User login
VTE Pathway Improves Outcomes for Uninsured Patients
A poster presented at HM12 in San Diego last April describes a standardized, systematic, multidisciplinary clinical pathway for treating acute VTE (venous thromboembolism) in an urban hospital serving a high proportion of the uninsured.3 Implementing the pathway in February 2011 “dramatically reduced hospital utilization and cost, particularly among uninsured patients,” who were previously shown to have increased length of stay, cost, and emergency department recidivism, says lead author Gregory Misky, MD, a hospitalist at the University of Colorado Denver.
The pathway—which aimed to standardize all VTE care from hospital presentation to post-discharge follow-up—contained multiple components, including education for staff, enhanced communication processes, written order sets, and a series of formal and informal meetings held with community providers, such as the clinics where these patients get their follow-up primary care. Dr. Misky collaborated with his university’s anticoagulation clinic to help identify primary-care physicians and clinics and arrange follow-up outpatient appointments much sooner than the patients could have obtained by themselves.
The prospective study compared 135 VTE patients presenting to the emergency department or admitted to a medicine service and receiving care under the pathway, compared with 234 VTE patients prior to its introduction. Length of stay dropped to 2.5 days from 4.2, and for uninsured patients it dropped even more, to 2.2 days from 5.5.
Dr. Misky says the data gathered since the San Diego conference “continue to show good results in resource utilization, particularly for the uninsured, with emergency department visits and readmissions slashed.” Readmissions have dropped to 5.2% from 9.8%—and to 3.5% from 11.6% for uninsured VTE patients. He suggests that the clinical pathway approach likely has implications for other diseases as well.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
A poster presented at HM12 in San Diego last April describes a standardized, systematic, multidisciplinary clinical pathway for treating acute VTE (venous thromboembolism) in an urban hospital serving a high proportion of the uninsured.3 Implementing the pathway in February 2011 “dramatically reduced hospital utilization and cost, particularly among uninsured patients,” who were previously shown to have increased length of stay, cost, and emergency department recidivism, says lead author Gregory Misky, MD, a hospitalist at the University of Colorado Denver.
The pathway—which aimed to standardize all VTE care from hospital presentation to post-discharge follow-up—contained multiple components, including education for staff, enhanced communication processes, written order sets, and a series of formal and informal meetings held with community providers, such as the clinics where these patients get their follow-up primary care. Dr. Misky collaborated with his university’s anticoagulation clinic to help identify primary-care physicians and clinics and arrange follow-up outpatient appointments much sooner than the patients could have obtained by themselves.
The prospective study compared 135 VTE patients presenting to the emergency department or admitted to a medicine service and receiving care under the pathway, compared with 234 VTE patients prior to its introduction. Length of stay dropped to 2.5 days from 4.2, and for uninsured patients it dropped even more, to 2.2 days from 5.5.
Dr. Misky says the data gathered since the San Diego conference “continue to show good results in resource utilization, particularly for the uninsured, with emergency department visits and readmissions slashed.” Readmissions have dropped to 5.2% from 9.8%—and to 3.5% from 11.6% for uninsured VTE patients. He suggests that the clinical pathway approach likely has implications for other diseases as well.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
A poster presented at HM12 in San Diego last April describes a standardized, systematic, multidisciplinary clinical pathway for treating acute VTE (venous thromboembolism) in an urban hospital serving a high proportion of the uninsured.3 Implementing the pathway in February 2011 “dramatically reduced hospital utilization and cost, particularly among uninsured patients,” who were previously shown to have increased length of stay, cost, and emergency department recidivism, says lead author Gregory Misky, MD, a hospitalist at the University of Colorado Denver.
The pathway—which aimed to standardize all VTE care from hospital presentation to post-discharge follow-up—contained multiple components, including education for staff, enhanced communication processes, written order sets, and a series of formal and informal meetings held with community providers, such as the clinics where these patients get their follow-up primary care. Dr. Misky collaborated with his university’s anticoagulation clinic to help identify primary-care physicians and clinics and arrange follow-up outpatient appointments much sooner than the patients could have obtained by themselves.
The prospective study compared 135 VTE patients presenting to the emergency department or admitted to a medicine service and receiving care under the pathway, compared with 234 VTE patients prior to its introduction. Length of stay dropped to 2.5 days from 4.2, and for uninsured patients it dropped even more, to 2.2 days from 5.5.
Dr. Misky says the data gathered since the San Diego conference “continue to show good results in resource utilization, particularly for the uninsured, with emergency department visits and readmissions slashed.” Readmissions have dropped to 5.2% from 9.8%—and to 3.5% from 11.6% for uninsured VTE patients. He suggests that the clinical pathway approach likely has implications for other diseases as well.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
ONLINE EXCLUSIVE: How to take the fear out of expanding a hospitalist group
Click here to listen to Brian Hazen, MD, medical director of Inova Fairfax Hospital Group in Fairfax, Va.
Click here to listen to Brian Hazen, MD, medical director of Inova Fairfax Hospital Group in Fairfax, Va.
Click here to listen to Brian Hazen, MD, medical director of Inova Fairfax Hospital Group in Fairfax, Va.
ONLINE EXCLUSIVE: American Pain Society Board Member Discusses Opioid Risks, Rewards, and Why Continuing Education is a Must
Click here to listen to Scott Strassels, PhD, PharmD, BCPS, an assistant professor in the College of Pharmacy at the University of Texas at Austin and a board member of the American Pain Society, discuss the risks and rewards of opioid therapies, and why continuing education is important for all clinicians.
Click here to listen to Scott Strassels, PhD, PharmD, BCPS, an assistant professor in the College of Pharmacy at the University of Texas at Austin and a board member of the American Pain Society, discuss the risks and rewards of opioid therapies, and why continuing education is important for all clinicians.
Click here to listen to Scott Strassels, PhD, PharmD, BCPS, an assistant professor in the College of Pharmacy at the University of Texas at Austin and a board member of the American Pain Society, discuss the risks and rewards of opioid therapies, and why continuing education is important for all clinicians.
How Hospitalists Can Improve the Care of Patients on Opioids
Pain is one of the chief complaints that results in patient admissions to the hospital. Hospitalists inevitably confront pain issues every day, says Joe A. Contreras, MD, FAAHPM, chair of the Pain and Palliative Medicine Institute at Hackensack University Medical Center in Hackensack, N.J. As a result, “it is expected that all physicians who take care of sick people have some baseline knowledge of opioids use,” Dr. Contreras says.
There is a preference on the public’s part and, consequently, from the physician’s perspective to treat pain with opioids, even though minor cases can be controlled without pharmacologic interventions, Dr. Contreras says. Patients might receive some relief from repositioning, hot or cold packs, extra pillows, Reiki therapy, and other soothing modalities. Additionally, hospitals can benefit from having a pain champion on staff to safely manage various situations.
A hospitalist should still obtain important and relevant information when a patient is admitted. This includes the pain medicine the patient is taking and how often, who prescribed it, whether it helps, and if the patient has experienced side effects.
“As the primary-care physician in the hospital,” Dr. Liao says, “the hospitalist is ultimately responsible.”
Special attention is needed during care transitions.
“This is when patients are most vulnerable,” says Beth B. Murinson, MS, MD, PhD, associate professor and director of pain education in the department of neurology at Johns Hopkins University School of Medicine in Baltimore.
These situations occur during transfers from the ED or recovery room to an inpatient unit, and from hospital to home or skilled nursing facility. Patients being discharged must be thoroughly informed about their opioid pain relievers, Dr. Murinson says, with instructions to store them in a secure place. TH
Susan Kreimer is a freelance writer in New York City.
Pain is one of the chief complaints that results in patient admissions to the hospital. Hospitalists inevitably confront pain issues every day, says Joe A. Contreras, MD, FAAHPM, chair of the Pain and Palliative Medicine Institute at Hackensack University Medical Center in Hackensack, N.J. As a result, “it is expected that all physicians who take care of sick people have some baseline knowledge of opioids use,” Dr. Contreras says.
There is a preference on the public’s part and, consequently, from the physician’s perspective to treat pain with opioids, even though minor cases can be controlled without pharmacologic interventions, Dr. Contreras says. Patients might receive some relief from repositioning, hot or cold packs, extra pillows, Reiki therapy, and other soothing modalities. Additionally, hospitals can benefit from having a pain champion on staff to safely manage various situations.
A hospitalist should still obtain important and relevant information when a patient is admitted. This includes the pain medicine the patient is taking and how often, who prescribed it, whether it helps, and if the patient has experienced side effects.
“As the primary-care physician in the hospital,” Dr. Liao says, “the hospitalist is ultimately responsible.”
Special attention is needed during care transitions.
“This is when patients are most vulnerable,” says Beth B. Murinson, MS, MD, PhD, associate professor and director of pain education in the department of neurology at Johns Hopkins University School of Medicine in Baltimore.
These situations occur during transfers from the ED or recovery room to an inpatient unit, and from hospital to home or skilled nursing facility. Patients being discharged must be thoroughly informed about their opioid pain relievers, Dr. Murinson says, with instructions to store them in a secure place. TH
Susan Kreimer is a freelance writer in New York City.
Pain is one of the chief complaints that results in patient admissions to the hospital. Hospitalists inevitably confront pain issues every day, says Joe A. Contreras, MD, FAAHPM, chair of the Pain and Palliative Medicine Institute at Hackensack University Medical Center in Hackensack, N.J. As a result, “it is expected that all physicians who take care of sick people have some baseline knowledge of opioids use,” Dr. Contreras says.
There is a preference on the public’s part and, consequently, from the physician’s perspective to treat pain with opioids, even though minor cases can be controlled without pharmacologic interventions, Dr. Contreras says. Patients might receive some relief from repositioning, hot or cold packs, extra pillows, Reiki therapy, and other soothing modalities. Additionally, hospitals can benefit from having a pain champion on staff to safely manage various situations.
A hospitalist should still obtain important and relevant information when a patient is admitted. This includes the pain medicine the patient is taking and how often, who prescribed it, whether it helps, and if the patient has experienced side effects.
“As the primary-care physician in the hospital,” Dr. Liao says, “the hospitalist is ultimately responsible.”
Special attention is needed during care transitions.
“This is when patients are most vulnerable,” says Beth B. Murinson, MS, MD, PhD, associate professor and director of pain education in the department of neurology at Johns Hopkins University School of Medicine in Baltimore.
These situations occur during transfers from the ED or recovery room to an inpatient unit, and from hospital to home or skilled nursing facility. Patients being discharged must be thoroughly informed about their opioid pain relievers, Dr. Murinson says, with instructions to store them in a secure place. TH
Susan Kreimer is a freelance writer in New York City.
Hospitalists Get Answers to Tough Healthcare Questions
When it comes to Medicare, the Affordable Care Act, and a host of other healthcare-reform-related topics, hospitalists have lots of good questions, such as:
- When does the Physician Value-Based Payment Modifier (VBPM) take effect? And will I be included?
- Which primary-care services are covered by the increased Medicaid payments?
- Are hospitalists eligible to bill for Medicare’s new CPT Transitional Care Management (TCM) codes? (see “New Codes Bridge Billing Gap,”).
Now, SHM’s Public Policy Committee has answered all of the above—and many more—in a set of three “Frequently Asked Questions” documents available at www.hospitalmedicine.org/advocacy. Each document goes in-depth on the most cutting-edge policy issues that are top of mind for hospitalists and the hospitals they serve on these issues:
The Physician Value-Based Payment Modifier (VBPM): The VBPM seeks to connect cost and quality of services in order to begin reimbursement for the value, rather than the quantity, of care. It combines the quality measuring in the Physician Quality Reporting System (PQRS), cost measures, and a payment adjustment for physicians. Measurement begins this year, and many hospitalists will be included.
Medicaid/Medicare parity regulation: On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulations implementing Section 1202 of the Affordable Care Act, which increases Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
New CPT Transitional Care Management (TCM) codes 99495-99496: CMS has created two new CPT Transitional Care Management (TCM) codes designed to improve care coordination and provide better incentives to ensure patients are seen in a physician’s office, rather than be at risk for readmission.
New Action: Getting Involved Just Got Easier
SHM’s Legislative Action Center also makes getting involved easier with a new grassroots outreach tool called Voter Voice. SHM’s first action alert on Voter Voice was sent to members in December. Hospitalists’ willingness to take a few minutes and contact their congressional leaders using Voter Voice increased SHM’s visibility to Congress by nearly five times compared with prior similar alerts.
Getting involved is easy and only takes a few seconds. You can use either your ZIP code to look up your members of Congress or search active legislation by keyword. SHM members can sign up for SHM Legislative Action Center alerts by entering their email address.
To download the new SHM advocacy FAQs or use the improved Legislative Action Center, visit www.hospitalmedicine.org/advocacy.
When it comes to Medicare, the Affordable Care Act, and a host of other healthcare-reform-related topics, hospitalists have lots of good questions, such as:
- When does the Physician Value-Based Payment Modifier (VBPM) take effect? And will I be included?
- Which primary-care services are covered by the increased Medicaid payments?
- Are hospitalists eligible to bill for Medicare’s new CPT Transitional Care Management (TCM) codes? (see “New Codes Bridge Billing Gap,”).
Now, SHM’s Public Policy Committee has answered all of the above—and many more—in a set of three “Frequently Asked Questions” documents available at www.hospitalmedicine.org/advocacy. Each document goes in-depth on the most cutting-edge policy issues that are top of mind for hospitalists and the hospitals they serve on these issues:
The Physician Value-Based Payment Modifier (VBPM): The VBPM seeks to connect cost and quality of services in order to begin reimbursement for the value, rather than the quantity, of care. It combines the quality measuring in the Physician Quality Reporting System (PQRS), cost measures, and a payment adjustment for physicians. Measurement begins this year, and many hospitalists will be included.
Medicaid/Medicare parity regulation: On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulations implementing Section 1202 of the Affordable Care Act, which increases Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
New CPT Transitional Care Management (TCM) codes 99495-99496: CMS has created two new CPT Transitional Care Management (TCM) codes designed to improve care coordination and provide better incentives to ensure patients are seen in a physician’s office, rather than be at risk for readmission.
New Action: Getting Involved Just Got Easier
SHM’s Legislative Action Center also makes getting involved easier with a new grassroots outreach tool called Voter Voice. SHM’s first action alert on Voter Voice was sent to members in December. Hospitalists’ willingness to take a few minutes and contact their congressional leaders using Voter Voice increased SHM’s visibility to Congress by nearly five times compared with prior similar alerts.
Getting involved is easy and only takes a few seconds. You can use either your ZIP code to look up your members of Congress or search active legislation by keyword. SHM members can sign up for SHM Legislative Action Center alerts by entering their email address.
To download the new SHM advocacy FAQs or use the improved Legislative Action Center, visit www.hospitalmedicine.org/advocacy.
When it comes to Medicare, the Affordable Care Act, and a host of other healthcare-reform-related topics, hospitalists have lots of good questions, such as:
- When does the Physician Value-Based Payment Modifier (VBPM) take effect? And will I be included?
- Which primary-care services are covered by the increased Medicaid payments?
- Are hospitalists eligible to bill for Medicare’s new CPT Transitional Care Management (TCM) codes? (see “New Codes Bridge Billing Gap,”).
Now, SHM’s Public Policy Committee has answered all of the above—and many more—in a set of three “Frequently Asked Questions” documents available at www.hospitalmedicine.org/advocacy. Each document goes in-depth on the most cutting-edge policy issues that are top of mind for hospitalists and the hospitals they serve on these issues:
The Physician Value-Based Payment Modifier (VBPM): The VBPM seeks to connect cost and quality of services in order to begin reimbursement for the value, rather than the quantity, of care. It combines the quality measuring in the Physician Quality Reporting System (PQRS), cost measures, and a payment adjustment for physicians. Measurement begins this year, and many hospitalists will be included.
Medicaid/Medicare parity regulation: On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulations implementing Section 1202 of the Affordable Care Act, which increases Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
New CPT Transitional Care Management (TCM) codes 99495-99496: CMS has created two new CPT Transitional Care Management (TCM) codes designed to improve care coordination and provide better incentives to ensure patients are seen in a physician’s office, rather than be at risk for readmission.
New Action: Getting Involved Just Got Easier
SHM’s Legislative Action Center also makes getting involved easier with a new grassroots outreach tool called Voter Voice. SHM’s first action alert on Voter Voice was sent to members in December. Hospitalists’ willingness to take a few minutes and contact their congressional leaders using Voter Voice increased SHM’s visibility to Congress by nearly five times compared with prior similar alerts.
Getting involved is easy and only takes a few seconds. You can use either your ZIP code to look up your members of Congress or search active legislation by keyword. SHM members can sign up for SHM Legislative Action Center alerts by entering their email address.
To download the new SHM advocacy FAQs or use the improved Legislative Action Center, visit www.hospitalmedicine.org/advocacy.
Local Factors Play Major Role in Determining Compensation Rates for Pediatric Hospitalists
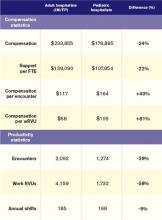
Although pediatricians make up less than 6% of the hospitalists surveyed by the Medical Group Management Association (MGMA), they represent a very different data profile from other specialties reported in SHM’s 2012 State of Hospital Medicine report.
The nonpediatric HM specialties (internal medicine, family medicine, and med/peds) have similar data profiles with regard to productivity and compensation statistics. They are all within 2% of the $233,855 “all adult hospitalists” median compensation. Although there is a bit more variability in the productivity data, all three groups are clustered within 10% of each other. The key to understanding their similarity is that they all serve mostly adult inpatients. While some of these physicians may also care for hospitalized children, I suspect this population is a small proportion of their daily workload.
Pediatric hospitalists only treat pediatric patients and differ significantly from adult hospitalists, as summarized in Table 1.
Pediatricians remain among the lowest-earning specialties nationally, whether in the office or on children’s wards. The key to understanding the differences between adult and pediatric hospitalists is that they derive their compensation and productivity expectations from two separate and distinct physician marketplaces. Adult hospitalists benefit from more than a decade of rapidly growing demand for their services, as well as higher compensation for their office-based counterparts. Meanwhile, the market for pediatric hospitalists remains smaller and more segmented, allowing local factors to drive compensation more than a national demand for their services would.
Pediatric hospitalists appear to earn about a quarter less than their adult counterparts while receiving a similarly lower amount of hospital financial support per provider. Pediatric hospitalists also appear to work less than adult hospitalists, reflected in fewer shifts annually and fewer hours per shift; 75% of adult hospitalist groups report shift lengths of 12 hours or more, compared with 48% of pediatric hospitalist groups. This may stem from the frequent lulls in census common to a community hospital pediatrics service, in contrast to more consistent demand posed by geriatric populations. Although pediatric hospitalists receive more compensation per encounter or wRVU, they cannot generate those encounters or work RVUs at the same clip as adult hospitalists. Pediatricians must hold a family meeting for every single patient, and even something as seemingly simple as obtaining intravenous access might consume 45 minutes of a hospitalist’s time.
Thus, pediatric hospitalists find themselves caught in the same market as other pediatric specialists. These providers remain undervalued compared to virtually all other physicians. Those who seek to improve their financial prospects likely need to work more shifts or generate more workload relative to the expectations of their pediatrician peers.
Personally, I can’t help but wonder what attention pediatric care might enjoy if kids had a vote, a pension, an entitlement program, and a lobby on K Street like their grandparents do.
Dr. Ahlstrom is clinical director of Hospitalists of Northern Michigan and a member of SHM’s Practice Analysis Committee.
Although pediatricians make up less than 6% of the hospitalists surveyed by the Medical Group Management Association (MGMA), they represent a very different data profile from other specialties reported in SHM’s 2012 State of Hospital Medicine report.
The nonpediatric HM specialties (internal medicine, family medicine, and med/peds) have similar data profiles with regard to productivity and compensation statistics. They are all within 2% of the $233,855 “all adult hospitalists” median compensation. Although there is a bit more variability in the productivity data, all three groups are clustered within 10% of each other. The key to understanding their similarity is that they all serve mostly adult inpatients. While some of these physicians may also care for hospitalized children, I suspect this population is a small proportion of their daily workload.
Pediatric hospitalists only treat pediatric patients and differ significantly from adult hospitalists, as summarized in Table 1.
Pediatricians remain among the lowest-earning specialties nationally, whether in the office or on children’s wards. The key to understanding the differences between adult and pediatric hospitalists is that they derive their compensation and productivity expectations from two separate and distinct physician marketplaces. Adult hospitalists benefit from more than a decade of rapidly growing demand for their services, as well as higher compensation for their office-based counterparts. Meanwhile, the market for pediatric hospitalists remains smaller and more segmented, allowing local factors to drive compensation more than a national demand for their services would.
Pediatric hospitalists appear to earn about a quarter less than their adult counterparts while receiving a similarly lower amount of hospital financial support per provider. Pediatric hospitalists also appear to work less than adult hospitalists, reflected in fewer shifts annually and fewer hours per shift; 75% of adult hospitalist groups report shift lengths of 12 hours or more, compared with 48% of pediatric hospitalist groups. This may stem from the frequent lulls in census common to a community hospital pediatrics service, in contrast to more consistent demand posed by geriatric populations. Although pediatric hospitalists receive more compensation per encounter or wRVU, they cannot generate those encounters or work RVUs at the same clip as adult hospitalists. Pediatricians must hold a family meeting for every single patient, and even something as seemingly simple as obtaining intravenous access might consume 45 minutes of a hospitalist’s time.
Thus, pediatric hospitalists find themselves caught in the same market as other pediatric specialists. These providers remain undervalued compared to virtually all other physicians. Those who seek to improve their financial prospects likely need to work more shifts or generate more workload relative to the expectations of their pediatrician peers.
Personally, I can’t help but wonder what attention pediatric care might enjoy if kids had a vote, a pension, an entitlement program, and a lobby on K Street like their grandparents do.
Dr. Ahlstrom is clinical director of Hospitalists of Northern Michigan and a member of SHM’s Practice Analysis Committee.
Although pediatricians make up less than 6% of the hospitalists surveyed by the Medical Group Management Association (MGMA), they represent a very different data profile from other specialties reported in SHM’s 2012 State of Hospital Medicine report.
The nonpediatric HM specialties (internal medicine, family medicine, and med/peds) have similar data profiles with regard to productivity and compensation statistics. They are all within 2% of the $233,855 “all adult hospitalists” median compensation. Although there is a bit more variability in the productivity data, all three groups are clustered within 10% of each other. The key to understanding their similarity is that they all serve mostly adult inpatients. While some of these physicians may also care for hospitalized children, I suspect this population is a small proportion of their daily workload.
Pediatric hospitalists only treat pediatric patients and differ significantly from adult hospitalists, as summarized in Table 1.
Pediatricians remain among the lowest-earning specialties nationally, whether in the office or on children’s wards. The key to understanding the differences between adult and pediatric hospitalists is that they derive their compensation and productivity expectations from two separate and distinct physician marketplaces. Adult hospitalists benefit from more than a decade of rapidly growing demand for their services, as well as higher compensation for their office-based counterparts. Meanwhile, the market for pediatric hospitalists remains smaller and more segmented, allowing local factors to drive compensation more than a national demand for their services would.
Pediatric hospitalists appear to earn about a quarter less than their adult counterparts while receiving a similarly lower amount of hospital financial support per provider. Pediatric hospitalists also appear to work less than adult hospitalists, reflected in fewer shifts annually and fewer hours per shift; 75% of adult hospitalist groups report shift lengths of 12 hours or more, compared with 48% of pediatric hospitalist groups. This may stem from the frequent lulls in census common to a community hospital pediatrics service, in contrast to more consistent demand posed by geriatric populations. Although pediatric hospitalists receive more compensation per encounter or wRVU, they cannot generate those encounters or work RVUs at the same clip as adult hospitalists. Pediatricians must hold a family meeting for every single patient, and even something as seemingly simple as obtaining intravenous access might consume 45 minutes of a hospitalist’s time.
Thus, pediatric hospitalists find themselves caught in the same market as other pediatric specialists. These providers remain undervalued compared to virtually all other physicians. Those who seek to improve their financial prospects likely need to work more shifts or generate more workload relative to the expectations of their pediatrician peers.
Personally, I can’t help but wonder what attention pediatric care might enjoy if kids had a vote, a pension, an entitlement program, and a lobby on K Street like their grandparents do.
Dr. Ahlstrom is clinical director of Hospitalists of Northern Michigan and a member of SHM’s Practice Analysis Committee.
Hospitalists to Unveil Patient Care Recommendations As Part of Choosing Wisely Campaign
This month, hospitalists will be a vital part of Choosing Wisely, an important public initiative from the American Board of Internal Medicine (ABIM) Foundation that identifies treatments and procedures that might be overused by caregivers.
On Feb. 21 in Washington, D.C., the ABIM Foundation, SHM, and more than a dozen other medical specialties will announce recommendations that, in the ABIM Foundation’s words, “represent specific, evidence-based recommendations physicians and patients should discuss to help make wise decisions about the most appropriate care based on their individual situation.” Hospitalists who helped SHM develop its recommendations will be in attendance to help field questions about SHM’s work with Choosing Wisely and its lists.
SHM has developed two lists of recommendations: one for adult HM and another for pediatric HM. SHM will make a special announcement Feb. 21 in The Hospitalist eWire with both lists and commentary for how hospitalists can have informed conversations with their patients about the lists. The Hospitalist will follow up with a feature story and other information about Choosing Wisely in its March issue.
As part of the campaign, the ABIM Foundation, SHM, and consumer magazine Consumer Reports have teamed up to develop material specifically designed to educate patients about the Choosing Wisely recommendations. Materials will be available on the ABIM Foundation and SHM websites.
SHM will continue the conversation about high-value care and working with patients to make wise decisions well beyond February and March. At HM13, SHM’s annual meeting in Washington, D.C., SHM will offer a pre-course on Choosing Wisely and its philosophy. The pre-course is May 16, the day before the official start of HM13.
For more information about Choosing Wisely, visit www.choosingwisely.org. To register for the Choosing Wisely pre-course at HM13, visit www.hospitalmedicine2013.org.
This month, hospitalists will be a vital part of Choosing Wisely, an important public initiative from the American Board of Internal Medicine (ABIM) Foundation that identifies treatments and procedures that might be overused by caregivers.
On Feb. 21 in Washington, D.C., the ABIM Foundation, SHM, and more than a dozen other medical specialties will announce recommendations that, in the ABIM Foundation’s words, “represent specific, evidence-based recommendations physicians and patients should discuss to help make wise decisions about the most appropriate care based on their individual situation.” Hospitalists who helped SHM develop its recommendations will be in attendance to help field questions about SHM’s work with Choosing Wisely and its lists.
SHM has developed two lists of recommendations: one for adult HM and another for pediatric HM. SHM will make a special announcement Feb. 21 in The Hospitalist eWire with both lists and commentary for how hospitalists can have informed conversations with their patients about the lists. The Hospitalist will follow up with a feature story and other information about Choosing Wisely in its March issue.
As part of the campaign, the ABIM Foundation, SHM, and consumer magazine Consumer Reports have teamed up to develop material specifically designed to educate patients about the Choosing Wisely recommendations. Materials will be available on the ABIM Foundation and SHM websites.
SHM will continue the conversation about high-value care and working with patients to make wise decisions well beyond February and March. At HM13, SHM’s annual meeting in Washington, D.C., SHM will offer a pre-course on Choosing Wisely and its philosophy. The pre-course is May 16, the day before the official start of HM13.
For more information about Choosing Wisely, visit www.choosingwisely.org. To register for the Choosing Wisely pre-course at HM13, visit www.hospitalmedicine2013.org.
This month, hospitalists will be a vital part of Choosing Wisely, an important public initiative from the American Board of Internal Medicine (ABIM) Foundation that identifies treatments and procedures that might be overused by caregivers.
On Feb. 21 in Washington, D.C., the ABIM Foundation, SHM, and more than a dozen other medical specialties will announce recommendations that, in the ABIM Foundation’s words, “represent specific, evidence-based recommendations physicians and patients should discuss to help make wise decisions about the most appropriate care based on their individual situation.” Hospitalists who helped SHM develop its recommendations will be in attendance to help field questions about SHM’s work with Choosing Wisely and its lists.
SHM has developed two lists of recommendations: one for adult HM and another for pediatric HM. SHM will make a special announcement Feb. 21 in The Hospitalist eWire with both lists and commentary for how hospitalists can have informed conversations with their patients about the lists. The Hospitalist will follow up with a feature story and other information about Choosing Wisely in its March issue.
As part of the campaign, the ABIM Foundation, SHM, and consumer magazine Consumer Reports have teamed up to develop material specifically designed to educate patients about the Choosing Wisely recommendations. Materials will be available on the ABIM Foundation and SHM websites.
SHM will continue the conversation about high-value care and working with patients to make wise decisions well beyond February and March. At HM13, SHM’s annual meeting in Washington, D.C., SHM will offer a pre-course on Choosing Wisely and its philosophy. The pre-course is May 16, the day before the official start of HM13.
For more information about Choosing Wisely, visit www.choosingwisely.org. To register for the Choosing Wisely pre-course at HM13, visit www.hospitalmedicine2013.org.
Hospitalist Rajan Gurunathan, MD, Stresses Commitment and Community
Rajan Gurunathan, MD, was an undergraduate student at Johns Hopkins University in Baltimore in the early 1990s weighing his career options.
“I went through a lot of permutations, actually,” he says. “Scientist, clinical researcher, doctor, physician/scientist—all of those things entered my mind at some point.”
He applied to dual-track MD and PhD programs, but ultimately decided that interacting with people—patients in particular—was the goal for him. He earned his medical degree from UMDNJ-Robert Wood Johnson Medical School in Camden, N.J., and completed his internship in the department of medicine at St. Luke’s-Roosevelt Hospital Center in New York City, not far from where he grew up as a child in northern New Jersey.
And he never left.

—Anthony Back, MD, professor of medicine, University of Washington, Seattle
Dr. Gurunathan has risen through the ranks at St. Luke’s-Roosevelt, from resident to chief resident to chief of the section of hospital medicine. He is a faculty member for the Clinical Quality Fellowship Program at the Great New York Hospital Association and an assistant clinical professor of medicine at Columbia University College of Physicians and Surgeons in New York.
His long tenure at St. Luke’s-Roosevelt has been “an incredible experience because I really get a sense and feeling of commitment from the community,” he adds. “I’ve seen it grow over time and see how the needs have changed and how the service the hospital has been able to provide has only grown over time.”
After several years of presenting posters at SHM’s annual meetings, Dr. Gurunathan joined Team Hospitalist in April 2012 to become an even more active member of his specialty.
QUESTION: When you started as an intern 15 years ago, did you expect that you’d still be at the same institution?
Answer: No, I wouldn’t have expected that at all. In fact, there was a time where I was briefly considering a general medicine fellowship at Johns Hopkins, and I was prepared to go there. And family circumstances, etc., made me decide not to move on and to make a commitment and join the department as faculty, first as a chief and then as faculty. And I was really lucky to have those opportunities, because while my course didn’t go exactly the way that I’d planned, I wouldn’t have changed a thing.
Q: When you now deal with the residents and younger staff members, what’s that experience like for you?
A: It’s a really neat experience, and often brings a chuckle to my face when I see that they’re frustrated about the same things, because I can certainly commiserate. But I can really also see the value of what they provide every day, and having been in their shoes, I know a little bit about what they’ve been through and the work that they do. So I have a real appreciation for that.
Q: What brought you to hospital medicine?
A: I’ve always enjoyed the collegiality of a hospital environment in terms of multiple disciplines working together in ways to help care for patients. It’s a paradox in the sense that it’s fascinating to see disease and be able to be impactful in that way, but it’s also unfortunate sometimes to see what people have to go through.
Q: Is there something specific about the setting that’s kept you in the academic world?
A: A lot of things, actually. As I mentioned, hospitals in general should have a collegial nature. Again, it’s a really nice place where people share a unique common goal of banding together and fighting a goal, and academic departments are the same. So it’s being with people with like-minded intellectual interests. And we’re fortunate enough to have a number of strong mentors within the department who have had a lot of clinical training and bring a lot of experience and a wealth of knowledge, and being able to utilize their experience and draw from their experiences only makes people better clinicians. And we’re fortunate enough to have a pretty supportive department in general where there is a lot of collegiality and camaraderie.
Q: As an administrator, what is the value of being an SHM member, to you?
A: I think what I’ve seen administratively is the changing face of healthcare and how hospitals are going to need to continue to transform with time due to things that are both regulatory- and quality-of-care-based, in terms of improving outcomes and keeping people healthy. SHM has really embraced [those changes] and taken them head-on for really important reasons, not only in terms of helping people adapt to the changing landscape, but also training them in the ways that we need to be thinking about problems now and in the future.
Q: You’ve attended multiple annual meetings and presented posters. What value have you taken out of them, and would you recommend the experience to others?
A: Absolutely. I think as people develop, it’s good to always learn new skills, and my clinical research is an area that I would actually like to build up. So I’ve had a little bit of exposure, and it’s been nice to be able to draw from the resources of SHM and be able to partake. We presented something last year, which was a really neat experience, and we’re looking to bring some new faculty this year and encourage them to get involved in the scholarship process. These are the kinds of things that can really help hone skills, and that’s a good thing.
Q: Once you’re inside the doors of a New York City hospital, is daily practice much different than anywhere else?
A: I would say yes and no. I would say no in that I think all hospitals are really neat places and really incredible places. I heard somebody say once at a talk that hospitals were places of refuge, and I really do believe that. That being said, I think there is something slightly unique about New York City in a lot of ways. Certainly the challenges that New York City hospitals face are somewhat unique in terms of patient population, difficulty in socioeconomic factors, insurance issues. I think they are really fun places to work, but they’re not for the faint of heart.
Richard Quinn is a freelance writer in New Jersey.
Rajan Gurunathan, MD, was an undergraduate student at Johns Hopkins University in Baltimore in the early 1990s weighing his career options.
“I went through a lot of permutations, actually,” he says. “Scientist, clinical researcher, doctor, physician/scientist—all of those things entered my mind at some point.”
He applied to dual-track MD and PhD programs, but ultimately decided that interacting with people—patients in particular—was the goal for him. He earned his medical degree from UMDNJ-Robert Wood Johnson Medical School in Camden, N.J., and completed his internship in the department of medicine at St. Luke’s-Roosevelt Hospital Center in New York City, not far from where he grew up as a child in northern New Jersey.
And he never left.

—Anthony Back, MD, professor of medicine, University of Washington, Seattle
Dr. Gurunathan has risen through the ranks at St. Luke’s-Roosevelt, from resident to chief resident to chief of the section of hospital medicine. He is a faculty member for the Clinical Quality Fellowship Program at the Great New York Hospital Association and an assistant clinical professor of medicine at Columbia University College of Physicians and Surgeons in New York.
His long tenure at St. Luke’s-Roosevelt has been “an incredible experience because I really get a sense and feeling of commitment from the community,” he adds. “I’ve seen it grow over time and see how the needs have changed and how the service the hospital has been able to provide has only grown over time.”
After several years of presenting posters at SHM’s annual meetings, Dr. Gurunathan joined Team Hospitalist in April 2012 to become an even more active member of his specialty.
QUESTION: When you started as an intern 15 years ago, did you expect that you’d still be at the same institution?
Answer: No, I wouldn’t have expected that at all. In fact, there was a time where I was briefly considering a general medicine fellowship at Johns Hopkins, and I was prepared to go there. And family circumstances, etc., made me decide not to move on and to make a commitment and join the department as faculty, first as a chief and then as faculty. And I was really lucky to have those opportunities, because while my course didn’t go exactly the way that I’d planned, I wouldn’t have changed a thing.
Q: When you now deal with the residents and younger staff members, what’s that experience like for you?
A: It’s a really neat experience, and often brings a chuckle to my face when I see that they’re frustrated about the same things, because I can certainly commiserate. But I can really also see the value of what they provide every day, and having been in their shoes, I know a little bit about what they’ve been through and the work that they do. So I have a real appreciation for that.
Q: What brought you to hospital medicine?
A: I’ve always enjoyed the collegiality of a hospital environment in terms of multiple disciplines working together in ways to help care for patients. It’s a paradox in the sense that it’s fascinating to see disease and be able to be impactful in that way, but it’s also unfortunate sometimes to see what people have to go through.
Q: Is there something specific about the setting that’s kept you in the academic world?
A: A lot of things, actually. As I mentioned, hospitals in general should have a collegial nature. Again, it’s a really nice place where people share a unique common goal of banding together and fighting a goal, and academic departments are the same. So it’s being with people with like-minded intellectual interests. And we’re fortunate enough to have a number of strong mentors within the department who have had a lot of clinical training and bring a lot of experience and a wealth of knowledge, and being able to utilize their experience and draw from their experiences only makes people better clinicians. And we’re fortunate enough to have a pretty supportive department in general where there is a lot of collegiality and camaraderie.
Q: As an administrator, what is the value of being an SHM member, to you?
A: I think what I’ve seen administratively is the changing face of healthcare and how hospitals are going to need to continue to transform with time due to things that are both regulatory- and quality-of-care-based, in terms of improving outcomes and keeping people healthy. SHM has really embraced [those changes] and taken them head-on for really important reasons, not only in terms of helping people adapt to the changing landscape, but also training them in the ways that we need to be thinking about problems now and in the future.
Q: You’ve attended multiple annual meetings and presented posters. What value have you taken out of them, and would you recommend the experience to others?
A: Absolutely. I think as people develop, it’s good to always learn new skills, and my clinical research is an area that I would actually like to build up. So I’ve had a little bit of exposure, and it’s been nice to be able to draw from the resources of SHM and be able to partake. We presented something last year, which was a really neat experience, and we’re looking to bring some new faculty this year and encourage them to get involved in the scholarship process. These are the kinds of things that can really help hone skills, and that’s a good thing.
Q: Once you’re inside the doors of a New York City hospital, is daily practice much different than anywhere else?
A: I would say yes and no. I would say no in that I think all hospitals are really neat places and really incredible places. I heard somebody say once at a talk that hospitals were places of refuge, and I really do believe that. That being said, I think there is something slightly unique about New York City in a lot of ways. Certainly the challenges that New York City hospitals face are somewhat unique in terms of patient population, difficulty in socioeconomic factors, insurance issues. I think they are really fun places to work, but they’re not for the faint of heart.
Richard Quinn is a freelance writer in New Jersey.
Rajan Gurunathan, MD, was an undergraduate student at Johns Hopkins University in Baltimore in the early 1990s weighing his career options.
“I went through a lot of permutations, actually,” he says. “Scientist, clinical researcher, doctor, physician/scientist—all of those things entered my mind at some point.”
He applied to dual-track MD and PhD programs, but ultimately decided that interacting with people—patients in particular—was the goal for him. He earned his medical degree from UMDNJ-Robert Wood Johnson Medical School in Camden, N.J., and completed his internship in the department of medicine at St. Luke’s-Roosevelt Hospital Center in New York City, not far from where he grew up as a child in northern New Jersey.
And he never left.

—Anthony Back, MD, professor of medicine, University of Washington, Seattle
Dr. Gurunathan has risen through the ranks at St. Luke’s-Roosevelt, from resident to chief resident to chief of the section of hospital medicine. He is a faculty member for the Clinical Quality Fellowship Program at the Great New York Hospital Association and an assistant clinical professor of medicine at Columbia University College of Physicians and Surgeons in New York.
His long tenure at St. Luke’s-Roosevelt has been “an incredible experience because I really get a sense and feeling of commitment from the community,” he adds. “I’ve seen it grow over time and see how the needs have changed and how the service the hospital has been able to provide has only grown over time.”
After several years of presenting posters at SHM’s annual meetings, Dr. Gurunathan joined Team Hospitalist in April 2012 to become an even more active member of his specialty.
QUESTION: When you started as an intern 15 years ago, did you expect that you’d still be at the same institution?
Answer: No, I wouldn’t have expected that at all. In fact, there was a time where I was briefly considering a general medicine fellowship at Johns Hopkins, and I was prepared to go there. And family circumstances, etc., made me decide not to move on and to make a commitment and join the department as faculty, first as a chief and then as faculty. And I was really lucky to have those opportunities, because while my course didn’t go exactly the way that I’d planned, I wouldn’t have changed a thing.
Q: When you now deal with the residents and younger staff members, what’s that experience like for you?
A: It’s a really neat experience, and often brings a chuckle to my face when I see that they’re frustrated about the same things, because I can certainly commiserate. But I can really also see the value of what they provide every day, and having been in their shoes, I know a little bit about what they’ve been through and the work that they do. So I have a real appreciation for that.
Q: What brought you to hospital medicine?
A: I’ve always enjoyed the collegiality of a hospital environment in terms of multiple disciplines working together in ways to help care for patients. It’s a paradox in the sense that it’s fascinating to see disease and be able to be impactful in that way, but it’s also unfortunate sometimes to see what people have to go through.
Q: Is there something specific about the setting that’s kept you in the academic world?
A: A lot of things, actually. As I mentioned, hospitals in general should have a collegial nature. Again, it’s a really nice place where people share a unique common goal of banding together and fighting a goal, and academic departments are the same. So it’s being with people with like-minded intellectual interests. And we’re fortunate enough to have a number of strong mentors within the department who have had a lot of clinical training and bring a lot of experience and a wealth of knowledge, and being able to utilize their experience and draw from their experiences only makes people better clinicians. And we’re fortunate enough to have a pretty supportive department in general where there is a lot of collegiality and camaraderie.
Q: As an administrator, what is the value of being an SHM member, to you?
A: I think what I’ve seen administratively is the changing face of healthcare and how hospitals are going to need to continue to transform with time due to things that are both regulatory- and quality-of-care-based, in terms of improving outcomes and keeping people healthy. SHM has really embraced [those changes] and taken them head-on for really important reasons, not only in terms of helping people adapt to the changing landscape, but also training them in the ways that we need to be thinking about problems now and in the future.
Q: You’ve attended multiple annual meetings and presented posters. What value have you taken out of them, and would you recommend the experience to others?
A: Absolutely. I think as people develop, it’s good to always learn new skills, and my clinical research is an area that I would actually like to build up. So I’ve had a little bit of exposure, and it’s been nice to be able to draw from the resources of SHM and be able to partake. We presented something last year, which was a really neat experience, and we’re looking to bring some new faculty this year and encourage them to get involved in the scholarship process. These are the kinds of things that can really help hone skills, and that’s a good thing.
Q: Once you’re inside the doors of a New York City hospital, is daily practice much different than anywhere else?
A: I would say yes and no. I would say no in that I think all hospitals are really neat places and really incredible places. I heard somebody say once at a talk that hospitals were places of refuge, and I really do believe that. That being said, I think there is something slightly unique about New York City in a lot of ways. Certainly the challenges that New York City hospitals face are somewhat unique in terms of patient population, difficulty in socioeconomic factors, insurance issues. I think they are really fun places to work, but they’re not for the faint of heart.
Richard Quinn is a freelance writer in New Jersey.
Hospitalists Spared Reduced Medicare Reimbursement Rates … For Now
The short-term compromise congressional leaders reached earlier this month on Draconian cuts to Medicare payments can only be viewed as a good thing for hospital medicine, says the head of SHM's Public Policy Committee. However, the fight is far from over.
"Just like everything else they've been doing, they're kicking the can down the road,” says committee chair Ron Greeno, MD, FCCP, MHM. "At least they kicked it a year this time, so that gives us a little bit of breathing room in terms of our physician practices being able to plan."
The American Taxpayer Relief Act of 2012 averts a 26.5% cut to Medicare payment rates and extends the current Medicare physician fee schedule through the end of this year. The downside is the one-year delay is to be paid for "largely through adjustments to payments for hospitals and non-physician providers, and reductions in Medicaid disproportionate share hospital payments," according to a report from SHM issued earlier this month.
Dr. Greeno agrees that by reducing hospital revenue, the compromise puts additional fiscal pressures on HM groups, but that is the reality of the political logjam in Washington. Still, SHM will continue to lobby for a long-term answer.
The decision has drawn criticism from hospital trade associations. Chip Kahn, president and CEO of the Federation of American Hospitals (FAH), described it as a plan to "rob hospital Peter to pay for fiscal cliff Paul." [PDF]
"This is all just another patch," Dr. Greeno says, "and it doesn't create the solution that everybody is looking for, which is basically repeal of the SGR and replacing it with something that creates the incentives needed to engage physicians in improving the healthcare system."
The compromise also does not address the budget sequester, which was delayed until the end of March. Without action on that front, SHM says providers will lose 2% from their Medicare payments. The sequestration also would reduce funding dedicated to medical research.
Visit our website for more information about efforts to repeal the SGR.
The short-term compromise congressional leaders reached earlier this month on Draconian cuts to Medicare payments can only be viewed as a good thing for hospital medicine, says the head of SHM's Public Policy Committee. However, the fight is far from over.
"Just like everything else they've been doing, they're kicking the can down the road,” says committee chair Ron Greeno, MD, FCCP, MHM. "At least they kicked it a year this time, so that gives us a little bit of breathing room in terms of our physician practices being able to plan."
The American Taxpayer Relief Act of 2012 averts a 26.5% cut to Medicare payment rates and extends the current Medicare physician fee schedule through the end of this year. The downside is the one-year delay is to be paid for "largely through adjustments to payments for hospitals and non-physician providers, and reductions in Medicaid disproportionate share hospital payments," according to a report from SHM issued earlier this month.
Dr. Greeno agrees that by reducing hospital revenue, the compromise puts additional fiscal pressures on HM groups, but that is the reality of the political logjam in Washington. Still, SHM will continue to lobby for a long-term answer.
The decision has drawn criticism from hospital trade associations. Chip Kahn, president and CEO of the Federation of American Hospitals (FAH), described it as a plan to "rob hospital Peter to pay for fiscal cliff Paul." [PDF]
"This is all just another patch," Dr. Greeno says, "and it doesn't create the solution that everybody is looking for, which is basically repeal of the SGR and replacing it with something that creates the incentives needed to engage physicians in improving the healthcare system."
The compromise also does not address the budget sequester, which was delayed until the end of March. Without action on that front, SHM says providers will lose 2% from their Medicare payments. The sequestration also would reduce funding dedicated to medical research.
Visit our website for more information about efforts to repeal the SGR.
The short-term compromise congressional leaders reached earlier this month on Draconian cuts to Medicare payments can only be viewed as a good thing for hospital medicine, says the head of SHM's Public Policy Committee. However, the fight is far from over.
"Just like everything else they've been doing, they're kicking the can down the road,” says committee chair Ron Greeno, MD, FCCP, MHM. "At least they kicked it a year this time, so that gives us a little bit of breathing room in terms of our physician practices being able to plan."
The American Taxpayer Relief Act of 2012 averts a 26.5% cut to Medicare payment rates and extends the current Medicare physician fee schedule through the end of this year. The downside is the one-year delay is to be paid for "largely through adjustments to payments for hospitals and non-physician providers, and reductions in Medicaid disproportionate share hospital payments," according to a report from SHM issued earlier this month.
Dr. Greeno agrees that by reducing hospital revenue, the compromise puts additional fiscal pressures on HM groups, but that is the reality of the political logjam in Washington. Still, SHM will continue to lobby for a long-term answer.
The decision has drawn criticism from hospital trade associations. Chip Kahn, president and CEO of the Federation of American Hospitals (FAH), described it as a plan to "rob hospital Peter to pay for fiscal cliff Paul." [PDF]
"This is all just another patch," Dr. Greeno says, "and it doesn't create the solution that everybody is looking for, which is basically repeal of the SGR and replacing it with something that creates the incentives needed to engage physicians in improving the healthcare system."
The compromise also does not address the budget sequester, which was delayed until the end of March. Without action on that front, SHM says providers will lose 2% from their Medicare payments. The sequestration also would reduce funding dedicated to medical research.
Visit our website for more information about efforts to repeal the SGR.
In the Literature: Research You Need to Know
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.