User login
Code Correctly
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.
Palliative-Care Payment
Many hospitalists provide palliative-care services to patients at the request of physicians within their own groups or from other specialists. Varying factors affect how hospitalists report these services—namely, the nature of the request and the type of service provided. Palliative-care programs can be quite costly as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives is pertinent.
Nature of the Request
Members of a palliative-care team often are called on to provide management options to assist in reducing pain and suffering associated with both terminal and nonterminal disease, thereby improving a patient’s quality of life. When a palliative-care specialist is asked to provide an opinion or advice, the initial service could qualify as a consultation. However, all requirements must be met in order to report the service as an inpatient consultation (codes 99251-99255).
There must be a written request from a qualified healthcare provider involved in the patient’s care (e.g., a physician, resident, or nurse practitioner). In the inpatient setting, this request can be documented as a physician order or in the assessment of the requesting provider’s progress note. Standing orders for consultation are not permitted. Ideally, the requesting provider should identify the reason for a consult to support the medical necessity of the service.
Additionally, the palliative-care physician renders and documents the service, then reports findings to the requesting physician. The consultant’s required written report does not have to be sent separately to the requesting physician. Because the requesting physician and the consultant share a common medical record in an inpatient setting, the consultant’s inpatient progress note suffices the “written report” requirement.
One concern about billing consultations involves the nature of the request. If the requesting physician documents the need for an opinion or advice from the palliative-care specialist, the service can be reported as a consultation. If, however, the request states consult for “medical management” or “palliative management,” it’s less likely that payors will consider the service a consultation. In the latter situation, it appears as if the requesting physician is not seeking an opinion or advice from the consultant to incorporate into his own plan of care for the patient and would rather the consultant take over that portion of patient care.
Recently revised billing policies prevent the consultant from billing consults under these circumstances. Without a sufficient request for consultation, the palliative-care specialist can only report “subsequent” hospital care services.1 Language that better supports the consultative nature of the request is:
- Consult for an opinion or advice on palliative measures;
- Consult for evaluation of palliative options; and
- Consult palliative care for treatment options.
Proper Documentation
The requesting physician can be in the same or different provider group as the consultant. The consultant must possess expertise in an area beyond that of the requesting provider. Because the specialty designation for most hospitalists is internal medicine, palliative-care claims could be scrutinized more closely. This does not necessarily occur when the requesting provider has a different two-digit specialty designation (e.g., internal medicine and gastroenterology).2 Scrutiny is more likely to occur when the requesting provider has the same internal-medicine designation as the palliative-care consultant, even if they are in different provider groups.
Payor concern escalates when physicians of the same designated specialty submit claims for the same patient on the same date. Having different primary diagnosis codes attached to each visit level does not necessarily help. The payor is likely to deny the second claim received, pending a review of documentation. If this happens, the provider who received the denial should submit a copy of both progress notes for the date in question. Hopefully, the distinction between the services is demonstrated in the documentation.
Service Type
Palliative services might involve obtaining and documenting the standard key components for visit-level selection: history, exam, and medical decision-making.3 However, the palliative-care specialist might spend more time providing counseling or coordination of care for a patient and family. When this occurs, the palliative-care specialist should not forget about the guidelines for reporting time-based services.4 Inpatient services may be reported on the basis of time, as long as a face-to-face service between the provider and the patient occurs. Consider the total time spent face to face with the patient, and the time spent obtaining, discussing, and coordinating patient care, while you are in the patient’s unit or floor.
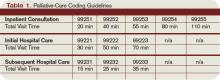
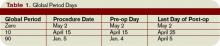
As a reminder, document the total time, the amount of time spent counseling, and the details of discussion and coordination. The physician may count the time spent counseling the patient’s family regarding the treatment and care, as long as the focus is not emotional support for the family, the meeting takes place in the patient’s unit or floor, and the patient is present, unless there is medically supported reason for which the patient is unable to participate (e.g., cognitive impairment). The palliative-care specialist can then select the visit level based on time.5 (See Table 1, above.) TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.10. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26, Section 10.8. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c26.pdf. Accessed Jan. 30, 2009.
3. Centers for Medicare and Medicaid Services. Documentation Guidelines for Evaluation and Management Services. CMS Web site. Available at: www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp. Accessed Jan. 30, 2009.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
Many hospitalists provide palliative-care services to patients at the request of physicians within their own groups or from other specialists. Varying factors affect how hospitalists report these services—namely, the nature of the request and the type of service provided. Palliative-care programs can be quite costly as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives is pertinent.
Nature of the Request
Members of a palliative-care team often are called on to provide management options to assist in reducing pain and suffering associated with both terminal and nonterminal disease, thereby improving a patient’s quality of life. When a palliative-care specialist is asked to provide an opinion or advice, the initial service could qualify as a consultation. However, all requirements must be met in order to report the service as an inpatient consultation (codes 99251-99255).
There must be a written request from a qualified healthcare provider involved in the patient’s care (e.g., a physician, resident, or nurse practitioner). In the inpatient setting, this request can be documented as a physician order or in the assessment of the requesting provider’s progress note. Standing orders for consultation are not permitted. Ideally, the requesting provider should identify the reason for a consult to support the medical necessity of the service.
Additionally, the palliative-care physician renders and documents the service, then reports findings to the requesting physician. The consultant’s required written report does not have to be sent separately to the requesting physician. Because the requesting physician and the consultant share a common medical record in an inpatient setting, the consultant’s inpatient progress note suffices the “written report” requirement.
One concern about billing consultations involves the nature of the request. If the requesting physician documents the need for an opinion or advice from the palliative-care specialist, the service can be reported as a consultation. If, however, the request states consult for “medical management” or “palliative management,” it’s less likely that payors will consider the service a consultation. In the latter situation, it appears as if the requesting physician is not seeking an opinion or advice from the consultant to incorporate into his own plan of care for the patient and would rather the consultant take over that portion of patient care.
Recently revised billing policies prevent the consultant from billing consults under these circumstances. Without a sufficient request for consultation, the palliative-care specialist can only report “subsequent” hospital care services.1 Language that better supports the consultative nature of the request is:
- Consult for an opinion or advice on palliative measures;
- Consult for evaluation of palliative options; and
- Consult palliative care for treatment options.
Proper Documentation
The requesting physician can be in the same or different provider group as the consultant. The consultant must possess expertise in an area beyond that of the requesting provider. Because the specialty designation for most hospitalists is internal medicine, palliative-care claims could be scrutinized more closely. This does not necessarily occur when the requesting provider has a different two-digit specialty designation (e.g., internal medicine and gastroenterology).2 Scrutiny is more likely to occur when the requesting provider has the same internal-medicine designation as the palliative-care consultant, even if they are in different provider groups.
Payor concern escalates when physicians of the same designated specialty submit claims for the same patient on the same date. Having different primary diagnosis codes attached to each visit level does not necessarily help. The payor is likely to deny the second claim received, pending a review of documentation. If this happens, the provider who received the denial should submit a copy of both progress notes for the date in question. Hopefully, the distinction between the services is demonstrated in the documentation.
Service Type
Palliative services might involve obtaining and documenting the standard key components for visit-level selection: history, exam, and medical decision-making.3 However, the palliative-care specialist might spend more time providing counseling or coordination of care for a patient and family. When this occurs, the palliative-care specialist should not forget about the guidelines for reporting time-based services.4 Inpatient services may be reported on the basis of time, as long as a face-to-face service between the provider and the patient occurs. Consider the total time spent face to face with the patient, and the time spent obtaining, discussing, and coordinating patient care, while you are in the patient’s unit or floor.
As a reminder, document the total time, the amount of time spent counseling, and the details of discussion and coordination. The physician may count the time spent counseling the patient’s family regarding the treatment and care, as long as the focus is not emotional support for the family, the meeting takes place in the patient’s unit or floor, and the patient is present, unless there is medically supported reason for which the patient is unable to participate (e.g., cognitive impairment). The palliative-care specialist can then select the visit level based on time.5 (See Table 1, above.) TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.10. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26, Section 10.8. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c26.pdf. Accessed Jan. 30, 2009.
3. Centers for Medicare and Medicaid Services. Documentation Guidelines for Evaluation and Management Services. CMS Web site. Available at: www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp. Accessed Jan. 30, 2009.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
Many hospitalists provide palliative-care services to patients at the request of physicians within their own groups or from other specialists. Varying factors affect how hospitalists report these services—namely, the nature of the request and the type of service provided. Palliative-care programs can be quite costly as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives is pertinent.
Nature of the Request
Members of a palliative-care team often are called on to provide management options to assist in reducing pain and suffering associated with both terminal and nonterminal disease, thereby improving a patient’s quality of life. When a palliative-care specialist is asked to provide an opinion or advice, the initial service could qualify as a consultation. However, all requirements must be met in order to report the service as an inpatient consultation (codes 99251-99255).
There must be a written request from a qualified healthcare provider involved in the patient’s care (e.g., a physician, resident, or nurse practitioner). In the inpatient setting, this request can be documented as a physician order or in the assessment of the requesting provider’s progress note. Standing orders for consultation are not permitted. Ideally, the requesting provider should identify the reason for a consult to support the medical necessity of the service.
Additionally, the palliative-care physician renders and documents the service, then reports findings to the requesting physician. The consultant’s required written report does not have to be sent separately to the requesting physician. Because the requesting physician and the consultant share a common medical record in an inpatient setting, the consultant’s inpatient progress note suffices the “written report” requirement.
One concern about billing consultations involves the nature of the request. If the requesting physician documents the need for an opinion or advice from the palliative-care specialist, the service can be reported as a consultation. If, however, the request states consult for “medical management” or “palliative management,” it’s less likely that payors will consider the service a consultation. In the latter situation, it appears as if the requesting physician is not seeking an opinion or advice from the consultant to incorporate into his own plan of care for the patient and would rather the consultant take over that portion of patient care.
Recently revised billing policies prevent the consultant from billing consults under these circumstances. Without a sufficient request for consultation, the palliative-care specialist can only report “subsequent” hospital care services.1 Language that better supports the consultative nature of the request is:
- Consult for an opinion or advice on palliative measures;
- Consult for evaluation of palliative options; and
- Consult palliative care for treatment options.
Proper Documentation
The requesting physician can be in the same or different provider group as the consultant. The consultant must possess expertise in an area beyond that of the requesting provider. Because the specialty designation for most hospitalists is internal medicine, palliative-care claims could be scrutinized more closely. This does not necessarily occur when the requesting provider has a different two-digit specialty designation (e.g., internal medicine and gastroenterology).2 Scrutiny is more likely to occur when the requesting provider has the same internal-medicine designation as the palliative-care consultant, even if they are in different provider groups.
Payor concern escalates when physicians of the same designated specialty submit claims for the same patient on the same date. Having different primary diagnosis codes attached to each visit level does not necessarily help. The payor is likely to deny the second claim received, pending a review of documentation. If this happens, the provider who received the denial should submit a copy of both progress notes for the date in question. Hopefully, the distinction between the services is demonstrated in the documentation.
Service Type
Palliative services might involve obtaining and documenting the standard key components for visit-level selection: history, exam, and medical decision-making.3 However, the palliative-care specialist might spend more time providing counseling or coordination of care for a patient and family. When this occurs, the palliative-care specialist should not forget about the guidelines for reporting time-based services.4 Inpatient services may be reported on the basis of time, as long as a face-to-face service between the provider and the patient occurs. Consider the total time spent face to face with the patient, and the time spent obtaining, discussing, and coordinating patient care, while you are in the patient’s unit or floor.
As a reminder, document the total time, the amount of time spent counseling, and the details of discussion and coordination. The physician may count the time spent counseling the patient’s family regarding the treatment and care, as long as the focus is not emotional support for the family, the meeting takes place in the patient’s unit or floor, and the patient is present, unless there is medically supported reason for which the patient is unable to participate (e.g., cognitive impairment). The palliative-care specialist can then select the visit level based on time.5 (See Table 1, above.) TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.10. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26, Section 10.8. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c26.pdf. Accessed Jan. 30, 2009.
3. Centers for Medicare and Medicaid Services. Documentation Guidelines for Evaluation and Management Services. CMS Web site. Available at: www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp. Accessed Jan. 30, 2009.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
Misunderstood Modifiers
Modifiers are two-digit representations used in conjunction with a service or procedure code (e.g., 99233-25) during claim submission to alert payors that the service or procedure was performed under a special circumstance. Modifiers can:
- Identify body areas;
- Distinguish multiple, separately identifiable services;
- Identify reduced or multiple services of the same or a different nature; or
- Categorize unusual events surrounding a particular service.1
Many questions arise over appropriate modifier use. Hospitalist misconceptions typically involve surgical comanagement or multiple services on the same day. Understanding when to use modifiers is imperative for proper claim submission and reimbursement.
Multiple Visits
Most hospitalists know payors allow reimbursement for only one visit per specialty, per patient, per day; however, some payors further limit coverage to a single service (i.e., a visit or a procedure) unless physician documentation demonstrates a medical necessity for each billed service. When two visits are performed on the same date by the same physician, or by two physicians of the same specialty within the same group, only one cumulative service should be reported.2
Consideration of two notes during visit-level selection does not authorize physicians to report a higher visit level (e.g., 99233 for two notes instead of 99232 for one note). If the cumulative documentation does not include the necessary elements of history, exam, or medical decision-making that are associated with 99233, the physician must report the lower visit level that accurately reflects the content of the progress note (for more information on documentation guidelines, visit www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp).
One exception to this “single cumulative service” rule occurs when a physician provides a typical inpatient service (e.g., admission or subsequent hospital care) for chronic obstructive bronchitis with acute exacerbation (diagnosis code 491.21) early in the day, and later the patient requires a second, more intense encounter for acute respiratory distress (diagnosis code 518.82) that meets the definition of critical care (99291). In this scenario, the physician is allowed to report both services on the same date, appending modifier 25 to the initial service (i.e., 99233-25) because each service was performed for distinct reasons.
If different physicians in the same provider group and specialty provided the initial and follow-up services, each physician reports the corresponding service in their own name with modifier 25 appended to the subsequent hospital care service (as above). Please note that physicians may not report both services if critical care is the initial service of the day. In this latter scenario, the physician reports critical-care codes (99291, 99292) for all of his or other group members’ encounters provided in one calendar day.3
Visits and Procedures
When a physician bills for a procedure and a visit (inpatient or outpatient) on the same day, most payors “bundle” the visit payment into that of the procedure. Some payors do provide separate payment for the visit, if the service is separately identifiable from the procedure (i.e., performed for a separate reason). To electronically demonstrate this on the claim form, the physician appends modifier 25 to the visit. Although not required, it is strongly suggested that, when possible, the primary diagnosis for the visit differs from the one used with the procedure. This will further distinguish the services. However, different diagnoses may not be possible when the physician evaluates the patient and decides, during the course of the evaluation, that a procedure is warranted. In this case, the physician may only have a single diagnosis to list with the procedure and the visit.
Payors may request documentation prior to payment to ensure that the visit is not associated with the required preprocedure history and physical. Modifier 57 is not to be confused with modifier 25. Modifier 57 indicates that the physician made the decision for “surgery” during the visit, but this modifier is used with preprocedural visits involving major surgical procedures (i.e., procedures associated with 90-day global periods). Since hospitalists do not perform major surgical procedures, they would not use this modifier with preprocedural visits.
Keep in mind that this “bundling” concept only applies when same-day visits and procedures are performed by the same physician or members of the same provider group with the same specialty designation. In other words, hospitalist visits are typically considered separate from procedures performed by a surgeon, and there is no need to append a modifier to visits on the same day as the surgeon’s procedure. The surgeon’s packaged payment includes preoperative visits after the decision for surgery is made beginning one day prior to surgery, and postoperative visits by the surgeon related to recovery from surgery, postoperative pain management, and discharge care.4 The surgeon is entitled to the full global payment if he provides the preoperative, intraoperative, and postoperative management.
If the surgeon relinquishes care and formally transfers the preoperative or postoperative management to another physician not associated with the surgical group, the other physician may bill for his portion of the perioperative management by appending modifier 56 (preop) or 55 (postop) to the procedure code. Unfortunately, the hospitalist is subject to the surgeon’s claim reporting. If the surgeon fails to solely report his intraoperative management (modifier 54 appended to the procedure code), the surgeon receives the full packaged payment. The payor will deny the hospitalist’s claim.
The payor is unlikely to retrieve money from one provider to pay another provider, unless a pattern of inappropriate claim submission is detected. Surgical intraoperative responsibilities are not typically reassigned to other provider groups unless special circumstances occur (e.g., geographical restrictions). Therefore, if the surgeon does not relinquish care but merely wants the hospitalist to assist in medical management, the hospitalist reports his medically necessary services with the appropriate inpatient visit code (subsequent hospital care, 99231-99233). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Holmes A. Appropriate Use of Modifiers In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2008:273-282.
2. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
3. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
4. Pohlig, C. Sort out surgical cases. The Hospitalist. 2008;12(8):19.
Modifiers are two-digit representations used in conjunction with a service or procedure code (e.g., 99233-25) during claim submission to alert payors that the service or procedure was performed under a special circumstance. Modifiers can:
- Identify body areas;
- Distinguish multiple, separately identifiable services;
- Identify reduced or multiple services of the same or a different nature; or
- Categorize unusual events surrounding a particular service.1
Many questions arise over appropriate modifier use. Hospitalist misconceptions typically involve surgical comanagement or multiple services on the same day. Understanding when to use modifiers is imperative for proper claim submission and reimbursement.
Multiple Visits
Most hospitalists know payors allow reimbursement for only one visit per specialty, per patient, per day; however, some payors further limit coverage to a single service (i.e., a visit or a procedure) unless physician documentation demonstrates a medical necessity for each billed service. When two visits are performed on the same date by the same physician, or by two physicians of the same specialty within the same group, only one cumulative service should be reported.2
Consideration of two notes during visit-level selection does not authorize physicians to report a higher visit level (e.g., 99233 for two notes instead of 99232 for one note). If the cumulative documentation does not include the necessary elements of history, exam, or medical decision-making that are associated with 99233, the physician must report the lower visit level that accurately reflects the content of the progress note (for more information on documentation guidelines, visit www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp).
One exception to this “single cumulative service” rule occurs when a physician provides a typical inpatient service (e.g., admission or subsequent hospital care) for chronic obstructive bronchitis with acute exacerbation (diagnosis code 491.21) early in the day, and later the patient requires a second, more intense encounter for acute respiratory distress (diagnosis code 518.82) that meets the definition of critical care (99291). In this scenario, the physician is allowed to report both services on the same date, appending modifier 25 to the initial service (i.e., 99233-25) because each service was performed for distinct reasons.
If different physicians in the same provider group and specialty provided the initial and follow-up services, each physician reports the corresponding service in their own name with modifier 25 appended to the subsequent hospital care service (as above). Please note that physicians may not report both services if critical care is the initial service of the day. In this latter scenario, the physician reports critical-care codes (99291, 99292) for all of his or other group members’ encounters provided in one calendar day.3
Visits and Procedures
When a physician bills for a procedure and a visit (inpatient or outpatient) on the same day, most payors “bundle” the visit payment into that of the procedure. Some payors do provide separate payment for the visit, if the service is separately identifiable from the procedure (i.e., performed for a separate reason). To electronically demonstrate this on the claim form, the physician appends modifier 25 to the visit. Although not required, it is strongly suggested that, when possible, the primary diagnosis for the visit differs from the one used with the procedure. This will further distinguish the services. However, different diagnoses may not be possible when the physician evaluates the patient and decides, during the course of the evaluation, that a procedure is warranted. In this case, the physician may only have a single diagnosis to list with the procedure and the visit.
Payors may request documentation prior to payment to ensure that the visit is not associated with the required preprocedure history and physical. Modifier 57 is not to be confused with modifier 25. Modifier 57 indicates that the physician made the decision for “surgery” during the visit, but this modifier is used with preprocedural visits involving major surgical procedures (i.e., procedures associated with 90-day global periods). Since hospitalists do not perform major surgical procedures, they would not use this modifier with preprocedural visits.
Keep in mind that this “bundling” concept only applies when same-day visits and procedures are performed by the same physician or members of the same provider group with the same specialty designation. In other words, hospitalist visits are typically considered separate from procedures performed by a surgeon, and there is no need to append a modifier to visits on the same day as the surgeon’s procedure. The surgeon’s packaged payment includes preoperative visits after the decision for surgery is made beginning one day prior to surgery, and postoperative visits by the surgeon related to recovery from surgery, postoperative pain management, and discharge care.4 The surgeon is entitled to the full global payment if he provides the preoperative, intraoperative, and postoperative management.
If the surgeon relinquishes care and formally transfers the preoperative or postoperative management to another physician not associated with the surgical group, the other physician may bill for his portion of the perioperative management by appending modifier 56 (preop) or 55 (postop) to the procedure code. Unfortunately, the hospitalist is subject to the surgeon’s claim reporting. If the surgeon fails to solely report his intraoperative management (modifier 54 appended to the procedure code), the surgeon receives the full packaged payment. The payor will deny the hospitalist’s claim.
The payor is unlikely to retrieve money from one provider to pay another provider, unless a pattern of inappropriate claim submission is detected. Surgical intraoperative responsibilities are not typically reassigned to other provider groups unless special circumstances occur (e.g., geographical restrictions). Therefore, if the surgeon does not relinquish care but merely wants the hospitalist to assist in medical management, the hospitalist reports his medically necessary services with the appropriate inpatient visit code (subsequent hospital care, 99231-99233). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Holmes A. Appropriate Use of Modifiers In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2008:273-282.
2. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
3. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
4. Pohlig, C. Sort out surgical cases. The Hospitalist. 2008;12(8):19.
Modifiers are two-digit representations used in conjunction with a service or procedure code (e.g., 99233-25) during claim submission to alert payors that the service or procedure was performed under a special circumstance. Modifiers can:
- Identify body areas;
- Distinguish multiple, separately identifiable services;
- Identify reduced or multiple services of the same or a different nature; or
- Categorize unusual events surrounding a particular service.1
Many questions arise over appropriate modifier use. Hospitalist misconceptions typically involve surgical comanagement or multiple services on the same day. Understanding when to use modifiers is imperative for proper claim submission and reimbursement.
Multiple Visits
Most hospitalists know payors allow reimbursement for only one visit per specialty, per patient, per day; however, some payors further limit coverage to a single service (i.e., a visit or a procedure) unless physician documentation demonstrates a medical necessity for each billed service. When two visits are performed on the same date by the same physician, or by two physicians of the same specialty within the same group, only one cumulative service should be reported.2
Consideration of two notes during visit-level selection does not authorize physicians to report a higher visit level (e.g., 99233 for two notes instead of 99232 for one note). If the cumulative documentation does not include the necessary elements of history, exam, or medical decision-making that are associated with 99233, the physician must report the lower visit level that accurately reflects the content of the progress note (for more information on documentation guidelines, visit www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp).
One exception to this “single cumulative service” rule occurs when a physician provides a typical inpatient service (e.g., admission or subsequent hospital care) for chronic obstructive bronchitis with acute exacerbation (diagnosis code 491.21) early in the day, and later the patient requires a second, more intense encounter for acute respiratory distress (diagnosis code 518.82) that meets the definition of critical care (99291). In this scenario, the physician is allowed to report both services on the same date, appending modifier 25 to the initial service (i.e., 99233-25) because each service was performed for distinct reasons.
If different physicians in the same provider group and specialty provided the initial and follow-up services, each physician reports the corresponding service in their own name with modifier 25 appended to the subsequent hospital care service (as above). Please note that physicians may not report both services if critical care is the initial service of the day. In this latter scenario, the physician reports critical-care codes (99291, 99292) for all of his or other group members’ encounters provided in one calendar day.3
Visits and Procedures
When a physician bills for a procedure and a visit (inpatient or outpatient) on the same day, most payors “bundle” the visit payment into that of the procedure. Some payors do provide separate payment for the visit, if the service is separately identifiable from the procedure (i.e., performed for a separate reason). To electronically demonstrate this on the claim form, the physician appends modifier 25 to the visit. Although not required, it is strongly suggested that, when possible, the primary diagnosis for the visit differs from the one used with the procedure. This will further distinguish the services. However, different diagnoses may not be possible when the physician evaluates the patient and decides, during the course of the evaluation, that a procedure is warranted. In this case, the physician may only have a single diagnosis to list with the procedure and the visit.
Payors may request documentation prior to payment to ensure that the visit is not associated with the required preprocedure history and physical. Modifier 57 is not to be confused with modifier 25. Modifier 57 indicates that the physician made the decision for “surgery” during the visit, but this modifier is used with preprocedural visits involving major surgical procedures (i.e., procedures associated with 90-day global periods). Since hospitalists do not perform major surgical procedures, they would not use this modifier with preprocedural visits.
Keep in mind that this “bundling” concept only applies when same-day visits and procedures are performed by the same physician or members of the same provider group with the same specialty designation. In other words, hospitalist visits are typically considered separate from procedures performed by a surgeon, and there is no need to append a modifier to visits on the same day as the surgeon’s procedure. The surgeon’s packaged payment includes preoperative visits after the decision for surgery is made beginning one day prior to surgery, and postoperative visits by the surgeon related to recovery from surgery, postoperative pain management, and discharge care.4 The surgeon is entitled to the full global payment if he provides the preoperative, intraoperative, and postoperative management.
If the surgeon relinquishes care and formally transfers the preoperative or postoperative management to another physician not associated with the surgical group, the other physician may bill for his portion of the perioperative management by appending modifier 56 (preop) or 55 (postop) to the procedure code. Unfortunately, the hospitalist is subject to the surgeon’s claim reporting. If the surgeon fails to solely report his intraoperative management (modifier 54 appended to the procedure code), the surgeon receives the full packaged payment. The payor will deny the hospitalist’s claim.
The payor is unlikely to retrieve money from one provider to pay another provider, unless a pattern of inappropriate claim submission is detected. Surgical intraoperative responsibilities are not typically reassigned to other provider groups unless special circumstances occur (e.g., geographical restrictions). Therefore, if the surgeon does not relinquish care but merely wants the hospitalist to assist in medical management, the hospitalist reports his medically necessary services with the appropriate inpatient visit code (subsequent hospital care, 99231-99233). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Holmes A. Appropriate Use of Modifiers In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2008:273-282.
2. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
3. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
4. Pohlig, C. Sort out surgical cases. The Hospitalist. 2008;12(8):19.
Eagle-Eye Your Payors
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
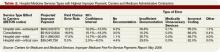
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.
Face-to-Face Improvement
The American Medical Association recently released Current Procedural Terminology (CPT) 2009. New, deleted, and revised codes went into effect Jan. 1. The biggest change to hospitalist billing involves prolonged care codes (99354-99357). CPT 2009 descriptor revisions make it possible for physicians to contribute non-face-to-face time toward prolonged care services.
Inpatient Prolonged Care
Previous versions of CPT defined code 99356 as the first hour of prolonged physician [inpatient] services requiring direct (face-to-face) patient contact beyond the usual services (reportable after the initial 30 minutes); and 99357 for each additional 30 minutes of prolonged [inpatient] care beyond the first hour (reportable after the first 15 minutes of each additional segment). CPT 2009 has changed prolonged care guidelines to be more consistent with other time-based services: all unit/floor time spent by the physician is considered when reporting 99356 and 99357.1
As with most other evaluation and management services, a face-to-face encounter still must occur. In addition to the time associated with the face-to-face encounter, count the time associated with all other physician activities occurring on the unit/floor (e.g., reviewing images, obtaining information involving overnight events, discussing management options with the family) directed toward an individual patient. The cumulative time spent by the billing provider on a single calendar day is considered for billing. Time spent by someone other than the billing provider cannot be credited toward prolonged care.
As example, a physician cares for a 65-year-old male with uncontrolled diabetes, diabetic nephropathy, and congestive heart failure. Early in the day, the physician rounds, spending a total of 20 minutes reviewing the overnight course of events on the unit, re-confirming the patient history, and performing an exam with the patient. Anticipating the patient’s needs, the physician discusses post-discharge options and care with the patient and his family for 45 minutes. After the discussion, the physician spends an additional 30 minutes relaying information to the team and coordinating care. Merely reporting the highest-level subsequent hospital care service (99233), does not capture the physician’s cumulative effort. It only would account for 40 of the 95 minutes spent throughout the day. In order to capture the remaining 55 minutes, the physician reports 99356 on the same claim form as 99233.
Do not report prolonged care codes on a separate claim form. Prolonged care codes do not represent an independent service. These codes are reported along with a primary service. They must appear as a separate line item on the claim form, which includes a code representing the primary service. For prolonged care in the inpatient setting, the primary service must be initial hospital care (99221-99223), subsequent hospital care (99231-99233), inpatient consultations (99251-99255), or nursing facility services (99304-99318). Additional examples of billable prolonged care services are in Section 30.6.15.1I of the Medicare manual, available at www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf.
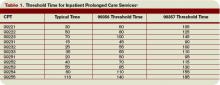
Threshold Time
Prolonged care guidelines refer to “threshold” time. Threshold time requires the physician to exceed the time requirements associated with the “primary” codes before reporting prolonged care. Table 1 identifies the typical times associated with inpatient services qualifying for prolonged care. The physician must exceed the typical time by a minimum of 30 minutes. (For example, 99232 + 99356 = 25 minutes + 30 minutes = 55 total minutes). Additionally, the physician must document the total time spent during the face-to-face portion of the encounter, and the additional unit or floor time in one cumulative note or in separate notes representing the physician services provided to the patient throughout the day.
Prolonged Outpatient Services
Prolonged care (99354-99355) provided to outpatients remains unchanged. Physicians only report personally provided face-to-face time with the patient. Time spent by other staff members does not count toward prolonged care.
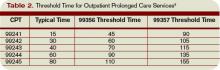
As with prolonged inpatient care, report 99354 and 99355 in addition to a primary service code. The companion outpatient codes are outpatient/office visits (99201-99205 or 99212–99215), outpatient consultation (99241–99245), domiciliary/custodial care (99324–99328 or 99334–99337), and home services (99341-99350). Hospitalists more often use outpatient prolonged care with office consultation codes for services provided in the emergency department, as appropriate.
Do not report 99354 or 99355 with observation care (99217-99220) or emergency department visits (99281-99288), since these service categories typically require prolonged periods of physician monitoring, thereby prohibiting use of prolonged care codes. As with inpatient-prolonged care, the concept of threshold time exists. Refer to Table 2 (pg. 25) for the typical threshold times associated with office consultation codes.
Medicare Consideration
Although CPT has offered revisions to this code, Medicare guidelines remain unchanged. The Medicare Claims Processing Manual still states: “In the case of prolonged hospital services, time spent reviewing charts or discussion of a patient with house medical staff and not with direct face-to-face contact with the patient, or waiting for test results, for changes in the patient’s condition, for end of a therapy, or for use of facilities, cannot be billed as prolonged services.”4 It is yet to be determined if the Centers for Medicare and Medicaid Services (CMS) will issue a transmittal to revise the current description in the processing manual. Physicians and staff may access past and present transmittal information at www.cms.hhs.gov/ Transmittals/.
As always, be sure to query payers about prolonged care services, since some non-Medicare insurers may not recognize these codes.
Modifier 21
Modifier 21 has been deleted from the CPT. Modifier 21 was appended to an appropriate visit code (e.g., 99232-21) when the face-to-face or floor/unit service(s) provided is prolonged or otherwise greater than usually required for the highest level of evaluation and management service within a given category.5 Since the descriptors for codes 99354-99357 have been revised to more consistently reflect the description formerly associated with modifier 21, there is no need to maintain its existence. Additionally, Medicare and most other payers did not recognize this modifier.
Code This Case
Question: A newly diagnosed diabetic requires extensive counseling regarding lifestyle changes, medication regime, the disease process, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient (15 minutes), and performs an abbreviated service (problem-focused history and exam). The attending physician asks the resident to assist him with the remaining counseling efforts and coordination of care (30 minutes).
Each physician documents his or her portion of the service. What visit level can the hospitalist report?
Answer: When two billing providers (i.e., two attending physicians) from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service, since 99356 must be reported on the same invoice as the primary visit code (e.g., 99231).6
The example above involves the resident’s time as well as the attending physician’s time. Documentation must be very clear to demonstrate the attending physician actively participated in the entire 45-minute service. Otherwise, only the attending may report the amount of time he actually spent providing the service.
Billing options for this scenario can vary. When the physician performs and documents the key components of history, exam, and decision making for the primary encounter, report 99231 (0.76 physician work relative value units; $33.90) and 99356 (1.71 physician work relative value units; $76.46) for the cumulative service. Alternatively, in those evaluation and management services for which the [primary] code level is selected based on time alone (i.e., history and exam was not performed or required), prolonged services may only be reported with the highest code level in that family of codes as the companion code.7
Therefore, this 45-minute service may be reported as 99233 (2.0 physician work relative value units; $86.92) since more than half of the total visit time was dedicated to counseling/coordi-nation of care (see Section 30.6.1B-C available at www. cms.hhs.gov/manuals/ downloads/clm104c12.pdf for additional information on billing for counseling/coordination of care time).
If a payer does not recognize prolonged care codes, only the latter billing option is possible. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 25-26.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1G. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
3. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1F. www.cms.hhs.gov/manuals/dowloads/ clm104c12.pdf. Accessed November 19, 2008.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf. Accessed November 19, 2008.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 457.
6. Pohlig, C. Bill by time spent on case. The Hospitalist. Jul 2008;19.
7. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1H. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
The American Medical Association recently released Current Procedural Terminology (CPT) 2009. New, deleted, and revised codes went into effect Jan. 1. The biggest change to hospitalist billing involves prolonged care codes (99354-99357). CPT 2009 descriptor revisions make it possible for physicians to contribute non-face-to-face time toward prolonged care services.
Inpatient Prolonged Care
Previous versions of CPT defined code 99356 as the first hour of prolonged physician [inpatient] services requiring direct (face-to-face) patient contact beyond the usual services (reportable after the initial 30 minutes); and 99357 for each additional 30 minutes of prolonged [inpatient] care beyond the first hour (reportable after the first 15 minutes of each additional segment). CPT 2009 has changed prolonged care guidelines to be more consistent with other time-based services: all unit/floor time spent by the physician is considered when reporting 99356 and 99357.1
As with most other evaluation and management services, a face-to-face encounter still must occur. In addition to the time associated with the face-to-face encounter, count the time associated with all other physician activities occurring on the unit/floor (e.g., reviewing images, obtaining information involving overnight events, discussing management options with the family) directed toward an individual patient. The cumulative time spent by the billing provider on a single calendar day is considered for billing. Time spent by someone other than the billing provider cannot be credited toward prolonged care.
As example, a physician cares for a 65-year-old male with uncontrolled diabetes, diabetic nephropathy, and congestive heart failure. Early in the day, the physician rounds, spending a total of 20 minutes reviewing the overnight course of events on the unit, re-confirming the patient history, and performing an exam with the patient. Anticipating the patient’s needs, the physician discusses post-discharge options and care with the patient and his family for 45 minutes. After the discussion, the physician spends an additional 30 minutes relaying information to the team and coordinating care. Merely reporting the highest-level subsequent hospital care service (99233), does not capture the physician’s cumulative effort. It only would account for 40 of the 95 minutes spent throughout the day. In order to capture the remaining 55 minutes, the physician reports 99356 on the same claim form as 99233.
Do not report prolonged care codes on a separate claim form. Prolonged care codes do not represent an independent service. These codes are reported along with a primary service. They must appear as a separate line item on the claim form, which includes a code representing the primary service. For prolonged care in the inpatient setting, the primary service must be initial hospital care (99221-99223), subsequent hospital care (99231-99233), inpatient consultations (99251-99255), or nursing facility services (99304-99318). Additional examples of billable prolonged care services are in Section 30.6.15.1I of the Medicare manual, available at www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf.
Threshold Time
Prolonged care guidelines refer to “threshold” time. Threshold time requires the physician to exceed the time requirements associated with the “primary” codes before reporting prolonged care. Table 1 identifies the typical times associated with inpatient services qualifying for prolonged care. The physician must exceed the typical time by a minimum of 30 minutes. (For example, 99232 + 99356 = 25 minutes + 30 minutes = 55 total minutes). Additionally, the physician must document the total time spent during the face-to-face portion of the encounter, and the additional unit or floor time in one cumulative note or in separate notes representing the physician services provided to the patient throughout the day.
Prolonged Outpatient Services
Prolonged care (99354-99355) provided to outpatients remains unchanged. Physicians only report personally provided face-to-face time with the patient. Time spent by other staff members does not count toward prolonged care.
As with prolonged inpatient care, report 99354 and 99355 in addition to a primary service code. The companion outpatient codes are outpatient/office visits (99201-99205 or 99212–99215), outpatient consultation (99241–99245), domiciliary/custodial care (99324–99328 or 99334–99337), and home services (99341-99350). Hospitalists more often use outpatient prolonged care with office consultation codes for services provided in the emergency department, as appropriate.
Do not report 99354 or 99355 with observation care (99217-99220) or emergency department visits (99281-99288), since these service categories typically require prolonged periods of physician monitoring, thereby prohibiting use of prolonged care codes. As with inpatient-prolonged care, the concept of threshold time exists. Refer to Table 2 (pg. 25) for the typical threshold times associated with office consultation codes.
Medicare Consideration
Although CPT has offered revisions to this code, Medicare guidelines remain unchanged. The Medicare Claims Processing Manual still states: “In the case of prolonged hospital services, time spent reviewing charts or discussion of a patient with house medical staff and not with direct face-to-face contact with the patient, or waiting for test results, for changes in the patient’s condition, for end of a therapy, or for use of facilities, cannot be billed as prolonged services.”4 It is yet to be determined if the Centers for Medicare and Medicaid Services (CMS) will issue a transmittal to revise the current description in the processing manual. Physicians and staff may access past and present transmittal information at www.cms.hhs.gov/ Transmittals/.
As always, be sure to query payers about prolonged care services, since some non-Medicare insurers may not recognize these codes.
Modifier 21
Modifier 21 has been deleted from the CPT. Modifier 21 was appended to an appropriate visit code (e.g., 99232-21) when the face-to-face or floor/unit service(s) provided is prolonged or otherwise greater than usually required for the highest level of evaluation and management service within a given category.5 Since the descriptors for codes 99354-99357 have been revised to more consistently reflect the description formerly associated with modifier 21, there is no need to maintain its existence. Additionally, Medicare and most other payers did not recognize this modifier.
Code This Case
Question: A newly diagnosed diabetic requires extensive counseling regarding lifestyle changes, medication regime, the disease process, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient (15 minutes), and performs an abbreviated service (problem-focused history and exam). The attending physician asks the resident to assist him with the remaining counseling efforts and coordination of care (30 minutes).
Each physician documents his or her portion of the service. What visit level can the hospitalist report?
Answer: When two billing providers (i.e., two attending physicians) from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service, since 99356 must be reported on the same invoice as the primary visit code (e.g., 99231).6
The example above involves the resident’s time as well as the attending physician’s time. Documentation must be very clear to demonstrate the attending physician actively participated in the entire 45-minute service. Otherwise, only the attending may report the amount of time he actually spent providing the service.
Billing options for this scenario can vary. When the physician performs and documents the key components of history, exam, and decision making for the primary encounter, report 99231 (0.76 physician work relative value units; $33.90) and 99356 (1.71 physician work relative value units; $76.46) for the cumulative service. Alternatively, in those evaluation and management services for which the [primary] code level is selected based on time alone (i.e., history and exam was not performed or required), prolonged services may only be reported with the highest code level in that family of codes as the companion code.7
Therefore, this 45-minute service may be reported as 99233 (2.0 physician work relative value units; $86.92) since more than half of the total visit time was dedicated to counseling/coordi-nation of care (see Section 30.6.1B-C available at www. cms.hhs.gov/manuals/ downloads/clm104c12.pdf for additional information on billing for counseling/coordination of care time).
If a payer does not recognize prolonged care codes, only the latter billing option is possible. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 25-26.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1G. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
3. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1F. www.cms.hhs.gov/manuals/dowloads/ clm104c12.pdf. Accessed November 19, 2008.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf. Accessed November 19, 2008.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 457.
6. Pohlig, C. Bill by time spent on case. The Hospitalist. Jul 2008;19.
7. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1H. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
The American Medical Association recently released Current Procedural Terminology (CPT) 2009. New, deleted, and revised codes went into effect Jan. 1. The biggest change to hospitalist billing involves prolonged care codes (99354-99357). CPT 2009 descriptor revisions make it possible for physicians to contribute non-face-to-face time toward prolonged care services.
Inpatient Prolonged Care
Previous versions of CPT defined code 99356 as the first hour of prolonged physician [inpatient] services requiring direct (face-to-face) patient contact beyond the usual services (reportable after the initial 30 minutes); and 99357 for each additional 30 minutes of prolonged [inpatient] care beyond the first hour (reportable after the first 15 minutes of each additional segment). CPT 2009 has changed prolonged care guidelines to be more consistent with other time-based services: all unit/floor time spent by the physician is considered when reporting 99356 and 99357.1
As with most other evaluation and management services, a face-to-face encounter still must occur. In addition to the time associated with the face-to-face encounter, count the time associated with all other physician activities occurring on the unit/floor (e.g., reviewing images, obtaining information involving overnight events, discussing management options with the family) directed toward an individual patient. The cumulative time spent by the billing provider on a single calendar day is considered for billing. Time spent by someone other than the billing provider cannot be credited toward prolonged care.
As example, a physician cares for a 65-year-old male with uncontrolled diabetes, diabetic nephropathy, and congestive heart failure. Early in the day, the physician rounds, spending a total of 20 minutes reviewing the overnight course of events on the unit, re-confirming the patient history, and performing an exam with the patient. Anticipating the patient’s needs, the physician discusses post-discharge options and care with the patient and his family for 45 minutes. After the discussion, the physician spends an additional 30 minutes relaying information to the team and coordinating care. Merely reporting the highest-level subsequent hospital care service (99233), does not capture the physician’s cumulative effort. It only would account for 40 of the 95 minutes spent throughout the day. In order to capture the remaining 55 minutes, the physician reports 99356 on the same claim form as 99233.
Do not report prolonged care codes on a separate claim form. Prolonged care codes do not represent an independent service. These codes are reported along with a primary service. They must appear as a separate line item on the claim form, which includes a code representing the primary service. For prolonged care in the inpatient setting, the primary service must be initial hospital care (99221-99223), subsequent hospital care (99231-99233), inpatient consultations (99251-99255), or nursing facility services (99304-99318). Additional examples of billable prolonged care services are in Section 30.6.15.1I of the Medicare manual, available at www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf.
Threshold Time
Prolonged care guidelines refer to “threshold” time. Threshold time requires the physician to exceed the time requirements associated with the “primary” codes before reporting prolonged care. Table 1 identifies the typical times associated with inpatient services qualifying for prolonged care. The physician must exceed the typical time by a minimum of 30 minutes. (For example, 99232 + 99356 = 25 minutes + 30 minutes = 55 total minutes). Additionally, the physician must document the total time spent during the face-to-face portion of the encounter, and the additional unit or floor time in one cumulative note or in separate notes representing the physician services provided to the patient throughout the day.
Prolonged Outpatient Services
Prolonged care (99354-99355) provided to outpatients remains unchanged. Physicians only report personally provided face-to-face time with the patient. Time spent by other staff members does not count toward prolonged care.
As with prolonged inpatient care, report 99354 and 99355 in addition to a primary service code. The companion outpatient codes are outpatient/office visits (99201-99205 or 99212–99215), outpatient consultation (99241–99245), domiciliary/custodial care (99324–99328 or 99334–99337), and home services (99341-99350). Hospitalists more often use outpatient prolonged care with office consultation codes for services provided in the emergency department, as appropriate.
Do not report 99354 or 99355 with observation care (99217-99220) or emergency department visits (99281-99288), since these service categories typically require prolonged periods of physician monitoring, thereby prohibiting use of prolonged care codes. As with inpatient-prolonged care, the concept of threshold time exists. Refer to Table 2 (pg. 25) for the typical threshold times associated with office consultation codes.
Medicare Consideration
Although CPT has offered revisions to this code, Medicare guidelines remain unchanged. The Medicare Claims Processing Manual still states: “In the case of prolonged hospital services, time spent reviewing charts or discussion of a patient with house medical staff and not with direct face-to-face contact with the patient, or waiting for test results, for changes in the patient’s condition, for end of a therapy, or for use of facilities, cannot be billed as prolonged services.”4 It is yet to be determined if the Centers for Medicare and Medicaid Services (CMS) will issue a transmittal to revise the current description in the processing manual. Physicians and staff may access past and present transmittal information at www.cms.hhs.gov/ Transmittals/.
As always, be sure to query payers about prolonged care services, since some non-Medicare insurers may not recognize these codes.
Modifier 21
Modifier 21 has been deleted from the CPT. Modifier 21 was appended to an appropriate visit code (e.g., 99232-21) when the face-to-face or floor/unit service(s) provided is prolonged or otherwise greater than usually required for the highest level of evaluation and management service within a given category.5 Since the descriptors for codes 99354-99357 have been revised to more consistently reflect the description formerly associated with modifier 21, there is no need to maintain its existence. Additionally, Medicare and most other payers did not recognize this modifier.
Code This Case
Question: A newly diagnosed diabetic requires extensive counseling regarding lifestyle changes, medication regime, the disease process, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient (15 minutes), and performs an abbreviated service (problem-focused history and exam). The attending physician asks the resident to assist him with the remaining counseling efforts and coordination of care (30 minutes).
Each physician documents his or her portion of the service. What visit level can the hospitalist report?
Answer: When two billing providers (i.e., two attending physicians) from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service, since 99356 must be reported on the same invoice as the primary visit code (e.g., 99231).6
The example above involves the resident’s time as well as the attending physician’s time. Documentation must be very clear to demonstrate the attending physician actively participated in the entire 45-minute service. Otherwise, only the attending may report the amount of time he actually spent providing the service.
Billing options for this scenario can vary. When the physician performs and documents the key components of history, exam, and decision making for the primary encounter, report 99231 (0.76 physician work relative value units; $33.90) and 99356 (1.71 physician work relative value units; $76.46) for the cumulative service. Alternatively, in those evaluation and management services for which the [primary] code level is selected based on time alone (i.e., history and exam was not performed or required), prolonged services may only be reported with the highest code level in that family of codes as the companion code.7
Therefore, this 45-minute service may be reported as 99233 (2.0 physician work relative value units; $86.92) since more than half of the total visit time was dedicated to counseling/coordi-nation of care (see Section 30.6.1B-C available at www. cms.hhs.gov/manuals/ downloads/clm104c12.pdf for additional information on billing for counseling/coordination of care time).
If a payer does not recognize prolonged care codes, only the latter billing option is possible. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 25-26.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1G. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
3. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1F. www.cms.hhs.gov/manuals/dowloads/ clm104c12.pdf. Accessed November 19, 2008.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf. Accessed November 19, 2008.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 457.
6. Pohlig, C. Bill by time spent on case. The Hospitalist. Jul 2008;19.
7. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1H. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
The Bare Necessities
Medicare reimburses for procedures and services deemed “reasonable and necessary.” By statute, Medicare only may pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury, or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g., colorectal cancer screening).1 Medical necessity is determined by evidence-based clinical standards of care, which guide the physician’s diagnostic and treatment process for certain patient populations, illnesses, or clinical circumstances.
National Coverage Determinations
The Centers for Medicare and Medicaid Services (CMS) develop national coverage determinations (NCDs) through an evidence-based process with opportunities for public participation. In some cases, CMS’ own research is supplemented by an outside technology assessment and/or consultation with the Medicare Evidence Development and Coverage Advisory Committee (MEDCAC).
All Medicare contractors must adhere to NCDs and cannot create additional limitations or guidelines. As an example, the NCD for pronouncement of death states an individual only is considered to have died as of the time he orshe is pronounced dead by a person who is legally authorized to make such a pronouncement, usually a physician; and medical services rendered up to and including pronouncement are considered reasonable and necessary.2 Further guidance authorizes physicians to report discharge day management codes (99238-99239) for the face-to-face pronouncement encounter.3 See the Medicare National Coverage Determination Manual (www.cms.hhs.gov/Manuals/ IOM/itemdetail.asp?filterType=none&filterByDID=-99&sortByDID=1&sort Order=ascending&itemID=CMS014961&intNumPerPage=10) for other applicable NCDs.
Local Coverage Determinations
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).4
An LCD, as established by Section 522 of the Benefits Improvement and Protection Act (BIPA), is a decision made by a fiscal intermediary or carrier to cover a particular service on an intermediary-wide or carrier-wide basis, in accordance with Section 1862(a)(1)(A) of the Social Security Act (i.e., a determination as to whether the service is reasonable and necessary).5 LCDs may vary by state, causing an inconsistent approach to medical coverage. Non-Medicare payers do not have to follow federal guidelines, unless the member participates in a Medicare managed care plan. A list of Medicare contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.
Certain payers develop coverage requirements for frequent or problematic procedures or services. Coverage requirements identify specific conditions (i.e., ICD-9-CM codes) for which the services or procedures are considered medically necessary. For example, echocardiography (99307) may not be considered medically necessary for a patient who presents with chest pain unless documentation also supports suspected acute myocardial ischemia and baseline electrocardiogram (ECG) is nondiagnostic; or in cases when the physician suspects aortic dissection.6
Medical Review Program
It is insufficient to develop billing compliance policies and standards without enforcement of these guidelines. In an effort to verify the appropriateness of claims and payment, CMS contracts with Medicare Administrative Contractors (MACs), Fiscal Intermediaries (FIs), and Program Safeguard Contractors (PSCs) to perform medical reviews. The goals of the Medical Review Program are reducing Medicare claims payment errors; decreased denials and increased timely payments; and increased educational opportunities.7
In order to determine which providers should be subject to medical review, contractors must analyze provider compliance with coverage and coding rules and take corrective action when necessary. The corrective action aims to modify behavior in need of change, collect overpayments, and deny improper payments.8 Several types of review exist:
- Prepayment review: The Medicare contractor requests medical records prior to payment;
- Postpayment review: The contractor requests medical records after payment has been received by the physician; this may result in upholding or reversing the initial payment determination;
- Probe review: The contractor requests medical records associated with 20 to 40 claims based upon provider-specific issues; and
- Comprehensive error rate testing (CERT) review: CMS measures the error rate and estimates improper claim payments by randomly selecting and reviewing a sample of claims for compliance.9
Prepayment reviews seem to be expanding as a response to the error rate for certain services. For example, high-level consultation services (99245 and 99255) have prompted review over the last several years to ensure documentation and medical necessity are appropriately supported and maintained. Hospitalists may have noticed a recent increase in prepayment record requests for subsequent hospital care (99232 or 99233) and discharge day management (99239) services. Responses to these and other record requests must be timely in order to prevent claim denial or repayment requests. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References:
1. Exclusions from coverage and Medicare as a secondary payer. Social Security Online. www.ssa.gov/ OP_Home/ssact/title18/1862.htm. Updated October 28, 2008. Accessed October 15, 2008.
2. Centers for Medicare and Medicaid Services. Medicare national coverage determination manual: chapter 1, part 1, section 70.4. www.cms.hhs.gov/manuals/ downloads/ncd103c1_Part1.pdf. Accessed October 14, 2008.
3. Centers for Medicare and Medicaid Services. Transmittal 1460: Subsequent hospital visits and hospital discharge day management services (Codes 99231-99239). www.cms.hhs.gov/transmittals/downloads/R1460CP.pdf. Accessed October 14, 2008.
4. Centers for Medicare and Medicaid Services. Medicare coverage determination process: overview. www. cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Updated August 5, 2008. Accessed October 15, 2008.
5. Centers for Medicare and Medicaid Services. Medicare coverage determination process: local coverage determinations. www.cms.hhs.gov/DeterminationProcess/ 04_LCDs.asp. Updated October 7, 2008. Accessed October 15, 2008.
6. Highmark Medicare Services. LCD L27536: transthoracic echocardiography. www.highmarkmedicareservices. com/policy/mac-ab/l27536-r3.html. Updated Septem-ber 23, 2008. Accessed October 16, 2008.
7. Centers for Medicare and Medicaid Services. The Medicare medical review program. www.cms. hhs.gov/MedicalReviewProcess/Downloads/mrfactsheet.pdf. Published September 2004. Accessed October 15, 2008.
8. Rudolph P, Shuren A. Dealing with Medicare. In: coding for chest medicine 2008. Northbrook, IL: Am Coll of Chest Physicians. 2008;23-35.
9. Centers for Medicare and Medicaid Services. Comprehensive error rate testing: overview. www. cms.hhs.gov/CERT/. Updated December 14, 2005. Accessed October 16, 2008.
10. Centers for Medicare and Medicaid Services. Medicare claims processing manual: chapter 12, section 30.6.10G. www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Updated July 9, 2008. Accessed October 16, 2008.
Medicare reimburses for procedures and services deemed “reasonable and necessary.” By statute, Medicare only may pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury, or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g., colorectal cancer screening).1 Medical necessity is determined by evidence-based clinical standards of care, which guide the physician’s diagnostic and treatment process for certain patient populations, illnesses, or clinical circumstances.
National Coverage Determinations
The Centers for Medicare and Medicaid Services (CMS) develop national coverage determinations (NCDs) through an evidence-based process with opportunities for public participation. In some cases, CMS’ own research is supplemented by an outside technology assessment and/or consultation with the Medicare Evidence Development and Coverage Advisory Committee (MEDCAC).
All Medicare contractors must adhere to NCDs and cannot create additional limitations or guidelines. As an example, the NCD for pronouncement of death states an individual only is considered to have died as of the time he orshe is pronounced dead by a person who is legally authorized to make such a pronouncement, usually a physician; and medical services rendered up to and including pronouncement are considered reasonable and necessary.2 Further guidance authorizes physicians to report discharge day management codes (99238-99239) for the face-to-face pronouncement encounter.3 See the Medicare National Coverage Determination Manual (www.cms.hhs.gov/Manuals/ IOM/itemdetail.asp?filterType=none&filterByDID=-99&sortByDID=1&sort Order=ascending&itemID=CMS014961&intNumPerPage=10) for other applicable NCDs.
Local Coverage Determinations
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).4
An LCD, as established by Section 522 of the Benefits Improvement and Protection Act (BIPA), is a decision made by a fiscal intermediary or carrier to cover a particular service on an intermediary-wide or carrier-wide basis, in accordance with Section 1862(a)(1)(A) of the Social Security Act (i.e., a determination as to whether the service is reasonable and necessary).5 LCDs may vary by state, causing an inconsistent approach to medical coverage. Non-Medicare payers do not have to follow federal guidelines, unless the member participates in a Medicare managed care plan. A list of Medicare contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.
Certain payers develop coverage requirements for frequent or problematic procedures or services. Coverage requirements identify specific conditions (i.e., ICD-9-CM codes) for which the services or procedures are considered medically necessary. For example, echocardiography (99307) may not be considered medically necessary for a patient who presents with chest pain unless documentation also supports suspected acute myocardial ischemia and baseline electrocardiogram (ECG) is nondiagnostic; or in cases when the physician suspects aortic dissection.6
Medical Review Program
It is insufficient to develop billing compliance policies and standards without enforcement of these guidelines. In an effort to verify the appropriateness of claims and payment, CMS contracts with Medicare Administrative Contractors (MACs), Fiscal Intermediaries (FIs), and Program Safeguard Contractors (PSCs) to perform medical reviews. The goals of the Medical Review Program are reducing Medicare claims payment errors; decreased denials and increased timely payments; and increased educational opportunities.7
In order to determine which providers should be subject to medical review, contractors must analyze provider compliance with coverage and coding rules and take corrective action when necessary. The corrective action aims to modify behavior in need of change, collect overpayments, and deny improper payments.8 Several types of review exist:
- Prepayment review: The Medicare contractor requests medical records prior to payment;
- Postpayment review: The contractor requests medical records after payment has been received by the physician; this may result in upholding or reversing the initial payment determination;
- Probe review: The contractor requests medical records associated with 20 to 40 claims based upon provider-specific issues; and
- Comprehensive error rate testing (CERT) review: CMS measures the error rate and estimates improper claim payments by randomly selecting and reviewing a sample of claims for compliance.9
Prepayment reviews seem to be expanding as a response to the error rate for certain services. For example, high-level consultation services (99245 and 99255) have prompted review over the last several years to ensure documentation and medical necessity are appropriately supported and maintained. Hospitalists may have noticed a recent increase in prepayment record requests for subsequent hospital care (99232 or 99233) and discharge day management (99239) services. Responses to these and other record requests must be timely in order to prevent claim denial or repayment requests. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References:
1. Exclusions from coverage and Medicare as a secondary payer. Social Security Online. www.ssa.gov/ OP_Home/ssact/title18/1862.htm. Updated October 28, 2008. Accessed October 15, 2008.
2. Centers for Medicare and Medicaid Services. Medicare national coverage determination manual: chapter 1, part 1, section 70.4. www.cms.hhs.gov/manuals/ downloads/ncd103c1_Part1.pdf. Accessed October 14, 2008.
3. Centers for Medicare and Medicaid Services. Transmittal 1460: Subsequent hospital visits and hospital discharge day management services (Codes 99231-99239). www.cms.hhs.gov/transmittals/downloads/R1460CP.pdf. Accessed October 14, 2008.
4. Centers for Medicare and Medicaid Services. Medicare coverage determination process: overview. www. cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Updated August 5, 2008. Accessed October 15, 2008.
5. Centers for Medicare and Medicaid Services. Medicare coverage determination process: local coverage determinations. www.cms.hhs.gov/DeterminationProcess/ 04_LCDs.asp. Updated October 7, 2008. Accessed October 15, 2008.
6. Highmark Medicare Services. LCD L27536: transthoracic echocardiography. www.highmarkmedicareservices. com/policy/mac-ab/l27536-r3.html. Updated Septem-ber 23, 2008. Accessed October 16, 2008.
7. Centers for Medicare and Medicaid Services. The Medicare medical review program. www.cms. hhs.gov/MedicalReviewProcess/Downloads/mrfactsheet.pdf. Published September 2004. Accessed October 15, 2008.
8. Rudolph P, Shuren A. Dealing with Medicare. In: coding for chest medicine 2008. Northbrook, IL: Am Coll of Chest Physicians. 2008;23-35.
9. Centers for Medicare and Medicaid Services. Comprehensive error rate testing: overview. www. cms.hhs.gov/CERT/. Updated December 14, 2005. Accessed October 16, 2008.
10. Centers for Medicare and Medicaid Services. Medicare claims processing manual: chapter 12, section 30.6.10G. www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Updated July 9, 2008. Accessed October 16, 2008.
Medicare reimburses for procedures and services deemed “reasonable and necessary.” By statute, Medicare only may pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury, or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g., colorectal cancer screening).1 Medical necessity is determined by evidence-based clinical standards of care, which guide the physician’s diagnostic and treatment process for certain patient populations, illnesses, or clinical circumstances.
National Coverage Determinations
The Centers for Medicare and Medicaid Services (CMS) develop national coverage determinations (NCDs) through an evidence-based process with opportunities for public participation. In some cases, CMS’ own research is supplemented by an outside technology assessment and/or consultation with the Medicare Evidence Development and Coverage Advisory Committee (MEDCAC).
All Medicare contractors must adhere to NCDs and cannot create additional limitations or guidelines. As an example, the NCD for pronouncement of death states an individual only is considered to have died as of the time he orshe is pronounced dead by a person who is legally authorized to make such a pronouncement, usually a physician; and medical services rendered up to and including pronouncement are considered reasonable and necessary.2 Further guidance authorizes physicians to report discharge day management codes (99238-99239) for the face-to-face pronouncement encounter.3 See the Medicare National Coverage Determination Manual (www.cms.hhs.gov/Manuals/ IOM/itemdetail.asp?filterType=none&filterByDID=-99&sortByDID=1&sort Order=ascending&itemID=CMS014961&intNumPerPage=10) for other applicable NCDs.
Local Coverage Determinations
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).4
An LCD, as established by Section 522 of the Benefits Improvement and Protection Act (BIPA), is a decision made by a fiscal intermediary or carrier to cover a particular service on an intermediary-wide or carrier-wide basis, in accordance with Section 1862(a)(1)(A) of the Social Security Act (i.e., a determination as to whether the service is reasonable and necessary).5 LCDs may vary by state, causing an inconsistent approach to medical coverage. Non-Medicare payers do not have to follow federal guidelines, unless the member participates in a Medicare managed care plan. A list of Medicare contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.
Certain payers develop coverage requirements for frequent or problematic procedures or services. Coverage requirements identify specific conditions (i.e., ICD-9-CM codes) for which the services or procedures are considered medically necessary. For example, echocardiography (99307) may not be considered medically necessary for a patient who presents with chest pain unless documentation also supports suspected acute myocardial ischemia and baseline electrocardiogram (ECG) is nondiagnostic; or in cases when the physician suspects aortic dissection.6
Medical Review Program
It is insufficient to develop billing compliance policies and standards without enforcement of these guidelines. In an effort to verify the appropriateness of claims and payment, CMS contracts with Medicare Administrative Contractors (MACs), Fiscal Intermediaries (FIs), and Program Safeguard Contractors (PSCs) to perform medical reviews. The goals of the Medical Review Program are reducing Medicare claims payment errors; decreased denials and increased timely payments; and increased educational opportunities.7
In order to determine which providers should be subject to medical review, contractors must analyze provider compliance with coverage and coding rules and take corrective action when necessary. The corrective action aims to modify behavior in need of change, collect overpayments, and deny improper payments.8 Several types of review exist:
- Prepayment review: The Medicare contractor requests medical records prior to payment;
- Postpayment review: The contractor requests medical records after payment has been received by the physician; this may result in upholding or reversing the initial payment determination;
- Probe review: The contractor requests medical records associated with 20 to 40 claims based upon provider-specific issues; and
- Comprehensive error rate testing (CERT) review: CMS measures the error rate and estimates improper claim payments by randomly selecting and reviewing a sample of claims for compliance.9
Prepayment reviews seem to be expanding as a response to the error rate for certain services. For example, high-level consultation services (99245 and 99255) have prompted review over the last several years to ensure documentation and medical necessity are appropriately supported and maintained. Hospitalists may have noticed a recent increase in prepayment record requests for subsequent hospital care (99232 or 99233) and discharge day management (99239) services. Responses to these and other record requests must be timely in order to prevent claim denial or repayment requests. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References:
1. Exclusions from coverage and Medicare as a secondary payer. Social Security Online. www.ssa.gov/ OP_Home/ssact/title18/1862.htm. Updated October 28, 2008. Accessed October 15, 2008.
2. Centers for Medicare and Medicaid Services. Medicare national coverage determination manual: chapter 1, part 1, section 70.4. www.cms.hhs.gov/manuals/ downloads/ncd103c1_Part1.pdf. Accessed October 14, 2008.
3. Centers for Medicare and Medicaid Services. Transmittal 1460: Subsequent hospital visits and hospital discharge day management services (Codes 99231-99239). www.cms.hhs.gov/transmittals/downloads/R1460CP.pdf. Accessed October 14, 2008.
4. Centers for Medicare and Medicaid Services. Medicare coverage determination process: overview. www. cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Updated August 5, 2008. Accessed October 15, 2008.
5. Centers for Medicare and Medicaid Services. Medicare coverage determination process: local coverage determinations. www.cms.hhs.gov/DeterminationProcess/ 04_LCDs.asp. Updated October 7, 2008. Accessed October 15, 2008.
6. Highmark Medicare Services. LCD L27536: transthoracic echocardiography. www.highmarkmedicareservices. com/policy/mac-ab/l27536-r3.html. Updated Septem-ber 23, 2008. Accessed October 16, 2008.
7. Centers for Medicare and Medicaid Services. The Medicare medical review program. www.cms. hhs.gov/MedicalReviewProcess/Downloads/mrfactsheet.pdf. Published September 2004. Accessed October 15, 2008.
8. Rudolph P, Shuren A. Dealing with Medicare. In: coding for chest medicine 2008. Northbrook, IL: Am Coll of Chest Physicians. 2008;23-35.
9. Centers for Medicare and Medicaid Services. Comprehensive error rate testing: overview. www. cms.hhs.gov/CERT/. Updated December 14, 2005. Accessed October 16, 2008.
10. Centers for Medicare and Medicaid Services. Medicare claims processing manual: chapter 12, section 30.6.10G. www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Updated July 9, 2008. Accessed October 16, 2008.
Reimbursement Rights
Recent changes in healthcare have forced academic medical centers to seek additional resources in the delivery of quality care. In response to internal and external pressures to minimize length of stay, adhere to limitations on the maximum number of admitted patients, focus on evidence-based care, and improve outcomes of care, hospitalists have incorporated non-physician providers (NPPs), such as acute care nurse practitioners (ACNPs), into their group practices.1
Whereas traditional nurse practitioners focus on the promotion of health and management of chronic illness, ACNPs focus on the care of acutely ill patients. Hospitalists utilize NPPs to expand medical service capacity and improve the efficiency and quality of patient care.2
Research indicates physician/nurse practitioner collaboration in the multidisciplinary management of hospitalized medical patients reduces length of stay and improves hospital profit without altering readmissions or mortality.3 Billing and documentation standards for NPP services must comply with current state and federal regulations. Hospitalist groups should become familiar with these guidelines prior to billing for NPP services involved in this patient care model.
The following highlights inpatient services provided by nurse practitioners (NPs) and physician assistants (PAs).
Covered Services
Medicare pays for services considered reasonable and necessary and not otherwise excluded from coverage. NPPs may provide any service permitted by the state scope of practice and performed in conjunction with the appropriate level of supervision or collaboration, as outlined in licensure or billing requirements. Being only limited by state and/or facility regulations, NPP services comprise visits or procedures typically rendered by ancillary staff or considered a physician service (a doctor of medicine, MD, or osteopathy, DO). Additionally, NPPs must meet the insurer-specified qualifications.
Independent Billing
Since 1998, designated NPPs are allowed to submit Medicare Part B claims for services, including procedures, provided in any inpatient or outpatient setting. For billing purposes, these “independent” services do not require physician involvement (e.g. physician initiation of care plan, physician-patient encounter, or physician presence on patient floor/unit) unless otherwise specified by state legislation or facility standards of practice. NPPs do not need to be employed by the physician group. The entity employing the physician group also may employ the NPP.
Claim requirements mandate the use of a national provider identifier (NPI) on all claims, therefore, all NPPs receive an NPI for claim submission. However, not all NPPs may directly bill Medicare or receive direct payment (e.g., physician assistant).1 In this situation, the NPP employer (i.e., physician or group), reports the service with the physician or group provider number and the NPP’s NPI included for identification of who actually provided the service.
Medicare Part B processes NPP claims reported under the independent billing option. Duplicate payments from any other Medicare Part A or Part B source is strictly prohibited and may result in refunds, fines and penalties. Generally, Medicare payment for NPP services is limited to 85% of the allowable physician rate. Financial impact of the 15% rate reduction is typically offset by the increase in physician time. Physicians may use this time to provide more comprehensive or complex services (admissions or consultations), potentially generating more revenue. Consistent with all provider documentation, NPP documentation must support the reported service.
Shared/Split Billing
The shared/split billing option first appeared in 2002 to address facility-based services provided to a single patient by an NPP and physician from the same group practice on the same calendar day. This option only applies to evaluation and management services provided in an emergency department, outpatient or inpatient hospital. It excludes consultations and critical care services. Unlike the independent billing option, the shared/split billing option only involves service provided by nurse practitioners, physician assistants, clinical nurse specialists, and certified nurse-midwives.
In order to qualify as a shared/split service, the NPP and the physician each must have a face-to-face encounter with the patient, although the extent of each provider’s involvement is left to provider discretion and/or local Medicare contractor requirements. The timing of each provider’s visit is irrelevant, as long as the two services are performed on the same date. For example, the NPP may see a hospital inpatient in the morning with a follow-up visit by the physician later in the day.4 When documenting, both the NPP and the physician should identify the name of the individual with whom the service is shared/split. This will allow for appropriate service capture, and ensure that the correct notes are sent to the payer in the event of claim denial and subsequent appeal. Each provider must document their portion of the rendered service and select the visit level supported by the cumulative encounter. The physician need not duplicate the elements performed and documented by the NPP, but merely perform and record the physician-determined critical or key portions. Do not confuse this billing option with teaching physician regulations. Physician and the specified NPPs cannot share or split a service with any other provider type (e.g., residents, medical or nursing students).
Only one claim may be submitted for a shared/split service. The physician may choose to report the service under his own name or under the NPP name. Reimbursement is dependent upon this selection. The physician name secures 100% of the Medicare allowable rate; the NPP name earns 85% of the allowable physician rate.
While the physician has the opportunity to report the service under his own name for the full service rate, the shared/split billing option requires the efforts of two individuals and may be an impractical approach for some physician groups.
“Incident-to”
Hospitalists, or their staff, may have encountered the term “incident-to” and wondered how this billing option applies to hospitalist services. “Incident-to” guidelines only apply to procedures and services performed in a private physician office. In this setting, the patient establishes care with the physician and the physician develops a patient-specific plan of care. Subsequent services may be provided to the established patient by the NPP, yet reported under the physician’s name for 100% of the allowable physician rate. “Incident-to” services cannot be reported by a hospitalist, since hospitalist services only take place in facility-based locations.
Summary
NPPs currently are involved in an extensive number of services within the hospital, and Medicare has two billing options for NPP services provided on behalf of or in conjunction with hospitalists. Each option involves specific rules and regulations with which NPPs and physician groups must comply.
Successful reporting requires understanding of and adherence to federal, state, and facility guidelines. It is important to identify NPP employment relationships, the NPP’s role in the provision of services, the state supervisory or collaborative rules, and local payer interpretations to prevent misrepresentation, misunderstanding, or erroneous reporting. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare benefit policy manual. www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed September 12, 2008.
2. Howie J, Erickson M. Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J of Critical Care. 2002;11:448-458.
3. Cowan M, Shapiro M, et al.. The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nursing Admin. 2006;36:79-85.
4. CMS. Medicare claims processing manual: Chapter 12, Section 30.6.1B. www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed September 14, 2008.
5. Pohlig C. Nonphysician providers in your practice. In: coding for chest medicine 2008. Northbrook, IL: Am Coll Chest Phy. 2008;249-254.
Recent changes in healthcare have forced academic medical centers to seek additional resources in the delivery of quality care. In response to internal and external pressures to minimize length of stay, adhere to limitations on the maximum number of admitted patients, focus on evidence-based care, and improve outcomes of care, hospitalists have incorporated non-physician providers (NPPs), such as acute care nurse practitioners (ACNPs), into their group practices.1
Whereas traditional nurse practitioners focus on the promotion of health and management of chronic illness, ACNPs focus on the care of acutely ill patients. Hospitalists utilize NPPs to expand medical service capacity and improve the efficiency and quality of patient care.2
Research indicates physician/nurse practitioner collaboration in the multidisciplinary management of hospitalized medical patients reduces length of stay and improves hospital profit without altering readmissions or mortality.3 Billing and documentation standards for NPP services must comply with current state and federal regulations. Hospitalist groups should become familiar with these guidelines prior to billing for NPP services involved in this patient care model.
The following highlights inpatient services provided by nurse practitioners (NPs) and physician assistants (PAs).
Covered Services
Medicare pays for services considered reasonable and necessary and not otherwise excluded from coverage. NPPs may provide any service permitted by the state scope of practice and performed in conjunction with the appropriate level of supervision or collaboration, as outlined in licensure or billing requirements. Being only limited by state and/or facility regulations, NPP services comprise visits or procedures typically rendered by ancillary staff or considered a physician service (a doctor of medicine, MD, or osteopathy, DO). Additionally, NPPs must meet the insurer-specified qualifications.
Independent Billing
Since 1998, designated NPPs are allowed to submit Medicare Part B claims for services, including procedures, provided in any inpatient or outpatient setting. For billing purposes, these “independent” services do not require physician involvement (e.g. physician initiation of care plan, physician-patient encounter, or physician presence on patient floor/unit) unless otherwise specified by state legislation or facility standards of practice. NPPs do not need to be employed by the physician group. The entity employing the physician group also may employ the NPP.
Claim requirements mandate the use of a national provider identifier (NPI) on all claims, therefore, all NPPs receive an NPI for claim submission. However, not all NPPs may directly bill Medicare or receive direct payment (e.g., physician assistant).1 In this situation, the NPP employer (i.e., physician or group), reports the service with the physician or group provider number and the NPP’s NPI included for identification of who actually provided the service.
Medicare Part B processes NPP claims reported under the independent billing option. Duplicate payments from any other Medicare Part A or Part B source is strictly prohibited and may result in refunds, fines and penalties. Generally, Medicare payment for NPP services is limited to 85% of the allowable physician rate. Financial impact of the 15% rate reduction is typically offset by the increase in physician time. Physicians may use this time to provide more comprehensive or complex services (admissions or consultations), potentially generating more revenue. Consistent with all provider documentation, NPP documentation must support the reported service.
Shared/Split Billing
The shared/split billing option first appeared in 2002 to address facility-based services provided to a single patient by an NPP and physician from the same group practice on the same calendar day. This option only applies to evaluation and management services provided in an emergency department, outpatient or inpatient hospital. It excludes consultations and critical care services. Unlike the independent billing option, the shared/split billing option only involves service provided by nurse practitioners, physician assistants, clinical nurse specialists, and certified nurse-midwives.
In order to qualify as a shared/split service, the NPP and the physician each must have a face-to-face encounter with the patient, although the extent of each provider’s involvement is left to provider discretion and/or local Medicare contractor requirements. The timing of each provider’s visit is irrelevant, as long as the two services are performed on the same date. For example, the NPP may see a hospital inpatient in the morning with a follow-up visit by the physician later in the day.4 When documenting, both the NPP and the physician should identify the name of the individual with whom the service is shared/split. This will allow for appropriate service capture, and ensure that the correct notes are sent to the payer in the event of claim denial and subsequent appeal. Each provider must document their portion of the rendered service and select the visit level supported by the cumulative encounter. The physician need not duplicate the elements performed and documented by the NPP, but merely perform and record the physician-determined critical or key portions. Do not confuse this billing option with teaching physician regulations. Physician and the specified NPPs cannot share or split a service with any other provider type (e.g., residents, medical or nursing students).
Only one claim may be submitted for a shared/split service. The physician may choose to report the service under his own name or under the NPP name. Reimbursement is dependent upon this selection. The physician name secures 100% of the Medicare allowable rate; the NPP name earns 85% of the allowable physician rate.
While the physician has the opportunity to report the service under his own name for the full service rate, the shared/split billing option requires the efforts of two individuals and may be an impractical approach for some physician groups.
“Incident-to”
Hospitalists, or their staff, may have encountered the term “incident-to” and wondered how this billing option applies to hospitalist services. “Incident-to” guidelines only apply to procedures and services performed in a private physician office. In this setting, the patient establishes care with the physician and the physician develops a patient-specific plan of care. Subsequent services may be provided to the established patient by the NPP, yet reported under the physician’s name for 100% of the allowable physician rate. “Incident-to” services cannot be reported by a hospitalist, since hospitalist services only take place in facility-based locations.
Summary
NPPs currently are involved in an extensive number of services within the hospital, and Medicare has two billing options for NPP services provided on behalf of or in conjunction with hospitalists. Each option involves specific rules and regulations with which NPPs and physician groups must comply.
Successful reporting requires understanding of and adherence to federal, state, and facility guidelines. It is important to identify NPP employment relationships, the NPP’s role in the provision of services, the state supervisory or collaborative rules, and local payer interpretations to prevent misrepresentation, misunderstanding, or erroneous reporting. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare benefit policy manual. www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed September 12, 2008.
2. Howie J, Erickson M. Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J of Critical Care. 2002;11:448-458.
3. Cowan M, Shapiro M, et al.. The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nursing Admin. 2006;36:79-85.
4. CMS. Medicare claims processing manual: Chapter 12, Section 30.6.1B. www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed September 14, 2008.
5. Pohlig C. Nonphysician providers in your practice. In: coding for chest medicine 2008. Northbrook, IL: Am Coll Chest Phy. 2008;249-254.
Recent changes in healthcare have forced academic medical centers to seek additional resources in the delivery of quality care. In response to internal and external pressures to minimize length of stay, adhere to limitations on the maximum number of admitted patients, focus on evidence-based care, and improve outcomes of care, hospitalists have incorporated non-physician providers (NPPs), such as acute care nurse practitioners (ACNPs), into their group practices.1
Whereas traditional nurse practitioners focus on the promotion of health and management of chronic illness, ACNPs focus on the care of acutely ill patients. Hospitalists utilize NPPs to expand medical service capacity and improve the efficiency and quality of patient care.2
Research indicates physician/nurse practitioner collaboration in the multidisciplinary management of hospitalized medical patients reduces length of stay and improves hospital profit without altering readmissions or mortality.3 Billing and documentation standards for NPP services must comply with current state and federal regulations. Hospitalist groups should become familiar with these guidelines prior to billing for NPP services involved in this patient care model.
The following highlights inpatient services provided by nurse practitioners (NPs) and physician assistants (PAs).
Covered Services
Medicare pays for services considered reasonable and necessary and not otherwise excluded from coverage. NPPs may provide any service permitted by the state scope of practice and performed in conjunction with the appropriate level of supervision or collaboration, as outlined in licensure or billing requirements. Being only limited by state and/or facility regulations, NPP services comprise visits or procedures typically rendered by ancillary staff or considered a physician service (a doctor of medicine, MD, or osteopathy, DO). Additionally, NPPs must meet the insurer-specified qualifications.
Independent Billing
Since 1998, designated NPPs are allowed to submit Medicare Part B claims for services, including procedures, provided in any inpatient or outpatient setting. For billing purposes, these “independent” services do not require physician involvement (e.g. physician initiation of care plan, physician-patient encounter, or physician presence on patient floor/unit) unless otherwise specified by state legislation or facility standards of practice. NPPs do not need to be employed by the physician group. The entity employing the physician group also may employ the NPP.
Claim requirements mandate the use of a national provider identifier (NPI) on all claims, therefore, all NPPs receive an NPI for claim submission. However, not all NPPs may directly bill Medicare or receive direct payment (e.g., physician assistant).1 In this situation, the NPP employer (i.e., physician or group), reports the service with the physician or group provider number and the NPP’s NPI included for identification of who actually provided the service.
Medicare Part B processes NPP claims reported under the independent billing option. Duplicate payments from any other Medicare Part A or Part B source is strictly prohibited and may result in refunds, fines and penalties. Generally, Medicare payment for NPP services is limited to 85% of the allowable physician rate. Financial impact of the 15% rate reduction is typically offset by the increase in physician time. Physicians may use this time to provide more comprehensive or complex services (admissions or consultations), potentially generating more revenue. Consistent with all provider documentation, NPP documentation must support the reported service.
Shared/Split Billing
The shared/split billing option first appeared in 2002 to address facility-based services provided to a single patient by an NPP and physician from the same group practice on the same calendar day. This option only applies to evaluation and management services provided in an emergency department, outpatient or inpatient hospital. It excludes consultations and critical care services. Unlike the independent billing option, the shared/split billing option only involves service provided by nurse practitioners, physician assistants, clinical nurse specialists, and certified nurse-midwives.
In order to qualify as a shared/split service, the NPP and the physician each must have a face-to-face encounter with the patient, although the extent of each provider’s involvement is left to provider discretion and/or local Medicare contractor requirements. The timing of each provider’s visit is irrelevant, as long as the two services are performed on the same date. For example, the NPP may see a hospital inpatient in the morning with a follow-up visit by the physician later in the day.4 When documenting, both the NPP and the physician should identify the name of the individual with whom the service is shared/split. This will allow for appropriate service capture, and ensure that the correct notes are sent to the payer in the event of claim denial and subsequent appeal. Each provider must document their portion of the rendered service and select the visit level supported by the cumulative encounter. The physician need not duplicate the elements performed and documented by the NPP, but merely perform and record the physician-determined critical or key portions. Do not confuse this billing option with teaching physician regulations. Physician and the specified NPPs cannot share or split a service with any other provider type (e.g., residents, medical or nursing students).
Only one claim may be submitted for a shared/split service. The physician may choose to report the service under his own name or under the NPP name. Reimbursement is dependent upon this selection. The physician name secures 100% of the Medicare allowable rate; the NPP name earns 85% of the allowable physician rate.
While the physician has the opportunity to report the service under his own name for the full service rate, the shared/split billing option requires the efforts of two individuals and may be an impractical approach for some physician groups.
“Incident-to”
Hospitalists, or their staff, may have encountered the term “incident-to” and wondered how this billing option applies to hospitalist services. “Incident-to” guidelines only apply to procedures and services performed in a private physician office. In this setting, the patient establishes care with the physician and the physician develops a patient-specific plan of care. Subsequent services may be provided to the established patient by the NPP, yet reported under the physician’s name for 100% of the allowable physician rate. “Incident-to” services cannot be reported by a hospitalist, since hospitalist services only take place in facility-based locations.
Summary
NPPs currently are involved in an extensive number of services within the hospital, and Medicare has two billing options for NPP services provided on behalf of or in conjunction with hospitalists. Each option involves specific rules and regulations with which NPPs and physician groups must comply.
Successful reporting requires understanding of and adherence to federal, state, and facility guidelines. It is important to identify NPP employment relationships, the NPP’s role in the provision of services, the state supervisory or collaborative rules, and local payer interpretations to prevent misrepresentation, misunderstanding, or erroneous reporting. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare benefit policy manual. www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed September 12, 2008.
2. Howie J, Erickson M. Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J of Critical Care. 2002;11:448-458.
3. Cowan M, Shapiro M, et al.. The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nursing Admin. 2006;36:79-85.
4. CMS. Medicare claims processing manual: Chapter 12, Section 30.6.1B. www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed September 14, 2008.
5. Pohlig C. Nonphysician providers in your practice. In: coding for chest medicine 2008. Northbrook, IL: Am Coll Chest Phy. 2008;249-254.
Know What to Document
Hospitalists who work in teaching hospitals need to understand the teaching physician (TP) rules, to know what qualifies for payment and how to document to receive that payment. TP services are payable when they are furnished by a physician who is not a resident or a resident with a teaching physician physically present during the critical or key portions of the service.
This article will focus on the documentation guidelines for inpatient services provided by the hospitalist in a teaching setting.
Evaluation and Management Services
Teaching physicians participate in evaluation and management (E/M) services with residents in several different ways. Below, three scenarios discuss documentation requirements:
Scenario One: The Stand-Alone Service. In this scenario, the teaching physician independently performs the entire service (i.e., all required elements of the billed visit) though the resident also may have seen the patient that same day. The TP may choose to document as if the care took place in a non-teaching setting. This documentation stands alone and independently supports the reported visit level.
Alternatively, the teaching physician may use the resident’s note. He or she does this by first documenting involvement in patient management and performance of the critical or key portion(s) of the service, and then linking to the resident’s note. The teaching physician selects the visit level based on the combined documentation (i.e., that of the teaching physician and the resident).
When referencing resident documentation, the teaching physician should use Medicare-approved linkage statements. Common examples include the following:
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note except the heart murmur is louder than documented, so I will obtain an echo to evaluate.”
Although all of these examples are acceptable, the last one best identifies the teaching physician’s involvement in patient management, which is a requirement of TP documentation.
Scenario Two: The Supervised Service. In this scenario, resident and teaching physician provide services simultaneously. The teaching physician either may supervise the resident’s performance of required service elements or personally perform some of them.
Documentation includes information about the teaching physician’s presence during the encounter, performance of the critical or key portions of the service and involvement in patient management, as well as a reference to the resident’s note. As in scenario one, the teaching physician selects the visit level based on the combined documentation.
Teaching physician statements associated with scenario two and accepted by Medicare reviewers include the following:
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Scenario two examples contain generalized statements considered acceptable for billing under teaching physician rules. Documenting patient-specific elements of the assessment and plan, however, not only demonstrate teaching physician involvement in patient care, but also evidence better quality of care.
Scenario Three: The Shared Service. In this case, the resident performs a portion or all of the required service elements without the teaching physician present and then documents the services. The teaching physician independently performs only the critical, or key, portions of the service and, as appropriate, discusses the case with the resident. Similar to scenario two, the TP references the resident’s note and documents presence during the encounter, performance of the critical or key portions of the service and involvement in patient management.
Remember, the teaching physician can not link to a resident note that does not exist. In other words, if the resident’s note is not available when the teaching physician is documenting, the note cannot be considered for billing purposes. When documented appropriately, as in the scenarios above, the teaching physician selects the visit level based on the combined documentation.
Medicare-approved linkage statements for use by teaching physicians in this scenario include the following:
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Documentation of teaching physician presence and participation provided solely by the resident is not sufficient to support the teaching physician service. Some examples of unacceptable documentation include:
- “Agree with above,” followed by legible countersignature or identity;
- “Rounded, Reviewed, Agree,” followed by legible countersignature or identity;
- “Discussed with resident. Agree,” followed by legible countersignature or identity;
- “Seen and agree,” followed by legible countersignature or identity;
- “Patient seen and evaluated,” followed by legible countersignature or identity; and
- Legible countersignature or identity alone.
Time-Based Services
Time-based E/M services require the teaching physician be present for the entire period for which the claim is made. Medical record documentation should reflect the teaching physician’s total visit time (i.e., spent on the unit/floor for inpatient services), including face-to-face time with the patient.
Time spent by the resident without the presence of the teaching physician does not count toward the teaching physician’s time, nor does time the TP spends teaching activities unrelated to patient care. Examples of time-based services typically provided by hospitalists include:
- Critical-care services (CPT codes 99291-99292);
- Hospital discharge day management (CPT codes 99238-99239);
- E/M codes in which counseling and/or coordination of care dominates (more than 50% of) the encounter, and time is considered the key or controlling factor to qualify for a particular level of E/M service; and
- Prolonged services (CPT codes 99358-99359).
Surgical Services
Surgical services, which are defined as minor or major, also are subject to teaching physician rules. Teaching physician regulations identify minor procedures as those that take five minutes or less to complete and involve relatively little decision making once the need for the service is determined. Appropriate billing and payment hinges on the teaching physician’s presence for the entire procedure. Documentation should include a statement of presence, written and signed by the teaching physician.
Services that require more than five minutes are considered major surgical services, requiring teaching physician presence only during the (physician-determined) critical and key portions of the procedure. However, the teaching physician must be available to return to the procedure area during the surgery’s entirety, and not be involved in another procedure. Arrangements must be made to have another qualified physician available should the teaching physician get called away. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References:
1. Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100, www.cms.hhs.gov/manuals/downloads/clm104c12.pdf.
2. Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2, www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf.
3. Centers for Medicare & Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents, www.cms.hhs.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf.
4. Manaker, S. Teaching Physician Regulations. Coding for Chest Medicine 2008, American College of Chest Physicians, 2008; 279-285.
5. Pohlig, C. Evaluation & Management Services: An Overview. Coding for Chest Medicine 2008, American College of Chest Physicians, 2008;57-69.
6. American Medical Association. cpt® 2008, Current Procedural Terminology Professional Edition. American Medical Association, 2007; 9-16.
Hospitalists who work in teaching hospitals need to understand the teaching physician (TP) rules, to know what qualifies for payment and how to document to receive that payment. TP services are payable when they are furnished by a physician who is not a resident or a resident with a teaching physician physically present during the critical or key portions of the service.
This article will focus on the documentation guidelines for inpatient services provided by the hospitalist in a teaching setting.
Evaluation and Management Services
Teaching physicians participate in evaluation and management (E/M) services with residents in several different ways. Below, three scenarios discuss documentation requirements:
Scenario One: The Stand-Alone Service. In this scenario, the teaching physician independently performs the entire service (i.e., all required elements of the billed visit) though the resident also may have seen the patient that same day. The TP may choose to document as if the care took place in a non-teaching setting. This documentation stands alone and independently supports the reported visit level.
Alternatively, the teaching physician may use the resident’s note. He or she does this by first documenting involvement in patient management and performance of the critical or key portion(s) of the service, and then linking to the resident’s note. The teaching physician selects the visit level based on the combined documentation (i.e., that of the teaching physician and the resident).
When referencing resident documentation, the teaching physician should use Medicare-approved linkage statements. Common examples include the following:
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note except the heart murmur is louder than documented, so I will obtain an echo to evaluate.”
Although all of these examples are acceptable, the last one best identifies the teaching physician’s involvement in patient management, which is a requirement of TP documentation.
Scenario Two: The Supervised Service. In this scenario, resident and teaching physician provide services simultaneously. The teaching physician either may supervise the resident’s performance of required service elements or personally perform some of them.
Documentation includes information about the teaching physician’s presence during the encounter, performance of the critical or key portions of the service and involvement in patient management, as well as a reference to the resident’s note. As in scenario one, the teaching physician selects the visit level based on the combined documentation.
Teaching physician statements associated with scenario two and accepted by Medicare reviewers include the following:
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Scenario two examples contain generalized statements considered acceptable for billing under teaching physician rules. Documenting patient-specific elements of the assessment and plan, however, not only demonstrate teaching physician involvement in patient care, but also evidence better quality of care.
Scenario Three: The Shared Service. In this case, the resident performs a portion or all of the required service elements without the teaching physician present and then documents the services. The teaching physician independently performs only the critical, or key, portions of the service and, as appropriate, discusses the case with the resident. Similar to scenario two, the TP references the resident’s note and documents presence during the encounter, performance of the critical or key portions of the service and involvement in patient management.
Remember, the teaching physician can not link to a resident note that does not exist. In other words, if the resident’s note is not available when the teaching physician is documenting, the note cannot be considered for billing purposes. When documented appropriately, as in the scenarios above, the teaching physician selects the visit level based on the combined documentation.
Medicare-approved linkage statements for use by teaching physicians in this scenario include the following:
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Documentation of teaching physician presence and participation provided solely by the resident is not sufficient to support the teaching physician service. Some examples of unacceptable documentation include:
- “Agree with above,” followed by legible countersignature or identity;
- “Rounded, Reviewed, Agree,” followed by legible countersignature or identity;
- “Discussed with resident. Agree,” followed by legible countersignature or identity;
- “Seen and agree,” followed by legible countersignature or identity;
- “Patient seen and evaluated,” followed by legible countersignature or identity; and
- Legible countersignature or identity alone.
Time-Based Services
Time-based E/M services require the teaching physician be present for the entire period for which the claim is made. Medical record documentation should reflect the teaching physician’s total visit time (i.e., spent on the unit/floor for inpatient services), including face-to-face time with the patient.
Time spent by the resident without the presence of the teaching physician does not count toward the teaching physician’s time, nor does time the TP spends teaching activities unrelated to patient care. Examples of time-based services typically provided by hospitalists include:
- Critical-care services (CPT codes 99291-99292);
- Hospital discharge day management (CPT codes 99238-99239);
- E/M codes in which counseling and/or coordination of care dominates (more than 50% of) the encounter, and time is considered the key or controlling factor to qualify for a particular level of E/M service; and
- Prolonged services (CPT codes 99358-99359).
Surgical Services
Surgical services, which are defined as minor or major, also are subject to teaching physician rules. Teaching physician regulations identify minor procedures as those that take five minutes or less to complete and involve relatively little decision making once the need for the service is determined. Appropriate billing and payment hinges on the teaching physician’s presence for the entire procedure. Documentation should include a statement of presence, written and signed by the teaching physician.
Services that require more than five minutes are considered major surgical services, requiring teaching physician presence only during the (physician-determined) critical and key portions of the procedure. However, the teaching physician must be available to return to the procedure area during the surgery’s entirety, and not be involved in another procedure. Arrangements must be made to have another qualified physician available should the teaching physician get called away. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References:
1. Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100, www.cms.hhs.gov/manuals/downloads/clm104c12.pdf.
2. Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2, www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf.
3. Centers for Medicare & Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents, www.cms.hhs.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf.
4. Manaker, S. Teaching Physician Regulations. Coding for Chest Medicine 2008, American College of Chest Physicians, 2008; 279-285.
5. Pohlig, C. Evaluation & Management Services: An Overview. Coding for Chest Medicine 2008, American College of Chest Physicians, 2008;57-69.
6. American Medical Association. cpt® 2008, Current Procedural Terminology Professional Edition. American Medical Association, 2007; 9-16.
Hospitalists who work in teaching hospitals need to understand the teaching physician (TP) rules, to know what qualifies for payment and how to document to receive that payment. TP services are payable when they are furnished by a physician who is not a resident or a resident with a teaching physician physically present during the critical or key portions of the service.
This article will focus on the documentation guidelines for inpatient services provided by the hospitalist in a teaching setting.
Evaluation and Management Services
Teaching physicians participate in evaluation and management (E/M) services with residents in several different ways. Below, three scenarios discuss documentation requirements:
Scenario One: The Stand-Alone Service. In this scenario, the teaching physician independently performs the entire service (i.e., all required elements of the billed visit) though the resident also may have seen the patient that same day. The TP may choose to document as if the care took place in a non-teaching setting. This documentation stands alone and independently supports the reported visit level.
Alternatively, the teaching physician may use the resident’s note. He or she does this by first documenting involvement in patient management and performance of the critical or key portion(s) of the service, and then linking to the resident’s note. The teaching physician selects the visit level based on the combined documentation (i.e., that of the teaching physician and the resident).
When referencing resident documentation, the teaching physician should use Medicare-approved linkage statements. Common examples include the following:
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note except the heart murmur is louder than documented, so I will obtain an echo to evaluate.”
Although all of these examples are acceptable, the last one best identifies the teaching physician’s involvement in patient management, which is a requirement of TP documentation.
Scenario Two: The Supervised Service. In this scenario, resident and teaching physician provide services simultaneously. The teaching physician either may supervise the resident’s performance of required service elements or personally perform some of them.
Documentation includes information about the teaching physician’s presence during the encounter, performance of the critical or key portions of the service and involvement in patient management, as well as a reference to the resident’s note. As in scenario one, the teaching physician selects the visit level based on the combined documentation.
Teaching physician statements associated with scenario two and accepted by Medicare reviewers include the following:
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Scenario two examples contain generalized statements considered acceptable for billing under teaching physician rules. Documenting patient-specific elements of the assessment and plan, however, not only demonstrate teaching physician involvement in patient care, but also evidence better quality of care.
Scenario Three: The Shared Service. In this case, the resident performs a portion or all of the required service elements without the teaching physician present and then documents the services. The teaching physician independently performs only the critical, or key, portions of the service and, as appropriate, discusses the case with the resident. Similar to scenario two, the TP references the resident’s note and documents presence during the encounter, performance of the critical or key portions of the service and involvement in patient management.
Remember, the teaching physician can not link to a resident note that does not exist. In other words, if the resident’s note is not available when the teaching physician is documenting, the note cannot be considered for billing purposes. When documented appropriately, as in the scenarios above, the teaching physician selects the visit level based on the combined documentation.
Medicare-approved linkage statements for use by teaching physicians in this scenario include the following:
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Documentation of teaching physician presence and participation provided solely by the resident is not sufficient to support the teaching physician service. Some examples of unacceptable documentation include:
- “Agree with above,” followed by legible countersignature or identity;
- “Rounded, Reviewed, Agree,” followed by legible countersignature or identity;
- “Discussed with resident. Agree,” followed by legible countersignature or identity;
- “Seen and agree,” followed by legible countersignature or identity;
- “Patient seen and evaluated,” followed by legible countersignature or identity; and
- Legible countersignature or identity alone.
Time-Based Services
Time-based E/M services require the teaching physician be present for the entire period for which the claim is made. Medical record documentation should reflect the teaching physician’s total visit time (i.e., spent on the unit/floor for inpatient services), including face-to-face time with the patient.
Time spent by the resident without the presence of the teaching physician does not count toward the teaching physician’s time, nor does time the TP spends teaching activities unrelated to patient care. Examples of time-based services typically provided by hospitalists include:
- Critical-care services (CPT codes 99291-99292);
- Hospital discharge day management (CPT codes 99238-99239);
- E/M codes in which counseling and/or coordination of care dominates (more than 50% of) the encounter, and time is considered the key or controlling factor to qualify for a particular level of E/M service; and
- Prolonged services (CPT codes 99358-99359).
Surgical Services
Surgical services, which are defined as minor or major, also are subject to teaching physician rules. Teaching physician regulations identify minor procedures as those that take five minutes or less to complete and involve relatively little decision making once the need for the service is determined. Appropriate billing and payment hinges on the teaching physician’s presence for the entire procedure. Documentation should include a statement of presence, written and signed by the teaching physician.
Services that require more than five minutes are considered major surgical services, requiring teaching physician presence only during the (physician-determined) critical and key portions of the procedure. However, the teaching physician must be available to return to the procedure area during the surgery’s entirety, and not be involved in another procedure. Arrangements must be made to have another qualified physician available should the teaching physician get called away. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References:
1. Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100, www.cms.hhs.gov/manuals/downloads/clm104c12.pdf.
2. Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2, www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf.
3. Centers for Medicare & Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents, www.cms.hhs.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf.
4. Manaker, S. Teaching Physician Regulations. Coding for Chest Medicine 2008, American College of Chest Physicians, 2008; 279-285.
5. Pohlig, C. Evaluation & Management Services: An Overview. Coding for Chest Medicine 2008, American College of Chest Physicians, 2008;57-69.
6. American Medical Association. cpt® 2008, Current Procedural Terminology Professional Edition. American Medical Association, 2007; 9-16.
The Observation Deck
Observation care provides a mechanism to evaluate and treat patients without the resource utilization and financial responsibility associated with an inpatient admission. Hospitalists may not understand the billing compliance risk and corresponding revenue implications when observation services (OBS) are not captured correctly.
Are OBS best reported with observation care codes (99218-99220, 99234-99236), office visit codes (99201-99215), or initial hospital care codes (99221-99223)? Code selection depends upon the patient’s registered status, the nature of the provided service, and the length of stay. Review the following information before reporting OBS to ensure an accurate claim submission.
Attending Physician Responsibilities
The physician-documented reason for observation substantiates the medical necessity for the OBS admission. Contractors often evaluate medical records to determine the consistency between the physician order (physician intent), the services actually provided (inpatient or outpatient), and the medical necessity of those services, including the medical appropriateness of the inpatient or observation stay.
Certain diagnoses and procedures generally do not support an inpatient admission and fall within the definitions of outpatient observation. Uncomplicated presentations of chest pain (rule out MI), mild asthma/COPD, mild CHF, syncope and decreased responsiveness, atrial arrhythmias, and renal colic all frequently are associated with the expectation of a brief (less than 24-hour) stay unless serious pathology is uncovered.2 Situations that do not meet the criteria for observation care are considered “not medically necessary” and separate payment is not permitted. Examples of circumstances that lack medical necessity include:
- Outpatient blood administration;
- Lack of/delay in patient transportation;
- Provision of a medical exam for patients who do not require skilled support;
- Routine preparation prior to and recovery after diagnostic testing;
- Routine recovery and post-operative care after ambulatory surgery;
- When used for the convenience of the physician, patient or patient’s family;
- While awaiting transfer to another facility;
- Duration of care exceeding 48 hours;
- When an overnight stay is planned prior to diagnostic testing;
- Standing orders following outpatient surgery;
- Services that would normally require inpatient stay;
- No physicians order to admit to observation;
- Observation following an uncomplicated treatment or procedure;
- Services that are not reasonable and necessary for care of the patient;
- Services provided concurrently with chemotherapy; and
- Inpatients discharged to outpatient observation status.3
The attending physician of record assumes responsibility for the patient’s admission to observation and is permitted to report observation care codes. In addition to the reason for admission, a medical record involving the observation stay must include dated and timed physician admitting orders outlining the care plan, physician progress notes, and discharge orders. This documentation must be added to any other record prepared as a result of an emergency department or outpatient clinic encounter. If physicians other than the admitting physician/group (i.e., physicians in different specialties) provide services to the patient during observation, they must use the appropriate outpatient visit (e.g., 99214) or consultation code (e.g., 99244).
Length of Stay4
In general, the duration of observation care services typically does not exceed 24 hours, although in some circumstances patients may require a second day. Observation care for greater than 48 hours without inpatient admission is not considered medically necessary but may be payable after medical review. When the stay spans two calendar days, physician billing is straightforward: Select an initial observation care code (99218-99220) for calendar day one and the observation discharge code (99217) for day two. Only the admitting physician/group may report the discharge service, when applicable. Documentation must demonstrate a face-to-face encounter by the physician for each date of service.
Should the stay only constitute one calendar day, the duration of care becomes a crucial factor in determining the code category. Standard OBS codes (99218-99220) are applicable if the patient stay is less than eight hours on any given date. The OBS discharge code (99217) is not reported in this instance, although the documentation should reflect the attending physician’s written order and appropriate discharge plan. Alternately, same day admit/discharge codes (99234-99236) apply to single-day stays lasting more than eight hours. The OBS discharge code (99217) also is not reported in this instance. Documentation must identify, at a minimum:
- Duration of the stay;
- Presence by the billing physician; and
- Physician performance of each service (i.e., both an admission and discharge note).
Inpatient Admission1,4-5
Sometimes the patient requires inpatient admission after initially being placed in observation. If the inpatient admission occurs on the same day as the OBS admission, only one service is reported (e.g., 99222). The physician need not redocument a complete history and physical (H&P) but merely write the new order for admission and update the OBS assessment with any relevant, new information.
Should the inpatient admission occur on the second calendar day of the OBS stay, the physician is able to report the initial observation care code (e.g., 99219) on day one, and the initial inpatient care code (e.g., 99223) on day two. However, the physician must meet the documentation guidelines for initial hospital care and redocument the H&P associated with the reported visit level. In the case of 99223, the physician must document a comprehensive history (only referring to the previous review of systems and histories, while rewriting the history of present illness) and high complexity decision making. If the physician chooses not to document to this extent, a subsequent hospital care code (99231-99233) is reasonable because the episode of care is a continuation from the observation phase.
Beware that some insurers may change the patient’s status for the entire episode of care. In other words, the conversion to inpatient status occurs on day two of the patient stay, but the insurer may convert the entire stay, including day one, to an inpatient status. Should this happen, the physician is responsible for reporting the visit category that corresponds with the patient’s status. Inpatient services codes are required for claim submission when the patient stay qualifies as an inpatient admission. Because these conversions occur with some frequency, it is advisable to hold claims intended for observation patients until the correct patient status can be confirmed by the utilization review team, and communicated to the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References
- 1. American Medical Association. cpt 2008, Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2007; 9-16 CPT codes, descriptions and other data only are copyright 2007 American Medical Association (AMA). All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the AMA.
- 2. Highmark Medicare Services. Local Coverage Determination L27548 Acute Care: Inpatient, Observation and Treatment Room Services. Available at www.highmarkmedicareservices.com/policy/mac-ab/127548.html. Accessed July 14, 2008.
- 3. Cigna. Healthcare Coverage Position: Observation Care. Available at www.cigna.com/customer_care/healthcare_ professional/coverage_positions/medical/mm_0411_coveragepositioncriteria_observation_care.pdf. Accessed July 12, 2008.
- 4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed July 13, 2008.
- 5. Pohlig C. Evaluation & Management Services: An Overview. Coding for Chest Medicine 2008. Northbrook, IL: American College of Chest Physicians, 2008; 57-69.
- 6. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 1, Section 50.3. Available at www.cms.hhs.gov/manuals/downloads/ clm104c01.pdf. Accessed July 13, 2008.
Observation care provides a mechanism to evaluate and treat patients without the resource utilization and financial responsibility associated with an inpatient admission. Hospitalists may not understand the billing compliance risk and corresponding revenue implications when observation services (OBS) are not captured correctly.
Are OBS best reported with observation care codes (99218-99220, 99234-99236), office visit codes (99201-99215), or initial hospital care codes (99221-99223)? Code selection depends upon the patient’s registered status, the nature of the provided service, and the length of stay. Review the following information before reporting OBS to ensure an accurate claim submission.
Attending Physician Responsibilities
The physician-documented reason for observation substantiates the medical necessity for the OBS admission. Contractors often evaluate medical records to determine the consistency between the physician order (physician intent), the services actually provided (inpatient or outpatient), and the medical necessity of those services, including the medical appropriateness of the inpatient or observation stay.
Certain diagnoses and procedures generally do not support an inpatient admission and fall within the definitions of outpatient observation. Uncomplicated presentations of chest pain (rule out MI), mild asthma/COPD, mild CHF, syncope and decreased responsiveness, atrial arrhythmias, and renal colic all frequently are associated with the expectation of a brief (less than 24-hour) stay unless serious pathology is uncovered.2 Situations that do not meet the criteria for observation care are considered “not medically necessary” and separate payment is not permitted. Examples of circumstances that lack medical necessity include:
- Outpatient blood administration;
- Lack of/delay in patient transportation;
- Provision of a medical exam for patients who do not require skilled support;
- Routine preparation prior to and recovery after diagnostic testing;
- Routine recovery and post-operative care after ambulatory surgery;
- When used for the convenience of the physician, patient or patient’s family;
- While awaiting transfer to another facility;
- Duration of care exceeding 48 hours;
- When an overnight stay is planned prior to diagnostic testing;
- Standing orders following outpatient surgery;
- Services that would normally require inpatient stay;
- No physicians order to admit to observation;
- Observation following an uncomplicated treatment or procedure;
- Services that are not reasonable and necessary for care of the patient;
- Services provided concurrently with chemotherapy; and
- Inpatients discharged to outpatient observation status.3
The attending physician of record assumes responsibility for the patient’s admission to observation and is permitted to report observation care codes. In addition to the reason for admission, a medical record involving the observation stay must include dated and timed physician admitting orders outlining the care plan, physician progress notes, and discharge orders. This documentation must be added to any other record prepared as a result of an emergency department or outpatient clinic encounter. If physicians other than the admitting physician/group (i.e., physicians in different specialties) provide services to the patient during observation, they must use the appropriate outpatient visit (e.g., 99214) or consultation code (e.g., 99244).
Length of Stay4
In general, the duration of observation care services typically does not exceed 24 hours, although in some circumstances patients may require a second day. Observation care for greater than 48 hours without inpatient admission is not considered medically necessary but may be payable after medical review. When the stay spans two calendar days, physician billing is straightforward: Select an initial observation care code (99218-99220) for calendar day one and the observation discharge code (99217) for day two. Only the admitting physician/group may report the discharge service, when applicable. Documentation must demonstrate a face-to-face encounter by the physician for each date of service.
Should the stay only constitute one calendar day, the duration of care becomes a crucial factor in determining the code category. Standard OBS codes (99218-99220) are applicable if the patient stay is less than eight hours on any given date. The OBS discharge code (99217) is not reported in this instance, although the documentation should reflect the attending physician’s written order and appropriate discharge plan. Alternately, same day admit/discharge codes (99234-99236) apply to single-day stays lasting more than eight hours. The OBS discharge code (99217) also is not reported in this instance. Documentation must identify, at a minimum:
- Duration of the stay;
- Presence by the billing physician; and
- Physician performance of each service (i.e., both an admission and discharge note).
Inpatient Admission1,4-5
Sometimes the patient requires inpatient admission after initially being placed in observation. If the inpatient admission occurs on the same day as the OBS admission, only one service is reported (e.g., 99222). The physician need not redocument a complete history and physical (H&P) but merely write the new order for admission and update the OBS assessment with any relevant, new information.
Should the inpatient admission occur on the second calendar day of the OBS stay, the physician is able to report the initial observation care code (e.g., 99219) on day one, and the initial inpatient care code (e.g., 99223) on day two. However, the physician must meet the documentation guidelines for initial hospital care and redocument the H&P associated with the reported visit level. In the case of 99223, the physician must document a comprehensive history (only referring to the previous review of systems and histories, while rewriting the history of present illness) and high complexity decision making. If the physician chooses not to document to this extent, a subsequent hospital care code (99231-99233) is reasonable because the episode of care is a continuation from the observation phase.
Beware that some insurers may change the patient’s status for the entire episode of care. In other words, the conversion to inpatient status occurs on day two of the patient stay, but the insurer may convert the entire stay, including day one, to an inpatient status. Should this happen, the physician is responsible for reporting the visit category that corresponds with the patient’s status. Inpatient services codes are required for claim submission when the patient stay qualifies as an inpatient admission. Because these conversions occur with some frequency, it is advisable to hold claims intended for observation patients until the correct patient status can be confirmed by the utilization review team, and communicated to the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References
- 1. American Medical Association. cpt 2008, Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2007; 9-16 CPT codes, descriptions and other data only are copyright 2007 American Medical Association (AMA). All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the AMA.
- 2. Highmark Medicare Services. Local Coverage Determination L27548 Acute Care: Inpatient, Observation and Treatment Room Services. Available at www.highmarkmedicareservices.com/policy/mac-ab/127548.html. Accessed July 14, 2008.
- 3. Cigna. Healthcare Coverage Position: Observation Care. Available at www.cigna.com/customer_care/healthcare_ professional/coverage_positions/medical/mm_0411_coveragepositioncriteria_observation_care.pdf. Accessed July 12, 2008.
- 4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed July 13, 2008.
- 5. Pohlig C. Evaluation & Management Services: An Overview. Coding for Chest Medicine 2008. Northbrook, IL: American College of Chest Physicians, 2008; 57-69.
- 6. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 1, Section 50.3. Available at www.cms.hhs.gov/manuals/downloads/ clm104c01.pdf. Accessed July 13, 2008.
Observation care provides a mechanism to evaluate and treat patients without the resource utilization and financial responsibility associated with an inpatient admission. Hospitalists may not understand the billing compliance risk and corresponding revenue implications when observation services (OBS) are not captured correctly.
Are OBS best reported with observation care codes (99218-99220, 99234-99236), office visit codes (99201-99215), or initial hospital care codes (99221-99223)? Code selection depends upon the patient’s registered status, the nature of the provided service, and the length of stay. Review the following information before reporting OBS to ensure an accurate claim submission.
Attending Physician Responsibilities
The physician-documented reason for observation substantiates the medical necessity for the OBS admission. Contractors often evaluate medical records to determine the consistency between the physician order (physician intent), the services actually provided (inpatient or outpatient), and the medical necessity of those services, including the medical appropriateness of the inpatient or observation stay.
Certain diagnoses and procedures generally do not support an inpatient admission and fall within the definitions of outpatient observation. Uncomplicated presentations of chest pain (rule out MI), mild asthma/COPD, mild CHF, syncope and decreased responsiveness, atrial arrhythmias, and renal colic all frequently are associated with the expectation of a brief (less than 24-hour) stay unless serious pathology is uncovered.2 Situations that do not meet the criteria for observation care are considered “not medically necessary” and separate payment is not permitted. Examples of circumstances that lack medical necessity include:
- Outpatient blood administration;
- Lack of/delay in patient transportation;
- Provision of a medical exam for patients who do not require skilled support;
- Routine preparation prior to and recovery after diagnostic testing;
- Routine recovery and post-operative care after ambulatory surgery;
- When used for the convenience of the physician, patient or patient’s family;
- While awaiting transfer to another facility;
- Duration of care exceeding 48 hours;
- When an overnight stay is planned prior to diagnostic testing;
- Standing orders following outpatient surgery;
- Services that would normally require inpatient stay;
- No physicians order to admit to observation;
- Observation following an uncomplicated treatment or procedure;
- Services that are not reasonable and necessary for care of the patient;
- Services provided concurrently with chemotherapy; and
- Inpatients discharged to outpatient observation status.3
The attending physician of record assumes responsibility for the patient’s admission to observation and is permitted to report observation care codes. In addition to the reason for admission, a medical record involving the observation stay must include dated and timed physician admitting orders outlining the care plan, physician progress notes, and discharge orders. This documentation must be added to any other record prepared as a result of an emergency department or outpatient clinic encounter. If physicians other than the admitting physician/group (i.e., physicians in different specialties) provide services to the patient during observation, they must use the appropriate outpatient visit (e.g., 99214) or consultation code (e.g., 99244).
Length of Stay4
In general, the duration of observation care services typically does not exceed 24 hours, although in some circumstances patients may require a second day. Observation care for greater than 48 hours without inpatient admission is not considered medically necessary but may be payable after medical review. When the stay spans two calendar days, physician billing is straightforward: Select an initial observation care code (99218-99220) for calendar day one and the observation discharge code (99217) for day two. Only the admitting physician/group may report the discharge service, when applicable. Documentation must demonstrate a face-to-face encounter by the physician for each date of service.
Should the stay only constitute one calendar day, the duration of care becomes a crucial factor in determining the code category. Standard OBS codes (99218-99220) are applicable if the patient stay is less than eight hours on any given date. The OBS discharge code (99217) is not reported in this instance, although the documentation should reflect the attending physician’s written order and appropriate discharge plan. Alternately, same day admit/discharge codes (99234-99236) apply to single-day stays lasting more than eight hours. The OBS discharge code (99217) also is not reported in this instance. Documentation must identify, at a minimum:
- Duration of the stay;
- Presence by the billing physician; and
- Physician performance of each service (i.e., both an admission and discharge note).
Inpatient Admission1,4-5
Sometimes the patient requires inpatient admission after initially being placed in observation. If the inpatient admission occurs on the same day as the OBS admission, only one service is reported (e.g., 99222). The physician need not redocument a complete history and physical (H&P) but merely write the new order for admission and update the OBS assessment with any relevant, new information.
Should the inpatient admission occur on the second calendar day of the OBS stay, the physician is able to report the initial observation care code (e.g., 99219) on day one, and the initial inpatient care code (e.g., 99223) on day two. However, the physician must meet the documentation guidelines for initial hospital care and redocument the H&P associated with the reported visit level. In the case of 99223, the physician must document a comprehensive history (only referring to the previous review of systems and histories, while rewriting the history of present illness) and high complexity decision making. If the physician chooses not to document to this extent, a subsequent hospital care code (99231-99233) is reasonable because the episode of care is a continuation from the observation phase.
Beware that some insurers may change the patient’s status for the entire episode of care. In other words, the conversion to inpatient status occurs on day two of the patient stay, but the insurer may convert the entire stay, including day one, to an inpatient status. Should this happen, the physician is responsible for reporting the visit category that corresponds with the patient’s status. Inpatient services codes are required for claim submission when the patient stay qualifies as an inpatient admission. Because these conversions occur with some frequency, it is advisable to hold claims intended for observation patients until the correct patient status can be confirmed by the utilization review team, and communicated to the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
References
- 1. American Medical Association. cpt 2008, Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2007; 9-16 CPT codes, descriptions and other data only are copyright 2007 American Medical Association (AMA). All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the AMA.
- 2. Highmark Medicare Services. Local Coverage Determination L27548 Acute Care: Inpatient, Observation and Treatment Room Services. Available at www.highmarkmedicareservices.com/policy/mac-ab/127548.html. Accessed July 14, 2008.
- 3. Cigna. Healthcare Coverage Position: Observation Care. Available at www.cigna.com/customer_care/healthcare_ professional/coverage_positions/medical/mm_0411_coveragepositioncriteria_observation_care.pdf. Accessed July 12, 2008.
- 4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed July 13, 2008.
- 5. Pohlig C. Evaluation & Management Services: An Overview. Coding for Chest Medicine 2008. Northbrook, IL: American College of Chest Physicians, 2008; 57-69.
- 6. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 1, Section 50.3. Available at www.cms.hhs.gov/manuals/downloads/ clm104c01.pdf. Accessed July 13, 2008.
Sort Out Surgical Cases
Hospitalists often are involved in the care of a surgical patient. Reimbursement for surgical procedures includes payment for pre-, intra-, and post-operative care.
Knowing the billing and coding responsibilities apart from those of the surgeon is imperative for the hospitalist’s accurate charge capture. There are several critical misconceptions in this regard:
- Hospitalists cannot bill for services when involved in a surgical case;
- Surgeons are not responsible for inpatient care if the patient is stable and does not require additional inpatient post-op visits; and
- Modifiers are not required for hospitalist claims unless the hospitalist reports under the same tax identification number as the surgeon.
Determine Global Period
Procedures are categorized as major or minor surgery. A global period is assigned to each procedure code, designating post-operative periods of zero, 10, or 90 days. Physician services during this global period are considered part of the packaged payment and not separately reimbursed.
The global period for any given CPT code can be identified in the Medicare Physician Fee Schedule and accessed at www.cms.hhs.gov/PfsLookup. In addition to zero, 10, and 90 days, services can be noted with:
- XXX, indicating the global period concept does not apply; or
- ZZZ, indicating an “add-on” procedure that must always be reported with the relevant primary procedure code; “add-on” procedures assume the global period of the primary procedure.
Major surgery routinely is allotted 90-day global periods. Therefore, the surgeon is responsible for the patient and must provide all related care one day prior to the surgery forward thru 90 postoperative days at no additional charge. Minor surgery, including endoscopy, has zero or 10-day postoperative periods, bundling all services on the surgical day only, or the surgical day and the subsequent 10 days, respectively (see Table 1, p. above).
The Surgeon Defined
Any qualified physician able to perform “surgical” services within his scope of practice is considered a “surgeon” for billing purposes. For example, a pulmonologist, or primary care physician, must meet the surgical billing and documentation requirements when performing bronchoscopies or uncomplicated incision-and-drainage services, respectively.
Surgical services easily are identified as any code included in range 20000-69999. This code series includes major, minor, and endoscopic procedures. The “surgeon” and all physicians in the same group practice (i.e., reporting services under the same tax identification number) with the same specialty designation must adhere to the global period billing rules.
Alternately, physicians with different specialty designations in the same group practice (e.g., multispecialty group that reports services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed upon) transfer of care did not occur. Information on physician specialty designations is available at www.highmarkmedicareservices.com/partb/refman/appendix-d.html.
Package Components
The following services are included in the surgeon’s packaged payment:
- Preoperative visits after the decision for surgery is made beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications, but not require additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Post-operative pain management provided by the surgeon.
Services not included are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery. Append modifier 57 to this visit if provided the day before or day of major surgery to alert the payer that the service resulted in the decision for surgery. Append modifier 25 to this visit if provided the day of minor surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care. This agreement may be in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record;
- Post-operative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery. These services only are payable after the patient has been discharged from the hospitalization in which the surgery occurred. Append modifier 24 to these unrelated post-op visits;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the post-operative period that do not result in repeat operations or treatment for complications;
- Treatment for post-operative complications that require a return trip to the operating room, catheterization lab, or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical care services (CPT codes 99291 and 99292) unrelated to the surgery in which a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon. Append modifier 24 to these unrelated critical care services (see Table 2, above).
Payer Variations
While Medicare does not require modifier usage by hospitalists providing medically necessary services on surgical cases, some private payers do. Their electronic claim systems may not differentiate services by non-surgical specialists, requiring all physicians to append the appropriate modifier depending on the reason and timing of the service (see “Key Modifiers” below). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Hospitalists often are involved in the care of a surgical patient. Reimbursement for surgical procedures includes payment for pre-, intra-, and post-operative care.
Knowing the billing and coding responsibilities apart from those of the surgeon is imperative for the hospitalist’s accurate charge capture. There are several critical misconceptions in this regard:
- Hospitalists cannot bill for services when involved in a surgical case;
- Surgeons are not responsible for inpatient care if the patient is stable and does not require additional inpatient post-op visits; and
- Modifiers are not required for hospitalist claims unless the hospitalist reports under the same tax identification number as the surgeon.
Determine Global Period
Procedures are categorized as major or minor surgery. A global period is assigned to each procedure code, designating post-operative periods of zero, 10, or 90 days. Physician services during this global period are considered part of the packaged payment and not separately reimbursed.
The global period for any given CPT code can be identified in the Medicare Physician Fee Schedule and accessed at www.cms.hhs.gov/PfsLookup. In addition to zero, 10, and 90 days, services can be noted with:
- XXX, indicating the global period concept does not apply; or
- ZZZ, indicating an “add-on” procedure that must always be reported with the relevant primary procedure code; “add-on” procedures assume the global period of the primary procedure.
Major surgery routinely is allotted 90-day global periods. Therefore, the surgeon is responsible for the patient and must provide all related care one day prior to the surgery forward thru 90 postoperative days at no additional charge. Minor surgery, including endoscopy, has zero or 10-day postoperative periods, bundling all services on the surgical day only, or the surgical day and the subsequent 10 days, respectively (see Table 1, p. above).
The Surgeon Defined
Any qualified physician able to perform “surgical” services within his scope of practice is considered a “surgeon” for billing purposes. For example, a pulmonologist, or primary care physician, must meet the surgical billing and documentation requirements when performing bronchoscopies or uncomplicated incision-and-drainage services, respectively.
Surgical services easily are identified as any code included in range 20000-69999. This code series includes major, minor, and endoscopic procedures. The “surgeon” and all physicians in the same group practice (i.e., reporting services under the same tax identification number) with the same specialty designation must adhere to the global period billing rules.
Alternately, physicians with different specialty designations in the same group practice (e.g., multispecialty group that reports services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed upon) transfer of care did not occur. Information on physician specialty designations is available at www.highmarkmedicareservices.com/partb/refman/appendix-d.html.
Package Components
The following services are included in the surgeon’s packaged payment:
- Preoperative visits after the decision for surgery is made beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications, but not require additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Post-operative pain management provided by the surgeon.
Services not included are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery. Append modifier 57 to this visit if provided the day before or day of major surgery to alert the payer that the service resulted in the decision for surgery. Append modifier 25 to this visit if provided the day of minor surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care. This agreement may be in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record;
- Post-operative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery. These services only are payable after the patient has been discharged from the hospitalization in which the surgery occurred. Append modifier 24 to these unrelated post-op visits;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the post-operative period that do not result in repeat operations or treatment for complications;
- Treatment for post-operative complications that require a return trip to the operating room, catheterization lab, or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical care services (CPT codes 99291 and 99292) unrelated to the surgery in which a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon. Append modifier 24 to these unrelated critical care services (see Table 2, above).
Payer Variations
While Medicare does not require modifier usage by hospitalists providing medically necessary services on surgical cases, some private payers do. Their electronic claim systems may not differentiate services by non-surgical specialists, requiring all physicians to append the appropriate modifier depending on the reason and timing of the service (see “Key Modifiers” below). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Hospitalists often are involved in the care of a surgical patient. Reimbursement for surgical procedures includes payment for pre-, intra-, and post-operative care.
Knowing the billing and coding responsibilities apart from those of the surgeon is imperative for the hospitalist’s accurate charge capture. There are several critical misconceptions in this regard:
- Hospitalists cannot bill for services when involved in a surgical case;
- Surgeons are not responsible for inpatient care if the patient is stable and does not require additional inpatient post-op visits; and
- Modifiers are not required for hospitalist claims unless the hospitalist reports under the same tax identification number as the surgeon.
Determine Global Period
Procedures are categorized as major or minor surgery. A global period is assigned to each procedure code, designating post-operative periods of zero, 10, or 90 days. Physician services during this global period are considered part of the packaged payment and not separately reimbursed.
The global period for any given CPT code can be identified in the Medicare Physician Fee Schedule and accessed at www.cms.hhs.gov/PfsLookup. In addition to zero, 10, and 90 days, services can be noted with:
- XXX, indicating the global period concept does not apply; or
- ZZZ, indicating an “add-on” procedure that must always be reported with the relevant primary procedure code; “add-on” procedures assume the global period of the primary procedure.
Major surgery routinely is allotted 90-day global periods. Therefore, the surgeon is responsible for the patient and must provide all related care one day prior to the surgery forward thru 90 postoperative days at no additional charge. Minor surgery, including endoscopy, has zero or 10-day postoperative periods, bundling all services on the surgical day only, or the surgical day and the subsequent 10 days, respectively (see Table 1, p. above).
The Surgeon Defined
Any qualified physician able to perform “surgical” services within his scope of practice is considered a “surgeon” for billing purposes. For example, a pulmonologist, or primary care physician, must meet the surgical billing and documentation requirements when performing bronchoscopies or uncomplicated incision-and-drainage services, respectively.
Surgical services easily are identified as any code included in range 20000-69999. This code series includes major, minor, and endoscopic procedures. The “surgeon” and all physicians in the same group practice (i.e., reporting services under the same tax identification number) with the same specialty designation must adhere to the global period billing rules.
Alternately, physicians with different specialty designations in the same group practice (e.g., multispecialty group that reports services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed upon) transfer of care did not occur. Information on physician specialty designations is available at www.highmarkmedicareservices.com/partb/refman/appendix-d.html.
Package Components
The following services are included in the surgeon’s packaged payment:
- Preoperative visits after the decision for surgery is made beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications, but not require additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Post-operative pain management provided by the surgeon.
Services not included are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery. Append modifier 57 to this visit if provided the day before or day of major surgery to alert the payer that the service resulted in the decision for surgery. Append modifier 25 to this visit if provided the day of minor surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care. This agreement may be in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record;
- Post-operative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery. These services only are payable after the patient has been discharged from the hospitalization in which the surgery occurred. Append modifier 24 to these unrelated post-op visits;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the post-operative period that do not result in repeat operations or treatment for complications;
- Treatment for post-operative complications that require a return trip to the operating room, catheterization lab, or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical care services (CPT codes 99291 and 99292) unrelated to the surgery in which a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon. Append modifier 24 to these unrelated critical care services (see Table 2, above).
Payer Variations
While Medicare does not require modifier usage by hospitalists providing medically necessary services on surgical cases, some private payers do. Their electronic claim systems may not differentiate services by non-surgical specialists, requiring all physicians to append the appropriate modifier depending on the reason and timing of the service (see “Key Modifiers” below). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.