User login
Hospitalist movers and shakers
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Survey insights: Unwrapping the compensation package
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
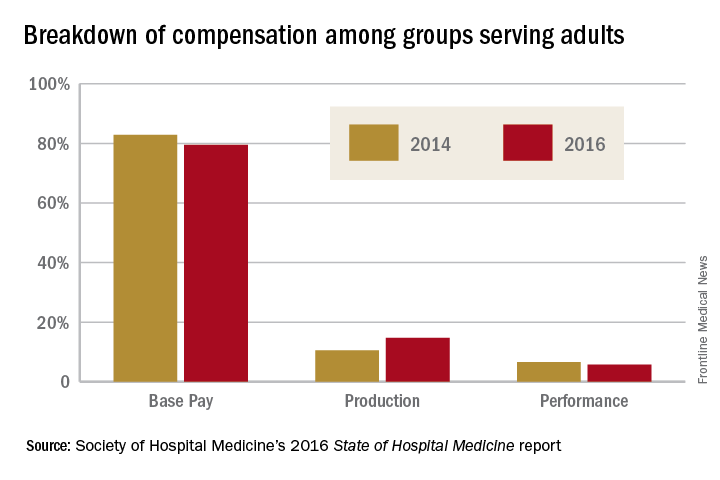
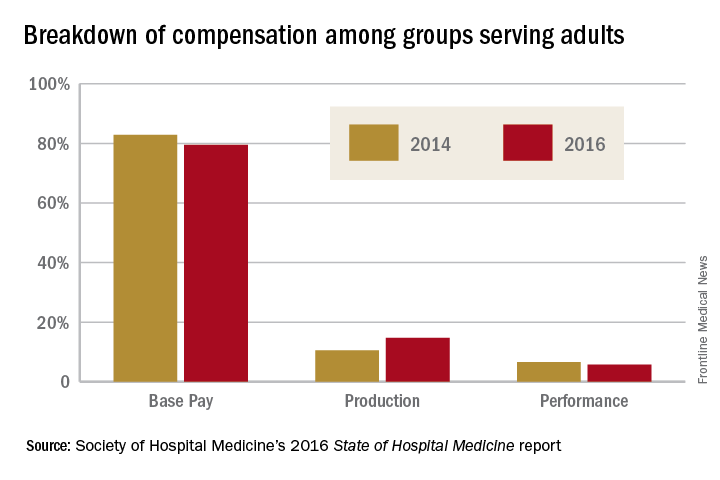
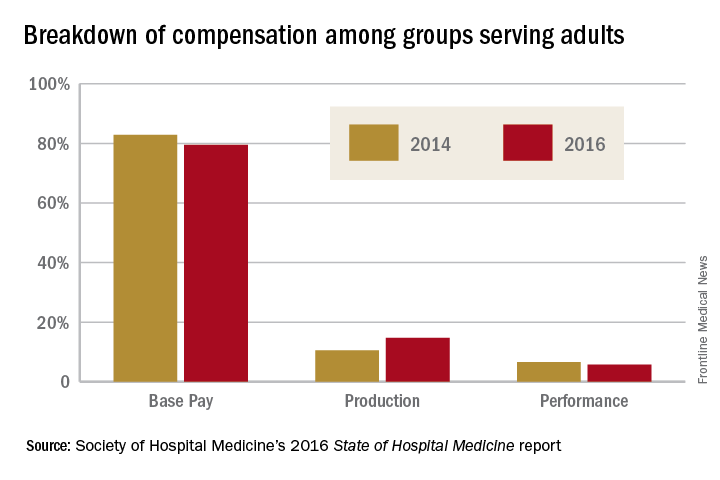
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
Set a goal, or two, or three
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
Hospitalist movers and shakers
O’Neil Pike, MD, SFHM, has been promoted to chief medical officer with healthcare staffing company Medicus Healthcare Solutions (MHS) of Windham, N.H. Formerly a hospitalist consultant and chief practice advisor with MHS, Dr. Pike is a practicing hospitalist and serves as an assistant professor of medicine at Geisinger Commonwealth School of Medicine in Scranton, Pa.
Timothy D. Bode, MD, MBA, SFHM, has been named appointed medical officer at Saint Thomas Rutherford Hospital in Murfreesboro, Tenn., as well as several regional hospitals in the Saint Thomas system. Previously, Dr. Bode served as senior vice president and CMO at Memorial Health in Jacksonville, Fla.
Joseph Perras, MD, has been named chief executive officer at Mt. Ascutney Hospital and Health Center (MAHHC) in Windsor, Vt. Dr. Perras will continue as the center’s CMO, as well. He previously held the role of MAHHC’s director of hospital medicine.
Alamjit Virk, MD, has been promoted to medical director of Emergency Medicine and Hospitalist Services at Martha’s Vineyard Hospital in Oak Bluffs, Mass. Dr. Virk was a MVH staff physician for a year and half prior to the elevation, and he previously served as an attending physician in emergency medicine at Emerson Hospital in Concord, Mass.
Business Moves
Dearborn County Hospital (DCH) in Lawrenceburg, Ind., has partnered with TriHealth to provide hospitalist services for its inpatients. TriHealth’s team of more than 30 hospitalists is led by chief of hospital medicine Bryan Strader, MD. TriHealth also provides care for patients at Ohio’s Bethesda North, Good Samaritan and Bethesda Butler Hospitals.
MidMichigan Medical Centers in Alma, Gladwin, and Midland have been recognized with Five Star Excellence Awards by national health care research leader Professional Research Consultants. Awards were received for excellence in providing patients discharge information and pain management.
Pediatric Associates, located in Broward County, Fla., has expanded its pediatric hospitalist program thanks to the success of a pilot program run at Palm Beach Children’s Hospital at St. Mary’s Medical Center (West Palm Beach). Jamilah Grant-Guimaraes, MD, FAAP, and Nina Phillips Bernstein, DO, FAAP, will provide care to Pediatrics Associates patients at Broward General Medical Center.
The University of Pennsylvania Health System announced that it will add Princeton HealthCare System (PHCS) to the UPHS family. Located just 40 miles from Philadelphia, PHCS serves more than 1.3 million people in central New Jersey and includes the University Medical Center of Princeton, which opened in 2012 in Plainsboro, N.J.
Lehigh Valley Health Network, based out of Allentown, Pa., has absorbed Pocono Health System (East Stroudsburg, Pa.) in a move effective Jan. 1. Under the deal’s terms, Pocono Medical Center (the system’s only hospital) now will be known as Lehigh Valley Hospital–Pocono. LVH also absorbs Pocono’s three health centers. LVH now operates 8 hospital campuses and 19 health centers.
O’Neil Pike, MD, SFHM, has been promoted to chief medical officer with healthcare staffing company Medicus Healthcare Solutions (MHS) of Windham, N.H. Formerly a hospitalist consultant and chief practice advisor with MHS, Dr. Pike is a practicing hospitalist and serves as an assistant professor of medicine at Geisinger Commonwealth School of Medicine in Scranton, Pa.
Timothy D. Bode, MD, MBA, SFHM, has been named appointed medical officer at Saint Thomas Rutherford Hospital in Murfreesboro, Tenn., as well as several regional hospitals in the Saint Thomas system. Previously, Dr. Bode served as senior vice president and CMO at Memorial Health in Jacksonville, Fla.
Joseph Perras, MD, has been named chief executive officer at Mt. Ascutney Hospital and Health Center (MAHHC) in Windsor, Vt. Dr. Perras will continue as the center’s CMO, as well. He previously held the role of MAHHC’s director of hospital medicine.
Alamjit Virk, MD, has been promoted to medical director of Emergency Medicine and Hospitalist Services at Martha’s Vineyard Hospital in Oak Bluffs, Mass. Dr. Virk was a MVH staff physician for a year and half prior to the elevation, and he previously served as an attending physician in emergency medicine at Emerson Hospital in Concord, Mass.
Business Moves
Dearborn County Hospital (DCH) in Lawrenceburg, Ind., has partnered with TriHealth to provide hospitalist services for its inpatients. TriHealth’s team of more than 30 hospitalists is led by chief of hospital medicine Bryan Strader, MD. TriHealth also provides care for patients at Ohio’s Bethesda North, Good Samaritan and Bethesda Butler Hospitals.
MidMichigan Medical Centers in Alma, Gladwin, and Midland have been recognized with Five Star Excellence Awards by national health care research leader Professional Research Consultants. Awards were received for excellence in providing patients discharge information and pain management.
Pediatric Associates, located in Broward County, Fla., has expanded its pediatric hospitalist program thanks to the success of a pilot program run at Palm Beach Children’s Hospital at St. Mary’s Medical Center (West Palm Beach). Jamilah Grant-Guimaraes, MD, FAAP, and Nina Phillips Bernstein, DO, FAAP, will provide care to Pediatrics Associates patients at Broward General Medical Center.
The University of Pennsylvania Health System announced that it will add Princeton HealthCare System (PHCS) to the UPHS family. Located just 40 miles from Philadelphia, PHCS serves more than 1.3 million people in central New Jersey and includes the University Medical Center of Princeton, which opened in 2012 in Plainsboro, N.J.
Lehigh Valley Health Network, based out of Allentown, Pa., has absorbed Pocono Health System (East Stroudsburg, Pa.) in a move effective Jan. 1. Under the deal’s terms, Pocono Medical Center (the system’s only hospital) now will be known as Lehigh Valley Hospital–Pocono. LVH also absorbs Pocono’s three health centers. LVH now operates 8 hospital campuses and 19 health centers.
O’Neil Pike, MD, SFHM, has been promoted to chief medical officer with healthcare staffing company Medicus Healthcare Solutions (MHS) of Windham, N.H. Formerly a hospitalist consultant and chief practice advisor with MHS, Dr. Pike is a practicing hospitalist and serves as an assistant professor of medicine at Geisinger Commonwealth School of Medicine in Scranton, Pa.
Timothy D. Bode, MD, MBA, SFHM, has been named appointed medical officer at Saint Thomas Rutherford Hospital in Murfreesboro, Tenn., as well as several regional hospitals in the Saint Thomas system. Previously, Dr. Bode served as senior vice president and CMO at Memorial Health in Jacksonville, Fla.
Joseph Perras, MD, has been named chief executive officer at Mt. Ascutney Hospital and Health Center (MAHHC) in Windsor, Vt. Dr. Perras will continue as the center’s CMO, as well. He previously held the role of MAHHC’s director of hospital medicine.
Alamjit Virk, MD, has been promoted to medical director of Emergency Medicine and Hospitalist Services at Martha’s Vineyard Hospital in Oak Bluffs, Mass. Dr. Virk was a MVH staff physician for a year and half prior to the elevation, and he previously served as an attending physician in emergency medicine at Emerson Hospital in Concord, Mass.
Business Moves
Dearborn County Hospital (DCH) in Lawrenceburg, Ind., has partnered with TriHealth to provide hospitalist services for its inpatients. TriHealth’s team of more than 30 hospitalists is led by chief of hospital medicine Bryan Strader, MD. TriHealth also provides care for patients at Ohio’s Bethesda North, Good Samaritan and Bethesda Butler Hospitals.
MidMichigan Medical Centers in Alma, Gladwin, and Midland have been recognized with Five Star Excellence Awards by national health care research leader Professional Research Consultants. Awards were received for excellence in providing patients discharge information and pain management.
Pediatric Associates, located in Broward County, Fla., has expanded its pediatric hospitalist program thanks to the success of a pilot program run at Palm Beach Children’s Hospital at St. Mary’s Medical Center (West Palm Beach). Jamilah Grant-Guimaraes, MD, FAAP, and Nina Phillips Bernstein, DO, FAAP, will provide care to Pediatrics Associates patients at Broward General Medical Center.
The University of Pennsylvania Health System announced that it will add Princeton HealthCare System (PHCS) to the UPHS family. Located just 40 miles from Philadelphia, PHCS serves more than 1.3 million people in central New Jersey and includes the University Medical Center of Princeton, which opened in 2012 in Plainsboro, N.J.
Lehigh Valley Health Network, based out of Allentown, Pa., has absorbed Pocono Health System (East Stroudsburg, Pa.) in a move effective Jan. 1. Under the deal’s terms, Pocono Medical Center (the system’s only hospital) now will be known as Lehigh Valley Hospital–Pocono. LVH also absorbs Pocono’s three health centers. LVH now operates 8 hospital campuses and 19 health centers.
Burnout: No laughing matter
Much has been written about burnout in U.S. physicians over the course of many years. Burnout is a syndrome that is exemplified by emotional exhaustion, depersonalization, and a low sense of personal accomplishment. It appears that hospitalists are particularly prone to burnout, being at the very front line of patient care. In addition, the prevalence of burnout appears to be getting worse. According to a survey from the American Medical Association, the prevalence of burnout in 2011 was 45%. Three years later in 2014 the prevalence was up to 55%.1,2
Although triggers for the onset and intensity of burnout likely vary by specialty, a recent Medscape Lifestyle Report found the most common causes of burnout among physicians included (see graphic):3
• Bureaucratic tasks.
• Work hours.
• Computerization.
• Compensation.

• Lower work satisfaction.
• Disrupted personal relationships.
• Substance misuse.
• Depression.
• Suicide.
Burnout also leads to lower productivity, higher job turnover, and early retirement. In addition, from a systems perspective, burnout is associated with higher medical errors, reduced quality of patient care, and lower patient satisfaction. And, at its most extreme, burnout is deadly: Sadly, every year, 300-400 physicians in the United States commit suicide. Female physicians are 2.3 times more likely to commit suicide than are female nonphysicians; for males, the risk is 1.4 times higher among physicians compared to the general population.1
Proactive approaches
Despite all these sobering statistics on the prevalence and outcomes of burnout among physicians, the ongoing question is, what can we do about it? Although awareness and recognition of burnout has grown substantially over time, successful interventions to prevent or mitigate burnout have not. Many potential interventions and ideas have surfaced and have been published, but none have had impressive impacts or have been adopted widely within or across institutions. According to a Modern Healthcare survey of approximately 100 health care CEOs, only about one-third reported that their organization had programs to address physician burnout, although about another one-third reported attempts to develop such programs.1
The good news is that at least there is a lot of activity around trying new interventions to reduce burnout, including in medical schools and graduate training programs. The thought is that if you can employ healthy resilience tactics during training, these can be carried throughout a career to diminish the risk and/or severity of burnout, despite any challenges that arise along the way.
Some of these interventions are aimed at individuals (to enhance personal resilience and coping skills) while others are aimed at the level of organizations (to reduce organizational stress and/or workload). A recent Modern Healthcare article found several good examples:1
• New York’s Albert Einstein College of Medicine’s WellMed program has been designed to help students develop healthy and balanced habits and attitudes, and to enhance their personal resilience, for the short and the long term.
• Baystate Health in Massachusetts hosts a physician leadership academy that offers training in communication, unconscious bias, strategy, and other management skills, to enhance individual resilience and organizational engagement.
• HealthPartners, a not-for-profit, Minnesota-based health care organization, has specific programs to engage physicians and allow them to have organizational impact, as well as programs to simplify technology use.
Organization efforts are key to prevent, treat
The key to reducing burnout does seem to be employing a combination of self-directed and organization-directed interventions, each of which enhances resilience and reduces workplace stressors (i.e., administrative tasks and workload). Specific to hospitalists, Leslie Flores, MBA, recently wrote about burnout at The Hospital Leader blog. Her list included several specific examples to reduce the top causes of burnout among busy hospitalists:4
• Modifying the skill mix in hospital medicine groups so that less costly support staff are doing much of the work not requiring a physician’s expertise, freeing up hospitalists to provide better care to more patients.
• Reducing unnecessary interruptions and the stress they cause, via both technology and process improvement.
• Paying deliberate attention to hospitalist personal and professional well-being.
• Adjusting hospitalist schedules and work flow so that hospitalists can be more efficient (that is, do less low-value work and re-work) and have better work-life balance.
• Ensuring that hospitalists have the training, clinical competencies, and support to comfortably perform in expanded clinical roles.
Many of these systemic solutions were recently validated as likely able to have an impact on burnout (and seem to be more effective than interventions focused on individual resilience).5 A recent meta-analysis found that physician-directed interventions were associated with small but significant reductions in burnout; these were primarily mindfulness-based stress reduction techniques, educational interventions targeting physicians self-confidence and communication skills, exercise, or a combination of these features. More impactful were organization-directed interventions, which were associated with more significant reductions in burnout; these were primarily aimed at reducing workload and enhancing teamwork and leadership.
In sum
It is important for all of us hospitalists to understand and try to mitigate burnout within our teams. Although individual-focused interventions can have some effect, most efforts should primarily be focused on system-based interventions, to reduce administrative burdens and workload. Through such system design and redesign, we can likely reduce burnout amongst our teams, and therefore improve the sustainability of our specialty.
References
1.http://www.modernhealthcare.com/article/20161029/MAGAZINE/310299983
2. http://www.mayoclinicproceedings.org/article/S0025-6196(15)00716-8/abstract
3.http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=5
4. http://blogs.hospitalmedicine.org/Blog/making-hospital-medicine-a-sustainable-specialty/
5.http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2588814
Much has been written about burnout in U.S. physicians over the course of many years. Burnout is a syndrome that is exemplified by emotional exhaustion, depersonalization, and a low sense of personal accomplishment. It appears that hospitalists are particularly prone to burnout, being at the very front line of patient care. In addition, the prevalence of burnout appears to be getting worse. According to a survey from the American Medical Association, the prevalence of burnout in 2011 was 45%. Three years later in 2014 the prevalence was up to 55%.1,2
Although triggers for the onset and intensity of burnout likely vary by specialty, a recent Medscape Lifestyle Report found the most common causes of burnout among physicians included (see graphic):3
• Bureaucratic tasks.
• Work hours.
• Computerization.
• Compensation.

• Lower work satisfaction.
• Disrupted personal relationships.
• Substance misuse.
• Depression.
• Suicide.
Burnout also leads to lower productivity, higher job turnover, and early retirement. In addition, from a systems perspective, burnout is associated with higher medical errors, reduced quality of patient care, and lower patient satisfaction. And, at its most extreme, burnout is deadly: Sadly, every year, 300-400 physicians in the United States commit suicide. Female physicians are 2.3 times more likely to commit suicide than are female nonphysicians; for males, the risk is 1.4 times higher among physicians compared to the general population.1
Proactive approaches
Despite all these sobering statistics on the prevalence and outcomes of burnout among physicians, the ongoing question is, what can we do about it? Although awareness and recognition of burnout has grown substantially over time, successful interventions to prevent or mitigate burnout have not. Many potential interventions and ideas have surfaced and have been published, but none have had impressive impacts or have been adopted widely within or across institutions. According to a Modern Healthcare survey of approximately 100 health care CEOs, only about one-third reported that their organization had programs to address physician burnout, although about another one-third reported attempts to develop such programs.1
The good news is that at least there is a lot of activity around trying new interventions to reduce burnout, including in medical schools and graduate training programs. The thought is that if you can employ healthy resilience tactics during training, these can be carried throughout a career to diminish the risk and/or severity of burnout, despite any challenges that arise along the way.
Some of these interventions are aimed at individuals (to enhance personal resilience and coping skills) while others are aimed at the level of organizations (to reduce organizational stress and/or workload). A recent Modern Healthcare article found several good examples:1
• New York’s Albert Einstein College of Medicine’s WellMed program has been designed to help students develop healthy and balanced habits and attitudes, and to enhance their personal resilience, for the short and the long term.
• Baystate Health in Massachusetts hosts a physician leadership academy that offers training in communication, unconscious bias, strategy, and other management skills, to enhance individual resilience and organizational engagement.
• HealthPartners, a not-for-profit, Minnesota-based health care organization, has specific programs to engage physicians and allow them to have organizational impact, as well as programs to simplify technology use.
Organization efforts are key to prevent, treat
The key to reducing burnout does seem to be employing a combination of self-directed and organization-directed interventions, each of which enhances resilience and reduces workplace stressors (i.e., administrative tasks and workload). Specific to hospitalists, Leslie Flores, MBA, recently wrote about burnout at The Hospital Leader blog. Her list included several specific examples to reduce the top causes of burnout among busy hospitalists:4
• Modifying the skill mix in hospital medicine groups so that less costly support staff are doing much of the work not requiring a physician’s expertise, freeing up hospitalists to provide better care to more patients.
• Reducing unnecessary interruptions and the stress they cause, via both technology and process improvement.
• Paying deliberate attention to hospitalist personal and professional well-being.
• Adjusting hospitalist schedules and work flow so that hospitalists can be more efficient (that is, do less low-value work and re-work) and have better work-life balance.
• Ensuring that hospitalists have the training, clinical competencies, and support to comfortably perform in expanded clinical roles.
Many of these systemic solutions were recently validated as likely able to have an impact on burnout (and seem to be more effective than interventions focused on individual resilience).5 A recent meta-analysis found that physician-directed interventions were associated with small but significant reductions in burnout; these were primarily mindfulness-based stress reduction techniques, educational interventions targeting physicians self-confidence and communication skills, exercise, or a combination of these features. More impactful were organization-directed interventions, which were associated with more significant reductions in burnout; these were primarily aimed at reducing workload and enhancing teamwork and leadership.
In sum
It is important for all of us hospitalists to understand and try to mitigate burnout within our teams. Although individual-focused interventions can have some effect, most efforts should primarily be focused on system-based interventions, to reduce administrative burdens and workload. Through such system design and redesign, we can likely reduce burnout amongst our teams, and therefore improve the sustainability of our specialty.
References
1.http://www.modernhealthcare.com/article/20161029/MAGAZINE/310299983
2. http://www.mayoclinicproceedings.org/article/S0025-6196(15)00716-8/abstract
3.http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=5
4. http://blogs.hospitalmedicine.org/Blog/making-hospital-medicine-a-sustainable-specialty/
5.http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2588814
Much has been written about burnout in U.S. physicians over the course of many years. Burnout is a syndrome that is exemplified by emotional exhaustion, depersonalization, and a low sense of personal accomplishment. It appears that hospitalists are particularly prone to burnout, being at the very front line of patient care. In addition, the prevalence of burnout appears to be getting worse. According to a survey from the American Medical Association, the prevalence of burnout in 2011 was 45%. Three years later in 2014 the prevalence was up to 55%.1,2
Although triggers for the onset and intensity of burnout likely vary by specialty, a recent Medscape Lifestyle Report found the most common causes of burnout among physicians included (see graphic):3
• Bureaucratic tasks.
• Work hours.
• Computerization.
• Compensation.

• Lower work satisfaction.
• Disrupted personal relationships.
• Substance misuse.
• Depression.
• Suicide.
Burnout also leads to lower productivity, higher job turnover, and early retirement. In addition, from a systems perspective, burnout is associated with higher medical errors, reduced quality of patient care, and lower patient satisfaction. And, at its most extreme, burnout is deadly: Sadly, every year, 300-400 physicians in the United States commit suicide. Female physicians are 2.3 times more likely to commit suicide than are female nonphysicians; for males, the risk is 1.4 times higher among physicians compared to the general population.1
Proactive approaches
Despite all these sobering statistics on the prevalence and outcomes of burnout among physicians, the ongoing question is, what can we do about it? Although awareness and recognition of burnout has grown substantially over time, successful interventions to prevent or mitigate burnout have not. Many potential interventions and ideas have surfaced and have been published, but none have had impressive impacts or have been adopted widely within or across institutions. According to a Modern Healthcare survey of approximately 100 health care CEOs, only about one-third reported that their organization had programs to address physician burnout, although about another one-third reported attempts to develop such programs.1
The good news is that at least there is a lot of activity around trying new interventions to reduce burnout, including in medical schools and graduate training programs. The thought is that if you can employ healthy resilience tactics during training, these can be carried throughout a career to diminish the risk and/or severity of burnout, despite any challenges that arise along the way.
Some of these interventions are aimed at individuals (to enhance personal resilience and coping skills) while others are aimed at the level of organizations (to reduce organizational stress and/or workload). A recent Modern Healthcare article found several good examples:1
• New York’s Albert Einstein College of Medicine’s WellMed program has been designed to help students develop healthy and balanced habits and attitudes, and to enhance their personal resilience, for the short and the long term.
• Baystate Health in Massachusetts hosts a physician leadership academy that offers training in communication, unconscious bias, strategy, and other management skills, to enhance individual resilience and organizational engagement.
• HealthPartners, a not-for-profit, Minnesota-based health care organization, has specific programs to engage physicians and allow them to have organizational impact, as well as programs to simplify technology use.
Organization efforts are key to prevent, treat
The key to reducing burnout does seem to be employing a combination of self-directed and organization-directed interventions, each of which enhances resilience and reduces workplace stressors (i.e., administrative tasks and workload). Specific to hospitalists, Leslie Flores, MBA, recently wrote about burnout at The Hospital Leader blog. Her list included several specific examples to reduce the top causes of burnout among busy hospitalists:4
• Modifying the skill mix in hospital medicine groups so that less costly support staff are doing much of the work not requiring a physician’s expertise, freeing up hospitalists to provide better care to more patients.
• Reducing unnecessary interruptions and the stress they cause, via both technology and process improvement.
• Paying deliberate attention to hospitalist personal and professional well-being.
• Adjusting hospitalist schedules and work flow so that hospitalists can be more efficient (that is, do less low-value work and re-work) and have better work-life balance.
• Ensuring that hospitalists have the training, clinical competencies, and support to comfortably perform in expanded clinical roles.
Many of these systemic solutions were recently validated as likely able to have an impact on burnout (and seem to be more effective than interventions focused on individual resilience).5 A recent meta-analysis found that physician-directed interventions were associated with small but significant reductions in burnout; these were primarily mindfulness-based stress reduction techniques, educational interventions targeting physicians self-confidence and communication skills, exercise, or a combination of these features. More impactful were organization-directed interventions, which were associated with more significant reductions in burnout; these were primarily aimed at reducing workload and enhancing teamwork and leadership.
In sum
It is important for all of us hospitalists to understand and try to mitigate burnout within our teams. Although individual-focused interventions can have some effect, most efforts should primarily be focused on system-based interventions, to reduce administrative burdens and workload. Through such system design and redesign, we can likely reduce burnout amongst our teams, and therefore improve the sustainability of our specialty.
References
1.http://www.modernhealthcare.com/article/20161029/MAGAZINE/310299983
2. http://www.mayoclinicproceedings.org/article/S0025-6196(15)00716-8/abstract
3.http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=5
4. http://blogs.hospitalmedicine.org/Blog/making-hospital-medicine-a-sustainable-specialty/
5.http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2588814
Don’t assume work is sole burnout determinant
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
Hot-button issue: physician burnout
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
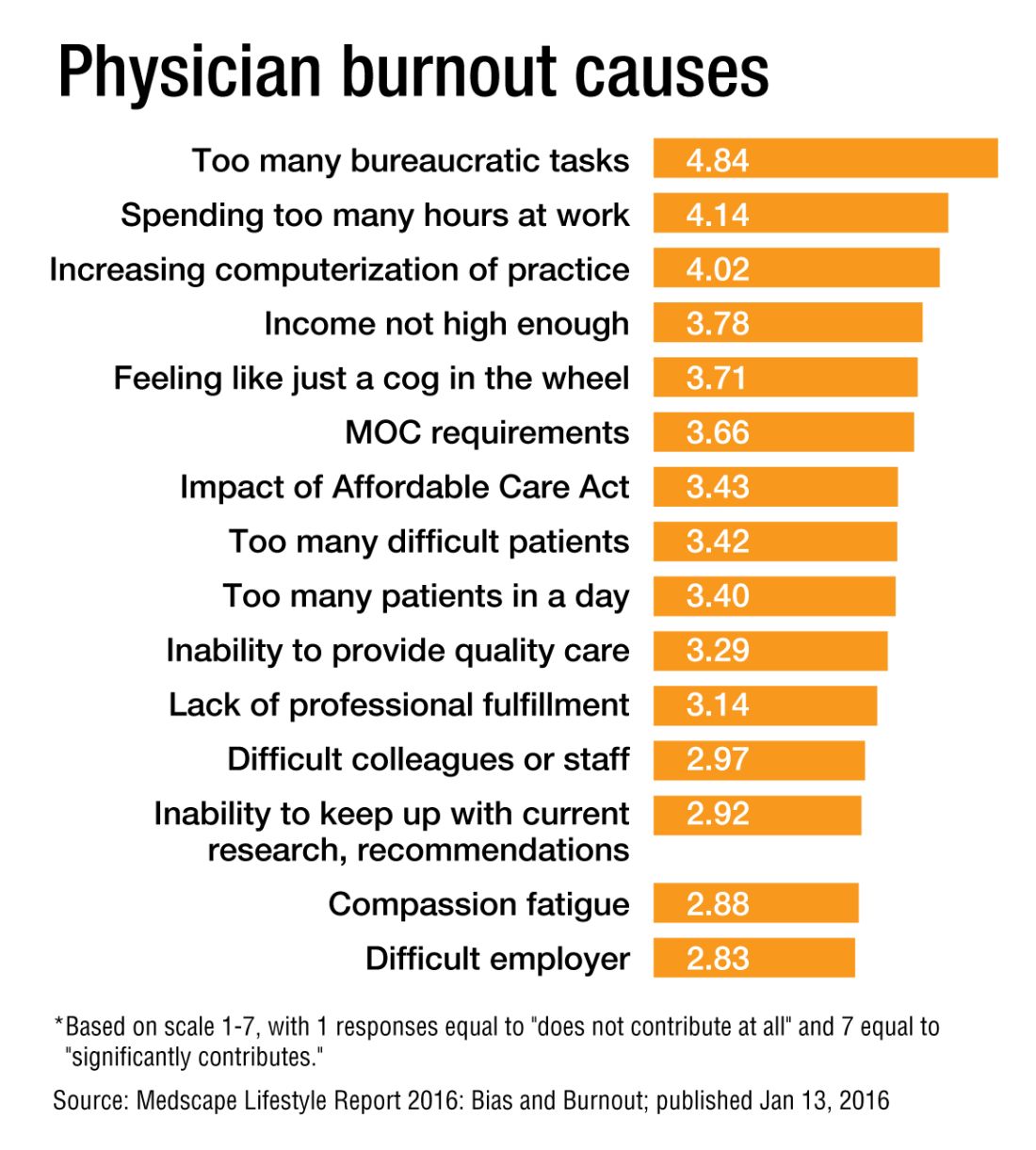
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
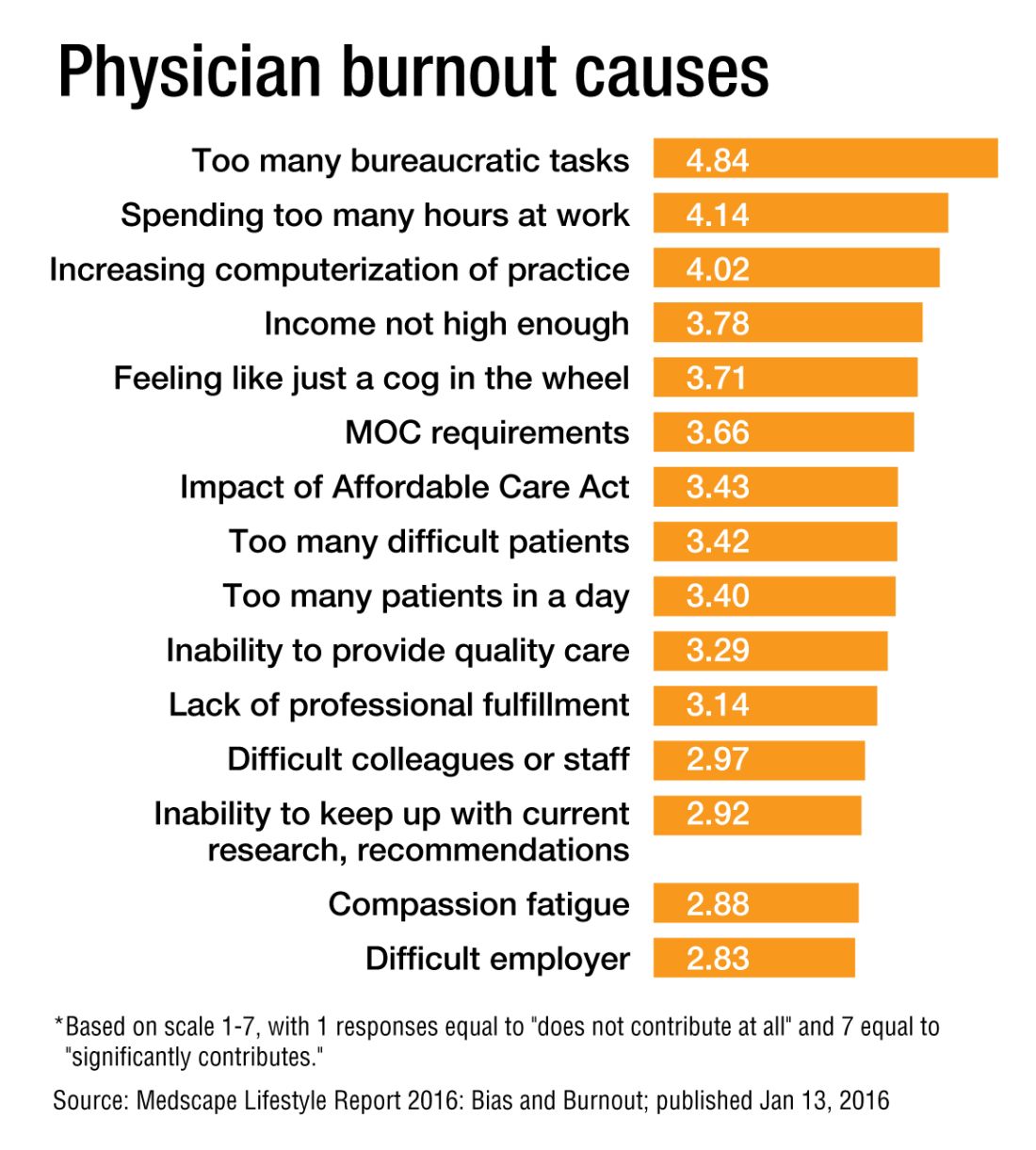
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
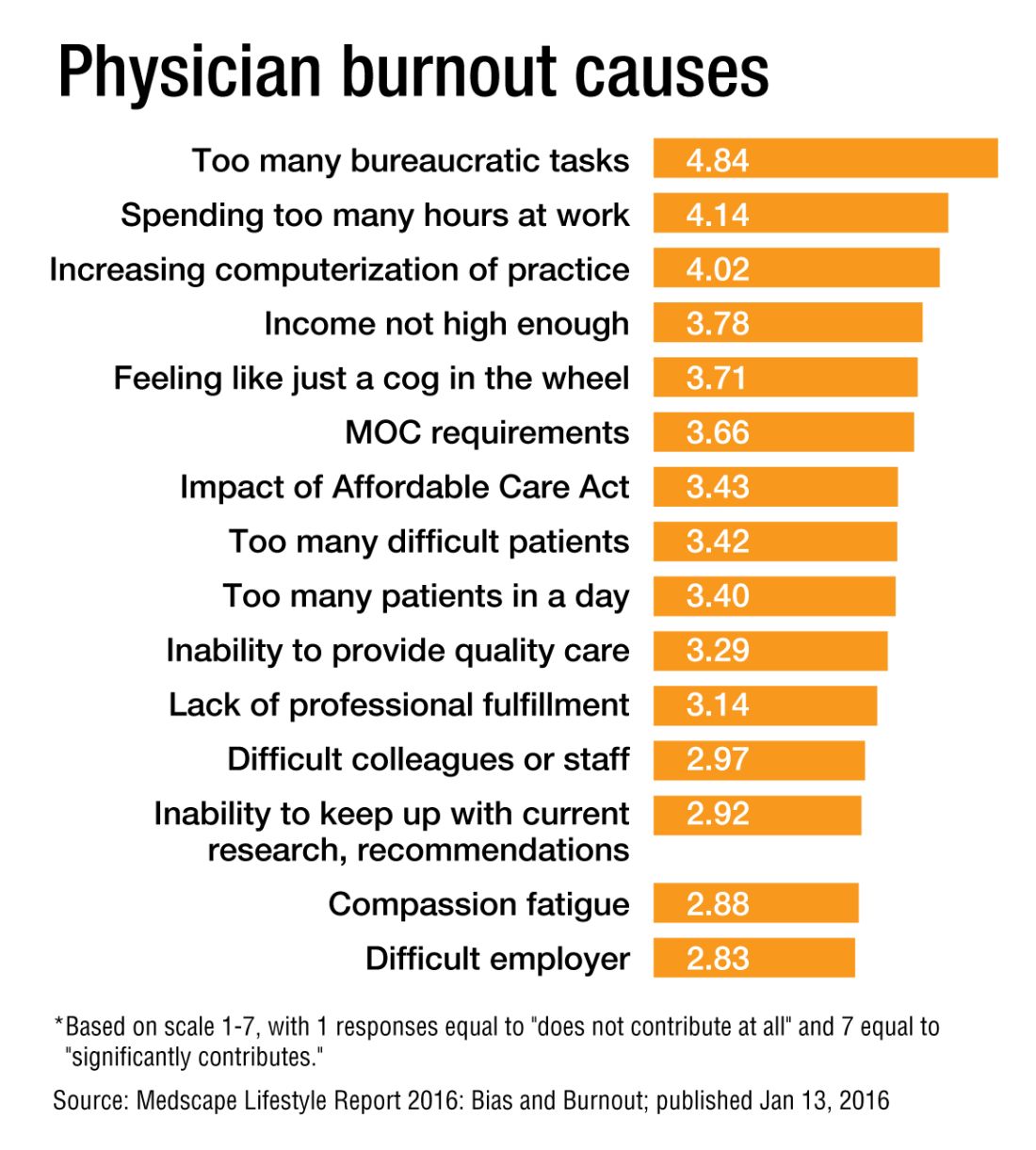
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Eight things hospitalists need to know about post-acute care
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC.
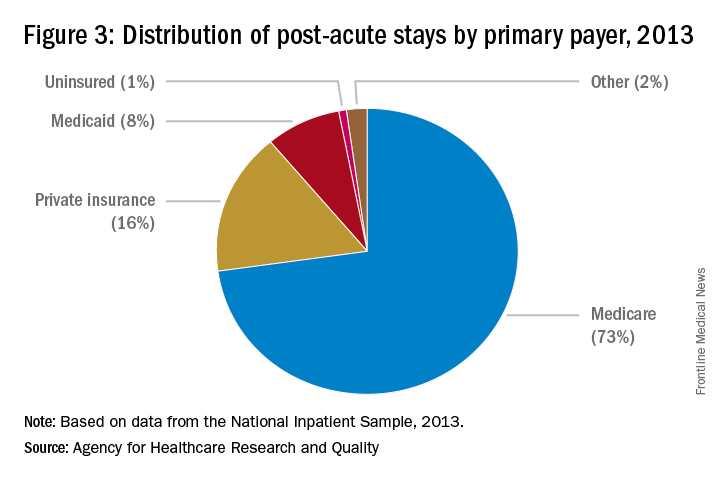
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC.
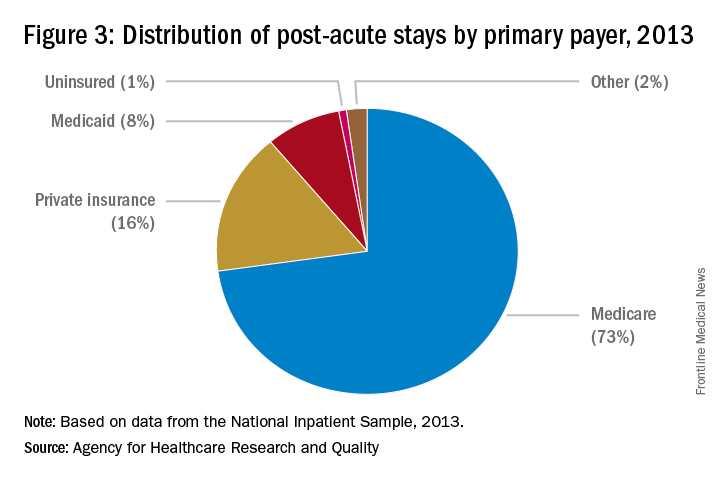
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC.
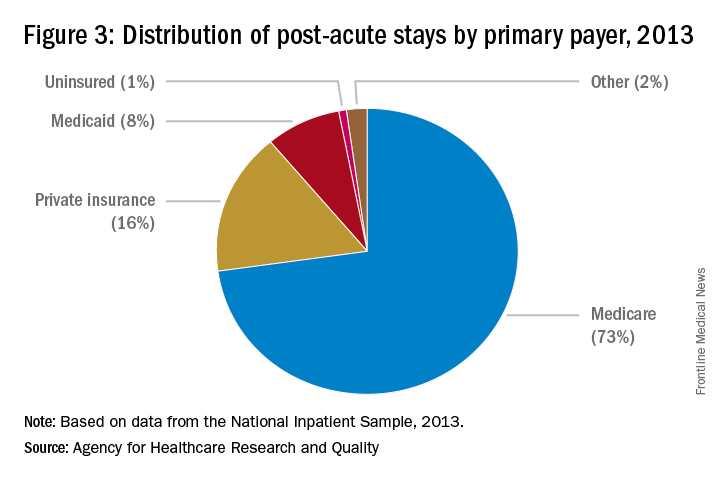
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Female physicians, lower mortality, lower readmissions: A case study
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
VIDEO: Tips & Strategies for the Hospital Medicine Job Search
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel