User login
Promoting treatment adherence in patients with bipolar disorder
Discuss this article at www.facebook.com/CurrentPsychiatry
Treatment nonadherence among patients with chronic illness is high, and bipolar disorder (BD) is no exception. Approximately 21% to 50% of patients with BD do not adhere to their recommended treatment regimen,1 which adds to the burden of illness and worsens prognosis.
Although treatment nonadherence is a concern with any psychiatric disorder, we focus on BD because of the high prevalence of the disorder, the lifelong nature of the illness, and its resulting disability. BD is challenging to treat even with motivated patients, and psychiatrists cannot count on individuals to follow their prescribed regimen just because they were told to do so. Choosing the best treatment for each patient is complicated, and as physicians, we need to learn how to connect with our patients, increase our insight into their concerns, and work collaboratively to find a treatment they can follow.
This article describes methods of assessing adherence, factors that affect adherence, and pharmacologic and psychosocial interventions to enhance adherence and improve outcomes.
What is adherence?
As the doctor-patient relationship and medical treatment evolved to become more patient-centered, so have the terms used to describe individuals’ treatment-related behavior. Compliance, a physician-centered term that mandates following instructions to achieve treatment goals, evolved to adherence, the extent to which a person fulfills their part of an agreed-upon treatment plan, followed by concordance, which describes a decision-making alliance between patient and provider that strongly considers patients’ input.
Adherence is considered adequate when it occurs at the minimum level necessary for the patient to respond to treatment and avoid relapse.2 Research on adherence in BD can be difficult to interpret because results may be influenced by:
- selection bias (patients who are adherent and insightful are more likely to consent to research)
- complications caused by polypharmacy and comorbidity
- investigators’ ability to choose the proper measure to delineate medication adherence attitudes and behaviors
- patients’ compliance with the adherence-enhancing interventions.2
Assessment methods. Several tools can be used to measure adherence to mental illness treatment. Attitudinal scales capture a person’s subjective feelings (such as being on a medication, insight, perceived strength of the therapeutic alliance, and level of stigma faced) and can reflect attitude change that may result from adherence-enhancing interventions. Adherence behavior scales may be convenient to administer in the office but tend to overestimate patients’ adherence (Table 1).3-7
Pill counts are inexpensive but patients can manipulate unused medication. Prescription refill counts are easy to obtain but do not confirm that the patient took the medication. Electronic medication monitors capture the time of specific doses and can calculate the adherence rate, but they are expensive and do not ensure that the medication was ingested. Measuring the drug in urine or blood is an objective measure of adherence and can serve as clinical guide to pharmacotherapy, but offers limited correlation with the amount of medication taken and is expensive. A combination of measures to estimate adherence may be best.2
Table 1
Tools for measuring adherence to medications
| Components/characteristics | Advantages | Disadvantages |
|---|---|---|
| Rating of Medication Influences3 | ||
| 19 items. Subscales: Reasons for adherence (prevention, influence of others, medication affinity), reasons for nonadherence (denial, dysphoria, logistical problems, label rejection, family influence, negative therapeutic alliance) | Valid, reliable. Correlates with other scales (DAI) | Developed on a population including only patients with schizophrenia treated with antipsychotics. Requires a trained rater |
| Drug Attitude Inventory4 | ||
| 30 items. Reflects patients’ attitudes about medication | Self-rated. High internal consistency. Accurately discriminates between adherent and nonadherent patients | Developed on a population including only patients with schizophrenia |
| Lithium Attitudes Questionnaire5 | ||
| 19 items. Areas of assessment: opposition to continue lithium, therapeutic effectiveness of lithium not accepted, difficulty with pill-taking routine, denial of illness severity, subcultural attitudes opposed to drug treatment, dissatisfaction with factual knowledge of lithium | Self-rated. Developed on patients with BD attending a lithium clinic. Good test/retest reliability for most items | The questionnaire is fairly long; shorter versions were adapted from original version |
| Medication Adherence Rating Scale6 | ||
| 10 items that assess medication adherence behavior, attitudes toward taking medication, negative side effects, attitudes toward psychotropic medication, measures adherence in past week | Self-rated. Validated on patients with various diagnoses, including BD. Correlates well with DAI, MAQ, and mood stabilizer drug levels (lithium and carbamazepine) | Validation methods may be limited by the other measures (for example, medication levels can be influenced by metabolism) |
| Brief Adherence Rating Scale7 | ||
| 3 items. Number of pills prescribed daily, days with no medication taken, and days with medication taken less than prescribed. Nonadherence defined as <70% of doses taken. Measures adherence in past month | Clinician–rated. Short. Good correlation with electronic medication monitoring. High internal reliability. Good test/retest reliability. Greater adherence on BARS correlates with lower psychotic symptom scores. Sensitive and specific in identifying nonadherence | Validation study only on patients with schizophrenia and schizoaffective disorder taking antipsychotics |
| BARS: Brief Adherence Rating Scale; BD: bipolar disorder; DAI: Drug Attitude Inventory; MAQ: Medication Adherence Questionnaire | ||
BD adherence studies
Treatment adherence in BD is challenged by the chronic remission-relapse pattern of the disorder. Manic episodes carry the highest risk of nonadherence.2 Scott and Pope8 evaluated self-reported adherence to mood stabilizers (lithium, carbamazepine, or valproate) among 98 patients with major depressive disorder and 78 with BD. They found that 32% of patients were partially adherent (defined as having missed >30% of doses in the past month) and >60% of these patients had sub-therapeutic plasma levels of mood stabilizers.
In a study of 106 BD outpatients treated with lithium who completed scales regarding their attitudes toward and knowledge of lithium and the Medication Adherence Rating Scale (MARS), 86% of patients had a therapeutic serum lithium level (.6 to 1.2 mEq/L), and knowledge of lithium was correlated with adherence.9 Jónsdóttir et al10 looked at medication adherence among 280 patients with schizophrenia and BD by comparing patient self-reports to provider reports and measuring serum drug concentrations; adherence was defined as having a serum concentration within the reference level for the specific medication. BD patients had an adherence rate of 66%, and self-reported adherence as measured by MARS and provider reports correlated with serum concentrations.
In a study of 71 adolescents with BD followed for 1 year after their first hospitalization for a manic or mixed episode, DelBello et al11 defined nonadherence as taking medication <25% of the time and partial adherence as taking medication 25% to 75% of the time. They found that 42% of patients were partially adherent and 23% were nonadherent.
Strakowski12 followed 46 adults from Taiwan and 96 from the United States for 1 year after their first manic or mixed episode and found that 79% of the Taiwanese patients and 50% of U.S. patients were adherent. Using the medication possession ratio (MPR)—which is calculated based the number of days between expected and actual prescription refills—to determine adherence, Sajatovic13 found that 54% of 44,637 veterans being treated for BD with lithium or anticonvulsants were fully adherent (MPR >.80), 25% were partially adherent (MPR >.50 to .80), and 21% were nonadherent (MPR ≤.50). In a survey of 131 randomly selected psychiatrists and 429 of their adult BD patients, Baldessarini14 found that 34% of patients reported missing ≥1 medication dose in past 10 days, but psychiatrists recognized only 18% of patients as nonadherent.
What affects adherence?
Although all BD patients share the same diagnosis, the factors that ultimately result in their medication adherence are as variable as the individuals themselves. Patients’ age, sex, culture, symptom severity, worldview, socioeconomic status, opinion of mental illness, and self-image influence their individual decisions on adhering to a prescribed medication regimen.1,15
Perception of medication efficacy. Not surprisingly, if a medication does not seem to decrease debilitating symptoms, a patient is unlikely to continue taking it. Patients with BD feel more affected by depressive symptoms than by manic symptoms, and have indicated that they are more likely to adhere to and view as successful treatments that reduce depressive symptoms.16,17
Tolerability. In an Internet-based survey, 469 patients with BD indicated that medication-related weight gain and cognitive impairment were the most important factors that affected adherence.16 Individuals’ concerns about possible side effects may contribute more to nonadherence than actually experiencing side effects.17 Concerns about long-term metabolic side effects from atypical antipsychotics also may limit adherence.17
Neurocognitive impairment. Whether caused by BD, aging, or a combination of these factors, deficits in memory, attention, and executive functioning can lead to unintentional nonadherence. In a study that assessed medication management ability among middle-aged and older adults, patients with BD were found to make 2.8 times more errors than healthy controls.18
Therapeutic alliance and psychoeducation. Patients’ expectations for pharmacotherapy vary from specific symptom relief to hopes for a complete cure, and their fears may be influenced by media and advertisements.17 Nonetheless a positive therapeutic alliance with the treating provider improves illness outcomes.19
A clinician’s ability to help patients build insight is invaluable for their current and future treatment. In a survey of 435 veterans with BD, nonadherence was greater among patients with limited insight about the role of medication in their illness.20 A study of 65 BD patients that evaluated insight into medication adherence at initial interview and 1 year later found that difficulty with adherence at the initial interview predicted future nonadherence and was correlated with lack of insight.21 Rosa et al9 found that BD patients in denial of their illness and those who had little psychoeducation were more frequently nonadherent with lithium treatment.
Other factors that may contribute to medication nonadherence in BD patients include comorbid substance abuse or personality disorders, both of which are associated with more frequent relapse.15 Marriage has a beneficial affect on adherence.15 A good support system may contribute to treatment adherence; in a study of 107 children and adolescents with BD, nonadherent patients were more likely to experience family dysfunction and have a parental history of psychiatric hospitalization.22
Adherence and BD course
Treatment adherence decreases the suicide rate among BD patients. Angst et al23 evaluated the rate of suicide among 406 patients with BD and unipolar depression who were followed for 40 years. They found that 11% committed suicide; untreated patients had significantly higher standardized mortality rates than of those who were treated with lithium, antipsychotics, or antidepressants. Other studies confirm this finding.15
Repeated relapse may predict poorer cognitive performance. Lopez-Jaramillo et al24 showed that patients with BD who had more manic episodes performed poorer on cognitive tests assessing attention, memory, and executive functioning compared with patients with less episodes and with normal subjects.
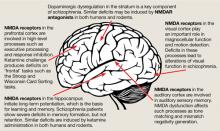
Medication adherence in BD is a priority because of potential neurodegeneration in BD and the neuroprotective effects of mood stabilizers and some atypical antipsychotics (Box).
As emerging studies document morphologic brain changes associated with bipolar disorder (BD), researchers have been relating these changes to the duration and progression of illness. A longer duration of illness is associated with a smaller total gray matter volume on brain MRI of BD patients compared with unipolar patients and normal controls.a Brain MRI analysis of grey and white matter in elderly patients with longstanding BD who underwent neuropsychological testing to rule out dementia showed a decreased concentration of grey matter in the anterior limbic areas as well as reduced fiber tract coherence in the corpus callosum when compared with normal controls.b
Additionally, microstructural brain changes have been associated with acute mood states, in particular bipolar depression.c Lithium, valproate, olanzapine, and clozapine are neuroprotective in cultures of human-derived neuroblastoma cells, by enhancing the cells’ proliferation and survival.d
Source:
a. Frey BN, Zunta-Soares GB, Caetano SC, et al. Illness duration and total brain gray matter in bipolar disorder: evidence for neurodegeneration? European Neuropsychopharm. 2008;18:717-722.
b. Haller S, Xekardaki A, Delaloye C, et al. Combined analysis of grey matter voxel-based morphometry and white matter tract-based spatial statistics in late-life bipolar disorder. J Psychiatry Neurosci. 2011;36(1):100140.
c. Zanetti MV, Jackowski MP, Versace A, et al. State-dependent microstructural white matter changes in bipolar I depression. Eur Arch Psychiatry Clin Neurosci. 2009;259(6):316-328.
d. Aubry J, Schwald M, Ballmann E, et al. Early effects of mood stabilizers on the Akt/GSK-3ß signaling pathway and on cell survival and proliferation. Psychopharmacology. 2009;205:419-429.
Increasing adherence
Pharmacologic strategies. Adherence in BD often is difficult when patients require a complex medication regimen to control their illness. Patients and clinicians may prefer to use once-daily dosing drug formulations, which can provide consistent serum levels and fewer adverse effects. Divalproex extended-release (ER) allows once-daily dosing and improved tolerability by reducing fluctuations in valproic acid serum concentrations compared with the delayed-release formulation. In a retrospective chart review,25 most patients (62%) who switched to divalproex ER from divalproex delayed-release preferred the ER formulation; 52% showed clinical improvement, 81% did not experience side effects, and 8% demonstrated higher adherence after switching.25 Similarly, an extended-release formulation of carbamazepine is approved for treating acute mania.
Many atypical antipsychotics are FDA-approved for acute mania, acute bipolar depression, and/or maintenance (Table 2). Long-acting injectable formulations (LAIs) may be used as maintenance treatment if nonadherence is an issue. LAI risperidone, which is FDA-approved for maintenance treatment of bipolar I disorder (BDI), was found to be safe and effective in stable BD patients who were switched from an oral antipsychotic.26 Asenapine is provided in a rapidly absorbed, sublingual form and is FDA-approved for treating acute mania or mixed episodes associated with BDI.27 Overall, however, only slightly more than one-half of BD patients are adherent to atypical antipsychotics.15
Although antidepressant use in BD is controversial, Sajatovic17 found 44% of depressed BDI patients were treated with antidepressants. Novel extended-release antidepressant formulations—including controlled-release fluvoxamine, paroxetine, extended-release bupropion and venlafaxine, once-weekly fluoxetine, rapidly dissolving mirtazapine, and transdermal selegiline—can optimize drug delivery, minimize side effects, and delay onset of action.1
Psychosocial strategies used in BD include psychoeducation, cognitive-behavioral therapy (CBT), family-focused interventions, and interpersonal and social rhythm therapy (IPSRT) (Table 3).28-30 Psychoeducation alone or combined with other interventions can decrease the risk of relapse and hospitalization and improve adherence.28 In a 2-year study of 50 euthymic BD patients treated with lithium who participated in a brief hospital-based psychoeducation program, Even et al31 found patients’ knowledge about lithium but not their attitudes changed significantly after the program. The changes persisted 2 years after the intervention, with a trend toward a decreased hospitalization rate.
Miklowitz32 reported on 293 BD patients randomized to receive collaborative care (3 psychoeducational sessions delivered over 6 weeks) or 1 of 3 types of intensive psychotherapy: CBT, IPSRT, or family-focused therapy. Attrition was similar for both groups. Compared with those receiving collaborative care, significantly more patients receiving intensive psychotherapy recovered after 1 year, and did so in shorter time.
In a 3-year, multi-site Veterans Administration (VA) study, 306 BD patients received psychoeducation and support from nurse care coordinators who were responsible for access, continuity of care, and information flow to psychiatrists or usual care according to VA guidelines.33 Compared with the usual care group, patients who received psychoeducation and support from nurse care coordinators had shorter duration of manic episodes and improved function and quality of life. A meta-analysis30 of 12 randomized controlled trials of CBT in BD showed a medium effect size of CBT on adherence at 6 months post-treatment.
Table 2
FDA-approved medications for adult bipolar disorder
| Bipolar disorder indication | Medications |
|---|---|
| Acute treatment of mania/mixed episodes | Aripiprazole,a,b asenapine,a carbamazepine extended release,a divalproex sodium,a lithium,a quetiapine,a risperidone,a-c ziprasidonea,b |
| Depressive episodes | Olanzapine/fluoxetine,a quetiapinea |
| Maintenance treatment | Aripiprazole (as monotherapy and as adjunct to lithium or divalproex sodium),a,b asenapine,d lamotrigine,a lithium,a olanzapine,a-c quetiapine (as adjunct to lithium or divalproex sodium),a risperidone,e ziprasidone (as adjunct to lithium or divalproex sodium)a |
| apill form bintramuscular for acute agitation cdisintegrating tablet dsublingual tablet elong-acting injectable | |
Table 3
Psychosocial interventions for bipolar disorder
| Intervention | Description | Results in bipolar disorder | Optimal stage of illness for intervention |
|---|---|---|---|
| Individual and family psycho-education28,29 | Strategies to educate the patient about the illness, medications, side effects, and relapse prevention | Decreases relapse, (particularly manic episodes) and hospitalizations. Increases adherence | Manic episodes |
| Cognitive-behavioral therapy28-30 | Focuses on understanding patient’s perceptions of illness and treatment. Equates resistance with exploring, rather than challenging resistance to take medication. Identifies and modifies negative automatic thoughts about medication. Motivation techniques useful in comorbid substance use | Decreases clinical symptoms. Increases adherence, quality of life, and social functioning | Depressive episodes |
| IPSRT28,29 | Uses motivational interviewing and CBT techniques to stabilize daily routines and resolve interpersonal problems | Prevents relapse | Depressive episodes |
| Family-focused therapy28,29 | A combination of psychoeducation, communication, and problem-solving skills training | Reduces mood symptoms, number of depressive relapses, and time depressed. Increases adherence | Depressive episodes |
| IPSRT: interpersonal and social rhythm therapy | |||
Related Resource
- Deegan PE. The importance of personal medicine: a qualitative study of resilience in people with psychiatric disabilities. Scand J Public Health Suppl. 2005;66:29-35.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Bupropion • Wellbutrin
- Carbamazepine • Carbatrol, Tegretol
- Carbamazepine extended- release • Equetro
- Clozapine • Clozaril
- Divalproex • Depakote, Depakote ER
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Paroxetine • Paxil
- Quetiapine • Seroquel, Seroquel XR
- Risperidone • Risperdal
- Risperidone long-acting injectable • Risperdal Consta
- Selegiline • Eldepryl, Emsam
- Valproate • Depacon
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Foster receives research/grant support from the American Psychiatric Foundation, the National Institute of Mental Health, and Sunovion Pharmaceuticals.
Dr. Sheehan and Ms. Johns report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Buckley PF, Foster AE, Patel NC, et al. Adherence to mental health treatment. New York, NY: Oxford University Press; 2009;1-10:53-69.
2. Velligan D, Sajatovic M, Valenstein M, et al. Methodological challenges in psychiatric treatment adherence research. Clin Schizophr Relat Psychoses. 2010;4(1):74-91.
3. Weiden P, Rapkin B, Mott T, et al. Rating of Medication Influences (ROMI) scale in schizophrenia. Schizophr Bull. 1994;20:297-310.
4. Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med. 1983;13(1):177-183.
5. Harvey NS. The development and descriptive use of the Lithium Attitudes Questionnaire. J Affect Disord. 1991;22(4):211-219.
6. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS). Schizophr Res. 2000;42:241-247.
7. Byerly MJ, Nazonezny PA, Rush AJ. The Brief Adherence Rating Scale (BARS) validated against electronic monitoring in assessing the antipsychotic medication adherence of outpatients with schizophrenia and schizoaffective disorder. Schizophr Res. 2008;100(1-3):60-69.
8. Scott J, Pope M. Non-adherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry. 2002;63:384-390.
9. Rosa AR, Marco M, Fachel JM, et al. Correlation between drug treatment adherence and lithium treatment attitudes and knowledge in bipolar patients. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:217-224.
10. Jónsdóttir H, Opjordsmoen S, Birkenaes A, et al. Medication adherence in outpatients with severe mental disorders, relation between self-reports and serum level. J Clin Psychopharmacol. 2010;30:169-175.
11. DelBello M, Hanserman D, Adler CM, et al. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007;164:582-590.
12. Strakowski SM, Tsai SY, DelBello MP, et al. Outcome following a first manic episode: cross national US and Taiwan comparison. Bipolar Disord. 2007;9:820-827.
13. Sajatovic M, Valenstein M, Blow F, et al. Treatment adherence with lithium and anticonvulsant medications among patients with bipolar disorder. Psychiatr Serv. 2007;58:855-863.
14. Baldessarini RJ, Perry R, Pike J. Factors associated with treatment nonadherence among US bipolar patients. Hum Psychopharmacol. 2008;23:95-105.
15. Berk L, Hallam KT, Colom F, et al. Enhancing medication adherence in patients with bipolar disorder. Hum Psychopharmacol. 2010;25(1):1-16.
16. Johnson FR, Ozdemir S, Manjunath R, et al. Factors that affect adherence to bipolar disorder treatments: a stated-preference approach. Med Care. 2007;45(6):545-552.
17. Sajatovic M, Jenkins JH, Cassidy KA, et al. Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. J Affect Disord. 2009;115(3):360-366.
18. Depp CA, Cain AE, Palmer BW, et al. Assessment of medication management ability in middle-aged and older adults with bipolar disorder. J Clin Psychopharmacol. 2008;28(2):225-229.
19. Gaudiano BA, Miller IW. Patients’ expectancies the alliance in pharmacotherapy, and treatment outcomes in bipolar disorder. J Consult Clin Psychol. 2006;74(4):671-676.
20. Copeland LA, Zeber JE, Salloum IM, et al. Treatment adherence and illness insight in veterans with bipolar disorder. J Nerv Ment Dis. 2008;196(1):16-21.
21. Yen CF, Chen CS, Ko CH, et al. Relationships between insight and medication adherence in outpatients with schizophrenia and bipolar disorder: prospective study. Psychiatry Clin Neurosci. 2005;59(4):403-409.
22. Drotar D, Greenley RN, Demeter CA, et al. Adherence to pharmacological treatment for juvenile bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):831-839.
23. Angst J, Angst F, Gerber-Werder R, et al. Suicide in 406 mood-disorder patients with and without long–term medication: a 40 to 44 years’ follow-up. Arch Suicide Res. 2005;9:279-300.
24. Lopez-Jaramillo C, Lopera-Vasquez J, Aurora G, et al. Effects of recurrence on the cognitive performance of patients with bipolar I disorder: implications for relapse prevention and treatment adherence. Bipolar Disord. 2010;12:557-567.
25. Minirth FB, Neal V. Assessment of patient preference and side effects in patients switched from divalproex sodium delayed release to divalproex sodium extended release. J Clin Psychopharmacol. 2005;25:99-101.
26. Han C, Lee MS, Pae CU, et al. Usefulness of long-acting injectable risperidone during 12-month maintenance therapy of bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1219-1223.
27. McIntyre RS, Cohen M, Zhao J, et al. Asenapine for long term treatment of bipolar disorder: a double blind 40-week extension study. J Affect Disord. 2010;126:358-365.
28. Velligan DI, Weiden PJ, Sajatovic M, et al. Strategies for addressing adherence problems in patients with serious and persistent mental illness: recommendations from expert consensus guidelines. J Psychiatr Pract. 2010;16(5):306-324.
29. Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry. 2008;165(11):1408-1419.
30. Szentagotai A, David D. The efficacy of cognitive-behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71(1):66-72.
31. Even C, Thuile J, Stern K, et al. Psychoeducation for patients with bipolar disorder receiving lithium: short and long term impact on locus of control and knowledge about lithium. J Affect Disord. 2010;123:299-302.
32. Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007;64:419-426.
33. Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder, part II. Impact on clinical outcome, function and costs. Psychiatr Serv. 2006;57:937-945.
Discuss this article at www.facebook.com/CurrentPsychiatry
Treatment nonadherence among patients with chronic illness is high, and bipolar disorder (BD) is no exception. Approximately 21% to 50% of patients with BD do not adhere to their recommended treatment regimen,1 which adds to the burden of illness and worsens prognosis.
Although treatment nonadherence is a concern with any psychiatric disorder, we focus on BD because of the high prevalence of the disorder, the lifelong nature of the illness, and its resulting disability. BD is challenging to treat even with motivated patients, and psychiatrists cannot count on individuals to follow their prescribed regimen just because they were told to do so. Choosing the best treatment for each patient is complicated, and as physicians, we need to learn how to connect with our patients, increase our insight into their concerns, and work collaboratively to find a treatment they can follow.
This article describes methods of assessing adherence, factors that affect adherence, and pharmacologic and psychosocial interventions to enhance adherence and improve outcomes.
What is adherence?
As the doctor-patient relationship and medical treatment evolved to become more patient-centered, so have the terms used to describe individuals’ treatment-related behavior. Compliance, a physician-centered term that mandates following instructions to achieve treatment goals, evolved to adherence, the extent to which a person fulfills their part of an agreed-upon treatment plan, followed by concordance, which describes a decision-making alliance between patient and provider that strongly considers patients’ input.
Adherence is considered adequate when it occurs at the minimum level necessary for the patient to respond to treatment and avoid relapse.2 Research on adherence in BD can be difficult to interpret because results may be influenced by:
- selection bias (patients who are adherent and insightful are more likely to consent to research)
- complications caused by polypharmacy and comorbidity
- investigators’ ability to choose the proper measure to delineate medication adherence attitudes and behaviors
- patients’ compliance with the adherence-enhancing interventions.2
Assessment methods. Several tools can be used to measure adherence to mental illness treatment. Attitudinal scales capture a person’s subjective feelings (such as being on a medication, insight, perceived strength of the therapeutic alliance, and level of stigma faced) and can reflect attitude change that may result from adherence-enhancing interventions. Adherence behavior scales may be convenient to administer in the office but tend to overestimate patients’ adherence (Table 1).3-7
Pill counts are inexpensive but patients can manipulate unused medication. Prescription refill counts are easy to obtain but do not confirm that the patient took the medication. Electronic medication monitors capture the time of specific doses and can calculate the adherence rate, but they are expensive and do not ensure that the medication was ingested. Measuring the drug in urine or blood is an objective measure of adherence and can serve as clinical guide to pharmacotherapy, but offers limited correlation with the amount of medication taken and is expensive. A combination of measures to estimate adherence may be best.2
Table 1
Tools for measuring adherence to medications
| Components/characteristics | Advantages | Disadvantages |
|---|---|---|
| Rating of Medication Influences3 | ||
| 19 items. Subscales: Reasons for adherence (prevention, influence of others, medication affinity), reasons for nonadherence (denial, dysphoria, logistical problems, label rejection, family influence, negative therapeutic alliance) | Valid, reliable. Correlates with other scales (DAI) | Developed on a population including only patients with schizophrenia treated with antipsychotics. Requires a trained rater |
| Drug Attitude Inventory4 | ||
| 30 items. Reflects patients’ attitudes about medication | Self-rated. High internal consistency. Accurately discriminates between adherent and nonadherent patients | Developed on a population including only patients with schizophrenia |
| Lithium Attitudes Questionnaire5 | ||
| 19 items. Areas of assessment: opposition to continue lithium, therapeutic effectiveness of lithium not accepted, difficulty with pill-taking routine, denial of illness severity, subcultural attitudes opposed to drug treatment, dissatisfaction with factual knowledge of lithium | Self-rated. Developed on patients with BD attending a lithium clinic. Good test/retest reliability for most items | The questionnaire is fairly long; shorter versions were adapted from original version |
| Medication Adherence Rating Scale6 | ||
| 10 items that assess medication adherence behavior, attitudes toward taking medication, negative side effects, attitudes toward psychotropic medication, measures adherence in past week | Self-rated. Validated on patients with various diagnoses, including BD. Correlates well with DAI, MAQ, and mood stabilizer drug levels (lithium and carbamazepine) | Validation methods may be limited by the other measures (for example, medication levels can be influenced by metabolism) |
| Brief Adherence Rating Scale7 | ||
| 3 items. Number of pills prescribed daily, days with no medication taken, and days with medication taken less than prescribed. Nonadherence defined as <70% of doses taken. Measures adherence in past month | Clinician–rated. Short. Good correlation with electronic medication monitoring. High internal reliability. Good test/retest reliability. Greater adherence on BARS correlates with lower psychotic symptom scores. Sensitive and specific in identifying nonadherence | Validation study only on patients with schizophrenia and schizoaffective disorder taking antipsychotics |
| BARS: Brief Adherence Rating Scale; BD: bipolar disorder; DAI: Drug Attitude Inventory; MAQ: Medication Adherence Questionnaire | ||
BD adherence studies
Treatment adherence in BD is challenged by the chronic remission-relapse pattern of the disorder. Manic episodes carry the highest risk of nonadherence.2 Scott and Pope8 evaluated self-reported adherence to mood stabilizers (lithium, carbamazepine, or valproate) among 98 patients with major depressive disorder and 78 with BD. They found that 32% of patients were partially adherent (defined as having missed >30% of doses in the past month) and >60% of these patients had sub-therapeutic plasma levels of mood stabilizers.
In a study of 106 BD outpatients treated with lithium who completed scales regarding their attitudes toward and knowledge of lithium and the Medication Adherence Rating Scale (MARS), 86% of patients had a therapeutic serum lithium level (.6 to 1.2 mEq/L), and knowledge of lithium was correlated with adherence.9 Jónsdóttir et al10 looked at medication adherence among 280 patients with schizophrenia and BD by comparing patient self-reports to provider reports and measuring serum drug concentrations; adherence was defined as having a serum concentration within the reference level for the specific medication. BD patients had an adherence rate of 66%, and self-reported adherence as measured by MARS and provider reports correlated with serum concentrations.
In a study of 71 adolescents with BD followed for 1 year after their first hospitalization for a manic or mixed episode, DelBello et al11 defined nonadherence as taking medication <25% of the time and partial adherence as taking medication 25% to 75% of the time. They found that 42% of patients were partially adherent and 23% were nonadherent.
Strakowski12 followed 46 adults from Taiwan and 96 from the United States for 1 year after their first manic or mixed episode and found that 79% of the Taiwanese patients and 50% of U.S. patients were adherent. Using the medication possession ratio (MPR)—which is calculated based the number of days between expected and actual prescription refills—to determine adherence, Sajatovic13 found that 54% of 44,637 veterans being treated for BD with lithium or anticonvulsants were fully adherent (MPR >.80), 25% were partially adherent (MPR >.50 to .80), and 21% were nonadherent (MPR ≤.50). In a survey of 131 randomly selected psychiatrists and 429 of their adult BD patients, Baldessarini14 found that 34% of patients reported missing ≥1 medication dose in past 10 days, but psychiatrists recognized only 18% of patients as nonadherent.
What affects adherence?
Although all BD patients share the same diagnosis, the factors that ultimately result in their medication adherence are as variable as the individuals themselves. Patients’ age, sex, culture, symptom severity, worldview, socioeconomic status, opinion of mental illness, and self-image influence their individual decisions on adhering to a prescribed medication regimen.1,15
Perception of medication efficacy. Not surprisingly, if a medication does not seem to decrease debilitating symptoms, a patient is unlikely to continue taking it. Patients with BD feel more affected by depressive symptoms than by manic symptoms, and have indicated that they are more likely to adhere to and view as successful treatments that reduce depressive symptoms.16,17
Tolerability. In an Internet-based survey, 469 patients with BD indicated that medication-related weight gain and cognitive impairment were the most important factors that affected adherence.16 Individuals’ concerns about possible side effects may contribute more to nonadherence than actually experiencing side effects.17 Concerns about long-term metabolic side effects from atypical antipsychotics also may limit adherence.17
Neurocognitive impairment. Whether caused by BD, aging, or a combination of these factors, deficits in memory, attention, and executive functioning can lead to unintentional nonadherence. In a study that assessed medication management ability among middle-aged and older adults, patients with BD were found to make 2.8 times more errors than healthy controls.18
Therapeutic alliance and psychoeducation. Patients’ expectations for pharmacotherapy vary from specific symptom relief to hopes for a complete cure, and their fears may be influenced by media and advertisements.17 Nonetheless a positive therapeutic alliance with the treating provider improves illness outcomes.19
A clinician’s ability to help patients build insight is invaluable for their current and future treatment. In a survey of 435 veterans with BD, nonadherence was greater among patients with limited insight about the role of medication in their illness.20 A study of 65 BD patients that evaluated insight into medication adherence at initial interview and 1 year later found that difficulty with adherence at the initial interview predicted future nonadherence and was correlated with lack of insight.21 Rosa et al9 found that BD patients in denial of their illness and those who had little psychoeducation were more frequently nonadherent with lithium treatment.
Other factors that may contribute to medication nonadherence in BD patients include comorbid substance abuse or personality disorders, both of which are associated with more frequent relapse.15 Marriage has a beneficial affect on adherence.15 A good support system may contribute to treatment adherence; in a study of 107 children and adolescents with BD, nonadherent patients were more likely to experience family dysfunction and have a parental history of psychiatric hospitalization.22
Adherence and BD course
Treatment adherence decreases the suicide rate among BD patients. Angst et al23 evaluated the rate of suicide among 406 patients with BD and unipolar depression who were followed for 40 years. They found that 11% committed suicide; untreated patients had significantly higher standardized mortality rates than of those who were treated with lithium, antipsychotics, or antidepressants. Other studies confirm this finding.15
Repeated relapse may predict poorer cognitive performance. Lopez-Jaramillo et al24 showed that patients with BD who had more manic episodes performed poorer on cognitive tests assessing attention, memory, and executive functioning compared with patients with less episodes and with normal subjects.
Medication adherence in BD is a priority because of potential neurodegeneration in BD and the neuroprotective effects of mood stabilizers and some atypical antipsychotics (Box).
As emerging studies document morphologic brain changes associated with bipolar disorder (BD), researchers have been relating these changes to the duration and progression of illness. A longer duration of illness is associated with a smaller total gray matter volume on brain MRI of BD patients compared with unipolar patients and normal controls.a Brain MRI analysis of grey and white matter in elderly patients with longstanding BD who underwent neuropsychological testing to rule out dementia showed a decreased concentration of grey matter in the anterior limbic areas as well as reduced fiber tract coherence in the corpus callosum when compared with normal controls.b
Additionally, microstructural brain changes have been associated with acute mood states, in particular bipolar depression.c Lithium, valproate, olanzapine, and clozapine are neuroprotective in cultures of human-derived neuroblastoma cells, by enhancing the cells’ proliferation and survival.d
Source:
a. Frey BN, Zunta-Soares GB, Caetano SC, et al. Illness duration and total brain gray matter in bipolar disorder: evidence for neurodegeneration? European Neuropsychopharm. 2008;18:717-722.
b. Haller S, Xekardaki A, Delaloye C, et al. Combined analysis of grey matter voxel-based morphometry and white matter tract-based spatial statistics in late-life bipolar disorder. J Psychiatry Neurosci. 2011;36(1):100140.
c. Zanetti MV, Jackowski MP, Versace A, et al. State-dependent microstructural white matter changes in bipolar I depression. Eur Arch Psychiatry Clin Neurosci. 2009;259(6):316-328.
d. Aubry J, Schwald M, Ballmann E, et al. Early effects of mood stabilizers on the Akt/GSK-3ß signaling pathway and on cell survival and proliferation. Psychopharmacology. 2009;205:419-429.
Increasing adherence
Pharmacologic strategies. Adherence in BD often is difficult when patients require a complex medication regimen to control their illness. Patients and clinicians may prefer to use once-daily dosing drug formulations, which can provide consistent serum levels and fewer adverse effects. Divalproex extended-release (ER) allows once-daily dosing and improved tolerability by reducing fluctuations in valproic acid serum concentrations compared with the delayed-release formulation. In a retrospective chart review,25 most patients (62%) who switched to divalproex ER from divalproex delayed-release preferred the ER formulation; 52% showed clinical improvement, 81% did not experience side effects, and 8% demonstrated higher adherence after switching.25 Similarly, an extended-release formulation of carbamazepine is approved for treating acute mania.
Many atypical antipsychotics are FDA-approved for acute mania, acute bipolar depression, and/or maintenance (Table 2). Long-acting injectable formulations (LAIs) may be used as maintenance treatment if nonadherence is an issue. LAI risperidone, which is FDA-approved for maintenance treatment of bipolar I disorder (BDI), was found to be safe and effective in stable BD patients who were switched from an oral antipsychotic.26 Asenapine is provided in a rapidly absorbed, sublingual form and is FDA-approved for treating acute mania or mixed episodes associated with BDI.27 Overall, however, only slightly more than one-half of BD patients are adherent to atypical antipsychotics.15
Although antidepressant use in BD is controversial, Sajatovic17 found 44% of depressed BDI patients were treated with antidepressants. Novel extended-release antidepressant formulations—including controlled-release fluvoxamine, paroxetine, extended-release bupropion and venlafaxine, once-weekly fluoxetine, rapidly dissolving mirtazapine, and transdermal selegiline—can optimize drug delivery, minimize side effects, and delay onset of action.1
Psychosocial strategies used in BD include psychoeducation, cognitive-behavioral therapy (CBT), family-focused interventions, and interpersonal and social rhythm therapy (IPSRT) (Table 3).28-30 Psychoeducation alone or combined with other interventions can decrease the risk of relapse and hospitalization and improve adherence.28 In a 2-year study of 50 euthymic BD patients treated with lithium who participated in a brief hospital-based psychoeducation program, Even et al31 found patients’ knowledge about lithium but not their attitudes changed significantly after the program. The changes persisted 2 years after the intervention, with a trend toward a decreased hospitalization rate.
Miklowitz32 reported on 293 BD patients randomized to receive collaborative care (3 psychoeducational sessions delivered over 6 weeks) or 1 of 3 types of intensive psychotherapy: CBT, IPSRT, or family-focused therapy. Attrition was similar for both groups. Compared with those receiving collaborative care, significantly more patients receiving intensive psychotherapy recovered after 1 year, and did so in shorter time.
In a 3-year, multi-site Veterans Administration (VA) study, 306 BD patients received psychoeducation and support from nurse care coordinators who were responsible for access, continuity of care, and information flow to psychiatrists or usual care according to VA guidelines.33 Compared with the usual care group, patients who received psychoeducation and support from nurse care coordinators had shorter duration of manic episodes and improved function and quality of life. A meta-analysis30 of 12 randomized controlled trials of CBT in BD showed a medium effect size of CBT on adherence at 6 months post-treatment.
Table 2
FDA-approved medications for adult bipolar disorder
| Bipolar disorder indication | Medications |
|---|---|
| Acute treatment of mania/mixed episodes | Aripiprazole,a,b asenapine,a carbamazepine extended release,a divalproex sodium,a lithium,a quetiapine,a risperidone,a-c ziprasidonea,b |
| Depressive episodes | Olanzapine/fluoxetine,a quetiapinea |
| Maintenance treatment | Aripiprazole (as monotherapy and as adjunct to lithium or divalproex sodium),a,b asenapine,d lamotrigine,a lithium,a olanzapine,a-c quetiapine (as adjunct to lithium or divalproex sodium),a risperidone,e ziprasidone (as adjunct to lithium or divalproex sodium)a |
| apill form bintramuscular for acute agitation cdisintegrating tablet dsublingual tablet elong-acting injectable | |
Table 3
Psychosocial interventions for bipolar disorder
| Intervention | Description | Results in bipolar disorder | Optimal stage of illness for intervention |
|---|---|---|---|
| Individual and family psycho-education28,29 | Strategies to educate the patient about the illness, medications, side effects, and relapse prevention | Decreases relapse, (particularly manic episodes) and hospitalizations. Increases adherence | Manic episodes |
| Cognitive-behavioral therapy28-30 | Focuses on understanding patient’s perceptions of illness and treatment. Equates resistance with exploring, rather than challenging resistance to take medication. Identifies and modifies negative automatic thoughts about medication. Motivation techniques useful in comorbid substance use | Decreases clinical symptoms. Increases adherence, quality of life, and social functioning | Depressive episodes |
| IPSRT28,29 | Uses motivational interviewing and CBT techniques to stabilize daily routines and resolve interpersonal problems | Prevents relapse | Depressive episodes |
| Family-focused therapy28,29 | A combination of psychoeducation, communication, and problem-solving skills training | Reduces mood symptoms, number of depressive relapses, and time depressed. Increases adherence | Depressive episodes |
| IPSRT: interpersonal and social rhythm therapy | |||
Related Resource
- Deegan PE. The importance of personal medicine: a qualitative study of resilience in people with psychiatric disabilities. Scand J Public Health Suppl. 2005;66:29-35.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Bupropion • Wellbutrin
- Carbamazepine • Carbatrol, Tegretol
- Carbamazepine extended- release • Equetro
- Clozapine • Clozaril
- Divalproex • Depakote, Depakote ER
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Paroxetine • Paxil
- Quetiapine • Seroquel, Seroquel XR
- Risperidone • Risperdal
- Risperidone long-acting injectable • Risperdal Consta
- Selegiline • Eldepryl, Emsam
- Valproate • Depacon
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Foster receives research/grant support from the American Psychiatric Foundation, the National Institute of Mental Health, and Sunovion Pharmaceuticals.
Dr. Sheehan and Ms. Johns report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Treatment nonadherence among patients with chronic illness is high, and bipolar disorder (BD) is no exception. Approximately 21% to 50% of patients with BD do not adhere to their recommended treatment regimen,1 which adds to the burden of illness and worsens prognosis.
Although treatment nonadherence is a concern with any psychiatric disorder, we focus on BD because of the high prevalence of the disorder, the lifelong nature of the illness, and its resulting disability. BD is challenging to treat even with motivated patients, and psychiatrists cannot count on individuals to follow their prescribed regimen just because they were told to do so. Choosing the best treatment for each patient is complicated, and as physicians, we need to learn how to connect with our patients, increase our insight into their concerns, and work collaboratively to find a treatment they can follow.
This article describes methods of assessing adherence, factors that affect adherence, and pharmacologic and psychosocial interventions to enhance adherence and improve outcomes.
What is adherence?
As the doctor-patient relationship and medical treatment evolved to become more patient-centered, so have the terms used to describe individuals’ treatment-related behavior. Compliance, a physician-centered term that mandates following instructions to achieve treatment goals, evolved to adherence, the extent to which a person fulfills their part of an agreed-upon treatment plan, followed by concordance, which describes a decision-making alliance between patient and provider that strongly considers patients’ input.
Adherence is considered adequate when it occurs at the minimum level necessary for the patient to respond to treatment and avoid relapse.2 Research on adherence in BD can be difficult to interpret because results may be influenced by:
- selection bias (patients who are adherent and insightful are more likely to consent to research)
- complications caused by polypharmacy and comorbidity
- investigators’ ability to choose the proper measure to delineate medication adherence attitudes and behaviors
- patients’ compliance with the adherence-enhancing interventions.2
Assessment methods. Several tools can be used to measure adherence to mental illness treatment. Attitudinal scales capture a person’s subjective feelings (such as being on a medication, insight, perceived strength of the therapeutic alliance, and level of stigma faced) and can reflect attitude change that may result from adherence-enhancing interventions. Adherence behavior scales may be convenient to administer in the office but tend to overestimate patients’ adherence (Table 1).3-7
Pill counts are inexpensive but patients can manipulate unused medication. Prescription refill counts are easy to obtain but do not confirm that the patient took the medication. Electronic medication monitors capture the time of specific doses and can calculate the adherence rate, but they are expensive and do not ensure that the medication was ingested. Measuring the drug in urine or blood is an objective measure of adherence and can serve as clinical guide to pharmacotherapy, but offers limited correlation with the amount of medication taken and is expensive. A combination of measures to estimate adherence may be best.2
Table 1
Tools for measuring adherence to medications
| Components/characteristics | Advantages | Disadvantages |
|---|---|---|
| Rating of Medication Influences3 | ||
| 19 items. Subscales: Reasons for adherence (prevention, influence of others, medication affinity), reasons for nonadherence (denial, dysphoria, logistical problems, label rejection, family influence, negative therapeutic alliance) | Valid, reliable. Correlates with other scales (DAI) | Developed on a population including only patients with schizophrenia treated with antipsychotics. Requires a trained rater |
| Drug Attitude Inventory4 | ||
| 30 items. Reflects patients’ attitudes about medication | Self-rated. High internal consistency. Accurately discriminates between adherent and nonadherent patients | Developed on a population including only patients with schizophrenia |
| Lithium Attitudes Questionnaire5 | ||
| 19 items. Areas of assessment: opposition to continue lithium, therapeutic effectiveness of lithium not accepted, difficulty with pill-taking routine, denial of illness severity, subcultural attitudes opposed to drug treatment, dissatisfaction with factual knowledge of lithium | Self-rated. Developed on patients with BD attending a lithium clinic. Good test/retest reliability for most items | The questionnaire is fairly long; shorter versions were adapted from original version |
| Medication Adherence Rating Scale6 | ||
| 10 items that assess medication adherence behavior, attitudes toward taking medication, negative side effects, attitudes toward psychotropic medication, measures adherence in past week | Self-rated. Validated on patients with various diagnoses, including BD. Correlates well with DAI, MAQ, and mood stabilizer drug levels (lithium and carbamazepine) | Validation methods may be limited by the other measures (for example, medication levels can be influenced by metabolism) |
| Brief Adherence Rating Scale7 | ||
| 3 items. Number of pills prescribed daily, days with no medication taken, and days with medication taken less than prescribed. Nonadherence defined as <70% of doses taken. Measures adherence in past month | Clinician–rated. Short. Good correlation with electronic medication monitoring. High internal reliability. Good test/retest reliability. Greater adherence on BARS correlates with lower psychotic symptom scores. Sensitive and specific in identifying nonadherence | Validation study only on patients with schizophrenia and schizoaffective disorder taking antipsychotics |
| BARS: Brief Adherence Rating Scale; BD: bipolar disorder; DAI: Drug Attitude Inventory; MAQ: Medication Adherence Questionnaire | ||
BD adherence studies
Treatment adherence in BD is challenged by the chronic remission-relapse pattern of the disorder. Manic episodes carry the highest risk of nonadherence.2 Scott and Pope8 evaluated self-reported adherence to mood stabilizers (lithium, carbamazepine, or valproate) among 98 patients with major depressive disorder and 78 with BD. They found that 32% of patients were partially adherent (defined as having missed >30% of doses in the past month) and >60% of these patients had sub-therapeutic plasma levels of mood stabilizers.
In a study of 106 BD outpatients treated with lithium who completed scales regarding their attitudes toward and knowledge of lithium and the Medication Adherence Rating Scale (MARS), 86% of patients had a therapeutic serum lithium level (.6 to 1.2 mEq/L), and knowledge of lithium was correlated with adherence.9 Jónsdóttir et al10 looked at medication adherence among 280 patients with schizophrenia and BD by comparing patient self-reports to provider reports and measuring serum drug concentrations; adherence was defined as having a serum concentration within the reference level for the specific medication. BD patients had an adherence rate of 66%, and self-reported adherence as measured by MARS and provider reports correlated with serum concentrations.
In a study of 71 adolescents with BD followed for 1 year after their first hospitalization for a manic or mixed episode, DelBello et al11 defined nonadherence as taking medication <25% of the time and partial adherence as taking medication 25% to 75% of the time. They found that 42% of patients were partially adherent and 23% were nonadherent.
Strakowski12 followed 46 adults from Taiwan and 96 from the United States for 1 year after their first manic or mixed episode and found that 79% of the Taiwanese patients and 50% of U.S. patients were adherent. Using the medication possession ratio (MPR)—which is calculated based the number of days between expected and actual prescription refills—to determine adherence, Sajatovic13 found that 54% of 44,637 veterans being treated for BD with lithium or anticonvulsants were fully adherent (MPR >.80), 25% were partially adherent (MPR >.50 to .80), and 21% were nonadherent (MPR ≤.50). In a survey of 131 randomly selected psychiatrists and 429 of their adult BD patients, Baldessarini14 found that 34% of patients reported missing ≥1 medication dose in past 10 days, but psychiatrists recognized only 18% of patients as nonadherent.
What affects adherence?
Although all BD patients share the same diagnosis, the factors that ultimately result in their medication adherence are as variable as the individuals themselves. Patients’ age, sex, culture, symptom severity, worldview, socioeconomic status, opinion of mental illness, and self-image influence their individual decisions on adhering to a prescribed medication regimen.1,15
Perception of medication efficacy. Not surprisingly, if a medication does not seem to decrease debilitating symptoms, a patient is unlikely to continue taking it. Patients with BD feel more affected by depressive symptoms than by manic symptoms, and have indicated that they are more likely to adhere to and view as successful treatments that reduce depressive symptoms.16,17
Tolerability. In an Internet-based survey, 469 patients with BD indicated that medication-related weight gain and cognitive impairment were the most important factors that affected adherence.16 Individuals’ concerns about possible side effects may contribute more to nonadherence than actually experiencing side effects.17 Concerns about long-term metabolic side effects from atypical antipsychotics also may limit adherence.17
Neurocognitive impairment. Whether caused by BD, aging, or a combination of these factors, deficits in memory, attention, and executive functioning can lead to unintentional nonadherence. In a study that assessed medication management ability among middle-aged and older adults, patients with BD were found to make 2.8 times more errors than healthy controls.18
Therapeutic alliance and psychoeducation. Patients’ expectations for pharmacotherapy vary from specific symptom relief to hopes for a complete cure, and their fears may be influenced by media and advertisements.17 Nonetheless a positive therapeutic alliance with the treating provider improves illness outcomes.19
A clinician’s ability to help patients build insight is invaluable for their current and future treatment. In a survey of 435 veterans with BD, nonadherence was greater among patients with limited insight about the role of medication in their illness.20 A study of 65 BD patients that evaluated insight into medication adherence at initial interview and 1 year later found that difficulty with adherence at the initial interview predicted future nonadherence and was correlated with lack of insight.21 Rosa et al9 found that BD patients in denial of their illness and those who had little psychoeducation were more frequently nonadherent with lithium treatment.
Other factors that may contribute to medication nonadherence in BD patients include comorbid substance abuse or personality disorders, both of which are associated with more frequent relapse.15 Marriage has a beneficial affect on adherence.15 A good support system may contribute to treatment adherence; in a study of 107 children and adolescents with BD, nonadherent patients were more likely to experience family dysfunction and have a parental history of psychiatric hospitalization.22
Adherence and BD course
Treatment adherence decreases the suicide rate among BD patients. Angst et al23 evaluated the rate of suicide among 406 patients with BD and unipolar depression who were followed for 40 years. They found that 11% committed suicide; untreated patients had significantly higher standardized mortality rates than of those who were treated with lithium, antipsychotics, or antidepressants. Other studies confirm this finding.15
Repeated relapse may predict poorer cognitive performance. Lopez-Jaramillo et al24 showed that patients with BD who had more manic episodes performed poorer on cognitive tests assessing attention, memory, and executive functioning compared with patients with less episodes and with normal subjects.
Medication adherence in BD is a priority because of potential neurodegeneration in BD and the neuroprotective effects of mood stabilizers and some atypical antipsychotics (Box).
As emerging studies document morphologic brain changes associated with bipolar disorder (BD), researchers have been relating these changes to the duration and progression of illness. A longer duration of illness is associated with a smaller total gray matter volume on brain MRI of BD patients compared with unipolar patients and normal controls.a Brain MRI analysis of grey and white matter in elderly patients with longstanding BD who underwent neuropsychological testing to rule out dementia showed a decreased concentration of grey matter in the anterior limbic areas as well as reduced fiber tract coherence in the corpus callosum when compared with normal controls.b
Additionally, microstructural brain changes have been associated with acute mood states, in particular bipolar depression.c Lithium, valproate, olanzapine, and clozapine are neuroprotective in cultures of human-derived neuroblastoma cells, by enhancing the cells’ proliferation and survival.d
Source:
a. Frey BN, Zunta-Soares GB, Caetano SC, et al. Illness duration and total brain gray matter in bipolar disorder: evidence for neurodegeneration? European Neuropsychopharm. 2008;18:717-722.
b. Haller S, Xekardaki A, Delaloye C, et al. Combined analysis of grey matter voxel-based morphometry and white matter tract-based spatial statistics in late-life bipolar disorder. J Psychiatry Neurosci. 2011;36(1):100140.
c. Zanetti MV, Jackowski MP, Versace A, et al. State-dependent microstructural white matter changes in bipolar I depression. Eur Arch Psychiatry Clin Neurosci. 2009;259(6):316-328.
d. Aubry J, Schwald M, Ballmann E, et al. Early effects of mood stabilizers on the Akt/GSK-3ß signaling pathway and on cell survival and proliferation. Psychopharmacology. 2009;205:419-429.
Increasing adherence
Pharmacologic strategies. Adherence in BD often is difficult when patients require a complex medication regimen to control their illness. Patients and clinicians may prefer to use once-daily dosing drug formulations, which can provide consistent serum levels and fewer adverse effects. Divalproex extended-release (ER) allows once-daily dosing and improved tolerability by reducing fluctuations in valproic acid serum concentrations compared with the delayed-release formulation. In a retrospective chart review,25 most patients (62%) who switched to divalproex ER from divalproex delayed-release preferred the ER formulation; 52% showed clinical improvement, 81% did not experience side effects, and 8% demonstrated higher adherence after switching.25 Similarly, an extended-release formulation of carbamazepine is approved for treating acute mania.
Many atypical antipsychotics are FDA-approved for acute mania, acute bipolar depression, and/or maintenance (Table 2). Long-acting injectable formulations (LAIs) may be used as maintenance treatment if nonadherence is an issue. LAI risperidone, which is FDA-approved for maintenance treatment of bipolar I disorder (BDI), was found to be safe and effective in stable BD patients who were switched from an oral antipsychotic.26 Asenapine is provided in a rapidly absorbed, sublingual form and is FDA-approved for treating acute mania or mixed episodes associated with BDI.27 Overall, however, only slightly more than one-half of BD patients are adherent to atypical antipsychotics.15
Although antidepressant use in BD is controversial, Sajatovic17 found 44% of depressed BDI patients were treated with antidepressants. Novel extended-release antidepressant formulations—including controlled-release fluvoxamine, paroxetine, extended-release bupropion and venlafaxine, once-weekly fluoxetine, rapidly dissolving mirtazapine, and transdermal selegiline—can optimize drug delivery, minimize side effects, and delay onset of action.1
Psychosocial strategies used in BD include psychoeducation, cognitive-behavioral therapy (CBT), family-focused interventions, and interpersonal and social rhythm therapy (IPSRT) (Table 3).28-30 Psychoeducation alone or combined with other interventions can decrease the risk of relapse and hospitalization and improve adherence.28 In a 2-year study of 50 euthymic BD patients treated with lithium who participated in a brief hospital-based psychoeducation program, Even et al31 found patients’ knowledge about lithium but not their attitudes changed significantly after the program. The changes persisted 2 years after the intervention, with a trend toward a decreased hospitalization rate.
Miklowitz32 reported on 293 BD patients randomized to receive collaborative care (3 psychoeducational sessions delivered over 6 weeks) or 1 of 3 types of intensive psychotherapy: CBT, IPSRT, or family-focused therapy. Attrition was similar for both groups. Compared with those receiving collaborative care, significantly more patients receiving intensive psychotherapy recovered after 1 year, and did so in shorter time.
In a 3-year, multi-site Veterans Administration (VA) study, 306 BD patients received psychoeducation and support from nurse care coordinators who were responsible for access, continuity of care, and information flow to psychiatrists or usual care according to VA guidelines.33 Compared with the usual care group, patients who received psychoeducation and support from nurse care coordinators had shorter duration of manic episodes and improved function and quality of life. A meta-analysis30 of 12 randomized controlled trials of CBT in BD showed a medium effect size of CBT on adherence at 6 months post-treatment.
Table 2
FDA-approved medications for adult bipolar disorder
| Bipolar disorder indication | Medications |
|---|---|
| Acute treatment of mania/mixed episodes | Aripiprazole,a,b asenapine,a carbamazepine extended release,a divalproex sodium,a lithium,a quetiapine,a risperidone,a-c ziprasidonea,b |
| Depressive episodes | Olanzapine/fluoxetine,a quetiapinea |
| Maintenance treatment | Aripiprazole (as monotherapy and as adjunct to lithium or divalproex sodium),a,b asenapine,d lamotrigine,a lithium,a olanzapine,a-c quetiapine (as adjunct to lithium or divalproex sodium),a risperidone,e ziprasidone (as adjunct to lithium or divalproex sodium)a |
| apill form bintramuscular for acute agitation cdisintegrating tablet dsublingual tablet elong-acting injectable | |
Table 3
Psychosocial interventions for bipolar disorder
| Intervention | Description | Results in bipolar disorder | Optimal stage of illness for intervention |
|---|---|---|---|
| Individual and family psycho-education28,29 | Strategies to educate the patient about the illness, medications, side effects, and relapse prevention | Decreases relapse, (particularly manic episodes) and hospitalizations. Increases adherence | Manic episodes |
| Cognitive-behavioral therapy28-30 | Focuses on understanding patient’s perceptions of illness and treatment. Equates resistance with exploring, rather than challenging resistance to take medication. Identifies and modifies negative automatic thoughts about medication. Motivation techniques useful in comorbid substance use | Decreases clinical symptoms. Increases adherence, quality of life, and social functioning | Depressive episodes |
| IPSRT28,29 | Uses motivational interviewing and CBT techniques to stabilize daily routines and resolve interpersonal problems | Prevents relapse | Depressive episodes |
| Family-focused therapy28,29 | A combination of psychoeducation, communication, and problem-solving skills training | Reduces mood symptoms, number of depressive relapses, and time depressed. Increases adherence | Depressive episodes |
| IPSRT: interpersonal and social rhythm therapy | |||
Related Resource
- Deegan PE. The importance of personal medicine: a qualitative study of resilience in people with psychiatric disabilities. Scand J Public Health Suppl. 2005;66:29-35.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Bupropion • Wellbutrin
- Carbamazepine • Carbatrol, Tegretol
- Carbamazepine extended- release • Equetro
- Clozapine • Clozaril
- Divalproex • Depakote, Depakote ER
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Paroxetine • Paxil
- Quetiapine • Seroquel, Seroquel XR
- Risperidone • Risperdal
- Risperidone long-acting injectable • Risperdal Consta
- Selegiline • Eldepryl, Emsam
- Valproate • Depacon
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Foster receives research/grant support from the American Psychiatric Foundation, the National Institute of Mental Health, and Sunovion Pharmaceuticals.
Dr. Sheehan and Ms. Johns report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Buckley PF, Foster AE, Patel NC, et al. Adherence to mental health treatment. New York, NY: Oxford University Press; 2009;1-10:53-69.
2. Velligan D, Sajatovic M, Valenstein M, et al. Methodological challenges in psychiatric treatment adherence research. Clin Schizophr Relat Psychoses. 2010;4(1):74-91.
3. Weiden P, Rapkin B, Mott T, et al. Rating of Medication Influences (ROMI) scale in schizophrenia. Schizophr Bull. 1994;20:297-310.
4. Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med. 1983;13(1):177-183.
5. Harvey NS. The development and descriptive use of the Lithium Attitudes Questionnaire. J Affect Disord. 1991;22(4):211-219.
6. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS). Schizophr Res. 2000;42:241-247.
7. Byerly MJ, Nazonezny PA, Rush AJ. The Brief Adherence Rating Scale (BARS) validated against electronic monitoring in assessing the antipsychotic medication adherence of outpatients with schizophrenia and schizoaffective disorder. Schizophr Res. 2008;100(1-3):60-69.
8. Scott J, Pope M. Non-adherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry. 2002;63:384-390.
9. Rosa AR, Marco M, Fachel JM, et al. Correlation between drug treatment adherence and lithium treatment attitudes and knowledge in bipolar patients. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:217-224.
10. Jónsdóttir H, Opjordsmoen S, Birkenaes A, et al. Medication adherence in outpatients with severe mental disorders, relation between self-reports and serum level. J Clin Psychopharmacol. 2010;30:169-175.
11. DelBello M, Hanserman D, Adler CM, et al. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007;164:582-590.
12. Strakowski SM, Tsai SY, DelBello MP, et al. Outcome following a first manic episode: cross national US and Taiwan comparison. Bipolar Disord. 2007;9:820-827.
13. Sajatovic M, Valenstein M, Blow F, et al. Treatment adherence with lithium and anticonvulsant medications among patients with bipolar disorder. Psychiatr Serv. 2007;58:855-863.
14. Baldessarini RJ, Perry R, Pike J. Factors associated with treatment nonadherence among US bipolar patients. Hum Psychopharmacol. 2008;23:95-105.
15. Berk L, Hallam KT, Colom F, et al. Enhancing medication adherence in patients with bipolar disorder. Hum Psychopharmacol. 2010;25(1):1-16.
16. Johnson FR, Ozdemir S, Manjunath R, et al. Factors that affect adherence to bipolar disorder treatments: a stated-preference approach. Med Care. 2007;45(6):545-552.
17. Sajatovic M, Jenkins JH, Cassidy KA, et al. Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. J Affect Disord. 2009;115(3):360-366.
18. Depp CA, Cain AE, Palmer BW, et al. Assessment of medication management ability in middle-aged and older adults with bipolar disorder. J Clin Psychopharmacol. 2008;28(2):225-229.
19. Gaudiano BA, Miller IW. Patients’ expectancies the alliance in pharmacotherapy, and treatment outcomes in bipolar disorder. J Consult Clin Psychol. 2006;74(4):671-676.
20. Copeland LA, Zeber JE, Salloum IM, et al. Treatment adherence and illness insight in veterans with bipolar disorder. J Nerv Ment Dis. 2008;196(1):16-21.
21. Yen CF, Chen CS, Ko CH, et al. Relationships between insight and medication adherence in outpatients with schizophrenia and bipolar disorder: prospective study. Psychiatry Clin Neurosci. 2005;59(4):403-409.
22. Drotar D, Greenley RN, Demeter CA, et al. Adherence to pharmacological treatment for juvenile bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):831-839.
23. Angst J, Angst F, Gerber-Werder R, et al. Suicide in 406 mood-disorder patients with and without long–term medication: a 40 to 44 years’ follow-up. Arch Suicide Res. 2005;9:279-300.
24. Lopez-Jaramillo C, Lopera-Vasquez J, Aurora G, et al. Effects of recurrence on the cognitive performance of patients with bipolar I disorder: implications for relapse prevention and treatment adherence. Bipolar Disord. 2010;12:557-567.
25. Minirth FB, Neal V. Assessment of patient preference and side effects in patients switched from divalproex sodium delayed release to divalproex sodium extended release. J Clin Psychopharmacol. 2005;25:99-101.
26. Han C, Lee MS, Pae CU, et al. Usefulness of long-acting injectable risperidone during 12-month maintenance therapy of bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1219-1223.
27. McIntyre RS, Cohen M, Zhao J, et al. Asenapine for long term treatment of bipolar disorder: a double blind 40-week extension study. J Affect Disord. 2010;126:358-365.
28. Velligan DI, Weiden PJ, Sajatovic M, et al. Strategies for addressing adherence problems in patients with serious and persistent mental illness: recommendations from expert consensus guidelines. J Psychiatr Pract. 2010;16(5):306-324.
29. Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry. 2008;165(11):1408-1419.
30. Szentagotai A, David D. The efficacy of cognitive-behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71(1):66-72.
31. Even C, Thuile J, Stern K, et al. Psychoeducation for patients with bipolar disorder receiving lithium: short and long term impact on locus of control and knowledge about lithium. J Affect Disord. 2010;123:299-302.
32. Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007;64:419-426.
33. Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder, part II. Impact on clinical outcome, function and costs. Psychiatr Serv. 2006;57:937-945.
1. Buckley PF, Foster AE, Patel NC, et al. Adherence to mental health treatment. New York, NY: Oxford University Press; 2009;1-10:53-69.
2. Velligan D, Sajatovic M, Valenstein M, et al. Methodological challenges in psychiatric treatment adherence research. Clin Schizophr Relat Psychoses. 2010;4(1):74-91.
3. Weiden P, Rapkin B, Mott T, et al. Rating of Medication Influences (ROMI) scale in schizophrenia. Schizophr Bull. 1994;20:297-310.
4. Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med. 1983;13(1):177-183.
5. Harvey NS. The development and descriptive use of the Lithium Attitudes Questionnaire. J Affect Disord. 1991;22(4):211-219.
6. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS). Schizophr Res. 2000;42:241-247.
7. Byerly MJ, Nazonezny PA, Rush AJ. The Brief Adherence Rating Scale (BARS) validated against electronic monitoring in assessing the antipsychotic medication adherence of outpatients with schizophrenia and schizoaffective disorder. Schizophr Res. 2008;100(1-3):60-69.
8. Scott J, Pope M. Non-adherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry. 2002;63:384-390.
9. Rosa AR, Marco M, Fachel JM, et al. Correlation between drug treatment adherence and lithium treatment attitudes and knowledge in bipolar patients. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:217-224.
10. Jónsdóttir H, Opjordsmoen S, Birkenaes A, et al. Medication adherence in outpatients with severe mental disorders, relation between self-reports and serum level. J Clin Psychopharmacol. 2010;30:169-175.
11. DelBello M, Hanserman D, Adler CM, et al. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007;164:582-590.
12. Strakowski SM, Tsai SY, DelBello MP, et al. Outcome following a first manic episode: cross national US and Taiwan comparison. Bipolar Disord. 2007;9:820-827.
13. Sajatovic M, Valenstein M, Blow F, et al. Treatment adherence with lithium and anticonvulsant medications among patients with bipolar disorder. Psychiatr Serv. 2007;58:855-863.
14. Baldessarini RJ, Perry R, Pike J. Factors associated with treatment nonadherence among US bipolar patients. Hum Psychopharmacol. 2008;23:95-105.
15. Berk L, Hallam KT, Colom F, et al. Enhancing medication adherence in patients with bipolar disorder. Hum Psychopharmacol. 2010;25(1):1-16.
16. Johnson FR, Ozdemir S, Manjunath R, et al. Factors that affect adherence to bipolar disorder treatments: a stated-preference approach. Med Care. 2007;45(6):545-552.
17. Sajatovic M, Jenkins JH, Cassidy KA, et al. Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. J Affect Disord. 2009;115(3):360-366.
18. Depp CA, Cain AE, Palmer BW, et al. Assessment of medication management ability in middle-aged and older adults with bipolar disorder. J Clin Psychopharmacol. 2008;28(2):225-229.
19. Gaudiano BA, Miller IW. Patients’ expectancies the alliance in pharmacotherapy, and treatment outcomes in bipolar disorder. J Consult Clin Psychol. 2006;74(4):671-676.
20. Copeland LA, Zeber JE, Salloum IM, et al. Treatment adherence and illness insight in veterans with bipolar disorder. J Nerv Ment Dis. 2008;196(1):16-21.
21. Yen CF, Chen CS, Ko CH, et al. Relationships between insight and medication adherence in outpatients with schizophrenia and bipolar disorder: prospective study. Psychiatry Clin Neurosci. 2005;59(4):403-409.
22. Drotar D, Greenley RN, Demeter CA, et al. Adherence to pharmacological treatment for juvenile bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):831-839.
23. Angst J, Angst F, Gerber-Werder R, et al. Suicide in 406 mood-disorder patients with and without long–term medication: a 40 to 44 years’ follow-up. Arch Suicide Res. 2005;9:279-300.
24. Lopez-Jaramillo C, Lopera-Vasquez J, Aurora G, et al. Effects of recurrence on the cognitive performance of patients with bipolar I disorder: implications for relapse prevention and treatment adherence. Bipolar Disord. 2010;12:557-567.
25. Minirth FB, Neal V. Assessment of patient preference and side effects in patients switched from divalproex sodium delayed release to divalproex sodium extended release. J Clin Psychopharmacol. 2005;25:99-101.
26. Han C, Lee MS, Pae CU, et al. Usefulness of long-acting injectable risperidone during 12-month maintenance therapy of bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1219-1223.
27. McIntyre RS, Cohen M, Zhao J, et al. Asenapine for long term treatment of bipolar disorder: a double blind 40-week extension study. J Affect Disord. 2010;126:358-365.
28. Velligan DI, Weiden PJ, Sajatovic M, et al. Strategies for addressing adherence problems in patients with serious and persistent mental illness: recommendations from expert consensus guidelines. J Psychiatr Pract. 2010;16(5):306-324.
29. Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry. 2008;165(11):1408-1419.
30. Szentagotai A, David D. The efficacy of cognitive-behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71(1):66-72.
31. Even C, Thuile J, Stern K, et al. Psychoeducation for patients with bipolar disorder receiving lithium: short and long term impact on locus of control and knowledge about lithium. J Affect Disord. 2010;123:299-302.
32. Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007;64:419-426.
33. Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder, part II. Impact on clinical outcome, function and costs. Psychiatr Serv. 2006;57:937-945.
How to prevent adverse drug events
Medication errors due to system-, provider-, or patient-related factors contribute significantly to increased costs, adverse drug events (ADEs), and morbidity and mortality.1 One study found >60% of ADEs that led to hospitalization could have been prevented by strategies such as adequate monitoring or appropriate prescribing.2 Psychiatrists have an opportunity to reduce rates of ADEs; however, the possibility of disease symptoms overlapping with these adverse events is 1 of many obstacles prescribing clinicians face.1 Prescribers also must contend with adverse effects of polypharmacy, which are common among psychiatric patients. Patient-related factors of concern include:
- seeing multiple prescribers
- medication nonadherence
- failure to communicate use of herbal or over-the-counter products
- lack of insight
- comorbid medical and psychiatric diagnoses, such as dementia.1
This article highlights potential ADEs and major medication safety concerns that may contribute to morbidity and mortality among patients taking psychotropics. Although many factors are beyond the prescribing clinician’s control—such as medication dispensing and administration errors—psychiatrists can substantially reduce ADEs. We will cover potential adverse events associated with key medications or medication classes, drug interactions with potentially devastating consequences, and strategies to minimize risks of ADEs, including enhanced awareness and monitoring (Table 1).
Table 1
How to avoid ADEs with psychotropics
| Establish a collaborative practice among physicians, pharmacists, nurses, and social workers to enhance patient care and reduce the risk of medication errors and negative outcomes |
| Educate patients to increase their understanding of psychiatric diseases and medications and increase compliance with therapy. This may lead the patient to self-monitor drug efficacy and adverse effects |
| Be aware of psychotropic medications’ ‘black-box’ warnings that guide their safe use |
| Pay particular attention to drugs with a narrow therapeutic index, such as lithium and tricyclic antidepressants, which have small safety margins and are lethal in overdose |
| Avoid using 1 drug to treat the side effects of another. Minimizing polypharmacy can reduce medication errors, DDIs, and ADEs |
| Remain vigilant for DDIs, which can be serious and life-threatening. Examples include sudden cardiac death from additive QTc prolongation effects and NMS. Early detection of NMS and discontinuing the offending agent(s) can help prevent patient morbidity and mortality |
| Stay up-to-date on literature and drug warnings to employ best practices and avoid potentially serious adverse and/or lethal outcomes |
| Encourage patients to disclose any prescription drugs, over-the-counter medications, and herbal therapies they are taking |
| Develop strategies to prevent ADEs, such as personal formularies, suicide assessments, prescribing limited quantities, ‘eyes on’ medication administration, therapeutic drug monitoring, utilizing databases and resources for drug information, and patient education |
| ADEs: adverse drug events; DDIs: drug-drug interactions; NMS: neuroleptic malignant syndrome |
Prescription drug overdose
Each year, unintentional drug overdoses account for >20,000 deaths in the United States.3 Prescription medications, particularly opioid analgesics, have contributed to the doubling of overdose mortality rates in recent years. A recent study reported that nearly 50% of unintentional drug overdose deaths were associated with psychotropics and one-third of these deaths were associated with benzodiazepines, many of which were not prescribed to the individual.4
The risk of mortality from intentional drug overdose also must be assessed. Tricyclic antidepressants (TCAs) are a particularly lethal class of medications in suicide attempts and may result in arrhythmias, coma, seizures, respiratory failure, and death.5 Venlafaxine and mirtazapine are associated with greater risk of death and toxicity in overdose, respectively, than selective serotonin reuptake inhibitors (SSRIs).6 Lithium toxicity in overdose may lead to bradycardia, seizure, coma, hyperventilation, serotonin syndrome, respiratory failure, or death.5 The risk of death with lithium or benzodiazepine monotherapy is low when these agents are taken as prescribed. However, prescribers must exercise caution when these agents are used in combination. Interactions involving drugs with a narrow therapeutic index—such as lithium and TCAs—are more likely to be clinically significant because small increases in drug concentration can lead to serious adverse effects or death. See Related Resources for a review article on appropriate use and monitoring of lithium.
Drug-drug interactions
Many Americans take multiple prescription and nonprescription drugs, and psychiatric patients are more likely than other individuals to have more complex medication regimens.7 This can result in polypharmacy and drug-drug interactions (DDIs), which can lead to undesired medication effects and serious, potentially fatal ADEs.
Pharmacokinetic interactions typically affect drug concentrations and occur when 1 drug interferes with the absorption, distribution, metabolism, or excretion of another drug. Many common pharmacokinetic interactions involve the liver cytochrome P450 (CYP) system, which is responsible for metabolizing many medications.8 DDIs can occur when CYP enzymes are modified by inhibitors or inducers, which can decrease or increase drug clearance, respectively. Table 2 5,7,9 provides examples of common CYP450 substrates, inhibitors, and inducers. Polymorphisms in the pharmacogenetics of CYP450 also can affect overall drug clearance and the impact of DDIs.8
Pharmacodynamic interactions are caused by additive or competing effects of multiple drugs. The most serious of these involve medications that increase a patient’s risk of serotonin syndrome or neuroleptic malignant syndrome (NMS); both are medical emergencies that require immediate hospitalization.
Although any medication with serotonergic activity can induce serotonin syndrome, combinations of serotonergic drugs in particular are associated with increased risk.10 Serotonin syndrome is characterized by hyperthermia, altered muscle tone, altered mental status, and autonomic instability; rhabdomyolysis and disseminated intravascular coagulation are potential lethal complications.10 A high index of suspicion can help clinicians rapidly detect serotonin syndrome, discontinue offending agents, and initiate supportive treatments.
NMS is a life-threatening complication of antipsychotics characterized by fever, delirium, muscle rigidity, autonomic instability, and abnormal laboratory findings that include elevated white blood count and increased creatinine kinase from muscle injury. In early stages, NMS may be mistaken for extrapyramidal symptoms. Although NMS can occur with any antipsychotic as monotherapy, additive antidopaminergic effects increase the risk. Patients with a compromised CNS as a result of mental retardation, traumatic brain injury, or metabolic abnormalities also are at increased risk of developing NMS.11
Other pharmacodynamic interactions involve medications that may have additive effects on prolonging QTc intervals. For example, TCAs are pro-arrhythmic and have quinidine-like effects, which can cause cardiac conduction abnormalities and prolonged PR and QTc intervals.12 Employ routine ECG monitoring when prescribing multiple medications known to cause QTc prolongation, such as TCAs (Table 3).13,14 The Arizona Center for Education and Research on Therapeutics (www.azcert.org) provides a searchable list of QT-prolonging drugs (see Related Resources).
Medications also can interact with food, disease states, and herbal supplements. Alcohol interacts with many CNS-active medications, including many psychotropics. Patients taking benzodiazepines may experience oversedation and respiratory depression from alcohol’s additive sedating effects.5 Advise patients to limit their alcohol intake while taking CNS-depressing psychotropics such as benzodiazepines, antipsychotics, and some antidepressants. Monoamine oxidase inhibitors (MAOIs) and tyramine-containing food—such as cheese, beer, preserved meat, and soy sauce—can lead to a dangerous hypertensive crisis that requires immediate medical intervention to prevent life-threatening complications.5 Hypertensive crisis may be more significant in patients who have pre-existing hypertension. Finally, herbal supplements also can interact with medications. Patients who take St. John’s wort for depressive symptoms might not realize that it can reduce the efficacy of other drugs or increase their risk of serotonin syndrome.9
Table 2
Cytochrome P450 substrates, inhibitors, and inducers
| 3A4 | 2D6 | 2C9 | 2C19 | 1A2 | |
|---|---|---|---|---|---|
| Substrates | Carbamazepine Citalopram Fluoxetine Haloperidol Mirtazapine Oxcarbazepine Quetiapine Sertraline Ziprasidone | Aripiprazole Citalopram Duloxetine Fluoxetine Haloperidol Mirtazapine Paroxetine Risperidone Sertraline Venlafaxine TCAs | Amitriptyline Carbamazepine Sertraline Valproic acid | Citalopram Clomipramine Sertraline Valproic acid | Carbamazepine Clozapine Olanzapine |
| Inhibitors | Amiodarone Aprepitant Azole antifungals Carbamazepine Cimetidine Diltiazem Erythromycin Fluoxetine (norfloxetine) Grapefruit juice Imatinib Paroxetine Ritonavir Sertraline Verapamil | Amiodarone Bupropion Cimetidine Duloxetine Fluoxetine Methadone Paroxetine Ritonavir Sertraline | Amiodarone Fluconazole Isoniazid Sertraline Trimethoprim-sulfamethoxazole Valproic acid | Cimetidine Fluoxetine Ketoconazole Omeprazole Sertraline Valproic acid | Amiodarone Cimetidine Fluoroquinolones |
| Inducers | Carbamazepine Phenobarbital Phenytoin Rifampin St. John’s wort | Rifampin | Phenobarbital Rifampin | Carbamazepine Rifampin | Nafcillin Phenobarbital Rifampin Smoking |
| TCAs: tricyclic antidepressants Source: References 5,7,9 | |||||
Table 3
Psychotropics associated with QT prolongation
| Class | Agents |
|---|---|
| Antidepressants | Mirtazapine, SNRIs (desvenlafaxine, venlafaxine), SSRIs (citalopram, fluoxetine, paroxetine, sertraline), TCAs (amitriptyline, clomipramine, desipramine, doxepin, imipramine, protriptyline, trimipramine), trazodone |
| Typical antipsychotics | Chlorpromazine, fluphenazine, haloperidol, perphenazine, thioridazine, trifluoperazine |
| Atypical antipsychotics | Aripiprazole, asenapine, clozapine, iloperidone, paliperidone, quetiapine, risperidone, ziprasidone |
| Mood stabilizers | Lithium |
| Miscellaneous agents | Amantadine, atomoxetine, chloral hydrate, diphenhydramine, galantamine |
| Stimulants | Amphetamine/dextroamphetamine products, methylphenidate/dexmethylphenidate |
| SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants Source: Adapted from references 13,14 | |
“Black-box” warnings issued by the FDA are included in the package insert to highlight a medication’s risks of dangerous and potentially lethal adverse effects. Table 4 highlights current black-box warnings for various psychotropics.5,14-16
Antidepressants and suicide. All medications with antidepressant indications carry a black-box warning for risk of suicidal ideation and behavior in children, adolescents, and young adults during the early months of medication therapy. This includes not only SSRIs and serotonin-norepinephrine reuptake inhibitors, but also anticonvulsants and atypical antipsychotics indicated for treating mood disorders. Monitor young patients carefully and advise family members to alert clinicians of any signs of suicidality or unusual behavior.
Lamotrigine and aseptic meningitis. Aseptic meningitis—inflammation of the meninges that is not caused by bacteria—is a rare but serious adverse effect of lamotrigine. Symptoms include headache, fever, stiff neck, nausea and vomiting, delirium, rash, and sensitivity to light.5 Forty cases of aseptic meningitis in children and adults were reported over 15 years, representing <.01% of all lamotrigine prescriptions.5 Most of these patients required hospitalization, but symptoms resolved after lamotrigine was discontinued. Prompt identification and management of aseptic meningitis are necessary to prevent permanent brain damage and death. Other complications of aseptic meningitis include long-term neurologic sequelae such as cognitive impairment, seizure disorders, and behavioral disturbances.
Table 4
Which psychotropics carry ‘black-box’ warnings?
| Warning | Class or medication affected | Comments |
|---|---|---|
| Suicidality | Antidepressants Antipsychotics indicated for mood disorders Anticonvulsants | See ‘Black-box warnings’ |
| Serious, life-threatening rashes such as Stevens-Johnson syndrome or toxic epidermal necrolysis | Lamotrigine Carbamazepine | Lamotrigine’s risk of severe dermatologic reactions necessitates slow titration during drug initiation Carbamazepine warning includes a recommendation for genetic screening in Asian patients because Stevens-Johnson syndrome is associated with the HLA-B*1502 allele found primarily in the Asian population |
| Increased mortality in elderly patients with dementia-related psychosis | Antipsychotics | A study of >10,000 geriatric patients with dementia showed mortality rates of 22.6% to 29.1% among those who took antipsychotics compared with 14.6% for patients taking other psychiatric medications. When antipsychotics are used in older adults, well-documented informed consent from the patient or substitute decision-maker is required |
| Other effects | Clozapine | Agranulocytosis occurs in 1% to 2% of clozapine patients, necessitating WBC/ANC monitoring Clozapine-induced myocarditis, generally accompanied by peripheral eosinophilia, usually occurs within the first 2 months of treatment, and can result in significant mortality from resultant cardiomyopathy. Early warning signs of fever, fatigue, and tachycardia are easily mistaken for the more benign effects of clozapine titration Seizures are more likely with higher doses. Cautious use is advised with patients who have an underlying seizure disorder Other cardiovascular and respiratory effects: Hypotension has been associated with rapid initial titration. Cardiac and respiratory arrest and circulatory collapse have occurred rarely. Respiratory complications are more likely when clozapine is used in combination with benzodiazepines |
| ANC: absolute neutrophil count; WBC: white blood cell Source: References 5,14-16 | ||
Other complications
Hematologic effects. All classes of psychotropics carry a risk (1 to 2 cases per year per 100,00 patients) of serious hematologic complications, including neutropenia, agranulocytosis, eosinophilia, thrombocytopenia, purpura, and anemia.17 Agranulocytosis has been associated most commonly with clozapine, carbamazepine, and typical antipsychotics.17 SSRIs, which are widely prescribed, are associated with increased risk of bruising and bleeding. Patients with bleeding or platelet disorders are at an increased risk for these complications.17
Seizures. Several classes of psychotropics are associated with an increased risk of seizures. Among antipsychotics, clozapine and chlorpromazine are the most seizurogenic.18 Among antidepressants, bupropion and clomipramine are most likely to lower seizure thresholds.18 Psychotropics’ seizure-inducing effects are dose-related. Vulnerability to seizures while taking psychotropics is related to having a history of epilepsy or brain injury.18 Seizures also can occur when benzodiazepines or anticonvulsants are withdrawn too quickly.
Heat stroke. Although a rare occurrence, psychotropics with anticholinergic side effects can contribute to heat stroke. Older patients are particularly vulnerable to the risk of body temperature dysregulation.19
Ketoacidosis and hyperosmolar coma. Medication-related deaths have occurred as a result of ketoacidosis and hyperosmolar coma associated with atypical antipsychotics. These hyperglycemia-related fatalities are most likely with clozapine and olanzapine.20
Hip fractures and falls. Geriatric patients are vulnerable to falls and resultant hip fractures related to use of TCAs, SSRIs, benzodiazepines, and antipsychotics. This is not a trivial matter; hip fractures increase the mortality rate by 12% to 20% in the year after the injury.21 The risk of falls is related to sedation, orthostatic hypotension, arrhythmias, and confusion associated with psychotropics.21,22
Akathisia and suicide. Unrecognized or undertreated akathisia is most commonly associated with antipsychotics, but also can occur with SSRIs. Although akathisia is commonly thought of as a motor syndrome of restlessness, patients may find the less-recognized psychic symptoms of increased inner turmoil and hallucinations just as distressing. This complex of symptoms is associated with an increased risk of suicide.23 If discontinuing the offending agent is not feasible, akathisia can be treated with beta blockers, benzodiazepines, or anticholinergics.24
Hepatotoxicity. Hepatotoxicity from psychotropics occurs in only a small percentage of patients, and can range from transient elevations in liver enzymes to fulminant liver failure. Adverse hepatic effects may be a manifestation of a hypersensitivity reaction accompanied by rash and eosinophilia.25 MAOIs and TCAs can cause cholestatic liver injury, whereas nefazodone has been associated with fulminant liver failure. Other psychotropics—including SSRIs, antipsychotics, benzodiazepines, and older antiepileptics—can cause negative hepatic effects but rarely are associated with acute liver failure.25,26 Although few medications can cause complete liver failure on their own, hepatotoxicity from medications may precipitate severe, potentially fatal outcomes in patients with underlying liver diseases such as hepatitis and cirrhosis. Additive hepatotoxicity from multiple medications also can be problematic. Although psychotropic-induced hepatotoxicity is rare, assess psychotropic doses in patients with liver dysfunction, because drug clearance may be altered, which increases the risk for other serious adverse events.25
Suicide assessment is key
Ongoing monitoring for current or developing suicidal ideation is an important strategy to prevent medication-related mortality in patients vulnerable to self-harm. Initial assessments and follow-up appointments should include a detailed inquiry about suicidal ideations, plans, and behaviors. Patients taking medications that carry black-box warnings for suicide risk should be seen frequently during the first few months of treatment. Patients receiving medications that are lethal in overdose (eg, lithium and TCAs) should be carefully screened for suicide risk. Prescribe medications in limited quantities or arrange for a family member to monitor the patient if necessary. Patients with a history of suicide attempts and current suicide plans may require close observation and initiating medications while hospitalized.
Other prevention strategies
Prescribing psychotropics in a manner that promotes mental well being while minimizing negative outcomes can be challenging. By developing a personal formulary of drugs commonly encountered and prescribed in their practice, psychiatrists can increase their awareness of serious safety concerns, potential DDIs, and appropriate use based on available literature.7,27
Medication histories and drug reconciliation—comparing a patient’s medication orders to all of the medications the patient has been taking—can help clinicians avoid making inappropriate dose adjustments, duplicating therapy, or prescribing medications patients previously have failed or did not tolerate. Establishing a collaborative practice environment with physicians, pharmacists, nurses, and social workers can minimize medication errors and risk of adverse outcomes by increasing communication regarding the patient’s treatment.7
Computerized drug databases and other electronic resources and consultation with pharmacists can help prescribers identify, avoid, and manage clinically significant DDIs.27 Medications could interact with other drugs as long as their effects persist in the body, which could be days to months after the drug is discontinued. Future research may lead to tools to identify patient pharmacogenetic profiles.
Recognizing psychotropic DDIs and adverse effects remains a challenge because of the complexity of the affected organ, the brain. Clinicians should be vigilant to changes in a patient’s presentation because they may be a manifestation of a medication side effect.7 Appropriate therapeutic drug monitoring should occur on a routine, scheduled basis. Closer monitoring may be necessary with dose changes, potential DDIs, signs and symptoms of toxicity/efficacy failure, and renal or hepatic function changes.
Lastly, patients’ education and involvement in their health care may increase their awareness, responsibility, and medication adherence. For challenging patients, family involvement and “eyes on” medication administration can increase adherence and prevent psychotropic misuse.
- Arizona Center for Education and Research on Therapeutics. Drugs that prolong the QT interval and/or induce Torsades de Pointes ventricular arrhythmia. www.azcert.org/medical-pros/drug-lists/drug-lists.cfm.
- Cates ME, Sims PJ. Therapeutic drug management of lithium. Am J Pharm Educ. 2005;69(5):88.
- Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
- Bishop JR, Bishop DL. How to prevent serotonin syndrome from drug-drug interactions. Current Psychiatry. 2011;10(3):81-83.
Drug Brand Names
- Amantadine • Symmetrel
- Amiodarone • Cordarone, Pacerone
- Amitriptyline • Elavil
- Amphetamine/dextroamphetamine • Adderall, others
- Aprepitant • Emend
- Aripiprazole • Abilify
- Asenapine • Saphris
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, Zyban
- Carbamazepine • Tegretol, others
- Chloral hydrate • Somnote
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clozapine • Clozaril
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Diltiazem • Cardia, others
- Diphenhydramine • Benadryl, others
- Doxepin • Sinequan, Silenor
- Duloxetine • Cymbalta
- Erythromycin • Ery-Tab, others
- Fluconazole • Diflucan
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Galantamine • Razadyne
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Imatinib • Gleevec
- Imipramine • Tofranil
- Isoniazid • Nydrazid, others
- Ketoconazole • Nizoral, others
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Methadone • Dolophine, Methadose
- Methylphenidate/ dexmethylphenidate • Ritalin, others
- Mirtazapine • Remeron
- Nafcillin • Nafcil, others
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Oxcarbazepine • Trileptal
- Paliperidone • Invega
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenobarbital • Luminal, others
- Phenytoin • Dilantin
- Protriptyline • Vivactil
- Quetiapine • Seroquel
- Rifampin • Rifadin, others
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimethoprim/Sulfamethoxazole • Bactrim, Septra
- Trimipramine • Surmontil
- Valproic acid • Depakote, others
- Venlafaxine • Effexor
- Verapamil • Calan, others
- Ziprasidone • Geodon
Disclosure
Drs. Yu and Bostwick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Casher is a speaker for AstraZeneca, Pfizer Inc, and Sunovion Pharmaceuticals.
1. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2004;24(7):595-609.
2. McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331-1336.
3. Centers for Disease Control and Prevention. Prescription drug overdose: state health agencies respond. 2008. Available at: http://www.cdc.gov/HomeandRecreationalSafety/pubs/RXReport_web-a.pdf. Accessed February 15 2011.
4. Toblin RL, Paulozzi LJ, Logan JE, et al. Mental illness and psychotropic drug use among prescription drug overdose deaths: a medical examiner chart review. J Clin Psychiatry. 2010;71(4):491-496.
5. Micromedex Healthcare Series (electronic version). 2011. Available at: http://www.micromedex.com. Accessed February 15 2011.
6. Hawton K, Bergen H, Simkin S, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354-358.
7. Preskorn SH, Flockhart D. 2010 guide to psychiatric drug interactions. Primary Psychiatry. 2009;16(12):45-74.
8. Lin JH, Lu AY. Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet. 1998;35(5):361-390.
9. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
10. Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
11. Dave M, Miceli K, Modha P. Psychiatric medicine. The psychiatrist’s guide to the treatment of common medical illnesses. Philadelphia PA: Lippincott Williams & Wilkins; 2007.
12. Mir S, Taylor D. The adverse effects of antidepressants. Curr Opin Psychiatry. 1997;10(2):88-94.
13. Drug-induced long QT interval. Pharmacist’s Letter/Prescriber’s Letter. 2010;26(4):260421.-
14. Drug-induced prolongation of the QT interval and torsades de pointes. 2011. Available at: http://online.factsandcomparisons.com. Accessed February 15 2011.
15. Kales HC, Valenstein M, Kim HM, et al. Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. Am J Psychiatry. 2007;164(10):1568-1576; quiz 1623.
16. Merrill DB, Ahmari SE, Bradford JM, et al. Myocarditis during clozapine treatment. Am J Psychiatry. 2006;163(2):204-208.
17. Oyesanmi O, Kunkel EJ, Monti DA, et al. Hematologic side effects of psychotropics. Psychosomatics. 1999;40(5):414-421.
18. Pisani F, Oteri G, Costa C, et al. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25(2):91-110.
19. Martin-Latry K, Goumy M, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalization. Eur Psychiatry. 2007;22:335-338.
20. Melkersson K, Dahl ML. Adverse metabolic effects associated with atypical antipsychotics: literature review and clinical implications. Drugs. 2004;64(7):701-723.
21. Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351(9112):1303-1307.
22. Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs. 2003;17(11):825-837.
23. Hirose S. The causes of underdiagnosing akathisia. Schizophr Bull. 2003;29(3):547-558.
24. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
25. Selim K, Kaplowitz N. Hepatotoxicity of psychotropic drugs. Hepatology. 1999;29(5):1347-1351.
26. Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002;22(2):169-183.
27. Sandson NB, Armstrong SC, Cozza KL. An overview of psychotropic drug-drug interactions. Psychosomatics. 2005;46(5):464-494.
Medication errors due to system-, provider-, or patient-related factors contribute significantly to increased costs, adverse drug events (ADEs), and morbidity and mortality.1 One study found >60% of ADEs that led to hospitalization could have been prevented by strategies such as adequate monitoring or appropriate prescribing.2 Psychiatrists have an opportunity to reduce rates of ADEs; however, the possibility of disease symptoms overlapping with these adverse events is 1 of many obstacles prescribing clinicians face.1 Prescribers also must contend with adverse effects of polypharmacy, which are common among psychiatric patients. Patient-related factors of concern include:
- seeing multiple prescribers
- medication nonadherence
- failure to communicate use of herbal or over-the-counter products
- lack of insight
- comorbid medical and psychiatric diagnoses, such as dementia.1
This article highlights potential ADEs and major medication safety concerns that may contribute to morbidity and mortality among patients taking psychotropics. Although many factors are beyond the prescribing clinician’s control—such as medication dispensing and administration errors—psychiatrists can substantially reduce ADEs. We will cover potential adverse events associated with key medications or medication classes, drug interactions with potentially devastating consequences, and strategies to minimize risks of ADEs, including enhanced awareness and monitoring (Table 1).
Table 1
How to avoid ADEs with psychotropics
| Establish a collaborative practice among physicians, pharmacists, nurses, and social workers to enhance patient care and reduce the risk of medication errors and negative outcomes |
| Educate patients to increase their understanding of psychiatric diseases and medications and increase compliance with therapy. This may lead the patient to self-monitor drug efficacy and adverse effects |
| Be aware of psychotropic medications’ ‘black-box’ warnings that guide their safe use |
| Pay particular attention to drugs with a narrow therapeutic index, such as lithium and tricyclic antidepressants, which have small safety margins and are lethal in overdose |
| Avoid using 1 drug to treat the side effects of another. Minimizing polypharmacy can reduce medication errors, DDIs, and ADEs |
| Remain vigilant for DDIs, which can be serious and life-threatening. Examples include sudden cardiac death from additive QTc prolongation effects and NMS. Early detection of NMS and discontinuing the offending agent(s) can help prevent patient morbidity and mortality |
| Stay up-to-date on literature and drug warnings to employ best practices and avoid potentially serious adverse and/or lethal outcomes |
| Encourage patients to disclose any prescription drugs, over-the-counter medications, and herbal therapies they are taking |
| Develop strategies to prevent ADEs, such as personal formularies, suicide assessments, prescribing limited quantities, ‘eyes on’ medication administration, therapeutic drug monitoring, utilizing databases and resources for drug information, and patient education |
| ADEs: adverse drug events; DDIs: drug-drug interactions; NMS: neuroleptic malignant syndrome |
Prescription drug overdose
Each year, unintentional drug overdoses account for >20,000 deaths in the United States.3 Prescription medications, particularly opioid analgesics, have contributed to the doubling of overdose mortality rates in recent years. A recent study reported that nearly 50% of unintentional drug overdose deaths were associated with psychotropics and one-third of these deaths were associated with benzodiazepines, many of which were not prescribed to the individual.4
The risk of mortality from intentional drug overdose also must be assessed. Tricyclic antidepressants (TCAs) are a particularly lethal class of medications in suicide attempts and may result in arrhythmias, coma, seizures, respiratory failure, and death.5 Venlafaxine and mirtazapine are associated with greater risk of death and toxicity in overdose, respectively, than selective serotonin reuptake inhibitors (SSRIs).6 Lithium toxicity in overdose may lead to bradycardia, seizure, coma, hyperventilation, serotonin syndrome, respiratory failure, or death.5 The risk of death with lithium or benzodiazepine monotherapy is low when these agents are taken as prescribed. However, prescribers must exercise caution when these agents are used in combination. Interactions involving drugs with a narrow therapeutic index—such as lithium and TCAs—are more likely to be clinically significant because small increases in drug concentration can lead to serious adverse effects or death. See Related Resources for a review article on appropriate use and monitoring of lithium.
Drug-drug interactions
Many Americans take multiple prescription and nonprescription drugs, and psychiatric patients are more likely than other individuals to have more complex medication regimens.7 This can result in polypharmacy and drug-drug interactions (DDIs), which can lead to undesired medication effects and serious, potentially fatal ADEs.
Pharmacokinetic interactions typically affect drug concentrations and occur when 1 drug interferes with the absorption, distribution, metabolism, or excretion of another drug. Many common pharmacokinetic interactions involve the liver cytochrome P450 (CYP) system, which is responsible for metabolizing many medications.8 DDIs can occur when CYP enzymes are modified by inhibitors or inducers, which can decrease or increase drug clearance, respectively. Table 2 5,7,9 provides examples of common CYP450 substrates, inhibitors, and inducers. Polymorphisms in the pharmacogenetics of CYP450 also can affect overall drug clearance and the impact of DDIs.8
Pharmacodynamic interactions are caused by additive or competing effects of multiple drugs. The most serious of these involve medications that increase a patient’s risk of serotonin syndrome or neuroleptic malignant syndrome (NMS); both are medical emergencies that require immediate hospitalization.
Although any medication with serotonergic activity can induce serotonin syndrome, combinations of serotonergic drugs in particular are associated with increased risk.10 Serotonin syndrome is characterized by hyperthermia, altered muscle tone, altered mental status, and autonomic instability; rhabdomyolysis and disseminated intravascular coagulation are potential lethal complications.10 A high index of suspicion can help clinicians rapidly detect serotonin syndrome, discontinue offending agents, and initiate supportive treatments.
NMS is a life-threatening complication of antipsychotics characterized by fever, delirium, muscle rigidity, autonomic instability, and abnormal laboratory findings that include elevated white blood count and increased creatinine kinase from muscle injury. In early stages, NMS may be mistaken for extrapyramidal symptoms. Although NMS can occur with any antipsychotic as monotherapy, additive antidopaminergic effects increase the risk. Patients with a compromised CNS as a result of mental retardation, traumatic brain injury, or metabolic abnormalities also are at increased risk of developing NMS.11
Other pharmacodynamic interactions involve medications that may have additive effects on prolonging QTc intervals. For example, TCAs are pro-arrhythmic and have quinidine-like effects, which can cause cardiac conduction abnormalities and prolonged PR and QTc intervals.12 Employ routine ECG monitoring when prescribing multiple medications known to cause QTc prolongation, such as TCAs (Table 3).13,14 The Arizona Center for Education and Research on Therapeutics (www.azcert.org) provides a searchable list of QT-prolonging drugs (see Related Resources).
Medications also can interact with food, disease states, and herbal supplements. Alcohol interacts with many CNS-active medications, including many psychotropics. Patients taking benzodiazepines may experience oversedation and respiratory depression from alcohol’s additive sedating effects.5 Advise patients to limit their alcohol intake while taking CNS-depressing psychotropics such as benzodiazepines, antipsychotics, and some antidepressants. Monoamine oxidase inhibitors (MAOIs) and tyramine-containing food—such as cheese, beer, preserved meat, and soy sauce—can lead to a dangerous hypertensive crisis that requires immediate medical intervention to prevent life-threatening complications.5 Hypertensive crisis may be more significant in patients who have pre-existing hypertension. Finally, herbal supplements also can interact with medications. Patients who take St. John’s wort for depressive symptoms might not realize that it can reduce the efficacy of other drugs or increase their risk of serotonin syndrome.9
Table 2
Cytochrome P450 substrates, inhibitors, and inducers
| 3A4 | 2D6 | 2C9 | 2C19 | 1A2 | |
|---|---|---|---|---|---|
| Substrates | Carbamazepine Citalopram Fluoxetine Haloperidol Mirtazapine Oxcarbazepine Quetiapine Sertraline Ziprasidone | Aripiprazole Citalopram Duloxetine Fluoxetine Haloperidol Mirtazapine Paroxetine Risperidone Sertraline Venlafaxine TCAs | Amitriptyline Carbamazepine Sertraline Valproic acid | Citalopram Clomipramine Sertraline Valproic acid | Carbamazepine Clozapine Olanzapine |
| Inhibitors | Amiodarone Aprepitant Azole antifungals Carbamazepine Cimetidine Diltiazem Erythromycin Fluoxetine (norfloxetine) Grapefruit juice Imatinib Paroxetine Ritonavir Sertraline Verapamil | Amiodarone Bupropion Cimetidine Duloxetine Fluoxetine Methadone Paroxetine Ritonavir Sertraline | Amiodarone Fluconazole Isoniazid Sertraline Trimethoprim-sulfamethoxazole Valproic acid | Cimetidine Fluoxetine Ketoconazole Omeprazole Sertraline Valproic acid | Amiodarone Cimetidine Fluoroquinolones |
| Inducers | Carbamazepine Phenobarbital Phenytoin Rifampin St. John’s wort | Rifampin | Phenobarbital Rifampin | Carbamazepine Rifampin | Nafcillin Phenobarbital Rifampin Smoking |
| TCAs: tricyclic antidepressants Source: References 5,7,9 | |||||
Table 3
Psychotropics associated with QT prolongation
| Class | Agents |
|---|---|
| Antidepressants | Mirtazapine, SNRIs (desvenlafaxine, venlafaxine), SSRIs (citalopram, fluoxetine, paroxetine, sertraline), TCAs (amitriptyline, clomipramine, desipramine, doxepin, imipramine, protriptyline, trimipramine), trazodone |
| Typical antipsychotics | Chlorpromazine, fluphenazine, haloperidol, perphenazine, thioridazine, trifluoperazine |
| Atypical antipsychotics | Aripiprazole, asenapine, clozapine, iloperidone, paliperidone, quetiapine, risperidone, ziprasidone |
| Mood stabilizers | Lithium |
| Miscellaneous agents | Amantadine, atomoxetine, chloral hydrate, diphenhydramine, galantamine |
| Stimulants | Amphetamine/dextroamphetamine products, methylphenidate/dexmethylphenidate |
| SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants Source: Adapted from references 13,14 | |
“Black-box” warnings issued by the FDA are included in the package insert to highlight a medication’s risks of dangerous and potentially lethal adverse effects. Table 4 highlights current black-box warnings for various psychotropics.5,14-16
Antidepressants and suicide. All medications with antidepressant indications carry a black-box warning for risk of suicidal ideation and behavior in children, adolescents, and young adults during the early months of medication therapy. This includes not only SSRIs and serotonin-norepinephrine reuptake inhibitors, but also anticonvulsants and atypical antipsychotics indicated for treating mood disorders. Monitor young patients carefully and advise family members to alert clinicians of any signs of suicidality or unusual behavior.
Lamotrigine and aseptic meningitis. Aseptic meningitis—inflammation of the meninges that is not caused by bacteria—is a rare but serious adverse effect of lamotrigine. Symptoms include headache, fever, stiff neck, nausea and vomiting, delirium, rash, and sensitivity to light.5 Forty cases of aseptic meningitis in children and adults were reported over 15 years, representing <.01% of all lamotrigine prescriptions.5 Most of these patients required hospitalization, but symptoms resolved after lamotrigine was discontinued. Prompt identification and management of aseptic meningitis are necessary to prevent permanent brain damage and death. Other complications of aseptic meningitis include long-term neurologic sequelae such as cognitive impairment, seizure disorders, and behavioral disturbances.
Table 4
Which psychotropics carry ‘black-box’ warnings?
| Warning | Class or medication affected | Comments |
|---|---|---|
| Suicidality | Antidepressants Antipsychotics indicated for mood disorders Anticonvulsants | See ‘Black-box warnings’ |
| Serious, life-threatening rashes such as Stevens-Johnson syndrome or toxic epidermal necrolysis | Lamotrigine Carbamazepine | Lamotrigine’s risk of severe dermatologic reactions necessitates slow titration during drug initiation Carbamazepine warning includes a recommendation for genetic screening in Asian patients because Stevens-Johnson syndrome is associated with the HLA-B*1502 allele found primarily in the Asian population |
| Increased mortality in elderly patients with dementia-related psychosis | Antipsychotics | A study of >10,000 geriatric patients with dementia showed mortality rates of 22.6% to 29.1% among those who took antipsychotics compared with 14.6% for patients taking other psychiatric medications. When antipsychotics are used in older adults, well-documented informed consent from the patient or substitute decision-maker is required |
| Other effects | Clozapine | Agranulocytosis occurs in 1% to 2% of clozapine patients, necessitating WBC/ANC monitoring Clozapine-induced myocarditis, generally accompanied by peripheral eosinophilia, usually occurs within the first 2 months of treatment, and can result in significant mortality from resultant cardiomyopathy. Early warning signs of fever, fatigue, and tachycardia are easily mistaken for the more benign effects of clozapine titration Seizures are more likely with higher doses. Cautious use is advised with patients who have an underlying seizure disorder Other cardiovascular and respiratory effects: Hypotension has been associated with rapid initial titration. Cardiac and respiratory arrest and circulatory collapse have occurred rarely. Respiratory complications are more likely when clozapine is used in combination with benzodiazepines |
| ANC: absolute neutrophil count; WBC: white blood cell Source: References 5,14-16 | ||
Other complications
Hematologic effects. All classes of psychotropics carry a risk (1 to 2 cases per year per 100,00 patients) of serious hematologic complications, including neutropenia, agranulocytosis, eosinophilia, thrombocytopenia, purpura, and anemia.17 Agranulocytosis has been associated most commonly with clozapine, carbamazepine, and typical antipsychotics.17 SSRIs, which are widely prescribed, are associated with increased risk of bruising and bleeding. Patients with bleeding or platelet disorders are at an increased risk for these complications.17
Seizures. Several classes of psychotropics are associated with an increased risk of seizures. Among antipsychotics, clozapine and chlorpromazine are the most seizurogenic.18 Among antidepressants, bupropion and clomipramine are most likely to lower seizure thresholds.18 Psychotropics’ seizure-inducing effects are dose-related. Vulnerability to seizures while taking psychotropics is related to having a history of epilepsy or brain injury.18 Seizures also can occur when benzodiazepines or anticonvulsants are withdrawn too quickly.
Heat stroke. Although a rare occurrence, psychotropics with anticholinergic side effects can contribute to heat stroke. Older patients are particularly vulnerable to the risk of body temperature dysregulation.19
Ketoacidosis and hyperosmolar coma. Medication-related deaths have occurred as a result of ketoacidosis and hyperosmolar coma associated with atypical antipsychotics. These hyperglycemia-related fatalities are most likely with clozapine and olanzapine.20
Hip fractures and falls. Geriatric patients are vulnerable to falls and resultant hip fractures related to use of TCAs, SSRIs, benzodiazepines, and antipsychotics. This is not a trivial matter; hip fractures increase the mortality rate by 12% to 20% in the year after the injury.21 The risk of falls is related to sedation, orthostatic hypotension, arrhythmias, and confusion associated with psychotropics.21,22
Akathisia and suicide. Unrecognized or undertreated akathisia is most commonly associated with antipsychotics, but also can occur with SSRIs. Although akathisia is commonly thought of as a motor syndrome of restlessness, patients may find the less-recognized psychic symptoms of increased inner turmoil and hallucinations just as distressing. This complex of symptoms is associated with an increased risk of suicide.23 If discontinuing the offending agent is not feasible, akathisia can be treated with beta blockers, benzodiazepines, or anticholinergics.24
Hepatotoxicity. Hepatotoxicity from psychotropics occurs in only a small percentage of patients, and can range from transient elevations in liver enzymes to fulminant liver failure. Adverse hepatic effects may be a manifestation of a hypersensitivity reaction accompanied by rash and eosinophilia.25 MAOIs and TCAs can cause cholestatic liver injury, whereas nefazodone has been associated with fulminant liver failure. Other psychotropics—including SSRIs, antipsychotics, benzodiazepines, and older antiepileptics—can cause negative hepatic effects but rarely are associated with acute liver failure.25,26 Although few medications can cause complete liver failure on their own, hepatotoxicity from medications may precipitate severe, potentially fatal outcomes in patients with underlying liver diseases such as hepatitis and cirrhosis. Additive hepatotoxicity from multiple medications also can be problematic. Although psychotropic-induced hepatotoxicity is rare, assess psychotropic doses in patients with liver dysfunction, because drug clearance may be altered, which increases the risk for other serious adverse events.25
Suicide assessment is key
Ongoing monitoring for current or developing suicidal ideation is an important strategy to prevent medication-related mortality in patients vulnerable to self-harm. Initial assessments and follow-up appointments should include a detailed inquiry about suicidal ideations, plans, and behaviors. Patients taking medications that carry black-box warnings for suicide risk should be seen frequently during the first few months of treatment. Patients receiving medications that are lethal in overdose (eg, lithium and TCAs) should be carefully screened for suicide risk. Prescribe medications in limited quantities or arrange for a family member to monitor the patient if necessary. Patients with a history of suicide attempts and current suicide plans may require close observation and initiating medications while hospitalized.
Other prevention strategies
Prescribing psychotropics in a manner that promotes mental well being while minimizing negative outcomes can be challenging. By developing a personal formulary of drugs commonly encountered and prescribed in their practice, psychiatrists can increase their awareness of serious safety concerns, potential DDIs, and appropriate use based on available literature.7,27
Medication histories and drug reconciliation—comparing a patient’s medication orders to all of the medications the patient has been taking—can help clinicians avoid making inappropriate dose adjustments, duplicating therapy, or prescribing medications patients previously have failed or did not tolerate. Establishing a collaborative practice environment with physicians, pharmacists, nurses, and social workers can minimize medication errors and risk of adverse outcomes by increasing communication regarding the patient’s treatment.7
Computerized drug databases and other electronic resources and consultation with pharmacists can help prescribers identify, avoid, and manage clinically significant DDIs.27 Medications could interact with other drugs as long as their effects persist in the body, which could be days to months after the drug is discontinued. Future research may lead to tools to identify patient pharmacogenetic profiles.
Recognizing psychotropic DDIs and adverse effects remains a challenge because of the complexity of the affected organ, the brain. Clinicians should be vigilant to changes in a patient’s presentation because they may be a manifestation of a medication side effect.7 Appropriate therapeutic drug monitoring should occur on a routine, scheduled basis. Closer monitoring may be necessary with dose changes, potential DDIs, signs and symptoms of toxicity/efficacy failure, and renal or hepatic function changes.
Lastly, patients’ education and involvement in their health care may increase their awareness, responsibility, and medication adherence. For challenging patients, family involvement and “eyes on” medication administration can increase adherence and prevent psychotropic misuse.
- Arizona Center for Education and Research on Therapeutics. Drugs that prolong the QT interval and/or induce Torsades de Pointes ventricular arrhythmia. www.azcert.org/medical-pros/drug-lists/drug-lists.cfm.
- Cates ME, Sims PJ. Therapeutic drug management of lithium. Am J Pharm Educ. 2005;69(5):88.
- Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
- Bishop JR, Bishop DL. How to prevent serotonin syndrome from drug-drug interactions. Current Psychiatry. 2011;10(3):81-83.
Drug Brand Names
- Amantadine • Symmetrel
- Amiodarone • Cordarone, Pacerone
- Amitriptyline • Elavil
- Amphetamine/dextroamphetamine • Adderall, others
- Aprepitant • Emend
- Aripiprazole • Abilify
- Asenapine • Saphris
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, Zyban
- Carbamazepine • Tegretol, others
- Chloral hydrate • Somnote
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clozapine • Clozaril
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Diltiazem • Cardia, others
- Diphenhydramine • Benadryl, others
- Doxepin • Sinequan, Silenor
- Duloxetine • Cymbalta
- Erythromycin • Ery-Tab, others
- Fluconazole • Diflucan
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Galantamine • Razadyne
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Imatinib • Gleevec
- Imipramine • Tofranil
- Isoniazid • Nydrazid, others
- Ketoconazole • Nizoral, others
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Methadone • Dolophine, Methadose
- Methylphenidate/ dexmethylphenidate • Ritalin, others
- Mirtazapine • Remeron
- Nafcillin • Nafcil, others
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Oxcarbazepine • Trileptal
- Paliperidone • Invega
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenobarbital • Luminal, others
- Phenytoin • Dilantin
- Protriptyline • Vivactil
- Quetiapine • Seroquel
- Rifampin • Rifadin, others
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimethoprim/Sulfamethoxazole • Bactrim, Septra
- Trimipramine • Surmontil
- Valproic acid • Depakote, others
- Venlafaxine • Effexor
- Verapamil • Calan, others
- Ziprasidone • Geodon
Disclosure
Drs. Yu and Bostwick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Casher is a speaker for AstraZeneca, Pfizer Inc, and Sunovion Pharmaceuticals.
Medication errors due to system-, provider-, or patient-related factors contribute significantly to increased costs, adverse drug events (ADEs), and morbidity and mortality.1 One study found >60% of ADEs that led to hospitalization could have been prevented by strategies such as adequate monitoring or appropriate prescribing.2 Psychiatrists have an opportunity to reduce rates of ADEs; however, the possibility of disease symptoms overlapping with these adverse events is 1 of many obstacles prescribing clinicians face.1 Prescribers also must contend with adverse effects of polypharmacy, which are common among psychiatric patients. Patient-related factors of concern include:
- seeing multiple prescribers
- medication nonadherence
- failure to communicate use of herbal or over-the-counter products
- lack of insight
- comorbid medical and psychiatric diagnoses, such as dementia.1
This article highlights potential ADEs and major medication safety concerns that may contribute to morbidity and mortality among patients taking psychotropics. Although many factors are beyond the prescribing clinician’s control—such as medication dispensing and administration errors—psychiatrists can substantially reduce ADEs. We will cover potential adverse events associated with key medications or medication classes, drug interactions with potentially devastating consequences, and strategies to minimize risks of ADEs, including enhanced awareness and monitoring (Table 1).
Table 1
How to avoid ADEs with psychotropics
| Establish a collaborative practice among physicians, pharmacists, nurses, and social workers to enhance patient care and reduce the risk of medication errors and negative outcomes |
| Educate patients to increase their understanding of psychiatric diseases and medications and increase compliance with therapy. This may lead the patient to self-monitor drug efficacy and adverse effects |
| Be aware of psychotropic medications’ ‘black-box’ warnings that guide their safe use |
| Pay particular attention to drugs with a narrow therapeutic index, such as lithium and tricyclic antidepressants, which have small safety margins and are lethal in overdose |
| Avoid using 1 drug to treat the side effects of another. Minimizing polypharmacy can reduce medication errors, DDIs, and ADEs |
| Remain vigilant for DDIs, which can be serious and life-threatening. Examples include sudden cardiac death from additive QTc prolongation effects and NMS. Early detection of NMS and discontinuing the offending agent(s) can help prevent patient morbidity and mortality |
| Stay up-to-date on literature and drug warnings to employ best practices and avoid potentially serious adverse and/or lethal outcomes |
| Encourage patients to disclose any prescription drugs, over-the-counter medications, and herbal therapies they are taking |
| Develop strategies to prevent ADEs, such as personal formularies, suicide assessments, prescribing limited quantities, ‘eyes on’ medication administration, therapeutic drug monitoring, utilizing databases and resources for drug information, and patient education |
| ADEs: adverse drug events; DDIs: drug-drug interactions; NMS: neuroleptic malignant syndrome |
Prescription drug overdose
Each year, unintentional drug overdoses account for >20,000 deaths in the United States.3 Prescription medications, particularly opioid analgesics, have contributed to the doubling of overdose mortality rates in recent years. A recent study reported that nearly 50% of unintentional drug overdose deaths were associated with psychotropics and one-third of these deaths were associated with benzodiazepines, many of which were not prescribed to the individual.4
The risk of mortality from intentional drug overdose also must be assessed. Tricyclic antidepressants (TCAs) are a particularly lethal class of medications in suicide attempts and may result in arrhythmias, coma, seizures, respiratory failure, and death.5 Venlafaxine and mirtazapine are associated with greater risk of death and toxicity in overdose, respectively, than selective serotonin reuptake inhibitors (SSRIs).6 Lithium toxicity in overdose may lead to bradycardia, seizure, coma, hyperventilation, serotonin syndrome, respiratory failure, or death.5 The risk of death with lithium or benzodiazepine monotherapy is low when these agents are taken as prescribed. However, prescribers must exercise caution when these agents are used in combination. Interactions involving drugs with a narrow therapeutic index—such as lithium and TCAs—are more likely to be clinically significant because small increases in drug concentration can lead to serious adverse effects or death. See Related Resources for a review article on appropriate use and monitoring of lithium.
Drug-drug interactions
Many Americans take multiple prescription and nonprescription drugs, and psychiatric patients are more likely than other individuals to have more complex medication regimens.7 This can result in polypharmacy and drug-drug interactions (DDIs), which can lead to undesired medication effects and serious, potentially fatal ADEs.
Pharmacokinetic interactions typically affect drug concentrations and occur when 1 drug interferes with the absorption, distribution, metabolism, or excretion of another drug. Many common pharmacokinetic interactions involve the liver cytochrome P450 (CYP) system, which is responsible for metabolizing many medications.8 DDIs can occur when CYP enzymes are modified by inhibitors or inducers, which can decrease or increase drug clearance, respectively. Table 2 5,7,9 provides examples of common CYP450 substrates, inhibitors, and inducers. Polymorphisms in the pharmacogenetics of CYP450 also can affect overall drug clearance and the impact of DDIs.8
Pharmacodynamic interactions are caused by additive or competing effects of multiple drugs. The most serious of these involve medications that increase a patient’s risk of serotonin syndrome or neuroleptic malignant syndrome (NMS); both are medical emergencies that require immediate hospitalization.
Although any medication with serotonergic activity can induce serotonin syndrome, combinations of serotonergic drugs in particular are associated with increased risk.10 Serotonin syndrome is characterized by hyperthermia, altered muscle tone, altered mental status, and autonomic instability; rhabdomyolysis and disseminated intravascular coagulation are potential lethal complications.10 A high index of suspicion can help clinicians rapidly detect serotonin syndrome, discontinue offending agents, and initiate supportive treatments.
NMS is a life-threatening complication of antipsychotics characterized by fever, delirium, muscle rigidity, autonomic instability, and abnormal laboratory findings that include elevated white blood count and increased creatinine kinase from muscle injury. In early stages, NMS may be mistaken for extrapyramidal symptoms. Although NMS can occur with any antipsychotic as monotherapy, additive antidopaminergic effects increase the risk. Patients with a compromised CNS as a result of mental retardation, traumatic brain injury, or metabolic abnormalities also are at increased risk of developing NMS.11
Other pharmacodynamic interactions involve medications that may have additive effects on prolonging QTc intervals. For example, TCAs are pro-arrhythmic and have quinidine-like effects, which can cause cardiac conduction abnormalities and prolonged PR and QTc intervals.12 Employ routine ECG monitoring when prescribing multiple medications known to cause QTc prolongation, such as TCAs (Table 3).13,14 The Arizona Center for Education and Research on Therapeutics (www.azcert.org) provides a searchable list of QT-prolonging drugs (see Related Resources).
Medications also can interact with food, disease states, and herbal supplements. Alcohol interacts with many CNS-active medications, including many psychotropics. Patients taking benzodiazepines may experience oversedation and respiratory depression from alcohol’s additive sedating effects.5 Advise patients to limit their alcohol intake while taking CNS-depressing psychotropics such as benzodiazepines, antipsychotics, and some antidepressants. Monoamine oxidase inhibitors (MAOIs) and tyramine-containing food—such as cheese, beer, preserved meat, and soy sauce—can lead to a dangerous hypertensive crisis that requires immediate medical intervention to prevent life-threatening complications.5 Hypertensive crisis may be more significant in patients who have pre-existing hypertension. Finally, herbal supplements also can interact with medications. Patients who take St. John’s wort for depressive symptoms might not realize that it can reduce the efficacy of other drugs or increase their risk of serotonin syndrome.9
Table 2
Cytochrome P450 substrates, inhibitors, and inducers
| 3A4 | 2D6 | 2C9 | 2C19 | 1A2 | |
|---|---|---|---|---|---|
| Substrates | Carbamazepine Citalopram Fluoxetine Haloperidol Mirtazapine Oxcarbazepine Quetiapine Sertraline Ziprasidone | Aripiprazole Citalopram Duloxetine Fluoxetine Haloperidol Mirtazapine Paroxetine Risperidone Sertraline Venlafaxine TCAs | Amitriptyline Carbamazepine Sertraline Valproic acid | Citalopram Clomipramine Sertraline Valproic acid | Carbamazepine Clozapine Olanzapine |
| Inhibitors | Amiodarone Aprepitant Azole antifungals Carbamazepine Cimetidine Diltiazem Erythromycin Fluoxetine (norfloxetine) Grapefruit juice Imatinib Paroxetine Ritonavir Sertraline Verapamil | Amiodarone Bupropion Cimetidine Duloxetine Fluoxetine Methadone Paroxetine Ritonavir Sertraline | Amiodarone Fluconazole Isoniazid Sertraline Trimethoprim-sulfamethoxazole Valproic acid | Cimetidine Fluoxetine Ketoconazole Omeprazole Sertraline Valproic acid | Amiodarone Cimetidine Fluoroquinolones |
| Inducers | Carbamazepine Phenobarbital Phenytoin Rifampin St. John’s wort | Rifampin | Phenobarbital Rifampin | Carbamazepine Rifampin | Nafcillin Phenobarbital Rifampin Smoking |
| TCAs: tricyclic antidepressants Source: References 5,7,9 | |||||
Table 3
Psychotropics associated with QT prolongation
| Class | Agents |
|---|---|
| Antidepressants | Mirtazapine, SNRIs (desvenlafaxine, venlafaxine), SSRIs (citalopram, fluoxetine, paroxetine, sertraline), TCAs (amitriptyline, clomipramine, desipramine, doxepin, imipramine, protriptyline, trimipramine), trazodone |
| Typical antipsychotics | Chlorpromazine, fluphenazine, haloperidol, perphenazine, thioridazine, trifluoperazine |
| Atypical antipsychotics | Aripiprazole, asenapine, clozapine, iloperidone, paliperidone, quetiapine, risperidone, ziprasidone |
| Mood stabilizers | Lithium |
| Miscellaneous agents | Amantadine, atomoxetine, chloral hydrate, diphenhydramine, galantamine |
| Stimulants | Amphetamine/dextroamphetamine products, methylphenidate/dexmethylphenidate |
| SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants Source: Adapted from references 13,14 | |
“Black-box” warnings issued by the FDA are included in the package insert to highlight a medication’s risks of dangerous and potentially lethal adverse effects. Table 4 highlights current black-box warnings for various psychotropics.5,14-16
Antidepressants and suicide. All medications with antidepressant indications carry a black-box warning for risk of suicidal ideation and behavior in children, adolescents, and young adults during the early months of medication therapy. This includes not only SSRIs and serotonin-norepinephrine reuptake inhibitors, but also anticonvulsants and atypical antipsychotics indicated for treating mood disorders. Monitor young patients carefully and advise family members to alert clinicians of any signs of suicidality or unusual behavior.
Lamotrigine and aseptic meningitis. Aseptic meningitis—inflammation of the meninges that is not caused by bacteria—is a rare but serious adverse effect of lamotrigine. Symptoms include headache, fever, stiff neck, nausea and vomiting, delirium, rash, and sensitivity to light.5 Forty cases of aseptic meningitis in children and adults were reported over 15 years, representing <.01% of all lamotrigine prescriptions.5 Most of these patients required hospitalization, but symptoms resolved after lamotrigine was discontinued. Prompt identification and management of aseptic meningitis are necessary to prevent permanent brain damage and death. Other complications of aseptic meningitis include long-term neurologic sequelae such as cognitive impairment, seizure disorders, and behavioral disturbances.
Table 4
Which psychotropics carry ‘black-box’ warnings?
| Warning | Class or medication affected | Comments |
|---|---|---|
| Suicidality | Antidepressants Antipsychotics indicated for mood disorders Anticonvulsants | See ‘Black-box warnings’ |
| Serious, life-threatening rashes such as Stevens-Johnson syndrome or toxic epidermal necrolysis | Lamotrigine Carbamazepine | Lamotrigine’s risk of severe dermatologic reactions necessitates slow titration during drug initiation Carbamazepine warning includes a recommendation for genetic screening in Asian patients because Stevens-Johnson syndrome is associated with the HLA-B*1502 allele found primarily in the Asian population |
| Increased mortality in elderly patients with dementia-related psychosis | Antipsychotics | A study of >10,000 geriatric patients with dementia showed mortality rates of 22.6% to 29.1% among those who took antipsychotics compared with 14.6% for patients taking other psychiatric medications. When antipsychotics are used in older adults, well-documented informed consent from the patient or substitute decision-maker is required |
| Other effects | Clozapine | Agranulocytosis occurs in 1% to 2% of clozapine patients, necessitating WBC/ANC monitoring Clozapine-induced myocarditis, generally accompanied by peripheral eosinophilia, usually occurs within the first 2 months of treatment, and can result in significant mortality from resultant cardiomyopathy. Early warning signs of fever, fatigue, and tachycardia are easily mistaken for the more benign effects of clozapine titration Seizures are more likely with higher doses. Cautious use is advised with patients who have an underlying seizure disorder Other cardiovascular and respiratory effects: Hypotension has been associated with rapid initial titration. Cardiac and respiratory arrest and circulatory collapse have occurred rarely. Respiratory complications are more likely when clozapine is used in combination with benzodiazepines |
| ANC: absolute neutrophil count; WBC: white blood cell Source: References 5,14-16 | ||
Other complications
Hematologic effects. All classes of psychotropics carry a risk (1 to 2 cases per year per 100,00 patients) of serious hematologic complications, including neutropenia, agranulocytosis, eosinophilia, thrombocytopenia, purpura, and anemia.17 Agranulocytosis has been associated most commonly with clozapine, carbamazepine, and typical antipsychotics.17 SSRIs, which are widely prescribed, are associated with increased risk of bruising and bleeding. Patients with bleeding or platelet disorders are at an increased risk for these complications.17
Seizures. Several classes of psychotropics are associated with an increased risk of seizures. Among antipsychotics, clozapine and chlorpromazine are the most seizurogenic.18 Among antidepressants, bupropion and clomipramine are most likely to lower seizure thresholds.18 Psychotropics’ seizure-inducing effects are dose-related. Vulnerability to seizures while taking psychotropics is related to having a history of epilepsy or brain injury.18 Seizures also can occur when benzodiazepines or anticonvulsants are withdrawn too quickly.
Heat stroke. Although a rare occurrence, psychotropics with anticholinergic side effects can contribute to heat stroke. Older patients are particularly vulnerable to the risk of body temperature dysregulation.19
Ketoacidosis and hyperosmolar coma. Medication-related deaths have occurred as a result of ketoacidosis and hyperosmolar coma associated with atypical antipsychotics. These hyperglycemia-related fatalities are most likely with clozapine and olanzapine.20
Hip fractures and falls. Geriatric patients are vulnerable to falls and resultant hip fractures related to use of TCAs, SSRIs, benzodiazepines, and antipsychotics. This is not a trivial matter; hip fractures increase the mortality rate by 12% to 20% in the year after the injury.21 The risk of falls is related to sedation, orthostatic hypotension, arrhythmias, and confusion associated with psychotropics.21,22
Akathisia and suicide. Unrecognized or undertreated akathisia is most commonly associated with antipsychotics, but also can occur with SSRIs. Although akathisia is commonly thought of as a motor syndrome of restlessness, patients may find the less-recognized psychic symptoms of increased inner turmoil and hallucinations just as distressing. This complex of symptoms is associated with an increased risk of suicide.23 If discontinuing the offending agent is not feasible, akathisia can be treated with beta blockers, benzodiazepines, or anticholinergics.24
Hepatotoxicity. Hepatotoxicity from psychotropics occurs in only a small percentage of patients, and can range from transient elevations in liver enzymes to fulminant liver failure. Adverse hepatic effects may be a manifestation of a hypersensitivity reaction accompanied by rash and eosinophilia.25 MAOIs and TCAs can cause cholestatic liver injury, whereas nefazodone has been associated with fulminant liver failure. Other psychotropics—including SSRIs, antipsychotics, benzodiazepines, and older antiepileptics—can cause negative hepatic effects but rarely are associated with acute liver failure.25,26 Although few medications can cause complete liver failure on their own, hepatotoxicity from medications may precipitate severe, potentially fatal outcomes in patients with underlying liver diseases such as hepatitis and cirrhosis. Additive hepatotoxicity from multiple medications also can be problematic. Although psychotropic-induced hepatotoxicity is rare, assess psychotropic doses in patients with liver dysfunction, because drug clearance may be altered, which increases the risk for other serious adverse events.25
Suicide assessment is key
Ongoing monitoring for current or developing suicidal ideation is an important strategy to prevent medication-related mortality in patients vulnerable to self-harm. Initial assessments and follow-up appointments should include a detailed inquiry about suicidal ideations, plans, and behaviors. Patients taking medications that carry black-box warnings for suicide risk should be seen frequently during the first few months of treatment. Patients receiving medications that are lethal in overdose (eg, lithium and TCAs) should be carefully screened for suicide risk. Prescribe medications in limited quantities or arrange for a family member to monitor the patient if necessary. Patients with a history of suicide attempts and current suicide plans may require close observation and initiating medications while hospitalized.
Other prevention strategies
Prescribing psychotropics in a manner that promotes mental well being while minimizing negative outcomes can be challenging. By developing a personal formulary of drugs commonly encountered and prescribed in their practice, psychiatrists can increase their awareness of serious safety concerns, potential DDIs, and appropriate use based on available literature.7,27
Medication histories and drug reconciliation—comparing a patient’s medication orders to all of the medications the patient has been taking—can help clinicians avoid making inappropriate dose adjustments, duplicating therapy, or prescribing medications patients previously have failed or did not tolerate. Establishing a collaborative practice environment with physicians, pharmacists, nurses, and social workers can minimize medication errors and risk of adverse outcomes by increasing communication regarding the patient’s treatment.7
Computerized drug databases and other electronic resources and consultation with pharmacists can help prescribers identify, avoid, and manage clinically significant DDIs.27 Medications could interact with other drugs as long as their effects persist in the body, which could be days to months after the drug is discontinued. Future research may lead to tools to identify patient pharmacogenetic profiles.
Recognizing psychotropic DDIs and adverse effects remains a challenge because of the complexity of the affected organ, the brain. Clinicians should be vigilant to changes in a patient’s presentation because they may be a manifestation of a medication side effect.7 Appropriate therapeutic drug monitoring should occur on a routine, scheduled basis. Closer monitoring may be necessary with dose changes, potential DDIs, signs and symptoms of toxicity/efficacy failure, and renal or hepatic function changes.
Lastly, patients’ education and involvement in their health care may increase their awareness, responsibility, and medication adherence. For challenging patients, family involvement and “eyes on” medication administration can increase adherence and prevent psychotropic misuse.
- Arizona Center for Education and Research on Therapeutics. Drugs that prolong the QT interval and/or induce Torsades de Pointes ventricular arrhythmia. www.azcert.org/medical-pros/drug-lists/drug-lists.cfm.
- Cates ME, Sims PJ. Therapeutic drug management of lithium. Am J Pharm Educ. 2005;69(5):88.
- Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
- Bishop JR, Bishop DL. How to prevent serotonin syndrome from drug-drug interactions. Current Psychiatry. 2011;10(3):81-83.
Drug Brand Names
- Amantadine • Symmetrel
- Amiodarone • Cordarone, Pacerone
- Amitriptyline • Elavil
- Amphetamine/dextroamphetamine • Adderall, others
- Aprepitant • Emend
- Aripiprazole • Abilify
- Asenapine • Saphris
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, Zyban
- Carbamazepine • Tegretol, others
- Chloral hydrate • Somnote
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clozapine • Clozaril
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Diltiazem • Cardia, others
- Diphenhydramine • Benadryl, others
- Doxepin • Sinequan, Silenor
- Duloxetine • Cymbalta
- Erythromycin • Ery-Tab, others
- Fluconazole • Diflucan
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Galantamine • Razadyne
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Imatinib • Gleevec
- Imipramine • Tofranil
- Isoniazid • Nydrazid, others
- Ketoconazole • Nizoral, others
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Methadone • Dolophine, Methadose
- Methylphenidate/ dexmethylphenidate • Ritalin, others
- Mirtazapine • Remeron
- Nafcillin • Nafcil, others
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Oxcarbazepine • Trileptal
- Paliperidone • Invega
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenobarbital • Luminal, others
- Phenytoin • Dilantin
- Protriptyline • Vivactil
- Quetiapine • Seroquel
- Rifampin • Rifadin, others
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimethoprim/Sulfamethoxazole • Bactrim, Septra
- Trimipramine • Surmontil
- Valproic acid • Depakote, others
- Venlafaxine • Effexor
- Verapamil • Calan, others
- Ziprasidone • Geodon
Disclosure
Drs. Yu and Bostwick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Casher is a speaker for AstraZeneca, Pfizer Inc, and Sunovion Pharmaceuticals.
1. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2004;24(7):595-609.
2. McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331-1336.
3. Centers for Disease Control and Prevention. Prescription drug overdose: state health agencies respond. 2008. Available at: http://www.cdc.gov/HomeandRecreationalSafety/pubs/RXReport_web-a.pdf. Accessed February 15 2011.
4. Toblin RL, Paulozzi LJ, Logan JE, et al. Mental illness and psychotropic drug use among prescription drug overdose deaths: a medical examiner chart review. J Clin Psychiatry. 2010;71(4):491-496.
5. Micromedex Healthcare Series (electronic version). 2011. Available at: http://www.micromedex.com. Accessed February 15 2011.
6. Hawton K, Bergen H, Simkin S, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354-358.
7. Preskorn SH, Flockhart D. 2010 guide to psychiatric drug interactions. Primary Psychiatry. 2009;16(12):45-74.
8. Lin JH, Lu AY. Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet. 1998;35(5):361-390.
9. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
10. Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
11. Dave M, Miceli K, Modha P. Psychiatric medicine. The psychiatrist’s guide to the treatment of common medical illnesses. Philadelphia PA: Lippincott Williams & Wilkins; 2007.
12. Mir S, Taylor D. The adverse effects of antidepressants. Curr Opin Psychiatry. 1997;10(2):88-94.
13. Drug-induced long QT interval. Pharmacist’s Letter/Prescriber’s Letter. 2010;26(4):260421.-
14. Drug-induced prolongation of the QT interval and torsades de pointes. 2011. Available at: http://online.factsandcomparisons.com. Accessed February 15 2011.
15. Kales HC, Valenstein M, Kim HM, et al. Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. Am J Psychiatry. 2007;164(10):1568-1576; quiz 1623.
16. Merrill DB, Ahmari SE, Bradford JM, et al. Myocarditis during clozapine treatment. Am J Psychiatry. 2006;163(2):204-208.
17. Oyesanmi O, Kunkel EJ, Monti DA, et al. Hematologic side effects of psychotropics. Psychosomatics. 1999;40(5):414-421.
18. Pisani F, Oteri G, Costa C, et al. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25(2):91-110.
19. Martin-Latry K, Goumy M, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalization. Eur Psychiatry. 2007;22:335-338.
20. Melkersson K, Dahl ML. Adverse metabolic effects associated with atypical antipsychotics: literature review and clinical implications. Drugs. 2004;64(7):701-723.
21. Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351(9112):1303-1307.
22. Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs. 2003;17(11):825-837.
23. Hirose S. The causes of underdiagnosing akathisia. Schizophr Bull. 2003;29(3):547-558.
24. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
25. Selim K, Kaplowitz N. Hepatotoxicity of psychotropic drugs. Hepatology. 1999;29(5):1347-1351.
26. Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002;22(2):169-183.
27. Sandson NB, Armstrong SC, Cozza KL. An overview of psychotropic drug-drug interactions. Psychosomatics. 2005;46(5):464-494.
1. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2004;24(7):595-609.
2. McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331-1336.
3. Centers for Disease Control and Prevention. Prescription drug overdose: state health agencies respond. 2008. Available at: http://www.cdc.gov/HomeandRecreationalSafety/pubs/RXReport_web-a.pdf. Accessed February 15 2011.
4. Toblin RL, Paulozzi LJ, Logan JE, et al. Mental illness and psychotropic drug use among prescription drug overdose deaths: a medical examiner chart review. J Clin Psychiatry. 2010;71(4):491-496.
5. Micromedex Healthcare Series (electronic version). 2011. Available at: http://www.micromedex.com. Accessed February 15 2011.
6. Hawton K, Bergen H, Simkin S, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354-358.
7. Preskorn SH, Flockhart D. 2010 guide to psychiatric drug interactions. Primary Psychiatry. 2009;16(12):45-74.
8. Lin JH, Lu AY. Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet. 1998;35(5):361-390.
9. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
10. Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
11. Dave M, Miceli K, Modha P. Psychiatric medicine. The psychiatrist’s guide to the treatment of common medical illnesses. Philadelphia PA: Lippincott Williams & Wilkins; 2007.
12. Mir S, Taylor D. The adverse effects of antidepressants. Curr Opin Psychiatry. 1997;10(2):88-94.
13. Drug-induced long QT interval. Pharmacist’s Letter/Prescriber’s Letter. 2010;26(4):260421.-
14. Drug-induced prolongation of the QT interval and torsades de pointes. 2011. Available at: http://online.factsandcomparisons.com. Accessed February 15 2011.
15. Kales HC, Valenstein M, Kim HM, et al. Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. Am J Psychiatry. 2007;164(10):1568-1576; quiz 1623.
16. Merrill DB, Ahmari SE, Bradford JM, et al. Myocarditis during clozapine treatment. Am J Psychiatry. 2006;163(2):204-208.
17. Oyesanmi O, Kunkel EJ, Monti DA, et al. Hematologic side effects of psychotropics. Psychosomatics. 1999;40(5):414-421.
18. Pisani F, Oteri G, Costa C, et al. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25(2):91-110.
19. Martin-Latry K, Goumy M, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalization. Eur Psychiatry. 2007;22:335-338.
20. Melkersson K, Dahl ML. Adverse metabolic effects associated with atypical antipsychotics: literature review and clinical implications. Drugs. 2004;64(7):701-723.
21. Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351(9112):1303-1307.
22. Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs. 2003;17(11):825-837.
23. Hirose S. The causes of underdiagnosing akathisia. Schizophr Bull. 2003;29(3):547-558.
24. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
25. Selim K, Kaplowitz N. Hepatotoxicity of psychotropic drugs. Hepatology. 1999;29(5):1347-1351.
26. Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002;22(2):169-183.
27. Sandson NB, Armstrong SC, Cozza KL. An overview of psychotropic drug-drug interactions. Psychosomatics. 2005;46(5):464-494.
Identifying and treating depression across the life span
Discuss this article at www.facebook.com/CurrentPsychiatry
Most clinical trials of major depressive disorder (MDD) have focused on diagnosis and treatment of adults, but many younger and older patients also suffer from this condition. The prevalence of MDD is estimated to be 2% in children and 6% in adolescents.1 Up to 25% of adults age >60 experience MDD, dysthymic disorder, or “minor” depression.2
Although diagnosis and treatment of depression is similar regardless of a patient’s age, younger and older patients may not exhibit typical depressive symptoms (Table 1).1,2 For example, older adults may be more likely to report a lack of emotions than depressed mood. Vigilance for these types of distinct clinical manifestations can improve early recognition and treatment. In addition, evidence suggests there are differences in MDD treatment for younger and older patients.
This article reviews common challenges in recognizing and treating MDD in children, adolescents, and older adults.
Table 1
Major depressive disorder: Age-related differences
| Children/adolescents | Adults | Older adults | |
|---|---|---|---|
| Prevalence | 2% in children; 6% in adolescents | 20% | 25% |
| Male-to-female ratio | 1:1 in children; 1:2 in adolescents | 1:2 | 1:2 |
| DSM-IV-TR criteria | Similar | Similar | Similar |
| Clinical features | Irritability, temper tantrums, somatic complaints, hypersomina, weight gain, auditory hallucinations, psychomotor agitation, separation anxiety, social phobia, panic disorder, drug abuse, poor self-esteem | Typical DSM-IV-TR features. Psychomotor retardation, middle and terminal insomnia | Irritability, motor agitation, restlessness, somatic complaints, diarrhea and constipation, decreased libido, cognitive impairment, delusions, anxiety, panic, worsening of medical comorbidities |
| Source: References 1,2 | |||
Varying clinical features
Children/adolescents. The clinical presentation of MDD in children and adolescents is similar to that of adults. Children usually display anxiety, irritability, temper tantrums, and somatic complaints before verbally expressing depressive feelings. Psychotic depression in children manifests more often as auditory hallucinations than delusions.1
Younger vs middle-age adults. Researchers who evaluated baseline clinical and sociodemographic information of 1,498 patients enrolled in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study found that the presentation of depressive symptoms in young adult patients (age 18 to 35) differed from those of middle-age (age 36 to 50) patients.3 Younger patients were more likely to be irritable, complain of weight gain and hypersomnia, and have a negative view of life and the future. They also were more likely to report previous suicide attempts and endorse symptoms consistent with generalized anxiety disorder, social phobia, panic disorder, and drug abuse. Middle-age patients had more depressive episodes, deceased libido, and middle insomnia, and more frequently reported gastrointestinal symptoms such as diarrhea or constipation.3
Older adults. In our experience, typical MDD mood symptoms often are absent in older patients. Frequently, we see somatic complaints, motor restlessness, or psychomotor retardation; these symptoms may be attributable to a concurrent medical illness. This in turn may worsen the physical illness, leading to social isolation and considerable medical morbidity.4
Pain plays an important role in depression, particularly in older adults. Chronic pain affects up to 65% of older adults who live in the community and up to 80% of those who are institutionalized.5 The most common causes of pain in these patients are osteoarthritis, osteoporosis, fibromyalgia, degenerative disk disease, lumbar spinal stenosis, and scoliosis. In addition, neuropathic pain, such as post-herpetic neuralgia and peripheral neuropathy, and injuries resulting from falls often cause long-lasting pain.6
The presence of pain tends to negatively affect recognizing and treating depression. Regardless of their age, when a patient presents with pain or depression, investigate and consider treating both conditions.7
Memory decline is likely to be depressed older adults’ chief complaint, and when objectively tested these patients often show cognitive impairment.8 Whether depressive symptoms in this age group are a reaction to early cognitive deficits or are an early symptom of neurodegeneration remains controversial.9 Some case-control studies have found a link between a history of depression and Alzheimer’s disease (AD).10,11 In general, older patients whose first episode of depression occurs in late life have a higher relative risk of developing some form of dementia; research suggests that 50% of late-life MDD patients will develop dementia within 5 years.12
Researchers have considered the possibility that mild cognitive impairment (MCI) and dementia are a continuum of depression. In 1 study, 29 patients with MCI and 31 with MCI and MDD were assessed annually for an average of 4.3 years.13 Thirty-six patients with MCI (60%) progressed to AD. Presence of depression at the time of MCI diagnosis did not predict conversion to AD but persistence of depression for 2 to 3 years and the presence of melancholic features were associated with higher risk for AD.
Alexopoulos et al14 proposed the “vascular hypothesis theory” that cerebrovascular disease can predispose patients, particularly older adults, to depressive symptoms (Table 2).14 Whether vascular depression is a subtype of MDD remains controversial.
Table 2
Features of vascular depression
| Onset after age 50 |
| Family history of mood disorders is less common |
| Apathy |
| Marked loss of interest in activities |
| Lack of insight |
| Executive dysfunction (problems with planning, organizing, sequencing, abstracting), impaired memory or speed of processing of information |
| History of hypertension, diabetes, or cardiovascular disease |
| May have a neurologic event such as stroke or transient ischemic attack |
| White or gray matter hyperintensities |
| Source: Reference 14 |
Course and prognosis
MDD has been characterized as a self-limited disease, with an average duration of 6 to 9 months. However, newer prospective studies suggest that a substantial number of patients recover more slowly or do not ever fully recover.15 Several factors, such as genetic/biologic vulnerability and psychosocial factors, influence the courses, prognosis, and risk of relapse/recurrence of MDD in all age groups.
Children and adolescents. The typical duration of a major depressive episode for clinically referred children and adolescents is 8 to 13 months.1,16 Approximately 90% of these patients’ major depressive episodes remit by 2 years, but up to 10% persist.1,16 Within 5 years of MDD onset, up to 70% of children and adolescents will experience a recurrence,17 a rate comparable to adults.
Anxiety disorders, panic disorders, phobias, substance abuse, conduct and oppositional disorders, and attention-deficit/hyperactivity disorder occur 2 to 6 times more frequently in children and adolescents with MDD.18,19 Children with MDD who have significant psychiatric and psychosocial comorbidity experience poorer outcomes.18
Older adults. Despite optimal treatment conditions, ≥50% of older patients fail to respond adequately to first-line antidepressant pharmacotherapy.20 Treatment-resistant MDD in older patients increases:
- nonadherence to treatment for comorbid medical disorders
- disability and cognitive impairment
- burden on caregivers
- risk for early mortality, including suicide.20
Differences in treatment
Although MDD often is recurrent, episodic, and in some patients chronic, in general earlier treatment and quicker response lead to better outcomes. A large, naturalistic German study of 795 inpatients with major depression found that early improvement (20% reduction in Hamilton Depression Rating Scale-21 score within the first 2 weeks) with antidepressant therapy may predict later response and remission.21
Regardless of a patient’s age, MDD treatment should begin with education. All patients should be involved in their treatment. Encourage patients to become familiar with their triggers and stressors, improve their coping skills, and adopt a healthy lifestyle, which includes a nutritious diet, frequent exercise, and adequate sleep. As maintenance treatment we recommend that patients participate in frequent socialization and activities (Table 3). Refer patients to self-help books, online help guides, and handouts from sources such as National Institute of Mental Health.22,23 Encourage patients to have patience and perseverance, and guide them through each step of recovery.
In addition to lifestyle modification, other treatment options for depression include pharmacotherapy, interpersonal psychotherapy, cognitive-behavioral therapy (CBT), and electroconvulsive therapy (ECT). All these modalities are effective for acute and maintenance treatment and should be considered when determining the best approach for each patient.
The effectiveness of antidepressants in general is comparable among and within classes.2 Base your initial selection on the patient’s previous response to antidepressants and the medication’s side effects profile and cost.
The benefits of exercise for all patients cannot be underestimated.24 Prescribe 20 to 30 minutes of daily exercise as part of recommended lifestyle changes. Writing “daily exercise” on a prescription pad can effectively remind patients that exercise needs to be taken as seriously as medication compliance.
Children and adolescents. For mild depression, supportive therapy seems to be as effective as CBT and medications.25 A randomized controlled trial of 439 depressed adolescents found that CBT plus fluoxetine conferred quicker benefit, but in the long run may not be any more efficacious than pharmacotherapy alone.25 Researchers also found that CBT plus fluoxetine was no more effective than pharmacotherapy alone for adolescents with moderate to severe depression.25
Older adults. Compared with younger patients, geriatric patients typically require lower antidepressant dosages to achieve a specific blood level, but the blood levels at which antidepressants are most effective appear to be similar.2 Older patients also may be more likely to relapse and less likely to achieve full response to antidepressants than younger patients.2 In older adults, amitriptyline, imipramine, and doxepin are not preferred because these agents may cause orthostatic hypotension and urinary retention.2 A depressed older adult who experiences weight loss might benefit from an antidepressant that improves appetite, such as mirtazapine.26 Some research suggests that maintenance antidepressant therapy in older patients experiencing a first-time episode of MDD should continue for up to 2 years.27
A meta-analysis of 12 studies of CBT in depressed adults age ≥60 with chronic pain found that CBT was effective at improving self-reported pain but had no significant effect on depressive symptoms, physical function, or medication use.6 ECT often is prescribed for depressed older adults because its safety and efficacy for these patients has been well documented.28 Other neuromodulation therapies include vagus nerve, repetitive transcranial magnetic stimulation, and deep brain stimulation, but none of these treatments have been extensively evaluated in older patients.
Table 3
Avoiding reoccurrence of depression—a ‘prescription’ for patients
| Take medication as prescribed until your doctor instructs you to stop |
| Eat 3 nutritious meals every day |
| Sleep 6 to 8 hours each night |
| Walk/exercise for 20 minutes every day |
| Relax and do breathing exercises as taught 3 times a day |
| Talk with a friend or family member each day |
| Develop a hobby |
| Remain active |
| See your doctor once a month |
Related Resource
- American Psychiatric Association. Treatment of patients with major depressive disorder. 3rd ed. www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx.
Drug Brand Names
- Amitriptyline • Elavil
- Doxepin • Aponal, Silenor
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Mirtazapine • Remeron
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Birmaher B, Brent D. AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503-1526.
2. American Psychiatric Association. Treatment of patients with major depressive disorder. 3rd ed. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx. Accessed April 4 2011.
3. Husain MM, Rush AJ, Sakheim HA. Age-related characteristics of major depression: a preliminary STAR*D report. Am J Geriatr Psychiatry. 2005;13(10):852-862.
4. Gonda X, Molnár E, Torzsa P, et al. Characteristics of depression in the elderly. Psychiatr Hung. 2009;24(3):166-174.
5. Gibson, SJ. Pain and aging: a comparison of the pain experience over the adult life span. In: Dostrovsky JO, Carr DB, Koltzenburg M, eds. Proceedings of the 10th World Congress on Pain. Progress in pain research and management. Seattle, WA: IASP Press; 2003:767–790.
6. Lunde LH, Nordhus IH, Pallesen H. The effectiveness of cognitive and behavioural treatment of chronic pain in the elderly: a quantitative review. J Clin Psychol Med Settings. 2009;16:254-262.
7. Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433-2445.
8. Reid LM, Machullich AM. Subjective memory complaints and cognitive impairment in older people. Dement Geriatr Cogn Disord. 2006;22(5-6):471-485.
9. Tsuno N, Homma A. What is the association between depression and Alzheimer’s disease? Expert Rev Neurother. 2009;9(11):]1667-1676.
10. Tsolaki M, Fountalakis K, Chantzi E, et al. Risk factors for clinically diagnosed Alzheimer’s disease: a case-control study of a Greek population. Int Psychogeriatr. 1997;9(3):327-341.
11. Speck CE, Kukull WA, Brenner DE, et al. History of depression as a risk factor for Alzheimer’s disease. Epidemiology. 1995;6(4):366-369.
12. Alexopoulos GS. Depression in elderly. Lancet. 2005;365:1961-1970.
13. Houde M, Bergman H, Whitehead V, et al. Predictive depression pattern in mild cognitive impairment. Int J Geriatr Psychiatry. 2008;23:1028-1033.
14. Alexopoulos GS, Meyers BS, Young RC, et al. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997;54(10):915-922.
15. Angst J, Gamma A, Rossler W, et al. Long-term depression versus episodic major depression: results from the prospective Zurich study of a community sample. J Affect Disord. 2009;115(1-2):112-121.
16. Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am. 2002;11(3):619-637 x.
17. Rao U, Ryan ND, Birmaher B, et al. Unipolar depression in adolescents: clinical outcome in adulthood. J Am Acad Child Adolesc Psychiatry. 1995;34:566-578.
18. Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psych Psychiatry. 1999;40(1):57-87.
19. Costello EJ, Pine DS, Hammen C, et al. Development and natural history of mood disorders. Biol Psychiatry. 2002;52(6):529-542.
20. Lenze EJ, Sheffrin M, Driscoll HC, et al. Incomplete response in late-life depression: getting to remission. Dialogues Clin Neurosci. 2008;10(4):419-430.
21. Henkel V, Seemuller F, Obermeier M, et al. Does early improvement triggered by antidepressant predict response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J Affect Disord. 2009;115(3):439-449.
22. National Institute of Mental Health. Depression. NIH publication No. 083561. 2008. Available at: http://www.nimh.nih.gov/health/publications/depression/complete-index.shtml. Accessed April 4 2011.
23. Helpguide.org. Depression. Available at: http://www.helpguide.org/topics/depression.htm. Accessed April 4, 2011.
24. Sidhu K, Vandana P, Balon R. Exercise prescription. A practical and effective therapy for depression. Current Psychiatry. 2009;8(6):39-51.
25. Curry J, Rohde P, Simons A, et al. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1427-1439.
26. Rajii TK, Mulsant BH, Lotrich FE, et al. Use of antidepressant in late-life depression. Drugs Aging. 2008;25(10):841-853.
27. Rush AJ, Trivedi MH, Weiniewski SR, et al. Acute and longer term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905-1917.
28. Van der Wurff FB, Stek ML, Hoogendijk WJ. The efficacy and safety of ECT in depressed older adults: a literature review. Int J Geriatr Psychiatry. 2003;18(10):894-904.
Discuss this article at www.facebook.com/CurrentPsychiatry
Most clinical trials of major depressive disorder (MDD) have focused on diagnosis and treatment of adults, but many younger and older patients also suffer from this condition. The prevalence of MDD is estimated to be 2% in children and 6% in adolescents.1 Up to 25% of adults age >60 experience MDD, dysthymic disorder, or “minor” depression.2
Although diagnosis and treatment of depression is similar regardless of a patient’s age, younger and older patients may not exhibit typical depressive symptoms (Table 1).1,2 For example, older adults may be more likely to report a lack of emotions than depressed mood. Vigilance for these types of distinct clinical manifestations can improve early recognition and treatment. In addition, evidence suggests there are differences in MDD treatment for younger and older patients.
This article reviews common challenges in recognizing and treating MDD in children, adolescents, and older adults.
Table 1
Major depressive disorder: Age-related differences
| Children/adolescents | Adults | Older adults | |
|---|---|---|---|
| Prevalence | 2% in children; 6% in adolescents | 20% | 25% |
| Male-to-female ratio | 1:1 in children; 1:2 in adolescents | 1:2 | 1:2 |
| DSM-IV-TR criteria | Similar | Similar | Similar |
| Clinical features | Irritability, temper tantrums, somatic complaints, hypersomina, weight gain, auditory hallucinations, psychomotor agitation, separation anxiety, social phobia, panic disorder, drug abuse, poor self-esteem | Typical DSM-IV-TR features. Psychomotor retardation, middle and terminal insomnia | Irritability, motor agitation, restlessness, somatic complaints, diarrhea and constipation, decreased libido, cognitive impairment, delusions, anxiety, panic, worsening of medical comorbidities |
| Source: References 1,2 | |||
Varying clinical features
Children/adolescents. The clinical presentation of MDD in children and adolescents is similar to that of adults. Children usually display anxiety, irritability, temper tantrums, and somatic complaints before verbally expressing depressive feelings. Psychotic depression in children manifests more often as auditory hallucinations than delusions.1
Younger vs middle-age adults. Researchers who evaluated baseline clinical and sociodemographic information of 1,498 patients enrolled in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study found that the presentation of depressive symptoms in young adult patients (age 18 to 35) differed from those of middle-age (age 36 to 50) patients.3 Younger patients were more likely to be irritable, complain of weight gain and hypersomnia, and have a negative view of life and the future. They also were more likely to report previous suicide attempts and endorse symptoms consistent with generalized anxiety disorder, social phobia, panic disorder, and drug abuse. Middle-age patients had more depressive episodes, deceased libido, and middle insomnia, and more frequently reported gastrointestinal symptoms such as diarrhea or constipation.3
Older adults. In our experience, typical MDD mood symptoms often are absent in older patients. Frequently, we see somatic complaints, motor restlessness, or psychomotor retardation; these symptoms may be attributable to a concurrent medical illness. This in turn may worsen the physical illness, leading to social isolation and considerable medical morbidity.4
Pain plays an important role in depression, particularly in older adults. Chronic pain affects up to 65% of older adults who live in the community and up to 80% of those who are institutionalized.5 The most common causes of pain in these patients are osteoarthritis, osteoporosis, fibromyalgia, degenerative disk disease, lumbar spinal stenosis, and scoliosis. In addition, neuropathic pain, such as post-herpetic neuralgia and peripheral neuropathy, and injuries resulting from falls often cause long-lasting pain.6
The presence of pain tends to negatively affect recognizing and treating depression. Regardless of their age, when a patient presents with pain or depression, investigate and consider treating both conditions.7
Memory decline is likely to be depressed older adults’ chief complaint, and when objectively tested these patients often show cognitive impairment.8 Whether depressive symptoms in this age group are a reaction to early cognitive deficits or are an early symptom of neurodegeneration remains controversial.9 Some case-control studies have found a link between a history of depression and Alzheimer’s disease (AD).10,11 In general, older patients whose first episode of depression occurs in late life have a higher relative risk of developing some form of dementia; research suggests that 50% of late-life MDD patients will develop dementia within 5 years.12
Researchers have considered the possibility that mild cognitive impairment (MCI) and dementia are a continuum of depression. In 1 study, 29 patients with MCI and 31 with MCI and MDD were assessed annually for an average of 4.3 years.13 Thirty-six patients with MCI (60%) progressed to AD. Presence of depression at the time of MCI diagnosis did not predict conversion to AD but persistence of depression for 2 to 3 years and the presence of melancholic features were associated with higher risk for AD.
Alexopoulos et al14 proposed the “vascular hypothesis theory” that cerebrovascular disease can predispose patients, particularly older adults, to depressive symptoms (Table 2).14 Whether vascular depression is a subtype of MDD remains controversial.
Table 2
Features of vascular depression
| Onset after age 50 |
| Family history of mood disorders is less common |
| Apathy |
| Marked loss of interest in activities |
| Lack of insight |
| Executive dysfunction (problems with planning, organizing, sequencing, abstracting), impaired memory or speed of processing of information |
| History of hypertension, diabetes, or cardiovascular disease |
| May have a neurologic event such as stroke or transient ischemic attack |
| White or gray matter hyperintensities |
| Source: Reference 14 |
Course and prognosis
MDD has been characterized as a self-limited disease, with an average duration of 6 to 9 months. However, newer prospective studies suggest that a substantial number of patients recover more slowly or do not ever fully recover.15 Several factors, such as genetic/biologic vulnerability and psychosocial factors, influence the courses, prognosis, and risk of relapse/recurrence of MDD in all age groups.
Children and adolescents. The typical duration of a major depressive episode for clinically referred children and adolescents is 8 to 13 months.1,16 Approximately 90% of these patients’ major depressive episodes remit by 2 years, but up to 10% persist.1,16 Within 5 years of MDD onset, up to 70% of children and adolescents will experience a recurrence,17 a rate comparable to adults.
Anxiety disorders, panic disorders, phobias, substance abuse, conduct and oppositional disorders, and attention-deficit/hyperactivity disorder occur 2 to 6 times more frequently in children and adolescents with MDD.18,19 Children with MDD who have significant psychiatric and psychosocial comorbidity experience poorer outcomes.18
Older adults. Despite optimal treatment conditions, ≥50% of older patients fail to respond adequately to first-line antidepressant pharmacotherapy.20 Treatment-resistant MDD in older patients increases:
- nonadherence to treatment for comorbid medical disorders
- disability and cognitive impairment
- burden on caregivers
- risk for early mortality, including suicide.20
Differences in treatment
Although MDD often is recurrent, episodic, and in some patients chronic, in general earlier treatment and quicker response lead to better outcomes. A large, naturalistic German study of 795 inpatients with major depression found that early improvement (20% reduction in Hamilton Depression Rating Scale-21 score within the first 2 weeks) with antidepressant therapy may predict later response and remission.21
Regardless of a patient’s age, MDD treatment should begin with education. All patients should be involved in their treatment. Encourage patients to become familiar with their triggers and stressors, improve their coping skills, and adopt a healthy lifestyle, which includes a nutritious diet, frequent exercise, and adequate sleep. As maintenance treatment we recommend that patients participate in frequent socialization and activities (Table 3). Refer patients to self-help books, online help guides, and handouts from sources such as National Institute of Mental Health.22,23 Encourage patients to have patience and perseverance, and guide them through each step of recovery.
In addition to lifestyle modification, other treatment options for depression include pharmacotherapy, interpersonal psychotherapy, cognitive-behavioral therapy (CBT), and electroconvulsive therapy (ECT). All these modalities are effective for acute and maintenance treatment and should be considered when determining the best approach for each patient.
The effectiveness of antidepressants in general is comparable among and within classes.2 Base your initial selection on the patient’s previous response to antidepressants and the medication’s side effects profile and cost.
The benefits of exercise for all patients cannot be underestimated.24 Prescribe 20 to 30 minutes of daily exercise as part of recommended lifestyle changes. Writing “daily exercise” on a prescription pad can effectively remind patients that exercise needs to be taken as seriously as medication compliance.
Children and adolescents. For mild depression, supportive therapy seems to be as effective as CBT and medications.25 A randomized controlled trial of 439 depressed adolescents found that CBT plus fluoxetine conferred quicker benefit, but in the long run may not be any more efficacious than pharmacotherapy alone.25 Researchers also found that CBT plus fluoxetine was no more effective than pharmacotherapy alone for adolescents with moderate to severe depression.25
Older adults. Compared with younger patients, geriatric patients typically require lower antidepressant dosages to achieve a specific blood level, but the blood levels at which antidepressants are most effective appear to be similar.2 Older patients also may be more likely to relapse and less likely to achieve full response to antidepressants than younger patients.2 In older adults, amitriptyline, imipramine, and doxepin are not preferred because these agents may cause orthostatic hypotension and urinary retention.2 A depressed older adult who experiences weight loss might benefit from an antidepressant that improves appetite, such as mirtazapine.26 Some research suggests that maintenance antidepressant therapy in older patients experiencing a first-time episode of MDD should continue for up to 2 years.27
A meta-analysis of 12 studies of CBT in depressed adults age ≥60 with chronic pain found that CBT was effective at improving self-reported pain but had no significant effect on depressive symptoms, physical function, or medication use.6 ECT often is prescribed for depressed older adults because its safety and efficacy for these patients has been well documented.28 Other neuromodulation therapies include vagus nerve, repetitive transcranial magnetic stimulation, and deep brain stimulation, but none of these treatments have been extensively evaluated in older patients.
Table 3
Avoiding reoccurrence of depression—a ‘prescription’ for patients
| Take medication as prescribed until your doctor instructs you to stop |
| Eat 3 nutritious meals every day |
| Sleep 6 to 8 hours each night |
| Walk/exercise for 20 minutes every day |
| Relax and do breathing exercises as taught 3 times a day |
| Talk with a friend or family member each day |
| Develop a hobby |
| Remain active |
| See your doctor once a month |
Related Resource
- American Psychiatric Association. Treatment of patients with major depressive disorder. 3rd ed. www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx.
Drug Brand Names
- Amitriptyline • Elavil
- Doxepin • Aponal, Silenor
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Mirtazapine • Remeron
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Most clinical trials of major depressive disorder (MDD) have focused on diagnosis and treatment of adults, but many younger and older patients also suffer from this condition. The prevalence of MDD is estimated to be 2% in children and 6% in adolescents.1 Up to 25% of adults age >60 experience MDD, dysthymic disorder, or “minor” depression.2
Although diagnosis and treatment of depression is similar regardless of a patient’s age, younger and older patients may not exhibit typical depressive symptoms (Table 1).1,2 For example, older adults may be more likely to report a lack of emotions than depressed mood. Vigilance for these types of distinct clinical manifestations can improve early recognition and treatment. In addition, evidence suggests there are differences in MDD treatment for younger and older patients.
This article reviews common challenges in recognizing and treating MDD in children, adolescents, and older adults.
Table 1
Major depressive disorder: Age-related differences
| Children/adolescents | Adults | Older adults | |
|---|---|---|---|
| Prevalence | 2% in children; 6% in adolescents | 20% | 25% |
| Male-to-female ratio | 1:1 in children; 1:2 in adolescents | 1:2 | 1:2 |
| DSM-IV-TR criteria | Similar | Similar | Similar |
| Clinical features | Irritability, temper tantrums, somatic complaints, hypersomina, weight gain, auditory hallucinations, psychomotor agitation, separation anxiety, social phobia, panic disorder, drug abuse, poor self-esteem | Typical DSM-IV-TR features. Psychomotor retardation, middle and terminal insomnia | Irritability, motor agitation, restlessness, somatic complaints, diarrhea and constipation, decreased libido, cognitive impairment, delusions, anxiety, panic, worsening of medical comorbidities |
| Source: References 1,2 | |||
Varying clinical features
Children/adolescents. The clinical presentation of MDD in children and adolescents is similar to that of adults. Children usually display anxiety, irritability, temper tantrums, and somatic complaints before verbally expressing depressive feelings. Psychotic depression in children manifests more often as auditory hallucinations than delusions.1
Younger vs middle-age adults. Researchers who evaluated baseline clinical and sociodemographic information of 1,498 patients enrolled in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study found that the presentation of depressive symptoms in young adult patients (age 18 to 35) differed from those of middle-age (age 36 to 50) patients.3 Younger patients were more likely to be irritable, complain of weight gain and hypersomnia, and have a negative view of life and the future. They also were more likely to report previous suicide attempts and endorse symptoms consistent with generalized anxiety disorder, social phobia, panic disorder, and drug abuse. Middle-age patients had more depressive episodes, deceased libido, and middle insomnia, and more frequently reported gastrointestinal symptoms such as diarrhea or constipation.3
Older adults. In our experience, typical MDD mood symptoms often are absent in older patients. Frequently, we see somatic complaints, motor restlessness, or psychomotor retardation; these symptoms may be attributable to a concurrent medical illness. This in turn may worsen the physical illness, leading to social isolation and considerable medical morbidity.4
Pain plays an important role in depression, particularly in older adults. Chronic pain affects up to 65% of older adults who live in the community and up to 80% of those who are institutionalized.5 The most common causes of pain in these patients are osteoarthritis, osteoporosis, fibromyalgia, degenerative disk disease, lumbar spinal stenosis, and scoliosis. In addition, neuropathic pain, such as post-herpetic neuralgia and peripheral neuropathy, and injuries resulting from falls often cause long-lasting pain.6
The presence of pain tends to negatively affect recognizing and treating depression. Regardless of their age, when a patient presents with pain or depression, investigate and consider treating both conditions.7
Memory decline is likely to be depressed older adults’ chief complaint, and when objectively tested these patients often show cognitive impairment.8 Whether depressive symptoms in this age group are a reaction to early cognitive deficits or are an early symptom of neurodegeneration remains controversial.9 Some case-control studies have found a link between a history of depression and Alzheimer’s disease (AD).10,11 In general, older patients whose first episode of depression occurs in late life have a higher relative risk of developing some form of dementia; research suggests that 50% of late-life MDD patients will develop dementia within 5 years.12
Researchers have considered the possibility that mild cognitive impairment (MCI) and dementia are a continuum of depression. In 1 study, 29 patients with MCI and 31 with MCI and MDD were assessed annually for an average of 4.3 years.13 Thirty-six patients with MCI (60%) progressed to AD. Presence of depression at the time of MCI diagnosis did not predict conversion to AD but persistence of depression for 2 to 3 years and the presence of melancholic features were associated with higher risk for AD.
Alexopoulos et al14 proposed the “vascular hypothesis theory” that cerebrovascular disease can predispose patients, particularly older adults, to depressive symptoms (Table 2).14 Whether vascular depression is a subtype of MDD remains controversial.
Table 2
Features of vascular depression
| Onset after age 50 |
| Family history of mood disorders is less common |
| Apathy |
| Marked loss of interest in activities |
| Lack of insight |
| Executive dysfunction (problems with planning, organizing, sequencing, abstracting), impaired memory or speed of processing of information |
| History of hypertension, diabetes, or cardiovascular disease |
| May have a neurologic event such as stroke or transient ischemic attack |
| White or gray matter hyperintensities |
| Source: Reference 14 |
Course and prognosis
MDD has been characterized as a self-limited disease, with an average duration of 6 to 9 months. However, newer prospective studies suggest that a substantial number of patients recover more slowly or do not ever fully recover.15 Several factors, such as genetic/biologic vulnerability and psychosocial factors, influence the courses, prognosis, and risk of relapse/recurrence of MDD in all age groups.
Children and adolescents. The typical duration of a major depressive episode for clinically referred children and adolescents is 8 to 13 months.1,16 Approximately 90% of these patients’ major depressive episodes remit by 2 years, but up to 10% persist.1,16 Within 5 years of MDD onset, up to 70% of children and adolescents will experience a recurrence,17 a rate comparable to adults.
Anxiety disorders, panic disorders, phobias, substance abuse, conduct and oppositional disorders, and attention-deficit/hyperactivity disorder occur 2 to 6 times more frequently in children and adolescents with MDD.18,19 Children with MDD who have significant psychiatric and psychosocial comorbidity experience poorer outcomes.18
Older adults. Despite optimal treatment conditions, ≥50% of older patients fail to respond adequately to first-line antidepressant pharmacotherapy.20 Treatment-resistant MDD in older patients increases:
- nonadherence to treatment for comorbid medical disorders
- disability and cognitive impairment
- burden on caregivers
- risk for early mortality, including suicide.20
Differences in treatment
Although MDD often is recurrent, episodic, and in some patients chronic, in general earlier treatment and quicker response lead to better outcomes. A large, naturalistic German study of 795 inpatients with major depression found that early improvement (20% reduction in Hamilton Depression Rating Scale-21 score within the first 2 weeks) with antidepressant therapy may predict later response and remission.21
Regardless of a patient’s age, MDD treatment should begin with education. All patients should be involved in their treatment. Encourage patients to become familiar with their triggers and stressors, improve their coping skills, and adopt a healthy lifestyle, which includes a nutritious diet, frequent exercise, and adequate sleep. As maintenance treatment we recommend that patients participate in frequent socialization and activities (Table 3). Refer patients to self-help books, online help guides, and handouts from sources such as National Institute of Mental Health.22,23 Encourage patients to have patience and perseverance, and guide them through each step of recovery.
In addition to lifestyle modification, other treatment options for depression include pharmacotherapy, interpersonal psychotherapy, cognitive-behavioral therapy (CBT), and electroconvulsive therapy (ECT). All these modalities are effective for acute and maintenance treatment and should be considered when determining the best approach for each patient.
The effectiveness of antidepressants in general is comparable among and within classes.2 Base your initial selection on the patient’s previous response to antidepressants and the medication’s side effects profile and cost.
The benefits of exercise for all patients cannot be underestimated.24 Prescribe 20 to 30 minutes of daily exercise as part of recommended lifestyle changes. Writing “daily exercise” on a prescription pad can effectively remind patients that exercise needs to be taken as seriously as medication compliance.
Children and adolescents. For mild depression, supportive therapy seems to be as effective as CBT and medications.25 A randomized controlled trial of 439 depressed adolescents found that CBT plus fluoxetine conferred quicker benefit, but in the long run may not be any more efficacious than pharmacotherapy alone.25 Researchers also found that CBT plus fluoxetine was no more effective than pharmacotherapy alone for adolescents with moderate to severe depression.25
Older adults. Compared with younger patients, geriatric patients typically require lower antidepressant dosages to achieve a specific blood level, but the blood levels at which antidepressants are most effective appear to be similar.2 Older patients also may be more likely to relapse and less likely to achieve full response to antidepressants than younger patients.2 In older adults, amitriptyline, imipramine, and doxepin are not preferred because these agents may cause orthostatic hypotension and urinary retention.2 A depressed older adult who experiences weight loss might benefit from an antidepressant that improves appetite, such as mirtazapine.26 Some research suggests that maintenance antidepressant therapy in older patients experiencing a first-time episode of MDD should continue for up to 2 years.27
A meta-analysis of 12 studies of CBT in depressed adults age ≥60 with chronic pain found that CBT was effective at improving self-reported pain but had no significant effect on depressive symptoms, physical function, or medication use.6 ECT often is prescribed for depressed older adults because its safety and efficacy for these patients has been well documented.28 Other neuromodulation therapies include vagus nerve, repetitive transcranial magnetic stimulation, and deep brain stimulation, but none of these treatments have been extensively evaluated in older patients.
Table 3
Avoiding reoccurrence of depression—a ‘prescription’ for patients
| Take medication as prescribed until your doctor instructs you to stop |
| Eat 3 nutritious meals every day |
| Sleep 6 to 8 hours each night |
| Walk/exercise for 20 minutes every day |
| Relax and do breathing exercises as taught 3 times a day |
| Talk with a friend or family member each day |
| Develop a hobby |
| Remain active |
| See your doctor once a month |
Related Resource
- American Psychiatric Association. Treatment of patients with major depressive disorder. 3rd ed. www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx.
Drug Brand Names
- Amitriptyline • Elavil
- Doxepin • Aponal, Silenor
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Mirtazapine • Remeron
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Birmaher B, Brent D. AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503-1526.
2. American Psychiatric Association. Treatment of patients with major depressive disorder. 3rd ed. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx. Accessed April 4 2011.
3. Husain MM, Rush AJ, Sakheim HA. Age-related characteristics of major depression: a preliminary STAR*D report. Am J Geriatr Psychiatry. 2005;13(10):852-862.
4. Gonda X, Molnár E, Torzsa P, et al. Characteristics of depression in the elderly. Psychiatr Hung. 2009;24(3):166-174.
5. Gibson, SJ. Pain and aging: a comparison of the pain experience over the adult life span. In: Dostrovsky JO, Carr DB, Koltzenburg M, eds. Proceedings of the 10th World Congress on Pain. Progress in pain research and management. Seattle, WA: IASP Press; 2003:767–790.
6. Lunde LH, Nordhus IH, Pallesen H. The effectiveness of cognitive and behavioural treatment of chronic pain in the elderly: a quantitative review. J Clin Psychol Med Settings. 2009;16:254-262.
7. Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433-2445.
8. Reid LM, Machullich AM. Subjective memory complaints and cognitive impairment in older people. Dement Geriatr Cogn Disord. 2006;22(5-6):471-485.
9. Tsuno N, Homma A. What is the association between depression and Alzheimer’s disease? Expert Rev Neurother. 2009;9(11):]1667-1676.
10. Tsolaki M, Fountalakis K, Chantzi E, et al. Risk factors for clinically diagnosed Alzheimer’s disease: a case-control study of a Greek population. Int Psychogeriatr. 1997;9(3):327-341.
11. Speck CE, Kukull WA, Brenner DE, et al. History of depression as a risk factor for Alzheimer’s disease. Epidemiology. 1995;6(4):366-369.
12. Alexopoulos GS. Depression in elderly. Lancet. 2005;365:1961-1970.
13. Houde M, Bergman H, Whitehead V, et al. Predictive depression pattern in mild cognitive impairment. Int J Geriatr Psychiatry. 2008;23:1028-1033.
14. Alexopoulos GS, Meyers BS, Young RC, et al. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997;54(10):915-922.
15. Angst J, Gamma A, Rossler W, et al. Long-term depression versus episodic major depression: results from the prospective Zurich study of a community sample. J Affect Disord. 2009;115(1-2):112-121.
16. Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am. 2002;11(3):619-637 x.
17. Rao U, Ryan ND, Birmaher B, et al. Unipolar depression in adolescents: clinical outcome in adulthood. J Am Acad Child Adolesc Psychiatry. 1995;34:566-578.
18. Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psych Psychiatry. 1999;40(1):57-87.
19. Costello EJ, Pine DS, Hammen C, et al. Development and natural history of mood disorders. Biol Psychiatry. 2002;52(6):529-542.
20. Lenze EJ, Sheffrin M, Driscoll HC, et al. Incomplete response in late-life depression: getting to remission. Dialogues Clin Neurosci. 2008;10(4):419-430.
21. Henkel V, Seemuller F, Obermeier M, et al. Does early improvement triggered by antidepressant predict response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J Affect Disord. 2009;115(3):439-449.
22. National Institute of Mental Health. Depression. NIH publication No. 083561. 2008. Available at: http://www.nimh.nih.gov/health/publications/depression/complete-index.shtml. Accessed April 4 2011.
23. Helpguide.org. Depression. Available at: http://www.helpguide.org/topics/depression.htm. Accessed April 4, 2011.
24. Sidhu K, Vandana P, Balon R. Exercise prescription. A practical and effective therapy for depression. Current Psychiatry. 2009;8(6):39-51.
25. Curry J, Rohde P, Simons A, et al. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1427-1439.
26. Rajii TK, Mulsant BH, Lotrich FE, et al. Use of antidepressant in late-life depression. Drugs Aging. 2008;25(10):841-853.
27. Rush AJ, Trivedi MH, Weiniewski SR, et al. Acute and longer term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905-1917.
28. Van der Wurff FB, Stek ML, Hoogendijk WJ. The efficacy and safety of ECT in depressed older adults: a literature review. Int J Geriatr Psychiatry. 2003;18(10):894-904.
1. Birmaher B, Brent D. AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503-1526.
2. American Psychiatric Association. Treatment of patients with major depressive disorder. 3rd ed. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx. Accessed April 4 2011.
3. Husain MM, Rush AJ, Sakheim HA. Age-related characteristics of major depression: a preliminary STAR*D report. Am J Geriatr Psychiatry. 2005;13(10):852-862.
4. Gonda X, Molnár E, Torzsa P, et al. Characteristics of depression in the elderly. Psychiatr Hung. 2009;24(3):166-174.
5. Gibson, SJ. Pain and aging: a comparison of the pain experience over the adult life span. In: Dostrovsky JO, Carr DB, Koltzenburg M, eds. Proceedings of the 10th World Congress on Pain. Progress in pain research and management. Seattle, WA: IASP Press; 2003:767–790.
6. Lunde LH, Nordhus IH, Pallesen H. The effectiveness of cognitive and behavioural treatment of chronic pain in the elderly: a quantitative review. J Clin Psychol Med Settings. 2009;16:254-262.
7. Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433-2445.
8. Reid LM, Machullich AM. Subjective memory complaints and cognitive impairment in older people. Dement Geriatr Cogn Disord. 2006;22(5-6):471-485.
9. Tsuno N, Homma A. What is the association between depression and Alzheimer’s disease? Expert Rev Neurother. 2009;9(11):]1667-1676.
10. Tsolaki M, Fountalakis K, Chantzi E, et al. Risk factors for clinically diagnosed Alzheimer’s disease: a case-control study of a Greek population. Int Psychogeriatr. 1997;9(3):327-341.
11. Speck CE, Kukull WA, Brenner DE, et al. History of depression as a risk factor for Alzheimer’s disease. Epidemiology. 1995;6(4):366-369.
12. Alexopoulos GS. Depression in elderly. Lancet. 2005;365:1961-1970.
13. Houde M, Bergman H, Whitehead V, et al. Predictive depression pattern in mild cognitive impairment. Int J Geriatr Psychiatry. 2008;23:1028-1033.
14. Alexopoulos GS, Meyers BS, Young RC, et al. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997;54(10):915-922.
15. Angst J, Gamma A, Rossler W, et al. Long-term depression versus episodic major depression: results from the prospective Zurich study of a community sample. J Affect Disord. 2009;115(1-2):112-121.
16. Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am. 2002;11(3):619-637 x.
17. Rao U, Ryan ND, Birmaher B, et al. Unipolar depression in adolescents: clinical outcome in adulthood. J Am Acad Child Adolesc Psychiatry. 1995;34:566-578.
18. Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psych Psychiatry. 1999;40(1):57-87.
19. Costello EJ, Pine DS, Hammen C, et al. Development and natural history of mood disorders. Biol Psychiatry. 2002;52(6):529-542.
20. Lenze EJ, Sheffrin M, Driscoll HC, et al. Incomplete response in late-life depression: getting to remission. Dialogues Clin Neurosci. 2008;10(4):419-430.
21. Henkel V, Seemuller F, Obermeier M, et al. Does early improvement triggered by antidepressant predict response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J Affect Disord. 2009;115(3):439-449.
22. National Institute of Mental Health. Depression. NIH publication No. 083561. 2008. Available at: http://www.nimh.nih.gov/health/publications/depression/complete-index.shtml. Accessed April 4 2011.
23. Helpguide.org. Depression. Available at: http://www.helpguide.org/topics/depression.htm. Accessed April 4, 2011.
24. Sidhu K, Vandana P, Balon R. Exercise prescription. A practical and effective therapy for depression. Current Psychiatry. 2009;8(6):39-51.
25. Curry J, Rohde P, Simons A, et al. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1427-1439.
26. Rajii TK, Mulsant BH, Lotrich FE, et al. Use of antidepressant in late-life depression. Drugs Aging. 2008;25(10):841-853.
27. Rush AJ, Trivedi MH, Weiniewski SR, et al. Acute and longer term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905-1917.
28. Van der Wurff FB, Stek ML, Hoogendijk WJ. The efficacy and safety of ECT in depressed older adults: a literature review. Int J Geriatr Psychiatry. 2003;18(10):894-904.
Treatment-resistant schizophrenia: What can we do about it?
Discuss this article at www.facebook.com/CurrentPsychiatry
Patients with treatment-resistant schizophrenia can be broadly defined to include any persons with residual symptoms that cause distress or impairment despite several treatment attempts. Unfortunately, this definition may include most of our patients with schizophrenia.
Clinical trial data on treatment-resistant schizophrenia can be contradictory, leaving “N of 1” empirical treatment trials for individual patients as the current state of the art. This article presents data from clinical trials for pharmacologic and nonpharmacologic options and offers recommendations to try to help our treatment-resistant patients.
Defining treatment resistance
Research reports regarding treatment-resistant or treatment-refractory schizophrenia have relied on operational criteria such as that found in the pivotal study for clozapine1:
- at least 3 periods of treatment in the preceding 5 years with neuroleptic agents from at least 2 different chemical classes at dosages equivalent to ≥1000 mg/d of chlorpromazine for 6 weeks, each without significant symptomatic relief, and
- no period of good functioning within the preceding 5 years.1 In that study, patients also underwent a prospective treatment trial with what we now know are high doses of haloperidol (up to 60 mg/d or higher) and benztropine mesylate (6 mg/d) for a period of 6 weeks to confirm lack of drug responsiveness. Other studies have more relaxed criteria, such as:
- persistent positive symptoms—hallucinations, delusions, or marked thought disorder—after at least 6 contiguous weeks of past or present treatment, with ≥1 typical antipsychotics at doses of ≥600 mg/d in chlorpromazine equivalents
- a poor level of functioning over the past 2 years, as defined by the lack of competitive employment or enrollment in an academic or vocational program and not having age-expected interpersonal relations with someone outside the biologic family with whom ongoing regular contacts were maintained.2
In this study, no prospective period of treatment to confirm lack of drug responsiveness was required.
The most clinically relevant definition of treatment resistance depends on the patient’s individual circumstances. For some patients, targeting positive symptoms is a high priority; for others it may be negative and cognitive symptoms; for others, it may be excitement. Moreover, families may complain of symptoms or behavior that are of little or no concern to your patient.
Although we desire treatment response and remission for our patients, definitions for remission and functional recovery are in flux. Proposed criteria define symptomatic remission as 6-month maintenance of simultaneous ratings of mild or less on delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms.3,4 Emsley et al4 note that reported remission rates vary widely across studies (17% to 88%) and that patients in remission do better than their non-remitted counterparts in several other outcome domains. Also, patients move in and out of remission over time. Predictors of remission include:
- early treatment response
- baseline symptom severity
- subjective well-being.4
Recovery is a more complex construct than remission and includes social outcomes. Although recovery lacks a standard definition, it is the implied goal of treatment. Anything short of recovery can be viewed as inadequate. If we set the bar at this height, many or most of the patients we treat for schizophrenia could be considered treatment-resistant.
Confounding factors
Before concluding that a patient is treatment-resistant, address medication adherence and possible substance use. Partial or nonadherence with antipsychotic treatment is common—approximately one-half of patients are nonadherent5—and associated with relapse and re-hospitalization.6 In addition, an estimated one-half of all individuals with schizophrenia also use substances.7
Be aware of the optimal dose for any particular antipsychotic and factors that can interfere with achieving adequate plasma levels. This means acknowledging that dosing ranges established during registration studies may not reflect the needs of day-to-day clinical practice.8 Pharmacokinetic interactions with other medications, such as carbamazepine or rifampin, can induce liver enzymes and result in subtherapeutic antipsychotic levels. Cigarette smoking also may have this effect. Lowered clozapine or olanzapine plasma levels have been observed in patients who resume smoking after being discharged from a non-smoking inpatient environment. Some antipsychotics, such as ziprasidone and lurasidone, must be taken with food in order to have sufficient bioavailability.9
What does a patient want?
Patients with schizophrenia often have limited insight into their psychotic symptoms.10 Savvy clinicians will attempt to leverage a patient’s insight into ancillary symptoms—such as impaired sleep, anxiety, and dysphoria—to encourage a therapeutic alliance and therefore adherence. If patients feel their concerns are not addressed, they may consider treatment inadequate even though the intensity of their hallucinations and delusions may have decreased.
Which antipsychotic is best?
Meta-analyses of randomized controlled trials (RCTs) of antipsychotic treatment for schizophrenia found that, although individual response will vary, clozapine generally has better efficacy that other antipsychotics.11-13 Olanzapine, risperidone, and amisulpride (which is not available in the United States) appear to be more efficacious than first-generation antipsychotics. Other second-generation antipsychotics do not consistently show greater efficacy than first-generation antipsychotics, although their tolerability profiles vary greatly.11-13
Antipsychotic monotherapy. More than 25 RCTs have focused on antipsychotic monotherapy for treatment-resistant patients; for a bibliography of these studies, click here. For the most part, clozapine has consistently demonstrated superiority over comparators. Because not all patients with schizophrenia can tolerate clozapine or are willing to have their blood monitored as required, other second-generation antipsychotics have been suggested as possible substitutes. Olanzapine has established superior efficacy to first-generation antipsychotics11-13 and perhaps comparable efficacy to clozapine in some studies.2,14-17 Risperidone appeared to be comparable to clozapine in some studies,18,19 whereas clozapine’s superiority was evident in others.14,20,21 Although an RCT found comparable efficacy for ziprasidone vs clozapine,22 patients enrolled in this study may not have been treatment-resistant regarding efficacy but instead could not tolerate prior treatments. Enrolling patients on the basis of poor efficacy and/or poor tolerability to their prior antipsychotic regimen also has complicated the interpretation of studies comparing olanzapine with clozapine16 and risperidone with clozapine.18
Antipsychotic combinations. Combinations of antipsychotics are used commonly when treating chronic schizophrenia.23 Of the approximately 20 RCTs of antipsychotic combination therapy, most tested clozapine combined with other second-generation antipsychotics, such as risperidone. For a bibliography of these studies, click here. Only 5 studies support a combination approach (Table 1).
Table 1
Antipsychotic combinations: Few studies support efficacy
| Study | Design | Patients | Results |
|---|---|---|---|
| Shiloh et al, 1997a | 10-week, double-blind, placebo-controlled | 28 patients nonresponsive to typical antipsychotics and partially responsive to clozapine received add-on sulpiride,* 600 mg/d, or placebo | The sulpiride group showed improvements in positive and negative symptoms |
| Josiassen et al, 2005b | 12-week, randomized, double-blind, placebo-controlled | 40 schizophrenia patients unresponsive or partially responsive to clozapine randomized to clozapine + placebo or clozapine + risperidone, 6 mg/d | Mean BPRS total and positive symptom subscale scores reduced in both groups but reductions were greater in the clozapine/risperidone group; reduction in SANS also was observed in the clozapine/risperidone group |
| Genç et al, 2007c | 8-week, randomized, single-blind | 56 treatment-resistant schizophrenia patients randomly assigned to clozapine + amisulpride* or clozapine + quetiapine | Both groups improved at week 8 as measured by BPRS, SANS, SAPS, and CGI; however, patients receiving amisulpride showed greater improvement |
| Muscatello et al, 2011d | 24-week, randomized, double-blind, placebo-controlled | 31 treatment-resistant schizophrenia patients receiving clozapine randomized to receive adjunctive aripiprazole or placebo | Aripiprazole showed beneficial effect on positive and general psychopathologic symptomatology, but no significant effects on executive cognitive function |
| Takahashi et al, 1999e | 8-week, randomized, single-blind, crossover | 10 neuroleptic-treated patients received add-on risperidone and mosapramine* | Both additions resulted in significant, yet modest, improvement; no significant difference in PANSS between risperidone and mosapramine |
| *Not available in the United States BPRS: Brief Psychiatric Rating Scale; CGI: Clinical Global Impression; PANSS: Positive and Negative Syndrome Scale; SANS: Scale for the Assessment of Negative Symptoms; SAPS: Scale for the Assessment of Positive Symptoms | |||
| Source: References a. Shiloh R, Zemishlany Z, Aizenberg D, et al. Sulpiride augmentation in people with schizophrenia partially responsive to clozapine. A double-blind, placebo-controlled study. Br J Psychiatry. 1997;171:569-573. b. Josiassen RC, Joseph A, Kohegyi E, et al. Clozapine augmented with risperidone in the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2005;162(1):130-136. c. Genç Y, Taner E, Candansayar S. Comparison of clozapine-amisulpride and clozapine-quetiapine combinations for patients with schizophrenia who are partially responsive to clozapine: a single-blind randomized study. Adv Ther. 2007;24(1):1-13. d. Muscatello MR, Bruno A, Pandolfo G, et al. Effect of aripiprazole augmentation of clozapine in schizophrenia: a double-blind, placebo-controlled study. Schizophr Res. 2011;127(1-3):93-99. e. Takahashi N, Terao T, Oga T, et al. Comparison of risperidone and mosapramine addition to neuroleptic treatment in chronic schizophrenia. Neuropsychobiology. 1999;39(2):81-85. | |||
What about augmentation?
Adjunctive non-antipsychotics also are commonly used when treating patients with chronic schizophrenia. For example, lithium and anticonvulsants are used in approximately one-half of all inpatients with schizophrenia in facilities operated by the State of New York Office of Mental Health.24,25 The evidence base for these agents as adjuncts to antipsychotics generally is weak.26 Specifically, early reports of benefit with adjunctive lithium have been negated by later studies. Similarly, large trials of adjunctive valproate and lamotrigine have failed to replicate early and promising efficacy signals from smaller trials, although the larger studies did not specifically target treatment-resistant schizophrenia.
Among mood stabilizers, lamotrigine may be the most promising for treatment-resistant schizophrenia. In a meta-analysis of clinical trials examining schizophrenia patients receiving clozapine (N=161) who were randomized to receive adjunctive lamotrigine or adjunctive placebo, lamotrigine was superior to placebo in total score for psychosis symptoms and scores for positive and negative symptoms.27
More than 125 published RCTs have studied a wide variety of adjunctive agents other than lithium or anticonvulsants for treating persistent schizophrenia symptoms (Table 2).
Only some of the approximately 40 RCTs regarding adjunctive antidepressants in patients with chronic schizophrenia focused on patients with ongoing depressive symptoms. For a bibliography of these studies, click here. In a meta-analysis measuring improvement of negative symptoms from 23 trials (N=819),28 the effect size was moderate in favor of antidepressants. Subgroup analysis revealed significant responses for fluoxetine, trazodone, and ritanserin.
More than 50 RCTs have focused on augmenting medications for cognitive dysfunction in chronic schizophrenia. Unfortunately, agents used to treat Alzheimer’s disease have shown disappointing results when tested in patients with schizophrenia, as have agents prescribed for attention-deficit/hyperactivity disorder (methylphenidate, guanfacine, atomoxetine) or agents used to promote alertness (modafinil and armodafinil).
Medications that act on glutamate receptors may offer another potential solution, although not in combination with clozapine.29
Other agents that require further study where ≥2 positive studies have been reported (with ≤2 negative studies) include celecoxib, neurosteroids and hormones, purinergic agents, serotonin 5-HT1A receptor agonists, and serotonin 5-HT3 receptor antagonists.
Table 2
Agents studied as adjuncts to antipsychotics
| Acetylsalicylic acid and nonsteroidal anti-inflammatory agents |
| Anticonvulsants and lithium |
| Antidepressants |
| Antiglucocorticoids |
| Agents used to treat attention-deficit/hyperactivity disorder |
| Beta blockers |
| Cholinesterase inhibitors and other agents used to treat Alzheimer’s disease |
| Experimental agents that act on glutamate receptors |
| GABAA receptor drugs |
| Neurosteroids and hormones |
| Omega-3 fatty acids |
| Opioid system agents |
| Peptides |
| Purinergic agents |
| Serotonin 5-HT1A receptor agonists |
| Serotonin 5-HT3 receptor antagonists |
| Wakefulness promoting agents |
Therapeutic neuromodulation
More than 10 RCTs of repetitive transcranial magnetic stimulation (rTMS) in patients with refractory symptoms of schizophrenia have been published; the results were mixed. For a bibliography of these studies, click here. In a meta-analysis of 9 trials (n=213),30 prefrontal rTMS for treating negative symptoms demonstrated a small-to-medium effect size. In another meta-analysis31 of all prospective studies of rTMS for negative symptoms and for auditory hallucinations and overall positive symptoms in refractory schizophrenia, the effect sizes showed moderate effects.
Fewer controlled trials are available for electroconvulsive therapy,32,33 but its use with clozapine appears encouraging.34
Psychological and behavioral intervention. Cognitive-behavioral therapy, although labor-intensive, can be helpful even in patients considered treatment-resistant (Table 3). These interventions generally are provided together with pharmacotherapy.
Complementary and alternative therapies. Patients and their families may ask about complementary and alternative therapies, particularly when conventional approaches have not been successful. A meta-analysis of 6 studies (n=828)35 that reviewed adjunctive use of ginkgo in patients with chronic schizophrenia found statistically significant moderate improvement in total and negative symptoms. Negative reports also are available, including a 5-month study of adjunctive megavitamins that did not demonstrate any benefits.36 In a review of 13 RCTs of acupuncture for schizophrenia, Lee et al found the overall methodological quality was too low to draw firm conclusions.37
Table 3
Cognitive-behavioral therapy for schizophrenia
| Study | Design | Patients | Results |
|---|---|---|---|
| Pinto et al, 1999a | 6-month, randomized controlled | 37 treatment-resistant schizophrenia patients were randomized to CBT plus social skills training or supportive therapy | Both groups showed statistically significant improvement on the BPRS, SAPS, and SANS; however, patients in the CBT group had lower BPRS and SAPS scores. No difference on SANS scores |
| Barretto et al, 2009b | 21-week, controlled (nonrandom-ized) | Patients refractory to clozapine were placed in a CBT or befriending control group | The CBT group showed significant improvement in PANSS total score and general psychopathology subscale score, as well as an improvement of QLS; improvement persisted at 6-month follow-up |
| BPRS: Brief Psychiatric Rating Scale; CBT: cognitive-behavioral therapy; PANSS: Positive and Negative Syndrome Scale; QLS: Quality of Life Scale; SANS: Scale for the Assessment of Negative Symptoms; SAPS: Scale for the Assessment of Positive Symptoms | |||
| Source: References a. Pinto A, La Pia S, Mennella R, et al. Cognitive-behavioral therapy and clozapine for clients with treatment-refractory schizophrenia. Psychiatr Serv. 1999;50(7):901-904. b. Barretto EM, Kayo M, Avrichir BS, et al. A preliminary controlled trial of cognitive behavioral therapy in clozapine-resistant schizophrenia. J Nerv Ment Dis. 2009;197(11):865-868. | |||
Clinical recommendations
Before declaring a patient with schizophrenia as treatment-resistant, ensure that an adequate trial of medication did take place. This includes consideration of adequate dosing and pharmacokinetic issues. Awareness of potential substance use and/or partial adherence or nonadherence also is critical because these factors can impact treatment response.
When prescribing for a treatment-resistant schizophrenia patient, identify specific target symptoms to better inform medication selection—especially for symptoms that the patient feels are important. For example, consider an antidepressant for patients who have negative or depressive symptoms. Also take into account other patient-centered concerns, such as tolerability issues that may have interfered with adherence and response in the past.
Clozapine remains the medication of choice for treatment-resistant schizophrenia. Despite dozens of RCTs of potential adjunctive agents for treatment-resistant schizophrenia, no single approach has consistently shown efficacy in reducing symptoms, improving cognition, or increasing a patient’s level of function. Individual response can vary, and our search for the “outlier” who does respond to an adjunctive agent can explain our use of these strategies in clinical practice.
Related Resources
- Cochrane Database of Systematic Reviews. www.cochrane.org/reviews. This database contains reviews of additional therapeutic options for patients with treatment-resistant schizophrenia. As of February 23, 2011, 157 reviews were available.
- Citrome L. Treatment-refractory schizophrenia: What it is and what’s been done about it. Neuropsychiatry. 2011. Epub ahead of print.
- Citrome L. Clozapine for schizophrenia. Life-threatening or life-saving treatment? Current Psychiatry. 2009;8(12):56-63.
Drug Brand Names
- Aripiprazole • Abilify
- Armodafinil • Nuvigil
- Atomoxetine • Strattera
- Benztropine mesylate • Cogentin
- Carbamazepine • Tegretol
- Celecoxib • Celebrex
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluoxetine • Prozac
- Guanfacine • Tenex
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid, others
- Lurasidone • Latuda
- Methylphenidate • Ritalin, Methylin, others
- Modafinil • Provigil
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Rifampin • Rifadin
- Risperidone • Risperdal
- Trazodone • Desyrel, Oleptro
- Valproate (Divalproex) • Depakote, Depakote ER
- Ziprasidone • Geodon
Disclosure
No writing assistance or external financial support was used for this article. Dr. Citrome is a consultant for, has received honoraria from, or has conducted clinical research supported by Abbott Laboratories, AstraZeneca Pharmaceuticals, Avanir Pharmaceuticals, Azur Pharma Inc., Barr Laboratories, Bristol-Myers Squibb, Eli Lilly and Company, Forest Research Institute, GlaxoSmithKline, Janssen Pharmaceuticals, Jazz Pharmaceuticals, Merck, Novartis, Pfizer Inc., Sunovion, Valeant Pharmaceuticals, and Vanda Pharmaceuticals.
1. Kane J, Honigfeld G, Singer J, et al. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988;45(9):789-796.
2. Volavka J, Czobor P, Sheitman B, et al. Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry. 2002;159(2):255-262.
3. Andreasen NC, Carpenter WT Jr, Kane JM, et al. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162(3):441-449.
4. Emsley R, Chiliza B, Asmal L, et al. The concepts of remission and recovery in schizophrenia. Curr Opin Psychiatry. 2011;24(2):114-121.
5. Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892-909.
6. Robinson DG, Woerner MG, Delman HM, et al. Pharmacological treatments for first-episode schizophrenia. Schizophr Bull. 2005;31(3):705-722.
7. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
8. Citrome L, Volavka J. Optimal dosing of atypical antipsychotics in adults: a review of the current evidence. Harv Rev Psychiatry. 2002;10(5):280-291.
9. Citrome L. Iloperidone asenapine and lurasidone. A brief overview of three new second-generation antipsychotics. Postgrad Med. 2011;123(2):153-162.
10. Lincoln TM, Lüllmann E, Rief W. Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr Bull. 2007;33(6):1324-1342.
11. Leucht S, Corves C, Arbter D, et al. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373(9657):31-41.
12. Leucht S, Komossa K, Rummel-Kluge C, et al. A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. 2009;166(2):152-163.
13. Leucht S, Arbter D, Engel RR, et al. How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials. Mol Psychiatry. 2009;14(4):429-447.
14. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610.
15. Tollefson GD, Birkett MA, Kiesler GM, et al. Double-blind comparison of olanzapine versus clozapine in schizophrenic patients clinically eligible for treatment with clozapine. Biol Psychiatry. 2001;49(1):52-63.
16. Bitter I, Dossenbach MR, Brook S, et al. Olanzapine versus clozapine in treatment-resistant or treatment-intolerant schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28(1):173-180.
17. Meltzer HY, Bobo WV, Roy A, et al. A randomized, double-blind comparison of clozapine and high-dose olanzapine in treatment-resistant patients with schizophrenia. J Clin Psychiatry. 2008;69(2):274-285.
18. Bondolfi G, Dufour H, Patris M, et al. Risperidone versus clozapine in treatment-resistant chronic schizophrenia: a randomized double-blind study. Am J Psychiatry. 1998;155(4):499-504.
19. Wahlbeck K, Cheine M, Tuisku K, et al. Risperidone versus clozapine in treatment-resistant schizophrenia: a randomized pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2000;24(6):911-922.
20. Breier AF, Malhotra AK, Su TP, et al. Clozapine and risperidone in chronic schizophrenia: effects on symptoms, parkinsonian side effects, and neuroendocrine response. Am J Psychiatry. 1999;156(2):294-298.
21. Azorin JM, Spiegel R, Remington G, et al. A double-blind comparative study of clozapine and risperidone in the management of severe chronic schizophrenia. Am J Psychiatry. 2001;158(8):1305-1313.
22. Sacchetti E, Galluzzo A, Valsecchi P, et al. Ziprasidone vs clozapine in schizophrenia patients refractory to multiple antipsychotic treatments: the MOZART study. Schizophr Res. 2009;113(1):112-121.
23. Jaffe AB, Levine J. Antipsychotic medication coprescribing in a large state hospital system. Pharmacoepidemiol Drug Saf. 2003;12(1):41-48.
24. Citrome L, Levine J, Allingham B. Changes in use of valproate and other mood stabilizers for patients with schizophrenia from 1994 to 1998. Psychiatr Serv. 2000;51(5):634-638.
25. Citrome L, Jaffe A, Levine J, et al. Use of mood stabilizers among patients with schizophrenia, 1994-2001. Psychiatr Serv. 2002;53(10):1212.-
26. Citrome L. Adjunctive lithium and anticonvulsants for the treatment of schizophrenia: what is the evidence? Expert Rev Neurother. 2009;9(1):55-71.
27. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2009;109(1-3):10-14.
28. Singh SP, Singh V, Kar N, et al. Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: meta-analysis. Br J Psychiatry. 2010;197(3):174-179.
29. Kantrowitz JT, Javitt DC. Thinking glutamatergically: changing concepts of schizophrenia based upon changing neurochemical models. Clin Schizophr Relat Psychoses. 2010;4(3):189-200.
30. Dlabac-de Lange JJ, Knegtering R, Aleman A, et al. Repetitive transcranial magnetic stimulation for negative symptoms of schizophrenia: review and meta-analysis. J Clin Psychiatry. 2010;71(4):411-418.
31. Freitas C, Fregni F, Pascual-Leone A. Meta-analysis of the effects of repetitive transcranial magnetic stimulation (rTMS) on negative and positive symptoms in schizophrenia. Schizophr Res. 2009;108(1-3):11-24.
32. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15(3):178-192.
33. Goswami U, Kumar U, Singh B. Efficacy of electroconvulsive therapy in treatment resistant schizophrenia: a double-blind study. Indian J Psychiatry. 2003;45(1):26-29.
34. Braga RJ, Petrides G. The combined use of electroconvulsive therapy and antipsychotics in patients with schizophrenia. J ECT. 2005;21(2):75-83.
35. Singh V, Singh SP, Chan K. Review and meta-analysis of usage of ginkgo as an adjunct therapy in chronic schizophrenia. Int J Neuropsychopharmacol. 2010;13(2):257-271.
36. Vaughan K, McConaghy N. Megavitamin and dietary treatment in schizophrenia: a randomised controlled trial. Aust N Z J Psychiatry. 1999;33(1):84-88.
37. Lee MS, Shin BC, Ronan P, et al. Acupuncture for schizophrenia: a systematic review and meta-analysis. Int J Clin Pract. 2009;63(11):1622-1633.
Discuss this article at www.facebook.com/CurrentPsychiatry
Patients with treatment-resistant schizophrenia can be broadly defined to include any persons with residual symptoms that cause distress or impairment despite several treatment attempts. Unfortunately, this definition may include most of our patients with schizophrenia.
Clinical trial data on treatment-resistant schizophrenia can be contradictory, leaving “N of 1” empirical treatment trials for individual patients as the current state of the art. This article presents data from clinical trials for pharmacologic and nonpharmacologic options and offers recommendations to try to help our treatment-resistant patients.
Defining treatment resistance
Research reports regarding treatment-resistant or treatment-refractory schizophrenia have relied on operational criteria such as that found in the pivotal study for clozapine1:
- at least 3 periods of treatment in the preceding 5 years with neuroleptic agents from at least 2 different chemical classes at dosages equivalent to ≥1000 mg/d of chlorpromazine for 6 weeks, each without significant symptomatic relief, and
- no period of good functioning within the preceding 5 years.1 In that study, patients also underwent a prospective treatment trial with what we now know are high doses of haloperidol (up to 60 mg/d or higher) and benztropine mesylate (6 mg/d) for a period of 6 weeks to confirm lack of drug responsiveness. Other studies have more relaxed criteria, such as:
- persistent positive symptoms—hallucinations, delusions, or marked thought disorder—after at least 6 contiguous weeks of past or present treatment, with ≥1 typical antipsychotics at doses of ≥600 mg/d in chlorpromazine equivalents
- a poor level of functioning over the past 2 years, as defined by the lack of competitive employment or enrollment in an academic or vocational program and not having age-expected interpersonal relations with someone outside the biologic family with whom ongoing regular contacts were maintained.2
In this study, no prospective period of treatment to confirm lack of drug responsiveness was required.
The most clinically relevant definition of treatment resistance depends on the patient’s individual circumstances. For some patients, targeting positive symptoms is a high priority; for others it may be negative and cognitive symptoms; for others, it may be excitement. Moreover, families may complain of symptoms or behavior that are of little or no concern to your patient.
Although we desire treatment response and remission for our patients, definitions for remission and functional recovery are in flux. Proposed criteria define symptomatic remission as 6-month maintenance of simultaneous ratings of mild or less on delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms.3,4 Emsley et al4 note that reported remission rates vary widely across studies (17% to 88%) and that patients in remission do better than their non-remitted counterparts in several other outcome domains. Also, patients move in and out of remission over time. Predictors of remission include:
- early treatment response
- baseline symptom severity
- subjective well-being.4
Recovery is a more complex construct than remission and includes social outcomes. Although recovery lacks a standard definition, it is the implied goal of treatment. Anything short of recovery can be viewed as inadequate. If we set the bar at this height, many or most of the patients we treat for schizophrenia could be considered treatment-resistant.
Confounding factors
Before concluding that a patient is treatment-resistant, address medication adherence and possible substance use. Partial or nonadherence with antipsychotic treatment is common—approximately one-half of patients are nonadherent5—and associated with relapse and re-hospitalization.6 In addition, an estimated one-half of all individuals with schizophrenia also use substances.7
Be aware of the optimal dose for any particular antipsychotic and factors that can interfere with achieving adequate plasma levels. This means acknowledging that dosing ranges established during registration studies may not reflect the needs of day-to-day clinical practice.8 Pharmacokinetic interactions with other medications, such as carbamazepine or rifampin, can induce liver enzymes and result in subtherapeutic antipsychotic levels. Cigarette smoking also may have this effect. Lowered clozapine or olanzapine plasma levels have been observed in patients who resume smoking after being discharged from a non-smoking inpatient environment. Some antipsychotics, such as ziprasidone and lurasidone, must be taken with food in order to have sufficient bioavailability.9
What does a patient want?
Patients with schizophrenia often have limited insight into their psychotic symptoms.10 Savvy clinicians will attempt to leverage a patient’s insight into ancillary symptoms—such as impaired sleep, anxiety, and dysphoria—to encourage a therapeutic alliance and therefore adherence. If patients feel their concerns are not addressed, they may consider treatment inadequate even though the intensity of their hallucinations and delusions may have decreased.
Which antipsychotic is best?
Meta-analyses of randomized controlled trials (RCTs) of antipsychotic treatment for schizophrenia found that, although individual response will vary, clozapine generally has better efficacy that other antipsychotics.11-13 Olanzapine, risperidone, and amisulpride (which is not available in the United States) appear to be more efficacious than first-generation antipsychotics. Other second-generation antipsychotics do not consistently show greater efficacy than first-generation antipsychotics, although their tolerability profiles vary greatly.11-13
Antipsychotic monotherapy. More than 25 RCTs have focused on antipsychotic monotherapy for treatment-resistant patients; for a bibliography of these studies, click here. For the most part, clozapine has consistently demonstrated superiority over comparators. Because not all patients with schizophrenia can tolerate clozapine or are willing to have their blood monitored as required, other second-generation antipsychotics have been suggested as possible substitutes. Olanzapine has established superior efficacy to first-generation antipsychotics11-13 and perhaps comparable efficacy to clozapine in some studies.2,14-17 Risperidone appeared to be comparable to clozapine in some studies,18,19 whereas clozapine’s superiority was evident in others.14,20,21 Although an RCT found comparable efficacy for ziprasidone vs clozapine,22 patients enrolled in this study may not have been treatment-resistant regarding efficacy but instead could not tolerate prior treatments. Enrolling patients on the basis of poor efficacy and/or poor tolerability to their prior antipsychotic regimen also has complicated the interpretation of studies comparing olanzapine with clozapine16 and risperidone with clozapine.18
Antipsychotic combinations. Combinations of antipsychotics are used commonly when treating chronic schizophrenia.23 Of the approximately 20 RCTs of antipsychotic combination therapy, most tested clozapine combined with other second-generation antipsychotics, such as risperidone. For a bibliography of these studies, click here. Only 5 studies support a combination approach (Table 1).
Table 1
Antipsychotic combinations: Few studies support efficacy
| Study | Design | Patients | Results |
|---|---|---|---|
| Shiloh et al, 1997a | 10-week, double-blind, placebo-controlled | 28 patients nonresponsive to typical antipsychotics and partially responsive to clozapine received add-on sulpiride,* 600 mg/d, or placebo | The sulpiride group showed improvements in positive and negative symptoms |
| Josiassen et al, 2005b | 12-week, randomized, double-blind, placebo-controlled | 40 schizophrenia patients unresponsive or partially responsive to clozapine randomized to clozapine + placebo or clozapine + risperidone, 6 mg/d | Mean BPRS total and positive symptom subscale scores reduced in both groups but reductions were greater in the clozapine/risperidone group; reduction in SANS also was observed in the clozapine/risperidone group |
| Genç et al, 2007c | 8-week, randomized, single-blind | 56 treatment-resistant schizophrenia patients randomly assigned to clozapine + amisulpride* or clozapine + quetiapine | Both groups improved at week 8 as measured by BPRS, SANS, SAPS, and CGI; however, patients receiving amisulpride showed greater improvement |
| Muscatello et al, 2011d | 24-week, randomized, double-blind, placebo-controlled | 31 treatment-resistant schizophrenia patients receiving clozapine randomized to receive adjunctive aripiprazole or placebo | Aripiprazole showed beneficial effect on positive and general psychopathologic symptomatology, but no significant effects on executive cognitive function |
| Takahashi et al, 1999e | 8-week, randomized, single-blind, crossover | 10 neuroleptic-treated patients received add-on risperidone and mosapramine* | Both additions resulted in significant, yet modest, improvement; no significant difference in PANSS between risperidone and mosapramine |
| *Not available in the United States BPRS: Brief Psychiatric Rating Scale; CGI: Clinical Global Impression; PANSS: Positive and Negative Syndrome Scale; SANS: Scale for the Assessment of Negative Symptoms; SAPS: Scale for the Assessment of Positive Symptoms | |||
| Source: References a. Shiloh R, Zemishlany Z, Aizenberg D, et al. Sulpiride augmentation in people with schizophrenia partially responsive to clozapine. A double-blind, placebo-controlled study. Br J Psychiatry. 1997;171:569-573. b. Josiassen RC, Joseph A, Kohegyi E, et al. Clozapine augmented with risperidone in the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2005;162(1):130-136. c. Genç Y, Taner E, Candansayar S. Comparison of clozapine-amisulpride and clozapine-quetiapine combinations for patients with schizophrenia who are partially responsive to clozapine: a single-blind randomized study. Adv Ther. 2007;24(1):1-13. d. Muscatello MR, Bruno A, Pandolfo G, et al. Effect of aripiprazole augmentation of clozapine in schizophrenia: a double-blind, placebo-controlled study. Schizophr Res. 2011;127(1-3):93-99. e. Takahashi N, Terao T, Oga T, et al. Comparison of risperidone and mosapramine addition to neuroleptic treatment in chronic schizophrenia. Neuropsychobiology. 1999;39(2):81-85. | |||
What about augmentation?
Adjunctive non-antipsychotics also are commonly used when treating patients with chronic schizophrenia. For example, lithium and anticonvulsants are used in approximately one-half of all inpatients with schizophrenia in facilities operated by the State of New York Office of Mental Health.24,25 The evidence base for these agents as adjuncts to antipsychotics generally is weak.26 Specifically, early reports of benefit with adjunctive lithium have been negated by later studies. Similarly, large trials of adjunctive valproate and lamotrigine have failed to replicate early and promising efficacy signals from smaller trials, although the larger studies did not specifically target treatment-resistant schizophrenia.
Among mood stabilizers, lamotrigine may be the most promising for treatment-resistant schizophrenia. In a meta-analysis of clinical trials examining schizophrenia patients receiving clozapine (N=161) who were randomized to receive adjunctive lamotrigine or adjunctive placebo, lamotrigine was superior to placebo in total score for psychosis symptoms and scores for positive and negative symptoms.27
More than 125 published RCTs have studied a wide variety of adjunctive agents other than lithium or anticonvulsants for treating persistent schizophrenia symptoms (Table 2).
Only some of the approximately 40 RCTs regarding adjunctive antidepressants in patients with chronic schizophrenia focused on patients with ongoing depressive symptoms. For a bibliography of these studies, click here. In a meta-analysis measuring improvement of negative symptoms from 23 trials (N=819),28 the effect size was moderate in favor of antidepressants. Subgroup analysis revealed significant responses for fluoxetine, trazodone, and ritanserin.
More than 50 RCTs have focused on augmenting medications for cognitive dysfunction in chronic schizophrenia. Unfortunately, agents used to treat Alzheimer’s disease have shown disappointing results when tested in patients with schizophrenia, as have agents prescribed for attention-deficit/hyperactivity disorder (methylphenidate, guanfacine, atomoxetine) or agents used to promote alertness (modafinil and armodafinil).
Medications that act on glutamate receptors may offer another potential solution, although not in combination with clozapine.29
Other agents that require further study where ≥2 positive studies have been reported (with ≤2 negative studies) include celecoxib, neurosteroids and hormones, purinergic agents, serotonin 5-HT1A receptor agonists, and serotonin 5-HT3 receptor antagonists.
Table 2
Agents studied as adjuncts to antipsychotics
| Acetylsalicylic acid and nonsteroidal anti-inflammatory agents |
| Anticonvulsants and lithium |
| Antidepressants |
| Antiglucocorticoids |
| Agents used to treat attention-deficit/hyperactivity disorder |
| Beta blockers |
| Cholinesterase inhibitors and other agents used to treat Alzheimer’s disease |
| Experimental agents that act on glutamate receptors |
| GABAA receptor drugs |
| Neurosteroids and hormones |
| Omega-3 fatty acids |
| Opioid system agents |
| Peptides |
| Purinergic agents |
| Serotonin 5-HT1A receptor agonists |
| Serotonin 5-HT3 receptor antagonists |
| Wakefulness promoting agents |
Therapeutic neuromodulation
More than 10 RCTs of repetitive transcranial magnetic stimulation (rTMS) in patients with refractory symptoms of schizophrenia have been published; the results were mixed. For a bibliography of these studies, click here. In a meta-analysis of 9 trials (n=213),30 prefrontal rTMS for treating negative symptoms demonstrated a small-to-medium effect size. In another meta-analysis31 of all prospective studies of rTMS for negative symptoms and for auditory hallucinations and overall positive symptoms in refractory schizophrenia, the effect sizes showed moderate effects.
Fewer controlled trials are available for electroconvulsive therapy,32,33 but its use with clozapine appears encouraging.34
Psychological and behavioral intervention. Cognitive-behavioral therapy, although labor-intensive, can be helpful even in patients considered treatment-resistant (Table 3). These interventions generally are provided together with pharmacotherapy.
Complementary and alternative therapies. Patients and their families may ask about complementary and alternative therapies, particularly when conventional approaches have not been successful. A meta-analysis of 6 studies (n=828)35 that reviewed adjunctive use of ginkgo in patients with chronic schizophrenia found statistically significant moderate improvement in total and negative symptoms. Negative reports also are available, including a 5-month study of adjunctive megavitamins that did not demonstrate any benefits.36 In a review of 13 RCTs of acupuncture for schizophrenia, Lee et al found the overall methodological quality was too low to draw firm conclusions.37
Table 3
Cognitive-behavioral therapy for schizophrenia
| Study | Design | Patients | Results |
|---|---|---|---|
| Pinto et al, 1999a | 6-month, randomized controlled | 37 treatment-resistant schizophrenia patients were randomized to CBT plus social skills training or supportive therapy | Both groups showed statistically significant improvement on the BPRS, SAPS, and SANS; however, patients in the CBT group had lower BPRS and SAPS scores. No difference on SANS scores |
| Barretto et al, 2009b | 21-week, controlled (nonrandom-ized) | Patients refractory to clozapine were placed in a CBT or befriending control group | The CBT group showed significant improvement in PANSS total score and general psychopathology subscale score, as well as an improvement of QLS; improvement persisted at 6-month follow-up |
| BPRS: Brief Psychiatric Rating Scale; CBT: cognitive-behavioral therapy; PANSS: Positive and Negative Syndrome Scale; QLS: Quality of Life Scale; SANS: Scale for the Assessment of Negative Symptoms; SAPS: Scale for the Assessment of Positive Symptoms | |||
| Source: References a. Pinto A, La Pia S, Mennella R, et al. Cognitive-behavioral therapy and clozapine for clients with treatment-refractory schizophrenia. Psychiatr Serv. 1999;50(7):901-904. b. Barretto EM, Kayo M, Avrichir BS, et al. A preliminary controlled trial of cognitive behavioral therapy in clozapine-resistant schizophrenia. J Nerv Ment Dis. 2009;197(11):865-868. | |||
Clinical recommendations
Before declaring a patient with schizophrenia as treatment-resistant, ensure that an adequate trial of medication did take place. This includes consideration of adequate dosing and pharmacokinetic issues. Awareness of potential substance use and/or partial adherence or nonadherence also is critical because these factors can impact treatment response.
When prescribing for a treatment-resistant schizophrenia patient, identify specific target symptoms to better inform medication selection—especially for symptoms that the patient feels are important. For example, consider an antidepressant for patients who have negative or depressive symptoms. Also take into account other patient-centered concerns, such as tolerability issues that may have interfered with adherence and response in the past.
Clozapine remains the medication of choice for treatment-resistant schizophrenia. Despite dozens of RCTs of potential adjunctive agents for treatment-resistant schizophrenia, no single approach has consistently shown efficacy in reducing symptoms, improving cognition, or increasing a patient’s level of function. Individual response can vary, and our search for the “outlier” who does respond to an adjunctive agent can explain our use of these strategies in clinical practice.
Related Resources
- Cochrane Database of Systematic Reviews. www.cochrane.org/reviews. This database contains reviews of additional therapeutic options for patients with treatment-resistant schizophrenia. As of February 23, 2011, 157 reviews were available.
- Citrome L. Treatment-refractory schizophrenia: What it is and what’s been done about it. Neuropsychiatry. 2011. Epub ahead of print.
- Citrome L. Clozapine for schizophrenia. Life-threatening or life-saving treatment? Current Psychiatry. 2009;8(12):56-63.
Drug Brand Names
- Aripiprazole • Abilify
- Armodafinil • Nuvigil
- Atomoxetine • Strattera
- Benztropine mesylate • Cogentin
- Carbamazepine • Tegretol
- Celecoxib • Celebrex
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluoxetine • Prozac
- Guanfacine • Tenex
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid, others
- Lurasidone • Latuda
- Methylphenidate • Ritalin, Methylin, others
- Modafinil • Provigil
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Rifampin • Rifadin
- Risperidone • Risperdal
- Trazodone • Desyrel, Oleptro
- Valproate (Divalproex) • Depakote, Depakote ER
- Ziprasidone • Geodon
Disclosure
No writing assistance or external financial support was used for this article. Dr. Citrome is a consultant for, has received honoraria from, or has conducted clinical research supported by Abbott Laboratories, AstraZeneca Pharmaceuticals, Avanir Pharmaceuticals, Azur Pharma Inc., Barr Laboratories, Bristol-Myers Squibb, Eli Lilly and Company, Forest Research Institute, GlaxoSmithKline, Janssen Pharmaceuticals, Jazz Pharmaceuticals, Merck, Novartis, Pfizer Inc., Sunovion, Valeant Pharmaceuticals, and Vanda Pharmaceuticals.
Discuss this article at www.facebook.com/CurrentPsychiatry
Patients with treatment-resistant schizophrenia can be broadly defined to include any persons with residual symptoms that cause distress or impairment despite several treatment attempts. Unfortunately, this definition may include most of our patients with schizophrenia.
Clinical trial data on treatment-resistant schizophrenia can be contradictory, leaving “N of 1” empirical treatment trials for individual patients as the current state of the art. This article presents data from clinical trials for pharmacologic and nonpharmacologic options and offers recommendations to try to help our treatment-resistant patients.
Defining treatment resistance
Research reports regarding treatment-resistant or treatment-refractory schizophrenia have relied on operational criteria such as that found in the pivotal study for clozapine1:
- at least 3 periods of treatment in the preceding 5 years with neuroleptic agents from at least 2 different chemical classes at dosages equivalent to ≥1000 mg/d of chlorpromazine for 6 weeks, each without significant symptomatic relief, and
- no period of good functioning within the preceding 5 years.1 In that study, patients also underwent a prospective treatment trial with what we now know are high doses of haloperidol (up to 60 mg/d or higher) and benztropine mesylate (6 mg/d) for a period of 6 weeks to confirm lack of drug responsiveness. Other studies have more relaxed criteria, such as:
- persistent positive symptoms—hallucinations, delusions, or marked thought disorder—after at least 6 contiguous weeks of past or present treatment, with ≥1 typical antipsychotics at doses of ≥600 mg/d in chlorpromazine equivalents
- a poor level of functioning over the past 2 years, as defined by the lack of competitive employment or enrollment in an academic or vocational program and not having age-expected interpersonal relations with someone outside the biologic family with whom ongoing regular contacts were maintained.2
In this study, no prospective period of treatment to confirm lack of drug responsiveness was required.
The most clinically relevant definition of treatment resistance depends on the patient’s individual circumstances. For some patients, targeting positive symptoms is a high priority; for others it may be negative and cognitive symptoms; for others, it may be excitement. Moreover, families may complain of symptoms or behavior that are of little or no concern to your patient.
Although we desire treatment response and remission for our patients, definitions for remission and functional recovery are in flux. Proposed criteria define symptomatic remission as 6-month maintenance of simultaneous ratings of mild or less on delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms.3,4 Emsley et al4 note that reported remission rates vary widely across studies (17% to 88%) and that patients in remission do better than their non-remitted counterparts in several other outcome domains. Also, patients move in and out of remission over time. Predictors of remission include:
- early treatment response
- baseline symptom severity
- subjective well-being.4
Recovery is a more complex construct than remission and includes social outcomes. Although recovery lacks a standard definition, it is the implied goal of treatment. Anything short of recovery can be viewed as inadequate. If we set the bar at this height, many or most of the patients we treat for schizophrenia could be considered treatment-resistant.
Confounding factors
Before concluding that a patient is treatment-resistant, address medication adherence and possible substance use. Partial or nonadherence with antipsychotic treatment is common—approximately one-half of patients are nonadherent5—and associated with relapse and re-hospitalization.6 In addition, an estimated one-half of all individuals with schizophrenia also use substances.7
Be aware of the optimal dose for any particular antipsychotic and factors that can interfere with achieving adequate plasma levels. This means acknowledging that dosing ranges established during registration studies may not reflect the needs of day-to-day clinical practice.8 Pharmacokinetic interactions with other medications, such as carbamazepine or rifampin, can induce liver enzymes and result in subtherapeutic antipsychotic levels. Cigarette smoking also may have this effect. Lowered clozapine or olanzapine plasma levels have been observed in patients who resume smoking after being discharged from a non-smoking inpatient environment. Some antipsychotics, such as ziprasidone and lurasidone, must be taken with food in order to have sufficient bioavailability.9
What does a patient want?
Patients with schizophrenia often have limited insight into their psychotic symptoms.10 Savvy clinicians will attempt to leverage a patient’s insight into ancillary symptoms—such as impaired sleep, anxiety, and dysphoria—to encourage a therapeutic alliance and therefore adherence. If patients feel their concerns are not addressed, they may consider treatment inadequate even though the intensity of their hallucinations and delusions may have decreased.
Which antipsychotic is best?
Meta-analyses of randomized controlled trials (RCTs) of antipsychotic treatment for schizophrenia found that, although individual response will vary, clozapine generally has better efficacy that other antipsychotics.11-13 Olanzapine, risperidone, and amisulpride (which is not available in the United States) appear to be more efficacious than first-generation antipsychotics. Other second-generation antipsychotics do not consistently show greater efficacy than first-generation antipsychotics, although their tolerability profiles vary greatly.11-13
Antipsychotic monotherapy. More than 25 RCTs have focused on antipsychotic monotherapy for treatment-resistant patients; for a bibliography of these studies, click here. For the most part, clozapine has consistently demonstrated superiority over comparators. Because not all patients with schizophrenia can tolerate clozapine or are willing to have their blood monitored as required, other second-generation antipsychotics have been suggested as possible substitutes. Olanzapine has established superior efficacy to first-generation antipsychotics11-13 and perhaps comparable efficacy to clozapine in some studies.2,14-17 Risperidone appeared to be comparable to clozapine in some studies,18,19 whereas clozapine’s superiority was evident in others.14,20,21 Although an RCT found comparable efficacy for ziprasidone vs clozapine,22 patients enrolled in this study may not have been treatment-resistant regarding efficacy but instead could not tolerate prior treatments. Enrolling patients on the basis of poor efficacy and/or poor tolerability to their prior antipsychotic regimen also has complicated the interpretation of studies comparing olanzapine with clozapine16 and risperidone with clozapine.18
Antipsychotic combinations. Combinations of antipsychotics are used commonly when treating chronic schizophrenia.23 Of the approximately 20 RCTs of antipsychotic combination therapy, most tested clozapine combined with other second-generation antipsychotics, such as risperidone. For a bibliography of these studies, click here. Only 5 studies support a combination approach (Table 1).
Table 1
Antipsychotic combinations: Few studies support efficacy
| Study | Design | Patients | Results |
|---|---|---|---|
| Shiloh et al, 1997a | 10-week, double-blind, placebo-controlled | 28 patients nonresponsive to typical antipsychotics and partially responsive to clozapine received add-on sulpiride,* 600 mg/d, or placebo | The sulpiride group showed improvements in positive and negative symptoms |
| Josiassen et al, 2005b | 12-week, randomized, double-blind, placebo-controlled | 40 schizophrenia patients unresponsive or partially responsive to clozapine randomized to clozapine + placebo or clozapine + risperidone, 6 mg/d | Mean BPRS total and positive symptom subscale scores reduced in both groups but reductions were greater in the clozapine/risperidone group; reduction in SANS also was observed in the clozapine/risperidone group |
| Genç et al, 2007c | 8-week, randomized, single-blind | 56 treatment-resistant schizophrenia patients randomly assigned to clozapine + amisulpride* or clozapine + quetiapine | Both groups improved at week 8 as measured by BPRS, SANS, SAPS, and CGI; however, patients receiving amisulpride showed greater improvement |
| Muscatello et al, 2011d | 24-week, randomized, double-blind, placebo-controlled | 31 treatment-resistant schizophrenia patients receiving clozapine randomized to receive adjunctive aripiprazole or placebo | Aripiprazole showed beneficial effect on positive and general psychopathologic symptomatology, but no significant effects on executive cognitive function |
| Takahashi et al, 1999e | 8-week, randomized, single-blind, crossover | 10 neuroleptic-treated patients received add-on risperidone and mosapramine* | Both additions resulted in significant, yet modest, improvement; no significant difference in PANSS between risperidone and mosapramine |
| *Not available in the United States BPRS: Brief Psychiatric Rating Scale; CGI: Clinical Global Impression; PANSS: Positive and Negative Syndrome Scale; SANS: Scale for the Assessment of Negative Symptoms; SAPS: Scale for the Assessment of Positive Symptoms | |||
| Source: References a. Shiloh R, Zemishlany Z, Aizenberg D, et al. Sulpiride augmentation in people with schizophrenia partially responsive to clozapine. A double-blind, placebo-controlled study. Br J Psychiatry. 1997;171:569-573. b. Josiassen RC, Joseph A, Kohegyi E, et al. Clozapine augmented with risperidone in the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2005;162(1):130-136. c. Genç Y, Taner E, Candansayar S. Comparison of clozapine-amisulpride and clozapine-quetiapine combinations for patients with schizophrenia who are partially responsive to clozapine: a single-blind randomized study. Adv Ther. 2007;24(1):1-13. d. Muscatello MR, Bruno A, Pandolfo G, et al. Effect of aripiprazole augmentation of clozapine in schizophrenia: a double-blind, placebo-controlled study. Schizophr Res. 2011;127(1-3):93-99. e. Takahashi N, Terao T, Oga T, et al. Comparison of risperidone and mosapramine addition to neuroleptic treatment in chronic schizophrenia. Neuropsychobiology. 1999;39(2):81-85. | |||
What about augmentation?
Adjunctive non-antipsychotics also are commonly used when treating patients with chronic schizophrenia. For example, lithium and anticonvulsants are used in approximately one-half of all inpatients with schizophrenia in facilities operated by the State of New York Office of Mental Health.24,25 The evidence base for these agents as adjuncts to antipsychotics generally is weak.26 Specifically, early reports of benefit with adjunctive lithium have been negated by later studies. Similarly, large trials of adjunctive valproate and lamotrigine have failed to replicate early and promising efficacy signals from smaller trials, although the larger studies did not specifically target treatment-resistant schizophrenia.
Among mood stabilizers, lamotrigine may be the most promising for treatment-resistant schizophrenia. In a meta-analysis of clinical trials examining schizophrenia patients receiving clozapine (N=161) who were randomized to receive adjunctive lamotrigine or adjunctive placebo, lamotrigine was superior to placebo in total score for psychosis symptoms and scores for positive and negative symptoms.27
More than 125 published RCTs have studied a wide variety of adjunctive agents other than lithium or anticonvulsants for treating persistent schizophrenia symptoms (Table 2).
Only some of the approximately 40 RCTs regarding adjunctive antidepressants in patients with chronic schizophrenia focused on patients with ongoing depressive symptoms. For a bibliography of these studies, click here. In a meta-analysis measuring improvement of negative symptoms from 23 trials (N=819),28 the effect size was moderate in favor of antidepressants. Subgroup analysis revealed significant responses for fluoxetine, trazodone, and ritanserin.
More than 50 RCTs have focused on augmenting medications for cognitive dysfunction in chronic schizophrenia. Unfortunately, agents used to treat Alzheimer’s disease have shown disappointing results when tested in patients with schizophrenia, as have agents prescribed for attention-deficit/hyperactivity disorder (methylphenidate, guanfacine, atomoxetine) or agents used to promote alertness (modafinil and armodafinil).
Medications that act on glutamate receptors may offer another potential solution, although not in combination with clozapine.29
Other agents that require further study where ≥2 positive studies have been reported (with ≤2 negative studies) include celecoxib, neurosteroids and hormones, purinergic agents, serotonin 5-HT1A receptor agonists, and serotonin 5-HT3 receptor antagonists.
Table 2
Agents studied as adjuncts to antipsychotics
| Acetylsalicylic acid and nonsteroidal anti-inflammatory agents |
| Anticonvulsants and lithium |
| Antidepressants |
| Antiglucocorticoids |
| Agents used to treat attention-deficit/hyperactivity disorder |
| Beta blockers |
| Cholinesterase inhibitors and other agents used to treat Alzheimer’s disease |
| Experimental agents that act on glutamate receptors |
| GABAA receptor drugs |
| Neurosteroids and hormones |
| Omega-3 fatty acids |
| Opioid system agents |
| Peptides |
| Purinergic agents |
| Serotonin 5-HT1A receptor agonists |
| Serotonin 5-HT3 receptor antagonists |
| Wakefulness promoting agents |
Therapeutic neuromodulation
More than 10 RCTs of repetitive transcranial magnetic stimulation (rTMS) in patients with refractory symptoms of schizophrenia have been published; the results were mixed. For a bibliography of these studies, click here. In a meta-analysis of 9 trials (n=213),30 prefrontal rTMS for treating negative symptoms demonstrated a small-to-medium effect size. In another meta-analysis31 of all prospective studies of rTMS for negative symptoms and for auditory hallucinations and overall positive symptoms in refractory schizophrenia, the effect sizes showed moderate effects.
Fewer controlled trials are available for electroconvulsive therapy,32,33 but its use with clozapine appears encouraging.34
Psychological and behavioral intervention. Cognitive-behavioral therapy, although labor-intensive, can be helpful even in patients considered treatment-resistant (Table 3). These interventions generally are provided together with pharmacotherapy.
Complementary and alternative therapies. Patients and their families may ask about complementary and alternative therapies, particularly when conventional approaches have not been successful. A meta-analysis of 6 studies (n=828)35 that reviewed adjunctive use of ginkgo in patients with chronic schizophrenia found statistically significant moderate improvement in total and negative symptoms. Negative reports also are available, including a 5-month study of adjunctive megavitamins that did not demonstrate any benefits.36 In a review of 13 RCTs of acupuncture for schizophrenia, Lee et al found the overall methodological quality was too low to draw firm conclusions.37
Table 3
Cognitive-behavioral therapy for schizophrenia
| Study | Design | Patients | Results |
|---|---|---|---|
| Pinto et al, 1999a | 6-month, randomized controlled | 37 treatment-resistant schizophrenia patients were randomized to CBT plus social skills training or supportive therapy | Both groups showed statistically significant improvement on the BPRS, SAPS, and SANS; however, patients in the CBT group had lower BPRS and SAPS scores. No difference on SANS scores |
| Barretto et al, 2009b | 21-week, controlled (nonrandom-ized) | Patients refractory to clozapine were placed in a CBT or befriending control group | The CBT group showed significant improvement in PANSS total score and general psychopathology subscale score, as well as an improvement of QLS; improvement persisted at 6-month follow-up |
| BPRS: Brief Psychiatric Rating Scale; CBT: cognitive-behavioral therapy; PANSS: Positive and Negative Syndrome Scale; QLS: Quality of Life Scale; SANS: Scale for the Assessment of Negative Symptoms; SAPS: Scale for the Assessment of Positive Symptoms | |||
| Source: References a. Pinto A, La Pia S, Mennella R, et al. Cognitive-behavioral therapy and clozapine for clients with treatment-refractory schizophrenia. Psychiatr Serv. 1999;50(7):901-904. b. Barretto EM, Kayo M, Avrichir BS, et al. A preliminary controlled trial of cognitive behavioral therapy in clozapine-resistant schizophrenia. J Nerv Ment Dis. 2009;197(11):865-868. | |||
Clinical recommendations
Before declaring a patient with schizophrenia as treatment-resistant, ensure that an adequate trial of medication did take place. This includes consideration of adequate dosing and pharmacokinetic issues. Awareness of potential substance use and/or partial adherence or nonadherence also is critical because these factors can impact treatment response.
When prescribing for a treatment-resistant schizophrenia patient, identify specific target symptoms to better inform medication selection—especially for symptoms that the patient feels are important. For example, consider an antidepressant for patients who have negative or depressive symptoms. Also take into account other patient-centered concerns, such as tolerability issues that may have interfered with adherence and response in the past.
Clozapine remains the medication of choice for treatment-resistant schizophrenia. Despite dozens of RCTs of potential adjunctive agents for treatment-resistant schizophrenia, no single approach has consistently shown efficacy in reducing symptoms, improving cognition, or increasing a patient’s level of function. Individual response can vary, and our search for the “outlier” who does respond to an adjunctive agent can explain our use of these strategies in clinical practice.
Related Resources
- Cochrane Database of Systematic Reviews. www.cochrane.org/reviews. This database contains reviews of additional therapeutic options for patients with treatment-resistant schizophrenia. As of February 23, 2011, 157 reviews were available.
- Citrome L. Treatment-refractory schizophrenia: What it is and what’s been done about it. Neuropsychiatry. 2011. Epub ahead of print.
- Citrome L. Clozapine for schizophrenia. Life-threatening or life-saving treatment? Current Psychiatry. 2009;8(12):56-63.
Drug Brand Names
- Aripiprazole • Abilify
- Armodafinil • Nuvigil
- Atomoxetine • Strattera
- Benztropine mesylate • Cogentin
- Carbamazepine • Tegretol
- Celecoxib • Celebrex
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluoxetine • Prozac
- Guanfacine • Tenex
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid, others
- Lurasidone • Latuda
- Methylphenidate • Ritalin, Methylin, others
- Modafinil • Provigil
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Rifampin • Rifadin
- Risperidone • Risperdal
- Trazodone • Desyrel, Oleptro
- Valproate (Divalproex) • Depakote, Depakote ER
- Ziprasidone • Geodon
Disclosure
No writing assistance or external financial support was used for this article. Dr. Citrome is a consultant for, has received honoraria from, or has conducted clinical research supported by Abbott Laboratories, AstraZeneca Pharmaceuticals, Avanir Pharmaceuticals, Azur Pharma Inc., Barr Laboratories, Bristol-Myers Squibb, Eli Lilly and Company, Forest Research Institute, GlaxoSmithKline, Janssen Pharmaceuticals, Jazz Pharmaceuticals, Merck, Novartis, Pfizer Inc., Sunovion, Valeant Pharmaceuticals, and Vanda Pharmaceuticals.
1. Kane J, Honigfeld G, Singer J, et al. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988;45(9):789-796.
2. Volavka J, Czobor P, Sheitman B, et al. Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry. 2002;159(2):255-262.
3. Andreasen NC, Carpenter WT Jr, Kane JM, et al. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162(3):441-449.
4. Emsley R, Chiliza B, Asmal L, et al. The concepts of remission and recovery in schizophrenia. Curr Opin Psychiatry. 2011;24(2):114-121.
5. Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892-909.
6. Robinson DG, Woerner MG, Delman HM, et al. Pharmacological treatments for first-episode schizophrenia. Schizophr Bull. 2005;31(3):705-722.
7. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
8. Citrome L, Volavka J. Optimal dosing of atypical antipsychotics in adults: a review of the current evidence. Harv Rev Psychiatry. 2002;10(5):280-291.
9. Citrome L. Iloperidone asenapine and lurasidone. A brief overview of three new second-generation antipsychotics. Postgrad Med. 2011;123(2):153-162.
10. Lincoln TM, Lüllmann E, Rief W. Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr Bull. 2007;33(6):1324-1342.
11. Leucht S, Corves C, Arbter D, et al. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373(9657):31-41.
12. Leucht S, Komossa K, Rummel-Kluge C, et al. A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. 2009;166(2):152-163.
13. Leucht S, Arbter D, Engel RR, et al. How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials. Mol Psychiatry. 2009;14(4):429-447.
14. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610.
15. Tollefson GD, Birkett MA, Kiesler GM, et al. Double-blind comparison of olanzapine versus clozapine in schizophrenic patients clinically eligible for treatment with clozapine. Biol Psychiatry. 2001;49(1):52-63.
16. Bitter I, Dossenbach MR, Brook S, et al. Olanzapine versus clozapine in treatment-resistant or treatment-intolerant schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28(1):173-180.
17. Meltzer HY, Bobo WV, Roy A, et al. A randomized, double-blind comparison of clozapine and high-dose olanzapine in treatment-resistant patients with schizophrenia. J Clin Psychiatry. 2008;69(2):274-285.
18. Bondolfi G, Dufour H, Patris M, et al. Risperidone versus clozapine in treatment-resistant chronic schizophrenia: a randomized double-blind study. Am J Psychiatry. 1998;155(4):499-504.
19. Wahlbeck K, Cheine M, Tuisku K, et al. Risperidone versus clozapine in treatment-resistant schizophrenia: a randomized pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2000;24(6):911-922.
20. Breier AF, Malhotra AK, Su TP, et al. Clozapine and risperidone in chronic schizophrenia: effects on symptoms, parkinsonian side effects, and neuroendocrine response. Am J Psychiatry. 1999;156(2):294-298.
21. Azorin JM, Spiegel R, Remington G, et al. A double-blind comparative study of clozapine and risperidone in the management of severe chronic schizophrenia. Am J Psychiatry. 2001;158(8):1305-1313.
22. Sacchetti E, Galluzzo A, Valsecchi P, et al. Ziprasidone vs clozapine in schizophrenia patients refractory to multiple antipsychotic treatments: the MOZART study. Schizophr Res. 2009;113(1):112-121.
23. Jaffe AB, Levine J. Antipsychotic medication coprescribing in a large state hospital system. Pharmacoepidemiol Drug Saf. 2003;12(1):41-48.
24. Citrome L, Levine J, Allingham B. Changes in use of valproate and other mood stabilizers for patients with schizophrenia from 1994 to 1998. Psychiatr Serv. 2000;51(5):634-638.
25. Citrome L, Jaffe A, Levine J, et al. Use of mood stabilizers among patients with schizophrenia, 1994-2001. Psychiatr Serv. 2002;53(10):1212.-
26. Citrome L. Adjunctive lithium and anticonvulsants for the treatment of schizophrenia: what is the evidence? Expert Rev Neurother. 2009;9(1):55-71.
27. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2009;109(1-3):10-14.
28. Singh SP, Singh V, Kar N, et al. Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: meta-analysis. Br J Psychiatry. 2010;197(3):174-179.
29. Kantrowitz JT, Javitt DC. Thinking glutamatergically: changing concepts of schizophrenia based upon changing neurochemical models. Clin Schizophr Relat Psychoses. 2010;4(3):189-200.
30. Dlabac-de Lange JJ, Knegtering R, Aleman A, et al. Repetitive transcranial magnetic stimulation for negative symptoms of schizophrenia: review and meta-analysis. J Clin Psychiatry. 2010;71(4):411-418.
31. Freitas C, Fregni F, Pascual-Leone A. Meta-analysis of the effects of repetitive transcranial magnetic stimulation (rTMS) on negative and positive symptoms in schizophrenia. Schizophr Res. 2009;108(1-3):11-24.
32. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15(3):178-192.
33. Goswami U, Kumar U, Singh B. Efficacy of electroconvulsive therapy in treatment resistant schizophrenia: a double-blind study. Indian J Psychiatry. 2003;45(1):26-29.
34. Braga RJ, Petrides G. The combined use of electroconvulsive therapy and antipsychotics in patients with schizophrenia. J ECT. 2005;21(2):75-83.
35. Singh V, Singh SP, Chan K. Review and meta-analysis of usage of ginkgo as an adjunct therapy in chronic schizophrenia. Int J Neuropsychopharmacol. 2010;13(2):257-271.
36. Vaughan K, McConaghy N. Megavitamin and dietary treatment in schizophrenia: a randomised controlled trial. Aust N Z J Psychiatry. 1999;33(1):84-88.
37. Lee MS, Shin BC, Ronan P, et al. Acupuncture for schizophrenia: a systematic review and meta-analysis. Int J Clin Pract. 2009;63(11):1622-1633.
1. Kane J, Honigfeld G, Singer J, et al. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988;45(9):789-796.
2. Volavka J, Czobor P, Sheitman B, et al. Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry. 2002;159(2):255-262.
3. Andreasen NC, Carpenter WT Jr, Kane JM, et al. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162(3):441-449.
4. Emsley R, Chiliza B, Asmal L, et al. The concepts of remission and recovery in schizophrenia. Curr Opin Psychiatry. 2011;24(2):114-121.
5. Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892-909.
6. Robinson DG, Woerner MG, Delman HM, et al. Pharmacological treatments for first-episode schizophrenia. Schizophr Bull. 2005;31(3):705-722.
7. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
8. Citrome L, Volavka J. Optimal dosing of atypical antipsychotics in adults: a review of the current evidence. Harv Rev Psychiatry. 2002;10(5):280-291.
9. Citrome L. Iloperidone asenapine and lurasidone. A brief overview of three new second-generation antipsychotics. Postgrad Med. 2011;123(2):153-162.
10. Lincoln TM, Lüllmann E, Rief W. Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr Bull. 2007;33(6):1324-1342.
11. Leucht S, Corves C, Arbter D, et al. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373(9657):31-41.
12. Leucht S, Komossa K, Rummel-Kluge C, et al. A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. 2009;166(2):152-163.
13. Leucht S, Arbter D, Engel RR, et al. How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials. Mol Psychiatry. 2009;14(4):429-447.
14. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610.
15. Tollefson GD, Birkett MA, Kiesler GM, et al. Double-blind comparison of olanzapine versus clozapine in schizophrenic patients clinically eligible for treatment with clozapine. Biol Psychiatry. 2001;49(1):52-63.
16. Bitter I, Dossenbach MR, Brook S, et al. Olanzapine versus clozapine in treatment-resistant or treatment-intolerant schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28(1):173-180.
17. Meltzer HY, Bobo WV, Roy A, et al. A randomized, double-blind comparison of clozapine and high-dose olanzapine in treatment-resistant patients with schizophrenia. J Clin Psychiatry. 2008;69(2):274-285.
18. Bondolfi G, Dufour H, Patris M, et al. Risperidone versus clozapine in treatment-resistant chronic schizophrenia: a randomized double-blind study. Am J Psychiatry. 1998;155(4):499-504.
19. Wahlbeck K, Cheine M, Tuisku K, et al. Risperidone versus clozapine in treatment-resistant schizophrenia: a randomized pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2000;24(6):911-922.
20. Breier AF, Malhotra AK, Su TP, et al. Clozapine and risperidone in chronic schizophrenia: effects on symptoms, parkinsonian side effects, and neuroendocrine response. Am J Psychiatry. 1999;156(2):294-298.
21. Azorin JM, Spiegel R, Remington G, et al. A double-blind comparative study of clozapine and risperidone in the management of severe chronic schizophrenia. Am J Psychiatry. 2001;158(8):1305-1313.
22. Sacchetti E, Galluzzo A, Valsecchi P, et al. Ziprasidone vs clozapine in schizophrenia patients refractory to multiple antipsychotic treatments: the MOZART study. Schizophr Res. 2009;113(1):112-121.
23. Jaffe AB, Levine J. Antipsychotic medication coprescribing in a large state hospital system. Pharmacoepidemiol Drug Saf. 2003;12(1):41-48.
24. Citrome L, Levine J, Allingham B. Changes in use of valproate and other mood stabilizers for patients with schizophrenia from 1994 to 1998. Psychiatr Serv. 2000;51(5):634-638.
25. Citrome L, Jaffe A, Levine J, et al. Use of mood stabilizers among patients with schizophrenia, 1994-2001. Psychiatr Serv. 2002;53(10):1212.-
26. Citrome L. Adjunctive lithium and anticonvulsants for the treatment of schizophrenia: what is the evidence? Expert Rev Neurother. 2009;9(1):55-71.
27. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2009;109(1-3):10-14.
28. Singh SP, Singh V, Kar N, et al. Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: meta-analysis. Br J Psychiatry. 2010;197(3):174-179.
29. Kantrowitz JT, Javitt DC. Thinking glutamatergically: changing concepts of schizophrenia based upon changing neurochemical models. Clin Schizophr Relat Psychoses. 2010;4(3):189-200.
30. Dlabac-de Lange JJ, Knegtering R, Aleman A, et al. Repetitive transcranial magnetic stimulation for negative symptoms of schizophrenia: review and meta-analysis. J Clin Psychiatry. 2010;71(4):411-418.
31. Freitas C, Fregni F, Pascual-Leone A. Meta-analysis of the effects of repetitive transcranial magnetic stimulation (rTMS) on negative and positive symptoms in schizophrenia. Schizophr Res. 2009;108(1-3):11-24.
32. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15(3):178-192.
33. Goswami U, Kumar U, Singh B. Efficacy of electroconvulsive therapy in treatment resistant schizophrenia: a double-blind study. Indian J Psychiatry. 2003;45(1):26-29.
34. Braga RJ, Petrides G. The combined use of electroconvulsive therapy and antipsychotics in patients with schizophrenia. J ECT. 2005;21(2):75-83.
35. Singh V, Singh SP, Chan K. Review and meta-analysis of usage of ginkgo as an adjunct therapy in chronic schizophrenia. Int J Neuropsychopharmacol. 2010;13(2):257-271.
36. Vaughan K, McConaghy N. Megavitamin and dietary treatment in schizophrenia: a randomised controlled trial. Aust N Z J Psychiatry. 1999;33(1):84-88.
37. Lee MS, Shin BC, Ronan P, et al. Acupuncture for schizophrenia: a systematic review and meta-analysis. Int J Clin Pract. 2009;63(11):1622-1633.
Does your patient have a psychiatric illness or nonverbal learning disorder?
Discuss this article at www.facebook.com/CurrentPsychiatry
Patients who present with impairment in academic, cognitive, social, and vocational functioning might be struggling with an unrecognized learning disorder. Ten percent of the US population has some form of learning disability, and up to 40% of those with learning disorders may meet diagnostic criteria for a psychiatric disorder.1,2 Some learning disorders affect a person’s ability to read, write, or do math, whereas less-recognized nonverbal learning disorder (NLD) impacts the social and emotional functioning of children, adolescents, and adults. Common features of NLD include:
- deficits in nonlinguistic information processing
- speech prosody deficits
- difficulty reading facial expressions
- associated impairment in interpersonal functioning.
The severity of these deficits varies among individuals with NLD. Patients may experience chronic low self-esteem, anxiety, and mood symptoms because of their limited ability to express their feelings within an appropriate social context. NLD may be first misdiagnosed as attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or Asperger’s disorder.
In this article we review the underlying neurophysiology of NLD and present a clinical approach to these patients, including the differential diagnosis and factors that will allow clinicians to distinguish NLD from psychiatric conditions with symptomatic and syndromic overlap. We also describe treatment for patients with NLD.
The learning process
Learning is a cognitive process of acquiring and processing information and experiences from the environment that allows us to acquire knowledge, skills, and social abilities. When we learn how to relate to others, we undergo neurophysiologic changes that subsequently influence behavior and the way we understand our environment. Deficits in learning processes or the ability to acquire relational skills result in impaired affect regulation in regard to others and may lead to low self-esteem, depression, anxiety, interpersonal conflict, and anger toward others. Learning influences a person’s ability to navigate social relationships and perform academically and occupationally.
The impact of learning deficits may be magnified in adulthood after an individual has suffered years of in-securities and poor self-esteem. Adults with learning disabilities often seek psychiatric treatment as a result of their disappointment about difficulties in relationships and work. NLD may coexist with or mimic other neuropsychiatric disorders. For example, problematic behavior within a family or at the workplace is a common reason for referral to a psychiatrist. These behaviors may be influenced by a patient’s NLD symptoms, which can complicate diagnosis and treatment.
Persons with NLD are at increased risk for depression because of failures in coping, loss of self-esteem, internalized psychopathology, and other social and emotional strains. In addition, individuals with NLD may experience multiple psychosocial impairments, including difficulty maintaining employment, achieving goals, and maintaining relationships.3
A variable presentation
NLD has been associated with right hemispheric dysfunction.3 For a description of the neurophysiology of NLD, see this article at CurrentPsychiatry.com. In childhood, NLD may present as deficits in:
- processing nonlinguistic information
- expressing or comprehending nonverbal components of language such as pitch, volume, or rate of speech (aprosodia)
- reading facial expressions
- social or emotional functioning, such as difficulty understanding social situations, violations of personal space, or difficulty learning from past emotional experiences.4
The extent of these deficits varies among patients. As children, patients with NLD often show strengths in rote verbal memory, spoken language mechanics or form, and word reading. These children may be hyperverbal and use language at a level higher than expected for their age group, which may mask some learning difficulties and delay diagnosis.
Throughout life, NLD manifests as difficulty interacting with peers. Children with NLD may have difficulty playing with others and making friends and as result may feel socially isolated. Without the critical skills of social reciprocity or understanding social context, NLD patients often have many superficial friendships but lack deep relationships.4,5
Patients with NLD may rely on their verbal skills for relating socially and relieving anxiety and tend to withdraw from social situations as they become aware of their deficits.
NLD can be characterized on the basis of primary, secondary, and tertiary deficits. Primary deficits in tactile and visual perception and complex psychomotor skills lead to secondary deficits in attention and exploratory behavior, which lead to tertiary deficits in memory and executive function.6
Given NLD’s variable presentation, clinicians must remain vigilant to this possible diagnosis in patients with a history of multiple pharmacotherapy or psychotherapy failures for axis I disorders. Using clues from symptoms described in Table 17 may provide information necessary to refer for formal psychoeducational testing to diagnose NLD. Early diagnosis can help target NLD symptoms and tailor treatment of comorbid psychopathology.7 NLD is a chronic disability and—similar to other learning disabilities—early, targeted interventions initiated by parents, teachers, and clinicians can improve outcomes.
Neuropsychological/psychoeducational testing. Traditionally, clinicians suspected NLD if a patient had a ≥10 point difference between performance intelligence quotient (IQ) and verbal IQ on the Wechsler Intelligence Scale for Children (WISC-III).8 However, the most recent version—the WISC-IV9—incorporates changes based on new neurologic models of cognitive functioning, and performance IQ and verbal IQ are no longer calculated. Thus, interpreting this split in IQ type with regard to NLD is no longer straightforward. IQ tests, such as the Woodcock-Johnson10 battery, which assesses visual-spatial thinking and fluid reasoning, may be particularly important in characterizing NLD deficits—especially when used in conjunction with other neuropsychological batteries, which may directly assess discrete abilities related to visual and spatial processing.
A thorough social and educational history, IQ testing, neuropsychological batteries, and a psychoeducational assessment can help determine the extent of cognitive deficits that may require accommodations at school or work and characterize the complex interplay of specific deficits and functioning.
Table 1
Clinical manifestation of nonverbal learning disorder
| Tactile-perceptual deficits and psychomotor coordination deficiencies, usually more marked on the left side |
| Visual-spatial organization deficits |
| Deficiencies in nonverbal problem solving, such as hypothesis testing and understanding cause-effect relationships |
| Difficulty adapting to novel situations and reliance on rote behaviors |
| Relative deficiencies in mechanical arithmetic with proficiencies in reading, word recognition, and spelling |
| Well developed rote verbal-memory skills |
| Verbosity characterized by poor pragmatics |
| Deficits in social perception, judgment, and interaction |
| Source: Reference 7 |
Differential diagnosis
ADHD. Patients diagnosed with ADHD or NLD may have a history of attention difficulties and hyperactivity. These clinical similarities may include restlessness, distractibility, impulsivity, and poor attention (Table 2).11,12 In adults, these features may attenuate and patients with NLD or ADHD could appear normoactive. Individuals with NLD demonstrate withdrawal, anxiety, and continued social skills deficits,13 whereas adult ADHD patients show persistent attention difficulties. Although both groups may have difficulty maintaining steady employment, NLD patients’ employment failures often are caused by cognitive and social difficulties as opposed to problems with attention.
The psychopathology of these 2 conditions differs in that ADHD is characterized primarily by prefrontal dysfunction.14 However, in a small study of children with NLD (N=20), all participants also met diagnostic criteria for ADHD; therefore, the true epidemiologic comorbidity is unknown.15
BD. Because patients with NLD may experience affective symptoms similar to those with BD, it is critical to clarify the temporal course of mood symptoms and understand the complex relationships between symptoms and external events (Table 2).11,12 In BD, mood symptoms are cyclical, punctuated by discrete periods of euthymia. In NLD affective symptoms are clearly linked to learning difficulties and impaired information processing. Research shows cognitive deficits in individuals with BD often persist during euthymic periods.16 Literature suggests that cognitive deficits in adult BD commonly involve verbal memory, executive function, and attention, whereas patients with NLD often have strong verbal memory.17,18
Individuals with BD may understand the intentions of others and—especially in periods of hypomania or mania—will engage others. In contrast, persons with NLD struggle to attract and engage friends, may be irritable when they misunderstand social cues, may be bullied or taken advantage of by others, and may struggle to communicate this problem to clinicians. NLD patients’ sense of frustration typically does not vary; a continuous depressed or anxious mood may improve briefly when they feel accepted in their environment. This pattern can be discerned from BD by strictly applying DSM-IV-TR criteria for variability in mood states.19 BD treatment may be complicated in patients with comorbid NLD. These patients may underreport adverse effects of medications, including metabolic effects and cognitive dulling, which results in a complicated and frustrating clinical course.20
Asperger’s disorder. Patients with NLD—a neuropsychological disorder—may present with social interaction difficulties that seem similar to those of Asperger’s disorder—a behavioral disorder. Overlapping behaviors, similar cognitive processes, and coexisting conditions may challenge even experienced clinicians (Table 3).21-23 However, impairments are more severe in Asperger’s disorder and will present as early as age 4. Patients with Asperger’s disorder show difficulty communicating characterized by unusual interactions, such as pedantic or 1-sided discussions of topics that are unusual for the patient’s age group and inattentiveness to social cues. By contrast, communication difficulties in children with NLD are not apparent until after they start school.
Both Asperger’s disorder and NLD patients will show noticeable variations in thought process that often are apparent in conversations. Individuals with Asperger’s disorder may have some concrete thinking, although they often express idiosyncratic thinking, whereas individuals with NLD often show concrete logic. An individual with NLD may be easily overwhelmed by peer group social interactions but remains emotionally aware of his or her shortcomings and may be able to handle 1-on-1 interactions. Individuals with Asperger’s disorder will demonstrate restrictive interests or repetitive behaviors, a characteristic typically not seen in individuals with NLD. Patients with Asperger’s disorder may have specific skills, such as expertise with directions and spatial reasoning, whereas individuals with NLD may get lost even when traveling to familiar places or may have difficulty relating directions. Both groups likely will have good reading skills but patients with NLD will have trouble comprehending and integrating the material, evident by difficulty with multiple choice questions or “story problems.” Individuals with either disorder may develop frustration and anger with their challenges.
In adults, many of these subtle differences in language and thought process may be masked by years of difficult and frustrating communication, making definitive diagnosis challenging. Semistructured interviews, such as the Autism Diagnostic Observation Schedule24 or the Gilliam Asperger’s Disorder Scale,25 may help in differentiating Asperger’s disorder from NLD. However, these 2 disorders may be comorbid, thus complicating the diagnostic process.21
Table 2
Differences among NLD, ADHD, and bipolar disorder
| Clinical features | NLD | ADHD | Bipolar disorder |
|---|---|---|---|
| Cognition | Impairment stable | Impairment fluctuates with attention | Impairment fluctuates with mood episodes |
| IQ | 1.5 to 2 standard deviations between verbal and performance IQ | Full scale IQ within one standard deviation of healthy subjects | Independent of disorder |
| Experiential learning | Deficits present | Successful with treatment | Experiences influence behavior |
| Social competency | Mostly aware of shortcomings, a degree of mind sharing, empathy | Generally good, attentive to others | Generally good, when manic patients are ‘the life of the party’ |
| Peer relationships | Often lack friends, victims of bullying | Often have friends | Often have friends |
| Motor coordination | Multiple impairments | No impairments (may be good at sports) | No impairments |
| ADHD: attention-deficit/hyperactivity disorder; IQ: intelligence quotient; NLD: nonverbal learning disorder Source: References 11,12 | |||
Table 3
Differences between NLD and Asperger’s disorder
| Clinical features | NLD | Asperger’s disorder |
|---|---|---|
| Spatial cognition | Poor sense of direction | Precise sense of direction |
| Reading and math comprehension | Good word recognition and ‘word attack,’ with poor reading comprehension | Good |
| Interests | Intense interest in 1 topic for short periods, frequent changes | Idiosyncratic, repetitive, inflexible |
| Social competency | Mostly aware of shortcomings, a degree of mind sharing, empathy | Blames others for social difficulties, poor empathy |
| Regulation of affect | Often impaired, unaware when infringing on others’ personal space | May be impaired when anxious; fear of being in close proximity to nonfamily members |
| NLD: nonverbal learning disorder Source: References 21-23 | ||
Treatment implications
The day-to-day care of patients with NLD and a comorbid psychiatric disorder may include systems-level interventions, supportive psychotherapy, and psychopharmacologic treatments that are informed by the comorbid condition (Table 4).7,26 Open, honest dialogue about strengths and challenges for individuals with NLD will help reframe expectations and frustrations. Early recognition of NLD may, in some cases, prevent internalized psychopathology and loss of self-esteem.27,28
Children and adolescents with NLD require early intervention to help them function socially and academically. Involving family and school personnel is important to develop accommodations to improve functioning. Comprehension problems associated with NLD often become more noticeable as the student moves into upper elementary grades, where abstract thinking and the ability to manage novelty (eg, unfamiliar content or situations) are required. Many students with NLD can manage rote memorization and concrete facts, but have trouble with inference, integration, and reasoning. Academically appropriate classroom placement, limited writing, and use of voice recognition software may aid success. Parents can help by teaching and modeling social skills such as appropriate expression of emotions, which can be facilitated by watching movies or attending group activities together.
Adults. Patients with NLD may be late for appointments and often forget what is discussed. They may be at increased risk for noncompliance with pharmacotherapy for comorbid disorders and may require written instructions, frequent reminders, and reviews of treatment plan. In addition, interactions with clinicians may seem shallow and unsatisfying, despite the clinician’s best efforts to empathize. The pattern of feeling misunderstood likely exists in the patient’s other relationships, including significant others and employers. Although no systemic evaluations exist, mindfulness-based therapies might help alleviate this deficit.29,30
Treatment plans may involve family-focused modalities where NLD patients learn to rely on family members to interpret others’ motives and intentions.31 Education of the patient and family and friends should emphasize the need for consistent daily schedules and frequent verbal feedback, such as taking turns in conversations. Academic accommodations in college are crucial for success. Education experts have advocated for increased use of technology for students with NLD, including voice recognition software, laptop computers, and audio recordings of class notes.32
Table 4
Treating patients with NLD
| Remember that treating patients with NLD can be challenging |
| Clinical neuropsychological and psychoeducational assessments often are necessary |
| Employ open dialogue with patient and family about need for multifaceted approach |
| Recognize a patient’s individual strengths and weaknesses |
| Suggest academic and workplace accommodations |
| Provide written instructions and discuss your patient’s understanding of them |
| Suggest the use of frequent visual cues and reminders of scheduled tasks and appointments |
| Provide supportive psychotherapy and review the treatment plan frequently |
| Recognize the increased risk of suicide and develop a safety plan appropriate to your patient’s cognitive abilities |
| NLD: nonverbal learning disorder Source: References 7,26 |
Related Resources
- Rourke BP. Syndrome of nonverbal learning disabilities: Neurodevelopmental manifestations. New York, NY: Guilford Press; 1995.
- NLD Line. www.nldline.com.
- NLD on the Web. www.nldontheweb.org.
- Massachusetts General Hospital school psychiatry program and Mood and Anxiety Disorders Institute resource center. www2.massgeneral.org/schoolpsychiatry.
Disclosures
Drs. Delgado and Wassenaar report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Strawn has received research support from the American Academy of Child and Adolescent Psychiatry and Eli Lilly and Company.
Acknowledgements
The authors acknowledge Drs. Michele Berg and Carleen Franz for their careful review of this manuscript and for their critiques, which have greatly improved this contribution.
Rourkea conceptualized nonverbal learning disorder (NLD) as being related to dysfunction in the right cerebral hemisphere with subsequent disruption of the cognitive functions modulated by that region. Difficulties associated with NLD were thought to be related to dysfunction in intermodal integration, a process that inherently depends on white matter connectivity.b
More recent data suggest that although right brain dysfunction may affect cognition, NLD patients likely exhibit dysfunction in multiple brain regions.c-e Nonetheless, right hemisphere lesions in adults often result in similar disturbances as those observed in patients with NLD (eg, visual-spatial integration, attention, nonverbal memory, and expression and integration of emotion).f,g Functional brain imaging studies and functional connectivity studies are needed to better elucidate the neurocircuitry of NLD.
References
a. Drummond CR, Ahmad SA, Rourke BP. Rules for the classification of younger children with nonverbal learning disabilities and basic phonological processing disabilities. Arch Clin Neuropsychol. 2005;(20):171-182.
b. McDonald BC. Recent developments in the application of the nonverbal learning disabilities model. Curr Psychiatry Rep. 2002;4(5):323-330.
c. McCann MV, Pongonis SJ, Golomb MR, et al. Like father, like son: periventricular nodular heterotopia and nonverbal learning disorder. J Child Neurol. 2008;23:950-953.
d. Carey ME, Barakat LP, Foley B, et al. Neuropsychological functioning and social functioning of survivors of pediatric brain tumors: evidence of nonverbal learning disability. Child Neuropsychol. 2001;7(4):265-272.
e. Denckla MB. Academic and extracurricular aspects of nonverbal learning disabilities. Psychiatric Annals. 1991;21: 717-724.
f. Gross-Tsur V, Shalev RS, Manor O, et al. Developmental right-hemisphere syndrome: clinical spectrum of the nonverbal learning disability. J Learn Disabil. 1995;28(2):80-86.
g. Mesulam M. Principles of behavioral and cognitive neurology. New York, NY: Oxford University Press; 2000.
1. Altarac M, Saroha E. Lifetime prevalence of learning disability among US children. Pediatrics. 2007;119(suppl 1):S77-S83.
2. Cooper S, Smiley E, Morrison J, et al. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry. 2007;190:27-35.
3. Rourke BP, Young GC, Leenaars AA. A childhood learning disability that predisposes those afflicted to adolescent and adult depression and suicide risk. J Learn Disabil. 1989;22(3):169-175.
4. Little SS. Nonverbal learning disabilities and socioemotional functioning: a review of recent literature. J Learn Disabil. 1993;26(10):653-665.
5. Hubbard A, Smith Myles B. NLDA. Nonverbal learning disabilities. 2005. Available at: http://www.partnerstx.org/Resources/LD/NVLD.html. Accessed August 11 2010.
6. Drummond CR, Ahmad SA, Rourke BP. Rules for the classification of younger children with nonverbal learning disabilities and basic phonological processing disabilities. Arch Clin Neuropsychol. 2005;(20):171-182.
7. Palombo J. Nonverbal learning disabilities: a clinical perspective. New York NY: W.W. Norton & Company, Inc; 2006.
8. Wechsler D. Wechsler Intelligence Scale for Children. 3rd edition. San Antonio TX: The Psychological Corporation; 1991.
9. Wechsler D. The WISC-IV technical and interpretive manual. San Antonio TX: The Psychological Corporation; 2003.
10. Woodcock RR, Shrank FA, McGrew KS, et al. Woodcock-Johnson III Normative Update technical manual. Itasca, IL: Riverside Publishing; 2007.
11. Frazier TW, Demaree HA, Youngstrom EA. Meta-analysis of intellectual and neuropsychological test performance in attention-deficit/hyperactivity disorder. Neuropsychology. 2004;18(3):543-555.
12. Torres IJ, Boudreau VG, Yatham LN. Neuropsychological functioning in euthymic bipolar disorder: a meta-analysis. Acta Psychiatr Scand Suppl. 2007;(434):17-26.
13. Rourke BP. Neuropsychology of learning disabilities: past and future. Learning Disability Quarterly. 2005;(28):111-114.
14. Dhar M, Been PH, Minderaa RB, et al. Information processing differences and similarities in adults with dyslexia and adults with attention deficit hyperactivity disorder during a Continuous Performance Test: a study of cortical potentials. Neuropsychologia. 2010;48:3045-3056.
15. Gross-Tsur V, Shalev RS, Manor O, et al. Developmental right-hemisphere syndrome: clinical spectrum of the nonverbal learning disability. J Learn Disabil. 1995;28(2):80-86.
16. Strakowski SM, Adler CM, Holland SK, et al. Abnormal FMRI brain activation in euthymic bipolar disorder patients during a counting Stroop interference task. Am J Psychiatry. 2005;162(9):1697-1705.
17. Goldberg JF, Chengappa KN. Identifying and treating cognitive impairment in bipolar disorder. Bipolar Disord. 2009;11(suppl 2):123-137.
18. McDonough-Ryan P, DelBello M, Shear PK, et al. Academic and cognitive abilities in children of parents with bipolar disorder: a test of the nonverbal learning disability model. J Clin Exp Neuropsychol. 2002;24(3):280-285.
19. Mokros HB, Poznanski EO, Merrick WA. Depression and learning disabilities in children: a test of an hypothesis. J Learn Disabil. 1989;22(4):230-233,244.
20. Vieta E. Maintenance therapy for bipolar disorder: current and future management options. Expert Rev Neurother. 2004;4(6 suppl 2):S35-S42.
21. Stein MT, Klin A, Miller K. When Asperger’s syndrome and a nonverbal learning disability look alike. Pediatrics. 2004;114(suppl 6):1458-1463.
22. Klin A, Volkmar FR, Sparrow SS, et al. Validity and neuropsychological characterization of Asperger syndrome: convergence with nonverbal learning disabilities syndrome. J Child Psychol Psychiatry. 1995;36(7):1127-1140.
23. Volkmar FR, Klin A. Asperger syndrome and nonverbal learning disabilities. In: Schopler E, Mesibov GB, Kunce LJ, eds. Asperger syndrome or high-functioning autism? New York, NY: Plenum Press; 1998:107–121.
24. Lord C, Rutter M, Goode S, et al. Autism diagnostic observation schedule: a standardized observation of communicative and social behavior. J Autism Dev Disord. 1989;19(2):185-212.
25. Gilliam JE. Gilliam Asperger’s disorder scale: second edition. Austin TX: Pro-Ed; 2005.
26. Pennington BF. Diagnosing learning disorders: a neuropsychological framework. 2nd ed. New York NY: The Guilford Press; 1998.
27. Sundheim ST, Voeller KK. Psychiatric implications of language disorders and learning disabilities: risks and management. J Child Neurol. 2004;19(10):814-826.
28. Fletcher J. Nonverbal learning disabilities and suicide: classification leads to prevention. J Learn Disabil. 1989;22(3):176-179.
29. Williams KA, Kolar MM, Reger BE, et al. Evaluation of a wellness-based mindfulness stress reduction intervention: a controlled trial. Am J Health Promot. 2001;15:422-432.
30. Sanders KM. Mindfulness and psychotherapy. Focus. 2010;8:19-24.
31. Fisher NJ, DeLuca JW. Verbal learning strategies of adults and adolescents with syndrome of NVLD. Child Neuropsychol. 1997;3(3):192-198.
32. Thompson S. Developing an educational plan for the student with NLD. 1998. Available at: http://www.ldonline.org/article/Developing_an_Educational_Plan_for_the_Student_with_NLD. Accessed March 25 2011.
Discuss this article at www.facebook.com/CurrentPsychiatry
Patients who present with impairment in academic, cognitive, social, and vocational functioning might be struggling with an unrecognized learning disorder. Ten percent of the US population has some form of learning disability, and up to 40% of those with learning disorders may meet diagnostic criteria for a psychiatric disorder.1,2 Some learning disorders affect a person’s ability to read, write, or do math, whereas less-recognized nonverbal learning disorder (NLD) impacts the social and emotional functioning of children, adolescents, and adults. Common features of NLD include:
- deficits in nonlinguistic information processing
- speech prosody deficits
- difficulty reading facial expressions
- associated impairment in interpersonal functioning.
The severity of these deficits varies among individuals with NLD. Patients may experience chronic low self-esteem, anxiety, and mood symptoms because of their limited ability to express their feelings within an appropriate social context. NLD may be first misdiagnosed as attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or Asperger’s disorder.
In this article we review the underlying neurophysiology of NLD and present a clinical approach to these patients, including the differential diagnosis and factors that will allow clinicians to distinguish NLD from psychiatric conditions with symptomatic and syndromic overlap. We also describe treatment for patients with NLD.
The learning process
Learning is a cognitive process of acquiring and processing information and experiences from the environment that allows us to acquire knowledge, skills, and social abilities. When we learn how to relate to others, we undergo neurophysiologic changes that subsequently influence behavior and the way we understand our environment. Deficits in learning processes or the ability to acquire relational skills result in impaired affect regulation in regard to others and may lead to low self-esteem, depression, anxiety, interpersonal conflict, and anger toward others. Learning influences a person’s ability to navigate social relationships and perform academically and occupationally.
The impact of learning deficits may be magnified in adulthood after an individual has suffered years of in-securities and poor self-esteem. Adults with learning disabilities often seek psychiatric treatment as a result of their disappointment about difficulties in relationships and work. NLD may coexist with or mimic other neuropsychiatric disorders. For example, problematic behavior within a family or at the workplace is a common reason for referral to a psychiatrist. These behaviors may be influenced by a patient’s NLD symptoms, which can complicate diagnosis and treatment.
Persons with NLD are at increased risk for depression because of failures in coping, loss of self-esteem, internalized psychopathology, and other social and emotional strains. In addition, individuals with NLD may experience multiple psychosocial impairments, including difficulty maintaining employment, achieving goals, and maintaining relationships.3
A variable presentation
NLD has been associated with right hemispheric dysfunction.3 For a description of the neurophysiology of NLD, see this article at CurrentPsychiatry.com. In childhood, NLD may present as deficits in:
- processing nonlinguistic information
- expressing or comprehending nonverbal components of language such as pitch, volume, or rate of speech (aprosodia)
- reading facial expressions
- social or emotional functioning, such as difficulty understanding social situations, violations of personal space, or difficulty learning from past emotional experiences.4
The extent of these deficits varies among patients. As children, patients with NLD often show strengths in rote verbal memory, spoken language mechanics or form, and word reading. These children may be hyperverbal and use language at a level higher than expected for their age group, which may mask some learning difficulties and delay diagnosis.
Throughout life, NLD manifests as difficulty interacting with peers. Children with NLD may have difficulty playing with others and making friends and as result may feel socially isolated. Without the critical skills of social reciprocity or understanding social context, NLD patients often have many superficial friendships but lack deep relationships.4,5
Patients with NLD may rely on their verbal skills for relating socially and relieving anxiety and tend to withdraw from social situations as they become aware of their deficits.
NLD can be characterized on the basis of primary, secondary, and tertiary deficits. Primary deficits in tactile and visual perception and complex psychomotor skills lead to secondary deficits in attention and exploratory behavior, which lead to tertiary deficits in memory and executive function.6
Given NLD’s variable presentation, clinicians must remain vigilant to this possible diagnosis in patients with a history of multiple pharmacotherapy or psychotherapy failures for axis I disorders. Using clues from symptoms described in Table 17 may provide information necessary to refer for formal psychoeducational testing to diagnose NLD. Early diagnosis can help target NLD symptoms and tailor treatment of comorbid psychopathology.7 NLD is a chronic disability and—similar to other learning disabilities—early, targeted interventions initiated by parents, teachers, and clinicians can improve outcomes.
Neuropsychological/psychoeducational testing. Traditionally, clinicians suspected NLD if a patient had a ≥10 point difference between performance intelligence quotient (IQ) and verbal IQ on the Wechsler Intelligence Scale for Children (WISC-III).8 However, the most recent version—the WISC-IV9—incorporates changes based on new neurologic models of cognitive functioning, and performance IQ and verbal IQ are no longer calculated. Thus, interpreting this split in IQ type with regard to NLD is no longer straightforward. IQ tests, such as the Woodcock-Johnson10 battery, which assesses visual-spatial thinking and fluid reasoning, may be particularly important in characterizing NLD deficits—especially when used in conjunction with other neuropsychological batteries, which may directly assess discrete abilities related to visual and spatial processing.
A thorough social and educational history, IQ testing, neuropsychological batteries, and a psychoeducational assessment can help determine the extent of cognitive deficits that may require accommodations at school or work and characterize the complex interplay of specific deficits and functioning.
Table 1
Clinical manifestation of nonverbal learning disorder
| Tactile-perceptual deficits and psychomotor coordination deficiencies, usually more marked on the left side |
| Visual-spatial organization deficits |
| Deficiencies in nonverbal problem solving, such as hypothesis testing and understanding cause-effect relationships |
| Difficulty adapting to novel situations and reliance on rote behaviors |
| Relative deficiencies in mechanical arithmetic with proficiencies in reading, word recognition, and spelling |
| Well developed rote verbal-memory skills |
| Verbosity characterized by poor pragmatics |
| Deficits in social perception, judgment, and interaction |
| Source: Reference 7 |
Differential diagnosis
ADHD. Patients diagnosed with ADHD or NLD may have a history of attention difficulties and hyperactivity. These clinical similarities may include restlessness, distractibility, impulsivity, and poor attention (Table 2).11,12 In adults, these features may attenuate and patients with NLD or ADHD could appear normoactive. Individuals with NLD demonstrate withdrawal, anxiety, and continued social skills deficits,13 whereas adult ADHD patients show persistent attention difficulties. Although both groups may have difficulty maintaining steady employment, NLD patients’ employment failures often are caused by cognitive and social difficulties as opposed to problems with attention.
The psychopathology of these 2 conditions differs in that ADHD is characterized primarily by prefrontal dysfunction.14 However, in a small study of children with NLD (N=20), all participants also met diagnostic criteria for ADHD; therefore, the true epidemiologic comorbidity is unknown.15
BD. Because patients with NLD may experience affective symptoms similar to those with BD, it is critical to clarify the temporal course of mood symptoms and understand the complex relationships between symptoms and external events (Table 2).11,12 In BD, mood symptoms are cyclical, punctuated by discrete periods of euthymia. In NLD affective symptoms are clearly linked to learning difficulties and impaired information processing. Research shows cognitive deficits in individuals with BD often persist during euthymic periods.16 Literature suggests that cognitive deficits in adult BD commonly involve verbal memory, executive function, and attention, whereas patients with NLD often have strong verbal memory.17,18
Individuals with BD may understand the intentions of others and—especially in periods of hypomania or mania—will engage others. In contrast, persons with NLD struggle to attract and engage friends, may be irritable when they misunderstand social cues, may be bullied or taken advantage of by others, and may struggle to communicate this problem to clinicians. NLD patients’ sense of frustration typically does not vary; a continuous depressed or anxious mood may improve briefly when they feel accepted in their environment. This pattern can be discerned from BD by strictly applying DSM-IV-TR criteria for variability in mood states.19 BD treatment may be complicated in patients with comorbid NLD. These patients may underreport adverse effects of medications, including metabolic effects and cognitive dulling, which results in a complicated and frustrating clinical course.20
Asperger’s disorder. Patients with NLD—a neuropsychological disorder—may present with social interaction difficulties that seem similar to those of Asperger’s disorder—a behavioral disorder. Overlapping behaviors, similar cognitive processes, and coexisting conditions may challenge even experienced clinicians (Table 3).21-23 However, impairments are more severe in Asperger’s disorder and will present as early as age 4. Patients with Asperger’s disorder show difficulty communicating characterized by unusual interactions, such as pedantic or 1-sided discussions of topics that are unusual for the patient’s age group and inattentiveness to social cues. By contrast, communication difficulties in children with NLD are not apparent until after they start school.
Both Asperger’s disorder and NLD patients will show noticeable variations in thought process that often are apparent in conversations. Individuals with Asperger’s disorder may have some concrete thinking, although they often express idiosyncratic thinking, whereas individuals with NLD often show concrete logic. An individual with NLD may be easily overwhelmed by peer group social interactions but remains emotionally aware of his or her shortcomings and may be able to handle 1-on-1 interactions. Individuals with Asperger’s disorder will demonstrate restrictive interests or repetitive behaviors, a characteristic typically not seen in individuals with NLD. Patients with Asperger’s disorder may have specific skills, such as expertise with directions and spatial reasoning, whereas individuals with NLD may get lost even when traveling to familiar places or may have difficulty relating directions. Both groups likely will have good reading skills but patients with NLD will have trouble comprehending and integrating the material, evident by difficulty with multiple choice questions or “story problems.” Individuals with either disorder may develop frustration and anger with their challenges.
In adults, many of these subtle differences in language and thought process may be masked by years of difficult and frustrating communication, making definitive diagnosis challenging. Semistructured interviews, such as the Autism Diagnostic Observation Schedule24 or the Gilliam Asperger’s Disorder Scale,25 may help in differentiating Asperger’s disorder from NLD. However, these 2 disorders may be comorbid, thus complicating the diagnostic process.21
Table 2
Differences among NLD, ADHD, and bipolar disorder
| Clinical features | NLD | ADHD | Bipolar disorder |
|---|---|---|---|
| Cognition | Impairment stable | Impairment fluctuates with attention | Impairment fluctuates with mood episodes |
| IQ | 1.5 to 2 standard deviations between verbal and performance IQ | Full scale IQ within one standard deviation of healthy subjects | Independent of disorder |
| Experiential learning | Deficits present | Successful with treatment | Experiences influence behavior |
| Social competency | Mostly aware of shortcomings, a degree of mind sharing, empathy | Generally good, attentive to others | Generally good, when manic patients are ‘the life of the party’ |
| Peer relationships | Often lack friends, victims of bullying | Often have friends | Often have friends |
| Motor coordination | Multiple impairments | No impairments (may be good at sports) | No impairments |
| ADHD: attention-deficit/hyperactivity disorder; IQ: intelligence quotient; NLD: nonverbal learning disorder Source: References 11,12 | |||
Table 3
Differences between NLD and Asperger’s disorder
| Clinical features | NLD | Asperger’s disorder |
|---|---|---|
| Spatial cognition | Poor sense of direction | Precise sense of direction |
| Reading and math comprehension | Good word recognition and ‘word attack,’ with poor reading comprehension | Good |
| Interests | Intense interest in 1 topic for short periods, frequent changes | Idiosyncratic, repetitive, inflexible |
| Social competency | Mostly aware of shortcomings, a degree of mind sharing, empathy | Blames others for social difficulties, poor empathy |
| Regulation of affect | Often impaired, unaware when infringing on others’ personal space | May be impaired when anxious; fear of being in close proximity to nonfamily members |
| NLD: nonverbal learning disorder Source: References 21-23 | ||
Treatment implications
The day-to-day care of patients with NLD and a comorbid psychiatric disorder may include systems-level interventions, supportive psychotherapy, and psychopharmacologic treatments that are informed by the comorbid condition (Table 4).7,26 Open, honest dialogue about strengths and challenges for individuals with NLD will help reframe expectations and frustrations. Early recognition of NLD may, in some cases, prevent internalized psychopathology and loss of self-esteem.27,28
Children and adolescents with NLD require early intervention to help them function socially and academically. Involving family and school personnel is important to develop accommodations to improve functioning. Comprehension problems associated with NLD often become more noticeable as the student moves into upper elementary grades, where abstract thinking and the ability to manage novelty (eg, unfamiliar content or situations) are required. Many students with NLD can manage rote memorization and concrete facts, but have trouble with inference, integration, and reasoning. Academically appropriate classroom placement, limited writing, and use of voice recognition software may aid success. Parents can help by teaching and modeling social skills such as appropriate expression of emotions, which can be facilitated by watching movies or attending group activities together.
Adults. Patients with NLD may be late for appointments and often forget what is discussed. They may be at increased risk for noncompliance with pharmacotherapy for comorbid disorders and may require written instructions, frequent reminders, and reviews of treatment plan. In addition, interactions with clinicians may seem shallow and unsatisfying, despite the clinician’s best efforts to empathize. The pattern of feeling misunderstood likely exists in the patient’s other relationships, including significant others and employers. Although no systemic evaluations exist, mindfulness-based therapies might help alleviate this deficit.29,30
Treatment plans may involve family-focused modalities where NLD patients learn to rely on family members to interpret others’ motives and intentions.31 Education of the patient and family and friends should emphasize the need for consistent daily schedules and frequent verbal feedback, such as taking turns in conversations. Academic accommodations in college are crucial for success. Education experts have advocated for increased use of technology for students with NLD, including voice recognition software, laptop computers, and audio recordings of class notes.32
Table 4
Treating patients with NLD
| Remember that treating patients with NLD can be challenging |
| Clinical neuropsychological and psychoeducational assessments often are necessary |
| Employ open dialogue with patient and family about need for multifaceted approach |
| Recognize a patient’s individual strengths and weaknesses |
| Suggest academic and workplace accommodations |
| Provide written instructions and discuss your patient’s understanding of them |
| Suggest the use of frequent visual cues and reminders of scheduled tasks and appointments |
| Provide supportive psychotherapy and review the treatment plan frequently |
| Recognize the increased risk of suicide and develop a safety plan appropriate to your patient’s cognitive abilities |
| NLD: nonverbal learning disorder Source: References 7,26 |
Related Resources
- Rourke BP. Syndrome of nonverbal learning disabilities: Neurodevelopmental manifestations. New York, NY: Guilford Press; 1995.
- NLD Line. www.nldline.com.
- NLD on the Web. www.nldontheweb.org.
- Massachusetts General Hospital school psychiatry program and Mood and Anxiety Disorders Institute resource center. www2.massgeneral.org/schoolpsychiatry.
Disclosures
Drs. Delgado and Wassenaar report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Strawn has received research support from the American Academy of Child and Adolescent Psychiatry and Eli Lilly and Company.
Acknowledgements
The authors acknowledge Drs. Michele Berg and Carleen Franz for their careful review of this manuscript and for their critiques, which have greatly improved this contribution.
Rourkea conceptualized nonverbal learning disorder (NLD) as being related to dysfunction in the right cerebral hemisphere with subsequent disruption of the cognitive functions modulated by that region. Difficulties associated with NLD were thought to be related to dysfunction in intermodal integration, a process that inherently depends on white matter connectivity.b
More recent data suggest that although right brain dysfunction may affect cognition, NLD patients likely exhibit dysfunction in multiple brain regions.c-e Nonetheless, right hemisphere lesions in adults often result in similar disturbances as those observed in patients with NLD (eg, visual-spatial integration, attention, nonverbal memory, and expression and integration of emotion).f,g Functional brain imaging studies and functional connectivity studies are needed to better elucidate the neurocircuitry of NLD.
References
a. Drummond CR, Ahmad SA, Rourke BP. Rules for the classification of younger children with nonverbal learning disabilities and basic phonological processing disabilities. Arch Clin Neuropsychol. 2005;(20):171-182.
b. McDonald BC. Recent developments in the application of the nonverbal learning disabilities model. Curr Psychiatry Rep. 2002;4(5):323-330.
c. McCann MV, Pongonis SJ, Golomb MR, et al. Like father, like son: periventricular nodular heterotopia and nonverbal learning disorder. J Child Neurol. 2008;23:950-953.
d. Carey ME, Barakat LP, Foley B, et al. Neuropsychological functioning and social functioning of survivors of pediatric brain tumors: evidence of nonverbal learning disability. Child Neuropsychol. 2001;7(4):265-272.
e. Denckla MB. Academic and extracurricular aspects of nonverbal learning disabilities. Psychiatric Annals. 1991;21: 717-724.
f. Gross-Tsur V, Shalev RS, Manor O, et al. Developmental right-hemisphere syndrome: clinical spectrum of the nonverbal learning disability. J Learn Disabil. 1995;28(2):80-86.
g. Mesulam M. Principles of behavioral and cognitive neurology. New York, NY: Oxford University Press; 2000.
Discuss this article at www.facebook.com/CurrentPsychiatry
Patients who present with impairment in academic, cognitive, social, and vocational functioning might be struggling with an unrecognized learning disorder. Ten percent of the US population has some form of learning disability, and up to 40% of those with learning disorders may meet diagnostic criteria for a psychiatric disorder.1,2 Some learning disorders affect a person’s ability to read, write, or do math, whereas less-recognized nonverbal learning disorder (NLD) impacts the social and emotional functioning of children, adolescents, and adults. Common features of NLD include:
- deficits in nonlinguistic information processing
- speech prosody deficits
- difficulty reading facial expressions
- associated impairment in interpersonal functioning.
The severity of these deficits varies among individuals with NLD. Patients may experience chronic low self-esteem, anxiety, and mood symptoms because of their limited ability to express their feelings within an appropriate social context. NLD may be first misdiagnosed as attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or Asperger’s disorder.
In this article we review the underlying neurophysiology of NLD and present a clinical approach to these patients, including the differential diagnosis and factors that will allow clinicians to distinguish NLD from psychiatric conditions with symptomatic and syndromic overlap. We also describe treatment for patients with NLD.
The learning process
Learning is a cognitive process of acquiring and processing information and experiences from the environment that allows us to acquire knowledge, skills, and social abilities. When we learn how to relate to others, we undergo neurophysiologic changes that subsequently influence behavior and the way we understand our environment. Deficits in learning processes or the ability to acquire relational skills result in impaired affect regulation in regard to others and may lead to low self-esteem, depression, anxiety, interpersonal conflict, and anger toward others. Learning influences a person’s ability to navigate social relationships and perform academically and occupationally.
The impact of learning deficits may be magnified in adulthood after an individual has suffered years of in-securities and poor self-esteem. Adults with learning disabilities often seek psychiatric treatment as a result of their disappointment about difficulties in relationships and work. NLD may coexist with or mimic other neuropsychiatric disorders. For example, problematic behavior within a family or at the workplace is a common reason for referral to a psychiatrist. These behaviors may be influenced by a patient’s NLD symptoms, which can complicate diagnosis and treatment.
Persons with NLD are at increased risk for depression because of failures in coping, loss of self-esteem, internalized psychopathology, and other social and emotional strains. In addition, individuals with NLD may experience multiple psychosocial impairments, including difficulty maintaining employment, achieving goals, and maintaining relationships.3
A variable presentation
NLD has been associated with right hemispheric dysfunction.3 For a description of the neurophysiology of NLD, see this article at CurrentPsychiatry.com. In childhood, NLD may present as deficits in:
- processing nonlinguistic information
- expressing or comprehending nonverbal components of language such as pitch, volume, or rate of speech (aprosodia)
- reading facial expressions
- social or emotional functioning, such as difficulty understanding social situations, violations of personal space, or difficulty learning from past emotional experiences.4
The extent of these deficits varies among patients. As children, patients with NLD often show strengths in rote verbal memory, spoken language mechanics or form, and word reading. These children may be hyperverbal and use language at a level higher than expected for their age group, which may mask some learning difficulties and delay diagnosis.
Throughout life, NLD manifests as difficulty interacting with peers. Children with NLD may have difficulty playing with others and making friends and as result may feel socially isolated. Without the critical skills of social reciprocity or understanding social context, NLD patients often have many superficial friendships but lack deep relationships.4,5
Patients with NLD may rely on their verbal skills for relating socially and relieving anxiety and tend to withdraw from social situations as they become aware of their deficits.
NLD can be characterized on the basis of primary, secondary, and tertiary deficits. Primary deficits in tactile and visual perception and complex psychomotor skills lead to secondary deficits in attention and exploratory behavior, which lead to tertiary deficits in memory and executive function.6
Given NLD’s variable presentation, clinicians must remain vigilant to this possible diagnosis in patients with a history of multiple pharmacotherapy or psychotherapy failures for axis I disorders. Using clues from symptoms described in Table 17 may provide information necessary to refer for formal psychoeducational testing to diagnose NLD. Early diagnosis can help target NLD symptoms and tailor treatment of comorbid psychopathology.7 NLD is a chronic disability and—similar to other learning disabilities—early, targeted interventions initiated by parents, teachers, and clinicians can improve outcomes.
Neuropsychological/psychoeducational testing. Traditionally, clinicians suspected NLD if a patient had a ≥10 point difference between performance intelligence quotient (IQ) and verbal IQ on the Wechsler Intelligence Scale for Children (WISC-III).8 However, the most recent version—the WISC-IV9—incorporates changes based on new neurologic models of cognitive functioning, and performance IQ and verbal IQ are no longer calculated. Thus, interpreting this split in IQ type with regard to NLD is no longer straightforward. IQ tests, such as the Woodcock-Johnson10 battery, which assesses visual-spatial thinking and fluid reasoning, may be particularly important in characterizing NLD deficits—especially when used in conjunction with other neuropsychological batteries, which may directly assess discrete abilities related to visual and spatial processing.
A thorough social and educational history, IQ testing, neuropsychological batteries, and a psychoeducational assessment can help determine the extent of cognitive deficits that may require accommodations at school or work and characterize the complex interplay of specific deficits and functioning.
Table 1
Clinical manifestation of nonverbal learning disorder
| Tactile-perceptual deficits and psychomotor coordination deficiencies, usually more marked on the left side |
| Visual-spatial organization deficits |
| Deficiencies in nonverbal problem solving, such as hypothesis testing and understanding cause-effect relationships |
| Difficulty adapting to novel situations and reliance on rote behaviors |
| Relative deficiencies in mechanical arithmetic with proficiencies in reading, word recognition, and spelling |
| Well developed rote verbal-memory skills |
| Verbosity characterized by poor pragmatics |
| Deficits in social perception, judgment, and interaction |
| Source: Reference 7 |
Differential diagnosis
ADHD. Patients diagnosed with ADHD or NLD may have a history of attention difficulties and hyperactivity. These clinical similarities may include restlessness, distractibility, impulsivity, and poor attention (Table 2).11,12 In adults, these features may attenuate and patients with NLD or ADHD could appear normoactive. Individuals with NLD demonstrate withdrawal, anxiety, and continued social skills deficits,13 whereas adult ADHD patients show persistent attention difficulties. Although both groups may have difficulty maintaining steady employment, NLD patients’ employment failures often are caused by cognitive and social difficulties as opposed to problems with attention.
The psychopathology of these 2 conditions differs in that ADHD is characterized primarily by prefrontal dysfunction.14 However, in a small study of children with NLD (N=20), all participants also met diagnostic criteria for ADHD; therefore, the true epidemiologic comorbidity is unknown.15
BD. Because patients with NLD may experience affective symptoms similar to those with BD, it is critical to clarify the temporal course of mood symptoms and understand the complex relationships between symptoms and external events (Table 2).11,12 In BD, mood symptoms are cyclical, punctuated by discrete periods of euthymia. In NLD affective symptoms are clearly linked to learning difficulties and impaired information processing. Research shows cognitive deficits in individuals with BD often persist during euthymic periods.16 Literature suggests that cognitive deficits in adult BD commonly involve verbal memory, executive function, and attention, whereas patients with NLD often have strong verbal memory.17,18
Individuals with BD may understand the intentions of others and—especially in periods of hypomania or mania—will engage others. In contrast, persons with NLD struggle to attract and engage friends, may be irritable when they misunderstand social cues, may be bullied or taken advantage of by others, and may struggle to communicate this problem to clinicians. NLD patients’ sense of frustration typically does not vary; a continuous depressed or anxious mood may improve briefly when they feel accepted in their environment. This pattern can be discerned from BD by strictly applying DSM-IV-TR criteria for variability in mood states.19 BD treatment may be complicated in patients with comorbid NLD. These patients may underreport adverse effects of medications, including metabolic effects and cognitive dulling, which results in a complicated and frustrating clinical course.20
Asperger’s disorder. Patients with NLD—a neuropsychological disorder—may present with social interaction difficulties that seem similar to those of Asperger’s disorder—a behavioral disorder. Overlapping behaviors, similar cognitive processes, and coexisting conditions may challenge even experienced clinicians (Table 3).21-23 However, impairments are more severe in Asperger’s disorder and will present as early as age 4. Patients with Asperger’s disorder show difficulty communicating characterized by unusual interactions, such as pedantic or 1-sided discussions of topics that are unusual for the patient’s age group and inattentiveness to social cues. By contrast, communication difficulties in children with NLD are not apparent until after they start school.
Both Asperger’s disorder and NLD patients will show noticeable variations in thought process that often are apparent in conversations. Individuals with Asperger’s disorder may have some concrete thinking, although they often express idiosyncratic thinking, whereas individuals with NLD often show concrete logic. An individual with NLD may be easily overwhelmed by peer group social interactions but remains emotionally aware of his or her shortcomings and may be able to handle 1-on-1 interactions. Individuals with Asperger’s disorder will demonstrate restrictive interests or repetitive behaviors, a characteristic typically not seen in individuals with NLD. Patients with Asperger’s disorder may have specific skills, such as expertise with directions and spatial reasoning, whereas individuals with NLD may get lost even when traveling to familiar places or may have difficulty relating directions. Both groups likely will have good reading skills but patients with NLD will have trouble comprehending and integrating the material, evident by difficulty with multiple choice questions or “story problems.” Individuals with either disorder may develop frustration and anger with their challenges.
In adults, many of these subtle differences in language and thought process may be masked by years of difficult and frustrating communication, making definitive diagnosis challenging. Semistructured interviews, such as the Autism Diagnostic Observation Schedule24 or the Gilliam Asperger’s Disorder Scale,25 may help in differentiating Asperger’s disorder from NLD. However, these 2 disorders may be comorbid, thus complicating the diagnostic process.21
Table 2
Differences among NLD, ADHD, and bipolar disorder
| Clinical features | NLD | ADHD | Bipolar disorder |
|---|---|---|---|
| Cognition | Impairment stable | Impairment fluctuates with attention | Impairment fluctuates with mood episodes |
| IQ | 1.5 to 2 standard deviations between verbal and performance IQ | Full scale IQ within one standard deviation of healthy subjects | Independent of disorder |
| Experiential learning | Deficits present | Successful with treatment | Experiences influence behavior |
| Social competency | Mostly aware of shortcomings, a degree of mind sharing, empathy | Generally good, attentive to others | Generally good, when manic patients are ‘the life of the party’ |
| Peer relationships | Often lack friends, victims of bullying | Often have friends | Often have friends |
| Motor coordination | Multiple impairments | No impairments (may be good at sports) | No impairments |
| ADHD: attention-deficit/hyperactivity disorder; IQ: intelligence quotient; NLD: nonverbal learning disorder Source: References 11,12 | |||
Table 3
Differences between NLD and Asperger’s disorder
| Clinical features | NLD | Asperger’s disorder |
|---|---|---|
| Spatial cognition | Poor sense of direction | Precise sense of direction |
| Reading and math comprehension | Good word recognition and ‘word attack,’ with poor reading comprehension | Good |
| Interests | Intense interest in 1 topic for short periods, frequent changes | Idiosyncratic, repetitive, inflexible |
| Social competency | Mostly aware of shortcomings, a degree of mind sharing, empathy | Blames others for social difficulties, poor empathy |
| Regulation of affect | Often impaired, unaware when infringing on others’ personal space | May be impaired when anxious; fear of being in close proximity to nonfamily members |
| NLD: nonverbal learning disorder Source: References 21-23 | ||
Treatment implications
The day-to-day care of patients with NLD and a comorbid psychiatric disorder may include systems-level interventions, supportive psychotherapy, and psychopharmacologic treatments that are informed by the comorbid condition (Table 4).7,26 Open, honest dialogue about strengths and challenges for individuals with NLD will help reframe expectations and frustrations. Early recognition of NLD may, in some cases, prevent internalized psychopathology and loss of self-esteem.27,28
Children and adolescents with NLD require early intervention to help them function socially and academically. Involving family and school personnel is important to develop accommodations to improve functioning. Comprehension problems associated with NLD often become more noticeable as the student moves into upper elementary grades, where abstract thinking and the ability to manage novelty (eg, unfamiliar content or situations) are required. Many students with NLD can manage rote memorization and concrete facts, but have trouble with inference, integration, and reasoning. Academically appropriate classroom placement, limited writing, and use of voice recognition software may aid success. Parents can help by teaching and modeling social skills such as appropriate expression of emotions, which can be facilitated by watching movies or attending group activities together.
Adults. Patients with NLD may be late for appointments and often forget what is discussed. They may be at increased risk for noncompliance with pharmacotherapy for comorbid disorders and may require written instructions, frequent reminders, and reviews of treatment plan. In addition, interactions with clinicians may seem shallow and unsatisfying, despite the clinician’s best efforts to empathize. The pattern of feeling misunderstood likely exists in the patient’s other relationships, including significant others and employers. Although no systemic evaluations exist, mindfulness-based therapies might help alleviate this deficit.29,30
Treatment plans may involve family-focused modalities where NLD patients learn to rely on family members to interpret others’ motives and intentions.31 Education of the patient and family and friends should emphasize the need for consistent daily schedules and frequent verbal feedback, such as taking turns in conversations. Academic accommodations in college are crucial for success. Education experts have advocated for increased use of technology for students with NLD, including voice recognition software, laptop computers, and audio recordings of class notes.32
Table 4
Treating patients with NLD
| Remember that treating patients with NLD can be challenging |
| Clinical neuropsychological and psychoeducational assessments often are necessary |
| Employ open dialogue with patient and family about need for multifaceted approach |
| Recognize a patient’s individual strengths and weaknesses |
| Suggest academic and workplace accommodations |
| Provide written instructions and discuss your patient’s understanding of them |
| Suggest the use of frequent visual cues and reminders of scheduled tasks and appointments |
| Provide supportive psychotherapy and review the treatment plan frequently |
| Recognize the increased risk of suicide and develop a safety plan appropriate to your patient’s cognitive abilities |
| NLD: nonverbal learning disorder Source: References 7,26 |
Related Resources
- Rourke BP. Syndrome of nonverbal learning disabilities: Neurodevelopmental manifestations. New York, NY: Guilford Press; 1995.
- NLD Line. www.nldline.com.
- NLD on the Web. www.nldontheweb.org.
- Massachusetts General Hospital school psychiatry program and Mood and Anxiety Disorders Institute resource center. www2.massgeneral.org/schoolpsychiatry.
Disclosures
Drs. Delgado and Wassenaar report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Strawn has received research support from the American Academy of Child and Adolescent Psychiatry and Eli Lilly and Company.
Acknowledgements
The authors acknowledge Drs. Michele Berg and Carleen Franz for their careful review of this manuscript and for their critiques, which have greatly improved this contribution.
Rourkea conceptualized nonverbal learning disorder (NLD) as being related to dysfunction in the right cerebral hemisphere with subsequent disruption of the cognitive functions modulated by that region. Difficulties associated with NLD were thought to be related to dysfunction in intermodal integration, a process that inherently depends on white matter connectivity.b
More recent data suggest that although right brain dysfunction may affect cognition, NLD patients likely exhibit dysfunction in multiple brain regions.c-e Nonetheless, right hemisphere lesions in adults often result in similar disturbances as those observed in patients with NLD (eg, visual-spatial integration, attention, nonverbal memory, and expression and integration of emotion).f,g Functional brain imaging studies and functional connectivity studies are needed to better elucidate the neurocircuitry of NLD.
References
a. Drummond CR, Ahmad SA, Rourke BP. Rules for the classification of younger children with nonverbal learning disabilities and basic phonological processing disabilities. Arch Clin Neuropsychol. 2005;(20):171-182.
b. McDonald BC. Recent developments in the application of the nonverbal learning disabilities model. Curr Psychiatry Rep. 2002;4(5):323-330.
c. McCann MV, Pongonis SJ, Golomb MR, et al. Like father, like son: periventricular nodular heterotopia and nonverbal learning disorder. J Child Neurol. 2008;23:950-953.
d. Carey ME, Barakat LP, Foley B, et al. Neuropsychological functioning and social functioning of survivors of pediatric brain tumors: evidence of nonverbal learning disability. Child Neuropsychol. 2001;7(4):265-272.
e. Denckla MB. Academic and extracurricular aspects of nonverbal learning disabilities. Psychiatric Annals. 1991;21: 717-724.
f. Gross-Tsur V, Shalev RS, Manor O, et al. Developmental right-hemisphere syndrome: clinical spectrum of the nonverbal learning disability. J Learn Disabil. 1995;28(2):80-86.
g. Mesulam M. Principles of behavioral and cognitive neurology. New York, NY: Oxford University Press; 2000.
1. Altarac M, Saroha E. Lifetime prevalence of learning disability among US children. Pediatrics. 2007;119(suppl 1):S77-S83.
2. Cooper S, Smiley E, Morrison J, et al. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry. 2007;190:27-35.
3. Rourke BP, Young GC, Leenaars AA. A childhood learning disability that predisposes those afflicted to adolescent and adult depression and suicide risk. J Learn Disabil. 1989;22(3):169-175.
4. Little SS. Nonverbal learning disabilities and socioemotional functioning: a review of recent literature. J Learn Disabil. 1993;26(10):653-665.
5. Hubbard A, Smith Myles B. NLDA. Nonverbal learning disabilities. 2005. Available at: http://www.partnerstx.org/Resources/LD/NVLD.html. Accessed August 11 2010.
6. Drummond CR, Ahmad SA, Rourke BP. Rules for the classification of younger children with nonverbal learning disabilities and basic phonological processing disabilities. Arch Clin Neuropsychol. 2005;(20):171-182.
7. Palombo J. Nonverbal learning disabilities: a clinical perspective. New York NY: W.W. Norton & Company, Inc; 2006.
8. Wechsler D. Wechsler Intelligence Scale for Children. 3rd edition. San Antonio TX: The Psychological Corporation; 1991.
9. Wechsler D. The WISC-IV technical and interpretive manual. San Antonio TX: The Psychological Corporation; 2003.
10. Woodcock RR, Shrank FA, McGrew KS, et al. Woodcock-Johnson III Normative Update technical manual. Itasca, IL: Riverside Publishing; 2007.
11. Frazier TW, Demaree HA, Youngstrom EA. Meta-analysis of intellectual and neuropsychological test performance in attention-deficit/hyperactivity disorder. Neuropsychology. 2004;18(3):543-555.
12. Torres IJ, Boudreau VG, Yatham LN. Neuropsychological functioning in euthymic bipolar disorder: a meta-analysis. Acta Psychiatr Scand Suppl. 2007;(434):17-26.
13. Rourke BP. Neuropsychology of learning disabilities: past and future. Learning Disability Quarterly. 2005;(28):111-114.
14. Dhar M, Been PH, Minderaa RB, et al. Information processing differences and similarities in adults with dyslexia and adults with attention deficit hyperactivity disorder during a Continuous Performance Test: a study of cortical potentials. Neuropsychologia. 2010;48:3045-3056.
15. Gross-Tsur V, Shalev RS, Manor O, et al. Developmental right-hemisphere syndrome: clinical spectrum of the nonverbal learning disability. J Learn Disabil. 1995;28(2):80-86.
16. Strakowski SM, Adler CM, Holland SK, et al. Abnormal FMRI brain activation in euthymic bipolar disorder patients during a counting Stroop interference task. Am J Psychiatry. 2005;162(9):1697-1705.
17. Goldberg JF, Chengappa KN. Identifying and treating cognitive impairment in bipolar disorder. Bipolar Disord. 2009;11(suppl 2):123-137.
18. McDonough-Ryan P, DelBello M, Shear PK, et al. Academic and cognitive abilities in children of parents with bipolar disorder: a test of the nonverbal learning disability model. J Clin Exp Neuropsychol. 2002;24(3):280-285.
19. Mokros HB, Poznanski EO, Merrick WA. Depression and learning disabilities in children: a test of an hypothesis. J Learn Disabil. 1989;22(4):230-233,244.
20. Vieta E. Maintenance therapy for bipolar disorder: current and future management options. Expert Rev Neurother. 2004;4(6 suppl 2):S35-S42.
21. Stein MT, Klin A, Miller K. When Asperger’s syndrome and a nonverbal learning disability look alike. Pediatrics. 2004;114(suppl 6):1458-1463.
22. Klin A, Volkmar FR, Sparrow SS, et al. Validity and neuropsychological characterization of Asperger syndrome: convergence with nonverbal learning disabilities syndrome. J Child Psychol Psychiatry. 1995;36(7):1127-1140.
23. Volkmar FR, Klin A. Asperger syndrome and nonverbal learning disabilities. In: Schopler E, Mesibov GB, Kunce LJ, eds. Asperger syndrome or high-functioning autism? New York, NY: Plenum Press; 1998:107–121.
24. Lord C, Rutter M, Goode S, et al. Autism diagnostic observation schedule: a standardized observation of communicative and social behavior. J Autism Dev Disord. 1989;19(2):185-212.
25. Gilliam JE. Gilliam Asperger’s disorder scale: second edition. Austin TX: Pro-Ed; 2005.
26. Pennington BF. Diagnosing learning disorders: a neuropsychological framework. 2nd ed. New York NY: The Guilford Press; 1998.
27. Sundheim ST, Voeller KK. Psychiatric implications of language disorders and learning disabilities: risks and management. J Child Neurol. 2004;19(10):814-826.
28. Fletcher J. Nonverbal learning disabilities and suicide: classification leads to prevention. J Learn Disabil. 1989;22(3):176-179.
29. Williams KA, Kolar MM, Reger BE, et al. Evaluation of a wellness-based mindfulness stress reduction intervention: a controlled trial. Am J Health Promot. 2001;15:422-432.
30. Sanders KM. Mindfulness and psychotherapy. Focus. 2010;8:19-24.
31. Fisher NJ, DeLuca JW. Verbal learning strategies of adults and adolescents with syndrome of NVLD. Child Neuropsychol. 1997;3(3):192-198.
32. Thompson S. Developing an educational plan for the student with NLD. 1998. Available at: http://www.ldonline.org/article/Developing_an_Educational_Plan_for_the_Student_with_NLD. Accessed March 25 2011.
1. Altarac M, Saroha E. Lifetime prevalence of learning disability among US children. Pediatrics. 2007;119(suppl 1):S77-S83.
2. Cooper S, Smiley E, Morrison J, et al. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry. 2007;190:27-35.
3. Rourke BP, Young GC, Leenaars AA. A childhood learning disability that predisposes those afflicted to adolescent and adult depression and suicide risk. J Learn Disabil. 1989;22(3):169-175.
4. Little SS. Nonverbal learning disabilities and socioemotional functioning: a review of recent literature. J Learn Disabil. 1993;26(10):653-665.
5. Hubbard A, Smith Myles B. NLDA. Nonverbal learning disabilities. 2005. Available at: http://www.partnerstx.org/Resources/LD/NVLD.html. Accessed August 11 2010.
6. Drummond CR, Ahmad SA, Rourke BP. Rules for the classification of younger children with nonverbal learning disabilities and basic phonological processing disabilities. Arch Clin Neuropsychol. 2005;(20):171-182.
7. Palombo J. Nonverbal learning disabilities: a clinical perspective. New York NY: W.W. Norton & Company, Inc; 2006.
8. Wechsler D. Wechsler Intelligence Scale for Children. 3rd edition. San Antonio TX: The Psychological Corporation; 1991.
9. Wechsler D. The WISC-IV technical and interpretive manual. San Antonio TX: The Psychological Corporation; 2003.
10. Woodcock RR, Shrank FA, McGrew KS, et al. Woodcock-Johnson III Normative Update technical manual. Itasca, IL: Riverside Publishing; 2007.
11. Frazier TW, Demaree HA, Youngstrom EA. Meta-analysis of intellectual and neuropsychological test performance in attention-deficit/hyperactivity disorder. Neuropsychology. 2004;18(3):543-555.
12. Torres IJ, Boudreau VG, Yatham LN. Neuropsychological functioning in euthymic bipolar disorder: a meta-analysis. Acta Psychiatr Scand Suppl. 2007;(434):17-26.
13. Rourke BP. Neuropsychology of learning disabilities: past and future. Learning Disability Quarterly. 2005;(28):111-114.
14. Dhar M, Been PH, Minderaa RB, et al. Information processing differences and similarities in adults with dyslexia and adults with attention deficit hyperactivity disorder during a Continuous Performance Test: a study of cortical potentials. Neuropsychologia. 2010;48:3045-3056.
15. Gross-Tsur V, Shalev RS, Manor O, et al. Developmental right-hemisphere syndrome: clinical spectrum of the nonverbal learning disability. J Learn Disabil. 1995;28(2):80-86.
16. Strakowski SM, Adler CM, Holland SK, et al. Abnormal FMRI brain activation in euthymic bipolar disorder patients during a counting Stroop interference task. Am J Psychiatry. 2005;162(9):1697-1705.
17. Goldberg JF, Chengappa KN. Identifying and treating cognitive impairment in bipolar disorder. Bipolar Disord. 2009;11(suppl 2):123-137.
18. McDonough-Ryan P, DelBello M, Shear PK, et al. Academic and cognitive abilities in children of parents with bipolar disorder: a test of the nonverbal learning disability model. J Clin Exp Neuropsychol. 2002;24(3):280-285.
19. Mokros HB, Poznanski EO, Merrick WA. Depression and learning disabilities in children: a test of an hypothesis. J Learn Disabil. 1989;22(4):230-233,244.
20. Vieta E. Maintenance therapy for bipolar disorder: current and future management options. Expert Rev Neurother. 2004;4(6 suppl 2):S35-S42.
21. Stein MT, Klin A, Miller K. When Asperger’s syndrome and a nonverbal learning disability look alike. Pediatrics. 2004;114(suppl 6):1458-1463.
22. Klin A, Volkmar FR, Sparrow SS, et al. Validity and neuropsychological characterization of Asperger syndrome: convergence with nonverbal learning disabilities syndrome. J Child Psychol Psychiatry. 1995;36(7):1127-1140.
23. Volkmar FR, Klin A. Asperger syndrome and nonverbal learning disabilities. In: Schopler E, Mesibov GB, Kunce LJ, eds. Asperger syndrome or high-functioning autism? New York, NY: Plenum Press; 1998:107–121.
24. Lord C, Rutter M, Goode S, et al. Autism diagnostic observation schedule: a standardized observation of communicative and social behavior. J Autism Dev Disord. 1989;19(2):185-212.
25. Gilliam JE. Gilliam Asperger’s disorder scale: second edition. Austin TX: Pro-Ed; 2005.
26. Pennington BF. Diagnosing learning disorders: a neuropsychological framework. 2nd ed. New York NY: The Guilford Press; 1998.
27. Sundheim ST, Voeller KK. Psychiatric implications of language disorders and learning disabilities: risks and management. J Child Neurol. 2004;19(10):814-826.
28. Fletcher J. Nonverbal learning disabilities and suicide: classification leads to prevention. J Learn Disabil. 1989;22(3):176-179.
29. Williams KA, Kolar MM, Reger BE, et al. Evaluation of a wellness-based mindfulness stress reduction intervention: a controlled trial. Am J Health Promot. 2001;15:422-432.
30. Sanders KM. Mindfulness and psychotherapy. Focus. 2010;8:19-24.
31. Fisher NJ, DeLuca JW. Verbal learning strategies of adults and adolescents with syndrome of NVLD. Child Neuropsychol. 1997;3(3):192-198.
32. Thompson S. Developing an educational plan for the student with NLD. 1998. Available at: http://www.ldonline.org/article/Developing_an_Educational_Plan_for_the_Student_with_NLD. Accessed March 25 2011.
Minimizing the impact of elevated prolactin in children and adolescents
Discuss this article at www.facebook.com/CurrentPsychiatry
Hyperprolactinemia—increased levels of prolactin (PRL) in the blood that may be caused by hypothyroidism, pituitary disorders, atypical antipsychotics, or other conditions and medications—has numerous physiologic manifestations, including amenorrhea, infertility, abnormal bone resorption, increased risk of breast cancer, and compromised immunity. Evaluation of hyperprolactinemia in patients taking psychotropics—particularly children and adolescents, in whom hyperprolactinemia’s adverse effects may be more pronounced—should include an examination for signs and symptoms of hyperprolactinemia and assessment to rule out other potential causes. This article reviews hyperprolactinemia’s causes, symptoms, evaluation, and treatment, with an emphasis on younger patients.
Causes of hyperprolactinemia
PRL is a circulating autocrine or paracrine factor (Box 1).1,2 Its primary biologic activities can be broadly divided into 4 areas: reproductive, metabolic, osmoregulatory, and immunoregulatory (Box 2).1,3-8
Hyperprolactinemia has numerous physiologic and iatrogenic causes (Table 1).9 Substantially increased serum PRL levels may be seen with:
- prolactinomas, which usually present as incidental findings on a brain CT or MRI or with symptoms of tumor mass
- a craniopharyngioma or other tumor that compresses the pituitary stalk or hypothalamus and interrupts the hypothalamic-dopa minergic inhibition of PRL release.10
Primary thyroid failure (hypothyroidism) can produce a compensatory increase in the discharge of central hypothalamic thyrotropin-releasing hormone, resulting in increased stimulation of PRL secretion.10
Medications can increase serum PRL (Table 2)9 and cause clinical symptoms similar to those of physiologically induced hyperprolactinemia.
Conventional antipsychotics. The anti-psychotic potency of phenothiazines, thioxanthenes, butyrophenones, and dibenzoxazepines generally parallels their potency in increasing PRL levels.9 Although a dose-response relationship between PRL concentrations and conventional antipsychotics is likely, immediate and pronounced increases in PRL can occur even with low doses.
Prospective studies have shown that 3 to 9 weeks of treatment with an antipsychotic such as chlorpromazine increased mean baseline PRL levels up to 10-fold, even at therapeutic doses.11 Conventional antipsychotics can cause marked increases in PRL, probably by blocking dopamine receptors in the tuberoinfundibular tract.12 The blockage of D2 receptors removes the main inhibitory influence on PRL secretion and is associated with increased PRL release.12
Atypical antipsychotics cause less elevation in PRL levels than conventional anti-psychotics. This may be because of their:
- highly selective mesolimbic and meso-cortical dopamine receptor antagonism, which spares dopamine blockade within the tuberoinfundibular tract
- relatively lower D2 receptor affinity.11
Risperidone and its active metabolite paliperidone (9-hydroxyrisperidone) have a high affinity for D2 receptors and thus have potent D2 antagonistic effects.12,13 At dosages of 8 mg/d to 11.8 mg/d, risperidone and paliperidone are associated with the greatest increase in PRL levels among atypical antipsychotics.14
The rate of risperidone metabolism depends on the patient’s cytochrome P (CYP) 2D6 liver enzyme genotype. “Extensive” CYP2D6 metabolizers convert risperidone rapidly into 9-hydroxyrisperidone, whereas “poor” CYP2D6 metabolizers convert it much more slowly. Six percent to 8% of white individuals and a very low percentage of Asians have little or no CYP2D6 activity and are “poor metabolizers.” CYP2D6 also is inhibited by various substrates and nonsubstrates, notably quinidine. Although extensive metabolizers have lower risperidone and higher 9-hydroxyrisperidone concentrations than poor metabolizers, the pharmacokinetics of the active moiety after single and multiple doses are similar in extensive and poor metabolizers.15
Clozapine, olanzapine, quetiapine, ziprasidone, and aripiprazole are associated with a much lower risk of PRL elevation than risperidone. In an 8-week open-label trial, aripiprazole (mean dose 9.4±4.2 mg/d), did not increase serum PRL in 15 children and adolescents.2
Ziprasidone may cause only transient PRL elevation.16 PRL abnormalities may be least likely with clozapine and quetiapine, possibly because of their relatively lower D2 receptor affinity. Amenorrhea, galactorrhea, or inhibition of ejaculation have not been reported with the use of these 2 antipsychotics.16 Patients who developed hyperprolactinemia on conventional anti-psychotics have been treated subsequently with clozapine without hyperprolactinemia recurrence.16 Iloperidone has been associated with decreased PRL levels.17
Antidepressants that work by blocking catecholamine reuptake also cause hyperprolactinemia. This increase may be related to the antidopaminergic, stimulatory effects of estrogen. Numerous cases of galactorrhea and amenorrhea have been reported with the use of selective serotonin reuptake inhibitors (SSRIs).16 Galactorrhea has been reported in women who took venlafaxine.12 Less is known about the effects of nefazodone or bupropion on serum PRL. Mirtazapine can decrease serum PRL in men, probably through indirect 5-HT1 agonist and 5-HT2 and 5-HT3 antagonist activity.16
PRL elevation is greater in children and adolescents than adults because of increased density of D2 receptors in the developing striatum and differential D2 receptor sensitivity in the tuberoinfundibular tract.16 Unfortunately, few studies have examined the consequences of elevated PRL in children and adolescents.
Prolactin (PRL) is a lactogenic polypeptide hormone with a structure that resembles human growth hormone and human placental lactogen. A single gene on chromosome 6 encodes PRL, which is composed of 199 amino acids.1
PRL is produced primarily by lactotroph cells in the anterior pituitary gland, but also is produced and is active in breast tissue and mammary glands, placenta and decidua, bone marrow cells, lymphocytes (T cells and B cells), and other tissues. It has >300 biologic activities.1
PRL acts primarily through receptors that belong to the large class-1 cytokine receptor superfamily. PRL receptors have multiple isoforms in many different tissues.
Like most anterior pituitary hormones, PRL is under dual regulation by hypothalamic hormones delivered via the hypothalamic-pituitary portal circulation. Its production is stimulated and inhibited by several molecular factors. Under most conditions the predominant signal for PRL secretion from the pituitary is under inhibitory control. This is primarily mediated by the neurotransmitter dopamine, which is a tonic inhibitor of PRL expression and thus prevents its release. Other inhibitors of PRL are triiodothyronine (T3) and somatostatin.2 Molecular stimulators of PRL production include thyrotropin-releasing factor, vasoactive intestinal peptide, peptide histidine isoleucine, gonadotropin-releasing hormone, and estrogen. These 5 molecular stimulators all enhance the growth of PRL-producing cells.1 The balance between these stimulatory and inhibitory signals determines the amount of PRL released from the anterior pituitary.
Prolactin (PRL) is best known for its regulatory role in reproductive processes. It inhibits secretion of the pituitary hormones (luteinizing hormone [LH] and follicle-stimulating hormone [FSH]), which are responsible for gonadal function. PRL also influences normal breast development, lactation following childbirth, and corpus luteum development. It plays a critical role in inducing and maintaining mammary epithelial cell growth and differentiation.1
A recently observed correlation between elevated plasma PRL and breast cancer development suggests a mitogenic action in breast tissue. A prospective, case-control study of 851 women from the Nurses’ Health Study cohort found a “modestly” increased relative risk of postmenopausal breast cancer associated with PRL plasma concentrations (1.34; 95% confidence interval, 1.02 to 1.76).3
PRL also acts as a physiologic sensor during lactation. It regulates ductal side branching and directly controls lobuloalveolar development and lactogenesis (synthesis of milk) in breast tissue. PRL is stimulated by suckling; it responds to demands for milk production by partitioning nutrients such as calcium away from adipose tissue and into the mammary glands.1,4
In reproduction, PRL can have a luteotropic or luteolytic action, depending on the stage of the reproductive cycle. It negatively modulates LH and FSH secretion by suppressing gonadotropin-releasing hormone and as a result suppresses ovulation during lactation.3 PRL also maintains luteal vascularization in early pregnancy.1
PRL also has a role in bone development and bone mass maintenance. It has a direct inhibitory effect on osteoblast function, possibly through an effect on estrogen.5 Although the mechanism is unclear, sustained plasma PRL elevation decreases bone formation, leading to reduced bone mineral density and increased risk of hip fracture.6
PRL is a stimulatory modulator of immune function and may be a “stress hormone.” It is widely produced by lymphocytes. PRL and its receptors are expressed on diverse bone marrow-derived human cell types, including B cells, T cells, monocytes, natural killer cells, and cluster of differentiation 34 (CD34) human stem cells.7 The widespread expression of PRL receptors on hematopoietic and immune cells implies a role in immunohematopoietic system development.
Other functions of PRL include regulation of pancreatic islets growth and function during the perinatal period; osmoregulation in mammary glands, amniotic membranes, and the intestinal epithelial membrane; and maintenance of positive calcium deposition.1 As a potent platelet aggregation co-activator, prolactin also may be a risk factor for both arterial and venous thrombosis.8
Table 1
Causes of hyperprolactinemia
| Iatrogenic causes |
|---|
| Conventional antipsychotics (phenothiazines, thioxanthenes, butyrophenones, dibenzoxazepines) |
| Atypical antipsychotics (risperidone, olanzapine, ziprasidone, clozapine, quetiapine, aripiprazole, paliperidone) |
| SSRIs (fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram) |
| Antiretroviral agents (ritonavir, indinavir, zidovudine) |
| Gastrointestinal agents (omeprazole, ranitidine, cimetidine, famotidine) |
| Other medications (oral contraceptives, verapamil, methyldopa, reserpine, triptorelin, bendroflumethiazide) |
| Other causes |
| Tumors (prolactinoma, craniopharyngioma, other cerebral tumor) |
| Ectopic prolactin synthesis (bronchial carcinoma, acromegaly, empty sella syndrome, polycystic ovarian syndrome) |
| Chronic renal failure |
| Primary thyroid failure |
| Physiological causes (pregnancy, lactation, stress, sleep, sexual intercourse, head injury, surgery) |
| SSRIs: selective serotonin reuptake inhibitors Source: Reference 9 |
Table 2
Relative risk of hyperprolactinemia with common psychotropics
| Medication | Effect on prolactin serum levels |
|---|---|
| Antipsychotics | |
| Phenothiazines | ++ |
| Butyrophenones | ++ |
| Thioxanthenes | ++ |
| Risperidone | ++ |
| Quetiapine | + |
| Olanzapine | + |
| Clozapine | 0 |
| Ziprasidone | 0 |
| Aripiprazole | 0 |
| SSRIs | |
| Paroxetine | +/- |
| Citalopram | +/- |
| Fluvoxamine | +/- |
| Fluoxetine | CR |
| 0: no hyperprolactinemia effect; +/-: increased but not to abnormal levels; +: increased to abnormal in small percentage of patients; ++: increased to abnormal in >50% of patients; CR: isolated case reports of hyperprolactinemia but generally no increase to abnormal SSRIs: selective serotonin reuptake inhibitors Source: Adapted from reference 9 | |
Clinical features
Adenomas. Primary hyperprolactinemia related to excessive secretion from the pituitary and other tissues causes multiple clinical effects, including:
- amenorrhea, oligomenorrhea, anovulatory cycles, galactorrhea, breast pain, breast enlargement, infertility, hirsutism, and loss of libido in females
- impotence, loss of libido, decrease in seminal fluid volume, galactorrhea, and gynecomastia in males.12
Preclinical studies of risperidone suggested an association with pituitary adenomas in female mice.18 To determine if there was a similar association in humans, Szarfman et al18 retrospectively evaluated data on 7 antipsychotics—aripiprazole, clozapine, olanzapine, quetiapine, risperidone, ziprasidone, and haloperidol—and found 77 pituitary tumors associated with use of these medications. Risperidone was associated with 54 of the pituitary tumors—including 3 in adolescents age 14 to 16. No pituitary tumors were reported with aripiprazole. Approximately one-half of the pituitary tumors were benign. Symptoms included visual field defects, headaches, pituitary hemorrhage, convulsions, and coma.
Other adverse effects reported in the study were hyperprolactinemia, galactorrhea, amenorrhea, and gynecomastia. The incidence of adverse effects with risperidone was >10-fold higher than with haloperidol or olanzapine and >25-fold higher than with clozapine, ziprasidone, quetiapine, and aripiprazole.
Hyperprolactinemia secondary to macroadenoma or microadenoma in children and adolescents is rare and difficult to diagnose because typically it is suspected only when symptoms of tumor expansion occur. The usual initial symptoms of microadenomas are menstrual disturbances and galactorrhea in girls and galactorrhea and gynecomastia in boys.19
Decreased bone mass. Long-term hyperprolactinemia may lead to delayed puberty, primary amenorrhea, short stature, infertility, and osteopenia and/or osteoporosis due to decreased bone mass density (BMD).16 The risk of osteoporosis and/or osteopenia is directly related to the duration of hyperprolactinemia. A serum PRL level twice the upper limit of normal can result in osteopenia.
Breast cancer risk may be increased in hyperprolactinemia because of the effects of PRL on breast tissue and mammary gland development. A study of premenopausal (n=235) and postmenopausal women (n=851) reported a positive correlation between elevated PRL levels and breast cancer risk.3 “Crosstalk” between PRL and estradiol in activating AP-1 activity may promote carcinogenesis. Furthermore, tamoxifen, a common treatment for breast cancer, lowers PRL concentrations.3
Not all patients with hyperprolactinemia develop problems. Whether hyperprolactinemia secondary to antipsychotic treatment adversely affects bone density or sexual maturation is unknown. Furthermore, sexual side effects—such as a decrease or loss of libido, erectile dysfunction, impotence, and ejaculatory or orgasmic difficulties—do not show a strong correlation with PRL levels.11
Effects of hyperprolactinemia may be more pronounced in adolescents because PRL synthesis and release are stimulated by estrogen. In adolescent females elevated estrogen levels can be related to:
- increased estrogen levels in menstruating females
- increased estrogen levels in females taking oral contraceptives.16
Therefore, adolescent females taking antipsychotics are at high risk for increased PRL levels and resultant effects. For example, the BMD of adolescent girls with 6 months of hypothalamic-pituitary-gonadal (HPG) axis dysfunction caused by hyperprolactinemia was reduced by 2 standard deviations (SDs) below the population mean.16 A BMD 1 SD below the mean age-population value may double the risk for fractures.16 Unfortunately, there are no studies that measure estrogen levels or BMDs of children taking psychotropics16 or that assess PRL in pubertal girls taking atypical antipsychotics or SSRIs.
Evaluation of hyperprolactinemia
Blood samples to measure PRL levels must be collected under standardized conditions. A morning fasting serum PRL level should be obtained between 8 am and 10 am (3 hours after waking up). It is best to avoid emotional stress or strenuous exercise for at least 30 minutes before the blood draw because these conditions can raise PRL. Avoid nipple stimulation for 24 hours before testing because this also can raise PRL levels. A woman having abnormal nipple discharge should not do anything to cause more discharge before the test. Serum PRL levels should be monitored every 6 months in pubertal girls taking psychotropics until they experience sexual maturity or regular menstrual cycles so that abnormalities can be identified early and irreversible BMD loss is minimized.16
Absolute PRL level is not useful in guiding treatment because it is not consistently correlated with adverse effects. However, the degree of change of serum PRL levels over time or the change of PRL levels from baseline may be important in diagnosing asymptomatic hyperprolactinemia.16 Suspect pathologic hyperprolactinemia in patients (except newborns and pregnant women) with plasma PRL levels consistently >15 to 25 ng/mL.12 This finding occurs in <1% of the population, but the rate is higher among individuals with specific symptoms attributable to hyperprolactinemia. For example, 9% of women with amenorrhea, 25% of women with galactorrhea, and 70% of women with both amenorrhea and galactorrhea have hyperprolactinemia. The prevalence is approximately 5% among men with impotence or infertility.10
If hyperprolactinemia is detected, the degree of PRL elevation can help determine etiology. In the absence of pregnancy and breastfeeding, a serum PRL level of >600 ng/mL is highly suggestive of a macroprolactinoma.12 PRL concentrations >250 ng/mL suggest a microprolactinoma or a nonfunctioning adenoma.12 Antipsychotics usually produce moderate PRL elevation (up to 6 times the upper limit of the reference range of 100 ng/mL).12 In 1 study, the median time to onset of galactorrhea was 20 days after initiating antipsychotics in female patients.12 Hyperprolactinemia-induced HPG axis dysfunction causes delayed pubertal development or loss of bone mineral deposit.16 Measuring BMD in children and adolescents with hyperprolactinemia is important during this critical time of skeletal development.16
Managing hyperprolactinemia
Before starting any antipsychotic, inform patients and families of possible side effects, including hyperprolactinemia. Educate them about recognizing the signs and symptoms of hyperprolactinemia (Table 3).12 Although PRL blood levels typically are not routinely measured in pubertal girls who take PRL-modulating agents, consider monitoring serum PRL levels every 6 months until patients achieve sexual maturity and menstrual cycle regularity.16
If laboratory testing detects elevated PRL levels in a child or adolescent, determine if the patient had sexual intercourse, nipple stimulation, stress (including venipuncture), sleep disturbances, seizures, head injury, or surgery before the blood sample was obtained. This information will help to determine if the PRL elevation is caused by one of these factors.
To treat hyperprolactinemia, address the underlying medical cause(s). If patients using antipsychotics have signs and symptoms of hyperprolactinemia, consider discontinuing the drug or reducing the dosage.11 If dose change fails to reduce hyperprolactinemia, consider a switch to a low-potency D2 agent or aripiprazole. Shim et al20 studied the effects of adjunctive treatment with aripiprazole on hyperprolactinemia and psychopathology in schizophrenia patients maintained on haloperidol. In this study, aripiprazole reversed hyperprolactinemia in both sexes but plasma levels of haloperidol were not significantly altered. The authors hypothesized that decreased PRL levels may have been the result of pharmacodynamic interaction at dopamine receptors rather than pharmacokinetic interaction between aripiprazole and haloperidol. Additional studies are needed to confirm these findings.
If a medication switch is contraindicated, pharmacologic treatment for hyperprolactinemia may be required.11 Bromocriptine, cabergoline, and amantadine have been used to treat hyperprolactinemia.11 Bromocriptine lowers PRL levels and restores normal gonadal function for men and women with hyperprolactinemia regardless of etiology, but may worsen psychiatric symptoms and can cause nausea, headaches, dizziness, and orthostatic hypotension.11 In a pilot study, amantadine, 300 mg/d, used to treat neuroleptic-induced extrapyramidal effects also decreased PRL levels and reduced galactorrhea.11
Osteoporosis can be minimized by exercising, taking adequate calcium and vitamin D, and avoiding caffeinated drinks.9 Simmons et al21 found bisphosphonate treatment in children and adolescents improved bone density and fragility within 2 to 4 years. Unfortunately, information about optimal duration and long-term effects of bisphosphonate therapy is limited.22
Surgical treatment may be necessary to remove a pituitary tumor that causes hyperprolactinemia. For some patients, referral to pediatric endocrinologist for further treatment may be needed.
Table 3
Presenting symptoms of hyperprolactinemia
| Adult females | Adult males | Prepubertal children (male and female) |
|---|---|---|
| Amenorrhea Anovulatory cycle Breast enlargement Breast pain Galactorrhea Hirsutism Infertility Loss of libido Oligomenorrhea | Decreased in seminal fluid volume Galactorrhea Gynecomastia Impotence Loss of libido | Delayed puberty Galactorrhea Gynecomastia Osteopenia or osteoporosis Primary amenorrhea (females only) Short stature |
| Source: Adapted from reference 12 | ||
Related Resources
- Ali J, Khemka M. Hyperprolactinemia: Monitoring children on long-term risperidone. Current Psychiatry. 2008;7(11):64-72.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bendroflumethiazide • Naturetin
- Bromocriptine • Parlodel
- Bupropion • Wellbutrin
- Cabergoline • Dostinex
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clozapine • Clozaril
- Famotidine • Pepcid
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Indinavir • Crixivan
- Methyldopa • Aldomet
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Paliperidone • Invega
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Quinidine • Quinidex
- Ranitidine • Zantac
- Reserpine • Serpasil
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Triptorelin • Trelstar
- Venlafaxine • Effexor
- Verapamil • Calan, Isoptin
- Zidovudine • Retrovir
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors wish to thank Yunyoung C. Chang, BS, for her assistance with this article.
1. Freeman ME, Kanyicska B, Lerant A, et al. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80(4):1523-1631.
2. Biederman J, Mick E, Spencer T, et al. An open-label trial of aripiprazole monotherapy in children and adolescents with bipolar disorder. CNS Spectr. 2007;12(9):683-689.
3. Tworoger SS, Eliassen AH, Rosner B, et al. Plasma prolactin concentrations and risk of postmenopausal breast cancer. Cancer Res. 2004;64(18):6814-6819.
4. Anantamongkol U, Takemura H, Suthiphongchai T, et al. Regulation of Ca2+ mobilization by prolactin in mammary gland cells: possible role of secretory pathway Ca2+- ATPase type 2. Biochem Biophy Res Commun. 2007;352(2):537-542.
5. Coss D, Yang L, Kuo CB, et al. Effects of prolactin on osteoblast alkaline phosphatase and bone formation in the developing rat. Am J Physiol Endocrinol Metab. 2000;279(6):1216-1225.
6. Meaney AM, O’Keane V. Bone mineral density changes over a year in young females with schizophrenia: relationship to medication and endocrine variables. Schizophr Res. 2007;93(1-3):136-143.
7. Richards SM, Murphy WJ. Use of human prolactin as a therapeutic protein to potentiate immunohematopoietic function. J Neuroimmunol. 2000;109(1):56-62.
8. Wallaschofski H, Donné M, Eigenthaler M, et al. PRL as a novel potent cofactor for platelet aggregation. J Clin Endocrinol Metab. 2001;86(12):5912-5919.
9. Molitch M. Medication-induced hyperprolactinemia. Mayo Clin Proc. 2005;80(8):1050-1057.
10. Serri O, Chik CL, Ur E, et al. Diagnosis and management of hyperprolactinemia. CMAJ. 2003;169(6):575-581.
11. Compton M, Miller A. Antipsychotic-induced hyper-prolactinemia and sexual dysfunction. Psychopharmacol Bull. 2002;36(1):143-164.
12. Haddad PM, Wieck A. Antipsychotic-induced hyper-prolactinaemia: mechanisms clinical features and management. Drugs. 2004;64(20):2291-2314.
13. Nussbaum A, Stroup T. Paliperidone for treatment of schizophrenia. Schizophr Bull. 2008;34(3):419-422.
14. Findling R, Kusumakar V, Daneman D, et al. Prolactin levels during long-term risperidone treatment in children and adolescents. J Clin Psychiatry. 2003;64(11):1362-1369.
15. Risperdal [package insert]. Titusville NJ: Ortho-McNeil-Janssen Pharmaceuticals, Inc; 2010.
16. Becker A, Epperson CN. Female puberty: clinical implications for the use for prolactin-modulating psychotropics. Child Adolesc Psychiatr N Am. 2006;15(1):207-220.
17. Weiden PJ, Cutler AJ, Polymeropoulos MH, et al. Safety profile of iloperidone: a pooled analysis of 6-week acute-phase pivotal trials. J Clin Psychopharmacol. 2008;28 (2 suppl 1):S12-S19.
18. Szarfman A, Tonning J, Levine J, et al. Atypical antipsychotics and pituitary tumors: a pharmacovigilance study. Pharmacotherapy. 2006;26(6):748-758.
19. Colao A, Loche S, Cappa M, et al. Prolactinoma in children and adolescents. Clinical presentation and long-term follow-up. J Clin Endocrinol Metab. 1998;83(8):2777-2780.
20. Shim JC, Shin JG, Kelly DL, et al. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: a placebo-controlled trial. Am J Psychiatry. 2007;164:1404-1410.
21. Simmons J, Zeitler P, Steelman J. Advances in the diagnosis and treatment of osteoporosis. Adv Pediatr. 2007;54:85-114.
22. Ward L, Tricco AC, Phuong P, et al. Bisphosphonate therapy for children and adolescents with secondary osteoporosis. Cochrane Database Syst Rev. 2007;(4):CD005324.-
Discuss this article at www.facebook.com/CurrentPsychiatry
Hyperprolactinemia—increased levels of prolactin (PRL) in the blood that may be caused by hypothyroidism, pituitary disorders, atypical antipsychotics, or other conditions and medications—has numerous physiologic manifestations, including amenorrhea, infertility, abnormal bone resorption, increased risk of breast cancer, and compromised immunity. Evaluation of hyperprolactinemia in patients taking psychotropics—particularly children and adolescents, in whom hyperprolactinemia’s adverse effects may be more pronounced—should include an examination for signs and symptoms of hyperprolactinemia and assessment to rule out other potential causes. This article reviews hyperprolactinemia’s causes, symptoms, evaluation, and treatment, with an emphasis on younger patients.
Causes of hyperprolactinemia
PRL is a circulating autocrine or paracrine factor (Box 1).1,2 Its primary biologic activities can be broadly divided into 4 areas: reproductive, metabolic, osmoregulatory, and immunoregulatory (Box 2).1,3-8
Hyperprolactinemia has numerous physiologic and iatrogenic causes (Table 1).9 Substantially increased serum PRL levels may be seen with:
- prolactinomas, which usually present as incidental findings on a brain CT or MRI or with symptoms of tumor mass
- a craniopharyngioma or other tumor that compresses the pituitary stalk or hypothalamus and interrupts the hypothalamic-dopa minergic inhibition of PRL release.10
Primary thyroid failure (hypothyroidism) can produce a compensatory increase in the discharge of central hypothalamic thyrotropin-releasing hormone, resulting in increased stimulation of PRL secretion.10
Medications can increase serum PRL (Table 2)9 and cause clinical symptoms similar to those of physiologically induced hyperprolactinemia.
Conventional antipsychotics. The anti-psychotic potency of phenothiazines, thioxanthenes, butyrophenones, and dibenzoxazepines generally parallels their potency in increasing PRL levels.9 Although a dose-response relationship between PRL concentrations and conventional antipsychotics is likely, immediate and pronounced increases in PRL can occur even with low doses.
Prospective studies have shown that 3 to 9 weeks of treatment with an antipsychotic such as chlorpromazine increased mean baseline PRL levels up to 10-fold, even at therapeutic doses.11 Conventional antipsychotics can cause marked increases in PRL, probably by blocking dopamine receptors in the tuberoinfundibular tract.12 The blockage of D2 receptors removes the main inhibitory influence on PRL secretion and is associated with increased PRL release.12
Atypical antipsychotics cause less elevation in PRL levels than conventional anti-psychotics. This may be because of their:
- highly selective mesolimbic and meso-cortical dopamine receptor antagonism, which spares dopamine blockade within the tuberoinfundibular tract
- relatively lower D2 receptor affinity.11
Risperidone and its active metabolite paliperidone (9-hydroxyrisperidone) have a high affinity for D2 receptors and thus have potent D2 antagonistic effects.12,13 At dosages of 8 mg/d to 11.8 mg/d, risperidone and paliperidone are associated with the greatest increase in PRL levels among atypical antipsychotics.14
The rate of risperidone metabolism depends on the patient’s cytochrome P (CYP) 2D6 liver enzyme genotype. “Extensive” CYP2D6 metabolizers convert risperidone rapidly into 9-hydroxyrisperidone, whereas “poor” CYP2D6 metabolizers convert it much more slowly. Six percent to 8% of white individuals and a very low percentage of Asians have little or no CYP2D6 activity and are “poor metabolizers.” CYP2D6 also is inhibited by various substrates and nonsubstrates, notably quinidine. Although extensive metabolizers have lower risperidone and higher 9-hydroxyrisperidone concentrations than poor metabolizers, the pharmacokinetics of the active moiety after single and multiple doses are similar in extensive and poor metabolizers.15
Clozapine, olanzapine, quetiapine, ziprasidone, and aripiprazole are associated with a much lower risk of PRL elevation than risperidone. In an 8-week open-label trial, aripiprazole (mean dose 9.4±4.2 mg/d), did not increase serum PRL in 15 children and adolescents.2
Ziprasidone may cause only transient PRL elevation.16 PRL abnormalities may be least likely with clozapine and quetiapine, possibly because of their relatively lower D2 receptor affinity. Amenorrhea, galactorrhea, or inhibition of ejaculation have not been reported with the use of these 2 antipsychotics.16 Patients who developed hyperprolactinemia on conventional anti-psychotics have been treated subsequently with clozapine without hyperprolactinemia recurrence.16 Iloperidone has been associated with decreased PRL levels.17
Antidepressants that work by blocking catecholamine reuptake also cause hyperprolactinemia. This increase may be related to the antidopaminergic, stimulatory effects of estrogen. Numerous cases of galactorrhea and amenorrhea have been reported with the use of selective serotonin reuptake inhibitors (SSRIs).16 Galactorrhea has been reported in women who took venlafaxine.12 Less is known about the effects of nefazodone or bupropion on serum PRL. Mirtazapine can decrease serum PRL in men, probably through indirect 5-HT1 agonist and 5-HT2 and 5-HT3 antagonist activity.16
PRL elevation is greater in children and adolescents than adults because of increased density of D2 receptors in the developing striatum and differential D2 receptor sensitivity in the tuberoinfundibular tract.16 Unfortunately, few studies have examined the consequences of elevated PRL in children and adolescents.
Prolactin (PRL) is a lactogenic polypeptide hormone with a structure that resembles human growth hormone and human placental lactogen. A single gene on chromosome 6 encodes PRL, which is composed of 199 amino acids.1
PRL is produced primarily by lactotroph cells in the anterior pituitary gland, but also is produced and is active in breast tissue and mammary glands, placenta and decidua, bone marrow cells, lymphocytes (T cells and B cells), and other tissues. It has >300 biologic activities.1
PRL acts primarily through receptors that belong to the large class-1 cytokine receptor superfamily. PRL receptors have multiple isoforms in many different tissues.
Like most anterior pituitary hormones, PRL is under dual regulation by hypothalamic hormones delivered via the hypothalamic-pituitary portal circulation. Its production is stimulated and inhibited by several molecular factors. Under most conditions the predominant signal for PRL secretion from the pituitary is under inhibitory control. This is primarily mediated by the neurotransmitter dopamine, which is a tonic inhibitor of PRL expression and thus prevents its release. Other inhibitors of PRL are triiodothyronine (T3) and somatostatin.2 Molecular stimulators of PRL production include thyrotropin-releasing factor, vasoactive intestinal peptide, peptide histidine isoleucine, gonadotropin-releasing hormone, and estrogen. These 5 molecular stimulators all enhance the growth of PRL-producing cells.1 The balance between these stimulatory and inhibitory signals determines the amount of PRL released from the anterior pituitary.
Prolactin (PRL) is best known for its regulatory role in reproductive processes. It inhibits secretion of the pituitary hormones (luteinizing hormone [LH] and follicle-stimulating hormone [FSH]), which are responsible for gonadal function. PRL also influences normal breast development, lactation following childbirth, and corpus luteum development. It plays a critical role in inducing and maintaining mammary epithelial cell growth and differentiation.1
A recently observed correlation between elevated plasma PRL and breast cancer development suggests a mitogenic action in breast tissue. A prospective, case-control study of 851 women from the Nurses’ Health Study cohort found a “modestly” increased relative risk of postmenopausal breast cancer associated with PRL plasma concentrations (1.34; 95% confidence interval, 1.02 to 1.76).3
PRL also acts as a physiologic sensor during lactation. It regulates ductal side branching and directly controls lobuloalveolar development and lactogenesis (synthesis of milk) in breast tissue. PRL is stimulated by suckling; it responds to demands for milk production by partitioning nutrients such as calcium away from adipose tissue and into the mammary glands.1,4
In reproduction, PRL can have a luteotropic or luteolytic action, depending on the stage of the reproductive cycle. It negatively modulates LH and FSH secretion by suppressing gonadotropin-releasing hormone and as a result suppresses ovulation during lactation.3 PRL also maintains luteal vascularization in early pregnancy.1
PRL also has a role in bone development and bone mass maintenance. It has a direct inhibitory effect on osteoblast function, possibly through an effect on estrogen.5 Although the mechanism is unclear, sustained plasma PRL elevation decreases bone formation, leading to reduced bone mineral density and increased risk of hip fracture.6
PRL is a stimulatory modulator of immune function and may be a “stress hormone.” It is widely produced by lymphocytes. PRL and its receptors are expressed on diverse bone marrow-derived human cell types, including B cells, T cells, monocytes, natural killer cells, and cluster of differentiation 34 (CD34) human stem cells.7 The widespread expression of PRL receptors on hematopoietic and immune cells implies a role in immunohematopoietic system development.
Other functions of PRL include regulation of pancreatic islets growth and function during the perinatal period; osmoregulation in mammary glands, amniotic membranes, and the intestinal epithelial membrane; and maintenance of positive calcium deposition.1 As a potent platelet aggregation co-activator, prolactin also may be a risk factor for both arterial and venous thrombosis.8
Table 1
Causes of hyperprolactinemia
| Iatrogenic causes |
|---|
| Conventional antipsychotics (phenothiazines, thioxanthenes, butyrophenones, dibenzoxazepines) |
| Atypical antipsychotics (risperidone, olanzapine, ziprasidone, clozapine, quetiapine, aripiprazole, paliperidone) |
| SSRIs (fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram) |
| Antiretroviral agents (ritonavir, indinavir, zidovudine) |
| Gastrointestinal agents (omeprazole, ranitidine, cimetidine, famotidine) |
| Other medications (oral contraceptives, verapamil, methyldopa, reserpine, triptorelin, bendroflumethiazide) |
| Other causes |
| Tumors (prolactinoma, craniopharyngioma, other cerebral tumor) |
| Ectopic prolactin synthesis (bronchial carcinoma, acromegaly, empty sella syndrome, polycystic ovarian syndrome) |
| Chronic renal failure |
| Primary thyroid failure |
| Physiological causes (pregnancy, lactation, stress, sleep, sexual intercourse, head injury, surgery) |
| SSRIs: selective serotonin reuptake inhibitors Source: Reference 9 |
Table 2
Relative risk of hyperprolactinemia with common psychotropics
| Medication | Effect on prolactin serum levels |
|---|---|
| Antipsychotics | |
| Phenothiazines | ++ |
| Butyrophenones | ++ |
| Thioxanthenes | ++ |
| Risperidone | ++ |
| Quetiapine | + |
| Olanzapine | + |
| Clozapine | 0 |
| Ziprasidone | 0 |
| Aripiprazole | 0 |
| SSRIs | |
| Paroxetine | +/- |
| Citalopram | +/- |
| Fluvoxamine | +/- |
| Fluoxetine | CR |
| 0: no hyperprolactinemia effect; +/-: increased but not to abnormal levels; +: increased to abnormal in small percentage of patients; ++: increased to abnormal in >50% of patients; CR: isolated case reports of hyperprolactinemia but generally no increase to abnormal SSRIs: selective serotonin reuptake inhibitors Source: Adapted from reference 9 | |
Clinical features
Adenomas. Primary hyperprolactinemia related to excessive secretion from the pituitary and other tissues causes multiple clinical effects, including:
- amenorrhea, oligomenorrhea, anovulatory cycles, galactorrhea, breast pain, breast enlargement, infertility, hirsutism, and loss of libido in females
- impotence, loss of libido, decrease in seminal fluid volume, galactorrhea, and gynecomastia in males.12
Preclinical studies of risperidone suggested an association with pituitary adenomas in female mice.18 To determine if there was a similar association in humans, Szarfman et al18 retrospectively evaluated data on 7 antipsychotics—aripiprazole, clozapine, olanzapine, quetiapine, risperidone, ziprasidone, and haloperidol—and found 77 pituitary tumors associated with use of these medications. Risperidone was associated with 54 of the pituitary tumors—including 3 in adolescents age 14 to 16. No pituitary tumors were reported with aripiprazole. Approximately one-half of the pituitary tumors were benign. Symptoms included visual field defects, headaches, pituitary hemorrhage, convulsions, and coma.
Other adverse effects reported in the study were hyperprolactinemia, galactorrhea, amenorrhea, and gynecomastia. The incidence of adverse effects with risperidone was >10-fold higher than with haloperidol or olanzapine and >25-fold higher than with clozapine, ziprasidone, quetiapine, and aripiprazole.
Hyperprolactinemia secondary to macroadenoma or microadenoma in children and adolescents is rare and difficult to diagnose because typically it is suspected only when symptoms of tumor expansion occur. The usual initial symptoms of microadenomas are menstrual disturbances and galactorrhea in girls and galactorrhea and gynecomastia in boys.19
Decreased bone mass. Long-term hyperprolactinemia may lead to delayed puberty, primary amenorrhea, short stature, infertility, and osteopenia and/or osteoporosis due to decreased bone mass density (BMD).16 The risk of osteoporosis and/or osteopenia is directly related to the duration of hyperprolactinemia. A serum PRL level twice the upper limit of normal can result in osteopenia.
Breast cancer risk may be increased in hyperprolactinemia because of the effects of PRL on breast tissue and mammary gland development. A study of premenopausal (n=235) and postmenopausal women (n=851) reported a positive correlation between elevated PRL levels and breast cancer risk.3 “Crosstalk” between PRL and estradiol in activating AP-1 activity may promote carcinogenesis. Furthermore, tamoxifen, a common treatment for breast cancer, lowers PRL concentrations.3
Not all patients with hyperprolactinemia develop problems. Whether hyperprolactinemia secondary to antipsychotic treatment adversely affects bone density or sexual maturation is unknown. Furthermore, sexual side effects—such as a decrease or loss of libido, erectile dysfunction, impotence, and ejaculatory or orgasmic difficulties—do not show a strong correlation with PRL levels.11
Effects of hyperprolactinemia may be more pronounced in adolescents because PRL synthesis and release are stimulated by estrogen. In adolescent females elevated estrogen levels can be related to:
- increased estrogen levels in menstruating females
- increased estrogen levels in females taking oral contraceptives.16
Therefore, adolescent females taking antipsychotics are at high risk for increased PRL levels and resultant effects. For example, the BMD of adolescent girls with 6 months of hypothalamic-pituitary-gonadal (HPG) axis dysfunction caused by hyperprolactinemia was reduced by 2 standard deviations (SDs) below the population mean.16 A BMD 1 SD below the mean age-population value may double the risk for fractures.16 Unfortunately, there are no studies that measure estrogen levels or BMDs of children taking psychotropics16 or that assess PRL in pubertal girls taking atypical antipsychotics or SSRIs.
Evaluation of hyperprolactinemia
Blood samples to measure PRL levels must be collected under standardized conditions. A morning fasting serum PRL level should be obtained between 8 am and 10 am (3 hours after waking up). It is best to avoid emotional stress or strenuous exercise for at least 30 minutes before the blood draw because these conditions can raise PRL. Avoid nipple stimulation for 24 hours before testing because this also can raise PRL levels. A woman having abnormal nipple discharge should not do anything to cause more discharge before the test. Serum PRL levels should be monitored every 6 months in pubertal girls taking psychotropics until they experience sexual maturity or regular menstrual cycles so that abnormalities can be identified early and irreversible BMD loss is minimized.16
Absolute PRL level is not useful in guiding treatment because it is not consistently correlated with adverse effects. However, the degree of change of serum PRL levels over time or the change of PRL levels from baseline may be important in diagnosing asymptomatic hyperprolactinemia.16 Suspect pathologic hyperprolactinemia in patients (except newborns and pregnant women) with plasma PRL levels consistently >15 to 25 ng/mL.12 This finding occurs in <1% of the population, but the rate is higher among individuals with specific symptoms attributable to hyperprolactinemia. For example, 9% of women with amenorrhea, 25% of women with galactorrhea, and 70% of women with both amenorrhea and galactorrhea have hyperprolactinemia. The prevalence is approximately 5% among men with impotence or infertility.10
If hyperprolactinemia is detected, the degree of PRL elevation can help determine etiology. In the absence of pregnancy and breastfeeding, a serum PRL level of >600 ng/mL is highly suggestive of a macroprolactinoma.12 PRL concentrations >250 ng/mL suggest a microprolactinoma or a nonfunctioning adenoma.12 Antipsychotics usually produce moderate PRL elevation (up to 6 times the upper limit of the reference range of 100 ng/mL).12 In 1 study, the median time to onset of galactorrhea was 20 days after initiating antipsychotics in female patients.12 Hyperprolactinemia-induced HPG axis dysfunction causes delayed pubertal development or loss of bone mineral deposit.16 Measuring BMD in children and adolescents with hyperprolactinemia is important during this critical time of skeletal development.16
Managing hyperprolactinemia
Before starting any antipsychotic, inform patients and families of possible side effects, including hyperprolactinemia. Educate them about recognizing the signs and symptoms of hyperprolactinemia (Table 3).12 Although PRL blood levels typically are not routinely measured in pubertal girls who take PRL-modulating agents, consider monitoring serum PRL levels every 6 months until patients achieve sexual maturity and menstrual cycle regularity.16
If laboratory testing detects elevated PRL levels in a child or adolescent, determine if the patient had sexual intercourse, nipple stimulation, stress (including venipuncture), sleep disturbances, seizures, head injury, or surgery before the blood sample was obtained. This information will help to determine if the PRL elevation is caused by one of these factors.
To treat hyperprolactinemia, address the underlying medical cause(s). If patients using antipsychotics have signs and symptoms of hyperprolactinemia, consider discontinuing the drug or reducing the dosage.11 If dose change fails to reduce hyperprolactinemia, consider a switch to a low-potency D2 agent or aripiprazole. Shim et al20 studied the effects of adjunctive treatment with aripiprazole on hyperprolactinemia and psychopathology in schizophrenia patients maintained on haloperidol. In this study, aripiprazole reversed hyperprolactinemia in both sexes but plasma levels of haloperidol were not significantly altered. The authors hypothesized that decreased PRL levels may have been the result of pharmacodynamic interaction at dopamine receptors rather than pharmacokinetic interaction between aripiprazole and haloperidol. Additional studies are needed to confirm these findings.
If a medication switch is contraindicated, pharmacologic treatment for hyperprolactinemia may be required.11 Bromocriptine, cabergoline, and amantadine have been used to treat hyperprolactinemia.11 Bromocriptine lowers PRL levels and restores normal gonadal function for men and women with hyperprolactinemia regardless of etiology, but may worsen psychiatric symptoms and can cause nausea, headaches, dizziness, and orthostatic hypotension.11 In a pilot study, amantadine, 300 mg/d, used to treat neuroleptic-induced extrapyramidal effects also decreased PRL levels and reduced galactorrhea.11
Osteoporosis can be minimized by exercising, taking adequate calcium and vitamin D, and avoiding caffeinated drinks.9 Simmons et al21 found bisphosphonate treatment in children and adolescents improved bone density and fragility within 2 to 4 years. Unfortunately, information about optimal duration and long-term effects of bisphosphonate therapy is limited.22
Surgical treatment may be necessary to remove a pituitary tumor that causes hyperprolactinemia. For some patients, referral to pediatric endocrinologist for further treatment may be needed.
Table 3
Presenting symptoms of hyperprolactinemia
| Adult females | Adult males | Prepubertal children (male and female) |
|---|---|---|
| Amenorrhea Anovulatory cycle Breast enlargement Breast pain Galactorrhea Hirsutism Infertility Loss of libido Oligomenorrhea | Decreased in seminal fluid volume Galactorrhea Gynecomastia Impotence Loss of libido | Delayed puberty Galactorrhea Gynecomastia Osteopenia or osteoporosis Primary amenorrhea (females only) Short stature |
| Source: Adapted from reference 12 | ||
Related Resources
- Ali J, Khemka M. Hyperprolactinemia: Monitoring children on long-term risperidone. Current Psychiatry. 2008;7(11):64-72.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bendroflumethiazide • Naturetin
- Bromocriptine • Parlodel
- Bupropion • Wellbutrin
- Cabergoline • Dostinex
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clozapine • Clozaril
- Famotidine • Pepcid
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Indinavir • Crixivan
- Methyldopa • Aldomet
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Paliperidone • Invega
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Quinidine • Quinidex
- Ranitidine • Zantac
- Reserpine • Serpasil
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Triptorelin • Trelstar
- Venlafaxine • Effexor
- Verapamil • Calan, Isoptin
- Zidovudine • Retrovir
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors wish to thank Yunyoung C. Chang, BS, for her assistance with this article.
Discuss this article at www.facebook.com/CurrentPsychiatry
Hyperprolactinemia—increased levels of prolactin (PRL) in the blood that may be caused by hypothyroidism, pituitary disorders, atypical antipsychotics, or other conditions and medications—has numerous physiologic manifestations, including amenorrhea, infertility, abnormal bone resorption, increased risk of breast cancer, and compromised immunity. Evaluation of hyperprolactinemia in patients taking psychotropics—particularly children and adolescents, in whom hyperprolactinemia’s adverse effects may be more pronounced—should include an examination for signs and symptoms of hyperprolactinemia and assessment to rule out other potential causes. This article reviews hyperprolactinemia’s causes, symptoms, evaluation, and treatment, with an emphasis on younger patients.
Causes of hyperprolactinemia
PRL is a circulating autocrine or paracrine factor (Box 1).1,2 Its primary biologic activities can be broadly divided into 4 areas: reproductive, metabolic, osmoregulatory, and immunoregulatory (Box 2).1,3-8
Hyperprolactinemia has numerous physiologic and iatrogenic causes (Table 1).9 Substantially increased serum PRL levels may be seen with:
- prolactinomas, which usually present as incidental findings on a brain CT or MRI or with symptoms of tumor mass
- a craniopharyngioma or other tumor that compresses the pituitary stalk or hypothalamus and interrupts the hypothalamic-dopa minergic inhibition of PRL release.10
Primary thyroid failure (hypothyroidism) can produce a compensatory increase in the discharge of central hypothalamic thyrotropin-releasing hormone, resulting in increased stimulation of PRL secretion.10
Medications can increase serum PRL (Table 2)9 and cause clinical symptoms similar to those of physiologically induced hyperprolactinemia.
Conventional antipsychotics. The anti-psychotic potency of phenothiazines, thioxanthenes, butyrophenones, and dibenzoxazepines generally parallels their potency in increasing PRL levels.9 Although a dose-response relationship between PRL concentrations and conventional antipsychotics is likely, immediate and pronounced increases in PRL can occur even with low doses.
Prospective studies have shown that 3 to 9 weeks of treatment with an antipsychotic such as chlorpromazine increased mean baseline PRL levels up to 10-fold, even at therapeutic doses.11 Conventional antipsychotics can cause marked increases in PRL, probably by blocking dopamine receptors in the tuberoinfundibular tract.12 The blockage of D2 receptors removes the main inhibitory influence on PRL secretion and is associated with increased PRL release.12
Atypical antipsychotics cause less elevation in PRL levels than conventional anti-psychotics. This may be because of their:
- highly selective mesolimbic and meso-cortical dopamine receptor antagonism, which spares dopamine blockade within the tuberoinfundibular tract
- relatively lower D2 receptor affinity.11
Risperidone and its active metabolite paliperidone (9-hydroxyrisperidone) have a high affinity for D2 receptors and thus have potent D2 antagonistic effects.12,13 At dosages of 8 mg/d to 11.8 mg/d, risperidone and paliperidone are associated with the greatest increase in PRL levels among atypical antipsychotics.14
The rate of risperidone metabolism depends on the patient’s cytochrome P (CYP) 2D6 liver enzyme genotype. “Extensive” CYP2D6 metabolizers convert risperidone rapidly into 9-hydroxyrisperidone, whereas “poor” CYP2D6 metabolizers convert it much more slowly. Six percent to 8% of white individuals and a very low percentage of Asians have little or no CYP2D6 activity and are “poor metabolizers.” CYP2D6 also is inhibited by various substrates and nonsubstrates, notably quinidine. Although extensive metabolizers have lower risperidone and higher 9-hydroxyrisperidone concentrations than poor metabolizers, the pharmacokinetics of the active moiety after single and multiple doses are similar in extensive and poor metabolizers.15
Clozapine, olanzapine, quetiapine, ziprasidone, and aripiprazole are associated with a much lower risk of PRL elevation than risperidone. In an 8-week open-label trial, aripiprazole (mean dose 9.4±4.2 mg/d), did not increase serum PRL in 15 children and adolescents.2
Ziprasidone may cause only transient PRL elevation.16 PRL abnormalities may be least likely with clozapine and quetiapine, possibly because of their relatively lower D2 receptor affinity. Amenorrhea, galactorrhea, or inhibition of ejaculation have not been reported with the use of these 2 antipsychotics.16 Patients who developed hyperprolactinemia on conventional anti-psychotics have been treated subsequently with clozapine without hyperprolactinemia recurrence.16 Iloperidone has been associated with decreased PRL levels.17
Antidepressants that work by blocking catecholamine reuptake also cause hyperprolactinemia. This increase may be related to the antidopaminergic, stimulatory effects of estrogen. Numerous cases of galactorrhea and amenorrhea have been reported with the use of selective serotonin reuptake inhibitors (SSRIs).16 Galactorrhea has been reported in women who took venlafaxine.12 Less is known about the effects of nefazodone or bupropion on serum PRL. Mirtazapine can decrease serum PRL in men, probably through indirect 5-HT1 agonist and 5-HT2 and 5-HT3 antagonist activity.16
PRL elevation is greater in children and adolescents than adults because of increased density of D2 receptors in the developing striatum and differential D2 receptor sensitivity in the tuberoinfundibular tract.16 Unfortunately, few studies have examined the consequences of elevated PRL in children and adolescents.
Prolactin (PRL) is a lactogenic polypeptide hormone with a structure that resembles human growth hormone and human placental lactogen. A single gene on chromosome 6 encodes PRL, which is composed of 199 amino acids.1
PRL is produced primarily by lactotroph cells in the anterior pituitary gland, but also is produced and is active in breast tissue and mammary glands, placenta and decidua, bone marrow cells, lymphocytes (T cells and B cells), and other tissues. It has >300 biologic activities.1
PRL acts primarily through receptors that belong to the large class-1 cytokine receptor superfamily. PRL receptors have multiple isoforms in many different tissues.
Like most anterior pituitary hormones, PRL is under dual regulation by hypothalamic hormones delivered via the hypothalamic-pituitary portal circulation. Its production is stimulated and inhibited by several molecular factors. Under most conditions the predominant signal for PRL secretion from the pituitary is under inhibitory control. This is primarily mediated by the neurotransmitter dopamine, which is a tonic inhibitor of PRL expression and thus prevents its release. Other inhibitors of PRL are triiodothyronine (T3) and somatostatin.2 Molecular stimulators of PRL production include thyrotropin-releasing factor, vasoactive intestinal peptide, peptide histidine isoleucine, gonadotropin-releasing hormone, and estrogen. These 5 molecular stimulators all enhance the growth of PRL-producing cells.1 The balance between these stimulatory and inhibitory signals determines the amount of PRL released from the anterior pituitary.
Prolactin (PRL) is best known for its regulatory role in reproductive processes. It inhibits secretion of the pituitary hormones (luteinizing hormone [LH] and follicle-stimulating hormone [FSH]), which are responsible for gonadal function. PRL also influences normal breast development, lactation following childbirth, and corpus luteum development. It plays a critical role in inducing and maintaining mammary epithelial cell growth and differentiation.1
A recently observed correlation between elevated plasma PRL and breast cancer development suggests a mitogenic action in breast tissue. A prospective, case-control study of 851 women from the Nurses’ Health Study cohort found a “modestly” increased relative risk of postmenopausal breast cancer associated with PRL plasma concentrations (1.34; 95% confidence interval, 1.02 to 1.76).3
PRL also acts as a physiologic sensor during lactation. It regulates ductal side branching and directly controls lobuloalveolar development and lactogenesis (synthesis of milk) in breast tissue. PRL is stimulated by suckling; it responds to demands for milk production by partitioning nutrients such as calcium away from adipose tissue and into the mammary glands.1,4
In reproduction, PRL can have a luteotropic or luteolytic action, depending on the stage of the reproductive cycle. It negatively modulates LH and FSH secretion by suppressing gonadotropin-releasing hormone and as a result suppresses ovulation during lactation.3 PRL also maintains luteal vascularization in early pregnancy.1
PRL also has a role in bone development and bone mass maintenance. It has a direct inhibitory effect on osteoblast function, possibly through an effect on estrogen.5 Although the mechanism is unclear, sustained plasma PRL elevation decreases bone formation, leading to reduced bone mineral density and increased risk of hip fracture.6
PRL is a stimulatory modulator of immune function and may be a “stress hormone.” It is widely produced by lymphocytes. PRL and its receptors are expressed on diverse bone marrow-derived human cell types, including B cells, T cells, monocytes, natural killer cells, and cluster of differentiation 34 (CD34) human stem cells.7 The widespread expression of PRL receptors on hematopoietic and immune cells implies a role in immunohematopoietic system development.
Other functions of PRL include regulation of pancreatic islets growth and function during the perinatal period; osmoregulation in mammary glands, amniotic membranes, and the intestinal epithelial membrane; and maintenance of positive calcium deposition.1 As a potent platelet aggregation co-activator, prolactin also may be a risk factor for both arterial and venous thrombosis.8
Table 1
Causes of hyperprolactinemia
| Iatrogenic causes |
|---|
| Conventional antipsychotics (phenothiazines, thioxanthenes, butyrophenones, dibenzoxazepines) |
| Atypical antipsychotics (risperidone, olanzapine, ziprasidone, clozapine, quetiapine, aripiprazole, paliperidone) |
| SSRIs (fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram) |
| Antiretroviral agents (ritonavir, indinavir, zidovudine) |
| Gastrointestinal agents (omeprazole, ranitidine, cimetidine, famotidine) |
| Other medications (oral contraceptives, verapamil, methyldopa, reserpine, triptorelin, bendroflumethiazide) |
| Other causes |
| Tumors (prolactinoma, craniopharyngioma, other cerebral tumor) |
| Ectopic prolactin synthesis (bronchial carcinoma, acromegaly, empty sella syndrome, polycystic ovarian syndrome) |
| Chronic renal failure |
| Primary thyroid failure |
| Physiological causes (pregnancy, lactation, stress, sleep, sexual intercourse, head injury, surgery) |
| SSRIs: selective serotonin reuptake inhibitors Source: Reference 9 |
Table 2
Relative risk of hyperprolactinemia with common psychotropics
| Medication | Effect on prolactin serum levels |
|---|---|
| Antipsychotics | |
| Phenothiazines | ++ |
| Butyrophenones | ++ |
| Thioxanthenes | ++ |
| Risperidone | ++ |
| Quetiapine | + |
| Olanzapine | + |
| Clozapine | 0 |
| Ziprasidone | 0 |
| Aripiprazole | 0 |
| SSRIs | |
| Paroxetine | +/- |
| Citalopram | +/- |
| Fluvoxamine | +/- |
| Fluoxetine | CR |
| 0: no hyperprolactinemia effect; +/-: increased but not to abnormal levels; +: increased to abnormal in small percentage of patients; ++: increased to abnormal in >50% of patients; CR: isolated case reports of hyperprolactinemia but generally no increase to abnormal SSRIs: selective serotonin reuptake inhibitors Source: Adapted from reference 9 | |
Clinical features
Adenomas. Primary hyperprolactinemia related to excessive secretion from the pituitary and other tissues causes multiple clinical effects, including:
- amenorrhea, oligomenorrhea, anovulatory cycles, galactorrhea, breast pain, breast enlargement, infertility, hirsutism, and loss of libido in females
- impotence, loss of libido, decrease in seminal fluid volume, galactorrhea, and gynecomastia in males.12
Preclinical studies of risperidone suggested an association with pituitary adenomas in female mice.18 To determine if there was a similar association in humans, Szarfman et al18 retrospectively evaluated data on 7 antipsychotics—aripiprazole, clozapine, olanzapine, quetiapine, risperidone, ziprasidone, and haloperidol—and found 77 pituitary tumors associated with use of these medications. Risperidone was associated with 54 of the pituitary tumors—including 3 in adolescents age 14 to 16. No pituitary tumors were reported with aripiprazole. Approximately one-half of the pituitary tumors were benign. Symptoms included visual field defects, headaches, pituitary hemorrhage, convulsions, and coma.
Other adverse effects reported in the study were hyperprolactinemia, galactorrhea, amenorrhea, and gynecomastia. The incidence of adverse effects with risperidone was >10-fold higher than with haloperidol or olanzapine and >25-fold higher than with clozapine, ziprasidone, quetiapine, and aripiprazole.
Hyperprolactinemia secondary to macroadenoma or microadenoma in children and adolescents is rare and difficult to diagnose because typically it is suspected only when symptoms of tumor expansion occur. The usual initial symptoms of microadenomas are menstrual disturbances and galactorrhea in girls and galactorrhea and gynecomastia in boys.19
Decreased bone mass. Long-term hyperprolactinemia may lead to delayed puberty, primary amenorrhea, short stature, infertility, and osteopenia and/or osteoporosis due to decreased bone mass density (BMD).16 The risk of osteoporosis and/or osteopenia is directly related to the duration of hyperprolactinemia. A serum PRL level twice the upper limit of normal can result in osteopenia.
Breast cancer risk may be increased in hyperprolactinemia because of the effects of PRL on breast tissue and mammary gland development. A study of premenopausal (n=235) and postmenopausal women (n=851) reported a positive correlation between elevated PRL levels and breast cancer risk.3 “Crosstalk” between PRL and estradiol in activating AP-1 activity may promote carcinogenesis. Furthermore, tamoxifen, a common treatment for breast cancer, lowers PRL concentrations.3
Not all patients with hyperprolactinemia develop problems. Whether hyperprolactinemia secondary to antipsychotic treatment adversely affects bone density or sexual maturation is unknown. Furthermore, sexual side effects—such as a decrease or loss of libido, erectile dysfunction, impotence, and ejaculatory or orgasmic difficulties—do not show a strong correlation with PRL levels.11
Effects of hyperprolactinemia may be more pronounced in adolescents because PRL synthesis and release are stimulated by estrogen. In adolescent females elevated estrogen levels can be related to:
- increased estrogen levels in menstruating females
- increased estrogen levels in females taking oral contraceptives.16
Therefore, adolescent females taking antipsychotics are at high risk for increased PRL levels and resultant effects. For example, the BMD of adolescent girls with 6 months of hypothalamic-pituitary-gonadal (HPG) axis dysfunction caused by hyperprolactinemia was reduced by 2 standard deviations (SDs) below the population mean.16 A BMD 1 SD below the mean age-population value may double the risk for fractures.16 Unfortunately, there are no studies that measure estrogen levels or BMDs of children taking psychotropics16 or that assess PRL in pubertal girls taking atypical antipsychotics or SSRIs.
Evaluation of hyperprolactinemia
Blood samples to measure PRL levels must be collected under standardized conditions. A morning fasting serum PRL level should be obtained between 8 am and 10 am (3 hours after waking up). It is best to avoid emotional stress or strenuous exercise for at least 30 minutes before the blood draw because these conditions can raise PRL. Avoid nipple stimulation for 24 hours before testing because this also can raise PRL levels. A woman having abnormal nipple discharge should not do anything to cause more discharge before the test. Serum PRL levels should be monitored every 6 months in pubertal girls taking psychotropics until they experience sexual maturity or regular menstrual cycles so that abnormalities can be identified early and irreversible BMD loss is minimized.16
Absolute PRL level is not useful in guiding treatment because it is not consistently correlated with adverse effects. However, the degree of change of serum PRL levels over time or the change of PRL levels from baseline may be important in diagnosing asymptomatic hyperprolactinemia.16 Suspect pathologic hyperprolactinemia in patients (except newborns and pregnant women) with plasma PRL levels consistently >15 to 25 ng/mL.12 This finding occurs in <1% of the population, but the rate is higher among individuals with specific symptoms attributable to hyperprolactinemia. For example, 9% of women with amenorrhea, 25% of women with galactorrhea, and 70% of women with both amenorrhea and galactorrhea have hyperprolactinemia. The prevalence is approximately 5% among men with impotence or infertility.10
If hyperprolactinemia is detected, the degree of PRL elevation can help determine etiology. In the absence of pregnancy and breastfeeding, a serum PRL level of >600 ng/mL is highly suggestive of a macroprolactinoma.12 PRL concentrations >250 ng/mL suggest a microprolactinoma or a nonfunctioning adenoma.12 Antipsychotics usually produce moderate PRL elevation (up to 6 times the upper limit of the reference range of 100 ng/mL).12 In 1 study, the median time to onset of galactorrhea was 20 days after initiating antipsychotics in female patients.12 Hyperprolactinemia-induced HPG axis dysfunction causes delayed pubertal development or loss of bone mineral deposit.16 Measuring BMD in children and adolescents with hyperprolactinemia is important during this critical time of skeletal development.16
Managing hyperprolactinemia
Before starting any antipsychotic, inform patients and families of possible side effects, including hyperprolactinemia. Educate them about recognizing the signs and symptoms of hyperprolactinemia (Table 3).12 Although PRL blood levels typically are not routinely measured in pubertal girls who take PRL-modulating agents, consider monitoring serum PRL levels every 6 months until patients achieve sexual maturity and menstrual cycle regularity.16
If laboratory testing detects elevated PRL levels in a child or adolescent, determine if the patient had sexual intercourse, nipple stimulation, stress (including venipuncture), sleep disturbances, seizures, head injury, or surgery before the blood sample was obtained. This information will help to determine if the PRL elevation is caused by one of these factors.
To treat hyperprolactinemia, address the underlying medical cause(s). If patients using antipsychotics have signs and symptoms of hyperprolactinemia, consider discontinuing the drug or reducing the dosage.11 If dose change fails to reduce hyperprolactinemia, consider a switch to a low-potency D2 agent or aripiprazole. Shim et al20 studied the effects of adjunctive treatment with aripiprazole on hyperprolactinemia and psychopathology in schizophrenia patients maintained on haloperidol. In this study, aripiprazole reversed hyperprolactinemia in both sexes but plasma levels of haloperidol were not significantly altered. The authors hypothesized that decreased PRL levels may have been the result of pharmacodynamic interaction at dopamine receptors rather than pharmacokinetic interaction between aripiprazole and haloperidol. Additional studies are needed to confirm these findings.
If a medication switch is contraindicated, pharmacologic treatment for hyperprolactinemia may be required.11 Bromocriptine, cabergoline, and amantadine have been used to treat hyperprolactinemia.11 Bromocriptine lowers PRL levels and restores normal gonadal function for men and women with hyperprolactinemia regardless of etiology, but may worsen psychiatric symptoms and can cause nausea, headaches, dizziness, and orthostatic hypotension.11 In a pilot study, amantadine, 300 mg/d, used to treat neuroleptic-induced extrapyramidal effects also decreased PRL levels and reduced galactorrhea.11
Osteoporosis can be minimized by exercising, taking adequate calcium and vitamin D, and avoiding caffeinated drinks.9 Simmons et al21 found bisphosphonate treatment in children and adolescents improved bone density and fragility within 2 to 4 years. Unfortunately, information about optimal duration and long-term effects of bisphosphonate therapy is limited.22
Surgical treatment may be necessary to remove a pituitary tumor that causes hyperprolactinemia. For some patients, referral to pediatric endocrinologist for further treatment may be needed.
Table 3
Presenting symptoms of hyperprolactinemia
| Adult females | Adult males | Prepubertal children (male and female) |
|---|---|---|
| Amenorrhea Anovulatory cycle Breast enlargement Breast pain Galactorrhea Hirsutism Infertility Loss of libido Oligomenorrhea | Decreased in seminal fluid volume Galactorrhea Gynecomastia Impotence Loss of libido | Delayed puberty Galactorrhea Gynecomastia Osteopenia or osteoporosis Primary amenorrhea (females only) Short stature |
| Source: Adapted from reference 12 | ||
Related Resources
- Ali J, Khemka M. Hyperprolactinemia: Monitoring children on long-term risperidone. Current Psychiatry. 2008;7(11):64-72.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bendroflumethiazide • Naturetin
- Bromocriptine • Parlodel
- Bupropion • Wellbutrin
- Cabergoline • Dostinex
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clozapine • Clozaril
- Famotidine • Pepcid
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Indinavir • Crixivan
- Methyldopa • Aldomet
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Paliperidone • Invega
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Quinidine • Quinidex
- Ranitidine • Zantac
- Reserpine • Serpasil
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Triptorelin • Trelstar
- Venlafaxine • Effexor
- Verapamil • Calan, Isoptin
- Zidovudine • Retrovir
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors wish to thank Yunyoung C. Chang, BS, for her assistance with this article.
1. Freeman ME, Kanyicska B, Lerant A, et al. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80(4):1523-1631.
2. Biederman J, Mick E, Spencer T, et al. An open-label trial of aripiprazole monotherapy in children and adolescents with bipolar disorder. CNS Spectr. 2007;12(9):683-689.
3. Tworoger SS, Eliassen AH, Rosner B, et al. Plasma prolactin concentrations and risk of postmenopausal breast cancer. Cancer Res. 2004;64(18):6814-6819.
4. Anantamongkol U, Takemura H, Suthiphongchai T, et al. Regulation of Ca2+ mobilization by prolactin in mammary gland cells: possible role of secretory pathway Ca2+- ATPase type 2. Biochem Biophy Res Commun. 2007;352(2):537-542.
5. Coss D, Yang L, Kuo CB, et al. Effects of prolactin on osteoblast alkaline phosphatase and bone formation in the developing rat. Am J Physiol Endocrinol Metab. 2000;279(6):1216-1225.
6. Meaney AM, O’Keane V. Bone mineral density changes over a year in young females with schizophrenia: relationship to medication and endocrine variables. Schizophr Res. 2007;93(1-3):136-143.
7. Richards SM, Murphy WJ. Use of human prolactin as a therapeutic protein to potentiate immunohematopoietic function. J Neuroimmunol. 2000;109(1):56-62.
8. Wallaschofski H, Donné M, Eigenthaler M, et al. PRL as a novel potent cofactor for platelet aggregation. J Clin Endocrinol Metab. 2001;86(12):5912-5919.
9. Molitch M. Medication-induced hyperprolactinemia. Mayo Clin Proc. 2005;80(8):1050-1057.
10. Serri O, Chik CL, Ur E, et al. Diagnosis and management of hyperprolactinemia. CMAJ. 2003;169(6):575-581.
11. Compton M, Miller A. Antipsychotic-induced hyper-prolactinemia and sexual dysfunction. Psychopharmacol Bull. 2002;36(1):143-164.
12. Haddad PM, Wieck A. Antipsychotic-induced hyper-prolactinaemia: mechanisms clinical features and management. Drugs. 2004;64(20):2291-2314.
13. Nussbaum A, Stroup T. Paliperidone for treatment of schizophrenia. Schizophr Bull. 2008;34(3):419-422.
14. Findling R, Kusumakar V, Daneman D, et al. Prolactin levels during long-term risperidone treatment in children and adolescents. J Clin Psychiatry. 2003;64(11):1362-1369.
15. Risperdal [package insert]. Titusville NJ: Ortho-McNeil-Janssen Pharmaceuticals, Inc; 2010.
16. Becker A, Epperson CN. Female puberty: clinical implications for the use for prolactin-modulating psychotropics. Child Adolesc Psychiatr N Am. 2006;15(1):207-220.
17. Weiden PJ, Cutler AJ, Polymeropoulos MH, et al. Safety profile of iloperidone: a pooled analysis of 6-week acute-phase pivotal trials. J Clin Psychopharmacol. 2008;28 (2 suppl 1):S12-S19.
18. Szarfman A, Tonning J, Levine J, et al. Atypical antipsychotics and pituitary tumors: a pharmacovigilance study. Pharmacotherapy. 2006;26(6):748-758.
19. Colao A, Loche S, Cappa M, et al. Prolactinoma in children and adolescents. Clinical presentation and long-term follow-up. J Clin Endocrinol Metab. 1998;83(8):2777-2780.
20. Shim JC, Shin JG, Kelly DL, et al. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: a placebo-controlled trial. Am J Psychiatry. 2007;164:1404-1410.
21. Simmons J, Zeitler P, Steelman J. Advances in the diagnosis and treatment of osteoporosis. Adv Pediatr. 2007;54:85-114.
22. Ward L, Tricco AC, Phuong P, et al. Bisphosphonate therapy for children and adolescents with secondary osteoporosis. Cochrane Database Syst Rev. 2007;(4):CD005324.-
1. Freeman ME, Kanyicska B, Lerant A, et al. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80(4):1523-1631.
2. Biederman J, Mick E, Spencer T, et al. An open-label trial of aripiprazole monotherapy in children and adolescents with bipolar disorder. CNS Spectr. 2007;12(9):683-689.
3. Tworoger SS, Eliassen AH, Rosner B, et al. Plasma prolactin concentrations and risk of postmenopausal breast cancer. Cancer Res. 2004;64(18):6814-6819.
4. Anantamongkol U, Takemura H, Suthiphongchai T, et al. Regulation of Ca2+ mobilization by prolactin in mammary gland cells: possible role of secretory pathway Ca2+- ATPase type 2. Biochem Biophy Res Commun. 2007;352(2):537-542.
5. Coss D, Yang L, Kuo CB, et al. Effects of prolactin on osteoblast alkaline phosphatase and bone formation in the developing rat. Am J Physiol Endocrinol Metab. 2000;279(6):1216-1225.
6. Meaney AM, O’Keane V. Bone mineral density changes over a year in young females with schizophrenia: relationship to medication and endocrine variables. Schizophr Res. 2007;93(1-3):136-143.
7. Richards SM, Murphy WJ. Use of human prolactin as a therapeutic protein to potentiate immunohematopoietic function. J Neuroimmunol. 2000;109(1):56-62.
8. Wallaschofski H, Donné M, Eigenthaler M, et al. PRL as a novel potent cofactor for platelet aggregation. J Clin Endocrinol Metab. 2001;86(12):5912-5919.
9. Molitch M. Medication-induced hyperprolactinemia. Mayo Clin Proc. 2005;80(8):1050-1057.
10. Serri O, Chik CL, Ur E, et al. Diagnosis and management of hyperprolactinemia. CMAJ. 2003;169(6):575-581.
11. Compton M, Miller A. Antipsychotic-induced hyper-prolactinemia and sexual dysfunction. Psychopharmacol Bull. 2002;36(1):143-164.
12. Haddad PM, Wieck A. Antipsychotic-induced hyper-prolactinaemia: mechanisms clinical features and management. Drugs. 2004;64(20):2291-2314.
13. Nussbaum A, Stroup T. Paliperidone for treatment of schizophrenia. Schizophr Bull. 2008;34(3):419-422.
14. Findling R, Kusumakar V, Daneman D, et al. Prolactin levels during long-term risperidone treatment in children and adolescents. J Clin Psychiatry. 2003;64(11):1362-1369.
15. Risperdal [package insert]. Titusville NJ: Ortho-McNeil-Janssen Pharmaceuticals, Inc; 2010.
16. Becker A, Epperson CN. Female puberty: clinical implications for the use for prolactin-modulating psychotropics. Child Adolesc Psychiatr N Am. 2006;15(1):207-220.
17. Weiden PJ, Cutler AJ, Polymeropoulos MH, et al. Safety profile of iloperidone: a pooled analysis of 6-week acute-phase pivotal trials. J Clin Psychopharmacol. 2008;28 (2 suppl 1):S12-S19.
18. Szarfman A, Tonning J, Levine J, et al. Atypical antipsychotics and pituitary tumors: a pharmacovigilance study. Pharmacotherapy. 2006;26(6):748-758.
19. Colao A, Loche S, Cappa M, et al. Prolactinoma in children and adolescents. Clinical presentation and long-term follow-up. J Clin Endocrinol Metab. 1998;83(8):2777-2780.
20. Shim JC, Shin JG, Kelly DL, et al. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: a placebo-controlled trial. Am J Psychiatry. 2007;164:1404-1410.
21. Simmons J, Zeitler P, Steelman J. Advances in the diagnosis and treatment of osteoporosis. Adv Pediatr. 2007;54:85-114.
22. Ward L, Tricco AC, Phuong P, et al. Bisphosphonate therapy for children and adolescents with secondary osteoporosis. Cochrane Database Syst Rev. 2007;(4):CD005324.-
Benzodiazepines and stimulants for patients with substance use disorders
Although benzodiazepines and stimulants have well-documented efficacy for numerous psychiatric disorders, psychiatrists hesitate to prescribe these medications to patients with substance use disorders (SUDs)—even to those with a comorbid condition that likely would respond to a benzodiazepine or stimulant—because of risk of abuse or dependence. Conventional practice typically has focused on treating active substance use first rather than using simultaneous treatments. Prejudice, fear, and misinformation can influence this decision.
We believe these cases lie on a continuum. At one extreme, ignoring a past or present SUD may lead a remitted patient toward relapse, or further delay recovery for an active user. At the other end, psychiatrists who overreact to a remote history of substance use may deprive patients of legitimate pharmacologic symptom relief. Most cases lie somewhere in the middle.
A literature review does not support the assertion that the use of these medications leads to future substance use or worsens active use, especially for stimulants. In fact, stepwise—as opposed to concurrent—treatment for both conditions actually may delay recovery and increase patients’ risk for morbidity.
We outline issues involved in these complex clinical situations, point out controversies, review relevant research data, and offer guidelines for treatment.
CASE 1 Panic disorder in sobriety
Since he was a teen, Mr. A, age 51, drank heavily, which cost him jobs and relationships. After being convicted for driving under the influence, he was court-ordered to attend a rehabilitation facility, where, as he describes it, he “finally turned [his] life around.” He followed up residential treatment with regular attendance at Alcoholics Anonymous meetings.
After 1 year of sobriety, Mr. A develops increasingly frequent episodes of intense anxiety with sweating, nausea, chest pain, and hyperventilation and is diagnosed with panic disorder. His internist prescribes alprazolam, 0.5 mg 3 times a day, which provides some symptom relief, and refers him for follow-up psychiatric care. At his first visit, Mr. A confides to his psychiatrist that he is taking much more than the prescribed dosage of alprazolam, even when he is not experiencing anxiety, and is contemplating “buying it on the street” if his dosage is not raised to “at least 3 mg 3 times a day.”
CASE 2 Anxiety in controlled psychosis
Ms. B, age 40, had her first psychotic break at age 18 and was diagnosed with schizophrenia. Since then, she has had multiple psychiatric hospitalizations, usually presenting with auditory hallucinations and a recurring delusion that the person who calls herself Ms. B’s mother is really an actress “playing” her mother. At times this delusion has led Ms. B to attack her “imposter” mother. Over several years Ms. B began to drink heavily, but recently achieved a few months of sobriety by attending dual-diagnosis groups at her local community mental health center and individual psychotherapy sessions with her case manager. Fortunately, Ms. B’s psychosis has been stabilized with risperidone long-acting injection, 25 mg every 2 weeks, which she tolerates well.
When her beloved calico cat passes away, Ms. B experiences intense anxiety. Ms. B’s friend tells her she “needs some Valium,” but her psychiatrist, case manager, and the other patients in her dual-diagnosis group are not sure this is a good idea.
Benzodiazepines
Pros. There are multiple legitimate uses of benzodiazepines in general medicine and psychiatric practice, based upon their considerable sedative/hypnotic, anxiolytic, anticonvulsant, and muscle-relaxant properties (Table 1).1
Recommendations regarding benzodiazepine use for anxious patients with a history of SUD are not clear-cut. First, it often is difficult to determine whether the patient truly has an anxiety disorder or is suffering anxiety symptoms secondary to substance use and/or withdrawal. In addition, even if a diagnosis of a separate anxiety disorder is established, psychiatrists debate how to treat such patients. Some clinicians maintain that benzodiazepines should be used only for acute detoxification, and that ongoing benzodiazepine use will lead to relapse or benzodiazepine dependence. However, in a prospective study of 545 alcohol use disorder (AUD) patients receiving benzodiazepines for anxiety disorders, Mueller et al2 found no association—at 12 months or at 12 years—between benzodiazepine use and AUD recurrence. Furthermore, there was no difference in benzodiazepine usage when comparing patients with and without an AUD.3
Table 1
Clinical uses of benzodiazepines
| Insomnia |
| Anxiety disorders (eg, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, social phobia, and obsessive-compulsive disorder) |
| Side effects of other psychiatric medications (eg, akathisia with antipsychotics or tremor with lithium) |
| Alcohol or benzodiazepine withdrawal |
| Acute agitation states, either as monotherapy or as adjuncts to antipsychotics or mood stabilizers |
| Catatonia |
| Source: Reference 1 |
Cons. Although widely prescribed—and despite their efficacy in numerous conditions— both acute or long-term benzodiazepine use frequently causes adverse effects.4 Patients may develop tolerance, which can lead to escalating dosages and/or to withdrawal symptoms when patients attempt to cut back. Benzodiazepines eventually become ineffective for sleep, and continued use can cause rebound insomnia. Also, with many patients taking benzodiazepines long-term, clinicians struggle to differentiate between “real” anxiety symptoms and subtle states of withdrawal from fluctuating benzodiazepine blood levels.5
Geriatric patients who take benzodiazepines are at risk for falls and hip fractures.4 Although older dementia patients are at particular risk for cognitive problems— including frank delirium—secondary to benzodiazepine use, patients of all ages are susceptible to these medications’ deleterious neurocognitive effects.
Benzodiazepines can lead to excessive sedation, thereby impairing performance at work or school, and have been implicated as a cause of motor vehicle accidents.6 Finally, a serious drawback to benzodiazepine use is possible lethality in overdose, especially when combined with alcohol.
Benzodiazepine prescribing should not be taken lightly. Always analyze the difference between benzodiazepines’ well-documented efficacy and their adverse effect profile. This risk-benefit analysis becomes much more complex for patients with SUDs.
Special considerations. Patients at higher risk for benzodiazepine abuse include those with:
- severe alcohol dependence (ie, long-term use, drinking since a young age [“Type II”])
- intravenous drug use
- comorbid alcoholism and antisocial personality disorder.7,8
Exercise special caution when considering benzodiazepines for patients with severe psychiatric illness such as schizophrenia-spectrum disorders, bipolar disorder, or severe depression. Patients with schizophrenia have high rates of alcohol, cocaine, cannabis, and benzodiazepine abuse.9,10 Bipolar disorder patients show similar vulnerability—up to 56% of patients screen positive for substance abuse or dependence.11 Vulnerability to addiction in severely ill psychiatric patients is thought to be related to several factors, including:
- use of drugs as self-medication
- genetic predisposition
- environment/lifestyle that supports substance abuse
- neurobiologic deficits that lead to lack of inhibition of reward-seeking behaviors.11
Bipolar disorder patients in particular score high on measures of sensation seeking, which leaves them vulnerable to abusing all classes of substances.12
In a 6-year study of 203 patients with severe psychiatric illnesses and SUDs, Brunette et al13 found that these patients were 2.5 times more likely than patients with severe psychiatric illness alone to abuse prescribed benzodiazepines. In an analysis of Medicaid records, Clark et al14 found similar vulnerability in patients with major depressive disorder (MDD) and SUD. Not only did these patients show a higher rate of benzodiazepine use than patients with MDD without SUD, but the dual-diagnosis group also gravitated toward more addictive high-potency/fast-acting benzodiazepines, such as alprazolam, estazolam, or triazolam.
Case discussion/suggestions. Initially, Mr. A may seem to be an appropriate candidate for closely monitored benzodiazepine use. However, he shows a pattern of misuse, likely related to his history of severe alcohol dependence and alprazolam use. This benzodiazepine is fast-acting and has a short half-life, and thus is highly reinforcing.
Similarly, Ms. B might benefit from benzodiazepine treatment. However, her history of schizophrenia and alcohol abuse makes her a risky candidate, and alternative treatments for anxiety symptoms should be considered. If prescribed at all, a benzodiazepine should be used only short-term (eg, 1 to 2 weeks).
In general, avoid prescribing benzodiazepines to most patients who have an ongoing or past SUD.15 Consider making an exception for SUD patients with comorbid anxiety disorders, with close monitoring of their benzodiazepine use. Clonazepam, chlordiazepoxide, clorazepate, and oxazepam may be less reinforcing for SUD patients than diazepam, lorazepam, alprazolam, estazolam, or triazolam.7,16 The drawbacks of benzodiazepines, especially in the situations described above, point to the need to find alternative treatments (Table 2).17 Keep in mind nonpharmacologic options, which completely avoid the risks of medication misuse and diversion. Cognitive-behavioral therapy (CBT), for instance, has well-documented efficacy in treating insomnia and anxiety disorders.18,19
Table 2
Alternatives to benzodiazepines for anxiety and/or insomnia
| Treatment option | Comments |
|---|---|
| CBT, relaxation techniques, sleep hygiene counseling | Many advantages to nonpharmacologic interventions (eg, fewer side effects, no risk of substance dependence) |
| Antihistamines (eg, diphenhydramine, 25 to 50 mg at bedtime* for sleep, or 2 to 3 times a day for anxiety) | Can be used for anxiety or insomnia; can cause confusion in older patients |
| Atypical antipsychotics | Off-label use; many agents in this class have metabolic side effects |
| SSRIs/SNRIs | First-line for many anxiety disorders, including panic disorder, GAD; possible weight gain and sexual side effects |
| Mirtazapine (7.5 to 30 mg at bedtime*) | Sedation side effect helps with sleep; weight gain and oversedation limit use |
| Trazodone (25 to 100 mg at bedtime*) | Commonly used off-label as a sleep aid |
| Monoamine oxidase inhibitors | May be useful for social phobia; dietary restrictions and side effects limit use |
| Doxepin (3 to 6 mg at bedtime) | Minimal anticholinergic and alpha-blockade side effects at this dose; FDA-approved for insomnia |
| Gabapentin (300 to 2,000 mg/d* in divided doses) | Off-label use, mild anxiolytic and sedative properties, relatively weight neutral |
| Beta blockers (eg, propranolol, 20 to 80 mg twice a day*) | Useful for peripheral manifestations of anxiety; may be effective for social phobias |
| Pregabalin (50 to 200 mg 3 times a day*) | Off-label use; industry-sponsored studies show comparable to SNRIs for anxiety |
| Non-benzodiazepine GABAA receptor modulators | Short-term option for primary insomnia, some abuse potential |
| Melatonin (1 to 3 mg at bedtime*) | Mild and ‘natural’ but not always an effective sleep aid |
| *Off-label approximate doses based on the authors’ clinical experience and consensus of the literature; agents listed may require slow titration and close monitoring for adverse effects CBT: cognitive-behavioral therapy; GABA: gamma-aminobutyric acid; GAD: generalized anxiety disorder; SNRI: serotoninnorepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor Source: Reference 17 | |
CASE 3 Adult ADHD and marijuana use
Mr. C, age 30, presents to a psychiatrist with ongoing complaints of inattention, fatigue, and difficulty staying organized. A self-report screen yields symptoms consistent with adult attention-deficit/hyperactivity disorder (ADHD). Mr. C’s school and job history and collateral history from his wife appear to corroborate his assertion that his symptoms have been lifelong. He later admits to regular marijuana use. After further discussion and full evaluation of his substance use, Mr. C is started on bupropion, titrated to 300 mg/d. After 2 months, despite faithful attendance at appointments and openness about his continued marijuana use, Mr. C’s symptoms remain unchanged. He asks about atomoxetine.
Stimulants
Pros. Despite many clinicians’ hesitance to prescribe controlled substances to patients with SUDs, psychostimulants should be considered in a variety of scenarios. Although nonstimulant options are available, stimulants consistently have demonstrated superior efficacy over other treatments and remain first-line agents for adult ADHD.20 Methylphenidate, mixed amphetamine salts, lisdexamfetamine, and atomoxetine are FDA-approved for adult ADHD. Both stimulant classes (methylphenidate and amphetamine-based products) are equally effective for ADHD. In addition, stimulants are used to treat narcolepsy, cognitive disorders such as traumatic brain injury, and as augmentation to antidepressants for MDD.
ADHD affects 5% to 12% of children, and >60% of patients remain symptomatic into adulthood and require continued treatment.21 In particular, problematic inattention may persist throughout adulthood. ADHD does not appear to be an independent risk factor for SUDs in children and adolescents.22 However, substance use increases sharply as ADHD patients enter late adolescence and adulthood, and eventually becomes a problem for 20% of adolescents and adults with ADHD. Conversely, 17% to 50% of patients with alcohol, cocaine, or opioid dependence have co-occurring ADHD.23
Withholding ADHD treatment based on concerns about future or increased current substance abuse is unfounded. A meta-analysis of 6 studies that included 674 medicated and 360 unmedicated patients with ADHD who were followed at least 4 years demonstrated that childhood treatment of ADHD with stimulants reduces the risk of developing alcohol and other drug disorders in adulthood.24 Regarding the effect stimulants have on active substance use, a 12-week, double-blind, randomized controlled trial of 48 cocaine-dependent adults with ADHD showed methylphenidate did not change cocaine abuse or craving, but did improve ADHD symptoms.25
Clinicians also must assess whether untreated ADHD symptoms impair patients’ work or other activities. Driving is a particular concern because ADHD is associated with risky driving habits, motor vehicle accidents, traffic violations, and driving license suspensions.26 In a study that administered cognitive tests to 27 adults with ADHD, methylphenidate treatment improved cognitive performance related to driving (eg, better visual-motor coordination under high-stress conditions, improved visual orientation, and sustained visual attention).27 It is likely this effect could be generalized to other activities where safety is important. Finally, appropriate stimulant treatment may improve participation in rehabilitative programs.
Cons. Despite their positive effects, stimulants can have adverse effects and consequences.28 In routinely prescribed dosages, methylphenidate and amphetamines can cause symptoms related to sympathetic activation, including anxiety, tics, anorexia/ weight loss, and sleep disturbance. A 5-year study of 79 school-age children prescribed methylphenidate, dextroamphetamine, or pemoline, which is no longer available in the United States, showed a significant association between adherence to stimulants and persistence of physiological (eg, headaches, insomnia, anorexia) and mood-related (eg, irritability, dysphoria) side effects.29 Stimulants’ sympathomimetic properties also can lead to dangerous drug-drug interactions with monoamine oxidase inhibitors. For both methylphenidate and amphetamines, overdose can lead to seizures, cardiac toxicity, dysrhythmias, and hyperthermia. All stimulants carry an FDA “black-box” warning that lists increased risk of cardiac complications, sudden death, and psychiatric complications such as psychosis or mania.30
Special considerations. All stimulants have potential for diversion or abuse. Pay close attention to these issues, especially in vulnerable populations and situations where rates of abuse and diversion are elevated. Among college students, white patients, fraternity/sorority members, and individuals with lower grade point averages may be at higher risk for nonmedical stimulant use.31 Adults who misuse or divert stimulants commonly have a history of substance abuse and conduct disorder.32 Short-acting stimulants are abused 4 times more often than extended-release preparations.33
If your ADHD patient has active substance use, be clear that continued substance use is likely to limit stimulants’ effectiveness. In patients who are actively using substances, it will be difficult to disentangle apparent nonresponse to stimulants from the negative cognitive effects of substance use.
Case discussion/suggestions. As Mr. C’s case illustrates, there are alternatives to stimulants for ADHD. For example, atomoxetine, a selective norepinephrine reuptake inhibitor, may be considered a first-line agent in patients with mostly inattentive ADHD symptoms and comorbid stimulant abuse, or for those in whom stimulants cause adverse effects such as mood lability or tics.34 Other alternatives to stimulants are listed in Table 3.35
Because Mr. C did not respond to bupropion, which presumably was tried first because of his ongoing substance use, he asked about atomoxetine. This agent is not addictive and there is no evidence that it leads to or exacerbates substance use. Depending on Mr. C’s symptom profile, atomoxetine might be a good choice. Continued monitoring of his marijuana use and frequent assessment of his motivation to quit are necessary. Psychoeducation about the cognitive effects of marijuana, including inattention and poor concentration, is important.
If Mr. C does not respond to atomoxetine, his psychiatrist will face a difficult decision. Setting Mr. C’s marijuana use aside, symptoms that do not respond to atomoxetine or a second-line agent are likely to respond to a stimulant. However, several issues must be addressed. If Mr. C’s motivation to stop using marijuana is low, how motivated is he to improve his ADHD symptoms? Next, would marijuana’s depressive/blunting effects counteract the anticipated benefit of a stimulant? Also, what is the risk that Mr. C might sell or exchange his stimulants to obtain marijuana? Assessing these complicated questions is key. Another important factor in Mr. C’s case is his wife’s involvement. Does she monitor his marijuana use? Would she be willing to supervise Mr. C’s stimulant use, and would he allow it?
Past or present SUDs are not an absolute contraindication to stimulant use. You should affirm the diagnosis and identify target symptoms. Consider nonstimulant alternatives if appropriate.
Table 3
Alternatives to stimulants for ADHD
| Treatment option | Comments |
|---|---|
| Atomoxetine | Effectiveness may be limited to inattentive type |
| Modafinil | Well-tolerated but expensive, limited evidence, no FDA indication; may be a consideration in ADHD + SUD |
| α2-adrenergic agonist (eg, clonidine or guanfacine) | Useful when hyperactivity/impulsivity symptoms predominate, or when stimulant-induced insomnia occurs |
| Bupropion | Some evidence of mild efficacy, especially useful if nicotine dependence also is a target for treatment |
| Psychotherapy | Can be useful as adjunctive treatment, but as monotherapy it is of little benefit in ADHD |
| ADHD: attention-deficit/hyperactivity disorder; SUD: substance abuse disorder Source: Reference 35 | |
Legal liabilities
Being aware of the medicolegal issues of benzodiazepine and/or stimulant prescribing is crucial because a court may find a psychiatrist liable for negative outcomes (eg, suicide) when controlled substances are prescribed to a patient with a history of addiction.36 The most prudent course is to weigh the pros and cons for each patient individually, taking into consideration the factors described above.8 This is consistent with guidelines from the American Psychiatric Association and the British Association for Psychopharmacology,37 both of which call for extreme caution in these cases.
Educate patients and caregivers about the risks of taking a controlled substance, including misuse, diversion, and theft. Provide and document explicit instructions that the patient will receive stimulants from only a single provider. Remind patients that state and federal authorities closely track controlled medications. Finally, a “stimulant contract” or “benzodiazepine contract,” similar to a pain or narcotic contact, may be useful to formally document discussions about appropriate medication use.
Related Resources
- National Institute on Drug Abuse. Prescription drugs: abuse and addiction. Research Report Series, 2005. http://drugabuse.gov/ResearchReports/Prescription/Prescription.html.
- Galanter M, Kleber HD. The American Psychiatric Publishing textbook of substance abuse treatment. 4th ed. Arlington, VA: American Psychiatric Publishing, Inc; 2008.
Drug Brand Names
- Alprazolam • Xanax
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, others
- Chlordiazepoxide • Librium
- Clonazepam • Klonopin
- Clonidine • Catapres
- Clorazepate • Tranxene
- Dextroamphetamine • Dexedrine
- Diazepam • Valium
- Diphenhydramine • Benadryl, others
- Doxepin • Silenor
- Estazolam • ProSom
- Gabapentin • Neurontin
- Guanfacine • Tenex, Intuniv
- Lisdexamfetamine • Vyvanse
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Methylphenidate • Ritalin, Concerta, others
- Mirtazapine • Remeron
- Mixed amphetamine salts • Adderall
- Modafinil • Provigil
- Oxazepam • Serax
- Pemoline • Cylert
- Propranolol • Inderal
- Trazodone • Desyrel, Oleptro
- Triazolam • Halcion
Disclosures
Dr. Casher is a speaker for AstraZeneca and Pfizer Inc.
Drs. Gih and Bess report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Ashton H. Guidelines for the rational use of benzodiazepines. When and what to use. Drugs. 1994;48(1):25.-
2. Mueller TI, Pagano ME, Rodriguez BF, et al. Long-term use of benzodiazepines in participants with comorbid anxiety and alcohol use disorders. Alcohol Clin Exp Res. 2005;29(8):1411-1418.
3. Mueller TI, Goldenberg IM, Gordon AL, et al. Benzodiazepine use in anxiety disordered patients with and without a history of alcoholism. J Clin Psychiatry. 1996;57(2):83-89.
4. Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005;(18):249-255.
5. Back SE, Brady KT. Anxiety disorders with comorbid substance use disorders: diagnostic and treatment considerations. Psychiatric Annals. 2008;38(11):724-729.
6. Walsh JM, Flegel R, Cangianelli LA, et al. Epidemiology of alcohol and other drug use among motor vehicle crash victims admitted to a trauma center. Traffic Inj Prev. 2004;5(3):254-260.
7. Ciraulo DA, Nace EP. Benzodiazepine treatment of anxiety or insomnia in substance abuse patients. Am J Addict. 2000;9(4):276-279;discussion 280–284.
8. Sattar S, Bhatia S. Benzodiazepines for substance abusers. Current Psychiatry. 2003;2(5):25-34.
9. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
10. Kendler KS, Gallagher TJ, Abelson JM, et al. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53(11):1022-1031
11. Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(suppl 7):5-9.
12. Bizzarri JV, Sbrana A, Rucci P, et al. The spectrum of substance abuse in bipolar disorder: reasons for use, sensation seeking and substance sensitivity. Bipolar Disord. 2007;9(3):213-220.
13. Brunette MF, Noordsy DL, Xie H, et al. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr Serv. 2003;54(10):1395-1401.
14. Clark RE, Xie H, Brunette MF, et al. Benzodiazepine prescription practices and substance abuse in persons with severe mental illness. J Clin Psychiatry. 2004;65(2):151-155.
15. Longo LP. Addiction: part I. Benzodiazepines—side effects abuse risk and alternatives. Am Fam Physician. 2000;61(7):2121-2128.
16. Ciraulo DA, Barnhill JG, Ciraulo AM, et al. Alterations in pharmacodynamics of anxiolytics in abstinent alcoholic men: subjective responses, abuse liability, and electroencephalographic effects of alprazolam, diazepam, and buspirone. J Clin Pharmacol. 1997;37(1):64-73.
17. Casher MI, Bess JD. Manual of inpatient psychiatry. Cambridge United Kingdom: Cambridge University Press; 2010.
18. Hofmann S, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
19. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
20. Wilens TE. Drug therapy for adults with attention-deficit hyperactivity disorder. Drugs. 2003;63(22):2395-2411.
21. Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
22. Biederman J, Wilens T, Mick E, et al. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;36(1):21-29.
23. Waid L, Johnson D, Anton R. Attention-deficit hyperactivity disorder and substance abuse. In: Kranzler HR Rounsaville BJ, eds. Dual diagnosis and treatment: substance abuse and comorbid medical and psychiatric disorders. vol 8. New York, NY: Marcel Dekker; 1998:393–425.
24. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
25. Schubiner H, Saules KK, Arfken CL, et al. Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol. 2002;10(3):286-294.
26. Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6 Pt 1):1089-1095.
27. Sobanski E, Sabljic D, Alm B, et al. Driving-related risks and impact of methylphenidate treatment on driving in adults with attention-deficit/hyperactivity disorder (ADHD). J Neural Transm. 2008;115(2):347-356.
28. Leonard BE, McCartan D, White J, et al. Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects. Hum Psychopharmacol. 2004;19(3):151-180.
29. Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004;43(5):559-567.
30. Schatzberg AF, Nemeroff CB. The American Psychiatric Publishing textbook of psychopharmacology. 4th ed. Arlington VA: American Psychiatric Publishing, Inc; 2009.
31. Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21-31.
32. Wilens TE, Gignac M, Swezey A, et al. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408-414.
33. Bright GM. Abuse of medications employed for the treatment of ADHD: results from a large-scale community survey. Medscape J Med. 2008;10(5):111.-
34. Biederman J, Spencer T, Wilens T. Evidence-based pharmacotherapy for attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2004;7(1):77-97.
35. Mann N, Bitsios P. Modafinil treatment of amphetamine abuse in adult ADHD. J Psychopharmacol. 2009;23(4):468-471.
36. Grant JE. Prudent prescribing for patients with addictions. Current Psychiatry. 2006;5(10):99-102.
37. Lingford-Hughes AR, Welch S, Nutt DJ. and the British Association for Psychopharmacology. Evidence-based guidelines for the pharmacological management of substance misuse addiction and comorbidity: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2004;18(3):293-335.
Although benzodiazepines and stimulants have well-documented efficacy for numerous psychiatric disorders, psychiatrists hesitate to prescribe these medications to patients with substance use disorders (SUDs)—even to those with a comorbid condition that likely would respond to a benzodiazepine or stimulant—because of risk of abuse or dependence. Conventional practice typically has focused on treating active substance use first rather than using simultaneous treatments. Prejudice, fear, and misinformation can influence this decision.
We believe these cases lie on a continuum. At one extreme, ignoring a past or present SUD may lead a remitted patient toward relapse, or further delay recovery for an active user. At the other end, psychiatrists who overreact to a remote history of substance use may deprive patients of legitimate pharmacologic symptom relief. Most cases lie somewhere in the middle.
A literature review does not support the assertion that the use of these medications leads to future substance use or worsens active use, especially for stimulants. In fact, stepwise—as opposed to concurrent—treatment for both conditions actually may delay recovery and increase patients’ risk for morbidity.
We outline issues involved in these complex clinical situations, point out controversies, review relevant research data, and offer guidelines for treatment.
CASE 1 Panic disorder in sobriety
Since he was a teen, Mr. A, age 51, drank heavily, which cost him jobs and relationships. After being convicted for driving under the influence, he was court-ordered to attend a rehabilitation facility, where, as he describes it, he “finally turned [his] life around.” He followed up residential treatment with regular attendance at Alcoholics Anonymous meetings.
After 1 year of sobriety, Mr. A develops increasingly frequent episodes of intense anxiety with sweating, nausea, chest pain, and hyperventilation and is diagnosed with panic disorder. His internist prescribes alprazolam, 0.5 mg 3 times a day, which provides some symptom relief, and refers him for follow-up psychiatric care. At his first visit, Mr. A confides to his psychiatrist that he is taking much more than the prescribed dosage of alprazolam, even when he is not experiencing anxiety, and is contemplating “buying it on the street” if his dosage is not raised to “at least 3 mg 3 times a day.”
CASE 2 Anxiety in controlled psychosis
Ms. B, age 40, had her first psychotic break at age 18 and was diagnosed with schizophrenia. Since then, she has had multiple psychiatric hospitalizations, usually presenting with auditory hallucinations and a recurring delusion that the person who calls herself Ms. B’s mother is really an actress “playing” her mother. At times this delusion has led Ms. B to attack her “imposter” mother. Over several years Ms. B began to drink heavily, but recently achieved a few months of sobriety by attending dual-diagnosis groups at her local community mental health center and individual psychotherapy sessions with her case manager. Fortunately, Ms. B’s psychosis has been stabilized with risperidone long-acting injection, 25 mg every 2 weeks, which she tolerates well.
When her beloved calico cat passes away, Ms. B experiences intense anxiety. Ms. B’s friend tells her she “needs some Valium,” but her psychiatrist, case manager, and the other patients in her dual-diagnosis group are not sure this is a good idea.
Benzodiazepines
Pros. There are multiple legitimate uses of benzodiazepines in general medicine and psychiatric practice, based upon their considerable sedative/hypnotic, anxiolytic, anticonvulsant, and muscle-relaxant properties (Table 1).1
Recommendations regarding benzodiazepine use for anxious patients with a history of SUD are not clear-cut. First, it often is difficult to determine whether the patient truly has an anxiety disorder or is suffering anxiety symptoms secondary to substance use and/or withdrawal. In addition, even if a diagnosis of a separate anxiety disorder is established, psychiatrists debate how to treat such patients. Some clinicians maintain that benzodiazepines should be used only for acute detoxification, and that ongoing benzodiazepine use will lead to relapse or benzodiazepine dependence. However, in a prospective study of 545 alcohol use disorder (AUD) patients receiving benzodiazepines for anxiety disorders, Mueller et al2 found no association—at 12 months or at 12 years—between benzodiazepine use and AUD recurrence. Furthermore, there was no difference in benzodiazepine usage when comparing patients with and without an AUD.3
Table 1
Clinical uses of benzodiazepines
| Insomnia |
| Anxiety disorders (eg, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, social phobia, and obsessive-compulsive disorder) |
| Side effects of other psychiatric medications (eg, akathisia with antipsychotics or tremor with lithium) |
| Alcohol or benzodiazepine withdrawal |
| Acute agitation states, either as monotherapy or as adjuncts to antipsychotics or mood stabilizers |
| Catatonia |
| Source: Reference 1 |
Cons. Although widely prescribed—and despite their efficacy in numerous conditions— both acute or long-term benzodiazepine use frequently causes adverse effects.4 Patients may develop tolerance, which can lead to escalating dosages and/or to withdrawal symptoms when patients attempt to cut back. Benzodiazepines eventually become ineffective for sleep, and continued use can cause rebound insomnia. Also, with many patients taking benzodiazepines long-term, clinicians struggle to differentiate between “real” anxiety symptoms and subtle states of withdrawal from fluctuating benzodiazepine blood levels.5
Geriatric patients who take benzodiazepines are at risk for falls and hip fractures.4 Although older dementia patients are at particular risk for cognitive problems— including frank delirium—secondary to benzodiazepine use, patients of all ages are susceptible to these medications’ deleterious neurocognitive effects.
Benzodiazepines can lead to excessive sedation, thereby impairing performance at work or school, and have been implicated as a cause of motor vehicle accidents.6 Finally, a serious drawback to benzodiazepine use is possible lethality in overdose, especially when combined with alcohol.
Benzodiazepine prescribing should not be taken lightly. Always analyze the difference between benzodiazepines’ well-documented efficacy and their adverse effect profile. This risk-benefit analysis becomes much more complex for patients with SUDs.
Special considerations. Patients at higher risk for benzodiazepine abuse include those with:
- severe alcohol dependence (ie, long-term use, drinking since a young age [“Type II”])
- intravenous drug use
- comorbid alcoholism and antisocial personality disorder.7,8
Exercise special caution when considering benzodiazepines for patients with severe psychiatric illness such as schizophrenia-spectrum disorders, bipolar disorder, or severe depression. Patients with schizophrenia have high rates of alcohol, cocaine, cannabis, and benzodiazepine abuse.9,10 Bipolar disorder patients show similar vulnerability—up to 56% of patients screen positive for substance abuse or dependence.11 Vulnerability to addiction in severely ill psychiatric patients is thought to be related to several factors, including:
- use of drugs as self-medication
- genetic predisposition
- environment/lifestyle that supports substance abuse
- neurobiologic deficits that lead to lack of inhibition of reward-seeking behaviors.11
Bipolar disorder patients in particular score high on measures of sensation seeking, which leaves them vulnerable to abusing all classes of substances.12
In a 6-year study of 203 patients with severe psychiatric illnesses and SUDs, Brunette et al13 found that these patients were 2.5 times more likely than patients with severe psychiatric illness alone to abuse prescribed benzodiazepines. In an analysis of Medicaid records, Clark et al14 found similar vulnerability in patients with major depressive disorder (MDD) and SUD. Not only did these patients show a higher rate of benzodiazepine use than patients with MDD without SUD, but the dual-diagnosis group also gravitated toward more addictive high-potency/fast-acting benzodiazepines, such as alprazolam, estazolam, or triazolam.
Case discussion/suggestions. Initially, Mr. A may seem to be an appropriate candidate for closely monitored benzodiazepine use. However, he shows a pattern of misuse, likely related to his history of severe alcohol dependence and alprazolam use. This benzodiazepine is fast-acting and has a short half-life, and thus is highly reinforcing.
Similarly, Ms. B might benefit from benzodiazepine treatment. However, her history of schizophrenia and alcohol abuse makes her a risky candidate, and alternative treatments for anxiety symptoms should be considered. If prescribed at all, a benzodiazepine should be used only short-term (eg, 1 to 2 weeks).
In general, avoid prescribing benzodiazepines to most patients who have an ongoing or past SUD.15 Consider making an exception for SUD patients with comorbid anxiety disorders, with close monitoring of their benzodiazepine use. Clonazepam, chlordiazepoxide, clorazepate, and oxazepam may be less reinforcing for SUD patients than diazepam, lorazepam, alprazolam, estazolam, or triazolam.7,16 The drawbacks of benzodiazepines, especially in the situations described above, point to the need to find alternative treatments (Table 2).17 Keep in mind nonpharmacologic options, which completely avoid the risks of medication misuse and diversion. Cognitive-behavioral therapy (CBT), for instance, has well-documented efficacy in treating insomnia and anxiety disorders.18,19
Table 2
Alternatives to benzodiazepines for anxiety and/or insomnia
| Treatment option | Comments |
|---|---|
| CBT, relaxation techniques, sleep hygiene counseling | Many advantages to nonpharmacologic interventions (eg, fewer side effects, no risk of substance dependence) |
| Antihistamines (eg, diphenhydramine, 25 to 50 mg at bedtime* for sleep, or 2 to 3 times a day for anxiety) | Can be used for anxiety or insomnia; can cause confusion in older patients |
| Atypical antipsychotics | Off-label use; many agents in this class have metabolic side effects |
| SSRIs/SNRIs | First-line for many anxiety disorders, including panic disorder, GAD; possible weight gain and sexual side effects |
| Mirtazapine (7.5 to 30 mg at bedtime*) | Sedation side effect helps with sleep; weight gain and oversedation limit use |
| Trazodone (25 to 100 mg at bedtime*) | Commonly used off-label as a sleep aid |
| Monoamine oxidase inhibitors | May be useful for social phobia; dietary restrictions and side effects limit use |
| Doxepin (3 to 6 mg at bedtime) | Minimal anticholinergic and alpha-blockade side effects at this dose; FDA-approved for insomnia |
| Gabapentin (300 to 2,000 mg/d* in divided doses) | Off-label use, mild anxiolytic and sedative properties, relatively weight neutral |
| Beta blockers (eg, propranolol, 20 to 80 mg twice a day*) | Useful for peripheral manifestations of anxiety; may be effective for social phobias |
| Pregabalin (50 to 200 mg 3 times a day*) | Off-label use; industry-sponsored studies show comparable to SNRIs for anxiety |
| Non-benzodiazepine GABAA receptor modulators | Short-term option for primary insomnia, some abuse potential |
| Melatonin (1 to 3 mg at bedtime*) | Mild and ‘natural’ but not always an effective sleep aid |
| *Off-label approximate doses based on the authors’ clinical experience and consensus of the literature; agents listed may require slow titration and close monitoring for adverse effects CBT: cognitive-behavioral therapy; GABA: gamma-aminobutyric acid; GAD: generalized anxiety disorder; SNRI: serotoninnorepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor Source: Reference 17 | |
CASE 3 Adult ADHD and marijuana use
Mr. C, age 30, presents to a psychiatrist with ongoing complaints of inattention, fatigue, and difficulty staying organized. A self-report screen yields symptoms consistent with adult attention-deficit/hyperactivity disorder (ADHD). Mr. C’s school and job history and collateral history from his wife appear to corroborate his assertion that his symptoms have been lifelong. He later admits to regular marijuana use. After further discussion and full evaluation of his substance use, Mr. C is started on bupropion, titrated to 300 mg/d. After 2 months, despite faithful attendance at appointments and openness about his continued marijuana use, Mr. C’s symptoms remain unchanged. He asks about atomoxetine.
Stimulants
Pros. Despite many clinicians’ hesitance to prescribe controlled substances to patients with SUDs, psychostimulants should be considered in a variety of scenarios. Although nonstimulant options are available, stimulants consistently have demonstrated superior efficacy over other treatments and remain first-line agents for adult ADHD.20 Methylphenidate, mixed amphetamine salts, lisdexamfetamine, and atomoxetine are FDA-approved for adult ADHD. Both stimulant classes (methylphenidate and amphetamine-based products) are equally effective for ADHD. In addition, stimulants are used to treat narcolepsy, cognitive disorders such as traumatic brain injury, and as augmentation to antidepressants for MDD.
ADHD affects 5% to 12% of children, and >60% of patients remain symptomatic into adulthood and require continued treatment.21 In particular, problematic inattention may persist throughout adulthood. ADHD does not appear to be an independent risk factor for SUDs in children and adolescents.22 However, substance use increases sharply as ADHD patients enter late adolescence and adulthood, and eventually becomes a problem for 20% of adolescents and adults with ADHD. Conversely, 17% to 50% of patients with alcohol, cocaine, or opioid dependence have co-occurring ADHD.23
Withholding ADHD treatment based on concerns about future or increased current substance abuse is unfounded. A meta-analysis of 6 studies that included 674 medicated and 360 unmedicated patients with ADHD who were followed at least 4 years demonstrated that childhood treatment of ADHD with stimulants reduces the risk of developing alcohol and other drug disorders in adulthood.24 Regarding the effect stimulants have on active substance use, a 12-week, double-blind, randomized controlled trial of 48 cocaine-dependent adults with ADHD showed methylphenidate did not change cocaine abuse or craving, but did improve ADHD symptoms.25
Clinicians also must assess whether untreated ADHD symptoms impair patients’ work or other activities. Driving is a particular concern because ADHD is associated with risky driving habits, motor vehicle accidents, traffic violations, and driving license suspensions.26 In a study that administered cognitive tests to 27 adults with ADHD, methylphenidate treatment improved cognitive performance related to driving (eg, better visual-motor coordination under high-stress conditions, improved visual orientation, and sustained visual attention).27 It is likely this effect could be generalized to other activities where safety is important. Finally, appropriate stimulant treatment may improve participation in rehabilitative programs.
Cons. Despite their positive effects, stimulants can have adverse effects and consequences.28 In routinely prescribed dosages, methylphenidate and amphetamines can cause symptoms related to sympathetic activation, including anxiety, tics, anorexia/ weight loss, and sleep disturbance. A 5-year study of 79 school-age children prescribed methylphenidate, dextroamphetamine, or pemoline, which is no longer available in the United States, showed a significant association between adherence to stimulants and persistence of physiological (eg, headaches, insomnia, anorexia) and mood-related (eg, irritability, dysphoria) side effects.29 Stimulants’ sympathomimetic properties also can lead to dangerous drug-drug interactions with monoamine oxidase inhibitors. For both methylphenidate and amphetamines, overdose can lead to seizures, cardiac toxicity, dysrhythmias, and hyperthermia. All stimulants carry an FDA “black-box” warning that lists increased risk of cardiac complications, sudden death, and psychiatric complications such as psychosis or mania.30
Special considerations. All stimulants have potential for diversion or abuse. Pay close attention to these issues, especially in vulnerable populations and situations where rates of abuse and diversion are elevated. Among college students, white patients, fraternity/sorority members, and individuals with lower grade point averages may be at higher risk for nonmedical stimulant use.31 Adults who misuse or divert stimulants commonly have a history of substance abuse and conduct disorder.32 Short-acting stimulants are abused 4 times more often than extended-release preparations.33
If your ADHD patient has active substance use, be clear that continued substance use is likely to limit stimulants’ effectiveness. In patients who are actively using substances, it will be difficult to disentangle apparent nonresponse to stimulants from the negative cognitive effects of substance use.
Case discussion/suggestions. As Mr. C’s case illustrates, there are alternatives to stimulants for ADHD. For example, atomoxetine, a selective norepinephrine reuptake inhibitor, may be considered a first-line agent in patients with mostly inattentive ADHD symptoms and comorbid stimulant abuse, or for those in whom stimulants cause adverse effects such as mood lability or tics.34 Other alternatives to stimulants are listed in Table 3.35
Because Mr. C did not respond to bupropion, which presumably was tried first because of his ongoing substance use, he asked about atomoxetine. This agent is not addictive and there is no evidence that it leads to or exacerbates substance use. Depending on Mr. C’s symptom profile, atomoxetine might be a good choice. Continued monitoring of his marijuana use and frequent assessment of his motivation to quit are necessary. Psychoeducation about the cognitive effects of marijuana, including inattention and poor concentration, is important.
If Mr. C does not respond to atomoxetine, his psychiatrist will face a difficult decision. Setting Mr. C’s marijuana use aside, symptoms that do not respond to atomoxetine or a second-line agent are likely to respond to a stimulant. However, several issues must be addressed. If Mr. C’s motivation to stop using marijuana is low, how motivated is he to improve his ADHD symptoms? Next, would marijuana’s depressive/blunting effects counteract the anticipated benefit of a stimulant? Also, what is the risk that Mr. C might sell or exchange his stimulants to obtain marijuana? Assessing these complicated questions is key. Another important factor in Mr. C’s case is his wife’s involvement. Does she monitor his marijuana use? Would she be willing to supervise Mr. C’s stimulant use, and would he allow it?
Past or present SUDs are not an absolute contraindication to stimulant use. You should affirm the diagnosis and identify target symptoms. Consider nonstimulant alternatives if appropriate.
Table 3
Alternatives to stimulants for ADHD
| Treatment option | Comments |
|---|---|
| Atomoxetine | Effectiveness may be limited to inattentive type |
| Modafinil | Well-tolerated but expensive, limited evidence, no FDA indication; may be a consideration in ADHD + SUD |
| α2-adrenergic agonist (eg, clonidine or guanfacine) | Useful when hyperactivity/impulsivity symptoms predominate, or when stimulant-induced insomnia occurs |
| Bupropion | Some evidence of mild efficacy, especially useful if nicotine dependence also is a target for treatment |
| Psychotherapy | Can be useful as adjunctive treatment, but as monotherapy it is of little benefit in ADHD |
| ADHD: attention-deficit/hyperactivity disorder; SUD: substance abuse disorder Source: Reference 35 | |
Legal liabilities
Being aware of the medicolegal issues of benzodiazepine and/or stimulant prescribing is crucial because a court may find a psychiatrist liable for negative outcomes (eg, suicide) when controlled substances are prescribed to a patient with a history of addiction.36 The most prudent course is to weigh the pros and cons for each patient individually, taking into consideration the factors described above.8 This is consistent with guidelines from the American Psychiatric Association and the British Association for Psychopharmacology,37 both of which call for extreme caution in these cases.
Educate patients and caregivers about the risks of taking a controlled substance, including misuse, diversion, and theft. Provide and document explicit instructions that the patient will receive stimulants from only a single provider. Remind patients that state and federal authorities closely track controlled medications. Finally, a “stimulant contract” or “benzodiazepine contract,” similar to a pain or narcotic contact, may be useful to formally document discussions about appropriate medication use.
Related Resources
- National Institute on Drug Abuse. Prescription drugs: abuse and addiction. Research Report Series, 2005. http://drugabuse.gov/ResearchReports/Prescription/Prescription.html.
- Galanter M, Kleber HD. The American Psychiatric Publishing textbook of substance abuse treatment. 4th ed. Arlington, VA: American Psychiatric Publishing, Inc; 2008.
Drug Brand Names
- Alprazolam • Xanax
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, others
- Chlordiazepoxide • Librium
- Clonazepam • Klonopin
- Clonidine • Catapres
- Clorazepate • Tranxene
- Dextroamphetamine • Dexedrine
- Diazepam • Valium
- Diphenhydramine • Benadryl, others
- Doxepin • Silenor
- Estazolam • ProSom
- Gabapentin • Neurontin
- Guanfacine • Tenex, Intuniv
- Lisdexamfetamine • Vyvanse
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Methylphenidate • Ritalin, Concerta, others
- Mirtazapine • Remeron
- Mixed amphetamine salts • Adderall
- Modafinil • Provigil
- Oxazepam • Serax
- Pemoline • Cylert
- Propranolol • Inderal
- Trazodone • Desyrel, Oleptro
- Triazolam • Halcion
Disclosures
Dr. Casher is a speaker for AstraZeneca and Pfizer Inc.
Drs. Gih and Bess report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Although benzodiazepines and stimulants have well-documented efficacy for numerous psychiatric disorders, psychiatrists hesitate to prescribe these medications to patients with substance use disorders (SUDs)—even to those with a comorbid condition that likely would respond to a benzodiazepine or stimulant—because of risk of abuse or dependence. Conventional practice typically has focused on treating active substance use first rather than using simultaneous treatments. Prejudice, fear, and misinformation can influence this decision.
We believe these cases lie on a continuum. At one extreme, ignoring a past or present SUD may lead a remitted patient toward relapse, or further delay recovery for an active user. At the other end, psychiatrists who overreact to a remote history of substance use may deprive patients of legitimate pharmacologic symptom relief. Most cases lie somewhere in the middle.
A literature review does not support the assertion that the use of these medications leads to future substance use or worsens active use, especially for stimulants. In fact, stepwise—as opposed to concurrent—treatment for both conditions actually may delay recovery and increase patients’ risk for morbidity.
We outline issues involved in these complex clinical situations, point out controversies, review relevant research data, and offer guidelines for treatment.
CASE 1 Panic disorder in sobriety
Since he was a teen, Mr. A, age 51, drank heavily, which cost him jobs and relationships. After being convicted for driving under the influence, he was court-ordered to attend a rehabilitation facility, where, as he describes it, he “finally turned [his] life around.” He followed up residential treatment with regular attendance at Alcoholics Anonymous meetings.
After 1 year of sobriety, Mr. A develops increasingly frequent episodes of intense anxiety with sweating, nausea, chest pain, and hyperventilation and is diagnosed with panic disorder. His internist prescribes alprazolam, 0.5 mg 3 times a day, which provides some symptom relief, and refers him for follow-up psychiatric care. At his first visit, Mr. A confides to his psychiatrist that he is taking much more than the prescribed dosage of alprazolam, even when he is not experiencing anxiety, and is contemplating “buying it on the street” if his dosage is not raised to “at least 3 mg 3 times a day.”
CASE 2 Anxiety in controlled psychosis
Ms. B, age 40, had her first psychotic break at age 18 and was diagnosed with schizophrenia. Since then, she has had multiple psychiatric hospitalizations, usually presenting with auditory hallucinations and a recurring delusion that the person who calls herself Ms. B’s mother is really an actress “playing” her mother. At times this delusion has led Ms. B to attack her “imposter” mother. Over several years Ms. B began to drink heavily, but recently achieved a few months of sobriety by attending dual-diagnosis groups at her local community mental health center and individual psychotherapy sessions with her case manager. Fortunately, Ms. B’s psychosis has been stabilized with risperidone long-acting injection, 25 mg every 2 weeks, which she tolerates well.
When her beloved calico cat passes away, Ms. B experiences intense anxiety. Ms. B’s friend tells her she “needs some Valium,” but her psychiatrist, case manager, and the other patients in her dual-diagnosis group are not sure this is a good idea.
Benzodiazepines
Pros. There are multiple legitimate uses of benzodiazepines in general medicine and psychiatric practice, based upon their considerable sedative/hypnotic, anxiolytic, anticonvulsant, and muscle-relaxant properties (Table 1).1
Recommendations regarding benzodiazepine use for anxious patients with a history of SUD are not clear-cut. First, it often is difficult to determine whether the patient truly has an anxiety disorder or is suffering anxiety symptoms secondary to substance use and/or withdrawal. In addition, even if a diagnosis of a separate anxiety disorder is established, psychiatrists debate how to treat such patients. Some clinicians maintain that benzodiazepines should be used only for acute detoxification, and that ongoing benzodiazepine use will lead to relapse or benzodiazepine dependence. However, in a prospective study of 545 alcohol use disorder (AUD) patients receiving benzodiazepines for anxiety disorders, Mueller et al2 found no association—at 12 months or at 12 years—between benzodiazepine use and AUD recurrence. Furthermore, there was no difference in benzodiazepine usage when comparing patients with and without an AUD.3
Table 1
Clinical uses of benzodiazepines
| Insomnia |
| Anxiety disorders (eg, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, social phobia, and obsessive-compulsive disorder) |
| Side effects of other psychiatric medications (eg, akathisia with antipsychotics or tremor with lithium) |
| Alcohol or benzodiazepine withdrawal |
| Acute agitation states, either as monotherapy or as adjuncts to antipsychotics or mood stabilizers |
| Catatonia |
| Source: Reference 1 |
Cons. Although widely prescribed—and despite their efficacy in numerous conditions— both acute or long-term benzodiazepine use frequently causes adverse effects.4 Patients may develop tolerance, which can lead to escalating dosages and/or to withdrawal symptoms when patients attempt to cut back. Benzodiazepines eventually become ineffective for sleep, and continued use can cause rebound insomnia. Also, with many patients taking benzodiazepines long-term, clinicians struggle to differentiate between “real” anxiety symptoms and subtle states of withdrawal from fluctuating benzodiazepine blood levels.5
Geriatric patients who take benzodiazepines are at risk for falls and hip fractures.4 Although older dementia patients are at particular risk for cognitive problems— including frank delirium—secondary to benzodiazepine use, patients of all ages are susceptible to these medications’ deleterious neurocognitive effects.
Benzodiazepines can lead to excessive sedation, thereby impairing performance at work or school, and have been implicated as a cause of motor vehicle accidents.6 Finally, a serious drawback to benzodiazepine use is possible lethality in overdose, especially when combined with alcohol.
Benzodiazepine prescribing should not be taken lightly. Always analyze the difference between benzodiazepines’ well-documented efficacy and their adverse effect profile. This risk-benefit analysis becomes much more complex for patients with SUDs.
Special considerations. Patients at higher risk for benzodiazepine abuse include those with:
- severe alcohol dependence (ie, long-term use, drinking since a young age [“Type II”])
- intravenous drug use
- comorbid alcoholism and antisocial personality disorder.7,8
Exercise special caution when considering benzodiazepines for patients with severe psychiatric illness such as schizophrenia-spectrum disorders, bipolar disorder, or severe depression. Patients with schizophrenia have high rates of alcohol, cocaine, cannabis, and benzodiazepine abuse.9,10 Bipolar disorder patients show similar vulnerability—up to 56% of patients screen positive for substance abuse or dependence.11 Vulnerability to addiction in severely ill psychiatric patients is thought to be related to several factors, including:
- use of drugs as self-medication
- genetic predisposition
- environment/lifestyle that supports substance abuse
- neurobiologic deficits that lead to lack of inhibition of reward-seeking behaviors.11
Bipolar disorder patients in particular score high on measures of sensation seeking, which leaves them vulnerable to abusing all classes of substances.12
In a 6-year study of 203 patients with severe psychiatric illnesses and SUDs, Brunette et al13 found that these patients were 2.5 times more likely than patients with severe psychiatric illness alone to abuse prescribed benzodiazepines. In an analysis of Medicaid records, Clark et al14 found similar vulnerability in patients with major depressive disorder (MDD) and SUD. Not only did these patients show a higher rate of benzodiazepine use than patients with MDD without SUD, but the dual-diagnosis group also gravitated toward more addictive high-potency/fast-acting benzodiazepines, such as alprazolam, estazolam, or triazolam.
Case discussion/suggestions. Initially, Mr. A may seem to be an appropriate candidate for closely monitored benzodiazepine use. However, he shows a pattern of misuse, likely related to his history of severe alcohol dependence and alprazolam use. This benzodiazepine is fast-acting and has a short half-life, and thus is highly reinforcing.
Similarly, Ms. B might benefit from benzodiazepine treatment. However, her history of schizophrenia and alcohol abuse makes her a risky candidate, and alternative treatments for anxiety symptoms should be considered. If prescribed at all, a benzodiazepine should be used only short-term (eg, 1 to 2 weeks).
In general, avoid prescribing benzodiazepines to most patients who have an ongoing or past SUD.15 Consider making an exception for SUD patients with comorbid anxiety disorders, with close monitoring of their benzodiazepine use. Clonazepam, chlordiazepoxide, clorazepate, and oxazepam may be less reinforcing for SUD patients than diazepam, lorazepam, alprazolam, estazolam, or triazolam.7,16 The drawbacks of benzodiazepines, especially in the situations described above, point to the need to find alternative treatments (Table 2).17 Keep in mind nonpharmacologic options, which completely avoid the risks of medication misuse and diversion. Cognitive-behavioral therapy (CBT), for instance, has well-documented efficacy in treating insomnia and anxiety disorders.18,19
Table 2
Alternatives to benzodiazepines for anxiety and/or insomnia
| Treatment option | Comments |
|---|---|
| CBT, relaxation techniques, sleep hygiene counseling | Many advantages to nonpharmacologic interventions (eg, fewer side effects, no risk of substance dependence) |
| Antihistamines (eg, diphenhydramine, 25 to 50 mg at bedtime* for sleep, or 2 to 3 times a day for anxiety) | Can be used for anxiety or insomnia; can cause confusion in older patients |
| Atypical antipsychotics | Off-label use; many agents in this class have metabolic side effects |
| SSRIs/SNRIs | First-line for many anxiety disorders, including panic disorder, GAD; possible weight gain and sexual side effects |
| Mirtazapine (7.5 to 30 mg at bedtime*) | Sedation side effect helps with sleep; weight gain and oversedation limit use |
| Trazodone (25 to 100 mg at bedtime*) | Commonly used off-label as a sleep aid |
| Monoamine oxidase inhibitors | May be useful for social phobia; dietary restrictions and side effects limit use |
| Doxepin (3 to 6 mg at bedtime) | Minimal anticholinergic and alpha-blockade side effects at this dose; FDA-approved for insomnia |
| Gabapentin (300 to 2,000 mg/d* in divided doses) | Off-label use, mild anxiolytic and sedative properties, relatively weight neutral |
| Beta blockers (eg, propranolol, 20 to 80 mg twice a day*) | Useful for peripheral manifestations of anxiety; may be effective for social phobias |
| Pregabalin (50 to 200 mg 3 times a day*) | Off-label use; industry-sponsored studies show comparable to SNRIs for anxiety |
| Non-benzodiazepine GABAA receptor modulators | Short-term option for primary insomnia, some abuse potential |
| Melatonin (1 to 3 mg at bedtime*) | Mild and ‘natural’ but not always an effective sleep aid |
| *Off-label approximate doses based on the authors’ clinical experience and consensus of the literature; agents listed may require slow titration and close monitoring for adverse effects CBT: cognitive-behavioral therapy; GABA: gamma-aminobutyric acid; GAD: generalized anxiety disorder; SNRI: serotoninnorepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor Source: Reference 17 | |
CASE 3 Adult ADHD and marijuana use
Mr. C, age 30, presents to a psychiatrist with ongoing complaints of inattention, fatigue, and difficulty staying organized. A self-report screen yields symptoms consistent with adult attention-deficit/hyperactivity disorder (ADHD). Mr. C’s school and job history and collateral history from his wife appear to corroborate his assertion that his symptoms have been lifelong. He later admits to regular marijuana use. After further discussion and full evaluation of his substance use, Mr. C is started on bupropion, titrated to 300 mg/d. After 2 months, despite faithful attendance at appointments and openness about his continued marijuana use, Mr. C’s symptoms remain unchanged. He asks about atomoxetine.
Stimulants
Pros. Despite many clinicians’ hesitance to prescribe controlled substances to patients with SUDs, psychostimulants should be considered in a variety of scenarios. Although nonstimulant options are available, stimulants consistently have demonstrated superior efficacy over other treatments and remain first-line agents for adult ADHD.20 Methylphenidate, mixed amphetamine salts, lisdexamfetamine, and atomoxetine are FDA-approved for adult ADHD. Both stimulant classes (methylphenidate and amphetamine-based products) are equally effective for ADHD. In addition, stimulants are used to treat narcolepsy, cognitive disorders such as traumatic brain injury, and as augmentation to antidepressants for MDD.
ADHD affects 5% to 12% of children, and >60% of patients remain symptomatic into adulthood and require continued treatment.21 In particular, problematic inattention may persist throughout adulthood. ADHD does not appear to be an independent risk factor for SUDs in children and adolescents.22 However, substance use increases sharply as ADHD patients enter late adolescence and adulthood, and eventually becomes a problem for 20% of adolescents and adults with ADHD. Conversely, 17% to 50% of patients with alcohol, cocaine, or opioid dependence have co-occurring ADHD.23
Withholding ADHD treatment based on concerns about future or increased current substance abuse is unfounded. A meta-analysis of 6 studies that included 674 medicated and 360 unmedicated patients with ADHD who were followed at least 4 years demonstrated that childhood treatment of ADHD with stimulants reduces the risk of developing alcohol and other drug disorders in adulthood.24 Regarding the effect stimulants have on active substance use, a 12-week, double-blind, randomized controlled trial of 48 cocaine-dependent adults with ADHD showed methylphenidate did not change cocaine abuse or craving, but did improve ADHD symptoms.25
Clinicians also must assess whether untreated ADHD symptoms impair patients’ work or other activities. Driving is a particular concern because ADHD is associated with risky driving habits, motor vehicle accidents, traffic violations, and driving license suspensions.26 In a study that administered cognitive tests to 27 adults with ADHD, methylphenidate treatment improved cognitive performance related to driving (eg, better visual-motor coordination under high-stress conditions, improved visual orientation, and sustained visual attention).27 It is likely this effect could be generalized to other activities where safety is important. Finally, appropriate stimulant treatment may improve participation in rehabilitative programs.
Cons. Despite their positive effects, stimulants can have adverse effects and consequences.28 In routinely prescribed dosages, methylphenidate and amphetamines can cause symptoms related to sympathetic activation, including anxiety, tics, anorexia/ weight loss, and sleep disturbance. A 5-year study of 79 school-age children prescribed methylphenidate, dextroamphetamine, or pemoline, which is no longer available in the United States, showed a significant association between adherence to stimulants and persistence of physiological (eg, headaches, insomnia, anorexia) and mood-related (eg, irritability, dysphoria) side effects.29 Stimulants’ sympathomimetic properties also can lead to dangerous drug-drug interactions with monoamine oxidase inhibitors. For both methylphenidate and amphetamines, overdose can lead to seizures, cardiac toxicity, dysrhythmias, and hyperthermia. All stimulants carry an FDA “black-box” warning that lists increased risk of cardiac complications, sudden death, and psychiatric complications such as psychosis or mania.30
Special considerations. All stimulants have potential for diversion or abuse. Pay close attention to these issues, especially in vulnerable populations and situations where rates of abuse and diversion are elevated. Among college students, white patients, fraternity/sorority members, and individuals with lower grade point averages may be at higher risk for nonmedical stimulant use.31 Adults who misuse or divert stimulants commonly have a history of substance abuse and conduct disorder.32 Short-acting stimulants are abused 4 times more often than extended-release preparations.33
If your ADHD patient has active substance use, be clear that continued substance use is likely to limit stimulants’ effectiveness. In patients who are actively using substances, it will be difficult to disentangle apparent nonresponse to stimulants from the negative cognitive effects of substance use.
Case discussion/suggestions. As Mr. C’s case illustrates, there are alternatives to stimulants for ADHD. For example, atomoxetine, a selective norepinephrine reuptake inhibitor, may be considered a first-line agent in patients with mostly inattentive ADHD symptoms and comorbid stimulant abuse, or for those in whom stimulants cause adverse effects such as mood lability or tics.34 Other alternatives to stimulants are listed in Table 3.35
Because Mr. C did not respond to bupropion, which presumably was tried first because of his ongoing substance use, he asked about atomoxetine. This agent is not addictive and there is no evidence that it leads to or exacerbates substance use. Depending on Mr. C’s symptom profile, atomoxetine might be a good choice. Continued monitoring of his marijuana use and frequent assessment of his motivation to quit are necessary. Psychoeducation about the cognitive effects of marijuana, including inattention and poor concentration, is important.
If Mr. C does not respond to atomoxetine, his psychiatrist will face a difficult decision. Setting Mr. C’s marijuana use aside, symptoms that do not respond to atomoxetine or a second-line agent are likely to respond to a stimulant. However, several issues must be addressed. If Mr. C’s motivation to stop using marijuana is low, how motivated is he to improve his ADHD symptoms? Next, would marijuana’s depressive/blunting effects counteract the anticipated benefit of a stimulant? Also, what is the risk that Mr. C might sell or exchange his stimulants to obtain marijuana? Assessing these complicated questions is key. Another important factor in Mr. C’s case is his wife’s involvement. Does she monitor his marijuana use? Would she be willing to supervise Mr. C’s stimulant use, and would he allow it?
Past or present SUDs are not an absolute contraindication to stimulant use. You should affirm the diagnosis and identify target symptoms. Consider nonstimulant alternatives if appropriate.
Table 3
Alternatives to stimulants for ADHD
| Treatment option | Comments |
|---|---|
| Atomoxetine | Effectiveness may be limited to inattentive type |
| Modafinil | Well-tolerated but expensive, limited evidence, no FDA indication; may be a consideration in ADHD + SUD |
| α2-adrenergic agonist (eg, clonidine or guanfacine) | Useful when hyperactivity/impulsivity symptoms predominate, or when stimulant-induced insomnia occurs |
| Bupropion | Some evidence of mild efficacy, especially useful if nicotine dependence also is a target for treatment |
| Psychotherapy | Can be useful as adjunctive treatment, but as monotherapy it is of little benefit in ADHD |
| ADHD: attention-deficit/hyperactivity disorder; SUD: substance abuse disorder Source: Reference 35 | |
Legal liabilities
Being aware of the medicolegal issues of benzodiazepine and/or stimulant prescribing is crucial because a court may find a psychiatrist liable for negative outcomes (eg, suicide) when controlled substances are prescribed to a patient with a history of addiction.36 The most prudent course is to weigh the pros and cons for each patient individually, taking into consideration the factors described above.8 This is consistent with guidelines from the American Psychiatric Association and the British Association for Psychopharmacology,37 both of which call for extreme caution in these cases.
Educate patients and caregivers about the risks of taking a controlled substance, including misuse, diversion, and theft. Provide and document explicit instructions that the patient will receive stimulants from only a single provider. Remind patients that state and federal authorities closely track controlled medications. Finally, a “stimulant contract” or “benzodiazepine contract,” similar to a pain or narcotic contact, may be useful to formally document discussions about appropriate medication use.
Related Resources
- National Institute on Drug Abuse. Prescription drugs: abuse and addiction. Research Report Series, 2005. http://drugabuse.gov/ResearchReports/Prescription/Prescription.html.
- Galanter M, Kleber HD. The American Psychiatric Publishing textbook of substance abuse treatment. 4th ed. Arlington, VA: American Psychiatric Publishing, Inc; 2008.
Drug Brand Names
- Alprazolam • Xanax
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, others
- Chlordiazepoxide • Librium
- Clonazepam • Klonopin
- Clonidine • Catapres
- Clorazepate • Tranxene
- Dextroamphetamine • Dexedrine
- Diazepam • Valium
- Diphenhydramine • Benadryl, others
- Doxepin • Silenor
- Estazolam • ProSom
- Gabapentin • Neurontin
- Guanfacine • Tenex, Intuniv
- Lisdexamfetamine • Vyvanse
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Methylphenidate • Ritalin, Concerta, others
- Mirtazapine • Remeron
- Mixed amphetamine salts • Adderall
- Modafinil • Provigil
- Oxazepam • Serax
- Pemoline • Cylert
- Propranolol • Inderal
- Trazodone • Desyrel, Oleptro
- Triazolam • Halcion
Disclosures
Dr. Casher is a speaker for AstraZeneca and Pfizer Inc.
Drs. Gih and Bess report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Ashton H. Guidelines for the rational use of benzodiazepines. When and what to use. Drugs. 1994;48(1):25.-
2. Mueller TI, Pagano ME, Rodriguez BF, et al. Long-term use of benzodiazepines in participants with comorbid anxiety and alcohol use disorders. Alcohol Clin Exp Res. 2005;29(8):1411-1418.
3. Mueller TI, Goldenberg IM, Gordon AL, et al. Benzodiazepine use in anxiety disordered patients with and without a history of alcoholism. J Clin Psychiatry. 1996;57(2):83-89.
4. Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005;(18):249-255.
5. Back SE, Brady KT. Anxiety disorders with comorbid substance use disorders: diagnostic and treatment considerations. Psychiatric Annals. 2008;38(11):724-729.
6. Walsh JM, Flegel R, Cangianelli LA, et al. Epidemiology of alcohol and other drug use among motor vehicle crash victims admitted to a trauma center. Traffic Inj Prev. 2004;5(3):254-260.
7. Ciraulo DA, Nace EP. Benzodiazepine treatment of anxiety or insomnia in substance abuse patients. Am J Addict. 2000;9(4):276-279;discussion 280–284.
8. Sattar S, Bhatia S. Benzodiazepines for substance abusers. Current Psychiatry. 2003;2(5):25-34.
9. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
10. Kendler KS, Gallagher TJ, Abelson JM, et al. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53(11):1022-1031
11. Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(suppl 7):5-9.
12. Bizzarri JV, Sbrana A, Rucci P, et al. The spectrum of substance abuse in bipolar disorder: reasons for use, sensation seeking and substance sensitivity. Bipolar Disord. 2007;9(3):213-220.
13. Brunette MF, Noordsy DL, Xie H, et al. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr Serv. 2003;54(10):1395-1401.
14. Clark RE, Xie H, Brunette MF, et al. Benzodiazepine prescription practices and substance abuse in persons with severe mental illness. J Clin Psychiatry. 2004;65(2):151-155.
15. Longo LP. Addiction: part I. Benzodiazepines—side effects abuse risk and alternatives. Am Fam Physician. 2000;61(7):2121-2128.
16. Ciraulo DA, Barnhill JG, Ciraulo AM, et al. Alterations in pharmacodynamics of anxiolytics in abstinent alcoholic men: subjective responses, abuse liability, and electroencephalographic effects of alprazolam, diazepam, and buspirone. J Clin Pharmacol. 1997;37(1):64-73.
17. Casher MI, Bess JD. Manual of inpatient psychiatry. Cambridge United Kingdom: Cambridge University Press; 2010.
18. Hofmann S, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
19. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
20. Wilens TE. Drug therapy for adults with attention-deficit hyperactivity disorder. Drugs. 2003;63(22):2395-2411.
21. Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
22. Biederman J, Wilens T, Mick E, et al. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;36(1):21-29.
23. Waid L, Johnson D, Anton R. Attention-deficit hyperactivity disorder and substance abuse. In: Kranzler HR Rounsaville BJ, eds. Dual diagnosis and treatment: substance abuse and comorbid medical and psychiatric disorders. vol 8. New York, NY: Marcel Dekker; 1998:393–425.
24. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
25. Schubiner H, Saules KK, Arfken CL, et al. Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol. 2002;10(3):286-294.
26. Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6 Pt 1):1089-1095.
27. Sobanski E, Sabljic D, Alm B, et al. Driving-related risks and impact of methylphenidate treatment on driving in adults with attention-deficit/hyperactivity disorder (ADHD). J Neural Transm. 2008;115(2):347-356.
28. Leonard BE, McCartan D, White J, et al. Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects. Hum Psychopharmacol. 2004;19(3):151-180.
29. Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004;43(5):559-567.
30. Schatzberg AF, Nemeroff CB. The American Psychiatric Publishing textbook of psychopharmacology. 4th ed. Arlington VA: American Psychiatric Publishing, Inc; 2009.
31. Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21-31.
32. Wilens TE, Gignac M, Swezey A, et al. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408-414.
33. Bright GM. Abuse of medications employed for the treatment of ADHD: results from a large-scale community survey. Medscape J Med. 2008;10(5):111.-
34. Biederman J, Spencer T, Wilens T. Evidence-based pharmacotherapy for attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2004;7(1):77-97.
35. Mann N, Bitsios P. Modafinil treatment of amphetamine abuse in adult ADHD. J Psychopharmacol. 2009;23(4):468-471.
36. Grant JE. Prudent prescribing for patients with addictions. Current Psychiatry. 2006;5(10):99-102.
37. Lingford-Hughes AR, Welch S, Nutt DJ. and the British Association for Psychopharmacology. Evidence-based guidelines for the pharmacological management of substance misuse addiction and comorbidity: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2004;18(3):293-335.
1. Ashton H. Guidelines for the rational use of benzodiazepines. When and what to use. Drugs. 1994;48(1):25.-
2. Mueller TI, Pagano ME, Rodriguez BF, et al. Long-term use of benzodiazepines in participants with comorbid anxiety and alcohol use disorders. Alcohol Clin Exp Res. 2005;29(8):1411-1418.
3. Mueller TI, Goldenberg IM, Gordon AL, et al. Benzodiazepine use in anxiety disordered patients with and without a history of alcoholism. J Clin Psychiatry. 1996;57(2):83-89.
4. Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005;(18):249-255.
5. Back SE, Brady KT. Anxiety disorders with comorbid substance use disorders: diagnostic and treatment considerations. Psychiatric Annals. 2008;38(11):724-729.
6. Walsh JM, Flegel R, Cangianelli LA, et al. Epidemiology of alcohol and other drug use among motor vehicle crash victims admitted to a trauma center. Traffic Inj Prev. 2004;5(3):254-260.
7. Ciraulo DA, Nace EP. Benzodiazepine treatment of anxiety or insomnia in substance abuse patients. Am J Addict. 2000;9(4):276-279;discussion 280–284.
8. Sattar S, Bhatia S. Benzodiazepines for substance abusers. Current Psychiatry. 2003;2(5):25-34.
9. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
10. Kendler KS, Gallagher TJ, Abelson JM, et al. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53(11):1022-1031
11. Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(suppl 7):5-9.
12. Bizzarri JV, Sbrana A, Rucci P, et al. The spectrum of substance abuse in bipolar disorder: reasons for use, sensation seeking and substance sensitivity. Bipolar Disord. 2007;9(3):213-220.
13. Brunette MF, Noordsy DL, Xie H, et al. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr Serv. 2003;54(10):1395-1401.
14. Clark RE, Xie H, Brunette MF, et al. Benzodiazepine prescription practices and substance abuse in persons with severe mental illness. J Clin Psychiatry. 2004;65(2):151-155.
15. Longo LP. Addiction: part I. Benzodiazepines—side effects abuse risk and alternatives. Am Fam Physician. 2000;61(7):2121-2128.
16. Ciraulo DA, Barnhill JG, Ciraulo AM, et al. Alterations in pharmacodynamics of anxiolytics in abstinent alcoholic men: subjective responses, abuse liability, and electroencephalographic effects of alprazolam, diazepam, and buspirone. J Clin Pharmacol. 1997;37(1):64-73.
17. Casher MI, Bess JD. Manual of inpatient psychiatry. Cambridge United Kingdom: Cambridge University Press; 2010.
18. Hofmann S, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
19. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
20. Wilens TE. Drug therapy for adults with attention-deficit hyperactivity disorder. Drugs. 2003;63(22):2395-2411.
21. Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
22. Biederman J, Wilens T, Mick E, et al. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;36(1):21-29.
23. Waid L, Johnson D, Anton R. Attention-deficit hyperactivity disorder and substance abuse. In: Kranzler HR Rounsaville BJ, eds. Dual diagnosis and treatment: substance abuse and comorbid medical and psychiatric disorders. vol 8. New York, NY: Marcel Dekker; 1998:393–425.
24. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
25. Schubiner H, Saules KK, Arfken CL, et al. Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol. 2002;10(3):286-294.
26. Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6 Pt 1):1089-1095.
27. Sobanski E, Sabljic D, Alm B, et al. Driving-related risks and impact of methylphenidate treatment on driving in adults with attention-deficit/hyperactivity disorder (ADHD). J Neural Transm. 2008;115(2):347-356.
28. Leonard BE, McCartan D, White J, et al. Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects. Hum Psychopharmacol. 2004;19(3):151-180.
29. Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004;43(5):559-567.
30. Schatzberg AF, Nemeroff CB. The American Psychiatric Publishing textbook of psychopharmacology. 4th ed. Arlington VA: American Psychiatric Publishing, Inc; 2009.
31. Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21-31.
32. Wilens TE, Gignac M, Swezey A, et al. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408-414.
33. Bright GM. Abuse of medications employed for the treatment of ADHD: results from a large-scale community survey. Medscape J Med. 2008;10(5):111.-
34. Biederman J, Spencer T, Wilens T. Evidence-based pharmacotherapy for attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2004;7(1):77-97.
35. Mann N, Bitsios P. Modafinil treatment of amphetamine abuse in adult ADHD. J Psychopharmacol. 2009;23(4):468-471.
36. Grant JE. Prudent prescribing for patients with addictions. Current Psychiatry. 2006;5(10):99-102.
37. Lingford-Hughes AR, Welch S, Nutt DJ. and the British Association for Psychopharmacology. Evidence-based guidelines for the pharmacological management of substance misuse addiction and comorbidity: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2004;18(3):293-335.
Glutamate: New hope for schizophrenia treatment
Discuss this article at www.facebook.com/CurrentPsychiatry
In patients with schizophrenia, positive symptoms typically respond to treatment, while negative and cognitive symptoms often persist and contribute to chronic disability.1 Schizophrenia also is associated with widespread neurocognitive deficits—including impairments in executive functioning, learning, memory, and processing speed—that are a core feature of the disorder and may precede illness onset.2
Current treatment is based on the dopamine model of schizophrenia, which proposes that dopaminergic dysfunction is the basis for symptoms and cognitive deficits.3 Although this model is effective in guiding treatment for some patients, most show persistent disability despite receiving the best available treatment. Over the last 2 decades, researchers have developed alternative conceptual models of schizophrenia based on the psychotomimetic effects of compounds such as phencyclidine (PCP) and ketamine.4 These compounds function primarily by blocking N-methyl-D-aspartate (NMDA)-type glutamate receptors (NMDARs), which has lead researchers to focus on glutamatergic neurotransmission and NMDARs as a basis for new drug development. This article describes the glutamatergic model of schizophrenia and its implications for future treatments.
Dopaminergic models
Since the discovery of chlorpromazine almost 60 years ago, the dopamine model of schizophrenia has been widely accepted. It has gone through several iterations but in general suggests that schizophrenia is caused by dopaminergic system dysfunction, particularly increased dopamine within subcortical brain regions such as the striatum or nucleus accumben.3 The ability of amphetamine or other dopaminergic agents to induce symptoms closely resembling positive symptoms supports this model, as do genetic studies that show dopamine-related genes are associated with schizophrenia.5 In addition, all antipsychotics block dopamine type 2 receptors.
Unfortunately, limitations of this model continue to limit treatment:
- Dopaminergic compounds such as amphetamine do not induce negative symptoms or cognitive deficits similar to those observed in schizophrenia.
- Dopamine receptor blockers do not reverse cognitive dysfunction or negative symptoms.
- Dopaminergic instability observed during acute decompensation appears to resolve after stabilization even without symptom remission.
- Although dopaminergic systems preferentially innervate frontal brain regions, cognitive deficits in schizophrenia appear to be widespread, involving sensory as well as frontal brain systems.
Thus, dopaminergic dysfunction appears to account for only a part of schizophrenia’s symptomatic and neurocognitive profile.
Glutamatergic model
Approximately 20 years ago, researchers proposed an alternate schizophrenia model based on the observed clinical actions of “dissociative anesthetics,” including PCP and ketamine. PCP was patented in 1953 as a surgical anesthetic, but serious side effects, such as hallucinations, agitation, and catatonic-like reactions, soon curtailed its clinical use. As early as 1959, some researchers noted similarities between PCP psychosis and schizophrenia.4,6
The binding site for PCP and other dissociative anesthetics (“PCP receptor”) was first described in 1979 and subsequently localized within the ion channel formed by the NMDAR. Glutamate is the primary excitatory neurotransmitter in the brain, and binds to NMDA and non-NMDA (eg, metabotropic or alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid [AMPA]) receptors. Binding of PCP prevents glutamate from activating NMDARs, which suggests that the pathogenesis of schizophrenia may be caused by dysfunction of NMDARs in particular or of the glutamatergic system in general. Unlike dopamine, the glutamatergic system is distributed throughout the brain and plays a prominent role in sensory processing and higher-level functions such as memory and executive functioning (Figure).6 Therefore, glutamatergic theories open new approaches for potential schizophrenia treatments, most of which are now entering clinical evaluation.
Figure: The wide reach of glutamatergic dysfunction
NMDA: N-methyl-D-aspartate; NMDAR: N-methyl-D-aspartate-type glutamate receptors
Source: Reference 6
Effects of NMDAR antagonists
In initial studies with PCP and ketamine in the early 1960s, researchers noted that these agents produced psychotic effects similar to schizophrenia symptoms.6 Further confirmation was obtained from retrospective studies of PCP abusers.6 It was not until the 1990s, however, that studies using modern operationalized symptom and neuropsychological rating scales were conducted. In those studies, healthy participants developed positive symptoms, negative symptoms, and cognitive dysfunction after receiving ketamine.7,8 Moreover, in these studies the balance between negative and positive symptoms was similar to that typically observed in schizophrenia, as was the pattern of cognitive dysfunction. Therefore, unlike dopaminergic agents, NMDAR antagonists appear to be able to produce the full constellation of symptoms and cognitive deficits associated with schizophrenia.
Similarly, ketamine worsened positive and negative symptoms in patients diagnosed with schizophrenia.9 Although acute challenge with NMDAR antagonists does not produce schizophrenia-like auditory hallucinations in healthy controls, it does induce sensory distortions similar to those seen in individuals with early schizophrenia and does exacerbate pre-existing hallucinations in schizophrenia patients.10 Thus, acute challenge with NMDAR antagonists appears to re-create a state similar to the earliest stages of schizophrenia.6
NMDAR antagonists also reproduce the widespread neuropsychological abnormalities of schizophrenia (Figure).6 Ketamine infusion results in the severity and type of disorganized thinking seen in schizophrenia. Given the importance of neurocognitive dysfunction to the conceptualization of schizophrenia, these findings further support a glutamatergic model.
Sensory processing deficits
A key difference between dopaminergic and glutamatergic models is prediction of sensory processing deficits. Traditionally, dopaminergic models have viewed cognitive deficits of schizophrenia as being driven “top down” from higher order brain regions such as the prefrontal cortex, or from local dysfunction within regions such as the striatum.11 In contrast, glutamatergic models predict that deficits also should be observed within sensory brain regions, such as the primary auditory and visual cortex.
Because of the focus on higher-level brain dysfunction, little research on sensory processing deficits was performed until recently. It has become increasingly clear that:
- patients with schizophrenia show severe deficits in early auditory and visual processing
- these deficits significantly contribute to patterns of cognitive dysfunction and psychosocial impairment.12,13
In the auditory system, patients show deficits in pitch perception and, specifically, the ability to match tones after a brief delay. Schizophrenia patients show dysfunction in a specific part of the visual system called the magnocellular visual system. Deficits in these regions lead to impaired ability to detect emotion based on vocal intonation or facial expression, among other deficits.
In addition, reading ability—which was once thought to be normal in patients with schizophrenia—has been found to be severely disturbed.14 As in developmental dyslexia, impairments relate to dysfunction of underlying auditory and visual brain regions. Administering NMDAR antagonists to humans or animals causes deficits in the auditory and visual system similar to those seen in schizophrenia, which confirms the importance of NMDA dysfunction.
Glutamate-based treatments
Because NMDAR antagonists can induce schizophrenia symptoms, the most straightforward approach for treatment is to develop compounds that stimulate glutamate or NMDAR function (Table). The NMDAR contains modulatory sites that may be appropriate targets for drug development, including one that binds the amino acids glycine and D-serine and a redox site that is sensitive to brain glutathione levels. Reductions in brain D-serine and glutathione levels have been reported in schizophrenia, which suggests that impaired NMDAR regulation may contribute directly to brain dysfunction.15 Other treatment approaches being developed include targeting glycine transporters, which indirectly regulate brain levels of glycine, or metabotropic glutamate receptors, which modulate both pre-synaptic glutamate release and post-synaptic NMDAR function.
Table
Glutamatergic drugs in development
| Target | Proposed mechanism | Proposed agents | Phase of development |
|---|---|---|---|
| Glycine/D-serine receptor | Allosteric modulator of the NMDA receptor | Glycine, D-serine, D-alanine, D-cycloserine | Phase II |
| Glycine-type I transport inhibitor | Blocks the reuptake of glycine, akin to SSRIs’ action on serotonin | Sarcosine, RG1678 | Phase II/III |
| Metabotropic glutamate type 2/3 (mGluR2/3) | Blocks presynaptic glutamate release | LY-2140023 | Phase II |
| Redox sensitive site | Allosteric modulator of the NMDA receptor | N-acetylcysteine | Phase II |
| D-amino acid oxidase (DAAO) inhibitors | Inhibits the enzyme that metabolizes D-serine | Remains in preclinical stage | |
| Tetrahydrobiopterin (BH4) | Indirectly modulates glutamatergic system | Remains in preclinical stage | |
| NMDA: N-methyl-D-aspartate; SSRIs: selective serotonin reuptake inhibitors | |||
Glycine/D-serine site agonists. To date, most studies have used glutamatergic drugs adjunctive to antipsychotics and targeted the glycine/D-serine modulatory site, in part because glycine and D-serine are natural compounds and therefore FDA approval for their use could be obtained without the extensive preclinical development usually required for new chemical entities.16 Unfortunately, these agents are less potent than traditional pharmaceuticals, and delivering optimal doses may be impossible. Nevertheless, positive studies with these compounds have provided proof-of-concept for development of agents with higher affinity and specificity.
Studies have used glycine administered at doses up to 60 g/d, D-serine up to 8 g/d, or D-alanine approximately 6 g/d. For glycine, 60 g/d is the highest dose that can be given because of concerns about tolerability and replacement of other essential amino acids. D-serine originally was tested at approximately 2 g/d with promising results, but a recent open-label trial suggested that higher doses may be more efficacious.17 D-serine doses are limited by potential renal toxicity, as demonstrated in rodents studies.
Although not all studies of glycine/D-serine site agonists have been positive, a recent meta-analysis suggests significant improvement in negative symptoms across studies.18 Variability in statistical results across studies is related primarily to degree of placebo effect within individual trials, with a mean improvement in negative symptoms of approximately 15%. Glycine/D-serine site agonists seem to be less effective when combined with clozapine, possibly because clozapine may already enhance the glutamatergic system and increase synaptic glycine levels.6
One study that evaluated effects of open-label glycine in individuals with schizophrenia symptoms observed a large effect-size improvement, including early remission in 3 of 10 patients.19 These data—if confirmed by double-blind trials—would indicate that glycine/d-serine site agonists might have utility in treating the schizophrenia prodrome.
Glycine transport inhibitors. A potential indirect approach to raising glycine levels in the brain is using GlyT1-type glycine transport inhibitors (GTIs). GlyT1 transporters are co-localized in brain with NMDARs and modulate local glycine levels. Rather than binding directly to the NMDAR glycine binding site, GTIs increase glycine levels in the synapse by preventing its removal by GlyT1 transporters. Their function is analogous to using selective serotonin reuptake inhibitors to increase serotonin levels in patients with depression.6
Sarcosine (N-methylglycine) is a naturally occurring GlyT1 inhibitor that has been used in early clinical trials in Taiwan. Initial studies with sarcosine showed efficacy similar to—and in some cases better than—that of direct glycine/D-serine site agonists when added to first-generation or non-clozapine second-generation antipsychotics.18 Sarcosine also has been found to be effective for acute treatment of schizophrenia.20 At present, however, sarcosine is not available for experimental use in the United States because of toxicity considerations.
Using high-affinity GTIs for schizophrenia was first proposed in the mid-1990s,6 but such compounds are only now entering clinical efficacy studies. Most recently, phase II results were presented for RG1678, a compound developed by Hoffman LaRoche.21 The study targeted persistent negative symptoms in patients receiving chronic antipsychotic treatment. Adding RG1678, 10 mg and 30 mg, to antipsychotics led to significant improvement in persistent negative symptoms vs placebo. These promising results are being followed up in phase III studies.
Other glutamatergic options. Few compounds are available to modulate NMDARs at sites other than the glycine/D-serine site. One study administered N-acetylcysteine, a glutathione precursor, as a potential treatment for persistent negative symptoms.22 Encouraging clinical results were observed in this double-blind study, along with improvement in electrophysiologic measures, negative symptoms, and overall functioning, but the study was limited by relatively high rates of noncompletion. Preclinical studies have combined D-serine with an inhibitor of D-amino acid oxidase to prevent D-serine breakdown.23 In rodents, this approach produces a 30-fold increase in D-serine potency.
Tetrahydrobiopterin (BH4) is a cofactor for enzymes responsible for the synthesis of dopamine and other monoamines, and presynaptic release of dopamine and glutamate. Reductions in BH4 levels have been reported in schizophrenia, which suggests that this compound may be etiologically important.24 Researchers have initiated a study of this compound in schizophrenia.
Other schizophrenia models propose that the crucial issue is not NMDA blockade but subsequent dysregulation of presynaptic glutamate release. Type 2/3 metabotropic glutamate receptors (mGluR2/3) are located on presynaptic glutamate terminals and inhibit presynaptic glutamate release. mGluR2/3 agonists have been shown to reverse ketamine’s effects in humans and in animal models,25,26 which suggests a potential role in schizophrenia treatment.
The first mGluR2/3 agonist entered into monotherapy clinical efficacy trials for schizophrenia was LY-2140023. In an initial trial, this compound showed significant efficacy in improving positive and negative symptoms, comparable to that of olanzapine.27 However, a follow-up study failed because of a large placebo effect,28 which leaves the efficacy question unresolved.
In contrast to mGluR2/3, type 5 metabotropic receptors (mGluR5) are co-localized with NMDA receptors and potentiate activation. Thus, mGluR5 agonists also may be effective for treating schizophrenia. These compounds remain in preclinical development. Other approaches, such as stimulating specific types of GABA receptors to overcome glutamatergic deficits, remain promising but have not been tested in definitive clinical trials.
Related Resources
- Kantrowitz JT, Javitt DC. N-methyl-D-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull. 2010; 83(3-4): 108-121.
- Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Kantrowitz JT, Javitt DC, eds. Handbook of neurochemistry and molecular neurobiology: schizophrenia. 3rd ed. New York, NY: Springer; 2009.
Drug Brand Names
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Ketamine • Ketalar
- Olanzapine • Zyprexa
Disclosures
Dr. Javitt receives grant/research support from Jazz Pharmaceuticals, Pfizer Inc., and Roche and is a consultant to AstraZeneca, Cypress, Eli Lilly and Company, NPS Pharmaceuticals, Sepracor, Solvay, Sunovion, and Takeda. He holds intellectual property rights for use of glycine, D-serine, and glycine transport inhibitors in treatment of schizophrenia and related disorders.
Dr. Kantrowitz receives grant/research support from Eli Lilly and Company, Jazz Pharmaceuticals, Pfizer Inc., Roche, and Sepracor.
Preparation of this manuscript was supported in part by National Institute of Health grants R01 DA03383, R37 MH49334, and P50 MH086385.
1. Fenton WS, McGlashan TH. Antecedents symptom progression, and long-term outcome of the deficit syndrome in schizophrenia. Am J Psychiatry. 1994;151(3):351-356.
2. Woodberry KA. Premorbid IQ in schizophrenia: a meta-analytic review. Am J Psychiatry. 2008;165(5):579-587.
3. Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III—the final common pathway. Schizophr Bull. 2009;35(3):549-562.
4. Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301-1308.
5. Egan MF, Goldberg TE, Kolachana BS, et al. Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. Proc Natl Acad Sci U S A. 2001;98:6917-6922.
6. Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Kantrowitz JT Javitt DC, eds. Handbook of neurochemistry and molecular neurobiology: schizophrenia. 3rd ed. New York, NY: Springer; 2009.
7. Krystal JH, Karper LP, Seibyl JP, et al. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry. 1994;51(3):199-214.
8. Krystal J, D’Souza DC, Mathalon D, et al. NMDA receptor antagonist effects, cortical glutamatergic function, and schizophrenia: toward a paradigm shift in medication development. Psychopharmacology. 2003;169(3-4):215-233.
9. Malhotra AK, Pinals DA, Adler CM, et al. Ketamine-induced exacerbation of psychotic symptoms and cognitive impairment in neuroleptic-free schizophrenics. Neuropsychopharmacology. 1997;17(3):141-150.
10. Lahti AC, Koffel B, LaPorte D, et al. Subanesthetic doses of ketamine stimulate psychosis in schizophrenia. Neuropsychopharmacology. 1995;13(1):9-19.
11. Lesh TA, Niendam TA, Minzenberg MJ, et al. Cognitive control deficits in schizophrenia: mechanisms and meaning. Neuropsychopharmacology. 2011;36(1):316-338.
12. Leitman DI, Laukka P, Juslin PN, et al. Getting the cue: sensory contributions to auditory emotion recognition impairments in schizophrenia. Schizophr Bull. 2010;36(3):545-556.
13. Butler PD, Abeles IY, Weiskopf NG, et al. Sensory contributions to impaired emotion processing in schizophrenia. Schizophr Bull. 2009;35(6):1095-1107.
14. Revheim N, Butler PD, Schechter I, et al. Reading impairment and visual processing deficits in schizophrenia. Schizophr Res. 2006;87(1-3):238-245.
15. Hashimoto K, Fukushima T, Shimizu E, et al. Decreased serum levels of D-serine in patients with schizophrenia: evidence in support of the N-methyl-D-aspartate receptor hypofunction hypothesis of schizophrenia. Arch Gen Psychiatry. 2003;60:572-576.
16. Javitt DC, Balla A, Burch S, et al. Reversal of phencyclidine-induced dopaminergic dysregulation by N-methyl-D-aspartate receptor/glycine-site agonists. Neuropsychopharmacology. 2004;29(2):300-307.
17. Kantrowitz JT, Malhotra AK, Cornblatt B, et al. High dose D-serine in the treatment of schizophrenia. Schizophr Res. 2010;121(1-3):125-130.
18. Tsai GE, Lin PY. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia a critical review and meta-analysis. Curr Pharm Des. 2010;16(5):522-537.
19. Woods SW, Thomas L, Tully E, et al. Effects of oral glycine in the schizophrenia prodrome. Schizophr Res. 2004;70(suppl 1):79.-
20. Lane HY, Liu YC, Huang CL, et al. Sarcosine (N-methylglycine) treatment for acute schizophrenia: a randomized, double-blind study. Biol Psychiatry. 2008;63(1):9-12.
21. Umbricht D, Yoo K, Youssef E, et al. Glycine transporter type 1 (GLYT1) inhibitor RG1678: positive results of the proof-of-concept study for the treatment of negative symptoms in schizophrenia. Neuropsychopharmacology. 2010;35:S320-S321.
22. Berk M, Copolov D, Dean O, et al. N-acetyl cysteine as a glutathione precursor for schizophrenia—a double-blind, randomized, placebo-controlled trial. Biol Psychiatry. 2008;64(5):361-368.
23. Smith SM, Uslaner JM, Hutson PH. The therapeutic potential of d-amino acid oxidase (DAAO) inhibitors. Open Med Chem J. 2010;4:3-9.
24. Richardson MA, Read LL, Reilly MA, et al. Analysis of plasma biopterin levels in psychiatric disorders suggests a common BH4 deficit in schizophrenia and schizoaffective disorder. Neurochem Res. 2007;32(1):107-113.
25. Moghaddam B, Adams BW. Reversal of phencyclidine effects by a group II metabotropic glutamate receptor agonist in rats. Science. 1998;281(5381):1349-1352.
26. Krystal JH, Abi-Saab W, Perry E, et al. Preliminary evidence of attenuation of the disruptive effects of the NMDA glutamate receptor antagonist, ketamine, on working memory by pretreatment with the group II metabotropic glutamate receptor agonist, LY354740, in healthy human subjects. Psychopharmacology (Berl). 2005;179(1):303-309.
27. Patil ST, Zhang L, Martenyi F, et al. Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial. Nat Med. 2007;13(9):1102-1107.
28. A multi-center, inpatient, phase 2, double-blind, placebo-controlled dose ranging study of LY2140023 in patients with DSM-IV schizophrenia. ClinicalTrials.gov identifier NCT00520923. Available at: http://clinicaltrials.gov/ct2/show/NCT00520923?intr=LY2140023&rank=1. Accessed February 23 2011.
Discuss this article at www.facebook.com/CurrentPsychiatry
In patients with schizophrenia, positive symptoms typically respond to treatment, while negative and cognitive symptoms often persist and contribute to chronic disability.1 Schizophrenia also is associated with widespread neurocognitive deficits—including impairments in executive functioning, learning, memory, and processing speed—that are a core feature of the disorder and may precede illness onset.2
Current treatment is based on the dopamine model of schizophrenia, which proposes that dopaminergic dysfunction is the basis for symptoms and cognitive deficits.3 Although this model is effective in guiding treatment for some patients, most show persistent disability despite receiving the best available treatment. Over the last 2 decades, researchers have developed alternative conceptual models of schizophrenia based on the psychotomimetic effects of compounds such as phencyclidine (PCP) and ketamine.4 These compounds function primarily by blocking N-methyl-D-aspartate (NMDA)-type glutamate receptors (NMDARs), which has lead researchers to focus on glutamatergic neurotransmission and NMDARs as a basis for new drug development. This article describes the glutamatergic model of schizophrenia and its implications for future treatments.
Dopaminergic models
Since the discovery of chlorpromazine almost 60 years ago, the dopamine model of schizophrenia has been widely accepted. It has gone through several iterations but in general suggests that schizophrenia is caused by dopaminergic system dysfunction, particularly increased dopamine within subcortical brain regions such as the striatum or nucleus accumben.3 The ability of amphetamine or other dopaminergic agents to induce symptoms closely resembling positive symptoms supports this model, as do genetic studies that show dopamine-related genes are associated with schizophrenia.5 In addition, all antipsychotics block dopamine type 2 receptors.
Unfortunately, limitations of this model continue to limit treatment:
- Dopaminergic compounds such as amphetamine do not induce negative symptoms or cognitive deficits similar to those observed in schizophrenia.
- Dopamine receptor blockers do not reverse cognitive dysfunction or negative symptoms.
- Dopaminergic instability observed during acute decompensation appears to resolve after stabilization even without symptom remission.
- Although dopaminergic systems preferentially innervate frontal brain regions, cognitive deficits in schizophrenia appear to be widespread, involving sensory as well as frontal brain systems.
Thus, dopaminergic dysfunction appears to account for only a part of schizophrenia’s symptomatic and neurocognitive profile.
Glutamatergic model
Approximately 20 years ago, researchers proposed an alternate schizophrenia model based on the observed clinical actions of “dissociative anesthetics,” including PCP and ketamine. PCP was patented in 1953 as a surgical anesthetic, but serious side effects, such as hallucinations, agitation, and catatonic-like reactions, soon curtailed its clinical use. As early as 1959, some researchers noted similarities between PCP psychosis and schizophrenia.4,6
The binding site for PCP and other dissociative anesthetics (“PCP receptor”) was first described in 1979 and subsequently localized within the ion channel formed by the NMDAR. Glutamate is the primary excitatory neurotransmitter in the brain, and binds to NMDA and non-NMDA (eg, metabotropic or alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid [AMPA]) receptors. Binding of PCP prevents glutamate from activating NMDARs, which suggests that the pathogenesis of schizophrenia may be caused by dysfunction of NMDARs in particular or of the glutamatergic system in general. Unlike dopamine, the glutamatergic system is distributed throughout the brain and plays a prominent role in sensory processing and higher-level functions such as memory and executive functioning (Figure).6 Therefore, glutamatergic theories open new approaches for potential schizophrenia treatments, most of which are now entering clinical evaluation.
Figure: The wide reach of glutamatergic dysfunction
NMDA: N-methyl-D-aspartate; NMDAR: N-methyl-D-aspartate-type glutamate receptors
Source: Reference 6
Effects of NMDAR antagonists
In initial studies with PCP and ketamine in the early 1960s, researchers noted that these agents produced psychotic effects similar to schizophrenia symptoms.6 Further confirmation was obtained from retrospective studies of PCP abusers.6 It was not until the 1990s, however, that studies using modern operationalized symptom and neuropsychological rating scales were conducted. In those studies, healthy participants developed positive symptoms, negative symptoms, and cognitive dysfunction after receiving ketamine.7,8 Moreover, in these studies the balance between negative and positive symptoms was similar to that typically observed in schizophrenia, as was the pattern of cognitive dysfunction. Therefore, unlike dopaminergic agents, NMDAR antagonists appear to be able to produce the full constellation of symptoms and cognitive deficits associated with schizophrenia.
Similarly, ketamine worsened positive and negative symptoms in patients diagnosed with schizophrenia.9 Although acute challenge with NMDAR antagonists does not produce schizophrenia-like auditory hallucinations in healthy controls, it does induce sensory distortions similar to those seen in individuals with early schizophrenia and does exacerbate pre-existing hallucinations in schizophrenia patients.10 Thus, acute challenge with NMDAR antagonists appears to re-create a state similar to the earliest stages of schizophrenia.6
NMDAR antagonists also reproduce the widespread neuropsychological abnormalities of schizophrenia (Figure).6 Ketamine infusion results in the severity and type of disorganized thinking seen in schizophrenia. Given the importance of neurocognitive dysfunction to the conceptualization of schizophrenia, these findings further support a glutamatergic model.
Sensory processing deficits
A key difference between dopaminergic and glutamatergic models is prediction of sensory processing deficits. Traditionally, dopaminergic models have viewed cognitive deficits of schizophrenia as being driven “top down” from higher order brain regions such as the prefrontal cortex, or from local dysfunction within regions such as the striatum.11 In contrast, glutamatergic models predict that deficits also should be observed within sensory brain regions, such as the primary auditory and visual cortex.
Because of the focus on higher-level brain dysfunction, little research on sensory processing deficits was performed until recently. It has become increasingly clear that:
- patients with schizophrenia show severe deficits in early auditory and visual processing
- these deficits significantly contribute to patterns of cognitive dysfunction and psychosocial impairment.12,13
In the auditory system, patients show deficits in pitch perception and, specifically, the ability to match tones after a brief delay. Schizophrenia patients show dysfunction in a specific part of the visual system called the magnocellular visual system. Deficits in these regions lead to impaired ability to detect emotion based on vocal intonation or facial expression, among other deficits.
In addition, reading ability—which was once thought to be normal in patients with schizophrenia—has been found to be severely disturbed.14 As in developmental dyslexia, impairments relate to dysfunction of underlying auditory and visual brain regions. Administering NMDAR antagonists to humans or animals causes deficits in the auditory and visual system similar to those seen in schizophrenia, which confirms the importance of NMDA dysfunction.
Glutamate-based treatments
Because NMDAR antagonists can induce schizophrenia symptoms, the most straightforward approach for treatment is to develop compounds that stimulate glutamate or NMDAR function (Table). The NMDAR contains modulatory sites that may be appropriate targets for drug development, including one that binds the amino acids glycine and D-serine and a redox site that is sensitive to brain glutathione levels. Reductions in brain D-serine and glutathione levels have been reported in schizophrenia, which suggests that impaired NMDAR regulation may contribute directly to brain dysfunction.15 Other treatment approaches being developed include targeting glycine transporters, which indirectly regulate brain levels of glycine, or metabotropic glutamate receptors, which modulate both pre-synaptic glutamate release and post-synaptic NMDAR function.
Table
Glutamatergic drugs in development
| Target | Proposed mechanism | Proposed agents | Phase of development |
|---|---|---|---|
| Glycine/D-serine receptor | Allosteric modulator of the NMDA receptor | Glycine, D-serine, D-alanine, D-cycloserine | Phase II |
| Glycine-type I transport inhibitor | Blocks the reuptake of glycine, akin to SSRIs’ action on serotonin | Sarcosine, RG1678 | Phase II/III |
| Metabotropic glutamate type 2/3 (mGluR2/3) | Blocks presynaptic glutamate release | LY-2140023 | Phase II |
| Redox sensitive site | Allosteric modulator of the NMDA receptor | N-acetylcysteine | Phase II |
| D-amino acid oxidase (DAAO) inhibitors | Inhibits the enzyme that metabolizes D-serine | Remains in preclinical stage | |
| Tetrahydrobiopterin (BH4) | Indirectly modulates glutamatergic system | Remains in preclinical stage | |
| NMDA: N-methyl-D-aspartate; SSRIs: selective serotonin reuptake inhibitors | |||
Glycine/D-serine site agonists. To date, most studies have used glutamatergic drugs adjunctive to antipsychotics and targeted the glycine/D-serine modulatory site, in part because glycine and D-serine are natural compounds and therefore FDA approval for their use could be obtained without the extensive preclinical development usually required for new chemical entities.16 Unfortunately, these agents are less potent than traditional pharmaceuticals, and delivering optimal doses may be impossible. Nevertheless, positive studies with these compounds have provided proof-of-concept for development of agents with higher affinity and specificity.
Studies have used glycine administered at doses up to 60 g/d, D-serine up to 8 g/d, or D-alanine approximately 6 g/d. For glycine, 60 g/d is the highest dose that can be given because of concerns about tolerability and replacement of other essential amino acids. D-serine originally was tested at approximately 2 g/d with promising results, but a recent open-label trial suggested that higher doses may be more efficacious.17 D-serine doses are limited by potential renal toxicity, as demonstrated in rodents studies.
Although not all studies of glycine/D-serine site agonists have been positive, a recent meta-analysis suggests significant improvement in negative symptoms across studies.18 Variability in statistical results across studies is related primarily to degree of placebo effect within individual trials, with a mean improvement in negative symptoms of approximately 15%. Glycine/D-serine site agonists seem to be less effective when combined with clozapine, possibly because clozapine may already enhance the glutamatergic system and increase synaptic glycine levels.6
One study that evaluated effects of open-label glycine in individuals with schizophrenia symptoms observed a large effect-size improvement, including early remission in 3 of 10 patients.19 These data—if confirmed by double-blind trials—would indicate that glycine/d-serine site agonists might have utility in treating the schizophrenia prodrome.
Glycine transport inhibitors. A potential indirect approach to raising glycine levels in the brain is using GlyT1-type glycine transport inhibitors (GTIs). GlyT1 transporters are co-localized in brain with NMDARs and modulate local glycine levels. Rather than binding directly to the NMDAR glycine binding site, GTIs increase glycine levels in the synapse by preventing its removal by GlyT1 transporters. Their function is analogous to using selective serotonin reuptake inhibitors to increase serotonin levels in patients with depression.6
Sarcosine (N-methylglycine) is a naturally occurring GlyT1 inhibitor that has been used in early clinical trials in Taiwan. Initial studies with sarcosine showed efficacy similar to—and in some cases better than—that of direct glycine/D-serine site agonists when added to first-generation or non-clozapine second-generation antipsychotics.18 Sarcosine also has been found to be effective for acute treatment of schizophrenia.20 At present, however, sarcosine is not available for experimental use in the United States because of toxicity considerations.
Using high-affinity GTIs for schizophrenia was first proposed in the mid-1990s,6 but such compounds are only now entering clinical efficacy studies. Most recently, phase II results were presented for RG1678, a compound developed by Hoffman LaRoche.21 The study targeted persistent negative symptoms in patients receiving chronic antipsychotic treatment. Adding RG1678, 10 mg and 30 mg, to antipsychotics led to significant improvement in persistent negative symptoms vs placebo. These promising results are being followed up in phase III studies.
Other glutamatergic options. Few compounds are available to modulate NMDARs at sites other than the glycine/D-serine site. One study administered N-acetylcysteine, a glutathione precursor, as a potential treatment for persistent negative symptoms.22 Encouraging clinical results were observed in this double-blind study, along with improvement in electrophysiologic measures, negative symptoms, and overall functioning, but the study was limited by relatively high rates of noncompletion. Preclinical studies have combined D-serine with an inhibitor of D-amino acid oxidase to prevent D-serine breakdown.23 In rodents, this approach produces a 30-fold increase in D-serine potency.
Tetrahydrobiopterin (BH4) is a cofactor for enzymes responsible for the synthesis of dopamine and other monoamines, and presynaptic release of dopamine and glutamate. Reductions in BH4 levels have been reported in schizophrenia, which suggests that this compound may be etiologically important.24 Researchers have initiated a study of this compound in schizophrenia.
Other schizophrenia models propose that the crucial issue is not NMDA blockade but subsequent dysregulation of presynaptic glutamate release. Type 2/3 metabotropic glutamate receptors (mGluR2/3) are located on presynaptic glutamate terminals and inhibit presynaptic glutamate release. mGluR2/3 agonists have been shown to reverse ketamine’s effects in humans and in animal models,25,26 which suggests a potential role in schizophrenia treatment.
The first mGluR2/3 agonist entered into monotherapy clinical efficacy trials for schizophrenia was LY-2140023. In an initial trial, this compound showed significant efficacy in improving positive and negative symptoms, comparable to that of olanzapine.27 However, a follow-up study failed because of a large placebo effect,28 which leaves the efficacy question unresolved.
In contrast to mGluR2/3, type 5 metabotropic receptors (mGluR5) are co-localized with NMDA receptors and potentiate activation. Thus, mGluR5 agonists also may be effective for treating schizophrenia. These compounds remain in preclinical development. Other approaches, such as stimulating specific types of GABA receptors to overcome glutamatergic deficits, remain promising but have not been tested in definitive clinical trials.
Related Resources
- Kantrowitz JT, Javitt DC. N-methyl-D-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull. 2010; 83(3-4): 108-121.
- Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Kantrowitz JT, Javitt DC, eds. Handbook of neurochemistry and molecular neurobiology: schizophrenia. 3rd ed. New York, NY: Springer; 2009.
Drug Brand Names
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Ketamine • Ketalar
- Olanzapine • Zyprexa
Disclosures
Dr. Javitt receives grant/research support from Jazz Pharmaceuticals, Pfizer Inc., and Roche and is a consultant to AstraZeneca, Cypress, Eli Lilly and Company, NPS Pharmaceuticals, Sepracor, Solvay, Sunovion, and Takeda. He holds intellectual property rights for use of glycine, D-serine, and glycine transport inhibitors in treatment of schizophrenia and related disorders.
Dr. Kantrowitz receives grant/research support from Eli Lilly and Company, Jazz Pharmaceuticals, Pfizer Inc., Roche, and Sepracor.
Preparation of this manuscript was supported in part by National Institute of Health grants R01 DA03383, R37 MH49334, and P50 MH086385.
Discuss this article at www.facebook.com/CurrentPsychiatry
In patients with schizophrenia, positive symptoms typically respond to treatment, while negative and cognitive symptoms often persist and contribute to chronic disability.1 Schizophrenia also is associated with widespread neurocognitive deficits—including impairments in executive functioning, learning, memory, and processing speed—that are a core feature of the disorder and may precede illness onset.2
Current treatment is based on the dopamine model of schizophrenia, which proposes that dopaminergic dysfunction is the basis for symptoms and cognitive deficits.3 Although this model is effective in guiding treatment for some patients, most show persistent disability despite receiving the best available treatment. Over the last 2 decades, researchers have developed alternative conceptual models of schizophrenia based on the psychotomimetic effects of compounds such as phencyclidine (PCP) and ketamine.4 These compounds function primarily by blocking N-methyl-D-aspartate (NMDA)-type glutamate receptors (NMDARs), which has lead researchers to focus on glutamatergic neurotransmission and NMDARs as a basis for new drug development. This article describes the glutamatergic model of schizophrenia and its implications for future treatments.
Dopaminergic models
Since the discovery of chlorpromazine almost 60 years ago, the dopamine model of schizophrenia has been widely accepted. It has gone through several iterations but in general suggests that schizophrenia is caused by dopaminergic system dysfunction, particularly increased dopamine within subcortical brain regions such as the striatum or nucleus accumben.3 The ability of amphetamine or other dopaminergic agents to induce symptoms closely resembling positive symptoms supports this model, as do genetic studies that show dopamine-related genes are associated with schizophrenia.5 In addition, all antipsychotics block dopamine type 2 receptors.
Unfortunately, limitations of this model continue to limit treatment:
- Dopaminergic compounds such as amphetamine do not induce negative symptoms or cognitive deficits similar to those observed in schizophrenia.
- Dopamine receptor blockers do not reverse cognitive dysfunction or negative symptoms.
- Dopaminergic instability observed during acute decompensation appears to resolve after stabilization even without symptom remission.
- Although dopaminergic systems preferentially innervate frontal brain regions, cognitive deficits in schizophrenia appear to be widespread, involving sensory as well as frontal brain systems.
Thus, dopaminergic dysfunction appears to account for only a part of schizophrenia’s symptomatic and neurocognitive profile.
Glutamatergic model
Approximately 20 years ago, researchers proposed an alternate schizophrenia model based on the observed clinical actions of “dissociative anesthetics,” including PCP and ketamine. PCP was patented in 1953 as a surgical anesthetic, but serious side effects, such as hallucinations, agitation, and catatonic-like reactions, soon curtailed its clinical use. As early as 1959, some researchers noted similarities between PCP psychosis and schizophrenia.4,6
The binding site for PCP and other dissociative anesthetics (“PCP receptor”) was first described in 1979 and subsequently localized within the ion channel formed by the NMDAR. Glutamate is the primary excitatory neurotransmitter in the brain, and binds to NMDA and non-NMDA (eg, metabotropic or alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid [AMPA]) receptors. Binding of PCP prevents glutamate from activating NMDARs, which suggests that the pathogenesis of schizophrenia may be caused by dysfunction of NMDARs in particular or of the glutamatergic system in general. Unlike dopamine, the glutamatergic system is distributed throughout the brain and plays a prominent role in sensory processing and higher-level functions such as memory and executive functioning (Figure).6 Therefore, glutamatergic theories open new approaches for potential schizophrenia treatments, most of which are now entering clinical evaluation.
Figure: The wide reach of glutamatergic dysfunction
NMDA: N-methyl-D-aspartate; NMDAR: N-methyl-D-aspartate-type glutamate receptors
Source: Reference 6
Effects of NMDAR antagonists
In initial studies with PCP and ketamine in the early 1960s, researchers noted that these agents produced psychotic effects similar to schizophrenia symptoms.6 Further confirmation was obtained from retrospective studies of PCP abusers.6 It was not until the 1990s, however, that studies using modern operationalized symptom and neuropsychological rating scales were conducted. In those studies, healthy participants developed positive symptoms, negative symptoms, and cognitive dysfunction after receiving ketamine.7,8 Moreover, in these studies the balance between negative and positive symptoms was similar to that typically observed in schizophrenia, as was the pattern of cognitive dysfunction. Therefore, unlike dopaminergic agents, NMDAR antagonists appear to be able to produce the full constellation of symptoms and cognitive deficits associated with schizophrenia.
Similarly, ketamine worsened positive and negative symptoms in patients diagnosed with schizophrenia.9 Although acute challenge with NMDAR antagonists does not produce schizophrenia-like auditory hallucinations in healthy controls, it does induce sensory distortions similar to those seen in individuals with early schizophrenia and does exacerbate pre-existing hallucinations in schizophrenia patients.10 Thus, acute challenge with NMDAR antagonists appears to re-create a state similar to the earliest stages of schizophrenia.6
NMDAR antagonists also reproduce the widespread neuropsychological abnormalities of schizophrenia (Figure).6 Ketamine infusion results in the severity and type of disorganized thinking seen in schizophrenia. Given the importance of neurocognitive dysfunction to the conceptualization of schizophrenia, these findings further support a glutamatergic model.
Sensory processing deficits
A key difference between dopaminergic and glutamatergic models is prediction of sensory processing deficits. Traditionally, dopaminergic models have viewed cognitive deficits of schizophrenia as being driven “top down” from higher order brain regions such as the prefrontal cortex, or from local dysfunction within regions such as the striatum.11 In contrast, glutamatergic models predict that deficits also should be observed within sensory brain regions, such as the primary auditory and visual cortex.
Because of the focus on higher-level brain dysfunction, little research on sensory processing deficits was performed until recently. It has become increasingly clear that:
- patients with schizophrenia show severe deficits in early auditory and visual processing
- these deficits significantly contribute to patterns of cognitive dysfunction and psychosocial impairment.12,13
In the auditory system, patients show deficits in pitch perception and, specifically, the ability to match tones after a brief delay. Schizophrenia patients show dysfunction in a specific part of the visual system called the magnocellular visual system. Deficits in these regions lead to impaired ability to detect emotion based on vocal intonation or facial expression, among other deficits.
In addition, reading ability—which was once thought to be normal in patients with schizophrenia—has been found to be severely disturbed.14 As in developmental dyslexia, impairments relate to dysfunction of underlying auditory and visual brain regions. Administering NMDAR antagonists to humans or animals causes deficits in the auditory and visual system similar to those seen in schizophrenia, which confirms the importance of NMDA dysfunction.
Glutamate-based treatments
Because NMDAR antagonists can induce schizophrenia symptoms, the most straightforward approach for treatment is to develop compounds that stimulate glutamate or NMDAR function (Table). The NMDAR contains modulatory sites that may be appropriate targets for drug development, including one that binds the amino acids glycine and D-serine and a redox site that is sensitive to brain glutathione levels. Reductions in brain D-serine and glutathione levels have been reported in schizophrenia, which suggests that impaired NMDAR regulation may contribute directly to brain dysfunction.15 Other treatment approaches being developed include targeting glycine transporters, which indirectly regulate brain levels of glycine, or metabotropic glutamate receptors, which modulate both pre-synaptic glutamate release and post-synaptic NMDAR function.
Table
Glutamatergic drugs in development
| Target | Proposed mechanism | Proposed agents | Phase of development |
|---|---|---|---|
| Glycine/D-serine receptor | Allosteric modulator of the NMDA receptor | Glycine, D-serine, D-alanine, D-cycloserine | Phase II |
| Glycine-type I transport inhibitor | Blocks the reuptake of glycine, akin to SSRIs’ action on serotonin | Sarcosine, RG1678 | Phase II/III |
| Metabotropic glutamate type 2/3 (mGluR2/3) | Blocks presynaptic glutamate release | LY-2140023 | Phase II |
| Redox sensitive site | Allosteric modulator of the NMDA receptor | N-acetylcysteine | Phase II |
| D-amino acid oxidase (DAAO) inhibitors | Inhibits the enzyme that metabolizes D-serine | Remains in preclinical stage | |
| Tetrahydrobiopterin (BH4) | Indirectly modulates glutamatergic system | Remains in preclinical stage | |
| NMDA: N-methyl-D-aspartate; SSRIs: selective serotonin reuptake inhibitors | |||
Glycine/D-serine site agonists. To date, most studies have used glutamatergic drugs adjunctive to antipsychotics and targeted the glycine/D-serine modulatory site, in part because glycine and D-serine are natural compounds and therefore FDA approval for their use could be obtained without the extensive preclinical development usually required for new chemical entities.16 Unfortunately, these agents are less potent than traditional pharmaceuticals, and delivering optimal doses may be impossible. Nevertheless, positive studies with these compounds have provided proof-of-concept for development of agents with higher affinity and specificity.
Studies have used glycine administered at doses up to 60 g/d, D-serine up to 8 g/d, or D-alanine approximately 6 g/d. For glycine, 60 g/d is the highest dose that can be given because of concerns about tolerability and replacement of other essential amino acids. D-serine originally was tested at approximately 2 g/d with promising results, but a recent open-label trial suggested that higher doses may be more efficacious.17 D-serine doses are limited by potential renal toxicity, as demonstrated in rodents studies.
Although not all studies of glycine/D-serine site agonists have been positive, a recent meta-analysis suggests significant improvement in negative symptoms across studies.18 Variability in statistical results across studies is related primarily to degree of placebo effect within individual trials, with a mean improvement in negative symptoms of approximately 15%. Glycine/D-serine site agonists seem to be less effective when combined with clozapine, possibly because clozapine may already enhance the glutamatergic system and increase synaptic glycine levels.6
One study that evaluated effects of open-label glycine in individuals with schizophrenia symptoms observed a large effect-size improvement, including early remission in 3 of 10 patients.19 These data—if confirmed by double-blind trials—would indicate that glycine/d-serine site agonists might have utility in treating the schizophrenia prodrome.
Glycine transport inhibitors. A potential indirect approach to raising glycine levels in the brain is using GlyT1-type glycine transport inhibitors (GTIs). GlyT1 transporters are co-localized in brain with NMDARs and modulate local glycine levels. Rather than binding directly to the NMDAR glycine binding site, GTIs increase glycine levels in the synapse by preventing its removal by GlyT1 transporters. Their function is analogous to using selective serotonin reuptake inhibitors to increase serotonin levels in patients with depression.6
Sarcosine (N-methylglycine) is a naturally occurring GlyT1 inhibitor that has been used in early clinical trials in Taiwan. Initial studies with sarcosine showed efficacy similar to—and in some cases better than—that of direct glycine/D-serine site agonists when added to first-generation or non-clozapine second-generation antipsychotics.18 Sarcosine also has been found to be effective for acute treatment of schizophrenia.20 At present, however, sarcosine is not available for experimental use in the United States because of toxicity considerations.
Using high-affinity GTIs for schizophrenia was first proposed in the mid-1990s,6 but such compounds are only now entering clinical efficacy studies. Most recently, phase II results were presented for RG1678, a compound developed by Hoffman LaRoche.21 The study targeted persistent negative symptoms in patients receiving chronic antipsychotic treatment. Adding RG1678, 10 mg and 30 mg, to antipsychotics led to significant improvement in persistent negative symptoms vs placebo. These promising results are being followed up in phase III studies.
Other glutamatergic options. Few compounds are available to modulate NMDARs at sites other than the glycine/D-serine site. One study administered N-acetylcysteine, a glutathione precursor, as a potential treatment for persistent negative symptoms.22 Encouraging clinical results were observed in this double-blind study, along with improvement in electrophysiologic measures, negative symptoms, and overall functioning, but the study was limited by relatively high rates of noncompletion. Preclinical studies have combined D-serine with an inhibitor of D-amino acid oxidase to prevent D-serine breakdown.23 In rodents, this approach produces a 30-fold increase in D-serine potency.
Tetrahydrobiopterin (BH4) is a cofactor for enzymes responsible for the synthesis of dopamine and other monoamines, and presynaptic release of dopamine and glutamate. Reductions in BH4 levels have been reported in schizophrenia, which suggests that this compound may be etiologically important.24 Researchers have initiated a study of this compound in schizophrenia.
Other schizophrenia models propose that the crucial issue is not NMDA blockade but subsequent dysregulation of presynaptic glutamate release. Type 2/3 metabotropic glutamate receptors (mGluR2/3) are located on presynaptic glutamate terminals and inhibit presynaptic glutamate release. mGluR2/3 agonists have been shown to reverse ketamine’s effects in humans and in animal models,25,26 which suggests a potential role in schizophrenia treatment.
The first mGluR2/3 agonist entered into monotherapy clinical efficacy trials for schizophrenia was LY-2140023. In an initial trial, this compound showed significant efficacy in improving positive and negative symptoms, comparable to that of olanzapine.27 However, a follow-up study failed because of a large placebo effect,28 which leaves the efficacy question unresolved.
In contrast to mGluR2/3, type 5 metabotropic receptors (mGluR5) are co-localized with NMDA receptors and potentiate activation. Thus, mGluR5 agonists also may be effective for treating schizophrenia. These compounds remain in preclinical development. Other approaches, such as stimulating specific types of GABA receptors to overcome glutamatergic deficits, remain promising but have not been tested in definitive clinical trials.
Related Resources
- Kantrowitz JT, Javitt DC. N-methyl-D-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull. 2010; 83(3-4): 108-121.
- Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Kantrowitz JT, Javitt DC, eds. Handbook of neurochemistry and molecular neurobiology: schizophrenia. 3rd ed. New York, NY: Springer; 2009.
Drug Brand Names
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Ketamine • Ketalar
- Olanzapine • Zyprexa
Disclosures
Dr. Javitt receives grant/research support from Jazz Pharmaceuticals, Pfizer Inc., and Roche and is a consultant to AstraZeneca, Cypress, Eli Lilly and Company, NPS Pharmaceuticals, Sepracor, Solvay, Sunovion, and Takeda. He holds intellectual property rights for use of glycine, D-serine, and glycine transport inhibitors in treatment of schizophrenia and related disorders.
Dr. Kantrowitz receives grant/research support from Eli Lilly and Company, Jazz Pharmaceuticals, Pfizer Inc., Roche, and Sepracor.
Preparation of this manuscript was supported in part by National Institute of Health grants R01 DA03383, R37 MH49334, and P50 MH086385.
1. Fenton WS, McGlashan TH. Antecedents symptom progression, and long-term outcome of the deficit syndrome in schizophrenia. Am J Psychiatry. 1994;151(3):351-356.
2. Woodberry KA. Premorbid IQ in schizophrenia: a meta-analytic review. Am J Psychiatry. 2008;165(5):579-587.
3. Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III—the final common pathway. Schizophr Bull. 2009;35(3):549-562.
4. Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301-1308.
5. Egan MF, Goldberg TE, Kolachana BS, et al. Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. Proc Natl Acad Sci U S A. 2001;98:6917-6922.
6. Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Kantrowitz JT Javitt DC, eds. Handbook of neurochemistry and molecular neurobiology: schizophrenia. 3rd ed. New York, NY: Springer; 2009.
7. Krystal JH, Karper LP, Seibyl JP, et al. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry. 1994;51(3):199-214.
8. Krystal J, D’Souza DC, Mathalon D, et al. NMDA receptor antagonist effects, cortical glutamatergic function, and schizophrenia: toward a paradigm shift in medication development. Psychopharmacology. 2003;169(3-4):215-233.
9. Malhotra AK, Pinals DA, Adler CM, et al. Ketamine-induced exacerbation of psychotic symptoms and cognitive impairment in neuroleptic-free schizophrenics. Neuropsychopharmacology. 1997;17(3):141-150.
10. Lahti AC, Koffel B, LaPorte D, et al. Subanesthetic doses of ketamine stimulate psychosis in schizophrenia. Neuropsychopharmacology. 1995;13(1):9-19.
11. Lesh TA, Niendam TA, Minzenberg MJ, et al. Cognitive control deficits in schizophrenia: mechanisms and meaning. Neuropsychopharmacology. 2011;36(1):316-338.
12. Leitman DI, Laukka P, Juslin PN, et al. Getting the cue: sensory contributions to auditory emotion recognition impairments in schizophrenia. Schizophr Bull. 2010;36(3):545-556.
13. Butler PD, Abeles IY, Weiskopf NG, et al. Sensory contributions to impaired emotion processing in schizophrenia. Schizophr Bull. 2009;35(6):1095-1107.
14. Revheim N, Butler PD, Schechter I, et al. Reading impairment and visual processing deficits in schizophrenia. Schizophr Res. 2006;87(1-3):238-245.
15. Hashimoto K, Fukushima T, Shimizu E, et al. Decreased serum levels of D-serine in patients with schizophrenia: evidence in support of the N-methyl-D-aspartate receptor hypofunction hypothesis of schizophrenia. Arch Gen Psychiatry. 2003;60:572-576.
16. Javitt DC, Balla A, Burch S, et al. Reversal of phencyclidine-induced dopaminergic dysregulation by N-methyl-D-aspartate receptor/glycine-site agonists. Neuropsychopharmacology. 2004;29(2):300-307.
17. Kantrowitz JT, Malhotra AK, Cornblatt B, et al. High dose D-serine in the treatment of schizophrenia. Schizophr Res. 2010;121(1-3):125-130.
18. Tsai GE, Lin PY. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia a critical review and meta-analysis. Curr Pharm Des. 2010;16(5):522-537.
19. Woods SW, Thomas L, Tully E, et al. Effects of oral glycine in the schizophrenia prodrome. Schizophr Res. 2004;70(suppl 1):79.-
20. Lane HY, Liu YC, Huang CL, et al. Sarcosine (N-methylglycine) treatment for acute schizophrenia: a randomized, double-blind study. Biol Psychiatry. 2008;63(1):9-12.
21. Umbricht D, Yoo K, Youssef E, et al. Glycine transporter type 1 (GLYT1) inhibitor RG1678: positive results of the proof-of-concept study for the treatment of negative symptoms in schizophrenia. Neuropsychopharmacology. 2010;35:S320-S321.
22. Berk M, Copolov D, Dean O, et al. N-acetyl cysteine as a glutathione precursor for schizophrenia—a double-blind, randomized, placebo-controlled trial. Biol Psychiatry. 2008;64(5):361-368.
23. Smith SM, Uslaner JM, Hutson PH. The therapeutic potential of d-amino acid oxidase (DAAO) inhibitors. Open Med Chem J. 2010;4:3-9.
24. Richardson MA, Read LL, Reilly MA, et al. Analysis of plasma biopterin levels in psychiatric disorders suggests a common BH4 deficit in schizophrenia and schizoaffective disorder. Neurochem Res. 2007;32(1):107-113.
25. Moghaddam B, Adams BW. Reversal of phencyclidine effects by a group II metabotropic glutamate receptor agonist in rats. Science. 1998;281(5381):1349-1352.
26. Krystal JH, Abi-Saab W, Perry E, et al. Preliminary evidence of attenuation of the disruptive effects of the NMDA glutamate receptor antagonist, ketamine, on working memory by pretreatment with the group II metabotropic glutamate receptor agonist, LY354740, in healthy human subjects. Psychopharmacology (Berl). 2005;179(1):303-309.
27. Patil ST, Zhang L, Martenyi F, et al. Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial. Nat Med. 2007;13(9):1102-1107.
28. A multi-center, inpatient, phase 2, double-blind, placebo-controlled dose ranging study of LY2140023 in patients with DSM-IV schizophrenia. ClinicalTrials.gov identifier NCT00520923. Available at: http://clinicaltrials.gov/ct2/show/NCT00520923?intr=LY2140023&rank=1. Accessed February 23 2011.
1. Fenton WS, McGlashan TH. Antecedents symptom progression, and long-term outcome of the deficit syndrome in schizophrenia. Am J Psychiatry. 1994;151(3):351-356.
2. Woodberry KA. Premorbid IQ in schizophrenia: a meta-analytic review. Am J Psychiatry. 2008;165(5):579-587.
3. Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III—the final common pathway. Schizophr Bull. 2009;35(3):549-562.
4. Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301-1308.
5. Egan MF, Goldberg TE, Kolachana BS, et al. Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. Proc Natl Acad Sci U S A. 2001;98:6917-6922.
6. Kantrowitz JT, Javitt DC. Glutamatergic approaches to the conceptualization and treatment of schizophrenia. In: Kantrowitz JT Javitt DC, eds. Handbook of neurochemistry and molecular neurobiology: schizophrenia. 3rd ed. New York, NY: Springer; 2009.
7. Krystal JH, Karper LP, Seibyl JP, et al. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry. 1994;51(3):199-214.
8. Krystal J, D’Souza DC, Mathalon D, et al. NMDA receptor antagonist effects, cortical glutamatergic function, and schizophrenia: toward a paradigm shift in medication development. Psychopharmacology. 2003;169(3-4):215-233.
9. Malhotra AK, Pinals DA, Adler CM, et al. Ketamine-induced exacerbation of psychotic symptoms and cognitive impairment in neuroleptic-free schizophrenics. Neuropsychopharmacology. 1997;17(3):141-150.
10. Lahti AC, Koffel B, LaPorte D, et al. Subanesthetic doses of ketamine stimulate psychosis in schizophrenia. Neuropsychopharmacology. 1995;13(1):9-19.
11. Lesh TA, Niendam TA, Minzenberg MJ, et al. Cognitive control deficits in schizophrenia: mechanisms and meaning. Neuropsychopharmacology. 2011;36(1):316-338.
12. Leitman DI, Laukka P, Juslin PN, et al. Getting the cue: sensory contributions to auditory emotion recognition impairments in schizophrenia. Schizophr Bull. 2010;36(3):545-556.
13. Butler PD, Abeles IY, Weiskopf NG, et al. Sensory contributions to impaired emotion processing in schizophrenia. Schizophr Bull. 2009;35(6):1095-1107.
14. Revheim N, Butler PD, Schechter I, et al. Reading impairment and visual processing deficits in schizophrenia. Schizophr Res. 2006;87(1-3):238-245.
15. Hashimoto K, Fukushima T, Shimizu E, et al. Decreased serum levels of D-serine in patients with schizophrenia: evidence in support of the N-methyl-D-aspartate receptor hypofunction hypothesis of schizophrenia. Arch Gen Psychiatry. 2003;60:572-576.
16. Javitt DC, Balla A, Burch S, et al. Reversal of phencyclidine-induced dopaminergic dysregulation by N-methyl-D-aspartate receptor/glycine-site agonists. Neuropsychopharmacology. 2004;29(2):300-307.
17. Kantrowitz JT, Malhotra AK, Cornblatt B, et al. High dose D-serine in the treatment of schizophrenia. Schizophr Res. 2010;121(1-3):125-130.
18. Tsai GE, Lin PY. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia a critical review and meta-analysis. Curr Pharm Des. 2010;16(5):522-537.
19. Woods SW, Thomas L, Tully E, et al. Effects of oral glycine in the schizophrenia prodrome. Schizophr Res. 2004;70(suppl 1):79.-
20. Lane HY, Liu YC, Huang CL, et al. Sarcosine (N-methylglycine) treatment for acute schizophrenia: a randomized, double-blind study. Biol Psychiatry. 2008;63(1):9-12.
21. Umbricht D, Yoo K, Youssef E, et al. Glycine transporter type 1 (GLYT1) inhibitor RG1678: positive results of the proof-of-concept study for the treatment of negative symptoms in schizophrenia. Neuropsychopharmacology. 2010;35:S320-S321.
22. Berk M, Copolov D, Dean O, et al. N-acetyl cysteine as a glutathione precursor for schizophrenia—a double-blind, randomized, placebo-controlled trial. Biol Psychiatry. 2008;64(5):361-368.
23. Smith SM, Uslaner JM, Hutson PH. The therapeutic potential of d-amino acid oxidase (DAAO) inhibitors. Open Med Chem J. 2010;4:3-9.
24. Richardson MA, Read LL, Reilly MA, et al. Analysis of plasma biopterin levels in psychiatric disorders suggests a common BH4 deficit in schizophrenia and schizoaffective disorder. Neurochem Res. 2007;32(1):107-113.
25. Moghaddam B, Adams BW. Reversal of phencyclidine effects by a group II metabotropic glutamate receptor agonist in rats. Science. 1998;281(5381):1349-1352.
26. Krystal JH, Abi-Saab W, Perry E, et al. Preliminary evidence of attenuation of the disruptive effects of the NMDA glutamate receptor antagonist, ketamine, on working memory by pretreatment with the group II metabotropic glutamate receptor agonist, LY354740, in healthy human subjects. Psychopharmacology (Berl). 2005;179(1):303-309.
27. Patil ST, Zhang L, Martenyi F, et al. Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial. Nat Med. 2007;13(9):1102-1107.
28. A multi-center, inpatient, phase 2, double-blind, placebo-controlled dose ranging study of LY2140023 in patients with DSM-IV schizophrenia. ClinicalTrials.gov identifier NCT00520923. Available at: http://clinicaltrials.gov/ct2/show/NCT00520923?intr=LY2140023&rank=1. Accessed February 23 2011.
Comorbid bipolar disorder and substance abuse: Evidence-based options
Discuss this article at www.facebook.com/CurrentPsychiatry
Among DSM axis I diagnoses, bipolar disorder (BD) has the highest rates of comorbid substance use disorders (SUDs).1-3 Approximately 60% of patients with bipolar I disorder have a lifetime diagnosis of an SUD.1 Excluding tobacco, alcohol is the substance most often abused by BD patients, followed by cannabis, amphetamines, and cocaine.1-3
BD patients with comorbid SUD usually exhibit more severe clinical presentations and poorer outcomes than their counterparts without SUDs. Compared with patients with BD alone, those with BD and SUD comorbidity (BD-SUD) experience earlier onset of mood symptoms; higher rates of anxiety disorders, suicide attempts, accidents, hospitalizations, and rapid cycling; more depressive episodes; and lower treatment compliance.4-9
Several treatment options are available for patients with BD-SUD, including psychotherapy modalities, medications primarily used to treat BD, and medications primarily used to treat SUDs. Evidence-based support for these treatments remains limited, and no treatment of choice has emerged. This article reviews evidence on the longer-term treatment of BD-SUD, including general strategies and specific psychosocial and pharmacologic interventions. Short-term treatment strategies, such as pharmacotherapy for detoxification, are outside the scope of this review.
General strategies
The causes of BD-SUD are complex. Evidence suggests that the presence of affective symptoms is associated with an increased risk for substance misuse. This should be kept in mind when treating a patient with BD-SUD because controlling mood symptoms probably will help control substance abuse. However, evidence also shows that SUDs may be independent of mood episodes. Therefore, treating only mood symptoms in the hope that doing so will control substance abuse may not be enough.
Because the negative impact of SUDs on BD outcome is well documented, inform patients that limiting their use of alcohol and/or drugs is vital to control their mood disorder. Efforts to educate, stimulate, and support patients to moderate or stop their alcohol and/or drug use are likely to result in positive changes.10 Therefore, treatment for BD-SUD should follow, in part, the same recommendations for treatment of SUDs in patients with no comorbid axis I disorders:
- identify the problem (ie, the existence of a comorbid SUD)
- share your concerns with your patient
- offer appropriate and specific treatments, such as detoxification and/or self-help and counseling programs.10
Because SUDs usually are chronic and relapsing conditions, periods of drug and/ or alcohol use should be expected and not considered a sign of treatment failure. In addition, integrating treatment for both conditions probably is better than managing each separately. Therefore, targeting BD symptoms with mood-stabilizing medications and substance abuse with nonpharmacologic modalities such as drug counseling likely will bring about the best results.
Compared with BD patients without comorbid SUD, BD-SUD patients have a 7-fold increased risk of antidepressantinduced mania.11 Therefore, antidepressants should be prescribed cautiously for patients with BD-SUD.
Integrated psychosocial therapy
BD-SUD patients may benefit from attending self-help programs such as Alcoholics Anonymous and Narcotics Anonymous, provided their mood is stable enough to allow them to participate. Other forms of psychotherapy for BD-SUD patients include standard group drug counseling and integrated group therapy that simultaneously addresses both conditions.
Integrated group therapy is based on the premise that changing maladaptive mood cognitions and behaviors will facilitate recovery from SUDs, and changing maladaptive substance use cognitions and behaviors will facilitate recovery from mood disorders.12 In a recent randomized controlled trial, 62 BD-SUD patients were blindly assigned to integrated group therapy or standard group drug counseling and followed for 3 months.12 Pharmacotherapy was prescribed as usual. Substance use decreased for both groups. However, compared with patients in the drug counseling group, those who participated in integrated group therapy spent fewer days using substances in general and alcohol in particular, fewer days using alcohol to intoxication, and had a shorter time from treatment initiation to the first abstinent month. There were no differences between groups in number of weeks in a mood episode.
Pharmacotherapy options
For a table that summarizes the dosages and indications of the medications used to treat BD-SUD that are described below, visit this article at CurrentPsychiatry.com.
Table
Medications used to treat substance use disorders in bipolar disorder patients*
| Drug | Dosages | FDA-approved indication(s) |
|---|---|---|
| Acamprosate | 1,998 mg/d | Maintenance of abstinence from alcohol in patients with alcohol dependence |
| Aripiprazole | 15 to 45 mg/d | Acute manic or mixed episode of bipolar disorder; augmentation therapy for major depressive disorder |
| Carbamazepine | 400 to 1,200 mg/d | Manic and mixed episodes associated with bipolar disorder |
| Disulfiram | 250 to 500 mg/d | Enforced sobriety in abstinent alcohol-dependence patients |
| Divalproex sodium | Initial dose: 750 mg/d Maximum dose: 60 mg/kg/d† | Manic episodes associated with bipolar disorder |
| Lamotrigine | 200 mg/d | Maintenance treatment of bipolar I disorder |
| Lithium | 900 to 1,800 mg/d for acute episodes 900 mg to 1,200 mg/d for maintenance‡. | Manic episodes associated with bipolar disorder; maintenance treatment of bipolar disorder |
| Naltrexone | 50 mg/d 380 mg/month | Alcohol dependence |
| Quetiapine | 300 mg/d for bipolar depression 400 to 800 mg/d for bipolar mania 400 to 800 mg/d for maintenance treatment of bipolar disorder | Depressive and acute manic episodes associated with bipolar I disorder; maintenance treatment of bipolar I disorder |
| Risperidone | 1 to 6 mg/d | Acute manic or mixed episodes associated with bipolar I disorder |
| * None of the medications cited in this table or the text have been specifically approved by the FDA for treating alcohol/drug abuse/dependence co-occurring with bipolar disorder †Dose should correspond to valproic acid therapeutic levels between 50 and 100 μg/mL ‡Dose should correspond to lithium therapeutic levels between 0.8 and 1.2 mEq/L for acute manic episode treatment and 0.6 and 1.0 mEq/L for maintenance treatment | ||
Lithium. Given its well-documented mood stabilizing effect, lithium would seem to be a reasonable option to treat BD-SUD patients, but scant evidence supports its role as an anti-alcohol or anti-drug medication (Table 1).13,14 Lithium’s efficacy was evaluated in a study of 25 adolescents suffering from mood disorders (mostly BD) and comorbid SUDs (mostly alcohol and cannabis) randomized to receive lithium or placebo for 6 weeks.13 Lithium was well tolerated and improved psychiatric symptoms. At week 3, patients receiving lithium produced fewer positive results on randomly administered urine drug screens than those receiving placebo.
However, lithium seems to have little efficacy in reducing cocaine use in cocaine-dependent patients with bipolar spectrum disorders.14 In an open-label study, 10 patients with a history of hypomania or cyclothymia received lithium monotherapy for 12 weeks. Although patients experienced improved mood symptoms and decreased cocaine use, the mean decrease was transitory and not statistically significant. Another factor that may limit lithium’s use for BD-SUD patients is that these patients are more likely to comply with valproate treatment than with lithium.15
Table 1
Lithium for BD patients with substance use disorders
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Geller et al, 199813 | Lithium vs placebo | Double-blind, placebo-controlled | Alcohol and cannabis use disorders | Decreased positive drug screen results |
| Nunes et al, 199014 | Lithium | Open label | Cocaine abuse | Nonsignificant decrease in cocaine use |
| BD: bipolar disorder | ||||
Anticonvulsants. In a double-blind, placebo-controlled study of 59 alcohol-dependent bipolar I disorder patients, lithium plus divalproex sodium was superior to lithium plus placebo in decreasing number of drinking days and number of drinks per day and in increasing periods of abstinence (Table 2).16-19 Divalproex sodium was well tolerated and liver function improved in the divalproex sodium group compared with the placebo group, which probably was a benefit of decreased alcohol consumption. In addition, there was a strong association between mood symptoms and alcohol use, which suggests that maximizing mood symptom treatment may decrease alcohol use. However, the divalproex sodium and placebo groups did not differ in measures of mood symptoms, which implies that divalproex sodium might exhibit a positive effect on drinking regardless of its mood-stabilizing properties.
Divalproex sodium also has been used to treat BD comorbid with cocaine dependence. In a small open-label study, 15 patients receiving divalproex sodium plus counseling for mood and substance use disorders were followed for 6 weeks.17 The 7 patients who completed the trial had significantly more cocaine-abstinent days, spent less money on cocaine, and experienced fewer manic and depressive symptoms. However, divalproex sodium’s effect on cocaine use cannot be determined solely from this study because there was no placebo control group.
Despite its widespread use as a mood stabilizer and potential use in alcohol detoxification, carbamazepine scarcely has been studied in BD-SUD patients. A double-blind, placebo-controlled study of 139 cocaine-dependent patients with BD or other affective disorders found that patients taking carbamazepine for 12 weeks experienced modest reductions in positive urine drug screens and increased time to cocaine use.18 They also reported less cocaine craving than patients taking placebo, and mood symptoms (mostly depressive) improved.
An open-label study used lamotrigine as adjunctive therapy or monotherapy for 62 cocaine-dependent BD patients followed for 36 weeks.19 There was some decrease in cocaine craving, money spent on cocaine, and rate of depressive and manic symptoms, but no effect on cocaine use. A placebo-controlled trial is necessary to confirm these modest effects.
No studies have evaluated the potential role of topiramate in treating BD-SUD, despite its FDA-approved indication for alcoholism treatment. Topiramate’s well-known safety and tolerability profile in BD patients make it an interesting option for those with co-occurring alcohol dependence.
Table 2
Studies suggest anticonvulsants may reduce alcohol, cocaine use in BD patients
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Salloum et al, 200516 | Divalproex sodium plus lithium vs placebo plus lithium | Double-blind, placebo-controlled | Alcohol dependence | Decreased number of drinking days and number of drinks per day and increased time of abstinence |
| Salloum et al, 200717 | Divalproex sodium | Open label | Cocaine dependence | Increased cocaine-abstinent days and decreased money spent on cocaine and cocaine use severity index |
| Brady et al,* 200218 | Carbamazepine vs placebo | Double-blind, placebo-controlled | Cocaine dependence | Decreased cocaine craving and cocaine use |
| Brown et al, 200619 | Lamotrigine | Open label | Cocaine dependence | Decreased cocaine craving and money spent on cocaine |
| *Sample included, but was not limited to, patients with BD BD: bipolar disorder | ||||
Atypical antipsychotics. In an open-label study, 16 weeks of quetiapine monotherapy effectively decreased alcohol consumption, alcohol craving, and psychotic and affective symptoms in 28 alcoholics with a variety of psychiatric diagnoses, including BD, schizoaffective disorder, and borderline personality disorder (Table 3).20-24 However, in a double-blind study of augmentation with quetiapine or placebo for 102 alcohol-dependent BD patients, no significant differences in alcohol use were found between groups.21
Quetiapine may be effective for treating BD patients with comorbid cocaine dependence. In an open-label study, 12 weeks of quetiapine augmentation in 17 cocaine-dependent BD patients was associated with decreased cocaine craving and improvement in depressive symptoms.22 In another open-label study, 80 BD patients with comorbid cocaine or amphetamine dependence were randomly assigned to receive quetiapine or risperidone as adjunctive therapy or monotherapy for 20 weeks.23 Both groups showed significantly decreased drug use and drug craving and improved mood. This study suggests that risperidone also may be an option for BD patients with comorbid cocaine or stimulant dependence.
A 20-week, open-label study of 20 BD-SUD patients found that switching patients from their previous antipsychotic to aripiprazole resulted in less cocaine craving, less alcohol craving, and less money spent on alcohol.24
Olanzapine has not been systematically studied in BD-SUD patients. Some case reports suggest that olanzapine may decrease cocaine craving and use in patients with schizoaffective disorder (bipolar type) and alcohol craving and use in BD patients with comorbid alcohol dependence.25
Table 3
Evidence of efficacy for antipsychotics for BD patients with SUDs
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Martinotti et al,* 200820 | Quetiapine | Open label | Alcohol dependence | Decreased alcohol consumption and alcohol craving |
| Brown et al, 200821 | Quetiapine vs placebo | Double-blind, placebo-controlled | Alcohol dependence | No difference between quetiapine and placebo in decreasing alcohol use and alcohol craving |
| Brown et al, 200222 | Quetiapine | Open label | Cocaine dependence | Decreased cocaine use and cocaine craving |
| Nejtek et al, 200823 | Risperidone vs quetiapine | Open label | Cocaine dependence and amphetamine dependence | Decreased drug use and drug craving |
| Brown et al, 200524 | Aripiprazole | Open label | Alcohol and cocaine dependence | Decreased alcohol and cocaine craving and money spent on alcohol |
| *Sample included, but was not limited to, patients with BD BD: bipolar disorder; SUDs: substance use disorders | ||||
SUD medications. Little evidence guides using medications indicated for treating SUDs—such as naltrexone, acamprosate, and disulfiram—as treatment for BD patients (Table 4).26-29 In an open-label trial of 34 BD patients with alcohol dependence, naltrexone was well tolerated and associated with decreased alcohol craving and use and modest improvement in manic and depressive symptoms.26
In a double-blind, placebo-controlled study, 50 alcohol-dependent BD patients treated with standard mood-stabilizing therapy and cognitive-behavioral therapy were randomized to receive add-on naltrexone, 50 mg/d, or placebo.27 Patients receiving naltrexone showed decreased alcohol consumption, although no measures were statistically significant. Effect sizes of alcohol use decrease and alcohol craving were moderate to large compared with placebo, which suggests that naltrexone may be effective for treating alcoholism in these patients.
Two other studies evaluated naltrexone and disulfiram in patients with BD or other mood disorders.28,29 Naltrexone was well tolerated, caused no serious adverse side effects, and was significantly more effective than placebo in decreasing drinking rates and increasing the number of abstinent days.28,29 Disulfiram was as effective as naltrexone, but the combination of both offered no advantage over use of either drug separately.
There are reports of a new-onset manic episode associated with naltrexone use in a patient with opioid dependence, and a manic episode triggered by naltrexone in a patient with BD with comorbid alcohol dependence.30,31 At both low and high doses, disulfiram is associated with induction of psychotic mania in alcoholic patients without a personal or family history of BD.32,33
We found no studies that evaluated treating BD patients who abused other substances, such as cannabis or opiates. We recommend that BD patients with these substance use disorders should be referred to treatment modalities that are condition-specific, such as psychotherapy for cannabis use disorders or methadone or naltrexone treatment for opiate dependence. More severe cases of comorbid SUD probably would benefit from a referral to or consultation with a SUD specialist.
Table 4
Naltrexone and disulfiram for BD patients with alcohol dependence
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Brown et al, 200626 | Naltrexone | Open label | Alcohol dependence | Decreased alcohol use and craving |
| Brown et al, 200927 | Naltrexone vs placebo | Double-blind, placebo-controlled | Alcohol dependence | Nonsignificant decrease in alcohol consumption |
| Petrakis et al, 200528 and 200729 | Naltrexone alone vs disulfiram alone vs naltrexone plus disulfiram | Double-blind, randomized, placebo-controlled | Alcohol dependence | More time in abstinence and decreased craving for both compounds |
| BD: bipolar disorder | ||||
Related Resource
- Tolliver BK. Bipolar disorder and substance abuse: Overcome the challenges of ‘dual diagnosis’ patients. Current Psychiatry. 2010; 9(8): 32-38.
Drug Brand Names
- Acamprosate • Campral
- Aripiprazole • Abilify
- Carbamazepine • Carbatrol, Equetro, others
- Disulfiram • Antabuse
- Divalproex sodium • Depakote,
- Depakote ER Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methadone • Dolophine
- Naltrexone • ReVia, Vivitrol
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Valproate • Depacon
Disclosures
Dr. Nery held a temporary work contract as a clinical research physician with Eli Lilly and Company Brazil from May 2009 to November 2009.
Dr. Soares was partly supported by National Institute of Health grants MH 68766, MH 69774, and RR 20571. He receives grant/research support from Bristol-Myers Squibb, Cephalon, GlaxoSmithKline, and Sunovion.
1. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
2. Kessler RC, Crum RM, Warner LA, et al. Lifetime cooccurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54(4):313-321.
3. Grant BF, Stinson FS, Hasin DS, et al. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66(10):1205-1215.
4. Feinman JA, Dunner DL. The effect of alcohol and substance abuse on the course of bipolar affective disorder. J Affect Disord. 1996;37(1):43-49.
5. Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3(4):181-188.
6. Frye MA, Altshuler LL, McElroy SL, et al. Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am J Psychiatry. 2003;160(5):883-889.
7. Khalsa HM, Salvatore P, Hennen J, et al. Suicidal events and accidents in 215 first-episode bipolar I disorder patients: predictive factors. J Affect Disord. 2008;106(1-2):179-184.
8. Baldessarini RJ, Perry R, Pike J. Factors associated with treatment nonadherence among US bipolar disorder patients. Hum Psychopharmacol. 2008;23(2):95-105.
9. Cardoso BM, Kauer Sant’Anna M, Dias VV, et al. The impact of co-morbid alcohol use disorder in bipolar patients. Alcohol. 2008;42(6):451-457.
10. Schuckit MA. Alcohol-use disorders. Lancet. 2009;373 (9662):492-501.
11. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry. 2002;63:791-795.
12. Weiss RD, Griffin ML, Kolodziej ME, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164(1):100-107.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry. 1998;37:171-178.
14. Nunes EV, McGrath PJ, Wager S, et al. Lithium treatment for cocaine abusers with bipolar spectrum disorders. Am J Psychiatry. 1990;147:655-657.
15. Weiss RD, Greenfield SF, Najavits LM, et al. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry. 1998;59:172-174.
16. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2005;62(1):37-45.
17. Salloum IM, Douaihy A, Cornelius JR, et al. Divalproex utility in bipolar disorder with co-occurring cocaine dependence: a pilot study. Addict Behav. 2007;32(2):410-405.
18. Brady KT, Sonne SC, Malcolm RJ, et al. Carbamazepine in the treatment of cocaine dependence: subtyping by affective disorder. Exp Clin Psychopharmacol. 2002;10:276-285.
19. Brown ES, Perantie DC, Dhanani N, et al. Lamotrigine for bipolar disorder and comorbid cocaine dependence: a replication and extension study. J Affect Disord. 2006;93(1-3):219-222.
20. Martinotti G, Andreoli S, Di Nicola M, et al. Quetiapine decreases alcohol consumption, craving, and psychiatric symptoms in dually diagnosed alcoholics. Hum Psychopharmacol. 2008;23(5):417-424.
21. Brown ES, Garza M, Carmody TJ. A randomized double-blind, placebo-controlled add-on trial of quetiapine in outpatients with bipolar disorder and alcohol use disorders. J Clin Psychiatry. 2008;69(5):701-705.
22. Brown ES, Nejtek VA, Perantie DC, et al. Quetiapine in bipolar disorder and cocaine dependence. Bipolar Disord. 2002;4(6):406-411.
23. Nejtek VA, Avila M, Chen LA, et al. Do atypical antipsychotics effectively treat co-occurring bipolar disorder and stimulant dependence? A randomized, double-blind trial. J Clin Psychiatry. 2008;69(8):1257-1266.
24. Brown ES, Jeffress J, Liggin JD, et al. Switching outpatients with bipolar or schizoaffective disorders and substance abuse from their current antipsychotic to aripiprazole. J Clin Psychiatry. 2005;66:756-760.
25. Sattar SP, Grant K, Bhatia S, et al. Potential use of olanzapine in treatment of substance dependence disorders. J Clin Psychopharmacol. 2003;23:413-415.
26. Brown ES, Beard L, Dobbs L, et al. Naltrexone in patients with bipolar disorder and alcohol dependence. Depress Anxiety. 2006;23(8):492-495.
27. Brown ES, Carmody TJ, Schmitz JM, et al. A randomized, double-blind, placebo-controlled pilot study of naltrexone in outpatients with bipolar disorder and alcohol dependence. Alcohol Clin Exp Res. 2009;33:1863-1869.
28. Petrakis IL, Poling J, Levinson C, et al. and the VA New England VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Biol Psychiatry. 2005;57(10):1128-1137.
29. Petrakis I, Ralevski E, Nich C, et al. and the VA VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and current depression. J Clin Psychopharmacol. 2007;27(2):160-165.
30. Sullivan MA, Nunes EV. New-onset mania and psychosis following heroin detoxification and naltrexone maintenance. Am J Addict. 2005;14(5):486-487.
31. Sonne SC, Brady KT. Naltrexone for individuals with comorbid bipolar disorder and alcohol dependence. J Clin Psychopharmacol. 2000;20(1):114-115.
32. Ceylan ME, Turkcan A, Mutlu E, et al. Manic episode with psychotic symptoms associated with high dose of disulfiram: a case report. J Clin Psychopharmacol. 2007;27(2):224-225.
33. Li MY, Shen YC. Manic episode with psychosis following a lower than recommended dosage regimen of disulfiram. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(1):311-312.
Discuss this article at www.facebook.com/CurrentPsychiatry
Among DSM axis I diagnoses, bipolar disorder (BD) has the highest rates of comorbid substance use disorders (SUDs).1-3 Approximately 60% of patients with bipolar I disorder have a lifetime diagnosis of an SUD.1 Excluding tobacco, alcohol is the substance most often abused by BD patients, followed by cannabis, amphetamines, and cocaine.1-3
BD patients with comorbid SUD usually exhibit more severe clinical presentations and poorer outcomes than their counterparts without SUDs. Compared with patients with BD alone, those with BD and SUD comorbidity (BD-SUD) experience earlier onset of mood symptoms; higher rates of anxiety disorders, suicide attempts, accidents, hospitalizations, and rapid cycling; more depressive episodes; and lower treatment compliance.4-9
Several treatment options are available for patients with BD-SUD, including psychotherapy modalities, medications primarily used to treat BD, and medications primarily used to treat SUDs. Evidence-based support for these treatments remains limited, and no treatment of choice has emerged. This article reviews evidence on the longer-term treatment of BD-SUD, including general strategies and specific psychosocial and pharmacologic interventions. Short-term treatment strategies, such as pharmacotherapy for detoxification, are outside the scope of this review.
General strategies
The causes of BD-SUD are complex. Evidence suggests that the presence of affective symptoms is associated with an increased risk for substance misuse. This should be kept in mind when treating a patient with BD-SUD because controlling mood symptoms probably will help control substance abuse. However, evidence also shows that SUDs may be independent of mood episodes. Therefore, treating only mood symptoms in the hope that doing so will control substance abuse may not be enough.
Because the negative impact of SUDs on BD outcome is well documented, inform patients that limiting their use of alcohol and/or drugs is vital to control their mood disorder. Efforts to educate, stimulate, and support patients to moderate or stop their alcohol and/or drug use are likely to result in positive changes.10 Therefore, treatment for BD-SUD should follow, in part, the same recommendations for treatment of SUDs in patients with no comorbid axis I disorders:
- identify the problem (ie, the existence of a comorbid SUD)
- share your concerns with your patient
- offer appropriate and specific treatments, such as detoxification and/or self-help and counseling programs.10
Because SUDs usually are chronic and relapsing conditions, periods of drug and/ or alcohol use should be expected and not considered a sign of treatment failure. In addition, integrating treatment for both conditions probably is better than managing each separately. Therefore, targeting BD symptoms with mood-stabilizing medications and substance abuse with nonpharmacologic modalities such as drug counseling likely will bring about the best results.
Compared with BD patients without comorbid SUD, BD-SUD patients have a 7-fold increased risk of antidepressantinduced mania.11 Therefore, antidepressants should be prescribed cautiously for patients with BD-SUD.
Integrated psychosocial therapy
BD-SUD patients may benefit from attending self-help programs such as Alcoholics Anonymous and Narcotics Anonymous, provided their mood is stable enough to allow them to participate. Other forms of psychotherapy for BD-SUD patients include standard group drug counseling and integrated group therapy that simultaneously addresses both conditions.
Integrated group therapy is based on the premise that changing maladaptive mood cognitions and behaviors will facilitate recovery from SUDs, and changing maladaptive substance use cognitions and behaviors will facilitate recovery from mood disorders.12 In a recent randomized controlled trial, 62 BD-SUD patients were blindly assigned to integrated group therapy or standard group drug counseling and followed for 3 months.12 Pharmacotherapy was prescribed as usual. Substance use decreased for both groups. However, compared with patients in the drug counseling group, those who participated in integrated group therapy spent fewer days using substances in general and alcohol in particular, fewer days using alcohol to intoxication, and had a shorter time from treatment initiation to the first abstinent month. There were no differences between groups in number of weeks in a mood episode.
Pharmacotherapy options
For a table that summarizes the dosages and indications of the medications used to treat BD-SUD that are described below, visit this article at CurrentPsychiatry.com.
Table
Medications used to treat substance use disorders in bipolar disorder patients*
| Drug | Dosages | FDA-approved indication(s) |
|---|---|---|
| Acamprosate | 1,998 mg/d | Maintenance of abstinence from alcohol in patients with alcohol dependence |
| Aripiprazole | 15 to 45 mg/d | Acute manic or mixed episode of bipolar disorder; augmentation therapy for major depressive disorder |
| Carbamazepine | 400 to 1,200 mg/d | Manic and mixed episodes associated with bipolar disorder |
| Disulfiram | 250 to 500 mg/d | Enforced sobriety in abstinent alcohol-dependence patients |
| Divalproex sodium | Initial dose: 750 mg/d Maximum dose: 60 mg/kg/d† | Manic episodes associated with bipolar disorder |
| Lamotrigine | 200 mg/d | Maintenance treatment of bipolar I disorder |
| Lithium | 900 to 1,800 mg/d for acute episodes 900 mg to 1,200 mg/d for maintenance‡. | Manic episodes associated with bipolar disorder; maintenance treatment of bipolar disorder |
| Naltrexone | 50 mg/d 380 mg/month | Alcohol dependence |
| Quetiapine | 300 mg/d for bipolar depression 400 to 800 mg/d for bipolar mania 400 to 800 mg/d for maintenance treatment of bipolar disorder | Depressive and acute manic episodes associated with bipolar I disorder; maintenance treatment of bipolar I disorder |
| Risperidone | 1 to 6 mg/d | Acute manic or mixed episodes associated with bipolar I disorder |
| * None of the medications cited in this table or the text have been specifically approved by the FDA for treating alcohol/drug abuse/dependence co-occurring with bipolar disorder †Dose should correspond to valproic acid therapeutic levels between 50 and 100 μg/mL ‡Dose should correspond to lithium therapeutic levels between 0.8 and 1.2 mEq/L for acute manic episode treatment and 0.6 and 1.0 mEq/L for maintenance treatment | ||
Lithium. Given its well-documented mood stabilizing effect, lithium would seem to be a reasonable option to treat BD-SUD patients, but scant evidence supports its role as an anti-alcohol or anti-drug medication (Table 1).13,14 Lithium’s efficacy was evaluated in a study of 25 adolescents suffering from mood disorders (mostly BD) and comorbid SUDs (mostly alcohol and cannabis) randomized to receive lithium or placebo for 6 weeks.13 Lithium was well tolerated and improved psychiatric symptoms. At week 3, patients receiving lithium produced fewer positive results on randomly administered urine drug screens than those receiving placebo.
However, lithium seems to have little efficacy in reducing cocaine use in cocaine-dependent patients with bipolar spectrum disorders.14 In an open-label study, 10 patients with a history of hypomania or cyclothymia received lithium monotherapy for 12 weeks. Although patients experienced improved mood symptoms and decreased cocaine use, the mean decrease was transitory and not statistically significant. Another factor that may limit lithium’s use for BD-SUD patients is that these patients are more likely to comply with valproate treatment than with lithium.15
Table 1
Lithium for BD patients with substance use disorders
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Geller et al, 199813 | Lithium vs placebo | Double-blind, placebo-controlled | Alcohol and cannabis use disorders | Decreased positive drug screen results |
| Nunes et al, 199014 | Lithium | Open label | Cocaine abuse | Nonsignificant decrease in cocaine use |
| BD: bipolar disorder | ||||
Anticonvulsants. In a double-blind, placebo-controlled study of 59 alcohol-dependent bipolar I disorder patients, lithium plus divalproex sodium was superior to lithium plus placebo in decreasing number of drinking days and number of drinks per day and in increasing periods of abstinence (Table 2).16-19 Divalproex sodium was well tolerated and liver function improved in the divalproex sodium group compared with the placebo group, which probably was a benefit of decreased alcohol consumption. In addition, there was a strong association between mood symptoms and alcohol use, which suggests that maximizing mood symptom treatment may decrease alcohol use. However, the divalproex sodium and placebo groups did not differ in measures of mood symptoms, which implies that divalproex sodium might exhibit a positive effect on drinking regardless of its mood-stabilizing properties.
Divalproex sodium also has been used to treat BD comorbid with cocaine dependence. In a small open-label study, 15 patients receiving divalproex sodium plus counseling for mood and substance use disorders were followed for 6 weeks.17 The 7 patients who completed the trial had significantly more cocaine-abstinent days, spent less money on cocaine, and experienced fewer manic and depressive symptoms. However, divalproex sodium’s effect on cocaine use cannot be determined solely from this study because there was no placebo control group.
Despite its widespread use as a mood stabilizer and potential use in alcohol detoxification, carbamazepine scarcely has been studied in BD-SUD patients. A double-blind, placebo-controlled study of 139 cocaine-dependent patients with BD or other affective disorders found that patients taking carbamazepine for 12 weeks experienced modest reductions in positive urine drug screens and increased time to cocaine use.18 They also reported less cocaine craving than patients taking placebo, and mood symptoms (mostly depressive) improved.
An open-label study used lamotrigine as adjunctive therapy or monotherapy for 62 cocaine-dependent BD patients followed for 36 weeks.19 There was some decrease in cocaine craving, money spent on cocaine, and rate of depressive and manic symptoms, but no effect on cocaine use. A placebo-controlled trial is necessary to confirm these modest effects.
No studies have evaluated the potential role of topiramate in treating BD-SUD, despite its FDA-approved indication for alcoholism treatment. Topiramate’s well-known safety and tolerability profile in BD patients make it an interesting option for those with co-occurring alcohol dependence.
Table 2
Studies suggest anticonvulsants may reduce alcohol, cocaine use in BD patients
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Salloum et al, 200516 | Divalproex sodium plus lithium vs placebo plus lithium | Double-blind, placebo-controlled | Alcohol dependence | Decreased number of drinking days and number of drinks per day and increased time of abstinence |
| Salloum et al, 200717 | Divalproex sodium | Open label | Cocaine dependence | Increased cocaine-abstinent days and decreased money spent on cocaine and cocaine use severity index |
| Brady et al,* 200218 | Carbamazepine vs placebo | Double-blind, placebo-controlled | Cocaine dependence | Decreased cocaine craving and cocaine use |
| Brown et al, 200619 | Lamotrigine | Open label | Cocaine dependence | Decreased cocaine craving and money spent on cocaine |
| *Sample included, but was not limited to, patients with BD BD: bipolar disorder | ||||
Atypical antipsychotics. In an open-label study, 16 weeks of quetiapine monotherapy effectively decreased alcohol consumption, alcohol craving, and psychotic and affective symptoms in 28 alcoholics with a variety of psychiatric diagnoses, including BD, schizoaffective disorder, and borderline personality disorder (Table 3).20-24 However, in a double-blind study of augmentation with quetiapine or placebo for 102 alcohol-dependent BD patients, no significant differences in alcohol use were found between groups.21
Quetiapine may be effective for treating BD patients with comorbid cocaine dependence. In an open-label study, 12 weeks of quetiapine augmentation in 17 cocaine-dependent BD patients was associated with decreased cocaine craving and improvement in depressive symptoms.22 In another open-label study, 80 BD patients with comorbid cocaine or amphetamine dependence were randomly assigned to receive quetiapine or risperidone as adjunctive therapy or monotherapy for 20 weeks.23 Both groups showed significantly decreased drug use and drug craving and improved mood. This study suggests that risperidone also may be an option for BD patients with comorbid cocaine or stimulant dependence.
A 20-week, open-label study of 20 BD-SUD patients found that switching patients from their previous antipsychotic to aripiprazole resulted in less cocaine craving, less alcohol craving, and less money spent on alcohol.24
Olanzapine has not been systematically studied in BD-SUD patients. Some case reports suggest that olanzapine may decrease cocaine craving and use in patients with schizoaffective disorder (bipolar type) and alcohol craving and use in BD patients with comorbid alcohol dependence.25
Table 3
Evidence of efficacy for antipsychotics for BD patients with SUDs
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Martinotti et al,* 200820 | Quetiapine | Open label | Alcohol dependence | Decreased alcohol consumption and alcohol craving |
| Brown et al, 200821 | Quetiapine vs placebo | Double-blind, placebo-controlled | Alcohol dependence | No difference between quetiapine and placebo in decreasing alcohol use and alcohol craving |
| Brown et al, 200222 | Quetiapine | Open label | Cocaine dependence | Decreased cocaine use and cocaine craving |
| Nejtek et al, 200823 | Risperidone vs quetiapine | Open label | Cocaine dependence and amphetamine dependence | Decreased drug use and drug craving |
| Brown et al, 200524 | Aripiprazole | Open label | Alcohol and cocaine dependence | Decreased alcohol and cocaine craving and money spent on alcohol |
| *Sample included, but was not limited to, patients with BD BD: bipolar disorder; SUDs: substance use disorders | ||||
SUD medications. Little evidence guides using medications indicated for treating SUDs—such as naltrexone, acamprosate, and disulfiram—as treatment for BD patients (Table 4).26-29 In an open-label trial of 34 BD patients with alcohol dependence, naltrexone was well tolerated and associated with decreased alcohol craving and use and modest improvement in manic and depressive symptoms.26
In a double-blind, placebo-controlled study, 50 alcohol-dependent BD patients treated with standard mood-stabilizing therapy and cognitive-behavioral therapy were randomized to receive add-on naltrexone, 50 mg/d, or placebo.27 Patients receiving naltrexone showed decreased alcohol consumption, although no measures were statistically significant. Effect sizes of alcohol use decrease and alcohol craving were moderate to large compared with placebo, which suggests that naltrexone may be effective for treating alcoholism in these patients.
Two other studies evaluated naltrexone and disulfiram in patients with BD or other mood disorders.28,29 Naltrexone was well tolerated, caused no serious adverse side effects, and was significantly more effective than placebo in decreasing drinking rates and increasing the number of abstinent days.28,29 Disulfiram was as effective as naltrexone, but the combination of both offered no advantage over use of either drug separately.
There are reports of a new-onset manic episode associated with naltrexone use in a patient with opioid dependence, and a manic episode triggered by naltrexone in a patient with BD with comorbid alcohol dependence.30,31 At both low and high doses, disulfiram is associated with induction of psychotic mania in alcoholic patients without a personal or family history of BD.32,33
We found no studies that evaluated treating BD patients who abused other substances, such as cannabis or opiates. We recommend that BD patients with these substance use disorders should be referred to treatment modalities that are condition-specific, such as psychotherapy for cannabis use disorders or methadone or naltrexone treatment for opiate dependence. More severe cases of comorbid SUD probably would benefit from a referral to or consultation with a SUD specialist.
Table 4
Naltrexone and disulfiram for BD patients with alcohol dependence
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Brown et al, 200626 | Naltrexone | Open label | Alcohol dependence | Decreased alcohol use and craving |
| Brown et al, 200927 | Naltrexone vs placebo | Double-blind, placebo-controlled | Alcohol dependence | Nonsignificant decrease in alcohol consumption |
| Petrakis et al, 200528 and 200729 | Naltrexone alone vs disulfiram alone vs naltrexone plus disulfiram | Double-blind, randomized, placebo-controlled | Alcohol dependence | More time in abstinence and decreased craving for both compounds |
| BD: bipolar disorder | ||||
Related Resource
- Tolliver BK. Bipolar disorder and substance abuse: Overcome the challenges of ‘dual diagnosis’ patients. Current Psychiatry. 2010; 9(8): 32-38.
Drug Brand Names
- Acamprosate • Campral
- Aripiprazole • Abilify
- Carbamazepine • Carbatrol, Equetro, others
- Disulfiram • Antabuse
- Divalproex sodium • Depakote,
- Depakote ER Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methadone • Dolophine
- Naltrexone • ReVia, Vivitrol
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Valproate • Depacon
Disclosures
Dr. Nery held a temporary work contract as a clinical research physician with Eli Lilly and Company Brazil from May 2009 to November 2009.
Dr. Soares was partly supported by National Institute of Health grants MH 68766, MH 69774, and RR 20571. He receives grant/research support from Bristol-Myers Squibb, Cephalon, GlaxoSmithKline, and Sunovion.
Discuss this article at www.facebook.com/CurrentPsychiatry
Among DSM axis I diagnoses, bipolar disorder (BD) has the highest rates of comorbid substance use disorders (SUDs).1-3 Approximately 60% of patients with bipolar I disorder have a lifetime diagnosis of an SUD.1 Excluding tobacco, alcohol is the substance most often abused by BD patients, followed by cannabis, amphetamines, and cocaine.1-3
BD patients with comorbid SUD usually exhibit more severe clinical presentations and poorer outcomes than their counterparts without SUDs. Compared with patients with BD alone, those with BD and SUD comorbidity (BD-SUD) experience earlier onset of mood symptoms; higher rates of anxiety disorders, suicide attempts, accidents, hospitalizations, and rapid cycling; more depressive episodes; and lower treatment compliance.4-9
Several treatment options are available for patients with BD-SUD, including psychotherapy modalities, medications primarily used to treat BD, and medications primarily used to treat SUDs. Evidence-based support for these treatments remains limited, and no treatment of choice has emerged. This article reviews evidence on the longer-term treatment of BD-SUD, including general strategies and specific psychosocial and pharmacologic interventions. Short-term treatment strategies, such as pharmacotherapy for detoxification, are outside the scope of this review.
General strategies
The causes of BD-SUD are complex. Evidence suggests that the presence of affective symptoms is associated with an increased risk for substance misuse. This should be kept in mind when treating a patient with BD-SUD because controlling mood symptoms probably will help control substance abuse. However, evidence also shows that SUDs may be independent of mood episodes. Therefore, treating only mood symptoms in the hope that doing so will control substance abuse may not be enough.
Because the negative impact of SUDs on BD outcome is well documented, inform patients that limiting their use of alcohol and/or drugs is vital to control their mood disorder. Efforts to educate, stimulate, and support patients to moderate or stop their alcohol and/or drug use are likely to result in positive changes.10 Therefore, treatment for BD-SUD should follow, in part, the same recommendations for treatment of SUDs in patients with no comorbid axis I disorders:
- identify the problem (ie, the existence of a comorbid SUD)
- share your concerns with your patient
- offer appropriate and specific treatments, such as detoxification and/or self-help and counseling programs.10
Because SUDs usually are chronic and relapsing conditions, periods of drug and/ or alcohol use should be expected and not considered a sign of treatment failure. In addition, integrating treatment for both conditions probably is better than managing each separately. Therefore, targeting BD symptoms with mood-stabilizing medications and substance abuse with nonpharmacologic modalities such as drug counseling likely will bring about the best results.
Compared with BD patients without comorbid SUD, BD-SUD patients have a 7-fold increased risk of antidepressantinduced mania.11 Therefore, antidepressants should be prescribed cautiously for patients with BD-SUD.
Integrated psychosocial therapy
BD-SUD patients may benefit from attending self-help programs such as Alcoholics Anonymous and Narcotics Anonymous, provided their mood is stable enough to allow them to participate. Other forms of psychotherapy for BD-SUD patients include standard group drug counseling and integrated group therapy that simultaneously addresses both conditions.
Integrated group therapy is based on the premise that changing maladaptive mood cognitions and behaviors will facilitate recovery from SUDs, and changing maladaptive substance use cognitions and behaviors will facilitate recovery from mood disorders.12 In a recent randomized controlled trial, 62 BD-SUD patients were blindly assigned to integrated group therapy or standard group drug counseling and followed for 3 months.12 Pharmacotherapy was prescribed as usual. Substance use decreased for both groups. However, compared with patients in the drug counseling group, those who participated in integrated group therapy spent fewer days using substances in general and alcohol in particular, fewer days using alcohol to intoxication, and had a shorter time from treatment initiation to the first abstinent month. There were no differences between groups in number of weeks in a mood episode.
Pharmacotherapy options
For a table that summarizes the dosages and indications of the medications used to treat BD-SUD that are described below, visit this article at CurrentPsychiatry.com.
Table
Medications used to treat substance use disorders in bipolar disorder patients*
| Drug | Dosages | FDA-approved indication(s) |
|---|---|---|
| Acamprosate | 1,998 mg/d | Maintenance of abstinence from alcohol in patients with alcohol dependence |
| Aripiprazole | 15 to 45 mg/d | Acute manic or mixed episode of bipolar disorder; augmentation therapy for major depressive disorder |
| Carbamazepine | 400 to 1,200 mg/d | Manic and mixed episodes associated with bipolar disorder |
| Disulfiram | 250 to 500 mg/d | Enforced sobriety in abstinent alcohol-dependence patients |
| Divalproex sodium | Initial dose: 750 mg/d Maximum dose: 60 mg/kg/d† | Manic episodes associated with bipolar disorder |
| Lamotrigine | 200 mg/d | Maintenance treatment of bipolar I disorder |
| Lithium | 900 to 1,800 mg/d for acute episodes 900 mg to 1,200 mg/d for maintenance‡. | Manic episodes associated with bipolar disorder; maintenance treatment of bipolar disorder |
| Naltrexone | 50 mg/d 380 mg/month | Alcohol dependence |
| Quetiapine | 300 mg/d for bipolar depression 400 to 800 mg/d for bipolar mania 400 to 800 mg/d for maintenance treatment of bipolar disorder | Depressive and acute manic episodes associated with bipolar I disorder; maintenance treatment of bipolar I disorder |
| Risperidone | 1 to 6 mg/d | Acute manic or mixed episodes associated with bipolar I disorder |
| * None of the medications cited in this table or the text have been specifically approved by the FDA for treating alcohol/drug abuse/dependence co-occurring with bipolar disorder †Dose should correspond to valproic acid therapeutic levels between 50 and 100 μg/mL ‡Dose should correspond to lithium therapeutic levels between 0.8 and 1.2 mEq/L for acute manic episode treatment and 0.6 and 1.0 mEq/L for maintenance treatment | ||
Lithium. Given its well-documented mood stabilizing effect, lithium would seem to be a reasonable option to treat BD-SUD patients, but scant evidence supports its role as an anti-alcohol or anti-drug medication (Table 1).13,14 Lithium’s efficacy was evaluated in a study of 25 adolescents suffering from mood disorders (mostly BD) and comorbid SUDs (mostly alcohol and cannabis) randomized to receive lithium or placebo for 6 weeks.13 Lithium was well tolerated and improved psychiatric symptoms. At week 3, patients receiving lithium produced fewer positive results on randomly administered urine drug screens than those receiving placebo.
However, lithium seems to have little efficacy in reducing cocaine use in cocaine-dependent patients with bipolar spectrum disorders.14 In an open-label study, 10 patients with a history of hypomania or cyclothymia received lithium monotherapy for 12 weeks. Although patients experienced improved mood symptoms and decreased cocaine use, the mean decrease was transitory and not statistically significant. Another factor that may limit lithium’s use for BD-SUD patients is that these patients are more likely to comply with valproate treatment than with lithium.15
Table 1
Lithium for BD patients with substance use disorders
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Geller et al, 199813 | Lithium vs placebo | Double-blind, placebo-controlled | Alcohol and cannabis use disorders | Decreased positive drug screen results |
| Nunes et al, 199014 | Lithium | Open label | Cocaine abuse | Nonsignificant decrease in cocaine use |
| BD: bipolar disorder | ||||
Anticonvulsants. In a double-blind, placebo-controlled study of 59 alcohol-dependent bipolar I disorder patients, lithium plus divalproex sodium was superior to lithium plus placebo in decreasing number of drinking days and number of drinks per day and in increasing periods of abstinence (Table 2).16-19 Divalproex sodium was well tolerated and liver function improved in the divalproex sodium group compared with the placebo group, which probably was a benefit of decreased alcohol consumption. In addition, there was a strong association between mood symptoms and alcohol use, which suggests that maximizing mood symptom treatment may decrease alcohol use. However, the divalproex sodium and placebo groups did not differ in measures of mood symptoms, which implies that divalproex sodium might exhibit a positive effect on drinking regardless of its mood-stabilizing properties.
Divalproex sodium also has been used to treat BD comorbid with cocaine dependence. In a small open-label study, 15 patients receiving divalproex sodium plus counseling for mood and substance use disorders were followed for 6 weeks.17 The 7 patients who completed the trial had significantly more cocaine-abstinent days, spent less money on cocaine, and experienced fewer manic and depressive symptoms. However, divalproex sodium’s effect on cocaine use cannot be determined solely from this study because there was no placebo control group.
Despite its widespread use as a mood stabilizer and potential use in alcohol detoxification, carbamazepine scarcely has been studied in BD-SUD patients. A double-blind, placebo-controlled study of 139 cocaine-dependent patients with BD or other affective disorders found that patients taking carbamazepine for 12 weeks experienced modest reductions in positive urine drug screens and increased time to cocaine use.18 They also reported less cocaine craving than patients taking placebo, and mood symptoms (mostly depressive) improved.
An open-label study used lamotrigine as adjunctive therapy or monotherapy for 62 cocaine-dependent BD patients followed for 36 weeks.19 There was some decrease in cocaine craving, money spent on cocaine, and rate of depressive and manic symptoms, but no effect on cocaine use. A placebo-controlled trial is necessary to confirm these modest effects.
No studies have evaluated the potential role of topiramate in treating BD-SUD, despite its FDA-approved indication for alcoholism treatment. Topiramate’s well-known safety and tolerability profile in BD patients make it an interesting option for those with co-occurring alcohol dependence.
Table 2
Studies suggest anticonvulsants may reduce alcohol, cocaine use in BD patients
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Salloum et al, 200516 | Divalproex sodium plus lithium vs placebo plus lithium | Double-blind, placebo-controlled | Alcohol dependence | Decreased number of drinking days and number of drinks per day and increased time of abstinence |
| Salloum et al, 200717 | Divalproex sodium | Open label | Cocaine dependence | Increased cocaine-abstinent days and decreased money spent on cocaine and cocaine use severity index |
| Brady et al,* 200218 | Carbamazepine vs placebo | Double-blind, placebo-controlled | Cocaine dependence | Decreased cocaine craving and cocaine use |
| Brown et al, 200619 | Lamotrigine | Open label | Cocaine dependence | Decreased cocaine craving and money spent on cocaine |
| *Sample included, but was not limited to, patients with BD BD: bipolar disorder | ||||
Atypical antipsychotics. In an open-label study, 16 weeks of quetiapine monotherapy effectively decreased alcohol consumption, alcohol craving, and psychotic and affective symptoms in 28 alcoholics with a variety of psychiatric diagnoses, including BD, schizoaffective disorder, and borderline personality disorder (Table 3).20-24 However, in a double-blind study of augmentation with quetiapine or placebo for 102 alcohol-dependent BD patients, no significant differences in alcohol use were found between groups.21
Quetiapine may be effective for treating BD patients with comorbid cocaine dependence. In an open-label study, 12 weeks of quetiapine augmentation in 17 cocaine-dependent BD patients was associated with decreased cocaine craving and improvement in depressive symptoms.22 In another open-label study, 80 BD patients with comorbid cocaine or amphetamine dependence were randomly assigned to receive quetiapine or risperidone as adjunctive therapy or monotherapy for 20 weeks.23 Both groups showed significantly decreased drug use and drug craving and improved mood. This study suggests that risperidone also may be an option for BD patients with comorbid cocaine or stimulant dependence.
A 20-week, open-label study of 20 BD-SUD patients found that switching patients from their previous antipsychotic to aripiprazole resulted in less cocaine craving, less alcohol craving, and less money spent on alcohol.24
Olanzapine has not been systematically studied in BD-SUD patients. Some case reports suggest that olanzapine may decrease cocaine craving and use in patients with schizoaffective disorder (bipolar type) and alcohol craving and use in BD patients with comorbid alcohol dependence.25
Table 3
Evidence of efficacy for antipsychotics for BD patients with SUDs
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Martinotti et al,* 200820 | Quetiapine | Open label | Alcohol dependence | Decreased alcohol consumption and alcohol craving |
| Brown et al, 200821 | Quetiapine vs placebo | Double-blind, placebo-controlled | Alcohol dependence | No difference between quetiapine and placebo in decreasing alcohol use and alcohol craving |
| Brown et al, 200222 | Quetiapine | Open label | Cocaine dependence | Decreased cocaine use and cocaine craving |
| Nejtek et al, 200823 | Risperidone vs quetiapine | Open label | Cocaine dependence and amphetamine dependence | Decreased drug use and drug craving |
| Brown et al, 200524 | Aripiprazole | Open label | Alcohol and cocaine dependence | Decreased alcohol and cocaine craving and money spent on alcohol |
| *Sample included, but was not limited to, patients with BD BD: bipolar disorder; SUDs: substance use disorders | ||||
SUD medications. Little evidence guides using medications indicated for treating SUDs—such as naltrexone, acamprosate, and disulfiram—as treatment for BD patients (Table 4).26-29 In an open-label trial of 34 BD patients with alcohol dependence, naltrexone was well tolerated and associated with decreased alcohol craving and use and modest improvement in manic and depressive symptoms.26
In a double-blind, placebo-controlled study, 50 alcohol-dependent BD patients treated with standard mood-stabilizing therapy and cognitive-behavioral therapy were randomized to receive add-on naltrexone, 50 mg/d, or placebo.27 Patients receiving naltrexone showed decreased alcohol consumption, although no measures were statistically significant. Effect sizes of alcohol use decrease and alcohol craving were moderate to large compared with placebo, which suggests that naltrexone may be effective for treating alcoholism in these patients.
Two other studies evaluated naltrexone and disulfiram in patients with BD or other mood disorders.28,29 Naltrexone was well tolerated, caused no serious adverse side effects, and was significantly more effective than placebo in decreasing drinking rates and increasing the number of abstinent days.28,29 Disulfiram was as effective as naltrexone, but the combination of both offered no advantage over use of either drug separately.
There are reports of a new-onset manic episode associated with naltrexone use in a patient with opioid dependence, and a manic episode triggered by naltrexone in a patient with BD with comorbid alcohol dependence.30,31 At both low and high doses, disulfiram is associated with induction of psychotic mania in alcoholic patients without a personal or family history of BD.32,33
We found no studies that evaluated treating BD patients who abused other substances, such as cannabis or opiates. We recommend that BD patients with these substance use disorders should be referred to treatment modalities that are condition-specific, such as psychotherapy for cannabis use disorders or methadone or naltrexone treatment for opiate dependence. More severe cases of comorbid SUD probably would benefit from a referral to or consultation with a SUD specialist.
Table 4
Naltrexone and disulfiram for BD patients with alcohol dependence
| Study | Intervention | Design | Substance use disorder | Results |
|---|---|---|---|---|
| Brown et al, 200626 | Naltrexone | Open label | Alcohol dependence | Decreased alcohol use and craving |
| Brown et al, 200927 | Naltrexone vs placebo | Double-blind, placebo-controlled | Alcohol dependence | Nonsignificant decrease in alcohol consumption |
| Petrakis et al, 200528 and 200729 | Naltrexone alone vs disulfiram alone vs naltrexone plus disulfiram | Double-blind, randomized, placebo-controlled | Alcohol dependence | More time in abstinence and decreased craving for both compounds |
| BD: bipolar disorder | ||||
Related Resource
- Tolliver BK. Bipolar disorder and substance abuse: Overcome the challenges of ‘dual diagnosis’ patients. Current Psychiatry. 2010; 9(8): 32-38.
Drug Brand Names
- Acamprosate • Campral
- Aripiprazole • Abilify
- Carbamazepine • Carbatrol, Equetro, others
- Disulfiram • Antabuse
- Divalproex sodium • Depakote,
- Depakote ER Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methadone • Dolophine
- Naltrexone • ReVia, Vivitrol
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Valproate • Depacon
Disclosures
Dr. Nery held a temporary work contract as a clinical research physician with Eli Lilly and Company Brazil from May 2009 to November 2009.
Dr. Soares was partly supported by National Institute of Health grants MH 68766, MH 69774, and RR 20571. He receives grant/research support from Bristol-Myers Squibb, Cephalon, GlaxoSmithKline, and Sunovion.
1. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
2. Kessler RC, Crum RM, Warner LA, et al. Lifetime cooccurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54(4):313-321.
3. Grant BF, Stinson FS, Hasin DS, et al. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66(10):1205-1215.
4. Feinman JA, Dunner DL. The effect of alcohol and substance abuse on the course of bipolar affective disorder. J Affect Disord. 1996;37(1):43-49.
5. Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3(4):181-188.
6. Frye MA, Altshuler LL, McElroy SL, et al. Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am J Psychiatry. 2003;160(5):883-889.
7. Khalsa HM, Salvatore P, Hennen J, et al. Suicidal events and accidents in 215 first-episode bipolar I disorder patients: predictive factors. J Affect Disord. 2008;106(1-2):179-184.
8. Baldessarini RJ, Perry R, Pike J. Factors associated with treatment nonadherence among US bipolar disorder patients. Hum Psychopharmacol. 2008;23(2):95-105.
9. Cardoso BM, Kauer Sant’Anna M, Dias VV, et al. The impact of co-morbid alcohol use disorder in bipolar patients. Alcohol. 2008;42(6):451-457.
10. Schuckit MA. Alcohol-use disorders. Lancet. 2009;373 (9662):492-501.
11. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry. 2002;63:791-795.
12. Weiss RD, Griffin ML, Kolodziej ME, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164(1):100-107.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry. 1998;37:171-178.
14. Nunes EV, McGrath PJ, Wager S, et al. Lithium treatment for cocaine abusers with bipolar spectrum disorders. Am J Psychiatry. 1990;147:655-657.
15. Weiss RD, Greenfield SF, Najavits LM, et al. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry. 1998;59:172-174.
16. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2005;62(1):37-45.
17. Salloum IM, Douaihy A, Cornelius JR, et al. Divalproex utility in bipolar disorder with co-occurring cocaine dependence: a pilot study. Addict Behav. 2007;32(2):410-405.
18. Brady KT, Sonne SC, Malcolm RJ, et al. Carbamazepine in the treatment of cocaine dependence: subtyping by affective disorder. Exp Clin Psychopharmacol. 2002;10:276-285.
19. Brown ES, Perantie DC, Dhanani N, et al. Lamotrigine for bipolar disorder and comorbid cocaine dependence: a replication and extension study. J Affect Disord. 2006;93(1-3):219-222.
20. Martinotti G, Andreoli S, Di Nicola M, et al. Quetiapine decreases alcohol consumption, craving, and psychiatric symptoms in dually diagnosed alcoholics. Hum Psychopharmacol. 2008;23(5):417-424.
21. Brown ES, Garza M, Carmody TJ. A randomized double-blind, placebo-controlled add-on trial of quetiapine in outpatients with bipolar disorder and alcohol use disorders. J Clin Psychiatry. 2008;69(5):701-705.
22. Brown ES, Nejtek VA, Perantie DC, et al. Quetiapine in bipolar disorder and cocaine dependence. Bipolar Disord. 2002;4(6):406-411.
23. Nejtek VA, Avila M, Chen LA, et al. Do atypical antipsychotics effectively treat co-occurring bipolar disorder and stimulant dependence? A randomized, double-blind trial. J Clin Psychiatry. 2008;69(8):1257-1266.
24. Brown ES, Jeffress J, Liggin JD, et al. Switching outpatients with bipolar or schizoaffective disorders and substance abuse from their current antipsychotic to aripiprazole. J Clin Psychiatry. 2005;66:756-760.
25. Sattar SP, Grant K, Bhatia S, et al. Potential use of olanzapine in treatment of substance dependence disorders. J Clin Psychopharmacol. 2003;23:413-415.
26. Brown ES, Beard L, Dobbs L, et al. Naltrexone in patients with bipolar disorder and alcohol dependence. Depress Anxiety. 2006;23(8):492-495.
27. Brown ES, Carmody TJ, Schmitz JM, et al. A randomized, double-blind, placebo-controlled pilot study of naltrexone in outpatients with bipolar disorder and alcohol dependence. Alcohol Clin Exp Res. 2009;33:1863-1869.
28. Petrakis IL, Poling J, Levinson C, et al. and the VA New England VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Biol Psychiatry. 2005;57(10):1128-1137.
29. Petrakis I, Ralevski E, Nich C, et al. and the VA VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and current depression. J Clin Psychopharmacol. 2007;27(2):160-165.
30. Sullivan MA, Nunes EV. New-onset mania and psychosis following heroin detoxification and naltrexone maintenance. Am J Addict. 2005;14(5):486-487.
31. Sonne SC, Brady KT. Naltrexone for individuals with comorbid bipolar disorder and alcohol dependence. J Clin Psychopharmacol. 2000;20(1):114-115.
32. Ceylan ME, Turkcan A, Mutlu E, et al. Manic episode with psychotic symptoms associated with high dose of disulfiram: a case report. J Clin Psychopharmacol. 2007;27(2):224-225.
33. Li MY, Shen YC. Manic episode with psychosis following a lower than recommended dosage regimen of disulfiram. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(1):311-312.
1. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
2. Kessler RC, Crum RM, Warner LA, et al. Lifetime cooccurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54(4):313-321.
3. Grant BF, Stinson FS, Hasin DS, et al. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66(10):1205-1215.
4. Feinman JA, Dunner DL. The effect of alcohol and substance abuse on the course of bipolar affective disorder. J Affect Disord. 1996;37(1):43-49.
5. Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3(4):181-188.
6. Frye MA, Altshuler LL, McElroy SL, et al. Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am J Psychiatry. 2003;160(5):883-889.
7. Khalsa HM, Salvatore P, Hennen J, et al. Suicidal events and accidents in 215 first-episode bipolar I disorder patients: predictive factors. J Affect Disord. 2008;106(1-2):179-184.
8. Baldessarini RJ, Perry R, Pike J. Factors associated with treatment nonadherence among US bipolar disorder patients. Hum Psychopharmacol. 2008;23(2):95-105.
9. Cardoso BM, Kauer Sant’Anna M, Dias VV, et al. The impact of co-morbid alcohol use disorder in bipolar patients. Alcohol. 2008;42(6):451-457.
10. Schuckit MA. Alcohol-use disorders. Lancet. 2009;373 (9662):492-501.
11. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry. 2002;63:791-795.
12. Weiss RD, Griffin ML, Kolodziej ME, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164(1):100-107.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry. 1998;37:171-178.
14. Nunes EV, McGrath PJ, Wager S, et al. Lithium treatment for cocaine abusers with bipolar spectrum disorders. Am J Psychiatry. 1990;147:655-657.
15. Weiss RD, Greenfield SF, Najavits LM, et al. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry. 1998;59:172-174.
16. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2005;62(1):37-45.
17. Salloum IM, Douaihy A, Cornelius JR, et al. Divalproex utility in bipolar disorder with co-occurring cocaine dependence: a pilot study. Addict Behav. 2007;32(2):410-405.
18. Brady KT, Sonne SC, Malcolm RJ, et al. Carbamazepine in the treatment of cocaine dependence: subtyping by affective disorder. Exp Clin Psychopharmacol. 2002;10:276-285.
19. Brown ES, Perantie DC, Dhanani N, et al. Lamotrigine for bipolar disorder and comorbid cocaine dependence: a replication and extension study. J Affect Disord. 2006;93(1-3):219-222.
20. Martinotti G, Andreoli S, Di Nicola M, et al. Quetiapine decreases alcohol consumption, craving, and psychiatric symptoms in dually diagnosed alcoholics. Hum Psychopharmacol. 2008;23(5):417-424.
21. Brown ES, Garza M, Carmody TJ. A randomized double-blind, placebo-controlled add-on trial of quetiapine in outpatients with bipolar disorder and alcohol use disorders. J Clin Psychiatry. 2008;69(5):701-705.
22. Brown ES, Nejtek VA, Perantie DC, et al. Quetiapine in bipolar disorder and cocaine dependence. Bipolar Disord. 2002;4(6):406-411.
23. Nejtek VA, Avila M, Chen LA, et al. Do atypical antipsychotics effectively treat co-occurring bipolar disorder and stimulant dependence? A randomized, double-blind trial. J Clin Psychiatry. 2008;69(8):1257-1266.
24. Brown ES, Jeffress J, Liggin JD, et al. Switching outpatients with bipolar or schizoaffective disorders and substance abuse from their current antipsychotic to aripiprazole. J Clin Psychiatry. 2005;66:756-760.
25. Sattar SP, Grant K, Bhatia S, et al. Potential use of olanzapine in treatment of substance dependence disorders. J Clin Psychopharmacol. 2003;23:413-415.
26. Brown ES, Beard L, Dobbs L, et al. Naltrexone in patients with bipolar disorder and alcohol dependence. Depress Anxiety. 2006;23(8):492-495.
27. Brown ES, Carmody TJ, Schmitz JM, et al. A randomized, double-blind, placebo-controlled pilot study of naltrexone in outpatients with bipolar disorder and alcohol dependence. Alcohol Clin Exp Res. 2009;33:1863-1869.
28. Petrakis IL, Poling J, Levinson C, et al. and the VA New England VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Biol Psychiatry. 2005;57(10):1128-1137.
29. Petrakis I, Ralevski E, Nich C, et al. and the VA VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and current depression. J Clin Psychopharmacol. 2007;27(2):160-165.
30. Sullivan MA, Nunes EV. New-onset mania and psychosis following heroin detoxification and naltrexone maintenance. Am J Addict. 2005;14(5):486-487.
31. Sonne SC, Brady KT. Naltrexone for individuals with comorbid bipolar disorder and alcohol dependence. J Clin Psychopharmacol. 2000;20(1):114-115.
32. Ceylan ME, Turkcan A, Mutlu E, et al. Manic episode with psychotic symptoms associated with high dose of disulfiram: a case report. J Clin Psychopharmacol. 2007;27(2):224-225.
33. Li MY, Shen YC. Manic episode with psychosis following a lower than recommended dosage regimen of disulfiram. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(1):311-312.
Subjective cognitive impairment: When to be concerned about ‘senior moments’
MS. F, age 66, requests genetic testing because she is concerned about mild memory difficulties, such as forgetting names and where she puts her keys or checkbook, and fears she may be developing Alzheimer’s disease (AD). Her mother and sister were diagnosed with AD in their early 60s. Ms. F has 20 years of education and reports no problems with driving, managing her finances, remembering to take her medications, or maintaining social activities, which her husband confirms.
Detailed questioning about anxiety and depressive symptoms reveals substantial worries about future cognitive decline and some concerns about her finances and her husband’s health. Ms. F says she occasionally feels down and has low energy but denies other depressive symptoms. She reports no sleep disturbances—including snoring and daytime sleepiness, which could indicate obstructive sleep apnea—which her husband confirms. Ms. F takes levothyroxine for hypothyroidism, atenolol for hypertension, aspirin and clopidogrel for coronary artery disease, and atorvastatin for hyperlipidemia. In addition, she provides a long list of over-the-counter (OTC) supplements—ginkgo, huperzine, ginseng, phosphatidylserine, B1, B12, folate, vitamin D, alpha-lipoic acid, and vinpocetine—that she takes to “protect” her brain from AD.
Subjective cognitive impairment (SCI) in older persons is a common condition with a largely unclear prognosis. Many older adults (age ≥65) express concern about mild cognitive problems—“senior moments”—such as word-finding difficulties and forgetfulness.1 Individuals may wonder if walking into a room only to forget why might be the first sign of dementia. Some older adults try to counteract these memory problems by engaging in brain exercises—including costly computer games—and taking OTC “brain-enhancing” vitamins, herbal remedies, and other supplements.
Although some clinicians may view SCI as benign, that is not always true (Table l).2-5 This article discusses the clinical significance of these mild cognitive complaints by examining:
- age-related cognitive decline (ARCD)
- SCI
- how SCI can be differentiated from more serious conditions, such as mild cognitive impairment (MCI) and early stages of AD and other dementias.
We also will discuss assessing and treating cognitive complaints. Although distinctions between SCI and ARCD may be controversial, evidence suggests clinicians need to adopt a more nuanced clinical approach.
Table 1
Why SCI should be taken seriously
| SCI may create emotional distress because patients are aware of decline in their ‘mental sharpness’ |
| SCI patients might consume unnecessary and potentially harmful OTC supplements touted to promote memory |
| Patients might limit their driving and financial management to avoid making mistakes |
| SCI might impair medication adherence2 |
| SCI may be an early sign of dementia3 |
| Patients’ worry about their self-perceived memory loss might predict dementia4 |
| SCI may predict nursing home placement5 |
| Addressing SCI gives health care providers an opportunity to address anxiety or depression that often accompany SCI |
| Evaluation of potential causes of SCI may uncover reversible conditions that can be treated |
| OTC: over-the-counter; SCI: subjective cognitive impairment |
‘Normal’ cognitive decline
ARCD is subtle decline in cognitive abilities, such as episodic memory, attention, and time needed to complete complex activities.6,7 Individuals with ARCD might not have subjective memory complaints or objective cognitive deficits, and their ability to live independently may not be compromised.7 The degree of decline in ARCD may be smaller than previously thought.8 Park9 summarizes 4 main mechanisms thought to underlie age-related declines in cognition:
- reduced speed of processing
- decreased working memory capabilities
- declining inhibitory control (eg, impaired complex attentional capabilities)
- sensory changes (eg, visual and auditory deficits).
ARCD traditionally is thought to result from predictable changes in the brain associated with aging, such as reduced brain volume in the hippocampus and frontal lobes, loss of myelin, loss of synapses, and cytoskeletal changes.7 However, not all older adults experience ARCD. Some remain highly functional in their later years and continue to actively engage in life well into very old age.6,9
Subjective cognitive impairment
One-quarter to one-half of community-dwelling older adults report subjective cognitive complaints, such as forgetfulness and word-finding difficulties.10 Patients with SCI do not show objective evidence of cognitive impairment on neuropsychological tests and their cognitive problems cause no functional decline.10
Preliminary evidence indicates that SCI may be a harbinger of further cognitive decline. Reisberg et al3 found that compared with patients without SCI, patients with SCI were 4.5 times more likely to develop MCI—cognitive difficulties that can be detected by cognitive tests, but do not cause functional decline—or dementia within 7 years.3 Studies also have suggested that SCI may be a pre-MCI stage of subsequent dementia.11-13 AD generally has a long (10 to 12 years) and progressive prodromal phase before dementia onset and is characterized by successive emergence of cognitive deficits, memory complaints, depressive symptoms, and functional impairment.14
In light of this research, we believe patients with SCI and other risk factors for AD, such as a family history of AD, may be at higher risk of further cognitive and functional decline compared with individuals with ARCD and no AD risk factors. Therefore, patients with SCI and other risk factors for AD (Table 2)15-19 may benefit from annual follow-up to determine if cognitive problems have progressed to MCI or AD.
SCI may be a response to subclinical alterations in neurobiology—a phenomenon known as reverse causality.20 Biomarkers, such as cerebrospinal fluid levels of ß-amyloid and phosphorylated tau, and amyloid imaging using positron emission tomography may help identify AD in SCI patients.21 In these patients, SCI is a misnomer because the cognitive impairment is real—not “subjective”—but current tests are not sensitive enough to detect the cognitive decline the patient has recognized. This group of patients should be differentiated from individuals who may perceive typical cognitive aging (ARCD) as pathologic and complain about it. In the future, biomarkers may help differentiate these 2 groups.
Table 2
Factors that increase SCI patients’ risk for dementia
| Family history of Alzheimer’s disease |
| Mild behavioral impairment |
| Slow gait |
| Depression |
| Rapid weight loss |
| Multiple subtle neurologic abnormalities |
| Vascular disease (eg, peripheral vascular disease, coronary artery disease, cerebrovascular disease) |
| SCI: subjective cognitive impairment Source: References 15-19 |
Mild cognitive impairment
MCI is similar to SCI because MCI patients may present with complaints of memory decline and other cognitive difficulties22 but neither condition is associated with significant impairment of daily activities.23 The key difference is that patients with MCI demonstrate impaired performance on objective cognitive tests whereas SCI patients do not.24 In our experience, office-based tests do not reliably differentiate the 2 conditions because many patients with SCI may show mild impairment in tests such as the Mini-Mental State Exam (MMSE)25 but comprehensive neuropsychological testing reveals no objective cognitive deficits. Neuropsychological testing is essential to reliably differentiate SCI from MCI.
The distinction between SCI and MCI is clinically relevant because evidence suggests that MCI patients have a near-term risk of developing dementia, particularly AD.22,23 In a longitudinal study of 76 individuals with MCI, 12% of patients progressed to AD each year compared with 1% to 2% of healthy older adults.26 Patients with MCI are at increased risk of delirium (especially during hospitalization), falls, medication errors, and difficulty managing their finances.24 Older adults with MCI also have increased mortality compared with older adults with normal cognitive functioning.22 Both SCI and MCI should be differentiated from mild dementia. Common dementias in older adults include:
- AD dementia
- Vascular dementia (may occur with or without AD)
- Lewy body dementia
- Frontotemporal dementia
- Parkinson’s disease dementia.
By definition, all dementia types are associated with impaired ability to perform daily activities and cognitive decline.27
Assessing cognitive complaints
Evaluation of older adults’ cognitive complaints should begin with a thorough history to elicit symptoms of anxiety, depression, physical complaints, and any associated functional decline; a physical exam; and a comprehensive mental status examination. This initial evaluation should be followed by routine and specific investigations as indicated (Table 3).22,24,28,29
In a 6-year study of 100 older adults with and without objective evidence of memory decline, both groups showed similar rates of cognitive complaints.30 Also, researchers found no relationship between individuals’ perception of their cognitive functioning and performance on neuropsychological testing. Mood, education level, and apolipoprotein E epsilon 4 genotype status also did not correlate with participants’ subjective cognitive complaints. These findings highlight the need for objective test data to determine whether older adults’ memory complaints reflect pathologic changes in cognition. After a thorough diagnostic workup, some patients complaining of memory decline will have no detectable evidence of cognitive dysfunction or an identifiable cause. However, others may have identifiable causes of memory impairment (Table 4)28,29,31,32—which could be treated—some will have MCI, and others may be in an early stage of dementia.
Table 3
Investigation of older adults with SCI
| Investigation | Rationale |
|---|---|
| Routine | |
| Neuropsychological testing | Delineation of cognitive syndromes (SCI vs MCI vs AD*) |
| Hematology (full blood count) | Screen for anemia |
| Biochemistry (electrolytes, renal function, liver function, thyroid function, B12, and folate) | Screen for treatable causes of cognitive complaints |
| For specific indication suggested by history, physical exam, or neuropsychological testing | |
| Neuroimaging | Generalized and regional imaging (eg, hippocampal atrophy, space occupying lesions) |
| Electroencephalography | Epilepsy/seizures (especially absence and complex partial) |
| Cardiac (eg, echocardiography) | May reveal cardiac arrhythmia or sources of emboli |
| Inflammatory markers (eg, ESR) | Screen for inflammatory processes |
| Treponemal serology | Tertiary syphilis |
| *Alzheimer’s disease and other dementias AD: Alzheimer’s disease; ESR: erythrocyte sedimentation rate; MCI: mild cognitive impairment; SCI: subjective cognitive impairment Source: References 22,24,28,29 | |
Table 4
Differential diagnosis of SCI
| Cause of cognitive impairment | Potential mechanism |
|---|---|
| ARCD | Allostatic load, ‘wear and tear’ from a lifetime of physiological or psychological stresses and adaptations |
| Anemia | Neuronal hypoxia |
| Alzheimer’s disease | Amyloid and/or tau-mediated neurotoxicity, neuroinflammation |
| Cerebrovascular disease | Neuronal ischemia and hypoxia, neuroinflammation |
| Vitamin deficiencies (eg, B1, B12, folate, D) | Impaired neuronal and neurotransmitter function |
| Inadequate protein intake | Impaired neuronal function |
| Anticholinergic drug use | Decreased cholinergic neurotransmission |
| Alcohol use | Direct neurotoxicity and indirect causes such as malnutrition or head injury |
| Depression, anxiety | Hippocampal dysfunction with or without atrophy |
| Obstructive sleep apnea | Neuronal hypoxia, neuroinflammation |
| Head injury | Neuronal and synaptic loss |
| ARCD: age-related cognitive decline; SCI: subjective cognitive impairment Source: References 28,29,31,32 | |
CASE CONTINUED: No measurable deficits
Ms. F’s medical history is remarkable for coronary artery disease, hypothyroidism, hypertension, hyperlipidemia, cataracts, arthritis, back surgery (secondary to spondylosis), and foot surgery. Ms. F denies a history of alcohol or illicit substance abuse. She smoked tobacco for 30 years (2 packs per day), but quit 5 years ago after her heart attack. Physical exam is unremarkable except for mild obesity (body mass index = 31 kg/m2).
Ms. F’s mental status exam reveals anxious mood and affect. Her recall is 2 out of 3 items. Her MMSE score is 29/30 (1 point lost on recall) and her Geriatric Depression Scale33 score is 2/15, indicating minimal depressive symptoms. On neuropsychological testing, Ms. F demonstrates high average intellectual abilities; compared with others her age, she performs within expectations on all measures. That is, she performs within the above-average to low-average range on measures of attention, working memory, speed of processing, expressive language, learning, memory, visual spatial abilities, executive functioning, and knowledge of basic health and safety information.
Enhancing neuroplasticity
We recommend neuroplasticity-based interventions to treat SCI and promote healthy brain aging.20,29 For a checklist clinicians can use to promote healthy brain aging and thus improve patients’ cognitive health see this article at CurrentPsychiatry. com. Table 51,29 lists cognitive strategies to improve memory and maintain cognitive vitality.
Enhancing brain plasticity and neurogenesis requires engaging older adults in demanding sensory, cognitive, and motor activities on an intensive basis.34 Therapeutic stimulation of neuroplasticity and neurogenesis might contribute to functional “repair” of the diseased adult brain before damage to whole neuronal networks has ensued.29 An important treatment component is reassuring patients with SCI that they do not have AD or MCI. Treating comorbid anxiety and depression and reversible causes of cognitive complaints is key to successful outcomes.
Table 5
Strategies to improve memory and maintain cognitive vitality
| Strategy | Description |
|---|---|
| Mindfulness | Focus on 1 task at a time rather than trying to multitask. Research shows that cognition is more efficient in this manner |
| Cognitive strategies | Use mnemonics (such as ROY G BIV to remember the colors of the rainbow). Make associations for information, such as when meeting someone new, relate their name to someone else you know well. Use cues such as memory notebooks to prompt information recall. Engage in learning new and challenging cognitive activities, such as a new language, a music instrument, or dance. Consider computer-based brain exercises |
| Rehearsal | Practice information you want to remember, such as repeating the information several times or writing it down |
| Be patient | Getting frustrated when you have memory difficulties makes it more challenging to remember information |
| Exercise (mental and physical) | Engage in mental activities, such as reading and crossword puzzles. Do something that you are interested in, rather than making it a chore. Research has demonstrated that physical exercise also aids memory |
| Diet | What is good for the heart is good for the brain. Fruits, vegetables, food rich in omega-3 fatty acids (eg, fatty fish such as salmon), whole grains, spices (eg, turmeric), and small amounts of tree nuts (eg, walnuts) are recommended as part of a balanced diet |
| Source: References 1,29 | |
CASE CONTINUED: Reassurance and risk reduction
Ms. F’s psychiatrist reassures her that she does not have AD. She receives genetic counseling and decides to forgo genetic testing. Her psychiatrist educates Ms. F about the risks of OTC supplements—especially increased risk of bleeding because she takes aspirin and clopidogrel—and lack of data supporting their use. Ms. F is counseled that a healthy lifestyle, including regular exercise, Mediterranean diet with increased intake of omega-3 fatty acids, learning new things, and being socially active, is the safest way to promote brain health. Over 3 months, Ms. F discontinues all supplements except the vitamins and omega-3, starts exercising, resumes piano lessons that she stopped 10 years ago, and becomes a vegetarian. She continues to have mild SCI but she says she is not bothered by it and feels satisfied that she is doing all she can to promote her brain health.
Related Resources
- Desai AK. Healthy brain aging: evidence based methods to preserve brain function and prevent dementia. Philadelphia, PA: W. B. Saunders; 2010.
- Doidge N. The brain that changes itself. New York, NY: Penguin Books; 2007.
- Vance DE, Roberson AJ, McGuinness TM, et al. How neuroplasticity and cognitive reserve protect cognitive functioning. J Psychosoc Nurs Ment Health Serv. 2010; 48: 1-8.
Brain Training Resources
- Weil A, Small G. The healthy brain kit. Boulder, CO: Sounds True, Inc.; 2007. Audio CDs, brain-training cards and workbooks.
- Posit Science. www.positscience.com.
- Sharp Brains. www.sharpbrains.com.
Drug Brand Names
- Atenolol • Tenormin
- Atorvastatin • Lipitor
- Clopidogrel • Plavix
- Levothyroxine • Levoxyl, Synthroid
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
Abhilash K. Desai, MD, discusses emerging research on biomarkers that may help clarify diagnosis.
1. Small GW. What we need to know about age related memory loss. BMJ. 2002;324:1502-1505.
2. Hayes TL, Larimer N, Adami A, et al. Medication adherence in healthy elders. J Aging Health. 2009;21(4):567-580.
3. Reisberg B, Shulman MB, Torossian C, et al. Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement. 2010;6(1):11-24.
4. Jessen F, Wiese B, Bachmann C, et al. Prediction of dementia by subjective memory impairments: effects of severity and temporal association with cognitive impairment. Arch Gen Psychiatry. 2010;67:414-422.
5. Waldorff FB, Siersma V, Waldemar G. Association between subjective memory complaints and nursing home placement: a four-year follow-up. Int J Geriatr Psychiatry. 2009;24(6):602-609.
6. Salthouse TA. Selective review of cognitive aging. J Int Neuropsychol Soc. 2010;16:754-760.
7. Anderton B. Ageing of the brain. Mech Ageing Dev. 2002;23:811-817.
8. Salthouse TA. Influence of age on practice effects in longitudinal neurocognitive change. Neuropsychology. 2010;24(5):563-572.
9. Park D, Schwarz N. Cognitive aging: a primer. Philadelphia PA: Taylor and Francis Group; 2000.
10. Reisberg B, Shulman MB. Commentary on “a roadmap for the prevention of dementia II: Leon Thal Symposium 2008.” Subjective cognitive impairment as an antecedent of Alzheimer’s dementia: policy import. Alzheimers Dement. 2009;5:154-156.
11. Reisberg B, Gauthier S. Current evidence for subjective cognitive impairment (SCI) as the pre-mild cognitive impairment (MCI) stage of subsequently manifest Alzheimer’s disease. Int Psychogeriatr. 2008;20(1):1-16.
12. Mosconi L, Pupi A, De Leon MJ. Brain glucose hypometabolism and oxidative stress in preclinical Alzheimer’s disease. Ann N Y Acad Sci. 2008;1147:180-195.
13. Ramakers IH, Visser PJ, Aalten P, et al. Symptoms of preclinical dementia in general practice up to five years before dementia diagnosis. Dement Geriatr Cogn Disord. 2007;24(4):300-306.
14. Amieva H, Le Goff M, Millet X, et al. Prodromal Alzheimer’s disease: successive emergence of the clinical symptoms. Ann Neurol. 2008;64(5):492-498.
15. Taragano FE, Allegri RF, Krupitzki H, et al. Mild behavioral impairment and risk of dementia: a prospective cohort study of 358 patients. J Clin Psychiatry. 2009;70(4):584-592.
16. Jayadev S, Steinbart EJ, Chi YY, et al. Conjugal Alzheimer disease: risk in children when both parents have Alzheimer disease. Arch Neurol. 2008;65(3):373-378.
17. Hajjar I, Yang F, Sorond F, et al. A novel aging phenotype of slow gait, impaired executive function, and depressive symptoms: relationship to blood pressure and other cardiovascular risks. J Gerontol A Biol Sci Med Sci. 2009;64(9):994-1001.
18. Yamamoto N, Yamanaka G, Ishikawa M, et al. Cardio-ankle vascular index as a predictor of cognitive impairment in community-dwelling elderly people: four-year follow-up. Dement Geriatr Cogn Disord. 2009;28(2):153-158.
19. Inzitari M, Pozzi C, Ferrucci L, et al. Subtle neurological abnormalities as risk factors for cognitive and functional decline, cerebrovascular events, and mortality in older community-dwelling adults. Arch Intern Med. 2008;168(12):1270-1276.
20. Shineman DW, Salthouse TA, Launer LJ, et al. Therapeutics of cognitive aging. Ann N Y Acad Sci. 2010;1191(suppl 1):E1-E10.
21. Dubois B, Feldman HH, Jacova C, et al. Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol. 2010;9:1118-1127.
22. Chertkow H, Massoud F, Nasreddine Z, et al. Diagnosis and treatment of dementia: 3. Mild cognitive impairment and cognitive impairment without dementia. CMAJ. 2008;178(10):1273-1285.
23. Rosenberg PB, Lyketsos C. Mild cognitive impairment: searching for the prodrome of Alzheimer’s disease. World Psychiatry. 2008;7(2):72-78.
24. Rosenberg PB, Johnston D, Lyketsos CG. A clinical approach to mild cognitive impairment. Am J Psychiatry. 2006;163(11):1884-1890.
25. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198.
26. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303-308.
27. Diagnostic and statistical manual of mental disorders. 4th ed text rev. Washington, DC: American Psychiatric Association; 2000:135–180.
28. Malhotra R, Desai AK. Healthy brain aging: what has sleep got to do with it? Clin Geriatr Med. 2010;26:45-56.
29. Desai AK, Grossberg GT, Chibnall JT. Healthy brain aging: a road map. Clin Geriatr Med. 2010;26:1-16.
30. Weaver Cargin J, Collie A, Masters C, et al. The nature of cognitive complaints in healthy older adults with and without objective memory decline. J Clin Exp Neuropsychol. 2008;30:245-257.
31. Wilson RS, Arnold SE, Schneider JA, et al. Chronic distress, age-related neuropathology, and late-life dementia. Psychosom Med. 2007;69:47-53.
32. Deal JA, Carlson MC, Xue Q, et al. Anemia and 9-year domain-specific cognitive decline in community-dwelling older women: the Women’s Health and Aging Study II. J Am Geriatr Soc. 2009;57(9):1604-1611.
33. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression scale: a preliminary report. J Psychiatr Res. 1983;17:37-49.
34. Mahncke HW, Bronstone A, Merzenich MM. Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Prog Brain Res. 2006;157:81-109.
MS. F, age 66, requests genetic testing because she is concerned about mild memory difficulties, such as forgetting names and where she puts her keys or checkbook, and fears she may be developing Alzheimer’s disease (AD). Her mother and sister were diagnosed with AD in their early 60s. Ms. F has 20 years of education and reports no problems with driving, managing her finances, remembering to take her medications, or maintaining social activities, which her husband confirms.
Detailed questioning about anxiety and depressive symptoms reveals substantial worries about future cognitive decline and some concerns about her finances and her husband’s health. Ms. F says she occasionally feels down and has low energy but denies other depressive symptoms. She reports no sleep disturbances—including snoring and daytime sleepiness, which could indicate obstructive sleep apnea—which her husband confirms. Ms. F takes levothyroxine for hypothyroidism, atenolol for hypertension, aspirin and clopidogrel for coronary artery disease, and atorvastatin for hyperlipidemia. In addition, she provides a long list of over-the-counter (OTC) supplements—ginkgo, huperzine, ginseng, phosphatidylserine, B1, B12, folate, vitamin D, alpha-lipoic acid, and vinpocetine—that she takes to “protect” her brain from AD.
Subjective cognitive impairment (SCI) in older persons is a common condition with a largely unclear prognosis. Many older adults (age ≥65) express concern about mild cognitive problems—“senior moments”—such as word-finding difficulties and forgetfulness.1 Individuals may wonder if walking into a room only to forget why might be the first sign of dementia. Some older adults try to counteract these memory problems by engaging in brain exercises—including costly computer games—and taking OTC “brain-enhancing” vitamins, herbal remedies, and other supplements.
Although some clinicians may view SCI as benign, that is not always true (Table l).2-5 This article discusses the clinical significance of these mild cognitive complaints by examining:
- age-related cognitive decline (ARCD)
- SCI
- how SCI can be differentiated from more serious conditions, such as mild cognitive impairment (MCI) and early stages of AD and other dementias.
We also will discuss assessing and treating cognitive complaints. Although distinctions between SCI and ARCD may be controversial, evidence suggests clinicians need to adopt a more nuanced clinical approach.
Table 1
Why SCI should be taken seriously
| SCI may create emotional distress because patients are aware of decline in their ‘mental sharpness’ |
| SCI patients might consume unnecessary and potentially harmful OTC supplements touted to promote memory |
| Patients might limit their driving and financial management to avoid making mistakes |
| SCI might impair medication adherence2 |
| SCI may be an early sign of dementia3 |
| Patients’ worry about their self-perceived memory loss might predict dementia4 |
| SCI may predict nursing home placement5 |
| Addressing SCI gives health care providers an opportunity to address anxiety or depression that often accompany SCI |
| Evaluation of potential causes of SCI may uncover reversible conditions that can be treated |
| OTC: over-the-counter; SCI: subjective cognitive impairment |
‘Normal’ cognitive decline
ARCD is subtle decline in cognitive abilities, such as episodic memory, attention, and time needed to complete complex activities.6,7 Individuals with ARCD might not have subjective memory complaints or objective cognitive deficits, and their ability to live independently may not be compromised.7 The degree of decline in ARCD may be smaller than previously thought.8 Park9 summarizes 4 main mechanisms thought to underlie age-related declines in cognition:
- reduced speed of processing
- decreased working memory capabilities
- declining inhibitory control (eg, impaired complex attentional capabilities)
- sensory changes (eg, visual and auditory deficits).
ARCD traditionally is thought to result from predictable changes in the brain associated with aging, such as reduced brain volume in the hippocampus and frontal lobes, loss of myelin, loss of synapses, and cytoskeletal changes.7 However, not all older adults experience ARCD. Some remain highly functional in their later years and continue to actively engage in life well into very old age.6,9
Subjective cognitive impairment
One-quarter to one-half of community-dwelling older adults report subjective cognitive complaints, such as forgetfulness and word-finding difficulties.10 Patients with SCI do not show objective evidence of cognitive impairment on neuropsychological tests and their cognitive problems cause no functional decline.10
Preliminary evidence indicates that SCI may be a harbinger of further cognitive decline. Reisberg et al3 found that compared with patients without SCI, patients with SCI were 4.5 times more likely to develop MCI—cognitive difficulties that can be detected by cognitive tests, but do not cause functional decline—or dementia within 7 years.3 Studies also have suggested that SCI may be a pre-MCI stage of subsequent dementia.11-13 AD generally has a long (10 to 12 years) and progressive prodromal phase before dementia onset and is characterized by successive emergence of cognitive deficits, memory complaints, depressive symptoms, and functional impairment.14
In light of this research, we believe patients with SCI and other risk factors for AD, such as a family history of AD, may be at higher risk of further cognitive and functional decline compared with individuals with ARCD and no AD risk factors. Therefore, patients with SCI and other risk factors for AD (Table 2)15-19 may benefit from annual follow-up to determine if cognitive problems have progressed to MCI or AD.
SCI may be a response to subclinical alterations in neurobiology—a phenomenon known as reverse causality.20 Biomarkers, such as cerebrospinal fluid levels of ß-amyloid and phosphorylated tau, and amyloid imaging using positron emission tomography may help identify AD in SCI patients.21 In these patients, SCI is a misnomer because the cognitive impairment is real—not “subjective”—but current tests are not sensitive enough to detect the cognitive decline the patient has recognized. This group of patients should be differentiated from individuals who may perceive typical cognitive aging (ARCD) as pathologic and complain about it. In the future, biomarkers may help differentiate these 2 groups.
Table 2
Factors that increase SCI patients’ risk for dementia
| Family history of Alzheimer’s disease |
| Mild behavioral impairment |
| Slow gait |
| Depression |
| Rapid weight loss |
| Multiple subtle neurologic abnormalities |
| Vascular disease (eg, peripheral vascular disease, coronary artery disease, cerebrovascular disease) |
| SCI: subjective cognitive impairment Source: References 15-19 |
Mild cognitive impairment
MCI is similar to SCI because MCI patients may present with complaints of memory decline and other cognitive difficulties22 but neither condition is associated with significant impairment of daily activities.23 The key difference is that patients with MCI demonstrate impaired performance on objective cognitive tests whereas SCI patients do not.24 In our experience, office-based tests do not reliably differentiate the 2 conditions because many patients with SCI may show mild impairment in tests such as the Mini-Mental State Exam (MMSE)25 but comprehensive neuropsychological testing reveals no objective cognitive deficits. Neuropsychological testing is essential to reliably differentiate SCI from MCI.
The distinction between SCI and MCI is clinically relevant because evidence suggests that MCI patients have a near-term risk of developing dementia, particularly AD.22,23 In a longitudinal study of 76 individuals with MCI, 12% of patients progressed to AD each year compared with 1% to 2% of healthy older adults.26 Patients with MCI are at increased risk of delirium (especially during hospitalization), falls, medication errors, and difficulty managing their finances.24 Older adults with MCI also have increased mortality compared with older adults with normal cognitive functioning.22 Both SCI and MCI should be differentiated from mild dementia. Common dementias in older adults include:
- AD dementia
- Vascular dementia (may occur with or without AD)
- Lewy body dementia
- Frontotemporal dementia
- Parkinson’s disease dementia.
By definition, all dementia types are associated with impaired ability to perform daily activities and cognitive decline.27
Assessing cognitive complaints
Evaluation of older adults’ cognitive complaints should begin with a thorough history to elicit symptoms of anxiety, depression, physical complaints, and any associated functional decline; a physical exam; and a comprehensive mental status examination. This initial evaluation should be followed by routine and specific investigations as indicated (Table 3).22,24,28,29
In a 6-year study of 100 older adults with and without objective evidence of memory decline, both groups showed similar rates of cognitive complaints.30 Also, researchers found no relationship between individuals’ perception of their cognitive functioning and performance on neuropsychological testing. Mood, education level, and apolipoprotein E epsilon 4 genotype status also did not correlate with participants’ subjective cognitive complaints. These findings highlight the need for objective test data to determine whether older adults’ memory complaints reflect pathologic changes in cognition. After a thorough diagnostic workup, some patients complaining of memory decline will have no detectable evidence of cognitive dysfunction or an identifiable cause. However, others may have identifiable causes of memory impairment (Table 4)28,29,31,32—which could be treated—some will have MCI, and others may be in an early stage of dementia.
Table 3
Investigation of older adults with SCI
| Investigation | Rationale |
|---|---|
| Routine | |
| Neuropsychological testing | Delineation of cognitive syndromes (SCI vs MCI vs AD*) |
| Hematology (full blood count) | Screen for anemia |
| Biochemistry (electrolytes, renal function, liver function, thyroid function, B12, and folate) | Screen for treatable causes of cognitive complaints |
| For specific indication suggested by history, physical exam, or neuropsychological testing | |
| Neuroimaging | Generalized and regional imaging (eg, hippocampal atrophy, space occupying lesions) |
| Electroencephalography | Epilepsy/seizures (especially absence and complex partial) |
| Cardiac (eg, echocardiography) | May reveal cardiac arrhythmia or sources of emboli |
| Inflammatory markers (eg, ESR) | Screen for inflammatory processes |
| Treponemal serology | Tertiary syphilis |
| *Alzheimer’s disease and other dementias AD: Alzheimer’s disease; ESR: erythrocyte sedimentation rate; MCI: mild cognitive impairment; SCI: subjective cognitive impairment Source: References 22,24,28,29 | |
Table 4
Differential diagnosis of SCI
| Cause of cognitive impairment | Potential mechanism |
|---|---|
| ARCD | Allostatic load, ‘wear and tear’ from a lifetime of physiological or psychological stresses and adaptations |
| Anemia | Neuronal hypoxia |
| Alzheimer’s disease | Amyloid and/or tau-mediated neurotoxicity, neuroinflammation |
| Cerebrovascular disease | Neuronal ischemia and hypoxia, neuroinflammation |
| Vitamin deficiencies (eg, B1, B12, folate, D) | Impaired neuronal and neurotransmitter function |
| Inadequate protein intake | Impaired neuronal function |
| Anticholinergic drug use | Decreased cholinergic neurotransmission |
| Alcohol use | Direct neurotoxicity and indirect causes such as malnutrition or head injury |
| Depression, anxiety | Hippocampal dysfunction with or without atrophy |
| Obstructive sleep apnea | Neuronal hypoxia, neuroinflammation |
| Head injury | Neuronal and synaptic loss |
| ARCD: age-related cognitive decline; SCI: subjective cognitive impairment Source: References 28,29,31,32 | |
CASE CONTINUED: No measurable deficits
Ms. F’s medical history is remarkable for coronary artery disease, hypothyroidism, hypertension, hyperlipidemia, cataracts, arthritis, back surgery (secondary to spondylosis), and foot surgery. Ms. F denies a history of alcohol or illicit substance abuse. She smoked tobacco for 30 years (2 packs per day), but quit 5 years ago after her heart attack. Physical exam is unremarkable except for mild obesity (body mass index = 31 kg/m2).
Ms. F’s mental status exam reveals anxious mood and affect. Her recall is 2 out of 3 items. Her MMSE score is 29/30 (1 point lost on recall) and her Geriatric Depression Scale33 score is 2/15, indicating minimal depressive symptoms. On neuropsychological testing, Ms. F demonstrates high average intellectual abilities; compared with others her age, she performs within expectations on all measures. That is, she performs within the above-average to low-average range on measures of attention, working memory, speed of processing, expressive language, learning, memory, visual spatial abilities, executive functioning, and knowledge of basic health and safety information.
Enhancing neuroplasticity
We recommend neuroplasticity-based interventions to treat SCI and promote healthy brain aging.20,29 For a checklist clinicians can use to promote healthy brain aging and thus improve patients’ cognitive health see this article at CurrentPsychiatry. com. Table 51,29 lists cognitive strategies to improve memory and maintain cognitive vitality.
Enhancing brain plasticity and neurogenesis requires engaging older adults in demanding sensory, cognitive, and motor activities on an intensive basis.34 Therapeutic stimulation of neuroplasticity and neurogenesis might contribute to functional “repair” of the diseased adult brain before damage to whole neuronal networks has ensued.29 An important treatment component is reassuring patients with SCI that they do not have AD or MCI. Treating comorbid anxiety and depression and reversible causes of cognitive complaints is key to successful outcomes.
Table 5
Strategies to improve memory and maintain cognitive vitality
| Strategy | Description |
|---|---|
| Mindfulness | Focus on 1 task at a time rather than trying to multitask. Research shows that cognition is more efficient in this manner |
| Cognitive strategies | Use mnemonics (such as ROY G BIV to remember the colors of the rainbow). Make associations for information, such as when meeting someone new, relate their name to someone else you know well. Use cues such as memory notebooks to prompt information recall. Engage in learning new and challenging cognitive activities, such as a new language, a music instrument, or dance. Consider computer-based brain exercises |
| Rehearsal | Practice information you want to remember, such as repeating the information several times or writing it down |
| Be patient | Getting frustrated when you have memory difficulties makes it more challenging to remember information |
| Exercise (mental and physical) | Engage in mental activities, such as reading and crossword puzzles. Do something that you are interested in, rather than making it a chore. Research has demonstrated that physical exercise also aids memory |
| Diet | What is good for the heart is good for the brain. Fruits, vegetables, food rich in omega-3 fatty acids (eg, fatty fish such as salmon), whole grains, spices (eg, turmeric), and small amounts of tree nuts (eg, walnuts) are recommended as part of a balanced diet |
| Source: References 1,29 | |
CASE CONTINUED: Reassurance and risk reduction
Ms. F’s psychiatrist reassures her that she does not have AD. She receives genetic counseling and decides to forgo genetic testing. Her psychiatrist educates Ms. F about the risks of OTC supplements—especially increased risk of bleeding because she takes aspirin and clopidogrel—and lack of data supporting their use. Ms. F is counseled that a healthy lifestyle, including regular exercise, Mediterranean diet with increased intake of omega-3 fatty acids, learning new things, and being socially active, is the safest way to promote brain health. Over 3 months, Ms. F discontinues all supplements except the vitamins and omega-3, starts exercising, resumes piano lessons that she stopped 10 years ago, and becomes a vegetarian. She continues to have mild SCI but she says she is not bothered by it and feels satisfied that she is doing all she can to promote her brain health.
Related Resources
- Desai AK. Healthy brain aging: evidence based methods to preserve brain function and prevent dementia. Philadelphia, PA: W. B. Saunders; 2010.
- Doidge N. The brain that changes itself. New York, NY: Penguin Books; 2007.
- Vance DE, Roberson AJ, McGuinness TM, et al. How neuroplasticity and cognitive reserve protect cognitive functioning. J Psychosoc Nurs Ment Health Serv. 2010; 48: 1-8.
Brain Training Resources
- Weil A, Small G. The healthy brain kit. Boulder, CO: Sounds True, Inc.; 2007. Audio CDs, brain-training cards and workbooks.
- Posit Science. www.positscience.com.
- Sharp Brains. www.sharpbrains.com.
Drug Brand Names
- Atenolol • Tenormin
- Atorvastatin • Lipitor
- Clopidogrel • Plavix
- Levothyroxine • Levoxyl, Synthroid
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
Abhilash K. Desai, MD, discusses emerging research on biomarkers that may help clarify diagnosis.
MS. F, age 66, requests genetic testing because she is concerned about mild memory difficulties, such as forgetting names and where she puts her keys or checkbook, and fears she may be developing Alzheimer’s disease (AD). Her mother and sister were diagnosed with AD in their early 60s. Ms. F has 20 years of education and reports no problems with driving, managing her finances, remembering to take her medications, or maintaining social activities, which her husband confirms.
Detailed questioning about anxiety and depressive symptoms reveals substantial worries about future cognitive decline and some concerns about her finances and her husband’s health. Ms. F says she occasionally feels down and has low energy but denies other depressive symptoms. She reports no sleep disturbances—including snoring and daytime sleepiness, which could indicate obstructive sleep apnea—which her husband confirms. Ms. F takes levothyroxine for hypothyroidism, atenolol for hypertension, aspirin and clopidogrel for coronary artery disease, and atorvastatin for hyperlipidemia. In addition, she provides a long list of over-the-counter (OTC) supplements—ginkgo, huperzine, ginseng, phosphatidylserine, B1, B12, folate, vitamin D, alpha-lipoic acid, and vinpocetine—that she takes to “protect” her brain from AD.
Subjective cognitive impairment (SCI) in older persons is a common condition with a largely unclear prognosis. Many older adults (age ≥65) express concern about mild cognitive problems—“senior moments”—such as word-finding difficulties and forgetfulness.1 Individuals may wonder if walking into a room only to forget why might be the first sign of dementia. Some older adults try to counteract these memory problems by engaging in brain exercises—including costly computer games—and taking OTC “brain-enhancing” vitamins, herbal remedies, and other supplements.
Although some clinicians may view SCI as benign, that is not always true (Table l).2-5 This article discusses the clinical significance of these mild cognitive complaints by examining:
- age-related cognitive decline (ARCD)
- SCI
- how SCI can be differentiated from more serious conditions, such as mild cognitive impairment (MCI) and early stages of AD and other dementias.
We also will discuss assessing and treating cognitive complaints. Although distinctions between SCI and ARCD may be controversial, evidence suggests clinicians need to adopt a more nuanced clinical approach.
Table 1
Why SCI should be taken seriously
| SCI may create emotional distress because patients are aware of decline in their ‘mental sharpness’ |
| SCI patients might consume unnecessary and potentially harmful OTC supplements touted to promote memory |
| Patients might limit their driving and financial management to avoid making mistakes |
| SCI might impair medication adherence2 |
| SCI may be an early sign of dementia3 |
| Patients’ worry about their self-perceived memory loss might predict dementia4 |
| SCI may predict nursing home placement5 |
| Addressing SCI gives health care providers an opportunity to address anxiety or depression that often accompany SCI |
| Evaluation of potential causes of SCI may uncover reversible conditions that can be treated |
| OTC: over-the-counter; SCI: subjective cognitive impairment |
‘Normal’ cognitive decline
ARCD is subtle decline in cognitive abilities, such as episodic memory, attention, and time needed to complete complex activities.6,7 Individuals with ARCD might not have subjective memory complaints or objective cognitive deficits, and their ability to live independently may not be compromised.7 The degree of decline in ARCD may be smaller than previously thought.8 Park9 summarizes 4 main mechanisms thought to underlie age-related declines in cognition:
- reduced speed of processing
- decreased working memory capabilities
- declining inhibitory control (eg, impaired complex attentional capabilities)
- sensory changes (eg, visual and auditory deficits).
ARCD traditionally is thought to result from predictable changes in the brain associated with aging, such as reduced brain volume in the hippocampus and frontal lobes, loss of myelin, loss of synapses, and cytoskeletal changes.7 However, not all older adults experience ARCD. Some remain highly functional in their later years and continue to actively engage in life well into very old age.6,9
Subjective cognitive impairment
One-quarter to one-half of community-dwelling older adults report subjective cognitive complaints, such as forgetfulness and word-finding difficulties.10 Patients with SCI do not show objective evidence of cognitive impairment on neuropsychological tests and their cognitive problems cause no functional decline.10
Preliminary evidence indicates that SCI may be a harbinger of further cognitive decline. Reisberg et al3 found that compared with patients without SCI, patients with SCI were 4.5 times more likely to develop MCI—cognitive difficulties that can be detected by cognitive tests, but do not cause functional decline—or dementia within 7 years.3 Studies also have suggested that SCI may be a pre-MCI stage of subsequent dementia.11-13 AD generally has a long (10 to 12 years) and progressive prodromal phase before dementia onset and is characterized by successive emergence of cognitive deficits, memory complaints, depressive symptoms, and functional impairment.14
In light of this research, we believe patients with SCI and other risk factors for AD, such as a family history of AD, may be at higher risk of further cognitive and functional decline compared with individuals with ARCD and no AD risk factors. Therefore, patients with SCI and other risk factors for AD (Table 2)15-19 may benefit from annual follow-up to determine if cognitive problems have progressed to MCI or AD.
SCI may be a response to subclinical alterations in neurobiology—a phenomenon known as reverse causality.20 Biomarkers, such as cerebrospinal fluid levels of ß-amyloid and phosphorylated tau, and amyloid imaging using positron emission tomography may help identify AD in SCI patients.21 In these patients, SCI is a misnomer because the cognitive impairment is real—not “subjective”—but current tests are not sensitive enough to detect the cognitive decline the patient has recognized. This group of patients should be differentiated from individuals who may perceive typical cognitive aging (ARCD) as pathologic and complain about it. In the future, biomarkers may help differentiate these 2 groups.
Table 2
Factors that increase SCI patients’ risk for dementia
| Family history of Alzheimer’s disease |
| Mild behavioral impairment |
| Slow gait |
| Depression |
| Rapid weight loss |
| Multiple subtle neurologic abnormalities |
| Vascular disease (eg, peripheral vascular disease, coronary artery disease, cerebrovascular disease) |
| SCI: subjective cognitive impairment Source: References 15-19 |
Mild cognitive impairment
MCI is similar to SCI because MCI patients may present with complaints of memory decline and other cognitive difficulties22 but neither condition is associated with significant impairment of daily activities.23 The key difference is that patients with MCI demonstrate impaired performance on objective cognitive tests whereas SCI patients do not.24 In our experience, office-based tests do not reliably differentiate the 2 conditions because many patients with SCI may show mild impairment in tests such as the Mini-Mental State Exam (MMSE)25 but comprehensive neuropsychological testing reveals no objective cognitive deficits. Neuropsychological testing is essential to reliably differentiate SCI from MCI.
The distinction between SCI and MCI is clinically relevant because evidence suggests that MCI patients have a near-term risk of developing dementia, particularly AD.22,23 In a longitudinal study of 76 individuals with MCI, 12% of patients progressed to AD each year compared with 1% to 2% of healthy older adults.26 Patients with MCI are at increased risk of delirium (especially during hospitalization), falls, medication errors, and difficulty managing their finances.24 Older adults with MCI also have increased mortality compared with older adults with normal cognitive functioning.22 Both SCI and MCI should be differentiated from mild dementia. Common dementias in older adults include:
- AD dementia
- Vascular dementia (may occur with or without AD)
- Lewy body dementia
- Frontotemporal dementia
- Parkinson’s disease dementia.
By definition, all dementia types are associated with impaired ability to perform daily activities and cognitive decline.27
Assessing cognitive complaints
Evaluation of older adults’ cognitive complaints should begin with a thorough history to elicit symptoms of anxiety, depression, physical complaints, and any associated functional decline; a physical exam; and a comprehensive mental status examination. This initial evaluation should be followed by routine and specific investigations as indicated (Table 3).22,24,28,29
In a 6-year study of 100 older adults with and without objective evidence of memory decline, both groups showed similar rates of cognitive complaints.30 Also, researchers found no relationship between individuals’ perception of their cognitive functioning and performance on neuropsychological testing. Mood, education level, and apolipoprotein E epsilon 4 genotype status also did not correlate with participants’ subjective cognitive complaints. These findings highlight the need for objective test data to determine whether older adults’ memory complaints reflect pathologic changes in cognition. After a thorough diagnostic workup, some patients complaining of memory decline will have no detectable evidence of cognitive dysfunction or an identifiable cause. However, others may have identifiable causes of memory impairment (Table 4)28,29,31,32—which could be treated—some will have MCI, and others may be in an early stage of dementia.
Table 3
Investigation of older adults with SCI
| Investigation | Rationale |
|---|---|
| Routine | |
| Neuropsychological testing | Delineation of cognitive syndromes (SCI vs MCI vs AD*) |
| Hematology (full blood count) | Screen for anemia |
| Biochemistry (electrolytes, renal function, liver function, thyroid function, B12, and folate) | Screen for treatable causes of cognitive complaints |
| For specific indication suggested by history, physical exam, or neuropsychological testing | |
| Neuroimaging | Generalized and regional imaging (eg, hippocampal atrophy, space occupying lesions) |
| Electroencephalography | Epilepsy/seizures (especially absence and complex partial) |
| Cardiac (eg, echocardiography) | May reveal cardiac arrhythmia or sources of emboli |
| Inflammatory markers (eg, ESR) | Screen for inflammatory processes |
| Treponemal serology | Tertiary syphilis |
| *Alzheimer’s disease and other dementias AD: Alzheimer’s disease; ESR: erythrocyte sedimentation rate; MCI: mild cognitive impairment; SCI: subjective cognitive impairment Source: References 22,24,28,29 | |
Table 4
Differential diagnosis of SCI
| Cause of cognitive impairment | Potential mechanism |
|---|---|
| ARCD | Allostatic load, ‘wear and tear’ from a lifetime of physiological or psychological stresses and adaptations |
| Anemia | Neuronal hypoxia |
| Alzheimer’s disease | Amyloid and/or tau-mediated neurotoxicity, neuroinflammation |
| Cerebrovascular disease | Neuronal ischemia and hypoxia, neuroinflammation |
| Vitamin deficiencies (eg, B1, B12, folate, D) | Impaired neuronal and neurotransmitter function |
| Inadequate protein intake | Impaired neuronal function |
| Anticholinergic drug use | Decreased cholinergic neurotransmission |
| Alcohol use | Direct neurotoxicity and indirect causes such as malnutrition or head injury |
| Depression, anxiety | Hippocampal dysfunction with or without atrophy |
| Obstructive sleep apnea | Neuronal hypoxia, neuroinflammation |
| Head injury | Neuronal and synaptic loss |
| ARCD: age-related cognitive decline; SCI: subjective cognitive impairment Source: References 28,29,31,32 | |
CASE CONTINUED: No measurable deficits
Ms. F’s medical history is remarkable for coronary artery disease, hypothyroidism, hypertension, hyperlipidemia, cataracts, arthritis, back surgery (secondary to spondylosis), and foot surgery. Ms. F denies a history of alcohol or illicit substance abuse. She smoked tobacco for 30 years (2 packs per day), but quit 5 years ago after her heart attack. Physical exam is unremarkable except for mild obesity (body mass index = 31 kg/m2).
Ms. F’s mental status exam reveals anxious mood and affect. Her recall is 2 out of 3 items. Her MMSE score is 29/30 (1 point lost on recall) and her Geriatric Depression Scale33 score is 2/15, indicating minimal depressive symptoms. On neuropsychological testing, Ms. F demonstrates high average intellectual abilities; compared with others her age, she performs within expectations on all measures. That is, she performs within the above-average to low-average range on measures of attention, working memory, speed of processing, expressive language, learning, memory, visual spatial abilities, executive functioning, and knowledge of basic health and safety information.
Enhancing neuroplasticity
We recommend neuroplasticity-based interventions to treat SCI and promote healthy brain aging.20,29 For a checklist clinicians can use to promote healthy brain aging and thus improve patients’ cognitive health see this article at CurrentPsychiatry. com. Table 51,29 lists cognitive strategies to improve memory and maintain cognitive vitality.
Enhancing brain plasticity and neurogenesis requires engaging older adults in demanding sensory, cognitive, and motor activities on an intensive basis.34 Therapeutic stimulation of neuroplasticity and neurogenesis might contribute to functional “repair” of the diseased adult brain before damage to whole neuronal networks has ensued.29 An important treatment component is reassuring patients with SCI that they do not have AD or MCI. Treating comorbid anxiety and depression and reversible causes of cognitive complaints is key to successful outcomes.
Table 5
Strategies to improve memory and maintain cognitive vitality
| Strategy | Description |
|---|---|
| Mindfulness | Focus on 1 task at a time rather than trying to multitask. Research shows that cognition is more efficient in this manner |
| Cognitive strategies | Use mnemonics (such as ROY G BIV to remember the colors of the rainbow). Make associations for information, such as when meeting someone new, relate their name to someone else you know well. Use cues such as memory notebooks to prompt information recall. Engage in learning new and challenging cognitive activities, such as a new language, a music instrument, or dance. Consider computer-based brain exercises |
| Rehearsal | Practice information you want to remember, such as repeating the information several times or writing it down |
| Be patient | Getting frustrated when you have memory difficulties makes it more challenging to remember information |
| Exercise (mental and physical) | Engage in mental activities, such as reading and crossword puzzles. Do something that you are interested in, rather than making it a chore. Research has demonstrated that physical exercise also aids memory |
| Diet | What is good for the heart is good for the brain. Fruits, vegetables, food rich in omega-3 fatty acids (eg, fatty fish such as salmon), whole grains, spices (eg, turmeric), and small amounts of tree nuts (eg, walnuts) are recommended as part of a balanced diet |
| Source: References 1,29 | |
CASE CONTINUED: Reassurance and risk reduction
Ms. F’s psychiatrist reassures her that she does not have AD. She receives genetic counseling and decides to forgo genetic testing. Her psychiatrist educates Ms. F about the risks of OTC supplements—especially increased risk of bleeding because she takes aspirin and clopidogrel—and lack of data supporting their use. Ms. F is counseled that a healthy lifestyle, including regular exercise, Mediterranean diet with increased intake of omega-3 fatty acids, learning new things, and being socially active, is the safest way to promote brain health. Over 3 months, Ms. F discontinues all supplements except the vitamins and omega-3, starts exercising, resumes piano lessons that she stopped 10 years ago, and becomes a vegetarian. She continues to have mild SCI but she says she is not bothered by it and feels satisfied that she is doing all she can to promote her brain health.
Related Resources
- Desai AK. Healthy brain aging: evidence based methods to preserve brain function and prevent dementia. Philadelphia, PA: W. B. Saunders; 2010.
- Doidge N. The brain that changes itself. New York, NY: Penguin Books; 2007.
- Vance DE, Roberson AJ, McGuinness TM, et al. How neuroplasticity and cognitive reserve protect cognitive functioning. J Psychosoc Nurs Ment Health Serv. 2010; 48: 1-8.
Brain Training Resources
- Weil A, Small G. The healthy brain kit. Boulder, CO: Sounds True, Inc.; 2007. Audio CDs, brain-training cards and workbooks.
- Posit Science. www.positscience.com.
- Sharp Brains. www.sharpbrains.com.
Drug Brand Names
- Atenolol • Tenormin
- Atorvastatin • Lipitor
- Clopidogrel • Plavix
- Levothyroxine • Levoxyl, Synthroid
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
Abhilash K. Desai, MD, discusses emerging research on biomarkers that may help clarify diagnosis.
1. Small GW. What we need to know about age related memory loss. BMJ. 2002;324:1502-1505.
2. Hayes TL, Larimer N, Adami A, et al. Medication adherence in healthy elders. J Aging Health. 2009;21(4):567-580.
3. Reisberg B, Shulman MB, Torossian C, et al. Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement. 2010;6(1):11-24.
4. Jessen F, Wiese B, Bachmann C, et al. Prediction of dementia by subjective memory impairments: effects of severity and temporal association with cognitive impairment. Arch Gen Psychiatry. 2010;67:414-422.
5. Waldorff FB, Siersma V, Waldemar G. Association between subjective memory complaints and nursing home placement: a four-year follow-up. Int J Geriatr Psychiatry. 2009;24(6):602-609.
6. Salthouse TA. Selective review of cognitive aging. J Int Neuropsychol Soc. 2010;16:754-760.
7. Anderton B. Ageing of the brain. Mech Ageing Dev. 2002;23:811-817.
8. Salthouse TA. Influence of age on practice effects in longitudinal neurocognitive change. Neuropsychology. 2010;24(5):563-572.
9. Park D, Schwarz N. Cognitive aging: a primer. Philadelphia PA: Taylor and Francis Group; 2000.
10. Reisberg B, Shulman MB. Commentary on “a roadmap for the prevention of dementia II: Leon Thal Symposium 2008.” Subjective cognitive impairment as an antecedent of Alzheimer’s dementia: policy import. Alzheimers Dement. 2009;5:154-156.
11. Reisberg B, Gauthier S. Current evidence for subjective cognitive impairment (SCI) as the pre-mild cognitive impairment (MCI) stage of subsequently manifest Alzheimer’s disease. Int Psychogeriatr. 2008;20(1):1-16.
12. Mosconi L, Pupi A, De Leon MJ. Brain glucose hypometabolism and oxidative stress in preclinical Alzheimer’s disease. Ann N Y Acad Sci. 2008;1147:180-195.
13. Ramakers IH, Visser PJ, Aalten P, et al. Symptoms of preclinical dementia in general practice up to five years before dementia diagnosis. Dement Geriatr Cogn Disord. 2007;24(4):300-306.
14. Amieva H, Le Goff M, Millet X, et al. Prodromal Alzheimer’s disease: successive emergence of the clinical symptoms. Ann Neurol. 2008;64(5):492-498.
15. Taragano FE, Allegri RF, Krupitzki H, et al. Mild behavioral impairment and risk of dementia: a prospective cohort study of 358 patients. J Clin Psychiatry. 2009;70(4):584-592.
16. Jayadev S, Steinbart EJ, Chi YY, et al. Conjugal Alzheimer disease: risk in children when both parents have Alzheimer disease. Arch Neurol. 2008;65(3):373-378.
17. Hajjar I, Yang F, Sorond F, et al. A novel aging phenotype of slow gait, impaired executive function, and depressive symptoms: relationship to blood pressure and other cardiovascular risks. J Gerontol A Biol Sci Med Sci. 2009;64(9):994-1001.
18. Yamamoto N, Yamanaka G, Ishikawa M, et al. Cardio-ankle vascular index as a predictor of cognitive impairment in community-dwelling elderly people: four-year follow-up. Dement Geriatr Cogn Disord. 2009;28(2):153-158.
19. Inzitari M, Pozzi C, Ferrucci L, et al. Subtle neurological abnormalities as risk factors for cognitive and functional decline, cerebrovascular events, and mortality in older community-dwelling adults. Arch Intern Med. 2008;168(12):1270-1276.
20. Shineman DW, Salthouse TA, Launer LJ, et al. Therapeutics of cognitive aging. Ann N Y Acad Sci. 2010;1191(suppl 1):E1-E10.
21. Dubois B, Feldman HH, Jacova C, et al. Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol. 2010;9:1118-1127.
22. Chertkow H, Massoud F, Nasreddine Z, et al. Diagnosis and treatment of dementia: 3. Mild cognitive impairment and cognitive impairment without dementia. CMAJ. 2008;178(10):1273-1285.
23. Rosenberg PB, Lyketsos C. Mild cognitive impairment: searching for the prodrome of Alzheimer’s disease. World Psychiatry. 2008;7(2):72-78.
24. Rosenberg PB, Johnston D, Lyketsos CG. A clinical approach to mild cognitive impairment. Am J Psychiatry. 2006;163(11):1884-1890.
25. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198.
26. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303-308.
27. Diagnostic and statistical manual of mental disorders. 4th ed text rev. Washington, DC: American Psychiatric Association; 2000:135–180.
28. Malhotra R, Desai AK. Healthy brain aging: what has sleep got to do with it? Clin Geriatr Med. 2010;26:45-56.
29. Desai AK, Grossberg GT, Chibnall JT. Healthy brain aging: a road map. Clin Geriatr Med. 2010;26:1-16.
30. Weaver Cargin J, Collie A, Masters C, et al. The nature of cognitive complaints in healthy older adults with and without objective memory decline. J Clin Exp Neuropsychol. 2008;30:245-257.
31. Wilson RS, Arnold SE, Schneider JA, et al. Chronic distress, age-related neuropathology, and late-life dementia. Psychosom Med. 2007;69:47-53.
32. Deal JA, Carlson MC, Xue Q, et al. Anemia and 9-year domain-specific cognitive decline in community-dwelling older women: the Women’s Health and Aging Study II. J Am Geriatr Soc. 2009;57(9):1604-1611.
33. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression scale: a preliminary report. J Psychiatr Res. 1983;17:37-49.
34. Mahncke HW, Bronstone A, Merzenich MM. Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Prog Brain Res. 2006;157:81-109.
1. Small GW. What we need to know about age related memory loss. BMJ. 2002;324:1502-1505.
2. Hayes TL, Larimer N, Adami A, et al. Medication adherence in healthy elders. J Aging Health. 2009;21(4):567-580.
3. Reisberg B, Shulman MB, Torossian C, et al. Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement. 2010;6(1):11-24.
4. Jessen F, Wiese B, Bachmann C, et al. Prediction of dementia by subjective memory impairments: effects of severity and temporal association with cognitive impairment. Arch Gen Psychiatry. 2010;67:414-422.
5. Waldorff FB, Siersma V, Waldemar G. Association between subjective memory complaints and nursing home placement: a four-year follow-up. Int J Geriatr Psychiatry. 2009;24(6):602-609.
6. Salthouse TA. Selective review of cognitive aging. J Int Neuropsychol Soc. 2010;16:754-760.
7. Anderton B. Ageing of the brain. Mech Ageing Dev. 2002;23:811-817.
8. Salthouse TA. Influence of age on practice effects in longitudinal neurocognitive change. Neuropsychology. 2010;24(5):563-572.
9. Park D, Schwarz N. Cognitive aging: a primer. Philadelphia PA: Taylor and Francis Group; 2000.
10. Reisberg B, Shulman MB. Commentary on “a roadmap for the prevention of dementia II: Leon Thal Symposium 2008.” Subjective cognitive impairment as an antecedent of Alzheimer’s dementia: policy import. Alzheimers Dement. 2009;5:154-156.
11. Reisberg B, Gauthier S. Current evidence for subjective cognitive impairment (SCI) as the pre-mild cognitive impairment (MCI) stage of subsequently manifest Alzheimer’s disease. Int Psychogeriatr. 2008;20(1):1-16.
12. Mosconi L, Pupi A, De Leon MJ. Brain glucose hypometabolism and oxidative stress in preclinical Alzheimer’s disease. Ann N Y Acad Sci. 2008;1147:180-195.
13. Ramakers IH, Visser PJ, Aalten P, et al. Symptoms of preclinical dementia in general practice up to five years before dementia diagnosis. Dement Geriatr Cogn Disord. 2007;24(4):300-306.
14. Amieva H, Le Goff M, Millet X, et al. Prodromal Alzheimer’s disease: successive emergence of the clinical symptoms. Ann Neurol. 2008;64(5):492-498.
15. Taragano FE, Allegri RF, Krupitzki H, et al. Mild behavioral impairment and risk of dementia: a prospective cohort study of 358 patients. J Clin Psychiatry. 2009;70(4):584-592.
16. Jayadev S, Steinbart EJ, Chi YY, et al. Conjugal Alzheimer disease: risk in children when both parents have Alzheimer disease. Arch Neurol. 2008;65(3):373-378.
17. Hajjar I, Yang F, Sorond F, et al. A novel aging phenotype of slow gait, impaired executive function, and depressive symptoms: relationship to blood pressure and other cardiovascular risks. J Gerontol A Biol Sci Med Sci. 2009;64(9):994-1001.
18. Yamamoto N, Yamanaka G, Ishikawa M, et al. Cardio-ankle vascular index as a predictor of cognitive impairment in community-dwelling elderly people: four-year follow-up. Dement Geriatr Cogn Disord. 2009;28(2):153-158.
19. Inzitari M, Pozzi C, Ferrucci L, et al. Subtle neurological abnormalities as risk factors for cognitive and functional decline, cerebrovascular events, and mortality in older community-dwelling adults. Arch Intern Med. 2008;168(12):1270-1276.
20. Shineman DW, Salthouse TA, Launer LJ, et al. Therapeutics of cognitive aging. Ann N Y Acad Sci. 2010;1191(suppl 1):E1-E10.
21. Dubois B, Feldman HH, Jacova C, et al. Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol. 2010;9:1118-1127.
22. Chertkow H, Massoud F, Nasreddine Z, et al. Diagnosis and treatment of dementia: 3. Mild cognitive impairment and cognitive impairment without dementia. CMAJ. 2008;178(10):1273-1285.
23. Rosenberg PB, Lyketsos C. Mild cognitive impairment: searching for the prodrome of Alzheimer’s disease. World Psychiatry. 2008;7(2):72-78.
24. Rosenberg PB, Johnston D, Lyketsos CG. A clinical approach to mild cognitive impairment. Am J Psychiatry. 2006;163(11):1884-1890.
25. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198.
26. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303-308.
27. Diagnostic and statistical manual of mental disorders. 4th ed text rev. Washington, DC: American Psychiatric Association; 2000:135–180.
28. Malhotra R, Desai AK. Healthy brain aging: what has sleep got to do with it? Clin Geriatr Med. 2010;26:45-56.
29. Desai AK, Grossberg GT, Chibnall JT. Healthy brain aging: a road map. Clin Geriatr Med. 2010;26:1-16.
30. Weaver Cargin J, Collie A, Masters C, et al. The nature of cognitive complaints in healthy older adults with and without objective memory decline. J Clin Exp Neuropsychol. 2008;30:245-257.
31. Wilson RS, Arnold SE, Schneider JA, et al. Chronic distress, age-related neuropathology, and late-life dementia. Psychosom Med. 2007;69:47-53.
32. Deal JA, Carlson MC, Xue Q, et al. Anemia and 9-year domain-specific cognitive decline in community-dwelling older women: the Women’s Health and Aging Study II. J Am Geriatr Soc. 2009;57(9):1604-1611.
33. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression scale: a preliminary report. J Psychiatr Res. 1983;17:37-49.
34. Mahncke HW, Bronstone A, Merzenich MM. Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Prog Brain Res. 2006;157:81-109.