User login
Don’t forget about OSHA
With the bewildering array of new bureaucracies that private practices are now forced to contend with, it is easy to forget about the older ones – especially the Occupational Health and Safety Administration (OSHA).
with all the applicable regulations. Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
For starters, do you have an official OSHA poster, enumerating employee rights and explaining how to file complaints? Every office must have one posted in plain site, and it is the first thing an OSHA inspector will look for. You can download one from OSHA’s Web site or order it at no charge by calling 800-321-OSHA.
Next, how old is your written exposure control plan for blood-borne pathogens? It should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, and your implementation of universal precautions – and it is supposed to be updated annually, to reflect changes in technology.
You need not adopt every new safety device as it comes on the market, but you should document which ones you are using – and which you pass up – and why. For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at your decision and why you feel that your current protocol is as good or better.
Review your list of hazardous substances, which all employees have a right to know about. Keep in mind that OSHA’s list includes alcohol, hydrogen peroxide, acetone, and other substances that you might not consider particularly dangerous, but are nevertheless classified as “hazardous.” (My favorite in that category is liquid nitrogen; it’s hard to envision anything less hazardous, since it evaporates instantly if spilled, and cannot injure skin, or anything else, without purposeful, sustained exposure – and is great, incidentally, for extinguishing small fires.) For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
Check out your building’s exits. Everyone must be able to evacuate your office quickly in case of fire or other emergencies. At a minimum, you (or the owner of the building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
You must provide all at-risk employees with hepatitis B vaccine at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars.
How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you do that? Because OSHA issues no citations during voluntary inspections, as long as you agree to remedy any violations they find.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
With the bewildering array of new bureaucracies that private practices are now forced to contend with, it is easy to forget about the older ones – especially the Occupational Health and Safety Administration (OSHA).
with all the applicable regulations. Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
For starters, do you have an official OSHA poster, enumerating employee rights and explaining how to file complaints? Every office must have one posted in plain site, and it is the first thing an OSHA inspector will look for. You can download one from OSHA’s Web site or order it at no charge by calling 800-321-OSHA.
Next, how old is your written exposure control plan for blood-borne pathogens? It should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, and your implementation of universal precautions – and it is supposed to be updated annually, to reflect changes in technology.
You need not adopt every new safety device as it comes on the market, but you should document which ones you are using – and which you pass up – and why. For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at your decision and why you feel that your current protocol is as good or better.
Review your list of hazardous substances, which all employees have a right to know about. Keep in mind that OSHA’s list includes alcohol, hydrogen peroxide, acetone, and other substances that you might not consider particularly dangerous, but are nevertheless classified as “hazardous.” (My favorite in that category is liquid nitrogen; it’s hard to envision anything less hazardous, since it evaporates instantly if spilled, and cannot injure skin, or anything else, without purposeful, sustained exposure – and is great, incidentally, for extinguishing small fires.) For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
Check out your building’s exits. Everyone must be able to evacuate your office quickly in case of fire or other emergencies. At a minimum, you (or the owner of the building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
You must provide all at-risk employees with hepatitis B vaccine at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars.
How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you do that? Because OSHA issues no citations during voluntary inspections, as long as you agree to remedy any violations they find.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
With the bewildering array of new bureaucracies that private practices are now forced to contend with, it is easy to forget about the older ones – especially the Occupational Health and Safety Administration (OSHA).
with all the applicable regulations. Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
For starters, do you have an official OSHA poster, enumerating employee rights and explaining how to file complaints? Every office must have one posted in plain site, and it is the first thing an OSHA inspector will look for. You can download one from OSHA’s Web site or order it at no charge by calling 800-321-OSHA.
Next, how old is your written exposure control plan for blood-borne pathogens? It should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, and your implementation of universal precautions – and it is supposed to be updated annually, to reflect changes in technology.
You need not adopt every new safety device as it comes on the market, but you should document which ones you are using – and which you pass up – and why. For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at your decision and why you feel that your current protocol is as good or better.
Review your list of hazardous substances, which all employees have a right to know about. Keep in mind that OSHA’s list includes alcohol, hydrogen peroxide, acetone, and other substances that you might not consider particularly dangerous, but are nevertheless classified as “hazardous.” (My favorite in that category is liquid nitrogen; it’s hard to envision anything less hazardous, since it evaporates instantly if spilled, and cannot injure skin, or anything else, without purposeful, sustained exposure – and is great, incidentally, for extinguishing small fires.) For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
Check out your building’s exits. Everyone must be able to evacuate your office quickly in case of fire or other emergencies. At a minimum, you (or the owner of the building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
You must provide all at-risk employees with hepatitis B vaccine at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars.
How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you do that? Because OSHA issues no citations during voluntary inspections, as long as you agree to remedy any violations they find.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Employment practices liability insurance
No matter how complete your insurance portfolio, there is one policy – one you probably have never heard of – that you should definitely consider adding to it.
A while ago, I spoke with a dermatologist in California who experienced every employer’s nightmare: he fired an incompetent employee, who promptly sued him for wrongful termination and accused him of sexual harassment to boot. The charges were completely false, and the employee’s transgressions were well documented; but he was not insured against a suit of that type, and defending it would have been prohibitively expensive. He was forced to settle it for a significant sum of money.
Disasters like that are becoming more common. Plaintiffs’ attorneys know that most small businesses, including medical practices, are not insured against internal liability actions – and that settlements are cheaper than litigation.
Fortunately, there is a relatively inexpensive alternative: not covered by conventional liability insurance. These include wrongful termination, sexual harassment, discrimination, breach of employment contract, negligent hiring or evaluation, failure to promote, wrongful discipline, mismanagement of benefits, and the ever-popular “emotional distress.”
EPLI coverage would have permitted the California dermatologist to mount a proper defense against his employee’s groundless charges. In fact, there is a better than even chance that the lawsuit would have been dropped, or never filed to begin with.
Some liability carriers are beginning to cover some employee-related issues in “umbrella” policies, so before looking into EPLI, check your current coverage. Then, as with all insurance, you should shop around for the best price and carefully read the policies on your short list. All EPLI policies cover litigation against your practice and its owners by employees, but some cover only full-timers. Try to obtain the broadest coverage possible so that claims from part-time, temporary, and seasonal employees, and, if possible, even applicants for employment and former employees, also are covered.
You should also look for the most comprehensive policy in terms of coverage. Almost every EPLI policy covers the allegations mentioned above, but some offer a more comprehensive list of covered acts, such as invasion of privacy and defamation of character.
Also be aware of precisely what each policy does not cover. Most exclude punitive damages and court-imposed fines, as well as criminal acts, fraud, and other clearly illegal conduct. For example, you would not be covered if you fired an employee because he or she refused to falsify insurance claims.
Depending on where you practice, it may be necessary to ask an employment attorney to evaluate your individual EPLI needs. An underwriter cannot anticipate every eventuality for you, particularly if he or she does not live in your area and is not familiar with employment conditions in your community.
As with any liability policy, try to get a clause added that permits you to choose your own defense attorney. Better still, pick a specific attorney or firm that you trust and have that counsel named in an endorsement to the policy. Otherwise, the insurance carrier will select an attorney from its own panel who may not consider your interests a higher priority than those of the insurer itself.
If you must accept the insurer’s choice of counsel, you should find out whether that attorney is experienced in employment law, which is a very specialized area. And just as with your malpractice policy, you will want to maintain as much control as possible over the settlement of claims. Ideally, no claim should be settled without your express permission.
As with any insurance policy you buy, be sure to choose an established carrier with ample experience in the field and solid financial strength. A low premium is no bargain if the carrier is new to EPLI or goes broke.
Above all, as with any insurance policy, make sure that you can live with the claims definition and exclusions in the policy you choose, and seek advice if you are unsure what your specific needs are before signing on the dotted line.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
No matter how complete your insurance portfolio, there is one policy – one you probably have never heard of – that you should definitely consider adding to it.
A while ago, I spoke with a dermatologist in California who experienced every employer’s nightmare: he fired an incompetent employee, who promptly sued him for wrongful termination and accused him of sexual harassment to boot. The charges were completely false, and the employee’s transgressions were well documented; but he was not insured against a suit of that type, and defending it would have been prohibitively expensive. He was forced to settle it for a significant sum of money.
Disasters like that are becoming more common. Plaintiffs’ attorneys know that most small businesses, including medical practices, are not insured against internal liability actions – and that settlements are cheaper than litigation.
Fortunately, there is a relatively inexpensive alternative: not covered by conventional liability insurance. These include wrongful termination, sexual harassment, discrimination, breach of employment contract, negligent hiring or evaluation, failure to promote, wrongful discipline, mismanagement of benefits, and the ever-popular “emotional distress.”
EPLI coverage would have permitted the California dermatologist to mount a proper defense against his employee’s groundless charges. In fact, there is a better than even chance that the lawsuit would have been dropped, or never filed to begin with.
Some liability carriers are beginning to cover some employee-related issues in “umbrella” policies, so before looking into EPLI, check your current coverage. Then, as with all insurance, you should shop around for the best price and carefully read the policies on your short list. All EPLI policies cover litigation against your practice and its owners by employees, but some cover only full-timers. Try to obtain the broadest coverage possible so that claims from part-time, temporary, and seasonal employees, and, if possible, even applicants for employment and former employees, also are covered.
You should also look for the most comprehensive policy in terms of coverage. Almost every EPLI policy covers the allegations mentioned above, but some offer a more comprehensive list of covered acts, such as invasion of privacy and defamation of character.
Also be aware of precisely what each policy does not cover. Most exclude punitive damages and court-imposed fines, as well as criminal acts, fraud, and other clearly illegal conduct. For example, you would not be covered if you fired an employee because he or she refused to falsify insurance claims.
Depending on where you practice, it may be necessary to ask an employment attorney to evaluate your individual EPLI needs. An underwriter cannot anticipate every eventuality for you, particularly if he or she does not live in your area and is not familiar with employment conditions in your community.
As with any liability policy, try to get a clause added that permits you to choose your own defense attorney. Better still, pick a specific attorney or firm that you trust and have that counsel named in an endorsement to the policy. Otherwise, the insurance carrier will select an attorney from its own panel who may not consider your interests a higher priority than those of the insurer itself.
If you must accept the insurer’s choice of counsel, you should find out whether that attorney is experienced in employment law, which is a very specialized area. And just as with your malpractice policy, you will want to maintain as much control as possible over the settlement of claims. Ideally, no claim should be settled without your express permission.
As with any insurance policy you buy, be sure to choose an established carrier with ample experience in the field and solid financial strength. A low premium is no bargain if the carrier is new to EPLI or goes broke.
Above all, as with any insurance policy, make sure that you can live with the claims definition and exclusions in the policy you choose, and seek advice if you are unsure what your specific needs are before signing on the dotted line.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
No matter how complete your insurance portfolio, there is one policy – one you probably have never heard of – that you should definitely consider adding to it.
A while ago, I spoke with a dermatologist in California who experienced every employer’s nightmare: he fired an incompetent employee, who promptly sued him for wrongful termination and accused him of sexual harassment to boot. The charges were completely false, and the employee’s transgressions were well documented; but he was not insured against a suit of that type, and defending it would have been prohibitively expensive. He was forced to settle it for a significant sum of money.
Disasters like that are becoming more common. Plaintiffs’ attorneys know that most small businesses, including medical practices, are not insured against internal liability actions – and that settlements are cheaper than litigation.
Fortunately, there is a relatively inexpensive alternative: not covered by conventional liability insurance. These include wrongful termination, sexual harassment, discrimination, breach of employment contract, negligent hiring or evaluation, failure to promote, wrongful discipline, mismanagement of benefits, and the ever-popular “emotional distress.”
EPLI coverage would have permitted the California dermatologist to mount a proper defense against his employee’s groundless charges. In fact, there is a better than even chance that the lawsuit would have been dropped, or never filed to begin with.
Some liability carriers are beginning to cover some employee-related issues in “umbrella” policies, so before looking into EPLI, check your current coverage. Then, as with all insurance, you should shop around for the best price and carefully read the policies on your short list. All EPLI policies cover litigation against your practice and its owners by employees, but some cover only full-timers. Try to obtain the broadest coverage possible so that claims from part-time, temporary, and seasonal employees, and, if possible, even applicants for employment and former employees, also are covered.
You should also look for the most comprehensive policy in terms of coverage. Almost every EPLI policy covers the allegations mentioned above, but some offer a more comprehensive list of covered acts, such as invasion of privacy and defamation of character.
Also be aware of precisely what each policy does not cover. Most exclude punitive damages and court-imposed fines, as well as criminal acts, fraud, and other clearly illegal conduct. For example, you would not be covered if you fired an employee because he or she refused to falsify insurance claims.
Depending on where you practice, it may be necessary to ask an employment attorney to evaluate your individual EPLI needs. An underwriter cannot anticipate every eventuality for you, particularly if he or she does not live in your area and is not familiar with employment conditions in your community.
As with any liability policy, try to get a clause added that permits you to choose your own defense attorney. Better still, pick a specific attorney or firm that you trust and have that counsel named in an endorsement to the policy. Otherwise, the insurance carrier will select an attorney from its own panel who may not consider your interests a higher priority than those of the insurer itself.
If you must accept the insurer’s choice of counsel, you should find out whether that attorney is experienced in employment law, which is a very specialized area. And just as with your malpractice policy, you will want to maintain as much control as possible over the settlement of claims. Ideally, no claim should be settled without your express permission.
As with any insurance policy you buy, be sure to choose an established carrier with ample experience in the field and solid financial strength. A low premium is no bargain if the carrier is new to EPLI or goes broke.
Above all, as with any insurance policy, make sure that you can live with the claims definition and exclusions in the policy you choose, and seek advice if you are unsure what your specific needs are before signing on the dotted line.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
MOC: ACOG’s role in developing a solution to the heated controversy
The American Board of Medical Specialties (ABMS) has decided to trade the phrase “maintenance of certification” (MOC) for “continuing board certification,” a seemingly minor change that has an important backstory. This is the story of how the physician community flexed its collective muscle and how the American College of Obstetricians and Gynecologists (ACOG) helped broker an important détente and pathway in a highly contentious issue.
Founded in 1933 as a nonprofit organization dedicated to maintaining high uniform standards among physicians, the ABMS and many of its specialty boards have found themselves, for more than a decade, under heavy fire from physicians (especially family physicians, internists, and surgeons), their 24 subspecialties, and the state medical societies representing them.
The ObGyn experience with the American Board of Obstetrics and Gynecology (ABOG), however, is better for a number of reasons. Historically, ABOG and ACOG have worked closely together, which is an anomaly among boards as many boards have an arms-length or even an antagonistic relationship with their specialty society.
The discussion below outlines physician concerns with the ABMS and related boards and describes efforts to address and rebuild the continuing board certification process.
Direct and indirect costs
Physicians are very concerned with the costs involved in MOC. Measurable costs include testing fees, while indirect costs include time, stress, travel to test centers, and threats to livelihood for failing a high-stakes examination. Physicians want the high-stakes exam eliminated.
Relevance to practice
Physicians often feel that the MOC has little relevance to their practice, which fuels a sense of resentment toward boards that they believe are dominated by physicians who no longer practice. Subspecialists feel farther away from general practice and the base exams. Generalists feel that the exams miss the points of their daily practice.
Lack of data to show improved quality of care
Physicians want to know that the MOC is worth their time, effort, and money because it improves patient care. To date, however, empirical or clinical data on patient outcomes are absent or ambiguous; most studies lack high-level data or do not investigate the MOC requirements. Physicians want to know what the best MOC practices are, what improves care, and that practices that make no difference will be discarded. In addition, they want timely knowledge alerts when evidence changes.
Relationship to licensing, employment, privileging, credentialing, and reimbursement
Hospitals, insurers, and states increasingly—and inappropriately—use board certification as the primary (sometimes only) default measure of a physician’s fitness for patient care. Physicians without board certification often are denied hospital privileges, inclusion in insurance panels, and even medical licenses. This changes certification from a voluntary physician self-improvement exercise into a can’t-earn-a-living-without-it cudgel.
Variation
Boards vary significantly in their MOC requirements and costs. The importance of an equal standard across all boards is a clear theme among physician concerns.
Role and authority of the ABMS and related boards
Many physicians are frustrated with the perceived autocratic nature of their boards—boards that lack transparency, do not solicit or allow input from practicing physicians, and are unresponsive to physician concerns.
According to Susan Ramin, MD, ABOG Associate Executive Director, ABOG is leading in a number of these areas, including:
- rapidly disseminating clinical information on emerging topics, such as Zika virus infection and opioid misuse
- offering physician choice of testing categories
- exempting high scorers from the secured written exam, which saved physicians a total of $881,000 in exam fees
- crediting physicians for what they already are doing, including serving on maternal mortality review committees, participating in registries, and participating in the Alliance for Innovation on Maternal Health (AIM)
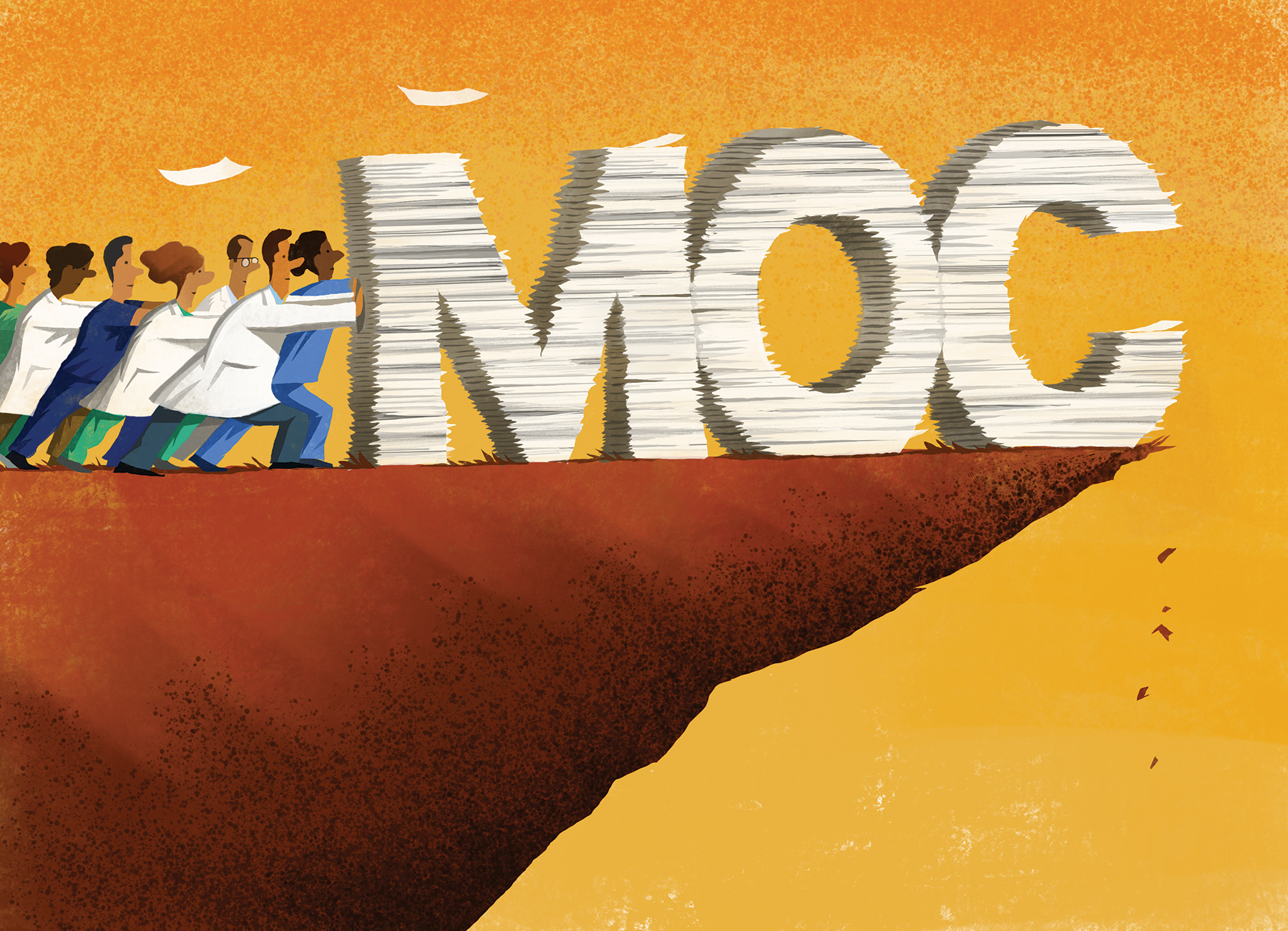
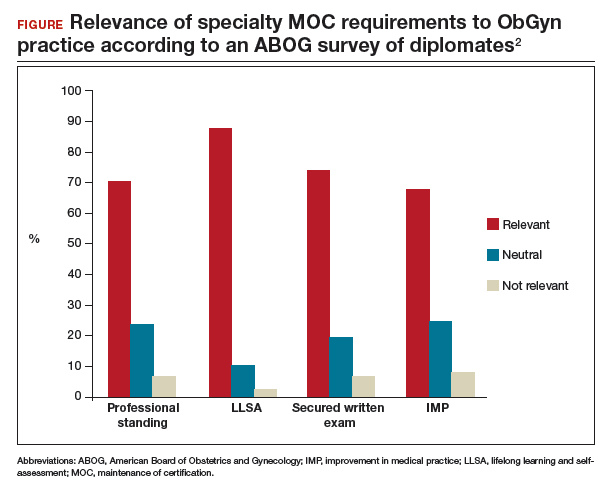
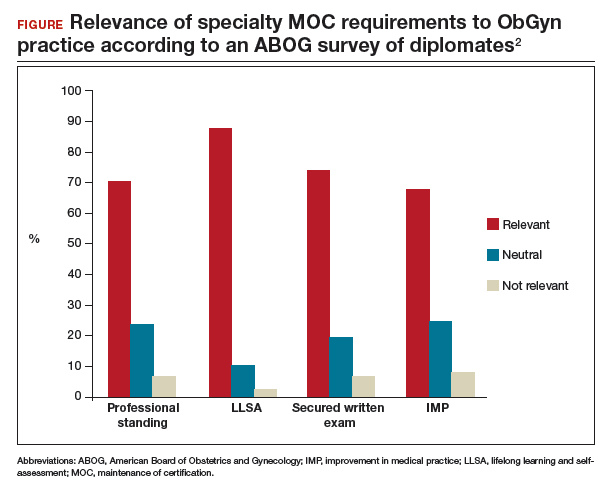
- providing Lifelong Learning and Self-Assessment (LLSA) articles that, according to 90% of diplomates surveyed, are beneficial to their clinical practice (FIGURE).1,2
Our colleague physicians are not so lucky. In a 2015 New England Journal of Medicine Perspective, one physician called out the American Board of Internal Medicine as “a private, self-appointed certifying organization,” a not-for-profit organization that has “grown into a $55-million-per-year business.”3 He concluded that “many physicians are waking up to the fact that our profession is increasingly controlled by people not directly involved in patient care who have lost contact with the realities of day-to-day clinical practice.”3
State and society responses to MOC requirements
Frustration with an inability to resolve these concerns has grown steadily, bubbling over into state governments. The American Medical Association developed “model state legislation intended to prohibit hospitals, health care insurers, and state boards of medicine and osteopathic medicine from requiring participation in MOC processes as a condition of credentialing, privileging, insurance panel participation, licensure, or licensure renewal.”4
Some states are proposing or have enacted legislation that prohibits the use of MOC as a criterion for licensure, privileging, employment, reimbursement, and/or insurance panel participation. Eight states (Arizona, Georgia, Kentucky, Maryland, Maine, Missouri, Oklahoma, Tennessee) have enacted laws to prohibit the use of MOC for initial and renewal licensure decisions. Many states are actively considering MOC-related legislation, including Alaska, Florida, Iowa, Indiana, Maryland, Massachusetts, Michigan, Missouri, New Hampshire, New York, Ohio, Oklahoma, Rhode Island, South Carolina, Tennessee, Utah, Washington, and Wisconsin.
Legislation is not the only outlet for physician frustration. Some medical specialty societies are considering dropping board certification as a membership requirement; physicians are exploring developing alternative boards; and some physicians are defying the board certification requirement altogether, with thousands signing anti-MOC petitions.
ACOG asserts importance of maintaining self-regulation
While other specialties are actively advocating state legislation, ACOG and ABOG have worked together to oppose state legislation, believing that physician self-regulation is paramount. In fact, in 2017, ACOG and ABOG issued a joint statement urging state lawmakers to “not interfere with our decades of successful self-regulation and to realize that each medical society has its own experience with its MOC program.”5
Negotiations lead to new initiative
This brings us to an interesting situation. ACOG’s Executive Vice President and CEO Hal Lawrence III, MD, was tapped (in his position as Chair of the Specialty Society CEO Consortium) to represent physician specialties in negotiations and discussions with the boards, which were represented by Lois Nora, MD, JD, President and CEO of the ABMS, and state medical societies, represented by Donald Palmisano Jr, JD, Executive Director and CEO of the Medical Association of Georgia. Many state medical societies, boards, and physician specialty organizations participated in these meetings.
Throughout months of debate, Dr. Lawrence urged his colleagues to stay at the table and do the hard work of reaching an agreement, rather than ask politicians to solve medicine’s problems. This approach was leveraged by the serious efforts and threats of state legislation, which brought the boards to the table. In August 2017, 41 state medical societies and 33 national medical specialty societies wrote to Dr. Nora expressing their concerns that “professional self-regulation is under attack. Concerns regarding the usefulness of the high-stakes exam, the exorbitant costs of the MOC process, and the lack of transparent communication from the certifying boards have led to damaging the MOC brand, and creating state-based attacks on the MOC process.”6
In December 2017, Dr. Lawrence and Mr. Palmisano led a meeting of principals from the national medical specialty societies and state medical societies with leaders of ABMS and 8 specialty boards, including ABOG, an opportunity to secure meaningful change. Dr. Lawrence began by stressing that the interests of physicians and patients would be best served by all parties coming together and collaborating on a meaningful solution, to repair trust and preserve physician self-regulation.
Dr. Ramin presented ABOG’s approach to continuous certification, lifelong learning, and self-assessment. The American Board of Urology and the American Board of Psychiatry and Neurology indicated that they were basing important changes in their MOC process on ABOG’s work, including using 5 modules (1 general and 4 specific to the physician’s practice) and multiple open-book mini-exams based on selected journal articles as an alternative to the 10-year MOC exam.
The Vision Initiative. At that meeting and others, the ABMS and other boards heard physicians’ candid and sometimes blunt concerns. Dr. Nora spoke to the recently announced Continuing Board Certification: Vision for the Future program, also known as the “Vision Initiative,” a process designed to fundamentally rebuild the continuing certification process with input and guidance from practicing physicians. Physician response seemed uniform: Seeing is believing.
Importantly, all participants at the December meeting agreed to work together to rebuild trust and ensure professionalism and professional self-regulation, reflected in this Statement of Shared Purpose:
ABMS certifying boards and national medical specialty societies will collaborate to resolve differences in the process of ongoing certification and to fulfill the principles of professional self-regulation, achieving appropriate standardization, and assuring that ongoing certification is relevant to the practices of physicians without undue burden. Furthermore, the boards and societies, and their organizations (ABMS and CMSS [Council of Medical Specialty Societies]), will undertake necessary changes in a timely manner, and will commit to ongoing communication with state medical associations to solicit their input.4
Two ObGyns participating in the Vision Initiative are Haywood Brown, MD, ACOG’s Immediate Past President, and George Wendel, MD, ABOG’s Executive Director. The Vision Initiative is composed of 3 parts. Part 1, Organization, is complete. The committee is currently working on part 2, Envisioning the Future, an information-gathering component that includes physician surveys, hearings, open solicited input, and identifying new and better approaches. After the final report is delivered to the ABMS in February 2019, part 3, Implementation, will begin.
The Vision Initiative offers physicians an important opportunity to help shape the future of continuing education and certification. ObGyns and other physicians should consider reviewing and commenting on the draft report, due in November, during the public comment period. Visit https://visioninitiative.org for more information and to sign up for email updates.

Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- American Board of Obstetrics and Gynecology. From pilot to permanent: ABOG's program offering an innovative pathway integrating lifelong learning and self-assessment and external assessment is approved. https://www.abog.org/new/ABOG_PilotToPermanent.aspx. Accessed July 6, 2018.
- Ramin S. American Board of Obstetrics and Gynecology MOC program. PowerPoint presentation; December 4, 2017.
- Teirstein PS. Boarded to death--why maintenance of certification is bad for doctors and patients. N Engl J Med. 2015;372(2):106-108.
- AMA Council on Medical Education. Executive summary. 2017. https://www.ama-assn.org/sites/default/files/media-browser/public/council-on-med-ed/a18-cme-02.pdf. Accessed July 6, 2018.
- American College of Obstetricians and Gynecologists. ACOG-ABOG joint statement: political interference in physician maintenance of skills threatens women's health care. https://www.acog.org/-/media/Departments/State-Legislative-Activities/2017ACOG-ABMS-MOC-Statement.pdf?dmc=1&ts=20180706T1615538746. Accessed July 6, 2018.
- Letter to Lois Nora, MD, JD. August 18, 2017. https://www.mainemed.com/sites/default/files/content/MOC%20Letter%20082117.pdf. Accessed July 6, 2018.
The American Board of Medical Specialties (ABMS) has decided to trade the phrase “maintenance of certification” (MOC) for “continuing board certification,” a seemingly minor change that has an important backstory. This is the story of how the physician community flexed its collective muscle and how the American College of Obstetricians and Gynecologists (ACOG) helped broker an important détente and pathway in a highly contentious issue.
Founded in 1933 as a nonprofit organization dedicated to maintaining high uniform standards among physicians, the ABMS and many of its specialty boards have found themselves, for more than a decade, under heavy fire from physicians (especially family physicians, internists, and surgeons), their 24 subspecialties, and the state medical societies representing them.
The ObGyn experience with the American Board of Obstetrics and Gynecology (ABOG), however, is better for a number of reasons. Historically, ABOG and ACOG have worked closely together, which is an anomaly among boards as many boards have an arms-length or even an antagonistic relationship with their specialty society.
The discussion below outlines physician concerns with the ABMS and related boards and describes efforts to address and rebuild the continuing board certification process.
Direct and indirect costs
Physicians are very concerned with the costs involved in MOC. Measurable costs include testing fees, while indirect costs include time, stress, travel to test centers, and threats to livelihood for failing a high-stakes examination. Physicians want the high-stakes exam eliminated.
Relevance to practice
Physicians often feel that the MOC has little relevance to their practice, which fuels a sense of resentment toward boards that they believe are dominated by physicians who no longer practice. Subspecialists feel farther away from general practice and the base exams. Generalists feel that the exams miss the points of their daily practice.
Lack of data to show improved quality of care
Physicians want to know that the MOC is worth their time, effort, and money because it improves patient care. To date, however, empirical or clinical data on patient outcomes are absent or ambiguous; most studies lack high-level data or do not investigate the MOC requirements. Physicians want to know what the best MOC practices are, what improves care, and that practices that make no difference will be discarded. In addition, they want timely knowledge alerts when evidence changes.
Relationship to licensing, employment, privileging, credentialing, and reimbursement
Hospitals, insurers, and states increasingly—and inappropriately—use board certification as the primary (sometimes only) default measure of a physician’s fitness for patient care. Physicians without board certification often are denied hospital privileges, inclusion in insurance panels, and even medical licenses. This changes certification from a voluntary physician self-improvement exercise into a can’t-earn-a-living-without-it cudgel.
Variation
Boards vary significantly in their MOC requirements and costs. The importance of an equal standard across all boards is a clear theme among physician concerns.
Role and authority of the ABMS and related boards
Many physicians are frustrated with the perceived autocratic nature of their boards—boards that lack transparency, do not solicit or allow input from practicing physicians, and are unresponsive to physician concerns.
According to Susan Ramin, MD, ABOG Associate Executive Director, ABOG is leading in a number of these areas, including:
- rapidly disseminating clinical information on emerging topics, such as Zika virus infection and opioid misuse
- offering physician choice of testing categories
- exempting high scorers from the secured written exam, which saved physicians a total of $881,000 in exam fees
- crediting physicians for what they already are doing, including serving on maternal mortality review committees, participating in registries, and participating in the Alliance for Innovation on Maternal Health (AIM)
- providing Lifelong Learning and Self-Assessment (LLSA) articles that, according to 90% of diplomates surveyed, are beneficial to their clinical practice (FIGURE).1,2
Our colleague physicians are not so lucky. In a 2015 New England Journal of Medicine Perspective, one physician called out the American Board of Internal Medicine as “a private, self-appointed certifying organization,” a not-for-profit organization that has “grown into a $55-million-per-year business.”3 He concluded that “many physicians are waking up to the fact that our profession is increasingly controlled by people not directly involved in patient care who have lost contact with the realities of day-to-day clinical practice.”3
State and society responses to MOC requirements
Frustration with an inability to resolve these concerns has grown steadily, bubbling over into state governments. The American Medical Association developed “model state legislation intended to prohibit hospitals, health care insurers, and state boards of medicine and osteopathic medicine from requiring participation in MOC processes as a condition of credentialing, privileging, insurance panel participation, licensure, or licensure renewal.”4
Some states are proposing or have enacted legislation that prohibits the use of MOC as a criterion for licensure, privileging, employment, reimbursement, and/or insurance panel participation. Eight states (Arizona, Georgia, Kentucky, Maryland, Maine, Missouri, Oklahoma, Tennessee) have enacted laws to prohibit the use of MOC for initial and renewal licensure decisions. Many states are actively considering MOC-related legislation, including Alaska, Florida, Iowa, Indiana, Maryland, Massachusetts, Michigan, Missouri, New Hampshire, New York, Ohio, Oklahoma, Rhode Island, South Carolina, Tennessee, Utah, Washington, and Wisconsin.
Legislation is not the only outlet for physician frustration. Some medical specialty societies are considering dropping board certification as a membership requirement; physicians are exploring developing alternative boards; and some physicians are defying the board certification requirement altogether, with thousands signing anti-MOC petitions.
ACOG asserts importance of maintaining self-regulation
While other specialties are actively advocating state legislation, ACOG and ABOG have worked together to oppose state legislation, believing that physician self-regulation is paramount. In fact, in 2017, ACOG and ABOG issued a joint statement urging state lawmakers to “not interfere with our decades of successful self-regulation and to realize that each medical society has its own experience with its MOC program.”5
Negotiations lead to new initiative
This brings us to an interesting situation. ACOG’s Executive Vice President and CEO Hal Lawrence III, MD, was tapped (in his position as Chair of the Specialty Society CEO Consortium) to represent physician specialties in negotiations and discussions with the boards, which were represented by Lois Nora, MD, JD, President and CEO of the ABMS, and state medical societies, represented by Donald Palmisano Jr, JD, Executive Director and CEO of the Medical Association of Georgia. Many state medical societies, boards, and physician specialty organizations participated in these meetings.
Throughout months of debate, Dr. Lawrence urged his colleagues to stay at the table and do the hard work of reaching an agreement, rather than ask politicians to solve medicine’s problems. This approach was leveraged by the serious efforts and threats of state legislation, which brought the boards to the table. In August 2017, 41 state medical societies and 33 national medical specialty societies wrote to Dr. Nora expressing their concerns that “professional self-regulation is under attack. Concerns regarding the usefulness of the high-stakes exam, the exorbitant costs of the MOC process, and the lack of transparent communication from the certifying boards have led to damaging the MOC brand, and creating state-based attacks on the MOC process.”6
In December 2017, Dr. Lawrence and Mr. Palmisano led a meeting of principals from the national medical specialty societies and state medical societies with leaders of ABMS and 8 specialty boards, including ABOG, an opportunity to secure meaningful change. Dr. Lawrence began by stressing that the interests of physicians and patients would be best served by all parties coming together and collaborating on a meaningful solution, to repair trust and preserve physician self-regulation.
Dr. Ramin presented ABOG’s approach to continuous certification, lifelong learning, and self-assessment. The American Board of Urology and the American Board of Psychiatry and Neurology indicated that they were basing important changes in their MOC process on ABOG’s work, including using 5 modules (1 general and 4 specific to the physician’s practice) and multiple open-book mini-exams based on selected journal articles as an alternative to the 10-year MOC exam.
The Vision Initiative. At that meeting and others, the ABMS and other boards heard physicians’ candid and sometimes blunt concerns. Dr. Nora spoke to the recently announced Continuing Board Certification: Vision for the Future program, also known as the “Vision Initiative,” a process designed to fundamentally rebuild the continuing certification process with input and guidance from practicing physicians. Physician response seemed uniform: Seeing is believing.
Importantly, all participants at the December meeting agreed to work together to rebuild trust and ensure professionalism and professional self-regulation, reflected in this Statement of Shared Purpose:
ABMS certifying boards and national medical specialty societies will collaborate to resolve differences in the process of ongoing certification and to fulfill the principles of professional self-regulation, achieving appropriate standardization, and assuring that ongoing certification is relevant to the practices of physicians without undue burden. Furthermore, the boards and societies, and their organizations (ABMS and CMSS [Council of Medical Specialty Societies]), will undertake necessary changes in a timely manner, and will commit to ongoing communication with state medical associations to solicit their input.4
Two ObGyns participating in the Vision Initiative are Haywood Brown, MD, ACOG’s Immediate Past President, and George Wendel, MD, ABOG’s Executive Director. The Vision Initiative is composed of 3 parts. Part 1, Organization, is complete. The committee is currently working on part 2, Envisioning the Future, an information-gathering component that includes physician surveys, hearings, open solicited input, and identifying new and better approaches. After the final report is delivered to the ABMS in February 2019, part 3, Implementation, will begin.
The Vision Initiative offers physicians an important opportunity to help shape the future of continuing education and certification. ObGyns and other physicians should consider reviewing and commenting on the draft report, due in November, during the public comment period. Visit https://visioninitiative.org for more information and to sign up for email updates.

Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The American Board of Medical Specialties (ABMS) has decided to trade the phrase “maintenance of certification” (MOC) for “continuing board certification,” a seemingly minor change that has an important backstory. This is the story of how the physician community flexed its collective muscle and how the American College of Obstetricians and Gynecologists (ACOG) helped broker an important détente and pathway in a highly contentious issue.
Founded in 1933 as a nonprofit organization dedicated to maintaining high uniform standards among physicians, the ABMS and many of its specialty boards have found themselves, for more than a decade, under heavy fire from physicians (especially family physicians, internists, and surgeons), their 24 subspecialties, and the state medical societies representing them.
The ObGyn experience with the American Board of Obstetrics and Gynecology (ABOG), however, is better for a number of reasons. Historically, ABOG and ACOG have worked closely together, which is an anomaly among boards as many boards have an arms-length or even an antagonistic relationship with their specialty society.
The discussion below outlines physician concerns with the ABMS and related boards and describes efforts to address and rebuild the continuing board certification process.
Direct and indirect costs
Physicians are very concerned with the costs involved in MOC. Measurable costs include testing fees, while indirect costs include time, stress, travel to test centers, and threats to livelihood for failing a high-stakes examination. Physicians want the high-stakes exam eliminated.
Relevance to practice
Physicians often feel that the MOC has little relevance to their practice, which fuels a sense of resentment toward boards that they believe are dominated by physicians who no longer practice. Subspecialists feel farther away from general practice and the base exams. Generalists feel that the exams miss the points of their daily practice.
Lack of data to show improved quality of care
Physicians want to know that the MOC is worth their time, effort, and money because it improves patient care. To date, however, empirical or clinical data on patient outcomes are absent or ambiguous; most studies lack high-level data or do not investigate the MOC requirements. Physicians want to know what the best MOC practices are, what improves care, and that practices that make no difference will be discarded. In addition, they want timely knowledge alerts when evidence changes.
Relationship to licensing, employment, privileging, credentialing, and reimbursement
Hospitals, insurers, and states increasingly—and inappropriately—use board certification as the primary (sometimes only) default measure of a physician’s fitness for patient care. Physicians without board certification often are denied hospital privileges, inclusion in insurance panels, and even medical licenses. This changes certification from a voluntary physician self-improvement exercise into a can’t-earn-a-living-without-it cudgel.
Variation
Boards vary significantly in their MOC requirements and costs. The importance of an equal standard across all boards is a clear theme among physician concerns.
Role and authority of the ABMS and related boards
Many physicians are frustrated with the perceived autocratic nature of their boards—boards that lack transparency, do not solicit or allow input from practicing physicians, and are unresponsive to physician concerns.
According to Susan Ramin, MD, ABOG Associate Executive Director, ABOG is leading in a number of these areas, including:
- rapidly disseminating clinical information on emerging topics, such as Zika virus infection and opioid misuse
- offering physician choice of testing categories
- exempting high scorers from the secured written exam, which saved physicians a total of $881,000 in exam fees
- crediting physicians for what they already are doing, including serving on maternal mortality review committees, participating in registries, and participating in the Alliance for Innovation on Maternal Health (AIM)
- providing Lifelong Learning and Self-Assessment (LLSA) articles that, according to 90% of diplomates surveyed, are beneficial to their clinical practice (FIGURE).1,2
Our colleague physicians are not so lucky. In a 2015 New England Journal of Medicine Perspective, one physician called out the American Board of Internal Medicine as “a private, self-appointed certifying organization,” a not-for-profit organization that has “grown into a $55-million-per-year business.”3 He concluded that “many physicians are waking up to the fact that our profession is increasingly controlled by people not directly involved in patient care who have lost contact with the realities of day-to-day clinical practice.”3
State and society responses to MOC requirements
Frustration with an inability to resolve these concerns has grown steadily, bubbling over into state governments. The American Medical Association developed “model state legislation intended to prohibit hospitals, health care insurers, and state boards of medicine and osteopathic medicine from requiring participation in MOC processes as a condition of credentialing, privileging, insurance panel participation, licensure, or licensure renewal.”4
Some states are proposing or have enacted legislation that prohibits the use of MOC as a criterion for licensure, privileging, employment, reimbursement, and/or insurance panel participation. Eight states (Arizona, Georgia, Kentucky, Maryland, Maine, Missouri, Oklahoma, Tennessee) have enacted laws to prohibit the use of MOC for initial and renewal licensure decisions. Many states are actively considering MOC-related legislation, including Alaska, Florida, Iowa, Indiana, Maryland, Massachusetts, Michigan, Missouri, New Hampshire, New York, Ohio, Oklahoma, Rhode Island, South Carolina, Tennessee, Utah, Washington, and Wisconsin.
Legislation is not the only outlet for physician frustration. Some medical specialty societies are considering dropping board certification as a membership requirement; physicians are exploring developing alternative boards; and some physicians are defying the board certification requirement altogether, with thousands signing anti-MOC petitions.
ACOG asserts importance of maintaining self-regulation
While other specialties are actively advocating state legislation, ACOG and ABOG have worked together to oppose state legislation, believing that physician self-regulation is paramount. In fact, in 2017, ACOG and ABOG issued a joint statement urging state lawmakers to “not interfere with our decades of successful self-regulation and to realize that each medical society has its own experience with its MOC program.”5
Negotiations lead to new initiative
This brings us to an interesting situation. ACOG’s Executive Vice President and CEO Hal Lawrence III, MD, was tapped (in his position as Chair of the Specialty Society CEO Consortium) to represent physician specialties in negotiations and discussions with the boards, which were represented by Lois Nora, MD, JD, President and CEO of the ABMS, and state medical societies, represented by Donald Palmisano Jr, JD, Executive Director and CEO of the Medical Association of Georgia. Many state medical societies, boards, and physician specialty organizations participated in these meetings.
Throughout months of debate, Dr. Lawrence urged his colleagues to stay at the table and do the hard work of reaching an agreement, rather than ask politicians to solve medicine’s problems. This approach was leveraged by the serious efforts and threats of state legislation, which brought the boards to the table. In August 2017, 41 state medical societies and 33 national medical specialty societies wrote to Dr. Nora expressing their concerns that “professional self-regulation is under attack. Concerns regarding the usefulness of the high-stakes exam, the exorbitant costs of the MOC process, and the lack of transparent communication from the certifying boards have led to damaging the MOC brand, and creating state-based attacks on the MOC process.”6
In December 2017, Dr. Lawrence and Mr. Palmisano led a meeting of principals from the national medical specialty societies and state medical societies with leaders of ABMS and 8 specialty boards, including ABOG, an opportunity to secure meaningful change. Dr. Lawrence began by stressing that the interests of physicians and patients would be best served by all parties coming together and collaborating on a meaningful solution, to repair trust and preserve physician self-regulation.
Dr. Ramin presented ABOG’s approach to continuous certification, lifelong learning, and self-assessment. The American Board of Urology and the American Board of Psychiatry and Neurology indicated that they were basing important changes in their MOC process on ABOG’s work, including using 5 modules (1 general and 4 specific to the physician’s practice) and multiple open-book mini-exams based on selected journal articles as an alternative to the 10-year MOC exam.
The Vision Initiative. At that meeting and others, the ABMS and other boards heard physicians’ candid and sometimes blunt concerns. Dr. Nora spoke to the recently announced Continuing Board Certification: Vision for the Future program, also known as the “Vision Initiative,” a process designed to fundamentally rebuild the continuing certification process with input and guidance from practicing physicians. Physician response seemed uniform: Seeing is believing.
Importantly, all participants at the December meeting agreed to work together to rebuild trust and ensure professionalism and professional self-regulation, reflected in this Statement of Shared Purpose:
ABMS certifying boards and national medical specialty societies will collaborate to resolve differences in the process of ongoing certification and to fulfill the principles of professional self-regulation, achieving appropriate standardization, and assuring that ongoing certification is relevant to the practices of physicians without undue burden. Furthermore, the boards and societies, and their organizations (ABMS and CMSS [Council of Medical Specialty Societies]), will undertake necessary changes in a timely manner, and will commit to ongoing communication with state medical associations to solicit their input.4
Two ObGyns participating in the Vision Initiative are Haywood Brown, MD, ACOG’s Immediate Past President, and George Wendel, MD, ABOG’s Executive Director. The Vision Initiative is composed of 3 parts. Part 1, Organization, is complete. The committee is currently working on part 2, Envisioning the Future, an information-gathering component that includes physician surveys, hearings, open solicited input, and identifying new and better approaches. After the final report is delivered to the ABMS in February 2019, part 3, Implementation, will begin.
The Vision Initiative offers physicians an important opportunity to help shape the future of continuing education and certification. ObGyns and other physicians should consider reviewing and commenting on the draft report, due in November, during the public comment period. Visit https://visioninitiative.org for more information and to sign up for email updates.

Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- American Board of Obstetrics and Gynecology. From pilot to permanent: ABOG's program offering an innovative pathway integrating lifelong learning and self-assessment and external assessment is approved. https://www.abog.org/new/ABOG_PilotToPermanent.aspx. Accessed July 6, 2018.
- Ramin S. American Board of Obstetrics and Gynecology MOC program. PowerPoint presentation; December 4, 2017.
- Teirstein PS. Boarded to death--why maintenance of certification is bad for doctors and patients. N Engl J Med. 2015;372(2):106-108.
- AMA Council on Medical Education. Executive summary. 2017. https://www.ama-assn.org/sites/default/files/media-browser/public/council-on-med-ed/a18-cme-02.pdf. Accessed July 6, 2018.
- American College of Obstetricians and Gynecologists. ACOG-ABOG joint statement: political interference in physician maintenance of skills threatens women's health care. https://www.acog.org/-/media/Departments/State-Legislative-Activities/2017ACOG-ABMS-MOC-Statement.pdf?dmc=1&ts=20180706T1615538746. Accessed July 6, 2018.
- Letter to Lois Nora, MD, JD. August 18, 2017. https://www.mainemed.com/sites/default/files/content/MOC%20Letter%20082117.pdf. Accessed July 6, 2018.
- American Board of Obstetrics and Gynecology. From pilot to permanent: ABOG's program offering an innovative pathway integrating lifelong learning and self-assessment and external assessment is approved. https://www.abog.org/new/ABOG_PilotToPermanent.aspx. Accessed July 6, 2018.
- Ramin S. American Board of Obstetrics and Gynecology MOC program. PowerPoint presentation; December 4, 2017.
- Teirstein PS. Boarded to death--why maintenance of certification is bad for doctors and patients. N Engl J Med. 2015;372(2):106-108.
- AMA Council on Medical Education. Executive summary. 2017. https://www.ama-assn.org/sites/default/files/media-browser/public/council-on-med-ed/a18-cme-02.pdf. Accessed July 6, 2018.
- American College of Obstetricians and Gynecologists. ACOG-ABOG joint statement: political interference in physician maintenance of skills threatens women's health care. https://www.acog.org/-/media/Departments/State-Legislative-Activities/2017ACOG-ABMS-MOC-Statement.pdf?dmc=1&ts=20180706T1615538746. Accessed July 6, 2018.
- Letter to Lois Nora, MD, JD. August 18, 2017. https://www.mainemed.com/sites/default/files/content/MOC%20Letter%20082117.pdf. Accessed July 6, 2018.
Title X and proposed changes: Take action now
The facts
Title X, a bill originally passed in 1970 under President Nixon, is the only federal grant program dedicated to providing family planning services as well as other preventive health care to primarily low-income patients. It is estimated that 70% of patients using Title X services are below the federal poverty level and more than 60% are uninsured or underinsured.1
In 2015 alone, Title X clinics served 3.8 million women, preventing 822,300 unintended pregnancies and 277,800 abortions.2 These clinics provide comprehensive family planning services including information, counseling, and referrals for abortion services. Title X clinics do not use the funding to provide abortion care, and no federal funding from Title X has ever been used to pay for abortions.

Proposed rule changes
The Trump Administration has proposed several new rules for Title X grant recipients.
Here are the main changes3:
- There must be a “financial and physical” separation between a clinic that is a Title X grant recipient and a facility where “abortion is a method of family planning.” This would prevent health centers that receive Title X funding from providing abortions at the same facility. This rule would predominantly affect health centers like Planned Parenthood. Although these clinics already have a financial separation from abortion care, there would not be a physical one in most situations and these clinics would lose Title X funding or be forced to stop providing abortion services.
- Providers who work at a clinic that receives Title X funding but provides abortions at a completely different facility may be ineligible for ongoing Title X grant money. In the new changes, “funds may not be used…to support the separate abortion business of Title X grant subrecipient.” The changes also propose to “protect Title X providers” from choosing between the health of their patients and their consciences. It plans to do this by removing the requirement to provide abortion counseling and referral and allows “non-directive” counseling.
- There would also be a requirement to encourage more parental involvement in minors’ decision making. While clinics already discuss parental involvement, the change would seek to increase the encouragement to young patients to involve parents. Most young patients do involve a parent or guardian in their care; however, many Title X clinics serve young patients who seek care confidentially. Patients seek confidential care due to a multitude of reasons, including history of abuse, lack of trust, and intimate partner violence.
- “A Title X project may not perform, promote, refer for, or support abortion as a method of family planning.” Although the rule does not prevent providers from discussing abortions, clinicians could offer little guidance if a patient opts for an abortion. Providers can give a list of “qualified, comprehensive health service providers” but may not disclose which, if any, of the providers perform abortions.
Take action
Title X provides important health care services to low-income, uninsured, and underinsured patients. These proposals put access to comprehensive health care for vulnerable populations at risk. Medical organizations including the American Medical Association and American College of Obstetricians and Gynecologists have made statements against the proposed changes to Title X. As ObGyns, we need to ensure our patients are fully informed and have access to all family planning and preventive health services.
Call or email your local representative and tell them you oppose the changes to Title X. Find your representatives here.
Follow ACOG’s Action Center on protecting Title X, which includes a flyer for your waiting room.
Send a message to the Health and Human Services Secretary. Submit a formal comment through July 31, 2018, on the Federal Registrar website expressing your thoughts with these proposed changes.
- Title X: Helping ensure access to high-quality care. National family planning website. https://www.nationalfamilyplanning.org/document.doc?id=514. Accessed July 25, 2018.
- Publicly Funded Contraceptive Services at U.S. Clinics, 2015. Guttmacher website. https://www.guttmacher.org/article/2018/06/domestic-gag-rule-and-more-administrations-proposed-changes-title-x. Accessed July 25, 2018.
- Compliance with statutory program integrity requirements. Federal register website. https://www.federalregister.gov/documents/2018/06/01/2018-11673/compliance-with-statutory-program-integrity-requirements. Accessed July 25, 2018.
The facts
Title X, a bill originally passed in 1970 under President Nixon, is the only federal grant program dedicated to providing family planning services as well as other preventive health care to primarily low-income patients. It is estimated that 70% of patients using Title X services are below the federal poverty level and more than 60% are uninsured or underinsured.1
In 2015 alone, Title X clinics served 3.8 million women, preventing 822,300 unintended pregnancies and 277,800 abortions.2 These clinics provide comprehensive family planning services including information, counseling, and referrals for abortion services. Title X clinics do not use the funding to provide abortion care, and no federal funding from Title X has ever been used to pay for abortions.

Proposed rule changes
The Trump Administration has proposed several new rules for Title X grant recipients.
Here are the main changes3:
- There must be a “financial and physical” separation between a clinic that is a Title X grant recipient and a facility where “abortion is a method of family planning.” This would prevent health centers that receive Title X funding from providing abortions at the same facility. This rule would predominantly affect health centers like Planned Parenthood. Although these clinics already have a financial separation from abortion care, there would not be a physical one in most situations and these clinics would lose Title X funding or be forced to stop providing abortion services.
- Providers who work at a clinic that receives Title X funding but provides abortions at a completely different facility may be ineligible for ongoing Title X grant money. In the new changes, “funds may not be used…to support the separate abortion business of Title X grant subrecipient.” The changes also propose to “protect Title X providers” from choosing between the health of their patients and their consciences. It plans to do this by removing the requirement to provide abortion counseling and referral and allows “non-directive” counseling.
- There would also be a requirement to encourage more parental involvement in minors’ decision making. While clinics already discuss parental involvement, the change would seek to increase the encouragement to young patients to involve parents. Most young patients do involve a parent or guardian in their care; however, many Title X clinics serve young patients who seek care confidentially. Patients seek confidential care due to a multitude of reasons, including history of abuse, lack of trust, and intimate partner violence.
- “A Title X project may not perform, promote, refer for, or support abortion as a method of family planning.” Although the rule does not prevent providers from discussing abortions, clinicians could offer little guidance if a patient opts for an abortion. Providers can give a list of “qualified, comprehensive health service providers” but may not disclose which, if any, of the providers perform abortions.
Take action
Title X provides important health care services to low-income, uninsured, and underinsured patients. These proposals put access to comprehensive health care for vulnerable populations at risk. Medical organizations including the American Medical Association and American College of Obstetricians and Gynecologists have made statements against the proposed changes to Title X. As ObGyns, we need to ensure our patients are fully informed and have access to all family planning and preventive health services.
Call or email your local representative and tell them you oppose the changes to Title X. Find your representatives here.
Follow ACOG’s Action Center on protecting Title X, which includes a flyer for your waiting room.
Send a message to the Health and Human Services Secretary. Submit a formal comment through July 31, 2018, on the Federal Registrar website expressing your thoughts with these proposed changes.
The facts
Title X, a bill originally passed in 1970 under President Nixon, is the only federal grant program dedicated to providing family planning services as well as other preventive health care to primarily low-income patients. It is estimated that 70% of patients using Title X services are below the federal poverty level and more than 60% are uninsured or underinsured.1
In 2015 alone, Title X clinics served 3.8 million women, preventing 822,300 unintended pregnancies and 277,800 abortions.2 These clinics provide comprehensive family planning services including information, counseling, and referrals for abortion services. Title X clinics do not use the funding to provide abortion care, and no federal funding from Title X has ever been used to pay for abortions.

Proposed rule changes
The Trump Administration has proposed several new rules for Title X grant recipients.
Here are the main changes3:
- There must be a “financial and physical” separation between a clinic that is a Title X grant recipient and a facility where “abortion is a method of family planning.” This would prevent health centers that receive Title X funding from providing abortions at the same facility. This rule would predominantly affect health centers like Planned Parenthood. Although these clinics already have a financial separation from abortion care, there would not be a physical one in most situations and these clinics would lose Title X funding or be forced to stop providing abortion services.
- Providers who work at a clinic that receives Title X funding but provides abortions at a completely different facility may be ineligible for ongoing Title X grant money. In the new changes, “funds may not be used…to support the separate abortion business of Title X grant subrecipient.” The changes also propose to “protect Title X providers” from choosing between the health of their patients and their consciences. It plans to do this by removing the requirement to provide abortion counseling and referral and allows “non-directive” counseling.
- There would also be a requirement to encourage more parental involvement in minors’ decision making. While clinics already discuss parental involvement, the change would seek to increase the encouragement to young patients to involve parents. Most young patients do involve a parent or guardian in their care; however, many Title X clinics serve young patients who seek care confidentially. Patients seek confidential care due to a multitude of reasons, including history of abuse, lack of trust, and intimate partner violence.
- “A Title X project may not perform, promote, refer for, or support abortion as a method of family planning.” Although the rule does not prevent providers from discussing abortions, clinicians could offer little guidance if a patient opts for an abortion. Providers can give a list of “qualified, comprehensive health service providers” but may not disclose which, if any, of the providers perform abortions.
Take action
Title X provides important health care services to low-income, uninsured, and underinsured patients. These proposals put access to comprehensive health care for vulnerable populations at risk. Medical organizations including the American Medical Association and American College of Obstetricians and Gynecologists have made statements against the proposed changes to Title X. As ObGyns, we need to ensure our patients are fully informed and have access to all family planning and preventive health services.
Call or email your local representative and tell them you oppose the changes to Title X. Find your representatives here.
Follow ACOG’s Action Center on protecting Title X, which includes a flyer for your waiting room.
Send a message to the Health and Human Services Secretary. Submit a formal comment through July 31, 2018, on the Federal Registrar website expressing your thoughts with these proposed changes.
- Title X: Helping ensure access to high-quality care. National family planning website. https://www.nationalfamilyplanning.org/document.doc?id=514. Accessed July 25, 2018.
- Publicly Funded Contraceptive Services at U.S. Clinics, 2015. Guttmacher website. https://www.guttmacher.org/article/2018/06/domestic-gag-rule-and-more-administrations-proposed-changes-title-x. Accessed July 25, 2018.
- Compliance with statutory program integrity requirements. Federal register website. https://www.federalregister.gov/documents/2018/06/01/2018-11673/compliance-with-statutory-program-integrity-requirements. Accessed July 25, 2018.
- Title X: Helping ensure access to high-quality care. National family planning website. https://www.nationalfamilyplanning.org/document.doc?id=514. Accessed July 25, 2018.
- Publicly Funded Contraceptive Services at U.S. Clinics, 2015. Guttmacher website. https://www.guttmacher.org/article/2018/06/domestic-gag-rule-and-more-administrations-proposed-changes-title-x. Accessed July 25, 2018.
- Compliance with statutory program integrity requirements. Federal register website. https://www.federalregister.gov/documents/2018/06/01/2018-11673/compliance-with-statutory-program-integrity-requirements. Accessed July 25, 2018.
Credit cards FAQ
After my last column on credit cards, I was (as usual) inundated with questions, comments, and requests for copies of the letter we give to patients explaining our credit card policy.
at www.mdedge.com/edermatologynews. If you have a question not addressed here, feel free to ask, either on the website or via email ([email protected]).
How do you safeguard the credit information you keep on file?
The same way we do medical information; it’s all covered by the same HIPAA rules. If you have an EHR, it can go in the chart with everything else; if not, I suggest a separate portable file that can be locked up each night.
How do you keep the info current, as cards do expire?
We check expiration dates at each visit, and ask for a new number or date if the card has expired or is close.
Don’t your patients object to signing, in effect, a blank check?
They’re not “signing a blank check.” All credit card contracts give cardholders the right to challenge any charge against their account.
There were some initial objections, mostly from devotees of the financial “old school.” But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well, by decreasing the bills they will receive and the checks they must write, most come around.
How do you handle patients who refuse to hand over a number, particularly those who say they have no credit cards?
We used to let refusers slide, but now we’ve made the policy mandatory. Patients who refuse without a good reason are asked, like any patient who refuses to cooperate with any standard office policy, to go elsewhere. Life’s too short. And “I don’t have any credit cards” does not count as a good reason. Nearly everyone has credit cards in this day and age. For the occasional patient who does not have a credit card, my office manager does have authority to make exceptions on a case-by-case basis, however.
One cosmetic surgeon I know asks “no credit card” patients to pay a lawyer-style “retainer,” which is held in escrow, and used to pay receivable amounts as they come due. When presented with that alternative, he told me, most of them suddenly remember that they do have a credit card after all.
What’s the difference between this and “balance billing”?
All the difference in the world. “Balance billing” is billing patients for the difference between your normal fee and the insurer’s authorized payment. If your office has contracted to accept that particular insurance, you can’t do that; but you can bill for the portion of the insurer-determined payment not paid by the insurer. (Many contracts stipulate that you must do so.) For example, your normal fee is $200; the insurer approves $100, and pays 80% of that. The other $20 is the patient’s responsibility, and that is what you charge to the credit card – instead of sending out a statement for that amount.
Since we instituted this policy, one patient has called to ask if it is legal, and one insurance company has inquired about it. How do you respond to such queries?
Of course it’s legal; you are entitled to collect what is owed to you. Ask those patients if they question the legality every time they check into a hotel or rent a car.
We have had no inquiries from insurers, but my response would be that it’s none of their business. Again, you have every right to bill for the patient-owed portion of your fees – in fact, Medicare and many private insurers consider it an illegal “inducement” if you don’t – and third parties have no right to dictate how you can or cannot collect it.
In the past, another popular practice management columnist advised against adopting this policy.
Despite multiple requests from me and others, that columnist – who owns a medical billing company – has never, to my knowledge, offered a single convincing argument in support of that position.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
After my last column on credit cards, I was (as usual) inundated with questions, comments, and requests for copies of the letter we give to patients explaining our credit card policy.
at www.mdedge.com/edermatologynews. If you have a question not addressed here, feel free to ask, either on the website or via email ([email protected]).
How do you safeguard the credit information you keep on file?
The same way we do medical information; it’s all covered by the same HIPAA rules. If you have an EHR, it can go in the chart with everything else; if not, I suggest a separate portable file that can be locked up each night.
How do you keep the info current, as cards do expire?
We check expiration dates at each visit, and ask for a new number or date if the card has expired or is close.
Don’t your patients object to signing, in effect, a blank check?
They’re not “signing a blank check.” All credit card contracts give cardholders the right to challenge any charge against their account.
There were some initial objections, mostly from devotees of the financial “old school.” But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well, by decreasing the bills they will receive and the checks they must write, most come around.
How do you handle patients who refuse to hand over a number, particularly those who say they have no credit cards?
We used to let refusers slide, but now we’ve made the policy mandatory. Patients who refuse without a good reason are asked, like any patient who refuses to cooperate with any standard office policy, to go elsewhere. Life’s too short. And “I don’t have any credit cards” does not count as a good reason. Nearly everyone has credit cards in this day and age. For the occasional patient who does not have a credit card, my office manager does have authority to make exceptions on a case-by-case basis, however.
One cosmetic surgeon I know asks “no credit card” patients to pay a lawyer-style “retainer,” which is held in escrow, and used to pay receivable amounts as they come due. When presented with that alternative, he told me, most of them suddenly remember that they do have a credit card after all.
What’s the difference between this and “balance billing”?
All the difference in the world. “Balance billing” is billing patients for the difference between your normal fee and the insurer’s authorized payment. If your office has contracted to accept that particular insurance, you can’t do that; but you can bill for the portion of the insurer-determined payment not paid by the insurer. (Many contracts stipulate that you must do so.) For example, your normal fee is $200; the insurer approves $100, and pays 80% of that. The other $20 is the patient’s responsibility, and that is what you charge to the credit card – instead of sending out a statement for that amount.
Since we instituted this policy, one patient has called to ask if it is legal, and one insurance company has inquired about it. How do you respond to such queries?
Of course it’s legal; you are entitled to collect what is owed to you. Ask those patients if they question the legality every time they check into a hotel or rent a car.
We have had no inquiries from insurers, but my response would be that it’s none of their business. Again, you have every right to bill for the patient-owed portion of your fees – in fact, Medicare and many private insurers consider it an illegal “inducement” if you don’t – and third parties have no right to dictate how you can or cannot collect it.
In the past, another popular practice management columnist advised against adopting this policy.
Despite multiple requests from me and others, that columnist – who owns a medical billing company – has never, to my knowledge, offered a single convincing argument in support of that position.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
After my last column on credit cards, I was (as usual) inundated with questions, comments, and requests for copies of the letter we give to patients explaining our credit card policy.
at www.mdedge.com/edermatologynews. If you have a question not addressed here, feel free to ask, either on the website or via email ([email protected]).
How do you safeguard the credit information you keep on file?
The same way we do medical information; it’s all covered by the same HIPAA rules. If you have an EHR, it can go in the chart with everything else; if not, I suggest a separate portable file that can be locked up each night.
How do you keep the info current, as cards do expire?
We check expiration dates at each visit, and ask for a new number or date if the card has expired or is close.
Don’t your patients object to signing, in effect, a blank check?
They’re not “signing a blank check.” All credit card contracts give cardholders the right to challenge any charge against their account.
There were some initial objections, mostly from devotees of the financial “old school.” But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well, by decreasing the bills they will receive and the checks they must write, most come around.
How do you handle patients who refuse to hand over a number, particularly those who say they have no credit cards?
We used to let refusers slide, but now we’ve made the policy mandatory. Patients who refuse without a good reason are asked, like any patient who refuses to cooperate with any standard office policy, to go elsewhere. Life’s too short. And “I don’t have any credit cards” does not count as a good reason. Nearly everyone has credit cards in this day and age. For the occasional patient who does not have a credit card, my office manager does have authority to make exceptions on a case-by-case basis, however.
One cosmetic surgeon I know asks “no credit card” patients to pay a lawyer-style “retainer,” which is held in escrow, and used to pay receivable amounts as they come due. When presented with that alternative, he told me, most of them suddenly remember that they do have a credit card after all.
What’s the difference between this and “balance billing”?
All the difference in the world. “Balance billing” is billing patients for the difference between your normal fee and the insurer’s authorized payment. If your office has contracted to accept that particular insurance, you can’t do that; but you can bill for the portion of the insurer-determined payment not paid by the insurer. (Many contracts stipulate that you must do so.) For example, your normal fee is $200; the insurer approves $100, and pays 80% of that. The other $20 is the patient’s responsibility, and that is what you charge to the credit card – instead of sending out a statement for that amount.
Since we instituted this policy, one patient has called to ask if it is legal, and one insurance company has inquired about it. How do you respond to such queries?
Of course it’s legal; you are entitled to collect what is owed to you. Ask those patients if they question the legality every time they check into a hotel or rent a car.
We have had no inquiries from insurers, but my response would be that it’s none of their business. Again, you have every right to bill for the patient-owed portion of your fees – in fact, Medicare and many private insurers consider it an illegal “inducement” if you don’t – and third parties have no right to dictate how you can or cannot collect it.
In the past, another popular practice management columnist advised against adopting this policy.
Despite multiple requests from me and others, that columnist – who owns a medical billing company – has never, to my knowledge, offered a single convincing argument in support of that position.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Stop extending credit
For as long as I have been writing this column, I have stressed that ; and yet, all these years later, AR is still the subject that generates the most questions.
Okay; let’s go over it one more time: Basically, physicians extend more credit than any business except banks. Despite what you may have read recently, banks are good at it, and they charge interest (and a myriad of fees) to do it. Doctors do it for free. Are we crazy? No business owner in his or her right mind allows customers to take away goods or services without paying for them; but doctors do it every day.
What to do? Common sense tells you to collect everything you can at the time of service; but some patients inevitably brandish the old “I forgot my checkbook” excuse and escape without paying. And the patient-owed portion of most insurance charges is often unknown, and unknowable, at the time of service.
That means you’ll need to send a bill; and every bill you send (or hire somebody to send) costs you a bundle. And when it arrives, it goes right to the bottom of your patient’s payment priority list. That is, each month your patients will pay their electric, water, gas, and telephone bills … and just about any other bill ... before getting around to yours. If there is no more money when your bill finally surfaces, that’s just too bad. The electric company can shut off their power; what can you do?
What we do is what every hotel, rental car agency, and many other businesses have done for years: We ask for a credit card number, keep it on file, and bill balances to it as they come in. Plastic runs the show everywhere you go – except in most medical offices.
New patients in my office receive a letter at their first visit explaining our policy. At the bottom is a brief consent for the patient to sign, and a place to write the credit card number and expiration date. (See below for a copy of our letter; feel free to use it as a template for creating your own.)
Do patients object? Some do – mostly older people, and fewer each year. But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well by decreasing the bills they will receive and the checks they must write, most come around. Make it an option at first if you wish; then, when everyone is accustomed to it, you can make it mandatory.
Do patients worry about confidentiality, or unauthorized use? They don’t anywhere else. They think nothing of handing a card to a waiter or waitress in a restaurant with no thought of what he or she might do with it in the kitchen. They hand cards over to hotel clerks, and never think to ask how long they keep the information or who has access to it. They blithely shoot their numbers into black holes on the Internet. We explain that we guard our patients’ financial information as carefully as we do their medical information. (If you have EHR, it can go in the chart with everything else; if not, I suggest a separate portable Rolodex-type file that can be locked up each night.)
Does it work? In only a year, our accounts receivable totals dropped by nearly 50%; after another year, they stabilized at 30%-35% of previous levels and have remained there ever since. When my accountant retired a few years ago, I hired a new one. Something must be wrong, he said nervously, after his first look at our books; AR totals are “never” that low in a practice with our level of volume. His eyes widened as I explained our system. “Why doesn’t every medical office do that?” he asked.
Why indeed? The business of health care delivery is being rocked to its very foundations as we speak. In my humble opinion, private practice will only survive those changes if physicians learn to do more of what we do best – treating patients – and leave the business of extending credit to the banks.
Patient consent form
This generic letter is intended to be used as an example for a letter you might draft for a similar purpose. We take no responsibility for your use of its content, either verbatim or altered, or for any inappropriate usage. Click on the attachment below for a printable copy of the letter.
To Our Patients:
As you know if you have ever checked into a hotel or rented a car, the first thing you are asked for is a credit card, which is imprinted and later used to pay your bill. This is an advantage for both you and the hotel or rental company, since it makes checkout easier, faster, and more efficient.
We have implemented a similar policy. You will be asked for a credit card number at the time you check in and the information will be held securely until your insurances have paid their portion and notified us of the amount of your share. At that time, any remaining balance owed by you will be charged to your credit card, and a copy of the charge will be mailed to you.
This will be an advantage to you, since you will no longer have to write out and mail us checks. It will be an advantage to us as well, since it will greatly decrease the number of statements that we have to generate and send out. The combination will benefit everybody in helping to keep the cost of health care down.
This in no way will compromise your ability to dispute a charge or question your insurance company’s determination of payment.
Copays due at the time of the visit will, of course, still be due at the time of the visit.
If you have any questions about this payment method, do not hesitate to ask.
Sincerely yours,
I authorize ********************, PA to charge outstanding balances on my account to the following credit card:
Visa Mastercard American Express Other: ____________________________
Account number _______________________Expiration Date ____________CVV_____
Name on card (please print) _________________________________________________
Signature _____________________________________ Date ______________________
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
For as long as I have been writing this column, I have stressed that ; and yet, all these years later, AR is still the subject that generates the most questions.
Okay; let’s go over it one more time: Basically, physicians extend more credit than any business except banks. Despite what you may have read recently, banks are good at it, and they charge interest (and a myriad of fees) to do it. Doctors do it for free. Are we crazy? No business owner in his or her right mind allows customers to take away goods or services without paying for them; but doctors do it every day.
What to do? Common sense tells you to collect everything you can at the time of service; but some patients inevitably brandish the old “I forgot my checkbook” excuse and escape without paying. And the patient-owed portion of most insurance charges is often unknown, and unknowable, at the time of service.
That means you’ll need to send a bill; and every bill you send (or hire somebody to send) costs you a bundle. And when it arrives, it goes right to the bottom of your patient’s payment priority list. That is, each month your patients will pay their electric, water, gas, and telephone bills … and just about any other bill ... before getting around to yours. If there is no more money when your bill finally surfaces, that’s just too bad. The electric company can shut off their power; what can you do?
What we do is what every hotel, rental car agency, and many other businesses have done for years: We ask for a credit card number, keep it on file, and bill balances to it as they come in. Plastic runs the show everywhere you go – except in most medical offices.
New patients in my office receive a letter at their first visit explaining our policy. At the bottom is a brief consent for the patient to sign, and a place to write the credit card number and expiration date. (See below for a copy of our letter; feel free to use it as a template for creating your own.)
Do patients object? Some do – mostly older people, and fewer each year. But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well by decreasing the bills they will receive and the checks they must write, most come around. Make it an option at first if you wish; then, when everyone is accustomed to it, you can make it mandatory.
Do patients worry about confidentiality, or unauthorized use? They don’t anywhere else. They think nothing of handing a card to a waiter or waitress in a restaurant with no thought of what he or she might do with it in the kitchen. They hand cards over to hotel clerks, and never think to ask how long they keep the information or who has access to it. They blithely shoot their numbers into black holes on the Internet. We explain that we guard our patients’ financial information as carefully as we do their medical information. (If you have EHR, it can go in the chart with everything else; if not, I suggest a separate portable Rolodex-type file that can be locked up each night.)
Does it work? In only a year, our accounts receivable totals dropped by nearly 50%; after another year, they stabilized at 30%-35% of previous levels and have remained there ever since. When my accountant retired a few years ago, I hired a new one. Something must be wrong, he said nervously, after his first look at our books; AR totals are “never” that low in a practice with our level of volume. His eyes widened as I explained our system. “Why doesn’t every medical office do that?” he asked.
Why indeed? The business of health care delivery is being rocked to its very foundations as we speak. In my humble opinion, private practice will only survive those changes if physicians learn to do more of what we do best – treating patients – and leave the business of extending credit to the banks.
Patient consent form
This generic letter is intended to be used as an example for a letter you might draft for a similar purpose. We take no responsibility for your use of its content, either verbatim or altered, or for any inappropriate usage. Click on the attachment below for a printable copy of the letter.
To Our Patients:
As you know if you have ever checked into a hotel or rented a car, the first thing you are asked for is a credit card, which is imprinted and later used to pay your bill. This is an advantage for both you and the hotel or rental company, since it makes checkout easier, faster, and more efficient.
We have implemented a similar policy. You will be asked for a credit card number at the time you check in and the information will be held securely until your insurances have paid their portion and notified us of the amount of your share. At that time, any remaining balance owed by you will be charged to your credit card, and a copy of the charge will be mailed to you.
This will be an advantage to you, since you will no longer have to write out and mail us checks. It will be an advantage to us as well, since it will greatly decrease the number of statements that we have to generate and send out. The combination will benefit everybody in helping to keep the cost of health care down.
This in no way will compromise your ability to dispute a charge or question your insurance company’s determination of payment.
Copays due at the time of the visit will, of course, still be due at the time of the visit.
If you have any questions about this payment method, do not hesitate to ask.
Sincerely yours,
I authorize ********************, PA to charge outstanding balances on my account to the following credit card:
Visa Mastercard American Express Other: ____________________________
Account number _______________________Expiration Date ____________CVV_____
Name on card (please print) _________________________________________________
Signature _____________________________________ Date ______________________
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
For as long as I have been writing this column, I have stressed that ; and yet, all these years later, AR is still the subject that generates the most questions.
Okay; let’s go over it one more time: Basically, physicians extend more credit than any business except banks. Despite what you may have read recently, banks are good at it, and they charge interest (and a myriad of fees) to do it. Doctors do it for free. Are we crazy? No business owner in his or her right mind allows customers to take away goods or services without paying for them; but doctors do it every day.
What to do? Common sense tells you to collect everything you can at the time of service; but some patients inevitably brandish the old “I forgot my checkbook” excuse and escape without paying. And the patient-owed portion of most insurance charges is often unknown, and unknowable, at the time of service.
That means you’ll need to send a bill; and every bill you send (or hire somebody to send) costs you a bundle. And when it arrives, it goes right to the bottom of your patient’s payment priority list. That is, each month your patients will pay their electric, water, gas, and telephone bills … and just about any other bill ... before getting around to yours. If there is no more money when your bill finally surfaces, that’s just too bad. The electric company can shut off their power; what can you do?
What we do is what every hotel, rental car agency, and many other businesses have done for years: We ask for a credit card number, keep it on file, and bill balances to it as they come in. Plastic runs the show everywhere you go – except in most medical offices.
New patients in my office receive a letter at their first visit explaining our policy. At the bottom is a brief consent for the patient to sign, and a place to write the credit card number and expiration date. (See below for a copy of our letter; feel free to use it as a template for creating your own.)
Do patients object? Some do – mostly older people, and fewer each year. But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well by decreasing the bills they will receive and the checks they must write, most come around. Make it an option at first if you wish; then, when everyone is accustomed to it, you can make it mandatory.
Do patients worry about confidentiality, or unauthorized use? They don’t anywhere else. They think nothing of handing a card to a waiter or waitress in a restaurant with no thought of what he or she might do with it in the kitchen. They hand cards over to hotel clerks, and never think to ask how long they keep the information or who has access to it. They blithely shoot their numbers into black holes on the Internet. We explain that we guard our patients’ financial information as carefully as we do their medical information. (If you have EHR, it can go in the chart with everything else; if not, I suggest a separate portable Rolodex-type file that can be locked up each night.)
Does it work? In only a year, our accounts receivable totals dropped by nearly 50%; after another year, they stabilized at 30%-35% of previous levels and have remained there ever since. When my accountant retired a few years ago, I hired a new one. Something must be wrong, he said nervously, after his first look at our books; AR totals are “never” that low in a practice with our level of volume. His eyes widened as I explained our system. “Why doesn’t every medical office do that?” he asked.
Why indeed? The business of health care delivery is being rocked to its very foundations as we speak. In my humble opinion, private practice will only survive those changes if physicians learn to do more of what we do best – treating patients – and leave the business of extending credit to the banks.
Patient consent form
This generic letter is intended to be used as an example for a letter you might draft for a similar purpose. We take no responsibility for your use of its content, either verbatim or altered, or for any inappropriate usage. Click on the attachment below for a printable copy of the letter.
To Our Patients:
As you know if you have ever checked into a hotel or rented a car, the first thing you are asked for is a credit card, which is imprinted and later used to pay your bill. This is an advantage for both you and the hotel or rental company, since it makes checkout easier, faster, and more efficient.
We have implemented a similar policy. You will be asked for a credit card number at the time you check in and the information will be held securely until your insurances have paid their portion and notified us of the amount of your share. At that time, any remaining balance owed by you will be charged to your credit card, and a copy of the charge will be mailed to you.
This will be an advantage to you, since you will no longer have to write out and mail us checks. It will be an advantage to us as well, since it will greatly decrease the number of statements that we have to generate and send out. The combination will benefit everybody in helping to keep the cost of health care down.
This in no way will compromise your ability to dispute a charge or question your insurance company’s determination of payment.
Copays due at the time of the visit will, of course, still be due at the time of the visit.
If you have any questions about this payment method, do not hesitate to ask.
Sincerely yours,
I authorize ********************, PA to charge outstanding balances on my account to the following credit card:
Visa Mastercard American Express Other: ____________________________
Account number _______________________Expiration Date ____________CVV_____
Name on card (please print) _________________________________________________
Signature _____________________________________ Date ______________________
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
Supreme Court case NIFLA v Becerra: What you need to know
On March 20, 2018, the United States Supreme Court heard arguments in National Institute of Family and Life Advocates (NIFLA) v Becerra. The Court is expected to issue its decision in June and the results could shape legislation around the country. Here is what you need to know.
The background
There are more than 4,000 Crisis Pregnancy Centers (CPCs) around the country, vastly out numbering abortion clinics.1 The services offered and the make-up of the staff who work in CPCs can vary. CPCs can be licensed to provide medical services, including urine pregnancy tests and ultrasounds, and may have clinicians on staff. Alternatively, other CPCs may be volunteer-run and provide counseling as well as supplies for women, including diapers and baby formula. Within CPCs, however, women are often given misleading and medically inaccurate information about abortion and contraception and are not provided with appropriate or timely referrals if they seek abortion care.
To ensure women have access to comprehensive reproductive health services, California passed the Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act in 2015. This act requires licensed clinics — which may include some CPCs — to notify patients that they may access state-funded prenatal care, family planning, and abortion services through a county health department phone number. Additionally, facilities that provide pregnancy testing and ultrasounds are required to notify clients if they do not employ a licensed medical professional.
In response, NIFLA sued the state of California, alleging that the law violated their freedom of speech by forcing them to communicate about abortion with women who visited their centers.
The case
NIFLA argues that California is violating CPCs’ freedom of speech by requiring them to post statements about medications and medical procedures they strongly oppose. According to NIFLA, if California wants to promote state-funded options, they should publicize that information and not require the CPCs to post it.
The State of California enacted the law to ensure that California women have timely access to all available health care services, including contraception and abortion, and are made aware that the clinic they visit does not offer licensed medical care. Women may not know of their publicly funded options and, without this law, CPCs could withhold that information or provide misleading information, delaying or preventing women from accessing care.
Possible outcomes
If the Supreme Court strikes down California’s FACT Act as a violation of the First Amendment, CPCs in that state would not be required to provide information about free or low-cost prenatal care, contraception, and abortion services or post, if appropriate, that they were an unlicensed facility. However, such a ruling could call into question laws in 18 other states that require doctors to give women false information about possible side effects and complications of abortion during the consent process. This case could provide precedent for physicians to assert that such requirements violate their freedom of speech.
If the Supreme Court upholds California’s FACT Act, this would likely lead to similar laws around the country requiring CPCs to disclose the availability of affordable contraception and abortion services in their state and the lack of licensed medical providers.
For more information, check out https://www.supremecourt.gov/
Acknowledgement
Special thanks to Sara Needleman Kline, Esq, Chief Legal Officer, American College of Obstetricians and Gynecologists, for aid with this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Dias E. The Abortion Battleground: Crisis Pregnancy Centers. Time Magazine. http://content.time.com/time/nation/article/0,8599,2008846,00.html. Published August 5, 2010. Accessed May 16, 2018.
On March 20, 2018, the United States Supreme Court heard arguments in National Institute of Family and Life Advocates (NIFLA) v Becerra. The Court is expected to issue its decision in June and the results could shape legislation around the country. Here is what you need to know.
The background
There are more than 4,000 Crisis Pregnancy Centers (CPCs) around the country, vastly out numbering abortion clinics.1 The services offered and the make-up of the staff who work in CPCs can vary. CPCs can be licensed to provide medical services, including urine pregnancy tests and ultrasounds, and may have clinicians on staff. Alternatively, other CPCs may be volunteer-run and provide counseling as well as supplies for women, including diapers and baby formula. Within CPCs, however, women are often given misleading and medically inaccurate information about abortion and contraception and are not provided with appropriate or timely referrals if they seek abortion care.
To ensure women have access to comprehensive reproductive health services, California passed the Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act in 2015. This act requires licensed clinics — which may include some CPCs — to notify patients that they may access state-funded prenatal care, family planning, and abortion services through a county health department phone number. Additionally, facilities that provide pregnancy testing and ultrasounds are required to notify clients if they do not employ a licensed medical professional.
In response, NIFLA sued the state of California, alleging that the law violated their freedom of speech by forcing them to communicate about abortion with women who visited their centers.
The case
NIFLA argues that California is violating CPCs’ freedom of speech by requiring them to post statements about medications and medical procedures they strongly oppose. According to NIFLA, if California wants to promote state-funded options, they should publicize that information and not require the CPCs to post it.
The State of California enacted the law to ensure that California women have timely access to all available health care services, including contraception and abortion, and are made aware that the clinic they visit does not offer licensed medical care. Women may not know of their publicly funded options and, without this law, CPCs could withhold that information or provide misleading information, delaying or preventing women from accessing care.
Possible outcomes
If the Supreme Court strikes down California’s FACT Act as a violation of the First Amendment, CPCs in that state would not be required to provide information about free or low-cost prenatal care, contraception, and abortion services or post, if appropriate, that they were an unlicensed facility. However, such a ruling could call into question laws in 18 other states that require doctors to give women false information about possible side effects and complications of abortion during the consent process. This case could provide precedent for physicians to assert that such requirements violate their freedom of speech.
If the Supreme Court upholds California’s FACT Act, this would likely lead to similar laws around the country requiring CPCs to disclose the availability of affordable contraception and abortion services in their state and the lack of licensed medical providers.
For more information, check out https://www.supremecourt.gov/
Acknowledgement
Special thanks to Sara Needleman Kline, Esq, Chief Legal Officer, American College of Obstetricians and Gynecologists, for aid with this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
On March 20, 2018, the United States Supreme Court heard arguments in National Institute of Family and Life Advocates (NIFLA) v Becerra. The Court is expected to issue its decision in June and the results could shape legislation around the country. Here is what you need to know.
The background
There are more than 4,000 Crisis Pregnancy Centers (CPCs) around the country, vastly out numbering abortion clinics.1 The services offered and the make-up of the staff who work in CPCs can vary. CPCs can be licensed to provide medical services, including urine pregnancy tests and ultrasounds, and may have clinicians on staff. Alternatively, other CPCs may be volunteer-run and provide counseling as well as supplies for women, including diapers and baby formula. Within CPCs, however, women are often given misleading and medically inaccurate information about abortion and contraception and are not provided with appropriate or timely referrals if they seek abortion care.
To ensure women have access to comprehensive reproductive health services, California passed the Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act in 2015. This act requires licensed clinics — which may include some CPCs — to notify patients that they may access state-funded prenatal care, family planning, and abortion services through a county health department phone number. Additionally, facilities that provide pregnancy testing and ultrasounds are required to notify clients if they do not employ a licensed medical professional.
In response, NIFLA sued the state of California, alleging that the law violated their freedom of speech by forcing them to communicate about abortion with women who visited their centers.
The case
NIFLA argues that California is violating CPCs’ freedom of speech by requiring them to post statements about medications and medical procedures they strongly oppose. According to NIFLA, if California wants to promote state-funded options, they should publicize that information and not require the CPCs to post it.
The State of California enacted the law to ensure that California women have timely access to all available health care services, including contraception and abortion, and are made aware that the clinic they visit does not offer licensed medical care. Women may not know of their publicly funded options and, without this law, CPCs could withhold that information or provide misleading information, delaying or preventing women from accessing care.
Possible outcomes
If the Supreme Court strikes down California’s FACT Act as a violation of the First Amendment, CPCs in that state would not be required to provide information about free or low-cost prenatal care, contraception, and abortion services or post, if appropriate, that they were an unlicensed facility. However, such a ruling could call into question laws in 18 other states that require doctors to give women false information about possible side effects and complications of abortion during the consent process. This case could provide precedent for physicians to assert that such requirements violate their freedom of speech.
If the Supreme Court upholds California’s FACT Act, this would likely lead to similar laws around the country requiring CPCs to disclose the availability of affordable contraception and abortion services in their state and the lack of licensed medical providers.
For more information, check out https://www.supremecourt.gov/
Acknowledgement
Special thanks to Sara Needleman Kline, Esq, Chief Legal Officer, American College of Obstetricians and Gynecologists, for aid with this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Dias E. The Abortion Battleground: Crisis Pregnancy Centers. Time Magazine. http://content.time.com/time/nation/article/0,8599,2008846,00.html. Published August 5, 2010. Accessed May 16, 2018.
- Dias E. The Abortion Battleground: Crisis Pregnancy Centers. Time Magazine. http://content.time.com/time/nation/article/0,8599,2008846,00.html. Published August 5, 2010. Accessed May 16, 2018.