User login
Bill by Time Spent on Case
In my recent columns, I addressed documentation guidelines with respect to the three key components: history, exam, and medical decision-making. However, time is considered the fourth key component.
Time-based billing places significant emphasis on the duration of the hospitalist-patient encounter more so than the detail or quality of the documentation. This month, I’ll focus on the guidelines for reporting inpatient hospital services based on time.
Counseling, Coordination
Hospitalists try to make their rounds as efficient as possible while still upholding a high standard of care. It is not unusual for a patient encounter to vary from the norm of updating the history, performing the necessary exam, and implementing the plan.
In fact, hospitalists often counsel patients with newly diagnosed conditions or when treatment options seem extensive and complicated. Based on these circumstances, physicians can document only a brief history and exam or none at all, since the bulk of the encounter focuses on medical decision-making, counseling, and coordination of care. Despite the minimal documentation compared with other physician services, it still is possible to report something more than the lowest service level (e.g., subsequent hospital care, 99231).
To use time as the determining factor for the visit level, more than 50% of the total visit time must involve counseling/coordination of care. The total visit time encompasses both the face-to-face time spent with the patient at the bedside and the additional time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers. Physicians providing care in academic settings cannot contribute teaching time toward the total visit time. Further, only the attending physician’s time counts.
Documentation
Hospitalists must document events during the patient encounter. There may be little or no history and an exam and counseling may dominate the entire visit.
Physicians must document both the counseling/coordination of care time and total visit time. The format may vary: “Total visit time = 25 minutes; more than 50% spent counseling/coordinating care,” or “20 of 25 minutes spent counseling/coordinating care.” Any given payer may prefer one documentation style over another. It always is best to query payers and review their documentation standards to determine the local preference.
In addition to the time, physicians must document the medical decision-making and details of the counseling/coordination of care. For example, patients with newly diagnosed diabetes need to be educated about their condition, lifestyle, and medication requirements. Physicians should include information regarding these factors in their progress notes as necessary.
Family Discussions
As noted in my previous article on critical care services (March 2008, p. 18), family discussions can contribute toward counseling/coordination of care time when:
- The patient is unable or clinically incompetent to participate in discussions;
- Time is spent on the unit/floor with family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; or
- The conversation bears directly on the management of the patient.
Prolonged Care
A physician makes his rounds in the morning. He cares for a 72-year-old female with diabetes, end-stage renal disease, and hypertension. In the afternoon, he returns to find the family waiting with questions. He spends an additional 30 minutes speaking at the bedside with the patient and family. The additional afternoon effort may be captured as prolonged care if both services are documented appropriately.
For inpatient services, CPT defines code 99356 as the first hour of prolonged physician services requiring face-to-face patient contact beyond the usual services (reportable after the initial 30 minutes). Code 99357 is used for each additional 30 minutes of prolonged care beyond the first hour (reportable after the first 15 minutes of each additional segment). Both codes are considered add-on codes and cannot be reported alone on a claim form; a primary code must be reported. Code 99357 must be used with 99356, and 99356 must be reported with one of the following inpatient service [primary] codes: 99221-99223, 99231-99233, or 99251-99255.
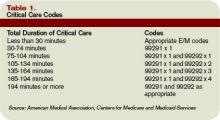
Prolonged care employs the concept of threshold time. This means total face-to-face physician visit time must exceed the time requirements associated with the primary codes by 30 minutes (e.g., 99232 plus 99356 = 25 minutes plus 30 minutes = 55 total face-to-face attending visit minutes). Accordingly, the physician must document the total face-to-face time spent during each portion of care in two separate notes or in one cumulative note. Be aware that this varies from the standard reporting of counseling and/or coordination of care time in that the physician must meet the threshold face-to-face-time requirements (see Table 1, left), making prolonged care services inefficient. When two providers from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service. To reiterate, 99356 must be reported on the same invoice as the primary visit code (e.g., 99232). Be sure once again to query payers, because most non-Medicare insurers do not recognize these codes. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
In my recent columns, I addressed documentation guidelines with respect to the three key components: history, exam, and medical decision-making. However, time is considered the fourth key component.
Time-based billing places significant emphasis on the duration of the hospitalist-patient encounter more so than the detail or quality of the documentation. This month, I’ll focus on the guidelines for reporting inpatient hospital services based on time.
Counseling, Coordination
Hospitalists try to make their rounds as efficient as possible while still upholding a high standard of care. It is not unusual for a patient encounter to vary from the norm of updating the history, performing the necessary exam, and implementing the plan.
In fact, hospitalists often counsel patients with newly diagnosed conditions or when treatment options seem extensive and complicated. Based on these circumstances, physicians can document only a brief history and exam or none at all, since the bulk of the encounter focuses on medical decision-making, counseling, and coordination of care. Despite the minimal documentation compared with other physician services, it still is possible to report something more than the lowest service level (e.g., subsequent hospital care, 99231).
To use time as the determining factor for the visit level, more than 50% of the total visit time must involve counseling/coordination of care. The total visit time encompasses both the face-to-face time spent with the patient at the bedside and the additional time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers. Physicians providing care in academic settings cannot contribute teaching time toward the total visit time. Further, only the attending physician’s time counts.
Documentation
Hospitalists must document events during the patient encounter. There may be little or no history and an exam and counseling may dominate the entire visit.
Physicians must document both the counseling/coordination of care time and total visit time. The format may vary: “Total visit time = 25 minutes; more than 50% spent counseling/coordinating care,” or “20 of 25 minutes spent counseling/coordinating care.” Any given payer may prefer one documentation style over another. It always is best to query payers and review their documentation standards to determine the local preference.
In addition to the time, physicians must document the medical decision-making and details of the counseling/coordination of care. For example, patients with newly diagnosed diabetes need to be educated about their condition, lifestyle, and medication requirements. Physicians should include information regarding these factors in their progress notes as necessary.
Family Discussions
As noted in my previous article on critical care services (March 2008, p. 18), family discussions can contribute toward counseling/coordination of care time when:
- The patient is unable or clinically incompetent to participate in discussions;
- Time is spent on the unit/floor with family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; or
- The conversation bears directly on the management of the patient.
Prolonged Care
A physician makes his rounds in the morning. He cares for a 72-year-old female with diabetes, end-stage renal disease, and hypertension. In the afternoon, he returns to find the family waiting with questions. He spends an additional 30 minutes speaking at the bedside with the patient and family. The additional afternoon effort may be captured as prolonged care if both services are documented appropriately.
For inpatient services, CPT defines code 99356 as the first hour of prolonged physician services requiring face-to-face patient contact beyond the usual services (reportable after the initial 30 minutes). Code 99357 is used for each additional 30 minutes of prolonged care beyond the first hour (reportable after the first 15 minutes of each additional segment). Both codes are considered add-on codes and cannot be reported alone on a claim form; a primary code must be reported. Code 99357 must be used with 99356, and 99356 must be reported with one of the following inpatient service [primary] codes: 99221-99223, 99231-99233, or 99251-99255.
Prolonged care employs the concept of threshold time. This means total face-to-face physician visit time must exceed the time requirements associated with the primary codes by 30 minutes (e.g., 99232 plus 99356 = 25 minutes plus 30 minutes = 55 total face-to-face attending visit minutes). Accordingly, the physician must document the total face-to-face time spent during each portion of care in two separate notes or in one cumulative note. Be aware that this varies from the standard reporting of counseling and/or coordination of care time in that the physician must meet the threshold face-to-face-time requirements (see Table 1, left), making prolonged care services inefficient. When two providers from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service. To reiterate, 99356 must be reported on the same invoice as the primary visit code (e.g., 99232). Be sure once again to query payers, because most non-Medicare insurers do not recognize these codes. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
In my recent columns, I addressed documentation guidelines with respect to the three key components: history, exam, and medical decision-making. However, time is considered the fourth key component.
Time-based billing places significant emphasis on the duration of the hospitalist-patient encounter more so than the detail or quality of the documentation. This month, I’ll focus on the guidelines for reporting inpatient hospital services based on time.
Counseling, Coordination
Hospitalists try to make their rounds as efficient as possible while still upholding a high standard of care. It is not unusual for a patient encounter to vary from the norm of updating the history, performing the necessary exam, and implementing the plan.
In fact, hospitalists often counsel patients with newly diagnosed conditions or when treatment options seem extensive and complicated. Based on these circumstances, physicians can document only a brief history and exam or none at all, since the bulk of the encounter focuses on medical decision-making, counseling, and coordination of care. Despite the minimal documentation compared with other physician services, it still is possible to report something more than the lowest service level (e.g., subsequent hospital care, 99231).
To use time as the determining factor for the visit level, more than 50% of the total visit time must involve counseling/coordination of care. The total visit time encompasses both the face-to-face time spent with the patient at the bedside and the additional time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers. Physicians providing care in academic settings cannot contribute teaching time toward the total visit time. Further, only the attending physician’s time counts.
Documentation
Hospitalists must document events during the patient encounter. There may be little or no history and an exam and counseling may dominate the entire visit.
Physicians must document both the counseling/coordination of care time and total visit time. The format may vary: “Total visit time = 25 minutes; more than 50% spent counseling/coordinating care,” or “20 of 25 minutes spent counseling/coordinating care.” Any given payer may prefer one documentation style over another. It always is best to query payers and review their documentation standards to determine the local preference.
In addition to the time, physicians must document the medical decision-making and details of the counseling/coordination of care. For example, patients with newly diagnosed diabetes need to be educated about their condition, lifestyle, and medication requirements. Physicians should include information regarding these factors in their progress notes as necessary.
Family Discussions
As noted in my previous article on critical care services (March 2008, p. 18), family discussions can contribute toward counseling/coordination of care time when:
- The patient is unable or clinically incompetent to participate in discussions;
- Time is spent on the unit/floor with family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; or
- The conversation bears directly on the management of the patient.
Prolonged Care
A physician makes his rounds in the morning. He cares for a 72-year-old female with diabetes, end-stage renal disease, and hypertension. In the afternoon, he returns to find the family waiting with questions. He spends an additional 30 minutes speaking at the bedside with the patient and family. The additional afternoon effort may be captured as prolonged care if both services are documented appropriately.
For inpatient services, CPT defines code 99356 as the first hour of prolonged physician services requiring face-to-face patient contact beyond the usual services (reportable after the initial 30 minutes). Code 99357 is used for each additional 30 minutes of prolonged care beyond the first hour (reportable after the first 15 minutes of each additional segment). Both codes are considered add-on codes and cannot be reported alone on a claim form; a primary code must be reported. Code 99357 must be used with 99356, and 99356 must be reported with one of the following inpatient service [primary] codes: 99221-99223, 99231-99233, or 99251-99255.
Prolonged care employs the concept of threshold time. This means total face-to-face physician visit time must exceed the time requirements associated with the primary codes by 30 minutes (e.g., 99232 plus 99356 = 25 minutes plus 30 minutes = 55 total face-to-face attending visit minutes). Accordingly, the physician must document the total face-to-face time spent during each portion of care in two separate notes or in one cumulative note. Be aware that this varies from the standard reporting of counseling and/or coordination of care time in that the physician must meet the threshold face-to-face-time requirements (see Table 1, left), making prolonged care services inefficient. When two providers from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service. To reiterate, 99356 must be reported on the same invoice as the primary visit code (e.g., 99232). Be sure once again to query payers, because most non-Medicare insurers do not recognize these codes. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Document Your Decisions
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
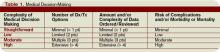
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Choose Your Exam Rules
Physicians only should perform patient examinations based upon the presenting problem and the standard of care. As mentioned in my previous column (April 2008, p. 21), the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA) set forth two sets of documentation guidelines. The biggest difference between them is the exam component.
1995 Guidelines
The 1995 guidelines distinguish 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).
Further, these guidelines let physicians document their findings in any manner while adhering to some simple rules:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems; and
- Elaborate on abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Guidelines
The 1997 guidelines comprise bulleted items—referred to as elements—that correspond to each organ system. Some elements specify numeric criterion that must be met to credit the physician for documentation of that element.
For example, the physician only receives credit for documentation of vital signs (an element of the constitutional system) when three measurements are referenced (e.g., blood pressure, heart rate, and respiratory rate). Documentation that does not include three measurements or only contains a single generalized comment (e.g., vital signs stable) cannot be credited to the physician in the 1997 guidelines—even though these same comments are credited when applying the 1995 guidelines.
This logic also applies to the lymphatic system. The physician must identify findings associated with at least two lymphatic areas examined (e.g., “no lymphadenopathy of the neck or axillae”).
Elements that do not contain numeric criterion but identify multiple components require documentation of at least one component. For example, one psychiatric element involves the assessment of the patient’s “mood and affect.” If the physician comments that the patient appears depressed but does not comment on a flat (or normal) affect, the physician still receives credit for this exam element.
Levels of Exam
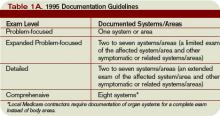
There are four levels of exam, determined by the number of elements documented in the progress note (see Tables 1A and 1B, p. below).
As with the history component, the physician must meet the requirements for a particular level of exam before assigning it. The most problematic feature of the 1995 guidelines involves the “detailed” exam. Both the expanded problem-focused and detailed exams involve two to seven systems/areas, but the detailed exam requires an “extended” exam of the affected system/area related to the presenting problem. Questions surround the number of elements needed to qualify as an “extended” exam of the affected system/area.
Does “regular rate and rhythm; normal S1, S2; no jugular venous distention; no murmur, gallop, or rub; peripheral pulses intact; no edema noted” constitute an “extended” exam of the cardiovascular system, or should there be an additional comment regarding the abdominal aorta? This decision is left to the discretion of the local Medicare contractor and/or the medical reviewer.
Since no other CMS directive has been provided, documentation of the detailed exam continues to be inconsistent. More importantly, review and audit of the detailed exam remains arbitrary. Some Medicare contractors suggest using the 1997 requirements for the detailed exam, while others create their own definition and corresponding number of exam elements needed for documentation of the detailed exam. This issue exemplifies the ambiguity for which the 1995 guidelines often are criticized.
Meanwhile, the 1997 guidelines often are criticized as too specific. While this may help the medical reviewer/auditor, it hinders the physician. Physicians are frequently frustrated trying to remember the explicit comments and number of elements associated with a particular level of exam.
One solution is documentation templates. Physicians can use paper or electronic templates that incorporate cues and prompts for normal exam findings, incorporating adequate space to elaborate abnormal findings.
Remember the physician has the option of utilizing either the 1995 or 1997 guidelines, depending upon which set he perceives as easier to implement.
Additionally, auditors must review physician documentation using both the 1995 and 1997 guidelines, and apply the most favorable result to the final audit score.
Each type of evaluation and management service identifies a specific level of exam that must be documented in the medical record before the associated CPT code is submitted on a claim.
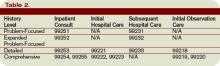
The most common visit categories provided by hospitalists and corresponding exam levels are outlined in Table 2 (above). Similar to the history component, other visit categories, such as critical care and discharge day management, do not have specified levels of exam or associated documentation requirements for physical exam elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Physicians only should perform patient examinations based upon the presenting problem and the standard of care. As mentioned in my previous column (April 2008, p. 21), the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA) set forth two sets of documentation guidelines. The biggest difference between them is the exam component.
1995 Guidelines
The 1995 guidelines distinguish 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).
Further, these guidelines let physicians document their findings in any manner while adhering to some simple rules:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems; and
- Elaborate on abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Guidelines
The 1997 guidelines comprise bulleted items—referred to as elements—that correspond to each organ system. Some elements specify numeric criterion that must be met to credit the physician for documentation of that element.
For example, the physician only receives credit for documentation of vital signs (an element of the constitutional system) when three measurements are referenced (e.g., blood pressure, heart rate, and respiratory rate). Documentation that does not include three measurements or only contains a single generalized comment (e.g., vital signs stable) cannot be credited to the physician in the 1997 guidelines—even though these same comments are credited when applying the 1995 guidelines.
This logic also applies to the lymphatic system. The physician must identify findings associated with at least two lymphatic areas examined (e.g., “no lymphadenopathy of the neck or axillae”).
Elements that do not contain numeric criterion but identify multiple components require documentation of at least one component. For example, one psychiatric element involves the assessment of the patient’s “mood and affect.” If the physician comments that the patient appears depressed but does not comment on a flat (or normal) affect, the physician still receives credit for this exam element.
Levels of Exam
There are four levels of exam, determined by the number of elements documented in the progress note (see Tables 1A and 1B, p. below).
As with the history component, the physician must meet the requirements for a particular level of exam before assigning it. The most problematic feature of the 1995 guidelines involves the “detailed” exam. Both the expanded problem-focused and detailed exams involve two to seven systems/areas, but the detailed exam requires an “extended” exam of the affected system/area related to the presenting problem. Questions surround the number of elements needed to qualify as an “extended” exam of the affected system/area.
Does “regular rate and rhythm; normal S1, S2; no jugular venous distention; no murmur, gallop, or rub; peripheral pulses intact; no edema noted” constitute an “extended” exam of the cardiovascular system, or should there be an additional comment regarding the abdominal aorta? This decision is left to the discretion of the local Medicare contractor and/or the medical reviewer.
Since no other CMS directive has been provided, documentation of the detailed exam continues to be inconsistent. More importantly, review and audit of the detailed exam remains arbitrary. Some Medicare contractors suggest using the 1997 requirements for the detailed exam, while others create their own definition and corresponding number of exam elements needed for documentation of the detailed exam. This issue exemplifies the ambiguity for which the 1995 guidelines often are criticized.
Meanwhile, the 1997 guidelines often are criticized as too specific. While this may help the medical reviewer/auditor, it hinders the physician. Physicians are frequently frustrated trying to remember the explicit comments and number of elements associated with a particular level of exam.
One solution is documentation templates. Physicians can use paper or electronic templates that incorporate cues and prompts for normal exam findings, incorporating adequate space to elaborate abnormal findings.
Remember the physician has the option of utilizing either the 1995 or 1997 guidelines, depending upon which set he perceives as easier to implement.
Additionally, auditors must review physician documentation using both the 1995 and 1997 guidelines, and apply the most favorable result to the final audit score.
Each type of evaluation and management service identifies a specific level of exam that must be documented in the medical record before the associated CPT code is submitted on a claim.
The most common visit categories provided by hospitalists and corresponding exam levels are outlined in Table 2 (above). Similar to the history component, other visit categories, such as critical care and discharge day management, do not have specified levels of exam or associated documentation requirements for physical exam elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Physicians only should perform patient examinations based upon the presenting problem and the standard of care. As mentioned in my previous column (April 2008, p. 21), the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA) set forth two sets of documentation guidelines. The biggest difference between them is the exam component.
1995 Guidelines
The 1995 guidelines distinguish 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).
Further, these guidelines let physicians document their findings in any manner while adhering to some simple rules:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems; and
- Elaborate on abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Guidelines
The 1997 guidelines comprise bulleted items—referred to as elements—that correspond to each organ system. Some elements specify numeric criterion that must be met to credit the physician for documentation of that element.
For example, the physician only receives credit for documentation of vital signs (an element of the constitutional system) when three measurements are referenced (e.g., blood pressure, heart rate, and respiratory rate). Documentation that does not include three measurements or only contains a single generalized comment (e.g., vital signs stable) cannot be credited to the physician in the 1997 guidelines—even though these same comments are credited when applying the 1995 guidelines.
This logic also applies to the lymphatic system. The physician must identify findings associated with at least two lymphatic areas examined (e.g., “no lymphadenopathy of the neck or axillae”).
Elements that do not contain numeric criterion but identify multiple components require documentation of at least one component. For example, one psychiatric element involves the assessment of the patient’s “mood and affect.” If the physician comments that the patient appears depressed but does not comment on a flat (or normal) affect, the physician still receives credit for this exam element.
Levels of Exam
There are four levels of exam, determined by the number of elements documented in the progress note (see Tables 1A and 1B, p. below).
As with the history component, the physician must meet the requirements for a particular level of exam before assigning it. The most problematic feature of the 1995 guidelines involves the “detailed” exam. Both the expanded problem-focused and detailed exams involve two to seven systems/areas, but the detailed exam requires an “extended” exam of the affected system/area related to the presenting problem. Questions surround the number of elements needed to qualify as an “extended” exam of the affected system/area.
Does “regular rate and rhythm; normal S1, S2; no jugular venous distention; no murmur, gallop, or rub; peripheral pulses intact; no edema noted” constitute an “extended” exam of the cardiovascular system, or should there be an additional comment regarding the abdominal aorta? This decision is left to the discretion of the local Medicare contractor and/or the medical reviewer.
Since no other CMS directive has been provided, documentation of the detailed exam continues to be inconsistent. More importantly, review and audit of the detailed exam remains arbitrary. Some Medicare contractors suggest using the 1997 requirements for the detailed exam, while others create their own definition and corresponding number of exam elements needed for documentation of the detailed exam. This issue exemplifies the ambiguity for which the 1995 guidelines often are criticized.
Meanwhile, the 1997 guidelines often are criticized as too specific. While this may help the medical reviewer/auditor, it hinders the physician. Physicians are frequently frustrated trying to remember the explicit comments and number of elements associated with a particular level of exam.
One solution is documentation templates. Physicians can use paper or electronic templates that incorporate cues and prompts for normal exam findings, incorporating adequate space to elaborate abnormal findings.
Remember the physician has the option of utilizing either the 1995 or 1997 guidelines, depending upon which set he perceives as easier to implement.
Additionally, auditors must review physician documentation using both the 1995 and 1997 guidelines, and apply the most favorable result to the final audit score.
Each type of evaluation and management service identifies a specific level of exam that must be documented in the medical record before the associated CPT code is submitted on a claim.
The most common visit categories provided by hospitalists and corresponding exam levels are outlined in Table 2 (above). Similar to the history component, other visit categories, such as critical care and discharge day management, do not have specified levels of exam or associated documentation requirements for physical exam elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Document Patient History
Documentation in the medical record serves many purposes: communication among healthcare professionals, evidence of patient care, and justification for provider claims.
Although these three aspects of documentation are intertwined, the first two prevent physicians from paying settlements involving malpractice allegations, while the last one assists in obtaining appropriate reimbursement for services rendered. This is the first of a three-part series that will focus on claim reporting and outline the documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) in conjunction with the American Medical Association (AMA).
1995, 1997 Guidelines
Two sets of documentation guidelines are in place, referred to as the 1995 and 1997 guidelines. Increased criticism of the ambiguity in the 1995 guidelines from auditors and providers inspired development of the 1997 guidelines.
While the 1997 guidelines were intended to create a more objective and unified approach to documentation, the level of specificity required brought criticism and frustration. But while the physician community balked, most auditors praised these efforts.
To satisfy all parties and allow physicians to document as they prefer, both sets of guidelines remain. Physicians can document according to either style, and auditors are obligated to review provider records against both sets of guidelines, selecting the final visit level with the set that best supports provider documentation.
Elements of History
Chief complaint (CC): The CC is the reason for the visit as stated in the patient’s own words. This must be present for each encounter, and should reference a specific condition or complaint (e.g., patient complains of abdominal pain).
History of present illness (HPI): This is a description of the present illness as it developed. It is typically formatted and documented with reference to location, quality, severity, timing, context, modifying factors, and associated signs/symptoms as related to the chief complaint. The HPI may be classified as brief (a comment on fewer than HPI elements) or extended (a comment on more than four HPI elements). Sample documentation of an extended HPI is: “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
The 1997 guidelines offer an alternate format for documenting the HPI. In contrast to the standard method above, the physician may list and status the patient’s chronic or inactive conditions. An extended HPI consists of the status of at least three chronic or inactive conditions (e.g., “Diabetes controlled by oral medication; extrinsic asthma without acute exacerbation in past six months; hypertension stable with pressures ranging from 130-140/80-90”). Failing to document the status negates the opportunity for the physician to receive HPI credit. Instead, he will receive credit for a past medical history.
The HPI should never be documented by ancillary staff (e.g., registered nurse, medical assistant, students). HPI might be documented by residents (e.g., residents, fellows, interns) or nonphysician providers (nurse practitioners and physician assistants) when utilizing the Teaching Physician Rules or Split-Shared Billing Rules, respectively (teaching Physician Rules and Split-Shared Billing Rules will be addressed in an upcoming issue).
Review of systems (ROS): This is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient:
- Constitutional;
- Eyes; ears, nose, mouth, throat;
- Cardiovascular;
- Respiratory;
- Gastrointestinal;
- Genitourinary;
- Musculoskeletal;
- Integumentary (including skin and/or breast);
- Neurological;
- Psychiatric;
- Endocrine;
- Hematologic/lymphatic; and
- Allergic/immunologic.
The ROS may be classified as brief (a comment on one system), expanded (a comment on two to nine systems), or complete (a comment on more than 10 systems).
Documentation of a complete ROS (more than 10 systems) can occur in two ways:
- The physician can individually document each system. For example: “No fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular); shortness of breath (respiratory); or belly pain (gastrointestinal); etc.”; or
- The physician can document the positive findings and pertinent negative findings related to the chief complaint, along with a comment that “all other systems are negative.” This latter statement is not accepted by all local Medicare contractors.
Information involving the ROS can be documented by anyone, including the patient. If documented by someone else (e.g., a medical student) other than residents under the Teaching Physician Rules or nonphysician providers under the Split-Shared Billing Rules, the physician should reference the documented ROS in his progress note. Re-documentation of the ROS is not necessary unless a revision is required.
Past, family, and social history (PFSH): Documentation of PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH can be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). Documentation that exemplifies a complete PFSH is: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
As with ROS, the PFSH can be documented by anyone, including the patient. If documented by someone else (e.g., a medical student) other than residents under the Teaching Physician Rules or nonphysician providers under the Split-Shared Billing Rules, the physician should reference the documented PFSH in his progress note. Re-documentation of the PFSH is not necessary unless a revision is required. It is important to note that while documentation of the PFSH is required when billing higher level consultations (99254-99255) or initial inpatient care (99221-99223), it is not required when reporting subsequent hospital care services (99231-99233).
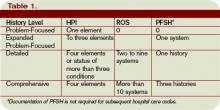
Levels of History
There are four levels of history, determined by the number of elements documented in the progress note (see Table 1, p. 21). The physician must meet all the requirements in a specific level of history before assigning it.
If all of the required elements in a given history level are not documented, the level assigned is that of the least documented element. For example, physician documentation may include four HPI elements and a complete PFSH, yet only eight ROS. The physician can only receive credit for a detailed history. If the physician submitted a claim for 99222 (initial hospital care requiring a comprehensive history, a comprehensive exam, and moderate-complexity decision making), documentation would not support the reported service due to the underdocumented ROS. Deficiencies in the ROS and family history are the most common physician documentation errors involving the history component.
A specific level of history is associated with each type of physician encounter, and must be documented accordingly (see Table 2, right). The most common visit categories provided by hospitalists that include documentation requirements for history are initial inpatient consultations, initial hospital care, subsequent hospital care, and initial observation care. Other visit categories, such as critical care and discharge day management, have neither associated levels of history nor documentation requirements for historical elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Documentation in the medical record serves many purposes: communication among healthcare professionals, evidence of patient care, and justification for provider claims.
Although these three aspects of documentation are intertwined, the first two prevent physicians from paying settlements involving malpractice allegations, while the last one assists in obtaining appropriate reimbursement for services rendered. This is the first of a three-part series that will focus on claim reporting and outline the documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) in conjunction with the American Medical Association (AMA).
1995, 1997 Guidelines
Two sets of documentation guidelines are in place, referred to as the 1995 and 1997 guidelines. Increased criticism of the ambiguity in the 1995 guidelines from auditors and providers inspired development of the 1997 guidelines.
While the 1997 guidelines were intended to create a more objective and unified approach to documentation, the level of specificity required brought criticism and frustration. But while the physician community balked, most auditors praised these efforts.
To satisfy all parties and allow physicians to document as they prefer, both sets of guidelines remain. Physicians can document according to either style, and auditors are obligated to review provider records against both sets of guidelines, selecting the final visit level with the set that best supports provider documentation.
Elements of History
Chief complaint (CC): The CC is the reason for the visit as stated in the patient’s own words. This must be present for each encounter, and should reference a specific condition or complaint (e.g., patient complains of abdominal pain).
History of present illness (HPI): This is a description of the present illness as it developed. It is typically formatted and documented with reference to location, quality, severity, timing, context, modifying factors, and associated signs/symptoms as related to the chief complaint. The HPI may be classified as brief (a comment on fewer than HPI elements) or extended (a comment on more than four HPI elements). Sample documentation of an extended HPI is: “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
The 1997 guidelines offer an alternate format for documenting the HPI. In contrast to the standard method above, the physician may list and status the patient’s chronic or inactive conditions. An extended HPI consists of the status of at least three chronic or inactive conditions (e.g., “Diabetes controlled by oral medication; extrinsic asthma without acute exacerbation in past six months; hypertension stable with pressures ranging from 130-140/80-90”). Failing to document the status negates the opportunity for the physician to receive HPI credit. Instead, he will receive credit for a past medical history.
The HPI should never be documented by ancillary staff (e.g., registered nurse, medical assistant, students). HPI might be documented by residents (e.g., residents, fellows, interns) or nonphysician providers (nurse practitioners and physician assistants) when utilizing the Teaching Physician Rules or Split-Shared Billing Rules, respectively (teaching Physician Rules and Split-Shared Billing Rules will be addressed in an upcoming issue).
Review of systems (ROS): This is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient:
- Constitutional;
- Eyes; ears, nose, mouth, throat;
- Cardiovascular;
- Respiratory;
- Gastrointestinal;
- Genitourinary;
- Musculoskeletal;
- Integumentary (including skin and/or breast);
- Neurological;
- Psychiatric;
- Endocrine;
- Hematologic/lymphatic; and
- Allergic/immunologic.
The ROS may be classified as brief (a comment on one system), expanded (a comment on two to nine systems), or complete (a comment on more than 10 systems).
Documentation of a complete ROS (more than 10 systems) can occur in two ways:
- The physician can individually document each system. For example: “No fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular); shortness of breath (respiratory); or belly pain (gastrointestinal); etc.”; or
- The physician can document the positive findings and pertinent negative findings related to the chief complaint, along with a comment that “all other systems are negative.” This latter statement is not accepted by all local Medicare contractors.
Information involving the ROS can be documented by anyone, including the patient. If documented by someone else (e.g., a medical student) other than residents under the Teaching Physician Rules or nonphysician providers under the Split-Shared Billing Rules, the physician should reference the documented ROS in his progress note. Re-documentation of the ROS is not necessary unless a revision is required.
Past, family, and social history (PFSH): Documentation of PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH can be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). Documentation that exemplifies a complete PFSH is: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
As with ROS, the PFSH can be documented by anyone, including the patient. If documented by someone else (e.g., a medical student) other than residents under the Teaching Physician Rules or nonphysician providers under the Split-Shared Billing Rules, the physician should reference the documented PFSH in his progress note. Re-documentation of the PFSH is not necessary unless a revision is required. It is important to note that while documentation of the PFSH is required when billing higher level consultations (99254-99255) or initial inpatient care (99221-99223), it is not required when reporting subsequent hospital care services (99231-99233).
Levels of History
There are four levels of history, determined by the number of elements documented in the progress note (see Table 1, p. 21). The physician must meet all the requirements in a specific level of history before assigning it.
If all of the required elements in a given history level are not documented, the level assigned is that of the least documented element. For example, physician documentation may include four HPI elements and a complete PFSH, yet only eight ROS. The physician can only receive credit for a detailed history. If the physician submitted a claim for 99222 (initial hospital care requiring a comprehensive history, a comprehensive exam, and moderate-complexity decision making), documentation would not support the reported service due to the underdocumented ROS. Deficiencies in the ROS and family history are the most common physician documentation errors involving the history component.
A specific level of history is associated with each type of physician encounter, and must be documented accordingly (see Table 2, right). The most common visit categories provided by hospitalists that include documentation requirements for history are initial inpatient consultations, initial hospital care, subsequent hospital care, and initial observation care. Other visit categories, such as critical care and discharge day management, have neither associated levels of history nor documentation requirements for historical elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Documentation in the medical record serves many purposes: communication among healthcare professionals, evidence of patient care, and justification for provider claims.
Although these three aspects of documentation are intertwined, the first two prevent physicians from paying settlements involving malpractice allegations, while the last one assists in obtaining appropriate reimbursement for services rendered. This is the first of a three-part series that will focus on claim reporting and outline the documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) in conjunction with the American Medical Association (AMA).
1995, 1997 Guidelines
Two sets of documentation guidelines are in place, referred to as the 1995 and 1997 guidelines. Increased criticism of the ambiguity in the 1995 guidelines from auditors and providers inspired development of the 1997 guidelines.
While the 1997 guidelines were intended to create a more objective and unified approach to documentation, the level of specificity required brought criticism and frustration. But while the physician community balked, most auditors praised these efforts.
To satisfy all parties and allow physicians to document as they prefer, both sets of guidelines remain. Physicians can document according to either style, and auditors are obligated to review provider records against both sets of guidelines, selecting the final visit level with the set that best supports provider documentation.
Elements of History
Chief complaint (CC): The CC is the reason for the visit as stated in the patient’s own words. This must be present for each encounter, and should reference a specific condition or complaint (e.g., patient complains of abdominal pain).
History of present illness (HPI): This is a description of the present illness as it developed. It is typically formatted and documented with reference to location, quality, severity, timing, context, modifying factors, and associated signs/symptoms as related to the chief complaint. The HPI may be classified as brief (a comment on fewer than HPI elements) or extended (a comment on more than four HPI elements). Sample documentation of an extended HPI is: “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
The 1997 guidelines offer an alternate format for documenting the HPI. In contrast to the standard method above, the physician may list and status the patient’s chronic or inactive conditions. An extended HPI consists of the status of at least three chronic or inactive conditions (e.g., “Diabetes controlled by oral medication; extrinsic asthma without acute exacerbation in past six months; hypertension stable with pressures ranging from 130-140/80-90”). Failing to document the status negates the opportunity for the physician to receive HPI credit. Instead, he will receive credit for a past medical history.
The HPI should never be documented by ancillary staff (e.g., registered nurse, medical assistant, students). HPI might be documented by residents (e.g., residents, fellows, interns) or nonphysician providers (nurse practitioners and physician assistants) when utilizing the Teaching Physician Rules or Split-Shared Billing Rules, respectively (teaching Physician Rules and Split-Shared Billing Rules will be addressed in an upcoming issue).
Review of systems (ROS): This is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient:
- Constitutional;
- Eyes; ears, nose, mouth, throat;
- Cardiovascular;
- Respiratory;
- Gastrointestinal;
- Genitourinary;
- Musculoskeletal;
- Integumentary (including skin and/or breast);
- Neurological;
- Psychiatric;
- Endocrine;
- Hematologic/lymphatic; and
- Allergic/immunologic.
The ROS may be classified as brief (a comment on one system), expanded (a comment on two to nine systems), or complete (a comment on more than 10 systems).
Documentation of a complete ROS (more than 10 systems) can occur in two ways:
- The physician can individually document each system. For example: “No fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular); shortness of breath (respiratory); or belly pain (gastrointestinal); etc.”; or
- The physician can document the positive findings and pertinent negative findings related to the chief complaint, along with a comment that “all other systems are negative.” This latter statement is not accepted by all local Medicare contractors.
Information involving the ROS can be documented by anyone, including the patient. If documented by someone else (e.g., a medical student) other than residents under the Teaching Physician Rules or nonphysician providers under the Split-Shared Billing Rules, the physician should reference the documented ROS in his progress note. Re-documentation of the ROS is not necessary unless a revision is required.
Past, family, and social history (PFSH): Documentation of PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH can be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). Documentation that exemplifies a complete PFSH is: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
As with ROS, the PFSH can be documented by anyone, including the patient. If documented by someone else (e.g., a medical student) other than residents under the Teaching Physician Rules or nonphysician providers under the Split-Shared Billing Rules, the physician should reference the documented PFSH in his progress note. Re-documentation of the PFSH is not necessary unless a revision is required. It is important to note that while documentation of the PFSH is required when billing higher level consultations (99254-99255) or initial inpatient care (99221-99223), it is not required when reporting subsequent hospital care services (99231-99233).
Levels of History
There are four levels of history, determined by the number of elements documented in the progress note (see Table 1, p. 21). The physician must meet all the requirements in a specific level of history before assigning it.
If all of the required elements in a given history level are not documented, the level assigned is that of the least documented element. For example, physician documentation may include four HPI elements and a complete PFSH, yet only eight ROS. The physician can only receive credit for a detailed history. If the physician submitted a claim for 99222 (initial hospital care requiring a comprehensive history, a comprehensive exam, and moderate-complexity decision making), documentation would not support the reported service due to the underdocumented ROS. Deficiencies in the ROS and family history are the most common physician documentation errors involving the history component.
A specific level of history is associated with each type of physician encounter, and must be documented accordingly (see Table 2, right). The most common visit categories provided by hospitalists that include documentation requirements for history are initial inpatient consultations, initial hospital care, subsequent hospital care, and initial observation care. Other visit categories, such as critical care and discharge day management, have neither associated levels of history nor documentation requirements for historical elements. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Report Critical Care
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Plan for Discharge
Discharge planning typically begins at the time of admission. Physicians and hospital staff manage the patient’s acute issues throughout the stay while simultaneously trying to anticipate the patient’s discharge needs. Physicians capture these associated efforts by reporting discharge day management codes 99238 or 99239.
Code Use
Use of discharge day management codes 99238-99239 is reserved for the admitting physician/group, unless a formal transfer of care occurs (e.g., patient is transferred from the intensive care unit by the critical care physician to the medical-surgical floor on the hospitalist’s service).
Report one discharge code per hospitalization, but only when the service occurs after the initial date of admission. Codes 99238 or 99239 are not permitted for use when the patient is admitted and discharged on the same calendar date. When this occurs, the physician selects from 99221-99223 (initial inpatient care) or 99234-99236 (admission and discharge on the same day). Choose 99234-99238 when the patient stay is eight or more hours on the same calendar day and the insurer accepts these codes.
Documentation must also reflect two components of service: the corresponding elements of both the admission and discharge. Alternately, if the patient stays less than eight hours, or the insurer does not recognize 99234-99236 (admission and discharge on the same day), report 9922x (initial inpatient care) as appropriate.
Don’t mistakenly report discharge services for merely dictating the discharge summary. Discharge day management, as with most payable evaluation and management (E/M) services, requires a face-to-face visit between the physician and the patient on discharge day.
The entire visit need not take place at the bedside and may include other discharge-related elements performed on the patient’s unit/floor such as discussions with other healthcare professionals, patient/caregiver instruction and coordination of follow-up care. The discharge code description indicates that a final examination of the patient is included, but only “as appropriate.” In other words, an exam may not occur, or may not be documented, yet this does not preclude the physician from reporting 99238-99239. However, inclusion of the exam in the discharge day documentation is the best way to justify that a face-to-face service occurred on discharge day. This may be included in the discharge summary or a separate progress note in the medical record.
Time-Based Service
Discharge day management codes reflect the time accumulated on a calendar date, ending when the patient physically leaves the hospital. Services performed in a location other than the patient’s unit/floor (e.g., dictating the discharge summary from the outpatient office), do not count toward the cumulative time. Additionally, discharge-related services performed by residents, students or ancillary staff (i.e., registered nurses), such as reviewing instructions with the patient, do not count toward the discharge service time.
To support the discharge day management claim, documentation should reference the discharge status and other clinically relevant information. Time is not required when documenting 99238 because this service code constitutes any amount of time up to and including 30 minutes. When reporting 99239, documentation must include the physician’s cumulative service time (more than 30 minutes).
Medicare currently initiates a prepayment review (i.e., request for documentation to review the service prior to any payment consideration) for claims involving 99239. Failure to respond to the prepayment request or failure to include the time component in the documentation often results in claim denial. Payment can be recovered only through the appeal process or claim correction, when applicable.
Rules For Surgery
Surgeons are prohibited from separately reporting inpatient postoperative services related to the surgery, including discharge day management (99238-99239). Additionally, when the surgeon admits a patient to the hospital and discharge services are performed postoperatively by the hospitalist, discharge day management is included in the surgical package.
The reasons are two-fold: If the surgeon transfers the remaining inpatient care to the hospitalist, these discharge services are considered part of the global surgical package.
If no transfer occurs (as the surgeon is typically responsible and paid for all care up to 90 days following surgery), only the admitting physician/group (i.e., the surgeon) may report discharge day management codes 99238-99239.
In the latter scenario, the hospitalist reports subsequent hospital care (99231-99233) for all medically necessary services involving the patient’s medical management, even if provided on the day of discharge.
Pronouncement of Death
One of the most underreported services involves pronouncement of death. A physician who performs this service may qualify to report discharge day management code 99238-99239. To pronounce death, the physician must examine the patient, thus satisfying the face-to-face visit requirement.
Additionally, the physician may have to coordinate the necessary services, speak with family members or other healthcare providers, and fill out the necessary documentation.
If performed on the patient’s unit/floor, these services count toward the cumulative discharge service time. Documentation must include the time (if reporting 99239) as well as the patient’s discharge status and clinically relevant information. Completion of the death certificate alone is not sufficient for billing. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Discharge planning typically begins at the time of admission. Physicians and hospital staff manage the patient’s acute issues throughout the stay while simultaneously trying to anticipate the patient’s discharge needs. Physicians capture these associated efforts by reporting discharge day management codes 99238 or 99239.
Code Use
Use of discharge day management codes 99238-99239 is reserved for the admitting physician/group, unless a formal transfer of care occurs (e.g., patient is transferred from the intensive care unit by the critical care physician to the medical-surgical floor on the hospitalist’s service).
Report one discharge code per hospitalization, but only when the service occurs after the initial date of admission. Codes 99238 or 99239 are not permitted for use when the patient is admitted and discharged on the same calendar date. When this occurs, the physician selects from 99221-99223 (initial inpatient care) or 99234-99236 (admission and discharge on the same day). Choose 99234-99238 when the patient stay is eight or more hours on the same calendar day and the insurer accepts these codes.
Documentation must also reflect two components of service: the corresponding elements of both the admission and discharge. Alternately, if the patient stays less than eight hours, or the insurer does not recognize 99234-99236 (admission and discharge on the same day), report 9922x (initial inpatient care) as appropriate.
Don’t mistakenly report discharge services for merely dictating the discharge summary. Discharge day management, as with most payable evaluation and management (E/M) services, requires a face-to-face visit between the physician and the patient on discharge day.
The entire visit need not take place at the bedside and may include other discharge-related elements performed on the patient’s unit/floor such as discussions with other healthcare professionals, patient/caregiver instruction and coordination of follow-up care. The discharge code description indicates that a final examination of the patient is included, but only “as appropriate.” In other words, an exam may not occur, or may not be documented, yet this does not preclude the physician from reporting 99238-99239. However, inclusion of the exam in the discharge day documentation is the best way to justify that a face-to-face service occurred on discharge day. This may be included in the discharge summary or a separate progress note in the medical record.
Time-Based Service
Discharge day management codes reflect the time accumulated on a calendar date, ending when the patient physically leaves the hospital. Services performed in a location other than the patient’s unit/floor (e.g., dictating the discharge summary from the outpatient office), do not count toward the cumulative time. Additionally, discharge-related services performed by residents, students or ancillary staff (i.e., registered nurses), such as reviewing instructions with the patient, do not count toward the discharge service time.
To support the discharge day management claim, documentation should reference the discharge status and other clinically relevant information. Time is not required when documenting 99238 because this service code constitutes any amount of time up to and including 30 minutes. When reporting 99239, documentation must include the physician’s cumulative service time (more than 30 minutes).
Medicare currently initiates a prepayment review (i.e., request for documentation to review the service prior to any payment consideration) for claims involving 99239. Failure to respond to the prepayment request or failure to include the time component in the documentation often results in claim denial. Payment can be recovered only through the appeal process or claim correction, when applicable.
Rules For Surgery
Surgeons are prohibited from separately reporting inpatient postoperative services related to the surgery, including discharge day management (99238-99239). Additionally, when the surgeon admits a patient to the hospital and discharge services are performed postoperatively by the hospitalist, discharge day management is included in the surgical package.
The reasons are two-fold: If the surgeon transfers the remaining inpatient care to the hospitalist, these discharge services are considered part of the global surgical package.
If no transfer occurs (as the surgeon is typically responsible and paid for all care up to 90 days following surgery), only the admitting physician/group (i.e., the surgeon) may report discharge day management codes 99238-99239.
In the latter scenario, the hospitalist reports subsequent hospital care (99231-99233) for all medically necessary services involving the patient’s medical management, even if provided on the day of discharge.
Pronouncement of Death
One of the most underreported services involves pronouncement of death. A physician who performs this service may qualify to report discharge day management code 99238-99239. To pronounce death, the physician must examine the patient, thus satisfying the face-to-face visit requirement.
Additionally, the physician may have to coordinate the necessary services, speak with family members or other healthcare providers, and fill out the necessary documentation.
If performed on the patient’s unit/floor, these services count toward the cumulative discharge service time. Documentation must include the time (if reporting 99239) as well as the patient’s discharge status and clinically relevant information. Completion of the death certificate alone is not sufficient for billing. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Discharge planning typically begins at the time of admission. Physicians and hospital staff manage the patient’s acute issues throughout the stay while simultaneously trying to anticipate the patient’s discharge needs. Physicians capture these associated efforts by reporting discharge day management codes 99238 or 99239.
Code Use
Use of discharge day management codes 99238-99239 is reserved for the admitting physician/group, unless a formal transfer of care occurs (e.g., patient is transferred from the intensive care unit by the critical care physician to the medical-surgical floor on the hospitalist’s service).
Report one discharge code per hospitalization, but only when the service occurs after the initial date of admission. Codes 99238 or 99239 are not permitted for use when the patient is admitted and discharged on the same calendar date. When this occurs, the physician selects from 99221-99223 (initial inpatient care) or 99234-99236 (admission and discharge on the same day). Choose 99234-99238 when the patient stay is eight or more hours on the same calendar day and the insurer accepts these codes.
Documentation must also reflect two components of service: the corresponding elements of both the admission and discharge. Alternately, if the patient stays less than eight hours, or the insurer does not recognize 99234-99236 (admission and discharge on the same day), report 9922x (initial inpatient care) as appropriate.
Don’t mistakenly report discharge services for merely dictating the discharge summary. Discharge day management, as with most payable evaluation and management (E/M) services, requires a face-to-face visit between the physician and the patient on discharge day.
The entire visit need not take place at the bedside and may include other discharge-related elements performed on the patient’s unit/floor such as discussions with other healthcare professionals, patient/caregiver instruction and coordination of follow-up care. The discharge code description indicates that a final examination of the patient is included, but only “as appropriate.” In other words, an exam may not occur, or may not be documented, yet this does not preclude the physician from reporting 99238-99239. However, inclusion of the exam in the discharge day documentation is the best way to justify that a face-to-face service occurred on discharge day. This may be included in the discharge summary or a separate progress note in the medical record.
Time-Based Service
Discharge day management codes reflect the time accumulated on a calendar date, ending when the patient physically leaves the hospital. Services performed in a location other than the patient’s unit/floor (e.g., dictating the discharge summary from the outpatient office), do not count toward the cumulative time. Additionally, discharge-related services performed by residents, students or ancillary staff (i.e., registered nurses), such as reviewing instructions with the patient, do not count toward the discharge service time.
To support the discharge day management claim, documentation should reference the discharge status and other clinically relevant information. Time is not required when documenting 99238 because this service code constitutes any amount of time up to and including 30 minutes. When reporting 99239, documentation must include the physician’s cumulative service time (more than 30 minutes).
Medicare currently initiates a prepayment review (i.e., request for documentation to review the service prior to any payment consideration) for claims involving 99239. Failure to respond to the prepayment request or failure to include the time component in the documentation often results in claim denial. Payment can be recovered only through the appeal process or claim correction, when applicable.
Rules For Surgery
Surgeons are prohibited from separately reporting inpatient postoperative services related to the surgery, including discharge day management (99238-99239). Additionally, when the surgeon admits a patient to the hospital and discharge services are performed postoperatively by the hospitalist, discharge day management is included in the surgical package.
The reasons are two-fold: If the surgeon transfers the remaining inpatient care to the hospitalist, these discharge services are considered part of the global surgical package.
If no transfer occurs (as the surgeon is typically responsible and paid for all care up to 90 days following surgery), only the admitting physician/group (i.e., the surgeon) may report discharge day management codes 99238-99239.
In the latter scenario, the hospitalist reports subsequent hospital care (99231-99233) for all medically necessary services involving the patient’s medical management, even if provided on the day of discharge.
Pronouncement of Death
One of the most underreported services involves pronouncement of death. A physician who performs this service may qualify to report discharge day management code 99238-99239. To pronounce death, the physician must examine the patient, thus satisfying the face-to-face visit requirement.
Additionally, the physician may have to coordinate the necessary services, speak with family members or other healthcare providers, and fill out the necessary documentation.
If performed on the patient’s unit/floor, these services count toward the cumulative discharge service time. Documentation must include the time (if reporting 99239) as well as the patient’s discharge status and clinically relevant information. Completion of the death certificate alone is not sufficient for billing. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Daily Care Conundrums
Subsequent hospital care, also known as daily care, presents a variety of daily-care scenarios that cause confusion for billing providers.
Subsequent hospital care codes are reported once per day after the initial patient encounter (e.g., admission or consultation service), but only when a face-to-face visit occurs between provider and patient.
The entire visit need not take place at the bedside. It may include other important elements performed on the patient’s unit/floor such as data review, discussions with other healthcare professionals, coordination of care, and family meetings. In addition, subsequent hospital care codes represent the cumulative evaluation and management service performed on a calendar date, even if the hospitalist evaluates the patient for different reasons or at different times throughout the day.
Concurrent Care
Traditionally, concurrent care occurs when physicians of different specialties and group practices participate in a patient’s care. Each physician manages a particular aspect while considering the patient’s overall condition.
When submitting claims for concurrent care services, each physician should report the appropriate subsequent hospital care code and the corresponding diagnosis each primarily manages. If billed correctly, each hospitalist will have a different primary diagnosis code and be more likely to receive payment.
Some managed-care payers require each hospitalist to append modifier 25 to their evaluation and management (E/M) visit code (99232-25) even though each submits claims under different tax identification numbers. Modifier 25 is a separately identifiable E/M service performed on the same day as a procedure or other E/M service. In this situation, Medicare is likely to reimburse as appropriate.
Payment by managed-care companies is less easily obtained: Payment for the first received claim is likely, and denial of any claim received beyond the first claim is inevitable. Appealing the denied claims with documentation for each hospitalist’s visit on a given date helps the payer understand the need for each service.
Group Practice
When concurrent care is provided by members of the same group practice, claim reporting becomes more complex. Physicians in the same group practice and specialty bill and are paid as though to a single physician. In other words, if two hospitalists evaluate a patient on the same day (e.g., one hospitalist sees the patient in the morning, and another one sees the patient in the afternoon), the efforts of each medically necessary evaluation and management service may be captured.
However, the billing mechanism used in this situation varies from the standard. Instead of reporting each service separately under each corresponding hospitalist’s name, the hospitalists select subsequent hospital care code 99231-99233 representing the combined visits and submit one appropriate code for the collective level of service.
The difficulty is selecting the name that will appear on the claim form. Solutions range from reporting the hospitalist who provided the first encounter of the day to identifying the hospitalist who provided the most extensive or best-documented encounter of the day. For productivity analysis, some practices develop an internal accounting system and credit each hospitalist for their medically necessary joint efforts. The latter option is a labor-intensive task for administrators.
Physicians in the same group practice but different specialties may bill and be paid without regard to their membership in the same group. For example, a hospitalist and an infectious disease specialist may be part of the same multispecialty group practice and bill under a group tax-identification number, yet qualify for separate payment.
This is permitted if each physician has a differing specialty code designation. Specialty codes are self-designated, two-digit representations that describe the kind of medicine physicians, non-physician practitioners, or other healthcare providers/suppliers practice. They are initially selected and registered with each payer during the enrollment process.
A list of qualifying specialty codes can be found at www.cms.hhs.gov/MedicareFeeforSvcPartsAB/Downloads/SpecialtyCodes2207.pdf.
Covering Physicians
Hospital inpatient situations involving physician coverage are complicated. If Dr. Richards sees the patient earlier in the day and Dr. Andrews, covering for Dr. Richards, sees the same patient later that same day, Dr. Andrews cannot be paid for the second visit.
Subsequent hospital care descriptors emphasize “per day” to account for all care provided during the calendar day. Insurers treat the covering physician as if he were the physician being covered. Services provided by each are handled in the same manner described above.
If each hospitalist is responsible for a different aspect of the patient’s care, payment is made for both visits if:
- The hospitalists are in different specialties and different group practices;
- The visits are billed with different diagnoses; and
- The patient is a Medicare beneficiary or a member of an insurance plan that adopts Medicare rules.
There are limited circumstances where concurrent care can be billed to Medicare by hospitalists of the same specialty (e.g., an internist and a hospitalist, one with significant and demonstrated expertise in pain management).
Each hospitalist must belong to a different group practice and submit claims under different tax identification numbers. The patient’s condition must require the expertise possessed by the “sub-specialist.” Payment will be denied in the initial claim determination. But formulating a Medicare appeal with documentation from both encounters can demonstrate the medical necessity and separateness of each service and help earn reimbursement—although it is not guaranteed.
Managed-care payment for two visits on the same day by physicians of the same registered specialty (e.g., internal medicine), regardless of sub-specialization, is highly unlikely. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Subsequent hospital care, also known as daily care, presents a variety of daily-care scenarios that cause confusion for billing providers.
Subsequent hospital care codes are reported once per day after the initial patient encounter (e.g., admission or consultation service), but only when a face-to-face visit occurs between provider and patient.
The entire visit need not take place at the bedside. It may include other important elements performed on the patient’s unit/floor such as data review, discussions with other healthcare professionals, coordination of care, and family meetings. In addition, subsequent hospital care codes represent the cumulative evaluation and management service performed on a calendar date, even if the hospitalist evaluates the patient for different reasons or at different times throughout the day.
Concurrent Care
Traditionally, concurrent care occurs when physicians of different specialties and group practices participate in a patient’s care. Each physician manages a particular aspect while considering the patient’s overall condition.
When submitting claims for concurrent care services, each physician should report the appropriate subsequent hospital care code and the corresponding diagnosis each primarily manages. If billed correctly, each hospitalist will have a different primary diagnosis code and be more likely to receive payment.
Some managed-care payers require each hospitalist to append modifier 25 to their evaluation and management (E/M) visit code (99232-25) even though each submits claims under different tax identification numbers. Modifier 25 is a separately identifiable E/M service performed on the same day as a procedure or other E/M service. In this situation, Medicare is likely to reimburse as appropriate.
Payment by managed-care companies is less easily obtained: Payment for the first received claim is likely, and denial of any claim received beyond the first claim is inevitable. Appealing the denied claims with documentation for each hospitalist’s visit on a given date helps the payer understand the need for each service.
Group Practice
When concurrent care is provided by members of the same group practice, claim reporting becomes more complex. Physicians in the same group practice and specialty bill and are paid as though to a single physician. In other words, if two hospitalists evaluate a patient on the same day (e.g., one hospitalist sees the patient in the morning, and another one sees the patient in the afternoon), the efforts of each medically necessary evaluation and management service may be captured.
However, the billing mechanism used in this situation varies from the standard. Instead of reporting each service separately under each corresponding hospitalist’s name, the hospitalists select subsequent hospital care code 99231-99233 representing the combined visits and submit one appropriate code for the collective level of service.
The difficulty is selecting the name that will appear on the claim form. Solutions range from reporting the hospitalist who provided the first encounter of the day to identifying the hospitalist who provided the most extensive or best-documented encounter of the day. For productivity analysis, some practices develop an internal accounting system and credit each hospitalist for their medically necessary joint efforts. The latter option is a labor-intensive task for administrators.
Physicians in the same group practice but different specialties may bill and be paid without regard to their membership in the same group. For example, a hospitalist and an infectious disease specialist may be part of the same multispecialty group practice and bill under a group tax-identification number, yet qualify for separate payment.
This is permitted if each physician has a differing specialty code designation. Specialty codes are self-designated, two-digit representations that describe the kind of medicine physicians, non-physician practitioners, or other healthcare providers/suppliers practice. They are initially selected and registered with each payer during the enrollment process.
A list of qualifying specialty codes can be found at www.cms.hhs.gov/MedicareFeeforSvcPartsAB/Downloads/SpecialtyCodes2207.pdf.
Covering Physicians
Hospital inpatient situations involving physician coverage are complicated. If Dr. Richards sees the patient earlier in the day and Dr. Andrews, covering for Dr. Richards, sees the same patient later that same day, Dr. Andrews cannot be paid for the second visit.
Subsequent hospital care descriptors emphasize “per day” to account for all care provided during the calendar day. Insurers treat the covering physician as if he were the physician being covered. Services provided by each are handled in the same manner described above.
If each hospitalist is responsible for a different aspect of the patient’s care, payment is made for both visits if:
- The hospitalists are in different specialties and different group practices;
- The visits are billed with different diagnoses; and
- The patient is a Medicare beneficiary or a member of an insurance plan that adopts Medicare rules.
There are limited circumstances where concurrent care can be billed to Medicare by hospitalists of the same specialty (e.g., an internist and a hospitalist, one with significant and demonstrated expertise in pain management).
Each hospitalist must belong to a different group practice and submit claims under different tax identification numbers. The patient’s condition must require the expertise possessed by the “sub-specialist.” Payment will be denied in the initial claim determination. But formulating a Medicare appeal with documentation from both encounters can demonstrate the medical necessity and separateness of each service and help earn reimbursement—although it is not guaranteed.
Managed-care payment for two visits on the same day by physicians of the same registered specialty (e.g., internal medicine), regardless of sub-specialization, is highly unlikely. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Subsequent hospital care, also known as daily care, presents a variety of daily-care scenarios that cause confusion for billing providers.
Subsequent hospital care codes are reported once per day after the initial patient encounter (e.g., admission or consultation service), but only when a face-to-face visit occurs between provider and patient.
The entire visit need not take place at the bedside. It may include other important elements performed on the patient’s unit/floor such as data review, discussions with other healthcare professionals, coordination of care, and family meetings. In addition, subsequent hospital care codes represent the cumulative evaluation and management service performed on a calendar date, even if the hospitalist evaluates the patient for different reasons or at different times throughout the day.
Concurrent Care
Traditionally, concurrent care occurs when physicians of different specialties and group practices participate in a patient’s care. Each physician manages a particular aspect while considering the patient’s overall condition.
When submitting claims for concurrent care services, each physician should report the appropriate subsequent hospital care code and the corresponding diagnosis each primarily manages. If billed correctly, each hospitalist will have a different primary diagnosis code and be more likely to receive payment.
Some managed-care payers require each hospitalist to append modifier 25 to their evaluation and management (E/M) visit code (99232-25) even though each submits claims under different tax identification numbers. Modifier 25 is a separately identifiable E/M service performed on the same day as a procedure or other E/M service. In this situation, Medicare is likely to reimburse as appropriate.
Payment by managed-care companies is less easily obtained: Payment for the first received claim is likely, and denial of any claim received beyond the first claim is inevitable. Appealing the denied claims with documentation for each hospitalist’s visit on a given date helps the payer understand the need for each service.
Group Practice
When concurrent care is provided by members of the same group practice, claim reporting becomes more complex. Physicians in the same group practice and specialty bill and are paid as though to a single physician. In other words, if two hospitalists evaluate a patient on the same day (e.g., one hospitalist sees the patient in the morning, and another one sees the patient in the afternoon), the efforts of each medically necessary evaluation and management service may be captured.
However, the billing mechanism used in this situation varies from the standard. Instead of reporting each service separately under each corresponding hospitalist’s name, the hospitalists select subsequent hospital care code 99231-99233 representing the combined visits and submit one appropriate code for the collective level of service.
The difficulty is selecting the name that will appear on the claim form. Solutions range from reporting the hospitalist who provided the first encounter of the day to identifying the hospitalist who provided the most extensive or best-documented encounter of the day. For productivity analysis, some practices develop an internal accounting system and credit each hospitalist for their medically necessary joint efforts. The latter option is a labor-intensive task for administrators.
Physicians in the same group practice but different specialties may bill and be paid without regard to their membership in the same group. For example, a hospitalist and an infectious disease specialist may be part of the same multispecialty group practice and bill under a group tax-identification number, yet qualify for separate payment.
This is permitted if each physician has a differing specialty code designation. Specialty codes are self-designated, two-digit representations that describe the kind of medicine physicians, non-physician practitioners, or other healthcare providers/suppliers practice. They are initially selected and registered with each payer during the enrollment process.
A list of qualifying specialty codes can be found at www.cms.hhs.gov/MedicareFeeforSvcPartsAB/Downloads/SpecialtyCodes2207.pdf.
Covering Physicians
Hospital inpatient situations involving physician coverage are complicated. If Dr. Richards sees the patient earlier in the day and Dr. Andrews, covering for Dr. Richards, sees the same patient later that same day, Dr. Andrews cannot be paid for the second visit.
Subsequent hospital care descriptors emphasize “per day” to account for all care provided during the calendar day. Insurers treat the covering physician as if he were the physician being covered. Services provided by each are handled in the same manner described above.
If each hospitalist is responsible for a different aspect of the patient’s care, payment is made for both visits if:
- The hospitalists are in different specialties and different group practices;
- The visits are billed with different diagnoses; and
- The patient is a Medicare beneficiary or a member of an insurance plan that adopts Medicare rules.
There are limited circumstances where concurrent care can be billed to Medicare by hospitalists of the same specialty (e.g., an internist and a hospitalist, one with significant and demonstrated expertise in pain management).
Each hospitalist must belong to a different group practice and submit claims under different tax identification numbers. The patient’s condition must require the expertise possessed by the “sub-specialist.” Payment will be denied in the initial claim determination. But formulating a Medicare appeal with documentation from both encounters can demonstrate the medical necessity and separateness of each service and help earn reimbursement—although it is not guaranteed.
Managed-care payment for two visits on the same day by physicians of the same registered specialty (e.g., internal medicine), regardless of sub-specialization, is highly unlikely. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
The Admission Consult
When consultation services occur in inpatient and outpatient settings, physicians report the code category that best corresponds to the patient’s registered status at the time of service:
- Inpatient consultation (99251-99255) for services provided to an inpatient (acute care, inpatient rehabilitation, inpatient psychiatric, long-term acute care, or skilled nursing); or
- Outpatient consultation (99241-99245) for services provided to an outpatient (office, emergency department [ED], or observation care).
Regardless of location, consultants must meet each requirement before submitting a claim for these services. This article focuses on the coding and billing nuances of inpatient consultation services; outpatient consultations provided in the ED or during observation care will be addressed in a future issue.
The Three R’s
Reason and request: Consultants (physicians or qualified non-physician providers) are asked to give an opinion or recommendation, a suggestion, direction, or counsel in the treatment of a patient’s condition because the consultant has expertise in a specific medical area beyond the requesting professional’s knowledge.
The requesting professional must be a physician or other qualified healthcare provider (e.g., nurse practitioner, physician assistant, resident acting under guidance of a teaching physician) currently involved in the patient’s care. Do not report consultation codes when a patient, family member, or third party requests a second opinion. Instead, select the most appropriate subsequent hospital care code (99231-99233).
The request must be documented in the patient’s medical record. The initial request may be a verbal interaction between the requesting provider and the consulting physician; however, when this occurs, the verbal conversation must be documented by both the consultant (in the progress note) and the requesting provider (in the plan of care or as a written order). Standing orders for consultation are prohibited. Clearly document the reason for the service: the patient’s condition, sign, or symptoms that prompted the consult request, ensuring the medical necessity of the service.
Try to avoid terminology, such as “Consult hospitalist for perioperative management.” This leads to the payer’s confusion about co-management issues. The documentation should reflect the true intent of the service: “Consult hospitalist for perioperative risk assessment.” If necessary, ask the requesting provider to clarify the request. The consultant should further explain the request in his/her own note.
Report: After the patient’s assessment, the consultant documents the service and prepares a written report for the requesting provider, which includes the written request, consultation evaluation, findings, and recommendations.
It is appropriate for the consultant to initiate diagnostic services and treatment at the initial consultation service or at a subsequent visit, yet still qualify as a consult. In the inpatient setting, it is acceptable for the consultant’s report to appear as an entry in the shared medical record without need to forward a separate document to the requesting provider.
Code Use
Inpatient consultation codes are reported once per hospitalization. If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99251-99255 are denied. This happens even when the consultant signs off and is re-consulted for a different problem during the same hospitalization.
A physician who provides patient services after the initial consultation reports subsequent hospital care codes 99231-99233 for each date in which a face-to-face encounter occurs.
A physician or qualified nonphysician provider may request a consultation from a member of the same group practice as long as the consultant possesses a legitimate expertise in a specific medical area beyond the requesting professional’s knowledge (e.g., a hospitalist may consult a member of his group who specializes in infectious disease).
This situation is likely to produce a rejected consult claim. In appealing the claim, submit notes from each member of the group (i.e., the requesting provider and the consultant) to demonstrate medical necessity and distinguish the expertise involved in each service. Medicare and payers who follow Medicare guidelines should reimburse the consult after the documentation is reviewed.
Co-management
Preoperative consults: Preoperative consultations are permitted when performed by any physician or qualified nonphysician provider at the request of a surgeon—as long as all requirements for performing and reporting the consultation codes are met. The service must be medically necessary and not provided for routine screening (i.e., consults for healthy patients scheduled for elective surgery).
Postoperative management: If a physician or qualified nonphysician provider who has performed a preoperative consultation is subsequently consulted and/or assumes responsibility for the complete or partial management of the patient’s condition(s) during the postoperative period, the appropriate subsequent hospital care code 99231-99233 is used.
Additionally, do not report consultation codes when the surgeon asks the hospitalist to take responsibility for the management of an aspect of the patient’s condition during the postoperative period (i.e., consult for postoperative management). In this situation, the surgeon is not asking the consultant for an opinion or advice for the surgeon’s use in treating the patient, and the surgeon is not expected to continue on the case. This constitutes concurrent care and is billed with the appropriate subsequent hospital care codes.
Alternately, the surgeon may continue on the case, not transferring the care for the remaining portion of the hospitalization to the hospitalist, and incorporating the hospitalist’s recommendations into his/her own care plan, subsequently retaining the hospitalist’s services in assisting with care. Because the transfer did not occur prior to the consultation, this situation may constitute an inpatient consultation and be reported as such.
Unfortunately, some local Medicare contractors do not recognize this latter distinction and prohibit reporting post-surgical involvement with 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
When consultation services occur in inpatient and outpatient settings, physicians report the code category that best corresponds to the patient’s registered status at the time of service:
- Inpatient consultation (99251-99255) for services provided to an inpatient (acute care, inpatient rehabilitation, inpatient psychiatric, long-term acute care, or skilled nursing); or
- Outpatient consultation (99241-99245) for services provided to an outpatient (office, emergency department [ED], or observation care).
Regardless of location, consultants must meet each requirement before submitting a claim for these services. This article focuses on the coding and billing nuances of inpatient consultation services; outpatient consultations provided in the ED or during observation care will be addressed in a future issue.
The Three R’s
Reason and request: Consultants (physicians or qualified non-physician providers) are asked to give an opinion or recommendation, a suggestion, direction, or counsel in the treatment of a patient’s condition because the consultant has expertise in a specific medical area beyond the requesting professional’s knowledge.
The requesting professional must be a physician or other qualified healthcare provider (e.g., nurse practitioner, physician assistant, resident acting under guidance of a teaching physician) currently involved in the patient’s care. Do not report consultation codes when a patient, family member, or third party requests a second opinion. Instead, select the most appropriate subsequent hospital care code (99231-99233).
The request must be documented in the patient’s medical record. The initial request may be a verbal interaction between the requesting provider and the consulting physician; however, when this occurs, the verbal conversation must be documented by both the consultant (in the progress note) and the requesting provider (in the plan of care or as a written order). Standing orders for consultation are prohibited. Clearly document the reason for the service: the patient’s condition, sign, or symptoms that prompted the consult request, ensuring the medical necessity of the service.
Try to avoid terminology, such as “Consult hospitalist for perioperative management.” This leads to the payer’s confusion about co-management issues. The documentation should reflect the true intent of the service: “Consult hospitalist for perioperative risk assessment.” If necessary, ask the requesting provider to clarify the request. The consultant should further explain the request in his/her own note.
Report: After the patient’s assessment, the consultant documents the service and prepares a written report for the requesting provider, which includes the written request, consultation evaluation, findings, and recommendations.
It is appropriate for the consultant to initiate diagnostic services and treatment at the initial consultation service or at a subsequent visit, yet still qualify as a consult. In the inpatient setting, it is acceptable for the consultant’s report to appear as an entry in the shared medical record without need to forward a separate document to the requesting provider.
Code Use
Inpatient consultation codes are reported once per hospitalization. If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99251-99255 are denied. This happens even when the consultant signs off and is re-consulted for a different problem during the same hospitalization.
A physician who provides patient services after the initial consultation reports subsequent hospital care codes 99231-99233 for each date in which a face-to-face encounter occurs.
A physician or qualified nonphysician provider may request a consultation from a member of the same group practice as long as the consultant possesses a legitimate expertise in a specific medical area beyond the requesting professional’s knowledge (e.g., a hospitalist may consult a member of his group who specializes in infectious disease).
This situation is likely to produce a rejected consult claim. In appealing the claim, submit notes from each member of the group (i.e., the requesting provider and the consultant) to demonstrate medical necessity and distinguish the expertise involved in each service. Medicare and payers who follow Medicare guidelines should reimburse the consult after the documentation is reviewed.
Co-management
Preoperative consults: Preoperative consultations are permitted when performed by any physician or qualified nonphysician provider at the request of a surgeon—as long as all requirements for performing and reporting the consultation codes are met. The service must be medically necessary and not provided for routine screening (i.e., consults for healthy patients scheduled for elective surgery).
Postoperative management: If a physician or qualified nonphysician provider who has performed a preoperative consultation is subsequently consulted and/or assumes responsibility for the complete or partial management of the patient’s condition(s) during the postoperative period, the appropriate subsequent hospital care code 99231-99233 is used.
Additionally, do not report consultation codes when the surgeon asks the hospitalist to take responsibility for the management of an aspect of the patient’s condition during the postoperative period (i.e., consult for postoperative management). In this situation, the surgeon is not asking the consultant for an opinion or advice for the surgeon’s use in treating the patient, and the surgeon is not expected to continue on the case. This constitutes concurrent care and is billed with the appropriate subsequent hospital care codes.
Alternately, the surgeon may continue on the case, not transferring the care for the remaining portion of the hospitalization to the hospitalist, and incorporating the hospitalist’s recommendations into his/her own care plan, subsequently retaining the hospitalist’s services in assisting with care. Because the transfer did not occur prior to the consultation, this situation may constitute an inpatient consultation and be reported as such.
Unfortunately, some local Medicare contractors do not recognize this latter distinction and prohibit reporting post-surgical involvement with 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
When consultation services occur in inpatient and outpatient settings, physicians report the code category that best corresponds to the patient’s registered status at the time of service:
- Inpatient consultation (99251-99255) for services provided to an inpatient (acute care, inpatient rehabilitation, inpatient psychiatric, long-term acute care, or skilled nursing); or
- Outpatient consultation (99241-99245) for services provided to an outpatient (office, emergency department [ED], or observation care).
Regardless of location, consultants must meet each requirement before submitting a claim for these services. This article focuses on the coding and billing nuances of inpatient consultation services; outpatient consultations provided in the ED or during observation care will be addressed in a future issue.
The Three R’s
Reason and request: Consultants (physicians or qualified non-physician providers) are asked to give an opinion or recommendation, a suggestion, direction, or counsel in the treatment of a patient’s condition because the consultant has expertise in a specific medical area beyond the requesting professional’s knowledge.
The requesting professional must be a physician or other qualified healthcare provider (e.g., nurse practitioner, physician assistant, resident acting under guidance of a teaching physician) currently involved in the patient’s care. Do not report consultation codes when a patient, family member, or third party requests a second opinion. Instead, select the most appropriate subsequent hospital care code (99231-99233).
The request must be documented in the patient’s medical record. The initial request may be a verbal interaction between the requesting provider and the consulting physician; however, when this occurs, the verbal conversation must be documented by both the consultant (in the progress note) and the requesting provider (in the plan of care or as a written order). Standing orders for consultation are prohibited. Clearly document the reason for the service: the patient’s condition, sign, or symptoms that prompted the consult request, ensuring the medical necessity of the service.
Try to avoid terminology, such as “Consult hospitalist for perioperative management.” This leads to the payer’s confusion about co-management issues. The documentation should reflect the true intent of the service: “Consult hospitalist for perioperative risk assessment.” If necessary, ask the requesting provider to clarify the request. The consultant should further explain the request in his/her own note.
Report: After the patient’s assessment, the consultant documents the service and prepares a written report for the requesting provider, which includes the written request, consultation evaluation, findings, and recommendations.
It is appropriate for the consultant to initiate diagnostic services and treatment at the initial consultation service or at a subsequent visit, yet still qualify as a consult. In the inpatient setting, it is acceptable for the consultant’s report to appear as an entry in the shared medical record without need to forward a separate document to the requesting provider.
Code Use
Inpatient consultation codes are reported once per hospitalization. If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99251-99255 are denied. This happens even when the consultant signs off and is re-consulted for a different problem during the same hospitalization.
A physician who provides patient services after the initial consultation reports subsequent hospital care codes 99231-99233 for each date in which a face-to-face encounter occurs.
A physician or qualified nonphysician provider may request a consultation from a member of the same group practice as long as the consultant possesses a legitimate expertise in a specific medical area beyond the requesting professional’s knowledge (e.g., a hospitalist may consult a member of his group who specializes in infectious disease).
This situation is likely to produce a rejected consult claim. In appealing the claim, submit notes from each member of the group (i.e., the requesting provider and the consultant) to demonstrate medical necessity and distinguish the expertise involved in each service. Medicare and payers who follow Medicare guidelines should reimburse the consult after the documentation is reviewed.
Co-management
Preoperative consults: Preoperative consultations are permitted when performed by any physician or qualified nonphysician provider at the request of a surgeon—as long as all requirements for performing and reporting the consultation codes are met. The service must be medically necessary and not provided for routine screening (i.e., consults for healthy patients scheduled for elective surgery).
Postoperative management: If a physician or qualified nonphysician provider who has performed a preoperative consultation is subsequently consulted and/or assumes responsibility for the complete or partial management of the patient’s condition(s) during the postoperative period, the appropriate subsequent hospital care code 99231-99233 is used.
Additionally, do not report consultation codes when the surgeon asks the hospitalist to take responsibility for the management of an aspect of the patient’s condition during the postoperative period (i.e., consult for postoperative management). In this situation, the surgeon is not asking the consultant for an opinion or advice for the surgeon’s use in treating the patient, and the surgeon is not expected to continue on the case. This constitutes concurrent care and is billed with the appropriate subsequent hospital care codes.
Alternately, the surgeon may continue on the case, not transferring the care for the remaining portion of the hospitalization to the hospitalist, and incorporating the hospitalist’s recommendations into his/her own care plan, subsequently retaining the hospitalist’s services in assisting with care. Because the transfer did not occur prior to the consultation, this situation may constitute an inpatient consultation and be reported as such.
Unfortunately, some local Medicare contractors do not recognize this latter distinction and prohibit reporting post-surgical involvement with 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Demystify Admissions
Physicians may encounter patients in various ways during the first few days of a hospitalization: admission services, consultations, and medical-surgical co-management.
Submitting claims for these services is often inconsistent and inaccurate because billing education is not a standard part of medical education.
In an attempt to clarify the rules and reduce frustration, I will address billing, coding, and reimbursement guidelines for each type of initial hospital encounter over the next several issues.
Definition
Initial Hospital Care (IHC) comprises all services related to the patient’s admission to an acute care facility. An acute care facility is any that registers inpatients but does not have a corresponding Current Procedural Terminology (CPT) code category for claim reporting. Acute care facilities also include “partial hospitals.”
For example, admissions to inpatient rehabilitation are reported with IHC codes 99221-99223, while nursing facility admissions have a designated category and are best reported with CPT codes 99304-99306 for Initial Nursing Facility Care.
Code Use
IHC codes are reported once per hospitalization and reserved for the physician/group assuming primary responsibility for the patient’s care during that time.
If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99221-99223 are denied or rejected pending review of documentation to ascertain the correct service date and responsible party. This is common because physicians confuse code description IHC with its true intent. They mistakenly report these codes for their first inpatient encounter, regardless of the encounter date or the admitting physician/group.
Specialists assisting in the patient’s management and not primarily responsible for the entire hospitalization report the code category that best reflects the performed service and documentation—as long as the selected category requirements are met. The physician selects from either Inpatient Consultation codes 99251-99255 or Subsequent Hospital Care (SHC) codes 99231-99233. Any physician who provides patient services after the initial encounter, including those by the responsible attending physician/group or a specialist concurrently involved in the patient’s care, reports SHC codes for each date in which a face-to-face encounter occurs.
When services begin in one location (e.g., physician’s office, emergency department, or observation) and end with an inpatient admission on the same calendar day, the physician reports only the most appropriate initial hospital care code. It is not necessary for the physician to duplicate the information from the earlier encounter for the admission service. Instead, the physician can forward a copy of the progress note from the earlier encounter to the inpatient chart, along with the documented decision for admission and pertinent information obtained throughout the day. Auditors consider the culmination of all chart entries in a given date when reviewed. When services begin in one location but end with an admission on different calendar day, the physician separately reports each service provided on each date: 99220 on Day 1 and 99223 on Day 2.
Intrafacility Transfers
Patients may receive different components of inpatient services within the same (uninterrupted) episode of care, all within the same building but treated as separate facility admissions (e.g., rehabilitation or long-term acute care).
It is unlikely the attending physician of record during the acute care phase will also be the attending physician during the second phase of care. Should this occur, Medicare contractors and those payers who follow Medicare guidelines permit the attending physician to separately report the acute care discharge (99238-99239) and the secondary admission (99221-99223), but only in the absence of a shared medical record (see Section 30.6.9.1D,www.cms.hhs.gov/manuals/downloads/clm104c12.pdf). If a common chart is used, the physician reports the secondary admission services as ongoing care, using SHC codes 99231-99233 instead.
Similarly, transfers occur within a single phase of care, such as transfers to and from a medical intensive care unit and a standard medical-surgical unit. Such transfers are not treated as separate admissions, and the receiving physician reports only the SHC codes because the IHC service was previously reported by the admitting physician/group. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia.
Physicians may encounter patients in various ways during the first few days of a hospitalization: admission services, consultations, and medical-surgical co-management.
Submitting claims for these services is often inconsistent and inaccurate because billing education is not a standard part of medical education.
In an attempt to clarify the rules and reduce frustration, I will address billing, coding, and reimbursement guidelines for each type of initial hospital encounter over the next several issues.
Definition
Initial Hospital Care (IHC) comprises all services related to the patient’s admission to an acute care facility. An acute care facility is any that registers inpatients but does not have a corresponding Current Procedural Terminology (CPT) code category for claim reporting. Acute care facilities also include “partial hospitals.”
For example, admissions to inpatient rehabilitation are reported with IHC codes 99221-99223, while nursing facility admissions have a designated category and are best reported with CPT codes 99304-99306 for Initial Nursing Facility Care.
Code Use
IHC codes are reported once per hospitalization and reserved for the physician/group assuming primary responsibility for the patient’s care during that time.
If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99221-99223 are denied or rejected pending review of documentation to ascertain the correct service date and responsible party. This is common because physicians confuse code description IHC with its true intent. They mistakenly report these codes for their first inpatient encounter, regardless of the encounter date or the admitting physician/group.
Specialists assisting in the patient’s management and not primarily responsible for the entire hospitalization report the code category that best reflects the performed service and documentation—as long as the selected category requirements are met. The physician selects from either Inpatient Consultation codes 99251-99255 or Subsequent Hospital Care (SHC) codes 99231-99233. Any physician who provides patient services after the initial encounter, including those by the responsible attending physician/group or a specialist concurrently involved in the patient’s care, reports SHC codes for each date in which a face-to-face encounter occurs.
When services begin in one location (e.g., physician’s office, emergency department, or observation) and end with an inpatient admission on the same calendar day, the physician reports only the most appropriate initial hospital care code. It is not necessary for the physician to duplicate the information from the earlier encounter for the admission service. Instead, the physician can forward a copy of the progress note from the earlier encounter to the inpatient chart, along with the documented decision for admission and pertinent information obtained throughout the day. Auditors consider the culmination of all chart entries in a given date when reviewed. When services begin in one location but end with an admission on different calendar day, the physician separately reports each service provided on each date: 99220 on Day 1 and 99223 on Day 2.
Intrafacility Transfers
Patients may receive different components of inpatient services within the same (uninterrupted) episode of care, all within the same building but treated as separate facility admissions (e.g., rehabilitation or long-term acute care).
It is unlikely the attending physician of record during the acute care phase will also be the attending physician during the second phase of care. Should this occur, Medicare contractors and those payers who follow Medicare guidelines permit the attending physician to separately report the acute care discharge (99238-99239) and the secondary admission (99221-99223), but only in the absence of a shared medical record (see Section 30.6.9.1D,www.cms.hhs.gov/manuals/downloads/clm104c12.pdf). If a common chart is used, the physician reports the secondary admission services as ongoing care, using SHC codes 99231-99233 instead.
Similarly, transfers occur within a single phase of care, such as transfers to and from a medical intensive care unit and a standard medical-surgical unit. Such transfers are not treated as separate admissions, and the receiving physician reports only the SHC codes because the IHC service was previously reported by the admitting physician/group. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia.
Physicians may encounter patients in various ways during the first few days of a hospitalization: admission services, consultations, and medical-surgical co-management.
Submitting claims for these services is often inconsistent and inaccurate because billing education is not a standard part of medical education.
In an attempt to clarify the rules and reduce frustration, I will address billing, coding, and reimbursement guidelines for each type of initial hospital encounter over the next several issues.
Definition
Initial Hospital Care (IHC) comprises all services related to the patient’s admission to an acute care facility. An acute care facility is any that registers inpatients but does not have a corresponding Current Procedural Terminology (CPT) code category for claim reporting. Acute care facilities also include “partial hospitals.”
For example, admissions to inpatient rehabilitation are reported with IHC codes 99221-99223, while nursing facility admissions have a designated category and are best reported with CPT codes 99304-99306 for Initial Nursing Facility Care.
Code Use
IHC codes are reported once per hospitalization and reserved for the physician/group assuming primary responsibility for the patient’s care during that time.
If reported more frequently, all claims within the same hospitalization subsequently reported with codes 99221-99223 are denied or rejected pending review of documentation to ascertain the correct service date and responsible party. This is common because physicians confuse code description IHC with its true intent. They mistakenly report these codes for their first inpatient encounter, regardless of the encounter date or the admitting physician/group.
Specialists assisting in the patient’s management and not primarily responsible for the entire hospitalization report the code category that best reflects the performed service and documentation—as long as the selected category requirements are met. The physician selects from either Inpatient Consultation codes 99251-99255 or Subsequent Hospital Care (SHC) codes 99231-99233. Any physician who provides patient services after the initial encounter, including those by the responsible attending physician/group or a specialist concurrently involved in the patient’s care, reports SHC codes for each date in which a face-to-face encounter occurs.
When services begin in one location (e.g., physician’s office, emergency department, or observation) and end with an inpatient admission on the same calendar day, the physician reports only the most appropriate initial hospital care code. It is not necessary for the physician to duplicate the information from the earlier encounter for the admission service. Instead, the physician can forward a copy of the progress note from the earlier encounter to the inpatient chart, along with the documented decision for admission and pertinent information obtained throughout the day. Auditors consider the culmination of all chart entries in a given date when reviewed. When services begin in one location but end with an admission on different calendar day, the physician separately reports each service provided on each date: 99220 on Day 1 and 99223 on Day 2.
Intrafacility Transfers
Patients may receive different components of inpatient services within the same (uninterrupted) episode of care, all within the same building but treated as separate facility admissions (e.g., rehabilitation or long-term acute care).
It is unlikely the attending physician of record during the acute care phase will also be the attending physician during the second phase of care. Should this occur, Medicare contractors and those payers who follow Medicare guidelines permit the attending physician to separately report the acute care discharge (99238-99239) and the secondary admission (99221-99223), but only in the absence of a shared medical record (see Section 30.6.9.1D,www.cms.hhs.gov/manuals/downloads/clm104c12.pdf). If a common chart is used, the physician reports the secondary admission services as ongoing care, using SHC codes 99231-99233 instead.
Similarly, transfers occur within a single phase of care, such as transfers to and from a medical intensive care unit and a standard medical-surgical unit. Such transfers are not treated as separate admissions, and the receiving physician reports only the SHC codes because the IHC service was previously reported by the admitting physician/group. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia.