User login
Providing Pain and Palliative Care Education Internationally
Volume 9, Issue 4, July-August 2011, Pages 129-133
How we do it
Judith A. Paice PhD, RN![]()
Available online 2 July 2011.
Article Outline
For many clinicians in oncology, educating other health-care professionals about cancer pain and palliative care is part of their professional life. The need for education exists across clinical settings around the world. Improved education is an urgent need as the prevalence of cancer is increasing. This burden is largely carried by the developing world, where resources are often limited.[1] Global educational efforts, including managing common symptoms, communication, care at the time of death, grief, and other topics, are imperative to reduce pain and suffering.[2] International training efforts require additional expertise and preparation beyond the standard teaching skills needed for all professional education.
The goal of international training efforts in pain and palliative care is to provide useful, culturally relevant programs while empowering participants to sustain these efforts in the long term. Global efforts in palliative care have demonstrated that sharing educational materials, resources, support and encouragement with our international colleagues can provide mentorship to go beyond simply attending a course to developing and expanding their own programs of palliative care in oncology.[3] and [4] To do this well, the following provides specific suggestions for before, during, and after international palliative care training experiences.
Do Your Homework
Before a course, it is essential to learn as much as possible about the region, the culture(s), and the health-care system. Several resources for this information are listed in Table 1. Additionally, speaking with colleagues who have traveled to the country or to those who have emigrated from the country can provide valuable insight. These individuals can provide a wealth of information to assist in developing an appropriate curriculum and specific presentations. As demographics vary, it is important to know the common cancers and other leading causes of death in the region. Issues that may be seen as “competing” issues HIV/AIDS, malaria, immunizations, lack of clean water, or maternal–infant mortality.[5] and [6] Literature, including fiction and nonfiction, as well as movies and other media, can enlighten the traveler regarding life in the region. Local consulates offer opportunities for learning, as do organizations such as the Council on Global Relations. There are rapid changes in global politics, health-care systems, and governments, so it is also vital to have current information.
| American Society for Clinical Oncology (ASCO) | Offers international cancer courses as well as fellowships and other awards. |
| Centers for Disease Control and Prevention (CDC), http://wwwnc.cdc.gov/travel/ | Provides information regarding common infectious illnesses, traveler's alerts. |
| Central Intelligence Agency (CIA), The World Factbook, https://www.cia.gov/library/publications/the-world-factbook/ | Excellent review of a country's political, demographic, geographic, and other attributes. |
| City of Hope Pain & Palliative Care Resource Center, http://prc.coh.org/ | Provides a clearinghouse that includes a wide array of resources and references to enhance pain and palliative care education and research. |
| End of Life Nursing Education Consortium (ELNEC), http://www.aacn.nche.edu/elnec/ | Includes relevant articles, resources, and a summary of current international ELNEC training programs. |
| International Association for Hospice and Palliative Care (IAHPC), http://www.hospicecare.com/ | Numerous global palliative care resources, including List of Essential Medicines, Global Directory of Educational Programs in Palliative Care, Global Directory of Palliative Care Providers/Services/Organizations, as well as Palliative Care in the Developing World: Principles and Practice. |
| International Association for the Study of Pain (IASP), http://www.iasp-pain.org/ | Strong emphasis on support of developing countries with research and educational grants; publishes a Guide to Pain Management in Low-Resource Settings offered without cost. |
| Open Society Institute–International Palliative Care Initiative, http://www.soros.org/initiatives/health/focus/ipci/about | Offers support for training, clinical care, and research in palliative care, alone and in collaboration with other organizations. |
| Pain & Policy Studies Group, http://www.painpolicy.wisc.edu/ | Excellent resource for information regarding opioid consumption by country as well as guidelines for policies that allow access to necessary medications. |
| U.S. Department of State, http://www.usembassy.gov/ Bureau of Consular Affairs, http://travel.state.gov/travel/travel_1744.html | Comprehensive lists of US embassies, consulates, and diplomatic missions; information to assist travelers from the United States to other countries, including visa requirements and safety alerts. |
| World Health Organization, http://www.who.int | Many useful resources, including Access to Analgesics and to other Controlled Medicines, as well as statistics regarding common illnesses by country. |
Health-Care Structure
Understand the existing health-care structure and what health care is available to all or for select populations. What is the extent of health-care services? Are there clinics for preventive care, or is most care obtained in the hospital? Is home care available with support from nurses and other professionals? Are emergency services available (eg, does the region have ambulances to transport and emergency departments to accept critically ill patients)? Where do patients obtain medications, and do they have to pay out of pocket for these? Do most people die in the hospital or at home? While websites and government sources are valuable, verify this information with clinicians since the clinical reality may be quite different.
Available Medications
To provide useful guidance in symptom management, it is necessary to have a list of available medications used to treat pain, nausea, dyspnea, constipation/diarrhea, wounds, and other symptoms commonly seen in oncology. Your presentation may need to be modified based upon these available drugs (Table 2). Where do patients obtain medications, and do they pay out of pocket for these? There are limitations on availability and access to opioids around the world.[7] Which opioids are available and actually used? What is the process for obtaining a supply of an opioid for a person with cancer? For example, in some countries, physicians can order only one week's worth of medication at a time. In other countries, patients must obtain opioids from the police station rather than a pharmacy. In several settings, only the patient, not family members, can pick up the medication from the dispensing site. And in a few countries, only parenteral opioids are available. It is also helpful to understand issues such as the prevalence of drug trafficking in the region and how this might affect local drug laws. Are traditional medicines, such as herbal therapies, or other techniques commonly used? It is helpful to be aware of these practices and incorporate them into teaching plans where appropriate.
Education of Health-Care Professionals
International education in palliative care should consider how physicians, nurses, pharmacists, and others are educated. Is the educational system very traditional and formal, with little interaction between students and teachers? Professionals trained in this manner may be less comfortable when faced with role-play, learning through discussion, or other Socratic educational methods. That does not mean that one should exclude these methods when planning the curriculum but, rather, be prepared for silence and possibly even discomfort when first introduced. Seek guidance from local educators as to what methods will be acceptable.
Who is included in the health-care team? Are psychologists available, and are chaplains considered part of health-care services? What is the relationship between physicians, nurses, and other team members? Is collegiality accepted, or is there a hierarchy that limits true teamwork? What is the status of physicians, nurses, and other professionals in the region? In some areas, physicians are highly regarded and financially compensated accordingly. In other parts of the world, physicians have very low social status, respect, and compensation. Within diverse cultures, compensation and acceptance of tips (or bribes) to see a patient or perform an intervention may be accepted practice. Attitudes toward work hours may differ from the Western perspective. In some cultures, socialization and development of personal relationships may be considered more important than other aspects of the workload.[8]
Planning in advance to know the targeted attendees is helpful. It is advisable to inquire if the hosts might consider inviting representatives from the ministry of health, the appropriate drug institutes, other key government officials, as well as medical, nursing, and pharmacy leaders who can become champions for access to pain relief and palliative care. Having multiple disciplines and leaders from health care and government at the same program can foster ongoing communication and understanding. Include chief educators as they can incorporate this content into their respective curricula.
Plan the Curriculum and the Program
The importance of cultural issues when developing content cannot be overstated.[9] Factors that might affect pain expression and language or cultural beliefs about death and dying will greatly impact content for teaching. Be aware of local religious and spiritual beliefs impacting pain and palliative care. Consider issues surrounding disclosure of diagnosis and prognosis. Autonomy may not be the prevailing perspective as seen in North America. Ensure that slides are culturally correct and that pictures and illustrations are appropriate. Having the host country leaders review the curriculum in advance is advisable. Avoid cartoons as these may not translate well. Use case examples, but ensure that they represent the types of patients and scenarios seen by the audience. It is also important to avoid being ethnocentric as Western medicine has much to learn from other approaches. It is very helpful to use case studies from the host country. In some settings, trainers will not have access to computers and projectors, limiting the role of PowerPoint slides. Paper presentations or the use of flip-charts may be more accessible.
Consider the need for translation and, if so, which type will be used. Simultaneous interpretation generally requires a sound booth and headphones for participants, and may be more expensive. Consecutive interpretation requires that the instructor present blocks of information, usually a sentence or two, followed by the interpreter providing the content in the appropriate language. This requires speakers to plan much shorter presentations with up to 50% less content being delivered. In either case, trained interpreters can benefit from seeing the slides in advance so they can prepare and clarify prior to the presentation.
When developing an agenda, inquire about the usual times for breaks and meals, as well as time for prayers or other activities. What is considered a “full day” varies around the world, as does the value of adhering rigidly to a schedule. International education generally means that the agenda is fluid; once you are actually in the country and providing the course, other needs may arise. A common mistake is trying to squeeze in too much content. Ask your host to meet prior to the program and, optimally, plan for time before the course to tour health-care facilities. Arrange for a time to meet with key medical, nursing, pharmacy, and governmental leaders who are not scheduled to attend the meeting but might somehow influence curricula and practice. In some settings, local media may be alerted to generate local interest in the topic. Communicate with your host about these opportunities so that arrangements can be made in advance.
For resource-poor countries, consider asking for donations from colleagues before leaving, including books, CDs, and medical supplies. Check local regulations first, particularly if bringing in medications or equipment. If sending books, some countries require high tariff fees to be paid by the receiver when accepting these packages, creating a financial burden for your hosts. Inquire ahead of time if they have to pay to accept these packages. Additionally, in some resource-poor countries, professionals do not have access to personal or work computers and internet café computers often do not have CD drives. Information on jump drives may be more easily accessible.
Finally, visiting educators may want to pack small gifts to give to hosts and others. These should be easily transported and may include items that represent your city or institution. We have also found bringing candy and small toys to be universally appreciated when visiting pediatric settings. A small portable color printer can be used to print photographs of pediatric patients as some of these children have never seen pictures of themselves. You can also print photographs of participants in the training courses.
Personal Considerations
Several months prior to departure, you should contact your traveler's health information resource to identify which vaccinations and what documents are needed to enter the country. To avoid lost time due to illness, ciprofloxacin and antidiarrheal medicines should be obtained before traveling. It is advisable to update your passport. Some countries require you to have sufficient blank pages in your passport to allow entry into their country. An entry fee paid in cash may be required upon arrival. Travelers should consider the political climate of the country and check the U.S. Department of State website (included in Table 1) for alerts or precautions.
Consider appropriate attire when packing. Clothing should reflect respect for the cultural and religious beliefs of the attendees.
During the Experience
It is very useful to meet with interpreters prior to the presentations to clarify any questions. Translation can be quite complicated. For example, a slide that used the term “caring” was interpreted as “romantic love,” and concepts about suffering and death can take on a cultural meaning. Check with interpreters regularly to determine if the speed of delivery is acceptable. Also, translators may have difficulty with this emotional content. In some instances, interpreters have become tearful and required debriefing after palliative care education events. Consider nonverbal communication and personal space. In some cultures, it may not be appropriate to shake hands or to use two hands. Gestures may have very different meanings in other cultures, so avoid these forms of communication. For example, the “OK” sign commonly used in North America, with the tip of the finger touching the tip of the thumb and the other three fingers extended, is considered an obscene gesture in Brazil.
When using teaching strategies other than lecture, respect that some students may not be comfortable at first with nontraditional approaches. Informal teaching strategies that are valued in North America may be viewed as of poor academic quality in other cultures. Debate and discussion, which may make it seem that the student is questioning a teacher's view, may be seen as disrespectful. At times, eliciting personal reflection and experience can engage the audience. For example, when introducing the topic of communication, health-care professionals in the audience can be asked the following questions:
- • If you had cancer, would you want to know?
• Would you want to know that you had a disease that you could die from?
Following these with “What do you tell your patients?” usually engenders excellent discussion.
We have also found that asking participants to do “homework” can be useful, particularly if the students have been quiet or reluctant to communicate during class. Suggested assignments might include listing the five top barriers to cancer pain management in your setting, describing a difficult death or a death that you made better, or related issues. Reticence to speak during class may be due to discomfort with language skills. Some students feel more comfortable sharing ideas in writing, and these assignments have yielded valuable stories that have helped us to understand their experiences and perspectives.
Since the goal of these educational efforts should be sustained, it is helpful to develop a plan for the future with students. Assist them in identifying goals, as well as action items to meet these goals. Allow time for individual meetings between faculty and students to fine-tune these efforts. This ensures that the educational experience will have a greater likelihood of translation into action. To provide practical assistance, if Internet access is available, spend time with small groups to demonstrate literature searches, useful websites, and other information that will foster continuity.
Faculty should meet after each day of training to modify the planned agenda as needed, to optimally meet the needs of the participants. This also provides needed time to debrief about the day's activities and provide support. Particularly when new to international education, the experience may be overwhelming as the status of health-care in developing countries can cause deep personal reflection.
Finally, celebrate. We have found that many students appreciate the opportunity to have some type of closing ceremony to receive certificates and pins, acknowledge their accomplishments, and encourage their future efforts.
Afterward
E-mail, voiceover Internet services, and videoconferencing software have significantly enhanced global communication. Faculty can make themselves available to the trainees after leaving the country using these technologies. Group conversations via e-mail can help solve problems, provide encouragement, and celebrate successes. Connect attendees with international professional organizations to support ongoing educational efforts. It is very useful to identify the leaders or champions and to plan ongoing support to help sustain their commitment. Many countries do not have professional organizations or support networks. These leaders can exist in isolation and suffer great personal sacrifice to lead palliative care efforts in their country.
Conclusion
When educating about pain and palliative care to a worldwide audience, never make assumptions, expect the unexpected, and be flexible. We have found many of these international teaching experiences to be some of the most exhilarating of our professional lives, providing insight to our own practices and creating lasting relationships with colleagues from around the globe. Ultimately, these efforts will improve care for people with cancer.
Acknowledgments
The authors acknowledge the American Association of Colleges of Nursing and the City of Hope for their ongoing support of the End-of-Life Nursing Education Consortium training activities, as well as the Oncology Nursing Society Foundation and the Open Society Institute for their support of international educational efforts. They also thank Marian Grant for her input.
References [Pub Med ID in Brackets]
1 A.L. Taylor, L.O. Gostin and K.A. Pagonis, Ensuring effective pain treatment: a national and global perspective, JAMA 299 (2008), pp. 89–91 [18167410].
2 K. Crane, Palliative care gains ground in developing countries, J Natl Cancer Inst 102 (21) (2010), pp. 1613–1615 [20966432].
3 J.A. Paice, B.R. Ferrell, N. Coyle, P. Coyne and M. Callaway, Global efforts to improve palliative care: the International End-of-Life Nursing Education Consortium training programme, J Adv Nurs 61 (2007), pp. 173–180 [18186909].
4 J.A. Paice, B. Ferrell, N. Coyle, P. Coyne and T. Smith, Living and dying in East Africa: implementing the End-of-Life Nursing Education Consortium curriculum in Tanzania, Clin J Oncol Nurs 14 (2010), pp. 161–166 [20350889].
5 C. Olweny, C. Sepulveda, A. Merriman, S. Fonn, M. Borok, T. Ngoma, A. Doh and J. Stjernsward, Desirable services and guidelines for the treatment and palliative care of HIV disease patients with cancer in Africa: a World Health Organization consultation, J Palliat Care 19 (2003), pp. 198–205 [14606333].
6 C. Sepulveda, V. Habiyatmbete, J. Amandua, M. Borok, E. Kikule, B. Mudanga and B. Solomon, Quality care at the end of life in Africa, BMJ 327 (2003), pp. 209–213 [12881267].
7 E.L. Krakauer, R. Wenk, R. Buitrago, P. Jenkins and W. Scholten, Opioid inaccessibility and its human consequences: reports from the field, J Pain Palliat Care Pharmacother 24 (2010), pp. 239–243 [20718644].
8 C.M. Bolin, Developing a postbasic gerontology program for international learners: considerations for the process, J Contin Educ Nurs 34 (2003), pp. 177–183 [12887229].
9 K.D. Meneses and C.H. Yarbro, Cultural perspectives of international breast health and breast cancer education, J Nurs Scholarsh 39 (2) (2007), pp. 105–112 [19058079].
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
![]()
Vitae
Dr. Paice is Director of the Cancer Pain Program, Division of Hematology-Oncology, Northwestern University, Feinberg School of Medicine, Chicago, Illinois.
Carma Erickson-Hurt is a faculty member at Grand Canyon University, Phoenix, Arizona.
Dr. Ferrell is a Professor and Research Scientist at the City of Hope National Medical Center, Duarte, California.
Nessa Coyle is on the Pain and Palliative Care Service, Department of Medicine, Memorial Sloan-Kettering Cancer Center, New York.
Dr. Coyne is Clinical Director of the Thomas Palliative Care Program, Virginia Commonwealth University/Massey Cancer Center, Richmond, Virginia.
Dr. Long is a geriatric nursing consultant and codirector of the Palliative Care for Advanced Dementia, Beatitudes Campus, Phoenix, Arizona.
Dr. Mazanec is a clinical nurse specialist at the University Hospitals Seidman Cancer Center, Cleveland, Ohio.
Pam Malloy is ELNEC Project Director, American Association of Colleges of Nursing, Washington, DC.
Dr. Smith is Professor of Medicine and Palliative Care Research, Virginia Commonwealth University/Massey Cancer Center, Richmond.
Volume 9, Issue 4, July-August 2011, Pages 129-133
How we do it
Judith A. Paice PhD, RN![]()
Available online 2 July 2011.
Article Outline
For many clinicians in oncology, educating other health-care professionals about cancer pain and palliative care is part of their professional life. The need for education exists across clinical settings around the world. Improved education is an urgent need as the prevalence of cancer is increasing. This burden is largely carried by the developing world, where resources are often limited.[1] Global educational efforts, including managing common symptoms, communication, care at the time of death, grief, and other topics, are imperative to reduce pain and suffering.[2] International training efforts require additional expertise and preparation beyond the standard teaching skills needed for all professional education.
The goal of international training efforts in pain and palliative care is to provide useful, culturally relevant programs while empowering participants to sustain these efforts in the long term. Global efforts in palliative care have demonstrated that sharing educational materials, resources, support and encouragement with our international colleagues can provide mentorship to go beyond simply attending a course to developing and expanding their own programs of palliative care in oncology.[3] and [4] To do this well, the following provides specific suggestions for before, during, and after international palliative care training experiences.
Do Your Homework
Before a course, it is essential to learn as much as possible about the region, the culture(s), and the health-care system. Several resources for this information are listed in Table 1. Additionally, speaking with colleagues who have traveled to the country or to those who have emigrated from the country can provide valuable insight. These individuals can provide a wealth of information to assist in developing an appropriate curriculum and specific presentations. As demographics vary, it is important to know the common cancers and other leading causes of death in the region. Issues that may be seen as “competing” issues HIV/AIDS, malaria, immunizations, lack of clean water, or maternal–infant mortality.[5] and [6] Literature, including fiction and nonfiction, as well as movies and other media, can enlighten the traveler regarding life in the region. Local consulates offer opportunities for learning, as do organizations such as the Council on Global Relations. There are rapid changes in global politics, health-care systems, and governments, so it is also vital to have current information.
| American Society for Clinical Oncology (ASCO) | Offers international cancer courses as well as fellowships and other awards. |
| Centers for Disease Control and Prevention (CDC), http://wwwnc.cdc.gov/travel/ | Provides information regarding common infectious illnesses, traveler's alerts. |
| Central Intelligence Agency (CIA), The World Factbook, https://www.cia.gov/library/publications/the-world-factbook/ | Excellent review of a country's political, demographic, geographic, and other attributes. |
| City of Hope Pain & Palliative Care Resource Center, http://prc.coh.org/ | Provides a clearinghouse that includes a wide array of resources and references to enhance pain and palliative care education and research. |
| End of Life Nursing Education Consortium (ELNEC), http://www.aacn.nche.edu/elnec/ | Includes relevant articles, resources, and a summary of current international ELNEC training programs. |
| International Association for Hospice and Palliative Care (IAHPC), http://www.hospicecare.com/ | Numerous global palliative care resources, including List of Essential Medicines, Global Directory of Educational Programs in Palliative Care, Global Directory of Palliative Care Providers/Services/Organizations, as well as Palliative Care in the Developing World: Principles and Practice. |
| International Association for the Study of Pain (IASP), http://www.iasp-pain.org/ | Strong emphasis on support of developing countries with research and educational grants; publishes a Guide to Pain Management in Low-Resource Settings offered without cost. |
| Open Society Institute–International Palliative Care Initiative, http://www.soros.org/initiatives/health/focus/ipci/about | Offers support for training, clinical care, and research in palliative care, alone and in collaboration with other organizations. |
| Pain & Policy Studies Group, http://www.painpolicy.wisc.edu/ | Excellent resource for information regarding opioid consumption by country as well as guidelines for policies that allow access to necessary medications. |
| U.S. Department of State, http://www.usembassy.gov/ Bureau of Consular Affairs, http://travel.state.gov/travel/travel_1744.html | Comprehensive lists of US embassies, consulates, and diplomatic missions; information to assist travelers from the United States to other countries, including visa requirements and safety alerts. |
| World Health Organization, http://www.who.int | Many useful resources, including Access to Analgesics and to other Controlled Medicines, as well as statistics regarding common illnesses by country. |
Health-Care Structure
Understand the existing health-care structure and what health care is available to all or for select populations. What is the extent of health-care services? Are there clinics for preventive care, or is most care obtained in the hospital? Is home care available with support from nurses and other professionals? Are emergency services available (eg, does the region have ambulances to transport and emergency departments to accept critically ill patients)? Where do patients obtain medications, and do they have to pay out of pocket for these? Do most people die in the hospital or at home? While websites and government sources are valuable, verify this information with clinicians since the clinical reality may be quite different.
Available Medications
To provide useful guidance in symptom management, it is necessary to have a list of available medications used to treat pain, nausea, dyspnea, constipation/diarrhea, wounds, and other symptoms commonly seen in oncology. Your presentation may need to be modified based upon these available drugs (Table 2). Where do patients obtain medications, and do they pay out of pocket for these? There are limitations on availability and access to opioids around the world.[7] Which opioids are available and actually used? What is the process for obtaining a supply of an opioid for a person with cancer? For example, in some countries, physicians can order only one week's worth of medication at a time. In other countries, patients must obtain opioids from the police station rather than a pharmacy. In several settings, only the patient, not family members, can pick up the medication from the dispensing site. And in a few countries, only parenteral opioids are available. It is also helpful to understand issues such as the prevalence of drug trafficking in the region and how this might affect local drug laws. Are traditional medicines, such as herbal therapies, or other techniques commonly used? It is helpful to be aware of these practices and incorporate them into teaching plans where appropriate.
Education of Health-Care Professionals
International education in palliative care should consider how physicians, nurses, pharmacists, and others are educated. Is the educational system very traditional and formal, with little interaction between students and teachers? Professionals trained in this manner may be less comfortable when faced with role-play, learning through discussion, or other Socratic educational methods. That does not mean that one should exclude these methods when planning the curriculum but, rather, be prepared for silence and possibly even discomfort when first introduced. Seek guidance from local educators as to what methods will be acceptable.
Who is included in the health-care team? Are psychologists available, and are chaplains considered part of health-care services? What is the relationship between physicians, nurses, and other team members? Is collegiality accepted, or is there a hierarchy that limits true teamwork? What is the status of physicians, nurses, and other professionals in the region? In some areas, physicians are highly regarded and financially compensated accordingly. In other parts of the world, physicians have very low social status, respect, and compensation. Within diverse cultures, compensation and acceptance of tips (or bribes) to see a patient or perform an intervention may be accepted practice. Attitudes toward work hours may differ from the Western perspective. In some cultures, socialization and development of personal relationships may be considered more important than other aspects of the workload.[8]
Planning in advance to know the targeted attendees is helpful. It is advisable to inquire if the hosts might consider inviting representatives from the ministry of health, the appropriate drug institutes, other key government officials, as well as medical, nursing, and pharmacy leaders who can become champions for access to pain relief and palliative care. Having multiple disciplines and leaders from health care and government at the same program can foster ongoing communication and understanding. Include chief educators as they can incorporate this content into their respective curricula.
Plan the Curriculum and the Program
The importance of cultural issues when developing content cannot be overstated.[9] Factors that might affect pain expression and language or cultural beliefs about death and dying will greatly impact content for teaching. Be aware of local religious and spiritual beliefs impacting pain and palliative care. Consider issues surrounding disclosure of diagnosis and prognosis. Autonomy may not be the prevailing perspective as seen in North America. Ensure that slides are culturally correct and that pictures and illustrations are appropriate. Having the host country leaders review the curriculum in advance is advisable. Avoid cartoons as these may not translate well. Use case examples, but ensure that they represent the types of patients and scenarios seen by the audience. It is also important to avoid being ethnocentric as Western medicine has much to learn from other approaches. It is very helpful to use case studies from the host country. In some settings, trainers will not have access to computers and projectors, limiting the role of PowerPoint slides. Paper presentations or the use of flip-charts may be more accessible.
Consider the need for translation and, if so, which type will be used. Simultaneous interpretation generally requires a sound booth and headphones for participants, and may be more expensive. Consecutive interpretation requires that the instructor present blocks of information, usually a sentence or two, followed by the interpreter providing the content in the appropriate language. This requires speakers to plan much shorter presentations with up to 50% less content being delivered. In either case, trained interpreters can benefit from seeing the slides in advance so they can prepare and clarify prior to the presentation.
When developing an agenda, inquire about the usual times for breaks and meals, as well as time for prayers or other activities. What is considered a “full day” varies around the world, as does the value of adhering rigidly to a schedule. International education generally means that the agenda is fluid; once you are actually in the country and providing the course, other needs may arise. A common mistake is trying to squeeze in too much content. Ask your host to meet prior to the program and, optimally, plan for time before the course to tour health-care facilities. Arrange for a time to meet with key medical, nursing, pharmacy, and governmental leaders who are not scheduled to attend the meeting but might somehow influence curricula and practice. In some settings, local media may be alerted to generate local interest in the topic. Communicate with your host about these opportunities so that arrangements can be made in advance.
For resource-poor countries, consider asking for donations from colleagues before leaving, including books, CDs, and medical supplies. Check local regulations first, particularly if bringing in medications or equipment. If sending books, some countries require high tariff fees to be paid by the receiver when accepting these packages, creating a financial burden for your hosts. Inquire ahead of time if they have to pay to accept these packages. Additionally, in some resource-poor countries, professionals do not have access to personal or work computers and internet café computers often do not have CD drives. Information on jump drives may be more easily accessible.
Finally, visiting educators may want to pack small gifts to give to hosts and others. These should be easily transported and may include items that represent your city or institution. We have also found bringing candy and small toys to be universally appreciated when visiting pediatric settings. A small portable color printer can be used to print photographs of pediatric patients as some of these children have never seen pictures of themselves. You can also print photographs of participants in the training courses.
Personal Considerations
Several months prior to departure, you should contact your traveler's health information resource to identify which vaccinations and what documents are needed to enter the country. To avoid lost time due to illness, ciprofloxacin and antidiarrheal medicines should be obtained before traveling. It is advisable to update your passport. Some countries require you to have sufficient blank pages in your passport to allow entry into their country. An entry fee paid in cash may be required upon arrival. Travelers should consider the political climate of the country and check the U.S. Department of State website (included in Table 1) for alerts or precautions.
Consider appropriate attire when packing. Clothing should reflect respect for the cultural and religious beliefs of the attendees.
During the Experience
It is very useful to meet with interpreters prior to the presentations to clarify any questions. Translation can be quite complicated. For example, a slide that used the term “caring” was interpreted as “romantic love,” and concepts about suffering and death can take on a cultural meaning. Check with interpreters regularly to determine if the speed of delivery is acceptable. Also, translators may have difficulty with this emotional content. In some instances, interpreters have become tearful and required debriefing after palliative care education events. Consider nonverbal communication and personal space. In some cultures, it may not be appropriate to shake hands or to use two hands. Gestures may have very different meanings in other cultures, so avoid these forms of communication. For example, the “OK” sign commonly used in North America, with the tip of the finger touching the tip of the thumb and the other three fingers extended, is considered an obscene gesture in Brazil.
When using teaching strategies other than lecture, respect that some students may not be comfortable at first with nontraditional approaches. Informal teaching strategies that are valued in North America may be viewed as of poor academic quality in other cultures. Debate and discussion, which may make it seem that the student is questioning a teacher's view, may be seen as disrespectful. At times, eliciting personal reflection and experience can engage the audience. For example, when introducing the topic of communication, health-care professionals in the audience can be asked the following questions:
- • If you had cancer, would you want to know?
• Would you want to know that you had a disease that you could die from?
Following these with “What do you tell your patients?” usually engenders excellent discussion.
We have also found that asking participants to do “homework” can be useful, particularly if the students have been quiet or reluctant to communicate during class. Suggested assignments might include listing the five top barriers to cancer pain management in your setting, describing a difficult death or a death that you made better, or related issues. Reticence to speak during class may be due to discomfort with language skills. Some students feel more comfortable sharing ideas in writing, and these assignments have yielded valuable stories that have helped us to understand their experiences and perspectives.
Since the goal of these educational efforts should be sustained, it is helpful to develop a plan for the future with students. Assist them in identifying goals, as well as action items to meet these goals. Allow time for individual meetings between faculty and students to fine-tune these efforts. This ensures that the educational experience will have a greater likelihood of translation into action. To provide practical assistance, if Internet access is available, spend time with small groups to demonstrate literature searches, useful websites, and other information that will foster continuity.
Faculty should meet after each day of training to modify the planned agenda as needed, to optimally meet the needs of the participants. This also provides needed time to debrief about the day's activities and provide support. Particularly when new to international education, the experience may be overwhelming as the status of health-care in developing countries can cause deep personal reflection.
Finally, celebrate. We have found that many students appreciate the opportunity to have some type of closing ceremony to receive certificates and pins, acknowledge their accomplishments, and encourage their future efforts.
Afterward
E-mail, voiceover Internet services, and videoconferencing software have significantly enhanced global communication. Faculty can make themselves available to the trainees after leaving the country using these technologies. Group conversations via e-mail can help solve problems, provide encouragement, and celebrate successes. Connect attendees with international professional organizations to support ongoing educational efforts. It is very useful to identify the leaders or champions and to plan ongoing support to help sustain their commitment. Many countries do not have professional organizations or support networks. These leaders can exist in isolation and suffer great personal sacrifice to lead palliative care efforts in their country.
Conclusion
When educating about pain and palliative care to a worldwide audience, never make assumptions, expect the unexpected, and be flexible. We have found many of these international teaching experiences to be some of the most exhilarating of our professional lives, providing insight to our own practices and creating lasting relationships with colleagues from around the globe. Ultimately, these efforts will improve care for people with cancer.
Acknowledgments
The authors acknowledge the American Association of Colleges of Nursing and the City of Hope for their ongoing support of the End-of-Life Nursing Education Consortium training activities, as well as the Oncology Nursing Society Foundation and the Open Society Institute for their support of international educational efforts. They also thank Marian Grant for her input.
References [Pub Med ID in Brackets]
1 A.L. Taylor, L.O. Gostin and K.A. Pagonis, Ensuring effective pain treatment: a national and global perspective, JAMA 299 (2008), pp. 89–91 [18167410].
2 K. Crane, Palliative care gains ground in developing countries, J Natl Cancer Inst 102 (21) (2010), pp. 1613–1615 [20966432].
3 J.A. Paice, B.R. Ferrell, N. Coyle, P. Coyne and M. Callaway, Global efforts to improve palliative care: the International End-of-Life Nursing Education Consortium training programme, J Adv Nurs 61 (2007), pp. 173–180 [18186909].
4 J.A. Paice, B. Ferrell, N. Coyle, P. Coyne and T. Smith, Living and dying in East Africa: implementing the End-of-Life Nursing Education Consortium curriculum in Tanzania, Clin J Oncol Nurs 14 (2010), pp. 161–166 [20350889].
5 C. Olweny, C. Sepulveda, A. Merriman, S. Fonn, M. Borok, T. Ngoma, A. Doh and J. Stjernsward, Desirable services and guidelines for the treatment and palliative care of HIV disease patients with cancer in Africa: a World Health Organization consultation, J Palliat Care 19 (2003), pp. 198–205 [14606333].
6 C. Sepulveda, V. Habiyatmbete, J. Amandua, M. Borok, E. Kikule, B. Mudanga and B. Solomon, Quality care at the end of life in Africa, BMJ 327 (2003), pp. 209–213 [12881267].
7 E.L. Krakauer, R. Wenk, R. Buitrago, P. Jenkins and W. Scholten, Opioid inaccessibility and its human consequences: reports from the field, J Pain Palliat Care Pharmacother 24 (2010), pp. 239–243 [20718644].
8 C.M. Bolin, Developing a postbasic gerontology program for international learners: considerations for the process, J Contin Educ Nurs 34 (2003), pp. 177–183 [12887229].
9 K.D. Meneses and C.H. Yarbro, Cultural perspectives of international breast health and breast cancer education, J Nurs Scholarsh 39 (2) (2007), pp. 105–112 [19058079].
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
![]()
Vitae
Dr. Paice is Director of the Cancer Pain Program, Division of Hematology-Oncology, Northwestern University, Feinberg School of Medicine, Chicago, Illinois.
Carma Erickson-Hurt is a faculty member at Grand Canyon University, Phoenix, Arizona.
Dr. Ferrell is a Professor and Research Scientist at the City of Hope National Medical Center, Duarte, California.
Nessa Coyle is on the Pain and Palliative Care Service, Department of Medicine, Memorial Sloan-Kettering Cancer Center, New York.
Dr. Coyne is Clinical Director of the Thomas Palliative Care Program, Virginia Commonwealth University/Massey Cancer Center, Richmond, Virginia.
Dr. Long is a geriatric nursing consultant and codirector of the Palliative Care for Advanced Dementia, Beatitudes Campus, Phoenix, Arizona.
Dr. Mazanec is a clinical nurse specialist at the University Hospitals Seidman Cancer Center, Cleveland, Ohio.
Pam Malloy is ELNEC Project Director, American Association of Colleges of Nursing, Washington, DC.
Dr. Smith is Professor of Medicine and Palliative Care Research, Virginia Commonwealth University/Massey Cancer Center, Richmond.
Volume 9, Issue 4, July-August 2011, Pages 129-133
How we do it
Judith A. Paice PhD, RN![]()
Available online 2 July 2011.
Article Outline
For many clinicians in oncology, educating other health-care professionals about cancer pain and palliative care is part of their professional life. The need for education exists across clinical settings around the world. Improved education is an urgent need as the prevalence of cancer is increasing. This burden is largely carried by the developing world, where resources are often limited.[1] Global educational efforts, including managing common symptoms, communication, care at the time of death, grief, and other topics, are imperative to reduce pain and suffering.[2] International training efforts require additional expertise and preparation beyond the standard teaching skills needed for all professional education.
The goal of international training efforts in pain and palliative care is to provide useful, culturally relevant programs while empowering participants to sustain these efforts in the long term. Global efforts in palliative care have demonstrated that sharing educational materials, resources, support and encouragement with our international colleagues can provide mentorship to go beyond simply attending a course to developing and expanding their own programs of palliative care in oncology.[3] and [4] To do this well, the following provides specific suggestions for before, during, and after international palliative care training experiences.
Do Your Homework
Before a course, it is essential to learn as much as possible about the region, the culture(s), and the health-care system. Several resources for this information are listed in Table 1. Additionally, speaking with colleagues who have traveled to the country or to those who have emigrated from the country can provide valuable insight. These individuals can provide a wealth of information to assist in developing an appropriate curriculum and specific presentations. As demographics vary, it is important to know the common cancers and other leading causes of death in the region. Issues that may be seen as “competing” issues HIV/AIDS, malaria, immunizations, lack of clean water, or maternal–infant mortality.[5] and [6] Literature, including fiction and nonfiction, as well as movies and other media, can enlighten the traveler regarding life in the region. Local consulates offer opportunities for learning, as do organizations such as the Council on Global Relations. There are rapid changes in global politics, health-care systems, and governments, so it is also vital to have current information.
| American Society for Clinical Oncology (ASCO) | Offers international cancer courses as well as fellowships and other awards. |
| Centers for Disease Control and Prevention (CDC), http://wwwnc.cdc.gov/travel/ | Provides information regarding common infectious illnesses, traveler's alerts. |
| Central Intelligence Agency (CIA), The World Factbook, https://www.cia.gov/library/publications/the-world-factbook/ | Excellent review of a country's political, demographic, geographic, and other attributes. |
| City of Hope Pain & Palliative Care Resource Center, http://prc.coh.org/ | Provides a clearinghouse that includes a wide array of resources and references to enhance pain and palliative care education and research. |
| End of Life Nursing Education Consortium (ELNEC), http://www.aacn.nche.edu/elnec/ | Includes relevant articles, resources, and a summary of current international ELNEC training programs. |
| International Association for Hospice and Palliative Care (IAHPC), http://www.hospicecare.com/ | Numerous global palliative care resources, including List of Essential Medicines, Global Directory of Educational Programs in Palliative Care, Global Directory of Palliative Care Providers/Services/Organizations, as well as Palliative Care in the Developing World: Principles and Practice. |
| International Association for the Study of Pain (IASP), http://www.iasp-pain.org/ | Strong emphasis on support of developing countries with research and educational grants; publishes a Guide to Pain Management in Low-Resource Settings offered without cost. |
| Open Society Institute–International Palliative Care Initiative, http://www.soros.org/initiatives/health/focus/ipci/about | Offers support for training, clinical care, and research in palliative care, alone and in collaboration with other organizations. |
| Pain & Policy Studies Group, http://www.painpolicy.wisc.edu/ | Excellent resource for information regarding opioid consumption by country as well as guidelines for policies that allow access to necessary medications. |
| U.S. Department of State, http://www.usembassy.gov/ Bureau of Consular Affairs, http://travel.state.gov/travel/travel_1744.html | Comprehensive lists of US embassies, consulates, and diplomatic missions; information to assist travelers from the United States to other countries, including visa requirements and safety alerts. |
| World Health Organization, http://www.who.int | Many useful resources, including Access to Analgesics and to other Controlled Medicines, as well as statistics regarding common illnesses by country. |
Health-Care Structure
Understand the existing health-care structure and what health care is available to all or for select populations. What is the extent of health-care services? Are there clinics for preventive care, or is most care obtained in the hospital? Is home care available with support from nurses and other professionals? Are emergency services available (eg, does the region have ambulances to transport and emergency departments to accept critically ill patients)? Where do patients obtain medications, and do they have to pay out of pocket for these? Do most people die in the hospital or at home? While websites and government sources are valuable, verify this information with clinicians since the clinical reality may be quite different.
Available Medications
To provide useful guidance in symptom management, it is necessary to have a list of available medications used to treat pain, nausea, dyspnea, constipation/diarrhea, wounds, and other symptoms commonly seen in oncology. Your presentation may need to be modified based upon these available drugs (Table 2). Where do patients obtain medications, and do they pay out of pocket for these? There are limitations on availability and access to opioids around the world.[7] Which opioids are available and actually used? What is the process for obtaining a supply of an opioid for a person with cancer? For example, in some countries, physicians can order only one week's worth of medication at a time. In other countries, patients must obtain opioids from the police station rather than a pharmacy. In several settings, only the patient, not family members, can pick up the medication from the dispensing site. And in a few countries, only parenteral opioids are available. It is also helpful to understand issues such as the prevalence of drug trafficking in the region and how this might affect local drug laws. Are traditional medicines, such as herbal therapies, or other techniques commonly used? It is helpful to be aware of these practices and incorporate them into teaching plans where appropriate.
Education of Health-Care Professionals
International education in palliative care should consider how physicians, nurses, pharmacists, and others are educated. Is the educational system very traditional and formal, with little interaction between students and teachers? Professionals trained in this manner may be less comfortable when faced with role-play, learning through discussion, or other Socratic educational methods. That does not mean that one should exclude these methods when planning the curriculum but, rather, be prepared for silence and possibly even discomfort when first introduced. Seek guidance from local educators as to what methods will be acceptable.
Who is included in the health-care team? Are psychologists available, and are chaplains considered part of health-care services? What is the relationship between physicians, nurses, and other team members? Is collegiality accepted, or is there a hierarchy that limits true teamwork? What is the status of physicians, nurses, and other professionals in the region? In some areas, physicians are highly regarded and financially compensated accordingly. In other parts of the world, physicians have very low social status, respect, and compensation. Within diverse cultures, compensation and acceptance of tips (or bribes) to see a patient or perform an intervention may be accepted practice. Attitudes toward work hours may differ from the Western perspective. In some cultures, socialization and development of personal relationships may be considered more important than other aspects of the workload.[8]
Planning in advance to know the targeted attendees is helpful. It is advisable to inquire if the hosts might consider inviting representatives from the ministry of health, the appropriate drug institutes, other key government officials, as well as medical, nursing, and pharmacy leaders who can become champions for access to pain relief and palliative care. Having multiple disciplines and leaders from health care and government at the same program can foster ongoing communication and understanding. Include chief educators as they can incorporate this content into their respective curricula.
Plan the Curriculum and the Program
The importance of cultural issues when developing content cannot be overstated.[9] Factors that might affect pain expression and language or cultural beliefs about death and dying will greatly impact content for teaching. Be aware of local religious and spiritual beliefs impacting pain and palliative care. Consider issues surrounding disclosure of diagnosis and prognosis. Autonomy may not be the prevailing perspective as seen in North America. Ensure that slides are culturally correct and that pictures and illustrations are appropriate. Having the host country leaders review the curriculum in advance is advisable. Avoid cartoons as these may not translate well. Use case examples, but ensure that they represent the types of patients and scenarios seen by the audience. It is also important to avoid being ethnocentric as Western medicine has much to learn from other approaches. It is very helpful to use case studies from the host country. In some settings, trainers will not have access to computers and projectors, limiting the role of PowerPoint slides. Paper presentations or the use of flip-charts may be more accessible.
Consider the need for translation and, if so, which type will be used. Simultaneous interpretation generally requires a sound booth and headphones for participants, and may be more expensive. Consecutive interpretation requires that the instructor present blocks of information, usually a sentence or two, followed by the interpreter providing the content in the appropriate language. This requires speakers to plan much shorter presentations with up to 50% less content being delivered. In either case, trained interpreters can benefit from seeing the slides in advance so they can prepare and clarify prior to the presentation.
When developing an agenda, inquire about the usual times for breaks and meals, as well as time for prayers or other activities. What is considered a “full day” varies around the world, as does the value of adhering rigidly to a schedule. International education generally means that the agenda is fluid; once you are actually in the country and providing the course, other needs may arise. A common mistake is trying to squeeze in too much content. Ask your host to meet prior to the program and, optimally, plan for time before the course to tour health-care facilities. Arrange for a time to meet with key medical, nursing, pharmacy, and governmental leaders who are not scheduled to attend the meeting but might somehow influence curricula and practice. In some settings, local media may be alerted to generate local interest in the topic. Communicate with your host about these opportunities so that arrangements can be made in advance.
For resource-poor countries, consider asking for donations from colleagues before leaving, including books, CDs, and medical supplies. Check local regulations first, particularly if bringing in medications or equipment. If sending books, some countries require high tariff fees to be paid by the receiver when accepting these packages, creating a financial burden for your hosts. Inquire ahead of time if they have to pay to accept these packages. Additionally, in some resource-poor countries, professionals do not have access to personal or work computers and internet café computers often do not have CD drives. Information on jump drives may be more easily accessible.
Finally, visiting educators may want to pack small gifts to give to hosts and others. These should be easily transported and may include items that represent your city or institution. We have also found bringing candy and small toys to be universally appreciated when visiting pediatric settings. A small portable color printer can be used to print photographs of pediatric patients as some of these children have never seen pictures of themselves. You can also print photographs of participants in the training courses.
Personal Considerations
Several months prior to departure, you should contact your traveler's health information resource to identify which vaccinations and what documents are needed to enter the country. To avoid lost time due to illness, ciprofloxacin and antidiarrheal medicines should be obtained before traveling. It is advisable to update your passport. Some countries require you to have sufficient blank pages in your passport to allow entry into their country. An entry fee paid in cash may be required upon arrival. Travelers should consider the political climate of the country and check the U.S. Department of State website (included in Table 1) for alerts or precautions.
Consider appropriate attire when packing. Clothing should reflect respect for the cultural and religious beliefs of the attendees.
During the Experience
It is very useful to meet with interpreters prior to the presentations to clarify any questions. Translation can be quite complicated. For example, a slide that used the term “caring” was interpreted as “romantic love,” and concepts about suffering and death can take on a cultural meaning. Check with interpreters regularly to determine if the speed of delivery is acceptable. Also, translators may have difficulty with this emotional content. In some instances, interpreters have become tearful and required debriefing after palliative care education events. Consider nonverbal communication and personal space. In some cultures, it may not be appropriate to shake hands or to use two hands. Gestures may have very different meanings in other cultures, so avoid these forms of communication. For example, the “OK” sign commonly used in North America, with the tip of the finger touching the tip of the thumb and the other three fingers extended, is considered an obscene gesture in Brazil.
When using teaching strategies other than lecture, respect that some students may not be comfortable at first with nontraditional approaches. Informal teaching strategies that are valued in North America may be viewed as of poor academic quality in other cultures. Debate and discussion, which may make it seem that the student is questioning a teacher's view, may be seen as disrespectful. At times, eliciting personal reflection and experience can engage the audience. For example, when introducing the topic of communication, health-care professionals in the audience can be asked the following questions:
- • If you had cancer, would you want to know?
• Would you want to know that you had a disease that you could die from?
Following these with “What do you tell your patients?” usually engenders excellent discussion.
We have also found that asking participants to do “homework” can be useful, particularly if the students have been quiet or reluctant to communicate during class. Suggested assignments might include listing the five top barriers to cancer pain management in your setting, describing a difficult death or a death that you made better, or related issues. Reticence to speak during class may be due to discomfort with language skills. Some students feel more comfortable sharing ideas in writing, and these assignments have yielded valuable stories that have helped us to understand their experiences and perspectives.
Since the goal of these educational efforts should be sustained, it is helpful to develop a plan for the future with students. Assist them in identifying goals, as well as action items to meet these goals. Allow time for individual meetings between faculty and students to fine-tune these efforts. This ensures that the educational experience will have a greater likelihood of translation into action. To provide practical assistance, if Internet access is available, spend time with small groups to demonstrate literature searches, useful websites, and other information that will foster continuity.
Faculty should meet after each day of training to modify the planned agenda as needed, to optimally meet the needs of the participants. This also provides needed time to debrief about the day's activities and provide support. Particularly when new to international education, the experience may be overwhelming as the status of health-care in developing countries can cause deep personal reflection.
Finally, celebrate. We have found that many students appreciate the opportunity to have some type of closing ceremony to receive certificates and pins, acknowledge their accomplishments, and encourage their future efforts.
Afterward
E-mail, voiceover Internet services, and videoconferencing software have significantly enhanced global communication. Faculty can make themselves available to the trainees after leaving the country using these technologies. Group conversations via e-mail can help solve problems, provide encouragement, and celebrate successes. Connect attendees with international professional organizations to support ongoing educational efforts. It is very useful to identify the leaders or champions and to plan ongoing support to help sustain their commitment. Many countries do not have professional organizations or support networks. These leaders can exist in isolation and suffer great personal sacrifice to lead palliative care efforts in their country.
Conclusion
When educating about pain and palliative care to a worldwide audience, never make assumptions, expect the unexpected, and be flexible. We have found many of these international teaching experiences to be some of the most exhilarating of our professional lives, providing insight to our own practices and creating lasting relationships with colleagues from around the globe. Ultimately, these efforts will improve care for people with cancer.
Acknowledgments
The authors acknowledge the American Association of Colleges of Nursing and the City of Hope for their ongoing support of the End-of-Life Nursing Education Consortium training activities, as well as the Oncology Nursing Society Foundation and the Open Society Institute for their support of international educational efforts. They also thank Marian Grant for her input.
References [Pub Med ID in Brackets]
1 A.L. Taylor, L.O. Gostin and K.A. Pagonis, Ensuring effective pain treatment: a national and global perspective, JAMA 299 (2008), pp. 89–91 [18167410].
2 K. Crane, Palliative care gains ground in developing countries, J Natl Cancer Inst 102 (21) (2010), pp. 1613–1615 [20966432].
3 J.A. Paice, B.R. Ferrell, N. Coyle, P. Coyne and M. Callaway, Global efforts to improve palliative care: the International End-of-Life Nursing Education Consortium training programme, J Adv Nurs 61 (2007), pp. 173–180 [18186909].
4 J.A. Paice, B. Ferrell, N. Coyle, P. Coyne and T. Smith, Living and dying in East Africa: implementing the End-of-Life Nursing Education Consortium curriculum in Tanzania, Clin J Oncol Nurs 14 (2010), pp. 161–166 [20350889].
5 C. Olweny, C. Sepulveda, A. Merriman, S. Fonn, M. Borok, T. Ngoma, A. Doh and J. Stjernsward, Desirable services and guidelines for the treatment and palliative care of HIV disease patients with cancer in Africa: a World Health Organization consultation, J Palliat Care 19 (2003), pp. 198–205 [14606333].
6 C. Sepulveda, V. Habiyatmbete, J. Amandua, M. Borok, E. Kikule, B. Mudanga and B. Solomon, Quality care at the end of life in Africa, BMJ 327 (2003), pp. 209–213 [12881267].
7 E.L. Krakauer, R. Wenk, R. Buitrago, P. Jenkins and W. Scholten, Opioid inaccessibility and its human consequences: reports from the field, J Pain Palliat Care Pharmacother 24 (2010), pp. 239–243 [20718644].
8 C.M. Bolin, Developing a postbasic gerontology program for international learners: considerations for the process, J Contin Educ Nurs 34 (2003), pp. 177–183 [12887229].
9 K.D. Meneses and C.H. Yarbro, Cultural perspectives of international breast health and breast cancer education, J Nurs Scholarsh 39 (2) (2007), pp. 105–112 [19058079].
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
![]()
Vitae
Dr. Paice is Director of the Cancer Pain Program, Division of Hematology-Oncology, Northwestern University, Feinberg School of Medicine, Chicago, Illinois.
Carma Erickson-Hurt is a faculty member at Grand Canyon University, Phoenix, Arizona.
Dr. Ferrell is a Professor and Research Scientist at the City of Hope National Medical Center, Duarte, California.
Nessa Coyle is on the Pain and Palliative Care Service, Department of Medicine, Memorial Sloan-Kettering Cancer Center, New York.
Dr. Coyne is Clinical Director of the Thomas Palliative Care Program, Virginia Commonwealth University/Massey Cancer Center, Richmond, Virginia.
Dr. Long is a geriatric nursing consultant and codirector of the Palliative Care for Advanced Dementia, Beatitudes Campus, Phoenix, Arizona.
Dr. Mazanec is a clinical nurse specialist at the University Hospitals Seidman Cancer Center, Cleveland, Ohio.
Pam Malloy is ELNEC Project Director, American Association of Colleges of Nursing, Washington, DC.
Dr. Smith is Professor of Medicine and Palliative Care Research, Virginia Commonwealth University/Massey Cancer Center, Richmond.
For many clinicians in oncology, educating other health-care professionals about cancer pain and palliative care is part of their professional life. The need for education exists across clinical settings around the world. Improved education is an urgent need as the prevalence of cancer is increasing.
How High Can Your Support Payments Go?
Last December, St. Peter’s Hospital, a 122-bed acute-care facility in Helena, Mont., crossed a symbolic line in the decade-long evolution of the financial payments that hospitals have provided to HM groups to make up the gap that exists between the expenses of running a hospitalist service and the professional fees that generate its revenue.
Hospital administrators asked the outpatient providers at the Helena Physicians’ Clinic to pay nearly $400,000 per year to support the in-house HM service at St. Peter’s, according to a series of stories in the local paper, the Helena Independent Record. The fee was never instituted and, in fact, some Helena patients and physicians have questioned whether the high-stakes payment was part of a broader campaign for the hospital to take over the clinic, a process that culminated in March with the hospital’s purchase of the clinic’s building.
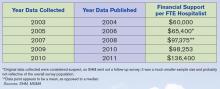
Still, the Montana case focused a spotlight on the doughnut hole of HM ledger sheets: hospital subsidies. More than 80% of HM groups took financial support from their host institutions in fiscal year 2010, according to new data from SHM and the Medical Group Management Association (MGMA), which will be released in September. And the amount of that support has more than doubled, from $60,000 per full-time equivalent (FTE) in 2003-2004 to $136,400 per FTE in the latest data, according to a presentation at HM11 in May.
HM leaders agree the growth is unsustainable, particularly in the new world of healthcare reform, but they also concur that satisfaction with the benefits a hospitalist service offers make it unlikely other institutions will implement a fee-for-service system similar to that of St. Peter’s (see “Pay to Play?,” p. 38). As hospital administrators struggle to dole out pieces of their ever-shrinking financial pie, hospitalists also agree that they will find it more and more difficult to ask their C-suite for continually larger payments (see Figure 1, “Growth in Hospitalist Financial Support,” p. 37). Even when portrayed as “investments” in physicians that provide more than clinical care (e.g. hospitalists assuming leadership roles on hospital committees and pushing quality-improvement initiatives), a hospital’s bottom line can only afford so much.
“It’s not sustainable,” says Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners in Minneapolis and an SHM board member. “I think hospitals are pretty much tapped out by and large.
“What we’ve been seeing is practices have been able to ramp up their productivity, but people have also found other revenue streams, be it perioperative clinics, be it trying to find direct subsidies from specialty practices, be it educational funds for teaching. … We’re kind of entering a time when payment reform of some sort is going to have to come into play.”
History Lesson
Support payments have been around since HM’s earliest days, Dr. Kealey says. From the outset, it was difficult for most practices to cover their own salaries and expenses with reimbursement to the charges that make up the bulk of the field’s billing opportunities. “The economics of the situation are such that it is pretty difficult for a hospitalist to cover their own salary with the standard E/M codes,” he adds.
Hospitals, though, quickly realized that hospitalist practices were a valuable presence and created a payment stream to help offset the difference.
John Laverty, DHA, vice president of hospital-based physicians at HCA Physician Services in Nashville, Tenn., says four main factors drive the need for the hospitalist subsidy:
- Physician productivity. How many patients can a practice see on a daily or a monthly basis? Most averages teeter between 15 and 20 patients per day, often less in academic models. There is a mathematical point at which a group can generate enough revenue to cover costs, but many HM leaders say that comes at the cost of quality care delivery and physician satisfaction.
- Nonclinical/non-revenue-generating activities performed by hospitalists. HM groups usually are involved in QI and patient-safety initiatives, which, while important, are not necessarily captured by billing codes. Some HM contracts call for compensation tied to those activities, but many still do not, leaving groups with a gap to cover.
- Payor mix. A particularly difficult mix with high charity care and uninsured patients can lower the average net collected revenue per visit. There also is the choice between being a Medicaid participating provider or a nonparticipating provider with managed-care payors. So-called “non-par” providers typically have the ability to negotiate higher rates.
- Expenses. “How rich is your benefit package for your physicians?” Laverty asks. “Do you provide a retirement plan? Health, dental and vision? … Do you pay for CME?”
Dr. Kealey says it’s not “impossible” to cover all of a hospitalist’s costs through professional fees; however, “it usually requires a hospitalist be in an area with a very good payor mix or a hospital of very high efficiency, where they can see lots of patients. And often, there might be a setup where they aren’t covering unproductive times or tasks.”
Another Point of View
Not everyone thinks the subsidy is a fait accompli. Jeff Taylor, president and chief operating officer of IPC: The Hospitalist Co., a national physician group practice based in North Hollywood, Calif., says subsidies do not need to be a factor in a practice’s bottom line. Taylor says that IPC generates just 5% of its revenues from subsidies, with the remaining 95% financed by professional fees.
He attributes much of that to the work schedule, particularly the popular model of seven days on clinical duty followed by seven days off. He says that model has led to increased practice costs that then require financial support from their hospital. The schedule’s popularity is fueled by the balance it offers physicians between their work and personal lives, Taylor says, but it also means that practitioners working under it lose two weeks a month of billing opportunities.
He’s right about the popularity, as more than 70% of hospitalist groups use a shift-based staffing model, according to the State of Hospital Medicine: 2010 Report Based on 2009 Data. The number of HM groups employing call-based and hybrid coverage (some shift, some call) is 30%.

—Todd Nelson, MBA, technical director, Healthcare Financial Management Association, Chicago
“There is nothing else inherent in hospital medicine that makes this expensive, other than scheduling,” Taylor says. “Absent a very difficult payor mix, it’s the scheduling and the number of days worked that drives the cost. … We have been saying that for years, but we haven’t seen much of a waver yet. Once hospitals realize—some of them are starting to get it—that it’s the underlying work schedule that drives cost, they’re not going to continue to do it.”
Todd Nelson, MBA, a technical director at the Healthcare Financial Management Association in Chicago, agrees that the upward trajectory of hospital support payments will have to end, likely in concert with the expected payment reform of the next five years. But, he adds, the mere fact that hospital administrators have allowed the payments to double suggests that they view the support as an investment. In return for that money, though, C-suite members should contract for and then demand adherence to performance measures, he notes.
“Many specialties say, ‘We’re valuable; help us out,’ ” says Nelson, a former chief financial officer at Grinnell Regional Medical Center in Iowa. “In the hospital world, you can’t just ‘help out.’ They need to be providing a service you’re paying them for.”
SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, could not agree more. “The way I view monies that are sent to a group for nonclinical work is exactly that,” he says. “It’s compensation for nonclinical work. Subsidy, to me, seems to mean that despite whatever you’re doing, you need some more to pay because you can’t make your ends meet. That’s not true. What that figure is, for my group and for the vast majority of groups in this country, is really compensation for nonclinical efforts.”
HM groups should take it upon themselves to discuss their value contribution with their chief financial officer, as many in that position view hospitalist services as a “cost center” rather than as a means to the end of better financial performance for the institution as a whole, says Beth Hawley, senior vice president with Brentwood, Tenn.-based Cogent HMG.
“You need to look at it from the viewpoint of your CFO,” she says. “It is really important to educate your CFO on the myriad ways that your hospitalist program can create value for the hospital.”

—Jeff Taylor, president, COO, IPC: The Hospitalist Co., North Hollywood, Calif.
Hospitalist John Bulger, DO, FACP, FHM, of Geisinger Medical Center in Danville, Pa., says such education should highlight the intangible values of HM services, but it also needs to include firm, eye-opening data points. Put another way: “Have true ROI [return on investment], not soft ROI,” he says.
Dr. Bulger suggests pointing out that what some call a subsidy, he views as simply a payment, no different from the lump-sum check a hospital or healthcare system might cut for the group running its ED, or the check it writes for a cardiology specialty.
“There’s a subsidy for all those groups, but it’s never been looked at as a subsidy,” he adds. “But from a business perspective, it’s the same thing.”
The Future of Support
The relative value, justification, and existence of the support aside, the question remains: What is its future?
“Subsidies are not going to go away, because you can’t recruit and retain physicians in this environment for the most part without them,” says Troy Ahlstrom, MD, SFHM, CFO of Hospitalists of Northern Michigan, a hospitalist-owned and -managed group based in Traverse City. “Especially not when physicians coming out of residency have a desire to maintain a reasonable work and personal life, with fewer shifts where possible, fewer patients per shift. And they also have income goals that they have to maintain with that because they’re coming out of training with larger debt loads than ever before. That’s the tricky part for CMS and the federal government moving forward.”
Nelson, however, says that the future of support will be tied to payment reform, as bundled payments, value-based purchasing (VBP), and other initiatives to reduce overall healthcare spending are implemented. He said HM and other specialties should keep in mind that the point of reform is less overall spending, which translates to less support for everyone.
“When the pie shrinks, the table manners change,” he adds. “People are going to have to figure out how to slice that pie.”
Accountable-care organizations (ACOs) could be one answer. An ACO is a type of healthcare delivery model being piloted by the Centers for Medicare & Medicaid Services (CMS), in which a group of providers band together to coordinate the care of beneficiaries (see “Quality over Quantity,” December 2009, p. 23). Reimbursement is shared by the group and is tied to the quality of care provided. Nelson says the model could significantly cut the need for support, as HM groups are allowed to share in the upside created by the ACO.
The program is set to go live Jan. 1, 2012, but a leading hospitalist already has questioned whether the proposed rules provide enough capitated risk and, therefore, whether the incentive is enough to spur adoption of the model and the potential support reductions it would bring.
“You can certainly start by taking a lower amount of risk, just upside risk,” Cogent HMG chief medical officer Ron Greeno, MD, FCCP, SFHM, told The Hospitalist eWire in April, when the proposed rules were issued. “But your plan should be not to stay there. Your plan should be to take more and more risk as soon as you can, as soon as you’re capable.”
Nelson says that the support can continue in some form or fashion in the new models as long as the hospital and its practitioners are integrated and looking to achieve the same goal.
“The reality is, from the hospital perspective, you need to make sure you’re getting some value,” he says. “What are they buying in exchange for that [payment]?” TH
Richard Quinn is a freelance writer based in New Jersey.
Last December, St. Peter’s Hospital, a 122-bed acute-care facility in Helena, Mont., crossed a symbolic line in the decade-long evolution of the financial payments that hospitals have provided to HM groups to make up the gap that exists between the expenses of running a hospitalist service and the professional fees that generate its revenue.
Hospital administrators asked the outpatient providers at the Helena Physicians’ Clinic to pay nearly $400,000 per year to support the in-house HM service at St. Peter’s, according to a series of stories in the local paper, the Helena Independent Record. The fee was never instituted and, in fact, some Helena patients and physicians have questioned whether the high-stakes payment was part of a broader campaign for the hospital to take over the clinic, a process that culminated in March with the hospital’s purchase of the clinic’s building.
Still, the Montana case focused a spotlight on the doughnut hole of HM ledger sheets: hospital subsidies. More than 80% of HM groups took financial support from their host institutions in fiscal year 2010, according to new data from SHM and the Medical Group Management Association (MGMA), which will be released in September. And the amount of that support has more than doubled, from $60,000 per full-time equivalent (FTE) in 2003-2004 to $136,400 per FTE in the latest data, according to a presentation at HM11 in May.
HM leaders agree the growth is unsustainable, particularly in the new world of healthcare reform, but they also concur that satisfaction with the benefits a hospitalist service offers make it unlikely other institutions will implement a fee-for-service system similar to that of St. Peter’s (see “Pay to Play?,” p. 38). As hospital administrators struggle to dole out pieces of their ever-shrinking financial pie, hospitalists also agree that they will find it more and more difficult to ask their C-suite for continually larger payments (see Figure 1, “Growth in Hospitalist Financial Support,” p. 37). Even when portrayed as “investments” in physicians that provide more than clinical care (e.g. hospitalists assuming leadership roles on hospital committees and pushing quality-improvement initiatives), a hospital’s bottom line can only afford so much.
“It’s not sustainable,” says Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners in Minneapolis and an SHM board member. “I think hospitals are pretty much tapped out by and large.
“What we’ve been seeing is practices have been able to ramp up their productivity, but people have also found other revenue streams, be it perioperative clinics, be it trying to find direct subsidies from specialty practices, be it educational funds for teaching. … We’re kind of entering a time when payment reform of some sort is going to have to come into play.”
History Lesson
Support payments have been around since HM’s earliest days, Dr. Kealey says. From the outset, it was difficult for most practices to cover their own salaries and expenses with reimbursement to the charges that make up the bulk of the field’s billing opportunities. “The economics of the situation are such that it is pretty difficult for a hospitalist to cover their own salary with the standard E/M codes,” he adds.
Hospitals, though, quickly realized that hospitalist practices were a valuable presence and created a payment stream to help offset the difference.
John Laverty, DHA, vice president of hospital-based physicians at HCA Physician Services in Nashville, Tenn., says four main factors drive the need for the hospitalist subsidy:
- Physician productivity. How many patients can a practice see on a daily or a monthly basis? Most averages teeter between 15 and 20 patients per day, often less in academic models. There is a mathematical point at which a group can generate enough revenue to cover costs, but many HM leaders say that comes at the cost of quality care delivery and physician satisfaction.
- Nonclinical/non-revenue-generating activities performed by hospitalists. HM groups usually are involved in QI and patient-safety initiatives, which, while important, are not necessarily captured by billing codes. Some HM contracts call for compensation tied to those activities, but many still do not, leaving groups with a gap to cover.
- Payor mix. A particularly difficult mix with high charity care and uninsured patients can lower the average net collected revenue per visit. There also is the choice between being a Medicaid participating provider or a nonparticipating provider with managed-care payors. So-called “non-par” providers typically have the ability to negotiate higher rates.
- Expenses. “How rich is your benefit package for your physicians?” Laverty asks. “Do you provide a retirement plan? Health, dental and vision? … Do you pay for CME?”
Dr. Kealey says it’s not “impossible” to cover all of a hospitalist’s costs through professional fees; however, “it usually requires a hospitalist be in an area with a very good payor mix or a hospital of very high efficiency, where they can see lots of patients. And often, there might be a setup where they aren’t covering unproductive times or tasks.”
Another Point of View
Not everyone thinks the subsidy is a fait accompli. Jeff Taylor, president and chief operating officer of IPC: The Hospitalist Co., a national physician group practice based in North Hollywood, Calif., says subsidies do not need to be a factor in a practice’s bottom line. Taylor says that IPC generates just 5% of its revenues from subsidies, with the remaining 95% financed by professional fees.
He attributes much of that to the work schedule, particularly the popular model of seven days on clinical duty followed by seven days off. He says that model has led to increased practice costs that then require financial support from their hospital. The schedule’s popularity is fueled by the balance it offers physicians between their work and personal lives, Taylor says, but it also means that practitioners working under it lose two weeks a month of billing opportunities.
He’s right about the popularity, as more than 70% of hospitalist groups use a shift-based staffing model, according to the State of Hospital Medicine: 2010 Report Based on 2009 Data. The number of HM groups employing call-based and hybrid coverage (some shift, some call) is 30%.

—Todd Nelson, MBA, technical director, Healthcare Financial Management Association, Chicago
“There is nothing else inherent in hospital medicine that makes this expensive, other than scheduling,” Taylor says. “Absent a very difficult payor mix, it’s the scheduling and the number of days worked that drives the cost. … We have been saying that for years, but we haven’t seen much of a waver yet. Once hospitals realize—some of them are starting to get it—that it’s the underlying work schedule that drives cost, they’re not going to continue to do it.”
Todd Nelson, MBA, a technical director at the Healthcare Financial Management Association in Chicago, agrees that the upward trajectory of hospital support payments will have to end, likely in concert with the expected payment reform of the next five years. But, he adds, the mere fact that hospital administrators have allowed the payments to double suggests that they view the support as an investment. In return for that money, though, C-suite members should contract for and then demand adherence to performance measures, he notes.
“Many specialties say, ‘We’re valuable; help us out,’ ” says Nelson, a former chief financial officer at Grinnell Regional Medical Center in Iowa. “In the hospital world, you can’t just ‘help out.’ They need to be providing a service you’re paying them for.”
SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, could not agree more. “The way I view monies that are sent to a group for nonclinical work is exactly that,” he says. “It’s compensation for nonclinical work. Subsidy, to me, seems to mean that despite whatever you’re doing, you need some more to pay because you can’t make your ends meet. That’s not true. What that figure is, for my group and for the vast majority of groups in this country, is really compensation for nonclinical efforts.”
HM groups should take it upon themselves to discuss their value contribution with their chief financial officer, as many in that position view hospitalist services as a “cost center” rather than as a means to the end of better financial performance for the institution as a whole, says Beth Hawley, senior vice president with Brentwood, Tenn.-based Cogent HMG.
“You need to look at it from the viewpoint of your CFO,” she says. “It is really important to educate your CFO on the myriad ways that your hospitalist program can create value for the hospital.”

—Jeff Taylor, president, COO, IPC: The Hospitalist Co., North Hollywood, Calif.
Hospitalist John Bulger, DO, FACP, FHM, of Geisinger Medical Center in Danville, Pa., says such education should highlight the intangible values of HM services, but it also needs to include firm, eye-opening data points. Put another way: “Have true ROI [return on investment], not soft ROI,” he says.
Dr. Bulger suggests pointing out that what some call a subsidy, he views as simply a payment, no different from the lump-sum check a hospital or healthcare system might cut for the group running its ED, or the check it writes for a cardiology specialty.
“There’s a subsidy for all those groups, but it’s never been looked at as a subsidy,” he adds. “But from a business perspective, it’s the same thing.”
The Future of Support
The relative value, justification, and existence of the support aside, the question remains: What is its future?
“Subsidies are not going to go away, because you can’t recruit and retain physicians in this environment for the most part without them,” says Troy Ahlstrom, MD, SFHM, CFO of Hospitalists of Northern Michigan, a hospitalist-owned and -managed group based in Traverse City. “Especially not when physicians coming out of residency have a desire to maintain a reasonable work and personal life, with fewer shifts where possible, fewer patients per shift. And they also have income goals that they have to maintain with that because they’re coming out of training with larger debt loads than ever before. That’s the tricky part for CMS and the federal government moving forward.”
Nelson, however, says that the future of support will be tied to payment reform, as bundled payments, value-based purchasing (VBP), and other initiatives to reduce overall healthcare spending are implemented. He said HM and other specialties should keep in mind that the point of reform is less overall spending, which translates to less support for everyone.
“When the pie shrinks, the table manners change,” he adds. “People are going to have to figure out how to slice that pie.”
Accountable-care organizations (ACOs) could be one answer. An ACO is a type of healthcare delivery model being piloted by the Centers for Medicare & Medicaid Services (CMS), in which a group of providers band together to coordinate the care of beneficiaries (see “Quality over Quantity,” December 2009, p. 23). Reimbursement is shared by the group and is tied to the quality of care provided. Nelson says the model could significantly cut the need for support, as HM groups are allowed to share in the upside created by the ACO.
The program is set to go live Jan. 1, 2012, but a leading hospitalist already has questioned whether the proposed rules provide enough capitated risk and, therefore, whether the incentive is enough to spur adoption of the model and the potential support reductions it would bring.
“You can certainly start by taking a lower amount of risk, just upside risk,” Cogent HMG chief medical officer Ron Greeno, MD, FCCP, SFHM, told The Hospitalist eWire in April, when the proposed rules were issued. “But your plan should be not to stay there. Your plan should be to take more and more risk as soon as you can, as soon as you’re capable.”
Nelson says that the support can continue in some form or fashion in the new models as long as the hospital and its practitioners are integrated and looking to achieve the same goal.
“The reality is, from the hospital perspective, you need to make sure you’re getting some value,” he says. “What are they buying in exchange for that [payment]?” TH
Richard Quinn is a freelance writer based in New Jersey.
Last December, St. Peter’s Hospital, a 122-bed acute-care facility in Helena, Mont., crossed a symbolic line in the decade-long evolution of the financial payments that hospitals have provided to HM groups to make up the gap that exists between the expenses of running a hospitalist service and the professional fees that generate its revenue.
Hospital administrators asked the outpatient providers at the Helena Physicians’ Clinic to pay nearly $400,000 per year to support the in-house HM service at St. Peter’s, according to a series of stories in the local paper, the Helena Independent Record. The fee was never instituted and, in fact, some Helena patients and physicians have questioned whether the high-stakes payment was part of a broader campaign for the hospital to take over the clinic, a process that culminated in March with the hospital’s purchase of the clinic’s building.
Still, the Montana case focused a spotlight on the doughnut hole of HM ledger sheets: hospital subsidies. More than 80% of HM groups took financial support from their host institutions in fiscal year 2010, according to new data from SHM and the Medical Group Management Association (MGMA), which will be released in September. And the amount of that support has more than doubled, from $60,000 per full-time equivalent (FTE) in 2003-2004 to $136,400 per FTE in the latest data, according to a presentation at HM11 in May.
HM leaders agree the growth is unsustainable, particularly in the new world of healthcare reform, but they also concur that satisfaction with the benefits a hospitalist service offers make it unlikely other institutions will implement a fee-for-service system similar to that of St. Peter’s (see “Pay to Play?,” p. 38). As hospital administrators struggle to dole out pieces of their ever-shrinking financial pie, hospitalists also agree that they will find it more and more difficult to ask their C-suite for continually larger payments (see Figure 1, “Growth in Hospitalist Financial Support,” p. 37). Even when portrayed as “investments” in physicians that provide more than clinical care (e.g. hospitalists assuming leadership roles on hospital committees and pushing quality-improvement initiatives), a hospital’s bottom line can only afford so much.
“It’s not sustainable,” says Burke Kealey, MD, SFHM, medical director of hospital specialties at HealthPartners in Minneapolis and an SHM board member. “I think hospitals are pretty much tapped out by and large.
“What we’ve been seeing is practices have been able to ramp up their productivity, but people have also found other revenue streams, be it perioperative clinics, be it trying to find direct subsidies from specialty practices, be it educational funds for teaching. … We’re kind of entering a time when payment reform of some sort is going to have to come into play.”
History Lesson
Support payments have been around since HM’s earliest days, Dr. Kealey says. From the outset, it was difficult for most practices to cover their own salaries and expenses with reimbursement to the charges that make up the bulk of the field’s billing opportunities. “The economics of the situation are such that it is pretty difficult for a hospitalist to cover their own salary with the standard E/M codes,” he adds.
Hospitals, though, quickly realized that hospitalist practices were a valuable presence and created a payment stream to help offset the difference.
John Laverty, DHA, vice president of hospital-based physicians at HCA Physician Services in Nashville, Tenn., says four main factors drive the need for the hospitalist subsidy:
- Physician productivity. How many patients can a practice see on a daily or a monthly basis? Most averages teeter between 15 and 20 patients per day, often less in academic models. There is a mathematical point at which a group can generate enough revenue to cover costs, but many HM leaders say that comes at the cost of quality care delivery and physician satisfaction.
- Nonclinical/non-revenue-generating activities performed by hospitalists. HM groups usually are involved in QI and patient-safety initiatives, which, while important, are not necessarily captured by billing codes. Some HM contracts call for compensation tied to those activities, but many still do not, leaving groups with a gap to cover.
- Payor mix. A particularly difficult mix with high charity care and uninsured patients can lower the average net collected revenue per visit. There also is the choice between being a Medicaid participating provider or a nonparticipating provider with managed-care payors. So-called “non-par” providers typically have the ability to negotiate higher rates.
- Expenses. “How rich is your benefit package for your physicians?” Laverty asks. “Do you provide a retirement plan? Health, dental and vision? … Do you pay for CME?”
Dr. Kealey says it’s not “impossible” to cover all of a hospitalist’s costs through professional fees; however, “it usually requires a hospitalist be in an area with a very good payor mix or a hospital of very high efficiency, where they can see lots of patients. And often, there might be a setup where they aren’t covering unproductive times or tasks.”
Another Point of View
Not everyone thinks the subsidy is a fait accompli. Jeff Taylor, president and chief operating officer of IPC: The Hospitalist Co., a national physician group practice based in North Hollywood, Calif., says subsidies do not need to be a factor in a practice’s bottom line. Taylor says that IPC generates just 5% of its revenues from subsidies, with the remaining 95% financed by professional fees.
He attributes much of that to the work schedule, particularly the popular model of seven days on clinical duty followed by seven days off. He says that model has led to increased practice costs that then require financial support from their hospital. The schedule’s popularity is fueled by the balance it offers physicians between their work and personal lives, Taylor says, but it also means that practitioners working under it lose two weeks a month of billing opportunities.
He’s right about the popularity, as more than 70% of hospitalist groups use a shift-based staffing model, according to the State of Hospital Medicine: 2010 Report Based on 2009 Data. The number of HM groups employing call-based and hybrid coverage (some shift, some call) is 30%.

—Todd Nelson, MBA, technical director, Healthcare Financial Management Association, Chicago
“There is nothing else inherent in hospital medicine that makes this expensive, other than scheduling,” Taylor says. “Absent a very difficult payor mix, it’s the scheduling and the number of days worked that drives the cost. … We have been saying that for years, but we haven’t seen much of a waver yet. Once hospitals realize—some of them are starting to get it—that it’s the underlying work schedule that drives cost, they’re not going to continue to do it.”
Todd Nelson, MBA, a technical director at the Healthcare Financial Management Association in Chicago, agrees that the upward trajectory of hospital support payments will have to end, likely in concert with the expected payment reform of the next five years. But, he adds, the mere fact that hospital administrators have allowed the payments to double suggests that they view the support as an investment. In return for that money, though, C-suite members should contract for and then demand adherence to performance measures, he notes.
“Many specialties say, ‘We’re valuable; help us out,’ ” says Nelson, a former chief financial officer at Grinnell Regional Medical Center in Iowa. “In the hospital world, you can’t just ‘help out.’ They need to be providing a service you’re paying them for.”
SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, could not agree more. “The way I view monies that are sent to a group for nonclinical work is exactly that,” he says. “It’s compensation for nonclinical work. Subsidy, to me, seems to mean that despite whatever you’re doing, you need some more to pay because you can’t make your ends meet. That’s not true. What that figure is, for my group and for the vast majority of groups in this country, is really compensation for nonclinical efforts.”
HM groups should take it upon themselves to discuss their value contribution with their chief financial officer, as many in that position view hospitalist services as a “cost center” rather than as a means to the end of better financial performance for the institution as a whole, says Beth Hawley, senior vice president with Brentwood, Tenn.-based Cogent HMG.
“You need to look at it from the viewpoint of your CFO,” she says. “It is really important to educate your CFO on the myriad ways that your hospitalist program can create value for the hospital.”

—Jeff Taylor, president, COO, IPC: The Hospitalist Co., North Hollywood, Calif.
Hospitalist John Bulger, DO, FACP, FHM, of Geisinger Medical Center in Danville, Pa., says such education should highlight the intangible values of HM services, but it also needs to include firm, eye-opening data points. Put another way: “Have true ROI [return on investment], not soft ROI,” he says.
Dr. Bulger suggests pointing out that what some call a subsidy, he views as simply a payment, no different from the lump-sum check a hospital or healthcare system might cut for the group running its ED, or the check it writes for a cardiology specialty.
“There’s a subsidy for all those groups, but it’s never been looked at as a subsidy,” he adds. “But from a business perspective, it’s the same thing.”
The Future of Support
The relative value, justification, and existence of the support aside, the question remains: What is its future?
“Subsidies are not going to go away, because you can’t recruit and retain physicians in this environment for the most part without them,” says Troy Ahlstrom, MD, SFHM, CFO of Hospitalists of Northern Michigan, a hospitalist-owned and -managed group based in Traverse City. “Especially not when physicians coming out of residency have a desire to maintain a reasonable work and personal life, with fewer shifts where possible, fewer patients per shift. And they also have income goals that they have to maintain with that because they’re coming out of training with larger debt loads than ever before. That’s the tricky part for CMS and the federal government moving forward.”
Nelson, however, says that the future of support will be tied to payment reform, as bundled payments, value-based purchasing (VBP), and other initiatives to reduce overall healthcare spending are implemented. He said HM and other specialties should keep in mind that the point of reform is less overall spending, which translates to less support for everyone.
“When the pie shrinks, the table manners change,” he adds. “People are going to have to figure out how to slice that pie.”
Accountable-care organizations (ACOs) could be one answer. An ACO is a type of healthcare delivery model being piloted by the Centers for Medicare & Medicaid Services (CMS), in which a group of providers band together to coordinate the care of beneficiaries (see “Quality over Quantity,” December 2009, p. 23). Reimbursement is shared by the group and is tied to the quality of care provided. Nelson says the model could significantly cut the need for support, as HM groups are allowed to share in the upside created by the ACO.
The program is set to go live Jan. 1, 2012, but a leading hospitalist already has questioned whether the proposed rules provide enough capitated risk and, therefore, whether the incentive is enough to spur adoption of the model and the potential support reductions it would bring.
“You can certainly start by taking a lower amount of risk, just upside risk,” Cogent HMG chief medical officer Ron Greeno, MD, FCCP, SFHM, told The Hospitalist eWire in April, when the proposed rules were issued. “But your plan should be not to stay there. Your plan should be to take more and more risk as soon as you can, as soon as you’re capable.”
Nelson says that the support can continue in some form or fashion in the new models as long as the hospital and its practitioners are integrated and looking to achieve the same goal.
“The reality is, from the hospital perspective, you need to make sure you’re getting some value,” he says. “What are they buying in exchange for that [payment]?” TH
Richard Quinn is a freelance writer based in New Jersey.
It Takes a Village
Gregory Misky, MD, has been a hospitalist for 12 years, first at a community hospital and for the past seven years at the University of Colorado Denver. In recent years, his frustration has grown over the challenges of discharge planning, care transitions, and preventing readmissions for vulnerable, disadvantaged patients, including the uninsured, underinsured, and medically indigent.
“There’s a big elephant in the room that we’re not talking about, and that elephant is having babies,” he says. “Access is such a big problem for these patients and, as a hospitalist, it’s just not OK to me anymore. I need to be proactive about finding solutions.”
Dr. Misky’s concerns led him to do research with mentor Eric Coleman, MD, the university’s creator of the Care Transitions Program (www.caretransitions.org), studying patients who lacked primary-care physicians (PCPs) or timely PCP follow-up, and their resulting higher rates of readmissions.1 Dr. Misky also helped develop care pathways, including post-discharge care, for VTE patients, a “common, costly, and dangerous” condition. He is working with a hospitalist colleague to explore how electronic health records (EHR) might be used to help trigger post-discharge follow-up for at-risk patients.
University of Colorado Hospital (UCH), a 425-bed urban academic tertiary-care center, is not the designated safety net hospital for metro Denver, yet 28% to 32% of patients discharged from its medical services are uninsured, Dr. Misky says. He finds that academic physicians at UCH are not always able to take on large numbers of uninsured patients in their clinics, given the productivity demands they face, while the hospital has not been able to participate in systemwide, comprehensive national models for improving care transitions, such as SHM’s Project BOOST (www.hospitalmedicine.org/boost) or Boston Medical Center’s Project RED (www.bu.edu/fammed/projectred/).
Dr. Misky is in discussions with local community services, such as the Metro Community Provider Network (MCPN) of clinics for underserved patients, and exploring the development of a collaborative model for integrating post-hospital care between UCH and MCPN. “A lot of our ideas are still very exploratory—trying to get the key providers to the table to talk about what these approaches might look like,” Dr. Misky explains. “I’ve been part of ongoing meetings, and I think similar kinds of conversations are happening at many levels at UCH, but there’s not a unified, consensus approach to care transitions—and that’s a problem. But I’m in the midst of it all, trying to highlight the issues and explore solutions.”
—Patricia Rutherford, RN, MS, vice president, Institute for Healthcare Improvement
Dr. Misky says every hospital-based provider—hospitalist, nurses, social workers—feels the same frustration and worry about the level of care when indigent patients are discharged to the community. Uninsured patients can run into problems post-hospitalization and return to the ED for their primary care because they lack other options, he says. “Without established liaisons to the community clinics,” he notes, “it can take three or four months for a new indigent patient to get seen at one.”
Disproportional Issues of the Uninsured
Hospitalists at San Francisco General Hospital, which is the safety-net provider for the Bay Area, are looking at similar issues, says Jeff Critchfield, MD, division chief of hospital medicine. “What we know about the uninsured is that they have a wealth of other challenges and barriers that they bring to the table,” he says. “First of all, un- and underinsured patients are more likely to have chronic illnesses, to be hospitalized for those illnesses, and then to be rehospitalized after discharge.”
Other issues disproportionally impacting uninsured or indigent patients include low literacy, low healthcare literacy, language barriers, cross-cultural barriers, substance abuse and mental health issues, homelessness or marginal housing, transportation barriers, and “social isolation, which also plagues our population and, I believe, places patients at risk, as does depression,” says Dr. Critchfield’s colleague Michelle Schneidermann, MD.
One-third of San Francisco General’s patients are uninsured and 40% have Medi-Cal (California’s version of Medicaid), which basically means they are underinsured.
“California has 19 safety-net hospitals, with 6% of the state’s inpatient beds but 50% of its uninsured population. So that’s what we do,” Dr. Critchfield says. But almost any hospital or hospitalist will see many of the same issues and problems, just not in the same proportions. “These are patients who can be most frustrating to hospitalists, requiring a disproportionate amount of our time,” he says, adding the greatest difficulty is helping these patients understand and follow post-discharge care plans. But if someone is ill enough to need acute hospitalization and is later discharged back to the street, readmission should not be a surprise. “We’ve done that experiment for many years, and we know how it turns out,” he says.
Dr. Schneidermann serves as medical director of San Francisco General’s medical respite program, a 45-bed emergency shelter that accepts homeless or marginally housed patients in need of follow-up care following discharge from any of the city’s acute-care hospitals. Research has shown that the programs can have a major effect on keeping discharged patients off the street, reducing their rates of rehospitalization by as much as 50%.2,3
“We know that homeless patients have longer lengths of hospital stay because their discharges are fraught with problems,” she says. A homeless patient hospitalized with a blood clot potentially could be kept in the hospital for a week while transitioning from heparin to Coumadin, while similar patients with community support might get discharged in a day.
“We are also fortunate to have a program called Healthy San Francisco,” which isn’t a health insurance program per se but since 2007 has provided access to outpatient, inpatient, and preventive care and medications for indigent patients, Dr. Schneidermann says. Sponsored by the city’s Department of Public Health, it is accessed through 32 medical homes located in both public and private clinics. The hospitalists’ goal is to have a follow-up appointment set with a receiving provider at the time of discharge. “It doesn’t always happen, but that’s the goal,” she explains. “Someone, by name, who has accepted the referral.”
Dr. Critchfield is running a randomized controlled trial of the hospital’s interventions to stem the tide of readmissions in patients 60 and older; many of these patients share the same indigent demographics of the rest of San Francisco General’s caseload, although most patients 65 and older qualify for Medicare. He describes the program as a hybrid of Project RED and Dr. Coleman’s Care Transitions Program, although it targets patients who speak English, Spanish, Cantonese, and Mandarin.
How many Americans are uninsured today is a moving target in the context of healthcare reform and its uncertain future, but the number increased to 53 million in 2007 from 42 million in 1998.4 The number of hospitalizations of uninsured patients also grew to 2.3 million from 1.8 million in the same time period, an increase of 31%, while total hospitalizations were increasing by 13%. A May 2011 research brief from the U.S. Department of Health and Human Services estimates that uncompensated costs of hospital care incurred for uninsured patients total $73 billion per year.5
The homeless in shelters or on the street number about 630,000 on any given evening, and 1.5 million Americans experienced homelessness last year, says Sabrina Edgington, MSSW, program and policy specialist at the National Health Care for the Homeless Council in Nashville, Tenn. That said, 30% of the U.S. homeless have health insurance. Uninsured patients are less likely to receive necessary diagnostic tests and labs while in the hospital, and they face limited access and longer wait times—even in the facilities that are willing to take them.7 Research published in the Journal of Hospital Medicine finds that uninsured or Medicaid patients with three common conditions are more likely to die in the hospital than insured patients.8 A 2008 national sample survey of physicians found that “most U.S. physicians limit their care of medically indigent patients.”9 Other recent research suggests that readmission rates are affected by race and by site of care—with hospitals serving a higher proportion of black patients also having higher readmission rates.10
“This is not a hospital problem—it’s a communitywide problem. So there’s not just a hospital solution; it will take the whole village,” says Patricia Rutherford, RN, MS, vice president of the Institute for Healthcare Improvement (IHI), which sponsors initiatives targeting care transitions.
The major national care-transitions programs that assist hospitals with addressing rehospitalizations all share similar objectives, Rutherford says, and all could be helpful in improving hospitals’ responses to indigent patients. The recognized programs include IHI’s STAAR (State Action on Avoidable Rehospitalizations: www.ihi.org/IHI/Programs), a multistate, multistakeholder quality improvement (QI) program; Project BOOST; Project RED; Dr. Coleman’s Care Transitions Project; the nursing-based Transitional Care Model (www.transitionalcare.info); and the American College of Cardiology’s Hospital to Home (www.cardiosource.org).

—Amy Boutwell, MD, MPP, hospitalist, Newton (Mass.) Wellesley Hospital, president, Collaborative Healthcare Strategies
Most of these “well-established, evidence-based interventions,” including BOOST, will be given preference in applications for grants from the federal Community-Based Care Transitions Program (CCTP). The program recently committed $500 million to support community-based coalitions that include hospitals that are working with community partners to create seamless care transitions. “It’s most important that hospitalists are integrally involved with these care-transition teams—if not leading them,” Rutherford says.
BOOST’s approach is built on a major change-management strategy to reconstruct hospitals’ care transitions and discharge processes from the ground up, says Tina Budnitz, MPH, the project’s director at SHM (see “Discharge Improvement,” p. 7.) “The first thing we do, we literally get out pens and paper and chart what happens before patients get into the hospital and what happens after they are discharged, all of the services that touch them—or should,” she says. “The planning process occurs on many levels, with all of the stakeholders in the community looking at the process map and seeing where people fall off and end up readmitted.”
—Jeff Critchfield, MD, division chief of hospital medicine, San Francisco General Hospital
SHM is planning to launch several new BOOST cohorts for participating hospitals this fall, along with a wider range of technical support, Budnitz says.
The Cross-Setting Team
Research on care transitions for uninsured or indigent patients “is not very robust,” observes Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Newton, Mass., former director of health policy at IHI and president of Collaborative Healthcare Strategies. “We don’t have the information we need, but there are great opportunities to improve our research base,” she explains.
Dr. Boutwell is a big fan of the “cross-setting team,” which brings together around a conference table professionals who work in different care settings, including the hospital, long-term care, and home-based care. She says it’s her job “to make sure patients are safe upon discharge, but if the community is under-resourced for primary-care physicians, if the patient is uninsured and we can’t find a PCP, the hospitalist and cross-setting team need to say, ‘We just can’t accept that.’ ”
A proper handoff should be done in a way that helps the patient and the physician providing the follow-up care. “But you won’t know what that is unless you ask the people you’re sending patients to how you’re doing,” she explains. “When we routinely review readmitted patients in cross-setting groups, it quickly breaks down the mindset that we in the hospital did everything we could have done to make the discharge successful.”
Dr. Boutwell recommends that hospitalists avoid thinking of these issues in a vacuum, as medical-clinical issues that only doctors can fix. “Because you can’t,” she says. “I would never ask an individual hospitalist to reduce readmissions. It requires a multidisciplinary, all-hands-on-deck approach by the hospital. This is different and more exciting than other quality-improvement efforts.” What’s more, she says, the day is coming—and soon—when failing to manage these readmissions will be a bad business proposition for the hospital (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
IHI’s STAAR Initiative is working with coalitions of providers in Massachusetts, Michigan, Ohio, and Washington. One of those coalitions, Detroit CARR (Community Action to Reduce Rehospitalizations), convened by MPRO, a Michigan-based quality-improvement organization, is a great example of a cross-continuum team involving five inner-city hospitals, Dr. Boutwell says.
“CARR has really dug deeply into the needs of vulnerable patients in one of America’s most economically challenged communities, with a high proportion of Medicaid, uninsured, and disabled patients” and a shrinking population, she says. Many rehospitalizations are related to socio-economics. “The CARR coalition is meeting with the homeless shelters, the food pantries, and the faith-based agencies,” she says. “They’re really getting at the root of significant issues in their community.”
Nancy Vecchioni, RN, MSN, CPHQ, vice present of Medicare operations at MPRO, says CARR involves more than just healthcare providers; it also brings community agencies together with them to take ownership of the patient. Organizations that a year ago weren’t talking to each other are now meeting regularly to focus on the most vulnerable patients, reviewing cases of rehospitalized homeless patients, and sharing their experiences. Rehospitalized patients are being interviewed, using a prepared script (see Figure 1, p. 34), which allows the patient to tell their story. The information is shared within the coalition.
Each hospital has its own transition team, with post-acute providers, physicians, home health agencies, and community service providers, Vecchioni says. For patients who can’t get in to see a PCP within five days of discharge, some hospitals are opening continuity clinics. Others give patients three- to 30-day supplies of needed medications. “There’s no magic bullet—it’s just a different way of looking at how we do this work,” she adds. “Every day we see new barriers. But we’ve already seen a 5% overall reduction in readmissions. And I think hospitalists can be the champions and leaders of these efforts.”
Hospitalists have to raise the bar for themselves, Dr. Schneidermann says, “doing our best while recognizing we can only do so much. There is a lot we can learn from geriatrics, starting with truly embracing the multidisciplinary team.” If hospitalists feel like they are functioning in isolation, she says, they need to look around. “Are these kinds of interdisciplinary meetings happening? If so, join them. If not, light a fire. Convert your frustrating experiences with patients into action.” TH
Larry Beresford is a freelance medical writer based in California.
References
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
- Kertesz SG, Posner MA, O’Connell JJ, et al. Post-hospital medical respite care and hospital readmission of homeless persons. J Prev Inter Community. 2009;37:129-142.
- Nagamine M, Stocks C, Merrill C. Trends in uninsured hospital stays, 1998-2007. Health Care Cost & Utilization Project (HCUP) Statistical Brief #88. May 2010.
- U.S. Department of Health and Human Services. ASPE Research Brief. The value of health insurance: few of the uninsured have adequate resources to pay potential hospital bills. May 2011.
- U.S. Department of Housing and Urban Development. The Annual Housing Assessment Report to Congress, 2009.
- Kellerman A, Coleman M. Care without Coverage: Too Little, Too Late. Report by Institute of Medicine, May 2002.
- Hasan O, Orav EJ, Hicks LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8):452-459.
- Chirayath HT, Wentworth AL. Constraints to caring: Service to medically indigent patients by allopathic and osteopathic physicians. J Health Care Poor Underserved. 2008;19:500-511.
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675-681.
- Buchanan D, Rohr L, Kehoe L, Glick SB, Jain S. Changing attitudes toward homeless people. J Gen Intern Med. 2004;19(5 Pt 2):566-568.
Gregory Misky, MD, has been a hospitalist for 12 years, first at a community hospital and for the past seven years at the University of Colorado Denver. In recent years, his frustration has grown over the challenges of discharge planning, care transitions, and preventing readmissions for vulnerable, disadvantaged patients, including the uninsured, underinsured, and medically indigent.
“There’s a big elephant in the room that we’re not talking about, and that elephant is having babies,” he says. “Access is such a big problem for these patients and, as a hospitalist, it’s just not OK to me anymore. I need to be proactive about finding solutions.”
Dr. Misky’s concerns led him to do research with mentor Eric Coleman, MD, the university’s creator of the Care Transitions Program (www.caretransitions.org), studying patients who lacked primary-care physicians (PCPs) or timely PCP follow-up, and their resulting higher rates of readmissions.1 Dr. Misky also helped develop care pathways, including post-discharge care, for VTE patients, a “common, costly, and dangerous” condition. He is working with a hospitalist colleague to explore how electronic health records (EHR) might be used to help trigger post-discharge follow-up for at-risk patients.
University of Colorado Hospital (UCH), a 425-bed urban academic tertiary-care center, is not the designated safety net hospital for metro Denver, yet 28% to 32% of patients discharged from its medical services are uninsured, Dr. Misky says. He finds that academic physicians at UCH are not always able to take on large numbers of uninsured patients in their clinics, given the productivity demands they face, while the hospital has not been able to participate in systemwide, comprehensive national models for improving care transitions, such as SHM’s Project BOOST (www.hospitalmedicine.org/boost) or Boston Medical Center’s Project RED (www.bu.edu/fammed/projectred/).
Dr. Misky is in discussions with local community services, such as the Metro Community Provider Network (MCPN) of clinics for underserved patients, and exploring the development of a collaborative model for integrating post-hospital care between UCH and MCPN. “A lot of our ideas are still very exploratory—trying to get the key providers to the table to talk about what these approaches might look like,” Dr. Misky explains. “I’ve been part of ongoing meetings, and I think similar kinds of conversations are happening at many levels at UCH, but there’s not a unified, consensus approach to care transitions—and that’s a problem. But I’m in the midst of it all, trying to highlight the issues and explore solutions.”
—Patricia Rutherford, RN, MS, vice president, Institute for Healthcare Improvement
Dr. Misky says every hospital-based provider—hospitalist, nurses, social workers—feels the same frustration and worry about the level of care when indigent patients are discharged to the community. Uninsured patients can run into problems post-hospitalization and return to the ED for their primary care because they lack other options, he says. “Without established liaisons to the community clinics,” he notes, “it can take three or four months for a new indigent patient to get seen at one.”
Disproportional Issues of the Uninsured
Hospitalists at San Francisco General Hospital, which is the safety-net provider for the Bay Area, are looking at similar issues, says Jeff Critchfield, MD, division chief of hospital medicine. “What we know about the uninsured is that they have a wealth of other challenges and barriers that they bring to the table,” he says. “First of all, un- and underinsured patients are more likely to have chronic illnesses, to be hospitalized for those illnesses, and then to be rehospitalized after discharge.”
Other issues disproportionally impacting uninsured or indigent patients include low literacy, low healthcare literacy, language barriers, cross-cultural barriers, substance abuse and mental health issues, homelessness or marginal housing, transportation barriers, and “social isolation, which also plagues our population and, I believe, places patients at risk, as does depression,” says Dr. Critchfield’s colleague Michelle Schneidermann, MD.
One-third of San Francisco General’s patients are uninsured and 40% have Medi-Cal (California’s version of Medicaid), which basically means they are underinsured.
“California has 19 safety-net hospitals, with 6% of the state’s inpatient beds but 50% of its uninsured population. So that’s what we do,” Dr. Critchfield says. But almost any hospital or hospitalist will see many of the same issues and problems, just not in the same proportions. “These are patients who can be most frustrating to hospitalists, requiring a disproportionate amount of our time,” he says, adding the greatest difficulty is helping these patients understand and follow post-discharge care plans. But if someone is ill enough to need acute hospitalization and is later discharged back to the street, readmission should not be a surprise. “We’ve done that experiment for many years, and we know how it turns out,” he says.
Dr. Schneidermann serves as medical director of San Francisco General’s medical respite program, a 45-bed emergency shelter that accepts homeless or marginally housed patients in need of follow-up care following discharge from any of the city’s acute-care hospitals. Research has shown that the programs can have a major effect on keeping discharged patients off the street, reducing their rates of rehospitalization by as much as 50%.2,3
“We know that homeless patients have longer lengths of hospital stay because their discharges are fraught with problems,” she says. A homeless patient hospitalized with a blood clot potentially could be kept in the hospital for a week while transitioning from heparin to Coumadin, while similar patients with community support might get discharged in a day.
“We are also fortunate to have a program called Healthy San Francisco,” which isn’t a health insurance program per se but since 2007 has provided access to outpatient, inpatient, and preventive care and medications for indigent patients, Dr. Schneidermann says. Sponsored by the city’s Department of Public Health, it is accessed through 32 medical homes located in both public and private clinics. The hospitalists’ goal is to have a follow-up appointment set with a receiving provider at the time of discharge. “It doesn’t always happen, but that’s the goal,” she explains. “Someone, by name, who has accepted the referral.”
Dr. Critchfield is running a randomized controlled trial of the hospital’s interventions to stem the tide of readmissions in patients 60 and older; many of these patients share the same indigent demographics of the rest of San Francisco General’s caseload, although most patients 65 and older qualify for Medicare. He describes the program as a hybrid of Project RED and Dr. Coleman’s Care Transitions Program, although it targets patients who speak English, Spanish, Cantonese, and Mandarin.
How many Americans are uninsured today is a moving target in the context of healthcare reform and its uncertain future, but the number increased to 53 million in 2007 from 42 million in 1998.4 The number of hospitalizations of uninsured patients also grew to 2.3 million from 1.8 million in the same time period, an increase of 31%, while total hospitalizations were increasing by 13%. A May 2011 research brief from the U.S. Department of Health and Human Services estimates that uncompensated costs of hospital care incurred for uninsured patients total $73 billion per year.5
The homeless in shelters or on the street number about 630,000 on any given evening, and 1.5 million Americans experienced homelessness last year, says Sabrina Edgington, MSSW, program and policy specialist at the National Health Care for the Homeless Council in Nashville, Tenn. That said, 30% of the U.S. homeless have health insurance. Uninsured patients are less likely to receive necessary diagnostic tests and labs while in the hospital, and they face limited access and longer wait times—even in the facilities that are willing to take them.7 Research published in the Journal of Hospital Medicine finds that uninsured or Medicaid patients with three common conditions are more likely to die in the hospital than insured patients.8 A 2008 national sample survey of physicians found that “most U.S. physicians limit their care of medically indigent patients.”9 Other recent research suggests that readmission rates are affected by race and by site of care—with hospitals serving a higher proportion of black patients also having higher readmission rates.10
“This is not a hospital problem—it’s a communitywide problem. So there’s not just a hospital solution; it will take the whole village,” says Patricia Rutherford, RN, MS, vice president of the Institute for Healthcare Improvement (IHI), which sponsors initiatives targeting care transitions.
The major national care-transitions programs that assist hospitals with addressing rehospitalizations all share similar objectives, Rutherford says, and all could be helpful in improving hospitals’ responses to indigent patients. The recognized programs include IHI’s STAAR (State Action on Avoidable Rehospitalizations: www.ihi.org/IHI/Programs), a multistate, multistakeholder quality improvement (QI) program; Project BOOST; Project RED; Dr. Coleman’s Care Transitions Project; the nursing-based Transitional Care Model (www.transitionalcare.info); and the American College of Cardiology’s Hospital to Home (www.cardiosource.org).

—Amy Boutwell, MD, MPP, hospitalist, Newton (Mass.) Wellesley Hospital, president, Collaborative Healthcare Strategies
Most of these “well-established, evidence-based interventions,” including BOOST, will be given preference in applications for grants from the federal Community-Based Care Transitions Program (CCTP). The program recently committed $500 million to support community-based coalitions that include hospitals that are working with community partners to create seamless care transitions. “It’s most important that hospitalists are integrally involved with these care-transition teams—if not leading them,” Rutherford says.
BOOST’s approach is built on a major change-management strategy to reconstruct hospitals’ care transitions and discharge processes from the ground up, says Tina Budnitz, MPH, the project’s director at SHM (see “Discharge Improvement,” p. 7.) “The first thing we do, we literally get out pens and paper and chart what happens before patients get into the hospital and what happens after they are discharged, all of the services that touch them—or should,” she says. “The planning process occurs on many levels, with all of the stakeholders in the community looking at the process map and seeing where people fall off and end up readmitted.”
—Jeff Critchfield, MD, division chief of hospital medicine, San Francisco General Hospital
SHM is planning to launch several new BOOST cohorts for participating hospitals this fall, along with a wider range of technical support, Budnitz says.
The Cross-Setting Team
Research on care transitions for uninsured or indigent patients “is not very robust,” observes Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Newton, Mass., former director of health policy at IHI and president of Collaborative Healthcare Strategies. “We don’t have the information we need, but there are great opportunities to improve our research base,” she explains.
Dr. Boutwell is a big fan of the “cross-setting team,” which brings together around a conference table professionals who work in different care settings, including the hospital, long-term care, and home-based care. She says it’s her job “to make sure patients are safe upon discharge, but if the community is under-resourced for primary-care physicians, if the patient is uninsured and we can’t find a PCP, the hospitalist and cross-setting team need to say, ‘We just can’t accept that.’ ”
A proper handoff should be done in a way that helps the patient and the physician providing the follow-up care. “But you won’t know what that is unless you ask the people you’re sending patients to how you’re doing,” she explains. “When we routinely review readmitted patients in cross-setting groups, it quickly breaks down the mindset that we in the hospital did everything we could have done to make the discharge successful.”
Dr. Boutwell recommends that hospitalists avoid thinking of these issues in a vacuum, as medical-clinical issues that only doctors can fix. “Because you can’t,” she says. “I would never ask an individual hospitalist to reduce readmissions. It requires a multidisciplinary, all-hands-on-deck approach by the hospital. This is different and more exciting than other quality-improvement efforts.” What’s more, she says, the day is coming—and soon—when failing to manage these readmissions will be a bad business proposition for the hospital (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
IHI’s STAAR Initiative is working with coalitions of providers in Massachusetts, Michigan, Ohio, and Washington. One of those coalitions, Detroit CARR (Community Action to Reduce Rehospitalizations), convened by MPRO, a Michigan-based quality-improvement organization, is a great example of a cross-continuum team involving five inner-city hospitals, Dr. Boutwell says.
“CARR has really dug deeply into the needs of vulnerable patients in one of America’s most economically challenged communities, with a high proportion of Medicaid, uninsured, and disabled patients” and a shrinking population, she says. Many rehospitalizations are related to socio-economics. “The CARR coalition is meeting with the homeless shelters, the food pantries, and the faith-based agencies,” she says. “They’re really getting at the root of significant issues in their community.”
Nancy Vecchioni, RN, MSN, CPHQ, vice present of Medicare operations at MPRO, says CARR involves more than just healthcare providers; it also brings community agencies together with them to take ownership of the patient. Organizations that a year ago weren’t talking to each other are now meeting regularly to focus on the most vulnerable patients, reviewing cases of rehospitalized homeless patients, and sharing their experiences. Rehospitalized patients are being interviewed, using a prepared script (see Figure 1, p. 34), which allows the patient to tell their story. The information is shared within the coalition.
Each hospital has its own transition team, with post-acute providers, physicians, home health agencies, and community service providers, Vecchioni says. For patients who can’t get in to see a PCP within five days of discharge, some hospitals are opening continuity clinics. Others give patients three- to 30-day supplies of needed medications. “There’s no magic bullet—it’s just a different way of looking at how we do this work,” she adds. “Every day we see new barriers. But we’ve already seen a 5% overall reduction in readmissions. And I think hospitalists can be the champions and leaders of these efforts.”
Hospitalists have to raise the bar for themselves, Dr. Schneidermann says, “doing our best while recognizing we can only do so much. There is a lot we can learn from geriatrics, starting with truly embracing the multidisciplinary team.” If hospitalists feel like they are functioning in isolation, she says, they need to look around. “Are these kinds of interdisciplinary meetings happening? If so, join them. If not, light a fire. Convert your frustrating experiences with patients into action.” TH
Larry Beresford is a freelance medical writer based in California.
References
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
- Kertesz SG, Posner MA, O’Connell JJ, et al. Post-hospital medical respite care and hospital readmission of homeless persons. J Prev Inter Community. 2009;37:129-142.
- Nagamine M, Stocks C, Merrill C. Trends in uninsured hospital stays, 1998-2007. Health Care Cost & Utilization Project (HCUP) Statistical Brief #88. May 2010.
- U.S. Department of Health and Human Services. ASPE Research Brief. The value of health insurance: few of the uninsured have adequate resources to pay potential hospital bills. May 2011.
- U.S. Department of Housing and Urban Development. The Annual Housing Assessment Report to Congress, 2009.
- Kellerman A, Coleman M. Care without Coverage: Too Little, Too Late. Report by Institute of Medicine, May 2002.
- Hasan O, Orav EJ, Hicks LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8):452-459.
- Chirayath HT, Wentworth AL. Constraints to caring: Service to medically indigent patients by allopathic and osteopathic physicians. J Health Care Poor Underserved. 2008;19:500-511.
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675-681.
- Buchanan D, Rohr L, Kehoe L, Glick SB, Jain S. Changing attitudes toward homeless people. J Gen Intern Med. 2004;19(5 Pt 2):566-568.
Gregory Misky, MD, has been a hospitalist for 12 years, first at a community hospital and for the past seven years at the University of Colorado Denver. In recent years, his frustration has grown over the challenges of discharge planning, care transitions, and preventing readmissions for vulnerable, disadvantaged patients, including the uninsured, underinsured, and medically indigent.
“There’s a big elephant in the room that we’re not talking about, and that elephant is having babies,” he says. “Access is such a big problem for these patients and, as a hospitalist, it’s just not OK to me anymore. I need to be proactive about finding solutions.”
Dr. Misky’s concerns led him to do research with mentor Eric Coleman, MD, the university’s creator of the Care Transitions Program (www.caretransitions.org), studying patients who lacked primary-care physicians (PCPs) or timely PCP follow-up, and their resulting higher rates of readmissions.1 Dr. Misky also helped develop care pathways, including post-discharge care, for VTE patients, a “common, costly, and dangerous” condition. He is working with a hospitalist colleague to explore how electronic health records (EHR) might be used to help trigger post-discharge follow-up for at-risk patients.
University of Colorado Hospital (UCH), a 425-bed urban academic tertiary-care center, is not the designated safety net hospital for metro Denver, yet 28% to 32% of patients discharged from its medical services are uninsured, Dr. Misky says. He finds that academic physicians at UCH are not always able to take on large numbers of uninsured patients in their clinics, given the productivity demands they face, while the hospital has not been able to participate in systemwide, comprehensive national models for improving care transitions, such as SHM’s Project BOOST (www.hospitalmedicine.org/boost) or Boston Medical Center’s Project RED (www.bu.edu/fammed/projectred/).
Dr. Misky is in discussions with local community services, such as the Metro Community Provider Network (MCPN) of clinics for underserved patients, and exploring the development of a collaborative model for integrating post-hospital care between UCH and MCPN. “A lot of our ideas are still very exploratory—trying to get the key providers to the table to talk about what these approaches might look like,” Dr. Misky explains. “I’ve been part of ongoing meetings, and I think similar kinds of conversations are happening at many levels at UCH, but there’s not a unified, consensus approach to care transitions—and that’s a problem. But I’m in the midst of it all, trying to highlight the issues and explore solutions.”
—Patricia Rutherford, RN, MS, vice president, Institute for Healthcare Improvement
Dr. Misky says every hospital-based provider—hospitalist, nurses, social workers—feels the same frustration and worry about the level of care when indigent patients are discharged to the community. Uninsured patients can run into problems post-hospitalization and return to the ED for their primary care because they lack other options, he says. “Without established liaisons to the community clinics,” he notes, “it can take three or four months for a new indigent patient to get seen at one.”
Disproportional Issues of the Uninsured
Hospitalists at San Francisco General Hospital, which is the safety-net provider for the Bay Area, are looking at similar issues, says Jeff Critchfield, MD, division chief of hospital medicine. “What we know about the uninsured is that they have a wealth of other challenges and barriers that they bring to the table,” he says. “First of all, un- and underinsured patients are more likely to have chronic illnesses, to be hospitalized for those illnesses, and then to be rehospitalized after discharge.”
Other issues disproportionally impacting uninsured or indigent patients include low literacy, low healthcare literacy, language barriers, cross-cultural barriers, substance abuse and mental health issues, homelessness or marginal housing, transportation barriers, and “social isolation, which also plagues our population and, I believe, places patients at risk, as does depression,” says Dr. Critchfield’s colleague Michelle Schneidermann, MD.
One-third of San Francisco General’s patients are uninsured and 40% have Medi-Cal (California’s version of Medicaid), which basically means they are underinsured.
“California has 19 safety-net hospitals, with 6% of the state’s inpatient beds but 50% of its uninsured population. So that’s what we do,” Dr. Critchfield says. But almost any hospital or hospitalist will see many of the same issues and problems, just not in the same proportions. “These are patients who can be most frustrating to hospitalists, requiring a disproportionate amount of our time,” he says, adding the greatest difficulty is helping these patients understand and follow post-discharge care plans. But if someone is ill enough to need acute hospitalization and is later discharged back to the street, readmission should not be a surprise. “We’ve done that experiment for many years, and we know how it turns out,” he says.
Dr. Schneidermann serves as medical director of San Francisco General’s medical respite program, a 45-bed emergency shelter that accepts homeless or marginally housed patients in need of follow-up care following discharge from any of the city’s acute-care hospitals. Research has shown that the programs can have a major effect on keeping discharged patients off the street, reducing their rates of rehospitalization by as much as 50%.2,3
“We know that homeless patients have longer lengths of hospital stay because their discharges are fraught with problems,” she says. A homeless patient hospitalized with a blood clot potentially could be kept in the hospital for a week while transitioning from heparin to Coumadin, while similar patients with community support might get discharged in a day.
“We are also fortunate to have a program called Healthy San Francisco,” which isn’t a health insurance program per se but since 2007 has provided access to outpatient, inpatient, and preventive care and medications for indigent patients, Dr. Schneidermann says. Sponsored by the city’s Department of Public Health, it is accessed through 32 medical homes located in both public and private clinics. The hospitalists’ goal is to have a follow-up appointment set with a receiving provider at the time of discharge. “It doesn’t always happen, but that’s the goal,” she explains. “Someone, by name, who has accepted the referral.”
Dr. Critchfield is running a randomized controlled trial of the hospital’s interventions to stem the tide of readmissions in patients 60 and older; many of these patients share the same indigent demographics of the rest of San Francisco General’s caseload, although most patients 65 and older qualify for Medicare. He describes the program as a hybrid of Project RED and Dr. Coleman’s Care Transitions Program, although it targets patients who speak English, Spanish, Cantonese, and Mandarin.
How many Americans are uninsured today is a moving target in the context of healthcare reform and its uncertain future, but the number increased to 53 million in 2007 from 42 million in 1998.4 The number of hospitalizations of uninsured patients also grew to 2.3 million from 1.8 million in the same time period, an increase of 31%, while total hospitalizations were increasing by 13%. A May 2011 research brief from the U.S. Department of Health and Human Services estimates that uncompensated costs of hospital care incurred for uninsured patients total $73 billion per year.5
The homeless in shelters or on the street number about 630,000 on any given evening, and 1.5 million Americans experienced homelessness last year, says Sabrina Edgington, MSSW, program and policy specialist at the National Health Care for the Homeless Council in Nashville, Tenn. That said, 30% of the U.S. homeless have health insurance. Uninsured patients are less likely to receive necessary diagnostic tests and labs while in the hospital, and they face limited access and longer wait times—even in the facilities that are willing to take them.7 Research published in the Journal of Hospital Medicine finds that uninsured or Medicaid patients with three common conditions are more likely to die in the hospital than insured patients.8 A 2008 national sample survey of physicians found that “most U.S. physicians limit their care of medically indigent patients.”9 Other recent research suggests that readmission rates are affected by race and by site of care—with hospitals serving a higher proportion of black patients also having higher readmission rates.10
“This is not a hospital problem—it’s a communitywide problem. So there’s not just a hospital solution; it will take the whole village,” says Patricia Rutherford, RN, MS, vice president of the Institute for Healthcare Improvement (IHI), which sponsors initiatives targeting care transitions.
The major national care-transitions programs that assist hospitals with addressing rehospitalizations all share similar objectives, Rutherford says, and all could be helpful in improving hospitals’ responses to indigent patients. The recognized programs include IHI’s STAAR (State Action on Avoidable Rehospitalizations: www.ihi.org/IHI/Programs), a multistate, multistakeholder quality improvement (QI) program; Project BOOST; Project RED; Dr. Coleman’s Care Transitions Project; the nursing-based Transitional Care Model (www.transitionalcare.info); and the American College of Cardiology’s Hospital to Home (www.cardiosource.org).

—Amy Boutwell, MD, MPP, hospitalist, Newton (Mass.) Wellesley Hospital, president, Collaborative Healthcare Strategies
Most of these “well-established, evidence-based interventions,” including BOOST, will be given preference in applications for grants from the federal Community-Based Care Transitions Program (CCTP). The program recently committed $500 million to support community-based coalitions that include hospitals that are working with community partners to create seamless care transitions. “It’s most important that hospitalists are integrally involved with these care-transition teams—if not leading them,” Rutherford says.
BOOST’s approach is built on a major change-management strategy to reconstruct hospitals’ care transitions and discharge processes from the ground up, says Tina Budnitz, MPH, the project’s director at SHM (see “Discharge Improvement,” p. 7.) “The first thing we do, we literally get out pens and paper and chart what happens before patients get into the hospital and what happens after they are discharged, all of the services that touch them—or should,” she says. “The planning process occurs on many levels, with all of the stakeholders in the community looking at the process map and seeing where people fall off and end up readmitted.”
—Jeff Critchfield, MD, division chief of hospital medicine, San Francisco General Hospital
SHM is planning to launch several new BOOST cohorts for participating hospitals this fall, along with a wider range of technical support, Budnitz says.
The Cross-Setting Team
Research on care transitions for uninsured or indigent patients “is not very robust,” observes Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Newton, Mass., former director of health policy at IHI and president of Collaborative Healthcare Strategies. “We don’t have the information we need, but there are great opportunities to improve our research base,” she explains.
Dr. Boutwell is a big fan of the “cross-setting team,” which brings together around a conference table professionals who work in different care settings, including the hospital, long-term care, and home-based care. She says it’s her job “to make sure patients are safe upon discharge, but if the community is under-resourced for primary-care physicians, if the patient is uninsured and we can’t find a PCP, the hospitalist and cross-setting team need to say, ‘We just can’t accept that.’ ”
A proper handoff should be done in a way that helps the patient and the physician providing the follow-up care. “But you won’t know what that is unless you ask the people you’re sending patients to how you’re doing,” she explains. “When we routinely review readmitted patients in cross-setting groups, it quickly breaks down the mindset that we in the hospital did everything we could have done to make the discharge successful.”
Dr. Boutwell recommends that hospitalists avoid thinking of these issues in a vacuum, as medical-clinical issues that only doctors can fix. “Because you can’t,” she says. “I would never ask an individual hospitalist to reduce readmissions. It requires a multidisciplinary, all-hands-on-deck approach by the hospital. This is different and more exciting than other quality-improvement efforts.” What’s more, she says, the day is coming—and soon—when failing to manage these readmissions will be a bad business proposition for the hospital (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
IHI’s STAAR Initiative is working with coalitions of providers in Massachusetts, Michigan, Ohio, and Washington. One of those coalitions, Detroit CARR (Community Action to Reduce Rehospitalizations), convened by MPRO, a Michigan-based quality-improvement organization, is a great example of a cross-continuum team involving five inner-city hospitals, Dr. Boutwell says.
“CARR has really dug deeply into the needs of vulnerable patients in one of America’s most economically challenged communities, with a high proportion of Medicaid, uninsured, and disabled patients” and a shrinking population, she says. Many rehospitalizations are related to socio-economics. “The CARR coalition is meeting with the homeless shelters, the food pantries, and the faith-based agencies,” she says. “They’re really getting at the root of significant issues in their community.”
Nancy Vecchioni, RN, MSN, CPHQ, vice present of Medicare operations at MPRO, says CARR involves more than just healthcare providers; it also brings community agencies together with them to take ownership of the patient. Organizations that a year ago weren’t talking to each other are now meeting regularly to focus on the most vulnerable patients, reviewing cases of rehospitalized homeless patients, and sharing their experiences. Rehospitalized patients are being interviewed, using a prepared script (see Figure 1, p. 34), which allows the patient to tell their story. The information is shared within the coalition.
Each hospital has its own transition team, with post-acute providers, physicians, home health agencies, and community service providers, Vecchioni says. For patients who can’t get in to see a PCP within five days of discharge, some hospitals are opening continuity clinics. Others give patients three- to 30-day supplies of needed medications. “There’s no magic bullet—it’s just a different way of looking at how we do this work,” she adds. “Every day we see new barriers. But we’ve already seen a 5% overall reduction in readmissions. And I think hospitalists can be the champions and leaders of these efforts.”
Hospitalists have to raise the bar for themselves, Dr. Schneidermann says, “doing our best while recognizing we can only do so much. There is a lot we can learn from geriatrics, starting with truly embracing the multidisciplinary team.” If hospitalists feel like they are functioning in isolation, she says, they need to look around. “Are these kinds of interdisciplinary meetings happening? If so, join them. If not, light a fire. Convert your frustrating experiences with patients into action.” TH
Larry Beresford is a freelance medical writer based in California.
References
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
- Kertesz SG, Posner MA, O’Connell JJ, et al. Post-hospital medical respite care and hospital readmission of homeless persons. J Prev Inter Community. 2009;37:129-142.
- Nagamine M, Stocks C, Merrill C. Trends in uninsured hospital stays, 1998-2007. Health Care Cost & Utilization Project (HCUP) Statistical Brief #88. May 2010.
- U.S. Department of Health and Human Services. ASPE Research Brief. The value of health insurance: few of the uninsured have adequate resources to pay potential hospital bills. May 2011.
- U.S. Department of Housing and Urban Development. The Annual Housing Assessment Report to Congress, 2009.
- Kellerman A, Coleman M. Care without Coverage: Too Little, Too Late. Report by Institute of Medicine, May 2002.
- Hasan O, Orav EJ, Hicks LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8):452-459.
- Chirayath HT, Wentworth AL. Constraints to caring: Service to medically indigent patients by allopathic and osteopathic physicians. J Health Care Poor Underserved. 2008;19:500-511.
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675-681.
- Buchanan D, Rohr L, Kehoe L, Glick SB, Jain S. Changing attitudes toward homeless people. J Gen Intern Med. 2004;19(5 Pt 2):566-568.
Red Flags within Documentation for Hospitalists
With the number of clinical hospitalists still growing, more patients are under HM care, which puts hospitalists at higher risk for lawsuits. The goal for a hospitalist should be to take care of their patients, but at the same point make a defensible medical record. Plaintiffs’ attorneys look for potential red flags in the medical record. Potential red flags could be illegibility, omissions of date and time, criticism of other healthcare providers, vague terminology, abbreviations, delayed entries, inconsistencies between healthcare providers, corrections, and opinions about the patient.
The medical record is a legal document that is required by law and regulatory bodies. It serves as a communication vehicle for healthcare providers; it tells the patient’s story as well as the care that has been received. It is used for implementing quality-improvement initiatives, determining appropriate level of care, and research and education. It also is the most credible evidence in a legal proceeding. Inaccurate or incomplete documentation can mean serious trouble.
The most common documentation error is illegible handwriting. It is well known throughout medicine that if it’s not documented, it has not been done. At the same time, what is not readable has not been done. Electronic health records (EHR) have minimized this problem; however, EHR is not universally available, and documentation could include both electronic and handwritten entries.
Common sense dictates that all records should be legible, but it is surprising the number of progress notes that are illegible. Physicians are encouraged to write in black ink, so that the notes are capable of being photocopied. Some colored inks can run when they become wet. Also, all entries should include the full date, time, and the name of the physician, as well as their title and designation, which should be printed alongside their signatures.
Correction fluid must not be used in any patient records. Corrections should be made with a single line drawn through them, initialed, dated, and timed, so the error can still be read. All entries should be in a chronological order, with no spaces between the entries. Extra words should not be squeezed onto a line; a line must be drawn through any empty space at the end of an entry. Ditto marks should never be used. Use of glue is not permitted in the medical record, unless some special pages have tabs to allow sheets to be attached to the notes.
No paper should be removed from the clinical file, other than for purposes of photocopying, and those should be returned immediately. Each page of the documentation should be sequentially numbered; if the pages are kept in separate sections, make sure that is clear. Each progress note should have three unique patient identifiers: patient name, date of birth, and a record number. Most hospitals use sticker systems or printable progress notes, which have taken care of this problem.
Notes from various specialties, including nursing records, should be documented in the patient chart. If any of these include discussions held outside of normal working hours, those entry notes should clearly state the time and location of the discussions and state that the entry is made retrospectively.
Leaving space to accommodate late documentation never is a good idea. If the space is too small and subsequent documentation is squeezed in, an attorney could allege that the squeeze documentation was added to cover something up. If the space is too large, the blank space remains unaccounted for. When a late entry is made several days later, it should include a rationale for the delay. Unexplained late entries, along with erased or obliterated entries, are serious red flags.
The clinical content of a progress note should state in full a legible and understandable history. This should include a full assessment, including the positive and negative findings, interventions, and outcomes, as well as initial and ongoing assessments by each provider. Legible instructions should be included for all treatment therapies and medications. These records should be factual, consistent, and accurate.
When physicians disagree among themselves, criticism of that should not be on the record. In fact, this variance should be documented in the chart and the provider making this decision should clearly document the processes that led to the decision.
It is unwise to include abbreviations. In cases where abbreviations are necessary, they should be spelled out fully the first time. Institutional policies should be followed for appropriate abbreviations. Jargon, meaningless phrases, irrelevant speculation, and offensive or subjective statements should not be written. Labels to describe a patient as obnoxious, belligerent, or rude can lead to serious allegations. In fact, direct quotes should be applied on the record. The patient’s refusal of treatment should be documented, including the patient’s stated reason for refusal, if provided, and any action taken by the provider, as well as patient education and notifying the patient and their family. Patients who refuse to accept treatment recommendations might bear partial responsibility for a subsequent injury, which is known as “contributory negligence.”
Vague terminology should be avoided (e.g. “Cl urine” could mean colored urine, clear urine, or cloudy urine) as it can be subject to interpretation. Institutional policies should be followed for reporting incident reports. Peer-review processes should be noted; however, do not indicate in the chart that an incident report has been filed or an event report has been completed. This can serve as a red flag and could give the plaintiff’s attorney the right to access the record.
Documentation red flags should be addressed on a daily basis. Progress notes should be catered not only to providing an accurate record of the physicians’ thought process, but as an assessment of the patient, keeping in mind that if this case is called into court three or four years later, the record will speak for itself.
Deepak Pahuja, MD, FACP,
hospitalist, director of CME,
Erie Physician Network Hospitalists,
St. Vincent Health Center, Erie, Pa.,
CEO, Aerolib Healthcare Solutions LLC;
Priyanka Chadha, MD,
cofounder, Aerolib Healthcare Solutions LLC
DRG Accuracy Increases Medicare Reimbursement, Reduces Risks
Clinical documentation integrity (CDI) programs started in the 1990s. Most of the programs were experimental pilots that assessed the impact on physician documentation and quality.
In 2007, the Centers for Medicare & Medicaid Services (CMS) implemented the Medicare Severity Diagnosis Related Group (DRG). The focus of the DRG system was severity of illness and mortality rates. Indicators such as present on admission (POA) and hospital-acquired condition (HCA) were added the next year to identify conditions noted when a patient was admitted into the hospital.
Currently, the purpose of the CDI program is to optimize the DRG by capturing conditions through clear, concise documentation and coding. Accuracy in reporting DRG assignments will increase Medicare reimbursement and reduce compliance risks. CDI program popularity has grown because of careful consideration of the benefits of implementation.
Are we ready for the change? Launching a CDI program is not an easy task. It takes courage, tenacity, patience, and a great plan. The success of a CDI program depends on one key element: buy-in by physicians at your facility. Yes, physicians. Physician resistance is high for two key reasons: time and education.
A physician’s focus primarily has been the care of the patient, with time allowed to clarify their working or discharge diagnosis and maintaining their patients in the hospital setting. That’s where a clinical documentation specialist (CDS) comes in. At Civista Medical Center in Maryland, color-coded worksheets are printed and attached to the patient’s medical record. The purpose of the worksheet is to trigger the physician to write specific documentation.
Education! Education! It cannot be stressed enough. Healthcare is a team effort. To achieve accurate and concise documentation, physicians must be educated about the importance of documentation. Nonspecific documentation leads to nonspecific coding of the medical record. Therefore, the true severity of illness, mortality rate, and intensity of service goes uncaptured. The lack of specificity in documentation affects the quality of patient care, compliance risk, data integrity, and reimbursement.
The implementation of a CDI program can be successful by enlisting internal support at your facility, including administration, physicians, and such ancillary staff members as case management. A clear, concise plan that includes physicians every step of the way will be imperative.
Consider the many avenues you might have to implement your query system, either by paper or electronically. If the coding department does not own the concurrent CDI query process, make sure they are involved in the process of establishing the program. In addition, provide feedback to various facility departments about the impact the CDI program is having on quality, integrity, and reimbursement. Include an ongoing program to educate the physicians on ICD 9-CM, as well as the forthcoming ICD 10, for a smoother transition.
Karen Stanley, RN, MBA,
White Plains, Md.
With the number of clinical hospitalists still growing, more patients are under HM care, which puts hospitalists at higher risk for lawsuits. The goal for a hospitalist should be to take care of their patients, but at the same point make a defensible medical record. Plaintiffs’ attorneys look for potential red flags in the medical record. Potential red flags could be illegibility, omissions of date and time, criticism of other healthcare providers, vague terminology, abbreviations, delayed entries, inconsistencies between healthcare providers, corrections, and opinions about the patient.
The medical record is a legal document that is required by law and regulatory bodies. It serves as a communication vehicle for healthcare providers; it tells the patient’s story as well as the care that has been received. It is used for implementing quality-improvement initiatives, determining appropriate level of care, and research and education. It also is the most credible evidence in a legal proceeding. Inaccurate or incomplete documentation can mean serious trouble.
The most common documentation error is illegible handwriting. It is well known throughout medicine that if it’s not documented, it has not been done. At the same time, what is not readable has not been done. Electronic health records (EHR) have minimized this problem; however, EHR is not universally available, and documentation could include both electronic and handwritten entries.
Common sense dictates that all records should be legible, but it is surprising the number of progress notes that are illegible. Physicians are encouraged to write in black ink, so that the notes are capable of being photocopied. Some colored inks can run when they become wet. Also, all entries should include the full date, time, and the name of the physician, as well as their title and designation, which should be printed alongside their signatures.
Correction fluid must not be used in any patient records. Corrections should be made with a single line drawn through them, initialed, dated, and timed, so the error can still be read. All entries should be in a chronological order, with no spaces between the entries. Extra words should not be squeezed onto a line; a line must be drawn through any empty space at the end of an entry. Ditto marks should never be used. Use of glue is not permitted in the medical record, unless some special pages have tabs to allow sheets to be attached to the notes.
No paper should be removed from the clinical file, other than for purposes of photocopying, and those should be returned immediately. Each page of the documentation should be sequentially numbered; if the pages are kept in separate sections, make sure that is clear. Each progress note should have three unique patient identifiers: patient name, date of birth, and a record number. Most hospitals use sticker systems or printable progress notes, which have taken care of this problem.
Notes from various specialties, including nursing records, should be documented in the patient chart. If any of these include discussions held outside of normal working hours, those entry notes should clearly state the time and location of the discussions and state that the entry is made retrospectively.
Leaving space to accommodate late documentation never is a good idea. If the space is too small and subsequent documentation is squeezed in, an attorney could allege that the squeeze documentation was added to cover something up. If the space is too large, the blank space remains unaccounted for. When a late entry is made several days later, it should include a rationale for the delay. Unexplained late entries, along with erased or obliterated entries, are serious red flags.
The clinical content of a progress note should state in full a legible and understandable history. This should include a full assessment, including the positive and negative findings, interventions, and outcomes, as well as initial and ongoing assessments by each provider. Legible instructions should be included for all treatment therapies and medications. These records should be factual, consistent, and accurate.
When physicians disagree among themselves, criticism of that should not be on the record. In fact, this variance should be documented in the chart and the provider making this decision should clearly document the processes that led to the decision.
It is unwise to include abbreviations. In cases where abbreviations are necessary, they should be spelled out fully the first time. Institutional policies should be followed for appropriate abbreviations. Jargon, meaningless phrases, irrelevant speculation, and offensive or subjective statements should not be written. Labels to describe a patient as obnoxious, belligerent, or rude can lead to serious allegations. In fact, direct quotes should be applied on the record. The patient’s refusal of treatment should be documented, including the patient’s stated reason for refusal, if provided, and any action taken by the provider, as well as patient education and notifying the patient and their family. Patients who refuse to accept treatment recommendations might bear partial responsibility for a subsequent injury, which is known as “contributory negligence.”
Vague terminology should be avoided (e.g. “Cl urine” could mean colored urine, clear urine, or cloudy urine) as it can be subject to interpretation. Institutional policies should be followed for reporting incident reports. Peer-review processes should be noted; however, do not indicate in the chart that an incident report has been filed or an event report has been completed. This can serve as a red flag and could give the plaintiff’s attorney the right to access the record.
Documentation red flags should be addressed on a daily basis. Progress notes should be catered not only to providing an accurate record of the physicians’ thought process, but as an assessment of the patient, keeping in mind that if this case is called into court three or four years later, the record will speak for itself.
Deepak Pahuja, MD, FACP,
hospitalist, director of CME,
Erie Physician Network Hospitalists,
St. Vincent Health Center, Erie, Pa.,
CEO, Aerolib Healthcare Solutions LLC;
Priyanka Chadha, MD,
cofounder, Aerolib Healthcare Solutions LLC
DRG Accuracy Increases Medicare Reimbursement, Reduces Risks
Clinical documentation integrity (CDI) programs started in the 1990s. Most of the programs were experimental pilots that assessed the impact on physician documentation and quality.
In 2007, the Centers for Medicare & Medicaid Services (CMS) implemented the Medicare Severity Diagnosis Related Group (DRG). The focus of the DRG system was severity of illness and mortality rates. Indicators such as present on admission (POA) and hospital-acquired condition (HCA) were added the next year to identify conditions noted when a patient was admitted into the hospital.
Currently, the purpose of the CDI program is to optimize the DRG by capturing conditions through clear, concise documentation and coding. Accuracy in reporting DRG assignments will increase Medicare reimbursement and reduce compliance risks. CDI program popularity has grown because of careful consideration of the benefits of implementation.
Are we ready for the change? Launching a CDI program is not an easy task. It takes courage, tenacity, patience, and a great plan. The success of a CDI program depends on one key element: buy-in by physicians at your facility. Yes, physicians. Physician resistance is high for two key reasons: time and education.
A physician’s focus primarily has been the care of the patient, with time allowed to clarify their working or discharge diagnosis and maintaining their patients in the hospital setting. That’s where a clinical documentation specialist (CDS) comes in. At Civista Medical Center in Maryland, color-coded worksheets are printed and attached to the patient’s medical record. The purpose of the worksheet is to trigger the physician to write specific documentation.
Education! Education! It cannot be stressed enough. Healthcare is a team effort. To achieve accurate and concise documentation, physicians must be educated about the importance of documentation. Nonspecific documentation leads to nonspecific coding of the medical record. Therefore, the true severity of illness, mortality rate, and intensity of service goes uncaptured. The lack of specificity in documentation affects the quality of patient care, compliance risk, data integrity, and reimbursement.
The implementation of a CDI program can be successful by enlisting internal support at your facility, including administration, physicians, and such ancillary staff members as case management. A clear, concise plan that includes physicians every step of the way will be imperative.
Consider the many avenues you might have to implement your query system, either by paper or electronically. If the coding department does not own the concurrent CDI query process, make sure they are involved in the process of establishing the program. In addition, provide feedback to various facility departments about the impact the CDI program is having on quality, integrity, and reimbursement. Include an ongoing program to educate the physicians on ICD 9-CM, as well as the forthcoming ICD 10, for a smoother transition.
Karen Stanley, RN, MBA,
White Plains, Md.
With the number of clinical hospitalists still growing, more patients are under HM care, which puts hospitalists at higher risk for lawsuits. The goal for a hospitalist should be to take care of their patients, but at the same point make a defensible medical record. Plaintiffs’ attorneys look for potential red flags in the medical record. Potential red flags could be illegibility, omissions of date and time, criticism of other healthcare providers, vague terminology, abbreviations, delayed entries, inconsistencies between healthcare providers, corrections, and opinions about the patient.
The medical record is a legal document that is required by law and regulatory bodies. It serves as a communication vehicle for healthcare providers; it tells the patient’s story as well as the care that has been received. It is used for implementing quality-improvement initiatives, determining appropriate level of care, and research and education. It also is the most credible evidence in a legal proceeding. Inaccurate or incomplete documentation can mean serious trouble.
The most common documentation error is illegible handwriting. It is well known throughout medicine that if it’s not documented, it has not been done. At the same time, what is not readable has not been done. Electronic health records (EHR) have minimized this problem; however, EHR is not universally available, and documentation could include both electronic and handwritten entries.
Common sense dictates that all records should be legible, but it is surprising the number of progress notes that are illegible. Physicians are encouraged to write in black ink, so that the notes are capable of being photocopied. Some colored inks can run when they become wet. Also, all entries should include the full date, time, and the name of the physician, as well as their title and designation, which should be printed alongside their signatures.
Correction fluid must not be used in any patient records. Corrections should be made with a single line drawn through them, initialed, dated, and timed, so the error can still be read. All entries should be in a chronological order, with no spaces between the entries. Extra words should not be squeezed onto a line; a line must be drawn through any empty space at the end of an entry. Ditto marks should never be used. Use of glue is not permitted in the medical record, unless some special pages have tabs to allow sheets to be attached to the notes.
No paper should be removed from the clinical file, other than for purposes of photocopying, and those should be returned immediately. Each page of the documentation should be sequentially numbered; if the pages are kept in separate sections, make sure that is clear. Each progress note should have three unique patient identifiers: patient name, date of birth, and a record number. Most hospitals use sticker systems or printable progress notes, which have taken care of this problem.
Notes from various specialties, including nursing records, should be documented in the patient chart. If any of these include discussions held outside of normal working hours, those entry notes should clearly state the time and location of the discussions and state that the entry is made retrospectively.
Leaving space to accommodate late documentation never is a good idea. If the space is too small and subsequent documentation is squeezed in, an attorney could allege that the squeeze documentation was added to cover something up. If the space is too large, the blank space remains unaccounted for. When a late entry is made several days later, it should include a rationale for the delay. Unexplained late entries, along with erased or obliterated entries, are serious red flags.
The clinical content of a progress note should state in full a legible and understandable history. This should include a full assessment, including the positive and negative findings, interventions, and outcomes, as well as initial and ongoing assessments by each provider. Legible instructions should be included for all treatment therapies and medications. These records should be factual, consistent, and accurate.
When physicians disagree among themselves, criticism of that should not be on the record. In fact, this variance should be documented in the chart and the provider making this decision should clearly document the processes that led to the decision.
It is unwise to include abbreviations. In cases where abbreviations are necessary, they should be spelled out fully the first time. Institutional policies should be followed for appropriate abbreviations. Jargon, meaningless phrases, irrelevant speculation, and offensive or subjective statements should not be written. Labels to describe a patient as obnoxious, belligerent, or rude can lead to serious allegations. In fact, direct quotes should be applied on the record. The patient’s refusal of treatment should be documented, including the patient’s stated reason for refusal, if provided, and any action taken by the provider, as well as patient education and notifying the patient and their family. Patients who refuse to accept treatment recommendations might bear partial responsibility for a subsequent injury, which is known as “contributory negligence.”
Vague terminology should be avoided (e.g. “Cl urine” could mean colored urine, clear urine, or cloudy urine) as it can be subject to interpretation. Institutional policies should be followed for reporting incident reports. Peer-review processes should be noted; however, do not indicate in the chart that an incident report has been filed or an event report has been completed. This can serve as a red flag and could give the plaintiff’s attorney the right to access the record.
Documentation red flags should be addressed on a daily basis. Progress notes should be catered not only to providing an accurate record of the physicians’ thought process, but as an assessment of the patient, keeping in mind that if this case is called into court three or four years later, the record will speak for itself.
Deepak Pahuja, MD, FACP,
hospitalist, director of CME,
Erie Physician Network Hospitalists,
St. Vincent Health Center, Erie, Pa.,
CEO, Aerolib Healthcare Solutions LLC;
Priyanka Chadha, MD,
cofounder, Aerolib Healthcare Solutions LLC
DRG Accuracy Increases Medicare Reimbursement, Reduces Risks
Clinical documentation integrity (CDI) programs started in the 1990s. Most of the programs were experimental pilots that assessed the impact on physician documentation and quality.
In 2007, the Centers for Medicare & Medicaid Services (CMS) implemented the Medicare Severity Diagnosis Related Group (DRG). The focus of the DRG system was severity of illness and mortality rates. Indicators such as present on admission (POA) and hospital-acquired condition (HCA) were added the next year to identify conditions noted when a patient was admitted into the hospital.
Currently, the purpose of the CDI program is to optimize the DRG by capturing conditions through clear, concise documentation and coding. Accuracy in reporting DRG assignments will increase Medicare reimbursement and reduce compliance risks. CDI program popularity has grown because of careful consideration of the benefits of implementation.
Are we ready for the change? Launching a CDI program is not an easy task. It takes courage, tenacity, patience, and a great plan. The success of a CDI program depends on one key element: buy-in by physicians at your facility. Yes, physicians. Physician resistance is high for two key reasons: time and education.
A physician’s focus primarily has been the care of the patient, with time allowed to clarify their working or discharge diagnosis and maintaining their patients in the hospital setting. That’s where a clinical documentation specialist (CDS) comes in. At Civista Medical Center in Maryland, color-coded worksheets are printed and attached to the patient’s medical record. The purpose of the worksheet is to trigger the physician to write specific documentation.
Education! Education! It cannot be stressed enough. Healthcare is a team effort. To achieve accurate and concise documentation, physicians must be educated about the importance of documentation. Nonspecific documentation leads to nonspecific coding of the medical record. Therefore, the true severity of illness, mortality rate, and intensity of service goes uncaptured. The lack of specificity in documentation affects the quality of patient care, compliance risk, data integrity, and reimbursement.
The implementation of a CDI program can be successful by enlisting internal support at your facility, including administration, physicians, and such ancillary staff members as case management. A clear, concise plan that includes physicians every step of the way will be imperative.
Consider the many avenues you might have to implement your query system, either by paper or electronically. If the coding department does not own the concurrent CDI query process, make sure they are involved in the process of establishing the program. In addition, provide feedback to various facility departments about the impact the CDI program is having on quality, integrity, and reimbursement. Include an ongoing program to educate the physicians on ICD 9-CM, as well as the forthcoming ICD 10, for a smoother transition.
Karen Stanley, RN, MBA,
White Plains, Md.
Team Hospitalist Seats New Members
Six hospitalists have joined Team Hospitalist, the only reader-involvement group of its kind in HM. Each of the new members has experience in the practice of HM; many offer specialized backgrounds in pediatrics, academics, and group administration. The new members will serve two-year terms on the 12-person board, and act as special editorial consultants to the magazine.
Femi Adewunmi, MD, MBA, CPE, SFHM
Senior hospitalist management consultant
Crosswalk Consulting Group
Raleigh, N.C.
Tracy E. Cardin, ACNP-BC
Section of Hospital Medicine
Department of General Medicine
University of Chicago Medical Center
Dan Hale, MD, FAAP
Pediatric hospitalist
Floating Hospital for Children
Tufts Medical Center
Boston
Larry W. Holder, MD, FACP
Medical director hospitalist services
Chief medical information officer
Decatur Memorial Hospital,
Illinois
Joshua D. Lenchus, DO, RPh, FACP, FHM
Assistant professor, division of hospital medicine Department of Medicine
University of Miami Miller School of Medicine
Associate program director
Jackson Memorial Hospital Internal Medicine Residency
Michelle Mourad, MD
Assistant professor and director of quality, division of hospital medicine
Department of Medicine
University of California at San Francisco Medical Center
Six hospitalists have joined Team Hospitalist, the only reader-involvement group of its kind in HM. Each of the new members has experience in the practice of HM; many offer specialized backgrounds in pediatrics, academics, and group administration. The new members will serve two-year terms on the 12-person board, and act as special editorial consultants to the magazine.
Femi Adewunmi, MD, MBA, CPE, SFHM
Senior hospitalist management consultant
Crosswalk Consulting Group
Raleigh, N.C.
Tracy E. Cardin, ACNP-BC
Section of Hospital Medicine
Department of General Medicine
University of Chicago Medical Center
Dan Hale, MD, FAAP
Pediatric hospitalist
Floating Hospital for Children
Tufts Medical Center
Boston
Larry W. Holder, MD, FACP
Medical director hospitalist services
Chief medical information officer
Decatur Memorial Hospital,
Illinois
Joshua D. Lenchus, DO, RPh, FACP, FHM
Assistant professor, division of hospital medicine Department of Medicine
University of Miami Miller School of Medicine
Associate program director
Jackson Memorial Hospital Internal Medicine Residency
Michelle Mourad, MD
Assistant professor and director of quality, division of hospital medicine
Department of Medicine
University of California at San Francisco Medical Center
Six hospitalists have joined Team Hospitalist, the only reader-involvement group of its kind in HM. Each of the new members has experience in the practice of HM; many offer specialized backgrounds in pediatrics, academics, and group administration. The new members will serve two-year terms on the 12-person board, and act as special editorial consultants to the magazine.
Femi Adewunmi, MD, MBA, CPE, SFHM
Senior hospitalist management consultant
Crosswalk Consulting Group
Raleigh, N.C.
Tracy E. Cardin, ACNP-BC
Section of Hospital Medicine
Department of General Medicine
University of Chicago Medical Center
Dan Hale, MD, FAAP
Pediatric hospitalist
Floating Hospital for Children
Tufts Medical Center
Boston
Larry W. Holder, MD, FACP
Medical director hospitalist services
Chief medical information officer
Decatur Memorial Hospital,
Illinois
Joshua D. Lenchus, DO, RPh, FACP, FHM
Assistant professor, division of hospital medicine Department of Medicine
University of Miami Miller School of Medicine
Associate program director
Jackson Memorial Hospital Internal Medicine Residency
Michelle Mourad, MD
Assistant professor and director of quality, division of hospital medicine
Department of Medicine
University of California at San Francisco Medical Center
Policy Corner: ACA provides multiple pathways to develop and support ACOs
“ACO” is probably the most common acronym to come out of the Affordable Care Act of 2010 (ACA). Over the last several months, much of the public dialogue has focused on the confusion surrounding the “ACO Proposed Rule.” And now there are three new ACO initiatives, which were announced in May by the Centers for Medicare & Medicaid Services (CMS).
So, what’s the difference? And what does it mean for hospitalists?
The ACA provides multiple pathways to develop and support ACOs, or accountable-care organizations. The proposed rule released in March 2011 was for the Medicare Shared Savings Program (MSSP). Through this program, healthcare providers can join together in ACOs to integrate and coordinate services in return for a share of any savings to the Medicare program. These ACOs will be rewarded for lowering growth in Medicare costs while meeting performance standards on quality of care and putting patients first.
Three other initiatives from the newly created Center for Medicare and Medicaid Innovation give providers a broad range of options and support, and reflect the varying needs of providers in embarking on delivery system reforms. They are:
- Pioneer ACO Model: Provides a faster path for mature ACOs that already have begun coordinating care for patients. This model is estimated to save Medicare as much as $430 million over three years through better managing care for beneficiaries and eliminating duplication. It is designed to move away from the fee-for-service (FFS) payment model more quickly than its MSSP counterpart. In year three of the program, Pioneer ACOs that have shown savings over the first two years will be eligible to move to a population-based payment model. The MSSP version is based completely on FFS.
- Advance Payment ACO Initiative: Would allow certain ACOs participating in the MSSP access to a portion of their shared savings up front, helping providers make the infrastructure and staff investments crucial to successful ACOs.
- Accelerated Development Learning Sessions: These sessions will provide the executive leadership teams from existing or emerging ACO entities the opportunity to learn about essential ACO functions and ways to build capacity needed to achieve better care, better health, and lower costs through integrated care models. Three sessions will be offered in the fall: San Francisco in September, Philadelphia in October, and Atlanta in November. For more info, visit https://acoregister.rti.org.
For more information about ACOs, visit www.healthcare.gov.
How hospitalists will be impacted under the ACO model is largely up to the individual hospitalists. Hospitalists are uniquely positioned to lead the system-level changes and quality-improvement (QI) efforts that will be critical to ACO success, and will bring significant value to the ACO model due to the central role that many hospitalists play in promoting team-based care, care coordination, and improving transitions of care. All of these roles are critical to delivering higher-quality care more efficiently.
CMS has provided detailed information on the above programs via Healthcare.gov. SHM submitted comments on the Medicare Shared Savings Program and the Advance Payment ACO Initiative, which can be found in the Advocacy section of www.hospitalmedicine.org under “SHM Letters.” TH
“ACO” is probably the most common acronym to come out of the Affordable Care Act of 2010 (ACA). Over the last several months, much of the public dialogue has focused on the confusion surrounding the “ACO Proposed Rule.” And now there are three new ACO initiatives, which were announced in May by the Centers for Medicare & Medicaid Services (CMS).
So, what’s the difference? And what does it mean for hospitalists?
The ACA provides multiple pathways to develop and support ACOs, or accountable-care organizations. The proposed rule released in March 2011 was for the Medicare Shared Savings Program (MSSP). Through this program, healthcare providers can join together in ACOs to integrate and coordinate services in return for a share of any savings to the Medicare program. These ACOs will be rewarded for lowering growth in Medicare costs while meeting performance standards on quality of care and putting patients first.
Three other initiatives from the newly created Center for Medicare and Medicaid Innovation give providers a broad range of options and support, and reflect the varying needs of providers in embarking on delivery system reforms. They are:
- Pioneer ACO Model: Provides a faster path for mature ACOs that already have begun coordinating care for patients. This model is estimated to save Medicare as much as $430 million over three years through better managing care for beneficiaries and eliminating duplication. It is designed to move away from the fee-for-service (FFS) payment model more quickly than its MSSP counterpart. In year three of the program, Pioneer ACOs that have shown savings over the first two years will be eligible to move to a population-based payment model. The MSSP version is based completely on FFS.
- Advance Payment ACO Initiative: Would allow certain ACOs participating in the MSSP access to a portion of their shared savings up front, helping providers make the infrastructure and staff investments crucial to successful ACOs.
- Accelerated Development Learning Sessions: These sessions will provide the executive leadership teams from existing or emerging ACO entities the opportunity to learn about essential ACO functions and ways to build capacity needed to achieve better care, better health, and lower costs through integrated care models. Three sessions will be offered in the fall: San Francisco in September, Philadelphia in October, and Atlanta in November. For more info, visit https://acoregister.rti.org.
For more information about ACOs, visit www.healthcare.gov.
How hospitalists will be impacted under the ACO model is largely up to the individual hospitalists. Hospitalists are uniquely positioned to lead the system-level changes and quality-improvement (QI) efforts that will be critical to ACO success, and will bring significant value to the ACO model due to the central role that many hospitalists play in promoting team-based care, care coordination, and improving transitions of care. All of these roles are critical to delivering higher-quality care more efficiently.
CMS has provided detailed information on the above programs via Healthcare.gov. SHM submitted comments on the Medicare Shared Savings Program and the Advance Payment ACO Initiative, which can be found in the Advocacy section of www.hospitalmedicine.org under “SHM Letters.” TH
“ACO” is probably the most common acronym to come out of the Affordable Care Act of 2010 (ACA). Over the last several months, much of the public dialogue has focused on the confusion surrounding the “ACO Proposed Rule.” And now there are three new ACO initiatives, which were announced in May by the Centers for Medicare & Medicaid Services (CMS).
So, what’s the difference? And what does it mean for hospitalists?
The ACA provides multiple pathways to develop and support ACOs, or accountable-care organizations. The proposed rule released in March 2011 was for the Medicare Shared Savings Program (MSSP). Through this program, healthcare providers can join together in ACOs to integrate and coordinate services in return for a share of any savings to the Medicare program. These ACOs will be rewarded for lowering growth in Medicare costs while meeting performance standards on quality of care and putting patients first.
Three other initiatives from the newly created Center for Medicare and Medicaid Innovation give providers a broad range of options and support, and reflect the varying needs of providers in embarking on delivery system reforms. They are:
- Pioneer ACO Model: Provides a faster path for mature ACOs that already have begun coordinating care for patients. This model is estimated to save Medicare as much as $430 million over three years through better managing care for beneficiaries and eliminating duplication. It is designed to move away from the fee-for-service (FFS) payment model more quickly than its MSSP counterpart. In year three of the program, Pioneer ACOs that have shown savings over the first two years will be eligible to move to a population-based payment model. The MSSP version is based completely on FFS.
- Advance Payment ACO Initiative: Would allow certain ACOs participating in the MSSP access to a portion of their shared savings up front, helping providers make the infrastructure and staff investments crucial to successful ACOs.
- Accelerated Development Learning Sessions: These sessions will provide the executive leadership teams from existing or emerging ACO entities the opportunity to learn about essential ACO functions and ways to build capacity needed to achieve better care, better health, and lower costs through integrated care models. Three sessions will be offered in the fall: San Francisco in September, Philadelphia in October, and Atlanta in November. For more info, visit https://acoregister.rti.org.
For more information about ACOs, visit www.healthcare.gov.
How hospitalists will be impacted under the ACO model is largely up to the individual hospitalists. Hospitalists are uniquely positioned to lead the system-level changes and quality-improvement (QI) efforts that will be critical to ACO success, and will bring significant value to the ACO model due to the central role that many hospitalists play in promoting team-based care, care coordination, and improving transitions of care. All of these roles are critical to delivering higher-quality care more efficiently.
CMS has provided detailed information on the above programs via Healthcare.gov. SHM submitted comments on the Medicare Shared Savings Program and the Advance Payment ACO Initiative, which can be found in the Advocacy section of www.hospitalmedicine.org under “SHM Letters.” TH
Discharge improvement
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
Dr. Hospitalist: Welcome to Hospital Medicine
I am a cardiologist who retired early and now would like to return to work after 10 years. I am grandfathered, as far as my board certification is concerned, for internal medicine, and was board-certified in cardiology, but I did not recertify when the time came to do so because I was retired. Approximately 80% of my time was spent doing inpatient care when I was practicing. I am seriously thinking about now returning to work as a hospitalist. Having been away from inpatient care for as long as I have, however, is of concern to me. I was wondering if you could suggest the best route to take to bring myself up to date.
Dr. C.E., Indiana
Dr. Hospitalist responds: Welcome back! As hospital medicine continues to grow, we’ve seen many new entrants who might have been out of clinical practice for a period of time. The good news is that there is no strict pathway back to practice, but that’s also the bad news. As you’ve indicated, your state license is active, which is a big first step.
There are a couple of ways to look at this issue. The first is addressing your own comfort level with current HM practice. Having been out of practice for a decade, certainly a lot has changed. As you note, your ABIM certification remains active, so retaking an exam is not necessary. You could consider a board review course, but these tend to focus strictly on how to succeed at the exam, not to bring you up to date in clinical practice. I think the same could be said for the Focused Practice in Hospital Medicine exam: You will gain certification, but passing the exam itself won’t bring your skills up to date. Additionally, the FPHM exam requires enrollment in the Maintenance of Certification through the ABIM. Although it’s highly recommended, it would better serve your needs in the long term, instead of getting recredentialed right now.
To start, your best bet is a clinically focused internal-medicine meeting. SHM and the American College of Physicians offer national meetings in the spring, and there are a number of regional HM meetings in the fall in San Francisco, Chicago, Boston, Atlanta, and Colorado (www.hospitalmedicine.org/events). Not only will you gain knowledge, but also CME credits, which most hospitals (and states) require for privileging.
The next hurdle, which is probably even more important, is the practice requirements for the hospital(s) where you’ll be working. By way of example, my hospital requires, for initial appointment, “documentation of inpatient services to at least 12 patients in the prior 12 months.” That is but one example, but it’s a reasonable starting point.
For sake of argument, let’s assume you can’t meet the criteria. Most hospitals will require a mentored relationship in which you will have to see and document a specified number of cases under the auspices of a supervising physician. That might mean 10 cases, or it could be 80 cases, but the hospital should be able to lay out the explicit criteria in advance. Once those cases have been signed off, then your file can return to credentialing for review. Beware: This whole process could take a lot longer than you might expect, so three to six months might be the expected timeline.
One other resource to note would be something like the Center for Personalized Education for Physicians (CPEP; www.cpepdoc.org/re-entry-program.cfm), which tailors education plans for physicians who are re-entering practice. Some hospitals will ask for a formal evaluation through this resource to obtain a structured response and skills evaluation. It’s applicable for any location, and it helps provide both sides with meeting the expectations.
Regardless of the requirements, you’re not alone. Ask around and you’ll find physicians who’ve gone through a similar scenario. We even had a physician in our group who had been out of clinical practice for a few years successfully navigate a full mentored process without too much trouble.
It might seem a little daunting, but it is entirely doable. TH
I am a cardiologist who retired early and now would like to return to work after 10 years. I am grandfathered, as far as my board certification is concerned, for internal medicine, and was board-certified in cardiology, but I did not recertify when the time came to do so because I was retired. Approximately 80% of my time was spent doing inpatient care when I was practicing. I am seriously thinking about now returning to work as a hospitalist. Having been away from inpatient care for as long as I have, however, is of concern to me. I was wondering if you could suggest the best route to take to bring myself up to date.
Dr. C.E., Indiana
Dr. Hospitalist responds: Welcome back! As hospital medicine continues to grow, we’ve seen many new entrants who might have been out of clinical practice for a period of time. The good news is that there is no strict pathway back to practice, but that’s also the bad news. As you’ve indicated, your state license is active, which is a big first step.
There are a couple of ways to look at this issue. The first is addressing your own comfort level with current HM practice. Having been out of practice for a decade, certainly a lot has changed. As you note, your ABIM certification remains active, so retaking an exam is not necessary. You could consider a board review course, but these tend to focus strictly on how to succeed at the exam, not to bring you up to date in clinical practice. I think the same could be said for the Focused Practice in Hospital Medicine exam: You will gain certification, but passing the exam itself won’t bring your skills up to date. Additionally, the FPHM exam requires enrollment in the Maintenance of Certification through the ABIM. Although it’s highly recommended, it would better serve your needs in the long term, instead of getting recredentialed right now.
To start, your best bet is a clinically focused internal-medicine meeting. SHM and the American College of Physicians offer national meetings in the spring, and there are a number of regional HM meetings in the fall in San Francisco, Chicago, Boston, Atlanta, and Colorado (www.hospitalmedicine.org/events). Not only will you gain knowledge, but also CME credits, which most hospitals (and states) require for privileging.
The next hurdle, which is probably even more important, is the practice requirements for the hospital(s) where you’ll be working. By way of example, my hospital requires, for initial appointment, “documentation of inpatient services to at least 12 patients in the prior 12 months.” That is but one example, but it’s a reasonable starting point.
For sake of argument, let’s assume you can’t meet the criteria. Most hospitals will require a mentored relationship in which you will have to see and document a specified number of cases under the auspices of a supervising physician. That might mean 10 cases, or it could be 80 cases, but the hospital should be able to lay out the explicit criteria in advance. Once those cases have been signed off, then your file can return to credentialing for review. Beware: This whole process could take a lot longer than you might expect, so three to six months might be the expected timeline.
One other resource to note would be something like the Center for Personalized Education for Physicians (CPEP; www.cpepdoc.org/re-entry-program.cfm), which tailors education plans for physicians who are re-entering practice. Some hospitals will ask for a formal evaluation through this resource to obtain a structured response and skills evaluation. It’s applicable for any location, and it helps provide both sides with meeting the expectations.
Regardless of the requirements, you’re not alone. Ask around and you’ll find physicians who’ve gone through a similar scenario. We even had a physician in our group who had been out of clinical practice for a few years successfully navigate a full mentored process without too much trouble.
It might seem a little daunting, but it is entirely doable. TH
I am a cardiologist who retired early and now would like to return to work after 10 years. I am grandfathered, as far as my board certification is concerned, for internal medicine, and was board-certified in cardiology, but I did not recertify when the time came to do so because I was retired. Approximately 80% of my time was spent doing inpatient care when I was practicing. I am seriously thinking about now returning to work as a hospitalist. Having been away from inpatient care for as long as I have, however, is of concern to me. I was wondering if you could suggest the best route to take to bring myself up to date.
Dr. C.E., Indiana
Dr. Hospitalist responds: Welcome back! As hospital medicine continues to grow, we’ve seen many new entrants who might have been out of clinical practice for a period of time. The good news is that there is no strict pathway back to practice, but that’s also the bad news. As you’ve indicated, your state license is active, which is a big first step.
There are a couple of ways to look at this issue. The first is addressing your own comfort level with current HM practice. Having been out of practice for a decade, certainly a lot has changed. As you note, your ABIM certification remains active, so retaking an exam is not necessary. You could consider a board review course, but these tend to focus strictly on how to succeed at the exam, not to bring you up to date in clinical practice. I think the same could be said for the Focused Practice in Hospital Medicine exam: You will gain certification, but passing the exam itself won’t bring your skills up to date. Additionally, the FPHM exam requires enrollment in the Maintenance of Certification through the ABIM. Although it’s highly recommended, it would better serve your needs in the long term, instead of getting recredentialed right now.
To start, your best bet is a clinically focused internal-medicine meeting. SHM and the American College of Physicians offer national meetings in the spring, and there are a number of regional HM meetings in the fall in San Francisco, Chicago, Boston, Atlanta, and Colorado (www.hospitalmedicine.org/events). Not only will you gain knowledge, but also CME credits, which most hospitals (and states) require for privileging.
The next hurdle, which is probably even more important, is the practice requirements for the hospital(s) where you’ll be working. By way of example, my hospital requires, for initial appointment, “documentation of inpatient services to at least 12 patients in the prior 12 months.” That is but one example, but it’s a reasonable starting point.
For sake of argument, let’s assume you can’t meet the criteria. Most hospitals will require a mentored relationship in which you will have to see and document a specified number of cases under the auspices of a supervising physician. That might mean 10 cases, or it could be 80 cases, but the hospital should be able to lay out the explicit criteria in advance. Once those cases have been signed off, then your file can return to credentialing for review. Beware: This whole process could take a lot longer than you might expect, so three to six months might be the expected timeline.
One other resource to note would be something like the Center for Personalized Education for Physicians (CPEP; www.cpepdoc.org/re-entry-program.cfm), which tailors education plans for physicians who are re-entering practice. Some hospitals will ask for a formal evaluation through this resource to obtain a structured response and skills evaluation. It’s applicable for any location, and it helps provide both sides with meeting the expectations.
Regardless of the requirements, you’re not alone. Ask around and you’ll find physicians who’ve gone through a similar scenario. We even had a physician in our group who had been out of clinical practice for a few years successfully navigate a full mentored process without too much trouble.
It might seem a little daunting, but it is entirely doable. TH
ONLINE EXCLUSIVE: Hospitalists discuss the time-honored tradition of hospital payments to HM groups
In the Literature: HM-Related Research You Need to Know
Literature at a Glance
A guide to this month’s studies
- Risks of preoperative tobacco use
- Timing of perioperative beta-blocker use and outcomes
- Continuous vs. bolus dose diuretics in CHF
- Outcomes of carotid endearterectomy and carotid artery stenting
- Protocol for low-risk chest pain
- Effect of esomeprazole on recurrent ulcer rates in clopidogrel users
- Effect of ICU QI project on hospital mortality
- Acute kidney injury risks after coronary angiography
Smokers Have Worse Perioperative Outcomes
Clinical question: Do current smokers have worse 30-day postoperative outcomes than nonsmokers after noncardiac surgery?
Background: Approximately 20% of adults in the U.S. smoke cigarettes, and a significant fraction of surgical patients are current smokers. Despite concerns that smoking is associated with worse postoperative outcomes, these increased risks have not been quantified across multiple outcomes.
Study design: Retrospective cohort study.
Setting: Surgical patients in 200 centers throughout the United States.
Synopsis: Data from the American College of Surgeons National Surgical Quality Improvement Program from 2005 to 2008 were acquired, and 391,006 patient records were reviewed. Postoperative morbidity and mortality were significantly greater in smokers. Current smokers had a 40% increased odds of death at 30 days compared to people who had never smoked (OR 1.38, 95% CI, 1.11-1.72). Current smokers also had significantly greater odds of pulmonary complications, including pneumonia (OR 2.09, 95% CI, 1.80-2.43), unplanned intubation (OR 1.87, 95% CI, 1.58-2.21), and mechanical ventilation (OR 1.53, 95% CI, 1.31-1.79).
Furthermore, current smokers had significantly greater odds of postoperative cardiac arrest (OR 1.57, 95% CI, 1.10-2.25), myocardial infarction (OR 1.80, 95% CI, 1.11-2.25), and stroke (OR 1.73, 95% CI, 1.18-2.53). Odds of infectious complications were increased in current smokers, including deep incisional infections (OR 1.42, 95% CI, 1.21-1.68), sepsis (OR 1.30, 95% CI, 1.20-1.60), and septic shock (OR 1.55, 95% CI, 1.29-1.87).
Limitations of this study include self-reporting of smoking habits and absence of detailed smoking history just before and after surgery.
Bottom line: Current smokers have significantly increased postoperative morbidity and mortality after noncardiac surgery.
Citation: Turan A, Mascha EJ, Roberman D, et al. Smoking and perioperative outcomes. Anesthesiology. 2011;114(4):837-846.
Chronic Beta-Blockade Reduces Postoperative Myocardial Ischemia
Clinical question: Does the timing of beta-blocker exposure affect cardiovascular outcomes in patients undergoing elective, noncardiac surgery?
Background: Several studies have demonstrated that beta-blockers are associated with decreased perioperative cardiovascular morbidity and mortality. Study designs have varied greatly, and differences in dosing and timing of beta-blocker administration have caused conflicting results. The question of when to initiate beta-blockers prior to surgery remains controversial.
Study design: Prospective cohort study.
Setting: Three academic medical centers in Canada.
Synopsis: Data from 1,398 patients who had elective, noncardiac surgery with either acute (n=436) or chronic (n=962) beta-blocker exposure were analyzed. Acute exposure was defined as receiving a beta-blocker for the first time within 48 hours after surgery, whereas chronic beta-blocker exposure was defined as receiving a beta-blocker seven to 10 days prior to surgery.
Patients with chronic beta-blocker exposure were more likely to have a history of coronary disease, heart failure, or hypertension and were more likely to be receiving statins, antiplatelet agents, and angiotensin-converting enzyme inhibitors. The primary outcome was a composite of major cardiac events, including myocardial infarction, nonfatal cardiac arrest, and 30-day mortality.
Major cardiac events occurred more often in patients with acute versus chronic beta-blocker exposure in both the entire cohort (8.3% vs. 4.7%) and in the propensity-matched cohort (8.0% vs. 3.0%). Myocardial infarction accounted for the majority of cardiac events.
There are several limitations of this study: The sample size was small, the beta-blocker and dosage used varied, and the indication and exact duration of chronic beta-blocker therapy was unknown.
Bottom line: Chronic beta-blocker therapy reduces major cardiac events compared with acute beta-blocker therapy in patients undergoing elective, noncardiac surgery.
Citation: Ellenberger C, Tait G, Beattie WS. Chronic beta-blockade is associated with a better outcome after elective noncardiac surgery than acute beta-blockade: a single-center propensity-matched cohort study. Anesthesiology. 2011;114(4):817-823.
Continuous and Bolus Dosing of Furosemide Provides Similar Outcomes in Heart Failure
Clinical question: Does continuous infusion compared to bolus dosing of furosemide improve clinical outcomes in patients with acute decompensated heart failure?
Background: Diuresis with furosemide is commonly used to manage acute decompensated heart failure, but it is uncertain which dosing strategy is optimal. Continuous infusion of furosemide has been proposed as a more effective method of diuresis compared with bolus dosing, especially when higher doses are required, but data comparing the two strategies are limited.
Study design: Randomized, double-blind, controlled trial.
Setting: Twenty-six clinical sites in the U.S. and Canada.
Synopsis: Researchers randomized 308 patients with acute decompensated heart failure to either continuous or bolus intravenous dosing, which was calculated as either the equivalent of their daily oral dose (low-dose strategy) or 2.5 times their daily dose (high-dose strategy). Mean ejection fraction was 35%. Primary endpoints were patients’ assessment of symptoms based on a visual-analogue scale quantified as area under the curve, as well as change in serum creatinine level at 72 hours.
No significant differences between the continuous and bolus dosing groups were evidenced in primary endpoints at 72 hours. Patients in the bolus group had more dose increases at 48 hours (21% vs. 11%, P=0.01). Patients in the high-dose group were more likely to change from intravenous to oral doses at 48 hours (31% vs. 17%, P<0.001) and had greater net fluid loss (4.9L vs. 3.6L, P=0.01). More patients in the high-dose versus low-dose group had an increase in creatinine ≥0.3 mg/dL (23% vs. 14%, P=0.04). Hospital length of stay, readmission, and mortality rates were similar between the groups.
Bottom line: Diuretic therapy administered by continuous infusion or bolus dosing in patients with acute decompensated heart failure have equivocal effects on patients’ symptoms and kidney function.
Citation: Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364(9):797-805.
Carotid Endarterectomy Is Better than Carotid Artery Stenting
Clinical question: How do the clinical outcomes of carotid artery stenting compare with those of carotid endarterectomy?
Background: Whether carotid artery stenting or carotid endarterectomy is the preferred therapy for patients with carotid artery stenosis has been highly controversial. This study was a meta-analysis of all available data from randomized trials comparing carotid endarterectomy to carotid artery stenting.
Study design: Meta-analysis.
Setting: Teaching and nonteaching hospitals.
Synopsis: Thirteen randomized trials were identified with 3,723 patients who had undergone endarterectomy and 3,754 patients who had undergone carotid artery stenting. Outcomes included stroke, myocardial infarction, cranial nerve injury, and death or stroke, and these outcomes were divided as either short-term (<30 days) or long-term (>1 year) outcomes.
Patients who had undergone carotid artery stenting had less risk of short-term myocardial infarction (OR 0.48, 95% CI, 0.29–9.78, P=0.003) and less risk of cranial nerve injury (OR 0.09, 95% CI, 0.05–0.16, P<0.001). However, carotid artery stenting had a significantly higher risk of short-term stroke and combined death or stroke, and also significantly higher long-term risk of stroke and combined death or stroke. The association between carotid artery stenting and stroke was stronger in the subgroup of patients >68 years but not in patients <68 years. There was no significant heterogeneity, and no significant modifying associations were revealed by meta-regression analysis.
Limitations include potentially unpublished small studies favoring carotid endarterectomy and a significant publication bias regarding short-term death.
Bottom line: Although carotid artery stenting has less short-term risk of myocardial infarction and cranial nerve injury, carotid endarterectomy has less short-term and long-term risks of stroke and death.
Citation: Economopoulus KP, Sergentanis TN, Tsivgoulis G, Mariolis AD, Stefanadis C. Carotid artery stenting versus carotid endarterectomy: a comprehensive meta-analysis of short-term and long-term outcomes. Stroke. 2011;42:687-692.
Chest Pain Protocol Can Identify Low-Risk Chest Pain in Emergency Departments
Clinical question: Can a two-hour accelerated diagnostic protocol (ADP) based on electrocardiogram, point-of-care biomarkers, and Thrombolysis in Myocardial Infarction (TIMI) score safely identify patients with chest pain at very low short-term risk of major cardiac events?
Background: Evaluation of patients presenting to EDs with chest pain utilize significant amounts of hospital resources. A safe, reproducible, and expeditious process to identify patients at low risk for short-term cardiac events is desired.
Study design: Prospective cohort study.
Setting: Fourteen urban EDs in nine countries across the Asia-Pacific region.
Synopsis: The study included 3,582 patients presenting to an ED with at least five minutes of chest pain suggestive of an acute coronary syndrome and for whom further evaluation with serial cardiac biomarkers was planned. A negative ADP was defined as TIMI score of 0, no new ischemic changes on initial electrocardiogram, and normal cardiac biomarkers at zero and two hours after arrival.
All components of the ADP were negative for 352 patients (9.8%). Only three low-risk patients (0.9%) by ADP had a major cardiac event during the 30-day follow-up period, yielding a negative predictive value of 99.1% (95% CI, 97.3-99.8%). Mean hospital stay for the low-risk group with a negative ADP was 43 hours with a median of 26 hours. The authors suggest that a 10% reduction in prolonged workups of patients with chest pain could be seen with implementation of this protocol.
Potential limitations include applicability only to a select cohort of patients with chest pain and the low specificity of the protocol.
Bottom line: A two-hour diagnostic protocol can help expedite discharge of patients with very-low-risk chest pain.
Citation: Than T, Cullen L, Reid CM, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): a prospective observational validation study. Lancet. 2011;337:1077-1084.
Esomeprazole Reduces Peptic Ulcer Recurrence in Patients on Clopidogrel
Clinical question: Does esomeprazole prevent recurrent peptic ulcers in patients with atherosclerosis on clopidogrel?
Background: Although clopidogrel is sometimes used as an alternative antiplatelet agent to aspirin, a significant rate of recurrent ulcer bleeding on clopidogrel has been described. No previous prospective trial has studied whether a proton-pump inhibitor (PPI) can reduce the risk of peptic ulcer recurrence or bleeding in atherosclerotic patients on clopidogrel.
Study design: Randomized controlled trial.
Setting: A single veterans hospital in Taiwan.
Synopsis: One hundred sixty-five patients were enrolled with a past history of peptic ulcer disease, no signs of ulcer recurrence by endoscopy, and current use of clopidogrel 37.5 mg to 75 mg per day. All patients had atherosclerosis and had been on clopidogrel for at least two weeks, without aspirin, corticosteroids, anticoagulants, or recent treatment with a PPI. Patients were randomized to clopidogrel 75 mg at night (n=82) or clopidogrel 75 mg at night plus esomeprazole 20 mg before breakfast. Follow-up endoscopy was performed at six months or as needed for symptoms.
Recurrence of ulcer was found in 1.2% of patients on clopidogrel plus esomeprazole versus 11.0% in patients on clopidogrel alone (95% CI, 2.6-17.0%; P=0.009). The pharmacodynamic study revealed no significant differences in platelet aggregation within or between treatment groups on day 1 or day 28. No significant differences were seen on the incidence of ischemic events in this setting, but the trial was underpowered to draw conclusions on this outcome.
An important limitation is that the findings of this study are applicable only to patients on clopidogrel monotherapy and not dual antiplatelet therapy.
Bottom line: A significant reduction in recurrent peptic ulcers is seen with the combination of esomeprazole plus clopidogrel, versus clopidogrel alone, in patients with atherosclerosis and a history of peptic ulcer disease.
Citation: Hsu PI, Lai KH, Liu CP. Esomeprazole with clopidogrel reduces peptic ulcer recurrence, compared with clopidogrel alone, in patients with atherosclerosis. Gastroenterology. 2011;140:791-798.
ICU Quality-Improvement Project Reduces Hospital Mortality
Clinical question: Does a quality-improvement (QI) project in the ICU reduce in-hospital mortality and length of stay among elderly adults?
Background: Previous studies have shown that ICU-acquired infections are associated with increased morbidity and mortality, and QI initiatives reduce hospital-acquired infections. However, it has not been demonstrated that QI projects in the ICU reduce in-hospital mortality or length of stay.
Study design: Retrospective cohort study.
Setting: Four hundred fifty-nine Midwestern hospitals.
Synopsis: This study included 238,937 adults age >65 who were hospitalized in an ICU from 2001 to 2006 at one of 95 hospitals invited to implement the Keystone ICU Project. The control group included 1,091,547 elderly adults at one of 364 hospitals not invited to participate in the project. The Keystone ICU Project implements evidence-based practices to reduce rates of catheter-related bloodstream infections and ventilator-associated pneumonia.
Hospital mortality was not significantly reduced during initiation or implementation of the project; however, a significant reduction in hospital mortality occurred in the study group during one to 12 months post-implementation (OR=0.83 vs. 0.88, P=0.041) and 13 to 22 months post-implementation (OR=0.76 vs. 0.84, P=0.007). In contrast, length of stay did not differ significantly between the two groups, but the study was underpowered for this outcome.
The study is limited by the complexity of the Keystone ICU Project, as well as the exclusion of smaller hospitals and nonelderly adults. The study is promising because implementing a QI project in the ICU is associated with no known harms and might confer a mortality benefit at a relatively low cost.
Bottom line: Elderly adults had lower in-hospital mortality after implementation of the Keystone QI project in ICUs.
Citation: Lipitz-Snyderman A, Steinwachs D, Needham DM, Colantuoni E, Morlock LL, Pronovost PJ. Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis. BMJ. 2011;342:d219.
Serious Long-Term Risks with Acute Kidney Injury after Coronary Angiography
Clinical question: Does postcoronary angiography acute kidney injury (AKI) increase the risk of poor long-term clinical outcomes?
Background: Previous studies have shown that AKI following coronary angiography increases the risk of poor short-term clinical outcomes, such as in-hospital myocardial infarction, prolonged hospital stay, and early mortality. Little is known about the long-term cardiovascular and renal outcomes following post-coronary angiography AKI.
Study design: Retrospective cohort study.
Setting: All coronary angiography centers in Alberta, Canada.
Synopsis: The study included 14,782 adults who were ≥18 years of age, underwent coronary angiography, had a baseline creatinine measurement, did not have end-stage renal disease (ESRD), and had a creatinine measurement within seven days after coronary angiography.
During a median follow-up period of 19.7 months, 1,099 (7.4%) patients developed stage 1 AKI and 321 (2.2%) developed stage 2 or 3 AKI. Mortality increased twofold with stage 1 AKI and >3-fold with stage 2 or 3 AKI. Risk of ESRD increased substantially by >11-fold in patients with stage 2 or 3 AKI. Risk of hospitalization for subsequent AKI, myocardial infarction, and heart failure also increased significantly following post-coronary angiography AKI.
Patients who experienced AKI were older, had more severe CAD, were more likely to have such comorbidities as DM, HTN, and heart failure, and had lower baseline GFRs. However, the underlying comorbidities do not completely explain the increased risk of poor long-term outcomes in the adjusted analysis.
Limitations include missing or underestimating mild cases of AKI, residual confounding from unmeasured variables, and inability of retrospective comparative studies to establish causality.
Bottom line: Adults with post-coronary angiography AKI are at increased risk of poor long-term cardiovascular and renal outcomes.
Citation: James MT, Ghali WA, Knudtson ML, et al. Associations between acute kidney injury and cardiovascular and renal outcomes after coronary angiography. Circulation. 2011;123(4):409-416. TH
Literature at a Glance
A guide to this month’s studies
- Risks of preoperative tobacco use
- Timing of perioperative beta-blocker use and outcomes
- Continuous vs. bolus dose diuretics in CHF
- Outcomes of carotid endearterectomy and carotid artery stenting
- Protocol for low-risk chest pain
- Effect of esomeprazole on recurrent ulcer rates in clopidogrel users
- Effect of ICU QI project on hospital mortality
- Acute kidney injury risks after coronary angiography
Smokers Have Worse Perioperative Outcomes
Clinical question: Do current smokers have worse 30-day postoperative outcomes than nonsmokers after noncardiac surgery?
Background: Approximately 20% of adults in the U.S. smoke cigarettes, and a significant fraction of surgical patients are current smokers. Despite concerns that smoking is associated with worse postoperative outcomes, these increased risks have not been quantified across multiple outcomes.
Study design: Retrospective cohort study.
Setting: Surgical patients in 200 centers throughout the United States.
Synopsis: Data from the American College of Surgeons National Surgical Quality Improvement Program from 2005 to 2008 were acquired, and 391,006 patient records were reviewed. Postoperative morbidity and mortality were significantly greater in smokers. Current smokers had a 40% increased odds of death at 30 days compared to people who had never smoked (OR 1.38, 95% CI, 1.11-1.72). Current smokers also had significantly greater odds of pulmonary complications, including pneumonia (OR 2.09, 95% CI, 1.80-2.43), unplanned intubation (OR 1.87, 95% CI, 1.58-2.21), and mechanical ventilation (OR 1.53, 95% CI, 1.31-1.79).
Furthermore, current smokers had significantly greater odds of postoperative cardiac arrest (OR 1.57, 95% CI, 1.10-2.25), myocardial infarction (OR 1.80, 95% CI, 1.11-2.25), and stroke (OR 1.73, 95% CI, 1.18-2.53). Odds of infectious complications were increased in current smokers, including deep incisional infections (OR 1.42, 95% CI, 1.21-1.68), sepsis (OR 1.30, 95% CI, 1.20-1.60), and septic shock (OR 1.55, 95% CI, 1.29-1.87).
Limitations of this study include self-reporting of smoking habits and absence of detailed smoking history just before and after surgery.
Bottom line: Current smokers have significantly increased postoperative morbidity and mortality after noncardiac surgery.
Citation: Turan A, Mascha EJ, Roberman D, et al. Smoking and perioperative outcomes. Anesthesiology. 2011;114(4):837-846.
Chronic Beta-Blockade Reduces Postoperative Myocardial Ischemia
Clinical question: Does the timing of beta-blocker exposure affect cardiovascular outcomes in patients undergoing elective, noncardiac surgery?
Background: Several studies have demonstrated that beta-blockers are associated with decreased perioperative cardiovascular morbidity and mortality. Study designs have varied greatly, and differences in dosing and timing of beta-blocker administration have caused conflicting results. The question of when to initiate beta-blockers prior to surgery remains controversial.
Study design: Prospective cohort study.
Setting: Three academic medical centers in Canada.
Synopsis: Data from 1,398 patients who had elective, noncardiac surgery with either acute (n=436) or chronic (n=962) beta-blocker exposure were analyzed. Acute exposure was defined as receiving a beta-blocker for the first time within 48 hours after surgery, whereas chronic beta-blocker exposure was defined as receiving a beta-blocker seven to 10 days prior to surgery.
Patients with chronic beta-blocker exposure were more likely to have a history of coronary disease, heart failure, or hypertension and were more likely to be receiving statins, antiplatelet agents, and angiotensin-converting enzyme inhibitors. The primary outcome was a composite of major cardiac events, including myocardial infarction, nonfatal cardiac arrest, and 30-day mortality.
Major cardiac events occurred more often in patients with acute versus chronic beta-blocker exposure in both the entire cohort (8.3% vs. 4.7%) and in the propensity-matched cohort (8.0% vs. 3.0%). Myocardial infarction accounted for the majority of cardiac events.
There are several limitations of this study: The sample size was small, the beta-blocker and dosage used varied, and the indication and exact duration of chronic beta-blocker therapy was unknown.
Bottom line: Chronic beta-blocker therapy reduces major cardiac events compared with acute beta-blocker therapy in patients undergoing elective, noncardiac surgery.
Citation: Ellenberger C, Tait G, Beattie WS. Chronic beta-blockade is associated with a better outcome after elective noncardiac surgery than acute beta-blockade: a single-center propensity-matched cohort study. Anesthesiology. 2011;114(4):817-823.
Continuous and Bolus Dosing of Furosemide Provides Similar Outcomes in Heart Failure
Clinical question: Does continuous infusion compared to bolus dosing of furosemide improve clinical outcomes in patients with acute decompensated heart failure?
Background: Diuresis with furosemide is commonly used to manage acute decompensated heart failure, but it is uncertain which dosing strategy is optimal. Continuous infusion of furosemide has been proposed as a more effective method of diuresis compared with bolus dosing, especially when higher doses are required, but data comparing the two strategies are limited.
Study design: Randomized, double-blind, controlled trial.
Setting: Twenty-six clinical sites in the U.S. and Canada.
Synopsis: Researchers randomized 308 patients with acute decompensated heart failure to either continuous or bolus intravenous dosing, which was calculated as either the equivalent of their daily oral dose (low-dose strategy) or 2.5 times their daily dose (high-dose strategy). Mean ejection fraction was 35%. Primary endpoints were patients’ assessment of symptoms based on a visual-analogue scale quantified as area under the curve, as well as change in serum creatinine level at 72 hours.
No significant differences between the continuous and bolus dosing groups were evidenced in primary endpoints at 72 hours. Patients in the bolus group had more dose increases at 48 hours (21% vs. 11%, P=0.01). Patients in the high-dose group were more likely to change from intravenous to oral doses at 48 hours (31% vs. 17%, P<0.001) and had greater net fluid loss (4.9L vs. 3.6L, P=0.01). More patients in the high-dose versus low-dose group had an increase in creatinine ≥0.3 mg/dL (23% vs. 14%, P=0.04). Hospital length of stay, readmission, and mortality rates were similar between the groups.
Bottom line: Diuretic therapy administered by continuous infusion or bolus dosing in patients with acute decompensated heart failure have equivocal effects on patients’ symptoms and kidney function.
Citation: Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364(9):797-805.
Carotid Endarterectomy Is Better than Carotid Artery Stenting
Clinical question: How do the clinical outcomes of carotid artery stenting compare with those of carotid endarterectomy?
Background: Whether carotid artery stenting or carotid endarterectomy is the preferred therapy for patients with carotid artery stenosis has been highly controversial. This study was a meta-analysis of all available data from randomized trials comparing carotid endarterectomy to carotid artery stenting.
Study design: Meta-analysis.
Setting: Teaching and nonteaching hospitals.
Synopsis: Thirteen randomized trials were identified with 3,723 patients who had undergone endarterectomy and 3,754 patients who had undergone carotid artery stenting. Outcomes included stroke, myocardial infarction, cranial nerve injury, and death or stroke, and these outcomes were divided as either short-term (<30 days) or long-term (>1 year) outcomes.
Patients who had undergone carotid artery stenting had less risk of short-term myocardial infarction (OR 0.48, 95% CI, 0.29–9.78, P=0.003) and less risk of cranial nerve injury (OR 0.09, 95% CI, 0.05–0.16, P<0.001). However, carotid artery stenting had a significantly higher risk of short-term stroke and combined death or stroke, and also significantly higher long-term risk of stroke and combined death or stroke. The association between carotid artery stenting and stroke was stronger in the subgroup of patients >68 years but not in patients <68 years. There was no significant heterogeneity, and no significant modifying associations were revealed by meta-regression analysis.
Limitations include potentially unpublished small studies favoring carotid endarterectomy and a significant publication bias regarding short-term death.
Bottom line: Although carotid artery stenting has less short-term risk of myocardial infarction and cranial nerve injury, carotid endarterectomy has less short-term and long-term risks of stroke and death.
Citation: Economopoulus KP, Sergentanis TN, Tsivgoulis G, Mariolis AD, Stefanadis C. Carotid artery stenting versus carotid endarterectomy: a comprehensive meta-analysis of short-term and long-term outcomes. Stroke. 2011;42:687-692.
Chest Pain Protocol Can Identify Low-Risk Chest Pain in Emergency Departments
Clinical question: Can a two-hour accelerated diagnostic protocol (ADP) based on electrocardiogram, point-of-care biomarkers, and Thrombolysis in Myocardial Infarction (TIMI) score safely identify patients with chest pain at very low short-term risk of major cardiac events?
Background: Evaluation of patients presenting to EDs with chest pain utilize significant amounts of hospital resources. A safe, reproducible, and expeditious process to identify patients at low risk for short-term cardiac events is desired.
Study design: Prospective cohort study.
Setting: Fourteen urban EDs in nine countries across the Asia-Pacific region.
Synopsis: The study included 3,582 patients presenting to an ED with at least five minutes of chest pain suggestive of an acute coronary syndrome and for whom further evaluation with serial cardiac biomarkers was planned. A negative ADP was defined as TIMI score of 0, no new ischemic changes on initial electrocardiogram, and normal cardiac biomarkers at zero and two hours after arrival.
All components of the ADP were negative for 352 patients (9.8%). Only three low-risk patients (0.9%) by ADP had a major cardiac event during the 30-day follow-up period, yielding a negative predictive value of 99.1% (95% CI, 97.3-99.8%). Mean hospital stay for the low-risk group with a negative ADP was 43 hours with a median of 26 hours. The authors suggest that a 10% reduction in prolonged workups of patients with chest pain could be seen with implementation of this protocol.
Potential limitations include applicability only to a select cohort of patients with chest pain and the low specificity of the protocol.
Bottom line: A two-hour diagnostic protocol can help expedite discharge of patients with very-low-risk chest pain.
Citation: Than T, Cullen L, Reid CM, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): a prospective observational validation study. Lancet. 2011;337:1077-1084.
Esomeprazole Reduces Peptic Ulcer Recurrence in Patients on Clopidogrel
Clinical question: Does esomeprazole prevent recurrent peptic ulcers in patients with atherosclerosis on clopidogrel?
Background: Although clopidogrel is sometimes used as an alternative antiplatelet agent to aspirin, a significant rate of recurrent ulcer bleeding on clopidogrel has been described. No previous prospective trial has studied whether a proton-pump inhibitor (PPI) can reduce the risk of peptic ulcer recurrence or bleeding in atherosclerotic patients on clopidogrel.
Study design: Randomized controlled trial.
Setting: A single veterans hospital in Taiwan.
Synopsis: One hundred sixty-five patients were enrolled with a past history of peptic ulcer disease, no signs of ulcer recurrence by endoscopy, and current use of clopidogrel 37.5 mg to 75 mg per day. All patients had atherosclerosis and had been on clopidogrel for at least two weeks, without aspirin, corticosteroids, anticoagulants, or recent treatment with a PPI. Patients were randomized to clopidogrel 75 mg at night (n=82) or clopidogrel 75 mg at night plus esomeprazole 20 mg before breakfast. Follow-up endoscopy was performed at six months or as needed for symptoms.
Recurrence of ulcer was found in 1.2% of patients on clopidogrel plus esomeprazole versus 11.0% in patients on clopidogrel alone (95% CI, 2.6-17.0%; P=0.009). The pharmacodynamic study revealed no significant differences in platelet aggregation within or between treatment groups on day 1 or day 28. No significant differences were seen on the incidence of ischemic events in this setting, but the trial was underpowered to draw conclusions on this outcome.
An important limitation is that the findings of this study are applicable only to patients on clopidogrel monotherapy and not dual antiplatelet therapy.
Bottom line: A significant reduction in recurrent peptic ulcers is seen with the combination of esomeprazole plus clopidogrel, versus clopidogrel alone, in patients with atherosclerosis and a history of peptic ulcer disease.
Citation: Hsu PI, Lai KH, Liu CP. Esomeprazole with clopidogrel reduces peptic ulcer recurrence, compared with clopidogrel alone, in patients with atherosclerosis. Gastroenterology. 2011;140:791-798.
ICU Quality-Improvement Project Reduces Hospital Mortality
Clinical question: Does a quality-improvement (QI) project in the ICU reduce in-hospital mortality and length of stay among elderly adults?
Background: Previous studies have shown that ICU-acquired infections are associated with increased morbidity and mortality, and QI initiatives reduce hospital-acquired infections. However, it has not been demonstrated that QI projects in the ICU reduce in-hospital mortality or length of stay.
Study design: Retrospective cohort study.
Setting: Four hundred fifty-nine Midwestern hospitals.
Synopsis: This study included 238,937 adults age >65 who were hospitalized in an ICU from 2001 to 2006 at one of 95 hospitals invited to implement the Keystone ICU Project. The control group included 1,091,547 elderly adults at one of 364 hospitals not invited to participate in the project. The Keystone ICU Project implements evidence-based practices to reduce rates of catheter-related bloodstream infections and ventilator-associated pneumonia.
Hospital mortality was not significantly reduced during initiation or implementation of the project; however, a significant reduction in hospital mortality occurred in the study group during one to 12 months post-implementation (OR=0.83 vs. 0.88, P=0.041) and 13 to 22 months post-implementation (OR=0.76 vs. 0.84, P=0.007). In contrast, length of stay did not differ significantly between the two groups, but the study was underpowered for this outcome.
The study is limited by the complexity of the Keystone ICU Project, as well as the exclusion of smaller hospitals and nonelderly adults. The study is promising because implementing a QI project in the ICU is associated with no known harms and might confer a mortality benefit at a relatively low cost.
Bottom line: Elderly adults had lower in-hospital mortality after implementation of the Keystone QI project in ICUs.
Citation: Lipitz-Snyderman A, Steinwachs D, Needham DM, Colantuoni E, Morlock LL, Pronovost PJ. Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis. BMJ. 2011;342:d219.
Serious Long-Term Risks with Acute Kidney Injury after Coronary Angiography
Clinical question: Does postcoronary angiography acute kidney injury (AKI) increase the risk of poor long-term clinical outcomes?
Background: Previous studies have shown that AKI following coronary angiography increases the risk of poor short-term clinical outcomes, such as in-hospital myocardial infarction, prolonged hospital stay, and early mortality. Little is known about the long-term cardiovascular and renal outcomes following post-coronary angiography AKI.
Study design: Retrospective cohort study.
Setting: All coronary angiography centers in Alberta, Canada.
Synopsis: The study included 14,782 adults who were ≥18 years of age, underwent coronary angiography, had a baseline creatinine measurement, did not have end-stage renal disease (ESRD), and had a creatinine measurement within seven days after coronary angiography.
During a median follow-up period of 19.7 months, 1,099 (7.4%) patients developed stage 1 AKI and 321 (2.2%) developed stage 2 or 3 AKI. Mortality increased twofold with stage 1 AKI and >3-fold with stage 2 or 3 AKI. Risk of ESRD increased substantially by >11-fold in patients with stage 2 or 3 AKI. Risk of hospitalization for subsequent AKI, myocardial infarction, and heart failure also increased significantly following post-coronary angiography AKI.
Patients who experienced AKI were older, had more severe CAD, were more likely to have such comorbidities as DM, HTN, and heart failure, and had lower baseline GFRs. However, the underlying comorbidities do not completely explain the increased risk of poor long-term outcomes in the adjusted analysis.
Limitations include missing or underestimating mild cases of AKI, residual confounding from unmeasured variables, and inability of retrospective comparative studies to establish causality.
Bottom line: Adults with post-coronary angiography AKI are at increased risk of poor long-term cardiovascular and renal outcomes.
Citation: James MT, Ghali WA, Knudtson ML, et al. Associations between acute kidney injury and cardiovascular and renal outcomes after coronary angiography. Circulation. 2011;123(4):409-416. TH
Literature at a Glance
A guide to this month’s studies
- Risks of preoperative tobacco use
- Timing of perioperative beta-blocker use and outcomes
- Continuous vs. bolus dose diuretics in CHF
- Outcomes of carotid endearterectomy and carotid artery stenting
- Protocol for low-risk chest pain
- Effect of esomeprazole on recurrent ulcer rates in clopidogrel users
- Effect of ICU QI project on hospital mortality
- Acute kidney injury risks after coronary angiography
Smokers Have Worse Perioperative Outcomes
Clinical question: Do current smokers have worse 30-day postoperative outcomes than nonsmokers after noncardiac surgery?
Background: Approximately 20% of adults in the U.S. smoke cigarettes, and a significant fraction of surgical patients are current smokers. Despite concerns that smoking is associated with worse postoperative outcomes, these increased risks have not been quantified across multiple outcomes.
Study design: Retrospective cohort study.
Setting: Surgical patients in 200 centers throughout the United States.
Synopsis: Data from the American College of Surgeons National Surgical Quality Improvement Program from 2005 to 2008 were acquired, and 391,006 patient records were reviewed. Postoperative morbidity and mortality were significantly greater in smokers. Current smokers had a 40% increased odds of death at 30 days compared to people who had never smoked (OR 1.38, 95% CI, 1.11-1.72). Current smokers also had significantly greater odds of pulmonary complications, including pneumonia (OR 2.09, 95% CI, 1.80-2.43), unplanned intubation (OR 1.87, 95% CI, 1.58-2.21), and mechanical ventilation (OR 1.53, 95% CI, 1.31-1.79).
Furthermore, current smokers had significantly greater odds of postoperative cardiac arrest (OR 1.57, 95% CI, 1.10-2.25), myocardial infarction (OR 1.80, 95% CI, 1.11-2.25), and stroke (OR 1.73, 95% CI, 1.18-2.53). Odds of infectious complications were increased in current smokers, including deep incisional infections (OR 1.42, 95% CI, 1.21-1.68), sepsis (OR 1.30, 95% CI, 1.20-1.60), and septic shock (OR 1.55, 95% CI, 1.29-1.87).
Limitations of this study include self-reporting of smoking habits and absence of detailed smoking history just before and after surgery.
Bottom line: Current smokers have significantly increased postoperative morbidity and mortality after noncardiac surgery.
Citation: Turan A, Mascha EJ, Roberman D, et al. Smoking and perioperative outcomes. Anesthesiology. 2011;114(4):837-846.
Chronic Beta-Blockade Reduces Postoperative Myocardial Ischemia
Clinical question: Does the timing of beta-blocker exposure affect cardiovascular outcomes in patients undergoing elective, noncardiac surgery?
Background: Several studies have demonstrated that beta-blockers are associated with decreased perioperative cardiovascular morbidity and mortality. Study designs have varied greatly, and differences in dosing and timing of beta-blocker administration have caused conflicting results. The question of when to initiate beta-blockers prior to surgery remains controversial.
Study design: Prospective cohort study.
Setting: Three academic medical centers in Canada.
Synopsis: Data from 1,398 patients who had elective, noncardiac surgery with either acute (n=436) or chronic (n=962) beta-blocker exposure were analyzed. Acute exposure was defined as receiving a beta-blocker for the first time within 48 hours after surgery, whereas chronic beta-blocker exposure was defined as receiving a beta-blocker seven to 10 days prior to surgery.
Patients with chronic beta-blocker exposure were more likely to have a history of coronary disease, heart failure, or hypertension and were more likely to be receiving statins, antiplatelet agents, and angiotensin-converting enzyme inhibitors. The primary outcome was a composite of major cardiac events, including myocardial infarction, nonfatal cardiac arrest, and 30-day mortality.
Major cardiac events occurred more often in patients with acute versus chronic beta-blocker exposure in both the entire cohort (8.3% vs. 4.7%) and in the propensity-matched cohort (8.0% vs. 3.0%). Myocardial infarction accounted for the majority of cardiac events.
There are several limitations of this study: The sample size was small, the beta-blocker and dosage used varied, and the indication and exact duration of chronic beta-blocker therapy was unknown.
Bottom line: Chronic beta-blocker therapy reduces major cardiac events compared with acute beta-blocker therapy in patients undergoing elective, noncardiac surgery.
Citation: Ellenberger C, Tait G, Beattie WS. Chronic beta-blockade is associated with a better outcome after elective noncardiac surgery than acute beta-blockade: a single-center propensity-matched cohort study. Anesthesiology. 2011;114(4):817-823.
Continuous and Bolus Dosing of Furosemide Provides Similar Outcomes in Heart Failure
Clinical question: Does continuous infusion compared to bolus dosing of furosemide improve clinical outcomes in patients with acute decompensated heart failure?
Background: Diuresis with furosemide is commonly used to manage acute decompensated heart failure, but it is uncertain which dosing strategy is optimal. Continuous infusion of furosemide has been proposed as a more effective method of diuresis compared with bolus dosing, especially when higher doses are required, but data comparing the two strategies are limited.
Study design: Randomized, double-blind, controlled trial.
Setting: Twenty-six clinical sites in the U.S. and Canada.
Synopsis: Researchers randomized 308 patients with acute decompensated heart failure to either continuous or bolus intravenous dosing, which was calculated as either the equivalent of their daily oral dose (low-dose strategy) or 2.5 times their daily dose (high-dose strategy). Mean ejection fraction was 35%. Primary endpoints were patients’ assessment of symptoms based on a visual-analogue scale quantified as area under the curve, as well as change in serum creatinine level at 72 hours.
No significant differences between the continuous and bolus dosing groups were evidenced in primary endpoints at 72 hours. Patients in the bolus group had more dose increases at 48 hours (21% vs. 11%, P=0.01). Patients in the high-dose group were more likely to change from intravenous to oral doses at 48 hours (31% vs. 17%, P<0.001) and had greater net fluid loss (4.9L vs. 3.6L, P=0.01). More patients in the high-dose versus low-dose group had an increase in creatinine ≥0.3 mg/dL (23% vs. 14%, P=0.04). Hospital length of stay, readmission, and mortality rates were similar between the groups.
Bottom line: Diuretic therapy administered by continuous infusion or bolus dosing in patients with acute decompensated heart failure have equivocal effects on patients’ symptoms and kidney function.
Citation: Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364(9):797-805.
Carotid Endarterectomy Is Better than Carotid Artery Stenting
Clinical question: How do the clinical outcomes of carotid artery stenting compare with those of carotid endarterectomy?
Background: Whether carotid artery stenting or carotid endarterectomy is the preferred therapy for patients with carotid artery stenosis has been highly controversial. This study was a meta-analysis of all available data from randomized trials comparing carotid endarterectomy to carotid artery stenting.
Study design: Meta-analysis.
Setting: Teaching and nonteaching hospitals.
Synopsis: Thirteen randomized trials were identified with 3,723 patients who had undergone endarterectomy and 3,754 patients who had undergone carotid artery stenting. Outcomes included stroke, myocardial infarction, cranial nerve injury, and death or stroke, and these outcomes were divided as either short-term (<30 days) or long-term (>1 year) outcomes.
Patients who had undergone carotid artery stenting had less risk of short-term myocardial infarction (OR 0.48, 95% CI, 0.29–9.78, P=0.003) and less risk of cranial nerve injury (OR 0.09, 95% CI, 0.05–0.16, P<0.001). However, carotid artery stenting had a significantly higher risk of short-term stroke and combined death or stroke, and also significantly higher long-term risk of stroke and combined death or stroke. The association between carotid artery stenting and stroke was stronger in the subgroup of patients >68 years but not in patients <68 years. There was no significant heterogeneity, and no significant modifying associations were revealed by meta-regression analysis.
Limitations include potentially unpublished small studies favoring carotid endarterectomy and a significant publication bias regarding short-term death.
Bottom line: Although carotid artery stenting has less short-term risk of myocardial infarction and cranial nerve injury, carotid endarterectomy has less short-term and long-term risks of stroke and death.
Citation: Economopoulus KP, Sergentanis TN, Tsivgoulis G, Mariolis AD, Stefanadis C. Carotid artery stenting versus carotid endarterectomy: a comprehensive meta-analysis of short-term and long-term outcomes. Stroke. 2011;42:687-692.
Chest Pain Protocol Can Identify Low-Risk Chest Pain in Emergency Departments
Clinical question: Can a two-hour accelerated diagnostic protocol (ADP) based on electrocardiogram, point-of-care biomarkers, and Thrombolysis in Myocardial Infarction (TIMI) score safely identify patients with chest pain at very low short-term risk of major cardiac events?
Background: Evaluation of patients presenting to EDs with chest pain utilize significant amounts of hospital resources. A safe, reproducible, and expeditious process to identify patients at low risk for short-term cardiac events is desired.
Study design: Prospective cohort study.
Setting: Fourteen urban EDs in nine countries across the Asia-Pacific region.
Synopsis: The study included 3,582 patients presenting to an ED with at least five minutes of chest pain suggestive of an acute coronary syndrome and for whom further evaluation with serial cardiac biomarkers was planned. A negative ADP was defined as TIMI score of 0, no new ischemic changes on initial electrocardiogram, and normal cardiac biomarkers at zero and two hours after arrival.
All components of the ADP were negative for 352 patients (9.8%). Only three low-risk patients (0.9%) by ADP had a major cardiac event during the 30-day follow-up period, yielding a negative predictive value of 99.1% (95% CI, 97.3-99.8%). Mean hospital stay for the low-risk group with a negative ADP was 43 hours with a median of 26 hours. The authors suggest that a 10% reduction in prolonged workups of patients with chest pain could be seen with implementation of this protocol.
Potential limitations include applicability only to a select cohort of patients with chest pain and the low specificity of the protocol.
Bottom line: A two-hour diagnostic protocol can help expedite discharge of patients with very-low-risk chest pain.
Citation: Than T, Cullen L, Reid CM, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): a prospective observational validation study. Lancet. 2011;337:1077-1084.
Esomeprazole Reduces Peptic Ulcer Recurrence in Patients on Clopidogrel
Clinical question: Does esomeprazole prevent recurrent peptic ulcers in patients with atherosclerosis on clopidogrel?
Background: Although clopidogrel is sometimes used as an alternative antiplatelet agent to aspirin, a significant rate of recurrent ulcer bleeding on clopidogrel has been described. No previous prospective trial has studied whether a proton-pump inhibitor (PPI) can reduce the risk of peptic ulcer recurrence or bleeding in atherosclerotic patients on clopidogrel.
Study design: Randomized controlled trial.
Setting: A single veterans hospital in Taiwan.
Synopsis: One hundred sixty-five patients were enrolled with a past history of peptic ulcer disease, no signs of ulcer recurrence by endoscopy, and current use of clopidogrel 37.5 mg to 75 mg per day. All patients had atherosclerosis and had been on clopidogrel for at least two weeks, without aspirin, corticosteroids, anticoagulants, or recent treatment with a PPI. Patients were randomized to clopidogrel 75 mg at night (n=82) or clopidogrel 75 mg at night plus esomeprazole 20 mg before breakfast. Follow-up endoscopy was performed at six months or as needed for symptoms.
Recurrence of ulcer was found in 1.2% of patients on clopidogrel plus esomeprazole versus 11.0% in patients on clopidogrel alone (95% CI, 2.6-17.0%; P=0.009). The pharmacodynamic study revealed no significant differences in platelet aggregation within or between treatment groups on day 1 or day 28. No significant differences were seen on the incidence of ischemic events in this setting, but the trial was underpowered to draw conclusions on this outcome.
An important limitation is that the findings of this study are applicable only to patients on clopidogrel monotherapy and not dual antiplatelet therapy.
Bottom line: A significant reduction in recurrent peptic ulcers is seen with the combination of esomeprazole plus clopidogrel, versus clopidogrel alone, in patients with atherosclerosis and a history of peptic ulcer disease.
Citation: Hsu PI, Lai KH, Liu CP. Esomeprazole with clopidogrel reduces peptic ulcer recurrence, compared with clopidogrel alone, in patients with atherosclerosis. Gastroenterology. 2011;140:791-798.
ICU Quality-Improvement Project Reduces Hospital Mortality
Clinical question: Does a quality-improvement (QI) project in the ICU reduce in-hospital mortality and length of stay among elderly adults?
Background: Previous studies have shown that ICU-acquired infections are associated with increased morbidity and mortality, and QI initiatives reduce hospital-acquired infections. However, it has not been demonstrated that QI projects in the ICU reduce in-hospital mortality or length of stay.
Study design: Retrospective cohort study.
Setting: Four hundred fifty-nine Midwestern hospitals.
Synopsis: This study included 238,937 adults age >65 who were hospitalized in an ICU from 2001 to 2006 at one of 95 hospitals invited to implement the Keystone ICU Project. The control group included 1,091,547 elderly adults at one of 364 hospitals not invited to participate in the project. The Keystone ICU Project implements evidence-based practices to reduce rates of catheter-related bloodstream infections and ventilator-associated pneumonia.
Hospital mortality was not significantly reduced during initiation or implementation of the project; however, a significant reduction in hospital mortality occurred in the study group during one to 12 months post-implementation (OR=0.83 vs. 0.88, P=0.041) and 13 to 22 months post-implementation (OR=0.76 vs. 0.84, P=0.007). In contrast, length of stay did not differ significantly between the two groups, but the study was underpowered for this outcome.
The study is limited by the complexity of the Keystone ICU Project, as well as the exclusion of smaller hospitals and nonelderly adults. The study is promising because implementing a QI project in the ICU is associated with no known harms and might confer a mortality benefit at a relatively low cost.
Bottom line: Elderly adults had lower in-hospital mortality after implementation of the Keystone QI project in ICUs.
Citation: Lipitz-Snyderman A, Steinwachs D, Needham DM, Colantuoni E, Morlock LL, Pronovost PJ. Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis. BMJ. 2011;342:d219.
Serious Long-Term Risks with Acute Kidney Injury after Coronary Angiography
Clinical question: Does postcoronary angiography acute kidney injury (AKI) increase the risk of poor long-term clinical outcomes?
Background: Previous studies have shown that AKI following coronary angiography increases the risk of poor short-term clinical outcomes, such as in-hospital myocardial infarction, prolonged hospital stay, and early mortality. Little is known about the long-term cardiovascular and renal outcomes following post-coronary angiography AKI.
Study design: Retrospective cohort study.
Setting: All coronary angiography centers in Alberta, Canada.
Synopsis: The study included 14,782 adults who were ≥18 years of age, underwent coronary angiography, had a baseline creatinine measurement, did not have end-stage renal disease (ESRD), and had a creatinine measurement within seven days after coronary angiography.
During a median follow-up period of 19.7 months, 1,099 (7.4%) patients developed stage 1 AKI and 321 (2.2%) developed stage 2 or 3 AKI. Mortality increased twofold with stage 1 AKI and >3-fold with stage 2 or 3 AKI. Risk of ESRD increased substantially by >11-fold in patients with stage 2 or 3 AKI. Risk of hospitalization for subsequent AKI, myocardial infarction, and heart failure also increased significantly following post-coronary angiography AKI.
Patients who experienced AKI were older, had more severe CAD, were more likely to have such comorbidities as DM, HTN, and heart failure, and had lower baseline GFRs. However, the underlying comorbidities do not completely explain the increased risk of poor long-term outcomes in the adjusted analysis.
Limitations include missing or underestimating mild cases of AKI, residual confounding from unmeasured variables, and inability of retrospective comparative studies to establish causality.
Bottom line: Adults with post-coronary angiography AKI are at increased risk of poor long-term cardiovascular and renal outcomes.
Citation: James MT, Ghali WA, Knudtson ML, et al. Associations between acute kidney injury and cardiovascular and renal outcomes after coronary angiography. Circulation. 2011;123(4):409-416. TH