User login
New First-Line Therapies for Migraine Prevention
This transcript has been edited for clarity.
Today I am going to talk about the position statement from the American Headache Society (AHS) “Calcitonin gene-related peptide [CGRP]–targeting therapies are a first-line option for the prevention of migraine”. This update is of critical importance because about three fourths of people with migraine get their care from a primary care clinician, not from a neurologist or a headache specialist. CGRP-targeting therapies have transformed migraine care at the specialty level, but many in primary care are not yet familiar with this class of medicines. Until this new statement was released, CGRPs were not viewed as first-line agents for migraine. That has now changed.
Two main types of therapy for people with migraine headache are: (1) acute or abortive therapy (when a headache develops, it is treated), and (2) preventive therapy. Preventive therapy is typically used when the patient has headaches on 4 or more days per month. Preventive therapy is aimed at reducing the frequency and severity of headaches. About 40% of patients with migraine qualify for preventive therapy, but only a minority are receiving it.
The armamentarium for preventive therapy of migraines had not changed in a long time — until now. First-line preventive therapy has traditionally consisted of three classes of agents: beta-blockers, tricyclic antidepressants, and topiramate. These medicines were developed for different therapeutic purposes, yet they work for migraines. These drugs may have off-target effects that can make them difficult to tolerate.
Based on new evidence, candesartan — an angiotensin receptor blocker (ARB) — is now also a first-line drug for migraine. This is good news, because ARBs are a drug class that we have a lot of experience with, are easy to use, and could be an excellent choice for people with concomitant hypertension or chronic kidney disease. The serotonin-norepinephrine reuptake inhibitors (venlafaxine and duloxetine) are also considered first-line agents for migraine treatment.
In the AHS’s new position statement, the two main drug classes are small-molecule CGRP receptor antagonists and monoclonal antibodies.
The role of the neuropeptide CGRP in migraine was originally discovered after finding that blood levels of CGRP were elevated during migraine attacks. This led to the discovery of agents that blocked CGRP, initially for acute treatment of migraine, and then for preventive therapy. Multiple clinical studies show the CGRP targeting therapies to be as or even more effective than traditional first-line agents at decreasing the number of migraine days per month.
The efficacy and safety of these agents have been demonstrated in both randomized trials and in real-world studies. Other important positive endpoints include fewer days of migraine, reduced acute medication use, and improvements in many quality-of-life outcomes. Studies also have shown that CGRP-targeting therapies are well tolerated and safe, with very few serious adverse events.
Furthermore, studies have shown the CGRP targeting therapies are effective in individuals who have failed multiple other first-line therapies. They fit now both as first-line agents and as agents that can be used in difficult-to-treat patients as well as in patients who struggle with acute medication overuse, which is often very challenging.
To quote from the AHS statement,
Side effects are uncommon and can include hypertension, constipation, and Raynaud phenomenon.
The position statement is strong and is based on a lot of evidence and clinical experience. CGRP-targeting therapies are now first-line agents for the prevention of migraine headache. We should learn more about and begin to feel comfortable using this class of agents because they stand to benefit our patients greatly. I’d suggest looking at the table below and picking one new agent to become familiar with so that you can add that agent to your toolbox. 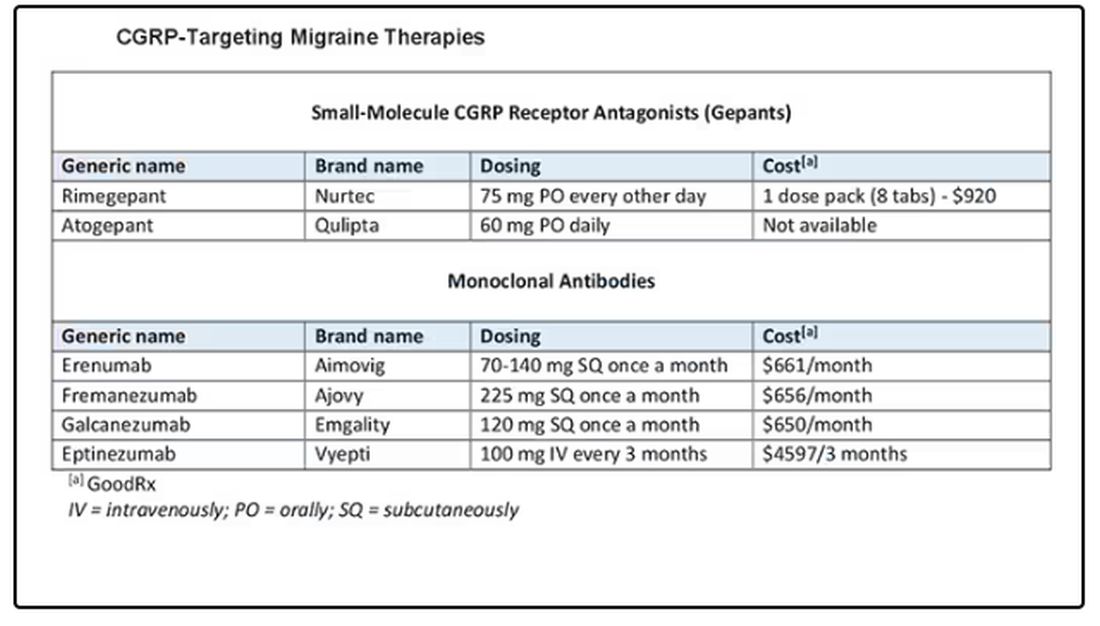
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, Pennsylvania, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, Bayer, and Teva.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Today I am going to talk about the position statement from the American Headache Society (AHS) “Calcitonin gene-related peptide [CGRP]–targeting therapies are a first-line option for the prevention of migraine”. This update is of critical importance because about three fourths of people with migraine get their care from a primary care clinician, not from a neurologist or a headache specialist. CGRP-targeting therapies have transformed migraine care at the specialty level, but many in primary care are not yet familiar with this class of medicines. Until this new statement was released, CGRPs were not viewed as first-line agents for migraine. That has now changed.
Two main types of therapy for people with migraine headache are: (1) acute or abortive therapy (when a headache develops, it is treated), and (2) preventive therapy. Preventive therapy is typically used when the patient has headaches on 4 or more days per month. Preventive therapy is aimed at reducing the frequency and severity of headaches. About 40% of patients with migraine qualify for preventive therapy, but only a minority are receiving it.
The armamentarium for preventive therapy of migraines had not changed in a long time — until now. First-line preventive therapy has traditionally consisted of three classes of agents: beta-blockers, tricyclic antidepressants, and topiramate. These medicines were developed for different therapeutic purposes, yet they work for migraines. These drugs may have off-target effects that can make them difficult to tolerate.
Based on new evidence, candesartan — an angiotensin receptor blocker (ARB) — is now also a first-line drug for migraine. This is good news, because ARBs are a drug class that we have a lot of experience with, are easy to use, and could be an excellent choice for people with concomitant hypertension or chronic kidney disease. The serotonin-norepinephrine reuptake inhibitors (venlafaxine and duloxetine) are also considered first-line agents for migraine treatment.
In the AHS’s new position statement, the two main drug classes are small-molecule CGRP receptor antagonists and monoclonal antibodies.
The role of the neuropeptide CGRP in migraine was originally discovered after finding that blood levels of CGRP were elevated during migraine attacks. This led to the discovery of agents that blocked CGRP, initially for acute treatment of migraine, and then for preventive therapy. Multiple clinical studies show the CGRP targeting therapies to be as or even more effective than traditional first-line agents at decreasing the number of migraine days per month.
The efficacy and safety of these agents have been demonstrated in both randomized trials and in real-world studies. Other important positive endpoints include fewer days of migraine, reduced acute medication use, and improvements in many quality-of-life outcomes. Studies also have shown that CGRP-targeting therapies are well tolerated and safe, with very few serious adverse events.
Furthermore, studies have shown the CGRP targeting therapies are effective in individuals who have failed multiple other first-line therapies. They fit now both as first-line agents and as agents that can be used in difficult-to-treat patients as well as in patients who struggle with acute medication overuse, which is often very challenging.
To quote from the AHS statement,
Side effects are uncommon and can include hypertension, constipation, and Raynaud phenomenon.
The position statement is strong and is based on a lot of evidence and clinical experience. CGRP-targeting therapies are now first-line agents for the prevention of migraine headache. We should learn more about and begin to feel comfortable using this class of agents because they stand to benefit our patients greatly. I’d suggest looking at the table below and picking one new agent to become familiar with so that you can add that agent to your toolbox. 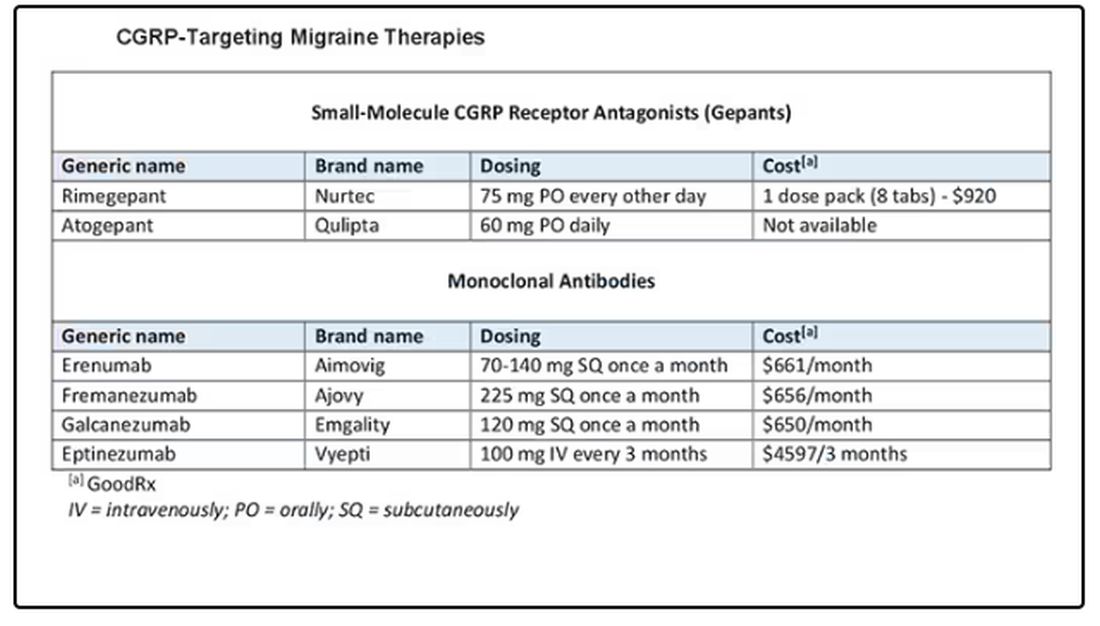
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, Pennsylvania, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, Bayer, and Teva.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Today I am going to talk about the position statement from the American Headache Society (AHS) “Calcitonin gene-related peptide [CGRP]–targeting therapies are a first-line option for the prevention of migraine”. This update is of critical importance because about three fourths of people with migraine get their care from a primary care clinician, not from a neurologist or a headache specialist. CGRP-targeting therapies have transformed migraine care at the specialty level, but many in primary care are not yet familiar with this class of medicines. Until this new statement was released, CGRPs were not viewed as first-line agents for migraine. That has now changed.
Two main types of therapy for people with migraine headache are: (1) acute or abortive therapy (when a headache develops, it is treated), and (2) preventive therapy. Preventive therapy is typically used when the patient has headaches on 4 or more days per month. Preventive therapy is aimed at reducing the frequency and severity of headaches. About 40% of patients with migraine qualify for preventive therapy, but only a minority are receiving it.
The armamentarium for preventive therapy of migraines had not changed in a long time — until now. First-line preventive therapy has traditionally consisted of three classes of agents: beta-blockers, tricyclic antidepressants, and topiramate. These medicines were developed for different therapeutic purposes, yet they work for migraines. These drugs may have off-target effects that can make them difficult to tolerate.
Based on new evidence, candesartan — an angiotensin receptor blocker (ARB) — is now also a first-line drug for migraine. This is good news, because ARBs are a drug class that we have a lot of experience with, are easy to use, and could be an excellent choice for people with concomitant hypertension or chronic kidney disease. The serotonin-norepinephrine reuptake inhibitors (venlafaxine and duloxetine) are also considered first-line agents for migraine treatment.
In the AHS’s new position statement, the two main drug classes are small-molecule CGRP receptor antagonists and monoclonal antibodies.
The role of the neuropeptide CGRP in migraine was originally discovered after finding that blood levels of CGRP were elevated during migraine attacks. This led to the discovery of agents that blocked CGRP, initially for acute treatment of migraine, and then for preventive therapy. Multiple clinical studies show the CGRP targeting therapies to be as or even more effective than traditional first-line agents at decreasing the number of migraine days per month.
The efficacy and safety of these agents have been demonstrated in both randomized trials and in real-world studies. Other important positive endpoints include fewer days of migraine, reduced acute medication use, and improvements in many quality-of-life outcomes. Studies also have shown that CGRP-targeting therapies are well tolerated and safe, with very few serious adverse events.
Furthermore, studies have shown the CGRP targeting therapies are effective in individuals who have failed multiple other first-line therapies. They fit now both as first-line agents and as agents that can be used in difficult-to-treat patients as well as in patients who struggle with acute medication overuse, which is often very challenging.
To quote from the AHS statement,
Side effects are uncommon and can include hypertension, constipation, and Raynaud phenomenon.
The position statement is strong and is based on a lot of evidence and clinical experience. CGRP-targeting therapies are now first-line agents for the prevention of migraine headache. We should learn more about and begin to feel comfortable using this class of agents because they stand to benefit our patients greatly. I’d suggest looking at the table below and picking one new agent to become familiar with so that you can add that agent to your toolbox. 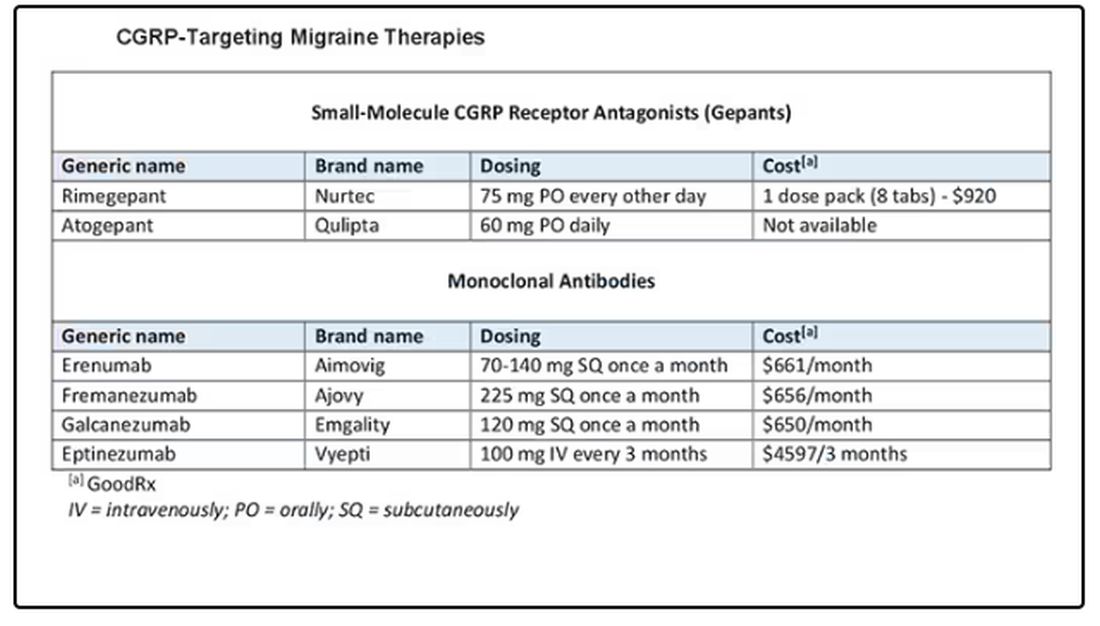
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, Pennsylvania, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, Bayer, and Teva.
A version of this article appeared on Medscape.com.
Does Headache Surgery Really Work? Neurologists Remain Unconvinced
Jeffrey E. Janis, MD, is on a mission. The professor of plastic surgery, surgery, neurosurgery, and neurology at The Ohio State University Wexner Medical Center, Columbus, Ohio, wants to convince neurologists of the safety and efficacy of nerve decompression surgery for treatment-resistant headache. However, many neurologists remain unconvinced.
There’s 24 years of evidence behind this surgical technique across hundreds of different studies with different study designs,” Dr. Janis said.
Yet this treatment approach — surgery on peripheral nerves rather than the brain or spinal cord — hasn’t garnered much support from neurologists. A scan of the agenda of topics at the recently held 2024 annual meeting of the American Headache Society showed few if any studies or presentations on this topic. And neurologists this news organization spoke to said they believe the surgery is experimental and unproven.
Experts do agree drugs don’t work for all patients with migraines. Up to 30% of patients don’t respond to the “laundry list of medications” available to treat the condition, said Dr. Janis.
Many patients have also tried, and failed, alternative treatment approaches such as massage, acupuncture, craniosacral therapy, transdermal patches, electrical stimulation, cryoablation, neurostimulation, and radiofrequency ablation.
If nothing else works, is surgery for headaches the answer?
Long-Held Theory
The idea that pinched, irritated, or compressed peripheral nerves can trigger migraine attacks has been around for nearly 25 years. Studies suggest that in addition to migraine, nerve compression can lead to other headache conditions, including occipital neuralgia, supraorbital neuralgia , and post-traumatic headaches.
This has led to the development of surgical techniques to deactivate various compression trigger sites — what Dr. Janis calls “pinch points” — which could involve muscles, bone, fascia, blood vessels, or scar tissue from prior trauma or surgery.
The procedure is predominantly performed by plastic surgeons, but to a lesser degree by neurosurgeons and ear, nose, and throat specialists.
Target nerves in surgical interventions include those in the frontal region of the head above the eye, temporal region, neck region, and nasal region. Affected areas are usually identified either through patient self-reports or by using a nerve block agent such as lidocaine or Botox at specific points, Dr. Janis noted. If pain subsides after an injection, that location is marked as a target.
One of the barriers to referring complicated patients for surgery is that neurologists evaluating migraine treatments “speak a different language” than surgeons performing the procedure, said Dr. Janis.
Neurologists tend to focus on reduction in monthly migraine days (MMD), while surgeons typically use the Migraine Headache Index that incorporates the frequency, intensity, and duration of migraine attacks.
“Rather than try to convince somebody to speak a different language, we thought, why don’t we just learn their language so we can build bridges and take down barriers,” said Dr. Janis, coauthor of a systematic review and meta-analysis published online recently in Plastic and Reconstructive Surgery.
Investigators examined 19 studies in the review, including five randomized controlled trials (RCTs), published from January 2020 to September 2023, with a total of 1603 participants who were mostly female and ranged in age from 9 to 72 years. Study follow-ups extended from 6 to 38 months. All but three studies were carried out in the United States, and six different compression sites were addressed during surgery.
Investigators found that across studies and by a number of measures, migraine frequency and severity improved after surgery.
Monthly migraine days decreased by 36%-92% and the number of overall migraine attacks per month dropped 25%-87.5%. Patients also reported decreases in attack duration of 41%-75% and intensity of 28%-82% across studies.
“Even using the neurologist-standard language of monthly migraine days, this surgery works,” said Dr. Janis. “Now this is documented both in the surgical literature and the nonsurgical literature.”
The most common complications were ecchymosis, hair loss or thinning, itching, dryness, and rhinorrhea, all of which Dr. Janis described as “fairly minor.” Major complications such as intraoperative bleeding and wound dehiscence were rare, occurring in 1% or less of participants.
‘One And Done?’
These surgeries are usually done on an outpatient basis and generally offer long-term results, Dr. Janis said.
“The idea is one and done,” he said. “The literature around this type of surgery says that whatever type of effect you get at 1 year is likely to be permanent.”
The American Society of Plastic Surgeons agrees. A 2018 position paper developed by experts and commissioned by the society reports that the intervention is safe and effective for appropriate patients, based on a comprehensive literature search and review of a large body of peer-reviewed scientific evidence.
“There is substantial, extensively replicated clinical data that demonstrates a significant reduction in [migraine headache] symptoms and frequency (even complete elimination of headache pain) following trigger site surgery,” the authors noted.
Pamela Blake, MD, a neurologist, board-certified headache specialist, and medical director at the Headache Center of River Oaks, Houston, is a proponent of what she said can be “lifesaving” headache surgery.
“If a doctor told you that you can either treat this problem with medications that you’ll need to take for the rest of your life or you can have a surgical procedure as an outpatient that has extremely low risk and has, in my experience, a 75% chance of reducing or eliminating your pain, you probably would be interested in surgery,” she said.
Continued Skepticism
However, other neurologists and clinicians appear doubtful about this intervention, including Hans-Christoph Diener, MD, PhD, professor of neurology and director, Essen Headache Centre, University of Duisburg-Essen in Germany.
During a debate on the topic a decade ago at the International Headache Congress, Dr. Diener argued that, as migraine is a complex multigene-related disorder of the brain, it doesn’t make sense that surgery would affect the epigenetics of 22 different genes.
Recently, he said that his views have not changed.
The topic remains controversial, and some neurologists are uncomfortable even openly discussing the procedure. Two clinicians who previously commented on this article later asked not to be included.
One neurologist, who asked to remain anonymous, said that Dr. Janis’s review article is “merely a review collecting 19 studies over the previous 10-plus years.”
Other limitations cited by this neurologist are the lack of consistency in procedures among the various studies and the inclusion of only four RCTs, the most recent of which was published 8 years ago, suggesting “the study was probably done closer to 9 or 10 years ago,” the neurologist said.
Dr. Blake suggested some neurologists’ reluctance could be due to limited background on the procedure, which she said isn’t widely discussed at headache meetings and is covered mostly in plastic surgery journals, not neurology literature. Access to surgery is further limited by a lack of specialists who perform the procedure and inconsistent insurance coverage.
A closer collaboration between neurologists and surgeons who perform the procedure could benefit patients, Dr. Blake noted.
“The headache doctor’s role is to identify who’s a candidate for surgery, who meets the criteria for nerve compression, and then follow that patient postoperatively, managing their medications, although usually we get them off their medications,” she added.
From Dr. Janis’s perspective, things are starting to change.
“I’m definitely seeing a greater comfort level among neurologists who are understanding where this sits in the algorithm for treatment, especially for complicated patients,” he said.
Dr. Janis receives royalties from Thieme and Springer Publishing. Dr. Blake reported no relevant conflicts. Dr. Diener received research support from the German Research Council; serves on the editorial boards of Cephalalgia, Lancet Neurology, and Drugs; and has received honoraria for participation in clinical trials, contribution to advisory boards, or oral presentations from AbbVie, Lilly, Lundbeck, Novartis, Pfizer, Teva, Weber & Weber, and WebMD.
A version of this article appeared on Medscape.com.
Jeffrey E. Janis, MD, is on a mission. The professor of plastic surgery, surgery, neurosurgery, and neurology at The Ohio State University Wexner Medical Center, Columbus, Ohio, wants to convince neurologists of the safety and efficacy of nerve decompression surgery for treatment-resistant headache. However, many neurologists remain unconvinced.
There’s 24 years of evidence behind this surgical technique across hundreds of different studies with different study designs,” Dr. Janis said.
Yet this treatment approach — surgery on peripheral nerves rather than the brain or spinal cord — hasn’t garnered much support from neurologists. A scan of the agenda of topics at the recently held 2024 annual meeting of the American Headache Society showed few if any studies or presentations on this topic. And neurologists this news organization spoke to said they believe the surgery is experimental and unproven.
Experts do agree drugs don’t work for all patients with migraines. Up to 30% of patients don’t respond to the “laundry list of medications” available to treat the condition, said Dr. Janis.
Many patients have also tried, and failed, alternative treatment approaches such as massage, acupuncture, craniosacral therapy, transdermal patches, electrical stimulation, cryoablation, neurostimulation, and radiofrequency ablation.
If nothing else works, is surgery for headaches the answer?
Long-Held Theory
The idea that pinched, irritated, or compressed peripheral nerves can trigger migraine attacks has been around for nearly 25 years. Studies suggest that in addition to migraine, nerve compression can lead to other headache conditions, including occipital neuralgia, supraorbital neuralgia , and post-traumatic headaches.
This has led to the development of surgical techniques to deactivate various compression trigger sites — what Dr. Janis calls “pinch points” — which could involve muscles, bone, fascia, blood vessels, or scar tissue from prior trauma or surgery.
The procedure is predominantly performed by plastic surgeons, but to a lesser degree by neurosurgeons and ear, nose, and throat specialists.
Target nerves in surgical interventions include those in the frontal region of the head above the eye, temporal region, neck region, and nasal region. Affected areas are usually identified either through patient self-reports or by using a nerve block agent such as lidocaine or Botox at specific points, Dr. Janis noted. If pain subsides after an injection, that location is marked as a target.
One of the barriers to referring complicated patients for surgery is that neurologists evaluating migraine treatments “speak a different language” than surgeons performing the procedure, said Dr. Janis.
Neurologists tend to focus on reduction in monthly migraine days (MMD), while surgeons typically use the Migraine Headache Index that incorporates the frequency, intensity, and duration of migraine attacks.
“Rather than try to convince somebody to speak a different language, we thought, why don’t we just learn their language so we can build bridges and take down barriers,” said Dr. Janis, coauthor of a systematic review and meta-analysis published online recently in Plastic and Reconstructive Surgery.
Investigators examined 19 studies in the review, including five randomized controlled trials (RCTs), published from January 2020 to September 2023, with a total of 1603 participants who were mostly female and ranged in age from 9 to 72 years. Study follow-ups extended from 6 to 38 months. All but three studies were carried out in the United States, and six different compression sites were addressed during surgery.
Investigators found that across studies and by a number of measures, migraine frequency and severity improved after surgery.
Monthly migraine days decreased by 36%-92% and the number of overall migraine attacks per month dropped 25%-87.5%. Patients also reported decreases in attack duration of 41%-75% and intensity of 28%-82% across studies.
“Even using the neurologist-standard language of monthly migraine days, this surgery works,” said Dr. Janis. “Now this is documented both in the surgical literature and the nonsurgical literature.”
The most common complications were ecchymosis, hair loss or thinning, itching, dryness, and rhinorrhea, all of which Dr. Janis described as “fairly minor.” Major complications such as intraoperative bleeding and wound dehiscence were rare, occurring in 1% or less of participants.
‘One And Done?’
These surgeries are usually done on an outpatient basis and generally offer long-term results, Dr. Janis said.
“The idea is one and done,” he said. “The literature around this type of surgery says that whatever type of effect you get at 1 year is likely to be permanent.”
The American Society of Plastic Surgeons agrees. A 2018 position paper developed by experts and commissioned by the society reports that the intervention is safe and effective for appropriate patients, based on a comprehensive literature search and review of a large body of peer-reviewed scientific evidence.
“There is substantial, extensively replicated clinical data that demonstrates a significant reduction in [migraine headache] symptoms and frequency (even complete elimination of headache pain) following trigger site surgery,” the authors noted.
Pamela Blake, MD, a neurologist, board-certified headache specialist, and medical director at the Headache Center of River Oaks, Houston, is a proponent of what she said can be “lifesaving” headache surgery.
“If a doctor told you that you can either treat this problem with medications that you’ll need to take for the rest of your life or you can have a surgical procedure as an outpatient that has extremely low risk and has, in my experience, a 75% chance of reducing or eliminating your pain, you probably would be interested in surgery,” she said.
Continued Skepticism
However, other neurologists and clinicians appear doubtful about this intervention, including Hans-Christoph Diener, MD, PhD, professor of neurology and director, Essen Headache Centre, University of Duisburg-Essen in Germany.
During a debate on the topic a decade ago at the International Headache Congress, Dr. Diener argued that, as migraine is a complex multigene-related disorder of the brain, it doesn’t make sense that surgery would affect the epigenetics of 22 different genes.
Recently, he said that his views have not changed.
The topic remains controversial, and some neurologists are uncomfortable even openly discussing the procedure. Two clinicians who previously commented on this article later asked not to be included.
One neurologist, who asked to remain anonymous, said that Dr. Janis’s review article is “merely a review collecting 19 studies over the previous 10-plus years.”
Other limitations cited by this neurologist are the lack of consistency in procedures among the various studies and the inclusion of only four RCTs, the most recent of which was published 8 years ago, suggesting “the study was probably done closer to 9 or 10 years ago,” the neurologist said.
Dr. Blake suggested some neurologists’ reluctance could be due to limited background on the procedure, which she said isn’t widely discussed at headache meetings and is covered mostly in plastic surgery journals, not neurology literature. Access to surgery is further limited by a lack of specialists who perform the procedure and inconsistent insurance coverage.
A closer collaboration between neurologists and surgeons who perform the procedure could benefit patients, Dr. Blake noted.
“The headache doctor’s role is to identify who’s a candidate for surgery, who meets the criteria for nerve compression, and then follow that patient postoperatively, managing their medications, although usually we get them off their medications,” she added.
From Dr. Janis’s perspective, things are starting to change.
“I’m definitely seeing a greater comfort level among neurologists who are understanding where this sits in the algorithm for treatment, especially for complicated patients,” he said.
Dr. Janis receives royalties from Thieme and Springer Publishing. Dr. Blake reported no relevant conflicts. Dr. Diener received research support from the German Research Council; serves on the editorial boards of Cephalalgia, Lancet Neurology, and Drugs; and has received honoraria for participation in clinical trials, contribution to advisory boards, or oral presentations from AbbVie, Lilly, Lundbeck, Novartis, Pfizer, Teva, Weber & Weber, and WebMD.
A version of this article appeared on Medscape.com.
Jeffrey E. Janis, MD, is on a mission. The professor of plastic surgery, surgery, neurosurgery, and neurology at The Ohio State University Wexner Medical Center, Columbus, Ohio, wants to convince neurologists of the safety and efficacy of nerve decompression surgery for treatment-resistant headache. However, many neurologists remain unconvinced.
There’s 24 years of evidence behind this surgical technique across hundreds of different studies with different study designs,” Dr. Janis said.
Yet this treatment approach — surgery on peripheral nerves rather than the brain or spinal cord — hasn’t garnered much support from neurologists. A scan of the agenda of topics at the recently held 2024 annual meeting of the American Headache Society showed few if any studies or presentations on this topic. And neurologists this news organization spoke to said they believe the surgery is experimental and unproven.
Experts do agree drugs don’t work for all patients with migraines. Up to 30% of patients don’t respond to the “laundry list of medications” available to treat the condition, said Dr. Janis.
Many patients have also tried, and failed, alternative treatment approaches such as massage, acupuncture, craniosacral therapy, transdermal patches, electrical stimulation, cryoablation, neurostimulation, and radiofrequency ablation.
If nothing else works, is surgery for headaches the answer?
Long-Held Theory
The idea that pinched, irritated, or compressed peripheral nerves can trigger migraine attacks has been around for nearly 25 years. Studies suggest that in addition to migraine, nerve compression can lead to other headache conditions, including occipital neuralgia, supraorbital neuralgia , and post-traumatic headaches.
This has led to the development of surgical techniques to deactivate various compression trigger sites — what Dr. Janis calls “pinch points” — which could involve muscles, bone, fascia, blood vessels, or scar tissue from prior trauma or surgery.
The procedure is predominantly performed by plastic surgeons, but to a lesser degree by neurosurgeons and ear, nose, and throat specialists.
Target nerves in surgical interventions include those in the frontal region of the head above the eye, temporal region, neck region, and nasal region. Affected areas are usually identified either through patient self-reports or by using a nerve block agent such as lidocaine or Botox at specific points, Dr. Janis noted. If pain subsides after an injection, that location is marked as a target.
One of the barriers to referring complicated patients for surgery is that neurologists evaluating migraine treatments “speak a different language” than surgeons performing the procedure, said Dr. Janis.
Neurologists tend to focus on reduction in monthly migraine days (MMD), while surgeons typically use the Migraine Headache Index that incorporates the frequency, intensity, and duration of migraine attacks.
“Rather than try to convince somebody to speak a different language, we thought, why don’t we just learn their language so we can build bridges and take down barriers,” said Dr. Janis, coauthor of a systematic review and meta-analysis published online recently in Plastic and Reconstructive Surgery.
Investigators examined 19 studies in the review, including five randomized controlled trials (RCTs), published from January 2020 to September 2023, with a total of 1603 participants who were mostly female and ranged in age from 9 to 72 years. Study follow-ups extended from 6 to 38 months. All but three studies were carried out in the United States, and six different compression sites were addressed during surgery.
Investigators found that across studies and by a number of measures, migraine frequency and severity improved after surgery.
Monthly migraine days decreased by 36%-92% and the number of overall migraine attacks per month dropped 25%-87.5%. Patients also reported decreases in attack duration of 41%-75% and intensity of 28%-82% across studies.
“Even using the neurologist-standard language of monthly migraine days, this surgery works,” said Dr. Janis. “Now this is documented both in the surgical literature and the nonsurgical literature.”
The most common complications were ecchymosis, hair loss or thinning, itching, dryness, and rhinorrhea, all of which Dr. Janis described as “fairly minor.” Major complications such as intraoperative bleeding and wound dehiscence were rare, occurring in 1% or less of participants.
‘One And Done?’
These surgeries are usually done on an outpatient basis and generally offer long-term results, Dr. Janis said.
“The idea is one and done,” he said. “The literature around this type of surgery says that whatever type of effect you get at 1 year is likely to be permanent.”
The American Society of Plastic Surgeons agrees. A 2018 position paper developed by experts and commissioned by the society reports that the intervention is safe and effective for appropriate patients, based on a comprehensive literature search and review of a large body of peer-reviewed scientific evidence.
“There is substantial, extensively replicated clinical data that demonstrates a significant reduction in [migraine headache] symptoms and frequency (even complete elimination of headache pain) following trigger site surgery,” the authors noted.
Pamela Blake, MD, a neurologist, board-certified headache specialist, and medical director at the Headache Center of River Oaks, Houston, is a proponent of what she said can be “lifesaving” headache surgery.
“If a doctor told you that you can either treat this problem with medications that you’ll need to take for the rest of your life or you can have a surgical procedure as an outpatient that has extremely low risk and has, in my experience, a 75% chance of reducing or eliminating your pain, you probably would be interested in surgery,” she said.
Continued Skepticism
However, other neurologists and clinicians appear doubtful about this intervention, including Hans-Christoph Diener, MD, PhD, professor of neurology and director, Essen Headache Centre, University of Duisburg-Essen in Germany.
During a debate on the topic a decade ago at the International Headache Congress, Dr. Diener argued that, as migraine is a complex multigene-related disorder of the brain, it doesn’t make sense that surgery would affect the epigenetics of 22 different genes.
Recently, he said that his views have not changed.
The topic remains controversial, and some neurologists are uncomfortable even openly discussing the procedure. Two clinicians who previously commented on this article later asked not to be included.
One neurologist, who asked to remain anonymous, said that Dr. Janis’s review article is “merely a review collecting 19 studies over the previous 10-plus years.”
Other limitations cited by this neurologist are the lack of consistency in procedures among the various studies and the inclusion of only four RCTs, the most recent of which was published 8 years ago, suggesting “the study was probably done closer to 9 or 10 years ago,” the neurologist said.
Dr. Blake suggested some neurologists’ reluctance could be due to limited background on the procedure, which she said isn’t widely discussed at headache meetings and is covered mostly in plastic surgery journals, not neurology literature. Access to surgery is further limited by a lack of specialists who perform the procedure and inconsistent insurance coverage.
A closer collaboration between neurologists and surgeons who perform the procedure could benefit patients, Dr. Blake noted.
“The headache doctor’s role is to identify who’s a candidate for surgery, who meets the criteria for nerve compression, and then follow that patient postoperatively, managing their medications, although usually we get them off their medications,” she added.
From Dr. Janis’s perspective, things are starting to change.
“I’m definitely seeing a greater comfort level among neurologists who are understanding where this sits in the algorithm for treatment, especially for complicated patients,” he said.
Dr. Janis receives royalties from Thieme and Springer Publishing. Dr. Blake reported no relevant conflicts. Dr. Diener received research support from the German Research Council; serves on the editorial boards of Cephalalgia, Lancet Neurology, and Drugs; and has received honoraria for participation in clinical trials, contribution to advisory boards, or oral presentations from AbbVie, Lilly, Lundbeck, Novartis, Pfizer, Teva, Weber & Weber, and WebMD.
A version of this article appeared on Medscape.com.
Commentary: Medication Overuse, Diet, and Parenting in Migraine, August 2024
MOH involves many of the same features as migraine headaches: photophobia, nausea, vomiting, and sleep disturbances.1 Additionally, patients with migraine and comorbid MOH are at a higher risk for anxiety, depression, and emotional stress. MOH is difficult to treat, and symptom relapse after treatment is common. Results of a retrospective analysis published in July 2024 in The Journal of Headache and Facial Pain confirmed the effectiveness of calcitonin gene-related peptide (CGRP) antibody treatment in a real-world setting among migraine patients who had MOH. The study included a total of 291 patients who had been treated with either erenumab, fremanezumab, or galcanezumab. The majority of patients experienced a significant decline in monthly headache days, monthly migraine days, and monthly acute medication intake at 1 year. The researchers found that only 15.4% of the patients who initially met the criterion of chronic migraine with MOH relapsed, meeting the criterion for chronic migraine/MOH at the end of the 1-year follow-up period.
Lifestyle factors, such as diet, should be addressed when discussing migraine therapy with patients. Dietary factors, including a low–glycemic index diet, have been associated with promising results in migraine control. Results of a 10,359-patient cross-sectional study published in 2023 in the journal Nutrition confirmed that the inflammatory potential of patients' diet is associated with severe headache or migraine in US adults.2 A more recent study, published in Frontiers in Nutrition in July 2024, examined dietary vitamin C intake of 13,445 individuals, of whom 20.42% had a severe headache or migraine. Vitamin C is a naturally occurring antioxidant and is also anti-inflammatory, found in foods such as citrus fruit, mangoes, strawberries, broccoli, and peppers. A subgroup analysis showed a significant association between vitamin C intake and severe headaches or migraines, with a reduced risk for severe headaches or migraines associated with an increased consumption of vitamin C. The authors noted that "each 1 mg/day increase in dietary vitamin C intake was significantly associated with a 6% lower risk for severe headache or migraine." Real-life application of this result for patients can involve encouraging patients to swap processed, low-nutrient foods in favor of fresh, nutrient-dense foods.
When treating migraine patients who are also parents, it is crucial to be persistent in searching for effective therapies to treat migraine and to treat or prevent MOH. According to a study published in 2018 in Headache, adolescents reported that parental migraine affected these factors in their lives: loss of parental support, reverse caregiving, emotional experience, interference with school, and missed activities and events.3 According to the authors of a more recent study, published in July 2024 in the Annals of General Psychiatry, parental migraine was significantly associated with an increased risk for attention-deficit/hyperactivity disorder, bipolar disorder, and depressive disorder among offspring of parents with migraine when compared with offspring of parents without migraine. The study authors noted that these outcomes could be the result of multiple factors, including psychosocial interactions, the burden of migraine on the family, and hereditary genetic traits. Nevertheless, even for offspring who may have a predisposition to these conditions because of genetic factors, effective treatment of parental migraine can relieve the day-to-day burden on the family, potentially reducing the effect of parental migraine on children. Parents who have migraine can become better equipped to provide attention to their children when their migraine symptoms are effectively treated. Furthermore, parents who have experienced improvement of their own migraine symptoms can offer hope and support if their children experience migraines, as migraine can be hereditary.
Additional References
1. Göçmez Yılmaz G, Ghouri R, et al. Complicated form of medication overuse headache is severe version of chronic migraine. J Clin Med. 2024;13(13):3696. doi: 10.3390/jcm13133696 Source
2. Liu H, Wang D, Wu F, et al. Association between inflammatory potential of diet and self-reported severe headache or migraine: A cross-sectional study of the National Health and Nutrition Examination Survey. Nutrition. 2023;113:112098. doi: 10.1016/j.nut.2023.112098 Source
3. Buse DC, Powers SW, Gelfand AA, et al. Adolescent perspectives on the burden of a parent's migraine: Results from the CaMEO Study. Headache. 2018;58(4):512-524. doi: 10.1111/head.13254 Source
MOH involves many of the same features as migraine headaches: photophobia, nausea, vomiting, and sleep disturbances.1 Additionally, patients with migraine and comorbid MOH are at a higher risk for anxiety, depression, and emotional stress. MOH is difficult to treat, and symptom relapse after treatment is common. Results of a retrospective analysis published in July 2024 in The Journal of Headache and Facial Pain confirmed the effectiveness of calcitonin gene-related peptide (CGRP) antibody treatment in a real-world setting among migraine patients who had MOH. The study included a total of 291 patients who had been treated with either erenumab, fremanezumab, or galcanezumab. The majority of patients experienced a significant decline in monthly headache days, monthly migraine days, and monthly acute medication intake at 1 year. The researchers found that only 15.4% of the patients who initially met the criterion of chronic migraine with MOH relapsed, meeting the criterion for chronic migraine/MOH at the end of the 1-year follow-up period.
Lifestyle factors, such as diet, should be addressed when discussing migraine therapy with patients. Dietary factors, including a low–glycemic index diet, have been associated with promising results in migraine control. Results of a 10,359-patient cross-sectional study published in 2023 in the journal Nutrition confirmed that the inflammatory potential of patients' diet is associated with severe headache or migraine in US adults.2 A more recent study, published in Frontiers in Nutrition in July 2024, examined dietary vitamin C intake of 13,445 individuals, of whom 20.42% had a severe headache or migraine. Vitamin C is a naturally occurring antioxidant and is also anti-inflammatory, found in foods such as citrus fruit, mangoes, strawberries, broccoli, and peppers. A subgroup analysis showed a significant association between vitamin C intake and severe headaches or migraines, with a reduced risk for severe headaches or migraines associated with an increased consumption of vitamin C. The authors noted that "each 1 mg/day increase in dietary vitamin C intake was significantly associated with a 6% lower risk for severe headache or migraine." Real-life application of this result for patients can involve encouraging patients to swap processed, low-nutrient foods in favor of fresh, nutrient-dense foods.
When treating migraine patients who are also parents, it is crucial to be persistent in searching for effective therapies to treat migraine and to treat or prevent MOH. According to a study published in 2018 in Headache, adolescents reported that parental migraine affected these factors in their lives: loss of parental support, reverse caregiving, emotional experience, interference with school, and missed activities and events.3 According to the authors of a more recent study, published in July 2024 in the Annals of General Psychiatry, parental migraine was significantly associated with an increased risk for attention-deficit/hyperactivity disorder, bipolar disorder, and depressive disorder among offspring of parents with migraine when compared with offspring of parents without migraine. The study authors noted that these outcomes could be the result of multiple factors, including psychosocial interactions, the burden of migraine on the family, and hereditary genetic traits. Nevertheless, even for offspring who may have a predisposition to these conditions because of genetic factors, effective treatment of parental migraine can relieve the day-to-day burden on the family, potentially reducing the effect of parental migraine on children. Parents who have migraine can become better equipped to provide attention to their children when their migraine symptoms are effectively treated. Furthermore, parents who have experienced improvement of their own migraine symptoms can offer hope and support if their children experience migraines, as migraine can be hereditary.
Additional References
1. Göçmez Yılmaz G, Ghouri R, et al. Complicated form of medication overuse headache is severe version of chronic migraine. J Clin Med. 2024;13(13):3696. doi: 10.3390/jcm13133696 Source
2. Liu H, Wang D, Wu F, et al. Association between inflammatory potential of diet and self-reported severe headache or migraine: A cross-sectional study of the National Health and Nutrition Examination Survey. Nutrition. 2023;113:112098. doi: 10.1016/j.nut.2023.112098 Source
3. Buse DC, Powers SW, Gelfand AA, et al. Adolescent perspectives on the burden of a parent's migraine: Results from the CaMEO Study. Headache. 2018;58(4):512-524. doi: 10.1111/head.13254 Source
MOH involves many of the same features as migraine headaches: photophobia, nausea, vomiting, and sleep disturbances.1 Additionally, patients with migraine and comorbid MOH are at a higher risk for anxiety, depression, and emotional stress. MOH is difficult to treat, and symptom relapse after treatment is common. Results of a retrospective analysis published in July 2024 in The Journal of Headache and Facial Pain confirmed the effectiveness of calcitonin gene-related peptide (CGRP) antibody treatment in a real-world setting among migraine patients who had MOH. The study included a total of 291 patients who had been treated with either erenumab, fremanezumab, or galcanezumab. The majority of patients experienced a significant decline in monthly headache days, monthly migraine days, and monthly acute medication intake at 1 year. The researchers found that only 15.4% of the patients who initially met the criterion of chronic migraine with MOH relapsed, meeting the criterion for chronic migraine/MOH at the end of the 1-year follow-up period.
Lifestyle factors, such as diet, should be addressed when discussing migraine therapy with patients. Dietary factors, including a low–glycemic index diet, have been associated with promising results in migraine control. Results of a 10,359-patient cross-sectional study published in 2023 in the journal Nutrition confirmed that the inflammatory potential of patients' diet is associated with severe headache or migraine in US adults.2 A more recent study, published in Frontiers in Nutrition in July 2024, examined dietary vitamin C intake of 13,445 individuals, of whom 20.42% had a severe headache or migraine. Vitamin C is a naturally occurring antioxidant and is also anti-inflammatory, found in foods such as citrus fruit, mangoes, strawberries, broccoli, and peppers. A subgroup analysis showed a significant association between vitamin C intake and severe headaches or migraines, with a reduced risk for severe headaches or migraines associated with an increased consumption of vitamin C. The authors noted that "each 1 mg/day increase in dietary vitamin C intake was significantly associated with a 6% lower risk for severe headache or migraine." Real-life application of this result for patients can involve encouraging patients to swap processed, low-nutrient foods in favor of fresh, nutrient-dense foods.
When treating migraine patients who are also parents, it is crucial to be persistent in searching for effective therapies to treat migraine and to treat or prevent MOH. According to a study published in 2018 in Headache, adolescents reported that parental migraine affected these factors in their lives: loss of parental support, reverse caregiving, emotional experience, interference with school, and missed activities and events.3 According to the authors of a more recent study, published in July 2024 in the Annals of General Psychiatry, parental migraine was significantly associated with an increased risk for attention-deficit/hyperactivity disorder, bipolar disorder, and depressive disorder among offspring of parents with migraine when compared with offspring of parents without migraine. The study authors noted that these outcomes could be the result of multiple factors, including psychosocial interactions, the burden of migraine on the family, and hereditary genetic traits. Nevertheless, even for offspring who may have a predisposition to these conditions because of genetic factors, effective treatment of parental migraine can relieve the day-to-day burden on the family, potentially reducing the effect of parental migraine on children. Parents who have migraine can become better equipped to provide attention to their children when their migraine symptoms are effectively treated. Furthermore, parents who have experienced improvement of their own migraine symptoms can offer hope and support if their children experience migraines, as migraine can be hereditary.
Additional References
1. Göçmez Yılmaz G, Ghouri R, et al. Complicated form of medication overuse headache is severe version of chronic migraine. J Clin Med. 2024;13(13):3696. doi: 10.3390/jcm13133696 Source
2. Liu H, Wang D, Wu F, et al. Association between inflammatory potential of diet and self-reported severe headache or migraine: A cross-sectional study of the National Health and Nutrition Examination Survey. Nutrition. 2023;113:112098. doi: 10.1016/j.nut.2023.112098 Source
3. Buse DC, Powers SW, Gelfand AA, et al. Adolescent perspectives on the burden of a parent's migraine: Results from the CaMEO Study. Headache. 2018;58(4):512-524. doi: 10.1111/head.13254 Source
Parental Migraine Ups Major Mental Disorder Risk in Offspring
Key clinical point: Parental migraine was associated with an increased risk for major mental disorders in the offspring, including attention deficit/hyperactivity disorder (ADHD), bipolar disorder, and depressive disorder.
Major finding: Offspring of parents with vs without migraine had a significantly higher risk for ADHD (hazard ratio [HR] 1.37; 95% CI 1.25-1.50), bipolar disorder (HR 1.35; 95% CI 1.06-1.71), and depressive disorder (HR 1.33; 95% CI 1.21-1.47). Sub-analyses revealed that only maternal migraine was a significant risk factor for these disorders.
Study details: This study used data from the Taiwan National Health Insurance Research Database and included 22,747 offspring of parents with migraine and 227,470 matched offspring of parents without migraine.
Disclosures: This study was supported by grants from the Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and Ministry of Science and Technology, Taiwan. The authors declared no conflicts of interest.
Source: Li D-J, Tsai S-J, Chen T-J, et al. Risk of major mental disorders in the offspring of parents with migraine. Ann Gen Psychiatry. 2024;23:23 (Jun 22). Doi: 10.1186/s12991-024-00508-y Source
Key clinical point: Parental migraine was associated with an increased risk for major mental disorders in the offspring, including attention deficit/hyperactivity disorder (ADHD), bipolar disorder, and depressive disorder.
Major finding: Offspring of parents with vs without migraine had a significantly higher risk for ADHD (hazard ratio [HR] 1.37; 95% CI 1.25-1.50), bipolar disorder (HR 1.35; 95% CI 1.06-1.71), and depressive disorder (HR 1.33; 95% CI 1.21-1.47). Sub-analyses revealed that only maternal migraine was a significant risk factor for these disorders.
Study details: This study used data from the Taiwan National Health Insurance Research Database and included 22,747 offspring of parents with migraine and 227,470 matched offspring of parents without migraine.
Disclosures: This study was supported by grants from the Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and Ministry of Science and Technology, Taiwan. The authors declared no conflicts of interest.
Source: Li D-J, Tsai S-J, Chen T-J, et al. Risk of major mental disorders in the offspring of parents with migraine. Ann Gen Psychiatry. 2024;23:23 (Jun 22). Doi: 10.1186/s12991-024-00508-y Source
Key clinical point: Parental migraine was associated with an increased risk for major mental disorders in the offspring, including attention deficit/hyperactivity disorder (ADHD), bipolar disorder, and depressive disorder.
Major finding: Offspring of parents with vs without migraine had a significantly higher risk for ADHD (hazard ratio [HR] 1.37; 95% CI 1.25-1.50), bipolar disorder (HR 1.35; 95% CI 1.06-1.71), and depressive disorder (HR 1.33; 95% CI 1.21-1.47). Sub-analyses revealed that only maternal migraine was a significant risk factor for these disorders.
Study details: This study used data from the Taiwan National Health Insurance Research Database and included 22,747 offspring of parents with migraine and 227,470 matched offspring of parents without migraine.
Disclosures: This study was supported by grants from the Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and Ministry of Science and Technology, Taiwan. The authors declared no conflicts of interest.
Source: Li D-J, Tsai S-J, Chen T-J, et al. Risk of major mental disorders in the offspring of parents with migraine. Ann Gen Psychiatry. 2024;23:23 (Jun 22). Doi: 10.1186/s12991-024-00508-y Source
Increasing Dietary Vitamin C Intake May Prevent Severe Headache or Migraine
Key clinical point: Dietary vitamin C intake was negatively associated with the risk for severe headache or migraine.
Major finding: Each 1 mg/day increase in dietary vitamin C intake was significantly associated with a 6% lower risk for severe headache or migraine (adjusted odd ratio [aOR] 0.94; P = .0007). This inverse association between dietary vitamin C intake and severe headache or migraine risk was significant in women (aOR 0.90; 95% CI 0.87-0.85) but not in men.
Study details: This cross-sectional study included 13,445 participants from the National Health and Nutrition Examination Survey, of whom 2745 (20.42%) had severe headache or migraine.
Disclosures: This study did not receive any specific funding. The authors declared no conflicts of interest.
Source: Zheng Y, Jin J, Wei C, Huang C. Association of dietary vitamin C consumption with severe headache or migraine among adults: A cross-sectional study of NHANES 1999–2004. Front Nutr. 2024;11:fnut.2024.1412031 (Jun 18). Doi: 10.3389/fnut.2024.1412031 Source
Key clinical point: Dietary vitamin C intake was negatively associated with the risk for severe headache or migraine.
Major finding: Each 1 mg/day increase in dietary vitamin C intake was significantly associated with a 6% lower risk for severe headache or migraine (adjusted odd ratio [aOR] 0.94; P = .0007). This inverse association between dietary vitamin C intake and severe headache or migraine risk was significant in women (aOR 0.90; 95% CI 0.87-0.85) but not in men.
Study details: This cross-sectional study included 13,445 participants from the National Health and Nutrition Examination Survey, of whom 2745 (20.42%) had severe headache or migraine.
Disclosures: This study did not receive any specific funding. The authors declared no conflicts of interest.
Source: Zheng Y, Jin J, Wei C, Huang C. Association of dietary vitamin C consumption with severe headache or migraine among adults: A cross-sectional study of NHANES 1999–2004. Front Nutr. 2024;11:fnut.2024.1412031 (Jun 18). Doi: 10.3389/fnut.2024.1412031 Source
Key clinical point: Dietary vitamin C intake was negatively associated with the risk for severe headache or migraine.
Major finding: Each 1 mg/day increase in dietary vitamin C intake was significantly associated with a 6% lower risk for severe headache or migraine (adjusted odd ratio [aOR] 0.94; P = .0007). This inverse association between dietary vitamin C intake and severe headache or migraine risk was significant in women (aOR 0.90; 95% CI 0.87-0.85) but not in men.
Study details: This cross-sectional study included 13,445 participants from the National Health and Nutrition Examination Survey, of whom 2745 (20.42%) had severe headache or migraine.
Disclosures: This study did not receive any specific funding. The authors declared no conflicts of interest.
Source: Zheng Y, Jin J, Wei C, Huang C. Association of dietary vitamin C consumption with severe headache or migraine among adults: A cross-sectional study of NHANES 1999–2004. Front Nutr. 2024;11:fnut.2024.1412031 (Jun 18). Doi: 10.3389/fnut.2024.1412031 Source
Sustained Benefits of CGRP Antibodies in Migraine and Medication Overuse Headache
Key clinical point: Prophylactic migraine therapy with calcitonin gene-related peptide (CGRP) antibodies showed sustained benefits in patients with migraine and medication overuse headache (MOH) or medication overuse (MO) for up to a year.
Major findings: All patients, including those with episodic migraine (EM) with MO, EM without MO, chronic migraine (CM) with MOH, or CM without MOH, had significant reductions in monthly headache days, monthly migraine days, and acute medication days at the last observation timepoint within the first year of CGRP therapy from baseline (all P < .0001). Relapse rates were lower (15.4%) in patients with CM with MOH after successful initiation of CGRP treatment.
Study details: This retrospective real-world analysis included 112 patients with EM (35 with MO and 77 without MO) and 179 patients with CM (109 with MOH and 70 without MOH).
Disclosures: This study was funded by Projekt DEAL. Some authors declared receiving travel fees, honoraria, or scientific support from or serving as consultants or advisors for various sources.
Source: Scheffler A, Basten J, Menzel L, et al. Persistent effectiveness of CGRP antibody therapy in migraine and comorbid medication overuse or medication overuse headache - a retrospective real-world analysis. J Headache Pain. 2024;25:109 (Jul 4). Doi: 10.1186/s10194-024-01813-3 Source
Key clinical point: Prophylactic migraine therapy with calcitonin gene-related peptide (CGRP) antibodies showed sustained benefits in patients with migraine and medication overuse headache (MOH) or medication overuse (MO) for up to a year.
Major findings: All patients, including those with episodic migraine (EM) with MO, EM without MO, chronic migraine (CM) with MOH, or CM without MOH, had significant reductions in monthly headache days, monthly migraine days, and acute medication days at the last observation timepoint within the first year of CGRP therapy from baseline (all P < .0001). Relapse rates were lower (15.4%) in patients with CM with MOH after successful initiation of CGRP treatment.
Study details: This retrospective real-world analysis included 112 patients with EM (35 with MO and 77 without MO) and 179 patients with CM (109 with MOH and 70 without MOH).
Disclosures: This study was funded by Projekt DEAL. Some authors declared receiving travel fees, honoraria, or scientific support from or serving as consultants or advisors for various sources.
Source: Scheffler A, Basten J, Menzel L, et al. Persistent effectiveness of CGRP antibody therapy in migraine and comorbid medication overuse or medication overuse headache - a retrospective real-world analysis. J Headache Pain. 2024;25:109 (Jul 4). Doi: 10.1186/s10194-024-01813-3 Source
Key clinical point: Prophylactic migraine therapy with calcitonin gene-related peptide (CGRP) antibodies showed sustained benefits in patients with migraine and medication overuse headache (MOH) or medication overuse (MO) for up to a year.
Major findings: All patients, including those with episodic migraine (EM) with MO, EM without MO, chronic migraine (CM) with MOH, or CM without MOH, had significant reductions in monthly headache days, monthly migraine days, and acute medication days at the last observation timepoint within the first year of CGRP therapy from baseline (all P < .0001). Relapse rates were lower (15.4%) in patients with CM with MOH after successful initiation of CGRP treatment.
Study details: This retrospective real-world analysis included 112 patients with EM (35 with MO and 77 without MO) and 179 patients with CM (109 with MOH and 70 without MOH).
Disclosures: This study was funded by Projekt DEAL. Some authors declared receiving travel fees, honoraria, or scientific support from or serving as consultants or advisors for various sources.
Source: Scheffler A, Basten J, Menzel L, et al. Persistent effectiveness of CGRP antibody therapy in migraine and comorbid medication overuse or medication overuse headache - a retrospective real-world analysis. J Headache Pain. 2024;25:109 (Jul 4). Doi: 10.1186/s10194-024-01813-3 Source
Neck Pain With Headache During Migraine Tied to Poor Migraine Health
Key clinical point: Patients with migraine who experienced neck pain with headache (NPWH) had a higher prevalence of disability, depression, anxiety, and allodynia, as well as a lower quality of life, greater work productivity losses, and poorer acute treatment optimization than those without NPWH.
Major findings: Patients with vs without NPWH showed a higher prevalence of moderate to severe disability (47.7% vs 28.9%), depression (40.2% vs 28.2%), anxiety (41.2% vs 29.2%), allodynia (54.0% vs 36.6%), and poor acute treatment optimization (61.1% vs 53.3%; P < .001 for all). They also had lower quality of life scores (60.0 vs 68.6) and higher work productivity loss scores (50.0 vs 30.0; P < .001 for both).
Study details: This analysis of the Chronic Migraine Epidemiology and Outcomes – International study included 14, 492 patients with migraine, of whom 9896 (68.3%) had NPWH.
Disclosures: This study was funded by Allergan (now AbbVie). One author declared being an employee or a stockholder of AbbVie. Several authors declared having ties with various sources, including AbbVie.
Source: Matharu M, Katsarava Z, Buse DC, et al. Characterizing neck pain during headache among people with migraine: Multicountry results from the Chronic Migraine Epidemiology and Outcomes – International (CaMEO-I) cross-sectional study. Headache. 2024;64:750-763 (Jun 22). Doi: 10.1111/head.14753 Source
Key clinical point: Patients with migraine who experienced neck pain with headache (NPWH) had a higher prevalence of disability, depression, anxiety, and allodynia, as well as a lower quality of life, greater work productivity losses, and poorer acute treatment optimization than those without NPWH.
Major findings: Patients with vs without NPWH showed a higher prevalence of moderate to severe disability (47.7% vs 28.9%), depression (40.2% vs 28.2%), anxiety (41.2% vs 29.2%), allodynia (54.0% vs 36.6%), and poor acute treatment optimization (61.1% vs 53.3%; P < .001 for all). They also had lower quality of life scores (60.0 vs 68.6) and higher work productivity loss scores (50.0 vs 30.0; P < .001 for both).
Study details: This analysis of the Chronic Migraine Epidemiology and Outcomes – International study included 14, 492 patients with migraine, of whom 9896 (68.3%) had NPWH.
Disclosures: This study was funded by Allergan (now AbbVie). One author declared being an employee or a stockholder of AbbVie. Several authors declared having ties with various sources, including AbbVie.
Source: Matharu M, Katsarava Z, Buse DC, et al. Characterizing neck pain during headache among people with migraine: Multicountry results from the Chronic Migraine Epidemiology and Outcomes – International (CaMEO-I) cross-sectional study. Headache. 2024;64:750-763 (Jun 22). Doi: 10.1111/head.14753 Source
Key clinical point: Patients with migraine who experienced neck pain with headache (NPWH) had a higher prevalence of disability, depression, anxiety, and allodynia, as well as a lower quality of life, greater work productivity losses, and poorer acute treatment optimization than those without NPWH.
Major findings: Patients with vs without NPWH showed a higher prevalence of moderate to severe disability (47.7% vs 28.9%), depression (40.2% vs 28.2%), anxiety (41.2% vs 29.2%), allodynia (54.0% vs 36.6%), and poor acute treatment optimization (61.1% vs 53.3%; P < .001 for all). They also had lower quality of life scores (60.0 vs 68.6) and higher work productivity loss scores (50.0 vs 30.0; P < .001 for both).
Study details: This analysis of the Chronic Migraine Epidemiology and Outcomes – International study included 14, 492 patients with migraine, of whom 9896 (68.3%) had NPWH.
Disclosures: This study was funded by Allergan (now AbbVie). One author declared being an employee or a stockholder of AbbVie. Several authors declared having ties with various sources, including AbbVie.
Source: Matharu M, Katsarava Z, Buse DC, et al. Characterizing neck pain during headache among people with migraine: Multicountry results from the Chronic Migraine Epidemiology and Outcomes – International (CaMEO-I) cross-sectional study. Headache. 2024;64:750-763 (Jun 22). Doi: 10.1111/head.14753 Source
Does Migraine Influence Serum Alpha-CGRP Levels in Patients With IBD?
Key clinical point: Patients with inflammatory bowel disease (IBD) and chronic migraine (CM) had higher serum levels of alpha-calcitonin gene-related peptide (CGRP) than patients with only IBD.
Major findings: The alpha-CGRP levels were significantly higher in patients with IBD (56.9 vs 37.2 pg/mL; P = .003) or CM (53.0 vs 37.2 pg/mL; P = .019) than healthy control participants without a history of IBD and CM. The levels of this peptide in the serum were further increased in patients with IBD and concomitant migraine compared with those with only IBD (70.9 vs 53.7 pg/mL; P = .046).
Study details: This cross-sectional study compared the serum CGRP levels in 96 patients with IBD, 50 patients with CM, and 50 healthy control participants without a history of IBD and CM.
Disclosures: This study was funded by Instituto de Salud Carlos III, Spain. The authors declared no conflicts of interest.
Source: Pascual-Mato M, Gárate G, González-Quintanilla V, et al. Differences in circulating alpha-calcitonin gene-related peptide levels in inflammatory bowel disease and its relation to migraine comorbidity: A cross-sectional study. Headache. 2024;64:849-858 (Jun 24). Doi: 10.1111/head.14768 Source
Key clinical point: Patients with inflammatory bowel disease (IBD) and chronic migraine (CM) had higher serum levels of alpha-calcitonin gene-related peptide (CGRP) than patients with only IBD.
Major findings: The alpha-CGRP levels were significantly higher in patients with IBD (56.9 vs 37.2 pg/mL; P = .003) or CM (53.0 vs 37.2 pg/mL; P = .019) than healthy control participants without a history of IBD and CM. The levels of this peptide in the serum were further increased in patients with IBD and concomitant migraine compared with those with only IBD (70.9 vs 53.7 pg/mL; P = .046).
Study details: This cross-sectional study compared the serum CGRP levels in 96 patients with IBD, 50 patients with CM, and 50 healthy control participants without a history of IBD and CM.
Disclosures: This study was funded by Instituto de Salud Carlos III, Spain. The authors declared no conflicts of interest.
Source: Pascual-Mato M, Gárate G, González-Quintanilla V, et al. Differences in circulating alpha-calcitonin gene-related peptide levels in inflammatory bowel disease and its relation to migraine comorbidity: A cross-sectional study. Headache. 2024;64:849-858 (Jun 24). Doi: 10.1111/head.14768 Source
Key clinical point: Patients with inflammatory bowel disease (IBD) and chronic migraine (CM) had higher serum levels of alpha-calcitonin gene-related peptide (CGRP) than patients with only IBD.
Major findings: The alpha-CGRP levels were significantly higher in patients with IBD (56.9 vs 37.2 pg/mL; P = .003) or CM (53.0 vs 37.2 pg/mL; P = .019) than healthy control participants without a history of IBD and CM. The levels of this peptide in the serum were further increased in patients with IBD and concomitant migraine compared with those with only IBD (70.9 vs 53.7 pg/mL; P = .046).
Study details: This cross-sectional study compared the serum CGRP levels in 96 patients with IBD, 50 patients with CM, and 50 healthy control participants without a history of IBD and CM.
Disclosures: This study was funded by Instituto de Salud Carlos III, Spain. The authors declared no conflicts of interest.
Source: Pascual-Mato M, Gárate G, González-Quintanilla V, et al. Differences in circulating alpha-calcitonin gene-related peptide levels in inflammatory bowel disease and its relation to migraine comorbidity: A cross-sectional study. Headache. 2024;64:849-858 (Jun 24). Doi: 10.1111/head.14768 Source
Long-term Eptinezumab Benefits Patients With Chronic Migraine and Medication-Overuse Headache
Key clinical point: Long-term eptinezumab treatment showed benefits in patients with chronic migraine (CM) who had concomitant medication-overuse headache (MOH).
Major findings: After eptinezumab treatment, the average number of headache days per 3 months reduced from 15.8 days (mean 47.5 headache days/month) at baseline to 3.8 days (mean 11.3 headache days/month) at 104 weeks, along with reductions observed in the Migraine Disability Assessment (mean change −51.9 points) and 6-item Headache Impact Test (mean change −9.7 points) scores. More than half (57.1%) the patients showed an improvement in their patient-identified most bothersome symptom at as early as 4 weeks.
Study details: This post hoc analysis of the PREVAIL study included 49 patients with CM and concomitant MOH.
Disclosures: This publication was supported by H. Lundbeck A/S, Copenhagen, Denmark. Two authors declared being employees of H. Lundbeck A/S. The other authors declared having ties with various sources, including H. Lundbeck A/S.
Source: Blumenfeld A, Kudrow D, McAllister P, et al. Long-term effectiveness of eptinezumab in the treatment of patients with chronic migraine and medication-overuse headache. Headache. 2024;64:738-749 (Jun 24). Doi: 10.1111/head.14767 Source
Key clinical point: Long-term eptinezumab treatment showed benefits in patients with chronic migraine (CM) who had concomitant medication-overuse headache (MOH).
Major findings: After eptinezumab treatment, the average number of headache days per 3 months reduced from 15.8 days (mean 47.5 headache days/month) at baseline to 3.8 days (mean 11.3 headache days/month) at 104 weeks, along with reductions observed in the Migraine Disability Assessment (mean change −51.9 points) and 6-item Headache Impact Test (mean change −9.7 points) scores. More than half (57.1%) the patients showed an improvement in their patient-identified most bothersome symptom at as early as 4 weeks.
Study details: This post hoc analysis of the PREVAIL study included 49 patients with CM and concomitant MOH.
Disclosures: This publication was supported by H. Lundbeck A/S, Copenhagen, Denmark. Two authors declared being employees of H. Lundbeck A/S. The other authors declared having ties with various sources, including H. Lundbeck A/S.
Source: Blumenfeld A, Kudrow D, McAllister P, et al. Long-term effectiveness of eptinezumab in the treatment of patients with chronic migraine and medication-overuse headache. Headache. 2024;64:738-749 (Jun 24). Doi: 10.1111/head.14767 Source
Key clinical point: Long-term eptinezumab treatment showed benefits in patients with chronic migraine (CM) who had concomitant medication-overuse headache (MOH).
Major findings: After eptinezumab treatment, the average number of headache days per 3 months reduced from 15.8 days (mean 47.5 headache days/month) at baseline to 3.8 days (mean 11.3 headache days/month) at 104 weeks, along with reductions observed in the Migraine Disability Assessment (mean change −51.9 points) and 6-item Headache Impact Test (mean change −9.7 points) scores. More than half (57.1%) the patients showed an improvement in their patient-identified most bothersome symptom at as early as 4 weeks.
Study details: This post hoc analysis of the PREVAIL study included 49 patients with CM and concomitant MOH.
Disclosures: This publication was supported by H. Lundbeck A/S, Copenhagen, Denmark. Two authors declared being employees of H. Lundbeck A/S. The other authors declared having ties with various sources, including H. Lundbeck A/S.
Source: Blumenfeld A, Kudrow D, McAllister P, et al. Long-term effectiveness of eptinezumab in the treatment of patients with chronic migraine and medication-overuse headache. Headache. 2024;64:738-749 (Jun 24). Doi: 10.1111/head.14767 Source
Patients with CGRP-Induced Migraine Attacks Can Benefit With Erenumab
Key clinical point: Calcitonin gene-related peptide (CGRP)–induced migraine attacks did not affect therapeutic response to erenumab in patients with migraine.
Major finding: Overall, a similar proportion of patients who experienced vs did not experience CGRP-induced migraine attacks had a ≥50% reduction in monthly migraine days during weeks 13-24 following erenumab treatment (61% vs 52%; odds ratio [OR] 1.42; P = .498). No significant differences were seen between the two patient groups that achieved a ≥50% reduction in monthly migraine or headache days of moderate to severe intensity (OR 1.25; P = .625).
Study details: This interim analysis of the REFORM study included 124 patients with migraine who received CGRP infusion on a single experimental day and subsequently a 24-week treatment with erenumab.
Disclosures: This study was funded by Novartis Pharma and the Lundbeck Foundation. Two authors declared being employees of or holding shares in Novartis Pharma AG. Several authors declared receiving personal fees from various sources, including Novartis, outside of the submitted work. One author is an associate editor for Cephalalgia.
Source: Al-Khazali HM, Ashina H, Christensen RH, et al. Hypersensitivity to CGRP as a predictive biomarker of migraine prevention with erenumab. Cephalalgia. 2024;44(6):3331024241258734 (Jun 11). Doi: 10.1177/03331024241258734 Source
Key clinical point: Calcitonin gene-related peptide (CGRP)–induced migraine attacks did not affect therapeutic response to erenumab in patients with migraine.
Major finding: Overall, a similar proportion of patients who experienced vs did not experience CGRP-induced migraine attacks had a ≥50% reduction in monthly migraine days during weeks 13-24 following erenumab treatment (61% vs 52%; odds ratio [OR] 1.42; P = .498). No significant differences were seen between the two patient groups that achieved a ≥50% reduction in monthly migraine or headache days of moderate to severe intensity (OR 1.25; P = .625).
Study details: This interim analysis of the REFORM study included 124 patients with migraine who received CGRP infusion on a single experimental day and subsequently a 24-week treatment with erenumab.
Disclosures: This study was funded by Novartis Pharma and the Lundbeck Foundation. Two authors declared being employees of or holding shares in Novartis Pharma AG. Several authors declared receiving personal fees from various sources, including Novartis, outside of the submitted work. One author is an associate editor for Cephalalgia.
Source: Al-Khazali HM, Ashina H, Christensen RH, et al. Hypersensitivity to CGRP as a predictive biomarker of migraine prevention with erenumab. Cephalalgia. 2024;44(6):3331024241258734 (Jun 11). Doi: 10.1177/03331024241258734 Source
Key clinical point: Calcitonin gene-related peptide (CGRP)–induced migraine attacks did not affect therapeutic response to erenumab in patients with migraine.
Major finding: Overall, a similar proportion of patients who experienced vs did not experience CGRP-induced migraine attacks had a ≥50% reduction in monthly migraine days during weeks 13-24 following erenumab treatment (61% vs 52%; odds ratio [OR] 1.42; P = .498). No significant differences were seen between the two patient groups that achieved a ≥50% reduction in monthly migraine or headache days of moderate to severe intensity (OR 1.25; P = .625).
Study details: This interim analysis of the REFORM study included 124 patients with migraine who received CGRP infusion on a single experimental day and subsequently a 24-week treatment with erenumab.
Disclosures: This study was funded by Novartis Pharma and the Lundbeck Foundation. Two authors declared being employees of or holding shares in Novartis Pharma AG. Several authors declared receiving personal fees from various sources, including Novartis, outside of the submitted work. One author is an associate editor for Cephalalgia.
Source: Al-Khazali HM, Ashina H, Christensen RH, et al. Hypersensitivity to CGRP as a predictive biomarker of migraine prevention with erenumab. Cephalalgia. 2024;44(6):3331024241258734 (Jun 11). Doi: 10.1177/03331024241258734 Source
