User login
Higher dose of mesalamine can decrease risk of relapse for patients with quiescent ulcerative colitis
Increasing dosages of mesalamine by 2.4 g/d for patients with quiescent ulcerative colitis can dramatically reduce concentrations of fecal calprotectin and ultimately decrease the likelihood of relapse, according to the results of a new Dose Escalation and Remission (DEAR) study published in the November issue of Clinical Gastroenterology and Hepatology (2014;12:1887-93.e3).
In an open-label, randomized controlled trial, 119 patients with quiescent ulcerative colitis (UC) in remission were screened for Simple Clinical Colitis Activity Index scores, fecal calprotectin (FC) of 50 mcg/gram, and intake of no more than 3 g of mesalamine per day between October 2008 and March 2012. These subjects were divided into four groups based on FC levels, with Group 1 comprising 58 representing a baseline of FC < 50 mcg/gram, and groups 2-4 having 61 individuals with elevated baseline FC levels. Group 1 patients were retained for an observational follow-up study but were not included in the randomized controlled trial.
Participants were either told to maintain their current medication regimen or were prescribed a multimatrix mesalamine of either 2.4 or 4.8 g/d for 6 weeks, depending on their initial FC levels, after which point FC levels were taken. Participants in Group 2 with FC < 50 mcg/g were kept in an observational follow-up study group, while the rest of the participants were randomly assigned to continue their 2.4 g/d regimen, or increase their intake to 4.8 g/d.
Individuals in Group 3 with FC levels greater than 50 mcg/g were randomly assigned to either the 2.4- or 4.8-g/d regimen for 6 weeks; after that point, those whose FC levels had decreased below 50 continued with their regimen while those whose FC levels remained high were upped to 4.8 g/d. Subjects in Group 4 who were not already on a multimatrix mesalamine regimen and whose FC levels were above 50 mcg/g were randomized to continue their medication or add 2.4 g/d of mesalamine; after 6 weeks, if FC levels remained above 50, the dosage was increased to 4.8 g/d.
The primary outcome of continued remission with FC no greater than 50 mcg/g was observed in 3.8% of controls and 26.9% of participants in the dose escalation group (P = .0496). Others within the same group experienced secondary outcomes of FC levels below 100 mcg/gram (P = .04) and below 200 mcg/g (P = .005). Furthermore, among patients who were in remission during the randomization phase of the study, relapse occurred far sooner in those whose FC was above 200 mcg/g than those whose FC levels were below that mark.
“Our study adds to the evidence supporting FC concentration as a valid biomarker for UC,” said lead authors Dr. Mark T. Osterman and Dr. Faten N. Aberra of the University of Pennsylvania’s department of medicine, Philadelphia. “Perhaps more importantly, our results offer a novel way to use FC testing to positively impact outcomes in UC. We demonstrated efficacy of intervention to reduce FC (a surrogate for mucosal inflammation) before symptoms develop in patients at potentially increased risk of relapse.”
Dr. Osterman is a consultant for AbbVie, Elan, Janssen, and UCB and receives research funding from UCB. Dr. Aberra is a consultant for Janssen and research investigator for Amgen, Janssen, and UCB. Other coauthors disclosed ties to numerous pharmaceutical companies.
Increasing dosages of mesalamine by 2.4 g/d for patients with quiescent ulcerative colitis can dramatically reduce concentrations of fecal calprotectin and ultimately decrease the likelihood of relapse, according to the results of a new Dose Escalation and Remission (DEAR) study published in the November issue of Clinical Gastroenterology and Hepatology (2014;12:1887-93.e3).
In an open-label, randomized controlled trial, 119 patients with quiescent ulcerative colitis (UC) in remission were screened for Simple Clinical Colitis Activity Index scores, fecal calprotectin (FC) of 50 mcg/gram, and intake of no more than 3 g of mesalamine per day between October 2008 and March 2012. These subjects were divided into four groups based on FC levels, with Group 1 comprising 58 representing a baseline of FC < 50 mcg/gram, and groups 2-4 having 61 individuals with elevated baseline FC levels. Group 1 patients were retained for an observational follow-up study but were not included in the randomized controlled trial.
Participants were either told to maintain their current medication regimen or were prescribed a multimatrix mesalamine of either 2.4 or 4.8 g/d for 6 weeks, depending on their initial FC levels, after which point FC levels were taken. Participants in Group 2 with FC < 50 mcg/g were kept in an observational follow-up study group, while the rest of the participants were randomly assigned to continue their 2.4 g/d regimen, or increase their intake to 4.8 g/d.
Individuals in Group 3 with FC levels greater than 50 mcg/g were randomly assigned to either the 2.4- or 4.8-g/d regimen for 6 weeks; after that point, those whose FC levels had decreased below 50 continued with their regimen while those whose FC levels remained high were upped to 4.8 g/d. Subjects in Group 4 who were not already on a multimatrix mesalamine regimen and whose FC levels were above 50 mcg/g were randomized to continue their medication or add 2.4 g/d of mesalamine; after 6 weeks, if FC levels remained above 50, the dosage was increased to 4.8 g/d.
The primary outcome of continued remission with FC no greater than 50 mcg/g was observed in 3.8% of controls and 26.9% of participants in the dose escalation group (P = .0496). Others within the same group experienced secondary outcomes of FC levels below 100 mcg/gram (P = .04) and below 200 mcg/g (P = .005). Furthermore, among patients who were in remission during the randomization phase of the study, relapse occurred far sooner in those whose FC was above 200 mcg/g than those whose FC levels were below that mark.
“Our study adds to the evidence supporting FC concentration as a valid biomarker for UC,” said lead authors Dr. Mark T. Osterman and Dr. Faten N. Aberra of the University of Pennsylvania’s department of medicine, Philadelphia. “Perhaps more importantly, our results offer a novel way to use FC testing to positively impact outcomes in UC. We demonstrated efficacy of intervention to reduce FC (a surrogate for mucosal inflammation) before symptoms develop in patients at potentially increased risk of relapse.”
Dr. Osterman is a consultant for AbbVie, Elan, Janssen, and UCB and receives research funding from UCB. Dr. Aberra is a consultant for Janssen and research investigator for Amgen, Janssen, and UCB. Other coauthors disclosed ties to numerous pharmaceutical companies.
Increasing dosages of mesalamine by 2.4 g/d for patients with quiescent ulcerative colitis can dramatically reduce concentrations of fecal calprotectin and ultimately decrease the likelihood of relapse, according to the results of a new Dose Escalation and Remission (DEAR) study published in the November issue of Clinical Gastroenterology and Hepatology (2014;12:1887-93.e3).
In an open-label, randomized controlled trial, 119 patients with quiescent ulcerative colitis (UC) in remission were screened for Simple Clinical Colitis Activity Index scores, fecal calprotectin (FC) of 50 mcg/gram, and intake of no more than 3 g of mesalamine per day between October 2008 and March 2012. These subjects were divided into four groups based on FC levels, with Group 1 comprising 58 representing a baseline of FC < 50 mcg/gram, and groups 2-4 having 61 individuals with elevated baseline FC levels. Group 1 patients were retained for an observational follow-up study but were not included in the randomized controlled trial.
Participants were either told to maintain their current medication regimen or were prescribed a multimatrix mesalamine of either 2.4 or 4.8 g/d for 6 weeks, depending on their initial FC levels, after which point FC levels were taken. Participants in Group 2 with FC < 50 mcg/g were kept in an observational follow-up study group, while the rest of the participants were randomly assigned to continue their 2.4 g/d regimen, or increase their intake to 4.8 g/d.
Individuals in Group 3 with FC levels greater than 50 mcg/g were randomly assigned to either the 2.4- or 4.8-g/d regimen for 6 weeks; after that point, those whose FC levels had decreased below 50 continued with their regimen while those whose FC levels remained high were upped to 4.8 g/d. Subjects in Group 4 who were not already on a multimatrix mesalamine regimen and whose FC levels were above 50 mcg/g were randomized to continue their medication or add 2.4 g/d of mesalamine; after 6 weeks, if FC levels remained above 50, the dosage was increased to 4.8 g/d.
The primary outcome of continued remission with FC no greater than 50 mcg/g was observed in 3.8% of controls and 26.9% of participants in the dose escalation group (P = .0496). Others within the same group experienced secondary outcomes of FC levels below 100 mcg/gram (P = .04) and below 200 mcg/g (P = .005). Furthermore, among patients who were in remission during the randomization phase of the study, relapse occurred far sooner in those whose FC was above 200 mcg/g than those whose FC levels were below that mark.
“Our study adds to the evidence supporting FC concentration as a valid biomarker for UC,” said lead authors Dr. Mark T. Osterman and Dr. Faten N. Aberra of the University of Pennsylvania’s department of medicine, Philadelphia. “Perhaps more importantly, our results offer a novel way to use FC testing to positively impact outcomes in UC. We demonstrated efficacy of intervention to reduce FC (a surrogate for mucosal inflammation) before symptoms develop in patients at potentially increased risk of relapse.”
Dr. Osterman is a consultant for AbbVie, Elan, Janssen, and UCB and receives research funding from UCB. Dr. Aberra is a consultant for Janssen and research investigator for Amgen, Janssen, and UCB. Other coauthors disclosed ties to numerous pharmaceutical companies.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Increasing mesalamine dosage by 2.4 g/d significantly decreases risk of relapse for patients with UC.
Major finding: 26.9% of subjects with dose increase experienced drop in fecal calprotectin level below 50 mcg/g.
Data source: Dose Escalation and Remission (DEAR) study; open-label, randomized controlled trial.
Disclosures: Dr. Osterman is a consultant for AbbVie, Elan, Janssen, and UCB and receives research funding from UCB. Dr. Aberra is a consultant for Janssen and research investigator for Amgen, Janssen, and UCB. Other coauthors disclosed ties to numerous pharmaceutical companies.
Hepatitis E virus mutation linked to ribavirin resistance
A mutation in the hepatitis E virus might contribute to ribavirin treatment failure in transplant recipients with chronic HEV infection, according to a small study published in the November issue of Gastroenterology.
The study is the first to find in vitro evidence for a virulence mutation in HEV, said Dr. Yannick Debing at the University of Leuven in Belgium, Dr. Annett Gisa at the Hanover Medical School in Germany, and their associates.
Courtesy: American Gastroenterological Association
The researchers studied 15 solid-organ transplant recipients who received ribavirin monotherapy for chronic HEV infection. Thirteen patients were successfully treated, but two with genotype 3c infections failed therapy. Viral RNA levels in both of these patients initially dropped and then rose, suggesting emerging resistance to ribavirin therapy, the investigators said (Gastroenterology 2014 Aug. 30 [doi: 10.1053/j.gastro.2014.08.040]).
When the researchers sequenced HEV genomes from the nonresponders, they found a G1634R mutation in HEV viral polymerase that conferred greater replication capacity compared with wild-type HEV, even after in vitro ribavirin treatment, they reported. “It may be interesting to assess the possible use of position 1634 as a prognostic marker, and accordingly to adjust the dose and duration of ribavirin therapy based on the presence of the G1634R variant,” Dr. Debing and his associates said.
The mutation consisted of a G-to-A nucleotide substitution in the C-terminal region of viral polymerase, the investigators said. By comparing HEV sequences in GenBank (an open-access collection of publicly available nucleotide sequences and their proteins), they found that G1634 was the most common amino acid sequence in genotype 3 HEV, while the K1634 sequence predominated in genotypes 1 and 4.
A subgenomic replicon of genotype 3 HEV with the 1634R mutation showed no increase in ribavirin sensitivity, compared with the wild-type replicon (50% effective concentration [EC50] values, 5.1 ± 4.1 mcM and 5.1 ± 3.7 mcM, respectively), the investigators said. But when they tested the 1634R variant in human hepatoma cells, they observed a 3.4-fold increase in luminescence signaling, compared with cells transfected with capped replicon RNA from wild-type HEV (P = .04). Greater luminescence indicated that the 1634R mutation increased viral replication, they said.
In addition, an HEV replicon with the K1634 mutation showed 2.7 times more luminescence compared with cells transfected with wild-type viral RNA (P = .07), the researchers reported.
The investigators next studied the effects of the 1634 R/K mutations on the full-length HEV genome. They introduced HEV with the two variants into human hepatoma cells, measured the amounts of viral RNA released, and found that both variants replicated at higher levels than did wild-type virus. When they treated these cells with 10- or 25-mcM ribavirin, replication levels dropped for the 1634 R/K variants and for wild-type virus, but remained at least twice as high for the variants, they said.
“The increased replication capacity of the mutant may have contributed to the persistent disease courses despite [ribavirin] treatment, although other patient- and virus-related factors could have contributed as well,” the investigators said.
The research was supported by the Research Foundation–Flanders, KU Leuven University, the Robert Koch Institute, Geconcerteerde Onderzoeksactie, the German Federal Ministry for Education and Research, and EU FP7 project SILVER. The authors reported having no conflicts of interest.
A mutation in the hepatitis E virus might contribute to ribavirin treatment failure in transplant recipients with chronic HEV infection, according to a small study published in the November issue of Gastroenterology.
The study is the first to find in vitro evidence for a virulence mutation in HEV, said Dr. Yannick Debing at the University of Leuven in Belgium, Dr. Annett Gisa at the Hanover Medical School in Germany, and their associates.
Courtesy: American Gastroenterological Association
The researchers studied 15 solid-organ transplant recipients who received ribavirin monotherapy for chronic HEV infection. Thirteen patients were successfully treated, but two with genotype 3c infections failed therapy. Viral RNA levels in both of these patients initially dropped and then rose, suggesting emerging resistance to ribavirin therapy, the investigators said (Gastroenterology 2014 Aug. 30 [doi: 10.1053/j.gastro.2014.08.040]).
When the researchers sequenced HEV genomes from the nonresponders, they found a G1634R mutation in HEV viral polymerase that conferred greater replication capacity compared with wild-type HEV, even after in vitro ribavirin treatment, they reported. “It may be interesting to assess the possible use of position 1634 as a prognostic marker, and accordingly to adjust the dose and duration of ribavirin therapy based on the presence of the G1634R variant,” Dr. Debing and his associates said.
The mutation consisted of a G-to-A nucleotide substitution in the C-terminal region of viral polymerase, the investigators said. By comparing HEV sequences in GenBank (an open-access collection of publicly available nucleotide sequences and their proteins), they found that G1634 was the most common amino acid sequence in genotype 3 HEV, while the K1634 sequence predominated in genotypes 1 and 4.
A subgenomic replicon of genotype 3 HEV with the 1634R mutation showed no increase in ribavirin sensitivity, compared with the wild-type replicon (50% effective concentration [EC50] values, 5.1 ± 4.1 mcM and 5.1 ± 3.7 mcM, respectively), the investigators said. But when they tested the 1634R variant in human hepatoma cells, they observed a 3.4-fold increase in luminescence signaling, compared with cells transfected with capped replicon RNA from wild-type HEV (P = .04). Greater luminescence indicated that the 1634R mutation increased viral replication, they said.
In addition, an HEV replicon with the K1634 mutation showed 2.7 times more luminescence compared with cells transfected with wild-type viral RNA (P = .07), the researchers reported.
The investigators next studied the effects of the 1634 R/K mutations on the full-length HEV genome. They introduced HEV with the two variants into human hepatoma cells, measured the amounts of viral RNA released, and found that both variants replicated at higher levels than did wild-type virus. When they treated these cells with 10- or 25-mcM ribavirin, replication levels dropped for the 1634 R/K variants and for wild-type virus, but remained at least twice as high for the variants, they said.
“The increased replication capacity of the mutant may have contributed to the persistent disease courses despite [ribavirin] treatment, although other patient- and virus-related factors could have contributed as well,” the investigators said.
The research was supported by the Research Foundation–Flanders, KU Leuven University, the Robert Koch Institute, Geconcerteerde Onderzoeksactie, the German Federal Ministry for Education and Research, and EU FP7 project SILVER. The authors reported having no conflicts of interest.
A mutation in the hepatitis E virus might contribute to ribavirin treatment failure in transplant recipients with chronic HEV infection, according to a small study published in the November issue of Gastroenterology.
The study is the first to find in vitro evidence for a virulence mutation in HEV, said Dr. Yannick Debing at the University of Leuven in Belgium, Dr. Annett Gisa at the Hanover Medical School in Germany, and their associates.
Courtesy: American Gastroenterological Association
The researchers studied 15 solid-organ transplant recipients who received ribavirin monotherapy for chronic HEV infection. Thirteen patients were successfully treated, but two with genotype 3c infections failed therapy. Viral RNA levels in both of these patients initially dropped and then rose, suggesting emerging resistance to ribavirin therapy, the investigators said (Gastroenterology 2014 Aug. 30 [doi: 10.1053/j.gastro.2014.08.040]).
When the researchers sequenced HEV genomes from the nonresponders, they found a G1634R mutation in HEV viral polymerase that conferred greater replication capacity compared with wild-type HEV, even after in vitro ribavirin treatment, they reported. “It may be interesting to assess the possible use of position 1634 as a prognostic marker, and accordingly to adjust the dose and duration of ribavirin therapy based on the presence of the G1634R variant,” Dr. Debing and his associates said.
The mutation consisted of a G-to-A nucleotide substitution in the C-terminal region of viral polymerase, the investigators said. By comparing HEV sequences in GenBank (an open-access collection of publicly available nucleotide sequences and their proteins), they found that G1634 was the most common amino acid sequence in genotype 3 HEV, while the K1634 sequence predominated in genotypes 1 and 4.
A subgenomic replicon of genotype 3 HEV with the 1634R mutation showed no increase in ribavirin sensitivity, compared with the wild-type replicon (50% effective concentration [EC50] values, 5.1 ± 4.1 mcM and 5.1 ± 3.7 mcM, respectively), the investigators said. But when they tested the 1634R variant in human hepatoma cells, they observed a 3.4-fold increase in luminescence signaling, compared with cells transfected with capped replicon RNA from wild-type HEV (P = .04). Greater luminescence indicated that the 1634R mutation increased viral replication, they said.
In addition, an HEV replicon with the K1634 mutation showed 2.7 times more luminescence compared with cells transfected with wild-type viral RNA (P = .07), the researchers reported.
The investigators next studied the effects of the 1634 R/K mutations on the full-length HEV genome. They introduced HEV with the two variants into human hepatoma cells, measured the amounts of viral RNA released, and found that both variants replicated at higher levels than did wild-type virus. When they treated these cells with 10- or 25-mcM ribavirin, replication levels dropped for the 1634 R/K variants and for wild-type virus, but remained at least twice as high for the variants, they said.
“The increased replication capacity of the mutant may have contributed to the persistent disease courses despite [ribavirin] treatment, although other patient- and virus-related factors could have contributed as well,” the investigators said.
The research was supported by the Research Foundation–Flanders, KU Leuven University, the Robert Koch Institute, Geconcerteerde Onderzoeksactie, the German Federal Ministry for Education and Research, and EU FP7 project SILVER. The authors reported having no conflicts of interest.
Key clinical point: A virulence mutation in the hepatitis E virus (HEV) was associated with ribavirin treatment failure.
Major finding: The mutation was associated with a 3.4-fold increase in luminescence signals, compared with wild-type HEV (P = .04), indicating greater viral replication.
Data source: Study of 15 solid-organ transplant recipients with chronic HEV infection.
Disclosures: The research was supported by the Research Foundation–Flanders, KU Leuven University, the Robert Koch Institute, Geconcerteerde Onderzoeksactie, the German Federal Ministry for Education and Research, and EU FP7 project SILVER. The authors reported having no conflicts of interest.
Topical steroid might improve mucosal integrity in eosinophilic esophagitis
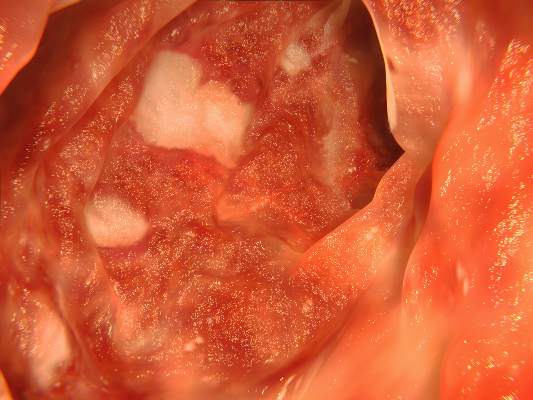
Topical steroid therapy improved some indicators of mucosal integrity in patients with eosinophilic esophagitis, but proton pump inhibitor therapy did not, according to two studies reported in the November issue of Clinical Gastroenterology and Hepatology.
The first study found that topical fluticasone therapy at a dose of 880 mcg twice daily for 2 months helped correct esophageal spongiosis, or dilated intercellular space, in patients with eosinophilic esophagitis (EoE). Spongiosis scores for treated patients were significantly lower than for untreated patients (0.4 vs. 1.3; P = .016), said Dr. David Katzka at the Mayo Clinic in Rochester, Minn. and his associates (Clin. Gastroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.039]).
In the study, histologic analyses also showed that improved spongiosis scores in treated patients correlated with increased density of two tight junction proteins, filaggrin (P = .001) and zonula occludens-3 (P = .016), said the investigators. These proteins might help regulate antigenic penetration of the esophageal mucosa and also could permit migration of white blood cells, they said. “Loss of tight junction regulators and dilation of intercellular spaces appear to be involved in the pathophysiology of EoE and could be targets for treatment,” the researchers concluded. But they also noted that their study did not examine the same patients before and after steroid therapy and did not look at desmosomes, intercellular junctions that past research has suggested might be affected in EoE.
For the second study, Dr. Bram van Rhijn and his associates at the Academic Medical Center in the Netherlands compared endoscopies of 16 patients with dysphagia and suspected (unconfirmed) EoE with 11 controls, both at baseline and after 8 weeks of high-dose esomeprazole treatment. Esophageal mucosal integrity was “severely impaired” in patients with confirmed EoE and in those with proton pump inhibitor–responsive eosinophilia (PPRE), the researchers said (Clin. Gasteroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.037]).
In both forms of disease, molecules as large as 40,000 daltons were able to pass through the compromised esophageal mucosa, Dr. Bram van Rhijn and his associates reported. “This size is similar to the size of most plant and animal food allergens to which EoE patients are sensitized,” they added. Esophageal permeability might increase the rate of immune exposure to allergens, thereby mediating EoE and PPRE, they said.
On mucosal functional tests, both EoE and PPRE were associated with reduced transepithelial electrical resistance and lower electrical tissue impedance, most notably in patients with EoE (P less than .001 for both, compared with controls), the investigators reported. Proton pump inhibitor treatment partially reversed these changes in patients with PPRE but showed no effect for patients with EoE, they said. This finding suggests that acid reflux might play a role in PPRE, but not in EOE, they concluded.
Dr. Katzka and his associates disclosed no funding sources and reported having no conflicts of interest. Dr. Rhijn and his associates were supported by the Netherlands Organization for Scientific Research. Two of Dr. Rhijn’s coauthors reported financial relationships with AstraZeneca, Endostim, Medical Measurement Systems, Shire, and GlaxoSmithKline.
In the past year, the topic of mucosal integrity in eosinophilic esophagitis has garnered growing attention. Epithelial permeability defects have been described in the pathogenesis of GI disorders, including inflammatory bowel disease and celiac sprue, as well as allergic disorders such as atopic dermatitis. In EoE, both experimental as well as clinical studies have shown an eosinophil-predominant inflammatory response to specific antigens, particularly common food allergens. Increased permeability may predispose genetically susceptible individuals to swallowed allergen penetration through the esophageal epithelium. Beneath the epithelial barrier, antigens have access to antigen presenting cells, including dendritic cells, leading to both allergic sensitization and perpetuation of the TH-2 chronic inflammatory response.
|
| Dr. Ikuo Hirano |
The article by Dr. Katzka and his colleagues supports the concept of epithelial barrier defects in EoE through the demonstration of reduced immunohistochemical expression of filaggrin, zonula occludens-3, and claudin-1, important tight junction proteins. Expression was increased in EoE patients treated with topical steroids. Similarly, the study by Dr. van Rhijn and his associates identified impaired mucosal integrity in EoE by a variety of techniques that included electron microscopic demonstration of dilated intercellular spaces, electrical tissue impedance as an in vivo biomarker, and in vitro transepithelial molecular flux in an Ussing chamber. Furthermore, they found that proton pump inhibitor therapy partially restored mucosal permeability defects to a greater degree in patients with PPI-responsive esophageal eosinophilia, compared with patients with EoE. These two studies substantiate studies from the Cincinnati group that previously identified reduced mRNA expression of filaggrin in esophageal mucosal biopsies as well as reduced expression of the intercellular adhesion molecule, desmoglein 1.
In spite of these novel data, the exact role of altered esophageal epithelial permeability in the pathogenesis of EoE is yet unclear. The reversibility of the defect with medical therapy argues against defective cell junction proteins as an intrinsic abnormality. Furthermore, the location of antigen presentation in EoE may occur through other routes such as the small intestine, nasal epithelium, or skin. In the meantime, these studies provide an important advance in our understanding of EoE and open the door to novel therapeutic approaches.
Dr. Ikuo Hirano, AGAF, is professor of medicine at Northwestern University, Chicago. He reported no conflicts of interest.
In the past year, the topic of mucosal integrity in eosinophilic esophagitis has garnered growing attention. Epithelial permeability defects have been described in the pathogenesis of GI disorders, including inflammatory bowel disease and celiac sprue, as well as allergic disorders such as atopic dermatitis. In EoE, both experimental as well as clinical studies have shown an eosinophil-predominant inflammatory response to specific antigens, particularly common food allergens. Increased permeability may predispose genetically susceptible individuals to swallowed allergen penetration through the esophageal epithelium. Beneath the epithelial barrier, antigens have access to antigen presenting cells, including dendritic cells, leading to both allergic sensitization and perpetuation of the TH-2 chronic inflammatory response.
|
| Dr. Ikuo Hirano |
The article by Dr. Katzka and his colleagues supports the concept of epithelial barrier defects in EoE through the demonstration of reduced immunohistochemical expression of filaggrin, zonula occludens-3, and claudin-1, important tight junction proteins. Expression was increased in EoE patients treated with topical steroids. Similarly, the study by Dr. van Rhijn and his associates identified impaired mucosal integrity in EoE by a variety of techniques that included electron microscopic demonstration of dilated intercellular spaces, electrical tissue impedance as an in vivo biomarker, and in vitro transepithelial molecular flux in an Ussing chamber. Furthermore, they found that proton pump inhibitor therapy partially restored mucosal permeability defects to a greater degree in patients with PPI-responsive esophageal eosinophilia, compared with patients with EoE. These two studies substantiate studies from the Cincinnati group that previously identified reduced mRNA expression of filaggrin in esophageal mucosal biopsies as well as reduced expression of the intercellular adhesion molecule, desmoglein 1.
In spite of these novel data, the exact role of altered esophageal epithelial permeability in the pathogenesis of EoE is yet unclear. The reversibility of the defect with medical therapy argues against defective cell junction proteins as an intrinsic abnormality. Furthermore, the location of antigen presentation in EoE may occur through other routes such as the small intestine, nasal epithelium, or skin. In the meantime, these studies provide an important advance in our understanding of EoE and open the door to novel therapeutic approaches.
Dr. Ikuo Hirano, AGAF, is professor of medicine at Northwestern University, Chicago. He reported no conflicts of interest.
In the past year, the topic of mucosal integrity in eosinophilic esophagitis has garnered growing attention. Epithelial permeability defects have been described in the pathogenesis of GI disorders, including inflammatory bowel disease and celiac sprue, as well as allergic disorders such as atopic dermatitis. In EoE, both experimental as well as clinical studies have shown an eosinophil-predominant inflammatory response to specific antigens, particularly common food allergens. Increased permeability may predispose genetically susceptible individuals to swallowed allergen penetration through the esophageal epithelium. Beneath the epithelial barrier, antigens have access to antigen presenting cells, including dendritic cells, leading to both allergic sensitization and perpetuation of the TH-2 chronic inflammatory response.
|
| Dr. Ikuo Hirano |
The article by Dr. Katzka and his colleagues supports the concept of epithelial barrier defects in EoE through the demonstration of reduced immunohistochemical expression of filaggrin, zonula occludens-3, and claudin-1, important tight junction proteins. Expression was increased in EoE patients treated with topical steroids. Similarly, the study by Dr. van Rhijn and his associates identified impaired mucosal integrity in EoE by a variety of techniques that included electron microscopic demonstration of dilated intercellular spaces, electrical tissue impedance as an in vivo biomarker, and in vitro transepithelial molecular flux in an Ussing chamber. Furthermore, they found that proton pump inhibitor therapy partially restored mucosal permeability defects to a greater degree in patients with PPI-responsive esophageal eosinophilia, compared with patients with EoE. These two studies substantiate studies from the Cincinnati group that previously identified reduced mRNA expression of filaggrin in esophageal mucosal biopsies as well as reduced expression of the intercellular adhesion molecule, desmoglein 1.
In spite of these novel data, the exact role of altered esophageal epithelial permeability in the pathogenesis of EoE is yet unclear. The reversibility of the defect with medical therapy argues against defective cell junction proteins as an intrinsic abnormality. Furthermore, the location of antigen presentation in EoE may occur through other routes such as the small intestine, nasal epithelium, or skin. In the meantime, these studies provide an important advance in our understanding of EoE and open the door to novel therapeutic approaches.
Dr. Ikuo Hirano, AGAF, is professor of medicine at Northwestern University, Chicago. He reported no conflicts of interest.
Topical steroid therapy improved some indicators of mucosal integrity in patients with eosinophilic esophagitis, but proton pump inhibitor therapy did not, according to two studies reported in the November issue of Clinical Gastroenterology and Hepatology.
The first study found that topical fluticasone therapy at a dose of 880 mcg twice daily for 2 months helped correct esophageal spongiosis, or dilated intercellular space, in patients with eosinophilic esophagitis (EoE). Spongiosis scores for treated patients were significantly lower than for untreated patients (0.4 vs. 1.3; P = .016), said Dr. David Katzka at the Mayo Clinic in Rochester, Minn. and his associates (Clin. Gastroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.039]).
In the study, histologic analyses also showed that improved spongiosis scores in treated patients correlated with increased density of two tight junction proteins, filaggrin (P = .001) and zonula occludens-3 (P = .016), said the investigators. These proteins might help regulate antigenic penetration of the esophageal mucosa and also could permit migration of white blood cells, they said. “Loss of tight junction regulators and dilation of intercellular spaces appear to be involved in the pathophysiology of EoE and could be targets for treatment,” the researchers concluded. But they also noted that their study did not examine the same patients before and after steroid therapy and did not look at desmosomes, intercellular junctions that past research has suggested might be affected in EoE.
For the second study, Dr. Bram van Rhijn and his associates at the Academic Medical Center in the Netherlands compared endoscopies of 16 patients with dysphagia and suspected (unconfirmed) EoE with 11 controls, both at baseline and after 8 weeks of high-dose esomeprazole treatment. Esophageal mucosal integrity was “severely impaired” in patients with confirmed EoE and in those with proton pump inhibitor–responsive eosinophilia (PPRE), the researchers said (Clin. Gasteroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.037]).
In both forms of disease, molecules as large as 40,000 daltons were able to pass through the compromised esophageal mucosa, Dr. Bram van Rhijn and his associates reported. “This size is similar to the size of most plant and animal food allergens to which EoE patients are sensitized,” they added. Esophageal permeability might increase the rate of immune exposure to allergens, thereby mediating EoE and PPRE, they said.
On mucosal functional tests, both EoE and PPRE were associated with reduced transepithelial electrical resistance and lower electrical tissue impedance, most notably in patients with EoE (P less than .001 for both, compared with controls), the investigators reported. Proton pump inhibitor treatment partially reversed these changes in patients with PPRE but showed no effect for patients with EoE, they said. This finding suggests that acid reflux might play a role in PPRE, but not in EOE, they concluded.
Dr. Katzka and his associates disclosed no funding sources and reported having no conflicts of interest. Dr. Rhijn and his associates were supported by the Netherlands Organization for Scientific Research. Two of Dr. Rhijn’s coauthors reported financial relationships with AstraZeneca, Endostim, Medical Measurement Systems, Shire, and GlaxoSmithKline.
Topical steroid therapy improved some indicators of mucosal integrity in patients with eosinophilic esophagitis, but proton pump inhibitor therapy did not, according to two studies reported in the November issue of Clinical Gastroenterology and Hepatology.
The first study found that topical fluticasone therapy at a dose of 880 mcg twice daily for 2 months helped correct esophageal spongiosis, or dilated intercellular space, in patients with eosinophilic esophagitis (EoE). Spongiosis scores for treated patients were significantly lower than for untreated patients (0.4 vs. 1.3; P = .016), said Dr. David Katzka at the Mayo Clinic in Rochester, Minn. and his associates (Clin. Gastroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.039]).
In the study, histologic analyses also showed that improved spongiosis scores in treated patients correlated with increased density of two tight junction proteins, filaggrin (P = .001) and zonula occludens-3 (P = .016), said the investigators. These proteins might help regulate antigenic penetration of the esophageal mucosa and also could permit migration of white blood cells, they said. “Loss of tight junction regulators and dilation of intercellular spaces appear to be involved in the pathophysiology of EoE and could be targets for treatment,” the researchers concluded. But they also noted that their study did not examine the same patients before and after steroid therapy and did not look at desmosomes, intercellular junctions that past research has suggested might be affected in EoE.
For the second study, Dr. Bram van Rhijn and his associates at the Academic Medical Center in the Netherlands compared endoscopies of 16 patients with dysphagia and suspected (unconfirmed) EoE with 11 controls, both at baseline and after 8 weeks of high-dose esomeprazole treatment. Esophageal mucosal integrity was “severely impaired” in patients with confirmed EoE and in those with proton pump inhibitor–responsive eosinophilia (PPRE), the researchers said (Clin. Gasteroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.037]).
In both forms of disease, molecules as large as 40,000 daltons were able to pass through the compromised esophageal mucosa, Dr. Bram van Rhijn and his associates reported. “This size is similar to the size of most plant and animal food allergens to which EoE patients are sensitized,” they added. Esophageal permeability might increase the rate of immune exposure to allergens, thereby mediating EoE and PPRE, they said.
On mucosal functional tests, both EoE and PPRE were associated with reduced transepithelial electrical resistance and lower electrical tissue impedance, most notably in patients with EoE (P less than .001 for both, compared with controls), the investigators reported. Proton pump inhibitor treatment partially reversed these changes in patients with PPRE but showed no effect for patients with EoE, they said. This finding suggests that acid reflux might play a role in PPRE, but not in EOE, they concluded.
Dr. Katzka and his associates disclosed no funding sources and reported having no conflicts of interest. Dr. Rhijn and his associates were supported by the Netherlands Organization for Scientific Research. Two of Dr. Rhijn’s coauthors reported financial relationships with AstraZeneca, Endostim, Medical Measurement Systems, Shire, and GlaxoSmithKline.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Topical steroids seemed to improve mucosal integrity in patients with eosinophilic esophagitis, but proton pump inhibitor therapy did not.
Major finding: Mean spongiosis score was significantly lower among treated vs. untreated patients (0.4 vs. 1.3; P = .016).
Data source: Immunohistochemistry, histology, endoscopy, and mucosal functional analyses of 57 subjects in two separate studies.
Disclosures: Dr. Katzka and associates disclosed no funding sources and reported having no conflicts of interest. Dr. Rhijn and associates were supported by the Netherlands Organization for Scientific Research. Two of Dr. Rhijn’s coauthors reported financial relationships with AstraZeneca, Endostim, Medical Measurement Systems, Shire, and GlaxoSmithKline.
Model could cut CT scans of patients with Crohn’s disease by 43%
A risk stratification model that determined whether patients with Crohn’s disease needed computed tomography cut scans of these patients in emergency departments by 43%, with a miss rate of only 0.8%, researchers reported online in Clinical Gastroenterology and Hepatology.
Computed tomography scans yield nonsignificant findings for almost one-third of patients with Crohn’s disease (CD) who present to emergency departments, said Dr. Shail Govani of the University of Michigan in Ann Arbor and his associates. By using their model to identify patients with serious gastrointestinal complications as opposed to straightforward intestinal inflammation, emergency departments could prevent more than 250 cancer cases and save more than $80 million per decade in the United States, the investigators added.
Source: American Gastroenterological Association
Patients with CD may be exposed to increasing cumulative radiation levels, and 30% of this exposure occurs in emergency departments, with 75% due to CT scans, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.036]).
For the study, the investigators retrospectively reviewed electronic medical records from the University of Michigan from 2000 through 2011, identifying 613 adults with CD who made 1,095 visits that included CT scans within 24 hours of presentation. The researchers then modeled associations between laboratory values and perforation, abscess, or other serious complications as opposed to intestinal inflammation.
Patients averaged 1.8 CT scans during the decade-long study period, and the overall rate of CT scans during that time rose from 63% to 87%, the investigators said. Only 16.8% of scans revealed a complication that would change clinical management, they reported.
Only C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were significantly associated with complications (odds ratio for CRP, 1.10; 95% confidence interval, 1.05-1.15; P less than .001; odds ratio for ESR, 1.02; 95% CI, 1.01-1.03; P less than .001), the researchers said. Adding ESR to 5 x CRP and not scanning patients with a resulting value of 10 or less would avoid CT scans in 18.5% of patients, they reported. But by using the more complex logistic regression model instead of the simpler equation, scans could be avoided for 43.0% of patients, with a miss rate of 0.8%, they said.
Based on the study, patients assessed as likely to have complications should undergo a standard CT scan of the abdomen and pelvis with nonbarium contrast to avoid barium peritonitis, said Dr. Govani and associates. Other patients should forego CT scans, have a consult with a gastroenterologist prior to further imaging, or undergo lower-radiation CT enterography, depending on presenting signs and probability of inflammation, they added.
The researchers said they were unable to construct good models that included obstruction as an outcome. Patients with suspected obstructions should have abdominal x-rays and then CT if an obstruction remained likely, they said.
"These models are limited in that they are retrospective and represent data from one center," the investigators added. "Although our internal validation with 10-fold cross-validation shows that these models have good performance characteristics, further external validation studies are needed to determine whether these models are generalizable to CD patients elsewhere."
The authors are prospectively testing the algorithms and hope to continue to validate and study them in emergency departments, they said.
The Inflammatory Bowel Disease Working Group, the Department of Veterans Affairs, and UCB supported the research. The authors reported having no conflicts of interest.
A risk stratification model that determined whether patients with Crohn’s disease needed computed tomography cut scans of these patients in emergency departments by 43%, with a miss rate of only 0.8%, researchers reported online in Clinical Gastroenterology and Hepatology.
Computed tomography scans yield nonsignificant findings for almost one-third of patients with Crohn’s disease (CD) who present to emergency departments, said Dr. Shail Govani of the University of Michigan in Ann Arbor and his associates. By using their model to identify patients with serious gastrointestinal complications as opposed to straightforward intestinal inflammation, emergency departments could prevent more than 250 cancer cases and save more than $80 million per decade in the United States, the investigators added.
Source: American Gastroenterological Association
Patients with CD may be exposed to increasing cumulative radiation levels, and 30% of this exposure occurs in emergency departments, with 75% due to CT scans, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.036]).
For the study, the investigators retrospectively reviewed electronic medical records from the University of Michigan from 2000 through 2011, identifying 613 adults with CD who made 1,095 visits that included CT scans within 24 hours of presentation. The researchers then modeled associations between laboratory values and perforation, abscess, or other serious complications as opposed to intestinal inflammation.
Patients averaged 1.8 CT scans during the decade-long study period, and the overall rate of CT scans during that time rose from 63% to 87%, the investigators said. Only 16.8% of scans revealed a complication that would change clinical management, they reported.
Only C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were significantly associated with complications (odds ratio for CRP, 1.10; 95% confidence interval, 1.05-1.15; P less than .001; odds ratio for ESR, 1.02; 95% CI, 1.01-1.03; P less than .001), the researchers said. Adding ESR to 5 x CRP and not scanning patients with a resulting value of 10 or less would avoid CT scans in 18.5% of patients, they reported. But by using the more complex logistic regression model instead of the simpler equation, scans could be avoided for 43.0% of patients, with a miss rate of 0.8%, they said.
Based on the study, patients assessed as likely to have complications should undergo a standard CT scan of the abdomen and pelvis with nonbarium contrast to avoid barium peritonitis, said Dr. Govani and associates. Other patients should forego CT scans, have a consult with a gastroenterologist prior to further imaging, or undergo lower-radiation CT enterography, depending on presenting signs and probability of inflammation, they added.
The researchers said they were unable to construct good models that included obstruction as an outcome. Patients with suspected obstructions should have abdominal x-rays and then CT if an obstruction remained likely, they said.
"These models are limited in that they are retrospective and represent data from one center," the investigators added. "Although our internal validation with 10-fold cross-validation shows that these models have good performance characteristics, further external validation studies are needed to determine whether these models are generalizable to CD patients elsewhere."
The authors are prospectively testing the algorithms and hope to continue to validate and study them in emergency departments, they said.
The Inflammatory Bowel Disease Working Group, the Department of Veterans Affairs, and UCB supported the research. The authors reported having no conflicts of interest.
A risk stratification model that determined whether patients with Crohn’s disease needed computed tomography cut scans of these patients in emergency departments by 43%, with a miss rate of only 0.8%, researchers reported online in Clinical Gastroenterology and Hepatology.
Computed tomography scans yield nonsignificant findings for almost one-third of patients with Crohn’s disease (CD) who present to emergency departments, said Dr. Shail Govani of the University of Michigan in Ann Arbor and his associates. By using their model to identify patients with serious gastrointestinal complications as opposed to straightforward intestinal inflammation, emergency departments could prevent more than 250 cancer cases and save more than $80 million per decade in the United States, the investigators added.
Source: American Gastroenterological Association
Patients with CD may be exposed to increasing cumulative radiation levels, and 30% of this exposure occurs in emergency departments, with 75% due to CT scans, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi:10.1016/j.cgh.2014.02.036]).
For the study, the investigators retrospectively reviewed electronic medical records from the University of Michigan from 2000 through 2011, identifying 613 adults with CD who made 1,095 visits that included CT scans within 24 hours of presentation. The researchers then modeled associations between laboratory values and perforation, abscess, or other serious complications as opposed to intestinal inflammation.
Patients averaged 1.8 CT scans during the decade-long study period, and the overall rate of CT scans during that time rose from 63% to 87%, the investigators said. Only 16.8% of scans revealed a complication that would change clinical management, they reported.
Only C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were significantly associated with complications (odds ratio for CRP, 1.10; 95% confidence interval, 1.05-1.15; P less than .001; odds ratio for ESR, 1.02; 95% CI, 1.01-1.03; P less than .001), the researchers said. Adding ESR to 5 x CRP and not scanning patients with a resulting value of 10 or less would avoid CT scans in 18.5% of patients, they reported. But by using the more complex logistic regression model instead of the simpler equation, scans could be avoided for 43.0% of patients, with a miss rate of 0.8%, they said.
Based on the study, patients assessed as likely to have complications should undergo a standard CT scan of the abdomen and pelvis with nonbarium contrast to avoid barium peritonitis, said Dr. Govani and associates. Other patients should forego CT scans, have a consult with a gastroenterologist prior to further imaging, or undergo lower-radiation CT enterography, depending on presenting signs and probability of inflammation, they added.
The researchers said they were unable to construct good models that included obstruction as an outcome. Patients with suspected obstructions should have abdominal x-rays and then CT if an obstruction remained likely, they said.
"These models are limited in that they are retrospective and represent data from one center," the investigators added. "Although our internal validation with 10-fold cross-validation shows that these models have good performance characteristics, further external validation studies are needed to determine whether these models are generalizable to CD patients elsewhere."
The authors are prospectively testing the algorithms and hope to continue to validate and study them in emergency departments, they said.
The Inflammatory Bowel Disease Working Group, the Department of Veterans Affairs, and UCB supported the research. The authors reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A risk-stratification model could cut the use of computed tomography scans in emergency department patients with Crohn’s disease by 43%, while missing less than 1% of emergencies.
Major finding: Adding ESR to 5 x CRP and not scanning patients with a resulting value of 10 or less would prevent unnecessary CT scans in 18.5% of patients.
Data source: Retrospective review of electronic medical records on 613 adults with Crohn’s disease who had 1,095 visits with CT scans at the University of Michigan from 2000 through 2011.
Disclosures: The Inflammatory Bowel Disease Working Group, the Department of Veterans Affairs, and UCB supported the research. The authors reported having no conflicts of interest.
MicroRNA test improved preop pancreatic cancer diagnosis
Cytology and a microRNA-based test identified pancreatic cancer 91% of the time in specimens obtained by endoscopic ultrasound-guided fine-needle aspiration – a substantial improvement, compared with cytology alone, researchers reported in the October issue of Clinical Gastroenterology and Hepatology.
The microRNA-based test could help reduce repeated fine-needle aspirations (FNAs) due to indeterminate cytologies, said Dr. Randall Brand of the University of Pittsburgh Medical Center and his associates. Correctly assessing pancreatic cancer before surgery also could help patients start neoadjuvant therapy sooner if appropriate, they noted.
Several microRNAs are expressed abnormally in patients with pancreatic ductal adenocarcinoma. The new test contains five of these sequences and is the first of its type for pancreatic cancer, the researchers said. To evaluate the assay, they assessed and compared relative quantitative polymerase chain reaction and cytology results from 95 formalin-fixed paraffin-embedded specimens and 228 endoscopic ultrasound-guided FNAs. Specimens were collected during routine visits by patients with solid pancreatic masses, the investigators said (Clin. Gastroenterol. Hepatol. 2014 October [doi:10.1016/j.cgh.2014.02.038]).
The test used together with cytology correctly identified pancreatic cancer in 91% of positive specimens (95% confidence interval, 85.6%-94.5%), while cytology alone had a sensitivity of 79% (95% CI, 72.2%-84.5%), the researchers reported. Cytology and the microRNA test each had positive predictive values greater than 99% (95% CI, 96%-100%), they added.
When used alone, the microRNA test had a diagnostic sensitivity of more than 82% and a specificity of 96% – better than cytology on the same specimens, the investigators said. And the test correctly found pancreatic cancer in 22 of 39 specimens previously assessed as benign, indeterminate, or nondiagnostic by cytology, they said.
The researchers separately assessed 46 specimens collected percutaneously instead of by endoscopic ultrasound-guided FNA and found much lower (58%) diagnostic sensitivity and a higher rate of technical failures, although specificity and predictive value still approached 90%, said the investigators. The percutaneous specimens all were collected from two study sites outside the United States, so further studies would need to validate whether a percutaneous approach could replace endoscopic ultrasound-guided FNA, they said.
Cytology and microRNA testing also had to be performed on different FNA specimens, a limitation that "could have contributed to some of the observed discrepancies between cytology and molecular results," the investigators said.
Pancreatic cancer remains notoriously difficult to treat, with overall 5-year survival rates of only about 6%. MicroRNA sequences are stable and can reliably be recovered from both formalin-fixed and FNA specimens, making them a "particularly promising" class of biomarkers for pancreatic and other cancers, the researchers said. Based on the study results, future studies should explore the test’s prognostic potential, such as for distinguishing patients with resectable tumors that are likely to progress early or to guide choice of therapies, they said.
The study was supported by Asuragen and by a grant from the German Federal Ministry of Education and Research. Dr. Brand and another author reported that they are on the clinical advisory board of Asuragen, and six of 27 coauthors reported being employees of the company. The rest reported no conflicts of interest.
The diagnosis of pancreas cancer is based on the results of clinical presentation, cross-sectional imaging, and endoscopic ultrasound (EUS) guided fine-needle aspiration (FNA). A definitive tissue diagnosis is often required before chemotherapy, radiation therapy, and surgery. Because of the greater sensitivity of EUS over CT scanning, EUS-guided FNA is often the procedure of choice. EUS-guided FNA is highly dependent on the identification of malignant cells in the FNA specimens. The presence of a dense peri-tumoral stroma containing fibroblasts often interferes with the aspiration and identification of malignant cells.
The cytological criteria for the diagnosis of pancreas adenocarcinoma with FNA requires the presence of a number of cellular features such as dark chromatin, large nuclei, and aggregates of atypical cells. Not surprisingly, cytologists adhere rigidly to the criteria for the diagnosis of adenocarcinoma resulting in a highly specific test with moderately high sensitivity. The sensitivity of EUS FNA for the diagnosis of pancreas cancer remains stubbornly imperfect, between 85% and 95%.
Brand et al. have presented the results of a large multicenter 3-year validation trial designed to determine the performance characteristics of a 5-microRNA-based classifier for the diagnosis of pancreas cancer on 228 EUS-FNA specimens. In the study, the false-negative rate for pancreas mass FNA was 20%. The results of the miRNA testing revealed a sensitivity of 83% and a false-negative rate of 17%. However, when both the cytology and the miRNA test were used in conjunction, the sensitivity increased to 91% with a specificity of 96%.
The use of molecular markers in the management of FNA cytology specimens provides an opportunity to objectify the findings of aspirated tissue analysis. With an objective test, the interpretation of specimens is not dependent upon the subjective findings of a cytologist. It seems likely that this type of testing will gradually improve FNA cytology.
Dr. William R. Brugge is director, Pancreas Biliary Center, Massachusetts General Hospital, Boston.
The diagnosis of pancreas cancer is based on the results of clinical presentation, cross-sectional imaging, and endoscopic ultrasound (EUS) guided fine-needle aspiration (FNA). A definitive tissue diagnosis is often required before chemotherapy, radiation therapy, and surgery. Because of the greater sensitivity of EUS over CT scanning, EUS-guided FNA is often the procedure of choice. EUS-guided FNA is highly dependent on the identification of malignant cells in the FNA specimens. The presence of a dense peri-tumoral stroma containing fibroblasts often interferes with the aspiration and identification of malignant cells.
The cytological criteria for the diagnosis of pancreas adenocarcinoma with FNA requires the presence of a number of cellular features such as dark chromatin, large nuclei, and aggregates of atypical cells. Not surprisingly, cytologists adhere rigidly to the criteria for the diagnosis of adenocarcinoma resulting in a highly specific test with moderately high sensitivity. The sensitivity of EUS FNA for the diagnosis of pancreas cancer remains stubbornly imperfect, between 85% and 95%.
Brand et al. have presented the results of a large multicenter 3-year validation trial designed to determine the performance characteristics of a 5-microRNA-based classifier for the diagnosis of pancreas cancer on 228 EUS-FNA specimens. In the study, the false-negative rate for pancreas mass FNA was 20%. The results of the miRNA testing revealed a sensitivity of 83% and a false-negative rate of 17%. However, when both the cytology and the miRNA test were used in conjunction, the sensitivity increased to 91% with a specificity of 96%.
The use of molecular markers in the management of FNA cytology specimens provides an opportunity to objectify the findings of aspirated tissue analysis. With an objective test, the interpretation of specimens is not dependent upon the subjective findings of a cytologist. It seems likely that this type of testing will gradually improve FNA cytology.
Dr. William R. Brugge is director, Pancreas Biliary Center, Massachusetts General Hospital, Boston.
The diagnosis of pancreas cancer is based on the results of clinical presentation, cross-sectional imaging, and endoscopic ultrasound (EUS) guided fine-needle aspiration (FNA). A definitive tissue diagnosis is often required before chemotherapy, radiation therapy, and surgery. Because of the greater sensitivity of EUS over CT scanning, EUS-guided FNA is often the procedure of choice. EUS-guided FNA is highly dependent on the identification of malignant cells in the FNA specimens. The presence of a dense peri-tumoral stroma containing fibroblasts often interferes with the aspiration and identification of malignant cells.
The cytological criteria for the diagnosis of pancreas adenocarcinoma with FNA requires the presence of a number of cellular features such as dark chromatin, large nuclei, and aggregates of atypical cells. Not surprisingly, cytologists adhere rigidly to the criteria for the diagnosis of adenocarcinoma resulting in a highly specific test with moderately high sensitivity. The sensitivity of EUS FNA for the diagnosis of pancreas cancer remains stubbornly imperfect, between 85% and 95%.
Brand et al. have presented the results of a large multicenter 3-year validation trial designed to determine the performance characteristics of a 5-microRNA-based classifier for the diagnosis of pancreas cancer on 228 EUS-FNA specimens. In the study, the false-negative rate for pancreas mass FNA was 20%. The results of the miRNA testing revealed a sensitivity of 83% and a false-negative rate of 17%. However, when both the cytology and the miRNA test were used in conjunction, the sensitivity increased to 91% with a specificity of 96%.
The use of molecular markers in the management of FNA cytology specimens provides an opportunity to objectify the findings of aspirated tissue analysis. With an objective test, the interpretation of specimens is not dependent upon the subjective findings of a cytologist. It seems likely that this type of testing will gradually improve FNA cytology.
Dr. William R. Brugge is director, Pancreas Biliary Center, Massachusetts General Hospital, Boston.
Cytology and a microRNA-based test identified pancreatic cancer 91% of the time in specimens obtained by endoscopic ultrasound-guided fine-needle aspiration – a substantial improvement, compared with cytology alone, researchers reported in the October issue of Clinical Gastroenterology and Hepatology.
The microRNA-based test could help reduce repeated fine-needle aspirations (FNAs) due to indeterminate cytologies, said Dr. Randall Brand of the University of Pittsburgh Medical Center and his associates. Correctly assessing pancreatic cancer before surgery also could help patients start neoadjuvant therapy sooner if appropriate, they noted.
Several microRNAs are expressed abnormally in patients with pancreatic ductal adenocarcinoma. The new test contains five of these sequences and is the first of its type for pancreatic cancer, the researchers said. To evaluate the assay, they assessed and compared relative quantitative polymerase chain reaction and cytology results from 95 formalin-fixed paraffin-embedded specimens and 228 endoscopic ultrasound-guided FNAs. Specimens were collected during routine visits by patients with solid pancreatic masses, the investigators said (Clin. Gastroenterol. Hepatol. 2014 October [doi:10.1016/j.cgh.2014.02.038]).
The test used together with cytology correctly identified pancreatic cancer in 91% of positive specimens (95% confidence interval, 85.6%-94.5%), while cytology alone had a sensitivity of 79% (95% CI, 72.2%-84.5%), the researchers reported. Cytology and the microRNA test each had positive predictive values greater than 99% (95% CI, 96%-100%), they added.
When used alone, the microRNA test had a diagnostic sensitivity of more than 82% and a specificity of 96% – better than cytology on the same specimens, the investigators said. And the test correctly found pancreatic cancer in 22 of 39 specimens previously assessed as benign, indeterminate, or nondiagnostic by cytology, they said.
The researchers separately assessed 46 specimens collected percutaneously instead of by endoscopic ultrasound-guided FNA and found much lower (58%) diagnostic sensitivity and a higher rate of technical failures, although specificity and predictive value still approached 90%, said the investigators. The percutaneous specimens all were collected from two study sites outside the United States, so further studies would need to validate whether a percutaneous approach could replace endoscopic ultrasound-guided FNA, they said.
Cytology and microRNA testing also had to be performed on different FNA specimens, a limitation that "could have contributed to some of the observed discrepancies between cytology and molecular results," the investigators said.
Pancreatic cancer remains notoriously difficult to treat, with overall 5-year survival rates of only about 6%. MicroRNA sequences are stable and can reliably be recovered from both formalin-fixed and FNA specimens, making them a "particularly promising" class of biomarkers for pancreatic and other cancers, the researchers said. Based on the study results, future studies should explore the test’s prognostic potential, such as for distinguishing patients with resectable tumors that are likely to progress early or to guide choice of therapies, they said.
The study was supported by Asuragen and by a grant from the German Federal Ministry of Education and Research. Dr. Brand and another author reported that they are on the clinical advisory board of Asuragen, and six of 27 coauthors reported being employees of the company. The rest reported no conflicts of interest.
Cytology and a microRNA-based test identified pancreatic cancer 91% of the time in specimens obtained by endoscopic ultrasound-guided fine-needle aspiration – a substantial improvement, compared with cytology alone, researchers reported in the October issue of Clinical Gastroenterology and Hepatology.
The microRNA-based test could help reduce repeated fine-needle aspirations (FNAs) due to indeterminate cytologies, said Dr. Randall Brand of the University of Pittsburgh Medical Center and his associates. Correctly assessing pancreatic cancer before surgery also could help patients start neoadjuvant therapy sooner if appropriate, they noted.
Several microRNAs are expressed abnormally in patients with pancreatic ductal adenocarcinoma. The new test contains five of these sequences and is the first of its type for pancreatic cancer, the researchers said. To evaluate the assay, they assessed and compared relative quantitative polymerase chain reaction and cytology results from 95 formalin-fixed paraffin-embedded specimens and 228 endoscopic ultrasound-guided FNAs. Specimens were collected during routine visits by patients with solid pancreatic masses, the investigators said (Clin. Gastroenterol. Hepatol. 2014 October [doi:10.1016/j.cgh.2014.02.038]).
The test used together with cytology correctly identified pancreatic cancer in 91% of positive specimens (95% confidence interval, 85.6%-94.5%), while cytology alone had a sensitivity of 79% (95% CI, 72.2%-84.5%), the researchers reported. Cytology and the microRNA test each had positive predictive values greater than 99% (95% CI, 96%-100%), they added.
When used alone, the microRNA test had a diagnostic sensitivity of more than 82% and a specificity of 96% – better than cytology on the same specimens, the investigators said. And the test correctly found pancreatic cancer in 22 of 39 specimens previously assessed as benign, indeterminate, or nondiagnostic by cytology, they said.
The researchers separately assessed 46 specimens collected percutaneously instead of by endoscopic ultrasound-guided FNA and found much lower (58%) diagnostic sensitivity and a higher rate of technical failures, although specificity and predictive value still approached 90%, said the investigators. The percutaneous specimens all were collected from two study sites outside the United States, so further studies would need to validate whether a percutaneous approach could replace endoscopic ultrasound-guided FNA, they said.
Cytology and microRNA testing also had to be performed on different FNA specimens, a limitation that "could have contributed to some of the observed discrepancies between cytology and molecular results," the investigators said.
Pancreatic cancer remains notoriously difficult to treat, with overall 5-year survival rates of only about 6%. MicroRNA sequences are stable and can reliably be recovered from both formalin-fixed and FNA specimens, making them a "particularly promising" class of biomarkers for pancreatic and other cancers, the researchers said. Based on the study results, future studies should explore the test’s prognostic potential, such as for distinguishing patients with resectable tumors that are likely to progress early or to guide choice of therapies, they said.
The study was supported by Asuragen and by a grant from the German Federal Ministry of Education and Research. Dr. Brand and another author reported that they are on the clinical advisory board of Asuragen, and six of 27 coauthors reported being employees of the company. The rest reported no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Cytology and a microRNA-based test were more sensitive than cytology alone in evaluating pancreatic cancer specimens obtained by endoscopic ultrasound-guided fine-needle aspiration.
Major finding: Using the microRNA test combined with cytology correctly identified pancreatic cancer almost 91% of the time (95% CI, 85.6%-94.5%), while cytology alone had a sensitivity of 79% (95% CI, 72.2%-84.5%).
Data source: Prospective, multicenter study of relative quantitative polymerase chain reaction and cytology results from 95 formalin-fixed paraffin-embedded samples and 228 specimens collected by endoscopic ultrasound-guided fine-needle aspirate.
Disclosures: The study was supported by Asuragen and by a grant from the German Federal Ministry of Education and Research. Dr. Brand and another author reported that they are on the clinical advisory board for Asuragen, and six of 27 coauthors reported being employees of the company. The rest reported no conflicts of interest.
Drug combinations found to increase upper gastrointestinal bleeding risk
Combining nonsteroidal anti-inflammatory drugs with selective serotonin reuptake inhibitors increased the risk of upper gastrointestinal bleeding by up to 190% beyond the baseline risk found for NSAID monotherapy, researchers reported in the October issue of Gastroenterology.
Patients also faced excess risks of upper GI bleeding when they took corticosteroids, aldosterone antagonists, or anticoagulants together with low-dose aspirin or nonselective NSAIDs, although the effect was not seen for COX-2 inhibitors, said Dr. Gwen Masclee at Erasmus Medical Center in Rotterdam, the Netherlands and her associates.
Source: American Gastroenterological Association
The findings should help clinicians tailor treatments to minimize chances of upper gastrointestinal bleeding, particularly for elderly patients who often take multiple drugs, the investigators said (Gastroenterology 2014 [doi:10.1053/j.gastro.2014.06.007]).
The researchers analyzed 114,835 cases of upper gastrointestinal bleeding, including all gastroduodenal ulcers and hemorrhages extracted from seven electronic health record databases from the Netherlands, Italy, and Denmark. Three databases included primary care data, and four were administrative claims data, the investigators said. Cases served as their own controls, they noted.
Monotherapy with prescription nonselective NSAIDs increased the chances of an upper gastrointestinal bleed by 4.3 times, compared with not using any of the drugs studied (95% confidence interval, 4.1-4.4), the researchers said. Notably, bleeding risk from taking either nonselective NSAIDs or corticosteroids was the same, they said, adding that previous studies have yielded inconsistent findings on the topic. The incidence ratios for monotherapy with low-dose aspirin and COX-2 inhibitors were slightly lower at 3.1 (95% CI, 2.9-3.2) and 2.9 (95% CI, 2.7-3.2), respectively, they added.
Combining nonselective NSAIDs, COX-2 inhibitors, or low-dose aspirin with SSRIs led to excess risks of upper gastrointestinal bleeding of 1.6 (95% CI, 0.5-2.6), 1.9 (95% CI, 0.2-3.4), and 0.49 (–0.05-1.03), respectively, the researchers reported. "From a biological point of view, this interaction seems plausible because SSRIs decrease the serotonin level, resulting in impaired thrombocyte aggregation and an increased risk of bleeding in general," they said.
Corticosteroids combined with nonselective NSAIDs led to the greatest increases in bleeding risk, with an incidence ratio of 12.8 (95% CI, 11.1-14.7), compared with nonuse of any drug studied, and an excess risk of 5.5 (3.7-7.3), compared with NSAID use alone, said the researchers. Adding aldosterone antagonists to nonselective NSAIDs led to an excess risk of 4.46, compared with using nonselective NSAIDs alone, they reported (95% CI, 1.79-7.13).
Because the study did not capture over-the-counter NSAID prescriptions, it could have underestimated use of these drugs, the investigators said. Also, changes in health or NSAID use during the study could have created residual confounding, although sensitivity analyses did not reveal problems, they reported. They added that misclassification of some data could have led them to underestimate risks. "Finally, we did not take any carryover effect or dose of drug exposure into account, which potentially limits the generalizability concerning causality of the associations," they concluded.
Five authors reported employment or other financial support from Erasmus University Medical Center, AstraZeneca, Janssen, PHARMO Institute, and the European Medicines Agency. The other authors reported no relevant conflicts of interests.
Gastrointestinal toxicity is the major issue limiting nonsteroidal anti-inflammatory use. The excess annual risk of upper gastrointestinal bleeding per 1,000 patients is about 1 with low-dose aspirin, about 2 with coxibs, and about 4-6 with traditional NSAIDs (ibuprofen, naproxen). However, the risk of upper gastrointestinal bleeding increases markedly with several factors, including the use of concomitant medications.
Ideally, large randomized trials comparing NSAIDs with and without a concomitant medication would inform our assessment of risk. However, few such trials are available, so we commonly rely on observational database studies, such as that of Masclee et al. These studies have the important benefit of large sample size and "real world" results, but also have potential limitations, including reliability of data (for example, accuracy of diagnostic coding) and potential bias because of unequal distribution of confounding factors between cases and controls.
Masclee et al. report significant synergy (more than additive risk) of traditional NSAIDs with corticosteroids, SSRIs, aldosterone antagonists, and antithrombotic agents other than low-dose aspirin (although risk was increased with traditional NSAIDs plus low-dose aspirin). Low-dose aspirin was synergistic with antithrombotic agents and corticosteroids, while coxibs were synergistic with low-dose aspirin and SSRIs.
The results of Masclee et al. support current North American guidelines, which suggest use of proton pump inhibitors or misoprostol for traditional NSAID users taking concomitant medications such as antithrombotics, corticosteroids, or SSRIs, and use of PPIs for low-dose-aspirin users taking antithrombotics or taking corticosteroids if greater than or equal to 60 years old. Their results also suggest further evaluation of aldosterone antagonists is warranted as another possible risk factor.
Dr. Loren Laine is professor of medicine, department of internal medicine, Yale University, New Haven, Conn. He is on the Data Safety Monitoring Boards of Eisai, BMS, and Bayer; and is a consultant for AstraZeneca.
Gastrointestinal toxicity is the major issue limiting nonsteroidal anti-inflammatory use. The excess annual risk of upper gastrointestinal bleeding per 1,000 patients is about 1 with low-dose aspirin, about 2 with coxibs, and about 4-6 with traditional NSAIDs (ibuprofen, naproxen). However, the risk of upper gastrointestinal bleeding increases markedly with several factors, including the use of concomitant medications.
Ideally, large randomized trials comparing NSAIDs with and without a concomitant medication would inform our assessment of risk. However, few such trials are available, so we commonly rely on observational database studies, such as that of Masclee et al. These studies have the important benefit of large sample size and "real world" results, but also have potential limitations, including reliability of data (for example, accuracy of diagnostic coding) and potential bias because of unequal distribution of confounding factors between cases and controls.
Masclee et al. report significant synergy (more than additive risk) of traditional NSAIDs with corticosteroids, SSRIs, aldosterone antagonists, and antithrombotic agents other than low-dose aspirin (although risk was increased with traditional NSAIDs plus low-dose aspirin). Low-dose aspirin was synergistic with antithrombotic agents and corticosteroids, while coxibs were synergistic with low-dose aspirin and SSRIs.
The results of Masclee et al. support current North American guidelines, which suggest use of proton pump inhibitors or misoprostol for traditional NSAID users taking concomitant medications such as antithrombotics, corticosteroids, or SSRIs, and use of PPIs for low-dose-aspirin users taking antithrombotics or taking corticosteroids if greater than or equal to 60 years old. Their results also suggest further evaluation of aldosterone antagonists is warranted as another possible risk factor.
Dr. Loren Laine is professor of medicine, department of internal medicine, Yale University, New Haven, Conn. He is on the Data Safety Monitoring Boards of Eisai, BMS, and Bayer; and is a consultant for AstraZeneca.
Gastrointestinal toxicity is the major issue limiting nonsteroidal anti-inflammatory use. The excess annual risk of upper gastrointestinal bleeding per 1,000 patients is about 1 with low-dose aspirin, about 2 with coxibs, and about 4-6 with traditional NSAIDs (ibuprofen, naproxen). However, the risk of upper gastrointestinal bleeding increases markedly with several factors, including the use of concomitant medications.
Ideally, large randomized trials comparing NSAIDs with and without a concomitant medication would inform our assessment of risk. However, few such trials are available, so we commonly rely on observational database studies, such as that of Masclee et al. These studies have the important benefit of large sample size and "real world" results, but also have potential limitations, including reliability of data (for example, accuracy of diagnostic coding) and potential bias because of unequal distribution of confounding factors between cases and controls.
Masclee et al. report significant synergy (more than additive risk) of traditional NSAIDs with corticosteroids, SSRIs, aldosterone antagonists, and antithrombotic agents other than low-dose aspirin (although risk was increased with traditional NSAIDs plus low-dose aspirin). Low-dose aspirin was synergistic with antithrombotic agents and corticosteroids, while coxibs were synergistic with low-dose aspirin and SSRIs.
The results of Masclee et al. support current North American guidelines, which suggest use of proton pump inhibitors or misoprostol for traditional NSAID users taking concomitant medications such as antithrombotics, corticosteroids, or SSRIs, and use of PPIs for low-dose-aspirin users taking antithrombotics or taking corticosteroids if greater than or equal to 60 years old. Their results also suggest further evaluation of aldosterone antagonists is warranted as another possible risk factor.
Dr. Loren Laine is professor of medicine, department of internal medicine, Yale University, New Haven, Conn. He is on the Data Safety Monitoring Boards of Eisai, BMS, and Bayer; and is a consultant for AstraZeneca.
Combining nonsteroidal anti-inflammatory drugs with selective serotonin reuptake inhibitors increased the risk of upper gastrointestinal bleeding by up to 190% beyond the baseline risk found for NSAID monotherapy, researchers reported in the October issue of Gastroenterology.
Patients also faced excess risks of upper GI bleeding when they took corticosteroids, aldosterone antagonists, or anticoagulants together with low-dose aspirin or nonselective NSAIDs, although the effect was not seen for COX-2 inhibitors, said Dr. Gwen Masclee at Erasmus Medical Center in Rotterdam, the Netherlands and her associates.
Source: American Gastroenterological Association
The findings should help clinicians tailor treatments to minimize chances of upper gastrointestinal bleeding, particularly for elderly patients who often take multiple drugs, the investigators said (Gastroenterology 2014 [doi:10.1053/j.gastro.2014.06.007]).
The researchers analyzed 114,835 cases of upper gastrointestinal bleeding, including all gastroduodenal ulcers and hemorrhages extracted from seven electronic health record databases from the Netherlands, Italy, and Denmark. Three databases included primary care data, and four were administrative claims data, the investigators said. Cases served as their own controls, they noted.
Monotherapy with prescription nonselective NSAIDs increased the chances of an upper gastrointestinal bleed by 4.3 times, compared with not using any of the drugs studied (95% confidence interval, 4.1-4.4), the researchers said. Notably, bleeding risk from taking either nonselective NSAIDs or corticosteroids was the same, they said, adding that previous studies have yielded inconsistent findings on the topic. The incidence ratios for monotherapy with low-dose aspirin and COX-2 inhibitors were slightly lower at 3.1 (95% CI, 2.9-3.2) and 2.9 (95% CI, 2.7-3.2), respectively, they added.
Combining nonselective NSAIDs, COX-2 inhibitors, or low-dose aspirin with SSRIs led to excess risks of upper gastrointestinal bleeding of 1.6 (95% CI, 0.5-2.6), 1.9 (95% CI, 0.2-3.4), and 0.49 (–0.05-1.03), respectively, the researchers reported. "From a biological point of view, this interaction seems plausible because SSRIs decrease the serotonin level, resulting in impaired thrombocyte aggregation and an increased risk of bleeding in general," they said.
Corticosteroids combined with nonselective NSAIDs led to the greatest increases in bleeding risk, with an incidence ratio of 12.8 (95% CI, 11.1-14.7), compared with nonuse of any drug studied, and an excess risk of 5.5 (3.7-7.3), compared with NSAID use alone, said the researchers. Adding aldosterone antagonists to nonselective NSAIDs led to an excess risk of 4.46, compared with using nonselective NSAIDs alone, they reported (95% CI, 1.79-7.13).
Because the study did not capture over-the-counter NSAID prescriptions, it could have underestimated use of these drugs, the investigators said. Also, changes in health or NSAID use during the study could have created residual confounding, although sensitivity analyses did not reveal problems, they reported. They added that misclassification of some data could have led them to underestimate risks. "Finally, we did not take any carryover effect or dose of drug exposure into account, which potentially limits the generalizability concerning causality of the associations," they concluded.
Five authors reported employment or other financial support from Erasmus University Medical Center, AstraZeneca, Janssen, PHARMO Institute, and the European Medicines Agency. The other authors reported no relevant conflicts of interests.
Combining nonsteroidal anti-inflammatory drugs with selective serotonin reuptake inhibitors increased the risk of upper gastrointestinal bleeding by up to 190% beyond the baseline risk found for NSAID monotherapy, researchers reported in the October issue of Gastroenterology.
Patients also faced excess risks of upper GI bleeding when they took corticosteroids, aldosterone antagonists, or anticoagulants together with low-dose aspirin or nonselective NSAIDs, although the effect was not seen for COX-2 inhibitors, said Dr. Gwen Masclee at Erasmus Medical Center in Rotterdam, the Netherlands and her associates.
Source: American Gastroenterological Association
The findings should help clinicians tailor treatments to minimize chances of upper gastrointestinal bleeding, particularly for elderly patients who often take multiple drugs, the investigators said (Gastroenterology 2014 [doi:10.1053/j.gastro.2014.06.007]).
The researchers analyzed 114,835 cases of upper gastrointestinal bleeding, including all gastroduodenal ulcers and hemorrhages extracted from seven electronic health record databases from the Netherlands, Italy, and Denmark. Three databases included primary care data, and four were administrative claims data, the investigators said. Cases served as their own controls, they noted.
Monotherapy with prescription nonselective NSAIDs increased the chances of an upper gastrointestinal bleed by 4.3 times, compared with not using any of the drugs studied (95% confidence interval, 4.1-4.4), the researchers said. Notably, bleeding risk from taking either nonselective NSAIDs or corticosteroids was the same, they said, adding that previous studies have yielded inconsistent findings on the topic. The incidence ratios for monotherapy with low-dose aspirin and COX-2 inhibitors were slightly lower at 3.1 (95% CI, 2.9-3.2) and 2.9 (95% CI, 2.7-3.2), respectively, they added.
Combining nonselective NSAIDs, COX-2 inhibitors, or low-dose aspirin with SSRIs led to excess risks of upper gastrointestinal bleeding of 1.6 (95% CI, 0.5-2.6), 1.9 (95% CI, 0.2-3.4), and 0.49 (–0.05-1.03), respectively, the researchers reported. "From a biological point of view, this interaction seems plausible because SSRIs decrease the serotonin level, resulting in impaired thrombocyte aggregation and an increased risk of bleeding in general," they said.
Corticosteroids combined with nonselective NSAIDs led to the greatest increases in bleeding risk, with an incidence ratio of 12.8 (95% CI, 11.1-14.7), compared with nonuse of any drug studied, and an excess risk of 5.5 (3.7-7.3), compared with NSAID use alone, said the researchers. Adding aldosterone antagonists to nonselective NSAIDs led to an excess risk of 4.46, compared with using nonselective NSAIDs alone, they reported (95% CI, 1.79-7.13).
Because the study did not capture over-the-counter NSAID prescriptions, it could have underestimated use of these drugs, the investigators said. Also, changes in health or NSAID use during the study could have created residual confounding, although sensitivity analyses did not reveal problems, they reported. They added that misclassification of some data could have led them to underestimate risks. "Finally, we did not take any carryover effect or dose of drug exposure into account, which potentially limits the generalizability concerning causality of the associations," they concluded.
Five authors reported employment or other financial support from Erasmus University Medical Center, AstraZeneca, Janssen, PHARMO Institute, and the European Medicines Agency. The other authors reported no relevant conflicts of interests.
FROM GASTROENTEROLOGY
Key clinical point: Excess risk of upper gastrointestinal bleeding occurred with combinations of NSAIDs and selective serotonin reuptake inhibitors, and with combinations of nonselective NSAIDs or low-dose aspirin with corticosteroids, aldosterone antagonists, or anticoagulants.
Major finding: Excess risks from combining SSRIs with nonselective NSAIDs, COX-2 inhibitors, or low-dose aspirin were 1.62 (95% CI, 0.58-2.66), 1.86 (95% CI, 0.28- 3.44), and 0.49 (95% CI, –0.05-1.03), respectively.
Data source: Case series analysis of 114,835 patients with upper gastrointestinal bleeding. Patients were identified from seven electronic health record databases from the Netherlands, Italy, and Denmark, and cases served as their own controls.
Disclosures: Five authors reported employment or other financial support from Erasmus University Medical Center, AstraZeneca, Janssen, PHARMO Institute, and the European Medicines Agency. The other authors reported no relevant conflicts of interests.
Pediatric IBD rose by more than 40% in 15 years
Pediatric inflammatory bowel disease grew by more than 40% in a 15-year period in Ontario, Canada, according to a retrospective cohort study published in the October issue of Gastroenterology.
Although rates of inflammatory bowel disease (IBD) rose in children and adolescents of all ages, the steepest increase occurred in children with very-early-onset IBD (VEO-IBD), defined as disease diagnosed before they were 10 years old, said Dr. Eric Benchimol at the University of Ottawa and his associates. But these patients also tended to use fewer health services and have fewer surgeries for IBD, compared with older children with the disease, the investigators said (Gastroenterology 2014 October [doi.org/10.1053/j.gastro.2014.06.023]).
Source: American Gastroenterological Association
The findings add to research indicating that VEO-IBD is a distinct form of IBD and indicate the need to assess subgroups of these patients to look at phenotype, genotype, intestinal microbiome, and treatment response, the investigators said.
For the study, researchers created a cohort based on an algorithm of health care visits that identified all children and adolescents in Ontario diagnosed with IBD before age 18 years. The analysis included 7,143 patients with IBD, among whom about 14% had VEO-IBD, the investigators reported.
The overall rate of IBD in children up to 18 years old increased from 9.4 to 13.2 cases per 100,000 population from 1994 through 2009 (P less than .0001), the researchers said. And the yearly increase in VEO-IBD averaged 7.4% – more than three times greater than the 2.2% average annual rise among children diagnosed at 10 years and older, the investigators reported.
But health care utilization trends did not mirror changes in incidence, Dr. Benchimol and associates reported. For example, children diagnosed before they were 6 years old had significantly fewer outpatient visits for IBD, compared with children diagnosed at 10 years and older (odds ratio for girls, 0.67; 95% confidence interval, 0.58-0.78; OR for boys, 0.86; 95% CI, 0.75-0.98). Furthermore, patients diagnosed before age 6 years were less likely to be hospitalized for IBD than were older children with the disease (hazard ratio for girls, 0.70; 95% CI, 0.56-0.87; HR for boys, 1.12; 95% CI, 0.94-1.33), the investigators said.
The likelihood of undergoing intestinal resection also was lower for children diagnosed before age 6 years with Crohn’s disease, compared with older girls (HR, 0.35; 95% CI, 0.16-0.78) and boys (HR, 0.59; 95% CI, 0.34-0.99), said the researchers. And patients diagnosed before age 6 years with ulcerative colitis were less likely to undergo colectomy than were older girls (HR, 0.88; 95% CI, 0.47-1.63) and boys (HR, 0.42; 95% CI, 0.21-0.85). In contrast, rates of IBD-related surgery and hospitalization were similar between children diagnosed at 6-9.9 years of age and those diagnosed at age 10 up to 18 years, the investigators said.
A cohort study from the United States also found a lower likelihood of surgery in children with VEO-IBD, the researchers noted. Large-bowel involvement without ileal disease is prominent in young children with IBD, and these patients might be unlikely to undergo resection because colectomy requires a permanent ostotomy, they added.
The work was supported by the American College of Gastroenterology, the Ontario Ministry of Health and Long-Term Care, the Canadian Institutes of Health Research, the Crohn’s and Colitis Foundation of Canada, the National Institutes of Health, the Wolpow Family Chair in IBD Treatment and Research, the Ontario Ministry of Research and Innovation, and the Leona M. and Harry B. Helmsley Charitable Trust. The authors reported no conflicts of interest.
Pediatric inflammatory bowel disease grew by more than 40% in a 15-year period in Ontario, Canada, according to a retrospective cohort study published in the October issue of Gastroenterology.
Although rates of inflammatory bowel disease (IBD) rose in children and adolescents of all ages, the steepest increase occurred in children with very-early-onset IBD (VEO-IBD), defined as disease diagnosed before they were 10 years old, said Dr. Eric Benchimol at the University of Ottawa and his associates. But these patients also tended to use fewer health services and have fewer surgeries for IBD, compared with older children with the disease, the investigators said (Gastroenterology 2014 October [doi.org/10.1053/j.gastro.2014.06.023]).
Source: American Gastroenterological Association
The findings add to research indicating that VEO-IBD is a distinct form of IBD and indicate the need to assess subgroups of these patients to look at phenotype, genotype, intestinal microbiome, and treatment response, the investigators said.
For the study, researchers created a cohort based on an algorithm of health care visits that identified all children and adolescents in Ontario diagnosed with IBD before age 18 years. The analysis included 7,143 patients with IBD, among whom about 14% had VEO-IBD, the investigators reported.
The overall rate of IBD in children up to 18 years old increased from 9.4 to 13.2 cases per 100,000 population from 1994 through 2009 (P less than .0001), the researchers said. And the yearly increase in VEO-IBD averaged 7.4% – more than three times greater than the 2.2% average annual rise among children diagnosed at 10 years and older, the investigators reported.
But health care utilization trends did not mirror changes in incidence, Dr. Benchimol and associates reported. For example, children diagnosed before they were 6 years old had significantly fewer outpatient visits for IBD, compared with children diagnosed at 10 years and older (odds ratio for girls, 0.67; 95% confidence interval, 0.58-0.78; OR for boys, 0.86; 95% CI, 0.75-0.98). Furthermore, patients diagnosed before age 6 years were less likely to be hospitalized for IBD than were older children with the disease (hazard ratio for girls, 0.70; 95% CI, 0.56-0.87; HR for boys, 1.12; 95% CI, 0.94-1.33), the investigators said.
The likelihood of undergoing intestinal resection also was lower for children diagnosed before age 6 years with Crohn’s disease, compared with older girls (HR, 0.35; 95% CI, 0.16-0.78) and boys (HR, 0.59; 95% CI, 0.34-0.99), said the researchers. And patients diagnosed before age 6 years with ulcerative colitis were less likely to undergo colectomy than were older girls (HR, 0.88; 95% CI, 0.47-1.63) and boys (HR, 0.42; 95% CI, 0.21-0.85). In contrast, rates of IBD-related surgery and hospitalization were similar between children diagnosed at 6-9.9 years of age and those diagnosed at age 10 up to 18 years, the investigators said.
A cohort study from the United States also found a lower likelihood of surgery in children with VEO-IBD, the researchers noted. Large-bowel involvement without ileal disease is prominent in young children with IBD, and these patients might be unlikely to undergo resection because colectomy requires a permanent ostotomy, they added.
The work was supported by the American College of Gastroenterology, the Ontario Ministry of Health and Long-Term Care, the Canadian Institutes of Health Research, the Crohn’s and Colitis Foundation of Canada, the National Institutes of Health, the Wolpow Family Chair in IBD Treatment and Research, the Ontario Ministry of Research and Innovation, and the Leona M. and Harry B. Helmsley Charitable Trust. The authors reported no conflicts of interest.
Pediatric inflammatory bowel disease grew by more than 40% in a 15-year period in Ontario, Canada, according to a retrospective cohort study published in the October issue of Gastroenterology.
Although rates of inflammatory bowel disease (IBD) rose in children and adolescents of all ages, the steepest increase occurred in children with very-early-onset IBD (VEO-IBD), defined as disease diagnosed before they were 10 years old, said Dr. Eric Benchimol at the University of Ottawa and his associates. But these patients also tended to use fewer health services and have fewer surgeries for IBD, compared with older children with the disease, the investigators said (Gastroenterology 2014 October [doi.org/10.1053/j.gastro.2014.06.023]).
Source: American Gastroenterological Association
The findings add to research indicating that VEO-IBD is a distinct form of IBD and indicate the need to assess subgroups of these patients to look at phenotype, genotype, intestinal microbiome, and treatment response, the investigators said.
For the study, researchers created a cohort based on an algorithm of health care visits that identified all children and adolescents in Ontario diagnosed with IBD before age 18 years. The analysis included 7,143 patients with IBD, among whom about 14% had VEO-IBD, the investigators reported.
The overall rate of IBD in children up to 18 years old increased from 9.4 to 13.2 cases per 100,000 population from 1994 through 2009 (P less than .0001), the researchers said. And the yearly increase in VEO-IBD averaged 7.4% – more than three times greater than the 2.2% average annual rise among children diagnosed at 10 years and older, the investigators reported.
But health care utilization trends did not mirror changes in incidence, Dr. Benchimol and associates reported. For example, children diagnosed before they were 6 years old had significantly fewer outpatient visits for IBD, compared with children diagnosed at 10 years and older (odds ratio for girls, 0.67; 95% confidence interval, 0.58-0.78; OR for boys, 0.86; 95% CI, 0.75-0.98). Furthermore, patients diagnosed before age 6 years were less likely to be hospitalized for IBD than were older children with the disease (hazard ratio for girls, 0.70; 95% CI, 0.56-0.87; HR for boys, 1.12; 95% CI, 0.94-1.33), the investigators said.
The likelihood of undergoing intestinal resection also was lower for children diagnosed before age 6 years with Crohn’s disease, compared with older girls (HR, 0.35; 95% CI, 0.16-0.78) and boys (HR, 0.59; 95% CI, 0.34-0.99), said the researchers. And patients diagnosed before age 6 years with ulcerative colitis were less likely to undergo colectomy than were older girls (HR, 0.88; 95% CI, 0.47-1.63) and boys (HR, 0.42; 95% CI, 0.21-0.85). In contrast, rates of IBD-related surgery and hospitalization were similar between children diagnosed at 6-9.9 years of age and those diagnosed at age 10 up to 18 years, the investigators said.
A cohort study from the United States also found a lower likelihood of surgery in children with VEO-IBD, the researchers noted. Large-bowel involvement without ileal disease is prominent in young children with IBD, and these patients might be unlikely to undergo resection because colectomy requires a permanent ostotomy, they added.
The work was supported by the American College of Gastroenterology, the Ontario Ministry of Health and Long-Term Care, the Canadian Institutes of Health Research, the Crohn’s and Colitis Foundation of Canada, the National Institutes of Health, the Wolpow Family Chair in IBD Treatment and Research, the Ontario Ministry of Research and Innovation, and the Leona M. and Harry B. Helmsley Charitable Trust. The authors reported no conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: Although the steepest rise in inflammatory bowel disease occurred in children diagnosed before age 10 years, children diagnosed before age 6 years had the lowest rates of IBD-related outpatient visits, hospitalizations, and surgeries.
Major finding: Rates of pediatric IBD increased by more than 40% between 1994 and 2009 in Ontario, Canada. Rates rose by an average of 7.4% annually in children diagnosed before age 10 years, compared with 2.2% for children diagnosed from 10 years to before 18 years of age. Rates of outpatient visits, hospitalizations, and IBD-related surgeries were significantly lower in children diagnosed before age 6 years, compared with children diagnosed at 10 years or older.
Data Source: Retrospective study of the Ontario Crohn’s and Colitis Cohort, which included 7,143 children and adolescents with IBD diagnosed between 1994 and 2009 in Ontario, Canada.
Disclosures: The work was supported by grants and researcher awards from the American College of Gastroenterology, the Ontario Ministry of Health and Long-Term Care, the Canadian Institutes of Health Research, the Crohn’s and Colitis Foundation of Canada, the National Institutes of Health, the Wolpow Family Chair in IBD Treatment and Research, the Ontario Ministry of Research and Innovation, and the Leona M. and Harry B. Helmsley Charitable Trust. The authors reported no conflicts of interest.
Gluten-free diet benefits patients with celiac disease serum markers
A gluten-free diet benefited asymptomatic patients with serologic markers for celiac disease in a prospective randomized study.
The findings support active screening for celiac disease in patients at risk for the disease, even if symptoms aren’t present, according to Dr. Kalle Kurppa of the University of Tampere (Finland) and Tampere University Hospital.
The report is in the September issue of Gastroenterology (doi.org/10.1053/j.gastro.2014.05.003).
After 1 year, 20 adults with endomysial antibodies (EmA) who were randomized to a gluten-free diet (GFD) experienced significant increases in mean mucosal villous height:crypt depth values, significantly decreased levels of celiac-associated antibodies, and greater improvement in gastrointestinal symptoms, compared with 20 patients randomized to a gluten-containing diet. For example, mean small bowel mucosal villous height:crypt depth increased from 1.0 to about 2.8 in the GFD group, and from 0.8 to about 0.9 in the gluten-containing diet group, and total Gastrointestinal Symptoms Rating Scale scores improved significantly (–0.4 difference in mean change from baseline, favoring a GFD), as did individual scores for diarrhea, indigestion, and reflux in the GFD group, wrote Dr. Kurppa and colleagues.
The patients in the GFD group also experienced reduced indigestion, reflux, and anxiety, and better health as measured by Psychological, General Health, and Well-Being scores and most Short Form–36 scores, they noted.
Only social function scores on the Short Form–36 improved more in the gluten-containing diet group (–8.3 difference in mean change from baseline, favoring a gluten-containing diet).
The subjects in both groups had a median age of 42 years, and the groups were similar with respect to sex, medical history, and associated conditions.
No differences were seen between the two groups with respect to laboratory test results, bone mineral density, or body composition, and the subjects in the GFD group did not report any negative effects or reactions to the diet. After trial completion, 92% reported adherence to the gluten-free diet, and 85% said they expected to remain on the diet, the investigators noted.
Because celiac disease affects 1%-2% of the population, but is difficult to detect because of clinical heterogeneity, wide-scale screening with noninvasive serologic testing is frequently suggested.
"However, the only current treatment of the condition, a lifelong strict gluten-free diet, is restrictive and difficult to maintain and thus the positive effects of the screening are not straightforward," the investigators noted, adding that results of prior studies exploring the benefits of a gluten-free diet have been inconsistent – particularly for asymptomatic patients.
Another problem is that wide-scale screening often detects asymptomatic seropositive subjects with only mild enteropathy or even normal small-bowel mucosa, and it is unclear whether these individuals actually suffer from a true gluten-induced clinical disease, they said.
"The results of this randomized study showed that screen-detected and even apparently asymptomatic EmA-positive patients benefit from a gluten-free diet as measured by extensive clinical, serologic, and histologic parameters," the investigators said.
The fact that subjects who considered themselves asymptomatic experienced improvement in the current study suggests that "the patients may in fact have accepted mild symptoms as normal and recognized them as abnormal only later when on the diet," they said.
The findings support active screening for celiac disease in patients at risk, but the potential consequences of screening – particularly on social functioning, should be considered on an individual basis, they said, adding that prospective studies are needed "to unravel whether screen-detected seropositive subjects with completely normal small-bowel mucosal histology should be treated."
This study was supported by the Academy of Finland Research Council for Health, the Competitive Research Funding of the Pirkanmaa Hospital District, the Sigrid Juselius Foundation, the Finnish Foundation for Research, the Yrjö Jahnsson Foundation, the Foundation for Pediatric Research, and the Finnish Celiac Society. The authors reported having no disclosures.
In 2004, the NIH Consensus Conference on Celiac Disease recommended that screening for celiac disease be evaluated, yet a decade later this remains a controversial issue. Available information regarding the morbidity of undiagnosed and untreated celiac disease is based almost entirely on clinically diagnosed disease. Although early detection and treatment may prevent complications, people with subclinical celiac disease are likely to remain well indefinitely on a normal diet without the logistical, social, and economic burdens of a gluten-free diet (GFD).
This key issue of whether diagnosis and treatment benefits those with minimally symptomatic celiac disease is addressed by Kurppa et al. in this issue of Gastroenterology, which describes the results of a randomized trial of treatment of celiac disease diagnosed through screening of individuals with a family history of the disease. In this study, endomysial antibody–positive individuals who adopted the GFD had improvement in intestinal histology, as well as gastrointestinal symptoms, which improved with treatment. Thus, even in a background of best practice case finding, screening detected patients with undetected celiac disease whose symptoms improved on the GFD.
|
|
This study provides some of the strongest data yet supporting celiac disease screening. At the same time, Finland is among the most celiac disease friendly countries in the world, although even here individuals who learned they had celiac disease through screening reported a deterioration of social function. However, while histology and symptoms did improve, they did not normalize. This suggests that celiac disease screening may improve gastrointestinal symptoms, but simultaneously worsen socialization, offer no overall change in health-related quality of life, and offer unknown long-term benefits. Until these uncertainties are addressed, widespread celiac disease screening is likely to remain a research endeavor only.
Dr. Daniel A. Leffler is director of research, The Celiac Center at BIDMC, director of quality assurance, division of gastroenterology, Beth Israel Deaconess Medical Center, Boston. Dr. Leffler has served as a consultant for or received research support from the National Institutes of Health, Sidney Frank Foundation, Inova Diagnostics, Prometheus Laboratories, Alba Therapeutics, Alvine Pharmaceuticals, Genzyme, Coranado Biosciences, and Bioline Rx.
In 2004, the NIH Consensus Conference on Celiac Disease recommended that screening for celiac disease be evaluated, yet a decade later this remains a controversial issue. Available information regarding the morbidity of undiagnosed and untreated celiac disease is based almost entirely on clinically diagnosed disease. Although early detection and treatment may prevent complications, people with subclinical celiac disease are likely to remain well indefinitely on a normal diet without the logistical, social, and economic burdens of a gluten-free diet (GFD).
This key issue of whether diagnosis and treatment benefits those with minimally symptomatic celiac disease is addressed by Kurppa et al. in this issue of Gastroenterology, which describes the results of a randomized trial of treatment of celiac disease diagnosed through screening of individuals with a family history of the disease. In this study, endomysial antibody–positive individuals who adopted the GFD had improvement in intestinal histology, as well as gastrointestinal symptoms, which improved with treatment. Thus, even in a background of best practice case finding, screening detected patients with undetected celiac disease whose symptoms improved on the GFD.
|
|
This study provides some of the strongest data yet supporting celiac disease screening. At the same time, Finland is among the most celiac disease friendly countries in the world, although even here individuals who learned they had celiac disease through screening reported a deterioration of social function. However, while histology and symptoms did improve, they did not normalize. This suggests that celiac disease screening may improve gastrointestinal symptoms, but simultaneously worsen socialization, offer no overall change in health-related quality of life, and offer unknown long-term benefits. Until these uncertainties are addressed, widespread celiac disease screening is likely to remain a research endeavor only.
Dr. Daniel A. Leffler is director of research, The Celiac Center at BIDMC, director of quality assurance, division of gastroenterology, Beth Israel Deaconess Medical Center, Boston. Dr. Leffler has served as a consultant for or received research support from the National Institutes of Health, Sidney Frank Foundation, Inova Diagnostics, Prometheus Laboratories, Alba Therapeutics, Alvine Pharmaceuticals, Genzyme, Coranado Biosciences, and Bioline Rx.
In 2004, the NIH Consensus Conference on Celiac Disease recommended that screening for celiac disease be evaluated, yet a decade later this remains a controversial issue. Available information regarding the morbidity of undiagnosed and untreated celiac disease is based almost entirely on clinically diagnosed disease. Although early detection and treatment may prevent complications, people with subclinical celiac disease are likely to remain well indefinitely on a normal diet without the logistical, social, and economic burdens of a gluten-free diet (GFD).
This key issue of whether diagnosis and treatment benefits those with minimally symptomatic celiac disease is addressed by Kurppa et al. in this issue of Gastroenterology, which describes the results of a randomized trial of treatment of celiac disease diagnosed through screening of individuals with a family history of the disease. In this study, endomysial antibody–positive individuals who adopted the GFD had improvement in intestinal histology, as well as gastrointestinal symptoms, which improved with treatment. Thus, even in a background of best practice case finding, screening detected patients with undetected celiac disease whose symptoms improved on the GFD.
|
|
This study provides some of the strongest data yet supporting celiac disease screening. At the same time, Finland is among the most celiac disease friendly countries in the world, although even here individuals who learned they had celiac disease through screening reported a deterioration of social function. However, while histology and symptoms did improve, they did not normalize. This suggests that celiac disease screening may improve gastrointestinal symptoms, but simultaneously worsen socialization, offer no overall change in health-related quality of life, and offer unknown long-term benefits. Until these uncertainties are addressed, widespread celiac disease screening is likely to remain a research endeavor only.
Dr. Daniel A. Leffler is director of research, The Celiac Center at BIDMC, director of quality assurance, division of gastroenterology, Beth Israel Deaconess Medical Center, Boston. Dr. Leffler has served as a consultant for or received research support from the National Institutes of Health, Sidney Frank Foundation, Inova Diagnostics, Prometheus Laboratories, Alba Therapeutics, Alvine Pharmaceuticals, Genzyme, Coranado Biosciences, and Bioline Rx.
A gluten-free diet benefited asymptomatic patients with serologic markers for celiac disease in a prospective randomized study.
The findings support active screening for celiac disease in patients at risk for the disease, even if symptoms aren’t present, according to Dr. Kalle Kurppa of the University of Tampere (Finland) and Tampere University Hospital.
The report is in the September issue of Gastroenterology (doi.org/10.1053/j.gastro.2014.05.003).
After 1 year, 20 adults with endomysial antibodies (EmA) who were randomized to a gluten-free diet (GFD) experienced significant increases in mean mucosal villous height:crypt depth values, significantly decreased levels of celiac-associated antibodies, and greater improvement in gastrointestinal symptoms, compared with 20 patients randomized to a gluten-containing diet. For example, mean small bowel mucosal villous height:crypt depth increased from 1.0 to about 2.8 in the GFD group, and from 0.8 to about 0.9 in the gluten-containing diet group, and total Gastrointestinal Symptoms Rating Scale scores improved significantly (–0.4 difference in mean change from baseline, favoring a GFD), as did individual scores for diarrhea, indigestion, and reflux in the GFD group, wrote Dr. Kurppa and colleagues.
The patients in the GFD group also experienced reduced indigestion, reflux, and anxiety, and better health as measured by Psychological, General Health, and Well-Being scores and most Short Form–36 scores, they noted.
Only social function scores on the Short Form–36 improved more in the gluten-containing diet group (–8.3 difference in mean change from baseline, favoring a gluten-containing diet).
The subjects in both groups had a median age of 42 years, and the groups were similar with respect to sex, medical history, and associated conditions.
No differences were seen between the two groups with respect to laboratory test results, bone mineral density, or body composition, and the subjects in the GFD group did not report any negative effects or reactions to the diet. After trial completion, 92% reported adherence to the gluten-free diet, and 85% said they expected to remain on the diet, the investigators noted.
Because celiac disease affects 1%-2% of the population, but is difficult to detect because of clinical heterogeneity, wide-scale screening with noninvasive serologic testing is frequently suggested.
"However, the only current treatment of the condition, a lifelong strict gluten-free diet, is restrictive and difficult to maintain and thus the positive effects of the screening are not straightforward," the investigators noted, adding that results of prior studies exploring the benefits of a gluten-free diet have been inconsistent – particularly for asymptomatic patients.
Another problem is that wide-scale screening often detects asymptomatic seropositive subjects with only mild enteropathy or even normal small-bowel mucosa, and it is unclear whether these individuals actually suffer from a true gluten-induced clinical disease, they said.
"The results of this randomized study showed that screen-detected and even apparently asymptomatic EmA-positive patients benefit from a gluten-free diet as measured by extensive clinical, serologic, and histologic parameters," the investigators said.
The fact that subjects who considered themselves asymptomatic experienced improvement in the current study suggests that "the patients may in fact have accepted mild symptoms as normal and recognized them as abnormal only later when on the diet," they said.
The findings support active screening for celiac disease in patients at risk, but the potential consequences of screening – particularly on social functioning, should be considered on an individual basis, they said, adding that prospective studies are needed "to unravel whether screen-detected seropositive subjects with completely normal small-bowel mucosal histology should be treated."
This study was supported by the Academy of Finland Research Council for Health, the Competitive Research Funding of the Pirkanmaa Hospital District, the Sigrid Juselius Foundation, the Finnish Foundation for Research, the Yrjö Jahnsson Foundation, the Foundation for Pediatric Research, and the Finnish Celiac Society. The authors reported having no disclosures.
A gluten-free diet benefited asymptomatic patients with serologic markers for celiac disease in a prospective randomized study.
The findings support active screening for celiac disease in patients at risk for the disease, even if symptoms aren’t present, according to Dr. Kalle Kurppa of the University of Tampere (Finland) and Tampere University Hospital.
The report is in the September issue of Gastroenterology (doi.org/10.1053/j.gastro.2014.05.003).
After 1 year, 20 adults with endomysial antibodies (EmA) who were randomized to a gluten-free diet (GFD) experienced significant increases in mean mucosal villous height:crypt depth values, significantly decreased levels of celiac-associated antibodies, and greater improvement in gastrointestinal symptoms, compared with 20 patients randomized to a gluten-containing diet. For example, mean small bowel mucosal villous height:crypt depth increased from 1.0 to about 2.8 in the GFD group, and from 0.8 to about 0.9 in the gluten-containing diet group, and total Gastrointestinal Symptoms Rating Scale scores improved significantly (–0.4 difference in mean change from baseline, favoring a GFD), as did individual scores for diarrhea, indigestion, and reflux in the GFD group, wrote Dr. Kurppa and colleagues.
The patients in the GFD group also experienced reduced indigestion, reflux, and anxiety, and better health as measured by Psychological, General Health, and Well-Being scores and most Short Form–36 scores, they noted.
Only social function scores on the Short Form–36 improved more in the gluten-containing diet group (–8.3 difference in mean change from baseline, favoring a gluten-containing diet).
The subjects in both groups had a median age of 42 years, and the groups were similar with respect to sex, medical history, and associated conditions.
No differences were seen between the two groups with respect to laboratory test results, bone mineral density, or body composition, and the subjects in the GFD group did not report any negative effects or reactions to the diet. After trial completion, 92% reported adherence to the gluten-free diet, and 85% said they expected to remain on the diet, the investigators noted.
Because celiac disease affects 1%-2% of the population, but is difficult to detect because of clinical heterogeneity, wide-scale screening with noninvasive serologic testing is frequently suggested.
"However, the only current treatment of the condition, a lifelong strict gluten-free diet, is restrictive and difficult to maintain and thus the positive effects of the screening are not straightforward," the investigators noted, adding that results of prior studies exploring the benefits of a gluten-free diet have been inconsistent – particularly for asymptomatic patients.
Another problem is that wide-scale screening often detects asymptomatic seropositive subjects with only mild enteropathy or even normal small-bowel mucosa, and it is unclear whether these individuals actually suffer from a true gluten-induced clinical disease, they said.
"The results of this randomized study showed that screen-detected and even apparently asymptomatic EmA-positive patients benefit from a gluten-free diet as measured by extensive clinical, serologic, and histologic parameters," the investigators said.
The fact that subjects who considered themselves asymptomatic experienced improvement in the current study suggests that "the patients may in fact have accepted mild symptoms as normal and recognized them as abnormal only later when on the diet," they said.
The findings support active screening for celiac disease in patients at risk, but the potential consequences of screening – particularly on social functioning, should be considered on an individual basis, they said, adding that prospective studies are needed "to unravel whether screen-detected seropositive subjects with completely normal small-bowel mucosal histology should be treated."
This study was supported by the Academy of Finland Research Council for Health, the Competitive Research Funding of the Pirkanmaa Hospital District, the Sigrid Juselius Foundation, the Finnish Foundation for Research, the Yrjö Jahnsson Foundation, the Foundation for Pediatric Research, and the Finnish Celiac Society. The authors reported having no disclosures.
FROM gastroenterology
Key clinical point: Asymptomatic patients with celiac serum markers may not be truly asymptomatic and will improve with a gluten-free diet.
Major finding: The difference in mean change from baseline for total GSRS scores was –0.4 favoring a GFD vs. a gluten-containing diet.
Data source: A prospective randomized study of 40 adults.
Disclosures: This study was supported by the Academy of Finland Research Council for Health, the Competitive Research Funding of the Pirkanmaa Hospital District, the Sigrid Juselius Foundation, the Finnish Foundation for Research, the Yrjö Jahnsson Foundation, the Foundation for Pediatric Research, and the Finnish Celiac Society. The authors reported having no disclosures.
VIDEO: Vedolizumab may benefit Crohn’s patients who fail anti-TNF therapy
Vedolizumab was not superior to placebo for inducing remission at 6 weeks in patients with Crohn’s disease who failed to respond to anti–tumor necrosis factor therapy, according to findings from the double-blind, phase III GEMINI 3 trial.
However, therapeutic benefit from the humanized, anti–alpha-4 beta-7 integrin, immunoglobulin G1 monoclonal antibody did become apparent by week 10, Dr. Bruce E. Sands of the Icahn School of Medicine at Mount Sinai, New York, and his colleagues report in the September issue of Gastroenterology (doi: 10.1053/j.gastro.2014.05.008).
Source: American Gastroenterological Association
The investigators randomized 315 patients with moderately to severely active Crohn’s disease who failed anti-TNF therapy to receive 300 mg of vedolizumab (158 patients) or placebo (157 patients) intravenously at weeks 0, 2, and 6. The results showed that 15.2% of the vedolizumab group was in remission at week 6, compared with 12.1% of the placebo group (relative risk, 1.2). At week 10, 26.6% of patients in the vedolizumab group, compared with 12.1% of those in the placebo group, were in remission (RR, 2.2), the investigators reported.
More patients in the vedolizumab group did, however, achieve at least a 100-point decrease in the Crohn’s Disease Activity Index (CDAI) score at both 6 weeks (39.2% vs. 22.3% of placebo patients; RR, 1.8) and 10 weeks (46.8% vs. 24.8%; RR, 1.4), they said.
The incidence and type of adverse events were similar in both groups.
GEMINI 3 was conducted between November 2010 and April 2012 at 107 sites in North America, Europe, Asia, Africa, and Australia. Participants were aged 18-80 years with moderately to severely active Crohn’s disease (defined in part by a CDAI score of 220-400 points), with known involvement of the ileum and/or colon at 3 or more months before enrollment.
Remission was defined by a CDAI score of 150 points or less.
Treatment with TNF antagonists has improved the care of patients with Crohn’s disease that is refractory to other treatments, but in controlled trials anti-TNF therapy failed in about two-thirds of patients. Treatment is also associated with an increased risk of serious infections in some patients. Natalizumab, another treatment used in Crohn’s disease, has been limited by its association with an increased risk of progressive multifocal leukoencephalopathy.
"Because of these limitations with TNF antagonists and natalizumab, therapies for patients with TNF antagonist failure are needed, and those that selectively inhibit lymphocyte trafficking to the gut may yield important safety benefits," the investigators said.
Vedolizumab was shown in the pivotal GEMINI 2 study to be safe and effective for induction and maintenance in patients with moderately to severely active Crohn’s disease who failed one or more prior therapies; GEMINI 3 specifically focuses on patients with prior TNF antagonist failure.
"The results of this short-term study support the safety of vedolizumab in patients with Crohn’s disease and are consistent with the drug’s postulated gut-selective mechanism of action," the investigators said.
Furthermore, several prespecified outcomes suggest that in addition to leading to clinical remission in the TNF antagonist–naive patients with Crohn’s disease, vedolizumab may lead to clinical remission at 10 weeks in those who failed TNF antagonist therapy.
"These clinically relevant response kinetics have potential implications for bridging induction therapy to vedolizumab maintenance therapy, which has established efficacy, in patients with this lifelong condition," they concluded.
This study was funded by Millennium Pharmaceuticals (doing business as Takeda Pharmaceuticals). Dr. Sands reported receiving consulting and advisory board fees, as well as clinical research/institutional grant support from AbbVie, Janssen, and Takeda. Detailed disclosures for all authors are available with the full text of the article.
Vedolizumab was not superior to placebo for inducing remission at 6 weeks in patients with Crohn’s disease who failed to respond to anti–tumor necrosis factor therapy, according to findings from the double-blind, phase III GEMINI 3 trial.
However, therapeutic benefit from the humanized, anti–alpha-4 beta-7 integrin, immunoglobulin G1 monoclonal antibody did become apparent by week 10, Dr. Bruce E. Sands of the Icahn School of Medicine at Mount Sinai, New York, and his colleagues report in the September issue of Gastroenterology (doi: 10.1053/j.gastro.2014.05.008).
Source: American Gastroenterological Association
The investigators randomized 315 patients with moderately to severely active Crohn’s disease who failed anti-TNF therapy to receive 300 mg of vedolizumab (158 patients) or placebo (157 patients) intravenously at weeks 0, 2, and 6. The results showed that 15.2% of the vedolizumab group was in remission at week 6, compared with 12.1% of the placebo group (relative risk, 1.2). At week 10, 26.6% of patients in the vedolizumab group, compared with 12.1% of those in the placebo group, were in remission (RR, 2.2), the investigators reported.
More patients in the vedolizumab group did, however, achieve at least a 100-point decrease in the Crohn’s Disease Activity Index (CDAI) score at both 6 weeks (39.2% vs. 22.3% of placebo patients; RR, 1.8) and 10 weeks (46.8% vs. 24.8%; RR, 1.4), they said.
The incidence and type of adverse events were similar in both groups.
GEMINI 3 was conducted between November 2010 and April 2012 at 107 sites in North America, Europe, Asia, Africa, and Australia. Participants were aged 18-80 years with moderately to severely active Crohn’s disease (defined in part by a CDAI score of 220-400 points), with known involvement of the ileum and/or colon at 3 or more months before enrollment.
Remission was defined by a CDAI score of 150 points or less.
Treatment with TNF antagonists has improved the care of patients with Crohn’s disease that is refractory to other treatments, but in controlled trials anti-TNF therapy failed in about two-thirds of patients. Treatment is also associated with an increased risk of serious infections in some patients. Natalizumab, another treatment used in Crohn’s disease, has been limited by its association with an increased risk of progressive multifocal leukoencephalopathy.
"Because of these limitations with TNF antagonists and natalizumab, therapies for patients with TNF antagonist failure are needed, and those that selectively inhibit lymphocyte trafficking to the gut may yield important safety benefits," the investigators said.
Vedolizumab was shown in the pivotal GEMINI 2 study to be safe and effective for induction and maintenance in patients with moderately to severely active Crohn’s disease who failed one or more prior therapies; GEMINI 3 specifically focuses on patients with prior TNF antagonist failure.
"The results of this short-term study support the safety of vedolizumab in patients with Crohn’s disease and are consistent with the drug’s postulated gut-selective mechanism of action," the investigators said.
Furthermore, several prespecified outcomes suggest that in addition to leading to clinical remission in the TNF antagonist–naive patients with Crohn’s disease, vedolizumab may lead to clinical remission at 10 weeks in those who failed TNF antagonist therapy.
"These clinically relevant response kinetics have potential implications for bridging induction therapy to vedolizumab maintenance therapy, which has established efficacy, in patients with this lifelong condition," they concluded.
This study was funded by Millennium Pharmaceuticals (doing business as Takeda Pharmaceuticals). Dr. Sands reported receiving consulting and advisory board fees, as well as clinical research/institutional grant support from AbbVie, Janssen, and Takeda. Detailed disclosures for all authors are available with the full text of the article.
Vedolizumab was not superior to placebo for inducing remission at 6 weeks in patients with Crohn’s disease who failed to respond to anti–tumor necrosis factor therapy, according to findings from the double-blind, phase III GEMINI 3 trial.
However, therapeutic benefit from the humanized, anti–alpha-4 beta-7 integrin, immunoglobulin G1 monoclonal antibody did become apparent by week 10, Dr. Bruce E. Sands of the Icahn School of Medicine at Mount Sinai, New York, and his colleagues report in the September issue of Gastroenterology (doi: 10.1053/j.gastro.2014.05.008).
Source: American Gastroenterological Association
The investigators randomized 315 patients with moderately to severely active Crohn’s disease who failed anti-TNF therapy to receive 300 mg of vedolizumab (158 patients) or placebo (157 patients) intravenously at weeks 0, 2, and 6. The results showed that 15.2% of the vedolizumab group was in remission at week 6, compared with 12.1% of the placebo group (relative risk, 1.2). At week 10, 26.6% of patients in the vedolizumab group, compared with 12.1% of those in the placebo group, were in remission (RR, 2.2), the investigators reported.
More patients in the vedolizumab group did, however, achieve at least a 100-point decrease in the Crohn’s Disease Activity Index (CDAI) score at both 6 weeks (39.2% vs. 22.3% of placebo patients; RR, 1.8) and 10 weeks (46.8% vs. 24.8%; RR, 1.4), they said.
The incidence and type of adverse events were similar in both groups.
GEMINI 3 was conducted between November 2010 and April 2012 at 107 sites in North America, Europe, Asia, Africa, and Australia. Participants were aged 18-80 years with moderately to severely active Crohn’s disease (defined in part by a CDAI score of 220-400 points), with known involvement of the ileum and/or colon at 3 or more months before enrollment.
Remission was defined by a CDAI score of 150 points or less.
Treatment with TNF antagonists has improved the care of patients with Crohn’s disease that is refractory to other treatments, but in controlled trials anti-TNF therapy failed in about two-thirds of patients. Treatment is also associated with an increased risk of serious infections in some patients. Natalizumab, another treatment used in Crohn’s disease, has been limited by its association with an increased risk of progressive multifocal leukoencephalopathy.
"Because of these limitations with TNF antagonists and natalizumab, therapies for patients with TNF antagonist failure are needed, and those that selectively inhibit lymphocyte trafficking to the gut may yield important safety benefits," the investigators said.
Vedolizumab was shown in the pivotal GEMINI 2 study to be safe and effective for induction and maintenance in patients with moderately to severely active Crohn’s disease who failed one or more prior therapies; GEMINI 3 specifically focuses on patients with prior TNF antagonist failure.
"The results of this short-term study support the safety of vedolizumab in patients with Crohn’s disease and are consistent with the drug’s postulated gut-selective mechanism of action," the investigators said.
Furthermore, several prespecified outcomes suggest that in addition to leading to clinical remission in the TNF antagonist–naive patients with Crohn’s disease, vedolizumab may lead to clinical remission at 10 weeks in those who failed TNF antagonist therapy.
"These clinically relevant response kinetics have potential implications for bridging induction therapy to vedolizumab maintenance therapy, which has established efficacy, in patients with this lifelong condition," they concluded.
This study was funded by Millennium Pharmaceuticals (doing business as Takeda Pharmaceuticals). Dr. Sands reported receiving consulting and advisory board fees, as well as clinical research/institutional grant support from AbbVie, Janssen, and Takeda. Detailed disclosures for all authors are available with the full text of the article.
FROM GASTROENTEROLOGY
Key clinical point: Vedolizumab seems to take longer than 6 weeks to work in patients with moderately to severely active Crohn’s disease.
Major finding: At 10 weeks, significantly more patients in the vedolizumab vs. placebo group were in remission (26.6% vs.12.1%; relative risk, 2.2).
Data source: The phase III, randomized, placebo-controlled, double-blind GEMINI 3 trial, which included 315 patients who failed anti-TNF therapy.
Disclosures: This study was funded by Millennium Pharmaceuticals (doing business as Takeda Pharmaceuticals). Dr. Sands reported receiving consulting and advisory board fees, as well as clinical research/institutional grant support from AbbVie, Janssen, and Takeda. Detailed disclosures for all authors are available with the full text of the article.
VIDEO: Systematic review: Anti-TNFs for IBD don’t up pediatric lymphoma risk
The risk of lymphoma is no greater in children with inflammatory bowel disease who are treated with anti–tumor necrosis factor therapy than in adults treated with anti-TNF therapies or in children treated with other therapies for IBD, according to findings from a systematic review.
The review, which included 65 studies involving a total of 5,528 patients with 9,516 patient-years of follow-up, also showed that the rate of serious infection was lower among children with IBD who were treated with anti-TNF agents than among those treated with steroids or among adults treated with anti-TNF agents, Dr. Parambir S. Dulai of Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his colleagues reported in the September issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2014.01.021).
Source: American Gastroenterological Association
Two patients developed lymphoma, for a rate of 2.1/10,000 patient-years of follow-up (PYF), which did not differ significantly from the expected rate among children (5.8/100,000 PYF), the rate among pediatric patients receiving thiopurine monotherapy (4.5/10,000), or the rate among adults treated with anti-TNF agents (6.1/10,000), the investigators found.
The rate of serious infections was 352/10,000 PYF in pediatric patients treated with anti-TNF agents as part of prospective studies included in the review, which was similar to the expected rate in those treated with immunomodulator therapy (333/10,000 PYF), and significantly lower than the expected rate in those treated with glucocorticoids (730/10,000 PYF) and adults treated with anti-TNF agents (654/10,000 PYF).
Of seven deaths that occurred among the patients, five were considered related to treatment (four cases of sepsis, one case of arrhythmia), for a rate of 5.3/10,000 PYF.
Although anti-TNF therapy is an effective treatment option for pediatric IBD, many physicians are hesitant about prescribing anti-TNFs to children because of concerns about infection and lymphoma risk based on the adult literature and case reports of hepatosplenic T-cell lymphoma. However, the findings of this pooled analysis suggest that such concerns may be unfounded.
Older age, sex, and duration of IBD have been linked with increased risk of lymphoproliferative disorders and could help explain the observed differences between adults and pediatric IBD patients with respect to lymphoma rates after anti-TNF exposure, the investigators said.
"Overall, the risk of serious infection, lymphoma, and death with anti-TNF therapy in pediatric IBD is very low," they wrote.
However, they noted that the study is limited by a number of factors, including short duration of per-person follow-up, which means that while the data are promising, they are "not definitive in answering the question of whether anti-TNF therapy is associated with an increased risk of lymphoma, particularly with long-term use," the investigators said.
Long-term follow-up studies are needed in children to assess whether lymphoma risk is exposure dependent – as suggested by the existing literature – rather than a cumulative risk that is dependent on duration of therapy, they added.
Dr. Dulai reported having no disclosures. Coauthor Dr. Corey Siegel reported serving as an advisory board member or consultant for, and/or receiving grant support from Abbvie, Janssen, UCB, and the Agency for Healthcare Research and Quality. Dr. Marla Dubinsky serves as a consultant for Abbvie, Janssen, UCB, and Takeda.
The risk of lymphoma is no greater in children with inflammatory bowel disease who are treated with anti–tumor necrosis factor therapy than in adults treated with anti-TNF therapies or in children treated with other therapies for IBD, according to findings from a systematic review.
The review, which included 65 studies involving a total of 5,528 patients with 9,516 patient-years of follow-up, also showed that the rate of serious infection was lower among children with IBD who were treated with anti-TNF agents than among those treated with steroids or among adults treated with anti-TNF agents, Dr. Parambir S. Dulai of Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his colleagues reported in the September issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2014.01.021).
Source: American Gastroenterological Association
Two patients developed lymphoma, for a rate of 2.1/10,000 patient-years of follow-up (PYF), which did not differ significantly from the expected rate among children (5.8/100,000 PYF), the rate among pediatric patients receiving thiopurine monotherapy (4.5/10,000), or the rate among adults treated with anti-TNF agents (6.1/10,000), the investigators found.
The rate of serious infections was 352/10,000 PYF in pediatric patients treated with anti-TNF agents as part of prospective studies included in the review, which was similar to the expected rate in those treated with immunomodulator therapy (333/10,000 PYF), and significantly lower than the expected rate in those treated with glucocorticoids (730/10,000 PYF) and adults treated with anti-TNF agents (654/10,000 PYF).
Of seven deaths that occurred among the patients, five were considered related to treatment (four cases of sepsis, one case of arrhythmia), for a rate of 5.3/10,000 PYF.
Although anti-TNF therapy is an effective treatment option for pediatric IBD, many physicians are hesitant about prescribing anti-TNFs to children because of concerns about infection and lymphoma risk based on the adult literature and case reports of hepatosplenic T-cell lymphoma. However, the findings of this pooled analysis suggest that such concerns may be unfounded.
Older age, sex, and duration of IBD have been linked with increased risk of lymphoproliferative disorders and could help explain the observed differences between adults and pediatric IBD patients with respect to lymphoma rates after anti-TNF exposure, the investigators said.
"Overall, the risk of serious infection, lymphoma, and death with anti-TNF therapy in pediatric IBD is very low," they wrote.
However, they noted that the study is limited by a number of factors, including short duration of per-person follow-up, which means that while the data are promising, they are "not definitive in answering the question of whether anti-TNF therapy is associated with an increased risk of lymphoma, particularly with long-term use," the investigators said.
Long-term follow-up studies are needed in children to assess whether lymphoma risk is exposure dependent – as suggested by the existing literature – rather than a cumulative risk that is dependent on duration of therapy, they added.
Dr. Dulai reported having no disclosures. Coauthor Dr. Corey Siegel reported serving as an advisory board member or consultant for, and/or receiving grant support from Abbvie, Janssen, UCB, and the Agency for Healthcare Research and Quality. Dr. Marla Dubinsky serves as a consultant for Abbvie, Janssen, UCB, and Takeda.
The risk of lymphoma is no greater in children with inflammatory bowel disease who are treated with anti–tumor necrosis factor therapy than in adults treated with anti-TNF therapies or in children treated with other therapies for IBD, according to findings from a systematic review.
The review, which included 65 studies involving a total of 5,528 patients with 9,516 patient-years of follow-up, also showed that the rate of serious infection was lower among children with IBD who were treated with anti-TNF agents than among those treated with steroids or among adults treated with anti-TNF agents, Dr. Parambir S. Dulai of Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his colleagues reported in the September issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2014.01.021).
Source: American Gastroenterological Association
Two patients developed lymphoma, for a rate of 2.1/10,000 patient-years of follow-up (PYF), which did not differ significantly from the expected rate among children (5.8/100,000 PYF), the rate among pediatric patients receiving thiopurine monotherapy (4.5/10,000), or the rate among adults treated with anti-TNF agents (6.1/10,000), the investigators found.
The rate of serious infections was 352/10,000 PYF in pediatric patients treated with anti-TNF agents as part of prospective studies included in the review, which was similar to the expected rate in those treated with immunomodulator therapy (333/10,000 PYF), and significantly lower than the expected rate in those treated with glucocorticoids (730/10,000 PYF) and adults treated with anti-TNF agents (654/10,000 PYF).
Of seven deaths that occurred among the patients, five were considered related to treatment (four cases of sepsis, one case of arrhythmia), for a rate of 5.3/10,000 PYF.
Although anti-TNF therapy is an effective treatment option for pediatric IBD, many physicians are hesitant about prescribing anti-TNFs to children because of concerns about infection and lymphoma risk based on the adult literature and case reports of hepatosplenic T-cell lymphoma. However, the findings of this pooled analysis suggest that such concerns may be unfounded.
Older age, sex, and duration of IBD have been linked with increased risk of lymphoproliferative disorders and could help explain the observed differences between adults and pediatric IBD patients with respect to lymphoma rates after anti-TNF exposure, the investigators said.
"Overall, the risk of serious infection, lymphoma, and death with anti-TNF therapy in pediatric IBD is very low," they wrote.
However, they noted that the study is limited by a number of factors, including short duration of per-person follow-up, which means that while the data are promising, they are "not definitive in answering the question of whether anti-TNF therapy is associated with an increased risk of lymphoma, particularly with long-term use," the investigators said.
Long-term follow-up studies are needed in children to assess whether lymphoma risk is exposure dependent – as suggested by the existing literature – rather than a cumulative risk that is dependent on duration of therapy, they added.
Dr. Dulai reported having no disclosures. Coauthor Dr. Corey Siegel reported serving as an advisory board member or consultant for, and/or receiving grant support from Abbvie, Janssen, UCB, and the Agency for Healthcare Research and Quality. Dr. Marla Dubinsky serves as a consultant for Abbvie, Janssen, UCB, and Takeda.
Key clinical point: Physicians should not be hesitant about prescribing anti-TNFs to children because of lymphoma risk.
Major finding: The rate of lymphoma in children with IBD who were treated with anti-TNF agents was 2.1/10,000 patient-years of follow-up, which did not differ significantly from the expected rate in children (5.8/100,000).
Data source: A systematic review of 65 studies involving 5,528 patients.
Disclosures: Dr. Dulai reported having no disclosures. Coauthor Dr. Corey Siegel reported serving as an advisory board member or consultant for, and/or receiving grant support from Abbvie, Janssen, UCB, and the Agency for Healthcare Research and Quality. Dr. Marla Dubinsky serves as a consultant for Abbvie, Janssen, UCB, and Takeda.