User login
Sarah Stella, MD, Has a Heart for Safety-Net Hospital Medicine
The best advice Sarah Stella, MD, ever received was simple: “You can’t cure everyone, but you can help everyone.” Why has the adage stuck with her?
Because the advice came from her dad, “and he’s been right about a lot of things before,” she says with a smile.
Dr. Stella got into medicine—clearly with her father’s blessing—to satisfy her “intense curiosity about my fellow human beings and to try to ease suffering.” She has risen to be an academic hospitalist at Denver Health and is one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Tell us about your training. What did you like most/dislike during the process?
Answer: I attended medical school at Michigan State College of Human Medicine. I appreciated their humanistic approach to medical education. I chose the University of Colorado for my internal medicine residency because I love the sunshine and the mountains and because I thought the large academic program would complement my community-based medical school training. I loved being able to easily access nature on my days off.
Q: What do you like most about working as a hospitalist?
A: Spending time with incredible patients and working to solve difficult problems alongside amazing colleagues. I also love the diversity of the work, being involved in direct patient care, teaching students and residents, being a part of committees, performing quality improvement research. I love the flexibility of the job, which allows me to spend time with my family and travel fairly frequently to far-flung places.
Q: Did you have a mentor during your training or early career?
A: My earliest mentor was my father, also a physician [an oncologist]. Some of my earliest medical memories are of going to the hospital with my dad, who also brought home petri dishes from the lab, which my brother and I then used to perform household science experiments. My dad taught me my first lessons about the scientific method and about the importance of a strong work ethic and mentorship. Since then, I have had many outstanding mentors and role models for various aspects of my training/career. During my time at Denver Health, Drs. Richard K. Albert and Marisha Burden have provided me with invaluable mentorship in my scholarly pursuits.
Q: Have you tried to mentor others? Why or why not?
A: I have really loved mentoring students and residents. It is among the most meaningful experiences of my career. Presently, I am a mentor for undergraduate students from underrepresented minority groups. The maturity, passion, and drive these students possess inspires me.
Q: Why is your mentoring focused on minorities? What is the appeal of that to you?
A: I mentor students and residents from all backgrounds. However, mentoring students from underrepresented minority groups is especially important to me. Ethnic minorities continue to have decreased access to healthcare and disproportionately high morbidity and mortality. In order to improve these disparities, we need to have more healthcare providers from these groups. Yet such students, while they may initially be attracted to a career in medicine, are much less likely to maintain their interest. The reasons for this are complicated but may be explained by differences in access to mentors to help guide and inspire them, write letters, etc.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Developing a rapport with patients. I try to use some techniques from social psychology to help me more easily. The hospital is a particularly depersonalizing place, so trying to see the person behind the patient does help.
Q: What aspect of patient care is most rewarding?
A: Really connecting with patients and seeing them thrive. Working at a safety-net hospital, I have the privilege of caring for some of the most underserved but some of the most gracious and beautiful people.
Q: Are you on teaching service? If so, what aspect of teaching in the 21st century is most difficult? And what is most enjoyable?
A: I do enjoy supervising medical students and residents at all levels and attend frequently on the medical wards. I particularly love teaching medical students because of their enthusiasm and curiosity. I love being reminded of basic pathophysiology by a thoughtfully asked question from a medical student. I am a big advocate of bedside rounding. Finding a way to do this efficiently and while teaching to all the levels on the team is challenging. Also, I still enjoy my own direct patient care activities and feel that they challenge me in a different way and make me a better teacher.
Q: Outside of patient care, tell us about your career interests.
A: My research has focused on understanding problems experienced by patients following hospital discharge and designing systems to help ameliorate them. On an institutional level, I serve on several committees, including the Utilization Review Committee, and a group aiming to improve collaboration between hospitalists and primary care physicians and improve discharge transitions. I have participated in several LEAN events aimed at understanding and improving various systems issues.
Q: When you aren’t working, what is important to you?
A: My family and friends, sunshine, and travel. My husband grew up in Papua, New Guinea, and Australia, and both of his parents are physicians, so he is very understanding and not the least bit grossed out when I regale him with stories involving bodily fluids. We have a beautiful, inquisitive 3-year-old daughter and her furry older sister, Ginger Wasabi Ninja. As the oldest of seven, I also love hanging out with my siblings.
Q: What SHM event has made the most lasting impression on you?
A: I really enjoyed HM16, particularly the keynote address by our U.S. Surgeon General and fellow hospitalist, Vivek Murthy, MD, who discussed the role hospitalists can play in public health. His message that we hospitalists should put as much of an effort into trying to improve health outside the walls of the hospital as we do within the walls really resonated with me and has encouraged me to get more involved in the community. TH
Richard Quinn is a freelance writer in New Jersey.
The best advice Sarah Stella, MD, ever received was simple: “You can’t cure everyone, but you can help everyone.” Why has the adage stuck with her?
Because the advice came from her dad, “and he’s been right about a lot of things before,” she says with a smile.
Dr. Stella got into medicine—clearly with her father’s blessing—to satisfy her “intense curiosity about my fellow human beings and to try to ease suffering.” She has risen to be an academic hospitalist at Denver Health and is one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Tell us about your training. What did you like most/dislike during the process?
Answer: I attended medical school at Michigan State College of Human Medicine. I appreciated their humanistic approach to medical education. I chose the University of Colorado for my internal medicine residency because I love the sunshine and the mountains and because I thought the large academic program would complement my community-based medical school training. I loved being able to easily access nature on my days off.
Q: What do you like most about working as a hospitalist?
A: Spending time with incredible patients and working to solve difficult problems alongside amazing colleagues. I also love the diversity of the work, being involved in direct patient care, teaching students and residents, being a part of committees, performing quality improvement research. I love the flexibility of the job, which allows me to spend time with my family and travel fairly frequently to far-flung places.
Q: Did you have a mentor during your training or early career?
A: My earliest mentor was my father, also a physician [an oncologist]. Some of my earliest medical memories are of going to the hospital with my dad, who also brought home petri dishes from the lab, which my brother and I then used to perform household science experiments. My dad taught me my first lessons about the scientific method and about the importance of a strong work ethic and mentorship. Since then, I have had many outstanding mentors and role models for various aspects of my training/career. During my time at Denver Health, Drs. Richard K. Albert and Marisha Burden have provided me with invaluable mentorship in my scholarly pursuits.
Q: Have you tried to mentor others? Why or why not?
A: I have really loved mentoring students and residents. It is among the most meaningful experiences of my career. Presently, I am a mentor for undergraduate students from underrepresented minority groups. The maturity, passion, and drive these students possess inspires me.
Q: Why is your mentoring focused on minorities? What is the appeal of that to you?
A: I mentor students and residents from all backgrounds. However, mentoring students from underrepresented minority groups is especially important to me. Ethnic minorities continue to have decreased access to healthcare and disproportionately high morbidity and mortality. In order to improve these disparities, we need to have more healthcare providers from these groups. Yet such students, while they may initially be attracted to a career in medicine, are much less likely to maintain their interest. The reasons for this are complicated but may be explained by differences in access to mentors to help guide and inspire them, write letters, etc.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Developing a rapport with patients. I try to use some techniques from social psychology to help me more easily. The hospital is a particularly depersonalizing place, so trying to see the person behind the patient does help.
Q: What aspect of patient care is most rewarding?
A: Really connecting with patients and seeing them thrive. Working at a safety-net hospital, I have the privilege of caring for some of the most underserved but some of the most gracious and beautiful people.
Q: Are you on teaching service? If so, what aspect of teaching in the 21st century is most difficult? And what is most enjoyable?
A: I do enjoy supervising medical students and residents at all levels and attend frequently on the medical wards. I particularly love teaching medical students because of their enthusiasm and curiosity. I love being reminded of basic pathophysiology by a thoughtfully asked question from a medical student. I am a big advocate of bedside rounding. Finding a way to do this efficiently and while teaching to all the levels on the team is challenging. Also, I still enjoy my own direct patient care activities and feel that they challenge me in a different way and make me a better teacher.
Q: Outside of patient care, tell us about your career interests.
A: My research has focused on understanding problems experienced by patients following hospital discharge and designing systems to help ameliorate them. On an institutional level, I serve on several committees, including the Utilization Review Committee, and a group aiming to improve collaboration between hospitalists and primary care physicians and improve discharge transitions. I have participated in several LEAN events aimed at understanding and improving various systems issues.
Q: When you aren’t working, what is important to you?
A: My family and friends, sunshine, and travel. My husband grew up in Papua, New Guinea, and Australia, and both of his parents are physicians, so he is very understanding and not the least bit grossed out when I regale him with stories involving bodily fluids. We have a beautiful, inquisitive 3-year-old daughter and her furry older sister, Ginger Wasabi Ninja. As the oldest of seven, I also love hanging out with my siblings.
Q: What SHM event has made the most lasting impression on you?
A: I really enjoyed HM16, particularly the keynote address by our U.S. Surgeon General and fellow hospitalist, Vivek Murthy, MD, who discussed the role hospitalists can play in public health. His message that we hospitalists should put as much of an effort into trying to improve health outside the walls of the hospital as we do within the walls really resonated with me and has encouraged me to get more involved in the community. TH
Richard Quinn is a freelance writer in New Jersey.
The best advice Sarah Stella, MD, ever received was simple: “You can’t cure everyone, but you can help everyone.” Why has the adage stuck with her?
Because the advice came from her dad, “and he’s been right about a lot of things before,” she says with a smile.
Dr. Stella got into medicine—clearly with her father’s blessing—to satisfy her “intense curiosity about my fellow human beings and to try to ease suffering.” She has risen to be an academic hospitalist at Denver Health and is one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Tell us about your training. What did you like most/dislike during the process?
Answer: I attended medical school at Michigan State College of Human Medicine. I appreciated their humanistic approach to medical education. I chose the University of Colorado for my internal medicine residency because I love the sunshine and the mountains and because I thought the large academic program would complement my community-based medical school training. I loved being able to easily access nature on my days off.
Q: What do you like most about working as a hospitalist?
A: Spending time with incredible patients and working to solve difficult problems alongside amazing colleagues. I also love the diversity of the work, being involved in direct patient care, teaching students and residents, being a part of committees, performing quality improvement research. I love the flexibility of the job, which allows me to spend time with my family and travel fairly frequently to far-flung places.
Q: Did you have a mentor during your training or early career?
A: My earliest mentor was my father, also a physician [an oncologist]. Some of my earliest medical memories are of going to the hospital with my dad, who also brought home petri dishes from the lab, which my brother and I then used to perform household science experiments. My dad taught me my first lessons about the scientific method and about the importance of a strong work ethic and mentorship. Since then, I have had many outstanding mentors and role models for various aspects of my training/career. During my time at Denver Health, Drs. Richard K. Albert and Marisha Burden have provided me with invaluable mentorship in my scholarly pursuits.
Q: Have you tried to mentor others? Why or why not?
A: I have really loved mentoring students and residents. It is among the most meaningful experiences of my career. Presently, I am a mentor for undergraduate students from underrepresented minority groups. The maturity, passion, and drive these students possess inspires me.
Q: Why is your mentoring focused on minorities? What is the appeal of that to you?
A: I mentor students and residents from all backgrounds. However, mentoring students from underrepresented minority groups is especially important to me. Ethnic minorities continue to have decreased access to healthcare and disproportionately high morbidity and mortality. In order to improve these disparities, we need to have more healthcare providers from these groups. Yet such students, while they may initially be attracted to a career in medicine, are much less likely to maintain their interest. The reasons for this are complicated but may be explained by differences in access to mentors to help guide and inspire them, write letters, etc.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Developing a rapport with patients. I try to use some techniques from social psychology to help me more easily. The hospital is a particularly depersonalizing place, so trying to see the person behind the patient does help.
Q: What aspect of patient care is most rewarding?
A: Really connecting with patients and seeing them thrive. Working at a safety-net hospital, I have the privilege of caring for some of the most underserved but some of the most gracious and beautiful people.
Q: Are you on teaching service? If so, what aspect of teaching in the 21st century is most difficult? And what is most enjoyable?
A: I do enjoy supervising medical students and residents at all levels and attend frequently on the medical wards. I particularly love teaching medical students because of their enthusiasm and curiosity. I love being reminded of basic pathophysiology by a thoughtfully asked question from a medical student. I am a big advocate of bedside rounding. Finding a way to do this efficiently and while teaching to all the levels on the team is challenging. Also, I still enjoy my own direct patient care activities and feel that they challenge me in a different way and make me a better teacher.
Q: Outside of patient care, tell us about your career interests.
A: My research has focused on understanding problems experienced by patients following hospital discharge and designing systems to help ameliorate them. On an institutional level, I serve on several committees, including the Utilization Review Committee, and a group aiming to improve collaboration between hospitalists and primary care physicians and improve discharge transitions. I have participated in several LEAN events aimed at understanding and improving various systems issues.
Q: When you aren’t working, what is important to you?
A: My family and friends, sunshine, and travel. My husband grew up in Papua, New Guinea, and Australia, and both of his parents are physicians, so he is very understanding and not the least bit grossed out when I regale him with stories involving bodily fluids. We have a beautiful, inquisitive 3-year-old daughter and her furry older sister, Ginger Wasabi Ninja. As the oldest of seven, I also love hanging out with my siblings.
Q: What SHM event has made the most lasting impression on you?
A: I really enjoyed HM16, particularly the keynote address by our U.S. Surgeon General and fellow hospitalist, Vivek Murthy, MD, who discussed the role hospitalists can play in public health. His message that we hospitalists should put as much of an effort into trying to improve health outside the walls of the hospital as we do within the walls really resonated with me and has encouraged me to get more involved in the community. TH
Richard Quinn is a freelance writer in New Jersey.
Tips for Communicating with Empathy
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each column will focus on how the contributor applies one of the “Key Communication” areas in practice.
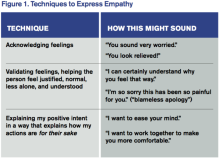
View a chart outlining key communication tactics
What I Say and Do
In interactions with patients and families, I make sure I communicate with empathy. By communicating with empathy, I mean not only listening for and understanding a patient’s experiences, concerns, and perspective but also communicating this understanding with my intention to help.
Why I Do It
Time constraints, endless to-do lists, and racing minds can eclipse empathic, attentive, and personalized care. When empathy is missing from the patient-clinician relationship, patients and clinicians suffer. Patients feel disengaged from their clinician; they remain anxious and lose trust. And physicians miss out on the gratification of feeling connected with patients and on achieving the best possible patient engagement and outcomes.
Physician empathy is associated with not only higher levels of patient satisfaction and survey scores but also with patient engagement, adherence to care plans, and positive health outcomes as well as physician job satisfaction.1–3
How I Do It
I start with mindfulness. I sustain eye contact, sit eye to eye, and give the person my undivided attention, listening to their words and nonverbal behavior—without judgment.
Then I draw on several techniques that express empathy. My favorites are these:
On a Personal Note
Albert Schweitzer said, “At times, our own light goes out and is rekindled by a spark from another person. Each of us has cause to think with deep gratitude of those who have lighted the flame within us.” Communicating with empathy, to me, is the spark that rekindles the lights of patients, families, and colleagues in our relationships with them. TH
Wendy Leebov is founder and partner in Language of Caring, LLC, author of The Language of Caring Guide for Physicians, and developer of the Language of Caring for Physicians web-based learning program. Reach her at [email protected].
References
- Leebov W, Rotering C. The Language of Caring Guide for Physicians: Communication Essentials for Patient-Centered Care. 2nd ed. Language of Caring, LLC; 2015.
- Butterfield S. New research links empathy to outcomes. ACP Internist website. Available at: http://www.acpinternist.org/archives/2013/03/empathy.htm. Accessed July 8, 2016.
- Hojat M, Louis D, Maio V, Gonnella J. Empathy and health care quality. Am J Medical Quality. 2013;28(1):6-7.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each column will focus on how the contributor applies one of the “Key Communication” areas in practice.
View a chart outlining key communication tactics
What I Say and Do
In interactions with patients and families, I make sure I communicate with empathy. By communicating with empathy, I mean not only listening for and understanding a patient’s experiences, concerns, and perspective but also communicating this understanding with my intention to help.
Why I Do It
Time constraints, endless to-do lists, and racing minds can eclipse empathic, attentive, and personalized care. When empathy is missing from the patient-clinician relationship, patients and clinicians suffer. Patients feel disengaged from their clinician; they remain anxious and lose trust. And physicians miss out on the gratification of feeling connected with patients and on achieving the best possible patient engagement and outcomes.
Physician empathy is associated with not only higher levels of patient satisfaction and survey scores but also with patient engagement, adherence to care plans, and positive health outcomes as well as physician job satisfaction.1–3
How I Do It
I start with mindfulness. I sustain eye contact, sit eye to eye, and give the person my undivided attention, listening to their words and nonverbal behavior—without judgment.
Then I draw on several techniques that express empathy. My favorites are these:
On a Personal Note
Albert Schweitzer said, “At times, our own light goes out and is rekindled by a spark from another person. Each of us has cause to think with deep gratitude of those who have lighted the flame within us.” Communicating with empathy, to me, is the spark that rekindles the lights of patients, families, and colleagues in our relationships with them. TH
Wendy Leebov is founder and partner in Language of Caring, LLC, author of The Language of Caring Guide for Physicians, and developer of the Language of Caring for Physicians web-based learning program. Reach her at [email protected].
References
- Leebov W, Rotering C. The Language of Caring Guide for Physicians: Communication Essentials for Patient-Centered Care. 2nd ed. Language of Caring, LLC; 2015.
- Butterfield S. New research links empathy to outcomes. ACP Internist website. Available at: http://www.acpinternist.org/archives/2013/03/empathy.htm. Accessed July 8, 2016.
- Hojat M, Louis D, Maio V, Gonnella J. Empathy and health care quality. Am J Medical Quality. 2013;28(1):6-7.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each column will focus on how the contributor applies one of the “Key Communication” areas in practice.
View a chart outlining key communication tactics
What I Say and Do
In interactions with patients and families, I make sure I communicate with empathy. By communicating with empathy, I mean not only listening for and understanding a patient’s experiences, concerns, and perspective but also communicating this understanding with my intention to help.
Why I Do It
Time constraints, endless to-do lists, and racing minds can eclipse empathic, attentive, and personalized care. When empathy is missing from the patient-clinician relationship, patients and clinicians suffer. Patients feel disengaged from their clinician; they remain anxious and lose trust. And physicians miss out on the gratification of feeling connected with patients and on achieving the best possible patient engagement and outcomes.
Physician empathy is associated with not only higher levels of patient satisfaction and survey scores but also with patient engagement, adherence to care plans, and positive health outcomes as well as physician job satisfaction.1–3
How I Do It
I start with mindfulness. I sustain eye contact, sit eye to eye, and give the person my undivided attention, listening to their words and nonverbal behavior—without judgment.
Then I draw on several techniques that express empathy. My favorites are these:
On a Personal Note
Albert Schweitzer said, “At times, our own light goes out and is rekindled by a spark from another person. Each of us has cause to think with deep gratitude of those who have lighted the flame within us.” Communicating with empathy, to me, is the spark that rekindles the lights of patients, families, and colleagues in our relationships with them. TH
Wendy Leebov is founder and partner in Language of Caring, LLC, author of The Language of Caring Guide for Physicians, and developer of the Language of Caring for Physicians web-based learning program. Reach her at [email protected].
References
- Leebov W, Rotering C. The Language of Caring Guide for Physicians: Communication Essentials for Patient-Centered Care. 2nd ed. Language of Caring, LLC; 2015.
- Butterfield S. New research links empathy to outcomes. ACP Internist website. Available at: http://www.acpinternist.org/archives/2013/03/empathy.htm. Accessed July 8, 2016.
- Hojat M, Louis D, Maio V, Gonnella J. Empathy and health care quality. Am J Medical Quality. 2013;28(1):6-7.
Should Physicians Care about Costs?
The healthcare industry is under major stress from steady declines in all sources of revenue. The drivers are multifactorial but include declining reimbursement from payors, a shift from fee-for-service to pay-for-performance, and state-by-state variability in patients covered by Medicaid, by high-deductible plans, or by being uninsured. In academic medical centers, rising overhead costs coupled with a reticence to raise student tuition and declining research funding streams have further compounded the situation.
Regardless of the actual numbers, all healthcare institutions are feeling the financial pinch. Most are intensely focused on cost-reduction efforts. The question is, what do physicians think about their role in these efforts, and what efforts will be most effective?
A recent survey of a large physician group practice found that many physicians do not know what their cost drivers are or do not think it is their role to participate in cost-reduction efforts.1 Of note, the group practice in the survey is a Pioneer Medicare accountable care organization (ACO) and participates in a combination of fee-for-service and capitated contracts.
Within the survey, the researchers embedded a cost-consciousness scale, which is a validated survey tool designed to assess daily cost consciousness. They also embedded other survey items to determine the physicians’ concerns for malpractice, comfort with diagnostic uncertainty, and perception of patient-family pressure for utilization of services. The average overall cost-consciousness score was 29 out of 44, with higher scores indicating more cost consciousness.
Almost all physicians agreed that they need to reduce unnecessary testing (97%), need to adhere to guidelines (98%), and have a responsibility to control costs (92%). However, 33% felt it was unfair for them to have to be both cost-conscious and concerned with the welfare of their patients.
Approximately a third of respondents also felt that there was too much emphasis on cost and that physicians are too busy to worry about costs.
More than a third (37%) said they did not have good knowledge about test-procedure cost within their system.
More than half of physicians felt pressure from patients to perform tests and procedures (from 68% of primary-care physicians, 58% of medical specialists, and 56% of surgical specialists) and felt pressure to refer to consultants (from 65% of primary-care physicians, 35% of medical specialists, and 34% of surgical specialists).
Based on this survey and other literature about physicians’ perceptions of their role and their ability to control costs, it is clear that the first step in understanding how to engage physicians in cost-reducing efforts is to understand what the drivers are for utilization and what the concerns are for reducing cost. Many hypothesize that the drivers to support the status quo include a fear of litigation, fear of missing a diagnosis, and patient demands for services. Another major driver of current utilization is that there is ongoing support for the status quo, as the majority of reimbursement for providers is still based on fee-for-service.
Change Efforts
One cost-reducing effort that has gained widespread enthusiasm from medical societies is the Choosing Wisely campaign. This campaign is an effort originally driven by the American Board of Internal Medicine (ABIM) Foundation to help physicians become aware of and reduce unnecessary utilization of resources. Each Choosing Wisely list is generated and endorsed by the relevant medical society and widely advertised to physicians via a variety of mechanisms. More than 70 medical societies have participated in the effort to date.
The recommendations are often widely accepted by those in the specialty since they are evidence-based and derived and advertised by their own specialty societies. In the survey mentioned above, almost all physicians agreed that their Choosing Wisely was a good source of guidance (ranging from 92% of surgical specialties to 97% of primary-care physicians). In order to drive the movement from the patient perspective, Consumer Reports has developed educational materials aimed at the consumer side of healthcare (ie, patients and families).
As Consumer Reports suggests, the first step to implementing cost-conscious care is to measure awareness of cost and causes of overutilization. By first understanding behaviors, a group can then work to impact such behaviors. It is highly likely that the drivers are different based on the specialty of the physician, the patient population being served, and the local healthcare market drivers. As such, there will not be a single, across-the-board solution to reducing unnecessary utilization of services (and therefore cost), but interventions will need to be tailored to different groups depending on the drivers of cost locally.
Depending on the issues within a group, successful interventions could include:
- Decision support tools (for appropriate use of consultants and diagnostic tests)
- Display of testing costs (not just at the time of ordering)
- Efforts aimed at patient education (both as general consumers as well as at the point of care)
- Malpractice reform to support physicians trying to balance cost consciousness with patient welfare
In Sum
We have a long way to go in engaging physicians in efforts to reduce unnecessary utilization and cost. I recommend that hospitalist practices utilize the survey tool used in this study to understand the perceived barriers and drivers of cost within their practice and work with their local administrative teams to better understand patterns of overutilization among their group. Then interventions can be designed to be evidence-based, tailored to local workflow, and both reliable and sustainable.
If done well, hospitalists can have a huge impact on utilization and cost and position their groups and their hospitals well to succeed in this cost-constrained era of healthcare. TH
References
- Colla CH, Kinsella EA, Morden NE, Meyers DJ, Rosenthal MB, Sequist TD. Physician perception of Choosing Wisely and drivers of overuse. Am J Manag Care. 2016;22(5):337-343.

The healthcare industry is under major stress from steady declines in all sources of revenue. The drivers are multifactorial but include declining reimbursement from payors, a shift from fee-for-service to pay-for-performance, and state-by-state variability in patients covered by Medicaid, by high-deductible plans, or by being uninsured. In academic medical centers, rising overhead costs coupled with a reticence to raise student tuition and declining research funding streams have further compounded the situation.
Regardless of the actual numbers, all healthcare institutions are feeling the financial pinch. Most are intensely focused on cost-reduction efforts. The question is, what do physicians think about their role in these efforts, and what efforts will be most effective?
A recent survey of a large physician group practice found that many physicians do not know what their cost drivers are or do not think it is their role to participate in cost-reduction efforts.1 Of note, the group practice in the survey is a Pioneer Medicare accountable care organization (ACO) and participates in a combination of fee-for-service and capitated contracts.
Within the survey, the researchers embedded a cost-consciousness scale, which is a validated survey tool designed to assess daily cost consciousness. They also embedded other survey items to determine the physicians’ concerns for malpractice, comfort with diagnostic uncertainty, and perception of patient-family pressure for utilization of services. The average overall cost-consciousness score was 29 out of 44, with higher scores indicating more cost consciousness.
Almost all physicians agreed that they need to reduce unnecessary testing (97%), need to adhere to guidelines (98%), and have a responsibility to control costs (92%). However, 33% felt it was unfair for them to have to be both cost-conscious and concerned with the welfare of their patients.
Approximately a third of respondents also felt that there was too much emphasis on cost and that physicians are too busy to worry about costs.
More than a third (37%) said they did not have good knowledge about test-procedure cost within their system.
More than half of physicians felt pressure from patients to perform tests and procedures (from 68% of primary-care physicians, 58% of medical specialists, and 56% of surgical specialists) and felt pressure to refer to consultants (from 65% of primary-care physicians, 35% of medical specialists, and 34% of surgical specialists).
Based on this survey and other literature about physicians’ perceptions of their role and their ability to control costs, it is clear that the first step in understanding how to engage physicians in cost-reducing efforts is to understand what the drivers are for utilization and what the concerns are for reducing cost. Many hypothesize that the drivers to support the status quo include a fear of litigation, fear of missing a diagnosis, and patient demands for services. Another major driver of current utilization is that there is ongoing support for the status quo, as the majority of reimbursement for providers is still based on fee-for-service.
Change Efforts
One cost-reducing effort that has gained widespread enthusiasm from medical societies is the Choosing Wisely campaign. This campaign is an effort originally driven by the American Board of Internal Medicine (ABIM) Foundation to help physicians become aware of and reduce unnecessary utilization of resources. Each Choosing Wisely list is generated and endorsed by the relevant medical society and widely advertised to physicians via a variety of mechanisms. More than 70 medical societies have participated in the effort to date.
The recommendations are often widely accepted by those in the specialty since they are evidence-based and derived and advertised by their own specialty societies. In the survey mentioned above, almost all physicians agreed that their Choosing Wisely was a good source of guidance (ranging from 92% of surgical specialties to 97% of primary-care physicians). In order to drive the movement from the patient perspective, Consumer Reports has developed educational materials aimed at the consumer side of healthcare (ie, patients and families).
As Consumer Reports suggests, the first step to implementing cost-conscious care is to measure awareness of cost and causes of overutilization. By first understanding behaviors, a group can then work to impact such behaviors. It is highly likely that the drivers are different based on the specialty of the physician, the patient population being served, and the local healthcare market drivers. As such, there will not be a single, across-the-board solution to reducing unnecessary utilization of services (and therefore cost), but interventions will need to be tailored to different groups depending on the drivers of cost locally.
Depending on the issues within a group, successful interventions could include:
- Decision support tools (for appropriate use of consultants and diagnostic tests)
- Display of testing costs (not just at the time of ordering)
- Efforts aimed at patient education (both as general consumers as well as at the point of care)
- Malpractice reform to support physicians trying to balance cost consciousness with patient welfare
In Sum
We have a long way to go in engaging physicians in efforts to reduce unnecessary utilization and cost. I recommend that hospitalist practices utilize the survey tool used in this study to understand the perceived barriers and drivers of cost within their practice and work with their local administrative teams to better understand patterns of overutilization among their group. Then interventions can be designed to be evidence-based, tailored to local workflow, and both reliable and sustainable.
If done well, hospitalists can have a huge impact on utilization and cost and position their groups and their hospitals well to succeed in this cost-constrained era of healthcare. TH
References
- Colla CH, Kinsella EA, Morden NE, Meyers DJ, Rosenthal MB, Sequist TD. Physician perception of Choosing Wisely and drivers of overuse. Am J Manag Care. 2016;22(5):337-343.

The healthcare industry is under major stress from steady declines in all sources of revenue. The drivers are multifactorial but include declining reimbursement from payors, a shift from fee-for-service to pay-for-performance, and state-by-state variability in patients covered by Medicaid, by high-deductible plans, or by being uninsured. In academic medical centers, rising overhead costs coupled with a reticence to raise student tuition and declining research funding streams have further compounded the situation.
Regardless of the actual numbers, all healthcare institutions are feeling the financial pinch. Most are intensely focused on cost-reduction efforts. The question is, what do physicians think about their role in these efforts, and what efforts will be most effective?
A recent survey of a large physician group practice found that many physicians do not know what their cost drivers are or do not think it is their role to participate in cost-reduction efforts.1 Of note, the group practice in the survey is a Pioneer Medicare accountable care organization (ACO) and participates in a combination of fee-for-service and capitated contracts.
Within the survey, the researchers embedded a cost-consciousness scale, which is a validated survey tool designed to assess daily cost consciousness. They also embedded other survey items to determine the physicians’ concerns for malpractice, comfort with diagnostic uncertainty, and perception of patient-family pressure for utilization of services. The average overall cost-consciousness score was 29 out of 44, with higher scores indicating more cost consciousness.
Almost all physicians agreed that they need to reduce unnecessary testing (97%), need to adhere to guidelines (98%), and have a responsibility to control costs (92%). However, 33% felt it was unfair for them to have to be both cost-conscious and concerned with the welfare of their patients.
Approximately a third of respondents also felt that there was too much emphasis on cost and that physicians are too busy to worry about costs.
More than a third (37%) said they did not have good knowledge about test-procedure cost within their system.
More than half of physicians felt pressure from patients to perform tests and procedures (from 68% of primary-care physicians, 58% of medical specialists, and 56% of surgical specialists) and felt pressure to refer to consultants (from 65% of primary-care physicians, 35% of medical specialists, and 34% of surgical specialists).
Based on this survey and other literature about physicians’ perceptions of their role and their ability to control costs, it is clear that the first step in understanding how to engage physicians in cost-reducing efforts is to understand what the drivers are for utilization and what the concerns are for reducing cost. Many hypothesize that the drivers to support the status quo include a fear of litigation, fear of missing a diagnosis, and patient demands for services. Another major driver of current utilization is that there is ongoing support for the status quo, as the majority of reimbursement for providers is still based on fee-for-service.
Change Efforts
One cost-reducing effort that has gained widespread enthusiasm from medical societies is the Choosing Wisely campaign. This campaign is an effort originally driven by the American Board of Internal Medicine (ABIM) Foundation to help physicians become aware of and reduce unnecessary utilization of resources. Each Choosing Wisely list is generated and endorsed by the relevant medical society and widely advertised to physicians via a variety of mechanisms. More than 70 medical societies have participated in the effort to date.
The recommendations are often widely accepted by those in the specialty since they are evidence-based and derived and advertised by their own specialty societies. In the survey mentioned above, almost all physicians agreed that their Choosing Wisely was a good source of guidance (ranging from 92% of surgical specialties to 97% of primary-care physicians). In order to drive the movement from the patient perspective, Consumer Reports has developed educational materials aimed at the consumer side of healthcare (ie, patients and families).
As Consumer Reports suggests, the first step to implementing cost-conscious care is to measure awareness of cost and causes of overutilization. By first understanding behaviors, a group can then work to impact such behaviors. It is highly likely that the drivers are different based on the specialty of the physician, the patient population being served, and the local healthcare market drivers. As such, there will not be a single, across-the-board solution to reducing unnecessary utilization of services (and therefore cost), but interventions will need to be tailored to different groups depending on the drivers of cost locally.
Depending on the issues within a group, successful interventions could include:
- Decision support tools (for appropriate use of consultants and diagnostic tests)
- Display of testing costs (not just at the time of ordering)
- Efforts aimed at patient education (both as general consumers as well as at the point of care)
- Malpractice reform to support physicians trying to balance cost consciousness with patient welfare
In Sum
We have a long way to go in engaging physicians in efforts to reduce unnecessary utilization and cost. I recommend that hospitalist practices utilize the survey tool used in this study to understand the perceived barriers and drivers of cost within their practice and work with their local administrative teams to better understand patterns of overutilization among their group. Then interventions can be designed to be evidence-based, tailored to local workflow, and both reliable and sustainable.
If done well, hospitalists can have a huge impact on utilization and cost and position their groups and their hospitals well to succeed in this cost-constrained era of healthcare. TH
References
- Colla CH, Kinsella EA, Morden NE, Meyers DJ, Rosenthal MB, Sequist TD. Physician perception of Choosing Wisely and drivers of overuse. Am J Manag Care. 2016;22(5):337-343.

Measure Hospitalist Engagement with SHM’s Engagement Benchmarking Service
One of the most important questions for leaders of HM groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
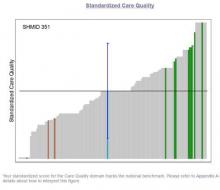
SHM has developed an Engagement Benchmarking Service to analyze engagement of hospitalists. The service evaluates relationships with leaders, care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization score in the various domains and where it falls within the national benchmark to help you determine what is working well and identify areas for improvement in your hospital medicine group.
Recruiting ends soon. Ensure hospitalists are engaged in your hospital medicine group by registering now for the next cohort at www.hospitalmedicine.org/pmad3.
One of the most important questions for leaders of HM groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
SHM has developed an Engagement Benchmarking Service to analyze engagement of hospitalists. The service evaluates relationships with leaders, care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization score in the various domains and where it falls within the national benchmark to help you determine what is working well and identify areas for improvement in your hospital medicine group.
Recruiting ends soon. Ensure hospitalists are engaged in your hospital medicine group by registering now for the next cohort at www.hospitalmedicine.org/pmad3.
One of the most important questions for leaders of HM groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
SHM has developed an Engagement Benchmarking Service to analyze engagement of hospitalists. The service evaluates relationships with leaders, care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization score in the various domains and where it falls within the national benchmark to help you determine what is working well and identify areas for improvement in your hospital medicine group.
Recruiting ends soon. Ensure hospitalists are engaged in your hospital medicine group by registering now for the next cohort at www.hospitalmedicine.org/pmad3.
SHM Leadership Academy: Learning Awaits in Mastering Teamwork Course
As the SHM Leadership Academy’s course director, I always find time to visit the Mastering Teamwork course because each year, even though it’s slightly different, it’s still exciting. In past meetings, I’ve learned from talented faculty how lessons in college football relate to practice, been provided guidance on how to recognize what makes me tick, and heard firsthand perspective on large-scale medical events like 9/11, Hurricane Katrina, and even the Boston Marathon tragedy. I always learn a few new things. As they say, repetition is the mother of learning, and the Mastering Teamwork course never fails to make that learning a lot of fun.
As a professor of medicine, I’ve always liked learning. But I truly enjoy learning when it’s fun and exciting. To me, this mixture of academia and excitement is the epitome of Mastering Teamwork. When two of the faculty, Mark Williams, MD, MHM, and Amit Prachand, MEng, needed to teach about teamwork, they decided to develop an interactive session. While in Hawaii, they constructed a “river” out of cardboard and props for Mastering Teamwork participants to navigate. It was a hands-on lesson in group dynamics. It was educational and, most of all, a hoot.
Kay Cannon, MBA, taught me that the skills I used in previous job levels may not be the drivers of my success in today’s job (or tomorrow’s), and Jeffrey Wiese, MD, MHM, and Lenny Marcus, PhD, are two of the best storytellers I know and have me on the edge of my seat every time I hear them speak. Their life experiences make excellent fodder for hospitalist leadership pearls and are more riveting than Downton Abbey (or whatever drama is your favorite).
I look forward to seeing everyone at Disney’s BoardWalk Inn in Lake Buena Vista, Florida, from October 24 to 27 to experience what I know will be a memorable, enjoyable learning experience for all.
To register, visit www.shmleadershipacademy.org. TH
Dr. Howell is SHM’s senior physician advisor and course director for SHM’s Leadership Academy.
As the SHM Leadership Academy’s course director, I always find time to visit the Mastering Teamwork course because each year, even though it’s slightly different, it’s still exciting. In past meetings, I’ve learned from talented faculty how lessons in college football relate to practice, been provided guidance on how to recognize what makes me tick, and heard firsthand perspective on large-scale medical events like 9/11, Hurricane Katrina, and even the Boston Marathon tragedy. I always learn a few new things. As they say, repetition is the mother of learning, and the Mastering Teamwork course never fails to make that learning a lot of fun.
As a professor of medicine, I’ve always liked learning. But I truly enjoy learning when it’s fun and exciting. To me, this mixture of academia and excitement is the epitome of Mastering Teamwork. When two of the faculty, Mark Williams, MD, MHM, and Amit Prachand, MEng, needed to teach about teamwork, they decided to develop an interactive session. While in Hawaii, they constructed a “river” out of cardboard and props for Mastering Teamwork participants to navigate. It was a hands-on lesson in group dynamics. It was educational and, most of all, a hoot.
Kay Cannon, MBA, taught me that the skills I used in previous job levels may not be the drivers of my success in today’s job (or tomorrow’s), and Jeffrey Wiese, MD, MHM, and Lenny Marcus, PhD, are two of the best storytellers I know and have me on the edge of my seat every time I hear them speak. Their life experiences make excellent fodder for hospitalist leadership pearls and are more riveting than Downton Abbey (or whatever drama is your favorite).
I look forward to seeing everyone at Disney’s BoardWalk Inn in Lake Buena Vista, Florida, from October 24 to 27 to experience what I know will be a memorable, enjoyable learning experience for all.
To register, visit www.shmleadershipacademy.org. TH
Dr. Howell is SHM’s senior physician advisor and course director for SHM’s Leadership Academy.
As the SHM Leadership Academy’s course director, I always find time to visit the Mastering Teamwork course because each year, even though it’s slightly different, it’s still exciting. In past meetings, I’ve learned from talented faculty how lessons in college football relate to practice, been provided guidance on how to recognize what makes me tick, and heard firsthand perspective on large-scale medical events like 9/11, Hurricane Katrina, and even the Boston Marathon tragedy. I always learn a few new things. As they say, repetition is the mother of learning, and the Mastering Teamwork course never fails to make that learning a lot of fun.
As a professor of medicine, I’ve always liked learning. But I truly enjoy learning when it’s fun and exciting. To me, this mixture of academia and excitement is the epitome of Mastering Teamwork. When two of the faculty, Mark Williams, MD, MHM, and Amit Prachand, MEng, needed to teach about teamwork, they decided to develop an interactive session. While in Hawaii, they constructed a “river” out of cardboard and props for Mastering Teamwork participants to navigate. It was a hands-on lesson in group dynamics. It was educational and, most of all, a hoot.
Kay Cannon, MBA, taught me that the skills I used in previous job levels may not be the drivers of my success in today’s job (or tomorrow’s), and Jeffrey Wiese, MD, MHM, and Lenny Marcus, PhD, are two of the best storytellers I know and have me on the edge of my seat every time I hear them speak. Their life experiences make excellent fodder for hospitalist leadership pearls and are more riveting than Downton Abbey (or whatever drama is your favorite).
I look forward to seeing everyone at Disney’s BoardWalk Inn in Lake Buena Vista, Florida, from October 24 to 27 to experience what I know will be a memorable, enjoyable learning experience for all.
To register, visit www.shmleadershipacademy.org. TH
Dr. Howell is SHM’s senior physician advisor and course director for SHM’s Leadership Academy.
Superbug Infections On the Rise With No Antibiotic Success Yet
NEW YORK - After two confirmed U.S. cases of a superbug that thwarts a last-resort antibiotic, infectious disease experts say they expect more cases in coming months because the bacterial gene behind it is likely far more widespread than previously believed.
Army scientists in May reported finding E. coli bacteria that harbor a gene which renders the antibiotic colistin useless. The gene, called mcr-1, was found in a urine sample of a Pennsylvania woman being treated for a urinary tract infection.
On Monday, researchers confirmed preliminary findings that E. coli carrying the same mcr-1 gene were found in a stored bacterial sample of a New York patient who had been treated for an infection last year, as well as in patient samples from nine other countries.
The report came from a global effort called the SENTRY Antimicrobial Surveillance Program, led by Mariana Castanheira of JMI Laboratories based in North Liberty, Iowa.
The mcr-1 superbug has been identified over the past six months in farm animals and people in about 20 countries, including China, Germany and Italy.
The bacteria can be transmitted by fecal contact and poor hygiene, which suggests a far wider likely presence than the documented cases so far, according to leading infectious disease experts.
Health officials fear the mcr-1 gene, carried by a highly mobile piece of DNA called a plasmid, will soon be found in bacteria already resistant to all or virtually all other types of antibiotics, potentially making infections untreatable.
"You can be sure (mcr-1) is already in the guts of people throughout the United States and will continue to spread," said Dr. Brad Spellberg, professor of medicine at the University of Southern California.
Dr. David Van Duin, an infectious disease expert at the University of North Carolina in Chapel Hill, said he expects more documented U.S. cases of mcr-1 in coming months because it is already here and will spread from abroad. "We will see a lot more of this gene."
Colistin causes kidney damage, but doctors have opted for it as other antibiotics increasingly fail. Its overuse, especially in overseas farm animals, has allowed bacteria to develop resistance to it.
PAST AND PRESENT INFECTIONS
To track the mcr-1 gene, U.S. hospitals are working together with state and federal agencies to test bacteria samples of patients that have recently been treated for infections. Many of the largest research hospitals are examining samples of antibiotic-resistant bacteria that have long been stored in their freezers.
Gautam Dantas, associate professor of pathology at Washington University Medical Center in St. Louis, has tested hundreds of U.S. samples of archived bacteria in recent months and has not yet detected mcr-1. But he expects dozens of confirmed cases of the gene will be documented by next year in the country, mostly among current patients.
The concern of many disease experts is that mcr-1 could soon show up in bacteria also resistant to carbapenems, one of the few remaining dependable classes of antibiotics. In that event, with colistin no longer a last-ditch option, some patients would have to rely on their immune systems to fight off infection.
"Within the next two to three years, it's going to be fairly routine for infections to occur in the United States for which we have no (effective) drugs available," Dantas said.
Castanheira also believes mcr-1 will find its way into carbapenem-resistant enterobacteriaceae (CRE).
In an interview, she said the resulting virtually impervious bacterium would likely spread slowly inside the United States because CRE themselves are not yet widespread in the country, giving drugmakers some time to create new antibiotics.
Beginning in August, the U.S. Centers for Disease Control and Prevention will use $21 million to expand surveillance at laboratories operated by all 50 state health departments and seven larger regional labs. The federal funding will help pay for more-sensitive equipment to test for antibiotic resistance in bacteria samples provided by hospitals.
Jean Patel, deputy director of the CDC's Office of Antimicrobial Resistance, said the effort will provide the CDC improved national surveillance of antibiotic-resistance trends, including any spread of mcr-1.
"This is data for action," she said, adding that special procedures to prevent infections from spreading in hospitals could be taken once a patient is identified with mcr-1 related infections or with multidrug-resistant bacteria.
SOURCE: http://bit.ly/29yFekw
Antimicrob Agents Chemother 2016.
NEW YORK - After two confirmed U.S. cases of a superbug that thwarts a last-resort antibiotic, infectious disease experts say they expect more cases in coming months because the bacterial gene behind it is likely far more widespread than previously believed.
Army scientists in May reported finding E. coli bacteria that harbor a gene which renders the antibiotic colistin useless. The gene, called mcr-1, was found in a urine sample of a Pennsylvania woman being treated for a urinary tract infection.
On Monday, researchers confirmed preliminary findings that E. coli carrying the same mcr-1 gene were found in a stored bacterial sample of a New York patient who had been treated for an infection last year, as well as in patient samples from nine other countries.
The report came from a global effort called the SENTRY Antimicrobial Surveillance Program, led by Mariana Castanheira of JMI Laboratories based in North Liberty, Iowa.
The mcr-1 superbug has been identified over the past six months in farm animals and people in about 20 countries, including China, Germany and Italy.
The bacteria can be transmitted by fecal contact and poor hygiene, which suggests a far wider likely presence than the documented cases so far, according to leading infectious disease experts.
Health officials fear the mcr-1 gene, carried by a highly mobile piece of DNA called a plasmid, will soon be found in bacteria already resistant to all or virtually all other types of antibiotics, potentially making infections untreatable.
"You can be sure (mcr-1) is already in the guts of people throughout the United States and will continue to spread," said Dr. Brad Spellberg, professor of medicine at the University of Southern California.
Dr. David Van Duin, an infectious disease expert at the University of North Carolina in Chapel Hill, said he expects more documented U.S. cases of mcr-1 in coming months because it is already here and will spread from abroad. "We will see a lot more of this gene."
Colistin causes kidney damage, but doctors have opted for it as other antibiotics increasingly fail. Its overuse, especially in overseas farm animals, has allowed bacteria to develop resistance to it.
PAST AND PRESENT INFECTIONS
To track the mcr-1 gene, U.S. hospitals are working together with state and federal agencies to test bacteria samples of patients that have recently been treated for infections. Many of the largest research hospitals are examining samples of antibiotic-resistant bacteria that have long been stored in their freezers.
Gautam Dantas, associate professor of pathology at Washington University Medical Center in St. Louis, has tested hundreds of U.S. samples of archived bacteria in recent months and has not yet detected mcr-1. But he expects dozens of confirmed cases of the gene will be documented by next year in the country, mostly among current patients.
The concern of many disease experts is that mcr-1 could soon show up in bacteria also resistant to carbapenems, one of the few remaining dependable classes of antibiotics. In that event, with colistin no longer a last-ditch option, some patients would have to rely on their immune systems to fight off infection.
"Within the next two to three years, it's going to be fairly routine for infections to occur in the United States for which we have no (effective) drugs available," Dantas said.
Castanheira also believes mcr-1 will find its way into carbapenem-resistant enterobacteriaceae (CRE).
In an interview, she said the resulting virtually impervious bacterium would likely spread slowly inside the United States because CRE themselves are not yet widespread in the country, giving drugmakers some time to create new antibiotics.
Beginning in August, the U.S. Centers for Disease Control and Prevention will use $21 million to expand surveillance at laboratories operated by all 50 state health departments and seven larger regional labs. The federal funding will help pay for more-sensitive equipment to test for antibiotic resistance in bacteria samples provided by hospitals.
Jean Patel, deputy director of the CDC's Office of Antimicrobial Resistance, said the effort will provide the CDC improved national surveillance of antibiotic-resistance trends, including any spread of mcr-1.
"This is data for action," she said, adding that special procedures to prevent infections from spreading in hospitals could be taken once a patient is identified with mcr-1 related infections or with multidrug-resistant bacteria.
SOURCE: http://bit.ly/29yFekw
Antimicrob Agents Chemother 2016.
NEW YORK - After two confirmed U.S. cases of a superbug that thwarts a last-resort antibiotic, infectious disease experts say they expect more cases in coming months because the bacterial gene behind it is likely far more widespread than previously believed.
Army scientists in May reported finding E. coli bacteria that harbor a gene which renders the antibiotic colistin useless. The gene, called mcr-1, was found in a urine sample of a Pennsylvania woman being treated for a urinary tract infection.
On Monday, researchers confirmed preliminary findings that E. coli carrying the same mcr-1 gene were found in a stored bacterial sample of a New York patient who had been treated for an infection last year, as well as in patient samples from nine other countries.
The report came from a global effort called the SENTRY Antimicrobial Surveillance Program, led by Mariana Castanheira of JMI Laboratories based in North Liberty, Iowa.
The mcr-1 superbug has been identified over the past six months in farm animals and people in about 20 countries, including China, Germany and Italy.
The bacteria can be transmitted by fecal contact and poor hygiene, which suggests a far wider likely presence than the documented cases so far, according to leading infectious disease experts.
Health officials fear the mcr-1 gene, carried by a highly mobile piece of DNA called a plasmid, will soon be found in bacteria already resistant to all or virtually all other types of antibiotics, potentially making infections untreatable.
"You can be sure (mcr-1) is already in the guts of people throughout the United States and will continue to spread," said Dr. Brad Spellberg, professor of medicine at the University of Southern California.
Dr. David Van Duin, an infectious disease expert at the University of North Carolina in Chapel Hill, said he expects more documented U.S. cases of mcr-1 in coming months because it is already here and will spread from abroad. "We will see a lot more of this gene."
Colistin causes kidney damage, but doctors have opted for it as other antibiotics increasingly fail. Its overuse, especially in overseas farm animals, has allowed bacteria to develop resistance to it.
PAST AND PRESENT INFECTIONS
To track the mcr-1 gene, U.S. hospitals are working together with state and federal agencies to test bacteria samples of patients that have recently been treated for infections. Many of the largest research hospitals are examining samples of antibiotic-resistant bacteria that have long been stored in their freezers.
Gautam Dantas, associate professor of pathology at Washington University Medical Center in St. Louis, has tested hundreds of U.S. samples of archived bacteria in recent months and has not yet detected mcr-1. But he expects dozens of confirmed cases of the gene will be documented by next year in the country, mostly among current patients.
The concern of many disease experts is that mcr-1 could soon show up in bacteria also resistant to carbapenems, one of the few remaining dependable classes of antibiotics. In that event, with colistin no longer a last-ditch option, some patients would have to rely on their immune systems to fight off infection.
"Within the next two to three years, it's going to be fairly routine for infections to occur in the United States for which we have no (effective) drugs available," Dantas said.
Castanheira also believes mcr-1 will find its way into carbapenem-resistant enterobacteriaceae (CRE).
In an interview, she said the resulting virtually impervious bacterium would likely spread slowly inside the United States because CRE themselves are not yet widespread in the country, giving drugmakers some time to create new antibiotics.
Beginning in August, the U.S. Centers for Disease Control and Prevention will use $21 million to expand surveillance at laboratories operated by all 50 state health departments and seven larger regional labs. The federal funding will help pay for more-sensitive equipment to test for antibiotic resistance in bacteria samples provided by hospitals.
Jean Patel, deputy director of the CDC's Office of Antimicrobial Resistance, said the effort will provide the CDC improved national surveillance of antibiotic-resistance trends, including any spread of mcr-1.
"This is data for action," she said, adding that special procedures to prevent infections from spreading in hospitals could be taken once a patient is identified with mcr-1 related infections or with multidrug-resistant bacteria.
SOURCE: http://bit.ly/29yFekw
Antimicrob Agents Chemother 2016.
Genetic Makeup Influences Risk of Diabetes: Study
CHICAGO - A study examining the genes of more than 120,000 people from Europe, Asia, Africa and the Americas has offered the clearest picture yet of the genes that drive type 2 diabetes.
The study, published July 11 in the journal Nature, puts to rest a decades-long debate over the genetics that influence the risk of diabetes, which affects one in 10 people over the course of their lifetime.
And it has identified more than a dozen specific genes directly involved in the development of type 2 diabetes that might serve as potential drug targets.
"There was a whole furious debate that arose about this," said Dr. Francis Collins, director of the National Institutes of Health, one of more than 300 scientists collaborating on the work.
Prior studies turned up more than 80 spots in the genome associated with the development of adult-onset diabetes, but most of these genetic errors were common, meaning they occurred frequently in the population, and they explained only a small fraction of disease risk.
These discoveries were based on genome-wide association studies or GWAS, which used gene chips that scan thousands of genes at a time. Researchers used these to scan DNA from large populations of individuals with a specific disease and compare them with DNA from similar groups of healthy people.
Critics, including geneticist Dr. David Goldstein at Columbia University, argued that such studies were a waste of resources because they only found common variants that explained just a small fraction of the risk for disease.
He said the really important drivers of common diseases such as diabetes and schizophrenia were more likely to be found in extremely rare genes, those occurring in individuals or in families, not those shared by large populations of people.
Goldstein "argued very persuasively that it was all about rare variants and we were all going down the wrong road looking at the common ones," Collins said in a telephone interview.
The new study took a deeper look, using next-generation sequencing to search the entire genetic code of 2,657 people with and without diabetes to assess the contribution of both rare and common genes driving diabetes.
They also sequenced all of the protein-making genes in 12,940 people, and used statistical methods to estimate risk in another 111,548 people with less complete DNA data.
They found that, indeed, most of the genetic risk for type 2 diabetes is caused by common mistakes in the genetic code, with each mistake contributing only a small portion of an individual's risk for developing the disease.
"What this study says quite definitively for diabetes is the vast majority of hereditary risk variants are in fact these common ones, and the rare ones, while they pop up here and there, are a much smaller contribution," Collins said.
The study also turned up more than a dozen examples where variants alter the way proteins are made, suggesting that these gene variants have some direct impact on the development of type 2 diabetes.
"These represent promising avenues for efforts to design new ways to treat or prevent the disease," said Mark McCarthy, a senior author of the study from Oxford University.
All of the data will be made publicly available online through the Accelerating Medicines Partnership, a public-private partnership between the NIH, the U.S. Food and Drug Administration, 10 drug companies and several nonprofits.
Goldstein said the work was "a careful, solid investigation" that does not change his view much overall, adding that it was time to "quit arguing."
"What I care about now is finding the exact variants that infer risk, and understanding how they do so," he said.
SOURCE: http://go.nature.com/29DlL5i
Nature 2016.
CHICAGO - A study examining the genes of more than 120,000 people from Europe, Asia, Africa and the Americas has offered the clearest picture yet of the genes that drive type 2 diabetes.
The study, published July 11 in the journal Nature, puts to rest a decades-long debate over the genetics that influence the risk of diabetes, which affects one in 10 people over the course of their lifetime.
And it has identified more than a dozen specific genes directly involved in the development of type 2 diabetes that might serve as potential drug targets.
"There was a whole furious debate that arose about this," said Dr. Francis Collins, director of the National Institutes of Health, one of more than 300 scientists collaborating on the work.
Prior studies turned up more than 80 spots in the genome associated with the development of adult-onset diabetes, but most of these genetic errors were common, meaning they occurred frequently in the population, and they explained only a small fraction of disease risk.
These discoveries were based on genome-wide association studies or GWAS, which used gene chips that scan thousands of genes at a time. Researchers used these to scan DNA from large populations of individuals with a specific disease and compare them with DNA from similar groups of healthy people.
Critics, including geneticist Dr. David Goldstein at Columbia University, argued that such studies were a waste of resources because they only found common variants that explained just a small fraction of the risk for disease.
He said the really important drivers of common diseases such as diabetes and schizophrenia were more likely to be found in extremely rare genes, those occurring in individuals or in families, not those shared by large populations of people.
Goldstein "argued very persuasively that it was all about rare variants and we were all going down the wrong road looking at the common ones," Collins said in a telephone interview.
The new study took a deeper look, using next-generation sequencing to search the entire genetic code of 2,657 people with and without diabetes to assess the contribution of both rare and common genes driving diabetes.
They also sequenced all of the protein-making genes in 12,940 people, and used statistical methods to estimate risk in another 111,548 people with less complete DNA data.
They found that, indeed, most of the genetic risk for type 2 diabetes is caused by common mistakes in the genetic code, with each mistake contributing only a small portion of an individual's risk for developing the disease.
"What this study says quite definitively for diabetes is the vast majority of hereditary risk variants are in fact these common ones, and the rare ones, while they pop up here and there, are a much smaller contribution," Collins said.
The study also turned up more than a dozen examples where variants alter the way proteins are made, suggesting that these gene variants have some direct impact on the development of type 2 diabetes.
"These represent promising avenues for efforts to design new ways to treat or prevent the disease," said Mark McCarthy, a senior author of the study from Oxford University.
All of the data will be made publicly available online through the Accelerating Medicines Partnership, a public-private partnership between the NIH, the U.S. Food and Drug Administration, 10 drug companies and several nonprofits.
Goldstein said the work was "a careful, solid investigation" that does not change his view much overall, adding that it was time to "quit arguing."
"What I care about now is finding the exact variants that infer risk, and understanding how they do so," he said.
SOURCE: http://go.nature.com/29DlL5i
Nature 2016.
CHICAGO - A study examining the genes of more than 120,000 people from Europe, Asia, Africa and the Americas has offered the clearest picture yet of the genes that drive type 2 diabetes.
The study, published July 11 in the journal Nature, puts to rest a decades-long debate over the genetics that influence the risk of diabetes, which affects one in 10 people over the course of their lifetime.
And it has identified more than a dozen specific genes directly involved in the development of type 2 diabetes that might serve as potential drug targets.
"There was a whole furious debate that arose about this," said Dr. Francis Collins, director of the National Institutes of Health, one of more than 300 scientists collaborating on the work.
Prior studies turned up more than 80 spots in the genome associated with the development of adult-onset diabetes, but most of these genetic errors were common, meaning they occurred frequently in the population, and they explained only a small fraction of disease risk.
These discoveries were based on genome-wide association studies or GWAS, which used gene chips that scan thousands of genes at a time. Researchers used these to scan DNA from large populations of individuals with a specific disease and compare them with DNA from similar groups of healthy people.
Critics, including geneticist Dr. David Goldstein at Columbia University, argued that such studies were a waste of resources because they only found common variants that explained just a small fraction of the risk for disease.
He said the really important drivers of common diseases such as diabetes and schizophrenia were more likely to be found in extremely rare genes, those occurring in individuals or in families, not those shared by large populations of people.
Goldstein "argued very persuasively that it was all about rare variants and we were all going down the wrong road looking at the common ones," Collins said in a telephone interview.
The new study took a deeper look, using next-generation sequencing to search the entire genetic code of 2,657 people with and without diabetes to assess the contribution of both rare and common genes driving diabetes.
They also sequenced all of the protein-making genes in 12,940 people, and used statistical methods to estimate risk in another 111,548 people with less complete DNA data.
They found that, indeed, most of the genetic risk for type 2 diabetes is caused by common mistakes in the genetic code, with each mistake contributing only a small portion of an individual's risk for developing the disease.
"What this study says quite definitively for diabetes is the vast majority of hereditary risk variants are in fact these common ones, and the rare ones, while they pop up here and there, are a much smaller contribution," Collins said.
The study also turned up more than a dozen examples where variants alter the way proteins are made, suggesting that these gene variants have some direct impact on the development of type 2 diabetes.
"These represent promising avenues for efforts to design new ways to treat or prevent the disease," said Mark McCarthy, a senior author of the study from Oxford University.
All of the data will be made publicly available online through the Accelerating Medicines Partnership, a public-private partnership between the NIH, the U.S. Food and Drug Administration, 10 drug companies and several nonprofits.
Goldstein said the work was "a careful, solid investigation" that does not change his view much overall, adding that it was time to "quit arguing."
"What I care about now is finding the exact variants that infer risk, and understanding how they do so," he said.
SOURCE: http://go.nature.com/29DlL5i
Nature 2016.
Australia Declares AIDS No Longer a Public Health Issue
SYDNEY - Australia declared on Monday the AIDS epidemic is no longer a public health issue there, a month after the United Nations adopted an ambitious target to eliminate the threat globally by 2030.
The government-backed Australian Federation of AIDS Organisations (AFAO) and top scientists said the number of people being diagnosed with AIDS in Australia was now so small it was no longer reported.
AIDS cases in Australia peaked in 1994, at 953 cases, according to the Kirby Institute for infection and immunity in society.
Since then, following the introduction of antiretroviral treatment, that prevent AIDS developing in people who are infected with the HIV virus, and awareness campaigns, AIDS diagnoses have declined sharply.
"Australia is incredibly fortunate to be in the position and its because of farsighted government policy," said Darryl O'Donnell, chief executive AFAO.
"We had community organizations of gay men, sex workers and drug users doing outreach campaigns that were extraordinarily effective," O'Donnell said.
A spokeswoman for the Federal Department of Health said while it was tremendous that AIDS was "not the automatic death sentence that it once was," approximately 1,100 cases of HIV are detected each year.
"We must not let down our guard."
Worldwide there are 36.7 million people living with HIV, according to the World Health Organisation, with 180,000 people dying from AIDS-related illness in the Asia-Pacific region last year.
The United Nations agreed a new declaration on ending the AIDS epidemic at a meeting in New York last month.
The UNAIDS Fast-Track approach to ending the AIDS epidemic has a set of time-bound targets, including reducing the number of people newly infected with HIV from 2.1 million in 2015 to fewer than 500,000 in 2020, reducing the number of people dying from AIDS-related illnesses from 1.1 million in 2015 to fewer than 500,000 in 2020 and eliminating HIV-related discrimination.
Andrew Grulich, head of the HIV Epidemiology and Prevention Program at the Kirby Institute, said other countries could learn from Australia.
"The thing that has characterized Australia is a partnership between all sectors involved," he said. "Community, research and the government - and having bipartisan political support."
SYDNEY - Australia declared on Monday the AIDS epidemic is no longer a public health issue there, a month after the United Nations adopted an ambitious target to eliminate the threat globally by 2030.
The government-backed Australian Federation of AIDS Organisations (AFAO) and top scientists said the number of people being diagnosed with AIDS in Australia was now so small it was no longer reported.
AIDS cases in Australia peaked in 1994, at 953 cases, according to the Kirby Institute for infection and immunity in society.
Since then, following the introduction of antiretroviral treatment, that prevent AIDS developing in people who are infected with the HIV virus, and awareness campaigns, AIDS diagnoses have declined sharply.
"Australia is incredibly fortunate to be in the position and its because of farsighted government policy," said Darryl O'Donnell, chief executive AFAO.
"We had community organizations of gay men, sex workers and drug users doing outreach campaigns that were extraordinarily effective," O'Donnell said.
A spokeswoman for the Federal Department of Health said while it was tremendous that AIDS was "not the automatic death sentence that it once was," approximately 1,100 cases of HIV are detected each year.
"We must not let down our guard."
Worldwide there are 36.7 million people living with HIV, according to the World Health Organisation, with 180,000 people dying from AIDS-related illness in the Asia-Pacific region last year.
The United Nations agreed a new declaration on ending the AIDS epidemic at a meeting in New York last month.
The UNAIDS Fast-Track approach to ending the AIDS epidemic has a set of time-bound targets, including reducing the number of people newly infected with HIV from 2.1 million in 2015 to fewer than 500,000 in 2020, reducing the number of people dying from AIDS-related illnesses from 1.1 million in 2015 to fewer than 500,000 in 2020 and eliminating HIV-related discrimination.
Andrew Grulich, head of the HIV Epidemiology and Prevention Program at the Kirby Institute, said other countries could learn from Australia.
"The thing that has characterized Australia is a partnership between all sectors involved," he said. "Community, research and the government - and having bipartisan political support."
SYDNEY - Australia declared on Monday the AIDS epidemic is no longer a public health issue there, a month after the United Nations adopted an ambitious target to eliminate the threat globally by 2030.
The government-backed Australian Federation of AIDS Organisations (AFAO) and top scientists said the number of people being diagnosed with AIDS in Australia was now so small it was no longer reported.
AIDS cases in Australia peaked in 1994, at 953 cases, according to the Kirby Institute for infection and immunity in society.
Since then, following the introduction of antiretroviral treatment, that prevent AIDS developing in people who are infected with the HIV virus, and awareness campaigns, AIDS diagnoses have declined sharply.
"Australia is incredibly fortunate to be in the position and its because of farsighted government policy," said Darryl O'Donnell, chief executive AFAO.
"We had community organizations of gay men, sex workers and drug users doing outreach campaigns that were extraordinarily effective," O'Donnell said.
A spokeswoman for the Federal Department of Health said while it was tremendous that AIDS was "not the automatic death sentence that it once was," approximately 1,100 cases of HIV are detected each year.
"We must not let down our guard."
Worldwide there are 36.7 million people living with HIV, according to the World Health Organisation, with 180,000 people dying from AIDS-related illness in the Asia-Pacific region last year.
The United Nations agreed a new declaration on ending the AIDS epidemic at a meeting in New York last month.
The UNAIDS Fast-Track approach to ending the AIDS epidemic has a set of time-bound targets, including reducing the number of people newly infected with HIV from 2.1 million in 2015 to fewer than 500,000 in 2020, reducing the number of people dying from AIDS-related illnesses from 1.1 million in 2015 to fewer than 500,000 in 2020 and eliminating HIV-related discrimination.
Andrew Grulich, head of the HIV Epidemiology and Prevention Program at the Kirby Institute, said other countries could learn from Australia.
"The thing that has characterized Australia is a partnership between all sectors involved," he said. "Community, research and the government - and having bipartisan political support."
Atrial Fibrillation Linked with Greater Alcohol Access
NEW YORK - Greater access to alcohol is linked with more atrial fibrillation but less myocardial infarction and congestive heart failure, researchers report.
Dr. Gregory M. Marcus, from the Division of Cardiology at the University of California, San Francisco, and colleagues conducted an observational cohort study of differences in health outcomes based on alcohol sales laws by county in Texas.
All patients were residents of Texas, 21 years old or older, and were admitted to hospitals in Texas between 2005 and 2010. More than 1 million patients were included in the analysis.
Of the counties, 47 were wet (no restrictions on the sale of alcohol) and 29 were dry (prohibition of alcohol sales). Seven of them changed from dry to wet during the study period.
The main cardiovascular outcomes were atrial fibrillation, acute myocardial infarction, and congestive heart failure.
After multivariable adjustment, wet county residents had a greater prevalence (odds ratio 1.05, p=0.007) and incidence (HR 1.07, p=0.014) of atrial fibrillation.
Prevalence of myocardial infarction was lower (OR 0.83, p<0.001), as was its incidence (HR 0.91, p=0.019). Prevalence of congestive heart failure was also lower (OR 0.87, p<0.001).
In the seven dry counties that changed their status to wet, the post-conversion interval (from dry to wet county status) was associated with greater odds of hospitalization for atrial fibrillation (OR 1.07, p=0.001) and congestive heart failure (OR 1.07, p<0.001).
The researchers found no difference in acute myocardial infarction (OR 0.99, p=0.746).
"Cardiovascular disease is the most common cause of death worldwide, and alcohol is the most widely consumed drug in the United States," said Dr. Rory Brett Weiner, a cardiologist at Massachusetts General Hospital in Boston.
He said that studying the impact of alcohol intake on incident cardiovascular disease is important for its public health implications.
"Differences in laws affecting access to alcohol are associated with changes in health outcomes, both harmful and protective," said Dr. Marcus, "but the study's findings shouldn't be used to change any specific legislation."
Dr. Weiner agreed. "The study design minimizes confounders commonly seen in prior research that relied on self-report," he said, "but it still doesn't provide conclusive evidence with regard to the use of alcohol and incident cardiovascular disease."
Dr. Weiner said that the study did not contain information on the level of individual alcohol exposure, and therefore, the impact of the 'dose' of alcohol on cardiovascular outcomes could not be ascertained.
"Based on the question at hand -- the impact of alcohol -- it's unlikely that a randomized controlled study will ever be performed," he said, "so analyses like the current one are important."
According to Dr. Marcus, "We still don't understand the mechanisms underlying the relationship between alcohol and cardiovascular disease, and have a long way to go to achieve the sort of personalized medicine needed to figure out how to counsel an individual patient on their particular "prescribed" amount, if any, of alcohol."
The National Institute on Alcohol Abuse and Alcoholism supported this research. Dr. Marcus reported research support from Medtronic and Pfizer and equity interest in InCarda.
SOURCE: http://bit.ly/1tlx1cx
BMJ 2016
NEW YORK - Greater access to alcohol is linked with more atrial fibrillation but less myocardial infarction and congestive heart failure, researchers report.
Dr. Gregory M. Marcus, from the Division of Cardiology at the University of California, San Francisco, and colleagues conducted an observational cohort study of differences in health outcomes based on alcohol sales laws by county in Texas.
All patients were residents of Texas, 21 years old or older, and were admitted to hospitals in Texas between 2005 and 2010. More than 1 million patients were included in the analysis.
Of the counties, 47 were wet (no restrictions on the sale of alcohol) and 29 were dry (prohibition of alcohol sales). Seven of them changed from dry to wet during the study period.
The main cardiovascular outcomes were atrial fibrillation, acute myocardial infarction, and congestive heart failure.
After multivariable adjustment, wet county residents had a greater prevalence (odds ratio 1.05, p=0.007) and incidence (HR 1.07, p=0.014) of atrial fibrillation.
Prevalence of myocardial infarction was lower (OR 0.83, p<0.001), as was its incidence (HR 0.91, p=0.019). Prevalence of congestive heart failure was also lower (OR 0.87, p<0.001).
In the seven dry counties that changed their status to wet, the post-conversion interval (from dry to wet county status) was associated with greater odds of hospitalization for atrial fibrillation (OR 1.07, p=0.001) and congestive heart failure (OR 1.07, p<0.001).
The researchers found no difference in acute myocardial infarction (OR 0.99, p=0.746).
"Cardiovascular disease is the most common cause of death worldwide, and alcohol is the most widely consumed drug in the United States," said Dr. Rory Brett Weiner, a cardiologist at Massachusetts General Hospital in Boston.
He said that studying the impact of alcohol intake on incident cardiovascular disease is important for its public health implications.
"Differences in laws affecting access to alcohol are associated with changes in health outcomes, both harmful and protective," said Dr. Marcus, "but the study's findings shouldn't be used to change any specific legislation."
Dr. Weiner agreed. "The study design minimizes confounders commonly seen in prior research that relied on self-report," he said, "but it still doesn't provide conclusive evidence with regard to the use of alcohol and incident cardiovascular disease."
Dr. Weiner said that the study did not contain information on the level of individual alcohol exposure, and therefore, the impact of the 'dose' of alcohol on cardiovascular outcomes could not be ascertained.
"Based on the question at hand -- the impact of alcohol -- it's unlikely that a randomized controlled study will ever be performed," he said, "so analyses like the current one are important."
According to Dr. Marcus, "We still don't understand the mechanisms underlying the relationship between alcohol and cardiovascular disease, and have a long way to go to achieve the sort of personalized medicine needed to figure out how to counsel an individual patient on their particular "prescribed" amount, if any, of alcohol."
The National Institute on Alcohol Abuse and Alcoholism supported this research. Dr. Marcus reported research support from Medtronic and Pfizer and equity interest in InCarda.
SOURCE: http://bit.ly/1tlx1cx
BMJ 2016
NEW YORK - Greater access to alcohol is linked with more atrial fibrillation but less myocardial infarction and congestive heart failure, researchers report.
Dr. Gregory M. Marcus, from the Division of Cardiology at the University of California, San Francisco, and colleagues conducted an observational cohort study of differences in health outcomes based on alcohol sales laws by county in Texas.
All patients were residents of Texas, 21 years old or older, and were admitted to hospitals in Texas between 2005 and 2010. More than 1 million patients were included in the analysis.
Of the counties, 47 were wet (no restrictions on the sale of alcohol) and 29 were dry (prohibition of alcohol sales). Seven of them changed from dry to wet during the study period.
The main cardiovascular outcomes were atrial fibrillation, acute myocardial infarction, and congestive heart failure.
After multivariable adjustment, wet county residents had a greater prevalence (odds ratio 1.05, p=0.007) and incidence (HR 1.07, p=0.014) of atrial fibrillation.
Prevalence of myocardial infarction was lower (OR 0.83, p<0.001), as was its incidence (HR 0.91, p=0.019). Prevalence of congestive heart failure was also lower (OR 0.87, p<0.001).
In the seven dry counties that changed their status to wet, the post-conversion interval (from dry to wet county status) was associated with greater odds of hospitalization for atrial fibrillation (OR 1.07, p=0.001) and congestive heart failure (OR 1.07, p<0.001).
The researchers found no difference in acute myocardial infarction (OR 0.99, p=0.746).
"Cardiovascular disease is the most common cause of death worldwide, and alcohol is the most widely consumed drug in the United States," said Dr. Rory Brett Weiner, a cardiologist at Massachusetts General Hospital in Boston.
He said that studying the impact of alcohol intake on incident cardiovascular disease is important for its public health implications.
"Differences in laws affecting access to alcohol are associated with changes in health outcomes, both harmful and protective," said Dr. Marcus, "but the study's findings shouldn't be used to change any specific legislation."
Dr. Weiner agreed. "The study design minimizes confounders commonly seen in prior research that relied on self-report," he said, "but it still doesn't provide conclusive evidence with regard to the use of alcohol and incident cardiovascular disease."
Dr. Weiner said that the study did not contain information on the level of individual alcohol exposure, and therefore, the impact of the 'dose' of alcohol on cardiovascular outcomes could not be ascertained.
"Based on the question at hand -- the impact of alcohol -- it's unlikely that a randomized controlled study will ever be performed," he said, "so analyses like the current one are important."
According to Dr. Marcus, "We still don't understand the mechanisms underlying the relationship between alcohol and cardiovascular disease, and have a long way to go to achieve the sort of personalized medicine needed to figure out how to counsel an individual patient on their particular "prescribed" amount, if any, of alcohol."
The National Institute on Alcohol Abuse and Alcoholism supported this research. Dr. Marcus reported research support from Medtronic and Pfizer and equity interest in InCarda.
SOURCE: http://bit.ly/1tlx1cx
BMJ 2016
Theranos Receives Biggest Blow as CMS Revokes Certificate for Government Payments
Theranos Inc founder and CEO Elizabeth Holmes, once touted as the Steve Jobs of biotech for her company's innovative blood-testing technology, has been barred by a U.S. regulator from owning or operating a lab for at least two years.
Dealing the biggest blow yet to the privately held company, the Centers for Medicare & Medicaid Services revoked a key certificate for its California lab and terminated the facility's approval to receive government payments.
Medicare is the government's medical insurance program for the elderly, while Medicaid is for the poor.
The sanctions, which also include an unspecified monetary penalty, come six months after the regulator sent a scathing letter to the company, saying its practices were jeopardizing patient health and safety.
Theranos said late on Thursday that it would continue to service its customers through its Arizona lab.
The company, once valued at $9 billion, was founded by Holmes in 2003 to develop an innovative blood testing device that would give quicker results using just one drop of blood.
However, its fortunes waned after the Wall Street Journal published a series of articles starting in October last year that suggested the devices were flawed and inaccurate.
Forbes magazine said last month that the company's value had fallen to about $800 million, while Holmes' own net worth had shrunk to zero from about $4.5 billion - a figure the magazine had said had made her the richest self-made woman in America.
"Everyone wanted her to succeed," Steve Brozak, president of WBB Securities, told Reuters, noting that the basic blood diagnostics sector has not had a significant advance in technology in 90 years.
Walgreens Boots Alliance terminated its relationship with the company last month and closed operations at all 40 Theranos Wellness Centers at its drug stores in Arizona.
Theranos is also facing a class action lawsuit filed in May accusing it of endangering customer health through "massive failures" that misrepresented test results.
The Palo Alto, California-based company is also being investigated by other federal and state agencies, including the U.S. Securities and Exchange Commission and the State Department of Health in Arizona.
Theranos Inc founder and CEO Elizabeth Holmes, once touted as the Steve Jobs of biotech for her company's innovative blood-testing technology, has been barred by a U.S. regulator from owning or operating a lab for at least two years.
Dealing the biggest blow yet to the privately held company, the Centers for Medicare & Medicaid Services revoked a key certificate for its California lab and terminated the facility's approval to receive government payments.
Medicare is the government's medical insurance program for the elderly, while Medicaid is for the poor.
The sanctions, which also include an unspecified monetary penalty, come six months after the regulator sent a scathing letter to the company, saying its practices were jeopardizing patient health and safety.
Theranos said late on Thursday that it would continue to service its customers through its Arizona lab.
The company, once valued at $9 billion, was founded by Holmes in 2003 to develop an innovative blood testing device that would give quicker results using just one drop of blood.
However, its fortunes waned after the Wall Street Journal published a series of articles starting in October last year that suggested the devices were flawed and inaccurate.
Forbes magazine said last month that the company's value had fallen to about $800 million, while Holmes' own net worth had shrunk to zero from about $4.5 billion - a figure the magazine had said had made her the richest self-made woman in America.
"Everyone wanted her to succeed," Steve Brozak, president of WBB Securities, told Reuters, noting that the basic blood diagnostics sector has not had a significant advance in technology in 90 years.
Walgreens Boots Alliance terminated its relationship with the company last month and closed operations at all 40 Theranos Wellness Centers at its drug stores in Arizona.
Theranos is also facing a class action lawsuit filed in May accusing it of endangering customer health through "massive failures" that misrepresented test results.
The Palo Alto, California-based company is also being investigated by other federal and state agencies, including the U.S. Securities and Exchange Commission and the State Department of Health in Arizona.
Theranos Inc founder and CEO Elizabeth Holmes, once touted as the Steve Jobs of biotech for her company's innovative blood-testing technology, has been barred by a U.S. regulator from owning or operating a lab for at least two years.
Dealing the biggest blow yet to the privately held company, the Centers for Medicare & Medicaid Services revoked a key certificate for its California lab and terminated the facility's approval to receive government payments.
Medicare is the government's medical insurance program for the elderly, while Medicaid is for the poor.
The sanctions, which also include an unspecified monetary penalty, come six months after the regulator sent a scathing letter to the company, saying its practices were jeopardizing patient health and safety.
Theranos said late on Thursday that it would continue to service its customers through its Arizona lab.
The company, once valued at $9 billion, was founded by Holmes in 2003 to develop an innovative blood testing device that would give quicker results using just one drop of blood.
However, its fortunes waned after the Wall Street Journal published a series of articles starting in October last year that suggested the devices were flawed and inaccurate.
Forbes magazine said last month that the company's value had fallen to about $800 million, while Holmes' own net worth had shrunk to zero from about $4.5 billion - a figure the magazine had said had made her the richest self-made woman in America.
"Everyone wanted her to succeed," Steve Brozak, president of WBB Securities, told Reuters, noting that the basic blood diagnostics sector has not had a significant advance in technology in 90 years.
Walgreens Boots Alliance terminated its relationship with the company last month and closed operations at all 40 Theranos Wellness Centers at its drug stores in Arizona.
Theranos is also facing a class action lawsuit filed in May accusing it of endangering customer health through "massive failures" that misrepresented test results.
The Palo Alto, California-based company is also being investigated by other federal and state agencies, including the U.S. Securities and Exchange Commission and the State Department of Health in Arizona.