User login
The Official Newspaper of the American Association for Thoracic Surgery
Nivolumab boosts 5-year survival in advanced NSCLC
Early data show that treatment with the immune checkpoint inhibitor nivolumab (Opdivo) resulted in a 5-year overall survival rate of 16% among patients with advanced non–small-cell lung cancer (NSCLC).
In comparison, the 5-year survival rate for patients with advanced lung and bronchus cancer, according to SEER data, is 4.3%, and for those with advanced NSCLC, 4.9%.
“This is the first report of the long-term survival rate in patients with metastatic NSCLC treated with an immune checkpoint inhibitor,” said Julie Brahmer, MD, of the Bloomberg Kimmel Institute for Cancer Immunotherapy at Johns Hopkins, Baltimore.
For a small subset of patients, immunotherapy can work for a very long time, explained Dr. Brahmer, who discussed her findings during a presscast at the annual meeting of the American Association for Cancer Research.
The 5-year overall survival rate that was reported in this study was much higher than what has been seen for this patient population who receive the standard of care. Statistics show that the majority of patients with advanced disease will die within a year of their diagnosis, Dr. Brahmer pointed out.
The findings presented at the meeting are updated results from the phase Ib CA209-003 dose-escalation cohort expansion trial that comprised 129 patients with heavily pretreated, advanced NSCLC . The cohort was randomized to receive nivolumab once every 2 weeks for up to 2 years at one of three dose levels: 1 mg/kg, 3 mg/kg, or 10 mg/kg.
A previous analysis of the data showed promising activity, and findings from subsequent clinical trials led to the approval of nivolumab for use in the second line setting of advanced NSCLC.
Dr. Brahmer now reported findings based on 5-year results of this phase Ib trial. “This analysis is based on a minimum follow up of 58 months,” she said.
The overall 5-year survival rates for squamous NSCLC were 16%, and the rates for nonsquamous were 15%.
At 1 year, overall survival was 42%. At 2 years, it was 24%, and at 3 years, 18%.
“After 3 years, the survival curve has plateaued out, which is similar to what has been seen in the past in other diseases treated with immunotherapy,” Dr. Brahmer noted.
Within the cohort, there were 16 patients who had survived for at least 5 years. Of this group, 12 achieved a partial response, 2 patients had stable disease, and 2 had progressive disease.
Dr. Brahmer pointed out that there was nothing different or unusual among the 16 patients who survived for 5 years, compared with the rest of the cohort. Their characteristics were similar to others in the study, most of them were former smokers, and they had very similar rates of different histologies.
One interesting note was that within that group, there were two patients with EGFR mutations. “We usually don’t expect them to do well with immunotherapy,” she said.
Dr. Brahmer received research funding from, and is an adviser to, Bristol-Myers Squibb, which funded the study.
Early data show that treatment with the immune checkpoint inhibitor nivolumab (Opdivo) resulted in a 5-year overall survival rate of 16% among patients with advanced non–small-cell lung cancer (NSCLC).
In comparison, the 5-year survival rate for patients with advanced lung and bronchus cancer, according to SEER data, is 4.3%, and for those with advanced NSCLC, 4.9%.
“This is the first report of the long-term survival rate in patients with metastatic NSCLC treated with an immune checkpoint inhibitor,” said Julie Brahmer, MD, of the Bloomberg Kimmel Institute for Cancer Immunotherapy at Johns Hopkins, Baltimore.
For a small subset of patients, immunotherapy can work for a very long time, explained Dr. Brahmer, who discussed her findings during a presscast at the annual meeting of the American Association for Cancer Research.
The 5-year overall survival rate that was reported in this study was much higher than what has been seen for this patient population who receive the standard of care. Statistics show that the majority of patients with advanced disease will die within a year of their diagnosis, Dr. Brahmer pointed out.
The findings presented at the meeting are updated results from the phase Ib CA209-003 dose-escalation cohort expansion trial that comprised 129 patients with heavily pretreated, advanced NSCLC . The cohort was randomized to receive nivolumab once every 2 weeks for up to 2 years at one of three dose levels: 1 mg/kg, 3 mg/kg, or 10 mg/kg.
A previous analysis of the data showed promising activity, and findings from subsequent clinical trials led to the approval of nivolumab for use in the second line setting of advanced NSCLC.
Dr. Brahmer now reported findings based on 5-year results of this phase Ib trial. “This analysis is based on a minimum follow up of 58 months,” she said.
The overall 5-year survival rates for squamous NSCLC were 16%, and the rates for nonsquamous were 15%.
At 1 year, overall survival was 42%. At 2 years, it was 24%, and at 3 years, 18%.
“After 3 years, the survival curve has plateaued out, which is similar to what has been seen in the past in other diseases treated with immunotherapy,” Dr. Brahmer noted.
Within the cohort, there were 16 patients who had survived for at least 5 years. Of this group, 12 achieved a partial response, 2 patients had stable disease, and 2 had progressive disease.
Dr. Brahmer pointed out that there was nothing different or unusual among the 16 patients who survived for 5 years, compared with the rest of the cohort. Their characteristics were similar to others in the study, most of them were former smokers, and they had very similar rates of different histologies.
One interesting note was that within that group, there were two patients with EGFR mutations. “We usually don’t expect them to do well with immunotherapy,” she said.
Dr. Brahmer received research funding from, and is an adviser to, Bristol-Myers Squibb, which funded the study.
Early data show that treatment with the immune checkpoint inhibitor nivolumab (Opdivo) resulted in a 5-year overall survival rate of 16% among patients with advanced non–small-cell lung cancer (NSCLC).
In comparison, the 5-year survival rate for patients with advanced lung and bronchus cancer, according to SEER data, is 4.3%, and for those with advanced NSCLC, 4.9%.
“This is the first report of the long-term survival rate in patients with metastatic NSCLC treated with an immune checkpoint inhibitor,” said Julie Brahmer, MD, of the Bloomberg Kimmel Institute for Cancer Immunotherapy at Johns Hopkins, Baltimore.
For a small subset of patients, immunotherapy can work for a very long time, explained Dr. Brahmer, who discussed her findings during a presscast at the annual meeting of the American Association for Cancer Research.
The 5-year overall survival rate that was reported in this study was much higher than what has been seen for this patient population who receive the standard of care. Statistics show that the majority of patients with advanced disease will die within a year of their diagnosis, Dr. Brahmer pointed out.
The findings presented at the meeting are updated results from the phase Ib CA209-003 dose-escalation cohort expansion trial that comprised 129 patients with heavily pretreated, advanced NSCLC . The cohort was randomized to receive nivolumab once every 2 weeks for up to 2 years at one of three dose levels: 1 mg/kg, 3 mg/kg, or 10 mg/kg.
A previous analysis of the data showed promising activity, and findings from subsequent clinical trials led to the approval of nivolumab for use in the second line setting of advanced NSCLC.
Dr. Brahmer now reported findings based on 5-year results of this phase Ib trial. “This analysis is based on a minimum follow up of 58 months,” she said.
The overall 5-year survival rates for squamous NSCLC were 16%, and the rates for nonsquamous were 15%.
At 1 year, overall survival was 42%. At 2 years, it was 24%, and at 3 years, 18%.
“After 3 years, the survival curve has plateaued out, which is similar to what has been seen in the past in other diseases treated with immunotherapy,” Dr. Brahmer noted.
Within the cohort, there were 16 patients who had survived for at least 5 years. Of this group, 12 achieved a partial response, 2 patients had stable disease, and 2 had progressive disease.
Dr. Brahmer pointed out that there was nothing different or unusual among the 16 patients who survived for 5 years, compared with the rest of the cohort. Their characteristics were similar to others in the study, most of them were former smokers, and they had very similar rates of different histologies.
One interesting note was that within that group, there were two patients with EGFR mutations. “We usually don’t expect them to do well with immunotherapy,” she said.
Dr. Brahmer received research funding from, and is an adviser to, Bristol-Myers Squibb, which funded the study.
Key clinical point: Treatment with nivolumab resulted in a 5-year overall survival rate that is much higher than what is reported for this patient population receiving standard-of-care treatment.
Major finding: Nivolumab yielded a 5-year survival rate of 16% in a cohort of patients with advanced NSCLC.
Data source: Updated results from a phase Ib study that included 129 patients with advanced NSCLC.
Disclosures: Dr. Brahmer received research funding from, and is an adviser to, Bristol-Myers Squibb, which funded the study.
Cell sheet transplantation improves ischemic cardiomyopathy at 1 year
For patients with ischemic cardiomyopathy (ICM), transplanting sheets of autologous myoblasts onto the epicardial surface was safe and led to “marked” improvements in functional and laboratory measures, investigators reported.
However, cell sheet transplantation was much less effective for patients with dilated cardiomyopathy in this phase I trial, wrote Shigeru Miyagawa, MD, PhD, of Osaka (Japan) University, and his associates in the Journal of the American Heart Association. The findings merit additional follow-up in larger clinical studies, the investigators asserted.
Heart failure remains life threatening even with the best approved treatments. Previously, the researchers transplanted scaffold-free sheets of autologous myoblasts derived from skeletal muscle into small and large animals with heart failure and found that this approach healed severely damaged myocardium. Transplantation caused secreted cytokines to induce native regeneration through paracrine effects, Dr. Miyagawa noted in a prior review article (BioMed Research International. 2013. doi: 10.1155/2013/583912).
To evaluate this approach in humans, the researchers transplanted 15 patients with ischemic cardiomyopathy and 12 patients with dilated cardiomyopathy (DCM). Patients were 20-75 years old, had ejection fractions under 35% and New York Heart Association (NYHA) classifications of II or more, and were responding inadequately to standard treatment with a beta-blocker or ACE inhibitor and an angiotensin receptor blocker. The sole intervention was transplantation of the cell sheet over the left ventricular-free wall during left thoracotomy (J Am Heart Assoc. 2017 Apr 5. doi: 10.1161/JAHA.116.003918). There were no major procedure-related complications during follow-up, the researchers said. For patients with ICM, NYHA classifications dropped significantly at 6 months, from 2.9 at baseline to 2.1 at 6 months and 1.9 at 1 year. Six-Minute Walk Test scores improved significantly, from 416 m at baseline to 475 m at 6 months to 484 m at 1 year. Transplantation also led to significant drops in serum brain natriuretic peptide levels (baseline average, 308 pg/mL; 6 months, 191 pg/mL; 1 year, 182 pg/mL). Additionally, ICM patients improved significantly on measures of pulmonary artery pressure, pulmonary capillary wedge pressure, pulmonary vein resistance, and left ventricular wall stress.
In contrast, DCM patients did not significantly improve based on the 6-Minute Walk Test, NYHA classification, or brain natriuretic peptide serum levels. Of 12, 3 progressed to NYHA functional class IV by 1-year follow-up and there were five cardiac deaths. There were no cardiac deaths in the ICM group. “It has been reported that regeneration mechanisms in cell sheet mainly depend on angiogenesis induced by secreted cytokines, so cell-sheet implantation may be more suitable for ICM patients, compared with DCM patients, considering pathophysiological aspects,” the researchers wrote.
The study was funded by grants from Regenerative Medicine for Clinical Application, Health and Labor Sciences Research, and the Japan Agency for Medical Research and Development. The investigators disclosed laboratory funding from Terumo for cooperative research in cell sheet.
For patients with ischemic cardiomyopathy (ICM), transplanting sheets of autologous myoblasts onto the epicardial surface was safe and led to “marked” improvements in functional and laboratory measures, investigators reported.
However, cell sheet transplantation was much less effective for patients with dilated cardiomyopathy in this phase I trial, wrote Shigeru Miyagawa, MD, PhD, of Osaka (Japan) University, and his associates in the Journal of the American Heart Association. The findings merit additional follow-up in larger clinical studies, the investigators asserted.
Heart failure remains life threatening even with the best approved treatments. Previously, the researchers transplanted scaffold-free sheets of autologous myoblasts derived from skeletal muscle into small and large animals with heart failure and found that this approach healed severely damaged myocardium. Transplantation caused secreted cytokines to induce native regeneration through paracrine effects, Dr. Miyagawa noted in a prior review article (BioMed Research International. 2013. doi: 10.1155/2013/583912).
To evaluate this approach in humans, the researchers transplanted 15 patients with ischemic cardiomyopathy and 12 patients with dilated cardiomyopathy (DCM). Patients were 20-75 years old, had ejection fractions under 35% and New York Heart Association (NYHA) classifications of II or more, and were responding inadequately to standard treatment with a beta-blocker or ACE inhibitor and an angiotensin receptor blocker. The sole intervention was transplantation of the cell sheet over the left ventricular-free wall during left thoracotomy (J Am Heart Assoc. 2017 Apr 5. doi: 10.1161/JAHA.116.003918). There were no major procedure-related complications during follow-up, the researchers said. For patients with ICM, NYHA classifications dropped significantly at 6 months, from 2.9 at baseline to 2.1 at 6 months and 1.9 at 1 year. Six-Minute Walk Test scores improved significantly, from 416 m at baseline to 475 m at 6 months to 484 m at 1 year. Transplantation also led to significant drops in serum brain natriuretic peptide levels (baseline average, 308 pg/mL; 6 months, 191 pg/mL; 1 year, 182 pg/mL). Additionally, ICM patients improved significantly on measures of pulmonary artery pressure, pulmonary capillary wedge pressure, pulmonary vein resistance, and left ventricular wall stress.
In contrast, DCM patients did not significantly improve based on the 6-Minute Walk Test, NYHA classification, or brain natriuretic peptide serum levels. Of 12, 3 progressed to NYHA functional class IV by 1-year follow-up and there were five cardiac deaths. There were no cardiac deaths in the ICM group. “It has been reported that regeneration mechanisms in cell sheet mainly depend on angiogenesis induced by secreted cytokines, so cell-sheet implantation may be more suitable for ICM patients, compared with DCM patients, considering pathophysiological aspects,” the researchers wrote.
The study was funded by grants from Regenerative Medicine for Clinical Application, Health and Labor Sciences Research, and the Japan Agency for Medical Research and Development. The investigators disclosed laboratory funding from Terumo for cooperative research in cell sheet.
For patients with ischemic cardiomyopathy (ICM), transplanting sheets of autologous myoblasts onto the epicardial surface was safe and led to “marked” improvements in functional and laboratory measures, investigators reported.
However, cell sheet transplantation was much less effective for patients with dilated cardiomyopathy in this phase I trial, wrote Shigeru Miyagawa, MD, PhD, of Osaka (Japan) University, and his associates in the Journal of the American Heart Association. The findings merit additional follow-up in larger clinical studies, the investigators asserted.
Heart failure remains life threatening even with the best approved treatments. Previously, the researchers transplanted scaffold-free sheets of autologous myoblasts derived from skeletal muscle into small and large animals with heart failure and found that this approach healed severely damaged myocardium. Transplantation caused secreted cytokines to induce native regeneration through paracrine effects, Dr. Miyagawa noted in a prior review article (BioMed Research International. 2013. doi: 10.1155/2013/583912).
To evaluate this approach in humans, the researchers transplanted 15 patients with ischemic cardiomyopathy and 12 patients with dilated cardiomyopathy (DCM). Patients were 20-75 years old, had ejection fractions under 35% and New York Heart Association (NYHA) classifications of II or more, and were responding inadequately to standard treatment with a beta-blocker or ACE inhibitor and an angiotensin receptor blocker. The sole intervention was transplantation of the cell sheet over the left ventricular-free wall during left thoracotomy (J Am Heart Assoc. 2017 Apr 5. doi: 10.1161/JAHA.116.003918). There were no major procedure-related complications during follow-up, the researchers said. For patients with ICM, NYHA classifications dropped significantly at 6 months, from 2.9 at baseline to 2.1 at 6 months and 1.9 at 1 year. Six-Minute Walk Test scores improved significantly, from 416 m at baseline to 475 m at 6 months to 484 m at 1 year. Transplantation also led to significant drops in serum brain natriuretic peptide levels (baseline average, 308 pg/mL; 6 months, 191 pg/mL; 1 year, 182 pg/mL). Additionally, ICM patients improved significantly on measures of pulmonary artery pressure, pulmonary capillary wedge pressure, pulmonary vein resistance, and left ventricular wall stress.
In contrast, DCM patients did not significantly improve based on the 6-Minute Walk Test, NYHA classification, or brain natriuretic peptide serum levels. Of 12, 3 progressed to NYHA functional class IV by 1-year follow-up and there were five cardiac deaths. There were no cardiac deaths in the ICM group. “It has been reported that regeneration mechanisms in cell sheet mainly depend on angiogenesis induced by secreted cytokines, so cell-sheet implantation may be more suitable for ICM patients, compared with DCM patients, considering pathophysiological aspects,” the researchers wrote.
The study was funded by grants from Regenerative Medicine for Clinical Application, Health and Labor Sciences Research, and the Japan Agency for Medical Research and Development. The investigators disclosed laboratory funding from Terumo for cooperative research in cell sheet.
Key clinical point: Transplanting a sheet of autologous myoblasts onto the epicardial surface was safe and was associated with functional and symptomatic improvements in patients with ischemic cardiomyopathy.
Major finding: Patients improved significantly on the 6-Minute Walk Test, New York Heart Classification, and on measures of brain natriuretic peptide, pulmonary artery pressure, pulmonary capillary wedge pressure, pulmonary vein resistance, and left ventricular wall stress. These effects did not extend to patients with dilated cardiomyopathy.
Data source: A phase I trial of 27 patients with ischemic or dilated cardiomyopathy.
Disclosures: The study was funded by grants from Regenerative Medicine for Clinical Application, Health and Labor Sciences Research, and the Japan Agency for Medical Research and Development. The investigators disclosed laboratory funding from Terumo for cooperative research in cell sheet.
Pushing the Boundaries of Conventional Surgery
With the myriad procedures and complications that thoracic surgeons are required to be familiar with, the Adult Cardiac Skills course, “100 Years of Training – More Skills Still Needed!” aims to shed some light on the more unconventional procedures that thoracic surgeons see less frequently.
The course will consist of sessions that will each highlight a specific topic: mitral valve repairs. imaging, coronary surgery, and “complex case presentations,” which will feature demonstrations of groundbreaking techniques for challenging presentations a surgeon could encounter.
The mitral valve repair session will focus on bileaflet and endoscopic mitral valve repair, along with talks on right perfusion management, transapical artificial chordae implantation, and using aortic valve repair on a bicuspid aortic valve. These talks – given by Patrick Perier, MD, of the Herz und Gefaess Klinik, Andrea Colli, MD, of the University of Padova, and David Fitzgerald, MD, of the Medical Center of South Carolina, among others – will each last about 15 minutes and will culminate in a panel discussion.
The following hour will be spent discussing imaging in cardiac surgery, where speakers such as Eric E. Roselli, MD, of the Cleveland Clinic, will discuss using imaging in TEVAR to facilitate aortic stenting. Wilson Y. Szeto, MD, of the University of Pennsylvania, will give a talk on transfemoral TAVR, and Mary Beth Brady, MD, of Johns Hopkins University, will discuss the use of transesophageal echocardiogram in thoracic surgery.
After lunch, the coronary surgery session will feature presentations on internal thoracic artery grafts – presented by course chair Dr. Zehr – along with discussions on hybrid revascularization and minimal access off-pump coronary artery bypass. And finally, the last session will highlight the most unusual and rare cases surgeons are likely to come across, such as redoing a mitral valve repair and operating on an infected aortic root. Dr. Zehr hopes the session will address some needs and questions for attendees to improve their practice. “What extra skill sets are necessary to do a few more mitral repairs than you’re already doing and to be a little bit more successful in aortic dissections? Or to know some of the subtleties between doing an open aortic valve versus a minimally invasive transapical or transcathetic aortic valve.”
With the myriad procedures and complications that thoracic surgeons are required to be familiar with, the Adult Cardiac Skills course, “100 Years of Training – More Skills Still Needed!” aims to shed some light on the more unconventional procedures that thoracic surgeons see less frequently.
The course will consist of sessions that will each highlight a specific topic: mitral valve repairs. imaging, coronary surgery, and “complex case presentations,” which will feature demonstrations of groundbreaking techniques for challenging presentations a surgeon could encounter.
The mitral valve repair session will focus on bileaflet and endoscopic mitral valve repair, along with talks on right perfusion management, transapical artificial chordae implantation, and using aortic valve repair on a bicuspid aortic valve. These talks – given by Patrick Perier, MD, of the Herz und Gefaess Klinik, Andrea Colli, MD, of the University of Padova, and David Fitzgerald, MD, of the Medical Center of South Carolina, among others – will each last about 15 minutes and will culminate in a panel discussion.
The following hour will be spent discussing imaging in cardiac surgery, where speakers such as Eric E. Roselli, MD, of the Cleveland Clinic, will discuss using imaging in TEVAR to facilitate aortic stenting. Wilson Y. Szeto, MD, of the University of Pennsylvania, will give a talk on transfemoral TAVR, and Mary Beth Brady, MD, of Johns Hopkins University, will discuss the use of transesophageal echocardiogram in thoracic surgery.
After lunch, the coronary surgery session will feature presentations on internal thoracic artery grafts – presented by course chair Dr. Zehr – along with discussions on hybrid revascularization and minimal access off-pump coronary artery bypass. And finally, the last session will highlight the most unusual and rare cases surgeons are likely to come across, such as redoing a mitral valve repair and operating on an infected aortic root. Dr. Zehr hopes the session will address some needs and questions for attendees to improve their practice. “What extra skill sets are necessary to do a few more mitral repairs than you’re already doing and to be a little bit more successful in aortic dissections? Or to know some of the subtleties between doing an open aortic valve versus a minimally invasive transapical or transcathetic aortic valve.”
With the myriad procedures and complications that thoracic surgeons are required to be familiar with, the Adult Cardiac Skills course, “100 Years of Training – More Skills Still Needed!” aims to shed some light on the more unconventional procedures that thoracic surgeons see less frequently.
The course will consist of sessions that will each highlight a specific topic: mitral valve repairs. imaging, coronary surgery, and “complex case presentations,” which will feature demonstrations of groundbreaking techniques for challenging presentations a surgeon could encounter.
The mitral valve repair session will focus on bileaflet and endoscopic mitral valve repair, along with talks on right perfusion management, transapical artificial chordae implantation, and using aortic valve repair on a bicuspid aortic valve. These talks – given by Patrick Perier, MD, of the Herz und Gefaess Klinik, Andrea Colli, MD, of the University of Padova, and David Fitzgerald, MD, of the Medical Center of South Carolina, among others – will each last about 15 minutes and will culminate in a panel discussion.
The following hour will be spent discussing imaging in cardiac surgery, where speakers such as Eric E. Roselli, MD, of the Cleveland Clinic, will discuss using imaging in TEVAR to facilitate aortic stenting. Wilson Y. Szeto, MD, of the University of Pennsylvania, will give a talk on transfemoral TAVR, and Mary Beth Brady, MD, of Johns Hopkins University, will discuss the use of transesophageal echocardiogram in thoracic surgery.
After lunch, the coronary surgery session will feature presentations on internal thoracic artery grafts – presented by course chair Dr. Zehr – along with discussions on hybrid revascularization and minimal access off-pump coronary artery bypass. And finally, the last session will highlight the most unusual and rare cases surgeons are likely to come across, such as redoing a mitral valve repair and operating on an infected aortic root. Dr. Zehr hopes the session will address some needs and questions for attendees to improve their practice. “What extra skill sets are necessary to do a few more mitral repairs than you’re already doing and to be a little bit more successful in aortic dissections? Or to know some of the subtleties between doing an open aortic valve versus a minimally invasive transapical or transcathetic aortic valve.”
Course Takes Aim at Innovative Approaches to Rare Congenital Heart Disease
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
Uptake of new heart failure drugs slow despite guidelines
SNOWMASS, COLO. – As William T. Abraham, MD, speaks to colleagues around the country about heart failure therapy, he has noticed that the first-in-class drug ivabradine remains below the radar of most physicians.
“I’ve found that this is an agent that very few people know about, even though it’s been FDA [Food and Drug Administration] approved for about 3 years. It’s used fairly extensively in Europe because that’s where the pivotal SHIFT trial was done, but not very much in the United States,” according to Dr. Abraham, professor of medicine, physiology, and cell biology and director of the division of cardiovascular medicine at Ohio State University in Columbus.
That’s likely to change as word spreads about the May 2016 update of the American College of Cardiology/American Heart Association Guideline for the Management of Heart Failure. The update incorporated evidence-based recommendations on the use of two important new heart failure medications: ivabradine (Corlanor), which received a moderate class IIa recommendation, meaning the drug “should be considered,” and sacubitril/valsartan (Entresto), which received the strongest class I recommendation.
In the right patients, these two oral medications improve heart failure morbidity and mortality significantly beyond what’s achievable with what has been the gold standard, guideline-directed medical therapy. Dr. Abraham described how to get started using the two medications at the Annual Cardiovascular Conference at Snowmass.
Ivabradine
Ivabradine is a selective inhibitor of the sinoatrial pacemaker modulating I(f) current. It acts by slowing the sinus rate without reducing myocardial contractility.
“This agent does one thing and one thing alone: It lowers heart rate,” the cardiologist explained.
And that, he added, was sufficient to significantly reduce the risks of death due to heart failure and recurrent hospitalization for worsening heart failure in the pivotal SHIFT trial.
SHIFT included 6,505 patients with moderate to severe heart failure with reduced left ventricular ejection fraction (LVEF) and a resting heart rate above 70 bpm despite background guideline-directed medical therapy. Participants were randomized double blind to ivabradine titrated to a maximum of 7.5 mg twice daily or placebo and followed for a median of about 23 months. The rate of death due to heart failure was 3% with ivabradine and 5% with placebo, for a statistically significant 26% relative risk reduction favoring ivabradine.
But the drug’s main benefit was in reducing recurrent hospitalizations for heart failure, an endpoint of particular interest to health policy officials given that heart failure hospitalizations chew up a substantial proportion of the Medicare budget. Ivabradine reduced first hospitalizations for heart failure during the study period by 25%, second hospitalizations by 34%, and third hospitalizations by 29% (Eur Heart J. 2012 Nov;33[22]:2813-20).
The ACC/AHA guideline update stresses the importance of reserving ivabradine for heart failure patients whose resting heart rate exceeds 70 bpm, despite being on their maximum tolerated dose of a beta-blocker, Dr. Abraham noted.
Ivabradine is contraindicated in the setting of acute decompensated heart failure, severe liver disease, or hypotension, in patients on any of the numerous agents that strongly inhibit the enzyme cytochrome P450 3A4, and in those who have sick sinus syndrome, have sinoatrial block, or are pacemaker dependent.
Sacubitril/valsartan
Sacubitril inhibits neprilysin, an enzyme that blocks the action of endogenous vasoactive peptides including bradykinin, substance P, and natriuretic peptides, all of which counter important maladaptive mechanisms in heart failure. Sacubitril has been combined with the angiotensin receptor blocker valsartan to form the first-in-class angiotensin receptor neprilysin inhibitor, or ARNI, formerly known as LCZ696 and now marketed as Entresto.
In the pivotal double-blind PARADIGM-HF trial, 8,442 patients with heart failure with reduced ejection fraction were randomized to the ARNI at 200 mg b.i.d. or to enalapril at 10 mg b.i.d. on top of background guideline-directed medical therapy. The trial was stopped early because of evidence of overwhelming benefit: a 20% relative risk reduction in cardiovascular death and a 21% decrease in the risk of heart failure hospitalizations in the sacubitril/valsartan group, as well as significant reductions in heart failure symptoms and physical limitations (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
The updated heart failure guidelines strongly recommend that patients with heart failure should be treated with either an ACE inhibitor, an angiotensin receptor blocker, or an ARNI. Further, patients who remain symptomatic on an ACE inhibitor or angiotensin receptor blocker should be switched to an ARNI; that’s a class Ib recommendation based upon the results of PARADIGM-HF.
In getting started using the ARNI, Dr. Abraham said it’s important to understand as background the selective nature of the PARADIGM-HF study design. During the single-blind run-in period of 5-8 weeks, roughly 10% of patients dropped out because they couldn’t tolerate enalapril at 10 mg b.i.d., and a similar percentage dropped out during the ARNI run-in. Thus, patients who couldn’t tolerate a low dose of an ACE inhibitor weren’t in the study. And patients capable of tolerating guideline-recommended full-dose ACE inhibitor therapy were not specifically sought for participation.
“So there are some unanswered questions about the ARNI. If you’re just getting started with this compound in treating your heart failure patients, my own feeling is you should maybe aim for the type of patient that was included in this trial: patients who could tolerate a moderate dose of an ACE inhibitor and had generally good blood pressure. That’s a great way to begin to get experience with this agent in heart failure,” the cardiologist advised.
He reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – As William T. Abraham, MD, speaks to colleagues around the country about heart failure therapy, he has noticed that the first-in-class drug ivabradine remains below the radar of most physicians.
“I’ve found that this is an agent that very few people know about, even though it’s been FDA [Food and Drug Administration] approved for about 3 years. It’s used fairly extensively in Europe because that’s where the pivotal SHIFT trial was done, but not very much in the United States,” according to Dr. Abraham, professor of medicine, physiology, and cell biology and director of the division of cardiovascular medicine at Ohio State University in Columbus.
That’s likely to change as word spreads about the May 2016 update of the American College of Cardiology/American Heart Association Guideline for the Management of Heart Failure. The update incorporated evidence-based recommendations on the use of two important new heart failure medications: ivabradine (Corlanor), which received a moderate class IIa recommendation, meaning the drug “should be considered,” and sacubitril/valsartan (Entresto), which received the strongest class I recommendation.
In the right patients, these two oral medications improve heart failure morbidity and mortality significantly beyond what’s achievable with what has been the gold standard, guideline-directed medical therapy. Dr. Abraham described how to get started using the two medications at the Annual Cardiovascular Conference at Snowmass.
Ivabradine
Ivabradine is a selective inhibitor of the sinoatrial pacemaker modulating I(f) current. It acts by slowing the sinus rate without reducing myocardial contractility.
“This agent does one thing and one thing alone: It lowers heart rate,” the cardiologist explained.
And that, he added, was sufficient to significantly reduce the risks of death due to heart failure and recurrent hospitalization for worsening heart failure in the pivotal SHIFT trial.
SHIFT included 6,505 patients with moderate to severe heart failure with reduced left ventricular ejection fraction (LVEF) and a resting heart rate above 70 bpm despite background guideline-directed medical therapy. Participants were randomized double blind to ivabradine titrated to a maximum of 7.5 mg twice daily or placebo and followed for a median of about 23 months. The rate of death due to heart failure was 3% with ivabradine and 5% with placebo, for a statistically significant 26% relative risk reduction favoring ivabradine.
But the drug’s main benefit was in reducing recurrent hospitalizations for heart failure, an endpoint of particular interest to health policy officials given that heart failure hospitalizations chew up a substantial proportion of the Medicare budget. Ivabradine reduced first hospitalizations for heart failure during the study period by 25%, second hospitalizations by 34%, and third hospitalizations by 29% (Eur Heart J. 2012 Nov;33[22]:2813-20).
The ACC/AHA guideline update stresses the importance of reserving ivabradine for heart failure patients whose resting heart rate exceeds 70 bpm, despite being on their maximum tolerated dose of a beta-blocker, Dr. Abraham noted.
Ivabradine is contraindicated in the setting of acute decompensated heart failure, severe liver disease, or hypotension, in patients on any of the numerous agents that strongly inhibit the enzyme cytochrome P450 3A4, and in those who have sick sinus syndrome, have sinoatrial block, or are pacemaker dependent.
Sacubitril/valsartan
Sacubitril inhibits neprilysin, an enzyme that blocks the action of endogenous vasoactive peptides including bradykinin, substance P, and natriuretic peptides, all of which counter important maladaptive mechanisms in heart failure. Sacubitril has been combined with the angiotensin receptor blocker valsartan to form the first-in-class angiotensin receptor neprilysin inhibitor, or ARNI, formerly known as LCZ696 and now marketed as Entresto.
In the pivotal double-blind PARADIGM-HF trial, 8,442 patients with heart failure with reduced ejection fraction were randomized to the ARNI at 200 mg b.i.d. or to enalapril at 10 mg b.i.d. on top of background guideline-directed medical therapy. The trial was stopped early because of evidence of overwhelming benefit: a 20% relative risk reduction in cardiovascular death and a 21% decrease in the risk of heart failure hospitalizations in the sacubitril/valsartan group, as well as significant reductions in heart failure symptoms and physical limitations (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
The updated heart failure guidelines strongly recommend that patients with heart failure should be treated with either an ACE inhibitor, an angiotensin receptor blocker, or an ARNI. Further, patients who remain symptomatic on an ACE inhibitor or angiotensin receptor blocker should be switched to an ARNI; that’s a class Ib recommendation based upon the results of PARADIGM-HF.
In getting started using the ARNI, Dr. Abraham said it’s important to understand as background the selective nature of the PARADIGM-HF study design. During the single-blind run-in period of 5-8 weeks, roughly 10% of patients dropped out because they couldn’t tolerate enalapril at 10 mg b.i.d., and a similar percentage dropped out during the ARNI run-in. Thus, patients who couldn’t tolerate a low dose of an ACE inhibitor weren’t in the study. And patients capable of tolerating guideline-recommended full-dose ACE inhibitor therapy were not specifically sought for participation.
“So there are some unanswered questions about the ARNI. If you’re just getting started with this compound in treating your heart failure patients, my own feeling is you should maybe aim for the type of patient that was included in this trial: patients who could tolerate a moderate dose of an ACE inhibitor and had generally good blood pressure. That’s a great way to begin to get experience with this agent in heart failure,” the cardiologist advised.
He reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – As William T. Abraham, MD, speaks to colleagues around the country about heart failure therapy, he has noticed that the first-in-class drug ivabradine remains below the radar of most physicians.
“I’ve found that this is an agent that very few people know about, even though it’s been FDA [Food and Drug Administration] approved for about 3 years. It’s used fairly extensively in Europe because that’s where the pivotal SHIFT trial was done, but not very much in the United States,” according to Dr. Abraham, professor of medicine, physiology, and cell biology and director of the division of cardiovascular medicine at Ohio State University in Columbus.
That’s likely to change as word spreads about the May 2016 update of the American College of Cardiology/American Heart Association Guideline for the Management of Heart Failure. The update incorporated evidence-based recommendations on the use of two important new heart failure medications: ivabradine (Corlanor), which received a moderate class IIa recommendation, meaning the drug “should be considered,” and sacubitril/valsartan (Entresto), which received the strongest class I recommendation.
In the right patients, these two oral medications improve heart failure morbidity and mortality significantly beyond what’s achievable with what has been the gold standard, guideline-directed medical therapy. Dr. Abraham described how to get started using the two medications at the Annual Cardiovascular Conference at Snowmass.
Ivabradine
Ivabradine is a selective inhibitor of the sinoatrial pacemaker modulating I(f) current. It acts by slowing the sinus rate without reducing myocardial contractility.
“This agent does one thing and one thing alone: It lowers heart rate,” the cardiologist explained.
And that, he added, was sufficient to significantly reduce the risks of death due to heart failure and recurrent hospitalization for worsening heart failure in the pivotal SHIFT trial.
SHIFT included 6,505 patients with moderate to severe heart failure with reduced left ventricular ejection fraction (LVEF) and a resting heart rate above 70 bpm despite background guideline-directed medical therapy. Participants were randomized double blind to ivabradine titrated to a maximum of 7.5 mg twice daily or placebo and followed for a median of about 23 months. The rate of death due to heart failure was 3% with ivabradine and 5% with placebo, for a statistically significant 26% relative risk reduction favoring ivabradine.
But the drug’s main benefit was in reducing recurrent hospitalizations for heart failure, an endpoint of particular interest to health policy officials given that heart failure hospitalizations chew up a substantial proportion of the Medicare budget. Ivabradine reduced first hospitalizations for heart failure during the study period by 25%, second hospitalizations by 34%, and third hospitalizations by 29% (Eur Heart J. 2012 Nov;33[22]:2813-20).
The ACC/AHA guideline update stresses the importance of reserving ivabradine for heart failure patients whose resting heart rate exceeds 70 bpm, despite being on their maximum tolerated dose of a beta-blocker, Dr. Abraham noted.
Ivabradine is contraindicated in the setting of acute decompensated heart failure, severe liver disease, or hypotension, in patients on any of the numerous agents that strongly inhibit the enzyme cytochrome P450 3A4, and in those who have sick sinus syndrome, have sinoatrial block, or are pacemaker dependent.
Sacubitril/valsartan
Sacubitril inhibits neprilysin, an enzyme that blocks the action of endogenous vasoactive peptides including bradykinin, substance P, and natriuretic peptides, all of which counter important maladaptive mechanisms in heart failure. Sacubitril has been combined with the angiotensin receptor blocker valsartan to form the first-in-class angiotensin receptor neprilysin inhibitor, or ARNI, formerly known as LCZ696 and now marketed as Entresto.
In the pivotal double-blind PARADIGM-HF trial, 8,442 patients with heart failure with reduced ejection fraction were randomized to the ARNI at 200 mg b.i.d. or to enalapril at 10 mg b.i.d. on top of background guideline-directed medical therapy. The trial was stopped early because of evidence of overwhelming benefit: a 20% relative risk reduction in cardiovascular death and a 21% decrease in the risk of heart failure hospitalizations in the sacubitril/valsartan group, as well as significant reductions in heart failure symptoms and physical limitations (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
The updated heart failure guidelines strongly recommend that patients with heart failure should be treated with either an ACE inhibitor, an angiotensin receptor blocker, or an ARNI. Further, patients who remain symptomatic on an ACE inhibitor or angiotensin receptor blocker should be switched to an ARNI; that’s a class Ib recommendation based upon the results of PARADIGM-HF.
In getting started using the ARNI, Dr. Abraham said it’s important to understand as background the selective nature of the PARADIGM-HF study design. During the single-blind run-in period of 5-8 weeks, roughly 10% of patients dropped out because they couldn’t tolerate enalapril at 10 mg b.i.d., and a similar percentage dropped out during the ARNI run-in. Thus, patients who couldn’t tolerate a low dose of an ACE inhibitor weren’t in the study. And patients capable of tolerating guideline-recommended full-dose ACE inhibitor therapy were not specifically sought for participation.
“So there are some unanswered questions about the ARNI. If you’re just getting started with this compound in treating your heart failure patients, my own feeling is you should maybe aim for the type of patient that was included in this trial: patients who could tolerate a moderate dose of an ACE inhibitor and had generally good blood pressure. That’s a great way to begin to get experience with this agent in heart failure,” the cardiologist advised.
He reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Boston - Rich History, Lively Cultural Scene
There is history around every corner in Boston. This vibrant city is rich with art, music, and dance institutions, theatre and cultural attractions, distinguished dining and nightlife venues, world-class shopping and championship sports teams that attract millions of visitors each year.
The city’s downtown neighborhoods, each with its own personality, offer endless unique experiences, and Boston’s proximity to other must-see sites all around New England make it one of the country’s most diverse and exciting locales.Each of the city’s neighborhoods has a remarkably different style and tone. From the Back Bay’s cosmopolitan streets and ornate Victorian townhouses to the aromas spilling into the narrow and jumbled 17th-century streets of Boston’s North End to the spirited and funky neighborhood squares of Cambridge – all within easy distance from one another.Boston is “America’s Walking City.” Even though it is one of the largest cities in the country, its accessibility is unparalleled. And while sightseeing on foot is easy, Boston also has an excellent public transportation system to help you get around.
Boston is also known as the mecca of medicine. Boston is home to some of the most prestigious hospitals and medical schools, physicians, and medical scientists in the world. Thoralf M. Sundt, III, MD, and the AATS Centennial Committee have organized an engaging social program for the AATS Centennial.
Tour 1: ITALIAN GASTRONOMY NORTH END MARKET TOUR
Sunday, April 30, 2017
10:30 a.m.– 1:15 p.m.
Cost: $95 per person
Tour 2: A VISIT TO THE ISABELLA STEWART GARDNER MUSEUM
Monday, May 1, 2017
12:15 p.m. – 2:45 p.m.
Cost: $85 per person
Enjoy the Gardners’ compilation of tapestries, exquisite antique furniture, and famous collections while hearing wonderful anecdotes about Mrs. Gardner’s sophisticated and eclectic life and the famous heist. A docent will be available to guidevisitors.
Tour 3: BEACON HILL CIRCLE “BEHIND THE BRAHMIN DOORS”
Tuesday, May 2, 2017
9:15 a.m. – 11:45 a.m.
Cost: $110 per person
*Preregistration for social events and tours are required. Tours require a minimum number of participants. All tours will depart from the Hynes Convention Center.
For additional visit information and things to do in Boston, go to https://www.bostonusa.com/things-to-do.
There is history around every corner in Boston. This vibrant city is rich with art, music, and dance institutions, theatre and cultural attractions, distinguished dining and nightlife venues, world-class shopping and championship sports teams that attract millions of visitors each year.
The city’s downtown neighborhoods, each with its own personality, offer endless unique experiences, and Boston’s proximity to other must-see sites all around New England make it one of the country’s most diverse and exciting locales.Each of the city’s neighborhoods has a remarkably different style and tone. From the Back Bay’s cosmopolitan streets and ornate Victorian townhouses to the aromas spilling into the narrow and jumbled 17th-century streets of Boston’s North End to the spirited and funky neighborhood squares of Cambridge – all within easy distance from one another.Boston is “America’s Walking City.” Even though it is one of the largest cities in the country, its accessibility is unparalleled. And while sightseeing on foot is easy, Boston also has an excellent public transportation system to help you get around.
Boston is also known as the mecca of medicine. Boston is home to some of the most prestigious hospitals and medical schools, physicians, and medical scientists in the world. Thoralf M. Sundt, III, MD, and the AATS Centennial Committee have organized an engaging social program for the AATS Centennial.
Tour 1: ITALIAN GASTRONOMY NORTH END MARKET TOUR
Sunday, April 30, 2017
10:30 a.m.– 1:15 p.m.
Cost: $95 per person
Tour 2: A VISIT TO THE ISABELLA STEWART GARDNER MUSEUM
Monday, May 1, 2017
12:15 p.m. – 2:45 p.m.
Cost: $85 per person
Enjoy the Gardners’ compilation of tapestries, exquisite antique furniture, and famous collections while hearing wonderful anecdotes about Mrs. Gardner’s sophisticated and eclectic life and the famous heist. A docent will be available to guidevisitors.
Tour 3: BEACON HILL CIRCLE “BEHIND THE BRAHMIN DOORS”
Tuesday, May 2, 2017
9:15 a.m. – 11:45 a.m.
Cost: $110 per person
*Preregistration for social events and tours are required. Tours require a minimum number of participants. All tours will depart from the Hynes Convention Center.
For additional visit information and things to do in Boston, go to https://www.bostonusa.com/things-to-do.
There is history around every corner in Boston. This vibrant city is rich with art, music, and dance institutions, theatre and cultural attractions, distinguished dining and nightlife venues, world-class shopping and championship sports teams that attract millions of visitors each year.
The city’s downtown neighborhoods, each with its own personality, offer endless unique experiences, and Boston’s proximity to other must-see sites all around New England make it one of the country’s most diverse and exciting locales.Each of the city’s neighborhoods has a remarkably different style and tone. From the Back Bay’s cosmopolitan streets and ornate Victorian townhouses to the aromas spilling into the narrow and jumbled 17th-century streets of Boston’s North End to the spirited and funky neighborhood squares of Cambridge – all within easy distance from one another.Boston is “America’s Walking City.” Even though it is one of the largest cities in the country, its accessibility is unparalleled. And while sightseeing on foot is easy, Boston also has an excellent public transportation system to help you get around.
Boston is also known as the mecca of medicine. Boston is home to some of the most prestigious hospitals and medical schools, physicians, and medical scientists in the world. Thoralf M. Sundt, III, MD, and the AATS Centennial Committee have organized an engaging social program for the AATS Centennial.
Tour 1: ITALIAN GASTRONOMY NORTH END MARKET TOUR
Sunday, April 30, 2017
10:30 a.m.– 1:15 p.m.
Cost: $95 per person
Tour 2: A VISIT TO THE ISABELLA STEWART GARDNER MUSEUM
Monday, May 1, 2017
12:15 p.m. – 2:45 p.m.
Cost: $85 per person
Enjoy the Gardners’ compilation of tapestries, exquisite antique furniture, and famous collections while hearing wonderful anecdotes about Mrs. Gardner’s sophisticated and eclectic life and the famous heist. A docent will be available to guidevisitors.
Tour 3: BEACON HILL CIRCLE “BEHIND THE BRAHMIN DOORS”
Tuesday, May 2, 2017
9:15 a.m. – 11:45 a.m.
Cost: $110 per person
*Preregistration for social events and tours are required. Tours require a minimum number of participants. All tours will depart from the Hynes Convention Center.
For additional visit information and things to do in Boston, go to https://www.bostonusa.com/things-to-do.
AATS Centennial Highlights
AATS Week 2017 is fast approaching, and we hope you are planning to participate in the wide variety of educational opportunities available across all areas of thoracic surgery.
The week opens with the two-day AATS Mitral Conclave, which will be held on Thursday, April 27, and Friday, April 28, in New York. You will have the chance to attend an exceptional program created by Director David H. Adams, MD, and the program com ntations, expert technique/video sessions and breakout sessions.
As we look back on the last 100 years and enter our second century as an Association for Thoracic Surgery, the 2017 meeting will provide again, as it always does, an extraordinary variety of educational opportunities across all areas of our specialty. The meeting’s theme of “Always Learning” is a testament to the drive for lifelong learning among attendees, and we commit to making certain that your time is well spent.
The meeting will include many of the most popular program components, including Saturday’s skills courses and Sunday’s Postgraduate Symposia. Saturday will also include hands-on sessions, the well-received Member for a Day Program as well as Survival Guide: Your First Night on Call. The abstract presentations were selected to provide you with new insights that are applicable to your practice and that benefit your patients as well as encourage rich discussions inside and outside of the sessions.
In addition to the programs with which you have become familiar, a number of sessions will be of interest to all members of the surgical team. The Association has long recognized the essential nature of a multidisciplinary approach to care of the cardiothoracic surgical patient as is reflected in the organization’s original membership roster, and the more recent addition of a postgraduate symposium for the Interprofessional Cardiothoracic Team. As always, we look forward to participation from nurses, perfusionists, anesthesiologists, and others in the program and as faculty. This year, we have taken another step forward by holding our meeting in conjunction with the American Society for ExtraCorporeal Technology (AmSECT) 55th International Conference.
It is fitting that we are holding such a historic meeting in a city like Boston, where you will be able to experience the city’s rich culture and history. We have planned a variety of special events and features in honor of the Centennial anniversary of the founding of the Association for Thoracic Surgery. I would like to thank meeting Co-Chairs, Robert D. Jaquiss. MD, and Bryan F. Meyers, MD, for their work to make this meeting represent the highest caliber in promoting leadership, scholarship, mentoring, excellence in patient care, integrity, and professionalism. Please visit the AATS website, watch your email for updates, and download the AATS Week Mobile App for all the information you need to make the most of the experience.
AATS Week 2017 is fast approaching, and we hope you are planning to participate in the wide variety of educational opportunities available across all areas of thoracic surgery.
The week opens with the two-day AATS Mitral Conclave, which will be held on Thursday, April 27, and Friday, April 28, in New York. You will have the chance to attend an exceptional program created by Director David H. Adams, MD, and the program com ntations, expert technique/video sessions and breakout sessions.
As we look back on the last 100 years and enter our second century as an Association for Thoracic Surgery, the 2017 meeting will provide again, as it always does, an extraordinary variety of educational opportunities across all areas of our specialty. The meeting’s theme of “Always Learning” is a testament to the drive for lifelong learning among attendees, and we commit to making certain that your time is well spent.
The meeting will include many of the most popular program components, including Saturday’s skills courses and Sunday’s Postgraduate Symposia. Saturday will also include hands-on sessions, the well-received Member for a Day Program as well as Survival Guide: Your First Night on Call. The abstract presentations were selected to provide you with new insights that are applicable to your practice and that benefit your patients as well as encourage rich discussions inside and outside of the sessions.
In addition to the programs with which you have become familiar, a number of sessions will be of interest to all members of the surgical team. The Association has long recognized the essential nature of a multidisciplinary approach to care of the cardiothoracic surgical patient as is reflected in the organization’s original membership roster, and the more recent addition of a postgraduate symposium for the Interprofessional Cardiothoracic Team. As always, we look forward to participation from nurses, perfusionists, anesthesiologists, and others in the program and as faculty. This year, we have taken another step forward by holding our meeting in conjunction with the American Society for ExtraCorporeal Technology (AmSECT) 55th International Conference.
It is fitting that we are holding such a historic meeting in a city like Boston, where you will be able to experience the city’s rich culture and history. We have planned a variety of special events and features in honor of the Centennial anniversary of the founding of the Association for Thoracic Surgery. I would like to thank meeting Co-Chairs, Robert D. Jaquiss. MD, and Bryan F. Meyers, MD, for their work to make this meeting represent the highest caliber in promoting leadership, scholarship, mentoring, excellence in patient care, integrity, and professionalism. Please visit the AATS website, watch your email for updates, and download the AATS Week Mobile App for all the information you need to make the most of the experience.
AATS Week 2017 is fast approaching, and we hope you are planning to participate in the wide variety of educational opportunities available across all areas of thoracic surgery.
The week opens with the two-day AATS Mitral Conclave, which will be held on Thursday, April 27, and Friday, April 28, in New York. You will have the chance to attend an exceptional program created by Director David H. Adams, MD, and the program com ntations, expert technique/video sessions and breakout sessions.
As we look back on the last 100 years and enter our second century as an Association for Thoracic Surgery, the 2017 meeting will provide again, as it always does, an extraordinary variety of educational opportunities across all areas of our specialty. The meeting’s theme of “Always Learning” is a testament to the drive for lifelong learning among attendees, and we commit to making certain that your time is well spent.
The meeting will include many of the most popular program components, including Saturday’s skills courses and Sunday’s Postgraduate Symposia. Saturday will also include hands-on sessions, the well-received Member for a Day Program as well as Survival Guide: Your First Night on Call. The abstract presentations were selected to provide you with new insights that are applicable to your practice and that benefit your patients as well as encourage rich discussions inside and outside of the sessions.
In addition to the programs with which you have become familiar, a number of sessions will be of interest to all members of the surgical team. The Association has long recognized the essential nature of a multidisciplinary approach to care of the cardiothoracic surgical patient as is reflected in the organization’s original membership roster, and the more recent addition of a postgraduate symposium for the Interprofessional Cardiothoracic Team. As always, we look forward to participation from nurses, perfusionists, anesthesiologists, and others in the program and as faculty. This year, we have taken another step forward by holding our meeting in conjunction with the American Society for ExtraCorporeal Technology (AmSECT) 55th International Conference.
It is fitting that we are holding such a historic meeting in a city like Boston, where you will be able to experience the city’s rich culture and history. We have planned a variety of special events and features in honor of the Centennial anniversary of the founding of the Association for Thoracic Surgery. I would like to thank meeting Co-Chairs, Robert D. Jaquiss. MD, and Bryan F. Meyers, MD, for their work to make this meeting represent the highest caliber in promoting leadership, scholarship, mentoring, excellence in patient care, integrity, and professionalism. Please visit the AATS website, watch your email for updates, and download the AATS Week Mobile App for all the information you need to make the most of the experience.
Senate committee moves Gorsuch nomination forward
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
What do doctors want from health reform?
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
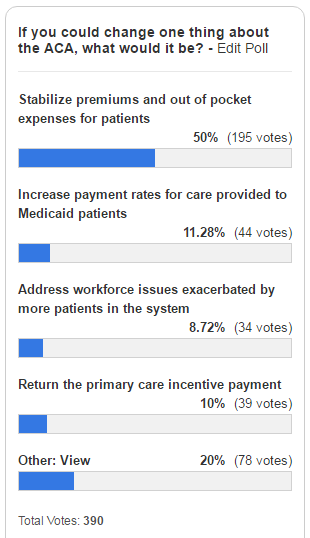
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
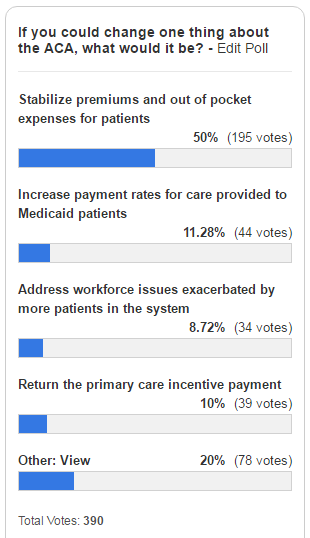
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
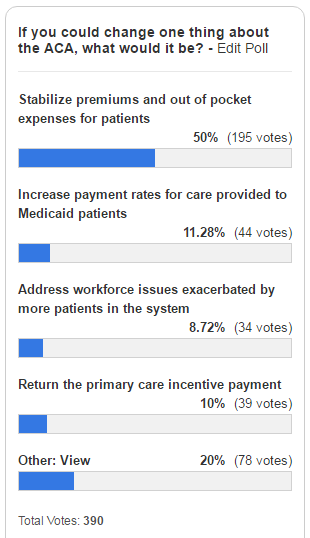
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.