User login
Using psychotropics safely in patients with HIV/AIDS: Watch for drug-drug interactions with antiretrovirals
Psychiatric patients—especially those with substance abuse disorders—are at high risk for HIV infection, which puts psychiatrists on the AIDS pandemic’s front lines.
In the wake of last month’s International AIDS Conference in Thailand, this article supplements American Psychiatric Association guidelines for managing patients with HIV/AIDS.1 Here is updated information on:
- who is at greatest risk for HIV infection today
- neuropsychiatric side effects of HIV medications
- in-office assessment of HIV-associated cognitive changes
- how to avoid psychotropic/antiretroviral interactions.
HIV and psychiatric patients
Psychiatric patients are among those at highest risk for HIV (Box).2-4 Cournos and McKinnon5 found that HIV seroprevalence among persons with severe mental illness was 4% to 23%compared with 0.4% in the general population.6 They defined severe mental illness as schizophrenia, schizoaffective disorder, major depression, or bipolar disorder accompanied by significant functional impairment, disruption of normal life tasks, periods of hospitalization, and need for psychotropics.
Infection rates varied with HIV geographic concentration, presence of comorbid substance use disorders, age, and ethnicity, but not psychiatric diagnosis. Unsafe sex and drug use (including noninjection) were associated with infection, and women were as likely to be infected as men.
Side effects and interactions
‘Triple therapy.’ Combining three antiretroviral agents—highly-active antiretroviral therapy (HAART) or “triple therapy”—is standard treatment for HIV infection in the United States. Initially, HAART was recommended for all patients with early-stage HIV, even if asymptomatic. This changed as antiretrovirals’ side effects—such as peripheral neuropathy with didanosine— and drug resistance from suboptimal adherence became apparent. Viral resistance develops if patients are <95% adherent to antiretroviral regimens.7
Antiretroviral therapy is usually started when:
- CD4 lymphocyte count is <200 cells/mm3 or abruptly decreasing
- plasma viral load is >55,000 copies/mL or abruptly increasing
- symptomatic AIDS emerges.
Psychiatric side effects. Psychiatric symptoms—such as depression, anxiety, confusion, psychosis, hallucinations, insomnia, and mania—are common side effects of antiretrovirals and other drugs used to treat HIV and its opportunistic infections and cancers (Table 1).8 Two antiretrovirals are of particular interest to psychiatrists:
Efavirenz is a non-nucleoside reverse transcriptase inhibitor that causes vivid dreams, especially when initiated.
AIDS death rates have declined in the United States since antiretroviral therapies were introduced in 1996, but the rate of new HIV infection has not changed.2 An estimated 850,000 to 950,000 Americans have HIV, and 25% do not know it.3
Changing demographics. Some 40,000 new HIV infections occur in the United States each year (70% among men), and one-half of the newly-infected are under age 25. African Americans and Hispanics represent 51% of total AIDS cases in men and 77% in women. From 1998 to 2002—the most recent data available from the Centers for Disease Control and Prevention (CDC)—AIDS incidence steadily decreased among whites and Hispanics but increased among blacks, Asian/Pacific Islanders, and American Indian/Alaska Natives.
Transmission routes. Approximately 60% of men with HIV are infected through male-to-male sex, 25% through IV drug use, and 15% through heterosexual sex. Unprotected anal sex appears to be occurring more frequently in some urban centers, particularly among young men who have sex with men.4 Approximately 75% of women with HIV are infected through heterosexual sex and 25% through IV drug use.
Ritonavir is a protease inhibitor that may inhibit psychotropics metabolized by cytochrome P450 3A4 and 2D6 isoenzymes.
Other HIV medications increase or decrease psychotropic blood levels via inhibition or induction of CYP isoenzymes (Table 2).9 When a patient is taking ritonavir or another protease inhibitor, reduced starting dosages of selective serotonin reuptake inhibitors (SSRIs) may be appropriate. Benzodiazepine dosages may need to be increased because of ritonavir induction of the enzyme glucuronosyltransferase.
Table 1
Psychiatric side effects of common HIV medications
| Drug | Side effects, by frequency |
|---|---|
| Acyclovir | Unknown: hallucination, confusion, thought insertion, insomnia |
| Amphotericin B | >5%: confusion, insomnia, somnolence; 1-5%: agitation, anxiety, depression, hallucination, nervousness, psychosis; Unkown: delirium |
| β-Lactam antibiotics | <1%: insomnia, somnolence, anxiety, nervousness, impaired concentration, confusion, nightmares, hallucination; Unkown: paranoia, mania |
| Trimethoprim/sulfamethoxazole | Unknown: hallucinations, depression, apathy, nervousness |
| Cycloserine Unknown: | psychosis, somnolence, depression, confusion, irritability, anxiety |
| Didanosine | Unknown: nervousness, anxiety, confusion, seizures, insomnia |
| Efavirenz | 13-16%: depression; 8-11%: anxiety; 2-6%: nervousness; >5%: headache, seizures, confusion; <2%: suicidal ideation and behavior, aggression |
| Unknown: | agitation, lability, neurosis, psychosis, insomnia, impaired concentration, somnolence, euphoria, amnesia, hallucination |
| Foscarnet | >5%: depression, confusion, anxiety; 1-5%: insomnia, somnolence, amnesia, nervousness, agitation, aggression, hallucination |
| Interferon-a | 6-19%: depression; 12-16%: irritability; 6-12%: insomnia; 3-8%: impaired concentration; >5%: anxiety: <5%: confusion, mania, aggression, delirium, lability, suicidal ideation, psychosis, personality disorder, alcohol intolerance |
| Isoniazid | Unknown: depression, agitation, hallucination, paranoia, anxiety, psychosis |
| Lamivudine | <11%: insomnia; <9%: mania, depressive disorders, dreams |
| Methotrexate | Unknown: cognitive and mood changes |
| Pentamidine | Unknown: confusion, lability, hallucination; Rare: anxiety, fatigue |
| Procarbazine | Unknown: hallucination, depression, nervousness, apprehension, mania, loss of appetite, insomnia, nightmares, confusion, malaise |
| Quinolones | <1%: somnolence, insomnia; Occasional: agitation, anxiety, depression, panic attacks, confusion, hallucination, aggression, psychosis, paranoia; |
| Rare: | suicidal ideation and suicide (no relationship with drug confirmed) |
| Stavudine | Unknown: confusion, depression, seizures, anxiety, mania, sleep problems |
| Sulfonamides | Unknown: psychosis, delirium, confusion, depression, hallucinations |
| Thiabendazole | Unknown: hallucination, fatigue, irritability, confusion, depression |
| Vinblastine | Unknown: depression |
| Vincristine | Unknown: hallucination |
| Zalcitabine | Unknown: acute psychosis, agitation, amnesia, anxiety, lability, euphoria, hallucination, insomnia, mania, paranoia, suicidal behavior, confusion, impaired concentration, somnolence, depression |
| Zidovudine | Unknown: Insomnia, vivid dreams, agitation, mania, hallucination, confusion |
Table 2
Psychotropic/HIV drug interactions, by cytochrome P-450 isoenzyme
| CYP 3A4 | CYP 2D6 | |
|---|---|---|
| Psychotropics primarily metabolized by isoenzyme | Benzodiazepines Buspirone Carbamazepine Citalopram Clomipramine Imipramine Trazodone | Fluoxetine Fluvoxamine Mirtazapine Antipsychotics (typical and atypical) Paroxetine Sertraline Tricyclics Venlafaxine |
| HIV drugs that inhibit isoenzyme | Protease inhibitors (esp. ritonavir and indinavir) Clarithromycin Erythromycin Itraconazole Ketoconazole Macrolide antibiotics | Protease inhibitors (esp. ritonavir and nelfinavir) |
| Possible clinical effect | Increased plasma levels and increased side effects; for benzodiazepines, sedation and decreased respiratory drive | Increased plasma levels and increased side effects; for tricyclics, increased risk for cardiac conduction delay |
| HIV drugs that induce isoenzyme | Nevirapine Efavirenz Glucocorticoids Rifampin Rifabutin | None |
| Possible clinical effect | Decreased psychotropic plasma levels, decreased effectiveness | None |
| Source: Adapted and reprinted with permission from reference 1, Table 16. Copyright 2000. American Psychiatric Association | ||
The FDA approved enfuvirtide—the first of the new fusion inhibitor class of antiretroviral agents—in March 2003. Enfuvirtide prevents HIV from entering the target CD4 lymphocyte in patients who show continued viral replication despite ongoing antiretroviral therapy. This agent requires twice-daily subcutaneous injections. Because enfuvirtide can be viewed as a medication of last resort, nonresponse may be especially disheartening to an AIDS patient.
Substances of abuse also interact with HIV medications. A lethal overdose of the street drug MDMA (“Ecstasy”) has been reported in a patient treated with ritonavir.10 MDMA is metabolized primarily via CYP 2D6. Other substances of abuse metabolized by CYP 2D6 or 3A4—such as amphetamines, ketamine, heroin, cocaine, and gamma-hydroxybutyrate—may cause toxic reactions in patients being treated with protease inhibitors.
Because substance abuse is a common comorbidity of HIV infection, warn patients that using recreational drugs with antiretroviral medications can cause adverse reactions. Extensive drug interaction lists are available on patient education and physician Web sites (see Related Resources).
Table 3
Diagnostic criteria for HIV-associated minor cognitive motor disorder
Probable diagnosis (must meet all four criteria)
A possible diagnosis of minor cognitive motor disorder can be given if criteria 1-3 are present and either:
|
| Source: Reprinted with permission from reference 14 |
Lipid and hyperglycemic side effects. Antivirals— especially protease inhibitors —appear to be associated with HIV lipodystrophy, which is associated with cosmetic and serum lipid changes as well as hyperglycemia.11 Facial wasting, buffalo humps, and central intra-abdominal obesity may occur, and elevated serum cholesterol and triglycerides often require treatment with cholesterollowering “statin” drugs.
Though it is unclear whether HIV lipodystrophy increases cardiovascular disease risk, carefully consider the potential effects of psychotropics associated with weight gain, hyper-glycemia, and elevated lipids in patients receiving antiretroviral therapy.
Hepatitis. Patients at risk for HIV infection are also at risk for viral hepatitis. One-quarter of persons with HIV are coinfected with hepatitis C, primarily through IV drug use.12 Alpha-interferon treatment of hepatitis B and C has been associated with depression. SSRI treatment—such as paroxetine, 20 mg/d—can ease depressive symptoms.13
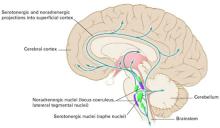
HIV-associated cognitive changes
Minor cognitive-motor disorder(Table 3) and HIV-associated dementia (Table 4) 14 are typically seen in late-stage HIV infections and are diagnoses of exclusion. Physical or neurologic examination in a patient with HIV/AIDS and altered mental status may show:
- focal deficits indicating a space-occupying lesion (eg, CNS lymphoma or toxoplasmosis)
- sensory changes that may indicate peripheral neuropathy
- ataxia or gait changes that may indicate myelopathy.
Useful neuropsychological tests include the HIV Dementia Rating Scale,15 Halstead finger-tapping test for motor speed,16 and the Trailmaking Test, which assesses psychomotor speed and sequencing ability.17
Antiretroviral therapy appears to reduce the risk of HIV-associated dementia. In a trial conducted at 42 AIDS Clinical Trials Group sites and 7 National Hemophilia Foundation sites, combination reverse transcriptase inhibitors helped preserve or improve neurologic function.18
Psychostimulants appear to improve HIV-induced brain impairment.19 Immune modulators—such as tumor necrosis factor-alpha blockers (eg, pentoxifylline)20 and interleukin-1 receptor blockers21 —have also been studied for possible beneficial effects on HIV brain disease.
HIV prevention
Because unprotected sex and IV substance use are the primary HIV transmission routes in the United States, assessing psychiatric patients’ sexual and substance use behaviors may help you prevent HIV infection. The CDC offers guidelines for HIV testing, counseling, and referral (see Related Resources).
To identify persons at risk for HIV infection, the CDC recommends asking open-ended questions about risk behaviors, such as: “What are you doing now or what have you done in the past that you think may put you at risk for HIV infection?”22
The shift of new HIV infection disproportionately into African-American and Hispanic populations suggests the need for more-intensive prevention and education in those communities. CDC guidelines emphasize the importance of using culturally sensitive language when asking about risk behavior. Some individuals may engage in same-sex behaviors but do not identify themselves as “homosexual” or “gay.” In some African-American communities, for example, being “on the down low” is used to describe men—oftentimes married—who have sex with men.
To incorporate HIV-prevention messages and brief behavioral interventions into clinical visits:
- speak with patients about sexual and drug use behaviors in simple, everyday language
- learn about interventions shown to be effective
- become familiar with community resources that address HIV risk reduction.23
Training. The CDC and Health Resources and Services Administration of the U.S. Department of Health and Human Services offer free training on risk screening and prevention, as well as opportunities for continuing medical education (see Related Resources).
Table 4
Diagnostic criteria for HIV-associated dementia
|
| Source: Reprinted with permission from reference 14 |
Advances in antibody testing
Psychiatrists play an important supportive role in encouraging HIV screening of at-risk patients of unknown serostatus and in counseling such patients before, during, and after test results are known.
Rapid lab tests. In 2002, the FDA approved a rapid, highly accurate HIV-1 screening test for serum specimens and in March 2004 approved the same test for screening oral fluid specimens. Test results with serum or an oral swab are available from a laboratory in approximately 20 minutes. In clinical studies submitted to the FDA, the OraQuick oral fluid test correctly identified 99.3% of persons infected with HIV-1 (sensitivity) and 99.9% of those not infected (specificity).
CDC guidelines for HIV counseling and testing have been revised to include rapid testing. Screening tests are most accurate at least 3 months after an HIV exposure—the time required for antibodies to develop. When counseling patients after a reactive test result, emphasize that the result is preliminary and further testing is needed to confirm the result. Counsel patients who have a negative result within 3 months of possible infection to be retested to guard against a possible false-negative result.
Home test kits. An FDA-approved consumer-controlled test kit—Home Access HIV-1 Test System24 —is sold at drug stores without a prescription. The customer pricks a finger with a special device, places drops of blood on a specially treated card, and mails the card to a licensed laboratory. Anonymous identification numbers are used when phoning for the results.
Customers may speak to a counselor before taking the test, while awaiting results, and when results are given. All individuals with a reactive test result are referred for a more-specific test and receive information and resources on treatment and support services.
Counseling the HIV patient
The psychological impact of positive HIV antibody test results on psychiatric patients has not been studied. Persons without psychiatric disorders commonly experience anxiety and depression immediately after learning of a positive result. Unless the patient has HIV-related physical symptoms, these psychological sequelae often return to baseline—similar to when the blood sample was drawn—within 2 weeks.25
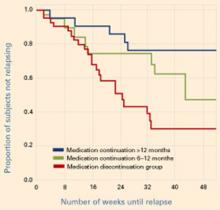
Patients need to know that a positive HIV test result is no longer associated with death within 2 to 3 years. During a 2-year period, for example, disease progression from HIV infection to AIDS decreased 7-fold among patients who started antiretroviral therapy with a CD4+ T-cell count >350 cells/mm3, compared with others who were monitored without therapy.26 This may be especially important to reinforce with newly-diagnosed patients unfamiliar with advances in HAART.
Medication adherence. To increase patients’ adherence to antiretroviral therapy:
- express interest that they are taking their medications
- use psychotherapy to help them solve problems that interfere with adherence.
Suicide risk. In the 1980s, significantly increased suicide rates were reported among HIV-infected persons. For example, the suicide rate in 1985 for New York City men ages 20 to 59 living with an AIDS diagnosis was 36 times higher than that of similar men without AIDS.27 A later study of HIV infection in New York male suicide victims from 1991 to 1993 suggested that HIV serostatus was associated with a modest increase—at most—in suicide risk. That study considered the interplay of other suicide risk factors, such as substance abuse.28
- Guidelines for HIV counseling, testing, and referral. Centers for Disease Control and Prevention. www.cdc.gov/mmwr/preview/mmwrhtml/rr5019a1.htm
- Training in HIV prevention and counseling. National Network of STD/HIV Prevention Training Centers (http://depts.washington.edu/nnptc) and AIDS Education and Training Centers National Resource Center (http://www.aids-ed.org)
- Rapid HIV testing. Centers for Disease Control and Prevention. http://www.cdc.gov/hiv/rapid_testing/
- Cytochrome P450 drug interaction table. Indiana University School of Medicine. Division of Clinical Pharmacology. www.drug-interactions.com
Drug brand names
- Buspirone • BuSpar
- Carbamazepine • Carbatrol
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Liang reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products
1. American Psychiatric Association. Practice guideline for the treatment of patients with HIV/AIDS. Am J Psychiatry. 2000 157 11(suppl). Also available at: www.psych.org/psych_pract/treatg/pg/hivaids_revisebook_index.cfm
2. Centers for Disease Control and Prevention National Center for HIV, STD, and TB Prevention. HIV AIDS Surveill Rep December 2001. Available at: http://www.cdc.gov/hiv/stats/hasr1302.htm
3. Centers for Disease Control and Prevention. HIV AIDS Surveill Rep 2002;14:148. Also available at: http://www.cdc.gov/hiv/stats/hasr1402/2002SurveillanceReport.pdf
4. Risk reduction: sex without condoms. HIV Counselor Perspectives [newsletter] 2001;10(2, March).
5. Cournos F, McKinnon K. HIV seroprevalence among people with severe mental illness in the United States: a critical review. Clin Psychol Rev 1997;17:259-69.
6. Steele FR. A moving target: CDC still trying to estimate HIV-1 prevalence. J NIH Res 1994;6:25-6.
7. Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000;133:21-30.
8. Grant I, Atkinson JH, Jr. Neuropsychiatric aspects of HIV infection and AIDS. In: Sadock BJ, Sadock VA (eds). Kaplan and Sadock’s comprehensive textbook of psychiatry. Philadelphia: Lippincott Williams & Wilkins, 1999;308-36.
9. Ayuso JL. Use of psychotropic drugs in patients with HIV infection. Drugs 1994;47:599-610.
10. Mirken B. Danger: possibly fatal interactions between ritonavir and “ecstasy,” some other psychoactive drugs. AIDS Treat News 1997;Feb 21(No 265):5.-
11. Miller KD, Jones E, Yanovski JA, et al. Visceral abdominal-fat accumulation associated with use of indinavir. Lancet 1998;351(9106):871-5.
12. Centers for Disease Control and Prevention. Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. MMWR 1998;47(No. RR-19):1-39.
13. Kraus MR, Schafer A, Faller H, et al. Paroxetine for the treatment of interferon-alpha-induced depression in chronic hepatitis C. Aliment Pharmacol Ther 2002;16(6):1091-9.
14. Nomenclature and research case definitions for neurologic manifestations of human immunodeficiency virus-type 1 (HIV-1) infection: report of a working group of the American Academy of Neurology AIDS Task Force. Neurology 1991;41:778-85.
15. Power C, Selnes OA, Grim JA, McArthur JC. HIV Dementia Scale: a rapid screening test. J Acquir Immune Defic Syndr Hum Retrovirol 1995 Mar 1;8(3):273-8.
16. Silberstein CH, McKegney FP, O'Dowd MA, et al. A prospective longitudinal study of neuropsychological and psychosocial factors in asymptomatic individuals at risk for HTLV-III/LAV infection in a methadone program: preliminary findings. Int J Neurosci 1987;32(3-4):669-76.
17. Reitan RM. Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills 1958;8:271-6.
18. Price RW, Yiannoutsos CT, Clifford DB, et al. Neurological outcomes in late HIV infection: adverse impact of neurological impairment on survival and protective effect of antiviral therapy. AIDS Clinical Trial Group and Neurological AIDS Research Consortium study team. AIDS 1999;13(13):1677-85.
19. Perry SW. Organic mental disorders caused by HIV: update on early diagnosis and treatment. Am J Psychiatry 1990;147(6):696-710.
20. Wilt SG, Milward E, Zhou JM, et al. In vitro evidence for a dual role of tumor necrosis factor-alpha in human immunodeficiency virus type 1 encephalopathy. Ann Neurol 1995;37(3):381-94.
21. Boven LA, Gomes L, Hery C, et al. Increased peroxynitrite activity in AIDS dementia complex: implications for the neuropathogenesis of HIV-1 infection. J Immunol 1999;162(7):4319-27.
22. Centers for Disease Control and Prevention. Revised guidelines for HIV counseling, testing, and referral. MMWR Nov. 9, 2001;50(RR19):1-58.
23. Centers for Disease Control and Prevention. Incorporating HIV prevention into the medical care of persons living with HIV. MMWR July 18, 2003;52(RR12):1-24. Also available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5212a1.htm
24. Food and Drug Administration. Home Access HIV-1 Test System: Summary of safety and effectiveness. Available at: http://www.fda.gov/cber/PMAsumm/P950002S.pdf
25. Perry SW, Jacobsberg LB, Fishman B. Psychological responses to serological testing for HIV. AIDS 1990;4(2):145-52.
26. Opravil M, Ledergerber B, Furrer H. et al and the Swiss HIV Cohort Study Clinical benefit of early initiation of HAART in patients with asymptomatic HIV and CD4 counts >350/mm 3 . Abstract LB-6. Chicago, IL: 8th Conference on Retroviruses and Opportunistic Infections, 2001.
27. Marzuk P, Tierney H, Tardiff K, et al. Increased risk of suicide in persons with AIDS. JAMA 1988;259:1333-7.
28. Marzuk PM, Tardiff K, Leon AC, et al. HIV seroprevalence among suicide victims in New York City, 1991-93. Am J Psychiatry 1997;154(6):1720-5.
Psychiatric patients—especially those with substance abuse disorders—are at high risk for HIV infection, which puts psychiatrists on the AIDS pandemic’s front lines.
In the wake of last month’s International AIDS Conference in Thailand, this article supplements American Psychiatric Association guidelines for managing patients with HIV/AIDS.1 Here is updated information on:
- who is at greatest risk for HIV infection today
- neuropsychiatric side effects of HIV medications
- in-office assessment of HIV-associated cognitive changes
- how to avoid psychotropic/antiretroviral interactions.
HIV and psychiatric patients
Psychiatric patients are among those at highest risk for HIV (Box).2-4 Cournos and McKinnon5 found that HIV seroprevalence among persons with severe mental illness was 4% to 23%compared with 0.4% in the general population.6 They defined severe mental illness as schizophrenia, schizoaffective disorder, major depression, or bipolar disorder accompanied by significant functional impairment, disruption of normal life tasks, periods of hospitalization, and need for psychotropics.
Infection rates varied with HIV geographic concentration, presence of comorbid substance use disorders, age, and ethnicity, but not psychiatric diagnosis. Unsafe sex and drug use (including noninjection) were associated with infection, and women were as likely to be infected as men.
Side effects and interactions
‘Triple therapy.’ Combining three antiretroviral agents—highly-active antiretroviral therapy (HAART) or “triple therapy”—is standard treatment for HIV infection in the United States. Initially, HAART was recommended for all patients with early-stage HIV, even if asymptomatic. This changed as antiretrovirals’ side effects—such as peripheral neuropathy with didanosine— and drug resistance from suboptimal adherence became apparent. Viral resistance develops if patients are <95% adherent to antiretroviral regimens.7
Antiretroviral therapy is usually started when:
- CD4 lymphocyte count is <200 cells/mm3 or abruptly decreasing
- plasma viral load is >55,000 copies/mL or abruptly increasing
- symptomatic AIDS emerges.
Psychiatric side effects. Psychiatric symptoms—such as depression, anxiety, confusion, psychosis, hallucinations, insomnia, and mania—are common side effects of antiretrovirals and other drugs used to treat HIV and its opportunistic infections and cancers (Table 1).8 Two antiretrovirals are of particular interest to psychiatrists:
Efavirenz is a non-nucleoside reverse transcriptase inhibitor that causes vivid dreams, especially when initiated.
AIDS death rates have declined in the United States since antiretroviral therapies were introduced in 1996, but the rate of new HIV infection has not changed.2 An estimated 850,000 to 950,000 Americans have HIV, and 25% do not know it.3
Changing demographics. Some 40,000 new HIV infections occur in the United States each year (70% among men), and one-half of the newly-infected are under age 25. African Americans and Hispanics represent 51% of total AIDS cases in men and 77% in women. From 1998 to 2002—the most recent data available from the Centers for Disease Control and Prevention (CDC)—AIDS incidence steadily decreased among whites and Hispanics but increased among blacks, Asian/Pacific Islanders, and American Indian/Alaska Natives.
Transmission routes. Approximately 60% of men with HIV are infected through male-to-male sex, 25% through IV drug use, and 15% through heterosexual sex. Unprotected anal sex appears to be occurring more frequently in some urban centers, particularly among young men who have sex with men.4 Approximately 75% of women with HIV are infected through heterosexual sex and 25% through IV drug use.
Ritonavir is a protease inhibitor that may inhibit psychotropics metabolized by cytochrome P450 3A4 and 2D6 isoenzymes.
Other HIV medications increase or decrease psychotropic blood levels via inhibition or induction of CYP isoenzymes (Table 2).9 When a patient is taking ritonavir or another protease inhibitor, reduced starting dosages of selective serotonin reuptake inhibitors (SSRIs) may be appropriate. Benzodiazepine dosages may need to be increased because of ritonavir induction of the enzyme glucuronosyltransferase.
Table 1
Psychiatric side effects of common HIV medications
| Drug | Side effects, by frequency |
|---|---|
| Acyclovir | Unknown: hallucination, confusion, thought insertion, insomnia |
| Amphotericin B | >5%: confusion, insomnia, somnolence; 1-5%: agitation, anxiety, depression, hallucination, nervousness, psychosis; Unkown: delirium |
| β-Lactam antibiotics | <1%: insomnia, somnolence, anxiety, nervousness, impaired concentration, confusion, nightmares, hallucination; Unkown: paranoia, mania |
| Trimethoprim/sulfamethoxazole | Unknown: hallucinations, depression, apathy, nervousness |
| Cycloserine Unknown: | psychosis, somnolence, depression, confusion, irritability, anxiety |
| Didanosine | Unknown: nervousness, anxiety, confusion, seizures, insomnia |
| Efavirenz | 13-16%: depression; 8-11%: anxiety; 2-6%: nervousness; >5%: headache, seizures, confusion; <2%: suicidal ideation and behavior, aggression |
| Unknown: | agitation, lability, neurosis, psychosis, insomnia, impaired concentration, somnolence, euphoria, amnesia, hallucination |
| Foscarnet | >5%: depression, confusion, anxiety; 1-5%: insomnia, somnolence, amnesia, nervousness, agitation, aggression, hallucination |
| Interferon-a | 6-19%: depression; 12-16%: irritability; 6-12%: insomnia; 3-8%: impaired concentration; >5%: anxiety: <5%: confusion, mania, aggression, delirium, lability, suicidal ideation, psychosis, personality disorder, alcohol intolerance |
| Isoniazid | Unknown: depression, agitation, hallucination, paranoia, anxiety, psychosis |
| Lamivudine | <11%: insomnia; <9%: mania, depressive disorders, dreams |
| Methotrexate | Unknown: cognitive and mood changes |
| Pentamidine | Unknown: confusion, lability, hallucination; Rare: anxiety, fatigue |
| Procarbazine | Unknown: hallucination, depression, nervousness, apprehension, mania, loss of appetite, insomnia, nightmares, confusion, malaise |
| Quinolones | <1%: somnolence, insomnia; Occasional: agitation, anxiety, depression, panic attacks, confusion, hallucination, aggression, psychosis, paranoia; |
| Rare: | suicidal ideation and suicide (no relationship with drug confirmed) |
| Stavudine | Unknown: confusion, depression, seizures, anxiety, mania, sleep problems |
| Sulfonamides | Unknown: psychosis, delirium, confusion, depression, hallucinations |
| Thiabendazole | Unknown: hallucination, fatigue, irritability, confusion, depression |
| Vinblastine | Unknown: depression |
| Vincristine | Unknown: hallucination |
| Zalcitabine | Unknown: acute psychosis, agitation, amnesia, anxiety, lability, euphoria, hallucination, insomnia, mania, paranoia, suicidal behavior, confusion, impaired concentration, somnolence, depression |
| Zidovudine | Unknown: Insomnia, vivid dreams, agitation, mania, hallucination, confusion |
Table 2
Psychotropic/HIV drug interactions, by cytochrome P-450 isoenzyme
| CYP 3A4 | CYP 2D6 | |
|---|---|---|
| Psychotropics primarily metabolized by isoenzyme | Benzodiazepines Buspirone Carbamazepine Citalopram Clomipramine Imipramine Trazodone | Fluoxetine Fluvoxamine Mirtazapine Antipsychotics (typical and atypical) Paroxetine Sertraline Tricyclics Venlafaxine |
| HIV drugs that inhibit isoenzyme | Protease inhibitors (esp. ritonavir and indinavir) Clarithromycin Erythromycin Itraconazole Ketoconazole Macrolide antibiotics | Protease inhibitors (esp. ritonavir and nelfinavir) |
| Possible clinical effect | Increased plasma levels and increased side effects; for benzodiazepines, sedation and decreased respiratory drive | Increased plasma levels and increased side effects; for tricyclics, increased risk for cardiac conduction delay |
| HIV drugs that induce isoenzyme | Nevirapine Efavirenz Glucocorticoids Rifampin Rifabutin | None |
| Possible clinical effect | Decreased psychotropic plasma levels, decreased effectiveness | None |
| Source: Adapted and reprinted with permission from reference 1, Table 16. Copyright 2000. American Psychiatric Association | ||
The FDA approved enfuvirtide—the first of the new fusion inhibitor class of antiretroviral agents—in March 2003. Enfuvirtide prevents HIV from entering the target CD4 lymphocyte in patients who show continued viral replication despite ongoing antiretroviral therapy. This agent requires twice-daily subcutaneous injections. Because enfuvirtide can be viewed as a medication of last resort, nonresponse may be especially disheartening to an AIDS patient.
Substances of abuse also interact with HIV medications. A lethal overdose of the street drug MDMA (“Ecstasy”) has been reported in a patient treated with ritonavir.10 MDMA is metabolized primarily via CYP 2D6. Other substances of abuse metabolized by CYP 2D6 or 3A4—such as amphetamines, ketamine, heroin, cocaine, and gamma-hydroxybutyrate—may cause toxic reactions in patients being treated with protease inhibitors.
Because substance abuse is a common comorbidity of HIV infection, warn patients that using recreational drugs with antiretroviral medications can cause adverse reactions. Extensive drug interaction lists are available on patient education and physician Web sites (see Related Resources).
Table 3
Diagnostic criteria for HIV-associated minor cognitive motor disorder
Probable diagnosis (must meet all four criteria)
A possible diagnosis of minor cognitive motor disorder can be given if criteria 1-3 are present and either:
|
| Source: Reprinted with permission from reference 14 |
Lipid and hyperglycemic side effects. Antivirals— especially protease inhibitors —appear to be associated with HIV lipodystrophy, which is associated with cosmetic and serum lipid changes as well as hyperglycemia.11 Facial wasting, buffalo humps, and central intra-abdominal obesity may occur, and elevated serum cholesterol and triglycerides often require treatment with cholesterollowering “statin” drugs.
Though it is unclear whether HIV lipodystrophy increases cardiovascular disease risk, carefully consider the potential effects of psychotropics associated with weight gain, hyper-glycemia, and elevated lipids in patients receiving antiretroviral therapy.
Hepatitis. Patients at risk for HIV infection are also at risk for viral hepatitis. One-quarter of persons with HIV are coinfected with hepatitis C, primarily through IV drug use.12 Alpha-interferon treatment of hepatitis B and C has been associated with depression. SSRI treatment—such as paroxetine, 20 mg/d—can ease depressive symptoms.13
HIV-associated cognitive changes
Minor cognitive-motor disorder(Table 3) and HIV-associated dementia (Table 4) 14 are typically seen in late-stage HIV infections and are diagnoses of exclusion. Physical or neurologic examination in a patient with HIV/AIDS and altered mental status may show:
- focal deficits indicating a space-occupying lesion (eg, CNS lymphoma or toxoplasmosis)
- sensory changes that may indicate peripheral neuropathy
- ataxia or gait changes that may indicate myelopathy.
Useful neuropsychological tests include the HIV Dementia Rating Scale,15 Halstead finger-tapping test for motor speed,16 and the Trailmaking Test, which assesses psychomotor speed and sequencing ability.17
Antiretroviral therapy appears to reduce the risk of HIV-associated dementia. In a trial conducted at 42 AIDS Clinical Trials Group sites and 7 National Hemophilia Foundation sites, combination reverse transcriptase inhibitors helped preserve or improve neurologic function.18
Psychostimulants appear to improve HIV-induced brain impairment.19 Immune modulators—such as tumor necrosis factor-alpha blockers (eg, pentoxifylline)20 and interleukin-1 receptor blockers21 —have also been studied for possible beneficial effects on HIV brain disease.
HIV prevention
Because unprotected sex and IV substance use are the primary HIV transmission routes in the United States, assessing psychiatric patients’ sexual and substance use behaviors may help you prevent HIV infection. The CDC offers guidelines for HIV testing, counseling, and referral (see Related Resources).
To identify persons at risk for HIV infection, the CDC recommends asking open-ended questions about risk behaviors, such as: “What are you doing now or what have you done in the past that you think may put you at risk for HIV infection?”22
The shift of new HIV infection disproportionately into African-American and Hispanic populations suggests the need for more-intensive prevention and education in those communities. CDC guidelines emphasize the importance of using culturally sensitive language when asking about risk behavior. Some individuals may engage in same-sex behaviors but do not identify themselves as “homosexual” or “gay.” In some African-American communities, for example, being “on the down low” is used to describe men—oftentimes married—who have sex with men.
To incorporate HIV-prevention messages and brief behavioral interventions into clinical visits:
- speak with patients about sexual and drug use behaviors in simple, everyday language
- learn about interventions shown to be effective
- become familiar with community resources that address HIV risk reduction.23
Training. The CDC and Health Resources and Services Administration of the U.S. Department of Health and Human Services offer free training on risk screening and prevention, as well as opportunities for continuing medical education (see Related Resources).
Table 4
Diagnostic criteria for HIV-associated dementia
|
| Source: Reprinted with permission from reference 14 |
Advances in antibody testing
Psychiatrists play an important supportive role in encouraging HIV screening of at-risk patients of unknown serostatus and in counseling such patients before, during, and after test results are known.
Rapid lab tests. In 2002, the FDA approved a rapid, highly accurate HIV-1 screening test for serum specimens and in March 2004 approved the same test for screening oral fluid specimens. Test results with serum or an oral swab are available from a laboratory in approximately 20 minutes. In clinical studies submitted to the FDA, the OraQuick oral fluid test correctly identified 99.3% of persons infected with HIV-1 (sensitivity) and 99.9% of those not infected (specificity).
CDC guidelines for HIV counseling and testing have been revised to include rapid testing. Screening tests are most accurate at least 3 months after an HIV exposure—the time required for antibodies to develop. When counseling patients after a reactive test result, emphasize that the result is preliminary and further testing is needed to confirm the result. Counsel patients who have a negative result within 3 months of possible infection to be retested to guard against a possible false-negative result.
Home test kits. An FDA-approved consumer-controlled test kit—Home Access HIV-1 Test System24 —is sold at drug stores without a prescription. The customer pricks a finger with a special device, places drops of blood on a specially treated card, and mails the card to a licensed laboratory. Anonymous identification numbers are used when phoning for the results.
Customers may speak to a counselor before taking the test, while awaiting results, and when results are given. All individuals with a reactive test result are referred for a more-specific test and receive information and resources on treatment and support services.
Counseling the HIV patient
The psychological impact of positive HIV antibody test results on psychiatric patients has not been studied. Persons without psychiatric disorders commonly experience anxiety and depression immediately after learning of a positive result. Unless the patient has HIV-related physical symptoms, these psychological sequelae often return to baseline—similar to when the blood sample was drawn—within 2 weeks.25
Patients need to know that a positive HIV test result is no longer associated with death within 2 to 3 years. During a 2-year period, for example, disease progression from HIV infection to AIDS decreased 7-fold among patients who started antiretroviral therapy with a CD4+ T-cell count >350 cells/mm3, compared with others who were monitored without therapy.26 This may be especially important to reinforce with newly-diagnosed patients unfamiliar with advances in HAART.
Medication adherence. To increase patients’ adherence to antiretroviral therapy:
- express interest that they are taking their medications
- use psychotherapy to help them solve problems that interfere with adherence.
Suicide risk. In the 1980s, significantly increased suicide rates were reported among HIV-infected persons. For example, the suicide rate in 1985 for New York City men ages 20 to 59 living with an AIDS diagnosis was 36 times higher than that of similar men without AIDS.27 A later study of HIV infection in New York male suicide victims from 1991 to 1993 suggested that HIV serostatus was associated with a modest increase—at most—in suicide risk. That study considered the interplay of other suicide risk factors, such as substance abuse.28
- Guidelines for HIV counseling, testing, and referral. Centers for Disease Control and Prevention. www.cdc.gov/mmwr/preview/mmwrhtml/rr5019a1.htm
- Training in HIV prevention and counseling. National Network of STD/HIV Prevention Training Centers (http://depts.washington.edu/nnptc) and AIDS Education and Training Centers National Resource Center (http://www.aids-ed.org)
- Rapid HIV testing. Centers for Disease Control and Prevention. http://www.cdc.gov/hiv/rapid_testing/
- Cytochrome P450 drug interaction table. Indiana University School of Medicine. Division of Clinical Pharmacology. www.drug-interactions.com
Drug brand names
- Buspirone • BuSpar
- Carbamazepine • Carbatrol
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Liang reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products
Psychiatric patients—especially those with substance abuse disorders—are at high risk for HIV infection, which puts psychiatrists on the AIDS pandemic’s front lines.
In the wake of last month’s International AIDS Conference in Thailand, this article supplements American Psychiatric Association guidelines for managing patients with HIV/AIDS.1 Here is updated information on:
- who is at greatest risk for HIV infection today
- neuropsychiatric side effects of HIV medications
- in-office assessment of HIV-associated cognitive changes
- how to avoid psychotropic/antiretroviral interactions.
HIV and psychiatric patients
Psychiatric patients are among those at highest risk for HIV (Box).2-4 Cournos and McKinnon5 found that HIV seroprevalence among persons with severe mental illness was 4% to 23%compared with 0.4% in the general population.6 They defined severe mental illness as schizophrenia, schizoaffective disorder, major depression, or bipolar disorder accompanied by significant functional impairment, disruption of normal life tasks, periods of hospitalization, and need for psychotropics.
Infection rates varied with HIV geographic concentration, presence of comorbid substance use disorders, age, and ethnicity, but not psychiatric diagnosis. Unsafe sex and drug use (including noninjection) were associated with infection, and women were as likely to be infected as men.
Side effects and interactions
‘Triple therapy.’ Combining three antiretroviral agents—highly-active antiretroviral therapy (HAART) or “triple therapy”—is standard treatment for HIV infection in the United States. Initially, HAART was recommended for all patients with early-stage HIV, even if asymptomatic. This changed as antiretrovirals’ side effects—such as peripheral neuropathy with didanosine— and drug resistance from suboptimal adherence became apparent. Viral resistance develops if patients are <95% adherent to antiretroviral regimens.7
Antiretroviral therapy is usually started when:
- CD4 lymphocyte count is <200 cells/mm3 or abruptly decreasing
- plasma viral load is >55,000 copies/mL or abruptly increasing
- symptomatic AIDS emerges.
Psychiatric side effects. Psychiatric symptoms—such as depression, anxiety, confusion, psychosis, hallucinations, insomnia, and mania—are common side effects of antiretrovirals and other drugs used to treat HIV and its opportunistic infections and cancers (Table 1).8 Two antiretrovirals are of particular interest to psychiatrists:
Efavirenz is a non-nucleoside reverse transcriptase inhibitor that causes vivid dreams, especially when initiated.
AIDS death rates have declined in the United States since antiretroviral therapies were introduced in 1996, but the rate of new HIV infection has not changed.2 An estimated 850,000 to 950,000 Americans have HIV, and 25% do not know it.3
Changing demographics. Some 40,000 new HIV infections occur in the United States each year (70% among men), and one-half of the newly-infected are under age 25. African Americans and Hispanics represent 51% of total AIDS cases in men and 77% in women. From 1998 to 2002—the most recent data available from the Centers for Disease Control and Prevention (CDC)—AIDS incidence steadily decreased among whites and Hispanics but increased among blacks, Asian/Pacific Islanders, and American Indian/Alaska Natives.
Transmission routes. Approximately 60% of men with HIV are infected through male-to-male sex, 25% through IV drug use, and 15% through heterosexual sex. Unprotected anal sex appears to be occurring more frequently in some urban centers, particularly among young men who have sex with men.4 Approximately 75% of women with HIV are infected through heterosexual sex and 25% through IV drug use.
Ritonavir is a protease inhibitor that may inhibit psychotropics metabolized by cytochrome P450 3A4 and 2D6 isoenzymes.
Other HIV medications increase or decrease psychotropic blood levels via inhibition or induction of CYP isoenzymes (Table 2).9 When a patient is taking ritonavir or another protease inhibitor, reduced starting dosages of selective serotonin reuptake inhibitors (SSRIs) may be appropriate. Benzodiazepine dosages may need to be increased because of ritonavir induction of the enzyme glucuronosyltransferase.
Table 1
Psychiatric side effects of common HIV medications
| Drug | Side effects, by frequency |
|---|---|
| Acyclovir | Unknown: hallucination, confusion, thought insertion, insomnia |
| Amphotericin B | >5%: confusion, insomnia, somnolence; 1-5%: agitation, anxiety, depression, hallucination, nervousness, psychosis; Unkown: delirium |
| β-Lactam antibiotics | <1%: insomnia, somnolence, anxiety, nervousness, impaired concentration, confusion, nightmares, hallucination; Unkown: paranoia, mania |
| Trimethoprim/sulfamethoxazole | Unknown: hallucinations, depression, apathy, nervousness |
| Cycloserine Unknown: | psychosis, somnolence, depression, confusion, irritability, anxiety |
| Didanosine | Unknown: nervousness, anxiety, confusion, seizures, insomnia |
| Efavirenz | 13-16%: depression; 8-11%: anxiety; 2-6%: nervousness; >5%: headache, seizures, confusion; <2%: suicidal ideation and behavior, aggression |
| Unknown: | agitation, lability, neurosis, psychosis, insomnia, impaired concentration, somnolence, euphoria, amnesia, hallucination |
| Foscarnet | >5%: depression, confusion, anxiety; 1-5%: insomnia, somnolence, amnesia, nervousness, agitation, aggression, hallucination |
| Interferon-a | 6-19%: depression; 12-16%: irritability; 6-12%: insomnia; 3-8%: impaired concentration; >5%: anxiety: <5%: confusion, mania, aggression, delirium, lability, suicidal ideation, psychosis, personality disorder, alcohol intolerance |
| Isoniazid | Unknown: depression, agitation, hallucination, paranoia, anxiety, psychosis |
| Lamivudine | <11%: insomnia; <9%: mania, depressive disorders, dreams |
| Methotrexate | Unknown: cognitive and mood changes |
| Pentamidine | Unknown: confusion, lability, hallucination; Rare: anxiety, fatigue |
| Procarbazine | Unknown: hallucination, depression, nervousness, apprehension, mania, loss of appetite, insomnia, nightmares, confusion, malaise |
| Quinolones | <1%: somnolence, insomnia; Occasional: agitation, anxiety, depression, panic attacks, confusion, hallucination, aggression, psychosis, paranoia; |
| Rare: | suicidal ideation and suicide (no relationship with drug confirmed) |
| Stavudine | Unknown: confusion, depression, seizures, anxiety, mania, sleep problems |
| Sulfonamides | Unknown: psychosis, delirium, confusion, depression, hallucinations |
| Thiabendazole | Unknown: hallucination, fatigue, irritability, confusion, depression |
| Vinblastine | Unknown: depression |
| Vincristine | Unknown: hallucination |
| Zalcitabine | Unknown: acute psychosis, agitation, amnesia, anxiety, lability, euphoria, hallucination, insomnia, mania, paranoia, suicidal behavior, confusion, impaired concentration, somnolence, depression |
| Zidovudine | Unknown: Insomnia, vivid dreams, agitation, mania, hallucination, confusion |
Table 2
Psychotropic/HIV drug interactions, by cytochrome P-450 isoenzyme
| CYP 3A4 | CYP 2D6 | |
|---|---|---|
| Psychotropics primarily metabolized by isoenzyme | Benzodiazepines Buspirone Carbamazepine Citalopram Clomipramine Imipramine Trazodone | Fluoxetine Fluvoxamine Mirtazapine Antipsychotics (typical and atypical) Paroxetine Sertraline Tricyclics Venlafaxine |
| HIV drugs that inhibit isoenzyme | Protease inhibitors (esp. ritonavir and indinavir) Clarithromycin Erythromycin Itraconazole Ketoconazole Macrolide antibiotics | Protease inhibitors (esp. ritonavir and nelfinavir) |
| Possible clinical effect | Increased plasma levels and increased side effects; for benzodiazepines, sedation and decreased respiratory drive | Increased plasma levels and increased side effects; for tricyclics, increased risk for cardiac conduction delay |
| HIV drugs that induce isoenzyme | Nevirapine Efavirenz Glucocorticoids Rifampin Rifabutin | None |
| Possible clinical effect | Decreased psychotropic plasma levels, decreased effectiveness | None |
| Source: Adapted and reprinted with permission from reference 1, Table 16. Copyright 2000. American Psychiatric Association | ||
The FDA approved enfuvirtide—the first of the new fusion inhibitor class of antiretroviral agents—in March 2003. Enfuvirtide prevents HIV from entering the target CD4 lymphocyte in patients who show continued viral replication despite ongoing antiretroviral therapy. This agent requires twice-daily subcutaneous injections. Because enfuvirtide can be viewed as a medication of last resort, nonresponse may be especially disheartening to an AIDS patient.
Substances of abuse also interact with HIV medications. A lethal overdose of the street drug MDMA (“Ecstasy”) has been reported in a patient treated with ritonavir.10 MDMA is metabolized primarily via CYP 2D6. Other substances of abuse metabolized by CYP 2D6 or 3A4—such as amphetamines, ketamine, heroin, cocaine, and gamma-hydroxybutyrate—may cause toxic reactions in patients being treated with protease inhibitors.
Because substance abuse is a common comorbidity of HIV infection, warn patients that using recreational drugs with antiretroviral medications can cause adverse reactions. Extensive drug interaction lists are available on patient education and physician Web sites (see Related Resources).
Table 3
Diagnostic criteria for HIV-associated minor cognitive motor disorder
Probable diagnosis (must meet all four criteria)
A possible diagnosis of minor cognitive motor disorder can be given if criteria 1-3 are present and either:
|
| Source: Reprinted with permission from reference 14 |
Lipid and hyperglycemic side effects. Antivirals— especially protease inhibitors —appear to be associated with HIV lipodystrophy, which is associated with cosmetic and serum lipid changes as well as hyperglycemia.11 Facial wasting, buffalo humps, and central intra-abdominal obesity may occur, and elevated serum cholesterol and triglycerides often require treatment with cholesterollowering “statin” drugs.
Though it is unclear whether HIV lipodystrophy increases cardiovascular disease risk, carefully consider the potential effects of psychotropics associated with weight gain, hyper-glycemia, and elevated lipids in patients receiving antiretroviral therapy.
Hepatitis. Patients at risk for HIV infection are also at risk for viral hepatitis. One-quarter of persons with HIV are coinfected with hepatitis C, primarily through IV drug use.12 Alpha-interferon treatment of hepatitis B and C has been associated with depression. SSRI treatment—such as paroxetine, 20 mg/d—can ease depressive symptoms.13
HIV-associated cognitive changes
Minor cognitive-motor disorder(Table 3) and HIV-associated dementia (Table 4) 14 are typically seen in late-stage HIV infections and are diagnoses of exclusion. Physical or neurologic examination in a patient with HIV/AIDS and altered mental status may show:
- focal deficits indicating a space-occupying lesion (eg, CNS lymphoma or toxoplasmosis)
- sensory changes that may indicate peripheral neuropathy
- ataxia or gait changes that may indicate myelopathy.
Useful neuropsychological tests include the HIV Dementia Rating Scale,15 Halstead finger-tapping test for motor speed,16 and the Trailmaking Test, which assesses psychomotor speed and sequencing ability.17
Antiretroviral therapy appears to reduce the risk of HIV-associated dementia. In a trial conducted at 42 AIDS Clinical Trials Group sites and 7 National Hemophilia Foundation sites, combination reverse transcriptase inhibitors helped preserve or improve neurologic function.18
Psychostimulants appear to improve HIV-induced brain impairment.19 Immune modulators—such as tumor necrosis factor-alpha blockers (eg, pentoxifylline)20 and interleukin-1 receptor blockers21 —have also been studied for possible beneficial effects on HIV brain disease.
HIV prevention
Because unprotected sex and IV substance use are the primary HIV transmission routes in the United States, assessing psychiatric patients’ sexual and substance use behaviors may help you prevent HIV infection. The CDC offers guidelines for HIV testing, counseling, and referral (see Related Resources).
To identify persons at risk for HIV infection, the CDC recommends asking open-ended questions about risk behaviors, such as: “What are you doing now or what have you done in the past that you think may put you at risk for HIV infection?”22
The shift of new HIV infection disproportionately into African-American and Hispanic populations suggests the need for more-intensive prevention and education in those communities. CDC guidelines emphasize the importance of using culturally sensitive language when asking about risk behavior. Some individuals may engage in same-sex behaviors but do not identify themselves as “homosexual” or “gay.” In some African-American communities, for example, being “on the down low” is used to describe men—oftentimes married—who have sex with men.
To incorporate HIV-prevention messages and brief behavioral interventions into clinical visits:
- speak with patients about sexual and drug use behaviors in simple, everyday language
- learn about interventions shown to be effective
- become familiar with community resources that address HIV risk reduction.23
Training. The CDC and Health Resources and Services Administration of the U.S. Department of Health and Human Services offer free training on risk screening and prevention, as well as opportunities for continuing medical education (see Related Resources).
Table 4
Diagnostic criteria for HIV-associated dementia
|
| Source: Reprinted with permission from reference 14 |
Advances in antibody testing
Psychiatrists play an important supportive role in encouraging HIV screening of at-risk patients of unknown serostatus and in counseling such patients before, during, and after test results are known.
Rapid lab tests. In 2002, the FDA approved a rapid, highly accurate HIV-1 screening test for serum specimens and in March 2004 approved the same test for screening oral fluid specimens. Test results with serum or an oral swab are available from a laboratory in approximately 20 minutes. In clinical studies submitted to the FDA, the OraQuick oral fluid test correctly identified 99.3% of persons infected with HIV-1 (sensitivity) and 99.9% of those not infected (specificity).
CDC guidelines for HIV counseling and testing have been revised to include rapid testing. Screening tests are most accurate at least 3 months after an HIV exposure—the time required for antibodies to develop. When counseling patients after a reactive test result, emphasize that the result is preliminary and further testing is needed to confirm the result. Counsel patients who have a negative result within 3 months of possible infection to be retested to guard against a possible false-negative result.
Home test kits. An FDA-approved consumer-controlled test kit—Home Access HIV-1 Test System24 —is sold at drug stores without a prescription. The customer pricks a finger with a special device, places drops of blood on a specially treated card, and mails the card to a licensed laboratory. Anonymous identification numbers are used when phoning for the results.
Customers may speak to a counselor before taking the test, while awaiting results, and when results are given. All individuals with a reactive test result are referred for a more-specific test and receive information and resources on treatment and support services.
Counseling the HIV patient
The psychological impact of positive HIV antibody test results on psychiatric patients has not been studied. Persons without psychiatric disorders commonly experience anxiety and depression immediately after learning of a positive result. Unless the patient has HIV-related physical symptoms, these psychological sequelae often return to baseline—similar to when the blood sample was drawn—within 2 weeks.25
Patients need to know that a positive HIV test result is no longer associated with death within 2 to 3 years. During a 2-year period, for example, disease progression from HIV infection to AIDS decreased 7-fold among patients who started antiretroviral therapy with a CD4+ T-cell count >350 cells/mm3, compared with others who were monitored without therapy.26 This may be especially important to reinforce with newly-diagnosed patients unfamiliar with advances in HAART.
Medication adherence. To increase patients’ adherence to antiretroviral therapy:
- express interest that they are taking their medications
- use psychotherapy to help them solve problems that interfere with adherence.
Suicide risk. In the 1980s, significantly increased suicide rates were reported among HIV-infected persons. For example, the suicide rate in 1985 for New York City men ages 20 to 59 living with an AIDS diagnosis was 36 times higher than that of similar men without AIDS.27 A later study of HIV infection in New York male suicide victims from 1991 to 1993 suggested that HIV serostatus was associated with a modest increase—at most—in suicide risk. That study considered the interplay of other suicide risk factors, such as substance abuse.28
- Guidelines for HIV counseling, testing, and referral. Centers for Disease Control and Prevention. www.cdc.gov/mmwr/preview/mmwrhtml/rr5019a1.htm
- Training in HIV prevention and counseling. National Network of STD/HIV Prevention Training Centers (http://depts.washington.edu/nnptc) and AIDS Education and Training Centers National Resource Center (http://www.aids-ed.org)
- Rapid HIV testing. Centers for Disease Control and Prevention. http://www.cdc.gov/hiv/rapid_testing/
- Cytochrome P450 drug interaction table. Indiana University School of Medicine. Division of Clinical Pharmacology. www.drug-interactions.com
Drug brand names
- Buspirone • BuSpar
- Carbamazepine • Carbatrol
- Citalopram • Celexa
- Clomipramine • Anafranil
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Liang reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products
1. American Psychiatric Association. Practice guideline for the treatment of patients with HIV/AIDS. Am J Psychiatry. 2000 157 11(suppl). Also available at: www.psych.org/psych_pract/treatg/pg/hivaids_revisebook_index.cfm
2. Centers for Disease Control and Prevention National Center for HIV, STD, and TB Prevention. HIV AIDS Surveill Rep December 2001. Available at: http://www.cdc.gov/hiv/stats/hasr1302.htm
3. Centers for Disease Control and Prevention. HIV AIDS Surveill Rep 2002;14:148. Also available at: http://www.cdc.gov/hiv/stats/hasr1402/2002SurveillanceReport.pdf
4. Risk reduction: sex without condoms. HIV Counselor Perspectives [newsletter] 2001;10(2, March).
5. Cournos F, McKinnon K. HIV seroprevalence among people with severe mental illness in the United States: a critical review. Clin Psychol Rev 1997;17:259-69.
6. Steele FR. A moving target: CDC still trying to estimate HIV-1 prevalence. J NIH Res 1994;6:25-6.
7. Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000;133:21-30.
8. Grant I, Atkinson JH, Jr. Neuropsychiatric aspects of HIV infection and AIDS. In: Sadock BJ, Sadock VA (eds). Kaplan and Sadock’s comprehensive textbook of psychiatry. Philadelphia: Lippincott Williams & Wilkins, 1999;308-36.
9. Ayuso JL. Use of psychotropic drugs in patients with HIV infection. Drugs 1994;47:599-610.
10. Mirken B. Danger: possibly fatal interactions between ritonavir and “ecstasy,” some other psychoactive drugs. AIDS Treat News 1997;Feb 21(No 265):5.-
11. Miller KD, Jones E, Yanovski JA, et al. Visceral abdominal-fat accumulation associated with use of indinavir. Lancet 1998;351(9106):871-5.
12. Centers for Disease Control and Prevention. Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. MMWR 1998;47(No. RR-19):1-39.
13. Kraus MR, Schafer A, Faller H, et al. Paroxetine for the treatment of interferon-alpha-induced depression in chronic hepatitis C. Aliment Pharmacol Ther 2002;16(6):1091-9.
14. Nomenclature and research case definitions for neurologic manifestations of human immunodeficiency virus-type 1 (HIV-1) infection: report of a working group of the American Academy of Neurology AIDS Task Force. Neurology 1991;41:778-85.
15. Power C, Selnes OA, Grim JA, McArthur JC. HIV Dementia Scale: a rapid screening test. J Acquir Immune Defic Syndr Hum Retrovirol 1995 Mar 1;8(3):273-8.
16. Silberstein CH, McKegney FP, O'Dowd MA, et al. A prospective longitudinal study of neuropsychological and psychosocial factors in asymptomatic individuals at risk for HTLV-III/LAV infection in a methadone program: preliminary findings. Int J Neurosci 1987;32(3-4):669-76.
17. Reitan RM. Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills 1958;8:271-6.
18. Price RW, Yiannoutsos CT, Clifford DB, et al. Neurological outcomes in late HIV infection: adverse impact of neurological impairment on survival and protective effect of antiviral therapy. AIDS Clinical Trial Group and Neurological AIDS Research Consortium study team. AIDS 1999;13(13):1677-85.
19. Perry SW. Organic mental disorders caused by HIV: update on early diagnosis and treatment. Am J Psychiatry 1990;147(6):696-710.
20. Wilt SG, Milward E, Zhou JM, et al. In vitro evidence for a dual role of tumor necrosis factor-alpha in human immunodeficiency virus type 1 encephalopathy. Ann Neurol 1995;37(3):381-94.
21. Boven LA, Gomes L, Hery C, et al. Increased peroxynitrite activity in AIDS dementia complex: implications for the neuropathogenesis of HIV-1 infection. J Immunol 1999;162(7):4319-27.
22. Centers for Disease Control and Prevention. Revised guidelines for HIV counseling, testing, and referral. MMWR Nov. 9, 2001;50(RR19):1-58.
23. Centers for Disease Control and Prevention. Incorporating HIV prevention into the medical care of persons living with HIV. MMWR July 18, 2003;52(RR12):1-24. Also available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5212a1.htm
24. Food and Drug Administration. Home Access HIV-1 Test System: Summary of safety and effectiveness. Available at: http://www.fda.gov/cber/PMAsumm/P950002S.pdf
25. Perry SW, Jacobsberg LB, Fishman B. Psychological responses to serological testing for HIV. AIDS 1990;4(2):145-52.
26. Opravil M, Ledergerber B, Furrer H. et al and the Swiss HIV Cohort Study Clinical benefit of early initiation of HAART in patients with asymptomatic HIV and CD4 counts >350/mm 3 . Abstract LB-6. Chicago, IL: 8th Conference on Retroviruses and Opportunistic Infections, 2001.
27. Marzuk P, Tierney H, Tardiff K, et al. Increased risk of suicide in persons with AIDS. JAMA 1988;259:1333-7.
28. Marzuk PM, Tardiff K, Leon AC, et al. HIV seroprevalence among suicide victims in New York City, 1991-93. Am J Psychiatry 1997;154(6):1720-5.
1. American Psychiatric Association. Practice guideline for the treatment of patients with HIV/AIDS. Am J Psychiatry. 2000 157 11(suppl). Also available at: www.psych.org/psych_pract/treatg/pg/hivaids_revisebook_index.cfm
2. Centers for Disease Control and Prevention National Center for HIV, STD, and TB Prevention. HIV AIDS Surveill Rep December 2001. Available at: http://www.cdc.gov/hiv/stats/hasr1302.htm
3. Centers for Disease Control and Prevention. HIV AIDS Surveill Rep 2002;14:148. Also available at: http://www.cdc.gov/hiv/stats/hasr1402/2002SurveillanceReport.pdf
4. Risk reduction: sex without condoms. HIV Counselor Perspectives [newsletter] 2001;10(2, March).
5. Cournos F, McKinnon K. HIV seroprevalence among people with severe mental illness in the United States: a critical review. Clin Psychol Rev 1997;17:259-69.
6. Steele FR. A moving target: CDC still trying to estimate HIV-1 prevalence. J NIH Res 1994;6:25-6.
7. Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000;133:21-30.
8. Grant I, Atkinson JH, Jr. Neuropsychiatric aspects of HIV infection and AIDS. In: Sadock BJ, Sadock VA (eds). Kaplan and Sadock’s comprehensive textbook of psychiatry. Philadelphia: Lippincott Williams & Wilkins, 1999;308-36.
9. Ayuso JL. Use of psychotropic drugs in patients with HIV infection. Drugs 1994;47:599-610.
10. Mirken B. Danger: possibly fatal interactions between ritonavir and “ecstasy,” some other psychoactive drugs. AIDS Treat News 1997;Feb 21(No 265):5.-
11. Miller KD, Jones E, Yanovski JA, et al. Visceral abdominal-fat accumulation associated with use of indinavir. Lancet 1998;351(9106):871-5.
12. Centers for Disease Control and Prevention. Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. MMWR 1998;47(No. RR-19):1-39.
13. Kraus MR, Schafer A, Faller H, et al. Paroxetine for the treatment of interferon-alpha-induced depression in chronic hepatitis C. Aliment Pharmacol Ther 2002;16(6):1091-9.
14. Nomenclature and research case definitions for neurologic manifestations of human immunodeficiency virus-type 1 (HIV-1) infection: report of a working group of the American Academy of Neurology AIDS Task Force. Neurology 1991;41:778-85.
15. Power C, Selnes OA, Grim JA, McArthur JC. HIV Dementia Scale: a rapid screening test. J Acquir Immune Defic Syndr Hum Retrovirol 1995 Mar 1;8(3):273-8.
16. Silberstein CH, McKegney FP, O'Dowd MA, et al. A prospective longitudinal study of neuropsychological and psychosocial factors in asymptomatic individuals at risk for HTLV-III/LAV infection in a methadone program: preliminary findings. Int J Neurosci 1987;32(3-4):669-76.
17. Reitan RM. Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills 1958;8:271-6.
18. Price RW, Yiannoutsos CT, Clifford DB, et al. Neurological outcomes in late HIV infection: adverse impact of neurological impairment on survival and protective effect of antiviral therapy. AIDS Clinical Trial Group and Neurological AIDS Research Consortium study team. AIDS 1999;13(13):1677-85.
19. Perry SW. Organic mental disorders caused by HIV: update on early diagnosis and treatment. Am J Psychiatry 1990;147(6):696-710.
20. Wilt SG, Milward E, Zhou JM, et al. In vitro evidence for a dual role of tumor necrosis factor-alpha in human immunodeficiency virus type 1 encephalopathy. Ann Neurol 1995;37(3):381-94.
21. Boven LA, Gomes L, Hery C, et al. Increased peroxynitrite activity in AIDS dementia complex: implications for the neuropathogenesis of HIV-1 infection. J Immunol 1999;162(7):4319-27.
22. Centers for Disease Control and Prevention. Revised guidelines for HIV counseling, testing, and referral. MMWR Nov. 9, 2001;50(RR19):1-58.
23. Centers for Disease Control and Prevention. Incorporating HIV prevention into the medical care of persons living with HIV. MMWR July 18, 2003;52(RR12):1-24. Also available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5212a1.htm
24. Food and Drug Administration. Home Access HIV-1 Test System: Summary of safety and effectiveness. Available at: http://www.fda.gov/cber/PMAsumm/P950002S.pdf
25. Perry SW, Jacobsberg LB, Fishman B. Psychological responses to serological testing for HIV. AIDS 1990;4(2):145-52.
26. Opravil M, Ledergerber B, Furrer H. et al and the Swiss HIV Cohort Study Clinical benefit of early initiation of HAART in patients with asymptomatic HIV and CD4 counts >350/mm 3 . Abstract LB-6. Chicago, IL: 8th Conference on Retroviruses and Opportunistic Infections, 2001.
27. Marzuk P, Tierney H, Tardiff K, et al. Increased risk of suicide in persons with AIDS. JAMA 1988;259:1333-7.
28. Marzuk PM, Tardiff K, Leon AC, et al. HIV seroprevalence among suicide victims in New York City, 1991-93. Am J Psychiatry 1997;154(6):1720-5.
Bedside psychotherapy: Brief and surprisingly effective
Bedside psychotherapy is not only possible but invaluable for some medical-surgical patients, despite hospitals’ distractions, lack of privacy, and short stays. If you are asked to evaluate a hospitalized patient, a 5-step strategy can help you:
- identify acute psychiatric problems that psychotherapy can help
- watch for common psychodynamic themes
- choose a beneficial psychotherapy
- integrate drug/psychotherapy, as needed
- quickly establish rapport by using an effective bedside manner.
Case report: A deeply wounded patient
Ms. T, age 45, was admitted to the trauma unit with gunshot wounds. Her estranged husband shot her during an argument and killed her 14-year-old son, who tried to help her.
She underwent multiple surgeries to repair internal organs and endured intense pain. She was medically stable after 10 days, and the surgical team called on the psychiatric consultation-liaison (C-L) service to evaluate her “depression.”
Table 1
5 steps to bedside psychotherapy
|
Ms. T told the psychiatrist she was having nightmares and re-experiencing the shootings. She felt overwhelming guilt and blamed herself for her son’s death. She reported hyperarousal, muscle tension, and palpitations. She also worried about facing her son’s killer in court.
The C-L psychiatrist felt Ms. T would benefit from medication and psychotherapy for anxiety while hospitalized.
Obstacles to bedside psychotherapy
Hospitalized patients do not usually seek psychiatric consultation but are referred by their physicians. Pain and injuries, medications, and illness can limit patients’ energy and motivation to participate in therapy, as well as their concentration and cognition. Moreover, bedside psychotherapy sessions are likely to be interrupted for blood draws, medical rounds, investigations, and procedures.
Despite these obstacles, medical patients are often receptive to psychiatric care.1 An alliance often develops within minutes, and the psychiatrist can achieve effective psychotherapy during a single bedside visit.2
The Academy of Psychosomatic Medicine considers psychotherapy a required skill for anyone who evaluates and treats psychiatric disorders in general medical settings.3
How to overcome obstacles
STEP 1. Identify when psychotherapy may help. Not every problem or patient benefits from bedside psychotherapy. The C-L psychiatrist’s first task is to identify:
- Problems that warrant psychotherapy. These may include depression, bereavement, adjustment disorder, maladaptive coping, anxiety related to medical procedures, acute stress disorder, posttraumatic stress disorder (PTSD), and demoralization.
- Patients likely to benefit. Look for evidence of ego strength, ability to interact in the first session, psychological-mindedness, ability to experience feeling, and absence of severe cognitive deficit.2
These patient traits are not prerequisites, however, and clinical judgment applies on a case-by-case basis.
Demoralization is the most common reason for psychiatric evaluation of medically-ill patients, though their physicians typically request a “depression” evaluation.4 Demoralization is an understandable response to serious illness or disabling, agonizing, or deforming treatment.5 Symptoms include anxiety, guilt, shame, depression, diminished self-worth, and possibly somatic complaints or preoccupation.6
Ms. T was experiencing survivor guilt—she blamed herself for her son’s death—and she described herself as feeling “lost.” Four strategies can treat demoralization (Table 2).
STEP 2. Watch for common psychodynamic themes, such as denial of illness, loss of control, dependency and regression, fear of abandonment, loss of identity, and fear of death.7 Other issues include survivor guilt, anger at the treatment team or family, and knowing someone who had a negative experience with the same illness or treatment.
Identifying these themes and integrating them into the treatment plan can improve outcomes. For example:
- Giving an empathic validation can help overcome fear of abandonment.
- Letting the patient choose the time when blood is drawn increases feelings of control.
Table 2
4 bedside strategies to treat demoralization
| Strategy | Examples |
|---|---|
| Validate the patient’s feeling and experience | Say, “I can see this is frustrating to you to be in the hospital so long,” or “You must feel as if everything is out of your control” |
| Reassure the patient that demoralization is a natural response to a difficult situation | Say, “I can imagine that anyone in your place would feel the same way,” or “It’s only natural to feel this way after what you’ve been through; this does not mean you have a mental illness or are ‘going crazy’” |
| Make simple gestures that promote an improved outlook | Use an effective bedside manner (Box 1) |
| Alleviate feelings of isolation, and foster a sense of hope | Use resilience-building questions (Box 2) |
STEP 3. Select appropriate psychotherapy. The psychiatrist’s challenge is to know:
- when to use which approach
- when to combine approaches
- what problems each approach targets.
A hospitalized medical patient often has a fluctuating course and may require more than one approach—or even a different approach at each visit. Thus, flexibility and creativity are keys to successful bedside psychotherapy.
STEP 4. Integrate psychotherapy with medication, as needed. Consider target symptoms for using psychotropics and how medication may help the patient attain treatment goals. Does the patient require medication to allow psychotherapy to occur?
STEP 5. Combine steps 1 to 4 with a good bedside manner. An empathetic approach will help most patients, no matter which psychotherapy model you use (Box 1).4,8,9
Case continued: First aid for the ego
The C-L psychiatrist diagnosed Ms. T as having acute stress disorder and identified four target symptoms: bereavement, demoralization, anxiety, and hyperarousal. During the initial interview, Ms. T appeared to be psychologically-minded and open to psychiatric intervention.
The psychiatrist considered her at high risk for PTSD and prescribed citalopram, 20 mg/d, because selective serotonin reuptake inhibitors may prevent PTSD. Ms. T was also given clonazepam, 0.25 mg as needed, for severe anxiety.
The psychiatrist visited her 20 to 30 minutes daily. Initial psychotherapy focused on supporting Ms. T’s ego. Resilience-building interviews—using questions to counter feelings of despair, meaninglessness, and sorrow—addressed her demoralization and grief. She regained some sense of meaning and hope by focusing on caring for her other son and on her family’s love. She also found a sense of peace through prayer and by visualizing her lost son safe in God’s hands.
The psychiatrist also taught her relaxation skills to manage her anxiety symptoms. These included abdominal breathing and guided imagery (picturing herself in a safe, comforting place).
- Start by attending to basic physical needs (help the patient get some water or move into a more comfortable position)
- Sit down, even for a brief session
- Smile and touch the patient when appropriate
- Ask “What troubles you most?”
- Inquire about the patient’s experience (ask what the medical illness or treatment was like, not just what happened)
- Look for opportunities to comment on the patient’s strength and accomplishments
- Avoid using confusing medical terms or psychiatric jargon
- Be sensitive to cross-cultural, spiritual, and religious issues, as well as culture-specific health beliefs
Psychotherapeutic options
Three psychotherapeutic approaches are particularly useful at bedside—supportive therapy and resilience-building, cognitive-behavioral therapy (CBT), and psychodynamic therapy.
Supportive therapy and resilience-building is the most common bedside model. Supportive therapy’s goal is to strengthen coping skills, thereby reducing anxiety and enhancing well-being, self-esteem, and function.
Fostering a good working relationship is the first priority.10 The therapist works to contain the patient’s anxiety and provide an “auxiliary ego” to supplement his or her reality testing, planning and judgment, and sense of self.2,10 Supportive techniques include suggestion, clarification, limit-setting, reinforcement, reassurance, and empathic listening.
Much of the work relies on positive transference to build the supportive relationship.8,10 Transference is interpreted only when negative transference disrupts treatment; the therapeutic goal is to decrease the patient’s anxiety. Resilience-building questions (Box 2)4,11 help identify the patient’s skills and competencies and mobilize his or her internal resources.
CBT attempts to identify, challenge, and correct a patient’s inaccurate or dysfunctional beliefs about illness, treatment, or self-image. For example:
- a patient with second-degree burns may be convinced she is the world’s ugliest person
- a patient facing an operation may believe he will be permanently disabled, as was his father after a similar procedure.
CBT can also help dispel beliefs that psychiatric treatment is for “crazy” people.
Behavioral therapy can help patients manage distress related to their medical care, such as shortness of breath while being weaned from a ventilator or arousal and anxiety related to procedures. Techniques that work in office settings—systematic desensitization, in vivo exposure, breathing exercises, progressive muscle relaxation, guided imagery, meditation, and hypnosis—also can be effective at bedside.12
Psychodynamic therapy. Patients can develop insight through psychodynamic therapy, even in brief therapeutic relationships. Useful bedside techniques include clarification, confrontation, and interpretation of behavior, conflict, and transference.
For example, a patient who survived heart surgery later developed depression and suicidal ideation. Psychiatric interview revealed she was experiencing survivor guilt because her mother had died from a heart attack. Emphatic clarification and validation of feelings often can help lift such a patient’s mood and allow a dialogue to begin.
A “psychodynamic life-narrative” approach1 can help treat depression in medically ill patients. The therapist first asks the patient to describe the illness’ meaning in his or her lifespan, then formulates a statement (the “narrative”) of its meaning at the moment. The narrative is intended to:
- create a new perspective
- increase self-esteem by emphasizing the patient’s strengths
- support coping mechanisms that worked in the past.
This approach also can help the patient understand that a psychiatric symptom is an understandable response when a previously successful adaptive method cannot be used.
Choosing a psychotherapy
Three factors—patient characteristics, therapist characteristics, and evidence—determine the psychotherapeutic approach.
Patient characteristics include ego functioning level and maturity, object relationship stability,13 history and experience of psychotherapeutic treatment, personality and coping style, and physical condition. For example:
- CBT and education may be effective for patients who cope through analytical thinking, controlling emotional expression, and managing situations.
- Psychodynamic methods may help those who cope through expressing feelings, self-reflection, and a wish to be understood.
Therapist characteristics include experience, preference, and degree of comfort in conducting each therapeutic approach, as well as time and schedule.
The goal of a resilience-building interview is to enable patients under stress to focus their attention and mobilize their emotions while answering each question.10,14 Here are sample questions, grouped by issues the psychiatrist wishes to address.
Countering isolation
- Who understands your situation?
- In whose presence do you feel peaceful?
Countering meaninglessness
- For whom or what does it matter that you continue to live?
Countering despair
- What keeps you from giving up on difficult days?
- From what sources do you draw hope?
Countering sorrow
- What sustains your capacity for joy in the midst of pain?
- What has this experience added to your life?
- Are there things that take your mind off your illness and comfort you?
Promoting resilience
- What part of you is strongest right now?
- What is still possible?
Promoting continuity of self/role preservation
- What should I know about you as a person that lies beyond this illness?
- How have you prevented this illness from taking charge of your life and identity?
- What did you do before you were sick that was important to you?
- What about yourself or your life are you most proud of?
- What have you learned about your life during your illness that you would want to pass along to others?
Evidence of efficacy. Psychiatric literature supports using CBT for depressive cognition in major depression,14 resilience-building interviews for demoralization,4 and behavioral therapy and relaxation for anxiety related to medical procedures.12
Case continued: Coming home
As Ms. T’s medical condition improved over several days and her discharge was planned, the psychiatrist began to emphasize practical issues, such as:
- limiting visitation to allow her time to grieve
- addressing her anxieties about outpatient treatment and moving in with her parents.
At discharge, Ms. T was taking citalopram, 40 mg/d, and clonazepam, 0.25 mg as needed. With this regimen, her nightmares and re-experiencing had decreased. The psychiatrist had treated Ms. T in the hospital for 21 days. She continued psychiatric care for acute stress disorder at a local outpatient center.
Related resources
- Academy of Psychosomatic Medicine. www.apm.org
- American Psychosomatic Society. www.psychosomatic.org
- Griffith JL, Griffith ME. Encountering the sacred in psychotherapy: how to talk with people about their spiritual lives. New York: Guilford Press, 2002.
- Dewan MJ, Steenbarger BN, Greenberg RP (eds). The art and science of brief psychotherapies: a practitioner’s guide. Washington, DC: American Psychiatric Publishing, 2004
Drug brand names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
Dr. Lolak reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgments
The author thanks James Griffith, MD, and Thomas Wise, MD, for their valuable contributions to this article.
1. Viederman M, Perry SW, 3rd. Use of a psychodynamic life narrative in the treatment of depression in the physically ill. Gen Hosp Psychiatry 1980;2(3):177-85.
2. Lipsitt D. Psychotherapy. In: Wise MG, Rundell JR (eds). Textbook of consultation-liaison psychiatry: psychiatry in the medically ill (2nd ed). Washington, DC: American Psychiatric Publishing, 2002;1027-51.
3. Bronheim HE, Fulop G, Kunkel EJ, et al. The Academy of Psychosomatic Medicine practice guidelines for psychiatric consultation in the general medical setting. Psychosomatics 1998;39(4):S8-S30.
4. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical Illness. In press.
5. Slavney PR. Diagnosing demoralization in consultation psychiatry. Psychosomatics 1999;40(4):325-9.
6. Goldberg RL, Green S. Medical psychotherapy. Am Fam Physician 1985;31(1):173-8.
7. Postone N. Psychotherapy with cancer patients. Am J Psychother 1998;52(4):412-24.
8. Muskin PR. The combined use of psychotherapy and pharmacotherapy in the medical setting. Psychiatr Clin North Am 1990;13(2):341-53.
9. Yager J. Specific components of bedside manner in the general hospital psychiatric consultation: 12 concrete suggestions. Psychosomatics 1989;30(2):209-12.
10. Ursano RJ, Silberman EK. Psychoanalysis, psychoanalytic psychotherapy, and supportive psychotherapy. In: Hales RE, Yudofsky SC (eds). Textbook of clinical psychiatry (4th ed). Washington, DC: American Psychiatric Publishing, 2003;1177-1203.
11. Chochinov HM. Dignity-conserving care—a new model for palliative care: helping the patient feel valued. JAMA 2002;287(17):2253-60.
12. Barrows KA, Jacobs BP. Mind-body medicine. An introduction and review of the literature. Med Clin North Am 2002;86(1):11-31.
13. O’Dowd MA, Gomez MF. Psychotherapy in consultation-liaison psychiatry. Am J Psychother 2001;55(1):122-32.
14. Wright JH, Beck AT, Thase ME. Cognitive therapy. In: Hales RE, Yudofsky SC (eds). Textbook of clinical psychiatry (4th ed). Washington, DC: American Psychiatric Publishing, 2003;1245-84.
Bedside psychotherapy is not only possible but invaluable for some medical-surgical patients, despite hospitals’ distractions, lack of privacy, and short stays. If you are asked to evaluate a hospitalized patient, a 5-step strategy can help you:
- identify acute psychiatric problems that psychotherapy can help
- watch for common psychodynamic themes
- choose a beneficial psychotherapy
- integrate drug/psychotherapy, as needed
- quickly establish rapport by using an effective bedside manner.
Case report: A deeply wounded patient
Ms. T, age 45, was admitted to the trauma unit with gunshot wounds. Her estranged husband shot her during an argument and killed her 14-year-old son, who tried to help her.
She underwent multiple surgeries to repair internal organs and endured intense pain. She was medically stable after 10 days, and the surgical team called on the psychiatric consultation-liaison (C-L) service to evaluate her “depression.”
Table 1
5 steps to bedside psychotherapy
|
Ms. T told the psychiatrist she was having nightmares and re-experiencing the shootings. She felt overwhelming guilt and blamed herself for her son’s death. She reported hyperarousal, muscle tension, and palpitations. She also worried about facing her son’s killer in court.
The C-L psychiatrist felt Ms. T would benefit from medication and psychotherapy for anxiety while hospitalized.
Obstacles to bedside psychotherapy
Hospitalized patients do not usually seek psychiatric consultation but are referred by their physicians. Pain and injuries, medications, and illness can limit patients’ energy and motivation to participate in therapy, as well as their concentration and cognition. Moreover, bedside psychotherapy sessions are likely to be interrupted for blood draws, medical rounds, investigations, and procedures.
Despite these obstacles, medical patients are often receptive to psychiatric care.1 An alliance often develops within minutes, and the psychiatrist can achieve effective psychotherapy during a single bedside visit.2
The Academy of Psychosomatic Medicine considers psychotherapy a required skill for anyone who evaluates and treats psychiatric disorders in general medical settings.3
How to overcome obstacles
STEP 1. Identify when psychotherapy may help. Not every problem or patient benefits from bedside psychotherapy. The C-L psychiatrist’s first task is to identify:
- Problems that warrant psychotherapy. These may include depression, bereavement, adjustment disorder, maladaptive coping, anxiety related to medical procedures, acute stress disorder, posttraumatic stress disorder (PTSD), and demoralization.
- Patients likely to benefit. Look for evidence of ego strength, ability to interact in the first session, psychological-mindedness, ability to experience feeling, and absence of severe cognitive deficit.2
These patient traits are not prerequisites, however, and clinical judgment applies on a case-by-case basis.
Demoralization is the most common reason for psychiatric evaluation of medically-ill patients, though their physicians typically request a “depression” evaluation.4 Demoralization is an understandable response to serious illness or disabling, agonizing, or deforming treatment.5 Symptoms include anxiety, guilt, shame, depression, diminished self-worth, and possibly somatic complaints or preoccupation.6
Ms. T was experiencing survivor guilt—she blamed herself for her son’s death—and she described herself as feeling “lost.” Four strategies can treat demoralization (Table 2).
STEP 2. Watch for common psychodynamic themes, such as denial of illness, loss of control, dependency and regression, fear of abandonment, loss of identity, and fear of death.7 Other issues include survivor guilt, anger at the treatment team or family, and knowing someone who had a negative experience with the same illness or treatment.
Identifying these themes and integrating them into the treatment plan can improve outcomes. For example:
- Giving an empathic validation can help overcome fear of abandonment.
- Letting the patient choose the time when blood is drawn increases feelings of control.
Table 2
4 bedside strategies to treat demoralization
| Strategy | Examples |
|---|---|
| Validate the patient’s feeling and experience | Say, “I can see this is frustrating to you to be in the hospital so long,” or “You must feel as if everything is out of your control” |
| Reassure the patient that demoralization is a natural response to a difficult situation | Say, “I can imagine that anyone in your place would feel the same way,” or “It’s only natural to feel this way after what you’ve been through; this does not mean you have a mental illness or are ‘going crazy’” |
| Make simple gestures that promote an improved outlook | Use an effective bedside manner (Box 1) |
| Alleviate feelings of isolation, and foster a sense of hope | Use resilience-building questions (Box 2) |
STEP 3. Select appropriate psychotherapy. The psychiatrist’s challenge is to know:
- when to use which approach
- when to combine approaches
- what problems each approach targets.
A hospitalized medical patient often has a fluctuating course and may require more than one approach—or even a different approach at each visit. Thus, flexibility and creativity are keys to successful bedside psychotherapy.
STEP 4. Integrate psychotherapy with medication, as needed. Consider target symptoms for using psychotropics and how medication may help the patient attain treatment goals. Does the patient require medication to allow psychotherapy to occur?
STEP 5. Combine steps 1 to 4 with a good bedside manner. An empathetic approach will help most patients, no matter which psychotherapy model you use (Box 1).4,8,9
Case continued: First aid for the ego
The C-L psychiatrist diagnosed Ms. T as having acute stress disorder and identified four target symptoms: bereavement, demoralization, anxiety, and hyperarousal. During the initial interview, Ms. T appeared to be psychologically-minded and open to psychiatric intervention.
The psychiatrist considered her at high risk for PTSD and prescribed citalopram, 20 mg/d, because selective serotonin reuptake inhibitors may prevent PTSD. Ms. T was also given clonazepam, 0.25 mg as needed, for severe anxiety.
The psychiatrist visited her 20 to 30 minutes daily. Initial psychotherapy focused on supporting Ms. T’s ego. Resilience-building interviews—using questions to counter feelings of despair, meaninglessness, and sorrow—addressed her demoralization and grief. She regained some sense of meaning and hope by focusing on caring for her other son and on her family’s love. She also found a sense of peace through prayer and by visualizing her lost son safe in God’s hands.
The psychiatrist also taught her relaxation skills to manage her anxiety symptoms. These included abdominal breathing and guided imagery (picturing herself in a safe, comforting place).
- Start by attending to basic physical needs (help the patient get some water or move into a more comfortable position)
- Sit down, even for a brief session
- Smile and touch the patient when appropriate
- Ask “What troubles you most?”
- Inquire about the patient’s experience (ask what the medical illness or treatment was like, not just what happened)
- Look for opportunities to comment on the patient’s strength and accomplishments
- Avoid using confusing medical terms or psychiatric jargon
- Be sensitive to cross-cultural, spiritual, and religious issues, as well as culture-specific health beliefs
Psychotherapeutic options
Three psychotherapeutic approaches are particularly useful at bedside—supportive therapy and resilience-building, cognitive-behavioral therapy (CBT), and psychodynamic therapy.
Supportive therapy and resilience-building is the most common bedside model. Supportive therapy’s goal is to strengthen coping skills, thereby reducing anxiety and enhancing well-being, self-esteem, and function.
Fostering a good working relationship is the first priority.10 The therapist works to contain the patient’s anxiety and provide an “auxiliary ego” to supplement his or her reality testing, planning and judgment, and sense of self.2,10 Supportive techniques include suggestion, clarification, limit-setting, reinforcement, reassurance, and empathic listening.
Much of the work relies on positive transference to build the supportive relationship.8,10 Transference is interpreted only when negative transference disrupts treatment; the therapeutic goal is to decrease the patient’s anxiety. Resilience-building questions (Box 2)4,11 help identify the patient’s skills and competencies and mobilize his or her internal resources.
CBT attempts to identify, challenge, and correct a patient’s inaccurate or dysfunctional beliefs about illness, treatment, or self-image. For example:
- a patient with second-degree burns may be convinced she is the world’s ugliest person
- a patient facing an operation may believe he will be permanently disabled, as was his father after a similar procedure.
CBT can also help dispel beliefs that psychiatric treatment is for “crazy” people.
Behavioral therapy can help patients manage distress related to their medical care, such as shortness of breath while being weaned from a ventilator or arousal and anxiety related to procedures. Techniques that work in office settings—systematic desensitization, in vivo exposure, breathing exercises, progressive muscle relaxation, guided imagery, meditation, and hypnosis—also can be effective at bedside.12
Psychodynamic therapy. Patients can develop insight through psychodynamic therapy, even in brief therapeutic relationships. Useful bedside techniques include clarification, confrontation, and interpretation of behavior, conflict, and transference.
For example, a patient who survived heart surgery later developed depression and suicidal ideation. Psychiatric interview revealed she was experiencing survivor guilt because her mother had died from a heart attack. Emphatic clarification and validation of feelings often can help lift such a patient’s mood and allow a dialogue to begin.
A “psychodynamic life-narrative” approach1 can help treat depression in medically ill patients. The therapist first asks the patient to describe the illness’ meaning in his or her lifespan, then formulates a statement (the “narrative”) of its meaning at the moment. The narrative is intended to:
- create a new perspective
- increase self-esteem by emphasizing the patient’s strengths
- support coping mechanisms that worked in the past.
This approach also can help the patient understand that a psychiatric symptom is an understandable response when a previously successful adaptive method cannot be used.
Choosing a psychotherapy
Three factors—patient characteristics, therapist characteristics, and evidence—determine the psychotherapeutic approach.
Patient characteristics include ego functioning level and maturity, object relationship stability,13 history and experience of psychotherapeutic treatment, personality and coping style, and physical condition. For example:
- CBT and education may be effective for patients who cope through analytical thinking, controlling emotional expression, and managing situations.
- Psychodynamic methods may help those who cope through expressing feelings, self-reflection, and a wish to be understood.
Therapist characteristics include experience, preference, and degree of comfort in conducting each therapeutic approach, as well as time and schedule.
The goal of a resilience-building interview is to enable patients under stress to focus their attention and mobilize their emotions while answering each question.10,14 Here are sample questions, grouped by issues the psychiatrist wishes to address.
Countering isolation
- Who understands your situation?
- In whose presence do you feel peaceful?
Countering meaninglessness
- For whom or what does it matter that you continue to live?
Countering despair
- What keeps you from giving up on difficult days?
- From what sources do you draw hope?
Countering sorrow
- What sustains your capacity for joy in the midst of pain?
- What has this experience added to your life?
- Are there things that take your mind off your illness and comfort you?
Promoting resilience
- What part of you is strongest right now?
- What is still possible?
Promoting continuity of self/role preservation
- What should I know about you as a person that lies beyond this illness?
- How have you prevented this illness from taking charge of your life and identity?
- What did you do before you were sick that was important to you?
- What about yourself or your life are you most proud of?
- What have you learned about your life during your illness that you would want to pass along to others?
Evidence of efficacy. Psychiatric literature supports using CBT for depressive cognition in major depression,14 resilience-building interviews for demoralization,4 and behavioral therapy and relaxation for anxiety related to medical procedures.12
Case continued: Coming home
As Ms. T’s medical condition improved over several days and her discharge was planned, the psychiatrist began to emphasize practical issues, such as:
- limiting visitation to allow her time to grieve
- addressing her anxieties about outpatient treatment and moving in with her parents.
At discharge, Ms. T was taking citalopram, 40 mg/d, and clonazepam, 0.25 mg as needed. With this regimen, her nightmares and re-experiencing had decreased. The psychiatrist had treated Ms. T in the hospital for 21 days. She continued psychiatric care for acute stress disorder at a local outpatient center.
Related resources
- Academy of Psychosomatic Medicine. www.apm.org
- American Psychosomatic Society. www.psychosomatic.org
- Griffith JL, Griffith ME. Encountering the sacred in psychotherapy: how to talk with people about their spiritual lives. New York: Guilford Press, 2002.
- Dewan MJ, Steenbarger BN, Greenberg RP (eds). The art and science of brief psychotherapies: a practitioner’s guide. Washington, DC: American Psychiatric Publishing, 2004
Drug brand names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
Dr. Lolak reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgments
The author thanks James Griffith, MD, and Thomas Wise, MD, for their valuable contributions to this article.
Bedside psychotherapy is not only possible but invaluable for some medical-surgical patients, despite hospitals’ distractions, lack of privacy, and short stays. If you are asked to evaluate a hospitalized patient, a 5-step strategy can help you:
- identify acute psychiatric problems that psychotherapy can help
- watch for common psychodynamic themes
- choose a beneficial psychotherapy
- integrate drug/psychotherapy, as needed
- quickly establish rapport by using an effective bedside manner.
Case report: A deeply wounded patient
Ms. T, age 45, was admitted to the trauma unit with gunshot wounds. Her estranged husband shot her during an argument and killed her 14-year-old son, who tried to help her.
She underwent multiple surgeries to repair internal organs and endured intense pain. She was medically stable after 10 days, and the surgical team called on the psychiatric consultation-liaison (C-L) service to evaluate her “depression.”
Table 1
5 steps to bedside psychotherapy
|
Ms. T told the psychiatrist she was having nightmares and re-experiencing the shootings. She felt overwhelming guilt and blamed herself for her son’s death. She reported hyperarousal, muscle tension, and palpitations. She also worried about facing her son’s killer in court.
The C-L psychiatrist felt Ms. T would benefit from medication and psychotherapy for anxiety while hospitalized.
Obstacles to bedside psychotherapy
Hospitalized patients do not usually seek psychiatric consultation but are referred by their physicians. Pain and injuries, medications, and illness can limit patients’ energy and motivation to participate in therapy, as well as their concentration and cognition. Moreover, bedside psychotherapy sessions are likely to be interrupted for blood draws, medical rounds, investigations, and procedures.
Despite these obstacles, medical patients are often receptive to psychiatric care.1 An alliance often develops within minutes, and the psychiatrist can achieve effective psychotherapy during a single bedside visit.2
The Academy of Psychosomatic Medicine considers psychotherapy a required skill for anyone who evaluates and treats psychiatric disorders in general medical settings.3
How to overcome obstacles
STEP 1. Identify when psychotherapy may help. Not every problem or patient benefits from bedside psychotherapy. The C-L psychiatrist’s first task is to identify:
- Problems that warrant psychotherapy. These may include depression, bereavement, adjustment disorder, maladaptive coping, anxiety related to medical procedures, acute stress disorder, posttraumatic stress disorder (PTSD), and demoralization.
- Patients likely to benefit. Look for evidence of ego strength, ability to interact in the first session, psychological-mindedness, ability to experience feeling, and absence of severe cognitive deficit.2
These patient traits are not prerequisites, however, and clinical judgment applies on a case-by-case basis.
Demoralization is the most common reason for psychiatric evaluation of medically-ill patients, though their physicians typically request a “depression” evaluation.4 Demoralization is an understandable response to serious illness or disabling, agonizing, or deforming treatment.5 Symptoms include anxiety, guilt, shame, depression, diminished self-worth, and possibly somatic complaints or preoccupation.6
Ms. T was experiencing survivor guilt—she blamed herself for her son’s death—and she described herself as feeling “lost.” Four strategies can treat demoralization (Table 2).
STEP 2. Watch for common psychodynamic themes, such as denial of illness, loss of control, dependency and regression, fear of abandonment, loss of identity, and fear of death.7 Other issues include survivor guilt, anger at the treatment team or family, and knowing someone who had a negative experience with the same illness or treatment.
Identifying these themes and integrating them into the treatment plan can improve outcomes. For example:
- Giving an empathic validation can help overcome fear of abandonment.
- Letting the patient choose the time when blood is drawn increases feelings of control.
Table 2
4 bedside strategies to treat demoralization
| Strategy | Examples |
|---|---|
| Validate the patient’s feeling and experience | Say, “I can see this is frustrating to you to be in the hospital so long,” or “You must feel as if everything is out of your control” |
| Reassure the patient that demoralization is a natural response to a difficult situation | Say, “I can imagine that anyone in your place would feel the same way,” or “It’s only natural to feel this way after what you’ve been through; this does not mean you have a mental illness or are ‘going crazy’” |
| Make simple gestures that promote an improved outlook | Use an effective bedside manner (Box 1) |
| Alleviate feelings of isolation, and foster a sense of hope | Use resilience-building questions (Box 2) |
STEP 3. Select appropriate psychotherapy. The psychiatrist’s challenge is to know:
- when to use which approach
- when to combine approaches
- what problems each approach targets.
A hospitalized medical patient often has a fluctuating course and may require more than one approach—or even a different approach at each visit. Thus, flexibility and creativity are keys to successful bedside psychotherapy.
STEP 4. Integrate psychotherapy with medication, as needed. Consider target symptoms for using psychotropics and how medication may help the patient attain treatment goals. Does the patient require medication to allow psychotherapy to occur?
STEP 5. Combine steps 1 to 4 with a good bedside manner. An empathetic approach will help most patients, no matter which psychotherapy model you use (Box 1).4,8,9
Case continued: First aid for the ego
The C-L psychiatrist diagnosed Ms. T as having acute stress disorder and identified four target symptoms: bereavement, demoralization, anxiety, and hyperarousal. During the initial interview, Ms. T appeared to be psychologically-minded and open to psychiatric intervention.
The psychiatrist considered her at high risk for PTSD and prescribed citalopram, 20 mg/d, because selective serotonin reuptake inhibitors may prevent PTSD. Ms. T was also given clonazepam, 0.25 mg as needed, for severe anxiety.
The psychiatrist visited her 20 to 30 minutes daily. Initial psychotherapy focused on supporting Ms. T’s ego. Resilience-building interviews—using questions to counter feelings of despair, meaninglessness, and sorrow—addressed her demoralization and grief. She regained some sense of meaning and hope by focusing on caring for her other son and on her family’s love. She also found a sense of peace through prayer and by visualizing her lost son safe in God’s hands.
The psychiatrist also taught her relaxation skills to manage her anxiety symptoms. These included abdominal breathing and guided imagery (picturing herself in a safe, comforting place).
- Start by attending to basic physical needs (help the patient get some water or move into a more comfortable position)
- Sit down, even for a brief session
- Smile and touch the patient when appropriate
- Ask “What troubles you most?”
- Inquire about the patient’s experience (ask what the medical illness or treatment was like, not just what happened)
- Look for opportunities to comment on the patient’s strength and accomplishments
- Avoid using confusing medical terms or psychiatric jargon
- Be sensitive to cross-cultural, spiritual, and religious issues, as well as culture-specific health beliefs
Psychotherapeutic options
Three psychotherapeutic approaches are particularly useful at bedside—supportive therapy and resilience-building, cognitive-behavioral therapy (CBT), and psychodynamic therapy.
Supportive therapy and resilience-building is the most common bedside model. Supportive therapy’s goal is to strengthen coping skills, thereby reducing anxiety and enhancing well-being, self-esteem, and function.
Fostering a good working relationship is the first priority.10 The therapist works to contain the patient’s anxiety and provide an “auxiliary ego” to supplement his or her reality testing, planning and judgment, and sense of self.2,10 Supportive techniques include suggestion, clarification, limit-setting, reinforcement, reassurance, and empathic listening.
Much of the work relies on positive transference to build the supportive relationship.8,10 Transference is interpreted only when negative transference disrupts treatment; the therapeutic goal is to decrease the patient’s anxiety. Resilience-building questions (Box 2)4,11 help identify the patient’s skills and competencies and mobilize his or her internal resources.
CBT attempts to identify, challenge, and correct a patient’s inaccurate or dysfunctional beliefs about illness, treatment, or self-image. For example:
- a patient with second-degree burns may be convinced she is the world’s ugliest person
- a patient facing an operation may believe he will be permanently disabled, as was his father after a similar procedure.
CBT can also help dispel beliefs that psychiatric treatment is for “crazy” people.
Behavioral therapy can help patients manage distress related to their medical care, such as shortness of breath while being weaned from a ventilator or arousal and anxiety related to procedures. Techniques that work in office settings—systematic desensitization, in vivo exposure, breathing exercises, progressive muscle relaxation, guided imagery, meditation, and hypnosis—also can be effective at bedside.12
Psychodynamic therapy. Patients can develop insight through psychodynamic therapy, even in brief therapeutic relationships. Useful bedside techniques include clarification, confrontation, and interpretation of behavior, conflict, and transference.
For example, a patient who survived heart surgery later developed depression and suicidal ideation. Psychiatric interview revealed she was experiencing survivor guilt because her mother had died from a heart attack. Emphatic clarification and validation of feelings often can help lift such a patient’s mood and allow a dialogue to begin.
A “psychodynamic life-narrative” approach1 can help treat depression in medically ill patients. The therapist first asks the patient to describe the illness’ meaning in his or her lifespan, then formulates a statement (the “narrative”) of its meaning at the moment. The narrative is intended to:
- create a new perspective
- increase self-esteem by emphasizing the patient’s strengths
- support coping mechanisms that worked in the past.
This approach also can help the patient understand that a psychiatric symptom is an understandable response when a previously successful adaptive method cannot be used.
Choosing a psychotherapy
Three factors—patient characteristics, therapist characteristics, and evidence—determine the psychotherapeutic approach.
Patient characteristics include ego functioning level and maturity, object relationship stability,13 history and experience of psychotherapeutic treatment, personality and coping style, and physical condition. For example:
- CBT and education may be effective for patients who cope through analytical thinking, controlling emotional expression, and managing situations.
- Psychodynamic methods may help those who cope through expressing feelings, self-reflection, and a wish to be understood.
Therapist characteristics include experience, preference, and degree of comfort in conducting each therapeutic approach, as well as time and schedule.
The goal of a resilience-building interview is to enable patients under stress to focus their attention and mobilize their emotions while answering each question.10,14 Here are sample questions, grouped by issues the psychiatrist wishes to address.
Countering isolation
- Who understands your situation?
- In whose presence do you feel peaceful?
Countering meaninglessness
- For whom or what does it matter that you continue to live?
Countering despair
- What keeps you from giving up on difficult days?
- From what sources do you draw hope?
Countering sorrow
- What sustains your capacity for joy in the midst of pain?
- What has this experience added to your life?
- Are there things that take your mind off your illness and comfort you?
Promoting resilience
- What part of you is strongest right now?
- What is still possible?
Promoting continuity of self/role preservation
- What should I know about you as a person that lies beyond this illness?
- How have you prevented this illness from taking charge of your life and identity?
- What did you do before you were sick that was important to you?
- What about yourself or your life are you most proud of?
- What have you learned about your life during your illness that you would want to pass along to others?
Evidence of efficacy. Psychiatric literature supports using CBT for depressive cognition in major depression,14 resilience-building interviews for demoralization,4 and behavioral therapy and relaxation for anxiety related to medical procedures.12
Case continued: Coming home
As Ms. T’s medical condition improved over several days and her discharge was planned, the psychiatrist began to emphasize practical issues, such as:
- limiting visitation to allow her time to grieve
- addressing her anxieties about outpatient treatment and moving in with her parents.
At discharge, Ms. T was taking citalopram, 40 mg/d, and clonazepam, 0.25 mg as needed. With this regimen, her nightmares and re-experiencing had decreased. The psychiatrist had treated Ms. T in the hospital for 21 days. She continued psychiatric care for acute stress disorder at a local outpatient center.
Related resources
- Academy of Psychosomatic Medicine. www.apm.org
- American Psychosomatic Society. www.psychosomatic.org
- Griffith JL, Griffith ME. Encountering the sacred in psychotherapy: how to talk with people about their spiritual lives. New York: Guilford Press, 2002.
- Dewan MJ, Steenbarger BN, Greenberg RP (eds). The art and science of brief psychotherapies: a practitioner’s guide. Washington, DC: American Psychiatric Publishing, 2004
Drug brand names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
Dr. Lolak reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgments
The author thanks James Griffith, MD, and Thomas Wise, MD, for their valuable contributions to this article.
1. Viederman M, Perry SW, 3rd. Use of a psychodynamic life narrative in the treatment of depression in the physically ill. Gen Hosp Psychiatry 1980;2(3):177-85.
2. Lipsitt D. Psychotherapy. In: Wise MG, Rundell JR (eds). Textbook of consultation-liaison psychiatry: psychiatry in the medically ill (2nd ed). Washington, DC: American Psychiatric Publishing, 2002;1027-51.
3. Bronheim HE, Fulop G, Kunkel EJ, et al. The Academy of Psychosomatic Medicine practice guidelines for psychiatric consultation in the general medical setting. Psychosomatics 1998;39(4):S8-S30.
4. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical Illness. In press.
5. Slavney PR. Diagnosing demoralization in consultation psychiatry. Psychosomatics 1999;40(4):325-9.
6. Goldberg RL, Green S. Medical psychotherapy. Am Fam Physician 1985;31(1):173-8.
7. Postone N. Psychotherapy with cancer patients. Am J Psychother 1998;52(4):412-24.
8. Muskin PR. The combined use of psychotherapy and pharmacotherapy in the medical setting. Psychiatr Clin North Am 1990;13(2):341-53.
9. Yager J. Specific components of bedside manner in the general hospital psychiatric consultation: 12 concrete suggestions. Psychosomatics 1989;30(2):209-12.
10. Ursano RJ, Silberman EK. Psychoanalysis, psychoanalytic psychotherapy, and supportive psychotherapy. In: Hales RE, Yudofsky SC (eds). Textbook of clinical psychiatry (4th ed). Washington, DC: American Psychiatric Publishing, 2003;1177-1203.
11. Chochinov HM. Dignity-conserving care—a new model for palliative care: helping the patient feel valued. JAMA 2002;287(17):2253-60.
12. Barrows KA, Jacobs BP. Mind-body medicine. An introduction and review of the literature. Med Clin North Am 2002;86(1):11-31.
13. O’Dowd MA, Gomez MF. Psychotherapy in consultation-liaison psychiatry. Am J Psychother 2001;55(1):122-32.
14. Wright JH, Beck AT, Thase ME. Cognitive therapy. In: Hales RE, Yudofsky SC (eds). Textbook of clinical psychiatry (4th ed). Washington, DC: American Psychiatric Publishing, 2003;1245-84.
1. Viederman M, Perry SW, 3rd. Use of a psychodynamic life narrative in the treatment of depression in the physically ill. Gen Hosp Psychiatry 1980;2(3):177-85.
2. Lipsitt D. Psychotherapy. In: Wise MG, Rundell JR (eds). Textbook of consultation-liaison psychiatry: psychiatry in the medically ill (2nd ed). Washington, DC: American Psychiatric Publishing, 2002;1027-51.
3. Bronheim HE, Fulop G, Kunkel EJ, et al. The Academy of Psychosomatic Medicine practice guidelines for psychiatric consultation in the general medical setting. Psychosomatics 1998;39(4):S8-S30.
4. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical Illness. In press.
5. Slavney PR. Diagnosing demoralization in consultation psychiatry. Psychosomatics 1999;40(4):325-9.
6. Goldberg RL, Green S. Medical psychotherapy. Am Fam Physician 1985;31(1):173-8.
7. Postone N. Psychotherapy with cancer patients. Am J Psychother 1998;52(4):412-24.
8. Muskin PR. The combined use of psychotherapy and pharmacotherapy in the medical setting. Psychiatr Clin North Am 1990;13(2):341-53.
9. Yager J. Specific components of bedside manner in the general hospital psychiatric consultation: 12 concrete suggestions. Psychosomatics 1989;30(2):209-12.
10. Ursano RJ, Silberman EK. Psychoanalysis, psychoanalytic psychotherapy, and supportive psychotherapy. In: Hales RE, Yudofsky SC (eds). Textbook of clinical psychiatry (4th ed). Washington, DC: American Psychiatric Publishing, 2003;1177-1203.
11. Chochinov HM. Dignity-conserving care—a new model for palliative care: helping the patient feel valued. JAMA 2002;287(17):2253-60.
12. Barrows KA, Jacobs BP. Mind-body medicine. An introduction and review of the literature. Med Clin North Am 2002;86(1):11-31.
13. O’Dowd MA, Gomez MF. Psychotherapy in consultation-liaison psychiatry. Am J Psychother 2001;55(1):122-32.
14. Wright JH, Beck AT, Thase ME. Cognitive therapy. In: Hales RE, Yudofsky SC (eds). Textbook of clinical psychiatry (4th ed). Washington, DC: American Psychiatric Publishing, 2003;1245-84.
High-dose antipsychotics: Desperation or data-driven?
When nothing else works, desperate clinicians are resorting to progressively more-tenuous and unpredictable treatments, trying to improve the lives of patients with refractory schizophrenia. High-dose antipsychotics is a common strategy.
Does boosting antipsychotic doses beyond the recommended range—but short of the neuroleptic threshold—enhance efficacy? This article attempts to answer that question by presenting the evidence on higher-than-recommended doses of atypical antipsychotics.
Lessons from neuroleptics
Up to 30% of patients with schizophrenia do not respond to antipsychotics and are considered “treatment refractory.”1 Even among those who do respond, improving symptoms by 20%—as research defines “treatment response”—does not necessarily yield clinical or functional improvement. Clozapine is the only atypical antipsychotic with well-established efficacy in these chronically ill patients,2 but its daunting side effects greatly curtail its use.
Before atypical antipsychotics, patients who did not respond to usual dosages of the typical neuroleptics were treated with higher dosages or switched to another drug class. Although many clinicians embraced high-dose neuroleptics, subsequent research discredited “rapid neuroleptization” in any clinical circumstance and showed that exceeding an antipsychotic’s neuroleptic threshold—the dose at which extrapyramidal side effects (EPS) occur—reduces its efficacy (Figure 1).3-5 In some instances, reducing neuroleptic dosages improves treatment-resistant patients’ symptoms and reduces druginduced side effects.6
Figure 1 Typical antipsychotics’ dose-response curve
Narrow therapeutic window between antipsychotic effect and neuroleptic threshold. Dotted line indicates declining efficacy.
Figure 2 Atypical antipsychotics’ dose-response curve
Wider therapeutic window with atypicals, compared with typical antipsychotics, as neuroleptic threshold (dotted line) moves right.Atypical antipsychotics are defined by their relative lack of EPS at recommended dosages (Figure 2). Because these agents can cause EPS if dosed too high, however, our historical habit of testing this dose limit risks losing “atypicality” and encountering other untoward events (Figure 3).
What is the safest, most effective dosage? Consider the evidence for each atypical antipsychotic.
Risperidone
Recommended dosage too high? When using atypicals at recommended doses, you are most likely to encounter the neuroleptic threshold with risperidone, with EPS risk increasing substantially at >6 mg/d.7 Post-approval studies set the most effective and safest dosage at approximately 4 mg/d, though this dosage was not studied in North American pre-approval trials. Dosages of 2 to 4 mg/d have been associated with more-favorable outcomes, suggesting that the initial recommendation to titrate to 6 mg/d within the first 3 days was ill-advised.8
In our study of patients with treatment-refractory schizophrenia,9 those treated with risperidone, 6 mg/d, improved significantly more after 4 weeks than did those receiving haloperidol, 15 mg/d, based on Brief Psychiatric Rating Scale (BPRS) scores. No additional benefit was seen after risperidone was increased to >6 mg/d at 8 weeks. Akathisia and tardive dyskinesia occurred significantly more often in the haloperidol group.
Conclusion. Some patients respond to higher-dose risperidone, but emerging EPS suggest the need to reduce the dosage rather than add an antiparkinsonian agent.
Figure 3 Unknown effects of high-dose atypical antipsychotic therapy
Dotted line indicates potential for greater antipsychotic effect with increasing dose.
Olanzapine
Mixed results. Case reports suggest that some patients who did not respond to previous antipsychotic trials or olanzapine, 20 mg/d, improved sig-nificantly—without substanial side effects—when olanzapine was increased up to 60 mg/d.10-14 Other case studies, however, report EPS, increased heart rate, increased transaminases, hyperprolactinemia, and prolonged QTc interval with high-dose olanzapine.14-16
In an open-label trial,17 43 patients with schizophrenia received olanzapine, up to 40 mg/d, after inadequate response to neuroleptics and risperidone or clozapine. Olanzapine was titrated to 20 mg/d by week 4 and increased 5 mg every 2 weeks if symptoms did not improve. After 14 weeks, improvement was modest and only 17% of patients met response criteria. However, >20 mg/d reduced symptoms more than did <20 mg/d, suggesting that high-dose olanzapine was more effective.
In a randomized trial,18 patients who did not respond to at least one atypical antipsychotic then received 8 weeks of fixed, standard-dose treatment with (mean dosages):
- haloperidol, 18.9 mg/d
- risperidone, 7.9 mg/d
- olanzapine, 19.6 mg/d
- clozapine, 401.6 mg/d.
Flexible dosing was then allowed for 6 weeks, and mean dosages were:
- haloperidol, 25.7 mg/d
- risperidone, 11.6 mg/d
- olanzapine, 30.4 mg/d
- clozapine, 526.6 mg/d.
Symptoms improved modestly at best for all medications, although patients taking olanzapine or clozapine improved significantly more than those treated with haloperidol as shown by mean changes in total Positive and Negative Syndrome Scale (PANSS) scores.
PANSS scores for olanzapine-treated patients showed additional improvement at week 14—when higher dosages were used—compared with week 8. This was not the case for the other medications, for which response plateaued. These findings suggest that high-dose risperidone and haloperidol are incrementally ineffective, but high-dose olanzapine could help some patients with refractory symptoms.
Results were different in a randomized, double-blind, 16-week, crossover study,19 when 13 patients with inadequate response to neuroleptics, risperidone, or conventional-dose olanzapine then received olanzapine, 50 mg/d, or clozapine, 450 mg/d. No olanzapine-treated patients and 20% of clozapine-treated patients met criteria for treatment response (20% improvement in BPRS score and final BPRS score <35 or 1-point improvement on Clinical Global Impressions-Severity of Illness scale).
Negative results don’t make headlines. Published clinical trials and case reports are subject to selective reporting of positive outcomes. Cases in which high-dose therapy proved ineffectivemay outnumber positive results but are less likely to be published.
Numbers don’t lie. Using high doses will almost always increase side effect risk and drug therapy costs, contributing to a poor risk-benefit ratio when efficacy remains unchanged. Resorting to an “if-it’s-not-working, double-it” strategy may seem reasonable, but two times zero is still zero.
Desperation warps perception. Clinicians tend to rely on observational experience. The desperation inherent in treating refractory patients, however, often creates a strong desire for improvement and therefore a potentially biased perception of outcome.
Likewise, patients may inaccurately portray themselves as improved to avoid disappointing their doctors. Controlled trials reduce these biases to better assess efficacy.
Antipsychotics work in 6 to 8 weeks. Improvements seen when pushing medications beyond recommended dosing may not be an effect of dose but of additional time on the medication. Antipsychotics usually take 6 to 8 weeks to produce maximal response, so high-dose therapy should not be started during this initial phase. This pace may not satisfy pressures for expedient stabilization and hospital discharge, but it is unrealistic to expect antipsychotics to work more quickly than they do.
Oversedation does not equal improvement. Patients who become excessively sedated from high-dose therapy or adjunctive medications may appear less psychotic but may not be so. The family or hospital staff may desire such sedation, but it can adversely affect the patient’s quality of life or medication adherence.
Polypharmacy clouds the issue. Many patients treated with high-dose antipsychotics are taking multiple agents, making it difficult to attribute improvement (or side effects) to any single one. A well-designed study of high-dose therapy would therefore:
- control for time
- examine concomitant medications’ effects
- determine whether “improvements” are related to sedation or reduced psychosis.
Medication may not need to change. When a patient decompensates, many forces pressure clinicians to change or add medications or increase dosages. Change may not be necessary, however, as nonadherence or substance abuse often trigger psychotic exacerbations. For example, Steingard et al27 added fluphenazine or placebo to antipsychotic regimens of newly hospitalized patients and found that increasing antipsychotic dosage did not improve outcome.
Subjects switching from clozapine to olanzapine tended to worsen, whereas those switching from olanzapine to clozapine tended to improve. Olanzapine-treated patients experienced more anticholinergic side effects and more weight gain than did clozapine-treated subjects.20
Conclusion. These mixed findings on high-dose olanzapine suggest questionable efficacy in patients with treatment-resistant schizophrenia and an uncertain risk of increased toxicity.
Quetiapine
Early placebo-controlled studies of quetiapine in schizophrenia concluded that statistically significant improvement begins at 150 mg/d and falls off after 600 mg/d.21 Although few high-dose quetiapine cases have been presented, clinical opinion holds that:
- most patients with chronic schizophrenia require 400 to 800 mg/d
- some treatment-refractory patients might benefit from >800 mg/d.
One patient responded to quetiapine, 1,600 mg/d, after not responding to olanzapine, 40 mg/d, and quetiapine, 800 mg/d. Constipation was the only reported side effect.22
Our group23 reported a series of 7 patients who responded (by clinician report) to quetiapine, 1,200 to 2,400 mg/d, after not responding to quetiapine, 800 mg/d, or to neuroleptics, risperidone, or olanzapine. Six responded to high-dose quetiapine and 1 to high-dose quetiapine plus risperidone, 2 mg/d; 4 received adjunctive dival-proex sodium, 1,500 to 3,000 mg/d. Psychopathology, violence, and behavioral disturbances were reduced throughout 5 to 14 months of monitoring. Side effects included sedation, orthostasis, and dysphagia.
When Nelson et al24 treated 13 subjects for 14 weeks with quetiapine, 1,000 to 1,400 mg/d, mean weight, glucose, total cholesterol, prolactin, and QTc interval duration did not change significantly. Heart rate increased significantly (though not to tachycardia), and headache, constipation, and lethargy were the most frequent side effects.
Summary. Although encouraging, these reports are preliminary, unpublished, and lack peer review. Controlled trials of high-dose quetiapine’s efficacy and safety are needed.
Ziprasidone and aripiprazole
No studies of high-dose ziprasidone or aripiprazole have been published. In premarketing trials:
- ziprasidone was studied at 200 mg/d and released with a maximum recommended dosage of 160 mg/d
- aripiprazole, 30 mg/d, was not more effective than 15 mg/d.25
Deutschman et al26 reviewed the charts of 31 patients who received ziprasidone, 240 to 320 mg/d, after an “incomplete” response to 160 mg/d. At the higher dosing:
- psychosis, affective symptoms, or anxiety improved in nearly one-half of patients
- 15% reported sedation, but most reported no side effects
- none developed QTc intervals >500 msec.
Caveats and precautions
These uncontrolled case reports and open-label studies do not “prove” efficacy or safety but reflect clinical practice. More than anything, they show that we need controlled trials to gauge high-dose antipsychotic therapy’s efficacy and safety and to curb our collective habit of relying on anecdotal experience and idiosyncratic beliefs.
Despite its side-effect profile, clozapine remains the treatment of choice for refractory schizophrenia. Given high-dose antipsychotic therapy’s uncertain efficacy and unknown risks, the evidence supports a clozapine trial before higher-than-recommended dosing is attempted.
Because educated guesswork plays a role in premarketing dosing studies, a medication’s optimal dose may be:
- overestimated (as with risperidone)
- underestimated (as perhaps with olanzapine and quetiapine).
Keep in mind some important caveats when you consider giving a patient high-dose antipsychotic therapy (Box).27 Of course, nonadherence is often the cause of apparent medication nonresponse. Increasing the dosage of a medication a patient is not taking rarely improves adherence. Interventions to enhance adherence—careful assessment, psychoeducation, and using longacting intramuscular medication—may be useful.
Related resources
- Marder SR, Essock SM, Miller AL, et al. The Mount Sinai Conference on the pharmacotherapy of schizophrenia. Schizophrenia Bull 2002;28:5-16.
- Practice guideline for the treatment of patients with schizophrenia (2nd ed). Am J Psychiatry 2004;161(suppl):1-56.
- Texas Medication Algorithm Project antipsychotic algorithm. http://www.mhmr.state.tx.us/centraloffice/medicaldirector/timascz1algo.pdf
Drug brand names
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Divalproex • Depakote
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosures
Dr. Pierre receives research support from Cephalon Inc., and is a consultant to and/or speaker for Pfizer Inc., Bristol-Myers Squibb Co., AstraZeneca Pharmaceuticals, and Janssen Pharmaceutica.
Dr. Donna Wirshing receives research support from, is a consultant to, and/or is a speaker for Bristol-Myers Squibb Co., Pfizer Inc., Eli Lilly & Co., Janssen Pharmaceutica, AstraZeneca Pharmaceuticals, and Abbott Laboratories.
Dr. William Wirshing receives research support from, is a consultant to, and/or is a speaker for Bristol-Myers Squibb Co., Pfizer Inc., Eli Lilly & Co., Janssen Pharmaceutica, and AstraZeneca Pharmaceuticals.
1. Conley RR, Buchanan RW. Evaluation of treatment-resistant schizophrenia. Schizophr Bull 1997;23:663-74.
2. Chakos M, Lieberman J, Hoffman E, et al. Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: A review and meta-analysis of randomized trials. Am J Psychiatry 2001;158:518-26.
3. Baldessarini RJ, Cohen BM, Teicher MH. Significance of neuroleptic dose and plasma level in the pharmacological treatment of psychoses. Arch Gen Psych 1988;45:79-91.
4. McEvoy JP, Hogarty GE, Steingard S. Optimal dose of neuroleptic in acute schizophrenia: A controlled study of the neuroleptic threshold and higher haloperidol dose. Arch Gen Psychiatry 1991;48:739-45.
5. Van Putten T, Marder SR, Mintz J, Poland R. Haloperidol plasma levels and clinical response: A therapeutic window relationship. Am J Psychiatry 1992;149:500-5.
6. Van Putten T, Marshall BD, Liberman R, et al. Systematic dosage reduction in treatment-resistant schizophrenic patients. Psychopharmacol Bull 1993;29:315-20.
7. Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry 1994;151:825-36.
8. Love RC, Conley RR, Kelly DL, Bartko JJ. A dose-outcome analysis of risperidone. J Clin Psychiatry 1999;60:771-5.
9. Wirshing DA, Marshall BD, Jr, Green MF, et al. Risperidone in treatment-refractory schizophrenia. Am J Psychiatry 1999;156:1374-9.
10. Fanous A, Lindenmayer JP. Schizophrenia and schizoaffective disorder treated with high doses of olanzapine. J Clin Psychopharmacol 1999;19:275-6.
11. Reich J. Use of high-dose olanzapine in refractory psychosis. Am J Psychiatry 1999;156:661.-
12. Dursun SM, Gardner DM, Bird DC, Flinn J. Olanzapine for patients with treatment-resistant schizophrenia: A naturalistic case-series outcome study. Can J Psychiatry 1999;44:701-4.
13. Lerner V. High-dose olanzapine for treatment-refractory schizophrenia. Clin Neuropharmacol 2003;26:58-61.
14. Sheitman BB, Lindgren JC, Early JE, Sved M. High-dose olanzapine for treatment-refractory schizophrenia. Am J Psychiatry 1997;154:1626.
15. Bronson BD, Lindenmayer JP. Adverse effects of high-dose olanzapine in treatment-refractory schizophrenia. J Clin Psychopharmacol 2000;20:383-4.
16. Dineen S, Withrow K, Voronovitch L, et al. QTc prolongation and high-dose olanzapine. Psychosomatics 2003;44:174-5.
17. Lindenmayer JP, Volavka J, Lieberman J, et al. Olanzapine for schizophrenia refractory to typical and atypical antipsychotics: An open-label, prospective trial. J Clin Psychopharmacol. 2001;21:448-53.
18. Volavka J, Czobor P, Sheitman B, et al. Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry 2002;159:255-62.
19. Conley RR, Kelly DL, Richardson CM, et al. The efficacy of high-dose olanzapine versus clozapine in treatment-resistant schizophrenia: A double-blind cross-over study. J Clin Psychopharmacol 2003;23:668-71.
20. Kelly DL, Conley RR, Richardson CM, et al. Adverse effects and laboratory parameters of high-dose olanzapine vs. clozapine in treatment-resistant schizophrenia. Ann Clin Psychiatry 2003;15:181-6.
21. Arvanitis LA, Miller BG. and the Seroquel Trial 13 Study Group. Multiple fixed doses of “Seroquel” (quetiapine) in patients with acute exacerbation of schizophrenia: A comparison with haloperidol and placebo. Biol Psychiatry 1997;42:233-46.
22. Bobes J, Garcia-Portilla MP, Saiz PA, et al. High degree of tolerability for monotherapy with high doses of quetiapine: A case report. J Clin Psychiatry 2002;63:1048-9.
23. Pierre JM, Wirshing DA, Cannell J, et al. High-dose quetiapine in treatment refractory schizophrenia (poster). Colorado Springs, CO: International Congress of Schizophrenia Research, 2003; abstracted in Schizophrenia Res 2003;60(supp):299.-
24. Nelson MW, Reynolds R, Kelly DL, et al. Safety and tolerability of high-dose quetiapine in treatment-refractory schizophrenia: Preliminary results from an open-label trial (poster). Colorado Springs, CO: International Congress of Schizophrenia Research, 2003; abstracted in Schizophrenia Res 2003;60(supp):363.-
25. Potkin SG, Saha AR, Kujawa MJ, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry 2003;60:681-90.
26. Deutschman DA, Deutschman DH. High-dose ziprasidone: effectiveness and tolerability in clinical practice (poster). Boston, MA: American Psychiatric Association Institute on Psychiatric Services annual meeting, 2003.
27. Steingard S, Allen M, Schooler MR. A study of pharmacologic treatment on medication-compliant schizophrenics who relapse. J Clin Psychiatry 1994;55:470-2.
When nothing else works, desperate clinicians are resorting to progressively more-tenuous and unpredictable treatments, trying to improve the lives of patients with refractory schizophrenia. High-dose antipsychotics is a common strategy.
Does boosting antipsychotic doses beyond the recommended range—but short of the neuroleptic threshold—enhance efficacy? This article attempts to answer that question by presenting the evidence on higher-than-recommended doses of atypical antipsychotics.
Lessons from neuroleptics
Up to 30% of patients with schizophrenia do not respond to antipsychotics and are considered “treatment refractory.”1 Even among those who do respond, improving symptoms by 20%—as research defines “treatment response”—does not necessarily yield clinical or functional improvement. Clozapine is the only atypical antipsychotic with well-established efficacy in these chronically ill patients,2 but its daunting side effects greatly curtail its use.
Before atypical antipsychotics, patients who did not respond to usual dosages of the typical neuroleptics were treated with higher dosages or switched to another drug class. Although many clinicians embraced high-dose neuroleptics, subsequent research discredited “rapid neuroleptization” in any clinical circumstance and showed that exceeding an antipsychotic’s neuroleptic threshold—the dose at which extrapyramidal side effects (EPS) occur—reduces its efficacy (Figure 1).3-5 In some instances, reducing neuroleptic dosages improves treatment-resistant patients’ symptoms and reduces druginduced side effects.6
Figure 1 Typical antipsychotics’ dose-response curve
Narrow therapeutic window between antipsychotic effect and neuroleptic threshold. Dotted line indicates declining efficacy.
Figure 2 Atypical antipsychotics’ dose-response curve
Wider therapeutic window with atypicals, compared with typical antipsychotics, as neuroleptic threshold (dotted line) moves right.Atypical antipsychotics are defined by their relative lack of EPS at recommended dosages (Figure 2). Because these agents can cause EPS if dosed too high, however, our historical habit of testing this dose limit risks losing “atypicality” and encountering other untoward events (Figure 3).
What is the safest, most effective dosage? Consider the evidence for each atypical antipsychotic.
Risperidone
Recommended dosage too high? When using atypicals at recommended doses, you are most likely to encounter the neuroleptic threshold with risperidone, with EPS risk increasing substantially at >6 mg/d.7 Post-approval studies set the most effective and safest dosage at approximately 4 mg/d, though this dosage was not studied in North American pre-approval trials. Dosages of 2 to 4 mg/d have been associated with more-favorable outcomes, suggesting that the initial recommendation to titrate to 6 mg/d within the first 3 days was ill-advised.8
In our study of patients with treatment-refractory schizophrenia,9 those treated with risperidone, 6 mg/d, improved significantly more after 4 weeks than did those receiving haloperidol, 15 mg/d, based on Brief Psychiatric Rating Scale (BPRS) scores. No additional benefit was seen after risperidone was increased to >6 mg/d at 8 weeks. Akathisia and tardive dyskinesia occurred significantly more often in the haloperidol group.
Conclusion. Some patients respond to higher-dose risperidone, but emerging EPS suggest the need to reduce the dosage rather than add an antiparkinsonian agent.
Figure 3 Unknown effects of high-dose atypical antipsychotic therapy
Dotted line indicates potential for greater antipsychotic effect with increasing dose.
Olanzapine
Mixed results. Case reports suggest that some patients who did not respond to previous antipsychotic trials or olanzapine, 20 mg/d, improved sig-nificantly—without substanial side effects—when olanzapine was increased up to 60 mg/d.10-14 Other case studies, however, report EPS, increased heart rate, increased transaminases, hyperprolactinemia, and prolonged QTc interval with high-dose olanzapine.14-16
In an open-label trial,17 43 patients with schizophrenia received olanzapine, up to 40 mg/d, after inadequate response to neuroleptics and risperidone or clozapine. Olanzapine was titrated to 20 mg/d by week 4 and increased 5 mg every 2 weeks if symptoms did not improve. After 14 weeks, improvement was modest and only 17% of patients met response criteria. However, >20 mg/d reduced symptoms more than did <20 mg/d, suggesting that high-dose olanzapine was more effective.
In a randomized trial,18 patients who did not respond to at least one atypical antipsychotic then received 8 weeks of fixed, standard-dose treatment with (mean dosages):
- haloperidol, 18.9 mg/d
- risperidone, 7.9 mg/d
- olanzapine, 19.6 mg/d
- clozapine, 401.6 mg/d.
Flexible dosing was then allowed for 6 weeks, and mean dosages were:
- haloperidol, 25.7 mg/d
- risperidone, 11.6 mg/d
- olanzapine, 30.4 mg/d
- clozapine, 526.6 mg/d.
Symptoms improved modestly at best for all medications, although patients taking olanzapine or clozapine improved significantly more than those treated with haloperidol as shown by mean changes in total Positive and Negative Syndrome Scale (PANSS) scores.
PANSS scores for olanzapine-treated patients showed additional improvement at week 14—when higher dosages were used—compared with week 8. This was not the case for the other medications, for which response plateaued. These findings suggest that high-dose risperidone and haloperidol are incrementally ineffective, but high-dose olanzapine could help some patients with refractory symptoms.
Results were different in a randomized, double-blind, 16-week, crossover study,19 when 13 patients with inadequate response to neuroleptics, risperidone, or conventional-dose olanzapine then received olanzapine, 50 mg/d, or clozapine, 450 mg/d. No olanzapine-treated patients and 20% of clozapine-treated patients met criteria for treatment response (20% improvement in BPRS score and final BPRS score <35 or 1-point improvement on Clinical Global Impressions-Severity of Illness scale).
Negative results don’t make headlines. Published clinical trials and case reports are subject to selective reporting of positive outcomes. Cases in which high-dose therapy proved ineffectivemay outnumber positive results but are less likely to be published.
Numbers don’t lie. Using high doses will almost always increase side effect risk and drug therapy costs, contributing to a poor risk-benefit ratio when efficacy remains unchanged. Resorting to an “if-it’s-not-working, double-it” strategy may seem reasonable, but two times zero is still zero.
Desperation warps perception. Clinicians tend to rely on observational experience. The desperation inherent in treating refractory patients, however, often creates a strong desire for improvement and therefore a potentially biased perception of outcome.
Likewise, patients may inaccurately portray themselves as improved to avoid disappointing their doctors. Controlled trials reduce these biases to better assess efficacy.
Antipsychotics work in 6 to 8 weeks. Improvements seen when pushing medications beyond recommended dosing may not be an effect of dose but of additional time on the medication. Antipsychotics usually take 6 to 8 weeks to produce maximal response, so high-dose therapy should not be started during this initial phase. This pace may not satisfy pressures for expedient stabilization and hospital discharge, but it is unrealistic to expect antipsychotics to work more quickly than they do.
Oversedation does not equal improvement. Patients who become excessively sedated from high-dose therapy or adjunctive medications may appear less psychotic but may not be so. The family or hospital staff may desire such sedation, but it can adversely affect the patient’s quality of life or medication adherence.
Polypharmacy clouds the issue. Many patients treated with high-dose antipsychotics are taking multiple agents, making it difficult to attribute improvement (or side effects) to any single one. A well-designed study of high-dose therapy would therefore:
- control for time
- examine concomitant medications’ effects
- determine whether “improvements” are related to sedation or reduced psychosis.
Medication may not need to change. When a patient decompensates, many forces pressure clinicians to change or add medications or increase dosages. Change may not be necessary, however, as nonadherence or substance abuse often trigger psychotic exacerbations. For example, Steingard et al27 added fluphenazine or placebo to antipsychotic regimens of newly hospitalized patients and found that increasing antipsychotic dosage did not improve outcome.
Subjects switching from clozapine to olanzapine tended to worsen, whereas those switching from olanzapine to clozapine tended to improve. Olanzapine-treated patients experienced more anticholinergic side effects and more weight gain than did clozapine-treated subjects.20
Conclusion. These mixed findings on high-dose olanzapine suggest questionable efficacy in patients with treatment-resistant schizophrenia and an uncertain risk of increased toxicity.
Quetiapine
Early placebo-controlled studies of quetiapine in schizophrenia concluded that statistically significant improvement begins at 150 mg/d and falls off after 600 mg/d.21 Although few high-dose quetiapine cases have been presented, clinical opinion holds that:
- most patients with chronic schizophrenia require 400 to 800 mg/d
- some treatment-refractory patients might benefit from >800 mg/d.
One patient responded to quetiapine, 1,600 mg/d, after not responding to olanzapine, 40 mg/d, and quetiapine, 800 mg/d. Constipation was the only reported side effect.22
Our group23 reported a series of 7 patients who responded (by clinician report) to quetiapine, 1,200 to 2,400 mg/d, after not responding to quetiapine, 800 mg/d, or to neuroleptics, risperidone, or olanzapine. Six responded to high-dose quetiapine and 1 to high-dose quetiapine plus risperidone, 2 mg/d; 4 received adjunctive dival-proex sodium, 1,500 to 3,000 mg/d. Psychopathology, violence, and behavioral disturbances were reduced throughout 5 to 14 months of monitoring. Side effects included sedation, orthostasis, and dysphagia.
When Nelson et al24 treated 13 subjects for 14 weeks with quetiapine, 1,000 to 1,400 mg/d, mean weight, glucose, total cholesterol, prolactin, and QTc interval duration did not change significantly. Heart rate increased significantly (though not to tachycardia), and headache, constipation, and lethargy were the most frequent side effects.
Summary. Although encouraging, these reports are preliminary, unpublished, and lack peer review. Controlled trials of high-dose quetiapine’s efficacy and safety are needed.
Ziprasidone and aripiprazole
No studies of high-dose ziprasidone or aripiprazole have been published. In premarketing trials:
- ziprasidone was studied at 200 mg/d and released with a maximum recommended dosage of 160 mg/d
- aripiprazole, 30 mg/d, was not more effective than 15 mg/d.25
Deutschman et al26 reviewed the charts of 31 patients who received ziprasidone, 240 to 320 mg/d, after an “incomplete” response to 160 mg/d. At the higher dosing:
- psychosis, affective symptoms, or anxiety improved in nearly one-half of patients
- 15% reported sedation, but most reported no side effects
- none developed QTc intervals >500 msec.
Caveats and precautions
These uncontrolled case reports and open-label studies do not “prove” efficacy or safety but reflect clinical practice. More than anything, they show that we need controlled trials to gauge high-dose antipsychotic therapy’s efficacy and safety and to curb our collective habit of relying on anecdotal experience and idiosyncratic beliefs.
Despite its side-effect profile, clozapine remains the treatment of choice for refractory schizophrenia. Given high-dose antipsychotic therapy’s uncertain efficacy and unknown risks, the evidence supports a clozapine trial before higher-than-recommended dosing is attempted.
Because educated guesswork plays a role in premarketing dosing studies, a medication’s optimal dose may be:
- overestimated (as with risperidone)
- underestimated (as perhaps with olanzapine and quetiapine).
Keep in mind some important caveats when you consider giving a patient high-dose antipsychotic therapy (Box).27 Of course, nonadherence is often the cause of apparent medication nonresponse. Increasing the dosage of a medication a patient is not taking rarely improves adherence. Interventions to enhance adherence—careful assessment, psychoeducation, and using longacting intramuscular medication—may be useful.
Related resources
- Marder SR, Essock SM, Miller AL, et al. The Mount Sinai Conference on the pharmacotherapy of schizophrenia. Schizophrenia Bull 2002;28:5-16.
- Practice guideline for the treatment of patients with schizophrenia (2nd ed). Am J Psychiatry 2004;161(suppl):1-56.
- Texas Medication Algorithm Project antipsychotic algorithm. http://www.mhmr.state.tx.us/centraloffice/medicaldirector/timascz1algo.pdf
Drug brand names
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Divalproex • Depakote
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosures
Dr. Pierre receives research support from Cephalon Inc., and is a consultant to and/or speaker for Pfizer Inc., Bristol-Myers Squibb Co., AstraZeneca Pharmaceuticals, and Janssen Pharmaceutica.
Dr. Donna Wirshing receives research support from, is a consultant to, and/or is a speaker for Bristol-Myers Squibb Co., Pfizer Inc., Eli Lilly & Co., Janssen Pharmaceutica, AstraZeneca Pharmaceuticals, and Abbott Laboratories.
Dr. William Wirshing receives research support from, is a consultant to, and/or is a speaker for Bristol-Myers Squibb Co., Pfizer Inc., Eli Lilly & Co., Janssen Pharmaceutica, and AstraZeneca Pharmaceuticals.
When nothing else works, desperate clinicians are resorting to progressively more-tenuous and unpredictable treatments, trying to improve the lives of patients with refractory schizophrenia. High-dose antipsychotics is a common strategy.
Does boosting antipsychotic doses beyond the recommended range—but short of the neuroleptic threshold—enhance efficacy? This article attempts to answer that question by presenting the evidence on higher-than-recommended doses of atypical antipsychotics.
Lessons from neuroleptics
Up to 30% of patients with schizophrenia do not respond to antipsychotics and are considered “treatment refractory.”1 Even among those who do respond, improving symptoms by 20%—as research defines “treatment response”—does not necessarily yield clinical or functional improvement. Clozapine is the only atypical antipsychotic with well-established efficacy in these chronically ill patients,2 but its daunting side effects greatly curtail its use.
Before atypical antipsychotics, patients who did not respond to usual dosages of the typical neuroleptics were treated with higher dosages or switched to another drug class. Although many clinicians embraced high-dose neuroleptics, subsequent research discredited “rapid neuroleptization” in any clinical circumstance and showed that exceeding an antipsychotic’s neuroleptic threshold—the dose at which extrapyramidal side effects (EPS) occur—reduces its efficacy (Figure 1).3-5 In some instances, reducing neuroleptic dosages improves treatment-resistant patients’ symptoms and reduces druginduced side effects.6
Figure 1 Typical antipsychotics’ dose-response curve
Narrow therapeutic window between antipsychotic effect and neuroleptic threshold. Dotted line indicates declining efficacy.
Figure 2 Atypical antipsychotics’ dose-response curve
Wider therapeutic window with atypicals, compared with typical antipsychotics, as neuroleptic threshold (dotted line) moves right.Atypical antipsychotics are defined by their relative lack of EPS at recommended dosages (Figure 2). Because these agents can cause EPS if dosed too high, however, our historical habit of testing this dose limit risks losing “atypicality” and encountering other untoward events (Figure 3).
What is the safest, most effective dosage? Consider the evidence for each atypical antipsychotic.
Risperidone
Recommended dosage too high? When using atypicals at recommended doses, you are most likely to encounter the neuroleptic threshold with risperidone, with EPS risk increasing substantially at >6 mg/d.7 Post-approval studies set the most effective and safest dosage at approximately 4 mg/d, though this dosage was not studied in North American pre-approval trials. Dosages of 2 to 4 mg/d have been associated with more-favorable outcomes, suggesting that the initial recommendation to titrate to 6 mg/d within the first 3 days was ill-advised.8
In our study of patients with treatment-refractory schizophrenia,9 those treated with risperidone, 6 mg/d, improved significantly more after 4 weeks than did those receiving haloperidol, 15 mg/d, based on Brief Psychiatric Rating Scale (BPRS) scores. No additional benefit was seen after risperidone was increased to >6 mg/d at 8 weeks. Akathisia and tardive dyskinesia occurred significantly more often in the haloperidol group.
Conclusion. Some patients respond to higher-dose risperidone, but emerging EPS suggest the need to reduce the dosage rather than add an antiparkinsonian agent.
Figure 3 Unknown effects of high-dose atypical antipsychotic therapy
Dotted line indicates potential for greater antipsychotic effect with increasing dose.
Olanzapine
Mixed results. Case reports suggest that some patients who did not respond to previous antipsychotic trials or olanzapine, 20 mg/d, improved sig-nificantly—without substanial side effects—when olanzapine was increased up to 60 mg/d.10-14 Other case studies, however, report EPS, increased heart rate, increased transaminases, hyperprolactinemia, and prolonged QTc interval with high-dose olanzapine.14-16
In an open-label trial,17 43 patients with schizophrenia received olanzapine, up to 40 mg/d, after inadequate response to neuroleptics and risperidone or clozapine. Olanzapine was titrated to 20 mg/d by week 4 and increased 5 mg every 2 weeks if symptoms did not improve. After 14 weeks, improvement was modest and only 17% of patients met response criteria. However, >20 mg/d reduced symptoms more than did <20 mg/d, suggesting that high-dose olanzapine was more effective.
In a randomized trial,18 patients who did not respond to at least one atypical antipsychotic then received 8 weeks of fixed, standard-dose treatment with (mean dosages):
- haloperidol, 18.9 mg/d
- risperidone, 7.9 mg/d
- olanzapine, 19.6 mg/d
- clozapine, 401.6 mg/d.
Flexible dosing was then allowed for 6 weeks, and mean dosages were:
- haloperidol, 25.7 mg/d
- risperidone, 11.6 mg/d
- olanzapine, 30.4 mg/d
- clozapine, 526.6 mg/d.
Symptoms improved modestly at best for all medications, although patients taking olanzapine or clozapine improved significantly more than those treated with haloperidol as shown by mean changes in total Positive and Negative Syndrome Scale (PANSS) scores.
PANSS scores for olanzapine-treated patients showed additional improvement at week 14—when higher dosages were used—compared with week 8. This was not the case for the other medications, for which response plateaued. These findings suggest that high-dose risperidone and haloperidol are incrementally ineffective, but high-dose olanzapine could help some patients with refractory symptoms.
Results were different in a randomized, double-blind, 16-week, crossover study,19 when 13 patients with inadequate response to neuroleptics, risperidone, or conventional-dose olanzapine then received olanzapine, 50 mg/d, or clozapine, 450 mg/d. No olanzapine-treated patients and 20% of clozapine-treated patients met criteria for treatment response (20% improvement in BPRS score and final BPRS score <35 or 1-point improvement on Clinical Global Impressions-Severity of Illness scale).
Negative results don’t make headlines. Published clinical trials and case reports are subject to selective reporting of positive outcomes. Cases in which high-dose therapy proved ineffectivemay outnumber positive results but are less likely to be published.
Numbers don’t lie. Using high doses will almost always increase side effect risk and drug therapy costs, contributing to a poor risk-benefit ratio when efficacy remains unchanged. Resorting to an “if-it’s-not-working, double-it” strategy may seem reasonable, but two times zero is still zero.
Desperation warps perception. Clinicians tend to rely on observational experience. The desperation inherent in treating refractory patients, however, often creates a strong desire for improvement and therefore a potentially biased perception of outcome.
Likewise, patients may inaccurately portray themselves as improved to avoid disappointing their doctors. Controlled trials reduce these biases to better assess efficacy.
Antipsychotics work in 6 to 8 weeks. Improvements seen when pushing medications beyond recommended dosing may not be an effect of dose but of additional time on the medication. Antipsychotics usually take 6 to 8 weeks to produce maximal response, so high-dose therapy should not be started during this initial phase. This pace may not satisfy pressures for expedient stabilization and hospital discharge, but it is unrealistic to expect antipsychotics to work more quickly than they do.
Oversedation does not equal improvement. Patients who become excessively sedated from high-dose therapy or adjunctive medications may appear less psychotic but may not be so. The family or hospital staff may desire such sedation, but it can adversely affect the patient’s quality of life or medication adherence.
Polypharmacy clouds the issue. Many patients treated with high-dose antipsychotics are taking multiple agents, making it difficult to attribute improvement (or side effects) to any single one. A well-designed study of high-dose therapy would therefore:
- control for time
- examine concomitant medications’ effects
- determine whether “improvements” are related to sedation or reduced psychosis.
Medication may not need to change. When a patient decompensates, many forces pressure clinicians to change or add medications or increase dosages. Change may not be necessary, however, as nonadherence or substance abuse often trigger psychotic exacerbations. For example, Steingard et al27 added fluphenazine or placebo to antipsychotic regimens of newly hospitalized patients and found that increasing antipsychotic dosage did not improve outcome.
Subjects switching from clozapine to olanzapine tended to worsen, whereas those switching from olanzapine to clozapine tended to improve. Olanzapine-treated patients experienced more anticholinergic side effects and more weight gain than did clozapine-treated subjects.20
Conclusion. These mixed findings on high-dose olanzapine suggest questionable efficacy in patients with treatment-resistant schizophrenia and an uncertain risk of increased toxicity.
Quetiapine
Early placebo-controlled studies of quetiapine in schizophrenia concluded that statistically significant improvement begins at 150 mg/d and falls off after 600 mg/d.21 Although few high-dose quetiapine cases have been presented, clinical opinion holds that:
- most patients with chronic schizophrenia require 400 to 800 mg/d
- some treatment-refractory patients might benefit from >800 mg/d.
One patient responded to quetiapine, 1,600 mg/d, after not responding to olanzapine, 40 mg/d, and quetiapine, 800 mg/d. Constipation was the only reported side effect.22
Our group23 reported a series of 7 patients who responded (by clinician report) to quetiapine, 1,200 to 2,400 mg/d, after not responding to quetiapine, 800 mg/d, or to neuroleptics, risperidone, or olanzapine. Six responded to high-dose quetiapine and 1 to high-dose quetiapine plus risperidone, 2 mg/d; 4 received adjunctive dival-proex sodium, 1,500 to 3,000 mg/d. Psychopathology, violence, and behavioral disturbances were reduced throughout 5 to 14 months of monitoring. Side effects included sedation, orthostasis, and dysphagia.
When Nelson et al24 treated 13 subjects for 14 weeks with quetiapine, 1,000 to 1,400 mg/d, mean weight, glucose, total cholesterol, prolactin, and QTc interval duration did not change significantly. Heart rate increased significantly (though not to tachycardia), and headache, constipation, and lethargy were the most frequent side effects.
Summary. Although encouraging, these reports are preliminary, unpublished, and lack peer review. Controlled trials of high-dose quetiapine’s efficacy and safety are needed.
Ziprasidone and aripiprazole
No studies of high-dose ziprasidone or aripiprazole have been published. In premarketing trials:
- ziprasidone was studied at 200 mg/d and released with a maximum recommended dosage of 160 mg/d
- aripiprazole, 30 mg/d, was not more effective than 15 mg/d.25
Deutschman et al26 reviewed the charts of 31 patients who received ziprasidone, 240 to 320 mg/d, after an “incomplete” response to 160 mg/d. At the higher dosing:
- psychosis, affective symptoms, or anxiety improved in nearly one-half of patients
- 15% reported sedation, but most reported no side effects
- none developed QTc intervals >500 msec.
Caveats and precautions
These uncontrolled case reports and open-label studies do not “prove” efficacy or safety but reflect clinical practice. More than anything, they show that we need controlled trials to gauge high-dose antipsychotic therapy’s efficacy and safety and to curb our collective habit of relying on anecdotal experience and idiosyncratic beliefs.
Despite its side-effect profile, clozapine remains the treatment of choice for refractory schizophrenia. Given high-dose antipsychotic therapy’s uncertain efficacy and unknown risks, the evidence supports a clozapine trial before higher-than-recommended dosing is attempted.
Because educated guesswork plays a role in premarketing dosing studies, a medication’s optimal dose may be:
- overestimated (as with risperidone)
- underestimated (as perhaps with olanzapine and quetiapine).
Keep in mind some important caveats when you consider giving a patient high-dose antipsychotic therapy (Box).27 Of course, nonadherence is often the cause of apparent medication nonresponse. Increasing the dosage of a medication a patient is not taking rarely improves adherence. Interventions to enhance adherence—careful assessment, psychoeducation, and using longacting intramuscular medication—may be useful.
Related resources
- Marder SR, Essock SM, Miller AL, et al. The Mount Sinai Conference on the pharmacotherapy of schizophrenia. Schizophrenia Bull 2002;28:5-16.
- Practice guideline for the treatment of patients with schizophrenia (2nd ed). Am J Psychiatry 2004;161(suppl):1-56.
- Texas Medication Algorithm Project antipsychotic algorithm. http://www.mhmr.state.tx.us/centraloffice/medicaldirector/timascz1algo.pdf
Drug brand names
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Divalproex • Depakote
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosures
Dr. Pierre receives research support from Cephalon Inc., and is a consultant to and/or speaker for Pfizer Inc., Bristol-Myers Squibb Co., AstraZeneca Pharmaceuticals, and Janssen Pharmaceutica.
Dr. Donna Wirshing receives research support from, is a consultant to, and/or is a speaker for Bristol-Myers Squibb Co., Pfizer Inc., Eli Lilly & Co., Janssen Pharmaceutica, AstraZeneca Pharmaceuticals, and Abbott Laboratories.
Dr. William Wirshing receives research support from, is a consultant to, and/or is a speaker for Bristol-Myers Squibb Co., Pfizer Inc., Eli Lilly & Co., Janssen Pharmaceutica, and AstraZeneca Pharmaceuticals.
1. Conley RR, Buchanan RW. Evaluation of treatment-resistant schizophrenia. Schizophr Bull 1997;23:663-74.
2. Chakos M, Lieberman J, Hoffman E, et al. Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: A review and meta-analysis of randomized trials. Am J Psychiatry 2001;158:518-26.
3. Baldessarini RJ, Cohen BM, Teicher MH. Significance of neuroleptic dose and plasma level in the pharmacological treatment of psychoses. Arch Gen Psych 1988;45:79-91.
4. McEvoy JP, Hogarty GE, Steingard S. Optimal dose of neuroleptic in acute schizophrenia: A controlled study of the neuroleptic threshold and higher haloperidol dose. Arch Gen Psychiatry 1991;48:739-45.
5. Van Putten T, Marder SR, Mintz J, Poland R. Haloperidol plasma levels and clinical response: A therapeutic window relationship. Am J Psychiatry 1992;149:500-5.
6. Van Putten T, Marshall BD, Liberman R, et al. Systematic dosage reduction in treatment-resistant schizophrenic patients. Psychopharmacol Bull 1993;29:315-20.
7. Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry 1994;151:825-36.
8. Love RC, Conley RR, Kelly DL, Bartko JJ. A dose-outcome analysis of risperidone. J Clin Psychiatry 1999;60:771-5.
9. Wirshing DA, Marshall BD, Jr, Green MF, et al. Risperidone in treatment-refractory schizophrenia. Am J Psychiatry 1999;156:1374-9.
10. Fanous A, Lindenmayer JP. Schizophrenia and schizoaffective disorder treated with high doses of olanzapine. J Clin Psychopharmacol 1999;19:275-6.
11. Reich J. Use of high-dose olanzapine in refractory psychosis. Am J Psychiatry 1999;156:661.-
12. Dursun SM, Gardner DM, Bird DC, Flinn J. Olanzapine for patients with treatment-resistant schizophrenia: A naturalistic case-series outcome study. Can J Psychiatry 1999;44:701-4.
13. Lerner V. High-dose olanzapine for treatment-refractory schizophrenia. Clin Neuropharmacol 2003;26:58-61.
14. Sheitman BB, Lindgren JC, Early JE, Sved M. High-dose olanzapine for treatment-refractory schizophrenia. Am J Psychiatry 1997;154:1626.
15. Bronson BD, Lindenmayer JP. Adverse effects of high-dose olanzapine in treatment-refractory schizophrenia. J Clin Psychopharmacol 2000;20:383-4.
16. Dineen S, Withrow K, Voronovitch L, et al. QTc prolongation and high-dose olanzapine. Psychosomatics 2003;44:174-5.
17. Lindenmayer JP, Volavka J, Lieberman J, et al. Olanzapine for schizophrenia refractory to typical and atypical antipsychotics: An open-label, prospective trial. J Clin Psychopharmacol. 2001;21:448-53.
18. Volavka J, Czobor P, Sheitman B, et al. Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry 2002;159:255-62.
19. Conley RR, Kelly DL, Richardson CM, et al. The efficacy of high-dose olanzapine versus clozapine in treatment-resistant schizophrenia: A double-blind cross-over study. J Clin Psychopharmacol 2003;23:668-71.
20. Kelly DL, Conley RR, Richardson CM, et al. Adverse effects and laboratory parameters of high-dose olanzapine vs. clozapine in treatment-resistant schizophrenia. Ann Clin Psychiatry 2003;15:181-6.
21. Arvanitis LA, Miller BG. and the Seroquel Trial 13 Study Group. Multiple fixed doses of “Seroquel” (quetiapine) in patients with acute exacerbation of schizophrenia: A comparison with haloperidol and placebo. Biol Psychiatry 1997;42:233-46.
22. Bobes J, Garcia-Portilla MP, Saiz PA, et al. High degree of tolerability for monotherapy with high doses of quetiapine: A case report. J Clin Psychiatry 2002;63:1048-9.
23. Pierre JM, Wirshing DA, Cannell J, et al. High-dose quetiapine in treatment refractory schizophrenia (poster). Colorado Springs, CO: International Congress of Schizophrenia Research, 2003; abstracted in Schizophrenia Res 2003;60(supp):299.-
24. Nelson MW, Reynolds R, Kelly DL, et al. Safety and tolerability of high-dose quetiapine in treatment-refractory schizophrenia: Preliminary results from an open-label trial (poster). Colorado Springs, CO: International Congress of Schizophrenia Research, 2003; abstracted in Schizophrenia Res 2003;60(supp):363.-
25. Potkin SG, Saha AR, Kujawa MJ, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry 2003;60:681-90.
26. Deutschman DA, Deutschman DH. High-dose ziprasidone: effectiveness and tolerability in clinical practice (poster). Boston, MA: American Psychiatric Association Institute on Psychiatric Services annual meeting, 2003.
27. Steingard S, Allen M, Schooler MR. A study of pharmacologic treatment on medication-compliant schizophrenics who relapse. J Clin Psychiatry 1994;55:470-2.
1. Conley RR, Buchanan RW. Evaluation of treatment-resistant schizophrenia. Schizophr Bull 1997;23:663-74.
2. Chakos M, Lieberman J, Hoffman E, et al. Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: A review and meta-analysis of randomized trials. Am J Psychiatry 2001;158:518-26.
3. Baldessarini RJ, Cohen BM, Teicher MH. Significance of neuroleptic dose and plasma level in the pharmacological treatment of psychoses. Arch Gen Psych 1988;45:79-91.
4. McEvoy JP, Hogarty GE, Steingard S. Optimal dose of neuroleptic in acute schizophrenia: A controlled study of the neuroleptic threshold and higher haloperidol dose. Arch Gen Psychiatry 1991;48:739-45.
5. Van Putten T, Marder SR, Mintz J, Poland R. Haloperidol plasma levels and clinical response: A therapeutic window relationship. Am J Psychiatry 1992;149:500-5.
6. Van Putten T, Marshall BD, Liberman R, et al. Systematic dosage reduction in treatment-resistant schizophrenic patients. Psychopharmacol Bull 1993;29:315-20.
7. Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry 1994;151:825-36.
8. Love RC, Conley RR, Kelly DL, Bartko JJ. A dose-outcome analysis of risperidone. J Clin Psychiatry 1999;60:771-5.
9. Wirshing DA, Marshall BD, Jr, Green MF, et al. Risperidone in treatment-refractory schizophrenia. Am J Psychiatry 1999;156:1374-9.
10. Fanous A, Lindenmayer JP. Schizophrenia and schizoaffective disorder treated with high doses of olanzapine. J Clin Psychopharmacol 1999;19:275-6.
11. Reich J. Use of high-dose olanzapine in refractory psychosis. Am J Psychiatry 1999;156:661.-
12. Dursun SM, Gardner DM, Bird DC, Flinn J. Olanzapine for patients with treatment-resistant schizophrenia: A naturalistic case-series outcome study. Can J Psychiatry 1999;44:701-4.
13. Lerner V. High-dose olanzapine for treatment-refractory schizophrenia. Clin Neuropharmacol 2003;26:58-61.
14. Sheitman BB, Lindgren JC, Early JE, Sved M. High-dose olanzapine for treatment-refractory schizophrenia. Am J Psychiatry 1997;154:1626.
15. Bronson BD, Lindenmayer JP. Adverse effects of high-dose olanzapine in treatment-refractory schizophrenia. J Clin Psychopharmacol 2000;20:383-4.
16. Dineen S, Withrow K, Voronovitch L, et al. QTc prolongation and high-dose olanzapine. Psychosomatics 2003;44:174-5.
17. Lindenmayer JP, Volavka J, Lieberman J, et al. Olanzapine for schizophrenia refractory to typical and atypical antipsychotics: An open-label, prospective trial. J Clin Psychopharmacol. 2001;21:448-53.
18. Volavka J, Czobor P, Sheitman B, et al. Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry 2002;159:255-62.
19. Conley RR, Kelly DL, Richardson CM, et al. The efficacy of high-dose olanzapine versus clozapine in treatment-resistant schizophrenia: A double-blind cross-over study. J Clin Psychopharmacol 2003;23:668-71.
20. Kelly DL, Conley RR, Richardson CM, et al. Adverse effects and laboratory parameters of high-dose olanzapine vs. clozapine in treatment-resistant schizophrenia. Ann Clin Psychiatry 2003;15:181-6.
21. Arvanitis LA, Miller BG. and the Seroquel Trial 13 Study Group. Multiple fixed doses of “Seroquel” (quetiapine) in patients with acute exacerbation of schizophrenia: A comparison with haloperidol and placebo. Biol Psychiatry 1997;42:233-46.
22. Bobes J, Garcia-Portilla MP, Saiz PA, et al. High degree of tolerability for monotherapy with high doses of quetiapine: A case report. J Clin Psychiatry 2002;63:1048-9.
23. Pierre JM, Wirshing DA, Cannell J, et al. High-dose quetiapine in treatment refractory schizophrenia (poster). Colorado Springs, CO: International Congress of Schizophrenia Research, 2003; abstracted in Schizophrenia Res 2003;60(supp):299.-
24. Nelson MW, Reynolds R, Kelly DL, et al. Safety and tolerability of high-dose quetiapine in treatment-refractory schizophrenia: Preliminary results from an open-label trial (poster). Colorado Springs, CO: International Congress of Schizophrenia Research, 2003; abstracted in Schizophrenia Res 2003;60(supp):363.-
25. Potkin SG, Saha AR, Kujawa MJ, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry 2003;60:681-90.
26. Deutschman DA, Deutschman DH. High-dose ziprasidone: effectiveness and tolerability in clinical practice (poster). Boston, MA: American Psychiatric Association Institute on Psychiatric Services annual meeting, 2003.
27. Steingard S, Allen M, Schooler MR. A study of pharmacologic treatment on medication-compliant schizophrenics who relapse. J Clin Psychiatry 1994;55:470-2.
Understanding the ‘joy’ of aggression
One of the most perplexing and shocking aspects of human behavior is the cruelty we can inflict on one another. Infamous events such as the Spanish Inquisition, slavery, lynching, conquest of the native Americans, and Nazi concentration camps are so sickening that many of us can barely tolerate hearing about them. How can people behave this way?
Recently, we’ve been shocked by photographs from the Abu Ghraib military prison in Iraq. American soldiers with unremarkable backgrounds—not Saddam’s henchmen—were shown humiliating and abusing Iraqi prisoners. Most remarkable was the joy on the Americans’ faces (Figure 1).
‘Good’ people, ‘bad’ circumstances
In experiments with college students, psychologists have shown that “regular” people can become sadistic under the right (or wrong) circumstances.1 One explanation is that it’s not just psychopaths who perpetrate crimes against humanity. Somehow, the psychopath within us all becomes unleashed.
Artificial situations such as the Stanford Prison Experiment (www.prisonexp.org) show that normal people can dissolve into cruelty but don’t explain why. A recent neuroscience experiment suggests a mechanism for this kind of aggression.
Figure 1 Deriving pleasure from abuse?
American soldiers appearing to enjoy themselves as they humiliate Iraqi prisoners in the Abu Ghraib military prison.
Source: Reprinted with permission of The New Yorker, which first published this photo.
Dopamine and aggression
The nucleus accumbens has been called the brain’s “pleasure center,” and dopamine is the neurotransmitter that activates it.2 Activities and substances that stimulate dopamine release include sex, gambling, and smoking as well as cocaine and alcohol. The good feeling a person gets from these activities/substances reinforces the behavior that produced the feeling. In some cases, problems develop when people cannot resist the urge for more.
Ferrari et al3 placed micropipettes in rats’ nucleus accumbens to measure extracellular dopamine before, during, and after an aggressive confrontation. When the rats were confronted with an intruder rat for 10 minutes, they attacked and bit the intruder an average of 5 times, despite being implanted, tethered, and sampled. During and after the fight, dopamine was increased in the rats’ nucleus accumbens (Figure 2). Clearly, fighting gave them a “squirt” of pleasure that lasted almost 2 hours.
If we can extrapolate from this study to humans, we may understand why people become aggressive. At some level, they enjoy it. The bully on the playground, the wife beater, the mean boss—they get pleasure from being aggressive. It’s not just serial killers.
It is important to acknowledge that other variables such as poor supervision and too much power affected the actions of American soldiers working as prison guards in Iraq. However, the neuroscientific studies show us that aggression can be pleasurable, and people often have a hard time resisting what feels good. This knowledge may help us treat war veterans struggling not only with traumatic memories of violence but also with socially and personally unacceptable feelings of pleasure.
Figure 2 A ‘squirt’ of dopamine during violence
A 10-minute fight increased extracellular dopamine levels in rats’ nucleus accumbens for approximately 2 hours, suggesting that aggressive behavior produced pleasure.
Source: Adapted and reprinted with permission from reference 3. Copyright 2003, Blackwell Publishing.
1. Shermer M. The science of good and evil: Why people cheat, gossip, care, share, and follow the Golden Rule. New York: Times Books, 2004.
2. Ikemoto S, Panksepp J. The role of nucleus accumbens dopamine in motivated behavior: a unifying interpretation with special reference to reward-seeking. Brain Res Brain Res Rev 1999;31(1):6-41.
3. Ferrari PF, van Erp AM, Tornatzky W, Miczek KA. Accumbal dopamine and serotonin in anticipation of the next aggressive episode in rats. Eur J Neurosci 2003;17:371-8.
One of the most perplexing and shocking aspects of human behavior is the cruelty we can inflict on one another. Infamous events such as the Spanish Inquisition, slavery, lynching, conquest of the native Americans, and Nazi concentration camps are so sickening that many of us can barely tolerate hearing about them. How can people behave this way?
Recently, we’ve been shocked by photographs from the Abu Ghraib military prison in Iraq. American soldiers with unremarkable backgrounds—not Saddam’s henchmen—were shown humiliating and abusing Iraqi prisoners. Most remarkable was the joy on the Americans’ faces (Figure 1).
‘Good’ people, ‘bad’ circumstances
In experiments with college students, psychologists have shown that “regular” people can become sadistic under the right (or wrong) circumstances.1 One explanation is that it’s not just psychopaths who perpetrate crimes against humanity. Somehow, the psychopath within us all becomes unleashed.
Artificial situations such as the Stanford Prison Experiment (www.prisonexp.org) show that normal people can dissolve into cruelty but don’t explain why. A recent neuroscience experiment suggests a mechanism for this kind of aggression.
Figure 1 Deriving pleasure from abuse?
American soldiers appearing to enjoy themselves as they humiliate Iraqi prisoners in the Abu Ghraib military prison.
Source: Reprinted with permission of The New Yorker, which first published this photo.
Dopamine and aggression
The nucleus accumbens has been called the brain’s “pleasure center,” and dopamine is the neurotransmitter that activates it.2 Activities and substances that stimulate dopamine release include sex, gambling, and smoking as well as cocaine and alcohol. The good feeling a person gets from these activities/substances reinforces the behavior that produced the feeling. In some cases, problems develop when people cannot resist the urge for more.
Ferrari et al3 placed micropipettes in rats’ nucleus accumbens to measure extracellular dopamine before, during, and after an aggressive confrontation. When the rats were confronted with an intruder rat for 10 minutes, they attacked and bit the intruder an average of 5 times, despite being implanted, tethered, and sampled. During and after the fight, dopamine was increased in the rats’ nucleus accumbens (Figure 2). Clearly, fighting gave them a “squirt” of pleasure that lasted almost 2 hours.
If we can extrapolate from this study to humans, we may understand why people become aggressive. At some level, they enjoy it. The bully on the playground, the wife beater, the mean boss—they get pleasure from being aggressive. It’s not just serial killers.
It is important to acknowledge that other variables such as poor supervision and too much power affected the actions of American soldiers working as prison guards in Iraq. However, the neuroscientific studies show us that aggression can be pleasurable, and people often have a hard time resisting what feels good. This knowledge may help us treat war veterans struggling not only with traumatic memories of violence but also with socially and personally unacceptable feelings of pleasure.
Figure 2 A ‘squirt’ of dopamine during violence
A 10-minute fight increased extracellular dopamine levels in rats’ nucleus accumbens for approximately 2 hours, suggesting that aggressive behavior produced pleasure.
Source: Adapted and reprinted with permission from reference 3. Copyright 2003, Blackwell Publishing.
One of the most perplexing and shocking aspects of human behavior is the cruelty we can inflict on one another. Infamous events such as the Spanish Inquisition, slavery, lynching, conquest of the native Americans, and Nazi concentration camps are so sickening that many of us can barely tolerate hearing about them. How can people behave this way?
Recently, we’ve been shocked by photographs from the Abu Ghraib military prison in Iraq. American soldiers with unremarkable backgrounds—not Saddam’s henchmen—were shown humiliating and abusing Iraqi prisoners. Most remarkable was the joy on the Americans’ faces (Figure 1).
‘Good’ people, ‘bad’ circumstances
In experiments with college students, psychologists have shown that “regular” people can become sadistic under the right (or wrong) circumstances.1 One explanation is that it’s not just psychopaths who perpetrate crimes against humanity. Somehow, the psychopath within us all becomes unleashed.
Artificial situations such as the Stanford Prison Experiment (www.prisonexp.org) show that normal people can dissolve into cruelty but don’t explain why. A recent neuroscience experiment suggests a mechanism for this kind of aggression.
Figure 1 Deriving pleasure from abuse?
American soldiers appearing to enjoy themselves as they humiliate Iraqi prisoners in the Abu Ghraib military prison.
Source: Reprinted with permission of The New Yorker, which first published this photo.
Dopamine and aggression
The nucleus accumbens has been called the brain’s “pleasure center,” and dopamine is the neurotransmitter that activates it.2 Activities and substances that stimulate dopamine release include sex, gambling, and smoking as well as cocaine and alcohol. The good feeling a person gets from these activities/substances reinforces the behavior that produced the feeling. In some cases, problems develop when people cannot resist the urge for more.
Ferrari et al3 placed micropipettes in rats’ nucleus accumbens to measure extracellular dopamine before, during, and after an aggressive confrontation. When the rats were confronted with an intruder rat for 10 minutes, they attacked and bit the intruder an average of 5 times, despite being implanted, tethered, and sampled. During and after the fight, dopamine was increased in the rats’ nucleus accumbens (Figure 2). Clearly, fighting gave them a “squirt” of pleasure that lasted almost 2 hours.
If we can extrapolate from this study to humans, we may understand why people become aggressive. At some level, they enjoy it. The bully on the playground, the wife beater, the mean boss—they get pleasure from being aggressive. It’s not just serial killers.
It is important to acknowledge that other variables such as poor supervision and too much power affected the actions of American soldiers working as prison guards in Iraq. However, the neuroscientific studies show us that aggression can be pleasurable, and people often have a hard time resisting what feels good. This knowledge may help us treat war veterans struggling not only with traumatic memories of violence but also with socially and personally unacceptable feelings of pleasure.
Figure 2 A ‘squirt’ of dopamine during violence
A 10-minute fight increased extracellular dopamine levels in rats’ nucleus accumbens for approximately 2 hours, suggesting that aggressive behavior produced pleasure.
Source: Adapted and reprinted with permission from reference 3. Copyright 2003, Blackwell Publishing.
1. Shermer M. The science of good and evil: Why people cheat, gossip, care, share, and follow the Golden Rule. New York: Times Books, 2004.
2. Ikemoto S, Panksepp J. The role of nucleus accumbens dopamine in motivated behavior: a unifying interpretation with special reference to reward-seeking. Brain Res Brain Res Rev 1999;31(1):6-41.
3. Ferrari PF, van Erp AM, Tornatzky W, Miczek KA. Accumbal dopamine and serotonin in anticipation of the next aggressive episode in rats. Eur J Neurosci 2003;17:371-8.
1. Shermer M. The science of good and evil: Why people cheat, gossip, care, share, and follow the Golden Rule. New York: Times Books, 2004.
2. Ikemoto S, Panksepp J. The role of nucleus accumbens dopamine in motivated behavior: a unifying interpretation with special reference to reward-seeking. Brain Res Brain Res Rev 1999;31(1):6-41.
3. Ferrari PF, van Erp AM, Tornatzky W, Miczek KA. Accumbal dopamine and serotonin in anticipation of the next aggressive episode in rats. Eur J Neurosci 2003;17:371-8.
Are psychostimulants useful in pervasive developmental disorders?
Psychostimulants benefit many patients with attention-deficit/hyperactivity disorder (ADHD)1 and thus might seem a logical choice to manage hyperactivity and inattention in youths with a pervasive developmental disorder (PDD). Some PDD patients do respond to psychostimulant therapy, but others worsen—and side effects are common.
Youths with PDDs often exhibit maladaptive behaviors—aggression, self-injury, irritability, hyperactivity, inattention—with repetitive activity patterns and fundamentally impaired social interaction and communication.2 To help you treat youths with PDD, we draw on the evidence, clinical experience, and our research to suggest psychostimulants’ role in a multimodal approach.
Targeting hyperactivity and inattentions
Step 1. Our approach begins with behavioral therapy (Figure), which includes identifying situations that trigger maladaptive behavior and environments that yield optimum behavior. The therapist assesses the child’s baseline attention and works with him or her to gradually increase it, using reinforcement and visual token boards.
Algorithm Suggested approach to hyperactivity and/or inattention in patients with PDDs

To set limits and expectations, the therapist introduces structure such as designating work and break areas and using visual schedules and timers to indicate activity duration. Minimizing distractions and understanding the child’s sensory needs may increase motivation and attention. Initially, the therapist allows numerous breaks and then may slowly decrease them as the child progresses. Tailoring work and play materials to the child’s interests can also help increase attention.
Step 2. Many patients will not respond to behavior therapy alone and will require added drug therapy. Based on evidence, we suggest starting with an alpha-2 adrenergic agonist. Guanfacine may be considered the drug of choice because of clonidine’s higher risk of adverse effects, such as hypotension and sedation. Obtain a baseline ECG with either agent, as clonidine has been associated with rare cardiovascular events.
Clonidine. Two small studies showed that clonidine may be of some benefit to patients with PDDs:
- Results were mixed in a 6-week, double-blind, placebo-controlled, crossover study of clonidine (4 to 10 μg/kg/d) in 8 autistic children ages 5 to 13.3 Teacher and parent rating instruments reflected significantly improved hyperactivity, irritability, and oppositional behavior. Clinician ratings, however, showed no significant difference between clonidine and placebo. Adverse effects with clonidine included hypotension, sedation, and decreased activity.
- In a 4-week, double-blind, placebo-con-trolled, crossover study of transdermal clonidine (0.16 to 0.48 mg/kg/d; mean: 3.6 μg/kg/d), clinician ratings showed significantly decreased hyperactivity, impulsivity, and anxiety in 9 autistic males ages 5 to 33. Sedation and fatigue were common adverse effects.
Guanfacine. In a recent retrospective review,5 we examined outcomes of 80 PDD patients ages 3 to 18 who received guanfacine (0.25 to 9 mg/d; mean: 2.6). Hyperactivity, inattention, and tics decreased in 19 patients (24%) treated for a mean 10 months.
Step 3. If clonidine or guanfacine fails to reduce hyperactivity and inattention, discontinue it and consider a psychostimulant trial.
Because psychostimulants’ efficacy in PDDs remains inconclusive, we suggest beginning with a low dosage and carefully monitoring the patient for worsening target symptoms and activation, such as emerging aggression or irritability.
Step 4. If hyperactivity and inattention remain prominent and treatment-refractory, we suggest that you discontinue the stimulant and consider an atypical antipsychotic trial. With the atypicals, monitor patients closely for adverse effects, including weight gain, extrapyramidal symptoms, and tardive dyskinesia. Fasting serum glucose and lipid profiles and liver function tests are recommended at least every 6 months and more often in individuals at risk for diabetes or hepatic disease.
Two studies provide evidence of atypicals’ efficacy in PDDs:
- In a 6-week open-label comparison,6 olanzapine significantly reduced hyperactivity and anger or uncooperativeness in 12 children with autistic disorder, but haloperidol did not. Average weight gain was 9 lbs in patients receiving olanzapine vs 3.2 lbs in those receiving haloperidol.
- An 8-week, double-blind study7 compared risperidone (0.5 to 3.5 mg/d; mean: 1.8) with placebo in 101 children and adolescents with autistic disorder. Response rates were 69% in the risperidone group and 12% in the control group. Risperidone reduced hyperactivity, aggression, agitation, and repetitive behavior. Adverse drug effects included weight gain (2.7 kg vs. 0.8 kg with placebo), increased appetite, and sedation.
Psychostimulant use in PDDs
Evidence is conflicting on psychostimulant use in patients with PDDs (Table). Early reviews suggested that stimulants were ineffective in PDDs and associated with adverse effects.8,9 Some preliminary studies supported that view, but recent reports have been mixed.
Dextroamphetamine. Campbell et al10 published a placebo-controlled study comparing triiodothyronine and dextroamphetamine (mean dosage, 4.8 mg/d; range 1.25 to 10 mg/d) in 16 children ages 3 to 6 (mean, 4.3 years) with diagnoses of autism, schizophrenia, and organic brain syndrome. All diagnostic groups worsened clinically with dextroamphetamine, and adverse effects—hyperactivity, worsened stereotypy, irritability, and decreased appetite—were common.
A subsequent case report11 found dex-troamphetamine effective when 2 patients ages 9 and 12 with PDD were treated with 10 and 5 mg/d, respectively. Hyperactivity, inattention, and impulsivity improved in both patients, and core PDD features did not worsen.
Levoamphetamine. In an 8-week, double-blind, crossover comparison with levodopa,12 levoamphetamine, 3.5 to 42 mg/d (mean, 13.4), worsened symptoms in 12 children ages 3 to 12 who had schizophrenia with autistic features. stereotypy emerged or increased in 9 of the 11 patients (82%) available for follow-up, and levoamphetamine was poorly tolerated.
Methylphenidate. In an early report, methylphenidate decreased hyperactivity and impulsivity in 9 of 15 children (60%) ages 2 to 13 with infantile autism.13 Dosages of 5 to 10 mg/d or 0.3 to 1 mg/kg/d were given for 2 to 60 weeks (mean, 26). Adverse effects included irritability, insomnia, and anorexia.
Table
Selected reports of stimulant use in pervasive developmental disorders
| Medication | Type of report | Dosage (mg/d); duration | Outcome | Adverse effects |
|---|---|---|---|---|
| Dextroamphetamine | Placebo-controlled10 (N=16) Case report11 (N=2) | Mean 4.8; N/A Mean 7.5; N/A | Clinical worsening Improved hyperactivity,inattention,impulsivity | Hyperactivity, irritability, decreased appetite, worsened stereotypy N/A |
| Levoamphetamine | Double-blind12 (N=12) | Mean 13.4 | Clinical worsening | Stereotypy emerged or worsened |
| Methylphenidate | Retrospective13 (N=15) Open-label14 (N=9) Case report15 (N=1) Double-blind, placebo-controlled, crossover16 (N=10) Double-blind, placebo-controlled, crossover17 (N=13) | 5 to 10; 26 weeks 10 to 50; 2 weeks 20; 4 weeks 20 mg/d for 2 weeks, 40 mg/d for 2 weeks 0.3 mg/kg and 0.6 mg/kg | Improved hyperactivity, impulsivity Improved hyperactivity Improved hyperactivity, concentration Modest benefit over placebo Improved hyperactivity, inattention | Irritability, insomnia, anorexia Initial mild insomnia Dysphoria, angry outbursts Statistically similar to placebo Social withdrawal, irritability |
| Methylphenidate, levoamphetamine, dextroamphetamine, or pemoline | Retrospective18 (N=195) | Various dosages, durations | Patients with, Asperger’s disorder were significantly more likely to respond | Agitation, dysphoria, irritability |
| N/A: not available | ||||
A subsequent open-label study and a case report also indicated that methylphenidate improved hyperactivity in patients with autistic disorder:
- In the 2-week, open-label study,14 9 patients ages 4 to 16 received methylphenidate, 10 to 50 mg/d. Two patients also received haloperidol, 4 and 5 mg/d. Hyperactivity improved significantly, as measured by the Conners Teacher Questionnaire.
- In the case report,15 one child, age 6, was. treated with methylphenidate, 10 mg bid, for 31 days. The drug significantly alleviated hyperactivity and improved concentration. Adverse effects included dysphoria and outbursts of anger.
Atomoxetine—a nonstimulant, selective norepinephrine reuptake inhibitor—has been approved to treat hyperactivity and inattention in ADHD, but no evidence has been published on its use in PDDs. A study of desipramine19 —also a norepinephrine reuptake inhibitor—may offer some insight into the possible efficacy and tolerability of atomoxetine in PDDs.
Desipramine (mean, 127 mg/d) was compared with the serotonin reuptake inhibitor clomipramine (mean, 153 mg/d) in a 10-week, double-blind, crossover study of 24 autistic patients ages 6 to 23. The agents were equally effective and superior to placebo in decreasing hyperactivity, although desipramine was associated with increased aggression and irritability.
Despite these results with desipramine, research is needed to understand atomoxetine’s potential role in treating hyperactivity and inattention in youths with PDDs.
Controlled trials. These early reports were followed by two double-blind, placebo-controlled, crossover studies of methylphenidate in children with autistic disorder.
- In the first trial,16 methylphenidate, 10 or 20 mg/d, improved irritability and hyperactivity in 10 children ages 7 to 11 but was only modestly more beneficial than placebo. Side-effect incidence—including decreased appetite, irritability, and insomnia—was similar during active and placebo treatments. Two patients required adjunctive haloperidol for prevailing behavioral problems.
- In the second trial,17 8 of 13 children (62%) ages 5 to 11 responded to methylphenidate, 0.3 and 0.6 mg/kg per dose. Hyperactivity and inattention improved significantly, as measured by a minimum 50% decrease in Conners Hyperactivity Index score. Ratings of stereotypy and inappropriate speech also decreased, but no changes were seen in the Child Autism Rating Scale. Adverse effects, which were more common with the 0.6 mg/kg dose, included social withdrawal and irritability.
Retrospective trial. Our group recently completed a retrospective study of 195 youth (mean age, 7.3 years; range, 2 to 19 years) with PDDs treated with a stimulant medication.18 As a whole, stimulants appeared ineffective.
Analysis of response by PDD subtype found that individuals with Asperger’s disorder—in contrast to those with autistic disorder or PDD not otherwise specified—were significantly more likely to respond to a stimulant medication. Gender, intelligence quotient (IQ), type of stimulant, and dosage did not significantly affect response. Adverse effects—including agitation, dysphoria, and irritability—occurred in 57.5% of the trials.
Atomoxetine. This nonstimulant medication has been approved for treating ADHD. However, research is needed to understand its use in patients with PDDs (Box)19
Summary. These mixed findings—combined with anecdotal reports from physicians describing the onset or exacerbation of hyperactivity, irritability, and aggression—indicate that much more evidence is needed regarding psychostimulant use in patients with PDDs.
To help meet this need, the National Institutes of Mental Health’s Research Units on Pediatric Psychopharmacology (RUPP) autism network recently completed a large, double-blind, placebo-controlled study to investigate methylphenidate’s efficacy and tolerability in PDDs. It is anticipated that the results will help us discern whether factors such as PDD subtype, patient age, dosage, or degree of mental retardation are associated with response.
Related resources
- Autism Society of America. www.autism-society.org
- McDougle CJ. Current and emerging therapeutics of autistic disorder and related pervasive developmental disorders. In: Davis KL, Charney D, Coyle JT, Nemeroff C (eds). Neuropsychopharmacology: The fifth generation of progress. Philadelphia: Lippincott Williams & Wilkins, 2002.
- McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, Charney DS, Leckman JF (eds). Pediatric psychopharmacology: Principles and practice.New York: Oxford University Press, 2002.
Drug brand names
- Atomoxetine • Strattera
- Clomipramine • Anafranil
- Clonidine • Catapres
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Guanfacine • Tenex
- Haloperidol • Haldol
- Levoamphetamine • Adderall
- Levodopa • Dopar, Laradopa
- Methylphenidate • Ritalin
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Risperidone • Risperdal
Disclosure
Dr. Stigler reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Posey receives research support from Janssen Pharmaceutica and Eli Lilly and Co. and is a speaker for Janssen Pharmaceutica.
Dr. McDougle receives research support from Janssen Pharmaceutica, Pfizer Inc., Eli Lilly and Co., and Bristol-Myers Squibb Co. He is a consultant to or speaker for Janssen Pharmaceutica, Pfizer Inc., Eli Lilly and Co., RepliGen Corp., and Bristol-Myers Squibb Co.
Acknowledgments
This work was supported in part by a Daniel X. Freedman Psychiatric Research Fellowship Award (Dr. Posey), a National Alliance for Research in Schizophrenia and Depression (NARSAD) Young Investigator Award (Dr. Posey), a Research Units on Pediatric Psychopharmacology Grant (U10MH66766-02) from the National Institute of Mental Health (NIMH) to Indiana University (Dr. McDougle, Dr. Stigler, and Dr. Posey), a Research Career Development Award (K23-MH068627-01) from the NIMH (Dr. Posey), a National Institutes of Health Clinical Research Center grant to Indiana University (M01-RR00750), and a Department of Housing and Urban Development (HUD) grant (B-01-SP-IN-0200) (Dr. McDougle).
1. Greenhill LL, Pliszka S, Dulcan MK, et al. Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry 2002;41(2 suppl):26S-49S.
2. Posey DJ, McDougle CJ. The pharmacotherapy of target symptoms associated with autistic disorder and other pervasive developmental disorders. Harv Rev Psychiatry 2000;8(2):45-63.
3. Jaselskis CA, Cook EH Jr, Fletcher KE, Leventhal BL. Clonidine treatment of hyperactive and impulsive children with autistic disorder. J Clin Psychopharmacol 1992;12(5):322-7.
4. Fankhauser MP, Karumanchi VC, German ML, et al. A double-blind, placebo-controlled study of the efficacy of transdermal clonidine in autism. J Clin Psychiatry 1992;53(3):77-82.
5. Posey DJ, Decker J, Sasher TM, et al. A retrospective analysis of guanfacine in the treatment of autism. J Child Adolesc.
6. Malone RP, Cater J, Sheikh RM, et al. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40(8):887-94.
7. McCracken JT, McGough J, Shah B, et al. Risperidone in children with autism and serious behavioral problems. N Engl J Med 2002;347(5):314-21.
8. Campbell M. Pharmacotherapy in early infantile autism. Biol Psychiatry 1975;10(4):399-423.
9. Aman MG. Stimulant drug effects in developmental disorders and hyperactivity—toward a resolution of disparate findings. J Autism Dev Disord 1982;12(4):385-98.
10. Campbell M, Fish B, David R, et al. Response to triiodothyronine and dextroamphetamine: a study of preschool schizophrenic children. J Autism Child Schizophr 1972;2(4):343-58.
11. Geller B, Guttmacher LB, Bleeg M. Coexistence of childhood onset pervasive developmental disorder and attention deficit disorder with hyperactivity. Am J Psychiatry 1981;138(3):388-9.
12. Campbell M, Small AM, Collins PJ, et al. Levodopa and levoamphetamine: a crossover study in young schizophrenic children. Curr Ther Res Clin Exp 1976;19(1):70-86.
13. Hoshino Y, Kumashiro H, Kaneko M, Takahashi Y. The effects of methylphenidate on early infantile autism and its relation to serum serotonin levels. Folia Psychiatr Neurol Jpn 1977;31(4):605-14.
14. Birmaher B, Quintana H, Greenhill LL. Methylphenidate treatment of hyperactive autistic children. J Am Acad Child Adolesc Psychiatry 1988;27(2):248-51.
15. Strayhorn JM Jr, Rapp N, Donina W, Strain PS. Randomized trial of methylphenidate for an autistic child. J Am Acad Child Adolesc Psychiatry 1988;27(2):244-7.
16. Quintana H, Birmaher B, Stedge D, et al. Use of methylphenidate in the treatment of children with autistic disorder. J Autism Dev Disord 1995;25(3):283-94.
17. Handen BL, Johnson CR, Lubetsky M. Efficacy of methylphenidate among children with autism and symptoms of attention-deficit hyperactivity disorder. J Autism Dev Disord 2000;30(3):245-55.
18. Stigler KA, Desmond LA, Posey DJ, et al. A naturalistic retrospective analysis of psychostimulants in pervasive developmental disorders. J Child Adolesc Psychopharmacol 2004;14(1):49-56.
19. Gordon CT, State RC, Nelson JE, et al. A double-blind comparison of clomipramine, desipramine, and placebo in the treatment of autistic disorder. Arch Gen Psychiatry 1993;50(6):441-7.
Psychostimulants benefit many patients with attention-deficit/hyperactivity disorder (ADHD)1 and thus might seem a logical choice to manage hyperactivity and inattention in youths with a pervasive developmental disorder (PDD). Some PDD patients do respond to psychostimulant therapy, but others worsen—and side effects are common.
Youths with PDDs often exhibit maladaptive behaviors—aggression, self-injury, irritability, hyperactivity, inattention—with repetitive activity patterns and fundamentally impaired social interaction and communication.2 To help you treat youths with PDD, we draw on the evidence, clinical experience, and our research to suggest psychostimulants’ role in a multimodal approach.
Targeting hyperactivity and inattentions
Step 1. Our approach begins with behavioral therapy (Figure), which includes identifying situations that trigger maladaptive behavior and environments that yield optimum behavior. The therapist assesses the child’s baseline attention and works with him or her to gradually increase it, using reinforcement and visual token boards.
Algorithm Suggested approach to hyperactivity and/or inattention in patients with PDDs

To set limits and expectations, the therapist introduces structure such as designating work and break areas and using visual schedules and timers to indicate activity duration. Minimizing distractions and understanding the child’s sensory needs may increase motivation and attention. Initially, the therapist allows numerous breaks and then may slowly decrease them as the child progresses. Tailoring work and play materials to the child’s interests can also help increase attention.
Step 2. Many patients will not respond to behavior therapy alone and will require added drug therapy. Based on evidence, we suggest starting with an alpha-2 adrenergic agonist. Guanfacine may be considered the drug of choice because of clonidine’s higher risk of adverse effects, such as hypotension and sedation. Obtain a baseline ECG with either agent, as clonidine has been associated with rare cardiovascular events.
Clonidine. Two small studies showed that clonidine may be of some benefit to patients with PDDs:
- Results were mixed in a 6-week, double-blind, placebo-controlled, crossover study of clonidine (4 to 10 μg/kg/d) in 8 autistic children ages 5 to 13.3 Teacher and parent rating instruments reflected significantly improved hyperactivity, irritability, and oppositional behavior. Clinician ratings, however, showed no significant difference between clonidine and placebo. Adverse effects with clonidine included hypotension, sedation, and decreased activity.
- In a 4-week, double-blind, placebo-con-trolled, crossover study of transdermal clonidine (0.16 to 0.48 mg/kg/d; mean: 3.6 μg/kg/d), clinician ratings showed significantly decreased hyperactivity, impulsivity, and anxiety in 9 autistic males ages 5 to 33. Sedation and fatigue were common adverse effects.
Guanfacine. In a recent retrospective review,5 we examined outcomes of 80 PDD patients ages 3 to 18 who received guanfacine (0.25 to 9 mg/d; mean: 2.6). Hyperactivity, inattention, and tics decreased in 19 patients (24%) treated for a mean 10 months.
Step 3. If clonidine or guanfacine fails to reduce hyperactivity and inattention, discontinue it and consider a psychostimulant trial.
Because psychostimulants’ efficacy in PDDs remains inconclusive, we suggest beginning with a low dosage and carefully monitoring the patient for worsening target symptoms and activation, such as emerging aggression or irritability.
Step 4. If hyperactivity and inattention remain prominent and treatment-refractory, we suggest that you discontinue the stimulant and consider an atypical antipsychotic trial. With the atypicals, monitor patients closely for adverse effects, including weight gain, extrapyramidal symptoms, and tardive dyskinesia. Fasting serum glucose and lipid profiles and liver function tests are recommended at least every 6 months and more often in individuals at risk for diabetes or hepatic disease.
Two studies provide evidence of atypicals’ efficacy in PDDs:
- In a 6-week open-label comparison,6 olanzapine significantly reduced hyperactivity and anger or uncooperativeness in 12 children with autistic disorder, but haloperidol did not. Average weight gain was 9 lbs in patients receiving olanzapine vs 3.2 lbs in those receiving haloperidol.
- An 8-week, double-blind study7 compared risperidone (0.5 to 3.5 mg/d; mean: 1.8) with placebo in 101 children and adolescents with autistic disorder. Response rates were 69% in the risperidone group and 12% in the control group. Risperidone reduced hyperactivity, aggression, agitation, and repetitive behavior. Adverse drug effects included weight gain (2.7 kg vs. 0.8 kg with placebo), increased appetite, and sedation.
Psychostimulant use in PDDs
Evidence is conflicting on psychostimulant use in patients with PDDs (Table). Early reviews suggested that stimulants were ineffective in PDDs and associated with adverse effects.8,9 Some preliminary studies supported that view, but recent reports have been mixed.
Dextroamphetamine. Campbell et al10 published a placebo-controlled study comparing triiodothyronine and dextroamphetamine (mean dosage, 4.8 mg/d; range 1.25 to 10 mg/d) in 16 children ages 3 to 6 (mean, 4.3 years) with diagnoses of autism, schizophrenia, and organic brain syndrome. All diagnostic groups worsened clinically with dextroamphetamine, and adverse effects—hyperactivity, worsened stereotypy, irritability, and decreased appetite—were common.
A subsequent case report11 found dex-troamphetamine effective when 2 patients ages 9 and 12 with PDD were treated with 10 and 5 mg/d, respectively. Hyperactivity, inattention, and impulsivity improved in both patients, and core PDD features did not worsen.
Levoamphetamine. In an 8-week, double-blind, crossover comparison with levodopa,12 levoamphetamine, 3.5 to 42 mg/d (mean, 13.4), worsened symptoms in 12 children ages 3 to 12 who had schizophrenia with autistic features. stereotypy emerged or increased in 9 of the 11 patients (82%) available for follow-up, and levoamphetamine was poorly tolerated.
Methylphenidate. In an early report, methylphenidate decreased hyperactivity and impulsivity in 9 of 15 children (60%) ages 2 to 13 with infantile autism.13 Dosages of 5 to 10 mg/d or 0.3 to 1 mg/kg/d were given for 2 to 60 weeks (mean, 26). Adverse effects included irritability, insomnia, and anorexia.
Table
Selected reports of stimulant use in pervasive developmental disorders
| Medication | Type of report | Dosage (mg/d); duration | Outcome | Adverse effects |
|---|---|---|---|---|
| Dextroamphetamine | Placebo-controlled10 (N=16) Case report11 (N=2) | Mean 4.8; N/A Mean 7.5; N/A | Clinical worsening Improved hyperactivity,inattention,impulsivity | Hyperactivity, irritability, decreased appetite, worsened stereotypy N/A |
| Levoamphetamine | Double-blind12 (N=12) | Mean 13.4 | Clinical worsening | Stereotypy emerged or worsened |
| Methylphenidate | Retrospective13 (N=15) Open-label14 (N=9) Case report15 (N=1) Double-blind, placebo-controlled, crossover16 (N=10) Double-blind, placebo-controlled, crossover17 (N=13) | 5 to 10; 26 weeks 10 to 50; 2 weeks 20; 4 weeks 20 mg/d for 2 weeks, 40 mg/d for 2 weeks 0.3 mg/kg and 0.6 mg/kg | Improved hyperactivity, impulsivity Improved hyperactivity Improved hyperactivity, concentration Modest benefit over placebo Improved hyperactivity, inattention | Irritability, insomnia, anorexia Initial mild insomnia Dysphoria, angry outbursts Statistically similar to placebo Social withdrawal, irritability |
| Methylphenidate, levoamphetamine, dextroamphetamine, or pemoline | Retrospective18 (N=195) | Various dosages, durations | Patients with, Asperger’s disorder were significantly more likely to respond | Agitation, dysphoria, irritability |
| N/A: not available | ||||
A subsequent open-label study and a case report also indicated that methylphenidate improved hyperactivity in patients with autistic disorder:
- In the 2-week, open-label study,14 9 patients ages 4 to 16 received methylphenidate, 10 to 50 mg/d. Two patients also received haloperidol, 4 and 5 mg/d. Hyperactivity improved significantly, as measured by the Conners Teacher Questionnaire.
- In the case report,15 one child, age 6, was. treated with methylphenidate, 10 mg bid, for 31 days. The drug significantly alleviated hyperactivity and improved concentration. Adverse effects included dysphoria and outbursts of anger.
Atomoxetine—a nonstimulant, selective norepinephrine reuptake inhibitor—has been approved to treat hyperactivity and inattention in ADHD, but no evidence has been published on its use in PDDs. A study of desipramine19 —also a norepinephrine reuptake inhibitor—may offer some insight into the possible efficacy and tolerability of atomoxetine in PDDs.
Desipramine (mean, 127 mg/d) was compared with the serotonin reuptake inhibitor clomipramine (mean, 153 mg/d) in a 10-week, double-blind, crossover study of 24 autistic patients ages 6 to 23. The agents were equally effective and superior to placebo in decreasing hyperactivity, although desipramine was associated with increased aggression and irritability.
Despite these results with desipramine, research is needed to understand atomoxetine’s potential role in treating hyperactivity and inattention in youths with PDDs.
Controlled trials. These early reports were followed by two double-blind, placebo-controlled, crossover studies of methylphenidate in children with autistic disorder.
- In the first trial,16 methylphenidate, 10 or 20 mg/d, improved irritability and hyperactivity in 10 children ages 7 to 11 but was only modestly more beneficial than placebo. Side-effect incidence—including decreased appetite, irritability, and insomnia—was similar during active and placebo treatments. Two patients required adjunctive haloperidol for prevailing behavioral problems.
- In the second trial,17 8 of 13 children (62%) ages 5 to 11 responded to methylphenidate, 0.3 and 0.6 mg/kg per dose. Hyperactivity and inattention improved significantly, as measured by a minimum 50% decrease in Conners Hyperactivity Index score. Ratings of stereotypy and inappropriate speech also decreased, but no changes were seen in the Child Autism Rating Scale. Adverse effects, which were more common with the 0.6 mg/kg dose, included social withdrawal and irritability.
Retrospective trial. Our group recently completed a retrospective study of 195 youth (mean age, 7.3 years; range, 2 to 19 years) with PDDs treated with a stimulant medication.18 As a whole, stimulants appeared ineffective.
Analysis of response by PDD subtype found that individuals with Asperger’s disorder—in contrast to those with autistic disorder or PDD not otherwise specified—were significantly more likely to respond to a stimulant medication. Gender, intelligence quotient (IQ), type of stimulant, and dosage did not significantly affect response. Adverse effects—including agitation, dysphoria, and irritability—occurred in 57.5% of the trials.
Atomoxetine. This nonstimulant medication has been approved for treating ADHD. However, research is needed to understand its use in patients with PDDs (Box)19
Summary. These mixed findings—combined with anecdotal reports from physicians describing the onset or exacerbation of hyperactivity, irritability, and aggression—indicate that much more evidence is needed regarding psychostimulant use in patients with PDDs.
To help meet this need, the National Institutes of Mental Health’s Research Units on Pediatric Psychopharmacology (RUPP) autism network recently completed a large, double-blind, placebo-controlled study to investigate methylphenidate’s efficacy and tolerability in PDDs. It is anticipated that the results will help us discern whether factors such as PDD subtype, patient age, dosage, or degree of mental retardation are associated with response.
Related resources
- Autism Society of America. www.autism-society.org
- McDougle CJ. Current and emerging therapeutics of autistic disorder and related pervasive developmental disorders. In: Davis KL, Charney D, Coyle JT, Nemeroff C (eds). Neuropsychopharmacology: The fifth generation of progress. Philadelphia: Lippincott Williams & Wilkins, 2002.
- McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, Charney DS, Leckman JF (eds). Pediatric psychopharmacology: Principles and practice.New York: Oxford University Press, 2002.
Drug brand names
- Atomoxetine • Strattera
- Clomipramine • Anafranil
- Clonidine • Catapres
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Guanfacine • Tenex
- Haloperidol • Haldol
- Levoamphetamine • Adderall
- Levodopa • Dopar, Laradopa
- Methylphenidate • Ritalin
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Risperidone • Risperdal
Disclosure
Dr. Stigler reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Posey receives research support from Janssen Pharmaceutica and Eli Lilly and Co. and is a speaker for Janssen Pharmaceutica.
Dr. McDougle receives research support from Janssen Pharmaceutica, Pfizer Inc., Eli Lilly and Co., and Bristol-Myers Squibb Co. He is a consultant to or speaker for Janssen Pharmaceutica, Pfizer Inc., Eli Lilly and Co., RepliGen Corp., and Bristol-Myers Squibb Co.
Acknowledgments
This work was supported in part by a Daniel X. Freedman Psychiatric Research Fellowship Award (Dr. Posey), a National Alliance for Research in Schizophrenia and Depression (NARSAD) Young Investigator Award (Dr. Posey), a Research Units on Pediatric Psychopharmacology Grant (U10MH66766-02) from the National Institute of Mental Health (NIMH) to Indiana University (Dr. McDougle, Dr. Stigler, and Dr. Posey), a Research Career Development Award (K23-MH068627-01) from the NIMH (Dr. Posey), a National Institutes of Health Clinical Research Center grant to Indiana University (M01-RR00750), and a Department of Housing and Urban Development (HUD) grant (B-01-SP-IN-0200) (Dr. McDougle).
Psychostimulants benefit many patients with attention-deficit/hyperactivity disorder (ADHD)1 and thus might seem a logical choice to manage hyperactivity and inattention in youths with a pervasive developmental disorder (PDD). Some PDD patients do respond to psychostimulant therapy, but others worsen—and side effects are common.
Youths with PDDs often exhibit maladaptive behaviors—aggression, self-injury, irritability, hyperactivity, inattention—with repetitive activity patterns and fundamentally impaired social interaction and communication.2 To help you treat youths with PDD, we draw on the evidence, clinical experience, and our research to suggest psychostimulants’ role in a multimodal approach.
Targeting hyperactivity and inattentions
Step 1. Our approach begins with behavioral therapy (Figure), which includes identifying situations that trigger maladaptive behavior and environments that yield optimum behavior. The therapist assesses the child’s baseline attention and works with him or her to gradually increase it, using reinforcement and visual token boards.
Algorithm Suggested approach to hyperactivity and/or inattention in patients with PDDs

To set limits and expectations, the therapist introduces structure such as designating work and break areas and using visual schedules and timers to indicate activity duration. Minimizing distractions and understanding the child’s sensory needs may increase motivation and attention. Initially, the therapist allows numerous breaks and then may slowly decrease them as the child progresses. Tailoring work and play materials to the child’s interests can also help increase attention.
Step 2. Many patients will not respond to behavior therapy alone and will require added drug therapy. Based on evidence, we suggest starting with an alpha-2 adrenergic agonist. Guanfacine may be considered the drug of choice because of clonidine’s higher risk of adverse effects, such as hypotension and sedation. Obtain a baseline ECG with either agent, as clonidine has been associated with rare cardiovascular events.
Clonidine. Two small studies showed that clonidine may be of some benefit to patients with PDDs:
- Results were mixed in a 6-week, double-blind, placebo-controlled, crossover study of clonidine (4 to 10 μg/kg/d) in 8 autistic children ages 5 to 13.3 Teacher and parent rating instruments reflected significantly improved hyperactivity, irritability, and oppositional behavior. Clinician ratings, however, showed no significant difference between clonidine and placebo. Adverse effects with clonidine included hypotension, sedation, and decreased activity.
- In a 4-week, double-blind, placebo-con-trolled, crossover study of transdermal clonidine (0.16 to 0.48 mg/kg/d; mean: 3.6 μg/kg/d), clinician ratings showed significantly decreased hyperactivity, impulsivity, and anxiety in 9 autistic males ages 5 to 33. Sedation and fatigue were common adverse effects.
Guanfacine. In a recent retrospective review,5 we examined outcomes of 80 PDD patients ages 3 to 18 who received guanfacine (0.25 to 9 mg/d; mean: 2.6). Hyperactivity, inattention, and tics decreased in 19 patients (24%) treated for a mean 10 months.
Step 3. If clonidine or guanfacine fails to reduce hyperactivity and inattention, discontinue it and consider a psychostimulant trial.
Because psychostimulants’ efficacy in PDDs remains inconclusive, we suggest beginning with a low dosage and carefully monitoring the patient for worsening target symptoms and activation, such as emerging aggression or irritability.
Step 4. If hyperactivity and inattention remain prominent and treatment-refractory, we suggest that you discontinue the stimulant and consider an atypical antipsychotic trial. With the atypicals, monitor patients closely for adverse effects, including weight gain, extrapyramidal symptoms, and tardive dyskinesia. Fasting serum glucose and lipid profiles and liver function tests are recommended at least every 6 months and more often in individuals at risk for diabetes or hepatic disease.
Two studies provide evidence of atypicals’ efficacy in PDDs:
- In a 6-week open-label comparison,6 olanzapine significantly reduced hyperactivity and anger or uncooperativeness in 12 children with autistic disorder, but haloperidol did not. Average weight gain was 9 lbs in patients receiving olanzapine vs 3.2 lbs in those receiving haloperidol.
- An 8-week, double-blind study7 compared risperidone (0.5 to 3.5 mg/d; mean: 1.8) with placebo in 101 children and adolescents with autistic disorder. Response rates were 69% in the risperidone group and 12% in the control group. Risperidone reduced hyperactivity, aggression, agitation, and repetitive behavior. Adverse drug effects included weight gain (2.7 kg vs. 0.8 kg with placebo), increased appetite, and sedation.
Psychostimulant use in PDDs
Evidence is conflicting on psychostimulant use in patients with PDDs (Table). Early reviews suggested that stimulants were ineffective in PDDs and associated with adverse effects.8,9 Some preliminary studies supported that view, but recent reports have been mixed.
Dextroamphetamine. Campbell et al10 published a placebo-controlled study comparing triiodothyronine and dextroamphetamine (mean dosage, 4.8 mg/d; range 1.25 to 10 mg/d) in 16 children ages 3 to 6 (mean, 4.3 years) with diagnoses of autism, schizophrenia, and organic brain syndrome. All diagnostic groups worsened clinically with dextroamphetamine, and adverse effects—hyperactivity, worsened stereotypy, irritability, and decreased appetite—were common.
A subsequent case report11 found dex-troamphetamine effective when 2 patients ages 9 and 12 with PDD were treated with 10 and 5 mg/d, respectively. Hyperactivity, inattention, and impulsivity improved in both patients, and core PDD features did not worsen.
Levoamphetamine. In an 8-week, double-blind, crossover comparison with levodopa,12 levoamphetamine, 3.5 to 42 mg/d (mean, 13.4), worsened symptoms in 12 children ages 3 to 12 who had schizophrenia with autistic features. stereotypy emerged or increased in 9 of the 11 patients (82%) available for follow-up, and levoamphetamine was poorly tolerated.
Methylphenidate. In an early report, methylphenidate decreased hyperactivity and impulsivity in 9 of 15 children (60%) ages 2 to 13 with infantile autism.13 Dosages of 5 to 10 mg/d or 0.3 to 1 mg/kg/d were given for 2 to 60 weeks (mean, 26). Adverse effects included irritability, insomnia, and anorexia.
Table
Selected reports of stimulant use in pervasive developmental disorders
| Medication | Type of report | Dosage (mg/d); duration | Outcome | Adverse effects |
|---|---|---|---|---|
| Dextroamphetamine | Placebo-controlled10 (N=16) Case report11 (N=2) | Mean 4.8; N/A Mean 7.5; N/A | Clinical worsening Improved hyperactivity,inattention,impulsivity | Hyperactivity, irritability, decreased appetite, worsened stereotypy N/A |
| Levoamphetamine | Double-blind12 (N=12) | Mean 13.4 | Clinical worsening | Stereotypy emerged or worsened |
| Methylphenidate | Retrospective13 (N=15) Open-label14 (N=9) Case report15 (N=1) Double-blind, placebo-controlled, crossover16 (N=10) Double-blind, placebo-controlled, crossover17 (N=13) | 5 to 10; 26 weeks 10 to 50; 2 weeks 20; 4 weeks 20 mg/d for 2 weeks, 40 mg/d for 2 weeks 0.3 mg/kg and 0.6 mg/kg | Improved hyperactivity, impulsivity Improved hyperactivity Improved hyperactivity, concentration Modest benefit over placebo Improved hyperactivity, inattention | Irritability, insomnia, anorexia Initial mild insomnia Dysphoria, angry outbursts Statistically similar to placebo Social withdrawal, irritability |
| Methylphenidate, levoamphetamine, dextroamphetamine, or pemoline | Retrospective18 (N=195) | Various dosages, durations | Patients with, Asperger’s disorder were significantly more likely to respond | Agitation, dysphoria, irritability |
| N/A: not available | ||||
A subsequent open-label study and a case report also indicated that methylphenidate improved hyperactivity in patients with autistic disorder:
- In the 2-week, open-label study,14 9 patients ages 4 to 16 received methylphenidate, 10 to 50 mg/d. Two patients also received haloperidol, 4 and 5 mg/d. Hyperactivity improved significantly, as measured by the Conners Teacher Questionnaire.
- In the case report,15 one child, age 6, was. treated with methylphenidate, 10 mg bid, for 31 days. The drug significantly alleviated hyperactivity and improved concentration. Adverse effects included dysphoria and outbursts of anger.
Atomoxetine—a nonstimulant, selective norepinephrine reuptake inhibitor—has been approved to treat hyperactivity and inattention in ADHD, but no evidence has been published on its use in PDDs. A study of desipramine19 —also a norepinephrine reuptake inhibitor—may offer some insight into the possible efficacy and tolerability of atomoxetine in PDDs.
Desipramine (mean, 127 mg/d) was compared with the serotonin reuptake inhibitor clomipramine (mean, 153 mg/d) in a 10-week, double-blind, crossover study of 24 autistic patients ages 6 to 23. The agents were equally effective and superior to placebo in decreasing hyperactivity, although desipramine was associated with increased aggression and irritability.
Despite these results with desipramine, research is needed to understand atomoxetine’s potential role in treating hyperactivity and inattention in youths with PDDs.
Controlled trials. These early reports were followed by two double-blind, placebo-controlled, crossover studies of methylphenidate in children with autistic disorder.
- In the first trial,16 methylphenidate, 10 or 20 mg/d, improved irritability and hyperactivity in 10 children ages 7 to 11 but was only modestly more beneficial than placebo. Side-effect incidence—including decreased appetite, irritability, and insomnia—was similar during active and placebo treatments. Two patients required adjunctive haloperidol for prevailing behavioral problems.
- In the second trial,17 8 of 13 children (62%) ages 5 to 11 responded to methylphenidate, 0.3 and 0.6 mg/kg per dose. Hyperactivity and inattention improved significantly, as measured by a minimum 50% decrease in Conners Hyperactivity Index score. Ratings of stereotypy and inappropriate speech also decreased, but no changes were seen in the Child Autism Rating Scale. Adverse effects, which were more common with the 0.6 mg/kg dose, included social withdrawal and irritability.
Retrospective trial. Our group recently completed a retrospective study of 195 youth (mean age, 7.3 years; range, 2 to 19 years) with PDDs treated with a stimulant medication.18 As a whole, stimulants appeared ineffective.
Analysis of response by PDD subtype found that individuals with Asperger’s disorder—in contrast to those with autistic disorder or PDD not otherwise specified—were significantly more likely to respond to a stimulant medication. Gender, intelligence quotient (IQ), type of stimulant, and dosage did not significantly affect response. Adverse effects—including agitation, dysphoria, and irritability—occurred in 57.5% of the trials.
Atomoxetine. This nonstimulant medication has been approved for treating ADHD. However, research is needed to understand its use in patients with PDDs (Box)19
Summary. These mixed findings—combined with anecdotal reports from physicians describing the onset or exacerbation of hyperactivity, irritability, and aggression—indicate that much more evidence is needed regarding psychostimulant use in patients with PDDs.
To help meet this need, the National Institutes of Mental Health’s Research Units on Pediatric Psychopharmacology (RUPP) autism network recently completed a large, double-blind, placebo-controlled study to investigate methylphenidate’s efficacy and tolerability in PDDs. It is anticipated that the results will help us discern whether factors such as PDD subtype, patient age, dosage, or degree of mental retardation are associated with response.
Related resources
- Autism Society of America. www.autism-society.org
- McDougle CJ. Current and emerging therapeutics of autistic disorder and related pervasive developmental disorders. In: Davis KL, Charney D, Coyle JT, Nemeroff C (eds). Neuropsychopharmacology: The fifth generation of progress. Philadelphia: Lippincott Williams & Wilkins, 2002.
- McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, Charney DS, Leckman JF (eds). Pediatric psychopharmacology: Principles and practice.New York: Oxford University Press, 2002.
Drug brand names
- Atomoxetine • Strattera
- Clomipramine • Anafranil
- Clonidine • Catapres
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Guanfacine • Tenex
- Haloperidol • Haldol
- Levoamphetamine • Adderall
- Levodopa • Dopar, Laradopa
- Methylphenidate • Ritalin
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Risperidone • Risperdal
Disclosure
Dr. Stigler reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Posey receives research support from Janssen Pharmaceutica and Eli Lilly and Co. and is a speaker for Janssen Pharmaceutica.
Dr. McDougle receives research support from Janssen Pharmaceutica, Pfizer Inc., Eli Lilly and Co., and Bristol-Myers Squibb Co. He is a consultant to or speaker for Janssen Pharmaceutica, Pfizer Inc., Eli Lilly and Co., RepliGen Corp., and Bristol-Myers Squibb Co.
Acknowledgments
This work was supported in part by a Daniel X. Freedman Psychiatric Research Fellowship Award (Dr. Posey), a National Alliance for Research in Schizophrenia and Depression (NARSAD) Young Investigator Award (Dr. Posey), a Research Units on Pediatric Psychopharmacology Grant (U10MH66766-02) from the National Institute of Mental Health (NIMH) to Indiana University (Dr. McDougle, Dr. Stigler, and Dr. Posey), a Research Career Development Award (K23-MH068627-01) from the NIMH (Dr. Posey), a National Institutes of Health Clinical Research Center grant to Indiana University (M01-RR00750), and a Department of Housing and Urban Development (HUD) grant (B-01-SP-IN-0200) (Dr. McDougle).
1. Greenhill LL, Pliszka S, Dulcan MK, et al. Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry 2002;41(2 suppl):26S-49S.
2. Posey DJ, McDougle CJ. The pharmacotherapy of target symptoms associated with autistic disorder and other pervasive developmental disorders. Harv Rev Psychiatry 2000;8(2):45-63.
3. Jaselskis CA, Cook EH Jr, Fletcher KE, Leventhal BL. Clonidine treatment of hyperactive and impulsive children with autistic disorder. J Clin Psychopharmacol 1992;12(5):322-7.
4. Fankhauser MP, Karumanchi VC, German ML, et al. A double-blind, placebo-controlled study of the efficacy of transdermal clonidine in autism. J Clin Psychiatry 1992;53(3):77-82.
5. Posey DJ, Decker J, Sasher TM, et al. A retrospective analysis of guanfacine in the treatment of autism. J Child Adolesc.
6. Malone RP, Cater J, Sheikh RM, et al. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40(8):887-94.
7. McCracken JT, McGough J, Shah B, et al. Risperidone in children with autism and serious behavioral problems. N Engl J Med 2002;347(5):314-21.
8. Campbell M. Pharmacotherapy in early infantile autism. Biol Psychiatry 1975;10(4):399-423.
9. Aman MG. Stimulant drug effects in developmental disorders and hyperactivity—toward a resolution of disparate findings. J Autism Dev Disord 1982;12(4):385-98.
10. Campbell M, Fish B, David R, et al. Response to triiodothyronine and dextroamphetamine: a study of preschool schizophrenic children. J Autism Child Schizophr 1972;2(4):343-58.
11. Geller B, Guttmacher LB, Bleeg M. Coexistence of childhood onset pervasive developmental disorder and attention deficit disorder with hyperactivity. Am J Psychiatry 1981;138(3):388-9.
12. Campbell M, Small AM, Collins PJ, et al. Levodopa and levoamphetamine: a crossover study in young schizophrenic children. Curr Ther Res Clin Exp 1976;19(1):70-86.
13. Hoshino Y, Kumashiro H, Kaneko M, Takahashi Y. The effects of methylphenidate on early infantile autism and its relation to serum serotonin levels. Folia Psychiatr Neurol Jpn 1977;31(4):605-14.
14. Birmaher B, Quintana H, Greenhill LL. Methylphenidate treatment of hyperactive autistic children. J Am Acad Child Adolesc Psychiatry 1988;27(2):248-51.
15. Strayhorn JM Jr, Rapp N, Donina W, Strain PS. Randomized trial of methylphenidate for an autistic child. J Am Acad Child Adolesc Psychiatry 1988;27(2):244-7.
16. Quintana H, Birmaher B, Stedge D, et al. Use of methylphenidate in the treatment of children with autistic disorder. J Autism Dev Disord 1995;25(3):283-94.
17. Handen BL, Johnson CR, Lubetsky M. Efficacy of methylphenidate among children with autism and symptoms of attention-deficit hyperactivity disorder. J Autism Dev Disord 2000;30(3):245-55.
18. Stigler KA, Desmond LA, Posey DJ, et al. A naturalistic retrospective analysis of psychostimulants in pervasive developmental disorders. J Child Adolesc Psychopharmacol 2004;14(1):49-56.
19. Gordon CT, State RC, Nelson JE, et al. A double-blind comparison of clomipramine, desipramine, and placebo in the treatment of autistic disorder. Arch Gen Psychiatry 1993;50(6):441-7.
1. Greenhill LL, Pliszka S, Dulcan MK, et al. Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry 2002;41(2 suppl):26S-49S.
2. Posey DJ, McDougle CJ. The pharmacotherapy of target symptoms associated with autistic disorder and other pervasive developmental disorders. Harv Rev Psychiatry 2000;8(2):45-63.
3. Jaselskis CA, Cook EH Jr, Fletcher KE, Leventhal BL. Clonidine treatment of hyperactive and impulsive children with autistic disorder. J Clin Psychopharmacol 1992;12(5):322-7.
4. Fankhauser MP, Karumanchi VC, German ML, et al. A double-blind, placebo-controlled study of the efficacy of transdermal clonidine in autism. J Clin Psychiatry 1992;53(3):77-82.
5. Posey DJ, Decker J, Sasher TM, et al. A retrospective analysis of guanfacine in the treatment of autism. J Child Adolesc.
6. Malone RP, Cater J, Sheikh RM, et al. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40(8):887-94.
7. McCracken JT, McGough J, Shah B, et al. Risperidone in children with autism and serious behavioral problems. N Engl J Med 2002;347(5):314-21.
8. Campbell M. Pharmacotherapy in early infantile autism. Biol Psychiatry 1975;10(4):399-423.
9. Aman MG. Stimulant drug effects in developmental disorders and hyperactivity—toward a resolution of disparate findings. J Autism Dev Disord 1982;12(4):385-98.
10. Campbell M, Fish B, David R, et al. Response to triiodothyronine and dextroamphetamine: a study of preschool schizophrenic children. J Autism Child Schizophr 1972;2(4):343-58.
11. Geller B, Guttmacher LB, Bleeg M. Coexistence of childhood onset pervasive developmental disorder and attention deficit disorder with hyperactivity. Am J Psychiatry 1981;138(3):388-9.
12. Campbell M, Small AM, Collins PJ, et al. Levodopa and levoamphetamine: a crossover study in young schizophrenic children. Curr Ther Res Clin Exp 1976;19(1):70-86.
13. Hoshino Y, Kumashiro H, Kaneko M, Takahashi Y. The effects of methylphenidate on early infantile autism and its relation to serum serotonin levels. Folia Psychiatr Neurol Jpn 1977;31(4):605-14.
14. Birmaher B, Quintana H, Greenhill LL. Methylphenidate treatment of hyperactive autistic children. J Am Acad Child Adolesc Psychiatry 1988;27(2):248-51.
15. Strayhorn JM Jr, Rapp N, Donina W, Strain PS. Randomized trial of methylphenidate for an autistic child. J Am Acad Child Adolesc Psychiatry 1988;27(2):244-7.
16. Quintana H, Birmaher B, Stedge D, et al. Use of methylphenidate in the treatment of children with autistic disorder. J Autism Dev Disord 1995;25(3):283-94.
17. Handen BL, Johnson CR, Lubetsky M. Efficacy of methylphenidate among children with autism and symptoms of attention-deficit hyperactivity disorder. J Autism Dev Disord 2000;30(3):245-55.
18. Stigler KA, Desmond LA, Posey DJ, et al. A naturalistic retrospective analysis of psychostimulants in pervasive developmental disorders. J Child Adolesc Psychopharmacol 2004;14(1):49-56.
19. Gordon CT, State RC, Nelson JE, et al. A double-blind comparison of clomipramine, desipramine, and placebo in the treatment of autistic disorder. Arch Gen Psychiatry 1993;50(6):441-7.
Recovery from schizophrenia: Fact or fiction?
Is it realistic for patients with schizophrenia to believe they can recover? Recent observational studies show that some do,1 even though all DSM editions have defined schizophrenia as a chronic disease with a poor outcome.2
Our understanding of schizophrenia is changing as we gain new insights into:
- mechanism of recovery
- efficacy of combined psychotherapeutic, psychosocial, and drug therapies for sustaining remission and recovery
- the value of long-term aftercare. This article examines evidence on:
- achieving recovery from schizophrenia
- factors associated with remission
- treatments that may help prevent relapse and lead to stable, lasting recovery.
What is ‘recovery’?
Diagnostic criteria. Recovery from schizophrenia has social, occupational, symptomatic, and psychostructural dimensions. For clinical practice, Liberman et al3 developed a useful set of 10 criteria for recovery (Table 1) by analyzing the literature and cases of 23 schizophrenia patients who returned to work or school with their symptoms under control.
Table 1
Recovery from schizophrenia: 10 clinical criteria
| Criteria | Characteristics of recovered patients* |
|---|---|
| Family relationships | 70% reported good or very good family relationships |
| Substance abuse | None reported illicit drug use in the past year, and two reported occasional alcohol consumption |
| Duration of untreated psychosis | Only 13% reported >1 year delay between symptom onset and treatment |
| Initial response to medication | 87% reported effective symptom control with their first antipsychotic medication |
| Adherence to treatment | All reported adherence to psychiatric care and medication regimens |
| Supportive therapy | 91% reported ongoing psychotherapy, and 78% reported that accessible and supportive psychiatrists and therapists aided their recovery |
| Cognitive abilities | Normal or near-normal functioning on tests of flexibility in solving problems, verbal working memory, and perceptual skills |
| Social skills | None showed more than very mild negative symptoms |
| Personal history | 70% graduated from college, 13% completed 2 years of college, and 3 of remaining 4 worked full time before becoming ill |
| Access to care | 91% received antipsychotics and psychotherapy, 48% social skills training, 57% family participation, 26% vocational rehabilitation, and 61% self-help groups |
| * Based on a study of 23 schizophrenia patients who returned to work or school with their symptoms under control. | |
| Source: Reference 3 | |
Recovery is not a smooth, linear progression. Even when patients attain remission, they often find it hard to make up for “lost life” during years of disability.4 Recovery also can be defined as social, emotional, and biological maturation. This definition considers recovery not as an end-state or cure but as a process of personal growth.5
Several groups proposed recently that recovery from schizophrenia includes four processes:
- finding hope
- re-establishing identity
- taking responsibility for recovery
- finding meaning6 and “getting on with life”7 (Box).
Long-tem vs short-term
Recovery has been studied in many populations, but the evidence is difficult to compare. Data quality is compromised by poorly-defined cohorts, weak study designs, and lack of clear definitions of recovery and its diagnostic criteria. Moreover, empirical evidence is lacking on recovery’s multidimensional nature, including psychosocial, biochemical, genetic, environmental, cultural, and ethnic correlates.
Long-term recovery. Recently, three studies of American populations diagnosed with schizophrenia detected trends toward long-term (>5 years) recovery.
U.S. populations. Modestin et al8 in 2003 re-evaluated diagnoses of 208 patients in Swiss psychiatrist Manfred Bleuler’s influential 1972 study on schizophrenia’s long-term course. Using DSM-III-R, DSM-IV, and International Statistical Classification of Diseases and Related Health Problems (ICD-10) criteria, the authors excluded about 30% of the original patients (most rediagnosed with schizoaffective disorder). Among those remaining, 12% to 15% showed long-term recovery and one-half had an undulating course with remissions.
In 1997, Stephens et al9 examined hospital records from 1913 to 1940 of 484 patients, mean age 27, hospitalized with schizophrenia. Using >5 years of follow-up data and DSM-IV criteria, the authors rated 13% as recovered and 58% unimproved.
Also in 1997, Harrow et al10 evaluated 74 patients diagnosed with schizophrenia by DSM-IV criteria at 2, 4.5, and 7.5 years. In this longitudinal study, one-third (32%) showed complete remission at one follow-up session, compared with 5% at all three evaluations.
This study suggested that schizophrenia patients show relatively poor functioning, compared with other psychotic patients. Over time, however, the likelihood of long-term remission appeared to increase. A similar pattern was seen in a sample of 658 Americans age >65 with schizophrenia diagnosed by DSM-III criteria. As these patients aged, 15% developed long-lasting remission.11
Elsewhere, empirical findings across 15 years from three Norwegian studies indicate that lasting recovery from schizophrenia—with symptom improvement and psychosocial adjustment—is rare (3% to 5% of patients).3 Similarly, only 4% of a Scandinavian sample of 301 patients attained complete, long-term remission during 3 to 39 years of follow-up.12
Across cultures, an international study13 evaluated 15- and 25-year outcomes in 1,633 patients diagnosed with schizophrenia. Approximately 50% had favorable outcomes—stable work, independent from support, no imprisonment, no substance abuse, no rehospitalization, improved social life—but heterogeneity was marked.
Ms J, 48, is in recovery from schizophrenia. She has a stable job as a Web designer, is married, and has learned to build and maintain social relationships. Much of her life, however, has been very different.
At age 15 she was diagnosed with schizophrenia, paranoid psychotic type, with occasional comorbid bipolar symptoms. Over the next 20 years, she was admitted to psychiatric hospitals six times for treatment. At age 36, she was hospitalized with psychosis, depressive symptoms, and insomnia. At that point, she was taking carbamazepine, 500 mg/d, for mood stabilization, and haloperidol, 50 mg/d.
Changing medications. Her psychiatriststarted olanzapine, 5 mg/d, and tapered off haloperidol, which appeared to be gradually becoming less effective while causing mood-related side effects. Ms. J’s psychosis persisted, however, with no response to olanzapine.
Her psychiatrist then tapered carbamazepine to 175 mg/d while starting lamotrigine, 150 to 300 mg/d. The rationale for switching mood stabilizers was that lamotrigine may be more effective than carbamazepine in controlling mixed bipolar states, provide a greater antidepressant effect, and cause fewer side effects.
Intensive treatment. Within 10 days, Ms J’s thought form and composition improved, and her psychiatrist immediately started psychotherapy and psychosocial guidance. Carbamazepine was withdrawn 3 months later, but Ms. J remained on olanzapine, 5 mg/d, and lamotrigine, 300 mg/d. With these medications, the paranoid psychosis went into remission.
After 5 months of intensive treatment, Ms. J was discharged. Outpatient treatment included weekly psychotherapy plus psychosocial guidance and social and coping training 6 times per month. These therapies —along with olanzapine, 5 mg/d, and carbamazepine, 300 mg/d—continue today.
Ms. J’s mental and emotional condition stabilized, and her cognitive abilities improved. Education and therapy helped reduce stress within her family. She has not been rehospitalized or suffered a serious relapse in 12 years.
Table 2
Psychosocial interventions for patients in recovery from schizophrenia*
|
| * Psychosocial interventions are most effective when combined with antipsychotic therapy and individualized psychotherapy |
Short-term course predicted long-term outcome, and local environment played a significant role in determining symptoms and social disability. The authors concluded that adequate early treatment and an optimum environment might lead to favorable long-term outcome.
In the United Kingdom, 14% of a sample of patients diagnosed by ICD-10 criteria achieved remission across a mean 8.5 years.14 In a study of Czechoslovakian patients (70 men, 50 women) with early-onset schizophrenia diagnosed by DSM-III-R criteria, 10% recovered during 13 to 42 years of follow-up.15
Short-term recovery. The McLean-Harvard first-episode project examined outcomes 6 months after schizophrenia diagnosis in 102 patients (55 men, 47 women). Sixty-five percent attained syndromal recovery (significant reduction of diagnostic features), whereas only 33% achieved functional recovery (increased social-emotional, vocational, and coping abilities).16
In Japan, 62 patients (33 men, 29 women; mean age 25) were followed for 13 years after a first hospitalization for schizophrenia. The authors reported an undulating course with recovery or a mild end-state in 53%, and a simple course of recovery and a moderate or severe end-state in 28%.17
Conclusions. The evidence suggests that early and lasting treatment of schizophrenic symptoms—even in recovered patients—might prevent frequent rehospitalizations. Thus, patients with schizophrenia must be followed carefully during and after recovery. Health care professionals, colleagues, friends, and relatives can help patients sustain recovery by watching for the earliest signs of deterioration and intervening before relapse occurs.
Strategies for recovery
Therapeutic factors. Many studies suggest psychosocial interventions (Table 2), psychotherapy, and medication are most effective in combination for stabilizing patients with schizophrenia and continuing their recovery. Other patient factors that may contribute to recovery include:
- quality of relationships with family, friends, and professional caregivers
- ability and motivation to use resources and take responsibility for one’s life
- spiritual and religious activities
- awareness that recovery is possible.
Sells et al18 noted that attempting to make new contacts outside of their former spheres (“positive withdrawal”) may allow schizophrenia patients to reconsider and ultimately recover a durable sense of self.
We at the W. Kahn Institute19 find that all these treatment strategies may be useful and even necessary to continue and stabilize recovery from schizophrenia. We feel they merit the attention of all professionals involved in recovered patients’ aftercare and guidance.
Table 3
Suggested antipsychotic dosages during schizophrenia recovery*
| Drug | Dosage (mg/d) | Potential side effects | Positive effects |
|---|---|---|---|
| Aripiprazole | 10 to 30 | Headache, anxiety, insomnia, lightheadedness | Reduced positive, negative symptoms |
| Clozapine | 300 to 900 | Withdrawal, blunted emotions, seizures, lack of motivation | Reduced positive symptoms |
| Haloperidol | 30 to 100 | Tardive dyskinesia, parkinsonian symptoms, insomnia, depressive reactions, confusion, drowsiness, hypertension | Reduced mania, hyperactivity, agitation |
| Olanzapine | 5 to 10 | Drowsiness, agitation, weight gain, involuntary movements, restlessness | Reduced positive, negative symptoms |
| Quetiapine | 25 to 100 | Dizziness, hypotension, increased cholesterol, weight gain | Reduced positive symptoms |
| Risperidone | 2.5 to 5 | Anxiety, nervousness, back pain, bleeding, dizziness, irregular blood pressure | Reduced positive, negative symptoms |
| Ziprasidone | 10 to 200 | Heart-rhythm irregularity, loss of consciousness, restlessness, weakness, drowsiness | Reduced positive symptoms |
| * Dosages are individualized and may vary among patients and situations, but most will be gradually reduced to minimum levels during remission. | |||
Social/vocational network. Family, friends, neighbors, and social workers play an important role in the patient’s development during recovery. They provide positive stimulation (such as physical activities and social or vocational engagements) and support.
To equip the patient’s network for this responsible task, provide them with training (such as in acceptance, empathy, feedback, and communication), education, and guidance. Support groups can enhance the social networks of patients whose own networks are too small to prevent social isolation or overburdening of members.
Vocational training and mediation also may be stabilizing. Religious activities are central to self-understanding and recovery for many psychiatric patients and may improve outcomes.20
Patient skills. To achieve stabilization and continue their recovery, patients must develop social interaction skills and coping strategies. Conversation training, for example, seems to help improve social interaction. Patients in remission must learn to:
- find or create low-stress, positively stimulating environments in which their recovery can flourish
- tolerate discomfort and stress
- overcome internalized stigma about recovery.
Patients also need to learn when and how to withdraw from hectic, stressful environments and from people who are overly emotional, patronizing, or hold unrealistic expectations about them.
Pharmacotherapy. Sound pharmacotherapy underlies rehabilitation and psychosocial treatment of patients in remission from schizophrenia.21 Healthy neurobiological functioning and equilibrium may help normalize social-emotional behavior and create opportunities to improve all life dimensions via psychotherapy, psychosocial guidance, education, and training.
Dosages often can be reduced during recovery, titrating gradually downward to reduce the risk of relapse. Suggested antipsychotic dosages during recovery are listed in Table 3. Be patient and consistent when adjusting dosages, guided by information in package inserts, from clinical trials, and in recent articles on specific medications. When introducing a medication, start with the lowest dosage and increase in small steps until symptoms are reduced and side effects are minimal.
Discontinuing antipsychotics. Is it therapeutically reasonable to discontinue antipsychotics after recovery? Probably not.
Relapse rates in unmedicated patients with schizophrenia appear extremely high—perhaps 8 or 9 out of 10 cases—even during remission. By comparison, relapse rates appear very low—perhaps 3 or 4 out of 10 cases—for remitted patients who remain on antipsychotics. Atypical antipsychotics or low doses of conventional agents are generally well-tolerated and safe in the long term.22
Patient monitoring. Patients in remission from schizophrenia benefit from:
- 24-hour phone lines to call for guidance, treatment, and quick interventions
- central, alert treatment coordination among psychiatrists, psychologists, social workers, therapists, vocational experts, and activity counselors.
Psychiatrists in solo or small-group settings may need to seek out these resources in their communities. The goal of this team approach—in cooperation with the patient’s social network—is to help the patient develop employment and social activities appropriate to his or her needs and capabilities.
Related resources
- Ascher-Svanuw H, Kraus A. Psychoeducational groups for patients with schizophrenia: a guide for practitioners. Gaithersburg, MD: Aspen Publishers, 1991.
- Suzuki T, Uchida H, Tanaka KF, et al. Revising polypharmacy to a single antipsychotic regimen for patients with chronic schizophrenia. Int J Neuropsychopharmacol 2004;7(2):133-42.
- American Psychiatric Association. Schizophrenia (patient/family information). www.psych.org/public_info/schizo.cfm
- Schizophrenia.com. Nonprofit Web community providing information, support, and education. www.schizophrenia.com
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Davidson L. Living outside mental illness: qualitative studies of recovery in schizophrenia. New York: New York University Press, 2003.
2. Kruger A. Schizophrenia: Recovery and hope. Psychiatr Rehabil J 2000;24(1):29-37.
3. Liberman RP, Kopelowicz A, Ventura J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. Int Rev Psychiatry 2002;14(4):256-72.
4. Torgalsboen AK, Rund BR. Lessons learned from three studies of recovery from schizophrenia. Int Rev Psychiatry 2002;14(4):312-17.
5. Boone EC. A qualitative investigation of the process of recovery in people experiencing schizophrenia. Dissert Abstr Int 1996;57 (5-B):3402.-
6. Andresen R, Oades L, Caputi P. The experience of recovery from schizophrenia: towards an empirically validated stage model. Aust NZ J Psychiatry 2003;37(5):586-94.
7. Noordsy D, Torrey W, Mueser K, et al. Recovery from severe mental illness: an interpersonal and functional outcome definition. Int Rev Psychiatry 2002;14(4):318-26.
8. Modestin J, Huber A, Satirli E, et al. Long-term course of schizophrenic illness: Bleuler’s study reconsidered. Am J Psychiatry 2003;160(12):2202-8.
9. Stephens JH, Richard P, McHugh PR. Long-term follow-up of patients hospitalized for schizophrenia, 1913 to1940. J Nerv Ment Dis 1997;185(12):715-21.
10. Harrow M, Sands JR, Silverstein ML, Goldberg JF. Course and outcome for schizophrenia versus other psychotic patients: a longitudinal study. Schizophr Bull 1997;23:287-303.
11. Craig TJ, Bregman Z. Late-onset schizophrenia-like illness. J Am Geriatr Soc 1988;36(2):104-7.
12. Opjordsmoen S. Long-term course and outcome in unipolar affective and schizoaffective psychoses. Acta Psychiatr Scand 1989;79(4):317-26.
13. Harris G, Hopper K, Craig T, et al. Recovery from psychotic illness: a 15- and 25-year international follow up study. Br J Psychiatry 2001;178:506-17.
14. Kiriakakis V, Bhatia KP, Quinn NP, Marsden CD. The natural history of tardive dystonia. A long-term follow-up study of 107 cases. Brain 1998;121(Pt 11):2053-66.
15. Mala E. Early onset schizophrenia. Cesk Slov Psychiatry 1993;89(5):259-71.
16. Tohen M, Strakowski SM, Zarate C, et al. The McLean-Harvard first episode project: 6-month symptomatic and functional outcome in affective and non-affective psychosis. Biol Psychiatry 2000;48(6):467-76.
17. Kobayashi T. Course types of first admission schizophrenia: A mean 13-year follow back study. Seishin Igaku Clin Psychiatry 2002;44(2):161-8.
18. Sells DJ, Stayner DA, Davidson L. Recovering the self in schizophrenia: An integrative review of qualitative studies. Psychiatr Q. 2004;75(1):87-97.
19. Martens WHJ, Kahn W, Oppenheimer C. Predictors and prevalence of recovery in schizophrenia. W. Kahn Institute of Theoretical Psychiatry and Neuroscience (WKITPN) Publication 36, 2001(5):113-26.
20. Fallot RD. The place of spirituality and religion in mental health services. In: Lamb HR (ed). Best of new directions for mental health services, 1979-2001. San Francisco: Jossey Bass, 2001:79-88.
21. Kane JM. Long-term treatment of schizophrenia: Moving from a relapse-prevention model to a recovery model. J Clin Psychiatry. 2003;64(11):1384-5.
22. Tauscher-Wisniewski S, Zipursky RB. The role of maintenance pharmacotherapy in achieving recovery from a first episode of schizophrenia. Int Rev Psychiatry. 2002;14(4):284-92.
Is it realistic for patients with schizophrenia to believe they can recover? Recent observational studies show that some do,1 even though all DSM editions have defined schizophrenia as a chronic disease with a poor outcome.2
Our understanding of schizophrenia is changing as we gain new insights into:
- mechanism of recovery
- efficacy of combined psychotherapeutic, psychosocial, and drug therapies for sustaining remission and recovery
- the value of long-term aftercare. This article examines evidence on:
- achieving recovery from schizophrenia
- factors associated with remission
- treatments that may help prevent relapse and lead to stable, lasting recovery.
What is ‘recovery’?
Diagnostic criteria. Recovery from schizophrenia has social, occupational, symptomatic, and psychostructural dimensions. For clinical practice, Liberman et al3 developed a useful set of 10 criteria for recovery (Table 1) by analyzing the literature and cases of 23 schizophrenia patients who returned to work or school with their symptoms under control.
Table 1
Recovery from schizophrenia: 10 clinical criteria
| Criteria | Characteristics of recovered patients* |
|---|---|
| Family relationships | 70% reported good or very good family relationships |
| Substance abuse | None reported illicit drug use in the past year, and two reported occasional alcohol consumption |
| Duration of untreated psychosis | Only 13% reported >1 year delay between symptom onset and treatment |
| Initial response to medication | 87% reported effective symptom control with their first antipsychotic medication |
| Adherence to treatment | All reported adherence to psychiatric care and medication regimens |
| Supportive therapy | 91% reported ongoing psychotherapy, and 78% reported that accessible and supportive psychiatrists and therapists aided their recovery |
| Cognitive abilities | Normal or near-normal functioning on tests of flexibility in solving problems, verbal working memory, and perceptual skills |
| Social skills | None showed more than very mild negative symptoms |
| Personal history | 70% graduated from college, 13% completed 2 years of college, and 3 of remaining 4 worked full time before becoming ill |
| Access to care | 91% received antipsychotics and psychotherapy, 48% social skills training, 57% family participation, 26% vocational rehabilitation, and 61% self-help groups |
| * Based on a study of 23 schizophrenia patients who returned to work or school with their symptoms under control. | |
| Source: Reference 3 | |
Recovery is not a smooth, linear progression. Even when patients attain remission, they often find it hard to make up for “lost life” during years of disability.4 Recovery also can be defined as social, emotional, and biological maturation. This definition considers recovery not as an end-state or cure but as a process of personal growth.5
Several groups proposed recently that recovery from schizophrenia includes four processes:
- finding hope
- re-establishing identity
- taking responsibility for recovery
- finding meaning6 and “getting on with life”7 (Box).
Long-tem vs short-term
Recovery has been studied in many populations, but the evidence is difficult to compare. Data quality is compromised by poorly-defined cohorts, weak study designs, and lack of clear definitions of recovery and its diagnostic criteria. Moreover, empirical evidence is lacking on recovery’s multidimensional nature, including psychosocial, biochemical, genetic, environmental, cultural, and ethnic correlates.
Long-term recovery. Recently, three studies of American populations diagnosed with schizophrenia detected trends toward long-term (>5 years) recovery.
U.S. populations. Modestin et al8 in 2003 re-evaluated diagnoses of 208 patients in Swiss psychiatrist Manfred Bleuler’s influential 1972 study on schizophrenia’s long-term course. Using DSM-III-R, DSM-IV, and International Statistical Classification of Diseases and Related Health Problems (ICD-10) criteria, the authors excluded about 30% of the original patients (most rediagnosed with schizoaffective disorder). Among those remaining, 12% to 15% showed long-term recovery and one-half had an undulating course with remissions.
In 1997, Stephens et al9 examined hospital records from 1913 to 1940 of 484 patients, mean age 27, hospitalized with schizophrenia. Using >5 years of follow-up data and DSM-IV criteria, the authors rated 13% as recovered and 58% unimproved.
Also in 1997, Harrow et al10 evaluated 74 patients diagnosed with schizophrenia by DSM-IV criteria at 2, 4.5, and 7.5 years. In this longitudinal study, one-third (32%) showed complete remission at one follow-up session, compared with 5% at all three evaluations.
This study suggested that schizophrenia patients show relatively poor functioning, compared with other psychotic patients. Over time, however, the likelihood of long-term remission appeared to increase. A similar pattern was seen in a sample of 658 Americans age >65 with schizophrenia diagnosed by DSM-III criteria. As these patients aged, 15% developed long-lasting remission.11
Elsewhere, empirical findings across 15 years from three Norwegian studies indicate that lasting recovery from schizophrenia—with symptom improvement and psychosocial adjustment—is rare (3% to 5% of patients).3 Similarly, only 4% of a Scandinavian sample of 301 patients attained complete, long-term remission during 3 to 39 years of follow-up.12
Across cultures, an international study13 evaluated 15- and 25-year outcomes in 1,633 patients diagnosed with schizophrenia. Approximately 50% had favorable outcomes—stable work, independent from support, no imprisonment, no substance abuse, no rehospitalization, improved social life—but heterogeneity was marked.
Ms J, 48, is in recovery from schizophrenia. She has a stable job as a Web designer, is married, and has learned to build and maintain social relationships. Much of her life, however, has been very different.
At age 15 she was diagnosed with schizophrenia, paranoid psychotic type, with occasional comorbid bipolar symptoms. Over the next 20 years, she was admitted to psychiatric hospitals six times for treatment. At age 36, she was hospitalized with psychosis, depressive symptoms, and insomnia. At that point, she was taking carbamazepine, 500 mg/d, for mood stabilization, and haloperidol, 50 mg/d.
Changing medications. Her psychiatriststarted olanzapine, 5 mg/d, and tapered off haloperidol, which appeared to be gradually becoming less effective while causing mood-related side effects. Ms. J’s psychosis persisted, however, with no response to olanzapine.
Her psychiatrist then tapered carbamazepine to 175 mg/d while starting lamotrigine, 150 to 300 mg/d. The rationale for switching mood stabilizers was that lamotrigine may be more effective than carbamazepine in controlling mixed bipolar states, provide a greater antidepressant effect, and cause fewer side effects.
Intensive treatment. Within 10 days, Ms J’s thought form and composition improved, and her psychiatrist immediately started psychotherapy and psychosocial guidance. Carbamazepine was withdrawn 3 months later, but Ms. J remained on olanzapine, 5 mg/d, and lamotrigine, 300 mg/d. With these medications, the paranoid psychosis went into remission.
After 5 months of intensive treatment, Ms. J was discharged. Outpatient treatment included weekly psychotherapy plus psychosocial guidance and social and coping training 6 times per month. These therapies —along with olanzapine, 5 mg/d, and carbamazepine, 300 mg/d—continue today.
Ms. J’s mental and emotional condition stabilized, and her cognitive abilities improved. Education and therapy helped reduce stress within her family. She has not been rehospitalized or suffered a serious relapse in 12 years.
Table 2
Psychosocial interventions for patients in recovery from schizophrenia*
|
| * Psychosocial interventions are most effective when combined with antipsychotic therapy and individualized psychotherapy |
Short-term course predicted long-term outcome, and local environment played a significant role in determining symptoms and social disability. The authors concluded that adequate early treatment and an optimum environment might lead to favorable long-term outcome.
In the United Kingdom, 14% of a sample of patients diagnosed by ICD-10 criteria achieved remission across a mean 8.5 years.14 In a study of Czechoslovakian patients (70 men, 50 women) with early-onset schizophrenia diagnosed by DSM-III-R criteria, 10% recovered during 13 to 42 years of follow-up.15
Short-term recovery. The McLean-Harvard first-episode project examined outcomes 6 months after schizophrenia diagnosis in 102 patients (55 men, 47 women). Sixty-five percent attained syndromal recovery (significant reduction of diagnostic features), whereas only 33% achieved functional recovery (increased social-emotional, vocational, and coping abilities).16
In Japan, 62 patients (33 men, 29 women; mean age 25) were followed for 13 years after a first hospitalization for schizophrenia. The authors reported an undulating course with recovery or a mild end-state in 53%, and a simple course of recovery and a moderate or severe end-state in 28%.17
Conclusions. The evidence suggests that early and lasting treatment of schizophrenic symptoms—even in recovered patients—might prevent frequent rehospitalizations. Thus, patients with schizophrenia must be followed carefully during and after recovery. Health care professionals, colleagues, friends, and relatives can help patients sustain recovery by watching for the earliest signs of deterioration and intervening before relapse occurs.
Strategies for recovery
Therapeutic factors. Many studies suggest psychosocial interventions (Table 2), psychotherapy, and medication are most effective in combination for stabilizing patients with schizophrenia and continuing their recovery. Other patient factors that may contribute to recovery include:
- quality of relationships with family, friends, and professional caregivers
- ability and motivation to use resources and take responsibility for one’s life
- spiritual and religious activities
- awareness that recovery is possible.
Sells et al18 noted that attempting to make new contacts outside of their former spheres (“positive withdrawal”) may allow schizophrenia patients to reconsider and ultimately recover a durable sense of self.
We at the W. Kahn Institute19 find that all these treatment strategies may be useful and even necessary to continue and stabilize recovery from schizophrenia. We feel they merit the attention of all professionals involved in recovered patients’ aftercare and guidance.
Table 3
Suggested antipsychotic dosages during schizophrenia recovery*
| Drug | Dosage (mg/d) | Potential side effects | Positive effects |
|---|---|---|---|
| Aripiprazole | 10 to 30 | Headache, anxiety, insomnia, lightheadedness | Reduced positive, negative symptoms |
| Clozapine | 300 to 900 | Withdrawal, blunted emotions, seizures, lack of motivation | Reduced positive symptoms |
| Haloperidol | 30 to 100 | Tardive dyskinesia, parkinsonian symptoms, insomnia, depressive reactions, confusion, drowsiness, hypertension | Reduced mania, hyperactivity, agitation |
| Olanzapine | 5 to 10 | Drowsiness, agitation, weight gain, involuntary movements, restlessness | Reduced positive, negative symptoms |
| Quetiapine | 25 to 100 | Dizziness, hypotension, increased cholesterol, weight gain | Reduced positive symptoms |
| Risperidone | 2.5 to 5 | Anxiety, nervousness, back pain, bleeding, dizziness, irregular blood pressure | Reduced positive, negative symptoms |
| Ziprasidone | 10 to 200 | Heart-rhythm irregularity, loss of consciousness, restlessness, weakness, drowsiness | Reduced positive symptoms |
| * Dosages are individualized and may vary among patients and situations, but most will be gradually reduced to minimum levels during remission. | |||
Social/vocational network. Family, friends, neighbors, and social workers play an important role in the patient’s development during recovery. They provide positive stimulation (such as physical activities and social or vocational engagements) and support.
To equip the patient’s network for this responsible task, provide them with training (such as in acceptance, empathy, feedback, and communication), education, and guidance. Support groups can enhance the social networks of patients whose own networks are too small to prevent social isolation or overburdening of members.
Vocational training and mediation also may be stabilizing. Religious activities are central to self-understanding and recovery for many psychiatric patients and may improve outcomes.20
Patient skills. To achieve stabilization and continue their recovery, patients must develop social interaction skills and coping strategies. Conversation training, for example, seems to help improve social interaction. Patients in remission must learn to:
- find or create low-stress, positively stimulating environments in which their recovery can flourish
- tolerate discomfort and stress
- overcome internalized stigma about recovery.
Patients also need to learn when and how to withdraw from hectic, stressful environments and from people who are overly emotional, patronizing, or hold unrealistic expectations about them.
Pharmacotherapy. Sound pharmacotherapy underlies rehabilitation and psychosocial treatment of patients in remission from schizophrenia.21 Healthy neurobiological functioning and equilibrium may help normalize social-emotional behavior and create opportunities to improve all life dimensions via psychotherapy, psychosocial guidance, education, and training.
Dosages often can be reduced during recovery, titrating gradually downward to reduce the risk of relapse. Suggested antipsychotic dosages during recovery are listed in Table 3. Be patient and consistent when adjusting dosages, guided by information in package inserts, from clinical trials, and in recent articles on specific medications. When introducing a medication, start with the lowest dosage and increase in small steps until symptoms are reduced and side effects are minimal.
Discontinuing antipsychotics. Is it therapeutically reasonable to discontinue antipsychotics after recovery? Probably not.
Relapse rates in unmedicated patients with schizophrenia appear extremely high—perhaps 8 or 9 out of 10 cases—even during remission. By comparison, relapse rates appear very low—perhaps 3 or 4 out of 10 cases—for remitted patients who remain on antipsychotics. Atypical antipsychotics or low doses of conventional agents are generally well-tolerated and safe in the long term.22
Patient monitoring. Patients in remission from schizophrenia benefit from:
- 24-hour phone lines to call for guidance, treatment, and quick interventions
- central, alert treatment coordination among psychiatrists, psychologists, social workers, therapists, vocational experts, and activity counselors.
Psychiatrists in solo or small-group settings may need to seek out these resources in their communities. The goal of this team approach—in cooperation with the patient’s social network—is to help the patient develop employment and social activities appropriate to his or her needs and capabilities.
Related resources
- Ascher-Svanuw H, Kraus A. Psychoeducational groups for patients with schizophrenia: a guide for practitioners. Gaithersburg, MD: Aspen Publishers, 1991.
- Suzuki T, Uchida H, Tanaka KF, et al. Revising polypharmacy to a single antipsychotic regimen for patients with chronic schizophrenia. Int J Neuropsychopharmacol 2004;7(2):133-42.
- American Psychiatric Association. Schizophrenia (patient/family information). www.psych.org/public_info/schizo.cfm
- Schizophrenia.com. Nonprofit Web community providing information, support, and education. www.schizophrenia.com
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Is it realistic for patients with schizophrenia to believe they can recover? Recent observational studies show that some do,1 even though all DSM editions have defined schizophrenia as a chronic disease with a poor outcome.2
Our understanding of schizophrenia is changing as we gain new insights into:
- mechanism of recovery
- efficacy of combined psychotherapeutic, psychosocial, and drug therapies for sustaining remission and recovery
- the value of long-term aftercare. This article examines evidence on:
- achieving recovery from schizophrenia
- factors associated with remission
- treatments that may help prevent relapse and lead to stable, lasting recovery.
What is ‘recovery’?
Diagnostic criteria. Recovery from schizophrenia has social, occupational, symptomatic, and psychostructural dimensions. For clinical practice, Liberman et al3 developed a useful set of 10 criteria for recovery (Table 1) by analyzing the literature and cases of 23 schizophrenia patients who returned to work or school with their symptoms under control.
Table 1
Recovery from schizophrenia: 10 clinical criteria
| Criteria | Characteristics of recovered patients* |
|---|---|
| Family relationships | 70% reported good or very good family relationships |
| Substance abuse | None reported illicit drug use in the past year, and two reported occasional alcohol consumption |
| Duration of untreated psychosis | Only 13% reported >1 year delay between symptom onset and treatment |
| Initial response to medication | 87% reported effective symptom control with their first antipsychotic medication |
| Adherence to treatment | All reported adherence to psychiatric care and medication regimens |
| Supportive therapy | 91% reported ongoing psychotherapy, and 78% reported that accessible and supportive psychiatrists and therapists aided their recovery |
| Cognitive abilities | Normal or near-normal functioning on tests of flexibility in solving problems, verbal working memory, and perceptual skills |
| Social skills | None showed more than very mild negative symptoms |
| Personal history | 70% graduated from college, 13% completed 2 years of college, and 3 of remaining 4 worked full time before becoming ill |
| Access to care | 91% received antipsychotics and psychotherapy, 48% social skills training, 57% family participation, 26% vocational rehabilitation, and 61% self-help groups |
| * Based on a study of 23 schizophrenia patients who returned to work or school with their symptoms under control. | |
| Source: Reference 3 | |
Recovery is not a smooth, linear progression. Even when patients attain remission, they often find it hard to make up for “lost life” during years of disability.4 Recovery also can be defined as social, emotional, and biological maturation. This definition considers recovery not as an end-state or cure but as a process of personal growth.5
Several groups proposed recently that recovery from schizophrenia includes four processes:
- finding hope
- re-establishing identity
- taking responsibility for recovery
- finding meaning6 and “getting on with life”7 (Box).
Long-tem vs short-term
Recovery has been studied in many populations, but the evidence is difficult to compare. Data quality is compromised by poorly-defined cohorts, weak study designs, and lack of clear definitions of recovery and its diagnostic criteria. Moreover, empirical evidence is lacking on recovery’s multidimensional nature, including psychosocial, biochemical, genetic, environmental, cultural, and ethnic correlates.
Long-term recovery. Recently, three studies of American populations diagnosed with schizophrenia detected trends toward long-term (>5 years) recovery.
U.S. populations. Modestin et al8 in 2003 re-evaluated diagnoses of 208 patients in Swiss psychiatrist Manfred Bleuler’s influential 1972 study on schizophrenia’s long-term course. Using DSM-III-R, DSM-IV, and International Statistical Classification of Diseases and Related Health Problems (ICD-10) criteria, the authors excluded about 30% of the original patients (most rediagnosed with schizoaffective disorder). Among those remaining, 12% to 15% showed long-term recovery and one-half had an undulating course with remissions.
In 1997, Stephens et al9 examined hospital records from 1913 to 1940 of 484 patients, mean age 27, hospitalized with schizophrenia. Using >5 years of follow-up data and DSM-IV criteria, the authors rated 13% as recovered and 58% unimproved.
Also in 1997, Harrow et al10 evaluated 74 patients diagnosed with schizophrenia by DSM-IV criteria at 2, 4.5, and 7.5 years. In this longitudinal study, one-third (32%) showed complete remission at one follow-up session, compared with 5% at all three evaluations.
This study suggested that schizophrenia patients show relatively poor functioning, compared with other psychotic patients. Over time, however, the likelihood of long-term remission appeared to increase. A similar pattern was seen in a sample of 658 Americans age >65 with schizophrenia diagnosed by DSM-III criteria. As these patients aged, 15% developed long-lasting remission.11
Elsewhere, empirical findings across 15 years from three Norwegian studies indicate that lasting recovery from schizophrenia—with symptom improvement and psychosocial adjustment—is rare (3% to 5% of patients).3 Similarly, only 4% of a Scandinavian sample of 301 patients attained complete, long-term remission during 3 to 39 years of follow-up.12
Across cultures, an international study13 evaluated 15- and 25-year outcomes in 1,633 patients diagnosed with schizophrenia. Approximately 50% had favorable outcomes—stable work, independent from support, no imprisonment, no substance abuse, no rehospitalization, improved social life—but heterogeneity was marked.
Ms J, 48, is in recovery from schizophrenia. She has a stable job as a Web designer, is married, and has learned to build and maintain social relationships. Much of her life, however, has been very different.
At age 15 she was diagnosed with schizophrenia, paranoid psychotic type, with occasional comorbid bipolar symptoms. Over the next 20 years, she was admitted to psychiatric hospitals six times for treatment. At age 36, she was hospitalized with psychosis, depressive symptoms, and insomnia. At that point, she was taking carbamazepine, 500 mg/d, for mood stabilization, and haloperidol, 50 mg/d.
Changing medications. Her psychiatriststarted olanzapine, 5 mg/d, and tapered off haloperidol, which appeared to be gradually becoming less effective while causing mood-related side effects. Ms. J’s psychosis persisted, however, with no response to olanzapine.
Her psychiatrist then tapered carbamazepine to 175 mg/d while starting lamotrigine, 150 to 300 mg/d. The rationale for switching mood stabilizers was that lamotrigine may be more effective than carbamazepine in controlling mixed bipolar states, provide a greater antidepressant effect, and cause fewer side effects.
Intensive treatment. Within 10 days, Ms J’s thought form and composition improved, and her psychiatrist immediately started psychotherapy and psychosocial guidance. Carbamazepine was withdrawn 3 months later, but Ms. J remained on olanzapine, 5 mg/d, and lamotrigine, 300 mg/d. With these medications, the paranoid psychosis went into remission.
After 5 months of intensive treatment, Ms. J was discharged. Outpatient treatment included weekly psychotherapy plus psychosocial guidance and social and coping training 6 times per month. These therapies —along with olanzapine, 5 mg/d, and carbamazepine, 300 mg/d—continue today.
Ms. J’s mental and emotional condition stabilized, and her cognitive abilities improved. Education and therapy helped reduce stress within her family. She has not been rehospitalized or suffered a serious relapse in 12 years.
Table 2
Psychosocial interventions for patients in recovery from schizophrenia*
|
| * Psychosocial interventions are most effective when combined with antipsychotic therapy and individualized psychotherapy |
Short-term course predicted long-term outcome, and local environment played a significant role in determining symptoms and social disability. The authors concluded that adequate early treatment and an optimum environment might lead to favorable long-term outcome.
In the United Kingdom, 14% of a sample of patients diagnosed by ICD-10 criteria achieved remission across a mean 8.5 years.14 In a study of Czechoslovakian patients (70 men, 50 women) with early-onset schizophrenia diagnosed by DSM-III-R criteria, 10% recovered during 13 to 42 years of follow-up.15
Short-term recovery. The McLean-Harvard first-episode project examined outcomes 6 months after schizophrenia diagnosis in 102 patients (55 men, 47 women). Sixty-five percent attained syndromal recovery (significant reduction of diagnostic features), whereas only 33% achieved functional recovery (increased social-emotional, vocational, and coping abilities).16
In Japan, 62 patients (33 men, 29 women; mean age 25) were followed for 13 years after a first hospitalization for schizophrenia. The authors reported an undulating course with recovery or a mild end-state in 53%, and a simple course of recovery and a moderate or severe end-state in 28%.17
Conclusions. The evidence suggests that early and lasting treatment of schizophrenic symptoms—even in recovered patients—might prevent frequent rehospitalizations. Thus, patients with schizophrenia must be followed carefully during and after recovery. Health care professionals, colleagues, friends, and relatives can help patients sustain recovery by watching for the earliest signs of deterioration and intervening before relapse occurs.
Strategies for recovery
Therapeutic factors. Many studies suggest psychosocial interventions (Table 2), psychotherapy, and medication are most effective in combination for stabilizing patients with schizophrenia and continuing their recovery. Other patient factors that may contribute to recovery include:
- quality of relationships with family, friends, and professional caregivers
- ability and motivation to use resources and take responsibility for one’s life
- spiritual and religious activities
- awareness that recovery is possible.
Sells et al18 noted that attempting to make new contacts outside of their former spheres (“positive withdrawal”) may allow schizophrenia patients to reconsider and ultimately recover a durable sense of self.
We at the W. Kahn Institute19 find that all these treatment strategies may be useful and even necessary to continue and stabilize recovery from schizophrenia. We feel they merit the attention of all professionals involved in recovered patients’ aftercare and guidance.
Table 3
Suggested antipsychotic dosages during schizophrenia recovery*
| Drug | Dosage (mg/d) | Potential side effects | Positive effects |
|---|---|---|---|
| Aripiprazole | 10 to 30 | Headache, anxiety, insomnia, lightheadedness | Reduced positive, negative symptoms |
| Clozapine | 300 to 900 | Withdrawal, blunted emotions, seizures, lack of motivation | Reduced positive symptoms |
| Haloperidol | 30 to 100 | Tardive dyskinesia, parkinsonian symptoms, insomnia, depressive reactions, confusion, drowsiness, hypertension | Reduced mania, hyperactivity, agitation |
| Olanzapine | 5 to 10 | Drowsiness, agitation, weight gain, involuntary movements, restlessness | Reduced positive, negative symptoms |
| Quetiapine | 25 to 100 | Dizziness, hypotension, increased cholesterol, weight gain | Reduced positive symptoms |
| Risperidone | 2.5 to 5 | Anxiety, nervousness, back pain, bleeding, dizziness, irregular blood pressure | Reduced positive, negative symptoms |
| Ziprasidone | 10 to 200 | Heart-rhythm irregularity, loss of consciousness, restlessness, weakness, drowsiness | Reduced positive symptoms |
| * Dosages are individualized and may vary among patients and situations, but most will be gradually reduced to minimum levels during remission. | |||
Social/vocational network. Family, friends, neighbors, and social workers play an important role in the patient’s development during recovery. They provide positive stimulation (such as physical activities and social or vocational engagements) and support.
To equip the patient’s network for this responsible task, provide them with training (such as in acceptance, empathy, feedback, and communication), education, and guidance. Support groups can enhance the social networks of patients whose own networks are too small to prevent social isolation or overburdening of members.
Vocational training and mediation also may be stabilizing. Religious activities are central to self-understanding and recovery for many psychiatric patients and may improve outcomes.20
Patient skills. To achieve stabilization and continue their recovery, patients must develop social interaction skills and coping strategies. Conversation training, for example, seems to help improve social interaction. Patients in remission must learn to:
- find or create low-stress, positively stimulating environments in which their recovery can flourish
- tolerate discomfort and stress
- overcome internalized stigma about recovery.
Patients also need to learn when and how to withdraw from hectic, stressful environments and from people who are overly emotional, patronizing, or hold unrealistic expectations about them.
Pharmacotherapy. Sound pharmacotherapy underlies rehabilitation and psychosocial treatment of patients in remission from schizophrenia.21 Healthy neurobiological functioning and equilibrium may help normalize social-emotional behavior and create opportunities to improve all life dimensions via psychotherapy, psychosocial guidance, education, and training.
Dosages often can be reduced during recovery, titrating gradually downward to reduce the risk of relapse. Suggested antipsychotic dosages during recovery are listed in Table 3. Be patient and consistent when adjusting dosages, guided by information in package inserts, from clinical trials, and in recent articles on specific medications. When introducing a medication, start with the lowest dosage and increase in small steps until symptoms are reduced and side effects are minimal.
Discontinuing antipsychotics. Is it therapeutically reasonable to discontinue antipsychotics after recovery? Probably not.
Relapse rates in unmedicated patients with schizophrenia appear extremely high—perhaps 8 or 9 out of 10 cases—even during remission. By comparison, relapse rates appear very low—perhaps 3 or 4 out of 10 cases—for remitted patients who remain on antipsychotics. Atypical antipsychotics or low doses of conventional agents are generally well-tolerated and safe in the long term.22
Patient monitoring. Patients in remission from schizophrenia benefit from:
- 24-hour phone lines to call for guidance, treatment, and quick interventions
- central, alert treatment coordination among psychiatrists, psychologists, social workers, therapists, vocational experts, and activity counselors.
Psychiatrists in solo or small-group settings may need to seek out these resources in their communities. The goal of this team approach—in cooperation with the patient’s social network—is to help the patient develop employment and social activities appropriate to his or her needs and capabilities.
Related resources
- Ascher-Svanuw H, Kraus A. Psychoeducational groups for patients with schizophrenia: a guide for practitioners. Gaithersburg, MD: Aspen Publishers, 1991.
- Suzuki T, Uchida H, Tanaka KF, et al. Revising polypharmacy to a single antipsychotic regimen for patients with chronic schizophrenia. Int J Neuropsychopharmacol 2004;7(2):133-42.
- American Psychiatric Association. Schizophrenia (patient/family information). www.psych.org/public_info/schizo.cfm
- Schizophrenia.com. Nonprofit Web community providing information, support, and education. www.schizophrenia.com
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Davidson L. Living outside mental illness: qualitative studies of recovery in schizophrenia. New York: New York University Press, 2003.
2. Kruger A. Schizophrenia: Recovery and hope. Psychiatr Rehabil J 2000;24(1):29-37.
3. Liberman RP, Kopelowicz A, Ventura J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. Int Rev Psychiatry 2002;14(4):256-72.
4. Torgalsboen AK, Rund BR. Lessons learned from three studies of recovery from schizophrenia. Int Rev Psychiatry 2002;14(4):312-17.
5. Boone EC. A qualitative investigation of the process of recovery in people experiencing schizophrenia. Dissert Abstr Int 1996;57 (5-B):3402.-
6. Andresen R, Oades L, Caputi P. The experience of recovery from schizophrenia: towards an empirically validated stage model. Aust NZ J Psychiatry 2003;37(5):586-94.
7. Noordsy D, Torrey W, Mueser K, et al. Recovery from severe mental illness: an interpersonal and functional outcome definition. Int Rev Psychiatry 2002;14(4):318-26.
8. Modestin J, Huber A, Satirli E, et al. Long-term course of schizophrenic illness: Bleuler’s study reconsidered. Am J Psychiatry 2003;160(12):2202-8.
9. Stephens JH, Richard P, McHugh PR. Long-term follow-up of patients hospitalized for schizophrenia, 1913 to1940. J Nerv Ment Dis 1997;185(12):715-21.
10. Harrow M, Sands JR, Silverstein ML, Goldberg JF. Course and outcome for schizophrenia versus other psychotic patients: a longitudinal study. Schizophr Bull 1997;23:287-303.
11. Craig TJ, Bregman Z. Late-onset schizophrenia-like illness. J Am Geriatr Soc 1988;36(2):104-7.
12. Opjordsmoen S. Long-term course and outcome in unipolar affective and schizoaffective psychoses. Acta Psychiatr Scand 1989;79(4):317-26.
13. Harris G, Hopper K, Craig T, et al. Recovery from psychotic illness: a 15- and 25-year international follow up study. Br J Psychiatry 2001;178:506-17.
14. Kiriakakis V, Bhatia KP, Quinn NP, Marsden CD. The natural history of tardive dystonia. A long-term follow-up study of 107 cases. Brain 1998;121(Pt 11):2053-66.
15. Mala E. Early onset schizophrenia. Cesk Slov Psychiatry 1993;89(5):259-71.
16. Tohen M, Strakowski SM, Zarate C, et al. The McLean-Harvard first episode project: 6-month symptomatic and functional outcome in affective and non-affective psychosis. Biol Psychiatry 2000;48(6):467-76.
17. Kobayashi T. Course types of first admission schizophrenia: A mean 13-year follow back study. Seishin Igaku Clin Psychiatry 2002;44(2):161-8.
18. Sells DJ, Stayner DA, Davidson L. Recovering the self in schizophrenia: An integrative review of qualitative studies. Psychiatr Q. 2004;75(1):87-97.
19. Martens WHJ, Kahn W, Oppenheimer C. Predictors and prevalence of recovery in schizophrenia. W. Kahn Institute of Theoretical Psychiatry and Neuroscience (WKITPN) Publication 36, 2001(5):113-26.
20. Fallot RD. The place of spirituality and religion in mental health services. In: Lamb HR (ed). Best of new directions for mental health services, 1979-2001. San Francisco: Jossey Bass, 2001:79-88.
21. Kane JM. Long-term treatment of schizophrenia: Moving from a relapse-prevention model to a recovery model. J Clin Psychiatry. 2003;64(11):1384-5.
22. Tauscher-Wisniewski S, Zipursky RB. The role of maintenance pharmacotherapy in achieving recovery from a first episode of schizophrenia. Int Rev Psychiatry. 2002;14(4):284-92.
1. Davidson L. Living outside mental illness: qualitative studies of recovery in schizophrenia. New York: New York University Press, 2003.
2. Kruger A. Schizophrenia: Recovery and hope. Psychiatr Rehabil J 2000;24(1):29-37.
3. Liberman RP, Kopelowicz A, Ventura J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. Int Rev Psychiatry 2002;14(4):256-72.
4. Torgalsboen AK, Rund BR. Lessons learned from three studies of recovery from schizophrenia. Int Rev Psychiatry 2002;14(4):312-17.
5. Boone EC. A qualitative investigation of the process of recovery in people experiencing schizophrenia. Dissert Abstr Int 1996;57 (5-B):3402.-
6. Andresen R, Oades L, Caputi P. The experience of recovery from schizophrenia: towards an empirically validated stage model. Aust NZ J Psychiatry 2003;37(5):586-94.
7. Noordsy D, Torrey W, Mueser K, et al. Recovery from severe mental illness: an interpersonal and functional outcome definition. Int Rev Psychiatry 2002;14(4):318-26.
8. Modestin J, Huber A, Satirli E, et al. Long-term course of schizophrenic illness: Bleuler’s study reconsidered. Am J Psychiatry 2003;160(12):2202-8.
9. Stephens JH, Richard P, McHugh PR. Long-term follow-up of patients hospitalized for schizophrenia, 1913 to1940. J Nerv Ment Dis 1997;185(12):715-21.
10. Harrow M, Sands JR, Silverstein ML, Goldberg JF. Course and outcome for schizophrenia versus other psychotic patients: a longitudinal study. Schizophr Bull 1997;23:287-303.
11. Craig TJ, Bregman Z. Late-onset schizophrenia-like illness. J Am Geriatr Soc 1988;36(2):104-7.
12. Opjordsmoen S. Long-term course and outcome in unipolar affective and schizoaffective psychoses. Acta Psychiatr Scand 1989;79(4):317-26.
13. Harris G, Hopper K, Craig T, et al. Recovery from psychotic illness: a 15- and 25-year international follow up study. Br J Psychiatry 2001;178:506-17.
14. Kiriakakis V, Bhatia KP, Quinn NP, Marsden CD. The natural history of tardive dystonia. A long-term follow-up study of 107 cases. Brain 1998;121(Pt 11):2053-66.
15. Mala E. Early onset schizophrenia. Cesk Slov Psychiatry 1993;89(5):259-71.
16. Tohen M, Strakowski SM, Zarate C, et al. The McLean-Harvard first episode project: 6-month symptomatic and functional outcome in affective and non-affective psychosis. Biol Psychiatry 2000;48(6):467-76.
17. Kobayashi T. Course types of first admission schizophrenia: A mean 13-year follow back study. Seishin Igaku Clin Psychiatry 2002;44(2):161-8.
18. Sells DJ, Stayner DA, Davidson L. Recovering the self in schizophrenia: An integrative review of qualitative studies. Psychiatr Q. 2004;75(1):87-97.
19. Martens WHJ, Kahn W, Oppenheimer C. Predictors and prevalence of recovery in schizophrenia. W. Kahn Institute of Theoretical Psychiatry and Neuroscience (WKITPN) Publication 36, 2001(5):113-26.
20. Fallot RD. The place of spirituality and religion in mental health services. In: Lamb HR (ed). Best of new directions for mental health services, 1979-2001. San Francisco: Jossey Bass, 2001:79-88.
21. Kane JM. Long-term treatment of schizophrenia: Moving from a relapse-prevention model to a recovery model. J Clin Psychiatry. 2003;64(11):1384-5.
22. Tauscher-Wisniewski S, Zipursky RB. The role of maintenance pharmacotherapy in achieving recovery from a first episode of schizophrenia. Int Rev Psychiatry. 2002;14(4):284-92.
Bipolar depression dilemma: Continue antidepressants after remission—or not?
Psychiatrists in the trenches are not alone in being unsure how to treat breakthrough bipolar depression. No panelist or other expert attending a recent American College of Neuropsychopharmacology symposium could definitively recommend:
- when to add an antidepressant to mood-stabilizer therapy
- whether to discontinue antidepressants after bipolar depression is stabilized.
Until controlled trials address these issues, we must use limited evidence to treat patients with bipolar depression. To help you meet this challenge, this article offers provisional suggestions based on recent published and unpublished reports.
Evidence for continuing
No published, randomized studies have examined how long to continue antidepressants after bipolar depression has stabilized. Until recently, conventional wisdom has been to discontinue antidepressants as soon as possible because of worries about antidepressant-induced mania. Then two case-controlled studies—one retrospective and one prospective—challenged that assumption.
Figure Reduced relapse rates in patients whose antidepressants were continued
In a prospective case-controlled study, patients with bipolar disorder who continued antidepressant treatment for 6 to 12 months or >12 months after depressive episode remission had lower relapse rates than those who discontinued antidepressants within 6 months.
Source: Reprinted with permission from reference 2. Copyright 2003. American Psychiatric AssociationUsing similar methodologies, Altshuler et al1,2 examined bipolar patients who remained in remission for 6 weeks on mood stabilizers plus adjunctive antidepressants. Those who continued the antidepressants were less likely to relapse into depression (without an increase in manic episodes) than those whose antidepressants were discontinued (Figure).
Relapse rates in the first study1 were 35% at 1 year in those who continued antidepressants and 68% in those who did not. In the second study,2 36% and 70% of patients, respectively, had relapsed at 1 year. In the latter study, those who continued to take antidepressants for at least 6 months—instead of at least 12 months—had intermediate depressive relapse rates (53% for 6 months vs. 24% for 12 months).
When interpreting these data, keep several caveats in mind. For one, patients were not randomly assigned to continue or discontinue antidepressants but were designated by patient and clinician choice. When comparing the two patient groups, however, the authors found no inherent differences in illness characteristics that might have biased the results.
More importantly, few patients initially treated with antidepressant augmentation responded well and remained in remission. In the prospective study, 549 of 1,078 patients in the Stanley Foundation Bipolar Network received an antidepressant for breakthrough depressive symptoms.2 Only 189 remained on antidepressants for 2 months, and only 84 (15%) of the original population remained in remission for 2 months.
Summary. A small subgroup of patients appears to respond well to antidepressants and sustains this response for 6 to 8 weeks. For this subset, continuing antidepressant therapy would appear to be an appropriate strategy, based on:
- a significantly reduced risk for depressive relapse
- no increased risk of switching to mania, which is the usual reason to terminate antidepressants early.
Subsequent evidence
One needs to assess these observations in light of an interim analysis reported halfway through a small, open, randomized study. Ghaemi et al3 found no significant difference in outcomes—regardless of rapid-cycling status—among 14 bipolar patients who remained on antidepressants and 19 who discontinued across an average 60 and 50 weeks, respectively.
Table
Evidence on continuing antidepressants in breakthrough bipolar depression
| Study | Design | Results |
|---|---|---|
| Altshuler et al 1 | Retrospective, case-control, 39 patients (1 year) | Relapse rates: 35% in patients who continued antidepressants after mood stabilization and and 68% in those who did not; study included no rapid-cyclers |
| Altshuler et al 2 | Prospective, case control 84 patients (1 year) | Relapse rates: 36% in patients who continued antidepressants after mood stabilization and 70% in those who did not; study included no rapid cyclers |
| Ghaemi et al 3 (unpublished) | Open, randomized 33 patients (approx. 1 yr) | Relapse rate: 50% within 20 weeks, whether or not patients continued antidepressants; one-third of patients were rapid cyclers |
A survival analysis initially suggested some benefit for continuing antidepressants, but this disappeared when the authors adjusted for potential confounding factors—which was not done in the Altshuler et al studies. Patients receiving short-term or long-term antidepressants had a similar number of depressive episodes per year (1.00 vs. 0.75 episodes/year, respectively). For some reason, nonrapid-cycling patients showed greater depressive morbidity than those with rapid cycling.
Rapid cyclers comprised 30% of patients who continued antidepressants and 37% of those who discontinued. This may explain the 50% relapse rate within 20 weeks in both groups. By comparison, the Altshuler et al studies included no rapid cyclers.1,2 More details on this unpublished data are expected.
Are antidepressants the answer?
The high relapse rate in patients taking mood stabilizers—with or without an antidepressant—and the Ghaemi et al data3 suggest that we need alternate antidepressant approaches to bipolar depression. Potential regimens—anticonvulsants, atypical antipsychotics, and other agents—merit further study. So far the evidence is mixed, and the most effective approaches are not well-delineated.
Anticonvulsants. Sachs et al4 reported that adding lamotrigine or lamotrigine plus an antidepressant to mood stabilizer therapy did not appear more effective in treating bipolar depression than simply maintaining the mood stabilizers.
Similarly, a small randomized, double-blind study in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) was stopped early because of low total response. Adjunctive lamotrigine (24%) and inositol (17%) appeared more effective than risperidone (5%) for refractory bipolar depression.
Antipsychotics. In an 8-week randomized trial by Tohen et al,5 833 patients with moderate to severe bipolar I depression were treated with olanzapine, olanzapine plus fluoxetine, or placebo. Core depression symptoms improved significantly more with olanzapine alone or with fluoxetine compared with placebo, as measured by mean changes in the Montgomery-Asberg Depression Rating Scale.
In a 6-month open trial, 192 patients whose bipolar I depression remitted with any of the three treatments6 continued olanzapine and then, if needed after the first week, the olanzapine/fluoxetine combination (OFC). Nearly two-thirds of patients (62%) remained without a depressive recurrence, and 94% remained without a manic recurrence while taking the OFC. These unpublished data indicate that the OFC provided greater prophylactic antimanic than antidepressant effects.
Calabrese et al7 recently presented unpublished data comparing the effects of quetiapine monotherapy, 300 or 600 mg/d, with placebo in patients with bipolar depression. Beginning in the first week of treatment, both quetiapine dosages produced significantly greater antidepressant, antianxiety, and anti-insomnia effects than placebo (P < 0.001). Remission rates with both dosages were >50%.
Summary. These first controlled studies of atypical antipsychotics in bipolar depression suggest that this drug class may have antidepressant as well as their demonstrated antimanic effects.
Recommendations—for now
Controlled clinical trials have not been conducted, and the evidence on using adjunctive antidepressants in bipolar depression is ambiguous.8-11 As a result, it is unclear when or how long to use antidepressants, and many of the inferences and suggestions in this paper remain highly provisional.
Initiating antidepressants. My personal treatment guidelines—and those of many other clinicians—are to use the unimodal antidepressants to augment mood stabilizers in bipolar patients experiencing breakthrough depression, as long as they have not had:
- ultra-rapid cycling (>4 episodes/week)
- antidepressant-induced cycle acceleration
- or multiple episodes of antidepressant-induced mania, despite co-treatment with mood stabilizers.
If any of these variables is present, I would instead add another mood stabilizer or an atypical antipsychotic.
Continuing antidepressants. If the patient remains stable for 2 months after the antidepressant is added—with no depression or manic occurrence—I would continue the antidepressant indefinitely, based on the Altshuler et al data.12
Mood charting.I also recommend that clinicians help patients develop an individual method for mood charting, such as that used in the National Institute of Mental Health Life Chart Method (NIMH-LCM)12,13 or the STEP-BD program.14 Goals of the 5-year STEP-BD are to:
- determine the most effective treatments and relapse prevention strategies for bipolar disorder
- evaluate the psychotropic benefit of anticonvulsants, atypical antipsychotics, cholinesterase inhibitors, and neurotransmitter precursors
- determine the benefit of psychotropic combinations.
Mood charts can provide a retrospective and prospective overview of a patient’s illness course and response to medications. Compared with patient recall, mood charts help clinicians evaluate more precisely the risk of switching and the risks and benefits of starting, continuing, or discontinuing antidepressants. Mood charts may be your most effective tool for managing a patient’s bipolar depression and achieving and maintaining long-term remission.
Summary. In the absence of consensus or guidelines for treating bipolar depression, I suggest:
- a conservative approach—ie, no changes in medication—when the patient remains well on a given regimen
- an aggressive—if not radical—series of treatments and revisions when the illness course remains problematic.
Many medication classes and adjunctive strategies are available for treating bipolar illness.15-18 I recommend that you continue to systematically explore adjunctive treatments and combinations until the patient improves or—even better—attains remission. Good response can be achieved—even in treatment-refractory patients ill for long periods or with recurrent bipolar depression—although complex combination therapy is often required.
Related resources
- National Institute of Mental Health-Life Chart Method. Retrospective and prospective mood-tracking charts for patients with bipolar disorder. www.bipolarnews.org
- Systematic Treatment Enhancement Program for Bipolar Depression (STEP-BD). National Institute of Mental Health. www.stepbd.org/research/
Drug brand names
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosure
Dr. Post is a consultant to Abbott Laboratories, Astra-Zeneca Pharmaceuticals, Bristol-Myers Squibb Co., Elan Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Novartis Pharmaceuticals Corp., Shire Pharmaceuticals, and UCB Pharma.
1. Altshuler L, Kiriakos L, Calcagno J, et al. The impact of antidepressant discontinuation versus antidepressant continuation on 1-year risk for relapse of bipolar depression: a retrospective chart review. J Clin Psychiatry 2001;62:612-16.
2. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
3. Ghaemi S, El-Mallakh R, Baldassano CF, et al. Antidepressant treatment in bipolar depression: Long-term outcome (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
4. Sachs GS. Mood stabilizers alone vs.mood stabilizers plus antidepressant in bipolar depression (symposium). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
5. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
6. Tohen M, Vieta E, Ketter TA, et al. Acute and long-term efficacy of olanzapine and olanzapine/fluoxetine combination for bipolar depression (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
7. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression (abstract). New York: American Psychiatric Association annual meeting, 2004.
8. Post RM, Denicoff KD, Leverich GS, et al. Presentations of depression in bipolar illness. Clin Neurosci Res 2002a;2:142-57.
9. Post RM, Leverich GS, Nolen WA, et al. A re-evaluation of the role of antidepressants in the treatment of bipolar depression: data from the Stanley Bipolar Treatment Network. Bipolar Disord 2003a;5:396-406.
10. Post RM, Speer AM, Leverich GS. Bipolar illness: Which critical treatment issues need studying? Clinical Approaches in Bipolar Disorders 2003b;2:24-30.
11. Goodwin GM. Bipolar disorder: is psychiatry’s Cinderella starting to get out a little more? Acta Neuropsychiatry 2000;12:105.-
12. Leverich GS, Post RM. Life charting the course of bipolar disorder. Current Review of Mood and Anxiety Disorders 1996;1:48-61.
13. Leverich GS, Post RM. Life charting of affective disorders. CNS Spectrums 1998;3:21-37.
14. Sachs GS, Thase ME, Otto MW, et al. Rationale, design, and methods of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2003;53:1028-42.
15. Post RM, Speer AM, Obrocea GV, Leverich GS. Acute and prophylactic effects of anticonvulsants in bipolar depression. Clin Neurosci Res 2002;2:228-51.
16. Post RM, Speer AM. A brief history of anticonvulsant use in affective disorders. In: Trimble MR, Schmitz B (eds). Seizures, affective disorders and anticonvulsant drugs Surrey, UK: Clarius Press 2002;53:81.-
17. Post RM, Speer AM, Leverich GS. Complex combination therapy: the evolution toward rational polypharmacy in lithium-resistant bipolar illness, In: Akiskal H, Tohen M (eds). 50 years: the psychopharmacology of bipolar illness London: John Wiley & Sons Ltd. 2004 (in press).
18. Post RM, Altshuler LL. Mood disorders: treatment of bipolar disorders. Sadock BJ, Sadock VA (eds). Kaplan & Sadock’s comprehensive textbook of psychiatry (8th ed) New York: Lippincott Williams & Wilkins, 2004 (in press).
Psychiatrists in the trenches are not alone in being unsure how to treat breakthrough bipolar depression. No panelist or other expert attending a recent American College of Neuropsychopharmacology symposium could definitively recommend:
- when to add an antidepressant to mood-stabilizer therapy
- whether to discontinue antidepressants after bipolar depression is stabilized.
Until controlled trials address these issues, we must use limited evidence to treat patients with bipolar depression. To help you meet this challenge, this article offers provisional suggestions based on recent published and unpublished reports.
Evidence for continuing
No published, randomized studies have examined how long to continue antidepressants after bipolar depression has stabilized. Until recently, conventional wisdom has been to discontinue antidepressants as soon as possible because of worries about antidepressant-induced mania. Then two case-controlled studies—one retrospective and one prospective—challenged that assumption.
Figure Reduced relapse rates in patients whose antidepressants were continued
In a prospective case-controlled study, patients with bipolar disorder who continued antidepressant treatment for 6 to 12 months or >12 months after depressive episode remission had lower relapse rates than those who discontinued antidepressants within 6 months.
Source: Reprinted with permission from reference 2. Copyright 2003. American Psychiatric AssociationUsing similar methodologies, Altshuler et al1,2 examined bipolar patients who remained in remission for 6 weeks on mood stabilizers plus adjunctive antidepressants. Those who continued the antidepressants were less likely to relapse into depression (without an increase in manic episodes) than those whose antidepressants were discontinued (Figure).
Relapse rates in the first study1 were 35% at 1 year in those who continued antidepressants and 68% in those who did not. In the second study,2 36% and 70% of patients, respectively, had relapsed at 1 year. In the latter study, those who continued to take antidepressants for at least 6 months—instead of at least 12 months—had intermediate depressive relapse rates (53% for 6 months vs. 24% for 12 months).
When interpreting these data, keep several caveats in mind. For one, patients were not randomly assigned to continue or discontinue antidepressants but were designated by patient and clinician choice. When comparing the two patient groups, however, the authors found no inherent differences in illness characteristics that might have biased the results.
More importantly, few patients initially treated with antidepressant augmentation responded well and remained in remission. In the prospective study, 549 of 1,078 patients in the Stanley Foundation Bipolar Network received an antidepressant for breakthrough depressive symptoms.2 Only 189 remained on antidepressants for 2 months, and only 84 (15%) of the original population remained in remission for 2 months.
Summary. A small subgroup of patients appears to respond well to antidepressants and sustains this response for 6 to 8 weeks. For this subset, continuing antidepressant therapy would appear to be an appropriate strategy, based on:
- a significantly reduced risk for depressive relapse
- no increased risk of switching to mania, which is the usual reason to terminate antidepressants early.
Subsequent evidence
One needs to assess these observations in light of an interim analysis reported halfway through a small, open, randomized study. Ghaemi et al3 found no significant difference in outcomes—regardless of rapid-cycling status—among 14 bipolar patients who remained on antidepressants and 19 who discontinued across an average 60 and 50 weeks, respectively.
Table
Evidence on continuing antidepressants in breakthrough bipolar depression
| Study | Design | Results |
|---|---|---|
| Altshuler et al 1 | Retrospective, case-control, 39 patients (1 year) | Relapse rates: 35% in patients who continued antidepressants after mood stabilization and and 68% in those who did not; study included no rapid-cyclers |
| Altshuler et al 2 | Prospective, case control 84 patients (1 year) | Relapse rates: 36% in patients who continued antidepressants after mood stabilization and 70% in those who did not; study included no rapid cyclers |
| Ghaemi et al 3 (unpublished) | Open, randomized 33 patients (approx. 1 yr) | Relapse rate: 50% within 20 weeks, whether or not patients continued antidepressants; one-third of patients were rapid cyclers |
A survival analysis initially suggested some benefit for continuing antidepressants, but this disappeared when the authors adjusted for potential confounding factors—which was not done in the Altshuler et al studies. Patients receiving short-term or long-term antidepressants had a similar number of depressive episodes per year (1.00 vs. 0.75 episodes/year, respectively). For some reason, nonrapid-cycling patients showed greater depressive morbidity than those with rapid cycling.
Rapid cyclers comprised 30% of patients who continued antidepressants and 37% of those who discontinued. This may explain the 50% relapse rate within 20 weeks in both groups. By comparison, the Altshuler et al studies included no rapid cyclers.1,2 More details on this unpublished data are expected.
Are antidepressants the answer?
The high relapse rate in patients taking mood stabilizers—with or without an antidepressant—and the Ghaemi et al data3 suggest that we need alternate antidepressant approaches to bipolar depression. Potential regimens—anticonvulsants, atypical antipsychotics, and other agents—merit further study. So far the evidence is mixed, and the most effective approaches are not well-delineated.
Anticonvulsants. Sachs et al4 reported that adding lamotrigine or lamotrigine plus an antidepressant to mood stabilizer therapy did not appear more effective in treating bipolar depression than simply maintaining the mood stabilizers.
Similarly, a small randomized, double-blind study in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) was stopped early because of low total response. Adjunctive lamotrigine (24%) and inositol (17%) appeared more effective than risperidone (5%) for refractory bipolar depression.
Antipsychotics. In an 8-week randomized trial by Tohen et al,5 833 patients with moderate to severe bipolar I depression were treated with olanzapine, olanzapine plus fluoxetine, or placebo. Core depression symptoms improved significantly more with olanzapine alone or with fluoxetine compared with placebo, as measured by mean changes in the Montgomery-Asberg Depression Rating Scale.
In a 6-month open trial, 192 patients whose bipolar I depression remitted with any of the three treatments6 continued olanzapine and then, if needed after the first week, the olanzapine/fluoxetine combination (OFC). Nearly two-thirds of patients (62%) remained without a depressive recurrence, and 94% remained without a manic recurrence while taking the OFC. These unpublished data indicate that the OFC provided greater prophylactic antimanic than antidepressant effects.
Calabrese et al7 recently presented unpublished data comparing the effects of quetiapine monotherapy, 300 or 600 mg/d, with placebo in patients with bipolar depression. Beginning in the first week of treatment, both quetiapine dosages produced significantly greater antidepressant, antianxiety, and anti-insomnia effects than placebo (P < 0.001). Remission rates with both dosages were >50%.
Summary. These first controlled studies of atypical antipsychotics in bipolar depression suggest that this drug class may have antidepressant as well as their demonstrated antimanic effects.
Recommendations—for now
Controlled clinical trials have not been conducted, and the evidence on using adjunctive antidepressants in bipolar depression is ambiguous.8-11 As a result, it is unclear when or how long to use antidepressants, and many of the inferences and suggestions in this paper remain highly provisional.
Initiating antidepressants. My personal treatment guidelines—and those of many other clinicians—are to use the unimodal antidepressants to augment mood stabilizers in bipolar patients experiencing breakthrough depression, as long as they have not had:
- ultra-rapid cycling (>4 episodes/week)
- antidepressant-induced cycle acceleration
- or multiple episodes of antidepressant-induced mania, despite co-treatment with mood stabilizers.
If any of these variables is present, I would instead add another mood stabilizer or an atypical antipsychotic.
Continuing antidepressants. If the patient remains stable for 2 months after the antidepressant is added—with no depression or manic occurrence—I would continue the antidepressant indefinitely, based on the Altshuler et al data.12
Mood charting.I also recommend that clinicians help patients develop an individual method for mood charting, such as that used in the National Institute of Mental Health Life Chart Method (NIMH-LCM)12,13 or the STEP-BD program.14 Goals of the 5-year STEP-BD are to:
- determine the most effective treatments and relapse prevention strategies for bipolar disorder
- evaluate the psychotropic benefit of anticonvulsants, atypical antipsychotics, cholinesterase inhibitors, and neurotransmitter precursors
- determine the benefit of psychotropic combinations.
Mood charts can provide a retrospective and prospective overview of a patient’s illness course and response to medications. Compared with patient recall, mood charts help clinicians evaluate more precisely the risk of switching and the risks and benefits of starting, continuing, or discontinuing antidepressants. Mood charts may be your most effective tool for managing a patient’s bipolar depression and achieving and maintaining long-term remission.
Summary. In the absence of consensus or guidelines for treating bipolar depression, I suggest:
- a conservative approach—ie, no changes in medication—when the patient remains well on a given regimen
- an aggressive—if not radical—series of treatments and revisions when the illness course remains problematic.
Many medication classes and adjunctive strategies are available for treating bipolar illness.15-18 I recommend that you continue to systematically explore adjunctive treatments and combinations until the patient improves or—even better—attains remission. Good response can be achieved—even in treatment-refractory patients ill for long periods or with recurrent bipolar depression—although complex combination therapy is often required.
Related resources
- National Institute of Mental Health-Life Chart Method. Retrospective and prospective mood-tracking charts for patients with bipolar disorder. www.bipolarnews.org
- Systematic Treatment Enhancement Program for Bipolar Depression (STEP-BD). National Institute of Mental Health. www.stepbd.org/research/
Drug brand names
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosure
Dr. Post is a consultant to Abbott Laboratories, Astra-Zeneca Pharmaceuticals, Bristol-Myers Squibb Co., Elan Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Novartis Pharmaceuticals Corp., Shire Pharmaceuticals, and UCB Pharma.
Psychiatrists in the trenches are not alone in being unsure how to treat breakthrough bipolar depression. No panelist or other expert attending a recent American College of Neuropsychopharmacology symposium could definitively recommend:
- when to add an antidepressant to mood-stabilizer therapy
- whether to discontinue antidepressants after bipolar depression is stabilized.
Until controlled trials address these issues, we must use limited evidence to treat patients with bipolar depression. To help you meet this challenge, this article offers provisional suggestions based on recent published and unpublished reports.
Evidence for continuing
No published, randomized studies have examined how long to continue antidepressants after bipolar depression has stabilized. Until recently, conventional wisdom has been to discontinue antidepressants as soon as possible because of worries about antidepressant-induced mania. Then two case-controlled studies—one retrospective and one prospective—challenged that assumption.
Figure Reduced relapse rates in patients whose antidepressants were continued
In a prospective case-controlled study, patients with bipolar disorder who continued antidepressant treatment for 6 to 12 months or >12 months after depressive episode remission had lower relapse rates than those who discontinued antidepressants within 6 months.
Source: Reprinted with permission from reference 2. Copyright 2003. American Psychiatric AssociationUsing similar methodologies, Altshuler et al1,2 examined bipolar patients who remained in remission for 6 weeks on mood stabilizers plus adjunctive antidepressants. Those who continued the antidepressants were less likely to relapse into depression (without an increase in manic episodes) than those whose antidepressants were discontinued (Figure).
Relapse rates in the first study1 were 35% at 1 year in those who continued antidepressants and 68% in those who did not. In the second study,2 36% and 70% of patients, respectively, had relapsed at 1 year. In the latter study, those who continued to take antidepressants for at least 6 months—instead of at least 12 months—had intermediate depressive relapse rates (53% for 6 months vs. 24% for 12 months).
When interpreting these data, keep several caveats in mind. For one, patients were not randomly assigned to continue or discontinue antidepressants but were designated by patient and clinician choice. When comparing the two patient groups, however, the authors found no inherent differences in illness characteristics that might have biased the results.
More importantly, few patients initially treated with antidepressant augmentation responded well and remained in remission. In the prospective study, 549 of 1,078 patients in the Stanley Foundation Bipolar Network received an antidepressant for breakthrough depressive symptoms.2 Only 189 remained on antidepressants for 2 months, and only 84 (15%) of the original population remained in remission for 2 months.
Summary. A small subgroup of patients appears to respond well to antidepressants and sustains this response for 6 to 8 weeks. For this subset, continuing antidepressant therapy would appear to be an appropriate strategy, based on:
- a significantly reduced risk for depressive relapse
- no increased risk of switching to mania, which is the usual reason to terminate antidepressants early.
Subsequent evidence
One needs to assess these observations in light of an interim analysis reported halfway through a small, open, randomized study. Ghaemi et al3 found no significant difference in outcomes—regardless of rapid-cycling status—among 14 bipolar patients who remained on antidepressants and 19 who discontinued across an average 60 and 50 weeks, respectively.
Table
Evidence on continuing antidepressants in breakthrough bipolar depression
| Study | Design | Results |
|---|---|---|
| Altshuler et al 1 | Retrospective, case-control, 39 patients (1 year) | Relapse rates: 35% in patients who continued antidepressants after mood stabilization and and 68% in those who did not; study included no rapid-cyclers |
| Altshuler et al 2 | Prospective, case control 84 patients (1 year) | Relapse rates: 36% in patients who continued antidepressants after mood stabilization and 70% in those who did not; study included no rapid cyclers |
| Ghaemi et al 3 (unpublished) | Open, randomized 33 patients (approx. 1 yr) | Relapse rate: 50% within 20 weeks, whether or not patients continued antidepressants; one-third of patients were rapid cyclers |
A survival analysis initially suggested some benefit for continuing antidepressants, but this disappeared when the authors adjusted for potential confounding factors—which was not done in the Altshuler et al studies. Patients receiving short-term or long-term antidepressants had a similar number of depressive episodes per year (1.00 vs. 0.75 episodes/year, respectively). For some reason, nonrapid-cycling patients showed greater depressive morbidity than those with rapid cycling.
Rapid cyclers comprised 30% of patients who continued antidepressants and 37% of those who discontinued. This may explain the 50% relapse rate within 20 weeks in both groups. By comparison, the Altshuler et al studies included no rapid cyclers.1,2 More details on this unpublished data are expected.
Are antidepressants the answer?
The high relapse rate in patients taking mood stabilizers—with or without an antidepressant—and the Ghaemi et al data3 suggest that we need alternate antidepressant approaches to bipolar depression. Potential regimens—anticonvulsants, atypical antipsychotics, and other agents—merit further study. So far the evidence is mixed, and the most effective approaches are not well-delineated.
Anticonvulsants. Sachs et al4 reported that adding lamotrigine or lamotrigine plus an antidepressant to mood stabilizer therapy did not appear more effective in treating bipolar depression than simply maintaining the mood stabilizers.
Similarly, a small randomized, double-blind study in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) was stopped early because of low total response. Adjunctive lamotrigine (24%) and inositol (17%) appeared more effective than risperidone (5%) for refractory bipolar depression.
Antipsychotics. In an 8-week randomized trial by Tohen et al,5 833 patients with moderate to severe bipolar I depression were treated with olanzapine, olanzapine plus fluoxetine, or placebo. Core depression symptoms improved significantly more with olanzapine alone or with fluoxetine compared with placebo, as measured by mean changes in the Montgomery-Asberg Depression Rating Scale.
In a 6-month open trial, 192 patients whose bipolar I depression remitted with any of the three treatments6 continued olanzapine and then, if needed after the first week, the olanzapine/fluoxetine combination (OFC). Nearly two-thirds of patients (62%) remained without a depressive recurrence, and 94% remained without a manic recurrence while taking the OFC. These unpublished data indicate that the OFC provided greater prophylactic antimanic than antidepressant effects.
Calabrese et al7 recently presented unpublished data comparing the effects of quetiapine monotherapy, 300 or 600 mg/d, with placebo in patients with bipolar depression. Beginning in the first week of treatment, both quetiapine dosages produced significantly greater antidepressant, antianxiety, and anti-insomnia effects than placebo (P < 0.001). Remission rates with both dosages were >50%.
Summary. These first controlled studies of atypical antipsychotics in bipolar depression suggest that this drug class may have antidepressant as well as their demonstrated antimanic effects.
Recommendations—for now
Controlled clinical trials have not been conducted, and the evidence on using adjunctive antidepressants in bipolar depression is ambiguous.8-11 As a result, it is unclear when or how long to use antidepressants, and many of the inferences and suggestions in this paper remain highly provisional.
Initiating antidepressants. My personal treatment guidelines—and those of many other clinicians—are to use the unimodal antidepressants to augment mood stabilizers in bipolar patients experiencing breakthrough depression, as long as they have not had:
- ultra-rapid cycling (>4 episodes/week)
- antidepressant-induced cycle acceleration
- or multiple episodes of antidepressant-induced mania, despite co-treatment with mood stabilizers.
If any of these variables is present, I would instead add another mood stabilizer or an atypical antipsychotic.
Continuing antidepressants. If the patient remains stable for 2 months after the antidepressant is added—with no depression or manic occurrence—I would continue the antidepressant indefinitely, based on the Altshuler et al data.12
Mood charting.I also recommend that clinicians help patients develop an individual method for mood charting, such as that used in the National Institute of Mental Health Life Chart Method (NIMH-LCM)12,13 or the STEP-BD program.14 Goals of the 5-year STEP-BD are to:
- determine the most effective treatments and relapse prevention strategies for bipolar disorder
- evaluate the psychotropic benefit of anticonvulsants, atypical antipsychotics, cholinesterase inhibitors, and neurotransmitter precursors
- determine the benefit of psychotropic combinations.
Mood charts can provide a retrospective and prospective overview of a patient’s illness course and response to medications. Compared with patient recall, mood charts help clinicians evaluate more precisely the risk of switching and the risks and benefits of starting, continuing, or discontinuing antidepressants. Mood charts may be your most effective tool for managing a patient’s bipolar depression and achieving and maintaining long-term remission.
Summary. In the absence of consensus or guidelines for treating bipolar depression, I suggest:
- a conservative approach—ie, no changes in medication—when the patient remains well on a given regimen
- an aggressive—if not radical—series of treatments and revisions when the illness course remains problematic.
Many medication classes and adjunctive strategies are available for treating bipolar illness.15-18 I recommend that you continue to systematically explore adjunctive treatments and combinations until the patient improves or—even better—attains remission. Good response can be achieved—even in treatment-refractory patients ill for long periods or with recurrent bipolar depression—although complex combination therapy is often required.
Related resources
- National Institute of Mental Health-Life Chart Method. Retrospective and prospective mood-tracking charts for patients with bipolar disorder. www.bipolarnews.org
- Systematic Treatment Enhancement Program for Bipolar Depression (STEP-BD). National Institute of Mental Health. www.stepbd.org/research/
Drug brand names
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosure
Dr. Post is a consultant to Abbott Laboratories, Astra-Zeneca Pharmaceuticals, Bristol-Myers Squibb Co., Elan Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Novartis Pharmaceuticals Corp., Shire Pharmaceuticals, and UCB Pharma.
1. Altshuler L, Kiriakos L, Calcagno J, et al. The impact of antidepressant discontinuation versus antidepressant continuation on 1-year risk for relapse of bipolar depression: a retrospective chart review. J Clin Psychiatry 2001;62:612-16.
2. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
3. Ghaemi S, El-Mallakh R, Baldassano CF, et al. Antidepressant treatment in bipolar depression: Long-term outcome (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
4. Sachs GS. Mood stabilizers alone vs.mood stabilizers plus antidepressant in bipolar depression (symposium). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
5. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
6. Tohen M, Vieta E, Ketter TA, et al. Acute and long-term efficacy of olanzapine and olanzapine/fluoxetine combination for bipolar depression (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
7. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression (abstract). New York: American Psychiatric Association annual meeting, 2004.
8. Post RM, Denicoff KD, Leverich GS, et al. Presentations of depression in bipolar illness. Clin Neurosci Res 2002a;2:142-57.
9. Post RM, Leverich GS, Nolen WA, et al. A re-evaluation of the role of antidepressants in the treatment of bipolar depression: data from the Stanley Bipolar Treatment Network. Bipolar Disord 2003a;5:396-406.
10. Post RM, Speer AM, Leverich GS. Bipolar illness: Which critical treatment issues need studying? Clinical Approaches in Bipolar Disorders 2003b;2:24-30.
11. Goodwin GM. Bipolar disorder: is psychiatry’s Cinderella starting to get out a little more? Acta Neuropsychiatry 2000;12:105.-
12. Leverich GS, Post RM. Life charting the course of bipolar disorder. Current Review of Mood and Anxiety Disorders 1996;1:48-61.
13. Leverich GS, Post RM. Life charting of affective disorders. CNS Spectrums 1998;3:21-37.
14. Sachs GS, Thase ME, Otto MW, et al. Rationale, design, and methods of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2003;53:1028-42.
15. Post RM, Speer AM, Obrocea GV, Leverich GS. Acute and prophylactic effects of anticonvulsants in bipolar depression. Clin Neurosci Res 2002;2:228-51.
16. Post RM, Speer AM. A brief history of anticonvulsant use in affective disorders. In: Trimble MR, Schmitz B (eds). Seizures, affective disorders and anticonvulsant drugs Surrey, UK: Clarius Press 2002;53:81.-
17. Post RM, Speer AM, Leverich GS. Complex combination therapy: the evolution toward rational polypharmacy in lithium-resistant bipolar illness, In: Akiskal H, Tohen M (eds). 50 years: the psychopharmacology of bipolar illness London: John Wiley & Sons Ltd. 2004 (in press).
18. Post RM, Altshuler LL. Mood disorders: treatment of bipolar disorders. Sadock BJ, Sadock VA (eds). Kaplan & Sadock’s comprehensive textbook of psychiatry (8th ed) New York: Lippincott Williams & Wilkins, 2004 (in press).
1. Altshuler L, Kiriakos L, Calcagno J, et al. The impact of antidepressant discontinuation versus antidepressant continuation on 1-year risk for relapse of bipolar depression: a retrospective chart review. J Clin Psychiatry 2001;62:612-16.
2. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
3. Ghaemi S, El-Mallakh R, Baldassano CF, et al. Antidepressant treatment in bipolar depression: Long-term outcome (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
4. Sachs GS. Mood stabilizers alone vs.mood stabilizers plus antidepressant in bipolar depression (symposium). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
5. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
6. Tohen M, Vieta E, Ketter TA, et al. Acute and long-term efficacy of olanzapine and olanzapine/fluoxetine combination for bipolar depression (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
7. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression (abstract). New York: American Psychiatric Association annual meeting, 2004.
8. Post RM, Denicoff KD, Leverich GS, et al. Presentations of depression in bipolar illness. Clin Neurosci Res 2002a;2:142-57.
9. Post RM, Leverich GS, Nolen WA, et al. A re-evaluation of the role of antidepressants in the treatment of bipolar depression: data from the Stanley Bipolar Treatment Network. Bipolar Disord 2003a;5:396-406.
10. Post RM, Speer AM, Leverich GS. Bipolar illness: Which critical treatment issues need studying? Clinical Approaches in Bipolar Disorders 2003b;2:24-30.
11. Goodwin GM. Bipolar disorder: is psychiatry’s Cinderella starting to get out a little more? Acta Neuropsychiatry 2000;12:105.-
12. Leverich GS, Post RM. Life charting the course of bipolar disorder. Current Review of Mood and Anxiety Disorders 1996;1:48-61.
13. Leverich GS, Post RM. Life charting of affective disorders. CNS Spectrums 1998;3:21-37.
14. Sachs GS, Thase ME, Otto MW, et al. Rationale, design, and methods of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2003;53:1028-42.
15. Post RM, Speer AM, Obrocea GV, Leverich GS. Acute and prophylactic effects of anticonvulsants in bipolar depression. Clin Neurosci Res 2002;2:228-51.
16. Post RM, Speer AM. A brief history of anticonvulsant use in affective disorders. In: Trimble MR, Schmitz B (eds). Seizures, affective disorders and anticonvulsant drugs Surrey, UK: Clarius Press 2002;53:81.-
17. Post RM, Speer AM, Leverich GS. Complex combination therapy: the evolution toward rational polypharmacy in lithium-resistant bipolar illness, In: Akiskal H, Tohen M (eds). 50 years: the psychopharmacology of bipolar illness London: John Wiley & Sons Ltd. 2004 (in press).
18. Post RM, Altshuler LL. Mood disorders: treatment of bipolar disorders. Sadock BJ, Sadock VA (eds). Kaplan & Sadock’s comprehensive textbook of psychiatry (8th ed) New York: Lippincott Williams & Wilkins, 2004 (in press).
Suicide risk assessment: Questions that reveal what you really need to know
You can make more-informed decisions about a patient’s acute suicide risk—such as over the phone at 3 AM—if you know what to ask the psychiatry resident or crisis worker. For suicide risk assessment—especially when you have not seen the patient—you need specific, high-yield questions to draw out danger signals from large amounts of data.
We are not suggesting that a short list of questions is sufficient for this extremely difficult task. Rather—because we recognize its complexity—we offer the questions we find most useful when evaluating patients with suicidal behaviors.
American Psychiatric Association practice guidelines1 provide a comprehensive discussion of assessing suicide risk. In addition, we teach clinicians we supervise to probe for high-risk and less-commonly explored “protective” factors.
High-risk factors
Mental health clinicians are more experienced in probing for high-risk factors than for protective factors. Because population studies offer limited help (Box 1),2 we ask clinicians these questions to evaluate the seriousness of a suicide attempt:
- Most studies of suicide risk factors focus on medium- to long-range risk
- Population-based risk factors (such as being Caucasian, over age 65, or depressed) apply to so many patients that their clinical usefulness is limited1
- Population-based risk factors often have high sensitivity but low specificity (recent loss is an important risk factor for attempting suicide, for example, but very few persons with a recent loss attempt suicide)
- In an acute situation, the positive predictive value of suicide risk factors—alone or in combination—is not known
Table
3 important questions to ask in overdose cases
|
What method was used? Methods other than taking an overdose or cutting the wrists may be more dangerous.
What amount was used? (in overdose or poisoning cases)
What treatment was needed? If the patient took an overdose of opioids and needs intubation, this indicates a relatively serious attempt. On the other hand, the psychiatric seriousness of an acetaminophen overdose depends on whether the patient realized the danger in taking high doses of acetaminophen. Additional questions can help determine the seriousness of suicide attempts by overdose (Table).
Was the attempt impulsive or planned? Planned attempts tend to be more serious.
What is the ‘risk-rescue ratio’? The potential lethality of the attempt and the likelihood of being saved must be evaluated together. Where did the attempt occur? In a setting where others were likely to intervene? Was the patient alone? Attempts in the presence of others may be considered less alarming.
What did the patient do immediately afterward? Did he tell anyone? How did he get to the hospital? Did he seek help on his own? Who called the ambulance?
How does the patient feel about the attempt now? Is she glad or disappointed she didn’t die? Does she regret the attempt?
Have there been past attempts? Does the patient have a history of suicide attempts or significant selfmutilation? If so, what was the most serious incident? Past attempts tend to predict future attempts.
Other considerations for patients who have attempted suicide and those who have not but are being evaluated for possible suicide risk include:
Mental state. To estimate a patient’s mental state and depth of negative affect, without having seen her yourself, three helpful questions are:
- Does she still look upset, depressed, or angry? Anger and agitation tend to increase risk.
- Can she smile or relax, even briefly?
- Does she feel things are likely to improve?
Access to firearms. Suicide by firearms accounts for 55% of all suicides.3 Does the patient have access to a gun and bullets? If so, get details. Does he now keep the gun on his person instead of in a locked cabinet, as he did earlier? We find that questions about guns are all too frequently omitted.
Contract for safety. Can the patient reliably contract not to harm himself and to call for help in a crisis? Although contracts for safety have limited value—as will be discussed—a patient’s refusal to contract for safety may indicate a higher suicide risk.
Some patients may refuse to contract for safety in order to be hospitalized for other reasons. They may say they can’t be sure what they will do if not admitted or declare that the clinician will be blamed for their death.
Protective factors
A patient’s high-risk clinical features must be balanced against factors that may reduce suicide risk.
How much social support? Can family or friends constantly stay with the patient, watch him closely, and get help if the situation worsens? This is the simplest and most relevant method to assess the availability of protective support.
How much mental health support? Does the patient have a good relationship with a psychiatrist or therapist who can see the patient soon?
Have circumstances changed? Has the stressor that led to suicidal behavior resolved, at least in part? For example, if a patient’s fight with her boyfriend led to her taking an overdose, have they made up?
Four common myths. Clinicians assessing patients for acute suicide risk often overestimate the protective value of some factors. They may tell you:
- The patient only tried to harm himself while he was intoxicated. He’s not intoxicated now and therefore is not at high risk. The patient will likely get intoxicated again, despite his protestations to the contrary. Substance intoxication and withdrawal tend to worsen depression and diminish inhibitions, making suicide more—not less—likely.
- The patient contracts for safety. A contract for safety may have some value,4 but its clinical and legal merits in suicide risk assessment are overestimated.5 We are concerned about how often we see clinicians judge that a contract for safety overrides numerous high-risk factors.
- The patient was only trying to get attention. It is difficult for mental health professionals—and even for patients—to reliably ascertain what motivates someone to attempt suicide. Multiple motivations and ambivalence are common.
- The patient is ‘just a borderline.’ Because patients with borderline personality disorder tend to make repeated suicide gestures, clinicians may not take their suicide attempts seriously. This statement reveals ignorance about the suffering of persons with borderline personality disorder; their rate of completed suicide is approximately 10%.6
- When a suicide assessment is inconclusive, draw two columns on a sheet of paper. List the patient’s high-risk factors on one side and protective factors on the other
- Seeing the information in black and white often helps clarify the assessment
- Consider both the number of factors in each column and your clinical sense of each factor’s importance and intensity. Place a check mark next to particularly important factors
- This balance sheet can remind you of further questions to ask and often reveals that either the high-risk or protective factors far outweigh the others in number and/or intensity
Practical advice
Distinguish short-term vs long-term risk. Based on the questions above, we often conclude that a patient is at high long-term risk of suicide, but the immediate risk is much lower. Acute hospitalization is unlikely to alleviate the long-term risk (though sometimes is the only way to get the patient into psychiatric treatment).
Consider the source. Never disregard the “gut feeling” of the person who interviewed the patient, but also factor in your assessment of that clinician’s judgment. Sometimes inexperienced staffs’ intuitions may derive more from countertransference than from objective assessment.
Write it down. In cases where suicide risk seems unclear, it may help to list a patient’s risk and protective factors (Box 2). We have found this technique to be a useful teaching tool as well.
Be flexible. Because no method for assessing shortterm suicide risk is foolproof, be ready to re-evaluate your assessment and—if you are unsure—to take action to protect the patient.
1. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160(11 suppl):1-60.
2. Fawcett J. Suicide risk factors in depressive disorders and in panic disorder. J Clin Psychiatry. 1992;53(suppl):9-13.
3. National Institute of Mental Health. Suicide facts. Available at: http://www.nimh.nih.gov/SuicidePrevention/suifact.cfm. Accessed June 3, 2004.
4. Stanford EJ, Goetz RR, Bloom JD. The no harm contract in the emergency assessment of suicidal risk. J Clin Psychiatry 1994;55(8):344-8.
5. Simon RI. The suicide prevention contract: clinical, legal, and risk management issues. J Am Acad Psychiatry Law 1999;27(3):445-50.
6. Paris J. Chronic suicidality among patients with borderline personality disorder. Psychiatr Serv 2002;53(6):738-42.
You can make more-informed decisions about a patient’s acute suicide risk—such as over the phone at 3 AM—if you know what to ask the psychiatry resident or crisis worker. For suicide risk assessment—especially when you have not seen the patient—you need specific, high-yield questions to draw out danger signals from large amounts of data.
We are not suggesting that a short list of questions is sufficient for this extremely difficult task. Rather—because we recognize its complexity—we offer the questions we find most useful when evaluating patients with suicidal behaviors.
American Psychiatric Association practice guidelines1 provide a comprehensive discussion of assessing suicide risk. In addition, we teach clinicians we supervise to probe for high-risk and less-commonly explored “protective” factors.
High-risk factors
Mental health clinicians are more experienced in probing for high-risk factors than for protective factors. Because population studies offer limited help (Box 1),2 we ask clinicians these questions to evaluate the seriousness of a suicide attempt:
- Most studies of suicide risk factors focus on medium- to long-range risk
- Population-based risk factors (such as being Caucasian, over age 65, or depressed) apply to so many patients that their clinical usefulness is limited1
- Population-based risk factors often have high sensitivity but low specificity (recent loss is an important risk factor for attempting suicide, for example, but very few persons with a recent loss attempt suicide)
- In an acute situation, the positive predictive value of suicide risk factors—alone or in combination—is not known
Table
3 important questions to ask in overdose cases
|
What method was used? Methods other than taking an overdose or cutting the wrists may be more dangerous.
What amount was used? (in overdose or poisoning cases)
What treatment was needed? If the patient took an overdose of opioids and needs intubation, this indicates a relatively serious attempt. On the other hand, the psychiatric seriousness of an acetaminophen overdose depends on whether the patient realized the danger in taking high doses of acetaminophen. Additional questions can help determine the seriousness of suicide attempts by overdose (Table).
Was the attempt impulsive or planned? Planned attempts tend to be more serious.
What is the ‘risk-rescue ratio’? The potential lethality of the attempt and the likelihood of being saved must be evaluated together. Where did the attempt occur? In a setting where others were likely to intervene? Was the patient alone? Attempts in the presence of others may be considered less alarming.
What did the patient do immediately afterward? Did he tell anyone? How did he get to the hospital? Did he seek help on his own? Who called the ambulance?
How does the patient feel about the attempt now? Is she glad or disappointed she didn’t die? Does she regret the attempt?
Have there been past attempts? Does the patient have a history of suicide attempts or significant selfmutilation? If so, what was the most serious incident? Past attempts tend to predict future attempts.
Other considerations for patients who have attempted suicide and those who have not but are being evaluated for possible suicide risk include:
Mental state. To estimate a patient’s mental state and depth of negative affect, without having seen her yourself, three helpful questions are:
- Does she still look upset, depressed, or angry? Anger and agitation tend to increase risk.
- Can she smile or relax, even briefly?
- Does she feel things are likely to improve?
Access to firearms. Suicide by firearms accounts for 55% of all suicides.3 Does the patient have access to a gun and bullets? If so, get details. Does he now keep the gun on his person instead of in a locked cabinet, as he did earlier? We find that questions about guns are all too frequently omitted.
Contract for safety. Can the patient reliably contract not to harm himself and to call for help in a crisis? Although contracts for safety have limited value—as will be discussed—a patient’s refusal to contract for safety may indicate a higher suicide risk.
Some patients may refuse to contract for safety in order to be hospitalized for other reasons. They may say they can’t be sure what they will do if not admitted or declare that the clinician will be blamed for their death.
Protective factors
A patient’s high-risk clinical features must be balanced against factors that may reduce suicide risk.
How much social support? Can family or friends constantly stay with the patient, watch him closely, and get help if the situation worsens? This is the simplest and most relevant method to assess the availability of protective support.
How much mental health support? Does the patient have a good relationship with a psychiatrist or therapist who can see the patient soon?
Have circumstances changed? Has the stressor that led to suicidal behavior resolved, at least in part? For example, if a patient’s fight with her boyfriend led to her taking an overdose, have they made up?
Four common myths. Clinicians assessing patients for acute suicide risk often overestimate the protective value of some factors. They may tell you:
- The patient only tried to harm himself while he was intoxicated. He’s not intoxicated now and therefore is not at high risk. The patient will likely get intoxicated again, despite his protestations to the contrary. Substance intoxication and withdrawal tend to worsen depression and diminish inhibitions, making suicide more—not less—likely.
- The patient contracts for safety. A contract for safety may have some value,4 but its clinical and legal merits in suicide risk assessment are overestimated.5 We are concerned about how often we see clinicians judge that a contract for safety overrides numerous high-risk factors.
- The patient was only trying to get attention. It is difficult for mental health professionals—and even for patients—to reliably ascertain what motivates someone to attempt suicide. Multiple motivations and ambivalence are common.
- The patient is ‘just a borderline.’ Because patients with borderline personality disorder tend to make repeated suicide gestures, clinicians may not take their suicide attempts seriously. This statement reveals ignorance about the suffering of persons with borderline personality disorder; their rate of completed suicide is approximately 10%.6
- When a suicide assessment is inconclusive, draw two columns on a sheet of paper. List the patient’s high-risk factors on one side and protective factors on the other
- Seeing the information in black and white often helps clarify the assessment
- Consider both the number of factors in each column and your clinical sense of each factor’s importance and intensity. Place a check mark next to particularly important factors
- This balance sheet can remind you of further questions to ask and often reveals that either the high-risk or protective factors far outweigh the others in number and/or intensity
Practical advice
Distinguish short-term vs long-term risk. Based on the questions above, we often conclude that a patient is at high long-term risk of suicide, but the immediate risk is much lower. Acute hospitalization is unlikely to alleviate the long-term risk (though sometimes is the only way to get the patient into psychiatric treatment).
Consider the source. Never disregard the “gut feeling” of the person who interviewed the patient, but also factor in your assessment of that clinician’s judgment. Sometimes inexperienced staffs’ intuitions may derive more from countertransference than from objective assessment.
Write it down. In cases where suicide risk seems unclear, it may help to list a patient’s risk and protective factors (Box 2). We have found this technique to be a useful teaching tool as well.
Be flexible. Because no method for assessing shortterm suicide risk is foolproof, be ready to re-evaluate your assessment and—if you are unsure—to take action to protect the patient.
You can make more-informed decisions about a patient’s acute suicide risk—such as over the phone at 3 AM—if you know what to ask the psychiatry resident or crisis worker. For suicide risk assessment—especially when you have not seen the patient—you need specific, high-yield questions to draw out danger signals from large amounts of data.
We are not suggesting that a short list of questions is sufficient for this extremely difficult task. Rather—because we recognize its complexity—we offer the questions we find most useful when evaluating patients with suicidal behaviors.
American Psychiatric Association practice guidelines1 provide a comprehensive discussion of assessing suicide risk. In addition, we teach clinicians we supervise to probe for high-risk and less-commonly explored “protective” factors.
High-risk factors
Mental health clinicians are more experienced in probing for high-risk factors than for protective factors. Because population studies offer limited help (Box 1),2 we ask clinicians these questions to evaluate the seriousness of a suicide attempt:
- Most studies of suicide risk factors focus on medium- to long-range risk
- Population-based risk factors (such as being Caucasian, over age 65, or depressed) apply to so many patients that their clinical usefulness is limited1
- Population-based risk factors often have high sensitivity but low specificity (recent loss is an important risk factor for attempting suicide, for example, but very few persons with a recent loss attempt suicide)
- In an acute situation, the positive predictive value of suicide risk factors—alone or in combination—is not known
Table
3 important questions to ask in overdose cases
|
What method was used? Methods other than taking an overdose or cutting the wrists may be more dangerous.
What amount was used? (in overdose or poisoning cases)
What treatment was needed? If the patient took an overdose of opioids and needs intubation, this indicates a relatively serious attempt. On the other hand, the psychiatric seriousness of an acetaminophen overdose depends on whether the patient realized the danger in taking high doses of acetaminophen. Additional questions can help determine the seriousness of suicide attempts by overdose (Table).
Was the attempt impulsive or planned? Planned attempts tend to be more serious.
What is the ‘risk-rescue ratio’? The potential lethality of the attempt and the likelihood of being saved must be evaluated together. Where did the attempt occur? In a setting where others were likely to intervene? Was the patient alone? Attempts in the presence of others may be considered less alarming.
What did the patient do immediately afterward? Did he tell anyone? How did he get to the hospital? Did he seek help on his own? Who called the ambulance?
How does the patient feel about the attempt now? Is she glad or disappointed she didn’t die? Does she regret the attempt?
Have there been past attempts? Does the patient have a history of suicide attempts or significant selfmutilation? If so, what was the most serious incident? Past attempts tend to predict future attempts.
Other considerations for patients who have attempted suicide and those who have not but are being evaluated for possible suicide risk include:
Mental state. To estimate a patient’s mental state and depth of negative affect, without having seen her yourself, three helpful questions are:
- Does she still look upset, depressed, or angry? Anger and agitation tend to increase risk.
- Can she smile or relax, even briefly?
- Does she feel things are likely to improve?
Access to firearms. Suicide by firearms accounts for 55% of all suicides.3 Does the patient have access to a gun and bullets? If so, get details. Does he now keep the gun on his person instead of in a locked cabinet, as he did earlier? We find that questions about guns are all too frequently omitted.
Contract for safety. Can the patient reliably contract not to harm himself and to call for help in a crisis? Although contracts for safety have limited value—as will be discussed—a patient’s refusal to contract for safety may indicate a higher suicide risk.
Some patients may refuse to contract for safety in order to be hospitalized for other reasons. They may say they can’t be sure what they will do if not admitted or declare that the clinician will be blamed for their death.
Protective factors
A patient’s high-risk clinical features must be balanced against factors that may reduce suicide risk.
How much social support? Can family or friends constantly stay with the patient, watch him closely, and get help if the situation worsens? This is the simplest and most relevant method to assess the availability of protective support.
How much mental health support? Does the patient have a good relationship with a psychiatrist or therapist who can see the patient soon?
Have circumstances changed? Has the stressor that led to suicidal behavior resolved, at least in part? For example, if a patient’s fight with her boyfriend led to her taking an overdose, have they made up?
Four common myths. Clinicians assessing patients for acute suicide risk often overestimate the protective value of some factors. They may tell you:
- The patient only tried to harm himself while he was intoxicated. He’s not intoxicated now and therefore is not at high risk. The patient will likely get intoxicated again, despite his protestations to the contrary. Substance intoxication and withdrawal tend to worsen depression and diminish inhibitions, making suicide more—not less—likely.
- The patient contracts for safety. A contract for safety may have some value,4 but its clinical and legal merits in suicide risk assessment are overestimated.5 We are concerned about how often we see clinicians judge that a contract for safety overrides numerous high-risk factors.
- The patient was only trying to get attention. It is difficult for mental health professionals—and even for patients—to reliably ascertain what motivates someone to attempt suicide. Multiple motivations and ambivalence are common.
- The patient is ‘just a borderline.’ Because patients with borderline personality disorder tend to make repeated suicide gestures, clinicians may not take their suicide attempts seriously. This statement reveals ignorance about the suffering of persons with borderline personality disorder; their rate of completed suicide is approximately 10%.6
- When a suicide assessment is inconclusive, draw two columns on a sheet of paper. List the patient’s high-risk factors on one side and protective factors on the other
- Seeing the information in black and white often helps clarify the assessment
- Consider both the number of factors in each column and your clinical sense of each factor’s importance and intensity. Place a check mark next to particularly important factors
- This balance sheet can remind you of further questions to ask and often reveals that either the high-risk or protective factors far outweigh the others in number and/or intensity
Practical advice
Distinguish short-term vs long-term risk. Based on the questions above, we often conclude that a patient is at high long-term risk of suicide, but the immediate risk is much lower. Acute hospitalization is unlikely to alleviate the long-term risk (though sometimes is the only way to get the patient into psychiatric treatment).
Consider the source. Never disregard the “gut feeling” of the person who interviewed the patient, but also factor in your assessment of that clinician’s judgment. Sometimes inexperienced staffs’ intuitions may derive more from countertransference than from objective assessment.
Write it down. In cases where suicide risk seems unclear, it may help to list a patient’s risk and protective factors (Box 2). We have found this technique to be a useful teaching tool as well.
Be flexible. Because no method for assessing shortterm suicide risk is foolproof, be ready to re-evaluate your assessment and—if you are unsure—to take action to protect the patient.
1. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160(11 suppl):1-60.
2. Fawcett J. Suicide risk factors in depressive disorders and in panic disorder. J Clin Psychiatry. 1992;53(suppl):9-13.
3. National Institute of Mental Health. Suicide facts. Available at: http://www.nimh.nih.gov/SuicidePrevention/suifact.cfm. Accessed June 3, 2004.
4. Stanford EJ, Goetz RR, Bloom JD. The no harm contract in the emergency assessment of suicidal risk. J Clin Psychiatry 1994;55(8):344-8.
5. Simon RI. The suicide prevention contract: clinical, legal, and risk management issues. J Am Acad Psychiatry Law 1999;27(3):445-50.
6. Paris J. Chronic suicidality among patients with borderline personality disorder. Psychiatr Serv 2002;53(6):738-42.
1. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160(11 suppl):1-60.
2. Fawcett J. Suicide risk factors in depressive disorders and in panic disorder. J Clin Psychiatry. 1992;53(suppl):9-13.
3. National Institute of Mental Health. Suicide facts. Available at: http://www.nimh.nih.gov/SuicidePrevention/suifact.cfm. Accessed June 3, 2004.
4. Stanford EJ, Goetz RR, Bloom JD. The no harm contract in the emergency assessment of suicidal risk. J Clin Psychiatry 1994;55(8):344-8.
5. Simon RI. The suicide prevention contract: clinical, legal, and risk management issues. J Am Acad Psychiatry Law 1999;27(3):445-50.
6. Paris J. Chronic suicidality among patients with borderline personality disorder. Psychiatr Serv 2002;53(6):738-42.
Is your patient’s dizziness psychogenic?
Dizziness is common among patients age 65 and older, and more than one-third have a psychiatric disorder that is caused by or is causing their dizziness.1
When older patients present with dizziness, psychiatrists may be asked to alleviate the psychological symptoms and help identify the underlying disease state.2
More than 60 medical and psychiatric disorders and many medications can cause dizziness. To help you sort through the possibilities, we offer:
- six diagnostic questions to rule out underlying medical problems
- lists of commonly used psychotropics and other drugs that may cause dizziness
- advice on treating depression, anxiety, and panic disorder in an older patient with dizziness while avoiding side effects and drug interactions.
Table 1
Four types of dizziness and their usual causes
| Vertigo Benign positional vertigo CNS cause—tumor, demyelination, neurodegenerative disorders Labyrinthitis Meniere’s disease Peripheral vestibulopathy (in 50% of cases) Vestibular neuronitis |
| Presyncope Arrhythmias Carotid sinus disease Hypoglycemia Neurocardiogenic syncope Organic heart disease Orthostatic hypotension Seizures Situational Transient ischemic attacks |
| Disequilibrium Balance and gait disorder Mixed CNS diseases (ischemic, degenerative) Neurodegenerative CNS disorders Presbystasis Sensorimotor dysfunction |
| Psychogenic lightheadedness Agoraphobia Anxiety Depression Panic disorder Hyperventilation |
| Source: Adapted from reference 6 |
Many causes of dizziness
The term “dizziness” is hard to define because of its nonspecific and variable symptom description, multiple causes, and lack of clear diagnostic and management guidelines. In clinical use, dizziness encompasses abnormal sensations relating to perception of the body’s relationship to space.
Some researchers believe dizziness is a distinct geriatric syndrome because numerous factors related to aging cause dizziness,2 including physiologic changes (presbystasis), accumulated impairment, disease states, and interactions between multiple medications.
Anxiety, somatization, panic disorder, and depression cause dizziness in the elderly, as do:
- peripheral vestibular disorders
- brainstem cerebrovascular accident
- diabetes mellitus
- neurologic disorders such as Parkinson’s disease
- and cardiovascular disorders.
Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants also have been shown to cause dizziness, as have numerous nonpsychotropic agents.
Recognizing patterns, testing hypotheses, and extending the diagnostic process over time can help you differentiate psychogenic from medicationinduced or neurologic dizziness.3 Because the presentation is so complex and the differential diagnosis so broad, algorithmic diagnosis is less effective than a flexible clinical approach that allows for uncertainty in evaluating initial symptoms.
Determining the cause
A thorough patient history and physical examination can uncover a cause of dizziness in 75% of cases.4 Look for duration of dizziness symptoms; history of heart disease, diabetes or other illnesses; family history of psychiatric disorders; and other illnesses among family members.
Ask the following six complaint-specific questions to help you narrow the differential diagnosis and rule out nonpsychiatric causes.5
1. WHAT TYPE OF DIZZINESS DOES THE PATIENT HAVE?
Four categories—vertigo, presyncope, disequilibrium, and lightheadedness—are used to classify dizziness (Table 1).6
Vertigo is a sense that the body or environment is Patients may feel as if the floor is tilting, sinking, rising or veering sideways, or they may feel pulled to one side.
Vertigo is commonly caused by peripheral vestibular disorders—including benign positional vertigo, Meniere’s disease, labyrinthitis, and vestibular neuronitis—and central vestibular disorders associated with cerebrovascular disease, tumors, demyelinating diseases, migraines, seizures, multiple sclerosis and other CNS diseases. Acute-onset vertigo and neurologic signs suggest brainstem infarction.
Nystagmus is usually present, horizontal, and may be rotational at times. A vertical-beating nystagmus points to a probable CNS cause and requires urgent neuroimaging and referral to a neurologist or otolaryngologist.
Presyncope describes near-fainting. A dimming of vision and roaring in the ears may precede presyncope.
Depending on its cause, presyncope may occur regardless of position or only when upright. Common causes include orthostatic hypotension, neurocardiogenic syncope, organic heart disease, arrhythmias, carotid sinus disease, seizures, hypoglycemia, and transient ischemic attacks.
Abrupt presyncopal attacks that occur regardless of position suggest a cardiovascular cause. If onset is gradual and not improved by lying down, suspect a cerebral metabolic cause such as hypoglycemia.
Syncope, like presyncope, often is traced to an underlying cardiovascular disease. Dizziness and syncope often coexist, and both can be multifactorial. Dizziness may precede or follow syncopal episodes.
Differentiating syncope and dizziness is important because many underlying causes of syncope can be fatal. By contrast, dizziness symptoms are usually benign and self-limiting.7
A thorough history is critical to distinguishing dizziness from presyncope. Assess medication effects—especially CNS-acting medications, cardiovascular drugs, antihypertensives, antibiotics, and over-the-counter medications such as dextromethorphan and acetaminophen compounds. Also check for dehydration.
Disequilibrium disorder signifies unsteadiness or a loss of balance primarily involving the lower extremities. Symptoms are evoked by walking or standing and relieved by sitting or lying down. Gait is abnormal and balance is compromised without abnormal head sensations.
Common causes include balance and gait disorders, sensorimotor dysfunction, presbystasis, neurodegenerative CNS disorders, and mixed ischemic and degenerative CNS diseases.
Vague lightheadedness is often associated with somatic symptoms such as headache. Some patients describe a floating sensation.
Lightheadedness is frequently associated with anxiety, panic disorder, depression, and somatization. Hyperventilation and agoraphobia are other common causes.
Multiple symptoms, multiple types. Classifying an older patient’s dizziness can be challenging because many patients report symptoms that suggest two or more subtypes.2 Also, patients often have trouble describing their dizziness symptoms, sometimes using terms such as “giddiness,” “wooziness,” or “confusion.”
To help patients explain dizziness symptoms more accurately, ask specific questions such as:
- Do you at times feel like you’re about to faint?
- Do you feel as if the room is moving?
- Do you sometimes feel as though you’re going to fall?
Table 2
Psychotropics that may cause dizziness
| Anti-Alzheimer’s medications Memantine, rivastigmine, tacrine |
| Anticonvulsants Phenytoin |
| Antidepressants Monoamine oxidase inhibitors (phenelzine, selegiline) Selective serotonin reuptake inhibitors (all) Tricyclics (amitriptyline, imipramine, nortriptyline, trazodone) Others (bupropion, buspirone, mirtazapine, nefazodone, venlafaxine) |
| Antipsychotics Typicals (chlorpromazine, fluphenazine, perphenazine, prochlorperazine, thioridazine, trifluoperazine) Atypicals (all except olanzapine) |
| Anxiolytics Alprazolam, chlordiazepoxide, clonazepam, diazepam, lorazepam, oxazepam |
| Hypnotics Estazolam, flurazepam, quazepam, temazepam, triazolam, zolpidem |
| Mood stabilizers Carbamazepine, divalproex/valproic acid, gabapentin, lamotrigine, oxcarbazepine |
| Source: Clinical Pharmacology version 2.11. Tampa, FL: Gold Standard MultiMedia, 2004. |
2. HOW DO DIZZINESS SYMPTOMS RELATE TO POSITION OR MOTION?
By reproducing dizziness symptoms, some quick-maneuver tests can help patients describe their symptoms and may reveal a medical cause.
Dix-Hallpike maneuver.3 Move the patient rapidly from a seated to prone position with the head below the horizontal plane and turned 45 degrees for 10 seconds; then have the patient sit up. Repeat with the head turned to the other side. If dizziness does not occur within a few seconds after each test, rule out benign positional vertigo.
Seated head turn, or head-thrust test, measures qualitative vestibular function.8 Move the head rapidly by 45 degrees in a brief, small-amplitude thrust to one side while the patient focuses on your nose; this gauges vestibularocular control. Repeat the test in the other direction. A refixation corrective saccade, occurring as the patient tries to fixate on the target, indicates a possible vestibular disorder.
‘Get-Up and Go’ test, which takes less than 10 seconds, measures balance in older patents.9 Have the patient stand up, walk 10 feet, turn around, walk back, and sit down. Watch for staggering, unsteadiness, and use of hands to balance. Onset of symptoms suggests dizziness brought on during activities of daily living and provides information on how dizziness is affecting the patient’s ability to function.
Romberg test. Have the patient stand with heels together, first with eyes open and then closed. Vision and proprioceptive signals are used to compensate for vestibular loss. Thus, a balance disturbance with eyes closed suggests vestibular or spinal proprioceptive problems and may predict risk of falls caused by inability to compensate.8
3. WHAT IS THE COURSE OF DIZZINESS?
Differentiating acute, sudden-onset dizziness from chronic, gradual-onset dizziness can help uncover the problem’s cause and seriousness. The latter often has a psychological cause or may point to vestibular or minor cardiovascular problems. Tinetti et al2 identified anxiety or depressive symptoms as risk factors among community-based older persons who reported dizziness episodes lasting 1 month.
Table 3
Recommended SSRI starting dosages for older patients
| SSRI | Starting dosage (mg/d) | Maximum dosage (mg/d) |
|---|---|---|
| Citalopram | 10 to 20 | 30 |
| Escitalopram | 10 | 10 |
| Fluoxetine* | 5 to 10 | 60 |
| Paroxetine | 5 | 40 |
| Sertraline | 25 to 50 | 200 |
| * Most patients will not need more than 20 mg/d. Dosages 40 mg/d should be divided into twice-daily doses. | ||
| Source: Adapted from Reuben DB, Herr K, Pacala JT, et al. Geriatrics at your fingertips (5th ed). Malden, MA: Blackwell Publishing, 2003:47. | ||
An acute presentation can suggest a panic disorder or acute anxiety state, but first rule out serious conditions such as acute myocardial infarction, arrhythmias, acute infections, GI bleeding, and carbon monoxide poisoning.
Also ask about:
- exacerbating and relieving factors. For example, positional changes, exercise or other physical activity, eating, or missing a meal can trigger presyncope. Also find out about situations that may bring on anxiety, panic, or phobia. Onset of dizziness following these situations may suggest psychogenesis.
- recent falls and injuries. Recurrent falls with presyncope suggest a probable orthostatic or cardiovascular diagnosis in older adults.
4. ANY PAST MEDICAL PROBLEMS?
Ask disease-specific questions. For example:
- Tinnitus or hearing loss could point to a vestibular disorder.
- Metabolic and cardiovascular disorders such as diabetes, ischemic heart disease, postural hypotension, and seizures can result in presyncope.
- Orthostasis, coronary ischemic events, hypoglycemia, and transient ischemic attacks may cause dizziness.
5. IS DIZZINESS RECURRENT?
Panic disorder, anxiety disorders, phobia, and psychogenic hyperventilation are commonly associated with chronic, recurrent dizziness episodes.
6. WHAT MEDICATIONS IS THE PATIENT TAKING?
All psychotropics are suspect when a patient presents with dizziness. When dizziness occurs after a dose or start of therapy, evaluate response to the medication and consider reducing the dosage or changing the medication. If symptoms persist, refer the patient back to the primary care physician to investigate for other causes of dizziness.
Psychotropics that may cause dizziness are listed in Table 2, For a list of other medications associated with dizziness, see this article at www.currentpsychiatry.com.
If the above strategies do not reveal a physical cause of dizziness despite multiple physical complaints, consider examining the patient for depression, anxiety, or panic disorder.
Treating a psychiatric cause
If dizziness is found to be psychogenic and the symptoms impede daily activities or contribute to functional decline, treat the psychiatric disorder but carefully weigh the risks and benefits of drug treatment.
Although SSRIs may cause dizziness, these agents are recommended first-line treatment for depression, anxiety, and/or phobia in older patients with dizziness because of their relative lack of anticholinergic action and side effects compared with other antidepressants or anxiolytics.
Coexisting medical symptoms may dictate choice of agent. For example, consider a sedating SSRI for a patient with sleep disturbances caused by dizziness or the psychiatric disorder; choose a nonsedating SSRI if the patient is sleeping normally.
Because SSRIs may cause weight loss, avoid giving them to patients with weight loss associated with dizziness or an underlying psychiatric illness. Mirtazapine, which is associated with weight gain, may offset weight loss. Start mirtazapine at 15 mg at bedtime for older patients.
Start low and go slow when prescribing an SSRI to an older patient. Dosing strategies applicable to younger patients should not be extrapolated to older patients, especially those with dizziness.
We have found that older patients respond well to minimum or below-normal SSRI dosages (Table 3). Titrate very slowly and instruct patients to report dizziness. Reduce the dosage if dizziness emerges.
If the patient does not respond to an SSRI or mirtazapine, consider a serotonin and norepinephrine reuptake inhibitor, which also has favorable anticholinergic and side-effect profiles.
Related resources
- WebMD Health—Dizziness: lightheadedness and vertigo. http://my.webMD.com/hw/health_guide_atoz/hw88500.asp.
- Sloane PD. Clinical research and geriatric dizziness: The blind men and the elephant. J Am Geriatr Soc 1999;47:113-14.
- Kroenke K, Hoffman RM, Einstadter D. How common are various forms of dizziness? A critical review. South Med J 2000;93:160-7.
Drug brand names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Carbamazepine • Tegretol
- Chlordiazepoxide • Librium
- Chlorpromazine • Thorazine
- Citalopram • Celexa
- Clonazepam • Klonopin
- Diazepam • Valium
- Divalproex/valproic acid • Depakote
- Escitalopram • Lexapro
- Estazolam • ProSom
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Flurazepam • Dalmane
- Gabapentin • Neurontin
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Memantine • Namenda
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Oxazepam • Serax
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenelzine • Nardil
- Phenytoin • Dilantin
- Prochlorperazine • Compazine
- Quazepam • Doral
- Rivastigmine • Exelon
- Selegiline • Eldepryl
- Sertraline • Zoloft
- Tacrine • Cognex
- Temazepam • Restoril
- Thioridazine • Mellaril
- Trazodone • Desyrel
- Triazolam • Halcion
- Trifluoperazine • Vesprin
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors thank Robert Cluxton, PharmD, University of Cincinnati College of Pharmacy, for helping to prepare this manuscript for publication.
1. Sloane PD, Hartman M, Mitchell CM. Psychological factors associated with chronic dizziness in patients aged 60 and older. J Am Geriatr Soc 1994;42:847-52.
2. Tinetti ME, Williams CS, Gill TM. Dizziness among older adults: a possible geriatric syndrome. Ann Intern Med 2000;132:337-44.
3. Sloane PD, Coeytaux RR, Beck RS, Dallara J. Dizziness: state of the science. Ann Intern Med 2001;134(9 pt 2):823-32.
4. Hoffman RM, Einstadter D, Kroenke K. Evaluating dizziness. Am J Med 1999;107:468-78.
5. Drachman DA. A 69-year-old man with chronic dizziness. JAMA 1998;280:2111-18.
6. Drachman DA, Hart CW. An approach to the dizzy patient. Neurology 1972;22:323-34.
7. Kapoor WN. Syncope. N Engl J Med 2000;343:1856-62.
8. Baloh RW. Hearing and equilibrium. In: Goldman L, Ansiello D (eds). Cecil textbook of medicine (22nd ed). Philadelphia: Saunders 2004;2436-42.
9. Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil 1986;67:387-9.
Dizziness is common among patients age 65 and older, and more than one-third have a psychiatric disorder that is caused by or is causing their dizziness.1
When older patients present with dizziness, psychiatrists may be asked to alleviate the psychological symptoms and help identify the underlying disease state.2
More than 60 medical and psychiatric disorders and many medications can cause dizziness. To help you sort through the possibilities, we offer:
- six diagnostic questions to rule out underlying medical problems
- lists of commonly used psychotropics and other drugs that may cause dizziness
- advice on treating depression, anxiety, and panic disorder in an older patient with dizziness while avoiding side effects and drug interactions.
Table 1
Four types of dizziness and their usual causes
| Vertigo Benign positional vertigo CNS cause—tumor, demyelination, neurodegenerative disorders Labyrinthitis Meniere’s disease Peripheral vestibulopathy (in 50% of cases) Vestibular neuronitis |
| Presyncope Arrhythmias Carotid sinus disease Hypoglycemia Neurocardiogenic syncope Organic heart disease Orthostatic hypotension Seizures Situational Transient ischemic attacks |
| Disequilibrium Balance and gait disorder Mixed CNS diseases (ischemic, degenerative) Neurodegenerative CNS disorders Presbystasis Sensorimotor dysfunction |
| Psychogenic lightheadedness Agoraphobia Anxiety Depression Panic disorder Hyperventilation |
| Source: Adapted from reference 6 |
Many causes of dizziness
The term “dizziness” is hard to define because of its nonspecific and variable symptom description, multiple causes, and lack of clear diagnostic and management guidelines. In clinical use, dizziness encompasses abnormal sensations relating to perception of the body’s relationship to space.
Some researchers believe dizziness is a distinct geriatric syndrome because numerous factors related to aging cause dizziness,2 including physiologic changes (presbystasis), accumulated impairment, disease states, and interactions between multiple medications.
Anxiety, somatization, panic disorder, and depression cause dizziness in the elderly, as do:
- peripheral vestibular disorders
- brainstem cerebrovascular accident
- diabetes mellitus
- neurologic disorders such as Parkinson’s disease
- and cardiovascular disorders.
Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants also have been shown to cause dizziness, as have numerous nonpsychotropic agents.
Recognizing patterns, testing hypotheses, and extending the diagnostic process over time can help you differentiate psychogenic from medicationinduced or neurologic dizziness.3 Because the presentation is so complex and the differential diagnosis so broad, algorithmic diagnosis is less effective than a flexible clinical approach that allows for uncertainty in evaluating initial symptoms.
Determining the cause
A thorough patient history and physical examination can uncover a cause of dizziness in 75% of cases.4 Look for duration of dizziness symptoms; history of heart disease, diabetes or other illnesses; family history of psychiatric disorders; and other illnesses among family members.
Ask the following six complaint-specific questions to help you narrow the differential diagnosis and rule out nonpsychiatric causes.5
1. WHAT TYPE OF DIZZINESS DOES THE PATIENT HAVE?
Four categories—vertigo, presyncope, disequilibrium, and lightheadedness—are used to classify dizziness (Table 1).6
Vertigo is a sense that the body or environment is Patients may feel as if the floor is tilting, sinking, rising or veering sideways, or they may feel pulled to one side.
Vertigo is commonly caused by peripheral vestibular disorders—including benign positional vertigo, Meniere’s disease, labyrinthitis, and vestibular neuronitis—and central vestibular disorders associated with cerebrovascular disease, tumors, demyelinating diseases, migraines, seizures, multiple sclerosis and other CNS diseases. Acute-onset vertigo and neurologic signs suggest brainstem infarction.
Nystagmus is usually present, horizontal, and may be rotational at times. A vertical-beating nystagmus points to a probable CNS cause and requires urgent neuroimaging and referral to a neurologist or otolaryngologist.
Presyncope describes near-fainting. A dimming of vision and roaring in the ears may precede presyncope.
Depending on its cause, presyncope may occur regardless of position or only when upright. Common causes include orthostatic hypotension, neurocardiogenic syncope, organic heart disease, arrhythmias, carotid sinus disease, seizures, hypoglycemia, and transient ischemic attacks.
Abrupt presyncopal attacks that occur regardless of position suggest a cardiovascular cause. If onset is gradual and not improved by lying down, suspect a cerebral metabolic cause such as hypoglycemia.
Syncope, like presyncope, often is traced to an underlying cardiovascular disease. Dizziness and syncope often coexist, and both can be multifactorial. Dizziness may precede or follow syncopal episodes.
Differentiating syncope and dizziness is important because many underlying causes of syncope can be fatal. By contrast, dizziness symptoms are usually benign and self-limiting.7
A thorough history is critical to distinguishing dizziness from presyncope. Assess medication effects—especially CNS-acting medications, cardiovascular drugs, antihypertensives, antibiotics, and over-the-counter medications such as dextromethorphan and acetaminophen compounds. Also check for dehydration.
Disequilibrium disorder signifies unsteadiness or a loss of balance primarily involving the lower extremities. Symptoms are evoked by walking or standing and relieved by sitting or lying down. Gait is abnormal and balance is compromised without abnormal head sensations.
Common causes include balance and gait disorders, sensorimotor dysfunction, presbystasis, neurodegenerative CNS disorders, and mixed ischemic and degenerative CNS diseases.
Vague lightheadedness is often associated with somatic symptoms such as headache. Some patients describe a floating sensation.
Lightheadedness is frequently associated with anxiety, panic disorder, depression, and somatization. Hyperventilation and agoraphobia are other common causes.
Multiple symptoms, multiple types. Classifying an older patient’s dizziness can be challenging because many patients report symptoms that suggest two or more subtypes.2 Also, patients often have trouble describing their dizziness symptoms, sometimes using terms such as “giddiness,” “wooziness,” or “confusion.”
To help patients explain dizziness symptoms more accurately, ask specific questions such as:
- Do you at times feel like you’re about to faint?
- Do you feel as if the room is moving?
- Do you sometimes feel as though you’re going to fall?
Table 2
Psychotropics that may cause dizziness
| Anti-Alzheimer’s medications Memantine, rivastigmine, tacrine |
| Anticonvulsants Phenytoin |
| Antidepressants Monoamine oxidase inhibitors (phenelzine, selegiline) Selective serotonin reuptake inhibitors (all) Tricyclics (amitriptyline, imipramine, nortriptyline, trazodone) Others (bupropion, buspirone, mirtazapine, nefazodone, venlafaxine) |
| Antipsychotics Typicals (chlorpromazine, fluphenazine, perphenazine, prochlorperazine, thioridazine, trifluoperazine) Atypicals (all except olanzapine) |
| Anxiolytics Alprazolam, chlordiazepoxide, clonazepam, diazepam, lorazepam, oxazepam |
| Hypnotics Estazolam, flurazepam, quazepam, temazepam, triazolam, zolpidem |
| Mood stabilizers Carbamazepine, divalproex/valproic acid, gabapentin, lamotrigine, oxcarbazepine |
| Source: Clinical Pharmacology version 2.11. Tampa, FL: Gold Standard MultiMedia, 2004. |
2. HOW DO DIZZINESS SYMPTOMS RELATE TO POSITION OR MOTION?
By reproducing dizziness symptoms, some quick-maneuver tests can help patients describe their symptoms and may reveal a medical cause.
Dix-Hallpike maneuver.3 Move the patient rapidly from a seated to prone position with the head below the horizontal plane and turned 45 degrees for 10 seconds; then have the patient sit up. Repeat with the head turned to the other side. If dizziness does not occur within a few seconds after each test, rule out benign positional vertigo.
Seated head turn, or head-thrust test, measures qualitative vestibular function.8 Move the head rapidly by 45 degrees in a brief, small-amplitude thrust to one side while the patient focuses on your nose; this gauges vestibularocular control. Repeat the test in the other direction. A refixation corrective saccade, occurring as the patient tries to fixate on the target, indicates a possible vestibular disorder.
‘Get-Up and Go’ test, which takes less than 10 seconds, measures balance in older patents.9 Have the patient stand up, walk 10 feet, turn around, walk back, and sit down. Watch for staggering, unsteadiness, and use of hands to balance. Onset of symptoms suggests dizziness brought on during activities of daily living and provides information on how dizziness is affecting the patient’s ability to function.
Romberg test. Have the patient stand with heels together, first with eyes open and then closed. Vision and proprioceptive signals are used to compensate for vestibular loss. Thus, a balance disturbance with eyes closed suggests vestibular or spinal proprioceptive problems and may predict risk of falls caused by inability to compensate.8
3. WHAT IS THE COURSE OF DIZZINESS?
Differentiating acute, sudden-onset dizziness from chronic, gradual-onset dizziness can help uncover the problem’s cause and seriousness. The latter often has a psychological cause or may point to vestibular or minor cardiovascular problems. Tinetti et al2 identified anxiety or depressive symptoms as risk factors among community-based older persons who reported dizziness episodes lasting 1 month.
Table 3
Recommended SSRI starting dosages for older patients
| SSRI | Starting dosage (mg/d) | Maximum dosage (mg/d) |
|---|---|---|
| Citalopram | 10 to 20 | 30 |
| Escitalopram | 10 | 10 |
| Fluoxetine* | 5 to 10 | 60 |
| Paroxetine | 5 | 40 |
| Sertraline | 25 to 50 | 200 |
| * Most patients will not need more than 20 mg/d. Dosages 40 mg/d should be divided into twice-daily doses. | ||
| Source: Adapted from Reuben DB, Herr K, Pacala JT, et al. Geriatrics at your fingertips (5th ed). Malden, MA: Blackwell Publishing, 2003:47. | ||
An acute presentation can suggest a panic disorder or acute anxiety state, but first rule out serious conditions such as acute myocardial infarction, arrhythmias, acute infections, GI bleeding, and carbon monoxide poisoning.
Also ask about:
- exacerbating and relieving factors. For example, positional changes, exercise or other physical activity, eating, or missing a meal can trigger presyncope. Also find out about situations that may bring on anxiety, panic, or phobia. Onset of dizziness following these situations may suggest psychogenesis.
- recent falls and injuries. Recurrent falls with presyncope suggest a probable orthostatic or cardiovascular diagnosis in older adults.
4. ANY PAST MEDICAL PROBLEMS?
Ask disease-specific questions. For example:
- Tinnitus or hearing loss could point to a vestibular disorder.
- Metabolic and cardiovascular disorders such as diabetes, ischemic heart disease, postural hypotension, and seizures can result in presyncope.
- Orthostasis, coronary ischemic events, hypoglycemia, and transient ischemic attacks may cause dizziness.
5. IS DIZZINESS RECURRENT?
Panic disorder, anxiety disorders, phobia, and psychogenic hyperventilation are commonly associated with chronic, recurrent dizziness episodes.
6. WHAT MEDICATIONS IS THE PATIENT TAKING?
All psychotropics are suspect when a patient presents with dizziness. When dizziness occurs after a dose or start of therapy, evaluate response to the medication and consider reducing the dosage or changing the medication. If symptoms persist, refer the patient back to the primary care physician to investigate for other causes of dizziness.
Psychotropics that may cause dizziness are listed in Table 2, For a list of other medications associated with dizziness, see this article at www.currentpsychiatry.com.
If the above strategies do not reveal a physical cause of dizziness despite multiple physical complaints, consider examining the patient for depression, anxiety, or panic disorder.
Treating a psychiatric cause
If dizziness is found to be psychogenic and the symptoms impede daily activities or contribute to functional decline, treat the psychiatric disorder but carefully weigh the risks and benefits of drug treatment.
Although SSRIs may cause dizziness, these agents are recommended first-line treatment for depression, anxiety, and/or phobia in older patients with dizziness because of their relative lack of anticholinergic action and side effects compared with other antidepressants or anxiolytics.
Coexisting medical symptoms may dictate choice of agent. For example, consider a sedating SSRI for a patient with sleep disturbances caused by dizziness or the psychiatric disorder; choose a nonsedating SSRI if the patient is sleeping normally.
Because SSRIs may cause weight loss, avoid giving them to patients with weight loss associated with dizziness or an underlying psychiatric illness. Mirtazapine, which is associated with weight gain, may offset weight loss. Start mirtazapine at 15 mg at bedtime for older patients.
Start low and go slow when prescribing an SSRI to an older patient. Dosing strategies applicable to younger patients should not be extrapolated to older patients, especially those with dizziness.
We have found that older patients respond well to minimum or below-normal SSRI dosages (Table 3). Titrate very slowly and instruct patients to report dizziness. Reduce the dosage if dizziness emerges.
If the patient does not respond to an SSRI or mirtazapine, consider a serotonin and norepinephrine reuptake inhibitor, which also has favorable anticholinergic and side-effect profiles.
Related resources
- WebMD Health—Dizziness: lightheadedness and vertigo. http://my.webMD.com/hw/health_guide_atoz/hw88500.asp.
- Sloane PD. Clinical research and geriatric dizziness: The blind men and the elephant. J Am Geriatr Soc 1999;47:113-14.
- Kroenke K, Hoffman RM, Einstadter D. How common are various forms of dizziness? A critical review. South Med J 2000;93:160-7.
Drug brand names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Carbamazepine • Tegretol
- Chlordiazepoxide • Librium
- Chlorpromazine • Thorazine
- Citalopram • Celexa
- Clonazepam • Klonopin
- Diazepam • Valium
- Divalproex/valproic acid • Depakote
- Escitalopram • Lexapro
- Estazolam • ProSom
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Flurazepam • Dalmane
- Gabapentin • Neurontin
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Memantine • Namenda
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Oxazepam • Serax
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenelzine • Nardil
- Phenytoin • Dilantin
- Prochlorperazine • Compazine
- Quazepam • Doral
- Rivastigmine • Exelon
- Selegiline • Eldepryl
- Sertraline • Zoloft
- Tacrine • Cognex
- Temazepam • Restoril
- Thioridazine • Mellaril
- Trazodone • Desyrel
- Triazolam • Halcion
- Trifluoperazine • Vesprin
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors thank Robert Cluxton, PharmD, University of Cincinnati College of Pharmacy, for helping to prepare this manuscript for publication.
Dizziness is common among patients age 65 and older, and more than one-third have a psychiatric disorder that is caused by or is causing their dizziness.1
When older patients present with dizziness, psychiatrists may be asked to alleviate the psychological symptoms and help identify the underlying disease state.2
More than 60 medical and psychiatric disorders and many medications can cause dizziness. To help you sort through the possibilities, we offer:
- six diagnostic questions to rule out underlying medical problems
- lists of commonly used psychotropics and other drugs that may cause dizziness
- advice on treating depression, anxiety, and panic disorder in an older patient with dizziness while avoiding side effects and drug interactions.
Table 1
Four types of dizziness and their usual causes
| Vertigo Benign positional vertigo CNS cause—tumor, demyelination, neurodegenerative disorders Labyrinthitis Meniere’s disease Peripheral vestibulopathy (in 50% of cases) Vestibular neuronitis |
| Presyncope Arrhythmias Carotid sinus disease Hypoglycemia Neurocardiogenic syncope Organic heart disease Orthostatic hypotension Seizures Situational Transient ischemic attacks |
| Disequilibrium Balance and gait disorder Mixed CNS diseases (ischemic, degenerative) Neurodegenerative CNS disorders Presbystasis Sensorimotor dysfunction |
| Psychogenic lightheadedness Agoraphobia Anxiety Depression Panic disorder Hyperventilation |
| Source: Adapted from reference 6 |
Many causes of dizziness
The term “dizziness” is hard to define because of its nonspecific and variable symptom description, multiple causes, and lack of clear diagnostic and management guidelines. In clinical use, dizziness encompasses abnormal sensations relating to perception of the body’s relationship to space.
Some researchers believe dizziness is a distinct geriatric syndrome because numerous factors related to aging cause dizziness,2 including physiologic changes (presbystasis), accumulated impairment, disease states, and interactions between multiple medications.
Anxiety, somatization, panic disorder, and depression cause dizziness in the elderly, as do:
- peripheral vestibular disorders
- brainstem cerebrovascular accident
- diabetes mellitus
- neurologic disorders such as Parkinson’s disease
- and cardiovascular disorders.
Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants also have been shown to cause dizziness, as have numerous nonpsychotropic agents.
Recognizing patterns, testing hypotheses, and extending the diagnostic process over time can help you differentiate psychogenic from medicationinduced or neurologic dizziness.3 Because the presentation is so complex and the differential diagnosis so broad, algorithmic diagnosis is less effective than a flexible clinical approach that allows for uncertainty in evaluating initial symptoms.
Determining the cause
A thorough patient history and physical examination can uncover a cause of dizziness in 75% of cases.4 Look for duration of dizziness symptoms; history of heart disease, diabetes or other illnesses; family history of psychiatric disorders; and other illnesses among family members.
Ask the following six complaint-specific questions to help you narrow the differential diagnosis and rule out nonpsychiatric causes.5
1. WHAT TYPE OF DIZZINESS DOES THE PATIENT HAVE?
Four categories—vertigo, presyncope, disequilibrium, and lightheadedness—are used to classify dizziness (Table 1).6
Vertigo is a sense that the body or environment is Patients may feel as if the floor is tilting, sinking, rising or veering sideways, or they may feel pulled to one side.
Vertigo is commonly caused by peripheral vestibular disorders—including benign positional vertigo, Meniere’s disease, labyrinthitis, and vestibular neuronitis—and central vestibular disorders associated with cerebrovascular disease, tumors, demyelinating diseases, migraines, seizures, multiple sclerosis and other CNS diseases. Acute-onset vertigo and neurologic signs suggest brainstem infarction.
Nystagmus is usually present, horizontal, and may be rotational at times. A vertical-beating nystagmus points to a probable CNS cause and requires urgent neuroimaging and referral to a neurologist or otolaryngologist.
Presyncope describes near-fainting. A dimming of vision and roaring in the ears may precede presyncope.
Depending on its cause, presyncope may occur regardless of position or only when upright. Common causes include orthostatic hypotension, neurocardiogenic syncope, organic heart disease, arrhythmias, carotid sinus disease, seizures, hypoglycemia, and transient ischemic attacks.
Abrupt presyncopal attacks that occur regardless of position suggest a cardiovascular cause. If onset is gradual and not improved by lying down, suspect a cerebral metabolic cause such as hypoglycemia.
Syncope, like presyncope, often is traced to an underlying cardiovascular disease. Dizziness and syncope often coexist, and both can be multifactorial. Dizziness may precede or follow syncopal episodes.
Differentiating syncope and dizziness is important because many underlying causes of syncope can be fatal. By contrast, dizziness symptoms are usually benign and self-limiting.7
A thorough history is critical to distinguishing dizziness from presyncope. Assess medication effects—especially CNS-acting medications, cardiovascular drugs, antihypertensives, antibiotics, and over-the-counter medications such as dextromethorphan and acetaminophen compounds. Also check for dehydration.
Disequilibrium disorder signifies unsteadiness or a loss of balance primarily involving the lower extremities. Symptoms are evoked by walking or standing and relieved by sitting or lying down. Gait is abnormal and balance is compromised without abnormal head sensations.
Common causes include balance and gait disorders, sensorimotor dysfunction, presbystasis, neurodegenerative CNS disorders, and mixed ischemic and degenerative CNS diseases.
Vague lightheadedness is often associated with somatic symptoms such as headache. Some patients describe a floating sensation.
Lightheadedness is frequently associated with anxiety, panic disorder, depression, and somatization. Hyperventilation and agoraphobia are other common causes.
Multiple symptoms, multiple types. Classifying an older patient’s dizziness can be challenging because many patients report symptoms that suggest two or more subtypes.2 Also, patients often have trouble describing their dizziness symptoms, sometimes using terms such as “giddiness,” “wooziness,” or “confusion.”
To help patients explain dizziness symptoms more accurately, ask specific questions such as:
- Do you at times feel like you’re about to faint?
- Do you feel as if the room is moving?
- Do you sometimes feel as though you’re going to fall?
Table 2
Psychotropics that may cause dizziness
| Anti-Alzheimer’s medications Memantine, rivastigmine, tacrine |
| Anticonvulsants Phenytoin |
| Antidepressants Monoamine oxidase inhibitors (phenelzine, selegiline) Selective serotonin reuptake inhibitors (all) Tricyclics (amitriptyline, imipramine, nortriptyline, trazodone) Others (bupropion, buspirone, mirtazapine, nefazodone, venlafaxine) |
| Antipsychotics Typicals (chlorpromazine, fluphenazine, perphenazine, prochlorperazine, thioridazine, trifluoperazine) Atypicals (all except olanzapine) |
| Anxiolytics Alprazolam, chlordiazepoxide, clonazepam, diazepam, lorazepam, oxazepam |
| Hypnotics Estazolam, flurazepam, quazepam, temazepam, triazolam, zolpidem |
| Mood stabilizers Carbamazepine, divalproex/valproic acid, gabapentin, lamotrigine, oxcarbazepine |
| Source: Clinical Pharmacology version 2.11. Tampa, FL: Gold Standard MultiMedia, 2004. |
2. HOW DO DIZZINESS SYMPTOMS RELATE TO POSITION OR MOTION?
By reproducing dizziness symptoms, some quick-maneuver tests can help patients describe their symptoms and may reveal a medical cause.
Dix-Hallpike maneuver.3 Move the patient rapidly from a seated to prone position with the head below the horizontal plane and turned 45 degrees for 10 seconds; then have the patient sit up. Repeat with the head turned to the other side. If dizziness does not occur within a few seconds after each test, rule out benign positional vertigo.
Seated head turn, or head-thrust test, measures qualitative vestibular function.8 Move the head rapidly by 45 degrees in a brief, small-amplitude thrust to one side while the patient focuses on your nose; this gauges vestibularocular control. Repeat the test in the other direction. A refixation corrective saccade, occurring as the patient tries to fixate on the target, indicates a possible vestibular disorder.
‘Get-Up and Go’ test, which takes less than 10 seconds, measures balance in older patents.9 Have the patient stand up, walk 10 feet, turn around, walk back, and sit down. Watch for staggering, unsteadiness, and use of hands to balance. Onset of symptoms suggests dizziness brought on during activities of daily living and provides information on how dizziness is affecting the patient’s ability to function.
Romberg test. Have the patient stand with heels together, first with eyes open and then closed. Vision and proprioceptive signals are used to compensate for vestibular loss. Thus, a balance disturbance with eyes closed suggests vestibular or spinal proprioceptive problems and may predict risk of falls caused by inability to compensate.8
3. WHAT IS THE COURSE OF DIZZINESS?
Differentiating acute, sudden-onset dizziness from chronic, gradual-onset dizziness can help uncover the problem’s cause and seriousness. The latter often has a psychological cause or may point to vestibular or minor cardiovascular problems. Tinetti et al2 identified anxiety or depressive symptoms as risk factors among community-based older persons who reported dizziness episodes lasting 1 month.
Table 3
Recommended SSRI starting dosages for older patients
| SSRI | Starting dosage (mg/d) | Maximum dosage (mg/d) |
|---|---|---|
| Citalopram | 10 to 20 | 30 |
| Escitalopram | 10 | 10 |
| Fluoxetine* | 5 to 10 | 60 |
| Paroxetine | 5 | 40 |
| Sertraline | 25 to 50 | 200 |
| * Most patients will not need more than 20 mg/d. Dosages 40 mg/d should be divided into twice-daily doses. | ||
| Source: Adapted from Reuben DB, Herr K, Pacala JT, et al. Geriatrics at your fingertips (5th ed). Malden, MA: Blackwell Publishing, 2003:47. | ||
An acute presentation can suggest a panic disorder or acute anxiety state, but first rule out serious conditions such as acute myocardial infarction, arrhythmias, acute infections, GI bleeding, and carbon monoxide poisoning.
Also ask about:
- exacerbating and relieving factors. For example, positional changes, exercise or other physical activity, eating, or missing a meal can trigger presyncope. Also find out about situations that may bring on anxiety, panic, or phobia. Onset of dizziness following these situations may suggest psychogenesis.
- recent falls and injuries. Recurrent falls with presyncope suggest a probable orthostatic or cardiovascular diagnosis in older adults.
4. ANY PAST MEDICAL PROBLEMS?
Ask disease-specific questions. For example:
- Tinnitus or hearing loss could point to a vestibular disorder.
- Metabolic and cardiovascular disorders such as diabetes, ischemic heart disease, postural hypotension, and seizures can result in presyncope.
- Orthostasis, coronary ischemic events, hypoglycemia, and transient ischemic attacks may cause dizziness.
5. IS DIZZINESS RECURRENT?
Panic disorder, anxiety disorders, phobia, and psychogenic hyperventilation are commonly associated with chronic, recurrent dizziness episodes.
6. WHAT MEDICATIONS IS THE PATIENT TAKING?
All psychotropics are suspect when a patient presents with dizziness. When dizziness occurs after a dose or start of therapy, evaluate response to the medication and consider reducing the dosage or changing the medication. If symptoms persist, refer the patient back to the primary care physician to investigate for other causes of dizziness.
Psychotropics that may cause dizziness are listed in Table 2, For a list of other medications associated with dizziness, see this article at www.currentpsychiatry.com.
If the above strategies do not reveal a physical cause of dizziness despite multiple physical complaints, consider examining the patient for depression, anxiety, or panic disorder.
Treating a psychiatric cause
If dizziness is found to be psychogenic and the symptoms impede daily activities or contribute to functional decline, treat the psychiatric disorder but carefully weigh the risks and benefits of drug treatment.
Although SSRIs may cause dizziness, these agents are recommended first-line treatment for depression, anxiety, and/or phobia in older patients with dizziness because of their relative lack of anticholinergic action and side effects compared with other antidepressants or anxiolytics.
Coexisting medical symptoms may dictate choice of agent. For example, consider a sedating SSRI for a patient with sleep disturbances caused by dizziness or the psychiatric disorder; choose a nonsedating SSRI if the patient is sleeping normally.
Because SSRIs may cause weight loss, avoid giving them to patients with weight loss associated with dizziness or an underlying psychiatric illness. Mirtazapine, which is associated with weight gain, may offset weight loss. Start mirtazapine at 15 mg at bedtime for older patients.
Start low and go slow when prescribing an SSRI to an older patient. Dosing strategies applicable to younger patients should not be extrapolated to older patients, especially those with dizziness.
We have found that older patients respond well to minimum or below-normal SSRI dosages (Table 3). Titrate very slowly and instruct patients to report dizziness. Reduce the dosage if dizziness emerges.
If the patient does not respond to an SSRI or mirtazapine, consider a serotonin and norepinephrine reuptake inhibitor, which also has favorable anticholinergic and side-effect profiles.
Related resources
- WebMD Health—Dizziness: lightheadedness and vertigo. http://my.webMD.com/hw/health_guide_atoz/hw88500.asp.
- Sloane PD. Clinical research and geriatric dizziness: The blind men and the elephant. J Am Geriatr Soc 1999;47:113-14.
- Kroenke K, Hoffman RM, Einstadter D. How common are various forms of dizziness? A critical review. South Med J 2000;93:160-7.
Drug brand names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Carbamazepine • Tegretol
- Chlordiazepoxide • Librium
- Chlorpromazine • Thorazine
- Citalopram • Celexa
- Clonazepam • Klonopin
- Diazepam • Valium
- Divalproex/valproic acid • Depakote
- Escitalopram • Lexapro
- Estazolam • ProSom
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Flurazepam • Dalmane
- Gabapentin • Neurontin
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Memantine • Namenda
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Nortriptyline • Pamelor
- Olanzapine • Zyprexa
- Oxazepam • Serax
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenelzine • Nardil
- Phenytoin • Dilantin
- Prochlorperazine • Compazine
- Quazepam • Doral
- Rivastigmine • Exelon
- Selegiline • Eldepryl
- Sertraline • Zoloft
- Tacrine • Cognex
- Temazepam • Restoril
- Thioridazine • Mellaril
- Trazodone • Desyrel
- Triazolam • Halcion
- Trifluoperazine • Vesprin
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The authors thank Robert Cluxton, PharmD, University of Cincinnati College of Pharmacy, for helping to prepare this manuscript for publication.
1. Sloane PD, Hartman M, Mitchell CM. Psychological factors associated with chronic dizziness in patients aged 60 and older. J Am Geriatr Soc 1994;42:847-52.
2. Tinetti ME, Williams CS, Gill TM. Dizziness among older adults: a possible geriatric syndrome. Ann Intern Med 2000;132:337-44.
3. Sloane PD, Coeytaux RR, Beck RS, Dallara J. Dizziness: state of the science. Ann Intern Med 2001;134(9 pt 2):823-32.
4. Hoffman RM, Einstadter D, Kroenke K. Evaluating dizziness. Am J Med 1999;107:468-78.
5. Drachman DA. A 69-year-old man with chronic dizziness. JAMA 1998;280:2111-18.
6. Drachman DA, Hart CW. An approach to the dizzy patient. Neurology 1972;22:323-34.
7. Kapoor WN. Syncope. N Engl J Med 2000;343:1856-62.
8. Baloh RW. Hearing and equilibrium. In: Goldman L, Ansiello D (eds). Cecil textbook of medicine (22nd ed). Philadelphia: Saunders 2004;2436-42.
9. Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil 1986;67:387-9.
1. Sloane PD, Hartman M, Mitchell CM. Psychological factors associated with chronic dizziness in patients aged 60 and older. J Am Geriatr Soc 1994;42:847-52.
2. Tinetti ME, Williams CS, Gill TM. Dizziness among older adults: a possible geriatric syndrome. Ann Intern Med 2000;132:337-44.
3. Sloane PD, Coeytaux RR, Beck RS, Dallara J. Dizziness: state of the science. Ann Intern Med 2001;134(9 pt 2):823-32.
4. Hoffman RM, Einstadter D, Kroenke K. Evaluating dizziness. Am J Med 1999;107:468-78.
5. Drachman DA. A 69-year-old man with chronic dizziness. JAMA 1998;280:2111-18.
6. Drachman DA, Hart CW. An approach to the dizzy patient. Neurology 1972;22:323-34.
7. Kapoor WN. Syncope. N Engl J Med 2000;343:1856-62.
8. Baloh RW. Hearing and equilibrium. In: Goldman L, Ansiello D (eds). Cecil textbook of medicine (22nd ed). Philadelphia: Saunders 2004;2436-42.
9. Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil 1986;67:387-9.
Post-stroke depression: Rapid action helps restore lost function
Patients with post-stroke depression (PSD) pose many clinical dilemmas: Is their depression a psychological reaction or a biological event? Are antidepressants effective for either type? Should antidepressants be given prophylactically after a stroke, even if the patient is not depressed?
Although the answers are not clear, this article describes a practical approach to stroke patients referred for psychiatric evaluation, including:
- strategies to distinguish reactive from endogenous depression
- issues that guide antidepressant selection
- benefits and risks of using medication to prevent depression after an acute stroke.
Reactive or endogenous depression?
Each year 500,000 to 600,000 Americans suffer strokes.1 Depression is the most common emotional sequela, reported in up to 40% of survivors within several months of an acute stroke.
Figure Possible mechanism for endogenous post-stroke depression
Anterior cerebrovascular lesions may block serotonergic and noradrenergic projections into the superficial cortex. The closer the lesion to the nuceli, the greater the pathway interruption, and the more severe the depression may be. Drawing represents nuclei in the brainstem, slightly enlarged, with their projections greatly simplified.
Source: Reference 8
Illustration for Current Psychiatry by Marcia Hartsock, CMIPSD is characterized as reactive (related to physical and psychosocial losses of stroke) or endogenous (a biologic consequence of stroke).
Reactive depression. Patients exhibit a constellation of emotional symptoms while attempting to cope with a new physical or cognitive deficit. This “catastrophic reaction”2 includes anxiety, crying, aggressive behavior, cursing, refusal, displacement, renouncement, and sometimes compensatory boasting.
In 62 stroke patients evaluated with the Catastrophic Reaction Scale:
- approximately 20% had a catastrophic reaction
- the reaction was significantly associated with major depression.
Anterior subcortical damage may be the common mechanism underlying both catastrophic reaction and major depression in stroke patients.3
Post-stroke emotional lability resembles PSD. This “pathologic emotion” or “emotional incontinence” can manifest as sudden, frequent, easily-provoked episodes of crying that are generally mood-congruent. Affected patients may also respond to nonemotional events with outbursts of pathologic crying or laughing.
The pathogenesis of post-stroke emotional lability is unclear, although biogenic amines may play a role. In a 6-week, double-blind trial, 28 patients with post-stroke pathologic laughter and crying were treated with nortriptyline or placebo. Symptoms improved significantly more with nortriptyline in both depressed and nondepressed patients, indicating that the response was not related simply to improved depressive symptoms.4
Endogenous depression. Robinson et al5 propose a neuroanatomic PSD model. They contend that major—but not minor—PSD correlates with the stroke lesion’s proximity to the left anterior frontal pole or underlying basal ganglia. Other investigators, however, question this anatomic distinction between major and minor PSD.
For example, Gainotti et al6 used their own Post-Stroke Depression Rating Scale to compare stroke patients without depression, with minor depression, or with major depressive disorder (MDD) and a group of nonstroke patients with functional MDD. They found that:
- the phenomenology of patients with major PSD was more similar to that of patients with minor PSD than to that of patients with functional major depression
- major and minor PSD were much more likely to be associated with reactive depression than with the endogenous form.
Other researchers disputed the neuroanatomic model after failing to confirm a correlation between PSD and the location of lesions in the left hemisphere.7
Most recently, a meta-analysis by Narushima et al8 suggested a moderately strong correlation between depressive symptom severity and the distance between the anterior border of a left-hemispheric lesion and the frontal pole during the first 6 months following a stroke. This group hypothesizes that more-anterior lesions interrupt the brain’s serotonergic and noradrenergic pathways (Figure) at a site closer to their origin—before they branch posteriorly into the superficial cortex. This interruption presumably increases serotonin and noradrenergic depletion, which is manifest as depression.
A common denominator? Two other recent studies suggest that depression may be a significant independent risk factor for stroke:
- A prospective study has assessed stroke risk factors in 2,800 Australians since 1988. Depression has been a significant stroke risk factor in men and women ages 70 and older.9
- A population-based study showed that depression predicted stroke across all strata in a cohort of 6,000 men and women ages 25 to 74. Subjects were stroke-free at enrollment and followed for up to 22 years.10
Table 1
How to evaluate a patient for post-stroke depression (PSD)
|
These observations—plus the fact that depression is a common sequela of stroke—suggest that stroke and depression may result from a common pathophysiology. Some evidence suggests that depression is a cerebrovascular disease. For example, stroke and depression are both associated with increased platelet reactivity (stickiness). However, platelet reactivity does not appear greater in patients who develop depression after a stroke than in those who do not.11
Table 2
Diagnostic criteria for mood disorder due to stroke*
|
| Specify type: |
| With depressive features: if the predominant mood is depressed but the full criteria are not met for a major depressive episode. |
| With major-depressive-like episode: if the full criteria are met (except criterion D) for a major depressive episode. |
| *DSM-IV-TR diagnostic criteria for mood disorder due to a general medical condition |
| Source: Adapted and reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision. Copyright 2000. American Psychiatric Association. |
A study of antidepressants’ effects on platelet dysfunction found that the selective serotonin reuptake inhibitors (SSRIs) paroxetine and sertraline may reverse platelet abnormalities, whereas the tricyclic nortriptyline does not.12
Summary. A biopsychosocial model helps explain the pathogenesis PSD, which may present as:
- a syndrome similar to MDD
- a relatively minor depression similar to dysthymic disorder
- a discrete phenomenon such as catastrophic reaction and emotional lability.
Evaluating patients for PSD
In the absence of PSD diagnostic guidelines, Table 1 provides a clinically useful approach. A comprehensive workup may suggest whether an individual’s depressive symptoms are endogenous or reactive, although this distinction may be subtle. Gathering information from other physicians, the patient, family, and caregivers may require more than one session.
Diagnostic criteria. Consult DSM-IV criteria for “mood disorder due to general medical condition” as they pertain to patients “with depressive features” (minor depression) or “with major depression-like episodes” (Table 2). In the initial evaluation, do not rely exclusively on instruments such as the Hamilton Depression Rating Scale for measuring depression, as patients with emotional lability may not meet the cut-off scores for depression. These scales may help monitor progress later during therapy.
Risk factors. Interview the patient, family, and caregivers to determine if the patient has possible risk factors for PSD:
- history of stroke
- personal or family history of depression
- loss of social activities
- major life event within 6 months of stroke
- cognitive impairment 1 month post-stroke.
Determine whether the patient’s stroke was precipitated by cocaine or other drug abuse. If so, address the cause.
Medical comorbidities. Consider the effect of medical comorbidities such as Parkinson’s disease, heart disease, or diabetes on the patient’s mood. Also rule out other metabolic causes of depression such as thyroid abnormalities, medication side effects, and vitamin B12 deficiency.
Table 3
Treating post-stroke depression with antidepressants
| TCAs | SSRIs | |
|---|---|---|
| Efficacy | Proven in double-blind, placebo-controlled trials One study found nortriptyline more effective than fluoxetine | Greater anxiolytic effect than TCAs (?) Overall less efficacious than TCAs (?) |
| Side effects | Alpha-adrenergic blockade, anticholinergic, antihistaminic, and cardiac effects | Drug interactions related to cytochrome P-450 isoenzyme inhibition Fluoxetine may prolong bleeding time |
| Overdose risk | Potentially fatal | Safe in overdose |
| Onset of action | Slower than SSRIs (?) | More rapid than TCAs (?) |
| Cost | Less expensive than SSRIs | More expensive than TCAs |
| (?) Not supported by controlled clinical trials | ||
| TCAs: Tricyclic antidepressants | ||
| SSRIs: Selective serotonin reuptake inhibitors | ||
Cognitive changes. Quantify any cognitive deficits with neuropsychological testing, such as the Mini-Mental State Examination. Also learn all you can about the patient’s premorbid personality for comparison with post-stroke behavior. Ask the nursing or rehabilitation staff about inpatients’ motivation and participation in care.
Social support. Determine if caregivers can provide transportation, medication monitoring, and other social support.
Treatment options
PSD calls for rapid, comprehensive treatment with antidepressants, psychotherapy, and help reintegrating into the community. Untreated PSD is associated with increased morbidity and mortality, whereas effective treatment improves functional outcomes.13
Antidepressants. Tricyclic antidepressants (desipramine, imipramine, and nortriptyline), SSRIs (citalopram and fluoxetine), and trazodone have been used to treat depression in stroke patients (Table 3) 14 Controlled studies suggest that:
- >60% of patients with PSD respond to medication
- they tolerate antidepressants well
- no antidepressant class has a distinct therapeutic advantage over others.
Antidepressants in other classes—such as venlafaxine, bupropion, and mirtazapine—have not been studied in patients with PSD.
Without strong evidence to guide the initial antidepressant choice, a pragmatic approach is to start with one or two agents with which you are most familiar. Consider side effects, potential drug-drug interactions, cost, and available formulations. A patient with post-stroke swallowing difficulties, for example, may benefit from a liquid form.
We do not have good data regarding the optimum starting dose and duration of therapy for any antidepressants in PSD. To minimize side effects, I recommend starting with low dosages, such as:
- fluoxetine, 10 mg/d
- sertraline, 25 to 50 mg/d
- nortriptyline, 10 to 25 mg/d.
Increase dosages gradually, watching for side effects and symptom improvement.
If treatment is effective, continue the antidepressant for at least 1 year. In patients with a history of depression, continue treatment longer to prevent depressive relapse.
Small, double-blind, controlled trials have used citalopram, fluoxetine, nortriptyline, or sertraline to treat post-stroke emotional lability.14 Compared with placebo, these agents all significantly reduced post-stroke emotionalism.
Psychostimulants such as methylphenidate and dextroamphetamine might be an effective alternative to antidepressants.15 They have a morerapid onset of action, better tolerability, and may be more effective in alleviating post-stroke apathy. Disadvantages include risks for tolerance, dependence, and psychiatric side effects.
As with antidepressants, start low and go slow to minimize side effects. You could start methylphenidate at 5 mg in the morning and increase to 20 to 30 mg/d before you decide—based on response—to continue or discontinue. After the dosage is stabilized, you could switch to a controlled-release formulation.
ECT. Although no controlled trials of electroconvulsive therapy for PSD have been reported, ECT can be an effective option for patients with treatment-resistant depression. Some retrospective studies16 have shown a good response among patients with PSD, although ECT may worsen stroke-related cognitive deficits.
rTMS. University of Iowa researchers recently completed a double-blind controlled trial evaluating the efficacy of repetitive transcranial magnetic stimulation (rTMS) in PSD. R.G. Robinson, MD (personal communication, 2003), reported that preliminary results are encouraging.
Psychotherapy. Cognitive-behavioral therapy—used alone patients or combined with medication—has yielded good results in some PSD studies. Controlled trials17,18 have shown that individual counseling, occupational therapy, leisure activities, and social work improve all aspects of PSD except mood.
Can be prevented?
Many patients who are not depressed during an initial post-stroke evaluation develop depression within 2 years.19 This raises the question: Can PSD be prevented by treating stroke patients prophylactically?
In a 12-week, randomized, double-blind trial,20 48 nondepressed post-stroke patients were treated with nortriptyline, fluoxetine, or placebo. Dosages were:
- nortriptyline—25 mg/d in week 1; 50 mg/d in weeks 2 and 3; 75 mg/d in weeks 4 to 6, and 100 mg/d in weeks 7 to 12
- fluoxetine—10 mg/d in weeks 1 to 3; 20 mg/d in weeks 4 to 6; 30 mg/d in weeks 7 to 9, and 40 mg/d in weeks 10 to 12.
After 3 months, the two antidepressants appeared comparable in efficacy and significantly more effective than placebo in preventing depression. Patients who had taken nortriptyline were more likely to develop depression during the subsequent 6 months than were patients in the other two groups, and their symptoms were more severe. However, the authors noted many study limitations, including small sample size and loss of some patients to follow-up.
In a randomized, double-blind study, prophylaxis with mianserin (not available in the United States) did not prevent post-stroke depression.21 For 1 year, 100 patients presenting with acute ischemic stroke received mianserin, 60 mg/d, or placebo. Monitoring at 2, 6, 12, and 18 months found no differences between the two groups with respect to PSD onset.
Recommendation. As with most aspects of PSD treatment, the issue of prophylaxis remains unsettled. I do not routinely start antidepressants in nondepressed stroke patients because evidence of benefit is lacking and any added medications increase the risk of side effects and drug-drug interactions.
Related resources
- National Institute of Neurological Disorders and Stroke. Stroke information page www.ninds.nih.gov/health_and_medical/disorders/stroke.htm
- Robinson RG. The clinical neuropsychiatry of stroke: cognitive, behavioral, and emotional disorders following vascular brain injury. New York: Cambridge University Press, 1998.
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrin
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Methylphenidate • Concerta, Ritalin
- Mirtazapine • Remeron
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Fozdar is a speaker for Eli Lilly and Company.
1. Heart and stroke statistical update. Dallas: American Heart Association, 2002.
2. Goldstein K. The organism:a holistic approach to biology derived from pathological data in man. New York: American Book Co, 1939.
3. Starkstein SE, Fedoroff JP, Price TR, et al. Catastrophic reaction after cerebrovascular lesions: frequency, correlates, and validation of a scale. J Neuropsychiatry Clin Neurosci 1993;5(2):189-94.
4. Robinson RG, Parikh RM, Lipsey JR, et al. Pathological laughing and crying following stroke: Validation of measurement scale and double-blind treatment study. Am J Psychiatry 1993;150:286-93.
5. Robinson RG, Kubos KL, Starr LB, et al. Mood changes in stroke patients: relationship to lesion location. Compr Psychiatry 1983;24(6):555-66.
6. Gainotti G, Azzoni A, Razzano C, et al. The Post-Stroke Depression Rating Scale: a test specifically devised to investigate affective disorders of stroke patients. J Clin Exp Neuropsychol 1997;19(3):340-56.
7. Carson AJ, MacHale S, Allen K, et al. Depression after stroke and lesion location: a systematic review. Lancet 2000;356(9224):122-6.
8. Narushima K, Kosier JT, Robinson RG. A reappraisal of poststroke depression, intra- and inter-hemispheric lesion location using meta-analysis. J Neuropsychiatry Clin Neurosci 2003;15(4):422-30.
9. Simons LA, McCallum J, Friedlander Y, Simons J. Risk factors for ischemic stroke: Dubbo Study of the elderly. Stroke 1998;29(7):1341-6.
10. Jonas BS, Mussolino ME. Symptoms of depression as a prospective risk factor for stroke. Psychosom Med 2000;62(4):463-71.
11. Cassidy EM, Walsh MT, O’Connor R, et al. Platelet surface glycoprotein expression in post-stroke depression: a preliminary study. Psychiatry Res 2003;118(2):175-81.
12. Pollock BG, Laghrissi-Thode F, Wagner WR. Evaluation of platelet activation in depressed patients with ischemic heart disease after paroxetine or nortriptyline treatment. J Clin Psychopharmacol 2000;20(2):137-40.
13. Everson SA, Roberts RE, Goldberg DE, Kaplan GA. Depressive symptoms and increased risk of stroke mortality over a 29-year period. Arch Intern Med 1998;158(10):1133-8.
14. Turner-Stokes L, Hassan N. Depression after stroke: a review of the evidence base to inform the development of an integrated care pathway. Part 2: Treatment alternatives. Clin Rehabil 2002;16(3):248-60.
15. Whyte EM, Mulsant BH. Post-stroke depression: epidemiology, pathophysiology, and biologic treatment. Biol Psychiatry 2002;52:253-64.
16. Currier M, Murray G, Welsh C. Electroconvulsive therapy for poststroke depressed geriatric patients. J Neuropsychiatry Clin Neurosci 1992;4(2):140-4.
17. Kemp BJ, Corgiat M, Gill C. Effects of brief cognitive behavioral group psychotherapy in older persons with and without disabling illness. Behav Health Ageing 1992;2:21-8.
18. Lincoln NB, Flannaghan T, Sutcliffe L, Rother L. Evaluation of cognitive behavioural treatment for depression after stroke: a pilot study. Clin Rehabil 1997;11(2):114-22.
19. Astrom M, Adolfsson R, Asplund K. Major depression in stroke patients: a 13-year longitudinal study. Stroke 1993;24:976-82.
20. Narushima K, Kosier JT, Robinson RG. Preventing poststroke depression: a 12-week double-blind randomized treatment trial and 21-month follow-up. J Nerv Ment Dis 2002;190(5):296-303.
21. Palomaki H, Kaste M, Berg A, et al. Prevention of poststroke depression: 1 year randomised placebo controlled double blind trial of mianserin with 6 month follow up after therapy. J Neurol Neurosurg Psychiatry 1999;66(4):490-4.
Patients with post-stroke depression (PSD) pose many clinical dilemmas: Is their depression a psychological reaction or a biological event? Are antidepressants effective for either type? Should antidepressants be given prophylactically after a stroke, even if the patient is not depressed?
Although the answers are not clear, this article describes a practical approach to stroke patients referred for psychiatric evaluation, including:
- strategies to distinguish reactive from endogenous depression
- issues that guide antidepressant selection
- benefits and risks of using medication to prevent depression after an acute stroke.
Reactive or endogenous depression?
Each year 500,000 to 600,000 Americans suffer strokes.1 Depression is the most common emotional sequela, reported in up to 40% of survivors within several months of an acute stroke.
Figure Possible mechanism for endogenous post-stroke depression
Anterior cerebrovascular lesions may block serotonergic and noradrenergic projections into the superficial cortex. The closer the lesion to the nuceli, the greater the pathway interruption, and the more severe the depression may be. Drawing represents nuclei in the brainstem, slightly enlarged, with their projections greatly simplified.
Source: Reference 8
Illustration for Current Psychiatry by Marcia Hartsock, CMIPSD is characterized as reactive (related to physical and psychosocial losses of stroke) or endogenous (a biologic consequence of stroke).
Reactive depression. Patients exhibit a constellation of emotional symptoms while attempting to cope with a new physical or cognitive deficit. This “catastrophic reaction”2 includes anxiety, crying, aggressive behavior, cursing, refusal, displacement, renouncement, and sometimes compensatory boasting.
In 62 stroke patients evaluated with the Catastrophic Reaction Scale:
- approximately 20% had a catastrophic reaction
- the reaction was significantly associated with major depression.
Anterior subcortical damage may be the common mechanism underlying both catastrophic reaction and major depression in stroke patients.3
Post-stroke emotional lability resembles PSD. This “pathologic emotion” or “emotional incontinence” can manifest as sudden, frequent, easily-provoked episodes of crying that are generally mood-congruent. Affected patients may also respond to nonemotional events with outbursts of pathologic crying or laughing.
The pathogenesis of post-stroke emotional lability is unclear, although biogenic amines may play a role. In a 6-week, double-blind trial, 28 patients with post-stroke pathologic laughter and crying were treated with nortriptyline or placebo. Symptoms improved significantly more with nortriptyline in both depressed and nondepressed patients, indicating that the response was not related simply to improved depressive symptoms.4
Endogenous depression. Robinson et al5 propose a neuroanatomic PSD model. They contend that major—but not minor—PSD correlates with the stroke lesion’s proximity to the left anterior frontal pole or underlying basal ganglia. Other investigators, however, question this anatomic distinction between major and minor PSD.
For example, Gainotti et al6 used their own Post-Stroke Depression Rating Scale to compare stroke patients without depression, with minor depression, or with major depressive disorder (MDD) and a group of nonstroke patients with functional MDD. They found that:
- the phenomenology of patients with major PSD was more similar to that of patients with minor PSD than to that of patients with functional major depression
- major and minor PSD were much more likely to be associated with reactive depression than with the endogenous form.
Other researchers disputed the neuroanatomic model after failing to confirm a correlation between PSD and the location of lesions in the left hemisphere.7
Most recently, a meta-analysis by Narushima et al8 suggested a moderately strong correlation between depressive symptom severity and the distance between the anterior border of a left-hemispheric lesion and the frontal pole during the first 6 months following a stroke. This group hypothesizes that more-anterior lesions interrupt the brain’s serotonergic and noradrenergic pathways (Figure) at a site closer to their origin—before they branch posteriorly into the superficial cortex. This interruption presumably increases serotonin and noradrenergic depletion, which is manifest as depression.
A common denominator? Two other recent studies suggest that depression may be a significant independent risk factor for stroke:
- A prospective study has assessed stroke risk factors in 2,800 Australians since 1988. Depression has been a significant stroke risk factor in men and women ages 70 and older.9
- A population-based study showed that depression predicted stroke across all strata in a cohort of 6,000 men and women ages 25 to 74. Subjects were stroke-free at enrollment and followed for up to 22 years.10
Table 1
How to evaluate a patient for post-stroke depression (PSD)
|
These observations—plus the fact that depression is a common sequela of stroke—suggest that stroke and depression may result from a common pathophysiology. Some evidence suggests that depression is a cerebrovascular disease. For example, stroke and depression are both associated with increased platelet reactivity (stickiness). However, platelet reactivity does not appear greater in patients who develop depression after a stroke than in those who do not.11
Table 2
Diagnostic criteria for mood disorder due to stroke*
|
| Specify type: |
| With depressive features: if the predominant mood is depressed but the full criteria are not met for a major depressive episode. |
| With major-depressive-like episode: if the full criteria are met (except criterion D) for a major depressive episode. |
| *DSM-IV-TR diagnostic criteria for mood disorder due to a general medical condition |
| Source: Adapted and reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision. Copyright 2000. American Psychiatric Association. |
A study of antidepressants’ effects on platelet dysfunction found that the selective serotonin reuptake inhibitors (SSRIs) paroxetine and sertraline may reverse platelet abnormalities, whereas the tricyclic nortriptyline does not.12
Summary. A biopsychosocial model helps explain the pathogenesis PSD, which may present as:
- a syndrome similar to MDD
- a relatively minor depression similar to dysthymic disorder
- a discrete phenomenon such as catastrophic reaction and emotional lability.
Evaluating patients for PSD
In the absence of PSD diagnostic guidelines, Table 1 provides a clinically useful approach. A comprehensive workup may suggest whether an individual’s depressive symptoms are endogenous or reactive, although this distinction may be subtle. Gathering information from other physicians, the patient, family, and caregivers may require more than one session.
Diagnostic criteria. Consult DSM-IV criteria for “mood disorder due to general medical condition” as they pertain to patients “with depressive features” (minor depression) or “with major depression-like episodes” (Table 2). In the initial evaluation, do not rely exclusively on instruments such as the Hamilton Depression Rating Scale for measuring depression, as patients with emotional lability may not meet the cut-off scores for depression. These scales may help monitor progress later during therapy.
Risk factors. Interview the patient, family, and caregivers to determine if the patient has possible risk factors for PSD:
- history of stroke
- personal or family history of depression
- loss of social activities
- major life event within 6 months of stroke
- cognitive impairment 1 month post-stroke.
Determine whether the patient’s stroke was precipitated by cocaine or other drug abuse. If so, address the cause.
Medical comorbidities. Consider the effect of medical comorbidities such as Parkinson’s disease, heart disease, or diabetes on the patient’s mood. Also rule out other metabolic causes of depression such as thyroid abnormalities, medication side effects, and vitamin B12 deficiency.
Table 3
Treating post-stroke depression with antidepressants
| TCAs | SSRIs | |
|---|---|---|
| Efficacy | Proven in double-blind, placebo-controlled trials One study found nortriptyline more effective than fluoxetine | Greater anxiolytic effect than TCAs (?) Overall less efficacious than TCAs (?) |
| Side effects | Alpha-adrenergic blockade, anticholinergic, antihistaminic, and cardiac effects | Drug interactions related to cytochrome P-450 isoenzyme inhibition Fluoxetine may prolong bleeding time |
| Overdose risk | Potentially fatal | Safe in overdose |
| Onset of action | Slower than SSRIs (?) | More rapid than TCAs (?) |
| Cost | Less expensive than SSRIs | More expensive than TCAs |
| (?) Not supported by controlled clinical trials | ||
| TCAs: Tricyclic antidepressants | ||
| SSRIs: Selective serotonin reuptake inhibitors | ||
Cognitive changes. Quantify any cognitive deficits with neuropsychological testing, such as the Mini-Mental State Examination. Also learn all you can about the patient’s premorbid personality for comparison with post-stroke behavior. Ask the nursing or rehabilitation staff about inpatients’ motivation and participation in care.
Social support. Determine if caregivers can provide transportation, medication monitoring, and other social support.
Treatment options
PSD calls for rapid, comprehensive treatment with antidepressants, psychotherapy, and help reintegrating into the community. Untreated PSD is associated with increased morbidity and mortality, whereas effective treatment improves functional outcomes.13
Antidepressants. Tricyclic antidepressants (desipramine, imipramine, and nortriptyline), SSRIs (citalopram and fluoxetine), and trazodone have been used to treat depression in stroke patients (Table 3) 14 Controlled studies suggest that:
- >60% of patients with PSD respond to medication
- they tolerate antidepressants well
- no antidepressant class has a distinct therapeutic advantage over others.
Antidepressants in other classes—such as venlafaxine, bupropion, and mirtazapine—have not been studied in patients with PSD.
Without strong evidence to guide the initial antidepressant choice, a pragmatic approach is to start with one or two agents with which you are most familiar. Consider side effects, potential drug-drug interactions, cost, and available formulations. A patient with post-stroke swallowing difficulties, for example, may benefit from a liquid form.
We do not have good data regarding the optimum starting dose and duration of therapy for any antidepressants in PSD. To minimize side effects, I recommend starting with low dosages, such as:
- fluoxetine, 10 mg/d
- sertraline, 25 to 50 mg/d
- nortriptyline, 10 to 25 mg/d.
Increase dosages gradually, watching for side effects and symptom improvement.
If treatment is effective, continue the antidepressant for at least 1 year. In patients with a history of depression, continue treatment longer to prevent depressive relapse.
Small, double-blind, controlled trials have used citalopram, fluoxetine, nortriptyline, or sertraline to treat post-stroke emotional lability.14 Compared with placebo, these agents all significantly reduced post-stroke emotionalism.
Psychostimulants such as methylphenidate and dextroamphetamine might be an effective alternative to antidepressants.15 They have a morerapid onset of action, better tolerability, and may be more effective in alleviating post-stroke apathy. Disadvantages include risks for tolerance, dependence, and psychiatric side effects.
As with antidepressants, start low and go slow to minimize side effects. You could start methylphenidate at 5 mg in the morning and increase to 20 to 30 mg/d before you decide—based on response—to continue or discontinue. After the dosage is stabilized, you could switch to a controlled-release formulation.
ECT. Although no controlled trials of electroconvulsive therapy for PSD have been reported, ECT can be an effective option for patients with treatment-resistant depression. Some retrospective studies16 have shown a good response among patients with PSD, although ECT may worsen stroke-related cognitive deficits.
rTMS. University of Iowa researchers recently completed a double-blind controlled trial evaluating the efficacy of repetitive transcranial magnetic stimulation (rTMS) in PSD. R.G. Robinson, MD (personal communication, 2003), reported that preliminary results are encouraging.
Psychotherapy. Cognitive-behavioral therapy—used alone patients or combined with medication—has yielded good results in some PSD studies. Controlled trials17,18 have shown that individual counseling, occupational therapy, leisure activities, and social work improve all aspects of PSD except mood.
Can be prevented?
Many patients who are not depressed during an initial post-stroke evaluation develop depression within 2 years.19 This raises the question: Can PSD be prevented by treating stroke patients prophylactically?
In a 12-week, randomized, double-blind trial,20 48 nondepressed post-stroke patients were treated with nortriptyline, fluoxetine, or placebo. Dosages were:
- nortriptyline—25 mg/d in week 1; 50 mg/d in weeks 2 and 3; 75 mg/d in weeks 4 to 6, and 100 mg/d in weeks 7 to 12
- fluoxetine—10 mg/d in weeks 1 to 3; 20 mg/d in weeks 4 to 6; 30 mg/d in weeks 7 to 9, and 40 mg/d in weeks 10 to 12.
After 3 months, the two antidepressants appeared comparable in efficacy and significantly more effective than placebo in preventing depression. Patients who had taken nortriptyline were more likely to develop depression during the subsequent 6 months than were patients in the other two groups, and their symptoms were more severe. However, the authors noted many study limitations, including small sample size and loss of some patients to follow-up.
In a randomized, double-blind study, prophylaxis with mianserin (not available in the United States) did not prevent post-stroke depression.21 For 1 year, 100 patients presenting with acute ischemic stroke received mianserin, 60 mg/d, or placebo. Monitoring at 2, 6, 12, and 18 months found no differences between the two groups with respect to PSD onset.
Recommendation. As with most aspects of PSD treatment, the issue of prophylaxis remains unsettled. I do not routinely start antidepressants in nondepressed stroke patients because evidence of benefit is lacking and any added medications increase the risk of side effects and drug-drug interactions.
Related resources
- National Institute of Neurological Disorders and Stroke. Stroke information page www.ninds.nih.gov/health_and_medical/disorders/stroke.htm
- Robinson RG. The clinical neuropsychiatry of stroke: cognitive, behavioral, and emotional disorders following vascular brain injury. New York: Cambridge University Press, 1998.
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrin
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Methylphenidate • Concerta, Ritalin
- Mirtazapine • Remeron
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Fozdar is a speaker for Eli Lilly and Company.
Patients with post-stroke depression (PSD) pose many clinical dilemmas: Is their depression a psychological reaction or a biological event? Are antidepressants effective for either type? Should antidepressants be given prophylactically after a stroke, even if the patient is not depressed?
Although the answers are not clear, this article describes a practical approach to stroke patients referred for psychiatric evaluation, including:
- strategies to distinguish reactive from endogenous depression
- issues that guide antidepressant selection
- benefits and risks of using medication to prevent depression after an acute stroke.
Reactive or endogenous depression?
Each year 500,000 to 600,000 Americans suffer strokes.1 Depression is the most common emotional sequela, reported in up to 40% of survivors within several months of an acute stroke.
Figure Possible mechanism for endogenous post-stroke depression
Anterior cerebrovascular lesions may block serotonergic and noradrenergic projections into the superficial cortex. The closer the lesion to the nuceli, the greater the pathway interruption, and the more severe the depression may be. Drawing represents nuclei in the brainstem, slightly enlarged, with their projections greatly simplified.
Source: Reference 8
Illustration for Current Psychiatry by Marcia Hartsock, CMIPSD is characterized as reactive (related to physical and psychosocial losses of stroke) or endogenous (a biologic consequence of stroke).
Reactive depression. Patients exhibit a constellation of emotional symptoms while attempting to cope with a new physical or cognitive deficit. This “catastrophic reaction”2 includes anxiety, crying, aggressive behavior, cursing, refusal, displacement, renouncement, and sometimes compensatory boasting.
In 62 stroke patients evaluated with the Catastrophic Reaction Scale:
- approximately 20% had a catastrophic reaction
- the reaction was significantly associated with major depression.
Anterior subcortical damage may be the common mechanism underlying both catastrophic reaction and major depression in stroke patients.3
Post-stroke emotional lability resembles PSD. This “pathologic emotion” or “emotional incontinence” can manifest as sudden, frequent, easily-provoked episodes of crying that are generally mood-congruent. Affected patients may also respond to nonemotional events with outbursts of pathologic crying or laughing.
The pathogenesis of post-stroke emotional lability is unclear, although biogenic amines may play a role. In a 6-week, double-blind trial, 28 patients with post-stroke pathologic laughter and crying were treated with nortriptyline or placebo. Symptoms improved significantly more with nortriptyline in both depressed and nondepressed patients, indicating that the response was not related simply to improved depressive symptoms.4
Endogenous depression. Robinson et al5 propose a neuroanatomic PSD model. They contend that major—but not minor—PSD correlates with the stroke lesion’s proximity to the left anterior frontal pole or underlying basal ganglia. Other investigators, however, question this anatomic distinction between major and minor PSD.
For example, Gainotti et al6 used their own Post-Stroke Depression Rating Scale to compare stroke patients without depression, with minor depression, or with major depressive disorder (MDD) and a group of nonstroke patients with functional MDD. They found that:
- the phenomenology of patients with major PSD was more similar to that of patients with minor PSD than to that of patients with functional major depression
- major and minor PSD were much more likely to be associated with reactive depression than with the endogenous form.
Other researchers disputed the neuroanatomic model after failing to confirm a correlation between PSD and the location of lesions in the left hemisphere.7
Most recently, a meta-analysis by Narushima et al8 suggested a moderately strong correlation between depressive symptom severity and the distance between the anterior border of a left-hemispheric lesion and the frontal pole during the first 6 months following a stroke. This group hypothesizes that more-anterior lesions interrupt the brain’s serotonergic and noradrenergic pathways (Figure) at a site closer to their origin—before they branch posteriorly into the superficial cortex. This interruption presumably increases serotonin and noradrenergic depletion, which is manifest as depression.
A common denominator? Two other recent studies suggest that depression may be a significant independent risk factor for stroke:
- A prospective study has assessed stroke risk factors in 2,800 Australians since 1988. Depression has been a significant stroke risk factor in men and women ages 70 and older.9
- A population-based study showed that depression predicted stroke across all strata in a cohort of 6,000 men and women ages 25 to 74. Subjects were stroke-free at enrollment and followed for up to 22 years.10
Table 1
How to evaluate a patient for post-stroke depression (PSD)
|
These observations—plus the fact that depression is a common sequela of stroke—suggest that stroke and depression may result from a common pathophysiology. Some evidence suggests that depression is a cerebrovascular disease. For example, stroke and depression are both associated with increased platelet reactivity (stickiness). However, platelet reactivity does not appear greater in patients who develop depression after a stroke than in those who do not.11
Table 2
Diagnostic criteria for mood disorder due to stroke*
|
| Specify type: |
| With depressive features: if the predominant mood is depressed but the full criteria are not met for a major depressive episode. |
| With major-depressive-like episode: if the full criteria are met (except criterion D) for a major depressive episode. |
| *DSM-IV-TR diagnostic criteria for mood disorder due to a general medical condition |
| Source: Adapted and reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision. Copyright 2000. American Psychiatric Association. |
A study of antidepressants’ effects on platelet dysfunction found that the selective serotonin reuptake inhibitors (SSRIs) paroxetine and sertraline may reverse platelet abnormalities, whereas the tricyclic nortriptyline does not.12
Summary. A biopsychosocial model helps explain the pathogenesis PSD, which may present as:
- a syndrome similar to MDD
- a relatively minor depression similar to dysthymic disorder
- a discrete phenomenon such as catastrophic reaction and emotional lability.
Evaluating patients for PSD
In the absence of PSD diagnostic guidelines, Table 1 provides a clinically useful approach. A comprehensive workup may suggest whether an individual’s depressive symptoms are endogenous or reactive, although this distinction may be subtle. Gathering information from other physicians, the patient, family, and caregivers may require more than one session.
Diagnostic criteria. Consult DSM-IV criteria for “mood disorder due to general medical condition” as they pertain to patients “with depressive features” (minor depression) or “with major depression-like episodes” (Table 2). In the initial evaluation, do not rely exclusively on instruments such as the Hamilton Depression Rating Scale for measuring depression, as patients with emotional lability may not meet the cut-off scores for depression. These scales may help monitor progress later during therapy.
Risk factors. Interview the patient, family, and caregivers to determine if the patient has possible risk factors for PSD:
- history of stroke
- personal or family history of depression
- loss of social activities
- major life event within 6 months of stroke
- cognitive impairment 1 month post-stroke.
Determine whether the patient’s stroke was precipitated by cocaine or other drug abuse. If so, address the cause.
Medical comorbidities. Consider the effect of medical comorbidities such as Parkinson’s disease, heart disease, or diabetes on the patient’s mood. Also rule out other metabolic causes of depression such as thyroid abnormalities, medication side effects, and vitamin B12 deficiency.
Table 3
Treating post-stroke depression with antidepressants
| TCAs | SSRIs | |
|---|---|---|
| Efficacy | Proven in double-blind, placebo-controlled trials One study found nortriptyline more effective than fluoxetine | Greater anxiolytic effect than TCAs (?) Overall less efficacious than TCAs (?) |
| Side effects | Alpha-adrenergic blockade, anticholinergic, antihistaminic, and cardiac effects | Drug interactions related to cytochrome P-450 isoenzyme inhibition Fluoxetine may prolong bleeding time |
| Overdose risk | Potentially fatal | Safe in overdose |
| Onset of action | Slower than SSRIs (?) | More rapid than TCAs (?) |
| Cost | Less expensive than SSRIs | More expensive than TCAs |
| (?) Not supported by controlled clinical trials | ||
| TCAs: Tricyclic antidepressants | ||
| SSRIs: Selective serotonin reuptake inhibitors | ||
Cognitive changes. Quantify any cognitive deficits with neuropsychological testing, such as the Mini-Mental State Examination. Also learn all you can about the patient’s premorbid personality for comparison with post-stroke behavior. Ask the nursing or rehabilitation staff about inpatients’ motivation and participation in care.
Social support. Determine if caregivers can provide transportation, medication monitoring, and other social support.
Treatment options
PSD calls for rapid, comprehensive treatment with antidepressants, psychotherapy, and help reintegrating into the community. Untreated PSD is associated with increased morbidity and mortality, whereas effective treatment improves functional outcomes.13
Antidepressants. Tricyclic antidepressants (desipramine, imipramine, and nortriptyline), SSRIs (citalopram and fluoxetine), and trazodone have been used to treat depression in stroke patients (Table 3) 14 Controlled studies suggest that:
- >60% of patients with PSD respond to medication
- they tolerate antidepressants well
- no antidepressant class has a distinct therapeutic advantage over others.
Antidepressants in other classes—such as venlafaxine, bupropion, and mirtazapine—have not been studied in patients with PSD.
Without strong evidence to guide the initial antidepressant choice, a pragmatic approach is to start with one or two agents with which you are most familiar. Consider side effects, potential drug-drug interactions, cost, and available formulations. A patient with post-stroke swallowing difficulties, for example, may benefit from a liquid form.
We do not have good data regarding the optimum starting dose and duration of therapy for any antidepressants in PSD. To minimize side effects, I recommend starting with low dosages, such as:
- fluoxetine, 10 mg/d
- sertraline, 25 to 50 mg/d
- nortriptyline, 10 to 25 mg/d.
Increase dosages gradually, watching for side effects and symptom improvement.
If treatment is effective, continue the antidepressant for at least 1 year. In patients with a history of depression, continue treatment longer to prevent depressive relapse.
Small, double-blind, controlled trials have used citalopram, fluoxetine, nortriptyline, or sertraline to treat post-stroke emotional lability.14 Compared with placebo, these agents all significantly reduced post-stroke emotionalism.
Psychostimulants such as methylphenidate and dextroamphetamine might be an effective alternative to antidepressants.15 They have a morerapid onset of action, better tolerability, and may be more effective in alleviating post-stroke apathy. Disadvantages include risks for tolerance, dependence, and psychiatric side effects.
As with antidepressants, start low and go slow to minimize side effects. You could start methylphenidate at 5 mg in the morning and increase to 20 to 30 mg/d before you decide—based on response—to continue or discontinue. After the dosage is stabilized, you could switch to a controlled-release formulation.
ECT. Although no controlled trials of electroconvulsive therapy for PSD have been reported, ECT can be an effective option for patients with treatment-resistant depression. Some retrospective studies16 have shown a good response among patients with PSD, although ECT may worsen stroke-related cognitive deficits.
rTMS. University of Iowa researchers recently completed a double-blind controlled trial evaluating the efficacy of repetitive transcranial magnetic stimulation (rTMS) in PSD. R.G. Robinson, MD (personal communication, 2003), reported that preliminary results are encouraging.
Psychotherapy. Cognitive-behavioral therapy—used alone patients or combined with medication—has yielded good results in some PSD studies. Controlled trials17,18 have shown that individual counseling, occupational therapy, leisure activities, and social work improve all aspects of PSD except mood.
Can be prevented?
Many patients who are not depressed during an initial post-stroke evaluation develop depression within 2 years.19 This raises the question: Can PSD be prevented by treating stroke patients prophylactically?
In a 12-week, randomized, double-blind trial,20 48 nondepressed post-stroke patients were treated with nortriptyline, fluoxetine, or placebo. Dosages were:
- nortriptyline—25 mg/d in week 1; 50 mg/d in weeks 2 and 3; 75 mg/d in weeks 4 to 6, and 100 mg/d in weeks 7 to 12
- fluoxetine—10 mg/d in weeks 1 to 3; 20 mg/d in weeks 4 to 6; 30 mg/d in weeks 7 to 9, and 40 mg/d in weeks 10 to 12.
After 3 months, the two antidepressants appeared comparable in efficacy and significantly more effective than placebo in preventing depression. Patients who had taken nortriptyline were more likely to develop depression during the subsequent 6 months than were patients in the other two groups, and their symptoms were more severe. However, the authors noted many study limitations, including small sample size and loss of some patients to follow-up.
In a randomized, double-blind study, prophylaxis with mianserin (not available in the United States) did not prevent post-stroke depression.21 For 1 year, 100 patients presenting with acute ischemic stroke received mianserin, 60 mg/d, or placebo. Monitoring at 2, 6, 12, and 18 months found no differences between the two groups with respect to PSD onset.
Recommendation. As with most aspects of PSD treatment, the issue of prophylaxis remains unsettled. I do not routinely start antidepressants in nondepressed stroke patients because evidence of benefit is lacking and any added medications increase the risk of side effects and drug-drug interactions.
Related resources
- National Institute of Neurological Disorders and Stroke. Stroke information page www.ninds.nih.gov/health_and_medical/disorders/stroke.htm
- Robinson RG. The clinical neuropsychiatry of stroke: cognitive, behavioral, and emotional disorders following vascular brain injury. New York: Cambridge University Press, 1998.
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrin
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Methylphenidate • Concerta, Ritalin
- Mirtazapine • Remeron
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Fozdar is a speaker for Eli Lilly and Company.
1. Heart and stroke statistical update. Dallas: American Heart Association, 2002.
2. Goldstein K. The organism:a holistic approach to biology derived from pathological data in man. New York: American Book Co, 1939.
3. Starkstein SE, Fedoroff JP, Price TR, et al. Catastrophic reaction after cerebrovascular lesions: frequency, correlates, and validation of a scale. J Neuropsychiatry Clin Neurosci 1993;5(2):189-94.
4. Robinson RG, Parikh RM, Lipsey JR, et al. Pathological laughing and crying following stroke: Validation of measurement scale and double-blind treatment study. Am J Psychiatry 1993;150:286-93.
5. Robinson RG, Kubos KL, Starr LB, et al. Mood changes in stroke patients: relationship to lesion location. Compr Psychiatry 1983;24(6):555-66.
6. Gainotti G, Azzoni A, Razzano C, et al. The Post-Stroke Depression Rating Scale: a test specifically devised to investigate affective disorders of stroke patients. J Clin Exp Neuropsychol 1997;19(3):340-56.
7. Carson AJ, MacHale S, Allen K, et al. Depression after stroke and lesion location: a systematic review. Lancet 2000;356(9224):122-6.
8. Narushima K, Kosier JT, Robinson RG. A reappraisal of poststroke depression, intra- and inter-hemispheric lesion location using meta-analysis. J Neuropsychiatry Clin Neurosci 2003;15(4):422-30.
9. Simons LA, McCallum J, Friedlander Y, Simons J. Risk factors for ischemic stroke: Dubbo Study of the elderly. Stroke 1998;29(7):1341-6.
10. Jonas BS, Mussolino ME. Symptoms of depression as a prospective risk factor for stroke. Psychosom Med 2000;62(4):463-71.
11. Cassidy EM, Walsh MT, O’Connor R, et al. Platelet surface glycoprotein expression in post-stroke depression: a preliminary study. Psychiatry Res 2003;118(2):175-81.
12. Pollock BG, Laghrissi-Thode F, Wagner WR. Evaluation of platelet activation in depressed patients with ischemic heart disease after paroxetine or nortriptyline treatment. J Clin Psychopharmacol 2000;20(2):137-40.
13. Everson SA, Roberts RE, Goldberg DE, Kaplan GA. Depressive symptoms and increased risk of stroke mortality over a 29-year period. Arch Intern Med 1998;158(10):1133-8.
14. Turner-Stokes L, Hassan N. Depression after stroke: a review of the evidence base to inform the development of an integrated care pathway. Part 2: Treatment alternatives. Clin Rehabil 2002;16(3):248-60.
15. Whyte EM, Mulsant BH. Post-stroke depression: epidemiology, pathophysiology, and biologic treatment. Biol Psychiatry 2002;52:253-64.
16. Currier M, Murray G, Welsh C. Electroconvulsive therapy for poststroke depressed geriatric patients. J Neuropsychiatry Clin Neurosci 1992;4(2):140-4.
17. Kemp BJ, Corgiat M, Gill C. Effects of brief cognitive behavioral group psychotherapy in older persons with and without disabling illness. Behav Health Ageing 1992;2:21-8.
18. Lincoln NB, Flannaghan T, Sutcliffe L, Rother L. Evaluation of cognitive behavioural treatment for depression after stroke: a pilot study. Clin Rehabil 1997;11(2):114-22.
19. Astrom M, Adolfsson R, Asplund K. Major depression in stroke patients: a 13-year longitudinal study. Stroke 1993;24:976-82.
20. Narushima K, Kosier JT, Robinson RG. Preventing poststroke depression: a 12-week double-blind randomized treatment trial and 21-month follow-up. J Nerv Ment Dis 2002;190(5):296-303.
21. Palomaki H, Kaste M, Berg A, et al. Prevention of poststroke depression: 1 year randomised placebo controlled double blind trial of mianserin with 6 month follow up after therapy. J Neurol Neurosurg Psychiatry 1999;66(4):490-4.
1. Heart and stroke statistical update. Dallas: American Heart Association, 2002.
2. Goldstein K. The organism:a holistic approach to biology derived from pathological data in man. New York: American Book Co, 1939.
3. Starkstein SE, Fedoroff JP, Price TR, et al. Catastrophic reaction after cerebrovascular lesions: frequency, correlates, and validation of a scale. J Neuropsychiatry Clin Neurosci 1993;5(2):189-94.
4. Robinson RG, Parikh RM, Lipsey JR, et al. Pathological laughing and crying following stroke: Validation of measurement scale and double-blind treatment study. Am J Psychiatry 1993;150:286-93.
5. Robinson RG, Kubos KL, Starr LB, et al. Mood changes in stroke patients: relationship to lesion location. Compr Psychiatry 1983;24(6):555-66.
6. Gainotti G, Azzoni A, Razzano C, et al. The Post-Stroke Depression Rating Scale: a test specifically devised to investigate affective disorders of stroke patients. J Clin Exp Neuropsychol 1997;19(3):340-56.
7. Carson AJ, MacHale S, Allen K, et al. Depression after stroke and lesion location: a systematic review. Lancet 2000;356(9224):122-6.
8. Narushima K, Kosier JT, Robinson RG. A reappraisal of poststroke depression, intra- and inter-hemispheric lesion location using meta-analysis. J Neuropsychiatry Clin Neurosci 2003;15(4):422-30.
9. Simons LA, McCallum J, Friedlander Y, Simons J. Risk factors for ischemic stroke: Dubbo Study of the elderly. Stroke 1998;29(7):1341-6.
10. Jonas BS, Mussolino ME. Symptoms of depression as a prospective risk factor for stroke. Psychosom Med 2000;62(4):463-71.
11. Cassidy EM, Walsh MT, O’Connor R, et al. Platelet surface glycoprotein expression in post-stroke depression: a preliminary study. Psychiatry Res 2003;118(2):175-81.
12. Pollock BG, Laghrissi-Thode F, Wagner WR. Evaluation of platelet activation in depressed patients with ischemic heart disease after paroxetine or nortriptyline treatment. J Clin Psychopharmacol 2000;20(2):137-40.
13. Everson SA, Roberts RE, Goldberg DE, Kaplan GA. Depressive symptoms and increased risk of stroke mortality over a 29-year period. Arch Intern Med 1998;158(10):1133-8.
14. Turner-Stokes L, Hassan N. Depression after stroke: a review of the evidence base to inform the development of an integrated care pathway. Part 2: Treatment alternatives. Clin Rehabil 2002;16(3):248-60.
15. Whyte EM, Mulsant BH. Post-stroke depression: epidemiology, pathophysiology, and biologic treatment. Biol Psychiatry 2002;52:253-64.
16. Currier M, Murray G, Welsh C. Electroconvulsive therapy for poststroke depressed geriatric patients. J Neuropsychiatry Clin Neurosci 1992;4(2):140-4.
17. Kemp BJ, Corgiat M, Gill C. Effects of brief cognitive behavioral group psychotherapy in older persons with and without disabling illness. Behav Health Ageing 1992;2:21-8.
18. Lincoln NB, Flannaghan T, Sutcliffe L, Rother L. Evaluation of cognitive behavioural treatment for depression after stroke: a pilot study. Clin Rehabil 1997;11(2):114-22.
19. Astrom M, Adolfsson R, Asplund K. Major depression in stroke patients: a 13-year longitudinal study. Stroke 1993;24:976-82.
20. Narushima K, Kosier JT, Robinson RG. Preventing poststroke depression: a 12-week double-blind randomized treatment trial and 21-month follow-up. J Nerv Ment Dis 2002;190(5):296-303.
21. Palomaki H, Kaste M, Berg A, et al. Prevention of poststroke depression: 1 year randomised placebo controlled double blind trial of mianserin with 6 month follow up after therapy. J Neurol Neurosurg Psychiatry 1999;66(4):490-4.