User login
Covered-stent TIPS tops large-volume paracentesis for cirrhosis survival
One-year survival without liver transplant was far more likely when transjugular intrahepatic portosystemic shunts (TIPS) with covered stents were used to treat cirrhosis with recurrent ascites, instead of ongoing large-volume paracenteses with albumin, in a 62-patient randomized trial from France.
“TIPS with covered stents ... should therefore be preferred to LVP [large-volume paracenteses] with volume expansion... These findings support TIPS as the first-line intervention,” said investigators led by gastroenterologist Christophe Bureau, MD, of Toulouse (France) University in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2016.09.016).
All 62 patients had at least two LVPs prior to the study; 29 were then randomized to covered transjugular intrahepatic portosystemic shunt (TIPS), and 33 to LVP and albumin as needed. All the patients were on a low-salt diet.
Twenty-seven TIPS patients (93%) were alive without a liver transplant at 1 year, versus 17 (52%) in the LVP group (P = .003). TIPS patients had a total of 32 paracenteses in the first year, versus 320 in the LVP group. Six paracentesis patients (18%) had portal hypertension–related bleeding, and six had hernia-related complications; none of the TIPS patients had either. LVP patients spent a mean of 35 days in the hospital, versus 17 days for the TIPS group (P = .04). The probability of remaining free of encephalopathy at 1 year was the same in both groups, at 65%.
It has been shown before that TIPS has the edge on LVP for reducing recurrence of tense ascites. However, early studies used uncovered stents and, due to their almost 80% risk of dysfunction, they did not show a significant benefit for survival. As a result, repeated paracenteses have been recommended as first-line treatment, with TIPS held in reserve for patients who need very frequent LVP.
Polytetrafluoroethylene-covered stents appear to have changed the equation, “owing to a substantial decrease in the rate of shunt dysfunction,” the investigators said.
The French results are a bit better than previous reports of covered TIPS. “This could be related to greater experience with the TIPS procedure;” there were no technical failures. The study also mostly included patients younger than 65 years with Child-Pugh class B disease and no prior encephalopathy – favorable factors that also may have contributed to the results. However, “we believe that the use of covered stents was the main determinant of the observed improvement in outcomes... TIPS with uncovered stent[s] should not be considered effective or recommended any longer for the long-term treatment of” portal hypertension, they said.
Cirrhosis in the trial was due almost entirely to alcohol abuse. About three-quarters of both groups reported abstinence while enrolled. The mean age was 56 years, and the majority of subjects were men.
The work was funded by the French Ministry of Health and supported by Gore, maker of the covered stent used in the study. Dr. Bureau and another author are Gore consultants.
One-year survival without liver transplant was far more likely when transjugular intrahepatic portosystemic shunts (TIPS) with covered stents were used to treat cirrhosis with recurrent ascites, instead of ongoing large-volume paracenteses with albumin, in a 62-patient randomized trial from France.
“TIPS with covered stents ... should therefore be preferred to LVP [large-volume paracenteses] with volume expansion... These findings support TIPS as the first-line intervention,” said investigators led by gastroenterologist Christophe Bureau, MD, of Toulouse (France) University in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2016.09.016).
All 62 patients had at least two LVPs prior to the study; 29 were then randomized to covered transjugular intrahepatic portosystemic shunt (TIPS), and 33 to LVP and albumin as needed. All the patients were on a low-salt diet.
Twenty-seven TIPS patients (93%) were alive without a liver transplant at 1 year, versus 17 (52%) in the LVP group (P = .003). TIPS patients had a total of 32 paracenteses in the first year, versus 320 in the LVP group. Six paracentesis patients (18%) had portal hypertension–related bleeding, and six had hernia-related complications; none of the TIPS patients had either. LVP patients spent a mean of 35 days in the hospital, versus 17 days for the TIPS group (P = .04). The probability of remaining free of encephalopathy at 1 year was the same in both groups, at 65%.
It has been shown before that TIPS has the edge on LVP for reducing recurrence of tense ascites. However, early studies used uncovered stents and, due to their almost 80% risk of dysfunction, they did not show a significant benefit for survival. As a result, repeated paracenteses have been recommended as first-line treatment, with TIPS held in reserve for patients who need very frequent LVP.
Polytetrafluoroethylene-covered stents appear to have changed the equation, “owing to a substantial decrease in the rate of shunt dysfunction,” the investigators said.
The French results are a bit better than previous reports of covered TIPS. “This could be related to greater experience with the TIPS procedure;” there were no technical failures. The study also mostly included patients younger than 65 years with Child-Pugh class B disease and no prior encephalopathy – favorable factors that also may have contributed to the results. However, “we believe that the use of covered stents was the main determinant of the observed improvement in outcomes... TIPS with uncovered stent[s] should not be considered effective or recommended any longer for the long-term treatment of” portal hypertension, they said.
Cirrhosis in the trial was due almost entirely to alcohol abuse. About three-quarters of both groups reported abstinence while enrolled. The mean age was 56 years, and the majority of subjects were men.
The work was funded by the French Ministry of Health and supported by Gore, maker of the covered stent used in the study. Dr. Bureau and another author are Gore consultants.
One-year survival without liver transplant was far more likely when transjugular intrahepatic portosystemic shunts (TIPS) with covered stents were used to treat cirrhosis with recurrent ascites, instead of ongoing large-volume paracenteses with albumin, in a 62-patient randomized trial from France.
“TIPS with covered stents ... should therefore be preferred to LVP [large-volume paracenteses] with volume expansion... These findings support TIPS as the first-line intervention,” said investigators led by gastroenterologist Christophe Bureau, MD, of Toulouse (France) University in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2016.09.016).
All 62 patients had at least two LVPs prior to the study; 29 were then randomized to covered transjugular intrahepatic portosystemic shunt (TIPS), and 33 to LVP and albumin as needed. All the patients were on a low-salt diet.
Twenty-seven TIPS patients (93%) were alive without a liver transplant at 1 year, versus 17 (52%) in the LVP group (P = .003). TIPS patients had a total of 32 paracenteses in the first year, versus 320 in the LVP group. Six paracentesis patients (18%) had portal hypertension–related bleeding, and six had hernia-related complications; none of the TIPS patients had either. LVP patients spent a mean of 35 days in the hospital, versus 17 days for the TIPS group (P = .04). The probability of remaining free of encephalopathy at 1 year was the same in both groups, at 65%.
It has been shown before that TIPS has the edge on LVP for reducing recurrence of tense ascites. However, early studies used uncovered stents and, due to their almost 80% risk of dysfunction, they did not show a significant benefit for survival. As a result, repeated paracenteses have been recommended as first-line treatment, with TIPS held in reserve for patients who need very frequent LVP.
Polytetrafluoroethylene-covered stents appear to have changed the equation, “owing to a substantial decrease in the rate of shunt dysfunction,” the investigators said.
The French results are a bit better than previous reports of covered TIPS. “This could be related to greater experience with the TIPS procedure;” there were no technical failures. The study also mostly included patients younger than 65 years with Child-Pugh class B disease and no prior encephalopathy – favorable factors that also may have contributed to the results. However, “we believe that the use of covered stents was the main determinant of the observed improvement in outcomes... TIPS with uncovered stent[s] should not be considered effective or recommended any longer for the long-term treatment of” portal hypertension, they said.
Cirrhosis in the trial was due almost entirely to alcohol abuse. About three-quarters of both groups reported abstinence while enrolled. The mean age was 56 years, and the majority of subjects were men.
The work was funded by the French Ministry of Health and supported by Gore, maker of the covered stent used in the study. Dr. Bureau and another author are Gore consultants.
FROM GASTROENTEROLOGY
Key clinical point:
Major finding: Twenty-seven TIPS patients (93%) were alive without a liver transplant at 1 year, versus 17 (52%) in the LVP group (P = .003).
Data source: Randomized trial with 62 patients.
Disclosures: The work was funded by the French Ministry of Health and supported by Gore, maker of the covered stent used in the study. The lead and one other investigator are Gore consultants.
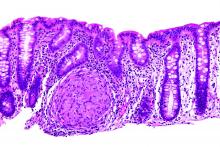
Fecal calprotectin tops CRP as Crohn’s marker
Stool calprotectin correlates with severity of small-bowel Crohn’s disease, as measured against balloon-assisted enteroscopy and computed tomography enterography, according to a review reported in the January issue of Clinical Gastroenterology and Hepatology of 89 patients at Toho University in Chiba, Japan.
Although the correlation was moderate, the findings suggest that fecal calprotectin (FC), with additional work, might turn out to be a good biomarker for tracking small-bowel Crohn’s disease (CD) and its response to tumor necrosis factor blockers. “Currently, it is not widely accepted that FC relates to disease activity in patients with small-intestinal CD,” said investigators led by Tsunetaka Arai of Toho University’s division of gastroenterology and hepatology (Clin Gastroenterol Hepatol. 2016 Aug 23. doi: 10.1016/j.cgh.2016.08.015).
Gastroenterologists need a decent biomarker for small-bowel Crohn’s because old-school endoscopy falls short. Adhesions and strictures block endoscopes, and sometimes scopes simply can’t reach the disease site.
Balloon-assisted enteroscopy (BAE) and computed tomography enterography (CTE) have emerged in recent years as alternatives, but, even so, the need persists for a noninvasive and inexpensive biomarker that’s better than the current standard of C-reactive protein (CRP), which can be thrown off by systemic inflammation, among other problems. The Toho investigators “believe that FC could be a relevant surrogate marker of disease activity in small-bowel CD.” Stool calprotectin paralleled disease activity in their study, while “neither the CDAI [CD activity index] score nor serum CRP showed similar correlation,” they said.
However, elevations in FC – a calcium- and zinc-binding protein released when neutrophils, monocytes, and macrophages inflame the intestinal mucosa – was independent of CD location, which signals the need for further investigation.
Meanwhile, the decent correlation between FC and CTE in the study “should [also] mean that” they could be used together to reliably define mucosal healing. CTE on its own “showed good correlation” with BAE; a CTE score/segment less than 2 [was] associated with endoscopic mucosal healing” on BAE, the investigators said.
The study subjects were an average of 32 years old, and had CD for 9 years; most were men. They had highly active disease at their first endoscopy (average CDAI of 120 points), and an average CRP of 1.09 mg/dL. Twenty-seven patients (30.3%) had small-bowel CD, 50 (56.2%) had ileocolonic CD, and 12 (13.5%) had colonic CD.
They all had endoscopic exams, BAE, and FC stool testing; those with strictures (17) went on to CTE; CTE detected every lesion despite the strictures.
The authors had no conflicts of interest.
Stool calprotectin correlates with severity of small-bowel Crohn’s disease, as measured against balloon-assisted enteroscopy and computed tomography enterography, according to a review reported in the January issue of Clinical Gastroenterology and Hepatology of 89 patients at Toho University in Chiba, Japan.
Although the correlation was moderate, the findings suggest that fecal calprotectin (FC), with additional work, might turn out to be a good biomarker for tracking small-bowel Crohn’s disease (CD) and its response to tumor necrosis factor blockers. “Currently, it is not widely accepted that FC relates to disease activity in patients with small-intestinal CD,” said investigators led by Tsunetaka Arai of Toho University’s division of gastroenterology and hepatology (Clin Gastroenterol Hepatol. 2016 Aug 23. doi: 10.1016/j.cgh.2016.08.015).
Gastroenterologists need a decent biomarker for small-bowel Crohn’s because old-school endoscopy falls short. Adhesions and strictures block endoscopes, and sometimes scopes simply can’t reach the disease site.
Balloon-assisted enteroscopy (BAE) and computed tomography enterography (CTE) have emerged in recent years as alternatives, but, even so, the need persists for a noninvasive and inexpensive biomarker that’s better than the current standard of C-reactive protein (CRP), which can be thrown off by systemic inflammation, among other problems. The Toho investigators “believe that FC could be a relevant surrogate marker of disease activity in small-bowel CD.” Stool calprotectin paralleled disease activity in their study, while “neither the CDAI [CD activity index] score nor serum CRP showed similar correlation,” they said.
However, elevations in FC – a calcium- and zinc-binding protein released when neutrophils, monocytes, and macrophages inflame the intestinal mucosa – was independent of CD location, which signals the need for further investigation.
Meanwhile, the decent correlation between FC and CTE in the study “should [also] mean that” they could be used together to reliably define mucosal healing. CTE on its own “showed good correlation” with BAE; a CTE score/segment less than 2 [was] associated with endoscopic mucosal healing” on BAE, the investigators said.
The study subjects were an average of 32 years old, and had CD for 9 years; most were men. They had highly active disease at their first endoscopy (average CDAI of 120 points), and an average CRP of 1.09 mg/dL. Twenty-seven patients (30.3%) had small-bowel CD, 50 (56.2%) had ileocolonic CD, and 12 (13.5%) had colonic CD.
They all had endoscopic exams, BAE, and FC stool testing; those with strictures (17) went on to CTE; CTE detected every lesion despite the strictures.
The authors had no conflicts of interest.
Stool calprotectin correlates with severity of small-bowel Crohn’s disease, as measured against balloon-assisted enteroscopy and computed tomography enterography, according to a review reported in the January issue of Clinical Gastroenterology and Hepatology of 89 patients at Toho University in Chiba, Japan.
Although the correlation was moderate, the findings suggest that fecal calprotectin (FC), with additional work, might turn out to be a good biomarker for tracking small-bowel Crohn’s disease (CD) and its response to tumor necrosis factor blockers. “Currently, it is not widely accepted that FC relates to disease activity in patients with small-intestinal CD,” said investigators led by Tsunetaka Arai of Toho University’s division of gastroenterology and hepatology (Clin Gastroenterol Hepatol. 2016 Aug 23. doi: 10.1016/j.cgh.2016.08.015).
Gastroenterologists need a decent biomarker for small-bowel Crohn’s because old-school endoscopy falls short. Adhesions and strictures block endoscopes, and sometimes scopes simply can’t reach the disease site.
Balloon-assisted enteroscopy (BAE) and computed tomography enterography (CTE) have emerged in recent years as alternatives, but, even so, the need persists for a noninvasive and inexpensive biomarker that’s better than the current standard of C-reactive protein (CRP), which can be thrown off by systemic inflammation, among other problems. The Toho investigators “believe that FC could be a relevant surrogate marker of disease activity in small-bowel CD.” Stool calprotectin paralleled disease activity in their study, while “neither the CDAI [CD activity index] score nor serum CRP showed similar correlation,” they said.
However, elevations in FC – a calcium- and zinc-binding protein released when neutrophils, monocytes, and macrophages inflame the intestinal mucosa – was independent of CD location, which signals the need for further investigation.
Meanwhile, the decent correlation between FC and CTE in the study “should [also] mean that” they could be used together to reliably define mucosal healing. CTE on its own “showed good correlation” with BAE; a CTE score/segment less than 2 [was] associated with endoscopic mucosal healing” on BAE, the investigators said.
The study subjects were an average of 32 years old, and had CD for 9 years; most were men. They had highly active disease at their first endoscopy (average CDAI of 120 points), and an average CRP of 1.09 mg/dL. Twenty-seven patients (30.3%) had small-bowel CD, 50 (56.2%) had ileocolonic CD, and 12 (13.5%) had colonic CD.
They all had endoscopic exams, BAE, and FC stool testing; those with strictures (17) went on to CTE; CTE detected every lesion despite the strictures.
The authors had no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:
Major finding: A fecal calprotectin cutoff of 215 mcg/g identified mucosal healing with 82.8% sensitivity, 71.4% specificity, and an AUC of 0.81.
Data source: Review of 89 Crohn’s patients
Disclosures: The investigators had no conflicts of interest.
Mobile health indexes accurately detected active inflammatory bowel disease
Mobile health indexes for remotely monitoring Crohn’s disease and ulcerative colitis accurately identified clinically active disease and changed significantly as disease activity did, researchers reported in the December issue of Clinical Gastroenterology and Hepatology.
The mobile health index for Crohn’s disease predicted clinical disease activity with an area under the receiver operating characteristic curve (AUC) of 0.90, Welmoed K. van Deen, MD, of the University of California, Los Angeles, and her associates wrote in Clinical Gastroenterology and Hepatology. The AUC for the ulcerative colitis index for ulcerative colitis was very similar, at 0.91. “The [mobile health indexes] are specifically designed for implementation on a mobile application, and are currently available to patients with IBD [inflammatory bowel disease] treated at the UCLA Center for IBD,” the researchers said. “Prospective, randomized studies need to assess the effect of remote monitoring on disease control, quality of life, patient satisfaction, and health care costs.”
Inspired by the lack of smartphone applications for remotely managing inflammatory bowel disease, the researchers administered comprehensive disease-specific questionnaires to 110 patients with Crohn’s disease and 109 patients with ulcerative colitis who visited the UCLA IBD center in 2013 and 2014. They compared patient-reported outcomes across 10 domains of disease activity with scores on a number of existing disease activity indexes, and used logistic regression to identify which self-reported outcomes best predicted disease activity in both Crohn’s disease and ulcerative colitis (Clin Gastroenterol Hepatol. 2015 Nov 18. doi: 10.1016/j.cgh.2015.10.035).
The resulting Crohn’s disease mobile health index asked how many liquid or “very soft” stools patients had per day, if they had abdominal pain, and how they would rate their well-being and level of disease control on scales ranging between 0 and 10. The ulcerative colitis mobile health index asked about number of stools the day before and had patients score abdominal pain, frequency of rectal bleeding, and level of disease control between 0 and 10. The researchers also validated each mobile health index in multicenter cohorts of 301 patients with Crohn’s disease and 265 patients with ulcerative colitis.
Each mobile health index detected clinical disease activity with about 90% accuracy, compared with standard measures, including the Crohn’s disease activity index and the Harvey Bradshaw index for Crohn’s disease, the partial Mayo score, the simple clinical colitis activity index, and the modified Truelove and Witts index for ulcerative colitis. But the mobile indexes detected endoscopic disease activity less accurately, with AUCs of 0.82 for ulcerative colitis and only 0.63 for Crohn’s disease. “As previously shown, ulcerative colitis clinical disease activity highly correlates with endoscopic disease activity, whereas correlation between Crohn’s disease symptoms and endoscopic findings is poor,” the researchers noted. However, both mobile indexes reliably detected changes in disease activity, varying significantly depending on whether patients were clinically improved, stable, or worse, regardless of whether they had Crohn’s disease (P = .003) or ulcerative colitis (P = .0025).
To explore intrapatient reliability, the researchers also compared initial and follow-up mobile health index results for subgroups of 40 Crohn’s disease patients tested a median of 21 hours apart, and 37 ulcerative colitis patients tested a median of 23 hours apart. In both cases, the intraclass correlation coefficient reached 0.94 (95% confidence interval, 0.89-0.97). “Cloud-based health technologies are predicted to revolutionize care delivery and patient engagement,” the investigators commented. “Patients can participate in their care by signaling meaningful health outcomes during year-round monitoring. Barriers for more widespread implementation of mobile health in inflammatory bowel disease care include policies affecting reimbursement and regulatory requirements, and privacy and security concerns.”
Genova Diagnostics provided stool collection kits and fecal calprotectin testing. The investigators had no disclosures.
To make mobile applications for inflammatory bowel disease valuable, it is critical to accurately capture disease activity in a consistent and reproducible manner. With this in mind, Dr. Van Deen and colleagues designed and evaluated specific “mobile health indexes” (mHIs) for patients with Crohn’s disease and ulcerative colitis.
Patients were invited to complete validated questionnaires assessing patient-reported outcomes (PROs) and clinical disease activity. PROs across 10 domains with the strongest correlation to clinical disease activity scores were identified and used to generate the mobile health indexes.
Strengths of this particular study include the prospective design that incorporated reliability assessments and independent validation cohorts. Potential weaknesses include patient recall bias, small sample size, and lack of knowledge on how language and numerical scales were interpreted across health literacy levels and cultural backgrounds. Nevertheless, these mobile health indexes have promise, both as disease-monitoring and engagement tools, whose clinical impact has yet to be fully realized.
Lauren K. Tormey, MD, is an assistant professor of medicine at the Geisel School of Medicine at Dartmouth and member of the Dartmouth-Hitchcock Inflammatory Bowel Disease Center in Lebanon, N.H. She discloses no conflicts.
To make mobile applications for inflammatory bowel disease valuable, it is critical to accurately capture disease activity in a consistent and reproducible manner. With this in mind, Dr. Van Deen and colleagues designed and evaluated specific “mobile health indexes” (mHIs) for patients with Crohn’s disease and ulcerative colitis.
Patients were invited to complete validated questionnaires assessing patient-reported outcomes (PROs) and clinical disease activity. PROs across 10 domains with the strongest correlation to clinical disease activity scores were identified and used to generate the mobile health indexes.
Strengths of this particular study include the prospective design that incorporated reliability assessments and independent validation cohorts. Potential weaknesses include patient recall bias, small sample size, and lack of knowledge on how language and numerical scales were interpreted across health literacy levels and cultural backgrounds. Nevertheless, these mobile health indexes have promise, both as disease-monitoring and engagement tools, whose clinical impact has yet to be fully realized.
Lauren K. Tormey, MD, is an assistant professor of medicine at the Geisel School of Medicine at Dartmouth and member of the Dartmouth-Hitchcock Inflammatory Bowel Disease Center in Lebanon, N.H. She discloses no conflicts.
To make mobile applications for inflammatory bowel disease valuable, it is critical to accurately capture disease activity in a consistent and reproducible manner. With this in mind, Dr. Van Deen and colleagues designed and evaluated specific “mobile health indexes” (mHIs) for patients with Crohn’s disease and ulcerative colitis.
Patients were invited to complete validated questionnaires assessing patient-reported outcomes (PROs) and clinical disease activity. PROs across 10 domains with the strongest correlation to clinical disease activity scores were identified and used to generate the mobile health indexes.
Strengths of this particular study include the prospective design that incorporated reliability assessments and independent validation cohorts. Potential weaknesses include patient recall bias, small sample size, and lack of knowledge on how language and numerical scales were interpreted across health literacy levels and cultural backgrounds. Nevertheless, these mobile health indexes have promise, both as disease-monitoring and engagement tools, whose clinical impact has yet to be fully realized.
Lauren K. Tormey, MD, is an assistant professor of medicine at the Geisel School of Medicine at Dartmouth and member of the Dartmouth-Hitchcock Inflammatory Bowel Disease Center in Lebanon, N.H. She discloses no conflicts.
Mobile health indexes for remotely monitoring Crohn’s disease and ulcerative colitis accurately identified clinically active disease and changed significantly as disease activity did, researchers reported in the December issue of Clinical Gastroenterology and Hepatology.
The mobile health index for Crohn’s disease predicted clinical disease activity with an area under the receiver operating characteristic curve (AUC) of 0.90, Welmoed K. van Deen, MD, of the University of California, Los Angeles, and her associates wrote in Clinical Gastroenterology and Hepatology. The AUC for the ulcerative colitis index for ulcerative colitis was very similar, at 0.91. “The [mobile health indexes] are specifically designed for implementation on a mobile application, and are currently available to patients with IBD [inflammatory bowel disease] treated at the UCLA Center for IBD,” the researchers said. “Prospective, randomized studies need to assess the effect of remote monitoring on disease control, quality of life, patient satisfaction, and health care costs.”
Inspired by the lack of smartphone applications for remotely managing inflammatory bowel disease, the researchers administered comprehensive disease-specific questionnaires to 110 patients with Crohn’s disease and 109 patients with ulcerative colitis who visited the UCLA IBD center in 2013 and 2014. They compared patient-reported outcomes across 10 domains of disease activity with scores on a number of existing disease activity indexes, and used logistic regression to identify which self-reported outcomes best predicted disease activity in both Crohn’s disease and ulcerative colitis (Clin Gastroenterol Hepatol. 2015 Nov 18. doi: 10.1016/j.cgh.2015.10.035).
The resulting Crohn’s disease mobile health index asked how many liquid or “very soft” stools patients had per day, if they had abdominal pain, and how they would rate their well-being and level of disease control on scales ranging between 0 and 10. The ulcerative colitis mobile health index asked about number of stools the day before and had patients score abdominal pain, frequency of rectal bleeding, and level of disease control between 0 and 10. The researchers also validated each mobile health index in multicenter cohorts of 301 patients with Crohn’s disease and 265 patients with ulcerative colitis.
Each mobile health index detected clinical disease activity with about 90% accuracy, compared with standard measures, including the Crohn’s disease activity index and the Harvey Bradshaw index for Crohn’s disease, the partial Mayo score, the simple clinical colitis activity index, and the modified Truelove and Witts index for ulcerative colitis. But the mobile indexes detected endoscopic disease activity less accurately, with AUCs of 0.82 for ulcerative colitis and only 0.63 for Crohn’s disease. “As previously shown, ulcerative colitis clinical disease activity highly correlates with endoscopic disease activity, whereas correlation between Crohn’s disease symptoms and endoscopic findings is poor,” the researchers noted. However, both mobile indexes reliably detected changes in disease activity, varying significantly depending on whether patients were clinically improved, stable, or worse, regardless of whether they had Crohn’s disease (P = .003) or ulcerative colitis (P = .0025).
To explore intrapatient reliability, the researchers also compared initial and follow-up mobile health index results for subgroups of 40 Crohn’s disease patients tested a median of 21 hours apart, and 37 ulcerative colitis patients tested a median of 23 hours apart. In both cases, the intraclass correlation coefficient reached 0.94 (95% confidence interval, 0.89-0.97). “Cloud-based health technologies are predicted to revolutionize care delivery and patient engagement,” the investigators commented. “Patients can participate in their care by signaling meaningful health outcomes during year-round monitoring. Barriers for more widespread implementation of mobile health in inflammatory bowel disease care include policies affecting reimbursement and regulatory requirements, and privacy and security concerns.”
Genova Diagnostics provided stool collection kits and fecal calprotectin testing. The investigators had no disclosures.
Mobile health indexes for remotely monitoring Crohn’s disease and ulcerative colitis accurately identified clinically active disease and changed significantly as disease activity did, researchers reported in the December issue of Clinical Gastroenterology and Hepatology.
The mobile health index for Crohn’s disease predicted clinical disease activity with an area under the receiver operating characteristic curve (AUC) of 0.90, Welmoed K. van Deen, MD, of the University of California, Los Angeles, and her associates wrote in Clinical Gastroenterology and Hepatology. The AUC for the ulcerative colitis index for ulcerative colitis was very similar, at 0.91. “The [mobile health indexes] are specifically designed for implementation on a mobile application, and are currently available to patients with IBD [inflammatory bowel disease] treated at the UCLA Center for IBD,” the researchers said. “Prospective, randomized studies need to assess the effect of remote monitoring on disease control, quality of life, patient satisfaction, and health care costs.”
Inspired by the lack of smartphone applications for remotely managing inflammatory bowel disease, the researchers administered comprehensive disease-specific questionnaires to 110 patients with Crohn’s disease and 109 patients with ulcerative colitis who visited the UCLA IBD center in 2013 and 2014. They compared patient-reported outcomes across 10 domains of disease activity with scores on a number of existing disease activity indexes, and used logistic regression to identify which self-reported outcomes best predicted disease activity in both Crohn’s disease and ulcerative colitis (Clin Gastroenterol Hepatol. 2015 Nov 18. doi: 10.1016/j.cgh.2015.10.035).
The resulting Crohn’s disease mobile health index asked how many liquid or “very soft” stools patients had per day, if they had abdominal pain, and how they would rate their well-being and level of disease control on scales ranging between 0 and 10. The ulcerative colitis mobile health index asked about number of stools the day before and had patients score abdominal pain, frequency of rectal bleeding, and level of disease control between 0 and 10. The researchers also validated each mobile health index in multicenter cohorts of 301 patients with Crohn’s disease and 265 patients with ulcerative colitis.
Each mobile health index detected clinical disease activity with about 90% accuracy, compared with standard measures, including the Crohn’s disease activity index and the Harvey Bradshaw index for Crohn’s disease, the partial Mayo score, the simple clinical colitis activity index, and the modified Truelove and Witts index for ulcerative colitis. But the mobile indexes detected endoscopic disease activity less accurately, with AUCs of 0.82 for ulcerative colitis and only 0.63 for Crohn’s disease. “As previously shown, ulcerative colitis clinical disease activity highly correlates with endoscopic disease activity, whereas correlation between Crohn’s disease symptoms and endoscopic findings is poor,” the researchers noted. However, both mobile indexes reliably detected changes in disease activity, varying significantly depending on whether patients were clinically improved, stable, or worse, regardless of whether they had Crohn’s disease (P = .003) or ulcerative colitis (P = .0025).
To explore intrapatient reliability, the researchers also compared initial and follow-up mobile health index results for subgroups of 40 Crohn’s disease patients tested a median of 21 hours apart, and 37 ulcerative colitis patients tested a median of 23 hours apart. In both cases, the intraclass correlation coefficient reached 0.94 (95% confidence interval, 0.89-0.97). “Cloud-based health technologies are predicted to revolutionize care delivery and patient engagement,” the investigators commented. “Patients can participate in their care by signaling meaningful health outcomes during year-round monitoring. Barriers for more widespread implementation of mobile health in inflammatory bowel disease care include policies affecting reimbursement and regulatory requirements, and privacy and security concerns.”
Genova Diagnostics provided stool collection kits and fecal calprotectin testing. The investigators had no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Two short mobile health indexes accurately identified disease activity in Crohn’s disease and ulcerative colitis.
Major finding: Areas under the receiver operating curve (AUC) were 0.91 for Crohn’s disease and 0.90 for ulcerative colitis when compared with standard measures of clinical disease activity.
Data source: A prospective, observational study of 110 patients with Crohn’s disease and 109 patients with ulcerative colitis.
Disclosures: Genova Diagnostics provided stool collection kits and fecal calprotectin testing. The investigators had no disclosures.
Second course of rifaximin edges out placebo in IBS-D trial
Patients with diarrhea-predominant irritable bowel syndrome (IBS-D) who responded to rifaximin but relapsed after completing treatment were significantly more likely to respond to a second course of the antibiotic than to placebo, according to a report in the December issue of Gastroenterology (2016 Aug 5. doi: 10.1053/j.gastro.2016.08.003).
A total of 38% of patients who received a second course of rifaximin met the primary endpoint in the randomized double-blinded trial, compared with 31.5% of the placebo group (P = .03), Dr. Anthony Lembo of Beth Israel Deaconess Medical Center, Boston, and his associates wrote in Gastroenterology. “Although this study had a positive outcome, questions remain regarding the role of nonsystemic antibiotics in the long term, particularly when patients with IBS-D may require years of symptom management,” they added. “Further research is needed to better understand the treatment algorithm in patients who may lose responsiveness to rifaximin.”
Rifaximin (Xifaxan) has been approved in the United States for treating IBS-D since 2015. The agent is an oral, minimally absorbed, broad-spectrum antibiotic that targets the gastrointestinal tract and has rarely been linked to “clinically relevant” antibiotic resistance, the researchers said. However, pivotal IBS-D trials had not investigated the durability of response to rifaximin or the efficacy and safety of repeat treatment, they noted. Therefore, they followed 1,074 patients with IBS-D who had responded to an open-label 2-week course of rifaximin dosed orally at 550 mg three times daily. By definition, these responders had met a combined primary endpoint that included at least a 30% decrease in abdominal pain and at least a 50% decrease in the frequency of loose stools during at least 2 of 4 weeks of follow-up.
In all, 692 (64%) responders relapsed up to 18 weeks after finishing the first rifaximin course, the investigators said. They randomly assigned 636 of these relapsers to double-blinded treatment with either placebo or a second course of rifaximin. In all, 125 of 328 patients (38.1%) in the rifaximin group again met the combined primary endpoint, compared with 97 of 308 patients (31.5%) in the placebo group (P = .03). Repeat rifaximin treatment also significantly outperformed placebo in terms of the individual abdominal pain endpoint (51% versus 42%, respectively; P = .02), but not the stool consistency endpoint (52% versus 50%).
“Adverse event rates were low and similar between groups,” the researchers said. Patients who received a second course of rifaximin most commonly developed nausea (3.7%), upper respiratory infection (3.7%), urinary tract infection (3.4%), and nasopharyngitis (3.0%). Four patients (1%) in each treatment group developed serious adverse events, none of which were deemed treatment related. One patient developed Clostridium difficile colitis 37 days after completing the second course of rifaximin. However, this patient had a past history of C. difficile infection, had tested negative for C. difficile toxins A and B at enrollment, and had completed a 10-day course of cefdinir for a urinary tract infection immediately before developing C. difficile colitis.
Salix Pharmaceuticals makes rifaximin and funded the study. Dr. Lembo and his coinvestigators disclosed ties to Salix.
Patients with diarrhea-predominant irritable bowel syndrome (IBS-D) who responded to rifaximin but relapsed after completing treatment were significantly more likely to respond to a second course of the antibiotic than to placebo, according to a report in the December issue of Gastroenterology (2016 Aug 5. doi: 10.1053/j.gastro.2016.08.003).
A total of 38% of patients who received a second course of rifaximin met the primary endpoint in the randomized double-blinded trial, compared with 31.5% of the placebo group (P = .03), Dr. Anthony Lembo of Beth Israel Deaconess Medical Center, Boston, and his associates wrote in Gastroenterology. “Although this study had a positive outcome, questions remain regarding the role of nonsystemic antibiotics in the long term, particularly when patients with IBS-D may require years of symptom management,” they added. “Further research is needed to better understand the treatment algorithm in patients who may lose responsiveness to rifaximin.”
Rifaximin (Xifaxan) has been approved in the United States for treating IBS-D since 2015. The agent is an oral, minimally absorbed, broad-spectrum antibiotic that targets the gastrointestinal tract and has rarely been linked to “clinically relevant” antibiotic resistance, the researchers said. However, pivotal IBS-D trials had not investigated the durability of response to rifaximin or the efficacy and safety of repeat treatment, they noted. Therefore, they followed 1,074 patients with IBS-D who had responded to an open-label 2-week course of rifaximin dosed orally at 550 mg three times daily. By definition, these responders had met a combined primary endpoint that included at least a 30% decrease in abdominal pain and at least a 50% decrease in the frequency of loose stools during at least 2 of 4 weeks of follow-up.
In all, 692 (64%) responders relapsed up to 18 weeks after finishing the first rifaximin course, the investigators said. They randomly assigned 636 of these relapsers to double-blinded treatment with either placebo or a second course of rifaximin. In all, 125 of 328 patients (38.1%) in the rifaximin group again met the combined primary endpoint, compared with 97 of 308 patients (31.5%) in the placebo group (P = .03). Repeat rifaximin treatment also significantly outperformed placebo in terms of the individual abdominal pain endpoint (51% versus 42%, respectively; P = .02), but not the stool consistency endpoint (52% versus 50%).
“Adverse event rates were low and similar between groups,” the researchers said. Patients who received a second course of rifaximin most commonly developed nausea (3.7%), upper respiratory infection (3.7%), urinary tract infection (3.4%), and nasopharyngitis (3.0%). Four patients (1%) in each treatment group developed serious adverse events, none of which were deemed treatment related. One patient developed Clostridium difficile colitis 37 days after completing the second course of rifaximin. However, this patient had a past history of C. difficile infection, had tested negative for C. difficile toxins A and B at enrollment, and had completed a 10-day course of cefdinir for a urinary tract infection immediately before developing C. difficile colitis.
Salix Pharmaceuticals makes rifaximin and funded the study. Dr. Lembo and his coinvestigators disclosed ties to Salix.
Patients with diarrhea-predominant irritable bowel syndrome (IBS-D) who responded to rifaximin but relapsed after completing treatment were significantly more likely to respond to a second course of the antibiotic than to placebo, according to a report in the December issue of Gastroenterology (2016 Aug 5. doi: 10.1053/j.gastro.2016.08.003).
A total of 38% of patients who received a second course of rifaximin met the primary endpoint in the randomized double-blinded trial, compared with 31.5% of the placebo group (P = .03), Dr. Anthony Lembo of Beth Israel Deaconess Medical Center, Boston, and his associates wrote in Gastroenterology. “Although this study had a positive outcome, questions remain regarding the role of nonsystemic antibiotics in the long term, particularly when patients with IBS-D may require years of symptom management,” they added. “Further research is needed to better understand the treatment algorithm in patients who may lose responsiveness to rifaximin.”
Rifaximin (Xifaxan) has been approved in the United States for treating IBS-D since 2015. The agent is an oral, minimally absorbed, broad-spectrum antibiotic that targets the gastrointestinal tract and has rarely been linked to “clinically relevant” antibiotic resistance, the researchers said. However, pivotal IBS-D trials had not investigated the durability of response to rifaximin or the efficacy and safety of repeat treatment, they noted. Therefore, they followed 1,074 patients with IBS-D who had responded to an open-label 2-week course of rifaximin dosed orally at 550 mg three times daily. By definition, these responders had met a combined primary endpoint that included at least a 30% decrease in abdominal pain and at least a 50% decrease in the frequency of loose stools during at least 2 of 4 weeks of follow-up.
In all, 692 (64%) responders relapsed up to 18 weeks after finishing the first rifaximin course, the investigators said. They randomly assigned 636 of these relapsers to double-blinded treatment with either placebo or a second course of rifaximin. In all, 125 of 328 patients (38.1%) in the rifaximin group again met the combined primary endpoint, compared with 97 of 308 patients (31.5%) in the placebo group (P = .03). Repeat rifaximin treatment also significantly outperformed placebo in terms of the individual abdominal pain endpoint (51% versus 42%, respectively; P = .02), but not the stool consistency endpoint (52% versus 50%).
“Adverse event rates were low and similar between groups,” the researchers said. Patients who received a second course of rifaximin most commonly developed nausea (3.7%), upper respiratory infection (3.7%), urinary tract infection (3.4%), and nasopharyngitis (3.0%). Four patients (1%) in each treatment group developed serious adverse events, none of which were deemed treatment related. One patient developed Clostridium difficile colitis 37 days after completing the second course of rifaximin. However, this patient had a past history of C. difficile infection, had tested negative for C. difficile toxins A and B at enrollment, and had completed a 10-day course of cefdinir for a urinary tract infection immediately before developing C. difficile colitis.
Salix Pharmaceuticals makes rifaximin and funded the study. Dr. Lembo and his coinvestigators disclosed ties to Salix.
FROM GASTROENTEROLOGY
Key clinical point: A second course of rifaximin may be merited in patients with diarrhea-predominant irritable bowel syndrome.
Major finding: In all, 38% of patients who received a second course of the antibiotic met the primary endpoint, compared with 31.5% of those who received placebo (P = .03),
Data source: A randomized, double-blind, phase III trial of 692 patients with IBS-D who relapsed after initially responding to a 2-week course of rifaximin.
Disclosures: Salix Pharmaceuticals, maker of rifaximin, funded the study. Dr. Lembo and his coinvestigators disclosed ties to Salix.
Yoga holds up to medications, walking for irritable bowel syndrome
Yoga may be a feasible and safe add-on therapy for patients with irritable bowel syndrome, based on a systematic review of six randomized controlled trials of 273 patients published in the December issue of Clinical Gastroenterology and Hepatology.
Yoga significantly outperformed no treatment and resembled pharmacologic therapies for IBS on measures of bowel symptoms, anxiety, and quality of life, said Dania Schumann of the University of Duisburg-Essen, Essen, Germany.
“Yoga also seems to be equally effective as a walking program in improving patient-reported outcomes,” she and her coinvestigators wrote. But “wide methodological heterogeneity” and a “mostly unclear risk of bias,” precluded a direct recommendation for yoga in IBS, they said. Nonetheless, “its practice need not be discouraged in this patient population, especially when [patients] believe that it benefits their health, quality of life, or IBS-related comorbidities.”
Experts have increasingly emphasized the role of stress, psychological disorders, and the bidirectional gut-brain axis in IBS, the reviewers noted. Because yoga had been found to cut stress and improve psychological functioning in past studies, they hypothesized that it also might improve IBS symptoms. By searching MEDLINE/Pubmed, the Cochrane Library, CAM-QUEST, CAMbase, and IndMED for studies of IBS and yoga, they identified 93 records, including six randomized controlled trials from India, the United States, and Canada. One trial defined IBS based on Rome I criteria, another used Rome II criteria, three used Rome III criteria, and the sixth trial relied solely on clinical and laboratory measures. Patients ranged in age from 14 to 44 years (median, 32 years), and most were female. They were allowed to continue their usual IBS care (Clin Gastroenterol Hepatol. 2016 Apr 22. doi: 10.1016/j.cgh.2016.04.026). Two trials compared 9-12 weeks of yoga with pharmacologic therapies. In one study, yoga and loperamide were associated with similar improvements in bowel symptoms, state anxiety, gastric motility, and other measures of autonomic reactivity. The second study found no significant differences in the colonic myoelectrical effects of yoga, placebo, and a regimen of psyllium husk, propantheline, and diazepam.
Three studies compared 4-12 weeks of Iyengar or hatha yoga with usual IBS care. Yoga outperformed standard care on measures of IBS symptoms, quality of life, psychological distress, and fatigue in two trials. The third study found a benefit for yoga after wait-listed controls joined the yoga intervention and the researchers combined their data with the other yoga group.
The sixth trial compared yoga with a walking program and found similar effects. Yoga was associated with significant improvements in abdominal pain, visceral sensitivity, and GI symptoms, while walking improved gastrointestinal symptoms, negative affect, and state anxiety. But at 6-month follow-up, walkers had fewer gastrointestinal symptoms than did the yoga group, perhaps because a walking program is easier to maintain at home, the reviewers noted.
Only one trial adequately performed adequate blinding during outcome assessments, and several others were at high risk of performance bias, reporting bias, and attrition bias, the reviewers said. The trials also did not adequately describe methods to randomize patients or conceal group allocations, and “selective reporting and high dropout rates [were] an issue,” they added.
Adverse events related to yoga included three cases of temporarily aggravated lower back pain and one fall after a participant slipped and hit his knee while in a headstand. However, only two trials assessed adverse events, the reviewers noted. “Future studies should ensure rigorous reporting of adverse events, and the correct use of terminology,” they said.
Because meditation, breathing exercises, and yoga seem to improve both stress and IBS symptoms, researchers should consider these practices when studying patients with “an increased gastrointestinal response to stress,” the reviewers concluded. “So far, the recent global guidelines of the World Gastroenterology Organization on IBS consider sufficient physical activity and relaxation techniques to be appropriate nonpharmacologic approaches.”
The reviewers did not report funding sources. They had no relevant conflicts of interest.
Yoga may be a feasible and safe add-on therapy for patients with irritable bowel syndrome, based on a systematic review of six randomized controlled trials of 273 patients published in the December issue of Clinical Gastroenterology and Hepatology.
Yoga significantly outperformed no treatment and resembled pharmacologic therapies for IBS on measures of bowel symptoms, anxiety, and quality of life, said Dania Schumann of the University of Duisburg-Essen, Essen, Germany.
“Yoga also seems to be equally effective as a walking program in improving patient-reported outcomes,” she and her coinvestigators wrote. But “wide methodological heterogeneity” and a “mostly unclear risk of bias,” precluded a direct recommendation for yoga in IBS, they said. Nonetheless, “its practice need not be discouraged in this patient population, especially when [patients] believe that it benefits their health, quality of life, or IBS-related comorbidities.”
Experts have increasingly emphasized the role of stress, psychological disorders, and the bidirectional gut-brain axis in IBS, the reviewers noted. Because yoga had been found to cut stress and improve psychological functioning in past studies, they hypothesized that it also might improve IBS symptoms. By searching MEDLINE/Pubmed, the Cochrane Library, CAM-QUEST, CAMbase, and IndMED for studies of IBS and yoga, they identified 93 records, including six randomized controlled trials from India, the United States, and Canada. One trial defined IBS based on Rome I criteria, another used Rome II criteria, three used Rome III criteria, and the sixth trial relied solely on clinical and laboratory measures. Patients ranged in age from 14 to 44 years (median, 32 years), and most were female. They were allowed to continue their usual IBS care (Clin Gastroenterol Hepatol. 2016 Apr 22. doi: 10.1016/j.cgh.2016.04.026). Two trials compared 9-12 weeks of yoga with pharmacologic therapies. In one study, yoga and loperamide were associated with similar improvements in bowel symptoms, state anxiety, gastric motility, and other measures of autonomic reactivity. The second study found no significant differences in the colonic myoelectrical effects of yoga, placebo, and a regimen of psyllium husk, propantheline, and diazepam.
Three studies compared 4-12 weeks of Iyengar or hatha yoga with usual IBS care. Yoga outperformed standard care on measures of IBS symptoms, quality of life, psychological distress, and fatigue in two trials. The third study found a benefit for yoga after wait-listed controls joined the yoga intervention and the researchers combined their data with the other yoga group.
The sixth trial compared yoga with a walking program and found similar effects. Yoga was associated with significant improvements in abdominal pain, visceral sensitivity, and GI symptoms, while walking improved gastrointestinal symptoms, negative affect, and state anxiety. But at 6-month follow-up, walkers had fewer gastrointestinal symptoms than did the yoga group, perhaps because a walking program is easier to maintain at home, the reviewers noted.
Only one trial adequately performed adequate blinding during outcome assessments, and several others were at high risk of performance bias, reporting bias, and attrition bias, the reviewers said. The trials also did not adequately describe methods to randomize patients or conceal group allocations, and “selective reporting and high dropout rates [were] an issue,” they added.
Adverse events related to yoga included three cases of temporarily aggravated lower back pain and one fall after a participant slipped and hit his knee while in a headstand. However, only two trials assessed adverse events, the reviewers noted. “Future studies should ensure rigorous reporting of adverse events, and the correct use of terminology,” they said.
Because meditation, breathing exercises, and yoga seem to improve both stress and IBS symptoms, researchers should consider these practices when studying patients with “an increased gastrointestinal response to stress,” the reviewers concluded. “So far, the recent global guidelines of the World Gastroenterology Organization on IBS consider sufficient physical activity and relaxation techniques to be appropriate nonpharmacologic approaches.”
The reviewers did not report funding sources. They had no relevant conflicts of interest.
Yoga may be a feasible and safe add-on therapy for patients with irritable bowel syndrome, based on a systematic review of six randomized controlled trials of 273 patients published in the December issue of Clinical Gastroenterology and Hepatology.
Yoga significantly outperformed no treatment and resembled pharmacologic therapies for IBS on measures of bowel symptoms, anxiety, and quality of life, said Dania Schumann of the University of Duisburg-Essen, Essen, Germany.
“Yoga also seems to be equally effective as a walking program in improving patient-reported outcomes,” she and her coinvestigators wrote. But “wide methodological heterogeneity” and a “mostly unclear risk of bias,” precluded a direct recommendation for yoga in IBS, they said. Nonetheless, “its practice need not be discouraged in this patient population, especially when [patients] believe that it benefits their health, quality of life, or IBS-related comorbidities.”
Experts have increasingly emphasized the role of stress, psychological disorders, and the bidirectional gut-brain axis in IBS, the reviewers noted. Because yoga had been found to cut stress and improve psychological functioning in past studies, they hypothesized that it also might improve IBS symptoms. By searching MEDLINE/Pubmed, the Cochrane Library, CAM-QUEST, CAMbase, and IndMED for studies of IBS and yoga, they identified 93 records, including six randomized controlled trials from India, the United States, and Canada. One trial defined IBS based on Rome I criteria, another used Rome II criteria, three used Rome III criteria, and the sixth trial relied solely on clinical and laboratory measures. Patients ranged in age from 14 to 44 years (median, 32 years), and most were female. They were allowed to continue their usual IBS care (Clin Gastroenterol Hepatol. 2016 Apr 22. doi: 10.1016/j.cgh.2016.04.026). Two trials compared 9-12 weeks of yoga with pharmacologic therapies. In one study, yoga and loperamide were associated with similar improvements in bowel symptoms, state anxiety, gastric motility, and other measures of autonomic reactivity. The second study found no significant differences in the colonic myoelectrical effects of yoga, placebo, and a regimen of psyllium husk, propantheline, and diazepam.
Three studies compared 4-12 weeks of Iyengar or hatha yoga with usual IBS care. Yoga outperformed standard care on measures of IBS symptoms, quality of life, psychological distress, and fatigue in two trials. The third study found a benefit for yoga after wait-listed controls joined the yoga intervention and the researchers combined their data with the other yoga group.
The sixth trial compared yoga with a walking program and found similar effects. Yoga was associated with significant improvements in abdominal pain, visceral sensitivity, and GI symptoms, while walking improved gastrointestinal symptoms, negative affect, and state anxiety. But at 6-month follow-up, walkers had fewer gastrointestinal symptoms than did the yoga group, perhaps because a walking program is easier to maintain at home, the reviewers noted.
Only one trial adequately performed adequate blinding during outcome assessments, and several others were at high risk of performance bias, reporting bias, and attrition bias, the reviewers said. The trials also did not adequately describe methods to randomize patients or conceal group allocations, and “selective reporting and high dropout rates [were] an issue,” they added.
Adverse events related to yoga included three cases of temporarily aggravated lower back pain and one fall after a participant slipped and hit his knee while in a headstand. However, only two trials assessed adverse events, the reviewers noted. “Future studies should ensure rigorous reporting of adverse events, and the correct use of terminology,” they said.
Because meditation, breathing exercises, and yoga seem to improve both stress and IBS symptoms, researchers should consider these practices when studying patients with “an increased gastrointestinal response to stress,” the reviewers concluded. “So far, the recent global guidelines of the World Gastroenterology Organization on IBS consider sufficient physical activity and relaxation techniques to be appropriate nonpharmacologic approaches.”
The reviewers did not report funding sources. They had no relevant conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Yoga may be an appropriate adjunctive therapy for patients with irritable bowel syndrome.
Major finding: Yoga outperformed no treatment on measures of gastrointestinal symptoms, anxiety, and quality of life, and was comparable to standard medications and a walking program.
Data source: A systematic review of six randomized controlled trials of 273 patients with irritable bowel syndrome.
Disclosures: The reviewers did not report funding sources. They had no relevant conflicts of interest.
VIDEO: No difference between PPI and H2RA for low-dose aspirin gastroprotection
Among patients on low-dose aspirin at risk for recurrent GI bleeding, there were slightly fewer GI bleeds or ulcers when patients were on the proton pump inhibitor rabeprazole (Aciphex) instead of the histamine2-receptor antagonist famotidine (Pepcid), but the difference was not statistically significant according to a study reported in the January issue of Gastroenterology.
SOURCE: American Gastroenterological Association
In a 270-subject, double-blind, randomized trial in Hong Kong and Japan led by Francis Chan, MD, of the Chinese University of Hong Kong, investigators found, “Among high-risk aspirin users, the incidence of recurrent bleeding is comparable with either use of PPI [proton pump inhibitor] or H2RA [H2-receptor antagonist].” However, “since a small difference in efficacy cannot be excluded, PPI probably remains the preferred treatment for long-term protection against upper GI bleeding in high-risk aspirin users” (Gastroenterology. 2016 Sep 15. doi: 10.1053/j.gastro.2016.09.006).
Even so, “our findings suggest that famotidine may be a reasonable alternative option for aspirin users who disfavor long-term PPI therapy,” they said.
Because of concerns about the long-term safety of PPIs, including the association between PPIs and increased risk of serious cardiovascular events in patients on clopidogrel (Plavix), clinicians have been looking for alternatives. The findings reassure that H2RAs are a reasonable choice; many clinicians have already turned to them.
All 270 subjects had previously had endoscopically confirmed ulcer bleeding while on low-dose aspirin (325 mg or less per day). “Considering clinicians will be most concerned with the adequacy of gastroprotective treatment effect in aspirin users with the highest risk, we exclusively enrolled patients with endoscopy-proven upper GI bleeding,” Dr. Chan and his colleagues said.
After the ulcers healed, the subjects resumed aspirin (80 mg) daily and were randomized to either famotidine 40 mg once daily (n = 132) or rabeprazole 20 mg daily (n = 138) for up to 12 months. Helicobacter pylori was eradicated prior to randomization in patients who tested positive. Subjects were evaluated every 2 months, with repeat endoscopy for symptoms of upper GI bleeding or significant drops in hemoglobin, as well as at the end of the study.
During the 12-month study period, upper GI bleeding recurred in one patient receiving rabeprazole (0.7%) and four receiving famotidine (3.1%; P = .16). The composite endpoint of recurrent bleeding or endoscopic ulcers at month 12 was reached by nine patients in the rabeprazole group (7.9%) and 13 receiving famotidine (12.4%; P = .26).
“Our findings indicate that both treatments are comparable in preventing recurrent upper GI bleeding in high-risk aspirin users, although a small difference in efficacy cannot be excluded,” the investigators said.
Over two-thirds of the subjects were men, and the mean age was 73 years. About a quarter in the PPI group and almost 40% in the H2RA group had H. pylori cleared before randomization.
The Research Grant Council of Hong Kong funded the work. Dr. Chan has served as a consultant to Pfizer, Eisai, Takeda, and Otsuka, and has received research grants from Pfizer and lecture fees from Pfizer, AstraZeneca, and Takeda. Several other authors reported similar industry disclosures.
Aspirin is widely used for primary and secondary prophylaxis of cardiovascular disease. Dr. Chan and colleagues present a randomized, controlled trial comparing rabeprazole 20 mg once a day to famotidine 40 mg once a day in preventing recurrent GI hemorrhage and endoscopic ulcers in low-dose (less than 325 mg) aspirin users. The authors conclude that no statistical difference was found between the two agents. The study contrasts with another study from Hong Kong, which found that proton pump inhibitors were more effective.
The authors are to be complimented on this important addition to the literature but the reader should not conclude that H2-receptor antagonists and proton pump inhibitors are equivalent in preventing recurrent bleeding from aspirin-induced ulcers.
Nimish Vakil, MD, AGAF, is clinical professor of medicine at the University of Wisconsin–Madison. He has consulted for Ironwood and AstraZeneca.
Aspirin is widely used for primary and secondary prophylaxis of cardiovascular disease. Dr. Chan and colleagues present a randomized, controlled trial comparing rabeprazole 20 mg once a day to famotidine 40 mg once a day in preventing recurrent GI hemorrhage and endoscopic ulcers in low-dose (less than 325 mg) aspirin users. The authors conclude that no statistical difference was found between the two agents. The study contrasts with another study from Hong Kong, which found that proton pump inhibitors were more effective.
The authors are to be complimented on this important addition to the literature but the reader should not conclude that H2-receptor antagonists and proton pump inhibitors are equivalent in preventing recurrent bleeding from aspirin-induced ulcers.
Nimish Vakil, MD, AGAF, is clinical professor of medicine at the University of Wisconsin–Madison. He has consulted for Ironwood and AstraZeneca.
Aspirin is widely used for primary and secondary prophylaxis of cardiovascular disease. Dr. Chan and colleagues present a randomized, controlled trial comparing rabeprazole 20 mg once a day to famotidine 40 mg once a day in preventing recurrent GI hemorrhage and endoscopic ulcers in low-dose (less than 325 mg) aspirin users. The authors conclude that no statistical difference was found between the two agents. The study contrasts with another study from Hong Kong, which found that proton pump inhibitors were more effective.
The authors are to be complimented on this important addition to the literature but the reader should not conclude that H2-receptor antagonists and proton pump inhibitors are equivalent in preventing recurrent bleeding from aspirin-induced ulcers.
Nimish Vakil, MD, AGAF, is clinical professor of medicine at the University of Wisconsin–Madison. He has consulted for Ironwood and AstraZeneca.
Among patients on low-dose aspirin at risk for recurrent GI bleeding, there were slightly fewer GI bleeds or ulcers when patients were on the proton pump inhibitor rabeprazole (Aciphex) instead of the histamine2-receptor antagonist famotidine (Pepcid), but the difference was not statistically significant according to a study reported in the January issue of Gastroenterology.
SOURCE: American Gastroenterological Association
In a 270-subject, double-blind, randomized trial in Hong Kong and Japan led by Francis Chan, MD, of the Chinese University of Hong Kong, investigators found, “Among high-risk aspirin users, the incidence of recurrent bleeding is comparable with either use of PPI [proton pump inhibitor] or H2RA [H2-receptor antagonist].” However, “since a small difference in efficacy cannot be excluded, PPI probably remains the preferred treatment for long-term protection against upper GI bleeding in high-risk aspirin users” (Gastroenterology. 2016 Sep 15. doi: 10.1053/j.gastro.2016.09.006).
Even so, “our findings suggest that famotidine may be a reasonable alternative option for aspirin users who disfavor long-term PPI therapy,” they said.
Because of concerns about the long-term safety of PPIs, including the association between PPIs and increased risk of serious cardiovascular events in patients on clopidogrel (Plavix), clinicians have been looking for alternatives. The findings reassure that H2RAs are a reasonable choice; many clinicians have already turned to them.
All 270 subjects had previously had endoscopically confirmed ulcer bleeding while on low-dose aspirin (325 mg or less per day). “Considering clinicians will be most concerned with the adequacy of gastroprotective treatment effect in aspirin users with the highest risk, we exclusively enrolled patients with endoscopy-proven upper GI bleeding,” Dr. Chan and his colleagues said.
After the ulcers healed, the subjects resumed aspirin (80 mg) daily and were randomized to either famotidine 40 mg once daily (n = 132) or rabeprazole 20 mg daily (n = 138) for up to 12 months. Helicobacter pylori was eradicated prior to randomization in patients who tested positive. Subjects were evaluated every 2 months, with repeat endoscopy for symptoms of upper GI bleeding or significant drops in hemoglobin, as well as at the end of the study.
During the 12-month study period, upper GI bleeding recurred in one patient receiving rabeprazole (0.7%) and four receiving famotidine (3.1%; P = .16). The composite endpoint of recurrent bleeding or endoscopic ulcers at month 12 was reached by nine patients in the rabeprazole group (7.9%) and 13 receiving famotidine (12.4%; P = .26).
“Our findings indicate that both treatments are comparable in preventing recurrent upper GI bleeding in high-risk aspirin users, although a small difference in efficacy cannot be excluded,” the investigators said.
Over two-thirds of the subjects were men, and the mean age was 73 years. About a quarter in the PPI group and almost 40% in the H2RA group had H. pylori cleared before randomization.
The Research Grant Council of Hong Kong funded the work. Dr. Chan has served as a consultant to Pfizer, Eisai, Takeda, and Otsuka, and has received research grants from Pfizer and lecture fees from Pfizer, AstraZeneca, and Takeda. Several other authors reported similar industry disclosures.
Among patients on low-dose aspirin at risk for recurrent GI bleeding, there were slightly fewer GI bleeds or ulcers when patients were on the proton pump inhibitor rabeprazole (Aciphex) instead of the histamine2-receptor antagonist famotidine (Pepcid), but the difference was not statistically significant according to a study reported in the January issue of Gastroenterology.
SOURCE: American Gastroenterological Association
In a 270-subject, double-blind, randomized trial in Hong Kong and Japan led by Francis Chan, MD, of the Chinese University of Hong Kong, investigators found, “Among high-risk aspirin users, the incidence of recurrent bleeding is comparable with either use of PPI [proton pump inhibitor] or H2RA [H2-receptor antagonist].” However, “since a small difference in efficacy cannot be excluded, PPI probably remains the preferred treatment for long-term protection against upper GI bleeding in high-risk aspirin users” (Gastroenterology. 2016 Sep 15. doi: 10.1053/j.gastro.2016.09.006).
Even so, “our findings suggest that famotidine may be a reasonable alternative option for aspirin users who disfavor long-term PPI therapy,” they said.
Because of concerns about the long-term safety of PPIs, including the association between PPIs and increased risk of serious cardiovascular events in patients on clopidogrel (Plavix), clinicians have been looking for alternatives. The findings reassure that H2RAs are a reasonable choice; many clinicians have already turned to them.
All 270 subjects had previously had endoscopically confirmed ulcer bleeding while on low-dose aspirin (325 mg or less per day). “Considering clinicians will be most concerned with the adequacy of gastroprotective treatment effect in aspirin users with the highest risk, we exclusively enrolled patients with endoscopy-proven upper GI bleeding,” Dr. Chan and his colleagues said.
After the ulcers healed, the subjects resumed aspirin (80 mg) daily and were randomized to either famotidine 40 mg once daily (n = 132) or rabeprazole 20 mg daily (n = 138) for up to 12 months. Helicobacter pylori was eradicated prior to randomization in patients who tested positive. Subjects were evaluated every 2 months, with repeat endoscopy for symptoms of upper GI bleeding or significant drops in hemoglobin, as well as at the end of the study.
During the 12-month study period, upper GI bleeding recurred in one patient receiving rabeprazole (0.7%) and four receiving famotidine (3.1%; P = .16). The composite endpoint of recurrent bleeding or endoscopic ulcers at month 12 was reached by nine patients in the rabeprazole group (7.9%) and 13 receiving famotidine (12.4%; P = .26).
“Our findings indicate that both treatments are comparable in preventing recurrent upper GI bleeding in high-risk aspirin users, although a small difference in efficacy cannot be excluded,” the investigators said.
Over two-thirds of the subjects were men, and the mean age was 73 years. About a quarter in the PPI group and almost 40% in the H2RA group had H. pylori cleared before randomization.
The Research Grant Council of Hong Kong funded the work. Dr. Chan has served as a consultant to Pfizer, Eisai, Takeda, and Otsuka, and has received research grants from Pfizer and lecture fees from Pfizer, AstraZeneca, and Takeda. Several other authors reported similar industry disclosures.
FROM GASTROENTEROLOGY
Key clinical point:
Major finding: During the 12-month study period, upper GI bleeding recurred in one patient receiving rabeprazole (0.7%) and four receiving famotidine (3.1%; P = .16). The composite endpoint of recurrent bleeding or endoscopic ulcers at month 12 was reached by nine patients in the rabeprazole group (7.9%) and 13 receiving famotidine (12.4%; P = .26).
Data source: A 270-subject, double-blind, randomized trial in Hong Kong and Japan.
Disclosures: The Research Grant Council of Hong Kong funded the work. The lead investigator has served as a consultant to Pfizer, Eisai, Takeda, and Otsuka, and has received research grants from Pfizer and lecture fees from Pfizer, AstraZeneca, and Takeda. Several other authors reported similar industry disclosures.
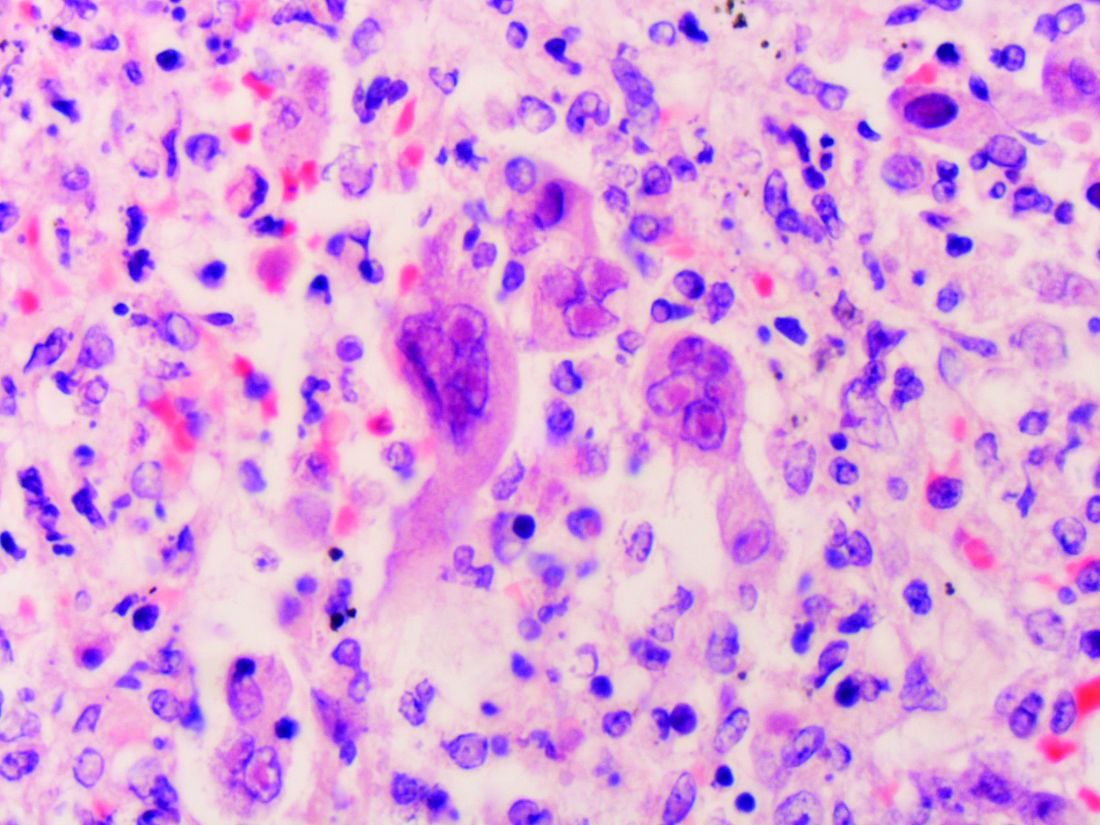
Increased death rate with platelets for aspirin/clopidogrel GI bleed
Patients with normal platelet counts who have a GI bleed while on antiplatelets were almost six times more likely to die in the hospital if they had a platelet transfusion in a retrospective cohort study from the Yale University in New Haven, Conn.
Ten of the 14 deaths in the 204 transfused patients – versus none of the 3 deaths in the 204 nontransfused patients - were due to bleeding, so it’s possible that the mortality difference was simply because patients with worse bleeding were more likely to get transfused. “On the other hand, the adjusted [odds ratios] for mortality (4.5-6.8 with different sensitivity analyses) [were] large, increasing the likelihood of a cause-and-effect relationship,” said investigators led by gastroenterologist Liam Zakko, MD, now at the Mayo Clinic in Rochester, Minn. (Clin Gastroenterol Hepatol. 2016 Jul 25. doi: 10.1016/j.cgh.2016.07.017).
Current guidelines suggest platelet transfusions are an option for antiplatelet patients with serious GI bleeds, but the Yale team found that they did not reduce rebleeding. “The observation of increased mortality without documentation of clinical benefit suggests a very cautious approach to the use of platelet transfusion. ... We do not support the use of platelet transfusions in patients with GI [bleeds] who are taking antiplatelet agents,” the investigators wrote.
Subjects in the two groups were matched for sex, age, and GI bleed location, and all had platelet counts above 100 × 109/L. Almost everyone was on aspirin for cardiovascular protection, and 30% were on also on clopidogrel.
Just over half in both groups had upper GI bleeds, and about 40% in each group had colonic bleeds. Transfused patients had more-severe bleeding, with overall lower blood pressure and lower hemoglobin; a larger proportion was admitted to the ICU.
On univariate analyses, platelet patients had more cardiovascular events (23% vs. 13%) while in the hospital. They were also more likely to stay in the hospital for more than 4 days (47% vs. 33%) and more likely to die while there (7% vs. 1%). On multivariable analysis, only the greater risk for death during admission remained statistically significant (odds ratio, 5.57; 95% confidence interval, 1.52-27.1). The adjusted odds ratio for recurrent bleeding was not significant.
Four patients in the platelet group died from cardiovascular causes. One patient in the control group had a fatal cardiovascular event.
Although counterintuitive, the authors said that it’s possible that platelet transfusions might actually increase the risk of severe and fatal GI bleeding. “Mechanisms by which platelet transfusion would increase mortality or [GI bleeding]–related mortality are not clear,” but “platelet transfusions are reported to be proinflammatory and alter recipient immunity,” they said.
At least for now, “the most prudent way to manage patients on antiplatelet agents with [GI bleeding] is to follow current evidence-based recommendations,” including early endoscopy, endoscopic hemostatic therapy for high-risk lesions, and intensive proton pump inhibitor therapy in patients with ulcers and high-risk endoscopic features.
“Although not based on high-quality evidence, we believe that hemostatic techniques that do not cause significant tissue damage (e.g., clips rather than thermal devices or sclerosants) should be used in patients on antiplatelet agents, especially if patients are expected to remain on these agents in the future,” they said.
The mean age in the study was 74 years, and about two-thirds of the subjects were men.
The authors had no disclosures.
The management of patients with gastrointestinal bleeding on antithrombotic drugs is a major challenge for gastroenterologists. Unfortunately, the use of aspirin alone has been shown to increase the risk of GI bleed twofold, and the addition of a thienopyridine additionally increases the risk of bleeding twofold. Furthermore, there is no available agent to reverse antiplatelet affects of these drugs, which irreversibly block platelet function for the life of the platelet (8-10 days). Current recommendations for the management of severe GI bleeding in patients receiving antithrombotic therapy include platelet transfusion, including those with a normal platelet count. However, this comes with a price as reversal of platelet function may increase the rate of cardiovascular events.
Zakko et al. performed a retrospective case-control study evaluating the role of platelet transfusion in patients presenting with GI bleeding. Patients were matched by age, sex, and the location of the GI bleed. Most patients included in the study were on low-dose aspirin and almost a third of the patients were taking both aspirin and a thienopyridine. Patients receiving platelet transfusions appeared to have more severe GI bleeding compared with matched controls, as patients receiving transfusion were more likely to have been hypotensive, tachycardic, have a low hemoglobin level, and require treatment in the intensive care unit (72% vs. 28%, P less than .0001). Patients receiving platelet transfusions were also more likely than matched controls to have recurrent GI bleeding as well as major cardiovascular adverse events, including myocardial infarction and inpatient death. After adjusting for patient characteristics, patients receiving platelet transfusions were more likely to have an increased risk of death (adjusted OR, 5.57; 95% CI, 1.52-27.1). The authors conclude that “the use of platelet transfusions in patients with GI bleeding who are taking antiplatelet agents without thrombocytopenia did not reduce rebleeding but was associated with higher mortality.”
Currently, there is no convincing evidence to support platelet transfusion in patients with bleeding on aspirin and/or a thienopyridine. Because the majority of the deaths were due to GI bleeding and not cardiovascular events, the observed increase in adverse events in patients receiving platelet transfusions likely reflects more severe GI bleeding in patients receiving platelet transfusions than in controls. We should avoid platelet transfusions and focus our management on achieving adequate resuscitation, use of proton pump inhibitors for patients with high-risk ulcers, and early endoscopy with endoscopic therapy for high-risk lesions.
John R. Saltzman, MD, AGAF, is director of endoscopy, Brigham and Women’s Hospital, professor of medicine, Harvard Medical School, Boston. He has no conflicts of interest.
The management of patients with gastrointestinal bleeding on antithrombotic drugs is a major challenge for gastroenterologists. Unfortunately, the use of aspirin alone has been shown to increase the risk of GI bleed twofold, and the addition of a thienopyridine additionally increases the risk of bleeding twofold. Furthermore, there is no available agent to reverse antiplatelet affects of these drugs, which irreversibly block platelet function for the life of the platelet (8-10 days). Current recommendations for the management of severe GI bleeding in patients receiving antithrombotic therapy include platelet transfusion, including those with a normal platelet count. However, this comes with a price as reversal of platelet function may increase the rate of cardiovascular events.
Zakko et al. performed a retrospective case-control study evaluating the role of platelet transfusion in patients presenting with GI bleeding. Patients were matched by age, sex, and the location of the GI bleed. Most patients included in the study were on low-dose aspirin and almost a third of the patients were taking both aspirin and a thienopyridine. Patients receiving platelet transfusions appeared to have more severe GI bleeding compared with matched controls, as patients receiving transfusion were more likely to have been hypotensive, tachycardic, have a low hemoglobin level, and require treatment in the intensive care unit (72% vs. 28%, P less than .0001). Patients receiving platelet transfusions were also more likely than matched controls to have recurrent GI bleeding as well as major cardiovascular adverse events, including myocardial infarction and inpatient death. After adjusting for patient characteristics, patients receiving platelet transfusions were more likely to have an increased risk of death (adjusted OR, 5.57; 95% CI, 1.52-27.1). The authors conclude that “the use of platelet transfusions in patients with GI bleeding who are taking antiplatelet agents without thrombocytopenia did not reduce rebleeding but was associated with higher mortality.”
Currently, there is no convincing evidence to support platelet transfusion in patients with bleeding on aspirin and/or a thienopyridine. Because the majority of the deaths were due to GI bleeding and not cardiovascular events, the observed increase in adverse events in patients receiving platelet transfusions likely reflects more severe GI bleeding in patients receiving platelet transfusions than in controls. We should avoid platelet transfusions and focus our management on achieving adequate resuscitation, use of proton pump inhibitors for patients with high-risk ulcers, and early endoscopy with endoscopic therapy for high-risk lesions.
John R. Saltzman, MD, AGAF, is director of endoscopy, Brigham and Women’s Hospital, professor of medicine, Harvard Medical School, Boston. He has no conflicts of interest.
The management of patients with gastrointestinal bleeding on antithrombotic drugs is a major challenge for gastroenterologists. Unfortunately, the use of aspirin alone has been shown to increase the risk of GI bleed twofold, and the addition of a thienopyridine additionally increases the risk of bleeding twofold. Furthermore, there is no available agent to reverse antiplatelet affects of these drugs, which irreversibly block platelet function for the life of the platelet (8-10 days). Current recommendations for the management of severe GI bleeding in patients receiving antithrombotic therapy include platelet transfusion, including those with a normal platelet count. However, this comes with a price as reversal of platelet function may increase the rate of cardiovascular events.
Zakko et al. performed a retrospective case-control study evaluating the role of platelet transfusion in patients presenting with GI bleeding. Patients were matched by age, sex, and the location of the GI bleed. Most patients included in the study were on low-dose aspirin and almost a third of the patients were taking both aspirin and a thienopyridine. Patients receiving platelet transfusions appeared to have more severe GI bleeding compared with matched controls, as patients receiving transfusion were more likely to have been hypotensive, tachycardic, have a low hemoglobin level, and require treatment in the intensive care unit (72% vs. 28%, P less than .0001). Patients receiving platelet transfusions were also more likely than matched controls to have recurrent GI bleeding as well as major cardiovascular adverse events, including myocardial infarction and inpatient death. After adjusting for patient characteristics, patients receiving platelet transfusions were more likely to have an increased risk of death (adjusted OR, 5.57; 95% CI, 1.52-27.1). The authors conclude that “the use of platelet transfusions in patients with GI bleeding who are taking antiplatelet agents without thrombocytopenia did not reduce rebleeding but was associated with higher mortality.”
Currently, there is no convincing evidence to support platelet transfusion in patients with bleeding on aspirin and/or a thienopyridine. Because the majority of the deaths were due to GI bleeding and not cardiovascular events, the observed increase in adverse events in patients receiving platelet transfusions likely reflects more severe GI bleeding in patients receiving platelet transfusions than in controls. We should avoid platelet transfusions and focus our management on achieving adequate resuscitation, use of proton pump inhibitors for patients with high-risk ulcers, and early endoscopy with endoscopic therapy for high-risk lesions.
John R. Saltzman, MD, AGAF, is director of endoscopy, Brigham and Women’s Hospital, professor of medicine, Harvard Medical School, Boston. He has no conflicts of interest.
Patients with normal platelet counts who have a GI bleed while on antiplatelets were almost six times more likely to die in the hospital if they had a platelet transfusion in a retrospective cohort study from the Yale University in New Haven, Conn.
Ten of the 14 deaths in the 204 transfused patients – versus none of the 3 deaths in the 204 nontransfused patients - were due to bleeding, so it’s possible that the mortality difference was simply because patients with worse bleeding were more likely to get transfused. “On the other hand, the adjusted [odds ratios] for mortality (4.5-6.8 with different sensitivity analyses) [were] large, increasing the likelihood of a cause-and-effect relationship,” said investigators led by gastroenterologist Liam Zakko, MD, now at the Mayo Clinic in Rochester, Minn. (Clin Gastroenterol Hepatol. 2016 Jul 25. doi: 10.1016/j.cgh.2016.07.017).
Current guidelines suggest platelet transfusions are an option for antiplatelet patients with serious GI bleeds, but the Yale team found that they did not reduce rebleeding. “The observation of increased mortality without documentation of clinical benefit suggests a very cautious approach to the use of platelet transfusion. ... We do not support the use of platelet transfusions in patients with GI [bleeds] who are taking antiplatelet agents,” the investigators wrote.
Subjects in the two groups were matched for sex, age, and GI bleed location, and all had platelet counts above 100 × 109/L. Almost everyone was on aspirin for cardiovascular protection, and 30% were on also on clopidogrel.
Just over half in both groups had upper GI bleeds, and about 40% in each group had colonic bleeds. Transfused patients had more-severe bleeding, with overall lower blood pressure and lower hemoglobin; a larger proportion was admitted to the ICU.
On univariate analyses, platelet patients had more cardiovascular events (23% vs. 13%) while in the hospital. They were also more likely to stay in the hospital for more than 4 days (47% vs. 33%) and more likely to die while there (7% vs. 1%). On multivariable analysis, only the greater risk for death during admission remained statistically significant (odds ratio, 5.57; 95% confidence interval, 1.52-27.1). The adjusted odds ratio for recurrent bleeding was not significant.
Four patients in the platelet group died from cardiovascular causes. One patient in the control group had a fatal cardiovascular event.
Although counterintuitive, the authors said that it’s possible that platelet transfusions might actually increase the risk of severe and fatal GI bleeding. “Mechanisms by which platelet transfusion would increase mortality or [GI bleeding]–related mortality are not clear,” but “platelet transfusions are reported to be proinflammatory and alter recipient immunity,” they said.
At least for now, “the most prudent way to manage patients on antiplatelet agents with [GI bleeding] is to follow current evidence-based recommendations,” including early endoscopy, endoscopic hemostatic therapy for high-risk lesions, and intensive proton pump inhibitor therapy in patients with ulcers and high-risk endoscopic features.
“Although not based on high-quality evidence, we believe that hemostatic techniques that do not cause significant tissue damage (e.g., clips rather than thermal devices or sclerosants) should be used in patients on antiplatelet agents, especially if patients are expected to remain on these agents in the future,” they said.
The mean age in the study was 74 years, and about two-thirds of the subjects were men.
The authors had no disclosures.
Patients with normal platelet counts who have a GI bleed while on antiplatelets were almost six times more likely to die in the hospital if they had a platelet transfusion in a retrospective cohort study from the Yale University in New Haven, Conn.
Ten of the 14 deaths in the 204 transfused patients – versus none of the 3 deaths in the 204 nontransfused patients - were due to bleeding, so it’s possible that the mortality difference was simply because patients with worse bleeding were more likely to get transfused. “On the other hand, the adjusted [odds ratios] for mortality (4.5-6.8 with different sensitivity analyses) [were] large, increasing the likelihood of a cause-and-effect relationship,” said investigators led by gastroenterologist Liam Zakko, MD, now at the Mayo Clinic in Rochester, Minn. (Clin Gastroenterol Hepatol. 2016 Jul 25. doi: 10.1016/j.cgh.2016.07.017).
Current guidelines suggest platelet transfusions are an option for antiplatelet patients with serious GI bleeds, but the Yale team found that they did not reduce rebleeding. “The observation of increased mortality without documentation of clinical benefit suggests a very cautious approach to the use of platelet transfusion. ... We do not support the use of platelet transfusions in patients with GI [bleeds] who are taking antiplatelet agents,” the investigators wrote.
Subjects in the two groups were matched for sex, age, and GI bleed location, and all had platelet counts above 100 × 109/L. Almost everyone was on aspirin for cardiovascular protection, and 30% were on also on clopidogrel.
Just over half in both groups had upper GI bleeds, and about 40% in each group had colonic bleeds. Transfused patients had more-severe bleeding, with overall lower blood pressure and lower hemoglobin; a larger proportion was admitted to the ICU.
On univariate analyses, platelet patients had more cardiovascular events (23% vs. 13%) while in the hospital. They were also more likely to stay in the hospital for more than 4 days (47% vs. 33%) and more likely to die while there (7% vs. 1%). On multivariable analysis, only the greater risk for death during admission remained statistically significant (odds ratio, 5.57; 95% confidence interval, 1.52-27.1). The adjusted odds ratio for recurrent bleeding was not significant.
Four patients in the platelet group died from cardiovascular causes. One patient in the control group had a fatal cardiovascular event.
Although counterintuitive, the authors said that it’s possible that platelet transfusions might actually increase the risk of severe and fatal GI bleeding. “Mechanisms by which platelet transfusion would increase mortality or [GI bleeding]–related mortality are not clear,” but “platelet transfusions are reported to be proinflammatory and alter recipient immunity,” they said.
At least for now, “the most prudent way to manage patients on antiplatelet agents with [GI bleeding] is to follow current evidence-based recommendations,” including early endoscopy, endoscopic hemostatic therapy for high-risk lesions, and intensive proton pump inhibitor therapy in patients with ulcers and high-risk endoscopic features.
“Although not based on high-quality evidence, we believe that hemostatic techniques that do not cause significant tissue damage (e.g., clips rather than thermal devices or sclerosants) should be used in patients on antiplatelet agents, especially if patients are expected to remain on these agents in the future,” they said.
The mean age in the study was 74 years, and about two-thirds of the subjects were men.
The authors had no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:
Major finding: Compared with those not transfused, the risk for death during admission remained statistically significant on multivariate analysis (OR, 5.57; 95% CI, 1.52-27.1).
Data source: Retrospective cohort study of 408 GI bleed patients
Disclosures: The authors had no disclosures.
Healthy relatives of IBD patients have intestinal dysbiosis
Healthy first-degree relatives of children and adolescents with inflammatory bowel disease had intestinal dysbiosis and an altered intestinal metabolome that correlated with one another and with the disease state, researchers reported in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
These findings suggest the existence of a “high-risk microbiome/metabolome” that may increase susceptibility to inflammatory bowel disease (IBD), Jonathan Jacobs, MD, of the University of California, Los Angeles, reported with his associates. Among the healthy relatives with dysbiosis, nearly one-third also had elevated levels of fecal calprotectin, a marker of intestinal inflammation that has been previously reported in family members of patients with ulcerative colitis, the researchers noted. “If validated, prospective identification of [high-risk individuals] creates the opportunity to prevent disease development by targeting the dysbiosis and/or its metabolic consequences in the intestine,” they wrote.
Participants in the study fell into one of two “operational taxonomic units” based on their microbial communities, the researchers said. The second taxonomic unit not only was associated with IBD, “but irrespective of disease status, had lower microbial diversity and characteristic shifts in microbial composition, including increased Enterobacteriaceae, consistent with dysbiosis.” Among 21 families in the study, 19 had at least one member in this group. Furthermore, tests of an independent pediatric cohort revealed this same taxonomic group characterized by low microbial diversity and associated with IBD.
Participants also fell into two distinct metabotypes, one of which was associated with IBD and had increased levels of bile acids and amino acid derivatives previously linked to Crohn’s disease, as well as elevated levels of taurine, tryptophan, serinyl tryptophan, and adrenic acid, an omega-6 fatty acid, the researchers said. Taxonomic units and metabolic groups correlated highly with one another among both IBD patients and healthy relatives (P = 3 × 10-8), suggesting a “functional relationship between the microbiome and the metabolome,” the investigators said. Additionally, although most healthy relatives had normal fecal calprotectin levels, those in the second operational taxonomic unit had about sixfold greater odds of elevated calprotectin, compared with those in the first group (P = .05).
“The existence of an IBD-associated operational taxonomic unit type and metabotype in healthy relatives suggests that dysbiosis with its associated metabolic products may be a preexisting trait that precedes the acquisition of [inflammatory bowel] disease,” the investigators concluded. “Validating this interpretation will require prospective longitudinal studies to assess the incidence of IBD in individuals stratified by operational taxonomic type, metabotype, and calprotectin, and to assess the stability of operational taxonomic unit types and metabotypes across time and diet.”
The research was supported by the Helmsley Charitable Trust, the Crohn’s and Colitis Foundation of America, the Fineberg Foundation, the United States Public Health Service, the National Institutes of Health, the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute, the European Union, and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics. The investigators had no conflicts of interest.
Numerous studies have established an association between intestinal dysbiosis and inflammatory bowel disease, and data from mouse models of colitis show that IBD-associated microbiota can exacerbate ongoing inflammation. Still, it is not clear that dysbiosis is either necessary or sufficient to trigger IBD – it could be that the microbiome must first be shaped by an inflammatory state on the host’s side before it can achieve a pathogenic signature and contribute to disease. New findings reported here speak to this question by demonstrating the presence of an IBD-like intestinal microbiome signature in a high-risk population, healthy first-degree relatives of IBD patients. The observation of dysbiosis in at-risk but asymptomatic individuals is an important step toward understanding the sequence of disease onset, raising the provocative possibility that, at least in some cases, dysbiosis is a predisease state, and could potentially be an instigator. The key next step will be longitudinal studies testing the predictive power of these findings. If healthy relatives with the IBD-associated microbiome signatures proceed to develop disease at an increased rate versus relatives with normal gut flora, these signatures would have potential clinical utility either as a screening and risk-assessment tool, or possibly as a target for preventative treatment.
Mark R. Frey, PhD, is assistant professor of pediatrics and biochemistry & molecular medicine at the Saban Research Institute at Children’s Hospital Los Angeles, University of Southern California, Los Angeles. He has no conflicts of interest to disclose.
Numerous studies have established an association between intestinal dysbiosis and inflammatory bowel disease, and data from mouse models of colitis show that IBD-associated microbiota can exacerbate ongoing inflammation. Still, it is not clear that dysbiosis is either necessary or sufficient to trigger IBD – it could be that the microbiome must first be shaped by an inflammatory state on the host’s side before it can achieve a pathogenic signature and contribute to disease. New findings reported here speak to this question by demonstrating the presence of an IBD-like intestinal microbiome signature in a high-risk population, healthy first-degree relatives of IBD patients. The observation of dysbiosis in at-risk but asymptomatic individuals is an important step toward understanding the sequence of disease onset, raising the provocative possibility that, at least in some cases, dysbiosis is a predisease state, and could potentially be an instigator. The key next step will be longitudinal studies testing the predictive power of these findings. If healthy relatives with the IBD-associated microbiome signatures proceed to develop disease at an increased rate versus relatives with normal gut flora, these signatures would have potential clinical utility either as a screening and risk-assessment tool, or possibly as a target for preventative treatment.
Mark R. Frey, PhD, is assistant professor of pediatrics and biochemistry & molecular medicine at the Saban Research Institute at Children’s Hospital Los Angeles, University of Southern California, Los Angeles. He has no conflicts of interest to disclose.
Numerous studies have established an association between intestinal dysbiosis and inflammatory bowel disease, and data from mouse models of colitis show that IBD-associated microbiota can exacerbate ongoing inflammation. Still, it is not clear that dysbiosis is either necessary or sufficient to trigger IBD – it could be that the microbiome must first be shaped by an inflammatory state on the host’s side before it can achieve a pathogenic signature and contribute to disease. New findings reported here speak to this question by demonstrating the presence of an IBD-like intestinal microbiome signature in a high-risk population, healthy first-degree relatives of IBD patients. The observation of dysbiosis in at-risk but asymptomatic individuals is an important step toward understanding the sequence of disease onset, raising the provocative possibility that, at least in some cases, dysbiosis is a predisease state, and could potentially be an instigator. The key next step will be longitudinal studies testing the predictive power of these findings. If healthy relatives with the IBD-associated microbiome signatures proceed to develop disease at an increased rate versus relatives with normal gut flora, these signatures would have potential clinical utility either as a screening and risk-assessment tool, or possibly as a target for preventative treatment.
Mark R. Frey, PhD, is assistant professor of pediatrics and biochemistry & molecular medicine at the Saban Research Institute at Children’s Hospital Los Angeles, University of Southern California, Los Angeles. He has no conflicts of interest to disclose.
Healthy first-degree relatives of children and adolescents with inflammatory bowel disease had intestinal dysbiosis and an altered intestinal metabolome that correlated with one another and with the disease state, researchers reported in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
These findings suggest the existence of a “high-risk microbiome/metabolome” that may increase susceptibility to inflammatory bowel disease (IBD), Jonathan Jacobs, MD, of the University of California, Los Angeles, reported with his associates. Among the healthy relatives with dysbiosis, nearly one-third also had elevated levels of fecal calprotectin, a marker of intestinal inflammation that has been previously reported in family members of patients with ulcerative colitis, the researchers noted. “If validated, prospective identification of [high-risk individuals] creates the opportunity to prevent disease development by targeting the dysbiosis and/or its metabolic consequences in the intestine,” they wrote.
Participants in the study fell into one of two “operational taxonomic units” based on their microbial communities, the researchers said. The second taxonomic unit not only was associated with IBD, “but irrespective of disease status, had lower microbial diversity and characteristic shifts in microbial composition, including increased Enterobacteriaceae, consistent with dysbiosis.” Among 21 families in the study, 19 had at least one member in this group. Furthermore, tests of an independent pediatric cohort revealed this same taxonomic group characterized by low microbial diversity and associated with IBD.
Participants also fell into two distinct metabotypes, one of which was associated with IBD and had increased levels of bile acids and amino acid derivatives previously linked to Crohn’s disease, as well as elevated levels of taurine, tryptophan, serinyl tryptophan, and adrenic acid, an omega-6 fatty acid, the researchers said. Taxonomic units and metabolic groups correlated highly with one another among both IBD patients and healthy relatives (P = 3 × 10-8), suggesting a “functional relationship between the microbiome and the metabolome,” the investigators said. Additionally, although most healthy relatives had normal fecal calprotectin levels, those in the second operational taxonomic unit had about sixfold greater odds of elevated calprotectin, compared with those in the first group (P = .05).
“The existence of an IBD-associated operational taxonomic unit type and metabotype in healthy relatives suggests that dysbiosis with its associated metabolic products may be a preexisting trait that precedes the acquisition of [inflammatory bowel] disease,” the investigators concluded. “Validating this interpretation will require prospective longitudinal studies to assess the incidence of IBD in individuals stratified by operational taxonomic type, metabotype, and calprotectin, and to assess the stability of operational taxonomic unit types and metabotypes across time and diet.”
The research was supported by the Helmsley Charitable Trust, the Crohn’s and Colitis Foundation of America, the Fineberg Foundation, the United States Public Health Service, the National Institutes of Health, the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute, the European Union, and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics. The investigators had no conflicts of interest.
Healthy first-degree relatives of children and adolescents with inflammatory bowel disease had intestinal dysbiosis and an altered intestinal metabolome that correlated with one another and with the disease state, researchers reported in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
These findings suggest the existence of a “high-risk microbiome/metabolome” that may increase susceptibility to inflammatory bowel disease (IBD), Jonathan Jacobs, MD, of the University of California, Los Angeles, reported with his associates. Among the healthy relatives with dysbiosis, nearly one-third also had elevated levels of fecal calprotectin, a marker of intestinal inflammation that has been previously reported in family members of patients with ulcerative colitis, the researchers noted. “If validated, prospective identification of [high-risk individuals] creates the opportunity to prevent disease development by targeting the dysbiosis and/or its metabolic consequences in the intestine,” they wrote.
Participants in the study fell into one of two “operational taxonomic units” based on their microbial communities, the researchers said. The second taxonomic unit not only was associated with IBD, “but irrespective of disease status, had lower microbial diversity and characteristic shifts in microbial composition, including increased Enterobacteriaceae, consistent with dysbiosis.” Among 21 families in the study, 19 had at least one member in this group. Furthermore, tests of an independent pediatric cohort revealed this same taxonomic group characterized by low microbial diversity and associated with IBD.
Participants also fell into two distinct metabotypes, one of which was associated with IBD and had increased levels of bile acids and amino acid derivatives previously linked to Crohn’s disease, as well as elevated levels of taurine, tryptophan, serinyl tryptophan, and adrenic acid, an omega-6 fatty acid, the researchers said. Taxonomic units and metabolic groups correlated highly with one another among both IBD patients and healthy relatives (P = 3 × 10-8), suggesting a “functional relationship between the microbiome and the metabolome,” the investigators said. Additionally, although most healthy relatives had normal fecal calprotectin levels, those in the second operational taxonomic unit had about sixfold greater odds of elevated calprotectin, compared with those in the first group (P = .05).
“The existence of an IBD-associated operational taxonomic unit type and metabotype in healthy relatives suggests that dysbiosis with its associated metabolic products may be a preexisting trait that precedes the acquisition of [inflammatory bowel] disease,” the investigators concluded. “Validating this interpretation will require prospective longitudinal studies to assess the incidence of IBD in individuals stratified by operational taxonomic type, metabotype, and calprotectin, and to assess the stability of operational taxonomic unit types and metabotypes across time and diet.”
The research was supported by the Helmsley Charitable Trust, the Crohn’s and Colitis Foundation of America, the Fineberg Foundation, the United States Public Health Service, the National Institutes of Health, the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute, the European Union, and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics. The investigators had no conflicts of interest.
Key clinical point: Healthy first-degree relatives of patients with remitted inflammatory bowel disease can have intestinal dysbiosis and an altered intestinal metabolome that may signify subclinical inflammation or a “pre-IBD” state.
Major finding: Nineteen of 21 families had at least one member whose microbial taxonomy and metabolome correlated with IBD.
Data source: A cross-sectional study of 21 pediatric and adolescent probands with inflammatory bowel disease, nine parents and six siblings with IBD, and 54 healthy first-degree relatives.
Disclosures: The research was supported by the Helmsley Charitable Trust, the Crohn’s and Colitis Foundation of America, the Fineberg Foundation, the United States Public Health Service, the National Institutes of Health, the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute, the European Union, and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics. The investigators had no conflicts of interest.
Interferon-free HCV treatment can lead to herpesvirus reactivation, experts say
Interferon-free direct-acting antiviral (DAA) regimens for chronic hepatitis C virus (HCV) infection can cause reactivation of herpesvirus, said the authors of a multicenter case series published in the November issue of Clinical Gastroenterology and Hepatology.
Reactivation occurred in 10 of 576 (2%) patients treated at three hospitals in Spain, reported Dr. Christie Perello of Puerta de Hierro University Hospital in Madrid, together with her associates. Clinicians who treat HCV should maintain a high degree of clinical suspicion for latent herpesvirus infection, particularly when patients are older or have undergone liver transplantation, and should consider varicella zoster virus vaccination before beginning DAA therapy in nontransplant patients, they said.
In all, 2% of patients had herpesvirus reactivations a median of 8 weeks after starting an interferon-free DAA regimen. Seven patients had cirrhosis, three were liver transplant recipients, and all achieved a sustained viral response. Seven patients were receiving sofosbuvir with ledipasvir, either with or without ribavirin; two patients were receiving ombitasvir with paritaprevir and ritonavir plus dasabuvir, with or without ribavirin; and one patient was receiving sofosbuvir with simeprevir plus ribavirin. Median age was 67 years. Seven cases involved cutaneous herpes, two involved ocular herpes, and one was herpes labialis. Two patients developed postherpetic neuralgia requiring gabapentin or pregabalin therapy, and one developed keratouveitis that was treated with valacyclovir (1 g every 8 hours for 7 days). Two other patients also received valacyclovir, three received famciclovir, and the remaining four received acyclovir. When the study was published, one patient, a 68-year-old male with postherpetic neuralgia, had residual symptoms even after undergoing antiviral therapy and nerve ablation. This patient was a liver transplantee and therefore was immunosuppressed, but like the others, he only developed herpesvirus reactivation after starting DAA HCV treatment, the researcher said.
In contrast, there were no reactivations among historical controls during a median of 37 months of follow-up. “Even when a causal relationship is not definitive, based on the temporal association and recent experience we conclude that the incidence of herpesvirus reactivation may be increased among patients on interferon-free regimens,” the researchers concluded. “More research is necessary in this new field because unexpected events might be arising in patients treated with direct-acting antivirals.”
The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.
Interferon-free direct-acting antiviral (DAA) regimens for chronic hepatitis C virus (HCV) infection can cause reactivation of herpesvirus, said the authors of a multicenter case series published in the November issue of Clinical Gastroenterology and Hepatology.
Reactivation occurred in 10 of 576 (2%) patients treated at three hospitals in Spain, reported Dr. Christie Perello of Puerta de Hierro University Hospital in Madrid, together with her associates. Clinicians who treat HCV should maintain a high degree of clinical suspicion for latent herpesvirus infection, particularly when patients are older or have undergone liver transplantation, and should consider varicella zoster virus vaccination before beginning DAA therapy in nontransplant patients, they said.
In all, 2% of patients had herpesvirus reactivations a median of 8 weeks after starting an interferon-free DAA regimen. Seven patients had cirrhosis, three were liver transplant recipients, and all achieved a sustained viral response. Seven patients were receiving sofosbuvir with ledipasvir, either with or without ribavirin; two patients were receiving ombitasvir with paritaprevir and ritonavir plus dasabuvir, with or without ribavirin; and one patient was receiving sofosbuvir with simeprevir plus ribavirin. Median age was 67 years. Seven cases involved cutaneous herpes, two involved ocular herpes, and one was herpes labialis. Two patients developed postherpetic neuralgia requiring gabapentin or pregabalin therapy, and one developed keratouveitis that was treated with valacyclovir (1 g every 8 hours for 7 days). Two other patients also received valacyclovir, three received famciclovir, and the remaining four received acyclovir. When the study was published, one patient, a 68-year-old male with postherpetic neuralgia, had residual symptoms even after undergoing antiviral therapy and nerve ablation. This patient was a liver transplantee and therefore was immunosuppressed, but like the others, he only developed herpesvirus reactivation after starting DAA HCV treatment, the researcher said.
In contrast, there were no reactivations among historical controls during a median of 37 months of follow-up. “Even when a causal relationship is not definitive, based on the temporal association and recent experience we conclude that the incidence of herpesvirus reactivation may be increased among patients on interferon-free regimens,” the researchers concluded. “More research is necessary in this new field because unexpected events might be arising in patients treated with direct-acting antivirals.”
The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.
Interferon-free direct-acting antiviral (DAA) regimens for chronic hepatitis C virus (HCV) infection can cause reactivation of herpesvirus, said the authors of a multicenter case series published in the November issue of Clinical Gastroenterology and Hepatology.
Reactivation occurred in 10 of 576 (2%) patients treated at three hospitals in Spain, reported Dr. Christie Perello of Puerta de Hierro University Hospital in Madrid, together with her associates. Clinicians who treat HCV should maintain a high degree of clinical suspicion for latent herpesvirus infection, particularly when patients are older or have undergone liver transplantation, and should consider varicella zoster virus vaccination before beginning DAA therapy in nontransplant patients, they said.
In all, 2% of patients had herpesvirus reactivations a median of 8 weeks after starting an interferon-free DAA regimen. Seven patients had cirrhosis, three were liver transplant recipients, and all achieved a sustained viral response. Seven patients were receiving sofosbuvir with ledipasvir, either with or without ribavirin; two patients were receiving ombitasvir with paritaprevir and ritonavir plus dasabuvir, with or without ribavirin; and one patient was receiving sofosbuvir with simeprevir plus ribavirin. Median age was 67 years. Seven cases involved cutaneous herpes, two involved ocular herpes, and one was herpes labialis. Two patients developed postherpetic neuralgia requiring gabapentin or pregabalin therapy, and one developed keratouveitis that was treated with valacyclovir (1 g every 8 hours for 7 days). Two other patients also received valacyclovir, three received famciclovir, and the remaining four received acyclovir. When the study was published, one patient, a 68-year-old male with postherpetic neuralgia, had residual symptoms even after undergoing antiviral therapy and nerve ablation. This patient was a liver transplantee and therefore was immunosuppressed, but like the others, he only developed herpesvirus reactivation after starting DAA HCV treatment, the researcher said.
In contrast, there were no reactivations among historical controls during a median of 37 months of follow-up. “Even when a causal relationship is not definitive, based on the temporal association and recent experience we conclude that the incidence of herpesvirus reactivation may be increased among patients on interferon-free regimens,” the researchers concluded. “More research is necessary in this new field because unexpected events might be arising in patients treated with direct-acting antivirals.”
The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.
Key clinical point: Latent herpesvirus infection may reactivate with interferon-free direct-acting antiviral treatment for chronic hepatitis C virus infection.
Major finding: In all, 2% of recipients of these regimens had herpesvirus reactivation a median of 8 weeks after starting treatment. Historical controls had no documented reactivations.
Data source: A multicenter retrospective study of 576 HCV-infected patients treated with interferon-free DAA regimens and 230 historical matched controls.
Disclosures: The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.
Study reinforces need to properly examine proximal large bowel during colonoscopy
Interval colorectal cancers were proximally located and had DNA mismatch repair deficiency significantly more often than did colorectal cancers in colonoscopy-naive patients, researchers reported in the November issue of Gastroenterology.
The findings underscore the need to effectively visualize the large colon to avoid missing lesions during colonoscopy, said Elena M. Stoffel, MD, MPH, of the University of Michigan Health System, Ann Arbor, and her associates. “Studies consistently show that colonoscopy affords less protection against proximal cancers, and DNA mismatch repair deficiency tumors are more frequent among proximal cancers,” they noted. But the proximal and distal colon also have different embryologic origins and gene expression profiles, “prompting some to suggest that these might be considered as two distinct organs. Whether the precursors of postcolonoscopy colorectal cancers are simply harder to detect or resect endoscopically, or whether their behavior differs on the basis of anatomic location or molecular subtype remains unclear,” they added.
A variety of quality-related factors contribute to the risk of postcolonoscopy or interval colorectal cancer, as do clinical characteristics such as older age at diagnosis, proximal tumor location, family history of colorectal cancer, and previous polypectomy, the investigators noted. To further explore the clinical and molecular correlates of postcolonoscopy tumors, they conducted a cross-sectional study of 10,365 colorectal cancers diagnosed in Denmark between 2007 and 2011 (Gastroenterology. 2016 Jul 18. doi: 10.1053/j.gastro.2016.07.010). A total of 725 (7%) of the colorectal cancers occurred after colonoscopy, the researchers determined. These lesions were significantly more often located in the proximal colon (odds ratio, 2.34; 95% confidence interval, 1.90-2.89) and were more likely to have DNA mismatch repair deficiency (OR, 1.26; 95% CI, 1.00-59) when compared with colorectal cancers diagnosed in patients with no prior colonoscopy. However, they also were significantly less likely to be metastatic at presentation (OR, 0.65; 95% CI, 0.48-0.89). Interval colorectal cancers were particularly likely to be located in the proximal colon and/or to have DNA mismatch repair deficiency when diagnosed 3-6 years after colonoscopy, but the excess burden of these characteristics persisted up to 10 years after colonoscopy, the researchers said.
Molecular analyses of 85 postcolonoscopy colorectal cancers from one hospital indicated that 24% had DNA mismatch repair deficiency. When considering only those tumors diagnosed within 10 years after colonoscopy, 27% had KRAS/NRAS mutations, 19% had BRAF mutations, and 19% had PIK3CA mutations. The 7% of tumors with molecular features of Lynch syndrome all occurred within 10 years after index colonoscopy and accounted for a third of cases of DNA mismatch repair deficiency, reflecting the role of this mutation pathway in Lynch syndrome and its tendency to rapidly progress, the investigators said.
Notably, 38% of colorectal cancers diagnosed within a year after colonoscopy involved an incomplete examination, compared with only 16% of cases diagnosed within 1-10 years after colonoscopy, they also reported. This finding and the clinical and molecular correlates of the interval cancers “supports the popular assumption that many cancers diagnosed soon after colonoscopy result from missed lesions,” they concluded. “However, the heterogeneity in clinical and molecular features of cancers diagnosed at different time intervals suggests postcolonoscopy colorectal cancers are likely multifactorial in their etiology and clinical behavior.”
The study was supported by the Danish Cancer Society, the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, M.D. Anderson Cancer Center, and a University of Texas Frederick Becker Distinguished University Chair in Cancer Research. The investigators had no disclosures.
Interval colorectal cancers were proximally located and had DNA mismatch repair deficiency significantly more often than did colorectal cancers in colonoscopy-naive patients, researchers reported in the November issue of Gastroenterology.
The findings underscore the need to effectively visualize the large colon to avoid missing lesions during colonoscopy, said Elena M. Stoffel, MD, MPH, of the University of Michigan Health System, Ann Arbor, and her associates. “Studies consistently show that colonoscopy affords less protection against proximal cancers, and DNA mismatch repair deficiency tumors are more frequent among proximal cancers,” they noted. But the proximal and distal colon also have different embryologic origins and gene expression profiles, “prompting some to suggest that these might be considered as two distinct organs. Whether the precursors of postcolonoscopy colorectal cancers are simply harder to detect or resect endoscopically, or whether their behavior differs on the basis of anatomic location or molecular subtype remains unclear,” they added.
A variety of quality-related factors contribute to the risk of postcolonoscopy or interval colorectal cancer, as do clinical characteristics such as older age at diagnosis, proximal tumor location, family history of colorectal cancer, and previous polypectomy, the investigators noted. To further explore the clinical and molecular correlates of postcolonoscopy tumors, they conducted a cross-sectional study of 10,365 colorectal cancers diagnosed in Denmark between 2007 and 2011 (Gastroenterology. 2016 Jul 18. doi: 10.1053/j.gastro.2016.07.010). A total of 725 (7%) of the colorectal cancers occurred after colonoscopy, the researchers determined. These lesions were significantly more often located in the proximal colon (odds ratio, 2.34; 95% confidence interval, 1.90-2.89) and were more likely to have DNA mismatch repair deficiency (OR, 1.26; 95% CI, 1.00-59) when compared with colorectal cancers diagnosed in patients with no prior colonoscopy. However, they also were significantly less likely to be metastatic at presentation (OR, 0.65; 95% CI, 0.48-0.89). Interval colorectal cancers were particularly likely to be located in the proximal colon and/or to have DNA mismatch repair deficiency when diagnosed 3-6 years after colonoscopy, but the excess burden of these characteristics persisted up to 10 years after colonoscopy, the researchers said.
Molecular analyses of 85 postcolonoscopy colorectal cancers from one hospital indicated that 24% had DNA mismatch repair deficiency. When considering only those tumors diagnosed within 10 years after colonoscopy, 27% had KRAS/NRAS mutations, 19% had BRAF mutations, and 19% had PIK3CA mutations. The 7% of tumors with molecular features of Lynch syndrome all occurred within 10 years after index colonoscopy and accounted for a third of cases of DNA mismatch repair deficiency, reflecting the role of this mutation pathway in Lynch syndrome and its tendency to rapidly progress, the investigators said.
Notably, 38% of colorectal cancers diagnosed within a year after colonoscopy involved an incomplete examination, compared with only 16% of cases diagnosed within 1-10 years after colonoscopy, they also reported. This finding and the clinical and molecular correlates of the interval cancers “supports the popular assumption that many cancers diagnosed soon after colonoscopy result from missed lesions,” they concluded. “However, the heterogeneity in clinical and molecular features of cancers diagnosed at different time intervals suggests postcolonoscopy colorectal cancers are likely multifactorial in their etiology and clinical behavior.”
The study was supported by the Danish Cancer Society, the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, M.D. Anderson Cancer Center, and a University of Texas Frederick Becker Distinguished University Chair in Cancer Research. The investigators had no disclosures.
Interval colorectal cancers were proximally located and had DNA mismatch repair deficiency significantly more often than did colorectal cancers in colonoscopy-naive patients, researchers reported in the November issue of Gastroenterology.
The findings underscore the need to effectively visualize the large colon to avoid missing lesions during colonoscopy, said Elena M. Stoffel, MD, MPH, of the University of Michigan Health System, Ann Arbor, and her associates. “Studies consistently show that colonoscopy affords less protection against proximal cancers, and DNA mismatch repair deficiency tumors are more frequent among proximal cancers,” they noted. But the proximal and distal colon also have different embryologic origins and gene expression profiles, “prompting some to suggest that these might be considered as two distinct organs. Whether the precursors of postcolonoscopy colorectal cancers are simply harder to detect or resect endoscopically, or whether their behavior differs on the basis of anatomic location or molecular subtype remains unclear,” they added.
A variety of quality-related factors contribute to the risk of postcolonoscopy or interval colorectal cancer, as do clinical characteristics such as older age at diagnosis, proximal tumor location, family history of colorectal cancer, and previous polypectomy, the investigators noted. To further explore the clinical and molecular correlates of postcolonoscopy tumors, they conducted a cross-sectional study of 10,365 colorectal cancers diagnosed in Denmark between 2007 and 2011 (Gastroenterology. 2016 Jul 18. doi: 10.1053/j.gastro.2016.07.010). A total of 725 (7%) of the colorectal cancers occurred after colonoscopy, the researchers determined. These lesions were significantly more often located in the proximal colon (odds ratio, 2.34; 95% confidence interval, 1.90-2.89) and were more likely to have DNA mismatch repair deficiency (OR, 1.26; 95% CI, 1.00-59) when compared with colorectal cancers diagnosed in patients with no prior colonoscopy. However, they also were significantly less likely to be metastatic at presentation (OR, 0.65; 95% CI, 0.48-0.89). Interval colorectal cancers were particularly likely to be located in the proximal colon and/or to have DNA mismatch repair deficiency when diagnosed 3-6 years after colonoscopy, but the excess burden of these characteristics persisted up to 10 years after colonoscopy, the researchers said.
Molecular analyses of 85 postcolonoscopy colorectal cancers from one hospital indicated that 24% had DNA mismatch repair deficiency. When considering only those tumors diagnosed within 10 years after colonoscopy, 27% had KRAS/NRAS mutations, 19% had BRAF mutations, and 19% had PIK3CA mutations. The 7% of tumors with molecular features of Lynch syndrome all occurred within 10 years after index colonoscopy and accounted for a third of cases of DNA mismatch repair deficiency, reflecting the role of this mutation pathway in Lynch syndrome and its tendency to rapidly progress, the investigators said.
Notably, 38% of colorectal cancers diagnosed within a year after colonoscopy involved an incomplete examination, compared with only 16% of cases diagnosed within 1-10 years after colonoscopy, they also reported. This finding and the clinical and molecular correlates of the interval cancers “supports the popular assumption that many cancers diagnosed soon after colonoscopy result from missed lesions,” they concluded. “However, the heterogeneity in clinical and molecular features of cancers diagnosed at different time intervals suggests postcolonoscopy colorectal cancers are likely multifactorial in their etiology and clinical behavior.”
The study was supported by the Danish Cancer Society, the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, M.D. Anderson Cancer Center, and a University of Texas Frederick Becker Distinguished University Chair in Cancer Research. The investigators had no disclosures.
FROM GASTROENTEROLOGY
Key clinical point: A large population-based study reinforced the need to properly examine the proximal large bowel during colonoscopy.
Major finding: Postcolonoscopy colorectal cancers were significantly more likely to be proximal (OR, 2.34) and to have DNA mismatch repair deficiency (OR, 1.26) compared with colorectal cancers diagnosed in patients with no prior colonoscopy.
Data source: A population-based, cross-sectional study of 10,365 newly diagnosed colorectal cancer cases.
Disclosures: The study was supported by the Danish Cancer Society, the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, M.D. Anderson Cancer Center, and a University of Texas Frederick Becker Distinguished University Chair in Cancer Research. The investigators had no disclosures.