User login
Multiple Sclerosis Hub
Escalate treatment to avoid MS relapses
BERLIN – Escalating treatment to a “highly effective” disease-modifying treatment (DMT) results in fewer relapses in patients with relapsing-remitting multiple sclerosis (RRMS) than does switching to another “moderately effective” therapy, according to data from a Danish cohort study.
The annualized relapse rate (ARR) was 0.23 for patients who switched to a highly effective DMT, defined as either natalizumab (Tysabri) or fingolimod (Gilenya), whereas the ARR was 0.35 in those who were switched to a moderately effective DMT, defined as an interferon-beta, glatiramer acetate (Copaxone), teriflunomide (Aubagio), or dimethyl fumarate (Tecfidera).
This resulted in a relapse-rate ratio of 0.67 (95% confidence interval [CI], 0.55-0.83) comparing high to moderate DMT, or a 33% lower relapse rate in the high DMT group, Thor Ameri Chalmer, MD, PhD, reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Chalmer, who works at the Danish Multiple Sclerosis Center at Rigshospitalet, the University of Copenhagen, reported that the time to first relapse and the likelihood for having recurrent relapses were all lowered by escalating treatment rather than switching treatment. Indeed, there was a 38% increase in the time to first relapse (hazard ratio [HR] = 0.62; 95% CI, 0.50-0.76) and a 31% reduction in recurrent relapses (HR = 0.69; 95% CI, 0.57-0.83).
However, there were “no clear differences” in the time to 3-month confirmed Expanded Disability Status Scale (EDSS) worsening and improvement, Dr. Chalmer said. The HR for time to first worsening in the 3-month confirmed EDSS was 0.86, and for recurrent worsening it was 0.86, but the 95% CI in both cases crossed over from 1.0 (0.65-1.14 and 0.71-1.05, respectively). There was no difference in the time to first improvement (HR = 1.23; 95% CI, 0.95-1.60).
“The aim of this study was to use data from the [Danish] MS Registry, find the patients who started on what we define as moderately effective DMT for the first time, and on this treatment experienced a disease breakthrough and then either switched to another moderately effective DMT or escalated to a highly effective DMT,” Dr. Chalmer explained.
Disease breakthrough was defined as at least one relapse occurring within 12 months of the treatment switch, or the treating neurologist defined the reason for switching as disease breakthrough. Dr. Chalmer acknowledged that this was one of the limitations of the observational study as patients could have been misclassified and switched treatment for another reason. The severity of the relapse was not recorded.
Data on more than 5,000 patients enrolled in the Danish Multiple Sclerosis Registry (DMSR) were considered, with a final propensity-match population of 788 included in the analysis; half had received highly effective DMT and half moderately effective DMT.
The DMSR contains data on virtually all patients with MS treated in Denmark, Dr. Chalmer observed; treatment with DMT is free of charge and it can be prescribed only in public MS clinics, he explained. Furthermore, all MS clinics are required to register information about treatment response at each clinical visit.
The mean age of patients in the study was 39 years, around 70% were female, and average disease duration was 5 years.
“I don’t see in your study what is really new,” Gilles Edan, MD, observed during a discussion. “We know that using more active, more efficient drugs gives more control on relapse.”
Dr. Edan, professor and head of the neurosciences department of University Hospital Pontchaillou, Rennes (France), added that these data “confirmed what has already been observed in the clinical trials.”
It is important to consider the safety and efficacy concerns on an individual level, Dr. Edan argued, questioning whether the more highly active drugs should be systematically used first-line rather than second-line in all patients with MS. He also noted that of course patients would need to be treated for very long periods.
Dr. Chalmer responded: “I agree some of the randomized trials have touched upon on this as well, but I think it’s really important to not just rely on one or two trials but to keep on doing the trials over and over again so that we show that we have the right results.”
Dr. Chalmer added that the present study looked only at efficacy and that the median follow-up time was 3.2 years. “Safety is important of course, but it was not the aim of this study.” Perhaps longer follow-up might have detected more differences in the EDSS outcomes, he added.
The study was funded by the Danish Multiple Sclerosis Society, the Foundation for Research in Neurology, Ejnar Jonassen, and Gangstedfonden. Dr. Chalmer disclosed he had received support for congress participation from Merck, Biogen, and Roche.
SOURCE: Chalmer T et al. Mult Scler. 2018;24(S2):99. Abstract 263.
BERLIN – Escalating treatment to a “highly effective” disease-modifying treatment (DMT) results in fewer relapses in patients with relapsing-remitting multiple sclerosis (RRMS) than does switching to another “moderately effective” therapy, according to data from a Danish cohort study.
The annualized relapse rate (ARR) was 0.23 for patients who switched to a highly effective DMT, defined as either natalizumab (Tysabri) or fingolimod (Gilenya), whereas the ARR was 0.35 in those who were switched to a moderately effective DMT, defined as an interferon-beta, glatiramer acetate (Copaxone), teriflunomide (Aubagio), or dimethyl fumarate (Tecfidera).
This resulted in a relapse-rate ratio of 0.67 (95% confidence interval [CI], 0.55-0.83) comparing high to moderate DMT, or a 33% lower relapse rate in the high DMT group, Thor Ameri Chalmer, MD, PhD, reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Chalmer, who works at the Danish Multiple Sclerosis Center at Rigshospitalet, the University of Copenhagen, reported that the time to first relapse and the likelihood for having recurrent relapses were all lowered by escalating treatment rather than switching treatment. Indeed, there was a 38% increase in the time to first relapse (hazard ratio [HR] = 0.62; 95% CI, 0.50-0.76) and a 31% reduction in recurrent relapses (HR = 0.69; 95% CI, 0.57-0.83).
However, there were “no clear differences” in the time to 3-month confirmed Expanded Disability Status Scale (EDSS) worsening and improvement, Dr. Chalmer said. The HR for time to first worsening in the 3-month confirmed EDSS was 0.86, and for recurrent worsening it was 0.86, but the 95% CI in both cases crossed over from 1.0 (0.65-1.14 and 0.71-1.05, respectively). There was no difference in the time to first improvement (HR = 1.23; 95% CI, 0.95-1.60).
“The aim of this study was to use data from the [Danish] MS Registry, find the patients who started on what we define as moderately effective DMT for the first time, and on this treatment experienced a disease breakthrough and then either switched to another moderately effective DMT or escalated to a highly effective DMT,” Dr. Chalmer explained.
Disease breakthrough was defined as at least one relapse occurring within 12 months of the treatment switch, or the treating neurologist defined the reason for switching as disease breakthrough. Dr. Chalmer acknowledged that this was one of the limitations of the observational study as patients could have been misclassified and switched treatment for another reason. The severity of the relapse was not recorded.
Data on more than 5,000 patients enrolled in the Danish Multiple Sclerosis Registry (DMSR) were considered, with a final propensity-match population of 788 included in the analysis; half had received highly effective DMT and half moderately effective DMT.
The DMSR contains data on virtually all patients with MS treated in Denmark, Dr. Chalmer observed; treatment with DMT is free of charge and it can be prescribed only in public MS clinics, he explained. Furthermore, all MS clinics are required to register information about treatment response at each clinical visit.
The mean age of patients in the study was 39 years, around 70% were female, and average disease duration was 5 years.
“I don’t see in your study what is really new,” Gilles Edan, MD, observed during a discussion. “We know that using more active, more efficient drugs gives more control on relapse.”
Dr. Edan, professor and head of the neurosciences department of University Hospital Pontchaillou, Rennes (France), added that these data “confirmed what has already been observed in the clinical trials.”
It is important to consider the safety and efficacy concerns on an individual level, Dr. Edan argued, questioning whether the more highly active drugs should be systematically used first-line rather than second-line in all patients with MS. He also noted that of course patients would need to be treated for very long periods.
Dr. Chalmer responded: “I agree some of the randomized trials have touched upon on this as well, but I think it’s really important to not just rely on one or two trials but to keep on doing the trials over and over again so that we show that we have the right results.”
Dr. Chalmer added that the present study looked only at efficacy and that the median follow-up time was 3.2 years. “Safety is important of course, but it was not the aim of this study.” Perhaps longer follow-up might have detected more differences in the EDSS outcomes, he added.
The study was funded by the Danish Multiple Sclerosis Society, the Foundation for Research in Neurology, Ejnar Jonassen, and Gangstedfonden. Dr. Chalmer disclosed he had received support for congress participation from Merck, Biogen, and Roche.
SOURCE: Chalmer T et al. Mult Scler. 2018;24(S2):99. Abstract 263.
BERLIN – Escalating treatment to a “highly effective” disease-modifying treatment (DMT) results in fewer relapses in patients with relapsing-remitting multiple sclerosis (RRMS) than does switching to another “moderately effective” therapy, according to data from a Danish cohort study.
The annualized relapse rate (ARR) was 0.23 for patients who switched to a highly effective DMT, defined as either natalizumab (Tysabri) or fingolimod (Gilenya), whereas the ARR was 0.35 in those who were switched to a moderately effective DMT, defined as an interferon-beta, glatiramer acetate (Copaxone), teriflunomide (Aubagio), or dimethyl fumarate (Tecfidera).
This resulted in a relapse-rate ratio of 0.67 (95% confidence interval [CI], 0.55-0.83) comparing high to moderate DMT, or a 33% lower relapse rate in the high DMT group, Thor Ameri Chalmer, MD, PhD, reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Chalmer, who works at the Danish Multiple Sclerosis Center at Rigshospitalet, the University of Copenhagen, reported that the time to first relapse and the likelihood for having recurrent relapses were all lowered by escalating treatment rather than switching treatment. Indeed, there was a 38% increase in the time to first relapse (hazard ratio [HR] = 0.62; 95% CI, 0.50-0.76) and a 31% reduction in recurrent relapses (HR = 0.69; 95% CI, 0.57-0.83).
However, there were “no clear differences” in the time to 3-month confirmed Expanded Disability Status Scale (EDSS) worsening and improvement, Dr. Chalmer said. The HR for time to first worsening in the 3-month confirmed EDSS was 0.86, and for recurrent worsening it was 0.86, but the 95% CI in both cases crossed over from 1.0 (0.65-1.14 and 0.71-1.05, respectively). There was no difference in the time to first improvement (HR = 1.23; 95% CI, 0.95-1.60).
“The aim of this study was to use data from the [Danish] MS Registry, find the patients who started on what we define as moderately effective DMT for the first time, and on this treatment experienced a disease breakthrough and then either switched to another moderately effective DMT or escalated to a highly effective DMT,” Dr. Chalmer explained.
Disease breakthrough was defined as at least one relapse occurring within 12 months of the treatment switch, or the treating neurologist defined the reason for switching as disease breakthrough. Dr. Chalmer acknowledged that this was one of the limitations of the observational study as patients could have been misclassified and switched treatment for another reason. The severity of the relapse was not recorded.
Data on more than 5,000 patients enrolled in the Danish Multiple Sclerosis Registry (DMSR) were considered, with a final propensity-match population of 788 included in the analysis; half had received highly effective DMT and half moderately effective DMT.
The DMSR contains data on virtually all patients with MS treated in Denmark, Dr. Chalmer observed; treatment with DMT is free of charge and it can be prescribed only in public MS clinics, he explained. Furthermore, all MS clinics are required to register information about treatment response at each clinical visit.
The mean age of patients in the study was 39 years, around 70% were female, and average disease duration was 5 years.
“I don’t see in your study what is really new,” Gilles Edan, MD, observed during a discussion. “We know that using more active, more efficient drugs gives more control on relapse.”
Dr. Edan, professor and head of the neurosciences department of University Hospital Pontchaillou, Rennes (France), added that these data “confirmed what has already been observed in the clinical trials.”
It is important to consider the safety and efficacy concerns on an individual level, Dr. Edan argued, questioning whether the more highly active drugs should be systematically used first-line rather than second-line in all patients with MS. He also noted that of course patients would need to be treated for very long periods.
Dr. Chalmer responded: “I agree some of the randomized trials have touched upon on this as well, but I think it’s really important to not just rely on one or two trials but to keep on doing the trials over and over again so that we show that we have the right results.”
Dr. Chalmer added that the present study looked only at efficacy and that the median follow-up time was 3.2 years. “Safety is important of course, but it was not the aim of this study.” Perhaps longer follow-up might have detected more differences in the EDSS outcomes, he added.
The study was funded by the Danish Multiple Sclerosis Society, the Foundation for Research in Neurology, Ejnar Jonassen, and Gangstedfonden. Dr. Chalmer disclosed he had received support for congress participation from Merck, Biogen, and Roche.
SOURCE: Chalmer T et al. Mult Scler. 2018;24(S2):99. Abstract 263.
REPORTING FROM ECTRIMS 2018
Higher BMI associated with greater loss of gray matter volume in MS
ATLANTA – Among patients with relapsing-remitting multiple sclerosis, higher body mass index, but not vitamin D status, appears to be related to greater loss of gray matter brain volume over time, results from a 5-year analysis showed.
“We had previously known that obesity is a risk factor for developing MS, and among those who already have the disease, obesity-related comorbidities are associated with increased morbidity and mortality,” lead study author Ellen M. Mowry, MD, said in an interview at the annual meeting of the American Neurological Association. “Loss of brain tissue, especially as measured by reduced volume of gray matter noted on brain MRI, is predictive of long-term disability in MS. While we await the results of confirmatory studies and randomized trials, this study adds to the growing body of evidence suggesting there may be a role for modification of lifestyle factors in mitigating longer-term MS-related disability risk.”
In an effort to determine if body mass index (BMI) or vitamin D status is associated with longer-term MRI measures of neurodegeneration, Dr. Mowry and her colleagues drew from 469 patients participating in a longitudinal MS cohort study at the University of California, San Francisco, known as EPIC. Participants had clinical evaluations, brain MRI, and blood draws annually and were followed for 5 years. The main outcomes of interest were BMI and serum 25-hydroxyvitamin D levels measured over the time period, and their relationship to brain volume.
At baseline, the mean age of patients was 42 years, 70% were female, their mean BMI was 25 kg/m2, and their mean serum vitamin D level was 27.8 ng/mL. Dr. Mowry, a neurologist at Johns Hopkins University, Baltimore, and her colleagues found that over time, each 1-kg/m2 higher BMI was independently associated with reduced gray matter in multivariate models (–1.1 mL; P = .001). In addition, each 1-kg/m2 higher BMI over time was independently associated with greater declines in normalized brain parenchymal brain volume (–1.1 mL; P = .039). Elevated vitamin D levels, however, did not appear to be meaningfully associated with brain volumes.
Dr. Mowry acknowledged certain limitations of the study, including its nonrandomized design. “Such a trial may be warranted but I believe will be challenging to conduct,” she said. “Also, this cohort was designed to assess the association of genes with brain MRI outcomes, and so the people included were racially homogeneous – only Caucasians were included. Since MS risk is especially high among African Americans in recent years, and African Americans appear overall to have a higher risk of long-term disability, it is important to evaluate these and other prognostic factors amongst a more representative group of people with MS.”
The study received funding support from the National Institutes of Health, GlaxoSmithKline, and Biogen. Dr. Mowry disclosed that she has received medication from Teva for use in a clinical trial. In addition, she has been the primary investigator for studies sponsored by Biogen and Sun Pharma, and has conducted investigator-initiated studies sponsored by Genzyme and Biogen.
SOURCE: Ann Neurol. 2018;84[S22]:S206-7. Abstract M250.
ATLANTA – Among patients with relapsing-remitting multiple sclerosis, higher body mass index, but not vitamin D status, appears to be related to greater loss of gray matter brain volume over time, results from a 5-year analysis showed.
“We had previously known that obesity is a risk factor for developing MS, and among those who already have the disease, obesity-related comorbidities are associated with increased morbidity and mortality,” lead study author Ellen M. Mowry, MD, said in an interview at the annual meeting of the American Neurological Association. “Loss of brain tissue, especially as measured by reduced volume of gray matter noted on brain MRI, is predictive of long-term disability in MS. While we await the results of confirmatory studies and randomized trials, this study adds to the growing body of evidence suggesting there may be a role for modification of lifestyle factors in mitigating longer-term MS-related disability risk.”
In an effort to determine if body mass index (BMI) or vitamin D status is associated with longer-term MRI measures of neurodegeneration, Dr. Mowry and her colleagues drew from 469 patients participating in a longitudinal MS cohort study at the University of California, San Francisco, known as EPIC. Participants had clinical evaluations, brain MRI, and blood draws annually and were followed for 5 years. The main outcomes of interest were BMI and serum 25-hydroxyvitamin D levels measured over the time period, and their relationship to brain volume.
At baseline, the mean age of patients was 42 years, 70% were female, their mean BMI was 25 kg/m2, and their mean serum vitamin D level was 27.8 ng/mL. Dr. Mowry, a neurologist at Johns Hopkins University, Baltimore, and her colleagues found that over time, each 1-kg/m2 higher BMI was independently associated with reduced gray matter in multivariate models (–1.1 mL; P = .001). In addition, each 1-kg/m2 higher BMI over time was independently associated with greater declines in normalized brain parenchymal brain volume (–1.1 mL; P = .039). Elevated vitamin D levels, however, did not appear to be meaningfully associated with brain volumes.
Dr. Mowry acknowledged certain limitations of the study, including its nonrandomized design. “Such a trial may be warranted but I believe will be challenging to conduct,” she said. “Also, this cohort was designed to assess the association of genes with brain MRI outcomes, and so the people included were racially homogeneous – only Caucasians were included. Since MS risk is especially high among African Americans in recent years, and African Americans appear overall to have a higher risk of long-term disability, it is important to evaluate these and other prognostic factors amongst a more representative group of people with MS.”
The study received funding support from the National Institutes of Health, GlaxoSmithKline, and Biogen. Dr. Mowry disclosed that she has received medication from Teva for use in a clinical trial. In addition, she has been the primary investigator for studies sponsored by Biogen and Sun Pharma, and has conducted investigator-initiated studies sponsored by Genzyme and Biogen.
SOURCE: Ann Neurol. 2018;84[S22]:S206-7. Abstract M250.
ATLANTA – Among patients with relapsing-remitting multiple sclerosis, higher body mass index, but not vitamin D status, appears to be related to greater loss of gray matter brain volume over time, results from a 5-year analysis showed.
“We had previously known that obesity is a risk factor for developing MS, and among those who already have the disease, obesity-related comorbidities are associated with increased morbidity and mortality,” lead study author Ellen M. Mowry, MD, said in an interview at the annual meeting of the American Neurological Association. “Loss of brain tissue, especially as measured by reduced volume of gray matter noted on brain MRI, is predictive of long-term disability in MS. While we await the results of confirmatory studies and randomized trials, this study adds to the growing body of evidence suggesting there may be a role for modification of lifestyle factors in mitigating longer-term MS-related disability risk.”
In an effort to determine if body mass index (BMI) or vitamin D status is associated with longer-term MRI measures of neurodegeneration, Dr. Mowry and her colleagues drew from 469 patients participating in a longitudinal MS cohort study at the University of California, San Francisco, known as EPIC. Participants had clinical evaluations, brain MRI, and blood draws annually and were followed for 5 years. The main outcomes of interest were BMI and serum 25-hydroxyvitamin D levels measured over the time period, and their relationship to brain volume.
At baseline, the mean age of patients was 42 years, 70% were female, their mean BMI was 25 kg/m2, and their mean serum vitamin D level was 27.8 ng/mL. Dr. Mowry, a neurologist at Johns Hopkins University, Baltimore, and her colleagues found that over time, each 1-kg/m2 higher BMI was independently associated with reduced gray matter in multivariate models (–1.1 mL; P = .001). In addition, each 1-kg/m2 higher BMI over time was independently associated with greater declines in normalized brain parenchymal brain volume (–1.1 mL; P = .039). Elevated vitamin D levels, however, did not appear to be meaningfully associated with brain volumes.
Dr. Mowry acknowledged certain limitations of the study, including its nonrandomized design. “Such a trial may be warranted but I believe will be challenging to conduct,” she said. “Also, this cohort was designed to assess the association of genes with brain MRI outcomes, and so the people included were racially homogeneous – only Caucasians were included. Since MS risk is especially high among African Americans in recent years, and African Americans appear overall to have a higher risk of long-term disability, it is important to evaluate these and other prognostic factors amongst a more representative group of people with MS.”
The study received funding support from the National Institutes of Health, GlaxoSmithKline, and Biogen. Dr. Mowry disclosed that she has received medication from Teva for use in a clinical trial. In addition, she has been the primary investigator for studies sponsored by Biogen and Sun Pharma, and has conducted investigator-initiated studies sponsored by Genzyme and Biogen.
SOURCE: Ann Neurol. 2018;84[S22]:S206-7. Abstract M250.
AT ANA 2018
Key clinical point: Higher body mass in MS patients appears to be related to greater brain atrophy over time.
Major finding: Over time, each 1-kg/m2 higher BMI was independently associated with reduced gray matter in multivariate models (–1.1 mL; P = .001).
Study details: An analysis of 469 patients participating in a longitudinal MS cohort study.
Disclosures: The study received funding support from the National Institutes of Health, GlaxoSmithKline, and Biogen. Dr. Mowry disclosed that she has received medication from Teva for use in a clinical trial. In addition, she has been the primary investigator for studies sponsored by Biogen and Sun Pharma, and has conducted investigator-initiated studies sponsored by Genzyme and Biogen.
Source: Ann Neurol. 2018;84[S22]:S206-7. Abstract M250.
Retinal thinning in aquaporin-4-positive NMOSD may occur without optic neuritis
BERLIN – Retinal thinning related to ganglion loss may be independent of optic neuritis attacks in patients with neuromyelitis optica spectrum disorders who have anti–aquaporin-4 antibodies.
These eyes exhibited an annual retinal volume loss of about 0.6 micrometers – 80 times higher than that of normal controls – even though they did not have a history of optic neuritis (ON), Frederike C. Oertel said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“The most likely explanation for this seems to be a disease-related primary retinopathy due to the high density of astrocytic cells in the retina and the afferent visual system,” said Ms. Oertel, a doctoral student at NeuroCure Clinical Research Center, Berlin.
The study appeared in the Journal of Neurology, Neurosurgery & Psychiatry (J Neurol Neurosurg Psychiatry. 2018 Jun 19. doi: 10.1136/jnnp-2018-318382).
A previous cross-sectional study by her group found retinal thinning and an alteration of foveal shape in anti–aquaporin-4 (anti-AQP4) positive patients with neuromyelitis optica spectrum disorders (NMOSD) independent of whether they had experienced a clinical attack of optic neuritis (Neurol Neuroimmunol Neuroinflamm. 2017 May;4[3]:e334). In these patients, the fovea changed shape from a characteristic steeply angled “V” to a broader, flatter “U” shape, she said.
In that 2017 paper, Ms. Oertel and her colleagues theorized that the relationship between the water-channel regulator AQP4 and astrocytes could be the root cause of these microstructural alterations.
“The parafoveal area is characterized by a high density of retinal astrocytic Müller cells, which express AQP4 and may thus serve as retinal targets in NMOSD,” they wrote. “Müller cells regulate the retinal water balance and have a relevant role in neurotransmitter and photopigment recycling, as well as in energy and lipid metabolism. Müller cell dysfunction or degeneration could thus lead to impaired retinal function including changes in water homeostasis. Of interest, both the initial cohort and the confirmatory cohort showed a mild increase of peripapillary retinal nerve fiber layer thickness, which could indicate tissue swelling. These findings are supported by animal studies showing retraction of astrocytic end feet in some and astrocyte death in other cases, suggesting a primary astrocytoma in NMOSD also outside acute lesions.”
The study Ms. Oertel presented at ECTRIMS looked at full retinal thickness using the same imaging tool, optical coherence tomography (OCT). The longitudinal cohort comprised 94 eyes in 51 anti–AQP4-IgG seropositive patients who had NMOSD; 60 of these eyes had experienced an optic neuritis attack and 34 had not. Most of the patients were female; the mean age was 47 years. They were compared against 28 age- and sex-matched healthy controls.
OCT measured combined ganglion cell and inner plexiform layer (GCIP), the peripapillary retinal nerve fiber layer (pRNFL), fovea thickness (FT), inner nuclear layer (INL), and total macular volume (TMV).
At baseline, ON eyes already displayed reduced GCIP, FT, and TMV, compared with healthy controls – but so had eyes that had not had ON. Over the follow-up period, eyes without ON continued to show thinning, even in the absence of a clinical attack. Although visual acuity didn’t change over time, the retinas continued to thin, losing an average of 0.6 micrometers each year, a rate 80 times greater than that seen in the control group.
“We saw this significant loss of the ganglion cell layer volume independent of ON, suggesting that retinal neurodegeneration is not dependent on ON in these patients,” Ms. Oertel said.
The results fit well into the group’s prior theory of astrocytic involvement. However, she added, “We still have to think about an alternative theory of drug-induced neuroaxonal damage and retrograde neuroaxonal degeneration.”
The project was supported with grants from the German Ministry for Education and Research. Ms. Oertel had no financial disclosures relevant to the work, but many coauthors reported financial relationships with industry.
BERLIN – Retinal thinning related to ganglion loss may be independent of optic neuritis attacks in patients with neuromyelitis optica spectrum disorders who have anti–aquaporin-4 antibodies.
These eyes exhibited an annual retinal volume loss of about 0.6 micrometers – 80 times higher than that of normal controls – even though they did not have a history of optic neuritis (ON), Frederike C. Oertel said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“The most likely explanation for this seems to be a disease-related primary retinopathy due to the high density of astrocytic cells in the retina and the afferent visual system,” said Ms. Oertel, a doctoral student at NeuroCure Clinical Research Center, Berlin.
The study appeared in the Journal of Neurology, Neurosurgery & Psychiatry (J Neurol Neurosurg Psychiatry. 2018 Jun 19. doi: 10.1136/jnnp-2018-318382).
A previous cross-sectional study by her group found retinal thinning and an alteration of foveal shape in anti–aquaporin-4 (anti-AQP4) positive patients with neuromyelitis optica spectrum disorders (NMOSD) independent of whether they had experienced a clinical attack of optic neuritis (Neurol Neuroimmunol Neuroinflamm. 2017 May;4[3]:e334). In these patients, the fovea changed shape from a characteristic steeply angled “V” to a broader, flatter “U” shape, she said.
In that 2017 paper, Ms. Oertel and her colleagues theorized that the relationship between the water-channel regulator AQP4 and astrocytes could be the root cause of these microstructural alterations.
“The parafoveal area is characterized by a high density of retinal astrocytic Müller cells, which express AQP4 and may thus serve as retinal targets in NMOSD,” they wrote. “Müller cells regulate the retinal water balance and have a relevant role in neurotransmitter and photopigment recycling, as well as in energy and lipid metabolism. Müller cell dysfunction or degeneration could thus lead to impaired retinal function including changes in water homeostasis. Of interest, both the initial cohort and the confirmatory cohort showed a mild increase of peripapillary retinal nerve fiber layer thickness, which could indicate tissue swelling. These findings are supported by animal studies showing retraction of astrocytic end feet in some and astrocyte death in other cases, suggesting a primary astrocytoma in NMOSD also outside acute lesions.”
The study Ms. Oertel presented at ECTRIMS looked at full retinal thickness using the same imaging tool, optical coherence tomography (OCT). The longitudinal cohort comprised 94 eyes in 51 anti–AQP4-IgG seropositive patients who had NMOSD; 60 of these eyes had experienced an optic neuritis attack and 34 had not. Most of the patients were female; the mean age was 47 years. They were compared against 28 age- and sex-matched healthy controls.
OCT measured combined ganglion cell and inner plexiform layer (GCIP), the peripapillary retinal nerve fiber layer (pRNFL), fovea thickness (FT), inner nuclear layer (INL), and total macular volume (TMV).
At baseline, ON eyes already displayed reduced GCIP, FT, and TMV, compared with healthy controls – but so had eyes that had not had ON. Over the follow-up period, eyes without ON continued to show thinning, even in the absence of a clinical attack. Although visual acuity didn’t change over time, the retinas continued to thin, losing an average of 0.6 micrometers each year, a rate 80 times greater than that seen in the control group.
“We saw this significant loss of the ganglion cell layer volume independent of ON, suggesting that retinal neurodegeneration is not dependent on ON in these patients,” Ms. Oertel said.
The results fit well into the group’s prior theory of astrocytic involvement. However, she added, “We still have to think about an alternative theory of drug-induced neuroaxonal damage and retrograde neuroaxonal degeneration.”
The project was supported with grants from the German Ministry for Education and Research. Ms. Oertel had no financial disclosures relevant to the work, but many coauthors reported financial relationships with industry.
BERLIN – Retinal thinning related to ganglion loss may be independent of optic neuritis attacks in patients with neuromyelitis optica spectrum disorders who have anti–aquaporin-4 antibodies.
These eyes exhibited an annual retinal volume loss of about 0.6 micrometers – 80 times higher than that of normal controls – even though they did not have a history of optic neuritis (ON), Frederike C. Oertel said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“The most likely explanation for this seems to be a disease-related primary retinopathy due to the high density of astrocytic cells in the retina and the afferent visual system,” said Ms. Oertel, a doctoral student at NeuroCure Clinical Research Center, Berlin.
The study appeared in the Journal of Neurology, Neurosurgery & Psychiatry (J Neurol Neurosurg Psychiatry. 2018 Jun 19. doi: 10.1136/jnnp-2018-318382).
A previous cross-sectional study by her group found retinal thinning and an alteration of foveal shape in anti–aquaporin-4 (anti-AQP4) positive patients with neuromyelitis optica spectrum disorders (NMOSD) independent of whether they had experienced a clinical attack of optic neuritis (Neurol Neuroimmunol Neuroinflamm. 2017 May;4[3]:e334). In these patients, the fovea changed shape from a characteristic steeply angled “V” to a broader, flatter “U” shape, she said.
In that 2017 paper, Ms. Oertel and her colleagues theorized that the relationship between the water-channel regulator AQP4 and astrocytes could be the root cause of these microstructural alterations.
“The parafoveal area is characterized by a high density of retinal astrocytic Müller cells, which express AQP4 and may thus serve as retinal targets in NMOSD,” they wrote. “Müller cells regulate the retinal water balance and have a relevant role in neurotransmitter and photopigment recycling, as well as in energy and lipid metabolism. Müller cell dysfunction or degeneration could thus lead to impaired retinal function including changes in water homeostasis. Of interest, both the initial cohort and the confirmatory cohort showed a mild increase of peripapillary retinal nerve fiber layer thickness, which could indicate tissue swelling. These findings are supported by animal studies showing retraction of astrocytic end feet in some and astrocyte death in other cases, suggesting a primary astrocytoma in NMOSD also outside acute lesions.”
The study Ms. Oertel presented at ECTRIMS looked at full retinal thickness using the same imaging tool, optical coherence tomography (OCT). The longitudinal cohort comprised 94 eyes in 51 anti–AQP4-IgG seropositive patients who had NMOSD; 60 of these eyes had experienced an optic neuritis attack and 34 had not. Most of the patients were female; the mean age was 47 years. They were compared against 28 age- and sex-matched healthy controls.
OCT measured combined ganglion cell and inner plexiform layer (GCIP), the peripapillary retinal nerve fiber layer (pRNFL), fovea thickness (FT), inner nuclear layer (INL), and total macular volume (TMV).
At baseline, ON eyes already displayed reduced GCIP, FT, and TMV, compared with healthy controls – but so had eyes that had not had ON. Over the follow-up period, eyes without ON continued to show thinning, even in the absence of a clinical attack. Although visual acuity didn’t change over time, the retinas continued to thin, losing an average of 0.6 micrometers each year, a rate 80 times greater than that seen in the control group.
“We saw this significant loss of the ganglion cell layer volume independent of ON, suggesting that retinal neurodegeneration is not dependent on ON in these patients,” Ms. Oertel said.
The results fit well into the group’s prior theory of astrocytic involvement. However, she added, “We still have to think about an alternative theory of drug-induced neuroaxonal damage and retrograde neuroaxonal degeneration.”
The project was supported with grants from the German Ministry for Education and Research. Ms. Oertel had no financial disclosures relevant to the work, but many coauthors reported financial relationships with industry.
REPORTING FROM ECTRIMS 2018
Key clinical point:
Major finding: Over 2.5 years retinas thinned an average of 0.6 micrometers annually.
Study details: The longitudinal study comprised 94 eyes.
Disclosures: The project was supported with grants from the German Ministry for Education and Research. Dr. Oertel had no conflicts of interest, but many coauthors reported financial relationships with industry.
Source: Oertel FC et al. ECTRIMS 2018, Abstract 212.
High-Dose Biotin for Progressive MS: Real-World Experience
Benefit was seen in primary and secondary progressive MS.
BERLIN—MD1003, a high-dose pharmaceutical grade biotin, is effective in the treatment of patients with progressive multiple sclerosis (MS), according to a report presented at ECTRIMS 2018. “This real-world study supports the growing body of evidence that MD1003 is an effective and safe treatment for progressive MS,” said lead author Jonathan Ciron, MD, of the Department of Neurology, CHU Toulouse, France, and colleagues.
In the 2016 MS-SPI study, MD1003 treatment was shown to be effective and well tolerated in patients with progressive MS. Notably, MD1003 reversed MS-related disease disability in 13% of patients with progressive MS. Based on these findings, MD1003 is currently being prescribed to patients with progressive MS in France under an expanded access program.
In the present study, Dr. Ciron and colleagues sought to determine the benefits, in terms of effectiveness and safety, of MD1003 in patients with primary progressive MS (PPMS) or secondary progressive MS (SPMS) in a clinical center.
MD1003 300 mg/day (100 mg tid) was prescribed to patients with PPMS or SPMS receiving care at a single center in France (CHU Toulouse) starting in January 2016. The following measures of effectiveness and safety were administered: Expanded Disability Status Scale (EDSS), timed 25-foot walk (T25W), nine-hole peg test (9-HPT), number of relapses, and gadolinium-enhancing lesions on T1-weighted images.
As of May 2018, a total of 220 patients received MD1003. The research team presented the results of the first 91 patients to complete one year of follow-up. At baseline, mean age was 59.5, 61.5% were female, 70.3% had SPMS, mean EDSS was 5.9, mean T25W was 50.7 seconds, 9-HPT in the dominant hand was 35.1 seconds, and the mean number of previous relapses was 5.1. After one year of treatment with MD1003, 19 (23%; n = 83 with data) patients experienced improvement in EDSS and 15 (23%; n = 66 with data) patients experienced 20% or greater improvement in T25W. Active disease, a clinically-defined relapse, or a gadolinium-enhancing T1 lesion was observed in nine (11%; n = 79 with data) patients. MD1003 was also well tolerated, the researchers noted.
Benefit was seen in primary and secondary progressive MS.
Benefit was seen in primary and secondary progressive MS.
BERLIN—MD1003, a high-dose pharmaceutical grade biotin, is effective in the treatment of patients with progressive multiple sclerosis (MS), according to a report presented at ECTRIMS 2018. “This real-world study supports the growing body of evidence that MD1003 is an effective and safe treatment for progressive MS,” said lead author Jonathan Ciron, MD, of the Department of Neurology, CHU Toulouse, France, and colleagues.
In the 2016 MS-SPI study, MD1003 treatment was shown to be effective and well tolerated in patients with progressive MS. Notably, MD1003 reversed MS-related disease disability in 13% of patients with progressive MS. Based on these findings, MD1003 is currently being prescribed to patients with progressive MS in France under an expanded access program.
In the present study, Dr. Ciron and colleagues sought to determine the benefits, in terms of effectiveness and safety, of MD1003 in patients with primary progressive MS (PPMS) or secondary progressive MS (SPMS) in a clinical center.
MD1003 300 mg/day (100 mg tid) was prescribed to patients with PPMS or SPMS receiving care at a single center in France (CHU Toulouse) starting in January 2016. The following measures of effectiveness and safety were administered: Expanded Disability Status Scale (EDSS), timed 25-foot walk (T25W), nine-hole peg test (9-HPT), number of relapses, and gadolinium-enhancing lesions on T1-weighted images.
As of May 2018, a total of 220 patients received MD1003. The research team presented the results of the first 91 patients to complete one year of follow-up. At baseline, mean age was 59.5, 61.5% were female, 70.3% had SPMS, mean EDSS was 5.9, mean T25W was 50.7 seconds, 9-HPT in the dominant hand was 35.1 seconds, and the mean number of previous relapses was 5.1. After one year of treatment with MD1003, 19 (23%; n = 83 with data) patients experienced improvement in EDSS and 15 (23%; n = 66 with data) patients experienced 20% or greater improvement in T25W. Active disease, a clinically-defined relapse, or a gadolinium-enhancing T1 lesion was observed in nine (11%; n = 79 with data) patients. MD1003 was also well tolerated, the researchers noted.
BERLIN—MD1003, a high-dose pharmaceutical grade biotin, is effective in the treatment of patients with progressive multiple sclerosis (MS), according to a report presented at ECTRIMS 2018. “This real-world study supports the growing body of evidence that MD1003 is an effective and safe treatment for progressive MS,” said lead author Jonathan Ciron, MD, of the Department of Neurology, CHU Toulouse, France, and colleagues.
In the 2016 MS-SPI study, MD1003 treatment was shown to be effective and well tolerated in patients with progressive MS. Notably, MD1003 reversed MS-related disease disability in 13% of patients with progressive MS. Based on these findings, MD1003 is currently being prescribed to patients with progressive MS in France under an expanded access program.
In the present study, Dr. Ciron and colleagues sought to determine the benefits, in terms of effectiveness and safety, of MD1003 in patients with primary progressive MS (PPMS) or secondary progressive MS (SPMS) in a clinical center.
MD1003 300 mg/day (100 mg tid) was prescribed to patients with PPMS or SPMS receiving care at a single center in France (CHU Toulouse) starting in January 2016. The following measures of effectiveness and safety were administered: Expanded Disability Status Scale (EDSS), timed 25-foot walk (T25W), nine-hole peg test (9-HPT), number of relapses, and gadolinium-enhancing lesions on T1-weighted images.
As of May 2018, a total of 220 patients received MD1003. The research team presented the results of the first 91 patients to complete one year of follow-up. At baseline, mean age was 59.5, 61.5% were female, 70.3% had SPMS, mean EDSS was 5.9, mean T25W was 50.7 seconds, 9-HPT in the dominant hand was 35.1 seconds, and the mean number of previous relapses was 5.1. After one year of treatment with MD1003, 19 (23%; n = 83 with data) patients experienced improvement in EDSS and 15 (23%; n = 66 with data) patients experienced 20% or greater improvement in T25W. Active disease, a clinically-defined relapse, or a gadolinium-enhancing T1 lesion was observed in nine (11%; n = 79 with data) patients. MD1003 was also well tolerated, the researchers noted.
Is a Unidimensional Cognitive Screen Sufficient for Patients With MS?
A unidimensional approach to evaluating cognitive deficits misses the variability and impact of the disease.
BERLIN—Cognitive impairment in patients with multiple sclerosis (MS) varies in presence and degree in a manner that is neither identified nor quantified by the Symbol Digit Modalities Test (SDMT), according to a study presented at ECTRIMS 2018. “A unidimensional score or measure is insufficient to adequately identify and appreciate the richness and variation of the combinations and degrees of cognitive impairment that occur in patients with MS and impact the appearance of meaningful cognitive-related disability,” said Mark Gudesblatt, MD, Medical Director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Islip, New York, and colleagues. “Better screening tools are required for evaluation of cognitive impairment in patients with MS.”
Cognitive impairment is common in people with MS. This impairment impacts economically important milestones and patient quality of life. Clinician and patient perceptions of the presence and degree of cognitive impairment are insufficiently sensitive measures, according to Dr. Gudesblatt. An increasing number of cognitive domains impaired greater than 1 standard deviation below age- and education-matched persons with MS has been shown to progressively impact self-reported driving, employment, and fall risk in patients with an EDSS score less than 6. Important cognitive disability in patients with MS can be unrelated to visible physical disability. Variability in the location and degree of MS plaque burden may differentially affect cognitive and physical ability, and many other factors may influence cognitive impairment in patients with MS. Routine cognitive screening in MS care is uncommon, Dr. Gudesblatt said. The SDMT, although frequently recommended, provides a single screening score that does not provide information about individual cognitive domains or the presence and degree of impairment across multiple cognitive domains or the accumulation of cognitive impairment.
Dr. Gudesblatt and colleagues conducted a retrospective review of consecutive patients with MS referred for screening with a multidomain computerized screening cognitive assessment battery (CAB) in the course of routine care who also underwent testing with the oral version of the SDMT on the same day. Their study included 113 patients with MS. The cohort had a mean age of 48.9, and 85% were female.
Within this patient sample, the SDMT defined cognitive function as follows: 68% normal classification, 14% low, 5% moderately low, and 12% very low. In this same patient group, the multidomain screening CAB identified the following domains of cognitive impairment greater than 1 standard deviation below normal values: memory (32%), executive function (25%), attention (28%), information processing speed (30%), visuospatial processing (20%), verbal function (23%), motor skills (20%), and a global summary screening score (24%). The multidimensional screening CAB in this same patient population further identified the number of cognitive domains impaired: zero domains, 36%; one domain, 24%; two domains, 11.5%; and three or more domains, 28%.
A unidimensional approach to evaluating cognitive deficits misses the variability and impact of the disease.
A unidimensional approach to evaluating cognitive deficits misses the variability and impact of the disease.
BERLIN—Cognitive impairment in patients with multiple sclerosis (MS) varies in presence and degree in a manner that is neither identified nor quantified by the Symbol Digit Modalities Test (SDMT), according to a study presented at ECTRIMS 2018. “A unidimensional score or measure is insufficient to adequately identify and appreciate the richness and variation of the combinations and degrees of cognitive impairment that occur in patients with MS and impact the appearance of meaningful cognitive-related disability,” said Mark Gudesblatt, MD, Medical Director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Islip, New York, and colleagues. “Better screening tools are required for evaluation of cognitive impairment in patients with MS.”
Cognitive impairment is common in people with MS. This impairment impacts economically important milestones and patient quality of life. Clinician and patient perceptions of the presence and degree of cognitive impairment are insufficiently sensitive measures, according to Dr. Gudesblatt. An increasing number of cognitive domains impaired greater than 1 standard deviation below age- and education-matched persons with MS has been shown to progressively impact self-reported driving, employment, and fall risk in patients with an EDSS score less than 6. Important cognitive disability in patients with MS can be unrelated to visible physical disability. Variability in the location and degree of MS plaque burden may differentially affect cognitive and physical ability, and many other factors may influence cognitive impairment in patients with MS. Routine cognitive screening in MS care is uncommon, Dr. Gudesblatt said. The SDMT, although frequently recommended, provides a single screening score that does not provide information about individual cognitive domains or the presence and degree of impairment across multiple cognitive domains or the accumulation of cognitive impairment.
Dr. Gudesblatt and colleagues conducted a retrospective review of consecutive patients with MS referred for screening with a multidomain computerized screening cognitive assessment battery (CAB) in the course of routine care who also underwent testing with the oral version of the SDMT on the same day. Their study included 113 patients with MS. The cohort had a mean age of 48.9, and 85% were female.
Within this patient sample, the SDMT defined cognitive function as follows: 68% normal classification, 14% low, 5% moderately low, and 12% very low. In this same patient group, the multidomain screening CAB identified the following domains of cognitive impairment greater than 1 standard deviation below normal values: memory (32%), executive function (25%), attention (28%), information processing speed (30%), visuospatial processing (20%), verbal function (23%), motor skills (20%), and a global summary screening score (24%). The multidimensional screening CAB in this same patient population further identified the number of cognitive domains impaired: zero domains, 36%; one domain, 24%; two domains, 11.5%; and three or more domains, 28%.
BERLIN—Cognitive impairment in patients with multiple sclerosis (MS) varies in presence and degree in a manner that is neither identified nor quantified by the Symbol Digit Modalities Test (SDMT), according to a study presented at ECTRIMS 2018. “A unidimensional score or measure is insufficient to adequately identify and appreciate the richness and variation of the combinations and degrees of cognitive impairment that occur in patients with MS and impact the appearance of meaningful cognitive-related disability,” said Mark Gudesblatt, MD, Medical Director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Islip, New York, and colleagues. “Better screening tools are required for evaluation of cognitive impairment in patients with MS.”
Cognitive impairment is common in people with MS. This impairment impacts economically important milestones and patient quality of life. Clinician and patient perceptions of the presence and degree of cognitive impairment are insufficiently sensitive measures, according to Dr. Gudesblatt. An increasing number of cognitive domains impaired greater than 1 standard deviation below age- and education-matched persons with MS has been shown to progressively impact self-reported driving, employment, and fall risk in patients with an EDSS score less than 6. Important cognitive disability in patients with MS can be unrelated to visible physical disability. Variability in the location and degree of MS plaque burden may differentially affect cognitive and physical ability, and many other factors may influence cognitive impairment in patients with MS. Routine cognitive screening in MS care is uncommon, Dr. Gudesblatt said. The SDMT, although frequently recommended, provides a single screening score that does not provide information about individual cognitive domains or the presence and degree of impairment across multiple cognitive domains or the accumulation of cognitive impairment.
Dr. Gudesblatt and colleagues conducted a retrospective review of consecutive patients with MS referred for screening with a multidomain computerized screening cognitive assessment battery (CAB) in the course of routine care who also underwent testing with the oral version of the SDMT on the same day. Their study included 113 patients with MS. The cohort had a mean age of 48.9, and 85% were female.
Within this patient sample, the SDMT defined cognitive function as follows: 68% normal classification, 14% low, 5% moderately low, and 12% very low. In this same patient group, the multidomain screening CAB identified the following domains of cognitive impairment greater than 1 standard deviation below normal values: memory (32%), executive function (25%), attention (28%), information processing speed (30%), visuospatial processing (20%), verbal function (23%), motor skills (20%), and a global summary screening score (24%). The multidimensional screening CAB in this same patient population further identified the number of cognitive domains impaired: zero domains, 36%; one domain, 24%; two domains, 11.5%; and three or more domains, 28%.
Novel IL-6 antibody slashes relapse rates in neuromyelitis optica
BERLIN – The monoclonal antibody satralizumab reduced by 62% relapses of neuromyelitis optica spectrum disorder (NMOSD) over 24 weeks, as compared with placebo.
Chugai Pharmaceuticals of Tokyo and Roche are codeveloping the molecule. Called a “recycling” antibody, it has been designed to have extended circulation in plasma, Dr. Yamamura said.
The SAkuraSky study randomized 83 patients to placebo or to subcutaneous satralizumab 120 mg at baseline and weeks 2 and 4, and then once a month for 20 months.
Patients in the study had either aquaporin-4–positive NMOSD or neuromyelitis optica with or without aquaporin-4 antibodies. They also had to have experienced at least two relapses in the past 2 years, at least one of which occurred in the last year. The primary endpoint was time to first relapse during the randomized phase.
Patients were a mean of about 42 years old. A total of 64% were diagnosed with neuromyelitis optica and the remainder with NMOSD, with a mean disease duration of about 5 years. Aquaporin-4 antibodies were present in 67%. The baseline annualized relapse rate was 1.4. Baseline medications included azathioprine, mycophenolate, and oral corticosteroids. Patients stayed on these throughout the study.
Relapse curves separated significantly by 36 weeks, with 89% of treated patients being relapse-free vs. 66% of placebo patients. At 96 weeks, the curves still favored satralizumab, with 77.6% vs. 58.7% without relapse. The trajectories held steady until the end of follow-up at 216 weeks (relapse-free rates 60% vs. 30%; HR 0.38). The difference amounted to a risk reduction of 62%.
The antibody was even more effective for aquaporin-4–positive patients. By 48 weeks, the relapse-free rates were 91.5% vs. 60%. By week 96, 91.5% of treated patients were still without relapse compared to 53.3% of placebo patients. By week 216, those numbers were about 70% vs. 20%, for a 79% risk reduction. Treatment was still significantly better than placebo for aquaporin negative patients, but the benefit was less dramatic (67% vs. 56%; RR 34%).
The rate of serious infections was similar between placebo and satralizumab (62% vs. 68%) with no serious opportunistic infections in either group. Injection site reactions were more common among patients taking satralizumab (12% vs. 5%). Neoplasms occurred in 7% of each group.
Development of the molecule will continue, Dr. Yamamura said.
Chugai Pharmaceuticals sponsored the study. Dr. Yamamura has served as a consultant for the company and reported financial ties with numerous other drug manufacturers.
SOURCE: Yamamura T et al. ECTRIMS 2018, Oral abstract 323
BERLIN – The monoclonal antibody satralizumab reduced by 62% relapses of neuromyelitis optica spectrum disorder (NMOSD) over 24 weeks, as compared with placebo.
Chugai Pharmaceuticals of Tokyo and Roche are codeveloping the molecule. Called a “recycling” antibody, it has been designed to have extended circulation in plasma, Dr. Yamamura said.
The SAkuraSky study randomized 83 patients to placebo or to subcutaneous satralizumab 120 mg at baseline and weeks 2 and 4, and then once a month for 20 months.
Patients in the study had either aquaporin-4–positive NMOSD or neuromyelitis optica with or without aquaporin-4 antibodies. They also had to have experienced at least two relapses in the past 2 years, at least one of which occurred in the last year. The primary endpoint was time to first relapse during the randomized phase.
Patients were a mean of about 42 years old. A total of 64% were diagnosed with neuromyelitis optica and the remainder with NMOSD, with a mean disease duration of about 5 years. Aquaporin-4 antibodies were present in 67%. The baseline annualized relapse rate was 1.4. Baseline medications included azathioprine, mycophenolate, and oral corticosteroids. Patients stayed on these throughout the study.
Relapse curves separated significantly by 36 weeks, with 89% of treated patients being relapse-free vs. 66% of placebo patients. At 96 weeks, the curves still favored satralizumab, with 77.6% vs. 58.7% without relapse. The trajectories held steady until the end of follow-up at 216 weeks (relapse-free rates 60% vs. 30%; HR 0.38). The difference amounted to a risk reduction of 62%.
The antibody was even more effective for aquaporin-4–positive patients. By 48 weeks, the relapse-free rates were 91.5% vs. 60%. By week 96, 91.5% of treated patients were still without relapse compared to 53.3% of placebo patients. By week 216, those numbers were about 70% vs. 20%, for a 79% risk reduction. Treatment was still significantly better than placebo for aquaporin negative patients, but the benefit was less dramatic (67% vs. 56%; RR 34%).
The rate of serious infections was similar between placebo and satralizumab (62% vs. 68%) with no serious opportunistic infections in either group. Injection site reactions were more common among patients taking satralizumab (12% vs. 5%). Neoplasms occurred in 7% of each group.
Development of the molecule will continue, Dr. Yamamura said.
Chugai Pharmaceuticals sponsored the study. Dr. Yamamura has served as a consultant for the company and reported financial ties with numerous other drug manufacturers.
SOURCE: Yamamura T et al. ECTRIMS 2018, Oral abstract 323
BERLIN – The monoclonal antibody satralizumab reduced by 62% relapses of neuromyelitis optica spectrum disorder (NMOSD) over 24 weeks, as compared with placebo.
Chugai Pharmaceuticals of Tokyo and Roche are codeveloping the molecule. Called a “recycling” antibody, it has been designed to have extended circulation in plasma, Dr. Yamamura said.
The SAkuraSky study randomized 83 patients to placebo or to subcutaneous satralizumab 120 mg at baseline and weeks 2 and 4, and then once a month for 20 months.
Patients in the study had either aquaporin-4–positive NMOSD or neuromyelitis optica with or without aquaporin-4 antibodies. They also had to have experienced at least two relapses in the past 2 years, at least one of which occurred in the last year. The primary endpoint was time to first relapse during the randomized phase.
Patients were a mean of about 42 years old. A total of 64% were diagnosed with neuromyelitis optica and the remainder with NMOSD, with a mean disease duration of about 5 years. Aquaporin-4 antibodies were present in 67%. The baseline annualized relapse rate was 1.4. Baseline medications included azathioprine, mycophenolate, and oral corticosteroids. Patients stayed on these throughout the study.
Relapse curves separated significantly by 36 weeks, with 89% of treated patients being relapse-free vs. 66% of placebo patients. At 96 weeks, the curves still favored satralizumab, with 77.6% vs. 58.7% without relapse. The trajectories held steady until the end of follow-up at 216 weeks (relapse-free rates 60% vs. 30%; HR 0.38). The difference amounted to a risk reduction of 62%.
The antibody was even more effective for aquaporin-4–positive patients. By 48 weeks, the relapse-free rates were 91.5% vs. 60%. By week 96, 91.5% of treated patients were still without relapse compared to 53.3% of placebo patients. By week 216, those numbers were about 70% vs. 20%, for a 79% risk reduction. Treatment was still significantly better than placebo for aquaporin negative patients, but the benefit was less dramatic (67% vs. 56%; RR 34%).
The rate of serious infections was similar between placebo and satralizumab (62% vs. 68%) with no serious opportunistic infections in either group. Injection site reactions were more common among patients taking satralizumab (12% vs. 5%). Neoplasms occurred in 7% of each group.
Development of the molecule will continue, Dr. Yamamura said.
Chugai Pharmaceuticals sponsored the study. Dr. Yamamura has served as a consultant for the company and reported financial ties with numerous other drug manufacturers.
SOURCE: Yamamura T et al. ECTRIMS 2018, Oral abstract 323
REPORTING FROM ECTRIMS 2018
Key clinical point: Satralizumab decreased relapse in all patients, but was more effective in those positive for aquaporin-4 antibodies.
Major finding: Compared with placebo, the antibody decreased relapse by 62% overall, and by 79% in aquaporin-4–positive patients.
Study details: A randomized, placebo-controlled study of 83 patients.
Disclosures: Chugai Pharmaceuticals sponsored the study. Dr. Yamamura has served as a consultant for the company and reported financial ties with numerous other drug manufacturers.
Source: Yamamura T et al. ECTRIMS 2018, Oral abstract 323.
Nf-L levels predictive of brain atrophy, disability in progressive MS
BERLIN – Neurofilament light chain (Nf-L) levels are higher in the plasma of patients with secondary progressive multiple sclerosis (SPMS) than primary progressive multiple sclerosis (PPMS) irrespective of age, according to an analysis of blood samples from two large phase 3 trials.
“Our data suggest that Nf-L should be considered as an informative endpoint for phase 2 studies in SPMS,” said the presenting study author Ludwig Kappos, MD, at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Much of the research on using Nf-L as a biomarker in MS to date has looked at patients with relapsing-remitting MS and the researchers wanted to see if Nf-L might be a useful biomarker in progressive MS because drug development in this area needs long-term and large trials to show an effect of a drug on disability. Conventional magnetic resonance imaging measures show only a modest association with disease evolution in SPMS and PPMS, and, as Nf-L is specific to neuronal damage, it should reflect damage to the brain and spinal cord, Dr. Kappos explained.
The aim of the study was to compare Nf-L levels in the two progressive subtypes of MS – SPMS and PPMS – and to see if it had any predictive value in determining the degree of brain atrophy or disability. Other objectives were to measure the sensitivity for Nf-L to detect treatment effects, and to estimate how big a sample size would be needed in a phase 2 study if it was used as a primary endpoint.
Blood samples from 1,830 patients who had participated in one of two phase 3 studies of siponimod in SPMS (EXPAND) and fingolimod (Gilyena) in PPMS (INFORMS). Nf-L levels were measured retrospectively in plasma using the SIMOA Nf-L immunoassay and categorized as being low (less than 30 pg/mL), medium (30-60 pg/mL), or high (greater than 60 pg/mL). Brain volume change on MRI was calculated using the SIENA (Structural Image Evaluation, using Normalization, of Atrophy) method, and disability changes assessed were evaluated by the Expanded Disability Status Scale (EDSS) score
“One of the confounders of measuring Nf-L is age,” Dr. Kappos acknowledged, “but we see a difference between SPMS and PPMS that is robust along the spectrum of ages.” The geometric mean of Nf-L at baseline was 32.1 pg/mL in patients with SPMS (n = 1,452) and 22.0 pg/mL in those with PPMS (n = 378).
Multiple regression analysis showed that, in both SPMS and PPMS patients, higher Nf-L levels were associated with older age and higher disease activity (increased EDSS score, more gadolinium-enhancing (Gd+) lesions and higher T2 lesion load).
Greater brain loss was seen at both 12 and 24 months in patients with high versus low Nf-L levels at baseline in both the SPMS and PPMS groups. For example, comparing high versus low Nf-L in SPMS, the mean brain volume change from baseline was –0.8% vs. –0.2% (P less than .0001) at 12 months and –1.5% vs. –0.5% at 24 months (P less than .0001). Corresponding values for PPMS were –0.8% vs. –0.4% (P = .0044) and –1.9% vs. –0.8% (P less than .0001).
Nf-L levels of 30 pg/mL were associated with a 32% increased risk of disability progression in patients with SPMS (P = .0055) and a 49% increased risk of disability progression in patients with PPMS (P = .0268).
In both groups of progressive MS patients, Nf-L levels were reduced in response to treatment at both 12 and 24 months, which remained significant.
“So, what about sample size calculation for a 1-year, phase 2 study with Nf-L as a primary endpoint?” Dr. Kappos queried. Assuming a reduction in Nf-L of 20% with a test drug, such a study would be likely to need to include 188 patients, or 94 patients per single arm to have 80% statistical power. To see a 30% reduction in Nf-L, fewer total and single-arm numbers would be needed, at 74 and 37 participants, respectively.
The study was funded by Novartis Pharma AG, Basel, Switzerland. Dr. Kappos disclosed that his institution (University Hospital Basel) had received steering committee, advisory board, and consultancy fees in the last 3 years that had been used exclusively for research support at the department from Novartis and a number of other pharmaceutical manufacturers. The Research of the MS Centre in Basel has been supported by grants from Bayer, Biogen, Novartis, the Swiss MS Society, the Swiss National Research Foundation, the European Union, and Roche Research Foundations.
SOURCE: Kuhle J et al. ECTRIMS 2018. Mult Scler. 2018;24(Suppl 2):111, Abstract 286.
BERLIN – Neurofilament light chain (Nf-L) levels are higher in the plasma of patients with secondary progressive multiple sclerosis (SPMS) than primary progressive multiple sclerosis (PPMS) irrespective of age, according to an analysis of blood samples from two large phase 3 trials.
“Our data suggest that Nf-L should be considered as an informative endpoint for phase 2 studies in SPMS,” said the presenting study author Ludwig Kappos, MD, at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Much of the research on using Nf-L as a biomarker in MS to date has looked at patients with relapsing-remitting MS and the researchers wanted to see if Nf-L might be a useful biomarker in progressive MS because drug development in this area needs long-term and large trials to show an effect of a drug on disability. Conventional magnetic resonance imaging measures show only a modest association with disease evolution in SPMS and PPMS, and, as Nf-L is specific to neuronal damage, it should reflect damage to the brain and spinal cord, Dr. Kappos explained.
The aim of the study was to compare Nf-L levels in the two progressive subtypes of MS – SPMS and PPMS – and to see if it had any predictive value in determining the degree of brain atrophy or disability. Other objectives were to measure the sensitivity for Nf-L to detect treatment effects, and to estimate how big a sample size would be needed in a phase 2 study if it was used as a primary endpoint.
Blood samples from 1,830 patients who had participated in one of two phase 3 studies of siponimod in SPMS (EXPAND) and fingolimod (Gilyena) in PPMS (INFORMS). Nf-L levels were measured retrospectively in plasma using the SIMOA Nf-L immunoassay and categorized as being low (less than 30 pg/mL), medium (30-60 pg/mL), or high (greater than 60 pg/mL). Brain volume change on MRI was calculated using the SIENA (Structural Image Evaluation, using Normalization, of Atrophy) method, and disability changes assessed were evaluated by the Expanded Disability Status Scale (EDSS) score
“One of the confounders of measuring Nf-L is age,” Dr. Kappos acknowledged, “but we see a difference between SPMS and PPMS that is robust along the spectrum of ages.” The geometric mean of Nf-L at baseline was 32.1 pg/mL in patients with SPMS (n = 1,452) and 22.0 pg/mL in those with PPMS (n = 378).
Multiple regression analysis showed that, in both SPMS and PPMS patients, higher Nf-L levels were associated with older age and higher disease activity (increased EDSS score, more gadolinium-enhancing (Gd+) lesions and higher T2 lesion load).
Greater brain loss was seen at both 12 and 24 months in patients with high versus low Nf-L levels at baseline in both the SPMS and PPMS groups. For example, comparing high versus low Nf-L in SPMS, the mean brain volume change from baseline was –0.8% vs. –0.2% (P less than .0001) at 12 months and –1.5% vs. –0.5% at 24 months (P less than .0001). Corresponding values for PPMS were –0.8% vs. –0.4% (P = .0044) and –1.9% vs. –0.8% (P less than .0001).
Nf-L levels of 30 pg/mL were associated with a 32% increased risk of disability progression in patients with SPMS (P = .0055) and a 49% increased risk of disability progression in patients with PPMS (P = .0268).
In both groups of progressive MS patients, Nf-L levels were reduced in response to treatment at both 12 and 24 months, which remained significant.
“So, what about sample size calculation for a 1-year, phase 2 study with Nf-L as a primary endpoint?” Dr. Kappos queried. Assuming a reduction in Nf-L of 20% with a test drug, such a study would be likely to need to include 188 patients, or 94 patients per single arm to have 80% statistical power. To see a 30% reduction in Nf-L, fewer total and single-arm numbers would be needed, at 74 and 37 participants, respectively.
The study was funded by Novartis Pharma AG, Basel, Switzerland. Dr. Kappos disclosed that his institution (University Hospital Basel) had received steering committee, advisory board, and consultancy fees in the last 3 years that had been used exclusively for research support at the department from Novartis and a number of other pharmaceutical manufacturers. The Research of the MS Centre in Basel has been supported by grants from Bayer, Biogen, Novartis, the Swiss MS Society, the Swiss National Research Foundation, the European Union, and Roche Research Foundations.
SOURCE: Kuhle J et al. ECTRIMS 2018. Mult Scler. 2018;24(Suppl 2):111, Abstract 286.
BERLIN – Neurofilament light chain (Nf-L) levels are higher in the plasma of patients with secondary progressive multiple sclerosis (SPMS) than primary progressive multiple sclerosis (PPMS) irrespective of age, according to an analysis of blood samples from two large phase 3 trials.
“Our data suggest that Nf-L should be considered as an informative endpoint for phase 2 studies in SPMS,” said the presenting study author Ludwig Kappos, MD, at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Much of the research on using Nf-L as a biomarker in MS to date has looked at patients with relapsing-remitting MS and the researchers wanted to see if Nf-L might be a useful biomarker in progressive MS because drug development in this area needs long-term and large trials to show an effect of a drug on disability. Conventional magnetic resonance imaging measures show only a modest association with disease evolution in SPMS and PPMS, and, as Nf-L is specific to neuronal damage, it should reflect damage to the brain and spinal cord, Dr. Kappos explained.
The aim of the study was to compare Nf-L levels in the two progressive subtypes of MS – SPMS and PPMS – and to see if it had any predictive value in determining the degree of brain atrophy or disability. Other objectives were to measure the sensitivity for Nf-L to detect treatment effects, and to estimate how big a sample size would be needed in a phase 2 study if it was used as a primary endpoint.
Blood samples from 1,830 patients who had participated in one of two phase 3 studies of siponimod in SPMS (EXPAND) and fingolimod (Gilyena) in PPMS (INFORMS). Nf-L levels were measured retrospectively in plasma using the SIMOA Nf-L immunoassay and categorized as being low (less than 30 pg/mL), medium (30-60 pg/mL), or high (greater than 60 pg/mL). Brain volume change on MRI was calculated using the SIENA (Structural Image Evaluation, using Normalization, of Atrophy) method, and disability changes assessed were evaluated by the Expanded Disability Status Scale (EDSS) score
“One of the confounders of measuring Nf-L is age,” Dr. Kappos acknowledged, “but we see a difference between SPMS and PPMS that is robust along the spectrum of ages.” The geometric mean of Nf-L at baseline was 32.1 pg/mL in patients with SPMS (n = 1,452) and 22.0 pg/mL in those with PPMS (n = 378).
Multiple regression analysis showed that, in both SPMS and PPMS patients, higher Nf-L levels were associated with older age and higher disease activity (increased EDSS score, more gadolinium-enhancing (Gd+) lesions and higher T2 lesion load).
Greater brain loss was seen at both 12 and 24 months in patients with high versus low Nf-L levels at baseline in both the SPMS and PPMS groups. For example, comparing high versus low Nf-L in SPMS, the mean brain volume change from baseline was –0.8% vs. –0.2% (P less than .0001) at 12 months and –1.5% vs. –0.5% at 24 months (P less than .0001). Corresponding values for PPMS were –0.8% vs. –0.4% (P = .0044) and –1.9% vs. –0.8% (P less than .0001).
Nf-L levels of 30 pg/mL were associated with a 32% increased risk of disability progression in patients with SPMS (P = .0055) and a 49% increased risk of disability progression in patients with PPMS (P = .0268).
In both groups of progressive MS patients, Nf-L levels were reduced in response to treatment at both 12 and 24 months, which remained significant.
“So, what about sample size calculation for a 1-year, phase 2 study with Nf-L as a primary endpoint?” Dr. Kappos queried. Assuming a reduction in Nf-L of 20% with a test drug, such a study would be likely to need to include 188 patients, or 94 patients per single arm to have 80% statistical power. To see a 30% reduction in Nf-L, fewer total and single-arm numbers would be needed, at 74 and 37 participants, respectively.
The study was funded by Novartis Pharma AG, Basel, Switzerland. Dr. Kappos disclosed that his institution (University Hospital Basel) had received steering committee, advisory board, and consultancy fees in the last 3 years that had been used exclusively for research support at the department from Novartis and a number of other pharmaceutical manufacturers. The Research of the MS Centre in Basel has been supported by grants from Bayer, Biogen, Novartis, the Swiss MS Society, the Swiss National Research Foundation, the European Union, and Roche Research Foundations.
SOURCE: Kuhle J et al. ECTRIMS 2018. Mult Scler. 2018;24(Suppl 2):111, Abstract 286.
REPORTING FROM ECTRIMS 2018
Key clinical point: Neurofilament light chain level was predictive of changes in brain atrophy, disability and sensitive to treatment effect in secondary progressive multiple sclerosis.
Major finding: Comparing high versus low baseline Nf-L in SPMS, the mean brain volume change from baseline was –0.8% vs. –0.2% (P less than .0001) at 12 months. Elevated Nf-L was associated with a 32% increase risk of disability progression.
Study details: Include study type and number of subjects.
Disclosures: The study was funded by Novartis Pharma AG, Basel, Switzerland. Dr. Kappos disclosed that his institution (University Hospital Basel) had received steering committee, advisory board, and consultancy fees in the last 3 years that had been used exclusively for research support at the department from Novartis and many other pharmaceutical manufacturers.
Source: Kuhle J et al. ECTRIMS 2018. Mult Scler. 2018;24(Suppl 2):111, Abstract 286.
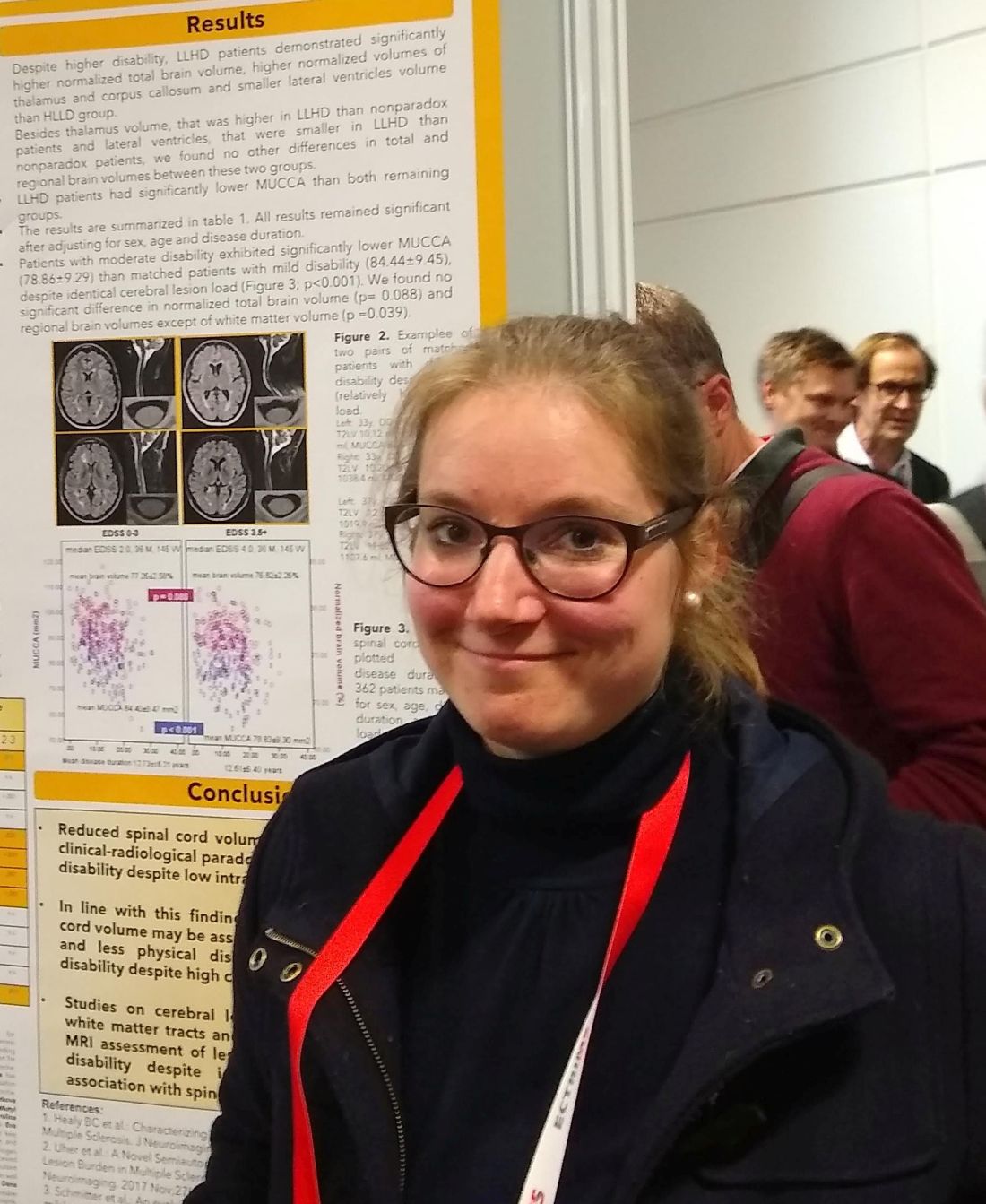
Low spinal cord volume linked to higher MS disability
BERLIN – Spinal cord volume deficits in patients with multiple sclerosis may contribute to clinical disability that appears out of proportion to lesion load on brain imaging, according to new research.
In a pool of 362 patients with mild to moderate MS-related disability but identical white matter lesion load identified by MRI, those with higher disability had significantly lower spinal cord volumes when compared against those with disability scores in the mild range (P less than .001).
Though brain MRI is a key tool used to track disease severity and progression in MS, some patients have relatively high disability but a low burden of white matter intracerebral lesions on MRI. Little is known about spinal cord volume in MS patients with pronounced dissociation between intracerebral lesion load and disability, Michaela Andelova, MD, said in an interview during a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Andelova, of Charles University, Prague, said that she and her colleagues hypothesized that spinal cord volume would differ between patients who had varying levels of disability, despite identical white matter lesion load.
To test this, she and her colleagues looked at records of 1,245 patients with relapsing-remitting MS. They divided them into three groups by severity of clinical disability, and also by extent of cerebral T2 hyperintense lesion load. The investigators identified a group of patients (n = 53) whose total volume of T2-weighted hyperintense lesions was less than 3 mL, but whose Expanded Disability Status Scale (EDSS) scores were at least 3.5; this was the low lesion load/high disability (LLHD) group.
Dr. Andelova and her colleagues then identified another group of patients (n = 71) who had a volume of T2-weighted hyperintensities that was greater than 9 mL, but whose EDSS score was less than 1.5. This was the high lesion load/low disability (HLLD) group.
The remaining patients (n = 1,121), who did not have these paradoxical associations, were analyzed separately.
For all patients, mean upper cervical cord area (MUCCA) was also measured. Using images acquired by a 3 T MRI scanner, MUCCA was calculated as the mean sum of spinal cord area in 21 slices centered at the C3/4 intervertebral disk, using an in-house, semiautomated method.
“Despite higher disability, LLHD patients demonstrated significantly higher normalized total brain volume, higher normalized volumes of thalamus and callosum, and smaller lateral ventricles than [the] HLLD group,” wrote Dr. Andelova and her collaborators.
However, the LLHD patients had MUCCA values that were significantly lower than the other groups: The nonparadoxical group’s mean MUCCA was 84.02 mm2, while the HLLD group had a mean MUCCA of 85.75 mm2. This difference was not statistically significant. By contrast, the LLHD group’s mean MUCCA was significantly smaller, at 80.40 mm2 (P = .023 versus nonparadoxical patients, and P = .007 versus HLLD patients).
Looking at the data another way, Dr. Andelova and her colleagues compared 362 evenly divided patients with moderate disability (EDSS 3.5-6.5) with matched patients who had mild MS-related disability (EDSS less than 3) and identical cerebral lesion loads. They found that MUCCA was significantly smaller in the moderate disability group (78.86 versus 84.44 mm2; P less than .001).
In addition to having identical lesions loads, the mild and moderate disability groups didn’t differ significantly in normalized total brain volume or regional brain volumes. The group with moderate disability did have slightly less white matter volume (P = .039), Dr. Andelova pointed out.
All differences found between groups retained statistical significance even after adjustment for such potential confounders as age, sex, and duration of disease, Dr. Andelova said.
“Reduced spinal cord volume may explain part of the clinical-radiological paradox in patients who have high disability despite low intracranial lesion load,” Dr. Andelova and her collaborators wrote. “In line with this finding, relatively preserved spinal cord volume may be associated with functional reserve and less physical disability in patients with low disability despite high cerebral lesion load.”
Further work looking more precisely at cerebral lesion distribution and quantitative MRI investigation of lesion distribution is in the works for Dr. Andelova and her collaborators. They are hoping to see some association between various distribution patterns and accelerated spinal atrophy.
The research was supported by the Czech government. Dr. Andelova and several of her collaborators reported financial relationships with pharmaceutical companies.
SOURCE: Andelova M et al. Mult Scler. 2018;24(Suppl 2):211, Abstract P477.
BERLIN – Spinal cord volume deficits in patients with multiple sclerosis may contribute to clinical disability that appears out of proportion to lesion load on brain imaging, according to new research.
In a pool of 362 patients with mild to moderate MS-related disability but identical white matter lesion load identified by MRI, those with higher disability had significantly lower spinal cord volumes when compared against those with disability scores in the mild range (P less than .001).
Though brain MRI is a key tool used to track disease severity and progression in MS, some patients have relatively high disability but a low burden of white matter intracerebral lesions on MRI. Little is known about spinal cord volume in MS patients with pronounced dissociation between intracerebral lesion load and disability, Michaela Andelova, MD, said in an interview during a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Andelova, of Charles University, Prague, said that she and her colleagues hypothesized that spinal cord volume would differ between patients who had varying levels of disability, despite identical white matter lesion load.
To test this, she and her colleagues looked at records of 1,245 patients with relapsing-remitting MS. They divided them into three groups by severity of clinical disability, and also by extent of cerebral T2 hyperintense lesion load. The investigators identified a group of patients (n = 53) whose total volume of T2-weighted hyperintense lesions was less than 3 mL, but whose Expanded Disability Status Scale (EDSS) scores were at least 3.5; this was the low lesion load/high disability (LLHD) group.
Dr. Andelova and her colleagues then identified another group of patients (n = 71) who had a volume of T2-weighted hyperintensities that was greater than 9 mL, but whose EDSS score was less than 1.5. This was the high lesion load/low disability (HLLD) group.
The remaining patients (n = 1,121), who did not have these paradoxical associations, were analyzed separately.
For all patients, mean upper cervical cord area (MUCCA) was also measured. Using images acquired by a 3 T MRI scanner, MUCCA was calculated as the mean sum of spinal cord area in 21 slices centered at the C3/4 intervertebral disk, using an in-house, semiautomated method.
“Despite higher disability, LLHD patients demonstrated significantly higher normalized total brain volume, higher normalized volumes of thalamus and callosum, and smaller lateral ventricles than [the] HLLD group,” wrote Dr. Andelova and her collaborators.
However, the LLHD patients had MUCCA values that were significantly lower than the other groups: The nonparadoxical group’s mean MUCCA was 84.02 mm2, while the HLLD group had a mean MUCCA of 85.75 mm2. This difference was not statistically significant. By contrast, the LLHD group’s mean MUCCA was significantly smaller, at 80.40 mm2 (P = .023 versus nonparadoxical patients, and P = .007 versus HLLD patients).
Looking at the data another way, Dr. Andelova and her colleagues compared 362 evenly divided patients with moderate disability (EDSS 3.5-6.5) with matched patients who had mild MS-related disability (EDSS less than 3) and identical cerebral lesion loads. They found that MUCCA was significantly smaller in the moderate disability group (78.86 versus 84.44 mm2; P less than .001).
In addition to having identical lesions loads, the mild and moderate disability groups didn’t differ significantly in normalized total brain volume or regional brain volumes. The group with moderate disability did have slightly less white matter volume (P = .039), Dr. Andelova pointed out.
All differences found between groups retained statistical significance even after adjustment for such potential confounders as age, sex, and duration of disease, Dr. Andelova said.
“Reduced spinal cord volume may explain part of the clinical-radiological paradox in patients who have high disability despite low intracranial lesion load,” Dr. Andelova and her collaborators wrote. “In line with this finding, relatively preserved spinal cord volume may be associated with functional reserve and less physical disability in patients with low disability despite high cerebral lesion load.”
Further work looking more precisely at cerebral lesion distribution and quantitative MRI investigation of lesion distribution is in the works for Dr. Andelova and her collaborators. They are hoping to see some association between various distribution patterns and accelerated spinal atrophy.
The research was supported by the Czech government. Dr. Andelova and several of her collaborators reported financial relationships with pharmaceutical companies.
SOURCE: Andelova M et al. Mult Scler. 2018;24(Suppl 2):211, Abstract P477.
BERLIN – Spinal cord volume deficits in patients with multiple sclerosis may contribute to clinical disability that appears out of proportion to lesion load on brain imaging, according to new research.
In a pool of 362 patients with mild to moderate MS-related disability but identical white matter lesion load identified by MRI, those with higher disability had significantly lower spinal cord volumes when compared against those with disability scores in the mild range (P less than .001).
Though brain MRI is a key tool used to track disease severity and progression in MS, some patients have relatively high disability but a low burden of white matter intracerebral lesions on MRI. Little is known about spinal cord volume in MS patients with pronounced dissociation between intracerebral lesion load and disability, Michaela Andelova, MD, said in an interview during a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Andelova, of Charles University, Prague, said that she and her colleagues hypothesized that spinal cord volume would differ between patients who had varying levels of disability, despite identical white matter lesion load.
To test this, she and her colleagues looked at records of 1,245 patients with relapsing-remitting MS. They divided them into three groups by severity of clinical disability, and also by extent of cerebral T2 hyperintense lesion load. The investigators identified a group of patients (n = 53) whose total volume of T2-weighted hyperintense lesions was less than 3 mL, but whose Expanded Disability Status Scale (EDSS) scores were at least 3.5; this was the low lesion load/high disability (LLHD) group.
Dr. Andelova and her colleagues then identified another group of patients (n = 71) who had a volume of T2-weighted hyperintensities that was greater than 9 mL, but whose EDSS score was less than 1.5. This was the high lesion load/low disability (HLLD) group.
The remaining patients (n = 1,121), who did not have these paradoxical associations, were analyzed separately.
For all patients, mean upper cervical cord area (MUCCA) was also measured. Using images acquired by a 3 T MRI scanner, MUCCA was calculated as the mean sum of spinal cord area in 21 slices centered at the C3/4 intervertebral disk, using an in-house, semiautomated method.
“Despite higher disability, LLHD patients demonstrated significantly higher normalized total brain volume, higher normalized volumes of thalamus and callosum, and smaller lateral ventricles than [the] HLLD group,” wrote Dr. Andelova and her collaborators.
However, the LLHD patients had MUCCA values that were significantly lower than the other groups: The nonparadoxical group’s mean MUCCA was 84.02 mm2, while the HLLD group had a mean MUCCA of 85.75 mm2. This difference was not statistically significant. By contrast, the LLHD group’s mean MUCCA was significantly smaller, at 80.40 mm2 (P = .023 versus nonparadoxical patients, and P = .007 versus HLLD patients).
Looking at the data another way, Dr. Andelova and her colleagues compared 362 evenly divided patients with moderate disability (EDSS 3.5-6.5) with matched patients who had mild MS-related disability (EDSS less than 3) and identical cerebral lesion loads. They found that MUCCA was significantly smaller in the moderate disability group (78.86 versus 84.44 mm2; P less than .001).
In addition to having identical lesions loads, the mild and moderate disability groups didn’t differ significantly in normalized total brain volume or regional brain volumes. The group with moderate disability did have slightly less white matter volume (P = .039), Dr. Andelova pointed out.
All differences found between groups retained statistical significance even after adjustment for such potential confounders as age, sex, and duration of disease, Dr. Andelova said.
“Reduced spinal cord volume may explain part of the clinical-radiological paradox in patients who have high disability despite low intracranial lesion load,” Dr. Andelova and her collaborators wrote. “In line with this finding, relatively preserved spinal cord volume may be associated with functional reserve and less physical disability in patients with low disability despite high cerebral lesion load.”
Further work looking more precisely at cerebral lesion distribution and quantitative MRI investigation of lesion distribution is in the works for Dr. Andelova and her collaborators. They are hoping to see some association between various distribution patterns and accelerated spinal atrophy.
The research was supported by the Czech government. Dr. Andelova and several of her collaborators reported financial relationships with pharmaceutical companies.
SOURCE: Andelova M et al. Mult Scler. 2018;24(Suppl 2):211, Abstract P477.
REPORTING FROM ECTRIMS 2018
Key clinical point:
Major finding: Moderate disability patients had lower spinal cord volumes than did those with mild disability but a similar intracerebral lesion load.
Study details: Retrospective study of 1,245 patients with relapsing-remitting MS.
Disclosures: The study was sponsored by a grant from the Czech government. Several authors, including Dr. Andelova, reported multiple financial relationships with pharmaceutical companies.
Source: Andelova M et al. Mult Scler. 2018;24(Suppl 2):211, Abstract P477.
Do Dimethyl Fumarate and Teriflunomide Have Equivalent Efficacy?
New T2 lesions are more likely on teriflunomide, which may contribute to its higher rate of discontinuation.
BERLIN—Dimethyl fumarate and teriflunomide have similar efficacy in terms of risk of relapse and worsening of Expanded Disability Status Scale (EDSS) score after one and two years of treatment, according to data presented at ECTRIMS 2018. Significantly more patients have new T2 lesions after two years of teriflunomide, however, compared with dimethyl fumarate, and this outcome may explain an increased treatment withdrawal for lack of efficacy among patients receiving teriflunomide.
Teriflunomide and dimethyl fumarate have been approved as first-line treatments for patients with relapsing-remitting multiple sclerosis (MS). To date, no randomized controlled nor observational studies have compared their relative efficacies. David A. Laplaud, MD, PhD, a team leader at the Center of Research in Transplantation and Immunology in Nantes, France, and colleagues conducted a study to compare the effects of teriflunomide and dimethyl fumarate on clinical and MRI outcomes in patients with relapsing-remitting MS from 34 MS centers participating in the French prospective national cohort of MS patients.
The investigators included 1,770 patients with relapsing-remitting MS in the study. In all, 713 participants received teriflunomide, and 1,057 received dimethyl fumarate. Participants were aged 18 to 65 and had an EDSS score of 0 to 5.5 and an available brain MRI performed within six months before treatment initiation. The outcomes under investigation were the proportion of patients with at least one relapse in the year and the two years following teriflunomide or dimethyl fumarate initiation, the proportion of patients with at least one new T2 lesion at one and two years, the number of patients with an increased EDSS score at one and two years, and reasons for treatment cessation at one and two years. For statistical analyses, the outcomes were modeled with propensity scores and logistic regressions by using weighted likelihood maximization and a robust variance estimator.
The confounder-adjusted proportion of patients with at least one relapse at one and two years of treatment was similar in the teriflunomide group and the dimethyl fumarate group (21.6% vs 20.2% for the first year, 30.4% vs 29.5% at two years). Likewise, a similar percentage of patients had an increase of EDSS score at one and two years in the teriflunomide group (27.4% and 41.6%, respectively) and the dimethyl fumarate group (27.1% and 40.6%, respectively). MRI comparisons, however, revealed that the confounder-adjusted proportion of patients with at least one new T2 lesion at two years was significantly lower in patients treated with dimethyl fumarate, compared with teriflunomide (60.8% vs 72.2%; odds ratio [OR], 0.6). The reason for treatment withdrawal at two years was lack of efficacy in 8.5% of patients who received dimethyl fumarate versus 14.5% of patients who received teriflunomide (OR, 0.54).
New T2 lesions are more likely on teriflunomide, which may contribute to its higher rate of discontinuation.
New T2 lesions are more likely on teriflunomide, which may contribute to its higher rate of discontinuation.
BERLIN—Dimethyl fumarate and teriflunomide have similar efficacy in terms of risk of relapse and worsening of Expanded Disability Status Scale (EDSS) score after one and two years of treatment, according to data presented at ECTRIMS 2018. Significantly more patients have new T2 lesions after two years of teriflunomide, however, compared with dimethyl fumarate, and this outcome may explain an increased treatment withdrawal for lack of efficacy among patients receiving teriflunomide.
Teriflunomide and dimethyl fumarate have been approved as first-line treatments for patients with relapsing-remitting multiple sclerosis (MS). To date, no randomized controlled nor observational studies have compared their relative efficacies. David A. Laplaud, MD, PhD, a team leader at the Center of Research in Transplantation and Immunology in Nantes, France, and colleagues conducted a study to compare the effects of teriflunomide and dimethyl fumarate on clinical and MRI outcomes in patients with relapsing-remitting MS from 34 MS centers participating in the French prospective national cohort of MS patients.
The investigators included 1,770 patients with relapsing-remitting MS in the study. In all, 713 participants received teriflunomide, and 1,057 received dimethyl fumarate. Participants were aged 18 to 65 and had an EDSS score of 0 to 5.5 and an available brain MRI performed within six months before treatment initiation. The outcomes under investigation were the proportion of patients with at least one relapse in the year and the two years following teriflunomide or dimethyl fumarate initiation, the proportion of patients with at least one new T2 lesion at one and two years, the number of patients with an increased EDSS score at one and two years, and reasons for treatment cessation at one and two years. For statistical analyses, the outcomes were modeled with propensity scores and logistic regressions by using weighted likelihood maximization and a robust variance estimator.
The confounder-adjusted proportion of patients with at least one relapse at one and two years of treatment was similar in the teriflunomide group and the dimethyl fumarate group (21.6% vs 20.2% for the first year, 30.4% vs 29.5% at two years). Likewise, a similar percentage of patients had an increase of EDSS score at one and two years in the teriflunomide group (27.4% and 41.6%, respectively) and the dimethyl fumarate group (27.1% and 40.6%, respectively). MRI comparisons, however, revealed that the confounder-adjusted proportion of patients with at least one new T2 lesion at two years was significantly lower in patients treated with dimethyl fumarate, compared with teriflunomide (60.8% vs 72.2%; odds ratio [OR], 0.6). The reason for treatment withdrawal at two years was lack of efficacy in 8.5% of patients who received dimethyl fumarate versus 14.5% of patients who received teriflunomide (OR, 0.54).
BERLIN—Dimethyl fumarate and teriflunomide have similar efficacy in terms of risk of relapse and worsening of Expanded Disability Status Scale (EDSS) score after one and two years of treatment, according to data presented at ECTRIMS 2018. Significantly more patients have new T2 lesions after two years of teriflunomide, however, compared with dimethyl fumarate, and this outcome may explain an increased treatment withdrawal for lack of efficacy among patients receiving teriflunomide.
Teriflunomide and dimethyl fumarate have been approved as first-line treatments for patients with relapsing-remitting multiple sclerosis (MS). To date, no randomized controlled nor observational studies have compared their relative efficacies. David A. Laplaud, MD, PhD, a team leader at the Center of Research in Transplantation and Immunology in Nantes, France, and colleagues conducted a study to compare the effects of teriflunomide and dimethyl fumarate on clinical and MRI outcomes in patients with relapsing-remitting MS from 34 MS centers participating in the French prospective national cohort of MS patients.
The investigators included 1,770 patients with relapsing-remitting MS in the study. In all, 713 participants received teriflunomide, and 1,057 received dimethyl fumarate. Participants were aged 18 to 65 and had an EDSS score of 0 to 5.5 and an available brain MRI performed within six months before treatment initiation. The outcomes under investigation were the proportion of patients with at least one relapse in the year and the two years following teriflunomide or dimethyl fumarate initiation, the proportion of patients with at least one new T2 lesion at one and two years, the number of patients with an increased EDSS score at one and two years, and reasons for treatment cessation at one and two years. For statistical analyses, the outcomes were modeled with propensity scores and logistic regressions by using weighted likelihood maximization and a robust variance estimator.
The confounder-adjusted proportion of patients with at least one relapse at one and two years of treatment was similar in the teriflunomide group and the dimethyl fumarate group (21.6% vs 20.2% for the first year, 30.4% vs 29.5% at two years). Likewise, a similar percentage of patients had an increase of EDSS score at one and two years in the teriflunomide group (27.4% and 41.6%, respectively) and the dimethyl fumarate group (27.1% and 40.6%, respectively). MRI comparisons, however, revealed that the confounder-adjusted proportion of patients with at least one new T2 lesion at two years was significantly lower in patients treated with dimethyl fumarate, compared with teriflunomide (60.8% vs 72.2%; odds ratio [OR], 0.6). The reason for treatment withdrawal at two years was lack of efficacy in 8.5% of patients who received dimethyl fumarate versus 14.5% of patients who received teriflunomide (OR, 0.54).
Cortical Damage at Onset May Indicate Risk of Secondary Progressive MS
This observation may aid patient stratification and guide the choice of appropriate therapy.
BERLIN—Widespread focal cortical damage at multiple sclerosis (MS) onset identifies patients likely to have frequent early relapses and a rapid development of progressive disease, which results from worsening global cortical pathology over time, according to a study presented at ECTRIMS 2018. The results provide a basis for patient stratification with the goal of therapeutic optimization. In addition, the data “highlight the importance of elucidating mechanisms involved in early cortical pathology,” according to the investigators.
Following Patients With Relapsing-Remitting MS
Among patients with relapsing-remitting MS, a high frequency of early relapses is associated with increased risk of developing severe disability, which suggests that early biologic mechanisms influence long-term disease evolution. Antonio Scalfari, MD, PhD, a consultant neurologist at Imperial College Healthcare in London, and colleagues sought to investigate the relationship between early cortical pathology, early relapses, and the risk of converting to secondary progressive MS.
Dr. Scalfari and colleagues examined 219 patients with relapsing-remitting MS. Participants had one (n = 116), two (n = 53), or three or more (n = 50) relapses during the first two years. Follow-up lasted for a mean of 7.9 years. The researchers assessed the number of cortical lesions and white matter lesions and the rate of cortical thinning using 3D double inversion recovery, 3D T1-weighted imaging, and Freesurfer analysis.
Cortical Lesions Predicted Cortical Thinning
During the observation period, 59 (27%) patients converted to secondary progressive MS in a mean of 6.1 years. At disease onset, the investigators detected 674 cortical lesions in 166 (76%) patients. A larger number of cortical lesions was associated with a significantly higher risk of secondary progressive MS. The hazard ratios (HR) for secondary progressive MS were 2.16 for patients with two lesions, 4.79 for patients with five lesions, and 12.3 for patients with seven lesions. A large number of cortical lesions also was associated with shorter latency to secondary progressive MS and a faster rate of global cortical thinning. The mean loss per year was 0.93% for patients with no lesions, 0.99% for patients with one to three lesions, 1.13% for patients with four to six lesions, and 1.33% for patients with seven or more lesions. In the group with no cortical lesions (n = 53), no patients entered the secondary progressive phase, and four reached an Expanded Disability Status Scale score of 4.
Patients with a high number of early relapses, compared with those with low and moderate numbers, had a larger volume of white matter lesions and cortical lesions at onset. The mean volumes of cortical lesions were 181.6 mm3, 386.8 mm3, and 544.0 mm3 for patients with one, two, and three or more early relapses, respectively. Patients with a high number of early relapses also accrued more cortical lesions (mean cortical lesion volumes were 118.8 mm3, 138.8 mm3, and 790.5 mm3 for patients with one, two, and three or more early relapses, respectively), had a faster rate of cortical atrophy (mean loss/year was 0.47%, 0.79%, and 0.94% for patients with one, two, and three or more early relapses, respectively), and entered the secondary progressive phase more rapidly.
In the multivariate model, older age at onset (HR, 1.97), a larger baseline cortical lesion (HR, 2.21) and white matter lesion (HR, 1.32) volume, early changes of global cortical thickness (HR, 1.36), and three or more early relapses (HR, 6.08) independently predicted a higher probability of secondary progressive MS.
This observation may aid patient stratification and guide the choice of appropriate therapy.
This observation may aid patient stratification and guide the choice of appropriate therapy.
BERLIN—Widespread focal cortical damage at multiple sclerosis (MS) onset identifies patients likely to have frequent early relapses and a rapid development of progressive disease, which results from worsening global cortical pathology over time, according to a study presented at ECTRIMS 2018. The results provide a basis for patient stratification with the goal of therapeutic optimization. In addition, the data “highlight the importance of elucidating mechanisms involved in early cortical pathology,” according to the investigators.
Following Patients With Relapsing-Remitting MS
Among patients with relapsing-remitting MS, a high frequency of early relapses is associated with increased risk of developing severe disability, which suggests that early biologic mechanisms influence long-term disease evolution. Antonio Scalfari, MD, PhD, a consultant neurologist at Imperial College Healthcare in London, and colleagues sought to investigate the relationship between early cortical pathology, early relapses, and the risk of converting to secondary progressive MS.
Dr. Scalfari and colleagues examined 219 patients with relapsing-remitting MS. Participants had one (n = 116), two (n = 53), or three or more (n = 50) relapses during the first two years. Follow-up lasted for a mean of 7.9 years. The researchers assessed the number of cortical lesions and white matter lesions and the rate of cortical thinning using 3D double inversion recovery, 3D T1-weighted imaging, and Freesurfer analysis.
Cortical Lesions Predicted Cortical Thinning
During the observation period, 59 (27%) patients converted to secondary progressive MS in a mean of 6.1 years. At disease onset, the investigators detected 674 cortical lesions in 166 (76%) patients. A larger number of cortical lesions was associated with a significantly higher risk of secondary progressive MS. The hazard ratios (HR) for secondary progressive MS were 2.16 for patients with two lesions, 4.79 for patients with five lesions, and 12.3 for patients with seven lesions. A large number of cortical lesions also was associated with shorter latency to secondary progressive MS and a faster rate of global cortical thinning. The mean loss per year was 0.93% for patients with no lesions, 0.99% for patients with one to three lesions, 1.13% for patients with four to six lesions, and 1.33% for patients with seven or more lesions. In the group with no cortical lesions (n = 53), no patients entered the secondary progressive phase, and four reached an Expanded Disability Status Scale score of 4.
Patients with a high number of early relapses, compared with those with low and moderate numbers, had a larger volume of white matter lesions and cortical lesions at onset. The mean volumes of cortical lesions were 181.6 mm3, 386.8 mm3, and 544.0 mm3 for patients with one, two, and three or more early relapses, respectively. Patients with a high number of early relapses also accrued more cortical lesions (mean cortical lesion volumes were 118.8 mm3, 138.8 mm3, and 790.5 mm3 for patients with one, two, and three or more early relapses, respectively), had a faster rate of cortical atrophy (mean loss/year was 0.47%, 0.79%, and 0.94% for patients with one, two, and three or more early relapses, respectively), and entered the secondary progressive phase more rapidly.
In the multivariate model, older age at onset (HR, 1.97), a larger baseline cortical lesion (HR, 2.21) and white matter lesion (HR, 1.32) volume, early changes of global cortical thickness (HR, 1.36), and three or more early relapses (HR, 6.08) independently predicted a higher probability of secondary progressive MS.
BERLIN—Widespread focal cortical damage at multiple sclerosis (MS) onset identifies patients likely to have frequent early relapses and a rapid development of progressive disease, which results from worsening global cortical pathology over time, according to a study presented at ECTRIMS 2018. The results provide a basis for patient stratification with the goal of therapeutic optimization. In addition, the data “highlight the importance of elucidating mechanisms involved in early cortical pathology,” according to the investigators.
Following Patients With Relapsing-Remitting MS
Among patients with relapsing-remitting MS, a high frequency of early relapses is associated with increased risk of developing severe disability, which suggests that early biologic mechanisms influence long-term disease evolution. Antonio Scalfari, MD, PhD, a consultant neurologist at Imperial College Healthcare in London, and colleagues sought to investigate the relationship between early cortical pathology, early relapses, and the risk of converting to secondary progressive MS.
Dr. Scalfari and colleagues examined 219 patients with relapsing-remitting MS. Participants had one (n = 116), two (n = 53), or three or more (n = 50) relapses during the first two years. Follow-up lasted for a mean of 7.9 years. The researchers assessed the number of cortical lesions and white matter lesions and the rate of cortical thinning using 3D double inversion recovery, 3D T1-weighted imaging, and Freesurfer analysis.
Cortical Lesions Predicted Cortical Thinning
During the observation period, 59 (27%) patients converted to secondary progressive MS in a mean of 6.1 years. At disease onset, the investigators detected 674 cortical lesions in 166 (76%) patients. A larger number of cortical lesions was associated with a significantly higher risk of secondary progressive MS. The hazard ratios (HR) for secondary progressive MS were 2.16 for patients with two lesions, 4.79 for patients with five lesions, and 12.3 for patients with seven lesions. A large number of cortical lesions also was associated with shorter latency to secondary progressive MS and a faster rate of global cortical thinning. The mean loss per year was 0.93% for patients with no lesions, 0.99% for patients with one to three lesions, 1.13% for patients with four to six lesions, and 1.33% for patients with seven or more lesions. In the group with no cortical lesions (n = 53), no patients entered the secondary progressive phase, and four reached an Expanded Disability Status Scale score of 4.
Patients with a high number of early relapses, compared with those with low and moderate numbers, had a larger volume of white matter lesions and cortical lesions at onset. The mean volumes of cortical lesions were 181.6 mm3, 386.8 mm3, and 544.0 mm3 for patients with one, two, and three or more early relapses, respectively. Patients with a high number of early relapses also accrued more cortical lesions (mean cortical lesion volumes were 118.8 mm3, 138.8 mm3, and 790.5 mm3 for patients with one, two, and three or more early relapses, respectively), had a faster rate of cortical atrophy (mean loss/year was 0.47%, 0.79%, and 0.94% for patients with one, two, and three or more early relapses, respectively), and entered the secondary progressive phase more rapidly.
In the multivariate model, older age at onset (HR, 1.97), a larger baseline cortical lesion (HR, 2.21) and white matter lesion (HR, 1.32) volume, early changes of global cortical thickness (HR, 1.36), and three or more early relapses (HR, 6.08) independently predicted a higher probability of secondary progressive MS.