User login
The Official Newspaper of the American Association for Thoracic Surgery
Coronary flow reserve reveals hidden cardiovascular risk
SNOWMASS, COLO. – Mounting evidence attests to the value of noninvasive measurement of coronary flow reserve as a means of classifying cardiovascular risk in patients with stable coronary artery disease (CAD) more accurately than is possible via coronary angiography or measurement of fractional flow reserve, Marcelo F. Di Carli, MD, reported at the Annual Cardiovascular Conference at Snowmass.
“We use CFR [coronary flow reserve] as a way to exclude coronary disease. It’s a good practical measure of multivessel ischemic CAD. When the CFR is normal, you can with high confidence exclude the possibility of high-risk CAD,” according to Dr. Di Carli, executive director of the cardiovascular imaging program and chief of the division of nuclear medicine and molecular imaging at Brigham and Women’s Hospital, Boston.
Most recently, he and his coinvestigators utilized CFR to provide new insight into the paradox that women have a higher cardiovascular disease death rate than men, even though their prevalence of obstructive CAD is lower.
Their NIH-sponsored study included 329 consecutive patients with a left ventricular ejection fraction greater than 40% – 43% of them women – who underwent coronary angiography several days after noninvasive assessment of CFR via myocardial perfusion positron emission tomography. The women had a lower burden of angiographic CAD and a lower pretest clinical risk score than the men. Nevertheless, during a median of 3 years of follow-up, the women had an adjusted twofold greater risk of the composite endpoint of cardiovascular death, nonfatal MI, or heart failure.
This excess cardiovascular risk in women was independently associated with a very low CFR, defined as less than 1.6. Dr. Di Carli and his coinvestigators calculated that this impaired CFR mediated 40% of the excess risk in women. Thus, a low CFR represents a novel hidden biologic risk for ischemic heart disease (Circulation. 2017 Feb 7;135[6]:566-77).
CFR is defined as the ratio of absolute coronary flow or myocardial perfusion between drug-induced hyperemia and rest. It can be quantified noninvasively using positron emission tomography or MRI.
CFR integrates into a single measure the three components of CAD: the focal stenosis, the diffuse atherosclerotic plaque typically present to a varying degree throughout a target vessel, and microvascular dysfunction.
CFR is a measure of coronary physiology, as is invasive fractional flow reserve (FFR). However, FFR measures only the severity of stenosis and extent of diffuse disease; it doesn’t assess microvascular dysfunction. This is a limitation because it means FFR can give false-negative readings in patients without significant obstructive coronary disease who have severe microvascular dysfunction.
As for angiography, Dr. Di Carli continued, it’s now evident that this purely anatomic assessment is of limited value as a marker of clinical risk and is inadequate to guide management decisions in the setting of stable CAD. After all, angiographically guided revascularization has not reduced cardiovascular events in clinical trials comparing it with optimal medical therapy, as in the COURAGE and BARI-2D trials.
“It’s clear that there’s been a paradigm shift in how we manage patients with stable CAD. For many years the coronary angiogram was the cornerstone of what we did: how we understand the symptoms, the patient’s risk, and ultimately how we proceed with treatment. But there is no benefit in basing treatment solely on what the lesions look like anatomically. That’s why we’ve turned to functional testing of coronary physiology,” he said.
CFR has opened a window on the importance of microvascular dysfunction, which is present in about half of patients with stable CAD and has been shown to predict cardiovascular risk independent of whether or not severe obstructive disease is present.
In an earlier study, Dr. Di Carli and coworkers demonstrated that quantification of CFR enhances stratification for risk of cardiac death among diabetes patients (Circulation. 2012 Oct 9;126[15]:1858-68). The study included 2,783 patients, of whom 1,172 were diabetic, who underwent measurement of CFR and were subsequently followed for a median of 1.4 years, during which 137 cardiac deaths occurred.
Diabetes patients without known CAD who had a low CFR had a high cardiac death rate of 2.8%/year, similar to the 2.0%/year rate in nondiabetic patients with a history of acute MI or revascularization. On the other hand, diabetes patients with a normal CFR and without known CAD had a cardiac mortality rate of only 0.3%/year, comparable to the 0.5% rate in nondiabetics without known CAD who had preserved systolic function and a normal stress perfusion study.
In the future, CFR may aid in decision making as to whether an individual with stable CAD is best treated by percutaneous coronary intervention, surgical revascularization, or guideline-directed medical therapy. For example, if CFR indicates the presence of an isolated severe focal stenosis, and this is confirmed by angiography and FFR, PCI may be the best option, while diffuse disease as demonstrated by CFR may be better treated surgically or using optimal medical therapy. But this needs to be established in prospective clinical trials, added Dr. Di Carli.
He reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – Mounting evidence attests to the value of noninvasive measurement of coronary flow reserve as a means of classifying cardiovascular risk in patients with stable coronary artery disease (CAD) more accurately than is possible via coronary angiography or measurement of fractional flow reserve, Marcelo F. Di Carli, MD, reported at the Annual Cardiovascular Conference at Snowmass.
“We use CFR [coronary flow reserve] as a way to exclude coronary disease. It’s a good practical measure of multivessel ischemic CAD. When the CFR is normal, you can with high confidence exclude the possibility of high-risk CAD,” according to Dr. Di Carli, executive director of the cardiovascular imaging program and chief of the division of nuclear medicine and molecular imaging at Brigham and Women’s Hospital, Boston.
Most recently, he and his coinvestigators utilized CFR to provide new insight into the paradox that women have a higher cardiovascular disease death rate than men, even though their prevalence of obstructive CAD is lower.
Their NIH-sponsored study included 329 consecutive patients with a left ventricular ejection fraction greater than 40% – 43% of them women – who underwent coronary angiography several days after noninvasive assessment of CFR via myocardial perfusion positron emission tomography. The women had a lower burden of angiographic CAD and a lower pretest clinical risk score than the men. Nevertheless, during a median of 3 years of follow-up, the women had an adjusted twofold greater risk of the composite endpoint of cardiovascular death, nonfatal MI, or heart failure.
This excess cardiovascular risk in women was independently associated with a very low CFR, defined as less than 1.6. Dr. Di Carli and his coinvestigators calculated that this impaired CFR mediated 40% of the excess risk in women. Thus, a low CFR represents a novel hidden biologic risk for ischemic heart disease (Circulation. 2017 Feb 7;135[6]:566-77).
CFR is defined as the ratio of absolute coronary flow or myocardial perfusion between drug-induced hyperemia and rest. It can be quantified noninvasively using positron emission tomography or MRI.
CFR integrates into a single measure the three components of CAD: the focal stenosis, the diffuse atherosclerotic plaque typically present to a varying degree throughout a target vessel, and microvascular dysfunction.
CFR is a measure of coronary physiology, as is invasive fractional flow reserve (FFR). However, FFR measures only the severity of stenosis and extent of diffuse disease; it doesn’t assess microvascular dysfunction. This is a limitation because it means FFR can give false-negative readings in patients without significant obstructive coronary disease who have severe microvascular dysfunction.
As for angiography, Dr. Di Carli continued, it’s now evident that this purely anatomic assessment is of limited value as a marker of clinical risk and is inadequate to guide management decisions in the setting of stable CAD. After all, angiographically guided revascularization has not reduced cardiovascular events in clinical trials comparing it with optimal medical therapy, as in the COURAGE and BARI-2D trials.
“It’s clear that there’s been a paradigm shift in how we manage patients with stable CAD. For many years the coronary angiogram was the cornerstone of what we did: how we understand the symptoms, the patient’s risk, and ultimately how we proceed with treatment. But there is no benefit in basing treatment solely on what the lesions look like anatomically. That’s why we’ve turned to functional testing of coronary physiology,” he said.
CFR has opened a window on the importance of microvascular dysfunction, which is present in about half of patients with stable CAD and has been shown to predict cardiovascular risk independent of whether or not severe obstructive disease is present.
In an earlier study, Dr. Di Carli and coworkers demonstrated that quantification of CFR enhances stratification for risk of cardiac death among diabetes patients (Circulation. 2012 Oct 9;126[15]:1858-68). The study included 2,783 patients, of whom 1,172 were diabetic, who underwent measurement of CFR and were subsequently followed for a median of 1.4 years, during which 137 cardiac deaths occurred.
Diabetes patients without known CAD who had a low CFR had a high cardiac death rate of 2.8%/year, similar to the 2.0%/year rate in nondiabetic patients with a history of acute MI or revascularization. On the other hand, diabetes patients with a normal CFR and without known CAD had a cardiac mortality rate of only 0.3%/year, comparable to the 0.5% rate in nondiabetics without known CAD who had preserved systolic function and a normal stress perfusion study.
In the future, CFR may aid in decision making as to whether an individual with stable CAD is best treated by percutaneous coronary intervention, surgical revascularization, or guideline-directed medical therapy. For example, if CFR indicates the presence of an isolated severe focal stenosis, and this is confirmed by angiography and FFR, PCI may be the best option, while diffuse disease as demonstrated by CFR may be better treated surgically or using optimal medical therapy. But this needs to be established in prospective clinical trials, added Dr. Di Carli.
He reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – Mounting evidence attests to the value of noninvasive measurement of coronary flow reserve as a means of classifying cardiovascular risk in patients with stable coronary artery disease (CAD) more accurately than is possible via coronary angiography or measurement of fractional flow reserve, Marcelo F. Di Carli, MD, reported at the Annual Cardiovascular Conference at Snowmass.
“We use CFR [coronary flow reserve] as a way to exclude coronary disease. It’s a good practical measure of multivessel ischemic CAD. When the CFR is normal, you can with high confidence exclude the possibility of high-risk CAD,” according to Dr. Di Carli, executive director of the cardiovascular imaging program and chief of the division of nuclear medicine and molecular imaging at Brigham and Women’s Hospital, Boston.
Most recently, he and his coinvestigators utilized CFR to provide new insight into the paradox that women have a higher cardiovascular disease death rate than men, even though their prevalence of obstructive CAD is lower.
Their NIH-sponsored study included 329 consecutive patients with a left ventricular ejection fraction greater than 40% – 43% of them women – who underwent coronary angiography several days after noninvasive assessment of CFR via myocardial perfusion positron emission tomography. The women had a lower burden of angiographic CAD and a lower pretest clinical risk score than the men. Nevertheless, during a median of 3 years of follow-up, the women had an adjusted twofold greater risk of the composite endpoint of cardiovascular death, nonfatal MI, or heart failure.
This excess cardiovascular risk in women was independently associated with a very low CFR, defined as less than 1.6. Dr. Di Carli and his coinvestigators calculated that this impaired CFR mediated 40% of the excess risk in women. Thus, a low CFR represents a novel hidden biologic risk for ischemic heart disease (Circulation. 2017 Feb 7;135[6]:566-77).
CFR is defined as the ratio of absolute coronary flow or myocardial perfusion between drug-induced hyperemia and rest. It can be quantified noninvasively using positron emission tomography or MRI.
CFR integrates into a single measure the three components of CAD: the focal stenosis, the diffuse atherosclerotic plaque typically present to a varying degree throughout a target vessel, and microvascular dysfunction.
CFR is a measure of coronary physiology, as is invasive fractional flow reserve (FFR). However, FFR measures only the severity of stenosis and extent of diffuse disease; it doesn’t assess microvascular dysfunction. This is a limitation because it means FFR can give false-negative readings in patients without significant obstructive coronary disease who have severe microvascular dysfunction.
As for angiography, Dr. Di Carli continued, it’s now evident that this purely anatomic assessment is of limited value as a marker of clinical risk and is inadequate to guide management decisions in the setting of stable CAD. After all, angiographically guided revascularization has not reduced cardiovascular events in clinical trials comparing it with optimal medical therapy, as in the COURAGE and BARI-2D trials.
“It’s clear that there’s been a paradigm shift in how we manage patients with stable CAD. For many years the coronary angiogram was the cornerstone of what we did: how we understand the symptoms, the patient’s risk, and ultimately how we proceed with treatment. But there is no benefit in basing treatment solely on what the lesions look like anatomically. That’s why we’ve turned to functional testing of coronary physiology,” he said.
CFR has opened a window on the importance of microvascular dysfunction, which is present in about half of patients with stable CAD and has been shown to predict cardiovascular risk independent of whether or not severe obstructive disease is present.
In an earlier study, Dr. Di Carli and coworkers demonstrated that quantification of CFR enhances stratification for risk of cardiac death among diabetes patients (Circulation. 2012 Oct 9;126[15]:1858-68). The study included 2,783 patients, of whom 1,172 were diabetic, who underwent measurement of CFR and were subsequently followed for a median of 1.4 years, during which 137 cardiac deaths occurred.
Diabetes patients without known CAD who had a low CFR had a high cardiac death rate of 2.8%/year, similar to the 2.0%/year rate in nondiabetic patients with a history of acute MI or revascularization. On the other hand, diabetes patients with a normal CFR and without known CAD had a cardiac mortality rate of only 0.3%/year, comparable to the 0.5% rate in nondiabetics without known CAD who had preserved systolic function and a normal stress perfusion study.
In the future, CFR may aid in decision making as to whether an individual with stable CAD is best treated by percutaneous coronary intervention, surgical revascularization, or guideline-directed medical therapy. For example, if CFR indicates the presence of an isolated severe focal stenosis, and this is confirmed by angiography and FFR, PCI may be the best option, while diffuse disease as demonstrated by CFR may be better treated surgically or using optimal medical therapy. But this needs to be established in prospective clinical trials, added Dr. Di Carli.
He reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Decision tool helps patients compare SAVR, TAVR
WASHINGTON – A decision-assistance tool will soon be available that is designed to help intermediate-risk patients with severe aortic stenosis and their physicians better compare each patient’s expected outcome from surgical or transcatheter valve replacement based on each patient’s individual clinical and demographic features.
The decision tool will be available as both a web-based calculator and a downloadable app. It is derived from the outcomes of 4,732 patients who underwent surgical aortic valve replacement (SAVR) during 2011-2013 and who were included in the registry maintained by the Society of Thoracic Surgeons (STS), as well as an equal number of closely matched patients who underwent transcatheter aortic valve replacement (TAVR) during 2014-2015 and entered in the Transcatheter Valve (TVT) registry run by STS and the American College of Cardiology. Tool development also used longer-term outcomes data collected through Medicare.
After receiving patient-specific data, the decision tool estimates the patient’s short-term and 1-year predicted risks for death and stroke and likelihood of being discharged home, as well as the predicted number of days the patient would remain alive and out of the hospital during the first postprocedural year, J. Matthew Brennan, MD, said at the annual meeting of the American College of Cardiology.
Cardiologists and cardiac surgeons “are desperately looking for something like this” because, currently, the only option is to estimate a patient’s risk after SAVR or TAVR using tools developed only from patients who underwent one of these procedures. The new tool gives clinicians and patients a way to compare the two options for an individual patient in a way that “minimizes the biases,” said Dr. Brennan, an interventional cardiologist at Duke University in Durham, N.C., and principal investigator for development of the website and the tool.
Dr. Brennan and his associates developed the decision assistance tool with funding from the Patient-Center Outcomes Research Institute, and it will be available online at no cost at valveadvice.org. The website was already up and running when Dr. Brennan announced the tool during the meeting, and it currently has patient-centered information about aortic valve disease and the options available for treating it. He expects the decision tool to be posted on the site by April or May.
The data he and his associates used to create the decision tool came from a total of more than 197,000 SAVR patients entered into the STS SAVR database during 2011-2013 and more than 25,000 TAVR patients enrolled in the TVT registry during 2014-2015. They used propensity score matching to identify 4,732 matched patients from each group. The patients averaged 81-82 years old, nearly half were women, and their average STS risk score was 5.5-5.8, which meant that patients fell in an intermediate-risk range by this criterion. Just over three-quarters of the TAVR patients had their procedure done via a transfemoral route.
The analysis showed that, overall, 1-year mortality and stroke rates following each type of procedure were not significantly different, and several subgroup analyses failed to identify any type of patient who fell outside this overall pattern. The TAVR patients had a stroke rate that continued to rise during 12-month follow-up, compared with a much flatter pattern among the SAVR patients. While this did not result in an excess stroke rate, the pattern over time suggested that TAVR patients may not have received optimal anticoagulant treatment during the year following their procedure, Dr. Brennan said. The number of months that patients were alive and not hospitalized was also very similar in the SAVR and TAVR groups.
While the 1-year outcomes were very similar, the periprocedural outcomes showed several statistically significant differences. In-hospital mortality was significantly higher in the SAVR patients at 5%, compared with 3% in the TAVR patients. The SAVR patients also were significantly more likely to develop a need for dialysis and a need for red cells and to have a doubled duration in their ICU stay and in their postprocedural length of hospitalization, compared with TAVR patients. On the other hand, TAVR patients were significantly more likely to need a new pacemaker while hospitalized and had a 10 times higher rate of major vascular complications. The stroke rates were very similar in both arms, Dr. Brennan reported.
According to Dr. Brennan, the most striking difference in hospital outcomes was the discharge destination for patients: 70% of TAVR patients went home after their procedural hospitalization, compared with 41% of the SAVR patients. Discharges home following periprocedural hospitalization were “substantially higher” with TAVR, he said.
Another notable feature of these data was how they contrasted with the 1-year outcomes reported from the German Aortic Valve Registry at the American Heart Association Scientific Sessions in November 2016. In the German registry, 1-year mortality after propensity-score adjustment was about 11% among SAVR patients and about 14% among TAVR patients treated with a transfemoral approach, a statistically significant difference, reported Nicolas Werner, MD, of the Ludwigshafen (Germany) Clinic.
“I think the reason we see a difference in the German data is they weren’t able to remove from their analysis the really high-risk patients” who preferentially underwent TAVR, suggested Dr. Brennan. “We had the ability to match patients who had equipoise for undergoing SAVR or TAVR. That’s why our results are more consistent with the findings from the TAVR clinical trials.”
“One of the most important findings from [Dr. Brennan’s] study is [that] it makes the German Registry results look like the outliers rather than the results from the TAVR clinical trials,” commented Howard C. Hermann, MD, professor of cardiovascular disease and director of the cardiac catheterization laboratories at the University of Pennsylvania in Philadelphia.
The data analysis and development of the valveadvice.org website and decision tool received no commercial support. Dr. Brennan had no disclosures. Dr. Hermann has received honoraria and research support from Edwards Pharmaceuticals, research support from Medtronic, and honoraria and research support from several other companies.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – A decision-assistance tool will soon be available that is designed to help intermediate-risk patients with severe aortic stenosis and their physicians better compare each patient’s expected outcome from surgical or transcatheter valve replacement based on each patient’s individual clinical and demographic features.
The decision tool will be available as both a web-based calculator and a downloadable app. It is derived from the outcomes of 4,732 patients who underwent surgical aortic valve replacement (SAVR) during 2011-2013 and who were included in the registry maintained by the Society of Thoracic Surgeons (STS), as well as an equal number of closely matched patients who underwent transcatheter aortic valve replacement (TAVR) during 2014-2015 and entered in the Transcatheter Valve (TVT) registry run by STS and the American College of Cardiology. Tool development also used longer-term outcomes data collected through Medicare.
After receiving patient-specific data, the decision tool estimates the patient’s short-term and 1-year predicted risks for death and stroke and likelihood of being discharged home, as well as the predicted number of days the patient would remain alive and out of the hospital during the first postprocedural year, J. Matthew Brennan, MD, said at the annual meeting of the American College of Cardiology.
Cardiologists and cardiac surgeons “are desperately looking for something like this” because, currently, the only option is to estimate a patient’s risk after SAVR or TAVR using tools developed only from patients who underwent one of these procedures. The new tool gives clinicians and patients a way to compare the two options for an individual patient in a way that “minimizes the biases,” said Dr. Brennan, an interventional cardiologist at Duke University in Durham, N.C., and principal investigator for development of the website and the tool.
Dr. Brennan and his associates developed the decision assistance tool with funding from the Patient-Center Outcomes Research Institute, and it will be available online at no cost at valveadvice.org. The website was already up and running when Dr. Brennan announced the tool during the meeting, and it currently has patient-centered information about aortic valve disease and the options available for treating it. He expects the decision tool to be posted on the site by April or May.
The data he and his associates used to create the decision tool came from a total of more than 197,000 SAVR patients entered into the STS SAVR database during 2011-2013 and more than 25,000 TAVR patients enrolled in the TVT registry during 2014-2015. They used propensity score matching to identify 4,732 matched patients from each group. The patients averaged 81-82 years old, nearly half were women, and their average STS risk score was 5.5-5.8, which meant that patients fell in an intermediate-risk range by this criterion. Just over three-quarters of the TAVR patients had their procedure done via a transfemoral route.
The analysis showed that, overall, 1-year mortality and stroke rates following each type of procedure were not significantly different, and several subgroup analyses failed to identify any type of patient who fell outside this overall pattern. The TAVR patients had a stroke rate that continued to rise during 12-month follow-up, compared with a much flatter pattern among the SAVR patients. While this did not result in an excess stroke rate, the pattern over time suggested that TAVR patients may not have received optimal anticoagulant treatment during the year following their procedure, Dr. Brennan said. The number of months that patients were alive and not hospitalized was also very similar in the SAVR and TAVR groups.
While the 1-year outcomes were very similar, the periprocedural outcomes showed several statistically significant differences. In-hospital mortality was significantly higher in the SAVR patients at 5%, compared with 3% in the TAVR patients. The SAVR patients also were significantly more likely to develop a need for dialysis and a need for red cells and to have a doubled duration in their ICU stay and in their postprocedural length of hospitalization, compared with TAVR patients. On the other hand, TAVR patients were significantly more likely to need a new pacemaker while hospitalized and had a 10 times higher rate of major vascular complications. The stroke rates were very similar in both arms, Dr. Brennan reported.
According to Dr. Brennan, the most striking difference in hospital outcomes was the discharge destination for patients: 70% of TAVR patients went home after their procedural hospitalization, compared with 41% of the SAVR patients. Discharges home following periprocedural hospitalization were “substantially higher” with TAVR, he said.
Another notable feature of these data was how they contrasted with the 1-year outcomes reported from the German Aortic Valve Registry at the American Heart Association Scientific Sessions in November 2016. In the German registry, 1-year mortality after propensity-score adjustment was about 11% among SAVR patients and about 14% among TAVR patients treated with a transfemoral approach, a statistically significant difference, reported Nicolas Werner, MD, of the Ludwigshafen (Germany) Clinic.
“I think the reason we see a difference in the German data is they weren’t able to remove from their analysis the really high-risk patients” who preferentially underwent TAVR, suggested Dr. Brennan. “We had the ability to match patients who had equipoise for undergoing SAVR or TAVR. That’s why our results are more consistent with the findings from the TAVR clinical trials.”
“One of the most important findings from [Dr. Brennan’s] study is [that] it makes the German Registry results look like the outliers rather than the results from the TAVR clinical trials,” commented Howard C. Hermann, MD, professor of cardiovascular disease and director of the cardiac catheterization laboratories at the University of Pennsylvania in Philadelphia.
The data analysis and development of the valveadvice.org website and decision tool received no commercial support. Dr. Brennan had no disclosures. Dr. Hermann has received honoraria and research support from Edwards Pharmaceuticals, research support from Medtronic, and honoraria and research support from several other companies.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – A decision-assistance tool will soon be available that is designed to help intermediate-risk patients with severe aortic stenosis and their physicians better compare each patient’s expected outcome from surgical or transcatheter valve replacement based on each patient’s individual clinical and demographic features.
The decision tool will be available as both a web-based calculator and a downloadable app. It is derived from the outcomes of 4,732 patients who underwent surgical aortic valve replacement (SAVR) during 2011-2013 and who were included in the registry maintained by the Society of Thoracic Surgeons (STS), as well as an equal number of closely matched patients who underwent transcatheter aortic valve replacement (TAVR) during 2014-2015 and entered in the Transcatheter Valve (TVT) registry run by STS and the American College of Cardiology. Tool development also used longer-term outcomes data collected through Medicare.
After receiving patient-specific data, the decision tool estimates the patient’s short-term and 1-year predicted risks for death and stroke and likelihood of being discharged home, as well as the predicted number of days the patient would remain alive and out of the hospital during the first postprocedural year, J. Matthew Brennan, MD, said at the annual meeting of the American College of Cardiology.
Cardiologists and cardiac surgeons “are desperately looking for something like this” because, currently, the only option is to estimate a patient’s risk after SAVR or TAVR using tools developed only from patients who underwent one of these procedures. The new tool gives clinicians and patients a way to compare the two options for an individual patient in a way that “minimizes the biases,” said Dr. Brennan, an interventional cardiologist at Duke University in Durham, N.C., and principal investigator for development of the website and the tool.
Dr. Brennan and his associates developed the decision assistance tool with funding from the Patient-Center Outcomes Research Institute, and it will be available online at no cost at valveadvice.org. The website was already up and running when Dr. Brennan announced the tool during the meeting, and it currently has patient-centered information about aortic valve disease and the options available for treating it. He expects the decision tool to be posted on the site by April or May.
The data he and his associates used to create the decision tool came from a total of more than 197,000 SAVR patients entered into the STS SAVR database during 2011-2013 and more than 25,000 TAVR patients enrolled in the TVT registry during 2014-2015. They used propensity score matching to identify 4,732 matched patients from each group. The patients averaged 81-82 years old, nearly half were women, and their average STS risk score was 5.5-5.8, which meant that patients fell in an intermediate-risk range by this criterion. Just over three-quarters of the TAVR patients had their procedure done via a transfemoral route.
The analysis showed that, overall, 1-year mortality and stroke rates following each type of procedure were not significantly different, and several subgroup analyses failed to identify any type of patient who fell outside this overall pattern. The TAVR patients had a stroke rate that continued to rise during 12-month follow-up, compared with a much flatter pattern among the SAVR patients. While this did not result in an excess stroke rate, the pattern over time suggested that TAVR patients may not have received optimal anticoagulant treatment during the year following their procedure, Dr. Brennan said. The number of months that patients were alive and not hospitalized was also very similar in the SAVR and TAVR groups.
While the 1-year outcomes were very similar, the periprocedural outcomes showed several statistically significant differences. In-hospital mortality was significantly higher in the SAVR patients at 5%, compared with 3% in the TAVR patients. The SAVR patients also were significantly more likely to develop a need for dialysis and a need for red cells and to have a doubled duration in their ICU stay and in their postprocedural length of hospitalization, compared with TAVR patients. On the other hand, TAVR patients were significantly more likely to need a new pacemaker while hospitalized and had a 10 times higher rate of major vascular complications. The stroke rates were very similar in both arms, Dr. Brennan reported.
According to Dr. Brennan, the most striking difference in hospital outcomes was the discharge destination for patients: 70% of TAVR patients went home after their procedural hospitalization, compared with 41% of the SAVR patients. Discharges home following periprocedural hospitalization were “substantially higher” with TAVR, he said.
Another notable feature of these data was how they contrasted with the 1-year outcomes reported from the German Aortic Valve Registry at the American Heart Association Scientific Sessions in November 2016. In the German registry, 1-year mortality after propensity-score adjustment was about 11% among SAVR patients and about 14% among TAVR patients treated with a transfemoral approach, a statistically significant difference, reported Nicolas Werner, MD, of the Ludwigshafen (Germany) Clinic.
“I think the reason we see a difference in the German data is they weren’t able to remove from their analysis the really high-risk patients” who preferentially underwent TAVR, suggested Dr. Brennan. “We had the ability to match patients who had equipoise for undergoing SAVR or TAVR. That’s why our results are more consistent with the findings from the TAVR clinical trials.”
“One of the most important findings from [Dr. Brennan’s] study is [that] it makes the German Registry results look like the outliers rather than the results from the TAVR clinical trials,” commented Howard C. Hermann, MD, professor of cardiovascular disease and director of the cardiac catheterization laboratories at the University of Pennsylvania in Philadelphia.
The data analysis and development of the valveadvice.org website and decision tool received no commercial support. Dr. Brennan had no disclosures. Dr. Hermann has received honoraria and research support from Edwards Pharmaceuticals, research support from Medtronic, and honoraria and research support from several other companies.
[email protected]
On Twitter @mitchelzoler
AT ACC 17
Key clinical point:
Major finding: In matched U.S. patients, TAVR led to 29% more patients being discharged home following their procedures, compared with SAVR.
Data source: Records for 9,464 U.S. patients who underwent TAVR or SAVR during 2011-2015.
Disclosures: Data analysis and development of the valveadvice.org website and decision tool received no commercial support. Dr. Brennan had no disclosures. Dr. Hermann has received honoraria and research support from Edwards Pharmaceuticals, research support from Medtronic, and honoraria and research support from several other companies.
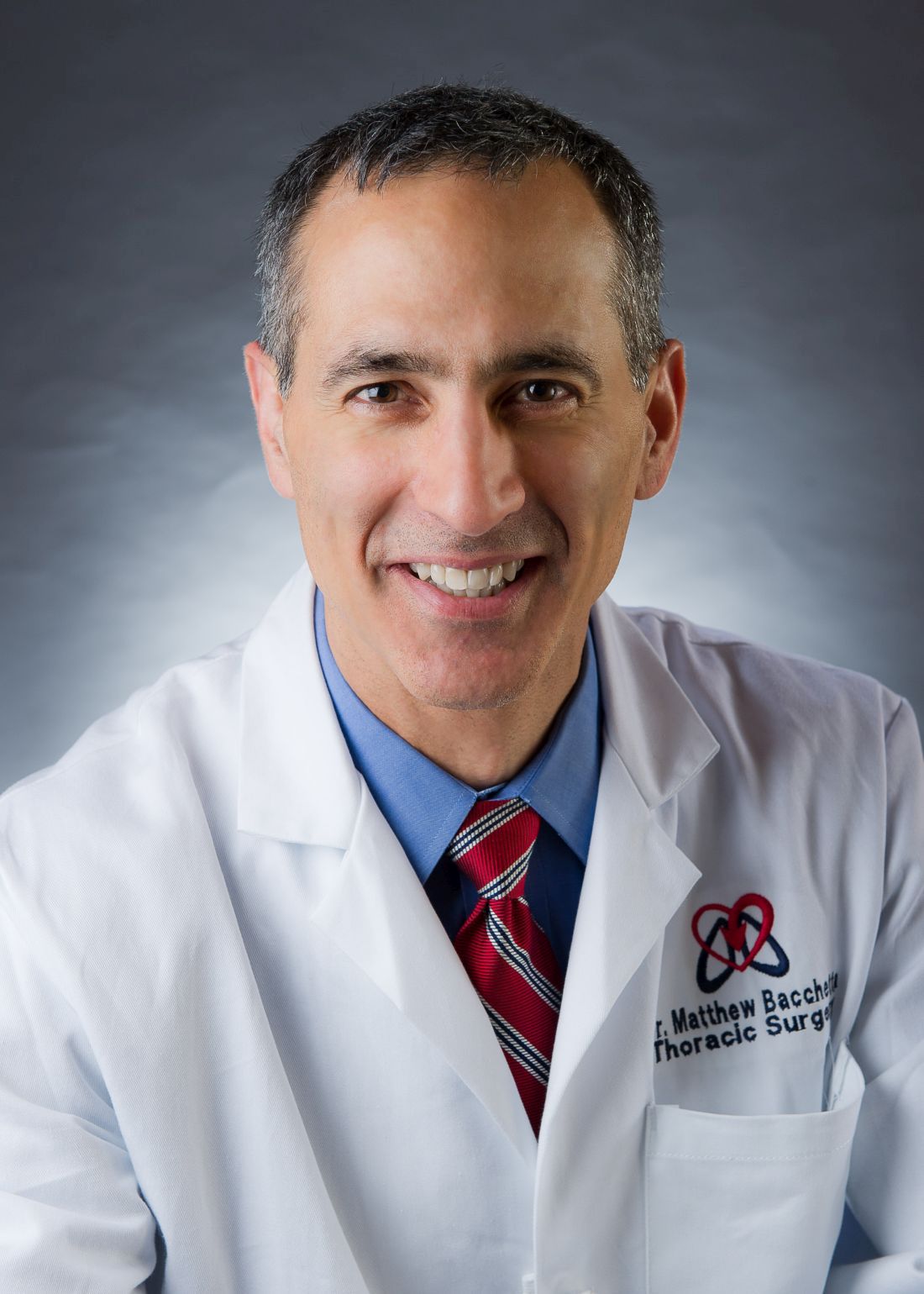
Transplantation and ECMO feature prominently at AATS
Saturday at the annual meeting of the American Association for Thoracic Surgery will feature a course dedicated to exploring novel techniques in heart and lung transplant, mechanical circulatory support, and ECMO, among other things.
“The schedule is pretty self-explanatory,” according to course chair Matthew D. Bacchetta, MD, of Columbia University in New York City. “We’ll be getting really good reviews from some of the best centers around the world.”
Following the talks on heart transplants will be a session on lung transplants. This session will include discussions on primary graft dysfunction, techniques for performing transplantations in patients with pulmonary hypertension, and a talk on bioengineered lungs, the latter of which will be given by Harold C. Ott, MD, of Massachusetts General Hospital.
“We’re going to get a very comprehensive update on the use of DCD lung transplantation, meaning donation after cardiac death, which is obviously a hot topic in our field right now,” explained Dr. Bacchetta. DCD will also be discussed in relation to heart transplants.
After lunch, mechanical circulatory support will take center-stage. Presentations will range from dealing with LVAD and BiVAD support, to avoiding and treating pump thrombosis, and techniques for troubleshooting implantable devices. Speakers include Emma Birks, MD, of the University of Louisville, Gert D. Victor Pretorius, MD, of the University of California in San Diego, and Nicholas G. Smedira, MD, of the Cleveland Clinic, among others.
The course will close with a session on extracorporeal membrane oxygenation (ECMO). Dr. Bacchetta will give a presentation on ECMO bridge to transplantation (BTT), while other talks will be about artificial lung development, ECMO transport, management of ambulation during ECMO, and Ex Vivo Lung Perfusion (EVLP). The session, and the course, will end just before 4:00 PM.
Dr. Bacchetta did not report any financial disclosures relevant to this course.
Saturday at the annual meeting of the American Association for Thoracic Surgery will feature a course dedicated to exploring novel techniques in heart and lung transplant, mechanical circulatory support, and ECMO, among other things.
“The schedule is pretty self-explanatory,” according to course chair Matthew D. Bacchetta, MD, of Columbia University in New York City. “We’ll be getting really good reviews from some of the best centers around the world.”
Following the talks on heart transplants will be a session on lung transplants. This session will include discussions on primary graft dysfunction, techniques for performing transplantations in patients with pulmonary hypertension, and a talk on bioengineered lungs, the latter of which will be given by Harold C. Ott, MD, of Massachusetts General Hospital.
“We’re going to get a very comprehensive update on the use of DCD lung transplantation, meaning donation after cardiac death, which is obviously a hot topic in our field right now,” explained Dr. Bacchetta. DCD will also be discussed in relation to heart transplants.
After lunch, mechanical circulatory support will take center-stage. Presentations will range from dealing with LVAD and BiVAD support, to avoiding and treating pump thrombosis, and techniques for troubleshooting implantable devices. Speakers include Emma Birks, MD, of the University of Louisville, Gert D. Victor Pretorius, MD, of the University of California in San Diego, and Nicholas G. Smedira, MD, of the Cleveland Clinic, among others.
The course will close with a session on extracorporeal membrane oxygenation (ECMO). Dr. Bacchetta will give a presentation on ECMO bridge to transplantation (BTT), while other talks will be about artificial lung development, ECMO transport, management of ambulation during ECMO, and Ex Vivo Lung Perfusion (EVLP). The session, and the course, will end just before 4:00 PM.
Dr. Bacchetta did not report any financial disclosures relevant to this course.
Saturday at the annual meeting of the American Association for Thoracic Surgery will feature a course dedicated to exploring novel techniques in heart and lung transplant, mechanical circulatory support, and ECMO, among other things.
“The schedule is pretty self-explanatory,” according to course chair Matthew D. Bacchetta, MD, of Columbia University in New York City. “We’ll be getting really good reviews from some of the best centers around the world.”
Following the talks on heart transplants will be a session on lung transplants. This session will include discussions on primary graft dysfunction, techniques for performing transplantations in patients with pulmonary hypertension, and a talk on bioengineered lungs, the latter of which will be given by Harold C. Ott, MD, of Massachusetts General Hospital.
“We’re going to get a very comprehensive update on the use of DCD lung transplantation, meaning donation after cardiac death, which is obviously a hot topic in our field right now,” explained Dr. Bacchetta. DCD will also be discussed in relation to heart transplants.
After lunch, mechanical circulatory support will take center-stage. Presentations will range from dealing with LVAD and BiVAD support, to avoiding and treating pump thrombosis, and techniques for troubleshooting implantable devices. Speakers include Emma Birks, MD, of the University of Louisville, Gert D. Victor Pretorius, MD, of the University of California in San Diego, and Nicholas G. Smedira, MD, of the Cleveland Clinic, among others.
The course will close with a session on extracorporeal membrane oxygenation (ECMO). Dr. Bacchetta will give a presentation on ECMO bridge to transplantation (BTT), while other talks will be about artificial lung development, ECMO transport, management of ambulation during ECMO, and Ex Vivo Lung Perfusion (EVLP). The session, and the course, will end just before 4:00 PM.
Dr. Bacchetta did not report any financial disclosures relevant to this course.
AATS/AmSECT Welcome Reception
The AATS and AmSECT Welcome Reception will be held on Sunday, April 30, from 5:00 p.m. to 7:00 p.m. in the Exhibit Hall of the Hynes Convention Center. Admission to this event is complimentary to all registered attendees and exhibitors of both the AATS and AmSECT meetings.
Join the AATS and AmSECT, for the official opening to this year’s meeting. Visit with valued exhibitors and supporters in the Exhibition Hall, where you will learn cutting-edge techniques, and discover groundbreaking new products while networking with other attendees.
In celebration of the Centennial for AATS, many exhibits will include historic artifacts in the field of cardiothoracic surgery for all to see. The AATS and AmSECT Exhibition offers a number of exciting learning opportunities:
AATS Mini Theaters: “Deep Dive” presentations of top abstracts from this year’s Annual Meeting as well as product demonstrations by from industry partners.
AATS Learning Center: Innovative surgical procedures as well as webcasts from other AATS events such as the Mitral Conclave meeting.
AmSECT Poster Presentations
AATS Resident Poster CompetitionThe Perioperative/Team-Based Care Poster Competition
The AATS and AmSECT Welcome Reception will be held on Sunday, April 30, from 5:00 p.m. to 7:00 p.m. in the Exhibit Hall of the Hynes Convention Center. Admission to this event is complimentary to all registered attendees and exhibitors of both the AATS and AmSECT meetings.
Join the AATS and AmSECT, for the official opening to this year’s meeting. Visit with valued exhibitors and supporters in the Exhibition Hall, where you will learn cutting-edge techniques, and discover groundbreaking new products while networking with other attendees.
In celebration of the Centennial for AATS, many exhibits will include historic artifacts in the field of cardiothoracic surgery for all to see. The AATS and AmSECT Exhibition offers a number of exciting learning opportunities:
AATS Mini Theaters: “Deep Dive” presentations of top abstracts from this year’s Annual Meeting as well as product demonstrations by from industry partners.
AATS Learning Center: Innovative surgical procedures as well as webcasts from other AATS events such as the Mitral Conclave meeting.
AmSECT Poster Presentations
AATS Resident Poster CompetitionThe Perioperative/Team-Based Care Poster Competition
The AATS and AmSECT Welcome Reception will be held on Sunday, April 30, from 5:00 p.m. to 7:00 p.m. in the Exhibit Hall of the Hynes Convention Center. Admission to this event is complimentary to all registered attendees and exhibitors of both the AATS and AmSECT meetings.
Join the AATS and AmSECT, for the official opening to this year’s meeting. Visit with valued exhibitors and supporters in the Exhibition Hall, where you will learn cutting-edge techniques, and discover groundbreaking new products while networking with other attendees.
In celebration of the Centennial for AATS, many exhibits will include historic artifacts in the field of cardiothoracic surgery for all to see. The AATS and AmSECT Exhibition offers a number of exciting learning opportunities:
AATS Mini Theaters: “Deep Dive” presentations of top abstracts from this year’s Annual Meeting as well as product demonstrations by from industry partners.
AATS Learning Center: Innovative surgical procedures as well as webcasts from other AATS events such as the Mitral Conclave meeting.
AmSECT Poster Presentations
AATS Resident Poster CompetitionThe Perioperative/Team-Based Care Poster Competition
Focus on Thoracic Tumor Management
Managing thoracic tumors will be the focus of a multifaceted course set to take place in Saturday morning’s “General Thoracic Skills: Management of Thoracic Tumors in 2017” session.
“Thoracic surgical approaches and techniques are in constant evolution,” said course chair Virginia R. Litle, MD, of the Boston Medical Center. “Less invasive approaches are available for diagnosing and staging thoracic malignancies, for preoperative planning and avoidance, and for management of complications, [so] we will hear from experts in the field about preoperative planning techniques that are increasingly available.”
Of particular interest will be a brief talk on the use of social media and what boundaries exist, if any, between clinicians and their patients. Brendon M. Stiles, MD, of New York Presbyterian Hospital, will discuss “responsible social media use,” an increasingly relevant concern for their use in health care.
The following session will cover innovative approaches to esophageal replacement, minimally invasive esophagectomy in both prone and lateral orientations, and segmental lung resections, along with talks about helping patients quit smoking and enrolling patients in clinical trials. Shanda H. Blackmon, MD, of the Mayo Clinic, will summarize 3-D printing for operative planning and Yolonda L. Colson, MD, of Brigham & Women’s Hospital, will outline experimental sentinel node mapping for non–small cell lung cancer.
After lunch, there will be an hour of presentations and discussion dedicated to imaging, which will include talks on the optimal surveillance imaging after stereotactic body radiation therapy, image-based therapy for ground glass opacities, and use of the hybrid operating room. The course’s final session will focus on rescue strategies for procedures such as esophagectomies, video and robot-assisted thoracic surgery, and postoperative air leaks in endobronchial valves.
“Management of clinical challenges such as creative esophageal replacement, vascular injuries during robotic surgery, and conduit revision after minimally invasive esophagectomies, will be of interest to thoracic surgeons,” Dr. Litle noted.
Managing thoracic tumors will be the focus of a multifaceted course set to take place in Saturday morning’s “General Thoracic Skills: Management of Thoracic Tumors in 2017” session.
“Thoracic surgical approaches and techniques are in constant evolution,” said course chair Virginia R. Litle, MD, of the Boston Medical Center. “Less invasive approaches are available for diagnosing and staging thoracic malignancies, for preoperative planning and avoidance, and for management of complications, [so] we will hear from experts in the field about preoperative planning techniques that are increasingly available.”
Of particular interest will be a brief talk on the use of social media and what boundaries exist, if any, between clinicians and their patients. Brendon M. Stiles, MD, of New York Presbyterian Hospital, will discuss “responsible social media use,” an increasingly relevant concern for their use in health care.
The following session will cover innovative approaches to esophageal replacement, minimally invasive esophagectomy in both prone and lateral orientations, and segmental lung resections, along with talks about helping patients quit smoking and enrolling patients in clinical trials. Shanda H. Blackmon, MD, of the Mayo Clinic, will summarize 3-D printing for operative planning and Yolonda L. Colson, MD, of Brigham & Women’s Hospital, will outline experimental sentinel node mapping for non–small cell lung cancer.
After lunch, there will be an hour of presentations and discussion dedicated to imaging, which will include talks on the optimal surveillance imaging after stereotactic body radiation therapy, image-based therapy for ground glass opacities, and use of the hybrid operating room. The course’s final session will focus on rescue strategies for procedures such as esophagectomies, video and robot-assisted thoracic surgery, and postoperative air leaks in endobronchial valves.
“Management of clinical challenges such as creative esophageal replacement, vascular injuries during robotic surgery, and conduit revision after minimally invasive esophagectomies, will be of interest to thoracic surgeons,” Dr. Litle noted.
Managing thoracic tumors will be the focus of a multifaceted course set to take place in Saturday morning’s “General Thoracic Skills: Management of Thoracic Tumors in 2017” session.
“Thoracic surgical approaches and techniques are in constant evolution,” said course chair Virginia R. Litle, MD, of the Boston Medical Center. “Less invasive approaches are available for diagnosing and staging thoracic malignancies, for preoperative planning and avoidance, and for management of complications, [so] we will hear from experts in the field about preoperative planning techniques that are increasingly available.”
Of particular interest will be a brief talk on the use of social media and what boundaries exist, if any, between clinicians and their patients. Brendon M. Stiles, MD, of New York Presbyterian Hospital, will discuss “responsible social media use,” an increasingly relevant concern for their use in health care.
The following session will cover innovative approaches to esophageal replacement, minimally invasive esophagectomy in both prone and lateral orientations, and segmental lung resections, along with talks about helping patients quit smoking and enrolling patients in clinical trials. Shanda H. Blackmon, MD, of the Mayo Clinic, will summarize 3-D printing for operative planning and Yolonda L. Colson, MD, of Brigham & Women’s Hospital, will outline experimental sentinel node mapping for non–small cell lung cancer.
After lunch, there will be an hour of presentations and discussion dedicated to imaging, which will include talks on the optimal surveillance imaging after stereotactic body radiation therapy, image-based therapy for ground glass opacities, and use of the hybrid operating room. The course’s final session will focus on rescue strategies for procedures such as esophagectomies, video and robot-assisted thoracic surgery, and postoperative air leaks in endobronchial valves.
“Management of clinical challenges such as creative esophageal replacement, vascular injuries during robotic surgery, and conduit revision after minimally invasive esophagectomies, will be of interest to thoracic surgeons,” Dr. Litle noted.
AmSECT Celebrates Collaboration
The American Society of ExtraCorporeal Technology (AmSECT) is excited to collaborate with AATS for a shared educational program.
Open communication is critical for a high-functioning team, ultimately leading to the best in patient care. During the AmSECT International Conference and AATS Centennial, there will be great opportunities for perfusionists, surgeons, and health care professionals to collaborate, learn together, and make connections. There will be collaborative parallel sessions during the didactic portion of the program on Saturday and Sunday. The combined sessions on Saturday and the Postgraduate Symposia on Sunday include educational content on adult and congenital practice, ethics, transplant and mechanical assist, teamwork, and communication.
[[{"fid":"193783","view_mode":"medstat_image_full_text","attributes":{"height":"73","width":"303","class":"media-element file-medstat-image-full-text","data-delta":"1"},"fields":{"format":"medstat_image_full_text","field_file_image_caption[und][0][value]":"","field_file_image_credit[und][0][value]":"","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_full_text","field_file_image_caption[und][0][value]":"","field_file_image_credit[und][0][value]":""}}}]]AmSECT President Kenny Shann says that AmSECT and the AATS have worked together to eliminate silos of care and bring surgeons and perfusionists together to learn. “We believe that better teams will lead to better outcomes. In my career, learning alongside members of the team, regardless of their specific role, has strengthened my ability to care for patients. Co-learning allows team members to develop a shared mental model and facilitates interdisciplinary communication, which will ultimately result in better patient care.”
Perfusionists: continue the power of collaboration after the Conference by becoming an AmSECT member. In a profession that embraces innovation and ingenuity, our community of connected perfusionists helps you keep up with changing demands and emerging technologies. As a member of AmSECT, you will be supporting efforts to help you do your job better. The AmSECT community focuses on developing practice documents, protocols, best practices, and other value-add guidelines. When the members of AmSECT come together, there is greater potential to meet new opportunities and practice expansions with unbiased results.
Go online to www.amsect.org to learn more and join today.
The American Society of ExtraCorporeal Technology (AmSECT) is excited to collaborate with AATS for a shared educational program.
Open communication is critical for a high-functioning team, ultimately leading to the best in patient care. During the AmSECT International Conference and AATS Centennial, there will be great opportunities for perfusionists, surgeons, and health care professionals to collaborate, learn together, and make connections. There will be collaborative parallel sessions during the didactic portion of the program on Saturday and Sunday. The combined sessions on Saturday and the Postgraduate Symposia on Sunday include educational content on adult and congenital practice, ethics, transplant and mechanical assist, teamwork, and communication.
[[{"fid":"193783","view_mode":"medstat_image_full_text","attributes":{"height":"73","width":"303","class":"media-element file-medstat-image-full-text","data-delta":"1"},"fields":{"format":"medstat_image_full_text","field_file_image_caption[und][0][value]":"","field_file_image_credit[und][0][value]":"","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_full_text","field_file_image_caption[und][0][value]":"","field_file_image_credit[und][0][value]":""}}}]]AmSECT President Kenny Shann says that AmSECT and the AATS have worked together to eliminate silos of care and bring surgeons and perfusionists together to learn. “We believe that better teams will lead to better outcomes. In my career, learning alongside members of the team, regardless of their specific role, has strengthened my ability to care for patients. Co-learning allows team members to develop a shared mental model and facilitates interdisciplinary communication, which will ultimately result in better patient care.”
Perfusionists: continue the power of collaboration after the Conference by becoming an AmSECT member. In a profession that embraces innovation and ingenuity, our community of connected perfusionists helps you keep up with changing demands and emerging technologies. As a member of AmSECT, you will be supporting efforts to help you do your job better. The AmSECT community focuses on developing practice documents, protocols, best practices, and other value-add guidelines. When the members of AmSECT come together, there is greater potential to meet new opportunities and practice expansions with unbiased results.
Go online to www.amsect.org to learn more and join today.
The American Society of ExtraCorporeal Technology (AmSECT) is excited to collaborate with AATS for a shared educational program.
Open communication is critical for a high-functioning team, ultimately leading to the best in patient care. During the AmSECT International Conference and AATS Centennial, there will be great opportunities for perfusionists, surgeons, and health care professionals to collaborate, learn together, and make connections. There will be collaborative parallel sessions during the didactic portion of the program on Saturday and Sunday. The combined sessions on Saturday and the Postgraduate Symposia on Sunday include educational content on adult and congenital practice, ethics, transplant and mechanical assist, teamwork, and communication.
[[{"fid":"193783","view_mode":"medstat_image_full_text","attributes":{"height":"73","width":"303","class":"media-element file-medstat-image-full-text","data-delta":"1"},"fields":{"format":"medstat_image_full_text","field_file_image_caption[und][0][value]":"","field_file_image_credit[und][0][value]":"","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_full_text","field_file_image_caption[und][0][value]":"","field_file_image_credit[und][0][value]":""}}}]]AmSECT President Kenny Shann says that AmSECT and the AATS have worked together to eliminate silos of care and bring surgeons and perfusionists together to learn. “We believe that better teams will lead to better outcomes. In my career, learning alongside members of the team, regardless of their specific role, has strengthened my ability to care for patients. Co-learning allows team members to develop a shared mental model and facilitates interdisciplinary communication, which will ultimately result in better patient care.”
Perfusionists: continue the power of collaboration after the Conference by becoming an AmSECT member. In a profession that embraces innovation and ingenuity, our community of connected perfusionists helps you keep up with changing demands and emerging technologies. As a member of AmSECT, you will be supporting efforts to help you do your job better. The AmSECT community focuses on developing practice documents, protocols, best practices, and other value-add guidelines. When the members of AmSECT come together, there is greater potential to meet new opportunities and practice expansions with unbiased results.
Go online to www.amsect.org to learn more and join today.
Get the 2017 Mobile App
You can get the full AATS meeting experience right in the palm of your hand with the AATS Week Mobile App. Available through the iTunes store, Android Market, and AATS website, the app gives you access to every detail of the AATS Mitral Conclave and the AATS Centennial.
The app features:
- My Schedule and My Notes, which allow you to add your own personalization.
- Complete up-to-date schedule of what is taking place.
- Interactive Exhibit Floor.
- Exhibitors list, with company descriptions, contact information and booth location.
- Floor plans for the New York Hilton Midtown and Boston Hynes Convention Center.
- General meeting information.
You can get the full AATS meeting experience right in the palm of your hand with the AATS Week Mobile App. Available through the iTunes store, Android Market, and AATS website, the app gives you access to every detail of the AATS Mitral Conclave and the AATS Centennial.
The app features:
- My Schedule and My Notes, which allow you to add your own personalization.
- Complete up-to-date schedule of what is taking place.
- Interactive Exhibit Floor.
- Exhibitors list, with company descriptions, contact information and booth location.
- Floor plans for the New York Hilton Midtown and Boston Hynes Convention Center.
- General meeting information.
You can get the full AATS meeting experience right in the palm of your hand with the AATS Week Mobile App. Available through the iTunes store, Android Market, and AATS website, the app gives you access to every detail of the AATS Mitral Conclave and the AATS Centennial.
The app features:
- My Schedule and My Notes, which allow you to add your own personalization.
- Complete up-to-date schedule of what is taking place.
- Interactive Exhibit Floor.
- Exhibitors list, with company descriptions, contact information and booth location.
- Floor plans for the New York Hilton Midtown and Boston Hynes Convention Center.
- General meeting information.
AATS Centennial Gala
This once-in-a-lifetime celebration of the 100th anniversary of AATS at the Centennial Gala will be held on Monday, May 1, at the famed Wang Theater at the Boch Center.
During this historic evening, the documentary film “In the Beginning” will be unveiled, which features an in-depth look at the formative years and challenges faced in cardiothoracic surgery and also includes interviews with Past Presidents and members of the Centennial Committee.
Buses depart from all meeting hotels (Sheraton, Marriott, and Westin) at 6:15 p.m.
This once-in-a-lifetime celebration of the 100th anniversary of AATS at the Centennial Gala will be held on Monday, May 1, at the famed Wang Theater at the Boch Center.
During this historic evening, the documentary film “In the Beginning” will be unveiled, which features an in-depth look at the formative years and challenges faced in cardiothoracic surgery and also includes interviews with Past Presidents and members of the Centennial Committee.
Buses depart from all meeting hotels (Sheraton, Marriott, and Westin) at 6:15 p.m.
This once-in-a-lifetime celebration of the 100th anniversary of AATS at the Centennial Gala will be held on Monday, May 1, at the famed Wang Theater at the Boch Center.
During this historic evening, the documentary film “In the Beginning” will be unveiled, which features an in-depth look at the formative years and challenges faced in cardiothoracic surgery and also includes interviews with Past Presidents and members of the Centennial Committee.
Buses depart from all meeting hotels (Sheraton, Marriott, and Westin) at 6:15 p.m.
Registration and Discount Package Information
Attendees may register for the Annual Meeting in three ways, although online registration is strongly encouraged.
1. Internet registration
Go to https://registration.experientevent.com/ShowAAT171/Attendee/Login.aspx
2. Register by phone
Call the AATS/Experient Customer Service Desk
(800) 424-5249 - Toll-free within the USA
(847) 996-5829 - International
3. Mail/fax registration
Send the meeting registration form, along with a check or credit card information, to:
AATS/Experient
5202 Presidents Court, Suite G100
Frederick, MD 21703
Fax: (301) 694-5124 (fax requires credit card information)
You cannot email a copy of your registration form.
Registration Cancellation Policy
Written requests for cancellations and refunds for registration must be received by April 26, 2017. Refunds will be subject to a $50 administrative fee and will be processed after the meeting. Refunds are not available after April 26, 2017. Requests can be sent to [email protected].
Information for International Travelers
Please be sure to check with your local embassy or consulate regarding the required travel documents for visiting Boston. Travel documents may take time to prepare in order to gain access to the United States. Refunds for registration fees will not be issued by the AATS if attendees are unable to travel into the United States due to inadequate travel documents.
For more information, please visit: http://travel.state.gov/content/visas/english/visit/visitor.html.
For information on what to expect if you are applying for a Visa to the United States and to review the Visa Application Guidelines, go to the U.S. Department of State’s website. Additionally, the International Visitors Office (IVO) of the National Academies has resources on all visa-related issues for the scientific community.
The AATS provides several documents that document your participation in the meeting. Official Letters of Invitation are available for meeting attendees. A personalized letter of invitation can be generated after you have been fully registered. Once your registration is fully paid and all verification documents have been received, a personalized letter of invitation can be generated for you. Please contact [email protected] with your request. Please note that you will receive an email confirmation, which you can also bring to your visa interview.
Please contact [email protected] with any further questions pertaining to invitation letters.
Attendees may register for the Annual Meeting in three ways, although online registration is strongly encouraged.
1. Internet registration
Go to https://registration.experientevent.com/ShowAAT171/Attendee/Login.aspx
2. Register by phone
Call the AATS/Experient Customer Service Desk
(800) 424-5249 - Toll-free within the USA
(847) 996-5829 - International
3. Mail/fax registration
Send the meeting registration form, along with a check or credit card information, to:
AATS/Experient
5202 Presidents Court, Suite G100
Frederick, MD 21703
Fax: (301) 694-5124 (fax requires credit card information)
You cannot email a copy of your registration form.
Registration Cancellation Policy
Written requests for cancellations and refunds for registration must be received by April 26, 2017. Refunds will be subject to a $50 administrative fee and will be processed after the meeting. Refunds are not available after April 26, 2017. Requests can be sent to [email protected].
Information for International Travelers
Please be sure to check with your local embassy or consulate regarding the required travel documents for visiting Boston. Travel documents may take time to prepare in order to gain access to the United States. Refunds for registration fees will not be issued by the AATS if attendees are unable to travel into the United States due to inadequate travel documents.
For more information, please visit: http://travel.state.gov/content/visas/english/visit/visitor.html.
For information on what to expect if you are applying for a Visa to the United States and to review the Visa Application Guidelines, go to the U.S. Department of State’s website. Additionally, the International Visitors Office (IVO) of the National Academies has resources on all visa-related issues for the scientific community.
The AATS provides several documents that document your participation in the meeting. Official Letters of Invitation are available for meeting attendees. A personalized letter of invitation can be generated after you have been fully registered. Once your registration is fully paid and all verification documents have been received, a personalized letter of invitation can be generated for you. Please contact [email protected] with your request. Please note that you will receive an email confirmation, which you can also bring to your visa interview.
Please contact [email protected] with any further questions pertaining to invitation letters.
Attendees may register for the Annual Meeting in three ways, although online registration is strongly encouraged.
1. Internet registration
Go to https://registration.experientevent.com/ShowAAT171/Attendee/Login.aspx
2. Register by phone
Call the AATS/Experient Customer Service Desk
(800) 424-5249 - Toll-free within the USA
(847) 996-5829 - International
3. Mail/fax registration
Send the meeting registration form, along with a check or credit card information, to:
AATS/Experient
5202 Presidents Court, Suite G100
Frederick, MD 21703
Fax: (301) 694-5124 (fax requires credit card information)
You cannot email a copy of your registration form.
Registration Cancellation Policy
Written requests for cancellations and refunds for registration must be received by April 26, 2017. Refunds will be subject to a $50 administrative fee and will be processed after the meeting. Refunds are not available after April 26, 2017. Requests can be sent to [email protected].
Information for International Travelers
Please be sure to check with your local embassy or consulate regarding the required travel documents for visiting Boston. Travel documents may take time to prepare in order to gain access to the United States. Refunds for registration fees will not be issued by the AATS if attendees are unable to travel into the United States due to inadequate travel documents.
For more information, please visit: http://travel.state.gov/content/visas/english/visit/visitor.html.
For information on what to expect if you are applying for a Visa to the United States and to review the Visa Application Guidelines, go to the U.S. Department of State’s website. Additionally, the International Visitors Office (IVO) of the National Academies has resources on all visa-related issues for the scientific community.
The AATS provides several documents that document your participation in the meeting. Official Letters of Invitation are available for meeting attendees. A personalized letter of invitation can be generated after you have been fully registered. Once your registration is fully paid and all verification documents have been received, a personalized letter of invitation can be generated for you. Please contact [email protected] with your request. Please note that you will receive an email confirmation, which you can also bring to your visa interview.
Please contact [email protected] with any further questions pertaining to invitation letters.