User login
Commentary: Adjuvant Chemotherapy in Stage II Colon Cancer, August 2022
This month brought us findings from DYNAMIC, a randomized trial of circulating tumor DNA (ctDNA), which aimed to provide guidance on the use of adjuvant chemotherapy in stage II colon cancer. This study has already been touted on oncology Twitter as a massive breakthrough for identifying patients with stage II colon cancer who would benefit from adjuvant chemotherapy. Does the reality live up to the hype? Let's break it down.
Patients with resected stage II colon cancer were eligible for enrollment. Two thirds of patients were randomly assigned to the ctDNA guidance arm, whereas the remaining third had chemotherapy guidance based on clinicopathologic high-risk features (T4, poor differentiation, < 12 lymph nodes in surgical sample, lymphovascular invasion, tumor perforation, or bowel obstruction). Chemotherapy choice was left up to the clinician and could be an oxaliplatin-based doublet or a single-agent fluoropyrimidine. The primary endpoint was recurrence-free survival at 2 years. A key secondary endpoint was chemotherapy treatment frequency by arm. A total of 459 patients were enrolled from 23 Australian centers over 4 years. Approximately 40% of patients were considered to be at high risk for recurrence on the basis of their tumors' clinicopathologic features. Approximately 20% of patients had tumors that were mismatch repair deficient.
There was no difference in 2-year recurrence-free survival between the two arms (93.5% vs 92.4%; 95% CI -4.1 to 6.2). This met criteria for noninferiority. However, chemotherapy administration in the two arms was markedly different. A significantly greater proportion of patients randomly assigned to the standard management arm received chemotherapy (28% vs 15%; relative risk [RR] 1.82; 95% CI 1.25-2.65). However, a significantly greater proportion of patients guided by ctDNA received an oxaliplatin-based doublet (62% vs 10%; RR 2.39; 95% CI 1.62-3.52). Clearly, when clinicians were presented with a positive ctDNA test, they overwhelmingly opted to give an oxaliplatin-based doublet rather than a single-agent fluoropyrimidine. Oxaliplatin's use in stage II colon cancer remains very controversial; it is oxaliplatin that causes most of the long-term toxicity associated with adjuvant chemotherapy for colorectal cancer. Although ctDNA testing might lower the total proportion of patients who received adjuvant treatment, it significantly raised the proportion who received oxaliplatin. I doubt this is a worthy trade-off.
Furthermore, clinicopathologic factors were still highly relevant in patients with ctDNA-negative results. Among ctDNA-negative patients, 3-year recurrence-free survival was higher in patients with clinicopathologic low-risk cancers than in those with high-risk cancers (96.7% vs 85.1%; hazard ratio 3.04; 95% CI 1.26-7.34). This strongly suggests that ctDNA testing is unlikely to replace clinicopathologic high-risk features in the real-world practice of clinical oncology. Rather, ctDNA testing will probably be added to the list of high-risk features, prompting use of more chemotherapy, not less, for stage II colon cancer.
A more useful study, in my opinion, should be performed in stage III colon cancer. Patients with stage III colon cancer receive chemotherapy without exception, although we know from MOSAIC that the absolute benefit of chemotherapy in stage III colon cancer is modest. What proportion of these patients who have a negative ctDNA test might be able to either forgo treatment completely or have treatment with a fluoropyrimidine only? That's something I would be very interested to find out.
This month brought us findings from DYNAMIC, a randomized trial of circulating tumor DNA (ctDNA), which aimed to provide guidance on the use of adjuvant chemotherapy in stage II colon cancer. This study has already been touted on oncology Twitter as a massive breakthrough for identifying patients with stage II colon cancer who would benefit from adjuvant chemotherapy. Does the reality live up to the hype? Let's break it down.
Patients with resected stage II colon cancer were eligible for enrollment. Two thirds of patients were randomly assigned to the ctDNA guidance arm, whereas the remaining third had chemotherapy guidance based on clinicopathologic high-risk features (T4, poor differentiation, < 12 lymph nodes in surgical sample, lymphovascular invasion, tumor perforation, or bowel obstruction). Chemotherapy choice was left up to the clinician and could be an oxaliplatin-based doublet or a single-agent fluoropyrimidine. The primary endpoint was recurrence-free survival at 2 years. A key secondary endpoint was chemotherapy treatment frequency by arm. A total of 459 patients were enrolled from 23 Australian centers over 4 years. Approximately 40% of patients were considered to be at high risk for recurrence on the basis of their tumors' clinicopathologic features. Approximately 20% of patients had tumors that were mismatch repair deficient.
There was no difference in 2-year recurrence-free survival between the two arms (93.5% vs 92.4%; 95% CI -4.1 to 6.2). This met criteria for noninferiority. However, chemotherapy administration in the two arms was markedly different. A significantly greater proportion of patients randomly assigned to the standard management arm received chemotherapy (28% vs 15%; relative risk [RR] 1.82; 95% CI 1.25-2.65). However, a significantly greater proportion of patients guided by ctDNA received an oxaliplatin-based doublet (62% vs 10%; RR 2.39; 95% CI 1.62-3.52). Clearly, when clinicians were presented with a positive ctDNA test, they overwhelmingly opted to give an oxaliplatin-based doublet rather than a single-agent fluoropyrimidine. Oxaliplatin's use in stage II colon cancer remains very controversial; it is oxaliplatin that causes most of the long-term toxicity associated with adjuvant chemotherapy for colorectal cancer. Although ctDNA testing might lower the total proportion of patients who received adjuvant treatment, it significantly raised the proportion who received oxaliplatin. I doubt this is a worthy trade-off.
Furthermore, clinicopathologic factors were still highly relevant in patients with ctDNA-negative results. Among ctDNA-negative patients, 3-year recurrence-free survival was higher in patients with clinicopathologic low-risk cancers than in those with high-risk cancers (96.7% vs 85.1%; hazard ratio 3.04; 95% CI 1.26-7.34). This strongly suggests that ctDNA testing is unlikely to replace clinicopathologic high-risk features in the real-world practice of clinical oncology. Rather, ctDNA testing will probably be added to the list of high-risk features, prompting use of more chemotherapy, not less, for stage II colon cancer.
A more useful study, in my opinion, should be performed in stage III colon cancer. Patients with stage III colon cancer receive chemotherapy without exception, although we know from MOSAIC that the absolute benefit of chemotherapy in stage III colon cancer is modest. What proportion of these patients who have a negative ctDNA test might be able to either forgo treatment completely or have treatment with a fluoropyrimidine only? That's something I would be very interested to find out.
This month brought us findings from DYNAMIC, a randomized trial of circulating tumor DNA (ctDNA), which aimed to provide guidance on the use of adjuvant chemotherapy in stage II colon cancer. This study has already been touted on oncology Twitter as a massive breakthrough for identifying patients with stage II colon cancer who would benefit from adjuvant chemotherapy. Does the reality live up to the hype? Let's break it down.
Patients with resected stage II colon cancer were eligible for enrollment. Two thirds of patients were randomly assigned to the ctDNA guidance arm, whereas the remaining third had chemotherapy guidance based on clinicopathologic high-risk features (T4, poor differentiation, < 12 lymph nodes in surgical sample, lymphovascular invasion, tumor perforation, or bowel obstruction). Chemotherapy choice was left up to the clinician and could be an oxaliplatin-based doublet or a single-agent fluoropyrimidine. The primary endpoint was recurrence-free survival at 2 years. A key secondary endpoint was chemotherapy treatment frequency by arm. A total of 459 patients were enrolled from 23 Australian centers over 4 years. Approximately 40% of patients were considered to be at high risk for recurrence on the basis of their tumors' clinicopathologic features. Approximately 20% of patients had tumors that were mismatch repair deficient.
There was no difference in 2-year recurrence-free survival between the two arms (93.5% vs 92.4%; 95% CI -4.1 to 6.2). This met criteria for noninferiority. However, chemotherapy administration in the two arms was markedly different. A significantly greater proportion of patients randomly assigned to the standard management arm received chemotherapy (28% vs 15%; relative risk [RR] 1.82; 95% CI 1.25-2.65). However, a significantly greater proportion of patients guided by ctDNA received an oxaliplatin-based doublet (62% vs 10%; RR 2.39; 95% CI 1.62-3.52). Clearly, when clinicians were presented with a positive ctDNA test, they overwhelmingly opted to give an oxaliplatin-based doublet rather than a single-agent fluoropyrimidine. Oxaliplatin's use in stage II colon cancer remains very controversial; it is oxaliplatin that causes most of the long-term toxicity associated with adjuvant chemotherapy for colorectal cancer. Although ctDNA testing might lower the total proportion of patients who received adjuvant treatment, it significantly raised the proportion who received oxaliplatin. I doubt this is a worthy trade-off.
Furthermore, clinicopathologic factors were still highly relevant in patients with ctDNA-negative results. Among ctDNA-negative patients, 3-year recurrence-free survival was higher in patients with clinicopathologic low-risk cancers than in those with high-risk cancers (96.7% vs 85.1%; hazard ratio 3.04; 95% CI 1.26-7.34). This strongly suggests that ctDNA testing is unlikely to replace clinicopathologic high-risk features in the real-world practice of clinical oncology. Rather, ctDNA testing will probably be added to the list of high-risk features, prompting use of more chemotherapy, not less, for stage II colon cancer.
A more useful study, in my opinion, should be performed in stage III colon cancer. Patients with stage III colon cancer receive chemotherapy without exception, although we know from MOSAIC that the absolute benefit of chemotherapy in stage III colon cancer is modest. What proportion of these patients who have a negative ctDNA test might be able to either forgo treatment completely or have treatment with a fluoropyrimidine only? That's something I would be very interested to find out.
Commentary: Exercise, Mental Health, and Checkpoint Inhibitors in PsA, August 2022
Biomechanical stress and trauma are important factors driving the development and progression of psoriatic arthritis (PsA). On the other hand, physical exercise is beneficial for patients with arthritis. However, there is concern that high-intensity interval training (HIIT) may worsen PsA. Hypothesizing that bone marrow edema changes could occur in patients with PsA after HIIT despite no reported changes in disease activity by clinical examination, Chronaiou and colleagues aimed to assess whether HIIT in PsA patients led to MRI-detectable changes in the axial skeleton. Comparing 19 PsA patients who went through 11 weeks of HIIT with 20 patients who had no change in physical exercise habits, they found no significant changes in bone marrow edema on MRI images of the spine after HIIT. Thus, the 11-week HIIT regimen may be safe in PsA.
Mental health problems are often underestimated in psoriatic disease. Lada and colleagues aimed to estimate the prevalence of depression in patients with psoriatic disease and determine whether PsA is associated with higher depression and anxiety in patients with psoriasis. Analyzing data from British Association of Dermatologists Biologic and Immunomodulators Register (BADBIR) participants (540 with psoriasis and 167 with both psoriasis and PsA) who had completed the Hospital Anxiety and Depression Scale (HADS), they found that the prevalence of depression was higher in patients with PsA (32%) than in patients without PsA (22.7%) using a HADS cutoff of 8 (odds ratio 1.66; 95% CI 1.13--2.43). Pain mediated the effect of PsA on depression and anxiety.
Inhibitors of interleukin (IL)-23 are safe and efficacious in the treatment of psoriasis and PsA. However, changes in composite PsA indices have not been investigated in detail. Using pooled data from the phase 3 DISCOVER-1 (n = 381) and DISCOVER-2 (n = 739) studies, Coates and colleagues demonstrated that a significantly higher proportion of patients receiving guselkumab every 4 or 8 weeks vs placebo achieved low disease activity according to the Disease Activity Index for PsA (DAPSA) at week 8 (19.8%/17.3% vs 8.1%), DAPSA remission at week 12 (4.3%/4.3% vs 0.5%), minimal disease activity at week 16 (14.7%/16.5% vs 4.6%; all P < .001), and very low disease activity at week 24 (6.4%/4.3% vs 1.3%; P < .05), with improvements maintained until week 52. Thus, compared with placebo, treatment with guselkumab leads to early and sustained benefits for patients with PsA.
Similarly, Ostor and colleagues demonstrated in the phase 3 KEEPsAKE2 trial, which included 443 patients with PsA, that, at week 24, patients receiving risankizumab report a significantly greater improvement in the mean pain index score (-14.7 vs -6.5; P < .001), fatigue score (4.9 vs 2.6; P < .01), patient's global assessment of disease activity (-16.5 vs -7.7; P < .001), general health status (0.09 vs 0.01; P < .001), and physical functioning (5.1 vs 2.0; P < .001) compared with placebo.
In another study, treatment with bimekizumab, an inhibitor of IL-17A and IL-17F, was associated with sustained improvement in patient-reported outcomes. Mease and colleagues report that, at week 48, there was a substantial improvement in mean arthritis pain (29.9 points), fatigue (2.4 points), Health Assessment Questionnaire-Disability Index (0.43 points), and Physical Component Summary score (9.1 points), with improvements sustained till week 152. High proportions of patients achieved the Patient Acceptable Symptom State at weeks 48 (75.2%) and 152 (65.0%). Thus, inhibitors of IL-23 and IL-17 have established efficacy in the treatment of PsA.
Biomechanical stress and trauma are important factors driving the development and progression of psoriatic arthritis (PsA). On the other hand, physical exercise is beneficial for patients with arthritis. However, there is concern that high-intensity interval training (HIIT) may worsen PsA. Hypothesizing that bone marrow edema changes could occur in patients with PsA after HIIT despite no reported changes in disease activity by clinical examination, Chronaiou and colleagues aimed to assess whether HIIT in PsA patients led to MRI-detectable changes in the axial skeleton. Comparing 19 PsA patients who went through 11 weeks of HIIT with 20 patients who had no change in physical exercise habits, they found no significant changes in bone marrow edema on MRI images of the spine after HIIT. Thus, the 11-week HIIT regimen may be safe in PsA.
Mental health problems are often underestimated in psoriatic disease. Lada and colleagues aimed to estimate the prevalence of depression in patients with psoriatic disease and determine whether PsA is associated with higher depression and anxiety in patients with psoriasis. Analyzing data from British Association of Dermatologists Biologic and Immunomodulators Register (BADBIR) participants (540 with psoriasis and 167 with both psoriasis and PsA) who had completed the Hospital Anxiety and Depression Scale (HADS), they found that the prevalence of depression was higher in patients with PsA (32%) than in patients without PsA (22.7%) using a HADS cutoff of 8 (odds ratio 1.66; 95% CI 1.13--2.43). Pain mediated the effect of PsA on depression and anxiety.
Inhibitors of interleukin (IL)-23 are safe and efficacious in the treatment of psoriasis and PsA. However, changes in composite PsA indices have not been investigated in detail. Using pooled data from the phase 3 DISCOVER-1 (n = 381) and DISCOVER-2 (n = 739) studies, Coates and colleagues demonstrated that a significantly higher proportion of patients receiving guselkumab every 4 or 8 weeks vs placebo achieved low disease activity according to the Disease Activity Index for PsA (DAPSA) at week 8 (19.8%/17.3% vs 8.1%), DAPSA remission at week 12 (4.3%/4.3% vs 0.5%), minimal disease activity at week 16 (14.7%/16.5% vs 4.6%; all P < .001), and very low disease activity at week 24 (6.4%/4.3% vs 1.3%; P < .05), with improvements maintained until week 52. Thus, compared with placebo, treatment with guselkumab leads to early and sustained benefits for patients with PsA.
Similarly, Ostor and colleagues demonstrated in the phase 3 KEEPsAKE2 trial, which included 443 patients with PsA, that, at week 24, patients receiving risankizumab report a significantly greater improvement in the mean pain index score (-14.7 vs -6.5; P < .001), fatigue score (4.9 vs 2.6; P < .01), patient's global assessment of disease activity (-16.5 vs -7.7; P < .001), general health status (0.09 vs 0.01; P < .001), and physical functioning (5.1 vs 2.0; P < .001) compared with placebo.
In another study, treatment with bimekizumab, an inhibitor of IL-17A and IL-17F, was associated with sustained improvement in patient-reported outcomes. Mease and colleagues report that, at week 48, there was a substantial improvement in mean arthritis pain (29.9 points), fatigue (2.4 points), Health Assessment Questionnaire-Disability Index (0.43 points), and Physical Component Summary score (9.1 points), with improvements sustained till week 152. High proportions of patients achieved the Patient Acceptable Symptom State at weeks 48 (75.2%) and 152 (65.0%). Thus, inhibitors of IL-23 and IL-17 have established efficacy in the treatment of PsA.
Biomechanical stress and trauma are important factors driving the development and progression of psoriatic arthritis (PsA). On the other hand, physical exercise is beneficial for patients with arthritis. However, there is concern that high-intensity interval training (HIIT) may worsen PsA. Hypothesizing that bone marrow edema changes could occur in patients with PsA after HIIT despite no reported changes in disease activity by clinical examination, Chronaiou and colleagues aimed to assess whether HIIT in PsA patients led to MRI-detectable changes in the axial skeleton. Comparing 19 PsA patients who went through 11 weeks of HIIT with 20 patients who had no change in physical exercise habits, they found no significant changes in bone marrow edema on MRI images of the spine after HIIT. Thus, the 11-week HIIT regimen may be safe in PsA.
Mental health problems are often underestimated in psoriatic disease. Lada and colleagues aimed to estimate the prevalence of depression in patients with psoriatic disease and determine whether PsA is associated with higher depression and anxiety in patients with psoriasis. Analyzing data from British Association of Dermatologists Biologic and Immunomodulators Register (BADBIR) participants (540 with psoriasis and 167 with both psoriasis and PsA) who had completed the Hospital Anxiety and Depression Scale (HADS), they found that the prevalence of depression was higher in patients with PsA (32%) than in patients without PsA (22.7%) using a HADS cutoff of 8 (odds ratio 1.66; 95% CI 1.13--2.43). Pain mediated the effect of PsA on depression and anxiety.
Inhibitors of interleukin (IL)-23 are safe and efficacious in the treatment of psoriasis and PsA. However, changes in composite PsA indices have not been investigated in detail. Using pooled data from the phase 3 DISCOVER-1 (n = 381) and DISCOVER-2 (n = 739) studies, Coates and colleagues demonstrated that a significantly higher proportion of patients receiving guselkumab every 4 or 8 weeks vs placebo achieved low disease activity according to the Disease Activity Index for PsA (DAPSA) at week 8 (19.8%/17.3% vs 8.1%), DAPSA remission at week 12 (4.3%/4.3% vs 0.5%), minimal disease activity at week 16 (14.7%/16.5% vs 4.6%; all P < .001), and very low disease activity at week 24 (6.4%/4.3% vs 1.3%; P < .05), with improvements maintained until week 52. Thus, compared with placebo, treatment with guselkumab leads to early and sustained benefits for patients with PsA.
Similarly, Ostor and colleagues demonstrated in the phase 3 KEEPsAKE2 trial, which included 443 patients with PsA, that, at week 24, patients receiving risankizumab report a significantly greater improvement in the mean pain index score (-14.7 vs -6.5; P < .001), fatigue score (4.9 vs 2.6; P < .01), patient's global assessment of disease activity (-16.5 vs -7.7; P < .001), general health status (0.09 vs 0.01; P < .001), and physical functioning (5.1 vs 2.0; P < .001) compared with placebo.
In another study, treatment with bimekizumab, an inhibitor of IL-17A and IL-17F, was associated with sustained improvement in patient-reported outcomes. Mease and colleagues report that, at week 48, there was a substantial improvement in mean arthritis pain (29.9 points), fatigue (2.4 points), Health Assessment Questionnaire-Disability Index (0.43 points), and Physical Component Summary score (9.1 points), with improvements sustained till week 152. High proportions of patients achieved the Patient Acceptable Symptom State at weeks 48 (75.2%) and 152 (65.0%). Thus, inhibitors of IL-23 and IL-17 have established efficacy in the treatment of PsA.
Mixed results for intensive home care for psychiatric crises
Intensive home treatment may offer an alternative to inpatient care for patients in acute psychiatric crisis – but the intervention is no outright substitute, new research suggests.
However, there was no difference between treatment groups in improvement in quality of life or patient satisfaction; and a reduction in symptom severity noted after 6 weeks of home treatment faded within 6 months.
“We found no differences in admission rates either, which suggests that intensive home treatment is not a substitute for inpatient care but a different treatment opportunity for psychiatric patients in crisis,” Jurgen Cornelis, MD, Arkin Institute for Mental Health, Amsterdam, and colleagues write.
The findings were published online in The Lancet Psychiatry.
Increasingly popular
“Intensive home treatment is increasingly popular as an alternative to hospitalization. It was developed to prevent or reduce levels of inpatient care and facilitate the transition between inpatient care and low-intensity outpatient care,” the investigators write.
However, there have previously been only two randomized controlled trials published that assessed this type of care, resulting in “somewhat conflicting findings,” they add.
For the current study, participants presented to psychiatric emergency wards at two medical centers in the Netherlands. They were included only if they were able to offer informed consent within 14 days.
The intensive home treatment group (n = 183) worked with a multidisciplinary team that designed a care plan tailored to their specific crisis. Treatment components included pharmacotherapy, up to three home visits each day, psychoeducation, brief supportive and cognitive behavioral therapy, social care, and support and empowerment of the patient’s informal care system.
The usual care group (n = 63) commonly received a combination of highly intensive inpatient treatment in the first phase and outpatient treatment up to two times a week in the second phase. Treatment included similar components as those in intensive home treatment.
The most common primary clinical diagnosis in both groups was mood disorder, followed by psychotic disorders, personality disorders, or anxiety disorders.
The home treatment group had a significantly higher total mean item score on the Brief Psychiatric Rating Scale (BPRS) at baseline (2.23 vs. 2.04, P = .04).
Mixed results
Results at 6 weeks showed the number of hospital days was 25.3% lower in the home treatment group, compared with those who received usual care.
That trend continued at 1 year, with the intensive home treatment group recording 36.6% fewer hospital days than the usual care group (mean, 42.5 days vs. 67 days, respectively; P = .03).
However, the number of patients who were admitted in the first 6 weeks and at 1 year stayed the same, as did the mean number of admissions per patient over 12 months.
The home treatment group reported significantly fewer symptoms on the BPRS depression and anxiety scale at 6 weeks, compared with the usual treatment group (P = .025), but that difference was not maintained after 6 months.
The number of adverse events, including suicide attempts, was similar between the groups. Three patients in the home treatment group and two in the usual care group died by suicide.
“Future research should focus on which components of intensive home treatment or hospitalization can be used when, for whom, and meet which goals, so that both hospital care and intensive home treatment can be used proportionally and efficiently for patients in psychiatric crisis,” the investigators write.
Not generalizable?
In an accompanying editorial, Claire Henderson, PhD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, noted that generalizing the study’s results to other countries could be problematic, especially to regions such as North America, which have shorter lengths of stay for psychiatric hospitalization.
“Future trials looking at intensive home treatment would be most informative if done in countries with relatively short lengths of stay, and without separate crisis services for people receiving assertive community treatment,” Dr. Henderson writes.
The study was funded by De Stichting tot Steun Vereniging voor Christelijke Verzorging van Geestes-en Zenuwzieken. The investigators and Dr. Henderson have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Intensive home treatment may offer an alternative to inpatient care for patients in acute psychiatric crisis – but the intervention is no outright substitute, new research suggests.
However, there was no difference between treatment groups in improvement in quality of life or patient satisfaction; and a reduction in symptom severity noted after 6 weeks of home treatment faded within 6 months.
“We found no differences in admission rates either, which suggests that intensive home treatment is not a substitute for inpatient care but a different treatment opportunity for psychiatric patients in crisis,” Jurgen Cornelis, MD, Arkin Institute for Mental Health, Amsterdam, and colleagues write.
The findings were published online in The Lancet Psychiatry.
Increasingly popular
“Intensive home treatment is increasingly popular as an alternative to hospitalization. It was developed to prevent or reduce levels of inpatient care and facilitate the transition between inpatient care and low-intensity outpatient care,” the investigators write.
However, there have previously been only two randomized controlled trials published that assessed this type of care, resulting in “somewhat conflicting findings,” they add.
For the current study, participants presented to psychiatric emergency wards at two medical centers in the Netherlands. They were included only if they were able to offer informed consent within 14 days.
The intensive home treatment group (n = 183) worked with a multidisciplinary team that designed a care plan tailored to their specific crisis. Treatment components included pharmacotherapy, up to three home visits each day, psychoeducation, brief supportive and cognitive behavioral therapy, social care, and support and empowerment of the patient’s informal care system.
The usual care group (n = 63) commonly received a combination of highly intensive inpatient treatment in the first phase and outpatient treatment up to two times a week in the second phase. Treatment included similar components as those in intensive home treatment.
The most common primary clinical diagnosis in both groups was mood disorder, followed by psychotic disorders, personality disorders, or anxiety disorders.
The home treatment group had a significantly higher total mean item score on the Brief Psychiatric Rating Scale (BPRS) at baseline (2.23 vs. 2.04, P = .04).
Mixed results
Results at 6 weeks showed the number of hospital days was 25.3% lower in the home treatment group, compared with those who received usual care.
That trend continued at 1 year, with the intensive home treatment group recording 36.6% fewer hospital days than the usual care group (mean, 42.5 days vs. 67 days, respectively; P = .03).
However, the number of patients who were admitted in the first 6 weeks and at 1 year stayed the same, as did the mean number of admissions per patient over 12 months.
The home treatment group reported significantly fewer symptoms on the BPRS depression and anxiety scale at 6 weeks, compared with the usual treatment group (P = .025), but that difference was not maintained after 6 months.
The number of adverse events, including suicide attempts, was similar between the groups. Three patients in the home treatment group and two in the usual care group died by suicide.
“Future research should focus on which components of intensive home treatment or hospitalization can be used when, for whom, and meet which goals, so that both hospital care and intensive home treatment can be used proportionally and efficiently for patients in psychiatric crisis,” the investigators write.
Not generalizable?
In an accompanying editorial, Claire Henderson, PhD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, noted that generalizing the study’s results to other countries could be problematic, especially to regions such as North America, which have shorter lengths of stay for psychiatric hospitalization.
“Future trials looking at intensive home treatment would be most informative if done in countries with relatively short lengths of stay, and without separate crisis services for people receiving assertive community treatment,” Dr. Henderson writes.
The study was funded by De Stichting tot Steun Vereniging voor Christelijke Verzorging van Geestes-en Zenuwzieken. The investigators and Dr. Henderson have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Intensive home treatment may offer an alternative to inpatient care for patients in acute psychiatric crisis – but the intervention is no outright substitute, new research suggests.
However, there was no difference between treatment groups in improvement in quality of life or patient satisfaction; and a reduction in symptom severity noted after 6 weeks of home treatment faded within 6 months.
“We found no differences in admission rates either, which suggests that intensive home treatment is not a substitute for inpatient care but a different treatment opportunity for psychiatric patients in crisis,” Jurgen Cornelis, MD, Arkin Institute for Mental Health, Amsterdam, and colleagues write.
The findings were published online in The Lancet Psychiatry.
Increasingly popular
“Intensive home treatment is increasingly popular as an alternative to hospitalization. It was developed to prevent or reduce levels of inpatient care and facilitate the transition between inpatient care and low-intensity outpatient care,” the investigators write.
However, there have previously been only two randomized controlled trials published that assessed this type of care, resulting in “somewhat conflicting findings,” they add.
For the current study, participants presented to psychiatric emergency wards at two medical centers in the Netherlands. They were included only if they were able to offer informed consent within 14 days.
The intensive home treatment group (n = 183) worked with a multidisciplinary team that designed a care plan tailored to their specific crisis. Treatment components included pharmacotherapy, up to three home visits each day, psychoeducation, brief supportive and cognitive behavioral therapy, social care, and support and empowerment of the patient’s informal care system.
The usual care group (n = 63) commonly received a combination of highly intensive inpatient treatment in the first phase and outpatient treatment up to two times a week in the second phase. Treatment included similar components as those in intensive home treatment.
The most common primary clinical diagnosis in both groups was mood disorder, followed by psychotic disorders, personality disorders, or anxiety disorders.
The home treatment group had a significantly higher total mean item score on the Brief Psychiatric Rating Scale (BPRS) at baseline (2.23 vs. 2.04, P = .04).
Mixed results
Results at 6 weeks showed the number of hospital days was 25.3% lower in the home treatment group, compared with those who received usual care.
That trend continued at 1 year, with the intensive home treatment group recording 36.6% fewer hospital days than the usual care group (mean, 42.5 days vs. 67 days, respectively; P = .03).
However, the number of patients who were admitted in the first 6 weeks and at 1 year stayed the same, as did the mean number of admissions per patient over 12 months.
The home treatment group reported significantly fewer symptoms on the BPRS depression and anxiety scale at 6 weeks, compared with the usual treatment group (P = .025), but that difference was not maintained after 6 months.
The number of adverse events, including suicide attempts, was similar between the groups. Three patients in the home treatment group and two in the usual care group died by suicide.
“Future research should focus on which components of intensive home treatment or hospitalization can be used when, for whom, and meet which goals, so that both hospital care and intensive home treatment can be used proportionally and efficiently for patients in psychiatric crisis,” the investigators write.
Not generalizable?
In an accompanying editorial, Claire Henderson, PhD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, noted that generalizing the study’s results to other countries could be problematic, especially to regions such as North America, which have shorter lengths of stay for psychiatric hospitalization.
“Future trials looking at intensive home treatment would be most informative if done in countries with relatively short lengths of stay, and without separate crisis services for people receiving assertive community treatment,” Dr. Henderson writes.
The study was funded by De Stichting tot Steun Vereniging voor Christelijke Verzorging van Geestes-en Zenuwzieken. The investigators and Dr. Henderson have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET PSYCHIATRY
Is Lp(a) a marker for aortic calcium onset?
Lipoprotein(a) has long been thought to be a potential marker of aortic valve disease, and the population-based Rotterdam Study in the Netherlands has reported that Lp(a) has a strong association with new-onset aortic valve calcium (AVC), but not necessarily with progression of aortic valve disease.
Reporting in the European Heart Journal, the study authors analyzed data on 922 participants in the Rotterdam Study whose Lp(a) was measured along with a computed tomography scan upon enrollment, followed by CT scan 14 years later. At baseline, 702 participants didn’t have AVC, but the follow-up scan identified new-onset AVC in 415 (59.1%).
The investigators found an association between Lp(a) concentration and baseline AVC, with an odds ratio of 1.43 for each 50 mg/dL higher Lp(a) (95% confidence interval, 1.15-1.79), as well as new-onset AVC, with an OR of 1.30 for each 50 mg/dL increase in Lp(a) (95% CI, 1.02-1.65). However, the study found no association between rising Lp(a) levels and AVC progression; it found only an association between baseline AVC score and progression (P < .001).
‘Trigger’ for calcification but not progression
“This suggests that Lp(a) is an important trigger in the initiation of aortic valve calcification, but once the valve is calcified, disease progression may be primarily driven by other factors such as the baseline calcium burden of the valve and likely other unknown factors,” senior study author Daniel Bos, MD, PhD, said in e-mailed comments.
Dr. Bos and coauthors claim this is the first study to show that even minor AVC progresses independently of Lp(a).
“There are previous studies that showed a possible relationship between Lp(a) [and] progression of aortic valve calcium,” he said. “Our study suggests that the most meaningful benefit of Lp(a) lowering may actually be prior to the onset of aortic valve calcification.”
While no treatments have been approved for lowering Lp(a), the study findings could be meaningful if trials, including the ongoing phase 3 Lp(a) HORIZON trial of the investigational antisense agent pelacarsen (NCT04023552), show promising results, Dr. Bos said. Citing Lp(a) HORIZON, he said, “If the study shows Lp(a) lowering leads to a reduction in incident cardiovascular disease, similar strategies may be applied to prevent, rather than slow down, progression of aortic valve calcification.”
Dr. Bos called the Rotterdam Study results “an important first pointer into that direction.” He added, “We will need randomized trials to provide a definitive answer to the question whether Lp(a) lowering may prevent aortic valve calcium.”
Focus on AVC is study ‘weakness’
The study findings raise a key question for clinical trials of investigative Lp(a)-lowering therapies as well as how to use those therapies to treat aortic valve disease, said Christie Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston.
The findings could be “problematic” for these clinical trials, he said. “This study is just looking at calcium progression,” Dr. Ballantyne noted. “What we want to know about clinically is the progression to aortic stenosis, and then in particular to progression from mild disease to moderate or severe disease, because once you get into more severe disease, one has to do an intervention with either surgery or TAVR [transcatheter aortic valve replacement].”
He considered the study’s focus on AVC rather than aortic valve function a weakness and noted that only 14 study participants had TAVR. “We’re going to need much bigger numbers to look into this question of progression, including progression to severe diseases,” he said.
However, the Rotterdam Study showed the importance of CT in evaluating AVC, which can easily be done in other trials to further explore the association between Lp(a) and AVC, Dr. Ballantyne said.
Dr. Bos has no relevant disclosures. Study coauthors disclosed relationships with Amgen, Sanofi, Reservlogix, Athera, Experio, Novartis and Ionis Pharmaceuticals. Dr. Ballantyne disclosed relationships with Amgen and Novartis.
Lipoprotein(a) has long been thought to be a potential marker of aortic valve disease, and the population-based Rotterdam Study in the Netherlands has reported that Lp(a) has a strong association with new-onset aortic valve calcium (AVC), but not necessarily with progression of aortic valve disease.
Reporting in the European Heart Journal, the study authors analyzed data on 922 participants in the Rotterdam Study whose Lp(a) was measured along with a computed tomography scan upon enrollment, followed by CT scan 14 years later. At baseline, 702 participants didn’t have AVC, but the follow-up scan identified new-onset AVC in 415 (59.1%).
The investigators found an association between Lp(a) concentration and baseline AVC, with an odds ratio of 1.43 for each 50 mg/dL higher Lp(a) (95% confidence interval, 1.15-1.79), as well as new-onset AVC, with an OR of 1.30 for each 50 mg/dL increase in Lp(a) (95% CI, 1.02-1.65). However, the study found no association between rising Lp(a) levels and AVC progression; it found only an association between baseline AVC score and progression (P < .001).
‘Trigger’ for calcification but not progression
“This suggests that Lp(a) is an important trigger in the initiation of aortic valve calcification, but once the valve is calcified, disease progression may be primarily driven by other factors such as the baseline calcium burden of the valve and likely other unknown factors,” senior study author Daniel Bos, MD, PhD, said in e-mailed comments.
Dr. Bos and coauthors claim this is the first study to show that even minor AVC progresses independently of Lp(a).
“There are previous studies that showed a possible relationship between Lp(a) [and] progression of aortic valve calcium,” he said. “Our study suggests that the most meaningful benefit of Lp(a) lowering may actually be prior to the onset of aortic valve calcification.”
While no treatments have been approved for lowering Lp(a), the study findings could be meaningful if trials, including the ongoing phase 3 Lp(a) HORIZON trial of the investigational antisense agent pelacarsen (NCT04023552), show promising results, Dr. Bos said. Citing Lp(a) HORIZON, he said, “If the study shows Lp(a) lowering leads to a reduction in incident cardiovascular disease, similar strategies may be applied to prevent, rather than slow down, progression of aortic valve calcification.”
Dr. Bos called the Rotterdam Study results “an important first pointer into that direction.” He added, “We will need randomized trials to provide a definitive answer to the question whether Lp(a) lowering may prevent aortic valve calcium.”
Focus on AVC is study ‘weakness’
The study findings raise a key question for clinical trials of investigative Lp(a)-lowering therapies as well as how to use those therapies to treat aortic valve disease, said Christie Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston.
The findings could be “problematic” for these clinical trials, he said. “This study is just looking at calcium progression,” Dr. Ballantyne noted. “What we want to know about clinically is the progression to aortic stenosis, and then in particular to progression from mild disease to moderate or severe disease, because once you get into more severe disease, one has to do an intervention with either surgery or TAVR [transcatheter aortic valve replacement].”
He considered the study’s focus on AVC rather than aortic valve function a weakness and noted that only 14 study participants had TAVR. “We’re going to need much bigger numbers to look into this question of progression, including progression to severe diseases,” he said.
However, the Rotterdam Study showed the importance of CT in evaluating AVC, which can easily be done in other trials to further explore the association between Lp(a) and AVC, Dr. Ballantyne said.
Dr. Bos has no relevant disclosures. Study coauthors disclosed relationships with Amgen, Sanofi, Reservlogix, Athera, Experio, Novartis and Ionis Pharmaceuticals. Dr. Ballantyne disclosed relationships with Amgen and Novartis.
Lipoprotein(a) has long been thought to be a potential marker of aortic valve disease, and the population-based Rotterdam Study in the Netherlands has reported that Lp(a) has a strong association with new-onset aortic valve calcium (AVC), but not necessarily with progression of aortic valve disease.
Reporting in the European Heart Journal, the study authors analyzed data on 922 participants in the Rotterdam Study whose Lp(a) was measured along with a computed tomography scan upon enrollment, followed by CT scan 14 years later. At baseline, 702 participants didn’t have AVC, but the follow-up scan identified new-onset AVC in 415 (59.1%).
The investigators found an association between Lp(a) concentration and baseline AVC, with an odds ratio of 1.43 for each 50 mg/dL higher Lp(a) (95% confidence interval, 1.15-1.79), as well as new-onset AVC, with an OR of 1.30 for each 50 mg/dL increase in Lp(a) (95% CI, 1.02-1.65). However, the study found no association between rising Lp(a) levels and AVC progression; it found only an association between baseline AVC score and progression (P < .001).
‘Trigger’ for calcification but not progression
“This suggests that Lp(a) is an important trigger in the initiation of aortic valve calcification, but once the valve is calcified, disease progression may be primarily driven by other factors such as the baseline calcium burden of the valve and likely other unknown factors,” senior study author Daniel Bos, MD, PhD, said in e-mailed comments.
Dr. Bos and coauthors claim this is the first study to show that even minor AVC progresses independently of Lp(a).
“There are previous studies that showed a possible relationship between Lp(a) [and] progression of aortic valve calcium,” he said. “Our study suggests that the most meaningful benefit of Lp(a) lowering may actually be prior to the onset of aortic valve calcification.”
While no treatments have been approved for lowering Lp(a), the study findings could be meaningful if trials, including the ongoing phase 3 Lp(a) HORIZON trial of the investigational antisense agent pelacarsen (NCT04023552), show promising results, Dr. Bos said. Citing Lp(a) HORIZON, he said, “If the study shows Lp(a) lowering leads to a reduction in incident cardiovascular disease, similar strategies may be applied to prevent, rather than slow down, progression of aortic valve calcification.”
Dr. Bos called the Rotterdam Study results “an important first pointer into that direction.” He added, “We will need randomized trials to provide a definitive answer to the question whether Lp(a) lowering may prevent aortic valve calcium.”
Focus on AVC is study ‘weakness’
The study findings raise a key question for clinical trials of investigative Lp(a)-lowering therapies as well as how to use those therapies to treat aortic valve disease, said Christie Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston.
The findings could be “problematic” for these clinical trials, he said. “This study is just looking at calcium progression,” Dr. Ballantyne noted. “What we want to know about clinically is the progression to aortic stenosis, and then in particular to progression from mild disease to moderate or severe disease, because once you get into more severe disease, one has to do an intervention with either surgery or TAVR [transcatheter aortic valve replacement].”
He considered the study’s focus on AVC rather than aortic valve function a weakness and noted that only 14 study participants had TAVR. “We’re going to need much bigger numbers to look into this question of progression, including progression to severe diseases,” he said.
However, the Rotterdam Study showed the importance of CT in evaluating AVC, which can easily be done in other trials to further explore the association between Lp(a) and AVC, Dr. Ballantyne said.
Dr. Bos has no relevant disclosures. Study coauthors disclosed relationships with Amgen, Sanofi, Reservlogix, Athera, Experio, Novartis and Ionis Pharmaceuticals. Dr. Ballantyne disclosed relationships with Amgen and Novartis.
FROM THE EUROPEAN HEART JOURNAL
AGA News – August 2022
Huge win for patients: CRC screening coverage continuum is complete
In a huge win for patients, Medicare will begin covering colonoscopies after a positive noninvasive stool test starting next year. Medicare was previously the only insurer who did not cover this critical prevention procedure.
This change comes after a year of advocacy led by AGA – including multiple meetings with senior officials at Health & Human Services and legislative pressure by members across the country.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities. Patients can now engage in CRC screening programs and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test,” says David Lieberman, MD, AGAF, who met with Centers for Medicare & Medicaid Services officials multiple times to push this policy forward. “AGA knows that increased participation in screening will further reduce the burden of colorectal cancer.”
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives. Importantly, the CMS proposed rule changes will lessen colorectal cancer disparities eliminating a financial burden for many patients,” says AGA president John Carethers, MD, AGAF, who met with CMS earlier this month to advocate for this change.
Thank you to everyone in the GI community who advocated for this important change!
CMS announced the coverage change as part of the 2023 Medicare proposed rule, which was released July 7, 2022. The rule must be finalized this Fall before taking effect Jan. 2, 2023.
What you need to know about proposed changes to Medicare payment policies
On July 7, CMS released the calendar year (CY) 2023 Medicare Physician Fee Schedule (MPFS) Proposed Rule. The rule will be posted in the Federal Register no later than July 11.
Good news!
In a win for patients and thanks to collective advocacy efforts from AGA and partner societies, CMS is proposing to expand the regulatory definition of “colorectal cancer screening tests” and waive cost sharing for a necessary follow-up colonoscopy after a positive stool-based screening test.
Looming cuts
The rule proposes 4% cuts to Medicare physician reimbursement through required decreases in the conversion factor and expiration of temporary fixes passed by Congress. AGA will continue to work with a coalition of national and state medical societies in urging Congress to prevent these cuts before Jan. 1, 2023.
What to know
CMS expands CRC screening in a proposal to waive cost-sharing for a follow-up colonoscopy to a positive stool-based colorectal cancer screening test and to cover the service for individuals 45 years of age and above.
Medicare payment cuts are looming with cuts to the proposed CY 2023 conversion factor.
Split/shared visits policy delayed until CY 2024.
Payment rates for new bariatric device codes proposed.
Don’t let insurance policies burden GI practices
Join us at AGA Advocacy Day on Thursday, Sept. 22, 2022, to virtually meet with your members of Congress to urge them to rein in insurance policies like prior authorization and step therapy.
If GI providers don’t have a seat at the table and engage with lawmakers, these decisions will be influenced by payers and other parties that do not have you or your patients’ best interests at heart.
AGA Advocacy Day is held shortly before the end of the fiscal year – prime time to educate policymakers and their staff about your everyday challenges and the reality of GI patient care in your state. We will also discuss the need for robust federal funding for GI research and the devastating impact that Medicare cuts could have on your practice.
Register today and AGA will take care of the rest, including scheduling your meetings and providing comprehensive advocacy training. Now more than ever, your voice needs to be heard on Capitol Hill.
Huge win for patients: CRC screening coverage continuum is complete
In a huge win for patients, Medicare will begin covering colonoscopies after a positive noninvasive stool test starting next year. Medicare was previously the only insurer who did not cover this critical prevention procedure.
This change comes after a year of advocacy led by AGA – including multiple meetings with senior officials at Health & Human Services and legislative pressure by members across the country.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities. Patients can now engage in CRC screening programs and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test,” says David Lieberman, MD, AGAF, who met with Centers for Medicare & Medicaid Services officials multiple times to push this policy forward. “AGA knows that increased participation in screening will further reduce the burden of colorectal cancer.”
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives. Importantly, the CMS proposed rule changes will lessen colorectal cancer disparities eliminating a financial burden for many patients,” says AGA president John Carethers, MD, AGAF, who met with CMS earlier this month to advocate for this change.
Thank you to everyone in the GI community who advocated for this important change!
CMS announced the coverage change as part of the 2023 Medicare proposed rule, which was released July 7, 2022. The rule must be finalized this Fall before taking effect Jan. 2, 2023.
What you need to know about proposed changes to Medicare payment policies
On July 7, CMS released the calendar year (CY) 2023 Medicare Physician Fee Schedule (MPFS) Proposed Rule. The rule will be posted in the Federal Register no later than July 11.
Good news!
In a win for patients and thanks to collective advocacy efforts from AGA and partner societies, CMS is proposing to expand the regulatory definition of “colorectal cancer screening tests” and waive cost sharing for a necessary follow-up colonoscopy after a positive stool-based screening test.
Looming cuts
The rule proposes 4% cuts to Medicare physician reimbursement through required decreases in the conversion factor and expiration of temporary fixes passed by Congress. AGA will continue to work with a coalition of national and state medical societies in urging Congress to prevent these cuts before Jan. 1, 2023.
What to know
CMS expands CRC screening in a proposal to waive cost-sharing for a follow-up colonoscopy to a positive stool-based colorectal cancer screening test and to cover the service for individuals 45 years of age and above.
Medicare payment cuts are looming with cuts to the proposed CY 2023 conversion factor.
Split/shared visits policy delayed until CY 2024.
Payment rates for new bariatric device codes proposed.
Don’t let insurance policies burden GI practices
Join us at AGA Advocacy Day on Thursday, Sept. 22, 2022, to virtually meet with your members of Congress to urge them to rein in insurance policies like prior authorization and step therapy.
If GI providers don’t have a seat at the table and engage with lawmakers, these decisions will be influenced by payers and other parties that do not have you or your patients’ best interests at heart.
AGA Advocacy Day is held shortly before the end of the fiscal year – prime time to educate policymakers and their staff about your everyday challenges and the reality of GI patient care in your state. We will also discuss the need for robust federal funding for GI research and the devastating impact that Medicare cuts could have on your practice.
Register today and AGA will take care of the rest, including scheduling your meetings and providing comprehensive advocacy training. Now more than ever, your voice needs to be heard on Capitol Hill.
Huge win for patients: CRC screening coverage continuum is complete
In a huge win for patients, Medicare will begin covering colonoscopies after a positive noninvasive stool test starting next year. Medicare was previously the only insurer who did not cover this critical prevention procedure.
This change comes after a year of advocacy led by AGA – including multiple meetings with senior officials at Health & Human Services and legislative pressure by members across the country.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities. Patients can now engage in CRC screening programs and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test,” says David Lieberman, MD, AGAF, who met with Centers for Medicare & Medicaid Services officials multiple times to push this policy forward. “AGA knows that increased participation in screening will further reduce the burden of colorectal cancer.”
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives. Importantly, the CMS proposed rule changes will lessen colorectal cancer disparities eliminating a financial burden for many patients,” says AGA president John Carethers, MD, AGAF, who met with CMS earlier this month to advocate for this change.
Thank you to everyone in the GI community who advocated for this important change!
CMS announced the coverage change as part of the 2023 Medicare proposed rule, which was released July 7, 2022. The rule must be finalized this Fall before taking effect Jan. 2, 2023.
What you need to know about proposed changes to Medicare payment policies
On July 7, CMS released the calendar year (CY) 2023 Medicare Physician Fee Schedule (MPFS) Proposed Rule. The rule will be posted in the Federal Register no later than July 11.
Good news!
In a win for patients and thanks to collective advocacy efforts from AGA and partner societies, CMS is proposing to expand the regulatory definition of “colorectal cancer screening tests” and waive cost sharing for a necessary follow-up colonoscopy after a positive stool-based screening test.
Looming cuts
The rule proposes 4% cuts to Medicare physician reimbursement through required decreases in the conversion factor and expiration of temporary fixes passed by Congress. AGA will continue to work with a coalition of national and state medical societies in urging Congress to prevent these cuts before Jan. 1, 2023.
What to know
CMS expands CRC screening in a proposal to waive cost-sharing for a follow-up colonoscopy to a positive stool-based colorectal cancer screening test and to cover the service for individuals 45 years of age and above.
Medicare payment cuts are looming with cuts to the proposed CY 2023 conversion factor.
Split/shared visits policy delayed until CY 2024.
Payment rates for new bariatric device codes proposed.
Don’t let insurance policies burden GI practices
Join us at AGA Advocacy Day on Thursday, Sept. 22, 2022, to virtually meet with your members of Congress to urge them to rein in insurance policies like prior authorization and step therapy.
If GI providers don’t have a seat at the table and engage with lawmakers, these decisions will be influenced by payers and other parties that do not have you or your patients’ best interests at heart.
AGA Advocacy Day is held shortly before the end of the fiscal year – prime time to educate policymakers and their staff about your everyday challenges and the reality of GI patient care in your state. We will also discuss the need for robust federal funding for GI research and the devastating impact that Medicare cuts could have on your practice.
Register today and AGA will take care of the rest, including scheduling your meetings and providing comprehensive advocacy training. Now more than ever, your voice needs to be heard on Capitol Hill.
Injectable HIV prevention better than pills in two trials
MONTREAL – , according to new data from two HIV Prevention Trials Network (HPTN) studies reported at the International AIDS Society Conference.
Follow-up data from the HPTN 084 trial, which compared the two regimens in 3,224 sub-Saharan persons who were assigned female sex at birth, show that three new HIV infections occurred in the CAB LA group in the 12 months since the study was unblinded, versus 20 new infections among the TDF-FTC group. That translates to an 89% lower risk of infection in the CAB LA arm across both the blinded and unblinded phases of the trial, said lead investigator Sinead Delany-Moretlwe, MD, PhD, director of research, Wits Reproductive Health and HIV Institute, the University of the Witwatersrand, Johannesburg, South Africa, during a press conference.
“The trial was designed with the assumption that both drugs were highly effective in preventing HIV infection but that, given the challenges with taking a pill a day, that injectable cabotegravir may offer an adherence advantage,” she said in an interview. “Our data appear to confirm this, as most of the participants in the TDF-FTC arm who became infected with HIV had evidence of poor or inconsistent use of PrEP.”
The study also found that pregnancy incidence increased “two- to threefold” between the blinded and the unblinded period, “and this emphasizes to us the desire of women to conceive safely, without the threat of HIV, and the importance of us continuing to evaluate the safety and pharmacology of cabotegravir in pregnant and breastfeeding women during open-label extension phase of HPTN 084, so that [they] are not excluded from access to this highly effective PrEP agent,” she said. To date, no congenital anomalies have been reported in babies born during the study.
In an update report from HPTN 083, which also showed superiority of CAB LA over TDF-FTC in cisgender men and transgender women (TGW), researchers reported the safety and efficacy of CAB LA use in TGW using gender-affirming hormone therapy (GAHT).
Among the 4,566 participants in HPTN 083, 570 were TGW, and of those, 58% used GAHT at baseline, reported Beatriz Grinsztejn, MD, PhD, head of the STD/AIDS Clinical Research Laboratory at the Instituto Nacional de Infectologicia/Fundação Oswaldo Cruz.
CAB LA drug concentrations measured in a subset of 53 TGW who received on-time CAB injections were comparable between those taking (n = 30) and those not taking GAHT (n = 23), “suggesting the lack of a gender-affirming hormone effect on CAB pharmacokinetics,” she said. “These are very promising results, as we all know that the use of gender-affirming hormone therapy is a major priority for our transgender women community, ... so the lack of drug-drug interaction is really a very important result.”
“Cabotegravir long-acting PrEP is now approved for all at-risk populations, including men who have sex with men, transgender women, and cisgender women, after the results of HPTN 083 and 084,” commented Monica Gandhi, MD, MPH, an infectious disease physician, professor of medicine, and associate chief in the division of HIV, infectious diseases, and global medicine at the University of California, San Francisco (UCSF).
Dr. Gandhi, who was not involved in either study, is also director of the UCSF Center for AIDS Research and medical director of the HIV Clinic (“Ward 86”) at San Francisco General Hospital. “The incredible efficacy of long-acting PrEP for cisgender women shown by HPTN 084 is game-changing for our practice, and we have already instituted CAB LA across a range of populations at Ward 86,” she said in an interview. “The durability of the 89% additional efficacy of CAB LA over oral TDF/FTC is thrilling and will lead to a greater use of long-acting options.”
She acknowledged that information on potential interactions of GAHT was needed from the HPTN 083 trial. “That cabotegravir levels did not change with the use of estradiol or spironolactone for gender-affirming therapy is important news for our practice and to reassure our TGW that they can safely and effectively use CAB LA for HIV prevention.”
The HPTN 084 and 083 trials were funded by the National Institutes for Allergy and Infectious Diseases. Dr. Delany-Moretlwe, Dr. Grinsztejn, and Dr. Gandhi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – , according to new data from two HIV Prevention Trials Network (HPTN) studies reported at the International AIDS Society Conference.
Follow-up data from the HPTN 084 trial, which compared the two regimens in 3,224 sub-Saharan persons who were assigned female sex at birth, show that three new HIV infections occurred in the CAB LA group in the 12 months since the study was unblinded, versus 20 new infections among the TDF-FTC group. That translates to an 89% lower risk of infection in the CAB LA arm across both the blinded and unblinded phases of the trial, said lead investigator Sinead Delany-Moretlwe, MD, PhD, director of research, Wits Reproductive Health and HIV Institute, the University of the Witwatersrand, Johannesburg, South Africa, during a press conference.
“The trial was designed with the assumption that both drugs were highly effective in preventing HIV infection but that, given the challenges with taking a pill a day, that injectable cabotegravir may offer an adherence advantage,” she said in an interview. “Our data appear to confirm this, as most of the participants in the TDF-FTC arm who became infected with HIV had evidence of poor or inconsistent use of PrEP.”
The study also found that pregnancy incidence increased “two- to threefold” between the blinded and the unblinded period, “and this emphasizes to us the desire of women to conceive safely, without the threat of HIV, and the importance of us continuing to evaluate the safety and pharmacology of cabotegravir in pregnant and breastfeeding women during open-label extension phase of HPTN 084, so that [they] are not excluded from access to this highly effective PrEP agent,” she said. To date, no congenital anomalies have been reported in babies born during the study.
In an update report from HPTN 083, which also showed superiority of CAB LA over TDF-FTC in cisgender men and transgender women (TGW), researchers reported the safety and efficacy of CAB LA use in TGW using gender-affirming hormone therapy (GAHT).
Among the 4,566 participants in HPTN 083, 570 were TGW, and of those, 58% used GAHT at baseline, reported Beatriz Grinsztejn, MD, PhD, head of the STD/AIDS Clinical Research Laboratory at the Instituto Nacional de Infectologicia/Fundação Oswaldo Cruz.
CAB LA drug concentrations measured in a subset of 53 TGW who received on-time CAB injections were comparable between those taking (n = 30) and those not taking GAHT (n = 23), “suggesting the lack of a gender-affirming hormone effect on CAB pharmacokinetics,” she said. “These are very promising results, as we all know that the use of gender-affirming hormone therapy is a major priority for our transgender women community, ... so the lack of drug-drug interaction is really a very important result.”
“Cabotegravir long-acting PrEP is now approved for all at-risk populations, including men who have sex with men, transgender women, and cisgender women, after the results of HPTN 083 and 084,” commented Monica Gandhi, MD, MPH, an infectious disease physician, professor of medicine, and associate chief in the division of HIV, infectious diseases, and global medicine at the University of California, San Francisco (UCSF).
Dr. Gandhi, who was not involved in either study, is also director of the UCSF Center for AIDS Research and medical director of the HIV Clinic (“Ward 86”) at San Francisco General Hospital. “The incredible efficacy of long-acting PrEP for cisgender women shown by HPTN 084 is game-changing for our practice, and we have already instituted CAB LA across a range of populations at Ward 86,” she said in an interview. “The durability of the 89% additional efficacy of CAB LA over oral TDF/FTC is thrilling and will lead to a greater use of long-acting options.”
She acknowledged that information on potential interactions of GAHT was needed from the HPTN 083 trial. “That cabotegravir levels did not change with the use of estradiol or spironolactone for gender-affirming therapy is important news for our practice and to reassure our TGW that they can safely and effectively use CAB LA for HIV prevention.”
The HPTN 084 and 083 trials were funded by the National Institutes for Allergy and Infectious Diseases. Dr. Delany-Moretlwe, Dr. Grinsztejn, and Dr. Gandhi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – , according to new data from two HIV Prevention Trials Network (HPTN) studies reported at the International AIDS Society Conference.
Follow-up data from the HPTN 084 trial, which compared the two regimens in 3,224 sub-Saharan persons who were assigned female sex at birth, show that three new HIV infections occurred in the CAB LA group in the 12 months since the study was unblinded, versus 20 new infections among the TDF-FTC group. That translates to an 89% lower risk of infection in the CAB LA arm across both the blinded and unblinded phases of the trial, said lead investigator Sinead Delany-Moretlwe, MD, PhD, director of research, Wits Reproductive Health and HIV Institute, the University of the Witwatersrand, Johannesburg, South Africa, during a press conference.
“The trial was designed with the assumption that both drugs were highly effective in preventing HIV infection but that, given the challenges with taking a pill a day, that injectable cabotegravir may offer an adherence advantage,” she said in an interview. “Our data appear to confirm this, as most of the participants in the TDF-FTC arm who became infected with HIV had evidence of poor or inconsistent use of PrEP.”
The study also found that pregnancy incidence increased “two- to threefold” between the blinded and the unblinded period, “and this emphasizes to us the desire of women to conceive safely, without the threat of HIV, and the importance of us continuing to evaluate the safety and pharmacology of cabotegravir in pregnant and breastfeeding women during open-label extension phase of HPTN 084, so that [they] are not excluded from access to this highly effective PrEP agent,” she said. To date, no congenital anomalies have been reported in babies born during the study.
In an update report from HPTN 083, which also showed superiority of CAB LA over TDF-FTC in cisgender men and transgender women (TGW), researchers reported the safety and efficacy of CAB LA use in TGW using gender-affirming hormone therapy (GAHT).
Among the 4,566 participants in HPTN 083, 570 were TGW, and of those, 58% used GAHT at baseline, reported Beatriz Grinsztejn, MD, PhD, head of the STD/AIDS Clinical Research Laboratory at the Instituto Nacional de Infectologicia/Fundação Oswaldo Cruz.
CAB LA drug concentrations measured in a subset of 53 TGW who received on-time CAB injections were comparable between those taking (n = 30) and those not taking GAHT (n = 23), “suggesting the lack of a gender-affirming hormone effect on CAB pharmacokinetics,” she said. “These are very promising results, as we all know that the use of gender-affirming hormone therapy is a major priority for our transgender women community, ... so the lack of drug-drug interaction is really a very important result.”
“Cabotegravir long-acting PrEP is now approved for all at-risk populations, including men who have sex with men, transgender women, and cisgender women, after the results of HPTN 083 and 084,” commented Monica Gandhi, MD, MPH, an infectious disease physician, professor of medicine, and associate chief in the division of HIV, infectious diseases, and global medicine at the University of California, San Francisco (UCSF).
Dr. Gandhi, who was not involved in either study, is also director of the UCSF Center for AIDS Research and medical director of the HIV Clinic (“Ward 86”) at San Francisco General Hospital. “The incredible efficacy of long-acting PrEP for cisgender women shown by HPTN 084 is game-changing for our practice, and we have already instituted CAB LA across a range of populations at Ward 86,” she said in an interview. “The durability of the 89% additional efficacy of CAB LA over oral TDF/FTC is thrilling and will lead to a greater use of long-acting options.”
She acknowledged that information on potential interactions of GAHT was needed from the HPTN 083 trial. “That cabotegravir levels did not change with the use of estradiol or spironolactone for gender-affirming therapy is important news for our practice and to reassure our TGW that they can safely and effectively use CAB LA for HIV prevention.”
The HPTN 084 and 083 trials were funded by the National Institutes for Allergy and Infectious Diseases. Dr. Delany-Moretlwe, Dr. Grinsztejn, and Dr. Gandhi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AIDS 2022
University to train ‘trip facilitators’ for psychedelic therapy
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.
Children and COVID: Weekly cases top 95,000, admissions continue to rise
New pediatric COVID-19 cases increased for the third straight week as a substantial number of children under age 5 years started to receive their second doses of the vaccine.
Despite the 3-week trend, however, there are some positive signs. The new-case count for the latest reporting week (July 22-28) was over 95,000, but the 3.9% increase over the previous week’s 92,000 cases is much smaller than that week’s (July 15-21) corresponding jump of almost 22% over the July 8-14 total (75,000), according to the American Academy of Pediatrics and the Children’s Hospital Association.
On the not-so-positive side is the trend in admissions among children aged 0-17 years, which continue to climb steadily and have nearly equaled the highest rate seen during the Delta surge in 2021. The rate on July 29 was 0.46 admissions per 100,000 population, and the highest rate over the course of the Delta surge was 0.47 per 100,000, but the all-time high from the Omicron surge – 1.25 per 100,000 in mid-January – is still a long way off, based on data from the Centers for Disease Control and Prevention.
A similar situation is occurring with emergency department visits, but there is differentiation by age group. Among those aged 0-11 years, visits with diagnosed COVID made up 6.5% of all their ED visits on July 25, which was well above the high (4.0%) during the Delta surge, the CDC said.
That is not the case, however, for the older children, for whom rates are rising more slowly. Those aged 12-15 have reached 3.4% so far this summer, as have the 16- to 17-years-olds, versus Delta highs last year of around 7%, the CDC said on its COVID Data Tracker. As with admissions, though, current rates are well below the all-time Omicron high points, the CDC data show.
Joining the ranks of the fully vaccinated
Over the last 2 weeks, the first children to receive the COVID vaccine after its approval for those under age 5 years have been coming back for their second doses. Almost 50,000, about 0.3% of all those in that age group, had done so by July 27. Just over 662,000, about 3.4% of the total under-5 population, have received at least one dose, the CDC said.
Meanwhile, analysis of “data from the first several weeks following availability of the vaccine in this age group indicate high variability across states,” the AAP said in its weekly vaccination report. In the District of Columbia, 20.7% of all children under age 5 have received an initial dose as of July 27, as have 15.5% of those in Vermont and 12.5% in Massachusetts. No other state was above 10%, but Mississippi, at 0.7%, was the only one below 1%.
The older children, obviously, have a head start, so their numbers are much higher. At the state level, Vermont has the highest initial dose rate, 69%, for those aged 5-11 years, while Alabama, Mississippi, and Wyoming, at 17%, are looking up at everyone else in the country. Among children aged 12-17 years, D.C. is the highest with 100% vaccination – Massachusetts and Rhode Island are at 98% – and Wyoming is the lowest with 40%, the AAP said.
New pediatric COVID-19 cases increased for the third straight week as a substantial number of children under age 5 years started to receive their second doses of the vaccine.
Despite the 3-week trend, however, there are some positive signs. The new-case count for the latest reporting week (July 22-28) was over 95,000, but the 3.9% increase over the previous week’s 92,000 cases is much smaller than that week’s (July 15-21) corresponding jump of almost 22% over the July 8-14 total (75,000), according to the American Academy of Pediatrics and the Children’s Hospital Association.
On the not-so-positive side is the trend in admissions among children aged 0-17 years, which continue to climb steadily and have nearly equaled the highest rate seen during the Delta surge in 2021. The rate on July 29 was 0.46 admissions per 100,000 population, and the highest rate over the course of the Delta surge was 0.47 per 100,000, but the all-time high from the Omicron surge – 1.25 per 100,000 in mid-January – is still a long way off, based on data from the Centers for Disease Control and Prevention.
A similar situation is occurring with emergency department visits, but there is differentiation by age group. Among those aged 0-11 years, visits with diagnosed COVID made up 6.5% of all their ED visits on July 25, which was well above the high (4.0%) during the Delta surge, the CDC said.
That is not the case, however, for the older children, for whom rates are rising more slowly. Those aged 12-15 have reached 3.4% so far this summer, as have the 16- to 17-years-olds, versus Delta highs last year of around 7%, the CDC said on its COVID Data Tracker. As with admissions, though, current rates are well below the all-time Omicron high points, the CDC data show.
Joining the ranks of the fully vaccinated
Over the last 2 weeks, the first children to receive the COVID vaccine after its approval for those under age 5 years have been coming back for their second doses. Almost 50,000, about 0.3% of all those in that age group, had done so by July 27. Just over 662,000, about 3.4% of the total under-5 population, have received at least one dose, the CDC said.
Meanwhile, analysis of “data from the first several weeks following availability of the vaccine in this age group indicate high variability across states,” the AAP said in its weekly vaccination report. In the District of Columbia, 20.7% of all children under age 5 have received an initial dose as of July 27, as have 15.5% of those in Vermont and 12.5% in Massachusetts. No other state was above 10%, but Mississippi, at 0.7%, was the only one below 1%.
The older children, obviously, have a head start, so their numbers are much higher. At the state level, Vermont has the highest initial dose rate, 69%, for those aged 5-11 years, while Alabama, Mississippi, and Wyoming, at 17%, are looking up at everyone else in the country. Among children aged 12-17 years, D.C. is the highest with 100% vaccination – Massachusetts and Rhode Island are at 98% – and Wyoming is the lowest with 40%, the AAP said.
New pediatric COVID-19 cases increased for the third straight week as a substantial number of children under age 5 years started to receive their second doses of the vaccine.
Despite the 3-week trend, however, there are some positive signs. The new-case count for the latest reporting week (July 22-28) was over 95,000, but the 3.9% increase over the previous week’s 92,000 cases is much smaller than that week’s (July 15-21) corresponding jump of almost 22% over the July 8-14 total (75,000), according to the American Academy of Pediatrics and the Children’s Hospital Association.
On the not-so-positive side is the trend in admissions among children aged 0-17 years, which continue to climb steadily and have nearly equaled the highest rate seen during the Delta surge in 2021. The rate on July 29 was 0.46 admissions per 100,000 population, and the highest rate over the course of the Delta surge was 0.47 per 100,000, but the all-time high from the Omicron surge – 1.25 per 100,000 in mid-January – is still a long way off, based on data from the Centers for Disease Control and Prevention.
A similar situation is occurring with emergency department visits, but there is differentiation by age group. Among those aged 0-11 years, visits with diagnosed COVID made up 6.5% of all their ED visits on July 25, which was well above the high (4.0%) during the Delta surge, the CDC said.
That is not the case, however, for the older children, for whom rates are rising more slowly. Those aged 12-15 have reached 3.4% so far this summer, as have the 16- to 17-years-olds, versus Delta highs last year of around 7%, the CDC said on its COVID Data Tracker. As with admissions, though, current rates are well below the all-time Omicron high points, the CDC data show.
Joining the ranks of the fully vaccinated
Over the last 2 weeks, the first children to receive the COVID vaccine after its approval for those under age 5 years have been coming back for their second doses. Almost 50,000, about 0.3% of all those in that age group, had done so by July 27. Just over 662,000, about 3.4% of the total under-5 population, have received at least one dose, the CDC said.
Meanwhile, analysis of “data from the first several weeks following availability of the vaccine in this age group indicate high variability across states,” the AAP said in its weekly vaccination report. In the District of Columbia, 20.7% of all children under age 5 have received an initial dose as of July 27, as have 15.5% of those in Vermont and 12.5% in Massachusetts. No other state was above 10%, but Mississippi, at 0.7%, was the only one below 1%.
The older children, obviously, have a head start, so their numbers are much higher. At the state level, Vermont has the highest initial dose rate, 69%, for those aged 5-11 years, while Alabama, Mississippi, and Wyoming, at 17%, are looking up at everyone else in the country. Among children aged 12-17 years, D.C. is the highest with 100% vaccination – Massachusetts and Rhode Island are at 98% – and Wyoming is the lowest with 40%, the AAP said.
Six specialties attracting the highest private equity acquisitions
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 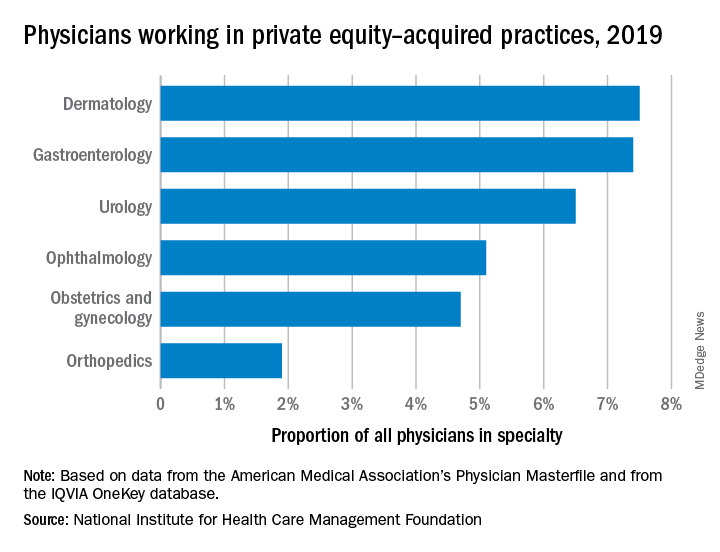
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 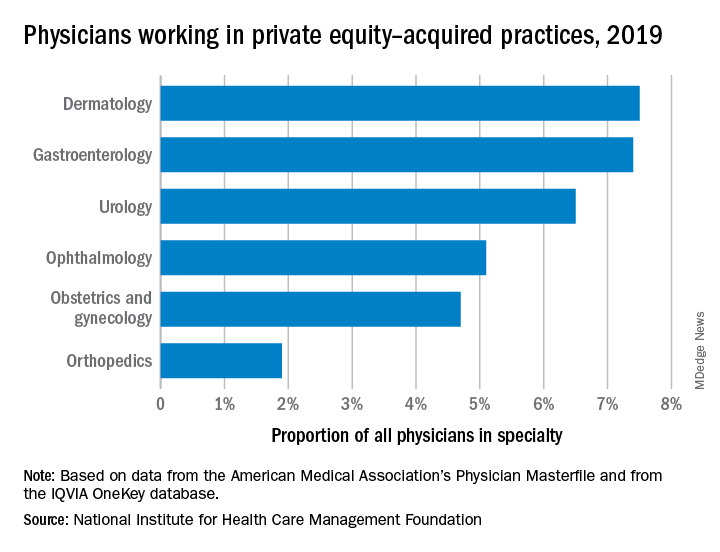
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 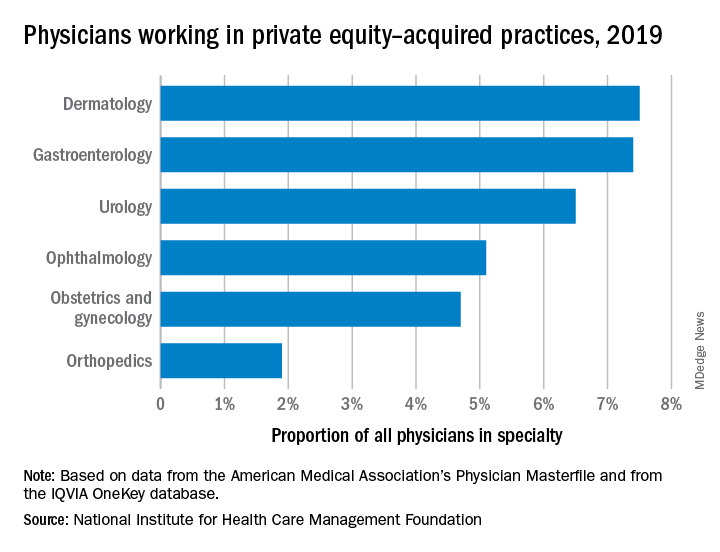
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
FROM JAMA HEALTH FORUM
Low calcium, potassium key risk factors for kidney stones
as well as their symptomatic recurrence, a population-based study of dietary factors shows.
“Our research is of particular importance as recommendations for preventing symptomatic recurrence of kidney stones has largely been based on dietary factors associated with the incidence rather than the recurrence of stone formation,” Api Chewcharat, MD, Mayo Clinic, Rochester, Minn., said in a video discussing the study.
“We recommend a daily intake of calcium of approximately 1,200 mg and a diet that is high in potassium, especially high in fruits and vegetables, in order to prevent both incident and recurrent symptomatic kidney stone formation,” he stressed.
The study was published online in Mayo Clinic Proceedings.
Lower dietary calcium, potassium, and fluid associated with increased incidence
Some 411 patients with incident symptomatic kidney stone formation were recruited. Diets were compared between them and 384 controls. Patients were seen at the Mayo Clinic in either Minnesota or Florida between Jan. 1, 2009, and Aug. 31, 2018. “Dietary factors were based on a Viocare food frequency questionnaire administered during a baseline in-person study visit,” Dr. Chewcharat and colleagues observed.
During a median follow-up of 4.1 years, 73 patients experienced a symptomatic recurrence. In a fully adjusted analysis, a dietary calcium intake less than 1,200 mg/d was associated with incident stone formation. Similarly, among participants with a fluid intake less than 3,400 mL/d – about nine 12-oz glasses of fluid – was also associated with incident stone formation, as was a lower intake of dietary potassium, caffeine, and phytate. Phytate is an antioxidant found in whole grains, nuts, and other foods that can increase calcium absorption and urinary calcium excretion.
After excluding patients who were taking either a thiazide diuretic or a calcium supplement, lower dietary calcium and potassium, fluid, and phytate intake remained significantly associated with incident stone formation.
However, only lower dietary calcium intake was associated with a higher risk for symptomatic recurrence, although a lower dietary potassium intake was also associated with a higher risk for symptomatic recurrence in an analysis that adjusted for body mass index, fluid, and energy intake.
As the authors suggested, patients may be less keen to adjust their diet to prevent the development of incident kidney stones. On the other hand, they may be much more willing to adjust their diet to prevent their symptomatic recurrence. The Department of Agriculture currently recommends that individuals get approximately 1,200 mg/d of dietary calcium which, given the study results, appears to be justified for the prevention of symptomatic stone recurrence.
A higher-calcium diet is associated with a higher urinary pH, and citrate confers an alkali load which helps protect against the formation of calcium oxalate stones. Foods that are high in potassium also contain more fluid, citrate, and phytate, which, again, have been reported to be protective against kidney stones. “Changing your diet to prevent kidney stones can be very difficult,” Andrew Rule, MD, a nephrologist at the Mayo Clinic said in a statement.
“Thus, knowing the dietary factors that are most important for preventing kidney stone recurrence can help patients and providers know what to prioritize,” he added.
The authors have no conflicts of interest to declare.
A version of this article first appeared on Medscape.com.
as well as their symptomatic recurrence, a population-based study of dietary factors shows.
“Our research is of particular importance as recommendations for preventing symptomatic recurrence of kidney stones has largely been based on dietary factors associated with the incidence rather than the recurrence of stone formation,” Api Chewcharat, MD, Mayo Clinic, Rochester, Minn., said in a video discussing the study.
“We recommend a daily intake of calcium of approximately 1,200 mg and a diet that is high in potassium, especially high in fruits and vegetables, in order to prevent both incident and recurrent symptomatic kidney stone formation,” he stressed.
The study was published online in Mayo Clinic Proceedings.
Lower dietary calcium, potassium, and fluid associated with increased incidence
Some 411 patients with incident symptomatic kidney stone formation were recruited. Diets were compared between them and 384 controls. Patients were seen at the Mayo Clinic in either Minnesota or Florida between Jan. 1, 2009, and Aug. 31, 2018. “Dietary factors were based on a Viocare food frequency questionnaire administered during a baseline in-person study visit,” Dr. Chewcharat and colleagues observed.
During a median follow-up of 4.1 years, 73 patients experienced a symptomatic recurrence. In a fully adjusted analysis, a dietary calcium intake less than 1,200 mg/d was associated with incident stone formation. Similarly, among participants with a fluid intake less than 3,400 mL/d – about nine 12-oz glasses of fluid – was also associated with incident stone formation, as was a lower intake of dietary potassium, caffeine, and phytate. Phytate is an antioxidant found in whole grains, nuts, and other foods that can increase calcium absorption and urinary calcium excretion.
After excluding patients who were taking either a thiazide diuretic or a calcium supplement, lower dietary calcium and potassium, fluid, and phytate intake remained significantly associated with incident stone formation.
However, only lower dietary calcium intake was associated with a higher risk for symptomatic recurrence, although a lower dietary potassium intake was also associated with a higher risk for symptomatic recurrence in an analysis that adjusted for body mass index, fluid, and energy intake.
As the authors suggested, patients may be less keen to adjust their diet to prevent the development of incident kidney stones. On the other hand, they may be much more willing to adjust their diet to prevent their symptomatic recurrence. The Department of Agriculture currently recommends that individuals get approximately 1,200 mg/d of dietary calcium which, given the study results, appears to be justified for the prevention of symptomatic stone recurrence.
A higher-calcium diet is associated with a higher urinary pH, and citrate confers an alkali load which helps protect against the formation of calcium oxalate stones. Foods that are high in potassium also contain more fluid, citrate, and phytate, which, again, have been reported to be protective against kidney stones. “Changing your diet to prevent kidney stones can be very difficult,” Andrew Rule, MD, a nephrologist at the Mayo Clinic said in a statement.
“Thus, knowing the dietary factors that are most important for preventing kidney stone recurrence can help patients and providers know what to prioritize,” he added.
The authors have no conflicts of interest to declare.
A version of this article first appeared on Medscape.com.
as well as their symptomatic recurrence, a population-based study of dietary factors shows.
“Our research is of particular importance as recommendations for preventing symptomatic recurrence of kidney stones has largely been based on dietary factors associated with the incidence rather than the recurrence of stone formation,” Api Chewcharat, MD, Mayo Clinic, Rochester, Minn., said in a video discussing the study.
“We recommend a daily intake of calcium of approximately 1,200 mg and a diet that is high in potassium, especially high in fruits and vegetables, in order to prevent both incident and recurrent symptomatic kidney stone formation,” he stressed.
The study was published online in Mayo Clinic Proceedings.
Lower dietary calcium, potassium, and fluid associated with increased incidence
Some 411 patients with incident symptomatic kidney stone formation were recruited. Diets were compared between them and 384 controls. Patients were seen at the Mayo Clinic in either Minnesota or Florida between Jan. 1, 2009, and Aug. 31, 2018. “Dietary factors were based on a Viocare food frequency questionnaire administered during a baseline in-person study visit,” Dr. Chewcharat and colleagues observed.
During a median follow-up of 4.1 years, 73 patients experienced a symptomatic recurrence. In a fully adjusted analysis, a dietary calcium intake less than 1,200 mg/d was associated with incident stone formation. Similarly, among participants with a fluid intake less than 3,400 mL/d – about nine 12-oz glasses of fluid – was also associated with incident stone formation, as was a lower intake of dietary potassium, caffeine, and phytate. Phytate is an antioxidant found in whole grains, nuts, and other foods that can increase calcium absorption and urinary calcium excretion.
After excluding patients who were taking either a thiazide diuretic or a calcium supplement, lower dietary calcium and potassium, fluid, and phytate intake remained significantly associated with incident stone formation.
However, only lower dietary calcium intake was associated with a higher risk for symptomatic recurrence, although a lower dietary potassium intake was also associated with a higher risk for symptomatic recurrence in an analysis that adjusted for body mass index, fluid, and energy intake.
As the authors suggested, patients may be less keen to adjust their diet to prevent the development of incident kidney stones. On the other hand, they may be much more willing to adjust their diet to prevent their symptomatic recurrence. The Department of Agriculture currently recommends that individuals get approximately 1,200 mg/d of dietary calcium which, given the study results, appears to be justified for the prevention of symptomatic stone recurrence.
A higher-calcium diet is associated with a higher urinary pH, and citrate confers an alkali load which helps protect against the formation of calcium oxalate stones. Foods that are high in potassium also contain more fluid, citrate, and phytate, which, again, have been reported to be protective against kidney stones. “Changing your diet to prevent kidney stones can be very difficult,” Andrew Rule, MD, a nephrologist at the Mayo Clinic said in a statement.
“Thus, knowing the dietary factors that are most important for preventing kidney stone recurrence can help patients and providers know what to prioritize,” he added.
The authors have no conflicts of interest to declare.
A version of this article first appeared on Medscape.com.
FROM MAYO CLINIC PRECEEDINGS









