User login
Tech-based cancer company raises access concerns
Oncologists are raising concerns about care access after the launch of a new company that links patients to cancer care options and clinical trials through mobile technology.
Driver, which began in September in the U.S. and China, is a global technology platform that allows patients to access treatment options across a broad network of cancer centers without leaving home. Cancer patients join the platform using a mobile app, through which Driver obtains the required consent to acquire medical records and tumor samples, and the company uses the information to recommend treatment options and clinical trials.
A separate app called Driver for Clinic enables oncologists who belong to Driver’s partner hospitals to manage their institution’s clinical trial information and quickly filter that information based on patients’ medical history to determine the patient’s eligibility for treatments.
Driver’s mission is to connect more patients to the best cancer treatments, regardless of location, said Will Polkinghorn, MD, Driver cofounder and CEO.
“Driver’s cofounders met at Harvard Medical School [in Boston] and saw firsthand the challenges of patients getting access to the latest, cutting-edge treatments available,” Dr. Polkinghorn said in an interview. “As doctors, [we] also witnessed how difficult it was for doctors to manage information in clinic and know about all the treatments that become available all around the world. Driver was created as a platform, with an app for the patient and an app for the doctor, to solve this broken marketplace.”
As part of the model, patients can review their recommended treatment options through video with an expert oncologist and select a hospital within Driver’s network for further evaluation. The company’s global network includes more than 30 leading U.S. cancer centers, including the Cleveland Clinic; multiple locations of the Mayo Clinic; the University of California, San Francisco; and Massachusetts General Hospital, Boston. The U.S. National Cancer Institute (NCI) and the Chinese National Cancer Center are founding members of Driver’s global network, according to the company.
Making more information and treatment options available is a positive for patients, said Walter Stadler, MD, chief of hematology/oncology and director of the genitourinary oncology program at the University of Chicago. However, he noted that the cost for patients to use Driver is prohibitive for many patients. Driver charges patients $3,000 up front and then a $20 monthly fee to use its service. Insurance does not subsidize the cost, nor does Driver help with travel or treatment costs, according to its website.
“It’s inequality of access,” Dr. Stadler said in an interview. “Many of us are very concerned that the clinical trials currently being conducted do not represent the general population well because they don’t represent patients with disparities … Here, we further exacerbate the problem by saying, ‘Okay, we’ll take the 5% of patients who can afford the service and expand their access, and the others, well, that’s not our problem.’ ”
Kashyap Patel, MD, secretary for the Community Oncology Alliance and CEO for the Carolina Blood and Cancer Care in Rock Hill, S.C., also sees positives and negatives about the business model. Using technology to link patients with care and clinical trials can help speed treatment and accelerate drug development, he said. But Driver’s network of large tertiary care centers in metropolitan areas poses challenges for rural cancer patients, he said.
“Access to clinical trials for patients residing in rural areas, as well as those getting their treatment in community based clinics, would not change,” Dr. Patel said in an interview. “Hence, challenges of social and demographic disparities and inequalities in clinical trial access and participation would be altered minimally. There is much greater need for such [platforms to include] community cancer clinics that would be more inclusive and encompass larger geographic areas where the majority of patients receive their care.”
Disadvantaged populations with limited access are not being overlooked by the company, according to Driver leaders. A branch of the company called Driver for All aims to increase access to optimal treatments for free through partnerships with local communities, Dr. Polkinghorn said. Driver for All has thus far partnered with Howard University Hospital in Washington to connect Howard patients to clinical trials at NCI. A partnership with Beijing Children’s Hospital and the Futang Research Center of Pediatric Development, meanwhile, is working to connect patients with rare-disease experts. Driver has funded 100% of the cost of these projects to date, according to its website.
Outside of Driver for All, Dr. Polkinghorn acknowledges that patients must bear the cost of Driver’s consumer products; however, the price should be viewed in context, he said.
“It’s important to remember that today, in order to be evaluated by 30 [plus] centers for treatment options, patients would need to fly to these centers, make appointments, and be seen by a doctor – this would require both time and resources for flights/hotels, which would cost much more than our sticker price,” he said. “So while $3,000 is a lot of money for some patients, Driver’s product is ultimately able to provide more visibility to options that simply would not be realistic today.”
James Gulley, MD, of the National Cancer Institute Center for Cancer Research, said any platform that can efficiently provide access to clinical trial options yields another source of information for patients to utilize in decision making with their health provider. Dr. Gulley, who heads the center’s genitourinary malignancies branch, declined to comment about access-to-care concerns with Driver’s model. He emphasized that patients who participate in NIH research studies are treated without charge.
“The key to finding better [cancer] treatment is to perform science-driven clinical trials,” Dr. Gulley said in an interview. “However, there are many barriers for enrollment in clinical trials. … As a government agency, NCI is open to partnering with any organization that seeks to improve access to clinical trials for cancer patients.”
NCI and Driver recently conducted a study to validate Driver’s platform; it showed that Driver’s technology successfully predicted the eligibility of patients in NCI Center for Cancer Research clinical trials. The study, presented at a recent American Society of Clinical Oncology meeting, evaluated Driver’s processing of 21 metastatic prostate cancer patients enrolled in a therapeutic NCI clinical trial within the last five years. Results showed Driver correctly predicted that 20 of the patients were “potentially eligible” for the trial in which they were enrolled, and that one was ineligible. Based on the study, a protocol is now in development for a new clinical study, which will seek to further determine the efficiency and accuracy of the clinical trial access program created by Driver, according to Dr. Gulley.
Charles Ryan, MD, director of the division of hematology, oncology, and transplantation for the University of Minnesota, Minneapolis, views Driver’s platform as a way to eliminate geographical barriers, which often keep patients from care, while at the same time enabling researchers to find the right patients for clinical trials.
“We need breakthrough technologies and opportunities for patients to be able to access the most successful and promising cancer treatments, regardless of where they live,” Dr. Ryan said in an interview. “Companies like Driver are attempting to bridge that gap by connecting patients to doctors at world class cancer institutes and direct them toward the best care for their particular condition.”
Driver’s model also allows researchers the opportunity to develop specific, unique treatment for less common cancers and remain optimistic that they can attract patients to receive such treatments as they are developed, Dr. Ryan said.
Dr. Stadler, however, worries that Driver may be giving patients the wrong perception that all it takes is a computer and medical records to determine their best treatment route.
“There’s a lot more subtlety to treatment decisions than most people would like to admit,” Dr. Stadler said. “It’s more than just a bunch of data from sophisticated laboratory tests and the written medical record. Obtaining objective information is the first step, but it’s far from the only step.”
Patients may have significant limitations in functional status that is apparent only during an in-person assessment, for example, he said. In other cases, family members may be essential in conveying information about a patient’s cognitive disabilities. Even when such information is documented, it is sometimes difficult to extract the full picture from the record alone, he said. Dr. Stadler is also bothered that the model requires physicians and hospitals to provide their skilled analyses to a for-profit company, which in turn, charges patients to review the information.
“This is our work,” he said. “I agree that patients should have the information, and I don’t mind sharing anything I have with patients, but now I’m going to share it with another business that essentially is competing with me in terms of providing guidance to patients.”
Oncologists are raising concerns about care access after the launch of a new company that links patients to cancer care options and clinical trials through mobile technology.
Driver, which began in September in the U.S. and China, is a global technology platform that allows patients to access treatment options across a broad network of cancer centers without leaving home. Cancer patients join the platform using a mobile app, through which Driver obtains the required consent to acquire medical records and tumor samples, and the company uses the information to recommend treatment options and clinical trials.
A separate app called Driver for Clinic enables oncologists who belong to Driver’s partner hospitals to manage their institution’s clinical trial information and quickly filter that information based on patients’ medical history to determine the patient’s eligibility for treatments.
Driver’s mission is to connect more patients to the best cancer treatments, regardless of location, said Will Polkinghorn, MD, Driver cofounder and CEO.
“Driver’s cofounders met at Harvard Medical School [in Boston] and saw firsthand the challenges of patients getting access to the latest, cutting-edge treatments available,” Dr. Polkinghorn said in an interview. “As doctors, [we] also witnessed how difficult it was for doctors to manage information in clinic and know about all the treatments that become available all around the world. Driver was created as a platform, with an app for the patient and an app for the doctor, to solve this broken marketplace.”
As part of the model, patients can review their recommended treatment options through video with an expert oncologist and select a hospital within Driver’s network for further evaluation. The company’s global network includes more than 30 leading U.S. cancer centers, including the Cleveland Clinic; multiple locations of the Mayo Clinic; the University of California, San Francisco; and Massachusetts General Hospital, Boston. The U.S. National Cancer Institute (NCI) and the Chinese National Cancer Center are founding members of Driver’s global network, according to the company.
Making more information and treatment options available is a positive for patients, said Walter Stadler, MD, chief of hematology/oncology and director of the genitourinary oncology program at the University of Chicago. However, he noted that the cost for patients to use Driver is prohibitive for many patients. Driver charges patients $3,000 up front and then a $20 monthly fee to use its service. Insurance does not subsidize the cost, nor does Driver help with travel or treatment costs, according to its website.
“It’s inequality of access,” Dr. Stadler said in an interview. “Many of us are very concerned that the clinical trials currently being conducted do not represent the general population well because they don’t represent patients with disparities … Here, we further exacerbate the problem by saying, ‘Okay, we’ll take the 5% of patients who can afford the service and expand their access, and the others, well, that’s not our problem.’ ”
Kashyap Patel, MD, secretary for the Community Oncology Alliance and CEO for the Carolina Blood and Cancer Care in Rock Hill, S.C., also sees positives and negatives about the business model. Using technology to link patients with care and clinical trials can help speed treatment and accelerate drug development, he said. But Driver’s network of large tertiary care centers in metropolitan areas poses challenges for rural cancer patients, he said.
“Access to clinical trials for patients residing in rural areas, as well as those getting their treatment in community based clinics, would not change,” Dr. Patel said in an interview. “Hence, challenges of social and demographic disparities and inequalities in clinical trial access and participation would be altered minimally. There is much greater need for such [platforms to include] community cancer clinics that would be more inclusive and encompass larger geographic areas where the majority of patients receive their care.”
Disadvantaged populations with limited access are not being overlooked by the company, according to Driver leaders. A branch of the company called Driver for All aims to increase access to optimal treatments for free through partnerships with local communities, Dr. Polkinghorn said. Driver for All has thus far partnered with Howard University Hospital in Washington to connect Howard patients to clinical trials at NCI. A partnership with Beijing Children’s Hospital and the Futang Research Center of Pediatric Development, meanwhile, is working to connect patients with rare-disease experts. Driver has funded 100% of the cost of these projects to date, according to its website.
Outside of Driver for All, Dr. Polkinghorn acknowledges that patients must bear the cost of Driver’s consumer products; however, the price should be viewed in context, he said.
“It’s important to remember that today, in order to be evaluated by 30 [plus] centers for treatment options, patients would need to fly to these centers, make appointments, and be seen by a doctor – this would require both time and resources for flights/hotels, which would cost much more than our sticker price,” he said. “So while $3,000 is a lot of money for some patients, Driver’s product is ultimately able to provide more visibility to options that simply would not be realistic today.”
James Gulley, MD, of the National Cancer Institute Center for Cancer Research, said any platform that can efficiently provide access to clinical trial options yields another source of information for patients to utilize in decision making with their health provider. Dr. Gulley, who heads the center’s genitourinary malignancies branch, declined to comment about access-to-care concerns with Driver’s model. He emphasized that patients who participate in NIH research studies are treated without charge.
“The key to finding better [cancer] treatment is to perform science-driven clinical trials,” Dr. Gulley said in an interview. “However, there are many barriers for enrollment in clinical trials. … As a government agency, NCI is open to partnering with any organization that seeks to improve access to clinical trials for cancer patients.”
NCI and Driver recently conducted a study to validate Driver’s platform; it showed that Driver’s technology successfully predicted the eligibility of patients in NCI Center for Cancer Research clinical trials. The study, presented at a recent American Society of Clinical Oncology meeting, evaluated Driver’s processing of 21 metastatic prostate cancer patients enrolled in a therapeutic NCI clinical trial within the last five years. Results showed Driver correctly predicted that 20 of the patients were “potentially eligible” for the trial in which they were enrolled, and that one was ineligible. Based on the study, a protocol is now in development for a new clinical study, which will seek to further determine the efficiency and accuracy of the clinical trial access program created by Driver, according to Dr. Gulley.
Charles Ryan, MD, director of the division of hematology, oncology, and transplantation for the University of Minnesota, Minneapolis, views Driver’s platform as a way to eliminate geographical barriers, which often keep patients from care, while at the same time enabling researchers to find the right patients for clinical trials.
“We need breakthrough technologies and opportunities for patients to be able to access the most successful and promising cancer treatments, regardless of where they live,” Dr. Ryan said in an interview. “Companies like Driver are attempting to bridge that gap by connecting patients to doctors at world class cancer institutes and direct them toward the best care for their particular condition.”
Driver’s model also allows researchers the opportunity to develop specific, unique treatment for less common cancers and remain optimistic that they can attract patients to receive such treatments as they are developed, Dr. Ryan said.
Dr. Stadler, however, worries that Driver may be giving patients the wrong perception that all it takes is a computer and medical records to determine their best treatment route.
“There’s a lot more subtlety to treatment decisions than most people would like to admit,” Dr. Stadler said. “It’s more than just a bunch of data from sophisticated laboratory tests and the written medical record. Obtaining objective information is the first step, but it’s far from the only step.”
Patients may have significant limitations in functional status that is apparent only during an in-person assessment, for example, he said. In other cases, family members may be essential in conveying information about a patient’s cognitive disabilities. Even when such information is documented, it is sometimes difficult to extract the full picture from the record alone, he said. Dr. Stadler is also bothered that the model requires physicians and hospitals to provide their skilled analyses to a for-profit company, which in turn, charges patients to review the information.
“This is our work,” he said. “I agree that patients should have the information, and I don’t mind sharing anything I have with patients, but now I’m going to share it with another business that essentially is competing with me in terms of providing guidance to patients.”
Oncologists are raising concerns about care access after the launch of a new company that links patients to cancer care options and clinical trials through mobile technology.
Driver, which began in September in the U.S. and China, is a global technology platform that allows patients to access treatment options across a broad network of cancer centers without leaving home. Cancer patients join the platform using a mobile app, through which Driver obtains the required consent to acquire medical records and tumor samples, and the company uses the information to recommend treatment options and clinical trials.
A separate app called Driver for Clinic enables oncologists who belong to Driver’s partner hospitals to manage their institution’s clinical trial information and quickly filter that information based on patients’ medical history to determine the patient’s eligibility for treatments.
Driver’s mission is to connect more patients to the best cancer treatments, regardless of location, said Will Polkinghorn, MD, Driver cofounder and CEO.
“Driver’s cofounders met at Harvard Medical School [in Boston] and saw firsthand the challenges of patients getting access to the latest, cutting-edge treatments available,” Dr. Polkinghorn said in an interview. “As doctors, [we] also witnessed how difficult it was for doctors to manage information in clinic and know about all the treatments that become available all around the world. Driver was created as a platform, with an app for the patient and an app for the doctor, to solve this broken marketplace.”
As part of the model, patients can review their recommended treatment options through video with an expert oncologist and select a hospital within Driver’s network for further evaluation. The company’s global network includes more than 30 leading U.S. cancer centers, including the Cleveland Clinic; multiple locations of the Mayo Clinic; the University of California, San Francisco; and Massachusetts General Hospital, Boston. The U.S. National Cancer Institute (NCI) and the Chinese National Cancer Center are founding members of Driver’s global network, according to the company.
Making more information and treatment options available is a positive for patients, said Walter Stadler, MD, chief of hematology/oncology and director of the genitourinary oncology program at the University of Chicago. However, he noted that the cost for patients to use Driver is prohibitive for many patients. Driver charges patients $3,000 up front and then a $20 monthly fee to use its service. Insurance does not subsidize the cost, nor does Driver help with travel or treatment costs, according to its website.
“It’s inequality of access,” Dr. Stadler said in an interview. “Many of us are very concerned that the clinical trials currently being conducted do not represent the general population well because they don’t represent patients with disparities … Here, we further exacerbate the problem by saying, ‘Okay, we’ll take the 5% of patients who can afford the service and expand their access, and the others, well, that’s not our problem.’ ”
Kashyap Patel, MD, secretary for the Community Oncology Alliance and CEO for the Carolina Blood and Cancer Care in Rock Hill, S.C., also sees positives and negatives about the business model. Using technology to link patients with care and clinical trials can help speed treatment and accelerate drug development, he said. But Driver’s network of large tertiary care centers in metropolitan areas poses challenges for rural cancer patients, he said.
“Access to clinical trials for patients residing in rural areas, as well as those getting their treatment in community based clinics, would not change,” Dr. Patel said in an interview. “Hence, challenges of social and demographic disparities and inequalities in clinical trial access and participation would be altered minimally. There is much greater need for such [platforms to include] community cancer clinics that would be more inclusive and encompass larger geographic areas where the majority of patients receive their care.”
Disadvantaged populations with limited access are not being overlooked by the company, according to Driver leaders. A branch of the company called Driver for All aims to increase access to optimal treatments for free through partnerships with local communities, Dr. Polkinghorn said. Driver for All has thus far partnered with Howard University Hospital in Washington to connect Howard patients to clinical trials at NCI. A partnership with Beijing Children’s Hospital and the Futang Research Center of Pediatric Development, meanwhile, is working to connect patients with rare-disease experts. Driver has funded 100% of the cost of these projects to date, according to its website.
Outside of Driver for All, Dr. Polkinghorn acknowledges that patients must bear the cost of Driver’s consumer products; however, the price should be viewed in context, he said.
“It’s important to remember that today, in order to be evaluated by 30 [plus] centers for treatment options, patients would need to fly to these centers, make appointments, and be seen by a doctor – this would require both time and resources for flights/hotels, which would cost much more than our sticker price,” he said. “So while $3,000 is a lot of money for some patients, Driver’s product is ultimately able to provide more visibility to options that simply would not be realistic today.”
James Gulley, MD, of the National Cancer Institute Center for Cancer Research, said any platform that can efficiently provide access to clinical trial options yields another source of information for patients to utilize in decision making with their health provider. Dr. Gulley, who heads the center’s genitourinary malignancies branch, declined to comment about access-to-care concerns with Driver’s model. He emphasized that patients who participate in NIH research studies are treated without charge.
“The key to finding better [cancer] treatment is to perform science-driven clinical trials,” Dr. Gulley said in an interview. “However, there are many barriers for enrollment in clinical trials. … As a government agency, NCI is open to partnering with any organization that seeks to improve access to clinical trials for cancer patients.”
NCI and Driver recently conducted a study to validate Driver’s platform; it showed that Driver’s technology successfully predicted the eligibility of patients in NCI Center for Cancer Research clinical trials. The study, presented at a recent American Society of Clinical Oncology meeting, evaluated Driver’s processing of 21 metastatic prostate cancer patients enrolled in a therapeutic NCI clinical trial within the last five years. Results showed Driver correctly predicted that 20 of the patients were “potentially eligible” for the trial in which they were enrolled, and that one was ineligible. Based on the study, a protocol is now in development for a new clinical study, which will seek to further determine the efficiency and accuracy of the clinical trial access program created by Driver, according to Dr. Gulley.
Charles Ryan, MD, director of the division of hematology, oncology, and transplantation for the University of Minnesota, Minneapolis, views Driver’s platform as a way to eliminate geographical barriers, which often keep patients from care, while at the same time enabling researchers to find the right patients for clinical trials.
“We need breakthrough technologies and opportunities for patients to be able to access the most successful and promising cancer treatments, regardless of where they live,” Dr. Ryan said in an interview. “Companies like Driver are attempting to bridge that gap by connecting patients to doctors at world class cancer institutes and direct them toward the best care for their particular condition.”
Driver’s model also allows researchers the opportunity to develop specific, unique treatment for less common cancers and remain optimistic that they can attract patients to receive such treatments as they are developed, Dr. Ryan said.
Dr. Stadler, however, worries that Driver may be giving patients the wrong perception that all it takes is a computer and medical records to determine their best treatment route.
“There’s a lot more subtlety to treatment decisions than most people would like to admit,” Dr. Stadler said. “It’s more than just a bunch of data from sophisticated laboratory tests and the written medical record. Obtaining objective information is the first step, but it’s far from the only step.”
Patients may have significant limitations in functional status that is apparent only during an in-person assessment, for example, he said. In other cases, family members may be essential in conveying information about a patient’s cognitive disabilities. Even when such information is documented, it is sometimes difficult to extract the full picture from the record alone, he said. Dr. Stadler is also bothered that the model requires physicians and hospitals to provide their skilled analyses to a for-profit company, which in turn, charges patients to review the information.
“This is our work,” he said. “I agree that patients should have the information, and I don’t mind sharing anything I have with patients, but now I’m going to share it with another business that essentially is competing with me in terms of providing guidance to patients.”
Be proactive with prophylaxis to tame VTE
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
FROM WORLD THROMBOSIS DAY 2018 WEBINAR
ESMO 2018: First look at immunotherapy as first-line treatment for HNSCC
for first-line treatment of recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) will be presented during a presidential symposium at the European Society for Medical Oncology Congress.
The drug is currently approved for second-line treatment of HNSCC. Merck, the maker of the anti–programmed cell death protein therapy, announced in July that the primary endpoint of overall survival as monotherapy in the first-line setting of advanced HNSCC had been met in patients whose tumors expressed programmed death–ligand 1.
More than 800 patients in KEYNOTE-048 were randomized to receive pembrolizumab as monotherapy or in combination with cisplatin or carboplatin and 5-FU, or cetuximab plus cisplatin or carboplatin and 5-FU.
The dual primary endpoints were overall survival and progression-free survival. The secondary endpoints of the study were PFS (at 6 months and 12 months), objective response rate, and time to deterioration in Quality of Life Global Health Status/Quality of Life Scales of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, according to the company.
Further details from the interim analysis of KEYNOTE-048 will be presented by Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn., during Presidential Symposium 3 at ESMO 2018 on Oct. 22 in Munich.
for first-line treatment of recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) will be presented during a presidential symposium at the European Society for Medical Oncology Congress.
The drug is currently approved for second-line treatment of HNSCC. Merck, the maker of the anti–programmed cell death protein therapy, announced in July that the primary endpoint of overall survival as monotherapy in the first-line setting of advanced HNSCC had been met in patients whose tumors expressed programmed death–ligand 1.
More than 800 patients in KEYNOTE-048 were randomized to receive pembrolizumab as monotherapy or in combination with cisplatin or carboplatin and 5-FU, or cetuximab plus cisplatin or carboplatin and 5-FU.
The dual primary endpoints were overall survival and progression-free survival. The secondary endpoints of the study were PFS (at 6 months and 12 months), objective response rate, and time to deterioration in Quality of Life Global Health Status/Quality of Life Scales of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, according to the company.
Further details from the interim analysis of KEYNOTE-048 will be presented by Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn., during Presidential Symposium 3 at ESMO 2018 on Oct. 22 in Munich.
for first-line treatment of recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) will be presented during a presidential symposium at the European Society for Medical Oncology Congress.
The drug is currently approved for second-line treatment of HNSCC. Merck, the maker of the anti–programmed cell death protein therapy, announced in July that the primary endpoint of overall survival as monotherapy in the first-line setting of advanced HNSCC had been met in patients whose tumors expressed programmed death–ligand 1.
More than 800 patients in KEYNOTE-048 were randomized to receive pembrolizumab as monotherapy or in combination with cisplatin or carboplatin and 5-FU, or cetuximab plus cisplatin or carboplatin and 5-FU.
The dual primary endpoints were overall survival and progression-free survival. The secondary endpoints of the study were PFS (at 6 months and 12 months), objective response rate, and time to deterioration in Quality of Life Global Health Status/Quality of Life Scales of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, according to the company.
Further details from the interim analysis of KEYNOTE-048 will be presented by Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn., during Presidential Symposium 3 at ESMO 2018 on Oct. 22 in Munich.
Low spinal cord volume linked to higher MS disability
BERLIN – Spinal cord volume deficits in patients with multiple sclerosis may contribute to clinical disability that appears out of proportion to lesion load on brain imaging, according to new research.
In a pool of 362 patients with mild to moderate MS-related disability but identical white matter lesion load identified by MRI, those with higher disability had significantly lower spinal cord volumes when compared against those with disability scores in the mild range (P less than .001).
Though brain MRI is a key tool used to track disease severity and progression in MS, some patients have relatively high disability but a low burden of white matter intracerebral lesions on MRI. Little is known about spinal cord volume in MS patients with pronounced dissociation between intracerebral lesion load and disability, Michaela Andelova, MD, said in an interview during a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Andelova, of Charles University, Prague, said that she and her colleagues hypothesized that spinal cord volume would differ between patients who had varying levels of disability, despite identical white matter lesion load.
To test this, she and her colleagues looked at records of 1,245 patients with relapsing-remitting MS. They divided them into three groups by severity of clinical disability, and also by extent of cerebral T2 hyperintense lesion load. The investigators identified a group of patients (n = 53) whose total volume of T2-weighted hyperintense lesions was less than 3 mL, but whose Expanded Disability Status Scale (EDSS) scores were at least 3.5; this was the low lesion load/high disability (LLHD) group.
Dr. Andelova and her colleagues then identified another group of patients (n = 71) who had a volume of T2-weighted hyperintensities that was greater than 9 mL, but whose EDSS score was less than 1.5. This was the high lesion load/low disability (HLLD) group.
The remaining patients (n = 1,121), who did not have these paradoxical associations, were analyzed separately.
For all patients, mean upper cervical cord area (MUCCA) was also measured. Using images acquired by a 3 T MRI scanner, MUCCA was calculated as the mean sum of spinal cord area in 21 slices centered at the C3/4 intervertebral disk, using an in-house, semiautomated method.
“Despite higher disability, LLHD patients demonstrated significantly higher normalized total brain volume, higher normalized volumes of thalamus and callosum, and smaller lateral ventricles than [the] HLLD group,” wrote Dr. Andelova and her collaborators.
However, the LLHD patients had MUCCA values that were significantly lower than the other groups: The nonparadoxical group’s mean MUCCA was 84.02 mm2, while the HLLD group had a mean MUCCA of 85.75 mm2. This difference was not statistically significant. By contrast, the LLHD group’s mean MUCCA was significantly smaller, at 80.40 mm2 (P = .023 versus nonparadoxical patients, and P = .007 versus HLLD patients).
Looking at the data another way, Dr. Andelova and her colleagues compared 362 evenly divided patients with moderate disability (EDSS 3.5-6.5) with matched patients who had mild MS-related disability (EDSS less than 3) and identical cerebral lesion loads. They found that MUCCA was significantly smaller in the moderate disability group (78.86 versus 84.44 mm2; P less than .001).
In addition to having identical lesions loads, the mild and moderate disability groups didn’t differ significantly in normalized total brain volume or regional brain volumes. The group with moderate disability did have slightly less white matter volume (P = .039), Dr. Andelova pointed out.
All differences found between groups retained statistical significance even after adjustment for such potential confounders as age, sex, and duration of disease, Dr. Andelova said.
“Reduced spinal cord volume may explain part of the clinical-radiological paradox in patients who have high disability despite low intracranial lesion load,” Dr. Andelova and her collaborators wrote. “In line with this finding, relatively preserved spinal cord volume may be associated with functional reserve and less physical disability in patients with low disability despite high cerebral lesion load.”
Further work looking more precisely at cerebral lesion distribution and quantitative MRI investigation of lesion distribution is in the works for Dr. Andelova and her collaborators. They are hoping to see some association between various distribution patterns and accelerated spinal atrophy.
The research was supported by the Czech government. Dr. Andelova and several of her collaborators reported financial relationships with pharmaceutical companies.
SOURCE: Andelova M et al. Mult Scler. 2018;24(Suppl 2):211, Abstract P477.
BERLIN – Spinal cord volume deficits in patients with multiple sclerosis may contribute to clinical disability that appears out of proportion to lesion load on brain imaging, according to new research.
In a pool of 362 patients with mild to moderate MS-related disability but identical white matter lesion load identified by MRI, those with higher disability had significantly lower spinal cord volumes when compared against those with disability scores in the mild range (P less than .001).
Though brain MRI is a key tool used to track disease severity and progression in MS, some patients have relatively high disability but a low burden of white matter intracerebral lesions on MRI. Little is known about spinal cord volume in MS patients with pronounced dissociation between intracerebral lesion load and disability, Michaela Andelova, MD, said in an interview during a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Andelova, of Charles University, Prague, said that she and her colleagues hypothesized that spinal cord volume would differ between patients who had varying levels of disability, despite identical white matter lesion load.
To test this, she and her colleagues looked at records of 1,245 patients with relapsing-remitting MS. They divided them into three groups by severity of clinical disability, and also by extent of cerebral T2 hyperintense lesion load. The investigators identified a group of patients (n = 53) whose total volume of T2-weighted hyperintense lesions was less than 3 mL, but whose Expanded Disability Status Scale (EDSS) scores were at least 3.5; this was the low lesion load/high disability (LLHD) group.
Dr. Andelova and her colleagues then identified another group of patients (n = 71) who had a volume of T2-weighted hyperintensities that was greater than 9 mL, but whose EDSS score was less than 1.5. This was the high lesion load/low disability (HLLD) group.
The remaining patients (n = 1,121), who did not have these paradoxical associations, were analyzed separately.
For all patients, mean upper cervical cord area (MUCCA) was also measured. Using images acquired by a 3 T MRI scanner, MUCCA was calculated as the mean sum of spinal cord area in 21 slices centered at the C3/4 intervertebral disk, using an in-house, semiautomated method.
“Despite higher disability, LLHD patients demonstrated significantly higher normalized total brain volume, higher normalized volumes of thalamus and callosum, and smaller lateral ventricles than [the] HLLD group,” wrote Dr. Andelova and her collaborators.
However, the LLHD patients had MUCCA values that were significantly lower than the other groups: The nonparadoxical group’s mean MUCCA was 84.02 mm2, while the HLLD group had a mean MUCCA of 85.75 mm2. This difference was not statistically significant. By contrast, the LLHD group’s mean MUCCA was significantly smaller, at 80.40 mm2 (P = .023 versus nonparadoxical patients, and P = .007 versus HLLD patients).
Looking at the data another way, Dr. Andelova and her colleagues compared 362 evenly divided patients with moderate disability (EDSS 3.5-6.5) with matched patients who had mild MS-related disability (EDSS less than 3) and identical cerebral lesion loads. They found that MUCCA was significantly smaller in the moderate disability group (78.86 versus 84.44 mm2; P less than .001).
In addition to having identical lesions loads, the mild and moderate disability groups didn’t differ significantly in normalized total brain volume or regional brain volumes. The group with moderate disability did have slightly less white matter volume (P = .039), Dr. Andelova pointed out.
All differences found between groups retained statistical significance even after adjustment for such potential confounders as age, sex, and duration of disease, Dr. Andelova said.
“Reduced spinal cord volume may explain part of the clinical-radiological paradox in patients who have high disability despite low intracranial lesion load,” Dr. Andelova and her collaborators wrote. “In line with this finding, relatively preserved spinal cord volume may be associated with functional reserve and less physical disability in patients with low disability despite high cerebral lesion load.”
Further work looking more precisely at cerebral lesion distribution and quantitative MRI investigation of lesion distribution is in the works for Dr. Andelova and her collaborators. They are hoping to see some association between various distribution patterns and accelerated spinal atrophy.
The research was supported by the Czech government. Dr. Andelova and several of her collaborators reported financial relationships with pharmaceutical companies.
SOURCE: Andelova M et al. Mult Scler. 2018;24(Suppl 2):211, Abstract P477.
BERLIN – Spinal cord volume deficits in patients with multiple sclerosis may contribute to clinical disability that appears out of proportion to lesion load on brain imaging, according to new research.
In a pool of 362 patients with mild to moderate MS-related disability but identical white matter lesion load identified by MRI, those with higher disability had significantly lower spinal cord volumes when compared against those with disability scores in the mild range (P less than .001).
Though brain MRI is a key tool used to track disease severity and progression in MS, some patients have relatively high disability but a low burden of white matter intracerebral lesions on MRI. Little is known about spinal cord volume in MS patients with pronounced dissociation between intracerebral lesion load and disability, Michaela Andelova, MD, said in an interview during a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Dr. Andelova, of Charles University, Prague, said that she and her colleagues hypothesized that spinal cord volume would differ between patients who had varying levels of disability, despite identical white matter lesion load.
To test this, she and her colleagues looked at records of 1,245 patients with relapsing-remitting MS. They divided them into three groups by severity of clinical disability, and also by extent of cerebral T2 hyperintense lesion load. The investigators identified a group of patients (n = 53) whose total volume of T2-weighted hyperintense lesions was less than 3 mL, but whose Expanded Disability Status Scale (EDSS) scores were at least 3.5; this was the low lesion load/high disability (LLHD) group.
Dr. Andelova and her colleagues then identified another group of patients (n = 71) who had a volume of T2-weighted hyperintensities that was greater than 9 mL, but whose EDSS score was less than 1.5. This was the high lesion load/low disability (HLLD) group.
The remaining patients (n = 1,121), who did not have these paradoxical associations, were analyzed separately.
For all patients, mean upper cervical cord area (MUCCA) was also measured. Using images acquired by a 3 T MRI scanner, MUCCA was calculated as the mean sum of spinal cord area in 21 slices centered at the C3/4 intervertebral disk, using an in-house, semiautomated method.
“Despite higher disability, LLHD patients demonstrated significantly higher normalized total brain volume, higher normalized volumes of thalamus and callosum, and smaller lateral ventricles than [the] HLLD group,” wrote Dr. Andelova and her collaborators.
However, the LLHD patients had MUCCA values that were significantly lower than the other groups: The nonparadoxical group’s mean MUCCA was 84.02 mm2, while the HLLD group had a mean MUCCA of 85.75 mm2. This difference was not statistically significant. By contrast, the LLHD group’s mean MUCCA was significantly smaller, at 80.40 mm2 (P = .023 versus nonparadoxical patients, and P = .007 versus HLLD patients).
Looking at the data another way, Dr. Andelova and her colleagues compared 362 evenly divided patients with moderate disability (EDSS 3.5-6.5) with matched patients who had mild MS-related disability (EDSS less than 3) and identical cerebral lesion loads. They found that MUCCA was significantly smaller in the moderate disability group (78.86 versus 84.44 mm2; P less than .001).
In addition to having identical lesions loads, the mild and moderate disability groups didn’t differ significantly in normalized total brain volume or regional brain volumes. The group with moderate disability did have slightly less white matter volume (P = .039), Dr. Andelova pointed out.
All differences found between groups retained statistical significance even after adjustment for such potential confounders as age, sex, and duration of disease, Dr. Andelova said.
“Reduced spinal cord volume may explain part of the clinical-radiological paradox in patients who have high disability despite low intracranial lesion load,” Dr. Andelova and her collaborators wrote. “In line with this finding, relatively preserved spinal cord volume may be associated with functional reserve and less physical disability in patients with low disability despite high cerebral lesion load.”
Further work looking more precisely at cerebral lesion distribution and quantitative MRI investigation of lesion distribution is in the works for Dr. Andelova and her collaborators. They are hoping to see some association between various distribution patterns and accelerated spinal atrophy.
The research was supported by the Czech government. Dr. Andelova and several of her collaborators reported financial relationships with pharmaceutical companies.
SOURCE: Andelova M et al. Mult Scler. 2018;24(Suppl 2):211, Abstract P477.
REPORTING FROM ECTRIMS 2018
Key clinical point:
Major finding: Moderate disability patients had lower spinal cord volumes than did those with mild disability but a similar intracerebral lesion load.
Study details: Retrospective study of 1,245 patients with relapsing-remitting MS.
Disclosures: The study was sponsored by a grant from the Czech government. Several authors, including Dr. Andelova, reported multiple financial relationships with pharmaceutical companies.
Source: Andelova M et al. Mult Scler. 2018;24(Suppl 2):211, Abstract P477.
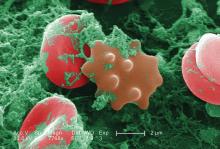
FDA approves DNA-based blood type test
The for use in transfusion.
It’s the second molecular test for blood compatibility but the first to report genotype in its results, according to an announcement from the agency.
The test is important because it evaluates patients – especially those who receive repeated blood transfusions for conditions such as sickle cell anemia – for non-ABO antigens, but it does so without using antisera, which is sometimes unavailable.
A study found comparable performance between the ID CORE XT, licensed serologic reagents, and DNA sequencing tests, according to the FDA.
The ID CORE XT test is marketed by Progenika Biopharma, a Grifols company.
More information can be found in the full FDA press announcement.
The for use in transfusion.
It’s the second molecular test for blood compatibility but the first to report genotype in its results, according to an announcement from the agency.
The test is important because it evaluates patients – especially those who receive repeated blood transfusions for conditions such as sickle cell anemia – for non-ABO antigens, but it does so without using antisera, which is sometimes unavailable.
A study found comparable performance between the ID CORE XT, licensed serologic reagents, and DNA sequencing tests, according to the FDA.
The ID CORE XT test is marketed by Progenika Biopharma, a Grifols company.
More information can be found in the full FDA press announcement.
The for use in transfusion.
It’s the second molecular test for blood compatibility but the first to report genotype in its results, according to an announcement from the agency.
The test is important because it evaluates patients – especially those who receive repeated blood transfusions for conditions such as sickle cell anemia – for non-ABO antigens, but it does so without using antisera, which is sometimes unavailable.
A study found comparable performance between the ID CORE XT, licensed serologic reagents, and DNA sequencing tests, according to the FDA.
The ID CORE XT test is marketed by Progenika Biopharma, a Grifols company.
More information can be found in the full FDA press announcement.
Oligoclonal bands, initial seizures increase risk of post-ADEM epilepsy in children
BERLIN – Children with acute disseminated encephalomyelitis have a significantly increased risk of subsequent epilepsy when it occurs with oligoclonal bands in cerebrospinal fluid and seizures at presentation, Thomas Rossor, MD, reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
But fortunately, the seizures of postacute disseminated encephalomyelitis (post-ADEM) epilepsy are relatively easy to control and not clinically devastating, said Dr. Rossor of Great Ormond Street Hospital, London.
Of the 12 who developed epilepsy in Dr. Rossor’s retrospective, multicenter review of 74 children with ADEM, 11 were well controlled on one drug and 1 on two drugs.
Pediatric ADEM is usually monophasic with good clinical outcome, he said. But a benign course is not set in stone: Up to 40% of children experience seizures during the acute presentation. “In contrast,” Dr. Rossor said, “adult patients with relapsing-remitting multiple sclerosis have the same risk of developing epilepsy as the general population.” Among adults with cortical encephalitis, antibodies against myelin oligodendrocyte glycoprotein (MOG) have been associated with seizures and the need for antiepileptic medications, he added.
That finding was part of what spurred Dr. Rossor’s study, which aimed to identify predictors of relapse and post-ADEM epilepsy in children. The patients in the review had a median age of 4.5 years. All were tested for anti-MOG antibodies, and most (about 68%) were positive. Oligoclonal bands in cerebrospinal fluid (CSF) occurred in 22%. The median follow-up period was 5 years.
A total of 41% (n = 31) relapsed after the initial acute phase. Among these, the final diagnosis included multiphasic disseminated encephalomyelitis (n = 19); ADEM-optic neuritis (n = 3); and neuromyelitis optica spectrum disorder (n = 6).
Of the 74 patients, 16 (22%) had seizures during the acute phase, and 12 (16%) developed post-ADEM epilepsy at a median of 3 months. The most common clinical characteristics with post-ADEM epilepsy included oligoclonal bands (57% vs. 13%), anti-MOG antibodies (92% vs. 16%), and seizures at presentation (50% vs. 16%). When these were entered into a regression model, oligoclonal bands and initial seizures significantly predicted epilepsy, increasing the risk by 20.7 and 13.5 times, respectively.
Since relapse is known to be associated with post-ADEM epilepsy, Dr. Rossor first looked at relapse risk. He conducted a multivariate analysis that included several clinical characteristics: age, prodrome, increased CSF white cells and protein, oligoclonal bands, anti-MOG antibodies, and seizures both at presentation and after the acute phase.
Anti-MOG antibodies were significantly more common among the relapsed patients than among the monophasic patients (87% vs. 53%). Seizures at presentation also were more common among the relapsed patients (32% vs. 14%). These two factors were entered into a binary regression analysis; only anti-MOG antibodies remained significantly associated with relapse, increasing the risk fivefold (odds ratio = 5.4; P = .007).
Anti-MOG antibodies also were associated with both earlier and more relapses. Overall, 40% of anti–MOG-antibody–positive patients relapsed by 24 months. In contrast, only 20% of anti–MOG-antibody–negative patients had relapsed by 24 months, and this number remained steady throughout the follow-up period.
By 96 months, almost all the anti–MOG-antibody–positive patients had relapsed, and some experienced many relapses. “In the antibody-negative group, four patients did relapse, but they had relatively few relapses. In the antibody-positive group, some had relatively few relapses, but several had 15, 20, or 25 clinical relapses in the follow-up period,” he said.
Dr. Rossor and his coauthors had no financial disclosures.
SOURCE: Rossor T et al. Mult Scler. 2018;24(Suppl 2):27. Abstract 62.
BERLIN – Children with acute disseminated encephalomyelitis have a significantly increased risk of subsequent epilepsy when it occurs with oligoclonal bands in cerebrospinal fluid and seizures at presentation, Thomas Rossor, MD, reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
But fortunately, the seizures of postacute disseminated encephalomyelitis (post-ADEM) epilepsy are relatively easy to control and not clinically devastating, said Dr. Rossor of Great Ormond Street Hospital, London.
Of the 12 who developed epilepsy in Dr. Rossor’s retrospective, multicenter review of 74 children with ADEM, 11 were well controlled on one drug and 1 on two drugs.
Pediatric ADEM is usually monophasic with good clinical outcome, he said. But a benign course is not set in stone: Up to 40% of children experience seizures during the acute presentation. “In contrast,” Dr. Rossor said, “adult patients with relapsing-remitting multiple sclerosis have the same risk of developing epilepsy as the general population.” Among adults with cortical encephalitis, antibodies against myelin oligodendrocyte glycoprotein (MOG) have been associated with seizures and the need for antiepileptic medications, he added.
That finding was part of what spurred Dr. Rossor’s study, which aimed to identify predictors of relapse and post-ADEM epilepsy in children. The patients in the review had a median age of 4.5 years. All were tested for anti-MOG antibodies, and most (about 68%) were positive. Oligoclonal bands in cerebrospinal fluid (CSF) occurred in 22%. The median follow-up period was 5 years.
A total of 41% (n = 31) relapsed after the initial acute phase. Among these, the final diagnosis included multiphasic disseminated encephalomyelitis (n = 19); ADEM-optic neuritis (n = 3); and neuromyelitis optica spectrum disorder (n = 6).
Of the 74 patients, 16 (22%) had seizures during the acute phase, and 12 (16%) developed post-ADEM epilepsy at a median of 3 months. The most common clinical characteristics with post-ADEM epilepsy included oligoclonal bands (57% vs. 13%), anti-MOG antibodies (92% vs. 16%), and seizures at presentation (50% vs. 16%). When these were entered into a regression model, oligoclonal bands and initial seizures significantly predicted epilepsy, increasing the risk by 20.7 and 13.5 times, respectively.
Since relapse is known to be associated with post-ADEM epilepsy, Dr. Rossor first looked at relapse risk. He conducted a multivariate analysis that included several clinical characteristics: age, prodrome, increased CSF white cells and protein, oligoclonal bands, anti-MOG antibodies, and seizures both at presentation and after the acute phase.
Anti-MOG antibodies were significantly more common among the relapsed patients than among the monophasic patients (87% vs. 53%). Seizures at presentation also were more common among the relapsed patients (32% vs. 14%). These two factors were entered into a binary regression analysis; only anti-MOG antibodies remained significantly associated with relapse, increasing the risk fivefold (odds ratio = 5.4; P = .007).
Anti-MOG antibodies also were associated with both earlier and more relapses. Overall, 40% of anti–MOG-antibody–positive patients relapsed by 24 months. In contrast, only 20% of anti–MOG-antibody–negative patients had relapsed by 24 months, and this number remained steady throughout the follow-up period.
By 96 months, almost all the anti–MOG-antibody–positive patients had relapsed, and some experienced many relapses. “In the antibody-negative group, four patients did relapse, but they had relatively few relapses. In the antibody-positive group, some had relatively few relapses, but several had 15, 20, or 25 clinical relapses in the follow-up period,” he said.
Dr. Rossor and his coauthors had no financial disclosures.
SOURCE: Rossor T et al. Mult Scler. 2018;24(Suppl 2):27. Abstract 62.
BERLIN – Children with acute disseminated encephalomyelitis have a significantly increased risk of subsequent epilepsy when it occurs with oligoclonal bands in cerebrospinal fluid and seizures at presentation, Thomas Rossor, MD, reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
But fortunately, the seizures of postacute disseminated encephalomyelitis (post-ADEM) epilepsy are relatively easy to control and not clinically devastating, said Dr. Rossor of Great Ormond Street Hospital, London.
Of the 12 who developed epilepsy in Dr. Rossor’s retrospective, multicenter review of 74 children with ADEM, 11 were well controlled on one drug and 1 on two drugs.
Pediatric ADEM is usually monophasic with good clinical outcome, he said. But a benign course is not set in stone: Up to 40% of children experience seizures during the acute presentation. “In contrast,” Dr. Rossor said, “adult patients with relapsing-remitting multiple sclerosis have the same risk of developing epilepsy as the general population.” Among adults with cortical encephalitis, antibodies against myelin oligodendrocyte glycoprotein (MOG) have been associated with seizures and the need for antiepileptic medications, he added.
That finding was part of what spurred Dr. Rossor’s study, which aimed to identify predictors of relapse and post-ADEM epilepsy in children. The patients in the review had a median age of 4.5 years. All were tested for anti-MOG antibodies, and most (about 68%) were positive. Oligoclonal bands in cerebrospinal fluid (CSF) occurred in 22%. The median follow-up period was 5 years.
A total of 41% (n = 31) relapsed after the initial acute phase. Among these, the final diagnosis included multiphasic disseminated encephalomyelitis (n = 19); ADEM-optic neuritis (n = 3); and neuromyelitis optica spectrum disorder (n = 6).
Of the 74 patients, 16 (22%) had seizures during the acute phase, and 12 (16%) developed post-ADEM epilepsy at a median of 3 months. The most common clinical characteristics with post-ADEM epilepsy included oligoclonal bands (57% vs. 13%), anti-MOG antibodies (92% vs. 16%), and seizures at presentation (50% vs. 16%). When these were entered into a regression model, oligoclonal bands and initial seizures significantly predicted epilepsy, increasing the risk by 20.7 and 13.5 times, respectively.
Since relapse is known to be associated with post-ADEM epilepsy, Dr. Rossor first looked at relapse risk. He conducted a multivariate analysis that included several clinical characteristics: age, prodrome, increased CSF white cells and protein, oligoclonal bands, anti-MOG antibodies, and seizures both at presentation and after the acute phase.
Anti-MOG antibodies were significantly more common among the relapsed patients than among the monophasic patients (87% vs. 53%). Seizures at presentation also were more common among the relapsed patients (32% vs. 14%). These two factors were entered into a binary regression analysis; only anti-MOG antibodies remained significantly associated with relapse, increasing the risk fivefold (odds ratio = 5.4; P = .007).
Anti-MOG antibodies also were associated with both earlier and more relapses. Overall, 40% of anti–MOG-antibody–positive patients relapsed by 24 months. In contrast, only 20% of anti–MOG-antibody–negative patients had relapsed by 24 months, and this number remained steady throughout the follow-up period.
By 96 months, almost all the anti–MOG-antibody–positive patients had relapsed, and some experienced many relapses. “In the antibody-negative group, four patients did relapse, but they had relatively few relapses. In the antibody-positive group, some had relatively few relapses, but several had 15, 20, or 25 clinical relapses in the follow-up period,” he said.
Dr. Rossor and his coauthors had no financial disclosures.
SOURCE: Rossor T et al. Mult Scler. 2018;24(Suppl 2):27. Abstract 62.
REPORTING FROM ECTRIMS 2018
Key clinical point: .
Major finding: Oligoclonal bands in CSF increased the risk of post-ADEM epilepsy by more than 20 times.
Study details: The retrospective cohort review comprised 74 children.
Disclosures: Dr. Rossor and his coauthors had no financial disclosures.
Source: Rossor T et al. Mult Scler. 2018;24(Suppl 2):27. Abstract 62.
Primary, metastatic ccRCC share mutational features
A comparison of the genomic landscapes of both primary and metastatic clear cell renal cell carcinoma (ccRCC) found no significant differences in gene expression or mutational burden between the disease states, suggesting that there is no single genetic driver of metastases, investigators reported.
An analysis of targeted next-generation sequencing of both primary tumors and metastases in two independent patient cohorts showed that only the gene encoding for the tumor suppressor TP53 was significantly more frequently mutated in metastases, compared with primary tumors, but this finding did not pass a false positive test (false discovery rate), noted Toni K. Choueiri, MD, from the Dana-Farber Cancer Institute in Boston, and his colleagues, in the British Journal of Cancer.
“No other gene had significant difference in the cohort frequency of mutations between the metastases and primary tumors. Mutation burden was not significantly different between the metastases and primary tumors or between metastatic sites,” they wrote.
Frequently mutated genes in ccRCC include VHL, the gene encoding for von Hippel–Lindau syndrome, as well as tumor suppressor genes such as PBRM1, SEDT2, BAP1 and KDM5C, but few mutations are clinically actionable, the investigators noted. “However, the value of genomic alterations will be determined by understanding the interactions between acquired genetic alterations, treatments received, heterogeneity, and the dynamics of mutations during evolution of disease.”
To see whether they could improve understanding of the genomic differences between primary and metastatic ccRCC and potentially develop personalized therapies, the investigators studied targeted next-generation sequencing data from two separate cohorts.
The first cohort included data on 349 ccRCC primary tumors and 229 unmatched cases of metastatic ccRCC from the Foundation Medicine database. The second, a validation cohort, included data on 177 ccRCC primary tumors and 80 metastases from patients treated at Dana-Farber. In each cohort, sequencing was performed on 275 genes and intronic regions in 30 genes for a total of 282 unique genes.
In cohort 1, which included tumor samples from 417 men and 169 women with a median age of 58 years, the frequency of mutations was similar in primary tumors and metastases. As noted before, mutations in TP53 were significantly more frequent in metastases than in primary tumors, detected in 14.85% versus 8.90% of samples, respectively (P = .031). This difference did not, however, pass the false discovery rate test (q = 0.21). Two other tumor suppressor genes, PBRM1 and KDM5C, were numerically but not significantly more frequent in metastases.
There were no differences in median tumor mutational burden between primary and metastatic samples and no difference in either mutations or mutational burden across different metastatic sites.
In cohort 2 there were no significantly different mutational frequencies between primary and metastatic samples for any gene and no differences in median tumor mutational burden.
An analysis comparing the frequency of gene mutations in primary tumors of patients in this cohort who went on to develop metastatic disease versus those of patients with only localized disease showed that, after a median follow-up of 21.9 months, there were no significant differences in either mutational frequency or tumor mutational burden.
“It is currently unknown if cohortwide genomic alterations in RCC metastases have a different genomic profile, including potential actionable mutations, compared to samples derived from the primary site. To our knowledge, our analysis is the largest genomic ccRCC study that compares cohortwide mutational differences between metastases and primary tumors,” the investigators wrote.
They acknowledged that because they did not match primary tumors with metastatic tumors in the same patients they were unable to evaluate how individual tumors evolve over time or how systemic therapies may alter the tumor genomic landscape.
Dr. Choueri is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, and Loker Pinard Funds for Kidney Cancer Research at the Dana-Farber Cancer Institute. Six of the study’s coauthors are employed by Foundation Medicine. The remaining authors declared no competing interests.
SOURCE: Choueiri TK et al. Br J Cancer. 2018 May;118(9):1238-42.
A comparison of the genomic landscapes of both primary and metastatic clear cell renal cell carcinoma (ccRCC) found no significant differences in gene expression or mutational burden between the disease states, suggesting that there is no single genetic driver of metastases, investigators reported.
An analysis of targeted next-generation sequencing of both primary tumors and metastases in two independent patient cohorts showed that only the gene encoding for the tumor suppressor TP53 was significantly more frequently mutated in metastases, compared with primary tumors, but this finding did not pass a false positive test (false discovery rate), noted Toni K. Choueiri, MD, from the Dana-Farber Cancer Institute in Boston, and his colleagues, in the British Journal of Cancer.
“No other gene had significant difference in the cohort frequency of mutations between the metastases and primary tumors. Mutation burden was not significantly different between the metastases and primary tumors or between metastatic sites,” they wrote.
Frequently mutated genes in ccRCC include VHL, the gene encoding for von Hippel–Lindau syndrome, as well as tumor suppressor genes such as PBRM1, SEDT2, BAP1 and KDM5C, but few mutations are clinically actionable, the investigators noted. “However, the value of genomic alterations will be determined by understanding the interactions between acquired genetic alterations, treatments received, heterogeneity, and the dynamics of mutations during evolution of disease.”
To see whether they could improve understanding of the genomic differences between primary and metastatic ccRCC and potentially develop personalized therapies, the investigators studied targeted next-generation sequencing data from two separate cohorts.
The first cohort included data on 349 ccRCC primary tumors and 229 unmatched cases of metastatic ccRCC from the Foundation Medicine database. The second, a validation cohort, included data on 177 ccRCC primary tumors and 80 metastases from patients treated at Dana-Farber. In each cohort, sequencing was performed on 275 genes and intronic regions in 30 genes for a total of 282 unique genes.
In cohort 1, which included tumor samples from 417 men and 169 women with a median age of 58 years, the frequency of mutations was similar in primary tumors and metastases. As noted before, mutations in TP53 were significantly more frequent in metastases than in primary tumors, detected in 14.85% versus 8.90% of samples, respectively (P = .031). This difference did not, however, pass the false discovery rate test (q = 0.21). Two other tumor suppressor genes, PBRM1 and KDM5C, were numerically but not significantly more frequent in metastases.
There were no differences in median tumor mutational burden between primary and metastatic samples and no difference in either mutations or mutational burden across different metastatic sites.
In cohort 2 there were no significantly different mutational frequencies between primary and metastatic samples for any gene and no differences in median tumor mutational burden.
An analysis comparing the frequency of gene mutations in primary tumors of patients in this cohort who went on to develop metastatic disease versus those of patients with only localized disease showed that, after a median follow-up of 21.9 months, there were no significant differences in either mutational frequency or tumor mutational burden.
“It is currently unknown if cohortwide genomic alterations in RCC metastases have a different genomic profile, including potential actionable mutations, compared to samples derived from the primary site. To our knowledge, our analysis is the largest genomic ccRCC study that compares cohortwide mutational differences between metastases and primary tumors,” the investigators wrote.
They acknowledged that because they did not match primary tumors with metastatic tumors in the same patients they were unable to evaluate how individual tumors evolve over time or how systemic therapies may alter the tumor genomic landscape.
Dr. Choueri is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, and Loker Pinard Funds for Kidney Cancer Research at the Dana-Farber Cancer Institute. Six of the study’s coauthors are employed by Foundation Medicine. The remaining authors declared no competing interests.
SOURCE: Choueiri TK et al. Br J Cancer. 2018 May;118(9):1238-42.
A comparison of the genomic landscapes of both primary and metastatic clear cell renal cell carcinoma (ccRCC) found no significant differences in gene expression or mutational burden between the disease states, suggesting that there is no single genetic driver of metastases, investigators reported.
An analysis of targeted next-generation sequencing of both primary tumors and metastases in two independent patient cohorts showed that only the gene encoding for the tumor suppressor TP53 was significantly more frequently mutated in metastases, compared with primary tumors, but this finding did not pass a false positive test (false discovery rate), noted Toni K. Choueiri, MD, from the Dana-Farber Cancer Institute in Boston, and his colleagues, in the British Journal of Cancer.
“No other gene had significant difference in the cohort frequency of mutations between the metastases and primary tumors. Mutation burden was not significantly different between the metastases and primary tumors or between metastatic sites,” they wrote.
Frequently mutated genes in ccRCC include VHL, the gene encoding for von Hippel–Lindau syndrome, as well as tumor suppressor genes such as PBRM1, SEDT2, BAP1 and KDM5C, but few mutations are clinically actionable, the investigators noted. “However, the value of genomic alterations will be determined by understanding the interactions between acquired genetic alterations, treatments received, heterogeneity, and the dynamics of mutations during evolution of disease.”
To see whether they could improve understanding of the genomic differences between primary and metastatic ccRCC and potentially develop personalized therapies, the investigators studied targeted next-generation sequencing data from two separate cohorts.
The first cohort included data on 349 ccRCC primary tumors and 229 unmatched cases of metastatic ccRCC from the Foundation Medicine database. The second, a validation cohort, included data on 177 ccRCC primary tumors and 80 metastases from patients treated at Dana-Farber. In each cohort, sequencing was performed on 275 genes and intronic regions in 30 genes for a total of 282 unique genes.
In cohort 1, which included tumor samples from 417 men and 169 women with a median age of 58 years, the frequency of mutations was similar in primary tumors and metastases. As noted before, mutations in TP53 were significantly more frequent in metastases than in primary tumors, detected in 14.85% versus 8.90% of samples, respectively (P = .031). This difference did not, however, pass the false discovery rate test (q = 0.21). Two other tumor suppressor genes, PBRM1 and KDM5C, were numerically but not significantly more frequent in metastases.
There were no differences in median tumor mutational burden between primary and metastatic samples and no difference in either mutations or mutational burden across different metastatic sites.
In cohort 2 there were no significantly different mutational frequencies between primary and metastatic samples for any gene and no differences in median tumor mutational burden.
An analysis comparing the frequency of gene mutations in primary tumors of patients in this cohort who went on to develop metastatic disease versus those of patients with only localized disease showed that, after a median follow-up of 21.9 months, there were no significant differences in either mutational frequency or tumor mutational burden.
“It is currently unknown if cohortwide genomic alterations in RCC metastases have a different genomic profile, including potential actionable mutations, compared to samples derived from the primary site. To our knowledge, our analysis is the largest genomic ccRCC study that compares cohortwide mutational differences between metastases and primary tumors,” the investigators wrote.
They acknowledged that because they did not match primary tumors with metastatic tumors in the same patients they were unable to evaluate how individual tumors evolve over time or how systemic therapies may alter the tumor genomic landscape.
Dr. Choueri is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, and Loker Pinard Funds for Kidney Cancer Research at the Dana-Farber Cancer Institute. Six of the study’s coauthors are employed by Foundation Medicine. The remaining authors declared no competing interests.
SOURCE: Choueiri TK et al. Br J Cancer. 2018 May;118(9):1238-42.
FROM THE BRITISH JOURNAL OF CANCER
Key clinical point: There does not appear to be a single-gene driver of metastases in patients with clear cell renal cell carcinoma.
Major finding: There were no significant differences in mutational frequency or tumor mutational burden between primary and metastatic clear cell renal cell carcinoma.
Study details: A targeted next-generation sequencing analysis of data from two independent patient cohorts.
Disclosures: Dr. Choueri is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, and Loker Pinard Funds for Kidney Cancer Research at the Dana-Farber Cancer Institute. Six of the study’s coauthors are employed by Foundation Medicine. The remaining authors reported no competing interests.
Source: Choueiri TK et al. Br J Cancer. 2018 May;118(9):1238-42.
Do Dimethyl Fumarate and Teriflunomide Have Equivalent Efficacy?
New T2 lesions are more likely on teriflunomide, which may contribute to its higher rate of discontinuation.
BERLIN—Dimethyl fumarate and teriflunomide have similar efficacy in terms of risk of relapse and worsening of Expanded Disability Status Scale (EDSS) score after one and two years of treatment, according to data presented at ECTRIMS 2018. Significantly more patients have new T2 lesions after two years of teriflunomide, however, compared with dimethyl fumarate, and this outcome may explain an increased treatment withdrawal for lack of efficacy among patients receiving teriflunomide.
Teriflunomide and dimethyl fumarate have been approved as first-line treatments for patients with relapsing-remitting multiple sclerosis (MS). To date, no randomized controlled nor observational studies have compared their relative efficacies. David A. Laplaud, MD, PhD, a team leader at the Center of Research in Transplantation and Immunology in Nantes, France, and colleagues conducted a study to compare the effects of teriflunomide and dimethyl fumarate on clinical and MRI outcomes in patients with relapsing-remitting MS from 34 MS centers participating in the French prospective national cohort of MS patients.
The investigators included 1,770 patients with relapsing-remitting MS in the study. In all, 713 participants received teriflunomide, and 1,057 received dimethyl fumarate. Participants were aged 18 to 65 and had an EDSS score of 0 to 5.5 and an available brain MRI performed within six months before treatment initiation. The outcomes under investigation were the proportion of patients with at least one relapse in the year and the two years following teriflunomide or dimethyl fumarate initiation, the proportion of patients with at least one new T2 lesion at one and two years, the number of patients with an increased EDSS score at one and two years, and reasons for treatment cessation at one and two years. For statistical analyses, the outcomes were modeled with propensity scores and logistic regressions by using weighted likelihood maximization and a robust variance estimator.
The confounder-adjusted proportion of patients with at least one relapse at one and two years of treatment was similar in the teriflunomide group and the dimethyl fumarate group (21.6% vs 20.2% for the first year, 30.4% vs 29.5% at two years). Likewise, a similar percentage of patients had an increase of EDSS score at one and two years in the teriflunomide group (27.4% and 41.6%, respectively) and the dimethyl fumarate group (27.1% and 40.6%, respectively). MRI comparisons, however, revealed that the confounder-adjusted proportion of patients with at least one new T2 lesion at two years was significantly lower in patients treated with dimethyl fumarate, compared with teriflunomide (60.8% vs 72.2%; odds ratio [OR], 0.6). The reason for treatment withdrawal at two years was lack of efficacy in 8.5% of patients who received dimethyl fumarate versus 14.5% of patients who received teriflunomide (OR, 0.54).
New T2 lesions are more likely on teriflunomide, which may contribute to its higher rate of discontinuation.
New T2 lesions are more likely on teriflunomide, which may contribute to its higher rate of discontinuation.
BERLIN—Dimethyl fumarate and teriflunomide have similar efficacy in terms of risk of relapse and worsening of Expanded Disability Status Scale (EDSS) score after one and two years of treatment, according to data presented at ECTRIMS 2018. Significantly more patients have new T2 lesions after two years of teriflunomide, however, compared with dimethyl fumarate, and this outcome may explain an increased treatment withdrawal for lack of efficacy among patients receiving teriflunomide.
Teriflunomide and dimethyl fumarate have been approved as first-line treatments for patients with relapsing-remitting multiple sclerosis (MS). To date, no randomized controlled nor observational studies have compared their relative efficacies. David A. Laplaud, MD, PhD, a team leader at the Center of Research in Transplantation and Immunology in Nantes, France, and colleagues conducted a study to compare the effects of teriflunomide and dimethyl fumarate on clinical and MRI outcomes in patients with relapsing-remitting MS from 34 MS centers participating in the French prospective national cohort of MS patients.
The investigators included 1,770 patients with relapsing-remitting MS in the study. In all, 713 participants received teriflunomide, and 1,057 received dimethyl fumarate. Participants were aged 18 to 65 and had an EDSS score of 0 to 5.5 and an available brain MRI performed within six months before treatment initiation. The outcomes under investigation were the proportion of patients with at least one relapse in the year and the two years following teriflunomide or dimethyl fumarate initiation, the proportion of patients with at least one new T2 lesion at one and two years, the number of patients with an increased EDSS score at one and two years, and reasons for treatment cessation at one and two years. For statistical analyses, the outcomes were modeled with propensity scores and logistic regressions by using weighted likelihood maximization and a robust variance estimator.
The confounder-adjusted proportion of patients with at least one relapse at one and two years of treatment was similar in the teriflunomide group and the dimethyl fumarate group (21.6% vs 20.2% for the first year, 30.4% vs 29.5% at two years). Likewise, a similar percentage of patients had an increase of EDSS score at one and two years in the teriflunomide group (27.4% and 41.6%, respectively) and the dimethyl fumarate group (27.1% and 40.6%, respectively). MRI comparisons, however, revealed that the confounder-adjusted proportion of patients with at least one new T2 lesion at two years was significantly lower in patients treated with dimethyl fumarate, compared with teriflunomide (60.8% vs 72.2%; odds ratio [OR], 0.6). The reason for treatment withdrawal at two years was lack of efficacy in 8.5% of patients who received dimethyl fumarate versus 14.5% of patients who received teriflunomide (OR, 0.54).
BERLIN—Dimethyl fumarate and teriflunomide have similar efficacy in terms of risk of relapse and worsening of Expanded Disability Status Scale (EDSS) score after one and two years of treatment, according to data presented at ECTRIMS 2018. Significantly more patients have new T2 lesions after two years of teriflunomide, however, compared with dimethyl fumarate, and this outcome may explain an increased treatment withdrawal for lack of efficacy among patients receiving teriflunomide.
Teriflunomide and dimethyl fumarate have been approved as first-line treatments for patients with relapsing-remitting multiple sclerosis (MS). To date, no randomized controlled nor observational studies have compared their relative efficacies. David A. Laplaud, MD, PhD, a team leader at the Center of Research in Transplantation and Immunology in Nantes, France, and colleagues conducted a study to compare the effects of teriflunomide and dimethyl fumarate on clinical and MRI outcomes in patients with relapsing-remitting MS from 34 MS centers participating in the French prospective national cohort of MS patients.
The investigators included 1,770 patients with relapsing-remitting MS in the study. In all, 713 participants received teriflunomide, and 1,057 received dimethyl fumarate. Participants were aged 18 to 65 and had an EDSS score of 0 to 5.5 and an available brain MRI performed within six months before treatment initiation. The outcomes under investigation were the proportion of patients with at least one relapse in the year and the two years following teriflunomide or dimethyl fumarate initiation, the proportion of patients with at least one new T2 lesion at one and two years, the number of patients with an increased EDSS score at one and two years, and reasons for treatment cessation at one and two years. For statistical analyses, the outcomes were modeled with propensity scores and logistic regressions by using weighted likelihood maximization and a robust variance estimator.
The confounder-adjusted proportion of patients with at least one relapse at one and two years of treatment was similar in the teriflunomide group and the dimethyl fumarate group (21.6% vs 20.2% for the first year, 30.4% vs 29.5% at two years). Likewise, a similar percentage of patients had an increase of EDSS score at one and two years in the teriflunomide group (27.4% and 41.6%, respectively) and the dimethyl fumarate group (27.1% and 40.6%, respectively). MRI comparisons, however, revealed that the confounder-adjusted proportion of patients with at least one new T2 lesion at two years was significantly lower in patients treated with dimethyl fumarate, compared with teriflunomide (60.8% vs 72.2%; odds ratio [OR], 0.6). The reason for treatment withdrawal at two years was lack of efficacy in 8.5% of patients who received dimethyl fumarate versus 14.5% of patients who received teriflunomide (OR, 0.54).
Task force advises behavioral intervention for obese adults
The U.S. Preventive Services Task Force advises clinicians to refer or offer intensive behavioral weight-loss interventions to obese adults, according to an updated recommendation statement published in JAMA.
Obesity affects more than one-third of U.S. adults, according to federal statistics. It carries increased risk for comorbidities including heart disease, diabetes, and various cancers, as well as increased risk of death among adults younger than 65 years, noted lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and members of the Task Force.
The B recommendation applies to obese adults; obesity was defined as a body mass index of 30 kg/m2 or higher. The evidence review focused on interventions for weight loss and weight maintenance that could be provided in primary care or referred from primary care, such as nutrition counseling, exercise strategies, and goal setting.
The Task Force found adequate evidence that behavior-based weight-loss interventions improved weight, reduced incidence of type 2 diabetes, and helped maintain weight loss after interventions ended.
The Task Force found small to no evidence of harm associated with any of the behavioral weight-loss interventions, which included group sessions, personal sessions, print-based interventions, and technology-based interventions (such as text messages). Although interventions that combined drug therapy with behavioral intervention resulted in greater weight loss over 12-18 months, compared with behavioral interventions alone, the attrition rates were high and data on weight-loss maintenance after discontinuation of the drugs were limited, the Task Force noted.
“As a result, the USPSTF encourages clinicians to promote behavioral interventions as the primary focus of effective interventions for weight loss in adults,” they wrote.
The Task Force acknowledged the need for future research in subgroups and to explore whether factors such as genetics and untreated conditions are barriers to behavior-based weight loss interventions.
In the evidence review published in JAMA, Erin S. LeBlanc, MD, of Kaiser Permanente in Portland, Ore., and her colleagues reviewed data from 122 randomized, controlled trials including more than 62,000 persons and 2 observational studies including more than 209,000 persons.
The researchers found behavioral interventions were associated with greater weight loss and less risk of developing diabetes, compared with control interventions.
Intensive behavioral interventions included counseling patients about healthy eating, encouraging physical activity, setting weight and health goals, and assisting with weight monitoring. The interventions ranged from text messaging to in-person sessions for individuals or groups. The average absolute weight loss in the trials included in the review ranged from –0.5 kg to –9.3 kg (–1.1 lb to –20.5 lb) for intervention patients and from +1.4 kg to –5.6 kg (+3.1 lb to –12.3 lb) in controls.
Limitations of the review included a lack of data on population subgroups and a lack of long-term data on weight and health outcomes, the researchers noted. However, the results support the value of behavior-based therapy for obesity treatment.
The final recommendation is consistent with the 2018 draft recommendation and updates the 2012 final recommendation on obesity management.
The researchers and Task Force members had no relevant financial conflicts to disclose.
SOURCE: U.S. Preventive Services Task Force. JAMA. 2018;320(11):1163-71. doi: 10.1001/jama.2018.13022.
In the USPSTF Recommendation Statement on Behavioral Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults the Task Force updates their 2012 statement and recommends that patients with obesity be referred for intensive, multicomponent behavioral weight loss interventions and weight loss maintenance. Reiterating the importance of intensive behavioral and lifestyle support is to be commended and should be the cornerstone of treatment for people with overweight disorders. As thoughtfully discussed in accompanying editorials by Haire-Joshu, Hill-Briggs, and Yanovski, moving from recommendation to reality will require access to high-quality programs for patients of all socioeconomic and ethnic backgrounds, less restrictive reimbursement for services, and broader involvement of the public health and food industry sectors.
However, the task force recommendations were limited in scope: they pertained to people with obesity defined as a BMI greater than 30 kg/m2, to those without diagnosed obesity-associated disorders, and to patients seen in a primary care setting. This lessens the impact of the report for a disease which continues to be epidemic in the United States. Leaving out the overweight pre-obese in whom efforts toward prevention are essential, as well as people with obesity who have coexisting comorbidities restricts the recommendations to one slice of the large obesity pie. As more high-quality data pertaining to a broader range of people impacted by overweight disorders become available, more expansive guidelines for treatment will be important.
Furthermore, while behavioral weight loss interventions are meaningful, they fall short for many in bringing about sustained efficacy. The primary care setting should include referral for appropriate patients to be evaluated for combined multidisciplinary behavioral and surgical, endoscopic, or pharmacologic therapies that can improve clinical outcomes for those refractory to behavioral weight loss interventions alone. Finally, tackling the obesity epidemic requires that health care providers across a broad range of specialties become involved in a coordinated effort to help our patients. As digestive disease specialists treating a myriad of obesity-related diseases from fatty liver to colorectal cancer, we too need to help address the underlying disease by providing obesity therapy within our practices or making referrals for its multidisciplinary treatment.
Sarah Streett, MD, AGAF, clinical associate professor of medicine, division of gastroenterology and hepatology, Stanford University School of Medicine, Stanford, Calif. She has no relevant disclosures.
In the USPSTF Recommendation Statement on Behavioral Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults the Task Force updates their 2012 statement and recommends that patients with obesity be referred for intensive, multicomponent behavioral weight loss interventions and weight loss maintenance. Reiterating the importance of intensive behavioral and lifestyle support is to be commended and should be the cornerstone of treatment for people with overweight disorders. As thoughtfully discussed in accompanying editorials by Haire-Joshu, Hill-Briggs, and Yanovski, moving from recommendation to reality will require access to high-quality programs for patients of all socioeconomic and ethnic backgrounds, less restrictive reimbursement for services, and broader involvement of the public health and food industry sectors.
However, the task force recommendations were limited in scope: they pertained to people with obesity defined as a BMI greater than 30 kg/m2, to those without diagnosed obesity-associated disorders, and to patients seen in a primary care setting. This lessens the impact of the report for a disease which continues to be epidemic in the United States. Leaving out the overweight pre-obese in whom efforts toward prevention are essential, as well as people with obesity who have coexisting comorbidities restricts the recommendations to one slice of the large obesity pie. As more high-quality data pertaining to a broader range of people impacted by overweight disorders become available, more expansive guidelines for treatment will be important.
Furthermore, while behavioral weight loss interventions are meaningful, they fall short for many in bringing about sustained efficacy. The primary care setting should include referral for appropriate patients to be evaluated for combined multidisciplinary behavioral and surgical, endoscopic, or pharmacologic therapies that can improve clinical outcomes for those refractory to behavioral weight loss interventions alone. Finally, tackling the obesity epidemic requires that health care providers across a broad range of specialties become involved in a coordinated effort to help our patients. As digestive disease specialists treating a myriad of obesity-related diseases from fatty liver to colorectal cancer, we too need to help address the underlying disease by providing obesity therapy within our practices or making referrals for its multidisciplinary treatment.
Sarah Streett, MD, AGAF, clinical associate professor of medicine, division of gastroenterology and hepatology, Stanford University School of Medicine, Stanford, Calif. She has no relevant disclosures.
In the USPSTF Recommendation Statement on Behavioral Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults the Task Force updates their 2012 statement and recommends that patients with obesity be referred for intensive, multicomponent behavioral weight loss interventions and weight loss maintenance. Reiterating the importance of intensive behavioral and lifestyle support is to be commended and should be the cornerstone of treatment for people with overweight disorders. As thoughtfully discussed in accompanying editorials by Haire-Joshu, Hill-Briggs, and Yanovski, moving from recommendation to reality will require access to high-quality programs for patients of all socioeconomic and ethnic backgrounds, less restrictive reimbursement for services, and broader involvement of the public health and food industry sectors.
However, the task force recommendations were limited in scope: they pertained to people with obesity defined as a BMI greater than 30 kg/m2, to those without diagnosed obesity-associated disorders, and to patients seen in a primary care setting. This lessens the impact of the report for a disease which continues to be epidemic in the United States. Leaving out the overweight pre-obese in whom efforts toward prevention are essential, as well as people with obesity who have coexisting comorbidities restricts the recommendations to one slice of the large obesity pie. As more high-quality data pertaining to a broader range of people impacted by overweight disorders become available, more expansive guidelines for treatment will be important.
Furthermore, while behavioral weight loss interventions are meaningful, they fall short for many in bringing about sustained efficacy. The primary care setting should include referral for appropriate patients to be evaluated for combined multidisciplinary behavioral and surgical, endoscopic, or pharmacologic therapies that can improve clinical outcomes for those refractory to behavioral weight loss interventions alone. Finally, tackling the obesity epidemic requires that health care providers across a broad range of specialties become involved in a coordinated effort to help our patients. As digestive disease specialists treating a myriad of obesity-related diseases from fatty liver to colorectal cancer, we too need to help address the underlying disease by providing obesity therapy within our practices or making referrals for its multidisciplinary treatment.
Sarah Streett, MD, AGAF, clinical associate professor of medicine, division of gastroenterology and hepatology, Stanford University School of Medicine, Stanford, Calif. She has no relevant disclosures.
The U.S. Preventive Services Task Force advises clinicians to refer or offer intensive behavioral weight-loss interventions to obese adults, according to an updated recommendation statement published in JAMA.
Obesity affects more than one-third of U.S. adults, according to federal statistics. It carries increased risk for comorbidities including heart disease, diabetes, and various cancers, as well as increased risk of death among adults younger than 65 years, noted lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and members of the Task Force.
The B recommendation applies to obese adults; obesity was defined as a body mass index of 30 kg/m2 or higher. The evidence review focused on interventions for weight loss and weight maintenance that could be provided in primary care or referred from primary care, such as nutrition counseling, exercise strategies, and goal setting.
The Task Force found adequate evidence that behavior-based weight-loss interventions improved weight, reduced incidence of type 2 diabetes, and helped maintain weight loss after interventions ended.
The Task Force found small to no evidence of harm associated with any of the behavioral weight-loss interventions, which included group sessions, personal sessions, print-based interventions, and technology-based interventions (such as text messages). Although interventions that combined drug therapy with behavioral intervention resulted in greater weight loss over 12-18 months, compared with behavioral interventions alone, the attrition rates were high and data on weight-loss maintenance after discontinuation of the drugs were limited, the Task Force noted.
“As a result, the USPSTF encourages clinicians to promote behavioral interventions as the primary focus of effective interventions for weight loss in adults,” they wrote.
The Task Force acknowledged the need for future research in subgroups and to explore whether factors such as genetics and untreated conditions are barriers to behavior-based weight loss interventions.
In the evidence review published in JAMA, Erin S. LeBlanc, MD, of Kaiser Permanente in Portland, Ore., and her colleagues reviewed data from 122 randomized, controlled trials including more than 62,000 persons and 2 observational studies including more than 209,000 persons.
The researchers found behavioral interventions were associated with greater weight loss and less risk of developing diabetes, compared with control interventions.
Intensive behavioral interventions included counseling patients about healthy eating, encouraging physical activity, setting weight and health goals, and assisting with weight monitoring. The interventions ranged from text messaging to in-person sessions for individuals or groups. The average absolute weight loss in the trials included in the review ranged from –0.5 kg to –9.3 kg (–1.1 lb to –20.5 lb) for intervention patients and from +1.4 kg to –5.6 kg (+3.1 lb to –12.3 lb) in controls.
Limitations of the review included a lack of data on population subgroups and a lack of long-term data on weight and health outcomes, the researchers noted. However, the results support the value of behavior-based therapy for obesity treatment.
The final recommendation is consistent with the 2018 draft recommendation and updates the 2012 final recommendation on obesity management.
The researchers and Task Force members had no relevant financial conflicts to disclose.
SOURCE: U.S. Preventive Services Task Force. JAMA. 2018;320(11):1163-71. doi: 10.1001/jama.2018.13022.
The U.S. Preventive Services Task Force advises clinicians to refer or offer intensive behavioral weight-loss interventions to obese adults, according to an updated recommendation statement published in JAMA.
Obesity affects more than one-third of U.S. adults, according to federal statistics. It carries increased risk for comorbidities including heart disease, diabetes, and various cancers, as well as increased risk of death among adults younger than 65 years, noted lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and members of the Task Force.
The B recommendation applies to obese adults; obesity was defined as a body mass index of 30 kg/m2 or higher. The evidence review focused on interventions for weight loss and weight maintenance that could be provided in primary care or referred from primary care, such as nutrition counseling, exercise strategies, and goal setting.
The Task Force found adequate evidence that behavior-based weight-loss interventions improved weight, reduced incidence of type 2 diabetes, and helped maintain weight loss after interventions ended.
The Task Force found small to no evidence of harm associated with any of the behavioral weight-loss interventions, which included group sessions, personal sessions, print-based interventions, and technology-based interventions (such as text messages). Although interventions that combined drug therapy with behavioral intervention resulted in greater weight loss over 12-18 months, compared with behavioral interventions alone, the attrition rates were high and data on weight-loss maintenance after discontinuation of the drugs were limited, the Task Force noted.
“As a result, the USPSTF encourages clinicians to promote behavioral interventions as the primary focus of effective interventions for weight loss in adults,” they wrote.
The Task Force acknowledged the need for future research in subgroups and to explore whether factors such as genetics and untreated conditions are barriers to behavior-based weight loss interventions.
In the evidence review published in JAMA, Erin S. LeBlanc, MD, of Kaiser Permanente in Portland, Ore., and her colleagues reviewed data from 122 randomized, controlled trials including more than 62,000 persons and 2 observational studies including more than 209,000 persons.
The researchers found behavioral interventions were associated with greater weight loss and less risk of developing diabetes, compared with control interventions.
Intensive behavioral interventions included counseling patients about healthy eating, encouraging physical activity, setting weight and health goals, and assisting with weight monitoring. The interventions ranged from text messaging to in-person sessions for individuals or groups. The average absolute weight loss in the trials included in the review ranged from –0.5 kg to –9.3 kg (–1.1 lb to –20.5 lb) for intervention patients and from +1.4 kg to –5.6 kg (+3.1 lb to –12.3 lb) in controls.
Limitations of the review included a lack of data on population subgroups and a lack of long-term data on weight and health outcomes, the researchers noted. However, the results support the value of behavior-based therapy for obesity treatment.
The final recommendation is consistent with the 2018 draft recommendation and updates the 2012 final recommendation on obesity management.
The researchers and Task Force members had no relevant financial conflicts to disclose.
SOURCE: U.S. Preventive Services Task Force. JAMA. 2018;320(11):1163-71. doi: 10.1001/jama.2018.13022.
FROM JAMA
Cortical Damage at Onset May Indicate Risk of Secondary Progressive MS
This observation may aid patient stratification and guide the choice of appropriate therapy.
BERLIN—Widespread focal cortical damage at multiple sclerosis (MS) onset identifies patients likely to have frequent early relapses and a rapid development of progressive disease, which results from worsening global cortical pathology over time, according to a study presented at ECTRIMS 2018. The results provide a basis for patient stratification with the goal of therapeutic optimization. In addition, the data “highlight the importance of elucidating mechanisms involved in early cortical pathology,” according to the investigators.
Following Patients With Relapsing-Remitting MS
Among patients with relapsing-remitting MS, a high frequency of early relapses is associated with increased risk of developing severe disability, which suggests that early biologic mechanisms influence long-term disease evolution. Antonio Scalfari, MD, PhD, a consultant neurologist at Imperial College Healthcare in London, and colleagues sought to investigate the relationship between early cortical pathology, early relapses, and the risk of converting to secondary progressive MS.
Dr. Scalfari and colleagues examined 219 patients with relapsing-remitting MS. Participants had one (n = 116), two (n = 53), or three or more (n = 50) relapses during the first two years. Follow-up lasted for a mean of 7.9 years. The researchers assessed the number of cortical lesions and white matter lesions and the rate of cortical thinning using 3D double inversion recovery, 3D T1-weighted imaging, and Freesurfer analysis.
Cortical Lesions Predicted Cortical Thinning
During the observation period, 59 (27%) patients converted to secondary progressive MS in a mean of 6.1 years. At disease onset, the investigators detected 674 cortical lesions in 166 (76%) patients. A larger number of cortical lesions was associated with a significantly higher risk of secondary progressive MS. The hazard ratios (HR) for secondary progressive MS were 2.16 for patients with two lesions, 4.79 for patients with five lesions, and 12.3 for patients with seven lesions. A large number of cortical lesions also was associated with shorter latency to secondary progressive MS and a faster rate of global cortical thinning. The mean loss per year was 0.93% for patients with no lesions, 0.99% for patients with one to three lesions, 1.13% for patients with four to six lesions, and 1.33% for patients with seven or more lesions. In the group with no cortical lesions (n = 53), no patients entered the secondary progressive phase, and four reached an Expanded Disability Status Scale score of 4.
Patients with a high number of early relapses, compared with those with low and moderate numbers, had a larger volume of white matter lesions and cortical lesions at onset. The mean volumes of cortical lesions were 181.6 mm3, 386.8 mm3, and 544.0 mm3 for patients with one, two, and three or more early relapses, respectively. Patients with a high number of early relapses also accrued more cortical lesions (mean cortical lesion volumes were 118.8 mm3, 138.8 mm3, and 790.5 mm3 for patients with one, two, and three or more early relapses, respectively), had a faster rate of cortical atrophy (mean loss/year was 0.47%, 0.79%, and 0.94% for patients with one, two, and three or more early relapses, respectively), and entered the secondary progressive phase more rapidly.
In the multivariate model, older age at onset (HR, 1.97), a larger baseline cortical lesion (HR, 2.21) and white matter lesion (HR, 1.32) volume, early changes of global cortical thickness (HR, 1.36), and three or more early relapses (HR, 6.08) independently predicted a higher probability of secondary progressive MS.
This observation may aid patient stratification and guide the choice of appropriate therapy.
This observation may aid patient stratification and guide the choice of appropriate therapy.
BERLIN—Widespread focal cortical damage at multiple sclerosis (MS) onset identifies patients likely to have frequent early relapses and a rapid development of progressive disease, which results from worsening global cortical pathology over time, according to a study presented at ECTRIMS 2018. The results provide a basis for patient stratification with the goal of therapeutic optimization. In addition, the data “highlight the importance of elucidating mechanisms involved in early cortical pathology,” according to the investigators.
Following Patients With Relapsing-Remitting MS
Among patients with relapsing-remitting MS, a high frequency of early relapses is associated with increased risk of developing severe disability, which suggests that early biologic mechanisms influence long-term disease evolution. Antonio Scalfari, MD, PhD, a consultant neurologist at Imperial College Healthcare in London, and colleagues sought to investigate the relationship between early cortical pathology, early relapses, and the risk of converting to secondary progressive MS.
Dr. Scalfari and colleagues examined 219 patients with relapsing-remitting MS. Participants had one (n = 116), two (n = 53), or three or more (n = 50) relapses during the first two years. Follow-up lasted for a mean of 7.9 years. The researchers assessed the number of cortical lesions and white matter lesions and the rate of cortical thinning using 3D double inversion recovery, 3D T1-weighted imaging, and Freesurfer analysis.
Cortical Lesions Predicted Cortical Thinning
During the observation period, 59 (27%) patients converted to secondary progressive MS in a mean of 6.1 years. At disease onset, the investigators detected 674 cortical lesions in 166 (76%) patients. A larger number of cortical lesions was associated with a significantly higher risk of secondary progressive MS. The hazard ratios (HR) for secondary progressive MS were 2.16 for patients with two lesions, 4.79 for patients with five lesions, and 12.3 for patients with seven lesions. A large number of cortical lesions also was associated with shorter latency to secondary progressive MS and a faster rate of global cortical thinning. The mean loss per year was 0.93% for patients with no lesions, 0.99% for patients with one to three lesions, 1.13% for patients with four to six lesions, and 1.33% for patients with seven or more lesions. In the group with no cortical lesions (n = 53), no patients entered the secondary progressive phase, and four reached an Expanded Disability Status Scale score of 4.
Patients with a high number of early relapses, compared with those with low and moderate numbers, had a larger volume of white matter lesions and cortical lesions at onset. The mean volumes of cortical lesions were 181.6 mm3, 386.8 mm3, and 544.0 mm3 for patients with one, two, and three or more early relapses, respectively. Patients with a high number of early relapses also accrued more cortical lesions (mean cortical lesion volumes were 118.8 mm3, 138.8 mm3, and 790.5 mm3 for patients with one, two, and three or more early relapses, respectively), had a faster rate of cortical atrophy (mean loss/year was 0.47%, 0.79%, and 0.94% for patients with one, two, and three or more early relapses, respectively), and entered the secondary progressive phase more rapidly.
In the multivariate model, older age at onset (HR, 1.97), a larger baseline cortical lesion (HR, 2.21) and white matter lesion (HR, 1.32) volume, early changes of global cortical thickness (HR, 1.36), and three or more early relapses (HR, 6.08) independently predicted a higher probability of secondary progressive MS.
BERLIN—Widespread focal cortical damage at multiple sclerosis (MS) onset identifies patients likely to have frequent early relapses and a rapid development of progressive disease, which results from worsening global cortical pathology over time, according to a study presented at ECTRIMS 2018. The results provide a basis for patient stratification with the goal of therapeutic optimization. In addition, the data “highlight the importance of elucidating mechanisms involved in early cortical pathology,” according to the investigators.
Following Patients With Relapsing-Remitting MS
Among patients with relapsing-remitting MS, a high frequency of early relapses is associated with increased risk of developing severe disability, which suggests that early biologic mechanisms influence long-term disease evolution. Antonio Scalfari, MD, PhD, a consultant neurologist at Imperial College Healthcare in London, and colleagues sought to investigate the relationship between early cortical pathology, early relapses, and the risk of converting to secondary progressive MS.
Dr. Scalfari and colleagues examined 219 patients with relapsing-remitting MS. Participants had one (n = 116), two (n = 53), or three or more (n = 50) relapses during the first two years. Follow-up lasted for a mean of 7.9 years. The researchers assessed the number of cortical lesions and white matter lesions and the rate of cortical thinning using 3D double inversion recovery, 3D T1-weighted imaging, and Freesurfer analysis.
Cortical Lesions Predicted Cortical Thinning
During the observation period, 59 (27%) patients converted to secondary progressive MS in a mean of 6.1 years. At disease onset, the investigators detected 674 cortical lesions in 166 (76%) patients. A larger number of cortical lesions was associated with a significantly higher risk of secondary progressive MS. The hazard ratios (HR) for secondary progressive MS were 2.16 for patients with two lesions, 4.79 for patients with five lesions, and 12.3 for patients with seven lesions. A large number of cortical lesions also was associated with shorter latency to secondary progressive MS and a faster rate of global cortical thinning. The mean loss per year was 0.93% for patients with no lesions, 0.99% for patients with one to three lesions, 1.13% for patients with four to six lesions, and 1.33% for patients with seven or more lesions. In the group with no cortical lesions (n = 53), no patients entered the secondary progressive phase, and four reached an Expanded Disability Status Scale score of 4.
Patients with a high number of early relapses, compared with those with low and moderate numbers, had a larger volume of white matter lesions and cortical lesions at onset. The mean volumes of cortical lesions were 181.6 mm3, 386.8 mm3, and 544.0 mm3 for patients with one, two, and three or more early relapses, respectively. Patients with a high number of early relapses also accrued more cortical lesions (mean cortical lesion volumes were 118.8 mm3, 138.8 mm3, and 790.5 mm3 for patients with one, two, and three or more early relapses, respectively), had a faster rate of cortical atrophy (mean loss/year was 0.47%, 0.79%, and 0.94% for patients with one, two, and three or more early relapses, respectively), and entered the secondary progressive phase more rapidly.
In the multivariate model, older age at onset (HR, 1.97), a larger baseline cortical lesion (HR, 2.21) and white matter lesion (HR, 1.32) volume, early changes of global cortical thickness (HR, 1.36), and three or more early relapses (HR, 6.08) independently predicted a higher probability of secondary progressive MS.