User login
Autism: A three-step practical approach to making the diagnosis
Autism and related pervasive developmental disorders (PDD) are increasingly being identified in children—and even in some adolescents and adults. As a result, psychiatry now recognizes that these debilitating disorders are more common than was once believed, with a prevalence as high as 1 in 250.
An accurate diagnosis can help families take advantage of the variety of treatments being offered and investigated for affected individuals (Box).1 As psychiatrists who primarily see patients with autism and PDD, we recommend a three-step diagnostic approach that includes:
- a comprehensive initial assessment to rule out medical or neurologic illnesses that can mimic or are associated with autism
- differentiating PDDs from other psychiatric disorders with similar symptoms
- distinguishing among the five PDD subtypes described in DSM-IV.2
Step 1: Comprehensive initial assessment
Assessment for possible PDD begins with a comprehensive history and examination. Most patients will be assessed in childhood, but milder symptoms of autism or Asperger’s disorder may go unrecognized initially and not be brought to a clinician’s attention until adolescence or even adulthood.
As PDDs are childhood-onset disorders, the logical approach emphasizes the developmental course and onset of symptoms. By definition, children with autism show evidence of the disorder by age 3. However, the diagnosis can often be made as early as age 18 to 24 months, when typically developing children exhibit a number of social and communicative milestones that are absent in autism.
History A thorough description of the mother’s pregnancy, labor, and delivery (if known) can help you determine whether intrauterine or perinatal events could be related to the patient’s presenting problem. These include infections and exposure to exogenous substances (e.g., alcohol) during the pregnancy, as well as complications during pregnancy and delivery (e.g., maternal bleeding, neonatal hypoxia).
A complete description of the child’s development including major milestones (e.g., sitting without support, walking, first words) can help distinguish among certain diagnoses and estimate the extent of developmental delay. Ask the parents what first concerned them about their child’s development, as children with autism most often present with delays in social or language milestones. Any developmental regression in acquired skills may implicate other neurologic processes and help distinguish among the subtypes of PDD.
Symptoms Review the symptoms of autism at length in all patients in whom you suspect a PDD. It is important to assess these symptoms in the context of the child’s overall developmental level. For example, a child with known mental retardation should be compared with peers of similar age and cognitive impairment.
Optimal treatment for autism and related pervasive developmental disorders (PDDs) involves the collaboration of many disciplines.
- All school-aged children who are diagnosed with a PDD should be evaluated by the local school system to determine eligibility for special education. For those who are eligible, an individualized educational plan (IEP) is established to outline specific educational objectives and how they will be met. This IEP will often recommend speech therapy, occupational therapy, and social skills training.
- Children with the disability of autism are guaranteed an appropriate education. Advocates are often available to assist parents in ensuring that their child’s educational needs are being met.
- Many families also make use of treatment offered outside the school, such as speech and occupational therapy. In addition, behavioral psychotherapy based on principles of applied behavioral analysis is often helpful. Certain specialty clinics offer social skills training and additional supports for families. Parent support groups can also be a crucial source of information and support (“Related resources”).
- Symptoms associated with autism such as aggression, irritability, hyperactivity, anxiety, and interfering repetitive phenomena may be reduced with appropriate psychopharmacologic treatment.2 In general, treatment is aimed at these associated target symptoms because no single drug treatment has been consistently shown to improve the core social and communication impairments.
Approximately 75% of persons with autism are diagnosed with mental retardation. A review of intellectual abilities and level of adaptive functioning can suggest the degree of mental retardation. A detailed family history is important because autism and other syndromes associated with mental retardation have varying degrees of heritability.
A thorough medical history, review of systems, and physical exam (with focus on the neurologic exam) can suggest the presence of medical conditions that could mimic or be associated with autism. The symptoms of autism are traditionally divided into three domains: social, communication, and repetitive behavior/narrow interests (Table 1):
- Social impairment includes problems with nonverbal behaviors such as eye contact, facial expressions, and “body language;” failure to develop peer relationships; lack of spontaneous seeking to share enjoyment, interests, or achievements with other people; and lack of social or emotional reciprocity.
- Communication impairment includes language delay, decreased communication with others, conversational impairment, echolalia, and lack of imaginative or social imitative play.
- Impairments in behavior, interests, and activity take the form of all-encompassing preoccupations, “need for sameness” and compulsive rituals, motor stereotypies, and preoccupation with parts of objects.
After the preliminary history and exam, you should have an initial impression as to whether a PDD may be present. Conditions that could mimic or co-exist with autism will then need to be evaluated (Table 2).
Hearing and vision testing Every child presenting with a language or cognitive delay should have an adequate hearing assessment, including an audiogram at the very least. If results are equivocal, then brainstem auditory-evoked responses are indicated to establish the auditory system’s integrity. Vision screening should be completed, and the child should be referred to an ophthalmologist if a problem is suspected.
IQ testing A child with cognitive delays, learning problems, or suspected PDD should be referred to an experienced psychologist for intelligence testing. Public school systems often provide this service. Intelligence testing can document mental retardation and offer important information about the child’s strengths and weaknesses in learning.
Speech and language assessment A speech and language pathologist should evaluate children with PDD and/or language problems for articulation, prosody, receptive and expressive language, and pragmatics.
Lab and genetic tests Laboratory investigation in a child with cognitive delays should include routine blood chemistries, CBC, thyroid function tests, and lead level. Screen for fragile X syndrome, as its symptoms overlap those of autism, and for disorders of amino acid and organic acid metabolism. Finally, consider a chromosome karyotype, especially in patients with dysmorphic features on physical exam.
Table 1
THE THREE DOMAINS OF IMPAIRMENT IN AUTISM
Impairment in social interaction
|
Impairment in communication
|
Restricted repetitive and stereotyped patterns of behavior, interests, and activities
|
| Adapted from DSM-IV-TR, American Psychiatric Association, 2000 |
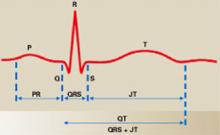
EEG Obtain a sleep-deprived electroencephalogram (EEG) in children with a history of significant language regression, episodic symptoms, or other indicators of possible seizures. Ideally, the EEG should include monitoring during sleep to help rule out acquired epileptic aphasia (Landau-Kleffner syndrome), a rare disorder associated with late-onset language regression. MRI of the brain is not routine but should be considered if indicated by the history or neurologic exam.
Consultations Consider consulting colleagues in neurology and medical genetics, especially when patients present with definite neurologic signs and symptoms or obvious dysmorphic features. These medical specialists are trained to screen for complex and rare syndromes that are sometimes associated with features of PDD.
Step 2. Is it PDD or another psychiatric disorder?
Psychiatric disorders that can be mistaken for PDD are listed in Table 3. The central feature of all PDDs is disturbance in social relatedness, and a diagnosis of PDD requires a history of significant social impairment.
Problems with social reciprocity in PDD are qualitatively different from the social impairment seen in other psychiatric disorders. For example, a child with attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) may have few friends because of a tendency to act impulsively and get into frequent conflicts with others. These social difficulties would not be considered indicative of PDD, as they typify those seen in children with ADHD and ODD.
Mental retardation Although mental retardation occurs in approximately 75% of persons with autism, most patients with mental retardation do not have autism. In assessing an individual with mental retardation for symptoms of PDD, consider the overall developmental level. It is not uncommon for individuals with mental retardation to have mild social problems, a history of language delay, and even motor stereotypies. These symptoms are considered indicative of PDD only when they are more severe than would be expected for the patient’s developmental level.
Table 2
TESTING OPTIONS FOR PATIENTS WITH PDD
| Hearing evaluation | Fragile X testing |
| Vision evaluation | Amino acids/organic acids |
| IQ testing | Chromosome karyotype |
| Speech/language evaluation | EEG |
| Chemistries, CBC, | Brain MRI |
| thyroid function tests | Neurology consultation |
| Lead level | Genetics consultation |
Table 3
DIFFERENTIAL DIAGNOSIS OF PDD
| Mental retardation |
| Reactive attachment disorder |
| Language disorders |
| Stereotypic movement disorder |
| Attention-deficit/hyperactivity disorder |
| Social phobia |
| Obsessive-compulsive disorder |
| Selective mutism |
| Schizophrenia |
| Personality disorders |
| Normality |
Other symptoms that are relatively specific to autism and PDD include lack of appropriate eye-to-eye gaze, abnormal speech prosody, echolalia, pronominal reversal, and narrow and circumscribed interests. The presence of these symptoms in excess should increase your suspicion of comorbid PDD.
RAD Reactive attachment disorder presents with abnormal social relatedness that can sometimes be confused with milder PDDs, especially in patients with comorbid mental retardation. In RAD, however, a history of severe neglect or abuse is thought to have caused the abnormal social relatedness. Placing the child in a caring and secure environment should improve many of the social deficits.
Language disorders are distinguished from PDDs by the absence of marked social impairment and lack of restricted interests and repetitive behaviors. In addition, children with primary language disorders often have intact nonverbal communication skills and make other attempts to communicate (e.g., through gesture, eye contact).
Stereotypic movement disorder can be seen in individuals with and without comorbid mental retardation. It is not diagnosed in the presence of autism, as these movements are thought to be part of the underlying disorder. The lack of social and communication impairments distinguishes stereotypic movement disorder from PDD.
ADHD Many children with autism and other PDDs have interfering symptoms of inattention, hyperactivity, and impulsivity. We usually do not give them an additional diagnosis of ADHD, as these symptoms are common in PDD. The pathophysiology of these symptoms may be different in ADHD and PDD, as evidenced by the frequent report of adverse effects following stimulant treatment of children with autism.2
Social phobia In higher functioning individuals with PDD, excessive social anxiety can sometimes be confused with social phobia. In social phobia, however, individuals usually do not exhibit marked problems with social relatedness and are able to interact normally with persons they know well and in some situations.
OCD Obsessive-compulsive disorder can occur in individuals with PDD but must be distinguished from the abnormal preoccupations and ritualistic behavior characteristic of autism. In autism, these activities often differ in quality from obsessions and compulsions.3 Furthermore, they usually are not associated with distress, and repetitive behaviors are not linked to a specific obsession.
Selective mutism is usually easy to distinguish from PDD because the affected child is typically able to talk in certain environments, such as at home. Also, the onset of selective mutism follows a period of normal social and communicative development.
Schizophrenia Autism was historically conceptualized as a type of childhood schizophrenia but is now thought to be distinct from the psychotic disorders. Schizophrenia with onset in childhood is much more rare than autism. Its onset usually occurs after several years of normal development, though some children with schizophrenia may have symptoms that resemble PDD early in their illness.4 Autistic persons may at times present with symptoms of a thought disorder. A diagnosis of schizophrenia usually is not made without evidence of prominent delusions and hallucinations.
Personality disorders PDDs are sometimes difficult to distinguish from personality disorders with similar features (e.g., schizotypal personality, schizoid personality). The social impairment in autistic and Asperger’s disorders is generally of earlier onset and greater severity than that seen in personality disorders. Those with personality disorders also typically lack stereotyped language or repetitive behaviors that are common in PDDs.
Table 4
CHARACTERISTIC FEATURES OF DSM-IV SUBTYPES OF PERVASIVE DEVELOPMENTAL DISORDERS
| Feature | Autistic disorder | Asperger’s disorder | Rett’s disorder | Childhood disintegrative disorder | Pervasive developmental disorder NOS* |
|---|---|---|---|---|---|
| Sex | Male:female ratio 4:1 | Male > female | Females only | Male > female | Male > female |
| Age of onset | < 3 years | Variable | 5-30 months | 2-10 years | Variable |
| Presence of regression | Mild regression in minority of patients | No | Yes | Yes | No |
| IQ | Most have mental retardation | Most have normal intellectual functioning | Severe mental retardation | Severe mental retardation | Variable |
| Social impairment | Yes | Yes | Yes | Yes | Yes |
| Communication impairment | Yes | No | Yes | Yes | Variable |
| Restricted interests/repetitive behaviors | Yes | Yes | Yes | Yes | Variable |
| Motor involvement | Usually not | Some have motor clumsiness | Gait and trunk ataxia; loss of purposeful hand movements | Loss of bowel/bladder control | Variable |
| *NOS: Not otherwise specified | |||||
Social awkwardness Finally, some of the PDDs that allow higher functioning (e.g., Asperger’s disorder and PDD not otherwise specified [NOS]) need to be distinguished from normal social awkwardness that can be common, especially in adolescence. The social impairment in PDD is marked and interferes with normal functioning and development.
Step 3. Which PDD is it?
DSM-IV describes five subtypes of PDD (autistic disorder, Asperger’s disorder, Rett’s disorder, childhood disintegrative disorder, and PDD NOS) that have in common problems with reciprocal social interaction (Table 4). For psychiatrists making the diagnosis, it is probably most difficult to differentiate the two most common types: autistic and Asperger’s disorders.
Autistic disorder is the prototypical PDD that is associated with abnormalities in reciprocal social interaction, qualitative impairments in communication, and narrow interests and repetitive behaviors (Table 1). By definition, symptoms of the disorder manifest by age 3.
Asperger’s disorder has several features that distinguish it from autistic disorder:
- Children with Asperger’s disorder do not have language delays. By definition, a child who has not developed single words by age 2 cannot be diagnosed with Asperger’s disorder.
- Early cognitive development in Asperger’s disorder is normal. Children with Asperger’s disorder are much more likely to have normal or above-average intellectual functioning than children with autistic disorder.
- Circumscribed interests and intense preoccupations are more common than motor stereotypies.
- Affected children may show verbal abilities that greatly exceed their visual-spatial skills. This may be apparent on individualized intelligence testing (i.e., verbal IQ > performance IQ) and clinically in the form of good language abilities but lagging fine-motor development (e.g., clumsiness).
Rett’s disorder occurs almost exclusively in girls, whereas autistic disorder is more common in boys. Following a brief period of normal development, affected girls experience deceleration of head growth, loss of previously acquired purposeful hand skills with subsequent development of stereotyped hand-wringing movements, loss of social engagement, onset of trunk and gait ataxia, and severe language and cognitive impairment. Genetic testing for mutations at MECP2 will be positive in most patients having all features of the classic phenotype.5
Childhood disintegrative disorder is thought to be more rare than autistic disorder. Following at least 2 years of normal development, affected children lose previously acquired skills. These can include play skills, language, social skills, bowel or bladder control, and motor skills. The children show impairments in social interaction, communication, and behavior of the type common to autistic disorder and often have severe mental retardation. The late onset of severe regression in development often prompts extensive neurologic evaluation, but a specific etiology is usually not found. The disorder is not diagnosed if full diagnostic criteria for autistic disorder are met (including onset of symptoms before age 3).
PDD NOS is diagnosed in many patients who are determined to have a significant impairment in social relatedness but do not meet full criteria for a specific PDD. Recent epidemiologic studies suggest that PDD NOS may be more common than autistic disorder.6 It may also be an appropriate designation for children with other proposed diagnostic constructs, such as nonverbal learning disabilities7 and multiple complex developmental disorders.8
Unfortunately, children diagnosed with PDD NOS instead of the better-recognized term “autism” may be denied appropriate social and financial services. When you inform others about the diagnosis of PDD NOS, it is important to emphasize to parents, schools, and funding agencies that PDD NOS is related to autism and should be considered one of the “autism spectrum disorders.” Children with PDDs or autism spectrum disorders will often benefit from similar treatment and educational interventions. In addition, their needs are equivalent for adequate insurance coverage and funding for specialized treatments.
- Cohen DJ, Volkmar FR (eds). Handbook of autism and pervasive developmental disorders (2nd ed). New York: Wiley, 1997.
- National Institute of Mental Health. Autism booklet. http://www.nimh.nih.gov/publicat/autism.cfm
- Autism Society of America http://www.autism-society.org Online Asperger Syndrome Information and Support (OASIS) http://www.udel.edu/bkirby/asperger
1. Posey DJ, McDougle CJ. The pharmacotherapy of target symptoms associated with autistic disorder and other pervasive developmental disorders. Harvard Rev Psychiatry 2000;8:45-63.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association, 2000.
3. McDougle CJ, Kresch LE, Goodman WK, et al. A case-controlled study of repetitive thoughts and behavior in adults with autistic disorder and obsessive-compulsive disorder. Am J Psychiatry 1995;152:772-7.
4. Kumra S. The diagnosis and treatment of children and adolescents with schizophrenia. “My mind is playing tricks on me.” Child Adolesc Psychiatr Clin N Am 2000;9:183-99.
5. Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature Genet 1999;23:185-8.
6. Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children. JAMA 2001;285:3093-9.
7. Rourke B. Nonverbal learning disabilities: The syndrome and the model. New York: Guilford Press, 1989.
8. Towbin KE, Dykens ED, Pearson GS, Cohen DJ. Conceptualizing “borderline syndrome of childhood” and “childhood schizophrenia” as a developmental disorder. J Am Acad Child Adolesc Psychiatry 1993;32:775-82.
Autism and related pervasive developmental disorders (PDD) are increasingly being identified in children—and even in some adolescents and adults. As a result, psychiatry now recognizes that these debilitating disorders are more common than was once believed, with a prevalence as high as 1 in 250.
An accurate diagnosis can help families take advantage of the variety of treatments being offered and investigated for affected individuals (Box).1 As psychiatrists who primarily see patients with autism and PDD, we recommend a three-step diagnostic approach that includes:
- a comprehensive initial assessment to rule out medical or neurologic illnesses that can mimic or are associated with autism
- differentiating PDDs from other psychiatric disorders with similar symptoms
- distinguishing among the five PDD subtypes described in DSM-IV.2
Step 1: Comprehensive initial assessment
Assessment for possible PDD begins with a comprehensive history and examination. Most patients will be assessed in childhood, but milder symptoms of autism or Asperger’s disorder may go unrecognized initially and not be brought to a clinician’s attention until adolescence or even adulthood.
As PDDs are childhood-onset disorders, the logical approach emphasizes the developmental course and onset of symptoms. By definition, children with autism show evidence of the disorder by age 3. However, the diagnosis can often be made as early as age 18 to 24 months, when typically developing children exhibit a number of social and communicative milestones that are absent in autism.
History A thorough description of the mother’s pregnancy, labor, and delivery (if known) can help you determine whether intrauterine or perinatal events could be related to the patient’s presenting problem. These include infections and exposure to exogenous substances (e.g., alcohol) during the pregnancy, as well as complications during pregnancy and delivery (e.g., maternal bleeding, neonatal hypoxia).
A complete description of the child’s development including major milestones (e.g., sitting without support, walking, first words) can help distinguish among certain diagnoses and estimate the extent of developmental delay. Ask the parents what first concerned them about their child’s development, as children with autism most often present with delays in social or language milestones. Any developmental regression in acquired skills may implicate other neurologic processes and help distinguish among the subtypes of PDD.
Symptoms Review the symptoms of autism at length in all patients in whom you suspect a PDD. It is important to assess these symptoms in the context of the child’s overall developmental level. For example, a child with known mental retardation should be compared with peers of similar age and cognitive impairment.
Optimal treatment for autism and related pervasive developmental disorders (PDDs) involves the collaboration of many disciplines.
- All school-aged children who are diagnosed with a PDD should be evaluated by the local school system to determine eligibility for special education. For those who are eligible, an individualized educational plan (IEP) is established to outline specific educational objectives and how they will be met. This IEP will often recommend speech therapy, occupational therapy, and social skills training.
- Children with the disability of autism are guaranteed an appropriate education. Advocates are often available to assist parents in ensuring that their child’s educational needs are being met.
- Many families also make use of treatment offered outside the school, such as speech and occupational therapy. In addition, behavioral psychotherapy based on principles of applied behavioral analysis is often helpful. Certain specialty clinics offer social skills training and additional supports for families. Parent support groups can also be a crucial source of information and support (“Related resources”).
- Symptoms associated with autism such as aggression, irritability, hyperactivity, anxiety, and interfering repetitive phenomena may be reduced with appropriate psychopharmacologic treatment.2 In general, treatment is aimed at these associated target symptoms because no single drug treatment has been consistently shown to improve the core social and communication impairments.
Approximately 75% of persons with autism are diagnosed with mental retardation. A review of intellectual abilities and level of adaptive functioning can suggest the degree of mental retardation. A detailed family history is important because autism and other syndromes associated with mental retardation have varying degrees of heritability.
A thorough medical history, review of systems, and physical exam (with focus on the neurologic exam) can suggest the presence of medical conditions that could mimic or be associated with autism. The symptoms of autism are traditionally divided into three domains: social, communication, and repetitive behavior/narrow interests (Table 1):
- Social impairment includes problems with nonverbal behaviors such as eye contact, facial expressions, and “body language;” failure to develop peer relationships; lack of spontaneous seeking to share enjoyment, interests, or achievements with other people; and lack of social or emotional reciprocity.
- Communication impairment includes language delay, decreased communication with others, conversational impairment, echolalia, and lack of imaginative or social imitative play.
- Impairments in behavior, interests, and activity take the form of all-encompassing preoccupations, “need for sameness” and compulsive rituals, motor stereotypies, and preoccupation with parts of objects.
After the preliminary history and exam, you should have an initial impression as to whether a PDD may be present. Conditions that could mimic or co-exist with autism will then need to be evaluated (Table 2).
Hearing and vision testing Every child presenting with a language or cognitive delay should have an adequate hearing assessment, including an audiogram at the very least. If results are equivocal, then brainstem auditory-evoked responses are indicated to establish the auditory system’s integrity. Vision screening should be completed, and the child should be referred to an ophthalmologist if a problem is suspected.
IQ testing A child with cognitive delays, learning problems, or suspected PDD should be referred to an experienced psychologist for intelligence testing. Public school systems often provide this service. Intelligence testing can document mental retardation and offer important information about the child’s strengths and weaknesses in learning.
Speech and language assessment A speech and language pathologist should evaluate children with PDD and/or language problems for articulation, prosody, receptive and expressive language, and pragmatics.
Lab and genetic tests Laboratory investigation in a child with cognitive delays should include routine blood chemistries, CBC, thyroid function tests, and lead level. Screen for fragile X syndrome, as its symptoms overlap those of autism, and for disorders of amino acid and organic acid metabolism. Finally, consider a chromosome karyotype, especially in patients with dysmorphic features on physical exam.
Table 1
THE THREE DOMAINS OF IMPAIRMENT IN AUTISM
Impairment in social interaction
|
Impairment in communication
|
Restricted repetitive and stereotyped patterns of behavior, interests, and activities
|
| Adapted from DSM-IV-TR, American Psychiatric Association, 2000 |
EEG Obtain a sleep-deprived electroencephalogram (EEG) in children with a history of significant language regression, episodic symptoms, or other indicators of possible seizures. Ideally, the EEG should include monitoring during sleep to help rule out acquired epileptic aphasia (Landau-Kleffner syndrome), a rare disorder associated with late-onset language regression. MRI of the brain is not routine but should be considered if indicated by the history or neurologic exam.
Consultations Consider consulting colleagues in neurology and medical genetics, especially when patients present with definite neurologic signs and symptoms or obvious dysmorphic features. These medical specialists are trained to screen for complex and rare syndromes that are sometimes associated with features of PDD.
Step 2. Is it PDD or another psychiatric disorder?
Psychiatric disorders that can be mistaken for PDD are listed in Table 3. The central feature of all PDDs is disturbance in social relatedness, and a diagnosis of PDD requires a history of significant social impairment.
Problems with social reciprocity in PDD are qualitatively different from the social impairment seen in other psychiatric disorders. For example, a child with attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) may have few friends because of a tendency to act impulsively and get into frequent conflicts with others. These social difficulties would not be considered indicative of PDD, as they typify those seen in children with ADHD and ODD.
Mental retardation Although mental retardation occurs in approximately 75% of persons with autism, most patients with mental retardation do not have autism. In assessing an individual with mental retardation for symptoms of PDD, consider the overall developmental level. It is not uncommon for individuals with mental retardation to have mild social problems, a history of language delay, and even motor stereotypies. These symptoms are considered indicative of PDD only when they are more severe than would be expected for the patient’s developmental level.
Table 2
TESTING OPTIONS FOR PATIENTS WITH PDD
| Hearing evaluation | Fragile X testing |
| Vision evaluation | Amino acids/organic acids |
| IQ testing | Chromosome karyotype |
| Speech/language evaluation | EEG |
| Chemistries, CBC, | Brain MRI |
| thyroid function tests | Neurology consultation |
| Lead level | Genetics consultation |
Table 3
DIFFERENTIAL DIAGNOSIS OF PDD
| Mental retardation |
| Reactive attachment disorder |
| Language disorders |
| Stereotypic movement disorder |
| Attention-deficit/hyperactivity disorder |
| Social phobia |
| Obsessive-compulsive disorder |
| Selective mutism |
| Schizophrenia |
| Personality disorders |
| Normality |
Other symptoms that are relatively specific to autism and PDD include lack of appropriate eye-to-eye gaze, abnormal speech prosody, echolalia, pronominal reversal, and narrow and circumscribed interests. The presence of these symptoms in excess should increase your suspicion of comorbid PDD.
RAD Reactive attachment disorder presents with abnormal social relatedness that can sometimes be confused with milder PDDs, especially in patients with comorbid mental retardation. In RAD, however, a history of severe neglect or abuse is thought to have caused the abnormal social relatedness. Placing the child in a caring and secure environment should improve many of the social deficits.
Language disorders are distinguished from PDDs by the absence of marked social impairment and lack of restricted interests and repetitive behaviors. In addition, children with primary language disorders often have intact nonverbal communication skills and make other attempts to communicate (e.g., through gesture, eye contact).
Stereotypic movement disorder can be seen in individuals with and without comorbid mental retardation. It is not diagnosed in the presence of autism, as these movements are thought to be part of the underlying disorder. The lack of social and communication impairments distinguishes stereotypic movement disorder from PDD.
ADHD Many children with autism and other PDDs have interfering symptoms of inattention, hyperactivity, and impulsivity. We usually do not give them an additional diagnosis of ADHD, as these symptoms are common in PDD. The pathophysiology of these symptoms may be different in ADHD and PDD, as evidenced by the frequent report of adverse effects following stimulant treatment of children with autism.2
Social phobia In higher functioning individuals with PDD, excessive social anxiety can sometimes be confused with social phobia. In social phobia, however, individuals usually do not exhibit marked problems with social relatedness and are able to interact normally with persons they know well and in some situations.
OCD Obsessive-compulsive disorder can occur in individuals with PDD but must be distinguished from the abnormal preoccupations and ritualistic behavior characteristic of autism. In autism, these activities often differ in quality from obsessions and compulsions.3 Furthermore, they usually are not associated with distress, and repetitive behaviors are not linked to a specific obsession.
Selective mutism is usually easy to distinguish from PDD because the affected child is typically able to talk in certain environments, such as at home. Also, the onset of selective mutism follows a period of normal social and communicative development.
Schizophrenia Autism was historically conceptualized as a type of childhood schizophrenia but is now thought to be distinct from the psychotic disorders. Schizophrenia with onset in childhood is much more rare than autism. Its onset usually occurs after several years of normal development, though some children with schizophrenia may have symptoms that resemble PDD early in their illness.4 Autistic persons may at times present with symptoms of a thought disorder. A diagnosis of schizophrenia usually is not made without evidence of prominent delusions and hallucinations.
Personality disorders PDDs are sometimes difficult to distinguish from personality disorders with similar features (e.g., schizotypal personality, schizoid personality). The social impairment in autistic and Asperger’s disorders is generally of earlier onset and greater severity than that seen in personality disorders. Those with personality disorders also typically lack stereotyped language or repetitive behaviors that are common in PDDs.
Table 4
CHARACTERISTIC FEATURES OF DSM-IV SUBTYPES OF PERVASIVE DEVELOPMENTAL DISORDERS
| Feature | Autistic disorder | Asperger’s disorder | Rett’s disorder | Childhood disintegrative disorder | Pervasive developmental disorder NOS* |
|---|---|---|---|---|---|
| Sex | Male:female ratio 4:1 | Male > female | Females only | Male > female | Male > female |
| Age of onset | < 3 years | Variable | 5-30 months | 2-10 years | Variable |
| Presence of regression | Mild regression in minority of patients | No | Yes | Yes | No |
| IQ | Most have mental retardation | Most have normal intellectual functioning | Severe mental retardation | Severe mental retardation | Variable |
| Social impairment | Yes | Yes | Yes | Yes | Yes |
| Communication impairment | Yes | No | Yes | Yes | Variable |
| Restricted interests/repetitive behaviors | Yes | Yes | Yes | Yes | Variable |
| Motor involvement | Usually not | Some have motor clumsiness | Gait and trunk ataxia; loss of purposeful hand movements | Loss of bowel/bladder control | Variable |
| *NOS: Not otherwise specified | |||||
Social awkwardness Finally, some of the PDDs that allow higher functioning (e.g., Asperger’s disorder and PDD not otherwise specified [NOS]) need to be distinguished from normal social awkwardness that can be common, especially in adolescence. The social impairment in PDD is marked and interferes with normal functioning and development.
Step 3. Which PDD is it?
DSM-IV describes five subtypes of PDD (autistic disorder, Asperger’s disorder, Rett’s disorder, childhood disintegrative disorder, and PDD NOS) that have in common problems with reciprocal social interaction (Table 4). For psychiatrists making the diagnosis, it is probably most difficult to differentiate the two most common types: autistic and Asperger’s disorders.
Autistic disorder is the prototypical PDD that is associated with abnormalities in reciprocal social interaction, qualitative impairments in communication, and narrow interests and repetitive behaviors (Table 1). By definition, symptoms of the disorder manifest by age 3.
Asperger’s disorder has several features that distinguish it from autistic disorder:
- Children with Asperger’s disorder do not have language delays. By definition, a child who has not developed single words by age 2 cannot be diagnosed with Asperger’s disorder.
- Early cognitive development in Asperger’s disorder is normal. Children with Asperger’s disorder are much more likely to have normal or above-average intellectual functioning than children with autistic disorder.
- Circumscribed interests and intense preoccupations are more common than motor stereotypies.
- Affected children may show verbal abilities that greatly exceed their visual-spatial skills. This may be apparent on individualized intelligence testing (i.e., verbal IQ > performance IQ) and clinically in the form of good language abilities but lagging fine-motor development (e.g., clumsiness).
Rett’s disorder occurs almost exclusively in girls, whereas autistic disorder is more common in boys. Following a brief period of normal development, affected girls experience deceleration of head growth, loss of previously acquired purposeful hand skills with subsequent development of stereotyped hand-wringing movements, loss of social engagement, onset of trunk and gait ataxia, and severe language and cognitive impairment. Genetic testing for mutations at MECP2 will be positive in most patients having all features of the classic phenotype.5
Childhood disintegrative disorder is thought to be more rare than autistic disorder. Following at least 2 years of normal development, affected children lose previously acquired skills. These can include play skills, language, social skills, bowel or bladder control, and motor skills. The children show impairments in social interaction, communication, and behavior of the type common to autistic disorder and often have severe mental retardation. The late onset of severe regression in development often prompts extensive neurologic evaluation, but a specific etiology is usually not found. The disorder is not diagnosed if full diagnostic criteria for autistic disorder are met (including onset of symptoms before age 3).
PDD NOS is diagnosed in many patients who are determined to have a significant impairment in social relatedness but do not meet full criteria for a specific PDD. Recent epidemiologic studies suggest that PDD NOS may be more common than autistic disorder.6 It may also be an appropriate designation for children with other proposed diagnostic constructs, such as nonverbal learning disabilities7 and multiple complex developmental disorders.8
Unfortunately, children diagnosed with PDD NOS instead of the better-recognized term “autism” may be denied appropriate social and financial services. When you inform others about the diagnosis of PDD NOS, it is important to emphasize to parents, schools, and funding agencies that PDD NOS is related to autism and should be considered one of the “autism spectrum disorders.” Children with PDDs or autism spectrum disorders will often benefit from similar treatment and educational interventions. In addition, their needs are equivalent for adequate insurance coverage and funding for specialized treatments.
- Cohen DJ, Volkmar FR (eds). Handbook of autism and pervasive developmental disorders (2nd ed). New York: Wiley, 1997.
- National Institute of Mental Health. Autism booklet. http://www.nimh.nih.gov/publicat/autism.cfm
- Autism Society of America http://www.autism-society.org Online Asperger Syndrome Information and Support (OASIS) http://www.udel.edu/bkirby/asperger
Autism and related pervasive developmental disorders (PDD) are increasingly being identified in children—and even in some adolescents and adults. As a result, psychiatry now recognizes that these debilitating disorders are more common than was once believed, with a prevalence as high as 1 in 250.
An accurate diagnosis can help families take advantage of the variety of treatments being offered and investigated for affected individuals (Box).1 As psychiatrists who primarily see patients with autism and PDD, we recommend a three-step diagnostic approach that includes:
- a comprehensive initial assessment to rule out medical or neurologic illnesses that can mimic or are associated with autism
- differentiating PDDs from other psychiatric disorders with similar symptoms
- distinguishing among the five PDD subtypes described in DSM-IV.2
Step 1: Comprehensive initial assessment
Assessment for possible PDD begins with a comprehensive history and examination. Most patients will be assessed in childhood, but milder symptoms of autism or Asperger’s disorder may go unrecognized initially and not be brought to a clinician’s attention until adolescence or even adulthood.
As PDDs are childhood-onset disorders, the logical approach emphasizes the developmental course and onset of symptoms. By definition, children with autism show evidence of the disorder by age 3. However, the diagnosis can often be made as early as age 18 to 24 months, when typically developing children exhibit a number of social and communicative milestones that are absent in autism.
History A thorough description of the mother’s pregnancy, labor, and delivery (if known) can help you determine whether intrauterine or perinatal events could be related to the patient’s presenting problem. These include infections and exposure to exogenous substances (e.g., alcohol) during the pregnancy, as well as complications during pregnancy and delivery (e.g., maternal bleeding, neonatal hypoxia).
A complete description of the child’s development including major milestones (e.g., sitting without support, walking, first words) can help distinguish among certain diagnoses and estimate the extent of developmental delay. Ask the parents what first concerned them about their child’s development, as children with autism most often present with delays in social or language milestones. Any developmental regression in acquired skills may implicate other neurologic processes and help distinguish among the subtypes of PDD.
Symptoms Review the symptoms of autism at length in all patients in whom you suspect a PDD. It is important to assess these symptoms in the context of the child’s overall developmental level. For example, a child with known mental retardation should be compared with peers of similar age and cognitive impairment.
Optimal treatment for autism and related pervasive developmental disorders (PDDs) involves the collaboration of many disciplines.
- All school-aged children who are diagnosed with a PDD should be evaluated by the local school system to determine eligibility for special education. For those who are eligible, an individualized educational plan (IEP) is established to outline specific educational objectives and how they will be met. This IEP will often recommend speech therapy, occupational therapy, and social skills training.
- Children with the disability of autism are guaranteed an appropriate education. Advocates are often available to assist parents in ensuring that their child’s educational needs are being met.
- Many families also make use of treatment offered outside the school, such as speech and occupational therapy. In addition, behavioral psychotherapy based on principles of applied behavioral analysis is often helpful. Certain specialty clinics offer social skills training and additional supports for families. Parent support groups can also be a crucial source of information and support (“Related resources”).
- Symptoms associated with autism such as aggression, irritability, hyperactivity, anxiety, and interfering repetitive phenomena may be reduced with appropriate psychopharmacologic treatment.2 In general, treatment is aimed at these associated target symptoms because no single drug treatment has been consistently shown to improve the core social and communication impairments.
Approximately 75% of persons with autism are diagnosed with mental retardation. A review of intellectual abilities and level of adaptive functioning can suggest the degree of mental retardation. A detailed family history is important because autism and other syndromes associated with mental retardation have varying degrees of heritability.
A thorough medical history, review of systems, and physical exam (with focus on the neurologic exam) can suggest the presence of medical conditions that could mimic or be associated with autism. The symptoms of autism are traditionally divided into three domains: social, communication, and repetitive behavior/narrow interests (Table 1):
- Social impairment includes problems with nonverbal behaviors such as eye contact, facial expressions, and “body language;” failure to develop peer relationships; lack of spontaneous seeking to share enjoyment, interests, or achievements with other people; and lack of social or emotional reciprocity.
- Communication impairment includes language delay, decreased communication with others, conversational impairment, echolalia, and lack of imaginative or social imitative play.
- Impairments in behavior, interests, and activity take the form of all-encompassing preoccupations, “need for sameness” and compulsive rituals, motor stereotypies, and preoccupation with parts of objects.
After the preliminary history and exam, you should have an initial impression as to whether a PDD may be present. Conditions that could mimic or co-exist with autism will then need to be evaluated (Table 2).
Hearing and vision testing Every child presenting with a language or cognitive delay should have an adequate hearing assessment, including an audiogram at the very least. If results are equivocal, then brainstem auditory-evoked responses are indicated to establish the auditory system’s integrity. Vision screening should be completed, and the child should be referred to an ophthalmologist if a problem is suspected.
IQ testing A child with cognitive delays, learning problems, or suspected PDD should be referred to an experienced psychologist for intelligence testing. Public school systems often provide this service. Intelligence testing can document mental retardation and offer important information about the child’s strengths and weaknesses in learning.
Speech and language assessment A speech and language pathologist should evaluate children with PDD and/or language problems for articulation, prosody, receptive and expressive language, and pragmatics.
Lab and genetic tests Laboratory investigation in a child with cognitive delays should include routine blood chemistries, CBC, thyroid function tests, and lead level. Screen for fragile X syndrome, as its symptoms overlap those of autism, and for disorders of amino acid and organic acid metabolism. Finally, consider a chromosome karyotype, especially in patients with dysmorphic features on physical exam.
Table 1
THE THREE DOMAINS OF IMPAIRMENT IN AUTISM
Impairment in social interaction
|
Impairment in communication
|
Restricted repetitive and stereotyped patterns of behavior, interests, and activities
|
| Adapted from DSM-IV-TR, American Psychiatric Association, 2000 |
EEG Obtain a sleep-deprived electroencephalogram (EEG) in children with a history of significant language regression, episodic symptoms, or other indicators of possible seizures. Ideally, the EEG should include monitoring during sleep to help rule out acquired epileptic aphasia (Landau-Kleffner syndrome), a rare disorder associated with late-onset language regression. MRI of the brain is not routine but should be considered if indicated by the history or neurologic exam.
Consultations Consider consulting colleagues in neurology and medical genetics, especially when patients present with definite neurologic signs and symptoms or obvious dysmorphic features. These medical specialists are trained to screen for complex and rare syndromes that are sometimes associated with features of PDD.
Step 2. Is it PDD or another psychiatric disorder?
Psychiatric disorders that can be mistaken for PDD are listed in Table 3. The central feature of all PDDs is disturbance in social relatedness, and a diagnosis of PDD requires a history of significant social impairment.
Problems with social reciprocity in PDD are qualitatively different from the social impairment seen in other psychiatric disorders. For example, a child with attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) may have few friends because of a tendency to act impulsively and get into frequent conflicts with others. These social difficulties would not be considered indicative of PDD, as they typify those seen in children with ADHD and ODD.
Mental retardation Although mental retardation occurs in approximately 75% of persons with autism, most patients with mental retardation do not have autism. In assessing an individual with mental retardation for symptoms of PDD, consider the overall developmental level. It is not uncommon for individuals with mental retardation to have mild social problems, a history of language delay, and even motor stereotypies. These symptoms are considered indicative of PDD only when they are more severe than would be expected for the patient’s developmental level.
Table 2
TESTING OPTIONS FOR PATIENTS WITH PDD
| Hearing evaluation | Fragile X testing |
| Vision evaluation | Amino acids/organic acids |
| IQ testing | Chromosome karyotype |
| Speech/language evaluation | EEG |
| Chemistries, CBC, | Brain MRI |
| thyroid function tests | Neurology consultation |
| Lead level | Genetics consultation |
Table 3
DIFFERENTIAL DIAGNOSIS OF PDD
| Mental retardation |
| Reactive attachment disorder |
| Language disorders |
| Stereotypic movement disorder |
| Attention-deficit/hyperactivity disorder |
| Social phobia |
| Obsessive-compulsive disorder |
| Selective mutism |
| Schizophrenia |
| Personality disorders |
| Normality |
Other symptoms that are relatively specific to autism and PDD include lack of appropriate eye-to-eye gaze, abnormal speech prosody, echolalia, pronominal reversal, and narrow and circumscribed interests. The presence of these symptoms in excess should increase your suspicion of comorbid PDD.
RAD Reactive attachment disorder presents with abnormal social relatedness that can sometimes be confused with milder PDDs, especially in patients with comorbid mental retardation. In RAD, however, a history of severe neglect or abuse is thought to have caused the abnormal social relatedness. Placing the child in a caring and secure environment should improve many of the social deficits.
Language disorders are distinguished from PDDs by the absence of marked social impairment and lack of restricted interests and repetitive behaviors. In addition, children with primary language disorders often have intact nonverbal communication skills and make other attempts to communicate (e.g., through gesture, eye contact).
Stereotypic movement disorder can be seen in individuals with and without comorbid mental retardation. It is not diagnosed in the presence of autism, as these movements are thought to be part of the underlying disorder. The lack of social and communication impairments distinguishes stereotypic movement disorder from PDD.
ADHD Many children with autism and other PDDs have interfering symptoms of inattention, hyperactivity, and impulsivity. We usually do not give them an additional diagnosis of ADHD, as these symptoms are common in PDD. The pathophysiology of these symptoms may be different in ADHD and PDD, as evidenced by the frequent report of adverse effects following stimulant treatment of children with autism.2
Social phobia In higher functioning individuals with PDD, excessive social anxiety can sometimes be confused with social phobia. In social phobia, however, individuals usually do not exhibit marked problems with social relatedness and are able to interact normally with persons they know well and in some situations.
OCD Obsessive-compulsive disorder can occur in individuals with PDD but must be distinguished from the abnormal preoccupations and ritualistic behavior characteristic of autism. In autism, these activities often differ in quality from obsessions and compulsions.3 Furthermore, they usually are not associated with distress, and repetitive behaviors are not linked to a specific obsession.
Selective mutism is usually easy to distinguish from PDD because the affected child is typically able to talk in certain environments, such as at home. Also, the onset of selective mutism follows a period of normal social and communicative development.
Schizophrenia Autism was historically conceptualized as a type of childhood schizophrenia but is now thought to be distinct from the psychotic disorders. Schizophrenia with onset in childhood is much more rare than autism. Its onset usually occurs after several years of normal development, though some children with schizophrenia may have symptoms that resemble PDD early in their illness.4 Autistic persons may at times present with symptoms of a thought disorder. A diagnosis of schizophrenia usually is not made without evidence of prominent delusions and hallucinations.
Personality disorders PDDs are sometimes difficult to distinguish from personality disorders with similar features (e.g., schizotypal personality, schizoid personality). The social impairment in autistic and Asperger’s disorders is generally of earlier onset and greater severity than that seen in personality disorders. Those with personality disorders also typically lack stereotyped language or repetitive behaviors that are common in PDDs.
Table 4
CHARACTERISTIC FEATURES OF DSM-IV SUBTYPES OF PERVASIVE DEVELOPMENTAL DISORDERS
| Feature | Autistic disorder | Asperger’s disorder | Rett’s disorder | Childhood disintegrative disorder | Pervasive developmental disorder NOS* |
|---|---|---|---|---|---|
| Sex | Male:female ratio 4:1 | Male > female | Females only | Male > female | Male > female |
| Age of onset | < 3 years | Variable | 5-30 months | 2-10 years | Variable |
| Presence of regression | Mild regression in minority of patients | No | Yes | Yes | No |
| IQ | Most have mental retardation | Most have normal intellectual functioning | Severe mental retardation | Severe mental retardation | Variable |
| Social impairment | Yes | Yes | Yes | Yes | Yes |
| Communication impairment | Yes | No | Yes | Yes | Variable |
| Restricted interests/repetitive behaviors | Yes | Yes | Yes | Yes | Variable |
| Motor involvement | Usually not | Some have motor clumsiness | Gait and trunk ataxia; loss of purposeful hand movements | Loss of bowel/bladder control | Variable |
| *NOS: Not otherwise specified | |||||
Social awkwardness Finally, some of the PDDs that allow higher functioning (e.g., Asperger’s disorder and PDD not otherwise specified [NOS]) need to be distinguished from normal social awkwardness that can be common, especially in adolescence. The social impairment in PDD is marked and interferes with normal functioning and development.
Step 3. Which PDD is it?
DSM-IV describes five subtypes of PDD (autistic disorder, Asperger’s disorder, Rett’s disorder, childhood disintegrative disorder, and PDD NOS) that have in common problems with reciprocal social interaction (Table 4). For psychiatrists making the diagnosis, it is probably most difficult to differentiate the two most common types: autistic and Asperger’s disorders.
Autistic disorder is the prototypical PDD that is associated with abnormalities in reciprocal social interaction, qualitative impairments in communication, and narrow interests and repetitive behaviors (Table 1). By definition, symptoms of the disorder manifest by age 3.
Asperger’s disorder has several features that distinguish it from autistic disorder:
- Children with Asperger’s disorder do not have language delays. By definition, a child who has not developed single words by age 2 cannot be diagnosed with Asperger’s disorder.
- Early cognitive development in Asperger’s disorder is normal. Children with Asperger’s disorder are much more likely to have normal or above-average intellectual functioning than children with autistic disorder.
- Circumscribed interests and intense preoccupations are more common than motor stereotypies.
- Affected children may show verbal abilities that greatly exceed their visual-spatial skills. This may be apparent on individualized intelligence testing (i.e., verbal IQ > performance IQ) and clinically in the form of good language abilities but lagging fine-motor development (e.g., clumsiness).
Rett’s disorder occurs almost exclusively in girls, whereas autistic disorder is more common in boys. Following a brief period of normal development, affected girls experience deceleration of head growth, loss of previously acquired purposeful hand skills with subsequent development of stereotyped hand-wringing movements, loss of social engagement, onset of trunk and gait ataxia, and severe language and cognitive impairment. Genetic testing for mutations at MECP2 will be positive in most patients having all features of the classic phenotype.5
Childhood disintegrative disorder is thought to be more rare than autistic disorder. Following at least 2 years of normal development, affected children lose previously acquired skills. These can include play skills, language, social skills, bowel or bladder control, and motor skills. The children show impairments in social interaction, communication, and behavior of the type common to autistic disorder and often have severe mental retardation. The late onset of severe regression in development often prompts extensive neurologic evaluation, but a specific etiology is usually not found. The disorder is not diagnosed if full diagnostic criteria for autistic disorder are met (including onset of symptoms before age 3).
PDD NOS is diagnosed in many patients who are determined to have a significant impairment in social relatedness but do not meet full criteria for a specific PDD. Recent epidemiologic studies suggest that PDD NOS may be more common than autistic disorder.6 It may also be an appropriate designation for children with other proposed diagnostic constructs, such as nonverbal learning disabilities7 and multiple complex developmental disorders.8
Unfortunately, children diagnosed with PDD NOS instead of the better-recognized term “autism” may be denied appropriate social and financial services. When you inform others about the diagnosis of PDD NOS, it is important to emphasize to parents, schools, and funding agencies that PDD NOS is related to autism and should be considered one of the “autism spectrum disorders.” Children with PDDs or autism spectrum disorders will often benefit from similar treatment and educational interventions. In addition, their needs are equivalent for adequate insurance coverage and funding for specialized treatments.
- Cohen DJ, Volkmar FR (eds). Handbook of autism and pervasive developmental disorders (2nd ed). New York: Wiley, 1997.
- National Institute of Mental Health. Autism booklet. http://www.nimh.nih.gov/publicat/autism.cfm
- Autism Society of America http://www.autism-society.org Online Asperger Syndrome Information and Support (OASIS) http://www.udel.edu/bkirby/asperger
1. Posey DJ, McDougle CJ. The pharmacotherapy of target symptoms associated with autistic disorder and other pervasive developmental disorders. Harvard Rev Psychiatry 2000;8:45-63.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association, 2000.
3. McDougle CJ, Kresch LE, Goodman WK, et al. A case-controlled study of repetitive thoughts and behavior in adults with autistic disorder and obsessive-compulsive disorder. Am J Psychiatry 1995;152:772-7.
4. Kumra S. The diagnosis and treatment of children and adolescents with schizophrenia. “My mind is playing tricks on me.” Child Adolesc Psychiatr Clin N Am 2000;9:183-99.
5. Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature Genet 1999;23:185-8.
6. Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children. JAMA 2001;285:3093-9.
7. Rourke B. Nonverbal learning disabilities: The syndrome and the model. New York: Guilford Press, 1989.
8. Towbin KE, Dykens ED, Pearson GS, Cohen DJ. Conceptualizing “borderline syndrome of childhood” and “childhood schizophrenia” as a developmental disorder. J Am Acad Child Adolesc Psychiatry 1993;32:775-82.
1. Posey DJ, McDougle CJ. The pharmacotherapy of target symptoms associated with autistic disorder and other pervasive developmental disorders. Harvard Rev Psychiatry 2000;8:45-63.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association, 2000.
3. McDougle CJ, Kresch LE, Goodman WK, et al. A case-controlled study of repetitive thoughts and behavior in adults with autistic disorder and obsessive-compulsive disorder. Am J Psychiatry 1995;152:772-7.
4. Kumra S. The diagnosis and treatment of children and adolescents with schizophrenia. “My mind is playing tricks on me.” Child Adolesc Psychiatr Clin N Am 2000;9:183-99.
5. Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature Genet 1999;23:185-8.
6. Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children. JAMA 2001;285:3093-9.
7. Rourke B. Nonverbal learning disabilities: The syndrome and the model. New York: Guilford Press, 1989.
8. Towbin KE, Dykens ED, Pearson GS, Cohen DJ. Conceptualizing “borderline syndrome of childhood” and “childhood schizophrenia” as a developmental disorder. J Am Acad Child Adolesc Psychiatry 1993;32:775-82.
Adolescent depression: Diagnostic skills can differentiate teen angst from psychopathology
Adolescents with depressive disorders tend to arrive in psychiatrists’ offices when their behavior has already been identified as problematic. Suicide attempts, academic failure, substance abuse, and family conflicts can all lead to teen psychiatric referrals. Other times, subtler changes in behavior may lead a family doctor or pediatrician to suspect depression and to send an adolescent to you for a psychiatric consultation.
The psychiatrist’s task is challenging. Adolescents are usually brought in by their worried parents and may not want to talk to a psychiatrist. Or they may be unable to accurately describe their internal states. Even people who know an adolescent well may not discern the emotions that drive his or her behavior. Adding to the mix are the recurrent nature of major depression in adolescents and the likelihood of complicating comorbid psychiatric conditions (Box).1-6
Based on clinical evidence, we offer advice to help you promptly identify and effectively treat adolescents with depressive disorders. We also provide preliminary information on two studies examining medication treatment, psychotherapy, and combined treatment for teens with major depression.
Adolescent depression disorders
Symptoms of depression in adolescents are similar to those in adults, and it is appropriate for psychiatrists to use DSM-IV diagnostic criteria for making the diagnosis. The three primary depressive disorders for both adults and adolescents are major depressive disorder (MDD), dysthymic disorder, and depressive disorder not otherwise specified (NOS).
Depression is relatively rare among children but becomes common after the onset of puberty. In particular, recurrent depression often starts in adolescence. Here are the statistics:
- Up to 9% of adolescents meet diagnostic criteria for major depressive disorder (MDD), and up to 25% suffer from it by their late teens.
- MDD affects boys and girls equally in childhood, but the prevalence seems to increase in girls after puberty.1,2
- Depression in adolescents is characterized by high rates of comorbid psychiatric conditions. In general, the younger the age of onset, the higher the rate of comorbid conduct disorder, attention-deficit/hyperactivity disorder, and/or anxiety disorder.3
- Adolescent depression tends to persist. An estimated 45 to 70% of children and adolescents with MDD have recurrent episodes.4 At particularly high risk for recurrence are adolescent girls with depression, adolescents with multiple MDD episodes, and adolescents with a family history of recurrent depression.
- As many as 50% of teens with MDD attempt suicide within 15 years of their initial episode, and more than 20% make recurrent attempts.4,5 No good estimates of the rate of completed suicide are available. One 15-year follow-up of a sample of depressed adolescents reported a suicide rate of 7.7%.5 Boys are much more likely to complete suicide than girls across all racial groups.6
Although the symptoms that make up the diagnostic criteria are similar for adults and teens, the behavioral manifestations and response to treatment may differ. The adolescent may present as irritable and angry, rather than overly sad. Impairments in functioning are likely to be related to decline in school performance, social withdrawal, or increased conflicts with peers and family.
As for treatment, certain antidepressant medications of proven efficacy in adults (i.e., tricyclics) do not seem to work for adolescents.
MDD is a time-limited episode of depressive symptoms severe enough to cause functional impairment, such as decline in school performance, social withdrawal, or increased conflicts with peers and family. Symptoms must be present at least 2 weeks.
Dysthymia is a chronic depression that is less severe than MDD and lasts 1 year or longer without sustained remission. It often begins early in childhood and may include periods of increased symptoms consistent with major depression (sometimes called “double depression”).
Depressive disorder NOS is a category of depression that, though clinically significant, does not meet the full criteria for severity, duration, or level of impairment of MDD or dysthymia.
Unless otherwise specified, the terms “depression” and “depressive disorder” in this article are used generically to include all three of these disorders.
Depressive disorders must be differentiated from bipolar disorder, which is characterized by least one prior episode of mania (for bipolar type I) or hypomania (for bipolar type II). The clinical picture of bipolar disorder in youths may differ from that seen in adults. For example, bipolar youth often present with dysphoric mood interspersed with frequent, short periods of intense emotional lability and irritability, rather than “classic” euphoria.
Diagnosis
To diagnose a depressive disorder in an adolescent, information is typically obtained from multiple sources, most commonly the teenage patient and at least one of the parents. Because several sources are involved, however, the information may be conflicting. For instance, the adolescent may contradict a parent’s report that he or she is having difficulties in school or has a substance abuse problem.
Interviewing skills and clinical judgment are required of the clinician in these situations. It is important to:
- obtain a complete description of the adolescent’s behavior and mood over time and as accurate a description as possible of when changes occurred
- assess comorbid conditions (particularly anxiety, attention-deficit/hyperactivity disorder [ADHD], conduct disorder, and substance abuse)
- differentiate between unipolar MDD and bipolar disorder
- evaluate the risk of suicide.
Table 1
DEPRESSION IN ADOLESCENTS AND ADULTS
| Similarities | Differences |
|---|---|
| Same types of diagnostic categories (i.e., major depression, dysthymia, depression NOS) | To diagnose dysthymia, minimum duration of mood disturbance must be 1 year in adolescents (2 years in adults) |
| Same diagnostic symptoms criteria | Mood is often irritable in adolescents (rather than depressed) |
| More common in females | |
| Suicide is more common among males | |
| Evidence of efficacy of SSRI antidepressants | No evidence of efficacy of tricyclic antidepressants in adolescent depression |
Interviewing Standardized diagnostic interviews, such as the Schedule for Affective Disorders and Schizophrenia for children (K-SADS), are commonly used to research adolescent depression but require special training and approximately 1 to 2 hours to administer. As an alternative, clinicians generally develop their own “semi-structured interview” to try to collect all the relevant information required for an accurate diagnosis.7
The interview should be conducted with the adolescent and the parent(s), first separately for ease of disclosure then together to reconcile any differences in the information they report. Open-ended questions and time for building rapport may facilitate disclosure from a reticent adolescent. At times, however, one must make the diagnosis by relying more on reports from others who know the child well. Building a trusting therapeutic relationship then becomes part of ongoing treatment.
Standardized measures In addition to the interview, standardized self-report and other-report measures can help:
- The Child Depression Rating Scale-Revised, commonly used in clinical research, can also be used in practice to quantify symptom severity and document treatment response. A score above 40 usually indicates major depression; a score below 28 indicates remission of depression.8-10
- The Beck Depression Inventory (BDI), a 21-item self-report questionnaire for adults, has reasonable reliability and validity for adolescents. Its modest specificity suggests that it may measure general distress and dysphoria, which is not specific to depressive disorders. The language may be too difficult for some younger adolescents and those with poor reading comprehension skills.
- The Children’s Depression Inventory, a version of the BDI for prepubertal children, can be considered for adolescents whose cognitive and/or reading skills are less mature.
- Achenbach’s Child Behavior Checklists and other standardized questionnaires can screen for comorbid psychopathology.
Assessing psychosocial stress, such as conflicts with parents or peers, school problems, or risk-taking behavior, is also important. Depressed youth often have family members with histories of depression, alcoholism, anxiety, and other psychiatric diagnoses. History of sexual abuse has been linked to depression.3 The depressed adolescent’s impaired functioning in school and at home may cause secondary stress, increasing the burden of illness and need for treatment.
Suicide risk Although suicide remains rare among adolescents in general, the rate of suicide among this age group has risen dramatically over the past decade, particularly among younger teens and preteens. In 1997, suicide was the third leading cause of death in adolescents after accidental injuries and homicide.
Adolescents with depressive disorders are at increased risk for suicide, and boys are more likely than girls to attempt and complete suicide. It is therefore imperative to assess and document suicide risk for each adolescent who presents with depressive symptoms.
After establishing a rapport, the most effective screening is a straightforward conversation with the adolescent about suicidal ideation, intent, and behavior. Assess the social context of support and psychopathology in the family, availability and accessibility of lethal suicide methods (e.g., firearms in the home), and presence of events that could influence imitative suicidal behavior (e.g., a friend’s suicide).6
Treatment
Approaches to adolescent depression include (in increasing order of intensity and complexity) watchful monitoring, nonspecific supportive therapy, pharmacotherapy, specific psychotherapy (i.e., cognitive-behavioral or interpersonal therapy), and combined treatment (e.g., psychotherapy plus pharmacotherapy, adolescent psychotherapy plus family therapy).
There are no clear-cut guidelines as to whether pharmacologic or psychosocial therapy should be offered first.11 In the community, patient and family preferences, past treatment response, and the clinician’s background and expertise influence the choice of treatment. As with adults, adolescents deemed at high risk for suicidal behavior must receive immediate attention from mental health professionals and must be monitored, usually in an inpatient setting.
Watchful monitoring means to wait and see if the youth improves spontaneously.
In some studies, nearly one-half (48%) of adolescents with depression were found to go into spontaneous remission within 8 weeks.12 Watchful monitoring, however, would leave most patients still depressed, and no predictors of spontaneous remission have been identified.
Table 2
SSRI DOSAGES FOUND TO BE EFFECTIVE IN ADOLESCENTS WITH MDD
| Drug | Dosage (per day) | Reference |
|---|---|---|
| Fluoxetine | 20 mg | Emslie et al, 1997 and 20018,9 |
| Citalopram | 20-40 mg | Wagner et al, 200110 |
| Paroxetine | 20-40 mg | Keller et al, 200114 |
| Sertraline | 50-200 mg | Donnelly et al, 200115 |
Because of the risks of suicide and social and academic impairment, monitoring alone is acceptable only for a few weeks, and only in cases where depression is mild and uncomplicated. In any case, “monitoring” requires that you periodically reassess the teen and be available for consultation between assessments.
Nonspecific supportive therapy Most psychotherapy provided in the community probably is nonspecific (i.e., not theoretically driven or conducted according to a treatment manual) and supportive (i.e., aimed at providing encouragement). This approach is known to be less effective than specific psychotherapies or antidepressant pharmacotherapy, but we have virtually no data comparing it with lack of treatment.
Nonspecific supportive therapy can be considered a reasonable first-step treatment for depressed teens without complicating risk factors.13 Specific treatment is indicated, however, if the adolescent does not improve in a few weeks.
Pharmacotherapy A few placebo-controlled clinical trials have studied the efficacy of selective serotonin reuptake inhibitors (SSRIs) in outpatient adolescents with major depression. It must be noted that practically all the available data relate to major depression, and no systematic studies have been done in dysthymia and other types of depression in this population.
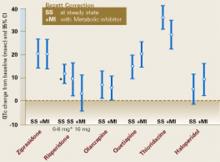
The SSRIs fluoxetine,8,9 citalopram,10 paroxetine,14 and sertraline15 can decrease symptoms of adolescent depression over 2 to 3 months when given at dosages similar to those used in adults (Table 2). At this time, there are no data that suggest the SSRI dosage must be different in younger (12-year-old) compared with older (18-year-old) adolescents, or in girls compared with boys.
The response rate (adolescents who were substantially improved at end of treatment) ranged from 52 to 65% with SSRI medication and 33 to 48% with a placebo. This means that one would need to treat about six adolescents in order to add one to those who would improve by taking a placebo. Thus, 6 is the number needed to treat (NNT), a common index used to make decisions in evidence-based medicine. As a comparison, the NNT is 1.5 for stimulant treatment of ADHD, indicating that stimulants are more effective in ADHD (i.e., the difference between an active drug and a placebo is greater) than SSRIs are in depression.
It must be noted that receiving a placebo in clinical trials of depression does not equal absence of treatment. Typically, research participants assigned to a placebo have weekly clinical contacts, so placebo treatment could be defined as “nonspecific clinical management.” In any case, the NNT for SSRIs in adolescent depression does not appear to be substantially different from that found in adults.
There is no evidence that tricyclic antidepressants, or TCAs, are more effective than a placebo in adolescents with depression. Considering TCAs’ side effects and potential cardiotoxicity in overdose, their use is not recommended in depressed adolescents. Other antidepressants, such as bupropion and venlafaxine, have been reported to be effective in open studies and clinical observations.
Antidepressants can trigger mania in persons predisposed to bipolar disorder. Before prescribing antidepressant medications, carefully evaluate depressed adolescents for present and past symptoms of mania or hypomania and check family history for possible bipolar disorder. During treatment, monitor the adolescent for signs that suggest emerging mania.
SSRIs and stimulant medications are commonly combined, as depression and ADHD often coexist. Clinical experience indicates that these medications can be safely combined in most cases, although no systematic studies of this combination have been performed in large, representative samples of teens. As with antidepressant monotherapy, adolescent patients must be monitored for signs of mania or hypomania.
Specific psychotherapy Among psychotherapies for depression, the best evidence of efficacy exists for cognitive-behavioral therapy (CBT), which attempts to correct cognitive distortions associated with depression and promotes healthy behaviors. In two clinical studies, CBT was more effective in depressed adolescents than no treatment (i.e., wait list), supportive therapy, or systemic behavior family therapy. About two-thirds of patients treated with CBT achieved remission from depressive symptoms.16,17
Interpersonal therapy (IPT) has been adapted for use in depressed adolescents.18 Its efficacy is supported by one controlled study that found greater improvement after 12 weekly IPT sessions than after once-monthly clinical contact.19 There is no convincing evidence that family therapies are effective in treating depression in adolescents or add much to the benefit of CBT.17
Combined treatment Research on combined treatments for adolescent depression has been limited. One study found that adding family therapy to CBT does not improve the adolescent’s depressive symptoms.8 Although no data are available on the combination of SSRI medication and CBT (or IPT), the National Institute of Mental Health is funding two studies on this important issue:
- The Treatment of Adolescents with Depression Study (TADS) is comparing the efficacy of fluoxetine plus CBT with that of fluoxetine or CBT alone in adolescents with major depression. The study, coordinated by John March, MD, of Duke University Medical Center, is being conducted with 432 teen subjects at 13 clinical sites.
- The Treatment of Resistant Depression in Adolescents (TORDIA) study is comparing the efficacy of antidepressant medication plus CBT to that of antidepressants alone in adolescents who have not improved on initial treatment with an SSRI. TORDIA, coordinated by David Brent, MD, University of Pittsburgh, is being conducted at six clinical sites.
Related resources
- National Institute of Mental Health. Child and Adolescent Mental Health. http://www.nimh.nih.gov/publicat/childmenu.cfm
- Depression in children and adolescents: A fact sheet for physicians. http://www.nimh.nih.gov/publicat/depchildresfact.cfm
- NIMH-funded treatment studies in adolescent depression:
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no affiliation or financial relationship with any of the companies whose products are mentioned in this article. The opinions and assertions contained in this article are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services or the National Institutes of Health.
1. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school. J Abnorm Psychol 1993;102:133-44.
2. Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
3. Jaffee SR, Moffitt TE, Caspi A, et al. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry 2002;58:215-22.
4. Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry 2000;157:1884-1591.
5. Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescents grow up. JAMA 2000;281:1707-13.
6. Pfeffer CR. Diagnosis of childhood and adolescent suicidal behavior: unmet needs for suicide prevention. Biol Psychiatry 2001;49:1055-61.
7. Carlson GA. The challenge of diagnosing depression in childhood and adolescence. J Affect Dis 2000;61(suppl 1):3-8.
8. Emslie GJ, Rush AJ, Weiberg WA, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54:1031-7.
9. Emslie GJ, Heligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents (poster presentation). Honolulu, Hawaii: American Academy of Child and Adolescent Psychiatry annual meeting, October 23-28, 2001.
10. Wagner KD, Robb AS, Findling R, Tiseo PJ. Citalopram is effective in the treatment of major depressive disorder in children and adolescents: results of a placebo-controlled (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
11. American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37:63S-83S.
12. Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry 1999;38:272-9.
13. Harrington R, Whittaker J, Shoebridge P, Campbell F. Systematic review of efficacy of cognitive behavior therapies in childhood and adolescent depressive disorder. BMJ 1998;316:1559-63.
14. Keller MB, Ryan ND, Birmaher B, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
15. Donnelly CL, Winokur A, Wholberg CJ. Efficacy and safety of sertraline in the treatment of pediatric major depressive disorder (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
16. Brent DA, Holder D, Kolko D, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Arch Gen Psychiatry 1997;54:877-85.
17. Harrington R, Whittaker J, Shoebridge P. Psychological treatment of depression in children and adolescents. A review of treatment research. Br J Psychiatry 1998;173:291-8.
18. Mufson L, Moreau D, Weissman MM, Klerman GL. Interpersonal psychotherapy for depressed adolescents. New York: Guilford Press, 1993.
19. Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 1999;56:573-9.
Adolescents with depressive disorders tend to arrive in psychiatrists’ offices when their behavior has already been identified as problematic. Suicide attempts, academic failure, substance abuse, and family conflicts can all lead to teen psychiatric referrals. Other times, subtler changes in behavior may lead a family doctor or pediatrician to suspect depression and to send an adolescent to you for a psychiatric consultation.
The psychiatrist’s task is challenging. Adolescents are usually brought in by their worried parents and may not want to talk to a psychiatrist. Or they may be unable to accurately describe their internal states. Even people who know an adolescent well may not discern the emotions that drive his or her behavior. Adding to the mix are the recurrent nature of major depression in adolescents and the likelihood of complicating comorbid psychiatric conditions (Box).1-6
Based on clinical evidence, we offer advice to help you promptly identify and effectively treat adolescents with depressive disorders. We also provide preliminary information on two studies examining medication treatment, psychotherapy, and combined treatment for teens with major depression.
Adolescent depression disorders
Symptoms of depression in adolescents are similar to those in adults, and it is appropriate for psychiatrists to use DSM-IV diagnostic criteria for making the diagnosis. The three primary depressive disorders for both adults and adolescents are major depressive disorder (MDD), dysthymic disorder, and depressive disorder not otherwise specified (NOS).
Depression is relatively rare among children but becomes common after the onset of puberty. In particular, recurrent depression often starts in adolescence. Here are the statistics:
- Up to 9% of adolescents meet diagnostic criteria for major depressive disorder (MDD), and up to 25% suffer from it by their late teens.
- MDD affects boys and girls equally in childhood, but the prevalence seems to increase in girls after puberty.1,2
- Depression in adolescents is characterized by high rates of comorbid psychiatric conditions. In general, the younger the age of onset, the higher the rate of comorbid conduct disorder, attention-deficit/hyperactivity disorder, and/or anxiety disorder.3
- Adolescent depression tends to persist. An estimated 45 to 70% of children and adolescents with MDD have recurrent episodes.4 At particularly high risk for recurrence are adolescent girls with depression, adolescents with multiple MDD episodes, and adolescents with a family history of recurrent depression.
- As many as 50% of teens with MDD attempt suicide within 15 years of their initial episode, and more than 20% make recurrent attempts.4,5 No good estimates of the rate of completed suicide are available. One 15-year follow-up of a sample of depressed adolescents reported a suicide rate of 7.7%.5 Boys are much more likely to complete suicide than girls across all racial groups.6
Although the symptoms that make up the diagnostic criteria are similar for adults and teens, the behavioral manifestations and response to treatment may differ. The adolescent may present as irritable and angry, rather than overly sad. Impairments in functioning are likely to be related to decline in school performance, social withdrawal, or increased conflicts with peers and family.
As for treatment, certain antidepressant medications of proven efficacy in adults (i.e., tricyclics) do not seem to work for adolescents.
MDD is a time-limited episode of depressive symptoms severe enough to cause functional impairment, such as decline in school performance, social withdrawal, or increased conflicts with peers and family. Symptoms must be present at least 2 weeks.
Dysthymia is a chronic depression that is less severe than MDD and lasts 1 year or longer without sustained remission. It often begins early in childhood and may include periods of increased symptoms consistent with major depression (sometimes called “double depression”).
Depressive disorder NOS is a category of depression that, though clinically significant, does not meet the full criteria for severity, duration, or level of impairment of MDD or dysthymia.
Unless otherwise specified, the terms “depression” and “depressive disorder” in this article are used generically to include all three of these disorders.
Depressive disorders must be differentiated from bipolar disorder, which is characterized by least one prior episode of mania (for bipolar type I) or hypomania (for bipolar type II). The clinical picture of bipolar disorder in youths may differ from that seen in adults. For example, bipolar youth often present with dysphoric mood interspersed with frequent, short periods of intense emotional lability and irritability, rather than “classic” euphoria.
Diagnosis
To diagnose a depressive disorder in an adolescent, information is typically obtained from multiple sources, most commonly the teenage patient and at least one of the parents. Because several sources are involved, however, the information may be conflicting. For instance, the adolescent may contradict a parent’s report that he or she is having difficulties in school or has a substance abuse problem.
Interviewing skills and clinical judgment are required of the clinician in these situations. It is important to:
- obtain a complete description of the adolescent’s behavior and mood over time and as accurate a description as possible of when changes occurred
- assess comorbid conditions (particularly anxiety, attention-deficit/hyperactivity disorder [ADHD], conduct disorder, and substance abuse)
- differentiate between unipolar MDD and bipolar disorder
- evaluate the risk of suicide.
Table 1
DEPRESSION IN ADOLESCENTS AND ADULTS
| Similarities | Differences |
|---|---|
| Same types of diagnostic categories (i.e., major depression, dysthymia, depression NOS) | To diagnose dysthymia, minimum duration of mood disturbance must be 1 year in adolescents (2 years in adults) |
| Same diagnostic symptoms criteria | Mood is often irritable in adolescents (rather than depressed) |
| More common in females | |
| Suicide is more common among males | |
| Evidence of efficacy of SSRI antidepressants | No evidence of efficacy of tricyclic antidepressants in adolescent depression |
Interviewing Standardized diagnostic interviews, such as the Schedule for Affective Disorders and Schizophrenia for children (K-SADS), are commonly used to research adolescent depression but require special training and approximately 1 to 2 hours to administer. As an alternative, clinicians generally develop their own “semi-structured interview” to try to collect all the relevant information required for an accurate diagnosis.7
The interview should be conducted with the adolescent and the parent(s), first separately for ease of disclosure then together to reconcile any differences in the information they report. Open-ended questions and time for building rapport may facilitate disclosure from a reticent adolescent. At times, however, one must make the diagnosis by relying more on reports from others who know the child well. Building a trusting therapeutic relationship then becomes part of ongoing treatment.
Standardized measures In addition to the interview, standardized self-report and other-report measures can help:
- The Child Depression Rating Scale-Revised, commonly used in clinical research, can also be used in practice to quantify symptom severity and document treatment response. A score above 40 usually indicates major depression; a score below 28 indicates remission of depression.8-10
- The Beck Depression Inventory (BDI), a 21-item self-report questionnaire for adults, has reasonable reliability and validity for adolescents. Its modest specificity suggests that it may measure general distress and dysphoria, which is not specific to depressive disorders. The language may be too difficult for some younger adolescents and those with poor reading comprehension skills.
- The Children’s Depression Inventory, a version of the BDI for prepubertal children, can be considered for adolescents whose cognitive and/or reading skills are less mature.
- Achenbach’s Child Behavior Checklists and other standardized questionnaires can screen for comorbid psychopathology.
Assessing psychosocial stress, such as conflicts with parents or peers, school problems, or risk-taking behavior, is also important. Depressed youth often have family members with histories of depression, alcoholism, anxiety, and other psychiatric diagnoses. History of sexual abuse has been linked to depression.3 The depressed adolescent’s impaired functioning in school and at home may cause secondary stress, increasing the burden of illness and need for treatment.
Suicide risk Although suicide remains rare among adolescents in general, the rate of suicide among this age group has risen dramatically over the past decade, particularly among younger teens and preteens. In 1997, suicide was the third leading cause of death in adolescents after accidental injuries and homicide.
Adolescents with depressive disorders are at increased risk for suicide, and boys are more likely than girls to attempt and complete suicide. It is therefore imperative to assess and document suicide risk for each adolescent who presents with depressive symptoms.
After establishing a rapport, the most effective screening is a straightforward conversation with the adolescent about suicidal ideation, intent, and behavior. Assess the social context of support and psychopathology in the family, availability and accessibility of lethal suicide methods (e.g., firearms in the home), and presence of events that could influence imitative suicidal behavior (e.g., a friend’s suicide).6
Treatment
Approaches to adolescent depression include (in increasing order of intensity and complexity) watchful monitoring, nonspecific supportive therapy, pharmacotherapy, specific psychotherapy (i.e., cognitive-behavioral or interpersonal therapy), and combined treatment (e.g., psychotherapy plus pharmacotherapy, adolescent psychotherapy plus family therapy).
There are no clear-cut guidelines as to whether pharmacologic or psychosocial therapy should be offered first.11 In the community, patient and family preferences, past treatment response, and the clinician’s background and expertise influence the choice of treatment. As with adults, adolescents deemed at high risk for suicidal behavior must receive immediate attention from mental health professionals and must be monitored, usually in an inpatient setting.
Watchful monitoring means to wait and see if the youth improves spontaneously.
In some studies, nearly one-half (48%) of adolescents with depression were found to go into spontaneous remission within 8 weeks.12 Watchful monitoring, however, would leave most patients still depressed, and no predictors of spontaneous remission have been identified.
Table 2
SSRI DOSAGES FOUND TO BE EFFECTIVE IN ADOLESCENTS WITH MDD
| Drug | Dosage (per day) | Reference |
|---|---|---|
| Fluoxetine | 20 mg | Emslie et al, 1997 and 20018,9 |
| Citalopram | 20-40 mg | Wagner et al, 200110 |
| Paroxetine | 20-40 mg | Keller et al, 200114 |
| Sertraline | 50-200 mg | Donnelly et al, 200115 |
Because of the risks of suicide and social and academic impairment, monitoring alone is acceptable only for a few weeks, and only in cases where depression is mild and uncomplicated. In any case, “monitoring” requires that you periodically reassess the teen and be available for consultation between assessments.
Nonspecific supportive therapy Most psychotherapy provided in the community probably is nonspecific (i.e., not theoretically driven or conducted according to a treatment manual) and supportive (i.e., aimed at providing encouragement). This approach is known to be less effective than specific psychotherapies or antidepressant pharmacotherapy, but we have virtually no data comparing it with lack of treatment.
Nonspecific supportive therapy can be considered a reasonable first-step treatment for depressed teens without complicating risk factors.13 Specific treatment is indicated, however, if the adolescent does not improve in a few weeks.
Pharmacotherapy A few placebo-controlled clinical trials have studied the efficacy of selective serotonin reuptake inhibitors (SSRIs) in outpatient adolescents with major depression. It must be noted that practically all the available data relate to major depression, and no systematic studies have been done in dysthymia and other types of depression in this population.
The SSRIs fluoxetine,8,9 citalopram,10 paroxetine,14 and sertraline15 can decrease symptoms of adolescent depression over 2 to 3 months when given at dosages similar to those used in adults (Table 2). At this time, there are no data that suggest the SSRI dosage must be different in younger (12-year-old) compared with older (18-year-old) adolescents, or in girls compared with boys.
The response rate (adolescents who were substantially improved at end of treatment) ranged from 52 to 65% with SSRI medication and 33 to 48% with a placebo. This means that one would need to treat about six adolescents in order to add one to those who would improve by taking a placebo. Thus, 6 is the number needed to treat (NNT), a common index used to make decisions in evidence-based medicine. As a comparison, the NNT is 1.5 for stimulant treatment of ADHD, indicating that stimulants are more effective in ADHD (i.e., the difference between an active drug and a placebo is greater) than SSRIs are in depression.
It must be noted that receiving a placebo in clinical trials of depression does not equal absence of treatment. Typically, research participants assigned to a placebo have weekly clinical contacts, so placebo treatment could be defined as “nonspecific clinical management.” In any case, the NNT for SSRIs in adolescent depression does not appear to be substantially different from that found in adults.
There is no evidence that tricyclic antidepressants, or TCAs, are more effective than a placebo in adolescents with depression. Considering TCAs’ side effects and potential cardiotoxicity in overdose, their use is not recommended in depressed adolescents. Other antidepressants, such as bupropion and venlafaxine, have been reported to be effective in open studies and clinical observations.
Antidepressants can trigger mania in persons predisposed to bipolar disorder. Before prescribing antidepressant medications, carefully evaluate depressed adolescents for present and past symptoms of mania or hypomania and check family history for possible bipolar disorder. During treatment, monitor the adolescent for signs that suggest emerging mania.
SSRIs and stimulant medications are commonly combined, as depression and ADHD often coexist. Clinical experience indicates that these medications can be safely combined in most cases, although no systematic studies of this combination have been performed in large, representative samples of teens. As with antidepressant monotherapy, adolescent patients must be monitored for signs of mania or hypomania.
Specific psychotherapy Among psychotherapies for depression, the best evidence of efficacy exists for cognitive-behavioral therapy (CBT), which attempts to correct cognitive distortions associated with depression and promotes healthy behaviors. In two clinical studies, CBT was more effective in depressed adolescents than no treatment (i.e., wait list), supportive therapy, or systemic behavior family therapy. About two-thirds of patients treated with CBT achieved remission from depressive symptoms.16,17
Interpersonal therapy (IPT) has been adapted for use in depressed adolescents.18 Its efficacy is supported by one controlled study that found greater improvement after 12 weekly IPT sessions than after once-monthly clinical contact.19 There is no convincing evidence that family therapies are effective in treating depression in adolescents or add much to the benefit of CBT.17
Combined treatment Research on combined treatments for adolescent depression has been limited. One study found that adding family therapy to CBT does not improve the adolescent’s depressive symptoms.8 Although no data are available on the combination of SSRI medication and CBT (or IPT), the National Institute of Mental Health is funding two studies on this important issue:
- The Treatment of Adolescents with Depression Study (TADS) is comparing the efficacy of fluoxetine plus CBT with that of fluoxetine or CBT alone in adolescents with major depression. The study, coordinated by John March, MD, of Duke University Medical Center, is being conducted with 432 teen subjects at 13 clinical sites.
- The Treatment of Resistant Depression in Adolescents (TORDIA) study is comparing the efficacy of antidepressant medication plus CBT to that of antidepressants alone in adolescents who have not improved on initial treatment with an SSRI. TORDIA, coordinated by David Brent, MD, University of Pittsburgh, is being conducted at six clinical sites.
Related resources
- National Institute of Mental Health. Child and Adolescent Mental Health. http://www.nimh.nih.gov/publicat/childmenu.cfm
- Depression in children and adolescents: A fact sheet for physicians. http://www.nimh.nih.gov/publicat/depchildresfact.cfm
- NIMH-funded treatment studies in adolescent depression:
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no affiliation or financial relationship with any of the companies whose products are mentioned in this article. The opinions and assertions contained in this article are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services or the National Institutes of Health.
Adolescents with depressive disorders tend to arrive in psychiatrists’ offices when their behavior has already been identified as problematic. Suicide attempts, academic failure, substance abuse, and family conflicts can all lead to teen psychiatric referrals. Other times, subtler changes in behavior may lead a family doctor or pediatrician to suspect depression and to send an adolescent to you for a psychiatric consultation.
The psychiatrist’s task is challenging. Adolescents are usually brought in by their worried parents and may not want to talk to a psychiatrist. Or they may be unable to accurately describe their internal states. Even people who know an adolescent well may not discern the emotions that drive his or her behavior. Adding to the mix are the recurrent nature of major depression in adolescents and the likelihood of complicating comorbid psychiatric conditions (Box).1-6
Based on clinical evidence, we offer advice to help you promptly identify and effectively treat adolescents with depressive disorders. We also provide preliminary information on two studies examining medication treatment, psychotherapy, and combined treatment for teens with major depression.
Adolescent depression disorders
Symptoms of depression in adolescents are similar to those in adults, and it is appropriate for psychiatrists to use DSM-IV diagnostic criteria for making the diagnosis. The three primary depressive disorders for both adults and adolescents are major depressive disorder (MDD), dysthymic disorder, and depressive disorder not otherwise specified (NOS).
Depression is relatively rare among children but becomes common after the onset of puberty. In particular, recurrent depression often starts in adolescence. Here are the statistics:
- Up to 9% of adolescents meet diagnostic criteria for major depressive disorder (MDD), and up to 25% suffer from it by their late teens.
- MDD affects boys and girls equally in childhood, but the prevalence seems to increase in girls after puberty.1,2
- Depression in adolescents is characterized by high rates of comorbid psychiatric conditions. In general, the younger the age of onset, the higher the rate of comorbid conduct disorder, attention-deficit/hyperactivity disorder, and/or anxiety disorder.3
- Adolescent depression tends to persist. An estimated 45 to 70% of children and adolescents with MDD have recurrent episodes.4 At particularly high risk for recurrence are adolescent girls with depression, adolescents with multiple MDD episodes, and adolescents with a family history of recurrent depression.
- As many as 50% of teens with MDD attempt suicide within 15 years of their initial episode, and more than 20% make recurrent attempts.4,5 No good estimates of the rate of completed suicide are available. One 15-year follow-up of a sample of depressed adolescents reported a suicide rate of 7.7%.5 Boys are much more likely to complete suicide than girls across all racial groups.6
Although the symptoms that make up the diagnostic criteria are similar for adults and teens, the behavioral manifestations and response to treatment may differ. The adolescent may present as irritable and angry, rather than overly sad. Impairments in functioning are likely to be related to decline in school performance, social withdrawal, or increased conflicts with peers and family.
As for treatment, certain antidepressant medications of proven efficacy in adults (i.e., tricyclics) do not seem to work for adolescents.
MDD is a time-limited episode of depressive symptoms severe enough to cause functional impairment, such as decline in school performance, social withdrawal, or increased conflicts with peers and family. Symptoms must be present at least 2 weeks.
Dysthymia is a chronic depression that is less severe than MDD and lasts 1 year or longer without sustained remission. It often begins early in childhood and may include periods of increased symptoms consistent with major depression (sometimes called “double depression”).
Depressive disorder NOS is a category of depression that, though clinically significant, does not meet the full criteria for severity, duration, or level of impairment of MDD or dysthymia.
Unless otherwise specified, the terms “depression” and “depressive disorder” in this article are used generically to include all three of these disorders.
Depressive disorders must be differentiated from bipolar disorder, which is characterized by least one prior episode of mania (for bipolar type I) or hypomania (for bipolar type II). The clinical picture of bipolar disorder in youths may differ from that seen in adults. For example, bipolar youth often present with dysphoric mood interspersed with frequent, short periods of intense emotional lability and irritability, rather than “classic” euphoria.
Diagnosis
To diagnose a depressive disorder in an adolescent, information is typically obtained from multiple sources, most commonly the teenage patient and at least one of the parents. Because several sources are involved, however, the information may be conflicting. For instance, the adolescent may contradict a parent’s report that he or she is having difficulties in school or has a substance abuse problem.
Interviewing skills and clinical judgment are required of the clinician in these situations. It is important to:
- obtain a complete description of the adolescent’s behavior and mood over time and as accurate a description as possible of when changes occurred
- assess comorbid conditions (particularly anxiety, attention-deficit/hyperactivity disorder [ADHD], conduct disorder, and substance abuse)
- differentiate between unipolar MDD and bipolar disorder
- evaluate the risk of suicide.
Table 1
DEPRESSION IN ADOLESCENTS AND ADULTS
| Similarities | Differences |
|---|---|
| Same types of diagnostic categories (i.e., major depression, dysthymia, depression NOS) | To diagnose dysthymia, minimum duration of mood disturbance must be 1 year in adolescents (2 years in adults) |
| Same diagnostic symptoms criteria | Mood is often irritable in adolescents (rather than depressed) |
| More common in females | |
| Suicide is more common among males | |
| Evidence of efficacy of SSRI antidepressants | No evidence of efficacy of tricyclic antidepressants in adolescent depression |
Interviewing Standardized diagnostic interviews, such as the Schedule for Affective Disorders and Schizophrenia for children (K-SADS), are commonly used to research adolescent depression but require special training and approximately 1 to 2 hours to administer. As an alternative, clinicians generally develop their own “semi-structured interview” to try to collect all the relevant information required for an accurate diagnosis.7
The interview should be conducted with the adolescent and the parent(s), first separately for ease of disclosure then together to reconcile any differences in the information they report. Open-ended questions and time for building rapport may facilitate disclosure from a reticent adolescent. At times, however, one must make the diagnosis by relying more on reports from others who know the child well. Building a trusting therapeutic relationship then becomes part of ongoing treatment.
Standardized measures In addition to the interview, standardized self-report and other-report measures can help:
- The Child Depression Rating Scale-Revised, commonly used in clinical research, can also be used in practice to quantify symptom severity and document treatment response. A score above 40 usually indicates major depression; a score below 28 indicates remission of depression.8-10
- The Beck Depression Inventory (BDI), a 21-item self-report questionnaire for adults, has reasonable reliability and validity for adolescents. Its modest specificity suggests that it may measure general distress and dysphoria, which is not specific to depressive disorders. The language may be too difficult for some younger adolescents and those with poor reading comprehension skills.
- The Children’s Depression Inventory, a version of the BDI for prepubertal children, can be considered for adolescents whose cognitive and/or reading skills are less mature.
- Achenbach’s Child Behavior Checklists and other standardized questionnaires can screen for comorbid psychopathology.
Assessing psychosocial stress, such as conflicts with parents or peers, school problems, or risk-taking behavior, is also important. Depressed youth often have family members with histories of depression, alcoholism, anxiety, and other psychiatric diagnoses. History of sexual abuse has been linked to depression.3 The depressed adolescent’s impaired functioning in school and at home may cause secondary stress, increasing the burden of illness and need for treatment.
Suicide risk Although suicide remains rare among adolescents in general, the rate of suicide among this age group has risen dramatically over the past decade, particularly among younger teens and preteens. In 1997, suicide was the third leading cause of death in adolescents after accidental injuries and homicide.
Adolescents with depressive disorders are at increased risk for suicide, and boys are more likely than girls to attempt and complete suicide. It is therefore imperative to assess and document suicide risk for each adolescent who presents with depressive symptoms.
After establishing a rapport, the most effective screening is a straightforward conversation with the adolescent about suicidal ideation, intent, and behavior. Assess the social context of support and psychopathology in the family, availability and accessibility of lethal suicide methods (e.g., firearms in the home), and presence of events that could influence imitative suicidal behavior (e.g., a friend’s suicide).6
Treatment
Approaches to adolescent depression include (in increasing order of intensity and complexity) watchful monitoring, nonspecific supportive therapy, pharmacotherapy, specific psychotherapy (i.e., cognitive-behavioral or interpersonal therapy), and combined treatment (e.g., psychotherapy plus pharmacotherapy, adolescent psychotherapy plus family therapy).
There are no clear-cut guidelines as to whether pharmacologic or psychosocial therapy should be offered first.11 In the community, patient and family preferences, past treatment response, and the clinician’s background and expertise influence the choice of treatment. As with adults, adolescents deemed at high risk for suicidal behavior must receive immediate attention from mental health professionals and must be monitored, usually in an inpatient setting.
Watchful monitoring means to wait and see if the youth improves spontaneously.
In some studies, nearly one-half (48%) of adolescents with depression were found to go into spontaneous remission within 8 weeks.12 Watchful monitoring, however, would leave most patients still depressed, and no predictors of spontaneous remission have been identified.
Table 2
SSRI DOSAGES FOUND TO BE EFFECTIVE IN ADOLESCENTS WITH MDD
| Drug | Dosage (per day) | Reference |
|---|---|---|
| Fluoxetine | 20 mg | Emslie et al, 1997 and 20018,9 |
| Citalopram | 20-40 mg | Wagner et al, 200110 |
| Paroxetine | 20-40 mg | Keller et al, 200114 |
| Sertraline | 50-200 mg | Donnelly et al, 200115 |
Because of the risks of suicide and social and academic impairment, monitoring alone is acceptable only for a few weeks, and only in cases where depression is mild and uncomplicated. In any case, “monitoring” requires that you periodically reassess the teen and be available for consultation between assessments.
Nonspecific supportive therapy Most psychotherapy provided in the community probably is nonspecific (i.e., not theoretically driven or conducted according to a treatment manual) and supportive (i.e., aimed at providing encouragement). This approach is known to be less effective than specific psychotherapies or antidepressant pharmacotherapy, but we have virtually no data comparing it with lack of treatment.
Nonspecific supportive therapy can be considered a reasonable first-step treatment for depressed teens without complicating risk factors.13 Specific treatment is indicated, however, if the adolescent does not improve in a few weeks.
Pharmacotherapy A few placebo-controlled clinical trials have studied the efficacy of selective serotonin reuptake inhibitors (SSRIs) in outpatient adolescents with major depression. It must be noted that practically all the available data relate to major depression, and no systematic studies have been done in dysthymia and other types of depression in this population.
The SSRIs fluoxetine,8,9 citalopram,10 paroxetine,14 and sertraline15 can decrease symptoms of adolescent depression over 2 to 3 months when given at dosages similar to those used in adults (Table 2). At this time, there are no data that suggest the SSRI dosage must be different in younger (12-year-old) compared with older (18-year-old) adolescents, or in girls compared with boys.
The response rate (adolescents who were substantially improved at end of treatment) ranged from 52 to 65% with SSRI medication and 33 to 48% with a placebo. This means that one would need to treat about six adolescents in order to add one to those who would improve by taking a placebo. Thus, 6 is the number needed to treat (NNT), a common index used to make decisions in evidence-based medicine. As a comparison, the NNT is 1.5 for stimulant treatment of ADHD, indicating that stimulants are more effective in ADHD (i.e., the difference between an active drug and a placebo is greater) than SSRIs are in depression.
It must be noted that receiving a placebo in clinical trials of depression does not equal absence of treatment. Typically, research participants assigned to a placebo have weekly clinical contacts, so placebo treatment could be defined as “nonspecific clinical management.” In any case, the NNT for SSRIs in adolescent depression does not appear to be substantially different from that found in adults.
There is no evidence that tricyclic antidepressants, or TCAs, are more effective than a placebo in adolescents with depression. Considering TCAs’ side effects and potential cardiotoxicity in overdose, their use is not recommended in depressed adolescents. Other antidepressants, such as bupropion and venlafaxine, have been reported to be effective in open studies and clinical observations.
Antidepressants can trigger mania in persons predisposed to bipolar disorder. Before prescribing antidepressant medications, carefully evaluate depressed adolescents for present and past symptoms of mania or hypomania and check family history for possible bipolar disorder. During treatment, monitor the adolescent for signs that suggest emerging mania.
SSRIs and stimulant medications are commonly combined, as depression and ADHD often coexist. Clinical experience indicates that these medications can be safely combined in most cases, although no systematic studies of this combination have been performed in large, representative samples of teens. As with antidepressant monotherapy, adolescent patients must be monitored for signs of mania or hypomania.
Specific psychotherapy Among psychotherapies for depression, the best evidence of efficacy exists for cognitive-behavioral therapy (CBT), which attempts to correct cognitive distortions associated with depression and promotes healthy behaviors. In two clinical studies, CBT was more effective in depressed adolescents than no treatment (i.e., wait list), supportive therapy, or systemic behavior family therapy. About two-thirds of patients treated with CBT achieved remission from depressive symptoms.16,17
Interpersonal therapy (IPT) has been adapted for use in depressed adolescents.18 Its efficacy is supported by one controlled study that found greater improvement after 12 weekly IPT sessions than after once-monthly clinical contact.19 There is no convincing evidence that family therapies are effective in treating depression in adolescents or add much to the benefit of CBT.17
Combined treatment Research on combined treatments for adolescent depression has been limited. One study found that adding family therapy to CBT does not improve the adolescent’s depressive symptoms.8 Although no data are available on the combination of SSRI medication and CBT (or IPT), the National Institute of Mental Health is funding two studies on this important issue:
- The Treatment of Adolescents with Depression Study (TADS) is comparing the efficacy of fluoxetine plus CBT with that of fluoxetine or CBT alone in adolescents with major depression. The study, coordinated by John March, MD, of Duke University Medical Center, is being conducted with 432 teen subjects at 13 clinical sites.
- The Treatment of Resistant Depression in Adolescents (TORDIA) study is comparing the efficacy of antidepressant medication plus CBT to that of antidepressants alone in adolescents who have not improved on initial treatment with an SSRI. TORDIA, coordinated by David Brent, MD, University of Pittsburgh, is being conducted at six clinical sites.
Related resources
- National Institute of Mental Health. Child and Adolescent Mental Health. http://www.nimh.nih.gov/publicat/childmenu.cfm
- Depression in children and adolescents: A fact sheet for physicians. http://www.nimh.nih.gov/publicat/depchildresfact.cfm
- NIMH-funded treatment studies in adolescent depression:
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no affiliation or financial relationship with any of the companies whose products are mentioned in this article. The opinions and assertions contained in this article are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services or the National Institutes of Health.
1. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school. J Abnorm Psychol 1993;102:133-44.
2. Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
3. Jaffee SR, Moffitt TE, Caspi A, et al. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry 2002;58:215-22.
4. Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry 2000;157:1884-1591.
5. Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescents grow up. JAMA 2000;281:1707-13.
6. Pfeffer CR. Diagnosis of childhood and adolescent suicidal behavior: unmet needs for suicide prevention. Biol Psychiatry 2001;49:1055-61.
7. Carlson GA. The challenge of diagnosing depression in childhood and adolescence. J Affect Dis 2000;61(suppl 1):3-8.
8. Emslie GJ, Rush AJ, Weiberg WA, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54:1031-7.
9. Emslie GJ, Heligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents (poster presentation). Honolulu, Hawaii: American Academy of Child and Adolescent Psychiatry annual meeting, October 23-28, 2001.
10. Wagner KD, Robb AS, Findling R, Tiseo PJ. Citalopram is effective in the treatment of major depressive disorder in children and adolescents: results of a placebo-controlled (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
11. American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37:63S-83S.
12. Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry 1999;38:272-9.
13. Harrington R, Whittaker J, Shoebridge P, Campbell F. Systematic review of efficacy of cognitive behavior therapies in childhood and adolescent depressive disorder. BMJ 1998;316:1559-63.
14. Keller MB, Ryan ND, Birmaher B, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
15. Donnelly CL, Winokur A, Wholberg CJ. Efficacy and safety of sertraline in the treatment of pediatric major depressive disorder (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
16. Brent DA, Holder D, Kolko D, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Arch Gen Psychiatry 1997;54:877-85.
17. Harrington R, Whittaker J, Shoebridge P. Psychological treatment of depression in children and adolescents. A review of treatment research. Br J Psychiatry 1998;173:291-8.
18. Mufson L, Moreau D, Weissman MM, Klerman GL. Interpersonal psychotherapy for depressed adolescents. New York: Guilford Press, 1993.
19. Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 1999;56:573-9.
1. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school. J Abnorm Psychol 1993;102:133-44.
2. Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
3. Jaffee SR, Moffitt TE, Caspi A, et al. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry 2002;58:215-22.
4. Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry 2000;157:1884-1591.
5. Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescents grow up. JAMA 2000;281:1707-13.
6. Pfeffer CR. Diagnosis of childhood and adolescent suicidal behavior: unmet needs for suicide prevention. Biol Psychiatry 2001;49:1055-61.
7. Carlson GA. The challenge of diagnosing depression in childhood and adolescence. J Affect Dis 2000;61(suppl 1):3-8.
8. Emslie GJ, Rush AJ, Weiberg WA, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54:1031-7.
9. Emslie GJ, Heligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents (poster presentation). Honolulu, Hawaii: American Academy of Child and Adolescent Psychiatry annual meeting, October 23-28, 2001.
10. Wagner KD, Robb AS, Findling R, Tiseo PJ. Citalopram is effective in the treatment of major depressive disorder in children and adolescents: results of a placebo-controlled (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
11. American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37:63S-83S.
12. Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry 1999;38:272-9.
13. Harrington R, Whittaker J, Shoebridge P, Campbell F. Systematic review of efficacy of cognitive behavior therapies in childhood and adolescent depressive disorder. BMJ 1998;316:1559-63.
14. Keller MB, Ryan ND, Birmaher B, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
15. Donnelly CL, Winokur A, Wholberg CJ. Efficacy and safety of sertraline in the treatment of pediatric major depressive disorder (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
16. Brent DA, Holder D, Kolko D, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Arch Gen Psychiatry 1997;54:877-85.
17. Harrington R, Whittaker J, Shoebridge P. Psychological treatment of depression in children and adolescents. A review of treatment research. Br J Psychiatry 1998;173:291-8.
18. Mufson L, Moreau D, Weissman MM, Klerman GL. Interpersonal psychotherapy for depressed adolescents. New York: Guilford Press, 1993.
19. Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 1999;56:573-9.
Adolescent depression: Diagnostic skills can differentiate teen angst from psychopathology
Adolescents with depressive disorders tend to arrive in psychiatrists’ offices when their behavior has already been identified as problematic. Suicide attempts, academic failure, substance abuse, and family conflicts can all lead to teen psychiatric referrals. Other times, subtler changes in behavior may lead a family doctor or pediatrician to suspect depression and to send an adolescent to you for a psychiatric consultation.
The psychiatrist’s task is challenging. Adolescents are usually brought in by their worried parents and may not want to talk to a psychiatrist. Or they may be unable to accurately describe their internal states. Even people who know an adolescent well may not discern the emotions that drive his or her behavior. Adding to the mix are the recurrent nature of major depression in adolescents and the likelihood of complicating comorbid psychiatric conditions (Box).1-6
Based on clinical evidence, we offer advice to help you promptly identify and effectively treat adolescents with depressive disorders. We also provide preliminary information on two studies examining medication treatment, psychotherapy, and combined treatment for teens with major depression.
Adolescent depression disorders
Symptoms of depression in adolescents are similar to those in adults, and it is appropriate for psychiatrists to use DSM-IV diagnostic criteria for making the diagnosis. The three primary depressive disorders for both adults and adolescents are major depressive disorder (MDD), dysthymic disorder, and depressive disorder not otherwise specified (NOS).
Depression is relatively rare among children but becomes common after the onset of puberty. In particular, recurrent depression often starts in adolescence. Here are the statistics:
- Up to 9% of adolescents meet diagnostic criteria for major depressive disorder (MDD), and up to 25% suffer from it by their late teens.
- MDD affects boys and girls equally in childhood, but the prevalence seems to increase in girls after puberty.1,2
- Depression in adolescents is characterized by high rates of comorbid psychiatric conditions. In general, the younger the age of onset, the higher the rate of comorbid conduct disorder, attention-deficit/hyperactivity disorder, and/or anxiety disorder.3
- Adolescent depression tends to persist. An estimated 45 to 70% of children and adolescents with MDD have recurrent episodes.4 At particularly high risk for recurrence are adolescent girls with depression, adolescents with multiple MDD episodes, and adolescents with a family history of recurrent depression.
- As many as 50% of teens with MDD attempt suicide within 15 years of their initial episode, and more than 20% make recurrent attempts.4,5 No good estimates of the rate of completed suicide are available. One 15-year follow-up of a sample of depressed adolescents reported a suicide rate of 7.7%.5 Boys are much more likely to complete suicide than girls across all racial groups.6
Although the symptoms that make up the diagnostic criteria are similar for adults and teens, the behavioral manifestations and response to treatment may differ. The adolescent may present as irritable and angry, rather than overly sad. Impairments in functioning are likely to be related to decline in school performance, social withdrawal, or increased conflicts with peers and family.
As for treatment, certain antidepressant medications of proven efficacy in adults (i.e., tricyclics) do not seem to work for adolescents.
MDD is a time-limited episode of depressive symptoms severe enough to cause functional impairment, such as decline in school performance, social withdrawal, or increased conflicts with peers and family. Symptoms must be present at least 2 weeks.
Dysthymia is a chronic depression that is less severe than MDD and lasts 1 year or longer without sustained remission. It often begins early in childhood and may include periods of increased symptoms consistent with major depression (sometimes called “double depression”).
Depressive disorder NOS is a category of depression that, though clinically significant, does not meet the full criteria for severity, duration, or level of impairment of MDD or dysthymia.
Unless otherwise specified, the terms “depression” and “depressive disorder” in this article are used generically to include all three of these disorders.
Depressive disorders must be differentiated from bipolar disorder, which is characterized by least one prior episode of mania (for bipolar type I) or hypomania (for bipolar type II). The clinical picture of bipolar disorder in youths may differ from that seen in adults. For example, bipolar youth often present with dysphoric mood interspersed with frequent, short periods of intense emotional lability and irritability, rather than “classic” euphoria.
Diagnosis
To diagnose a depressive disorder in an adolescent, information is typically obtained from multiple sources, most commonly the teenage patient and at least one of the parents. Because several sources are involved, however, the information may be conflicting. For instance, the adolescent may contradict a parent’s report that he or she is having difficulties in school or has a substance abuse problem.
Interviewing skills and clinical judgment are required of the clinician in these situations. It is important to:
- obtain a complete description of the adolescent’s behavior and mood over time and as accurate a description as possible of when changes occurred
- assess comorbid conditions (particularly anxiety, attention-deficit/hyperactivity disorder [ADHD], conduct disorder, and substance abuse)
- differentiate between unipolar MDD and bipolar disorder
- evaluate the risk of suicide.
Table 1
DEPRESSION IN ADOLESCENTS AND ADULTS
| Similarities | Differences |
|---|---|
| Same types of diagnostic categories (i.e., major depression, dysthymia, depression NOS) | To diagnose dysthymia, minimum duration of mood disturbance must be 1 year in adolescents (2 years in adults) |
| Same diagnostic symptoms criteria | Mood is often irritable in adolescents (rather than depressed) |
| More common in females | |
| Suicide is more common among males | |
| Evidence of efficacy of SSRI antidepressants | No evidence of efficacy of tricyclic antidepressants in adolescent depression |
Interviewing Standardized diagnostic interviews, such as the Schedule for Affective Disorders and Schizophrenia for children (K-SADS), are commonly used to research adolescent depression but require special training and approximately 1 to 2 hours to administer. As an alternative, clinicians generally develop their own “semi-structured interview” to try to collect all the relevant information required for an accurate diagnosis.7
The interview should be conducted with the adolescent and the parent(s), first separately for ease of disclosure then together to reconcile any differences in the information they report. Open-ended questions and time for building rapport may facilitate disclosure from a reticent adolescent. At times, however, one must make the diagnosis by relying more on reports from others who know the child well. Building a trusting therapeutic relationship then becomes part of ongoing treatment.
Standardized measures In addition to the interview, standardized self-report and other-report measures can help:
- The Child Depression Rating Scale-Revised, commonly used in clinical research, can also be used in practice to quantify symptom severity and document treatment response. A score above 40 usually indicates major depression; a score below 28 indicates remission of depression.8-10
- The Beck Depression Inventory (BDI), a 21-item self-report questionnaire for adults, has reasonable reliability and validity for adolescents. Its modest specificity suggests that it may measure general distress and dysphoria, which is not specific to depressive disorders. The language may be too difficult for some younger adolescents and those with poor reading comprehension skills.
- The Children’s Depression Inventory, a version of the BDI for prepubertal children, can be considered for adolescents whose cognitive and/or reading skills are less mature.
- Achenbach’s Child Behavior Checklists and other standardized questionnaires can screen for comorbid psychopathology.
Assessing psychosocial stress, such as conflicts with parents or peers, school problems, or risk-taking behavior, is also important. Depressed youth often have family members with histories of depression, alcoholism, anxiety, and other psychiatric diagnoses. History of sexual abuse has been linked to depression.3 The depressed adolescent’s impaired functioning in school and at home may cause secondary stress, increasing the burden of illness and need for treatment.
Suicide risk Although suicide remains rare among adolescents in general, the rate of suicide among this age group has risen dramatically over the past decade, particularly among younger teens and preteens. In 1997, suicide was the third leading cause of death in adolescents after accidental injuries and homicide.
Adolescents with depressive disorders are at increased risk for suicide, and boys are more likely than girls to attempt and complete suicide. It is therefore imperative to assess and document suicide risk for each adolescent who presents with depressive symptoms.
After establishing a rapport, the most effective screening is a straightforward conversation with the adolescent about suicidal ideation, intent, and behavior. Assess the social context of support and psychopathology in the family, availability and accessibility of lethal suicide methods (e.g., firearms in the home), and presence of events that could influence imitative suicidal behavior (e.g., a friend’s suicide).6
Treatment
Approaches to adolescent depression include (in increasing order of intensity and complexity) watchful monitoring, nonspecific supportive therapy, pharmacotherapy, specific psychotherapy (i.e., cognitive-behavioral or interpersonal therapy), and combined treatment (e.g., psychotherapy plus pharmacotherapy, adolescent psychotherapy plus family therapy).
There are no clear-cut guidelines as to whether pharmacologic or psychosocial therapy should be offered first.11 In the community, patient and family preferences, past treatment response, and the clinician’s background and expertise influence the choice of treatment. As with adults, adolescents deemed at high risk for suicidal behavior must receive immediate attention from mental health professionals and must be monitored, usually in an inpatient setting.
Watchful monitoring means to wait and see if the youth improves spontaneously.
In some studies, nearly one-half (48%) of adolescents with depression were found to go into spontaneous remission within 8 weeks.12 Watchful monitoring, however, would leave most patients still depressed, and no predictors of spontaneous remission have been identified.
Table 2
SSRI DOSAGES FOUND TO BE EFFECTIVE IN ADOLESCENTS WITH MDD
| Drug | Dosage (per day) | Reference |
|---|---|---|
| Fluoxetine | 20 mg | Emslie et al, 1997 and 20018,9 |
| Citalopram | 20-40 mg | Wagner et al, 200110 |
| Paroxetine | 20-40 mg | Keller et al, 200114 |
| Sertraline | 50-200 mg | Donnelly et al, 200115 |
Because of the risks of suicide and social and academic impairment, monitoring alone is acceptable only for a few weeks, and only in cases where depression is mild and uncomplicated. In any case, “monitoring” requires that you periodically reassess the teen and be available for consultation between assessments.
Nonspecific supportive therapy Most psychotherapy provided in the community probably is nonspecific (i.e., not theoretically driven or conducted according to a treatment manual) and supportive (i.e., aimed at providing encouragement). This approach is known to be less effective than specific psychotherapies or antidepressant pharmacotherapy, but we have virtually no data comparing it with lack of treatment.
Nonspecific supportive therapy can be considered a reasonable first-step treatment for depressed teens without complicating risk factors.13 Specific treatment is indicated, however, if the adolescent does not improve in a few weeks.
Pharmacotherapy A few placebo-controlled clinical trials have studied the efficacy of selective serotonin reuptake inhibitors (SSRIs) in outpatient adolescents with major depression. It must be noted that practically all the available data relate to major depression, and no systematic studies have been done in dysthymia and other types of depression in this population.
The SSRIs fluoxetine,8,9 citalopram,10 paroxetine,14 and sertraline15 can decrease symptoms of adolescent depression over 2 to 3 months when given at dosages similar to those used in adults (Table 2). At this time, there are no data that suggest the SSRI dosage must be different in younger (12-year-old) compared with older (18-year-old) adolescents, or in girls compared with boys.
The response rate (adolescents who were substantially improved at end of treatment) ranged from 52 to 65% with SSRI medication and 33 to 48% with a placebo. This means that one would need to treat about six adolescents in order to add one to those who would improve by taking a placebo. Thus, 6 is the number needed to treat (NNT), a common index used to make decisions in evidence-based medicine. As a comparison, the NNT is 1.5 for stimulant treatment of ADHD, indicating that stimulants are more effective in ADHD (i.e., the difference between an active drug and a placebo is greater) than SSRIs are in depression.
It must be noted that receiving a placebo in clinical trials of depression does not equal absence of treatment. Typically, research participants assigned to a placebo have weekly clinical contacts, so placebo treatment could be defined as “nonspecific clinical management.” In any case, the NNT for SSRIs in adolescent depression does not appear to be substantially different from that found in adults.
There is no evidence that tricyclic antidepressants, or TCAs, are more effective than a placebo in adolescents with depression. Considering TCAs’ side effects and potential cardiotoxicity in overdose, their use is not recommended in depressed adolescents. Other antidepressants, such as bupropion and venlafaxine, have been reported to be effective in open studies and clinical observations.
Antidepressants can trigger mania in persons predisposed to bipolar disorder. Before prescribing antidepressant medications, carefully evaluate depressed adolescents for present and past symptoms of mania or hypomania and check family history for possible bipolar disorder. During treatment, monitor the adolescent for signs that suggest emerging mania.
SSRIs and stimulant medications are commonly combined, as depression and ADHD often coexist. Clinical experience indicates that these medications can be safely combined in most cases, although no systematic studies of this combination have been performed in large, representative samples of teens. As with antidepressant monotherapy, adolescent patients must be monitored for signs of mania or hypomania.
Specific psychotherapy Among psychotherapies for depression, the best evidence of efficacy exists for cognitive-behavioral therapy (CBT), which attempts to correct cognitive distortions associated with depression and promotes healthy behaviors. In two clinical studies, CBT was more effective in depressed adolescents than no treatment (i.e., wait list), supportive therapy, or systemic behavior family therapy. About two-thirds of patients treated with CBT achieved remission from depressive symptoms.16,17
Interpersonal therapy (IPT) has been adapted for use in depressed adolescents.18 Its efficacy is supported by one controlled study that found greater improvement after 12 weekly IPT sessions than after once-monthly clinical contact.19 There is no convincing evidence that family therapies are effective in treating depression in adolescents or add much to the benefit of CBT.17
Combined treatment Research on combined treatments for adolescent depression has been limited. One study found that adding family therapy to CBT does not improve the adolescent’s depressive symptoms.8 Although no data are available on the combination of SSRI medication and CBT (or IPT), the National Institute of Mental Health is funding two studies on this important issue:
- The Treatment of Adolescents with Depression Study (TADS) is comparing the efficacy of fluoxetine plus CBT with that of fluoxetine or CBT alone in adolescents with major depression. The study, coordinated by John March, MD, of Duke University Medical Center, is being conducted with 432 teen subjects at 13 clinical sites.
- The Treatment of Resistant Depression in Adolescents (TORDIA) study is comparing the efficacy of antidepressant medication plus CBT to that of antidepressants alone in adolescents who have not improved on initial treatment with an SSRI. TORDIA, coordinated by David Brent, MD, University of Pittsburgh, is being conducted at six clinical sites.
Related resources
- National Institute of Mental Health. Child and Adolescent Mental Health. http://www.nimh.nih.gov/publicat/childmenu.cfm
- Depression in children and adolescents: A fact sheet for physicians. http://www.nimh.nih.gov/publicat/depchildresfact.cfm
- NIMH-funded treatment studies in adolescent depression:
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no affiliation or financial relationship with any of the companies whose products are mentioned in this article. The opinions and assertions contained in this article are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services or the National Institutes of Health.
1. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school. J Abnorm Psychol 1993;102:133-44.
2. Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
3. Jaffee SR, Moffitt TE, Caspi A, et al. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry 2002;58:215-22.
4. Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry 2000;157:1884-1591.
5. Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescents grow up. JAMA 2000;281:1707-13.
6. Pfeffer CR. Diagnosis of childhood and adolescent suicidal behavior: unmet needs for suicide prevention. Biol Psychiatry 2001;49:1055-61.
7. Carlson GA. The challenge of diagnosing depression in childhood and adolescence. J Affect Dis 2000;61(suppl 1):3-8.
8. Emslie GJ, Rush AJ, Weiberg WA, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54:1031-7.
9. Emslie GJ, Heligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents (poster presentation). Honolulu, Hawaii: American Academy of Child and Adolescent Psychiatry annual meeting, October 23-28, 2001.
10. Wagner KD, Robb AS, Findling R, Tiseo PJ. Citalopram is effective in the treatment of major depressive disorder in children and adolescents: results of a placebo-controlled (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
11. American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37:63S-83S.
12. Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry 1999;38:272-9.
13. Harrington R, Whittaker J, Shoebridge P, Campbell F. Systematic review of efficacy of cognitive behavior therapies in childhood and adolescent depressive disorder. BMJ 1998;316:1559-63.
14. Keller MB, Ryan ND, Birmaher B, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
15. Donnelly CL, Winokur A, Wholberg CJ. Efficacy and safety of sertraline in the treatment of pediatric major depressive disorder (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
16. Brent DA, Holder D, Kolko D, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Arch Gen Psychiatry 1997;54:877-85.
17. Harrington R, Whittaker J, Shoebridge P. Psychological treatment of depression in children and adolescents. A review of treatment research. Br J Psychiatry 1998;173:291-8.
18. Mufson L, Moreau D, Weissman MM, Klerman GL. Interpersonal psychotherapy for depressed adolescents. New York: Guilford Press, 1993.
19. Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 1999;56:573-9.
Adolescents with depressive disorders tend to arrive in psychiatrists’ offices when their behavior has already been identified as problematic. Suicide attempts, academic failure, substance abuse, and family conflicts can all lead to teen psychiatric referrals. Other times, subtler changes in behavior may lead a family doctor or pediatrician to suspect depression and to send an adolescent to you for a psychiatric consultation.
The psychiatrist’s task is challenging. Adolescents are usually brought in by their worried parents and may not want to talk to a psychiatrist. Or they may be unable to accurately describe their internal states. Even people who know an adolescent well may not discern the emotions that drive his or her behavior. Adding to the mix are the recurrent nature of major depression in adolescents and the likelihood of complicating comorbid psychiatric conditions (Box).1-6
Based on clinical evidence, we offer advice to help you promptly identify and effectively treat adolescents with depressive disorders. We also provide preliminary information on two studies examining medication treatment, psychotherapy, and combined treatment for teens with major depression.
Adolescent depression disorders
Symptoms of depression in adolescents are similar to those in adults, and it is appropriate for psychiatrists to use DSM-IV diagnostic criteria for making the diagnosis. The three primary depressive disorders for both adults and adolescents are major depressive disorder (MDD), dysthymic disorder, and depressive disorder not otherwise specified (NOS).
Depression is relatively rare among children but becomes common after the onset of puberty. In particular, recurrent depression often starts in adolescence. Here are the statistics:
- Up to 9% of adolescents meet diagnostic criteria for major depressive disorder (MDD), and up to 25% suffer from it by their late teens.
- MDD affects boys and girls equally in childhood, but the prevalence seems to increase in girls after puberty.1,2
- Depression in adolescents is characterized by high rates of comorbid psychiatric conditions. In general, the younger the age of onset, the higher the rate of comorbid conduct disorder, attention-deficit/hyperactivity disorder, and/or anxiety disorder.3
- Adolescent depression tends to persist. An estimated 45 to 70% of children and adolescents with MDD have recurrent episodes.4 At particularly high risk for recurrence are adolescent girls with depression, adolescents with multiple MDD episodes, and adolescents with a family history of recurrent depression.
- As many as 50% of teens with MDD attempt suicide within 15 years of their initial episode, and more than 20% make recurrent attempts.4,5 No good estimates of the rate of completed suicide are available. One 15-year follow-up of a sample of depressed adolescents reported a suicide rate of 7.7%.5 Boys are much more likely to complete suicide than girls across all racial groups.6
Although the symptoms that make up the diagnostic criteria are similar for adults and teens, the behavioral manifestations and response to treatment may differ. The adolescent may present as irritable and angry, rather than overly sad. Impairments in functioning are likely to be related to decline in school performance, social withdrawal, or increased conflicts with peers and family.
As for treatment, certain antidepressant medications of proven efficacy in adults (i.e., tricyclics) do not seem to work for adolescents.
MDD is a time-limited episode of depressive symptoms severe enough to cause functional impairment, such as decline in school performance, social withdrawal, or increased conflicts with peers and family. Symptoms must be present at least 2 weeks.
Dysthymia is a chronic depression that is less severe than MDD and lasts 1 year or longer without sustained remission. It often begins early in childhood and may include periods of increased symptoms consistent with major depression (sometimes called “double depression”).
Depressive disorder NOS is a category of depression that, though clinically significant, does not meet the full criteria for severity, duration, or level of impairment of MDD or dysthymia.
Unless otherwise specified, the terms “depression” and “depressive disorder” in this article are used generically to include all three of these disorders.
Depressive disorders must be differentiated from bipolar disorder, which is characterized by least one prior episode of mania (for bipolar type I) or hypomania (for bipolar type II). The clinical picture of bipolar disorder in youths may differ from that seen in adults. For example, bipolar youth often present with dysphoric mood interspersed with frequent, short periods of intense emotional lability and irritability, rather than “classic” euphoria.
Diagnosis
To diagnose a depressive disorder in an adolescent, information is typically obtained from multiple sources, most commonly the teenage patient and at least one of the parents. Because several sources are involved, however, the information may be conflicting. For instance, the adolescent may contradict a parent’s report that he or she is having difficulties in school or has a substance abuse problem.
Interviewing skills and clinical judgment are required of the clinician in these situations. It is important to:
- obtain a complete description of the adolescent’s behavior and mood over time and as accurate a description as possible of when changes occurred
- assess comorbid conditions (particularly anxiety, attention-deficit/hyperactivity disorder [ADHD], conduct disorder, and substance abuse)
- differentiate between unipolar MDD and bipolar disorder
- evaluate the risk of suicide.
Table 1
DEPRESSION IN ADOLESCENTS AND ADULTS
| Similarities | Differences |
|---|---|
| Same types of diagnostic categories (i.e., major depression, dysthymia, depression NOS) | To diagnose dysthymia, minimum duration of mood disturbance must be 1 year in adolescents (2 years in adults) |
| Same diagnostic symptoms criteria | Mood is often irritable in adolescents (rather than depressed) |
| More common in females | |
| Suicide is more common among males | |
| Evidence of efficacy of SSRI antidepressants | No evidence of efficacy of tricyclic antidepressants in adolescent depression |
Interviewing Standardized diagnostic interviews, such as the Schedule for Affective Disorders and Schizophrenia for children (K-SADS), are commonly used to research adolescent depression but require special training and approximately 1 to 2 hours to administer. As an alternative, clinicians generally develop their own “semi-structured interview” to try to collect all the relevant information required for an accurate diagnosis.7
The interview should be conducted with the adolescent and the parent(s), first separately for ease of disclosure then together to reconcile any differences in the information they report. Open-ended questions and time for building rapport may facilitate disclosure from a reticent adolescent. At times, however, one must make the diagnosis by relying more on reports from others who know the child well. Building a trusting therapeutic relationship then becomes part of ongoing treatment.
Standardized measures In addition to the interview, standardized self-report and other-report measures can help:
- The Child Depression Rating Scale-Revised, commonly used in clinical research, can also be used in practice to quantify symptom severity and document treatment response. A score above 40 usually indicates major depression; a score below 28 indicates remission of depression.8-10
- The Beck Depression Inventory (BDI), a 21-item self-report questionnaire for adults, has reasonable reliability and validity for adolescents. Its modest specificity suggests that it may measure general distress and dysphoria, which is not specific to depressive disorders. The language may be too difficult for some younger adolescents and those with poor reading comprehension skills.
- The Children’s Depression Inventory, a version of the BDI for prepubertal children, can be considered for adolescents whose cognitive and/or reading skills are less mature.
- Achenbach’s Child Behavior Checklists and other standardized questionnaires can screen for comorbid psychopathology.
Assessing psychosocial stress, such as conflicts with parents or peers, school problems, or risk-taking behavior, is also important. Depressed youth often have family members with histories of depression, alcoholism, anxiety, and other psychiatric diagnoses. History of sexual abuse has been linked to depression.3 The depressed adolescent’s impaired functioning in school and at home may cause secondary stress, increasing the burden of illness and need for treatment.
Suicide risk Although suicide remains rare among adolescents in general, the rate of suicide among this age group has risen dramatically over the past decade, particularly among younger teens and preteens. In 1997, suicide was the third leading cause of death in adolescents after accidental injuries and homicide.
Adolescents with depressive disorders are at increased risk for suicide, and boys are more likely than girls to attempt and complete suicide. It is therefore imperative to assess and document suicide risk for each adolescent who presents with depressive symptoms.
After establishing a rapport, the most effective screening is a straightforward conversation with the adolescent about suicidal ideation, intent, and behavior. Assess the social context of support and psychopathology in the family, availability and accessibility of lethal suicide methods (e.g., firearms in the home), and presence of events that could influence imitative suicidal behavior (e.g., a friend’s suicide).6
Treatment
Approaches to adolescent depression include (in increasing order of intensity and complexity) watchful monitoring, nonspecific supportive therapy, pharmacotherapy, specific psychotherapy (i.e., cognitive-behavioral or interpersonal therapy), and combined treatment (e.g., psychotherapy plus pharmacotherapy, adolescent psychotherapy plus family therapy).
There are no clear-cut guidelines as to whether pharmacologic or psychosocial therapy should be offered first.11 In the community, patient and family preferences, past treatment response, and the clinician’s background and expertise influence the choice of treatment. As with adults, adolescents deemed at high risk for suicidal behavior must receive immediate attention from mental health professionals and must be monitored, usually in an inpatient setting.
Watchful monitoring means to wait and see if the youth improves spontaneously.
In some studies, nearly one-half (48%) of adolescents with depression were found to go into spontaneous remission within 8 weeks.12 Watchful monitoring, however, would leave most patients still depressed, and no predictors of spontaneous remission have been identified.
Table 2
SSRI DOSAGES FOUND TO BE EFFECTIVE IN ADOLESCENTS WITH MDD
| Drug | Dosage (per day) | Reference |
|---|---|---|
| Fluoxetine | 20 mg | Emslie et al, 1997 and 20018,9 |
| Citalopram | 20-40 mg | Wagner et al, 200110 |
| Paroxetine | 20-40 mg | Keller et al, 200114 |
| Sertraline | 50-200 mg | Donnelly et al, 200115 |
Because of the risks of suicide and social and academic impairment, monitoring alone is acceptable only for a few weeks, and only in cases where depression is mild and uncomplicated. In any case, “monitoring” requires that you periodically reassess the teen and be available for consultation between assessments.
Nonspecific supportive therapy Most psychotherapy provided in the community probably is nonspecific (i.e., not theoretically driven or conducted according to a treatment manual) and supportive (i.e., aimed at providing encouragement). This approach is known to be less effective than specific psychotherapies or antidepressant pharmacotherapy, but we have virtually no data comparing it with lack of treatment.
Nonspecific supportive therapy can be considered a reasonable first-step treatment for depressed teens without complicating risk factors.13 Specific treatment is indicated, however, if the adolescent does not improve in a few weeks.
Pharmacotherapy A few placebo-controlled clinical trials have studied the efficacy of selective serotonin reuptake inhibitors (SSRIs) in outpatient adolescents with major depression. It must be noted that practically all the available data relate to major depression, and no systematic studies have been done in dysthymia and other types of depression in this population.
The SSRIs fluoxetine,8,9 citalopram,10 paroxetine,14 and sertraline15 can decrease symptoms of adolescent depression over 2 to 3 months when given at dosages similar to those used in adults (Table 2). At this time, there are no data that suggest the SSRI dosage must be different in younger (12-year-old) compared with older (18-year-old) adolescents, or in girls compared with boys.
The response rate (adolescents who were substantially improved at end of treatment) ranged from 52 to 65% with SSRI medication and 33 to 48% with a placebo. This means that one would need to treat about six adolescents in order to add one to those who would improve by taking a placebo. Thus, 6 is the number needed to treat (NNT), a common index used to make decisions in evidence-based medicine. As a comparison, the NNT is 1.5 for stimulant treatment of ADHD, indicating that stimulants are more effective in ADHD (i.e., the difference between an active drug and a placebo is greater) than SSRIs are in depression.
It must be noted that receiving a placebo in clinical trials of depression does not equal absence of treatment. Typically, research participants assigned to a placebo have weekly clinical contacts, so placebo treatment could be defined as “nonspecific clinical management.” In any case, the NNT for SSRIs in adolescent depression does not appear to be substantially different from that found in adults.
There is no evidence that tricyclic antidepressants, or TCAs, are more effective than a placebo in adolescents with depression. Considering TCAs’ side effects and potential cardiotoxicity in overdose, their use is not recommended in depressed adolescents. Other antidepressants, such as bupropion and venlafaxine, have been reported to be effective in open studies and clinical observations.
Antidepressants can trigger mania in persons predisposed to bipolar disorder. Before prescribing antidepressant medications, carefully evaluate depressed adolescents for present and past symptoms of mania or hypomania and check family history for possible bipolar disorder. During treatment, monitor the adolescent for signs that suggest emerging mania.
SSRIs and stimulant medications are commonly combined, as depression and ADHD often coexist. Clinical experience indicates that these medications can be safely combined in most cases, although no systematic studies of this combination have been performed in large, representative samples of teens. As with antidepressant monotherapy, adolescent patients must be monitored for signs of mania or hypomania.
Specific psychotherapy Among psychotherapies for depression, the best evidence of efficacy exists for cognitive-behavioral therapy (CBT), which attempts to correct cognitive distortions associated with depression and promotes healthy behaviors. In two clinical studies, CBT was more effective in depressed adolescents than no treatment (i.e., wait list), supportive therapy, or systemic behavior family therapy. About two-thirds of patients treated with CBT achieved remission from depressive symptoms.16,17
Interpersonal therapy (IPT) has been adapted for use in depressed adolescents.18 Its efficacy is supported by one controlled study that found greater improvement after 12 weekly IPT sessions than after once-monthly clinical contact.19 There is no convincing evidence that family therapies are effective in treating depression in adolescents or add much to the benefit of CBT.17
Combined treatment Research on combined treatments for adolescent depression has been limited. One study found that adding family therapy to CBT does not improve the adolescent’s depressive symptoms.8 Although no data are available on the combination of SSRI medication and CBT (or IPT), the National Institute of Mental Health is funding two studies on this important issue:
- The Treatment of Adolescents with Depression Study (TADS) is comparing the efficacy of fluoxetine plus CBT with that of fluoxetine or CBT alone in adolescents with major depression. The study, coordinated by John March, MD, of Duke University Medical Center, is being conducted with 432 teen subjects at 13 clinical sites.
- The Treatment of Resistant Depression in Adolescents (TORDIA) study is comparing the efficacy of antidepressant medication plus CBT to that of antidepressants alone in adolescents who have not improved on initial treatment with an SSRI. TORDIA, coordinated by David Brent, MD, University of Pittsburgh, is being conducted at six clinical sites.
Related resources
- National Institute of Mental Health. Child and Adolescent Mental Health. http://www.nimh.nih.gov/publicat/childmenu.cfm
- Depression in children and adolescents: A fact sheet for physicians. http://www.nimh.nih.gov/publicat/depchildresfact.cfm
- NIMH-funded treatment studies in adolescent depression:
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no affiliation or financial relationship with any of the companies whose products are mentioned in this article. The opinions and assertions contained in this article are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services or the National Institutes of Health.
Adolescents with depressive disorders tend to arrive in psychiatrists’ offices when their behavior has already been identified as problematic. Suicide attempts, academic failure, substance abuse, and family conflicts can all lead to teen psychiatric referrals. Other times, subtler changes in behavior may lead a family doctor or pediatrician to suspect depression and to send an adolescent to you for a psychiatric consultation.
The psychiatrist’s task is challenging. Adolescents are usually brought in by their worried parents and may not want to talk to a psychiatrist. Or they may be unable to accurately describe their internal states. Even people who know an adolescent well may not discern the emotions that drive his or her behavior. Adding to the mix are the recurrent nature of major depression in adolescents and the likelihood of complicating comorbid psychiatric conditions (Box).1-6
Based on clinical evidence, we offer advice to help you promptly identify and effectively treat adolescents with depressive disorders. We also provide preliminary information on two studies examining medication treatment, psychotherapy, and combined treatment for teens with major depression.
Adolescent depression disorders
Symptoms of depression in adolescents are similar to those in adults, and it is appropriate for psychiatrists to use DSM-IV diagnostic criteria for making the diagnosis. The three primary depressive disorders for both adults and adolescents are major depressive disorder (MDD), dysthymic disorder, and depressive disorder not otherwise specified (NOS).
Depression is relatively rare among children but becomes common after the onset of puberty. In particular, recurrent depression often starts in adolescence. Here are the statistics:
- Up to 9% of adolescents meet diagnostic criteria for major depressive disorder (MDD), and up to 25% suffer from it by their late teens.
- MDD affects boys and girls equally in childhood, but the prevalence seems to increase in girls after puberty.1,2
- Depression in adolescents is characterized by high rates of comorbid psychiatric conditions. In general, the younger the age of onset, the higher the rate of comorbid conduct disorder, attention-deficit/hyperactivity disorder, and/or anxiety disorder.3
- Adolescent depression tends to persist. An estimated 45 to 70% of children and adolescents with MDD have recurrent episodes.4 At particularly high risk for recurrence are adolescent girls with depression, adolescents with multiple MDD episodes, and adolescents with a family history of recurrent depression.
- As many as 50% of teens with MDD attempt suicide within 15 years of their initial episode, and more than 20% make recurrent attempts.4,5 No good estimates of the rate of completed suicide are available. One 15-year follow-up of a sample of depressed adolescents reported a suicide rate of 7.7%.5 Boys are much more likely to complete suicide than girls across all racial groups.6
Although the symptoms that make up the diagnostic criteria are similar for adults and teens, the behavioral manifestations and response to treatment may differ. The adolescent may present as irritable and angry, rather than overly sad. Impairments in functioning are likely to be related to decline in school performance, social withdrawal, or increased conflicts with peers and family.
As for treatment, certain antidepressant medications of proven efficacy in adults (i.e., tricyclics) do not seem to work for adolescents.
MDD is a time-limited episode of depressive symptoms severe enough to cause functional impairment, such as decline in school performance, social withdrawal, or increased conflicts with peers and family. Symptoms must be present at least 2 weeks.
Dysthymia is a chronic depression that is less severe than MDD and lasts 1 year or longer without sustained remission. It often begins early in childhood and may include periods of increased symptoms consistent with major depression (sometimes called “double depression”).
Depressive disorder NOS is a category of depression that, though clinically significant, does not meet the full criteria for severity, duration, or level of impairment of MDD or dysthymia.
Unless otherwise specified, the terms “depression” and “depressive disorder” in this article are used generically to include all three of these disorders.
Depressive disorders must be differentiated from bipolar disorder, which is characterized by least one prior episode of mania (for bipolar type I) or hypomania (for bipolar type II). The clinical picture of bipolar disorder in youths may differ from that seen in adults. For example, bipolar youth often present with dysphoric mood interspersed with frequent, short periods of intense emotional lability and irritability, rather than “classic” euphoria.
Diagnosis
To diagnose a depressive disorder in an adolescent, information is typically obtained from multiple sources, most commonly the teenage patient and at least one of the parents. Because several sources are involved, however, the information may be conflicting. For instance, the adolescent may contradict a parent’s report that he or she is having difficulties in school or has a substance abuse problem.
Interviewing skills and clinical judgment are required of the clinician in these situations. It is important to:
- obtain a complete description of the adolescent’s behavior and mood over time and as accurate a description as possible of when changes occurred
- assess comorbid conditions (particularly anxiety, attention-deficit/hyperactivity disorder [ADHD], conduct disorder, and substance abuse)
- differentiate between unipolar MDD and bipolar disorder
- evaluate the risk of suicide.
Table 1
DEPRESSION IN ADOLESCENTS AND ADULTS
| Similarities | Differences |
|---|---|
| Same types of diagnostic categories (i.e., major depression, dysthymia, depression NOS) | To diagnose dysthymia, minimum duration of mood disturbance must be 1 year in adolescents (2 years in adults) |
| Same diagnostic symptoms criteria | Mood is often irritable in adolescents (rather than depressed) |
| More common in females | |
| Suicide is more common among males | |
| Evidence of efficacy of SSRI antidepressants | No evidence of efficacy of tricyclic antidepressants in adolescent depression |
Interviewing Standardized diagnostic interviews, such as the Schedule for Affective Disorders and Schizophrenia for children (K-SADS), are commonly used to research adolescent depression but require special training and approximately 1 to 2 hours to administer. As an alternative, clinicians generally develop their own “semi-structured interview” to try to collect all the relevant information required for an accurate diagnosis.7
The interview should be conducted with the adolescent and the parent(s), first separately for ease of disclosure then together to reconcile any differences in the information they report. Open-ended questions and time for building rapport may facilitate disclosure from a reticent adolescent. At times, however, one must make the diagnosis by relying more on reports from others who know the child well. Building a trusting therapeutic relationship then becomes part of ongoing treatment.
Standardized measures In addition to the interview, standardized self-report and other-report measures can help:
- The Child Depression Rating Scale-Revised, commonly used in clinical research, can also be used in practice to quantify symptom severity and document treatment response. A score above 40 usually indicates major depression; a score below 28 indicates remission of depression.8-10
- The Beck Depression Inventory (BDI), a 21-item self-report questionnaire for adults, has reasonable reliability and validity for adolescents. Its modest specificity suggests that it may measure general distress and dysphoria, which is not specific to depressive disorders. The language may be too difficult for some younger adolescents and those with poor reading comprehension skills.
- The Children’s Depression Inventory, a version of the BDI for prepubertal children, can be considered for adolescents whose cognitive and/or reading skills are less mature.
- Achenbach’s Child Behavior Checklists and other standardized questionnaires can screen for comorbid psychopathology.
Assessing psychosocial stress, such as conflicts with parents or peers, school problems, or risk-taking behavior, is also important. Depressed youth often have family members with histories of depression, alcoholism, anxiety, and other psychiatric diagnoses. History of sexual abuse has been linked to depression.3 The depressed adolescent’s impaired functioning in school and at home may cause secondary stress, increasing the burden of illness and need for treatment.
Suicide risk Although suicide remains rare among adolescents in general, the rate of suicide among this age group has risen dramatically over the past decade, particularly among younger teens and preteens. In 1997, suicide was the third leading cause of death in adolescents after accidental injuries and homicide.
Adolescents with depressive disorders are at increased risk for suicide, and boys are more likely than girls to attempt and complete suicide. It is therefore imperative to assess and document suicide risk for each adolescent who presents with depressive symptoms.
After establishing a rapport, the most effective screening is a straightforward conversation with the adolescent about suicidal ideation, intent, and behavior. Assess the social context of support and psychopathology in the family, availability and accessibility of lethal suicide methods (e.g., firearms in the home), and presence of events that could influence imitative suicidal behavior (e.g., a friend’s suicide).6
Treatment
Approaches to adolescent depression include (in increasing order of intensity and complexity) watchful monitoring, nonspecific supportive therapy, pharmacotherapy, specific psychotherapy (i.e., cognitive-behavioral or interpersonal therapy), and combined treatment (e.g., psychotherapy plus pharmacotherapy, adolescent psychotherapy plus family therapy).
There are no clear-cut guidelines as to whether pharmacologic or psychosocial therapy should be offered first.11 In the community, patient and family preferences, past treatment response, and the clinician’s background and expertise influence the choice of treatment. As with adults, adolescents deemed at high risk for suicidal behavior must receive immediate attention from mental health professionals and must be monitored, usually in an inpatient setting.
Watchful monitoring means to wait and see if the youth improves spontaneously.
In some studies, nearly one-half (48%) of adolescents with depression were found to go into spontaneous remission within 8 weeks.12 Watchful monitoring, however, would leave most patients still depressed, and no predictors of spontaneous remission have been identified.
Table 2
SSRI DOSAGES FOUND TO BE EFFECTIVE IN ADOLESCENTS WITH MDD
| Drug | Dosage (per day) | Reference |
|---|---|---|
| Fluoxetine | 20 mg | Emslie et al, 1997 and 20018,9 |
| Citalopram | 20-40 mg | Wagner et al, 200110 |
| Paroxetine | 20-40 mg | Keller et al, 200114 |
| Sertraline | 50-200 mg | Donnelly et al, 200115 |
Because of the risks of suicide and social and academic impairment, monitoring alone is acceptable only for a few weeks, and only in cases where depression is mild and uncomplicated. In any case, “monitoring” requires that you periodically reassess the teen and be available for consultation between assessments.
Nonspecific supportive therapy Most psychotherapy provided in the community probably is nonspecific (i.e., not theoretically driven or conducted according to a treatment manual) and supportive (i.e., aimed at providing encouragement). This approach is known to be less effective than specific psychotherapies or antidepressant pharmacotherapy, but we have virtually no data comparing it with lack of treatment.
Nonspecific supportive therapy can be considered a reasonable first-step treatment for depressed teens without complicating risk factors.13 Specific treatment is indicated, however, if the adolescent does not improve in a few weeks.
Pharmacotherapy A few placebo-controlled clinical trials have studied the efficacy of selective serotonin reuptake inhibitors (SSRIs) in outpatient adolescents with major depression. It must be noted that practically all the available data relate to major depression, and no systematic studies have been done in dysthymia and other types of depression in this population.
The SSRIs fluoxetine,8,9 citalopram,10 paroxetine,14 and sertraline15 can decrease symptoms of adolescent depression over 2 to 3 months when given at dosages similar to those used in adults (Table 2). At this time, there are no data that suggest the SSRI dosage must be different in younger (12-year-old) compared with older (18-year-old) adolescents, or in girls compared with boys.
The response rate (adolescents who were substantially improved at end of treatment) ranged from 52 to 65% with SSRI medication and 33 to 48% with a placebo. This means that one would need to treat about six adolescents in order to add one to those who would improve by taking a placebo. Thus, 6 is the number needed to treat (NNT), a common index used to make decisions in evidence-based medicine. As a comparison, the NNT is 1.5 for stimulant treatment of ADHD, indicating that stimulants are more effective in ADHD (i.e., the difference between an active drug and a placebo is greater) than SSRIs are in depression.
It must be noted that receiving a placebo in clinical trials of depression does not equal absence of treatment. Typically, research participants assigned to a placebo have weekly clinical contacts, so placebo treatment could be defined as “nonspecific clinical management.” In any case, the NNT for SSRIs in adolescent depression does not appear to be substantially different from that found in adults.
There is no evidence that tricyclic antidepressants, or TCAs, are more effective than a placebo in adolescents with depression. Considering TCAs’ side effects and potential cardiotoxicity in overdose, their use is not recommended in depressed adolescents. Other antidepressants, such as bupropion and venlafaxine, have been reported to be effective in open studies and clinical observations.
Antidepressants can trigger mania in persons predisposed to bipolar disorder. Before prescribing antidepressant medications, carefully evaluate depressed adolescents for present and past symptoms of mania or hypomania and check family history for possible bipolar disorder. During treatment, monitor the adolescent for signs that suggest emerging mania.
SSRIs and stimulant medications are commonly combined, as depression and ADHD often coexist. Clinical experience indicates that these medications can be safely combined in most cases, although no systematic studies of this combination have been performed in large, representative samples of teens. As with antidepressant monotherapy, adolescent patients must be monitored for signs of mania or hypomania.
Specific psychotherapy Among psychotherapies for depression, the best evidence of efficacy exists for cognitive-behavioral therapy (CBT), which attempts to correct cognitive distortions associated with depression and promotes healthy behaviors. In two clinical studies, CBT was more effective in depressed adolescents than no treatment (i.e., wait list), supportive therapy, or systemic behavior family therapy. About two-thirds of patients treated with CBT achieved remission from depressive symptoms.16,17
Interpersonal therapy (IPT) has been adapted for use in depressed adolescents.18 Its efficacy is supported by one controlled study that found greater improvement after 12 weekly IPT sessions than after once-monthly clinical contact.19 There is no convincing evidence that family therapies are effective in treating depression in adolescents or add much to the benefit of CBT.17
Combined treatment Research on combined treatments for adolescent depression has been limited. One study found that adding family therapy to CBT does not improve the adolescent’s depressive symptoms.8 Although no data are available on the combination of SSRI medication and CBT (or IPT), the National Institute of Mental Health is funding two studies on this important issue:
- The Treatment of Adolescents with Depression Study (TADS) is comparing the efficacy of fluoxetine plus CBT with that of fluoxetine or CBT alone in adolescents with major depression. The study, coordinated by John March, MD, of Duke University Medical Center, is being conducted with 432 teen subjects at 13 clinical sites.
- The Treatment of Resistant Depression in Adolescents (TORDIA) study is comparing the efficacy of antidepressant medication plus CBT to that of antidepressants alone in adolescents who have not improved on initial treatment with an SSRI. TORDIA, coordinated by David Brent, MD, University of Pittsburgh, is being conducted at six clinical sites.
Related resources
- National Institute of Mental Health. Child and Adolescent Mental Health. http://www.nimh.nih.gov/publicat/childmenu.cfm
- Depression in children and adolescents: A fact sheet for physicians. http://www.nimh.nih.gov/publicat/depchildresfact.cfm
- NIMH-funded treatment studies in adolescent depression:
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no affiliation or financial relationship with any of the companies whose products are mentioned in this article. The opinions and assertions contained in this article are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services or the National Institutes of Health.
1. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school. J Abnorm Psychol 1993;102:133-44.
2. Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
3. Jaffee SR, Moffitt TE, Caspi A, et al. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry 2002;58:215-22.
4. Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry 2000;157:1884-1591.
5. Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescents grow up. JAMA 2000;281:1707-13.
6. Pfeffer CR. Diagnosis of childhood and adolescent suicidal behavior: unmet needs for suicide prevention. Biol Psychiatry 2001;49:1055-61.
7. Carlson GA. The challenge of diagnosing depression in childhood and adolescence. J Affect Dis 2000;61(suppl 1):3-8.
8. Emslie GJ, Rush AJ, Weiberg WA, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54:1031-7.
9. Emslie GJ, Heligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents (poster presentation). Honolulu, Hawaii: American Academy of Child and Adolescent Psychiatry annual meeting, October 23-28, 2001.
10. Wagner KD, Robb AS, Findling R, Tiseo PJ. Citalopram is effective in the treatment of major depressive disorder in children and adolescents: results of a placebo-controlled (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
11. American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37:63S-83S.
12. Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry 1999;38:272-9.
13. Harrington R, Whittaker J, Shoebridge P, Campbell F. Systematic review of efficacy of cognitive behavior therapies in childhood and adolescent depressive disorder. BMJ 1998;316:1559-63.
14. Keller MB, Ryan ND, Birmaher B, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
15. Donnelly CL, Winokur A, Wholberg CJ. Efficacy and safety of sertraline in the treatment of pediatric major depressive disorder (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
16. Brent DA, Holder D, Kolko D, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Arch Gen Psychiatry 1997;54:877-85.
17. Harrington R, Whittaker J, Shoebridge P. Psychological treatment of depression in children and adolescents. A review of treatment research. Br J Psychiatry 1998;173:291-8.
18. Mufson L, Moreau D, Weissman MM, Klerman GL. Interpersonal psychotherapy for depressed adolescents. New York: Guilford Press, 1993.
19. Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 1999;56:573-9.
1. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school. J Abnorm Psychol 1993;102:133-44.
2. Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiological perspective. Biol Psychiatry 2001;49:1002-14.
3. Jaffee SR, Moffitt TE, Caspi A, et al. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry 2002;58:215-22.
4. Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry 2000;157:1884-1591.
5. Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescents grow up. JAMA 2000;281:1707-13.
6. Pfeffer CR. Diagnosis of childhood and adolescent suicidal behavior: unmet needs for suicide prevention. Biol Psychiatry 2001;49:1055-61.
7. Carlson GA. The challenge of diagnosing depression in childhood and adolescence. J Affect Dis 2000;61(suppl 1):3-8.
8. Emslie GJ, Rush AJ, Weiberg WA, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997;54:1031-7.
9. Emslie GJ, Heligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents (poster presentation). Honolulu, Hawaii: American Academy of Child and Adolescent Psychiatry annual meeting, October 23-28, 2001.
10. Wagner KD, Robb AS, Findling R, Tiseo PJ. Citalopram is effective in the treatment of major depressive disorder in children and adolescents: results of a placebo-controlled (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
11. American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37:63S-83S.
12. Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry 1999;38:272-9.
13. Harrington R, Whittaker J, Shoebridge P, Campbell F. Systematic review of efficacy of cognitive behavior therapies in childhood and adolescent depressive disorder. BMJ 1998;316:1559-63.
14. Keller MB, Ryan ND, Birmaher B, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2001;40:762-72.
15. Donnelly CL, Winokur A, Wholberg CJ. Efficacy and safety of sertraline in the treatment of pediatric major depressive disorder (poster presentation). Waikoloa, Hawaii: American College of Neuropsychopharmacology annual meeting, December 9-13, 2001.
16. Brent DA, Holder D, Kolko D, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Arch Gen Psychiatry 1997;54:877-85.
17. Harrington R, Whittaker J, Shoebridge P. Psychological treatment of depression in children and adolescents. A review of treatment research. Br J Psychiatry 1998;173:291-8.
18. Mufson L, Moreau D, Weissman MM, Klerman GL. Interpersonal psychotherapy for depressed adolescents. New York: Guilford Press, 1993.
19. Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 1999;56:573-9.
Tricyclics: Still solid performers for the savvy psychiatrist
Recent practice guidelines generally do not position tricyclic antidepressants (TCAs) as first-line therapies because of concerns about side effects and safety issues.1-3 Yet these agents have important clinical uses—both for approved and off-label indications—and diverse pharmacologic properties that distinguish them from each other as well as from many of the “newer antidepressants.”
Eleven TCAs are available in the United States (Table 1). Here’s what the evidence says about when and how to use them to treat a variety of psychiatric disorders, along with our recommendations on how to reduce the risk of side effects.
Indications and off-label uses
TCAs’ pharmacologic properties make them very versatile (Box 1).4 Major depression and anxiety disorders (such as obsessive compulsive disorder [OCD]) are the principal FDA-approved indications for TCAs. Other approved indications are anxiety (doxepin) and childhood enuresis (imipramine). Common off-label uses supported by scientific literature include panic disorder, social phobia, insomnia, posttraumatic stress disorder (PTSD), generalized anxiety disorder (GAD), attention-deficit/hyperactivity disorder (ADHD), migraine headache, chronic pain syndromes, premature ejaculation, substance abuse disorders, and eating disorders, to name a few.
Major depression To treat major depressive disorder, the American Psychiatric Association recommends selective serotonin reuptake inhibitors (SSRIs), bupropion, venlafaxine, and the secondary amine TCAs desipramine and nortriptyline as “optimal” first-line therapy for most patients.1 The Texas Medication Algorithm Project recommends SSRIs, bupropion, nefazodone, venlafaxine, or mirtazapine as first-line therapy and lists TCAs as second- or third-line therapy for patients with partial or no response to initial therapy.2
Table 1
THERAPEUTIC DOSAGE RANGE
| Generic name | Brand names | Therapeutic dosage range (mg/d) |
|---|---|---|
| Amitriptyline | Elavil, Endep | 150-300 |
| Amoxapine | Asendin | 150-450 |
| Clomipramine | Anafranil | 100-250 |
| Desipramine | Norpramin, Pertofane | 150-300 |
| Doxepin | Sinequan Adapin | 150-300 |
| Imipramine | Tofranil, Tofranil PM Janimine, Sk-Pramine | 150-300 |
| Maprotiline | Ludiomil | 150-200 |
| Nortriptyline | Pamelor Aventyl | 50-150 |
| Protriptyline | Vivactil | 15-60 |
| Trimipramine | Surmontil | 150-300 |
| Trazodone | Desyrel | 50-600 |
| * Dosage ranges are approximate. Dosage needs to be tailored by individual patient needs. The elderly, children, and the medically compromised may require lower dosages. | ||
The tricyclic antidepresants are a broad class of drugs that can be divided, based on the number of rings in their nucleus, into tricyclics and tetracyclics. The tricyclics can be further classified into tertiary and secondary amines, based on the number of methyl groups on the side chain. In addition, some clinicians include trazodone—an antidepressant chemically unrelated to tricyclic, tetracyclic, or other known antidepressant agents—in the broad class of TCAs.
TCAs were initially hypothesized to block the reuptake of norepinephrine (NE) or serotonin (5HT), thereby increasing the levels of these neurotransmitters at the postsynaptic receptor. More recent theories include effects on pre- and postsynaptic receptors and other neurotransmitters, such as histamine and acetylcholine, which explain the various side effects of TCAs.
The relative norepinephrine-reuptake-blocking effects versus serotonin-reuptake-blocking effects of the TCAs and each drug’s biochemical effects are summarized in Table 2. Except for clomipramine, TCAs are relatively weak 5HT reuptake blockers.
Although recommended as first-line therapies, SSRIs and other newer antidepressants exhibit no greater efficacy than TCAs in treating major depression.5,6 Three major meta-analyses7-9 reported no significant difference in efficacy between the two antidepressant classes. In the largest,9 published by the U.S. Department of Health and Human Services, 50% of inpatients and 52% of outpatients responded to TCAs, whereas 54% of inpatients and 47% of outpatients responded to SSRIs. Compared with SSRIs, TCAs also may be associated with higher rates of remission.7,8
Clomipramine—approved for OCD—has been used for decades to treat depression and resistant depression. Two meta-analyses by the Danish University Antidepressant Group7,8 showed that clomipramine produced a “significantly better therapeutic effect” compared with citalopram and paroxetine. In three major studies,5,7,8 TCAs showed greater effectiveness than SSRIs in treating melancholic depression.
The anticholinergic side effects of TCAs have been perceived to cause higher patient dropout and discontinuation rates, but studies have shown mixed results. In one meta-analysis comparing SSRIs and TCAs, the difference in dropout rates due to adverse effects was less significant than previously reported. When total dropout rates for any reason were examined, the difference was less than was originally expected.10
OCD In clinical practice, most patients with OCD are started on an SSRI. Clomipramine is another valuable option, however, especially for patients who fail one or more therapeutic trials with SSRIs. Clomipramine may produce significant therapeutic benefit in patients with OCD, possibly because of its potent 5-HT reuptake properties. In one study, patients with OCD symptoms who received clomipramine improved more than those receiving SSRIs when each class was compared with placebo.11
Panic disorder Although not approved for panic disorder, imipramine and desipramine provide effective treatment, even in nondepressed patients.12 Doses and plasma levels are the same as those used for treating depression. Start low (e.g., imipramine, 10 to 20 mg/d; desipramine, 10 to 25 mg/d) and increase gradually over several weeks to typical therapeutic dosages (Table 1). Do not escalate too rapidly, as this may increase anxiety or precipitate a panic attack. Uses in children TCAs have been used to treat children with ADHD, OCD, enuresis, and depression. The American Academy of Child and Adolescent Psychiatry (AACAP) does not recommend TCAs as first-line treatment for youths requiring pharmacotherapy for depressive disorders but acknowledges that some youths with depression may respond better to TCAs than to other medications.3
Imipramine is the only TCA indicated for nocturnal enuresis, but its exact mechanism of action is not known. The benefit may be secondary to imipramine’s anticholinergic effect or to changes in sleep architecture. Recommended bedtime doses for children with enuresis are:
- 25 to 50 mg under age 12;
- up to 75 mg age 12 and older.
TCAs are an option for children with ADHD, especially if ADHD is present with comorbid depression or anxiety disorder. However, because at least four cases of sudden cardiac death have been reported in children taking desipramine, it is prudent to monitor cardiac function when children are started on TCAs. AACAP guidelines recommend obtaining a baseline ECG, resting blood pressure, and pulse (supine or sitting, then standing), with regular monitoring of the child’s weight during TCA therapy.
Combination therapy Few controlled studies have tested TCAs as combination therapy. Trazodone can be used as an adjunct to SSRIs and monoamine oxidase inhibitors (MAOIs) for patients with insomnia. TCAs are used as an adjunct to treat resistant depression and OCD13,14 (e.g., clomipramine added to fluvoxamine to treat OCD).15 Serum level monitoring is recommended when TCAs are used as adjuncts.
Other uses TCAs play a role in the prophylactic treatment of premature ejaculation and migraine headaches, probably because of their serotonergic (5HT2) effect. In patients with migraine and depression, a trial of a TCA such as amitriptyline may be warranted.
TCAs are widely used to manage neuropathic pain,16 although the exact mechanism of action is unknown. Because depression is commonly associated with pain, the effect may result from the agents’ action on depression, or TCAs may possess direct analgesic action.
Trazodone, 25 to 100 mg at bedtime, is widely used for insomnia, alone or as an adjunct with other classes of antidepressants—even in combination with MAOIs. Nortriptyline has been shown to be safe and effective for post-stroke and geriatric types of depression.17
TCAs are also used for a host of other medical, psychiatric, and neurologic problems, such as social phobia, PTSD, GAD, substance abuse disorders, and eating disorders.18 Only a few controlled studies have tested TCAs for these indications.
Side effects
Although TCAs have shown efficacy in many clinical situations, their use is associated with potentially serious side effects, which may include anticholinergic effects, sedation, weight gain, CNS toxicity, orthostatic hypotension, cardiovascular toxicity, delirium, and risk of suicide by overdose. The risk of side effects can be reduced with careful prescribing practices (Box 2).
Anticholinergic effects, sedation TCAs vary in their anticholinergic activity (Table 2). Tertiary amine TCAs such as amitriptyline and protriptyline may cause dry mouth, constipation, urinary hesitancy, and blurred vision in some patients, and confusion in elderly or demented patients. Secondary amine TCAs such as nortriptyline or desipramine are less anticholinergic and less likely to cause these side effects.
Peripheral anticholinergic side effects can be managed with bethanacol—a cholinergic drug—in dosages of 25 to 50 mg tid or qid. Dry mouth can be treated with pilocarpine, 5 mg bid to qid, or oral bethanacol (5- to 10-mg tablets sublingually), artificial saliva drops, sugarless candy/gum, or mouthwash.
- Obtain a baseline ECG for patients of all ages before starting TCA therapy.
- When dosing TCAs, start low and go slow to maximize efficacy and minimize side effects, especially in the elderly patient.
- In the elderly, avoid highly anticholinergic TCAs such as amitriptyline or protriptyline, which can cause delirium. Choose a TCA with low anticholinergic properties, such as desipramine or nortriptyline.
- For patients who are intolerant of the anticholinergic and sedative properties of amitriptyline or protriptyline, consider switching to desipramine or nortriptyline.
- If a patient develops a toxic effect mediated by either the cardiovascular or central nervous system, discontinue the TCA or reduce the dosage.
- In patients at risk for suicide by overdose, consider dispensing less than a 2-week supply. In case of overdose, cardiac monitoring for at least 24 hours may be indicated.
Table 2
BIOCHEMICAL EFFECTS OF TRICYCLICS AND OTHER ANTIDEPRESSANTS
| POTENCY | SIDE EFFECTS | |||||
|---|---|---|---|---|---|---|
| NE reuptake blockade | 5HT reuptake blockade | DA reuptake blockade | 5HT blockade | Muscorinic blockade | Histamine blockade | |
| TCAs | ||||||
| Tertiary amines | ||||||
| Amitriptyline | ♦♦ | ♦♦ | ○ | ♦ | ♦♦♦ | ♦♦ |
| Imipramine | ♦♦♦ | ♦♦♦ | ○ | ○ | ♦♦ | ♦ |
| Doxepin | ♦♦ | ♦♦ | ○ | ♦ | ♦♦ | ♦♦♦ |
| Clomipramine | ♦♦x | ♦♦♦ | ○ | ♦ | ♦ | ♦♦ |
| Trimipramine | ♦ | ♦ | ○ | ♦ | ♦♦ | ♦♦♦ |
| Secondary amines | ||||||
| Nortriptyline | ♦♦ | ♦♦ | ○ | ♦ | ♦ | ♦ |
| Desipramine | ♦♦♦ | ♦ | ○ | - | ♦ | ♦ |
| Protriptyline | ♦♦♦ | ♦ | ○ | ♦ | ♦♦♦ | ♦ |
| Tetracyclics | ||||||
| Maprotiline | ♦♦ | ♦ | ○ | ○ | ♦ | ♦♦ |
| Amoxapine | ♦♦ | ♦ | ○ | ♦♦♦ | ♦ | ♦ |
| Other | ||||||
| Trazodone | ○ | ♦ | ○ | ♦♦ | ○ | ○ |
| SSRIs | ||||||
| Fluoxetine | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Sertraline | ○ | ♦♦♦ | ♦ | ○ | ○ | ○ |
| Paroxetine | ♦ | ♦♦♦ | ○ | ○ | ♦ | ○ |
| Fluvoxamine | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Citalopram | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Receptor modulators/reuptake inhibitors | ||||||
| Nefazodone | ♦/○ | ♦ | ○ | ♦♦♦ | ○ | ○ |
| Mirtazapine | ♦* | ♦ | ○ | ♦♦♦ | ○ | ♦♦♦ |
| Norepinephrine/dopamine modulators | ||||||
| Bupropion | ♦/○ | ○ | ♦/○ | ○ | ○ | ○ |
| Serotonin/norepinephrine reuptake inhibitors | ||||||
| Venlafaxine | ♦♦* | ♦♦♦ | ♦* | ○ | ○ | ○ |
| Strength effect on a scale from ○(no effect) to ♦♦♦(marked effect); ♦/○(marginal effect) | ||||||
| NE: norepinephrine; 5HT: serotonin; DA: dopamine * Dose-dependent x Includes metabolite, desmethyl clomipramine | ||||||
Table 3
APPROXIMATE THERAPEUTIC PLASMA LEVEL RANGES
| TCA | Blood level (ng/ml) |
|---|---|
| Amitriptyline | 100-250 |
| Amoxapine | Unknown |
| Clomipramine | Unknown |
| Desipramine | Unknown |
| Doxepin | 120-250 |
| Imipramine | 150-300 |
| Maprotiline | 150-250 |
| Nortriptyline | 50-150 |
| Protriptyline | 75-250 |
| Trimipramine | Unknown |
| Trazodone | Unknown |
| + Only nortriptyline has a clear therapeutic window. The others are either approximate or unknown. | |
Sedation is a common side effect caused by the antihistaminic properties of some TCAs (Table 2). Agents with this effect (e.g., doxepin), when given once daily at bedtime, can benefit patients with concomitant sleep disturbance.
Weight gain Patients being treated with TCAs often gain weight, most likely because of carbohydrate craving associated with H2 blockade. Patient education, monitoring of weight, and dietary counseling may be necessary during TCA use. Regular exercise is recommended, although depressed patients often lack the motivation and energy to exercise.
Cardiovascular toxicity All TCAs have potential cardiovascular effects (Table 3), which are seen on an ECG as increased PR, QRS, or QTc intervals, especially at higher dosages or in patients with pre-existing cardiac disease.19 Orthostatic hypotension is among the most common cardiovascular side effects, particularly in the elderly, and may result in falls or other injuries.
A baseline ECG is recommended before starting TCA therapy, especially in depressed patients with cardiac conduction delays (primary or secondary to concomitant medications). Routine ECGs should be used to monitor patients:
- with pre-existing cardiac disease;
- taking higher-than-recommended dosages of a TCA;
- taking other medications that may affect cardiac conduction.
When in doubt, obtaining a cardiology consultation is recommended.
CNS effects Signs of CNS toxicity include confusion, memory impairment, delirium, seizures, coma, and eventual respiratory depression.20 Risk factors include toxic TCA plasma levels, elderly patient age, and concomitant use of other medications, such as psychotropics (neuroleptics), anticholinergics, and antihistamines. CNS toxicity may be difficult to diagnose, as it may initially resemble worsening of depressed mood. Confusion or worsening of memory or cognitive function are predictors of CNS toxicity.
A patient with anticholinergic-related delirium should be monitored on a medical unit. A trial of physostigmine may be warranted to confirm the diagnosis.
Neurologic symptoms Maprotiline and clomipramine have been associated with an increased risk of seizures. Use reduced dosages in patients with a history of seizures or concomitant use of medications that may increase maprotiline or clomipramine levels or decrease the seizure threshold (e.g., other antidepressants, withdrawal from benzodiazepines). Amoxapine has been associated with extrapyramidal symptoms secondary to a neuroleptic metabolite.
Overdose The severity of adverse side effects often depends upon drug concentration. An overdose of as little as a 2-week supply of a TCA can cause potentially fatal arrhythmias.
Priapism Trazodone has been associated with priapism, which has an incidence rate of 1/6,000 in patients taking this drug. Priapism is a medical emergency that requires prompt treatment.
Administration
TCAs are well-absorbed following oral administration and reach peak plasma levels in 2 to 6 hours. The average half-life of approximately 24 hours often allows therapeutic levels to be achieved with once-daily dosing at bedtime (Table 3).
TCAs are metabolized primarily by the cytochrome P-450 2D6 (CYP2D6) isoenzyme. Patients differ by a factor of 30- to 40-fold in their rate of metabolism of some TCAs, depending on individual genotypes.
The 7 to 9% of Caucasians classified as poor metabolizers at CYP2D6 require much lower-than-usual dosages of secondary amine TCAs.21 he 50% of Asians who are intermediate metabolizers require one-half the usual dosage. Tailor therapy to the individual patient, starting low, checking plasma levels, and monitoring for side effects.
For patients who would benefit from TCAs’ H1 anxiolytic effects, start with bid or tid dosing and later switch to once daily after achieving efficacy.
When using TCAs, start low and go slow to maximize efficacy and minimize side effects, especially in the elderly patient. The goal is to treat the patient, not to achieve target serum levels. The most favorable results have been demonstrated when patients are maintained at the dosages to which they respond when their disorder is in the acute stage.17
Symptoms usually improve after 2 weeks of TCA therapy, and up to 6 weeks may be required for a clinically significant effect. For many depressed patients, symptoms of insomnia, anxiety, and poor appetite improve within the first few days.
Monitoring serum levels
Serum levels are useful for monitoring treatment, compliance, and toxicity.22 Because the most accurate TCA serum levels are found at steady state, check the level after the patient has been on TCA therapy for at least 5 days and 8 to 12 hours after the last dose. Serum levels may also guide dosage increases in patients who exhibit a partial response to therapy.
Table 4
DRUGS THAT INTERACT WITH TCAs
| Anticholinergic agents |
| Barbiturates |
| Cimetidine |
| Disulfiram |
| ETOH |
| Flecainide |
| Guanethidine |
| Haloperidol |
| MAOIs |
| Methylphenidate |
| Phenothiazines |
| Phenytoin |
| Propafenone |
| Quinidine |
| SSRIs (e.g., fluoxetine, sertraline, paroxetine) |
| Sympathomimetic drugs (e.g., norepinephrine, epinephrine) |
| Warfarin |
Nortriptyline has a therapeutic window between 50 and 150 ng/mL. Patients who do not respond to serum levels higher than 150 ng/mL may respond when the dosage is reduced and the serum level falls to within that range. If response is adequate and without side effects, however, there is no need to reduce the dose. Other, less clear therapeutic windows have been described for other TCAs (Table 3).
TCA metabolism is affected by age and interaction with other drugs. Closely monitor serum levels in elderly and medically compromised patients, especially during dosage increases. Pay particular attention to other medications that may affect serum levels23 (Table 4). SSRIs, particularly fluoxetine and paroxetine, may affect TCA plasma levels because of their potent inhibition of CYP2D6.
Individualize dosing and serum level monitoring. For example, the patient who is clinically tolerating a TCA and has a normal ECG does not require a serum level measurement, unless medically indicated.
Discontinuing tricyclics
When discontinuing a TCA, taper the dosage no more rapidly than 25 to 50 mg every 2 to 3 days. Abrupt discontinuation can cause cholinergic rebound, with symptoms such as nausea, cramping, headache, vomiting, and sweating. “Rebound hypomania” or “mania” have been reported with abrupt cessation of TCAs,24 especially in patients with bipolar disorder. If the etiology of rebound symptoms is unclear (i.e., medical versus psychiatric), re-administering the discontinued TCA should relieve the symptoms and confirm a diagnosis of discontinuation.
Related resources
- Schatzberg AF, Cole JO, DeBattista C. Antidepressants. Manual of clinical psychopharmacology (3rd ed). Washington, DC: American Psychiatric Press, 1997.
- Janicak PG, Davis JM, Preskorn SH, Ayd Jr. FJ. Principles and practice of psychopharmacotherapy (2nd ed). Baltimore: Lippincott Williams & Wilkins, 1997.
- PDR Psychotropic Prescribing Guide (2nd ed). Montvale, NJ: Medical Economics, 1999.
- National Library of Medicine, MedlinePlus Health Information: Antidepressants, tricyclics (http://www.nlm.nih.gov/medlineplus/druginfo/antidepressantstricyclicsystem202055.html)
Drug brand names
See table 1 for tricyclic drug brand names. Others mentioned in this article include:
- Bupropion • Wellbutrin
- Cimetidine • Tagamet
- Citalopram • Celexa
- Disulfiram • Antabuse
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Guanethidine • Ismelin
- Methylphenidate • Concerta, Ritalin
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Phenytoin • Dilantin
Disclosure
Dr. Zajecka reports that he receives grant/research support from, serves as a consultant to, and is on the speaker’s bureau of Bristol-Myers Squibb and Eli Lilly and Co.; receives grant/research support from Cephalon Inc., GlaxoSmithKline, Lichtwer Pharma, Merck and Co., MIICRO Inc., Otsuka Pharmaceuticals, Parke-Davis, Pfizer Inc., and Wyeth-Ayerst Pharmaceuticals; serves as a consultant to Abbott Laboratories; and is on the speaker’s bureau of Abbott Laboratories, Pfizer/Roerig, GlaxoSmithKline, Pharmacia, and Wyeth-Ayerst Pharmaceuticals.
Dr. Tummala reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. American Psychiatric Association Practice guideline for the treatment of patients with major depressive disorder. Am J Psychiatry 2000;157(4 suppl):1-45.
2. Texas Implementation of Medication Algorithms (TIMA) Strategies for the treatment of major depression (nonpsychotic). Texas Department of Mental Health and Mental Retardation, 1999 (www.mhmr.state.tx.us/centraloffice/medicaldirector/TIMA.html).
3. American Academy of Child and Adolescent Psychiatry Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37(10 suppl):63S-83S.
4. Richelson EJ. Pharmacology of antidepressants. Mayo Clin Proc 2001;76:511-27.
5. Roose SP, Glassman AH, Attia E, Woodring S. Comparative efficacy of selective serotonin reuptake inhibitors and tricyclics in the treatment of melancholia. Am J Psychiatry 1994;151:1735-9.
6. Nierenberg AA. The treatment of severe depression: is there an efficacy gap between SSRI and TCA antidepressant generations? J Clin Psychiatry 1994;55(suppl A):55-9,98-100.
7. Danish University Antidepressant Group Citalopram: clinical effect profile in comparison with clomipramine. A controlled multicenter study. Psychopharmacology 1986;90:131-8.
8. Danish University Antidepressant Group Paroxetine: a selective serotonin reuptake inhibitor showing better tolerance but weaker antidepressant effect than clomipraine in a controlled multicenter study. J Affect Disord 1990;18:289-99.
9. U.S. Department of Health and Human Services Depression Guideline Panel. Depression in Primary Care, vol. 2: Treatment of Major Depression. Rockville, Md: U.S. Department of Health and Human Services, 1993.
10. Song F, Freemantle N, Sheldon TA, et al. Selective serotonin reuptake inhibitors: meta-analysis of efficacy and acceptability. Br Med J 1993;306:683-7.
11. Piccinelli M, Pini S, Bellantuono C, Wilkinson G. Efficacy of drug treatment in obsessive-compulsive disorder: a meta-analytic review. Br J Psychiatry 1995;166:424-43.
12. Lydiard RB, Morton WA, Emmanuel NP, Zealberg JJ. Placebo-controlled, double-blind study of the clinical and metabolic effects of desipramine in panic disorder Psychopharmacol Bull. 1993;29(2):183-8.
13. Zajecka JM, Fawcett J. Antidepressant combination and potentiation. Psychiatr Med 1999;9(1):55-75.
14. Zajecka JM, Jeffriess H, Fawcett J. The efficacy of fluoxetine combined with a heterocyclic antidepressant in treatment-resistant depression: a retrospective analysis J Clin Psychiatry 1995;56:338-43.
15. Figueroa Y, Rosenberg DR, Birmaher B, Keshavan MS. Combination treatment with clomipramine and selective serotonin reuptake inhibitors for obsessive-compulsive disorder in children and adolescents. J Child Adolesc Psychopharmacol 1998;8(1):61-7.
16. Spiegel K, Kalb R, Pasternak GW. Analgesic activity of tricyclic antidepressants. Ann Neurol 1983;13:462-5.
17. Schatzberg AF, Cole JO, DeBattista C, eds Manual of clinical psychopharmacology. 3rd ed. Washington, DC: American Psychiatric Publishing, 1997.
18. Pope HG, Hudson JI, Jonas JM. Bulimia treated with imipramine: a placebo controlled, double-blind study. Am J Psychiatry 1983;140:554-8.
19. Roose SP, Glassman AH, Giardina GV, et al. Tricyclic antidepressants in depressed patients with cardiac conduction disease. Arch Gen Psychiatry 1987;44:273-5.
20. Preskorn SH, Jerkovich GS. Central nervous system toxicity of tricyclic antidepressants: phenomenology, course, risk factors, and role of therapeutic drug monitoring. J Clin Psychopharmacology. 1990;10:88-95.
21. Potter WZ, Husseini KM, Rudorfer MV. Tricyclics and tetracyclics. In: Schatzberg AF, Nemeroff CB, eds. The American Psychiatric Press Textbook of Psychopharmacology. 2nd ed. Washington, DC: American Psychiatric Publishing, 1998.
22. Preskorn SH. Tricyclic antidepressants: The whys and hows of therapeutic drug monitoring. J Clin Psychiatry 1989;50(7, suppl):34-42.
23. Bell IR, Cole JO. Fluoxetine induces elevation of desipramine levels and exacerbation of geriatric nonpsychotic depression. J Clin Psychopharmacol 1988;8:447-8.
24. Nelson JC, Shottenfeld RS, Conrad CD. Hypomania after desipramine withdrawal. Am J Psychiatry 1983;140:624-5.
Recent practice guidelines generally do not position tricyclic antidepressants (TCAs) as first-line therapies because of concerns about side effects and safety issues.1-3 Yet these agents have important clinical uses—both for approved and off-label indications—and diverse pharmacologic properties that distinguish them from each other as well as from many of the “newer antidepressants.”
Eleven TCAs are available in the United States (Table 1). Here’s what the evidence says about when and how to use them to treat a variety of psychiatric disorders, along with our recommendations on how to reduce the risk of side effects.
Indications and off-label uses
TCAs’ pharmacologic properties make them very versatile (Box 1).4 Major depression and anxiety disorders (such as obsessive compulsive disorder [OCD]) are the principal FDA-approved indications for TCAs. Other approved indications are anxiety (doxepin) and childhood enuresis (imipramine). Common off-label uses supported by scientific literature include panic disorder, social phobia, insomnia, posttraumatic stress disorder (PTSD), generalized anxiety disorder (GAD), attention-deficit/hyperactivity disorder (ADHD), migraine headache, chronic pain syndromes, premature ejaculation, substance abuse disorders, and eating disorders, to name a few.
Major depression To treat major depressive disorder, the American Psychiatric Association recommends selective serotonin reuptake inhibitors (SSRIs), bupropion, venlafaxine, and the secondary amine TCAs desipramine and nortriptyline as “optimal” first-line therapy for most patients.1 The Texas Medication Algorithm Project recommends SSRIs, bupropion, nefazodone, venlafaxine, or mirtazapine as first-line therapy and lists TCAs as second- or third-line therapy for patients with partial or no response to initial therapy.2
Table 1
THERAPEUTIC DOSAGE RANGE
| Generic name | Brand names | Therapeutic dosage range (mg/d) |
|---|---|---|
| Amitriptyline | Elavil, Endep | 150-300 |
| Amoxapine | Asendin | 150-450 |
| Clomipramine | Anafranil | 100-250 |
| Desipramine | Norpramin, Pertofane | 150-300 |
| Doxepin | Sinequan Adapin | 150-300 |
| Imipramine | Tofranil, Tofranil PM Janimine, Sk-Pramine | 150-300 |
| Maprotiline | Ludiomil | 150-200 |
| Nortriptyline | Pamelor Aventyl | 50-150 |
| Protriptyline | Vivactil | 15-60 |
| Trimipramine | Surmontil | 150-300 |
| Trazodone | Desyrel | 50-600 |
| * Dosage ranges are approximate. Dosage needs to be tailored by individual patient needs. The elderly, children, and the medically compromised may require lower dosages. | ||
The tricyclic antidepresants are a broad class of drugs that can be divided, based on the number of rings in their nucleus, into tricyclics and tetracyclics. The tricyclics can be further classified into tertiary and secondary amines, based on the number of methyl groups on the side chain. In addition, some clinicians include trazodone—an antidepressant chemically unrelated to tricyclic, tetracyclic, or other known antidepressant agents—in the broad class of TCAs.
TCAs were initially hypothesized to block the reuptake of norepinephrine (NE) or serotonin (5HT), thereby increasing the levels of these neurotransmitters at the postsynaptic receptor. More recent theories include effects on pre- and postsynaptic receptors and other neurotransmitters, such as histamine and acetylcholine, which explain the various side effects of TCAs.
The relative norepinephrine-reuptake-blocking effects versus serotonin-reuptake-blocking effects of the TCAs and each drug’s biochemical effects are summarized in Table 2. Except for clomipramine, TCAs are relatively weak 5HT reuptake blockers.
Although recommended as first-line therapies, SSRIs and other newer antidepressants exhibit no greater efficacy than TCAs in treating major depression.5,6 Three major meta-analyses7-9 reported no significant difference in efficacy between the two antidepressant classes. In the largest,9 published by the U.S. Department of Health and Human Services, 50% of inpatients and 52% of outpatients responded to TCAs, whereas 54% of inpatients and 47% of outpatients responded to SSRIs. Compared with SSRIs, TCAs also may be associated with higher rates of remission.7,8
Clomipramine—approved for OCD—has been used for decades to treat depression and resistant depression. Two meta-analyses by the Danish University Antidepressant Group7,8 showed that clomipramine produced a “significantly better therapeutic effect” compared with citalopram and paroxetine. In three major studies,5,7,8 TCAs showed greater effectiveness than SSRIs in treating melancholic depression.
The anticholinergic side effects of TCAs have been perceived to cause higher patient dropout and discontinuation rates, but studies have shown mixed results. In one meta-analysis comparing SSRIs and TCAs, the difference in dropout rates due to adverse effects was less significant than previously reported. When total dropout rates for any reason were examined, the difference was less than was originally expected.10
OCD In clinical practice, most patients with OCD are started on an SSRI. Clomipramine is another valuable option, however, especially for patients who fail one or more therapeutic trials with SSRIs. Clomipramine may produce significant therapeutic benefit in patients with OCD, possibly because of its potent 5-HT reuptake properties. In one study, patients with OCD symptoms who received clomipramine improved more than those receiving SSRIs when each class was compared with placebo.11
Panic disorder Although not approved for panic disorder, imipramine and desipramine provide effective treatment, even in nondepressed patients.12 Doses and plasma levels are the same as those used for treating depression. Start low (e.g., imipramine, 10 to 20 mg/d; desipramine, 10 to 25 mg/d) and increase gradually over several weeks to typical therapeutic dosages (Table 1). Do not escalate too rapidly, as this may increase anxiety or precipitate a panic attack. Uses in children TCAs have been used to treat children with ADHD, OCD, enuresis, and depression. The American Academy of Child and Adolescent Psychiatry (AACAP) does not recommend TCAs as first-line treatment for youths requiring pharmacotherapy for depressive disorders but acknowledges that some youths with depression may respond better to TCAs than to other medications.3
Imipramine is the only TCA indicated for nocturnal enuresis, but its exact mechanism of action is not known. The benefit may be secondary to imipramine’s anticholinergic effect or to changes in sleep architecture. Recommended bedtime doses for children with enuresis are:
- 25 to 50 mg under age 12;
- up to 75 mg age 12 and older.
TCAs are an option for children with ADHD, especially if ADHD is present with comorbid depression or anxiety disorder. However, because at least four cases of sudden cardiac death have been reported in children taking desipramine, it is prudent to monitor cardiac function when children are started on TCAs. AACAP guidelines recommend obtaining a baseline ECG, resting blood pressure, and pulse (supine or sitting, then standing), with regular monitoring of the child’s weight during TCA therapy.
Combination therapy Few controlled studies have tested TCAs as combination therapy. Trazodone can be used as an adjunct to SSRIs and monoamine oxidase inhibitors (MAOIs) for patients with insomnia. TCAs are used as an adjunct to treat resistant depression and OCD13,14 (e.g., clomipramine added to fluvoxamine to treat OCD).15 Serum level monitoring is recommended when TCAs are used as adjuncts.
Other uses TCAs play a role in the prophylactic treatment of premature ejaculation and migraine headaches, probably because of their serotonergic (5HT2) effect. In patients with migraine and depression, a trial of a TCA such as amitriptyline may be warranted.
TCAs are widely used to manage neuropathic pain,16 although the exact mechanism of action is unknown. Because depression is commonly associated with pain, the effect may result from the agents’ action on depression, or TCAs may possess direct analgesic action.
Trazodone, 25 to 100 mg at bedtime, is widely used for insomnia, alone or as an adjunct with other classes of antidepressants—even in combination with MAOIs. Nortriptyline has been shown to be safe and effective for post-stroke and geriatric types of depression.17
TCAs are also used for a host of other medical, psychiatric, and neurologic problems, such as social phobia, PTSD, GAD, substance abuse disorders, and eating disorders.18 Only a few controlled studies have tested TCAs for these indications.
Side effects
Although TCAs have shown efficacy in many clinical situations, their use is associated with potentially serious side effects, which may include anticholinergic effects, sedation, weight gain, CNS toxicity, orthostatic hypotension, cardiovascular toxicity, delirium, and risk of suicide by overdose. The risk of side effects can be reduced with careful prescribing practices (Box 2).
Anticholinergic effects, sedation TCAs vary in their anticholinergic activity (Table 2). Tertiary amine TCAs such as amitriptyline and protriptyline may cause dry mouth, constipation, urinary hesitancy, and blurred vision in some patients, and confusion in elderly or demented patients. Secondary amine TCAs such as nortriptyline or desipramine are less anticholinergic and less likely to cause these side effects.
Peripheral anticholinergic side effects can be managed with bethanacol—a cholinergic drug—in dosages of 25 to 50 mg tid or qid. Dry mouth can be treated with pilocarpine, 5 mg bid to qid, or oral bethanacol (5- to 10-mg tablets sublingually), artificial saliva drops, sugarless candy/gum, or mouthwash.
- Obtain a baseline ECG for patients of all ages before starting TCA therapy.
- When dosing TCAs, start low and go slow to maximize efficacy and minimize side effects, especially in the elderly patient.
- In the elderly, avoid highly anticholinergic TCAs such as amitriptyline or protriptyline, which can cause delirium. Choose a TCA with low anticholinergic properties, such as desipramine or nortriptyline.
- For patients who are intolerant of the anticholinergic and sedative properties of amitriptyline or protriptyline, consider switching to desipramine or nortriptyline.
- If a patient develops a toxic effect mediated by either the cardiovascular or central nervous system, discontinue the TCA or reduce the dosage.
- In patients at risk for suicide by overdose, consider dispensing less than a 2-week supply. In case of overdose, cardiac monitoring for at least 24 hours may be indicated.
Table 2
BIOCHEMICAL EFFECTS OF TRICYCLICS AND OTHER ANTIDEPRESSANTS
| POTENCY | SIDE EFFECTS | |||||
|---|---|---|---|---|---|---|
| NE reuptake blockade | 5HT reuptake blockade | DA reuptake blockade | 5HT blockade | Muscorinic blockade | Histamine blockade | |
| TCAs | ||||||
| Tertiary amines | ||||||
| Amitriptyline | ♦♦ | ♦♦ | ○ | ♦ | ♦♦♦ | ♦♦ |
| Imipramine | ♦♦♦ | ♦♦♦ | ○ | ○ | ♦♦ | ♦ |
| Doxepin | ♦♦ | ♦♦ | ○ | ♦ | ♦♦ | ♦♦♦ |
| Clomipramine | ♦♦x | ♦♦♦ | ○ | ♦ | ♦ | ♦♦ |
| Trimipramine | ♦ | ♦ | ○ | ♦ | ♦♦ | ♦♦♦ |
| Secondary amines | ||||||
| Nortriptyline | ♦♦ | ♦♦ | ○ | ♦ | ♦ | ♦ |
| Desipramine | ♦♦♦ | ♦ | ○ | - | ♦ | ♦ |
| Protriptyline | ♦♦♦ | ♦ | ○ | ♦ | ♦♦♦ | ♦ |
| Tetracyclics | ||||||
| Maprotiline | ♦♦ | ♦ | ○ | ○ | ♦ | ♦♦ |
| Amoxapine | ♦♦ | ♦ | ○ | ♦♦♦ | ♦ | ♦ |
| Other | ||||||
| Trazodone | ○ | ♦ | ○ | ♦♦ | ○ | ○ |
| SSRIs | ||||||
| Fluoxetine | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Sertraline | ○ | ♦♦♦ | ♦ | ○ | ○ | ○ |
| Paroxetine | ♦ | ♦♦♦ | ○ | ○ | ♦ | ○ |
| Fluvoxamine | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Citalopram | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Receptor modulators/reuptake inhibitors | ||||||
| Nefazodone | ♦/○ | ♦ | ○ | ♦♦♦ | ○ | ○ |
| Mirtazapine | ♦* | ♦ | ○ | ♦♦♦ | ○ | ♦♦♦ |
| Norepinephrine/dopamine modulators | ||||||
| Bupropion | ♦/○ | ○ | ♦/○ | ○ | ○ | ○ |
| Serotonin/norepinephrine reuptake inhibitors | ||||||
| Venlafaxine | ♦♦* | ♦♦♦ | ♦* | ○ | ○ | ○ |
| Strength effect on a scale from ○(no effect) to ♦♦♦(marked effect); ♦/○(marginal effect) | ||||||
| NE: norepinephrine; 5HT: serotonin; DA: dopamine * Dose-dependent x Includes metabolite, desmethyl clomipramine | ||||||
Table 3
APPROXIMATE THERAPEUTIC PLASMA LEVEL RANGES
| TCA | Blood level (ng/ml) |
|---|---|
| Amitriptyline | 100-250 |
| Amoxapine | Unknown |
| Clomipramine | Unknown |
| Desipramine | Unknown |
| Doxepin | 120-250 |
| Imipramine | 150-300 |
| Maprotiline | 150-250 |
| Nortriptyline | 50-150 |
| Protriptyline | 75-250 |
| Trimipramine | Unknown |
| Trazodone | Unknown |
| + Only nortriptyline has a clear therapeutic window. The others are either approximate or unknown. | |
Sedation is a common side effect caused by the antihistaminic properties of some TCAs (Table 2). Agents with this effect (e.g., doxepin), when given once daily at bedtime, can benefit patients with concomitant sleep disturbance.
Weight gain Patients being treated with TCAs often gain weight, most likely because of carbohydrate craving associated with H2 blockade. Patient education, monitoring of weight, and dietary counseling may be necessary during TCA use. Regular exercise is recommended, although depressed patients often lack the motivation and energy to exercise.
Cardiovascular toxicity All TCAs have potential cardiovascular effects (Table 3), which are seen on an ECG as increased PR, QRS, or QTc intervals, especially at higher dosages or in patients with pre-existing cardiac disease.19 Orthostatic hypotension is among the most common cardiovascular side effects, particularly in the elderly, and may result in falls or other injuries.
A baseline ECG is recommended before starting TCA therapy, especially in depressed patients with cardiac conduction delays (primary or secondary to concomitant medications). Routine ECGs should be used to monitor patients:
- with pre-existing cardiac disease;
- taking higher-than-recommended dosages of a TCA;
- taking other medications that may affect cardiac conduction.
When in doubt, obtaining a cardiology consultation is recommended.
CNS effects Signs of CNS toxicity include confusion, memory impairment, delirium, seizures, coma, and eventual respiratory depression.20 Risk factors include toxic TCA plasma levels, elderly patient age, and concomitant use of other medications, such as psychotropics (neuroleptics), anticholinergics, and antihistamines. CNS toxicity may be difficult to diagnose, as it may initially resemble worsening of depressed mood. Confusion or worsening of memory or cognitive function are predictors of CNS toxicity.
A patient with anticholinergic-related delirium should be monitored on a medical unit. A trial of physostigmine may be warranted to confirm the diagnosis.
Neurologic symptoms Maprotiline and clomipramine have been associated with an increased risk of seizures. Use reduced dosages in patients with a history of seizures or concomitant use of medications that may increase maprotiline or clomipramine levels or decrease the seizure threshold (e.g., other antidepressants, withdrawal from benzodiazepines). Amoxapine has been associated with extrapyramidal symptoms secondary to a neuroleptic metabolite.
Overdose The severity of adverse side effects often depends upon drug concentration. An overdose of as little as a 2-week supply of a TCA can cause potentially fatal arrhythmias.
Priapism Trazodone has been associated with priapism, which has an incidence rate of 1/6,000 in patients taking this drug. Priapism is a medical emergency that requires prompt treatment.
Administration
TCAs are well-absorbed following oral administration and reach peak plasma levels in 2 to 6 hours. The average half-life of approximately 24 hours often allows therapeutic levels to be achieved with once-daily dosing at bedtime (Table 3).
TCAs are metabolized primarily by the cytochrome P-450 2D6 (CYP2D6) isoenzyme. Patients differ by a factor of 30- to 40-fold in their rate of metabolism of some TCAs, depending on individual genotypes.
The 7 to 9% of Caucasians classified as poor metabolizers at CYP2D6 require much lower-than-usual dosages of secondary amine TCAs.21 he 50% of Asians who are intermediate metabolizers require one-half the usual dosage. Tailor therapy to the individual patient, starting low, checking plasma levels, and monitoring for side effects.
For patients who would benefit from TCAs’ H1 anxiolytic effects, start with bid or tid dosing and later switch to once daily after achieving efficacy.
When using TCAs, start low and go slow to maximize efficacy and minimize side effects, especially in the elderly patient. The goal is to treat the patient, not to achieve target serum levels. The most favorable results have been demonstrated when patients are maintained at the dosages to which they respond when their disorder is in the acute stage.17
Symptoms usually improve after 2 weeks of TCA therapy, and up to 6 weeks may be required for a clinically significant effect. For many depressed patients, symptoms of insomnia, anxiety, and poor appetite improve within the first few days.
Monitoring serum levels
Serum levels are useful for monitoring treatment, compliance, and toxicity.22 Because the most accurate TCA serum levels are found at steady state, check the level after the patient has been on TCA therapy for at least 5 days and 8 to 12 hours after the last dose. Serum levels may also guide dosage increases in patients who exhibit a partial response to therapy.
Table 4
DRUGS THAT INTERACT WITH TCAs
| Anticholinergic agents |
| Barbiturates |
| Cimetidine |
| Disulfiram |
| ETOH |
| Flecainide |
| Guanethidine |
| Haloperidol |
| MAOIs |
| Methylphenidate |
| Phenothiazines |
| Phenytoin |
| Propafenone |
| Quinidine |
| SSRIs (e.g., fluoxetine, sertraline, paroxetine) |
| Sympathomimetic drugs (e.g., norepinephrine, epinephrine) |
| Warfarin |
Nortriptyline has a therapeutic window between 50 and 150 ng/mL. Patients who do not respond to serum levels higher than 150 ng/mL may respond when the dosage is reduced and the serum level falls to within that range. If response is adequate and without side effects, however, there is no need to reduce the dose. Other, less clear therapeutic windows have been described for other TCAs (Table 3).
TCA metabolism is affected by age and interaction with other drugs. Closely monitor serum levels in elderly and medically compromised patients, especially during dosage increases. Pay particular attention to other medications that may affect serum levels23 (Table 4). SSRIs, particularly fluoxetine and paroxetine, may affect TCA plasma levels because of their potent inhibition of CYP2D6.
Individualize dosing and serum level monitoring. For example, the patient who is clinically tolerating a TCA and has a normal ECG does not require a serum level measurement, unless medically indicated.
Discontinuing tricyclics
When discontinuing a TCA, taper the dosage no more rapidly than 25 to 50 mg every 2 to 3 days. Abrupt discontinuation can cause cholinergic rebound, with symptoms such as nausea, cramping, headache, vomiting, and sweating. “Rebound hypomania” or “mania” have been reported with abrupt cessation of TCAs,24 especially in patients with bipolar disorder. If the etiology of rebound symptoms is unclear (i.e., medical versus psychiatric), re-administering the discontinued TCA should relieve the symptoms and confirm a diagnosis of discontinuation.
Related resources
- Schatzberg AF, Cole JO, DeBattista C. Antidepressants. Manual of clinical psychopharmacology (3rd ed). Washington, DC: American Psychiatric Press, 1997.
- Janicak PG, Davis JM, Preskorn SH, Ayd Jr. FJ. Principles and practice of psychopharmacotherapy (2nd ed). Baltimore: Lippincott Williams & Wilkins, 1997.
- PDR Psychotropic Prescribing Guide (2nd ed). Montvale, NJ: Medical Economics, 1999.
- National Library of Medicine, MedlinePlus Health Information: Antidepressants, tricyclics (http://www.nlm.nih.gov/medlineplus/druginfo/antidepressantstricyclicsystem202055.html)
Drug brand names
See table 1 for tricyclic drug brand names. Others mentioned in this article include:
- Bupropion • Wellbutrin
- Cimetidine • Tagamet
- Citalopram • Celexa
- Disulfiram • Antabuse
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Guanethidine • Ismelin
- Methylphenidate • Concerta, Ritalin
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Phenytoin • Dilantin
Disclosure
Dr. Zajecka reports that he receives grant/research support from, serves as a consultant to, and is on the speaker’s bureau of Bristol-Myers Squibb and Eli Lilly and Co.; receives grant/research support from Cephalon Inc., GlaxoSmithKline, Lichtwer Pharma, Merck and Co., MIICRO Inc., Otsuka Pharmaceuticals, Parke-Davis, Pfizer Inc., and Wyeth-Ayerst Pharmaceuticals; serves as a consultant to Abbott Laboratories; and is on the speaker’s bureau of Abbott Laboratories, Pfizer/Roerig, GlaxoSmithKline, Pharmacia, and Wyeth-Ayerst Pharmaceuticals.
Dr. Tummala reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Recent practice guidelines generally do not position tricyclic antidepressants (TCAs) as first-line therapies because of concerns about side effects and safety issues.1-3 Yet these agents have important clinical uses—both for approved and off-label indications—and diverse pharmacologic properties that distinguish them from each other as well as from many of the “newer antidepressants.”
Eleven TCAs are available in the United States (Table 1). Here’s what the evidence says about when and how to use them to treat a variety of psychiatric disorders, along with our recommendations on how to reduce the risk of side effects.
Indications and off-label uses
TCAs’ pharmacologic properties make them very versatile (Box 1).4 Major depression and anxiety disorders (such as obsessive compulsive disorder [OCD]) are the principal FDA-approved indications for TCAs. Other approved indications are anxiety (doxepin) and childhood enuresis (imipramine). Common off-label uses supported by scientific literature include panic disorder, social phobia, insomnia, posttraumatic stress disorder (PTSD), generalized anxiety disorder (GAD), attention-deficit/hyperactivity disorder (ADHD), migraine headache, chronic pain syndromes, premature ejaculation, substance abuse disorders, and eating disorders, to name a few.
Major depression To treat major depressive disorder, the American Psychiatric Association recommends selective serotonin reuptake inhibitors (SSRIs), bupropion, venlafaxine, and the secondary amine TCAs desipramine and nortriptyline as “optimal” first-line therapy for most patients.1 The Texas Medication Algorithm Project recommends SSRIs, bupropion, nefazodone, venlafaxine, or mirtazapine as first-line therapy and lists TCAs as second- or third-line therapy for patients with partial or no response to initial therapy.2
Table 1
THERAPEUTIC DOSAGE RANGE
| Generic name | Brand names | Therapeutic dosage range (mg/d) |
|---|---|---|
| Amitriptyline | Elavil, Endep | 150-300 |
| Amoxapine | Asendin | 150-450 |
| Clomipramine | Anafranil | 100-250 |
| Desipramine | Norpramin, Pertofane | 150-300 |
| Doxepin | Sinequan Adapin | 150-300 |
| Imipramine | Tofranil, Tofranil PM Janimine, Sk-Pramine | 150-300 |
| Maprotiline | Ludiomil | 150-200 |
| Nortriptyline | Pamelor Aventyl | 50-150 |
| Protriptyline | Vivactil | 15-60 |
| Trimipramine | Surmontil | 150-300 |
| Trazodone | Desyrel | 50-600 |
| * Dosage ranges are approximate. Dosage needs to be tailored by individual patient needs. The elderly, children, and the medically compromised may require lower dosages. | ||
The tricyclic antidepresants are a broad class of drugs that can be divided, based on the number of rings in their nucleus, into tricyclics and tetracyclics. The tricyclics can be further classified into tertiary and secondary amines, based on the number of methyl groups on the side chain. In addition, some clinicians include trazodone—an antidepressant chemically unrelated to tricyclic, tetracyclic, or other known antidepressant agents—in the broad class of TCAs.
TCAs were initially hypothesized to block the reuptake of norepinephrine (NE) or serotonin (5HT), thereby increasing the levels of these neurotransmitters at the postsynaptic receptor. More recent theories include effects on pre- and postsynaptic receptors and other neurotransmitters, such as histamine and acetylcholine, which explain the various side effects of TCAs.
The relative norepinephrine-reuptake-blocking effects versus serotonin-reuptake-blocking effects of the TCAs and each drug’s biochemical effects are summarized in Table 2. Except for clomipramine, TCAs are relatively weak 5HT reuptake blockers.
Although recommended as first-line therapies, SSRIs and other newer antidepressants exhibit no greater efficacy than TCAs in treating major depression.5,6 Three major meta-analyses7-9 reported no significant difference in efficacy between the two antidepressant classes. In the largest,9 published by the U.S. Department of Health and Human Services, 50% of inpatients and 52% of outpatients responded to TCAs, whereas 54% of inpatients and 47% of outpatients responded to SSRIs. Compared with SSRIs, TCAs also may be associated with higher rates of remission.7,8
Clomipramine—approved for OCD—has been used for decades to treat depression and resistant depression. Two meta-analyses by the Danish University Antidepressant Group7,8 showed that clomipramine produced a “significantly better therapeutic effect” compared with citalopram and paroxetine. In three major studies,5,7,8 TCAs showed greater effectiveness than SSRIs in treating melancholic depression.
The anticholinergic side effects of TCAs have been perceived to cause higher patient dropout and discontinuation rates, but studies have shown mixed results. In one meta-analysis comparing SSRIs and TCAs, the difference in dropout rates due to adverse effects was less significant than previously reported. When total dropout rates for any reason were examined, the difference was less than was originally expected.10
OCD In clinical practice, most patients with OCD are started on an SSRI. Clomipramine is another valuable option, however, especially for patients who fail one or more therapeutic trials with SSRIs. Clomipramine may produce significant therapeutic benefit in patients with OCD, possibly because of its potent 5-HT reuptake properties. In one study, patients with OCD symptoms who received clomipramine improved more than those receiving SSRIs when each class was compared with placebo.11
Panic disorder Although not approved for panic disorder, imipramine and desipramine provide effective treatment, even in nondepressed patients.12 Doses and plasma levels are the same as those used for treating depression. Start low (e.g., imipramine, 10 to 20 mg/d; desipramine, 10 to 25 mg/d) and increase gradually over several weeks to typical therapeutic dosages (Table 1). Do not escalate too rapidly, as this may increase anxiety or precipitate a panic attack. Uses in children TCAs have been used to treat children with ADHD, OCD, enuresis, and depression. The American Academy of Child and Adolescent Psychiatry (AACAP) does not recommend TCAs as first-line treatment for youths requiring pharmacotherapy for depressive disorders but acknowledges that some youths with depression may respond better to TCAs than to other medications.3
Imipramine is the only TCA indicated for nocturnal enuresis, but its exact mechanism of action is not known. The benefit may be secondary to imipramine’s anticholinergic effect or to changes in sleep architecture. Recommended bedtime doses for children with enuresis are:
- 25 to 50 mg under age 12;
- up to 75 mg age 12 and older.
TCAs are an option for children with ADHD, especially if ADHD is present with comorbid depression or anxiety disorder. However, because at least four cases of sudden cardiac death have been reported in children taking desipramine, it is prudent to monitor cardiac function when children are started on TCAs. AACAP guidelines recommend obtaining a baseline ECG, resting blood pressure, and pulse (supine or sitting, then standing), with regular monitoring of the child’s weight during TCA therapy.
Combination therapy Few controlled studies have tested TCAs as combination therapy. Trazodone can be used as an adjunct to SSRIs and monoamine oxidase inhibitors (MAOIs) for patients with insomnia. TCAs are used as an adjunct to treat resistant depression and OCD13,14 (e.g., clomipramine added to fluvoxamine to treat OCD).15 Serum level monitoring is recommended when TCAs are used as adjuncts.
Other uses TCAs play a role in the prophylactic treatment of premature ejaculation and migraine headaches, probably because of their serotonergic (5HT2) effect. In patients with migraine and depression, a trial of a TCA such as amitriptyline may be warranted.
TCAs are widely used to manage neuropathic pain,16 although the exact mechanism of action is unknown. Because depression is commonly associated with pain, the effect may result from the agents’ action on depression, or TCAs may possess direct analgesic action.
Trazodone, 25 to 100 mg at bedtime, is widely used for insomnia, alone or as an adjunct with other classes of antidepressants—even in combination with MAOIs. Nortriptyline has been shown to be safe and effective for post-stroke and geriatric types of depression.17
TCAs are also used for a host of other medical, psychiatric, and neurologic problems, such as social phobia, PTSD, GAD, substance abuse disorders, and eating disorders.18 Only a few controlled studies have tested TCAs for these indications.
Side effects
Although TCAs have shown efficacy in many clinical situations, their use is associated with potentially serious side effects, which may include anticholinergic effects, sedation, weight gain, CNS toxicity, orthostatic hypotension, cardiovascular toxicity, delirium, and risk of suicide by overdose. The risk of side effects can be reduced with careful prescribing practices (Box 2).
Anticholinergic effects, sedation TCAs vary in their anticholinergic activity (Table 2). Tertiary amine TCAs such as amitriptyline and protriptyline may cause dry mouth, constipation, urinary hesitancy, and blurred vision in some patients, and confusion in elderly or demented patients. Secondary amine TCAs such as nortriptyline or desipramine are less anticholinergic and less likely to cause these side effects.
Peripheral anticholinergic side effects can be managed with bethanacol—a cholinergic drug—in dosages of 25 to 50 mg tid or qid. Dry mouth can be treated with pilocarpine, 5 mg bid to qid, or oral bethanacol (5- to 10-mg tablets sublingually), artificial saliva drops, sugarless candy/gum, or mouthwash.
- Obtain a baseline ECG for patients of all ages before starting TCA therapy.
- When dosing TCAs, start low and go slow to maximize efficacy and minimize side effects, especially in the elderly patient.
- In the elderly, avoid highly anticholinergic TCAs such as amitriptyline or protriptyline, which can cause delirium. Choose a TCA with low anticholinergic properties, such as desipramine or nortriptyline.
- For patients who are intolerant of the anticholinergic and sedative properties of amitriptyline or protriptyline, consider switching to desipramine or nortriptyline.
- If a patient develops a toxic effect mediated by either the cardiovascular or central nervous system, discontinue the TCA or reduce the dosage.
- In patients at risk for suicide by overdose, consider dispensing less than a 2-week supply. In case of overdose, cardiac monitoring for at least 24 hours may be indicated.
Table 2
BIOCHEMICAL EFFECTS OF TRICYCLICS AND OTHER ANTIDEPRESSANTS
| POTENCY | SIDE EFFECTS | |||||
|---|---|---|---|---|---|---|
| NE reuptake blockade | 5HT reuptake blockade | DA reuptake blockade | 5HT blockade | Muscorinic blockade | Histamine blockade | |
| TCAs | ||||||
| Tertiary amines | ||||||
| Amitriptyline | ♦♦ | ♦♦ | ○ | ♦ | ♦♦♦ | ♦♦ |
| Imipramine | ♦♦♦ | ♦♦♦ | ○ | ○ | ♦♦ | ♦ |
| Doxepin | ♦♦ | ♦♦ | ○ | ♦ | ♦♦ | ♦♦♦ |
| Clomipramine | ♦♦x | ♦♦♦ | ○ | ♦ | ♦ | ♦♦ |
| Trimipramine | ♦ | ♦ | ○ | ♦ | ♦♦ | ♦♦♦ |
| Secondary amines | ||||||
| Nortriptyline | ♦♦ | ♦♦ | ○ | ♦ | ♦ | ♦ |
| Desipramine | ♦♦♦ | ♦ | ○ | - | ♦ | ♦ |
| Protriptyline | ♦♦♦ | ♦ | ○ | ♦ | ♦♦♦ | ♦ |
| Tetracyclics | ||||||
| Maprotiline | ♦♦ | ♦ | ○ | ○ | ♦ | ♦♦ |
| Amoxapine | ♦♦ | ♦ | ○ | ♦♦♦ | ♦ | ♦ |
| Other | ||||||
| Trazodone | ○ | ♦ | ○ | ♦♦ | ○ | ○ |
| SSRIs | ||||||
| Fluoxetine | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Sertraline | ○ | ♦♦♦ | ♦ | ○ | ○ | ○ |
| Paroxetine | ♦ | ♦♦♦ | ○ | ○ | ♦ | ○ |
| Fluvoxamine | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Citalopram | ○ | ♦♦♦ | ○ | ○ | ○ | ○ |
| Receptor modulators/reuptake inhibitors | ||||||
| Nefazodone | ♦/○ | ♦ | ○ | ♦♦♦ | ○ | ○ |
| Mirtazapine | ♦* | ♦ | ○ | ♦♦♦ | ○ | ♦♦♦ |
| Norepinephrine/dopamine modulators | ||||||
| Bupropion | ♦/○ | ○ | ♦/○ | ○ | ○ | ○ |
| Serotonin/norepinephrine reuptake inhibitors | ||||||
| Venlafaxine | ♦♦* | ♦♦♦ | ♦* | ○ | ○ | ○ |
| Strength effect on a scale from ○(no effect) to ♦♦♦(marked effect); ♦/○(marginal effect) | ||||||
| NE: norepinephrine; 5HT: serotonin; DA: dopamine * Dose-dependent x Includes metabolite, desmethyl clomipramine | ||||||
Table 3
APPROXIMATE THERAPEUTIC PLASMA LEVEL RANGES
| TCA | Blood level (ng/ml) |
|---|---|
| Amitriptyline | 100-250 |
| Amoxapine | Unknown |
| Clomipramine | Unknown |
| Desipramine | Unknown |
| Doxepin | 120-250 |
| Imipramine | 150-300 |
| Maprotiline | 150-250 |
| Nortriptyline | 50-150 |
| Protriptyline | 75-250 |
| Trimipramine | Unknown |
| Trazodone | Unknown |
| + Only nortriptyline has a clear therapeutic window. The others are either approximate or unknown. | |
Sedation is a common side effect caused by the antihistaminic properties of some TCAs (Table 2). Agents with this effect (e.g., doxepin), when given once daily at bedtime, can benefit patients with concomitant sleep disturbance.
Weight gain Patients being treated with TCAs often gain weight, most likely because of carbohydrate craving associated with H2 blockade. Patient education, monitoring of weight, and dietary counseling may be necessary during TCA use. Regular exercise is recommended, although depressed patients often lack the motivation and energy to exercise.
Cardiovascular toxicity All TCAs have potential cardiovascular effects (Table 3), which are seen on an ECG as increased PR, QRS, or QTc intervals, especially at higher dosages or in patients with pre-existing cardiac disease.19 Orthostatic hypotension is among the most common cardiovascular side effects, particularly in the elderly, and may result in falls or other injuries.
A baseline ECG is recommended before starting TCA therapy, especially in depressed patients with cardiac conduction delays (primary or secondary to concomitant medications). Routine ECGs should be used to monitor patients:
- with pre-existing cardiac disease;
- taking higher-than-recommended dosages of a TCA;
- taking other medications that may affect cardiac conduction.
When in doubt, obtaining a cardiology consultation is recommended.
CNS effects Signs of CNS toxicity include confusion, memory impairment, delirium, seizures, coma, and eventual respiratory depression.20 Risk factors include toxic TCA plasma levels, elderly patient age, and concomitant use of other medications, such as psychotropics (neuroleptics), anticholinergics, and antihistamines. CNS toxicity may be difficult to diagnose, as it may initially resemble worsening of depressed mood. Confusion or worsening of memory or cognitive function are predictors of CNS toxicity.
A patient with anticholinergic-related delirium should be monitored on a medical unit. A trial of physostigmine may be warranted to confirm the diagnosis.
Neurologic symptoms Maprotiline and clomipramine have been associated with an increased risk of seizures. Use reduced dosages in patients with a history of seizures or concomitant use of medications that may increase maprotiline or clomipramine levels or decrease the seizure threshold (e.g., other antidepressants, withdrawal from benzodiazepines). Amoxapine has been associated with extrapyramidal symptoms secondary to a neuroleptic metabolite.
Overdose The severity of adverse side effects often depends upon drug concentration. An overdose of as little as a 2-week supply of a TCA can cause potentially fatal arrhythmias.
Priapism Trazodone has been associated with priapism, which has an incidence rate of 1/6,000 in patients taking this drug. Priapism is a medical emergency that requires prompt treatment.
Administration
TCAs are well-absorbed following oral administration and reach peak plasma levels in 2 to 6 hours. The average half-life of approximately 24 hours often allows therapeutic levels to be achieved with once-daily dosing at bedtime (Table 3).
TCAs are metabolized primarily by the cytochrome P-450 2D6 (CYP2D6) isoenzyme. Patients differ by a factor of 30- to 40-fold in their rate of metabolism of some TCAs, depending on individual genotypes.
The 7 to 9% of Caucasians classified as poor metabolizers at CYP2D6 require much lower-than-usual dosages of secondary amine TCAs.21 he 50% of Asians who are intermediate metabolizers require one-half the usual dosage. Tailor therapy to the individual patient, starting low, checking plasma levels, and monitoring for side effects.
For patients who would benefit from TCAs’ H1 anxiolytic effects, start with bid or tid dosing and later switch to once daily after achieving efficacy.
When using TCAs, start low and go slow to maximize efficacy and minimize side effects, especially in the elderly patient. The goal is to treat the patient, not to achieve target serum levels. The most favorable results have been demonstrated when patients are maintained at the dosages to which they respond when their disorder is in the acute stage.17
Symptoms usually improve after 2 weeks of TCA therapy, and up to 6 weeks may be required for a clinically significant effect. For many depressed patients, symptoms of insomnia, anxiety, and poor appetite improve within the first few days.
Monitoring serum levels
Serum levels are useful for monitoring treatment, compliance, and toxicity.22 Because the most accurate TCA serum levels are found at steady state, check the level after the patient has been on TCA therapy for at least 5 days and 8 to 12 hours after the last dose. Serum levels may also guide dosage increases in patients who exhibit a partial response to therapy.
Table 4
DRUGS THAT INTERACT WITH TCAs
| Anticholinergic agents |
| Barbiturates |
| Cimetidine |
| Disulfiram |
| ETOH |
| Flecainide |
| Guanethidine |
| Haloperidol |
| MAOIs |
| Methylphenidate |
| Phenothiazines |
| Phenytoin |
| Propafenone |
| Quinidine |
| SSRIs (e.g., fluoxetine, sertraline, paroxetine) |
| Sympathomimetic drugs (e.g., norepinephrine, epinephrine) |
| Warfarin |
Nortriptyline has a therapeutic window between 50 and 150 ng/mL. Patients who do not respond to serum levels higher than 150 ng/mL may respond when the dosage is reduced and the serum level falls to within that range. If response is adequate and without side effects, however, there is no need to reduce the dose. Other, less clear therapeutic windows have been described for other TCAs (Table 3).
TCA metabolism is affected by age and interaction with other drugs. Closely monitor serum levels in elderly and medically compromised patients, especially during dosage increases. Pay particular attention to other medications that may affect serum levels23 (Table 4). SSRIs, particularly fluoxetine and paroxetine, may affect TCA plasma levels because of their potent inhibition of CYP2D6.
Individualize dosing and serum level monitoring. For example, the patient who is clinically tolerating a TCA and has a normal ECG does not require a serum level measurement, unless medically indicated.
Discontinuing tricyclics
When discontinuing a TCA, taper the dosage no more rapidly than 25 to 50 mg every 2 to 3 days. Abrupt discontinuation can cause cholinergic rebound, with symptoms such as nausea, cramping, headache, vomiting, and sweating. “Rebound hypomania” or “mania” have been reported with abrupt cessation of TCAs,24 especially in patients with bipolar disorder. If the etiology of rebound symptoms is unclear (i.e., medical versus psychiatric), re-administering the discontinued TCA should relieve the symptoms and confirm a diagnosis of discontinuation.
Related resources
- Schatzberg AF, Cole JO, DeBattista C. Antidepressants. Manual of clinical psychopharmacology (3rd ed). Washington, DC: American Psychiatric Press, 1997.
- Janicak PG, Davis JM, Preskorn SH, Ayd Jr. FJ. Principles and practice of psychopharmacotherapy (2nd ed). Baltimore: Lippincott Williams & Wilkins, 1997.
- PDR Psychotropic Prescribing Guide (2nd ed). Montvale, NJ: Medical Economics, 1999.
- National Library of Medicine, MedlinePlus Health Information: Antidepressants, tricyclics (http://www.nlm.nih.gov/medlineplus/druginfo/antidepressantstricyclicsystem202055.html)
Drug brand names
See table 1 for tricyclic drug brand names. Others mentioned in this article include:
- Bupropion • Wellbutrin
- Cimetidine • Tagamet
- Citalopram • Celexa
- Disulfiram • Antabuse
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Guanethidine • Ismelin
- Methylphenidate • Concerta, Ritalin
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Phenytoin • Dilantin
Disclosure
Dr. Zajecka reports that he receives grant/research support from, serves as a consultant to, and is on the speaker’s bureau of Bristol-Myers Squibb and Eli Lilly and Co.; receives grant/research support from Cephalon Inc., GlaxoSmithKline, Lichtwer Pharma, Merck and Co., MIICRO Inc., Otsuka Pharmaceuticals, Parke-Davis, Pfizer Inc., and Wyeth-Ayerst Pharmaceuticals; serves as a consultant to Abbott Laboratories; and is on the speaker’s bureau of Abbott Laboratories, Pfizer/Roerig, GlaxoSmithKline, Pharmacia, and Wyeth-Ayerst Pharmaceuticals.
Dr. Tummala reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. American Psychiatric Association Practice guideline for the treatment of patients with major depressive disorder. Am J Psychiatry 2000;157(4 suppl):1-45.
2. Texas Implementation of Medication Algorithms (TIMA) Strategies for the treatment of major depression (nonpsychotic). Texas Department of Mental Health and Mental Retardation, 1999 (www.mhmr.state.tx.us/centraloffice/medicaldirector/TIMA.html).
3. American Academy of Child and Adolescent Psychiatry Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37(10 suppl):63S-83S.
4. Richelson EJ. Pharmacology of antidepressants. Mayo Clin Proc 2001;76:511-27.
5. Roose SP, Glassman AH, Attia E, Woodring S. Comparative efficacy of selective serotonin reuptake inhibitors and tricyclics in the treatment of melancholia. Am J Psychiatry 1994;151:1735-9.
6. Nierenberg AA. The treatment of severe depression: is there an efficacy gap between SSRI and TCA antidepressant generations? J Clin Psychiatry 1994;55(suppl A):55-9,98-100.
7. Danish University Antidepressant Group Citalopram: clinical effect profile in comparison with clomipramine. A controlled multicenter study. Psychopharmacology 1986;90:131-8.
8. Danish University Antidepressant Group Paroxetine: a selective serotonin reuptake inhibitor showing better tolerance but weaker antidepressant effect than clomipraine in a controlled multicenter study. J Affect Disord 1990;18:289-99.
9. U.S. Department of Health and Human Services Depression Guideline Panel. Depression in Primary Care, vol. 2: Treatment of Major Depression. Rockville, Md: U.S. Department of Health and Human Services, 1993.
10. Song F, Freemantle N, Sheldon TA, et al. Selective serotonin reuptake inhibitors: meta-analysis of efficacy and acceptability. Br Med J 1993;306:683-7.
11. Piccinelli M, Pini S, Bellantuono C, Wilkinson G. Efficacy of drug treatment in obsessive-compulsive disorder: a meta-analytic review. Br J Psychiatry 1995;166:424-43.
12. Lydiard RB, Morton WA, Emmanuel NP, Zealberg JJ. Placebo-controlled, double-blind study of the clinical and metabolic effects of desipramine in panic disorder Psychopharmacol Bull. 1993;29(2):183-8.
13. Zajecka JM, Fawcett J. Antidepressant combination and potentiation. Psychiatr Med 1999;9(1):55-75.
14. Zajecka JM, Jeffriess H, Fawcett J. The efficacy of fluoxetine combined with a heterocyclic antidepressant in treatment-resistant depression: a retrospective analysis J Clin Psychiatry 1995;56:338-43.
15. Figueroa Y, Rosenberg DR, Birmaher B, Keshavan MS. Combination treatment with clomipramine and selective serotonin reuptake inhibitors for obsessive-compulsive disorder in children and adolescents. J Child Adolesc Psychopharmacol 1998;8(1):61-7.
16. Spiegel K, Kalb R, Pasternak GW. Analgesic activity of tricyclic antidepressants. Ann Neurol 1983;13:462-5.
17. Schatzberg AF, Cole JO, DeBattista C, eds Manual of clinical psychopharmacology. 3rd ed. Washington, DC: American Psychiatric Publishing, 1997.
18. Pope HG, Hudson JI, Jonas JM. Bulimia treated with imipramine: a placebo controlled, double-blind study. Am J Psychiatry 1983;140:554-8.
19. Roose SP, Glassman AH, Giardina GV, et al. Tricyclic antidepressants in depressed patients with cardiac conduction disease. Arch Gen Psychiatry 1987;44:273-5.
20. Preskorn SH, Jerkovich GS. Central nervous system toxicity of tricyclic antidepressants: phenomenology, course, risk factors, and role of therapeutic drug monitoring. J Clin Psychopharmacology. 1990;10:88-95.
21. Potter WZ, Husseini KM, Rudorfer MV. Tricyclics and tetracyclics. In: Schatzberg AF, Nemeroff CB, eds. The American Psychiatric Press Textbook of Psychopharmacology. 2nd ed. Washington, DC: American Psychiatric Publishing, 1998.
22. Preskorn SH. Tricyclic antidepressants: The whys and hows of therapeutic drug monitoring. J Clin Psychiatry 1989;50(7, suppl):34-42.
23. Bell IR, Cole JO. Fluoxetine induces elevation of desipramine levels and exacerbation of geriatric nonpsychotic depression. J Clin Psychopharmacol 1988;8:447-8.
24. Nelson JC, Shottenfeld RS, Conrad CD. Hypomania after desipramine withdrawal. Am J Psychiatry 1983;140:624-5.
1. American Psychiatric Association Practice guideline for the treatment of patients with major depressive disorder. Am J Psychiatry 2000;157(4 suppl):1-45.
2. Texas Implementation of Medication Algorithms (TIMA) Strategies for the treatment of major depression (nonpsychotic). Texas Department of Mental Health and Mental Retardation, 1999 (www.mhmr.state.tx.us/centraloffice/medicaldirector/TIMA.html).
3. American Academy of Child and Adolescent Psychiatry Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998;37(10 suppl):63S-83S.
4. Richelson EJ. Pharmacology of antidepressants. Mayo Clin Proc 2001;76:511-27.
5. Roose SP, Glassman AH, Attia E, Woodring S. Comparative efficacy of selective serotonin reuptake inhibitors and tricyclics in the treatment of melancholia. Am J Psychiatry 1994;151:1735-9.
6. Nierenberg AA. The treatment of severe depression: is there an efficacy gap between SSRI and TCA antidepressant generations? J Clin Psychiatry 1994;55(suppl A):55-9,98-100.
7. Danish University Antidepressant Group Citalopram: clinical effect profile in comparison with clomipramine. A controlled multicenter study. Psychopharmacology 1986;90:131-8.
8. Danish University Antidepressant Group Paroxetine: a selective serotonin reuptake inhibitor showing better tolerance but weaker antidepressant effect than clomipraine in a controlled multicenter study. J Affect Disord 1990;18:289-99.
9. U.S. Department of Health and Human Services Depression Guideline Panel. Depression in Primary Care, vol. 2: Treatment of Major Depression. Rockville, Md: U.S. Department of Health and Human Services, 1993.
10. Song F, Freemantle N, Sheldon TA, et al. Selective serotonin reuptake inhibitors: meta-analysis of efficacy and acceptability. Br Med J 1993;306:683-7.
11. Piccinelli M, Pini S, Bellantuono C, Wilkinson G. Efficacy of drug treatment in obsessive-compulsive disorder: a meta-analytic review. Br J Psychiatry 1995;166:424-43.
12. Lydiard RB, Morton WA, Emmanuel NP, Zealberg JJ. Placebo-controlled, double-blind study of the clinical and metabolic effects of desipramine in panic disorder Psychopharmacol Bull. 1993;29(2):183-8.
13. Zajecka JM, Fawcett J. Antidepressant combination and potentiation. Psychiatr Med 1999;9(1):55-75.
14. Zajecka JM, Jeffriess H, Fawcett J. The efficacy of fluoxetine combined with a heterocyclic antidepressant in treatment-resistant depression: a retrospective analysis J Clin Psychiatry 1995;56:338-43.
15. Figueroa Y, Rosenberg DR, Birmaher B, Keshavan MS. Combination treatment with clomipramine and selective serotonin reuptake inhibitors for obsessive-compulsive disorder in children and adolescents. J Child Adolesc Psychopharmacol 1998;8(1):61-7.
16. Spiegel K, Kalb R, Pasternak GW. Analgesic activity of tricyclic antidepressants. Ann Neurol 1983;13:462-5.
17. Schatzberg AF, Cole JO, DeBattista C, eds Manual of clinical psychopharmacology. 3rd ed. Washington, DC: American Psychiatric Publishing, 1997.
18. Pope HG, Hudson JI, Jonas JM. Bulimia treated with imipramine: a placebo controlled, double-blind study. Am J Psychiatry 1983;140:554-8.
19. Roose SP, Glassman AH, Giardina GV, et al. Tricyclic antidepressants in depressed patients with cardiac conduction disease. Arch Gen Psychiatry 1987;44:273-5.
20. Preskorn SH, Jerkovich GS. Central nervous system toxicity of tricyclic antidepressants: phenomenology, course, risk factors, and role of therapeutic drug monitoring. J Clin Psychopharmacology. 1990;10:88-95.
21. Potter WZ, Husseini KM, Rudorfer MV. Tricyclics and tetracyclics. In: Schatzberg AF, Nemeroff CB, eds. The American Psychiatric Press Textbook of Psychopharmacology. 2nd ed. Washington, DC: American Psychiatric Publishing, 1998.
22. Preskorn SH. Tricyclic antidepressants: The whys and hows of therapeutic drug monitoring. J Clin Psychiatry 1989;50(7, suppl):34-42.
23. Bell IR, Cole JO. Fluoxetine induces elevation of desipramine levels and exacerbation of geriatric nonpsychotic depression. J Clin Psychopharmacol 1988;8:447-8.
24. Nelson JC, Shottenfeld RS, Conrad CD. Hypomania after desipramine withdrawal. Am J Psychiatry 1983;140:624-5.
Substance abuse: 12 principles to more effective outpatient treatment
Outpatient treatment of substance abuse is changing as research and experience teach us more about the nature of addictive illness and the principles of recovery. The recommended approach now emphasizes ease of access, chronic rather than acute treatment, and collaboration rather than confrontation.
As psychiatrists, we should be familiar with these changes, so that we can offer our addicted patients effective treatment and referrals. In particular, those of us who lead multidisciplinary teams in mental health clinics and outpatient programs need strategies that will help us make sound clinical decisions on detoxification, medical or psychiatric stabilization, and rehabilitation goals.
A new protocol that addresses these needs is being developed by a consensus panel of the Center for Substance Abuse and Treatment (Box 1).1,2 Two of us (RFF, RR) are members of that panel, and we all are recognized experts in the outpatient treatment of addicted individuals, with combined experience of more than 70 years. Based on available evidence and expert opinion, we offer you 12 principles of outpatient substance dependence treatment that can help you achieve the most favorable results (Table 1).
Many Americans are seeking outpatient treatment for substance dependence, according to recent federal surveys. In 1999, at least 1 million people were admitted to state-funded outpatient substance abuse treatment programs,1 and an additional unknown number sought treatment from psychiatrists in private practice. Outpatient treatment, including intensive outpatient care, is the most common form of treatment and is offered at 82% of all addiction treatment facilities.2
A federally-sponsored national consensus panel on intensive outpatient treatment of substance abuse is revising the existing Treatment Improvement Protocol (TIP) on Intensive Outpatient Treatment. Dr. Forman is the chair and Dr. Rawson is a member of the consensus panel. The draft TIP is under review and planned for release in 2003 by the Center for Substance Abuse Treatment, a center of the Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.
Principle 1: Open the doors wider
Outpatient clinics were once considered inappropriate for addicted individuals with significant psychosocial problems (such as homelessness) or co-occurring psychiatric disorders. Successful outpatient treatment was thought possible only for high-functioning, employed addicts who were free of significant psychiatric comorbidity.
Today, it is accepted that outpatients with a wide range of biopsychosocial problems can be effectively treated IF they receive case management and housing support and their co-occurring medical and psychiatric conditions are stabilized.
Efforts to ease the addicted patient into treatment should begin the moment a potential patient or family member seeks help. The pleasure that substance abusers derive from drug use makes them typically ambivalent about stopping their compulsive behaviors, and delays or obstacles to admission lead to “no shows” and drop-outs.3 Admissions increase when patients are given appointments the day they call for help.
From the initial outpatient encounter, the patient should feel like a welcomed participant who is responsible for his or her recovery. Access to outpatient programs increases when:
- child-care assistance is provided as needed;
- hours of operation are designed for the patient’s (rather than the staff’s) convenience;
- transportation assistance is provided, particularly for adolescents;
- the treatment plan is flexible and individualized to meet each patient’s specific needs.
Principle 2: Do a comprehensive initial evaluation
The open-door approach is most successful when the psychiatrist performs a comprehensive initial psychiatric and medical evaluation and works closely with a specialized treatment team. The initial medical and psychiatric evaluation is beyond the scope of this article and has been previously reviewed.4 Determining the need for medical detoxification is a priority during this phase of treatment.
Drug use patterns The treating physician should maintain a high index of suspicion for conditions associated with drug use. Cocaine causes seizures and cardiac arrhythmias, as well as vasoconstriction that leads to tissue necrosis (i.e., myocardial infarction, stroke, spontaneous abortion, and renal failure). Alcohol abuse affects brain, liver, cardiac, and endocrine tissue. Heroin produces acute overdose through respiratory depression, and its IV route of administration increases the risk of AIDS, viral hepatitis, pneumonia, sepsis, and endocarditis.
Function Structured interviews such as the Addiction Severity Index (ASI)5 can be used to assess functional impairment. Because addicted patients may be reluctant to disclose sensitive personal information, it is important to collect collateral information from family and friends, laboratory tests, and medical records.
Psychiatric concerns Many psychiatric syndromes are caused by substance abuse. Cocaine intoxication is often associated with psychosis (paranoia, auditory and tactile hallucinations), panic anxiety, and aggressiveness, whereas cocaine withdrawal produces depressed mood. Depression is also highly associated with chronic alcohol and opiate dependence. Withdrawal from opioids, alcohol, and sedatives produces anxiety.
Patients with bipolar disorder, major depression, panic anxiety, and schizophrenia who present with co-occurring addiction require coordinated and simultaneous stabilization of their addictive and psychiatric disorders.
Table 1
12 PRINCIPLES OF EFFECTIVE OUTPATIENT ADDICTION TREATMENT
|
Principle 3: Build on existing motivation
That an addicted patient must “hit bottom” before successful treatment may begin is a common misconception. In truth, studies find similar outcomes in individuals who enter treatment voluntarily and those who are externally pressured or legally coerced.6 Regardless of patients’ motivation when they enter treatment, they are likely to alternate over time between being more and less motivated. For this reason, it is necessary to remind them why they sought treatment and to use existing external pressures.
For example, with the patient’s consent it would be valuable to maintain contact with a parole officer who mandated a patient’s substance-abuse treatment. Likewise, patients entering treatment under threat of divorce should be asked to consent to family contact and should receive family therapy. Families often provide useful clinical information and can exert powerful influence when the patient’s motivation wanes. A patient’s refusal to allow contact with family (or other important sources of collateral information) often represents resistance that should be explored clinically and addressed.
With open dialogue, resistance to treatment can be reduced with education, peer groups, and family therapy. Motivational enhancement and interviewing work described by Miller, Procaska, and DiClemente7,8 is designed to reduce treatment resistance in a respectful and clinically effective manner while avoiding confrontation that might provoke dropout and relapse.
Principle 4: Forge a therapeutic alliance
A therapeutic alliance produces positive outcomes in substance-dependent outpatients.9-11 A recent National Institute on Drug Abuse (NIDA) therapy manual notes that a therapeutic alliance exists when the patient perceives that:
- the clinician accepts and respects him or her;
- the patient’s problems can be overcome by working together with the clinician;
- the clinician understands what the patient is hoping to get out of treatment.12
Clinicians can help forge this therapeutic alliance by being active listeners, by being empathic and nonjudgmental, and by approaching treatment as an active collaboration.12
Principle 5: Make retention a priority
It is simple but true: you cannot treat a patient who has dropped out.
Treatment retention is associated with better outcomes13,14 and is a key indicator of the performance of an outpatient treatment program. High drop-out rates are demoralizing to patients who remain in treatment and to the clinicians who must document so-called “3-day treatments.” Because admission and initial evaluation of patients is labor-intensive, premature attrition is costly and time-consuming. Strategies to increase retention are listed in Table 2.
Table 2
STRATEGIES TO RETAIN PATIENTS IN TREATMENT
|
Clinicians can improve retention by tolerating different rates of change and levels of motivation. Individuals adopt new behaviors at different rates. You might become frustrated when patients do not immediately “buy” a particular version of recovery. Patients, however, often drop out when they feel they are being “force-fed” recommendations for sacrifice and major lifestyle changes that make no sense to them (at least not at the moment).
Principle 6: Provide ongoing care
Addiction is a complex biopsychosocial problem that requires long-term treatment. Even after extended abstinence, substance abusers experience craving and are vulnerable to relapse.
Addicts often enter outpatient treatment with psychosocial, medical, and psychiatric problems. Transformation from active addiction to full functioning in society requires sustained and conscientious effort by the patient, support system, and treatment team. Like asthma, diabetes, and other chronic diseases, addiction requires ongoing care.15
Unlike other chronic conditions, however, addiction is pleasure-reinforced, and addicted individuals are particularly at risk for relapse. Ongoing care may interrupt a relapse or at least interrupt it sooner than if no ongoing treatment were provided.
Substance dependence treatment for less than 90 days is of little or no use, and treatment lasting significantly longer often is indicated, according to the NIDA.16 When patients complete an intensive treatment phase, they should be evaluated for readiness to transfer to less-intensive care, with gradual transition from several therapeutic contacts per week, to weekly contact, to semimonthly contact, and so on. The concept of “graduation” should clearly convey not an ending but a “commencement” or beginning, as it does in college.
Unfortunately, the long-term approach to substance dependence is undermined by managed care organizations’ insistence on brief treatments. Also, regulations that view addiction as an acute episode may require that patient charts be closed at the end of intensive treatment. Such failures to appreciate the chronic nature of addiction undermine access to treatment and service delivery and contribute to recidivism and medical, social, criminal, and economic consequences associated with active addiction.
Principle 7: Match services with treatment needs
Outcomes improve when treatment services meet individual needs.17 Medical, psychiatric, psychosocial, legal, and housing problems can distract patients from the work of therapy. It is important to match each patient’s problems and needs with appropriate treatment settings, interventions, and services, according to the NIDA’s Principles of Drug Addiction Treatment.16 Creating flexible, responsive programs means more work for the treatment team, but it enhances the quality of care.
Treating concomitant psychiatric illness often requires innovations in outpatient treatment programs. For example, psychiatrists must avoid undermining treatment by inappropriately prescribing addictive agents such as benzodiazepines. At the same time, drug counselors may benefit from education about the potential benefits of medications in treating co-occuring disorders and craving. Coordinated delivery of psychiatric and rehabilitative treatment requires open communication in regularly scheduled multidisciplinary team meetings.
Principle 8: Monitor abstinence
Routine urine drug screens, Breathalyzer tests—administered at least weekly— and/or other laboratory tests to confirm self-reported abstinence can improve treatment outcomes. Regular drug and alcohol monitoring provides an objective indicator of progress, serves as a deterrent, and can help motivate the patient to withstand drug urges.
Individuals attempting abstinence from one substance have better outcomes if they abstain from all addictive substances18 (although tobacco use is controversial and requires further research). Even so, patients often continue to use addictive substances during treatment. Patients struggling with abstinence should not be discharged from treatment programs for manifesting the symptoms for which they are seeking treatment.
Substance-dependent individuals progress at different rates during treatment, and creative strategies to enhance motivation and retention can ultimately produce positive results. Outpatient clinics should consider different treatment tracks for patients at different stages of readiness for recovery.
- Substance Abuse and Mental Health Services Administration and Center for Substance Abuse Treatment www.health.org
- National Institute on Drug Abuse www.nida.nih.gov
- National Institute on Alcohol Abuse and Alcoholism www.niaaa.nih.gov
- Center on Addiction and Substance Abuse www.casacolumbia.org
- Join Together (an organization that advocates community-based efforts to reduce, prevent, and treat substance abuse) www.jointogether.org
- 12-step resources www.onlinerecovery.org and www.healingresource.org
Principle 9: Use 12-step and other community supports
Patients who participate in 12-step programs and treatments have better outcomes than those who do not.19-21 Still, patients in early recovery may find it difficult to join community-based support groups, such as Alcoholics Anonymous (AA). Patients are often ambivalent about—or strongly opposed to—joining AA because of embarrassment, negative experiences, or inadequate preparation for joining a 12-step fellowship. Substance abusers who are ambivalent about recovery often dispute 12-step directives on total abstinence, sweeping lifestyle changes, and the need to “give up control” over treatment recommendations. Common issues in early recovery include:
- how to select a 12-step home group and a sponsor;
- how to overcome uneasiness associated with being in a 12-step group;
- how to address any discomfort the patient may feel with the religious nature of 12-step meetings.22
Patients’ resistance to 12-step treatment should be explored and addressed. Sometimes all they need is encouragement and help in finding a sponsor. Those with more difficult concerns may need a different approach. For example, social phobia is common in alcoholics and can be exacerbated by 12-step meetings; symptoms often respond to beta-adrenergic blockade. Patients with schizophrenia and those with paranoid features often do poorly in 12-step treatment if their paranoid symptoms cannot be successfully managed.
Principle 10: Manage medications
To avoid drug interactions, all prescribers involved with the patient’s care should coordinate their medication management efforts. Many substance abusers suffer from co-occurring psychiatric conditions23 for which psychiatric medications are standard treatment.24,25 In addition, medical detoxification is often necessary for heroin, alcohol, and sedative/hypnotic-dependent individuals. These treatments, which are beyond the scope of this article, are best integrated with drug rehabilitation.
Various medications for addiction have been reported to improve outcome:
- Agonist treatment with methadone, a long-acting opioid, can reduce heroin use, crime, and the risk of illnesses such as AIDS and viral hepatitis that are associated with IV drug use.
- Buprenorphine, a partial opioid receptor agonist with similar benefits, may soon be approved for the treatment of opiate dependence in outpatient settings.26
- Naltrexone, an opioid receptor antagonist, has long been proposed as a treatment for opiate dependence and has been shown to be effective in alcoholism.27
No effective pharmacologic treatment is available for cocaine dependence, although this is the focus of extensive government-sponsored research.
Principle 11: Educate about addiction and recovery
A wealth of accurate, free information about addiction and recovery is available through Web sites (Box 2) and other sources.
Ideally, outpatients in early recovery should be oriented in how to refuse offers of addictive substances, stress management, relapse prevention, information about the biology of addiction, 12-step fellowship integration, and appropriate use of medications.
Principle 12: Involve families in treatment
Treatment outcomes improve when addicts’ families are involved in the recovery process.28,29 Some family members enable addictive behavior by purchasing drugs for their relatives or providing money for this purpose, while other families are knowledgeable about treatment and can be a vital force supporting the recovery process
Treatment can help modify unhealthy behavior patterns that some families develop to compensate for a substance abuser’s actions. Because substance use disorders often run in families, try to assess not only the identified patient but also others in the patient’s life.
Related resources
- Center for Substance Abuse Treatment (http://www.health.org/)
- Miller WR. Enhancing motivation for change in substance abuse treatment. CSAT treatment improvement protocol #35. U.S. Department of Health and Human Services, 1999.
- Rawson R. Treatment for stimulant use disorders. CSAT treatment improvement protocol #33. U.S. Department of Health and Human Services, 1999.
- Mercer DE, Woody GE. An individual drug counseling approach to treat cocaine addiction: The Collaborative Cocaine Treatment Study model. NIDA manual #3. Therapy manuals for drug addiction. U.S. Department of Health and Human Services, 1999.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
1. Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment episode data set (TEDS): 1994-1999. National admissions to substance abuse treatment services. DASIS series: S-14. DHHS publication no. (SMA) 01-3550. Rockville, MD: Department of Health and Human Services, 2001.
2. Substance Abuse and Mental Health Services Administration, Office of Applied Studies. 1999 uniform facility data set. DASIS series: S-12. Rockville, MD: Department of Health and Human Services, 2001.
3. Festinger DS, Lamb RJ, Kirby KC, Marlowe DB. The accelerated intake: a method for increasing initial attendance to outpatient cocaine treatment. J Applied Behav Analysis 1996;29(3):387-9.
4. Dackis CA, Gold MS. Psychiatric hospitals for treatment of dual diagnosis. In: Lowinson JH, ed. Substance abuse: A comprehensive textbook. 2nd ed. Baltimore: Williams & Wilkins, 1992;467-85.
5. McLellan AT, Luborsky L, et al. An improved diagnostic instrument for substance abuse patients, The Addiction Severity Index. J Nervous Mental Dis 1980;168:26-33.
6. Marlowe DB, Kirby KC, et al. Assessment of coercive and noncoercive pressures to enter drug abuse treatment. Drug & Alcohol Dependence 1996;42(2):77-84.
7. Prochaska JO, DiClemente CC. The transtheoretical approach: crossing traditional boundaries of therapy. Homewood, IL: Dow Jones, Irwin, 1984.
8. Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press, 1991.
9. National Institute on Drug Abuse. Beyond the therapeutic alliance: keeping the drug-dependent individual in treatment. Research monograph 165, NTIS 97-181606, Rockville, MD: National Institutes of Health, 1997.
10. Connors GJ, DiClemente CC, Dermen KH, et al. Predicting the therapeutic alliance in alcoholism treatment. J Studies Alcohol 2000;61(1):139-49.
11. Barber JP, Luborsky L, Gallop R, et al. Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. J Consult Clin Psychol 2001;69(1):119-24.
12. Mercer D, Woody G. Individual drug counseling. National Institute on Drug Abuse (NIDA) manual #3: Therapy manuals for drug addiction. (NIH pub. no. 99-4380). Bethesda, MD: National Institutes of Health, 1999.
13. McKay JR, Alterman AI, McLellan AT, Snider EC. Treatment goals, continuity of care, and outcome in a day hospital substance abuse rehabilitation program. Am J Psychiatry 1994;151(2):254-9.
14. Simpson DD, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychol Addictive Behaviors 1998;11(4):294-307.
15. McLellan T, Kleber H, O’Brien C. Drug dependence, a chronic medical illness: implications for treatment, insurance and outcomes evaluation. JAMA 2000;284:1689-95.
16. National Institute on Drug Abuse. Principles of drug addiction treatment: a research-based guide (NIH publication no. 00-4180). Rockville, MD: National Institutes of Health, 1999.
17. McLellan AT, Hagan TA, Levine M, et al. Supplemental social services improve outcomes in public addiction treatment. Addiction 1998;93:1489-99.
18. Hughes JR. Treatment of smoking cessation in smokers with past alcohol/drug problems. J Substance Abuse Treatment 1993;10:181-7.
19. DuPont RL, Shiraki S. Recent research in twelve step programs. In: Miller NS, ed. Principles of Addiction Medicine Chevy Chase, MD: American Society of Addiction Medicine, 1994.
20. Crits-Christoph P, Siqueland L, Blaine J, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry 1999;57(6):493-502.
21. McCrady BS, Miller WR (eds) Research on Alcoholics Anonymous New Brunswick, NJ: Rutgers Center of Alcohol Studies, 1993.
22. Nowinski J, Baker S, Carroll KM. Twelve-Step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. NIAAA Project MATCH Monograph Series, vol. 1. DHHS Pub. No. (ADM)92-1893. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, 1992.
23. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA 1990;264(19):2511-18.
24. Carroll KM. Integrating psychotherapy and pharmacotherapy in substance abuse treatment. In: Rotgers F, Keller DS, Morgenstern J, eds. Treating substance abuse: theory and technique. New York: Guilford Press, 1996.
25. Carroll KM, Nich C, Ball SA, et al. Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction (in press).
26. Ling W, Wesson DR, Charuvastra C, Klett CJ. A controlled trial comparing buprenorphine and methadone maintenance in opioid dependence. Arch Gen Psychiatry 1996;53:401-7.
27. Volpicelli JR, Alterman AI, Hayashida M, O’Brien CP. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry 1992;49:876-80.
28. McCrady BS, Noel NE, Abrams DB, et al. Comparative effectiveness of three types of spouse involvement in outpatient behavioral alcoholism treatment. J Studies Alcohol 1986;47:459-67.
29. Szapocznik J, Williams RA. Brief strategic family therapy: twenty-five years of interplay among theory, research and practice in adolescent behavior problems and drug abuse. Clin Child Family Psychol Rev 2000;3(2):117-34.
Outpatient treatment of substance abuse is changing as research and experience teach us more about the nature of addictive illness and the principles of recovery. The recommended approach now emphasizes ease of access, chronic rather than acute treatment, and collaboration rather than confrontation.
As psychiatrists, we should be familiar with these changes, so that we can offer our addicted patients effective treatment and referrals. In particular, those of us who lead multidisciplinary teams in mental health clinics and outpatient programs need strategies that will help us make sound clinical decisions on detoxification, medical or psychiatric stabilization, and rehabilitation goals.
A new protocol that addresses these needs is being developed by a consensus panel of the Center for Substance Abuse and Treatment (Box 1).1,2 Two of us (RFF, RR) are members of that panel, and we all are recognized experts in the outpatient treatment of addicted individuals, with combined experience of more than 70 years. Based on available evidence and expert opinion, we offer you 12 principles of outpatient substance dependence treatment that can help you achieve the most favorable results (Table 1).
Many Americans are seeking outpatient treatment for substance dependence, according to recent federal surveys. In 1999, at least 1 million people were admitted to state-funded outpatient substance abuse treatment programs,1 and an additional unknown number sought treatment from psychiatrists in private practice. Outpatient treatment, including intensive outpatient care, is the most common form of treatment and is offered at 82% of all addiction treatment facilities.2
A federally-sponsored national consensus panel on intensive outpatient treatment of substance abuse is revising the existing Treatment Improvement Protocol (TIP) on Intensive Outpatient Treatment. Dr. Forman is the chair and Dr. Rawson is a member of the consensus panel. The draft TIP is under review and planned for release in 2003 by the Center for Substance Abuse Treatment, a center of the Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.
Principle 1: Open the doors wider
Outpatient clinics were once considered inappropriate for addicted individuals with significant psychosocial problems (such as homelessness) or co-occurring psychiatric disorders. Successful outpatient treatment was thought possible only for high-functioning, employed addicts who were free of significant psychiatric comorbidity.
Today, it is accepted that outpatients with a wide range of biopsychosocial problems can be effectively treated IF they receive case management and housing support and their co-occurring medical and psychiatric conditions are stabilized.
Efforts to ease the addicted patient into treatment should begin the moment a potential patient or family member seeks help. The pleasure that substance abusers derive from drug use makes them typically ambivalent about stopping their compulsive behaviors, and delays or obstacles to admission lead to “no shows” and drop-outs.3 Admissions increase when patients are given appointments the day they call for help.
From the initial outpatient encounter, the patient should feel like a welcomed participant who is responsible for his or her recovery. Access to outpatient programs increases when:
- child-care assistance is provided as needed;
- hours of operation are designed for the patient’s (rather than the staff’s) convenience;
- transportation assistance is provided, particularly for adolescents;
- the treatment plan is flexible and individualized to meet each patient’s specific needs.
Principle 2: Do a comprehensive initial evaluation
The open-door approach is most successful when the psychiatrist performs a comprehensive initial psychiatric and medical evaluation and works closely with a specialized treatment team. The initial medical and psychiatric evaluation is beyond the scope of this article and has been previously reviewed.4 Determining the need for medical detoxification is a priority during this phase of treatment.
Drug use patterns The treating physician should maintain a high index of suspicion for conditions associated with drug use. Cocaine causes seizures and cardiac arrhythmias, as well as vasoconstriction that leads to tissue necrosis (i.e., myocardial infarction, stroke, spontaneous abortion, and renal failure). Alcohol abuse affects brain, liver, cardiac, and endocrine tissue. Heroin produces acute overdose through respiratory depression, and its IV route of administration increases the risk of AIDS, viral hepatitis, pneumonia, sepsis, and endocarditis.
Function Structured interviews such as the Addiction Severity Index (ASI)5 can be used to assess functional impairment. Because addicted patients may be reluctant to disclose sensitive personal information, it is important to collect collateral information from family and friends, laboratory tests, and medical records.
Psychiatric concerns Many psychiatric syndromes are caused by substance abuse. Cocaine intoxication is often associated with psychosis (paranoia, auditory and tactile hallucinations), panic anxiety, and aggressiveness, whereas cocaine withdrawal produces depressed mood. Depression is also highly associated with chronic alcohol and opiate dependence. Withdrawal from opioids, alcohol, and sedatives produces anxiety.
Patients with bipolar disorder, major depression, panic anxiety, and schizophrenia who present with co-occurring addiction require coordinated and simultaneous stabilization of their addictive and psychiatric disorders.
Table 1
12 PRINCIPLES OF EFFECTIVE OUTPATIENT ADDICTION TREATMENT
|
Principle 3: Build on existing motivation
That an addicted patient must “hit bottom” before successful treatment may begin is a common misconception. In truth, studies find similar outcomes in individuals who enter treatment voluntarily and those who are externally pressured or legally coerced.6 Regardless of patients’ motivation when they enter treatment, they are likely to alternate over time between being more and less motivated. For this reason, it is necessary to remind them why they sought treatment and to use existing external pressures.
For example, with the patient’s consent it would be valuable to maintain contact with a parole officer who mandated a patient’s substance-abuse treatment. Likewise, patients entering treatment under threat of divorce should be asked to consent to family contact and should receive family therapy. Families often provide useful clinical information and can exert powerful influence when the patient’s motivation wanes. A patient’s refusal to allow contact with family (or other important sources of collateral information) often represents resistance that should be explored clinically and addressed.
With open dialogue, resistance to treatment can be reduced with education, peer groups, and family therapy. Motivational enhancement and interviewing work described by Miller, Procaska, and DiClemente7,8 is designed to reduce treatment resistance in a respectful and clinically effective manner while avoiding confrontation that might provoke dropout and relapse.
Principle 4: Forge a therapeutic alliance
A therapeutic alliance produces positive outcomes in substance-dependent outpatients.9-11 A recent National Institute on Drug Abuse (NIDA) therapy manual notes that a therapeutic alliance exists when the patient perceives that:
- the clinician accepts and respects him or her;
- the patient’s problems can be overcome by working together with the clinician;
- the clinician understands what the patient is hoping to get out of treatment.12
Clinicians can help forge this therapeutic alliance by being active listeners, by being empathic and nonjudgmental, and by approaching treatment as an active collaboration.12
Principle 5: Make retention a priority
It is simple but true: you cannot treat a patient who has dropped out.
Treatment retention is associated with better outcomes13,14 and is a key indicator of the performance of an outpatient treatment program. High drop-out rates are demoralizing to patients who remain in treatment and to the clinicians who must document so-called “3-day treatments.” Because admission and initial evaluation of patients is labor-intensive, premature attrition is costly and time-consuming. Strategies to increase retention are listed in Table 2.
Table 2
STRATEGIES TO RETAIN PATIENTS IN TREATMENT
|
Clinicians can improve retention by tolerating different rates of change and levels of motivation. Individuals adopt new behaviors at different rates. You might become frustrated when patients do not immediately “buy” a particular version of recovery. Patients, however, often drop out when they feel they are being “force-fed” recommendations for sacrifice and major lifestyle changes that make no sense to them (at least not at the moment).
Principle 6: Provide ongoing care
Addiction is a complex biopsychosocial problem that requires long-term treatment. Even after extended abstinence, substance abusers experience craving and are vulnerable to relapse.
Addicts often enter outpatient treatment with psychosocial, medical, and psychiatric problems. Transformation from active addiction to full functioning in society requires sustained and conscientious effort by the patient, support system, and treatment team. Like asthma, diabetes, and other chronic diseases, addiction requires ongoing care.15
Unlike other chronic conditions, however, addiction is pleasure-reinforced, and addicted individuals are particularly at risk for relapse. Ongoing care may interrupt a relapse or at least interrupt it sooner than if no ongoing treatment were provided.
Substance dependence treatment for less than 90 days is of little or no use, and treatment lasting significantly longer often is indicated, according to the NIDA.16 When patients complete an intensive treatment phase, they should be evaluated for readiness to transfer to less-intensive care, with gradual transition from several therapeutic contacts per week, to weekly contact, to semimonthly contact, and so on. The concept of “graduation” should clearly convey not an ending but a “commencement” or beginning, as it does in college.
Unfortunately, the long-term approach to substance dependence is undermined by managed care organizations’ insistence on brief treatments. Also, regulations that view addiction as an acute episode may require that patient charts be closed at the end of intensive treatment. Such failures to appreciate the chronic nature of addiction undermine access to treatment and service delivery and contribute to recidivism and medical, social, criminal, and economic consequences associated with active addiction.
Principle 7: Match services with treatment needs
Outcomes improve when treatment services meet individual needs.17 Medical, psychiatric, psychosocial, legal, and housing problems can distract patients from the work of therapy. It is important to match each patient’s problems and needs with appropriate treatment settings, interventions, and services, according to the NIDA’s Principles of Drug Addiction Treatment.16 Creating flexible, responsive programs means more work for the treatment team, but it enhances the quality of care.
Treating concomitant psychiatric illness often requires innovations in outpatient treatment programs. For example, psychiatrists must avoid undermining treatment by inappropriately prescribing addictive agents such as benzodiazepines. At the same time, drug counselors may benefit from education about the potential benefits of medications in treating co-occuring disorders and craving. Coordinated delivery of psychiatric and rehabilitative treatment requires open communication in regularly scheduled multidisciplinary team meetings.
Principle 8: Monitor abstinence
Routine urine drug screens, Breathalyzer tests—administered at least weekly— and/or other laboratory tests to confirm self-reported abstinence can improve treatment outcomes. Regular drug and alcohol monitoring provides an objective indicator of progress, serves as a deterrent, and can help motivate the patient to withstand drug urges.
Individuals attempting abstinence from one substance have better outcomes if they abstain from all addictive substances18 (although tobacco use is controversial and requires further research). Even so, patients often continue to use addictive substances during treatment. Patients struggling with abstinence should not be discharged from treatment programs for manifesting the symptoms for which they are seeking treatment.
Substance-dependent individuals progress at different rates during treatment, and creative strategies to enhance motivation and retention can ultimately produce positive results. Outpatient clinics should consider different treatment tracks for patients at different stages of readiness for recovery.
- Substance Abuse and Mental Health Services Administration and Center for Substance Abuse Treatment www.health.org
- National Institute on Drug Abuse www.nida.nih.gov
- National Institute on Alcohol Abuse and Alcoholism www.niaaa.nih.gov
- Center on Addiction and Substance Abuse www.casacolumbia.org
- Join Together (an organization that advocates community-based efforts to reduce, prevent, and treat substance abuse) www.jointogether.org
- 12-step resources www.onlinerecovery.org and www.healingresource.org
Principle 9: Use 12-step and other community supports
Patients who participate in 12-step programs and treatments have better outcomes than those who do not.19-21 Still, patients in early recovery may find it difficult to join community-based support groups, such as Alcoholics Anonymous (AA). Patients are often ambivalent about—or strongly opposed to—joining AA because of embarrassment, negative experiences, or inadequate preparation for joining a 12-step fellowship. Substance abusers who are ambivalent about recovery often dispute 12-step directives on total abstinence, sweeping lifestyle changes, and the need to “give up control” over treatment recommendations. Common issues in early recovery include:
- how to select a 12-step home group and a sponsor;
- how to overcome uneasiness associated with being in a 12-step group;
- how to address any discomfort the patient may feel with the religious nature of 12-step meetings.22
Patients’ resistance to 12-step treatment should be explored and addressed. Sometimes all they need is encouragement and help in finding a sponsor. Those with more difficult concerns may need a different approach. For example, social phobia is common in alcoholics and can be exacerbated by 12-step meetings; symptoms often respond to beta-adrenergic blockade. Patients with schizophrenia and those with paranoid features often do poorly in 12-step treatment if their paranoid symptoms cannot be successfully managed.
Principle 10: Manage medications
To avoid drug interactions, all prescribers involved with the patient’s care should coordinate their medication management efforts. Many substance abusers suffer from co-occurring psychiatric conditions23 for which psychiatric medications are standard treatment.24,25 In addition, medical detoxification is often necessary for heroin, alcohol, and sedative/hypnotic-dependent individuals. These treatments, which are beyond the scope of this article, are best integrated with drug rehabilitation.
Various medications for addiction have been reported to improve outcome:
- Agonist treatment with methadone, a long-acting opioid, can reduce heroin use, crime, and the risk of illnesses such as AIDS and viral hepatitis that are associated with IV drug use.
- Buprenorphine, a partial opioid receptor agonist with similar benefits, may soon be approved for the treatment of opiate dependence in outpatient settings.26
- Naltrexone, an opioid receptor antagonist, has long been proposed as a treatment for opiate dependence and has been shown to be effective in alcoholism.27
No effective pharmacologic treatment is available for cocaine dependence, although this is the focus of extensive government-sponsored research.
Principle 11: Educate about addiction and recovery
A wealth of accurate, free information about addiction and recovery is available through Web sites (Box 2) and other sources.
Ideally, outpatients in early recovery should be oriented in how to refuse offers of addictive substances, stress management, relapse prevention, information about the biology of addiction, 12-step fellowship integration, and appropriate use of medications.
Principle 12: Involve families in treatment
Treatment outcomes improve when addicts’ families are involved in the recovery process.28,29 Some family members enable addictive behavior by purchasing drugs for their relatives or providing money for this purpose, while other families are knowledgeable about treatment and can be a vital force supporting the recovery process
Treatment can help modify unhealthy behavior patterns that some families develop to compensate for a substance abuser’s actions. Because substance use disorders often run in families, try to assess not only the identified patient but also others in the patient’s life.
Related resources
- Center for Substance Abuse Treatment (http://www.health.org/)
- Miller WR. Enhancing motivation for change in substance abuse treatment. CSAT treatment improvement protocol #35. U.S. Department of Health and Human Services, 1999.
- Rawson R. Treatment for stimulant use disorders. CSAT treatment improvement protocol #33. U.S. Department of Health and Human Services, 1999.
- Mercer DE, Woody GE. An individual drug counseling approach to treat cocaine addiction: The Collaborative Cocaine Treatment Study model. NIDA manual #3. Therapy manuals for drug addiction. U.S. Department of Health and Human Services, 1999.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
Outpatient treatment of substance abuse is changing as research and experience teach us more about the nature of addictive illness and the principles of recovery. The recommended approach now emphasizes ease of access, chronic rather than acute treatment, and collaboration rather than confrontation.
As psychiatrists, we should be familiar with these changes, so that we can offer our addicted patients effective treatment and referrals. In particular, those of us who lead multidisciplinary teams in mental health clinics and outpatient programs need strategies that will help us make sound clinical decisions on detoxification, medical or psychiatric stabilization, and rehabilitation goals.
A new protocol that addresses these needs is being developed by a consensus panel of the Center for Substance Abuse and Treatment (Box 1).1,2 Two of us (RFF, RR) are members of that panel, and we all are recognized experts in the outpatient treatment of addicted individuals, with combined experience of more than 70 years. Based on available evidence and expert opinion, we offer you 12 principles of outpatient substance dependence treatment that can help you achieve the most favorable results (Table 1).
Many Americans are seeking outpatient treatment for substance dependence, according to recent federal surveys. In 1999, at least 1 million people were admitted to state-funded outpatient substance abuse treatment programs,1 and an additional unknown number sought treatment from psychiatrists in private practice. Outpatient treatment, including intensive outpatient care, is the most common form of treatment and is offered at 82% of all addiction treatment facilities.2
A federally-sponsored national consensus panel on intensive outpatient treatment of substance abuse is revising the existing Treatment Improvement Protocol (TIP) on Intensive Outpatient Treatment. Dr. Forman is the chair and Dr. Rawson is a member of the consensus panel. The draft TIP is under review and planned for release in 2003 by the Center for Substance Abuse Treatment, a center of the Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.
Principle 1: Open the doors wider
Outpatient clinics were once considered inappropriate for addicted individuals with significant psychosocial problems (such as homelessness) or co-occurring psychiatric disorders. Successful outpatient treatment was thought possible only for high-functioning, employed addicts who were free of significant psychiatric comorbidity.
Today, it is accepted that outpatients with a wide range of biopsychosocial problems can be effectively treated IF they receive case management and housing support and their co-occurring medical and psychiatric conditions are stabilized.
Efforts to ease the addicted patient into treatment should begin the moment a potential patient or family member seeks help. The pleasure that substance abusers derive from drug use makes them typically ambivalent about stopping their compulsive behaviors, and delays or obstacles to admission lead to “no shows” and drop-outs.3 Admissions increase when patients are given appointments the day they call for help.
From the initial outpatient encounter, the patient should feel like a welcomed participant who is responsible for his or her recovery. Access to outpatient programs increases when:
- child-care assistance is provided as needed;
- hours of operation are designed for the patient’s (rather than the staff’s) convenience;
- transportation assistance is provided, particularly for adolescents;
- the treatment plan is flexible and individualized to meet each patient’s specific needs.
Principle 2: Do a comprehensive initial evaluation
The open-door approach is most successful when the psychiatrist performs a comprehensive initial psychiatric and medical evaluation and works closely with a specialized treatment team. The initial medical and psychiatric evaluation is beyond the scope of this article and has been previously reviewed.4 Determining the need for medical detoxification is a priority during this phase of treatment.
Drug use patterns The treating physician should maintain a high index of suspicion for conditions associated with drug use. Cocaine causes seizures and cardiac arrhythmias, as well as vasoconstriction that leads to tissue necrosis (i.e., myocardial infarction, stroke, spontaneous abortion, and renal failure). Alcohol abuse affects brain, liver, cardiac, and endocrine tissue. Heroin produces acute overdose through respiratory depression, and its IV route of administration increases the risk of AIDS, viral hepatitis, pneumonia, sepsis, and endocarditis.
Function Structured interviews such as the Addiction Severity Index (ASI)5 can be used to assess functional impairment. Because addicted patients may be reluctant to disclose sensitive personal information, it is important to collect collateral information from family and friends, laboratory tests, and medical records.
Psychiatric concerns Many psychiatric syndromes are caused by substance abuse. Cocaine intoxication is often associated with psychosis (paranoia, auditory and tactile hallucinations), panic anxiety, and aggressiveness, whereas cocaine withdrawal produces depressed mood. Depression is also highly associated with chronic alcohol and opiate dependence. Withdrawal from opioids, alcohol, and sedatives produces anxiety.
Patients with bipolar disorder, major depression, panic anxiety, and schizophrenia who present with co-occurring addiction require coordinated and simultaneous stabilization of their addictive and psychiatric disorders.
Table 1
12 PRINCIPLES OF EFFECTIVE OUTPATIENT ADDICTION TREATMENT
|
Principle 3: Build on existing motivation
That an addicted patient must “hit bottom” before successful treatment may begin is a common misconception. In truth, studies find similar outcomes in individuals who enter treatment voluntarily and those who are externally pressured or legally coerced.6 Regardless of patients’ motivation when they enter treatment, they are likely to alternate over time between being more and less motivated. For this reason, it is necessary to remind them why they sought treatment and to use existing external pressures.
For example, with the patient’s consent it would be valuable to maintain contact with a parole officer who mandated a patient’s substance-abuse treatment. Likewise, patients entering treatment under threat of divorce should be asked to consent to family contact and should receive family therapy. Families often provide useful clinical information and can exert powerful influence when the patient’s motivation wanes. A patient’s refusal to allow contact with family (or other important sources of collateral information) often represents resistance that should be explored clinically and addressed.
With open dialogue, resistance to treatment can be reduced with education, peer groups, and family therapy. Motivational enhancement and interviewing work described by Miller, Procaska, and DiClemente7,8 is designed to reduce treatment resistance in a respectful and clinically effective manner while avoiding confrontation that might provoke dropout and relapse.
Principle 4: Forge a therapeutic alliance
A therapeutic alliance produces positive outcomes in substance-dependent outpatients.9-11 A recent National Institute on Drug Abuse (NIDA) therapy manual notes that a therapeutic alliance exists when the patient perceives that:
- the clinician accepts and respects him or her;
- the patient’s problems can be overcome by working together with the clinician;
- the clinician understands what the patient is hoping to get out of treatment.12
Clinicians can help forge this therapeutic alliance by being active listeners, by being empathic and nonjudgmental, and by approaching treatment as an active collaboration.12
Principle 5: Make retention a priority
It is simple but true: you cannot treat a patient who has dropped out.
Treatment retention is associated with better outcomes13,14 and is a key indicator of the performance of an outpatient treatment program. High drop-out rates are demoralizing to patients who remain in treatment and to the clinicians who must document so-called “3-day treatments.” Because admission and initial evaluation of patients is labor-intensive, premature attrition is costly and time-consuming. Strategies to increase retention are listed in Table 2.
Table 2
STRATEGIES TO RETAIN PATIENTS IN TREATMENT
|
Clinicians can improve retention by tolerating different rates of change and levels of motivation. Individuals adopt new behaviors at different rates. You might become frustrated when patients do not immediately “buy” a particular version of recovery. Patients, however, often drop out when they feel they are being “force-fed” recommendations for sacrifice and major lifestyle changes that make no sense to them (at least not at the moment).
Principle 6: Provide ongoing care
Addiction is a complex biopsychosocial problem that requires long-term treatment. Even after extended abstinence, substance abusers experience craving and are vulnerable to relapse.
Addicts often enter outpatient treatment with psychosocial, medical, and psychiatric problems. Transformation from active addiction to full functioning in society requires sustained and conscientious effort by the patient, support system, and treatment team. Like asthma, diabetes, and other chronic diseases, addiction requires ongoing care.15
Unlike other chronic conditions, however, addiction is pleasure-reinforced, and addicted individuals are particularly at risk for relapse. Ongoing care may interrupt a relapse or at least interrupt it sooner than if no ongoing treatment were provided.
Substance dependence treatment for less than 90 days is of little or no use, and treatment lasting significantly longer often is indicated, according to the NIDA.16 When patients complete an intensive treatment phase, they should be evaluated for readiness to transfer to less-intensive care, with gradual transition from several therapeutic contacts per week, to weekly contact, to semimonthly contact, and so on. The concept of “graduation” should clearly convey not an ending but a “commencement” or beginning, as it does in college.
Unfortunately, the long-term approach to substance dependence is undermined by managed care organizations’ insistence on brief treatments. Also, regulations that view addiction as an acute episode may require that patient charts be closed at the end of intensive treatment. Such failures to appreciate the chronic nature of addiction undermine access to treatment and service delivery and contribute to recidivism and medical, social, criminal, and economic consequences associated with active addiction.
Principle 7: Match services with treatment needs
Outcomes improve when treatment services meet individual needs.17 Medical, psychiatric, psychosocial, legal, and housing problems can distract patients from the work of therapy. It is important to match each patient’s problems and needs with appropriate treatment settings, interventions, and services, according to the NIDA’s Principles of Drug Addiction Treatment.16 Creating flexible, responsive programs means more work for the treatment team, but it enhances the quality of care.
Treating concomitant psychiatric illness often requires innovations in outpatient treatment programs. For example, psychiatrists must avoid undermining treatment by inappropriately prescribing addictive agents such as benzodiazepines. At the same time, drug counselors may benefit from education about the potential benefits of medications in treating co-occuring disorders and craving. Coordinated delivery of psychiatric and rehabilitative treatment requires open communication in regularly scheduled multidisciplinary team meetings.
Principle 8: Monitor abstinence
Routine urine drug screens, Breathalyzer tests—administered at least weekly— and/or other laboratory tests to confirm self-reported abstinence can improve treatment outcomes. Regular drug and alcohol monitoring provides an objective indicator of progress, serves as a deterrent, and can help motivate the patient to withstand drug urges.
Individuals attempting abstinence from one substance have better outcomes if they abstain from all addictive substances18 (although tobacco use is controversial and requires further research). Even so, patients often continue to use addictive substances during treatment. Patients struggling with abstinence should not be discharged from treatment programs for manifesting the symptoms for which they are seeking treatment.
Substance-dependent individuals progress at different rates during treatment, and creative strategies to enhance motivation and retention can ultimately produce positive results. Outpatient clinics should consider different treatment tracks for patients at different stages of readiness for recovery.
- Substance Abuse and Mental Health Services Administration and Center for Substance Abuse Treatment www.health.org
- National Institute on Drug Abuse www.nida.nih.gov
- National Institute on Alcohol Abuse and Alcoholism www.niaaa.nih.gov
- Center on Addiction and Substance Abuse www.casacolumbia.org
- Join Together (an organization that advocates community-based efforts to reduce, prevent, and treat substance abuse) www.jointogether.org
- 12-step resources www.onlinerecovery.org and www.healingresource.org
Principle 9: Use 12-step and other community supports
Patients who participate in 12-step programs and treatments have better outcomes than those who do not.19-21 Still, patients in early recovery may find it difficult to join community-based support groups, such as Alcoholics Anonymous (AA). Patients are often ambivalent about—or strongly opposed to—joining AA because of embarrassment, negative experiences, or inadequate preparation for joining a 12-step fellowship. Substance abusers who are ambivalent about recovery often dispute 12-step directives on total abstinence, sweeping lifestyle changes, and the need to “give up control” over treatment recommendations. Common issues in early recovery include:
- how to select a 12-step home group and a sponsor;
- how to overcome uneasiness associated with being in a 12-step group;
- how to address any discomfort the patient may feel with the religious nature of 12-step meetings.22
Patients’ resistance to 12-step treatment should be explored and addressed. Sometimes all they need is encouragement and help in finding a sponsor. Those with more difficult concerns may need a different approach. For example, social phobia is common in alcoholics and can be exacerbated by 12-step meetings; symptoms often respond to beta-adrenergic blockade. Patients with schizophrenia and those with paranoid features often do poorly in 12-step treatment if their paranoid symptoms cannot be successfully managed.
Principle 10: Manage medications
To avoid drug interactions, all prescribers involved with the patient’s care should coordinate their medication management efforts. Many substance abusers suffer from co-occurring psychiatric conditions23 for which psychiatric medications are standard treatment.24,25 In addition, medical detoxification is often necessary for heroin, alcohol, and sedative/hypnotic-dependent individuals. These treatments, which are beyond the scope of this article, are best integrated with drug rehabilitation.
Various medications for addiction have been reported to improve outcome:
- Agonist treatment with methadone, a long-acting opioid, can reduce heroin use, crime, and the risk of illnesses such as AIDS and viral hepatitis that are associated with IV drug use.
- Buprenorphine, a partial opioid receptor agonist with similar benefits, may soon be approved for the treatment of opiate dependence in outpatient settings.26
- Naltrexone, an opioid receptor antagonist, has long been proposed as a treatment for opiate dependence and has been shown to be effective in alcoholism.27
No effective pharmacologic treatment is available for cocaine dependence, although this is the focus of extensive government-sponsored research.
Principle 11: Educate about addiction and recovery
A wealth of accurate, free information about addiction and recovery is available through Web sites (Box 2) and other sources.
Ideally, outpatients in early recovery should be oriented in how to refuse offers of addictive substances, stress management, relapse prevention, information about the biology of addiction, 12-step fellowship integration, and appropriate use of medications.
Principle 12: Involve families in treatment
Treatment outcomes improve when addicts’ families are involved in the recovery process.28,29 Some family members enable addictive behavior by purchasing drugs for their relatives or providing money for this purpose, while other families are knowledgeable about treatment and can be a vital force supporting the recovery process
Treatment can help modify unhealthy behavior patterns that some families develop to compensate for a substance abuser’s actions. Because substance use disorders often run in families, try to assess not only the identified patient but also others in the patient’s life.
Related resources
- Center for Substance Abuse Treatment (http://www.health.org/)
- Miller WR. Enhancing motivation for change in substance abuse treatment. CSAT treatment improvement protocol #35. U.S. Department of Health and Human Services, 1999.
- Rawson R. Treatment for stimulant use disorders. CSAT treatment improvement protocol #33. U.S. Department of Health and Human Services, 1999.
- Mercer DE, Woody GE. An individual drug counseling approach to treat cocaine addiction: The Collaborative Cocaine Treatment Study model. NIDA manual #3. Therapy manuals for drug addiction. U.S. Department of Health and Human Services, 1999.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
1. Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment episode data set (TEDS): 1994-1999. National admissions to substance abuse treatment services. DASIS series: S-14. DHHS publication no. (SMA) 01-3550. Rockville, MD: Department of Health and Human Services, 2001.
2. Substance Abuse and Mental Health Services Administration, Office of Applied Studies. 1999 uniform facility data set. DASIS series: S-12. Rockville, MD: Department of Health and Human Services, 2001.
3. Festinger DS, Lamb RJ, Kirby KC, Marlowe DB. The accelerated intake: a method for increasing initial attendance to outpatient cocaine treatment. J Applied Behav Analysis 1996;29(3):387-9.
4. Dackis CA, Gold MS. Psychiatric hospitals for treatment of dual diagnosis. In: Lowinson JH, ed. Substance abuse: A comprehensive textbook. 2nd ed. Baltimore: Williams & Wilkins, 1992;467-85.
5. McLellan AT, Luborsky L, et al. An improved diagnostic instrument for substance abuse patients, The Addiction Severity Index. J Nervous Mental Dis 1980;168:26-33.
6. Marlowe DB, Kirby KC, et al. Assessment of coercive and noncoercive pressures to enter drug abuse treatment. Drug & Alcohol Dependence 1996;42(2):77-84.
7. Prochaska JO, DiClemente CC. The transtheoretical approach: crossing traditional boundaries of therapy. Homewood, IL: Dow Jones, Irwin, 1984.
8. Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press, 1991.
9. National Institute on Drug Abuse. Beyond the therapeutic alliance: keeping the drug-dependent individual in treatment. Research monograph 165, NTIS 97-181606, Rockville, MD: National Institutes of Health, 1997.
10. Connors GJ, DiClemente CC, Dermen KH, et al. Predicting the therapeutic alliance in alcoholism treatment. J Studies Alcohol 2000;61(1):139-49.
11. Barber JP, Luborsky L, Gallop R, et al. Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. J Consult Clin Psychol 2001;69(1):119-24.
12. Mercer D, Woody G. Individual drug counseling. National Institute on Drug Abuse (NIDA) manual #3: Therapy manuals for drug addiction. (NIH pub. no. 99-4380). Bethesda, MD: National Institutes of Health, 1999.
13. McKay JR, Alterman AI, McLellan AT, Snider EC. Treatment goals, continuity of care, and outcome in a day hospital substance abuse rehabilitation program. Am J Psychiatry 1994;151(2):254-9.
14. Simpson DD, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychol Addictive Behaviors 1998;11(4):294-307.
15. McLellan T, Kleber H, O’Brien C. Drug dependence, a chronic medical illness: implications for treatment, insurance and outcomes evaluation. JAMA 2000;284:1689-95.
16. National Institute on Drug Abuse. Principles of drug addiction treatment: a research-based guide (NIH publication no. 00-4180). Rockville, MD: National Institutes of Health, 1999.
17. McLellan AT, Hagan TA, Levine M, et al. Supplemental social services improve outcomes in public addiction treatment. Addiction 1998;93:1489-99.
18. Hughes JR. Treatment of smoking cessation in smokers with past alcohol/drug problems. J Substance Abuse Treatment 1993;10:181-7.
19. DuPont RL, Shiraki S. Recent research in twelve step programs. In: Miller NS, ed. Principles of Addiction Medicine Chevy Chase, MD: American Society of Addiction Medicine, 1994.
20. Crits-Christoph P, Siqueland L, Blaine J, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry 1999;57(6):493-502.
21. McCrady BS, Miller WR (eds) Research on Alcoholics Anonymous New Brunswick, NJ: Rutgers Center of Alcohol Studies, 1993.
22. Nowinski J, Baker S, Carroll KM. Twelve-Step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. NIAAA Project MATCH Monograph Series, vol. 1. DHHS Pub. No. (ADM)92-1893. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, 1992.
23. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA 1990;264(19):2511-18.
24. Carroll KM. Integrating psychotherapy and pharmacotherapy in substance abuse treatment. In: Rotgers F, Keller DS, Morgenstern J, eds. Treating substance abuse: theory and technique. New York: Guilford Press, 1996.
25. Carroll KM, Nich C, Ball SA, et al. Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction (in press).
26. Ling W, Wesson DR, Charuvastra C, Klett CJ. A controlled trial comparing buprenorphine and methadone maintenance in opioid dependence. Arch Gen Psychiatry 1996;53:401-7.
27. Volpicelli JR, Alterman AI, Hayashida M, O’Brien CP. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry 1992;49:876-80.
28. McCrady BS, Noel NE, Abrams DB, et al. Comparative effectiveness of three types of spouse involvement in outpatient behavioral alcoholism treatment. J Studies Alcohol 1986;47:459-67.
29. Szapocznik J, Williams RA. Brief strategic family therapy: twenty-five years of interplay among theory, research and practice in adolescent behavior problems and drug abuse. Clin Child Family Psychol Rev 2000;3(2):117-34.
1. Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment episode data set (TEDS): 1994-1999. National admissions to substance abuse treatment services. DASIS series: S-14. DHHS publication no. (SMA) 01-3550. Rockville, MD: Department of Health and Human Services, 2001.
2. Substance Abuse and Mental Health Services Administration, Office of Applied Studies. 1999 uniform facility data set. DASIS series: S-12. Rockville, MD: Department of Health and Human Services, 2001.
3. Festinger DS, Lamb RJ, Kirby KC, Marlowe DB. The accelerated intake: a method for increasing initial attendance to outpatient cocaine treatment. J Applied Behav Analysis 1996;29(3):387-9.
4. Dackis CA, Gold MS. Psychiatric hospitals for treatment of dual diagnosis. In: Lowinson JH, ed. Substance abuse: A comprehensive textbook. 2nd ed. Baltimore: Williams & Wilkins, 1992;467-85.
5. McLellan AT, Luborsky L, et al. An improved diagnostic instrument for substance abuse patients, The Addiction Severity Index. J Nervous Mental Dis 1980;168:26-33.
6. Marlowe DB, Kirby KC, et al. Assessment of coercive and noncoercive pressures to enter drug abuse treatment. Drug & Alcohol Dependence 1996;42(2):77-84.
7. Prochaska JO, DiClemente CC. The transtheoretical approach: crossing traditional boundaries of therapy. Homewood, IL: Dow Jones, Irwin, 1984.
8. Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press, 1991.
9. National Institute on Drug Abuse. Beyond the therapeutic alliance: keeping the drug-dependent individual in treatment. Research monograph 165, NTIS 97-181606, Rockville, MD: National Institutes of Health, 1997.
10. Connors GJ, DiClemente CC, Dermen KH, et al. Predicting the therapeutic alliance in alcoholism treatment. J Studies Alcohol 2000;61(1):139-49.
11. Barber JP, Luborsky L, Gallop R, et al. Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. J Consult Clin Psychol 2001;69(1):119-24.
12. Mercer D, Woody G. Individual drug counseling. National Institute on Drug Abuse (NIDA) manual #3: Therapy manuals for drug addiction. (NIH pub. no. 99-4380). Bethesda, MD: National Institutes of Health, 1999.
13. McKay JR, Alterman AI, McLellan AT, Snider EC. Treatment goals, continuity of care, and outcome in a day hospital substance abuse rehabilitation program. Am J Psychiatry 1994;151(2):254-9.
14. Simpson DD, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychol Addictive Behaviors 1998;11(4):294-307.
15. McLellan T, Kleber H, O’Brien C. Drug dependence, a chronic medical illness: implications for treatment, insurance and outcomes evaluation. JAMA 2000;284:1689-95.
16. National Institute on Drug Abuse. Principles of drug addiction treatment: a research-based guide (NIH publication no. 00-4180). Rockville, MD: National Institutes of Health, 1999.
17. McLellan AT, Hagan TA, Levine M, et al. Supplemental social services improve outcomes in public addiction treatment. Addiction 1998;93:1489-99.
18. Hughes JR. Treatment of smoking cessation in smokers with past alcohol/drug problems. J Substance Abuse Treatment 1993;10:181-7.
19. DuPont RL, Shiraki S. Recent research in twelve step programs. In: Miller NS, ed. Principles of Addiction Medicine Chevy Chase, MD: American Society of Addiction Medicine, 1994.
20. Crits-Christoph P, Siqueland L, Blaine J, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry 1999;57(6):493-502.
21. McCrady BS, Miller WR (eds) Research on Alcoholics Anonymous New Brunswick, NJ: Rutgers Center of Alcohol Studies, 1993.
22. Nowinski J, Baker S, Carroll KM. Twelve-Step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. NIAAA Project MATCH Monograph Series, vol. 1. DHHS Pub. No. (ADM)92-1893. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, 1992.
23. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA 1990;264(19):2511-18.
24. Carroll KM. Integrating psychotherapy and pharmacotherapy in substance abuse treatment. In: Rotgers F, Keller DS, Morgenstern J, eds. Treating substance abuse: theory and technique. New York: Guilford Press, 1996.
25. Carroll KM, Nich C, Ball SA, et al. Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction (in press).
26. Ling W, Wesson DR, Charuvastra C, Klett CJ. A controlled trial comparing buprenorphine and methadone maintenance in opioid dependence. Arch Gen Psychiatry 1996;53:401-7.
27. Volpicelli JR, Alterman AI, Hayashida M, O’Brien CP. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry 1992;49:876-80.
28. McCrady BS, Noel NE, Abrams DB, et al. Comparative effectiveness of three types of spouse involvement in outpatient behavioral alcoholism treatment. J Studies Alcohol 1986;47:459-67.
29. Szapocznik J, Williams RA. Brief strategic family therapy: twenty-five years of interplay among theory, research and practice in adolescent behavior problems and drug abuse. Clin Child Family Psychol Rev 2000;3(2):117-34.
MAO inhibitors: An option worth trying in treatment-resistant cases
Many fully trained psychiatrists, even psychopharmacologists, have rarely prescribed a monoamine oxidase inhibitor (MAOI), afraid of the possible consequences. One Boston-area psychiatrist who plans to retire soon has 12 patients who have been doing well for years on MAOIs. Before he called us, no psychiatrist in the area was willing to accept these patients who intended to stay on MAOIs.
Despite their potential side effects, the older MAOIs (phenelzine, tranylcypromine, isocarboxazid, and selegiline) have all been proven effective in depression; some studies have found them more effective than tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs).1,2 In our experience, MAOIs succeed in at least one-half the depressed patients who have failed on other antidepressants, and they are highly useful in treatment-resistant depressions and related disorders. Further, hypertensive crises are rare, and dietary restrictions are often exaggerated.
Drawing from the evidence and from our nearly 50 years’ experience in the use of MAOIs, we hope to acquaint or re-acquaint you with how to use these agents safely and to maximum effect.
When to use an MAOI
Reviews, meta-analyses, and more than 250 controlled studies have addressed MAOIs in psychiatric conditions.
The bulk of the literature reports a response rate of about 70% in various types of depression and anxiety.3 Unfortunately, because of the absence of major federal or industry funding, the findings are difficult to integrate, with most investigators testing different MAOIs on different subpopulations. This type of fragmented research, however, is not unique to MAOIs.
We at McLean have found MAOIs useful as second-line agents—and occasionally as first-line agents—in treating depression. We also use them as third-, fourth-, or fifth-line agents because we see many patients who have failed to respond to or tolerate several other antidepressants or whose response to other antidepressants has faded.
MAOIs are effective for a range of clinical presentations in inpatients and outpatients—depressive disorders (endogenous and atypical, unipolar and bipolar, neurasthenic and phobic), anxiety disorders (panic disorder and social phobia), and conditions as far afield as borderline personality disorder and the negative symptoms of schizophrenia.4
In controlled trials, many investigators have shown an MAOI to be more effective in some clinical conditions than a tricyclic and than a placebo.5 For example:
- A group at Columbia University studied phenelzine in various permutations of atypical depression (rejection sensitivity, overeating, oversleeping, mood reactivity, severe lack of physical energy).6
- Davidson et al studied isocarboxazid in anxious depression.7
- Thase and Himmelhoch studied tranylcypromine in anergic and bipolar depressions.8
- Liebowitz followed up with studies of phenelzine and tranylcypromine in social phobia.9
- At Yale, early studies were done with phenelzine in posttraumatic stress disorder (PTSD).10
- The British have generally argued for use of MAOIs in mixed anxiety and depression.11
- The magisterial text Manic Depressive Illness recommends MAOIs as first-line treatment for bipolar depression.12
All of these studies yielded clinically and statistically substantial results with modest adverse effects.
The enzymes MAO-A and MAO-B were identified in the 1950s. MAO-A occurs mainly in the intestine and brain, and the enzyme preferentially oxidizes (inactivates) serotonin and norepinephrine. MAO-B occurs in the brain and in platelets as well as in other tissues, and it inactivates phenylethylamine and benzylamine. Both enzymes metabolize tyramine and dopamine. The older MAOIs (phenelzine, tranylcypromine, isocarboxazid and high-dose selegiline) are irreversible MAO A and B inhibitors and block the actions of both enzymes from 14 to 28 days while new MAO enzymes are being resynthesized.
The actions of all MAOIs are presumed to be mediated by the blocking of the metabolism of intra- and extraneuronal biogenic amines, leading to increased brain levels of serotonin, norepinephrine, and dopamine.13 Even in the 1950s, when work with MAOIs was just beginning, these biogenic amines were suspected of being low or underactive in depression.
Research offers no real clues as to which enzyme is more important to inhibit or which of the various brain chemicals increased during MAOI therapy are crucial to clinical improvement. Two small studies suggest that decreasing the synthesis of brain serotonin will produce a temporary return of symptoms in patients clinically improved on MAOIs.14,15
The hypertensive crisis caused by tyramine has been shown to result from the inhibition of MAO-A, not MAO-B. More recent studies show effects of most MAOIs on receptors as well as enzymes. The basis or bases for MAO inhibitor actions may be more complex or different than anticipated.16
Characteristics of each agent
In the United States, a psychiatrist interested in using an MAOI for depressed patients can choose from among four agents. These older MAOIs are irreversible blockers of the enzymes MAO-A and MAO-B (Box 1).13-16
Tranylcypromine has been found effective in patients hospitalized with endogenous depressions.17 Most clinicians experienced with MAOIs prefer this agent because it triggers weight gain to a much lesser degree than other MAOIs. Tranylcypromine can cause insomnia and a greater increase in tyramine sensitivity than other MAOIs, which therefore brings a greater risk of hypertensive crisis.
Phenelzine has the advantage that the effective dosage for depression is probably now known—more than 1 mg/kg body weight—although in three earlier large negative controlled studies, the effective dosage was not known and too little was given for too short a period. Weight gain and hypotension may be more common with this drug than with other MAOIs.
Isocarboxazid is the least studied but has been shown to be effective, with an average 41% drug-placebo difference in two studies.16 One of us (JOC) preferred it for several years, based on good responses in a handful of treatment-resistant patients.
Selegiline is used in low dosages for parkinsonism. At higher dosages (more than 20 mg/d), selegiline is a good antidepressant but is no longer MAO-B selective—inhibiting both the MAO-B and MAO-A enzymes and thus requiring the usual dietary restrictions. One of us (JAB) routinely maintains bipolar patients with mild baseline depression or lethargy on a mood stabilizer plus a low dosage (5 to 10 mg/d) of selegiline. With this combination, patients are more satisfied and compliant with the mood stabilizer regimen and require no dietary restrictions.
Overall, there may be a special clinical benefit to phenelzine in the more anxious, easily distressed patient and to tranylcypromine or selegiline in the more sluggish, lethargic patient. But probably the soundest way to choose MAOIs is if other, more standard treatments have not worked.
Combinations with other antidepressants
We have found all antidepressants that do not involve significant serotonin reuptake inhibition (e.g., bupropion, trazodone, and tricyclics other than clomipramine) can be safely administered with MAOIs. Combination therapy is worth considering because it may be effective when other approaches have failed.
For a patient switching from an SSRI, a trial of one of these other antidepressants may be appropriate before undertaking MAOI therapy, simply because it avoids the SSRI washout period. Normally, patients should be off fluoxetine for 5 weeks, other SSRIs or clomipramine for 2 weeks, and venlafaxine for 1 week before starting an MAOI.
With the exception of clomipramine, TCAs generally are safe with MAOIs, although the Physician’s Desk Reference warns against adding a TCA to an MAOI. We know of one death and one case of delirium when parenteral imipramine was given to a patient who had been on a MAOI for some time unbeknownst to the MD giving the injection. Both amitriptyline (and by extension, nortriptyline) and trimipramine have been given along with an MAOI in controlled studies with no special adverse effects.18 Both drugs, and probably doxepin, are good hypnotics and seem safe in combination, although one should begin with a low dosage (e.g., 25 mg hs) if the patient is improving on an MAOI but is bothered by insomnia.
Table 1
RECOMMENDED MAOI DOSAGE RANGES
| Drug | Dosage range |
|---|---|
| Isocarboxazid | 20 to 80 mg/d |
| Moclobemide* | 300 to 900 mg/d |
| Phenelzine | 30 to 90 mg/d |
| Selegiline | 15 to 60 mg/d |
| Tranylcypromine | 20 to 100 mg/d |
| * Available in Canada but not in the United States | |
Trazodone is frequently employed as a remedy for MAOI-induced insomnia.19 Mirtazapine can be used safely in combination with MAOIs, and the agent has been reported to acutely treat serotonin syndrome.20
Determining dosage
Failure to understand the required effective dosages of MAOIs led to many early treatment failures and fueled clinicians’ perception that drugs in this class were ineffective. The senior author had to hospitalize a depressed man who had failed to improve on 30 mg/d of phenelzine for 10 days. The author later learned that a dose of more than 1 mg/kg per day for 3 to 4 weeks was necessary for response.
A rule of thumb is to start with one MAOI pill the first day and increase the dosage by one pill every 4 to 7 days until these levels are reached:
- 1 mg/kg/d for phenelzine;
- 40 mg/d for tranylcypromine and isocarboxazid;
- 45 mg/d for selegiline.
Reduce the dosage if side effects occur, or increase it if improvement is not noted in 1 to 2 months. We’ve tried starting patients on the 1 mg/kg dose of phenelzine the first day and elicited rapid and severe insomnia. Other intolerable side effects can also emerge from too-rapid dosage escalation. Clinical experience suggests the dosage ranges shown in Table 1.
Avoiding MAOI-related hypertension
We believe two factors have contributed to disuse of MAOIs by U.S. psychiatrists and slow development of new MAOIs here. These are the fear of severe hypertensive crisis and often vastly inflated MAOI dietary restrictions. In our practice, we provide patients receiving MAOIs with a reasonable list developed at the University of Toronto that explains foods to be avoided and alternatives that are allowed (Table 2).21
Table 2
DIETARY INSTRUCTIONS WITH MAOIs
| Several foods and beverages contain tyramine and may interact with your medication. You MUST follow the dietary instructions below, from the day before you start taking the medication until 2 weeks after you stop taking the medication. | Note: All foods must be fresh or properly frozen. If you are not aware of the storage conditions of a particular food, AVOID that food. |
| Food to avoid | Food allowed |
| Cheese | |
| All matured or aged cheese All casseroles made with cheeses (i.e., pizza, lasagna, etc.) | Fresh cottage cheese, cream cheese, ricotta cheese, and processed cheese slices. All fresh milk products that have been properly stored (i.e., sour cream, yogurt, ice cream) |
| Meat, fish, and poultry | |
| Fermented/dry sausage (pepperoni, salami, mortadella, summer sausage) Improperly stored meat, fish, poultry Improperly stored pickled herring | All fresh packaged or processed meat (e.g., chicken loaf, hot dogs), fish, or poultry. Store in refrigerator immediately, and eat as soon as possible |
| Fruits and vegetables | |
| Fava or broad bean pods (not beans) Banana peel | Raspberries up to a maximum of one-quarter pound at one time Banana pulp All others |
| Beverages | |
| All on-tap beer | Alcohol: No more than two bottled or canned beers or 4-fl. oz. glasses of red or white wine per day. This applies to nonalcoholic beer also. Red wine may produce headache unrelated to a rise in blood pressure |
| Miscellaneous | |
| Marmite-concentrated yeast extract Sauerkraut Soy sauce and other soy bean condiments | Other concentrated yeast extract (e.g., brewer’s yeast) Soy milk |
| Reprinted with permission of the department of pharmacy, Sunnybrook and Women’s College Health Science Center, North York, Ontario, Canada. Copyright 1994 | |
In experience, tyramine-associated hypertensive crisis in patients receiving the older MAOIs is rare, often very painful, and time-limited. Data on incidence of hypertensive crises with any MAOI is inadequate, except for a negligible incidence with low-dose selegiline and moclobemide (a reversible MAOI available in Canada but not in the United States). Most reported cases have involved tranylcypromine,22 which causes the greatest increase in sensitivity to tyramine, the basis of the dietary interaction with MAOIs.23 Specifically with tranylcypromine, transient hypertension can occur in the absence of dietary indiscretion or drug interaction.24,25
Food-associated hypertensive reactions are more common but unpredictable. A patient at McLean who had eaten cheese without trouble for 4 years while taking tranylcypromine in Europe mysteriously developed a severe headache after one bit of cheddar in the United States; she never tried an MAOI again. Another patient who took tranylcypromine for months at dosages exceeding 100 mg/d (but never took the tyramine restriction seriously) suffered a frightening pulsatile headache after a Chinese restaurant meal with soy sauce.
In our experience, oral adrenergic drugs (e.g., pseudoephedrine) can cause symptomatic hypertensive crises in patients taking MAOIs. Some over-the-counter cold preparations may contain an adrenergic decongestant, but it may not be listed clearly on the bottle. Cough syrup with codeine is preferable to OTC cough syrups that contain dextromethorphan. Patients should be urged to check labels and ask the pharmacist.
Advise patients taking MAOIs to purchase a blood pressure cuff or finger sphygmomanometer and learn how to take their own blood pressure. If they experience a “normal” headache and their systolic blood pressure is not elevated by at least 30 mm Hg, they are not having a “cheese reaction” and do not need to worry. MAOI headaches are typically unmistakable (they feel as if one’s head is splitting apart), and blood pressure is markedly elevated.
We give patients starting on MAOIs 10-mg tablets of nifedipine and advise them that if symptoms suggesting a hypertensive crisis appear, they should bite into one tablet to release the fluid inside and then swallow it. We tell patients to repeat this in 15 minutes if the headache is not receding; if the headache persists, they should visit the emergency ward or the internist’s office for observation.
Although there has been concern about the risk of MI or stroke with the hypotensive effect of nifedipine, we believe it is still the best option for acute severe hypertension in patients who do not have chronic hypertension. Chlorpromazine tablets (50 mg) also will stop the headache and lower blood pressure but will leave the patient groggy for about 24 hours, with possible extrapyramidal symptoms.
In the rare instance that a hypertensive crisis occurs, the “official” labeling recommendation is to give IV phentolamine, but we find emergency rooms either no longer stock the drug or do not remember to do this. Send any patient who is hurting and panicky to an ER, and call to suggest what the attending might do (i.e., IV phentolamine or oral nifedipine or chlorpromazine, or the emergency physician’s preference for hypertensive crisis).
Avoiding other MAOI-related side effects
Orthostatic hypotension is the most common early side effect of phenelzine and isocarboxazid. Clinically significant hypotension is best managed via dosage adjustment. If that fails, add Na Cl, 1 to 2 grams bid with increased fluids. If that doesn’t work, administer fludrocortisone, 0.1 to 0.4 mg/d. If that fails, administer d-amphetamine, starting with 2.5 to 5 mg/d, and observe carefully for hypertension.
An altered diurnal sleep cycle is another MAOI-related side effect. Some patients get extremely drowsy in the late afternoon but then may have insomnia at night.26 Attempts to alter this odd cycle by changing the timing of administration have generally not helped. We add a stimulant—pemoline (18.75 to 35.5 mg), d-amphetamine (2.5 to 5 mg), methylphenidate (5 to 10 mg), or modafinil (50 to 100 mg)—either in the morning or during afternoon sleepiness, with good effect and no hypertensive crises. We supervise the effect on blood pressure of the first few doses. Another helpful alternative has been to administer trazodone at night to initiate sleep.
Efforts over the years have been aimed at developing MAOIs that do not cause the tyramine reaction. One approach—devising reversible inhibitors of monoamine oxidase, which can be displaced from the MAO enzyme by tyramine—has resulted in two drugs (moclobemide and toloxatone) that are available in other parts of the world but not in the United States.27
Brofaromine, a reversible MAOI and an SSRI, looked promising in its clinical trials in Europe and the United States but was withdrawn from development by its manufacturer. A more recent approach to averting the MAOI-associated hypertensive interaction with dietary tyramine has been to deliver the drug parenterally, to spare the gut’s MAO-A.
Selegiline awaits Food and Drug Administration approval to be marketed in the United States as a transdermal preparation.28 The agent in this form would have several virtues, including a more stable blood level than the oral preparation and no clinically meaningful inhibition of intestinal MAO and thus no hypertensive crises.
MAOIs are adrenergic agonists, and dry mouth and constipation can occur as side effects; these can be treated with bethanechol. Edema also occurs, mainly with isocarboxazid and phenelzine, and responds in most cases to modest diuretic doses, such as hydrochlorothiazide, 50 mg/d.
The now-recognized trouble reaching orgasm on SSRIs was first reported to us by women on phenelzine, and this side effect is as difficult to treat with MAOIs as it is with other antidepressants. We have found that sexual dysfunction is less likely to occur with tranylcypromine and selegiline than other MAOIs.
Toward safer MAOIs
Newer reversible MAOIs are in development, and two agents are available (although not in the United States). Delivery systems that reduce the risk of hypertensive crisis also may soon be available (Box 2).27,28
Related resources
- Amsterdam JD, Chopra M. Monoamine oxidase inhibitors revisited. Psychiatric Ann2001;31(6):361-70.
- Treatment with antidepressants. In: Janicak PG, Davis JM, Preskorn SH, Ayd FJ, eds. Principles and practice of psychopharmacotherapy. 3rd ed. Philadelphia: Lippincott, Williams & Wilkins, 2001:215-326.
- Kennedy SH, ed. Clinical Advances in Monoamine Oxidase Inhibitor Therapies. Progress in Psychiatry Series. Washington, DC: American Psychiatric Press, 1994.
Drug brand names
- Isocarboxazide • Marplan
- Moclobemide • Aurorix, Manerix
- Phenelzine • Nardil
- Selegiline • Eldepryl
- Tranylcypromine • Parnate
Disclosure
Dr. Cole reports that he has served as a consultant to SmithKline Beecham Pharmaceuticals, manufacturer of tranylcypromine, and to Somerset Pharmaceuticals, manufacturer of selegiline in the United States. He also has participated in clinical studies of selegiline.
Dr. Bodkin reports that he has served as a consultant to Somerset Pharmaceuticals and has been principal investigator in several multicenter trials of selegiline.
1. Thase ME, Mallinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depression; IV; a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry 1992;149:195-8.
2. Thase ME, Trivedi MH, Rush AJ. MAOIs in the contemporary treatment of depression. Neuropsychopharmacol 1995;12(3):185-219.
3. Angst J, Amrein R, Stahl M. Moclobemide and tricyclic antidepressants in severe depression: meta-analysis and prospective studies. J Clin Psychopharmacology 1995;4(52):165-235.
4. Bodkin JA, Cohen BM, Cannon S, Salomon MS, Zornberg GL, Cole JO. Selegiline treatment of negative symptoms of schizophrenia and schizoaffective disorder: an open trial investigating the role of dopamine. J Nerv Ment Dis 1996;184:295-301.
5. Hudson JL, Pope HG. Affective spectrum disorder: does antidepressant response identify a family of disorders with a common pathophysiology? Am J Psychiatry 1990;147(15):552-64.
6. McGrath PJ, Stewart JW, Quitkin FM. The use of MAOIs for treating atypical depression. Psychiatric Ann 2001;31(6):371-5.
7. Davidson J, Giller EL, Zisook S, et al. An efficacy study of isocarboxazid and placebo in depression, and its relationship to depressive nosology. Arch Gen Psychiatry 1988;45:120-7.
8. Himmelhoch JM, Thase ME, Mallinger AG, Houck P. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry 1991;148(7):910-6.
9. Leibowitz MR, Heimberg RG, Schneier FR, et al. Cognitive-behavioral group therapy versus phenelzine in social phobia: long-term outcome. Depress Anxiety 1999;10(3):89-98.
10. Kosten TR, Frank JB, Dan E, McDougle CJ, Giller EL, Jr. Pharmacotherapy for posttraumatic stress disorder using phenelzine or imipramine. J Nerv Ment Dis 1991;179(6):366-70.
11. Pare CM. The present status of monoamine oxidase inhibitors. Br J Psychiatry 1985;146:576-84.
12. Goodwin FK, Jamison KR. Manic Depressive Illness. New York, Oxford University Press, 1990.
13. Glue P, Coupland N, Nutt DJ. Pharmacological basis for the therapeutic activity of MAOIs. In: Kennedy SH, ed. Clinical advances in monoamine oxidase inhibitor therapies. Progress in psychiatry, No. 43 Washington, DC: American Psychiatric Press, 1994;1-31.
14. Shopsin B, Friedman E, Gershon S. Parachlorophenylalanine reversal of tranylcypromine effects in depressed patients. Arch Gen Psychiatry 1976;33:881-91.
15. Delgado PL, Charney DS, Price LH, et al. Serotonin function and the mechanism of action of antidepressant treatment: reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan. Arch Gen Psychiatry 1990;47:411-18.
16. Shader R, Greenblatt D. The reappearance of a monoamine oxidase inhibitor (isocarboxazid). J Clin Psychopharmacol 1999;19(2):105-6.
17. McGrath PJ, Quitkin FM, Harrison W, et al. Treatment of melancholia with tranyl cypromine. Am J Psychiatry 1984;141:288-9.
18. White K, Simpson G. Combined MAOI-tricyclic antidepressant treatment: a reevaluation. J Clin Psychopharmacol 1981;1:264-82.
19. Nierenberg AA, Keck PE, Jr. Management of MAOI-associated insomnia with trazadone. J Clin Psychopharmacol 1989;9(1):42-5.
20. Hoes MJ, Zeijpveld JH. Mirtazapine as a treatment for serotonin syndrome. Pharmacopsychiatry 1996;29(2):81.-
21. Shulman KI, Walker SE. A reevaluation of dietary restrictions for irreversible MAOIs. Psychiatric Ann 2001;31(6):378-84.
22. Healy D. The Antidepressant Era. Cambridge, MA: Harvard University Press, 1997.
23. Bieck PR, Antonin K-H. Tyramine potentiation during treatment with MAOIs. In: Kennedy SH, ed. Clinical advances in monoamine oxidase inhibitor therapies. Progress in psychiatry, No. 43. Washington, DC: American Psychiatric Press, 1994;83-110.
24. Keck PE, Carter WP, et al. Acute cardiovascular effects of tranylcypromine: correlation with plasma drug, metabolite, norepinephrine and MHPG levels. J Clin Psychiatry 1991;92(6):250-4.
25. Keck PE, Pope HG, Jr, Nierenberg AA. Autoinduction of hypertensive reactions by tranylcypromine? J Clin Psychopharmacol 1989;9(1):148-51.
26. Teicher MH, Cohen BM, Baldessarini RJ, Cole JO. Severe daytime somnolence in patients treated with an MAOI. AmJ. Psychiatry 1988;145(12):1552-6.
27. Lotufo-Neto F, Trivedi M, Thase ME. Meta-analysis of the reversible inhibitors of monoamine oxidase Type A moclobemide and brofaromine for the treatment of depression. Neuropsychopharmacology 1999;20:226-47.
28. Bodkin JA, Kwon AE. Selegiline and other atypical monoamine oxidase inhibitors in depression. Psychiatric Ann 2001;31(6):385-91.
Many fully trained psychiatrists, even psychopharmacologists, have rarely prescribed a monoamine oxidase inhibitor (MAOI), afraid of the possible consequences. One Boston-area psychiatrist who plans to retire soon has 12 patients who have been doing well for years on MAOIs. Before he called us, no psychiatrist in the area was willing to accept these patients who intended to stay on MAOIs.
Despite their potential side effects, the older MAOIs (phenelzine, tranylcypromine, isocarboxazid, and selegiline) have all been proven effective in depression; some studies have found them more effective than tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs).1,2 In our experience, MAOIs succeed in at least one-half the depressed patients who have failed on other antidepressants, and they are highly useful in treatment-resistant depressions and related disorders. Further, hypertensive crises are rare, and dietary restrictions are often exaggerated.
Drawing from the evidence and from our nearly 50 years’ experience in the use of MAOIs, we hope to acquaint or re-acquaint you with how to use these agents safely and to maximum effect.
When to use an MAOI
Reviews, meta-analyses, and more than 250 controlled studies have addressed MAOIs in psychiatric conditions.
The bulk of the literature reports a response rate of about 70% in various types of depression and anxiety.3 Unfortunately, because of the absence of major federal or industry funding, the findings are difficult to integrate, with most investigators testing different MAOIs on different subpopulations. This type of fragmented research, however, is not unique to MAOIs.
We at McLean have found MAOIs useful as second-line agents—and occasionally as first-line agents—in treating depression. We also use them as third-, fourth-, or fifth-line agents because we see many patients who have failed to respond to or tolerate several other antidepressants or whose response to other antidepressants has faded.
MAOIs are effective for a range of clinical presentations in inpatients and outpatients—depressive disorders (endogenous and atypical, unipolar and bipolar, neurasthenic and phobic), anxiety disorders (panic disorder and social phobia), and conditions as far afield as borderline personality disorder and the negative symptoms of schizophrenia.4
In controlled trials, many investigators have shown an MAOI to be more effective in some clinical conditions than a tricyclic and than a placebo.5 For example:
- A group at Columbia University studied phenelzine in various permutations of atypical depression (rejection sensitivity, overeating, oversleeping, mood reactivity, severe lack of physical energy).6
- Davidson et al studied isocarboxazid in anxious depression.7
- Thase and Himmelhoch studied tranylcypromine in anergic and bipolar depressions.8
- Liebowitz followed up with studies of phenelzine and tranylcypromine in social phobia.9
- At Yale, early studies were done with phenelzine in posttraumatic stress disorder (PTSD).10
- The British have generally argued for use of MAOIs in mixed anxiety and depression.11
- The magisterial text Manic Depressive Illness recommends MAOIs as first-line treatment for bipolar depression.12
All of these studies yielded clinically and statistically substantial results with modest adverse effects.
The enzymes MAO-A and MAO-B were identified in the 1950s. MAO-A occurs mainly in the intestine and brain, and the enzyme preferentially oxidizes (inactivates) serotonin and norepinephrine. MAO-B occurs in the brain and in platelets as well as in other tissues, and it inactivates phenylethylamine and benzylamine. Both enzymes metabolize tyramine and dopamine. The older MAOIs (phenelzine, tranylcypromine, isocarboxazid and high-dose selegiline) are irreversible MAO A and B inhibitors and block the actions of both enzymes from 14 to 28 days while new MAO enzymes are being resynthesized.
The actions of all MAOIs are presumed to be mediated by the blocking of the metabolism of intra- and extraneuronal biogenic amines, leading to increased brain levels of serotonin, norepinephrine, and dopamine.13 Even in the 1950s, when work with MAOIs was just beginning, these biogenic amines were suspected of being low or underactive in depression.
Research offers no real clues as to which enzyme is more important to inhibit or which of the various brain chemicals increased during MAOI therapy are crucial to clinical improvement. Two small studies suggest that decreasing the synthesis of brain serotonin will produce a temporary return of symptoms in patients clinically improved on MAOIs.14,15
The hypertensive crisis caused by tyramine has been shown to result from the inhibition of MAO-A, not MAO-B. More recent studies show effects of most MAOIs on receptors as well as enzymes. The basis or bases for MAO inhibitor actions may be more complex or different than anticipated.16
Characteristics of each agent
In the United States, a psychiatrist interested in using an MAOI for depressed patients can choose from among four agents. These older MAOIs are irreversible blockers of the enzymes MAO-A and MAO-B (Box 1).13-16
Tranylcypromine has been found effective in patients hospitalized with endogenous depressions.17 Most clinicians experienced with MAOIs prefer this agent because it triggers weight gain to a much lesser degree than other MAOIs. Tranylcypromine can cause insomnia and a greater increase in tyramine sensitivity than other MAOIs, which therefore brings a greater risk of hypertensive crisis.
Phenelzine has the advantage that the effective dosage for depression is probably now known—more than 1 mg/kg body weight—although in three earlier large negative controlled studies, the effective dosage was not known and too little was given for too short a period. Weight gain and hypotension may be more common with this drug than with other MAOIs.
Isocarboxazid is the least studied but has been shown to be effective, with an average 41% drug-placebo difference in two studies.16 One of us (JOC) preferred it for several years, based on good responses in a handful of treatment-resistant patients.
Selegiline is used in low dosages for parkinsonism. At higher dosages (more than 20 mg/d), selegiline is a good antidepressant but is no longer MAO-B selective—inhibiting both the MAO-B and MAO-A enzymes and thus requiring the usual dietary restrictions. One of us (JAB) routinely maintains bipolar patients with mild baseline depression or lethargy on a mood stabilizer plus a low dosage (5 to 10 mg/d) of selegiline. With this combination, patients are more satisfied and compliant with the mood stabilizer regimen and require no dietary restrictions.
Overall, there may be a special clinical benefit to phenelzine in the more anxious, easily distressed patient and to tranylcypromine or selegiline in the more sluggish, lethargic patient. But probably the soundest way to choose MAOIs is if other, more standard treatments have not worked.
Combinations with other antidepressants
We have found all antidepressants that do not involve significant serotonin reuptake inhibition (e.g., bupropion, trazodone, and tricyclics other than clomipramine) can be safely administered with MAOIs. Combination therapy is worth considering because it may be effective when other approaches have failed.
For a patient switching from an SSRI, a trial of one of these other antidepressants may be appropriate before undertaking MAOI therapy, simply because it avoids the SSRI washout period. Normally, patients should be off fluoxetine for 5 weeks, other SSRIs or clomipramine for 2 weeks, and venlafaxine for 1 week before starting an MAOI.
With the exception of clomipramine, TCAs generally are safe with MAOIs, although the Physician’s Desk Reference warns against adding a TCA to an MAOI. We know of one death and one case of delirium when parenteral imipramine was given to a patient who had been on a MAOI for some time unbeknownst to the MD giving the injection. Both amitriptyline (and by extension, nortriptyline) and trimipramine have been given along with an MAOI in controlled studies with no special adverse effects.18 Both drugs, and probably doxepin, are good hypnotics and seem safe in combination, although one should begin with a low dosage (e.g., 25 mg hs) if the patient is improving on an MAOI but is bothered by insomnia.
Table 1
RECOMMENDED MAOI DOSAGE RANGES
| Drug | Dosage range |
|---|---|
| Isocarboxazid | 20 to 80 mg/d |
| Moclobemide* | 300 to 900 mg/d |
| Phenelzine | 30 to 90 mg/d |
| Selegiline | 15 to 60 mg/d |
| Tranylcypromine | 20 to 100 mg/d |
| * Available in Canada but not in the United States | |
Trazodone is frequently employed as a remedy for MAOI-induced insomnia.19 Mirtazapine can be used safely in combination with MAOIs, and the agent has been reported to acutely treat serotonin syndrome.20
Determining dosage
Failure to understand the required effective dosages of MAOIs led to many early treatment failures and fueled clinicians’ perception that drugs in this class were ineffective. The senior author had to hospitalize a depressed man who had failed to improve on 30 mg/d of phenelzine for 10 days. The author later learned that a dose of more than 1 mg/kg per day for 3 to 4 weeks was necessary for response.
A rule of thumb is to start with one MAOI pill the first day and increase the dosage by one pill every 4 to 7 days until these levels are reached:
- 1 mg/kg/d for phenelzine;
- 40 mg/d for tranylcypromine and isocarboxazid;
- 45 mg/d for selegiline.
Reduce the dosage if side effects occur, or increase it if improvement is not noted in 1 to 2 months. We’ve tried starting patients on the 1 mg/kg dose of phenelzine the first day and elicited rapid and severe insomnia. Other intolerable side effects can also emerge from too-rapid dosage escalation. Clinical experience suggests the dosage ranges shown in Table 1.
Avoiding MAOI-related hypertension
We believe two factors have contributed to disuse of MAOIs by U.S. psychiatrists and slow development of new MAOIs here. These are the fear of severe hypertensive crisis and often vastly inflated MAOI dietary restrictions. In our practice, we provide patients receiving MAOIs with a reasonable list developed at the University of Toronto that explains foods to be avoided and alternatives that are allowed (Table 2).21
Table 2
DIETARY INSTRUCTIONS WITH MAOIs
| Several foods and beverages contain tyramine and may interact with your medication. You MUST follow the dietary instructions below, from the day before you start taking the medication until 2 weeks after you stop taking the medication. | Note: All foods must be fresh or properly frozen. If you are not aware of the storage conditions of a particular food, AVOID that food. |
| Food to avoid | Food allowed |
| Cheese | |
| All matured or aged cheese All casseroles made with cheeses (i.e., pizza, lasagna, etc.) | Fresh cottage cheese, cream cheese, ricotta cheese, and processed cheese slices. All fresh milk products that have been properly stored (i.e., sour cream, yogurt, ice cream) |
| Meat, fish, and poultry | |
| Fermented/dry sausage (pepperoni, salami, mortadella, summer sausage) Improperly stored meat, fish, poultry Improperly stored pickled herring | All fresh packaged or processed meat (e.g., chicken loaf, hot dogs), fish, or poultry. Store in refrigerator immediately, and eat as soon as possible |
| Fruits and vegetables | |
| Fava or broad bean pods (not beans) Banana peel | Raspberries up to a maximum of one-quarter pound at one time Banana pulp All others |
| Beverages | |
| All on-tap beer | Alcohol: No more than two bottled or canned beers or 4-fl. oz. glasses of red or white wine per day. This applies to nonalcoholic beer also. Red wine may produce headache unrelated to a rise in blood pressure |
| Miscellaneous | |
| Marmite-concentrated yeast extract Sauerkraut Soy sauce and other soy bean condiments | Other concentrated yeast extract (e.g., brewer’s yeast) Soy milk |
| Reprinted with permission of the department of pharmacy, Sunnybrook and Women’s College Health Science Center, North York, Ontario, Canada. Copyright 1994 | |
In experience, tyramine-associated hypertensive crisis in patients receiving the older MAOIs is rare, often very painful, and time-limited. Data on incidence of hypertensive crises with any MAOI is inadequate, except for a negligible incidence with low-dose selegiline and moclobemide (a reversible MAOI available in Canada but not in the United States). Most reported cases have involved tranylcypromine,22 which causes the greatest increase in sensitivity to tyramine, the basis of the dietary interaction with MAOIs.23 Specifically with tranylcypromine, transient hypertension can occur in the absence of dietary indiscretion or drug interaction.24,25
Food-associated hypertensive reactions are more common but unpredictable. A patient at McLean who had eaten cheese without trouble for 4 years while taking tranylcypromine in Europe mysteriously developed a severe headache after one bit of cheddar in the United States; she never tried an MAOI again. Another patient who took tranylcypromine for months at dosages exceeding 100 mg/d (but never took the tyramine restriction seriously) suffered a frightening pulsatile headache after a Chinese restaurant meal with soy sauce.
In our experience, oral adrenergic drugs (e.g., pseudoephedrine) can cause symptomatic hypertensive crises in patients taking MAOIs. Some over-the-counter cold preparations may contain an adrenergic decongestant, but it may not be listed clearly on the bottle. Cough syrup with codeine is preferable to OTC cough syrups that contain dextromethorphan. Patients should be urged to check labels and ask the pharmacist.
Advise patients taking MAOIs to purchase a blood pressure cuff or finger sphygmomanometer and learn how to take their own blood pressure. If they experience a “normal” headache and their systolic blood pressure is not elevated by at least 30 mm Hg, they are not having a “cheese reaction” and do not need to worry. MAOI headaches are typically unmistakable (they feel as if one’s head is splitting apart), and blood pressure is markedly elevated.
We give patients starting on MAOIs 10-mg tablets of nifedipine and advise them that if symptoms suggesting a hypertensive crisis appear, they should bite into one tablet to release the fluid inside and then swallow it. We tell patients to repeat this in 15 minutes if the headache is not receding; if the headache persists, they should visit the emergency ward or the internist’s office for observation.
Although there has been concern about the risk of MI or stroke with the hypotensive effect of nifedipine, we believe it is still the best option for acute severe hypertension in patients who do not have chronic hypertension. Chlorpromazine tablets (50 mg) also will stop the headache and lower blood pressure but will leave the patient groggy for about 24 hours, with possible extrapyramidal symptoms.
In the rare instance that a hypertensive crisis occurs, the “official” labeling recommendation is to give IV phentolamine, but we find emergency rooms either no longer stock the drug or do not remember to do this. Send any patient who is hurting and panicky to an ER, and call to suggest what the attending might do (i.e., IV phentolamine or oral nifedipine or chlorpromazine, or the emergency physician’s preference for hypertensive crisis).
Avoiding other MAOI-related side effects
Orthostatic hypotension is the most common early side effect of phenelzine and isocarboxazid. Clinically significant hypotension is best managed via dosage adjustment. If that fails, add Na Cl, 1 to 2 grams bid with increased fluids. If that doesn’t work, administer fludrocortisone, 0.1 to 0.4 mg/d. If that fails, administer d-amphetamine, starting with 2.5 to 5 mg/d, and observe carefully for hypertension.
An altered diurnal sleep cycle is another MAOI-related side effect. Some patients get extremely drowsy in the late afternoon but then may have insomnia at night.26 Attempts to alter this odd cycle by changing the timing of administration have generally not helped. We add a stimulant—pemoline (18.75 to 35.5 mg), d-amphetamine (2.5 to 5 mg), methylphenidate (5 to 10 mg), or modafinil (50 to 100 mg)—either in the morning or during afternoon sleepiness, with good effect and no hypertensive crises. We supervise the effect on blood pressure of the first few doses. Another helpful alternative has been to administer trazodone at night to initiate sleep.
Efforts over the years have been aimed at developing MAOIs that do not cause the tyramine reaction. One approach—devising reversible inhibitors of monoamine oxidase, which can be displaced from the MAO enzyme by tyramine—has resulted in two drugs (moclobemide and toloxatone) that are available in other parts of the world but not in the United States.27
Brofaromine, a reversible MAOI and an SSRI, looked promising in its clinical trials in Europe and the United States but was withdrawn from development by its manufacturer. A more recent approach to averting the MAOI-associated hypertensive interaction with dietary tyramine has been to deliver the drug parenterally, to spare the gut’s MAO-A.
Selegiline awaits Food and Drug Administration approval to be marketed in the United States as a transdermal preparation.28 The agent in this form would have several virtues, including a more stable blood level than the oral preparation and no clinically meaningful inhibition of intestinal MAO and thus no hypertensive crises.
MAOIs are adrenergic agonists, and dry mouth and constipation can occur as side effects; these can be treated with bethanechol. Edema also occurs, mainly with isocarboxazid and phenelzine, and responds in most cases to modest diuretic doses, such as hydrochlorothiazide, 50 mg/d.
The now-recognized trouble reaching orgasm on SSRIs was first reported to us by women on phenelzine, and this side effect is as difficult to treat with MAOIs as it is with other antidepressants. We have found that sexual dysfunction is less likely to occur with tranylcypromine and selegiline than other MAOIs.
Toward safer MAOIs
Newer reversible MAOIs are in development, and two agents are available (although not in the United States). Delivery systems that reduce the risk of hypertensive crisis also may soon be available (Box 2).27,28
Related resources
- Amsterdam JD, Chopra M. Monoamine oxidase inhibitors revisited. Psychiatric Ann2001;31(6):361-70.
- Treatment with antidepressants. In: Janicak PG, Davis JM, Preskorn SH, Ayd FJ, eds. Principles and practice of psychopharmacotherapy. 3rd ed. Philadelphia: Lippincott, Williams & Wilkins, 2001:215-326.
- Kennedy SH, ed. Clinical Advances in Monoamine Oxidase Inhibitor Therapies. Progress in Psychiatry Series. Washington, DC: American Psychiatric Press, 1994.
Drug brand names
- Isocarboxazide • Marplan
- Moclobemide • Aurorix, Manerix
- Phenelzine • Nardil
- Selegiline • Eldepryl
- Tranylcypromine • Parnate
Disclosure
Dr. Cole reports that he has served as a consultant to SmithKline Beecham Pharmaceuticals, manufacturer of tranylcypromine, and to Somerset Pharmaceuticals, manufacturer of selegiline in the United States. He also has participated in clinical studies of selegiline.
Dr. Bodkin reports that he has served as a consultant to Somerset Pharmaceuticals and has been principal investigator in several multicenter trials of selegiline.
Many fully trained psychiatrists, even psychopharmacologists, have rarely prescribed a monoamine oxidase inhibitor (MAOI), afraid of the possible consequences. One Boston-area psychiatrist who plans to retire soon has 12 patients who have been doing well for years on MAOIs. Before he called us, no psychiatrist in the area was willing to accept these patients who intended to stay on MAOIs.
Despite their potential side effects, the older MAOIs (phenelzine, tranylcypromine, isocarboxazid, and selegiline) have all been proven effective in depression; some studies have found them more effective than tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs).1,2 In our experience, MAOIs succeed in at least one-half the depressed patients who have failed on other antidepressants, and they are highly useful in treatment-resistant depressions and related disorders. Further, hypertensive crises are rare, and dietary restrictions are often exaggerated.
Drawing from the evidence and from our nearly 50 years’ experience in the use of MAOIs, we hope to acquaint or re-acquaint you with how to use these agents safely and to maximum effect.
When to use an MAOI
Reviews, meta-analyses, and more than 250 controlled studies have addressed MAOIs in psychiatric conditions.
The bulk of the literature reports a response rate of about 70% in various types of depression and anxiety.3 Unfortunately, because of the absence of major federal or industry funding, the findings are difficult to integrate, with most investigators testing different MAOIs on different subpopulations. This type of fragmented research, however, is not unique to MAOIs.
We at McLean have found MAOIs useful as second-line agents—and occasionally as first-line agents—in treating depression. We also use them as third-, fourth-, or fifth-line agents because we see many patients who have failed to respond to or tolerate several other antidepressants or whose response to other antidepressants has faded.
MAOIs are effective for a range of clinical presentations in inpatients and outpatients—depressive disorders (endogenous and atypical, unipolar and bipolar, neurasthenic and phobic), anxiety disorders (panic disorder and social phobia), and conditions as far afield as borderline personality disorder and the negative symptoms of schizophrenia.4
In controlled trials, many investigators have shown an MAOI to be more effective in some clinical conditions than a tricyclic and than a placebo.5 For example:
- A group at Columbia University studied phenelzine in various permutations of atypical depression (rejection sensitivity, overeating, oversleeping, mood reactivity, severe lack of physical energy).6
- Davidson et al studied isocarboxazid in anxious depression.7
- Thase and Himmelhoch studied tranylcypromine in anergic and bipolar depressions.8
- Liebowitz followed up with studies of phenelzine and tranylcypromine in social phobia.9
- At Yale, early studies were done with phenelzine in posttraumatic stress disorder (PTSD).10
- The British have generally argued for use of MAOIs in mixed anxiety and depression.11
- The magisterial text Manic Depressive Illness recommends MAOIs as first-line treatment for bipolar depression.12
All of these studies yielded clinically and statistically substantial results with modest adverse effects.
The enzymes MAO-A and MAO-B were identified in the 1950s. MAO-A occurs mainly in the intestine and brain, and the enzyme preferentially oxidizes (inactivates) serotonin and norepinephrine. MAO-B occurs in the brain and in platelets as well as in other tissues, and it inactivates phenylethylamine and benzylamine. Both enzymes metabolize tyramine and dopamine. The older MAOIs (phenelzine, tranylcypromine, isocarboxazid and high-dose selegiline) are irreversible MAO A and B inhibitors and block the actions of both enzymes from 14 to 28 days while new MAO enzymes are being resynthesized.
The actions of all MAOIs are presumed to be mediated by the blocking of the metabolism of intra- and extraneuronal biogenic amines, leading to increased brain levels of serotonin, norepinephrine, and dopamine.13 Even in the 1950s, when work with MAOIs was just beginning, these biogenic amines were suspected of being low or underactive in depression.
Research offers no real clues as to which enzyme is more important to inhibit or which of the various brain chemicals increased during MAOI therapy are crucial to clinical improvement. Two small studies suggest that decreasing the synthesis of brain serotonin will produce a temporary return of symptoms in patients clinically improved on MAOIs.14,15
The hypertensive crisis caused by tyramine has been shown to result from the inhibition of MAO-A, not MAO-B. More recent studies show effects of most MAOIs on receptors as well as enzymes. The basis or bases for MAO inhibitor actions may be more complex or different than anticipated.16
Characteristics of each agent
In the United States, a psychiatrist interested in using an MAOI for depressed patients can choose from among four agents. These older MAOIs are irreversible blockers of the enzymes MAO-A and MAO-B (Box 1).13-16
Tranylcypromine has been found effective in patients hospitalized with endogenous depressions.17 Most clinicians experienced with MAOIs prefer this agent because it triggers weight gain to a much lesser degree than other MAOIs. Tranylcypromine can cause insomnia and a greater increase in tyramine sensitivity than other MAOIs, which therefore brings a greater risk of hypertensive crisis.
Phenelzine has the advantage that the effective dosage for depression is probably now known—more than 1 mg/kg body weight—although in three earlier large negative controlled studies, the effective dosage was not known and too little was given for too short a period. Weight gain and hypotension may be more common with this drug than with other MAOIs.
Isocarboxazid is the least studied but has been shown to be effective, with an average 41% drug-placebo difference in two studies.16 One of us (JOC) preferred it for several years, based on good responses in a handful of treatment-resistant patients.
Selegiline is used in low dosages for parkinsonism. At higher dosages (more than 20 mg/d), selegiline is a good antidepressant but is no longer MAO-B selective—inhibiting both the MAO-B and MAO-A enzymes and thus requiring the usual dietary restrictions. One of us (JAB) routinely maintains bipolar patients with mild baseline depression or lethargy on a mood stabilizer plus a low dosage (5 to 10 mg/d) of selegiline. With this combination, patients are more satisfied and compliant with the mood stabilizer regimen and require no dietary restrictions.
Overall, there may be a special clinical benefit to phenelzine in the more anxious, easily distressed patient and to tranylcypromine or selegiline in the more sluggish, lethargic patient. But probably the soundest way to choose MAOIs is if other, more standard treatments have not worked.
Combinations with other antidepressants
We have found all antidepressants that do not involve significant serotonin reuptake inhibition (e.g., bupropion, trazodone, and tricyclics other than clomipramine) can be safely administered with MAOIs. Combination therapy is worth considering because it may be effective when other approaches have failed.
For a patient switching from an SSRI, a trial of one of these other antidepressants may be appropriate before undertaking MAOI therapy, simply because it avoids the SSRI washout period. Normally, patients should be off fluoxetine for 5 weeks, other SSRIs or clomipramine for 2 weeks, and venlafaxine for 1 week before starting an MAOI.
With the exception of clomipramine, TCAs generally are safe with MAOIs, although the Physician’s Desk Reference warns against adding a TCA to an MAOI. We know of one death and one case of delirium when parenteral imipramine was given to a patient who had been on a MAOI for some time unbeknownst to the MD giving the injection. Both amitriptyline (and by extension, nortriptyline) and trimipramine have been given along with an MAOI in controlled studies with no special adverse effects.18 Both drugs, and probably doxepin, are good hypnotics and seem safe in combination, although one should begin with a low dosage (e.g., 25 mg hs) if the patient is improving on an MAOI but is bothered by insomnia.
Table 1
RECOMMENDED MAOI DOSAGE RANGES
| Drug | Dosage range |
|---|---|
| Isocarboxazid | 20 to 80 mg/d |
| Moclobemide* | 300 to 900 mg/d |
| Phenelzine | 30 to 90 mg/d |
| Selegiline | 15 to 60 mg/d |
| Tranylcypromine | 20 to 100 mg/d |
| * Available in Canada but not in the United States | |
Trazodone is frequently employed as a remedy for MAOI-induced insomnia.19 Mirtazapine can be used safely in combination with MAOIs, and the agent has been reported to acutely treat serotonin syndrome.20
Determining dosage
Failure to understand the required effective dosages of MAOIs led to many early treatment failures and fueled clinicians’ perception that drugs in this class were ineffective. The senior author had to hospitalize a depressed man who had failed to improve on 30 mg/d of phenelzine for 10 days. The author later learned that a dose of more than 1 mg/kg per day for 3 to 4 weeks was necessary for response.
A rule of thumb is to start with one MAOI pill the first day and increase the dosage by one pill every 4 to 7 days until these levels are reached:
- 1 mg/kg/d for phenelzine;
- 40 mg/d for tranylcypromine and isocarboxazid;
- 45 mg/d for selegiline.
Reduce the dosage if side effects occur, or increase it if improvement is not noted in 1 to 2 months. We’ve tried starting patients on the 1 mg/kg dose of phenelzine the first day and elicited rapid and severe insomnia. Other intolerable side effects can also emerge from too-rapid dosage escalation. Clinical experience suggests the dosage ranges shown in Table 1.
Avoiding MAOI-related hypertension
We believe two factors have contributed to disuse of MAOIs by U.S. psychiatrists and slow development of new MAOIs here. These are the fear of severe hypertensive crisis and often vastly inflated MAOI dietary restrictions. In our practice, we provide patients receiving MAOIs with a reasonable list developed at the University of Toronto that explains foods to be avoided and alternatives that are allowed (Table 2).21
Table 2
DIETARY INSTRUCTIONS WITH MAOIs
| Several foods and beverages contain tyramine and may interact with your medication. You MUST follow the dietary instructions below, from the day before you start taking the medication until 2 weeks after you stop taking the medication. | Note: All foods must be fresh or properly frozen. If you are not aware of the storage conditions of a particular food, AVOID that food. |
| Food to avoid | Food allowed |
| Cheese | |
| All matured or aged cheese All casseroles made with cheeses (i.e., pizza, lasagna, etc.) | Fresh cottage cheese, cream cheese, ricotta cheese, and processed cheese slices. All fresh milk products that have been properly stored (i.e., sour cream, yogurt, ice cream) |
| Meat, fish, and poultry | |
| Fermented/dry sausage (pepperoni, salami, mortadella, summer sausage) Improperly stored meat, fish, poultry Improperly stored pickled herring | All fresh packaged or processed meat (e.g., chicken loaf, hot dogs), fish, or poultry. Store in refrigerator immediately, and eat as soon as possible |
| Fruits and vegetables | |
| Fava or broad bean pods (not beans) Banana peel | Raspberries up to a maximum of one-quarter pound at one time Banana pulp All others |
| Beverages | |
| All on-tap beer | Alcohol: No more than two bottled or canned beers or 4-fl. oz. glasses of red or white wine per day. This applies to nonalcoholic beer also. Red wine may produce headache unrelated to a rise in blood pressure |
| Miscellaneous | |
| Marmite-concentrated yeast extract Sauerkraut Soy sauce and other soy bean condiments | Other concentrated yeast extract (e.g., brewer’s yeast) Soy milk |
| Reprinted with permission of the department of pharmacy, Sunnybrook and Women’s College Health Science Center, North York, Ontario, Canada. Copyright 1994 | |
In experience, tyramine-associated hypertensive crisis in patients receiving the older MAOIs is rare, often very painful, and time-limited. Data on incidence of hypertensive crises with any MAOI is inadequate, except for a negligible incidence with low-dose selegiline and moclobemide (a reversible MAOI available in Canada but not in the United States). Most reported cases have involved tranylcypromine,22 which causes the greatest increase in sensitivity to tyramine, the basis of the dietary interaction with MAOIs.23 Specifically with tranylcypromine, transient hypertension can occur in the absence of dietary indiscretion or drug interaction.24,25
Food-associated hypertensive reactions are more common but unpredictable. A patient at McLean who had eaten cheese without trouble for 4 years while taking tranylcypromine in Europe mysteriously developed a severe headache after one bit of cheddar in the United States; she never tried an MAOI again. Another patient who took tranylcypromine for months at dosages exceeding 100 mg/d (but never took the tyramine restriction seriously) suffered a frightening pulsatile headache after a Chinese restaurant meal with soy sauce.
In our experience, oral adrenergic drugs (e.g., pseudoephedrine) can cause symptomatic hypertensive crises in patients taking MAOIs. Some over-the-counter cold preparations may contain an adrenergic decongestant, but it may not be listed clearly on the bottle. Cough syrup with codeine is preferable to OTC cough syrups that contain dextromethorphan. Patients should be urged to check labels and ask the pharmacist.
Advise patients taking MAOIs to purchase a blood pressure cuff or finger sphygmomanometer and learn how to take their own blood pressure. If they experience a “normal” headache and their systolic blood pressure is not elevated by at least 30 mm Hg, they are not having a “cheese reaction” and do not need to worry. MAOI headaches are typically unmistakable (they feel as if one’s head is splitting apart), and blood pressure is markedly elevated.
We give patients starting on MAOIs 10-mg tablets of nifedipine and advise them that if symptoms suggesting a hypertensive crisis appear, they should bite into one tablet to release the fluid inside and then swallow it. We tell patients to repeat this in 15 minutes if the headache is not receding; if the headache persists, they should visit the emergency ward or the internist’s office for observation.
Although there has been concern about the risk of MI or stroke with the hypotensive effect of nifedipine, we believe it is still the best option for acute severe hypertension in patients who do not have chronic hypertension. Chlorpromazine tablets (50 mg) also will stop the headache and lower blood pressure but will leave the patient groggy for about 24 hours, with possible extrapyramidal symptoms.
In the rare instance that a hypertensive crisis occurs, the “official” labeling recommendation is to give IV phentolamine, but we find emergency rooms either no longer stock the drug or do not remember to do this. Send any patient who is hurting and panicky to an ER, and call to suggest what the attending might do (i.e., IV phentolamine or oral nifedipine or chlorpromazine, or the emergency physician’s preference for hypertensive crisis).
Avoiding other MAOI-related side effects
Orthostatic hypotension is the most common early side effect of phenelzine and isocarboxazid. Clinically significant hypotension is best managed via dosage adjustment. If that fails, add Na Cl, 1 to 2 grams bid with increased fluids. If that doesn’t work, administer fludrocortisone, 0.1 to 0.4 mg/d. If that fails, administer d-amphetamine, starting with 2.5 to 5 mg/d, and observe carefully for hypertension.
An altered diurnal sleep cycle is another MAOI-related side effect. Some patients get extremely drowsy in the late afternoon but then may have insomnia at night.26 Attempts to alter this odd cycle by changing the timing of administration have generally not helped. We add a stimulant—pemoline (18.75 to 35.5 mg), d-amphetamine (2.5 to 5 mg), methylphenidate (5 to 10 mg), or modafinil (50 to 100 mg)—either in the morning or during afternoon sleepiness, with good effect and no hypertensive crises. We supervise the effect on blood pressure of the first few doses. Another helpful alternative has been to administer trazodone at night to initiate sleep.
Efforts over the years have been aimed at developing MAOIs that do not cause the tyramine reaction. One approach—devising reversible inhibitors of monoamine oxidase, which can be displaced from the MAO enzyme by tyramine—has resulted in two drugs (moclobemide and toloxatone) that are available in other parts of the world but not in the United States.27
Brofaromine, a reversible MAOI and an SSRI, looked promising in its clinical trials in Europe and the United States but was withdrawn from development by its manufacturer. A more recent approach to averting the MAOI-associated hypertensive interaction with dietary tyramine has been to deliver the drug parenterally, to spare the gut’s MAO-A.
Selegiline awaits Food and Drug Administration approval to be marketed in the United States as a transdermal preparation.28 The agent in this form would have several virtues, including a more stable blood level than the oral preparation and no clinically meaningful inhibition of intestinal MAO and thus no hypertensive crises.
MAOIs are adrenergic agonists, and dry mouth and constipation can occur as side effects; these can be treated with bethanechol. Edema also occurs, mainly with isocarboxazid and phenelzine, and responds in most cases to modest diuretic doses, such as hydrochlorothiazide, 50 mg/d.
The now-recognized trouble reaching orgasm on SSRIs was first reported to us by women on phenelzine, and this side effect is as difficult to treat with MAOIs as it is with other antidepressants. We have found that sexual dysfunction is less likely to occur with tranylcypromine and selegiline than other MAOIs.
Toward safer MAOIs
Newer reversible MAOIs are in development, and two agents are available (although not in the United States). Delivery systems that reduce the risk of hypertensive crisis also may soon be available (Box 2).27,28
Related resources
- Amsterdam JD, Chopra M. Monoamine oxidase inhibitors revisited. Psychiatric Ann2001;31(6):361-70.
- Treatment with antidepressants. In: Janicak PG, Davis JM, Preskorn SH, Ayd FJ, eds. Principles and practice of psychopharmacotherapy. 3rd ed. Philadelphia: Lippincott, Williams & Wilkins, 2001:215-326.
- Kennedy SH, ed. Clinical Advances in Monoamine Oxidase Inhibitor Therapies. Progress in Psychiatry Series. Washington, DC: American Psychiatric Press, 1994.
Drug brand names
- Isocarboxazide • Marplan
- Moclobemide • Aurorix, Manerix
- Phenelzine • Nardil
- Selegiline • Eldepryl
- Tranylcypromine • Parnate
Disclosure
Dr. Cole reports that he has served as a consultant to SmithKline Beecham Pharmaceuticals, manufacturer of tranylcypromine, and to Somerset Pharmaceuticals, manufacturer of selegiline in the United States. He also has participated in clinical studies of selegiline.
Dr. Bodkin reports that he has served as a consultant to Somerset Pharmaceuticals and has been principal investigator in several multicenter trials of selegiline.
1. Thase ME, Mallinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depression; IV; a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry 1992;149:195-8.
2. Thase ME, Trivedi MH, Rush AJ. MAOIs in the contemporary treatment of depression. Neuropsychopharmacol 1995;12(3):185-219.
3. Angst J, Amrein R, Stahl M. Moclobemide and tricyclic antidepressants in severe depression: meta-analysis and prospective studies. J Clin Psychopharmacology 1995;4(52):165-235.
4. Bodkin JA, Cohen BM, Cannon S, Salomon MS, Zornberg GL, Cole JO. Selegiline treatment of negative symptoms of schizophrenia and schizoaffective disorder: an open trial investigating the role of dopamine. J Nerv Ment Dis 1996;184:295-301.
5. Hudson JL, Pope HG. Affective spectrum disorder: does antidepressant response identify a family of disorders with a common pathophysiology? Am J Psychiatry 1990;147(15):552-64.
6. McGrath PJ, Stewart JW, Quitkin FM. The use of MAOIs for treating atypical depression. Psychiatric Ann 2001;31(6):371-5.
7. Davidson J, Giller EL, Zisook S, et al. An efficacy study of isocarboxazid and placebo in depression, and its relationship to depressive nosology. Arch Gen Psychiatry 1988;45:120-7.
8. Himmelhoch JM, Thase ME, Mallinger AG, Houck P. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry 1991;148(7):910-6.
9. Leibowitz MR, Heimberg RG, Schneier FR, et al. Cognitive-behavioral group therapy versus phenelzine in social phobia: long-term outcome. Depress Anxiety 1999;10(3):89-98.
10. Kosten TR, Frank JB, Dan E, McDougle CJ, Giller EL, Jr. Pharmacotherapy for posttraumatic stress disorder using phenelzine or imipramine. J Nerv Ment Dis 1991;179(6):366-70.
11. Pare CM. The present status of monoamine oxidase inhibitors. Br J Psychiatry 1985;146:576-84.
12. Goodwin FK, Jamison KR. Manic Depressive Illness. New York, Oxford University Press, 1990.
13. Glue P, Coupland N, Nutt DJ. Pharmacological basis for the therapeutic activity of MAOIs. In: Kennedy SH, ed. Clinical advances in monoamine oxidase inhibitor therapies. Progress in psychiatry, No. 43 Washington, DC: American Psychiatric Press, 1994;1-31.
14. Shopsin B, Friedman E, Gershon S. Parachlorophenylalanine reversal of tranylcypromine effects in depressed patients. Arch Gen Psychiatry 1976;33:881-91.
15. Delgado PL, Charney DS, Price LH, et al. Serotonin function and the mechanism of action of antidepressant treatment: reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan. Arch Gen Psychiatry 1990;47:411-18.
16. Shader R, Greenblatt D. The reappearance of a monoamine oxidase inhibitor (isocarboxazid). J Clin Psychopharmacol 1999;19(2):105-6.
17. McGrath PJ, Quitkin FM, Harrison W, et al. Treatment of melancholia with tranyl cypromine. Am J Psychiatry 1984;141:288-9.
18. White K, Simpson G. Combined MAOI-tricyclic antidepressant treatment: a reevaluation. J Clin Psychopharmacol 1981;1:264-82.
19. Nierenberg AA, Keck PE, Jr. Management of MAOI-associated insomnia with trazadone. J Clin Psychopharmacol 1989;9(1):42-5.
20. Hoes MJ, Zeijpveld JH. Mirtazapine as a treatment for serotonin syndrome. Pharmacopsychiatry 1996;29(2):81.-
21. Shulman KI, Walker SE. A reevaluation of dietary restrictions for irreversible MAOIs. Psychiatric Ann 2001;31(6):378-84.
22. Healy D. The Antidepressant Era. Cambridge, MA: Harvard University Press, 1997.
23. Bieck PR, Antonin K-H. Tyramine potentiation during treatment with MAOIs. In: Kennedy SH, ed. Clinical advances in monoamine oxidase inhibitor therapies. Progress in psychiatry, No. 43. Washington, DC: American Psychiatric Press, 1994;83-110.
24. Keck PE, Carter WP, et al. Acute cardiovascular effects of tranylcypromine: correlation with plasma drug, metabolite, norepinephrine and MHPG levels. J Clin Psychiatry 1991;92(6):250-4.
25. Keck PE, Pope HG, Jr, Nierenberg AA. Autoinduction of hypertensive reactions by tranylcypromine? J Clin Psychopharmacol 1989;9(1):148-51.
26. Teicher MH, Cohen BM, Baldessarini RJ, Cole JO. Severe daytime somnolence in patients treated with an MAOI. AmJ. Psychiatry 1988;145(12):1552-6.
27. Lotufo-Neto F, Trivedi M, Thase ME. Meta-analysis of the reversible inhibitors of monoamine oxidase Type A moclobemide and brofaromine for the treatment of depression. Neuropsychopharmacology 1999;20:226-47.
28. Bodkin JA, Kwon AE. Selegiline and other atypical monoamine oxidase inhibitors in depression. Psychiatric Ann 2001;31(6):385-91.
1. Thase ME, Mallinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depression; IV; a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry 1992;149:195-8.
2. Thase ME, Trivedi MH, Rush AJ. MAOIs in the contemporary treatment of depression. Neuropsychopharmacol 1995;12(3):185-219.
3. Angst J, Amrein R, Stahl M. Moclobemide and tricyclic antidepressants in severe depression: meta-analysis and prospective studies. J Clin Psychopharmacology 1995;4(52):165-235.
4. Bodkin JA, Cohen BM, Cannon S, Salomon MS, Zornberg GL, Cole JO. Selegiline treatment of negative symptoms of schizophrenia and schizoaffective disorder: an open trial investigating the role of dopamine. J Nerv Ment Dis 1996;184:295-301.
5. Hudson JL, Pope HG. Affective spectrum disorder: does antidepressant response identify a family of disorders with a common pathophysiology? Am J Psychiatry 1990;147(15):552-64.
6. McGrath PJ, Stewart JW, Quitkin FM. The use of MAOIs for treating atypical depression. Psychiatric Ann 2001;31(6):371-5.
7. Davidson J, Giller EL, Zisook S, et al. An efficacy study of isocarboxazid and placebo in depression, and its relationship to depressive nosology. Arch Gen Psychiatry 1988;45:120-7.
8. Himmelhoch JM, Thase ME, Mallinger AG, Houck P. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry 1991;148(7):910-6.
9. Leibowitz MR, Heimberg RG, Schneier FR, et al. Cognitive-behavioral group therapy versus phenelzine in social phobia: long-term outcome. Depress Anxiety 1999;10(3):89-98.
10. Kosten TR, Frank JB, Dan E, McDougle CJ, Giller EL, Jr. Pharmacotherapy for posttraumatic stress disorder using phenelzine or imipramine. J Nerv Ment Dis 1991;179(6):366-70.
11. Pare CM. The present status of monoamine oxidase inhibitors. Br J Psychiatry 1985;146:576-84.
12. Goodwin FK, Jamison KR. Manic Depressive Illness. New York, Oxford University Press, 1990.
13. Glue P, Coupland N, Nutt DJ. Pharmacological basis for the therapeutic activity of MAOIs. In: Kennedy SH, ed. Clinical advances in monoamine oxidase inhibitor therapies. Progress in psychiatry, No. 43 Washington, DC: American Psychiatric Press, 1994;1-31.
14. Shopsin B, Friedman E, Gershon S. Parachlorophenylalanine reversal of tranylcypromine effects in depressed patients. Arch Gen Psychiatry 1976;33:881-91.
15. Delgado PL, Charney DS, Price LH, et al. Serotonin function and the mechanism of action of antidepressant treatment: reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan. Arch Gen Psychiatry 1990;47:411-18.
16. Shader R, Greenblatt D. The reappearance of a monoamine oxidase inhibitor (isocarboxazid). J Clin Psychopharmacol 1999;19(2):105-6.
17. McGrath PJ, Quitkin FM, Harrison W, et al. Treatment of melancholia with tranyl cypromine. Am J Psychiatry 1984;141:288-9.
18. White K, Simpson G. Combined MAOI-tricyclic antidepressant treatment: a reevaluation. J Clin Psychopharmacol 1981;1:264-82.
19. Nierenberg AA, Keck PE, Jr. Management of MAOI-associated insomnia with trazadone. J Clin Psychopharmacol 1989;9(1):42-5.
20. Hoes MJ, Zeijpveld JH. Mirtazapine as a treatment for serotonin syndrome. Pharmacopsychiatry 1996;29(2):81.-
21. Shulman KI, Walker SE. A reevaluation of dietary restrictions for irreversible MAOIs. Psychiatric Ann 2001;31(6):378-84.
22. Healy D. The Antidepressant Era. Cambridge, MA: Harvard University Press, 1997.
23. Bieck PR, Antonin K-H. Tyramine potentiation during treatment with MAOIs. In: Kennedy SH, ed. Clinical advances in monoamine oxidase inhibitor therapies. Progress in psychiatry, No. 43. Washington, DC: American Psychiatric Press, 1994;83-110.
24. Keck PE, Carter WP, et al. Acute cardiovascular effects of tranylcypromine: correlation with plasma drug, metabolite, norepinephrine and MHPG levels. J Clin Psychiatry 1991;92(6):250-4.
25. Keck PE, Pope HG, Jr, Nierenberg AA. Autoinduction of hypertensive reactions by tranylcypromine? J Clin Psychopharmacol 1989;9(1):148-51.
26. Teicher MH, Cohen BM, Baldessarini RJ, Cole JO. Severe daytime somnolence in patients treated with an MAOI. AmJ. Psychiatry 1988;145(12):1552-6.
27. Lotufo-Neto F, Trivedi M, Thase ME. Meta-analysis of the reversible inhibitors of monoamine oxidase Type A moclobemide and brofaromine for the treatment of depression. Neuropsychopharmacology 1999;20:226-47.
28. Bodkin JA, Kwon AE. Selegiline and other atypical monoamine oxidase inhibitors in depression. Psychiatric Ann 2001;31(6):385-91.
Antidepressants for fibromyalgia: Latest word on the link to depression and anxiety
Patients with fibromyalgia often resist being referred to a psychiatrist because they fear being told their pain and other somatic symptoms are “all in their heads.” Evidence is mounting that they may be literally correct—the symptoms of fibromyalgia appear to have a physiologic connection with the central nervous system. Abnormal CNS activity, including sleep patterns, response to stress, pain processing, and neurotransmitter levels, has been documented in patients with fibromyalgia.
As psychiatrists, we can reassure these patients—and their primary care physicians and rheumatologists—that we are in a position to help because we:
- have expertise in assessing mood and anxiety disorders and in managing antidepressants, the medication physicians most commonly prescribe for fibromyalgia;
- are skilled in the use of the anticonvulsant gabapentin, which is being used in fibromyalgia for its analgesic and sedative effects;
- can offer much-needed support through psychotherapy, as chronic pain and other fibromyalgia-related symptoms create great stress in these patients’ lives.
Antidepressants are showing promise as an effective treatment for pain, fatigue, and depression in patients with fibromyalgia in studies by our group and others. The following information can help you stay current with the newest understandings of this ailment.
Table 1
CRITERIA FOR DIAGNOSING FIBROMYALGIA
| 1. | History of widespread pain |
| Definition Pain in the right and left side of the body, pain above and below the waist, axial skeletal pain (cervical spine or anterior chest or thoracic spine or low back). In this definition, shoulder and buttock pain is considered as pain for each involved side. “Low back” pain is considered lower segment pain. | |
| 2. | Pain in 11 of 18 tender point sites on digital palpation |
| Definition Pain, on digital palpation, must be present in at least 11 of the following 18 tender points: | |
| Occiput Bilateral, at the suboccipital muscle insertion | |
| Low cervical Bilateral, at the anterior aspects of the intertransverse spaces at C5-C7 | |
| Trapezius Bilateral, at the midpoint of the upper border | |
| Supraspinatus Bilateral, at origins, above the scapula spine near the medial border | |
| Second rib Bilateral, at the second costochondral junctions, just lateral to the junctions on upper surfaces | |
| Lateral epicondyle Bilateral, 2 cm distal to the epicondyles | |
| Gluteal Bilateral, in upper outer quadrants of buttocks in anterior fold of muscle | |
| Greater trochanter Bilateral, posterior to the trochanteric prominence | |
| Knee Bilateral, at the medial fat pad proximal to the joint line | |
| Digital palpation should be performed with an approximate force of 4 kg. For a tender point to be considered “positive” the patient must state that the palpation was painful. “Tender” is not to be considered “painful” Source: American College of Rheumatology1 | |
Figure 1 LOCATION OF FIBROMYALGIA TENDER POINTS
To palpate tender point sites, pressure is applied with the thumb pad perpendicularly to each site and the force increased by 1 kg per second until 4 kg of pressure is achieved. Whitening of the thumbnail bed usually occurs when applying the 4-kg force.
Mood disorders in fibromyalgia
A diagnosis of fibromyalgia requires the finding of widespread pain and tenderness at specific anatomic points (Table 1, Figure 1).1 Most patients also report fatigue, sleep disturbance, and morning stiffness (Box 1).2-5 American College of Rheumatology criteria do not require exclusionary tests such as radiographs and blood tests for the diagnosis.
Primary care physicians are increasingly making the diagnosis themselves and referring patients to rheumatologists only when conditions other than fibromyalgia are suspected. The differential diagnosis is broad, and other rheumatic and nonrheumatic disorders have similar symptoms, require different treatment, and affect fibromyalgia management (Table 2).6
Patients with fibromyalgia often report symptoms of major depressive disorder, such as depressed mood, anxiety, fatigue, and insomnia.7 Many psychological studies of such patients have documented increased rates of depressive symptoms.8 Depression and anxiety symptoms are common and frequently severe, even among individuals with fibromyalgia in the general population.9
Patients’ mood and anxiety disorders correlate highly with the number of medically unexplained symptoms and are associated with functional disability.10 The presence of psychological symptoms predicts persistent fibromyalgia symptoms,11 and psychological distress is strongly associated with symptom severity.12
Evidence for a CNS link
CNS mechanisms appear to contribute to the development of clinical findings in fibromyalgia.
Abnormal sleep A qualitative defect in sleep has been identified in patients with fibromyalgia.13 This sleep abnormality consists of inappropriate intrusion of alpha waves (normally seen during wakefulness or REM sleep) into deep sleep (usually characterized by delta waves).13 Some researchers believe alpha-delta sleep intrusion is associated with the chronic musculoskeletal pain and fatigue of fibromyalgia and, in turn, is mediated by an abnormality in central serotonergic neurotransmission.14 This sleep abnormality is not specific to fibromyalgia and can be found in other conditions, however.15 Debate continues regarding the role of sleep dysregulation in the pathophysiology of fibromyalgia.
Fibromyalgia is more common in women than men, with an estimated prevalence of 2% in the general population (3.4% in women and 0.5% in men). Its prevalence increases with age, rising sharply in middle age and then dropping off after age 80.2
Fibromyalgia is seen most often in women ages 50 and older.2 It occurs in 5% to 6% of patients presenting to general medical and family practice clinics and in 15% to 20% of patients presenting to rheumatologists, making it one of the most common diagnoses in office-based rheumatology practices.
American College of Rheumatology criteria may require only widespread pain and tenderness for a diagnosis of fibromyalgia, but most patients (73% to 85%) also report fatigue, sleep disturbance, and morning stiffness. Many (45% to 69%) report “pain all over,” paresthesias, headache, and anxiety. Co-occurring irritable bowel syndrome, sicca symptoms, and Raynaud’s phenomenon are less common (<35%).1 Patients with fibromyalgia also have high lifetime rates of other comorbid disorders, including migraine, chronic fatigue syndrome, and mood and anxiety disorders. Some patients report weakness, forgetfulness, difficulties in concentration, urinary frequency, history of dysmenorrhea, and restless legs.
Fibromyalgia is chronic, debilitating, and often leads to substantial functional impairment.3 Most patients with fibromyalgia do not display significant improvement over an average of 7 years of treatment.4 Patients with fibromyalgia report lower quality of well-being than patients with diagnoses of chronic obstructive pulmonary disease, rheumatoid arthritis, atrial fibrillation, advanced cancer, and several other chronic diseases.5
Stress response Stress appears to precipitate or exacerbate fibromyalgia symptoms in many patients.16 For example, fibromyalgia appears to be associated with victimization (adult and childhood sexual, physical, and emotional trauma), and this stress may trigger the development of fibromyalgia in some patients.17
Patients with fibromyalgia appear to develop disturbances in the two major stress-response systems: the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system.16 Although the interpretation of these disturbances is still debated, some researchers suggest that the available data point to reduction in CNS corticotropin releasing hormone (CRH), the key mediator in the HPA axis.18,19 CRH is also a behaviorally active peptide that leads to physiologic and behavioral arousal when administered centrally to animals.18 CRH reduction could contribute to the clinical features of fibromyalgia (e.g., fatigue) either directly or indirectly by causing a relative glucocorticoid deficiency.18,19
Table 2
DIFFERENTIAL DIAGNOSIS OF FIBROMYALGIA
| Rheumatic disorders | Nonrheumatic disorders |
|---|---|
| Rheumatoid arthritis | Hypothyroidism |
| Systemic lupus erythematosus | Sleep apnea |
| Polyarticular osteoarthritis | Hepatitis |
| Polymyalgia rheumatica | Cushing’s syndrome |
| Addison’s disease | |
| Hyperparathyroidism | |
| Adapted from Clauw DJ. Fibromyalgia syndrome: an update on current understanding and medical management. Rheumatol Grand Rds 2000;3:1-9. | |
Fibromyalgia is also associated with moderate basal hypocortisolism.18,19 A relative glucocorticoid deficiency could contribute to fibromyalgia’s characteristic fatigue, arthralgias, myalgias, and disturbances in mood and sleep.18 This deficiency may also cause some of the immunologic disturbances seen with fibromyalgia.18,19
Atypical depression, which shares such features of fibromyalgia as profound lethargy, is also associated with inappropriately normal or reduced activation of the HPA axis and a functional deficit in the release of hypothalamic CRH.18 The unifying feature of HPA axis activity in both atypical depression and fibromyalgia may be a shared hypofunctioning.18 A more complete understanding of the neuroendocrine changes in fibromyalgia awaits further study.
Pain processing Aberrant CNS processing of pain may also play a role in fibromyalgia.16,20 Fibromyalgia is sometimes precipitated by physical trauma.21 A traumatic injury may start a process in susceptible individuals that leads to an enhanced central processing of painful stimuli characteristic of central sensitization.22 Patients with fibromyalgia often develop an increased response to painful stimuli (hyeralgesia) and experience pain from normally nonnoxious stimuli (allodynia).20
Substance P, an important nociceptive neurotransmitter, may have a role in generating central sensitization.23 Elevated concentrations of substance P have been found in the cerebrospinal fluid (CSF) of individuals with fibromyalgia.24 Substance P also inhibits CRH release and may contribute to low CRH activity in fibromyalgia.16
Neurotransmitter defects A functional reduction in serotonergic activity has been demonstrated in patients with fibromyalgia. Schwarz et al25 found a strong negative correlation between serum concentrations of the primary serotonin metabolite, 5-hydroxyindoleacetic acid (5-HIAA), and substance P, pain, and insomnia. Evidence also exists of reduced concentrations of the primary norepinephrine metabolite, 3-methoxy-4-hydroxyphenethylene (MHPG), in the CSF of patients with fibromyalgia.26 Reduced serotonin and norepinephrine levels in descending pain-inhibitory pathways may cause the allodynia and hyperalgesia of fibromyalgia.
Pharmacologic treatment
Most studies of pharmacologic treatment of fibromyalgia have examined antidepressants for three reasons:
- There is evidence of the successful use of antidepressants in other chronic pain conditions.27
- These agents are effective for treating mood and anxiety disorders, which frequently occur in patients with fibromyalgia and may share a common physiologic abnormality.28
- Antidepressants might enhance the activity of neurotransmitters such as serotonin and norepinephrine in the descending inhibitory pain pathways, leading to reduced pain perception.29
Tricyclics In randomized, controlled trials, tricyclic medications (including the muscle relaxant cyclobenzaprine) appear to be moderately effective in improving fibromyalgia symptoms. Two meta-analyses of trials of tricyclic medications (amitriptyline, dothiepin, cyclobenzaprine, clomipramine, and maprotiline) have found similar results.30,31 Our group found the greatest effect on measures of sleep improvement, which may be due in part to tricyclics’ sedative properties.30 Many patients with fibromyalgia, however, cannot tolerate the sedative and other side effects associated with tricyclic agents, even though low dosages (e.g., 25 mg/d of amitriptyline) have typically been used in clinical trials.
SSRIs. Selective serotonin reuptake inhibitors, although likely to be better tolerated than tricyclics, have been examined in only five placebo-controlled trials in fibromyalgia: two with citalopram, and three with fluoxetine. One citalopram study found no significant differences in efficacy between citalopram and a placebo,32 but the other reported significant improvement in one measure of pain and a significant decrease in depressive symptoms compared with the placebo group.33 No significant differences were found between groups in the global assessment of improvement.
The initial fluoxetine trial in fibromyalgia treatment did not reveal a significant therapeutic effect over a placebo,34 although the study was limited by a high (57%) placebo dropout rate, small sample size (42 subjects), brief duration (3 to 6 weeks after treatment), and restriction of fluoxetine dosage to 20 mg/d. In the two other controlled trials, including one which we recently conducted, fluoxetine was superior to a placebo in reducing pain and other fibromyalgia-associated symptoms.35,36
In our 12-week investigation (a randomized, placebocontrolled, parallel-group, flexible-dose trial), 60 subjects with fibromyalgia received fluoxetine 20 to 80 mg/d or a placebo.36 Those receiving fluoxetine (mean dosage 45 ±25 mg/d) displayed significantly greater reduction in pain, fatigue, and depression compared with those receiving the placebo. The effect of fluoxetine on pain remained significant after we adjusted for change in depression.
Sertraline was evaluated in an open study of 47 fibromyalgia patients at dosages of 25 to 200 mg/d for 6 weeks. Nearly two-thirds (63%) assessed the efficacy of sertraline as good or very good in the treatment of their symptoms.37 Paroxetine effectively reduced fibromyalgia symptoms in a single-blind study at dosages of 20 mg/d for 3 months.38
SNRIs Venlafaxine, a dual serotonin and norepinephrine reuptake inhibitor, has shown promise in the treatment of fibromyalgia in a preliminary open trial conducted by our group.39 Venlafaxine at a mean dosage of 167 mg/d resulted in significant improvement in fibromyalgia symptoms and quality of life compared with baseline. Notably, lifetime comorbid depressive and anxiety disorders were common in this sample, and their presence predicted response of fibromyalgia symptoms to venlafaxine.
Gabapentin Although no studies have been published on fibromyalgia treatment with this anticonvulsant, gabapentin has been found to exert substantial analgesic effects in controlled studies of other kinds of pain, including diabetic neuropathy, post-herpetic neuralgia, and migraines.40-42 There are also anecdotal reports of its successful use in fibromyalgia.2
Nonpharmacologic treatment
Cardiovascular fitness training, regional sympathetic block, electromyographic biofeedback, hypnotherapy, and electroacupuncture have been reported to have modest efficacy for fibromyalgia symptoms in short-term, randomized controlled trials.43-46 Other studies, however, have not replicated the efficacy of these treatments.
Cognitive-behavioral therapy has shown promise in preliminary studies.47,48 Cognitive restructuring techniques that challenge negative thoughts and promote an active, positive, problem-solving approach to pain were found to be important components of fibromyalgia therapy, as were relaxation training, aerobic exercise and stretching, pacing of activities, and family education.47
Recommendations
Based on our group’s experience and the limited data available, the following are recommendations for the pharmacologic treatment of fibromyalgia:
- Consider a trial of antidepressant medication for patients with a history of mood (unipolar) or anxiety disorders. First try an SSRI or an SNRI because many patients do not tolerate tricyclics. Use antidepressant therapeutic dosages and an adequate duration of treatment (at least 6 weeks).
- If symptoms do not respond to an adequate trial of first-line medications, treatment with tricyclics appears warranted. Although studies have focused mostly on tertiary amine tricyclics (e.g., amitriptyline), secondary amine agents (e.g., nortriptyline) may be just as effective and better tolerated, allowing for titration to higher dosages.
- Consider combination therapy when needed. For example, in patients who experience relief of pain, fatigue, and depressed mood with fluoxetine but continue to have insomnia, gabapentin can be added at night. Begin with 100 mg/d and increase by 100 mg/d until you see improvement or intolerance. Another option is trazodone, beginning with 50 mg hs. If you add a low-dose tricyclic to an SSRI, be aware of pharmacokinetic interaction and monitor tricyclic levels.
- Gabapentin alone, although it has not been studied in controlled trials of fibromyalgia, may be an option for patients who do not respond to antidepressants. Other pain conditions treated with gabapentin have required dosages of 1,600 to 2,400 mg/d to achieve substantial analgesic effects.
Cardiovascular fitness training is a potentially important component of fibromyalgia treatment. Many patients, however, have difficulty getting started because of increased pain after exercise and disabling fatigue. Treatment with medications as recommended may provide enough relief for patients to start an exercise program. Remind patients to start slowly, increasing the frequency and intensity of exercise as their endurance improves.
Because stress and a history of psychological trauma contribute to the onset and exacerbation of symptoms in some patients, cognitive-behavioral therapy is recommended as an adjunctive treatment as appropriate.
Related resources
- American Fibromyalgia Syndrome Association, Inc. www.afsafund.org
- Arnold LM, et al. Antidepressant treatment of fibromyalgia. A metaanalysis and review. Psychosomatics 2000;41:104-13.
- Kranzler JD, Gendreau JF, Rao SG. The psychopharmacology of fibromyalgia: a drug development perspective. Psychopharmacol Bull 2002;36:165-213.
Drug brand names
- Amitriptyline • Elavil
- Citalopram • Celexa
- Clomipramine • Anafranil
- Cyclobenzaprine • Flexeril
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Maprotiline • Ludiomil
- Nortriptyline • Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
The author reports that she receives research support from Eli Lilly & Co. and Pfizer Inc. and serves as a consultant and member of the speakers’ bureaus for both of those companies.
1. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum 1990;33:160-72.
2. Wolfe F, Ross K, Anderson J, et al. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 1995;38:19-28.
3. White KP, Speechley M, Harth M, et al. Comparing self-reported function and work disability in 100 community cases of fibromyalgia syndrome versus controls in London, Ontario. The London fibromyalgia epidemiology study. Arthritis Rheum 1999;42:76-83.
4. Wolfe F, Anderson J, Harkness D, et al. Health status and disease severity in fibromyalgia. Arthritis Rheum 1997;40:1571-9.
5. Kaplan RM, Schmidt SM, Cronan TA. Quality of well being in patients with fibromyalgia. J Rheumatol 2000;27:785-9.
6. Clauw DJ. Fibromyalgia syndrome: an update on current understanding and medical management. Rheumatol Grand Rds 2000;3:1-9.
7. Yunus MB, Masi AT, Aldag JC. A controlled study of primary fibromyalgia syndrome: Clinical features and association with other functional syndromes. J Rheumatol 1989;16:62-71.
8. Wolfe F, Cathey MA, Kleinheksel SM, et al. Psychological status in primary fibrositis and fibrositis associated with rheumatoid arthritis. J Rheumatol 1984;11:500-6.
9. White KP, Nielson WR, Harth M, et al. Chronic widespread musculoskeletal pain with or without fibromyalgia: Psychological distress in a representative community adult sample. J Rheumatol 2002;29:588-94.
10. Walker EA, Keegan D, Gardner G, et al. Psychosocial factors in fibromyalgia and rheumatoid arthritis: I. Psychiatric diagnoses and functional disability. Psychosomatic Med 1997;59:565-71.
11. MacFarlane GJ, Thomas E, Papageorgiou AC, et al. The natural history of chroninc pain in the community: A better prognosis than in the clinic? J Rheumatol 1996;23:1617-20.
12. Aaron LA, Bradley LA, Alarcón GS, et al. Psychiatric diagnoses in patients with fibromyalgia are related to health care-seeking behavior rather than to illness. Arthritis Rheum 1996;39:436-45.
13. Moldofsky H, Scarisbrick P, England R, et al. Musculoskeletal symptoms and non-REM sleep disturbance in patients with “fibrositis syndrome” and healthy subjects. Psychosom Med 1975;37:341-5.
14. Moldofsky H, Scarisbrick P. Induction of neurasthenic musculoskeletal pain syndrome by selective sleep stage deprivation. Psychosom Med 1975;38:35-44.
15. Schneider-Helmert D, Whitehouse I, Kumar A, et al. Insomnia and alpha sleep in chronic non-organic pain as compared to primary insomnia. Neuropsychobiology 2001;43:54-8.
16. Pillemer SR, Bradley LA, Crofford LJ, et al. The neuroscience and endocrinology of fibromyalgia. Arthritis Rheum 1997;40:1928-39.
17. Walker EA, Keegan D, Gardner G, et al. Psychosocial factors in fibromyalgia and rheumatoid arthritis: II. Sexual, physical, and emotional abuse and neglect. Psychosomatic Med 1997;59:572-7.
18. Demitrack MA, Crofford LJ. Hypothalamic-pituitary-adrenal axis dysregulation in fibromyalgia and chronic fatigue syndrome: An overview and hypothesis. J Musculoskeletal Pain 1995;3:67-73.
19. Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 2000;25:1-35.
20. Bennett RM. Emerging concepts in the neurobiology of chronic pain: Evidence of abnormal sensory processing in fibromyalgia. Mayo Clin Proc 1999;74:385-98.
21. Weigent DA, Bradley LA, Blalock JE, et al. Current concepts in the pathophysiology of abnormal pain perception in fibromyalgia. Am J Med Sci 1998;315:405-12.
22. Baranauskas G, Nistri A. Sensitization of pain pathways in the spinal cord: cellular mechanisms. Prog Neurobiol 1998;7:309-38.
23. Watkins LR, Wiertelak EP, Furness LE, et al. Illness-induced hyperalgesia is mediated by spinal neuropeptides and excitatory amino acids. Brain Res 1994;664:17-24.
24. Russell IJ, Orr MD, Littman B, et al. Elevated cerebrospinal fluid levels of substance P in patients with fibromyalgia syndrome. Arthritis Rheum 1994;37:1593-1601.
25. Schwarz MJ, Spath M, Muller-Bardorff H, et al. Relationship of substance P, 5-hydroxyindole acetic acid and tryptophan in serum of fibromyalgia patients. Neurosci Lett 1999;259:196-8.
26. Russell IJ, Vaeroy H, Javors M, Nyberg F. Cerebrospinal fluid biogenic amine metabolites in fibromyalgia/fibrositis syndrome and rheumatoid arthritis. Arthrits Rheum 1993;35(5):550-6.
27. Fishbain D. Evidence-based data on pain relief with antidepressants. Ann Med 2000;32:305-16.
28. Hudson JI, Goldenberg DL, Pope HG, et al. Comorbidity of fibromyalgia with medical and psychiatric disorders. Am J Med 1992;92:363-7.
29. Basbaum AI, Fields HL. Endogenous pain control systems: Brainstem pathways and endorphin circuitry. Ann Rev Neurosci 1984;7:309-38.
30. Arnold LM, Keck PE, Jr, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000;41:104-13.
31. O’Malley PG, Balden E, Tomkins G, et al. Treatment of fibromyalgia with antidepressants. A meta-analysis. J Gen Intern Med 2000;15:659-66.
32. Nørregaard J, Volkmann H, Danneskiold-Samsø B. A randomized controlled trial of citalopram in the treatment of fibromyalgia. Pain 1995;61:445-9.
33. Anderberg UM, Marteinsdottir I, von Knokrring L. Citalopram in patients with fibromyalgia-A randomized, double-blind, placebo-controlled study. Eur J Pain 2000;4:27-35.
34. Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994;23(5):255-9.
35. Goldenberg DL, Mayskiy M, Mossey C, et al. A randomized, double-blind crossover trial of fluoxetine and amitriptyline in the treatment of fibromyalgia. Arthritis Rheum 1996;39:1852-9.
36. Arnold LM, Hess EV, Hudson JI, et al. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002;112:191-7.
37. Syuertsen JO, Smedsrud T, Lane RM. An open study of sertraline in fibromyalgia syndrome. Eur Neuropsychopharmacol 1995;5:315.-
38. Giordano N, Geraci S, et al. Efficacy and tolerability of paroxetine in patients with fibromyalgia syndrome: A single blind study. Curr Ther Res 1999;60:696-702.
39. Dwight MM, Arnold LM, O’Brien H, et al. An open clinical trial of venlafaxine treatment of fibromyalgia. Psychosomatics 1998;39:14-17.
40. Backonja M, Beydoun A, Edwards KR, et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: A randomized controlled trial. JAMA 1998;280:1831-6.
41. Rice AS, Maton S. Gabapentin in postherpetic neuralgia: A randomized, doubleblind, placebo controlled study. Pain 2001;94:215-24.
42. Mathew NT, Rapoport A, Saper J, et al. Efficacy of gabapentin in migraine prophylaxis. Headache 2001;41:119-28.
43. Ferraccioli G, Ghirelli L, Scita F, et al. EMG-biofeedback training in fibromyalgia syndrome. J Rheumatol 1987;14:820-5.
44. McCain GA, Bell DA, Mai FM, et al. A controlled study of the effects of a supervised cardiovascular fitness training program on the manifestations of primary fibromyalgia. Arthritis Rheum 1988;31:1135-41.
45. Haanen HCM, Hoenderdos HTW, van Romande LKJ, et al. Controlled trial of hypnotherapy in the treatment of refractory fibromyalgia. J Rheumatol 1991;18:72-5.
46. Deluze C, Bosia L, Irbs A, et al. Electroacupuncture in fibromyalgia: Results of a controlled trial. BMJ 1992;1249-52.
47. Nielson WR, Walker C, McCain GA. Cognitive behavioral treatment of fibromyalgia syndrome preliminary findings. J Rheumatol 1992;19:98-103.
Patients with fibromyalgia often resist being referred to a psychiatrist because they fear being told their pain and other somatic symptoms are “all in their heads.” Evidence is mounting that they may be literally correct—the symptoms of fibromyalgia appear to have a physiologic connection with the central nervous system. Abnormal CNS activity, including sleep patterns, response to stress, pain processing, and neurotransmitter levels, has been documented in patients with fibromyalgia.
As psychiatrists, we can reassure these patients—and their primary care physicians and rheumatologists—that we are in a position to help because we:
- have expertise in assessing mood and anxiety disorders and in managing antidepressants, the medication physicians most commonly prescribe for fibromyalgia;
- are skilled in the use of the anticonvulsant gabapentin, which is being used in fibromyalgia for its analgesic and sedative effects;
- can offer much-needed support through psychotherapy, as chronic pain and other fibromyalgia-related symptoms create great stress in these patients’ lives.
Antidepressants are showing promise as an effective treatment for pain, fatigue, and depression in patients with fibromyalgia in studies by our group and others. The following information can help you stay current with the newest understandings of this ailment.
Table 1
CRITERIA FOR DIAGNOSING FIBROMYALGIA
| 1. | History of widespread pain |
| Definition Pain in the right and left side of the body, pain above and below the waist, axial skeletal pain (cervical spine or anterior chest or thoracic spine or low back). In this definition, shoulder and buttock pain is considered as pain for each involved side. “Low back” pain is considered lower segment pain. | |
| 2. | Pain in 11 of 18 tender point sites on digital palpation |
| Definition Pain, on digital palpation, must be present in at least 11 of the following 18 tender points: | |
| Occiput Bilateral, at the suboccipital muscle insertion | |
| Low cervical Bilateral, at the anterior aspects of the intertransverse spaces at C5-C7 | |
| Trapezius Bilateral, at the midpoint of the upper border | |
| Supraspinatus Bilateral, at origins, above the scapula spine near the medial border | |
| Second rib Bilateral, at the second costochondral junctions, just lateral to the junctions on upper surfaces | |
| Lateral epicondyle Bilateral, 2 cm distal to the epicondyles | |
| Gluteal Bilateral, in upper outer quadrants of buttocks in anterior fold of muscle | |
| Greater trochanter Bilateral, posterior to the trochanteric prominence | |
| Knee Bilateral, at the medial fat pad proximal to the joint line | |
| Digital palpation should be performed with an approximate force of 4 kg. For a tender point to be considered “positive” the patient must state that the palpation was painful. “Tender” is not to be considered “painful” Source: American College of Rheumatology1 | |
Figure 1 LOCATION OF FIBROMYALGIA TENDER POINTS
To palpate tender point sites, pressure is applied with the thumb pad perpendicularly to each site and the force increased by 1 kg per second until 4 kg of pressure is achieved. Whitening of the thumbnail bed usually occurs when applying the 4-kg force.
Mood disorders in fibromyalgia
A diagnosis of fibromyalgia requires the finding of widespread pain and tenderness at specific anatomic points (Table 1, Figure 1).1 Most patients also report fatigue, sleep disturbance, and morning stiffness (Box 1).2-5 American College of Rheumatology criteria do not require exclusionary tests such as radiographs and blood tests for the diagnosis.
Primary care physicians are increasingly making the diagnosis themselves and referring patients to rheumatologists only when conditions other than fibromyalgia are suspected. The differential diagnosis is broad, and other rheumatic and nonrheumatic disorders have similar symptoms, require different treatment, and affect fibromyalgia management (Table 2).6
Patients with fibromyalgia often report symptoms of major depressive disorder, such as depressed mood, anxiety, fatigue, and insomnia.7 Many psychological studies of such patients have documented increased rates of depressive symptoms.8 Depression and anxiety symptoms are common and frequently severe, even among individuals with fibromyalgia in the general population.9
Patients’ mood and anxiety disorders correlate highly with the number of medically unexplained symptoms and are associated with functional disability.10 The presence of psychological symptoms predicts persistent fibromyalgia symptoms,11 and psychological distress is strongly associated with symptom severity.12
Evidence for a CNS link
CNS mechanisms appear to contribute to the development of clinical findings in fibromyalgia.
Abnormal sleep A qualitative defect in sleep has been identified in patients with fibromyalgia.13 This sleep abnormality consists of inappropriate intrusion of alpha waves (normally seen during wakefulness or REM sleep) into deep sleep (usually characterized by delta waves).13 Some researchers believe alpha-delta sleep intrusion is associated with the chronic musculoskeletal pain and fatigue of fibromyalgia and, in turn, is mediated by an abnormality in central serotonergic neurotransmission.14 This sleep abnormality is not specific to fibromyalgia and can be found in other conditions, however.15 Debate continues regarding the role of sleep dysregulation in the pathophysiology of fibromyalgia.
Fibromyalgia is more common in women than men, with an estimated prevalence of 2% in the general population (3.4% in women and 0.5% in men). Its prevalence increases with age, rising sharply in middle age and then dropping off after age 80.2
Fibromyalgia is seen most often in women ages 50 and older.2 It occurs in 5% to 6% of patients presenting to general medical and family practice clinics and in 15% to 20% of patients presenting to rheumatologists, making it one of the most common diagnoses in office-based rheumatology practices.
American College of Rheumatology criteria may require only widespread pain and tenderness for a diagnosis of fibromyalgia, but most patients (73% to 85%) also report fatigue, sleep disturbance, and morning stiffness. Many (45% to 69%) report “pain all over,” paresthesias, headache, and anxiety. Co-occurring irritable bowel syndrome, sicca symptoms, and Raynaud’s phenomenon are less common (<35%).1 Patients with fibromyalgia also have high lifetime rates of other comorbid disorders, including migraine, chronic fatigue syndrome, and mood and anxiety disorders. Some patients report weakness, forgetfulness, difficulties in concentration, urinary frequency, history of dysmenorrhea, and restless legs.
Fibromyalgia is chronic, debilitating, and often leads to substantial functional impairment.3 Most patients with fibromyalgia do not display significant improvement over an average of 7 years of treatment.4 Patients with fibromyalgia report lower quality of well-being than patients with diagnoses of chronic obstructive pulmonary disease, rheumatoid arthritis, atrial fibrillation, advanced cancer, and several other chronic diseases.5
Stress response Stress appears to precipitate or exacerbate fibromyalgia symptoms in many patients.16 For example, fibromyalgia appears to be associated with victimization (adult and childhood sexual, physical, and emotional trauma), and this stress may trigger the development of fibromyalgia in some patients.17
Patients with fibromyalgia appear to develop disturbances in the two major stress-response systems: the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system.16 Although the interpretation of these disturbances is still debated, some researchers suggest that the available data point to reduction in CNS corticotropin releasing hormone (CRH), the key mediator in the HPA axis.18,19 CRH is also a behaviorally active peptide that leads to physiologic and behavioral arousal when administered centrally to animals.18 CRH reduction could contribute to the clinical features of fibromyalgia (e.g., fatigue) either directly or indirectly by causing a relative glucocorticoid deficiency.18,19
Table 2
DIFFERENTIAL DIAGNOSIS OF FIBROMYALGIA
| Rheumatic disorders | Nonrheumatic disorders |
|---|---|
| Rheumatoid arthritis | Hypothyroidism |
| Systemic lupus erythematosus | Sleep apnea |
| Polyarticular osteoarthritis | Hepatitis |
| Polymyalgia rheumatica | Cushing’s syndrome |
| Addison’s disease | |
| Hyperparathyroidism | |
| Adapted from Clauw DJ. Fibromyalgia syndrome: an update on current understanding and medical management. Rheumatol Grand Rds 2000;3:1-9. | |
Fibromyalgia is also associated with moderate basal hypocortisolism.18,19 A relative glucocorticoid deficiency could contribute to fibromyalgia’s characteristic fatigue, arthralgias, myalgias, and disturbances in mood and sleep.18 This deficiency may also cause some of the immunologic disturbances seen with fibromyalgia.18,19
Atypical depression, which shares such features of fibromyalgia as profound lethargy, is also associated with inappropriately normal or reduced activation of the HPA axis and a functional deficit in the release of hypothalamic CRH.18 The unifying feature of HPA axis activity in both atypical depression and fibromyalgia may be a shared hypofunctioning.18 A more complete understanding of the neuroendocrine changes in fibromyalgia awaits further study.
Pain processing Aberrant CNS processing of pain may also play a role in fibromyalgia.16,20 Fibromyalgia is sometimes precipitated by physical trauma.21 A traumatic injury may start a process in susceptible individuals that leads to an enhanced central processing of painful stimuli characteristic of central sensitization.22 Patients with fibromyalgia often develop an increased response to painful stimuli (hyeralgesia) and experience pain from normally nonnoxious stimuli (allodynia).20
Substance P, an important nociceptive neurotransmitter, may have a role in generating central sensitization.23 Elevated concentrations of substance P have been found in the cerebrospinal fluid (CSF) of individuals with fibromyalgia.24 Substance P also inhibits CRH release and may contribute to low CRH activity in fibromyalgia.16
Neurotransmitter defects A functional reduction in serotonergic activity has been demonstrated in patients with fibromyalgia. Schwarz et al25 found a strong negative correlation between serum concentrations of the primary serotonin metabolite, 5-hydroxyindoleacetic acid (5-HIAA), and substance P, pain, and insomnia. Evidence also exists of reduced concentrations of the primary norepinephrine metabolite, 3-methoxy-4-hydroxyphenethylene (MHPG), in the CSF of patients with fibromyalgia.26 Reduced serotonin and norepinephrine levels in descending pain-inhibitory pathways may cause the allodynia and hyperalgesia of fibromyalgia.
Pharmacologic treatment
Most studies of pharmacologic treatment of fibromyalgia have examined antidepressants for three reasons:
- There is evidence of the successful use of antidepressants in other chronic pain conditions.27
- These agents are effective for treating mood and anxiety disorders, which frequently occur in patients with fibromyalgia and may share a common physiologic abnormality.28
- Antidepressants might enhance the activity of neurotransmitters such as serotonin and norepinephrine in the descending inhibitory pain pathways, leading to reduced pain perception.29
Tricyclics In randomized, controlled trials, tricyclic medications (including the muscle relaxant cyclobenzaprine) appear to be moderately effective in improving fibromyalgia symptoms. Two meta-analyses of trials of tricyclic medications (amitriptyline, dothiepin, cyclobenzaprine, clomipramine, and maprotiline) have found similar results.30,31 Our group found the greatest effect on measures of sleep improvement, which may be due in part to tricyclics’ sedative properties.30 Many patients with fibromyalgia, however, cannot tolerate the sedative and other side effects associated with tricyclic agents, even though low dosages (e.g., 25 mg/d of amitriptyline) have typically been used in clinical trials.
SSRIs. Selective serotonin reuptake inhibitors, although likely to be better tolerated than tricyclics, have been examined in only five placebo-controlled trials in fibromyalgia: two with citalopram, and three with fluoxetine. One citalopram study found no significant differences in efficacy between citalopram and a placebo,32 but the other reported significant improvement in one measure of pain and a significant decrease in depressive symptoms compared with the placebo group.33 No significant differences were found between groups in the global assessment of improvement.
The initial fluoxetine trial in fibromyalgia treatment did not reveal a significant therapeutic effect over a placebo,34 although the study was limited by a high (57%) placebo dropout rate, small sample size (42 subjects), brief duration (3 to 6 weeks after treatment), and restriction of fluoxetine dosage to 20 mg/d. In the two other controlled trials, including one which we recently conducted, fluoxetine was superior to a placebo in reducing pain and other fibromyalgia-associated symptoms.35,36
In our 12-week investigation (a randomized, placebocontrolled, parallel-group, flexible-dose trial), 60 subjects with fibromyalgia received fluoxetine 20 to 80 mg/d or a placebo.36 Those receiving fluoxetine (mean dosage 45 ±25 mg/d) displayed significantly greater reduction in pain, fatigue, and depression compared with those receiving the placebo. The effect of fluoxetine on pain remained significant after we adjusted for change in depression.
Sertraline was evaluated in an open study of 47 fibromyalgia patients at dosages of 25 to 200 mg/d for 6 weeks. Nearly two-thirds (63%) assessed the efficacy of sertraline as good or very good in the treatment of their symptoms.37 Paroxetine effectively reduced fibromyalgia symptoms in a single-blind study at dosages of 20 mg/d for 3 months.38
SNRIs Venlafaxine, a dual serotonin and norepinephrine reuptake inhibitor, has shown promise in the treatment of fibromyalgia in a preliminary open trial conducted by our group.39 Venlafaxine at a mean dosage of 167 mg/d resulted in significant improvement in fibromyalgia symptoms and quality of life compared with baseline. Notably, lifetime comorbid depressive and anxiety disorders were common in this sample, and their presence predicted response of fibromyalgia symptoms to venlafaxine.
Gabapentin Although no studies have been published on fibromyalgia treatment with this anticonvulsant, gabapentin has been found to exert substantial analgesic effects in controlled studies of other kinds of pain, including diabetic neuropathy, post-herpetic neuralgia, and migraines.40-42 There are also anecdotal reports of its successful use in fibromyalgia.2
Nonpharmacologic treatment
Cardiovascular fitness training, regional sympathetic block, electromyographic biofeedback, hypnotherapy, and electroacupuncture have been reported to have modest efficacy for fibromyalgia symptoms in short-term, randomized controlled trials.43-46 Other studies, however, have not replicated the efficacy of these treatments.
Cognitive-behavioral therapy has shown promise in preliminary studies.47,48 Cognitive restructuring techniques that challenge negative thoughts and promote an active, positive, problem-solving approach to pain were found to be important components of fibromyalgia therapy, as were relaxation training, aerobic exercise and stretching, pacing of activities, and family education.47
Recommendations
Based on our group’s experience and the limited data available, the following are recommendations for the pharmacologic treatment of fibromyalgia:
- Consider a trial of antidepressant medication for patients with a history of mood (unipolar) or anxiety disorders. First try an SSRI or an SNRI because many patients do not tolerate tricyclics. Use antidepressant therapeutic dosages and an adequate duration of treatment (at least 6 weeks).
- If symptoms do not respond to an adequate trial of first-line medications, treatment with tricyclics appears warranted. Although studies have focused mostly on tertiary amine tricyclics (e.g., amitriptyline), secondary amine agents (e.g., nortriptyline) may be just as effective and better tolerated, allowing for titration to higher dosages.
- Consider combination therapy when needed. For example, in patients who experience relief of pain, fatigue, and depressed mood with fluoxetine but continue to have insomnia, gabapentin can be added at night. Begin with 100 mg/d and increase by 100 mg/d until you see improvement or intolerance. Another option is trazodone, beginning with 50 mg hs. If you add a low-dose tricyclic to an SSRI, be aware of pharmacokinetic interaction and monitor tricyclic levels.
- Gabapentin alone, although it has not been studied in controlled trials of fibromyalgia, may be an option for patients who do not respond to antidepressants. Other pain conditions treated with gabapentin have required dosages of 1,600 to 2,400 mg/d to achieve substantial analgesic effects.
Cardiovascular fitness training is a potentially important component of fibromyalgia treatment. Many patients, however, have difficulty getting started because of increased pain after exercise and disabling fatigue. Treatment with medications as recommended may provide enough relief for patients to start an exercise program. Remind patients to start slowly, increasing the frequency and intensity of exercise as their endurance improves.
Because stress and a history of psychological trauma contribute to the onset and exacerbation of symptoms in some patients, cognitive-behavioral therapy is recommended as an adjunctive treatment as appropriate.
Related resources
- American Fibromyalgia Syndrome Association, Inc. www.afsafund.org
- Arnold LM, et al. Antidepressant treatment of fibromyalgia. A metaanalysis and review. Psychosomatics 2000;41:104-13.
- Kranzler JD, Gendreau JF, Rao SG. The psychopharmacology of fibromyalgia: a drug development perspective. Psychopharmacol Bull 2002;36:165-213.
Drug brand names
- Amitriptyline • Elavil
- Citalopram • Celexa
- Clomipramine • Anafranil
- Cyclobenzaprine • Flexeril
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Maprotiline • Ludiomil
- Nortriptyline • Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
The author reports that she receives research support from Eli Lilly & Co. and Pfizer Inc. and serves as a consultant and member of the speakers’ bureaus for both of those companies.
Patients with fibromyalgia often resist being referred to a psychiatrist because they fear being told their pain and other somatic symptoms are “all in their heads.” Evidence is mounting that they may be literally correct—the symptoms of fibromyalgia appear to have a physiologic connection with the central nervous system. Abnormal CNS activity, including sleep patterns, response to stress, pain processing, and neurotransmitter levels, has been documented in patients with fibromyalgia.
As psychiatrists, we can reassure these patients—and their primary care physicians and rheumatologists—that we are in a position to help because we:
- have expertise in assessing mood and anxiety disorders and in managing antidepressants, the medication physicians most commonly prescribe for fibromyalgia;
- are skilled in the use of the anticonvulsant gabapentin, which is being used in fibromyalgia for its analgesic and sedative effects;
- can offer much-needed support through psychotherapy, as chronic pain and other fibromyalgia-related symptoms create great stress in these patients’ lives.
Antidepressants are showing promise as an effective treatment for pain, fatigue, and depression in patients with fibromyalgia in studies by our group and others. The following information can help you stay current with the newest understandings of this ailment.
Table 1
CRITERIA FOR DIAGNOSING FIBROMYALGIA
| 1. | History of widespread pain |
| Definition Pain in the right and left side of the body, pain above and below the waist, axial skeletal pain (cervical spine or anterior chest or thoracic spine or low back). In this definition, shoulder and buttock pain is considered as pain for each involved side. “Low back” pain is considered lower segment pain. | |
| 2. | Pain in 11 of 18 tender point sites on digital palpation |
| Definition Pain, on digital palpation, must be present in at least 11 of the following 18 tender points: | |
| Occiput Bilateral, at the suboccipital muscle insertion | |
| Low cervical Bilateral, at the anterior aspects of the intertransverse spaces at C5-C7 | |
| Trapezius Bilateral, at the midpoint of the upper border | |
| Supraspinatus Bilateral, at origins, above the scapula spine near the medial border | |
| Second rib Bilateral, at the second costochondral junctions, just lateral to the junctions on upper surfaces | |
| Lateral epicondyle Bilateral, 2 cm distal to the epicondyles | |
| Gluteal Bilateral, in upper outer quadrants of buttocks in anterior fold of muscle | |
| Greater trochanter Bilateral, posterior to the trochanteric prominence | |
| Knee Bilateral, at the medial fat pad proximal to the joint line | |
| Digital palpation should be performed with an approximate force of 4 kg. For a tender point to be considered “positive” the patient must state that the palpation was painful. “Tender” is not to be considered “painful” Source: American College of Rheumatology1 | |
Figure 1 LOCATION OF FIBROMYALGIA TENDER POINTS
To palpate tender point sites, pressure is applied with the thumb pad perpendicularly to each site and the force increased by 1 kg per second until 4 kg of pressure is achieved. Whitening of the thumbnail bed usually occurs when applying the 4-kg force.
Mood disorders in fibromyalgia
A diagnosis of fibromyalgia requires the finding of widespread pain and tenderness at specific anatomic points (Table 1, Figure 1).1 Most patients also report fatigue, sleep disturbance, and morning stiffness (Box 1).2-5 American College of Rheumatology criteria do not require exclusionary tests such as radiographs and blood tests for the diagnosis.
Primary care physicians are increasingly making the diagnosis themselves and referring patients to rheumatologists only when conditions other than fibromyalgia are suspected. The differential diagnosis is broad, and other rheumatic and nonrheumatic disorders have similar symptoms, require different treatment, and affect fibromyalgia management (Table 2).6
Patients with fibromyalgia often report symptoms of major depressive disorder, such as depressed mood, anxiety, fatigue, and insomnia.7 Many psychological studies of such patients have documented increased rates of depressive symptoms.8 Depression and anxiety symptoms are common and frequently severe, even among individuals with fibromyalgia in the general population.9
Patients’ mood and anxiety disorders correlate highly with the number of medically unexplained symptoms and are associated with functional disability.10 The presence of psychological symptoms predicts persistent fibromyalgia symptoms,11 and psychological distress is strongly associated with symptom severity.12
Evidence for a CNS link
CNS mechanisms appear to contribute to the development of clinical findings in fibromyalgia.
Abnormal sleep A qualitative defect in sleep has been identified in patients with fibromyalgia.13 This sleep abnormality consists of inappropriate intrusion of alpha waves (normally seen during wakefulness or REM sleep) into deep sleep (usually characterized by delta waves).13 Some researchers believe alpha-delta sleep intrusion is associated with the chronic musculoskeletal pain and fatigue of fibromyalgia and, in turn, is mediated by an abnormality in central serotonergic neurotransmission.14 This sleep abnormality is not specific to fibromyalgia and can be found in other conditions, however.15 Debate continues regarding the role of sleep dysregulation in the pathophysiology of fibromyalgia.
Fibromyalgia is more common in women than men, with an estimated prevalence of 2% in the general population (3.4% in women and 0.5% in men). Its prevalence increases with age, rising sharply in middle age and then dropping off after age 80.2
Fibromyalgia is seen most often in women ages 50 and older.2 It occurs in 5% to 6% of patients presenting to general medical and family practice clinics and in 15% to 20% of patients presenting to rheumatologists, making it one of the most common diagnoses in office-based rheumatology practices.
American College of Rheumatology criteria may require only widespread pain and tenderness for a diagnosis of fibromyalgia, but most patients (73% to 85%) also report fatigue, sleep disturbance, and morning stiffness. Many (45% to 69%) report “pain all over,” paresthesias, headache, and anxiety. Co-occurring irritable bowel syndrome, sicca symptoms, and Raynaud’s phenomenon are less common (<35%).1 Patients with fibromyalgia also have high lifetime rates of other comorbid disorders, including migraine, chronic fatigue syndrome, and mood and anxiety disorders. Some patients report weakness, forgetfulness, difficulties in concentration, urinary frequency, history of dysmenorrhea, and restless legs.
Fibromyalgia is chronic, debilitating, and often leads to substantial functional impairment.3 Most patients with fibromyalgia do not display significant improvement over an average of 7 years of treatment.4 Patients with fibromyalgia report lower quality of well-being than patients with diagnoses of chronic obstructive pulmonary disease, rheumatoid arthritis, atrial fibrillation, advanced cancer, and several other chronic diseases.5
Stress response Stress appears to precipitate or exacerbate fibromyalgia symptoms in many patients.16 For example, fibromyalgia appears to be associated with victimization (adult and childhood sexual, physical, and emotional trauma), and this stress may trigger the development of fibromyalgia in some patients.17
Patients with fibromyalgia appear to develop disturbances in the two major stress-response systems: the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system.16 Although the interpretation of these disturbances is still debated, some researchers suggest that the available data point to reduction in CNS corticotropin releasing hormone (CRH), the key mediator in the HPA axis.18,19 CRH is also a behaviorally active peptide that leads to physiologic and behavioral arousal when administered centrally to animals.18 CRH reduction could contribute to the clinical features of fibromyalgia (e.g., fatigue) either directly or indirectly by causing a relative glucocorticoid deficiency.18,19
Table 2
DIFFERENTIAL DIAGNOSIS OF FIBROMYALGIA
| Rheumatic disorders | Nonrheumatic disorders |
|---|---|
| Rheumatoid arthritis | Hypothyroidism |
| Systemic lupus erythematosus | Sleep apnea |
| Polyarticular osteoarthritis | Hepatitis |
| Polymyalgia rheumatica | Cushing’s syndrome |
| Addison’s disease | |
| Hyperparathyroidism | |
| Adapted from Clauw DJ. Fibromyalgia syndrome: an update on current understanding and medical management. Rheumatol Grand Rds 2000;3:1-9. | |
Fibromyalgia is also associated with moderate basal hypocortisolism.18,19 A relative glucocorticoid deficiency could contribute to fibromyalgia’s characteristic fatigue, arthralgias, myalgias, and disturbances in mood and sleep.18 This deficiency may also cause some of the immunologic disturbances seen with fibromyalgia.18,19
Atypical depression, which shares such features of fibromyalgia as profound lethargy, is also associated with inappropriately normal or reduced activation of the HPA axis and a functional deficit in the release of hypothalamic CRH.18 The unifying feature of HPA axis activity in both atypical depression and fibromyalgia may be a shared hypofunctioning.18 A more complete understanding of the neuroendocrine changes in fibromyalgia awaits further study.
Pain processing Aberrant CNS processing of pain may also play a role in fibromyalgia.16,20 Fibromyalgia is sometimes precipitated by physical trauma.21 A traumatic injury may start a process in susceptible individuals that leads to an enhanced central processing of painful stimuli characteristic of central sensitization.22 Patients with fibromyalgia often develop an increased response to painful stimuli (hyeralgesia) and experience pain from normally nonnoxious stimuli (allodynia).20
Substance P, an important nociceptive neurotransmitter, may have a role in generating central sensitization.23 Elevated concentrations of substance P have been found in the cerebrospinal fluid (CSF) of individuals with fibromyalgia.24 Substance P also inhibits CRH release and may contribute to low CRH activity in fibromyalgia.16
Neurotransmitter defects A functional reduction in serotonergic activity has been demonstrated in patients with fibromyalgia. Schwarz et al25 found a strong negative correlation between serum concentrations of the primary serotonin metabolite, 5-hydroxyindoleacetic acid (5-HIAA), and substance P, pain, and insomnia. Evidence also exists of reduced concentrations of the primary norepinephrine metabolite, 3-methoxy-4-hydroxyphenethylene (MHPG), in the CSF of patients with fibromyalgia.26 Reduced serotonin and norepinephrine levels in descending pain-inhibitory pathways may cause the allodynia and hyperalgesia of fibromyalgia.
Pharmacologic treatment
Most studies of pharmacologic treatment of fibromyalgia have examined antidepressants for three reasons:
- There is evidence of the successful use of antidepressants in other chronic pain conditions.27
- These agents are effective for treating mood and anxiety disorders, which frequently occur in patients with fibromyalgia and may share a common physiologic abnormality.28
- Antidepressants might enhance the activity of neurotransmitters such as serotonin and norepinephrine in the descending inhibitory pain pathways, leading to reduced pain perception.29
Tricyclics In randomized, controlled trials, tricyclic medications (including the muscle relaxant cyclobenzaprine) appear to be moderately effective in improving fibromyalgia symptoms. Two meta-analyses of trials of tricyclic medications (amitriptyline, dothiepin, cyclobenzaprine, clomipramine, and maprotiline) have found similar results.30,31 Our group found the greatest effect on measures of sleep improvement, which may be due in part to tricyclics’ sedative properties.30 Many patients with fibromyalgia, however, cannot tolerate the sedative and other side effects associated with tricyclic agents, even though low dosages (e.g., 25 mg/d of amitriptyline) have typically been used in clinical trials.
SSRIs. Selective serotonin reuptake inhibitors, although likely to be better tolerated than tricyclics, have been examined in only five placebo-controlled trials in fibromyalgia: two with citalopram, and three with fluoxetine. One citalopram study found no significant differences in efficacy between citalopram and a placebo,32 but the other reported significant improvement in one measure of pain and a significant decrease in depressive symptoms compared with the placebo group.33 No significant differences were found between groups in the global assessment of improvement.
The initial fluoxetine trial in fibromyalgia treatment did not reveal a significant therapeutic effect over a placebo,34 although the study was limited by a high (57%) placebo dropout rate, small sample size (42 subjects), brief duration (3 to 6 weeks after treatment), and restriction of fluoxetine dosage to 20 mg/d. In the two other controlled trials, including one which we recently conducted, fluoxetine was superior to a placebo in reducing pain and other fibromyalgia-associated symptoms.35,36
In our 12-week investigation (a randomized, placebocontrolled, parallel-group, flexible-dose trial), 60 subjects with fibromyalgia received fluoxetine 20 to 80 mg/d or a placebo.36 Those receiving fluoxetine (mean dosage 45 ±25 mg/d) displayed significantly greater reduction in pain, fatigue, and depression compared with those receiving the placebo. The effect of fluoxetine on pain remained significant after we adjusted for change in depression.
Sertraline was evaluated in an open study of 47 fibromyalgia patients at dosages of 25 to 200 mg/d for 6 weeks. Nearly two-thirds (63%) assessed the efficacy of sertraline as good or very good in the treatment of their symptoms.37 Paroxetine effectively reduced fibromyalgia symptoms in a single-blind study at dosages of 20 mg/d for 3 months.38
SNRIs Venlafaxine, a dual serotonin and norepinephrine reuptake inhibitor, has shown promise in the treatment of fibromyalgia in a preliminary open trial conducted by our group.39 Venlafaxine at a mean dosage of 167 mg/d resulted in significant improvement in fibromyalgia symptoms and quality of life compared with baseline. Notably, lifetime comorbid depressive and anxiety disorders were common in this sample, and their presence predicted response of fibromyalgia symptoms to venlafaxine.
Gabapentin Although no studies have been published on fibromyalgia treatment with this anticonvulsant, gabapentin has been found to exert substantial analgesic effects in controlled studies of other kinds of pain, including diabetic neuropathy, post-herpetic neuralgia, and migraines.40-42 There are also anecdotal reports of its successful use in fibromyalgia.2
Nonpharmacologic treatment
Cardiovascular fitness training, regional sympathetic block, electromyographic biofeedback, hypnotherapy, and electroacupuncture have been reported to have modest efficacy for fibromyalgia symptoms in short-term, randomized controlled trials.43-46 Other studies, however, have not replicated the efficacy of these treatments.
Cognitive-behavioral therapy has shown promise in preliminary studies.47,48 Cognitive restructuring techniques that challenge negative thoughts and promote an active, positive, problem-solving approach to pain were found to be important components of fibromyalgia therapy, as were relaxation training, aerobic exercise and stretching, pacing of activities, and family education.47
Recommendations
Based on our group’s experience and the limited data available, the following are recommendations for the pharmacologic treatment of fibromyalgia:
- Consider a trial of antidepressant medication for patients with a history of mood (unipolar) or anxiety disorders. First try an SSRI or an SNRI because many patients do not tolerate tricyclics. Use antidepressant therapeutic dosages and an adequate duration of treatment (at least 6 weeks).
- If symptoms do not respond to an adequate trial of first-line medications, treatment with tricyclics appears warranted. Although studies have focused mostly on tertiary amine tricyclics (e.g., amitriptyline), secondary amine agents (e.g., nortriptyline) may be just as effective and better tolerated, allowing for titration to higher dosages.
- Consider combination therapy when needed. For example, in patients who experience relief of pain, fatigue, and depressed mood with fluoxetine but continue to have insomnia, gabapentin can be added at night. Begin with 100 mg/d and increase by 100 mg/d until you see improvement or intolerance. Another option is trazodone, beginning with 50 mg hs. If you add a low-dose tricyclic to an SSRI, be aware of pharmacokinetic interaction and monitor tricyclic levels.
- Gabapentin alone, although it has not been studied in controlled trials of fibromyalgia, may be an option for patients who do not respond to antidepressants. Other pain conditions treated with gabapentin have required dosages of 1,600 to 2,400 mg/d to achieve substantial analgesic effects.
Cardiovascular fitness training is a potentially important component of fibromyalgia treatment. Many patients, however, have difficulty getting started because of increased pain after exercise and disabling fatigue. Treatment with medications as recommended may provide enough relief for patients to start an exercise program. Remind patients to start slowly, increasing the frequency and intensity of exercise as their endurance improves.
Because stress and a history of psychological trauma contribute to the onset and exacerbation of symptoms in some patients, cognitive-behavioral therapy is recommended as an adjunctive treatment as appropriate.
Related resources
- American Fibromyalgia Syndrome Association, Inc. www.afsafund.org
- Arnold LM, et al. Antidepressant treatment of fibromyalgia. A metaanalysis and review. Psychosomatics 2000;41:104-13.
- Kranzler JD, Gendreau JF, Rao SG. The psychopharmacology of fibromyalgia: a drug development perspective. Psychopharmacol Bull 2002;36:165-213.
Drug brand names
- Amitriptyline • Elavil
- Citalopram • Celexa
- Clomipramine • Anafranil
- Cyclobenzaprine • Flexeril
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Maprotiline • Ludiomil
- Nortriptyline • Pamelor
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
The author reports that she receives research support from Eli Lilly & Co. and Pfizer Inc. and serves as a consultant and member of the speakers’ bureaus for both of those companies.
1. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum 1990;33:160-72.
2. Wolfe F, Ross K, Anderson J, et al. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 1995;38:19-28.
3. White KP, Speechley M, Harth M, et al. Comparing self-reported function and work disability in 100 community cases of fibromyalgia syndrome versus controls in London, Ontario. The London fibromyalgia epidemiology study. Arthritis Rheum 1999;42:76-83.
4. Wolfe F, Anderson J, Harkness D, et al. Health status and disease severity in fibromyalgia. Arthritis Rheum 1997;40:1571-9.
5. Kaplan RM, Schmidt SM, Cronan TA. Quality of well being in patients with fibromyalgia. J Rheumatol 2000;27:785-9.
6. Clauw DJ. Fibromyalgia syndrome: an update on current understanding and medical management. Rheumatol Grand Rds 2000;3:1-9.
7. Yunus MB, Masi AT, Aldag JC. A controlled study of primary fibromyalgia syndrome: Clinical features and association with other functional syndromes. J Rheumatol 1989;16:62-71.
8. Wolfe F, Cathey MA, Kleinheksel SM, et al. Psychological status in primary fibrositis and fibrositis associated with rheumatoid arthritis. J Rheumatol 1984;11:500-6.
9. White KP, Nielson WR, Harth M, et al. Chronic widespread musculoskeletal pain with or without fibromyalgia: Psychological distress in a representative community adult sample. J Rheumatol 2002;29:588-94.
10. Walker EA, Keegan D, Gardner G, et al. Psychosocial factors in fibromyalgia and rheumatoid arthritis: I. Psychiatric diagnoses and functional disability. Psychosomatic Med 1997;59:565-71.
11. MacFarlane GJ, Thomas E, Papageorgiou AC, et al. The natural history of chroninc pain in the community: A better prognosis than in the clinic? J Rheumatol 1996;23:1617-20.
12. Aaron LA, Bradley LA, Alarcón GS, et al. Psychiatric diagnoses in patients with fibromyalgia are related to health care-seeking behavior rather than to illness. Arthritis Rheum 1996;39:436-45.
13. Moldofsky H, Scarisbrick P, England R, et al. Musculoskeletal symptoms and non-REM sleep disturbance in patients with “fibrositis syndrome” and healthy subjects. Psychosom Med 1975;37:341-5.
14. Moldofsky H, Scarisbrick P. Induction of neurasthenic musculoskeletal pain syndrome by selective sleep stage deprivation. Psychosom Med 1975;38:35-44.
15. Schneider-Helmert D, Whitehouse I, Kumar A, et al. Insomnia and alpha sleep in chronic non-organic pain as compared to primary insomnia. Neuropsychobiology 2001;43:54-8.
16. Pillemer SR, Bradley LA, Crofford LJ, et al. The neuroscience and endocrinology of fibromyalgia. Arthritis Rheum 1997;40:1928-39.
17. Walker EA, Keegan D, Gardner G, et al. Psychosocial factors in fibromyalgia and rheumatoid arthritis: II. Sexual, physical, and emotional abuse and neglect. Psychosomatic Med 1997;59:572-7.
18. Demitrack MA, Crofford LJ. Hypothalamic-pituitary-adrenal axis dysregulation in fibromyalgia and chronic fatigue syndrome: An overview and hypothesis. J Musculoskeletal Pain 1995;3:67-73.
19. Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 2000;25:1-35.
20. Bennett RM. Emerging concepts in the neurobiology of chronic pain: Evidence of abnormal sensory processing in fibromyalgia. Mayo Clin Proc 1999;74:385-98.
21. Weigent DA, Bradley LA, Blalock JE, et al. Current concepts in the pathophysiology of abnormal pain perception in fibromyalgia. Am J Med Sci 1998;315:405-12.
22. Baranauskas G, Nistri A. Sensitization of pain pathways in the spinal cord: cellular mechanisms. Prog Neurobiol 1998;7:309-38.
23. Watkins LR, Wiertelak EP, Furness LE, et al. Illness-induced hyperalgesia is mediated by spinal neuropeptides and excitatory amino acids. Brain Res 1994;664:17-24.
24. Russell IJ, Orr MD, Littman B, et al. Elevated cerebrospinal fluid levels of substance P in patients with fibromyalgia syndrome. Arthritis Rheum 1994;37:1593-1601.
25. Schwarz MJ, Spath M, Muller-Bardorff H, et al. Relationship of substance P, 5-hydroxyindole acetic acid and tryptophan in serum of fibromyalgia patients. Neurosci Lett 1999;259:196-8.
26. Russell IJ, Vaeroy H, Javors M, Nyberg F. Cerebrospinal fluid biogenic amine metabolites in fibromyalgia/fibrositis syndrome and rheumatoid arthritis. Arthrits Rheum 1993;35(5):550-6.
27. Fishbain D. Evidence-based data on pain relief with antidepressants. Ann Med 2000;32:305-16.
28. Hudson JI, Goldenberg DL, Pope HG, et al. Comorbidity of fibromyalgia with medical and psychiatric disorders. Am J Med 1992;92:363-7.
29. Basbaum AI, Fields HL. Endogenous pain control systems: Brainstem pathways and endorphin circuitry. Ann Rev Neurosci 1984;7:309-38.
30. Arnold LM, Keck PE, Jr, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000;41:104-13.
31. O’Malley PG, Balden E, Tomkins G, et al. Treatment of fibromyalgia with antidepressants. A meta-analysis. J Gen Intern Med 2000;15:659-66.
32. Nørregaard J, Volkmann H, Danneskiold-Samsø B. A randomized controlled trial of citalopram in the treatment of fibromyalgia. Pain 1995;61:445-9.
33. Anderberg UM, Marteinsdottir I, von Knokrring L. Citalopram in patients with fibromyalgia-A randomized, double-blind, placebo-controlled study. Eur J Pain 2000;4:27-35.
34. Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994;23(5):255-9.
35. Goldenberg DL, Mayskiy M, Mossey C, et al. A randomized, double-blind crossover trial of fluoxetine and amitriptyline in the treatment of fibromyalgia. Arthritis Rheum 1996;39:1852-9.
36. Arnold LM, Hess EV, Hudson JI, et al. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002;112:191-7.
37. Syuertsen JO, Smedsrud T, Lane RM. An open study of sertraline in fibromyalgia syndrome. Eur Neuropsychopharmacol 1995;5:315.-
38. Giordano N, Geraci S, et al. Efficacy and tolerability of paroxetine in patients with fibromyalgia syndrome: A single blind study. Curr Ther Res 1999;60:696-702.
39. Dwight MM, Arnold LM, O’Brien H, et al. An open clinical trial of venlafaxine treatment of fibromyalgia. Psychosomatics 1998;39:14-17.
40. Backonja M, Beydoun A, Edwards KR, et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: A randomized controlled trial. JAMA 1998;280:1831-6.
41. Rice AS, Maton S. Gabapentin in postherpetic neuralgia: A randomized, doubleblind, placebo controlled study. Pain 2001;94:215-24.
42. Mathew NT, Rapoport A, Saper J, et al. Efficacy of gabapentin in migraine prophylaxis. Headache 2001;41:119-28.
43. Ferraccioli G, Ghirelli L, Scita F, et al. EMG-biofeedback training in fibromyalgia syndrome. J Rheumatol 1987;14:820-5.
44. McCain GA, Bell DA, Mai FM, et al. A controlled study of the effects of a supervised cardiovascular fitness training program on the manifestations of primary fibromyalgia. Arthritis Rheum 1988;31:1135-41.
45. Haanen HCM, Hoenderdos HTW, van Romande LKJ, et al. Controlled trial of hypnotherapy in the treatment of refractory fibromyalgia. J Rheumatol 1991;18:72-5.
46. Deluze C, Bosia L, Irbs A, et al. Electroacupuncture in fibromyalgia: Results of a controlled trial. BMJ 1992;1249-52.
47. Nielson WR, Walker C, McCain GA. Cognitive behavioral treatment of fibromyalgia syndrome preliminary findings. J Rheumatol 1992;19:98-103.
1. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum 1990;33:160-72.
2. Wolfe F, Ross K, Anderson J, et al. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 1995;38:19-28.
3. White KP, Speechley M, Harth M, et al. Comparing self-reported function and work disability in 100 community cases of fibromyalgia syndrome versus controls in London, Ontario. The London fibromyalgia epidemiology study. Arthritis Rheum 1999;42:76-83.
4. Wolfe F, Anderson J, Harkness D, et al. Health status and disease severity in fibromyalgia. Arthritis Rheum 1997;40:1571-9.
5. Kaplan RM, Schmidt SM, Cronan TA. Quality of well being in patients with fibromyalgia. J Rheumatol 2000;27:785-9.
6. Clauw DJ. Fibromyalgia syndrome: an update on current understanding and medical management. Rheumatol Grand Rds 2000;3:1-9.
7. Yunus MB, Masi AT, Aldag JC. A controlled study of primary fibromyalgia syndrome: Clinical features and association with other functional syndromes. J Rheumatol 1989;16:62-71.
8. Wolfe F, Cathey MA, Kleinheksel SM, et al. Psychological status in primary fibrositis and fibrositis associated with rheumatoid arthritis. J Rheumatol 1984;11:500-6.
9. White KP, Nielson WR, Harth M, et al. Chronic widespread musculoskeletal pain with or without fibromyalgia: Psychological distress in a representative community adult sample. J Rheumatol 2002;29:588-94.
10. Walker EA, Keegan D, Gardner G, et al. Psychosocial factors in fibromyalgia and rheumatoid arthritis: I. Psychiatric diagnoses and functional disability. Psychosomatic Med 1997;59:565-71.
11. MacFarlane GJ, Thomas E, Papageorgiou AC, et al. The natural history of chroninc pain in the community: A better prognosis than in the clinic? J Rheumatol 1996;23:1617-20.
12. Aaron LA, Bradley LA, Alarcón GS, et al. Psychiatric diagnoses in patients with fibromyalgia are related to health care-seeking behavior rather than to illness. Arthritis Rheum 1996;39:436-45.
13. Moldofsky H, Scarisbrick P, England R, et al. Musculoskeletal symptoms and non-REM sleep disturbance in patients with “fibrositis syndrome” and healthy subjects. Psychosom Med 1975;37:341-5.
14. Moldofsky H, Scarisbrick P. Induction of neurasthenic musculoskeletal pain syndrome by selective sleep stage deprivation. Psychosom Med 1975;38:35-44.
15. Schneider-Helmert D, Whitehouse I, Kumar A, et al. Insomnia and alpha sleep in chronic non-organic pain as compared to primary insomnia. Neuropsychobiology 2001;43:54-8.
16. Pillemer SR, Bradley LA, Crofford LJ, et al. The neuroscience and endocrinology of fibromyalgia. Arthritis Rheum 1997;40:1928-39.
17. Walker EA, Keegan D, Gardner G, et al. Psychosocial factors in fibromyalgia and rheumatoid arthritis: II. Sexual, physical, and emotional abuse and neglect. Psychosomatic Med 1997;59:572-7.
18. Demitrack MA, Crofford LJ. Hypothalamic-pituitary-adrenal axis dysregulation in fibromyalgia and chronic fatigue syndrome: An overview and hypothesis. J Musculoskeletal Pain 1995;3:67-73.
19. Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 2000;25:1-35.
20. Bennett RM. Emerging concepts in the neurobiology of chronic pain: Evidence of abnormal sensory processing in fibromyalgia. Mayo Clin Proc 1999;74:385-98.
21. Weigent DA, Bradley LA, Blalock JE, et al. Current concepts in the pathophysiology of abnormal pain perception in fibromyalgia. Am J Med Sci 1998;315:405-12.
22. Baranauskas G, Nistri A. Sensitization of pain pathways in the spinal cord: cellular mechanisms. Prog Neurobiol 1998;7:309-38.
23. Watkins LR, Wiertelak EP, Furness LE, et al. Illness-induced hyperalgesia is mediated by spinal neuropeptides and excitatory amino acids. Brain Res 1994;664:17-24.
24. Russell IJ, Orr MD, Littman B, et al. Elevated cerebrospinal fluid levels of substance P in patients with fibromyalgia syndrome. Arthritis Rheum 1994;37:1593-1601.
25. Schwarz MJ, Spath M, Muller-Bardorff H, et al. Relationship of substance P, 5-hydroxyindole acetic acid and tryptophan in serum of fibromyalgia patients. Neurosci Lett 1999;259:196-8.
26. Russell IJ, Vaeroy H, Javors M, Nyberg F. Cerebrospinal fluid biogenic amine metabolites in fibromyalgia/fibrositis syndrome and rheumatoid arthritis. Arthrits Rheum 1993;35(5):550-6.
27. Fishbain D. Evidence-based data on pain relief with antidepressants. Ann Med 2000;32:305-16.
28. Hudson JI, Goldenberg DL, Pope HG, et al. Comorbidity of fibromyalgia with medical and psychiatric disorders. Am J Med 1992;92:363-7.
29. Basbaum AI, Fields HL. Endogenous pain control systems: Brainstem pathways and endorphin circuitry. Ann Rev Neurosci 1984;7:309-38.
30. Arnold LM, Keck PE, Jr, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000;41:104-13.
31. O’Malley PG, Balden E, Tomkins G, et al. Treatment of fibromyalgia with antidepressants. A meta-analysis. J Gen Intern Med 2000;15:659-66.
32. Nørregaard J, Volkmann H, Danneskiold-Samsø B. A randomized controlled trial of citalopram in the treatment of fibromyalgia. Pain 1995;61:445-9.
33. Anderberg UM, Marteinsdottir I, von Knokrring L. Citalopram in patients with fibromyalgia-A randomized, double-blind, placebo-controlled study. Eur J Pain 2000;4:27-35.
34. Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994;23(5):255-9.
35. Goldenberg DL, Mayskiy M, Mossey C, et al. A randomized, double-blind crossover trial of fluoxetine and amitriptyline in the treatment of fibromyalgia. Arthritis Rheum 1996;39:1852-9.
36. Arnold LM, Hess EV, Hudson JI, et al. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002;112:191-7.
37. Syuertsen JO, Smedsrud T, Lane RM. An open study of sertraline in fibromyalgia syndrome. Eur Neuropsychopharmacol 1995;5:315.-
38. Giordano N, Geraci S, et al. Efficacy and tolerability of paroxetine in patients with fibromyalgia syndrome: A single blind study. Curr Ther Res 1999;60:696-702.
39. Dwight MM, Arnold LM, O’Brien H, et al. An open clinical trial of venlafaxine treatment of fibromyalgia. Psychosomatics 1998;39:14-17.
40. Backonja M, Beydoun A, Edwards KR, et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: A randomized controlled trial. JAMA 1998;280:1831-6.
41. Rice AS, Maton S. Gabapentin in postherpetic neuralgia: A randomized, doubleblind, placebo controlled study. Pain 2001;94:215-24.
42. Mathew NT, Rapoport A, Saper J, et al. Efficacy of gabapentin in migraine prophylaxis. Headache 2001;41:119-28.
43. Ferraccioli G, Ghirelli L, Scita F, et al. EMG-biofeedback training in fibromyalgia syndrome. J Rheumatol 1987;14:820-5.
44. McCain GA, Bell DA, Mai FM, et al. A controlled study of the effects of a supervised cardiovascular fitness training program on the manifestations of primary fibromyalgia. Arthritis Rheum 1988;31:1135-41.
45. Haanen HCM, Hoenderdos HTW, van Romande LKJ, et al. Controlled trial of hypnotherapy in the treatment of refractory fibromyalgia. J Rheumatol 1991;18:72-5.
46. Deluze C, Bosia L, Irbs A, et al. Electroacupuncture in fibromyalgia: Results of a controlled trial. BMJ 1992;1249-52.
47. Nielson WR, Walker C, McCain GA. Cognitive behavioral treatment of fibromyalgia syndrome preliminary findings. J Rheumatol 1992;19:98-103.
Strategies to prevent fatal arrhythmias in patients taking antipsychotics
Before approving the antipsychotic agent ziprasidone last year, the Food and Drug Administration required specific safety data on whether the drug might cause the life-threatening arrhythmia known as torsade de pointes.
The FDA’s action, which delayed the drug’s approval for 3 years, underscores growing concern about the risk of cardiovascular effects with the use of antipsychotic and other agents known to prolong the cardiac QT interval. This concern has led to withdrawal of some drugs before reaching the market (e.g., the atypical neuroleptic sertindole), the addition of “black box” warnings in the labeling of some antipsychotics, and withdrawal from the market of antihistamines terfenadine and astemizole and the GI stimulant cisapride.
Torsade de pointes is a polymorphic ventricular tachycardia (VT), a rare arrhythmia that can cause sudden death. Because torsade can occur with the use of some antipsychotics, the psychiatrist needs to consider cardiovascular safety when selecting among available agents. To help with these decisions, here is information about the documented and potential electrocardiographic features of commonly prescribed antipsychotic drugs, as well as background on QT interval prolongation and torsade de pointes.
Torsade de pointes
Named for a ballet movement, torsade de pointes describes bursts of “twisting of the points,” a variation of the morphology of the QRS vector about the isoelectric axis from positive to net negative and back again. As seen on an ECG (Figure 1), the first beat of torsade de pointes is a normal ventricular complex preceded by a P wave. This is followed by a premature ventricular contraction (PVC) with a short coupling interval. After a compensatory pause, a second normal beat is followed by a second PVC, which is the first beat of a polymorphic VT. We know tachycardia is present because the ventricular beats appear close together. We know the arrhythmia is ventricular in origin because the ventricular complexes are wide. Finally, we note the ventricular complexes vary in configuration—that is, the shape (morphology) varies from beat to beat.
Figure 1 Typical ECG features of torsade de pointes
Sinus beat with normal ventricular complex (1) followed by premature ventricular contraction (PVC) (2) with short coupling interval. After a long pause (long refractory period), another sinus beat (3) is followed by another PVC (4) with a short coupling interval. The second PVC (4) is the first beat of polymorphic ventricular tachycardiaIn torsade, the stimulus for the VT moves within the ventricle, changing its shape from beat to beat. This multifocal VT differs from the more common unifocal VT, in which all the QRS complexes appear the same.
Drug-induced torsade de pointes
Although the term torsade de pointes was first described in 1966,1 the drug-induced form of this arrhythmia has been recognized for nearly a century.
Quinidine Around 1920, cardiologists first used quinidine to help restore normal sinus rhythm in patients with atrial fibrillation, most commonly due to rheumatic heart disease.2
In 1964, Selzer and Wray3 studied the use of quinidine to convert atrial fibrillation to normal sinus rhythm in more than 200 patients seen during 4 years in a cardiopulmonary clinic. In a subgroup of eight patients, these researchers documented 10 reactions (including five documented episodes of ventricular fibrillation/ventricular flutter) among 36 syncopal episodes that developed within 1 to 6.5 hours of quinidine administration. Symptoms were nonspecific and included nausea, faintness, and feeling ill. It is now recognized that torsade de pointes was the principal rhythm disturbance in those eight patients. Syncope usually occurs early in treatment and may be found in 5% to 10% of patients taking quinidine.
TCAs and antipsychotics Tricyclic antidepressants (TCAs) and antipsychotics that have quinidine-like properties (e.g., thioridazine) also may be associated with QT interval prolongation and torsade de pointes.4-9 In high doses (particularly in overdose), TCAs may induce widening of the QRS complex. Fowler et al reported episodes of VT in five patients taking thioridazine—one of whom died.10
Mehtonen et al reported sudden unexpected deaths associated with antipsychotic or antidepressant drugs among 31 women and 18 men in a survey of autopsies performed from 1985 to 1988 in Finland. The authors documented therapeutic use of phenothiazines in all but 3 of the 49 cases. Thioridazine was involved in more than half the deaths. In 15 of the deaths, thioridazine was the only antipsychotic drug taken. Drugs other than thioridazine were documented in only 5 of the 49 sudden cardiac deaths.11
Figure 2 Normal ECG in sinus rhythm
In this typical lead II of a surface ECG, the P wave (atrial depolarization) leads to right and left atrial contraction and the QRS complex (ventricular depolarization) leads to left and right ventricular contraction. The ST segment represents isoelectric ventricular repolarization, and the T wave represents directional repolarization. The QT interval includes both ventricular depolarization (QRS complex) and ventricular repolarization (JT interval, or ST segment plus T wave).
QT interval as a marker for torsade
The incidence of torsade is unknown, but it is an uncommon cardiac abnormality. In the United States, torsade probably accounts for less than 5% of the 300,000 sudden cardiac deaths that occur each year. Because torsade de pointes is rare, regulatory agencies and clinicians use the QT interval as a surrogate ECG marker for risk of torsade de pointes. Heart rate can affect the QT interval, so various formulae are used to correct the QT interval for heart rate (QTc).
What is the QT interval? In a normal ECG (Figure 2), the P wave derives from right and left atrial electrical depolarization. The pacemaker of the heart is located in the sino-atrial node (SAN) in the superior portion of the right atrium. From the SAN, electrical signals travel down three intra-atrial pathways, activating the right atrium, then travel to the atrioventricular node (AVN). Bachmann’s bundle—a fourth atrial pathway—passes from the SAN to depolarize the left atrium. From the AVN, the electrical signal travels through the left and right bundle branches to activate their respective ventricles.
Electrical depolarization of the left and right ventricles produces the QRS complex. Most of the electrical forces making up this complex arise in the left ventricle, which is much larger than the right ventricle.
The electrical circuitry of the heart activates the left and right atria in such a fashion that these chambers eject blood into their respective ventricles just before these chambers contract. Optimal ventricular filling maximizes ventricular ejection of blood (Starling’s law). Ventricular repolarization (JT interval—electrical recovery) follows ventricular depolarization. On the surface ECG, the JT interval consists of an isoelectric event—the ST segment running from the end of the QRS complex to the beginning of the T wave—and the T wave itself (directional electrical recovery).
The QT interval, then, consists of both ventricular depolarization (QRS complex) and ventricular repolarization (JT interval). Ventricular repolarization makes up by far the greater portion of the QT interval.
Correcting the QT interval (QTc) In 1920, Bazett noted that as the heart rate slowed, the QT interval lengthened.12 From personal and reported observations, he derived an equation called the Bazett formula that corrects (or normalizes) the QT interval to a heart rate of 60 beats/min (QTc). In the Bazett formula, the QTc interval is the measured QT interval divided by the square root of the RR interval (time between sequential QRS complexes—the determinant of heart rate) measured in seconds (QTc = QT/RR).
The Bazett formula is most widely used to estimate the QTc interval, although at least 20 other formulae have been developed in response to the original’s perceived inadequacies.13-15 Bazett’s formula is used in most automated interpretations of the ECG.
Up to age 55, the normal QTc interval ranges from 350 to 430 msec for men and 350 to 450 msec for women, and it tends to increase with age. Most cases of torsade occur when the QT or QTc interval is greater than 500 msec.14 A QTc interval between 450 and 500 msec is cause for concern; a QTc interval that exceeds 500 msec is cause for alarm.
Factors that cause variations in QTc
Factors that can affect the QTc interval and increase the risk of torsade de pointes include electrolyte imbalances, medication use and overdose, cardiac disease, liver disease, endocrine disorders such as diabetes and hypothyroidism, and CNS injury (Table 1).
Table 1
Risk factors contributing to QTc interval prolongation
| Risk factor | Causes/implications |
|---|---|
| Sex (female) | QT intervals longer in women than in men QT interval longer during first half of menstrual cycle |
| Age (elderly) | Increased risk for CAD Multiple medications Pharmacokinetic/pharmacodynamic changes |
| Electrolyte imbalance Hypokalemia, hypomagnesemia Hypocalcemia | Diuretic use Excessive vomiting or diarrhea Postprandial hypokalemia |
| Congenital long QT syndrome | Associated with torsade and sudden death |
| Cardiac disease, with history of acute or chronic myocardial ischemia, CHF, cardiac arrhythmias, bradycardia | Increased risk of cardiac arrhythmias |
| Drugs known to prolong QTc interval | May potentiate QTc prolongation |
| Medication overdose with drugs that prolong the QTc interval | QTc prolongation generally dose-dependent |
| Concomitant medications, liver disease | Adverse events with cytochrome P-450 enzyme system inhibition, leading to increased drug levels that can increase QT interval |
| Endocrine/metabolic disorders Diabetes, obesity Hypothyroidism, pituitary insufficiency | Via electrolytes or cardiovascular disease |
| CNS injury Stroke, infection, trauma | Via autonomic nervous system dysfunction |
Circadian patterns The QTc interval varies throughout the 24-hour day, with nocturnal values about 20 msec greater than daytime measurements. These differences are driven by changes in autonomic (sympathetic and parasympathetic) tone.16,17 In 20 normal subjects, circadian variability was 76 ± 19 msec (range 35 to 108 msec) from day to night.17 This circadian variation may be accentuated in patients with cardiovascular disease.
Sex. At birth, QTc interval measurements do no vary by sex.18 At puberty, however, the male QTc interval shortens and remains shorter than its female counterpart by about 20 msec until age 50 to 55, coincident with a decline in male testosterone levels. This sex difference appears to be androgen driven. About 70% of torsade de pointes cases occur in women.18
Menstrual cycle QTc interval measurements are stable throughout the menstrual cycle if quinidine-like drugs are not given.
Variations were seen, however, when Rodriguez et al studied the effect of IV low-dose ibutilide (an antiarrhythmic agent known to prolong the QT interval) on the QTc intervals of 58 healthy subjects (38 men and 20 women, ages 21 to 40). During 1 month, men were studied once and women studied three times, coincident with the three phases of the menstrual cycle. The greatest increase in QTc intervals measurements occurred in women during the first half of their menstrual cycles.19
Age and cardiovascular disease Two congenital long QT syndromes may be associated with sudden death, mostly in children and young adults:
- The Jervell and Lange-Nielsen syndrome is marked by severe congenital deafness and autosomal recessive inheritance.
- The Romano-Ward syndrome has normal hearing and autosomal dominant inheritance.20
Congenital long QT syndrome (LQTS) occurs in about one in 5,000 births and accounts for about 3,000 to 4,000 deaths per year in the United States. Nine percent of pediatric LQTS subjects present with sudden cardiac death. More than 71% of patients will die before age 15 if not treated.
Elderly persons tend to have longer QTc intervals than do younger subjects, even when both groups are free of cardiovascular disease.21 Also, age-matched subjects with cardiovascular disease tend to have longer QTc intervals than do those free of cardiovascular disease.
Electrolytes Electrolyte disturbances, particularly hypokalemia and hypomagnesemia, may contribute to or even cause QT interval prolongation.22
Hypokalemia prolongs the cardiac action potential and may cause early afterdepolarization, leading to torsade.23 Low potassium levels reduce the net outward potassium current during phase 3 of the cardiac action potential. Hypomagnesemia may contribute to gross U wave alternans, lengthening the cardiac action potential and setting the stage for torsade.24 Various factors may contribute to electrolyte disturbances, including use of diuretics and excessive vomiting and diarrhea. Even postprandial states may induce hypokalemia.
Intensive exercise and agitation may be associated with hypokalemia.25 Serum potassium may be lower in severely agitated patients (3.59 mmol/L) than in mildly agitated patients (3.79 mmol/L). The mean QTc interval of psychiatric emergency patients may be prolonged (453±40 msec),5 with QTc intervals of psychiatric inpatients longer than those of psychiatric outpatients. Altered potassium states probably explain these observations. Mechanisms that link exercise and agitation with hypokalemia remain to be elucidated.
Metabolic factors Drugs may alter phase 3 potassium flow, thereby disrupting the synchrony of action of individual cardiac cells during repolarization. This change may induce early afterdepolarizations and torsade.23
Five percent to 10% of Americans of European descent have genetic profiles that make them poor metabolizers of drugs that are metabolized by the cytochrome P-450 isoenzyme 2D6. The Pfizer Inc. 054 study assessed the potential for metabolic inhibitors such as paroxetine to raise antipsychotic drug levels in these patients and induce QTc interval prolongation.26
In response to FDA concerns about QTc interval prolongation associated with the use of ziprasidone, Pfizer studied the potential for QTc interval prolongation when antipsychotics are given with and without metabolic inhibitors of cytochrome P-450 isoenzymes 2D6 (paroxetine), 3A4 (ketoconazole), and 1A2 (fluvoxamine). The study population of 183 subjects (mean age:men, 37.1 years, women 38.8 years) was three-quarters young men with schizophrenia, in good health otherwise and possessing normal ECGs—i.e., patients with a low risk of developing cardiac arrhythmias.
Figure 3 Antipsychotic drugs and QTc interval changes
Six antipsychotic drugs and QTc interval changes from baseline when given with and without metabolic inhibitors. QTc interval changes (in msec) when given without a metabolic inhibitor were ziprasidone, 20.3; risperidone, 11.6; olanzapine, 6.8; quetiapine, 14.5; thioridazine, 35.6; and haloperidol 4.7.
Reprinted from: “FDA Psychopharmacological Drugs Advisory Committee. 19 July 2000. Briefing Documents for Zeldox Capsules (Ziprasidone HCL). Pfizer.” Available from Central Research Division, Pfizer, Inc., Eastern Point Road, Groton, CT 06340, (860) 441-4100.Over the course of about 1 week, daily doses were escalated to ziprasidone, 160 mg; risperidone, 8 mg and 16 mg; olanzapine, 20 mg; quetiapine, 750 mg; thioridazine, 300 mg; and haloperidol, 15 mg. Thioridazine (35.6 msec) and ziprasidone (20.3 msec) showed the greatest QTc interval increase following drug administration (Figure 3). Co-administration of a metabolic inhibitor did not further prolong the QTc interval for these two drugs.
Of the six drugs studied, only thioridazine and ziprasidone showed QTc interval increases 5% compared with baseline measurements.
Co-administration of a metabolic inhibitor caused the greatest increase in QTc intervals for quetiapine (from 14.5 to 19.7 msec). This value closely approached the steady-state ziprasidone measurement (20.3 msec). Because quetiapine is more likely than the other antipsychotic drugs studied to increase heart rate, it may be argued that the Bazett formula’s limitations in estimating the QTc interval at higher heart rates contributed to the quetiapine study findings.
Table 2
Relative risk of QTc interval prolongation with common antipsychotic agents
| Risk level | Agent |
|---|---|
| ECG required or strongly recommended before prescribing (most commonly associated with QTc interval prolongation and torsade de pointes) | Thioridazine Mesoridazine Droperidol Pimozide Haloperidol in large doses IV (commonly ≥ 100 mg/d) |
| Mild to moderate risk of QTc interval prolongation (~20 msec) when prescribed alone or with a metabolic inhibitor | Quetiapine Ziprasidone Chlorpromazine |
| Little or no risk of QTc interval prolongation (~20 msec) when prescribed alone or with a metabolic inhibitor | Haloperidol (oral) Olanzapine Risperidone Clozapine |
Recommendations
Taking a careful history is key to cardiovascular assessment before prescribing an antipsychotic. An ECG is indicated for patients with:
- Personal or family history of syncope or sudden death;
- Personal history of angina pectoris, myocardial infarction, congestive heart failure, cardiac arrhythmias, hypokalemia, hypomagnesemia, or significant cardiac risk factors.
The relative cardiovascular risks associated with antipsychotic agents are shown in Table 2.
An ECG also is required or strongly recommended before prescribing the antipsychotic drugs most commonly associated with QT prolongation and torsade de pointes—droperidol, haloperidol in large doses IV (commonly 100 mg/d), mesoridazine, pimozide, and thioridazine.
The FDA has strengthened the warning labels required for these agents, adding “black box” warnings about the risks of prolonged QTc intervals, torsade de pointes, and sudden death for droperidol, mesoridazine, and thioridazine. Thioridazine, for example, is indicated only for patients with schizophrenia who fail to show an acceptable response to other antipsychotic drugs. Its use is contraindicated in patients who take:
- fluvoxamine, propranolol, and pindolol;
- any drug that inhibits the cytochrome P-450 2D6 isoenzyme (e.g., fluoxetine, paroxetine);
- agents known to prolong the QTc interval.
Use of thioridazine also is contraindicated in patients known to have reduced levels of the cytochrome P450 2D6 isozyme, as well as in patients with congenital LQTS or a history of cardiac arrhythmias. Psychiatrists are advised to read the warnings and prescribing information in the labeling of all antipsychotics for potential cardiovascular side effects.
When the psychiatrist receives a report of suspected QTc interval prolongation on a patient’s ECG, the following steps are recommended:
- Obtain another ECG.
- Assess serum potassium, magnesium, calcium, and thyroid hormone levels.
In patients with confirmed QTc interval prolongation, any complaint of palpitations, presyncope, or syncope are grounds for urgent referral to a cardiologist.
Related resources
- European Society of Cardiology guidelines: www.escardio.org/scinfo/Guidelines/Haverkamp.pdf
- Sudden Arrhythmia Death Syndromes Foundation (SADSF): www.sads.org (800) 786-7723.
- Drugs that prolong the QT interval and/or induce torsade de pointes. Georgetown Center for Education and Research Therapeutics: www.torsades.org
1. Dessertenne F. Tachycardie ventriculaire a deux foyers opposes variables. Arch Mal Coeur Vaiss 1966;59(2):263-72.
2. Clark-Kennedy AE. Quinidine in the treatment of auricular fibrillation. Quart J Med 1922;16:204-35.
3. Selzer A, Wray W. Quinidine syncope. Paroxysmal ventricular fibrillation occurring during treatment of chronic atrial arrhythmias. Circulation 1964;30:17-26.
4. Reilly JG, Ayis SA, Ferrier IN, Jones SJ, Thomas SHL. QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet 2000;355:1048-52.
5. Hatta K, Takahashi T, Nakamura H, Yamashiro H, Yonezawa Y. Prolonged QT interval in acute psychotic patients. Psychiatry Res 2000;94(3):279-85.
6. Welch R. Antipsychotic agents and QT changes. J Psychiatry Neurosci 2000;25(2):154-60.
7. Fayek M, Kingsbury SJ, Zada J, Simpson GM. Cardiac effects of antipsychotic medications. Psychiatr Serv 2001;52(5):607-9.
8. Kelly HG, Fay JE, Laverty SG. Thioridazine hydrochloride (Mellaril): its effect on the electrocardiogram and a report of two fatalities with electrocardiographic abnormalities. Can Med Assoc J 1963;89:546-54.
9. Donatini B, LeBlaye I, Krupp P. Transient cardiac pacing is insufficiently used to treat arrhythmia associated with thioridazine. Cardiology 1992;81(6):340-1.
10. Fowler NO, McCall D, et al. Electrocardiographic changes and cardiac arrhythmias in patients receiving psychotropic drugs. Am J Cardiol 1976;37:223-30.
11. Mehtonen OP, Aranko K, Malkonen L, Vapaatalo H. A survey of sudden death associated with the use of antipsychotic or antidepressant drugs: 49 cases in Finland. Acta Psychiatr Scand 1991;84:58-64.
12 Bazett HC. An analysis of the time-relations of electrocardiograms. Heart 1920;7:353-70.
13. Funck-Brentano C, Jaillon P. Rate-corrected QT interval: techniques and limitations. Am J Cardiol 1993;72(suppl):17B-22B.
14. Bednar MM, et al. The QT Interval. Prog Cardiovas Dis 2001;43(5, pt 2):1-45.
15. Malik M. Problems of heart rate correction in assessment of drug-induced QT interval prolongation. J Cardiovasc Electrophysiol 2001;12(4):411-20.
16. Browne K, Prystowsky E, Heger JJ, Chilson DA, Zipes DP. Prolongation of the Q-T interval in man during sleep. Am J Cardiol 1983;52(1):55-9.
17. Morganroth J, Brozovich FV, McDonald JT, Jacobs RA. Variability of the QT measurement in healthy men, with implications for selection of an abnormal QT value to predict drug toxicity and proarrhythmia. Am J Cardiol 1991;67(8):774-6.
18. Woosley R, Sketch MH. Gender and drug-induced torsade de pointes. Bethesda, Md: American College of Cardiology, 1998; ACCEL 30, No. 2.
19. Rodriguez I, Kilborn MJ, Liu XK, Pezzullo JC, Woosley RL. Drug-induced QT prolongation in women during the menstrual cycle. JAMA 2001;285(10):1322-6.
20. Vincent GM. Long QT syndrome. Cardiology Clinics 1999;18:309-25.
21. Khan SP, Dahlvani S, Vieweg WVR, Bernardo NL, Lewis RE. Electrocardiographic QT interval in a geropsychiatric inpatient population: a preliminary study. Med Psychiatr 1998;1:71-4.
22. Compton SJ, Lux RL, Ramsey MR, et al. Genetically defined therapy of inherited long-QT syndrome. Correction of abnormal repolarization by potassium. Circulation 1996;94(5):1018-22.
23. Tan HL, Hou CJY, Lauer MR, Sung RJ. Electrophysiologic mechanisms of the long QT interval syndromes and torsade de pointes. Ann Intern Med 1995;122(9):701-14.
24. Jackman WM, Friday KJ, Anderson JL, et al. The long QT syndromes: a critical review, new clinical observations, and a unifying hypothesis. Prog Cardiovas Dis 1988;31(2):115-72.
25. Hatta K, Takahashi T, Nakamura H, et al. Hypokalemia and agitation in acute psychotic patients. Psychiatry Res 1999;86(1):85-8.
26. Food and Drug Administration Advisory Committee: Zeldox capsules (ziprasidone): summary of efficacy and safety and overall benefit risk relationship. Bethesda, Md: Food and Drug Administration, July 19, 2000.
Before approving the antipsychotic agent ziprasidone last year, the Food and Drug Administration required specific safety data on whether the drug might cause the life-threatening arrhythmia known as torsade de pointes.
The FDA’s action, which delayed the drug’s approval for 3 years, underscores growing concern about the risk of cardiovascular effects with the use of antipsychotic and other agents known to prolong the cardiac QT interval. This concern has led to withdrawal of some drugs before reaching the market (e.g., the atypical neuroleptic sertindole), the addition of “black box” warnings in the labeling of some antipsychotics, and withdrawal from the market of antihistamines terfenadine and astemizole and the GI stimulant cisapride.
Torsade de pointes is a polymorphic ventricular tachycardia (VT), a rare arrhythmia that can cause sudden death. Because torsade can occur with the use of some antipsychotics, the psychiatrist needs to consider cardiovascular safety when selecting among available agents. To help with these decisions, here is information about the documented and potential electrocardiographic features of commonly prescribed antipsychotic drugs, as well as background on QT interval prolongation and torsade de pointes.
Torsade de pointes
Named for a ballet movement, torsade de pointes describes bursts of “twisting of the points,” a variation of the morphology of the QRS vector about the isoelectric axis from positive to net negative and back again. As seen on an ECG (Figure 1), the first beat of torsade de pointes is a normal ventricular complex preceded by a P wave. This is followed by a premature ventricular contraction (PVC) with a short coupling interval. After a compensatory pause, a second normal beat is followed by a second PVC, which is the first beat of a polymorphic VT. We know tachycardia is present because the ventricular beats appear close together. We know the arrhythmia is ventricular in origin because the ventricular complexes are wide. Finally, we note the ventricular complexes vary in configuration—that is, the shape (morphology) varies from beat to beat.
Figure 1 Typical ECG features of torsade de pointes
Sinus beat with normal ventricular complex (1) followed by premature ventricular contraction (PVC) (2) with short coupling interval. After a long pause (long refractory period), another sinus beat (3) is followed by another PVC (4) with a short coupling interval. The second PVC (4) is the first beat of polymorphic ventricular tachycardiaIn torsade, the stimulus for the VT moves within the ventricle, changing its shape from beat to beat. This multifocal VT differs from the more common unifocal VT, in which all the QRS complexes appear the same.
Drug-induced torsade de pointes
Although the term torsade de pointes was first described in 1966,1 the drug-induced form of this arrhythmia has been recognized for nearly a century.
Quinidine Around 1920, cardiologists first used quinidine to help restore normal sinus rhythm in patients with atrial fibrillation, most commonly due to rheumatic heart disease.2
In 1964, Selzer and Wray3 studied the use of quinidine to convert atrial fibrillation to normal sinus rhythm in more than 200 patients seen during 4 years in a cardiopulmonary clinic. In a subgroup of eight patients, these researchers documented 10 reactions (including five documented episodes of ventricular fibrillation/ventricular flutter) among 36 syncopal episodes that developed within 1 to 6.5 hours of quinidine administration. Symptoms were nonspecific and included nausea, faintness, and feeling ill. It is now recognized that torsade de pointes was the principal rhythm disturbance in those eight patients. Syncope usually occurs early in treatment and may be found in 5% to 10% of patients taking quinidine.
TCAs and antipsychotics Tricyclic antidepressants (TCAs) and antipsychotics that have quinidine-like properties (e.g., thioridazine) also may be associated with QT interval prolongation and torsade de pointes.4-9 In high doses (particularly in overdose), TCAs may induce widening of the QRS complex. Fowler et al reported episodes of VT in five patients taking thioridazine—one of whom died.10
Mehtonen et al reported sudden unexpected deaths associated with antipsychotic or antidepressant drugs among 31 women and 18 men in a survey of autopsies performed from 1985 to 1988 in Finland. The authors documented therapeutic use of phenothiazines in all but 3 of the 49 cases. Thioridazine was involved in more than half the deaths. In 15 of the deaths, thioridazine was the only antipsychotic drug taken. Drugs other than thioridazine were documented in only 5 of the 49 sudden cardiac deaths.11
Figure 2 Normal ECG in sinus rhythm
In this typical lead II of a surface ECG, the P wave (atrial depolarization) leads to right and left atrial contraction and the QRS complex (ventricular depolarization) leads to left and right ventricular contraction. The ST segment represents isoelectric ventricular repolarization, and the T wave represents directional repolarization. The QT interval includes both ventricular depolarization (QRS complex) and ventricular repolarization (JT interval, or ST segment plus T wave).
QT interval as a marker for torsade
The incidence of torsade is unknown, but it is an uncommon cardiac abnormality. In the United States, torsade probably accounts for less than 5% of the 300,000 sudden cardiac deaths that occur each year. Because torsade de pointes is rare, regulatory agencies and clinicians use the QT interval as a surrogate ECG marker for risk of torsade de pointes. Heart rate can affect the QT interval, so various formulae are used to correct the QT interval for heart rate (QTc).
What is the QT interval? In a normal ECG (Figure 2), the P wave derives from right and left atrial electrical depolarization. The pacemaker of the heart is located in the sino-atrial node (SAN) in the superior portion of the right atrium. From the SAN, electrical signals travel down three intra-atrial pathways, activating the right atrium, then travel to the atrioventricular node (AVN). Bachmann’s bundle—a fourth atrial pathway—passes from the SAN to depolarize the left atrium. From the AVN, the electrical signal travels through the left and right bundle branches to activate their respective ventricles.
Electrical depolarization of the left and right ventricles produces the QRS complex. Most of the electrical forces making up this complex arise in the left ventricle, which is much larger than the right ventricle.
The electrical circuitry of the heart activates the left and right atria in such a fashion that these chambers eject blood into their respective ventricles just before these chambers contract. Optimal ventricular filling maximizes ventricular ejection of blood (Starling’s law). Ventricular repolarization (JT interval—electrical recovery) follows ventricular depolarization. On the surface ECG, the JT interval consists of an isoelectric event—the ST segment running from the end of the QRS complex to the beginning of the T wave—and the T wave itself (directional electrical recovery).
The QT interval, then, consists of both ventricular depolarization (QRS complex) and ventricular repolarization (JT interval). Ventricular repolarization makes up by far the greater portion of the QT interval.
Correcting the QT interval (QTc) In 1920, Bazett noted that as the heart rate slowed, the QT interval lengthened.12 From personal and reported observations, he derived an equation called the Bazett formula that corrects (or normalizes) the QT interval to a heart rate of 60 beats/min (QTc). In the Bazett formula, the QTc interval is the measured QT interval divided by the square root of the RR interval (time between sequential QRS complexes—the determinant of heart rate) measured in seconds (QTc = QT/RR).
The Bazett formula is most widely used to estimate the QTc interval, although at least 20 other formulae have been developed in response to the original’s perceived inadequacies.13-15 Bazett’s formula is used in most automated interpretations of the ECG.
Up to age 55, the normal QTc interval ranges from 350 to 430 msec for men and 350 to 450 msec for women, and it tends to increase with age. Most cases of torsade occur when the QT or QTc interval is greater than 500 msec.14 A QTc interval between 450 and 500 msec is cause for concern; a QTc interval that exceeds 500 msec is cause for alarm.
Factors that cause variations in QTc
Factors that can affect the QTc interval and increase the risk of torsade de pointes include electrolyte imbalances, medication use and overdose, cardiac disease, liver disease, endocrine disorders such as diabetes and hypothyroidism, and CNS injury (Table 1).
Table 1
Risk factors contributing to QTc interval prolongation
| Risk factor | Causes/implications |
|---|---|
| Sex (female) | QT intervals longer in women than in men QT interval longer during first half of menstrual cycle |
| Age (elderly) | Increased risk for CAD Multiple medications Pharmacokinetic/pharmacodynamic changes |
| Electrolyte imbalance Hypokalemia, hypomagnesemia Hypocalcemia | Diuretic use Excessive vomiting or diarrhea Postprandial hypokalemia |
| Congenital long QT syndrome | Associated with torsade and sudden death |
| Cardiac disease, with history of acute or chronic myocardial ischemia, CHF, cardiac arrhythmias, bradycardia | Increased risk of cardiac arrhythmias |
| Drugs known to prolong QTc interval | May potentiate QTc prolongation |
| Medication overdose with drugs that prolong the QTc interval | QTc prolongation generally dose-dependent |
| Concomitant medications, liver disease | Adverse events with cytochrome P-450 enzyme system inhibition, leading to increased drug levels that can increase QT interval |
| Endocrine/metabolic disorders Diabetes, obesity Hypothyroidism, pituitary insufficiency | Via electrolytes or cardiovascular disease |
| CNS injury Stroke, infection, trauma | Via autonomic nervous system dysfunction |
Circadian patterns The QTc interval varies throughout the 24-hour day, with nocturnal values about 20 msec greater than daytime measurements. These differences are driven by changes in autonomic (sympathetic and parasympathetic) tone.16,17 In 20 normal subjects, circadian variability was 76 ± 19 msec (range 35 to 108 msec) from day to night.17 This circadian variation may be accentuated in patients with cardiovascular disease.
Sex. At birth, QTc interval measurements do no vary by sex.18 At puberty, however, the male QTc interval shortens and remains shorter than its female counterpart by about 20 msec until age 50 to 55, coincident with a decline in male testosterone levels. This sex difference appears to be androgen driven. About 70% of torsade de pointes cases occur in women.18
Menstrual cycle QTc interval measurements are stable throughout the menstrual cycle if quinidine-like drugs are not given.
Variations were seen, however, when Rodriguez et al studied the effect of IV low-dose ibutilide (an antiarrhythmic agent known to prolong the QT interval) on the QTc intervals of 58 healthy subjects (38 men and 20 women, ages 21 to 40). During 1 month, men were studied once and women studied three times, coincident with the three phases of the menstrual cycle. The greatest increase in QTc intervals measurements occurred in women during the first half of their menstrual cycles.19
Age and cardiovascular disease Two congenital long QT syndromes may be associated with sudden death, mostly in children and young adults:
- The Jervell and Lange-Nielsen syndrome is marked by severe congenital deafness and autosomal recessive inheritance.
- The Romano-Ward syndrome has normal hearing and autosomal dominant inheritance.20
Congenital long QT syndrome (LQTS) occurs in about one in 5,000 births and accounts for about 3,000 to 4,000 deaths per year in the United States. Nine percent of pediatric LQTS subjects present with sudden cardiac death. More than 71% of patients will die before age 15 if not treated.
Elderly persons tend to have longer QTc intervals than do younger subjects, even when both groups are free of cardiovascular disease.21 Also, age-matched subjects with cardiovascular disease tend to have longer QTc intervals than do those free of cardiovascular disease.
Electrolytes Electrolyte disturbances, particularly hypokalemia and hypomagnesemia, may contribute to or even cause QT interval prolongation.22
Hypokalemia prolongs the cardiac action potential and may cause early afterdepolarization, leading to torsade.23 Low potassium levels reduce the net outward potassium current during phase 3 of the cardiac action potential. Hypomagnesemia may contribute to gross U wave alternans, lengthening the cardiac action potential and setting the stage for torsade.24 Various factors may contribute to electrolyte disturbances, including use of diuretics and excessive vomiting and diarrhea. Even postprandial states may induce hypokalemia.
Intensive exercise and agitation may be associated with hypokalemia.25 Serum potassium may be lower in severely agitated patients (3.59 mmol/L) than in mildly agitated patients (3.79 mmol/L). The mean QTc interval of psychiatric emergency patients may be prolonged (453±40 msec),5 with QTc intervals of psychiatric inpatients longer than those of psychiatric outpatients. Altered potassium states probably explain these observations. Mechanisms that link exercise and agitation with hypokalemia remain to be elucidated.
Metabolic factors Drugs may alter phase 3 potassium flow, thereby disrupting the synchrony of action of individual cardiac cells during repolarization. This change may induce early afterdepolarizations and torsade.23
Five percent to 10% of Americans of European descent have genetic profiles that make them poor metabolizers of drugs that are metabolized by the cytochrome P-450 isoenzyme 2D6. The Pfizer Inc. 054 study assessed the potential for metabolic inhibitors such as paroxetine to raise antipsychotic drug levels in these patients and induce QTc interval prolongation.26
In response to FDA concerns about QTc interval prolongation associated with the use of ziprasidone, Pfizer studied the potential for QTc interval prolongation when antipsychotics are given with and without metabolic inhibitors of cytochrome P-450 isoenzymes 2D6 (paroxetine), 3A4 (ketoconazole), and 1A2 (fluvoxamine). The study population of 183 subjects (mean age:men, 37.1 years, women 38.8 years) was three-quarters young men with schizophrenia, in good health otherwise and possessing normal ECGs—i.e., patients with a low risk of developing cardiac arrhythmias.
Figure 3 Antipsychotic drugs and QTc interval changes
Six antipsychotic drugs and QTc interval changes from baseline when given with and without metabolic inhibitors. QTc interval changes (in msec) when given without a metabolic inhibitor were ziprasidone, 20.3; risperidone, 11.6; olanzapine, 6.8; quetiapine, 14.5; thioridazine, 35.6; and haloperidol 4.7.
Reprinted from: “FDA Psychopharmacological Drugs Advisory Committee. 19 July 2000. Briefing Documents for Zeldox Capsules (Ziprasidone HCL). Pfizer.” Available from Central Research Division, Pfizer, Inc., Eastern Point Road, Groton, CT 06340, (860) 441-4100.Over the course of about 1 week, daily doses were escalated to ziprasidone, 160 mg; risperidone, 8 mg and 16 mg; olanzapine, 20 mg; quetiapine, 750 mg; thioridazine, 300 mg; and haloperidol, 15 mg. Thioridazine (35.6 msec) and ziprasidone (20.3 msec) showed the greatest QTc interval increase following drug administration (Figure 3). Co-administration of a metabolic inhibitor did not further prolong the QTc interval for these two drugs.
Of the six drugs studied, only thioridazine and ziprasidone showed QTc interval increases 5% compared with baseline measurements.
Co-administration of a metabolic inhibitor caused the greatest increase in QTc intervals for quetiapine (from 14.5 to 19.7 msec). This value closely approached the steady-state ziprasidone measurement (20.3 msec). Because quetiapine is more likely than the other antipsychotic drugs studied to increase heart rate, it may be argued that the Bazett formula’s limitations in estimating the QTc interval at higher heart rates contributed to the quetiapine study findings.
Table 2
Relative risk of QTc interval prolongation with common antipsychotic agents
| Risk level | Agent |
|---|---|
| ECG required or strongly recommended before prescribing (most commonly associated with QTc interval prolongation and torsade de pointes) | Thioridazine Mesoridazine Droperidol Pimozide Haloperidol in large doses IV (commonly ≥ 100 mg/d) |
| Mild to moderate risk of QTc interval prolongation (~20 msec) when prescribed alone or with a metabolic inhibitor | Quetiapine Ziprasidone Chlorpromazine |
| Little or no risk of QTc interval prolongation (~20 msec) when prescribed alone or with a metabolic inhibitor | Haloperidol (oral) Olanzapine Risperidone Clozapine |
Recommendations
Taking a careful history is key to cardiovascular assessment before prescribing an antipsychotic. An ECG is indicated for patients with:
- Personal or family history of syncope or sudden death;
- Personal history of angina pectoris, myocardial infarction, congestive heart failure, cardiac arrhythmias, hypokalemia, hypomagnesemia, or significant cardiac risk factors.
The relative cardiovascular risks associated with antipsychotic agents are shown in Table 2.
An ECG also is required or strongly recommended before prescribing the antipsychotic drugs most commonly associated with QT prolongation and torsade de pointes—droperidol, haloperidol in large doses IV (commonly 100 mg/d), mesoridazine, pimozide, and thioridazine.
The FDA has strengthened the warning labels required for these agents, adding “black box” warnings about the risks of prolonged QTc intervals, torsade de pointes, and sudden death for droperidol, mesoridazine, and thioridazine. Thioridazine, for example, is indicated only for patients with schizophrenia who fail to show an acceptable response to other antipsychotic drugs. Its use is contraindicated in patients who take:
- fluvoxamine, propranolol, and pindolol;
- any drug that inhibits the cytochrome P-450 2D6 isoenzyme (e.g., fluoxetine, paroxetine);
- agents known to prolong the QTc interval.
Use of thioridazine also is contraindicated in patients known to have reduced levels of the cytochrome P450 2D6 isozyme, as well as in patients with congenital LQTS or a history of cardiac arrhythmias. Psychiatrists are advised to read the warnings and prescribing information in the labeling of all antipsychotics for potential cardiovascular side effects.
When the psychiatrist receives a report of suspected QTc interval prolongation on a patient’s ECG, the following steps are recommended:
- Obtain another ECG.
- Assess serum potassium, magnesium, calcium, and thyroid hormone levels.
In patients with confirmed QTc interval prolongation, any complaint of palpitations, presyncope, or syncope are grounds for urgent referral to a cardiologist.
Related resources
- European Society of Cardiology guidelines: www.escardio.org/scinfo/Guidelines/Haverkamp.pdf
- Sudden Arrhythmia Death Syndromes Foundation (SADSF): www.sads.org (800) 786-7723.
- Drugs that prolong the QT interval and/or induce torsade de pointes. Georgetown Center for Education and Research Therapeutics: www.torsades.org
Before approving the antipsychotic agent ziprasidone last year, the Food and Drug Administration required specific safety data on whether the drug might cause the life-threatening arrhythmia known as torsade de pointes.
The FDA’s action, which delayed the drug’s approval for 3 years, underscores growing concern about the risk of cardiovascular effects with the use of antipsychotic and other agents known to prolong the cardiac QT interval. This concern has led to withdrawal of some drugs before reaching the market (e.g., the atypical neuroleptic sertindole), the addition of “black box” warnings in the labeling of some antipsychotics, and withdrawal from the market of antihistamines terfenadine and astemizole and the GI stimulant cisapride.
Torsade de pointes is a polymorphic ventricular tachycardia (VT), a rare arrhythmia that can cause sudden death. Because torsade can occur with the use of some antipsychotics, the psychiatrist needs to consider cardiovascular safety when selecting among available agents. To help with these decisions, here is information about the documented and potential electrocardiographic features of commonly prescribed antipsychotic drugs, as well as background on QT interval prolongation and torsade de pointes.
Torsade de pointes
Named for a ballet movement, torsade de pointes describes bursts of “twisting of the points,” a variation of the morphology of the QRS vector about the isoelectric axis from positive to net negative and back again. As seen on an ECG (Figure 1), the first beat of torsade de pointes is a normal ventricular complex preceded by a P wave. This is followed by a premature ventricular contraction (PVC) with a short coupling interval. After a compensatory pause, a second normal beat is followed by a second PVC, which is the first beat of a polymorphic VT. We know tachycardia is present because the ventricular beats appear close together. We know the arrhythmia is ventricular in origin because the ventricular complexes are wide. Finally, we note the ventricular complexes vary in configuration—that is, the shape (morphology) varies from beat to beat.
Figure 1 Typical ECG features of torsade de pointes
Sinus beat with normal ventricular complex (1) followed by premature ventricular contraction (PVC) (2) with short coupling interval. After a long pause (long refractory period), another sinus beat (3) is followed by another PVC (4) with a short coupling interval. The second PVC (4) is the first beat of polymorphic ventricular tachycardiaIn torsade, the stimulus for the VT moves within the ventricle, changing its shape from beat to beat. This multifocal VT differs from the more common unifocal VT, in which all the QRS complexes appear the same.
Drug-induced torsade de pointes
Although the term torsade de pointes was first described in 1966,1 the drug-induced form of this arrhythmia has been recognized for nearly a century.
Quinidine Around 1920, cardiologists first used quinidine to help restore normal sinus rhythm in patients with atrial fibrillation, most commonly due to rheumatic heart disease.2
In 1964, Selzer and Wray3 studied the use of quinidine to convert atrial fibrillation to normal sinus rhythm in more than 200 patients seen during 4 years in a cardiopulmonary clinic. In a subgroup of eight patients, these researchers documented 10 reactions (including five documented episodes of ventricular fibrillation/ventricular flutter) among 36 syncopal episodes that developed within 1 to 6.5 hours of quinidine administration. Symptoms were nonspecific and included nausea, faintness, and feeling ill. It is now recognized that torsade de pointes was the principal rhythm disturbance in those eight patients. Syncope usually occurs early in treatment and may be found in 5% to 10% of patients taking quinidine.
TCAs and antipsychotics Tricyclic antidepressants (TCAs) and antipsychotics that have quinidine-like properties (e.g., thioridazine) also may be associated with QT interval prolongation and torsade de pointes.4-9 In high doses (particularly in overdose), TCAs may induce widening of the QRS complex. Fowler et al reported episodes of VT in five patients taking thioridazine—one of whom died.10
Mehtonen et al reported sudden unexpected deaths associated with antipsychotic or antidepressant drugs among 31 women and 18 men in a survey of autopsies performed from 1985 to 1988 in Finland. The authors documented therapeutic use of phenothiazines in all but 3 of the 49 cases. Thioridazine was involved in more than half the deaths. In 15 of the deaths, thioridazine was the only antipsychotic drug taken. Drugs other than thioridazine were documented in only 5 of the 49 sudden cardiac deaths.11
Figure 2 Normal ECG in sinus rhythm
In this typical lead II of a surface ECG, the P wave (atrial depolarization) leads to right and left atrial contraction and the QRS complex (ventricular depolarization) leads to left and right ventricular contraction. The ST segment represents isoelectric ventricular repolarization, and the T wave represents directional repolarization. The QT interval includes both ventricular depolarization (QRS complex) and ventricular repolarization (JT interval, or ST segment plus T wave).
QT interval as a marker for torsade
The incidence of torsade is unknown, but it is an uncommon cardiac abnormality. In the United States, torsade probably accounts for less than 5% of the 300,000 sudden cardiac deaths that occur each year. Because torsade de pointes is rare, regulatory agencies and clinicians use the QT interval as a surrogate ECG marker for risk of torsade de pointes. Heart rate can affect the QT interval, so various formulae are used to correct the QT interval for heart rate (QTc).
What is the QT interval? In a normal ECG (Figure 2), the P wave derives from right and left atrial electrical depolarization. The pacemaker of the heart is located in the sino-atrial node (SAN) in the superior portion of the right atrium. From the SAN, electrical signals travel down three intra-atrial pathways, activating the right atrium, then travel to the atrioventricular node (AVN). Bachmann’s bundle—a fourth atrial pathway—passes from the SAN to depolarize the left atrium. From the AVN, the electrical signal travels through the left and right bundle branches to activate their respective ventricles.
Electrical depolarization of the left and right ventricles produces the QRS complex. Most of the electrical forces making up this complex arise in the left ventricle, which is much larger than the right ventricle.
The electrical circuitry of the heart activates the left and right atria in such a fashion that these chambers eject blood into their respective ventricles just before these chambers contract. Optimal ventricular filling maximizes ventricular ejection of blood (Starling’s law). Ventricular repolarization (JT interval—electrical recovery) follows ventricular depolarization. On the surface ECG, the JT interval consists of an isoelectric event—the ST segment running from the end of the QRS complex to the beginning of the T wave—and the T wave itself (directional electrical recovery).
The QT interval, then, consists of both ventricular depolarization (QRS complex) and ventricular repolarization (JT interval). Ventricular repolarization makes up by far the greater portion of the QT interval.
Correcting the QT interval (QTc) In 1920, Bazett noted that as the heart rate slowed, the QT interval lengthened.12 From personal and reported observations, he derived an equation called the Bazett formula that corrects (or normalizes) the QT interval to a heart rate of 60 beats/min (QTc). In the Bazett formula, the QTc interval is the measured QT interval divided by the square root of the RR interval (time between sequential QRS complexes—the determinant of heart rate) measured in seconds (QTc = QT/RR).
The Bazett formula is most widely used to estimate the QTc interval, although at least 20 other formulae have been developed in response to the original’s perceived inadequacies.13-15 Bazett’s formula is used in most automated interpretations of the ECG.
Up to age 55, the normal QTc interval ranges from 350 to 430 msec for men and 350 to 450 msec for women, and it tends to increase with age. Most cases of torsade occur when the QT or QTc interval is greater than 500 msec.14 A QTc interval between 450 and 500 msec is cause for concern; a QTc interval that exceeds 500 msec is cause for alarm.
Factors that cause variations in QTc
Factors that can affect the QTc interval and increase the risk of torsade de pointes include electrolyte imbalances, medication use and overdose, cardiac disease, liver disease, endocrine disorders such as diabetes and hypothyroidism, and CNS injury (Table 1).
Table 1
Risk factors contributing to QTc interval prolongation
| Risk factor | Causes/implications |
|---|---|
| Sex (female) | QT intervals longer in women than in men QT interval longer during first half of menstrual cycle |
| Age (elderly) | Increased risk for CAD Multiple medications Pharmacokinetic/pharmacodynamic changes |
| Electrolyte imbalance Hypokalemia, hypomagnesemia Hypocalcemia | Diuretic use Excessive vomiting or diarrhea Postprandial hypokalemia |
| Congenital long QT syndrome | Associated with torsade and sudden death |
| Cardiac disease, with history of acute or chronic myocardial ischemia, CHF, cardiac arrhythmias, bradycardia | Increased risk of cardiac arrhythmias |
| Drugs known to prolong QTc interval | May potentiate QTc prolongation |
| Medication overdose with drugs that prolong the QTc interval | QTc prolongation generally dose-dependent |
| Concomitant medications, liver disease | Adverse events with cytochrome P-450 enzyme system inhibition, leading to increased drug levels that can increase QT interval |
| Endocrine/metabolic disorders Diabetes, obesity Hypothyroidism, pituitary insufficiency | Via electrolytes or cardiovascular disease |
| CNS injury Stroke, infection, trauma | Via autonomic nervous system dysfunction |
Circadian patterns The QTc interval varies throughout the 24-hour day, with nocturnal values about 20 msec greater than daytime measurements. These differences are driven by changes in autonomic (sympathetic and parasympathetic) tone.16,17 In 20 normal subjects, circadian variability was 76 ± 19 msec (range 35 to 108 msec) from day to night.17 This circadian variation may be accentuated in patients with cardiovascular disease.
Sex. At birth, QTc interval measurements do no vary by sex.18 At puberty, however, the male QTc interval shortens and remains shorter than its female counterpart by about 20 msec until age 50 to 55, coincident with a decline in male testosterone levels. This sex difference appears to be androgen driven. About 70% of torsade de pointes cases occur in women.18
Menstrual cycle QTc interval measurements are stable throughout the menstrual cycle if quinidine-like drugs are not given.
Variations were seen, however, when Rodriguez et al studied the effect of IV low-dose ibutilide (an antiarrhythmic agent known to prolong the QT interval) on the QTc intervals of 58 healthy subjects (38 men and 20 women, ages 21 to 40). During 1 month, men were studied once and women studied three times, coincident with the three phases of the menstrual cycle. The greatest increase in QTc intervals measurements occurred in women during the first half of their menstrual cycles.19
Age and cardiovascular disease Two congenital long QT syndromes may be associated with sudden death, mostly in children and young adults:
- The Jervell and Lange-Nielsen syndrome is marked by severe congenital deafness and autosomal recessive inheritance.
- The Romano-Ward syndrome has normal hearing and autosomal dominant inheritance.20
Congenital long QT syndrome (LQTS) occurs in about one in 5,000 births and accounts for about 3,000 to 4,000 deaths per year in the United States. Nine percent of pediatric LQTS subjects present with sudden cardiac death. More than 71% of patients will die before age 15 if not treated.
Elderly persons tend to have longer QTc intervals than do younger subjects, even when both groups are free of cardiovascular disease.21 Also, age-matched subjects with cardiovascular disease tend to have longer QTc intervals than do those free of cardiovascular disease.
Electrolytes Electrolyte disturbances, particularly hypokalemia and hypomagnesemia, may contribute to or even cause QT interval prolongation.22
Hypokalemia prolongs the cardiac action potential and may cause early afterdepolarization, leading to torsade.23 Low potassium levels reduce the net outward potassium current during phase 3 of the cardiac action potential. Hypomagnesemia may contribute to gross U wave alternans, lengthening the cardiac action potential and setting the stage for torsade.24 Various factors may contribute to electrolyte disturbances, including use of diuretics and excessive vomiting and diarrhea. Even postprandial states may induce hypokalemia.
Intensive exercise and agitation may be associated with hypokalemia.25 Serum potassium may be lower in severely agitated patients (3.59 mmol/L) than in mildly agitated patients (3.79 mmol/L). The mean QTc interval of psychiatric emergency patients may be prolonged (453±40 msec),5 with QTc intervals of psychiatric inpatients longer than those of psychiatric outpatients. Altered potassium states probably explain these observations. Mechanisms that link exercise and agitation with hypokalemia remain to be elucidated.
Metabolic factors Drugs may alter phase 3 potassium flow, thereby disrupting the synchrony of action of individual cardiac cells during repolarization. This change may induce early afterdepolarizations and torsade.23
Five percent to 10% of Americans of European descent have genetic profiles that make them poor metabolizers of drugs that are metabolized by the cytochrome P-450 isoenzyme 2D6. The Pfizer Inc. 054 study assessed the potential for metabolic inhibitors such as paroxetine to raise antipsychotic drug levels in these patients and induce QTc interval prolongation.26
In response to FDA concerns about QTc interval prolongation associated with the use of ziprasidone, Pfizer studied the potential for QTc interval prolongation when antipsychotics are given with and without metabolic inhibitors of cytochrome P-450 isoenzymes 2D6 (paroxetine), 3A4 (ketoconazole), and 1A2 (fluvoxamine). The study population of 183 subjects (mean age:men, 37.1 years, women 38.8 years) was three-quarters young men with schizophrenia, in good health otherwise and possessing normal ECGs—i.e., patients with a low risk of developing cardiac arrhythmias.
Figure 3 Antipsychotic drugs and QTc interval changes
Six antipsychotic drugs and QTc interval changes from baseline when given with and without metabolic inhibitors. QTc interval changes (in msec) when given without a metabolic inhibitor were ziprasidone, 20.3; risperidone, 11.6; olanzapine, 6.8; quetiapine, 14.5; thioridazine, 35.6; and haloperidol 4.7.
Reprinted from: “FDA Psychopharmacological Drugs Advisory Committee. 19 July 2000. Briefing Documents for Zeldox Capsules (Ziprasidone HCL). Pfizer.” Available from Central Research Division, Pfizer, Inc., Eastern Point Road, Groton, CT 06340, (860) 441-4100.Over the course of about 1 week, daily doses were escalated to ziprasidone, 160 mg; risperidone, 8 mg and 16 mg; olanzapine, 20 mg; quetiapine, 750 mg; thioridazine, 300 mg; and haloperidol, 15 mg. Thioridazine (35.6 msec) and ziprasidone (20.3 msec) showed the greatest QTc interval increase following drug administration (Figure 3). Co-administration of a metabolic inhibitor did not further prolong the QTc interval for these two drugs.
Of the six drugs studied, only thioridazine and ziprasidone showed QTc interval increases 5% compared with baseline measurements.
Co-administration of a metabolic inhibitor caused the greatest increase in QTc intervals for quetiapine (from 14.5 to 19.7 msec). This value closely approached the steady-state ziprasidone measurement (20.3 msec). Because quetiapine is more likely than the other antipsychotic drugs studied to increase heart rate, it may be argued that the Bazett formula’s limitations in estimating the QTc interval at higher heart rates contributed to the quetiapine study findings.
Table 2
Relative risk of QTc interval prolongation with common antipsychotic agents
| Risk level | Agent |
|---|---|
| ECG required or strongly recommended before prescribing (most commonly associated with QTc interval prolongation and torsade de pointes) | Thioridazine Mesoridazine Droperidol Pimozide Haloperidol in large doses IV (commonly ≥ 100 mg/d) |
| Mild to moderate risk of QTc interval prolongation (~20 msec) when prescribed alone or with a metabolic inhibitor | Quetiapine Ziprasidone Chlorpromazine |
| Little or no risk of QTc interval prolongation (~20 msec) when prescribed alone or with a metabolic inhibitor | Haloperidol (oral) Olanzapine Risperidone Clozapine |
Recommendations
Taking a careful history is key to cardiovascular assessment before prescribing an antipsychotic. An ECG is indicated for patients with:
- Personal or family history of syncope or sudden death;
- Personal history of angina pectoris, myocardial infarction, congestive heart failure, cardiac arrhythmias, hypokalemia, hypomagnesemia, or significant cardiac risk factors.
The relative cardiovascular risks associated with antipsychotic agents are shown in Table 2.
An ECG also is required or strongly recommended before prescribing the antipsychotic drugs most commonly associated with QT prolongation and torsade de pointes—droperidol, haloperidol in large doses IV (commonly 100 mg/d), mesoridazine, pimozide, and thioridazine.
The FDA has strengthened the warning labels required for these agents, adding “black box” warnings about the risks of prolonged QTc intervals, torsade de pointes, and sudden death for droperidol, mesoridazine, and thioridazine. Thioridazine, for example, is indicated only for patients with schizophrenia who fail to show an acceptable response to other antipsychotic drugs. Its use is contraindicated in patients who take:
- fluvoxamine, propranolol, and pindolol;
- any drug that inhibits the cytochrome P-450 2D6 isoenzyme (e.g., fluoxetine, paroxetine);
- agents known to prolong the QTc interval.
Use of thioridazine also is contraindicated in patients known to have reduced levels of the cytochrome P450 2D6 isozyme, as well as in patients with congenital LQTS or a history of cardiac arrhythmias. Psychiatrists are advised to read the warnings and prescribing information in the labeling of all antipsychotics for potential cardiovascular side effects.
When the psychiatrist receives a report of suspected QTc interval prolongation on a patient’s ECG, the following steps are recommended:
- Obtain another ECG.
- Assess serum potassium, magnesium, calcium, and thyroid hormone levels.
In patients with confirmed QTc interval prolongation, any complaint of palpitations, presyncope, or syncope are grounds for urgent referral to a cardiologist.
Related resources
- European Society of Cardiology guidelines: www.escardio.org/scinfo/Guidelines/Haverkamp.pdf
- Sudden Arrhythmia Death Syndromes Foundation (SADSF): www.sads.org (800) 786-7723.
- Drugs that prolong the QT interval and/or induce torsade de pointes. Georgetown Center for Education and Research Therapeutics: www.torsades.org
1. Dessertenne F. Tachycardie ventriculaire a deux foyers opposes variables. Arch Mal Coeur Vaiss 1966;59(2):263-72.
2. Clark-Kennedy AE. Quinidine in the treatment of auricular fibrillation. Quart J Med 1922;16:204-35.
3. Selzer A, Wray W. Quinidine syncope. Paroxysmal ventricular fibrillation occurring during treatment of chronic atrial arrhythmias. Circulation 1964;30:17-26.
4. Reilly JG, Ayis SA, Ferrier IN, Jones SJ, Thomas SHL. QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet 2000;355:1048-52.
5. Hatta K, Takahashi T, Nakamura H, Yamashiro H, Yonezawa Y. Prolonged QT interval in acute psychotic patients. Psychiatry Res 2000;94(3):279-85.
6. Welch R. Antipsychotic agents and QT changes. J Psychiatry Neurosci 2000;25(2):154-60.
7. Fayek M, Kingsbury SJ, Zada J, Simpson GM. Cardiac effects of antipsychotic medications. Psychiatr Serv 2001;52(5):607-9.
8. Kelly HG, Fay JE, Laverty SG. Thioridazine hydrochloride (Mellaril): its effect on the electrocardiogram and a report of two fatalities with electrocardiographic abnormalities. Can Med Assoc J 1963;89:546-54.
9. Donatini B, LeBlaye I, Krupp P. Transient cardiac pacing is insufficiently used to treat arrhythmia associated with thioridazine. Cardiology 1992;81(6):340-1.
10. Fowler NO, McCall D, et al. Electrocardiographic changes and cardiac arrhythmias in patients receiving psychotropic drugs. Am J Cardiol 1976;37:223-30.
11. Mehtonen OP, Aranko K, Malkonen L, Vapaatalo H. A survey of sudden death associated with the use of antipsychotic or antidepressant drugs: 49 cases in Finland. Acta Psychiatr Scand 1991;84:58-64.
12 Bazett HC. An analysis of the time-relations of electrocardiograms. Heart 1920;7:353-70.
13. Funck-Brentano C, Jaillon P. Rate-corrected QT interval: techniques and limitations. Am J Cardiol 1993;72(suppl):17B-22B.
14. Bednar MM, et al. The QT Interval. Prog Cardiovas Dis 2001;43(5, pt 2):1-45.
15. Malik M. Problems of heart rate correction in assessment of drug-induced QT interval prolongation. J Cardiovasc Electrophysiol 2001;12(4):411-20.
16. Browne K, Prystowsky E, Heger JJ, Chilson DA, Zipes DP. Prolongation of the Q-T interval in man during sleep. Am J Cardiol 1983;52(1):55-9.
17. Morganroth J, Brozovich FV, McDonald JT, Jacobs RA. Variability of the QT measurement in healthy men, with implications for selection of an abnormal QT value to predict drug toxicity and proarrhythmia. Am J Cardiol 1991;67(8):774-6.
18. Woosley R, Sketch MH. Gender and drug-induced torsade de pointes. Bethesda, Md: American College of Cardiology, 1998; ACCEL 30, No. 2.
19. Rodriguez I, Kilborn MJ, Liu XK, Pezzullo JC, Woosley RL. Drug-induced QT prolongation in women during the menstrual cycle. JAMA 2001;285(10):1322-6.
20. Vincent GM. Long QT syndrome. Cardiology Clinics 1999;18:309-25.
21. Khan SP, Dahlvani S, Vieweg WVR, Bernardo NL, Lewis RE. Electrocardiographic QT interval in a geropsychiatric inpatient population: a preliminary study. Med Psychiatr 1998;1:71-4.
22. Compton SJ, Lux RL, Ramsey MR, et al. Genetically defined therapy of inherited long-QT syndrome. Correction of abnormal repolarization by potassium. Circulation 1996;94(5):1018-22.
23. Tan HL, Hou CJY, Lauer MR, Sung RJ. Electrophysiologic mechanisms of the long QT interval syndromes and torsade de pointes. Ann Intern Med 1995;122(9):701-14.
24. Jackman WM, Friday KJ, Anderson JL, et al. The long QT syndromes: a critical review, new clinical observations, and a unifying hypothesis. Prog Cardiovas Dis 1988;31(2):115-72.
25. Hatta K, Takahashi T, Nakamura H, et al. Hypokalemia and agitation in acute psychotic patients. Psychiatry Res 1999;86(1):85-8.
26. Food and Drug Administration Advisory Committee: Zeldox capsules (ziprasidone): summary of efficacy and safety and overall benefit risk relationship. Bethesda, Md: Food and Drug Administration, July 19, 2000.
1. Dessertenne F. Tachycardie ventriculaire a deux foyers opposes variables. Arch Mal Coeur Vaiss 1966;59(2):263-72.
2. Clark-Kennedy AE. Quinidine in the treatment of auricular fibrillation. Quart J Med 1922;16:204-35.
3. Selzer A, Wray W. Quinidine syncope. Paroxysmal ventricular fibrillation occurring during treatment of chronic atrial arrhythmias. Circulation 1964;30:17-26.
4. Reilly JG, Ayis SA, Ferrier IN, Jones SJ, Thomas SHL. QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet 2000;355:1048-52.
5. Hatta K, Takahashi T, Nakamura H, Yamashiro H, Yonezawa Y. Prolonged QT interval in acute psychotic patients. Psychiatry Res 2000;94(3):279-85.
6. Welch R. Antipsychotic agents and QT changes. J Psychiatry Neurosci 2000;25(2):154-60.
7. Fayek M, Kingsbury SJ, Zada J, Simpson GM. Cardiac effects of antipsychotic medications. Psychiatr Serv 2001;52(5):607-9.
8. Kelly HG, Fay JE, Laverty SG. Thioridazine hydrochloride (Mellaril): its effect on the electrocardiogram and a report of two fatalities with electrocardiographic abnormalities. Can Med Assoc J 1963;89:546-54.
9. Donatini B, LeBlaye I, Krupp P. Transient cardiac pacing is insufficiently used to treat arrhythmia associated with thioridazine. Cardiology 1992;81(6):340-1.
10. Fowler NO, McCall D, et al. Electrocardiographic changes and cardiac arrhythmias in patients receiving psychotropic drugs. Am J Cardiol 1976;37:223-30.
11. Mehtonen OP, Aranko K, Malkonen L, Vapaatalo H. A survey of sudden death associated with the use of antipsychotic or antidepressant drugs: 49 cases in Finland. Acta Psychiatr Scand 1991;84:58-64.
12 Bazett HC. An analysis of the time-relations of electrocardiograms. Heart 1920;7:353-70.
13. Funck-Brentano C, Jaillon P. Rate-corrected QT interval: techniques and limitations. Am J Cardiol 1993;72(suppl):17B-22B.
14. Bednar MM, et al. The QT Interval. Prog Cardiovas Dis 2001;43(5, pt 2):1-45.
15. Malik M. Problems of heart rate correction in assessment of drug-induced QT interval prolongation. J Cardiovasc Electrophysiol 2001;12(4):411-20.
16. Browne K, Prystowsky E, Heger JJ, Chilson DA, Zipes DP. Prolongation of the Q-T interval in man during sleep. Am J Cardiol 1983;52(1):55-9.
17. Morganroth J, Brozovich FV, McDonald JT, Jacobs RA. Variability of the QT measurement in healthy men, with implications for selection of an abnormal QT value to predict drug toxicity and proarrhythmia. Am J Cardiol 1991;67(8):774-6.
18. Woosley R, Sketch MH. Gender and drug-induced torsade de pointes. Bethesda, Md: American College of Cardiology, 1998; ACCEL 30, No. 2.
19. Rodriguez I, Kilborn MJ, Liu XK, Pezzullo JC, Woosley RL. Drug-induced QT prolongation in women during the menstrual cycle. JAMA 2001;285(10):1322-6.
20. Vincent GM. Long QT syndrome. Cardiology Clinics 1999;18:309-25.
21. Khan SP, Dahlvani S, Vieweg WVR, Bernardo NL, Lewis RE. Electrocardiographic QT interval in a geropsychiatric inpatient population: a preliminary study. Med Psychiatr 1998;1:71-4.
22. Compton SJ, Lux RL, Ramsey MR, et al. Genetically defined therapy of inherited long-QT syndrome. Correction of abnormal repolarization by potassium. Circulation 1996;94(5):1018-22.
23. Tan HL, Hou CJY, Lauer MR, Sung RJ. Electrophysiologic mechanisms of the long QT interval syndromes and torsade de pointes. Ann Intern Med 1995;122(9):701-14.
24. Jackman WM, Friday KJ, Anderson JL, et al. The long QT syndromes: a critical review, new clinical observations, and a unifying hypothesis. Prog Cardiovas Dis 1988;31(2):115-72.
25. Hatta K, Takahashi T, Nakamura H, et al. Hypokalemia and agitation in acute psychotic patients. Psychiatry Res 1999;86(1):85-8.
26. Food and Drug Administration Advisory Committee: Zeldox capsules (ziprasidone): summary of efficacy and safety and overall benefit risk relationship. Bethesda, Md: Food and Drug Administration, July 19, 2000.
Psychiatric illness or thyroid disease? Don’t be misled by false lab tests
Psychiatrists commonly order thyroid testing and are often the first to confront abnormal thyroid test results. As thyroid testing has become more sophisticated and sensitive (Box 1), the interpretation and management of abnormal or slightly abnormal results has become increasingly complex. What’s more, older individuals, hospitalized patients, and those with psychiatric illness often present with subtle laboratory abnormalities.
Hyperthyroidism and hypothyroidism are highly prevalent disorders, especially in women and the elderly. Thyroid dysfunction is the second most common endocrine disorder after diabetes among elders. In the three cases that follow, some of the problems and solutions in dealing with thyroid testing are presented.
Case 1: Depression and thyroid abnormalities
J.R., 67, has a history of hypertension. She was referred for evaluation of depressive symptoms. She reports 3 months of increasing fatigue, lethargy, and poor motivation. Her weight has increased by 10 pounds over this period. Her physical exam, ECG, and chest x-ray are normal. She is well groomed and slightly overweight. Her medications have not changed recently and include hydrochlorothiazide 25 mg/d and an aspirin a day.
J.R. reports no history of treatment for psychiatric illness, denies current use of alcohol, tobacco, or illicit drugs, exhibits no abnormal movements or psychomotor changes, and her speech is articulate. Her mood is depressed, and her affect is restricted. She is not suicidal or homicidal, and her exam reveals no psychotic features.
Challenge Patients with thyroid abnormalities often present with psychiatric complaints. Classically, hypothyroidism can present like a depressive episode with similar symptoms of fatigue, anhedonia, weight gain, and sleep disturbance. Patients with hypothyroidism, however, may have physical complaints as well, which should alert the clinician to an underlying thyroid disorder. Typical physical complaints include hair loss, weight gain, dry skin, cold intolerance, constipation, muscle cramps, and joint pains. Women may also complain of menstrual disturbances such as menorrhagia, and may have trouble with fertility.
An elevated or decreased TSH suggests thyroid dysfunction and should always be evaluated.
A low free T4 confirms the diagnosis of hypothyroidism. A low total T3 or free T3 is not always present but is associated with severe forms of hypothyroidism. The hallmark of hyperthyroidism is an elevated free T4 level or free T3 level or both. In a primary thyroid disorder, the TSH is below 0.1 U/L or undetectable.
Here is a description of these tests and what they mean:
- TSH (thyroid-stimulating hormone) is a pituitary hormone that acts on the thyroid gland to increase thyroid hormone secretion. Measurement of TSH is the most sensitive test to screen for hypothyroidism and hyperthyroidism as long as a second-generation assay is used (0.05 mIU/L). Thyroid testing should always begin just with the TSH test. Ordering a free T4 test at the same time is redundant and costly.
- T4 (thyroxine) is best and most accurately measured in its unbound free form. Of all the tests that measure thyroxine, free T4 most accurately reflects unbound thyroid hormone, which is physiologically active. Also, several variables (e.g. pregnancy, disease states, medications) alter total T4 levels by increasing or decreasing thyroid binding hormones. A free T4 test should always follow an abnormal TSH.
- T3 (triiodothyronine) is produced in the thyroid and in peripheral tissues via the enzymatic conversion of T4. Like T4, it is bound and unbound in the serum by thyroid binding globulin, and either form can be measured. T3 should be measured when the TSH is abnormal but the free T4 is within normal limits.
- T3 resin uptake is used to calculate indirectly free T4 and should only be ordered if a free T4 test is unavailable.
- Thyroid antibody tests can help uncover the underlying cause of thyroid dysfunction. These tests lack sensitivity and specificity and should not be used to rule out cancer. Thyroid peroxidase antibodies (antithyroglobulin) and antimicrosomal antibodies are associated with Hashimoto’s thyroiditis and Graves’ disease. Thyroid-stimulating immunoglobulin (TSI) or thyroid-stimulating hormone receptor antibodies are almost always unique to Graves’ disease.
- A radioactive iodine uptake thyroid scan (RAIU) is the best test to determine the cause of hyperthyroidism. Uptake is elevated in most common conditions causing hyperthyroidism, but the pattern of uptake differs. In the context of hyperthyroidism, absent uptake should raise a red flag for nonfunctioning nodules that can be either benign or malignant. A thyroid scan is unhelpful and should not be ordered in working up hypothyroidism.
- Thyroid ultrasound can characterize gland size and nodularity but cannot distinguish benign from malignant masses.
- Fine-needle aspiration biopsy (FNAB) is the best test to distinguish benign and malignant nodules.
What makes the diagnosis difficult and often missed is that some patients have hypothyroidism with minimal or no symptoms. This is especially true in elders because many of the signs and symptoms of hypothyroidism are attributed to “normal” aging. In one recent review of women older than 70 who were screened in an office-based setting, 2% were diagnosed with unsuspected overt hypothyroidism.1 Because classical exam and laboratory findings associated with hypothyroidism tend to present later in the disorder, many patients with thyroid dysfunction have “normal” exams.
Exam findings associated with a hypo-functioning thyroid may include an enlarged thyroid gland (goiter) or nonpalpable gland, non-pitting edema (myxedema), sinus bradycardia, decrease in body temperature, and delayed relaxation of the deep tendon reflexes. Secondary laboratory abnormalities associated with hypothyroidism include normacytic anemia and elevated lipoproteins. Without specific thyroid testing, a “normal” physical does not rule out thyroid dysfunction.
Hyperthyroidism can also manifest as a depression in elders, known as “apathetic hyperthyroidism.” Patients report decreased cognition, depression, and fatigue, and often experience unexplained weight loss, muscle weakness, or atrial fibrillation. Therefore, elderly patients presenting with depression may have a hyper- or hypo-functioning thyroid.
Case 1 concluded The treating psychiatrist diagnosed the patient with major depression. In addition to treatment with an antidepressant, the patient underwent laboratory testing, including a complete blood count, metabolic panel, and TSH (thyroid stimulating hormone). Test results were normal except for a TSH of 64 mU/L, consistent with hypothyroidism. The patient was referred to her primary care physician to begin thyroid hormone replacement.
Comment Although psychiatric symptoms may be caused by clinically important thyroid dysfunction, thyroid function testing may uncover abnormalities of questionable clinical significance. The prevalence of abnormal thyroid hormone levels in hospitalized psychiatric patients ranges from 3% to 32%.2 High thyroid levels (free T4 index and total T4) are associated with acutely psychotic patients such as those with schizophrenia, affective psychosis, and amphetamine abuses. Most studies show that these changes are transient and often normalize with correction of the psychiatric condition, usually within 10 days. Many researchers believe these findings are consistent with euthyroid sick syndrome (Box 2).3
Depressed patients and those with bipolar disorder often present with altered measures of the hypothalamic-pituitary-thyroid (HPT) axis. These abnormalities include mildly elevated or depressed T3, T4 and TSH levels and are not indicative of true thyroid dysfunction (Table 1). It has been debated whether these patients differ in prognosis from psychiatric patients without such abnormalities, although data in depressed patients suggest equivalent outcomes.4 Furthermore, there is no clear evidence that thyroid supplementation benefits depressed patients with mildly elevated TSH with normal T4 and T3 values.5
The prevalence of thyroid disorders in the general population depends largely on the age, sex, and iodine consumption of the population studied. Women in general face a greater risk of overt thyroid dysfunction than do men, and elders face a greater risk than do the young. High dietary iodine consumption is associated with autoimmune hypothyroidism, especially in the aged. Iodine deficiency facilitates the development of hyperthyroidism secondary to toxic nodular goiter.
Table 1
INTERPRETING TEST RESULTS
| Cause | TSH | Free T4 | Free T3 |
|---|---|---|---|
| Hypothyroidism | Increased | Decreased | Normal or decreased |
| Hypothyroidism | Decreased | Increased | Increased |
| Subclinical hypothyroidism | Increased | Normal | Normal |
| Subclinical hypothyroidism | Decreased | Normal | Normal |
| Euthyroid sick syndrome | Normal or decreased | Normal or decreased | Decreased |
| Hypothalamic pituitary disorder | Decreased | Decreased | Normal or decreased |
| Hypothalamic pituitary disorder | Increased | Increased | Normal or decreased |
A number of other risk factors should also clue the clinician to thyroid dysfunction (Table 2).
Case 2: Subclinical thyroid abnormalities
S.J., 34, has a history of panic disorder that has been well controlled with a selective serotonin reuptake inhibitor (SSRI). He is referred to a primary care physician for an annual physical exam. His blood pressure is elevated as it has been on several occasions over the past year. His physical exam is otherwise normal. Laboratory and ECG test results are normal, except for an elevated TSH at 12 mU/L. Follow-up free T4 and free T3 tests are within normal limits. S.J. agrees to eat less salt to address his hypertension.
Challenge An elevated or decreased TSH with a normal thyroxine level (Table 1) is referred to as a “subclinical” thyroid disorder, which is more common than overt thyroid disorders. Women and elders are at greatest risk for subclinical hypothyroidism. In patients older than 60, the rate can be as high as 17% in women and 15% in men.6 The rate largely depends on the number of patients receiving exogenous thyroid hormone—16% in populations including individuals receiving exogenous thyroid hormone and as low as 0.6-1.1% in populations without such patients.1 Chronic subclinical hypothyroidism or mild thyroid failure is the most common condition found in thyroid function screening.
Table 2
WHEN TO CONSIDER THYROID DYSFUNCTION
|
Although patients with subclinical abnormalities appear to be symptom-free, there are clinical implications for these patients. Subclinical hyperthyroidism in the elderly increases the risk for atrial fibrillation and osteoporosis. Postmenopausal women with chronically low TSH measures have lower bone density, especially in cortical bone (e.g., the forearm and hip). Subclinical hypothyroidism is associated with lipid abnormalities and progression to overt hypothyroidism. More recently it has become apparent that this “subclinical” syndrome is not as symptom-free as once assumed, with dry skin, cold intolerance, and easy fatigability more common than in euthyroid patients.7
Case 2 concluded Three months later, repeat testing reveals a negative thyroid antibody test, a TSH elevated to 9 mU/L, and a free T4 and fasting lipid profile within normal limits. S.J. and his physician discuss the pros and cons of thyroid replacement and decide to retest his thyroid function in 6 months with a repeat TSH.
Comment Should individuals with subclinical disorders be treated? How frequently should their thyroid function tests be monitored? The answers vary greatly among clinicians.
Some experts argue that treatment improves behavioral function and decreases lipid levels. Some clinicians take a “wait and see” approach because values can normalize in approximately 10% of patients.6,8 Others treat based on presence of symptoms and risk of progression to overt thyroid failure (Table 2). If treatment is elected, only partial supplementation is usually needed. Most clinicians will start with a dose of 25 ug/d of T4 with adjustment every 6 to 8 weeks until the TSH is normalized.
Unless subclinical hyperthyroidism is secondary to over-replacement with exogenous thyroid hormone, this condtion can be more difficult to treat than subclinical hypothyroidism. Antithyroid therapy should be discussed with patients who have symptoms suggestive of hyperthyroidism, osteoporosis, recurrent atrial fibrillation, or thyroid gland nodules. Consultation with an endocrinologist can help clarify the risks and benefits and determine the specific antithyroid treatment appropriate for each patient.
Case 3: Medications and thyroid abnormalities
R.K., 56, has a long history of bipolar disorder. Upon presenting to his psychiatrist for routine follow-up, he reports a lack of energy but denies other symptoms of mania or depression. He periodically leaves work early or takes a short nap in his office to combat the fatigue. He feels that this may simply be part of “getting old.” He denies any new medical problems and has seen his family physician in the last year. He states that he has been compliant with his medications, lithium and olanzapine. He appears slightly withdrawn and blunted but otherwise there are no abnormal features.
His lithium level, thyroid function, or kidney function had not been checked for 7 months. Subsequent testing reveals an elevated TSH (50 mU/L), a normal kidney profile, and a lithium level in the therapeutic range.
Challenge In psychiatric settings, lithium carbonate is the drug most commonly associated with decreased thyroid function. Lithium interferes with both thyroid hormone synthesis and secretion. One-half of those taking lithium chronically develop goiter, and 40% develop subclinical or overt hypothyroidism.9-11
Many patients treated with lithium test positive for antithyroid antibodies. It is unclear if this finding represents a chronic autoimmune thyroiditis or is secondary to lithium treatment itself. In any case, patients taking lithium face an increased risk of thyroid failure. Other risk factors for thyroid failure include female gender and duration of treatment. Lithium dosage does not seem to be related to risk.
Clinicians differ on the frequency of thyroid monitoring for patients taking lithium. For patients without a history of thyroid dysfunction, annual TSH testing is likely sufficient.
Other medications affecting thyroid hormone production include methimazole, propylthiouracil, and iodide-containing drugs and dyes. Methimazole and propylthiouracil are given to patients intentionally with overt hyperthyroidism and interfere with hormone synthesis. Patients receiving medications or dyes containing iodide may also be susceptible to hypothyroidism. These agents are partially deiodinated after they are given and therefore can cause transient or prolonged decreases in thyroid production.
In consultative work, psychiatrists often confront abnormal thyroid tests in critically ill patients. Euthyroid sick syndrome can be a challenge to distinguish from ill patients with true thyroid or pituitary dysfunction. This syndrome is common in hospitalized patients and has been documented in more than 50% of patients in some settings.14
Abnormal thyroid tests are observed in a variety of medical conditions including heart failure, myocardial infarction, renal failure, liver disease, infections, stress, trauma, starvation, and autoimmune disorders. There is considerable debate about the meaning of these test abnormalities, and to date no conclusive intervention to correct abnormalities has proven to be consistently effective in ill patients.
The complex results of testing contribute to the confusion. An isolated low T3 is the most common lab abnormality found in nonthyroidal illness, related to a decrease in T4 enzymatic conversion to T3. Many disease states decrease this enzyme’s (5’-deiodinase) activity. Unlike T3, TSH and T4 levels stay within normal limits in mild to moderately ill patients.
In patients who are moderately ill or who have been ill for a longer time, T4 levels fall with T3. In more severe and critically ill patients, the TSH level can decrease as well.
T4 can be elevated in sick patients without thyroid dysfunction. With this pattern, the TSH and T3 levels are normal or high. The clinical meaning of these abnormalities is unclear. Some studies suggest that the degree of thyroid hormone suppression correlates with disease severity and prognosis. Both decreased T3 and T4 levels have been shown to correlate with mortality in some disease states.15 Debate remains as to whether these findings represent a maladaptive process or a protective response to illness.
III patients with hyperthyroidism generally have an elevated serum free T4 and T3 with an undetectable TSH. Ill patients with true hypothyroidism will have a TSH greater than 20 to 30 mU/ml with suppressed T4 and T3 levels. Diagnosis is more difficult when TSH levels are mildly abnormal or when the clinician is trying to distinguish secondary hypothyroidism from the low T3, T4, and TSH pattern found in many critically ill patients. Secondary testing or clinical findings such as an enlarged gland, the presence of thyroid antibodies, or abnormalities in other pituitary hormones may point to an underlying thyroid or pituitary problem in ill patients.
Some oral cholecystographic agents and the antiarrhythmic medication amiodarone are excreted slowly and can be associated with more prolonged decreases in thyroid hormone production. Iodide and medications containing iodide may precipitate a longer enduring hypothyroidism in patients with chronic autoimmune thyroiditis and in those with hyperthyroidism who have received radioactive iodine therapy or have undergone partial thyroidectomy.
The cholesterol-lowering bile acid sequestrants colestipol and cholestyramine can also inhibit thyroid reabsorption from the intestine, potentially leading to hypothyroidism. Patients dependent on exogenous T4 or who have an underlying decreased thyroid function may develop hypothyroidism.
Table 3
WHICH MEDICATIONS CAN CAUSE THYROID DYSFUNCTION?
| Drugs that increase thyroid hormone secretion Iodide-containing medication Amiodarone Providone-iodine antiseptics X-ray contrast media containing iodine | Drugs that increase hepatic metabolism of T4 and T3 Phenobarbital Rifampin Phenytoin Carbamazepine |
| Drugs that decrease TBG,* causing a relative increase in unbound thyroid Androgens Anabolic steroids | Drugs that decrease T4 absorption Colestipol Cholestyramine Aluminum hydroxide Ferrous sulfate Sucralfate |
| Drugs that decrease thyroid hormone secretion Lithium carbonate Iodide Amiodarone | Drugs that increase TBG,* causing a relative decrease in unbound thyroid Estrogens Tamoxifen Heroin and methadone |
| *Thyroxine-binding globulin Table adapted from: Surks MI, Sievert R. Drugs and thyroid function. N Engl J Med 1995;333(25):1688-94. | |
Drugs that alter thyroid hormone metabolism can also be problematic. Although thyroid hormone is metabolized mostly by deiodination, it also undergoes glucuronidation and sulfation. Phenobarbital, rifampin, phenytoin, and carbamazepine all increase T4 and T3 metabolism by inducing these hepatic enzymes. In patients with no thyroid disease, phenytoin and carbamazepine can decrease circulating free T4 levels by 20% to 40%.12 Patients receiving T4 replacement may need their dosage increased or risk hypothyroidism if placed on one of these medications (Table 3).
Several medications alter total T4 and T3 levels by increasing or decreasing thyroid-binding proteins. Examples include estrogens, androgens, anabolic steroids, methadone, and heroin. Most thyroid hormone circulates as bound, but it is the unbound form that is active in peripheral tissues. Patients thus can experience changes in the binding proteins, while the proportion of unbound (“free”) hormone at the tissue level remains unaffected.
Because this unbound form remains relatively unchanged, the patient with normal thyroid function remains euthyroid despite alterations in total thyroid levels. When patients with hypothyroidism start one of these medications, their replacement hormone dosage may need to be adjusted.
Related resources
- American Association of Clinical Endocrinologists. www.aace.com
- Clinical practice guidelines for evaluation and treatment of hypothyroidism and hyperthyroidism. Position statement on subclinical hypothyroidism and pregnancy
- Thyroid Federation International. www.thyroid-fed.org
- Online videos regarding thyroid disease (patient-directed). Patient handouts on thyroid disease
- Jameson JL, Weetman AP. Disorders of the thyroid gland. In: Harrison’s Principles of Internal Medicine. 15th ed. New York: McGraw-Hill; 2001:2060-84
Drug brand names
- Amiodorone • Pacerone, Cordarone
- Colestipol • Colestid
- Methimazole • Tapazole
- Olanzapine • Zyprexa, Zyprexa Zydis
- Rifampin • Rifadin, Rimactane
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article.
1. Helfand M, Redfern CC. Screening for thyroid disease: an update. Ann Intern Med 1998;129(2):144-58.
2. Arem R, Cusi K. Thyroid function testing in psychiatric illness usefulness and limitations. Trends Endocrinol Metab 1997;8:282-87.
3. Nader S, Warner MD, Doyle S, Peabody CA. Euthyroid sick syndrome in psychiatric inpatients. Biol Psychiatry 1996;40(12):1288-93.
4. Fava M, Labbate LA, Abraham ME. Hypothyroidism and hyperthyroidism in major depression. J Clin Psychiatry 1995;56(5):186-92.
5. Jackson IM. The thyroid axis and depression. Thyroid 1998;8(10):951-56.
6. Samuels MH. Subclinical thyroid disease in the elderly. Thyroid 1998;8(9):803-13.
7. Staub JJ, Althaus BU, Engler H, Ryff AS, Trabucco P, Marquardt K, et al. Spectrum of subclinical and overt hypothyroidism: effect on thyrotropin, prolactin, and thyroid reserve, and metabolic impact on peripheral target tissues. Am J Med 1992;92(6):631-42.
8. Ayala AR, Wartofsky L. Minimally symptomatic (subclinical) hypothyroidism. Endocrinologist 1997;7:44-50.
9. Spaulding SW, Burrow GN, Bermudez F, Himmelhoch JM. The inhibitory effect of lithium on thyroid hormone release in both euthyroid and thyrotoxic patients. J Clin Endocrinol Metab 1972;35(6):905-11.
10. Perrild H, Hegedus L Baastrup PC, Kayser L, Kastberg S. Thyroid function and ultrasonically determined thyroid size in patients receiving long-term lithium treatment. Am J Psychiatry 1990;147(11):1518-21.
11. Bocchetta A, Bernardi F, Peditzi M. Thyroid abnormalities during lithium treatment. Acta Psychiatr Scand 1991;83(3):193-98.
12. Surks MI, Sievert R. Drugs and thyroid function. N Engl J Med 1995;333(25):1688-94.
13. Mandel SJ, Larsen PR, Seely EW, Brent GA. Increased need for thyroxine during pregnancy in women with primary hypothyroidism. N Engl J Med 1990;323(2):91-6.
14. Chopra IJ. Clinical review 86: euthyroid sick syndrome: is it a misnomer? J Clin Endocrinol Metab 1997;82(2):329-34.
15. Camacho PM, Dwarkanathan AA. Sick euthyroid syndrome, what to do when thyroid function tests are abnormal in critically ill patients. Postgrad Med 1999;105(4):215-19.
16. Woeber KA. Update of management of hyperthyroidism and hypothyroidism. Arch Fam Med 2000;9(8):743-47.
Psychiatrists commonly order thyroid testing and are often the first to confront abnormal thyroid test results. As thyroid testing has become more sophisticated and sensitive (Box 1), the interpretation and management of abnormal or slightly abnormal results has become increasingly complex. What’s more, older individuals, hospitalized patients, and those with psychiatric illness often present with subtle laboratory abnormalities.
Hyperthyroidism and hypothyroidism are highly prevalent disorders, especially in women and the elderly. Thyroid dysfunction is the second most common endocrine disorder after diabetes among elders. In the three cases that follow, some of the problems and solutions in dealing with thyroid testing are presented.
Case 1: Depression and thyroid abnormalities
J.R., 67, has a history of hypertension. She was referred for evaluation of depressive symptoms. She reports 3 months of increasing fatigue, lethargy, and poor motivation. Her weight has increased by 10 pounds over this period. Her physical exam, ECG, and chest x-ray are normal. She is well groomed and slightly overweight. Her medications have not changed recently and include hydrochlorothiazide 25 mg/d and an aspirin a day.
J.R. reports no history of treatment for psychiatric illness, denies current use of alcohol, tobacco, or illicit drugs, exhibits no abnormal movements or psychomotor changes, and her speech is articulate. Her mood is depressed, and her affect is restricted. She is not suicidal or homicidal, and her exam reveals no psychotic features.
Challenge Patients with thyroid abnormalities often present with psychiatric complaints. Classically, hypothyroidism can present like a depressive episode with similar symptoms of fatigue, anhedonia, weight gain, and sleep disturbance. Patients with hypothyroidism, however, may have physical complaints as well, which should alert the clinician to an underlying thyroid disorder. Typical physical complaints include hair loss, weight gain, dry skin, cold intolerance, constipation, muscle cramps, and joint pains. Women may also complain of menstrual disturbances such as menorrhagia, and may have trouble with fertility.
An elevated or decreased TSH suggests thyroid dysfunction and should always be evaluated.
A low free T4 confirms the diagnosis of hypothyroidism. A low total T3 or free T3 is not always present but is associated with severe forms of hypothyroidism. The hallmark of hyperthyroidism is an elevated free T4 level or free T3 level or both. In a primary thyroid disorder, the TSH is below 0.1 U/L or undetectable.
Here is a description of these tests and what they mean:
- TSH (thyroid-stimulating hormone) is a pituitary hormone that acts on the thyroid gland to increase thyroid hormone secretion. Measurement of TSH is the most sensitive test to screen for hypothyroidism and hyperthyroidism as long as a second-generation assay is used (0.05 mIU/L). Thyroid testing should always begin just with the TSH test. Ordering a free T4 test at the same time is redundant and costly.
- T4 (thyroxine) is best and most accurately measured in its unbound free form. Of all the tests that measure thyroxine, free T4 most accurately reflects unbound thyroid hormone, which is physiologically active. Also, several variables (e.g. pregnancy, disease states, medications) alter total T4 levels by increasing or decreasing thyroid binding hormones. A free T4 test should always follow an abnormal TSH.
- T3 (triiodothyronine) is produced in the thyroid and in peripheral tissues via the enzymatic conversion of T4. Like T4, it is bound and unbound in the serum by thyroid binding globulin, and either form can be measured. T3 should be measured when the TSH is abnormal but the free T4 is within normal limits.
- T3 resin uptake is used to calculate indirectly free T4 and should only be ordered if a free T4 test is unavailable.
- Thyroid antibody tests can help uncover the underlying cause of thyroid dysfunction. These tests lack sensitivity and specificity and should not be used to rule out cancer. Thyroid peroxidase antibodies (antithyroglobulin) and antimicrosomal antibodies are associated with Hashimoto’s thyroiditis and Graves’ disease. Thyroid-stimulating immunoglobulin (TSI) or thyroid-stimulating hormone receptor antibodies are almost always unique to Graves’ disease.
- A radioactive iodine uptake thyroid scan (RAIU) is the best test to determine the cause of hyperthyroidism. Uptake is elevated in most common conditions causing hyperthyroidism, but the pattern of uptake differs. In the context of hyperthyroidism, absent uptake should raise a red flag for nonfunctioning nodules that can be either benign or malignant. A thyroid scan is unhelpful and should not be ordered in working up hypothyroidism.
- Thyroid ultrasound can characterize gland size and nodularity but cannot distinguish benign from malignant masses.
- Fine-needle aspiration biopsy (FNAB) is the best test to distinguish benign and malignant nodules.
What makes the diagnosis difficult and often missed is that some patients have hypothyroidism with minimal or no symptoms. This is especially true in elders because many of the signs and symptoms of hypothyroidism are attributed to “normal” aging. In one recent review of women older than 70 who were screened in an office-based setting, 2% were diagnosed with unsuspected overt hypothyroidism.1 Because classical exam and laboratory findings associated with hypothyroidism tend to present later in the disorder, many patients with thyroid dysfunction have “normal” exams.
Exam findings associated with a hypo-functioning thyroid may include an enlarged thyroid gland (goiter) or nonpalpable gland, non-pitting edema (myxedema), sinus bradycardia, decrease in body temperature, and delayed relaxation of the deep tendon reflexes. Secondary laboratory abnormalities associated with hypothyroidism include normacytic anemia and elevated lipoproteins. Without specific thyroid testing, a “normal” physical does not rule out thyroid dysfunction.
Hyperthyroidism can also manifest as a depression in elders, known as “apathetic hyperthyroidism.” Patients report decreased cognition, depression, and fatigue, and often experience unexplained weight loss, muscle weakness, or atrial fibrillation. Therefore, elderly patients presenting with depression may have a hyper- or hypo-functioning thyroid.
Case 1 concluded The treating psychiatrist diagnosed the patient with major depression. In addition to treatment with an antidepressant, the patient underwent laboratory testing, including a complete blood count, metabolic panel, and TSH (thyroid stimulating hormone). Test results were normal except for a TSH of 64 mU/L, consistent with hypothyroidism. The patient was referred to her primary care physician to begin thyroid hormone replacement.
Comment Although psychiatric symptoms may be caused by clinically important thyroid dysfunction, thyroid function testing may uncover abnormalities of questionable clinical significance. The prevalence of abnormal thyroid hormone levels in hospitalized psychiatric patients ranges from 3% to 32%.2 High thyroid levels (free T4 index and total T4) are associated with acutely psychotic patients such as those with schizophrenia, affective psychosis, and amphetamine abuses. Most studies show that these changes are transient and often normalize with correction of the psychiatric condition, usually within 10 days. Many researchers believe these findings are consistent with euthyroid sick syndrome (Box 2).3
Depressed patients and those with bipolar disorder often present with altered measures of the hypothalamic-pituitary-thyroid (HPT) axis. These abnormalities include mildly elevated or depressed T3, T4 and TSH levels and are not indicative of true thyroid dysfunction (Table 1). It has been debated whether these patients differ in prognosis from psychiatric patients without such abnormalities, although data in depressed patients suggest equivalent outcomes.4 Furthermore, there is no clear evidence that thyroid supplementation benefits depressed patients with mildly elevated TSH with normal T4 and T3 values.5
The prevalence of thyroid disorders in the general population depends largely on the age, sex, and iodine consumption of the population studied. Women in general face a greater risk of overt thyroid dysfunction than do men, and elders face a greater risk than do the young. High dietary iodine consumption is associated with autoimmune hypothyroidism, especially in the aged. Iodine deficiency facilitates the development of hyperthyroidism secondary to toxic nodular goiter.
Table 1
INTERPRETING TEST RESULTS
| Cause | TSH | Free T4 | Free T3 |
|---|---|---|---|
| Hypothyroidism | Increased | Decreased | Normal or decreased |
| Hypothyroidism | Decreased | Increased | Increased |
| Subclinical hypothyroidism | Increased | Normal | Normal |
| Subclinical hypothyroidism | Decreased | Normal | Normal |
| Euthyroid sick syndrome | Normal or decreased | Normal or decreased | Decreased |
| Hypothalamic pituitary disorder | Decreased | Decreased | Normal or decreased |
| Hypothalamic pituitary disorder | Increased | Increased | Normal or decreased |
A number of other risk factors should also clue the clinician to thyroid dysfunction (Table 2).
Case 2: Subclinical thyroid abnormalities
S.J., 34, has a history of panic disorder that has been well controlled with a selective serotonin reuptake inhibitor (SSRI). He is referred to a primary care physician for an annual physical exam. His blood pressure is elevated as it has been on several occasions over the past year. His physical exam is otherwise normal. Laboratory and ECG test results are normal, except for an elevated TSH at 12 mU/L. Follow-up free T4 and free T3 tests are within normal limits. S.J. agrees to eat less salt to address his hypertension.
Challenge An elevated or decreased TSH with a normal thyroxine level (Table 1) is referred to as a “subclinical” thyroid disorder, which is more common than overt thyroid disorders. Women and elders are at greatest risk for subclinical hypothyroidism. In patients older than 60, the rate can be as high as 17% in women and 15% in men.6 The rate largely depends on the number of patients receiving exogenous thyroid hormone—16% in populations including individuals receiving exogenous thyroid hormone and as low as 0.6-1.1% in populations without such patients.1 Chronic subclinical hypothyroidism or mild thyroid failure is the most common condition found in thyroid function screening.
Table 2
WHEN TO CONSIDER THYROID DYSFUNCTION
|
Although patients with subclinical abnormalities appear to be symptom-free, there are clinical implications for these patients. Subclinical hyperthyroidism in the elderly increases the risk for atrial fibrillation and osteoporosis. Postmenopausal women with chronically low TSH measures have lower bone density, especially in cortical bone (e.g., the forearm and hip). Subclinical hypothyroidism is associated with lipid abnormalities and progression to overt hypothyroidism. More recently it has become apparent that this “subclinical” syndrome is not as symptom-free as once assumed, with dry skin, cold intolerance, and easy fatigability more common than in euthyroid patients.7
Case 2 concluded Three months later, repeat testing reveals a negative thyroid antibody test, a TSH elevated to 9 mU/L, and a free T4 and fasting lipid profile within normal limits. S.J. and his physician discuss the pros and cons of thyroid replacement and decide to retest his thyroid function in 6 months with a repeat TSH.
Comment Should individuals with subclinical disorders be treated? How frequently should their thyroid function tests be monitored? The answers vary greatly among clinicians.
Some experts argue that treatment improves behavioral function and decreases lipid levels. Some clinicians take a “wait and see” approach because values can normalize in approximately 10% of patients.6,8 Others treat based on presence of symptoms and risk of progression to overt thyroid failure (Table 2). If treatment is elected, only partial supplementation is usually needed. Most clinicians will start with a dose of 25 ug/d of T4 with adjustment every 6 to 8 weeks until the TSH is normalized.
Unless subclinical hyperthyroidism is secondary to over-replacement with exogenous thyroid hormone, this condtion can be more difficult to treat than subclinical hypothyroidism. Antithyroid therapy should be discussed with patients who have symptoms suggestive of hyperthyroidism, osteoporosis, recurrent atrial fibrillation, or thyroid gland nodules. Consultation with an endocrinologist can help clarify the risks and benefits and determine the specific antithyroid treatment appropriate for each patient.
Case 3: Medications and thyroid abnormalities
R.K., 56, has a long history of bipolar disorder. Upon presenting to his psychiatrist for routine follow-up, he reports a lack of energy but denies other symptoms of mania or depression. He periodically leaves work early or takes a short nap in his office to combat the fatigue. He feels that this may simply be part of “getting old.” He denies any new medical problems and has seen his family physician in the last year. He states that he has been compliant with his medications, lithium and olanzapine. He appears slightly withdrawn and blunted but otherwise there are no abnormal features.
His lithium level, thyroid function, or kidney function had not been checked for 7 months. Subsequent testing reveals an elevated TSH (50 mU/L), a normal kidney profile, and a lithium level in the therapeutic range.
Challenge In psychiatric settings, lithium carbonate is the drug most commonly associated with decreased thyroid function. Lithium interferes with both thyroid hormone synthesis and secretion. One-half of those taking lithium chronically develop goiter, and 40% develop subclinical or overt hypothyroidism.9-11
Many patients treated with lithium test positive for antithyroid antibodies. It is unclear if this finding represents a chronic autoimmune thyroiditis or is secondary to lithium treatment itself. In any case, patients taking lithium face an increased risk of thyroid failure. Other risk factors for thyroid failure include female gender and duration of treatment. Lithium dosage does not seem to be related to risk.
Clinicians differ on the frequency of thyroid monitoring for patients taking lithium. For patients without a history of thyroid dysfunction, annual TSH testing is likely sufficient.
Other medications affecting thyroid hormone production include methimazole, propylthiouracil, and iodide-containing drugs and dyes. Methimazole and propylthiouracil are given to patients intentionally with overt hyperthyroidism and interfere with hormone synthesis. Patients receiving medications or dyes containing iodide may also be susceptible to hypothyroidism. These agents are partially deiodinated after they are given and therefore can cause transient or prolonged decreases in thyroid production.
In consultative work, psychiatrists often confront abnormal thyroid tests in critically ill patients. Euthyroid sick syndrome can be a challenge to distinguish from ill patients with true thyroid or pituitary dysfunction. This syndrome is common in hospitalized patients and has been documented in more than 50% of patients in some settings.14
Abnormal thyroid tests are observed in a variety of medical conditions including heart failure, myocardial infarction, renal failure, liver disease, infections, stress, trauma, starvation, and autoimmune disorders. There is considerable debate about the meaning of these test abnormalities, and to date no conclusive intervention to correct abnormalities has proven to be consistently effective in ill patients.
The complex results of testing contribute to the confusion. An isolated low T3 is the most common lab abnormality found in nonthyroidal illness, related to a decrease in T4 enzymatic conversion to T3. Many disease states decrease this enzyme’s (5’-deiodinase) activity. Unlike T3, TSH and T4 levels stay within normal limits in mild to moderately ill patients.
In patients who are moderately ill or who have been ill for a longer time, T4 levels fall with T3. In more severe and critically ill patients, the TSH level can decrease as well.
T4 can be elevated in sick patients without thyroid dysfunction. With this pattern, the TSH and T3 levels are normal or high. The clinical meaning of these abnormalities is unclear. Some studies suggest that the degree of thyroid hormone suppression correlates with disease severity and prognosis. Both decreased T3 and T4 levels have been shown to correlate with mortality in some disease states.15 Debate remains as to whether these findings represent a maladaptive process or a protective response to illness.
III patients with hyperthyroidism generally have an elevated serum free T4 and T3 with an undetectable TSH. Ill patients with true hypothyroidism will have a TSH greater than 20 to 30 mU/ml with suppressed T4 and T3 levels. Diagnosis is more difficult when TSH levels are mildly abnormal or when the clinician is trying to distinguish secondary hypothyroidism from the low T3, T4, and TSH pattern found in many critically ill patients. Secondary testing or clinical findings such as an enlarged gland, the presence of thyroid antibodies, or abnormalities in other pituitary hormones may point to an underlying thyroid or pituitary problem in ill patients.
Some oral cholecystographic agents and the antiarrhythmic medication amiodarone are excreted slowly and can be associated with more prolonged decreases in thyroid hormone production. Iodide and medications containing iodide may precipitate a longer enduring hypothyroidism in patients with chronic autoimmune thyroiditis and in those with hyperthyroidism who have received radioactive iodine therapy or have undergone partial thyroidectomy.
The cholesterol-lowering bile acid sequestrants colestipol and cholestyramine can also inhibit thyroid reabsorption from the intestine, potentially leading to hypothyroidism. Patients dependent on exogenous T4 or who have an underlying decreased thyroid function may develop hypothyroidism.
Table 3
WHICH MEDICATIONS CAN CAUSE THYROID DYSFUNCTION?
| Drugs that increase thyroid hormone secretion Iodide-containing medication Amiodarone Providone-iodine antiseptics X-ray contrast media containing iodine | Drugs that increase hepatic metabolism of T4 and T3 Phenobarbital Rifampin Phenytoin Carbamazepine |
| Drugs that decrease TBG,* causing a relative increase in unbound thyroid Androgens Anabolic steroids | Drugs that decrease T4 absorption Colestipol Cholestyramine Aluminum hydroxide Ferrous sulfate Sucralfate |
| Drugs that decrease thyroid hormone secretion Lithium carbonate Iodide Amiodarone | Drugs that increase TBG,* causing a relative decrease in unbound thyroid Estrogens Tamoxifen Heroin and methadone |
| *Thyroxine-binding globulin Table adapted from: Surks MI, Sievert R. Drugs and thyroid function. N Engl J Med 1995;333(25):1688-94. | |
Drugs that alter thyroid hormone metabolism can also be problematic. Although thyroid hormone is metabolized mostly by deiodination, it also undergoes glucuronidation and sulfation. Phenobarbital, rifampin, phenytoin, and carbamazepine all increase T4 and T3 metabolism by inducing these hepatic enzymes. In patients with no thyroid disease, phenytoin and carbamazepine can decrease circulating free T4 levels by 20% to 40%.12 Patients receiving T4 replacement may need their dosage increased or risk hypothyroidism if placed on one of these medications (Table 3).
Several medications alter total T4 and T3 levels by increasing or decreasing thyroid-binding proteins. Examples include estrogens, androgens, anabolic steroids, methadone, and heroin. Most thyroid hormone circulates as bound, but it is the unbound form that is active in peripheral tissues. Patients thus can experience changes in the binding proteins, while the proportion of unbound (“free”) hormone at the tissue level remains unaffected.
Because this unbound form remains relatively unchanged, the patient with normal thyroid function remains euthyroid despite alterations in total thyroid levels. When patients with hypothyroidism start one of these medications, their replacement hormone dosage may need to be adjusted.
Related resources
- American Association of Clinical Endocrinologists. www.aace.com
- Clinical practice guidelines for evaluation and treatment of hypothyroidism and hyperthyroidism. Position statement on subclinical hypothyroidism and pregnancy
- Thyroid Federation International. www.thyroid-fed.org
- Online videos regarding thyroid disease (patient-directed). Patient handouts on thyroid disease
- Jameson JL, Weetman AP. Disorders of the thyroid gland. In: Harrison’s Principles of Internal Medicine. 15th ed. New York: McGraw-Hill; 2001:2060-84
Drug brand names
- Amiodorone • Pacerone, Cordarone
- Colestipol • Colestid
- Methimazole • Tapazole
- Olanzapine • Zyprexa, Zyprexa Zydis
- Rifampin • Rifadin, Rimactane
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article.
Psychiatrists commonly order thyroid testing and are often the first to confront abnormal thyroid test results. As thyroid testing has become more sophisticated and sensitive (Box 1), the interpretation and management of abnormal or slightly abnormal results has become increasingly complex. What’s more, older individuals, hospitalized patients, and those with psychiatric illness often present with subtle laboratory abnormalities.
Hyperthyroidism and hypothyroidism are highly prevalent disorders, especially in women and the elderly. Thyroid dysfunction is the second most common endocrine disorder after diabetes among elders. In the three cases that follow, some of the problems and solutions in dealing with thyroid testing are presented.
Case 1: Depression and thyroid abnormalities
J.R., 67, has a history of hypertension. She was referred for evaluation of depressive symptoms. She reports 3 months of increasing fatigue, lethargy, and poor motivation. Her weight has increased by 10 pounds over this period. Her physical exam, ECG, and chest x-ray are normal. She is well groomed and slightly overweight. Her medications have not changed recently and include hydrochlorothiazide 25 mg/d and an aspirin a day.
J.R. reports no history of treatment for psychiatric illness, denies current use of alcohol, tobacco, or illicit drugs, exhibits no abnormal movements or psychomotor changes, and her speech is articulate. Her mood is depressed, and her affect is restricted. She is not suicidal or homicidal, and her exam reveals no psychotic features.
Challenge Patients with thyroid abnormalities often present with psychiatric complaints. Classically, hypothyroidism can present like a depressive episode with similar symptoms of fatigue, anhedonia, weight gain, and sleep disturbance. Patients with hypothyroidism, however, may have physical complaints as well, which should alert the clinician to an underlying thyroid disorder. Typical physical complaints include hair loss, weight gain, dry skin, cold intolerance, constipation, muscle cramps, and joint pains. Women may also complain of menstrual disturbances such as menorrhagia, and may have trouble with fertility.
An elevated or decreased TSH suggests thyroid dysfunction and should always be evaluated.
A low free T4 confirms the diagnosis of hypothyroidism. A low total T3 or free T3 is not always present but is associated with severe forms of hypothyroidism. The hallmark of hyperthyroidism is an elevated free T4 level or free T3 level or both. In a primary thyroid disorder, the TSH is below 0.1 U/L or undetectable.
Here is a description of these tests and what they mean:
- TSH (thyroid-stimulating hormone) is a pituitary hormone that acts on the thyroid gland to increase thyroid hormone secretion. Measurement of TSH is the most sensitive test to screen for hypothyroidism and hyperthyroidism as long as a second-generation assay is used (0.05 mIU/L). Thyroid testing should always begin just with the TSH test. Ordering a free T4 test at the same time is redundant and costly.
- T4 (thyroxine) is best and most accurately measured in its unbound free form. Of all the tests that measure thyroxine, free T4 most accurately reflects unbound thyroid hormone, which is physiologically active. Also, several variables (e.g. pregnancy, disease states, medications) alter total T4 levels by increasing or decreasing thyroid binding hormones. A free T4 test should always follow an abnormal TSH.
- T3 (triiodothyronine) is produced in the thyroid and in peripheral tissues via the enzymatic conversion of T4. Like T4, it is bound and unbound in the serum by thyroid binding globulin, and either form can be measured. T3 should be measured when the TSH is abnormal but the free T4 is within normal limits.
- T3 resin uptake is used to calculate indirectly free T4 and should only be ordered if a free T4 test is unavailable.
- Thyroid antibody tests can help uncover the underlying cause of thyroid dysfunction. These tests lack sensitivity and specificity and should not be used to rule out cancer. Thyroid peroxidase antibodies (antithyroglobulin) and antimicrosomal antibodies are associated with Hashimoto’s thyroiditis and Graves’ disease. Thyroid-stimulating immunoglobulin (TSI) or thyroid-stimulating hormone receptor antibodies are almost always unique to Graves’ disease.
- A radioactive iodine uptake thyroid scan (RAIU) is the best test to determine the cause of hyperthyroidism. Uptake is elevated in most common conditions causing hyperthyroidism, but the pattern of uptake differs. In the context of hyperthyroidism, absent uptake should raise a red flag for nonfunctioning nodules that can be either benign or malignant. A thyroid scan is unhelpful and should not be ordered in working up hypothyroidism.
- Thyroid ultrasound can characterize gland size and nodularity but cannot distinguish benign from malignant masses.
- Fine-needle aspiration biopsy (FNAB) is the best test to distinguish benign and malignant nodules.
What makes the diagnosis difficult and often missed is that some patients have hypothyroidism with minimal or no symptoms. This is especially true in elders because many of the signs and symptoms of hypothyroidism are attributed to “normal” aging. In one recent review of women older than 70 who were screened in an office-based setting, 2% were diagnosed with unsuspected overt hypothyroidism.1 Because classical exam and laboratory findings associated with hypothyroidism tend to present later in the disorder, many patients with thyroid dysfunction have “normal” exams.
Exam findings associated with a hypo-functioning thyroid may include an enlarged thyroid gland (goiter) or nonpalpable gland, non-pitting edema (myxedema), sinus bradycardia, decrease in body temperature, and delayed relaxation of the deep tendon reflexes. Secondary laboratory abnormalities associated with hypothyroidism include normacytic anemia and elevated lipoproteins. Without specific thyroid testing, a “normal” physical does not rule out thyroid dysfunction.
Hyperthyroidism can also manifest as a depression in elders, known as “apathetic hyperthyroidism.” Patients report decreased cognition, depression, and fatigue, and often experience unexplained weight loss, muscle weakness, or atrial fibrillation. Therefore, elderly patients presenting with depression may have a hyper- or hypo-functioning thyroid.
Case 1 concluded The treating psychiatrist diagnosed the patient with major depression. In addition to treatment with an antidepressant, the patient underwent laboratory testing, including a complete blood count, metabolic panel, and TSH (thyroid stimulating hormone). Test results were normal except for a TSH of 64 mU/L, consistent with hypothyroidism. The patient was referred to her primary care physician to begin thyroid hormone replacement.
Comment Although psychiatric symptoms may be caused by clinically important thyroid dysfunction, thyroid function testing may uncover abnormalities of questionable clinical significance. The prevalence of abnormal thyroid hormone levels in hospitalized psychiatric patients ranges from 3% to 32%.2 High thyroid levels (free T4 index and total T4) are associated with acutely psychotic patients such as those with schizophrenia, affective psychosis, and amphetamine abuses. Most studies show that these changes are transient and often normalize with correction of the psychiatric condition, usually within 10 days. Many researchers believe these findings are consistent with euthyroid sick syndrome (Box 2).3
Depressed patients and those with bipolar disorder often present with altered measures of the hypothalamic-pituitary-thyroid (HPT) axis. These abnormalities include mildly elevated or depressed T3, T4 and TSH levels and are not indicative of true thyroid dysfunction (Table 1). It has been debated whether these patients differ in prognosis from psychiatric patients without such abnormalities, although data in depressed patients suggest equivalent outcomes.4 Furthermore, there is no clear evidence that thyroid supplementation benefits depressed patients with mildly elevated TSH with normal T4 and T3 values.5
The prevalence of thyroid disorders in the general population depends largely on the age, sex, and iodine consumption of the population studied. Women in general face a greater risk of overt thyroid dysfunction than do men, and elders face a greater risk than do the young. High dietary iodine consumption is associated with autoimmune hypothyroidism, especially in the aged. Iodine deficiency facilitates the development of hyperthyroidism secondary to toxic nodular goiter.
Table 1
INTERPRETING TEST RESULTS
| Cause | TSH | Free T4 | Free T3 |
|---|---|---|---|
| Hypothyroidism | Increased | Decreased | Normal or decreased |
| Hypothyroidism | Decreased | Increased | Increased |
| Subclinical hypothyroidism | Increased | Normal | Normal |
| Subclinical hypothyroidism | Decreased | Normal | Normal |
| Euthyroid sick syndrome | Normal or decreased | Normal or decreased | Decreased |
| Hypothalamic pituitary disorder | Decreased | Decreased | Normal or decreased |
| Hypothalamic pituitary disorder | Increased | Increased | Normal or decreased |
A number of other risk factors should also clue the clinician to thyroid dysfunction (Table 2).
Case 2: Subclinical thyroid abnormalities
S.J., 34, has a history of panic disorder that has been well controlled with a selective serotonin reuptake inhibitor (SSRI). He is referred to a primary care physician for an annual physical exam. His blood pressure is elevated as it has been on several occasions over the past year. His physical exam is otherwise normal. Laboratory and ECG test results are normal, except for an elevated TSH at 12 mU/L. Follow-up free T4 and free T3 tests are within normal limits. S.J. agrees to eat less salt to address his hypertension.
Challenge An elevated or decreased TSH with a normal thyroxine level (Table 1) is referred to as a “subclinical” thyroid disorder, which is more common than overt thyroid disorders. Women and elders are at greatest risk for subclinical hypothyroidism. In patients older than 60, the rate can be as high as 17% in women and 15% in men.6 The rate largely depends on the number of patients receiving exogenous thyroid hormone—16% in populations including individuals receiving exogenous thyroid hormone and as low as 0.6-1.1% in populations without such patients.1 Chronic subclinical hypothyroidism or mild thyroid failure is the most common condition found in thyroid function screening.
Table 2
WHEN TO CONSIDER THYROID DYSFUNCTION
|
Although patients with subclinical abnormalities appear to be symptom-free, there are clinical implications for these patients. Subclinical hyperthyroidism in the elderly increases the risk for atrial fibrillation and osteoporosis. Postmenopausal women with chronically low TSH measures have lower bone density, especially in cortical bone (e.g., the forearm and hip). Subclinical hypothyroidism is associated with lipid abnormalities and progression to overt hypothyroidism. More recently it has become apparent that this “subclinical” syndrome is not as symptom-free as once assumed, with dry skin, cold intolerance, and easy fatigability more common than in euthyroid patients.7
Case 2 concluded Three months later, repeat testing reveals a negative thyroid antibody test, a TSH elevated to 9 mU/L, and a free T4 and fasting lipid profile within normal limits. S.J. and his physician discuss the pros and cons of thyroid replacement and decide to retest his thyroid function in 6 months with a repeat TSH.
Comment Should individuals with subclinical disorders be treated? How frequently should their thyroid function tests be monitored? The answers vary greatly among clinicians.
Some experts argue that treatment improves behavioral function and decreases lipid levels. Some clinicians take a “wait and see” approach because values can normalize in approximately 10% of patients.6,8 Others treat based on presence of symptoms and risk of progression to overt thyroid failure (Table 2). If treatment is elected, only partial supplementation is usually needed. Most clinicians will start with a dose of 25 ug/d of T4 with adjustment every 6 to 8 weeks until the TSH is normalized.
Unless subclinical hyperthyroidism is secondary to over-replacement with exogenous thyroid hormone, this condtion can be more difficult to treat than subclinical hypothyroidism. Antithyroid therapy should be discussed with patients who have symptoms suggestive of hyperthyroidism, osteoporosis, recurrent atrial fibrillation, or thyroid gland nodules. Consultation with an endocrinologist can help clarify the risks and benefits and determine the specific antithyroid treatment appropriate for each patient.
Case 3: Medications and thyroid abnormalities
R.K., 56, has a long history of bipolar disorder. Upon presenting to his psychiatrist for routine follow-up, he reports a lack of energy but denies other symptoms of mania or depression. He periodically leaves work early or takes a short nap in his office to combat the fatigue. He feels that this may simply be part of “getting old.” He denies any new medical problems and has seen his family physician in the last year. He states that he has been compliant with his medications, lithium and olanzapine. He appears slightly withdrawn and blunted but otherwise there are no abnormal features.
His lithium level, thyroid function, or kidney function had not been checked for 7 months. Subsequent testing reveals an elevated TSH (50 mU/L), a normal kidney profile, and a lithium level in the therapeutic range.
Challenge In psychiatric settings, lithium carbonate is the drug most commonly associated with decreased thyroid function. Lithium interferes with both thyroid hormone synthesis and secretion. One-half of those taking lithium chronically develop goiter, and 40% develop subclinical or overt hypothyroidism.9-11
Many patients treated with lithium test positive for antithyroid antibodies. It is unclear if this finding represents a chronic autoimmune thyroiditis or is secondary to lithium treatment itself. In any case, patients taking lithium face an increased risk of thyroid failure. Other risk factors for thyroid failure include female gender and duration of treatment. Lithium dosage does not seem to be related to risk.
Clinicians differ on the frequency of thyroid monitoring for patients taking lithium. For patients without a history of thyroid dysfunction, annual TSH testing is likely sufficient.
Other medications affecting thyroid hormone production include methimazole, propylthiouracil, and iodide-containing drugs and dyes. Methimazole and propylthiouracil are given to patients intentionally with overt hyperthyroidism and interfere with hormone synthesis. Patients receiving medications or dyes containing iodide may also be susceptible to hypothyroidism. These agents are partially deiodinated after they are given and therefore can cause transient or prolonged decreases in thyroid production.
In consultative work, psychiatrists often confront abnormal thyroid tests in critically ill patients. Euthyroid sick syndrome can be a challenge to distinguish from ill patients with true thyroid or pituitary dysfunction. This syndrome is common in hospitalized patients and has been documented in more than 50% of patients in some settings.14
Abnormal thyroid tests are observed in a variety of medical conditions including heart failure, myocardial infarction, renal failure, liver disease, infections, stress, trauma, starvation, and autoimmune disorders. There is considerable debate about the meaning of these test abnormalities, and to date no conclusive intervention to correct abnormalities has proven to be consistently effective in ill patients.
The complex results of testing contribute to the confusion. An isolated low T3 is the most common lab abnormality found in nonthyroidal illness, related to a decrease in T4 enzymatic conversion to T3. Many disease states decrease this enzyme’s (5’-deiodinase) activity. Unlike T3, TSH and T4 levels stay within normal limits in mild to moderately ill patients.
In patients who are moderately ill or who have been ill for a longer time, T4 levels fall with T3. In more severe and critically ill patients, the TSH level can decrease as well.
T4 can be elevated in sick patients without thyroid dysfunction. With this pattern, the TSH and T3 levels are normal or high. The clinical meaning of these abnormalities is unclear. Some studies suggest that the degree of thyroid hormone suppression correlates with disease severity and prognosis. Both decreased T3 and T4 levels have been shown to correlate with mortality in some disease states.15 Debate remains as to whether these findings represent a maladaptive process or a protective response to illness.
III patients with hyperthyroidism generally have an elevated serum free T4 and T3 with an undetectable TSH. Ill patients with true hypothyroidism will have a TSH greater than 20 to 30 mU/ml with suppressed T4 and T3 levels. Diagnosis is more difficult when TSH levels are mildly abnormal or when the clinician is trying to distinguish secondary hypothyroidism from the low T3, T4, and TSH pattern found in many critically ill patients. Secondary testing or clinical findings such as an enlarged gland, the presence of thyroid antibodies, or abnormalities in other pituitary hormones may point to an underlying thyroid or pituitary problem in ill patients.
Some oral cholecystographic agents and the antiarrhythmic medication amiodarone are excreted slowly and can be associated with more prolonged decreases in thyroid hormone production. Iodide and medications containing iodide may precipitate a longer enduring hypothyroidism in patients with chronic autoimmune thyroiditis and in those with hyperthyroidism who have received radioactive iodine therapy or have undergone partial thyroidectomy.
The cholesterol-lowering bile acid sequestrants colestipol and cholestyramine can also inhibit thyroid reabsorption from the intestine, potentially leading to hypothyroidism. Patients dependent on exogenous T4 or who have an underlying decreased thyroid function may develop hypothyroidism.
Table 3
WHICH MEDICATIONS CAN CAUSE THYROID DYSFUNCTION?
| Drugs that increase thyroid hormone secretion Iodide-containing medication Amiodarone Providone-iodine antiseptics X-ray contrast media containing iodine | Drugs that increase hepatic metabolism of T4 and T3 Phenobarbital Rifampin Phenytoin Carbamazepine |
| Drugs that decrease TBG,* causing a relative increase in unbound thyroid Androgens Anabolic steroids | Drugs that decrease T4 absorption Colestipol Cholestyramine Aluminum hydroxide Ferrous sulfate Sucralfate |
| Drugs that decrease thyroid hormone secretion Lithium carbonate Iodide Amiodarone | Drugs that increase TBG,* causing a relative decrease in unbound thyroid Estrogens Tamoxifen Heroin and methadone |
| *Thyroxine-binding globulin Table adapted from: Surks MI, Sievert R. Drugs and thyroid function. N Engl J Med 1995;333(25):1688-94. | |
Drugs that alter thyroid hormone metabolism can also be problematic. Although thyroid hormone is metabolized mostly by deiodination, it also undergoes glucuronidation and sulfation. Phenobarbital, rifampin, phenytoin, and carbamazepine all increase T4 and T3 metabolism by inducing these hepatic enzymes. In patients with no thyroid disease, phenytoin and carbamazepine can decrease circulating free T4 levels by 20% to 40%.12 Patients receiving T4 replacement may need their dosage increased or risk hypothyroidism if placed on one of these medications (Table 3).
Several medications alter total T4 and T3 levels by increasing or decreasing thyroid-binding proteins. Examples include estrogens, androgens, anabolic steroids, methadone, and heroin. Most thyroid hormone circulates as bound, but it is the unbound form that is active in peripheral tissues. Patients thus can experience changes in the binding proteins, while the proportion of unbound (“free”) hormone at the tissue level remains unaffected.
Because this unbound form remains relatively unchanged, the patient with normal thyroid function remains euthyroid despite alterations in total thyroid levels. When patients with hypothyroidism start one of these medications, their replacement hormone dosage may need to be adjusted.
Related resources
- American Association of Clinical Endocrinologists. www.aace.com
- Clinical practice guidelines for evaluation and treatment of hypothyroidism and hyperthyroidism. Position statement on subclinical hypothyroidism and pregnancy
- Thyroid Federation International. www.thyroid-fed.org
- Online videos regarding thyroid disease (patient-directed). Patient handouts on thyroid disease
- Jameson JL, Weetman AP. Disorders of the thyroid gland. In: Harrison’s Principles of Internal Medicine. 15th ed. New York: McGraw-Hill; 2001:2060-84
Drug brand names
- Amiodorone • Pacerone, Cordarone
- Colestipol • Colestid
- Methimazole • Tapazole
- Olanzapine • Zyprexa, Zyprexa Zydis
- Rifampin • Rifadin, Rimactane
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article.
1. Helfand M, Redfern CC. Screening for thyroid disease: an update. Ann Intern Med 1998;129(2):144-58.
2. Arem R, Cusi K. Thyroid function testing in psychiatric illness usefulness and limitations. Trends Endocrinol Metab 1997;8:282-87.
3. Nader S, Warner MD, Doyle S, Peabody CA. Euthyroid sick syndrome in psychiatric inpatients. Biol Psychiatry 1996;40(12):1288-93.
4. Fava M, Labbate LA, Abraham ME. Hypothyroidism and hyperthyroidism in major depression. J Clin Psychiatry 1995;56(5):186-92.
5. Jackson IM. The thyroid axis and depression. Thyroid 1998;8(10):951-56.
6. Samuels MH. Subclinical thyroid disease in the elderly. Thyroid 1998;8(9):803-13.
7. Staub JJ, Althaus BU, Engler H, Ryff AS, Trabucco P, Marquardt K, et al. Spectrum of subclinical and overt hypothyroidism: effect on thyrotropin, prolactin, and thyroid reserve, and metabolic impact on peripheral target tissues. Am J Med 1992;92(6):631-42.
8. Ayala AR, Wartofsky L. Minimally symptomatic (subclinical) hypothyroidism. Endocrinologist 1997;7:44-50.
9. Spaulding SW, Burrow GN, Bermudez F, Himmelhoch JM. The inhibitory effect of lithium on thyroid hormone release in both euthyroid and thyrotoxic patients. J Clin Endocrinol Metab 1972;35(6):905-11.
10. Perrild H, Hegedus L Baastrup PC, Kayser L, Kastberg S. Thyroid function and ultrasonically determined thyroid size in patients receiving long-term lithium treatment. Am J Psychiatry 1990;147(11):1518-21.
11. Bocchetta A, Bernardi F, Peditzi M. Thyroid abnormalities during lithium treatment. Acta Psychiatr Scand 1991;83(3):193-98.
12. Surks MI, Sievert R. Drugs and thyroid function. N Engl J Med 1995;333(25):1688-94.
13. Mandel SJ, Larsen PR, Seely EW, Brent GA. Increased need for thyroxine during pregnancy in women with primary hypothyroidism. N Engl J Med 1990;323(2):91-6.
14. Chopra IJ. Clinical review 86: euthyroid sick syndrome: is it a misnomer? J Clin Endocrinol Metab 1997;82(2):329-34.
15. Camacho PM, Dwarkanathan AA. Sick euthyroid syndrome, what to do when thyroid function tests are abnormal in critically ill patients. Postgrad Med 1999;105(4):215-19.
16. Woeber KA. Update of management of hyperthyroidism and hypothyroidism. Arch Fam Med 2000;9(8):743-47.
1. Helfand M, Redfern CC. Screening for thyroid disease: an update. Ann Intern Med 1998;129(2):144-58.
2. Arem R, Cusi K. Thyroid function testing in psychiatric illness usefulness and limitations. Trends Endocrinol Metab 1997;8:282-87.
3. Nader S, Warner MD, Doyle S, Peabody CA. Euthyroid sick syndrome in psychiatric inpatients. Biol Psychiatry 1996;40(12):1288-93.
4. Fava M, Labbate LA, Abraham ME. Hypothyroidism and hyperthyroidism in major depression. J Clin Psychiatry 1995;56(5):186-92.
5. Jackson IM. The thyroid axis and depression. Thyroid 1998;8(10):951-56.
6. Samuels MH. Subclinical thyroid disease in the elderly. Thyroid 1998;8(9):803-13.
7. Staub JJ, Althaus BU, Engler H, Ryff AS, Trabucco P, Marquardt K, et al. Spectrum of subclinical and overt hypothyroidism: effect on thyrotropin, prolactin, and thyroid reserve, and metabolic impact on peripheral target tissues. Am J Med 1992;92(6):631-42.
8. Ayala AR, Wartofsky L. Minimally symptomatic (subclinical) hypothyroidism. Endocrinologist 1997;7:44-50.
9. Spaulding SW, Burrow GN, Bermudez F, Himmelhoch JM. The inhibitory effect of lithium on thyroid hormone release in both euthyroid and thyrotoxic patients. J Clin Endocrinol Metab 1972;35(6):905-11.
10. Perrild H, Hegedus L Baastrup PC, Kayser L, Kastberg S. Thyroid function and ultrasonically determined thyroid size in patients receiving long-term lithium treatment. Am J Psychiatry 1990;147(11):1518-21.
11. Bocchetta A, Bernardi F, Peditzi M. Thyroid abnormalities during lithium treatment. Acta Psychiatr Scand 1991;83(3):193-98.
12. Surks MI, Sievert R. Drugs and thyroid function. N Engl J Med 1995;333(25):1688-94.
13. Mandel SJ, Larsen PR, Seely EW, Brent GA. Increased need for thyroxine during pregnancy in women with primary hypothyroidism. N Engl J Med 1990;323(2):91-6.
14. Chopra IJ. Clinical review 86: euthyroid sick syndrome: is it a misnomer? J Clin Endocrinol Metab 1997;82(2):329-34.
15. Camacho PM, Dwarkanathan AA. Sick euthyroid syndrome, what to do when thyroid function tests are abnormal in critically ill patients. Postgrad Med 1999;105(4):215-19.
16. Woeber KA. Update of management of hyperthyroidism and hypothyroidism. Arch Fam Med 2000;9(8):743-47.
Postpartum depression: Is there an Andrea Yates in your practice?
Women face increased vulnerability to the onset of major depression during the childbearing years. Between 12% and 16% of women experience a major depressive episode in the postpartum period.1 Postpartum depression (PPD) can have severe and long-lasting consequences for maternal and infant functioning.2 If left untreated, it can impair maternal-infant bonding and infant attachment and can hinder the child’s cognitive and emotional development.
Based on our experience in caring for women with PPD, this article is intended to help you detect and diagnose PPD more quickly and make appropriate treatment recommendations to family physicians, obstetricians/gynecologists, and other clinicians. We will review the key risk factors for PPD, address screening and diagnostic strategies, and look at the latest evidence on psychosocial and pharmacologic treatment.
Risk factors
Key risk factors, such as a history of PPD or depression, have been identified as predictors of PPD (Table 1).3,4 In the diagnostic criteria for depression, the DSM-IV includes a specifier that states the onset of PPD must occur within 4 weeks after giving birth.5 Our clinical experience, however, indicates that PPD can occur up to 1 year after giving birth. The essential feature of major depressive disorder, according to the DSM-IV, is “a clinical course that is characterized by one or more Major Depressive Episodes” (Table 2).
PPD is often associated with comorbid anxiety disorders, which manifest in many ways. Panic attacks are often the first indication of an existing or impending depression. A small percentage of women will experience intrusive obsessional thoughts of harming their infants.
Andrea Yates, 37, of Harris County, Texas, was convicted of two counts of murder in the June 2001 bathtub drownings of her five children. The jury deliberated less than 4 hours to reach the verdict March 12. The next day, she was sentenced to life in prison. She had pleaded not guilty by reason of insanity.
It is not known why Mrs. Yates discontinued her antipsychotic medication a few weeks prior to this tragedy and why those around her did not heed the numerous warning signs of her mental illness.
Roughly 30% of women with postpartum depression experience thoughts of suicide or infanticide/homicide. Mrs. Yates showed evidence of such thoughts shortly after the birth of her first child, but she did not receive psychiatric care until her third child was born. Although she was hospitalized several times, no follow-up psychiatric care was provided. It was reported that she twice attempted suicide.
During the trial, defense attorneys presented testimony by psychiatrists that Mrs. Yates was suffering postpartum psychosis and schizoaffective disorder. Her severe illness produced the delusional belief that killing the children would save them from eternal damnation. Prosecutors convinced the jury that Mrs. Yates, although ill, was capable of distinguishing right from wrong at the time of the slayings and therefore did not meet the strict Texas standard for insanity.
Mental illness during pregnancy or the postpartum period is poorly understood by new mothers and their families. The verdict and sentence in this case represent an enormous step backward.
The media treatment of Andrea Yates and her imprisonment—rather than hospitalization for proper treatment of her mental illness—may deter mothers from telling their physicians about any negative feelings they may be experiencing. As a result, women who could benefit from treatment of depressive illness will not be identified, and they and their children will be at risk.
Shaila Misri, MD, FRCPC
Xanthoula Kostaras, BSc
Table 1
RISK FACTORS FOR POSTPARTUM DEPRESSION
| Major factors | Contributing factors |
|---|---|
|
|
Screening and diagnosis
Many women will not report depressive symptoms to their primary care physicians or obstetricians during the routine postpartum visit. This reticence by mothers to volunteer any negative information about themselves may be due to the brevity of the typical postpartum visit or its usual focus on the welfare of the infant.
A recent study of 391 outpatients in an obstetrical practice demonstrates the value of using a screening instrument to identify possible PPD cases during the 6-week follow-up visit. When the women were screened with the standardized Edinburgh Postnatal Depression Scale (EPDS), the rate of detection of PPD was 35.4%, whereas the rate of spontaneous detection was 6.3%.6
The EPDS (Box 1), a 10-item self-report questionnaire developed by Cox and colleagues, is used specifically to detect PPD.7 A minimum score of 12 or 13 warrants a diagnosis of PPD. The EPDS can be used as a screening tool at 6 to 8 weeks postpartum and can be repeated over several visits to track symptoms. This tool has been validated, computerized, and translated into more than 12 languages and can be copied and used free of charge.
A new screening tool, the Postpartum Depression Screening Scale (PDSS), was recently developed and validated by Beck and colleagues to help clinicians identify and respond to PPD as early as possible.8 Depressive symptoms are rated on a 5-point scale, and the total score is used to determine overall severity of depressive symptoms. Higher PDSS scores correspond to increasing severity of symptoms and indicate that the patient should be referred for additional evaluation. The PDSS is published by Western Psychological Services (www.wpspublish.com).
Psychosis in PPD
Psychotic depression in the postpartum period is sometimes associated with chronic mood disorders, especially untreated depression. The most prevalent psychotic features include paranoid delusions that incorporate the newborn. Hallucinations are rare. Psychotic depression places the postpartum patient at a heightened risk for suicide and/or infanticide and is considered a medical emergency that requires immediate hospitalization and treatment to ensure the safety of the infant and the ill mother (see “Andrea Yates: Warning signs were ignored,”).
If a patient with psychotic PPD is experiencing delusions centered on harming her infant, a family member or members should assume responsibility for the child’s care, and the patient should not be left alone with the infant. When the mother is hospitalized, visitation between the mother and infant should be restricted, particularly if the infant’s presence precipitates anxiety in the mother. The goal of hospitalization is to achieve symptom remission and stability in the mother so that bonding and attachment can occur. Maternal-infant bonding is difficult, if not impossible, if the mother is out of touch with reality.
Treating mild to moderate PPD
Psychosocial therapies are first-line treatment for mild-to-moderate PPD symptoms or when a patient refuses pharmacotherapy. These therapies include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), group therapy, family and/or marital therapy, supportive psychotherapy, and peer support groups. Psychosocial therapies also should be used as adjunctive treatments to pharmacotherapy.
Table 2
DSM-IV CRITERIA FOR A MAJOR DEPRESSIVE EPISODE
|
CBT. A preliminary study examining short-term cognitive-behavioral counseling for postpartum depressed women reported that participants who received six CBT sessions showed the same degree of improvement in functioning as did a group receiving fluoxetine. Both groups showed greatly improved functioning when compared with a group that received a placebo.9
IPT. In pregnant and postpartum women, the focus of IPT is on role transitions and the acquisition of skills applicable to motherhood. Preliminary studies of IPT in pregnant and postpartum women have shown encouraging results.10 A recent controlled study of 99 women provided additional evidence that IPT helps decrease depressive symptoms and promote social adjustment in women with moderate PPD.11
Group therapy. One of the most valuable benefits of group therapy in PPD treatment is that it may help women who are feeling socially isolated to increase their support networks. Several psychosocial therapy methods may be adapted to a group model, including interpersonal and supportive psychotherapy.
Family and marital therapy. The roles of the partner and family are critical to treating women with mood and anxiety disorders during pregnancy or the postpartum period. A recent study found that postpartum depressed women recover more rapidly and appreciate their partners’ contribution to the relationship more when the partner is supportive.12
Supportive psychotherapy involves offering patients and their families support, reassurance, and psychoeducation. This type of therapy is used to augment other psychosocial interventions and/or pharmacotherapy. In some cases, supportive therapy may be the only treatment a woman receives if her depressive symptoms are too severe for her to engage in CBT or IPT and she refuses pharmacotherapy. Then supportive psychotherapy is used to monitor her mental state.
Peer-support groups. Several groups formed by consumers and health care providers offer support and education to women with reproductive-associated mood and anxiety disorders. (See “Related resources,”).
Pharmacologic treatment
Pharmacotherapy is indicated in women with moderate-to-severe symptoms who do not respond to psychosocial treatment alone. Because all psychotropic medications are excreted in breast milk and passed on to the nursing infant, one must weigh the potential risks of the infant’s exposure to medication against the risks of untreated maternal depression.
Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) are used most commonly to treat PPD. Monoamine oxidase inhibitors (MAOIs) are not recommended as they have been reported to exacerbate hypertension, and their extensive interaction profiles with food and other medications can complicate treatment. Further, only limited evidence is available on the effects of MAOIs during pregnancy and the postpartum period.
- Ask the mother to underline the response that comes closest to how she has been feeling in the previous 7 days.
- All 10 items must be completed.
- Avoid the possibility of the mother discussing her answers with others.
- The mother should complete the scale herself, unless she has limited English or difficulty with reading.
- The EPDS may be used at 6 to 8 weeks postnatal. A visit to the child health clinic, a postnatal check-up, or a home visit may provide suitable opportunities for its completion.
As you have recently had a baby, we would like to know how you are feeling. Please CHECK the answer that comes closest to how you have felt IN THE PAST 7 DAYS, not just how you feel today.
- I have been able to laugh and see the funny side of things.
- I have looked forward with enjoyment to things.
- * I have blamed myself unnecessarily when things went wrong.
- I have been anxious or worried for no good reason.
- * I have felt scared or panicky without a good reason.
- * Things have been getting on top of me.
- * I have been so unhappy that I have had difficulty sleeping.
- * I have felt sad or miserable.
- * I have been so unhappy that I have been crying.
- * The thought of harming myself has occurred to me.
Responses to statements 1, 2, and 4 are scored 0, 1, 2, and 3 according to increasing severity of symptoms, and statements marked with an asterisk (*) are reverse-scored (3, 2, 1, and 0). Total score is calculated by adding the scores of all 10 items. A score of 12 or 13 has been found to identify most women with a diagnosis of PPD.
Adapted from Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-6.
Table 3
SSRI DRUG THERAPY FOR POSTPARTUM DEPRESSION
| Medication | Starting daily dosage (mg) | Maximum daily dosage (mg) | Precautions |
|---|---|---|---|
| Fluoxetine | 10 | 80 | Very long half-life of active metabolite may lead to accumulation in infants Inform parents of possible side effects, and include a pediatrician in routine clinical evaluations of the infant |
| Sertraline | 25 | 300 | Benign neonatal sleep myoclonus has been documented in one case of sertraline exposure during breast-feeding Inform parents of possible side effects, and include a pediatrician in routine clinical evaluations of the infant |
| Paroxetine | 10 | 60 | No adverse effects have been reported |
| Fluvoxamine | 50 | 300 | Data limited |
| Citalopram | 10 | 60 | Data limited |
Use of SSRIs
The literature on use of SSRIs in lactating women has expanded rapidly in recent years (Table 3). But because these agents have been on the market a relatively short time, the long-term developmental effects of infants’ exposure to SSRIs through breast milk have yet to be evaluated. Fluoxetineis the SSRI with the most published data on use by breast-feeding women. To date, nine studies have reported the outcomes of a total of 57 infants exposed to fluoxetine during breast feeding.13,14 Norfluoxetine, the potent metabolite of fluoxetine, has a long half-life that may predispose to accumulation in the serum of nursing infants.
Adverse effects such as colic, fussiness, crying, seizure activity, and reduced weight gain have been reported in two cases.15,16 The remaining studies on the use of fluoxetine by breast-feeding women have reported low drug levels in both mothers and infants, and no other adverse effects have been documented.
Sertraline. To date, seven published reports of sertraline exposure have documented 46 infant outcomes. In all of these reports, sertraline and its weak metabolite have been detected in low or trace amounts in the sera of nursing infants.13,14,17-19 A recent study of 19 breast-feeding mother-infant pairs found that platelet serotonin uptake in these infants was unaltered, despite the detection of low serum levels of sertraline and its metabolite.19
Paroxetine. Paroxetine is also excreted into the breast milk of lactating women, although—unlike the other SSRI medications—the agent does not have an active metabolite that could potentially accumulate in the serum of nursing infants. Five reports totaling 60 infant outcomes have been published regarding paroxetine exposure during breast feeding. Low or undetectable serum levels were reported in all of the infants, and no adverse effects were noted.13,14,20
Fluvoxamine, citalopram. Two small case studies of fluvoxamine have each reported very low drug levels in breast milk and no adverse events in the exposed infants.21,22 Only three case studies examining five infants exposed to citalopram during breast feeding have been published.13 As information is limited regarding the effects of these medications on nursing infants, caution is advised when prescribing either agent to breast-feeding women.
Use of TCAs and other antidepressants
TCAs are useful for treating PPD when SSRIs have failed or the patient has shown a previous good response to TCAs. All TCAs are excreted into breast milk in low concentrations, and a wide range of infant serum levels have been reported.
No adverse effects have been documented for infant exposure to amitriptyline, clomipramine, desipramine, imipramine, or nortriptyline.13,14,23,24 The active metabolite of doxepin has the longest half-life (37 hours) among the TCAs and may be potentially hazardous to nursing infants because of high serum accumulations. Because two reports have associated doxepin exposure with respiratory distress, poor sucking, drowsiness, and vomiting in infants, the use of medications with a shorter half-life and better-documented effects in infants is recommended.13
Limited evidence is available on the use of newer antidepressants such as bupropion, trazodone, and nefazodone by breast-feeding women.25-27 When possible, therefore, such patients should be prescribed an antidepressant with more documented use in breast-feeding mothers.
Venlafaxine is a newer antidepressant that inhibits reuptake of both serotonin and norepinephrine. The only case report published to date regarding venlafaxine levels in nursing infants found high drug levels in the sera of three exposed infants but no adverse effects.28
Use of antipsychotics, ECT
Postpartum psychosis is rare and requires immediate intervention. Treatment with antipsychotics is one of the most effective methods for controlling a psychotic episode. Most women with postpartum psychosis will be too disorganized to consider breast-feeding, but for those who may wish to breast-feed, a discussion with her partner about infant exposure issues is recommended.
Effects of infant exposure through breast milk to the typical antipsychotics (e.g., chlorpromazine, trifluoperazine, haloperidol) include drowsiness, lethargy, and possible developmental delays.13 Nursing infants should be monitored for sedation and other adverse effects during long-term maternal use of these medications.
Evidence on the use of atypical antipsychotics during breast-feeding is limited. One report described cardiomegaly, jaundice, and sedation in one of three infants exposed to olanzapine through breast milk. But the effects could not be attributed directly to breast milk, as that infant was exposed both in utero and during breast-feeding.13
One report of a nursing infant exposed to risperidone indicated no adverse effects,29 and there is no published data on quetiapine use during breast-feeding.
ECT If the patient with psychotic PPD cannot tolerate or does not respond to antipsychotic medication, electroconvulsive therapy (ECT) may be indicated. ECT in the postpartum period is safe for both mother and infant. It is particularly useful when rapid treatment is imperative, such as severe depression with psychotic symptoms, acute mania, and in mothers who are at risk for suicide or infanticide.30
Management guidelines for PPD
Based on our experience and the available evidence, we offer these recommendations to psychiatrists managing patients with PPD:
- During the initial psychiatric assessment, use screening tools such as the EPDS or the PDSS to assist with diagnosis and to identify symptom patterns.
- Next, schedule a conjoint visit with the patient’s partner, family members, and/or social supports. Provide educational materials about PPD and exchange information about treatment options to help the patient make informed decisions. Reading lists, appropriate research articles, lists of local resources, and Web sites can increase awareness about PPD and drive home the importance of compliance with treatment.
- If pharmacotherapy is to be used, discuss honestly and openly the medication’s benefits and potential risks for both mother and infant in the short and long term.
- Outline a treatment plan with the patient and her partner. This should include 6 weeks of treatment during the acute phase, as well as maintenance and long-term therapy.
- If applicable, discuss with the woman and her partner pregnancy planning during pharmacotherapy. In women who experience repeated episodes of depression, discontinuing an antidepressant during pregnancy almost always results in relapse of depressive symptoms.
- Misri S. Shouldn’t I Be Happy? Emotional problems of pregnant and postpartum women. . New York: Free Press, 1995.
- Sichel D, Driscoll JW. Women’s moods: What every woman must know about hormones, the brain, and emotional health. . New York: William Morrow & Co., 1999.
- Depression After Delivery, Inc. www.depressionafterdelivery.com or 1-800-944-4773 (4PPD)
- Postpartum Support International. www.postpartum.net
- Pacific Postpartum Support Society. www.postpartum.org
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Clomipramine • Anafranil
- Desipramine • Norpramin
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Nefazodone • Serzone
- Nortriptyline • Aventyl
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Misri reports that she receives grant/research support from and serves on the speaker’s bureau of GlaxoSmithKline Canada, receives research/grant support from Wyeth-Ayerst Pharmaceuticals, and has lectured for Eli Lilly & Co., AstraZeneca, and Janssen-Ortho.
Ms. Kostaras reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. O’Hara MW, Swain AM. Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry 1996;8:37-54.
2. Weinberg MK, Tronick EZ. The impact of maternal psychiatric illness on infant development. J Clin Psychiatry 1998;59(suppl 2):53-61.
3. O’Hara MW. Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry 1986;43:569-73.
4. Beck CT. Predictors of postpartum depression: an update. Nursing Res 2001;50(5):275-85.
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text revision. Washington, DC, American Psychiatric Association, 2000.
6. Evins GG, Theofrastous JP, Galvin SL. Postpartum depression: a comparison of screening and routine clinical evaluation. Am J Obstet Gynecol 2000;182(5):1080-2.
7. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10 –item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6.
8. Beck CT, Gable RK. Further validation of the postpartum depression screening scale. Nursing Res 2001;50(3):155-64.
9. Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive-behavioural counselling in the treatment of postnatal depression. BMJ 1997;314(7085):932-6.
10. Stuart S, O’Hara MW. Interpersonal psychotherapy for postpartum depression: a treatment program. J Psychother Pract Res 1995;4:18-29.
11. O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 2000;57(11):1039-45.
12. Misri S, Kostaras X, Fox D, Kostaras D. The impact of partner support in the treatment of postpartum depression. Can J Psychiatry 2000;45(6):554-8.
13. Burt VK, Suri R, Altshuler L, et al. The use of psychotropic medications during breast-feeding. Am J Psychiatry 2001;158(7):1001-9.
14. Birnbaum CS, Cohen LS, et al. Serum concentrations of antidepressants and benzodiazepines in nursing infants: a case series (electronic article). Pediatrics 1999;104(1):www.pediatrics.org/cgi/content/full/104/1/e11
15. Lester BM, Cucca J, Andreozzi L, et al. Possible association between fluoxetine hydrochloride and colic in an infant. J Am Acad Child Adolesc Psychiatry 1993;32(6):1253-5.
16. Chambers CD, Anderson PO, Thomas RG, et al. Weight gain in infants breastfed by mothers who take fluoxetine (electronic article). Pediatrics 1999;104(5):http://www.pediatrics.org/cgi/content/full/104/5/e61
17. Epperson CN, Anderson GM, McDougle CJ. Sertraline and breast feeding (letter). N Engl J Med 1997;336(16):1189-90.
18. Wisner KL, Perel JM, Blumer J. Serum sertraline and n-desmethylsertraline levels in breast-feeding mother-infant pairs. Am J Psychiatry 1998;155(5):690-2.
19. Epperson N, Czarkowski KA, Ward-O’Brien D, et al. Maternal sertraline treatment and serotonin transport in breast-feeding mother-infant pairs. Am J Psychiatry 2001;158(10):1631-7.
20. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61(11):828-32.
21. Wright S, Dawling S, Ashford JJ. Excretion of fluvoxamine in breast milk (letter). Br J Clin Pharmacol 1991;31:209.-
22. Piontek CM, Wisner KL, Perel JM, Peindl KS. Serum fluvoxamine levels in breastfed infants. J Clin Psychiatry 2001;62(2):111-3.
23. Wisner KL, Perel JM, Foglia JP. Serum clomipramine and metabolite levels in four nursing mother-infant pairs. J Clin Psychiatry 1995;56(1):17-20.
24. Altshuler LL, Burt VK, McMullen M, Hendrick V. Breastfeeding and sertraline: a 24-hour analysis. J Clin Psychiatry 1995;56(6):243-5.
25. Briggs GG, Samson JH, Ambrose PJ, Schroeder DH. Excretion of bupropion in breast milk. Ann Pharmacother 1993;27(4):431-3.
26. Verbeeck RK, Ross SG, McKenna EA. Excretion of trazodone in breast milk. Br J Clin Pharmacol 1986;22:367-70.
27. Yapp P, Ilett KF, Kristensen JH, et al. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34(11):1269-72.
28. Illett KF, Hackett LP, Dusci LJ, et al. Distribution and excretion of venlafaxine and O-desmethylvenlafaxine in human milk. Br J Clin Pharmacol 1998;45:459-62.
29. Hill RC, McIvor RJ, Wojnar-Horton RE, et al. Risperidone distribution and excretion in human milk: case report and estimated infant exposure during breast-feeding (letter). J Clin Psychopharmacol 2000;20(2):285-6.
30. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiat 1994;45:444-50.
Women face increased vulnerability to the onset of major depression during the childbearing years. Between 12% and 16% of women experience a major depressive episode in the postpartum period.1 Postpartum depression (PPD) can have severe and long-lasting consequences for maternal and infant functioning.2 If left untreated, it can impair maternal-infant bonding and infant attachment and can hinder the child’s cognitive and emotional development.
Based on our experience in caring for women with PPD, this article is intended to help you detect and diagnose PPD more quickly and make appropriate treatment recommendations to family physicians, obstetricians/gynecologists, and other clinicians. We will review the key risk factors for PPD, address screening and diagnostic strategies, and look at the latest evidence on psychosocial and pharmacologic treatment.
Risk factors
Key risk factors, such as a history of PPD or depression, have been identified as predictors of PPD (Table 1).3,4 In the diagnostic criteria for depression, the DSM-IV includes a specifier that states the onset of PPD must occur within 4 weeks after giving birth.5 Our clinical experience, however, indicates that PPD can occur up to 1 year after giving birth. The essential feature of major depressive disorder, according to the DSM-IV, is “a clinical course that is characterized by one or more Major Depressive Episodes” (Table 2).
PPD is often associated with comorbid anxiety disorders, which manifest in many ways. Panic attacks are often the first indication of an existing or impending depression. A small percentage of women will experience intrusive obsessional thoughts of harming their infants.
Andrea Yates, 37, of Harris County, Texas, was convicted of two counts of murder in the June 2001 bathtub drownings of her five children. The jury deliberated less than 4 hours to reach the verdict March 12. The next day, she was sentenced to life in prison. She had pleaded not guilty by reason of insanity.
It is not known why Mrs. Yates discontinued her antipsychotic medication a few weeks prior to this tragedy and why those around her did not heed the numerous warning signs of her mental illness.
Roughly 30% of women with postpartum depression experience thoughts of suicide or infanticide/homicide. Mrs. Yates showed evidence of such thoughts shortly after the birth of her first child, but she did not receive psychiatric care until her third child was born. Although she was hospitalized several times, no follow-up psychiatric care was provided. It was reported that she twice attempted suicide.
During the trial, defense attorneys presented testimony by psychiatrists that Mrs. Yates was suffering postpartum psychosis and schizoaffective disorder. Her severe illness produced the delusional belief that killing the children would save them from eternal damnation. Prosecutors convinced the jury that Mrs. Yates, although ill, was capable of distinguishing right from wrong at the time of the slayings and therefore did not meet the strict Texas standard for insanity.
Mental illness during pregnancy or the postpartum period is poorly understood by new mothers and their families. The verdict and sentence in this case represent an enormous step backward.
The media treatment of Andrea Yates and her imprisonment—rather than hospitalization for proper treatment of her mental illness—may deter mothers from telling their physicians about any negative feelings they may be experiencing. As a result, women who could benefit from treatment of depressive illness will not be identified, and they and their children will be at risk.
Shaila Misri, MD, FRCPC
Xanthoula Kostaras, BSc
Table 1
RISK FACTORS FOR POSTPARTUM DEPRESSION
| Major factors | Contributing factors |
|---|---|
|
|
Screening and diagnosis
Many women will not report depressive symptoms to their primary care physicians or obstetricians during the routine postpartum visit. This reticence by mothers to volunteer any negative information about themselves may be due to the brevity of the typical postpartum visit or its usual focus on the welfare of the infant.
A recent study of 391 outpatients in an obstetrical practice demonstrates the value of using a screening instrument to identify possible PPD cases during the 6-week follow-up visit. When the women were screened with the standardized Edinburgh Postnatal Depression Scale (EPDS), the rate of detection of PPD was 35.4%, whereas the rate of spontaneous detection was 6.3%.6
The EPDS (Box 1), a 10-item self-report questionnaire developed by Cox and colleagues, is used specifically to detect PPD.7 A minimum score of 12 or 13 warrants a diagnosis of PPD. The EPDS can be used as a screening tool at 6 to 8 weeks postpartum and can be repeated over several visits to track symptoms. This tool has been validated, computerized, and translated into more than 12 languages and can be copied and used free of charge.
A new screening tool, the Postpartum Depression Screening Scale (PDSS), was recently developed and validated by Beck and colleagues to help clinicians identify and respond to PPD as early as possible.8 Depressive symptoms are rated on a 5-point scale, and the total score is used to determine overall severity of depressive symptoms. Higher PDSS scores correspond to increasing severity of symptoms and indicate that the patient should be referred for additional evaluation. The PDSS is published by Western Psychological Services (www.wpspublish.com).
Psychosis in PPD
Psychotic depression in the postpartum period is sometimes associated with chronic mood disorders, especially untreated depression. The most prevalent psychotic features include paranoid delusions that incorporate the newborn. Hallucinations are rare. Psychotic depression places the postpartum patient at a heightened risk for suicide and/or infanticide and is considered a medical emergency that requires immediate hospitalization and treatment to ensure the safety of the infant and the ill mother (see “Andrea Yates: Warning signs were ignored,”).
If a patient with psychotic PPD is experiencing delusions centered on harming her infant, a family member or members should assume responsibility for the child’s care, and the patient should not be left alone with the infant. When the mother is hospitalized, visitation between the mother and infant should be restricted, particularly if the infant’s presence precipitates anxiety in the mother. The goal of hospitalization is to achieve symptom remission and stability in the mother so that bonding and attachment can occur. Maternal-infant bonding is difficult, if not impossible, if the mother is out of touch with reality.
Treating mild to moderate PPD
Psychosocial therapies are first-line treatment for mild-to-moderate PPD symptoms or when a patient refuses pharmacotherapy. These therapies include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), group therapy, family and/or marital therapy, supportive psychotherapy, and peer support groups. Psychosocial therapies also should be used as adjunctive treatments to pharmacotherapy.
Table 2
DSM-IV CRITERIA FOR A MAJOR DEPRESSIVE EPISODE
|
CBT. A preliminary study examining short-term cognitive-behavioral counseling for postpartum depressed women reported that participants who received six CBT sessions showed the same degree of improvement in functioning as did a group receiving fluoxetine. Both groups showed greatly improved functioning when compared with a group that received a placebo.9
IPT. In pregnant and postpartum women, the focus of IPT is on role transitions and the acquisition of skills applicable to motherhood. Preliminary studies of IPT in pregnant and postpartum women have shown encouraging results.10 A recent controlled study of 99 women provided additional evidence that IPT helps decrease depressive symptoms and promote social adjustment in women with moderate PPD.11
Group therapy. One of the most valuable benefits of group therapy in PPD treatment is that it may help women who are feeling socially isolated to increase their support networks. Several psychosocial therapy methods may be adapted to a group model, including interpersonal and supportive psychotherapy.
Family and marital therapy. The roles of the partner and family are critical to treating women with mood and anxiety disorders during pregnancy or the postpartum period. A recent study found that postpartum depressed women recover more rapidly and appreciate their partners’ contribution to the relationship more when the partner is supportive.12
Supportive psychotherapy involves offering patients and their families support, reassurance, and psychoeducation. This type of therapy is used to augment other psychosocial interventions and/or pharmacotherapy. In some cases, supportive therapy may be the only treatment a woman receives if her depressive symptoms are too severe for her to engage in CBT or IPT and she refuses pharmacotherapy. Then supportive psychotherapy is used to monitor her mental state.
Peer-support groups. Several groups formed by consumers and health care providers offer support and education to women with reproductive-associated mood and anxiety disorders. (See “Related resources,”).
Pharmacologic treatment
Pharmacotherapy is indicated in women with moderate-to-severe symptoms who do not respond to psychosocial treatment alone. Because all psychotropic medications are excreted in breast milk and passed on to the nursing infant, one must weigh the potential risks of the infant’s exposure to medication against the risks of untreated maternal depression.
Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) are used most commonly to treat PPD. Monoamine oxidase inhibitors (MAOIs) are not recommended as they have been reported to exacerbate hypertension, and their extensive interaction profiles with food and other medications can complicate treatment. Further, only limited evidence is available on the effects of MAOIs during pregnancy and the postpartum period.
- Ask the mother to underline the response that comes closest to how she has been feeling in the previous 7 days.
- All 10 items must be completed.
- Avoid the possibility of the mother discussing her answers with others.
- The mother should complete the scale herself, unless she has limited English or difficulty with reading.
- The EPDS may be used at 6 to 8 weeks postnatal. A visit to the child health clinic, a postnatal check-up, or a home visit may provide suitable opportunities for its completion.
As you have recently had a baby, we would like to know how you are feeling. Please CHECK the answer that comes closest to how you have felt IN THE PAST 7 DAYS, not just how you feel today.
- I have been able to laugh and see the funny side of things.
- I have looked forward with enjoyment to things.
- * I have blamed myself unnecessarily when things went wrong.
- I have been anxious or worried for no good reason.
- * I have felt scared or panicky without a good reason.
- * Things have been getting on top of me.
- * I have been so unhappy that I have had difficulty sleeping.
- * I have felt sad or miserable.
- * I have been so unhappy that I have been crying.
- * The thought of harming myself has occurred to me.
Responses to statements 1, 2, and 4 are scored 0, 1, 2, and 3 according to increasing severity of symptoms, and statements marked with an asterisk (*) are reverse-scored (3, 2, 1, and 0). Total score is calculated by adding the scores of all 10 items. A score of 12 or 13 has been found to identify most women with a diagnosis of PPD.
Adapted from Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-6.
Table 3
SSRI DRUG THERAPY FOR POSTPARTUM DEPRESSION
| Medication | Starting daily dosage (mg) | Maximum daily dosage (mg) | Precautions |
|---|---|---|---|
| Fluoxetine | 10 | 80 | Very long half-life of active metabolite may lead to accumulation in infants Inform parents of possible side effects, and include a pediatrician in routine clinical evaluations of the infant |
| Sertraline | 25 | 300 | Benign neonatal sleep myoclonus has been documented in one case of sertraline exposure during breast-feeding Inform parents of possible side effects, and include a pediatrician in routine clinical evaluations of the infant |
| Paroxetine | 10 | 60 | No adverse effects have been reported |
| Fluvoxamine | 50 | 300 | Data limited |
| Citalopram | 10 | 60 | Data limited |
Use of SSRIs
The literature on use of SSRIs in lactating women has expanded rapidly in recent years (Table 3). But because these agents have been on the market a relatively short time, the long-term developmental effects of infants’ exposure to SSRIs through breast milk have yet to be evaluated. Fluoxetineis the SSRI with the most published data on use by breast-feeding women. To date, nine studies have reported the outcomes of a total of 57 infants exposed to fluoxetine during breast feeding.13,14 Norfluoxetine, the potent metabolite of fluoxetine, has a long half-life that may predispose to accumulation in the serum of nursing infants.
Adverse effects such as colic, fussiness, crying, seizure activity, and reduced weight gain have been reported in two cases.15,16 The remaining studies on the use of fluoxetine by breast-feeding women have reported low drug levels in both mothers and infants, and no other adverse effects have been documented.
Sertraline. To date, seven published reports of sertraline exposure have documented 46 infant outcomes. In all of these reports, sertraline and its weak metabolite have been detected in low or trace amounts in the sera of nursing infants.13,14,17-19 A recent study of 19 breast-feeding mother-infant pairs found that platelet serotonin uptake in these infants was unaltered, despite the detection of low serum levels of sertraline and its metabolite.19
Paroxetine. Paroxetine is also excreted into the breast milk of lactating women, although—unlike the other SSRI medications—the agent does not have an active metabolite that could potentially accumulate in the serum of nursing infants. Five reports totaling 60 infant outcomes have been published regarding paroxetine exposure during breast feeding. Low or undetectable serum levels were reported in all of the infants, and no adverse effects were noted.13,14,20
Fluvoxamine, citalopram. Two small case studies of fluvoxamine have each reported very low drug levels in breast milk and no adverse events in the exposed infants.21,22 Only three case studies examining five infants exposed to citalopram during breast feeding have been published.13 As information is limited regarding the effects of these medications on nursing infants, caution is advised when prescribing either agent to breast-feeding women.
Use of TCAs and other antidepressants
TCAs are useful for treating PPD when SSRIs have failed or the patient has shown a previous good response to TCAs. All TCAs are excreted into breast milk in low concentrations, and a wide range of infant serum levels have been reported.
No adverse effects have been documented for infant exposure to amitriptyline, clomipramine, desipramine, imipramine, or nortriptyline.13,14,23,24 The active metabolite of doxepin has the longest half-life (37 hours) among the TCAs and may be potentially hazardous to nursing infants because of high serum accumulations. Because two reports have associated doxepin exposure with respiratory distress, poor sucking, drowsiness, and vomiting in infants, the use of medications with a shorter half-life and better-documented effects in infants is recommended.13
Limited evidence is available on the use of newer antidepressants such as bupropion, trazodone, and nefazodone by breast-feeding women.25-27 When possible, therefore, such patients should be prescribed an antidepressant with more documented use in breast-feeding mothers.
Venlafaxine is a newer antidepressant that inhibits reuptake of both serotonin and norepinephrine. The only case report published to date regarding venlafaxine levels in nursing infants found high drug levels in the sera of three exposed infants but no adverse effects.28
Use of antipsychotics, ECT
Postpartum psychosis is rare and requires immediate intervention. Treatment with antipsychotics is one of the most effective methods for controlling a psychotic episode. Most women with postpartum psychosis will be too disorganized to consider breast-feeding, but for those who may wish to breast-feed, a discussion with her partner about infant exposure issues is recommended.
Effects of infant exposure through breast milk to the typical antipsychotics (e.g., chlorpromazine, trifluoperazine, haloperidol) include drowsiness, lethargy, and possible developmental delays.13 Nursing infants should be monitored for sedation and other adverse effects during long-term maternal use of these medications.
Evidence on the use of atypical antipsychotics during breast-feeding is limited. One report described cardiomegaly, jaundice, and sedation in one of three infants exposed to olanzapine through breast milk. But the effects could not be attributed directly to breast milk, as that infant was exposed both in utero and during breast-feeding.13
One report of a nursing infant exposed to risperidone indicated no adverse effects,29 and there is no published data on quetiapine use during breast-feeding.
ECT If the patient with psychotic PPD cannot tolerate or does not respond to antipsychotic medication, electroconvulsive therapy (ECT) may be indicated. ECT in the postpartum period is safe for both mother and infant. It is particularly useful when rapid treatment is imperative, such as severe depression with psychotic symptoms, acute mania, and in mothers who are at risk for suicide or infanticide.30
Management guidelines for PPD
Based on our experience and the available evidence, we offer these recommendations to psychiatrists managing patients with PPD:
- During the initial psychiatric assessment, use screening tools such as the EPDS or the PDSS to assist with diagnosis and to identify symptom patterns.
- Next, schedule a conjoint visit with the patient’s partner, family members, and/or social supports. Provide educational materials about PPD and exchange information about treatment options to help the patient make informed decisions. Reading lists, appropriate research articles, lists of local resources, and Web sites can increase awareness about PPD and drive home the importance of compliance with treatment.
- If pharmacotherapy is to be used, discuss honestly and openly the medication’s benefits and potential risks for both mother and infant in the short and long term.
- Outline a treatment plan with the patient and her partner. This should include 6 weeks of treatment during the acute phase, as well as maintenance and long-term therapy.
- If applicable, discuss with the woman and her partner pregnancy planning during pharmacotherapy. In women who experience repeated episodes of depression, discontinuing an antidepressant during pregnancy almost always results in relapse of depressive symptoms.
- Misri S. Shouldn’t I Be Happy? Emotional problems of pregnant and postpartum women. . New York: Free Press, 1995.
- Sichel D, Driscoll JW. Women’s moods: What every woman must know about hormones, the brain, and emotional health. . New York: William Morrow & Co., 1999.
- Depression After Delivery, Inc. www.depressionafterdelivery.com or 1-800-944-4773 (4PPD)
- Postpartum Support International. www.postpartum.net
- Pacific Postpartum Support Society. www.postpartum.org
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Clomipramine • Anafranil
- Desipramine • Norpramin
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Nefazodone • Serzone
- Nortriptyline • Aventyl
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Misri reports that she receives grant/research support from and serves on the speaker’s bureau of GlaxoSmithKline Canada, receives research/grant support from Wyeth-Ayerst Pharmaceuticals, and has lectured for Eli Lilly & Co., AstraZeneca, and Janssen-Ortho.
Ms. Kostaras reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Women face increased vulnerability to the onset of major depression during the childbearing years. Between 12% and 16% of women experience a major depressive episode in the postpartum period.1 Postpartum depression (PPD) can have severe and long-lasting consequences for maternal and infant functioning.2 If left untreated, it can impair maternal-infant bonding and infant attachment and can hinder the child’s cognitive and emotional development.
Based on our experience in caring for women with PPD, this article is intended to help you detect and diagnose PPD more quickly and make appropriate treatment recommendations to family physicians, obstetricians/gynecologists, and other clinicians. We will review the key risk factors for PPD, address screening and diagnostic strategies, and look at the latest evidence on psychosocial and pharmacologic treatment.
Risk factors
Key risk factors, such as a history of PPD or depression, have been identified as predictors of PPD (Table 1).3,4 In the diagnostic criteria for depression, the DSM-IV includes a specifier that states the onset of PPD must occur within 4 weeks after giving birth.5 Our clinical experience, however, indicates that PPD can occur up to 1 year after giving birth. The essential feature of major depressive disorder, according to the DSM-IV, is “a clinical course that is characterized by one or more Major Depressive Episodes” (Table 2).
PPD is often associated with comorbid anxiety disorders, which manifest in many ways. Panic attacks are often the first indication of an existing or impending depression. A small percentage of women will experience intrusive obsessional thoughts of harming their infants.
Andrea Yates, 37, of Harris County, Texas, was convicted of two counts of murder in the June 2001 bathtub drownings of her five children. The jury deliberated less than 4 hours to reach the verdict March 12. The next day, she was sentenced to life in prison. She had pleaded not guilty by reason of insanity.
It is not known why Mrs. Yates discontinued her antipsychotic medication a few weeks prior to this tragedy and why those around her did not heed the numerous warning signs of her mental illness.
Roughly 30% of women with postpartum depression experience thoughts of suicide or infanticide/homicide. Mrs. Yates showed evidence of such thoughts shortly after the birth of her first child, but she did not receive psychiatric care until her third child was born. Although she was hospitalized several times, no follow-up psychiatric care was provided. It was reported that she twice attempted suicide.
During the trial, defense attorneys presented testimony by psychiatrists that Mrs. Yates was suffering postpartum psychosis and schizoaffective disorder. Her severe illness produced the delusional belief that killing the children would save them from eternal damnation. Prosecutors convinced the jury that Mrs. Yates, although ill, was capable of distinguishing right from wrong at the time of the slayings and therefore did not meet the strict Texas standard for insanity.
Mental illness during pregnancy or the postpartum period is poorly understood by new mothers and their families. The verdict and sentence in this case represent an enormous step backward.
The media treatment of Andrea Yates and her imprisonment—rather than hospitalization for proper treatment of her mental illness—may deter mothers from telling their physicians about any negative feelings they may be experiencing. As a result, women who could benefit from treatment of depressive illness will not be identified, and they and their children will be at risk.
Shaila Misri, MD, FRCPC
Xanthoula Kostaras, BSc
Table 1
RISK FACTORS FOR POSTPARTUM DEPRESSION
| Major factors | Contributing factors |
|---|---|
|
|
Screening and diagnosis
Many women will not report depressive symptoms to their primary care physicians or obstetricians during the routine postpartum visit. This reticence by mothers to volunteer any negative information about themselves may be due to the brevity of the typical postpartum visit or its usual focus on the welfare of the infant.
A recent study of 391 outpatients in an obstetrical practice demonstrates the value of using a screening instrument to identify possible PPD cases during the 6-week follow-up visit. When the women were screened with the standardized Edinburgh Postnatal Depression Scale (EPDS), the rate of detection of PPD was 35.4%, whereas the rate of spontaneous detection was 6.3%.6
The EPDS (Box 1), a 10-item self-report questionnaire developed by Cox and colleagues, is used specifically to detect PPD.7 A minimum score of 12 or 13 warrants a diagnosis of PPD. The EPDS can be used as a screening tool at 6 to 8 weeks postpartum and can be repeated over several visits to track symptoms. This tool has been validated, computerized, and translated into more than 12 languages and can be copied and used free of charge.
A new screening tool, the Postpartum Depression Screening Scale (PDSS), was recently developed and validated by Beck and colleagues to help clinicians identify and respond to PPD as early as possible.8 Depressive symptoms are rated on a 5-point scale, and the total score is used to determine overall severity of depressive symptoms. Higher PDSS scores correspond to increasing severity of symptoms and indicate that the patient should be referred for additional evaluation. The PDSS is published by Western Psychological Services (www.wpspublish.com).
Psychosis in PPD
Psychotic depression in the postpartum period is sometimes associated with chronic mood disorders, especially untreated depression. The most prevalent psychotic features include paranoid delusions that incorporate the newborn. Hallucinations are rare. Psychotic depression places the postpartum patient at a heightened risk for suicide and/or infanticide and is considered a medical emergency that requires immediate hospitalization and treatment to ensure the safety of the infant and the ill mother (see “Andrea Yates: Warning signs were ignored,”).
If a patient with psychotic PPD is experiencing delusions centered on harming her infant, a family member or members should assume responsibility for the child’s care, and the patient should not be left alone with the infant. When the mother is hospitalized, visitation between the mother and infant should be restricted, particularly if the infant’s presence precipitates anxiety in the mother. The goal of hospitalization is to achieve symptom remission and stability in the mother so that bonding and attachment can occur. Maternal-infant bonding is difficult, if not impossible, if the mother is out of touch with reality.
Treating mild to moderate PPD
Psychosocial therapies are first-line treatment for mild-to-moderate PPD symptoms or when a patient refuses pharmacotherapy. These therapies include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), group therapy, family and/or marital therapy, supportive psychotherapy, and peer support groups. Psychosocial therapies also should be used as adjunctive treatments to pharmacotherapy.
Table 2
DSM-IV CRITERIA FOR A MAJOR DEPRESSIVE EPISODE
|
CBT. A preliminary study examining short-term cognitive-behavioral counseling for postpartum depressed women reported that participants who received six CBT sessions showed the same degree of improvement in functioning as did a group receiving fluoxetine. Both groups showed greatly improved functioning when compared with a group that received a placebo.9
IPT. In pregnant and postpartum women, the focus of IPT is on role transitions and the acquisition of skills applicable to motherhood. Preliminary studies of IPT in pregnant and postpartum women have shown encouraging results.10 A recent controlled study of 99 women provided additional evidence that IPT helps decrease depressive symptoms and promote social adjustment in women with moderate PPD.11
Group therapy. One of the most valuable benefits of group therapy in PPD treatment is that it may help women who are feeling socially isolated to increase their support networks. Several psychosocial therapy methods may be adapted to a group model, including interpersonal and supportive psychotherapy.
Family and marital therapy. The roles of the partner and family are critical to treating women with mood and anxiety disorders during pregnancy or the postpartum period. A recent study found that postpartum depressed women recover more rapidly and appreciate their partners’ contribution to the relationship more when the partner is supportive.12
Supportive psychotherapy involves offering patients and their families support, reassurance, and psychoeducation. This type of therapy is used to augment other psychosocial interventions and/or pharmacotherapy. In some cases, supportive therapy may be the only treatment a woman receives if her depressive symptoms are too severe for her to engage in CBT or IPT and she refuses pharmacotherapy. Then supportive psychotherapy is used to monitor her mental state.
Peer-support groups. Several groups formed by consumers and health care providers offer support and education to women with reproductive-associated mood and anxiety disorders. (See “Related resources,”).
Pharmacologic treatment
Pharmacotherapy is indicated in women with moderate-to-severe symptoms who do not respond to psychosocial treatment alone. Because all psychotropic medications are excreted in breast milk and passed on to the nursing infant, one must weigh the potential risks of the infant’s exposure to medication against the risks of untreated maternal depression.
Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) are used most commonly to treat PPD. Monoamine oxidase inhibitors (MAOIs) are not recommended as they have been reported to exacerbate hypertension, and their extensive interaction profiles with food and other medications can complicate treatment. Further, only limited evidence is available on the effects of MAOIs during pregnancy and the postpartum period.
- Ask the mother to underline the response that comes closest to how she has been feeling in the previous 7 days.
- All 10 items must be completed.
- Avoid the possibility of the mother discussing her answers with others.
- The mother should complete the scale herself, unless she has limited English or difficulty with reading.
- The EPDS may be used at 6 to 8 weeks postnatal. A visit to the child health clinic, a postnatal check-up, or a home visit may provide suitable opportunities for its completion.
As you have recently had a baby, we would like to know how you are feeling. Please CHECK the answer that comes closest to how you have felt IN THE PAST 7 DAYS, not just how you feel today.
- I have been able to laugh and see the funny side of things.
- I have looked forward with enjoyment to things.
- * I have blamed myself unnecessarily when things went wrong.
- I have been anxious or worried for no good reason.
- * I have felt scared or panicky without a good reason.
- * Things have been getting on top of me.
- * I have been so unhappy that I have had difficulty sleeping.
- * I have felt sad or miserable.
- * I have been so unhappy that I have been crying.
- * The thought of harming myself has occurred to me.
Responses to statements 1, 2, and 4 are scored 0, 1, 2, and 3 according to increasing severity of symptoms, and statements marked with an asterisk (*) are reverse-scored (3, 2, 1, and 0). Total score is calculated by adding the scores of all 10 items. A score of 12 or 13 has been found to identify most women with a diagnosis of PPD.
Adapted from Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-6.
Table 3
SSRI DRUG THERAPY FOR POSTPARTUM DEPRESSION
| Medication | Starting daily dosage (mg) | Maximum daily dosage (mg) | Precautions |
|---|---|---|---|
| Fluoxetine | 10 | 80 | Very long half-life of active metabolite may lead to accumulation in infants Inform parents of possible side effects, and include a pediatrician in routine clinical evaluations of the infant |
| Sertraline | 25 | 300 | Benign neonatal sleep myoclonus has been documented in one case of sertraline exposure during breast-feeding Inform parents of possible side effects, and include a pediatrician in routine clinical evaluations of the infant |
| Paroxetine | 10 | 60 | No adverse effects have been reported |
| Fluvoxamine | 50 | 300 | Data limited |
| Citalopram | 10 | 60 | Data limited |
Use of SSRIs
The literature on use of SSRIs in lactating women has expanded rapidly in recent years (Table 3). But because these agents have been on the market a relatively short time, the long-term developmental effects of infants’ exposure to SSRIs through breast milk have yet to be evaluated. Fluoxetineis the SSRI with the most published data on use by breast-feeding women. To date, nine studies have reported the outcomes of a total of 57 infants exposed to fluoxetine during breast feeding.13,14 Norfluoxetine, the potent metabolite of fluoxetine, has a long half-life that may predispose to accumulation in the serum of nursing infants.
Adverse effects such as colic, fussiness, crying, seizure activity, and reduced weight gain have been reported in two cases.15,16 The remaining studies on the use of fluoxetine by breast-feeding women have reported low drug levels in both mothers and infants, and no other adverse effects have been documented.
Sertraline. To date, seven published reports of sertraline exposure have documented 46 infant outcomes. In all of these reports, sertraline and its weak metabolite have been detected in low or trace amounts in the sera of nursing infants.13,14,17-19 A recent study of 19 breast-feeding mother-infant pairs found that platelet serotonin uptake in these infants was unaltered, despite the detection of low serum levels of sertraline and its metabolite.19
Paroxetine. Paroxetine is also excreted into the breast milk of lactating women, although—unlike the other SSRI medications—the agent does not have an active metabolite that could potentially accumulate in the serum of nursing infants. Five reports totaling 60 infant outcomes have been published regarding paroxetine exposure during breast feeding. Low or undetectable serum levels were reported in all of the infants, and no adverse effects were noted.13,14,20
Fluvoxamine, citalopram. Two small case studies of fluvoxamine have each reported very low drug levels in breast milk and no adverse events in the exposed infants.21,22 Only three case studies examining five infants exposed to citalopram during breast feeding have been published.13 As information is limited regarding the effects of these medications on nursing infants, caution is advised when prescribing either agent to breast-feeding women.
Use of TCAs and other antidepressants
TCAs are useful for treating PPD when SSRIs have failed or the patient has shown a previous good response to TCAs. All TCAs are excreted into breast milk in low concentrations, and a wide range of infant serum levels have been reported.
No adverse effects have been documented for infant exposure to amitriptyline, clomipramine, desipramine, imipramine, or nortriptyline.13,14,23,24 The active metabolite of doxepin has the longest half-life (37 hours) among the TCAs and may be potentially hazardous to nursing infants because of high serum accumulations. Because two reports have associated doxepin exposure with respiratory distress, poor sucking, drowsiness, and vomiting in infants, the use of medications with a shorter half-life and better-documented effects in infants is recommended.13
Limited evidence is available on the use of newer antidepressants such as bupropion, trazodone, and nefazodone by breast-feeding women.25-27 When possible, therefore, such patients should be prescribed an antidepressant with more documented use in breast-feeding mothers.
Venlafaxine is a newer antidepressant that inhibits reuptake of both serotonin and norepinephrine. The only case report published to date regarding venlafaxine levels in nursing infants found high drug levels in the sera of three exposed infants but no adverse effects.28
Use of antipsychotics, ECT
Postpartum psychosis is rare and requires immediate intervention. Treatment with antipsychotics is one of the most effective methods for controlling a psychotic episode. Most women with postpartum psychosis will be too disorganized to consider breast-feeding, but for those who may wish to breast-feed, a discussion with her partner about infant exposure issues is recommended.
Effects of infant exposure through breast milk to the typical antipsychotics (e.g., chlorpromazine, trifluoperazine, haloperidol) include drowsiness, lethargy, and possible developmental delays.13 Nursing infants should be monitored for sedation and other adverse effects during long-term maternal use of these medications.
Evidence on the use of atypical antipsychotics during breast-feeding is limited. One report described cardiomegaly, jaundice, and sedation in one of three infants exposed to olanzapine through breast milk. But the effects could not be attributed directly to breast milk, as that infant was exposed both in utero and during breast-feeding.13
One report of a nursing infant exposed to risperidone indicated no adverse effects,29 and there is no published data on quetiapine use during breast-feeding.
ECT If the patient with psychotic PPD cannot tolerate or does not respond to antipsychotic medication, electroconvulsive therapy (ECT) may be indicated. ECT in the postpartum period is safe for both mother and infant. It is particularly useful when rapid treatment is imperative, such as severe depression with psychotic symptoms, acute mania, and in mothers who are at risk for suicide or infanticide.30
Management guidelines for PPD
Based on our experience and the available evidence, we offer these recommendations to psychiatrists managing patients with PPD:
- During the initial psychiatric assessment, use screening tools such as the EPDS or the PDSS to assist with diagnosis and to identify symptom patterns.
- Next, schedule a conjoint visit with the patient’s partner, family members, and/or social supports. Provide educational materials about PPD and exchange information about treatment options to help the patient make informed decisions. Reading lists, appropriate research articles, lists of local resources, and Web sites can increase awareness about PPD and drive home the importance of compliance with treatment.
- If pharmacotherapy is to be used, discuss honestly and openly the medication’s benefits and potential risks for both mother and infant in the short and long term.
- Outline a treatment plan with the patient and her partner. This should include 6 weeks of treatment during the acute phase, as well as maintenance and long-term therapy.
- If applicable, discuss with the woman and her partner pregnancy planning during pharmacotherapy. In women who experience repeated episodes of depression, discontinuing an antidepressant during pregnancy almost always results in relapse of depressive symptoms.
- Misri S. Shouldn’t I Be Happy? Emotional problems of pregnant and postpartum women. . New York: Free Press, 1995.
- Sichel D, Driscoll JW. Women’s moods: What every woman must know about hormones, the brain, and emotional health. . New York: William Morrow & Co., 1999.
- Depression After Delivery, Inc. www.depressionafterdelivery.com or 1-800-944-4773 (4PPD)
- Postpartum Support International. www.postpartum.net
- Pacific Postpartum Support Society. www.postpartum.org
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Clomipramine • Anafranil
- Desipramine • Norpramin
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Nefazodone • Serzone
- Nortriptyline • Aventyl
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
Dr. Misri reports that she receives grant/research support from and serves on the speaker’s bureau of GlaxoSmithKline Canada, receives research/grant support from Wyeth-Ayerst Pharmaceuticals, and has lectured for Eli Lilly & Co., AstraZeneca, and Janssen-Ortho.
Ms. Kostaras reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. O’Hara MW, Swain AM. Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry 1996;8:37-54.
2. Weinberg MK, Tronick EZ. The impact of maternal psychiatric illness on infant development. J Clin Psychiatry 1998;59(suppl 2):53-61.
3. O’Hara MW. Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry 1986;43:569-73.
4. Beck CT. Predictors of postpartum depression: an update. Nursing Res 2001;50(5):275-85.
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text revision. Washington, DC, American Psychiatric Association, 2000.
6. Evins GG, Theofrastous JP, Galvin SL. Postpartum depression: a comparison of screening and routine clinical evaluation. Am J Obstet Gynecol 2000;182(5):1080-2.
7. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10 –item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6.
8. Beck CT, Gable RK. Further validation of the postpartum depression screening scale. Nursing Res 2001;50(3):155-64.
9. Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive-behavioural counselling in the treatment of postnatal depression. BMJ 1997;314(7085):932-6.
10. Stuart S, O’Hara MW. Interpersonal psychotherapy for postpartum depression: a treatment program. J Psychother Pract Res 1995;4:18-29.
11. O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 2000;57(11):1039-45.
12. Misri S, Kostaras X, Fox D, Kostaras D. The impact of partner support in the treatment of postpartum depression. Can J Psychiatry 2000;45(6):554-8.
13. Burt VK, Suri R, Altshuler L, et al. The use of psychotropic medications during breast-feeding. Am J Psychiatry 2001;158(7):1001-9.
14. Birnbaum CS, Cohen LS, et al. Serum concentrations of antidepressants and benzodiazepines in nursing infants: a case series (electronic article). Pediatrics 1999;104(1):www.pediatrics.org/cgi/content/full/104/1/e11
15. Lester BM, Cucca J, Andreozzi L, et al. Possible association between fluoxetine hydrochloride and colic in an infant. J Am Acad Child Adolesc Psychiatry 1993;32(6):1253-5.
16. Chambers CD, Anderson PO, Thomas RG, et al. Weight gain in infants breastfed by mothers who take fluoxetine (electronic article). Pediatrics 1999;104(5):http://www.pediatrics.org/cgi/content/full/104/5/e61
17. Epperson CN, Anderson GM, McDougle CJ. Sertraline and breast feeding (letter). N Engl J Med 1997;336(16):1189-90.
18. Wisner KL, Perel JM, Blumer J. Serum sertraline and n-desmethylsertraline levels in breast-feeding mother-infant pairs. Am J Psychiatry 1998;155(5):690-2.
19. Epperson N, Czarkowski KA, Ward-O’Brien D, et al. Maternal sertraline treatment and serotonin transport in breast-feeding mother-infant pairs. Am J Psychiatry 2001;158(10):1631-7.
20. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61(11):828-32.
21. Wright S, Dawling S, Ashford JJ. Excretion of fluvoxamine in breast milk (letter). Br J Clin Pharmacol 1991;31:209.-
22. Piontek CM, Wisner KL, Perel JM, Peindl KS. Serum fluvoxamine levels in breastfed infants. J Clin Psychiatry 2001;62(2):111-3.
23. Wisner KL, Perel JM, Foglia JP. Serum clomipramine and metabolite levels in four nursing mother-infant pairs. J Clin Psychiatry 1995;56(1):17-20.
24. Altshuler LL, Burt VK, McMullen M, Hendrick V. Breastfeeding and sertraline: a 24-hour analysis. J Clin Psychiatry 1995;56(6):243-5.
25. Briggs GG, Samson JH, Ambrose PJ, Schroeder DH. Excretion of bupropion in breast milk. Ann Pharmacother 1993;27(4):431-3.
26. Verbeeck RK, Ross SG, McKenna EA. Excretion of trazodone in breast milk. Br J Clin Pharmacol 1986;22:367-70.
27. Yapp P, Ilett KF, Kristensen JH, et al. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34(11):1269-72.
28. Illett KF, Hackett LP, Dusci LJ, et al. Distribution and excretion of venlafaxine and O-desmethylvenlafaxine in human milk. Br J Clin Pharmacol 1998;45:459-62.
29. Hill RC, McIvor RJ, Wojnar-Horton RE, et al. Risperidone distribution and excretion in human milk: case report and estimated infant exposure during breast-feeding (letter). J Clin Psychopharmacol 2000;20(2):285-6.
30. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiat 1994;45:444-50.
1. O’Hara MW, Swain AM. Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry 1996;8:37-54.
2. Weinberg MK, Tronick EZ. The impact of maternal psychiatric illness on infant development. J Clin Psychiatry 1998;59(suppl 2):53-61.
3. O’Hara MW. Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry 1986;43:569-73.
4. Beck CT. Predictors of postpartum depression: an update. Nursing Res 2001;50(5):275-85.
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text revision. Washington, DC, American Psychiatric Association, 2000.
6. Evins GG, Theofrastous JP, Galvin SL. Postpartum depression: a comparison of screening and routine clinical evaluation. Am J Obstet Gynecol 2000;182(5):1080-2.
7. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10 –item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6.
8. Beck CT, Gable RK. Further validation of the postpartum depression screening scale. Nursing Res 2001;50(3):155-64.
9. Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive-behavioural counselling in the treatment of postnatal depression. BMJ 1997;314(7085):932-6.
10. Stuart S, O’Hara MW. Interpersonal psychotherapy for postpartum depression: a treatment program. J Psychother Pract Res 1995;4:18-29.
11. O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 2000;57(11):1039-45.
12. Misri S, Kostaras X, Fox D, Kostaras D. The impact of partner support in the treatment of postpartum depression. Can J Psychiatry 2000;45(6):554-8.
13. Burt VK, Suri R, Altshuler L, et al. The use of psychotropic medications during breast-feeding. Am J Psychiatry 2001;158(7):1001-9.
14. Birnbaum CS, Cohen LS, et al. Serum concentrations of antidepressants and benzodiazepines in nursing infants: a case series (electronic article). Pediatrics 1999;104(1):www.pediatrics.org/cgi/content/full/104/1/e11
15. Lester BM, Cucca J, Andreozzi L, et al. Possible association between fluoxetine hydrochloride and colic in an infant. J Am Acad Child Adolesc Psychiatry 1993;32(6):1253-5.
16. Chambers CD, Anderson PO, Thomas RG, et al. Weight gain in infants breastfed by mothers who take fluoxetine (electronic article). Pediatrics 1999;104(5):http://www.pediatrics.org/cgi/content/full/104/5/e61
17. Epperson CN, Anderson GM, McDougle CJ. Sertraline and breast feeding (letter). N Engl J Med 1997;336(16):1189-90.
18. Wisner KL, Perel JM, Blumer J. Serum sertraline and n-desmethylsertraline levels in breast-feeding mother-infant pairs. Am J Psychiatry 1998;155(5):690-2.
19. Epperson N, Czarkowski KA, Ward-O’Brien D, et al. Maternal sertraline treatment and serotonin transport in breast-feeding mother-infant pairs. Am J Psychiatry 2001;158(10):1631-7.
20. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61(11):828-32.
21. Wright S, Dawling S, Ashford JJ. Excretion of fluvoxamine in breast milk (letter). Br J Clin Pharmacol 1991;31:209.-
22. Piontek CM, Wisner KL, Perel JM, Peindl KS. Serum fluvoxamine levels in breastfed infants. J Clin Psychiatry 2001;62(2):111-3.
23. Wisner KL, Perel JM, Foglia JP. Serum clomipramine and metabolite levels in four nursing mother-infant pairs. J Clin Psychiatry 1995;56(1):17-20.
24. Altshuler LL, Burt VK, McMullen M, Hendrick V. Breastfeeding and sertraline: a 24-hour analysis. J Clin Psychiatry 1995;56(6):243-5.
25. Briggs GG, Samson JH, Ambrose PJ, Schroeder DH. Excretion of bupropion in breast milk. Ann Pharmacother 1993;27(4):431-3.
26. Verbeeck RK, Ross SG, McKenna EA. Excretion of trazodone in breast milk. Br J Clin Pharmacol 1986;22:367-70.
27. Yapp P, Ilett KF, Kristensen JH, et al. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34(11):1269-72.
28. Illett KF, Hackett LP, Dusci LJ, et al. Distribution and excretion of venlafaxine and O-desmethylvenlafaxine in human milk. Br J Clin Pharmacol 1998;45:459-62.
29. Hill RC, McIvor RJ, Wojnar-Horton RE, et al. Risperidone distribution and excretion in human milk: case report and estimated infant exposure during breast-feeding (letter). J Clin Psychopharmacol 2000;20(2):285-6.
30. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiat 1994;45:444-50.