User login
Mepolizumab shows efficacy in bronchiectasis with eosinophilia
PARIS – according to a small case series of patients presented as a late-breaking study at the annual congress of the European Respiratory Society.
“The message is that it is important to think of all of the etiologies and treatable traits in patients with bronchiectasis, and do not forget eosinophilia, because this can be treated,” reported Jessica Rademacher, MD, of the Clinic for Pulmonology at Hannover (Germany) Medical School.
Mepolizumab is a monoclonal antibody that targets interleukin-5, an important signaling protein for eosinophil recruitment, and is approved for use in asthma with eosinophilia. Larger, controlled trials are needed to confirm its efficacy in bronchiectasis, but the clinical improvements after 6 months of treatment in a series of 12 patients at Dr. Rademacher’s center were impressive.
Bronchiectasis patients were selected for treatment with mepolizumab if they had been poorly controlled on conventional therapies and they had an eosinophil count of greater than 300 cells/mm3. Of 328 patients with bronchiectasis that are being followed at Dr. Rademacher’s center, 7% met these criteria. Dr. Rademacher presented data on 12 who had been followed for at least 6 months.
In these patients, the median eosinophil count fell from a median baseline of 1,000 cells/mm3 to 100 cells/mm3 at 6 months (P = .0012). The median annualized rate of exacerbations fell from three per year to one per year, and the median Modified Medical Research Council Dyspnea Scale score fell from 2 to 0 (P = .004).
“There was a steroid-sparing effect in all seven patients who were taking oral corticosteroids at baseline. Five stopped oral steroids completely,” Dr. Rademacher reported.
A visual analog scale ranging from 1 to 10 with higher scores representing improvement showed patient-rated quality of life improved from 4 to 6.5 (P = .01). Dr. Rademacher emphasized this outcome because “improved quality of life is really what we are trying to achieve.”
Mepolizumab was well tolerated. In one patient who developed pneumonia, mepolizumab was discontinued, but it was restarted when the infection resolved, because the pneumonia was not considered mepolizumab related.
Although Dr. Rademacher acknowledged the possibility that at least some of the patients in this case series had overlapping asthma, she emphasized that they were selected from a referral population that had a comprehensive workup and that this overlap has been rarely reported.
There is evidence that anti–interleukin-5 therapies such as mepolizumab are effective in respiratory diseases when eosinophilia is present, according to Dr. Rademacher. For example, she cited reports of clinical improvement in chronic obstructive pulmonary disease and granulomatosis with polyangiitis patients with high eosinophil counts. In bronchiectasis, which has many causes, it may be particularly important to select relevant targets.
“There is an important variability in the presentation of bronchiectasis. Not all these patients have reduced lung function,” she said. Rather, the most significant symptoms for a patient may be sputum or cough. She suggested that the goals are to identify underlying causes of symptoms and which may be treatable.
According to these data, eosinophilia may be one of the treatable causes in a small but significant proportion of patients with bronchiectasis. A trial of mepolizumab may be reasonable in patients inadequately controlled on inhaled anti-inflammatory drugs. “If they do not profit from this therapy, then stop,” she added.
Dr. Rademacher acknowledged that data from this small case series are “not enough to say that [mepolizumab] is an option for these patients,” but she believes the consistency of benefit in this small series will encourage the trials needed to confirm that this approach is safe and effective.
Dr. Rademacher reported no disclosures relevant to the report.
PARIS – according to a small case series of patients presented as a late-breaking study at the annual congress of the European Respiratory Society.
“The message is that it is important to think of all of the etiologies and treatable traits in patients with bronchiectasis, and do not forget eosinophilia, because this can be treated,” reported Jessica Rademacher, MD, of the Clinic for Pulmonology at Hannover (Germany) Medical School.
Mepolizumab is a monoclonal antibody that targets interleukin-5, an important signaling protein for eosinophil recruitment, and is approved for use in asthma with eosinophilia. Larger, controlled trials are needed to confirm its efficacy in bronchiectasis, but the clinical improvements after 6 months of treatment in a series of 12 patients at Dr. Rademacher’s center were impressive.
Bronchiectasis patients were selected for treatment with mepolizumab if they had been poorly controlled on conventional therapies and they had an eosinophil count of greater than 300 cells/mm3. Of 328 patients with bronchiectasis that are being followed at Dr. Rademacher’s center, 7% met these criteria. Dr. Rademacher presented data on 12 who had been followed for at least 6 months.
In these patients, the median eosinophil count fell from a median baseline of 1,000 cells/mm3 to 100 cells/mm3 at 6 months (P = .0012). The median annualized rate of exacerbations fell from three per year to one per year, and the median Modified Medical Research Council Dyspnea Scale score fell from 2 to 0 (P = .004).
“There was a steroid-sparing effect in all seven patients who were taking oral corticosteroids at baseline. Five stopped oral steroids completely,” Dr. Rademacher reported.
A visual analog scale ranging from 1 to 10 with higher scores representing improvement showed patient-rated quality of life improved from 4 to 6.5 (P = .01). Dr. Rademacher emphasized this outcome because “improved quality of life is really what we are trying to achieve.”
Mepolizumab was well tolerated. In one patient who developed pneumonia, mepolizumab was discontinued, but it was restarted when the infection resolved, because the pneumonia was not considered mepolizumab related.
Although Dr. Rademacher acknowledged the possibility that at least some of the patients in this case series had overlapping asthma, she emphasized that they were selected from a referral population that had a comprehensive workup and that this overlap has been rarely reported.
There is evidence that anti–interleukin-5 therapies such as mepolizumab are effective in respiratory diseases when eosinophilia is present, according to Dr. Rademacher. For example, she cited reports of clinical improvement in chronic obstructive pulmonary disease and granulomatosis with polyangiitis patients with high eosinophil counts. In bronchiectasis, which has many causes, it may be particularly important to select relevant targets.
“There is an important variability in the presentation of bronchiectasis. Not all these patients have reduced lung function,” she said. Rather, the most significant symptoms for a patient may be sputum or cough. She suggested that the goals are to identify underlying causes of symptoms and which may be treatable.
According to these data, eosinophilia may be one of the treatable causes in a small but significant proportion of patients with bronchiectasis. A trial of mepolizumab may be reasonable in patients inadequately controlled on inhaled anti-inflammatory drugs. “If they do not profit from this therapy, then stop,” she added.
Dr. Rademacher acknowledged that data from this small case series are “not enough to say that [mepolizumab] is an option for these patients,” but she believes the consistency of benefit in this small series will encourage the trials needed to confirm that this approach is safe and effective.
Dr. Rademacher reported no disclosures relevant to the report.
PARIS – according to a small case series of patients presented as a late-breaking study at the annual congress of the European Respiratory Society.
“The message is that it is important to think of all of the etiologies and treatable traits in patients with bronchiectasis, and do not forget eosinophilia, because this can be treated,” reported Jessica Rademacher, MD, of the Clinic for Pulmonology at Hannover (Germany) Medical School.
Mepolizumab is a monoclonal antibody that targets interleukin-5, an important signaling protein for eosinophil recruitment, and is approved for use in asthma with eosinophilia. Larger, controlled trials are needed to confirm its efficacy in bronchiectasis, but the clinical improvements after 6 months of treatment in a series of 12 patients at Dr. Rademacher’s center were impressive.
Bronchiectasis patients were selected for treatment with mepolizumab if they had been poorly controlled on conventional therapies and they had an eosinophil count of greater than 300 cells/mm3. Of 328 patients with bronchiectasis that are being followed at Dr. Rademacher’s center, 7% met these criteria. Dr. Rademacher presented data on 12 who had been followed for at least 6 months.
In these patients, the median eosinophil count fell from a median baseline of 1,000 cells/mm3 to 100 cells/mm3 at 6 months (P = .0012). The median annualized rate of exacerbations fell from three per year to one per year, and the median Modified Medical Research Council Dyspnea Scale score fell from 2 to 0 (P = .004).
“There was a steroid-sparing effect in all seven patients who were taking oral corticosteroids at baseline. Five stopped oral steroids completely,” Dr. Rademacher reported.
A visual analog scale ranging from 1 to 10 with higher scores representing improvement showed patient-rated quality of life improved from 4 to 6.5 (P = .01). Dr. Rademacher emphasized this outcome because “improved quality of life is really what we are trying to achieve.”
Mepolizumab was well tolerated. In one patient who developed pneumonia, mepolizumab was discontinued, but it was restarted when the infection resolved, because the pneumonia was not considered mepolizumab related.
Although Dr. Rademacher acknowledged the possibility that at least some of the patients in this case series had overlapping asthma, she emphasized that they were selected from a referral population that had a comprehensive workup and that this overlap has been rarely reported.
There is evidence that anti–interleukin-5 therapies such as mepolizumab are effective in respiratory diseases when eosinophilia is present, according to Dr. Rademacher. For example, she cited reports of clinical improvement in chronic obstructive pulmonary disease and granulomatosis with polyangiitis patients with high eosinophil counts. In bronchiectasis, which has many causes, it may be particularly important to select relevant targets.
“There is an important variability in the presentation of bronchiectasis. Not all these patients have reduced lung function,” she said. Rather, the most significant symptoms for a patient may be sputum or cough. She suggested that the goals are to identify underlying causes of symptoms and which may be treatable.
According to these data, eosinophilia may be one of the treatable causes in a small but significant proportion of patients with bronchiectasis. A trial of mepolizumab may be reasonable in patients inadequately controlled on inhaled anti-inflammatory drugs. “If they do not profit from this therapy, then stop,” she added.
Dr. Rademacher acknowledged that data from this small case series are “not enough to say that [mepolizumab] is an option for these patients,” but she believes the consistency of benefit in this small series will encourage the trials needed to confirm that this approach is safe and effective.
Dr. Rademacher reported no disclosures relevant to the report.
REPORTING FROM THE Ers congress 2018
Key clinical point: Although tested in a small case series, mepolizumab was highly effective for bronchiectasis presenting with eosinophilia.
Major finding: At 6 months, the median Modified Medical Research Council Dyspnea Scale score decreased from 2 at baseline to 0 (P = .004).
Study details: A case series of 12 patients from a single center.
Disclosures: Dr. Rademacher reported no financial relationships relevant to this report.
Macitentan brought down arterial pressure in PoPH trial
PARIS – In a multicenter, placebo-controlled including the primary endpoint of pulmonary vascular resistance, according to a late-breaking presentation at the annual congress of the European Respiratory Society.
“This is the first randomized, controlled trial that enrolled only patients with PoPH, and it demonstrates that a therapy used in pulmonary arterial hypertension improves hemodynamics in PoPH,” reported Olivier Sitbon, MD, of the Centre des Maladies Vasculaires Pulmonaires, Université de Paris–Sud, Clamart, France.
PoPH, defined by accompanying portal hypertension, is a variant on pulmonary arterial hypertension (PAH). Liver dysfunction is common but not required for a diagnosis. Although patients often receive therapies known to be effective in PAH, such as drugs in the endothelin receptor antagonist class, prostanoids, or phosphodiesterase-5 inhibitors, there “are very limited data” demonstrating efficacy of any drug specifically for patients with PoPH, according to Dr. Sitbon. One reason is that PoPH has been an exclusion criterion in large PAH treatment trials.
In PORTICO, a double-blind trial presented by Dr. Sitbon, 85 PoPH patients were randomized to 10 mg macitentan or placebo. Essentially, all were in World Health Organization functional class II or III with a median 6-minute walk distance (6MWD) of about 385 meters. During the trial, patients were permitted to remain on baseline therapies, including prostanoids and phosphodiesterase-5 inhibitors when doses had been stable for at least 3 months prior to randomization.
The primary endpoint was change in pulmonary vascular resistance (PVR) at 12 weeks. Other hemodynamic changes, such as change in cardiac index and total pulmonary resistance, were included in secondary endpoints along with change in WHO class and change in 6MWD.
When compared at 12 weeks with a model-adjusted ratio of geometric means, the ratio of PVR for the treatment to experimental arms was 0.65, which was a 35% relative improvement (P less than .0001) with macitentan.
The relative reduction from baseline in total arterial pressure was also highly significant favoring macitentan (–199.8 vs. –18.3 dyne/sec per cm–5; P less than .0001). Mean pulmonary pressure was slightly increased at the end of 12 weeks relative to baseline in the placebo group (+0.4 mm Hg) but fell 6.4 mm Hg in the treatment group (P less than .0001). In addition, cardiac index improved substantially on macitentan but not on placebo (0.6 vs. 0.1 L/min per m2; P = .0009).
However, there were no significant differences at the end of 12 weeks between groups for change from baseline in WHO functional class or 6MWD. Change in hepatic venous pressure gradient was evaluated in patients with liver disease, but macitentan was not associated with any effect on this parameter.
Macitentan was well tolerated overall. Although one patient experienced a equal to or greater than three times the upper limit of normal elevation of liver enzymes, Dr. Sitbon reported that there were no other hepatic safety concerns. Overall, he characterized the safety of macitentan in PoPH as “consistent with that previously observed in PAH.”
Larger and longer-term trials are needed to evaluate the impact of treatment on clinical events, but Dr. Sitbon indicated that these results demonstrate acceptable safety and tolerability and a favorable effect on hemodynamics. He further suggested that this randomized study provides a first step toward establishing an evidence-based treatment in this disease.
Dr. Sitbon reported financial relationships with Bayer, GlaxoSmithKline, and Actelion, the sponsor of this trial.
PARIS – In a multicenter, placebo-controlled including the primary endpoint of pulmonary vascular resistance, according to a late-breaking presentation at the annual congress of the European Respiratory Society.
“This is the first randomized, controlled trial that enrolled only patients with PoPH, and it demonstrates that a therapy used in pulmonary arterial hypertension improves hemodynamics in PoPH,” reported Olivier Sitbon, MD, of the Centre des Maladies Vasculaires Pulmonaires, Université de Paris–Sud, Clamart, France.
PoPH, defined by accompanying portal hypertension, is a variant on pulmonary arterial hypertension (PAH). Liver dysfunction is common but not required for a diagnosis. Although patients often receive therapies known to be effective in PAH, such as drugs in the endothelin receptor antagonist class, prostanoids, or phosphodiesterase-5 inhibitors, there “are very limited data” demonstrating efficacy of any drug specifically for patients with PoPH, according to Dr. Sitbon. One reason is that PoPH has been an exclusion criterion in large PAH treatment trials.
In PORTICO, a double-blind trial presented by Dr. Sitbon, 85 PoPH patients were randomized to 10 mg macitentan or placebo. Essentially, all were in World Health Organization functional class II or III with a median 6-minute walk distance (6MWD) of about 385 meters. During the trial, patients were permitted to remain on baseline therapies, including prostanoids and phosphodiesterase-5 inhibitors when doses had been stable for at least 3 months prior to randomization.
The primary endpoint was change in pulmonary vascular resistance (PVR) at 12 weeks. Other hemodynamic changes, such as change in cardiac index and total pulmonary resistance, were included in secondary endpoints along with change in WHO class and change in 6MWD.
When compared at 12 weeks with a model-adjusted ratio of geometric means, the ratio of PVR for the treatment to experimental arms was 0.65, which was a 35% relative improvement (P less than .0001) with macitentan.
The relative reduction from baseline in total arterial pressure was also highly significant favoring macitentan (–199.8 vs. –18.3 dyne/sec per cm–5; P less than .0001). Mean pulmonary pressure was slightly increased at the end of 12 weeks relative to baseline in the placebo group (+0.4 mm Hg) but fell 6.4 mm Hg in the treatment group (P less than .0001). In addition, cardiac index improved substantially on macitentan but not on placebo (0.6 vs. 0.1 L/min per m2; P = .0009).
However, there were no significant differences at the end of 12 weeks between groups for change from baseline in WHO functional class or 6MWD. Change in hepatic venous pressure gradient was evaluated in patients with liver disease, but macitentan was not associated with any effect on this parameter.
Macitentan was well tolerated overall. Although one patient experienced a equal to or greater than three times the upper limit of normal elevation of liver enzymes, Dr. Sitbon reported that there were no other hepatic safety concerns. Overall, he characterized the safety of macitentan in PoPH as “consistent with that previously observed in PAH.”
Larger and longer-term trials are needed to evaluate the impact of treatment on clinical events, but Dr. Sitbon indicated that these results demonstrate acceptable safety and tolerability and a favorable effect on hemodynamics. He further suggested that this randomized study provides a first step toward establishing an evidence-based treatment in this disease.
Dr. Sitbon reported financial relationships with Bayer, GlaxoSmithKline, and Actelion, the sponsor of this trial.
PARIS – In a multicenter, placebo-controlled including the primary endpoint of pulmonary vascular resistance, according to a late-breaking presentation at the annual congress of the European Respiratory Society.
“This is the first randomized, controlled trial that enrolled only patients with PoPH, and it demonstrates that a therapy used in pulmonary arterial hypertension improves hemodynamics in PoPH,” reported Olivier Sitbon, MD, of the Centre des Maladies Vasculaires Pulmonaires, Université de Paris–Sud, Clamart, France.
PoPH, defined by accompanying portal hypertension, is a variant on pulmonary arterial hypertension (PAH). Liver dysfunction is common but not required for a diagnosis. Although patients often receive therapies known to be effective in PAH, such as drugs in the endothelin receptor antagonist class, prostanoids, or phosphodiesterase-5 inhibitors, there “are very limited data” demonstrating efficacy of any drug specifically for patients with PoPH, according to Dr. Sitbon. One reason is that PoPH has been an exclusion criterion in large PAH treatment trials.
In PORTICO, a double-blind trial presented by Dr. Sitbon, 85 PoPH patients were randomized to 10 mg macitentan or placebo. Essentially, all were in World Health Organization functional class II or III with a median 6-minute walk distance (6MWD) of about 385 meters. During the trial, patients were permitted to remain on baseline therapies, including prostanoids and phosphodiesterase-5 inhibitors when doses had been stable for at least 3 months prior to randomization.
The primary endpoint was change in pulmonary vascular resistance (PVR) at 12 weeks. Other hemodynamic changes, such as change in cardiac index and total pulmonary resistance, were included in secondary endpoints along with change in WHO class and change in 6MWD.
When compared at 12 weeks with a model-adjusted ratio of geometric means, the ratio of PVR for the treatment to experimental arms was 0.65, which was a 35% relative improvement (P less than .0001) with macitentan.
The relative reduction from baseline in total arterial pressure was also highly significant favoring macitentan (–199.8 vs. –18.3 dyne/sec per cm–5; P less than .0001). Mean pulmonary pressure was slightly increased at the end of 12 weeks relative to baseline in the placebo group (+0.4 mm Hg) but fell 6.4 mm Hg in the treatment group (P less than .0001). In addition, cardiac index improved substantially on macitentan but not on placebo (0.6 vs. 0.1 L/min per m2; P = .0009).
However, there were no significant differences at the end of 12 weeks between groups for change from baseline in WHO functional class or 6MWD. Change in hepatic venous pressure gradient was evaluated in patients with liver disease, but macitentan was not associated with any effect on this parameter.
Macitentan was well tolerated overall. Although one patient experienced a equal to or greater than three times the upper limit of normal elevation of liver enzymes, Dr. Sitbon reported that there were no other hepatic safety concerns. Overall, he characterized the safety of macitentan in PoPH as “consistent with that previously observed in PAH.”
Larger and longer-term trials are needed to evaluate the impact of treatment on clinical events, but Dr. Sitbon indicated that these results demonstrate acceptable safety and tolerability and a favorable effect on hemodynamics. He further suggested that this randomized study provides a first step toward establishing an evidence-based treatment in this disease.
Dr. Sitbon reported financial relationships with Bayer, GlaxoSmithKline, and Actelion, the sponsor of this trial.
Key clinical point: Compared with placebo, macitentan improves hemodynamic parameters in patients with portopulmonary hypertension.
Major finding: In a 12-week trial, macitentan reduced pulmonary vascular resistance by 35% (P less than 0.0001).
Study details: A double-blind, multicenter, placebo-controlled trial.
Disclosures: Dr. Sitbon reported financial relationships with Bayer, GlaxoSmithKline, and Actelion, the sponsor of this trial.
Nasal cannula device may be an option for severe COPD
PARIS – As an alternative to noninvasive ventilator devices (NIV), a battery-powered high-flow nasal cannula delivering heated air improves exercise tolerance as measured with the 6-minute walking distance (6MWD), according to a crossover trial presented at the annual congress of the European Respiratory Society.
Not least important, these preliminary results show treatment with the device to be well tolerated, a potential advantage over NIV, according to Ms. Rossi, who cited published studies suggesting up to 35% of patients are intolerant to ambulatory NIV therapy.
In the study, 12 clinically stable COPD patients with a 6MWD of less than 300 m and dyspnea at a low level of exertion were enrolled. In random order on 2 consecutive days, patients were evaluated with the 6MWD test while fitted with the high-flow nasal cannula (HFNC) or while breathing room air.
The HFNC device delivers heated and humidified oxygen, which has been previously shown by the same group to improve oxygen saturation (Respir Med. 2016;118:128-32). In this study, the oxygen fraction (FiO2) of the air delivered by the proprietary HFNC device, marketed under the name AIRVO2 (Fisher & Paykel), was the same as the room air during the control exam.
In both tests, the patients performed the 6MWD while pushing a cart holding the device and the battery power source.
The mean 6MWD was 306 m using HFNC versus 267 m during the control test (P less than .05), even though the mean and nadir blood oxygenation (SpO2) levels were the same. However, the postexertion respiratory rate was significantly lower (P less than .05) when HFNC was used, Ms. Rossi reported. The inspiratory capacity was unchanged.
The improved levels of oxygen saturation (SaO2) demonstrated previously with high flows of humidified oxygen provided the basis for this preliminary crossover study, but a larger multicenter randomized trial was initiated last year. In that study with a planned enrollment of 160 COPD patients, the comparison will be between HFNC and usual oxygen delivered by a venturi mask. The primary outcome of the study, which will be completed early in 2019, is endurance improvement.
“COPD patients with severe dyspnea are frequently unable to achieve a workload that leads to improved exercise tolerance, with a result of reduced daily physical activities,” Ms. Rossi explained. She indicated that the HFNC, which is now being evaluated at several institutions, might be an important alternative to NIV in permitting patients to achieve adequate mobility.
The device is likely to be improved with technological advances, according to Ms. Rossi. She acknowledged that the current battery is heavy and the duration of the charge is relatively short, but she characterized this device as “good fit” for patients with very severe COPD. Only 8% of patients failed to complete this study.
Dr. Rossi reports no financial relationships relevant to this study.
PARIS – As an alternative to noninvasive ventilator devices (NIV), a battery-powered high-flow nasal cannula delivering heated air improves exercise tolerance as measured with the 6-minute walking distance (6MWD), according to a crossover trial presented at the annual congress of the European Respiratory Society.
Not least important, these preliminary results show treatment with the device to be well tolerated, a potential advantage over NIV, according to Ms. Rossi, who cited published studies suggesting up to 35% of patients are intolerant to ambulatory NIV therapy.
In the study, 12 clinically stable COPD patients with a 6MWD of less than 300 m and dyspnea at a low level of exertion were enrolled. In random order on 2 consecutive days, patients were evaluated with the 6MWD test while fitted with the high-flow nasal cannula (HFNC) or while breathing room air.
The HFNC device delivers heated and humidified oxygen, which has been previously shown by the same group to improve oxygen saturation (Respir Med. 2016;118:128-32). In this study, the oxygen fraction (FiO2) of the air delivered by the proprietary HFNC device, marketed under the name AIRVO2 (Fisher & Paykel), was the same as the room air during the control exam.
In both tests, the patients performed the 6MWD while pushing a cart holding the device and the battery power source.
The mean 6MWD was 306 m using HFNC versus 267 m during the control test (P less than .05), even though the mean and nadir blood oxygenation (SpO2) levels were the same. However, the postexertion respiratory rate was significantly lower (P less than .05) when HFNC was used, Ms. Rossi reported. The inspiratory capacity was unchanged.
The improved levels of oxygen saturation (SaO2) demonstrated previously with high flows of humidified oxygen provided the basis for this preliminary crossover study, but a larger multicenter randomized trial was initiated last year. In that study with a planned enrollment of 160 COPD patients, the comparison will be between HFNC and usual oxygen delivered by a venturi mask. The primary outcome of the study, which will be completed early in 2019, is endurance improvement.
“COPD patients with severe dyspnea are frequently unable to achieve a workload that leads to improved exercise tolerance, with a result of reduced daily physical activities,” Ms. Rossi explained. She indicated that the HFNC, which is now being evaluated at several institutions, might be an important alternative to NIV in permitting patients to achieve adequate mobility.
The device is likely to be improved with technological advances, according to Ms. Rossi. She acknowledged that the current battery is heavy and the duration of the charge is relatively short, but she characterized this device as “good fit” for patients with very severe COPD. Only 8% of patients failed to complete this study.
Dr. Rossi reports no financial relationships relevant to this study.
PARIS – As an alternative to noninvasive ventilator devices (NIV), a battery-powered high-flow nasal cannula delivering heated air improves exercise tolerance as measured with the 6-minute walking distance (6MWD), according to a crossover trial presented at the annual congress of the European Respiratory Society.
Not least important, these preliminary results show treatment with the device to be well tolerated, a potential advantage over NIV, according to Ms. Rossi, who cited published studies suggesting up to 35% of patients are intolerant to ambulatory NIV therapy.
In the study, 12 clinically stable COPD patients with a 6MWD of less than 300 m and dyspnea at a low level of exertion were enrolled. In random order on 2 consecutive days, patients were evaluated with the 6MWD test while fitted with the high-flow nasal cannula (HFNC) or while breathing room air.
The HFNC device delivers heated and humidified oxygen, which has been previously shown by the same group to improve oxygen saturation (Respir Med. 2016;118:128-32). In this study, the oxygen fraction (FiO2) of the air delivered by the proprietary HFNC device, marketed under the name AIRVO2 (Fisher & Paykel), was the same as the room air during the control exam.
In both tests, the patients performed the 6MWD while pushing a cart holding the device and the battery power source.
The mean 6MWD was 306 m using HFNC versus 267 m during the control test (P less than .05), even though the mean and nadir blood oxygenation (SpO2) levels were the same. However, the postexertion respiratory rate was significantly lower (P less than .05) when HFNC was used, Ms. Rossi reported. The inspiratory capacity was unchanged.
The improved levels of oxygen saturation (SaO2) demonstrated previously with high flows of humidified oxygen provided the basis for this preliminary crossover study, but a larger multicenter randomized trial was initiated last year. In that study with a planned enrollment of 160 COPD patients, the comparison will be between HFNC and usual oxygen delivered by a venturi mask. The primary outcome of the study, which will be completed early in 2019, is endurance improvement.
“COPD patients with severe dyspnea are frequently unable to achieve a workload that leads to improved exercise tolerance, with a result of reduced daily physical activities,” Ms. Rossi explained. She indicated that the HFNC, which is now being evaluated at several institutions, might be an important alternative to NIV in permitting patients to achieve adequate mobility.
The device is likely to be improved with technological advances, according to Ms. Rossi. She acknowledged that the current battery is heavy and the duration of the charge is relatively short, but she characterized this device as “good fit” for patients with very severe COPD. Only 8% of patients failed to complete this study.
Dr. Rossi reports no financial relationships relevant to this study.
REPORTNG FROM THE ERS CONGRESS 2018
Key clinical point: A battery-powered high-flow nasal cannula device improved the exercise capacity of patients with severe COPD.
Major finding: In a crossover study, the high-flow nasal cannula relative to no device increased mean 6-minute walking distance 39 m (15%).
Study details: Prospective crossover study.
Disclosures: Dr. Rossi reports no financial relationships relevant to this study.
New valve to treat emphysema-related hyperinflation demonstrates efficacy
PARIS – A patients with hyperinflation provides acceptable safety and clinically significant improvement in lung function at 12 months, according to results from a multicenter trial presented as a late-breaker at the annual congress of the European Respiratory Society.
Six-month results have been presented previously, but the 12-month results suggest that lung volume reduction associated with placement of the valves provides “durable effectiveness in appropriately selected hyperinflated emphysema patients,” according to Gerard Criner, MD, chair of the thoracic medicine department at Temple University, Philadelphia.
In this randomized controlled trial, called EMPROVE, 172 emphysema patients with severe dyspnea were randomized in a 2:1 fashion to receive a proprietary endobronchial valve or medical therapy alone. The valve, marketed under the brand name Spiration Valve System (SVS), is currently indicated for the treatment of air leaks after lung surgery.
“The valve serves to block airflow from edematous lungs with the objective of blocking hyperinflation and improving lung function,” Dr. Criner explained. The valves are retrievable, if necessary, with bronchoscopy.
High resolution computed tomography (HRCT) was used to identify emphysema obstruction and target valve placement to the most diseased lobes. The average number of valves placed per patient was slightly less than four. Most of the valves (70%) were placed in an upper lobe.
When reported at 6 months, the responder rate, defined as at least 15% improvement in forced expiratory volume in 1 second (FEV1) was 36.8% and 10% in the SVS and control groups, respectively, a difference of 25.7% that Dr. Criner reported as statistically significant although he did not provide P values. At 12 months, the rates were 37.2% and 5.1%, respectively, demonstrating a persistent effect.
Thoracic adverse events were higher at both 6 months (31% vs. 11.9%) and 12 months (21.4% vs. 10.6%) in the treatment group relative to the control group. At 6 months, pneumothorax, which Dr. Criner characterized as “a recognized marker of target lobe volume reduction,” was the only event that occurred significantly more commonly (14.2% vs. 0%) in the SVS group.
Between 6 and 12 months, there were no pneumothorax events in either arm. The higher numerical rates of thoracic adverse events in the treatment arm were acute exacerbations (13.6% vs. 8.5%) and pneumonia in nontreated lobes (7.8% vs. 2.1%), but these rates were not statistically different.
At 6 months, there was a numerically higher rate of all-cause mortality in the treatment group (5.3% vs. 1.7%) but the rate was numerically lower between 6 and 12 months (2.9% vs. 6.4%). The differences were not significantly different at either time point or overall.
A significant reduction in hyperinflation favoring valve placement was accompanied by improvement in objective measures of lung function, such as FEV1, and dyspnea, as measured with the Modified Medical Research Council (mMRC) Dyspnea Scale, at 6 and 12 months. These improvements translated into persistent quality of life benefits as measured with the St. George Respiratory Questionnaire (SGRQ). At 12 months, the SGRQ changes from baseline were a 5.5-point reduction and a four-point gain in the treatment and control groups, respectively. This absolute difference of 9.5 points is slightly more modest than the 13-point difference at 6 months (–8 vs. +5 points), but demonstrates a durable effect, Dr. Criner reported.
According to Dr. Criner, EMPROVE reinforces the principle that HRCT is effective “for selecting the lobe for therapy and which patients may benefit,” but the most important message from the 12-month results is persistent clinical benefit.
The endobronchial values “provide statistically and clinically meaningful improvements in FEV1, reductions in lobe volume and dyspnea, and improvements in quality of life with an acceptable safety profile,” Dr. Criner reported.
On June 29, 2018, the Food and Drug Administration approved the first endobronchial valve for treatment of emphysema. This valve, marketed under the name Zephyr, was approved on the basis of the pivotal LIBERATE trial, also led by Dr. Criner and published earlier this year (Am J Respir Crit Care Med. 2018 May 22. doi: 10.1164/rccm.201803-0590OC.). The results of EMPROVE are consistent with previous evidence that a one-way valve, by preventing air from entering diseased lobes of patients with emphysema to exacerbate hyperinflation, improves lung function and reduces clinical symptoms.
Dr. Criner reports financial relationships with Olympus, the sponsor of this trial.
PARIS – A patients with hyperinflation provides acceptable safety and clinically significant improvement in lung function at 12 months, according to results from a multicenter trial presented as a late-breaker at the annual congress of the European Respiratory Society.
Six-month results have been presented previously, but the 12-month results suggest that lung volume reduction associated with placement of the valves provides “durable effectiveness in appropriately selected hyperinflated emphysema patients,” according to Gerard Criner, MD, chair of the thoracic medicine department at Temple University, Philadelphia.
In this randomized controlled trial, called EMPROVE, 172 emphysema patients with severe dyspnea were randomized in a 2:1 fashion to receive a proprietary endobronchial valve or medical therapy alone. The valve, marketed under the brand name Spiration Valve System (SVS), is currently indicated for the treatment of air leaks after lung surgery.
“The valve serves to block airflow from edematous lungs with the objective of blocking hyperinflation and improving lung function,” Dr. Criner explained. The valves are retrievable, if necessary, with bronchoscopy.
High resolution computed tomography (HRCT) was used to identify emphysema obstruction and target valve placement to the most diseased lobes. The average number of valves placed per patient was slightly less than four. Most of the valves (70%) were placed in an upper lobe.
When reported at 6 months, the responder rate, defined as at least 15% improvement in forced expiratory volume in 1 second (FEV1) was 36.8% and 10% in the SVS and control groups, respectively, a difference of 25.7% that Dr. Criner reported as statistically significant although he did not provide P values. At 12 months, the rates were 37.2% and 5.1%, respectively, demonstrating a persistent effect.
Thoracic adverse events were higher at both 6 months (31% vs. 11.9%) and 12 months (21.4% vs. 10.6%) in the treatment group relative to the control group. At 6 months, pneumothorax, which Dr. Criner characterized as “a recognized marker of target lobe volume reduction,” was the only event that occurred significantly more commonly (14.2% vs. 0%) in the SVS group.
Between 6 and 12 months, there were no pneumothorax events in either arm. The higher numerical rates of thoracic adverse events in the treatment arm were acute exacerbations (13.6% vs. 8.5%) and pneumonia in nontreated lobes (7.8% vs. 2.1%), but these rates were not statistically different.
At 6 months, there was a numerically higher rate of all-cause mortality in the treatment group (5.3% vs. 1.7%) but the rate was numerically lower between 6 and 12 months (2.9% vs. 6.4%). The differences were not significantly different at either time point or overall.
A significant reduction in hyperinflation favoring valve placement was accompanied by improvement in objective measures of lung function, such as FEV1, and dyspnea, as measured with the Modified Medical Research Council (mMRC) Dyspnea Scale, at 6 and 12 months. These improvements translated into persistent quality of life benefits as measured with the St. George Respiratory Questionnaire (SGRQ). At 12 months, the SGRQ changes from baseline were a 5.5-point reduction and a four-point gain in the treatment and control groups, respectively. This absolute difference of 9.5 points is slightly more modest than the 13-point difference at 6 months (–8 vs. +5 points), but demonstrates a durable effect, Dr. Criner reported.
According to Dr. Criner, EMPROVE reinforces the principle that HRCT is effective “for selecting the lobe for therapy and which patients may benefit,” but the most important message from the 12-month results is persistent clinical benefit.
The endobronchial values “provide statistically and clinically meaningful improvements in FEV1, reductions in lobe volume and dyspnea, and improvements in quality of life with an acceptable safety profile,” Dr. Criner reported.
On June 29, 2018, the Food and Drug Administration approved the first endobronchial valve for treatment of emphysema. This valve, marketed under the name Zephyr, was approved on the basis of the pivotal LIBERATE trial, also led by Dr. Criner and published earlier this year (Am J Respir Crit Care Med. 2018 May 22. doi: 10.1164/rccm.201803-0590OC.). The results of EMPROVE are consistent with previous evidence that a one-way valve, by preventing air from entering diseased lobes of patients with emphysema to exacerbate hyperinflation, improves lung function and reduces clinical symptoms.
Dr. Criner reports financial relationships with Olympus, the sponsor of this trial.
PARIS – A patients with hyperinflation provides acceptable safety and clinically significant improvement in lung function at 12 months, according to results from a multicenter trial presented as a late-breaker at the annual congress of the European Respiratory Society.
Six-month results have been presented previously, but the 12-month results suggest that lung volume reduction associated with placement of the valves provides “durable effectiveness in appropriately selected hyperinflated emphysema patients,” according to Gerard Criner, MD, chair of the thoracic medicine department at Temple University, Philadelphia.
In this randomized controlled trial, called EMPROVE, 172 emphysema patients with severe dyspnea were randomized in a 2:1 fashion to receive a proprietary endobronchial valve or medical therapy alone. The valve, marketed under the brand name Spiration Valve System (SVS), is currently indicated for the treatment of air leaks after lung surgery.
“The valve serves to block airflow from edematous lungs with the objective of blocking hyperinflation and improving lung function,” Dr. Criner explained. The valves are retrievable, if necessary, with bronchoscopy.
High resolution computed tomography (HRCT) was used to identify emphysema obstruction and target valve placement to the most diseased lobes. The average number of valves placed per patient was slightly less than four. Most of the valves (70%) were placed in an upper lobe.
When reported at 6 months, the responder rate, defined as at least 15% improvement in forced expiratory volume in 1 second (FEV1) was 36.8% and 10% in the SVS and control groups, respectively, a difference of 25.7% that Dr. Criner reported as statistically significant although he did not provide P values. At 12 months, the rates were 37.2% and 5.1%, respectively, demonstrating a persistent effect.
Thoracic adverse events were higher at both 6 months (31% vs. 11.9%) and 12 months (21.4% vs. 10.6%) in the treatment group relative to the control group. At 6 months, pneumothorax, which Dr. Criner characterized as “a recognized marker of target lobe volume reduction,” was the only event that occurred significantly more commonly (14.2% vs. 0%) in the SVS group.
Between 6 and 12 months, there were no pneumothorax events in either arm. The higher numerical rates of thoracic adverse events in the treatment arm were acute exacerbations (13.6% vs. 8.5%) and pneumonia in nontreated lobes (7.8% vs. 2.1%), but these rates were not statistically different.
At 6 months, there was a numerically higher rate of all-cause mortality in the treatment group (5.3% vs. 1.7%) but the rate was numerically lower between 6 and 12 months (2.9% vs. 6.4%). The differences were not significantly different at either time point or overall.
A significant reduction in hyperinflation favoring valve placement was accompanied by improvement in objective measures of lung function, such as FEV1, and dyspnea, as measured with the Modified Medical Research Council (mMRC) Dyspnea Scale, at 6 and 12 months. These improvements translated into persistent quality of life benefits as measured with the St. George Respiratory Questionnaire (SGRQ). At 12 months, the SGRQ changes from baseline were a 5.5-point reduction and a four-point gain in the treatment and control groups, respectively. This absolute difference of 9.5 points is slightly more modest than the 13-point difference at 6 months (–8 vs. +5 points), but demonstrates a durable effect, Dr. Criner reported.
According to Dr. Criner, EMPROVE reinforces the principle that HRCT is effective “for selecting the lobe for therapy and which patients may benefit,” but the most important message from the 12-month results is persistent clinical benefit.
The endobronchial values “provide statistically and clinically meaningful improvements in FEV1, reductions in lobe volume and dyspnea, and improvements in quality of life with an acceptable safety profile,” Dr. Criner reported.
On June 29, 2018, the Food and Drug Administration approved the first endobronchial valve for treatment of emphysema. This valve, marketed under the name Zephyr, was approved on the basis of the pivotal LIBERATE trial, also led by Dr. Criner and published earlier this year (Am J Respir Crit Care Med. 2018 May 22. doi: 10.1164/rccm.201803-0590OC.). The results of EMPROVE are consistent with previous evidence that a one-way valve, by preventing air from entering diseased lobes of patients with emphysema to exacerbate hyperinflation, improves lung function and reduces clinical symptoms.
Dr. Criner reports financial relationships with Olympus, the sponsor of this trial.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point: A one-way valve developed for postoperative air leaks was found effective against emphysema-related hyperinflation.
Major finding: At 12 months, the FEV1 response rate (at least a 15% improvement) was observed in 37.2% of valve-treated patients and 5.1% of controls.
Study details: Randomized, multicenter trial.
Disclosures: Dr. Criner reports financial relationships with Olympus, the sponsor of this trial.
Source: European Respiratory Society 2018 International Congress.
Targeted lung denervation for COPD found safe and effective
PARIS – In a sham-controlled randomized trial that enrolled patients with moderate to severe was not only found safe, which was the primary goal of the study, but effective, according to data presented at the annual congress of the European Respiratory Society.
Within the first year of follow-up, “the positive benefit in those randomized to TLD persisted with a more than 50% reduction in the number of patients hospitalized for respiratory complications,” reported Dirk-Jan Slebos, MD, department of lung diseases and tuberculosis, University of Gröningen, the Netherlands.
In this phase 2 trial, called AIRFLOW-2, 82 patients were randomized to receive TLD, which ablates nerves with radiofrequency energy, or a sham procedure. The study enrolled patients with moderate to severe COPD and forced expiratory volume in 1 second of 30%-60% predicted. All patients were treated with the long-acting muscarinic antagonist (LAMA) tiotropium.
The primary endpoint was a composite of respiratory-related adverse events, such as respiratory failure, worsening bronchitis, or worsening dyspnea. Secondary endpoints included serious adverse events of any kind as well as a variety of measures of efficacy, including changes in quality of life as measured with standardized tools such as the St. George’s Respiratory Questionnaire (SGRQ).
Within 6 months of the procedure, 71% of those randomized to the sham procedure and 32% of those treated with TLD experienced one of the predefined respiratory adverse events (P = .0008). At 1 year, 25% of patients in the sham group versus 12% in the TLD group were hospitalized for an exacerbation (P = .039). In addition to achieving greater improvement in several of the individual symptoms, such as dyspnea, those randomized to TLD also achieved numerical improvements in SGRQ scores (–8.3 vs. –3.8) at 12 months.
Gastrointestinal adverse events were more common in the TLD group (15% vs. 5%). Although the higher rate of GI events, which included nausea, bloating, and abdominal discomfort, did not reach statistical significance, it was attributed to off-target exposure of nerves in the GI system to the radiofrequency energy.
“We are improving our imaging process in order to implement additional measures to avoid these nerves,” said Dr. Slebos, who added that this potential risk can be modified. In this study, all of the GI symptoms resolved.
Dr. Slebos emphasized that the 12-month follow-up permitted the study to “confirm that TLD is safe and technically feasible with no late-onset safety signals.” It has set the stage for AIRFLOW-3, a phase 3 trial that is expected to lead to regulatory approval of the catheter if it shows similar safety and efficacy.
The principle of TLD is to deliver energy to ablate parasympathetic pulmonary nerves. The exact mechanism of benefit has not been proved, but it is believed that inhibiting release of acetylcholine that induces smooth muscle constriction has several beneficial downstream effects, including prevention of hyperinflation and reduced mucus production. AIRFLOW-3, like AIRFLOW-2, will evaluate a proprietary catheter developed for this purpose.
“TLD will not replace pharmaceutical therapy. Rather, it appears to have a synergistic effect,” explained Dr. Slebos, who said the procedure is performed on an outpatient basis. The average procedure time for TLD in AIRFLOW-2 was 42 minutes.
The first human study of TLD, also led by Dr. Slebos, was published in 2015. While several subsequent patient series support efficacy and benefit, Daiana Stolz, MD, Clinic for Respiratory Medicine and Pulmonary Cell Research, University of Basel (Switzerland), called the data from this sham-controlled trial “really exciting and important.” However, she said, the larger AIRFLOW-3 trial is needed “to confirm this is an effective and safe treatment.”
Dr. Slebos receives consultancy fees from Aeris Therapeutics, Boston Scientific, Broncus Technologies, CSA Medical. Olympus, Portaero, PulmonX, PneumRx/BTG, and Nuvaira, which provided the funding for this study.
PARIS – In a sham-controlled randomized trial that enrolled patients with moderate to severe was not only found safe, which was the primary goal of the study, but effective, according to data presented at the annual congress of the European Respiratory Society.
Within the first year of follow-up, “the positive benefit in those randomized to TLD persisted with a more than 50% reduction in the number of patients hospitalized for respiratory complications,” reported Dirk-Jan Slebos, MD, department of lung diseases and tuberculosis, University of Gröningen, the Netherlands.
In this phase 2 trial, called AIRFLOW-2, 82 patients were randomized to receive TLD, which ablates nerves with radiofrequency energy, or a sham procedure. The study enrolled patients with moderate to severe COPD and forced expiratory volume in 1 second of 30%-60% predicted. All patients were treated with the long-acting muscarinic antagonist (LAMA) tiotropium.
The primary endpoint was a composite of respiratory-related adverse events, such as respiratory failure, worsening bronchitis, or worsening dyspnea. Secondary endpoints included serious adverse events of any kind as well as a variety of measures of efficacy, including changes in quality of life as measured with standardized tools such as the St. George’s Respiratory Questionnaire (SGRQ).
Within 6 months of the procedure, 71% of those randomized to the sham procedure and 32% of those treated with TLD experienced one of the predefined respiratory adverse events (P = .0008). At 1 year, 25% of patients in the sham group versus 12% in the TLD group were hospitalized for an exacerbation (P = .039). In addition to achieving greater improvement in several of the individual symptoms, such as dyspnea, those randomized to TLD also achieved numerical improvements in SGRQ scores (–8.3 vs. –3.8) at 12 months.
Gastrointestinal adverse events were more common in the TLD group (15% vs. 5%). Although the higher rate of GI events, which included nausea, bloating, and abdominal discomfort, did not reach statistical significance, it was attributed to off-target exposure of nerves in the GI system to the radiofrequency energy.
“We are improving our imaging process in order to implement additional measures to avoid these nerves,” said Dr. Slebos, who added that this potential risk can be modified. In this study, all of the GI symptoms resolved.
Dr. Slebos emphasized that the 12-month follow-up permitted the study to “confirm that TLD is safe and technically feasible with no late-onset safety signals.” It has set the stage for AIRFLOW-3, a phase 3 trial that is expected to lead to regulatory approval of the catheter if it shows similar safety and efficacy.
The principle of TLD is to deliver energy to ablate parasympathetic pulmonary nerves. The exact mechanism of benefit has not been proved, but it is believed that inhibiting release of acetylcholine that induces smooth muscle constriction has several beneficial downstream effects, including prevention of hyperinflation and reduced mucus production. AIRFLOW-3, like AIRFLOW-2, will evaluate a proprietary catheter developed for this purpose.
“TLD will not replace pharmaceutical therapy. Rather, it appears to have a synergistic effect,” explained Dr. Slebos, who said the procedure is performed on an outpatient basis. The average procedure time for TLD in AIRFLOW-2 was 42 minutes.
The first human study of TLD, also led by Dr. Slebos, was published in 2015. While several subsequent patient series support efficacy and benefit, Daiana Stolz, MD, Clinic for Respiratory Medicine and Pulmonary Cell Research, University of Basel (Switzerland), called the data from this sham-controlled trial “really exciting and important.” However, she said, the larger AIRFLOW-3 trial is needed “to confirm this is an effective and safe treatment.”
Dr. Slebos receives consultancy fees from Aeris Therapeutics, Boston Scientific, Broncus Technologies, CSA Medical. Olympus, Portaero, PulmonX, PneumRx/BTG, and Nuvaira, which provided the funding for this study.
PARIS – In a sham-controlled randomized trial that enrolled patients with moderate to severe was not only found safe, which was the primary goal of the study, but effective, according to data presented at the annual congress of the European Respiratory Society.
Within the first year of follow-up, “the positive benefit in those randomized to TLD persisted with a more than 50% reduction in the number of patients hospitalized for respiratory complications,” reported Dirk-Jan Slebos, MD, department of lung diseases and tuberculosis, University of Gröningen, the Netherlands.
In this phase 2 trial, called AIRFLOW-2, 82 patients were randomized to receive TLD, which ablates nerves with radiofrequency energy, or a sham procedure. The study enrolled patients with moderate to severe COPD and forced expiratory volume in 1 second of 30%-60% predicted. All patients were treated with the long-acting muscarinic antagonist (LAMA) tiotropium.
The primary endpoint was a composite of respiratory-related adverse events, such as respiratory failure, worsening bronchitis, or worsening dyspnea. Secondary endpoints included serious adverse events of any kind as well as a variety of measures of efficacy, including changes in quality of life as measured with standardized tools such as the St. George’s Respiratory Questionnaire (SGRQ).
Within 6 months of the procedure, 71% of those randomized to the sham procedure and 32% of those treated with TLD experienced one of the predefined respiratory adverse events (P = .0008). At 1 year, 25% of patients in the sham group versus 12% in the TLD group were hospitalized for an exacerbation (P = .039). In addition to achieving greater improvement in several of the individual symptoms, such as dyspnea, those randomized to TLD also achieved numerical improvements in SGRQ scores (–8.3 vs. –3.8) at 12 months.
Gastrointestinal adverse events were more common in the TLD group (15% vs. 5%). Although the higher rate of GI events, which included nausea, bloating, and abdominal discomfort, did not reach statistical significance, it was attributed to off-target exposure of nerves in the GI system to the radiofrequency energy.
“We are improving our imaging process in order to implement additional measures to avoid these nerves,” said Dr. Slebos, who added that this potential risk can be modified. In this study, all of the GI symptoms resolved.
Dr. Slebos emphasized that the 12-month follow-up permitted the study to “confirm that TLD is safe and technically feasible with no late-onset safety signals.” It has set the stage for AIRFLOW-3, a phase 3 trial that is expected to lead to regulatory approval of the catheter if it shows similar safety and efficacy.
The principle of TLD is to deliver energy to ablate parasympathetic pulmonary nerves. The exact mechanism of benefit has not been proved, but it is believed that inhibiting release of acetylcholine that induces smooth muscle constriction has several beneficial downstream effects, including prevention of hyperinflation and reduced mucus production. AIRFLOW-3, like AIRFLOW-2, will evaluate a proprietary catheter developed for this purpose.
“TLD will not replace pharmaceutical therapy. Rather, it appears to have a synergistic effect,” explained Dr. Slebos, who said the procedure is performed on an outpatient basis. The average procedure time for TLD in AIRFLOW-2 was 42 minutes.
The first human study of TLD, also led by Dr. Slebos, was published in 2015. While several subsequent patient series support efficacy and benefit, Daiana Stolz, MD, Clinic for Respiratory Medicine and Pulmonary Cell Research, University of Basel (Switzerland), called the data from this sham-controlled trial “really exciting and important.” However, she said, the larger AIRFLOW-3 trial is needed “to confirm this is an effective and safe treatment.”
Dr. Slebos receives consultancy fees from Aeris Therapeutics, Boston Scientific, Broncus Technologies, CSA Medical. Olympus, Portaero, PulmonX, PneumRx/BTG, and Nuvaira, which provided the funding for this study.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point: Targeted lung denervation (TLD) in patients with moderate to severe COPD is safe and associated with improved disease control.
Major finding: In 1 year of follow-up, 12% of those treated with TLD versus 25% of sham patients had a severe exacerbation.
Study details: Randomized, sham-controlled trial.
Disclosures: Dr. Slebos receives consultancy fees from Aeris Therapeutics, Boston Scientific, Broncus Technologies, CSA Medical, Olympus, Portaero, PulmonX, PneumRx/BTG, and Nuvaira, which provided the funding for this study.
Source: European Respiratory Society 2018 International Congress.
Point-of-care test for respiratory viruses lowers antibiotic use
Routine testing in the ED is advocated
PARIS – Using a point-of-care test for viral pathogens, hospital admissions were avoided in about a third of emergency department patients with suspected respiratory infection when other clinical signs also suggested a low risk of a bacterial pathogen, according to a single-center experience presented at the annual congress of the European Respiratory Society.
“We found that when patients had point-of-care respiratory viral testing soon after they were admitted to the emergency department, we were able to reduce unnecessary admission and improve bed flow in our center,” reported Kay Roy, MBBS, consultant physician in respiratory medicine, West Hertfordshire (England) Hospital NHS Trust.
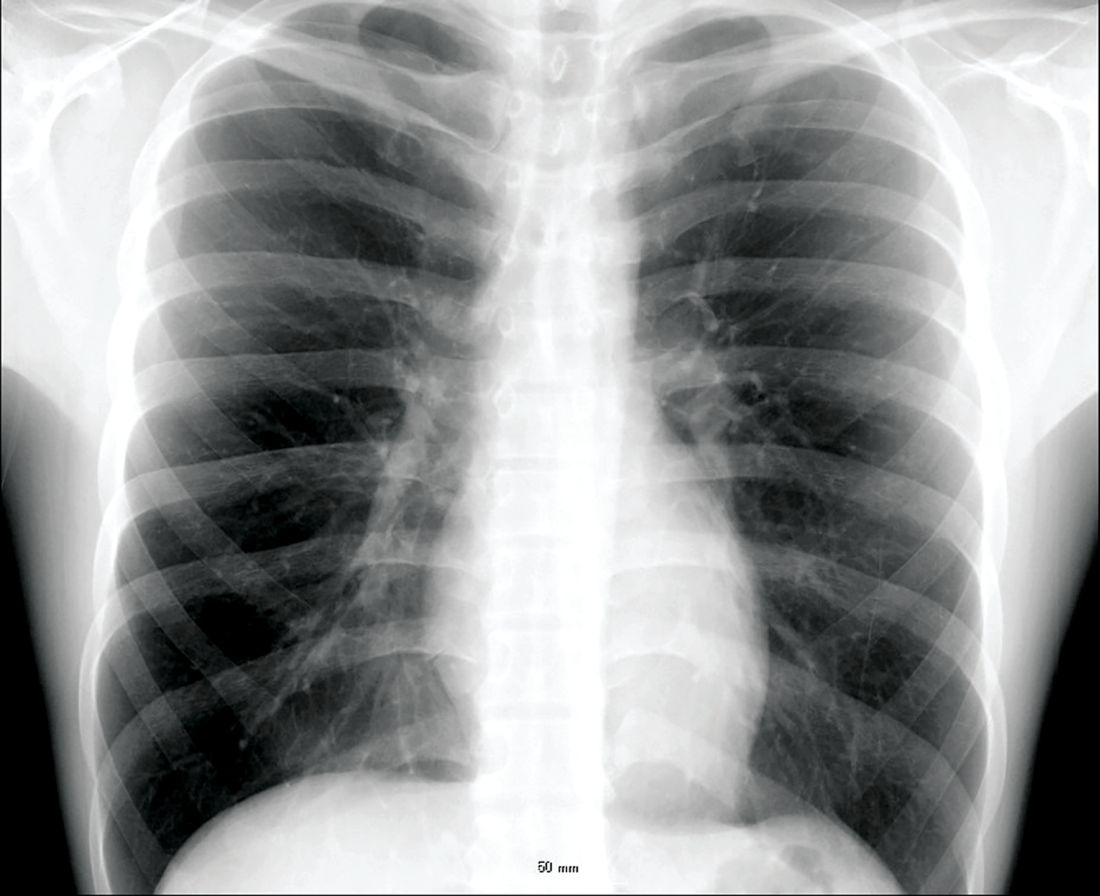
In a protocol that was launched at Dr. Kay’s institution in January 2018, the point-of-care viral test was combined with other clinical factors, particularly chest x-rays and elevated C-reactive protein (CRP), to determine whether patients had a viral pathogen and whether they could be discharged without antibiotics.
“Clinical judgment will always be required in individual patient decisions regarding antibiotic avoidance and early discharge,” Dr. Roy maintained. “But the point-of-care viral assay can be integrated into a strategy that permits more informed and rapid decision-making.”
This assertion is supported by the experience using a protocol anchored with the point-of-care viral test over a 4-month period. During this time, 901 patients with respiratory symptoms suspected of having a viral etiology were evaluated with the proprietary point-of-care device called FilmArray (bioMérieux).
From a sample taken with a nasopharyngeal swab, the test can identify a broad array of viruses using polymerase chain reaction technology in less than 45 minutes. However, the ED protocol for considering discharge without antibiotics requires additional evidence that the pathogen is viral, including a normal chest x-ray and a CRP less than 50 mg/L.
Of the 901 patients tested, a substantial proportion of whom had chronic obstructive pulmonary disease (COPD) or asthma, 507 (56%) tested positive for at least one virus, including influenza, rhinoviruses, coronaviruses, and adenovirus. Of these, 239 had normal chest x-rays and CRPs less than 50 mg/L. Because of the severity of symptoms or other clinical considerations, 154 patients were admitted, but 85 (36% of those meeting protocol criteria) were discharged without an antibiotic prescription.
“Antibiotics were continued in 90% of the patients who had an abnormal chest x-ray and abnormal CRP,” Dr. Roy reported. However, an objective strategy that permits clinicians to discharge patients at very low risk of a bacterial infection has many advantages even if it applies to a relatively modest proportion of those tested, according to Dr. Roy.
“Each respiratory admission can cost around [2,000 pounds] at our center,” reported Dr. Kay, referring to a figure equivalent to more than $2,600. In addition, she said that avoiding hospitalization frees up hospital beds and facilitates improved antimicrobial stewardship, which is vital to stem resistance.
Avoiding antibiotic use in patients with viral respiratory infections also is relevant to improved antibiotic stewardship in the community. For this reason, a randomized trial with a similar protocol involving the point-of-care viral test is planned in the outpatient setting. According to Dr. Roy, this will involve a community hub to which patients can be referred for testing and clinical evaluation.
“We hope that the quality of care can be improved with the point-of-care test for respiratory viruses as well as helping to reduce antibiotic resistance,” Dr. Roy said.
This approach is promising, according to Tobias Welte, MD, of the department of respiratory medicine at Hannover (Germany) Medical School, but he cautioned that it is not a standard approach.
“The protocol described by Dr. Roy will have to be compared to guidelines and recommended best clinical practice to confirm its usefulness,” he said, while conceding that any strategy that reduces unnecessary hospitalizations deserves further evaluation.
Routine testing in the ED is advocated
Routine testing in the ED is advocated
PARIS – Using a point-of-care test for viral pathogens, hospital admissions were avoided in about a third of emergency department patients with suspected respiratory infection when other clinical signs also suggested a low risk of a bacterial pathogen, according to a single-center experience presented at the annual congress of the European Respiratory Society.
“We found that when patients had point-of-care respiratory viral testing soon after they were admitted to the emergency department, we were able to reduce unnecessary admission and improve bed flow in our center,” reported Kay Roy, MBBS, consultant physician in respiratory medicine, West Hertfordshire (England) Hospital NHS Trust.
In a protocol that was launched at Dr. Kay’s institution in January 2018, the point-of-care viral test was combined with other clinical factors, particularly chest x-rays and elevated C-reactive protein (CRP), to determine whether patients had a viral pathogen and whether they could be discharged without antibiotics.
“Clinical judgment will always be required in individual patient decisions regarding antibiotic avoidance and early discharge,” Dr. Roy maintained. “But the point-of-care viral assay can be integrated into a strategy that permits more informed and rapid decision-making.”
This assertion is supported by the experience using a protocol anchored with the point-of-care viral test over a 4-month period. During this time, 901 patients with respiratory symptoms suspected of having a viral etiology were evaluated with the proprietary point-of-care device called FilmArray (bioMérieux).
From a sample taken with a nasopharyngeal swab, the test can identify a broad array of viruses using polymerase chain reaction technology in less than 45 minutes. However, the ED protocol for considering discharge without antibiotics requires additional evidence that the pathogen is viral, including a normal chest x-ray and a CRP less than 50 mg/L.
Of the 901 patients tested, a substantial proportion of whom had chronic obstructive pulmonary disease (COPD) or asthma, 507 (56%) tested positive for at least one virus, including influenza, rhinoviruses, coronaviruses, and adenovirus. Of these, 239 had normal chest x-rays and CRPs less than 50 mg/L. Because of the severity of symptoms or other clinical considerations, 154 patients were admitted, but 85 (36% of those meeting protocol criteria) were discharged without an antibiotic prescription.
“Antibiotics were continued in 90% of the patients who had an abnormal chest x-ray and abnormal CRP,” Dr. Roy reported. However, an objective strategy that permits clinicians to discharge patients at very low risk of a bacterial infection has many advantages even if it applies to a relatively modest proportion of those tested, according to Dr. Roy.
“Each respiratory admission can cost around [2,000 pounds] at our center,” reported Dr. Kay, referring to a figure equivalent to more than $2,600. In addition, she said that avoiding hospitalization frees up hospital beds and facilitates improved antimicrobial stewardship, which is vital to stem resistance.
Avoiding antibiotic use in patients with viral respiratory infections also is relevant to improved antibiotic stewardship in the community. For this reason, a randomized trial with a similar protocol involving the point-of-care viral test is planned in the outpatient setting. According to Dr. Roy, this will involve a community hub to which patients can be referred for testing and clinical evaluation.
“We hope that the quality of care can be improved with the point-of-care test for respiratory viruses as well as helping to reduce antibiotic resistance,” Dr. Roy said.
This approach is promising, according to Tobias Welte, MD, of the department of respiratory medicine at Hannover (Germany) Medical School, but he cautioned that it is not a standard approach.
“The protocol described by Dr. Roy will have to be compared to guidelines and recommended best clinical practice to confirm its usefulness,” he said, while conceding that any strategy that reduces unnecessary hospitalizations deserves further evaluation.
PARIS – Using a point-of-care test for viral pathogens, hospital admissions were avoided in about a third of emergency department patients with suspected respiratory infection when other clinical signs also suggested a low risk of a bacterial pathogen, according to a single-center experience presented at the annual congress of the European Respiratory Society.
“We found that when patients had point-of-care respiratory viral testing soon after they were admitted to the emergency department, we were able to reduce unnecessary admission and improve bed flow in our center,” reported Kay Roy, MBBS, consultant physician in respiratory medicine, West Hertfordshire (England) Hospital NHS Trust.
In a protocol that was launched at Dr. Kay’s institution in January 2018, the point-of-care viral test was combined with other clinical factors, particularly chest x-rays and elevated C-reactive protein (CRP), to determine whether patients had a viral pathogen and whether they could be discharged without antibiotics.
“Clinical judgment will always be required in individual patient decisions regarding antibiotic avoidance and early discharge,” Dr. Roy maintained. “But the point-of-care viral assay can be integrated into a strategy that permits more informed and rapid decision-making.”
This assertion is supported by the experience using a protocol anchored with the point-of-care viral test over a 4-month period. During this time, 901 patients with respiratory symptoms suspected of having a viral etiology were evaluated with the proprietary point-of-care device called FilmArray (bioMérieux).
From a sample taken with a nasopharyngeal swab, the test can identify a broad array of viruses using polymerase chain reaction technology in less than 45 minutes. However, the ED protocol for considering discharge without antibiotics requires additional evidence that the pathogen is viral, including a normal chest x-ray and a CRP less than 50 mg/L.
Of the 901 patients tested, a substantial proportion of whom had chronic obstructive pulmonary disease (COPD) or asthma, 507 (56%) tested positive for at least one virus, including influenza, rhinoviruses, coronaviruses, and adenovirus. Of these, 239 had normal chest x-rays and CRPs less than 50 mg/L. Because of the severity of symptoms or other clinical considerations, 154 patients were admitted, but 85 (36% of those meeting protocol criteria) were discharged without an antibiotic prescription.
“Antibiotics were continued in 90% of the patients who had an abnormal chest x-ray and abnormal CRP,” Dr. Roy reported. However, an objective strategy that permits clinicians to discharge patients at very low risk of a bacterial infection has many advantages even if it applies to a relatively modest proportion of those tested, according to Dr. Roy.
“Each respiratory admission can cost around [2,000 pounds] at our center,” reported Dr. Kay, referring to a figure equivalent to more than $2,600. In addition, she said that avoiding hospitalization frees up hospital beds and facilitates improved antimicrobial stewardship, which is vital to stem resistance.
Avoiding antibiotic use in patients with viral respiratory infections also is relevant to improved antibiotic stewardship in the community. For this reason, a randomized trial with a similar protocol involving the point-of-care viral test is planned in the outpatient setting. According to Dr. Roy, this will involve a community hub to which patients can be referred for testing and clinical evaluation.
“We hope that the quality of care can be improved with the point-of-care test for respiratory viruses as well as helping to reduce antibiotic resistance,” Dr. Roy said.
This approach is promising, according to Tobias Welte, MD, of the department of respiratory medicine at Hannover (Germany) Medical School, but he cautioned that it is not a standard approach.
“The protocol described by Dr. Roy will have to be compared to guidelines and recommended best clinical practice to confirm its usefulness,” he said, while conceding that any strategy that reduces unnecessary hospitalizations deserves further evaluation.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point:
Major finding: Of patients with a negative chest x-ray and low CRP level, 36% avoided hospital admission due to a positive test for a virus.
Study details: A case series.
Disclosures: Dr. Roy reports no financial relationships relevant to this study.
Troponin I: Powerful all-cause mortality risk marker in COPD
PARIS – High relative even after researchers adjusted for all major cardiovascular and COPD prognostic indicators, according to a late-breaker presentation at the annual congress of the European Respiratory Society.
Troponin I is detectable in the plasma of most patients with COPD, but relative increases in troponin I correlate with greater relative increases in most cardiovascular and COPD risk factors, according to Benjamin Waschki, MD, Pulmonary Research Institute, LungenClinic, Grosshansdorf, Germany.
The relationship between increased troponin I and increased all-cause mortality was observed in an on-going prospective multicenter cohort of COPD patients followed at 31 centers in Germany. The cohort is called COSYCONET and it began in 2010. The current analysis evaluated 2,020 COPD patients without regard to stage of disease.
There were 136 deaths over the course of follow-up. Without adjustment, the hazard ratio (HR) for death was more than twofold higher in the highest quartile of troponin I (equal to or greater than 6.6 ng/mL), when compared with the lowest (under 2.5 ng/mL) (HR, 2.42; P less than .001). Graphically, the mortality curves for each of the quartiles began to separate at about 12 months, widening in a stepwise manner for greater likelihood of death from the lowest to highest quartiles.
The risk of death from any cause remained elevated for the highest relative to lowest troponin I quartiles after adjusting for cardiovascular risk factors and after adjusting for COPD severity. Again, there was a distinct stepwise separation of the mortality curves for each higher troponin quartile,
Of particular importance, troponin I remained predictive beyond the BODE index, which is a currently employed prognostic mortality predictor in COPD, according to Dr. Waschki. When defining elevated troponin as greater than 6 ng/ML and a high BODE score as greater than 4, mortality was higher for those with a high BODE and low troponin than a high troponin and low BODE, (P less than .001), but a high troponin I was associated with a higher risk of mortality when BODE was low (P less than .001). Moreover, when both troponin I and BODE were elevated, all-cause mortality was more than doubled, relative to those without either risk factor (HR, 2.56; P = .003), Dr. Waschki reported.
After researchers adjusted for major cardiovascular risk factors, such as history of MI and renal impairment, and for major COPD risk factors, such as 6-minute walk test and BODE index, those in the highest quartile had a more than 50% greater risk of death relative to those in the lower quartile over the 3 years of follow-up (HR, 1.69; P = .007), according to Dr. Waschki.
Although troponin I is best known for its diagnostic role in MI, it is now being evaluated as a risk stratifier for many chronic diseases, such as heart failure and chronic kidney disease, explained Dr. Waschki in providing background for this study. He reported that many groups are looking at this as a marker of risk in a variety of chronic diseases.
In fact, a group working independently published a study in COPD just weeks before the ERS Congress that was complementary to those presented by Dr. Waschki. In this study, the goal was to evaluate troponin I as a predictor of cardiovascular events and cardiovascular death (Adamson PD et al. J Am Coll Cardiol 2018;72:1126-37). Performed as a subgroup analysis of 1,599 COPD patients participating in a large treatment trial, there was an almost fourfold increase in the risk of cardiovascular events (HR, 3.7; P = .012) when those in the highest quintile of troponin I (greater than 7.7 ng/ML) were compared with those in the lowest quintile (less than 2.3 ng/mL).
When compared for cardiovascular death, the highest quintile, relative to the lowest quintile, had a more than 20-fold increased risk of cardiovascular death (HR 20.1; P = .005). In the Adamson et al. study, which evaluated inhaled therapies for COPD, treatment response had no impact on troponin I levels or on the risk of cardiovascular events or death.
Based on this study and his own data, Dr. Waschki believes troponin I, which is readily ordered laboratory value, appears to be a useful tool for identifying COPD patients at high risk of death.
“The major message is that after adjusting for all known COPD and cardiovascular risk factors, troponin I remains a significant independent predictor of mortality,” he said.
Dr. Waschki reports no relevant conflicts of interest.
PARIS – High relative even after researchers adjusted for all major cardiovascular and COPD prognostic indicators, according to a late-breaker presentation at the annual congress of the European Respiratory Society.
Troponin I is detectable in the plasma of most patients with COPD, but relative increases in troponin I correlate with greater relative increases in most cardiovascular and COPD risk factors, according to Benjamin Waschki, MD, Pulmonary Research Institute, LungenClinic, Grosshansdorf, Germany.
The relationship between increased troponin I and increased all-cause mortality was observed in an on-going prospective multicenter cohort of COPD patients followed at 31 centers in Germany. The cohort is called COSYCONET and it began in 2010. The current analysis evaluated 2,020 COPD patients without regard to stage of disease.
There were 136 deaths over the course of follow-up. Without adjustment, the hazard ratio (HR) for death was more than twofold higher in the highest quartile of troponin I (equal to or greater than 6.6 ng/mL), when compared with the lowest (under 2.5 ng/mL) (HR, 2.42; P less than .001). Graphically, the mortality curves for each of the quartiles began to separate at about 12 months, widening in a stepwise manner for greater likelihood of death from the lowest to highest quartiles.
The risk of death from any cause remained elevated for the highest relative to lowest troponin I quartiles after adjusting for cardiovascular risk factors and after adjusting for COPD severity. Again, there was a distinct stepwise separation of the mortality curves for each higher troponin quartile,
Of particular importance, troponin I remained predictive beyond the BODE index, which is a currently employed prognostic mortality predictor in COPD, according to Dr. Waschki. When defining elevated troponin as greater than 6 ng/ML and a high BODE score as greater than 4, mortality was higher for those with a high BODE and low troponin than a high troponin and low BODE, (P less than .001), but a high troponin I was associated with a higher risk of mortality when BODE was low (P less than .001). Moreover, when both troponin I and BODE were elevated, all-cause mortality was more than doubled, relative to those without either risk factor (HR, 2.56; P = .003), Dr. Waschki reported.
After researchers adjusted for major cardiovascular risk factors, such as history of MI and renal impairment, and for major COPD risk factors, such as 6-minute walk test and BODE index, those in the highest quartile had a more than 50% greater risk of death relative to those in the lower quartile over the 3 years of follow-up (HR, 1.69; P = .007), according to Dr. Waschki.
Although troponin I is best known for its diagnostic role in MI, it is now being evaluated as a risk stratifier for many chronic diseases, such as heart failure and chronic kidney disease, explained Dr. Waschki in providing background for this study. He reported that many groups are looking at this as a marker of risk in a variety of chronic diseases.
In fact, a group working independently published a study in COPD just weeks before the ERS Congress that was complementary to those presented by Dr. Waschki. In this study, the goal was to evaluate troponin I as a predictor of cardiovascular events and cardiovascular death (Adamson PD et al. J Am Coll Cardiol 2018;72:1126-37). Performed as a subgroup analysis of 1,599 COPD patients participating in a large treatment trial, there was an almost fourfold increase in the risk of cardiovascular events (HR, 3.7; P = .012) when those in the highest quintile of troponin I (greater than 7.7 ng/ML) were compared with those in the lowest quintile (less than 2.3 ng/mL).
When compared for cardiovascular death, the highest quintile, relative to the lowest quintile, had a more than 20-fold increased risk of cardiovascular death (HR 20.1; P = .005). In the Adamson et al. study, which evaluated inhaled therapies for COPD, treatment response had no impact on troponin I levels or on the risk of cardiovascular events or death.
Based on this study and his own data, Dr. Waschki believes troponin I, which is readily ordered laboratory value, appears to be a useful tool for identifying COPD patients at high risk of death.
“The major message is that after adjusting for all known COPD and cardiovascular risk factors, troponin I remains a significant independent predictor of mortality,” he said.
Dr. Waschki reports no relevant conflicts of interest.
PARIS – High relative even after researchers adjusted for all major cardiovascular and COPD prognostic indicators, according to a late-breaker presentation at the annual congress of the European Respiratory Society.
Troponin I is detectable in the plasma of most patients with COPD, but relative increases in troponin I correlate with greater relative increases in most cardiovascular and COPD risk factors, according to Benjamin Waschki, MD, Pulmonary Research Institute, LungenClinic, Grosshansdorf, Germany.
The relationship between increased troponin I and increased all-cause mortality was observed in an on-going prospective multicenter cohort of COPD patients followed at 31 centers in Germany. The cohort is called COSYCONET and it began in 2010. The current analysis evaluated 2,020 COPD patients without regard to stage of disease.
There were 136 deaths over the course of follow-up. Without adjustment, the hazard ratio (HR) for death was more than twofold higher in the highest quartile of troponin I (equal to or greater than 6.6 ng/mL), when compared with the lowest (under 2.5 ng/mL) (HR, 2.42; P less than .001). Graphically, the mortality curves for each of the quartiles began to separate at about 12 months, widening in a stepwise manner for greater likelihood of death from the lowest to highest quartiles.
The risk of death from any cause remained elevated for the highest relative to lowest troponin I quartiles after adjusting for cardiovascular risk factors and after adjusting for COPD severity. Again, there was a distinct stepwise separation of the mortality curves for each higher troponin quartile,
Of particular importance, troponin I remained predictive beyond the BODE index, which is a currently employed prognostic mortality predictor in COPD, according to Dr. Waschki. When defining elevated troponin as greater than 6 ng/ML and a high BODE score as greater than 4, mortality was higher for those with a high BODE and low troponin than a high troponin and low BODE, (P less than .001), but a high troponin I was associated with a higher risk of mortality when BODE was low (P less than .001). Moreover, when both troponin I and BODE were elevated, all-cause mortality was more than doubled, relative to those without either risk factor (HR, 2.56; P = .003), Dr. Waschki reported.
After researchers adjusted for major cardiovascular risk factors, such as history of MI and renal impairment, and for major COPD risk factors, such as 6-minute walk test and BODE index, those in the highest quartile had a more than 50% greater risk of death relative to those in the lower quartile over the 3 years of follow-up (HR, 1.69; P = .007), according to Dr. Waschki.
Although troponin I is best known for its diagnostic role in MI, it is now being evaluated as a risk stratifier for many chronic diseases, such as heart failure and chronic kidney disease, explained Dr. Waschki in providing background for this study. He reported that many groups are looking at this as a marker of risk in a variety of chronic diseases.
In fact, a group working independently published a study in COPD just weeks before the ERS Congress that was complementary to those presented by Dr. Waschki. In this study, the goal was to evaluate troponin I as a predictor of cardiovascular events and cardiovascular death (Adamson PD et al. J Am Coll Cardiol 2018;72:1126-37). Performed as a subgroup analysis of 1,599 COPD patients participating in a large treatment trial, there was an almost fourfold increase in the risk of cardiovascular events (HR, 3.7; P = .012) when those in the highest quintile of troponin I (greater than 7.7 ng/ML) were compared with those in the lowest quintile (less than 2.3 ng/mL).
When compared for cardiovascular death, the highest quintile, relative to the lowest quintile, had a more than 20-fold increased risk of cardiovascular death (HR 20.1; P = .005). In the Adamson et al. study, which evaluated inhaled therapies for COPD, treatment response had no impact on troponin I levels or on the risk of cardiovascular events or death.
Based on this study and his own data, Dr. Waschki believes troponin I, which is readily ordered laboratory value, appears to be a useful tool for identifying COPD patients at high risk of death.
“The major message is that after adjusting for all known COPD and cardiovascular risk factors, troponin I remains a significant independent predictor of mortality,” he said.
Dr. Waschki reports no relevant conflicts of interest.
REPORTING FROM ERS CONGRESS 2018
Key clinical point: Elevated troponin I identifies COPD patients with increased mortality risk independent of all other clinical risk markers.
Major finding: With high troponin I levels, all-cause mortality was increased 69% after researchers adjusted for other risk markers.
Study details: Analysis drawn from on-going multicenter cohort study
Disclosures: Dr. Waschki reports no relevant conflicts of interest.
Global bronchial thermoplasty registry for asthma documents benefits
PARIS – A global registry to track the safety and efficacy of shows benefits comparable to those previously reported in randomized trials, according to 1-year results presented at the annual congress of the European Respiratory Society.
Bronchothermoplasty has been Food and Drug Administration approved since 2010, but joint 2014 guidelines from the ERS and the American Thoracic Society (ATS) recommended that this procedure be restricted to patients participating in a registry, making these findings an important part of an ongoing assessment, according to Alfons Torrego Fernández, MD, of the pulmonology service at Hospital de la Santa Creu i Sant Pau, Barcelona.
The BT Global Registry (BTGR), created at the end of 2014, involves 18 centers in Europe, South Africa, and Australia. Dr. Fernandez provided data on 123 of the 157 patients enrolled by the end of 2016. All had at least 1 year of follow-up.
Compared with the year prior to bronchial thermoplasty, the proportion of patients with severe exacerbations in the year following this procedure fell from 90.3% to 59.6%, a 34% reduction (P less than .001). The proportion of patients requiring oral corticosteroids fell from 47.8% to 23.5%, a reduction of more than 50%.
Relative to the year prior to bronchial thermoplasty, “there was also a reduction in emergency room visits [21.1% vs. 54.6%] and hospitalizations [20.2% vs. 43%] as well as a reduction in the need for asthma maintenance medications,” Dr. Fernandez reported.
On the Asthma Control Questionnaire (ACQ), quality of life (QOL) was improved on average by 1.2 points from the prior year (4.48 vs. 3.26; P less than .05), according to Dr. Fernandez. The proportion of patients who achieved at least a 0.5-point increase in the ACQ, a level that Dr. Fernandez said is considered clinically relevant, was 67.1%.
However, when lung function measures such as forced expiratory volume in one second and fractional exhaled nitric oxide taken 1 year after bronchothermoplasty were compared with the same measures taken prior to this treatment, there was no significant improvement, according to Dr. Fernandez.
Bronchial thermoplasty involves the use of thermal energy delivered through a bronchoscope to reduce airway smooth muscle mass, thereby eliminating a source of airway restriction. Although nearly 70% of severe asthma patients in this BTGR derived an improvement in quality of life, 30% did not. Asked if the registry has provided any insight about who does or does not respond, Dr. Fernandez acknowledged that this is “the key question,” but added that “no specific profile or biomarker” has yet been identified.
“These are early results, but a 2-year follow-up is planned,” he said.
Although the technical aspects of bronchial thermoplasty “are quite well standardized,” Dr. Fernandez acknowledged that there might be a learning curve that favors experienced operators. He reported that outcomes between high- and low-volume centers in BTGR have not yet been compared. However, he maintained that “these results in real-life patients confirm that severe asthma patients can benefit” from this therapy as shown previously in sham-controlled trials.
Dr. Fernandez reported having no conflicts of interest. The registry is funded by Boston Scientific.
PARIS – A global registry to track the safety and efficacy of shows benefits comparable to those previously reported in randomized trials, according to 1-year results presented at the annual congress of the European Respiratory Society.
Bronchothermoplasty has been Food and Drug Administration approved since 2010, but joint 2014 guidelines from the ERS and the American Thoracic Society (ATS) recommended that this procedure be restricted to patients participating in a registry, making these findings an important part of an ongoing assessment, according to Alfons Torrego Fernández, MD, of the pulmonology service at Hospital de la Santa Creu i Sant Pau, Barcelona.
The BT Global Registry (BTGR), created at the end of 2014, involves 18 centers in Europe, South Africa, and Australia. Dr. Fernandez provided data on 123 of the 157 patients enrolled by the end of 2016. All had at least 1 year of follow-up.
Compared with the year prior to bronchial thermoplasty, the proportion of patients with severe exacerbations in the year following this procedure fell from 90.3% to 59.6%, a 34% reduction (P less than .001). The proportion of patients requiring oral corticosteroids fell from 47.8% to 23.5%, a reduction of more than 50%.
Relative to the year prior to bronchial thermoplasty, “there was also a reduction in emergency room visits [21.1% vs. 54.6%] and hospitalizations [20.2% vs. 43%] as well as a reduction in the need for asthma maintenance medications,” Dr. Fernandez reported.
On the Asthma Control Questionnaire (ACQ), quality of life (QOL) was improved on average by 1.2 points from the prior year (4.48 vs. 3.26; P less than .05), according to Dr. Fernandez. The proportion of patients who achieved at least a 0.5-point increase in the ACQ, a level that Dr. Fernandez said is considered clinically relevant, was 67.1%.
However, when lung function measures such as forced expiratory volume in one second and fractional exhaled nitric oxide taken 1 year after bronchothermoplasty were compared with the same measures taken prior to this treatment, there was no significant improvement, according to Dr. Fernandez.
Bronchial thermoplasty involves the use of thermal energy delivered through a bronchoscope to reduce airway smooth muscle mass, thereby eliminating a source of airway restriction. Although nearly 70% of severe asthma patients in this BTGR derived an improvement in quality of life, 30% did not. Asked if the registry has provided any insight about who does or does not respond, Dr. Fernandez acknowledged that this is “the key question,” but added that “no specific profile or biomarker” has yet been identified.
“These are early results, but a 2-year follow-up is planned,” he said.
Although the technical aspects of bronchial thermoplasty “are quite well standardized,” Dr. Fernandez acknowledged that there might be a learning curve that favors experienced operators. He reported that outcomes between high- and low-volume centers in BTGR have not yet been compared. However, he maintained that “these results in real-life patients confirm that severe asthma patients can benefit” from this therapy as shown previously in sham-controlled trials.
Dr. Fernandez reported having no conflicts of interest. The registry is funded by Boston Scientific.
PARIS – A global registry to track the safety and efficacy of shows benefits comparable to those previously reported in randomized trials, according to 1-year results presented at the annual congress of the European Respiratory Society.
Bronchothermoplasty has been Food and Drug Administration approved since 2010, but joint 2014 guidelines from the ERS and the American Thoracic Society (ATS) recommended that this procedure be restricted to patients participating in a registry, making these findings an important part of an ongoing assessment, according to Alfons Torrego Fernández, MD, of the pulmonology service at Hospital de la Santa Creu i Sant Pau, Barcelona.
The BT Global Registry (BTGR), created at the end of 2014, involves 18 centers in Europe, South Africa, and Australia. Dr. Fernandez provided data on 123 of the 157 patients enrolled by the end of 2016. All had at least 1 year of follow-up.
Compared with the year prior to bronchial thermoplasty, the proportion of patients with severe exacerbations in the year following this procedure fell from 90.3% to 59.6%, a 34% reduction (P less than .001). The proportion of patients requiring oral corticosteroids fell from 47.8% to 23.5%, a reduction of more than 50%.
Relative to the year prior to bronchial thermoplasty, “there was also a reduction in emergency room visits [21.1% vs. 54.6%] and hospitalizations [20.2% vs. 43%] as well as a reduction in the need for asthma maintenance medications,” Dr. Fernandez reported.
On the Asthma Control Questionnaire (ACQ), quality of life (QOL) was improved on average by 1.2 points from the prior year (4.48 vs. 3.26; P less than .05), according to Dr. Fernandez. The proportion of patients who achieved at least a 0.5-point increase in the ACQ, a level that Dr. Fernandez said is considered clinically relevant, was 67.1%.
However, when lung function measures such as forced expiratory volume in one second and fractional exhaled nitric oxide taken 1 year after bronchothermoplasty were compared with the same measures taken prior to this treatment, there was no significant improvement, according to Dr. Fernandez.
Bronchial thermoplasty involves the use of thermal energy delivered through a bronchoscope to reduce airway smooth muscle mass, thereby eliminating a source of airway restriction. Although nearly 70% of severe asthma patients in this BTGR derived an improvement in quality of life, 30% did not. Asked if the registry has provided any insight about who does or does not respond, Dr. Fernandez acknowledged that this is “the key question,” but added that “no specific profile or biomarker” has yet been identified.
“These are early results, but a 2-year follow-up is planned,” he said.
Although the technical aspects of bronchial thermoplasty “are quite well standardized,” Dr. Fernandez acknowledged that there might be a learning curve that favors experienced operators. He reported that outcomes between high- and low-volume centers in BTGR have not yet been compared. However, he maintained that “these results in real-life patients confirm that severe asthma patients can benefit” from this therapy as shown previously in sham-controlled trials.
Dr. Fernandez reported having no conflicts of interest. The registry is funded by Boston Scientific.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point: In a global registry, bronchothermoplasty provided improvement in real-world severe asthma consistent with clinical trials.
Major finding: At 1 year, severe asthma exacerbations were reduced 34% (P less than .001) relative to the year before treatment.
Study details: Open-label observational study.
Disclosures: Dr. Fernandez reported having no conflicts of interest. The registry is funded by Boston Scientific.
Sildenafil added to nintedanib offers no benefit in IPF patients
PARIS – Despite the promise of in IPF patients who have significantly impaired gas exchange did not improve quality of life (QOL), according to a randomized trial presented at the annual congress of the European Respiratory Society and simultaneously published in the New England Journal of Medicine (2018 Sep 15. doi: 10.1056/NEJMoa18117).
“Sildenafil and nintedanib in combination were well tolerated, but there was no significant benefit for these two drugs relative to nintedanib alone in patients with IPF and severe gas exchange impairment,” reported Fernando J. Martinez, MD, of the department of internal medicine, Cornell University, New York.In the multicenter INSTAGE trial, 274 IPF patients with impaired gas exchange, defined as diffusing capacity of the lungs for carbon monoxide of 35% or less, were randomized to 20 mg of sildenafil or placebo three times daily. Both groups received 150 mg twice daily of nintedanib, which is approved for the treatment of IPF.
The primary endpoint of the study was change from baseline in the St. George’s Respiratory Questionnaire (SGRQ), a 50-item quality of life (QOL) survey that captures the impact of symptoms on activities and well-being. With lower scores representing improved QOL, Dr. Martinez reported that a change of 4 or more points is considered to be clinically meaningful.
At week 12, the SGRQ score fell by 1.28 points in the group that received sildenafil and by 0.77 points in the group randomized to placebo, a difference that did not approach significance (P = .72). There was also no significant difference after 12 weeks of treatment in dyspnea, a secondary endpoint measured with the University of California, San Diego Shortness of Breath Questionnaire (UCSD-SOBQ).
When both measures were reassessed after 24 weeks of treatment, the slight persistent numerical advantage in the sildenafil arm remained statistically and clinically insignificant, according to Dr. Martinez. Rates of acute exacerbations (7.3% vs. 7.4%) and all-cause mortality (10.2% vs. 11.0%) were also reported to be similar in the experimental and control arms, respectively.
Nintedanib, which has been shown to slow decline in forced vital capacity in patients with IPF, inhibits tyrosine kinases involved in IPF progression. However, it has not been associated with an improvement in QOL in this population.
In contrast, sildenafil, a phosphodiesterase-5 inhibitor that relaxes smooth muscle, has been associated with an improvement in both SGRQ score and in dyspnea in a large IPF trial even though it failed the primary endpoint of an improvement in the 6-minute walk test (N Engl J Med 2010;363:620-28).
The hypothesis of the INSTAGE trial was that combining sildenafil with nintedanib in patients with severely impaired gas exchange might have an additive or synergistic effect for IPF symptom control by providing two distinct mechanisms of action.
This was not seen, according to Dr. Martinez. Although those receiving the combination had “a lower risk of an absolute 5-percentage-point decline in FVC of the predicted value or death than those who received nintedanib alone,” Dr. Martinez said this was not a study endpoint, and was of unclear clinical significance. Rather, although nintedanib and sildenafil were well tolerated when taken together, Dr. Martinez concluded that this trial was unable to show any definitive clinical benefit from this combination.
Dr. Martinez has financial relationships with AstraZeneca, Boehringer-Ingelheim, Cheisi, ConCert, Genentech, GlaxoSmithKline, Inova, Novartis, Roche, Sunovion, Theravance, and Teva.
.
PARIS – Despite the promise of in IPF patients who have significantly impaired gas exchange did not improve quality of life (QOL), according to a randomized trial presented at the annual congress of the European Respiratory Society and simultaneously published in the New England Journal of Medicine (2018 Sep 15. doi: 10.1056/NEJMoa18117).
“Sildenafil and nintedanib in combination were well tolerated, but there was no significant benefit for these two drugs relative to nintedanib alone in patients with IPF and severe gas exchange impairment,” reported Fernando J. Martinez, MD, of the department of internal medicine, Cornell University, New York.In the multicenter INSTAGE trial, 274 IPF patients with impaired gas exchange, defined as diffusing capacity of the lungs for carbon monoxide of 35% or less, were randomized to 20 mg of sildenafil or placebo three times daily. Both groups received 150 mg twice daily of nintedanib, which is approved for the treatment of IPF.
The primary endpoint of the study was change from baseline in the St. George’s Respiratory Questionnaire (SGRQ), a 50-item quality of life (QOL) survey that captures the impact of symptoms on activities and well-being. With lower scores representing improved QOL, Dr. Martinez reported that a change of 4 or more points is considered to be clinically meaningful.
At week 12, the SGRQ score fell by 1.28 points in the group that received sildenafil and by 0.77 points in the group randomized to placebo, a difference that did not approach significance (P = .72). There was also no significant difference after 12 weeks of treatment in dyspnea, a secondary endpoint measured with the University of California, San Diego Shortness of Breath Questionnaire (UCSD-SOBQ).
When both measures were reassessed after 24 weeks of treatment, the slight persistent numerical advantage in the sildenafil arm remained statistically and clinically insignificant, according to Dr. Martinez. Rates of acute exacerbations (7.3% vs. 7.4%) and all-cause mortality (10.2% vs. 11.0%) were also reported to be similar in the experimental and control arms, respectively.
Nintedanib, which has been shown to slow decline in forced vital capacity in patients with IPF, inhibits tyrosine kinases involved in IPF progression. However, it has not been associated with an improvement in QOL in this population.
In contrast, sildenafil, a phosphodiesterase-5 inhibitor that relaxes smooth muscle, has been associated with an improvement in both SGRQ score and in dyspnea in a large IPF trial even though it failed the primary endpoint of an improvement in the 6-minute walk test (N Engl J Med 2010;363:620-28).
The hypothesis of the INSTAGE trial was that combining sildenafil with nintedanib in patients with severely impaired gas exchange might have an additive or synergistic effect for IPF symptom control by providing two distinct mechanisms of action.
This was not seen, according to Dr. Martinez. Although those receiving the combination had “a lower risk of an absolute 5-percentage-point decline in FVC of the predicted value or death than those who received nintedanib alone,” Dr. Martinez said this was not a study endpoint, and was of unclear clinical significance. Rather, although nintedanib and sildenafil were well tolerated when taken together, Dr. Martinez concluded that this trial was unable to show any definitive clinical benefit from this combination.
Dr. Martinez has financial relationships with AstraZeneca, Boehringer-Ingelheim, Cheisi, ConCert, Genentech, GlaxoSmithKline, Inova, Novartis, Roche, Sunovion, Theravance, and Teva.
.
PARIS – Despite the promise of in IPF patients who have significantly impaired gas exchange did not improve quality of life (QOL), according to a randomized trial presented at the annual congress of the European Respiratory Society and simultaneously published in the New England Journal of Medicine (2018 Sep 15. doi: 10.1056/NEJMoa18117).
“Sildenafil and nintedanib in combination were well tolerated, but there was no significant benefit for these two drugs relative to nintedanib alone in patients with IPF and severe gas exchange impairment,” reported Fernando J. Martinez, MD, of the department of internal medicine, Cornell University, New York.In the multicenter INSTAGE trial, 274 IPF patients with impaired gas exchange, defined as diffusing capacity of the lungs for carbon monoxide of 35% or less, were randomized to 20 mg of sildenafil or placebo three times daily. Both groups received 150 mg twice daily of nintedanib, which is approved for the treatment of IPF.
The primary endpoint of the study was change from baseline in the St. George’s Respiratory Questionnaire (SGRQ), a 50-item quality of life (QOL) survey that captures the impact of symptoms on activities and well-being. With lower scores representing improved QOL, Dr. Martinez reported that a change of 4 or more points is considered to be clinically meaningful.
At week 12, the SGRQ score fell by 1.28 points in the group that received sildenafil and by 0.77 points in the group randomized to placebo, a difference that did not approach significance (P = .72). There was also no significant difference after 12 weeks of treatment in dyspnea, a secondary endpoint measured with the University of California, San Diego Shortness of Breath Questionnaire (UCSD-SOBQ).
When both measures were reassessed after 24 weeks of treatment, the slight persistent numerical advantage in the sildenafil arm remained statistically and clinically insignificant, according to Dr. Martinez. Rates of acute exacerbations (7.3% vs. 7.4%) and all-cause mortality (10.2% vs. 11.0%) were also reported to be similar in the experimental and control arms, respectively.
Nintedanib, which has been shown to slow decline in forced vital capacity in patients with IPF, inhibits tyrosine kinases involved in IPF progression. However, it has not been associated with an improvement in QOL in this population.
In contrast, sildenafil, a phosphodiesterase-5 inhibitor that relaxes smooth muscle, has been associated with an improvement in both SGRQ score and in dyspnea in a large IPF trial even though it failed the primary endpoint of an improvement in the 6-minute walk test (N Engl J Med 2010;363:620-28).
The hypothesis of the INSTAGE trial was that combining sildenafil with nintedanib in patients with severely impaired gas exchange might have an additive or synergistic effect for IPF symptom control by providing two distinct mechanisms of action.
This was not seen, according to Dr. Martinez. Although those receiving the combination had “a lower risk of an absolute 5-percentage-point decline in FVC of the predicted value or death than those who received nintedanib alone,” Dr. Martinez said this was not a study endpoint, and was of unclear clinical significance. Rather, although nintedanib and sildenafil were well tolerated when taken together, Dr. Martinez concluded that this trial was unable to show any definitive clinical benefit from this combination.
Dr. Martinez has financial relationships with AstraZeneca, Boehringer-Ingelheim, Cheisi, ConCert, Genentech, GlaxoSmithKline, Inova, Novartis, Roche, Sunovion, Theravance, and Teva.
.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point: Sildenafil does not improve quality of life in patients with idiopathic pulmonary fibrosis who are taking nintedanib.
Major finding: At week 12, the modest QOL benefit with sildenafil plus nintedanib relative to nintedanib alone was statistically insignificant.
Study details: Randomized double-blind multicenter trial.
Disclosures: Dr. Kolb has financial relationships with Alkermes, Actelion, Boehringer-Ingelheim, GlaxoSmithKline, Gilead, Prometic, RespiVert, Roche and Synairgen.
Dupilumab efficacy extends to chronic rhinosinusitis/nasal polyposis
PARIS – Severe asthma patients with chronic rhinosinusitis (CRS), nasal polyposis (NP), or both derive more protection from severe exacerbations with the monoclonal antibody dupilumab than do those who do not have these comorbidities, according to a post hoc analysis of a phase 3 trial presented at the annual congress of the European Respiratory Society.
“Dupilumab reduced rates of severe exacerbations and improved FEV1 [forced expiratory volume in 1 second] in patients in asthma patients with or without CRS/NP. In those with CRS/NP, dupilumab reduced symptoms associated with these comorbidities,” reported Ian Pavord, MBBS, statutory chair in respiratory medicine at University of Oxford (England).
The data were drawn from the phase 3 Liberty Asthma Quest trial, which was published earlier this year in the New England Journal of Medicine (2018;378:2486-96). In that study, both the 200-mg and 300-mg dose of dupilumab (Dupixent) administered every 2 weeks was associated with about a 50% reduction in the annualized rate of severe exacerbations relative to placebo (P less than .001 for both doses).
In this new post hoc analysis, response in the 382 patients who entered the study with a history of CRS/NP was compared with the 1,520 without CRS/NP. In the CRS/NP patients, the reductions relative to placebo in the rates of severe exacerbations, defined as 3 or more days of systemic glucocorticoids or visit to an emergency department leading to treatment with systemic glucocorticoids, were 63% and 61% for the 200-mg and 300-mg doses of dupilumab, respectively (both P less than .001).
In the non-CRS/NP arms, the reductions relative to placebo were 42% and 40%, respectively (both P less than .001). The greater relative reductions in the CRS/NP patients were achieved even though they were older (mean age approximately 52 vs. 47 years for non-CRS/NP patients), had a significantly greater number of exacerbations in the past year (P = .027), and had higher baseline fractional exhaled nitric oxide and eosinophil levels (both P less than .001), Dr. Pavord reported.
“The greater asthma severity in the CRS/NP patients in this trial is consistent with that reported previously by others,” Dr. Pavord said.
Although the greater asthma severity may have provided a larger margin for benefit, Dr. Pavord also reported that there were improvements in CRS/NP-specific symptoms as measured with the 22-item Sino-Nasal Outcome Test (SNOT-22). By week 12, the total score reduction in SNOT-22 was approximately 15 points (P less than .05) from baseline for both the 200-mg and 300-mg dupilumab doses. This was significantly greater (P less than .05) relative to modest SNOT-22 reductions in the placebo arms (P less than .05). After 52 weeks, the reduction In SNOT-22 scores were sustained, providing an even greater statistical advantage over placebo (P less than .001).
In addition to greater protection against severe exacerbations and CRS/NP-specific symptoms, dupilumab may offer specific improvements on CRS/NP pathology, according to Dr. Pavord. Although imaging was not part of this study, he noted in particular that previous studies with dupilumab as well as other biologics have shown shrinkage of nasal polyps with treatment.
Dupilumab was similarly well tolerated in those with and without CRS/NP. The most common adverse event was injection site reactions in both groups, Dr. Pavord said.
Calling CRS and NP “important comorbidities” in severe asthma patients, Dr. Pavord said that this analysis should be reassuring for those who with CRS/NP who are being considered for dupilumab. Already approved for treatment of atopic dermatitis, dupilumab, which binds to interleukin-4 (IL-4) and IL-13 receptors, is currently under review for the treatment of moderate to severe asthma.
Dr. Pavord has financial relationships with Aerocrine, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Knapp, Merck Sharpe, Novartis, Knapp Teva, RespiVert, and Schering-Plough.
PARIS – Severe asthma patients with chronic rhinosinusitis (CRS), nasal polyposis (NP), or both derive more protection from severe exacerbations with the monoclonal antibody dupilumab than do those who do not have these comorbidities, according to a post hoc analysis of a phase 3 trial presented at the annual congress of the European Respiratory Society.
“Dupilumab reduced rates of severe exacerbations and improved FEV1 [forced expiratory volume in 1 second] in patients in asthma patients with or without CRS/NP. In those with CRS/NP, dupilumab reduced symptoms associated with these comorbidities,” reported Ian Pavord, MBBS, statutory chair in respiratory medicine at University of Oxford (England).
The data were drawn from the phase 3 Liberty Asthma Quest trial, which was published earlier this year in the New England Journal of Medicine (2018;378:2486-96). In that study, both the 200-mg and 300-mg dose of dupilumab (Dupixent) administered every 2 weeks was associated with about a 50% reduction in the annualized rate of severe exacerbations relative to placebo (P less than .001 for both doses).
In this new post hoc analysis, response in the 382 patients who entered the study with a history of CRS/NP was compared with the 1,520 without CRS/NP. In the CRS/NP patients, the reductions relative to placebo in the rates of severe exacerbations, defined as 3 or more days of systemic glucocorticoids or visit to an emergency department leading to treatment with systemic glucocorticoids, were 63% and 61% for the 200-mg and 300-mg doses of dupilumab, respectively (both P less than .001).
In the non-CRS/NP arms, the reductions relative to placebo were 42% and 40%, respectively (both P less than .001). The greater relative reductions in the CRS/NP patients were achieved even though they were older (mean age approximately 52 vs. 47 years for non-CRS/NP patients), had a significantly greater number of exacerbations in the past year (P = .027), and had higher baseline fractional exhaled nitric oxide and eosinophil levels (both P less than .001), Dr. Pavord reported.
“The greater asthma severity in the CRS/NP patients in this trial is consistent with that reported previously by others,” Dr. Pavord said.
Although the greater asthma severity may have provided a larger margin for benefit, Dr. Pavord also reported that there were improvements in CRS/NP-specific symptoms as measured with the 22-item Sino-Nasal Outcome Test (SNOT-22). By week 12, the total score reduction in SNOT-22 was approximately 15 points (P less than .05) from baseline for both the 200-mg and 300-mg dupilumab doses. This was significantly greater (P less than .05) relative to modest SNOT-22 reductions in the placebo arms (P less than .05). After 52 weeks, the reduction In SNOT-22 scores were sustained, providing an even greater statistical advantage over placebo (P less than .001).
In addition to greater protection against severe exacerbations and CRS/NP-specific symptoms, dupilumab may offer specific improvements on CRS/NP pathology, according to Dr. Pavord. Although imaging was not part of this study, he noted in particular that previous studies with dupilumab as well as other biologics have shown shrinkage of nasal polyps with treatment.
Dupilumab was similarly well tolerated in those with and without CRS/NP. The most common adverse event was injection site reactions in both groups, Dr. Pavord said.
Calling CRS and NP “important comorbidities” in severe asthma patients, Dr. Pavord said that this analysis should be reassuring for those who with CRS/NP who are being considered for dupilumab. Already approved for treatment of atopic dermatitis, dupilumab, which binds to interleukin-4 (IL-4) and IL-13 receptors, is currently under review for the treatment of moderate to severe asthma.
Dr. Pavord has financial relationships with Aerocrine, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Knapp, Merck Sharpe, Novartis, Knapp Teva, RespiVert, and Schering-Plough.
PARIS – Severe asthma patients with chronic rhinosinusitis (CRS), nasal polyposis (NP), or both derive more protection from severe exacerbations with the monoclonal antibody dupilumab than do those who do not have these comorbidities, according to a post hoc analysis of a phase 3 trial presented at the annual congress of the European Respiratory Society.
“Dupilumab reduced rates of severe exacerbations and improved FEV1 [forced expiratory volume in 1 second] in patients in asthma patients with or without CRS/NP. In those with CRS/NP, dupilumab reduced symptoms associated with these comorbidities,” reported Ian Pavord, MBBS, statutory chair in respiratory medicine at University of Oxford (England).
The data were drawn from the phase 3 Liberty Asthma Quest trial, which was published earlier this year in the New England Journal of Medicine (2018;378:2486-96). In that study, both the 200-mg and 300-mg dose of dupilumab (Dupixent) administered every 2 weeks was associated with about a 50% reduction in the annualized rate of severe exacerbations relative to placebo (P less than .001 for both doses).
In this new post hoc analysis, response in the 382 patients who entered the study with a history of CRS/NP was compared with the 1,520 without CRS/NP. In the CRS/NP patients, the reductions relative to placebo in the rates of severe exacerbations, defined as 3 or more days of systemic glucocorticoids or visit to an emergency department leading to treatment with systemic glucocorticoids, were 63% and 61% for the 200-mg and 300-mg doses of dupilumab, respectively (both P less than .001).
In the non-CRS/NP arms, the reductions relative to placebo were 42% and 40%, respectively (both P less than .001). The greater relative reductions in the CRS/NP patients were achieved even though they were older (mean age approximately 52 vs. 47 years for non-CRS/NP patients), had a significantly greater number of exacerbations in the past year (P = .027), and had higher baseline fractional exhaled nitric oxide and eosinophil levels (both P less than .001), Dr. Pavord reported.
“The greater asthma severity in the CRS/NP patients in this trial is consistent with that reported previously by others,” Dr. Pavord said.
Although the greater asthma severity may have provided a larger margin for benefit, Dr. Pavord also reported that there were improvements in CRS/NP-specific symptoms as measured with the 22-item Sino-Nasal Outcome Test (SNOT-22). By week 12, the total score reduction in SNOT-22 was approximately 15 points (P less than .05) from baseline for both the 200-mg and 300-mg dupilumab doses. This was significantly greater (P less than .05) relative to modest SNOT-22 reductions in the placebo arms (P less than .05). After 52 weeks, the reduction In SNOT-22 scores were sustained, providing an even greater statistical advantage over placebo (P less than .001).
In addition to greater protection against severe exacerbations and CRS/NP-specific symptoms, dupilumab may offer specific improvements on CRS/NP pathology, according to Dr. Pavord. Although imaging was not part of this study, he noted in particular that previous studies with dupilumab as well as other biologics have shown shrinkage of nasal polyps with treatment.
Dupilumab was similarly well tolerated in those with and without CRS/NP. The most common adverse event was injection site reactions in both groups, Dr. Pavord said.
Calling CRS and NP “important comorbidities” in severe asthma patients, Dr. Pavord said that this analysis should be reassuring for those who with CRS/NP who are being considered for dupilumab. Already approved for treatment of atopic dermatitis, dupilumab, which binds to interleukin-4 (IL-4) and IL-13 receptors, is currently under review for the treatment of moderate to severe asthma.
Dr. Pavord has financial relationships with Aerocrine, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Knapp, Merck Sharpe, Novartis, Knapp Teva, RespiVert, and Schering-Plough.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point: In asthma patients with chronic rhinosinusitis and/or nasal polyposis (CRS/NP), dupilumab reduces exacerbations.
Major finding: At 52 weeks, severe exacerbations were reduced 61% in CRS/NP patients and 40% in non-CRS/NP patients (both P less than .001).
Study details: Post hoc analysis of phase 3 trial.
Disclosures: Dr. Pavord has financial relationships with Aerocrine, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Knapp, Merck Sharpe, Novartis, Knapp Teva, RespiVert, and Schering-Plough.