupilumab is an anti–IL-4 and anti–IL-13 biologic whose most recent study results showed a severe exacerbations rate 50% lower than placebo (N Engl J Med. 2018 Jun 28;378[26]:2486-96.). Patients with higher baseline levels of eosinophils had the best response, although some patients showed hypereosinophilia following dupilumab therapy.
The study had a low number of adolescents enrolled, however, and more data on predictive biomarkers are needed. Dupilumab also requires a twice-monthly administration.
“It could be potentially better than those currently available due to additional effect on FEV1,” Dr. Szefler said, but cost and safety may determine how dupilumab is recommended and used, including possible use for early intervention.
As development in biologics for pediatric asthma continues to grow, questions about best practices for management remain, such as what age is best for starting biologics, what strategies are most safe and effective, and what risks and benefits exist for each strategy. Questions also remain regarding the risk factors for asthma and what early intervention strategies might change the disease’s natural history.
“Look at asthma in children as a chronic disease that can result in potentially preventable adverse respiratory outcomes in adulthood,” Dr. Szefler said. He recommended monitoring children’s lung function over time and using “measures of clinical outcomes, lung function, and biomarkers to assess potential benefits of biologic therapy.”
Dr. Szefler has served on the advisory board for Regeneron and Sanofi, and he has consulted for AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, GlaxoSmithKline, Novartis, and Propeller Health.
ORLANDO – The goal of treatment is the same for all asthma cases, regardless of severity: “to enable a patient to achieve and maintain control over their asthma,” according to Stanley J. Szefler, MD, a professor of pediatrics at the University of Colorado at Denver, Aurora.
That goal includes “reducing the risk of exacerbations, emergency department visits, hospitalizations, and progression as well as reducing impairments, including symptoms, functional limitations, poor quality of life, and other manifestations of asthma,” Dr. Szefler, also director of the Children’s Hospital of Colorado pediatric asthma research program, told colleagues at the annual meeting of the American Academy of Pediatrics.
Severe asthma challenges
These aims are more difficult with severe asthma, defined by the World Health Organization as “the current level of clinical control and risks which can result in frequent severe exacerbations and/or adverse reactions to medications and/or chronic morbidity,” Dr. Szefler explained. Severe asthma includes untreated severe asthma, difficult-to-treat asthma, and treatment-resistant severe asthma, whether controlled on high-dose medication or not.
Allergen sensitization, viral respiratory infections, and respiratory irritants (such as air pollution and smoking) are common features of severe asthma in children. Also common are challenges specific to management: poor medication adherence, poor technique for inhaled medications, and undertreatment. Poor management can lead to repeated exacerbations, adverse effects from drugs, disease progression, possible development of chronic obstructive pulmonary disease (COPD), and early mortality.
The National Heart, Lung, and Blood Institute EPR-3 guidelines for treatment of pediatric asthma recommend a stepwise approach to therapy, starting with short-acting beta2-agonists as needed (SABA p.r.n.). The clinician then assesses the patient’s symptoms, exacerbations, side effects, quality of life, and lung function to determine whether the asthma is well managed or requires inhaled corticosteroids, or another therapy in moving through the steps. Each step also involves patient education, environmental control, and management of the child’s comorbidities.
It is not until steps 5 and 6 that the guidelines advise considering the biologic omalizumab for patients who have allergies. But other biologic options exist as well. Four biologics currently approved for treating asthma include omalizumab, mepolizumab, benralizumab, and reslizumab, but reslizumab is approved only for patients at least 18 years old.
Biologics for pediatric asthma
Omalizumab, which targets IgE, is appropriate for patients at least 6 years old in whom inhaled corticosteroids could not adequately control the symptoms of moderate to-severe persistent asthma. Dosing of omalizumab is a subcutaneous injection every 2-4 weeks based on pretreatment serum IgE and body weight using a dosing table that starts at 0.016 mg/kg/IgE (IU/mL). Maximum dose is 375 mg every 2 weeks in the United States and 600 mg every 2 weeks in the European Union.
The advantages of an anti-IgE drug are its use only once a month and its substantial effect on reducing exacerbations in a clearly identified population. However, these drugs are costly and require supervised administration, Dr. Szefler noted. They also carry a risk of anaphylaxis in less than 0.2% of patients, requiring the patient to be monitored after first administration and to carry an injectable epinephrine after omalizumab administration as a precaution for late-occurring anaphylaxis.
Mepolizumab is an anti–interleukin (IL)–5 drug used in patients at least 12 years old with severe persistent asthma that’s inadequately controlled with inhaled corticosteroids. Peripheral blood counts of eosinophilia determine if a patient has an eosinophilic phenotype, which has the best response to mepolizumab. People with at least 150 cells per microliter at baseline or at least 300 cells per microliter within the past year have shown a good response to mepolizumab. Dosing is 100 mg subcutaneously every 4 weeks.
For patients with atopic asthma, mepolizumab is effective in reducing the daily oral corticosteroid dose and the number of both annual exacerbations and exacerbations requiring hospitalization or an emergency visit. Other benefits of mepolizumab include increasing the time to a first exacerbation, the pre- and postbronchodilator forced expiratory volume in one second (FEV1) and overall quality of life.
Patient reductions in exacerbations while taking mepolizumab were associated with eosinophil count but not IgE, atopic status, FEV1 or bronchodilator response in the DREAM study (Lancet. 2012 Aug 18;380[9842]:651-9.).
Two safety considerations with mepolizumab include an increased risk of shingles and the risk of a preexisting helminth infection getting worse. Providers should screen for helminth infection and might consider a herpes zoster vaccination prior to starting therapy, Dr. Szefler said.
Benralizumab is an anti-IL5Ra for use in people at least 12 years old with severe persistent asthma and an eosinophilic phenotype (at least 300 cells per microliter). Dosing begins with three subcutaneous injections of 30 mg every 4 weeks, followed by administration every 8 weeks thereafter.
Benralizumab’s clinical effects include reduced exacerbations and oral corticosteroid use, and improved asthma symptom scores and prebronchodilator FEV1. Higher serum eosinophils and a history of more frequent exacerbations are both biomarkers for reduced exacerbations with benralizumab treatment.
Dupilumab: New kid on the block
The newest biologic for asthma is dupilumab, approved Oct. 19, 2018, by the Food and Drug Administration as the only asthma biologic that patients can administer at home. Dupilumab is an anti–IL-4 and anti–IL-13 biologic whose most recent study results showed a severe exacerbations rate 50% lower than placebo (N Engl J Med. 2018 Jun 28;378[26]:2486-96.). Patients with higher baseline levels of eosinophils had the best response, although some patients showed hypereosinophilia following dupilumab therapy.
The study had a low number of adolescents enrolled, however, and more data on predictive biomarkers are needed. Dupilumab also requires a twice-monthly administration.
“It could be potentially better than those currently available due to additional effect on FEV1,” Dr. Szefler said, but cost and safety may determine how dupilumab is recommended and used, including possible use for early intervention.
As development in biologics for pediatric asthma continues to grow, questions about best practices for management remain, such as what age is best for starting biologics, what strategies are most safe and effective, and what risks and benefits exist for each strategy. Questions also remain regarding the risk factors for asthma and what early intervention strategies might change the disease’s natural history.
“Look at asthma in children as a chronic disease that can result in potentially preventable adverse respiratory outcomes in adulthood,” Dr. Szefler said. He recommended monitoring children’s lung function over time and using “measures of clinical outcomes, lung function, and biomarkers to assess potential benefits of biologic therapy.”
Dr. Szefler has served on the advisory board for Regeneron and Sanofi, and he has consulted for AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, GlaxoSmithKline, Novartis, and Propeller Health.
ORLANDO – The goal of treatment is the same for all asthma cases, regardless of severity: “to enable a patient to achieve and maintain control over their asthma,” according to Stanley J. Szefler, MD, a professor of pediatrics at the University of Colorado at Denver, Aurora.
That goal includes “reducing the risk of exacerbations, emergency department visits, hospitalizations, and progression as well as reducing impairments, including symptoms, functional limitations, poor quality of life, and other manifestations of asthma,” Dr. Szefler, also director of the Children’s Hospital of Colorado pediatric asthma research program, told colleagues at the annual meeting of the American Academy of Pediatrics.
Severe asthma challenges
These aims are more difficult with severe asthma, defined by the World Health Organization as “the current level of clinical control and risks which can result in frequent severe exacerbations and/or adverse reactions to medications and/or chronic morbidity,” Dr. Szefler explained. Severe asthma includes untreated severe asthma, difficult-to-treat asthma, and treatment-resistant severe asthma, whether controlled on high-dose medication or not.
Allergen sensitization, viral respiratory infections, and respiratory irritants (such as air pollution and smoking) are common features of severe asthma in children. Also common are challenges specific to management: poor medication adherence, poor technique for inhaled medications, and undertreatment. Poor management can lead to repeated exacerbations, adverse effects from drugs, disease progression, possible development of chronic obstructive pulmonary disease (COPD), and early mortality.
The National Heart, Lung, and Blood Institute EPR-3 guidelines for treatment of pediatric asthma recommend a stepwise approach to therapy, starting with short-acting beta2-agonists as needed (SABA p.r.n.). The clinician then assesses the patient’s symptoms, exacerbations, side effects, quality of life, and lung function to determine whether the asthma is well managed or requires inhaled corticosteroids, or another therapy in moving through the steps. Each step also involves patient education, environmental control, and management of the child’s comorbidities.
It is not until steps 5 and 6 that the guidelines advise considering the biologic omalizumab for patients who have allergies. But other biologic options exist as well. Four biologics currently approved for treating asthma include omalizumab, mepolizumab, benralizumab, and reslizumab, but reslizumab is approved only for patients at least 18 years old.
Biologics for pediatric asthma
Omalizumab, which targets IgE, is appropriate for patients at least 6 years old in whom inhaled corticosteroids could not adequately control the symptoms of moderate to-severe persistent asthma. Dosing of omalizumab is a subcutaneous injection every 2-4 weeks based on pretreatment serum IgE and body weight using a dosing table that starts at 0.016 mg/kg/IgE (IU/mL). Maximum dose is 375 mg every 2 weeks in the United States and 600 mg every 2 weeks in the European Union.
The advantages of an anti-IgE drug are its use only once a month and its substantial effect on reducing exacerbations in a clearly identified population. However, these drugs are costly and require supervised administration, Dr. Szefler noted. They also carry a risk of anaphylaxis in less than 0.2% of patients, requiring the patient to be monitored after first administration and to carry an injectable epinephrine after omalizumab administration as a precaution for late-occurring anaphylaxis.
Mepolizumab is an anti–interleukin (IL)–5 drug used in patients at least 12 years old with severe persistent asthma that’s inadequately controlled with inhaled corticosteroids. Peripheral blood counts of eosinophilia determine if a patient has an eosinophilic phenotype, which has the best response to mepolizumab. People with at least 150 cells per microliter at baseline or at least 300 cells per microliter within the past year have shown a good response to mepolizumab. Dosing is 100 mg subcutaneously every 4 weeks.
For patients with atopic asthma, mepolizumab is effective in reducing the daily oral corticosteroid dose and the number of both annual exacerbations and exacerbations requiring hospitalization or an emergency visit. Other benefits of mepolizumab include increasing the time to a first exacerbation, the pre- and postbronchodilator forced expiratory volume in one second (FEV1) and overall quality of life.
Patient reductions in exacerbations while taking mepolizumab were associated with eosinophil count but not IgE, atopic status, FEV1 or bronchodilator response in the DREAM study (Lancet. 2012 Aug 18;380[9842]:651-9.).
Two safety considerations with mepolizumab include an increased risk of shingles and the risk of a preexisting helminth infection getting worse. Providers should screen for helminth infection and might consider a herpes zoster vaccination prior to starting therapy, Dr. Szefler said.
Benralizumab is an anti-IL5Ra for use in people at least 12 years old with severe persistent asthma and an eosinophilic phenotype (at least 300 cells per microliter). Dosing begins with three subcutaneous injections of 30 mg every 4 weeks, followed by administration every 8 weeks thereafter.
Benralizumab’s clinical effects include reduced exacerbations and oral corticosteroid use, and improved asthma symptom scores and prebronchodilator FEV1. Higher serum eosinophils and a history of more frequent exacerbations are both biomarkers for reduced exacerbations with benralizumab treatment.
Dupilumab: New kid on the block
The newest biologic for asthma is dupilumab, approved Oct. 19, 2018, by the Food and Drug Administration as the only asthma biologic that patients can administer at home. Dupilumab is an anti–IL-4 and anti–IL-13 biologic whose most recent study results showed a severe exacerbations rate 50% lower than placebo (N Engl J Med. 2018 Jun 28;378[26]:2486-96.). Patients with higher baseline levels of eosinophils had the best response, although some patients showed hypereosinophilia following dupilumab therapy.
The study had a low number of adolescents enrolled, however, and more data on predictive biomarkers are needed. Dupilumab also requires a twice-monthly administration.
“It could be potentially better than those currently available due to additional effect on FEV1,” Dr. Szefler said, but cost and safety may determine how dupilumab is recommended and used, including possible use for early intervention.
As development in biologics for pediatric asthma continues to grow, questions about best practices for management remain, such as what age is best for starting biologics, what strategies are most safe and effective, and what risks and benefits exist for each strategy. Questions also remain regarding the risk factors for asthma and what early intervention strategies might change the disease’s natural history.
“Look at asthma in children as a chronic disease that can result in potentially preventable adverse respiratory outcomes in adulthood,” Dr. Szefler said. He recommended monitoring children’s lung function over time and using “measures of clinical outcomes, lung function, and biomarkers to assess potential benefits of biologic therapy.”
Dr. Szefler has served on the advisory board for Regeneron and Sanofi, and he has consulted for AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, GlaxoSmithKline, Novartis, and Propeller Health.
EXPERT ANALYSIS FROM AAP 18
Child gun deaths lowest in states with strictest firearm laws
ORLANDO – and laws restricting children’s access to firearms are linked to reduced pediatric firearm suicide rates, according to research.
“State-level legislation could play an important role in reducing pediatric firearm-related deaths,” concluded Jordan S. Taylor, MD, of Stanford (Calif.) University and his colleagues.
Dr. Taylor earned top honors among the American Academy of Pediatrics (AAP) Council on Injury, Violence and Poison Prevention research abstracts when he presented his findings at the annual meeting of the American Academy of Pediatrics.
Firearm injuries account for the second leading cause of death among U.S. children: 3,155 youth ages 19 years and younger died from gunshot injuries in 2016, and more than 17,000 were injured. Yet state laws governing the purchase, ownership, carriage, and storage of guns vary widely across the country. Dr. Taylor and his colleagues conducted two studies to assess the effects of firearm legislation on firearm-related injuries and deaths in U.S. children.
In their first study, they analyzed pediatric inpatient admissions for firearm injuries in 2012 relative to the stringency of state firearm legislation. They relied on five data sources for the analysis: the Kids’ Inpatient Database (KID), the Healthcare Cost and Utilization Project, the Agency for Healthcare Research and Quality, the U.S. Census Bureau, and the 2013 Brady scorecard.
The Brady scorecard provides scores for each state based on the presence and strictness of firearm-related laws, including legislation on background checks, ability of dangerous individuals to purchase guns, trafficking laws, and laws governing the sales, carrying, and purchasing of firearms.
The 10 states with the strictest laws (highest Brady scores) are California, Connecticut, Delaware, Hawaii, Illinois, Maryland, Massachusetts, New Jersey, New York, and Rhode Island. The 10 states with the lowest scores (least-strict legislation) are Alaska, Arizona, Arkansas, Florida, Kentucky, Louisiana, Montana, Nevada, Virginia, and Wyoming.
Among the 6,941 youth (aged 0-20 years) hospitalized in 2012 for firearm injuries, 7% died. More than a third of these (36%) occurred in the South, 25% in the Midwest, 22% in the West, and 17% in the Northeast.
Children most likely to be injured were boys, older children, black and Latino children, and children living in low-income zip codes.
The Midwest and South, which have lower average Brady scores (more lax legislation on guns), had 8.30 injuries per 100,000 children, compared with 7.54 injuries per 100,000 children in the Northeast and West, which have higher average Brady scores (more stringent gun laws). This was a difference of 0.76 injuries per 100,000 children (95% confidence interval, 0.38-1.13; P less than 0.001).
Then the researchers conducted a second analysis that looked specifically at firearm mortality within the context of both child access prevention (CAP) laws and states’ Brady scores. CAP laws include safe storage laws and gun lock laws, for example.
This analysis used the Web-Based Injury Statistics Query and Reporting System to capture pediatric firearm deaths from 2014-2015 and compared these to the 2014 Brady scores and CAP laws.
An estimated 2,715 child gun deaths occurred during the study period, of which 62% were homicides and 31% were suicides. The researchers identified “a significant negative correlation between states’ firearm legislation stringency and pediatric firearm mortality (Spearman correlation coefficient = –0.66) and between presence of CAP laws and firearm suicide rates (Spearman correlation coefficient = –0.56).”
Dr. Taylor said in an interview, “states that have both types of child access prevention laws [had] suicide rates four times lower than states that did not have either of those.”
Positive correlations also showed up between unemployment rate and firearm homicide rate (Spearman correlation coefficient = 0.55) and teen tobacco use and firearm suicide rate (Spearman correlation coefficient = 0.50).
The association between Brady scores and pediatric mortality from firearms remained significant after adjustment for poverty, unemployment, and substance abuse (P less than .01). Similarly, the association between the pediatric firearm suicide rate and CAP laws remained significant after controlling for socioeconomic factors and other firearm legislation (P less than .01).
In a video interview, Dr. Taylor discussed his research findings and their importance in clinical practice.
“It’s absolutely important for pediatricians to talk to families about firearms in their home and also in the homes of their friends that they visit,” Dr. Taylor said. “We try to approach it as a public health issue similar to seat belts and car seats.”
No external funding was used, and Dr. Taylor reported no conflicts of interest.
ORLANDO – and laws restricting children’s access to firearms are linked to reduced pediatric firearm suicide rates, according to research.
“State-level legislation could play an important role in reducing pediatric firearm-related deaths,” concluded Jordan S. Taylor, MD, of Stanford (Calif.) University and his colleagues.
Dr. Taylor earned top honors among the American Academy of Pediatrics (AAP) Council on Injury, Violence and Poison Prevention research abstracts when he presented his findings at the annual meeting of the American Academy of Pediatrics.
Firearm injuries account for the second leading cause of death among U.S. children: 3,155 youth ages 19 years and younger died from gunshot injuries in 2016, and more than 17,000 were injured. Yet state laws governing the purchase, ownership, carriage, and storage of guns vary widely across the country. Dr. Taylor and his colleagues conducted two studies to assess the effects of firearm legislation on firearm-related injuries and deaths in U.S. children.
In their first study, they analyzed pediatric inpatient admissions for firearm injuries in 2012 relative to the stringency of state firearm legislation. They relied on five data sources for the analysis: the Kids’ Inpatient Database (KID), the Healthcare Cost and Utilization Project, the Agency for Healthcare Research and Quality, the U.S. Census Bureau, and the 2013 Brady scorecard.
The Brady scorecard provides scores for each state based on the presence and strictness of firearm-related laws, including legislation on background checks, ability of dangerous individuals to purchase guns, trafficking laws, and laws governing the sales, carrying, and purchasing of firearms.
The 10 states with the strictest laws (highest Brady scores) are California, Connecticut, Delaware, Hawaii, Illinois, Maryland, Massachusetts, New Jersey, New York, and Rhode Island. The 10 states with the lowest scores (least-strict legislation) are Alaska, Arizona, Arkansas, Florida, Kentucky, Louisiana, Montana, Nevada, Virginia, and Wyoming.
Among the 6,941 youth (aged 0-20 years) hospitalized in 2012 for firearm injuries, 7% died. More than a third of these (36%) occurred in the South, 25% in the Midwest, 22% in the West, and 17% in the Northeast.
Children most likely to be injured were boys, older children, black and Latino children, and children living in low-income zip codes.
The Midwest and South, which have lower average Brady scores (more lax legislation on guns), had 8.30 injuries per 100,000 children, compared with 7.54 injuries per 100,000 children in the Northeast and West, which have higher average Brady scores (more stringent gun laws). This was a difference of 0.76 injuries per 100,000 children (95% confidence interval, 0.38-1.13; P less than 0.001).
Then the researchers conducted a second analysis that looked specifically at firearm mortality within the context of both child access prevention (CAP) laws and states’ Brady scores. CAP laws include safe storage laws and gun lock laws, for example.
This analysis used the Web-Based Injury Statistics Query and Reporting System to capture pediatric firearm deaths from 2014-2015 and compared these to the 2014 Brady scores and CAP laws.
An estimated 2,715 child gun deaths occurred during the study period, of which 62% were homicides and 31% were suicides. The researchers identified “a significant negative correlation between states’ firearm legislation stringency and pediatric firearm mortality (Spearman correlation coefficient = –0.66) and between presence of CAP laws and firearm suicide rates (Spearman correlation coefficient = –0.56).”
Dr. Taylor said in an interview, “states that have both types of child access prevention laws [had] suicide rates four times lower than states that did not have either of those.”
Positive correlations also showed up between unemployment rate and firearm homicide rate (Spearman correlation coefficient = 0.55) and teen tobacco use and firearm suicide rate (Spearman correlation coefficient = 0.50).
The association between Brady scores and pediatric mortality from firearms remained significant after adjustment for poverty, unemployment, and substance abuse (P less than .01). Similarly, the association between the pediatric firearm suicide rate and CAP laws remained significant after controlling for socioeconomic factors and other firearm legislation (P less than .01).
In a video interview, Dr. Taylor discussed his research findings and their importance in clinical practice.
“It’s absolutely important for pediatricians to talk to families about firearms in their home and also in the homes of their friends that they visit,” Dr. Taylor said. “We try to approach it as a public health issue similar to seat belts and car seats.”
No external funding was used, and Dr. Taylor reported no conflicts of interest.
ORLANDO – and laws restricting children’s access to firearms are linked to reduced pediatric firearm suicide rates, according to research.
“State-level legislation could play an important role in reducing pediatric firearm-related deaths,” concluded Jordan S. Taylor, MD, of Stanford (Calif.) University and his colleagues.
Dr. Taylor earned top honors among the American Academy of Pediatrics (AAP) Council on Injury, Violence and Poison Prevention research abstracts when he presented his findings at the annual meeting of the American Academy of Pediatrics.
Firearm injuries account for the second leading cause of death among U.S. children: 3,155 youth ages 19 years and younger died from gunshot injuries in 2016, and more than 17,000 were injured. Yet state laws governing the purchase, ownership, carriage, and storage of guns vary widely across the country. Dr. Taylor and his colleagues conducted two studies to assess the effects of firearm legislation on firearm-related injuries and deaths in U.S. children.
In their first study, they analyzed pediatric inpatient admissions for firearm injuries in 2012 relative to the stringency of state firearm legislation. They relied on five data sources for the analysis: the Kids’ Inpatient Database (KID), the Healthcare Cost and Utilization Project, the Agency for Healthcare Research and Quality, the U.S. Census Bureau, and the 2013 Brady scorecard.
The Brady scorecard provides scores for each state based on the presence and strictness of firearm-related laws, including legislation on background checks, ability of dangerous individuals to purchase guns, trafficking laws, and laws governing the sales, carrying, and purchasing of firearms.
The 10 states with the strictest laws (highest Brady scores) are California, Connecticut, Delaware, Hawaii, Illinois, Maryland, Massachusetts, New Jersey, New York, and Rhode Island. The 10 states with the lowest scores (least-strict legislation) are Alaska, Arizona, Arkansas, Florida, Kentucky, Louisiana, Montana, Nevada, Virginia, and Wyoming.
Among the 6,941 youth (aged 0-20 years) hospitalized in 2012 for firearm injuries, 7% died. More than a third of these (36%) occurred in the South, 25% in the Midwest, 22% in the West, and 17% in the Northeast.
Children most likely to be injured were boys, older children, black and Latino children, and children living in low-income zip codes.
The Midwest and South, which have lower average Brady scores (more lax legislation on guns), had 8.30 injuries per 100,000 children, compared with 7.54 injuries per 100,000 children in the Northeast and West, which have higher average Brady scores (more stringent gun laws). This was a difference of 0.76 injuries per 100,000 children (95% confidence interval, 0.38-1.13; P less than 0.001).
Then the researchers conducted a second analysis that looked specifically at firearm mortality within the context of both child access prevention (CAP) laws and states’ Brady scores. CAP laws include safe storage laws and gun lock laws, for example.
This analysis used the Web-Based Injury Statistics Query and Reporting System to capture pediatric firearm deaths from 2014-2015 and compared these to the 2014 Brady scores and CAP laws.
An estimated 2,715 child gun deaths occurred during the study period, of which 62% were homicides and 31% were suicides. The researchers identified “a significant negative correlation between states’ firearm legislation stringency and pediatric firearm mortality (Spearman correlation coefficient = –0.66) and between presence of CAP laws and firearm suicide rates (Spearman correlation coefficient = –0.56).”
Dr. Taylor said in an interview, “states that have both types of child access prevention laws [had] suicide rates four times lower than states that did not have either of those.”
Positive correlations also showed up between unemployment rate and firearm homicide rate (Spearman correlation coefficient = 0.55) and teen tobacco use and firearm suicide rate (Spearman correlation coefficient = 0.50).
The association between Brady scores and pediatric mortality from firearms remained significant after adjustment for poverty, unemployment, and substance abuse (P less than .01). Similarly, the association between the pediatric firearm suicide rate and CAP laws remained significant after controlling for socioeconomic factors and other firearm legislation (P less than .01).
In a video interview, Dr. Taylor discussed his research findings and their importance in clinical practice.
“It’s absolutely important for pediatricians to talk to families about firearms in their home and also in the homes of their friends that they visit,” Dr. Taylor said. “We try to approach it as a public health issue similar to seat belts and car seats.”
No external funding was used, and Dr. Taylor reported no conflicts of interest.
REPORTING FROM AAP 2018
Key clinical point: Stricter state firearm legislation was associated with reduced firearm-related pediatric mortality.
Major finding: 8.3 injuries per 100,000 children occurred in the Midwest and South, compared with 7.5 injuries per 100,000 children in the Northeast and West.
Study details: The findings are based on two separate analyses that analyzed state Brady scores along with 6,941 firearm-related hospitalizations in 2012 and 2,715 pediatric deaths from firearms in 2014-2015.
Disclosures: No external funding was used, and Dr. Taylor reported no conflicts of interest.
Sofa and bed injuries very common among young children
ORLANDO – Injuries related to beds and sofas in children aged under 5 years occur more than twice as frequently than injuries related to stairs, according to new research.
“Findings from our analysis reveal that it is an important source of injury to young children and a leading cause of trauma to infants,” concluded David S. Liu, of Baylor College of Medicine, Houston, who presented the findings at the annual meeting of the American Academy of Pediatrics.
“The rate of bed- and sofa-related injuries is increasing, which underscores the need for increased prevention efforts, including parental education and improved safety design, to decrease soft furniture injuries among young children,” Mr. Liu and his colleagues wrote.
The researchers used the National Electronic Injury Surveillance System of the U.S. Consumer Product Safety Commission to conduct a retrospective analysis of injuries related to sofas and beds from 2007 to 2016.
They found that an estimated 2.3 million children aged under 5 years were treated for injuries related to soft furniture during those years, an average of 230,026 injuries a year, or 115 injuries per 10,000 children. To the surprise of the researchers, injuries related to beds and sofas were the most common types of accidental injury in that age group, occurring 2.5 times more often than stair-related injuries, which occurred at a rate of 47 per 10,000 population.
Boys were slightly more likely to be injured, making up 56% of all the cases. Soft tissue/internal organ injuries were most common, comprising 28% of all injuries, followed by lacerations in 24% of cases, abrasions in 15%, and fractures in 14%.
More than half the children (61%) sustained injuries to the head or face, and 3% were hospitalized for their injuries. Although infants (under 1 year old) only accounted for 28% of children injured, they were twice as likely to be hospitalized than older children.
The researchers also identified increases in injuries over the time period studied. Bed-related injuries increased 17% from 2007 to 2016, and sofa/couch-related injuries increased 17% during that period.
Although the vast majority of children were treated and released, approximately 4% of children were admitted or treated and transferred to another facility. Overall, an estimated 3,361 children died during the 9-year period, translating to a little over 370 children a year.
In a video interview, Mr. Liu discussed the implications of these findings.
“We know how dangerous car accidents and staircases are, and we often recommend car seats and stair gates for those,” Mr. Liu said. “Obviously we can’t put a gate or a barrier on every single sofa, couch, and bed in America, so as clinicians and parents, the best we can do is keep aware of how dangerous these items are. Just because of their soft nature doesn’t mean they’re inherently safer.”
The researchers reported no disclosures and the research received no external funding.
ORLANDO – Injuries related to beds and sofas in children aged under 5 years occur more than twice as frequently than injuries related to stairs, according to new research.
“Findings from our analysis reveal that it is an important source of injury to young children and a leading cause of trauma to infants,” concluded David S. Liu, of Baylor College of Medicine, Houston, who presented the findings at the annual meeting of the American Academy of Pediatrics.
“The rate of bed- and sofa-related injuries is increasing, which underscores the need for increased prevention efforts, including parental education and improved safety design, to decrease soft furniture injuries among young children,” Mr. Liu and his colleagues wrote.
The researchers used the National Electronic Injury Surveillance System of the U.S. Consumer Product Safety Commission to conduct a retrospective analysis of injuries related to sofas and beds from 2007 to 2016.
They found that an estimated 2.3 million children aged under 5 years were treated for injuries related to soft furniture during those years, an average of 230,026 injuries a year, or 115 injuries per 10,000 children. To the surprise of the researchers, injuries related to beds and sofas were the most common types of accidental injury in that age group, occurring 2.5 times more often than stair-related injuries, which occurred at a rate of 47 per 10,000 population.
Boys were slightly more likely to be injured, making up 56% of all the cases. Soft tissue/internal organ injuries were most common, comprising 28% of all injuries, followed by lacerations in 24% of cases, abrasions in 15%, and fractures in 14%.
More than half the children (61%) sustained injuries to the head or face, and 3% were hospitalized for their injuries. Although infants (under 1 year old) only accounted for 28% of children injured, they were twice as likely to be hospitalized than older children.
The researchers also identified increases in injuries over the time period studied. Bed-related injuries increased 17% from 2007 to 2016, and sofa/couch-related injuries increased 17% during that period.
Although the vast majority of children were treated and released, approximately 4% of children were admitted or treated and transferred to another facility. Overall, an estimated 3,361 children died during the 9-year period, translating to a little over 370 children a year.
In a video interview, Mr. Liu discussed the implications of these findings.
“We know how dangerous car accidents and staircases are, and we often recommend car seats and stair gates for those,” Mr. Liu said. “Obviously we can’t put a gate or a barrier on every single sofa, couch, and bed in America, so as clinicians and parents, the best we can do is keep aware of how dangerous these items are. Just because of their soft nature doesn’t mean they’re inherently safer.”
The researchers reported no disclosures and the research received no external funding.
ORLANDO – Injuries related to beds and sofas in children aged under 5 years occur more than twice as frequently than injuries related to stairs, according to new research.
“Findings from our analysis reveal that it is an important source of injury to young children and a leading cause of trauma to infants,” concluded David S. Liu, of Baylor College of Medicine, Houston, who presented the findings at the annual meeting of the American Academy of Pediatrics.
“The rate of bed- and sofa-related injuries is increasing, which underscores the need for increased prevention efforts, including parental education and improved safety design, to decrease soft furniture injuries among young children,” Mr. Liu and his colleagues wrote.
The researchers used the National Electronic Injury Surveillance System of the U.S. Consumer Product Safety Commission to conduct a retrospective analysis of injuries related to sofas and beds from 2007 to 2016.
They found that an estimated 2.3 million children aged under 5 years were treated for injuries related to soft furniture during those years, an average of 230,026 injuries a year, or 115 injuries per 10,000 children. To the surprise of the researchers, injuries related to beds and sofas were the most common types of accidental injury in that age group, occurring 2.5 times more often than stair-related injuries, which occurred at a rate of 47 per 10,000 population.
Boys were slightly more likely to be injured, making up 56% of all the cases. Soft tissue/internal organ injuries were most common, comprising 28% of all injuries, followed by lacerations in 24% of cases, abrasions in 15%, and fractures in 14%.
More than half the children (61%) sustained injuries to the head or face, and 3% were hospitalized for their injuries. Although infants (under 1 year old) only accounted for 28% of children injured, they were twice as likely to be hospitalized than older children.
The researchers also identified increases in injuries over the time period studied. Bed-related injuries increased 17% from 2007 to 2016, and sofa/couch-related injuries increased 17% during that period.
Although the vast majority of children were treated and released, approximately 4% of children were admitted or treated and transferred to another facility. Overall, an estimated 3,361 children died during the 9-year period, translating to a little over 370 children a year.
In a video interview, Mr. Liu discussed the implications of these findings.
“We know how dangerous car accidents and staircases are, and we often recommend car seats and stair gates for those,” Mr. Liu said. “Obviously we can’t put a gate or a barrier on every single sofa, couch, and bed in America, so as clinicians and parents, the best we can do is keep aware of how dangerous these items are. Just because of their soft nature doesn’t mean they’re inherently safer.”
The researchers reported no disclosures and the research received no external funding.
REPORTING FROM AAP 2018
Key clinical point: Injuries from beds and sofas/couches are common in children aged under 5 years, occurring 2.5 times more frequently than stairs-related injuries.
Major finding: An estimated 115 bed/sofa-related injuries per 10,000 children occur every year.
Study details: The findings are based on a retrospective analysis of injuries related to sofas and beds from 2007 to 2016.
Disclosures: The researchers reported no disclosures and the research received no external funding.
AAP speaker emphasizes importance of understanding patients’ ‘lived experience’
ORLANDO – Pediatricians who learn about their patients’ lived experience have the potential to encourage patients and help them overcome biases, assumptions, and barriers of opioid use disorder, Tamela Milan said at the American Academy of Pediatrics annual meeting.
After her five children were taken into state welfare custody and she began a sixth pregnancy while struggling with opioid use disorder and as a survivor of domestic violence, Ms. Milan’s pediatrician was the one to encourage her to take steps to improve her life. She went on to regain custody of her children and complete college, and has given back by working in community health programs for over 20 years.
In a video interview, Ms. Milan said she would not have been able to overcome these barriers had it not been for the support of her pediatrician, who saw her as a person instead of a mother with opioid use disorder.
“I’ve been on both sides of the fence,” Ms. Milan said. “As someone who’s had to receive treatment and to provide it, it’s really important that we start looking at people for who they are and where they are.”
Tamela Milan has no relevant conflicts of interest.
ORLANDO – Pediatricians who learn about their patients’ lived experience have the potential to encourage patients and help them overcome biases, assumptions, and barriers of opioid use disorder, Tamela Milan said at the American Academy of Pediatrics annual meeting.
After her five children were taken into state welfare custody and she began a sixth pregnancy while struggling with opioid use disorder and as a survivor of domestic violence, Ms. Milan’s pediatrician was the one to encourage her to take steps to improve her life. She went on to regain custody of her children and complete college, and has given back by working in community health programs for over 20 years.
In a video interview, Ms. Milan said she would not have been able to overcome these barriers had it not been for the support of her pediatrician, who saw her as a person instead of a mother with opioid use disorder.
“I’ve been on both sides of the fence,” Ms. Milan said. “As someone who’s had to receive treatment and to provide it, it’s really important that we start looking at people for who they are and where they are.”
Tamela Milan has no relevant conflicts of interest.
ORLANDO – Pediatricians who learn about their patients’ lived experience have the potential to encourage patients and help them overcome biases, assumptions, and barriers of opioid use disorder, Tamela Milan said at the American Academy of Pediatrics annual meeting.
After her five children were taken into state welfare custody and she began a sixth pregnancy while struggling with opioid use disorder and as a survivor of domestic violence, Ms. Milan’s pediatrician was the one to encourage her to take steps to improve her life. She went on to regain custody of her children and complete college, and has given back by working in community health programs for over 20 years.
In a video interview, Ms. Milan said she would not have been able to overcome these barriers had it not been for the support of her pediatrician, who saw her as a person instead of a mother with opioid use disorder.
“I’ve been on both sides of the fence,” Ms. Milan said. “As someone who’s had to receive treatment and to provide it, it’s really important that we start looking at people for who they are and where they are.”
Tamela Milan has no relevant conflicts of interest.
REPORTING FROM AAP 2018
A paradigm shift in medical research is necessary
ORLANDO – What doctors think they know to be true in medicine has changed dramatically in the past several decades and will be different again in the decades to come, leaving them with a dilemma, according to Kevin T. Powell, MD, PhD, a pediatric hospitalist in St. Louis. If half of what doctors teach or know in medicine today will ultimately end up not being true, how do they know what to believe or accept?
While there is not a single satisfactory answer to that question, researchers can select research that gets doctors closer to reliable findings and steer them away from the barrage of poor-quality research that emerges from the current publish-or-perish system, Dr. Powell told his colleagues at the annual meeting of the American Academy of Pediatrics.
During his talk, Dr. Powell discussed the challenges and flaws with medical research as it is currently conducted, citing Doug Altman’s writings on these problems as early as 1994.
“The poor quality of much medical research is widely acknowledged, yet disturbingly the leaders of the medical profession seem only minimally concerned about the problem and make no apparent effort to find a solution,” wrote Mr. Altman, an English medical statistician (BMJ. 1994;308:283).
“We need less research, better research, and research done for the right reasons,” Mr. Altman concluded. “Abandoning using the number of publications as a measure of ability would be a start.”
In an interview, Dr. Powell described an unfortunate consequence of the publish-or-perish pressure in academic medicine: A glut of short-term, small studies with little clinical utility that researchers can complete in 1 or 2 years rather than the large, multicenter studies that take several years – and produce higher-quality findings – but cannot be turned into as many publications.
“We’re generating a lot of medical research findings that end up being false,” he said. “It’s a random walk in terms of getting to the truth rather than having an accurate process of getting to truth through evidence-based medicine.”
But he was hopeful, not cynical, about the way forward. By persuading people that medical research has changed for the worse over time and can change into something better, Dr. Powell saw potential for future research resulting in the same sort of public health achievements that research produced in the past, such as big reductions in smoking or sudden infant death syndrome.
Dr. Powell concluded his talk with a riff on Martin Luther’s 95 Theses, the 9.5 Theses, for a reformation of evidence-based medicine that together address the various shortcomings he discussed.
1. Recognize academic promotion as a bias, just like drug money.
2. Don’t confound statistically significant and clinically significant.
3. Use only significant figures.
4. Use the phrase “we did not DETECT a difference” and include power calculations.
5. Use confidence intervals instead of P values.
6. Use number needed to harm and number needed to treat instead of relative risk.
7. Absence of proof is not proof of absence. When there is insufficient randomized, controlled trial evidence, have an independent party estimate an effect based on non-RCT articles.
8. Any article implying clinical practice should change must include a counterpoint and a benefit cost analysis. Consider both effectiveness and safety.
9. Use postmarketing peer review.
9.5. Beware of research based on surveys.
Dr. Powell reported no relevant financial disclosures.
ORLANDO – What doctors think they know to be true in medicine has changed dramatically in the past several decades and will be different again in the decades to come, leaving them with a dilemma, according to Kevin T. Powell, MD, PhD, a pediatric hospitalist in St. Louis. If half of what doctors teach or know in medicine today will ultimately end up not being true, how do they know what to believe or accept?
While there is not a single satisfactory answer to that question, researchers can select research that gets doctors closer to reliable findings and steer them away from the barrage of poor-quality research that emerges from the current publish-or-perish system, Dr. Powell told his colleagues at the annual meeting of the American Academy of Pediatrics.
During his talk, Dr. Powell discussed the challenges and flaws with medical research as it is currently conducted, citing Doug Altman’s writings on these problems as early as 1994.
“The poor quality of much medical research is widely acknowledged, yet disturbingly the leaders of the medical profession seem only minimally concerned about the problem and make no apparent effort to find a solution,” wrote Mr. Altman, an English medical statistician (BMJ. 1994;308:283).
“We need less research, better research, and research done for the right reasons,” Mr. Altman concluded. “Abandoning using the number of publications as a measure of ability would be a start.”
In an interview, Dr. Powell described an unfortunate consequence of the publish-or-perish pressure in academic medicine: A glut of short-term, small studies with little clinical utility that researchers can complete in 1 or 2 years rather than the large, multicenter studies that take several years – and produce higher-quality findings – but cannot be turned into as many publications.
“We’re generating a lot of medical research findings that end up being false,” he said. “It’s a random walk in terms of getting to the truth rather than having an accurate process of getting to truth through evidence-based medicine.”
But he was hopeful, not cynical, about the way forward. By persuading people that medical research has changed for the worse over time and can change into something better, Dr. Powell saw potential for future research resulting in the same sort of public health achievements that research produced in the past, such as big reductions in smoking or sudden infant death syndrome.
Dr. Powell concluded his talk with a riff on Martin Luther’s 95 Theses, the 9.5 Theses, for a reformation of evidence-based medicine that together address the various shortcomings he discussed.
1. Recognize academic promotion as a bias, just like drug money.
2. Don’t confound statistically significant and clinically significant.
3. Use only significant figures.
4. Use the phrase “we did not DETECT a difference” and include power calculations.
5. Use confidence intervals instead of P values.
6. Use number needed to harm and number needed to treat instead of relative risk.
7. Absence of proof is not proof of absence. When there is insufficient randomized, controlled trial evidence, have an independent party estimate an effect based on non-RCT articles.
8. Any article implying clinical practice should change must include a counterpoint and a benefit cost analysis. Consider both effectiveness and safety.
9. Use postmarketing peer review.
9.5. Beware of research based on surveys.
Dr. Powell reported no relevant financial disclosures.
ORLANDO – What doctors think they know to be true in medicine has changed dramatically in the past several decades and will be different again in the decades to come, leaving them with a dilemma, according to Kevin T. Powell, MD, PhD, a pediatric hospitalist in St. Louis. If half of what doctors teach or know in medicine today will ultimately end up not being true, how do they know what to believe or accept?
While there is not a single satisfactory answer to that question, researchers can select research that gets doctors closer to reliable findings and steer them away from the barrage of poor-quality research that emerges from the current publish-or-perish system, Dr. Powell told his colleagues at the annual meeting of the American Academy of Pediatrics.
During his talk, Dr. Powell discussed the challenges and flaws with medical research as it is currently conducted, citing Doug Altman’s writings on these problems as early as 1994.
“The poor quality of much medical research is widely acknowledged, yet disturbingly the leaders of the medical profession seem only minimally concerned about the problem and make no apparent effort to find a solution,” wrote Mr. Altman, an English medical statistician (BMJ. 1994;308:283).
“We need less research, better research, and research done for the right reasons,” Mr. Altman concluded. “Abandoning using the number of publications as a measure of ability would be a start.”
In an interview, Dr. Powell described an unfortunate consequence of the publish-or-perish pressure in academic medicine: A glut of short-term, small studies with little clinical utility that researchers can complete in 1 or 2 years rather than the large, multicenter studies that take several years – and produce higher-quality findings – but cannot be turned into as many publications.
“We’re generating a lot of medical research findings that end up being false,” he said. “It’s a random walk in terms of getting to the truth rather than having an accurate process of getting to truth through evidence-based medicine.”
But he was hopeful, not cynical, about the way forward. By persuading people that medical research has changed for the worse over time and can change into something better, Dr. Powell saw potential for future research resulting in the same sort of public health achievements that research produced in the past, such as big reductions in smoking or sudden infant death syndrome.
Dr. Powell concluded his talk with a riff on Martin Luther’s 95 Theses, the 9.5 Theses, for a reformation of evidence-based medicine that together address the various shortcomings he discussed.
1. Recognize academic promotion as a bias, just like drug money.
2. Don’t confound statistically significant and clinically significant.
3. Use only significant figures.
4. Use the phrase “we did not DETECT a difference” and include power calculations.
5. Use confidence intervals instead of P values.
6. Use number needed to harm and number needed to treat instead of relative risk.
7. Absence of proof is not proof of absence. When there is insufficient randomized, controlled trial evidence, have an independent party estimate an effect based on non-RCT articles.
8. Any article implying clinical practice should change must include a counterpoint and a benefit cost analysis. Consider both effectiveness and safety.
9. Use postmarketing peer review.
9.5. Beware of research based on surveys.
Dr. Powell reported no relevant financial disclosures.
EXPERT ANALYSIS FROM AAP 18
Sandy Hook Promise: Four programs help people recognize signs of a threat
ORLANDO – “The caretaker of all living things” – that was the good-natured moniker 7-year-old Daniel Barden had earned from his family – according to his dad, Mark Barden. Daniel would pick up black ants and take them outside “to be with their families,” even when the ant bit his fingers.
A walk down the sidewalk after a rain would take three times longer than it should because Daniel stopped to pick up every worm on the pavement and put it in the grass, lest it dry out in the sun, Mr. Barden said with a chuckle at the annual meeting of the American Academy of Pediatrics.
Daniel was his youngest and full of pure joy, Mr. Barden said, but that ended with his son’s murder during the Sandy Hook Elementary mass shooting Dec. 14, 2012. To honor his son and work to reduce the likelihood of similar mass shootings, Mr. Barden, now the managing director of Sandy Hook Promise in Newtown, Conn., shared with the pediatrician audience the work of the organization formed by Sandy Hook parents to attempt to prevent gun violence before it happens.
“We’re moms and dads and a couple of families who have lost loved ones in that tragedy, and we are growing as an organization,” Mr. Barden said. “Our basic, most fundamental objective is to prevent other families from living with the pain I will live with for the rest of my life.”
Their mission involves “creating a culture engaged and committed to identifying, intervening, and getting help for individuals who may be at risk of hurting themselves or others,” Mr. Barden said.
Sandy Hook Promise accomplishes this goal by educating and empowering communities through their four programs: Start with Hello, SOS Suicide Prevention Program, SaySomething, and Safety Assessment & Intervention. The organization delivers these programs through multiple platforms, including national and local trainers, digital curriculum downloads, interactive online training videos, and using multilingual presenters and English and Spanish materials.
The organization also especially works with schools and student’s clubs to change their culture and feel empowered to speak up and do their part to prevent gun violence too.
These programs resulted from extensive qualitative and quantitative research that Sandy Hook Promise conducted after the shooting with academic researchers, law enforcement, educators, school administrators, mental health professionals, and social movement experts.
“As we see these stories play themselves out over and over again, we start to reveal the story of somebody who didn’t just snap overnight,” Mr. Barden said. Signs that a person may be at risk for committing mass violence include suicidality, preoccupation with weapons, talking about committing violent acts, and general signs of depression and anxiety. “If we can train people how to not only recognize but to look for those signs, we can make a sustainable difference,” he said.
Most mass shootings are planned at least 6 months in advance, he said. About 80% of school shooters tell someone about their plans, and 69% tell multiple people. Similarly, up to 70% of people who die by suicide tell someone they plan to do it or give some other warning sign.
Further, more than a third of violent threats and bullying occurs electronically, so students are well equipped to watch for the signs and report them if they know how and feel comfortable doing so.
Mr. Barden outlined the goals of each of the four Sandy Hook Promise programs.
Start With Hello
This program “teaches youth how to identify and minimize social isolation, marginalization, and rejection in order to create an inclusive, connected community,” Mr. Barden explained. The goals of the program are to reduce bullying, foster socialization, increase engagement, and change a culture from within.
SOS Signs of Suicide
This is Sandy Hook Promise’s newest program and is built on a program developed by the Federal Bureau of Investigation following the Virginia Tech shooting and adapted for school-based applications.
“It also develops a multidisciplinary team within the school who acts as various touch points who know how to recognize a potential warning sign and then triage that information and take steps to get to the root cause of that behavior and not just bandage the wound,” Mr. Barden explained.
SaySomething
The organization’s flagship program does the most to recruit student involvement in recognizing the signs of a potential threat, particularly in social media, and report the individual and their behavior to a trusted adult or through Sandy Hook Promise’s Anonymous Reporting System.
“The kids take this one, and they run with it and do amazing things with it,” Mr. Barden said, noting that it particularly helps students recognize warning signs on social media. “We have growing evidence of kids following this model, and we’ve already prevented mass shootings and numerous suicides with this.”
Safety Assessment & Intervention (SAI) program
This program “trains a multidisciplinary team how to identify, assess, and respond to threats and observed at-risk behaviors,” Mr. Barden said. SAI aims to create a safer, more open school environment with less violence, bullying, and threats. That includes reducing educators’ fear and anxiety, and leading students to have a more positive view of teachers and staff.
Students can report tips to the Anonymous Reporting System through the website, calling the hot line or via a free mobile app. Regardless of the method, the anonymous tips go to a 24/7 multilingual crisis center and, if needed, law enforcement. The crisis center contacts the appropriate school official via text, email, or a phone call, and the case is tracked in real time until it’s addressed, resolved, and closed.
All of these programs are freely available to any school or institution who wants to use them, Mr. Barden said, because the organization does not want cost to get in the way of any school or community that is taking advantage of tools to reduce the risk of violence.
In fact, more than 3.5 million youth and adults in more than 7,000 schools in every state have been trained in these programs, helping hundreds of youth access mental health and wellness help, he said. The program has reduced truancy, bullying, and other forms of violence and victimization, and it has intervened in multiple school shooting plans across the United States.
Mr. Barden wrapped up his address with his gratitude for pediatricians’ willingness to be partners in reducing gun violence.
“I want to tell you how much it means to me that you took the time to come here and listen to my story and the work I’m doing,” he said, “and how proud I am to be able to share it with you, and how proud I am to be able to honor that little kid who truly was the caretaker of all living things and to continue that spirit in his honor and in his absence.”
ORLANDO – “The caretaker of all living things” – that was the good-natured moniker 7-year-old Daniel Barden had earned from his family – according to his dad, Mark Barden. Daniel would pick up black ants and take them outside “to be with their families,” even when the ant bit his fingers.
A walk down the sidewalk after a rain would take three times longer than it should because Daniel stopped to pick up every worm on the pavement and put it in the grass, lest it dry out in the sun, Mr. Barden said with a chuckle at the annual meeting of the American Academy of Pediatrics.
Daniel was his youngest and full of pure joy, Mr. Barden said, but that ended with his son’s murder during the Sandy Hook Elementary mass shooting Dec. 14, 2012. To honor his son and work to reduce the likelihood of similar mass shootings, Mr. Barden, now the managing director of Sandy Hook Promise in Newtown, Conn., shared with the pediatrician audience the work of the organization formed by Sandy Hook parents to attempt to prevent gun violence before it happens.
“We’re moms and dads and a couple of families who have lost loved ones in that tragedy, and we are growing as an organization,” Mr. Barden said. “Our basic, most fundamental objective is to prevent other families from living with the pain I will live with for the rest of my life.”
Their mission involves “creating a culture engaged and committed to identifying, intervening, and getting help for individuals who may be at risk of hurting themselves or others,” Mr. Barden said.
Sandy Hook Promise accomplishes this goal by educating and empowering communities through their four programs: Start with Hello, SOS Suicide Prevention Program, SaySomething, and Safety Assessment & Intervention. The organization delivers these programs through multiple platforms, including national and local trainers, digital curriculum downloads, interactive online training videos, and using multilingual presenters and English and Spanish materials.
The organization also especially works with schools and student’s clubs to change their culture and feel empowered to speak up and do their part to prevent gun violence too.
These programs resulted from extensive qualitative and quantitative research that Sandy Hook Promise conducted after the shooting with academic researchers, law enforcement, educators, school administrators, mental health professionals, and social movement experts.
“As we see these stories play themselves out over and over again, we start to reveal the story of somebody who didn’t just snap overnight,” Mr. Barden said. Signs that a person may be at risk for committing mass violence include suicidality, preoccupation with weapons, talking about committing violent acts, and general signs of depression and anxiety. “If we can train people how to not only recognize but to look for those signs, we can make a sustainable difference,” he said.
Most mass shootings are planned at least 6 months in advance, he said. About 80% of school shooters tell someone about their plans, and 69% tell multiple people. Similarly, up to 70% of people who die by suicide tell someone they plan to do it or give some other warning sign.
Further, more than a third of violent threats and bullying occurs electronically, so students are well equipped to watch for the signs and report them if they know how and feel comfortable doing so.
Mr. Barden outlined the goals of each of the four Sandy Hook Promise programs.
Start With Hello
This program “teaches youth how to identify and minimize social isolation, marginalization, and rejection in order to create an inclusive, connected community,” Mr. Barden explained. The goals of the program are to reduce bullying, foster socialization, increase engagement, and change a culture from within.
SOS Signs of Suicide
This is Sandy Hook Promise’s newest program and is built on a program developed by the Federal Bureau of Investigation following the Virginia Tech shooting and adapted for school-based applications.
“It also develops a multidisciplinary team within the school who acts as various touch points who know how to recognize a potential warning sign and then triage that information and take steps to get to the root cause of that behavior and not just bandage the wound,” Mr. Barden explained.
SaySomething
The organization’s flagship program does the most to recruit student involvement in recognizing the signs of a potential threat, particularly in social media, and report the individual and their behavior to a trusted adult or through Sandy Hook Promise’s Anonymous Reporting System.
“The kids take this one, and they run with it and do amazing things with it,” Mr. Barden said, noting that it particularly helps students recognize warning signs on social media. “We have growing evidence of kids following this model, and we’ve already prevented mass shootings and numerous suicides with this.”
Safety Assessment & Intervention (SAI) program
This program “trains a multidisciplinary team how to identify, assess, and respond to threats and observed at-risk behaviors,” Mr. Barden said. SAI aims to create a safer, more open school environment with less violence, bullying, and threats. That includes reducing educators’ fear and anxiety, and leading students to have a more positive view of teachers and staff.
Students can report tips to the Anonymous Reporting System through the website, calling the hot line or via a free mobile app. Regardless of the method, the anonymous tips go to a 24/7 multilingual crisis center and, if needed, law enforcement. The crisis center contacts the appropriate school official via text, email, or a phone call, and the case is tracked in real time until it’s addressed, resolved, and closed.
All of these programs are freely available to any school or institution who wants to use them, Mr. Barden said, because the organization does not want cost to get in the way of any school or community that is taking advantage of tools to reduce the risk of violence.
In fact, more than 3.5 million youth and adults in more than 7,000 schools in every state have been trained in these programs, helping hundreds of youth access mental health and wellness help, he said. The program has reduced truancy, bullying, and other forms of violence and victimization, and it has intervened in multiple school shooting plans across the United States.
Mr. Barden wrapped up his address with his gratitude for pediatricians’ willingness to be partners in reducing gun violence.
“I want to tell you how much it means to me that you took the time to come here and listen to my story and the work I’m doing,” he said, “and how proud I am to be able to share it with you, and how proud I am to be able to honor that little kid who truly was the caretaker of all living things and to continue that spirit in his honor and in his absence.”
ORLANDO – “The caretaker of all living things” – that was the good-natured moniker 7-year-old Daniel Barden had earned from his family – according to his dad, Mark Barden. Daniel would pick up black ants and take them outside “to be with their families,” even when the ant bit his fingers.
A walk down the sidewalk after a rain would take three times longer than it should because Daniel stopped to pick up every worm on the pavement and put it in the grass, lest it dry out in the sun, Mr. Barden said with a chuckle at the annual meeting of the American Academy of Pediatrics.
Daniel was his youngest and full of pure joy, Mr. Barden said, but that ended with his son’s murder during the Sandy Hook Elementary mass shooting Dec. 14, 2012. To honor his son and work to reduce the likelihood of similar mass shootings, Mr. Barden, now the managing director of Sandy Hook Promise in Newtown, Conn., shared with the pediatrician audience the work of the organization formed by Sandy Hook parents to attempt to prevent gun violence before it happens.
“We’re moms and dads and a couple of families who have lost loved ones in that tragedy, and we are growing as an organization,” Mr. Barden said. “Our basic, most fundamental objective is to prevent other families from living with the pain I will live with for the rest of my life.”
Their mission involves “creating a culture engaged and committed to identifying, intervening, and getting help for individuals who may be at risk of hurting themselves or others,” Mr. Barden said.
Sandy Hook Promise accomplishes this goal by educating and empowering communities through their four programs: Start with Hello, SOS Suicide Prevention Program, SaySomething, and Safety Assessment & Intervention. The organization delivers these programs through multiple platforms, including national and local trainers, digital curriculum downloads, interactive online training videos, and using multilingual presenters and English and Spanish materials.
The organization also especially works with schools and student’s clubs to change their culture and feel empowered to speak up and do their part to prevent gun violence too.
These programs resulted from extensive qualitative and quantitative research that Sandy Hook Promise conducted after the shooting with academic researchers, law enforcement, educators, school administrators, mental health professionals, and social movement experts.
“As we see these stories play themselves out over and over again, we start to reveal the story of somebody who didn’t just snap overnight,” Mr. Barden said. Signs that a person may be at risk for committing mass violence include suicidality, preoccupation with weapons, talking about committing violent acts, and general signs of depression and anxiety. “If we can train people how to not only recognize but to look for those signs, we can make a sustainable difference,” he said.
Most mass shootings are planned at least 6 months in advance, he said. About 80% of school shooters tell someone about their plans, and 69% tell multiple people. Similarly, up to 70% of people who die by suicide tell someone they plan to do it or give some other warning sign.
Further, more than a third of violent threats and bullying occurs electronically, so students are well equipped to watch for the signs and report them if they know how and feel comfortable doing so.
Mr. Barden outlined the goals of each of the four Sandy Hook Promise programs.
Start With Hello
This program “teaches youth how to identify and minimize social isolation, marginalization, and rejection in order to create an inclusive, connected community,” Mr. Barden explained. The goals of the program are to reduce bullying, foster socialization, increase engagement, and change a culture from within.
SOS Signs of Suicide
This is Sandy Hook Promise’s newest program and is built on a program developed by the Federal Bureau of Investigation following the Virginia Tech shooting and adapted for school-based applications.
“It also develops a multidisciplinary team within the school who acts as various touch points who know how to recognize a potential warning sign and then triage that information and take steps to get to the root cause of that behavior and not just bandage the wound,” Mr. Barden explained.
SaySomething
The organization’s flagship program does the most to recruit student involvement in recognizing the signs of a potential threat, particularly in social media, and report the individual and their behavior to a trusted adult or through Sandy Hook Promise’s Anonymous Reporting System.
“The kids take this one, and they run with it and do amazing things with it,” Mr. Barden said, noting that it particularly helps students recognize warning signs on social media. “We have growing evidence of kids following this model, and we’ve already prevented mass shootings and numerous suicides with this.”
Safety Assessment & Intervention (SAI) program
This program “trains a multidisciplinary team how to identify, assess, and respond to threats and observed at-risk behaviors,” Mr. Barden said. SAI aims to create a safer, more open school environment with less violence, bullying, and threats. That includes reducing educators’ fear and anxiety, and leading students to have a more positive view of teachers and staff.
Students can report tips to the Anonymous Reporting System through the website, calling the hot line or via a free mobile app. Regardless of the method, the anonymous tips go to a 24/7 multilingual crisis center and, if needed, law enforcement. The crisis center contacts the appropriate school official via text, email, or a phone call, and the case is tracked in real time until it’s addressed, resolved, and closed.
All of these programs are freely available to any school or institution who wants to use them, Mr. Barden said, because the organization does not want cost to get in the way of any school or community that is taking advantage of tools to reduce the risk of violence.
In fact, more than 3.5 million youth and adults in more than 7,000 schools in every state have been trained in these programs, helping hundreds of youth access mental health and wellness help, he said. The program has reduced truancy, bullying, and other forms of violence and victimization, and it has intervened in multiple school shooting plans across the United States.
Mr. Barden wrapped up his address with his gratitude for pediatricians’ willingness to be partners in reducing gun violence.
“I want to tell you how much it means to me that you took the time to come here and listen to my story and the work I’m doing,” he said, “and how proud I am to be able to share it with you, and how proud I am to be able to honor that little kid who truly was the caretaker of all living things and to continue that spirit in his honor and in his absence.”
EXPERT ANALYSIS FROM AAP 18
Assess ADHD at developmental age, rather than chronological
ORLANDO – said David O. Childers, MD, chief of the division of developmental pediatrics at the University of Florida in Jacksonville.
“That is a huge consideration, and the vast majority of pediatricians don’t understand that,” Dr. Childers said at the annual meeting of the American Academy of Pediatrics.
A diagnosis of ADHD in children should be reserved for situations in which the symptoms clearly interfere with how they function in social, academic, and occupational settings. ADHD should not be diagnosed in children who exhibit hostility, defiance, a failure to understand, or who have oppositional defiant disorder (ODD). In addition, ADHD in children often overlaps with other conditions, such as learning disabilities, ODD, anxiety, depression, poor self-esteem, conduct disorder, motor coordination problems, and encopresis and enuresis.
One mistake you can make is starting the medication too young in patients who exhibit symptoms of ADHD. Receptive language relative to developmental age should be taken into consideration when deciding whether to treat very young patients. “If the voice in your head is at a 3-year-old level, that’s going to be your behavior picture regardless of your chronological age,” Dr. Childers said.
You also can misdiagnose ADHD in young patients because you don’t recognize behavioral phenotypes and diagnoses that are similar to ADHD. Extreme prematurity, global developmental delay, fetal alcohol syndrome, spina bifida, genetic syndrome, intellectual and learning disabilities, closed head injuries, and depression all can mimic ADHD symptoms. “Everything that wheezes is not asthma, and everything that is ‘hyper’ or ‘drifty’ is not ADHD,” he noted.
Another mistake is considering mixed amphetamine salts (MAS) the same as methylphenidate (MPH), Dr. Childers said. MAS has 5 mg of active isomer versus 2.5 mg in MPH doses, and patients could see side effects from the increased potency in MAS in the form of appetite suppression and tics. You should start with a low dose of the medication and titrate up until patients get the most out of the medication to avoid situations in which patients report a change in personality or that the treatment is not effective.
“The medicine should never change a kid’s personality,” Dr. Childers said. “We are not here to treat the kid to the point of hyperactivity management; we’re here to treat for attention.”
In cases where patients ask for the short-acting medication rather than long-acting stimulant, remember that short-acting medication for ADHD has a higher potential for abuse. “Medication diversion is real. It does occur,” he said.
Establishing a basal sleep history and whether the child has insomnia is important before prescribing ADHD medication. Dr. Childers noted he uses a short-acting stimulant as an off-label treatment to treat some of his patients with insomnia, but he said to be aware of side effects like headache, abdominal pain, anorexia, and tics, as well as cardiac issues.
You also should rethink your diagnosis if the medication is not having an effect after two trials of a stimulant, Dr. Childers noted, and when a child has conditions like anxiety and depression that can mimic ADHD symptoms, a stimulant will increase irritability and have a paradoxical response to the medication. Inattentive ADHD can be missed in adolescent patients who struggle academically until they fall behind their peers, which can result in developing depression that complicates treatment, he said.
A learning disorder also can be mistaken for ADHD in children and presents in different ways depending on what grade the child is in. As a child ages and learns how to read, he or she will begin to fall behind as learning through reading becomes more complex. Learning disorders should be ruled out before treating for ADHD because, if the child improves after taking a stimulant, it could be more difficult to find a diagnosis of learning disorder later, Dr. Childers noted.
Bipolar disorder can be overdiagnosed in children; in these patients, the most likely diagnoses are ADHD and ODD, he said. According to a 2004 National Alliance of Mental Illness fact sheet, approximately 7% of patients in caseloads for federally funded studies in psychiatric facilities met the criteria for bipolar disorder, but the lifelong prevalence of the disease is between 1% and 1.6%.
“Bipolar disorder is frequently oppositional defiant disorder, and the word ‘no’ can be a trigger,” Dr. Childers said.
Dr. Childers reported no relevant conflicts of interest.
ORLANDO – said David O. Childers, MD, chief of the division of developmental pediatrics at the University of Florida in Jacksonville.
“That is a huge consideration, and the vast majority of pediatricians don’t understand that,” Dr. Childers said at the annual meeting of the American Academy of Pediatrics.
A diagnosis of ADHD in children should be reserved for situations in which the symptoms clearly interfere with how they function in social, academic, and occupational settings. ADHD should not be diagnosed in children who exhibit hostility, defiance, a failure to understand, or who have oppositional defiant disorder (ODD). In addition, ADHD in children often overlaps with other conditions, such as learning disabilities, ODD, anxiety, depression, poor self-esteem, conduct disorder, motor coordination problems, and encopresis and enuresis.
One mistake you can make is starting the medication too young in patients who exhibit symptoms of ADHD. Receptive language relative to developmental age should be taken into consideration when deciding whether to treat very young patients. “If the voice in your head is at a 3-year-old level, that’s going to be your behavior picture regardless of your chronological age,” Dr. Childers said.
You also can misdiagnose ADHD in young patients because you don’t recognize behavioral phenotypes and diagnoses that are similar to ADHD. Extreme prematurity, global developmental delay, fetal alcohol syndrome, spina bifida, genetic syndrome, intellectual and learning disabilities, closed head injuries, and depression all can mimic ADHD symptoms. “Everything that wheezes is not asthma, and everything that is ‘hyper’ or ‘drifty’ is not ADHD,” he noted.
Another mistake is considering mixed amphetamine salts (MAS) the same as methylphenidate (MPH), Dr. Childers said. MAS has 5 mg of active isomer versus 2.5 mg in MPH doses, and patients could see side effects from the increased potency in MAS in the form of appetite suppression and tics. You should start with a low dose of the medication and titrate up until patients get the most out of the medication to avoid situations in which patients report a change in personality or that the treatment is not effective.
“The medicine should never change a kid’s personality,” Dr. Childers said. “We are not here to treat the kid to the point of hyperactivity management; we’re here to treat for attention.”
In cases where patients ask for the short-acting medication rather than long-acting stimulant, remember that short-acting medication for ADHD has a higher potential for abuse. “Medication diversion is real. It does occur,” he said.
Establishing a basal sleep history and whether the child has insomnia is important before prescribing ADHD medication. Dr. Childers noted he uses a short-acting stimulant as an off-label treatment to treat some of his patients with insomnia, but he said to be aware of side effects like headache, abdominal pain, anorexia, and tics, as well as cardiac issues.
You also should rethink your diagnosis if the medication is not having an effect after two trials of a stimulant, Dr. Childers noted, and when a child has conditions like anxiety and depression that can mimic ADHD symptoms, a stimulant will increase irritability and have a paradoxical response to the medication. Inattentive ADHD can be missed in adolescent patients who struggle academically until they fall behind their peers, which can result in developing depression that complicates treatment, he said.
A learning disorder also can be mistaken for ADHD in children and presents in different ways depending on what grade the child is in. As a child ages and learns how to read, he or she will begin to fall behind as learning through reading becomes more complex. Learning disorders should be ruled out before treating for ADHD because, if the child improves after taking a stimulant, it could be more difficult to find a diagnosis of learning disorder later, Dr. Childers noted.
Bipolar disorder can be overdiagnosed in children; in these patients, the most likely diagnoses are ADHD and ODD, he said. According to a 2004 National Alliance of Mental Illness fact sheet, approximately 7% of patients in caseloads for federally funded studies in psychiatric facilities met the criteria for bipolar disorder, but the lifelong prevalence of the disease is between 1% and 1.6%.
“Bipolar disorder is frequently oppositional defiant disorder, and the word ‘no’ can be a trigger,” Dr. Childers said.
Dr. Childers reported no relevant conflicts of interest.
ORLANDO – said David O. Childers, MD, chief of the division of developmental pediatrics at the University of Florida in Jacksonville.
“That is a huge consideration, and the vast majority of pediatricians don’t understand that,” Dr. Childers said at the annual meeting of the American Academy of Pediatrics.
A diagnosis of ADHD in children should be reserved for situations in which the symptoms clearly interfere with how they function in social, academic, and occupational settings. ADHD should not be diagnosed in children who exhibit hostility, defiance, a failure to understand, or who have oppositional defiant disorder (ODD). In addition, ADHD in children often overlaps with other conditions, such as learning disabilities, ODD, anxiety, depression, poor self-esteem, conduct disorder, motor coordination problems, and encopresis and enuresis.
One mistake you can make is starting the medication too young in patients who exhibit symptoms of ADHD. Receptive language relative to developmental age should be taken into consideration when deciding whether to treat very young patients. “If the voice in your head is at a 3-year-old level, that’s going to be your behavior picture regardless of your chronological age,” Dr. Childers said.
You also can misdiagnose ADHD in young patients because you don’t recognize behavioral phenotypes and diagnoses that are similar to ADHD. Extreme prematurity, global developmental delay, fetal alcohol syndrome, spina bifida, genetic syndrome, intellectual and learning disabilities, closed head injuries, and depression all can mimic ADHD symptoms. “Everything that wheezes is not asthma, and everything that is ‘hyper’ or ‘drifty’ is not ADHD,” he noted.
Another mistake is considering mixed amphetamine salts (MAS) the same as methylphenidate (MPH), Dr. Childers said. MAS has 5 mg of active isomer versus 2.5 mg in MPH doses, and patients could see side effects from the increased potency in MAS in the form of appetite suppression and tics. You should start with a low dose of the medication and titrate up until patients get the most out of the medication to avoid situations in which patients report a change in personality or that the treatment is not effective.
“The medicine should never change a kid’s personality,” Dr. Childers said. “We are not here to treat the kid to the point of hyperactivity management; we’re here to treat for attention.”
In cases where patients ask for the short-acting medication rather than long-acting stimulant, remember that short-acting medication for ADHD has a higher potential for abuse. “Medication diversion is real. It does occur,” he said.
Establishing a basal sleep history and whether the child has insomnia is important before prescribing ADHD medication. Dr. Childers noted he uses a short-acting stimulant as an off-label treatment to treat some of his patients with insomnia, but he said to be aware of side effects like headache, abdominal pain, anorexia, and tics, as well as cardiac issues.
You also should rethink your diagnosis if the medication is not having an effect after two trials of a stimulant, Dr. Childers noted, and when a child has conditions like anxiety and depression that can mimic ADHD symptoms, a stimulant will increase irritability and have a paradoxical response to the medication. Inattentive ADHD can be missed in adolescent patients who struggle academically until they fall behind their peers, which can result in developing depression that complicates treatment, he said.
A learning disorder also can be mistaken for ADHD in children and presents in different ways depending on what grade the child is in. As a child ages and learns how to read, he or she will begin to fall behind as learning through reading becomes more complex. Learning disorders should be ruled out before treating for ADHD because, if the child improves after taking a stimulant, it could be more difficult to find a diagnosis of learning disorder later, Dr. Childers noted.
Bipolar disorder can be overdiagnosed in children; in these patients, the most likely diagnoses are ADHD and ODD, he said. According to a 2004 National Alliance of Mental Illness fact sheet, approximately 7% of patients in caseloads for federally funded studies in psychiatric facilities met the criteria for bipolar disorder, but the lifelong prevalence of the disease is between 1% and 1.6%.
“Bipolar disorder is frequently oppositional defiant disorder, and the word ‘no’ can be a trigger,” Dr. Childers said.
Dr. Childers reported no relevant conflicts of interest.
EXPERT ANALYSIS FROM AAP 18
New pediatric therapies show promise for influenza, multidrug-resistant pathogens
ORLANDO – John S. Bradley, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Bradley, director of the division of infectious diseases at Rady Children’s Hospital–San Diego, discussed a therapy for influenza, baloxavir, which was recently approved as a fast-acting single-dose medication and currently is under study in children. Also, a recent double-blind, phase 3 trial in the New England Journal of Medicine recruited patients as young as 12 years old. In the study, patients in the intervention group resolved their fever in median 25 hours, compared with 42 hours in the placebo group. Baloxavir better reduced viral load at day 2, compared with oseltamivir and placebo, but there was a similar alleviation of symptoms between both groups. There was a greater incidence of nausea and vomiting among the oseltamivir group, while the baloxavir group had a higher rate of diarrhea (N Engl J Med 2018;379:913-23).
However, Dr. Bradley noted baloxavir is much more expensive than oseltamivir, which may not justify the better tolerance of the drug for influenza treatment.
You don’t get better with it faster, so I’m not going to be recommending you all run to baloxavir this flu season for kids 12 years of age and older,” Dr. Bradley said. “I think oseltamivir is still fine, unless we end up with oseltamivir resistance.”
Solithromycin, an intravenous and oral fluoroketolide, has shown promising results against gram-positive and gram-negative pathogens for community-acquired pneumonia and other infections. During the drug’s study period, Cempra sold solithromycin to Melinta. However, one trial showed elevated liver functions in a higher number of patients than expected, and the Food and Drug Administration asked Melinta to conduct additional studies. Investigations on solithromycin have currently stopped until Melinta secures funding. “Until they get better resources, this particular drug is on hold, but you’ll see it again, I’m sure,” said Dr. Bradley, who also is professor and chief of the division of infectious diseases at the University of California, San Diego.
Dr. Bradley also discussed the efficacy of tedizolid, a protein synthesis inhibitor similar to linezolid approved in adults for the treatment of skin infections. He noted tedizolid is more active than linezolid, but the treatment course is a shorter dose for a shorter amount of time. Compared with linezolid, which can cause thrombocytopenia or neutropenia if taken for more than 10 days to 14 days, there also are fewer side effects.
“The tedizolid is much, much safer,” Dr. Bradley said, who added that trials for efficacy of tedizolid are currently underway in pediatric patients. “We’re hoping that will end up being the pediatric oxazolidinone.”
Other investigative therapies approved for adults and under study for use in children include ceftazidime/avibactam for treatment of urinary tract and complicated intra-abdominal infections, which is effective against meropenem-resistant Enterobacteriaceae and resistant Escherichia coli with extended-spectrum beta-lactamases (ESBL); ceftolozane/tazobactam has also been approved for adults, is pending approval in pediatric patients, and is active against ESBLs such as Pseudomonas; and meropenem/vaborbactam, which is active against Klebsiella pneumoniae carbapenemase (KPC)–producing isolates. Plazomicin, an aminoglycoside similar to gentamicin used to treat KPC-producing isolates, is stable against enzymes that degrade gentamicin and tobramycin.
Therapies currently under study for adults and being considered for children include imipenem/relebactam for treatment against E. coli, Enterobacter species, and KPC-producing isolates, and cefiderocol, a siderophore cephalosporin antibiotic – commonly described as a “Trojan horse” antibiotic because it binds to iron and is actively transported into the organism – is effective against Pseudomonas and has finished phase 2 trials in adults, with researchers looking to do single-dose trials in children, Dr. Bradley noted.
More experimentally, phage therapy for multidrug-resistant Acinetobacter baumannii proved effective in a 68-year-old patient with necrotizing pancreatitis who continued to deteriorate over a 4-month period despite multiple courses of antibiotics and attempted drainage of a pancreatic pseudocyst. Researchers selected a phage-specific bacterium with specificity for A. baumannii and cured him. “This is like science fiction,” Dr. Bradley said.
Dr. Bradley reported no relevant conflicts of interest.
ORLANDO – John S. Bradley, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Bradley, director of the division of infectious diseases at Rady Children’s Hospital–San Diego, discussed a therapy for influenza, baloxavir, which was recently approved as a fast-acting single-dose medication and currently is under study in children. Also, a recent double-blind, phase 3 trial in the New England Journal of Medicine recruited patients as young as 12 years old. In the study, patients in the intervention group resolved their fever in median 25 hours, compared with 42 hours in the placebo group. Baloxavir better reduced viral load at day 2, compared with oseltamivir and placebo, but there was a similar alleviation of symptoms between both groups. There was a greater incidence of nausea and vomiting among the oseltamivir group, while the baloxavir group had a higher rate of diarrhea (N Engl J Med 2018;379:913-23).
However, Dr. Bradley noted baloxavir is much more expensive than oseltamivir, which may not justify the better tolerance of the drug for influenza treatment.
You don’t get better with it faster, so I’m not going to be recommending you all run to baloxavir this flu season for kids 12 years of age and older,” Dr. Bradley said. “I think oseltamivir is still fine, unless we end up with oseltamivir resistance.”
Solithromycin, an intravenous and oral fluoroketolide, has shown promising results against gram-positive and gram-negative pathogens for community-acquired pneumonia and other infections. During the drug’s study period, Cempra sold solithromycin to Melinta. However, one trial showed elevated liver functions in a higher number of patients than expected, and the Food and Drug Administration asked Melinta to conduct additional studies. Investigations on solithromycin have currently stopped until Melinta secures funding. “Until they get better resources, this particular drug is on hold, but you’ll see it again, I’m sure,” said Dr. Bradley, who also is professor and chief of the division of infectious diseases at the University of California, San Diego.
Dr. Bradley also discussed the efficacy of tedizolid, a protein synthesis inhibitor similar to linezolid approved in adults for the treatment of skin infections. He noted tedizolid is more active than linezolid, but the treatment course is a shorter dose for a shorter amount of time. Compared with linezolid, which can cause thrombocytopenia or neutropenia if taken for more than 10 days to 14 days, there also are fewer side effects.
“The tedizolid is much, much safer,” Dr. Bradley said, who added that trials for efficacy of tedizolid are currently underway in pediatric patients. “We’re hoping that will end up being the pediatric oxazolidinone.”
Other investigative therapies approved for adults and under study for use in children include ceftazidime/avibactam for treatment of urinary tract and complicated intra-abdominal infections, which is effective against meropenem-resistant Enterobacteriaceae and resistant Escherichia coli with extended-spectrum beta-lactamases (ESBL); ceftolozane/tazobactam has also been approved for adults, is pending approval in pediatric patients, and is active against ESBLs such as Pseudomonas; and meropenem/vaborbactam, which is active against Klebsiella pneumoniae carbapenemase (KPC)–producing isolates. Plazomicin, an aminoglycoside similar to gentamicin used to treat KPC-producing isolates, is stable against enzymes that degrade gentamicin and tobramycin.
Therapies currently under study for adults and being considered for children include imipenem/relebactam for treatment against E. coli, Enterobacter species, and KPC-producing isolates, and cefiderocol, a siderophore cephalosporin antibiotic – commonly described as a “Trojan horse” antibiotic because it binds to iron and is actively transported into the organism – is effective against Pseudomonas and has finished phase 2 trials in adults, with researchers looking to do single-dose trials in children, Dr. Bradley noted.
More experimentally, phage therapy for multidrug-resistant Acinetobacter baumannii proved effective in a 68-year-old patient with necrotizing pancreatitis who continued to deteriorate over a 4-month period despite multiple courses of antibiotics and attempted drainage of a pancreatic pseudocyst. Researchers selected a phage-specific bacterium with specificity for A. baumannii and cured him. “This is like science fiction,” Dr. Bradley said.
Dr. Bradley reported no relevant conflicts of interest.
ORLANDO – John S. Bradley, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Bradley, director of the division of infectious diseases at Rady Children’s Hospital–San Diego, discussed a therapy for influenza, baloxavir, which was recently approved as a fast-acting single-dose medication and currently is under study in children. Also, a recent double-blind, phase 3 trial in the New England Journal of Medicine recruited patients as young as 12 years old. In the study, patients in the intervention group resolved their fever in median 25 hours, compared with 42 hours in the placebo group. Baloxavir better reduced viral load at day 2, compared with oseltamivir and placebo, but there was a similar alleviation of symptoms between both groups. There was a greater incidence of nausea and vomiting among the oseltamivir group, while the baloxavir group had a higher rate of diarrhea (N Engl J Med 2018;379:913-23).
However, Dr. Bradley noted baloxavir is much more expensive than oseltamivir, which may not justify the better tolerance of the drug for influenza treatment.
You don’t get better with it faster, so I’m not going to be recommending you all run to baloxavir this flu season for kids 12 years of age and older,” Dr. Bradley said. “I think oseltamivir is still fine, unless we end up with oseltamivir resistance.”
Solithromycin, an intravenous and oral fluoroketolide, has shown promising results against gram-positive and gram-negative pathogens for community-acquired pneumonia and other infections. During the drug’s study period, Cempra sold solithromycin to Melinta. However, one trial showed elevated liver functions in a higher number of patients than expected, and the Food and Drug Administration asked Melinta to conduct additional studies. Investigations on solithromycin have currently stopped until Melinta secures funding. “Until they get better resources, this particular drug is on hold, but you’ll see it again, I’m sure,” said Dr. Bradley, who also is professor and chief of the division of infectious diseases at the University of California, San Diego.
Dr. Bradley also discussed the efficacy of tedizolid, a protein synthesis inhibitor similar to linezolid approved in adults for the treatment of skin infections. He noted tedizolid is more active than linezolid, but the treatment course is a shorter dose for a shorter amount of time. Compared with linezolid, which can cause thrombocytopenia or neutropenia if taken for more than 10 days to 14 days, there also are fewer side effects.
“The tedizolid is much, much safer,” Dr. Bradley said, who added that trials for efficacy of tedizolid are currently underway in pediatric patients. “We’re hoping that will end up being the pediatric oxazolidinone.”
Other investigative therapies approved for adults and under study for use in children include ceftazidime/avibactam for treatment of urinary tract and complicated intra-abdominal infections, which is effective against meropenem-resistant Enterobacteriaceae and resistant Escherichia coli with extended-spectrum beta-lactamases (ESBL); ceftolozane/tazobactam has also been approved for adults, is pending approval in pediatric patients, and is active against ESBLs such as Pseudomonas; and meropenem/vaborbactam, which is active against Klebsiella pneumoniae carbapenemase (KPC)–producing isolates. Plazomicin, an aminoglycoside similar to gentamicin used to treat KPC-producing isolates, is stable against enzymes that degrade gentamicin and tobramycin.
Therapies currently under study for adults and being considered for children include imipenem/relebactam for treatment against E. coli, Enterobacter species, and KPC-producing isolates, and cefiderocol, a siderophore cephalosporin antibiotic – commonly described as a “Trojan horse” antibiotic because it binds to iron and is actively transported into the organism – is effective against Pseudomonas and has finished phase 2 trials in adults, with researchers looking to do single-dose trials in children, Dr. Bradley noted.
More experimentally, phage therapy for multidrug-resistant Acinetobacter baumannii proved effective in a 68-year-old patient with necrotizing pancreatitis who continued to deteriorate over a 4-month period despite multiple courses of antibiotics and attempted drainage of a pancreatic pseudocyst. Researchers selected a phage-specific bacterium with specificity for A. baumannii and cured him. “This is like science fiction,” Dr. Bradley said.
Dr. Bradley reported no relevant conflicts of interest.
EXPERT ANALYSIS FROM AAP 18
Team approach needed to tackle complex care for fostered, adopted children
ORLANDO – Children in foster care or who are adopted are at a higher risk of developing medical conditions, and a team approach is needed when caring for these children with a focus on medical, developmental, and mental health, Judith K. Eckerle, MD, said at the annual meeting of the American Academy of Pediatrics.
“One of the things that I’m advocating more these days is [that] we don’t operate as physicians or medical people in a vacuum. We certainly have to operate within a team approach, and that really is the best approach for these kids,” said Dr. Eckerle, a pediatrician who specializes in neurobehavioral development and is director of the Adoption Medicine Clinic at the University of Minnesota, Minneapolis.
Recognizing how early adversity is associated with conditions such as growth, brain development, motor skills, cognition, mental health, attachment, stress sensitivity, sensory processing, language, and chromosome structure can help in the medical assessment of these patients. Dr. Eckerle noted that these issues can even present in children with no early adversity who are adopted or placed into healthy foster environments.
“What we’ve learned is, we’ve just seen dozens if not hundreds of kids now in the exact same scenario who are having exactly the same types of bonding, or attachment or stress issues, as kids who did spend those few years in a really neglectful or orphanage scenarios,” Dr. Eckerle said.
“The majority of adopted and foster care kids do great in the end,” she emphasized. “As a group, they can do beautifully, but we just have to be cognizant of the things that we should be looking for and not just gloss over them so we’re not missing things along the way.”
At her institution, Dr. Eckerle said a medical assessment for new foster care or adoption patients begins with explaining the exam process with the parent and child before the child is screened by an occupational therapist. During the screening, the occupational therapist will screen the child for signs of developmental delay such as delay in gross or fine motor skills, speech, cognition, musculoskeletal, psychosocial, and sensory processing, as well as in school-based, self-care, and functional skills.
While the child is out of the room, Dr. Eckerle will ask whether the parent has any concerns about the child. After that, she will check the child’s eyes, heart, and ears to make sure they are healthy; during the end of the exam, she may order lab tests based on any concerns about prenatal or foster care trauma. Adolescents and children in whom sexual abuse is suspected should be screened for hepatitis B, hepatitis C, syphilis, and HIV.
International adoptees should undergo ova and parasite screening and the Giardia antigen test. International adoptees as well as those who had contact with the homeless or prison systems should undergo QuantiFERON-TB Gold testing for tuberculosis, and children aged under 5 years should receive targeted tuberculin skin testing. She said her center also screens children for intellectual disability, fetal alcohol spectrum disorder, short stature, and precocious puberty.
Lastly, the child is seen by a pediatric psychologist for additional screening. Dr. Eckerle noted the most common diagnoses seen at her center are reactive attachment disorder, oppositional defiant disorder, conduct disorder, pervasive development delay, autism, learning disabilities, emotional or behavioral problems, and ADHD. With regard to mental health, doctors should help a caregiver understand a child with a mental health conditions and consider pairing with a pediatric psychologist to offer evidence-based interventions for children aged under 5 years, such as child-parent psychotherapy, circle of security, and attachment biobehavioral catch-up, and offer trauma-focused cognitive behavioral therapy in children aged between 4 and 5 years.
Bad behavior often is misinterpreted as dishonesty and willful misconduct on the part of the child, but instead could be a neurodevelopmental or mental health problem, Dr. Eckerle noted. For example, a parent might interpret a child who takes a sparkling watch off of a teacher’s desk as stealing, but the child may not yet understand the concept of ownership. “Reframing these things will lead to the goal of helping that parent understand the child.”
Above all, Dr. Eckerle said she emphasizes what will happen after the exam with children she sees to establish a routine, as many children she sees have gone through multiple foster environments. It also is important to let parents know the exam is just a first step and they likely will not receive a diagnosis that day, particularly with out-of-state or international families. “I want them to have appropriate expectations that we’re not going to cure or solve or fix everything the second that they leave that room, but that we are starting the process and we are on the right track.”
Dr. Eckerle reported no conflicts of interest.
ORLANDO – Children in foster care or who are adopted are at a higher risk of developing medical conditions, and a team approach is needed when caring for these children with a focus on medical, developmental, and mental health, Judith K. Eckerle, MD, said at the annual meeting of the American Academy of Pediatrics.
“One of the things that I’m advocating more these days is [that] we don’t operate as physicians or medical people in a vacuum. We certainly have to operate within a team approach, and that really is the best approach for these kids,” said Dr. Eckerle, a pediatrician who specializes in neurobehavioral development and is director of the Adoption Medicine Clinic at the University of Minnesota, Minneapolis.
Recognizing how early adversity is associated with conditions such as growth, brain development, motor skills, cognition, mental health, attachment, stress sensitivity, sensory processing, language, and chromosome structure can help in the medical assessment of these patients. Dr. Eckerle noted that these issues can even present in children with no early adversity who are adopted or placed into healthy foster environments.
“What we’ve learned is, we’ve just seen dozens if not hundreds of kids now in the exact same scenario who are having exactly the same types of bonding, or attachment or stress issues, as kids who did spend those few years in a really neglectful or orphanage scenarios,” Dr. Eckerle said.
“The majority of adopted and foster care kids do great in the end,” she emphasized. “As a group, they can do beautifully, but we just have to be cognizant of the things that we should be looking for and not just gloss over them so we’re not missing things along the way.”
At her institution, Dr. Eckerle said a medical assessment for new foster care or adoption patients begins with explaining the exam process with the parent and child before the child is screened by an occupational therapist. During the screening, the occupational therapist will screen the child for signs of developmental delay such as delay in gross or fine motor skills, speech, cognition, musculoskeletal, psychosocial, and sensory processing, as well as in school-based, self-care, and functional skills.
While the child is out of the room, Dr. Eckerle will ask whether the parent has any concerns about the child. After that, she will check the child’s eyes, heart, and ears to make sure they are healthy; during the end of the exam, she may order lab tests based on any concerns about prenatal or foster care trauma. Adolescents and children in whom sexual abuse is suspected should be screened for hepatitis B, hepatitis C, syphilis, and HIV.
International adoptees should undergo ova and parasite screening and the Giardia antigen test. International adoptees as well as those who had contact with the homeless or prison systems should undergo QuantiFERON-TB Gold testing for tuberculosis, and children aged under 5 years should receive targeted tuberculin skin testing. She said her center also screens children for intellectual disability, fetal alcohol spectrum disorder, short stature, and precocious puberty.
Lastly, the child is seen by a pediatric psychologist for additional screening. Dr. Eckerle noted the most common diagnoses seen at her center are reactive attachment disorder, oppositional defiant disorder, conduct disorder, pervasive development delay, autism, learning disabilities, emotional or behavioral problems, and ADHD. With regard to mental health, doctors should help a caregiver understand a child with a mental health conditions and consider pairing with a pediatric psychologist to offer evidence-based interventions for children aged under 5 years, such as child-parent psychotherapy, circle of security, and attachment biobehavioral catch-up, and offer trauma-focused cognitive behavioral therapy in children aged between 4 and 5 years.
Bad behavior often is misinterpreted as dishonesty and willful misconduct on the part of the child, but instead could be a neurodevelopmental or mental health problem, Dr. Eckerle noted. For example, a parent might interpret a child who takes a sparkling watch off of a teacher’s desk as stealing, but the child may not yet understand the concept of ownership. “Reframing these things will lead to the goal of helping that parent understand the child.”
Above all, Dr. Eckerle said she emphasizes what will happen after the exam with children she sees to establish a routine, as many children she sees have gone through multiple foster environments. It also is important to let parents know the exam is just a first step and they likely will not receive a diagnosis that day, particularly with out-of-state or international families. “I want them to have appropriate expectations that we’re not going to cure or solve or fix everything the second that they leave that room, but that we are starting the process and we are on the right track.”
Dr. Eckerle reported no conflicts of interest.
ORLANDO – Children in foster care or who are adopted are at a higher risk of developing medical conditions, and a team approach is needed when caring for these children with a focus on medical, developmental, and mental health, Judith K. Eckerle, MD, said at the annual meeting of the American Academy of Pediatrics.
“One of the things that I’m advocating more these days is [that] we don’t operate as physicians or medical people in a vacuum. We certainly have to operate within a team approach, and that really is the best approach for these kids,” said Dr. Eckerle, a pediatrician who specializes in neurobehavioral development and is director of the Adoption Medicine Clinic at the University of Minnesota, Minneapolis.
Recognizing how early adversity is associated with conditions such as growth, brain development, motor skills, cognition, mental health, attachment, stress sensitivity, sensory processing, language, and chromosome structure can help in the medical assessment of these patients. Dr. Eckerle noted that these issues can even present in children with no early adversity who are adopted or placed into healthy foster environments.
“What we’ve learned is, we’ve just seen dozens if not hundreds of kids now in the exact same scenario who are having exactly the same types of bonding, or attachment or stress issues, as kids who did spend those few years in a really neglectful or orphanage scenarios,” Dr. Eckerle said.
“The majority of adopted and foster care kids do great in the end,” she emphasized. “As a group, they can do beautifully, but we just have to be cognizant of the things that we should be looking for and not just gloss over them so we’re not missing things along the way.”
At her institution, Dr. Eckerle said a medical assessment for new foster care or adoption patients begins with explaining the exam process with the parent and child before the child is screened by an occupational therapist. During the screening, the occupational therapist will screen the child for signs of developmental delay such as delay in gross or fine motor skills, speech, cognition, musculoskeletal, psychosocial, and sensory processing, as well as in school-based, self-care, and functional skills.
While the child is out of the room, Dr. Eckerle will ask whether the parent has any concerns about the child. After that, she will check the child’s eyes, heart, and ears to make sure they are healthy; during the end of the exam, she may order lab tests based on any concerns about prenatal or foster care trauma. Adolescents and children in whom sexual abuse is suspected should be screened for hepatitis B, hepatitis C, syphilis, and HIV.
International adoptees should undergo ova and parasite screening and the Giardia antigen test. International adoptees as well as those who had contact with the homeless or prison systems should undergo QuantiFERON-TB Gold testing for tuberculosis, and children aged under 5 years should receive targeted tuberculin skin testing. She said her center also screens children for intellectual disability, fetal alcohol spectrum disorder, short stature, and precocious puberty.
Lastly, the child is seen by a pediatric psychologist for additional screening. Dr. Eckerle noted the most common diagnoses seen at her center are reactive attachment disorder, oppositional defiant disorder, conduct disorder, pervasive development delay, autism, learning disabilities, emotional or behavioral problems, and ADHD. With regard to mental health, doctors should help a caregiver understand a child with a mental health conditions and consider pairing with a pediatric psychologist to offer evidence-based interventions for children aged under 5 years, such as child-parent psychotherapy, circle of security, and attachment biobehavioral catch-up, and offer trauma-focused cognitive behavioral therapy in children aged between 4 and 5 years.
Bad behavior often is misinterpreted as dishonesty and willful misconduct on the part of the child, but instead could be a neurodevelopmental or mental health problem, Dr. Eckerle noted. For example, a parent might interpret a child who takes a sparkling watch off of a teacher’s desk as stealing, but the child may not yet understand the concept of ownership. “Reframing these things will lead to the goal of helping that parent understand the child.”
Above all, Dr. Eckerle said she emphasizes what will happen after the exam with children she sees to establish a routine, as many children she sees have gone through multiple foster environments. It also is important to let parents know the exam is just a first step and they likely will not receive a diagnosis that day, particularly with out-of-state or international families. “I want them to have appropriate expectations that we’re not going to cure or solve or fix everything the second that they leave that room, but that we are starting the process and we are on the right track.”
Dr. Eckerle reported no conflicts of interest.
EXPERT ANALYSIS FROM AAP 18
Children are vulnerable to diseases emerging because of climate change
ORLANDO – “Expect the unexpected” when considering the health impacts of climate change on children, Susan Pacheo, MD, advised in her presentation at the annual meeting of the American Academy of Pediatrics.
“We don’t know what we’re going to see, and we need to be ready,” said Dr. Pacheo of the University of Texas, Houston.
Climate change is categorized by an increase in droughts, fires, storms, floods, mudslides, and extreme temperatures. According to the Centers for Disease Control and Prevention, the impacts of climate change on human health are multiple, but can include an increased rate of infectious disease, respiratory conditions, injury, cardiovascular-related health issues, malnutrition, and mental health problems.
These problems can especially target children, Dr. Pacheo noted. “Kids are vulnerable. You’ve heard this, you’ve experienced this, you see this every day in your pediatric population.”
Children are more vulnerable because of the increased exposure they have to the environment. They spend more time outdoors, they are closer to the ground, and they are likely to put objects in their mouth. Children also tend to swallow more water when swimming, compared with adults. A 2014 study by de Man et al. found that children exposed to storm sewers and combined sewers swallowed 1.7 mL of water per exposure event and that the risk of infection from pathogens such as noroviruses, enteroviruses, Campylobacter jejuni, Cryptosporidium, and Giardia was 23%-33% per event, compared with 0.016 mL of water per exposure in adults and a mean infection risk of 0.58%-3.90% per event (Water Research. 2014 Jan 1. doi: 10.1016/j.watres.2013.09.022).
In addition, socioeconomic status and built environment as well as a child’s immature lung development and higher respiratory rate can lead to children being impacted by factors such as air pollution. Poverty, access to medical care, and the structure and dynamics of family also can affect children.
“We need to do something because this is a problem of social justice and we, as pediatricians, are advocates of the vulnerable,” Dr. Pacheo said.
Expect to see an increase in the number of vector-borne, airborne, and pollution-related disease, as well as water- and food-borne diseases, as a result of climate change, in addition to other issues such as hand, foot, and mouth disease and antibiotic resistance, she noted. As historically colder parts of the world continue to have milder winters, disease-carrying insects such as ticks and mosquitoes will expand their habitats and transmission of diseases such as Zika virus, malaria, dengue fever, and chikungunya will increase.
Leptospirosis and Naegleria fowleri, the latter which can cause primary amebic meningoencephalitis, are also becoming more common. Food-borne illnesses like vibriosis are being seen in more northern areas of the world like Alaska, and ciguatera fish poisoning is expected to be more prevalent in the southeastern United States and Gulf of Mexico, Dr. Pacheo said.
Air pollution carries a risk of respiratory diseases, pneumonia, and bronchiolitis, with a 2017 systematic review by Nhung et al. finding increased exposure to ambient air pollution markers such as sulfur dioxide, ozone, nitrogen dioxide, and carbon monoxide was associated with pneumonia in children (Environ Pollut. 2017 Jul 25. doi: 10.1016/j.envpol.2017.07.063). Coccidioidomycosis, or valley fever, is caused by inhaling a fungus in the soil and is associated with dust storms primarily in the southwestern United States. Warmer temperatures also have caused toxic algae blooms that have killed marine life and caused respiratory distress; children should not go near or play in water when algae blooms are growing, she noted.
Recent studies have linked an increase in temperature with incidence of Escherichia coli, with a 2016 study by Philipsborn et al. showing a 1° Celsius increase in mean monthly temperature was associated with an 8% increase in incidence of diarrheagenic E. coli (J Infect Dis. 2016 Feb 29. doi: 10.1093/infdis/jiw081). The incidence of hand, foot, and mouth disease also is linked to temperature and humidity, with a 2018 study by Cheng et al. showing a 1° Celsius increase in temperature and humidity was significantly associated with hand, foot, and mouth disease (Sci Total Environ. 2018 Jan 12. doi: 10.1016/j.scitotenv.2018.01.006). Rates of influenza are controlled by the changing environment as well, and increasing the number of vaccinations will help lower the number of influenza cases.
“We need to be advocates, we need to educate ourselves like we’re doing now so that we can educate our patients and to create a plan for preparedness,” Dr. Pacheo said.
She reported no relevant conflicts of interest.
ORLANDO – “Expect the unexpected” when considering the health impacts of climate change on children, Susan Pacheo, MD, advised in her presentation at the annual meeting of the American Academy of Pediatrics.
“We don’t know what we’re going to see, and we need to be ready,” said Dr. Pacheo of the University of Texas, Houston.
Climate change is categorized by an increase in droughts, fires, storms, floods, mudslides, and extreme temperatures. According to the Centers for Disease Control and Prevention, the impacts of climate change on human health are multiple, but can include an increased rate of infectious disease, respiratory conditions, injury, cardiovascular-related health issues, malnutrition, and mental health problems.
These problems can especially target children, Dr. Pacheo noted. “Kids are vulnerable. You’ve heard this, you’ve experienced this, you see this every day in your pediatric population.”
Children are more vulnerable because of the increased exposure they have to the environment. They spend more time outdoors, they are closer to the ground, and they are likely to put objects in their mouth. Children also tend to swallow more water when swimming, compared with adults. A 2014 study by de Man et al. found that children exposed to storm sewers and combined sewers swallowed 1.7 mL of water per exposure event and that the risk of infection from pathogens such as noroviruses, enteroviruses, Campylobacter jejuni, Cryptosporidium, and Giardia was 23%-33% per event, compared with 0.016 mL of water per exposure in adults and a mean infection risk of 0.58%-3.90% per event (Water Research. 2014 Jan 1. doi: 10.1016/j.watres.2013.09.022).
In addition, socioeconomic status and built environment as well as a child’s immature lung development and higher respiratory rate can lead to children being impacted by factors such as air pollution. Poverty, access to medical care, and the structure and dynamics of family also can affect children.
“We need to do something because this is a problem of social justice and we, as pediatricians, are advocates of the vulnerable,” Dr. Pacheo said.
Expect to see an increase in the number of vector-borne, airborne, and pollution-related disease, as well as water- and food-borne diseases, as a result of climate change, in addition to other issues such as hand, foot, and mouth disease and antibiotic resistance, she noted. As historically colder parts of the world continue to have milder winters, disease-carrying insects such as ticks and mosquitoes will expand their habitats and transmission of diseases such as Zika virus, malaria, dengue fever, and chikungunya will increase.
Leptospirosis and Naegleria fowleri, the latter which can cause primary amebic meningoencephalitis, are also becoming more common. Food-borne illnesses like vibriosis are being seen in more northern areas of the world like Alaska, and ciguatera fish poisoning is expected to be more prevalent in the southeastern United States and Gulf of Mexico, Dr. Pacheo said.
Air pollution carries a risk of respiratory diseases, pneumonia, and bronchiolitis, with a 2017 systematic review by Nhung et al. finding increased exposure to ambient air pollution markers such as sulfur dioxide, ozone, nitrogen dioxide, and carbon monoxide was associated with pneumonia in children (Environ Pollut. 2017 Jul 25. doi: 10.1016/j.envpol.2017.07.063). Coccidioidomycosis, or valley fever, is caused by inhaling a fungus in the soil and is associated with dust storms primarily in the southwestern United States. Warmer temperatures also have caused toxic algae blooms that have killed marine life and caused respiratory distress; children should not go near or play in water when algae blooms are growing, she noted.
Recent studies have linked an increase in temperature with incidence of Escherichia coli, with a 2016 study by Philipsborn et al. showing a 1° Celsius increase in mean monthly temperature was associated with an 8% increase in incidence of diarrheagenic E. coli (J Infect Dis. 2016 Feb 29. doi: 10.1093/infdis/jiw081). The incidence of hand, foot, and mouth disease also is linked to temperature and humidity, with a 2018 study by Cheng et al. showing a 1° Celsius increase in temperature and humidity was significantly associated with hand, foot, and mouth disease (Sci Total Environ. 2018 Jan 12. doi: 10.1016/j.scitotenv.2018.01.006). Rates of influenza are controlled by the changing environment as well, and increasing the number of vaccinations will help lower the number of influenza cases.
“We need to be advocates, we need to educate ourselves like we’re doing now so that we can educate our patients and to create a plan for preparedness,” Dr. Pacheo said.
She reported no relevant conflicts of interest.
ORLANDO – “Expect the unexpected” when considering the health impacts of climate change on children, Susan Pacheo, MD, advised in her presentation at the annual meeting of the American Academy of Pediatrics.
“We don’t know what we’re going to see, and we need to be ready,” said Dr. Pacheo of the University of Texas, Houston.
Climate change is categorized by an increase in droughts, fires, storms, floods, mudslides, and extreme temperatures. According to the Centers for Disease Control and Prevention, the impacts of climate change on human health are multiple, but can include an increased rate of infectious disease, respiratory conditions, injury, cardiovascular-related health issues, malnutrition, and mental health problems.
These problems can especially target children, Dr. Pacheo noted. “Kids are vulnerable. You’ve heard this, you’ve experienced this, you see this every day in your pediatric population.”
Children are more vulnerable because of the increased exposure they have to the environment. They spend more time outdoors, they are closer to the ground, and they are likely to put objects in their mouth. Children also tend to swallow more water when swimming, compared with adults. A 2014 study by de Man et al. found that children exposed to storm sewers and combined sewers swallowed 1.7 mL of water per exposure event and that the risk of infection from pathogens such as noroviruses, enteroviruses, Campylobacter jejuni, Cryptosporidium, and Giardia was 23%-33% per event, compared with 0.016 mL of water per exposure in adults and a mean infection risk of 0.58%-3.90% per event (Water Research. 2014 Jan 1. doi: 10.1016/j.watres.2013.09.022).
In addition, socioeconomic status and built environment as well as a child’s immature lung development and higher respiratory rate can lead to children being impacted by factors such as air pollution. Poverty, access to medical care, and the structure and dynamics of family also can affect children.
“We need to do something because this is a problem of social justice and we, as pediatricians, are advocates of the vulnerable,” Dr. Pacheo said.
Expect to see an increase in the number of vector-borne, airborne, and pollution-related disease, as well as water- and food-borne diseases, as a result of climate change, in addition to other issues such as hand, foot, and mouth disease and antibiotic resistance, she noted. As historically colder parts of the world continue to have milder winters, disease-carrying insects such as ticks and mosquitoes will expand their habitats and transmission of diseases such as Zika virus, malaria, dengue fever, and chikungunya will increase.
Leptospirosis and Naegleria fowleri, the latter which can cause primary amebic meningoencephalitis, are also becoming more common. Food-borne illnesses like vibriosis are being seen in more northern areas of the world like Alaska, and ciguatera fish poisoning is expected to be more prevalent in the southeastern United States and Gulf of Mexico, Dr. Pacheo said.
Air pollution carries a risk of respiratory diseases, pneumonia, and bronchiolitis, with a 2017 systematic review by Nhung et al. finding increased exposure to ambient air pollution markers such as sulfur dioxide, ozone, nitrogen dioxide, and carbon monoxide was associated with pneumonia in children (Environ Pollut. 2017 Jul 25. doi: 10.1016/j.envpol.2017.07.063). Coccidioidomycosis, or valley fever, is caused by inhaling a fungus in the soil and is associated with dust storms primarily in the southwestern United States. Warmer temperatures also have caused toxic algae blooms that have killed marine life and caused respiratory distress; children should not go near or play in water when algae blooms are growing, she noted.
Recent studies have linked an increase in temperature with incidence of Escherichia coli, with a 2016 study by Philipsborn et al. showing a 1° Celsius increase in mean monthly temperature was associated with an 8% increase in incidence of diarrheagenic E. coli (J Infect Dis. 2016 Feb 29. doi: 10.1093/infdis/jiw081). The incidence of hand, foot, and mouth disease also is linked to temperature and humidity, with a 2018 study by Cheng et al. showing a 1° Celsius increase in temperature and humidity was significantly associated with hand, foot, and mouth disease (Sci Total Environ. 2018 Jan 12. doi: 10.1016/j.scitotenv.2018.01.006). Rates of influenza are controlled by the changing environment as well, and increasing the number of vaccinations will help lower the number of influenza cases.
“We need to be advocates, we need to educate ourselves like we’re doing now so that we can educate our patients and to create a plan for preparedness,” Dr. Pacheo said.
She reported no relevant conflicts of interest.
EXPERT ANALYSIS FROM AAP 2018