User login
For some SUD patients, kratom may be a self-treatment tool
SAN DIEGO – New research suggests that some patients with substance use disorder are turning to the herbal supplement kratom in an effort to reduce their use of heroin and prescription pain killers.
“Some, but not all, heroin users are utilizing kratom as an opioidlike drug with less risks, primarily as a drug substitute or to help abstain from IV heroin and prescription opiate use,” lead author Kirsten Elin Smith, a PhD student at the University of Louisville and an associate at the University of Kentucky’s Center on Drug and Alcohol Research, said in an interview. “Kratom appears as less risky due to the fact that it is not readily injectable.”
Kratom, a plant-based herbal product that’s available over the counter, produces an opioidlike effect. When the Food and Drug Administration declared in February 2018 that scientific evidence shows that kratom indeed is an opioid, the agency also warned that the drug could lead to abuse, addiction, and death. Several U.S. states and the District of Columbia have banned it, as have some cities and counties. In addition, the Drug Enforcement Administration has put kratom on its list of Drugs and Chemicals of Concern.
Nevertheless, some substance users view kratom as helpful and are open to using it, Ms. Smith and her colleagues reported in Drug and Alcohol Dependence.
“There seem to be three categories of substance-using individuals with some relationship to kratom: Those who use kratom inconsistently and as needed when there isn’t an alternative, those who tried it once and just didn’t find much benefit in it, and didn’t try it again, and those who have been using it regularly/daily as a long-term replacement for opioids, including IV heroin use,” Ms. Smith said.
For the new research, Ms. Smith and her colleagues surveyed 478 polysubstance users at five residential recovery centers in Kentucky. The average age of subjects was 35, 58% were male, 85% were white, and 48% were employed. About 85% of the participants were referred to programs by correctional facilities. Twenty-one percent reported ever using kratom, and 10% reported use within the last 12 months.
What do the findings mean? Along with anecdotal reports now being documented, they suggest the use of kratom by heroin users as a “possible harm-reduction” aid, Ms. Smith said at the meeting.
“These men and women are not necessarily getting kratom on a Friday night and saying, ‘This is going to be a great time.’ ” In the interview, she added that “this shows that substance-using individuals are, above all else, pragmatic.”
“It is unlikely that the majority of these users are consuming kratom primarily for achieving recreational ‘highs,’ ” Ms. Smith and her colleagues wrote in the article.
She added during her presentation that kratom is inexpensive and primarily legal. “If it were going to catch on as a serious drug of abuse, we would have expected to have a kratom epidemic already – but we do not.”
As for the big picture, Ms. Smith said in the interview that
Going forward, Ms. Smith said, she and a colleague plan to document the lives of regular kratom users in an effort to understand the progression from heroin and other drugs to kratom. They also want to know what the users would do if kratom is banned.
“These will be case studies in Kentucky, New Mexico, and possibly somewhere in the Northeast,” she said. “Since data will be collected locally, I think it would be helpful to try and obtain samples of kratom that the individuals report using so it can be analyzed. There may be variation between kratom purchased online vs. local vendors, which needs to be documented as well.”
Ms. Smith reported funding from the University of Louisville Graduate Student Research Fund, and another author was supported by the National Institute on Drug Abuse. The authors reported no relevant disclosures.
SOURCE: Smith KE et al. CPDD 2018. Drug and Alcohol Depend. 2017 Nov 1. 180:340-8.
SAN DIEGO – New research suggests that some patients with substance use disorder are turning to the herbal supplement kratom in an effort to reduce their use of heroin and prescription pain killers.
“Some, but not all, heroin users are utilizing kratom as an opioidlike drug with less risks, primarily as a drug substitute or to help abstain from IV heroin and prescription opiate use,” lead author Kirsten Elin Smith, a PhD student at the University of Louisville and an associate at the University of Kentucky’s Center on Drug and Alcohol Research, said in an interview. “Kratom appears as less risky due to the fact that it is not readily injectable.”
Kratom, a plant-based herbal product that’s available over the counter, produces an opioidlike effect. When the Food and Drug Administration declared in February 2018 that scientific evidence shows that kratom indeed is an opioid, the agency also warned that the drug could lead to abuse, addiction, and death. Several U.S. states and the District of Columbia have banned it, as have some cities and counties. In addition, the Drug Enforcement Administration has put kratom on its list of Drugs and Chemicals of Concern.
Nevertheless, some substance users view kratom as helpful and are open to using it, Ms. Smith and her colleagues reported in Drug and Alcohol Dependence.
“There seem to be three categories of substance-using individuals with some relationship to kratom: Those who use kratom inconsistently and as needed when there isn’t an alternative, those who tried it once and just didn’t find much benefit in it, and didn’t try it again, and those who have been using it regularly/daily as a long-term replacement for opioids, including IV heroin use,” Ms. Smith said.
For the new research, Ms. Smith and her colleagues surveyed 478 polysubstance users at five residential recovery centers in Kentucky. The average age of subjects was 35, 58% were male, 85% were white, and 48% were employed. About 85% of the participants were referred to programs by correctional facilities. Twenty-one percent reported ever using kratom, and 10% reported use within the last 12 months.
What do the findings mean? Along with anecdotal reports now being documented, they suggest the use of kratom by heroin users as a “possible harm-reduction” aid, Ms. Smith said at the meeting.
“These men and women are not necessarily getting kratom on a Friday night and saying, ‘This is going to be a great time.’ ” In the interview, she added that “this shows that substance-using individuals are, above all else, pragmatic.”
“It is unlikely that the majority of these users are consuming kratom primarily for achieving recreational ‘highs,’ ” Ms. Smith and her colleagues wrote in the article.
She added during her presentation that kratom is inexpensive and primarily legal. “If it were going to catch on as a serious drug of abuse, we would have expected to have a kratom epidemic already – but we do not.”
As for the big picture, Ms. Smith said in the interview that
Going forward, Ms. Smith said, she and a colleague plan to document the lives of regular kratom users in an effort to understand the progression from heroin and other drugs to kratom. They also want to know what the users would do if kratom is banned.
“These will be case studies in Kentucky, New Mexico, and possibly somewhere in the Northeast,” she said. “Since data will be collected locally, I think it would be helpful to try and obtain samples of kratom that the individuals report using so it can be analyzed. There may be variation between kratom purchased online vs. local vendors, which needs to be documented as well.”
Ms. Smith reported funding from the University of Louisville Graduate Student Research Fund, and another author was supported by the National Institute on Drug Abuse. The authors reported no relevant disclosures.
SOURCE: Smith KE et al. CPDD 2018. Drug and Alcohol Depend. 2017 Nov 1. 180:340-8.
SAN DIEGO – New research suggests that some patients with substance use disorder are turning to the herbal supplement kratom in an effort to reduce their use of heroin and prescription pain killers.
“Some, but not all, heroin users are utilizing kratom as an opioidlike drug with less risks, primarily as a drug substitute or to help abstain from IV heroin and prescription opiate use,” lead author Kirsten Elin Smith, a PhD student at the University of Louisville and an associate at the University of Kentucky’s Center on Drug and Alcohol Research, said in an interview. “Kratom appears as less risky due to the fact that it is not readily injectable.”
Kratom, a plant-based herbal product that’s available over the counter, produces an opioidlike effect. When the Food and Drug Administration declared in February 2018 that scientific evidence shows that kratom indeed is an opioid, the agency also warned that the drug could lead to abuse, addiction, and death. Several U.S. states and the District of Columbia have banned it, as have some cities and counties. In addition, the Drug Enforcement Administration has put kratom on its list of Drugs and Chemicals of Concern.
Nevertheless, some substance users view kratom as helpful and are open to using it, Ms. Smith and her colleagues reported in Drug and Alcohol Dependence.
“There seem to be three categories of substance-using individuals with some relationship to kratom: Those who use kratom inconsistently and as needed when there isn’t an alternative, those who tried it once and just didn’t find much benefit in it, and didn’t try it again, and those who have been using it regularly/daily as a long-term replacement for opioids, including IV heroin use,” Ms. Smith said.
For the new research, Ms. Smith and her colleagues surveyed 478 polysubstance users at five residential recovery centers in Kentucky. The average age of subjects was 35, 58% were male, 85% were white, and 48% were employed. About 85% of the participants were referred to programs by correctional facilities. Twenty-one percent reported ever using kratom, and 10% reported use within the last 12 months.
What do the findings mean? Along with anecdotal reports now being documented, they suggest the use of kratom by heroin users as a “possible harm-reduction” aid, Ms. Smith said at the meeting.
“These men and women are not necessarily getting kratom on a Friday night and saying, ‘This is going to be a great time.’ ” In the interview, she added that “this shows that substance-using individuals are, above all else, pragmatic.”
“It is unlikely that the majority of these users are consuming kratom primarily for achieving recreational ‘highs,’ ” Ms. Smith and her colleagues wrote in the article.
She added during her presentation that kratom is inexpensive and primarily legal. “If it were going to catch on as a serious drug of abuse, we would have expected to have a kratom epidemic already – but we do not.”
As for the big picture, Ms. Smith said in the interview that
Going forward, Ms. Smith said, she and a colleague plan to document the lives of regular kratom users in an effort to understand the progression from heroin and other drugs to kratom. They also want to know what the users would do if kratom is banned.
“These will be case studies in Kentucky, New Mexico, and possibly somewhere in the Northeast,” she said. “Since data will be collected locally, I think it would be helpful to try and obtain samples of kratom that the individuals report using so it can be analyzed. There may be variation between kratom purchased online vs. local vendors, which needs to be documented as well.”
Ms. Smith reported funding from the University of Louisville Graduate Student Research Fund, and another author was supported by the National Institute on Drug Abuse. The authors reported no relevant disclosures.
SOURCE: Smith KE et al. CPDD 2018. Drug and Alcohol Depend. 2017 Nov 1. 180:340-8.
REPORTING FROM CPDD 2018
Key clinical point: Some polysubstance users might be taking the herb kratom for harm reduction.
Major finding: Nearly 74% of recent kratom users also reported using the addiction drug buprenorphine on a nonprescription basis, even though few prefer it.
Study details: Survey of 478 polysubstance users at five residential recovery centers in Kentucky.
Disclosures: Ms. Smith reported individual funding from the University of Louisville Graduate Student Research Fund, and another author was supported by the National Institute on Drug Abuse. The authors reported no relevant disclosures.
Source: Smith KE et al. CPDD 2018. Drug And Alcohol Depend. 2017 Nov 1. 180:340-8.
Private Facebook chats show promise as depression, cannabis use intervention
SAN DIEGO – A pair of small studies suggest that cyber-based interventions with private online meeting areas – like those available on Facebook – could help lift depression and encourage less marijuana use in young people with cannabis use disorder.
“Even individuals who are not looking to quit their use of cannabis have some degree of ambivalence about the extent of their use of it,” said study researcher Suzette Glasner, PhD, in an interview. “When given tools to explore the consequences of their use and change if they want to, they do find reasons and effective ways to change or reduce their use – even if they don’t quit completely.”
Research shows that nearly one-third of cannabis users in 2012-2013 showed signs of cannabis use disorder (JAMA Psychiatry. 2015 Dec; 72[12]:1235-42).
For the first study, researchers recruited 26 participants who were diagnosed with major depressive disorder and cannabis use disorder (all had used marijuana on at least 40 of the previous 90 days). After a brief in-person intervention session, they received 9 therapy sessions via computer and brief weekly check-ins by clinicians over 10 weeks.
The average age of the participants was 29, and 54% were women. They reported that their average depression severity fell from 13 to 6 at 14-week follow-up, based on the Patient Health Questionnaire-9 scale. Cannabis use also declined.
For the separate Facebook study, an additional 18 participants received access to a private Facebook group that included daily posts reinforcing the program. The average age of this group was 27, and 56% were women.
The posts asked questions about topics such as “your fears about cutting back” and feelings that are “triggers” for cannabis use. One post directed users to details about mindfulness activities, and another asked users to describe on a scale of 1-10 how important it is for them to cut back.
Participants responded with praise for the private group, offering comments such as “the Facebook group is really helpful and offers a lot of support,” “it’s nice throughout the day to have uplifting Facebook notifications,” and “I like the tips, the positive feedback and the feeling that we’re in it together, not alone.”
Dr. Glasner said. “The Facebook approach enables those addicted to cannabis, for whom motivation for many things – including socializing – may be lacking, to utilize social support, without having to leave the comfort of their home or wherever they might isolate when they’re using cannabis heavily.”
She added that “this social support may be inspiring, motivating, and reassuring to them,” letting them know that they’re not alone in experiencing an addiction whose existence is sometimes doubted.
Dr. Glasner said she next plans a large randomized trial to evaluate the efficacy of the Facebook intervention and its mechanisms of action.
After her presentation at the meeting, Dr. Glasner was asked about the ongoing concerns regarding privacy on Facebook. “When I funded and started this study, it was nearly 2 years ago, and it wasn’t as large of a concern,” she said. “We may need to look to utilize a social media platform that may not be Facebook: ‘We have one to support you, but it’s not Facebook.’”
In a related presentation at the meeting, another researcher reported success using 80 interactive texts over 4 weeks to reach out to participants in an intervention programs targeting cannabis use disorder.
The National Institute on Drug Abuse funded the study. Dr. Glasner is author of The Addiction Recovery Skills Workbook: Changing Addictive Behaviors Using CBT, Mindfulness, and Motivational Interviewing Techniques (Oakland, Calif.: New Harbinger Publications, 2015). The authors reported no relevant disclosures.
SAN DIEGO – A pair of small studies suggest that cyber-based interventions with private online meeting areas – like those available on Facebook – could help lift depression and encourage less marijuana use in young people with cannabis use disorder.
“Even individuals who are not looking to quit their use of cannabis have some degree of ambivalence about the extent of their use of it,” said study researcher Suzette Glasner, PhD, in an interview. “When given tools to explore the consequences of their use and change if they want to, they do find reasons and effective ways to change or reduce their use – even if they don’t quit completely.”
Research shows that nearly one-third of cannabis users in 2012-2013 showed signs of cannabis use disorder (JAMA Psychiatry. 2015 Dec; 72[12]:1235-42).
For the first study, researchers recruited 26 participants who were diagnosed with major depressive disorder and cannabis use disorder (all had used marijuana on at least 40 of the previous 90 days). After a brief in-person intervention session, they received 9 therapy sessions via computer and brief weekly check-ins by clinicians over 10 weeks.
The average age of the participants was 29, and 54% were women. They reported that their average depression severity fell from 13 to 6 at 14-week follow-up, based on the Patient Health Questionnaire-9 scale. Cannabis use also declined.
For the separate Facebook study, an additional 18 participants received access to a private Facebook group that included daily posts reinforcing the program. The average age of this group was 27, and 56% were women.
The posts asked questions about topics such as “your fears about cutting back” and feelings that are “triggers” for cannabis use. One post directed users to details about mindfulness activities, and another asked users to describe on a scale of 1-10 how important it is for them to cut back.
Participants responded with praise for the private group, offering comments such as “the Facebook group is really helpful and offers a lot of support,” “it’s nice throughout the day to have uplifting Facebook notifications,” and “I like the tips, the positive feedback and the feeling that we’re in it together, not alone.”
Dr. Glasner said. “The Facebook approach enables those addicted to cannabis, for whom motivation for many things – including socializing – may be lacking, to utilize social support, without having to leave the comfort of their home or wherever they might isolate when they’re using cannabis heavily.”
She added that “this social support may be inspiring, motivating, and reassuring to them,” letting them know that they’re not alone in experiencing an addiction whose existence is sometimes doubted.
Dr. Glasner said she next plans a large randomized trial to evaluate the efficacy of the Facebook intervention and its mechanisms of action.
After her presentation at the meeting, Dr. Glasner was asked about the ongoing concerns regarding privacy on Facebook. “When I funded and started this study, it was nearly 2 years ago, and it wasn’t as large of a concern,” she said. “We may need to look to utilize a social media platform that may not be Facebook: ‘We have one to support you, but it’s not Facebook.’”
In a related presentation at the meeting, another researcher reported success using 80 interactive texts over 4 weeks to reach out to participants in an intervention programs targeting cannabis use disorder.
The National Institute on Drug Abuse funded the study. Dr. Glasner is author of The Addiction Recovery Skills Workbook: Changing Addictive Behaviors Using CBT, Mindfulness, and Motivational Interviewing Techniques (Oakland, Calif.: New Harbinger Publications, 2015). The authors reported no relevant disclosures.
SAN DIEGO – A pair of small studies suggest that cyber-based interventions with private online meeting areas – like those available on Facebook – could help lift depression and encourage less marijuana use in young people with cannabis use disorder.
“Even individuals who are not looking to quit their use of cannabis have some degree of ambivalence about the extent of their use of it,” said study researcher Suzette Glasner, PhD, in an interview. “When given tools to explore the consequences of their use and change if they want to, they do find reasons and effective ways to change or reduce their use – even if they don’t quit completely.”
Research shows that nearly one-third of cannabis users in 2012-2013 showed signs of cannabis use disorder (JAMA Psychiatry. 2015 Dec; 72[12]:1235-42).
For the first study, researchers recruited 26 participants who were diagnosed with major depressive disorder and cannabis use disorder (all had used marijuana on at least 40 of the previous 90 days). After a brief in-person intervention session, they received 9 therapy sessions via computer and brief weekly check-ins by clinicians over 10 weeks.
The average age of the participants was 29, and 54% were women. They reported that their average depression severity fell from 13 to 6 at 14-week follow-up, based on the Patient Health Questionnaire-9 scale. Cannabis use also declined.
For the separate Facebook study, an additional 18 participants received access to a private Facebook group that included daily posts reinforcing the program. The average age of this group was 27, and 56% were women.
The posts asked questions about topics such as “your fears about cutting back” and feelings that are “triggers” for cannabis use. One post directed users to details about mindfulness activities, and another asked users to describe on a scale of 1-10 how important it is for them to cut back.
Participants responded with praise for the private group, offering comments such as “the Facebook group is really helpful and offers a lot of support,” “it’s nice throughout the day to have uplifting Facebook notifications,” and “I like the tips, the positive feedback and the feeling that we’re in it together, not alone.”
Dr. Glasner said. “The Facebook approach enables those addicted to cannabis, for whom motivation for many things – including socializing – may be lacking, to utilize social support, without having to leave the comfort of their home or wherever they might isolate when they’re using cannabis heavily.”
She added that “this social support may be inspiring, motivating, and reassuring to them,” letting them know that they’re not alone in experiencing an addiction whose existence is sometimes doubted.
Dr. Glasner said she next plans a large randomized trial to evaluate the efficacy of the Facebook intervention and its mechanisms of action.
After her presentation at the meeting, Dr. Glasner was asked about the ongoing concerns regarding privacy on Facebook. “When I funded and started this study, it was nearly 2 years ago, and it wasn’t as large of a concern,” she said. “We may need to look to utilize a social media platform that may not be Facebook: ‘We have one to support you, but it’s not Facebook.’”
In a related presentation at the meeting, another researcher reported success using 80 interactive texts over 4 weeks to reach out to participants in an intervention programs targeting cannabis use disorder.
The National Institute on Drug Abuse funded the study. Dr. Glasner is author of The Addiction Recovery Skills Workbook: Changing Addictive Behaviors Using CBT, Mindfulness, and Motivational Interviewing Techniques (Oakland, Calif.: New Harbinger Publications, 2015). The authors reported no relevant disclosures.
REPORTING FROM CPDD 2018
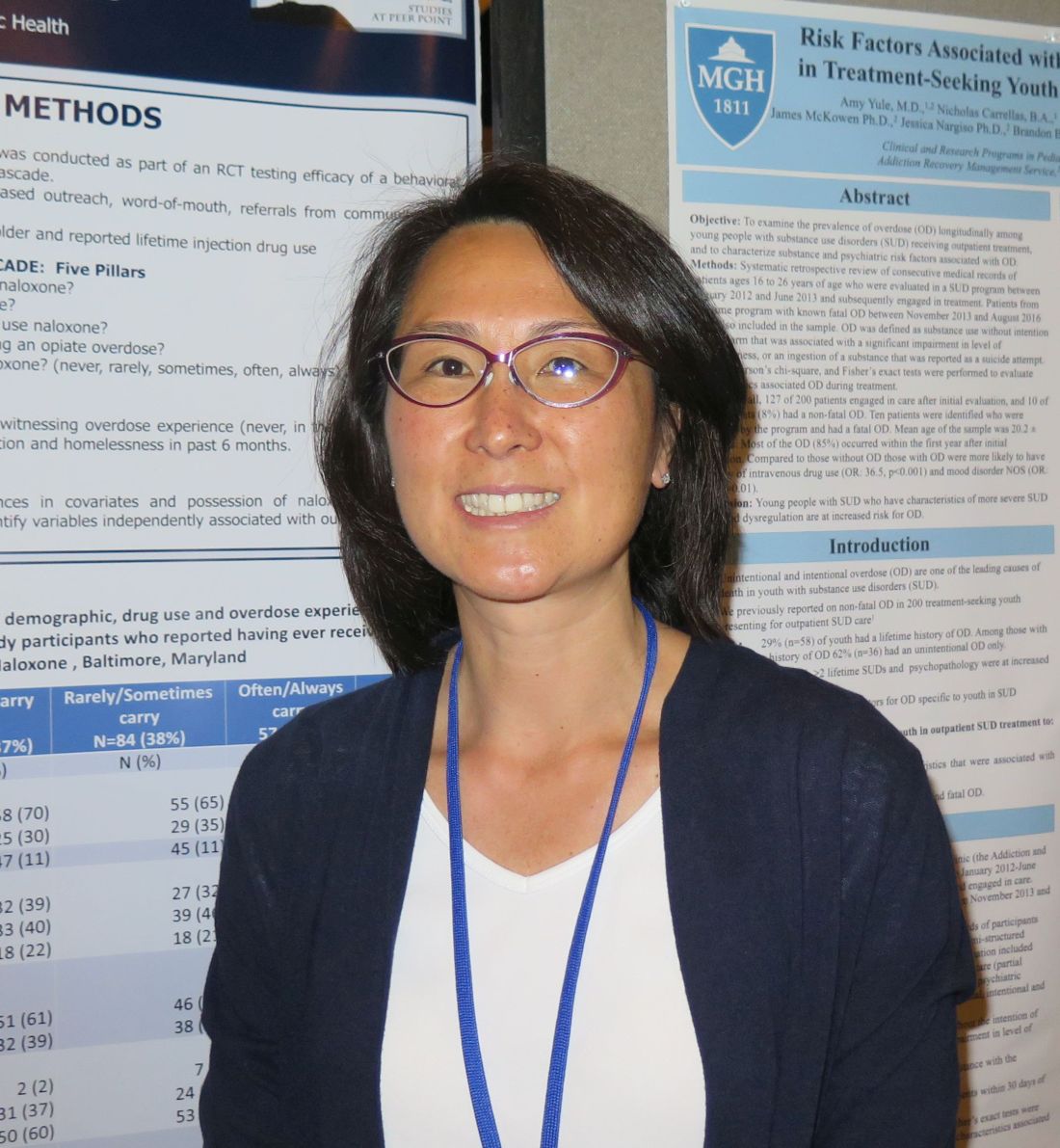
Watch for substance use risks among never-deployed reservists
SAN DIEGO – Reserve soldiers who have never been deployed are just as likely to have poor outcomes related to mental health and substance use as their peers who have been deployed, results from a novel survey suggest.
“We tend to focus on screening and intervention efforts for soldiers who have been deployed and who have experienced combat, but we should also focus our intervention and screening efforts on soldiers who have never been deployed,” lead study author Rachel A. Hoopsick, MPH, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “Both are at risk for substance use and mental illness.”
Measures included the Non-Deployment Emotions Questionnaire, the Alcohol Use Disorders Identification Test, the National Institute on Drug Abuse Modified Alcohol, Smoking and Substance Involvement Screening Test 2.0, and the Marital Adjustment Test. The researchers used separate models to examine the relationship between nondeployment emotions and alcohol problems, frequent heavy drinking, current nonmedical use of prescription drugs, and current illicit drug use, and controlled for years of military service, number of military friends in the social network, and marital satisfaction.
Ms. Hoopsick reported results from 121 never-deployed, male soldiers who completed the survey at baseline and at a 1-year follow-up. Their mean age was 30 years, 76% were non-Hispanic white, and 84% had at least some college education. In addition, the soldiers had served a mean of 5.5 years, had a mean of 0.6 military friends in the social network, and had a mean marital satisfaction score of 114 out of 158 possible points.
On responses to the Non-Deployment Emotions Questionnaire, 65% of nondeployed soldiers felt guilt, 56% felt decreased value within his unit, 50% felt decreased camaraderie within his unit, and 50% felt decreased connectedness within his unit for having never been deployed. “We did anticipate that some of these soldiers were going to have poor outcomes related to their nondeployment emotions, but it was surprising to see how many of the soldiers did express having negative emotions related to having never been deployed,” Ms. Hoopsick said. After the researchers controlled for years of military service, the number of military friends in the soldier’s social network, and marital satisfaction, more negative nondeployment emotions were associated with a greater likelihood of alcohol problems (adjusted risk ratio, 1.06), frequent heavy drinking (ARR, 1.03), and current nonmedical use of prescription drugs (ARR, 1.21).
She acknowledged certain limitations of the study, including its cross-sectional nature. she said.
The National Institute on Drug Abuse provided funding to Ms. Hoopsick’s mentor and coauthor, Gregory G. Homish, PhD, and the study received additional funding from the National Center for Advancing Translational Sciences and the Health Resources and Services Administration.
SAN DIEGO – Reserve soldiers who have never been deployed are just as likely to have poor outcomes related to mental health and substance use as their peers who have been deployed, results from a novel survey suggest.
“We tend to focus on screening and intervention efforts for soldiers who have been deployed and who have experienced combat, but we should also focus our intervention and screening efforts on soldiers who have never been deployed,” lead study author Rachel A. Hoopsick, MPH, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “Both are at risk for substance use and mental illness.”
Measures included the Non-Deployment Emotions Questionnaire, the Alcohol Use Disorders Identification Test, the National Institute on Drug Abuse Modified Alcohol, Smoking and Substance Involvement Screening Test 2.0, and the Marital Adjustment Test. The researchers used separate models to examine the relationship between nondeployment emotions and alcohol problems, frequent heavy drinking, current nonmedical use of prescription drugs, and current illicit drug use, and controlled for years of military service, number of military friends in the social network, and marital satisfaction.
Ms. Hoopsick reported results from 121 never-deployed, male soldiers who completed the survey at baseline and at a 1-year follow-up. Their mean age was 30 years, 76% were non-Hispanic white, and 84% had at least some college education. In addition, the soldiers had served a mean of 5.5 years, had a mean of 0.6 military friends in the social network, and had a mean marital satisfaction score of 114 out of 158 possible points.
On responses to the Non-Deployment Emotions Questionnaire, 65% of nondeployed soldiers felt guilt, 56% felt decreased value within his unit, 50% felt decreased camaraderie within his unit, and 50% felt decreased connectedness within his unit for having never been deployed. “We did anticipate that some of these soldiers were going to have poor outcomes related to their nondeployment emotions, but it was surprising to see how many of the soldiers did express having negative emotions related to having never been deployed,” Ms. Hoopsick said. After the researchers controlled for years of military service, the number of military friends in the soldier’s social network, and marital satisfaction, more negative nondeployment emotions were associated with a greater likelihood of alcohol problems (adjusted risk ratio, 1.06), frequent heavy drinking (ARR, 1.03), and current nonmedical use of prescription drugs (ARR, 1.21).
She acknowledged certain limitations of the study, including its cross-sectional nature. she said.
The National Institute on Drug Abuse provided funding to Ms. Hoopsick’s mentor and coauthor, Gregory G. Homish, PhD, and the study received additional funding from the National Center for Advancing Translational Sciences and the Health Resources and Services Administration.
SAN DIEGO – Reserve soldiers who have never been deployed are just as likely to have poor outcomes related to mental health and substance use as their peers who have been deployed, results from a novel survey suggest.
“We tend to focus on screening and intervention efforts for soldiers who have been deployed and who have experienced combat, but we should also focus our intervention and screening efforts on soldiers who have never been deployed,” lead study author Rachel A. Hoopsick, MPH, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “Both are at risk for substance use and mental illness.”
Measures included the Non-Deployment Emotions Questionnaire, the Alcohol Use Disorders Identification Test, the National Institute on Drug Abuse Modified Alcohol, Smoking and Substance Involvement Screening Test 2.0, and the Marital Adjustment Test. The researchers used separate models to examine the relationship between nondeployment emotions and alcohol problems, frequent heavy drinking, current nonmedical use of prescription drugs, and current illicit drug use, and controlled for years of military service, number of military friends in the social network, and marital satisfaction.
Ms. Hoopsick reported results from 121 never-deployed, male soldiers who completed the survey at baseline and at a 1-year follow-up. Their mean age was 30 years, 76% were non-Hispanic white, and 84% had at least some college education. In addition, the soldiers had served a mean of 5.5 years, had a mean of 0.6 military friends in the social network, and had a mean marital satisfaction score of 114 out of 158 possible points.
On responses to the Non-Deployment Emotions Questionnaire, 65% of nondeployed soldiers felt guilt, 56% felt decreased value within his unit, 50% felt decreased camaraderie within his unit, and 50% felt decreased connectedness within his unit for having never been deployed. “We did anticipate that some of these soldiers were going to have poor outcomes related to their nondeployment emotions, but it was surprising to see how many of the soldiers did express having negative emotions related to having never been deployed,” Ms. Hoopsick said. After the researchers controlled for years of military service, the number of military friends in the soldier’s social network, and marital satisfaction, more negative nondeployment emotions were associated with a greater likelihood of alcohol problems (adjusted risk ratio, 1.06), frequent heavy drinking (ARR, 1.03), and current nonmedical use of prescription drugs (ARR, 1.21).
She acknowledged certain limitations of the study, including its cross-sectional nature. she said.
The National Institute on Drug Abuse provided funding to Ms. Hoopsick’s mentor and coauthor, Gregory G. Homish, PhD, and the study received additional funding from the National Center for Advancing Translational Sciences and the Health Resources and Services Administration.
REPORTING FROM CPDD 2018
Key clinical point: All military personnel, regardless of deployment status, could be at risk for substance use.
Major finding:. More negative nondeployment emotions were associated with a greater likelihood of alcohol problems (adjusted risk ratio, 1.06), frequent heavy drinking (ARR, 1.03), and current nonmedical use of prescription drugs (ARR, 1.21).
Study details: Responses from 121 never-deployed, male U.S. Army Reserve/National Guard soldiers who completed surveys at baseline and at a 1-year follow-up.
Disclosures: The National Institute on Drug Abuse provided funding to Ms. Hoopsick’s mentor and coauthor, Gregory G. Homish, PhD, and the study received additional funding from the National Center for Advancing Translational Sciences and the Health Resources and Services Administration.
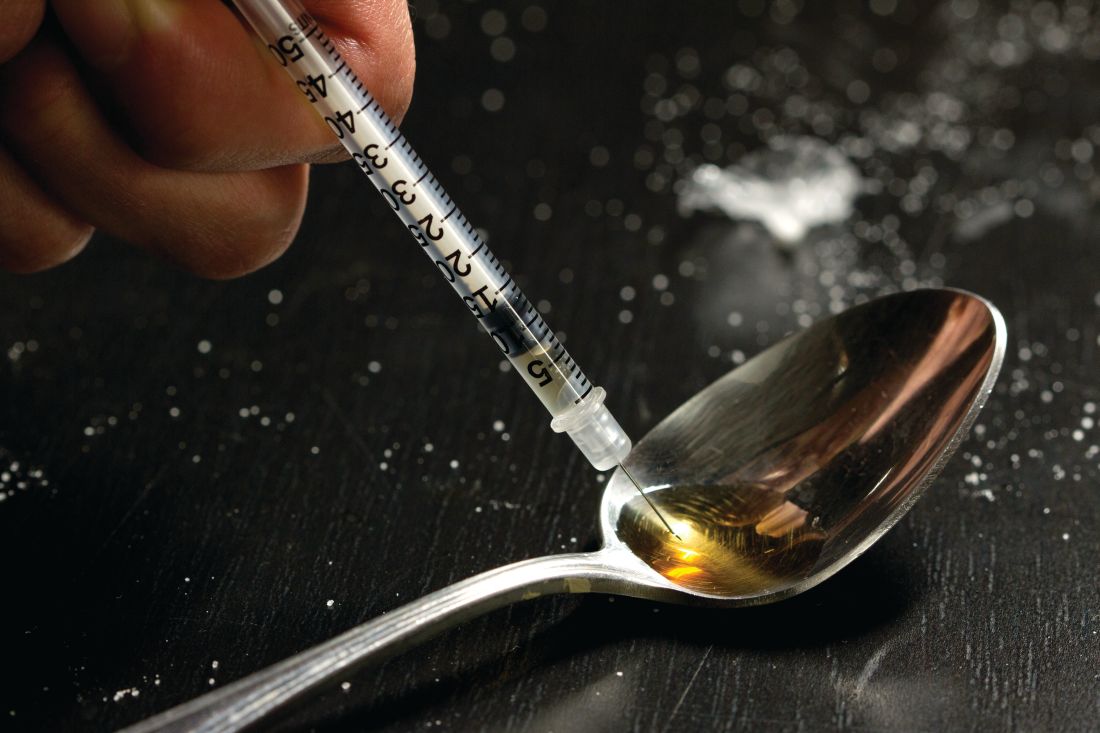
A call for ‘changing the social norms’ on naloxone
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
AT CPDD 2018
Key clinical point: Increasing possession of naloxone among people who use opiates is essential.
Major finding:. Carrying naloxone often or always was significantly associated with several variables, including female sex (odds ratio, 2.77) and having ever used naloxone during an overdose (OR, 4.33).
Study details: A cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use.
Disclosures: The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
Do free meals to physicians affect opioid prescribing?
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
REPORTING FROM CPDD 2018
Key clinical point: Opioid marketing appears to affect physician prescribing practices.
Major finding: Physicians who received opioid marketing payments and meals in 2014 prescribed an adjusted 9% more opioids in 2015 than did their opioid-prescribing colleagues.
Study details: Retrospective 2014-2015 analysis of 369,139 opioid-prescribing physicians in a Medicare Part D database.
Disclosures: Dr. Hadland reported funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reported funding from NIDA. No additional relevant disclosures were reported.
Source: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
Maternal use of pot and tobacco may boost birth defect risk
SAN DIEGO – New research suggests that pregnant users of both cannabis and tobacco may put their unborn children at higher risk of birth defects and small head circumference than if they used either alone.
Researchers also found that 13% of pregnant Medicaid recipients surveyed reported using both cannabis and tobacco within the past month.
, especially if they smoke tobacco, said study lead author Victoria H. Coleman-Cowger, PhD, of the research organization Battelle, in an interview.
In some cases, in fact, pregnant women might think that marijuana is healthier than regular cigarettes, said Dr. Coleman-Cowger. She observed this phenomenon while conducting a smoking intervention study at a prenatal clinic that largely served poor, African American women.
“I learned that many participants were also smoking cannabis and felt that there was lower risk associated with cannabis use than with tobacco use,” she said. “Some women were decreasing their use of tobacco during pregnancy but increasing their use of cannabis.”
Dr. Coleman-Cowger’s observations at the clinic inspired the new study, which reports the findings of a convenience survey of 500 pregnant women.
The mean age in the group was 28, and 71% were black. Two-thirds were employed, and 29% were college graduates.
By comparison, the 45 women in the co-user group – who reported both cannabis and tobacco use in the past month – were 93% black, 42% employed, and 7% college graduates. (An additional 39 women reported tobacco use only, and 60 reported cannabis use only.)
Co-use also was correlated with “never married, being in the first trimester of pregnancy, not wanting to be pregnant when they were, past-month other substance use, and more frequent use of both cannabis and tobacco than either exclusive group,” Dr. Coleman-Cowger said.
In adjusted models, co-users were more likely (odds ratio, 5.7; P = .05) to give birth to babies with small head circumference than nonusers. The risks of giving birth to babies with small head circumference also were more likely among the tobacco-only users (OR, 4.8; P = .05) and cannabis-only users (OR, 2.0; P = .05), compared with nonusers. Birth defects also were more likely in the co-user group.
The study did not allow researchers to speculate on whether co-use may multiply risk vs. cannabis or tobacco use alone.
Dr. Coleman-Cowger said in light of the small sample size, the results should be interpreted with caution. One possible confounder is quantity of use, she said. “We did not assess quantity of use, but given our finding that frequency of use is higher among the co-use group, it could be that the co-use group is simply using more of each substance and thus impacting the health consequences.”
Current clinical practice guidelines do not suggest screening for cannabis use in pregnant women. But Dr. Coleman-Cowger said it’s “particularly important when tobacco use has been identified, though in states where substance use is considered child abuse, professional judgment should be utilized in terms of the legal implications of asking about use.”
More research is planned to better understand issues like quantity of use, and reasons why pregnant women co-use cannabis and tobacco, Dr. Coleman-Cowger said.
The National Institute on Drug Abuse funded the study, which Dr. Coleman-Cowger said is part of a larger project “to compare and validate screeners that assess prescription drug misuse and illicit drug use during pregnancy.” The study authors report no relevant disclosures.
SAN DIEGO – New research suggests that pregnant users of both cannabis and tobacco may put their unborn children at higher risk of birth defects and small head circumference than if they used either alone.
Researchers also found that 13% of pregnant Medicaid recipients surveyed reported using both cannabis and tobacco within the past month.
, especially if they smoke tobacco, said study lead author Victoria H. Coleman-Cowger, PhD, of the research organization Battelle, in an interview.
In some cases, in fact, pregnant women might think that marijuana is healthier than regular cigarettes, said Dr. Coleman-Cowger. She observed this phenomenon while conducting a smoking intervention study at a prenatal clinic that largely served poor, African American women.
“I learned that many participants were also smoking cannabis and felt that there was lower risk associated with cannabis use than with tobacco use,” she said. “Some women were decreasing their use of tobacco during pregnancy but increasing their use of cannabis.”
Dr. Coleman-Cowger’s observations at the clinic inspired the new study, which reports the findings of a convenience survey of 500 pregnant women.
The mean age in the group was 28, and 71% were black. Two-thirds were employed, and 29% were college graduates.
By comparison, the 45 women in the co-user group – who reported both cannabis and tobacco use in the past month – were 93% black, 42% employed, and 7% college graduates. (An additional 39 women reported tobacco use only, and 60 reported cannabis use only.)
Co-use also was correlated with “never married, being in the first trimester of pregnancy, not wanting to be pregnant when they were, past-month other substance use, and more frequent use of both cannabis and tobacco than either exclusive group,” Dr. Coleman-Cowger said.
In adjusted models, co-users were more likely (odds ratio, 5.7; P = .05) to give birth to babies with small head circumference than nonusers. The risks of giving birth to babies with small head circumference also were more likely among the tobacco-only users (OR, 4.8; P = .05) and cannabis-only users (OR, 2.0; P = .05), compared with nonusers. Birth defects also were more likely in the co-user group.
The study did not allow researchers to speculate on whether co-use may multiply risk vs. cannabis or tobacco use alone.
Dr. Coleman-Cowger said in light of the small sample size, the results should be interpreted with caution. One possible confounder is quantity of use, she said. “We did not assess quantity of use, but given our finding that frequency of use is higher among the co-use group, it could be that the co-use group is simply using more of each substance and thus impacting the health consequences.”
Current clinical practice guidelines do not suggest screening for cannabis use in pregnant women. But Dr. Coleman-Cowger said it’s “particularly important when tobacco use has been identified, though in states where substance use is considered child abuse, professional judgment should be utilized in terms of the legal implications of asking about use.”
More research is planned to better understand issues like quantity of use, and reasons why pregnant women co-use cannabis and tobacco, Dr. Coleman-Cowger said.
The National Institute on Drug Abuse funded the study, which Dr. Coleman-Cowger said is part of a larger project “to compare and validate screeners that assess prescription drug misuse and illicit drug use during pregnancy.” The study authors report no relevant disclosures.
SAN DIEGO – New research suggests that pregnant users of both cannabis and tobacco may put their unborn children at higher risk of birth defects and small head circumference than if they used either alone.
Researchers also found that 13% of pregnant Medicaid recipients surveyed reported using both cannabis and tobacco within the past month.
, especially if they smoke tobacco, said study lead author Victoria H. Coleman-Cowger, PhD, of the research organization Battelle, in an interview.
In some cases, in fact, pregnant women might think that marijuana is healthier than regular cigarettes, said Dr. Coleman-Cowger. She observed this phenomenon while conducting a smoking intervention study at a prenatal clinic that largely served poor, African American women.
“I learned that many participants were also smoking cannabis and felt that there was lower risk associated with cannabis use than with tobacco use,” she said. “Some women were decreasing their use of tobacco during pregnancy but increasing their use of cannabis.”
Dr. Coleman-Cowger’s observations at the clinic inspired the new study, which reports the findings of a convenience survey of 500 pregnant women.
The mean age in the group was 28, and 71% were black. Two-thirds were employed, and 29% were college graduates.
By comparison, the 45 women in the co-user group – who reported both cannabis and tobacco use in the past month – were 93% black, 42% employed, and 7% college graduates. (An additional 39 women reported tobacco use only, and 60 reported cannabis use only.)
Co-use also was correlated with “never married, being in the first trimester of pregnancy, not wanting to be pregnant when they were, past-month other substance use, and more frequent use of both cannabis and tobacco than either exclusive group,” Dr. Coleman-Cowger said.
In adjusted models, co-users were more likely (odds ratio, 5.7; P = .05) to give birth to babies with small head circumference than nonusers. The risks of giving birth to babies with small head circumference also were more likely among the tobacco-only users (OR, 4.8; P = .05) and cannabis-only users (OR, 2.0; P = .05), compared with nonusers. Birth defects also were more likely in the co-user group.
The study did not allow researchers to speculate on whether co-use may multiply risk vs. cannabis or tobacco use alone.
Dr. Coleman-Cowger said in light of the small sample size, the results should be interpreted with caution. One possible confounder is quantity of use, she said. “We did not assess quantity of use, but given our finding that frequency of use is higher among the co-use group, it could be that the co-use group is simply using more of each substance and thus impacting the health consequences.”
Current clinical practice guidelines do not suggest screening for cannabis use in pregnant women. But Dr. Coleman-Cowger said it’s “particularly important when tobacco use has been identified, though in states where substance use is considered child abuse, professional judgment should be utilized in terms of the legal implications of asking about use.”
More research is planned to better understand issues like quantity of use, and reasons why pregnant women co-use cannabis and tobacco, Dr. Coleman-Cowger said.
The National Institute on Drug Abuse funded the study, which Dr. Coleman-Cowger said is part of a larger project “to compare and validate screeners that assess prescription drug misuse and illicit drug use during pregnancy.” The study authors report no relevant disclosures.
REPORTING FROM CPDD 2018
Key clinical point: Couse of cannabis and tobacco by pregnant mothers may pose more risk to unborn children than use of either alone.
Major finding: Cousers had a higher risk of giving birth to children with birth detects and small head circumference than tobacco-only or cannabis-only users. In adjusted models, cousers were more likely (odds ratio, 5.7; P = .05) to give birth to babies with small head circumference than nonusers. The risks of giving birth to babies with small head circumference also were more likely among the tobacco-only users (OR, 4.8; P = .05) and cannabis-only users (OR, 2.0; P = .05), compared with nonusers.
Study details: Survey of 500 pregnant Medicaid recipients.
Disclosures: The National Institute on Drug Abuse funded the study. The study authors report no relevant disclosures.
Mobile app engages individuals with opioid use disorders
SAN DIEGO – Individuals with opioid use disorder generally embraced the idea of using a novel mobile application to learn about recovery options and medication-assisted treatment, according to results from a pilot study.
“We found that, after participants engaged with our mobile app, their interest for recovery and attitudes about recovery improved,” lead study author Patricia Cavazos-Rehg, PhD, of the department of psychiatry at Washington University in St. Louis, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “We were not expecting results to be so positive, and these findings are very promising because they suggest that individuals may not have interest in or be reluctant to engage in treatment. But we can engage them with a tool that will get them interested and move them toward treatment recovery.”
Dr. Cavazos-Rehg and her associates set out to examine the effectiveness of a mobile application called “uMAT-R,” which includes evidence-based health information about opioid use disorder recovery and medication-assisted treatment (MAT). The app is being develop in partnership with iTether, an Arizona-based mobile health software company. Material for the user is derived from the Substance Abuse and Mental Health Services Administration’s online handbook, “Decisions in Recovery: Treatment for Opioid Disorders,” and is divided into consumer-friendly content modules that provide information on MAT, including costs, latest research findings, and potential side effects.
For the study, researchers recruited 161 individuals 18 years of age and older from three opioid-focused groups on Reddit to pilot the use of uMAT-R. To be eligible, they had to be a U.S. resident, be fluent in English, have misused opioids in the past 30 days, and not currently be using medication-assisted treatment. Participants had access to the app for 1 month, and the researchers administered a baseline questionnaire that assessed demographics, opioid dependence, and history of treatment. They also administered pre- and postapplication engagement questionnaires that assessed attitudes toward MAT, treatment interest, and usefulness of the app.
Of the 161 invited participants, 44 downloaded the app, and 26 completed all content modules and all pre- and postapp assessments. The median age of the 26 participants was 28 years; 65% were male, and 88% were non-Hispanic white. Nearly all (96%) met criteria for opioid dependence, and 12% had received treatment for opioid misuse in the past 6 months. Dr. Cavazos-Rehg and her associates found that only 32% expressed interest in starting treatment for their opioid use disorder before using the app, compared with 48% after using the app, a difference that reached statistical significance (P = 0.046). Feedback from participants was mostly positive. For example, 92% agreed that the app includes useful tips on how to make life better; 88% would consult the app if they had to make a decision about their recovery; 88% believed the app has a positive outlook; 84% said the app helped them have a better understanding of options for recovery, and 84% said they learned something new from the app.
In addition, scores on the MAT attitudes scale rose from a mean of 3.3 to a mean of 3.5 (P = 0.044).
“,” Dr. Cavazos-Rehg said. “We want to develop a mobile app that will teach individuals who have opioid use disorder about their recovery options so that we can nudge them towards considering recovery, and our findings indicate some success with this goal.”
Next, she and her associates plan to pair use of the app with traditional in-person care among pregnant women with opioid use disorders. “Even if people are engaged in treatment, they still only see a therapist or a clinician once or twice a week,” she said. “We want to be able to use a mobile health treatment to support their needs while they are outside of treatment.”
The study was funded by a grant from the National Institutes of Health. Dr. Cavazos-Rehg reported having no financial disclosures.
SAN DIEGO – Individuals with opioid use disorder generally embraced the idea of using a novel mobile application to learn about recovery options and medication-assisted treatment, according to results from a pilot study.
“We found that, after participants engaged with our mobile app, their interest for recovery and attitudes about recovery improved,” lead study author Patricia Cavazos-Rehg, PhD, of the department of psychiatry at Washington University in St. Louis, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “We were not expecting results to be so positive, and these findings are very promising because they suggest that individuals may not have interest in or be reluctant to engage in treatment. But we can engage them with a tool that will get them interested and move them toward treatment recovery.”
Dr. Cavazos-Rehg and her associates set out to examine the effectiveness of a mobile application called “uMAT-R,” which includes evidence-based health information about opioid use disorder recovery and medication-assisted treatment (MAT). The app is being develop in partnership with iTether, an Arizona-based mobile health software company. Material for the user is derived from the Substance Abuse and Mental Health Services Administration’s online handbook, “Decisions in Recovery: Treatment for Opioid Disorders,” and is divided into consumer-friendly content modules that provide information on MAT, including costs, latest research findings, and potential side effects.
For the study, researchers recruited 161 individuals 18 years of age and older from three opioid-focused groups on Reddit to pilot the use of uMAT-R. To be eligible, they had to be a U.S. resident, be fluent in English, have misused opioids in the past 30 days, and not currently be using medication-assisted treatment. Participants had access to the app for 1 month, and the researchers administered a baseline questionnaire that assessed demographics, opioid dependence, and history of treatment. They also administered pre- and postapplication engagement questionnaires that assessed attitudes toward MAT, treatment interest, and usefulness of the app.
Of the 161 invited participants, 44 downloaded the app, and 26 completed all content modules and all pre- and postapp assessments. The median age of the 26 participants was 28 years; 65% were male, and 88% were non-Hispanic white. Nearly all (96%) met criteria for opioid dependence, and 12% had received treatment for opioid misuse in the past 6 months. Dr. Cavazos-Rehg and her associates found that only 32% expressed interest in starting treatment for their opioid use disorder before using the app, compared with 48% after using the app, a difference that reached statistical significance (P = 0.046). Feedback from participants was mostly positive. For example, 92% agreed that the app includes useful tips on how to make life better; 88% would consult the app if they had to make a decision about their recovery; 88% believed the app has a positive outlook; 84% said the app helped them have a better understanding of options for recovery, and 84% said they learned something new from the app.
In addition, scores on the MAT attitudes scale rose from a mean of 3.3 to a mean of 3.5 (P = 0.044).
“,” Dr. Cavazos-Rehg said. “We want to develop a mobile app that will teach individuals who have opioid use disorder about their recovery options so that we can nudge them towards considering recovery, and our findings indicate some success with this goal.”
Next, she and her associates plan to pair use of the app with traditional in-person care among pregnant women with opioid use disorders. “Even if people are engaged in treatment, they still only see a therapist or a clinician once or twice a week,” she said. “We want to be able to use a mobile health treatment to support their needs while they are outside of treatment.”
The study was funded by a grant from the National Institutes of Health. Dr. Cavazos-Rehg reported having no financial disclosures.
SAN DIEGO – Individuals with opioid use disorder generally embraced the idea of using a novel mobile application to learn about recovery options and medication-assisted treatment, according to results from a pilot study.
“We found that, after participants engaged with our mobile app, their interest for recovery and attitudes about recovery improved,” lead study author Patricia Cavazos-Rehg, PhD, of the department of psychiatry at Washington University in St. Louis, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “We were not expecting results to be so positive, and these findings are very promising because they suggest that individuals may not have interest in or be reluctant to engage in treatment. But we can engage them with a tool that will get them interested and move them toward treatment recovery.”
Dr. Cavazos-Rehg and her associates set out to examine the effectiveness of a mobile application called “uMAT-R,” which includes evidence-based health information about opioid use disorder recovery and medication-assisted treatment (MAT). The app is being develop in partnership with iTether, an Arizona-based mobile health software company. Material for the user is derived from the Substance Abuse and Mental Health Services Administration’s online handbook, “Decisions in Recovery: Treatment for Opioid Disorders,” and is divided into consumer-friendly content modules that provide information on MAT, including costs, latest research findings, and potential side effects.
For the study, researchers recruited 161 individuals 18 years of age and older from three opioid-focused groups on Reddit to pilot the use of uMAT-R. To be eligible, they had to be a U.S. resident, be fluent in English, have misused opioids in the past 30 days, and not currently be using medication-assisted treatment. Participants had access to the app for 1 month, and the researchers administered a baseline questionnaire that assessed demographics, opioid dependence, and history of treatment. They also administered pre- and postapplication engagement questionnaires that assessed attitudes toward MAT, treatment interest, and usefulness of the app.
Of the 161 invited participants, 44 downloaded the app, and 26 completed all content modules and all pre- and postapp assessments. The median age of the 26 participants was 28 years; 65% were male, and 88% were non-Hispanic white. Nearly all (96%) met criteria for opioid dependence, and 12% had received treatment for opioid misuse in the past 6 months. Dr. Cavazos-Rehg and her associates found that only 32% expressed interest in starting treatment for their opioid use disorder before using the app, compared with 48% after using the app, a difference that reached statistical significance (P = 0.046). Feedback from participants was mostly positive. For example, 92% agreed that the app includes useful tips on how to make life better; 88% would consult the app if they had to make a decision about their recovery; 88% believed the app has a positive outlook; 84% said the app helped them have a better understanding of options for recovery, and 84% said they learned something new from the app.
In addition, scores on the MAT attitudes scale rose from a mean of 3.3 to a mean of 3.5 (P = 0.044).
“,” Dr. Cavazos-Rehg said. “We want to develop a mobile app that will teach individuals who have opioid use disorder about their recovery options so that we can nudge them towards considering recovery, and our findings indicate some success with this goal.”
Next, she and her associates plan to pair use of the app with traditional in-person care among pregnant women with opioid use disorders. “Even if people are engaged in treatment, they still only see a therapist or a clinician once or twice a week,” she said. “We want to be able to use a mobile health treatment to support their needs while they are outside of treatment.”
The study was funded by a grant from the National Institutes of Health. Dr. Cavazos-Rehg reported having no financial disclosures.
REPORTING FROM CPDD 2018
Key clinical point: Social media can be leveraged to connect individuals with opioid use disorder to a mobile app that encourages recovery.
Major finding:. Only 32% expressed interest in starting treatment for their opioid use disorder before using the app, compared with 48% after using the app, a difference that reached statistical significance (P = 0.046).
Study details: A study of 26 opioid users who piloted the use of a mobile app.
Disclosures: The study was funded by a grant from the National Institutes of Health. Dr. Cavazos-Rehg reported having no financial disclosures.
High-dose opioid prescribing linked to heroin use risk among U.S. veterans
SAN DIEGO – High-dose opioid prescribing is associated with an increased risk of heroin use among U.S. veterans, a prospective study showed.
“Despite evidence linking increased risk of opioid use disorder with specific opioid prescribing patterns, the relationship between these practices and heroin use is less understood,” researchers led by Geetanjoli Banerjee wrote in an abstract presented during the annual meeting of the College on Problems of Drug Dependence. “Understanding the relationship between prescription opioid use and initiation of heroin use among veterans is particularly important, as this population has both a higher underlying prevalence of substance abuse disorders and pain conditions.”
Ms. Banerjee, a graduate student at Brown University, Providence, R.I., and her associates examined data from 3,570 individuals enrolled in the Veterans Aging Cohort Study without nonmedical use or prescription opioids or heroin use in the year prior to baseline, and who received more than one prescription opioid from the VA during follow-up. between 2002 and 2012.
Among the 3,833 eligible participants, the proportion who were prescribed high-dose opioids (defined as a morphine equivalent daily dose of 90 mg or greater) did not change significantly between 2002 and 2012, and ranged from 4.4% to 5.9% (P = .22). The researchers also found that the 10-year incidence rate of recent heroin use was 8.15 event per 1,000 person-years. The time to recent heroin use differed significantly between participants with and without prior receipt of a high-dose prescription at baseline (P less than .001). Multivariable Cox regression analysis showed that prior receipt of a high-dose opioid prescription was associated with recent heroin use (adjusted hazard ratio, 2.54).
“Among patients who report no past year illicit use of opioids at baseline and who are receiving prescription opioids from the VA, receipt of high-dose prescription opioid increased the risk of subsequent heroin use,” the researchers concluded. “Patients receiving high-dose opioids, ages 50-56, with a history of HCV infection, injecting, opioid use disorder, or recent stimulant use should be screened for heroin use.”
They acknowledged certain limitations of the study, including its self-reported design and the fact that VA pharmacy data do not capture opioid prescriptions filled outside of the VA.
The study was funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Drug Abuse. Ms. Banerjee reported having no financial disclosures.
SAN DIEGO – High-dose opioid prescribing is associated with an increased risk of heroin use among U.S. veterans, a prospective study showed.
“Despite evidence linking increased risk of opioid use disorder with specific opioid prescribing patterns, the relationship between these practices and heroin use is less understood,” researchers led by Geetanjoli Banerjee wrote in an abstract presented during the annual meeting of the College on Problems of Drug Dependence. “Understanding the relationship between prescription opioid use and initiation of heroin use among veterans is particularly important, as this population has both a higher underlying prevalence of substance abuse disorders and pain conditions.”
Ms. Banerjee, a graduate student at Brown University, Providence, R.I., and her associates examined data from 3,570 individuals enrolled in the Veterans Aging Cohort Study without nonmedical use or prescription opioids or heroin use in the year prior to baseline, and who received more than one prescription opioid from the VA during follow-up. between 2002 and 2012.
Among the 3,833 eligible participants, the proportion who were prescribed high-dose opioids (defined as a morphine equivalent daily dose of 90 mg or greater) did not change significantly between 2002 and 2012, and ranged from 4.4% to 5.9% (P = .22). The researchers also found that the 10-year incidence rate of recent heroin use was 8.15 event per 1,000 person-years. The time to recent heroin use differed significantly between participants with and without prior receipt of a high-dose prescription at baseline (P less than .001). Multivariable Cox regression analysis showed that prior receipt of a high-dose opioid prescription was associated with recent heroin use (adjusted hazard ratio, 2.54).
“Among patients who report no past year illicit use of opioids at baseline and who are receiving prescription opioids from the VA, receipt of high-dose prescription opioid increased the risk of subsequent heroin use,” the researchers concluded. “Patients receiving high-dose opioids, ages 50-56, with a history of HCV infection, injecting, opioid use disorder, or recent stimulant use should be screened for heroin use.”
They acknowledged certain limitations of the study, including its self-reported design and the fact that VA pharmacy data do not capture opioid prescriptions filled outside of the VA.
The study was funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Drug Abuse. Ms. Banerjee reported having no financial disclosures.
SAN DIEGO – High-dose opioid prescribing is associated with an increased risk of heroin use among U.S. veterans, a prospective study showed.
“Despite evidence linking increased risk of opioid use disorder with specific opioid prescribing patterns, the relationship between these practices and heroin use is less understood,” researchers led by Geetanjoli Banerjee wrote in an abstract presented during the annual meeting of the College on Problems of Drug Dependence. “Understanding the relationship between prescription opioid use and initiation of heroin use among veterans is particularly important, as this population has both a higher underlying prevalence of substance abuse disorders and pain conditions.”
Ms. Banerjee, a graduate student at Brown University, Providence, R.I., and her associates examined data from 3,570 individuals enrolled in the Veterans Aging Cohort Study without nonmedical use or prescription opioids or heroin use in the year prior to baseline, and who received more than one prescription opioid from the VA during follow-up. between 2002 and 2012.
Among the 3,833 eligible participants, the proportion who were prescribed high-dose opioids (defined as a morphine equivalent daily dose of 90 mg or greater) did not change significantly between 2002 and 2012, and ranged from 4.4% to 5.9% (P = .22). The researchers also found that the 10-year incidence rate of recent heroin use was 8.15 event per 1,000 person-years. The time to recent heroin use differed significantly between participants with and without prior receipt of a high-dose prescription at baseline (P less than .001). Multivariable Cox regression analysis showed that prior receipt of a high-dose opioid prescription was associated with recent heroin use (adjusted hazard ratio, 2.54).
“Among patients who report no past year illicit use of opioids at baseline and who are receiving prescription opioids from the VA, receipt of high-dose prescription opioid increased the risk of subsequent heroin use,” the researchers concluded. “Patients receiving high-dose opioids, ages 50-56, with a history of HCV infection, injecting, opioid use disorder, or recent stimulant use should be screened for heroin use.”
They acknowledged certain limitations of the study, including its self-reported design and the fact that VA pharmacy data do not capture opioid prescriptions filled outside of the VA.
The study was funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Drug Abuse. Ms. Banerjee reported having no financial disclosures.
REPORTING CPDD 2018
Key clinical point: Screen patients who receive high-dose opioids and meet several other criteria for heroin use.
Major finding:. On multivariate Cox regression, prior prescription of high-dose opioids was an independent predictor of recent heroin use (adjusted hazard ratio, 2.54).
Study details: A prospective analysis of 3,833 participants in the Veterans Aging Cohort Study.
Disclosures: The study was funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Drug Abuse. Ms. Banerjee reported having no financial disclosures.