User login
Pediatric hospitalist certification beset by gender bias concerns
Are women unfairly penalized?
More than 1,625 pediatricians have applied to take the first pediatric hospitalist certification exam in November 2019, and approximately 93% of them have been accepted, according to a statement from the American Board of Pediatrics.
It was the rejection of the 7%, however, that set off a firestorm on the electronic discussion board for American Academy of Pediatrics (AAP) hospital medicine this summer, and led to a petition to the board to revise its eligibility requirements, ensure that the requirements are fair to women, and bring transparency to its decision process. The petition has more than 1,400 signatures.
Seattle Children’s Hospital and Yale New Haven (Conn.) Children’s Hospital have both said they will not consider board certification in hiring decisions until the situation is resolved.
The American Board of Pediatrics (ABP) declined an interview request pending its formal response to the Aug. 6 petition, but in a statement to this news organization, executive vice president Suzanne Woods, MD, said, “The percentage of women and men meeting the eligibility requirements for the exam did not differ. We stress this point because a concern about possible gender bias appears to have been the principal reason for this ... petition, and we wanted to offer immediate reassurance that no unintended bias has occurred.”
“We are carefully considering the requests and will release detailed data to hospitalists on the AAP’s [pediatric hospital medicine (PHM) electronic discussion board] ... and on the ABP’s website. We are conferring with ABP PHM subboard members as well as leaders from our volunteer community. We expect to provide a thoughtful response within the next 3 weeks,” Dr. Woods said in the Aug. 15 statement.
“Case-by-case” exceptions
The backstory is that, for better or worse depending on who you talk to, pediatric hospital medicine is becoming a board certified subspecialty. A fellowship will be required to sit for the exam after a few years, which is standard for subspecialties.
What’s generated concern is how the board is grandfathering current pediatric hospitalists into certification via a “practice pathway” until the fellowship requirement takes hold after 2023.
To qualify for the November test, hospitalists had to complete 4 years of full-time practice by June 30, 2019, which has been understood to mean 48 months of continual employment. At least 50% of that time had to be devoted to “professional activities ... related to the care of hospitalized children,” and at least 25% of that “devoted to direct patient care.” Assuming about 2,000 work hours per year, it translated to “450-500 hours” of direct patient care “per year over the most recent four years” to sit for the test, the board said.
“For individuals who have interrupted practice during the most recent four years for family leave or other such circumstances, an exception may be considered if there is substantial prior experience in pediatric hospital medicine. ... Such exceptions are made at the discretion of the ABP and will be considered on a case-by-case basis.” Specific criteria for exceptions were not spelled out.
In the end, there were more than a few surprises when denial letters went out in recent months, and scores of appeals have been filed. There’s “a lot of tension and a lot of confusion” about why some people with practice gaps during the 4 years were approved, but others were denied. There’s been “a lack of transparency on the ABP’s part,” said H. Barrett Fromme, MD, section chief of pediatric hospital medicine and a professor of pediatrics at the University of Chicago.
“The standard has to be reasonable”
There are concerns about the availability of fellowship slots and other issues, but the 4-year rule – instead of averaging clinical hours over 4 or 5 years, for instance – is the main sticking point. It’s a gender issue because “women take maternity; women move with their spouse; women take care of elders; women tend to be in these roles that require time off” more than men do, Dr. Fromme said.
Until the board releases its data, the gender breakdown of the denials and the degree to which practice gaps due to such issues led to them is unknown. There’s concern that women have been unfairly penalized.
The storm was set off on the discussion board this summer by stories from physicians such as Chandani DeZure, MD, a pediatric hospitalist currently working in the neonatal ICU at Stanford (Calif.) University. She was denied a seat at the table in November, appealed, and was denied again.
She was a full-time pediatric hospitalist at Children’s National Medical Center in Washington, from 2014, when she graduated residency, until Oct. 2018, when her husband, also a doctor, was offered a promising research position in California, and “we decided to take it,” Dr. DeZure said.
They moved to California with their young son in November. Dr. DeZure got her California medical license in 6 weeks, was hired by Stanford in January, and started her new postion in mid-April.
Because of the move, she worked only 3.5 years in the board’s 4 year practice window, but, as is common with young physicians, that time was spent in direct patient care, for a total of over 6,000 hours.
“How is that not good enough? How is a person that worked 500 hours with patients for 4 years” – for a total of 2,000 hours – “better qualified than someone who worked 100% for 3 and a half years? Nobody is saying there shouldn’t be a standard, but the standard has to be reasonable,” Dr. DeZure said.
“Illegal regardless of intent”
It’s situations like Dr. DeZure’s that led to the petition. One of demands is that ABP “revise the practice pathway criteria to be more inclusive of applicants with interrupted practice and varied clinical experience, to include clear-cut parameters rather than considering these applications on a closed-door ‘case-by-case basis...at the discretion of the ABP.’ ” Also, the petition asks the board to “clarify the appeals process and improve responsiveness to appeals and inquiries regarding denials.”
As ABP noted in its statement, however, the major demand is that the board “facilitate a timely analysis to determine if gender bias is present.” The petition noted that signers “do not suspect intentional bias on the part of the ABP; however, if gender bias is present it is unethical and potentially illegal regardless of intent.”
For now, the perception is that the board has “a hard 48-month rule” with not many exceptions; there are people who are “very concerned that, ‘Oh my gosh, I can’t have children for 4 years because I won’t be able to sit for the boards.’ No one should ever have to have that in their head,” Dr. Fromme said. At this point, it seems that 3 months off for maternity is being grandfathered in, but perhaps not 6 months for a second child; no one knows for sure.
Dr. DeZure, meanwhile, continues to study for the board exam, just in case.
Looking back over the past year, she said “I could have somehow picked up one shift a week moonlighting that would have kept me eligible, but the [board] didn’t respond to me” when contacted about her situation during the California move.
“The other option was for me was to live cross country from my husband with a small child,” she said.
Are women unfairly penalized?
Are women unfairly penalized?
More than 1,625 pediatricians have applied to take the first pediatric hospitalist certification exam in November 2019, and approximately 93% of them have been accepted, according to a statement from the American Board of Pediatrics.
It was the rejection of the 7%, however, that set off a firestorm on the electronic discussion board for American Academy of Pediatrics (AAP) hospital medicine this summer, and led to a petition to the board to revise its eligibility requirements, ensure that the requirements are fair to women, and bring transparency to its decision process. The petition has more than 1,400 signatures.
Seattle Children’s Hospital and Yale New Haven (Conn.) Children’s Hospital have both said they will not consider board certification in hiring decisions until the situation is resolved.
The American Board of Pediatrics (ABP) declined an interview request pending its formal response to the Aug. 6 petition, but in a statement to this news organization, executive vice president Suzanne Woods, MD, said, “The percentage of women and men meeting the eligibility requirements for the exam did not differ. We stress this point because a concern about possible gender bias appears to have been the principal reason for this ... petition, and we wanted to offer immediate reassurance that no unintended bias has occurred.”
“We are carefully considering the requests and will release detailed data to hospitalists on the AAP’s [pediatric hospital medicine (PHM) electronic discussion board] ... and on the ABP’s website. We are conferring with ABP PHM subboard members as well as leaders from our volunteer community. We expect to provide a thoughtful response within the next 3 weeks,” Dr. Woods said in the Aug. 15 statement.
“Case-by-case” exceptions
The backstory is that, for better or worse depending on who you talk to, pediatric hospital medicine is becoming a board certified subspecialty. A fellowship will be required to sit for the exam after a few years, which is standard for subspecialties.
What’s generated concern is how the board is grandfathering current pediatric hospitalists into certification via a “practice pathway” until the fellowship requirement takes hold after 2023.
To qualify for the November test, hospitalists had to complete 4 years of full-time practice by June 30, 2019, which has been understood to mean 48 months of continual employment. At least 50% of that time had to be devoted to “professional activities ... related to the care of hospitalized children,” and at least 25% of that “devoted to direct patient care.” Assuming about 2,000 work hours per year, it translated to “450-500 hours” of direct patient care “per year over the most recent four years” to sit for the test, the board said.
“For individuals who have interrupted practice during the most recent four years for family leave or other such circumstances, an exception may be considered if there is substantial prior experience in pediatric hospital medicine. ... Such exceptions are made at the discretion of the ABP and will be considered on a case-by-case basis.” Specific criteria for exceptions were not spelled out.
In the end, there were more than a few surprises when denial letters went out in recent months, and scores of appeals have been filed. There’s “a lot of tension and a lot of confusion” about why some people with practice gaps during the 4 years were approved, but others were denied. There’s been “a lack of transparency on the ABP’s part,” said H. Barrett Fromme, MD, section chief of pediatric hospital medicine and a professor of pediatrics at the University of Chicago.
“The standard has to be reasonable”
There are concerns about the availability of fellowship slots and other issues, but the 4-year rule – instead of averaging clinical hours over 4 or 5 years, for instance – is the main sticking point. It’s a gender issue because “women take maternity; women move with their spouse; women take care of elders; women tend to be in these roles that require time off” more than men do, Dr. Fromme said.
Until the board releases its data, the gender breakdown of the denials and the degree to which practice gaps due to such issues led to them is unknown. There’s concern that women have been unfairly penalized.
The storm was set off on the discussion board this summer by stories from physicians such as Chandani DeZure, MD, a pediatric hospitalist currently working in the neonatal ICU at Stanford (Calif.) University. She was denied a seat at the table in November, appealed, and was denied again.
She was a full-time pediatric hospitalist at Children’s National Medical Center in Washington, from 2014, when she graduated residency, until Oct. 2018, when her husband, also a doctor, was offered a promising research position in California, and “we decided to take it,” Dr. DeZure said.
They moved to California with their young son in November. Dr. DeZure got her California medical license in 6 weeks, was hired by Stanford in January, and started her new postion in mid-April.
Because of the move, she worked only 3.5 years in the board’s 4 year practice window, but, as is common with young physicians, that time was spent in direct patient care, for a total of over 6,000 hours.
“How is that not good enough? How is a person that worked 500 hours with patients for 4 years” – for a total of 2,000 hours – “better qualified than someone who worked 100% for 3 and a half years? Nobody is saying there shouldn’t be a standard, but the standard has to be reasonable,” Dr. DeZure said.
“Illegal regardless of intent”
It’s situations like Dr. DeZure’s that led to the petition. One of demands is that ABP “revise the practice pathway criteria to be more inclusive of applicants with interrupted practice and varied clinical experience, to include clear-cut parameters rather than considering these applications on a closed-door ‘case-by-case basis...at the discretion of the ABP.’ ” Also, the petition asks the board to “clarify the appeals process and improve responsiveness to appeals and inquiries regarding denials.”
As ABP noted in its statement, however, the major demand is that the board “facilitate a timely analysis to determine if gender bias is present.” The petition noted that signers “do not suspect intentional bias on the part of the ABP; however, if gender bias is present it is unethical and potentially illegal regardless of intent.”
For now, the perception is that the board has “a hard 48-month rule” with not many exceptions; there are people who are “very concerned that, ‘Oh my gosh, I can’t have children for 4 years because I won’t be able to sit for the boards.’ No one should ever have to have that in their head,” Dr. Fromme said. At this point, it seems that 3 months off for maternity is being grandfathered in, but perhaps not 6 months for a second child; no one knows for sure.
Dr. DeZure, meanwhile, continues to study for the board exam, just in case.
Looking back over the past year, she said “I could have somehow picked up one shift a week moonlighting that would have kept me eligible, but the [board] didn’t respond to me” when contacted about her situation during the California move.
“The other option was for me was to live cross country from my husband with a small child,” she said.
More than 1,625 pediatricians have applied to take the first pediatric hospitalist certification exam in November 2019, and approximately 93% of them have been accepted, according to a statement from the American Board of Pediatrics.
It was the rejection of the 7%, however, that set off a firestorm on the electronic discussion board for American Academy of Pediatrics (AAP) hospital medicine this summer, and led to a petition to the board to revise its eligibility requirements, ensure that the requirements are fair to women, and bring transparency to its decision process. The petition has more than 1,400 signatures.
Seattle Children’s Hospital and Yale New Haven (Conn.) Children’s Hospital have both said they will not consider board certification in hiring decisions until the situation is resolved.
The American Board of Pediatrics (ABP) declined an interview request pending its formal response to the Aug. 6 petition, but in a statement to this news organization, executive vice president Suzanne Woods, MD, said, “The percentage of women and men meeting the eligibility requirements for the exam did not differ. We stress this point because a concern about possible gender bias appears to have been the principal reason for this ... petition, and we wanted to offer immediate reassurance that no unintended bias has occurred.”
“We are carefully considering the requests and will release detailed data to hospitalists on the AAP’s [pediatric hospital medicine (PHM) electronic discussion board] ... and on the ABP’s website. We are conferring with ABP PHM subboard members as well as leaders from our volunteer community. We expect to provide a thoughtful response within the next 3 weeks,” Dr. Woods said in the Aug. 15 statement.
“Case-by-case” exceptions
The backstory is that, for better or worse depending on who you talk to, pediatric hospital medicine is becoming a board certified subspecialty. A fellowship will be required to sit for the exam after a few years, which is standard for subspecialties.
What’s generated concern is how the board is grandfathering current pediatric hospitalists into certification via a “practice pathway” until the fellowship requirement takes hold after 2023.
To qualify for the November test, hospitalists had to complete 4 years of full-time practice by June 30, 2019, which has been understood to mean 48 months of continual employment. At least 50% of that time had to be devoted to “professional activities ... related to the care of hospitalized children,” and at least 25% of that “devoted to direct patient care.” Assuming about 2,000 work hours per year, it translated to “450-500 hours” of direct patient care “per year over the most recent four years” to sit for the test, the board said.
“For individuals who have interrupted practice during the most recent four years for family leave or other such circumstances, an exception may be considered if there is substantial prior experience in pediatric hospital medicine. ... Such exceptions are made at the discretion of the ABP and will be considered on a case-by-case basis.” Specific criteria for exceptions were not spelled out.
In the end, there were more than a few surprises when denial letters went out in recent months, and scores of appeals have been filed. There’s “a lot of tension and a lot of confusion” about why some people with practice gaps during the 4 years were approved, but others were denied. There’s been “a lack of transparency on the ABP’s part,” said H. Barrett Fromme, MD, section chief of pediatric hospital medicine and a professor of pediatrics at the University of Chicago.
“The standard has to be reasonable”
There are concerns about the availability of fellowship slots and other issues, but the 4-year rule – instead of averaging clinical hours over 4 or 5 years, for instance – is the main sticking point. It’s a gender issue because “women take maternity; women move with their spouse; women take care of elders; women tend to be in these roles that require time off” more than men do, Dr. Fromme said.
Until the board releases its data, the gender breakdown of the denials and the degree to which practice gaps due to such issues led to them is unknown. There’s concern that women have been unfairly penalized.
The storm was set off on the discussion board this summer by stories from physicians such as Chandani DeZure, MD, a pediatric hospitalist currently working in the neonatal ICU at Stanford (Calif.) University. She was denied a seat at the table in November, appealed, and was denied again.
She was a full-time pediatric hospitalist at Children’s National Medical Center in Washington, from 2014, when she graduated residency, until Oct. 2018, when her husband, also a doctor, was offered a promising research position in California, and “we decided to take it,” Dr. DeZure said.
They moved to California with their young son in November. Dr. DeZure got her California medical license in 6 weeks, was hired by Stanford in January, and started her new postion in mid-April.
Because of the move, she worked only 3.5 years in the board’s 4 year practice window, but, as is common with young physicians, that time was spent in direct patient care, for a total of over 6,000 hours.
“How is that not good enough? How is a person that worked 500 hours with patients for 4 years” – for a total of 2,000 hours – “better qualified than someone who worked 100% for 3 and a half years? Nobody is saying there shouldn’t be a standard, but the standard has to be reasonable,” Dr. DeZure said.
“Illegal regardless of intent”
It’s situations like Dr. DeZure’s that led to the petition. One of demands is that ABP “revise the practice pathway criteria to be more inclusive of applicants with interrupted practice and varied clinical experience, to include clear-cut parameters rather than considering these applications on a closed-door ‘case-by-case basis...at the discretion of the ABP.’ ” Also, the petition asks the board to “clarify the appeals process and improve responsiveness to appeals and inquiries regarding denials.”
As ABP noted in its statement, however, the major demand is that the board “facilitate a timely analysis to determine if gender bias is present.” The petition noted that signers “do not suspect intentional bias on the part of the ABP; however, if gender bias is present it is unethical and potentially illegal regardless of intent.”
For now, the perception is that the board has “a hard 48-month rule” with not many exceptions; there are people who are “very concerned that, ‘Oh my gosh, I can’t have children for 4 years because I won’t be able to sit for the boards.’ No one should ever have to have that in their head,” Dr. Fromme said. At this point, it seems that 3 months off for maternity is being grandfathered in, but perhaps not 6 months for a second child; no one knows for sure.
Dr. DeZure, meanwhile, continues to study for the board exam, just in case.
Looking back over the past year, she said “I could have somehow picked up one shift a week moonlighting that would have kept me eligible, but the [board] didn’t respond to me” when contacted about her situation during the California move.
“The other option was for me was to live cross country from my husband with a small child,” she said.
Treating children with Kawasaki disease and coronary enlargement
IVIG plus steroids or infliximab, or IVIG alone?
Clinical question
Does use of corticosteroids or infliximab in addition to intravenous immunoglobulin improve cardiac outcomes in children with Kawasaki disease and enlarged coronary arteries?
Background
Kawasaki disease is a medium-vessel vasculitis primarily of young children. While the underlying cause remains unknown, treatment with intravenous immunoglobulin (IVIG) substantially lowers the risk of coronary artery aneurysms (CAA), the most serious sequelae of Kawasaki disease. Recent studies have suggested that – in cases of high-risk or treatment-resistant Kawasaki disease – using an immunomodulator, such as a corticosteroid or a TNF-alpha blocker, may improve outcomes, though these studies involved relatively small and homogeneous patient populations. It is unknown if these medications could prevent progression of CAA.
Study design
Retrospective multicenter study.
Setting
Two freestanding children’s hospitals and one mother-child hospital.
Synopsis
The study identified 121 children diagnosed with Kawasaki disease with CAA (z score 2.5-10) from 2008 through 2017 treated at the three study hospitals. Children with giant CAA at the time of diagnosis (z score greater than 10) or significant preexisting congenital heart disease were excluded.
All study hospitals had protocols for treatment of Kawasaki disease: Center 1 used IVIG and corticosteroids, Center 2 used IVIG and infliximab, and Center 3 used IVIG alone. Patients at all centers also received aspirin. Center 1 used methylprednisolone IV initially, changing to oral prednisolone after clinical improvement. The researchers reviewed the charts of each patient and classified them as having complete or incomplete Kawasaki disease. They assigned z scores for CAA size based on both initial and follow-up echocardiograms. The primary outcome was change in z score of CAA over the first year.
The population of patients treated at each center was significantly different. Center 1 reported older patients (median age 2.6 vs. 2.0 and 1.1), as well as a higher rate of male patients (83% vs. 77% and 58%). However, there was no difference in baseline z scores between centers. Patients who initially received IVIG and corticosteroids were less likely to require additional therapy because of persistent fever versus those receiving IVIG only, or IVIG and infliximab (0% vs. 21% vs. 14%, P = .03).
Patients receiving IVIG and corticosteroids, or IVIG and infliximab, were less likely to have progression of CAA size, with 23% and 24% having an increase in z score of more than 1 versus 58% of those who received IVIG alone. No group had significant differences in maximum z score, the rate of giant aneurysms, or the rate of regression of CAA.
Bottom line
Using IVIG + corticosteroids or IVIG + infliximab versus IVIG alone for children with Kawasaki disease with coronary artery aneurysms decreases the rate of aneurysm enlargement.
Citation
Dionne A et al. Treatment intensification in patients with Kawasaki disease and coronary aneurysm at diagnosis. Pediatrics. May 2019:e20183341. doi: 10.1542/peds.2018-3341.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
IVIG plus steroids or infliximab, or IVIG alone?
IVIG plus steroids or infliximab, or IVIG alone?
Clinical question
Does use of corticosteroids or infliximab in addition to intravenous immunoglobulin improve cardiac outcomes in children with Kawasaki disease and enlarged coronary arteries?
Background
Kawasaki disease is a medium-vessel vasculitis primarily of young children. While the underlying cause remains unknown, treatment with intravenous immunoglobulin (IVIG) substantially lowers the risk of coronary artery aneurysms (CAA), the most serious sequelae of Kawasaki disease. Recent studies have suggested that – in cases of high-risk or treatment-resistant Kawasaki disease – using an immunomodulator, such as a corticosteroid or a TNF-alpha blocker, may improve outcomes, though these studies involved relatively small and homogeneous patient populations. It is unknown if these medications could prevent progression of CAA.
Study design
Retrospective multicenter study.
Setting
Two freestanding children’s hospitals and one mother-child hospital.
Synopsis
The study identified 121 children diagnosed with Kawasaki disease with CAA (z score 2.5-10) from 2008 through 2017 treated at the three study hospitals. Children with giant CAA at the time of diagnosis (z score greater than 10) or significant preexisting congenital heart disease were excluded.
All study hospitals had protocols for treatment of Kawasaki disease: Center 1 used IVIG and corticosteroids, Center 2 used IVIG and infliximab, and Center 3 used IVIG alone. Patients at all centers also received aspirin. Center 1 used methylprednisolone IV initially, changing to oral prednisolone after clinical improvement. The researchers reviewed the charts of each patient and classified them as having complete or incomplete Kawasaki disease. They assigned z scores for CAA size based on both initial and follow-up echocardiograms. The primary outcome was change in z score of CAA over the first year.
The population of patients treated at each center was significantly different. Center 1 reported older patients (median age 2.6 vs. 2.0 and 1.1), as well as a higher rate of male patients (83% vs. 77% and 58%). However, there was no difference in baseline z scores between centers. Patients who initially received IVIG and corticosteroids were less likely to require additional therapy because of persistent fever versus those receiving IVIG only, or IVIG and infliximab (0% vs. 21% vs. 14%, P = .03).
Patients receiving IVIG and corticosteroids, or IVIG and infliximab, were less likely to have progression of CAA size, with 23% and 24% having an increase in z score of more than 1 versus 58% of those who received IVIG alone. No group had significant differences in maximum z score, the rate of giant aneurysms, or the rate of regression of CAA.
Bottom line
Using IVIG + corticosteroids or IVIG + infliximab versus IVIG alone for children with Kawasaki disease with coronary artery aneurysms decreases the rate of aneurysm enlargement.
Citation
Dionne A et al. Treatment intensification in patients with Kawasaki disease and coronary aneurysm at diagnosis. Pediatrics. May 2019:e20183341. doi: 10.1542/peds.2018-3341.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
Clinical question
Does use of corticosteroids or infliximab in addition to intravenous immunoglobulin improve cardiac outcomes in children with Kawasaki disease and enlarged coronary arteries?
Background
Kawasaki disease is a medium-vessel vasculitis primarily of young children. While the underlying cause remains unknown, treatment with intravenous immunoglobulin (IVIG) substantially lowers the risk of coronary artery aneurysms (CAA), the most serious sequelae of Kawasaki disease. Recent studies have suggested that – in cases of high-risk or treatment-resistant Kawasaki disease – using an immunomodulator, such as a corticosteroid or a TNF-alpha blocker, may improve outcomes, though these studies involved relatively small and homogeneous patient populations. It is unknown if these medications could prevent progression of CAA.
Study design
Retrospective multicenter study.
Setting
Two freestanding children’s hospitals and one mother-child hospital.
Synopsis
The study identified 121 children diagnosed with Kawasaki disease with CAA (z score 2.5-10) from 2008 through 2017 treated at the three study hospitals. Children with giant CAA at the time of diagnosis (z score greater than 10) or significant preexisting congenital heart disease were excluded.
All study hospitals had protocols for treatment of Kawasaki disease: Center 1 used IVIG and corticosteroids, Center 2 used IVIG and infliximab, and Center 3 used IVIG alone. Patients at all centers also received aspirin. Center 1 used methylprednisolone IV initially, changing to oral prednisolone after clinical improvement. The researchers reviewed the charts of each patient and classified them as having complete or incomplete Kawasaki disease. They assigned z scores for CAA size based on both initial and follow-up echocardiograms. The primary outcome was change in z score of CAA over the first year.
The population of patients treated at each center was significantly different. Center 1 reported older patients (median age 2.6 vs. 2.0 and 1.1), as well as a higher rate of male patients (83% vs. 77% and 58%). However, there was no difference in baseline z scores between centers. Patients who initially received IVIG and corticosteroids were less likely to require additional therapy because of persistent fever versus those receiving IVIG only, or IVIG and infliximab (0% vs. 21% vs. 14%, P = .03).
Patients receiving IVIG and corticosteroids, or IVIG and infliximab, were less likely to have progression of CAA size, with 23% and 24% having an increase in z score of more than 1 versus 58% of those who received IVIG alone. No group had significant differences in maximum z score, the rate of giant aneurysms, or the rate of regression of CAA.
Bottom line
Using IVIG + corticosteroids or IVIG + infliximab versus IVIG alone for children with Kawasaki disease with coronary artery aneurysms decreases the rate of aneurysm enlargement.
Citation
Dionne A et al. Treatment intensification in patients with Kawasaki disease and coronary aneurysm at diagnosis. Pediatrics. May 2019:e20183341. doi: 10.1542/peds.2018-3341.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
Obtain proper reimbursements with more effective documentation and coding
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
Am I still a hospitalist?
HM as a force for change
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.
HM as a force for change
HM as a force for change
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.
To be, or not to be ... on backup?
A staffing backup system is essential
It was late 2011. We were a practice of around 20 physicians, and just starting to integrate advanced practice providers into our practice. Our average daily census was about 100 patients and slightly more than 50% of our services were resident services.
My boss, colleague, friend, and mentor – Charles “Chuck” Sargent, MD, and I were on service together early one Saturday morning; Chuck gets a phone call that one of our colleagues was ill. With just 10 physicians working and 10 off, it was an ordeal for Chuck to call all 10 colleagues. Unlike most times, no one could come to moonlight that day. In the end Chuck and I took care of our colleague’s patients.
Yes, it was an exhausting few days, but illness and family needs do not come announced. Now, close to a decade later, we are a practice of 70 physicians and 16 advanced practice providers, our average daily census is about 270 patients, and we have two backup physicians every day – known as Jeopardy-1 and Jeopardy-2. Paternity leave, maternity leave, minor illness, minor trauma, surgery, and family needs are common for our practice. We considered it a good year when we utilized our Jeopardy-1 and Jeopardy-2 for 10% and 1% respectively; and for the past year with a lot of needs, we employed Jeopardy-1 and Jeopardy-2 for 25% and 10%, respectively.
A staffing backup system is a necessary tool for almost every practice. Not having a formal backup system doesn’t mean you don’t need one or you don’t have one – it is just called “no formal backup system.” The Society of Hospital Medicine’s State of Hospital Medicine Reports (SoHM) have been providing data about staffing backup systems every other year. Backup systems come in three flavors. The first system is no formal backup, which means the leaders of the program scramble for coverage every time there is a need. The second is a voluntary backup system in which clinicians volunteer to be on a backup schedule, and the third is a mandatory system in which all or most clinicians are required to be on the backup schedule.
The cumulative data reported in the 2014, 2016, and 2018 SoHM for hospital medicine groups serving adults only, children only, and both adults and children (weighted for number of groups reporting), suggests that 48.3% of respondent practices had no formal backup system, 31.7% had a voluntary system, and 20% had a mandatory backup system.
When we look at different populations served, the trend of “no formal backup system” responses is in decline. The 2014, 2016, and 2018 SoHM reports for hospital medicine groups serving adults, children, and both adults and children, reinforce such trends. The SoHM 2018 report shows 65.6% of hospital medicine groups serving children, 41.6% of groups serving adults, and only 25% of groups serving both adults and children have “no formal backup system.” Our medicine-pediatrics colleagues seem to be leading the trend and have already deduced that, for a solid practice, a backup system is a necessity.
It is also important to see the trend of “no formal backup system” based on geographic area, employer type, academic status, or total number of full-time employees. As we would have predicted, the larger the group the more likely they are to have a backup system. For academic practices a similar trend was seen; they had a higher percentage of some type of backup system year after year.
When it comes to compensation for backup work, four patterns were explored by the SoHM over the years. The most common type of arrangement was “no additional compensation for being on the backup schedule, but additional compensation was provided when called into work.” This kind of arrangement would be easiest to negotiate when the hospitalist and the employer sit across a table. There is nothing at risk for the employer when there isn’t a need, or when there is a need to fill a shift.
The least common method was “additional compensation for being on the backup schedule, but no additional compensation if called into work.” From employers’ perspectives, this is an extra expense and is not ideal for the hospitalist either. In the middle of the pack were “no additional compensation associated with the backup plan” (the second most common model), while the third most common model was “additional compensation for being on the backup schedule, as well as additional compensation if called into work.”
Once you have seen one hospital medicine practice, you have seen one hospital medicine practice. There are different needs for every group, and the backup system – as well its compensation model – has to be designed for it. Thankfully, the SoHM reports reveal the patterns and trends so that we don’t have to reinvent the wheel. For our practice, we decreased a week of clinical service for 2 weeks a year of backup. Every time we activate our backup system, the person coming in receives extra compensation or a similar shift off. In the long run, our backup system didn’t kill us, but rather made us stronger as a group.
Dr. Chadha is interim division chief in the division of hospital medicine at the University of Kentucky HealthCare in Lexington. He actively leads efforts of recruiting, scheduling, practice analysis, and operation of the group. He is a first-time member of the SHM Practice Analysis Committee. Ms. Babb is administrative support associate in the division of hospital medicine at University of Kentucky HealthCare.
A staffing backup system is essential
A staffing backup system is essential
It was late 2011. We were a practice of around 20 physicians, and just starting to integrate advanced practice providers into our practice. Our average daily census was about 100 patients and slightly more than 50% of our services were resident services.
My boss, colleague, friend, and mentor – Charles “Chuck” Sargent, MD, and I were on service together early one Saturday morning; Chuck gets a phone call that one of our colleagues was ill. With just 10 physicians working and 10 off, it was an ordeal for Chuck to call all 10 colleagues. Unlike most times, no one could come to moonlight that day. In the end Chuck and I took care of our colleague’s patients.
Yes, it was an exhausting few days, but illness and family needs do not come announced. Now, close to a decade later, we are a practice of 70 physicians and 16 advanced practice providers, our average daily census is about 270 patients, and we have two backup physicians every day – known as Jeopardy-1 and Jeopardy-2. Paternity leave, maternity leave, minor illness, minor trauma, surgery, and family needs are common for our practice. We considered it a good year when we utilized our Jeopardy-1 and Jeopardy-2 for 10% and 1% respectively; and for the past year with a lot of needs, we employed Jeopardy-1 and Jeopardy-2 for 25% and 10%, respectively.
A staffing backup system is a necessary tool for almost every practice. Not having a formal backup system doesn’t mean you don’t need one or you don’t have one – it is just called “no formal backup system.” The Society of Hospital Medicine’s State of Hospital Medicine Reports (SoHM) have been providing data about staffing backup systems every other year. Backup systems come in three flavors. The first system is no formal backup, which means the leaders of the program scramble for coverage every time there is a need. The second is a voluntary backup system in which clinicians volunteer to be on a backup schedule, and the third is a mandatory system in which all or most clinicians are required to be on the backup schedule.
The cumulative data reported in the 2014, 2016, and 2018 SoHM for hospital medicine groups serving adults only, children only, and both adults and children (weighted for number of groups reporting), suggests that 48.3% of respondent practices had no formal backup system, 31.7% had a voluntary system, and 20% had a mandatory backup system.
When we look at different populations served, the trend of “no formal backup system” responses is in decline. The 2014, 2016, and 2018 SoHM reports for hospital medicine groups serving adults, children, and both adults and children, reinforce such trends. The SoHM 2018 report shows 65.6% of hospital medicine groups serving children, 41.6% of groups serving adults, and only 25% of groups serving both adults and children have “no formal backup system.” Our medicine-pediatrics colleagues seem to be leading the trend and have already deduced that, for a solid practice, a backup system is a necessity.
It is also important to see the trend of “no formal backup system” based on geographic area, employer type, academic status, or total number of full-time employees. As we would have predicted, the larger the group the more likely they are to have a backup system. For academic practices a similar trend was seen; they had a higher percentage of some type of backup system year after year.
When it comes to compensation for backup work, four patterns were explored by the SoHM over the years. The most common type of arrangement was “no additional compensation for being on the backup schedule, but additional compensation was provided when called into work.” This kind of arrangement would be easiest to negotiate when the hospitalist and the employer sit across a table. There is nothing at risk for the employer when there isn’t a need, or when there is a need to fill a shift.
The least common method was “additional compensation for being on the backup schedule, but no additional compensation if called into work.” From employers’ perspectives, this is an extra expense and is not ideal for the hospitalist either. In the middle of the pack were “no additional compensation associated with the backup plan” (the second most common model), while the third most common model was “additional compensation for being on the backup schedule, as well as additional compensation if called into work.”
Once you have seen one hospital medicine practice, you have seen one hospital medicine practice. There are different needs for every group, and the backup system – as well its compensation model – has to be designed for it. Thankfully, the SoHM reports reveal the patterns and trends so that we don’t have to reinvent the wheel. For our practice, we decreased a week of clinical service for 2 weeks a year of backup. Every time we activate our backup system, the person coming in receives extra compensation or a similar shift off. In the long run, our backup system didn’t kill us, but rather made us stronger as a group.
Dr. Chadha is interim division chief in the division of hospital medicine at the University of Kentucky HealthCare in Lexington. He actively leads efforts of recruiting, scheduling, practice analysis, and operation of the group. He is a first-time member of the SHM Practice Analysis Committee. Ms. Babb is administrative support associate in the division of hospital medicine at University of Kentucky HealthCare.
It was late 2011. We were a practice of around 20 physicians, and just starting to integrate advanced practice providers into our practice. Our average daily census was about 100 patients and slightly more than 50% of our services were resident services.
My boss, colleague, friend, and mentor – Charles “Chuck” Sargent, MD, and I were on service together early one Saturday morning; Chuck gets a phone call that one of our colleagues was ill. With just 10 physicians working and 10 off, it was an ordeal for Chuck to call all 10 colleagues. Unlike most times, no one could come to moonlight that day. In the end Chuck and I took care of our colleague’s patients.
Yes, it was an exhausting few days, but illness and family needs do not come announced. Now, close to a decade later, we are a practice of 70 physicians and 16 advanced practice providers, our average daily census is about 270 patients, and we have two backup physicians every day – known as Jeopardy-1 and Jeopardy-2. Paternity leave, maternity leave, minor illness, minor trauma, surgery, and family needs are common for our practice. We considered it a good year when we utilized our Jeopardy-1 and Jeopardy-2 for 10% and 1% respectively; and for the past year with a lot of needs, we employed Jeopardy-1 and Jeopardy-2 for 25% and 10%, respectively.
A staffing backup system is a necessary tool for almost every practice. Not having a formal backup system doesn’t mean you don’t need one or you don’t have one – it is just called “no formal backup system.” The Society of Hospital Medicine’s State of Hospital Medicine Reports (SoHM) have been providing data about staffing backup systems every other year. Backup systems come in three flavors. The first system is no formal backup, which means the leaders of the program scramble for coverage every time there is a need. The second is a voluntary backup system in which clinicians volunteer to be on a backup schedule, and the third is a mandatory system in which all or most clinicians are required to be on the backup schedule.
The cumulative data reported in the 2014, 2016, and 2018 SoHM for hospital medicine groups serving adults only, children only, and both adults and children (weighted for number of groups reporting), suggests that 48.3% of respondent practices had no formal backup system, 31.7% had a voluntary system, and 20% had a mandatory backup system.
When we look at different populations served, the trend of “no formal backup system” responses is in decline. The 2014, 2016, and 2018 SoHM reports for hospital medicine groups serving adults, children, and both adults and children, reinforce such trends. The SoHM 2018 report shows 65.6% of hospital medicine groups serving children, 41.6% of groups serving adults, and only 25% of groups serving both adults and children have “no formal backup system.” Our medicine-pediatrics colleagues seem to be leading the trend and have already deduced that, for a solid practice, a backup system is a necessity.
It is also important to see the trend of “no formal backup system” based on geographic area, employer type, academic status, or total number of full-time employees. As we would have predicted, the larger the group the more likely they are to have a backup system. For academic practices a similar trend was seen; they had a higher percentage of some type of backup system year after year.
When it comes to compensation for backup work, four patterns were explored by the SoHM over the years. The most common type of arrangement was “no additional compensation for being on the backup schedule, but additional compensation was provided when called into work.” This kind of arrangement would be easiest to negotiate when the hospitalist and the employer sit across a table. There is nothing at risk for the employer when there isn’t a need, or when there is a need to fill a shift.
The least common method was “additional compensation for being on the backup schedule, but no additional compensation if called into work.” From employers’ perspectives, this is an extra expense and is not ideal for the hospitalist either. In the middle of the pack were “no additional compensation associated with the backup plan” (the second most common model), while the third most common model was “additional compensation for being on the backup schedule, as well as additional compensation if called into work.”
Once you have seen one hospital medicine practice, you have seen one hospital medicine practice. There are different needs for every group, and the backup system – as well its compensation model – has to be designed for it. Thankfully, the SoHM reports reveal the patterns and trends so that we don’t have to reinvent the wheel. For our practice, we decreased a week of clinical service for 2 weeks a year of backup. Every time we activate our backup system, the person coming in receives extra compensation or a similar shift off. In the long run, our backup system didn’t kill us, but rather made us stronger as a group.
Dr. Chadha is interim division chief in the division of hospital medicine at the University of Kentucky HealthCare in Lexington. He actively leads efforts of recruiting, scheduling, practice analysis, and operation of the group. He is a first-time member of the SHM Practice Analysis Committee. Ms. Babb is administrative support associate in the division of hospital medicine at University of Kentucky HealthCare.
Social determinants of health gaining prominence
Fragmented, essentializing, simplistic. That’s how students at Perelman School of Medicine at the University of Pennsylvania, Philadelphia, described their required course on cultural competence. Lectures and discussions about cultural groups and communication issues weren’t providing them with the skills they needed to navigate doctor-patient relationships.
Their criticism was a wake-up call that Horace Delisser, MD, associate dean for diversity and inclusion at the school, took to heart. He enlisted medical students to help reinvent the curriculum. The result, Introduction to Medicine and Society, launched in 2013 and described in an article published in 2017 (Acad Med. 2017;92[3]:335-43), emphasizes self-awareness and reflection about one’s own biases and the adoption of a less hierarchical and more respectful “other-oriented” approach to the patient relationship.
The course examines social determinants of health (SDHs) – the influences of society, government, culture, and health systems. Students analyze how health and health outcomes are affected by a patient’s income, education, and living and working conditions, as well as access to healthy food, safe water, and transportation.
A host of policy makers, advisory groups, and organized medicine groups have called in recent years for educational efforts to boost all physicians’ working knowledge of health inequities and SDHs.
Dr. Delisser, associate professor of medicine who also practices as a pulmonologist at the Harron Lung Center in the Perelman Center for Advanced Medicine, said SDHs play into daily care.
Consider the patient who is chronically late for appointments. “It may not be an issue of the patient being disinterested in their health care, but maybe the public transportation system is unreliable, or maybe the patient has to take two buses and a subway to get there. I need [this knowledge] to inform my care and to engage my patient. I need to know, ‘what does it take for you to get here?’ That factors into how I [make the care plan],” said Dr. Delisser.
Malika Fair, MD, MPH, who teaches a longitudinal professional development class at George Washington University, Washington, and is senior director of health equity partnerships and programs at the American Association of Medical Colleges, provided the example of how her medical students intervened during their rotation in the emergency department on behalf of a newly-diagnosed patient with diabetes who had been unable to fill a prescribed medication. After determining where the patient lived, the students ensured that she had transportation and was able to get the needed medication at a local grocery store. They asked about her barriers to healthy eating, researched local grocery stores, and made practical recommendations that the patient was amenable to implementing. They identified a clinic closer to the patient’s home, and worked with her on making an appointment at a time when she could take off from work.
“Because of their training, these students were able to identify and address social risks in their first month on the ward,” said Dr. Fair, who also practices emergency medicine. They had learned about how to ask about food access and how safe it was for the patient to walk and exercise in her neighborhood.
At Perelman, most students work in student-led community clinics, and some fourth-year students participate in an elective rotation as apprentices to community health workers, learning to address SDHs and develop the cultural humility that they learned about in the classroom. The rotation was similarly created in 2013 and is described in a 2018 article (J Health Care Poor Underserved. 2018;29[2]:581-90).“Being a good physician involves being technically competent as well as what I call relationally competent,” Dr. Delisser said. “And [this involves] being aware that my relationship with a patient doesn’t exist in a vacuum ... that there’s a bigger, broader social and structural context that I need to know and understand. I [then need] to use that to inform how I mediate and empower that relationship.”
Aletha Maybank, MD, who became the American Medical Association’s first chief health equity officer earlier this year, explained that “the medical profession had a very strong social context at one point in time,” but this was dampened by the Flexner Report of 1910.*
The report revolutionized medical education by increasing its rigor, but “it was really focused on clinical and basic science and took out the social context, the context of what medicine is about,” said Dr. Maybank, a pediatrician with a board certification in preventive medicine/public health. “[Now] we’re asking, how do we revolutionize medical education again at this point in time, recognizing the confluence of information and data that we now have available to us about inequities and disparities ... and the sense of urgency from students.”
Students driving practice change
Students nationally are “the most important” drivers of the increasing focus on SDHs in medical education, according to Dr. Fair. “They are demanding experiences to learn about the entire patient. We know that only 20% of a patient’s health is dependent on their health care. Our students are demanding education about the other 80%.”
More and more, communities are identifying needs and “students will then come up with initiatives to meet those needs,” Dr. Fair said.
Others interviewed for this story predicted this trend will only intensify, since not-for-profit hospitals are required under the Affordable Care Act regulations to assess community health needs every few years and to intervene accordingly.
Education on health care systems is also advancing. Penn State University, for instance, utilized a million-dollar grant from the AMA’s Accelerating Change in Medical Education initiative to design and implement a 4-year curriculum on the health system sciences that started in 2014. The curriculum includes an immersive experience in patient navigation.
“Students were taught to be patient navigators, and they were assigned within the clinical context to work on issues like, why are [patients] having trouble getting their medications?” said Susan E. Skochelak, MD, MPH, who leads the 6-year-old Accelerating Change initiative as vice president for medical education at the AMA.
From the start, she noted, students at Penn State are encouraged to question inequities, social and structural barriers to health, and faults in the health care system. “The message given at their white coat ceremony is ‘Welcome to medicine. Now that you’re here, you’re a member of the health care team, and we want you to speak up if you think there are things that need to be addressed. We want you to tell us when the system is working and not working,’ ” said Dr Skochelak, who previously served as the senior associate dean for academic affairs at the University of Wisconsin School of Medicine and Public Health, where she had been a tenured professor of family medicine.
Tomorrow’s physician partners
Approximately 80% of medical school graduates who participated in the AAMC’s 2018 survey of graduates said they had received significant training on health disparities—up from 71% in 2014.
“There’s a huge amount [of innovation] happening, but on the flip side, there’s not really a set of accepted tools and practices, and certainly no robust evaluation [of the training],” said Philip M. Alberti, PhD, senior director for health equity research and policy at the American Association of Medical Colleges. A recently published review (J Gen Intern Med. 2019;34[5]:720-30) shows growing interest in the teaching of SDHs in undergraduate medical education but variable content, strategies, and instructional practices.
Health care systems and practicing physicians are still very much feeling their way with SDHs. Screening tools are being developed and tested, and academic medical centers are trying to determine their roles in addressing issues such as transportation and housing – and what funding and structural levers can be pulled to fulfill these roles. “As we learn more about [these issues], it will become clearer what the right baseline set of competencies might be for all physicians,” Dr. Alberti noted.
In the meantime, some basic expectations for medical education are taking root officially. The National Board of Medical Examiners, with whom the AMA has partnered in its Accelerating Change initiative, has included questions in the United States Medical Licensing Examination on population health and SDHs, and plans to add more exam content on these topics and on health systems science, said Dr. Skochelak.
And through its site visit program (the Clinical Learning Environment Review program), the Accreditation Council for Graduate Medical Education has “made it pretty clear that there’s an expectation that residents and fellows are learning about the health system’s approach to identifying and addressing health care disparities – and that they’re given opportunities to develop quality improvement initiatives that target those disparities,” Dr. Alberti said.
In hopes of achieving consistency across medical specialties and in national accreditation and board certifications exams, the American Association of Medical Colleges is developing its first set of competencies in quality improvement and patient safety, with health equity being one of these competencies’ domains .
The competencies are tiered for medical school graduates, residency graduates, and faculty physicians who are 3-5 years post residency. At this point in time, said Dr. Alberti, the consensus among medical educators has been that physicians “need to be able to understand and consider [social, economic, and structural] contexts when they’re seeing patients, when they’re developing care plans, when they’re talking with caregivers, and when they’re looking at their own quality data.”
Elisabeth Poorman, MD, MPH, an internist at UW Medicine in Kent, Washington, said she worries that the passion of medical students for SDHs will too often be crushed, especially during residency and with immersion in the productivity-focused health care system. Studies show a drop in mental wellness and empathy and a rise in cynicism as training advances, said Dr. Poorman, who also writes about health care and issues of equity and serves on the editorial advisory board of Internal Medicine News.
With similar concerns, the AMA has recently launched a “Reimagining Residency” initiative that aims to improve transitions from medical school to residency and the wellness of residents and faculty, and expand educational content relating to SDHs.
Dr. Fair is optimistic that new physicians’ knowledge of SDHs will permeate medical practices.
“Physicians who are out practicing are going to be working with our graduates, and they’re going to be asking in [job] interviews, do you have flexible hours for patients? What community partnerships do you have? Are there other professionals on staff to help us address social determinants of health? What data [relating to SDHs] are you collecting?” she said.
Correction, 8/26/2019: An earlier version of this story misstated the title of Aletha Maybank, MD. Dr. Maybank's correct title is the first chief health equity officer of the American Medical Association.
Fragmented, essentializing, simplistic. That’s how students at Perelman School of Medicine at the University of Pennsylvania, Philadelphia, described their required course on cultural competence. Lectures and discussions about cultural groups and communication issues weren’t providing them with the skills they needed to navigate doctor-patient relationships.
Their criticism was a wake-up call that Horace Delisser, MD, associate dean for diversity and inclusion at the school, took to heart. He enlisted medical students to help reinvent the curriculum. The result, Introduction to Medicine and Society, launched in 2013 and described in an article published in 2017 (Acad Med. 2017;92[3]:335-43), emphasizes self-awareness and reflection about one’s own biases and the adoption of a less hierarchical and more respectful “other-oriented” approach to the patient relationship.
The course examines social determinants of health (SDHs) – the influences of society, government, culture, and health systems. Students analyze how health and health outcomes are affected by a patient’s income, education, and living and working conditions, as well as access to healthy food, safe water, and transportation.
A host of policy makers, advisory groups, and organized medicine groups have called in recent years for educational efforts to boost all physicians’ working knowledge of health inequities and SDHs.
Dr. Delisser, associate professor of medicine who also practices as a pulmonologist at the Harron Lung Center in the Perelman Center for Advanced Medicine, said SDHs play into daily care.
Consider the patient who is chronically late for appointments. “It may not be an issue of the patient being disinterested in their health care, but maybe the public transportation system is unreliable, or maybe the patient has to take two buses and a subway to get there. I need [this knowledge] to inform my care and to engage my patient. I need to know, ‘what does it take for you to get here?’ That factors into how I [make the care plan],” said Dr. Delisser.
Malika Fair, MD, MPH, who teaches a longitudinal professional development class at George Washington University, Washington, and is senior director of health equity partnerships and programs at the American Association of Medical Colleges, provided the example of how her medical students intervened during their rotation in the emergency department on behalf of a newly-diagnosed patient with diabetes who had been unable to fill a prescribed medication. After determining where the patient lived, the students ensured that she had transportation and was able to get the needed medication at a local grocery store. They asked about her barriers to healthy eating, researched local grocery stores, and made practical recommendations that the patient was amenable to implementing. They identified a clinic closer to the patient’s home, and worked with her on making an appointment at a time when she could take off from work.
“Because of their training, these students were able to identify and address social risks in their first month on the ward,” said Dr. Fair, who also practices emergency medicine. They had learned about how to ask about food access and how safe it was for the patient to walk and exercise in her neighborhood.
At Perelman, most students work in student-led community clinics, and some fourth-year students participate in an elective rotation as apprentices to community health workers, learning to address SDHs and develop the cultural humility that they learned about in the classroom. The rotation was similarly created in 2013 and is described in a 2018 article (J Health Care Poor Underserved. 2018;29[2]:581-90).“Being a good physician involves being technically competent as well as what I call relationally competent,” Dr. Delisser said. “And [this involves] being aware that my relationship with a patient doesn’t exist in a vacuum ... that there’s a bigger, broader social and structural context that I need to know and understand. I [then need] to use that to inform how I mediate and empower that relationship.”
Aletha Maybank, MD, who became the American Medical Association’s first chief health equity officer earlier this year, explained that “the medical profession had a very strong social context at one point in time,” but this was dampened by the Flexner Report of 1910.*
The report revolutionized medical education by increasing its rigor, but “it was really focused on clinical and basic science and took out the social context, the context of what medicine is about,” said Dr. Maybank, a pediatrician with a board certification in preventive medicine/public health. “[Now] we’re asking, how do we revolutionize medical education again at this point in time, recognizing the confluence of information and data that we now have available to us about inequities and disparities ... and the sense of urgency from students.”
Students driving practice change
Students nationally are “the most important” drivers of the increasing focus on SDHs in medical education, according to Dr. Fair. “They are demanding experiences to learn about the entire patient. We know that only 20% of a patient’s health is dependent on their health care. Our students are demanding education about the other 80%.”
More and more, communities are identifying needs and “students will then come up with initiatives to meet those needs,” Dr. Fair said.
Others interviewed for this story predicted this trend will only intensify, since not-for-profit hospitals are required under the Affordable Care Act regulations to assess community health needs every few years and to intervene accordingly.
Education on health care systems is also advancing. Penn State University, for instance, utilized a million-dollar grant from the AMA’s Accelerating Change in Medical Education initiative to design and implement a 4-year curriculum on the health system sciences that started in 2014. The curriculum includes an immersive experience in patient navigation.
“Students were taught to be patient navigators, and they were assigned within the clinical context to work on issues like, why are [patients] having trouble getting their medications?” said Susan E. Skochelak, MD, MPH, who leads the 6-year-old Accelerating Change initiative as vice president for medical education at the AMA.
From the start, she noted, students at Penn State are encouraged to question inequities, social and structural barriers to health, and faults in the health care system. “The message given at their white coat ceremony is ‘Welcome to medicine. Now that you’re here, you’re a member of the health care team, and we want you to speak up if you think there are things that need to be addressed. We want you to tell us when the system is working and not working,’ ” said Dr Skochelak, who previously served as the senior associate dean for academic affairs at the University of Wisconsin School of Medicine and Public Health, where she had been a tenured professor of family medicine.
Tomorrow’s physician partners
Approximately 80% of medical school graduates who participated in the AAMC’s 2018 survey of graduates said they had received significant training on health disparities—up from 71% in 2014.
“There’s a huge amount [of innovation] happening, but on the flip side, there’s not really a set of accepted tools and practices, and certainly no robust evaluation [of the training],” said Philip M. Alberti, PhD, senior director for health equity research and policy at the American Association of Medical Colleges. A recently published review (J Gen Intern Med. 2019;34[5]:720-30) shows growing interest in the teaching of SDHs in undergraduate medical education but variable content, strategies, and instructional practices.
Health care systems and practicing physicians are still very much feeling their way with SDHs. Screening tools are being developed and tested, and academic medical centers are trying to determine their roles in addressing issues such as transportation and housing – and what funding and structural levers can be pulled to fulfill these roles. “As we learn more about [these issues], it will become clearer what the right baseline set of competencies might be for all physicians,” Dr. Alberti noted.
In the meantime, some basic expectations for medical education are taking root officially. The National Board of Medical Examiners, with whom the AMA has partnered in its Accelerating Change initiative, has included questions in the United States Medical Licensing Examination on population health and SDHs, and plans to add more exam content on these topics and on health systems science, said Dr. Skochelak.
And through its site visit program (the Clinical Learning Environment Review program), the Accreditation Council for Graduate Medical Education has “made it pretty clear that there’s an expectation that residents and fellows are learning about the health system’s approach to identifying and addressing health care disparities – and that they’re given opportunities to develop quality improvement initiatives that target those disparities,” Dr. Alberti said.
In hopes of achieving consistency across medical specialties and in national accreditation and board certifications exams, the American Association of Medical Colleges is developing its first set of competencies in quality improvement and patient safety, with health equity being one of these competencies’ domains .
The competencies are tiered for medical school graduates, residency graduates, and faculty physicians who are 3-5 years post residency. At this point in time, said Dr. Alberti, the consensus among medical educators has been that physicians “need to be able to understand and consider [social, economic, and structural] contexts when they’re seeing patients, when they’re developing care plans, when they’re talking with caregivers, and when they’re looking at their own quality data.”
Elisabeth Poorman, MD, MPH, an internist at UW Medicine in Kent, Washington, said she worries that the passion of medical students for SDHs will too often be crushed, especially during residency and with immersion in the productivity-focused health care system. Studies show a drop in mental wellness and empathy and a rise in cynicism as training advances, said Dr. Poorman, who also writes about health care and issues of equity and serves on the editorial advisory board of Internal Medicine News.
With similar concerns, the AMA has recently launched a “Reimagining Residency” initiative that aims to improve transitions from medical school to residency and the wellness of residents and faculty, and expand educational content relating to SDHs.
Dr. Fair is optimistic that new physicians’ knowledge of SDHs will permeate medical practices.
“Physicians who are out practicing are going to be working with our graduates, and they’re going to be asking in [job] interviews, do you have flexible hours for patients? What community partnerships do you have? Are there other professionals on staff to help us address social determinants of health? What data [relating to SDHs] are you collecting?” she said.
Correction, 8/26/2019: An earlier version of this story misstated the title of Aletha Maybank, MD. Dr. Maybank's correct title is the first chief health equity officer of the American Medical Association.
Fragmented, essentializing, simplistic. That’s how students at Perelman School of Medicine at the University of Pennsylvania, Philadelphia, described their required course on cultural competence. Lectures and discussions about cultural groups and communication issues weren’t providing them with the skills they needed to navigate doctor-patient relationships.
Their criticism was a wake-up call that Horace Delisser, MD, associate dean for diversity and inclusion at the school, took to heart. He enlisted medical students to help reinvent the curriculum. The result, Introduction to Medicine and Society, launched in 2013 and described in an article published in 2017 (Acad Med. 2017;92[3]:335-43), emphasizes self-awareness and reflection about one’s own biases and the adoption of a less hierarchical and more respectful “other-oriented” approach to the patient relationship.
The course examines social determinants of health (SDHs) – the influences of society, government, culture, and health systems. Students analyze how health and health outcomes are affected by a patient’s income, education, and living and working conditions, as well as access to healthy food, safe water, and transportation.
A host of policy makers, advisory groups, and organized medicine groups have called in recent years for educational efforts to boost all physicians’ working knowledge of health inequities and SDHs.
Dr. Delisser, associate professor of medicine who also practices as a pulmonologist at the Harron Lung Center in the Perelman Center for Advanced Medicine, said SDHs play into daily care.
Consider the patient who is chronically late for appointments. “It may not be an issue of the patient being disinterested in their health care, but maybe the public transportation system is unreliable, or maybe the patient has to take two buses and a subway to get there. I need [this knowledge] to inform my care and to engage my patient. I need to know, ‘what does it take for you to get here?’ That factors into how I [make the care plan],” said Dr. Delisser.
Malika Fair, MD, MPH, who teaches a longitudinal professional development class at George Washington University, Washington, and is senior director of health equity partnerships and programs at the American Association of Medical Colleges, provided the example of how her medical students intervened during their rotation in the emergency department on behalf of a newly-diagnosed patient with diabetes who had been unable to fill a prescribed medication. After determining where the patient lived, the students ensured that she had transportation and was able to get the needed medication at a local grocery store. They asked about her barriers to healthy eating, researched local grocery stores, and made practical recommendations that the patient was amenable to implementing. They identified a clinic closer to the patient’s home, and worked with her on making an appointment at a time when she could take off from work.
“Because of their training, these students were able to identify and address social risks in their first month on the ward,” said Dr. Fair, who also practices emergency medicine. They had learned about how to ask about food access and how safe it was for the patient to walk and exercise in her neighborhood.
At Perelman, most students work in student-led community clinics, and some fourth-year students participate in an elective rotation as apprentices to community health workers, learning to address SDHs and develop the cultural humility that they learned about in the classroom. The rotation was similarly created in 2013 and is described in a 2018 article (J Health Care Poor Underserved. 2018;29[2]:581-90).“Being a good physician involves being technically competent as well as what I call relationally competent,” Dr. Delisser said. “And [this involves] being aware that my relationship with a patient doesn’t exist in a vacuum ... that there’s a bigger, broader social and structural context that I need to know and understand. I [then need] to use that to inform how I mediate and empower that relationship.”
Aletha Maybank, MD, who became the American Medical Association’s first chief health equity officer earlier this year, explained that “the medical profession had a very strong social context at one point in time,” but this was dampened by the Flexner Report of 1910.*
The report revolutionized medical education by increasing its rigor, but “it was really focused on clinical and basic science and took out the social context, the context of what medicine is about,” said Dr. Maybank, a pediatrician with a board certification in preventive medicine/public health. “[Now] we’re asking, how do we revolutionize medical education again at this point in time, recognizing the confluence of information and data that we now have available to us about inequities and disparities ... and the sense of urgency from students.”
Students driving practice change
Students nationally are “the most important” drivers of the increasing focus on SDHs in medical education, according to Dr. Fair. “They are demanding experiences to learn about the entire patient. We know that only 20% of a patient’s health is dependent on their health care. Our students are demanding education about the other 80%.”
More and more, communities are identifying needs and “students will then come up with initiatives to meet those needs,” Dr. Fair said.
Others interviewed for this story predicted this trend will only intensify, since not-for-profit hospitals are required under the Affordable Care Act regulations to assess community health needs every few years and to intervene accordingly.
Education on health care systems is also advancing. Penn State University, for instance, utilized a million-dollar grant from the AMA’s Accelerating Change in Medical Education initiative to design and implement a 4-year curriculum on the health system sciences that started in 2014. The curriculum includes an immersive experience in patient navigation.
“Students were taught to be patient navigators, and they were assigned within the clinical context to work on issues like, why are [patients] having trouble getting their medications?” said Susan E. Skochelak, MD, MPH, who leads the 6-year-old Accelerating Change initiative as vice president for medical education at the AMA.
From the start, she noted, students at Penn State are encouraged to question inequities, social and structural barriers to health, and faults in the health care system. “The message given at their white coat ceremony is ‘Welcome to medicine. Now that you’re here, you’re a member of the health care team, and we want you to speak up if you think there are things that need to be addressed. We want you to tell us when the system is working and not working,’ ” said Dr Skochelak, who previously served as the senior associate dean for academic affairs at the University of Wisconsin School of Medicine and Public Health, where she had been a tenured professor of family medicine.
Tomorrow’s physician partners
Approximately 80% of medical school graduates who participated in the AAMC’s 2018 survey of graduates said they had received significant training on health disparities—up from 71% in 2014.
“There’s a huge amount [of innovation] happening, but on the flip side, there’s not really a set of accepted tools and practices, and certainly no robust evaluation [of the training],” said Philip M. Alberti, PhD, senior director for health equity research and policy at the American Association of Medical Colleges. A recently published review (J Gen Intern Med. 2019;34[5]:720-30) shows growing interest in the teaching of SDHs in undergraduate medical education but variable content, strategies, and instructional practices.
Health care systems and practicing physicians are still very much feeling their way with SDHs. Screening tools are being developed and tested, and academic medical centers are trying to determine their roles in addressing issues such as transportation and housing – and what funding and structural levers can be pulled to fulfill these roles. “As we learn more about [these issues], it will become clearer what the right baseline set of competencies might be for all physicians,” Dr. Alberti noted.
In the meantime, some basic expectations for medical education are taking root officially. The National Board of Medical Examiners, with whom the AMA has partnered in its Accelerating Change initiative, has included questions in the United States Medical Licensing Examination on population health and SDHs, and plans to add more exam content on these topics and on health systems science, said Dr. Skochelak.
And through its site visit program (the Clinical Learning Environment Review program), the Accreditation Council for Graduate Medical Education has “made it pretty clear that there’s an expectation that residents and fellows are learning about the health system’s approach to identifying and addressing health care disparities – and that they’re given opportunities to develop quality improvement initiatives that target those disparities,” Dr. Alberti said.
In hopes of achieving consistency across medical specialties and in national accreditation and board certifications exams, the American Association of Medical Colleges is developing its first set of competencies in quality improvement and patient safety, with health equity being one of these competencies’ domains .
The competencies are tiered for medical school graduates, residency graduates, and faculty physicians who are 3-5 years post residency. At this point in time, said Dr. Alberti, the consensus among medical educators has been that physicians “need to be able to understand and consider [social, economic, and structural] contexts when they’re seeing patients, when they’re developing care plans, when they’re talking with caregivers, and when they’re looking at their own quality data.”
Elisabeth Poorman, MD, MPH, an internist at UW Medicine in Kent, Washington, said she worries that the passion of medical students for SDHs will too often be crushed, especially during residency and with immersion in the productivity-focused health care system. Studies show a drop in mental wellness and empathy and a rise in cynicism as training advances, said Dr. Poorman, who also writes about health care and issues of equity and serves on the editorial advisory board of Internal Medicine News.
With similar concerns, the AMA has recently launched a “Reimagining Residency” initiative that aims to improve transitions from medical school to residency and the wellness of residents and faculty, and expand educational content relating to SDHs.
Dr. Fair is optimistic that new physicians’ knowledge of SDHs will permeate medical practices.
“Physicians who are out practicing are going to be working with our graduates, and they’re going to be asking in [job] interviews, do you have flexible hours for patients? What community partnerships do you have? Are there other professionals on staff to help us address social determinants of health? What data [relating to SDHs] are you collecting?” she said.
Correction, 8/26/2019: An earlier version of this story misstated the title of Aletha Maybank, MD. Dr. Maybank's correct title is the first chief health equity officer of the American Medical Association.
How to nearly eliminate CLABSIs in children’s hospitals
SEATTLE – Levine Children’s Hospital, in Charlotte, N.C., dropped its central line–associated bloodstream infection rate from 1.13 per 1,000 line days to 0.67 in just a few months, with a mix of common sense steps and public accountability.
Levine Children’s was at about the 50th percentile for CLABSIs, compared with other children’s hospitals, but dropped to the 10th percentile after the changes. There were 21 CLABSIs in 2017, but only 12 in 2018. The hospital went 6 straight months without a CLABSI after the changes were made. The efforts saved about $300,000 and 63 patient days.
“We really had great success,” said Kayla S. Koch, MD, a pediatric hospitalist at Levine Children’s, who presented the findings at Pediatric Hospital Medicine.
Hospital units had been working to reduce CLABSIs, but they were each doing their own thing. “Many of our units were already dabbling, so we just sort of brought them together. We standardized the process and got everyone on the same page,” said copresenter Ketan P. Nadkarni, MD, also a pediatric hospitalist at Levine Children’s.
It wasn’t hard to get buy-in. “I don’t think the units were aware that everyone was doing it differently,” and were on board once the problem was explained. Also, using the same approach throughout the hospital made it easier for nurses and physicians moving between units, he said.
Each morning, the nurse supervisor and patient nurse would partner up at the bedside to check that central venous lines were set up correctly. They examined the alcohol disinfectant caps to make sure they were clean; determined that children were getting chlorhexidine gluconate baths; checked the dressings for bleeding and soiling; noted in the electronic medical record why the patient had a central line; and discussed with hospitalists if it were still needed. Problems were addressed immediately.
These quality processes were all tracked on wall racks placed in plain sight on each unit, including the neonatal and pediatric ICUs. Each central line patient had a card that listed what needed to be done, with a green stripe on one side and a red stripe on the other. If everything was done right, the green side faced out; if even one thing was done wrong, the red side was displayed, for all to see. It brought accountability to the process, the presenters said at the meeting sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The wall rack also had the central line audit schedule, plus diagrams that showed every failed item, the reason for it, and the unit’s compliance rate. Anyone walking by could see at a glance how the unit was doing that day and overall.
The number of dressing options was reduced from 10 to 2, a SorbaView SHIELD and a Tegaderm-like dressing, which made it easier to standardize the efforts. A protocol also was put in place to reinforce oozing dressings, instead of automatically changing them. “We were doing too many changes,” Dr. Koch said.
Compliance with the bundle was almost 90%. Staff “really got into it, and it was great to see,” she said.
The “initial success was almost unexpected, and so dramatic.” The goal now is to sustain the improvements, and roll them out to radiology and other places were central lines are placed, Dr. Nadkarni said.
There was no external funding, and the investigators had no disclosures.
SEATTLE – Levine Children’s Hospital, in Charlotte, N.C., dropped its central line–associated bloodstream infection rate from 1.13 per 1,000 line days to 0.67 in just a few months, with a mix of common sense steps and public accountability.
Levine Children’s was at about the 50th percentile for CLABSIs, compared with other children’s hospitals, but dropped to the 10th percentile after the changes. There were 21 CLABSIs in 2017, but only 12 in 2018. The hospital went 6 straight months without a CLABSI after the changes were made. The efforts saved about $300,000 and 63 patient days.
“We really had great success,” said Kayla S. Koch, MD, a pediatric hospitalist at Levine Children’s, who presented the findings at Pediatric Hospital Medicine.
Hospital units had been working to reduce CLABSIs, but they were each doing their own thing. “Many of our units were already dabbling, so we just sort of brought them together. We standardized the process and got everyone on the same page,” said copresenter Ketan P. Nadkarni, MD, also a pediatric hospitalist at Levine Children’s.
It wasn’t hard to get buy-in. “I don’t think the units were aware that everyone was doing it differently,” and were on board once the problem was explained. Also, using the same approach throughout the hospital made it easier for nurses and physicians moving between units, he said.
Each morning, the nurse supervisor and patient nurse would partner up at the bedside to check that central venous lines were set up correctly. They examined the alcohol disinfectant caps to make sure they were clean; determined that children were getting chlorhexidine gluconate baths; checked the dressings for bleeding and soiling; noted in the electronic medical record why the patient had a central line; and discussed with hospitalists if it were still needed. Problems were addressed immediately.
These quality processes were all tracked on wall racks placed in plain sight on each unit, including the neonatal and pediatric ICUs. Each central line patient had a card that listed what needed to be done, with a green stripe on one side and a red stripe on the other. If everything was done right, the green side faced out; if even one thing was done wrong, the red side was displayed, for all to see. It brought accountability to the process, the presenters said at the meeting sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The wall rack also had the central line audit schedule, plus diagrams that showed every failed item, the reason for it, and the unit’s compliance rate. Anyone walking by could see at a glance how the unit was doing that day and overall.
The number of dressing options was reduced from 10 to 2, a SorbaView SHIELD and a Tegaderm-like dressing, which made it easier to standardize the efforts. A protocol also was put in place to reinforce oozing dressings, instead of automatically changing them. “We were doing too many changes,” Dr. Koch said.
Compliance with the bundle was almost 90%. Staff “really got into it, and it was great to see,” she said.
The “initial success was almost unexpected, and so dramatic.” The goal now is to sustain the improvements, and roll them out to radiology and other places were central lines are placed, Dr. Nadkarni said.
There was no external funding, and the investigators had no disclosures.
SEATTLE – Levine Children’s Hospital, in Charlotte, N.C., dropped its central line–associated bloodstream infection rate from 1.13 per 1,000 line days to 0.67 in just a few months, with a mix of common sense steps and public accountability.
Levine Children’s was at about the 50th percentile for CLABSIs, compared with other children’s hospitals, but dropped to the 10th percentile after the changes. There were 21 CLABSIs in 2017, but only 12 in 2018. The hospital went 6 straight months without a CLABSI after the changes were made. The efforts saved about $300,000 and 63 patient days.
“We really had great success,” said Kayla S. Koch, MD, a pediatric hospitalist at Levine Children’s, who presented the findings at Pediatric Hospital Medicine.
Hospital units had been working to reduce CLABSIs, but they were each doing their own thing. “Many of our units were already dabbling, so we just sort of brought them together. We standardized the process and got everyone on the same page,” said copresenter Ketan P. Nadkarni, MD, also a pediatric hospitalist at Levine Children’s.
It wasn’t hard to get buy-in. “I don’t think the units were aware that everyone was doing it differently,” and were on board once the problem was explained. Also, using the same approach throughout the hospital made it easier for nurses and physicians moving between units, he said.
Each morning, the nurse supervisor and patient nurse would partner up at the bedside to check that central venous lines were set up correctly. They examined the alcohol disinfectant caps to make sure they were clean; determined that children were getting chlorhexidine gluconate baths; checked the dressings for bleeding and soiling; noted in the electronic medical record why the patient had a central line; and discussed with hospitalists if it were still needed. Problems were addressed immediately.
These quality processes were all tracked on wall racks placed in plain sight on each unit, including the neonatal and pediatric ICUs. Each central line patient had a card that listed what needed to be done, with a green stripe on one side and a red stripe on the other. If everything was done right, the green side faced out; if even one thing was done wrong, the red side was displayed, for all to see. It brought accountability to the process, the presenters said at the meeting sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The wall rack also had the central line audit schedule, plus diagrams that showed every failed item, the reason for it, and the unit’s compliance rate. Anyone walking by could see at a glance how the unit was doing that day and overall.
The number of dressing options was reduced from 10 to 2, a SorbaView SHIELD and a Tegaderm-like dressing, which made it easier to standardize the efforts. A protocol also was put in place to reinforce oozing dressings, instead of automatically changing them. “We were doing too many changes,” Dr. Koch said.
Compliance with the bundle was almost 90%. Staff “really got into it, and it was great to see,” she said.
The “initial success was almost unexpected, and so dramatic.” The goal now is to sustain the improvements, and roll them out to radiology and other places were central lines are placed, Dr. Nadkarni said.
There was no external funding, and the investigators had no disclosures.
REPORTING FROM PHM 2019
Procalcitonin advocated to help rule out bacterial infections
SEATTLE – Procalcitonin, a marker of bacterial infection, rises and peaks sooner than C-reactive protein (CRP), and is especially useful to help rule out invasive bacterial infections in young infants and pediatric community acquired pneumonia due to typical bacteria, according to a presentation at the 2019 Pediatric Hospital Medicine Conference.
It’s “excellent for identifying low risk patients” and has the potential to decrease lumbar punctures and antibiotic exposure, but “the specificity isn’t great,” so there’s the potential for false positives, said Russell McCulloh, MD, a pediatric infectious disease specialist at the University of Nebraska Medical Center, Omaha.
There was great interest in procalcitonin at the meeting; the presentation room was packed, with a line out the door. It’s used mostly in Europe at this point. Testing is available in many U.S. hospitals, but a large majority of audience members, when polled, said they don’t currently use it in clinical practice, and that it’s not a part of diagnostic algorithms at their institutions.
Levels of procalcitonin, a calcitonin precursor normally produced by the thyroid, are low or undetectable in healthy people, but inflammation, be it from infectious or noninfectious causes, triggers production by parenchymal cells throughout the body.
Levels began to rise as early as 2.5 hours after healthy subjects in one study were injected with bacterial endotoxins, and peaked as early as 6 hours; CRP, in contrast, started to rise after 12 hours, and peaked at 30 hours. Procalcitonin levels also seem to correlate with bacterial load and severity of infection, said Nivedita Srinivas, MD, a pediatric infectious disease specialist at Stanford (Calif.) University (J Pediatr Intensive Care. 2016 Dec;5[4]:162-71).
Due to time, the presenters focused their talk on community acquired pneumonia (CAP) and invasive bacterial infections (IBI) in young infants, meaning essentially bacteremia and meningitis.
Different studies use different cutoffs, but a procalcitonin below, for instance, 0.5 ng/mL is “certainly more sensitive [for IBI] than any single biomarker we currently use,” including CRP, white blood cells, and absolute neutrophil count (ANC). “If it’s negative, you’re really confident it’s negative,” but “a positive test does not necessarily indicate the presence of IBI,” Dr. McCulloh said (Pediatrics. 2012 Nov;130[5]:815-22).
“Procalcitonin works really well as part of a validated step-wise rule” that includes, for instance, CRP and ANC; “I think that’s where its utility is. On its own, it is not a substitute for you examining the patient and doing your basic risk stratification, but it may enhance your decision making incrementally above what we currently have,” he said.
Meanwhile, in a study of 532 children a median age of 2.4 years with radiographically confirmed CAP, procalcitonin levels were a median of 6.1 ng/mL in children whose pneumonia was caused by Streptococcus pneumoniae or other typical bacteria, and no child infected with typical bacteria had a level under 0.1 ng/mL. Below that level, “you can be very sure you do not have typical bacteria pneumonia,” said Marie Wang, MD, also a pediatric infectious disease specialist at Stanford (J Pediatric Infect Dis Soc. 2018 Feb 19;7[1]:46-53).
As procalcitonin levels went up, the likelihood of having bacterial pneumonia increased; at 2 ng/mL, 26% of subjects were infected with typical bacteria, “but even in that group, 58% still had viral infection, so you are still detecting a lot of viral” disease, she said.
Prolcalcitonin-guided therapy – antibiotics until patients fall below a level of 0.25 ng/ml, for instance – has also been associated with decreased antibiotic exposure (Respir Med. 2011 Dec;105[12]:1939-45).
The speakers had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
SEATTLE – Procalcitonin, a marker of bacterial infection, rises and peaks sooner than C-reactive protein (CRP), and is especially useful to help rule out invasive bacterial infections in young infants and pediatric community acquired pneumonia due to typical bacteria, according to a presentation at the 2019 Pediatric Hospital Medicine Conference.
It’s “excellent for identifying low risk patients” and has the potential to decrease lumbar punctures and antibiotic exposure, but “the specificity isn’t great,” so there’s the potential for false positives, said Russell McCulloh, MD, a pediatric infectious disease specialist at the University of Nebraska Medical Center, Omaha.
There was great interest in procalcitonin at the meeting; the presentation room was packed, with a line out the door. It’s used mostly in Europe at this point. Testing is available in many U.S. hospitals, but a large majority of audience members, when polled, said they don’t currently use it in clinical practice, and that it’s not a part of diagnostic algorithms at their institutions.
Levels of procalcitonin, a calcitonin precursor normally produced by the thyroid, are low or undetectable in healthy people, but inflammation, be it from infectious or noninfectious causes, triggers production by parenchymal cells throughout the body.
Levels began to rise as early as 2.5 hours after healthy subjects in one study were injected with bacterial endotoxins, and peaked as early as 6 hours; CRP, in contrast, started to rise after 12 hours, and peaked at 30 hours. Procalcitonin levels also seem to correlate with bacterial load and severity of infection, said Nivedita Srinivas, MD, a pediatric infectious disease specialist at Stanford (Calif.) University (J Pediatr Intensive Care. 2016 Dec;5[4]:162-71).
Due to time, the presenters focused their talk on community acquired pneumonia (CAP) and invasive bacterial infections (IBI) in young infants, meaning essentially bacteremia and meningitis.
Different studies use different cutoffs, but a procalcitonin below, for instance, 0.5 ng/mL is “certainly more sensitive [for IBI] than any single biomarker we currently use,” including CRP, white blood cells, and absolute neutrophil count (ANC). “If it’s negative, you’re really confident it’s negative,” but “a positive test does not necessarily indicate the presence of IBI,” Dr. McCulloh said (Pediatrics. 2012 Nov;130[5]:815-22).
“Procalcitonin works really well as part of a validated step-wise rule” that includes, for instance, CRP and ANC; “I think that’s where its utility is. On its own, it is not a substitute for you examining the patient and doing your basic risk stratification, but it may enhance your decision making incrementally above what we currently have,” he said.
Meanwhile, in a study of 532 children a median age of 2.4 years with radiographically confirmed CAP, procalcitonin levels were a median of 6.1 ng/mL in children whose pneumonia was caused by Streptococcus pneumoniae or other typical bacteria, and no child infected with typical bacteria had a level under 0.1 ng/mL. Below that level, “you can be very sure you do not have typical bacteria pneumonia,” said Marie Wang, MD, also a pediatric infectious disease specialist at Stanford (J Pediatric Infect Dis Soc. 2018 Feb 19;7[1]:46-53).
As procalcitonin levels went up, the likelihood of having bacterial pneumonia increased; at 2 ng/mL, 26% of subjects were infected with typical bacteria, “but even in that group, 58% still had viral infection, so you are still detecting a lot of viral” disease, she said.
Prolcalcitonin-guided therapy – antibiotics until patients fall below a level of 0.25 ng/ml, for instance – has also been associated with decreased antibiotic exposure (Respir Med. 2011 Dec;105[12]:1939-45).
The speakers had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
SEATTLE – Procalcitonin, a marker of bacterial infection, rises and peaks sooner than C-reactive protein (CRP), and is especially useful to help rule out invasive bacterial infections in young infants and pediatric community acquired pneumonia due to typical bacteria, according to a presentation at the 2019 Pediatric Hospital Medicine Conference.
It’s “excellent for identifying low risk patients” and has the potential to decrease lumbar punctures and antibiotic exposure, but “the specificity isn’t great,” so there’s the potential for false positives, said Russell McCulloh, MD, a pediatric infectious disease specialist at the University of Nebraska Medical Center, Omaha.
There was great interest in procalcitonin at the meeting; the presentation room was packed, with a line out the door. It’s used mostly in Europe at this point. Testing is available in many U.S. hospitals, but a large majority of audience members, when polled, said they don’t currently use it in clinical practice, and that it’s not a part of diagnostic algorithms at their institutions.
Levels of procalcitonin, a calcitonin precursor normally produced by the thyroid, are low or undetectable in healthy people, but inflammation, be it from infectious or noninfectious causes, triggers production by parenchymal cells throughout the body.
Levels began to rise as early as 2.5 hours after healthy subjects in one study were injected with bacterial endotoxins, and peaked as early as 6 hours; CRP, in contrast, started to rise after 12 hours, and peaked at 30 hours. Procalcitonin levels also seem to correlate with bacterial load and severity of infection, said Nivedita Srinivas, MD, a pediatric infectious disease specialist at Stanford (Calif.) University (J Pediatr Intensive Care. 2016 Dec;5[4]:162-71).
Due to time, the presenters focused their talk on community acquired pneumonia (CAP) and invasive bacterial infections (IBI) in young infants, meaning essentially bacteremia and meningitis.
Different studies use different cutoffs, but a procalcitonin below, for instance, 0.5 ng/mL is “certainly more sensitive [for IBI] than any single biomarker we currently use,” including CRP, white blood cells, and absolute neutrophil count (ANC). “If it’s negative, you’re really confident it’s negative,” but “a positive test does not necessarily indicate the presence of IBI,” Dr. McCulloh said (Pediatrics. 2012 Nov;130[5]:815-22).
“Procalcitonin works really well as part of a validated step-wise rule” that includes, for instance, CRP and ANC; “I think that’s where its utility is. On its own, it is not a substitute for you examining the patient and doing your basic risk stratification, but it may enhance your decision making incrementally above what we currently have,” he said.
Meanwhile, in a study of 532 children a median age of 2.4 years with radiographically confirmed CAP, procalcitonin levels were a median of 6.1 ng/mL in children whose pneumonia was caused by Streptococcus pneumoniae or other typical bacteria, and no child infected with typical bacteria had a level under 0.1 ng/mL. Below that level, “you can be very sure you do not have typical bacteria pneumonia,” said Marie Wang, MD, also a pediatric infectious disease specialist at Stanford (J Pediatric Infect Dis Soc. 2018 Feb 19;7[1]:46-53).
As procalcitonin levels went up, the likelihood of having bacterial pneumonia increased; at 2 ng/mL, 26% of subjects were infected with typical bacteria, “but even in that group, 58% still had viral infection, so you are still detecting a lot of viral” disease, she said.
Prolcalcitonin-guided therapy – antibiotics until patients fall below a level of 0.25 ng/ml, for instance – has also been associated with decreased antibiotic exposure (Respir Med. 2011 Dec;105[12]:1939-45).
The speakers had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
EXPERT ANALYSIS FROM PHM 2019
PTSD in the inpatient setting
A problem hiding in plain sight
“I need to get out of here! I haven’t gotten any sleep, my medications never come on time, and I feel like a pincushion. I am leaving NOW!” The commotion interrupts your intern’s meticulous presentation as your team quickly files into the room. You find a disheveled, visibly frustrated man tearing at his intravenous line, surrounded by his half-eaten breakfast and multiple urinals filled to various levels. His IV pump is beeping, and telemetry wires hang haphazardly off his chest.
Mr. Smith had been admitted for a heart failure exacerbation. You’d been making steady progress with diuresis but are now faced with a likely discharge against medical advice if you can’t defuse the situation.
As hospitalists, this scenario might feel eerily familiar. Perhaps Mr. Smith had enough of being in the hospital and just wanted to go home to see his dog, or maybe the food was not up to his standards.
However, his next line stops your team dead in its tracks. “I feel like I am in Vietnam all over again. I am tied up with all these wires and feel like a prisoner! Please let me go.” It turns out that Mr. Smith had a comorbidity that was overlooked during his initial intake: posttraumatic stress disorder.
Impact of PTSD
PTSD is a diagnosis characterized by intrusive recurrent thoughts, dreams, or flashbacks that follow exposure to a traumatic event or series of events (see Table 1). While more common among veterans (for example, Vietnam veterans have an estimated lifetime prevalence of PTSD of 30.9% for men and 26.9% for women),1 a national survey of U.S. households estimated the lifetime prevalence of PTSD among adult Americans to be 6.8%.2 PTSD is often underdiagnosed and underreported by patients in the outpatient setting, leading to underrecognition and undertreatment of these patients in the inpatient setting.
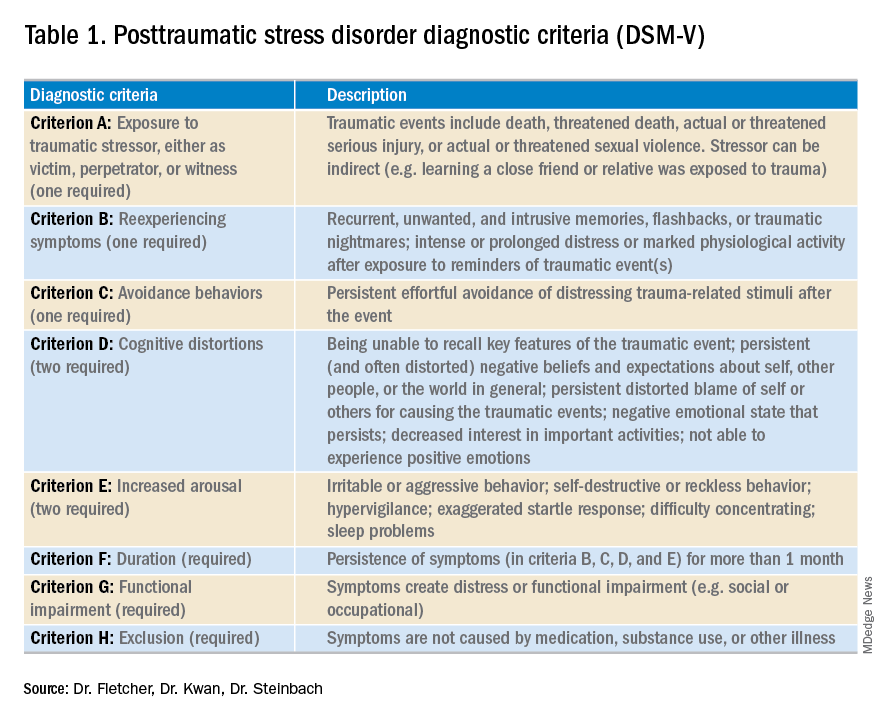
Although it may not be surprising that patients with PTSD use more mental health services, they are also more likely to use nonmental health services. In one study, total utilization of outpatient nonmental health services was 91% greater in veterans with PTSD, and these patients were three times more likely to be hospitalized than those without any mental health diagnoses.3 Additionally, they are likely to present later and stay longer when compared with patients without PTSD. One study estimated the cost of PTSD-related hospitalization in the United States from 2002 to 2011 as being $34.9 billion.4 Notably, close to 95% of hospitalizations in this study listed PTSD as a secondary rather than primary diagnosis, suggesting that the vast majority of these admitted patients are cared for by frontline providers who are not trained mental health professionals.
How PTSD manifests in the hospital
But, how exactly can the hospital environment contribute to decompensation of PTSD symptoms? Unfortunately, there is little empiric data to guide us. Based on what we do know of PTSD, we offer the following hypotheses.
Patients with PTSD may feel a loss of control or helplessness when admitted to the inpatient setting. For example, they cannot control when they receive their medications or when they get their meals. The act of showering or going outside requires approval. In addition, they might perceive they are being “ordered around” by staff and may be carted off to a study without knowing why the study is being done in the first place.
Triggers in the hospital environment may contribute to PTSD flares. Think about the loud, beeping IV pump that constantly goes off at random intervals, disrupting sleep. What about a blood draw in the early morning where the phlebotomist sticks a needle into the arm of a sleeping patient? Or the well-intentioned provider doing prerounds who wakes a sleeping patient with a shake of the shoulder or some other form of physical touch? The multidisciplinary team crowding around their hospital bed? For a patient suffering from PTSD, any of these could easily set off a cascade of escalating symptoms.
Knowing that these triggers exist, can anything be done to ameliorate their effects? We propose some practical suggestions for improving the hospital experience for patients with PTSD.
Strategies to combat PTSD in the inpatient setting
Perhaps the most practical place to start is with preserving sleep in hospitalized patients with PTSD. The majority of patients with PTSD have sleep disturbances, and interrupted sleep routines in these patients can exacerbate nightmares and underlying psychiatric issues.5 Therefore, we should strive to avoid unnecessary awakenings.
While this principle holds true for all hospitalized patients, it must be especially prioritized in patients with PTSD. Ask yourself these questions during your next admission: Must intravenous fluids run 24 hours a day, or could they be stopped at 6 p.m.? Are vital signs needed overnight? Could the last dose of furosemide occur at 4 p.m. to avoid nocturia?
Another strategy involves bedtime routines. Many of these patients may already follow a home sleep routine as part of their chronic PTSD management. To honor these habits in the hospital might mean that staff encourage turning the lights and the television off at a designated time. Additionally, the literature suggests music therapy can have a significant impact on enhanced sleep quality. When available, music therapy may reduce insomnia and decrease the amount of time prior to falling asleep.6
Other methods to counteract PTSD fall under the general principle of “trauma-informed care.” Trauma-informed care comprises practices promoting a culture of safety, empowerment, and healing.7 It is a mindful and sensitive approach that acknowledges the pervasive nature of trauma exposure, the reality of ongoing adverse effects in trauma survivors, and the fact that recovery is highly personal and complex.8
By definition, patients with PTSD have endured some traumatic event. Therefore, ideal care teams will ask patients about things that may trigger their anxiety and then work to mitigate them. For example, some patients with PTSD have a severe startle response when woken up by someone touching them. When patients feel that they can share their concerns with their care team and their team honors that observation by waking them in a different way, trust and control may be gained. This process of asking for patient guidance and adjusting accordingly is consistent with a trauma-informed care approach.9 A true trauma-informed care approach involves the entire practice environment but examining and adjusting our own behavior and assumptions are good places to start.
Summary of recommended treatments
Psychotherapy is preferable over pharmacotherapy, but both can be combined as needed. Individual trauma-focused psychotherapies utilizing a primary component of exposure and/or cognitive restructuring have strong evidence for effectiveness but are primarily outpatient based.
For pharmacologic treatment, selective serotonin reuptake inhibitors (for example, sertraline, paroxetine, or fluoxetine) and serotonin norepinephrine reuptake inhibitors (for example, venlafaxine) monotherapy have strong evidence for effectiveness and can be started while inpatient. However, these medications typically take weeks to produce benefits. Recent trials studying prazosin, an alpha1-adrenergic receptor antagonist used to alleviate nightmares associated with PTSD, have demonstrated inefficacy or even harm,leading experts to caution against its use.10,11 Finally, benzodiazepine and atypical antipsychotic usage should be restricted and used as a last resort.12
In summary, PTSD is common among veterans and nonveterans. While hospitalists may rarely admit patients because of their PTSD, they will often take care of patients who have PTSD as a comorbidity. Therefore, understanding the basics of PTSD and how hospitalization may exacerbate its symptoms can meaningfully improve care for these patients.
Dr. Fletcher is a hospitalist at the Milwaukee Veterans Affairs Medical Center and Froedtert Hospital in Wauwatosa, Wis. She is professor of internal medicine and program director for the internal medicine residency program at the Medical College of Wisconsin, Milwaukee. She is also faculty mentor for the VA’s Chief Resident for Quality and Safety. Dr. Kwan is a hospitalist at the VA San Diego Healthcare System and is associate professor at the University of California, San Diego, in the division of hospital medicine. He serves as an associate clerkship director of both the internal medicine clerkship and the medicine subinternship. He is the chair of SHM’s Physicians in Training committee. Dr. Steinbach is chief of hospital medicine at the Atlanta VA Medical Center and assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Kang HK et al. Posttraumatic stress disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157(2):141-8.
2. Kessler RC et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005; 62(6):593-602.
3. Cohen BE et al. Mental health diagnoses and utilization of VA nonmental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
4. Haviland MG et al. Posttraumatic stress disorder–related hospitalizations in the United States (2002-2011): Rates, co-occurring illnesses, suicidal ideation/self-harm, and hospital charges. J Nerv Ment Dis. 2016; 204(2):78-86.
5. Aurora RN et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
6. Blanaru M et al. The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment Illn. 2012;4(2):e13.
7. Tello M. (2018, Oct 16). Trauma-informed care: What it is, and why it’s important. Retrieved March 18, 2019, from https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562.
8. Harris M et al. Using trauma theory to design service systems. San Francisco: 2001.
9. Substance abuse and mental health services administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS publication no. SMA 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
10. Raskind MA et al. Trial of prazosin for posttraumatic stress disorder in military veterans. N Engl J Med. 2018 Feb 8;378(6):507-7.
11. McCall WV et al. A pilot, randomized clinical trial of bedtime doses of prazosin versus placebo in suicidal posttraumatic stress disorder patients with nightmares. J Clin Psychopharmacol. 2018 Dec;38(6):618-21.
12. U.S. Department of Veterans Affairs/U.S. Department of Defense. Clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction 2017. Accessed February 18, 2019.
A problem hiding in plain sight
A problem hiding in plain sight
“I need to get out of here! I haven’t gotten any sleep, my medications never come on time, and I feel like a pincushion. I am leaving NOW!” The commotion interrupts your intern’s meticulous presentation as your team quickly files into the room. You find a disheveled, visibly frustrated man tearing at his intravenous line, surrounded by his half-eaten breakfast and multiple urinals filled to various levels. His IV pump is beeping, and telemetry wires hang haphazardly off his chest.
Mr. Smith had been admitted for a heart failure exacerbation. You’d been making steady progress with diuresis but are now faced with a likely discharge against medical advice if you can’t defuse the situation.
As hospitalists, this scenario might feel eerily familiar. Perhaps Mr. Smith had enough of being in the hospital and just wanted to go home to see his dog, or maybe the food was not up to his standards.
However, his next line stops your team dead in its tracks. “I feel like I am in Vietnam all over again. I am tied up with all these wires and feel like a prisoner! Please let me go.” It turns out that Mr. Smith had a comorbidity that was overlooked during his initial intake: posttraumatic stress disorder.
Impact of PTSD
PTSD is a diagnosis characterized by intrusive recurrent thoughts, dreams, or flashbacks that follow exposure to a traumatic event or series of events (see Table 1). While more common among veterans (for example, Vietnam veterans have an estimated lifetime prevalence of PTSD of 30.9% for men and 26.9% for women),1 a national survey of U.S. households estimated the lifetime prevalence of PTSD among adult Americans to be 6.8%.2 PTSD is often underdiagnosed and underreported by patients in the outpatient setting, leading to underrecognition and undertreatment of these patients in the inpatient setting.
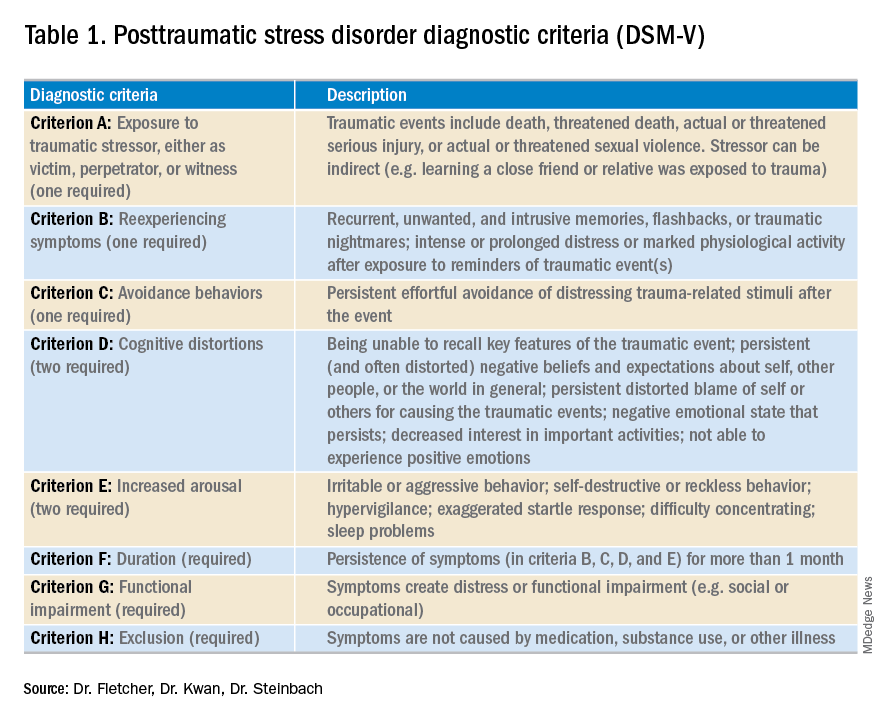
Although it may not be surprising that patients with PTSD use more mental health services, they are also more likely to use nonmental health services. In one study, total utilization of outpatient nonmental health services was 91% greater in veterans with PTSD, and these patients were three times more likely to be hospitalized than those without any mental health diagnoses.3 Additionally, they are likely to present later and stay longer when compared with patients without PTSD. One study estimated the cost of PTSD-related hospitalization in the United States from 2002 to 2011 as being $34.9 billion.4 Notably, close to 95% of hospitalizations in this study listed PTSD as a secondary rather than primary diagnosis, suggesting that the vast majority of these admitted patients are cared for by frontline providers who are not trained mental health professionals.
How PTSD manifests in the hospital
But, how exactly can the hospital environment contribute to decompensation of PTSD symptoms? Unfortunately, there is little empiric data to guide us. Based on what we do know of PTSD, we offer the following hypotheses.
Patients with PTSD may feel a loss of control or helplessness when admitted to the inpatient setting. For example, they cannot control when they receive their medications or when they get their meals. The act of showering or going outside requires approval. In addition, they might perceive they are being “ordered around” by staff and may be carted off to a study without knowing why the study is being done in the first place.
Triggers in the hospital environment may contribute to PTSD flares. Think about the loud, beeping IV pump that constantly goes off at random intervals, disrupting sleep. What about a blood draw in the early morning where the phlebotomist sticks a needle into the arm of a sleeping patient? Or the well-intentioned provider doing prerounds who wakes a sleeping patient with a shake of the shoulder or some other form of physical touch? The multidisciplinary team crowding around their hospital bed? For a patient suffering from PTSD, any of these could easily set off a cascade of escalating symptoms.
Knowing that these triggers exist, can anything be done to ameliorate their effects? We propose some practical suggestions for improving the hospital experience for patients with PTSD.
Strategies to combat PTSD in the inpatient setting
Perhaps the most practical place to start is with preserving sleep in hospitalized patients with PTSD. The majority of patients with PTSD have sleep disturbances, and interrupted sleep routines in these patients can exacerbate nightmares and underlying psychiatric issues.5 Therefore, we should strive to avoid unnecessary awakenings.
While this principle holds true for all hospitalized patients, it must be especially prioritized in patients with PTSD. Ask yourself these questions during your next admission: Must intravenous fluids run 24 hours a day, or could they be stopped at 6 p.m.? Are vital signs needed overnight? Could the last dose of furosemide occur at 4 p.m. to avoid nocturia?
Another strategy involves bedtime routines. Many of these patients may already follow a home sleep routine as part of their chronic PTSD management. To honor these habits in the hospital might mean that staff encourage turning the lights and the television off at a designated time. Additionally, the literature suggests music therapy can have a significant impact on enhanced sleep quality. When available, music therapy may reduce insomnia and decrease the amount of time prior to falling asleep.6
Other methods to counteract PTSD fall under the general principle of “trauma-informed care.” Trauma-informed care comprises practices promoting a culture of safety, empowerment, and healing.7 It is a mindful and sensitive approach that acknowledges the pervasive nature of trauma exposure, the reality of ongoing adverse effects in trauma survivors, and the fact that recovery is highly personal and complex.8
By definition, patients with PTSD have endured some traumatic event. Therefore, ideal care teams will ask patients about things that may trigger their anxiety and then work to mitigate them. For example, some patients with PTSD have a severe startle response when woken up by someone touching them. When patients feel that they can share their concerns with their care team and their team honors that observation by waking them in a different way, trust and control may be gained. This process of asking for patient guidance and adjusting accordingly is consistent with a trauma-informed care approach.9 A true trauma-informed care approach involves the entire practice environment but examining and adjusting our own behavior and assumptions are good places to start.
Summary of recommended treatments
Psychotherapy is preferable over pharmacotherapy, but both can be combined as needed. Individual trauma-focused psychotherapies utilizing a primary component of exposure and/or cognitive restructuring have strong evidence for effectiveness but are primarily outpatient based.
For pharmacologic treatment, selective serotonin reuptake inhibitors (for example, sertraline, paroxetine, or fluoxetine) and serotonin norepinephrine reuptake inhibitors (for example, venlafaxine) monotherapy have strong evidence for effectiveness and can be started while inpatient. However, these medications typically take weeks to produce benefits. Recent trials studying prazosin, an alpha1-adrenergic receptor antagonist used to alleviate nightmares associated with PTSD, have demonstrated inefficacy or even harm,leading experts to caution against its use.10,11 Finally, benzodiazepine and atypical antipsychotic usage should be restricted and used as a last resort.12
In summary, PTSD is common among veterans and nonveterans. While hospitalists may rarely admit patients because of their PTSD, they will often take care of patients who have PTSD as a comorbidity. Therefore, understanding the basics of PTSD and how hospitalization may exacerbate its symptoms can meaningfully improve care for these patients.
Dr. Fletcher is a hospitalist at the Milwaukee Veterans Affairs Medical Center and Froedtert Hospital in Wauwatosa, Wis. She is professor of internal medicine and program director for the internal medicine residency program at the Medical College of Wisconsin, Milwaukee. She is also faculty mentor for the VA’s Chief Resident for Quality and Safety. Dr. Kwan is a hospitalist at the VA San Diego Healthcare System and is associate professor at the University of California, San Diego, in the division of hospital medicine. He serves as an associate clerkship director of both the internal medicine clerkship and the medicine subinternship. He is the chair of SHM’s Physicians in Training committee. Dr. Steinbach is chief of hospital medicine at the Atlanta VA Medical Center and assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Kang HK et al. Posttraumatic stress disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157(2):141-8.
2. Kessler RC et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005; 62(6):593-602.
3. Cohen BE et al. Mental health diagnoses and utilization of VA nonmental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
4. Haviland MG et al. Posttraumatic stress disorder–related hospitalizations in the United States (2002-2011): Rates, co-occurring illnesses, suicidal ideation/self-harm, and hospital charges. J Nerv Ment Dis. 2016; 204(2):78-86.
5. Aurora RN et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
6. Blanaru M et al. The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment Illn. 2012;4(2):e13.
7. Tello M. (2018, Oct 16). Trauma-informed care: What it is, and why it’s important. Retrieved March 18, 2019, from https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562.
8. Harris M et al. Using trauma theory to design service systems. San Francisco: 2001.
9. Substance abuse and mental health services administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS publication no. SMA 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
10. Raskind MA et al. Trial of prazosin for posttraumatic stress disorder in military veterans. N Engl J Med. 2018 Feb 8;378(6):507-7.
11. McCall WV et al. A pilot, randomized clinical trial of bedtime doses of prazosin versus placebo in suicidal posttraumatic stress disorder patients with nightmares. J Clin Psychopharmacol. 2018 Dec;38(6):618-21.
12. U.S. Department of Veterans Affairs/U.S. Department of Defense. Clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction 2017. Accessed February 18, 2019.
“I need to get out of here! I haven’t gotten any sleep, my medications never come on time, and I feel like a pincushion. I am leaving NOW!” The commotion interrupts your intern’s meticulous presentation as your team quickly files into the room. You find a disheveled, visibly frustrated man tearing at his intravenous line, surrounded by his half-eaten breakfast and multiple urinals filled to various levels. His IV pump is beeping, and telemetry wires hang haphazardly off his chest.
Mr. Smith had been admitted for a heart failure exacerbation. You’d been making steady progress with diuresis but are now faced with a likely discharge against medical advice if you can’t defuse the situation.
As hospitalists, this scenario might feel eerily familiar. Perhaps Mr. Smith had enough of being in the hospital and just wanted to go home to see his dog, or maybe the food was not up to his standards.
However, his next line stops your team dead in its tracks. “I feel like I am in Vietnam all over again. I am tied up with all these wires and feel like a prisoner! Please let me go.” It turns out that Mr. Smith had a comorbidity that was overlooked during his initial intake: posttraumatic stress disorder.
Impact of PTSD
PTSD is a diagnosis characterized by intrusive recurrent thoughts, dreams, or flashbacks that follow exposure to a traumatic event or series of events (see Table 1). While more common among veterans (for example, Vietnam veterans have an estimated lifetime prevalence of PTSD of 30.9% for men and 26.9% for women),1 a national survey of U.S. households estimated the lifetime prevalence of PTSD among adult Americans to be 6.8%.2 PTSD is often underdiagnosed and underreported by patients in the outpatient setting, leading to underrecognition and undertreatment of these patients in the inpatient setting.
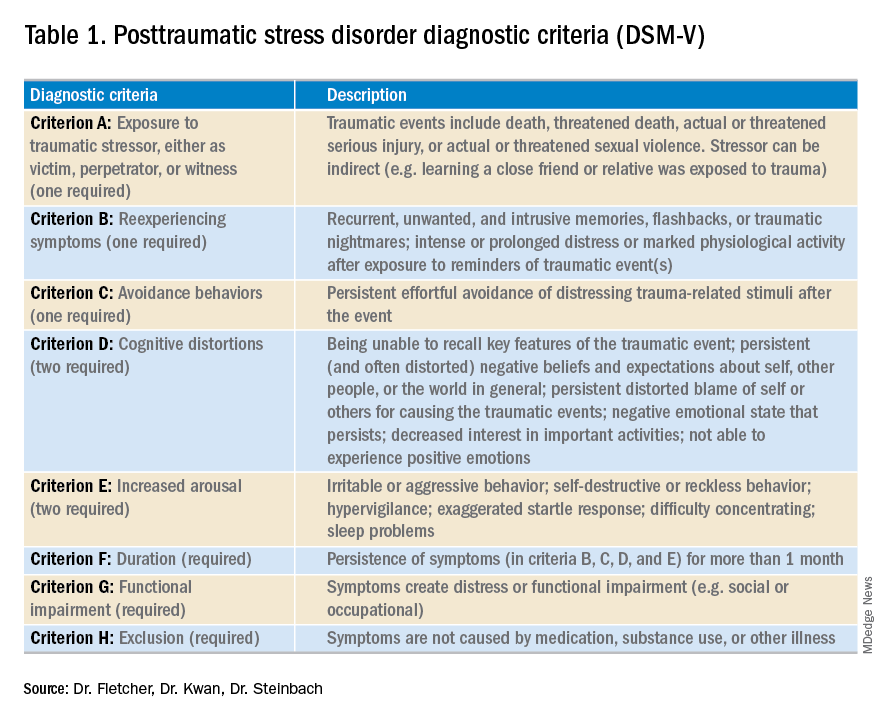
Although it may not be surprising that patients with PTSD use more mental health services, they are also more likely to use nonmental health services. In one study, total utilization of outpatient nonmental health services was 91% greater in veterans with PTSD, and these patients were three times more likely to be hospitalized than those without any mental health diagnoses.3 Additionally, they are likely to present later and stay longer when compared with patients without PTSD. One study estimated the cost of PTSD-related hospitalization in the United States from 2002 to 2011 as being $34.9 billion.4 Notably, close to 95% of hospitalizations in this study listed PTSD as a secondary rather than primary diagnosis, suggesting that the vast majority of these admitted patients are cared for by frontline providers who are not trained mental health professionals.
How PTSD manifests in the hospital
But, how exactly can the hospital environment contribute to decompensation of PTSD symptoms? Unfortunately, there is little empiric data to guide us. Based on what we do know of PTSD, we offer the following hypotheses.
Patients with PTSD may feel a loss of control or helplessness when admitted to the inpatient setting. For example, they cannot control when they receive their medications or when they get their meals. The act of showering or going outside requires approval. In addition, they might perceive they are being “ordered around” by staff and may be carted off to a study without knowing why the study is being done in the first place.
Triggers in the hospital environment may contribute to PTSD flares. Think about the loud, beeping IV pump that constantly goes off at random intervals, disrupting sleep. What about a blood draw in the early morning where the phlebotomist sticks a needle into the arm of a sleeping patient? Or the well-intentioned provider doing prerounds who wakes a sleeping patient with a shake of the shoulder or some other form of physical touch? The multidisciplinary team crowding around their hospital bed? For a patient suffering from PTSD, any of these could easily set off a cascade of escalating symptoms.
Knowing that these triggers exist, can anything be done to ameliorate their effects? We propose some practical suggestions for improving the hospital experience for patients with PTSD.
Strategies to combat PTSD in the inpatient setting
Perhaps the most practical place to start is with preserving sleep in hospitalized patients with PTSD. The majority of patients with PTSD have sleep disturbances, and interrupted sleep routines in these patients can exacerbate nightmares and underlying psychiatric issues.5 Therefore, we should strive to avoid unnecessary awakenings.
While this principle holds true for all hospitalized patients, it must be especially prioritized in patients with PTSD. Ask yourself these questions during your next admission: Must intravenous fluids run 24 hours a day, or could they be stopped at 6 p.m.? Are vital signs needed overnight? Could the last dose of furosemide occur at 4 p.m. to avoid nocturia?
Another strategy involves bedtime routines. Many of these patients may already follow a home sleep routine as part of their chronic PTSD management. To honor these habits in the hospital might mean that staff encourage turning the lights and the television off at a designated time. Additionally, the literature suggests music therapy can have a significant impact on enhanced sleep quality. When available, music therapy may reduce insomnia and decrease the amount of time prior to falling asleep.6
Other methods to counteract PTSD fall under the general principle of “trauma-informed care.” Trauma-informed care comprises practices promoting a culture of safety, empowerment, and healing.7 It is a mindful and sensitive approach that acknowledges the pervasive nature of trauma exposure, the reality of ongoing adverse effects in trauma survivors, and the fact that recovery is highly personal and complex.8
By definition, patients with PTSD have endured some traumatic event. Therefore, ideal care teams will ask patients about things that may trigger their anxiety and then work to mitigate them. For example, some patients with PTSD have a severe startle response when woken up by someone touching them. When patients feel that they can share their concerns with their care team and their team honors that observation by waking them in a different way, trust and control may be gained. This process of asking for patient guidance and adjusting accordingly is consistent with a trauma-informed care approach.9 A true trauma-informed care approach involves the entire practice environment but examining and adjusting our own behavior and assumptions are good places to start.
Summary of recommended treatments
Psychotherapy is preferable over pharmacotherapy, but both can be combined as needed. Individual trauma-focused psychotherapies utilizing a primary component of exposure and/or cognitive restructuring have strong evidence for effectiveness but are primarily outpatient based.
For pharmacologic treatment, selective serotonin reuptake inhibitors (for example, sertraline, paroxetine, or fluoxetine) and serotonin norepinephrine reuptake inhibitors (for example, venlafaxine) monotherapy have strong evidence for effectiveness and can be started while inpatient. However, these medications typically take weeks to produce benefits. Recent trials studying prazosin, an alpha1-adrenergic receptor antagonist used to alleviate nightmares associated with PTSD, have demonstrated inefficacy or even harm,leading experts to caution against its use.10,11 Finally, benzodiazepine and atypical antipsychotic usage should be restricted and used as a last resort.12
In summary, PTSD is common among veterans and nonveterans. While hospitalists may rarely admit patients because of their PTSD, they will often take care of patients who have PTSD as a comorbidity. Therefore, understanding the basics of PTSD and how hospitalization may exacerbate its symptoms can meaningfully improve care for these patients.
Dr. Fletcher is a hospitalist at the Milwaukee Veterans Affairs Medical Center and Froedtert Hospital in Wauwatosa, Wis. She is professor of internal medicine and program director for the internal medicine residency program at the Medical College of Wisconsin, Milwaukee. She is also faculty mentor for the VA’s Chief Resident for Quality and Safety. Dr. Kwan is a hospitalist at the VA San Diego Healthcare System and is associate professor at the University of California, San Diego, in the division of hospital medicine. He serves as an associate clerkship director of both the internal medicine clerkship and the medicine subinternship. He is the chair of SHM’s Physicians in Training committee. Dr. Steinbach is chief of hospital medicine at the Atlanta VA Medical Center and assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Kang HK et al. Posttraumatic stress disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157(2):141-8.
2. Kessler RC et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005; 62(6):593-602.
3. Cohen BE et al. Mental health diagnoses and utilization of VA nonmental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
4. Haviland MG et al. Posttraumatic stress disorder–related hospitalizations in the United States (2002-2011): Rates, co-occurring illnesses, suicidal ideation/self-harm, and hospital charges. J Nerv Ment Dis. 2016; 204(2):78-86.
5. Aurora RN et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
6. Blanaru M et al. The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment Illn. 2012;4(2):e13.
7. Tello M. (2018, Oct 16). Trauma-informed care: What it is, and why it’s important. Retrieved March 18, 2019, from https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562.
8. Harris M et al. Using trauma theory to design service systems. San Francisco: 2001.
9. Substance abuse and mental health services administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS publication no. SMA 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
10. Raskind MA et al. Trial of prazosin for posttraumatic stress disorder in military veterans. N Engl J Med. 2018 Feb 8;378(6):507-7.
11. McCall WV et al. A pilot, randomized clinical trial of bedtime doses of prazosin versus placebo in suicidal posttraumatic stress disorder patients with nightmares. J Clin Psychopharmacol. 2018 Dec;38(6):618-21.
12. U.S. Department of Veterans Affairs/U.S. Department of Defense. Clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction 2017. Accessed February 18, 2019.
The changing landscape of medical education
A brave new world
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”
A brave new world
A brave new world
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”