User login
Wedding dermatology
Planning a wedding doesn’t just involve decisions on venues, vows, guests, food, and décor, but also on the betrothed couple’s appearance. Memories and photographs from this day last a lifetime, so it is understandable that people may want to and feel pressured to look their best on this important day – which along with the pressures of planning a wedding, can lead to unnecessary stress, increased cortisol, and unexpected acne and other skin issues.
Because of a complete absence of wedding skin recommendations in the dermatology literature, Winklemann R et al. recently published a paper titled “Wedding Dermatology: A proposed timeline to optimize skin clearance and the avoidance of a true dermatologic emergency” (SKIN The Journal of Cutaneous Medicine 2019 Mar;3[2]:159-60). He focused on acne, using the American Academy of Dermatology acne treatment guidelines and expert opinion, they point out that other than intralesional corticosteroids (which take 0-14 days to have an effect), the majority of acne treatments require at least 3-12 months to achieve clearance or improvement.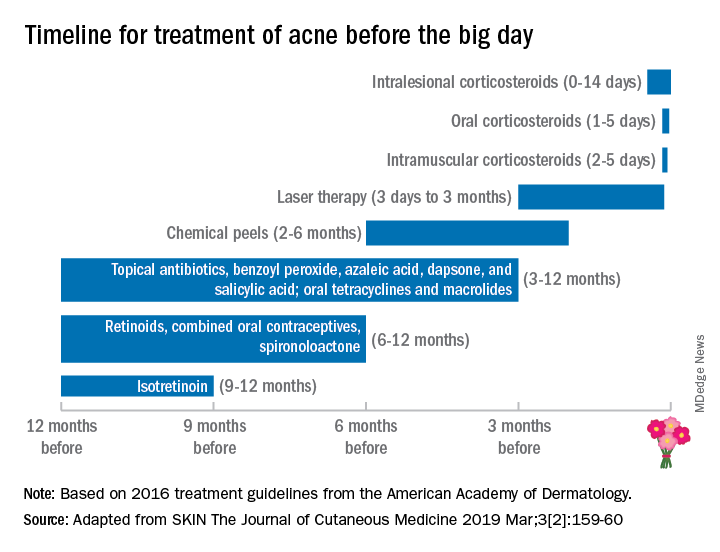
This proposed treatment timeline makes sense given that skin cell turnover on the face takes about 6-8 weeks; therefore, it may take that long for acne lesions to resolve or for treatment to have an effect.
Besides acne treatment, cosmetic treatments also have varying healing times and may require multiple sessions with time in between treatments for optimal results. For instance, treatment of photoaging with intense pulsed light or nonablative fractionated resurfacing may require three to six treatments, typically spaced 1 month apart.
Botulinum toxin treatments may take up to 2 weeks to kick in fully, then last 3-4 months. While the lead time for botulinum toxin to kick in is relatively short, I advise people not to get their first botulinum toxin 2 weeks before their wedding. Sometimes, having this treatment 4-6 weeks prior to the wedding date provides enough time for botulinum toxin to kick in – and to start wearing off to the point that the patient has the desired cosmetic effect, but still has some movement for the desired emotional facial expressions on the wedding day. Some patients also may require touch-ups, optimally at the 2-week window, once the botulinum toxin effect has fully kicked in.
With any injectable, there may be bruising and swelling that can take a week or so to heal, even when the bruises are treated with pulse dye laser used to make bruises resolve more quickly. Even a facial may result in blemishes that take a few days to 1-2 weeks to heal, especially with extractions. As such, a facial, especially a hydrafacial, may be beneficial before one’s wedding, but I would recommend having them done at least once or twice to assess an individual’s recovery time (if any) prior to the actual wedding date.
Treatment needs will vary considerably depending on the patient’s baseline skin health. As dermatologists, our patients depend greatly on us to help them look and feel their best, especially during a time when they are about to embark on a new journey like marriage. Patients need to be given realistic treatment options and time frames to achieve their goals. Whether the goal is treating acne or acne scars, starting or fine-tuning cosmetic treatments, or deciding on a skin-care regimen, the bottom line is making an appointment with the dermatologist early – 6-12 months in advance, if possible – to figure out the right plan.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Planning a wedding doesn’t just involve decisions on venues, vows, guests, food, and décor, but also on the betrothed couple’s appearance. Memories and photographs from this day last a lifetime, so it is understandable that people may want to and feel pressured to look their best on this important day – which along with the pressures of planning a wedding, can lead to unnecessary stress, increased cortisol, and unexpected acne and other skin issues.
Because of a complete absence of wedding skin recommendations in the dermatology literature, Winklemann R et al. recently published a paper titled “Wedding Dermatology: A proposed timeline to optimize skin clearance and the avoidance of a true dermatologic emergency” (SKIN The Journal of Cutaneous Medicine 2019 Mar;3[2]:159-60). He focused on acne, using the American Academy of Dermatology acne treatment guidelines and expert opinion, they point out that other than intralesional corticosteroids (which take 0-14 days to have an effect), the majority of acne treatments require at least 3-12 months to achieve clearance or improvement.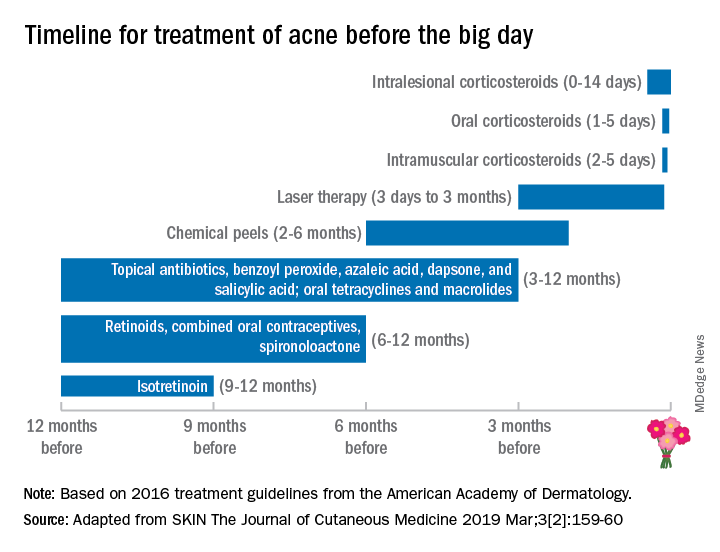
This proposed treatment timeline makes sense given that skin cell turnover on the face takes about 6-8 weeks; therefore, it may take that long for acne lesions to resolve or for treatment to have an effect.
Besides acne treatment, cosmetic treatments also have varying healing times and may require multiple sessions with time in between treatments for optimal results. For instance, treatment of photoaging with intense pulsed light or nonablative fractionated resurfacing may require three to six treatments, typically spaced 1 month apart.
Botulinum toxin treatments may take up to 2 weeks to kick in fully, then last 3-4 months. While the lead time for botulinum toxin to kick in is relatively short, I advise people not to get their first botulinum toxin 2 weeks before their wedding. Sometimes, having this treatment 4-6 weeks prior to the wedding date provides enough time for botulinum toxin to kick in – and to start wearing off to the point that the patient has the desired cosmetic effect, but still has some movement for the desired emotional facial expressions on the wedding day. Some patients also may require touch-ups, optimally at the 2-week window, once the botulinum toxin effect has fully kicked in.
With any injectable, there may be bruising and swelling that can take a week or so to heal, even when the bruises are treated with pulse dye laser used to make bruises resolve more quickly. Even a facial may result in blemishes that take a few days to 1-2 weeks to heal, especially with extractions. As such, a facial, especially a hydrafacial, may be beneficial before one’s wedding, but I would recommend having them done at least once or twice to assess an individual’s recovery time (if any) prior to the actual wedding date.
Treatment needs will vary considerably depending on the patient’s baseline skin health. As dermatologists, our patients depend greatly on us to help them look and feel their best, especially during a time when they are about to embark on a new journey like marriage. Patients need to be given realistic treatment options and time frames to achieve their goals. Whether the goal is treating acne or acne scars, starting or fine-tuning cosmetic treatments, or deciding on a skin-care regimen, the bottom line is making an appointment with the dermatologist early – 6-12 months in advance, if possible – to figure out the right plan.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Planning a wedding doesn’t just involve decisions on venues, vows, guests, food, and décor, but also on the betrothed couple’s appearance. Memories and photographs from this day last a lifetime, so it is understandable that people may want to and feel pressured to look their best on this important day – which along with the pressures of planning a wedding, can lead to unnecessary stress, increased cortisol, and unexpected acne and other skin issues.
Because of a complete absence of wedding skin recommendations in the dermatology literature, Winklemann R et al. recently published a paper titled “Wedding Dermatology: A proposed timeline to optimize skin clearance and the avoidance of a true dermatologic emergency” (SKIN The Journal of Cutaneous Medicine 2019 Mar;3[2]:159-60). He focused on acne, using the American Academy of Dermatology acne treatment guidelines and expert opinion, they point out that other than intralesional corticosteroids (which take 0-14 days to have an effect), the majority of acne treatments require at least 3-12 months to achieve clearance or improvement.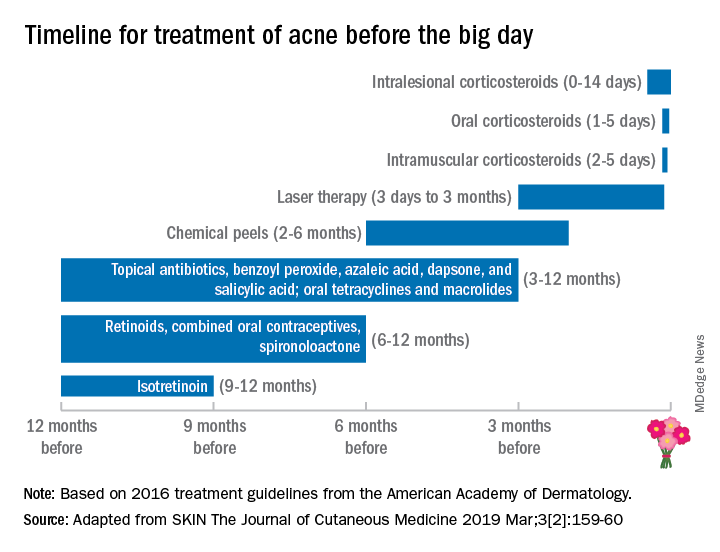
This proposed treatment timeline makes sense given that skin cell turnover on the face takes about 6-8 weeks; therefore, it may take that long for acne lesions to resolve or for treatment to have an effect.
Besides acne treatment, cosmetic treatments also have varying healing times and may require multiple sessions with time in between treatments for optimal results. For instance, treatment of photoaging with intense pulsed light or nonablative fractionated resurfacing may require three to six treatments, typically spaced 1 month apart.
Botulinum toxin treatments may take up to 2 weeks to kick in fully, then last 3-4 months. While the lead time for botulinum toxin to kick in is relatively short, I advise people not to get their first botulinum toxin 2 weeks before their wedding. Sometimes, having this treatment 4-6 weeks prior to the wedding date provides enough time for botulinum toxin to kick in – and to start wearing off to the point that the patient has the desired cosmetic effect, but still has some movement for the desired emotional facial expressions on the wedding day. Some patients also may require touch-ups, optimally at the 2-week window, once the botulinum toxin effect has fully kicked in.
With any injectable, there may be bruising and swelling that can take a week or so to heal, even when the bruises are treated with pulse dye laser used to make bruises resolve more quickly. Even a facial may result in blemishes that take a few days to 1-2 weeks to heal, especially with extractions. As such, a facial, especially a hydrafacial, may be beneficial before one’s wedding, but I would recommend having them done at least once or twice to assess an individual’s recovery time (if any) prior to the actual wedding date.
Treatment needs will vary considerably depending on the patient’s baseline skin health. As dermatologists, our patients depend greatly on us to help them look and feel their best, especially during a time when they are about to embark on a new journey like marriage. Patients need to be given realistic treatment options and time frames to achieve their goals. Whether the goal is treating acne or acne scars, starting or fine-tuning cosmetic treatments, or deciding on a skin-care regimen, the bottom line is making an appointment with the dermatologist early – 6-12 months in advance, if possible – to figure out the right plan.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Probiotic, prebiotic, and postbiotic skin care
A decade ago, I gave my senior expert talk at the University of California, San Francisco, department of dermatology on skin care and brought up the controversial topic that sterile or clean skin is bad. At the time, I initiated the conversation on the Today, I not only preach this message to my patients, but I also practice the “less-is-more” philosophy every day. It is my hope that this brief summary of the skin microbiome and the importance of skin bacteria will affect the development of the next generation of skin care products.
The normal human skin is a microbiome colonized by 10,000-1,000,000 bacteria units/cm2 that prevent the growth of pathogenic organisms and maintain the immunity of the skin. The diversity and type of skin bacteria (that is, Staphylococcus or Propionibacterium acnes), as well as their concentration, varies by person, body location, and environment. Symbiotic with bacteria on the skin are yeasts, such as Malassezia, and parasites, such as Demodex. When the composition and diversity of microorganisms are disrupted, the skin can no longer protect its barrier functions, leading to pathogenic bacterial infections, altered skin pH, decreased production of antimicrobial peptides, and increased inflammation. The microbiome also serves to shield the skin from environmental stressors, such as free radicals, UV radiation, and pollution.
What can lead to disruption of our skin is hygiene. Over-washing; stripping of the skin with lathering cleaner; overexfoliation; long, hot showers; and the use of products with antibacterial properties have increased over the last 50 years, and so has skin disease. The removal of these microorganisms, either by overcleansing or with antibiotic use, disrupts the microflora and leads to pH-imbalanced and inflamed skin. Our microflora contains prebiotics, probiotics, and postbiotics. Prebiotics are the “fertilizer” or “food,” so to speak, that encourages these essential microorganisms to grow; probiotics are the microorganisms themselves; and postbiotics are the chemical byproducts of bacteria, such as antimicrobial peptides and fragments of dead bacterial cells that remain on the skin.
Skin care tailored to our unique microbiome is in its infancy. On the frontier of microflora-rich skin care are organisms like Bifidobacterium longum, which increases the skin’s resistance to temperature and product-related irritation. Streptococcus thermophilus has been shown to increase the production of ceramides in the skin, which could help atopic dermatitis. Lactobacillus paracasei has been shown to inhibit the neuropeptide substance P, which increases inflammation and oil production. Enterococcus faecalis, Streptococcus salivarius, and Lactobacillus plantarum have all been shown to decrease Propionibacterium acnes. Bacillus coagulans and Bifidobacterium breve have been shown to decrease free radicals and protect against UV rays.
Probiotic, prebiotic, and postbiotic skin care, however, does have its challenges. Probiotics are live bacteria, and thus need refrigeration. These products are also not intended for use in anyone who is immunosuppressed or neutropenic. Another complexity in the development of probiotic, prebiotic, and postbiotic skin care is that each person may have a different need in terms of their skin microflora and that microflora is inherently different in different body parts. Furthermore, people with skin inflammation may require a different concentration or population of that flora.
In 2007, the National Institutes of Health initiated the Human Microbiome Project, and in 2016, the White House announced the creation of a new National Microbiome Initiative (NMI). Through this research, the identification and importance of our gut bacteria has led to a vast increase in development and near obsession with probiotic supplements, foods, and drinks (examples include Kombucha tea, kimchi, miso, and Kefir). Although oral consumption of prebiotics and probiotics may prove to be helpful, the skin does have its own unique flora and will benefit from targeted skin care. In the meantime, fostering the skins’s microflora is as important or more important than the replacement of it. My recommendations include using “microflora friendly” products that are lather-free, cream- or oil-based cleansers with acidic pH’s, and moisturizing heavily and consistently. I recommend staying away from antibacterial wipes, antibacterial soaps, and sanitizers.
Fostering this bacterial rich environment will help maintain your skin integrity. Squeaky clean skin is damaged skin.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Al-Ghazzewi F et al. Benef Microbes. 2014 Jun 1;5(2):99-107.
Baquerizo Nole K et al. J Am Acad Dermatol. 2014 Oct;71(4):814-21.
Chen Y et al. J Am Acad Dermatol. 2013 Jul;69(1):143-55.e3.
Grice E et al. Nat Rev Microbiol. 2011 Apr;9(4):244-53.
Kong H et al. J Invest Dermatol. 2012 Mar;132(3, part 2):933-9.
Hutkins R et al. Curr Opin Biotechnol. 2016 Feb;37:1-7.
Kober MM et al. Int J Womens Dermatol. 2015 Apr 6;1(2):85-9.
Maquire M. et al. Arch Dermatol Res. 2017 Aug;309(6):411-421.
Sugimoto S. et al. Photodermatol. Photoimmunol. Photomed. 2012 Dec;28(6): 312-9.
A decade ago, I gave my senior expert talk at the University of California, San Francisco, department of dermatology on skin care and brought up the controversial topic that sterile or clean skin is bad. At the time, I initiated the conversation on the Today, I not only preach this message to my patients, but I also practice the “less-is-more” philosophy every day. It is my hope that this brief summary of the skin microbiome and the importance of skin bacteria will affect the development of the next generation of skin care products.
The normal human skin is a microbiome colonized by 10,000-1,000,000 bacteria units/cm2 that prevent the growth of pathogenic organisms and maintain the immunity of the skin. The diversity and type of skin bacteria (that is, Staphylococcus or Propionibacterium acnes), as well as their concentration, varies by person, body location, and environment. Symbiotic with bacteria on the skin are yeasts, such as Malassezia, and parasites, such as Demodex. When the composition and diversity of microorganisms are disrupted, the skin can no longer protect its barrier functions, leading to pathogenic bacterial infections, altered skin pH, decreased production of antimicrobial peptides, and increased inflammation. The microbiome also serves to shield the skin from environmental stressors, such as free radicals, UV radiation, and pollution.
What can lead to disruption of our skin is hygiene. Over-washing; stripping of the skin with lathering cleaner; overexfoliation; long, hot showers; and the use of products with antibacterial properties have increased over the last 50 years, and so has skin disease. The removal of these microorganisms, either by overcleansing or with antibiotic use, disrupts the microflora and leads to pH-imbalanced and inflamed skin. Our microflora contains prebiotics, probiotics, and postbiotics. Prebiotics are the “fertilizer” or “food,” so to speak, that encourages these essential microorganisms to grow; probiotics are the microorganisms themselves; and postbiotics are the chemical byproducts of bacteria, such as antimicrobial peptides and fragments of dead bacterial cells that remain on the skin.
Skin care tailored to our unique microbiome is in its infancy. On the frontier of microflora-rich skin care are organisms like Bifidobacterium longum, which increases the skin’s resistance to temperature and product-related irritation. Streptococcus thermophilus has been shown to increase the production of ceramides in the skin, which could help atopic dermatitis. Lactobacillus paracasei has been shown to inhibit the neuropeptide substance P, which increases inflammation and oil production. Enterococcus faecalis, Streptococcus salivarius, and Lactobacillus plantarum have all been shown to decrease Propionibacterium acnes. Bacillus coagulans and Bifidobacterium breve have been shown to decrease free radicals and protect against UV rays.
Probiotic, prebiotic, and postbiotic skin care, however, does have its challenges. Probiotics are live bacteria, and thus need refrigeration. These products are also not intended for use in anyone who is immunosuppressed or neutropenic. Another complexity in the development of probiotic, prebiotic, and postbiotic skin care is that each person may have a different need in terms of their skin microflora and that microflora is inherently different in different body parts. Furthermore, people with skin inflammation may require a different concentration or population of that flora.
In 2007, the National Institutes of Health initiated the Human Microbiome Project, and in 2016, the White House announced the creation of a new National Microbiome Initiative (NMI). Through this research, the identification and importance of our gut bacteria has led to a vast increase in development and near obsession with probiotic supplements, foods, and drinks (examples include Kombucha tea, kimchi, miso, and Kefir). Although oral consumption of prebiotics and probiotics may prove to be helpful, the skin does have its own unique flora and will benefit from targeted skin care. In the meantime, fostering the skins’s microflora is as important or more important than the replacement of it. My recommendations include using “microflora friendly” products that are lather-free, cream- or oil-based cleansers with acidic pH’s, and moisturizing heavily and consistently. I recommend staying away from antibacterial wipes, antibacterial soaps, and sanitizers.
Fostering this bacterial rich environment will help maintain your skin integrity. Squeaky clean skin is damaged skin.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Al-Ghazzewi F et al. Benef Microbes. 2014 Jun 1;5(2):99-107.
Baquerizo Nole K et al. J Am Acad Dermatol. 2014 Oct;71(4):814-21.
Chen Y et al. J Am Acad Dermatol. 2013 Jul;69(1):143-55.e3.
Grice E et al. Nat Rev Microbiol. 2011 Apr;9(4):244-53.
Kong H et al. J Invest Dermatol. 2012 Mar;132(3, part 2):933-9.
Hutkins R et al. Curr Opin Biotechnol. 2016 Feb;37:1-7.
Kober MM et al. Int J Womens Dermatol. 2015 Apr 6;1(2):85-9.
Maquire M. et al. Arch Dermatol Res. 2017 Aug;309(6):411-421.
Sugimoto S. et al. Photodermatol. Photoimmunol. Photomed. 2012 Dec;28(6): 312-9.
A decade ago, I gave my senior expert talk at the University of California, San Francisco, department of dermatology on skin care and brought up the controversial topic that sterile or clean skin is bad. At the time, I initiated the conversation on the Today, I not only preach this message to my patients, but I also practice the “less-is-more” philosophy every day. It is my hope that this brief summary of the skin microbiome and the importance of skin bacteria will affect the development of the next generation of skin care products.
The normal human skin is a microbiome colonized by 10,000-1,000,000 bacteria units/cm2 that prevent the growth of pathogenic organisms and maintain the immunity of the skin. The diversity and type of skin bacteria (that is, Staphylococcus or Propionibacterium acnes), as well as their concentration, varies by person, body location, and environment. Symbiotic with bacteria on the skin are yeasts, such as Malassezia, and parasites, such as Demodex. When the composition and diversity of microorganisms are disrupted, the skin can no longer protect its barrier functions, leading to pathogenic bacterial infections, altered skin pH, decreased production of antimicrobial peptides, and increased inflammation. The microbiome also serves to shield the skin from environmental stressors, such as free radicals, UV radiation, and pollution.
What can lead to disruption of our skin is hygiene. Over-washing; stripping of the skin with lathering cleaner; overexfoliation; long, hot showers; and the use of products with antibacterial properties have increased over the last 50 years, and so has skin disease. The removal of these microorganisms, either by overcleansing or with antibiotic use, disrupts the microflora and leads to pH-imbalanced and inflamed skin. Our microflora contains prebiotics, probiotics, and postbiotics. Prebiotics are the “fertilizer” or “food,” so to speak, that encourages these essential microorganisms to grow; probiotics are the microorganisms themselves; and postbiotics are the chemical byproducts of bacteria, such as antimicrobial peptides and fragments of dead bacterial cells that remain on the skin.
Skin care tailored to our unique microbiome is in its infancy. On the frontier of microflora-rich skin care are organisms like Bifidobacterium longum, which increases the skin’s resistance to temperature and product-related irritation. Streptococcus thermophilus has been shown to increase the production of ceramides in the skin, which could help atopic dermatitis. Lactobacillus paracasei has been shown to inhibit the neuropeptide substance P, which increases inflammation and oil production. Enterococcus faecalis, Streptococcus salivarius, and Lactobacillus plantarum have all been shown to decrease Propionibacterium acnes. Bacillus coagulans and Bifidobacterium breve have been shown to decrease free radicals and protect against UV rays.
Probiotic, prebiotic, and postbiotic skin care, however, does have its challenges. Probiotics are live bacteria, and thus need refrigeration. These products are also not intended for use in anyone who is immunosuppressed or neutropenic. Another complexity in the development of probiotic, prebiotic, and postbiotic skin care is that each person may have a different need in terms of their skin microflora and that microflora is inherently different in different body parts. Furthermore, people with skin inflammation may require a different concentration or population of that flora.
In 2007, the National Institutes of Health initiated the Human Microbiome Project, and in 2016, the White House announced the creation of a new National Microbiome Initiative (NMI). Through this research, the identification and importance of our gut bacteria has led to a vast increase in development and near obsession with probiotic supplements, foods, and drinks (examples include Kombucha tea, kimchi, miso, and Kefir). Although oral consumption of prebiotics and probiotics may prove to be helpful, the skin does have its own unique flora and will benefit from targeted skin care. In the meantime, fostering the skins’s microflora is as important or more important than the replacement of it. My recommendations include using “microflora friendly” products that are lather-free, cream- or oil-based cleansers with acidic pH’s, and moisturizing heavily and consistently. I recommend staying away from antibacterial wipes, antibacterial soaps, and sanitizers.
Fostering this bacterial rich environment will help maintain your skin integrity. Squeaky clean skin is damaged skin.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Al-Ghazzewi F et al. Benef Microbes. 2014 Jun 1;5(2):99-107.
Baquerizo Nole K et al. J Am Acad Dermatol. 2014 Oct;71(4):814-21.
Chen Y et al. J Am Acad Dermatol. 2013 Jul;69(1):143-55.e3.
Grice E et al. Nat Rev Microbiol. 2011 Apr;9(4):244-53.
Kong H et al. J Invest Dermatol. 2012 Mar;132(3, part 2):933-9.
Hutkins R et al. Curr Opin Biotechnol. 2016 Feb;37:1-7.
Kober MM et al. Int J Womens Dermatol. 2015 Apr 6;1(2):85-9.
Maquire M. et al. Arch Dermatol Res. 2017 Aug;309(6):411-421.
Sugimoto S. et al. Photodermatol. Photoimmunol. Photomed. 2012 Dec;28(6): 312-9.
Winter exfoliation: A multicultural approach
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Knee and elbow rejuvenation
The cosmetic industry improves techniques for tightening faces, hands, necks, and decolletes; meanwhile, sagging elbows and knees, once ignored, also are a visible sign of aging. Modifying techniques commonly used for the face and neck can yield significant improvements in the elbows and knees. The elbows and knees naturally have looser skin to allow for joint movement; over time, the skin over these joints is exposed to sun damage, friction, and recurrent extension and flexion, which cause skin laxity and aging.
A combination approach addressing skin texture, collagen damage, rhytides, and fat deposition is the most effective method for knee and elbow rejuvenation.
For knees and elbows with loose skin and rhytides, in-office noninvasive and minimally invasive radio-frequency and light energy treatments are helpful in increasing collagen production and tissue tightening. Similarly, microfocused ultrasound has been shown to be a safe and effective skin tightening treatment for the knees. In comparison to the face, however, the skin around the elbows and knees can be thinner and has fewer sebaceous glands. Caution should be used particularly with minimally invasive radio-frequency techniques in order to protect the epidermal skin. Often, treatments have to be repeated to give optimal results, which are not apparent until 3-6 months after the initial procedure.
For knee skin with severe laxity, a comprehensive approach using polydioxanone (PDO) or poly-l-lactic acid (PLLA) threads in both the upper thighs and circumferentially around the knees provides collagen production and tightening of the loose skin. Treatment of the upper thighs is essential in providing a vector that lifts the skin of the knees. Treatments can be repeated, with results seen after 90 days. Thread lifts of the knees and thighs are highly effective, noninvasive procedures with little to no downtime and can be used for severe skin laxity, wrinkling, and thinning of the knee skin.
Loose, roughened knee and elbow skin can also be treated with nonablative factional resurfacing, radio-frequency microneedling, or a series of monthly treatments with PLLA and hyaluronic acid fillers injected in the superficial to mid-dermis. Both fractional resurfacing and dermal filler injections help stimulate collagen production and improve both fine rhytides and dermatoheliosis.
Adipose tissue around the knees can be treated with monthly deoxycholic acid injections (for a video of this procedure, go to https://drive.google.com/file/d/1rhw-nESy15AoDhKUrc25DDjKEun7RL4i/view). The volume of injection, however, is significantly higher than that recommended in the submental area. Two to four times the volume is needed per knee over a series of 3-6 treatments, depending on the amount of fat in the knees.
Cryolipolysis is also an effective option for fat pockets around the knees; however, in my experience, it can be difficult to fit the applicators onto the area of concern appropriately unless smaller applicators are applied.
With the increasing demand for body rejuvenation techniques, providers are adapting techniques used for the face and neck to lift, tighten, thin, and sculpt the knees and elbows. A combination approach using lasers, ultrasound, fillers, threads, and cryolipolysis can be effective for these areas. Results are obtainable when repeat treatments are performed; however, one must be patient because results are not seen for 6 months or more.
Dr. Lily Talakoub and Dr. Naissan Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Macedo O. et al. J Am Acad Dermatol. 2014;70(Suppl 1), Abstract P800, page AB193.
The cosmetic industry improves techniques for tightening faces, hands, necks, and decolletes; meanwhile, sagging elbows and knees, once ignored, also are a visible sign of aging. Modifying techniques commonly used for the face and neck can yield significant improvements in the elbows and knees. The elbows and knees naturally have looser skin to allow for joint movement; over time, the skin over these joints is exposed to sun damage, friction, and recurrent extension and flexion, which cause skin laxity and aging.
A combination approach addressing skin texture, collagen damage, rhytides, and fat deposition is the most effective method for knee and elbow rejuvenation.
For knees and elbows with loose skin and rhytides, in-office noninvasive and minimally invasive radio-frequency and light energy treatments are helpful in increasing collagen production and tissue tightening. Similarly, microfocused ultrasound has been shown to be a safe and effective skin tightening treatment for the knees. In comparison to the face, however, the skin around the elbows and knees can be thinner and has fewer sebaceous glands. Caution should be used particularly with minimally invasive radio-frequency techniques in order to protect the epidermal skin. Often, treatments have to be repeated to give optimal results, which are not apparent until 3-6 months after the initial procedure.
For knee skin with severe laxity, a comprehensive approach using polydioxanone (PDO) or poly-l-lactic acid (PLLA) threads in both the upper thighs and circumferentially around the knees provides collagen production and tightening of the loose skin. Treatment of the upper thighs is essential in providing a vector that lifts the skin of the knees. Treatments can be repeated, with results seen after 90 days. Thread lifts of the knees and thighs are highly effective, noninvasive procedures with little to no downtime and can be used for severe skin laxity, wrinkling, and thinning of the knee skin.
Loose, roughened knee and elbow skin can also be treated with nonablative factional resurfacing, radio-frequency microneedling, or a series of monthly treatments with PLLA and hyaluronic acid fillers injected in the superficial to mid-dermis. Both fractional resurfacing and dermal filler injections help stimulate collagen production and improve both fine rhytides and dermatoheliosis.
Adipose tissue around the knees can be treated with monthly deoxycholic acid injections (for a video of this procedure, go to https://drive.google.com/file/d/1rhw-nESy15AoDhKUrc25DDjKEun7RL4i/view). The volume of injection, however, is significantly higher than that recommended in the submental area. Two to four times the volume is needed per knee over a series of 3-6 treatments, depending on the amount of fat in the knees.
Cryolipolysis is also an effective option for fat pockets around the knees; however, in my experience, it can be difficult to fit the applicators onto the area of concern appropriately unless smaller applicators are applied.
With the increasing demand for body rejuvenation techniques, providers are adapting techniques used for the face and neck to lift, tighten, thin, and sculpt the knees and elbows. A combination approach using lasers, ultrasound, fillers, threads, and cryolipolysis can be effective for these areas. Results are obtainable when repeat treatments are performed; however, one must be patient because results are not seen for 6 months or more.
Dr. Lily Talakoub and Dr. Naissan Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Macedo O. et al. J Am Acad Dermatol. 2014;70(Suppl 1), Abstract P800, page AB193.
The cosmetic industry improves techniques for tightening faces, hands, necks, and decolletes; meanwhile, sagging elbows and knees, once ignored, also are a visible sign of aging. Modifying techniques commonly used for the face and neck can yield significant improvements in the elbows and knees. The elbows and knees naturally have looser skin to allow for joint movement; over time, the skin over these joints is exposed to sun damage, friction, and recurrent extension and flexion, which cause skin laxity and aging.
A combination approach addressing skin texture, collagen damage, rhytides, and fat deposition is the most effective method for knee and elbow rejuvenation.
For knees and elbows with loose skin and rhytides, in-office noninvasive and minimally invasive radio-frequency and light energy treatments are helpful in increasing collagen production and tissue tightening. Similarly, microfocused ultrasound has been shown to be a safe and effective skin tightening treatment for the knees. In comparison to the face, however, the skin around the elbows and knees can be thinner and has fewer sebaceous glands. Caution should be used particularly with minimally invasive radio-frequency techniques in order to protect the epidermal skin. Often, treatments have to be repeated to give optimal results, which are not apparent until 3-6 months after the initial procedure.
For knee skin with severe laxity, a comprehensive approach using polydioxanone (PDO) or poly-l-lactic acid (PLLA) threads in both the upper thighs and circumferentially around the knees provides collagen production and tightening of the loose skin. Treatment of the upper thighs is essential in providing a vector that lifts the skin of the knees. Treatments can be repeated, with results seen after 90 days. Thread lifts of the knees and thighs are highly effective, noninvasive procedures with little to no downtime and can be used for severe skin laxity, wrinkling, and thinning of the knee skin.
Loose, roughened knee and elbow skin can also be treated with nonablative factional resurfacing, radio-frequency microneedling, or a series of monthly treatments with PLLA and hyaluronic acid fillers injected in the superficial to mid-dermis. Both fractional resurfacing and dermal filler injections help stimulate collagen production and improve both fine rhytides and dermatoheliosis.
Adipose tissue around the knees can be treated with monthly deoxycholic acid injections (for a video of this procedure, go to https://drive.google.com/file/d/1rhw-nESy15AoDhKUrc25DDjKEun7RL4i/view). The volume of injection, however, is significantly higher than that recommended in the submental area. Two to four times the volume is needed per knee over a series of 3-6 treatments, depending on the amount of fat in the knees.
Cryolipolysis is also an effective option for fat pockets around the knees; however, in my experience, it can be difficult to fit the applicators onto the area of concern appropriately unless smaller applicators are applied.
With the increasing demand for body rejuvenation techniques, providers are adapting techniques used for the face and neck to lift, tighten, thin, and sculpt the knees and elbows. A combination approach using lasers, ultrasound, fillers, threads, and cryolipolysis can be effective for these areas. Results are obtainable when repeat treatments are performed; however, one must be patient because results are not seen for 6 months or more.
Dr. Lily Talakoub and Dr. Naissan Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Macedo O. et al. J Am Acad Dermatol. 2014;70(Suppl 1), Abstract P800, page AB193.
Integrative dermatology
In October of this year, the , and practitioners of Ayurvedic, Naturopathic, and traditional Chinese medicine (TCM), in one place. This was the first time in the United States that practitioners from these different areas of medicine were brought together to discuss and learn different approaches to skin care and treatment of dermatologic diseases.
Of all the medical specialties, it is presumed that dermatology is the most inherently holistic. By examining the hair, skin, and nails, we are able to diagnose internal organ diseases such as liver failure (jaundice, veins on stomach), thyroid disease (madarosis), sarcoidosis, and infectious diseases (cutaneous manifestations of HIV), diabetes (acanthosis nigricans, tripe palm), polycystic ovary syndrome (acne, hirsutism), and porphyria, just to name a few. We are also able to treat cutaneous conditions, such as psoriasis, with biologic medications, treatment that in turn, also benefits internal manifestations such as joint, cardiovascular, and metabolic disease. In TCM and Ayurveda, the skin, hair, body type, and tongue can also be analyzed to diagnose and treat disease.
Salves and skin care routines that would be considered natural or holistic have been “prescribed” by Western dermatologists with an MD license for many years. Most medicines initially come from nature, and it is only in the past century, with the boom in the pharmaceutical industry and development of synthetic prescription medications, that people have forgotten this. Some of this boom has been needed to treat enormous populations, as natural resources can be scarce, and in some cases, only an extract of the plant may be needed for treatment, where other elements may be ineffective or even harmful.
Domeboro solution, Epsom salt soaks, and wet to dry soaks are used to draw out and treat infections. Bleach baths are often used to decrease bacterial load and calm inflammation when treating eczema. In Mohs surgery, Fredrick Mohs initially used a zinc chloride paste on nonmelanoma skin cancers in between stages, before frozen section processing and cosmetic reconstruction made Mohs what it is today. In the days of Hippocrates, food was medicine. If you were “red in the face” your blood was deemed too acidic and alkaline-forming foods or “cold foods” were given. This has now again come full circle with rosacea and evidence supporting a link between disease flares or improvement related to foods and the gut microbiome.
On a photography trip to Wyoming, I learned how Native Americans in the United States wiped the white powder from the bark of aspen trees on their skin and used it as sunscreen. In Mongolia, I learned how fat from a sheep’s bottom was used in beauty skin care routines. It is from native and nomadic people that we can often learn how effective natural methods can be used, especially in cases where the treatment regimens may not be written down. With Ayurveda and TCM, we are lucky that textbooks thousands of years old and professors and schools are available to educate us about these ancient practices.
The rediscovery of ancient treatments through the study of ethnobotany, Ayurveda, and TCM has been fascinating, as most of these approaches focus not just on the skin, but on treating the patient as a whole, inside and out (often depending on the discipline treating mind, body, and spirit), with the effects ultimately benefiting the skin. With the many advances in Western medicine over the past 2,000 years, starting with Hippocrates, it will be interesting to see how we, in the field of dermatology, can still learn from and potentially integrate medicine that originated 3,000-5,000 plus years ago in Ayurveda and 2,000-plus years ago in TCM that is still practiced today. In the future, we hope to have more columns about these specialties and how they are used in skin and beauty.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
In October of this year, the , and practitioners of Ayurvedic, Naturopathic, and traditional Chinese medicine (TCM), in one place. This was the first time in the United States that practitioners from these different areas of medicine were brought together to discuss and learn different approaches to skin care and treatment of dermatologic diseases.
Of all the medical specialties, it is presumed that dermatology is the most inherently holistic. By examining the hair, skin, and nails, we are able to diagnose internal organ diseases such as liver failure (jaundice, veins on stomach), thyroid disease (madarosis), sarcoidosis, and infectious diseases (cutaneous manifestations of HIV), diabetes (acanthosis nigricans, tripe palm), polycystic ovary syndrome (acne, hirsutism), and porphyria, just to name a few. We are also able to treat cutaneous conditions, such as psoriasis, with biologic medications, treatment that in turn, also benefits internal manifestations such as joint, cardiovascular, and metabolic disease. In TCM and Ayurveda, the skin, hair, body type, and tongue can also be analyzed to diagnose and treat disease.
Salves and skin care routines that would be considered natural or holistic have been “prescribed” by Western dermatologists with an MD license for many years. Most medicines initially come from nature, and it is only in the past century, with the boom in the pharmaceutical industry and development of synthetic prescription medications, that people have forgotten this. Some of this boom has been needed to treat enormous populations, as natural resources can be scarce, and in some cases, only an extract of the plant may be needed for treatment, where other elements may be ineffective or even harmful.
Domeboro solution, Epsom salt soaks, and wet to dry soaks are used to draw out and treat infections. Bleach baths are often used to decrease bacterial load and calm inflammation when treating eczema. In Mohs surgery, Fredrick Mohs initially used a zinc chloride paste on nonmelanoma skin cancers in between stages, before frozen section processing and cosmetic reconstruction made Mohs what it is today. In the days of Hippocrates, food was medicine. If you were “red in the face” your blood was deemed too acidic and alkaline-forming foods or “cold foods” were given. This has now again come full circle with rosacea and evidence supporting a link between disease flares or improvement related to foods and the gut microbiome.
On a photography trip to Wyoming, I learned how Native Americans in the United States wiped the white powder from the bark of aspen trees on their skin and used it as sunscreen. In Mongolia, I learned how fat from a sheep’s bottom was used in beauty skin care routines. It is from native and nomadic people that we can often learn how effective natural methods can be used, especially in cases where the treatment regimens may not be written down. With Ayurveda and TCM, we are lucky that textbooks thousands of years old and professors and schools are available to educate us about these ancient practices.
The rediscovery of ancient treatments through the study of ethnobotany, Ayurveda, and TCM has been fascinating, as most of these approaches focus not just on the skin, but on treating the patient as a whole, inside and out (often depending on the discipline treating mind, body, and spirit), with the effects ultimately benefiting the skin. With the many advances in Western medicine over the past 2,000 years, starting with Hippocrates, it will be interesting to see how we, in the field of dermatology, can still learn from and potentially integrate medicine that originated 3,000-5,000 plus years ago in Ayurveda and 2,000-plus years ago in TCM that is still practiced today. In the future, we hope to have more columns about these specialties and how they are used in skin and beauty.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
In October of this year, the , and practitioners of Ayurvedic, Naturopathic, and traditional Chinese medicine (TCM), in one place. This was the first time in the United States that practitioners from these different areas of medicine were brought together to discuss and learn different approaches to skin care and treatment of dermatologic diseases.
Of all the medical specialties, it is presumed that dermatology is the most inherently holistic. By examining the hair, skin, and nails, we are able to diagnose internal organ diseases such as liver failure (jaundice, veins on stomach), thyroid disease (madarosis), sarcoidosis, and infectious diseases (cutaneous manifestations of HIV), diabetes (acanthosis nigricans, tripe palm), polycystic ovary syndrome (acne, hirsutism), and porphyria, just to name a few. We are also able to treat cutaneous conditions, such as psoriasis, with biologic medications, treatment that in turn, also benefits internal manifestations such as joint, cardiovascular, and metabolic disease. In TCM and Ayurveda, the skin, hair, body type, and tongue can also be analyzed to diagnose and treat disease.
Salves and skin care routines that would be considered natural or holistic have been “prescribed” by Western dermatologists with an MD license for many years. Most medicines initially come from nature, and it is only in the past century, with the boom in the pharmaceutical industry and development of synthetic prescription medications, that people have forgotten this. Some of this boom has been needed to treat enormous populations, as natural resources can be scarce, and in some cases, only an extract of the plant may be needed for treatment, where other elements may be ineffective or even harmful.
Domeboro solution, Epsom salt soaks, and wet to dry soaks are used to draw out and treat infections. Bleach baths are often used to decrease bacterial load and calm inflammation when treating eczema. In Mohs surgery, Fredrick Mohs initially used a zinc chloride paste on nonmelanoma skin cancers in between stages, before frozen section processing and cosmetic reconstruction made Mohs what it is today. In the days of Hippocrates, food was medicine. If you were “red in the face” your blood was deemed too acidic and alkaline-forming foods or “cold foods” were given. This has now again come full circle with rosacea and evidence supporting a link between disease flares or improvement related to foods and the gut microbiome.
On a photography trip to Wyoming, I learned how Native Americans in the United States wiped the white powder from the bark of aspen trees on their skin and used it as sunscreen. In Mongolia, I learned how fat from a sheep’s bottom was used in beauty skin care routines. It is from native and nomadic people that we can often learn how effective natural methods can be used, especially in cases where the treatment regimens may not be written down. With Ayurveda and TCM, we are lucky that textbooks thousands of years old and professors and schools are available to educate us about these ancient practices.
The rediscovery of ancient treatments through the study of ethnobotany, Ayurveda, and TCM has been fascinating, as most of these approaches focus not just on the skin, but on treating the patient as a whole, inside and out (often depending on the discipline treating mind, body, and spirit), with the effects ultimately benefiting the skin. With the many advances in Western medicine over the past 2,000 years, starting with Hippocrates, it will be interesting to see how we, in the field of dermatology, can still learn from and potentially integrate medicine that originated 3,000-5,000 plus years ago in Ayurveda and 2,000-plus years ago in TCM that is still practiced today. In the future, we hope to have more columns about these specialties and how they are used in skin and beauty.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Hypopigmentation
Hypopigmentation or depigmentation of the skin is very challenging to treat. The loss of melanin in the skin is often a frustrating problem, resulting from acne, burn scars, vitiligo, topically applied chemicals, or cryotherapy. To date, there is no universally accepted treatment that restores skin pigmentation. In our clinic, the induction of trauma to the skin via a series of microneedling or subcision treatments has shown promise in increasing the pigmentation of skin with localized hypo- or depigmented patches.

to improve the appearance of fine lines, acne scars, photoaging, stretch marks, enlarged pores, and other cosmetic issues characterized by loss of collagen or altered collagen remodeling. The skin-needling technique involves fine sterile needles 0.1 mm–2.5 mm in length that repeatedly pierce the stratum corneum producing microscopic “holes” in the dermis. These microscopic wounds lead to the release of growth factors stimulating the formation of new collagen, elastin, and neovascularization in the dermis. Similar to microneedling, subcision uses repeat trauma to the dermis and subcutis through the insertion and repeat movement of a needle.
In our practice, patients presenting with hypopigmentation of the skin from a variety of causes have been treated with a series of five subcision or microneedling procedures, resulting in rapid repigmentation of the skin with minimal to no side effects. Trauma to the skin causes regenerative mechanisms and wound healing. The release of cytokines that induce neoangiogenesis, neocollagenesis, and the deposition of hemosiderin from dermal bleeding induce the activation of melanocytes and stimulate skin pigmentation.
Subcision and microneedling are safe, effective, in-office procedures with vast indications that now can be applied to depigmented and hypopigmented skin. Patients have little to no downtime and results are permanent.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Dermatol Surg. 1995 Jun;21(6):543-9.
Aesthet Plast Surg. 1997 Jan-Feb;21(1):48-51.
Oral Maxillofac Surg Clin North Am. 2005 Feb;17(1):51-63.
Plast Reconstr Surg. 2008 Apr;121(4):1421-9.
Clin Dermatol. 2008 Mar-Apr;26(2):192-9.Plast Reconstr Surg. 2008 Nov;122(5):1553-63.
J Dermatolog Treat. 2012 Apr;23(2):144-52.
J Cutan Aesthet Surg. 2009 Jan;2(1):26-30.
J Cutan Aesthet Surg. 2009 Jul;2(2):110-1.
J Cosmet Dermatol. 2014 Sep;13(3):180-7.J Am Acad Dermatol. 2016 Nov;75(5):e195-e197.
Hypopigmentation or depigmentation of the skin is very challenging to treat. The loss of melanin in the skin is often a frustrating problem, resulting from acne, burn scars, vitiligo, topically applied chemicals, or cryotherapy. To date, there is no universally accepted treatment that restores skin pigmentation. In our clinic, the induction of trauma to the skin via a series of microneedling or subcision treatments has shown promise in increasing the pigmentation of skin with localized hypo- or depigmented patches.

to improve the appearance of fine lines, acne scars, photoaging, stretch marks, enlarged pores, and other cosmetic issues characterized by loss of collagen or altered collagen remodeling. The skin-needling technique involves fine sterile needles 0.1 mm–2.5 mm in length that repeatedly pierce the stratum corneum producing microscopic “holes” in the dermis. These microscopic wounds lead to the release of growth factors stimulating the formation of new collagen, elastin, and neovascularization in the dermis. Similar to microneedling, subcision uses repeat trauma to the dermis and subcutis through the insertion and repeat movement of a needle.
In our practice, patients presenting with hypopigmentation of the skin from a variety of causes have been treated with a series of five subcision or microneedling procedures, resulting in rapid repigmentation of the skin with minimal to no side effects. Trauma to the skin causes regenerative mechanisms and wound healing. The release of cytokines that induce neoangiogenesis, neocollagenesis, and the deposition of hemosiderin from dermal bleeding induce the activation of melanocytes and stimulate skin pigmentation.
Subcision and microneedling are safe, effective, in-office procedures with vast indications that now can be applied to depigmented and hypopigmented skin. Patients have little to no downtime and results are permanent.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Dermatol Surg. 1995 Jun;21(6):543-9.
Aesthet Plast Surg. 1997 Jan-Feb;21(1):48-51.
Oral Maxillofac Surg Clin North Am. 2005 Feb;17(1):51-63.
Plast Reconstr Surg. 2008 Apr;121(4):1421-9.
Clin Dermatol. 2008 Mar-Apr;26(2):192-9.Plast Reconstr Surg. 2008 Nov;122(5):1553-63.
J Dermatolog Treat. 2012 Apr;23(2):144-52.
J Cutan Aesthet Surg. 2009 Jan;2(1):26-30.
J Cutan Aesthet Surg. 2009 Jul;2(2):110-1.
J Cosmet Dermatol. 2014 Sep;13(3):180-7.J Am Acad Dermatol. 2016 Nov;75(5):e195-e197.
Hypopigmentation or depigmentation of the skin is very challenging to treat. The loss of melanin in the skin is often a frustrating problem, resulting from acne, burn scars, vitiligo, topically applied chemicals, or cryotherapy. To date, there is no universally accepted treatment that restores skin pigmentation. In our clinic, the induction of trauma to the skin via a series of microneedling or subcision treatments has shown promise in increasing the pigmentation of skin with localized hypo- or depigmented patches.

to improve the appearance of fine lines, acne scars, photoaging, stretch marks, enlarged pores, and other cosmetic issues characterized by loss of collagen or altered collagen remodeling. The skin-needling technique involves fine sterile needles 0.1 mm–2.5 mm in length that repeatedly pierce the stratum corneum producing microscopic “holes” in the dermis. These microscopic wounds lead to the release of growth factors stimulating the formation of new collagen, elastin, and neovascularization in the dermis. Similar to microneedling, subcision uses repeat trauma to the dermis and subcutis through the insertion and repeat movement of a needle.
In our practice, patients presenting with hypopigmentation of the skin from a variety of causes have been treated with a series of five subcision or microneedling procedures, resulting in rapid repigmentation of the skin with minimal to no side effects. Trauma to the skin causes regenerative mechanisms and wound healing. The release of cytokines that induce neoangiogenesis, neocollagenesis, and the deposition of hemosiderin from dermal bleeding induce the activation of melanocytes and stimulate skin pigmentation.
Subcision and microneedling are safe, effective, in-office procedures with vast indications that now can be applied to depigmented and hypopigmented skin. Patients have little to no downtime and results are permanent.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Dermatol Surg. 1995 Jun;21(6):543-9.
Aesthet Plast Surg. 1997 Jan-Feb;21(1):48-51.
Oral Maxillofac Surg Clin North Am. 2005 Feb;17(1):51-63.
Plast Reconstr Surg. 2008 Apr;121(4):1421-9.
Clin Dermatol. 2008 Mar-Apr;26(2):192-9.Plast Reconstr Surg. 2008 Nov;122(5):1553-63.
J Dermatolog Treat. 2012 Apr;23(2):144-52.
J Cutan Aesthet Surg. 2009 Jan;2(1):26-30.
J Cutan Aesthet Surg. 2009 Jul;2(2):110-1.
J Cosmet Dermatol. 2014 Sep;13(3):180-7.J Am Acad Dermatol. 2016 Nov;75(5):e195-e197.
Whole body cryotherapy
.
WBC has been purported to manage pain, reduce inflammation, and speed up recovery after injury, as well as relieve sore muscles after exercise, aid in weight loss, and improve mood. There have also been claims that it can treat acne, eczema, and psoriasis – even multiple sclerosis, fibromyalgia, and rheumatoid arthritis. It has been used as a beauty aid to reduce pore size and reduce wrinkles. Its popularity has exploded as centers are advertised on discount sites such as Groupon and Living Social, and it is now available as classes in the popular exercise app ClassPass as “Whole Body Cryotherapy” or a “CryoBeauty Facial.”
Despite these claims and popularity, research studies have yet to prove that WBC can deliver any of these benefits. The American Academy of Dermatology has released a statement for consumers that does not support its use. Because of the lack of research, WBC has not been cleared by the Food and Drug Administration for treating any medical indication.
Its popularity has to stem from somewhere. In many cultures, cold therapy has been used for health benefits for centuries. For example, Turkish, Russian, Finnish, Roman, and Chinese spas offer cold baths at 50 degrees Fahrenheit after heat therapy (saunas, baths) as a form of hydrotherapy to alter circulation for health benefits, with the goal of releasing toxins with heat, then closing pores and bringing the circulation back to the body’s core with cold therapy. Cold ice baths and ice packs are used by athletes routinely after games, practices, and injuries to reduce inflammation. How is WBC different?
With WBC, a person who is nearly nude enters a cold chamber of minus 200 degrees Fahrenheit, in sessions that typically last 2-4 minutes.
While the majority of those who engage in WBC have not had complications, the AAD statement refers to a Finnish study that found that 16% of individuals exposed to WBC had mild frostbite. In 2011, U.S. sprinter and Olympic gold medalist Justin Gatlin developed frostbite on both feet after a WBC session. Additional WBC-related complications that have been reported include a frozen limb (a frozen arm in a woman in Dallas in 2013, after a 3-minute session, manifesting as painful swelling, blisters, and third-degree burns – a more severe type of frostbite), and cold panniculitis (JAAD Case Rep. 2018;4:344-5). Others include eye injuries, temporary loss of memory, and even death due to suffocation, reported in 2015, of a staff member at a cryotherapy center outside of Las Vegas who went into a tank alone after hours when no one else was around.
Cryotherapy, when delivered to specific areas of the skin by a dermatologist, is a useful low-risk treatment. Postinflammatory pigment alteration can occur, but there has been great success in using the treatment locally for warts, actinic keratoses, and other benign skin growths, when it is done done by trained professionals. Granted, while localized cryotherapy to treat a skin growth is not the same as whole body cryotherapy, the same types of complication risks should be considered, including postinflammatory pigment alteration, particularly in skin of color, as cryotherapy can be toxic to melanocytes.
Before it is completely discounted, if it makes the person feel good or better, perhaps if the patient and practitioner are aware of the risks and how to identify and manage them, cold therapy could be useful. I once had a patient who described great relief with WBC after a Fraxel laser treatment, when her face felt like it was “on fire” despite refrigerated topical Biafine, cold air, and ice packs. As with most treatments, if someone feels better, they often look better.
While medical or aesthetic benefits of WBC have not been proved and WBC has definite risks, if the procedure is done in an appropriate and responsible way, perhaps the benefit could outweigh the informed risks for some patients. Claims should not be advertised until they are proven, so that patients are not misinformed. The same is true of chemical peels, microneedling, hyperbaric oxygen, and vitamin drips, which are provided over the counter in nonmedical settings for health and beauty uses. Medical history should be taken into account with WBC by the facility and the practitioner, including history of blood clots, smoking, vasculitis, Raynaud’s disease, autoimmune conditions, neuropathy, and prior history of frostbite. Perhaps these should be contraindications to WBC and mechanisms should be in place to manage complications should they occur. Better regulation of WBC is needed so that the procedure can be done effectively and safely.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
.
WBC has been purported to manage pain, reduce inflammation, and speed up recovery after injury, as well as relieve sore muscles after exercise, aid in weight loss, and improve mood. There have also been claims that it can treat acne, eczema, and psoriasis – even multiple sclerosis, fibromyalgia, and rheumatoid arthritis. It has been used as a beauty aid to reduce pore size and reduce wrinkles. Its popularity has exploded as centers are advertised on discount sites such as Groupon and Living Social, and it is now available as classes in the popular exercise app ClassPass as “Whole Body Cryotherapy” or a “CryoBeauty Facial.”
Despite these claims and popularity, research studies have yet to prove that WBC can deliver any of these benefits. The American Academy of Dermatology has released a statement for consumers that does not support its use. Because of the lack of research, WBC has not been cleared by the Food and Drug Administration for treating any medical indication.
Its popularity has to stem from somewhere. In many cultures, cold therapy has been used for health benefits for centuries. For example, Turkish, Russian, Finnish, Roman, and Chinese spas offer cold baths at 50 degrees Fahrenheit after heat therapy (saunas, baths) as a form of hydrotherapy to alter circulation for health benefits, with the goal of releasing toxins with heat, then closing pores and bringing the circulation back to the body’s core with cold therapy. Cold ice baths and ice packs are used by athletes routinely after games, practices, and injuries to reduce inflammation. How is WBC different?
With WBC, a person who is nearly nude enters a cold chamber of minus 200 degrees Fahrenheit, in sessions that typically last 2-4 minutes.
While the majority of those who engage in WBC have not had complications, the AAD statement refers to a Finnish study that found that 16% of individuals exposed to WBC had mild frostbite. In 2011, U.S. sprinter and Olympic gold medalist Justin Gatlin developed frostbite on both feet after a WBC session. Additional WBC-related complications that have been reported include a frozen limb (a frozen arm in a woman in Dallas in 2013, after a 3-minute session, manifesting as painful swelling, blisters, and third-degree burns – a more severe type of frostbite), and cold panniculitis (JAAD Case Rep. 2018;4:344-5). Others include eye injuries, temporary loss of memory, and even death due to suffocation, reported in 2015, of a staff member at a cryotherapy center outside of Las Vegas who went into a tank alone after hours when no one else was around.
Cryotherapy, when delivered to specific areas of the skin by a dermatologist, is a useful low-risk treatment. Postinflammatory pigment alteration can occur, but there has been great success in using the treatment locally for warts, actinic keratoses, and other benign skin growths, when it is done done by trained professionals. Granted, while localized cryotherapy to treat a skin growth is not the same as whole body cryotherapy, the same types of complication risks should be considered, including postinflammatory pigment alteration, particularly in skin of color, as cryotherapy can be toxic to melanocytes.
Before it is completely discounted, if it makes the person feel good or better, perhaps if the patient and practitioner are aware of the risks and how to identify and manage them, cold therapy could be useful. I once had a patient who described great relief with WBC after a Fraxel laser treatment, when her face felt like it was “on fire” despite refrigerated topical Biafine, cold air, and ice packs. As with most treatments, if someone feels better, they often look better.
While medical or aesthetic benefits of WBC have not been proved and WBC has definite risks, if the procedure is done in an appropriate and responsible way, perhaps the benefit could outweigh the informed risks for some patients. Claims should not be advertised until they are proven, so that patients are not misinformed. The same is true of chemical peels, microneedling, hyperbaric oxygen, and vitamin drips, which are provided over the counter in nonmedical settings for health and beauty uses. Medical history should be taken into account with WBC by the facility and the practitioner, including history of blood clots, smoking, vasculitis, Raynaud’s disease, autoimmune conditions, neuropathy, and prior history of frostbite. Perhaps these should be contraindications to WBC and mechanisms should be in place to manage complications should they occur. Better regulation of WBC is needed so that the procedure can be done effectively and safely.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
.
WBC has been purported to manage pain, reduce inflammation, and speed up recovery after injury, as well as relieve sore muscles after exercise, aid in weight loss, and improve mood. There have also been claims that it can treat acne, eczema, and psoriasis – even multiple sclerosis, fibromyalgia, and rheumatoid arthritis. It has been used as a beauty aid to reduce pore size and reduce wrinkles. Its popularity has exploded as centers are advertised on discount sites such as Groupon and Living Social, and it is now available as classes in the popular exercise app ClassPass as “Whole Body Cryotherapy” or a “CryoBeauty Facial.”
Despite these claims and popularity, research studies have yet to prove that WBC can deliver any of these benefits. The American Academy of Dermatology has released a statement for consumers that does not support its use. Because of the lack of research, WBC has not been cleared by the Food and Drug Administration for treating any medical indication.
Its popularity has to stem from somewhere. In many cultures, cold therapy has been used for health benefits for centuries. For example, Turkish, Russian, Finnish, Roman, and Chinese spas offer cold baths at 50 degrees Fahrenheit after heat therapy (saunas, baths) as a form of hydrotherapy to alter circulation for health benefits, with the goal of releasing toxins with heat, then closing pores and bringing the circulation back to the body’s core with cold therapy. Cold ice baths and ice packs are used by athletes routinely after games, practices, and injuries to reduce inflammation. How is WBC different?
With WBC, a person who is nearly nude enters a cold chamber of minus 200 degrees Fahrenheit, in sessions that typically last 2-4 minutes.
While the majority of those who engage in WBC have not had complications, the AAD statement refers to a Finnish study that found that 16% of individuals exposed to WBC had mild frostbite. In 2011, U.S. sprinter and Olympic gold medalist Justin Gatlin developed frostbite on both feet after a WBC session. Additional WBC-related complications that have been reported include a frozen limb (a frozen arm in a woman in Dallas in 2013, after a 3-minute session, manifesting as painful swelling, blisters, and third-degree burns – a more severe type of frostbite), and cold panniculitis (JAAD Case Rep. 2018;4:344-5). Others include eye injuries, temporary loss of memory, and even death due to suffocation, reported in 2015, of a staff member at a cryotherapy center outside of Las Vegas who went into a tank alone after hours when no one else was around.
Cryotherapy, when delivered to specific areas of the skin by a dermatologist, is a useful low-risk treatment. Postinflammatory pigment alteration can occur, but there has been great success in using the treatment locally for warts, actinic keratoses, and other benign skin growths, when it is done done by trained professionals. Granted, while localized cryotherapy to treat a skin growth is not the same as whole body cryotherapy, the same types of complication risks should be considered, including postinflammatory pigment alteration, particularly in skin of color, as cryotherapy can be toxic to melanocytes.
Before it is completely discounted, if it makes the person feel good or better, perhaps if the patient and practitioner are aware of the risks and how to identify and manage them, cold therapy could be useful. I once had a patient who described great relief with WBC after a Fraxel laser treatment, when her face felt like it was “on fire” despite refrigerated topical Biafine, cold air, and ice packs. As with most treatments, if someone feels better, they often look better.
While medical or aesthetic benefits of WBC have not been proved and WBC has definite risks, if the procedure is done in an appropriate and responsible way, perhaps the benefit could outweigh the informed risks for some patients. Claims should not be advertised until they are proven, so that patients are not misinformed. The same is true of chemical peels, microneedling, hyperbaric oxygen, and vitamin drips, which are provided over the counter in nonmedical settings for health and beauty uses. Medical history should be taken into account with WBC by the facility and the practitioner, including history of blood clots, smoking, vasculitis, Raynaud’s disease, autoimmune conditions, neuropathy, and prior history of frostbite. Perhaps these should be contraindications to WBC and mechanisms should be in place to manage complications should they occur. Better regulation of WBC is needed so that the procedure can be done effectively and safely.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Treating the effects of bruxism with botulinum toxin
Bruxism is grinding and clenching of the teeth with unconscious contractions of the temporal and masseter muscles while awake or during sleep. Bruxism occurs in 8%-16% of the population and is often an underdiagnosed condition that not only leads to dental problems but also to pain in the teeth, jaw, temporomandibular joint, and neck; headaches; and potentially, to tooth loss.
Although the pathogenesis of bruxism remains unclear, multiple factors, such as physical or psychological stress, malocclusion, sleep disorders and medication side effects, can cause bruxism. Treatment can be difficult given psychogenic and neurogenic components, and bruxism can be resistant to medical and behavioral therapy. There are various treatment options for bruxism, including oral splints; medications, such as muscle relaxants; antidepressants; and botulinum toxin. Multiple studies have shown that botulinum toxin injections into the masseter and temporalis muscles result in relaxation of the muscles and improvement of bruxism and the pain associated with chronic clenching and grinding.
In a recent study by Al-Wayli, 50 subjects who reported nocturnal bruxism were randomized to receive botulinum toxin versus conventional treatment (pharmacotherapy or oral splints). After 3 weeks, 2 months, 6 months, and 1 year, patients who received botulinum toxin had significantly less pain after only one treatment than did the traditional treatment group. Similarly, in a study by Lee et al., subjects randomized to receive botulinum toxin versus a placebo saline injections showed not only decreased pain but also decreased bruxism seen with nocturnal electromyography.
In our clinic, Botulinum toxin when injected into the temporalis and masseter muscles also helps with tension headaches and migraines related to clenching of the jaw. Albeit effective, the dose of botulinum toxin used in the aforementioned studies ranged between 25 U and 40 U of botulinum toxin and were lower than what we have found to be effective. Our patients receive 50 U botulinum toxin in each masseter muscle (100 U total). In a small minority of our patients, the temporalis muscle also needed 15-20 U per side as well. Clinical improvement starts within 3-5 days, and patients can expect to have relaxation of the muscle and decreased pain for 6 months. Side effects include mild swelling and bruising. Rarely, if the injection is not performed properly, the risorius muscle may be paralyzed, leading to an asymmetric smile. In addition, if the botulinum toxin is underdosed, the pain may not completely subside and the patient may report some symptoms returning within a couple of weeks of the initial treatment. Most patients also report thinning of the face and jaw, which is a much anticipated and appreciated result. Masseter hypertrophy with and without bruxism is treated similarly with botulinum toxin to sculpt the lower face.
Bruxism is a growing problem leading to facial pain, headaches, migraines, and significant dental pathology. Traditional treatments have been ineffective at treating the pain and masseter hypertrophy associated with chronic grinding and clenching. Botulinum toxin is a safe, effective, treatment with little downtime or side effects for treating both the neurogenic and muscular components of bruxism.
Dr. Lily Talakoub and Dr. Naissan Wesley and are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to them at [email protected]. They had no relevant disclosures.
References
Al-Wayli H. J Clin Exp Dent. 2017 Jan 1;9(1):e112-e117.
Asutay F et al. Pain Res Manag. 2017;2017:6264146. doi: 10.1155/2017/6264146.
Lee SJ et al. Am J Phys Med Rehabil. 2010 Jan;89(1):16-23.
Santamato A et al. J Chiropr Med. 2010 Sep;9(3):132-7.
Shetty S et al. J Indian Prosthodont Soc. 2010 Sep;10(3):141-8.
Tan EK et al. J Am Dent Assoc. 2000 Feb;131(2):211-6.
Bruxism is grinding and clenching of the teeth with unconscious contractions of the temporal and masseter muscles while awake or during sleep. Bruxism occurs in 8%-16% of the population and is often an underdiagnosed condition that not only leads to dental problems but also to pain in the teeth, jaw, temporomandibular joint, and neck; headaches; and potentially, to tooth loss.
Although the pathogenesis of bruxism remains unclear, multiple factors, such as physical or psychological stress, malocclusion, sleep disorders and medication side effects, can cause bruxism. Treatment can be difficult given psychogenic and neurogenic components, and bruxism can be resistant to medical and behavioral therapy. There are various treatment options for bruxism, including oral splints; medications, such as muscle relaxants; antidepressants; and botulinum toxin. Multiple studies have shown that botulinum toxin injections into the masseter and temporalis muscles result in relaxation of the muscles and improvement of bruxism and the pain associated with chronic clenching and grinding.
In a recent study by Al-Wayli, 50 subjects who reported nocturnal bruxism were randomized to receive botulinum toxin versus conventional treatment (pharmacotherapy or oral splints). After 3 weeks, 2 months, 6 months, and 1 year, patients who received botulinum toxin had significantly less pain after only one treatment than did the traditional treatment group. Similarly, in a study by Lee et al., subjects randomized to receive botulinum toxin versus a placebo saline injections showed not only decreased pain but also decreased bruxism seen with nocturnal electromyography.
In our clinic, Botulinum toxin when injected into the temporalis and masseter muscles also helps with tension headaches and migraines related to clenching of the jaw. Albeit effective, the dose of botulinum toxin used in the aforementioned studies ranged between 25 U and 40 U of botulinum toxin and were lower than what we have found to be effective. Our patients receive 50 U botulinum toxin in each masseter muscle (100 U total). In a small minority of our patients, the temporalis muscle also needed 15-20 U per side as well. Clinical improvement starts within 3-5 days, and patients can expect to have relaxation of the muscle and decreased pain for 6 months. Side effects include mild swelling and bruising. Rarely, if the injection is not performed properly, the risorius muscle may be paralyzed, leading to an asymmetric smile. In addition, if the botulinum toxin is underdosed, the pain may not completely subside and the patient may report some symptoms returning within a couple of weeks of the initial treatment. Most patients also report thinning of the face and jaw, which is a much anticipated and appreciated result. Masseter hypertrophy with and without bruxism is treated similarly with botulinum toxin to sculpt the lower face.
Bruxism is a growing problem leading to facial pain, headaches, migraines, and significant dental pathology. Traditional treatments have been ineffective at treating the pain and masseter hypertrophy associated with chronic grinding and clenching. Botulinum toxin is a safe, effective, treatment with little downtime or side effects for treating both the neurogenic and muscular components of bruxism.
Dr. Lily Talakoub and Dr. Naissan Wesley and are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to them at [email protected]. They had no relevant disclosures.
References
Al-Wayli H. J Clin Exp Dent. 2017 Jan 1;9(1):e112-e117.
Asutay F et al. Pain Res Manag. 2017;2017:6264146. doi: 10.1155/2017/6264146.
Lee SJ et al. Am J Phys Med Rehabil. 2010 Jan;89(1):16-23.
Santamato A et al. J Chiropr Med. 2010 Sep;9(3):132-7.
Shetty S et al. J Indian Prosthodont Soc. 2010 Sep;10(3):141-8.
Tan EK et al. J Am Dent Assoc. 2000 Feb;131(2):211-6.
Bruxism is grinding and clenching of the teeth with unconscious contractions of the temporal and masseter muscles while awake or during sleep. Bruxism occurs in 8%-16% of the population and is often an underdiagnosed condition that not only leads to dental problems but also to pain in the teeth, jaw, temporomandibular joint, and neck; headaches; and potentially, to tooth loss.
Although the pathogenesis of bruxism remains unclear, multiple factors, such as physical or psychological stress, malocclusion, sleep disorders and medication side effects, can cause bruxism. Treatment can be difficult given psychogenic and neurogenic components, and bruxism can be resistant to medical and behavioral therapy. There are various treatment options for bruxism, including oral splints; medications, such as muscle relaxants; antidepressants; and botulinum toxin. Multiple studies have shown that botulinum toxin injections into the masseter and temporalis muscles result in relaxation of the muscles and improvement of bruxism and the pain associated with chronic clenching and grinding.
In a recent study by Al-Wayli, 50 subjects who reported nocturnal bruxism were randomized to receive botulinum toxin versus conventional treatment (pharmacotherapy or oral splints). After 3 weeks, 2 months, 6 months, and 1 year, patients who received botulinum toxin had significantly less pain after only one treatment than did the traditional treatment group. Similarly, in a study by Lee et al., subjects randomized to receive botulinum toxin versus a placebo saline injections showed not only decreased pain but also decreased bruxism seen with nocturnal electromyography.
In our clinic, Botulinum toxin when injected into the temporalis and masseter muscles also helps with tension headaches and migraines related to clenching of the jaw. Albeit effective, the dose of botulinum toxin used in the aforementioned studies ranged between 25 U and 40 U of botulinum toxin and were lower than what we have found to be effective. Our patients receive 50 U botulinum toxin in each masseter muscle (100 U total). In a small minority of our patients, the temporalis muscle also needed 15-20 U per side as well. Clinical improvement starts within 3-5 days, and patients can expect to have relaxation of the muscle and decreased pain for 6 months. Side effects include mild swelling and bruising. Rarely, if the injection is not performed properly, the risorius muscle may be paralyzed, leading to an asymmetric smile. In addition, if the botulinum toxin is underdosed, the pain may not completely subside and the patient may report some symptoms returning within a couple of weeks of the initial treatment. Most patients also report thinning of the face and jaw, which is a much anticipated and appreciated result. Masseter hypertrophy with and without bruxism is treated similarly with botulinum toxin to sculpt the lower face.
Bruxism is a growing problem leading to facial pain, headaches, migraines, and significant dental pathology. Traditional treatments have been ineffective at treating the pain and masseter hypertrophy associated with chronic grinding and clenching. Botulinum toxin is a safe, effective, treatment with little downtime or side effects for treating both the neurogenic and muscular components of bruxism.
Dr. Lily Talakoub and Dr. Naissan Wesley and are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to them at [email protected]. They had no relevant disclosures.
References
Al-Wayli H. J Clin Exp Dent. 2017 Jan 1;9(1):e112-e117.
Asutay F et al. Pain Res Manag. 2017;2017:6264146. doi: 10.1155/2017/6264146.
Lee SJ et al. Am J Phys Med Rehabil. 2010 Jan;89(1):16-23.
Santamato A et al. J Chiropr Med. 2010 Sep;9(3):132-7.
Shetty S et al. J Indian Prosthodont Soc. 2010 Sep;10(3):141-8.
Tan EK et al. J Am Dent Assoc. 2000 Feb;131(2):211-6.
Fish pedicures
A letter published in JAMA Dermatology describes an otherwise healthy woman in her 20s who experienced nail abnormalities some months after having a fish pedicure. Onychomadesis, or transverse splitting of the nail plate, occurs when the nail matrix has arrested in producing the nail plate. It can be thought of as more severe form of Beau’s lines, in which the nail itself actually breaks and separates from the proximal nail plate and eventually sheds.
Fish pedicures have a long-standing history in Mediterranean and Middle Eastern cultures for aiding such skin conditions as psoriasis and helping to remove scaly skin. The Garra rufa fish are nonmigratory freshwater fish native to the Persian Gulf and Eastern Mediterranean. Suction allows them to attach to rocks and eat plankton. These “doctor fish,” as they are nicknamed, when placed in a warm bath of 25°C to 30°C, will also eat human skin when starved of their natural food source. As the JAMA Dermatology letter mentions, this was demonstrated in a study in Kangal, Turkey, where Garra rufa fish were used to improve psoriasis by feeding on psoriasis plaques but not normal skin. After 3 weeks of therapy with Garra rufa in 67 patients, there was a 72% reduction in the Psoriasis Area and Severity Index (PASI) score from baseline (Evid Based Complement Alternat Med. 2006 Dec;3[4]:483-8).
Popular in the United States and Europe about a decade ago, fish pedicures have now been banned in 10 U.S. states and in some parts of Europe. While the trend in the United States has waned, fish pedicures have recently become more popular in vacation destinations, such as the Caribbean. The inherent concern of fish pedicures is risk of infection as the same fish are used successively and cannot be adequately sanitized between people.
Two cases of staphylococcus infections and one of Mycobacterium marinum have been reported after fish pedicures. Whether these infections were caused by the fish or the water source, however, remains to be determined. If the fish were transmitting infections, it seems that more infections would likely have been reported, considering the widespread popularity in the past. I, like Antonella Tosti, MD, who commented in a CNN report on the JAMA Dermatology case, also doubt that the fish pedicure alone caused onychomadesis in this woman. In order for onychomadesis to occur, there would have had to have been significant trauma to all 10 nails at the matrix. Would the fish been able to have caused the same amount of trauma to all 10 nails in one setting? While it is possible, I believe a more likely explanation would be an alternate endogenous or exogenous source.
Traditional medicine has been used to enhance beauty and cure ailments for thousands of years before the advent of modern medicine as demonstrated by the Kangal study. Before discounting fish pedicures completely, perhaps some thought should also be given to how this practice affects wildlife and the fish. The CNN report refers to a 2011 investigation by the U.K.’s Fish Health Inspectorate, which “found a bacterial outbreak among thousands of these fish, which had been transported from Indonesia to the United Kingdom pedicure spas. Fish were found with bulging eyes, many hemorrhaging around the gills and mouth. The culprit was found to be a streptococcal bacteria, a strain that is associated with fish like tilapia, according to David Verner-Jeffreys, a senior microbiologist at the Centre for Environment, Fisheries and Aquaculture Science in the U.K.”
Whether or not these fish would pose any risk to humans is unknown, but certainly, this practice adversely affects the welfare of the fish and their environment. The overharvesting of these fish has led the Turkish government to introduce legal protections for the country’s Garra rufa in an attempt to combat overfishing and exploitation.
Perhaps fish pedicures solely for aesthetic reasons should not be practiced because of the potential infection risk – as well as the harm (to both humans and fish) and overharvesting of the fish. If used properly, these fish, however, could be an aid in treating certain skin pathologies.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
A letter published in JAMA Dermatology describes an otherwise healthy woman in her 20s who experienced nail abnormalities some months after having a fish pedicure. Onychomadesis, or transverse splitting of the nail plate, occurs when the nail matrix has arrested in producing the nail plate. It can be thought of as more severe form of Beau’s lines, in which the nail itself actually breaks and separates from the proximal nail plate and eventually sheds.
Fish pedicures have a long-standing history in Mediterranean and Middle Eastern cultures for aiding such skin conditions as psoriasis and helping to remove scaly skin. The Garra rufa fish are nonmigratory freshwater fish native to the Persian Gulf and Eastern Mediterranean. Suction allows them to attach to rocks and eat plankton. These “doctor fish,” as they are nicknamed, when placed in a warm bath of 25°C to 30°C, will also eat human skin when starved of their natural food source. As the JAMA Dermatology letter mentions, this was demonstrated in a study in Kangal, Turkey, where Garra rufa fish were used to improve psoriasis by feeding on psoriasis plaques but not normal skin. After 3 weeks of therapy with Garra rufa in 67 patients, there was a 72% reduction in the Psoriasis Area and Severity Index (PASI) score from baseline (Evid Based Complement Alternat Med. 2006 Dec;3[4]:483-8).
Popular in the United States and Europe about a decade ago, fish pedicures have now been banned in 10 U.S. states and in some parts of Europe. While the trend in the United States has waned, fish pedicures have recently become more popular in vacation destinations, such as the Caribbean. The inherent concern of fish pedicures is risk of infection as the same fish are used successively and cannot be adequately sanitized between people.
Two cases of staphylococcus infections and one of Mycobacterium marinum have been reported after fish pedicures. Whether these infections were caused by the fish or the water source, however, remains to be determined. If the fish were transmitting infections, it seems that more infections would likely have been reported, considering the widespread popularity in the past. I, like Antonella Tosti, MD, who commented in a CNN report on the JAMA Dermatology case, also doubt that the fish pedicure alone caused onychomadesis in this woman. In order for onychomadesis to occur, there would have had to have been significant trauma to all 10 nails at the matrix. Would the fish been able to have caused the same amount of trauma to all 10 nails in one setting? While it is possible, I believe a more likely explanation would be an alternate endogenous or exogenous source.
Traditional medicine has been used to enhance beauty and cure ailments for thousands of years before the advent of modern medicine as demonstrated by the Kangal study. Before discounting fish pedicures completely, perhaps some thought should also be given to how this practice affects wildlife and the fish. The CNN report refers to a 2011 investigation by the U.K.’s Fish Health Inspectorate, which “found a bacterial outbreak among thousands of these fish, which had been transported from Indonesia to the United Kingdom pedicure spas. Fish were found with bulging eyes, many hemorrhaging around the gills and mouth. The culprit was found to be a streptococcal bacteria, a strain that is associated with fish like tilapia, according to David Verner-Jeffreys, a senior microbiologist at the Centre for Environment, Fisheries and Aquaculture Science in the U.K.”
Whether or not these fish would pose any risk to humans is unknown, but certainly, this practice adversely affects the welfare of the fish and their environment. The overharvesting of these fish has led the Turkish government to introduce legal protections for the country’s Garra rufa in an attempt to combat overfishing and exploitation.
Perhaps fish pedicures solely for aesthetic reasons should not be practiced because of the potential infection risk – as well as the harm (to both humans and fish) and overharvesting of the fish. If used properly, these fish, however, could be an aid in treating certain skin pathologies.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
A letter published in JAMA Dermatology describes an otherwise healthy woman in her 20s who experienced nail abnormalities some months after having a fish pedicure. Onychomadesis, or transverse splitting of the nail plate, occurs when the nail matrix has arrested in producing the nail plate. It can be thought of as more severe form of Beau’s lines, in which the nail itself actually breaks and separates from the proximal nail plate and eventually sheds.
Fish pedicures have a long-standing history in Mediterranean and Middle Eastern cultures for aiding such skin conditions as psoriasis and helping to remove scaly skin. The Garra rufa fish are nonmigratory freshwater fish native to the Persian Gulf and Eastern Mediterranean. Suction allows them to attach to rocks and eat plankton. These “doctor fish,” as they are nicknamed, when placed in a warm bath of 25°C to 30°C, will also eat human skin when starved of their natural food source. As the JAMA Dermatology letter mentions, this was demonstrated in a study in Kangal, Turkey, where Garra rufa fish were used to improve psoriasis by feeding on psoriasis plaques but not normal skin. After 3 weeks of therapy with Garra rufa in 67 patients, there was a 72% reduction in the Psoriasis Area and Severity Index (PASI) score from baseline (Evid Based Complement Alternat Med. 2006 Dec;3[4]:483-8).
Popular in the United States and Europe about a decade ago, fish pedicures have now been banned in 10 U.S. states and in some parts of Europe. While the trend in the United States has waned, fish pedicures have recently become more popular in vacation destinations, such as the Caribbean. The inherent concern of fish pedicures is risk of infection as the same fish are used successively and cannot be adequately sanitized between people.
Two cases of staphylococcus infections and one of Mycobacterium marinum have been reported after fish pedicures. Whether these infections were caused by the fish or the water source, however, remains to be determined. If the fish were transmitting infections, it seems that more infections would likely have been reported, considering the widespread popularity in the past. I, like Antonella Tosti, MD, who commented in a CNN report on the JAMA Dermatology case, also doubt that the fish pedicure alone caused onychomadesis in this woman. In order for onychomadesis to occur, there would have had to have been significant trauma to all 10 nails at the matrix. Would the fish been able to have caused the same amount of trauma to all 10 nails in one setting? While it is possible, I believe a more likely explanation would be an alternate endogenous or exogenous source.
Traditional medicine has been used to enhance beauty and cure ailments for thousands of years before the advent of modern medicine as demonstrated by the Kangal study. Before discounting fish pedicures completely, perhaps some thought should also be given to how this practice affects wildlife and the fish. The CNN report refers to a 2011 investigation by the U.K.’s Fish Health Inspectorate, which “found a bacterial outbreak among thousands of these fish, which had been transported from Indonesia to the United Kingdom pedicure spas. Fish were found with bulging eyes, many hemorrhaging around the gills and mouth. The culprit was found to be a streptococcal bacteria, a strain that is associated with fish like tilapia, according to David Verner-Jeffreys, a senior microbiologist at the Centre for Environment, Fisheries and Aquaculture Science in the U.K.”
Whether or not these fish would pose any risk to humans is unknown, but certainly, this practice adversely affects the welfare of the fish and their environment. The overharvesting of these fish has led the Turkish government to introduce legal protections for the country’s Garra rufa in an attempt to combat overfishing and exploitation.
Perhaps fish pedicures solely for aesthetic reasons should not be practiced because of the potential infection risk – as well as the harm (to both humans and fish) and overharvesting of the fish. If used properly, these fish, however, could be an aid in treating certain skin pathologies.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
The magic of microblading
The use of permanent cosmetics dates back thousands of years in history. and has rapidly become one of the most popular cosmetic procedures in the United States. However, it has not completely replaced traditional eyebrow micropigmentation techniques: Many people may not be candidates for microblading because of how the pigment is manually deposited in the skin through tiny “tears” in the skin with this procedure.
The use of microblading has increased exponentially since 2015, as reflected by the millions of searches on popular social media sites. With the increase in the popularity and volume of tattoo artists performing these procedures, there has also been an increase in side effects and complications from microblading provided by poorly trained and unlicensed “artists,” a problem facilitated by the absence of adequate training requirements and/or regulatory oversight in many states.
Microblading is a revolutionary technique that can transform the lives of patients with hypotrichosis of the eyebrows, trichotillomania, eyebrow loss due to internal disease (such as thyroid disease), chemotherapy-induced eyebrow loss, or alopecia – or simply those seeking it for cosmetic improvement. The art of shaping the eyebrow depends on the natural growth of the brow (if any), facial symmetry, and meticulous measurement and mapping of the brow position based on facial landmarks and bone structure. The color of pigment selection is based on Fitzpatrick skin type and skin color undertones.
While dermatologists usually do not perform microblading, we may see patients with these complications. Practitioners treating patients who have had eyebrow microblading should also be aware of how to prevent premature fading of the eyebrow tattoo pigment. Tattooed eyebrows should be covered with petroleum jelly prior to the use of alpha hydroxy acids, vitamin C, chemical peels, hydroquinone, or retinols because these preparations can fade the pigment rapidly even if applied far from the microblading site. Any UV exposure, heat (such as steam from a facial), LED light exposure, or radio frequency can fade the pigment and exacerbate postinflammatory hyperpigmentation. Patients who have a history of hypertrophic scarring or keloids or are using isotretinoin concurrently should avoid microblading entirely. Resurfacing lasers and intense pulsed-light lasers should be used with caution as these aesthetic procedures will cause fading of the eyebrow pigment even if applied at a considerable distance from the eyebrow. Microbladed eyebrows should be covered with 20% zinc oxide paste prior to the use of any intense pulsed-light or resurfacing lasers.
The pigment used in eyebrow colors also may be composed of a mixture of iron oxide pigments, which should not be removed with traditional Q-switched lasers, with which not only is there potential for the pigment to darken but also postinflammatory hyper- or hypopigmentation to occur as well. Hairs can be singed, and the light absorbed by the pigment chromophore in the hair follicle can permanently damage the follicle, leading to hair loss in the area.
Despite the absolute precision and aggressive safety precautions needed for microblading, there are wide state-to-state variations in training and regulatory oversight. Infectious diseases, poor treatment outcomes, and unsterile conditions are just a few of the horrific consequences of unlicensed and untrained tattoo artists. Regulations should be imposed in every state to protect consumers and prevent serious medical complications related to microblading.
Like other cosmetic treatments, cheaper is never better.
Dr. Talakoub and Dr. Wesley and are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. They had no relevant disclosures. Write to them at [email protected]. This column was written with the help and professional expertise of Emily Joy, a cosmetic tattoo artist and the founder of Dollistic in McLean.
The use of permanent cosmetics dates back thousands of years in history. and has rapidly become one of the most popular cosmetic procedures in the United States. However, it has not completely replaced traditional eyebrow micropigmentation techniques: Many people may not be candidates for microblading because of how the pigment is manually deposited in the skin through tiny “tears” in the skin with this procedure.
The use of microblading has increased exponentially since 2015, as reflected by the millions of searches on popular social media sites. With the increase in the popularity and volume of tattoo artists performing these procedures, there has also been an increase in side effects and complications from microblading provided by poorly trained and unlicensed “artists,” a problem facilitated by the absence of adequate training requirements and/or regulatory oversight in many states.
Microblading is a revolutionary technique that can transform the lives of patients with hypotrichosis of the eyebrows, trichotillomania, eyebrow loss due to internal disease (such as thyroid disease), chemotherapy-induced eyebrow loss, or alopecia – or simply those seeking it for cosmetic improvement. The art of shaping the eyebrow depends on the natural growth of the brow (if any), facial symmetry, and meticulous measurement and mapping of the brow position based on facial landmarks and bone structure. The color of pigment selection is based on Fitzpatrick skin type and skin color undertones.
While dermatologists usually do not perform microblading, we may see patients with these complications. Practitioners treating patients who have had eyebrow microblading should also be aware of how to prevent premature fading of the eyebrow tattoo pigment. Tattooed eyebrows should be covered with petroleum jelly prior to the use of alpha hydroxy acids, vitamin C, chemical peels, hydroquinone, or retinols because these preparations can fade the pigment rapidly even if applied far from the microblading site. Any UV exposure, heat (such as steam from a facial), LED light exposure, or radio frequency can fade the pigment and exacerbate postinflammatory hyperpigmentation. Patients who have a history of hypertrophic scarring or keloids or are using isotretinoin concurrently should avoid microblading entirely. Resurfacing lasers and intense pulsed-light lasers should be used with caution as these aesthetic procedures will cause fading of the eyebrow pigment even if applied at a considerable distance from the eyebrow. Microbladed eyebrows should be covered with 20% zinc oxide paste prior to the use of any intense pulsed-light or resurfacing lasers.
The pigment used in eyebrow colors also may be composed of a mixture of iron oxide pigments, which should not be removed with traditional Q-switched lasers, with which not only is there potential for the pigment to darken but also postinflammatory hyper- or hypopigmentation to occur as well. Hairs can be singed, and the light absorbed by the pigment chromophore in the hair follicle can permanently damage the follicle, leading to hair loss in the area.
Despite the absolute precision and aggressive safety precautions needed for microblading, there are wide state-to-state variations in training and regulatory oversight. Infectious diseases, poor treatment outcomes, and unsterile conditions are just a few of the horrific consequences of unlicensed and untrained tattoo artists. Regulations should be imposed in every state to protect consumers and prevent serious medical complications related to microblading.
Like other cosmetic treatments, cheaper is never better.
Dr. Talakoub and Dr. Wesley and are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. They had no relevant disclosures. Write to them at [email protected]. This column was written with the help and professional expertise of Emily Joy, a cosmetic tattoo artist and the founder of Dollistic in McLean.
The use of permanent cosmetics dates back thousands of years in history. and has rapidly become one of the most popular cosmetic procedures in the United States. However, it has not completely replaced traditional eyebrow micropigmentation techniques: Many people may not be candidates for microblading because of how the pigment is manually deposited in the skin through tiny “tears” in the skin with this procedure.
The use of microblading has increased exponentially since 2015, as reflected by the millions of searches on popular social media sites. With the increase in the popularity and volume of tattoo artists performing these procedures, there has also been an increase in side effects and complications from microblading provided by poorly trained and unlicensed “artists,” a problem facilitated by the absence of adequate training requirements and/or regulatory oversight in many states.
Microblading is a revolutionary technique that can transform the lives of patients with hypotrichosis of the eyebrows, trichotillomania, eyebrow loss due to internal disease (such as thyroid disease), chemotherapy-induced eyebrow loss, or alopecia – or simply those seeking it for cosmetic improvement. The art of shaping the eyebrow depends on the natural growth of the brow (if any), facial symmetry, and meticulous measurement and mapping of the brow position based on facial landmarks and bone structure. The color of pigment selection is based on Fitzpatrick skin type and skin color undertones.
While dermatologists usually do not perform microblading, we may see patients with these complications. Practitioners treating patients who have had eyebrow microblading should also be aware of how to prevent premature fading of the eyebrow tattoo pigment. Tattooed eyebrows should be covered with petroleum jelly prior to the use of alpha hydroxy acids, vitamin C, chemical peels, hydroquinone, or retinols because these preparations can fade the pigment rapidly even if applied far from the microblading site. Any UV exposure, heat (such as steam from a facial), LED light exposure, or radio frequency can fade the pigment and exacerbate postinflammatory hyperpigmentation. Patients who have a history of hypertrophic scarring or keloids or are using isotretinoin concurrently should avoid microblading entirely. Resurfacing lasers and intense pulsed-light lasers should be used with caution as these aesthetic procedures will cause fading of the eyebrow pigment even if applied at a considerable distance from the eyebrow. Microbladed eyebrows should be covered with 20% zinc oxide paste prior to the use of any intense pulsed-light or resurfacing lasers.
The pigment used in eyebrow colors also may be composed of a mixture of iron oxide pigments, which should not be removed with traditional Q-switched lasers, with which not only is there potential for the pigment to darken but also postinflammatory hyper- or hypopigmentation to occur as well. Hairs can be singed, and the light absorbed by the pigment chromophore in the hair follicle can permanently damage the follicle, leading to hair loss in the area.
Despite the absolute precision and aggressive safety precautions needed for microblading, there are wide state-to-state variations in training and regulatory oversight. Infectious diseases, poor treatment outcomes, and unsterile conditions are just a few of the horrific consequences of unlicensed and untrained tattoo artists. Regulations should be imposed in every state to protect consumers and prevent serious medical complications related to microblading.
Like other cosmetic treatments, cheaper is never better.
Dr. Talakoub and Dr. Wesley and are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. They had no relevant disclosures. Write to them at [email protected]. This column was written with the help and professional expertise of Emily Joy, a cosmetic tattoo artist and the founder of Dollistic in McLean.

















